Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Soliman A, Parwani A. Epithelioid angiomyolipoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumorepitheliodaml.html. Accessed December 4th, 2024.
Definition / general
- Epithelioid angiomyolipoma (EAML) is a distinct rare subtype of angiomyolipoma with unique histological features
- EAML is characterized by the presence of at least 80% epithelioid cells, which is defined by round to polygonal cells with abundant pink to amphophilic to focally clear cytoplasm
Essential features
- Rare mesenchymal tumor first reported in 1995 (Int J Surg Pathol 1995;2:539)
- In contrast to other angiomyolipomas, EAML have malignant potential
- Presence of at least 80% epithelial component required for EAML diagnosis
- EAML shows positive staining with melanocytic markers, smooth muscle markers and cathepsin K, while negative for PAX8 and cytokeratins
Terminology
- Pure epithelioid PEComa of the kidney
- Traditionally, the term epithelioid angiomyolipoma is used for tumors in the kidney; at other sites, the term epithelioid PEComa is used
ICD coding
- ICD-O: 8860/1 - angiomyolipoma, epithelioid
- ICD-11
- 2F35 & XH0QR3 - benign neoplasm of urinary organs & angiomyolipoma, epithelioid
- 2B5F.2 & XH0QR3 - sarcoma, not elsewhere classified of other specified sites & angiomyolipoma, epithelioid
Epidemiology
- Rare in clinical practice
- Incidence rate among renal tumor is 1% and among renal angiomyolipoma is 4.6 - 7.7% (Mod Pathol 2013;26:1355)
- Mean patient age is 50 years (range: 30 - 80 years) and there is no sex predilection; EAMLs represent 4.6% of all resected angiomyolipomas (Mod Pathol 2013;26:1355)
Sites
- Kidney
Etiology
- Tuberous sclerosis complex (TSC)
- More than half of TSC patients have renal angiomyolipoma
- Mutations in the TSC1 gene on chromosome 9q34 and the TSC2 gene on chromosome 16p13 are identified in both TSC primary disease and sporadic EAML cases
- These proteins interact to form heterodimers with GTPase activity
- Dysfunctional hamartin and tuberin complexes lead to increased RHEB-GTP, activating the mTORC1 pathway, promoting cell growth and vascular smooth muscle differentiation (Nat Rev Neprol 2018;14:704, Nephrol Dial Transplant 2019;34:502, J Pathol 2008;214:387, Urol Case Rep 2022;45:102204)
- TFE3 gene rearrangements
- Rare EAML cases exhibit rearrangements of the TFE3 gene (Am J Surg Pathol 2010;34:1395)
- TFE3 is a transcription factor that regulates gene expression in the transforming growth factor β signaling pathway
- It activates mTOR signaling, promoting tumorigenesis
- EAML with TFE3 rearrangement is considered a unique subtype of PEComa (Oncol Clin Pract 2020;16:22, Am J Surg Pathol 2010;34:1395, J Pathol 2008;214:387, Clin Neprol Case Stud 2018;6:11)
- Genetic mutations in EAML: TSC2 is a common pathogenic factor, while TP53, ATRX and RB1 mutations are frequently noted in malignant cases (J Urol 2021;206:e708)
Clinical features
- Patients with small EAML may be asymptomatic but larger tumors tend to be symptomatic, often found during physical examination
- Depending on the size and location, it may present with fatigue, fever, low back pain, abdominal pain, hematuria, bleeding, dysuria and renal dysfunction; renal rupture may rarely occur (Urol Case Rep 2021;38:101645)
- It is known to cause paraneoplastic syndromes like high erythrocyte sedimentation rate (ESR), high platelet count and disruption of the immune system (J Int Med Res 2021;49:3000605211032493, Kaohsiung J Med Sci 2022;38:925)
Diagnosis
- Imaging: CT scan, MRI (World J Surg Oncol 2015;13:280, Asian J Surg 2020;43:967)
- Biopsy
- Histopathological examination and immunostaining
- Genetic testing
Radiology description
- Ultrasound: lack of specific findings (Abdom Radiol (NY) 2018;43:880)
- Computed tomography (CT) scan
- Shows irregular mixed density mass shadows (usually > 45 HU) with heterogeneous enhancement, "fast in and fast out" type on contrast enhanced CT scan (Abdom Imaging 2014;39:588, World J Surg Oncol 2015;13:280)
- Features suggestive of malignancy: large tumor size > 9 cm, necrosis, metastases, extrarenal extension, formation of tumor thrombus in a vein (Sci Rep 2015;5:10030)
- Magnetic resonance imaging (MRI): T2 hypointense reticular enhancement and "fast in and fast out" attributes (Kaohsiung J Med Sci 2022;38:925)
- Unlike conventional angiomyolipomas, EAML may have a reduced amount of fat within the tumor tissue; this can make it more challenging to differentiate from other kidney tumors using imaging techniques like CT scans and MRIs
Radiology images
Prognostic factors
- EAML has the potential to be malignant, recur and metastasize; however, the observed variation in its aggressive behavior, ranging from 5 - 66%, should be considered (Am J Surg Pathol 2010;34:715, Am J Surg Pathol 2011;35:161, Clin Neprol Case Stud 2018;6:11, Urol Case Rep 2018;18:52)
- The following factors have been correlated with poor prognosis: epithelial nuclear atypia ≥ 70%, mitotic count ≥ 2 per 10 high power fields, atypical mitoses, necrosis, epithelial cells > 70% or atypical epithelial cells > 60% (Am J Surg Pathol 2010;34:715, Sci Rep 2015;5:10030)
- Risk stratification model, based on prognostic parameters (presence of tuberous sclerosis complex, tumor necrosis, extrarenal extension or renal vein invasion, carcinoma-like histology and tumor size > 7.0 cm), classifies tumors into 3 distinct categories (Am J Surg Pathol 2011;35:161)
- Low risk (0 - 1 parameter)
- Intermediate risk (2 - 3 parameters)
- High risk (≥ 4 parameters)
- For patients possessing at least 3 adverse parameters, a substantial 80% experienced disease progression (Am J Surg Pathol 2011;35:161)
- Recent risk model has been suggested using different parameters (pT3 - pT4 stage, presence of necrosis, severe nuclear atypia, presence of atypical mitoses, mitotic count ≥ 2, Ki67 ≥ 10% and negative SMA expression) (BMC Urol 2022;22:148)
- Mutant p53 expression may be an adverse prognostic indicator for renal EAML (Diagn Pathol 2023;18:14)
Case reports
- 12 year old boy presented with episodic mild to moderate pain in the left flank for 1 month (J Kidney Cancer VHL 2021;8:20)
- 34 year old woman was complaining of acute left flank pain (Oncol Lett 2023;26:409)
- 40 year old man with a history of tuberous sclerosis presented with 5 months of painless gross hematuria (Urol Case Rep 2022;45:102204)
- 40 year old woman presented with complaints of right abdominal pain with tumor thrombus in inferior vena cava (IVC) and right atrium (Autops Case Rep 2020;10:e2020190)
- 57 year old man with lung effusion and 2 lung nodules (J Kidney Cancer VHL 2022;9:13)
Treatment
- Solid renal lesions > 4 cm should be treated promptly (Onco Targets Ther 2014;7:823)
- Surgical treatment: mainstay is surgical resection
- Radical nephrectomy for tumors ≥ 4 cm; partial nephrectomy for tumors < 4 cm
- Intraoperative frozen pathological examination aids differentiation from renal cancer
- Interventional therapies (selective arterial embolization [SAE], ablation) for hemorrhage or surgery intolerance are considered when renal AML is > 4 cm or clinical symptoms are present (Asian J Surg 2020;43:967, Ann Transl Med 2019;7:766)
- Medical therapy: for noncandidate patients for surgery
- mTOR Inhibitors (e.g., rapamycin, everolimus) target TSC1 / TSC2 gene mutations but resistance and pathway changes can occur
- Combination therapies (e.g., mTOR inhibitors with exemestane) effective for specific mutations (Clin Cancer Res 2020;26:5534)
- Angiogenesis inhibitors (bevacizumab, pizopanib, sorafenib) for TFE3 associated EAML (Front Oncol 2021;11:641376, Front Oncol 2020;10:582087)
- PD-1 antibodies enhance T cell infiltration, inhibit tumor growth and are effective in EAML with TSC gene mutation (Ann Transl Med 2019;7:766, J Immunother Cancer 2018;6:97, Kaohsiung J Med Sci 2022;38:925)
Gross description
- Large nodular or irregularly infiltrative in gross view, soft in texture, heterogeneous, partially cystic appearance with a grayish tan to grayish brown cut surface
- Hemorrhage and necrosis may be seen
- Potential extension into the renal vein or IVC may also occur
- EAML could involve lymph nodes; however, in some cases, it does not represent metastatic disease (Am J Surg Pathol 2010;34:715, Am J Surg Pathol 2011;35:161, Transl Androl Urol 2021;10:1506)
Gross images
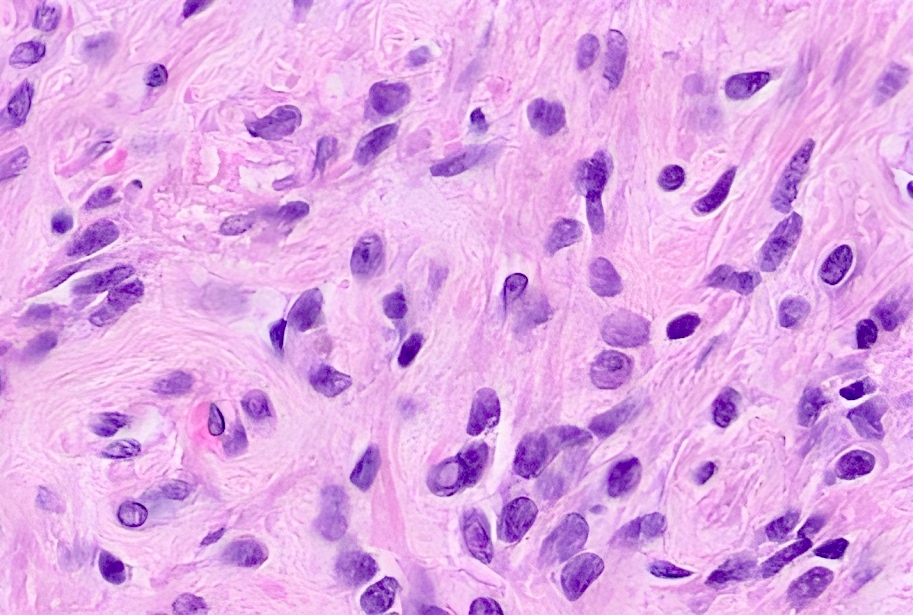
Frozen section description
- Usually sheets of polygonal to plump spindle cells with abundant pink, granular cytoplasm
- Significant nuclear pleomorphism with nuclear inclusions and nucleoli
- Areas with admixed adipocytes and abnormal vessels help in the diagnosis
- References: Appl Immunohistochem Mol Morphol 2004;12:277, Int J Clin Exp Med 2015;8:21252
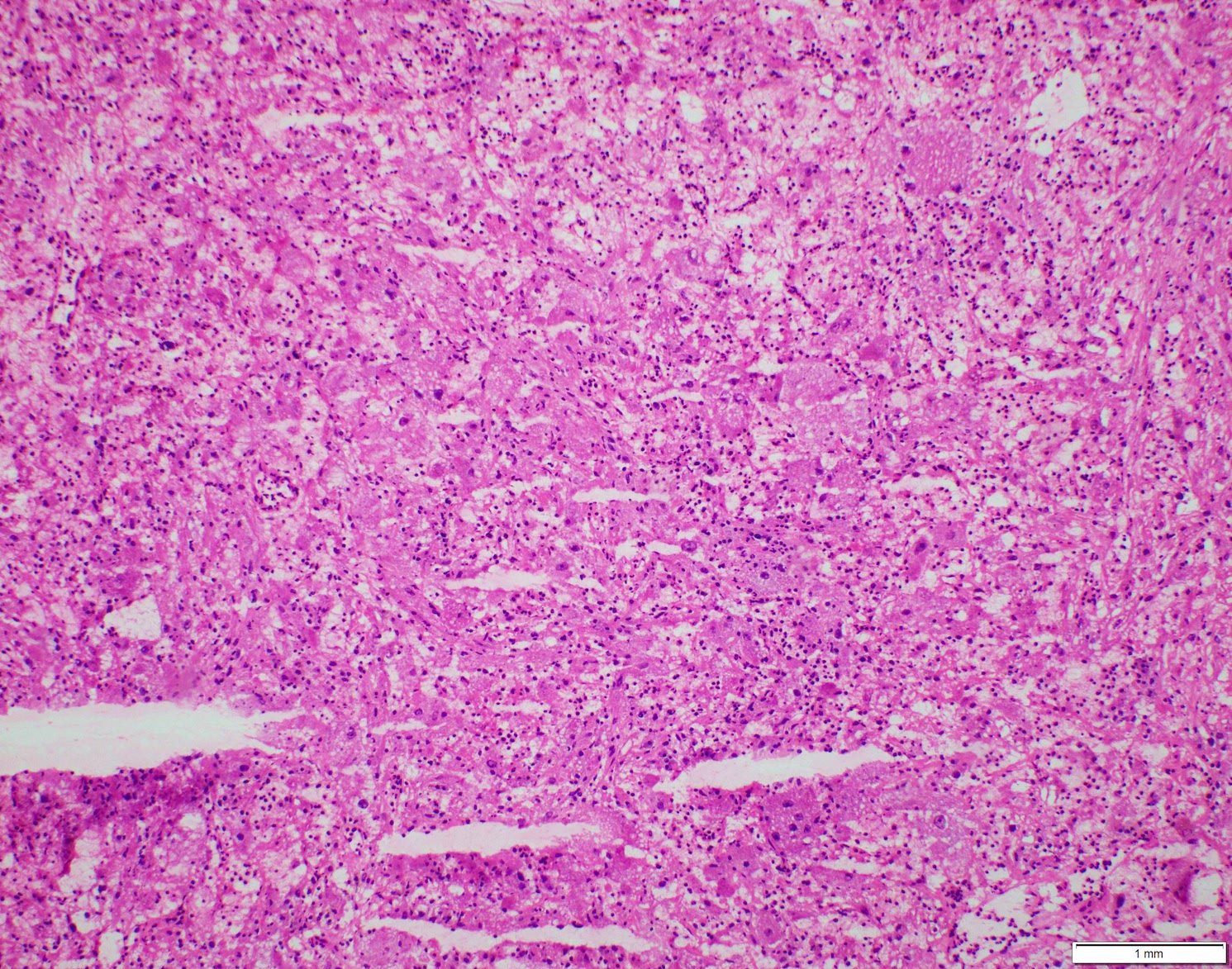
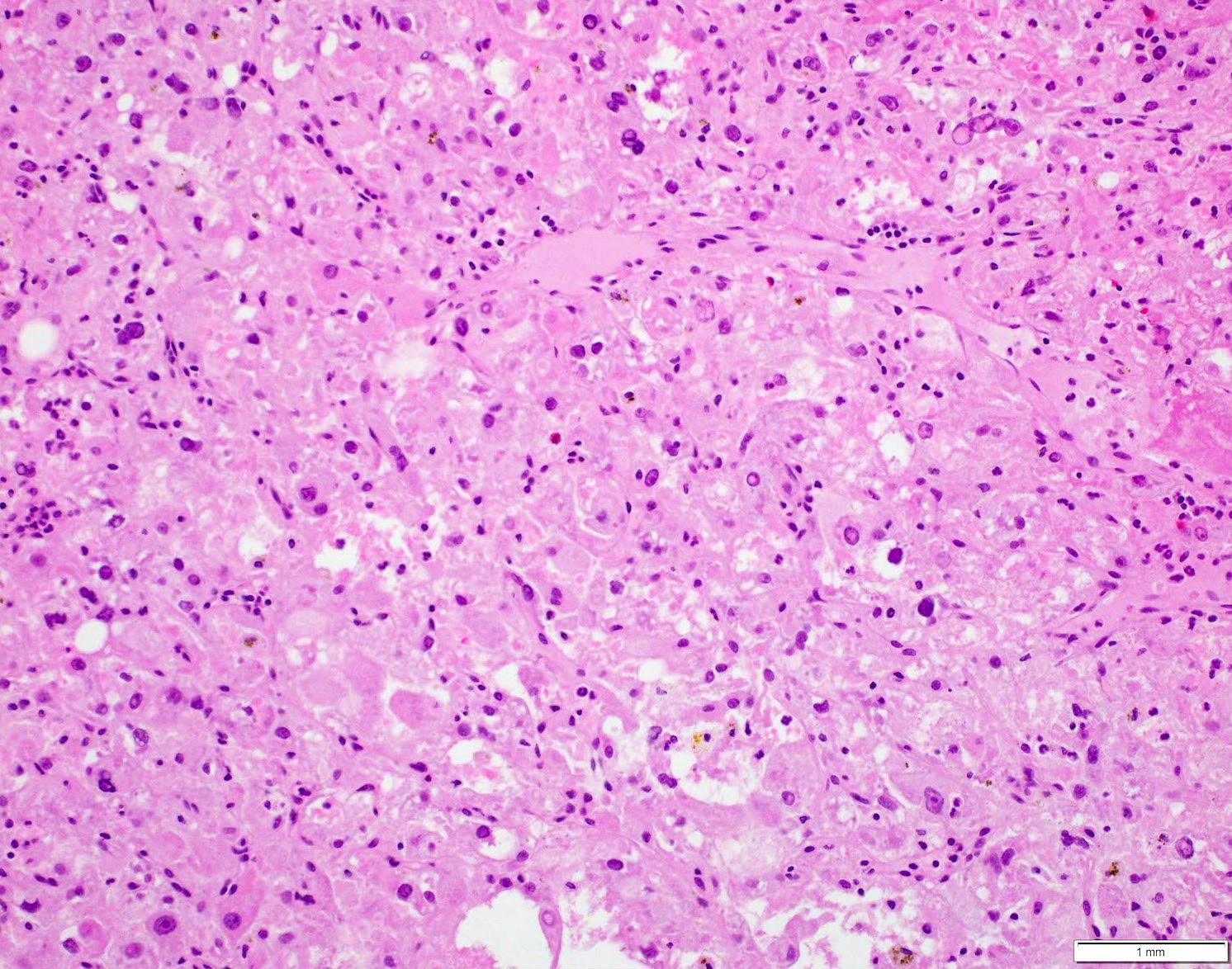
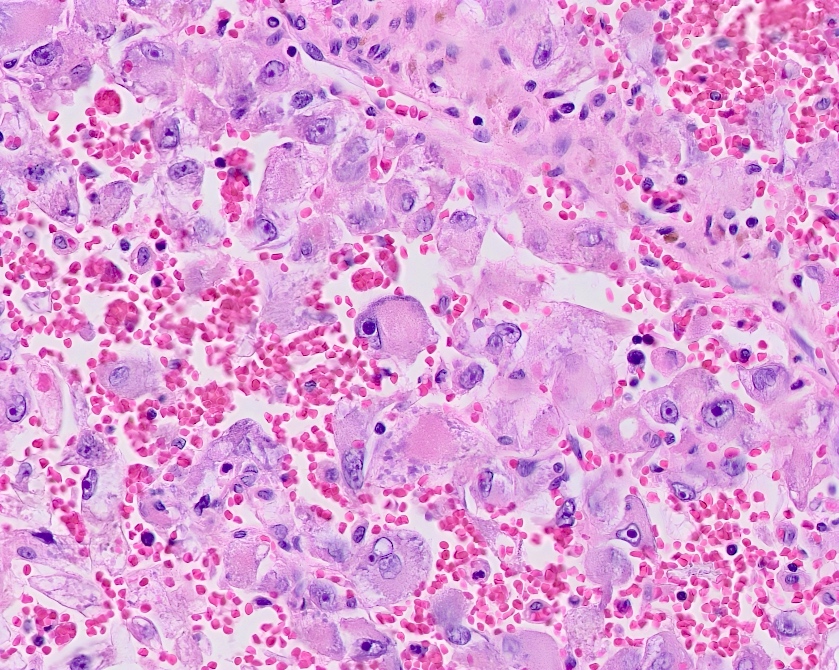
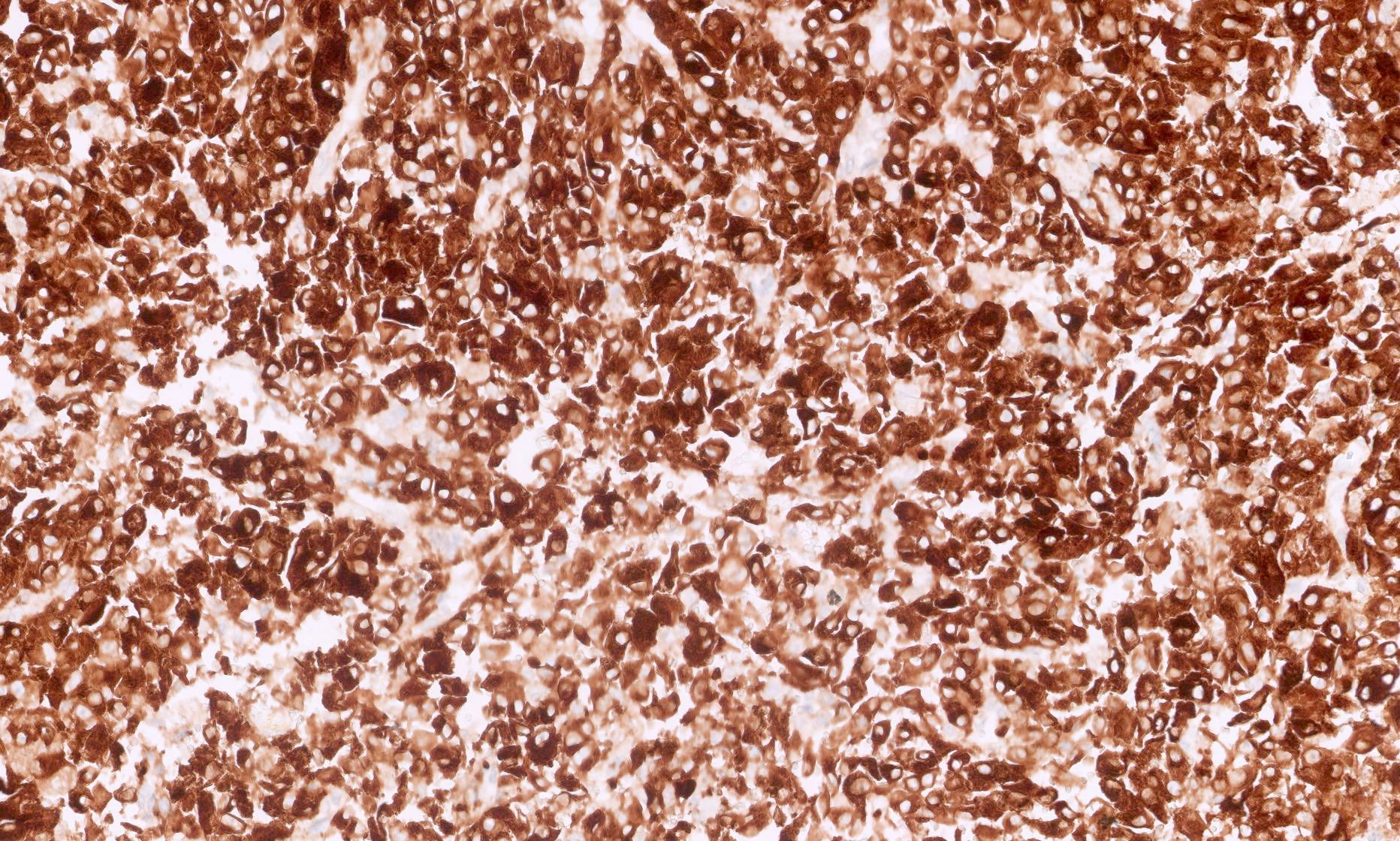
Microscopic (histologic) description
- According to WHO, more than 80% epithelial cells is required to diagnose EAML
- Malignant features on core needle biopsy: epithelial nuclear atypia ≥ 70%, mitotic count ≥ 2 per 10 high power fields, atypical mitoses, necrosis, epithelial cells > 70% or atypical epithelial cells > 60% (Kaohsiung J Med Sci 2022;38:925, Am J Surg Pathol 2010;34:715, Sci Rep 2015;5:10030)
- 2 distinct histologic patterns were described as follows
- Carcinoma-like growth pattern
- This pattern is characterized by the presence of large, polygonal cells with densely eosinophilic cytoplasm, diffusely atypical nuclei and prominent nucleoli
- These cells are arranged in cohesive nests, broad alveoli and compartmentalized sheets that are separated by thin vascular septa
- In some cases, intranuclear inclusions, nuclear degeneration and multinucleation are observed
- Mitotic activity is variable, with some cases showing > 2 mitotic figures per high power field (HPF), while the majority do not exhibit mitosis; atypical mitosis is not observed
- Hemorrhage and necrosis may be present to varying degrees
- Combination of prominent nucleoli, intranuclear inclusions and large, discohesive cells with eosinophilic cytoplasm gives the tumor cells a ganglion cell-like appearance
- Epithelioid and plump spindled cells in diffuse growth
- This pattern consists of epithelioid and plump spindled cells that are densely packed in diffuse sheets with homogenous growth without separation by vascular septa unlike the carcinoma-like pattern
- Cells are relatively uniform with epithelioid features, clear to granular, feathery eosinophilic cytoplasm and may lack atypia throughout; nuclei exhibit vesicular chromatin, prominent nucleoli, with intranuclear inclusion being less commonly observed
- Multinucleated giant cells may be present, either singly or in groups, areas of hemorrhage are often absent in this pattern (Am J Surg Pathol 2011;35:161)
- Carcinoma-like growth pattern
- *Besides those 2 patterns, morphology of a papillary component has been described; the papillae are by epithelioid cells containing abundant eosinophilic cytoplasm and round nuclei with conspicuous eosinophilic macronucleoli and perinucleolar halos (Int J Surg Pathol 2023 May 9 [Epub ahead of print])
Microscopic (histologic) images
Cytology description
- Round to plump spindle cells with indistinct cell borders
- Displaced eccentric nuclei with a voluminous, frothy cytoplasm and occasional nuclear pseudoinclusions (Diagn Cytopathol 2000;23:192, J Am Soc Cytopathol 2023;12:142)
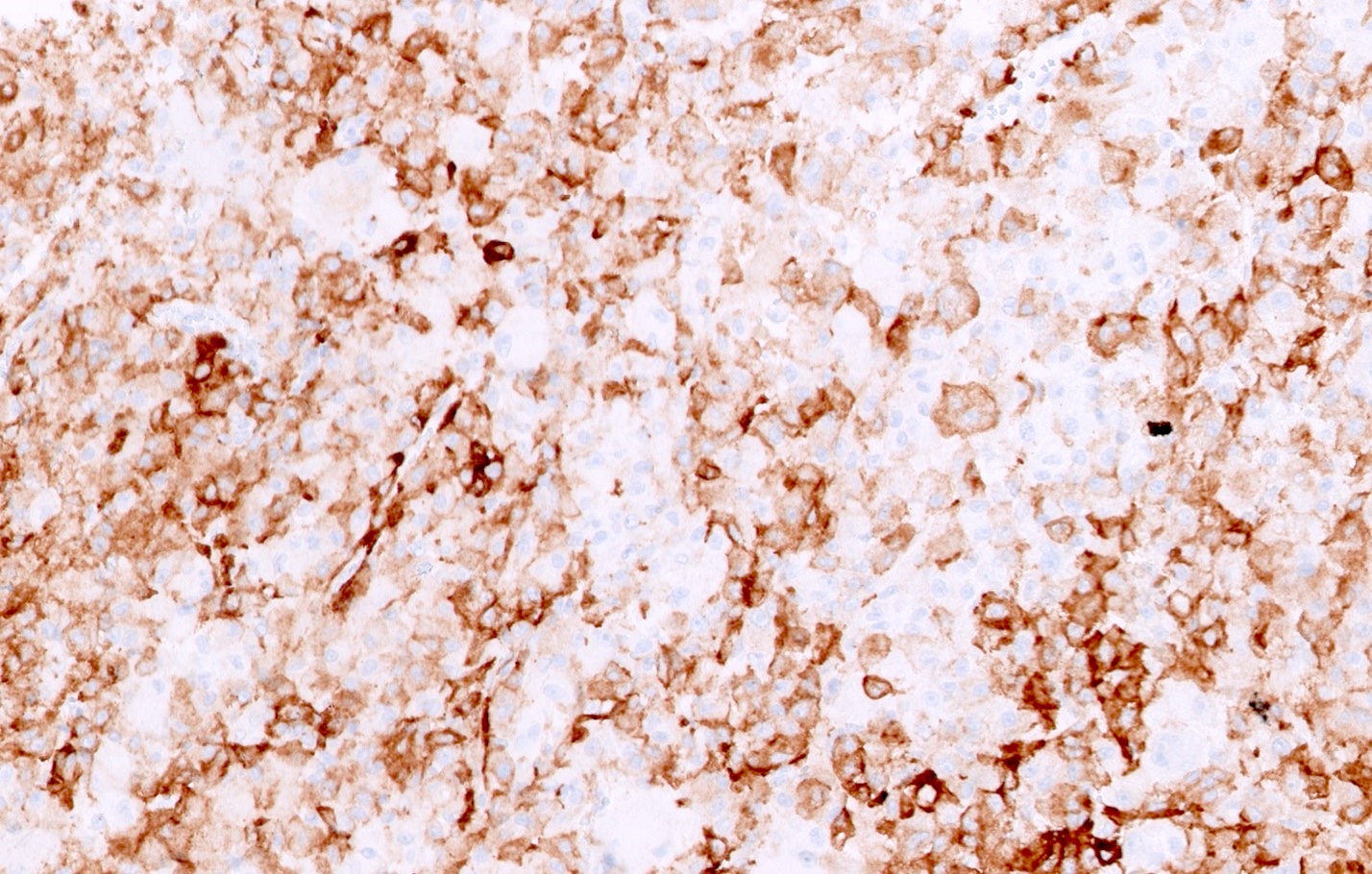
Positive stains
- HMB45, HMB50, MelanA, microphthalmia transcription factor (MITF), NKI-C3, SMA (variable), tyrosinase (Histopathology 2018;72:441, Kaohsiung J Med Sci 2022;38:925)
- Cathepsin K, expressed in all PEComas (Am J Surg Pathol 2018;42:1370)
- PNL2 has a higher sensitivity for differentiating PEComa from other renal tumors (85% versus 81%) and has specificity in malignant PEComa (89% versus 81%) (Histopathology 2018;72:441)
- Ki67 ≥ 10% correlates significantly with malignancy (BMC Urol 2022;22:148)
- GPNMB (J Pathol 2022;257:158)
Negative stains
- Cytokeratin, S100, PAX8
- Parvalbumin, unlike in other PEComa (Virchows Arch 2021;478:785)
Electron microscopy description
- Presence of glycogen, mitochondria and prominent electron dense, membrane bound granules (60 - 250 nm)
- Absence of melanosomes or premelanosomes (Am J Surg Pathol 1998;22:663)
Molecular / cytogenetics description
- Alteration in mTOR signaling pathway (including TSC2, mTOR and RICTOR) (Am J Surg Pathol 1998;22:663)
- Rarely, TFE3 gene rearrangement has been described in EAMLs (Med Mol Morphol 2012;45:234, Am J Surg Pathol 2016;40:723)
- Alterations of 5 tumor suppressor genes (TP53, ATRX, RB1, APC and NF1) have been reported (Diagn Pathol 2023;18:14, Arch Pathol Lab Med 2023;147:817)
Molecular / cytogenetics images
Sample pathology report
- Kidney, left, radical nephrectomy:
- Epithelioid angiomyolipoma, 6.5 cm, involving renal parenchyma and extending into sinus fat (see comment)
- Surgical margins, negative for tumor
- Comment: Focal necrosis (5%) is present. Immunohistochemical stains show the tumor to be positive for cathepsin K, MelanA and HMB45, supporting the diagnosis.
Differential diagnosis
- Clear cell renal cell carcinoma:
- Chromophobe renal cell carcinoma:
- Oncocytoma:
- Usually, small solid nests of tumor cells but can also show micro and macrocystic architecture
- Abundant granular eosinophilic cytoplasm with uniformly round nuclei with smooth nuclear border
- Can show some degenerative type nuclear atypia
- Positive for PAX8, CD117
- Negative for CK7, HMB45, MelanA and cathepsin K
- MITF translocation associated renal cell carcinoma:
- Renal cell carcinoma, unclassified type with oncocytic features:
- Positive for PAX8 and usually cytokeratins, while negative for cathepsin K, HMB45 and MelanA
- Malignant melanoma:
- Adipocytes and abnormal vessels are not seen in melanoma
- Positive for S100, SOX10, MelanA, HMB45 and PRAME
- Negative for cathepsin K, SMA and cytokeratins
- Epithelioid angiosarcoma:
- Positive for CD31, CD34, ERG or FLI1; may stain for cytokeratins
- Negative for cathepsin K, MelanA and HMB45
- Dedifferentiated liposarcoma:
- Well differentiated liposarcoma component may be identified
- Positive for CDK4, MDM2 by immunohistochemical stain
- CDK4 and MDM2 amplification by FISH
- Negative for HMB45, MelanA and cathepsin K
- Urothelial carcinoma with extensive sarcomatoid differentiation:
- Positive for vimentin, OSCAR cytokeratin, CK7 and PAX8 (variable)
- Eosinophilic solid and cystic RCC (ESC RCC):
- Positive for PAX8 and cytokeratin 20, however, could also express melanA, cathepsin K or HMB45 (Hum Pathol 2018:80:65)
- Usually have substantial cystic component
Additional references
- WHO Classification of Tumours Editorial Board: Urinary and Male Genital Tumours, 5th Edition, 2022, Investig Clin Urol 2018;59:357, Am J Surg Pathol 2001;25:65, Br J Radiol 2018;91:20170533, Urol Oncol 2022;40:18, Cancers (Basel) 2021;13:2441, Clin Genitourin Cancer 2020;18:e5, Pan Afr Med J 2020;37:210, Kaohsiung J Med Sci 2019;35:33
Board review style question #1
Which of the following is true in epithelioid angiomyolipoma?
- Positive for cathepsin K, HMB45, MelanA and MITF
- Positive for PAX8
- Positive for S100, SOX10, HMB45 and MelanA
- Positivity for TFE3 immunohistochemical stain usually correlates with TFE3 gene rearrangement
Board review style answer #1
A. Positive for cathepsin K, HMB45, MelanA and MITF. Angiomyolipomas are positive for melanoma markers including cathepsin K, HMB45, MelanA and MITF; however, they are negative for S100 and SOX10. Answer D is incorrect because TFE3 gene rearrangement is extremely uncommon in epithelioid angiomyolipoma. Positivity of TFE3 immunohistochemical stain does not correlate with TFE3 gene rearrangement. Answer C is incorrect because malignant melanoma is positive for S100, SOX10, HMB45 and MelanA. Answer B is incorrect because angiomyolipomas are negative for PAX8 and cytokeratins.
Comment Here
Reference: Epithelioid angiomyolipoma
Comment Here
Reference: Epithelioid angiomyolipoma
Board review style question #2
A radiological image of 40 year old man complaining of painless gross hematuria and left flank pain showed left renal mass with a central stellate scar measuring 16 x 14 x 11 cm. Left nephrectomy revealed a tumor with morphology depicted in the image above. Necrosis was present in ~30% of tumor cells. Immunohistochemistry showed diffuse strong staining for HMB45, MelanA and focal moderate staining for SMA. The tumor cells showed negative staining for EMA, AE1 / AE3, CK7, S100 and desmin. Which of the following genetic syndromes can be associated with this entity?
- Birt-Hogg-Dubé syndrome
- Succinate dehydrogenase deficiency
- Tuberous sclerosis complex
- Von Hippel-Lindau syndrome
Board review style answer #2
C. Tuberous sclerosis complex. Tuberous sclerosis complex (TSC) is an autosomal dominant genetic disorder resulting from inactivating losses of TSC1 (9q34) or TSC2 (16p13.3) genes. This is characterized by mental retardation, seizures and the development of neoplasms such as angiomyolipoma, subependymal giant cell tumors, cutaneous angiofibromas, cardiac rhabdomyomas, lymphangioleiomyomatosis and pulmonary multifocal micronodular hyperplasia. Answers A, B and D are incorrect because they are not associated with renal epithelioid angiomyolipoma (EAML).
Comment Here
Reference: Epithelioid angiomyolipoma
Comment Here
Reference: Epithelioid angiomyolipoma
Board review style question #3
Which is a true feature of epithelioid angiomyolipoma (EAML)?
- Diagnosis requires at least 20% epithelioid cells
- They are a common (> 10%) variant of angiomyolipoma
- Tumors are almost always associated with tuberous sclerosis
- Tumors may have malignant behavior
Board review style answer #3
D. Tumors may have malignant behavior. EAML has the potential to be malignant and recur and metastasize. Answer B is incorrect because it is a distinct rare subtype of angiomyolipoma with unique histological features.
Answer A is incorrect because EAML is characterized by the presence of at least 80% epithelioid cells. Answer C is incorrect because more than half of tuberous sclerosis (TSC) patients have renal angiomyolipoma but this does not imply it is always associated with TSC.
Comment Here
Reference: Epithelioid angiomyolipoma
Comment Here
Reference: Epithelioid angiomyolipoma