Table of Contents
Definition / general | Essential features | Physiology | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hashimoto H. Histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorhistology.html. Accessed April 26th, 2024.
Definition / general
- Lung: organ participating in and in charge of respiration, namely, gas exchange
- Lung histology: basic microscopic structures of the unaffected lung (i.e. nonneoplastic, noninflammatory and nondegenerated lung tissue)
Essential features
- Bronchus has cartilage and bronchial glands, while bronchiole lacks them (Mills: Histology for Pathologists, 5th Edition, 2019)
- Bronchi and bronchioles up to terminal bronchioles are pure conducting airways, while respiratory bronchioles and alveoli play a role in gas exchange
- There are 2 different definitions of a lobule (secondary lobule), namely, Miller's definition and Reid's definition (Radiology 2006;239:322)
- Miller: small lung units separated by interlobular septa and pulmonary veins, according to lung anatomy (Radiology 2006;239:322)
- Reid: an approximately equal sized unit (about 10 mm in diameter) of areas containing 3 to 5 acini, regardless of the interlobular septum, on the basis of bronchography (Radiology 2006;239:322)
- The term "primary pulmonary lobule," which indicates alveolar structures distal to respiratory bronchioles, is not commonly used; therefore, a lobule usually means a secondary lobule (Radiology 2006;239:322)
- Pulmonary acinus is defined as the largest unit participating in gas exchange, although there are different definitions of acinus (Radiology 2006;239:322)
- One definition of the acinus is a lung unit supplied by a single terminal bronchiole; the other is a lung unit supplied by a respiratory bronchiole
Physiology
- Ciliated cell: transports foreign bodies and mucous stream from the bronchus or bronchiole toward the proximal airway (Mills: Histology for Pathologists, 5th Edition, 2019)
- Mucous cell (goblet cell): secretes sulfomucin
- Basal cell: acts as a stem cell differentiating into other cells
- Neuroendocrine cell (Kulchitsky cell): secretes hormones (e.g. catecholamine, serotonin and gastrin releasing peptide) (Lowe: Stevens & Lowe's Human Histology, 4th Edition, 2014)
- Club cell (formerly Clara cell): plays a key role in lung remodeling, secretes surfactant and repairs airway epithelium
- Type I alveolar epithelium: responsible for respiration; namely, taking oxygen from the outside into the body and transporting carbon dioxide in the opposite direction
- Type II alveolar epithelium: secretes surfactant and plays a role as a precursor cell of type I alveolar epithelium (Lung Cancer 1994;10:S53)
- Pulmonary artery: supplies hypooxgenic blood into the lung in order to exchange the gas between airway and blood
- Bronchial artery: feeds bronchial wall, bronchiole wall and other connective tissue except alveolar septum with oxygen rich blood (Pawlina: Histology - A Text and Atlas, 8th Edition, 2018)
- Pulmonary vein: transports oxygen rich blood from the lungs to the left atrium
- Lymphatics: dual system, namely, flow along bronchovascular bundle from hilum and flow along interlobular septum from visceral pleura
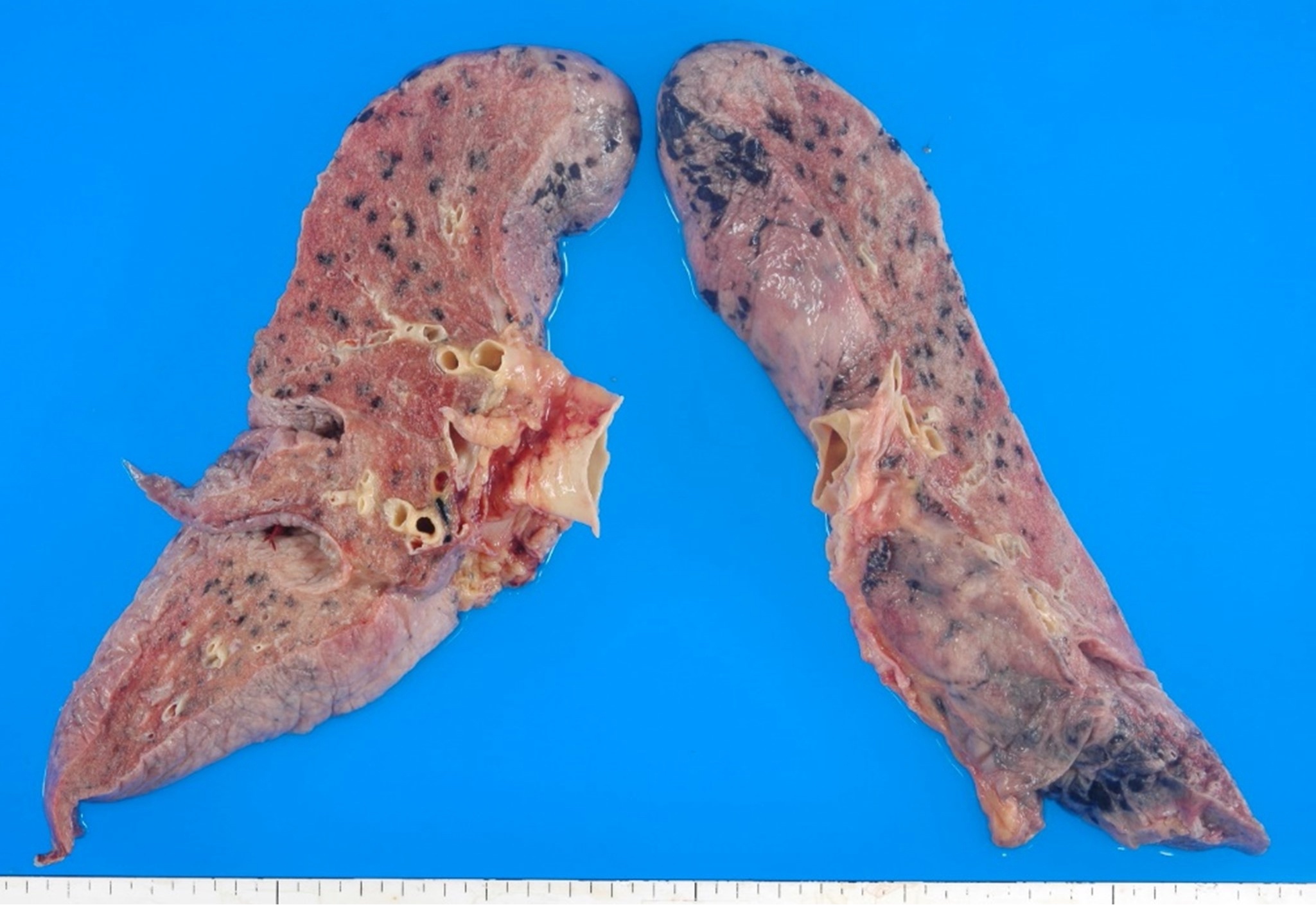
Gross description
- Location: periphery of the pulmonary hilum
- Lungs consist of the branched bronchus (airways) and vasculatures
- Broncho (bronchiolo) vascular bundle: includes bronchus (bronchiole) and pulmonary artery (peripheral branch) located in the center of pulmonary lobe (or lobule)
- Pulmonary vein: located in the interlobular septum (Katzenstein: Diagnostic Atlas of Non-Neoplastic Lung Disease, 1st Edition, 2016)
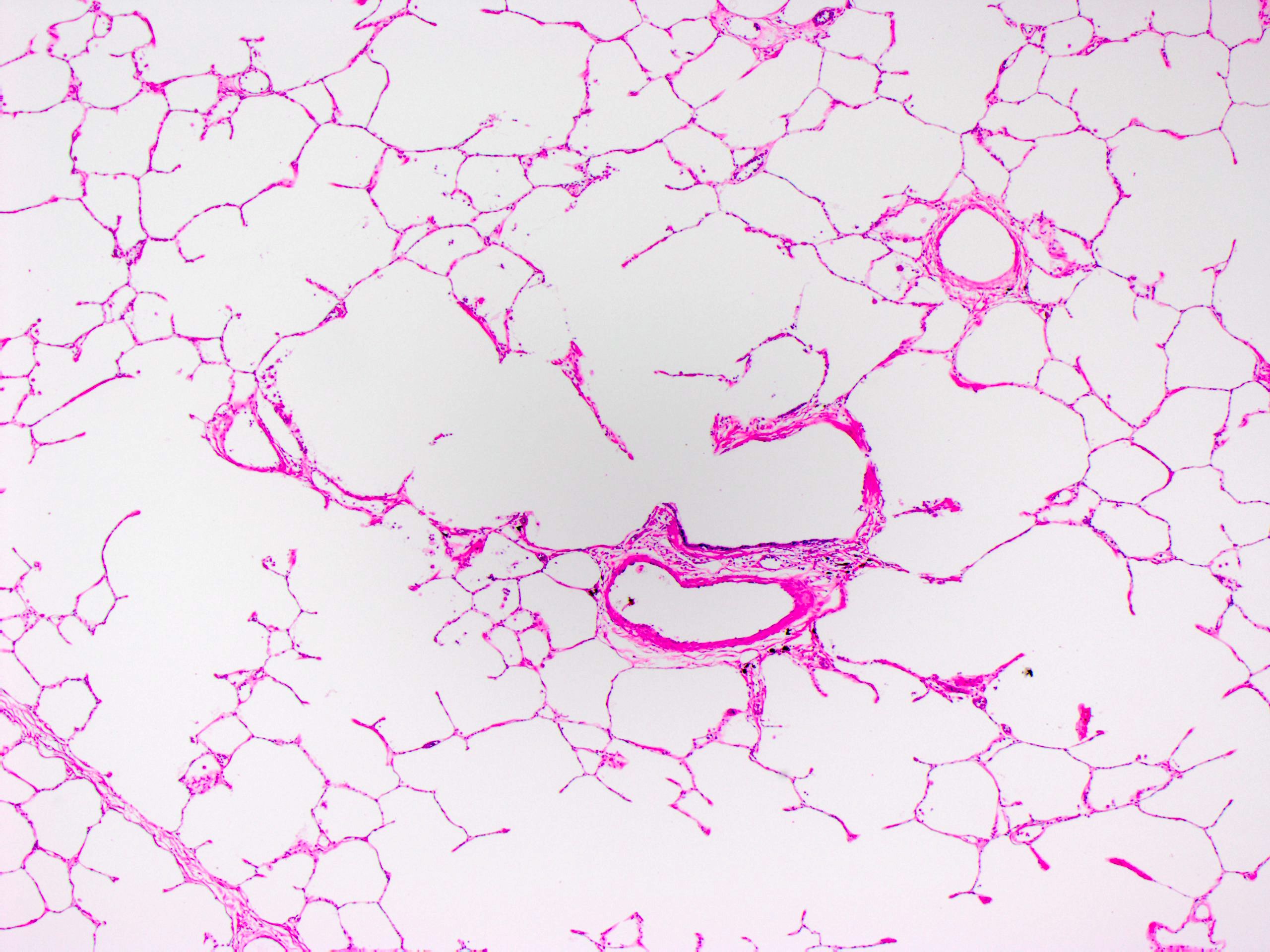
- Peripheral lung: shows sponge-like appearance with fine wall reflecting the microscopic appearance of alveoli
Microscopic (histologic) description
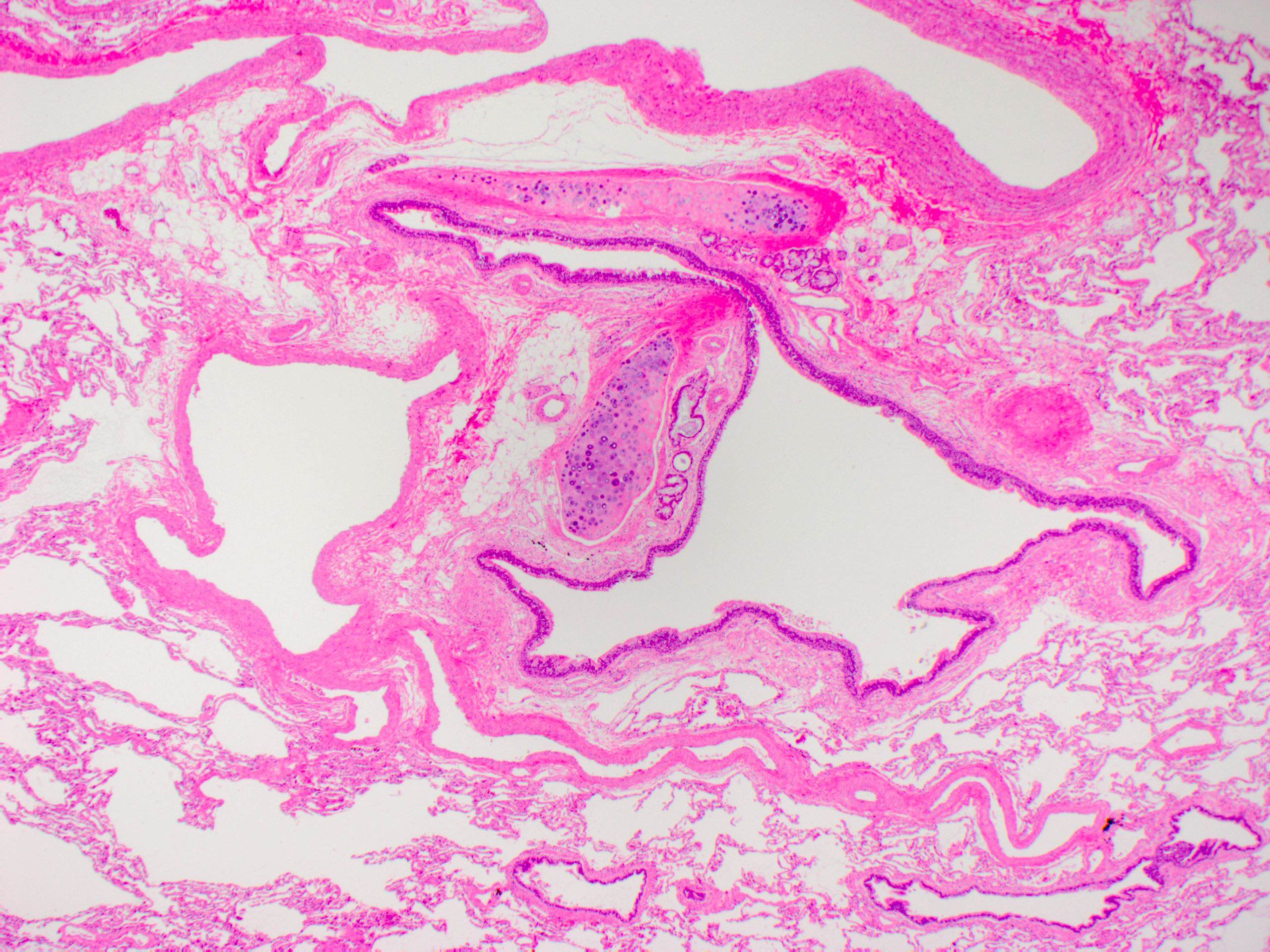
- Bronchus:
- Airway lined by pseudostratified ciliated epithelium
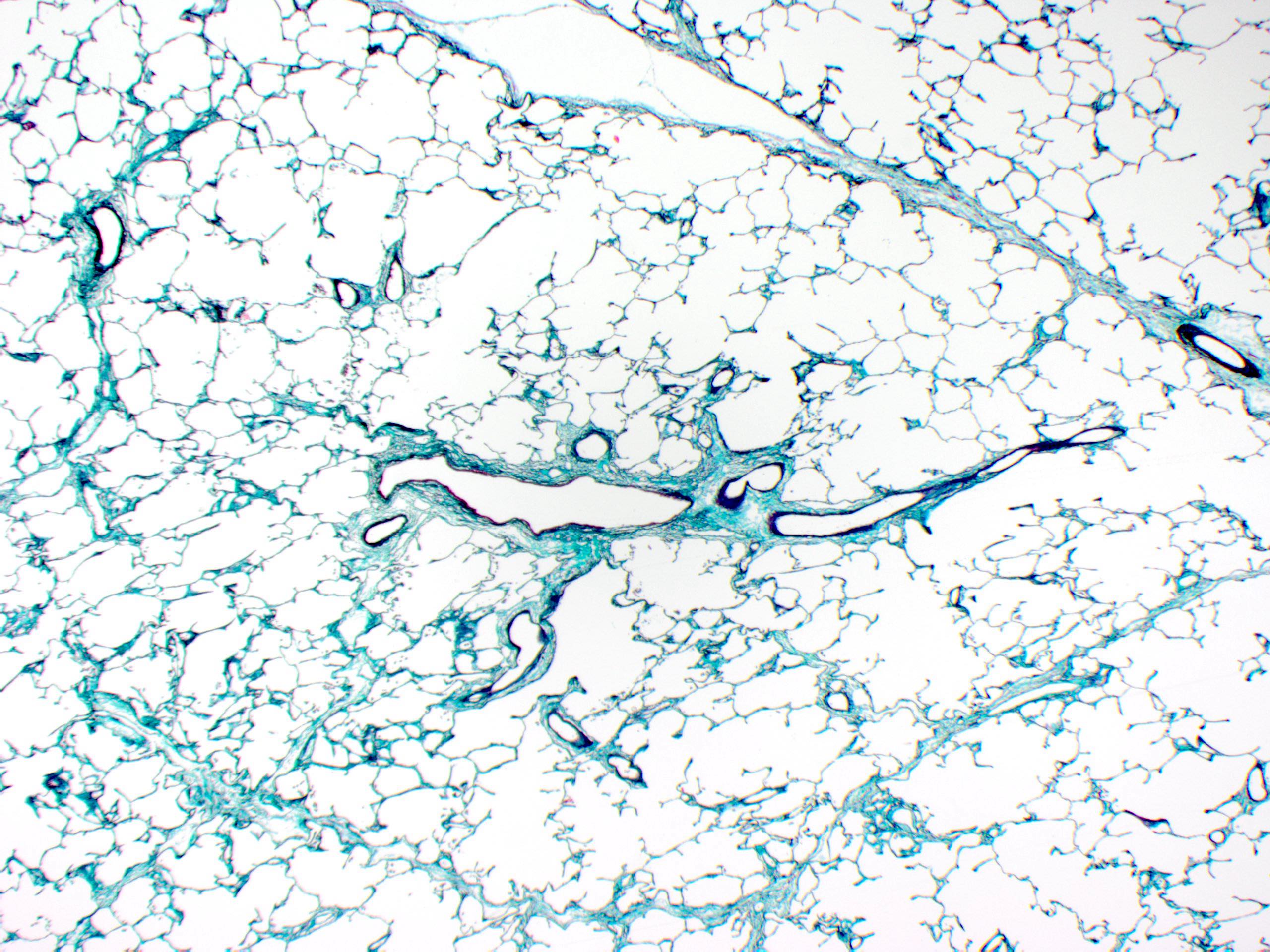
- Mucosal and submucosal layer are separated by elastic membrane confirmed by elastic staining (e.g. elastica Masson staining and elastica van Gieson staining), although it is not clearly observed by H&E staining alone
- Bronchial glands exist in the submucosa; cartilage and annular muscular layer exist in the wall between submucosa and adventitia
- References: Pawlina: Histology - A Text and Atlas, 8th Edition, 2018, Lowe: Stevens & Lowe's Human Histology, 4th Edition, 2014
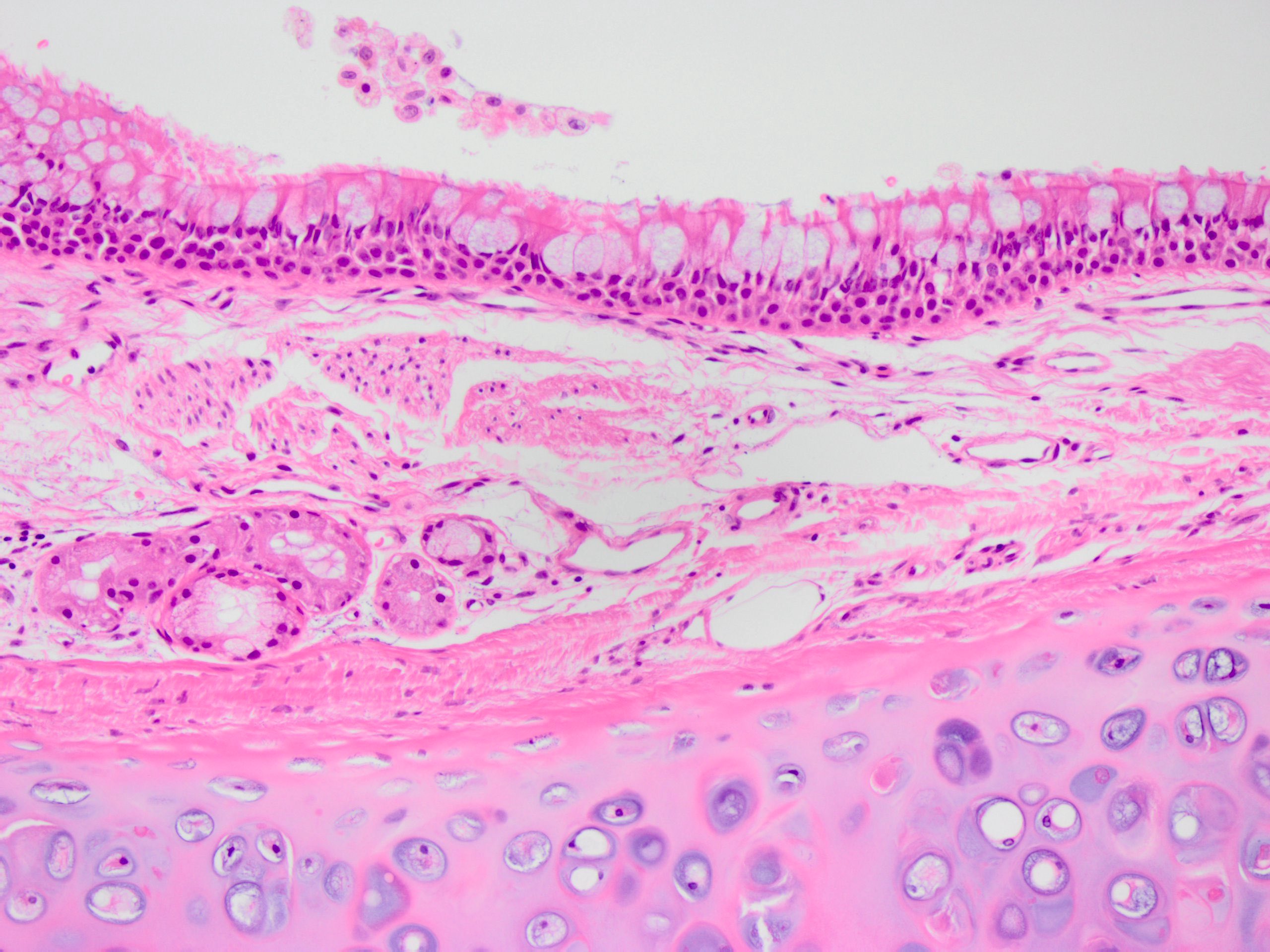
- Bronchiole:
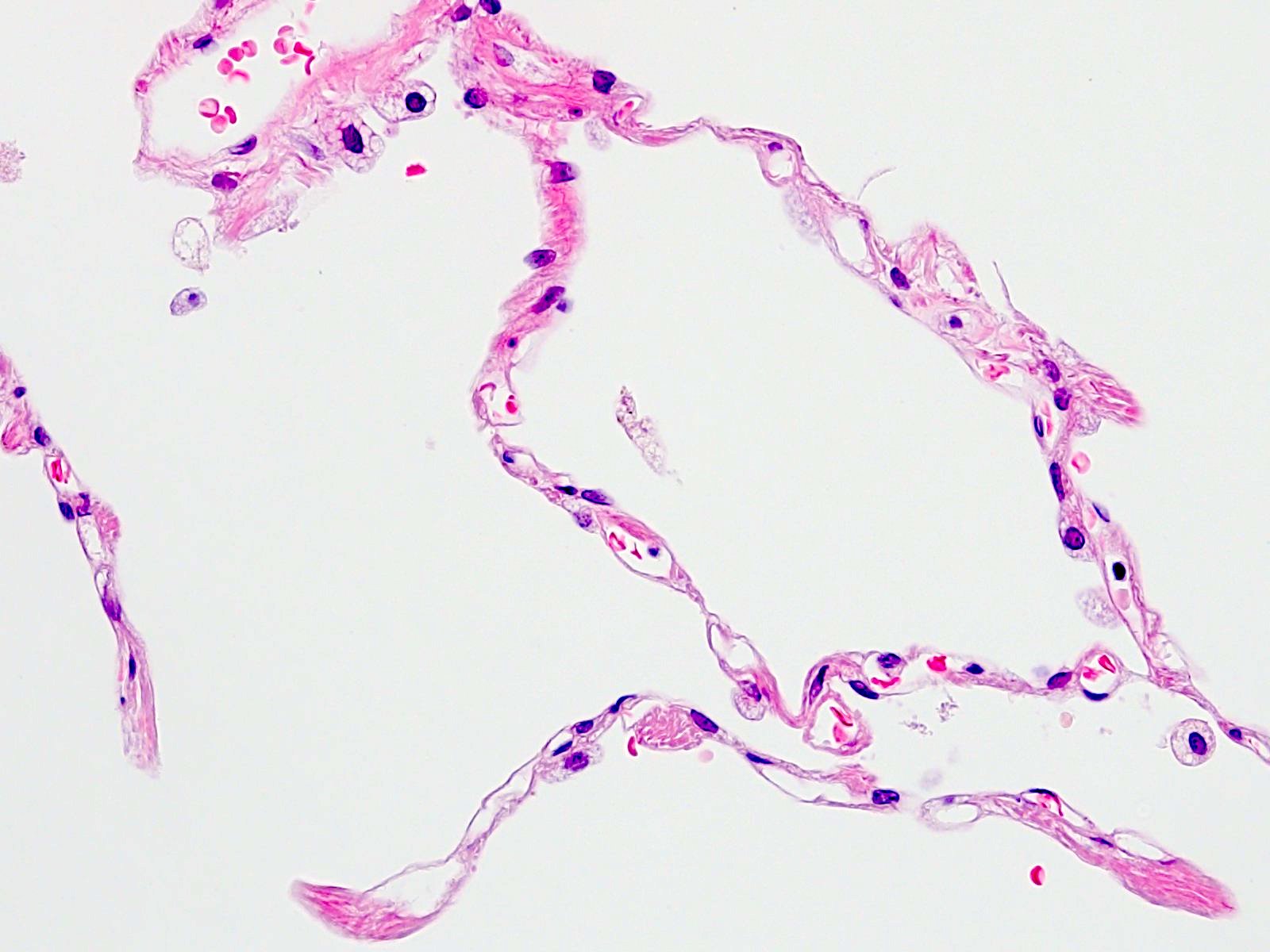
- Small airway, usually 1 mm in diameter or less, lined by single layer of ciliated epithelium
- Lacks bronchial glands and cartilage
- Ciliated cell:
- Tall columnar epithelium, with cilia on the edge of airway side
- Height becomes shorter as bronchiole heads toward periphery
- Reference: Mills: Histology for Pathologists, 5th Edition, 2019
- Mucous cell (goblet cell):
- Tall columnar epithelium with clear cytoplasm containing mucin, lacking cilia
- Basal cell:
- Laying on the basal membrane of bronchus or bronchiole with high nucleocytoplasmic ratio (Lung Cancer 1994;10:S53)
- Neuroendocrine cell (Kulchitsky cell):
- Laying scattered on the basal membrane with granular scant cytoplasm and relatively high nucleocytoplasmic ratio
- Usually difficult to distinguish from basal cell only by H&E staining
- Club cell (formerly Clara cell):
- Toll epithelial cell, no cytoplasmic mucin, no cilia
- Number of club cells increase as bronchiole heads toward periphery
- Bronchial gland:
- Mixed gland composed of both serous and mucinous epithelium
- Its duct opens to bronchial lumen
- Interlobular septum:
- Fibrous tissue separating Miller's secondary lung lobule, which contains pulmonary vein and lymphatic vessel
- Note that not every secondary lobule is separated by this septum
- Bronchovascular bundle:
- Fibrous tissue connecting from pulmonary hilum, which contains bronchus, pulmonary artery, bronchial artery and lymphatic vessel
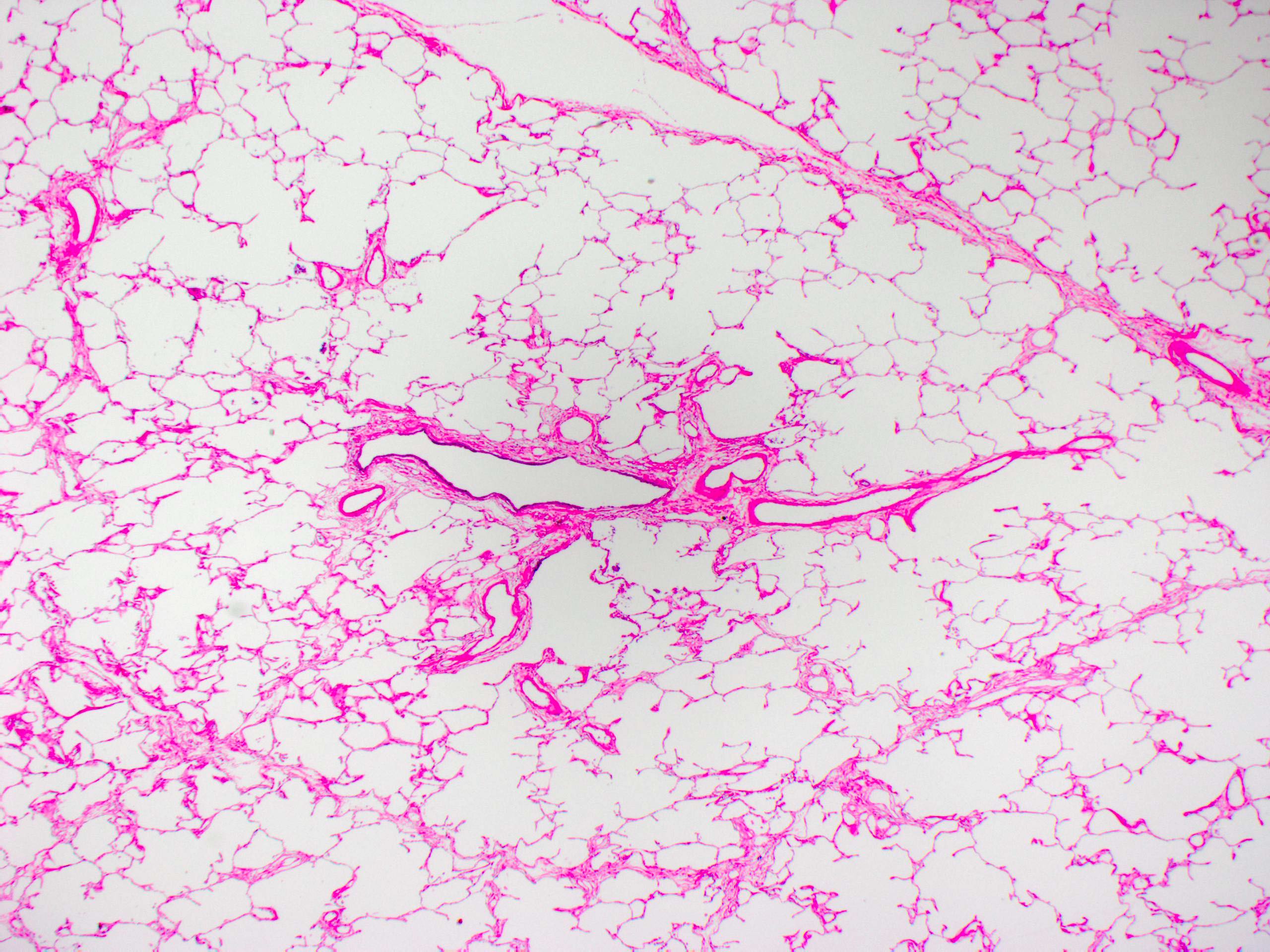
- Alveolar duct:
- Terminal airway opening to alveolus, of which alveolar entrance rings constitute the walls
- Alveolar entrance rings contain elastic fibers and smooth muscles
- Alveolus:
- Sac-like structure lined by alveolar epithelium
- Alveolar septum contains pulmonary capillaries
- Strictly speaking, alveolar structure is not sac shaped but is a polyhedral architecture
- Type I alveolar epithelium (pneumocyte):
- Thin flat epithelium covering about 90 - 95% of alveolar lumen in area, about 40% of all alveolar epithelia in number
- Type II alveolar epithelium (pneumocyte):
- Cuboid epithelium covering 5 - 10% of the alveolar lumen in area, about 60% of all alveolar epithelia in number
- Pulmonary artery:
- Elastic artery in the central (hilar) side and muscular artery in the peripheral (alveolar) side
- Runs in the bronchovascular bundle along bronchus
- Lumen size is almost similar to bronchus beside it
- This muscular artery often contains abundant elastic fiber in the tunica media
- Reference: Katzenstein: Diagnostic Atlas of Non-Neoplastic Lung Disease, 1st Edition, 2016
- Pulmonary vein:
- Vein composed of collagenous fiber, smooth muscle and elastic fiber in various rates
- The central part contains a lot of elastic fiber but there is less in the periphery
- Runs in the interlobular septum or periphery of Miller's secondary lung lobule
- Bronchial artery:
- Muscular artery supplied by thoracic aorta or costal artery
- Size is far smaller than bronchus beside it
- Lymphatic vessel:
- Thin vasculature lined by endothelia
- Runs with bronchovascular bundle or interlobular septum
- Anthracotic pigment:
- Black pigment, which usually is deposited in the bronchovascular (or bronchiolovascular) bundle and pleura
Microscopic (histologic) images
Positive stains
- Mucous cell (goblet cell): MUC2 and MUC5AC
- Basal cell: cytokeratin 5/6, cytokeratin 34 beta E12, p63 and p40
- Neuroendocrine cell (Kulchitsky cell): CD56, synaptophysin and chromogranin A (Mills: Histology for Pathologists, 5th Edition, 2019)
- Alveolar epithelium: cytokeratin 7
- Type II alveolar epithelium: TTF1, surfactant apoprotein A (SP-A) and napsin A
Negative stains
- Mucous cell (goblet cell): MUC6
- Basal cell: TTF1
- Alveolar epithelium: cytokeratin 20, cytokeratin 5/6, cytokeratin 34 beta E12 and p40
Electron microscopy description
- Club cell (formerly Clara cell): elevated higher than ciliated cells nearby (Lowe: Stevens & Lowe's Human Histology, 4th Edition, 2014)
- Type I alveolar epithelium: fewer organelles
- Type II alveolar epithelium: lamellar body and electron dense vesicles in the cytoplasm; microvilli on the alveolar surface
Additional references
Board review style question #1
Which of the following is expressed in the alveolar epithelium?
- Cytokeratin 5/6
- Cytokeratin 7
- Cytokeratin 20
- p40
Board review style answer #1
B. Alveolar epithelium expresses cytokeratin 7 but does not express cytokeratin 20, high molecular weight cytokeratins (e.g. cytokeratin 5/6 and 34 beta E12) or p40.
Comment Here
Reference: Lung nontumor - Normal histology
Comment Here
Reference: Lung nontumor - Normal histology
Board review style question #2
Board review style answer #2
C. Bronchiole. A bronchiolovascular bundle, including terminal bronchiole, is located in the center of Miller's secondary lung lobule. A bronchiole lacks bronchial glands and cartilage.
Comment Here
Reference: Lung nontumor - Normal histology
Comment Here
Reference: Lung nontumor - Normal histology