Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Carreon CK, Putra J. Cardiac (congestive) hepatopathy and Fontan associated liver disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverCHF.html. Accessed April 24th, 2024.
Definition / general
- Manifestations of chronic, passive congestion of the liver in the setting of heart failure or other heart defects (Clin Liver Dis (Hoboken) 2016;8:68)
Essential features
- Congestive hepatopathy can result from various cardiac diseases
- Similar hepatic manifestations following Fontan palliation in congenital heart defects is recognized as Fontan associated liver disease (Int J Mol Sci 2020;21:9420, Semin Thorac Cardiovasc Surg 2022;34:653, Pediatr Radiol 2021;51:2598)
Terminology
- Hepatic venous outflow obstruction
- Chronic passive congestion of the liver
- Congestive hepatopathy
- Cardiac hepatopathy
- Cardiac sclerosis
- Cardiac cirrhosis
ICD coding
Epidemiology
- Any cause of right sided heart failure can lead to congestive hepatopathy
- Widespread use of heart transplantation and major advances in medical and surgical management have significantly altered the profile of patients with congestive hepatopathy (Int J Mol Sci 2020;21:9420)
- Cases due to noncongenital heart failure are declining
- Cases following Fontan surgery (Fontan associated liver disease) are on the rise
Sites
- Liver
Pathophysiology
- Hepatic manifestations result from passive venous congestion / impaired hepatic venous drainage, secondary to chronic right sided heart failure (Int J Mol Sci 2020;21:9420)
- Fontan associated liver disease (FALD) (Int J Mol Sci 2020;21:9420):
- Functional structural alterations in the liver following Fontan creation (total cavopulmonary connection achieved by implanting a surgical shunt to divert blood from the inferior and superior vena cava to the pulmonary arteries) passively carry blood to the functionally single ventricular chamber
- Bypass leads to chronic hepatic venous congestion, secondary to high pressure nonpulsatile flow in the inferior vena cava
- Lack of subpulmonary ventricle also leads to diminished cardiac preload for the systemic ventricle, resulting in chronically low cardiac output
- FALD's natural history is poorly understood; at present, there are no methods to identify or predict patients that will eventually develop clinically significant advanced liver disease
Etiology
- Right sided heart failure or right ventricular failure (RVF), whether primary or secondary
- In the adult population, RVF is usually a result of left ventricular failure (Interact Cardiovasc Thorac Surg 2018;27:921)
- Primary RVF (Card Fail Rev 2019;5:140):
- Chronic conditions leading to pressure overload
- Congenital heart defects (pulmonic stenosis, those with right ventricular outflow obstruction or RV exposed to systemic pressure)
- Chronic conditions leading to volume overload (Card Fail Rev 2019;5:140):
- Valvular insufficiency involving tricuspid or pulmonic valves
- Congenital heart disease with left to right shunt (atrial septal defect, anomalous pulmonary venous return)
- Fontan associated liver disease (Int J Mol Sci 2020;21:9420):
- Recognized consequence of Fontan palliation in patients born with univentricular physiology, congenital heart disease
- Intrinsic RV myocardial disease / injury (Interact Cardiovasc Thorac Surg 2018;27:921):
- Ischemia or infarct
- Infiltrative disease (e.g., sarcoidosis, tumor, amyloidosis)
- Arrhythmogenic right ventricular dysplasia
- Cardiomyopathy
- Microvascular disease
- Impaired RV filling (Interact Cardiovasc Thorac Surg 2018;27:921):
- Constrictive pericarditis
- Tricuspid stenosis
- Systemic vasodilatory shock
- Cardiac tamponade
- Superior vena cava syndrome
- Hypovolemia
Clinical features
- Usually asymptomatic and in such a scenario, passive liver congestion may be incidentally discovered through abnormalities in routine laboratory evaluations (Clin Liver Dis (Hoboken) 2016;8:68)
- When symptomatic, patients may experience
- Dull right upper quadrant pain
- Jaundice
- Clinical stigmata of portal hypertension are generally absent until cirrhosis ensues (Clin Liver Dis 2002;6:947)
- Progressive dyspnea
- Hepatomegaly
- Gastroesophageal varices
- Ascites
- Hepatojugular reflux
- Peripheral edema
Diagnosis
- Diagnosis is often made by abnormal laboratory workup (see Laboratory findings)
- Liver biopsy may be performed if liver tests are persistently abnormal after heart failure treatment or as part of the heart or combined heart / liver transplant workup
Laboratory
- Unconjugated hyperbilirubinemia (total bilirubin < 3 mg/dL [51.31 micromol/L])
- Elevated aminotransferases (< 2 - 3 fold)
- Mild hypoalbuminemia in 30 - 50% of patients (Clin Liver Dis 2002;6:947)
- Prolonged prothrombin time / international normalized ratio (PT / INR)
- Ascitic fluid may show high serum to ascites albumin concentration gradient (JAMA 2016;316:340)
- Gradients ≥ 1.1 g/dL (11 g/L) are specific for ascites due to portal hypertension (the serum albumin concentration minus the ascitic albumin concentration [SAAG]) (JAMA 2016;316:340)
- High ascitic total protein content (typically > 2.5 g/dL [25 g/L]) plus a SAAG ≥ 1.1 g/dL (11 g/L) suggests congestive hepatopathy and differentiates portal hypertension from cirrhosis (typically total protein < 2.5 g/dL [25 g/L] plus a SAAG ≥ 1.1 g/dL [11 g/L])
Radiology description
- Ultrasound (US) may be used to evaluate hemodynamic properties of the liver in patients with congestive hepatopathy (CH)
- Doppler US is the most cost effective and expeditious modality for assessing blood flow direction and velocity in the hepatic vasculature
- Common US findings of CH (Acta Radiol Diagn (Stockh) 1982;23:361, Am J Cardiol 1984;53:579):
- Dilated inferior vena cava
- Dilated hepatic veins
- Degree of dilatation correlates with the severity of heart failure
- CT and MR imaging can show a number of characteristic findings helpful for the diagnosis of CH (Diagn Interv Radiol 2020;26:541)
- Hepatomegaly in acute congestion
- Atrophic nodular liver in patients with chronic congestion and cirrhosis
- As seen on the US, the inferior vena cava and hepatic veins are dilated; in severe cases, venous shunts can be observed between the hepatic veins
- Increased prevalence of hyperenhancing hepatic nodules that appear similar to focal nodular hyperplasia
- Presence of cirrhosis increases the risk for hepatocellular carcinoma in patients with CH; this diagnosis must be taken into consideration
- Reference: Radiographics 2016;36:1024
Prognostic factors
- Clinical outcome generally depends on the severity of underlying cardiac disease; progression to cirrhosis does not necessarily correlate with worse prognosis and reversibility may be achieved by optimization of cardiac function (Clin Liver Dis (Hoboken) 2016;8:68)
Case reports
- 7 year old girl with Fontan associated liver disease and hepatic adenomatosis (Pediatr Cardiol 2010;31:861)
- 36 year old woman with focal nodular hyperplasia in the setting of Fontan associated liver disease (Korean J Intern Med 2022;37:480)
- 40 year old man with Fontan associated liver disease and ruptured hepatocellular carcinoma (SAGE Open Med Case Rep 2020;8:2050313X20922030)
Treatment
- Management of the underlying heart condition with optimization of cardiac output
- Treatment options include diuresis, left ventricular assist device (LVAD) implantation and liver transplantation (Clin Liver Dis (Hoboken) 2016;8:68)
Gross description
- Sinusoidal congestion resulting in a classic nutmeg appearance
- Advanced fibrosis may lead to a firm and nodular cut surface
- Reference: Clin Liver Dis (Hoboken) 2016;8:68
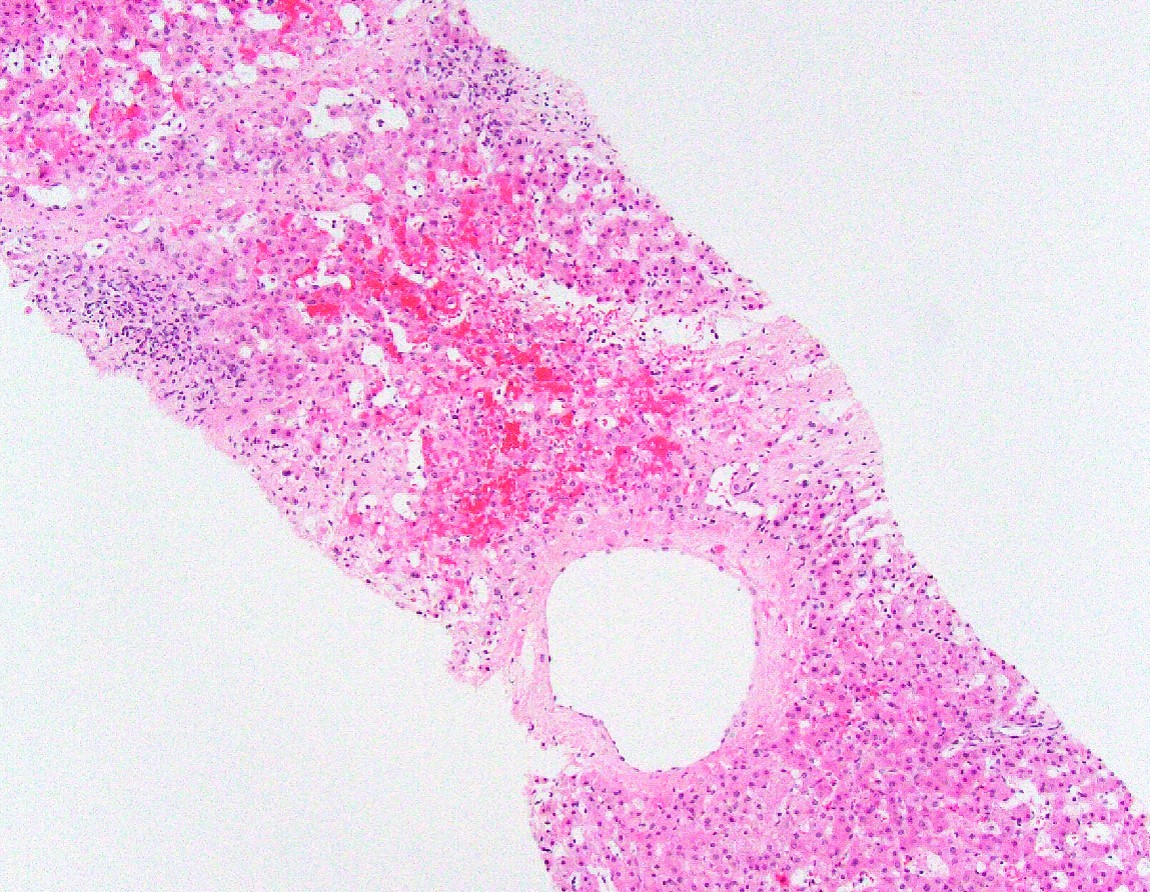
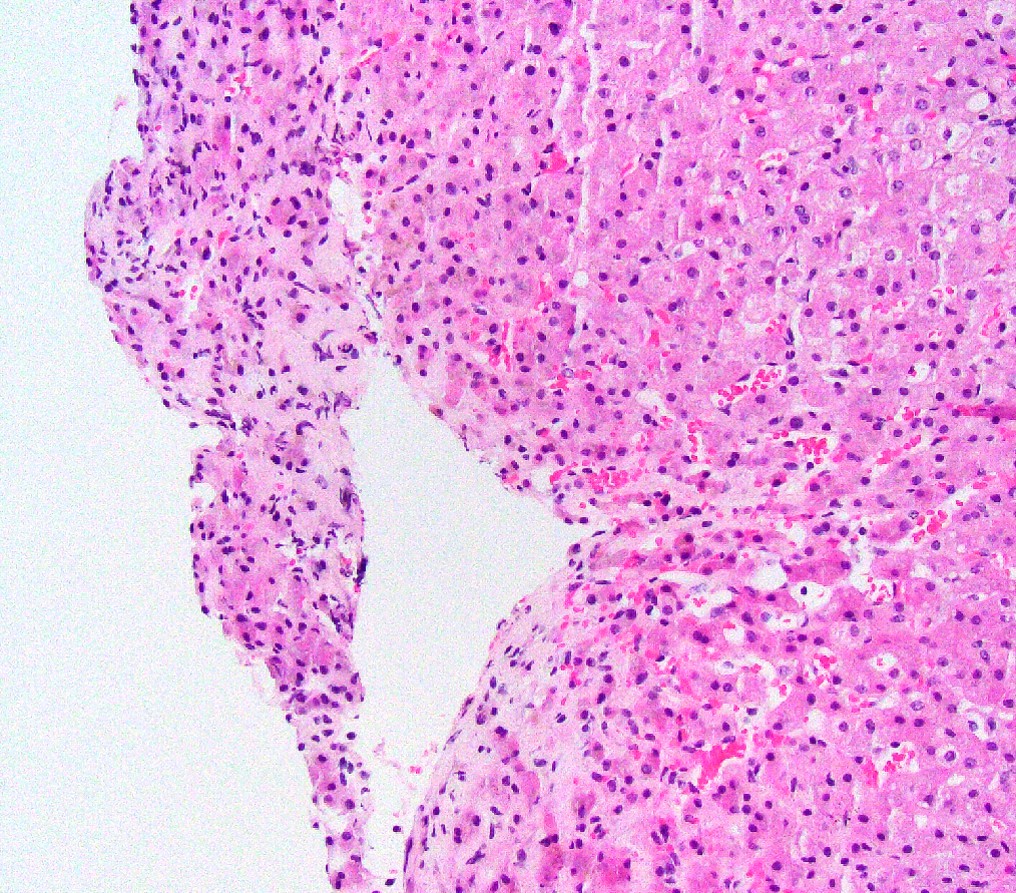
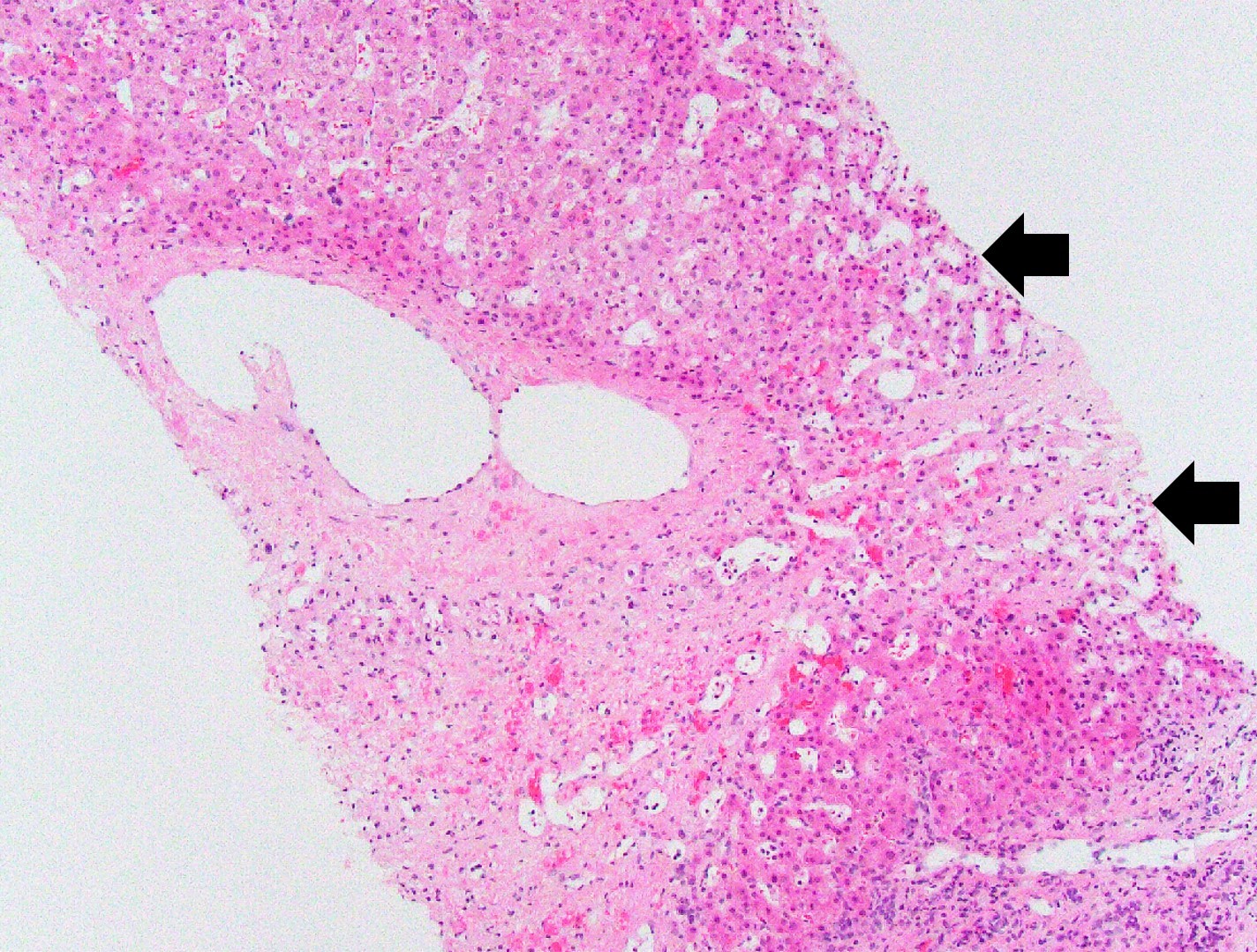
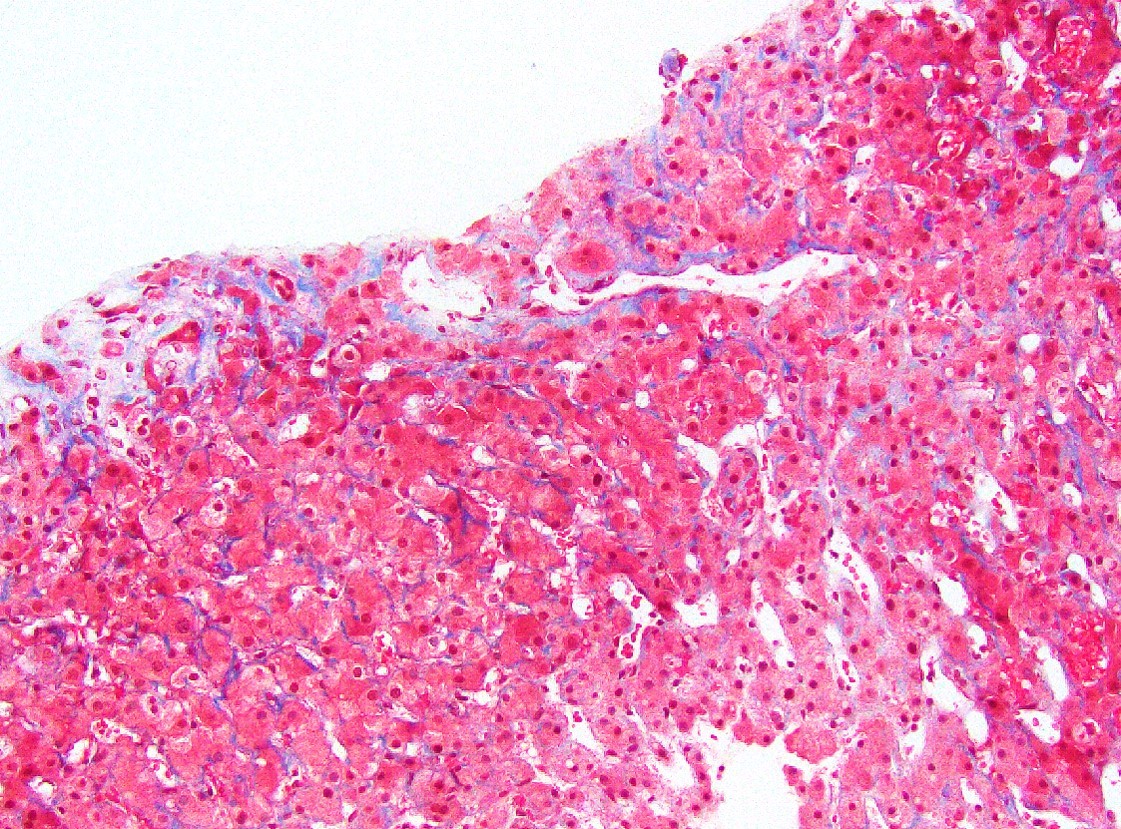
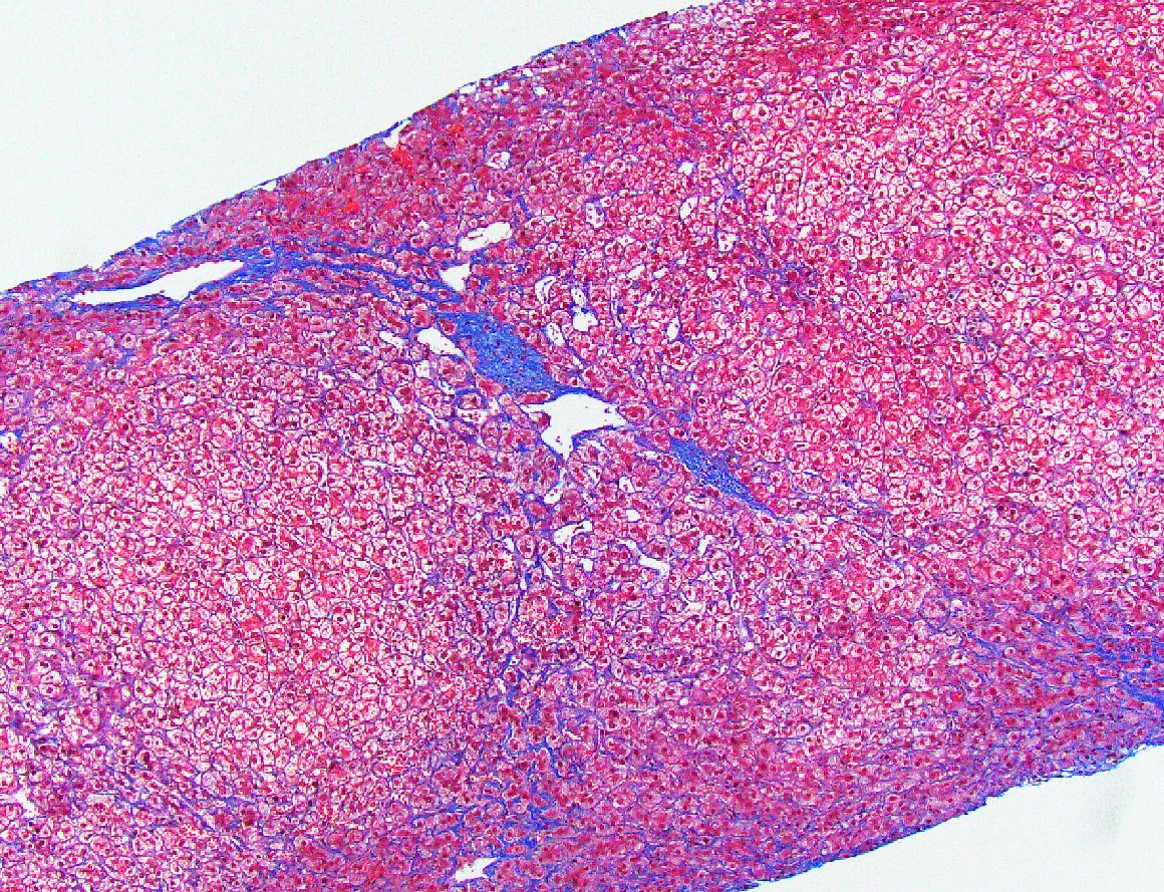
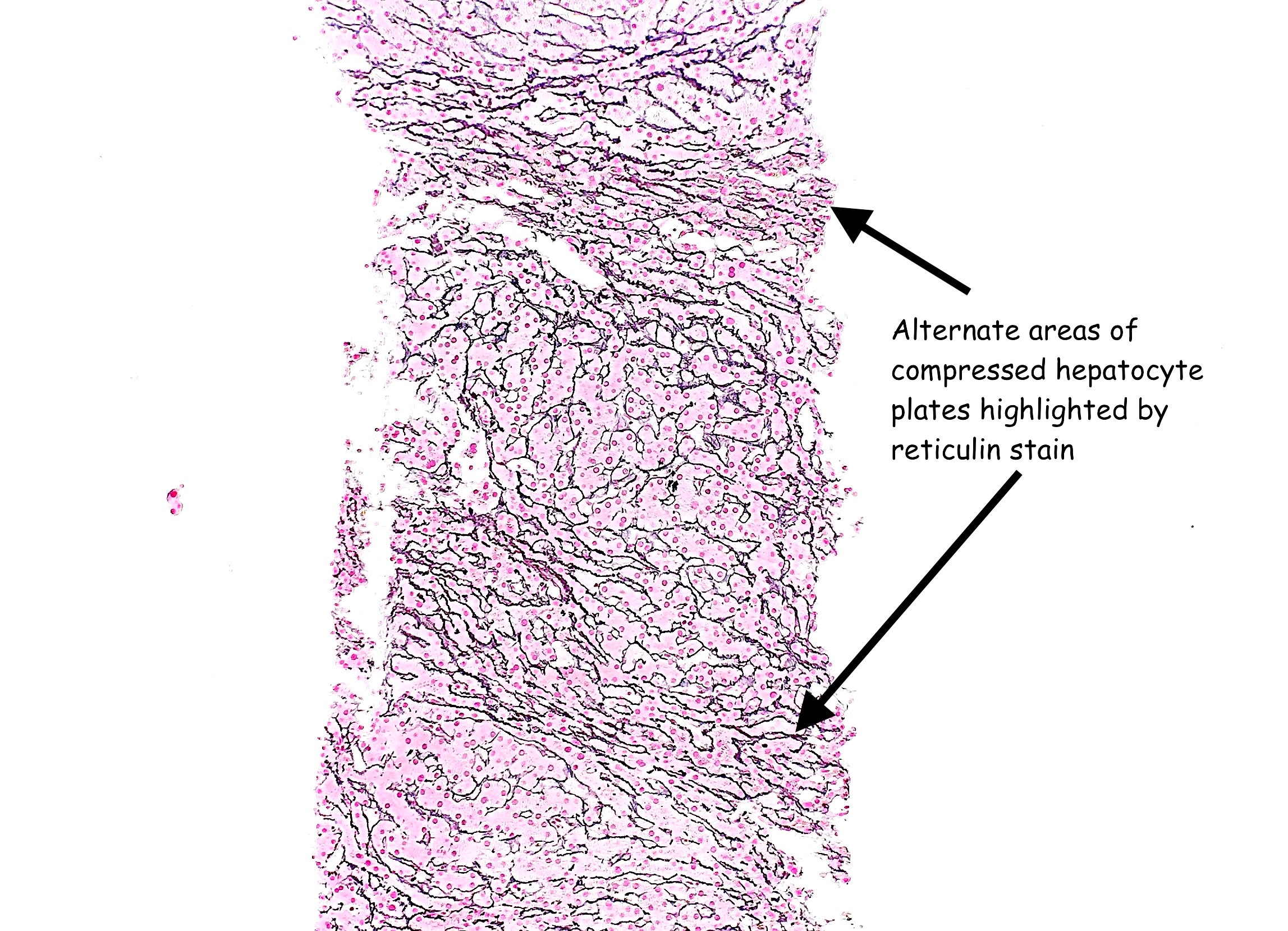
Microscopic (histologic) description
- Sinusoidal dilatation and congestion
- Centrilobular hepatocyte atrophy or dropout
- Centrilobular and perisinusoidal fibrosis (heterogeneous distribution but generally starts in zone 3 hepatocytes)
- Portal fibrosis in up to 75% of cases
- Minimal portal inflammation and ductular reaction
- Nodular regenerative hyperplasia (Rev Esp Cardiol (Engl Ed) 2018;71:192)
- Hepatocellular carcinoma may arise in the setting of cirrhosis (J Thorac Cardiovasc Surg 2005;129:1348, JHEP Rep 2021;3:100249)
- Focal nodular hyperplasia and hepatic adenoma may also occur (JACC Case Rep 2019;1:175, J Thorac Cardiovasc Surg 2005;129:1348, Pediatr Cardiol 2010;31:861)
- Pseudoground glass and eosinophilic cytoplasmic inclusions (Torbenson: Biopsy Interpretation of the Liver, 4th Edition, 2021, Mod Pathol 2000;13:679)
- Congestive hepatic fibrosis score shows a good correlation with the right atrial pressure (Mod Pathol 2014;27:1552):
- Score 0: no fibrosis
- Score 1: central zone fibrosis
- Score 2A: central zone and mild portal fibrosis, with accentuation at central zone
- Score 2B: at least moderate portal fibrosis and central zone fibrosis, with accentuation at portal zone
- Score 3: bridging fibrosis
- Score 4: cirrhosis
Microscopic (histologic) images
Positive stains
- Special stains for fibrosis evaluation: Masson trichrome or Sirius red
- Special stain for nodular regenerative hyperplasia and fibrosis evaluation: reticulin
Sample pathology report
- Liver, biopsy:
- Liver with patchy sinusoidal dilatation and congestion, in keeping with Fontan associated liver disease (congestive hepatopathy)
- Heterogeneous degree of fibrosis with portal, perivenular and perisinusoidal fibrosis with focal portal to central bridging fibrosis (congestive hepatic fibrosis score 2A-3 of 4)
- No significant portal inflammation, lobular activity, steatosis or cholestasis
Differential diagnosis
- Budd-Chiari syndrome:
- Centrilobular hepatocyte necrosis is more common
- Sinusoidal obstruction syndrome:
- Marked centrilobular hemorrhagic necrosis in the early phase and occlusion of the central veins by fibrous tissue in later stages of the disease
- Ischemia:
- Centrilobular coagulative hepatocyte necrosis is more common
Additional references
Board review style question #1
Which of the following histologic features is typical of congestive hepatopathy?
- Bile duct injury
- Feathery degeneration of hepatocytes
- Microvesicular steatosis
- Obliterated portal veins
- Perisinusoidal fibrosis
Board review style answer #1
E. Perisinusoidal fibrosis
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease
Board review style question #2
Board review style answer #2
C. Constrictive pericarditis
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease