Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Evason KJ. Chronic hepatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverchronichepgeneral.html. Accessed November 28th, 2024.
Definition / general
- Liver injury occurring for at least 6 months as a result of hepatocyte based injury and inflammation, most commonly due to viral or autoimmune hepatitis (Am J Surg Pathol 1995;19:1409)
Essential features
- Viral infection, deregulated inflammatory cells or other insults leading to chronic hepatocyte injury and hepatic stellate cell activation (Middle East J Dig Dis 2016;8:166, Physiol Rev 2008;88:125)
- Morphologically characterized by fibrosis, which is frequently accompanied by portal inflammation with interface activity or lobular necroinflammatory activity (Am J Surg Pathol 1995;19:1409)
- Progressive portal based fibrosis ultimately leads to liver cirrhosis (end stage liver disease) (Clin Liver Dis (Hoboken) 2021;17:222)
- Distinct etiology and morphology from steatohepatitis and biliary disorders, though all may be associated with chronic liver injury and cirrhosis (Am J Surg Pathol 1995;19:1409)
Terminology
- Chronic active hepatitis
- Chronic persistent hepatitis
- Chronic lobular hepatitis (Am J Surg Pathol 1995;19:1409)
ICD coding
- ICD-10:
- B18.0 - chronic viral hepatitis B with delta agent
- B18.1 - chronic viral hepatitis B without delta agent
- B18.2 - chronic viral hepatitis C
- B18.8 - other chronic viral hepatitis
- B18.9 - chronic viral hepatitis, unspecified
- K73.0 - chronic persistent hepatitis, not elsewhere classified
- K73.1 - chronic lobular hepatitis, not elsewhere classified
- K73.2 - chronic active hepatitis, not elsewhere classified
- K73.8 - other chronic hepatitis, not elsewhere classified
- K73.9 - chronic hepatitis, unspecified
Epidemiology
- Dependent on underlying etiology
Sites
- Liver parenchyma
Pathophysiology
- Hepatocytes are injured by viral infection, drugs, deregulated inflammatory cells or abnormal accumulation of metabolites, leading to activation of hepatic stellate cells, which produce increased extracellular matrix resulting in fibrosis (Middle East J Dig Dis 2016;8:166, Physiol Rev 2008;88:125)
Etiology
- Chronic viral hepatitis
- Hepatitis B virus (HBV)
- Hepatitis C virus (HCV)
- Hepatitis D virus (HDV)
- Autoimmune hepatitis
- Metabolic disease
- Drug induced chronic hepatitis (rare) (J Clin Pathol 2009;62:481)
- Lisinopril
- Sulfonamides
- Trazodone
- Uracil
- Tegafur
- Tamoxifen
- Methotrexate
- Minocycline
- Clometacin
- Methyldopa
- Nitrofurantoin
Clinical features
- May lack symptoms until end stage (cirrhosis)
- Associated signs and symptoms include (World J Gastroenterol 2022;28:5910):
- General: fatigue (most common), malaise, mild discomfort in the right upper quadrant, anorexia
- Impaired biliary tract function: jaundice, pruritus
- Portal hypertension: gastroesophageal varices, ascites, edema, splenomegaly
- Impaired hepatocyte metabolism: spider angiomata, hepatic encephalopathy, easy bleeding / bruising
Diagnosis
- Clinicopathologic diagnosis requires integration of clinical history (including associated signs and symptoms described above), laboratory testing and biopsy results (Am J Surg Pathol 1995;19:1409)
- Ongoing liver injury lasting at least 6 months (Am J Surg Pathol 1995;19:1409)
- Longstanding clinical signs / symptoms or laboratory abnormalities
- Fibrosis represents pathologic correlate of chronic liver injury
- Biopsy is gold standard for determining grade and stage
- Laboratory testing is essential for determining etiology
- Transient elastography (FibroScan) can also be used to estimate stage / extent of fibrosis (World J Gastroenterol 2014;20:11033, World J Gastroenterol 2014;20:2854)
Laboratory
- Serological testing for hepatitis B, C and D and autoantibodies (may be positive, depending on etiology)
- Aminotransferase levels (AST, ALT may be elevated)
- Several serum markers for evaluating liver fibrosis have been proposed but none are widely used (World J Gastroenterol 2014;20:11033, World J Gastroenterol 2014;20:2854)
Radiology description
- MRI and CT findings in cirrhosis
- Surface and parenchymal nodularity
- Hypertrophy of the caudate lobe and lateral segments of the left lobe
- Atrophy of the posterior segments of the right lobe
- Ultrasound findings in cirrhosis
- Surface nodularity
- Course and heterogeneous echotexture
- Segmental hypertrophy / atrophy
- Doppler flow changes indicative of portal hypertension
- Splenomegaly
- Ascites (Radiopaedia: Cirrhosis [Accessed 28 February 2023])
Prognostic factors
- Amount of fibrosis (stage) is a key predictor of progression to end stage liver disease (cirrhosis) and adverse clinical outcomes (i.e., a need for liver transplant or liver related death in patients with hepatitis C) (World J Gastroenterol 2014;20:2854, Hepatology 2010;51:585)
- Amount of inflammation (grade) is associated with fibrosis progression (stage) in patients with hepatitis C (Pathol Int 2002;52:683)
- Rate of progression to end stage liver disease depends on many other factors including age, sex, underlying etiology of liver injury and response to treatment (J Interferon Cytokine Res 2017;37:97, Gut Liver 2016;10:429)
Case reports
- 28 year old man with acute on chronic liver failure and hemolysis (EJIFCC 2019;30:99)
- 46 year old man with HBV cirrhosis and dermatomyositis (World J Clin Cases 2019;7:1206)
- 55 year old man with jaundice (N Engl J Med 2019;380:1955)
- 56 year old man with Guillain-Barré syndrome and chronic active hepatitis C (BMC Infect Dis 2019;19:636)
- 72 year old man successfully treated for HBV, HCV and HEV (J Infect Public Health 2020;13:149)
Treatment
- Dependent on underlying etiology
Gross description
- In cirrhosis, the liver is generally firm and demonstrates a micronodular or macronodular pattern
- Color ranges from beefy red (normal) to dark green (cholestasis) or yellow (steatosis) (World J Gastroenterol 2016;22:1357)
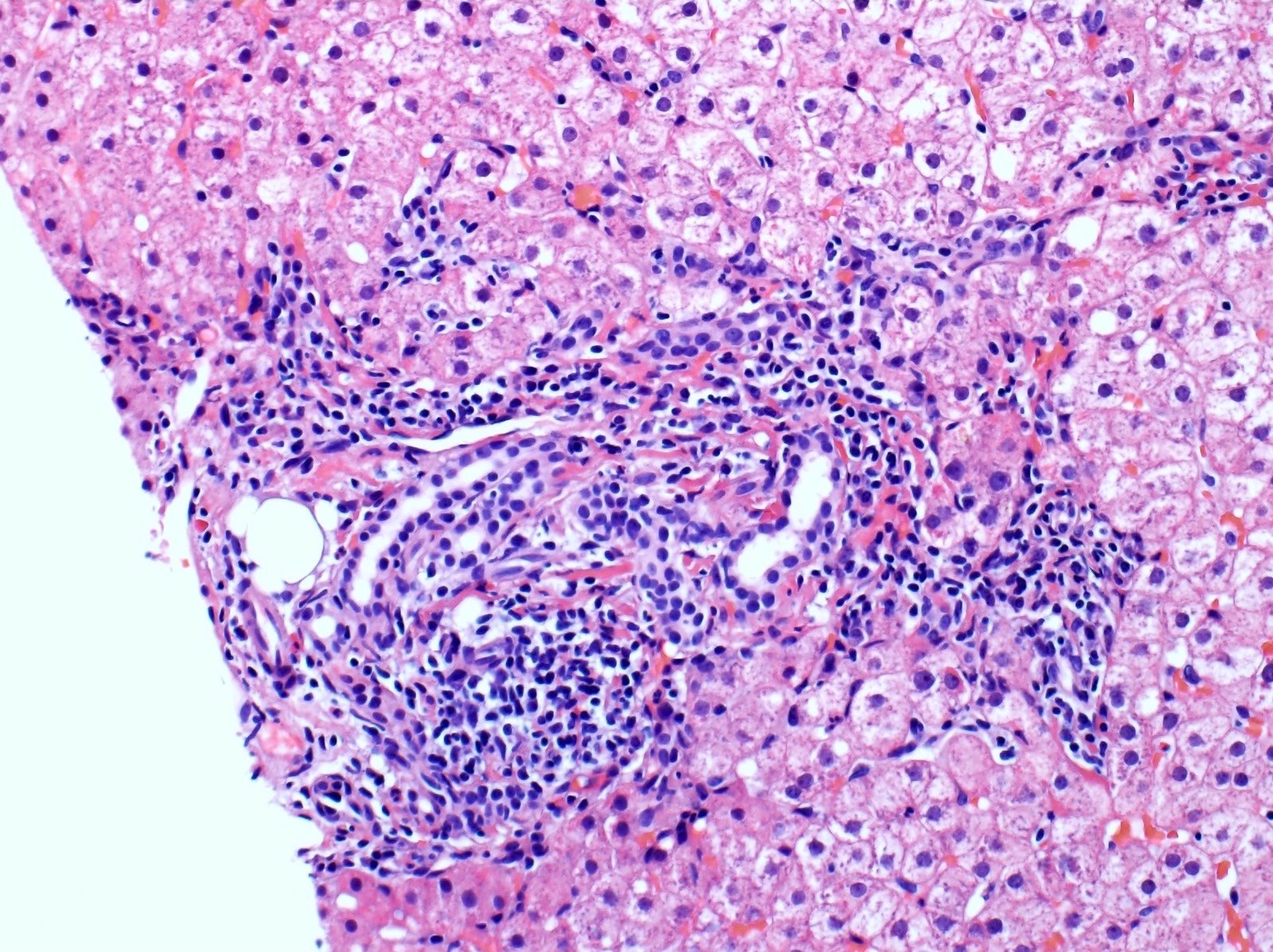
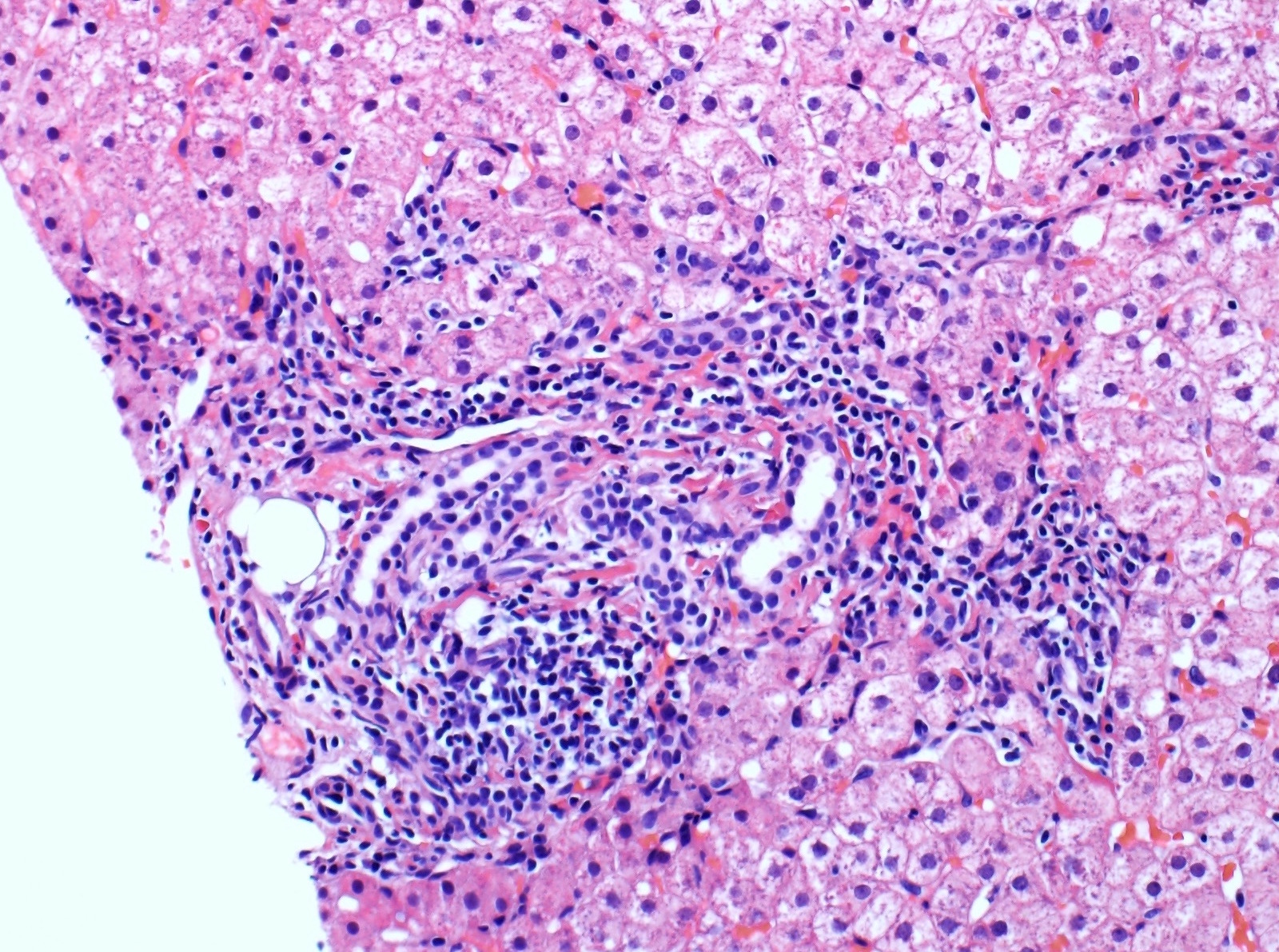
Microscopic (histologic) description
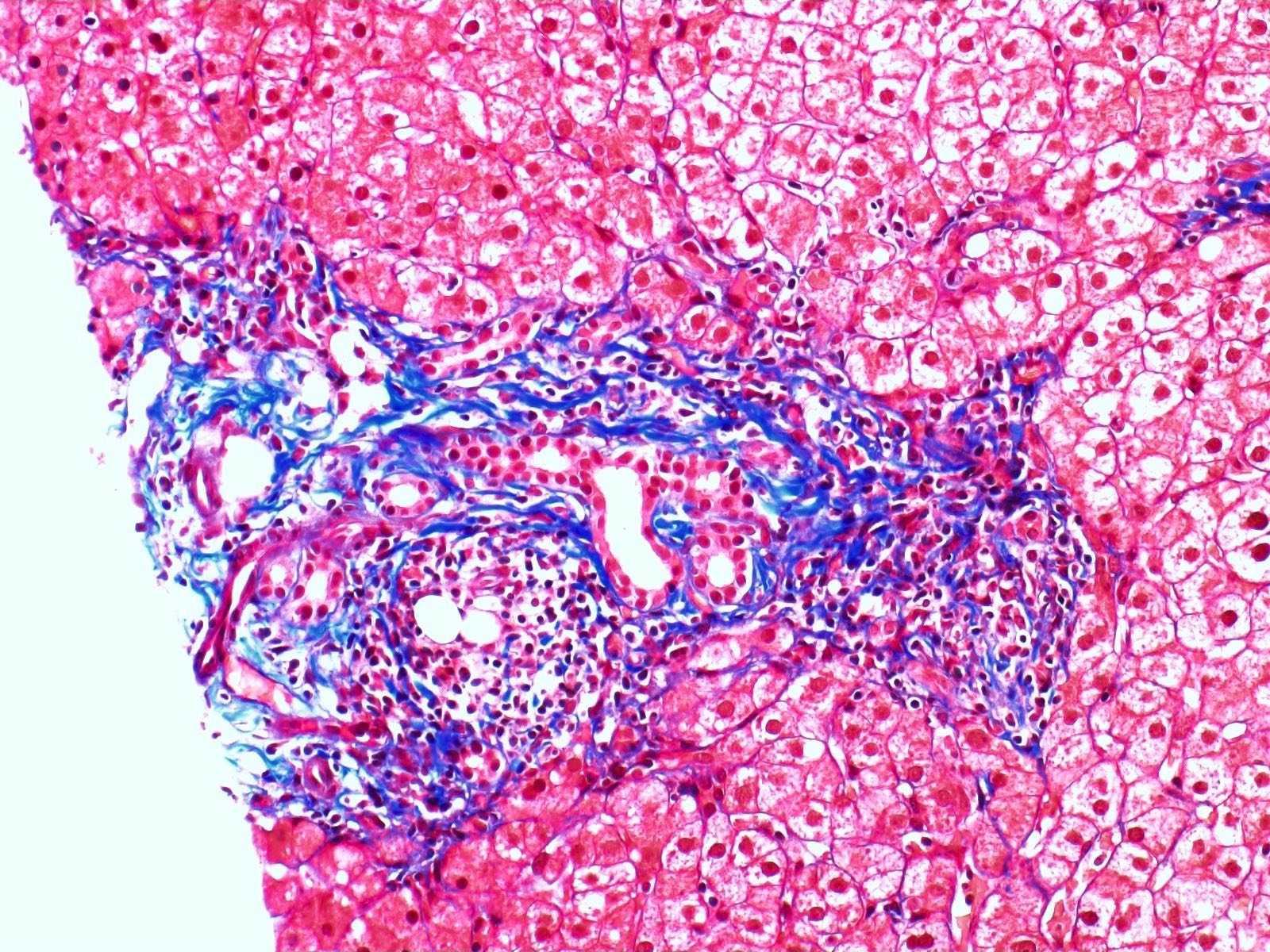
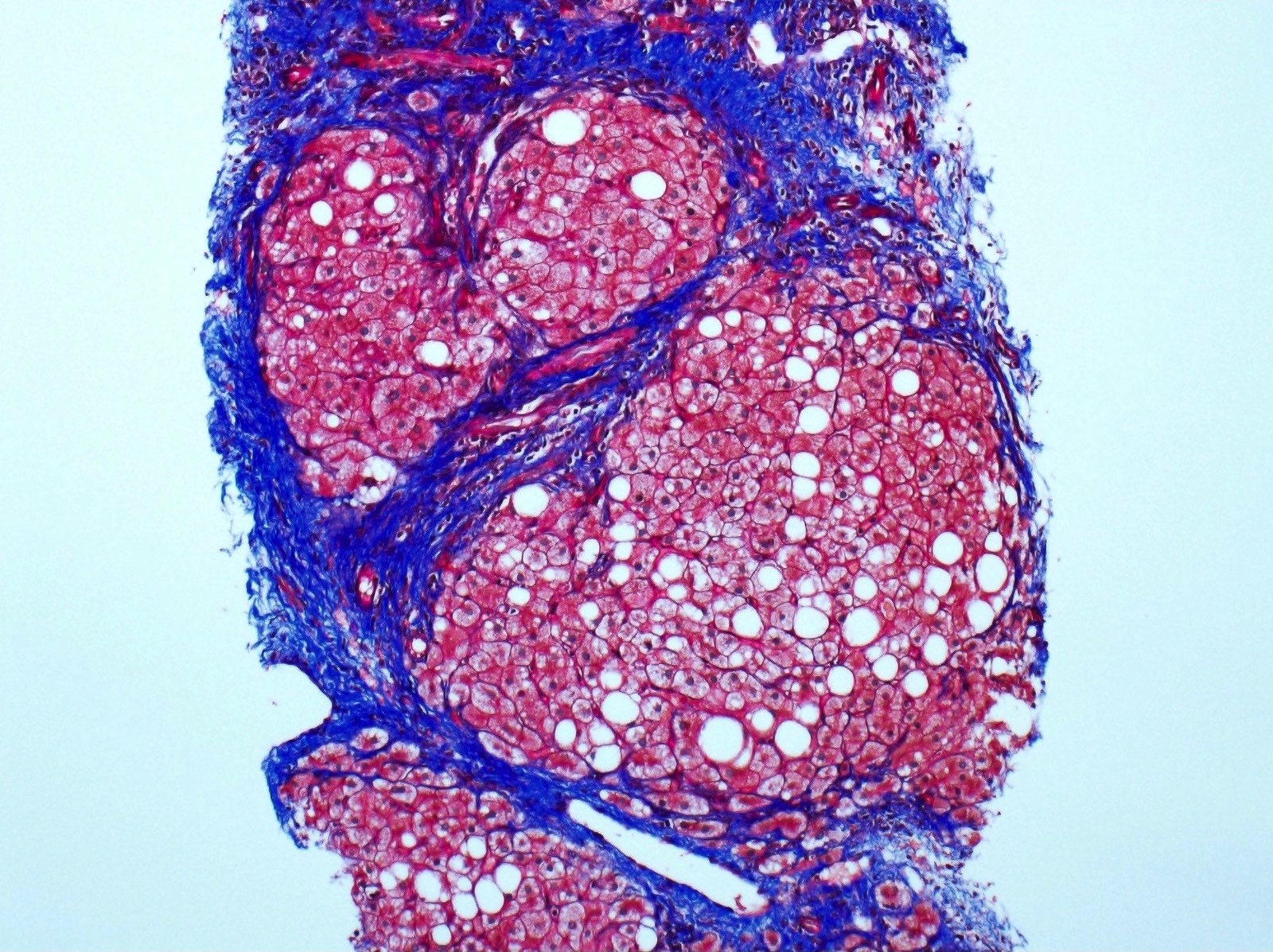
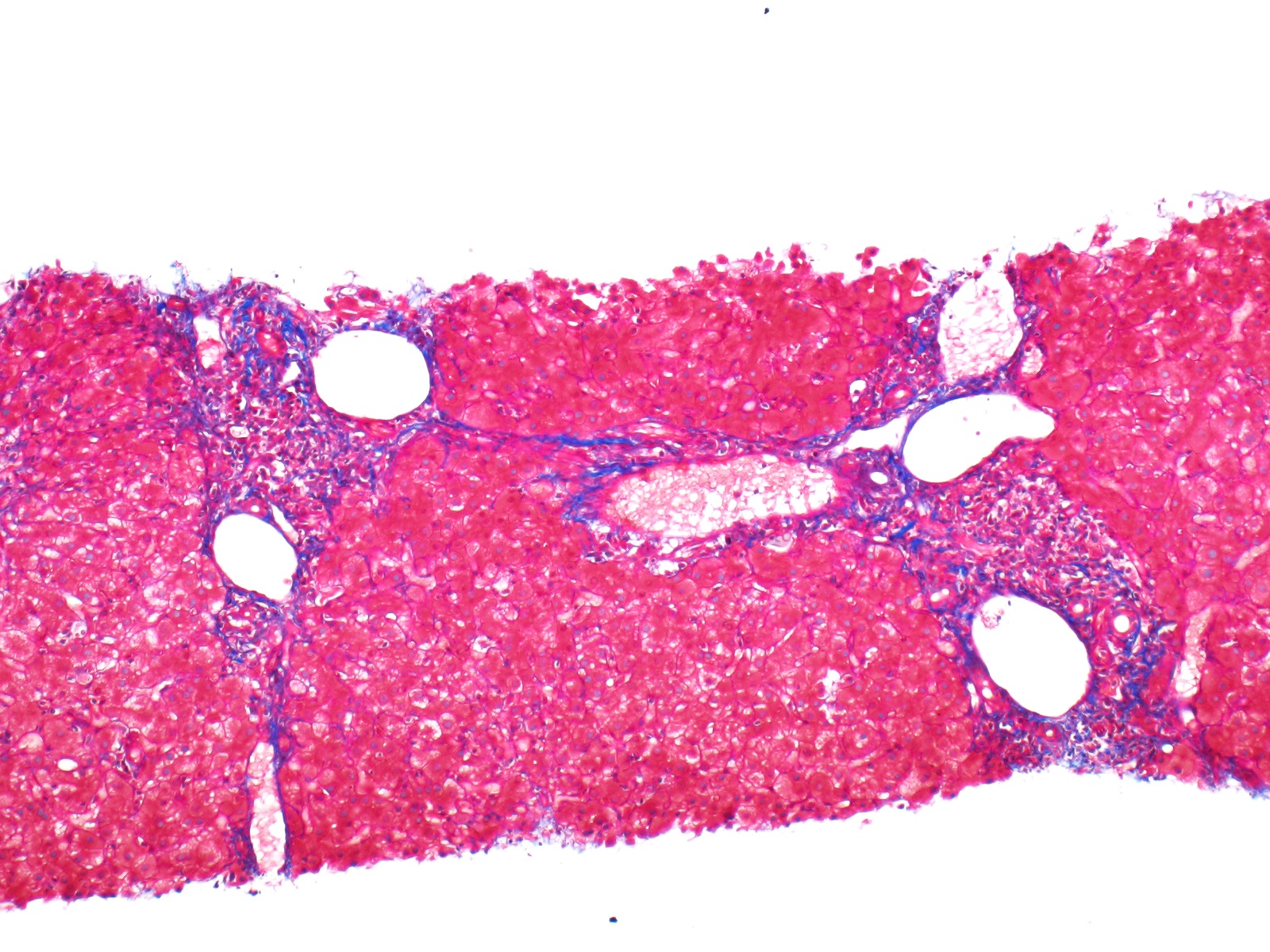
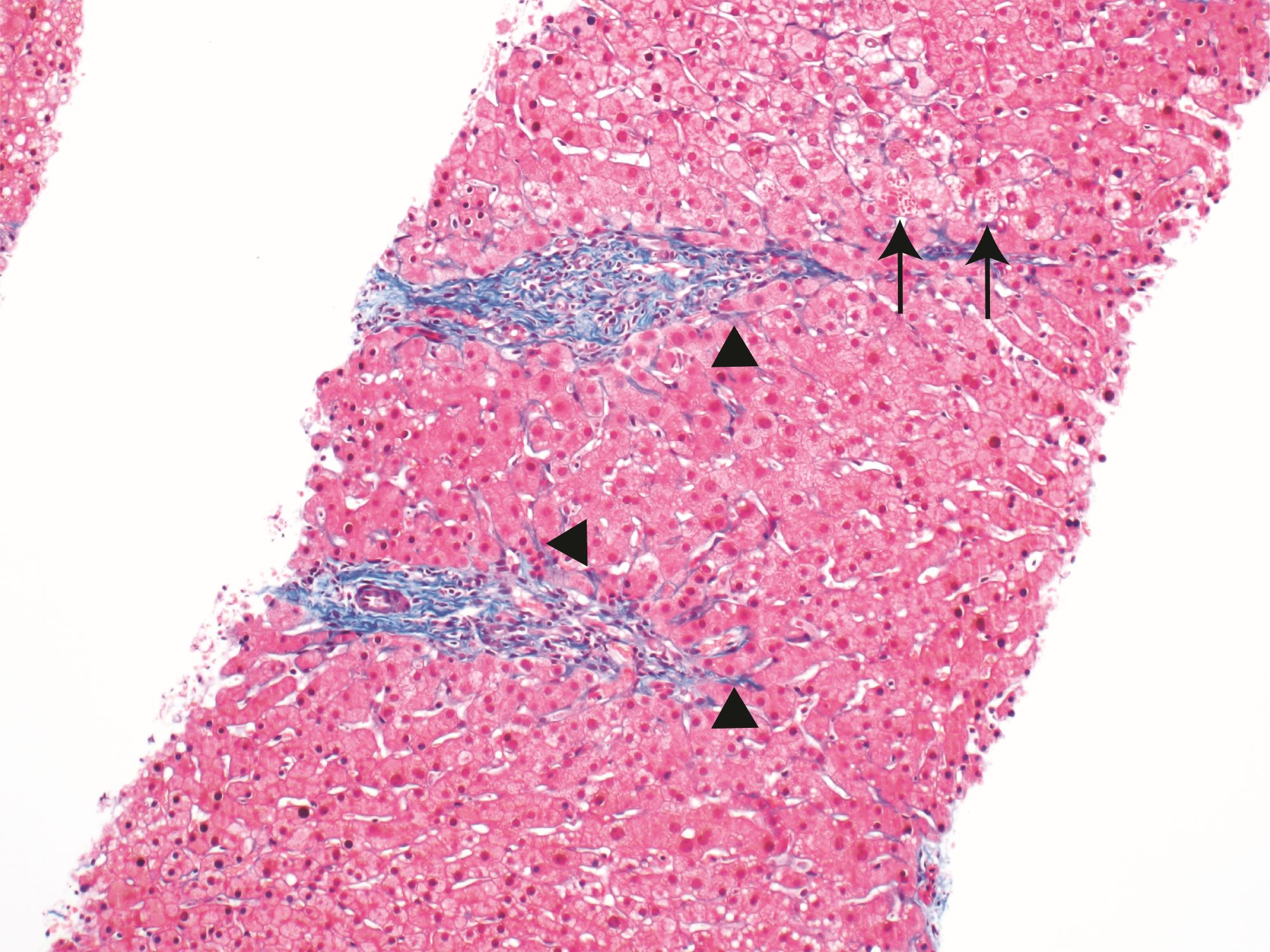
- Fibrosis
- Required for pathologic diagnosis of chronic hepatitis in the absence of clinically confirmed chronic liver disease
- Progressive fibrosis of the limiting plate leads to enlargement of portal tracts and stellate periportal fibrous extension
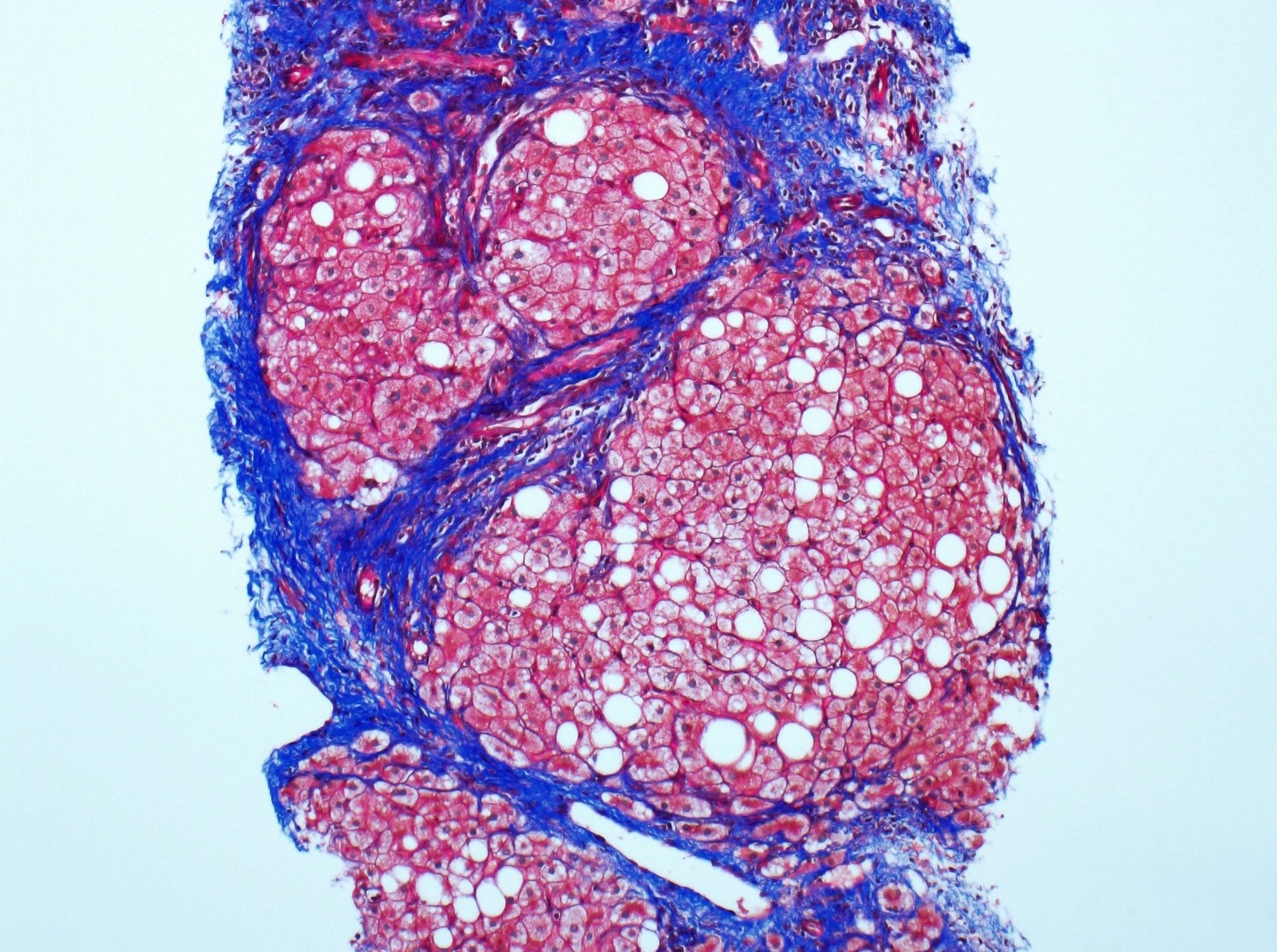
- May lead to portal - portal or portal - central fibrous bridging, culminating in cirrhosis, which is usually micronodular (nodules < 3 mm in diameter) or mixed micronodular and macronodular type
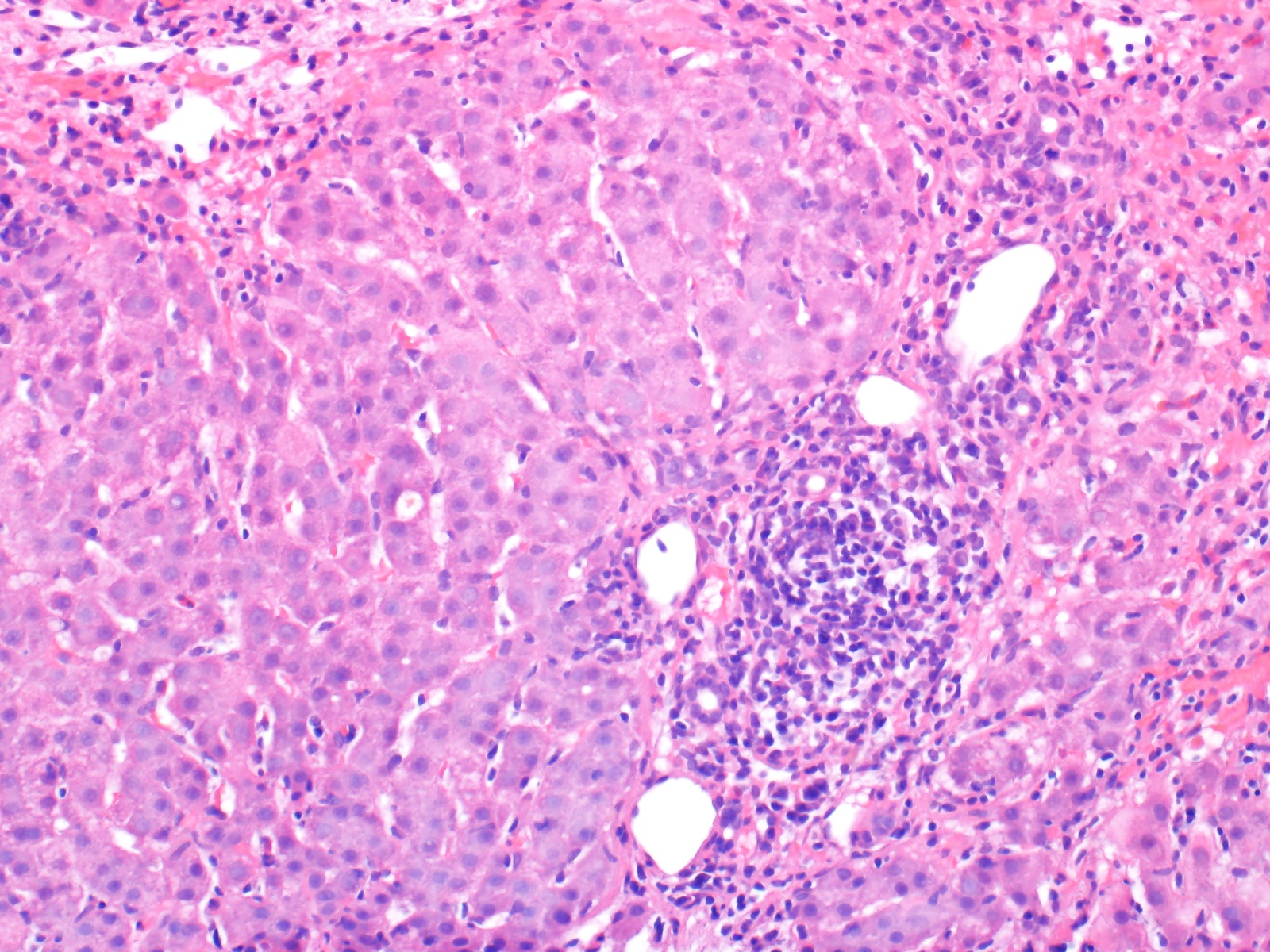
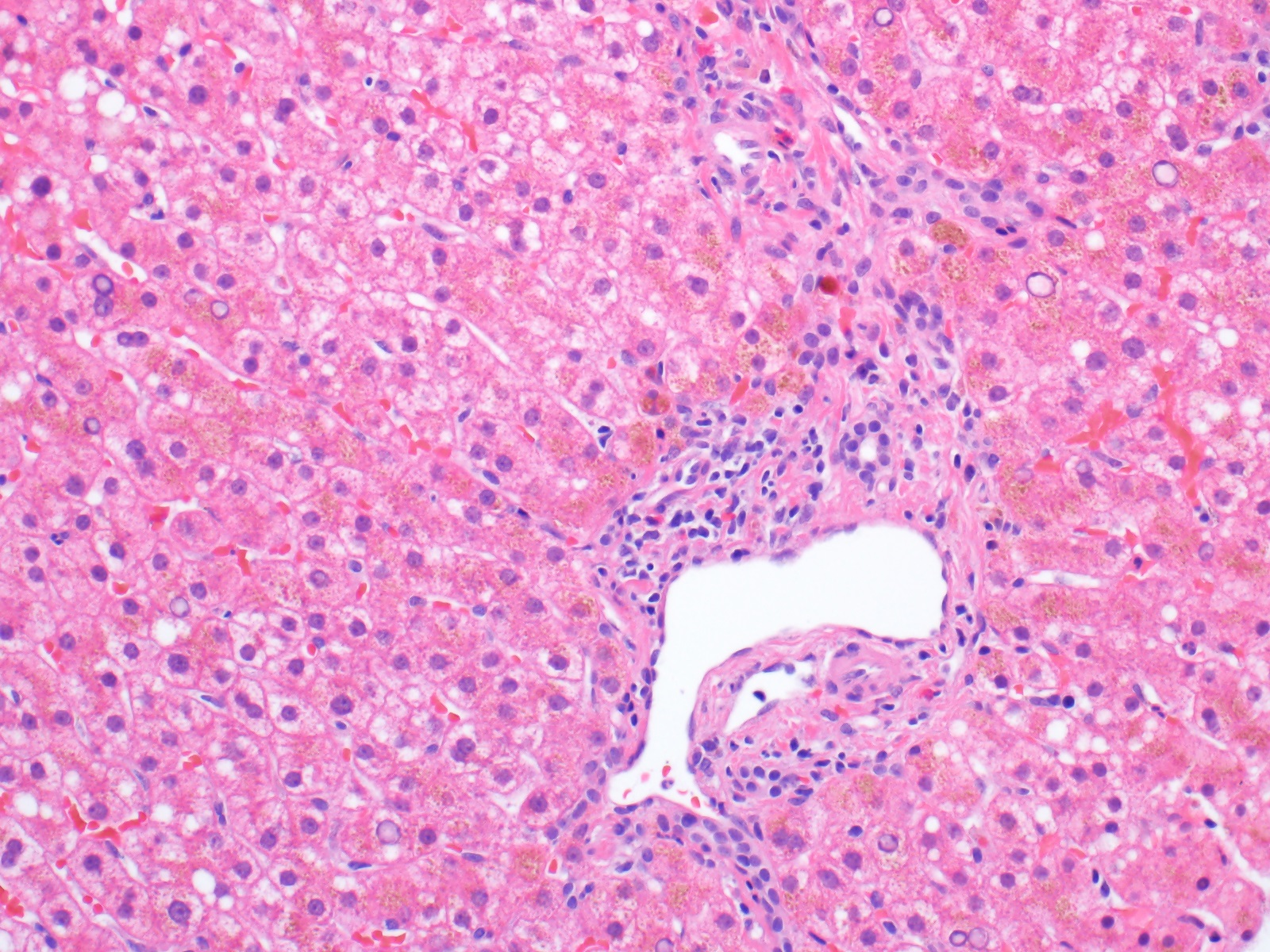
- Portal inflammation
- Mononuclear infiltration of portal tracts (mostly CD4+ T lymphocytes with some plasma cells)
- Lymphoid aggregates or follicles may be present (most common in hepatitis C infection)
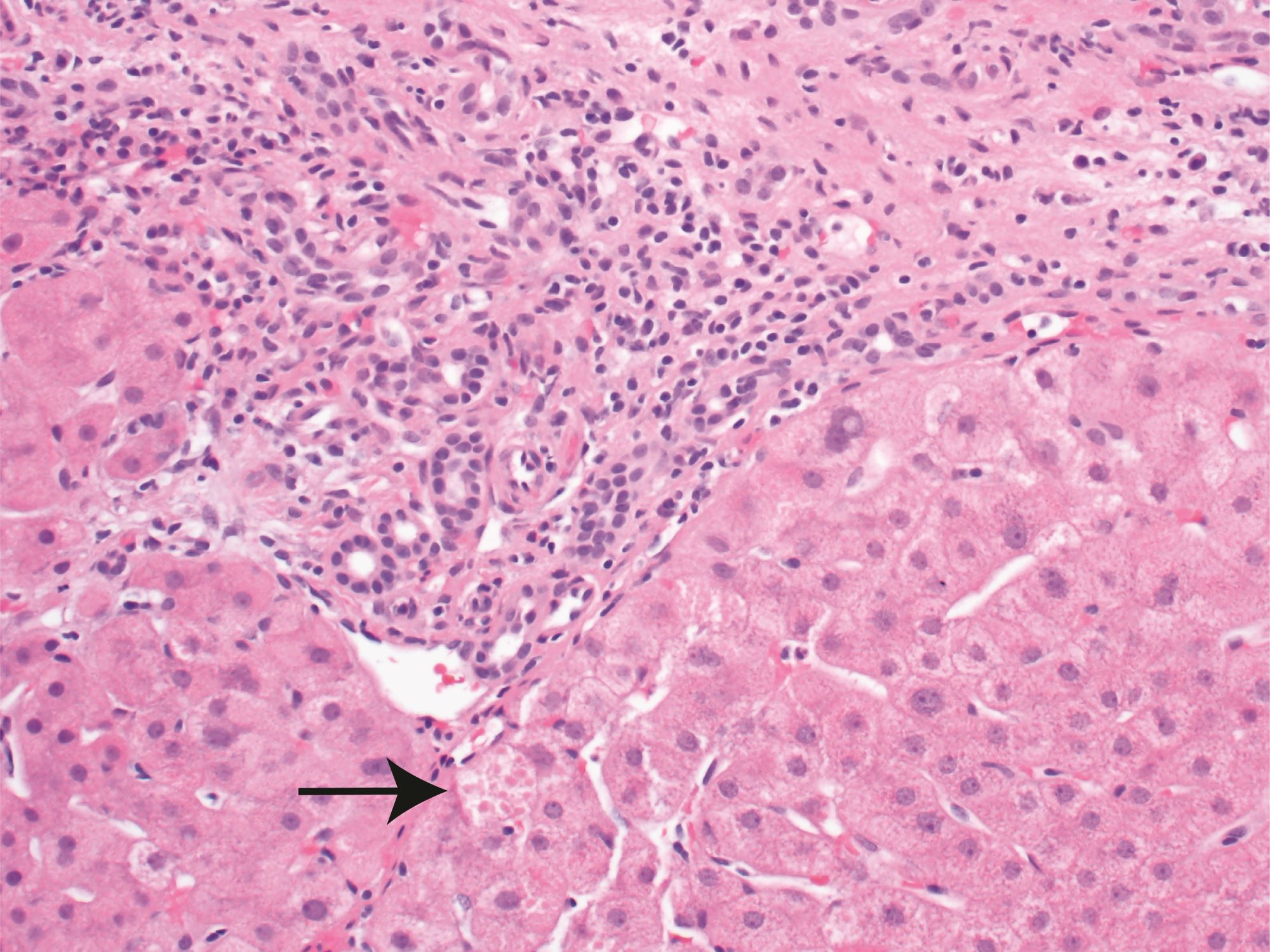
- Interface hepatitis
- Previously called piecemeal necrosis
- Hepatocyte apoptosis and inflammation at the stromal - parenchymal interface (interface of portal tract and lobule)
- Mononuclear infiltrate (mostly CD8+ T lymphocytes)
- Lobular hepatitis
- Mononuclear infiltrate of the hepatic parenchyma (lobules)
- Apoptotic / necrotic hepatocytes (Councilman bodies) in zones 2 and 3
- Reference: Am J Surg Pathol 1995;19:1409
Microscopic (histologic) images
Virtual slides
Positive stains
- Trichrome stain can help with the assessment of the amount of scarring and fibrosis present (stage)
Sample pathology report
- Liver, core biopsy:
- Chronic hepatitis with mild portal and lobular necroinflammatory activity (grade 2, scale 0 - 4, Batts-Ludwig methodology) and periportal fibrosis (stage 2, scale 0 - 4, Batts-Ludwig methodology), consistent with clinical history of chronic hepatitis C
Differential diagnosis
- Primary biliary cholangitis (PBC):
- Can have portal based inflammation with interface activity and lobular activity
- Florid duct lesions not seen in chronic hepatitis
- Clinical history may include elevated alkaline phosphatase, gamma glutamyl transpeptidase, serum IgM and antimitochondrial autoantibodies
- Lymphoma or leukemia infiltrating into the liver:
- Can have portal lymphocytic inflammation
- Lacks interface hepatitis and portal based fibrosis
- May have monomorphism and marked atypia of the infiltrating cells
- Chronic steatohepatitis:
- Can have portal and lobular lymphocytic inflammation
- Has steatosis / fat (may also be seen in chronic hepatitis)
- Centrizonal, pericellular fibrosis not seen in chronic hepatitis
- May be morphologically indistinguishable from chronic hepatitis at late stage (cirrhosis)
- Active hepatitis with bridging necrosis:
- Has portal inflammation with interface activity and lobular inflammation
- Bridging necrosis can cause a nodular appearance from low power, mimicking bridging fibrosis or cirrhosis
- Trichrome staining is paler in zones of dropout / necrosis than in fibrous areas
Additional references
Board review style question #1
- An asymptomatic 35 year old woman has elevated serum aminotransferases (aspartate aminotransferase [AST] and alanine aminotransferase [ALT]). A liver biopsy was performed. What is the most likely underlying etiology of these findings?
- Alcoholic liver disease
- Infection with hepatitis C
- Oxaliplatin induced liver injury
- Tylenol overdose
- Valproic acid associated liver injury
Board review style answer #1
Board review style question #2
Board review style answer #2