Table of Contents
Definition / general | Embryology | Physiology | Accessory lobe | Diagrams / tables | Clinical images | Microscopic (histologic) images | VideosCite this page: Arora K. Anatomy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livernormalanatomy.html. Accessed April 24th, 2024.
Definition / general
- 1,200 - 1,600 g
- Dual blood supply of portal vein (2/3) and hepatic artery (1/3) via porta hepatis (common hepatic bile duct exists in same region)
- Blood exits liver via left and right hepatic veins to inferior vena cava
- Divided into right and left lobes by Cantlie line projecting between gallbladder fossa and vena cava and defined by middle hepatic vein
- Right lobe is divided into anterior and posterior segments by right hepatic vein
- Left lobe is divided into medial and lateral segments by left hepatic vein
- Intrahepatic biliary tree: classified into intrahepatic large bile ducts (grossly visible with fibrous ductal wall and peribiliary glands) and small bile ducts
- Regional lymph nodes: hilar, hepatoduodenal ligament, caval
Embryology
- Arises at embryonic junction (septum transversum): where ectoderm of amnion meets endoderm of yolk sac (externally) and where foregut meets midgut (internally); mesenchymal structure of transverse septum provides support so blood vessels and liver can form in underlying splanchnic mesoderm (UNSW Embryology: Gastrointestinal Tract - Liver Development [Accessed 23 October 2017])
- Hepatic diverticulum buds from ventral foregut at end of third week, grows into primitive septum transversum
- Liver forms from endodermal cells of diverticulum, termed hepatoblasts and mesenchyme
- Blood supply primarily from umbilical vein; also portal vein and hepatic artery
- Placenta clears wastes in bile and absorbs nutrients and umbilical vein blood bypasses liver via ductus venosus
- All elements of the biliary tree are recognizable by week 5, although bile duct system not complete until after birth; derived from endoderm (large ducts) and embryonic ductal plate (smaller intrahepatic ducts) (Dig Surg 2010;27:87)
- Hematopoietic cells are present in embryonic / fetal liver but absent at term
Physiology
Bile:
Bile acids:
Images hosted on other servers:
Bile acid circulation:
Jaundice:
Bilirubin:
- Liver produces about 500 ml/day of bile
- Promotes dietary fat absorption via detergent action of bile salts; eliminates waste products (bilirubin, excess cholesterol, xenobiotics) that are insufficiently water soluble to be excreted into urine
Bile acids:
- Carboxylate steroid molecules, derived from cholesterol, that promote bile flow and secretion of phospholipid and cholesterol
- Primary bile acids are cholic acid and chenodeoxycholic acid, secreted as taurine and glycine conjugates; two secondary ones (deoxycholic and lithocholic acid) are formed in the colon by bacterial action
Images hosted on other servers:
Bile acid circulation:
- All bile acids are reabsorbed via sodium bile acid cotransporter in apical membrane of ileal enterocytes and transported back to liver
- Enterohepatic circulation of bile acids maintains a large endogenous pool of bile acids for digestive and excretory purposes
Jaundice:
- Also called icterus
- Discoloration of skin and sclera due to disruption of bile formation by either retention of pigmented bilirubin or block in bilirubin secretion (cholestasis)
Bilirubin:
- End product of heme degradation
- 200 mg produced daily from old red blood cells broken down via monocyte phagocytic system in spleen, liver, marrow
- Also from turnover of P450 cytochromes and premature destruction of marrow red blood cells (with ineffective erthyropoiesis)
- Red blood cells are broken down and produce hemoglobin
- Globin proteins are removed, leaving heme molecule
- Heme is converted to biliverdin via heme oxygenase
- Biliverdin is converted to bilirubin via biliverdin reductase
- Bilirubin is bound to serum albumin since it is insoluble in blood at physiologic pH; the % unbound increases in severe hemolytic disease or if protein binding drugs displace bilirubin
- Hepatocytes take in bilirubin at sinusoidal membrane, conjugate it with glucuronic acid using bilirubin uridine diphosphate glucuronosyltransferase (UGT) in endoplasmic reticulum, then bilirubin is excreted into bile
- Bacteria have beta glucuronidases which deconjugate and degrade bilirubin to colorless urobilinogens, excreted in feces as stercobilin, a brown pigment that colors stools
- 20% of urobilinogens are reabsorbed in ileum / colon, returned to liver, reexcreted into bile
- Some urobilinogen is reabsorbed and excreted by the kidney, oxidized to urobilin - a pigment that gives amber color to urine
Accessory lobe
- May appear clinically as hepatic mass
- Anterior abdominal wall defects are frequently associated with accessory hepatic lobes
- Can present with torsion (Surg Radiol Anat 2011;33:819)
Diagrams / tables
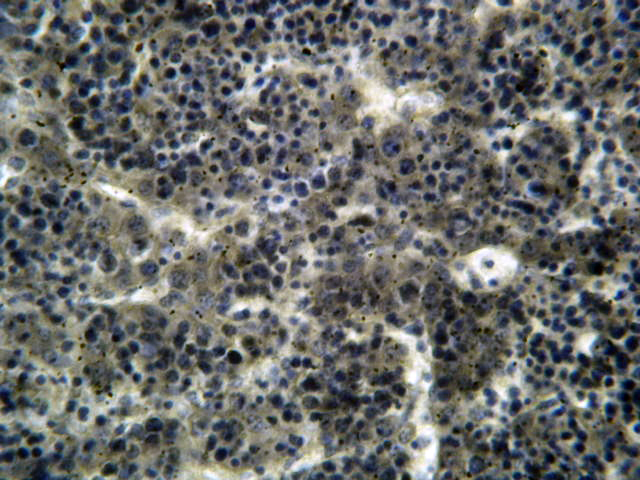
Microscopic (histologic) images
Videos
Development of foregut related to the peritoneum