Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chan AWH. Drug / toxin induced hepatitis-acetaminophen. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverdrugtoxinacetaminophen.html. Accessed April 17th, 2024.
Definition / general
- Intentional or unintentional overdose of acetaminophen, also known as paracetamol and N-acetyl-p-aminophenol, leading to liver injury
Essential features
- Acute hepatic necrosis related to acetaminophen overdose
- Acetaminophen overdose is one of the most common intentional or unintentional drug overdoses
- Acute liver failure associated with acetaminophen overdose is one of the most frequent causes of liver transplantation
ICD coding
- ICD-10
- X40 - accidental poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics
- X60 - intentional self poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics
- Y10 - poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics, undetermined intent
- ICD-11
- PB24 - unintentional exposure to or harmful effects of analgesics, antipyretics or nonsteroidal anti-inflammatory drugs
- PC94 - intentional self harm by exposure to or harmful effects of analgesics, antipyretics or nonsteroidal anti-inflammatory drugs
- PH44 - exposure to or harmful effects of undetermined intent of analgesics, antipyretics or nonsteroidal anti-inflammatory drugs
Epidemiology
- Acetaminophen is one of most used analgesic and antipyretic drugs, either as a standalone medication or combined with other medications (prescription or over the counter)
- In the U.S., 43 million adults take some form of acetaminophen
- 7.5% take over the counter acetaminophen at least weekly (Expert Rev Clin Pharmacol 2014;7:341)
- Acetaminophen overdose may lead to hepatotoxicity and annually accounts for > 80,000 emergency department visits, > 30,000 hospitalizations and 42% of all cases of acute liver failure in the U.S. (Arch Toxicol 2015;89:193)
- 61.8% of overdoses were unintentional but 30.5% were associated with a suicide attempt (J Clin Gastroenterol 2016;50:85)
- For acetaminophen overdoses, 30.3% were with this drug only, 14.1% were with a combination containing diphenhydramine and 56.6% were with a combination containing an opioid (J Clin Gastroenterol 2016;50:85)
Pathophysiology
- Normally, < 10% of acetaminophen is metabolized by the cytochrome p450 system in the liver to generate N-acetyl-p-benzoquinone imine (NAPQI)
- NAPQI is then quickly metabolized to nontoxic metabolites by glutathione
- NAPQI may accumulate, secondary to acetaminophen overdose, due to upregulation of the cytochrome p450 system (through chronic use of alcohol, isoniazid, rifampicin or phenobarbital) or depletion of glutathione (due to malnutrition or chronic liver disease), which leads to hepatotoxicity through mitochondrial dysfunction, cell death and modulation of the innate immune system (Arch Toxicol 2015;89:193)
Etiology
- Intentional or unintentional overdose of acetaminophen
- Maximal recommended dosage is 4 g/day (adult) or 50 - 75 mg/kg/day (children) (Cleve Clin J Med 2010;77:19)
Clinical features
- Most overdose patients are asymptomatic initially but progress to acute liver failure if untreated
- Initial presentation of acute liver failure includes abdominal pain, fatigue, anorexia and fever
- Later presentation includes jaundice, coagulopathy and encephalopathy, which may be complicated by shock, pulmonary edema and acute renal failure (Arch Toxicol 2015;89:193)
- Of those who developed acute liver failure, 7.1% required liver transplantation, 29.3% required hemodialysis and 16.7% died (J Clin Gastroenterol 2016;50:85)
Diagnosis
- Combination of drug history, liver biochemistry and serum acetaminophen
Laboratory
- Liver biochemistry
- Serum acetaminophen
Prognostic factors
- Factors associated with poor clinical outcome include older age, unintentional overdose, repeated supratherapeutic doses, excessive alcohol consumption, chronic liver disease (Arch Toxicol 2015;89:193)
Case reports
- 14 year old girl with acetaminophen induced Stevens-Johnson syndrome and acute liver failure (J Dermatol 2021;48:1423)
- 24 year old woman with acetaminophen associated fulminant hepatorenal syndrome (Clin Case Rep 2021;9:e04037)
- 36 year old woman with acetaminophen associated acute liver failure (Am J Case Rep 2023;24:e938500)
- 43 year old woman with delayed acetaminophen absorption associated acute liver failure (Case Rep Crit Care 2022;2022:3672248)
- 60 year old woman with intravenous acetaminophen associated acute liver failure (BMJ Case Rep 2022;15:e251305)
Treatment
- Activated charcoal minimizes GI absorption of acetaminophen if administered within 4 hours of an acute overdose (Arch Toxicol 2015;89:193)
- N-acetylcysteine minimizes hepatotoxicity by replenishing glutathione stores (Arch Toxicol 2015;89:193)
- Liver transplantation is the last resort for patients progressing to acute liver failure despite N-acetylcysteine
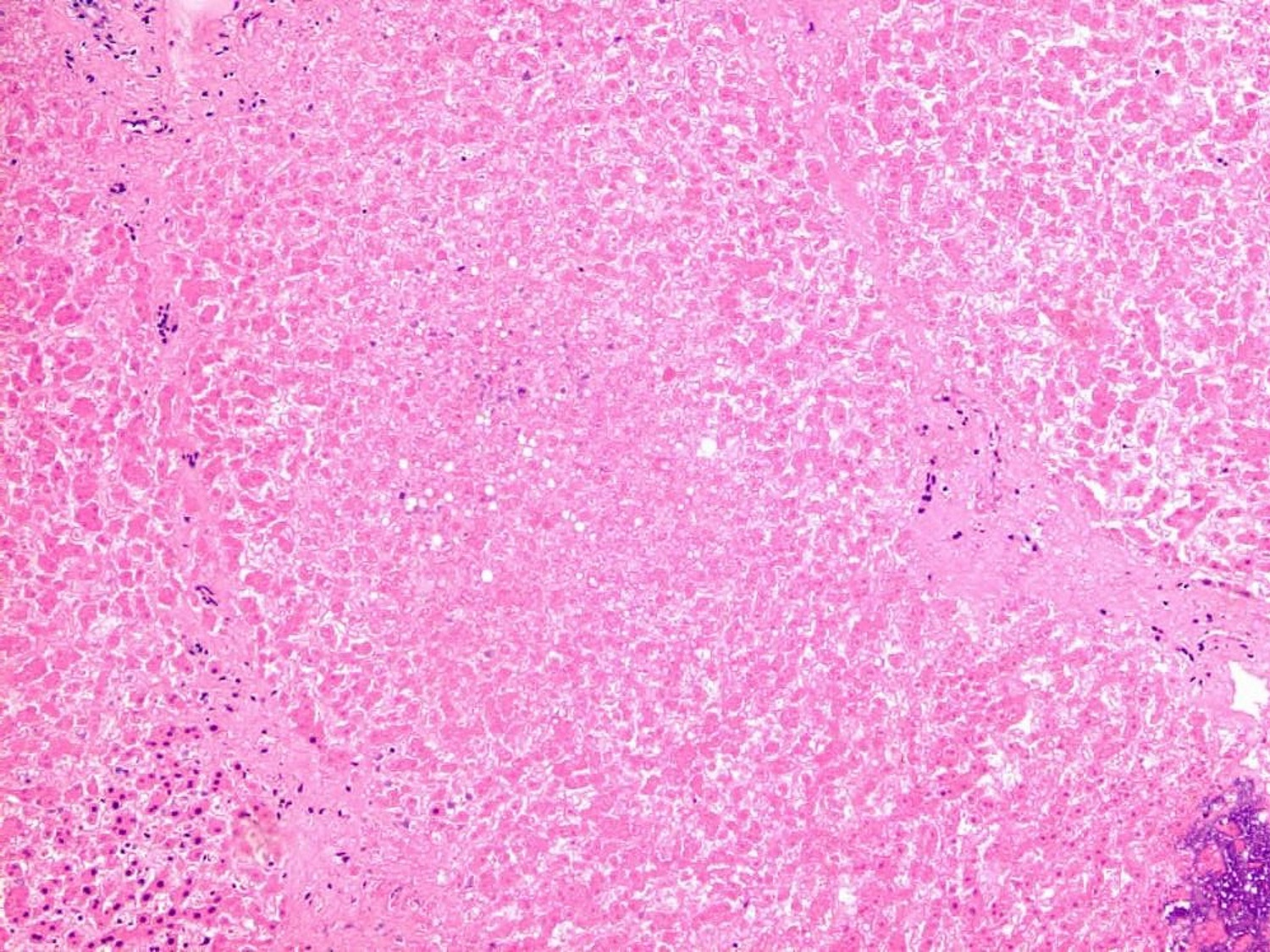
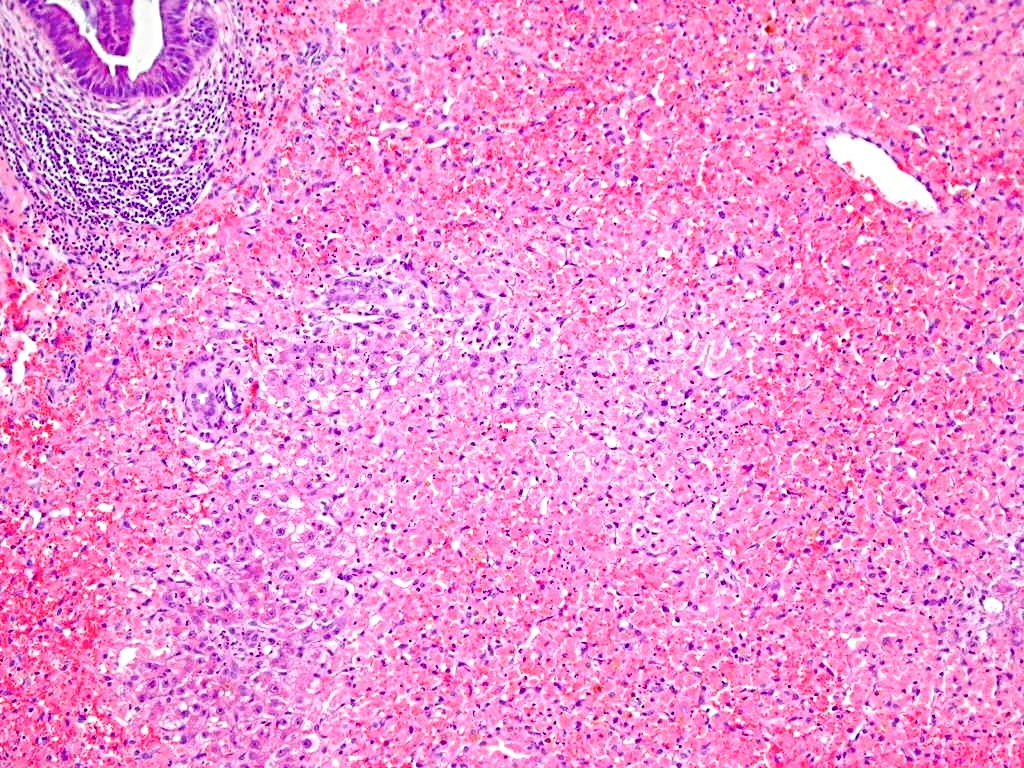
Microscopic (histologic) description
- Acute hepatic necrosis characterized by extensive zone 3 or panacinar necrosis with minimal inflammatory infiltrate
Microscopic (histologic) images
Sample pathology report
- Liver, recipient explant, hepatectomy:
- Acute hepatocellular necrosis (see comment)
- Comment: Extensive panacinar hepatocellular necrosis is accompanied by minimal inflammatory infiltrate and ductular necrosis. Provided by known drug history of acetaminophen overdose, the overall features are consistent with acetaminophen overdose associated liver failure.
Differential diagnosis
- Nonhepatotropic viral hepatitis (e.g., herpes simplex virus and adenovirus):
- Correlate with drug history and viral serology / PCR tests
- Histology shows viral inclusions, which could be highlighted by immunostains
- Other drug / toxin induced liver injury:
- Correlate with drug history and serum acetaminophen level
- Vascular disorders (e.g., shock, acute Budd-Chiari syndrome):
- Correlate with drug history and serum acetaminophen level
- Histology shows sinusoidal congestion and zone 3 / panacinar hemorrhagic necrosis
Additional references
Board review style question #1
Board review style answer #1
D. Zone 3 / panacinar hepatocellular necrosis. Zone 3 / panacinar hepatocellular necrosis is the typical pathological feature of acetaminophen associated liver injury. Answers A - C are incorrect because antibiotics (e.g., amoxicillin / clavulanate), oral contraceptive and iron overdose are typical drugs / toxins leading to acute cholestatic injury, bland cholestasis and zone 1 hepatocellular necrosis, respectively.
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen
Board review style question #2
Which of the following is associated with a better prognosis in acetaminophen induced liver injury?
- Chronic hepatitis B
- Cirrhosis
- Excessive alcohol consumption
- Younger age
Board review style answer #2
D. Younger age. Answers A - C are incorrect because older age rather than younger age, excessive alcohol consumption and chronic liver disease are associated poorer outcome of acetaminophen induced liver injury.
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen