Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnostic criteria | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Immunofluorescence images | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Davis D. Sjögren syndrome. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneysjogrensyndrome.html. Accessed April 1st, 2025.
Definition / general
- Autoimmune disease characterized by lymphoplasmacytic inflammation in exocrine glands, leading to dry eyes and mouth (sicca syndrome) (Nat Rev Nephrol 2016;12:82)
Essential features
- Renal disease is present in < 10% of patients with Sjögren syndrome (Nat Rev Nephrol 2016;12:82)
- Usually manifests as plasma cell rich tubulointerstitial nephritis
ICD coding
- ICD-10: N16.4 - Renal tubulointerstitial disorders in systemic connective tissue disorders
Epidemiology
- Primary Sjögren syndrome affects 0.01 - 0.1% of population (Ann Rheum Dis 2015;74:1983)
- F:M = 9:1
- Peak incidence at age 50 (N Engl J Med 2018;378:931)
- Renal involvement in 5 - 14% of Sjögren patients in European studies and 30% in a Chinese study (Nat Rev Nephrol 2016;12:82)
Sites
- Kidney, mouth, eyes
Pathophysiology
- Genetic predisposition plus environmental factors (Nat Rev Nephrol 2016;12:82)
- Injury to salivary gland and local presentation of autoantigens with T and B cell activation
- Release of type 1 and type 2 interferons promoting T cells, continuous B cell activation and antibody production
- Renal disease may be caused by tubulointerstitial infiltration by lymphocytes and plasma cells or by autoantibodies to tubular epitopes, some with associated distal renal tubular acidosis (RTA) (Nat Rev Nephrol 2016;12:82)
- Renal disease may be caused by immune complexes (commonly cryoglobulins) in the glomerulus, leading to a membranoproliferative glomerulonephritis (Nat Rev Nephrol 2016;12:82)
Etiology
- Likely multifactorial with genetic component and viral or exogenous instigator (Nat Rev Nephrol 2016;12:82)
Clinical features
- Renal involvement occurs 2 - 7 years after primary Sjögren syndrome diagnosis (Nat Rev Nephrol 2016;12:82)
- Tubulointerstitial nephritis:
- Present in 67% of Sjögren patients undergoing renal biopsy
- Lymphoplasmacytic infiltrate with chronic and active damage of tubules and interstitium
- Damage may lead to electrolyte disturbances associated with distal renal tubular acidosis and diabetes insipidus and more rarely Fanconi / proximal tubular acidosis or acquired Gitelman or Bartter syndrome (renal hypokalemia with secondary hyperaldosteronism) (Nat Rev Nephrol 2016;12:82, Rheumatology (Oxford) 2015;54:1541)
- Cryoglobulinemic membranoproliferative glomerulonephritis (MPGN):
- 5 - 30% of patients of Sjögren patients undergoing renal biopsy
- Due to continuous B cell activation and subsequent immune complex formation with already circulating autoantigens (Nat Rev Nephrol 2016;12:82, Rheumatology (Oxford) 2015;54:1541)
- Often a mixed (type 2 or 3) cryoglobulin with an IgM (rheumatoid factor) directed against the Fc portion of IgG but may be monoclonal (type 1 cryoglobulin) if associated with lymphoproliferative disorder (Arthritis Rheum 2013;65:2945)
Diagnostic criteria
- Sjögren syndrome has classic triad of sicca syndrome (dry eyes and mouth), fatigue and pain (N Engl J Med 2018;378:931, Nat Rev Nephrol 2016;12:82)
- If symptomatic, kidney biopsy (Rheumatology (Oxford) 2017;56:362)
- Tubulointerstitial nephritis
- Immune complex mediated glomerulonephritis
- Rule out other autoimmune diseases
Laboratory
- Anti-Ro (SSA) antibodies in 66% of patients
- Anti-La (SSB) antibodies relatively specific
- Rheumatoid factor positive in 50% of patients
- dsDNA usually negative (N Engl J Med 2018;378:931)
Prognostic factors
- Tubulointerstitial nephritis is generally associated with less severe manifestations and better prognosis than membranoproliferative glomerulonephritis but more likely to remain undetected and can lead to chronic kidney disease (Arthritis Rheum 2013;65:2945, Nat Rev Nephrol 2016;12:82)
- Glomerular disease is more likely to be symptomatic and treated earlier (Nat Rev Nephrol 2016;12:82)
Case reports
- 24 year old woman with diabetes insipidus and renal tubular acidosis (Am J Case Rep 2017;18:622)
- 37 year old woman with acute interstitial nephritis, renal tubular acidosis and thin basement membrane nephropathy (Medicine (Baltimore) 2020;99:e21644)
- 44 year old woman with distal renal tubular acidosis (BMJ Case Rep 2019;12:e230402)
- 44 year old man with cryoglobulinemic glomerulonephritis and spontaneous kidney rupture (Int Med Case Rep J 2016;9:77)
- 47 year old woman presenting with hypophosphatemic osteomalacia (Medicine (Baltimore) 2017;96:e6493)
Treatment
- Tubulointerstitial nephritis:
- Immunosuppression or immunomodulation (Nat Rev Nephrol 2016;12:82, Int J Med Sci 2017;14:191, BMC Musculoskelet Disord 2016;17:2)
- Membranoproliferative glomerulonephritis due to cryoglobulinemia:
- Immunosuppression or immunomodulation (Nat Rev Nephrol 2016;12:82)
Microscopic (histologic) description
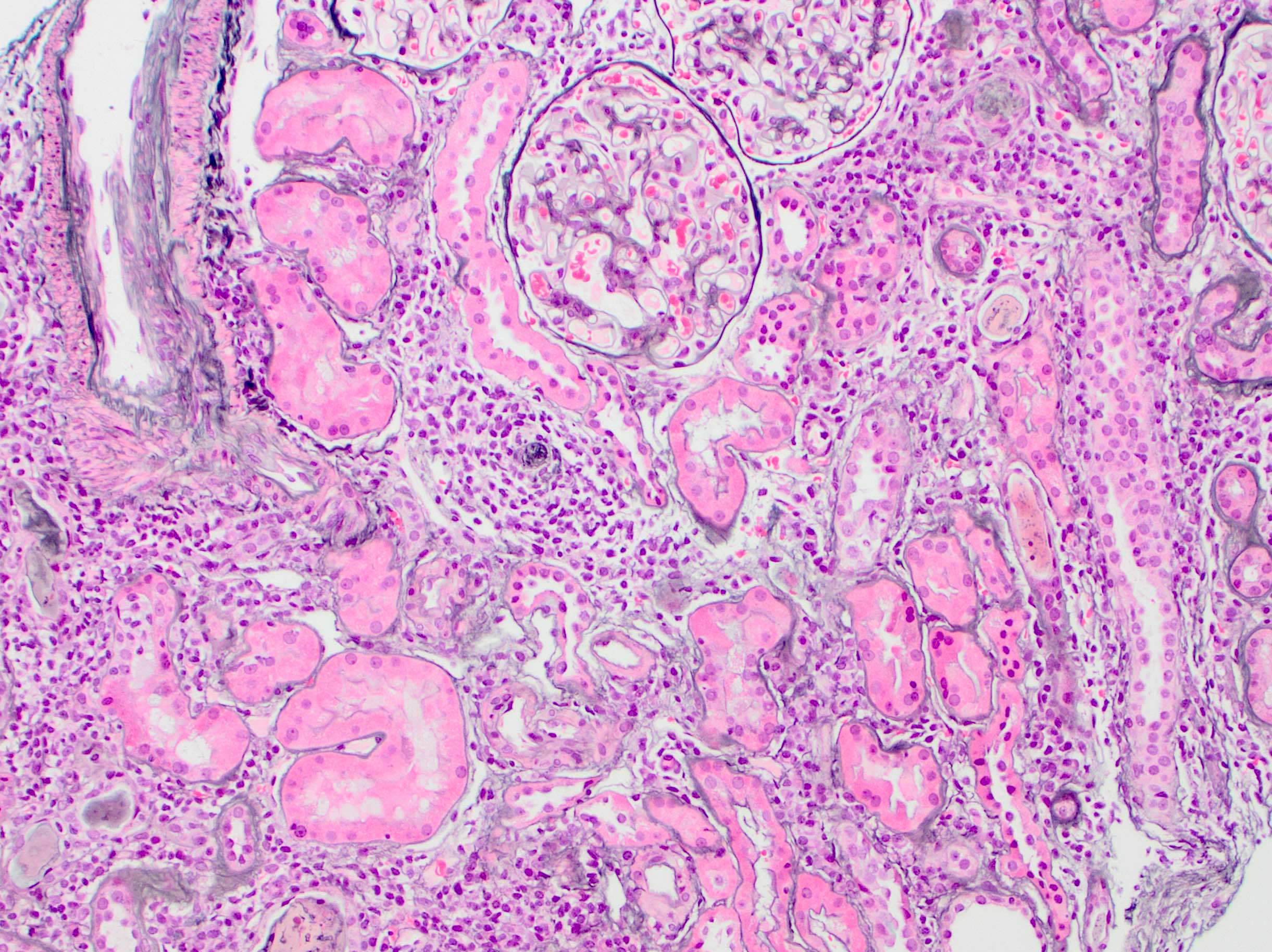
- Tubulointerstitial nephritis:
- Plasma cell rich interstitial inflammation with tubulitis, mixed B and T cells (Am J Kidney Dis 2017;69:e29)
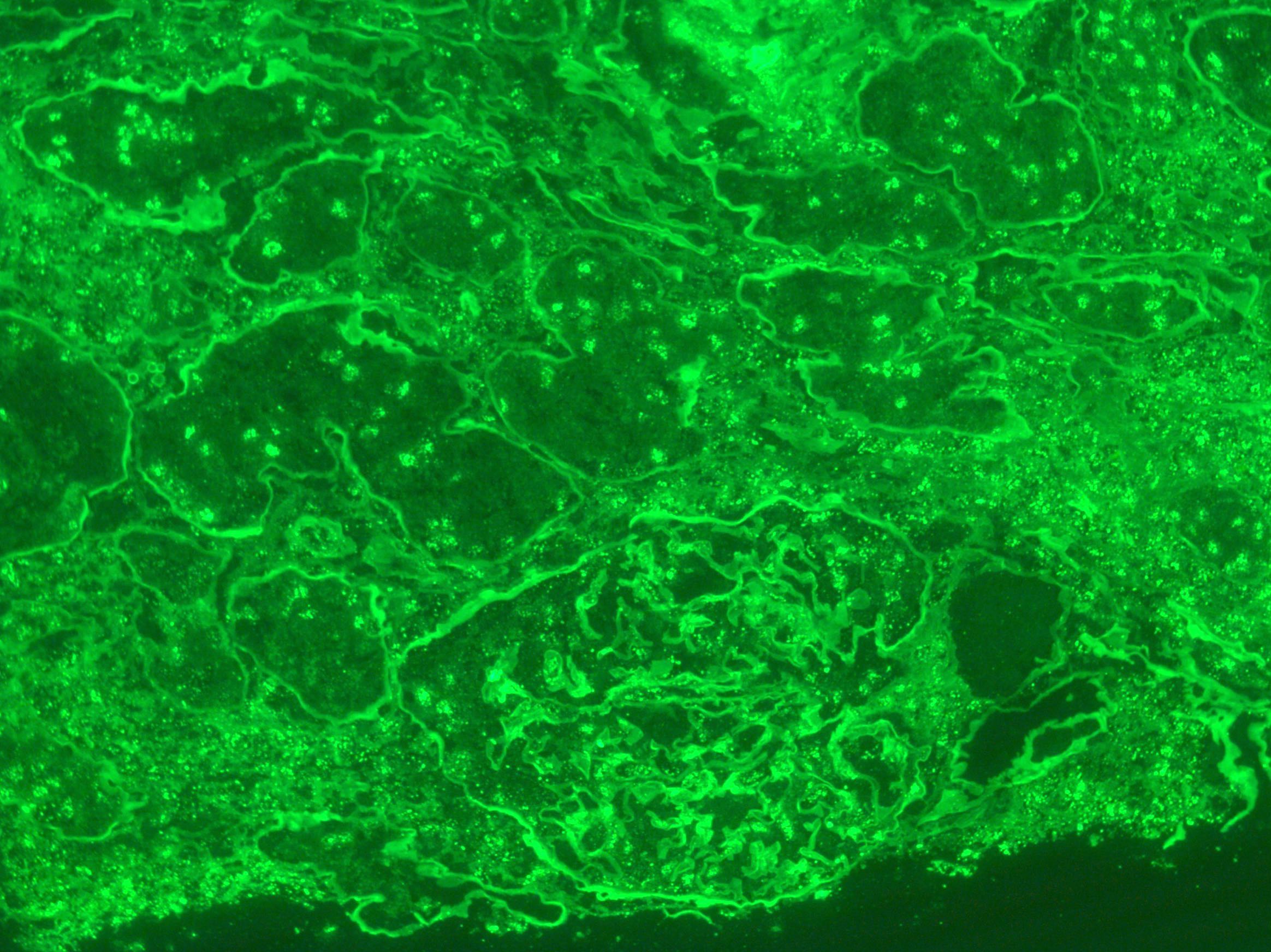
- May have tubular basement membrane or interstitial immune deposits detectable by immunofluorescence microscopy
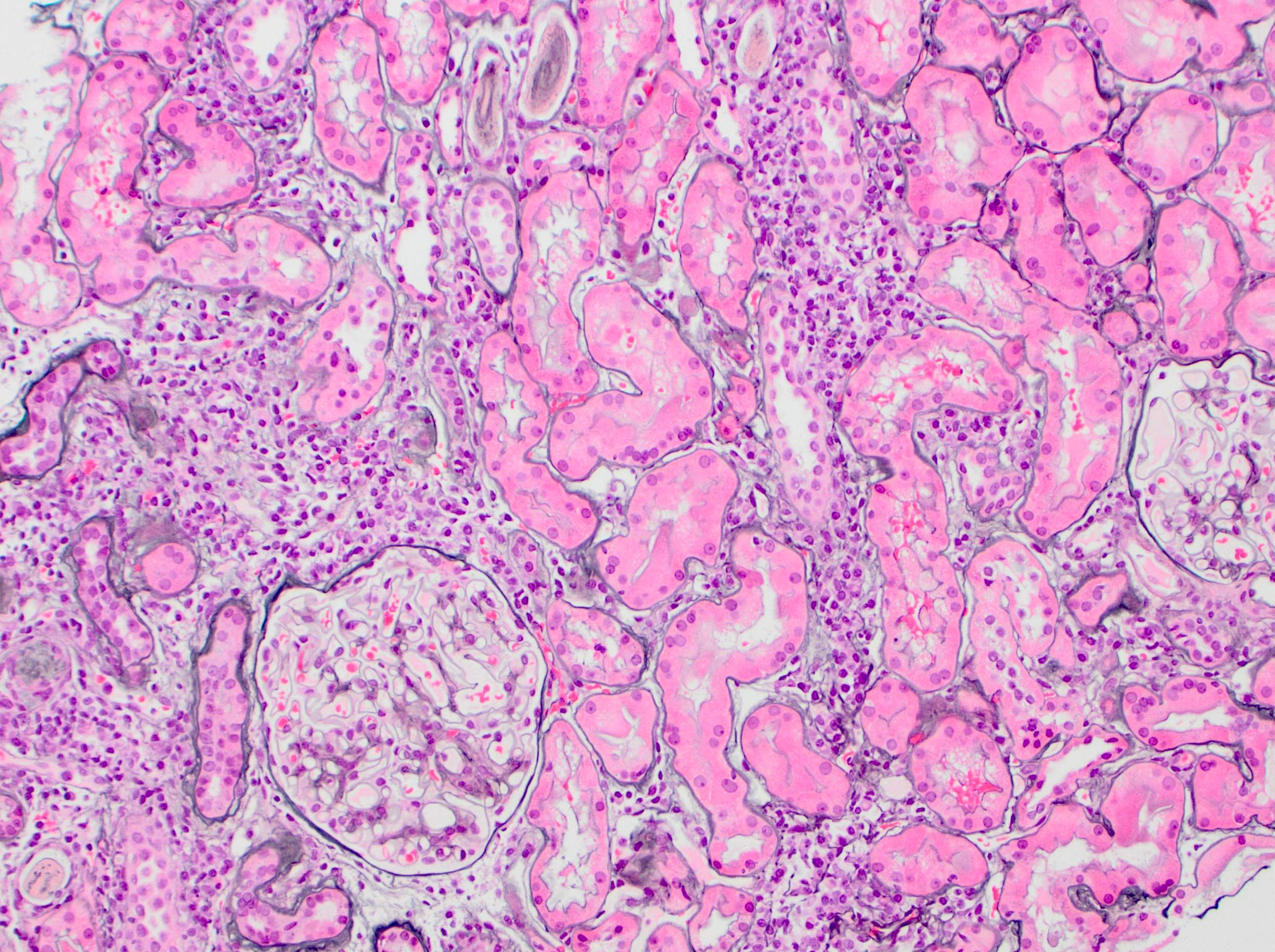
- Membranoproliferative glomerulonephritis:
- Mesangial expansion due to increased matrix and cellularity
- Endocapillary hypercellularity with occlusion of capillary lumina due to endothelial cell swelling and influx of leukocytes
- Duplication of glomerular basement membranes (tram tracking)
- Immune complex deposition, often of IgG and IgM, in mesangial and subendothelial regions of peripheral capillary loops
- Cryoglobulin plugs of immune complexes in capillary microvasculature
- References: Nephrol Dial Transplant 2015;30:1363, Nat Rev Nephrol 2016;12:82, Rheumatology (Oxford) 2017;56:362
Microscopic (histologic) images
Positive stains
- Jones silver stain, periodic acid Schiff and trichrome highlight basement membranes and renal architecture
- T, B and plasma cell markers dependent upon makeup of lymphocytic infiltrate (Rom J Morphol Embryol 2017;58:409)
Negative stains
- IgG4 low
Sample pathology report
- Left kidney, biopsy:
- Plasma cell rich tubulointerstitial nephritis (see comment)
- Comment: This patient’s renal insufficiency is due to a chronic and active, plasma cell rich tubulointerstial nephritis. Although not specific to etiology, in the provided clinical context of Sjögren syndrome with anti-Ro / SSA and anti-La / SSB antibodies, the findings are consistent with Sjögren associated tubulointerstitial nephritis. There is no significant eosinophilic infiltrate to suggest a hypersensitivity reaction, nor IgG4 positive plasma cells to suggest IgG4 related tubulointerstitial nephritis. There is no evidence of a glomerulonephritis nor immune complex deposition process. Chronic injury is mild. (Microscopic description, Immunofluorescence microscopy and Electron microscopy descriptions should also be reported.)
Differential diagnosis
- IgG4 related disease (J Am Soc Nephrol 2011;22:1343):
- Lacks female predominance
- Has expansile storiform fibrosis
- Abundant IgG4+ plasma cells by immunohistochemistry
- Different criteria for systemic disease, including elevated serum levels of IgG4 or IgG
- Drug induced allergic interstitial nephritis:
- Eosinophils more common
- Tubular basement membrane or interstitial immune deposits less common
- Correlate with clinical history
- Sarcoidosis:
- Granulomas more common
- Correlate with clinical history
- Hepatitis C and other causes of cryoglobulinemic glomerulonephritis:
- Determine whether the glomerular immune deposits are monoclonal (type 1 cryoglobulin, associated with a lymphoproliferative disorder) or polyclonal (type 2 or 3 cryoglobulin)
- Correlate with clinical and laboratory findings, rheumatoid factor and circulating cryoglobulins
- Reference: Nat Rev Nephrol 2016;12:82
Board review style question #1
Board review style answer #1
Board review style question #2
A middle aged woman presents with trouble swallowing food, feelings of fatigue and complaints of ill fitting contact lenses. Autoimmune testing shows antibodies to Ro (SSA) and La (SSB). If this patient later develops nocturia and polydipsia, renal biopsy is most likely to show
- Increase in IgG4+ plasma cells
- Lymphoplasmacytic tubulointerstitial nephritis
- Membranous nephropathy
- Pseudotumoral infiltrate
Board review style answer #2