Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Choy B. Hybrid oncocytic chromophobe tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumoroncocyticchromhybrid.html. Accessed December 23rd, 2024.
Definition / general
- Hybrid oncocytic chromophobe tumor (HOCT) is a renal neoplasm with overlapping features of both renal oncocytoma and chromophobe renal cell carcinoma (ChRCC)
Essential features
- Demonstrates intermediate morphologic and immunophenotypic features between renal oncocytoma and chromophobe RCC (Histol Histopathol 2013;28:1257)
- Classified as a subtype of ChRCC in the 2016 World Health Organization (WHO) Classification but recent molecular data suggest HOCT to be distinct from renal oncocytoma and ChRCC (Mod Pathol 2019;32:1698, Ann Transl Med 2019;7:S356)
- Described in 3 clinical settings: in association with renal oncocytosis, in association with Birt-Hogg-Dubé syndrome and in sporadic cases; recent Genitourinary Pathology Society (GUPS) recommendation for the term hybrid oncocytic tumor to be reserved for hereditary cases (Am J Surg Pathol 1999;23:1094, Am J Surg Pathol 2010;34:620, Am J Surg Pathol 2002;26:1542, Arch Pathol Lab Med 2006;130:1865, Virchows Arch 2010;456:355, Mod Pathol 2021;34:1392)
Terminology
- Hybrid oncocytic chromophobe tumor - GUPS recommends the term to be reserved for hereditary cases
- Other nonsyndromic tumors with borderlines features could be designated “oncocytic renal neoplasms of low malignant potential, not further classified”
Epidemiology
- Typically adults between fourth and eighth decades, slight M > F (Am J Surg Pathol 1999;23:1094, Am J Surg Pathol 2002;26:1542, Am J Surg Pathol 2010;34:620, Virchows Arch 2010;456:355)
- Described in patients with renal oncocytosis, patients with Birt-Hogg-Dubé syndrome and in sporadic cases
Sites
- Kidney
Clinical features
- Patients with Birt-Hogg-Dubé syndrome are predisposed to develop fibrofolliculomas, pulmonary cysts leading to increased risk of spontaneous pneumothorax (Am J Surg Pathol 2002;26:1542, Arch Pathol Lab Med 2006;130:1865)
- No specific symptoms in patients with oncocytosis or in sporadic cases (Histol Histopathol 2013;28:1257)
- Sporadic cases - nonspecific symptoms
Diagnosis
- Diagnosis by histologic examination of tissue
Radiology description
- CT (J Comput Assist Tomogr 2016;40:513):
- Solid and well circumscribed
- Central stellate hypodensity in 33%, heterogenous appearance 42%
- No calcifications seen
- Mean attenuation values: 25.7 Hounsfield units (HU, noncontrast), 77.4 HU (arterial), 124.8 HU (venous), 76.8 HU (delayed); tumor to cortex ratios for 2 enhanced phases (arterial and venous): 0.56 and 0.79, respectively
- Positive on 99mTc sestamibi SPECT / CT, similar to renal oncocytoma and ChRCC (Eur Urol 2016;69:413)
Radiology images
Prognostic factors
- Indolent behavior
- Rare reports of distant metastasis and unclassified renal cell carcinoma arising from HOCT (Mod Pathol 2019;32:1698, Int J Surg Pathol 2009;17:158)
Case reports
- 48 year old woman with multiple renal hybrid oncocytic tumors and Birt-Hogg-Dubé syndrome (Acta Cytol 2006;50:584)
- 48 year old woman with multiple HOCTs and schwannomas (Medicine (Baltimore) 2017;96:e8939)
- 55 year old woman with HOCTs presenting with tumor infection and rupture (Urol Case Rep 2020;33:101304)
- 69 year old woman with 4 cm HOCT (Exp Mol Pathol 2018;105:352)
Treatment
- Nephrectomy (total or partial) (Am J Surg Pathol 2013;37:1469, Eur Urol 2010;57:661)
- Surveillance may be considered (Eur Urol 2010;57:661)
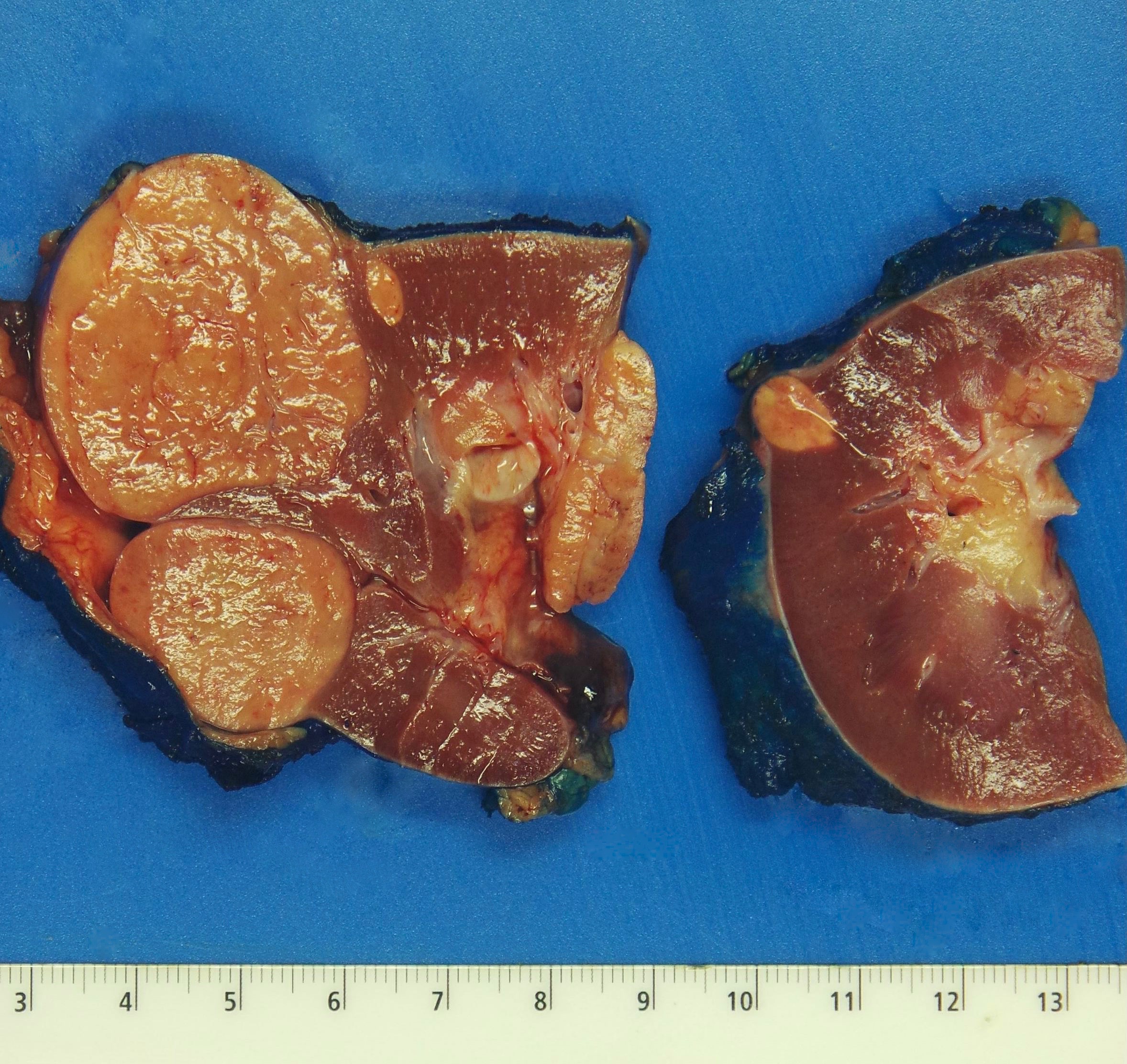
Gross description
- Multiple and bilateral tumors in patients with renal oncocytosis or Birt-Hogg-Dubé syndrome, more frequently unifocal / solitary in sporadic cases (Am J Surg Pathol 1999;23:1094, Am J Surg Pathol 2002;26:1542, Virchows Arch 2010;456:355)
- Well circumscribed, nonencapsulated
- Homogeneous tan to brown cut surfaces
- No necrosis
- No gross invasion into adipose tissue or vessels
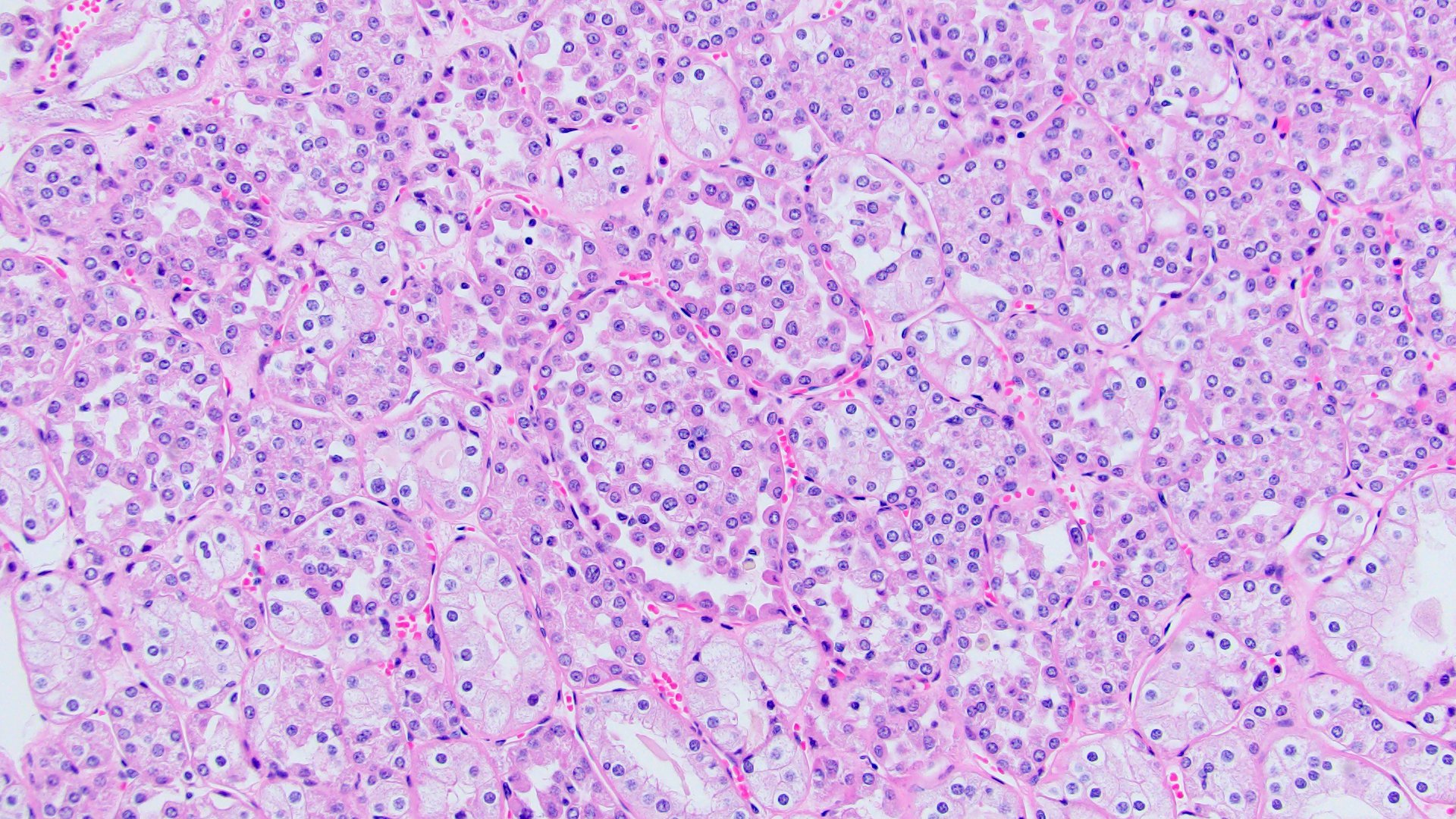
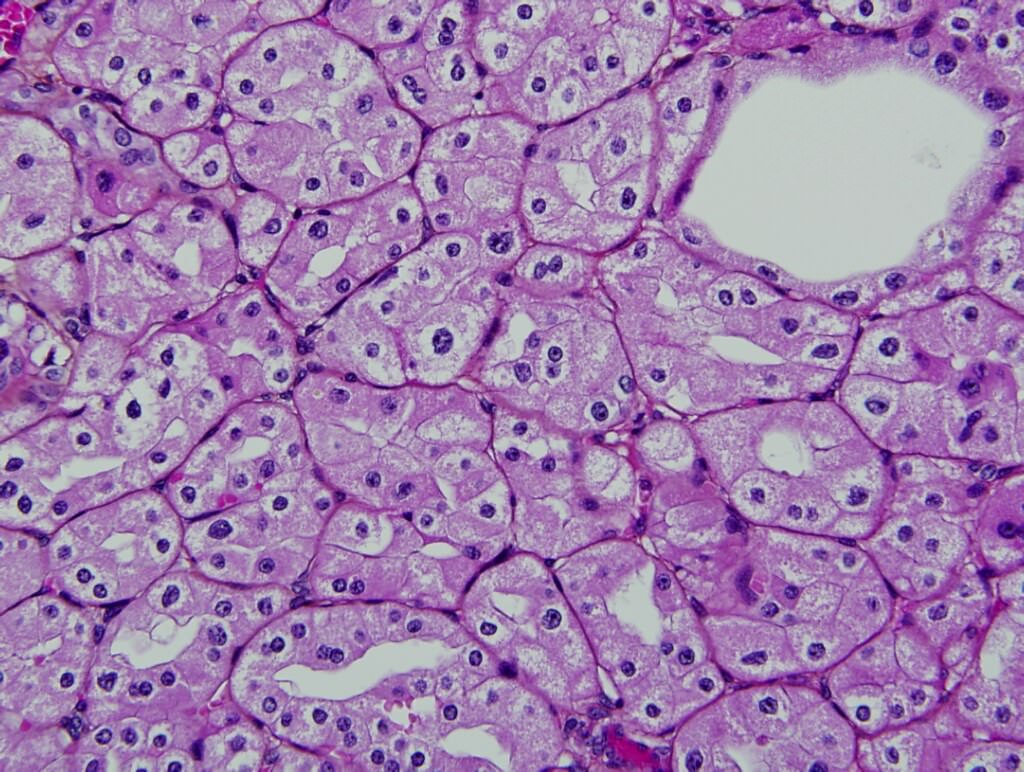
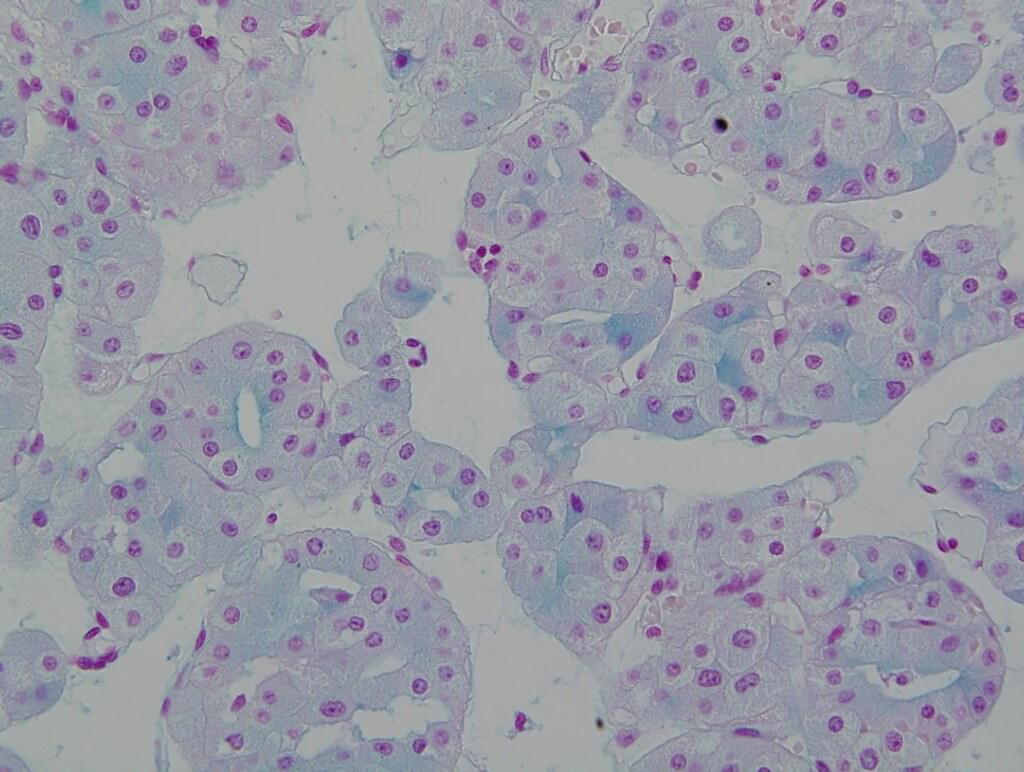
Microscopic (histologic) description
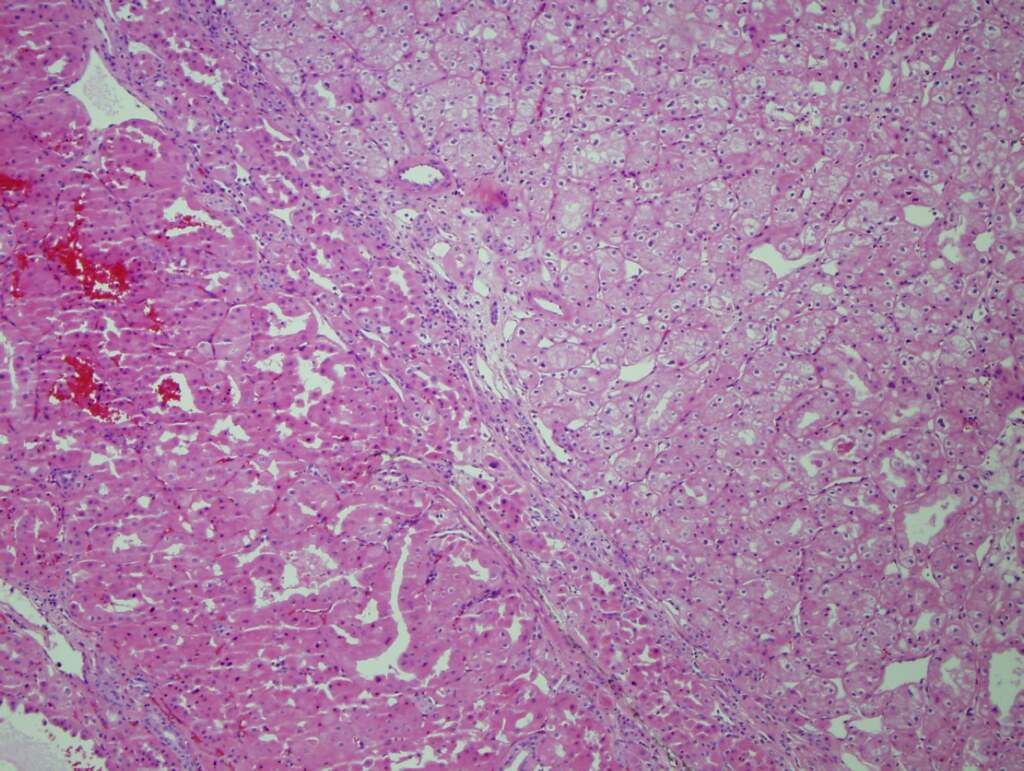
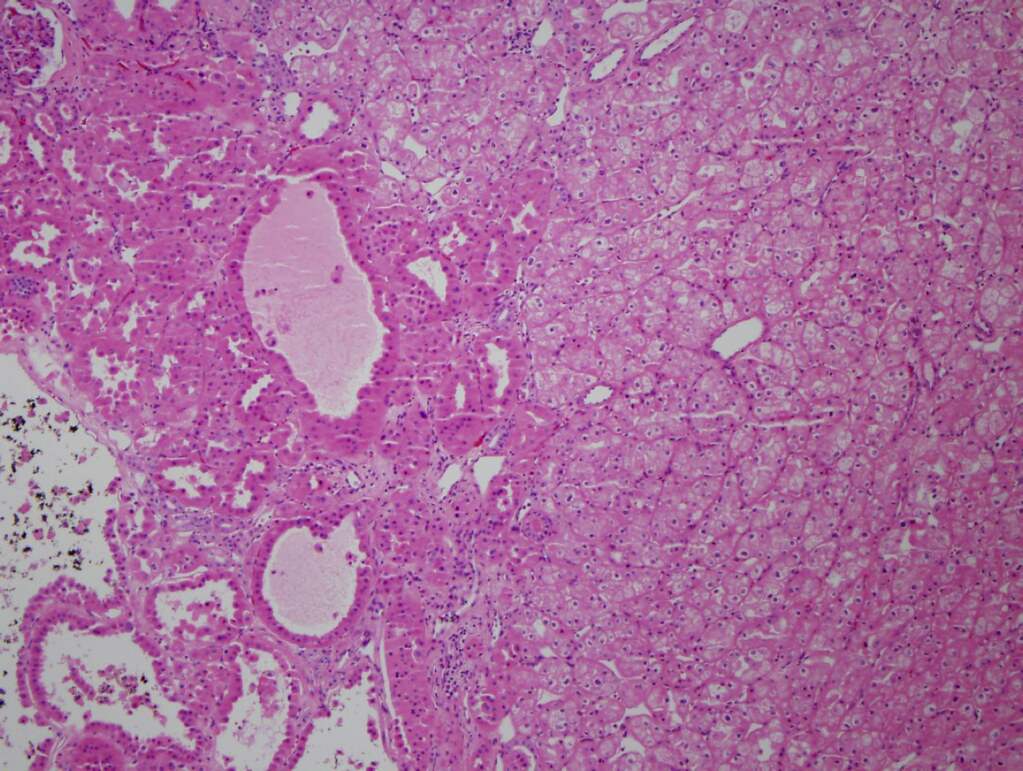
- 2 general morphologic appearances have been described (Am J Surg Pathol 1999;23:1094, Am J Surg Pathol 2002;26:1542, Eur Urol 2010;57:661, Am J Surg Pathol 2010;34:620, Virchows Arch 2010;456:355, Virchows Arch 2013;462:633, Hum Pathol 2020;104:18)
- Tumors with oncocytic cells with morphologic features between renal oncocytoma and chromophobe renal cell carcinoma
- Nuclei with slight atypia, binucleation, eosinophilic cytoplasm, perinuclear halo / cytoplasmic clearing but no raisinoid nuclei
- More commonly reported in sporadic HOCTs
- Or tumors with more discrete renal oncocytoma-like and chromophobe renal cell carcinoma-like areas (mosaic-like pattern)
- Rare foci with abrupt transition
- More frequently reported in syndromic HOCTs
- Tumors with oncocytic cells with morphologic features between renal oncocytoma and chromophobe renal cell carcinoma
- Arranged in mostly solid alveolar pattern
Microscopic (histologic) images
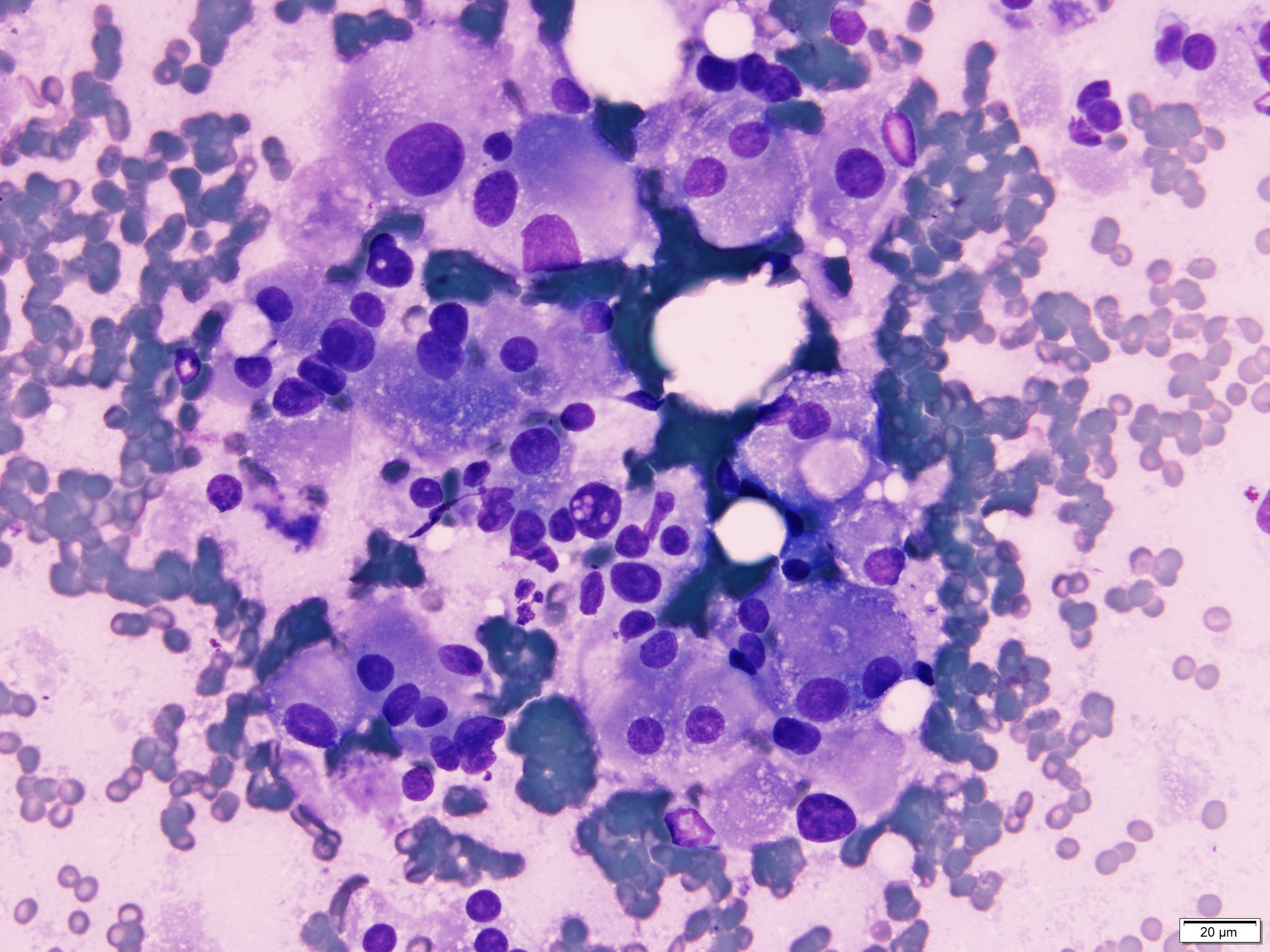
Cytology description
- Sheets of oncocytic cells with low nuclear / cytoplasmic ratios and uniform round nuclei (Acta Cytol 2006;50:584)
- Tumor cells with clear cytoplasm and slightly larger, irregular nuclei (Acta Cytol 2006;50:584)
- HOCT cells are larger in size with more cytoplasm and less uniform in size and shape than renal oncocytoma (Cancer Cytopathol 2020;128:962)
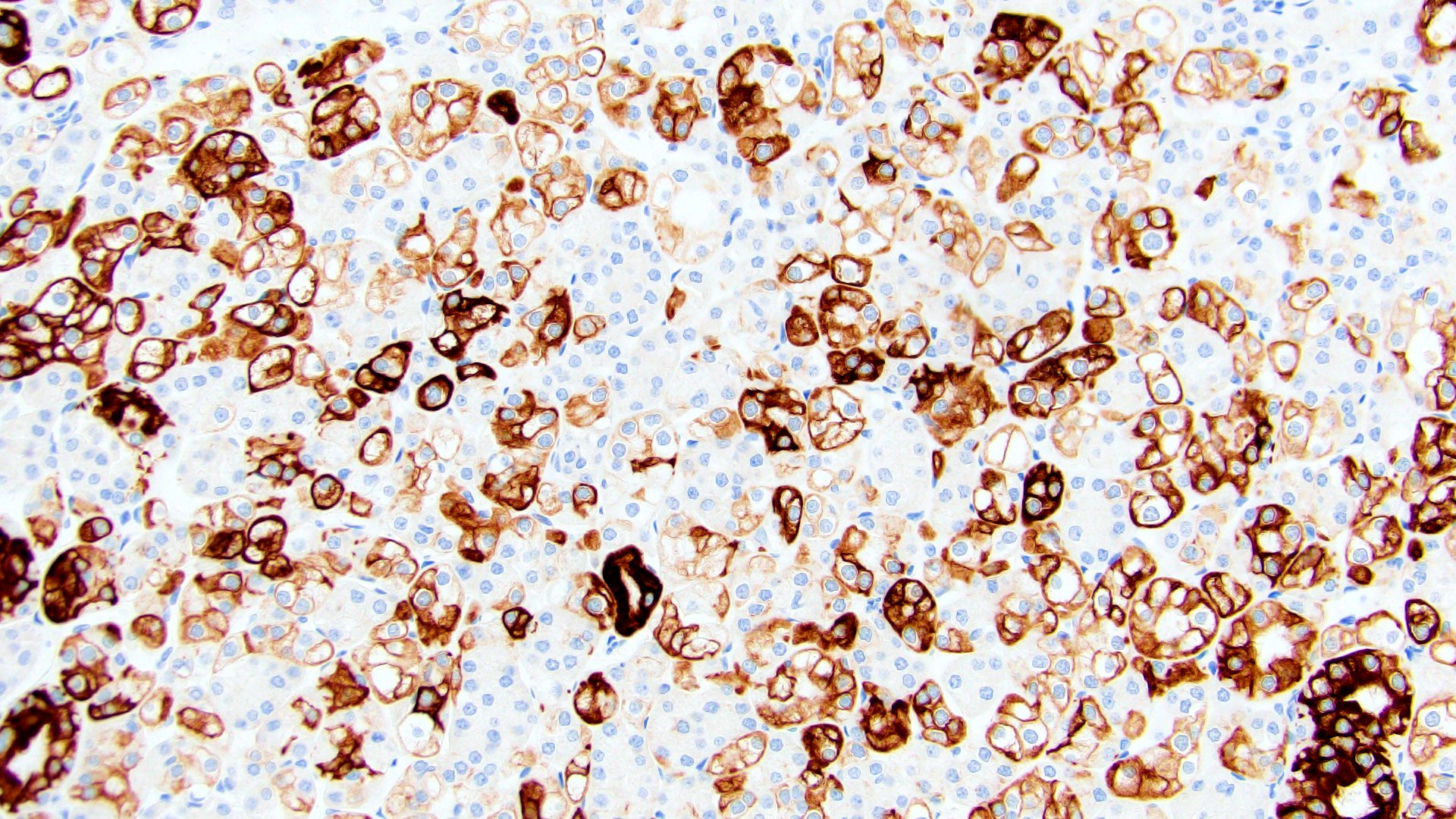
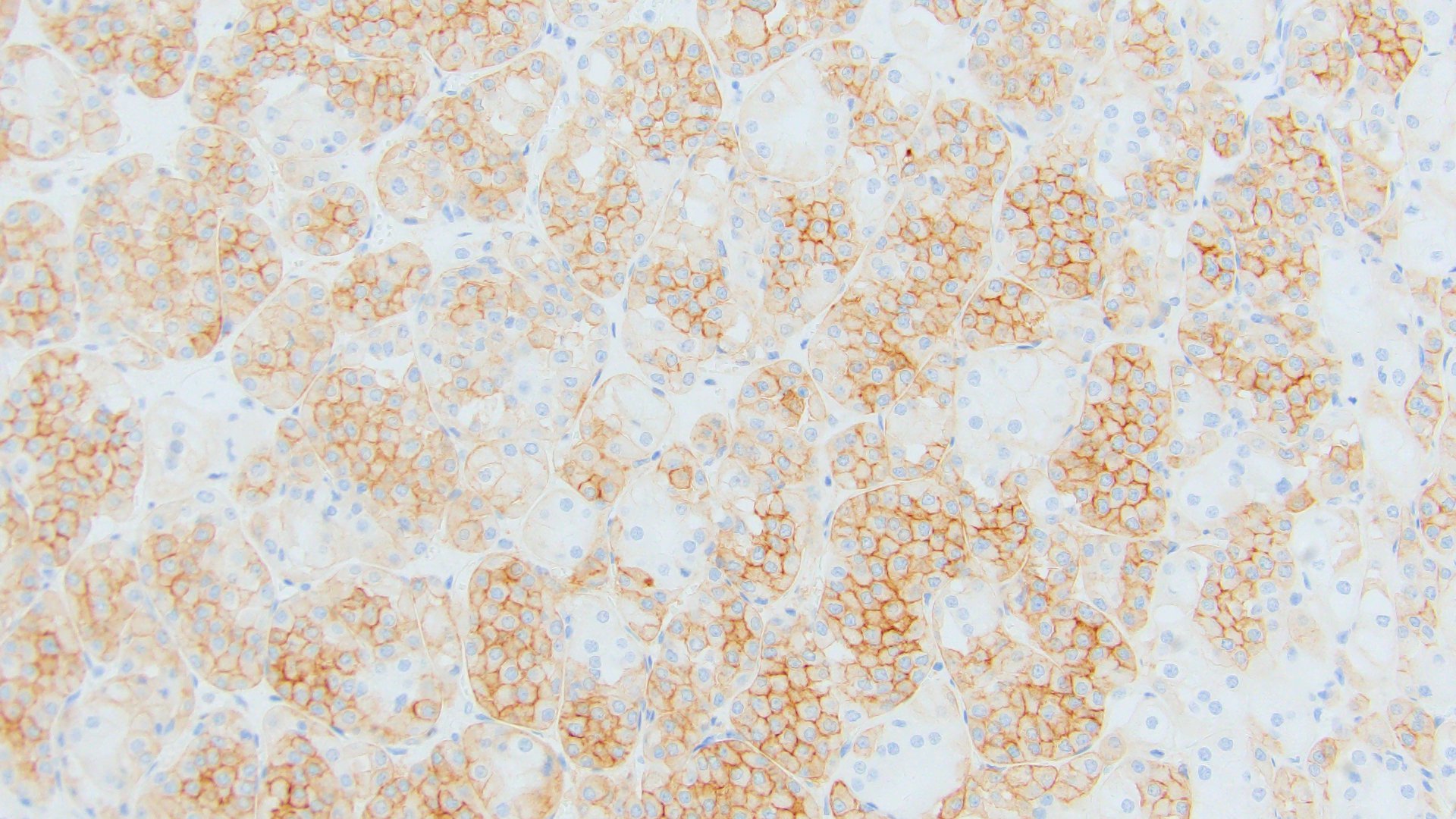
Positive stains
- Variable amount of oncocytic tumor cells with:
- Hale colloidal iron (apical to diffuse) (Virchows Arch 2013;462:633)
- CK7, AE1 / AE3, parvalbumin, antimitochondrial antigen, EMA, E-cadherin (most), CD117 (Histol Histopathol 2013;28:1257, Virchows Arch 2010;456:355)
- S100A1, CD82 (Pathol Int 2015;65:126)
Negative stains
Electron microscopy description
- Tumor cells with numerous mitochondria of varying sizes (Virchows Arch 2010;456:355)
- Sparse microvesicles with amorphic lamellar content
- Infrequently, small intracytoplasmatic tubuli covered by microvilli may be observed
Molecular / cytogenetics description
- Assessment of DNA copy number alterations showed conflicting results:
- Petersson et al.: 14 sporadic HOCTs (Virchows Arch 2010;456:355)
- Monosomy or polysomy in all cases analyzed (most common - chromosome 20 monosomy), distinct from cytogenetic anomalies commonly found in renal oncocytoma and ChRCC
- Poté et al.: 12 HOCTs: 10 sporadic, 2 Birt-Hogg-Dubé cases (Virchows Arch 2013;462:633)
- No chromosome imbalance in 58%
- Chromosome 1 deletions in 33%, similar to renal oncocytoma
- Petersson et al.: 14 sporadic HOCTs (Virchows Arch 2010;456:355)
- Assessment of DNA copy number alterations, as well as mutational and transcriptomic profile compared with renal oncocytoma and ChRCC:
- Ruiz-Cordero et al.: 27 HOCTs: 25 sporadic, 2 Birt-Hogg-Dubé cases (Mod Pathol 2019;32:1698)
- Low mutational frequency and absence of mutations in driver genes that are frequently seen in renal oncocytoma and ChRCC
- Copy number alterations primarily involving losses in chromosomes 1 and X / Y and ~40% lack chromosomal gains or losses - more similar to alteration profile of renal oncocytoma than ChRCC
- Gene expression profile intermediate between renal oncocytoma and ChRCC
- Ruiz-Cordero et al.: 27 HOCTs: 25 sporadic, 2 Birt-Hogg-Dubé cases (Mod Pathol 2019;32:1698)
- Tumor microdissection showed conflicting results:
- Poté et al.: (Virchows Arch 2013;462:633)
- No differences in renal oncocytoma-like and ChRCC-like areas using comparative genomic hybridization
- Pires-Luis et al.: (Exp Mol Pathol 2018;105:352)
- Higher miR-21 expression by microRNA analysis and focal multiple tetrasomies by FISH analysis in renal oncocytoma-like areas and higher relative miR-141 and miR200b expression and no chromosomal alterations in ChRCC-like areas
- Poté et al.: (Virchows Arch 2013;462:633)
- Tumors morphologically predicted to be HOCT were cytogenetically heterogenous and classified into 3 groups: renal oncocytoma (27%) renal oncocytoma variants (46%) and ChRCC (27%) (Hum Pathol 2020;104:18)
Sample pathology report
- Right kidney, partial nephrectomy:
- Hybrid oncocytic chromophobe tumors, measuring 3.5 and 2.3 cm in greatest dimensions (see comment)
- Surgical margins, negative for tumor
- Comment: The specimens contain a mixture of tumor cells demonstrating morphologic features that overlap with those of renal oncocytoma and chromophobe renal cell carcinoma. Given the patient's clinical history these are consistent with hybrid oncocytic chromophobe tumors associated with Birt-Hogg-Dubé syndrome.
Differential diagnosis
- Chromophobe renal cell carcinoma, eosinophilic variant:
- Oncocytic tumor cells with raisinoid nuclei and koilocytic atypia, including frequent binucleation and perinuclear halos
- Diffuse staining for Hale colloidal iron, CK7 and CD117
- Renal oncocytoma:
- No koilocytic atypia but some degenerative type atypia can be seen
- Negative or only focally positive for Hale colloidal iron and CK7
- Positive for S100A1
- Low grade oncocytic tumors (LOT):
- Provisional entity (Histopathology 2019;75:174, Mod Pathol 2021;34:1167)
- Oncocytic cells with round nuclei, perinuclear halos can be seen
- Archipelagenous cord-like architecture
- Positive for CK7 and negative for CD117
- Clear cell renal cell carcinoma:
- Tumor cells with clear to granular / eosinophilic cytoplasm with intervening vessels
- Diffuse membranous CAIX staining
- MiTF associated renal cell carcinoma:
- Variably morphology; TFEB t6;11 can demonstrate oncocytoma-like areas
- Positive for TFE3 or TFEB and cathepsin K
- Succinate dehydrogenase (SDH) deficient renal cell carcinoma:
- Classic presentation shows flocculent cytoplasmic vacuoles with pale eosinophilic appearance
- Loss of SDHB staining
- Epithelioid angiomyolipoma:
Board review style question #1
A patient with a history of Birt-Hogg-Dubé syndrome undergoes a partial nephrectomy. Gross examination of the specimen shows multiple well circumscribed tan-brown masses. H&E sections show the above histologic features. What is the likely diagnosis?
- Clear cell renal cell carcinoma
- Epithelioid angiomyolipoma
- Hybrid oncocytic chromophobe tumor
- Succinate dehydrogenase (SDH) deficient renal cell carcinoma
Board review style answer #1
C. Hybrid oncocytic chromophobe tumor
The patient's history of Birt-Hogg-Dubé syndrome and the macroscopic and microscopic findings support the diagnosis of hybrid oncocytic chromophobe tumor. Clear cell renal cell carcinoma has clear to granular tumor cells with intervening blood vessels. Epithelioid angiomyolipoma may contain areas admixed with adipocyte and vessels. Succinate dehydrogenase (SDH) deficient renal cell carcinoma demonstrates flocculent cytoplasmic vacuoles with pale eosinophilic appearance.
Immunohistochemistry can be used to confirm the diagnosis. While hybrid oncocytic chromophobe tumor is positive for CD117, the other choices are negative for CD117. Additionally, clear cell renal cell carcinoma is diffusely positive for CAIX, epithelioid angiomyolipoma is positive for Melan A and HMB45 and SDH deficient renal cell carcinoma shows loss of SDHB staining.
Comment Here
Reference: Hybrid oncocytic chromophobe tumor
The patient's history of Birt-Hogg-Dubé syndrome and the macroscopic and microscopic findings support the diagnosis of hybrid oncocytic chromophobe tumor. Clear cell renal cell carcinoma has clear to granular tumor cells with intervening blood vessels. Epithelioid angiomyolipoma may contain areas admixed with adipocyte and vessels. Succinate dehydrogenase (SDH) deficient renal cell carcinoma demonstrates flocculent cytoplasmic vacuoles with pale eosinophilic appearance.
Immunohistochemistry can be used to confirm the diagnosis. While hybrid oncocytic chromophobe tumor is positive for CD117, the other choices are negative for CD117. Additionally, clear cell renal cell carcinoma is diffusely positive for CAIX, epithelioid angiomyolipoma is positive for Melan A and HMB45 and SDH deficient renal cell carcinoma shows loss of SDHB staining.
Comment Here
Reference: Hybrid oncocytic chromophobe tumor
Board review style question #2
A patient has a history of skin lesions and spontaneous pneumothorax, now presenting with multiple and bilateral renal tumors. He underwent a partial nephrectomy, which revealed a hybrid oncocytic chromophobe tumor. Which of the following syndromes does the patient most likely have?
- Beckwith-Wiedemann syndrome
- Birt-Hogg-Dubé syndrome
- Tuberous sclerosis
- von Hippel-Lindau
Board review style answer #2
B. Birt-Hogg-Dubé syndrome
Explanation: A small percentage of kidney tumors are associated with hereditary syndromes. Birt-Hogg-Dubé syndrome is associated with hybrid oncocytic chromophobe tumor. Beckwith-Wiedemann syndrome is associated with Wilms tumor, while von Hippel-Lindau syndrome is associated with renal cell carcinoma. Angiomyolipoma, hereditary papillary renal cell carcinoma and familial renal oncocytoma are seen in patients with tuberous sclerosis.
Comment Here
Reference: Hybrid oncocytic chromophobe tumor
Explanation: A small percentage of kidney tumors are associated with hereditary syndromes. Birt-Hogg-Dubé syndrome is associated with hybrid oncocytic chromophobe tumor. Beckwith-Wiedemann syndrome is associated with Wilms tumor, while von Hippel-Lindau syndrome is associated with renal cell carcinoma. Angiomyolipoma, hereditary papillary renal cell carcinoma and familial renal oncocytoma are seen in patients with tuberous sclerosis.
Comment Here
Reference: Hybrid oncocytic chromophobe tumor