Table of Contents
Definition / general | Epidemiology | Etiology | Clinical features | Morphology | Immunophenotype | Genetics | Cell of origin | Prognostic factors | Treatment | Case reports | Microscopic (histologic) images | Electron microscopy images | Molecular / cytogenetics description | Differential diagnosisCite this page: Mihova D. Ambiguous lineage NOS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/leukemiaambiguouslin.html. Accessed March 30th, 2025.
Definition / general
- Acute leukemias in which the morphologic, cytochemical and immuno-phenotypic features of the blasts:
- Lack sufficient evidence to classify as myeloid or lymphoid origin
- Or, have morphologic and / or immunophenotypic characteristics of both myeloid and lymphoid cells
- Or, have both B and T lineages (acute bilineal leukemia and acute biphenotypic leukemia)
Acute leukemias of ambiguous lineage include the following:- Acute undifferentiated acute leukemia
- Mixed phenotype acute leukemia with t(9;22)(q34;q112.); BCR-ABL1
- Mixed phenotype acute leukemia with t(v;11q23); MLL rearranged
- Mixed phenotype acute leukemia, B/myeloid, NOS
- Mixed phenotype acute leukemia, T/myeloid, NOS
- Mixed phenotype acute leukemia, NOS rare types
- Other acute leukemias of ambiguous lineage
Epidemiology
- < 4% of all acute leukemias, more frequent in adults
Etiology
- Unknown
Clinical features
- Related to bone marrow failure: fatigue, infections, bleeding
Morphology
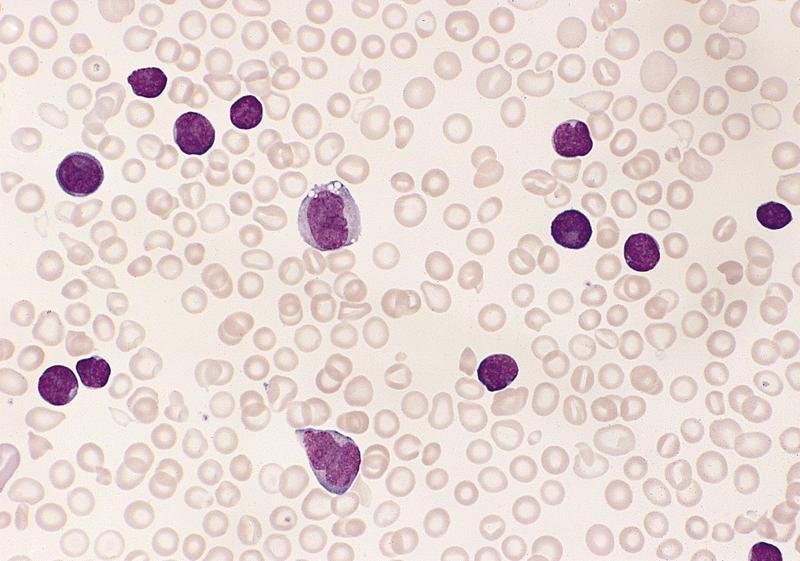
- Acute undifferentiated leukemia
- Leukemic cells lack any differentiating features
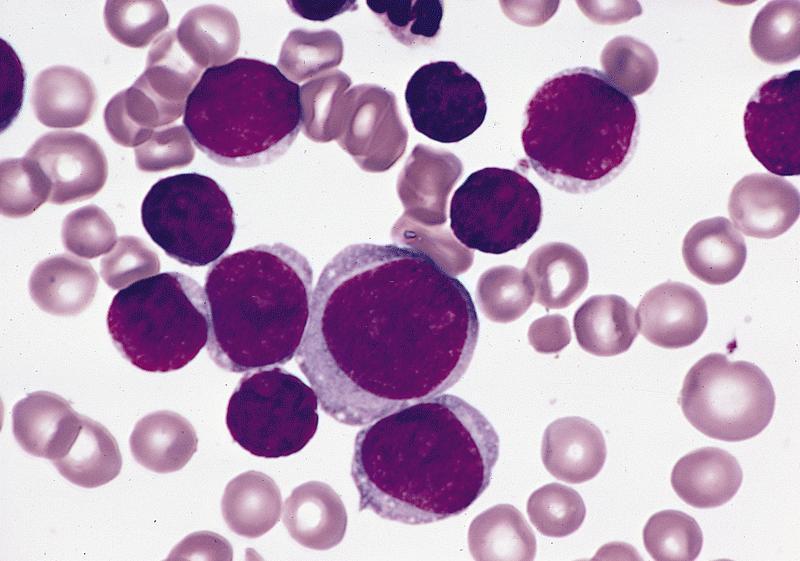
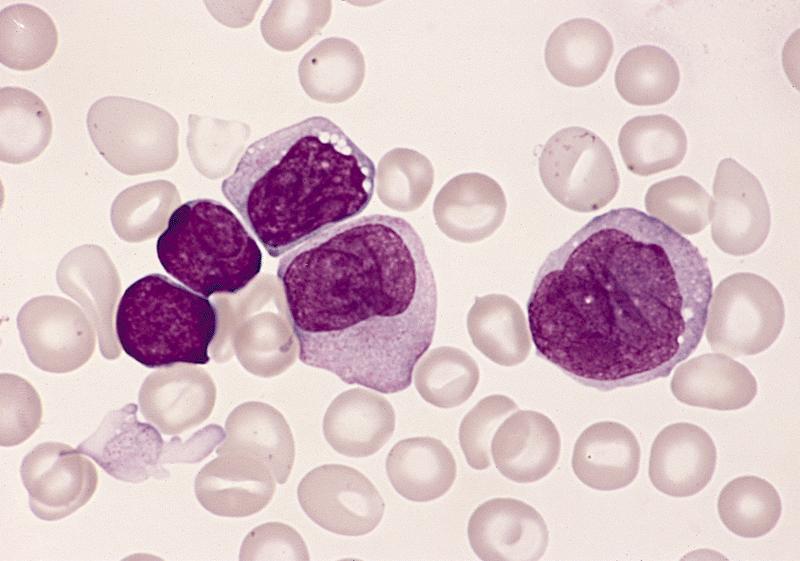
- Acute biphenotypic and acute bilineal leukemias
- May present as one subtype of AML with features of ALL (B, T or B and T)
Immunophenotype
Undifferentiated acute leukemia:
Bilineal acute leukemia
Biphenotypic acute leukemia
- Leukemias lack specific lineage markers
- cCD79a, cCD22, CD3 and MPO
- Generally don’t express more than one lineage associated marker
- Often express HLA-DR, CD34, CD38, may express TdT and CD7
Bilineal acute leukemia
- Dual population of blasts, each with distinct lineage: positive for myeloid, lymphoid or B and T-cell markers (Leukemia 2007;21:2264)
- May evolve into biphenotypic acute leukemia (Atlas of Genetics and Cytogenetics: Biphenotypic Acute Leukaemia (BAL) [Accessed 13 April 2018])
Biphenotypic acute leukemia
- Blasts co-express myeloid and T or B lineage markers
- Or, concurrent B and T lineage markers
- Rarely co-express markers for myeloid, T and B lineages
- Co-expression of one or two cross-lineage (nonspecific) markers is not sufficient for biphenotypic leukemia; e.g. myeloid antigen positive ALL or Lymphoid antigen positive AML
- Lineage switch after therapeutic intervention
- Possible expansion of pre-existing minor population of blasts of different lineage following therapeutic suppression of the major population
- Possible lineage instability
Genetics
- High degree of cytogenetic abnormalities
- 1/3 of cases have Ph chromosome
- t(4;11)(q21;q23) or 11q23, typically have CD10(–) precursor B lymphoid component
- T/myeloid biphenotypic or bilineal leukemia can have complex karyotype
Cell of origin
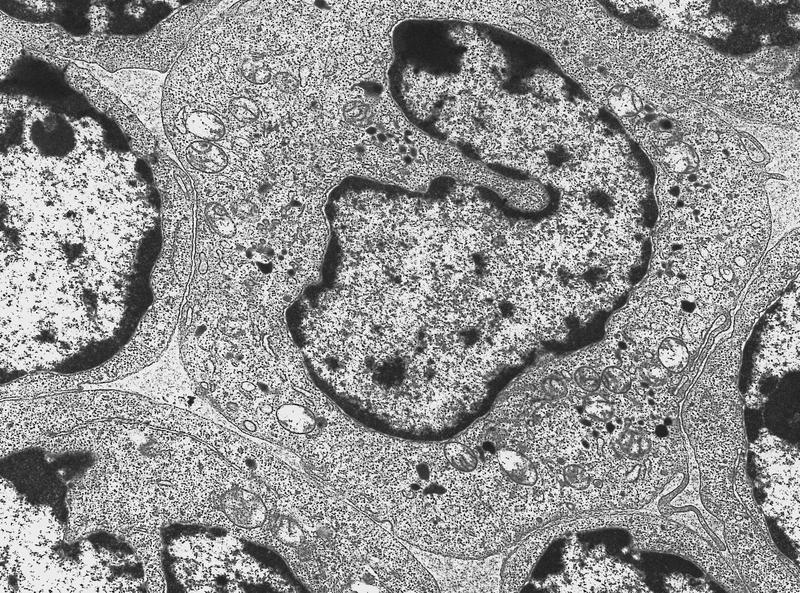
- Multipotent progenitor stem cell
Prognostic factors
- Unfavorable, particularly in adults
- t(4;11) or Ph particularly unfavorable
Treatment
- Usually aggressive chemotherapy or bone marrow transplant
Case reports
- 5 year old boy with t(9;17)(p11;q11) (Leuk Lymphoma 1997;25:179)
- 20 year old woman with myeloid, B cell and NK phenotype (Arch Pathol Lab Med 2003;127:E93)
- 80 year old man with blasts coexpressing CD79a and myeloid markers (Arch Pathol Lab Med 2003;127:356)
- Due to transformation of essential thrombocythemia (Am J Hematol 2006;81:624)
Microscopic (histologic) images
Molecular / cytogenetics description
- Many cases have IgH and TCR rearrangements or deletions
Differential diagnosis
- For biphenotypic acute leukemia
- Myeloid antigen positive ALL
- Lymphoid antigen positive AML
- For undifferentiated acute leukemia
- Minimally differentiated AML
- Unusual precursor-B-cell or T-cell ALL