Table of Contents
Definition / general | Essential features | Acute hepatitis pattern | Almost normal / near normal liver | Hepatitic pattern of injury | Resolving hepatitis pattern | Fatty liver | Cholestatic patterns | Bland lobular cholestasis | Bland ductular cholestasis or cholangitis lenta | Biliary obstruction pattern | Ductopenia | Chronic biliary / cholestatic injury / cholestatic hepatitis pattern | Cytoplasmic changes / abnormal deposition | Bland lobular necrosis | Granulomatous inflammation | Vascular injury pattern | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Patel KS, Windon AL. Diagnostic patterns-differential diagnosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverdiagnosticpatterns.html. Accessed April 26th, 2024.
Definition / general
- Identification of histologic features that define different patterns of liver injury to formulate appropriate differential diagnoses
Essential features
- Almost normal / near normal liver: minimal to absent histological findings but must look for changes in portal triad and lobules (cytoplasmic inclusions, steatosis, cholestasis, sinusoidal changes and altered hepatic plate architecture)
- Acute hepatitis pattern: mild to marked lobular inflammation and portal inflammation with hepatocyte necrosis
- Chronic hepatitis pattern: prominent chronic inflammatory infiltrate with occasional germinal centers in portal tracts with variable interface activity and less lobular inflammation than in acute hepatitis
- Resolving hepatitis pattern: scattered clusters of Kupffer cells and pigmented, ceroid laden, portal based macrophages with minimal chronic inflammation and hepatocyte regeneration
- Fatty liver - steatohepatitic pattern: more severe form of steatosis with hepatocyte ballooning, Mallory hyaline, lobular inflammation or fibrosis
- Cholestatic patterns: characterized by intracytoplasmic bile (hepatocanalicular cholestasis) and changes of chronic cholestasis
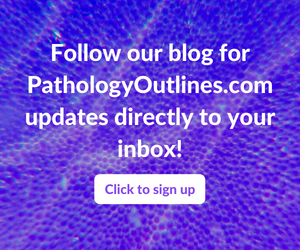
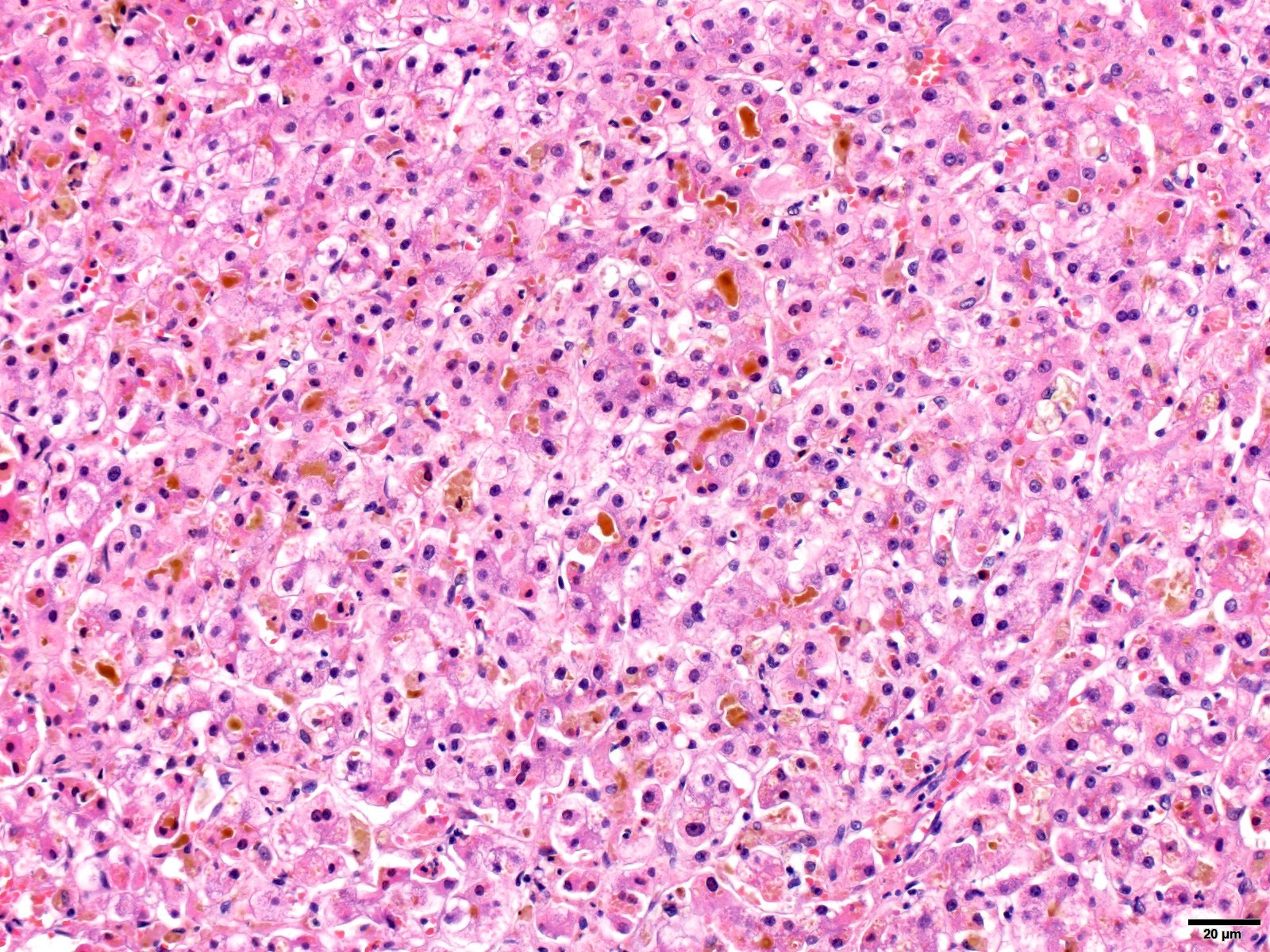
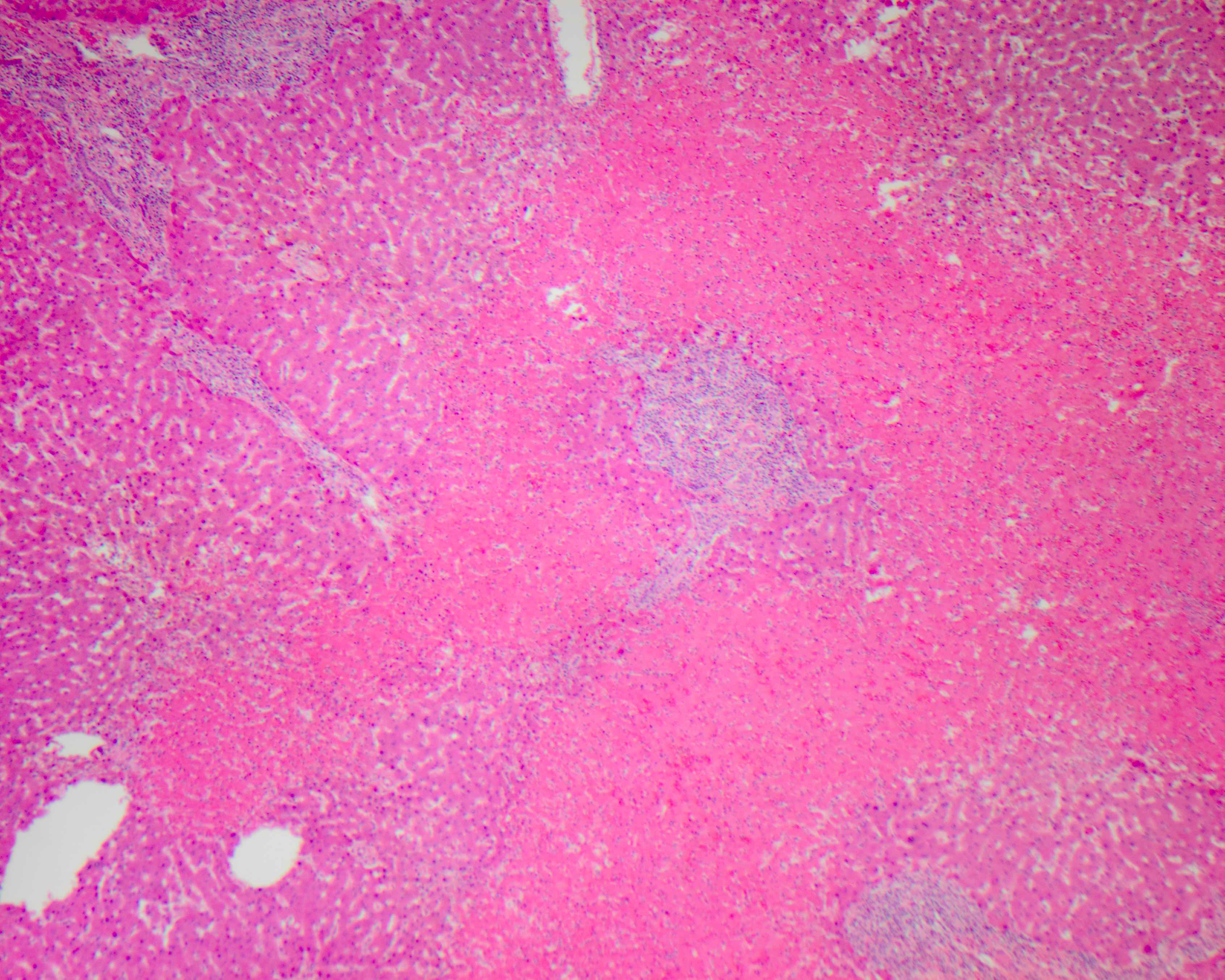
Acute hepatitis pattern
- Acute liver failure is an abrupt onset of liver disease or worsening liver function, either de novo or superimposed onto chronic liver disease
- Features of acute hepatitis pattern can overlap with other forms of hepatitis (chronic panlobular, cholestatic)
- Clinically, it is divided as hyperacute, acute and subacute liver failure, based on the duration of clinical presentation to development of serious symptoms, such as encephalopathy and coagulopathy
- Histologic pattern of injury can range from mild to marked lobular inflammation and hepatocyte necrosis
- Acute liver failure is associated commonly with drug induced liver injury (acetaminophen toxicity, idiosyncratic drug reactions), acute viral hepatitis, nonhepatotropic viruses (adenovirus, herpes simplex virus [HSV], cytomegalovirus [CMV], Epstein-Barr virus [EBV]), other infections (tick borne diseases, malaria), autoimmune hepatitis and Wilson disease
- Advanced fibrosis and percentage of necrosis in acute hepatitis have prognostic significance, with advanced fibrosis and > 25% necrosis indicating a worse prognosis (World J Gastroenterol 2017;23:4303)
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
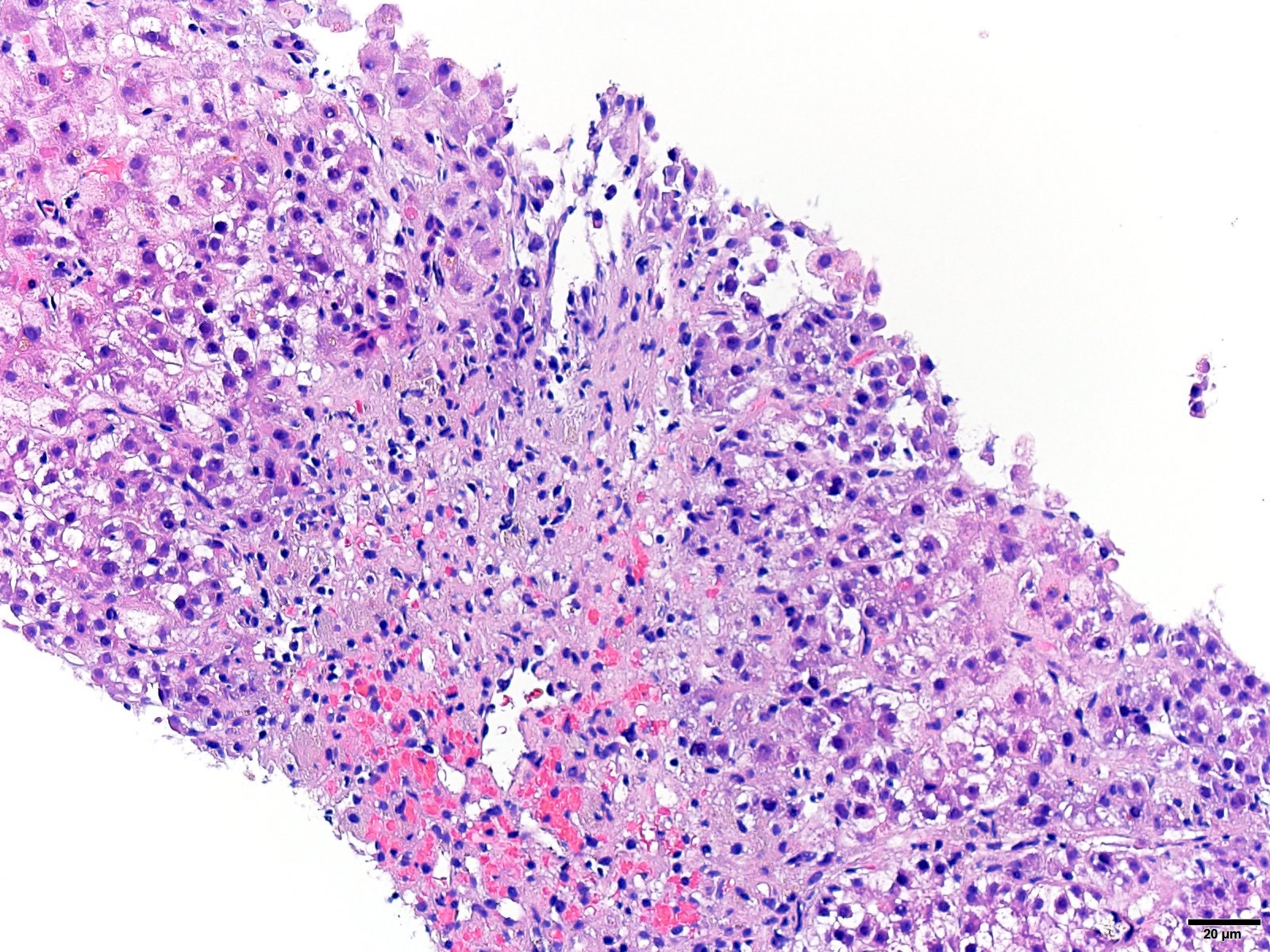
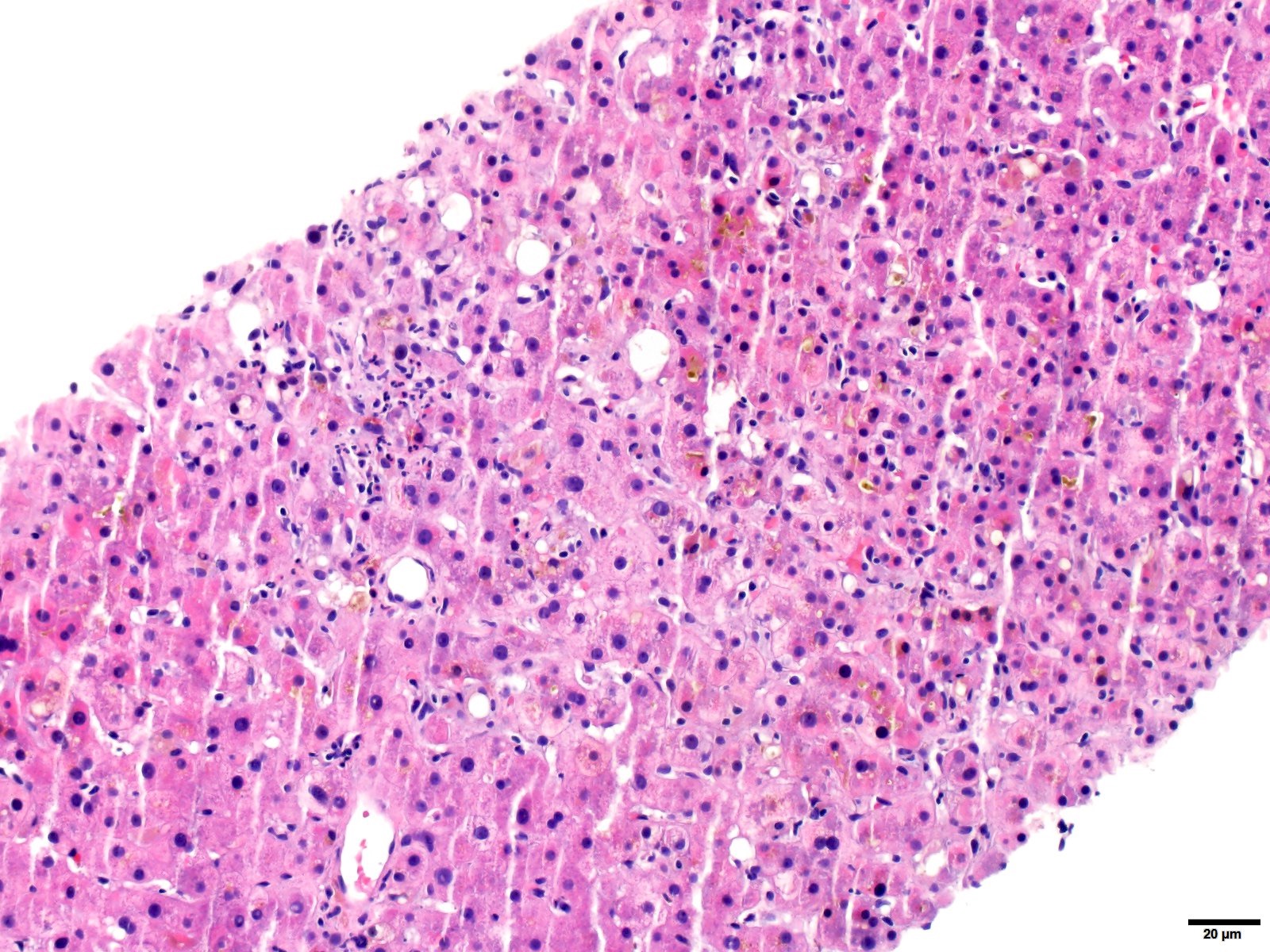
Almost normal / near normal liver
- Biopsies are usually prompted by unexplained abnormal liver enzymes, abnormal imaging or clinical presentations indicating liver etiology (portal hypertension, ascites)
- This pattern can be very challenging because of a broad differential diagnosis and potential to overlook subtle histologic findings leading to misdiagnosis
- Histologic findings are minimal to absent and there is no significant lobular or portal inflammation, fatty change, cholestasis or fibrosis
- It is still important to look for changes in the portal triad (bile ducts, hepatic arteries, portal veins) and in the lobules (cytoplasmic inclusions, steatosis, cholestasis, sinusoidal changes and altered hepatic plate architecture)
- Differential diagnosis for an almost normal liver biopsy includes systemic conditions (amyloidosis, Crohn's disease, celiac disease, thyroid disease, hypervitaminosis A), vascular disorders (portal venopathy, nodular regenerative hyperplasia and hepatoportal sclerosis, low grade or intermittent ischemic injury), genetic and metabolic conditions, drug effects, infection (sepsis, hepatotropic and nonhepatotropic viruses) and malignancy (leukemia, lymphoma)
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
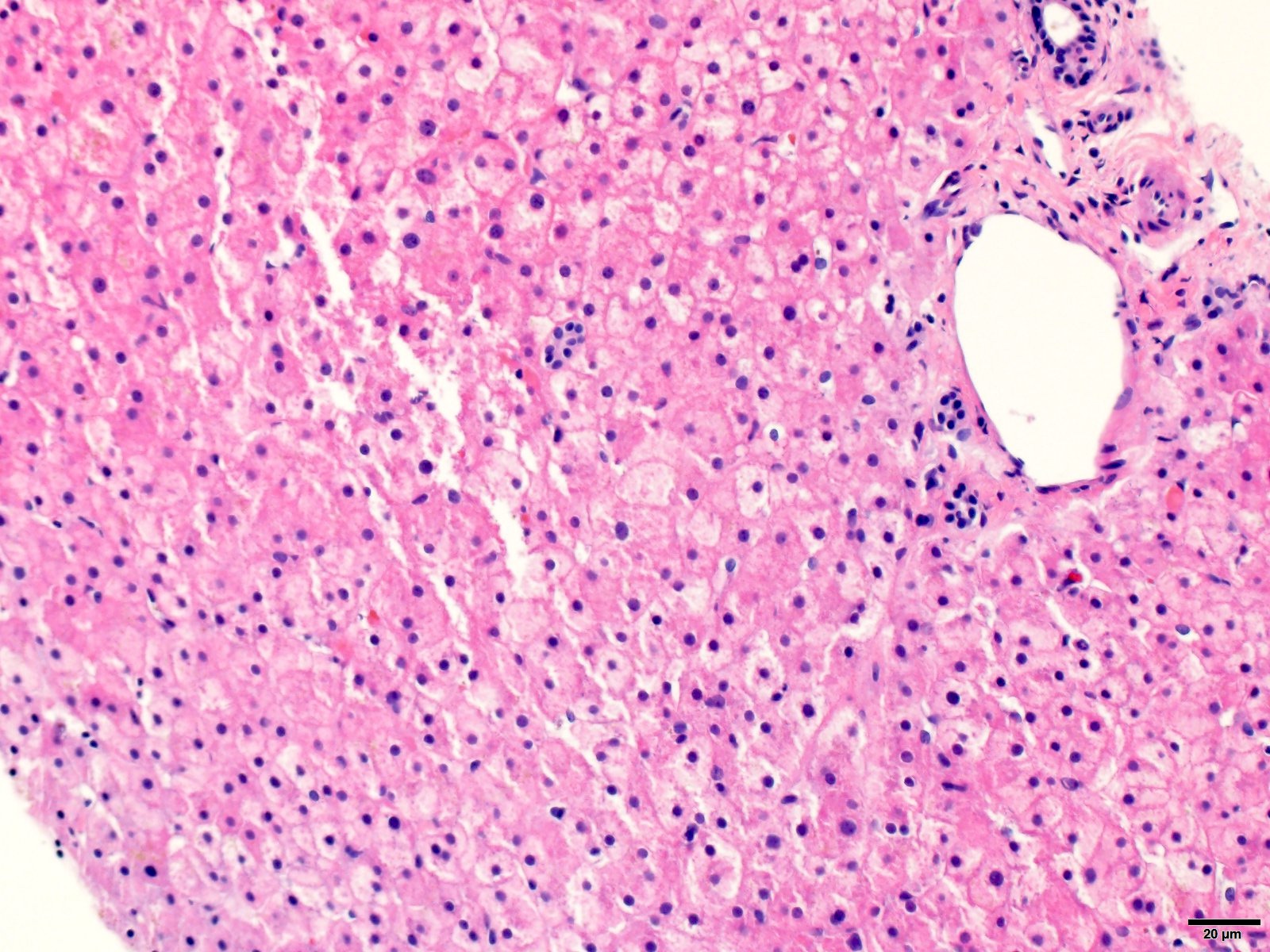
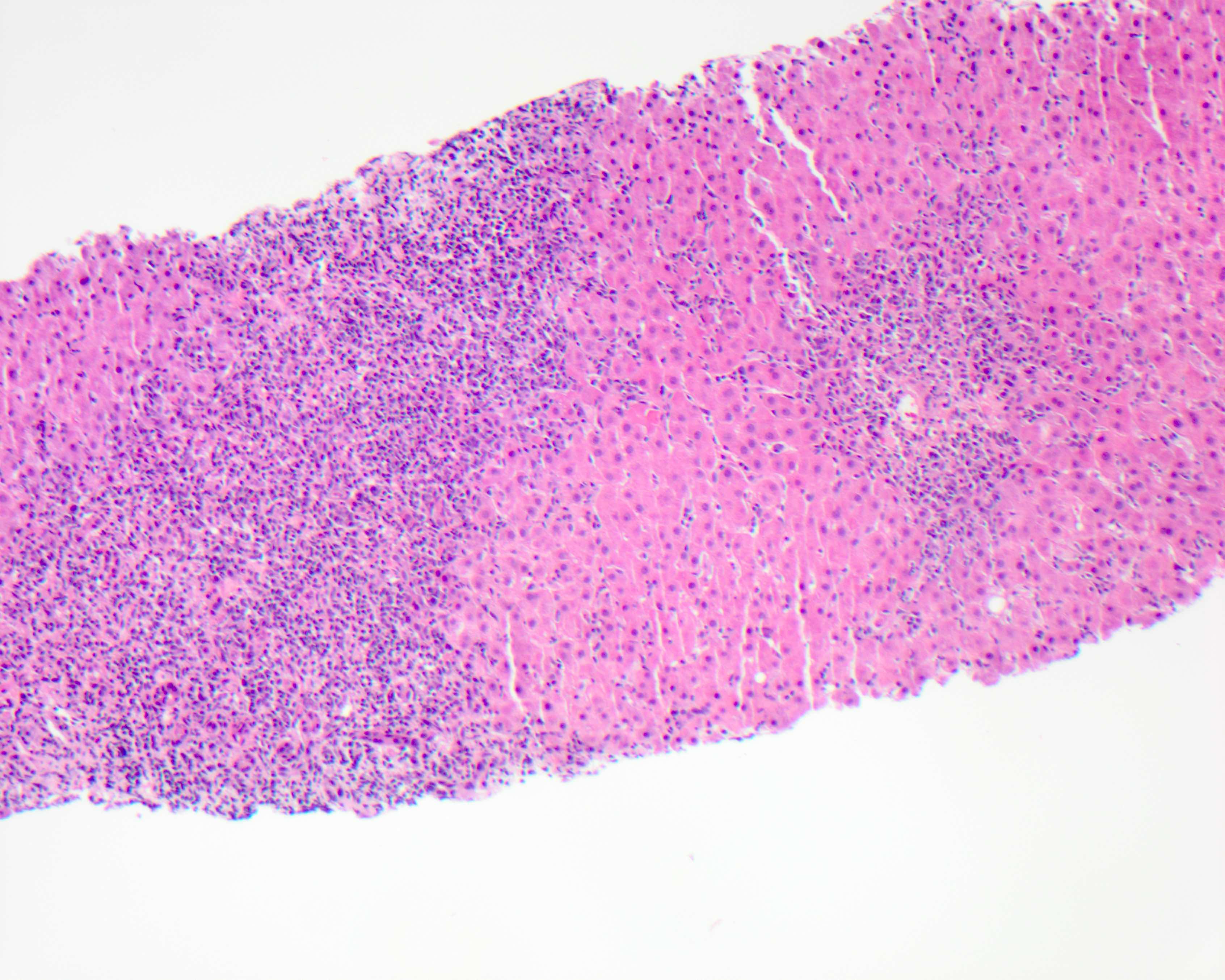
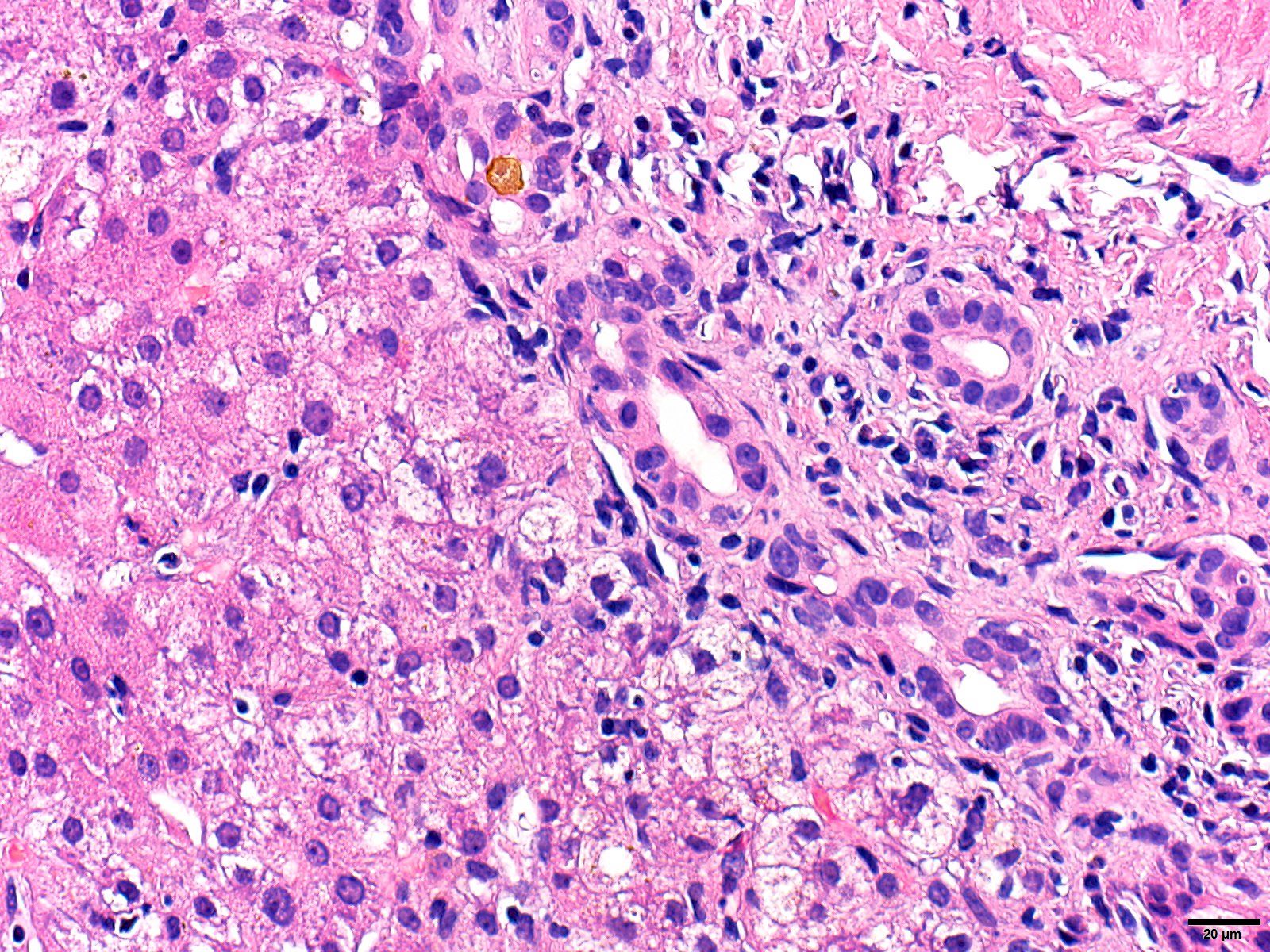
Hepatitic pattern of injury
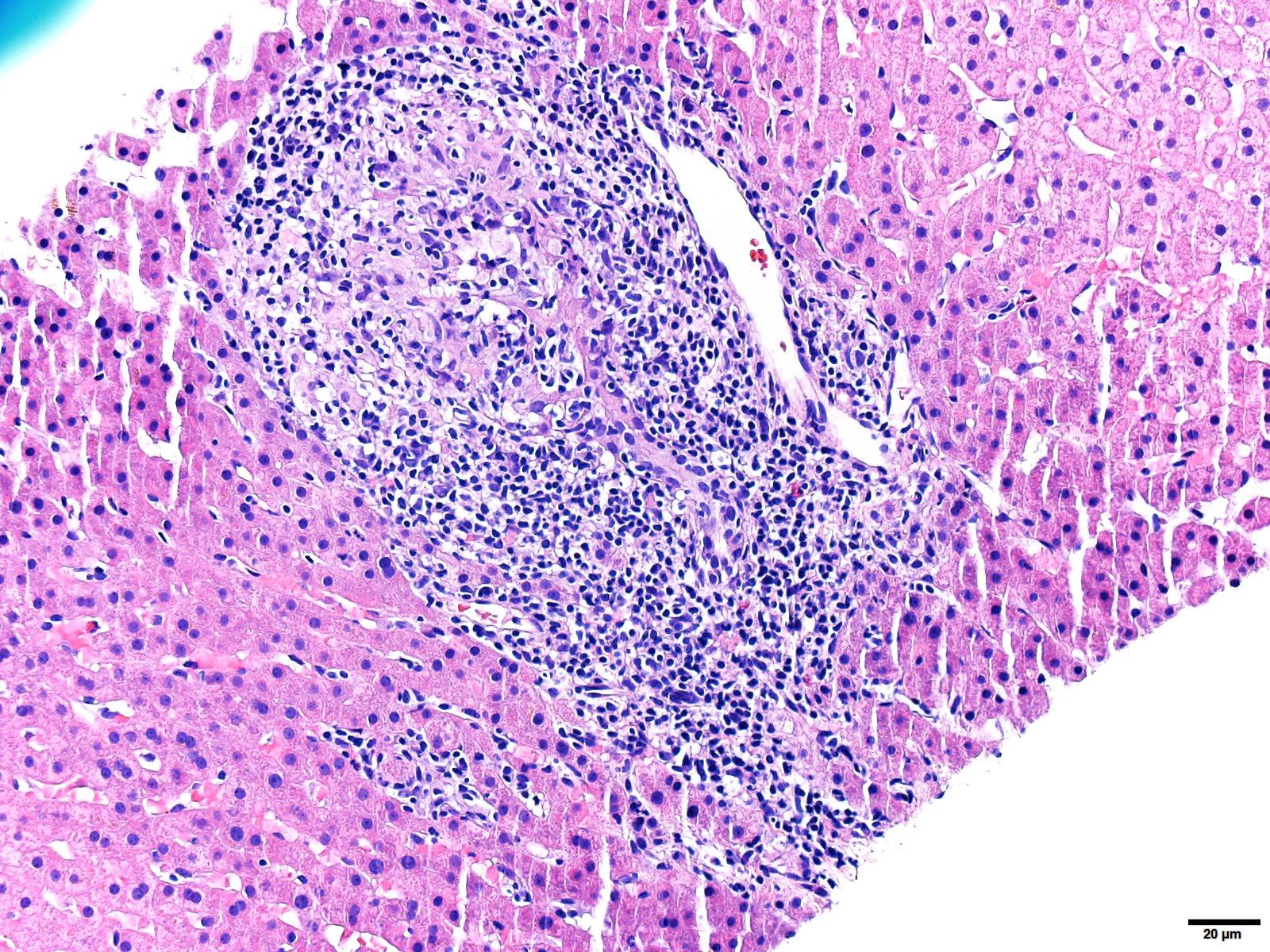
- Chronic hepatitis pattern is characterized by a prominent chronic inflammatory infiltrate with occasional germinal centers in the portal tracts, with varying amounts of interface activity
- Lobular inflammation is typically not as pronounced as what is seen in acute hepatitis
- Varying degrees of fibrosis might be present, depending on the length and severity of the chronic injury
- Acute and chronic hepatitis are clinical terms defined by the length of time of liver enzyme elevations
- Common diseases with the chronic hepatitic pattern of injury are chronic viral hepatitis (B and C), autoimmune hepatitis, primary biliary cholangitis, drug reactions and acute cellular rejection
- Plasma cell predominant / autoimmune pattern shows dense portal inflammation with increased plasma cells, scattered eosinophils and brisk interface activity
- It is commonly seen in autoimmune hepatitis, primary biliary cholangitis, drug induced liver injury (nitrofurtantoin, minocycline, methyldopa) and occasionally in viral hepatitis A, B and C
- Giant cell predominant pattern is characterized by the presence of large, multinucleated hepatocytes throughout the lobules
- Referred to as postinfantile (adult) type giant cell hepatitis
- Associated conditions include neonatal cholestasis in pediatric patients, autoimmune hepatitis, systemic diseases like systemic lupus erythematosis, immune thrombocytopenic purpura (ITP) and infections with CMV, HHV6, EBV, HIV
- Panacinar / panlobular pattern refers to a moderate lymphocytic or lymphoplasmacytic inflammatory infiltrate involving both portal tracts and hepatic lobules in a diffuse and uniform manner and may represent either an acute process or an acute flare of a chronic disease
- Associated conditions include acute viral hepatitis (nonhepatotropic), acute flare of chronic viral hepatitis (hepatitis B), drug induced liver injury and autoimmune hepatitis
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
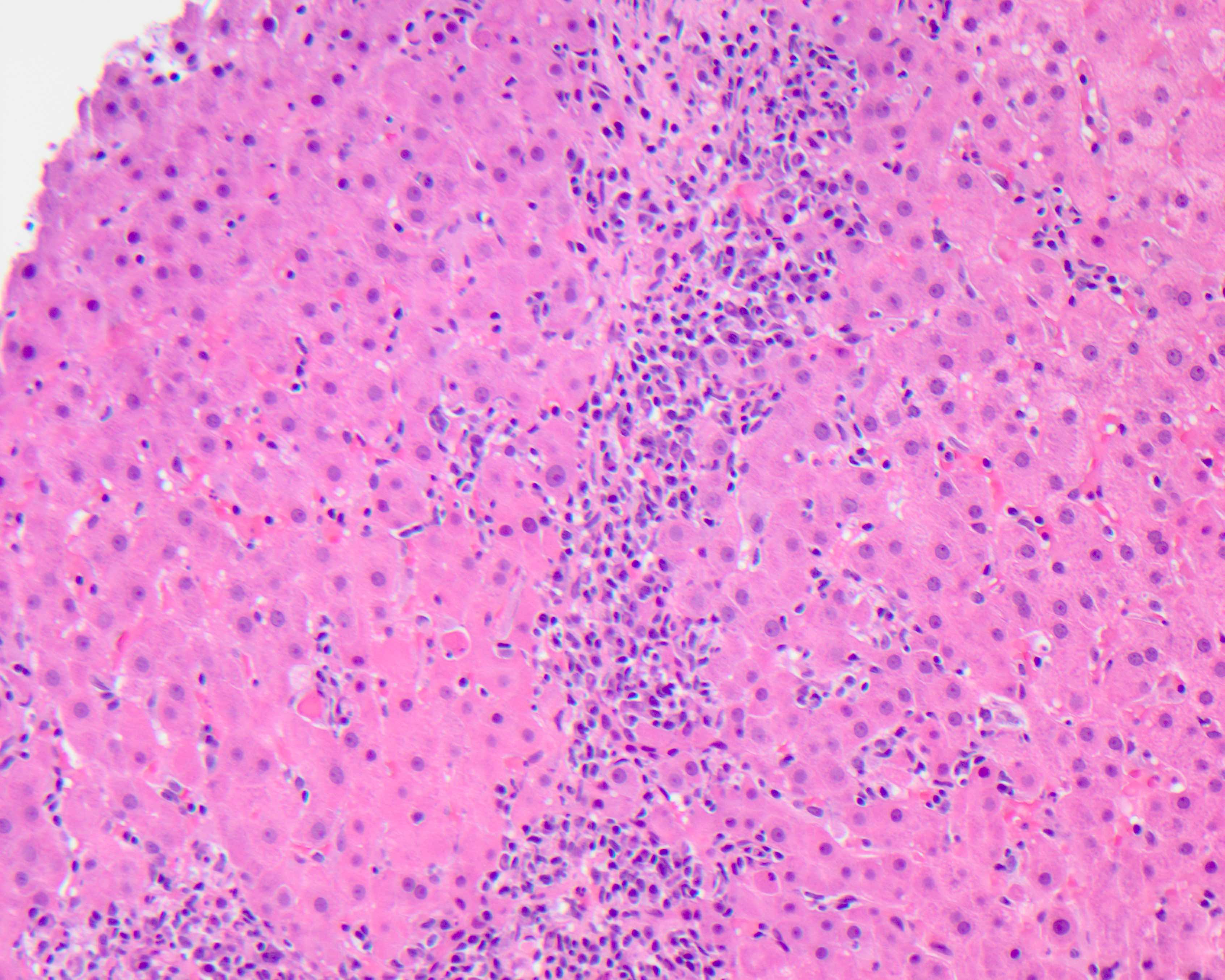
Resolving hepatitis pattern
- Resolving hepatitis pattern of injury consists of scattered clusters of Kupffer cells and pigmented, ceroid laden, portal based macrophages with minimal chronic inflammation and hepatocyte regeneration
- Common causes include acute self limited viral infection or an idiosyncratic drug reaction, where the drug was stopped before the liver biopsy was performed
- PASD special stain can highlight the clusters of pigmented macrophages in sites of prior mild lobular injury
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
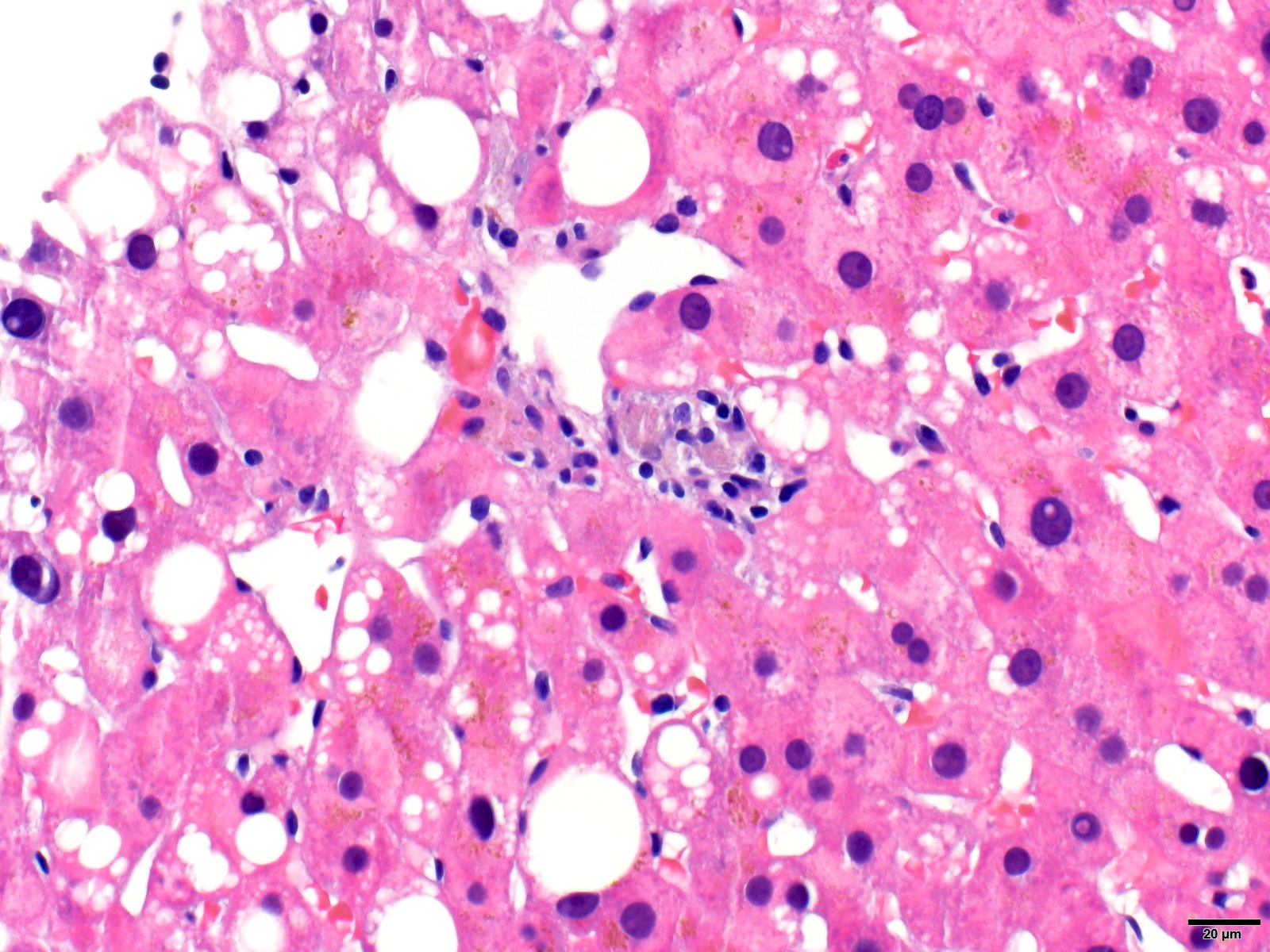
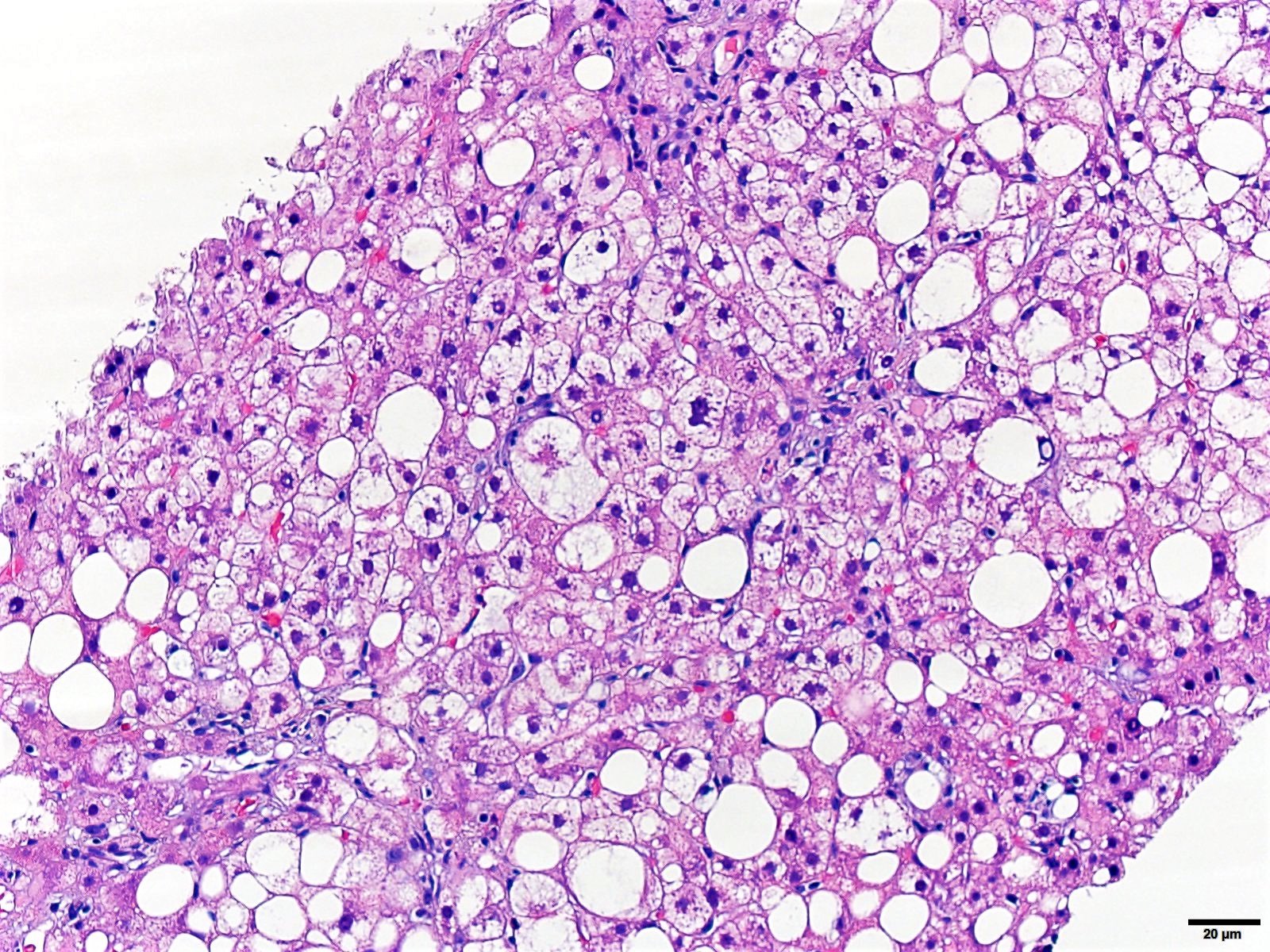
Fatty liver
- Fatty liver disease results from the accumulation of fat droplets in the cytoplasm of hepatocytes (steatosis), with varying amounts of associated inflammation, hepatocyte injury and fibrosis (steatohepatitis)
- Steatosis is subdivided into macrovesicular (large and small droplet) and microvesicular patterns
- Steatosis is graded by a semiquantitative approach: minimal (< 5%), mild (5 - 33%), moderate (34 - 66%) and marked (> 67%)
- Steatohepatitic pattern is a more severe form of steatosis and includes additional features of hepatocyte injury (hepatocyte ballooning, Mallory hyaline), lobular inflammation or fibrosis
- Common etiologies of macrovesicular steatosis and steatohepatitis include metabolic syndrome, alcohol use, drug effect (amiodarone toxicity, methotrexate, steroids), Wilson disease and neoplasm (hepatic adenoma, steatohepatitic variant of hepatocellular carcinoma)
- Microvesicular steatosis is rarer and can occur in acute fatty liver of pregnancy, HELLP syndrome, Reye syndrome, medication toxicity (tetracycline, valproic acid), alcoholic foamy degeneration and mitochondrial toxicity / dysfunction
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Cholestatic patterns
- Pattern of injury characterized by intracytoplasmic bile (hepatocanalicular cholestasis) and changes of chronic cholestasis, with or without inflammation and obstructive features
- Cholate stasis refers to hepatocyte injury (periportal hepatocyte swelling / feathery degeneration, with or without Mallory hyaline)
Bland lobular cholestasis
- In this pattern, the major finding is hepatocanalicular / lobular cholestasis, usually in a zone 3 distribution, without significant inflammation or changes of biliary obstruction; typically there is no ductopenia or evidence of advanced fibrosis
- Bile plugs are found in both the hepatocytes and in the bile canaliculi
- This pattern is seen in drug related liver injury, severe systemic illness, sepsis and paraneoplastic syndromes (lymphomas)
Bland ductular cholestasis or cholangitis lenta
Biliary obstruction pattern
- Biliary obstructive pattern is characterized by changes in the portal tracts, including bile ductular proliferation, mild mixed inflammation (neutrophils and lymphocytes) and portal edema
- Degree of changes correlates roughly with the acuity and severity of the obstruction
- Lobular cholestasis can range from absent to marked, depending on the duration and severity of the obstruction, with accompanying minimal to mild lobular inflammation
- Common etiologies of this pattern include downstream biliary obstruction from strictures, stones, tumors, ischemia, infection, vascular outflow disease, severe acute hepatitis and biliary atresia
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Ductopenia
- Ductopenia is defined as the loss of bile ducts in at least 50% of portal tracts in an adequate biopsy
- True ductopenia is usually associated with significantly elevated alkaline phosphatase levels
- Ductopenia is commonly associated with Alagille syndrome, primary sclerosing cholangitis, strictures, stones, tumors, primary biliary cholangitis, chronic liver allograft rejection, graft versus host disease, ischemic cholangiopathy, drug effect and paraneoplastic syndromes (Hodgkin, T cell lymphomas)
- Immunohistochemical stain for cytokeratin 7 is an excellent tool to evaluate for ductopenia; additionally, a copper stain can highlight copper deposition in the periportal hepatocytes, which can be seen in most cases of established ductopenia
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Chronic biliary / cholestatic injury / cholestatic hepatitis pattern
- This is a nonspecific overlapping pattern used when the overall findings are not sufficient for a diagnosis of the biliary obstructive pattern and do not fit for bland lobular cholestasis or ductopenia
- Bile ductular proliferation can range from absent to mild and patchy, with associated mild bile duct lymphocytosis and injury, mild nonspecific portal inflammation, absent to minimal lobular inflammation and lobular cholestasis
- This pattern is seen most commonly in drug reactions and viral infections and may also been seen in early stage primary biliary cholangitis or primary sclerosing cholangitis
- These subtle and equivocal histologic changes are best supported by immunohistochemistry with cytokeratin 7, which helps assess bile duct loss and identification of proliferating intermediate hepatocytes, a feature of chronic cholestasis
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Cytoplasmic changes / abnormal deposition
- Most cytoplasmic changes are classified as either diffuse cytoplasmic clearing or distinct cytoplasmic inclusions
- Diffuse cytoplasmic clearing usually results from glycogen accumulation, seen in poorly controlled diabetes, glycogen storage disease and urea cycle defects
- Ground glass change is characterized as large pale inclusions occupying the majority of the cytoplasm and is commonly seen in chronic hepatitis B or drug effects
- Smaller, more eosinophilic inclusions in zone 1 hepatocytes are seen in alpha-1 antitrypsin deficiency
- Smaller eosinophilic inclusions in zone 3 hepatocytes are seen in chronic passive congestion of the liver
Bland lobular necrosis
- Bland lobular necrosis is the result of direct liver injury that is not immune mediated and has relatively little or no inflammation
- Bland lobular necrosis pattern of injury is associated with larger areas of necrosis and is distinct from spotty necrosis, usually seen in other hepatitic patterns of injury
- Zone 3 hepatocyte necrosis is commonly seen in drug reactions (acetaminophen) toxins and ischemia
- Isolated zone 1 and zone 2 patterns of necrosis are rare and are associated with heavy metal toxicity, industrial chemicals, poisons and hepatitis A
- Punched out necrosis is a pattern of somewhat round, well circumscribed, azonal areas of necrosis, most commonly viral in origin (HSV, varicella zoster virus, adenovirus)
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Granulomatous inflammation
- Single or numerous necrotizing or nonnecrotizing granulomas can be found in the portal tracts or lobules
- Common conditions with granulomatous inflammation include primary biliary cholangitis, sarcoidosis, drug effect, infection (mycobacterial, bacterial, fungal) and paraneoplastic syndrome
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
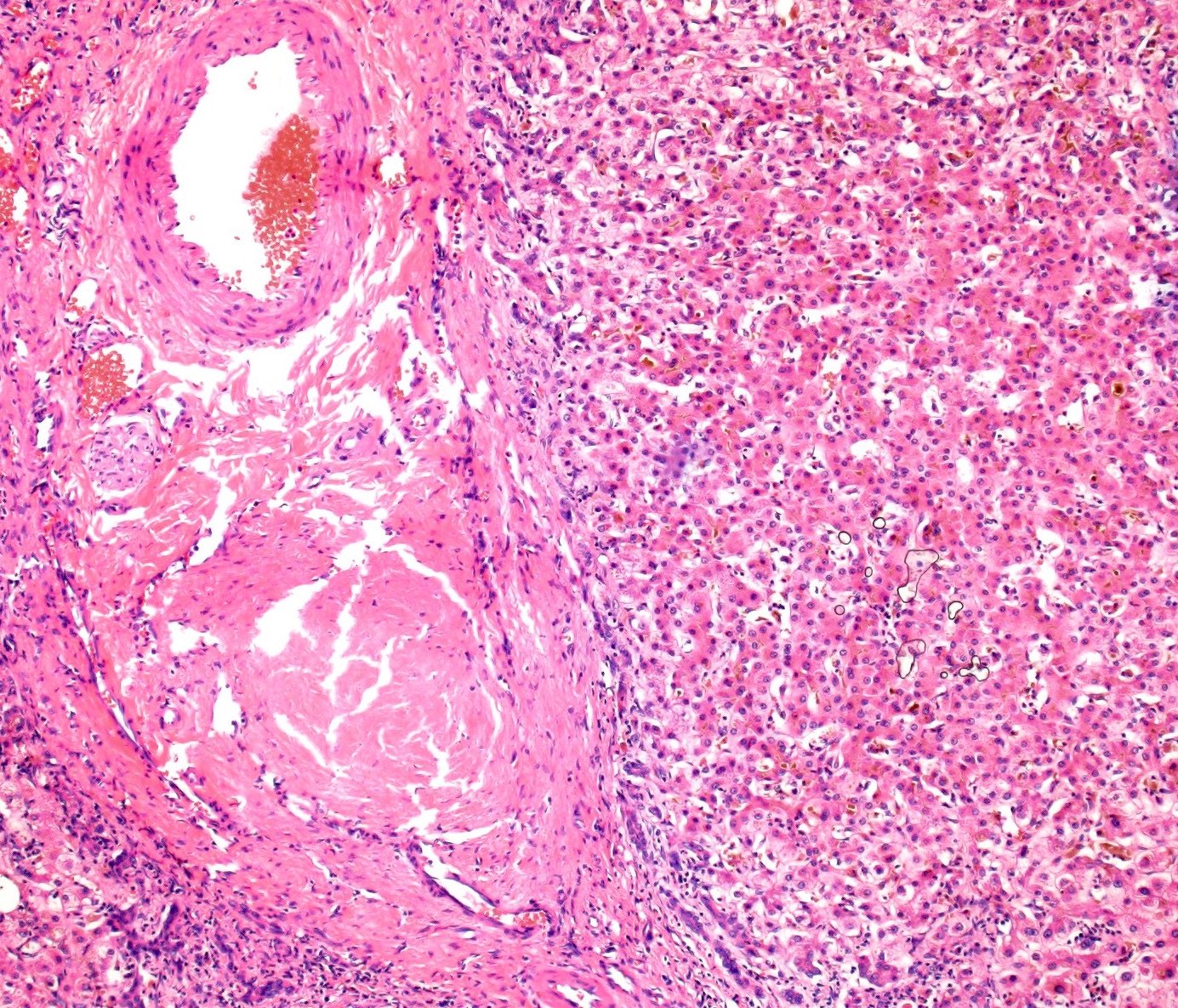
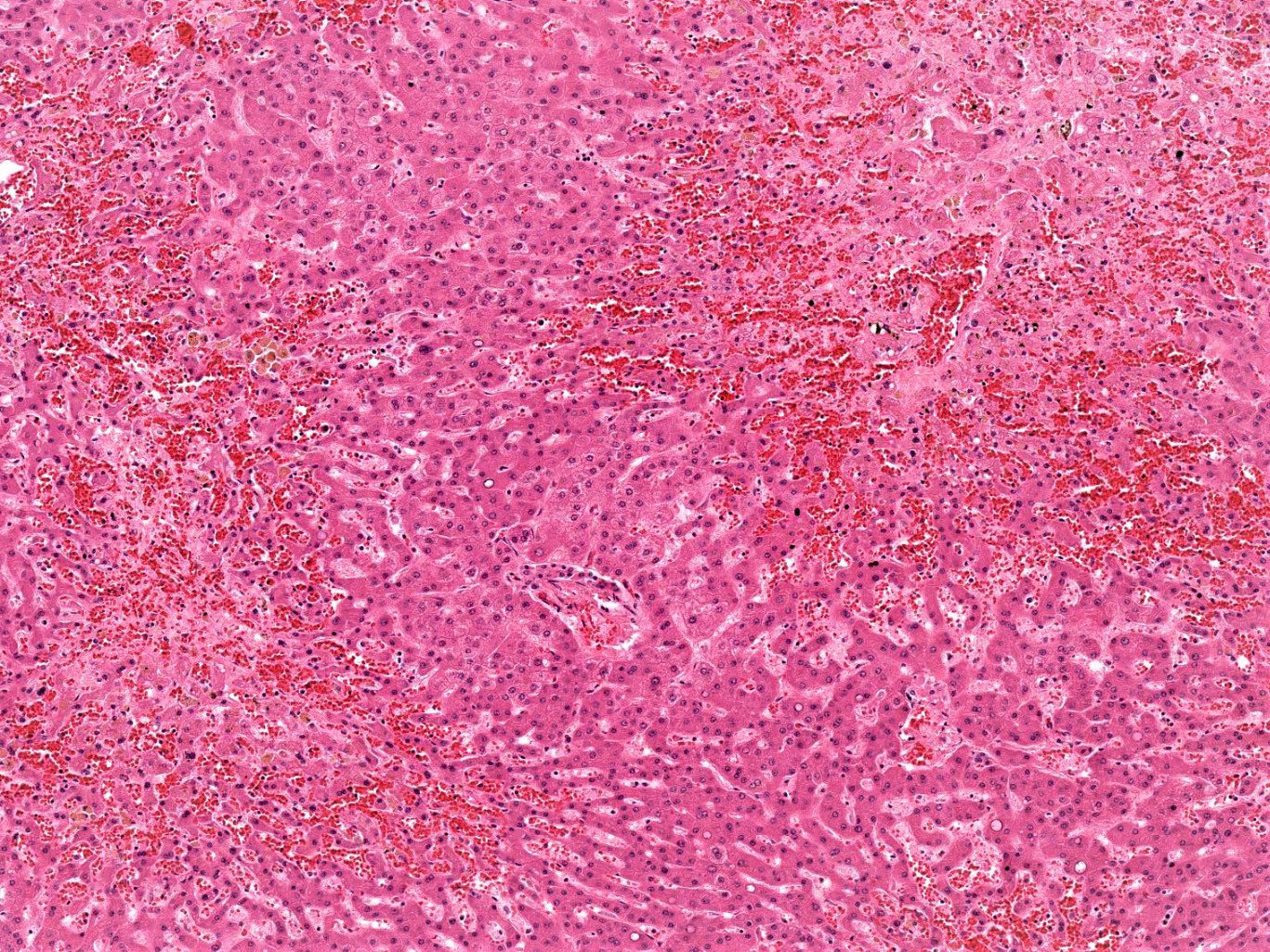
Vascular injury pattern
- Vascular diseases resulting in hepatic injury are classified as hepatic arterial disease, portal vein disease, sinusoidal disease, peliosis hepatitis or hepatic vein disease
- Most common pattern is vascular outflow disease, usually from cardiac disease or thrombosis of the hepatic veins or vena cava, presenting with zone 3 predominant sinusoidal dilatation, congestion and zone 3 fibrosis
- Portal vein disease is more subtle, with findings of varying degrees of herniation, atrophy, loss and fibrosis of the portal veins, with or without associated nodular regenerative hyperplasia of the lobules
- Hepatic arterial disease is very uncommon, with low grade or intermittent arterial obstruction leading to bland lobular spotty necrosis with little or no inflammation
- Peliosis hepatitis refers to irregular blood filled cysts without any endothelial lining and is a histologic finding in debilitating illnesses, like tuberculosis, AIDS, cancer, malnutrition and medications, like estrogens / androgens
- See Nodular regenerative hyperplasia
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Additional references
- Torbenson: Biopsy Interpretation of the Liver, 3rd Edition, 2015, Saxena: Practical Hepatic Pathology - A Diagnostic Approach, 1st Edition, 2011, Torbenson: Atlas of Liver Pathology - A Pattern Based Approach, 1st Edition, 2020, Torbenson: Surgical Pathology of the Liver, 1st Edition, 2018, Burt: MacSween's Pathology of the Liver, 7th Edition, 2018, Lefkowitch: Scheuer's Liver Biopsy Interpretation, 9th Edition, 2016
Board review style question #1
Board review style answer #1
A. Cytokeratin 7. The image shows bile ductular proliferation, usually highlighted by cytokeratin 7 immunohistochemical stain.
Comment Here
Reference: Diagnostic patterns-differential diagnosis
Comment Here
Reference: Diagnostic patterns-differential diagnosis
Board review style question #2
Peliosis hepatis is commonly associated with which condition?
- Estrogen intake
- HSV
- Inborn errors of metabolism
- Obesity
- Reye syndrome
Board review style answer #2
A. Estrogen intake. Peliosis hepatitis refers to irregular blood filled cysts, without any endothelial lining and is a histologic finding in debilitating illnesses, like tuberculosis, AIDS, cancer, malnutrition and medications, like estrogens / androgens.
Comment Here
Reference: Diagnostic patterns-differential diagnosis
Comment Here
Reference: Diagnostic patterns-differential diagnosis