Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Murshed KA, Taha NM, Akhtar M. Crescentic glomerulonephritis overview. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyrpgn.html. Accessed December 22nd, 2024.
Definition / general
- Rapidly progressive glomerulonephritis (RPGN) is a clinical syndrome, not a pathologic diagnosis
- Often presents with a rapid decline in kidney function, hematuria, proteinuria, oliguria or hypertenison
- Often crescentic glomerulonephritis (CGN) is characterized by glomerular crescents in > 50% of glomeruli
Essential features
- Often crescent formation in > 50% of the glomeruli
- Immunofluorescence and serologic findings distinguish etiology:
- Antiglomerular basement membrane (GBM) disease is characterized by circulating anti-GBM antibody, linear staining for immunoglobulin (Ig) G on immunofluorescence microscopy and absent electron dense deposits on electron microscopy
- Immune complex mediated glomerulonephritis (GN) occurs in various glomerulonephritis (lupus, IgAN) and is characterized by granular staining for Ig and complements immunofluorescence with electron dense deposits on electron microscopy
- Pauci-immune complex mediated / vasculitic type glomerulonephritis is frequently associated with circulating antineutrophil cytoplasmic antibody (ANCA) and is characterized by negative or scanty Ig deposits on immunofluorescence (pauci-immune complex pattern) and electron microscopy
Terminology
- Rapidly progressive nephritic syndrome
- Rapidly progressive nephritic syndrome, diffuse crescentic glomerulonephritis
- Rapidly progressive nephritic syndrome with extracapillary glomerulonephritis
ICD coding
Epidemiology
- CGN accounts for < 10% of all patients presenting with primary glomerulopathy
- M:F = 1:1, more common in white population, rare in Africans
- Bimodal age distribution: first peak around age 30 and second after 60
- Pauci-immune complex glomerulonephritis is the most common subtype of CGN in adults (Kidney Int 2003;63:1164)
- Anti-GBM disease is the most aggressive form of CGN (Kidney Int 2003;63:1164)
Sites
- Kidney
- Kidney and lung (pulmonary renal syndrome, Goodpasture’s syndrome)
- Systemic, including various organs such as skin, lung, gastrointestinal and nervous system, if associated with vasculitis and connective tissue disease
Pathophysiology
- For pathophysiology of crescents, endothelial injury is a key driver, which leads to breaks and rupture of GBM (J Pathol 2012;228:482)
- This triggers coagulation cascade within Bowman space, ultimately leading to fibrin deposition
- Fibrin stimulates parietal epithelial cells to proliferate, resulting in formation of cellular crescents
- Cellular crescents lead to increase in counter pressure, collapse of glomerular tuft and tubular outflow obstruction
- This will result in decline in the single nephron glomerular filtration rate
- Multilevel growth of parietal epithelial cells may lead to epithelial - mesenchymal transition in cell phenotype, which leads to the formation of fibrocellular and fibrous crescents (Curr Opin Nephrol Hypertens 2020;29:302)
Etiology
- Anti-GBM disease: circulating antibodies directed against the noncollagenous domain of alpha 3 chain of type IV collagen
- Immune complex mediated crescentic GN: secondary to immune complex deposition in conditions such as postinfectious GN, lupus nephritis, membranoproliferative GN, IgA nephropathy and cryoglobulinemia
- Pauci-immune complex crescentic GN: 80 - 90% are associated with ANCA
- ANCA associated vasculitis includes granulomatosis with polyangiitis, microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis or renal limited vasculitis (J Am Soc Nephrol 2010;21:1628)
- Variety of drugs may also cause the disease (hydralazine, penicillamine, rifampicin)
- Mixed antibody patterns may also occur (anti-GBM + ANCA, antidouble stranded DNA + ANCA, antidouble stranded DNA + anti-GBM)
Clinical features
- Rapid deterioration of renal function over short period (days to weeks)
- Acute nephritic syndrome: (Clin Exp Nephrol 2016;20:322)
- Oliguria
- Hypertension
- Hematuria, macroscopic and less frequently microscopic
- Proteinuria
Diagnosis
- Clinicopathological diagnosis, mainly achieved on renal biopsy
Laboratory
- Elevated serum creatinine and blood urea nitrogen (BUN) (Clin Exp Nephrol 2016;20:322)
- Elevated C reactive protein (CRP) and erythrocyte sedimentation rate (ESR)
- Hematuria
- Red blood cell casts
- Proteinuria (usually nonnephrotic range)
- Complement levels
- Autoantibodies (J Am Soc Nephrol 2016;27:1278)
- Anti-GBM antibody
- ANCA, antimyeloperoxidase (pANCA) and antiproteinase 3 (cANCA)
- Antidouble stranded DNA antibody
Prognostic factors
- Best predictor of outcome for all types of crescentic glomerulonephritis is the severity of renal failure at time of initiation of therapy (Kidney Int 2003;63:1164)
- Dialysis dependency at presentation is considered a poor prognostic sign
- Cellular crescents are usually reversible with prompt and aggressive treatment or may resolve spontaneously in postinfectious GN
- Fibrocellular and fibrous crescents are irreversible in terms of potential recovery of single nephron glomerular filtration rate (Curr Opin Nephrol Hypertens 2020;29:302)
Case reports
- 26 year old woman with necrotizing CGN related to sarcoidosis (J Med Case Rep 2015;9:282)
- 59 year old man presented with membranous nephropathy with crescents (J Am Soc Nephrol 2011;22:1804)
- 68 year old woman with CGN due to coexistent anti-GBM disease and fibrillary glomerulonephritis (Clin Kidney J 2016;9:97)
- 74 year old woman with systemic lupus erythematosus presented with RPGN secondary to IgA nephropathy (Case Rep Nephrol 2019;2019:8354823)
Treatment
- Anti-GBM disease: plasmapheresis and immunosuppressive agents (glucocorticoids and cyclophosphamide)
- Immune complex mediated crescentic GN: depends on the underlying etiology
- Pauci-immune complex crescentic GN: immunosuppressive agents, rituximab (Clin J Am Soc Nephrol 2017;12:1162)
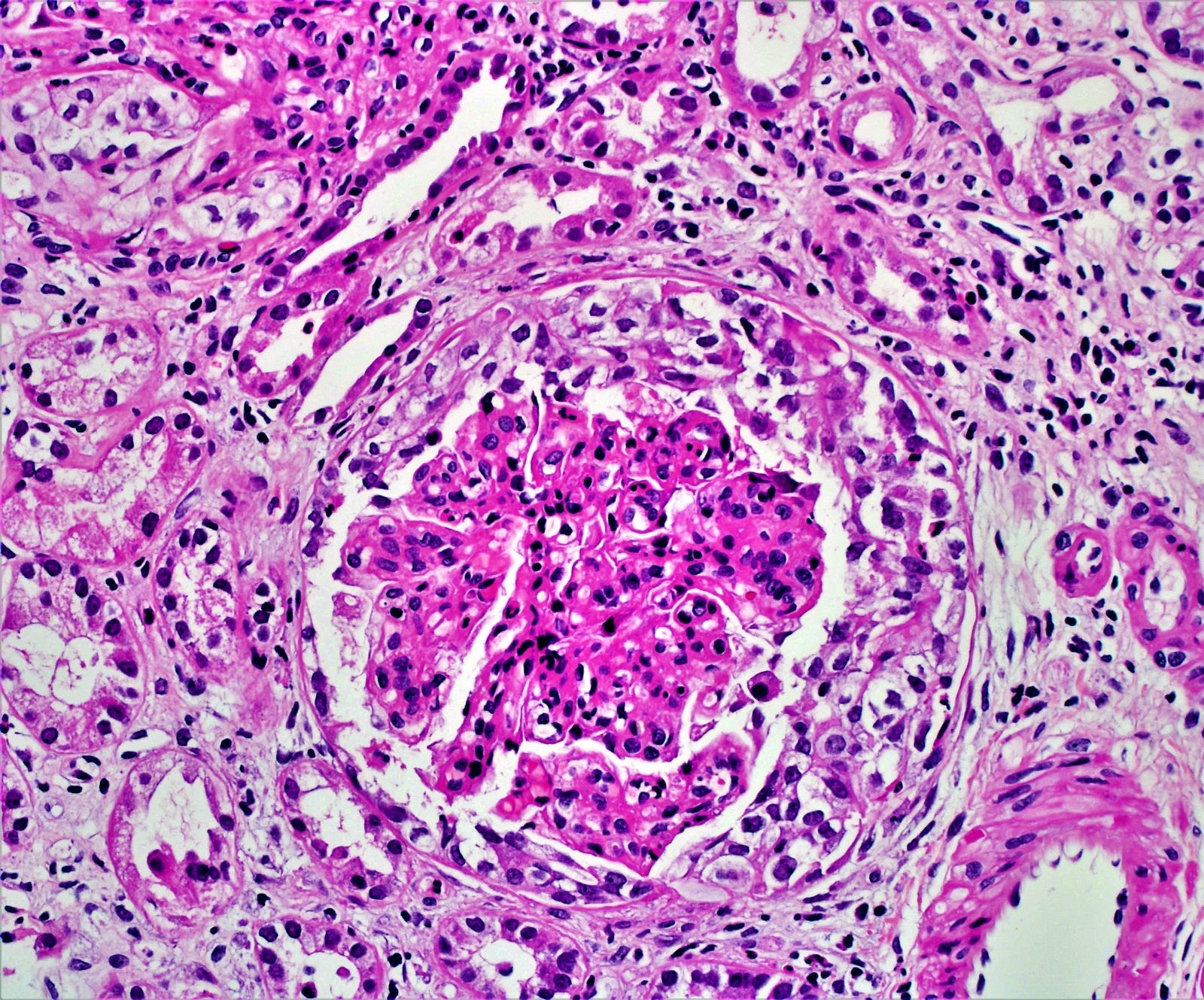
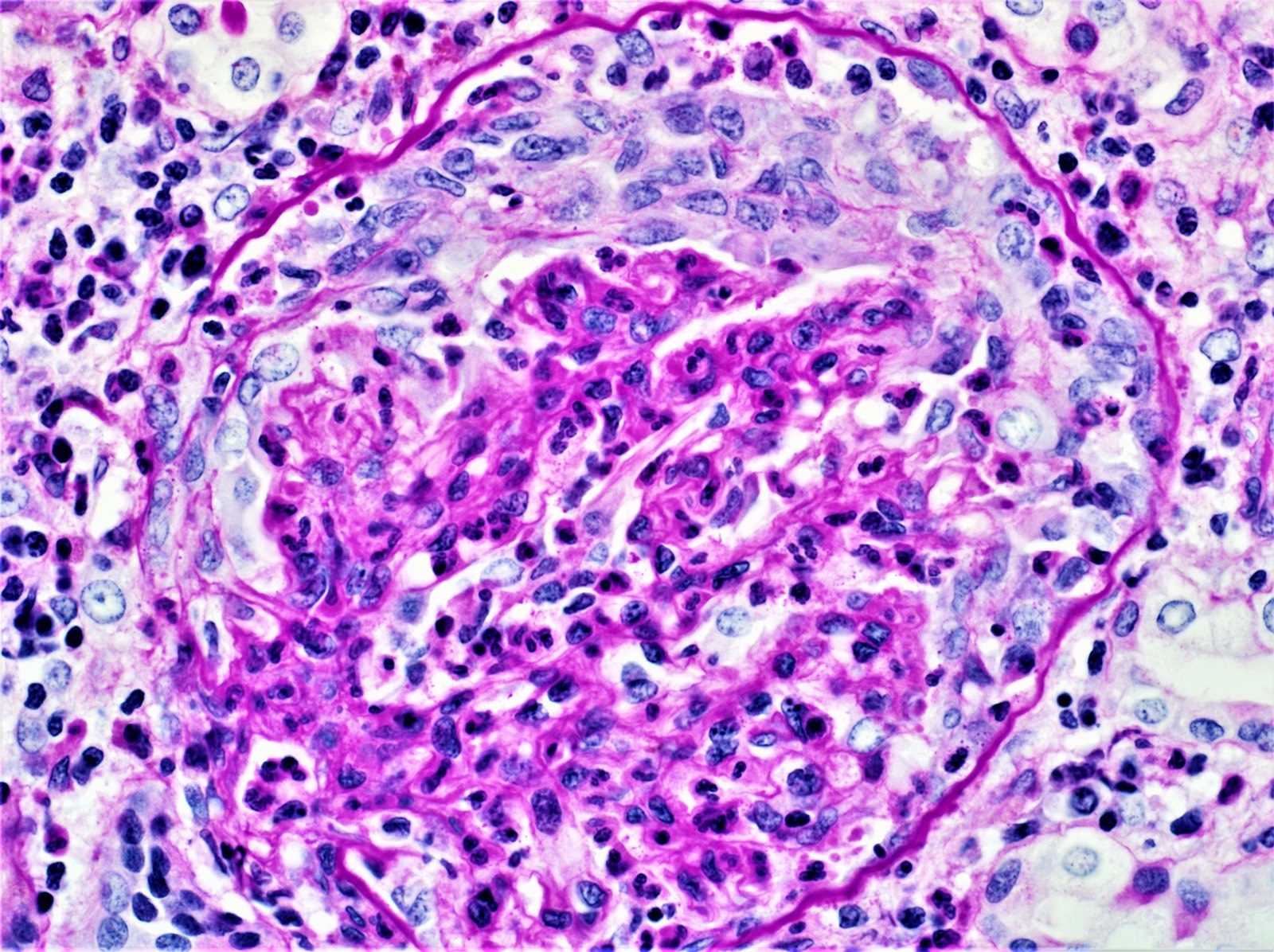
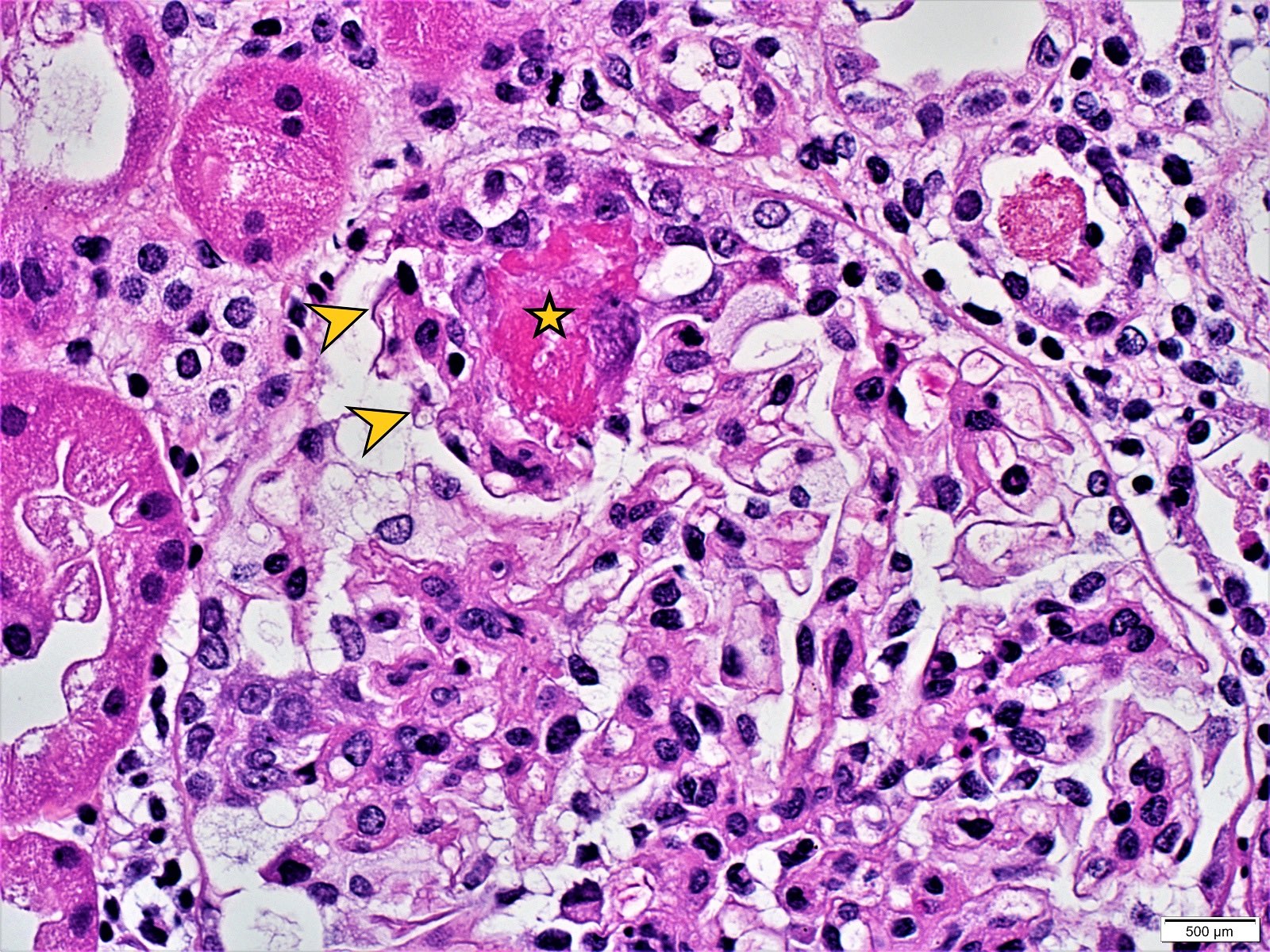
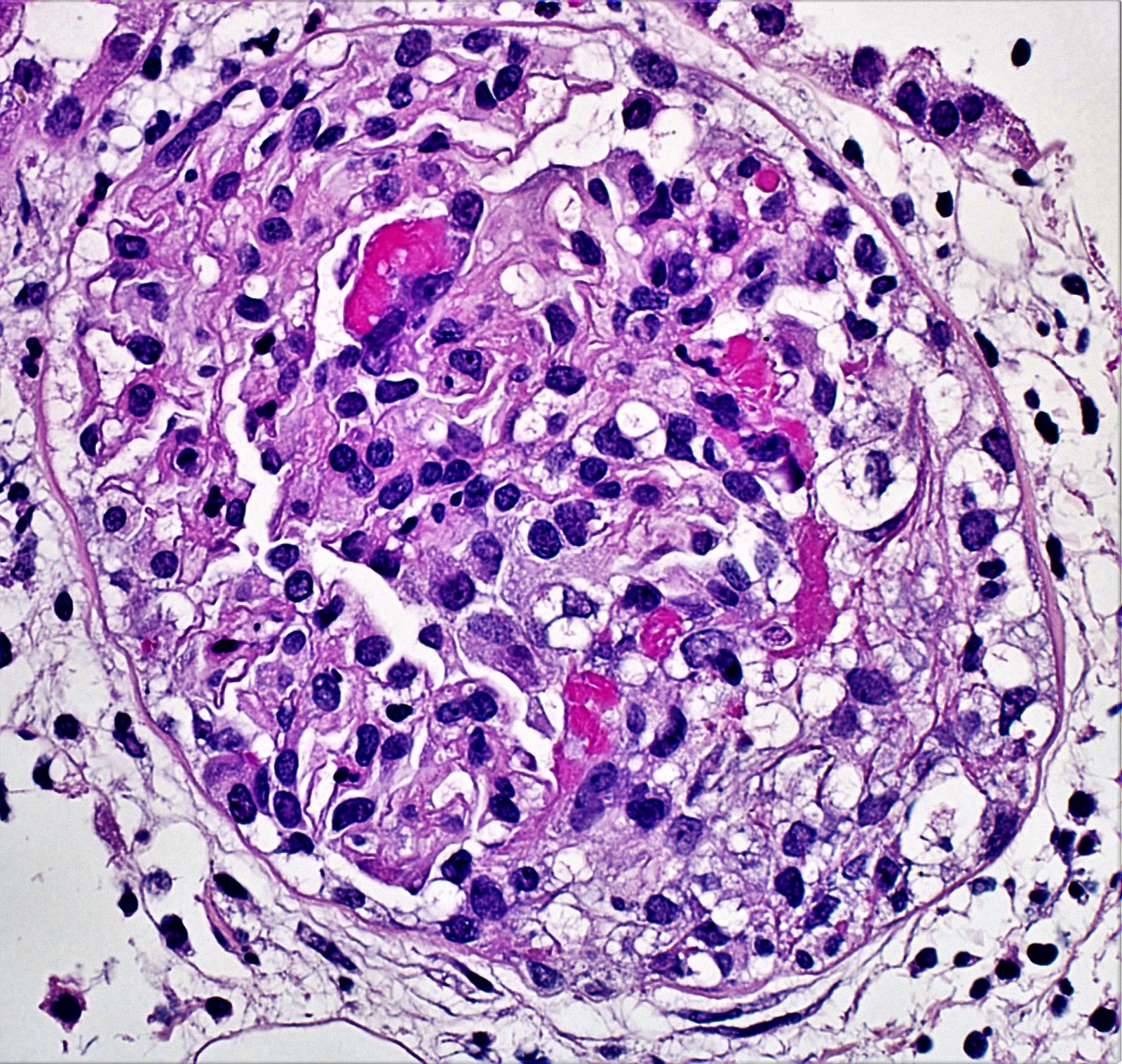
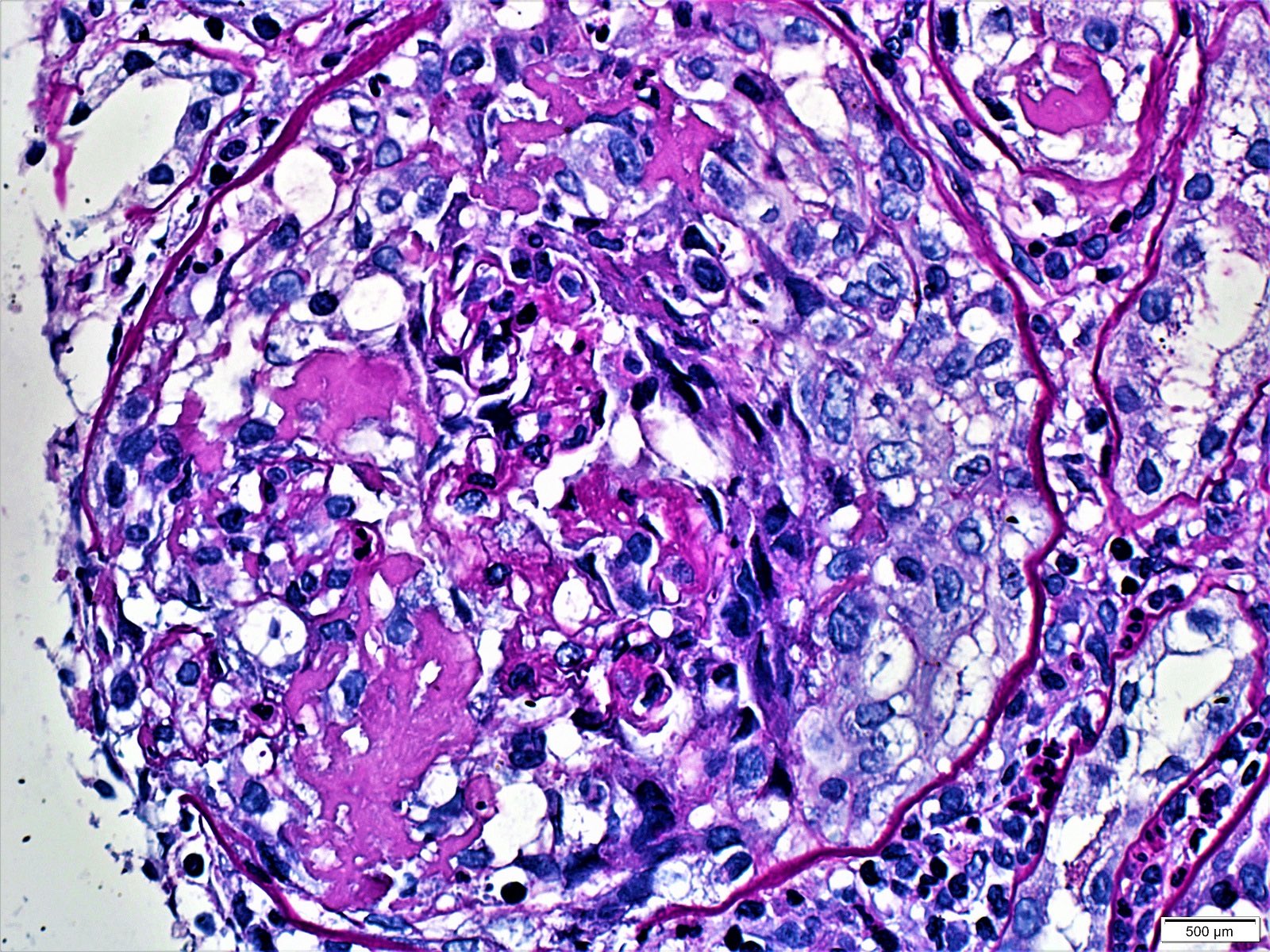
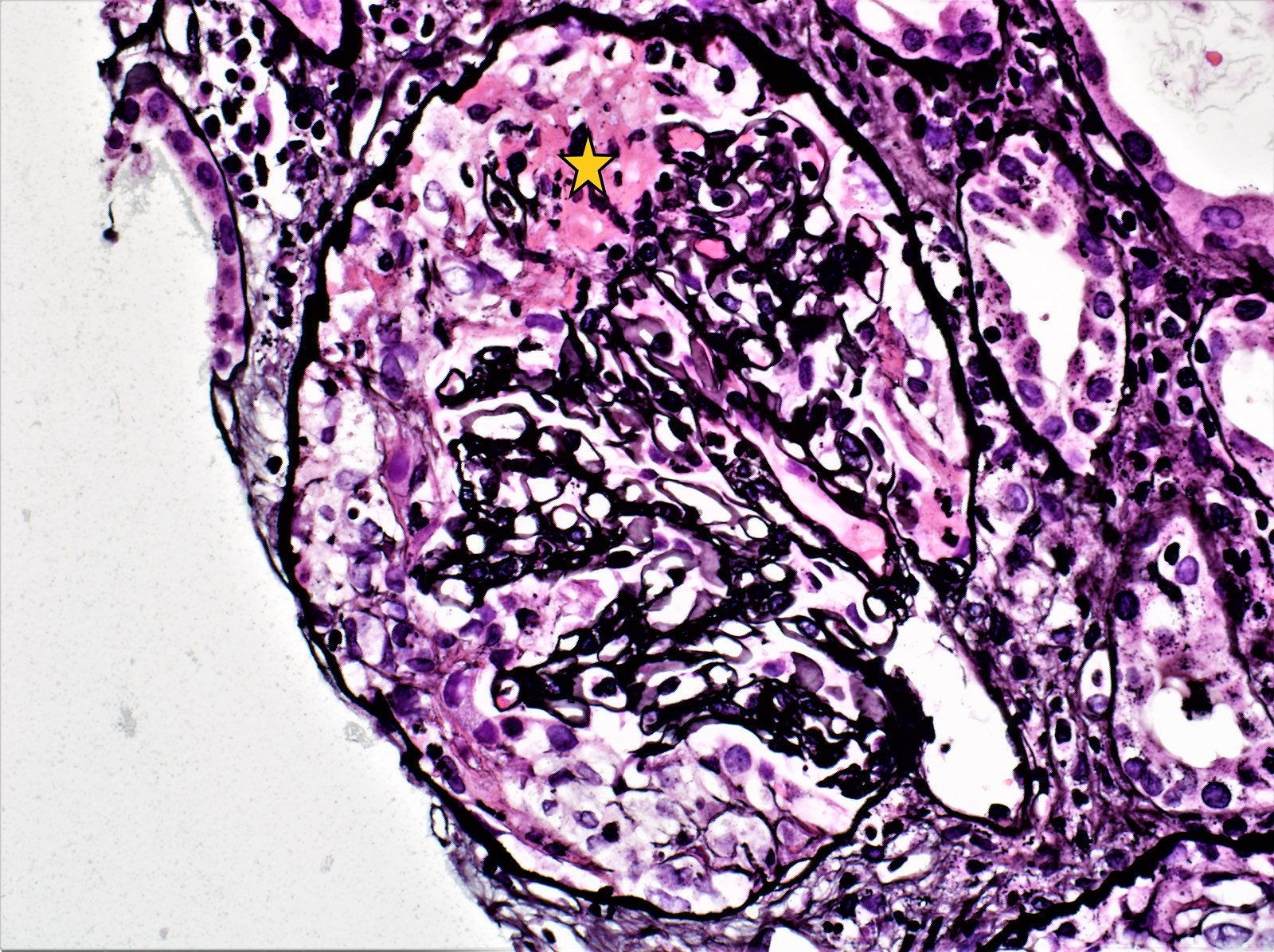
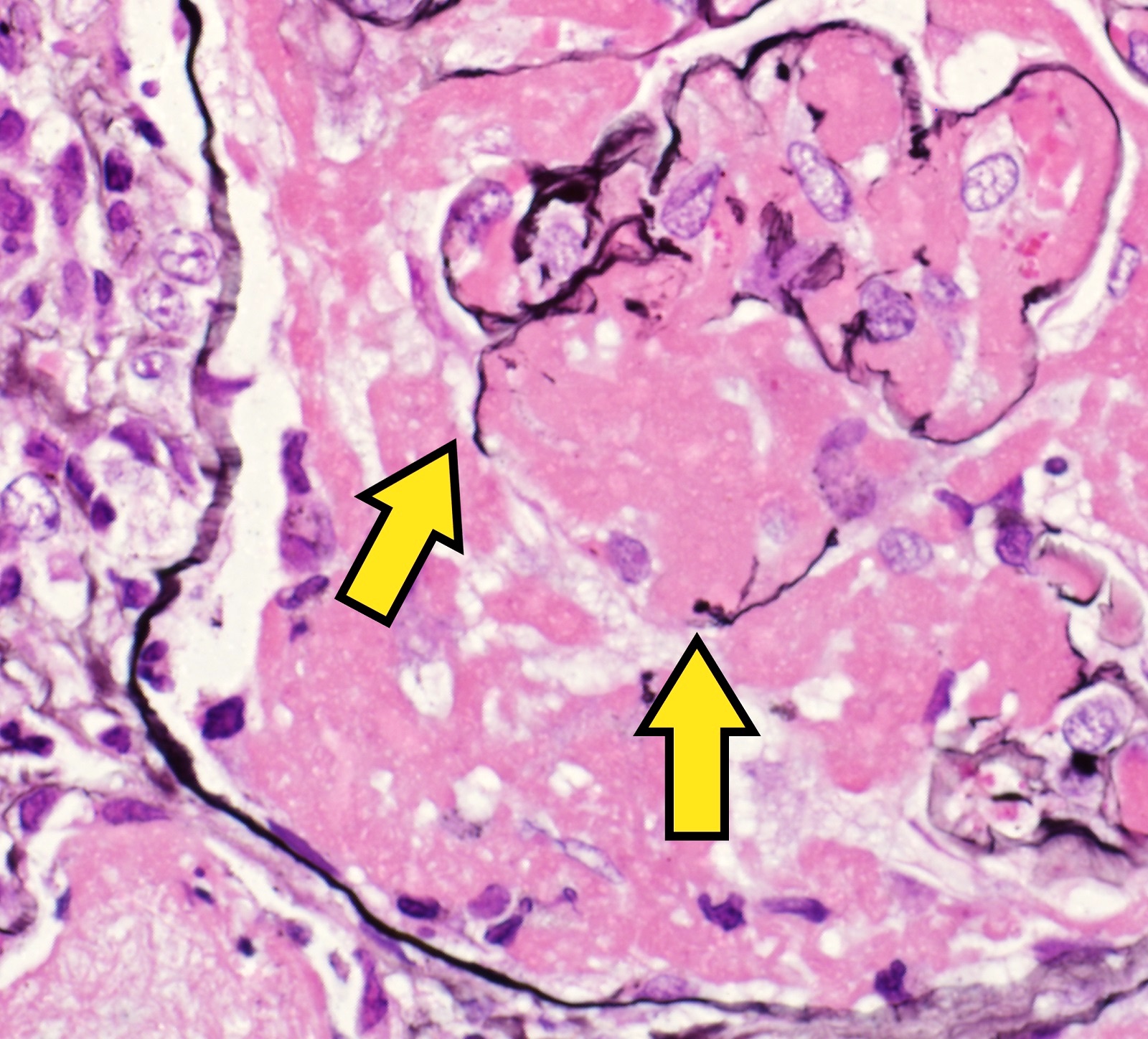
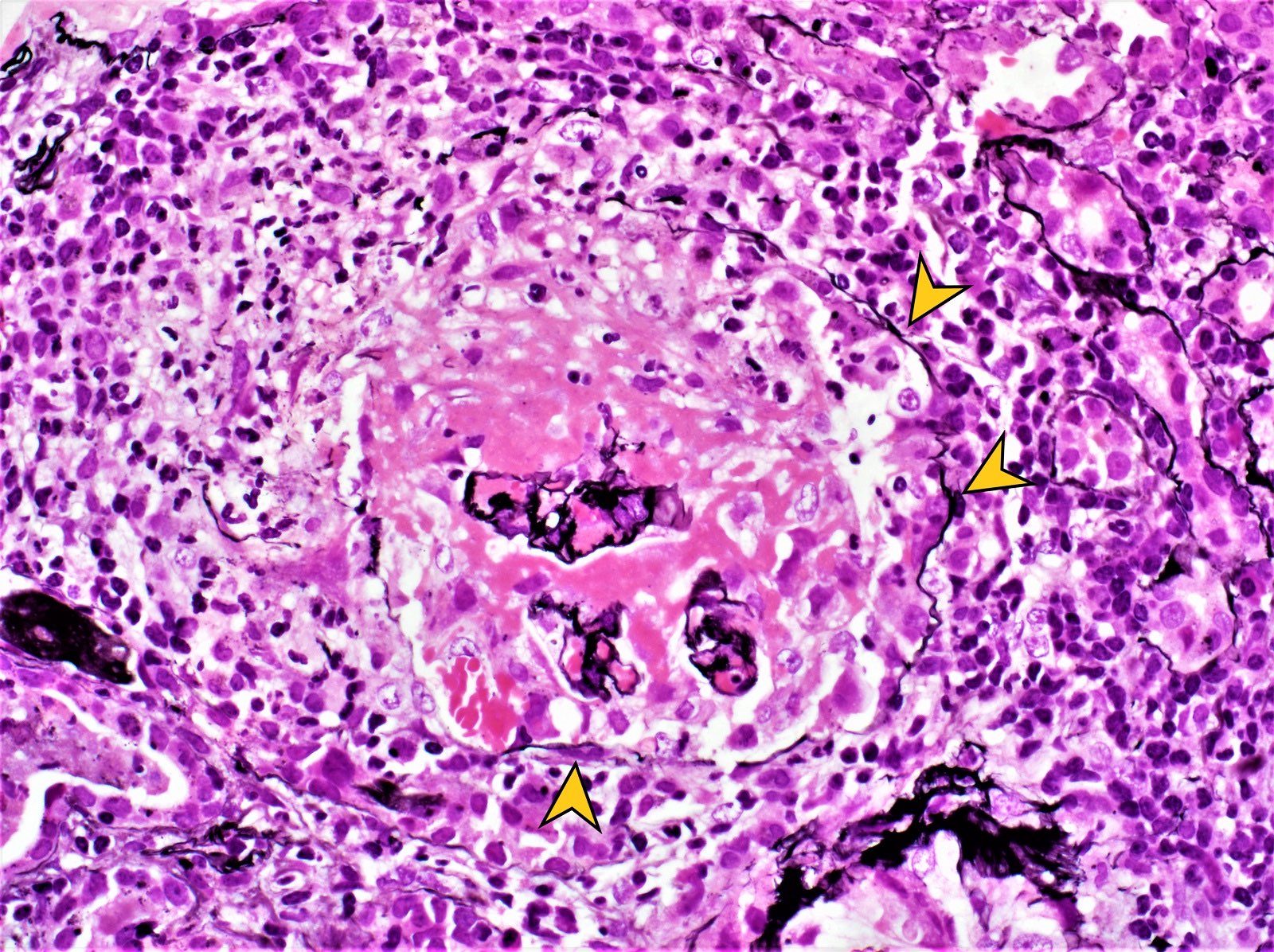
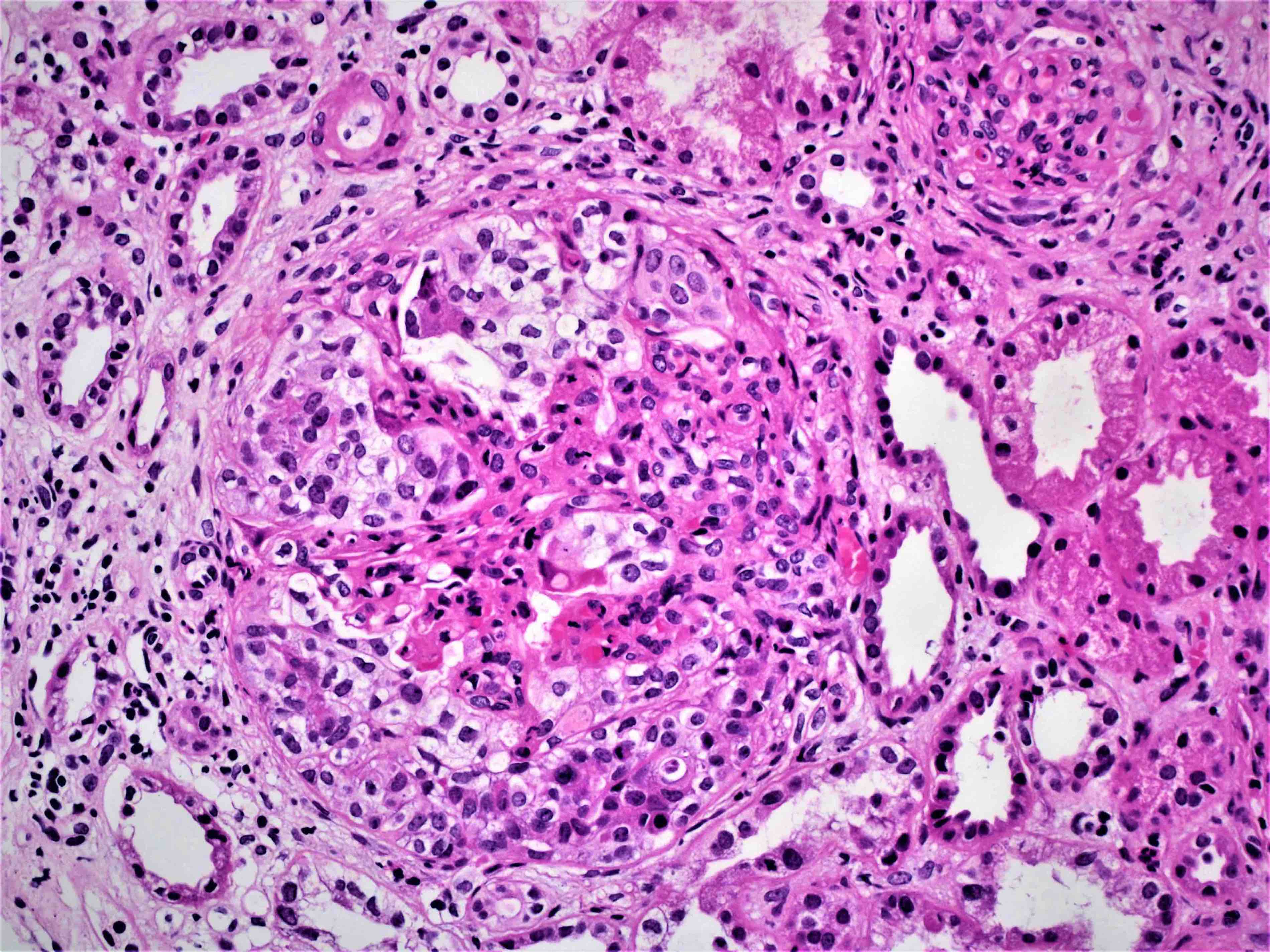
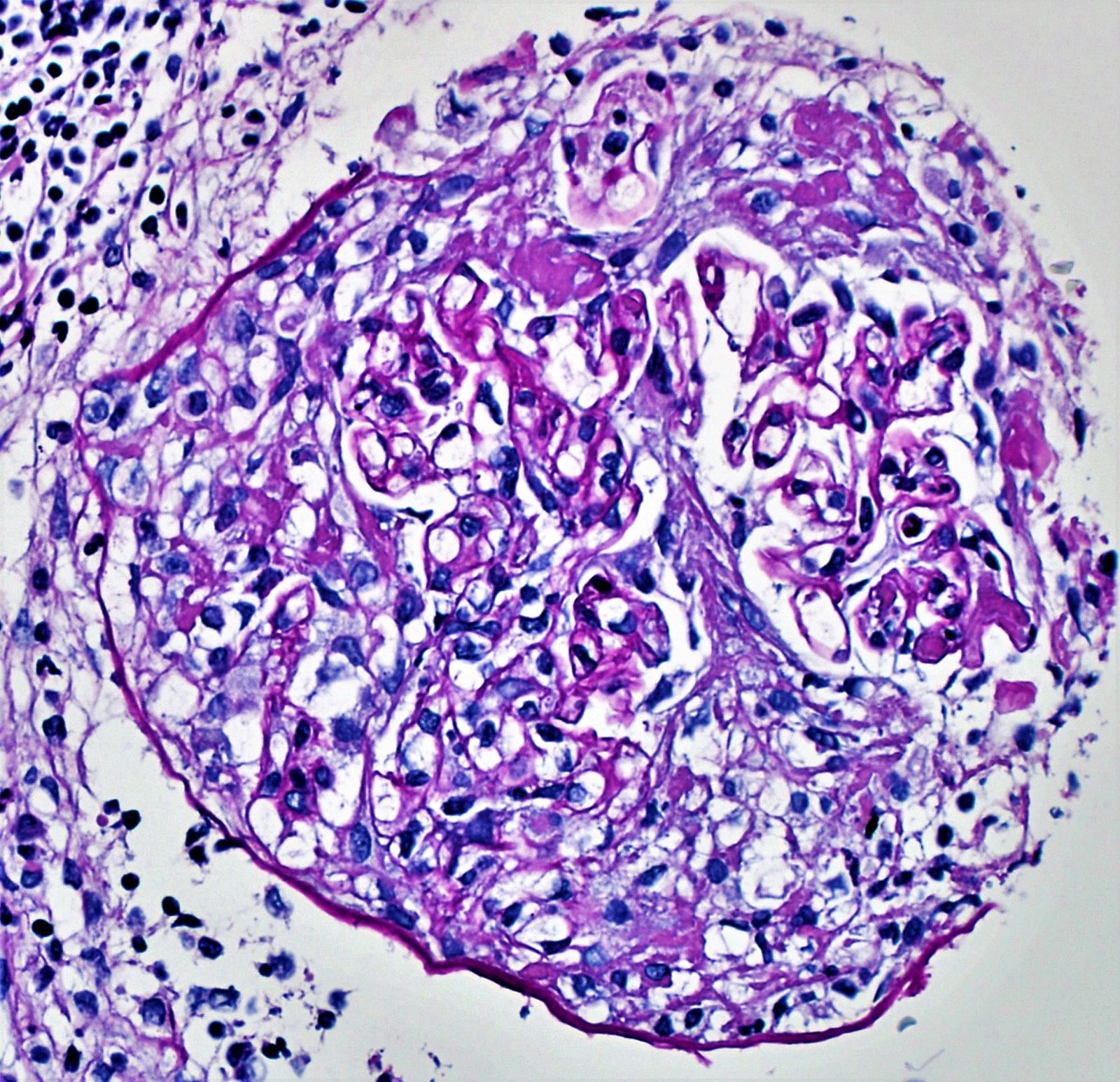
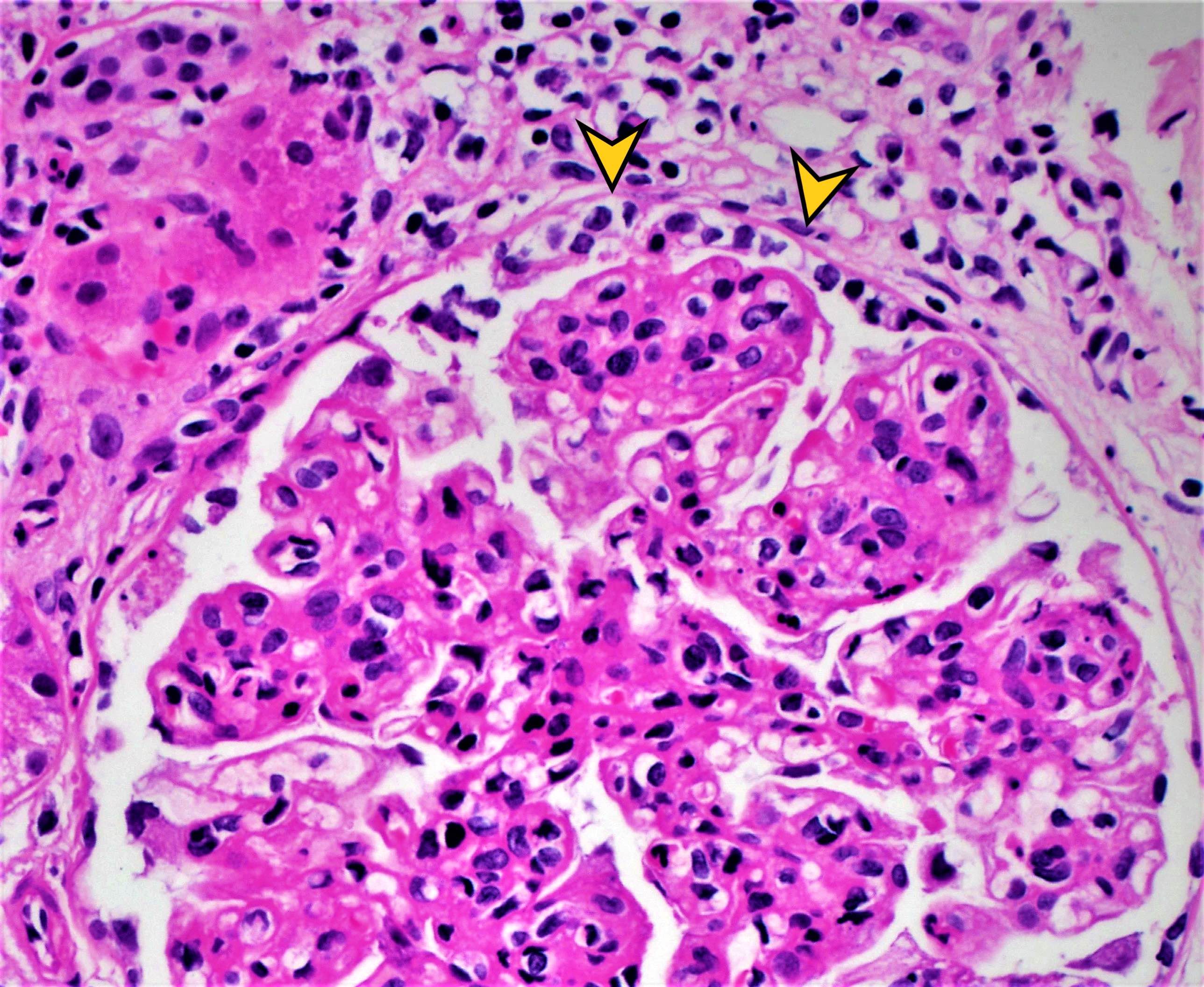
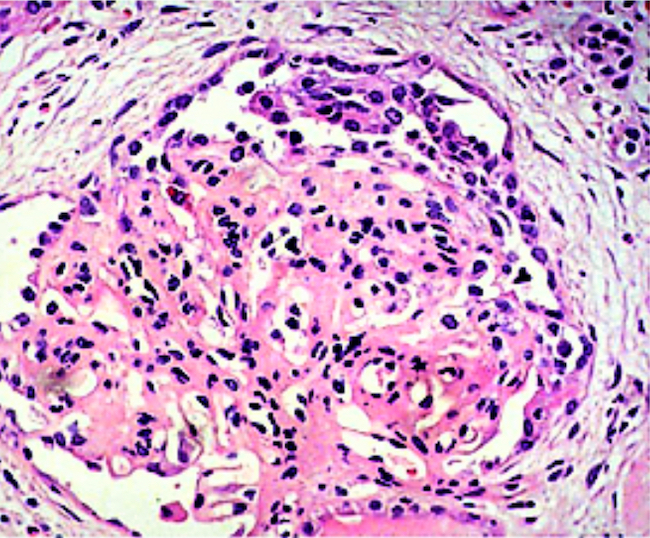
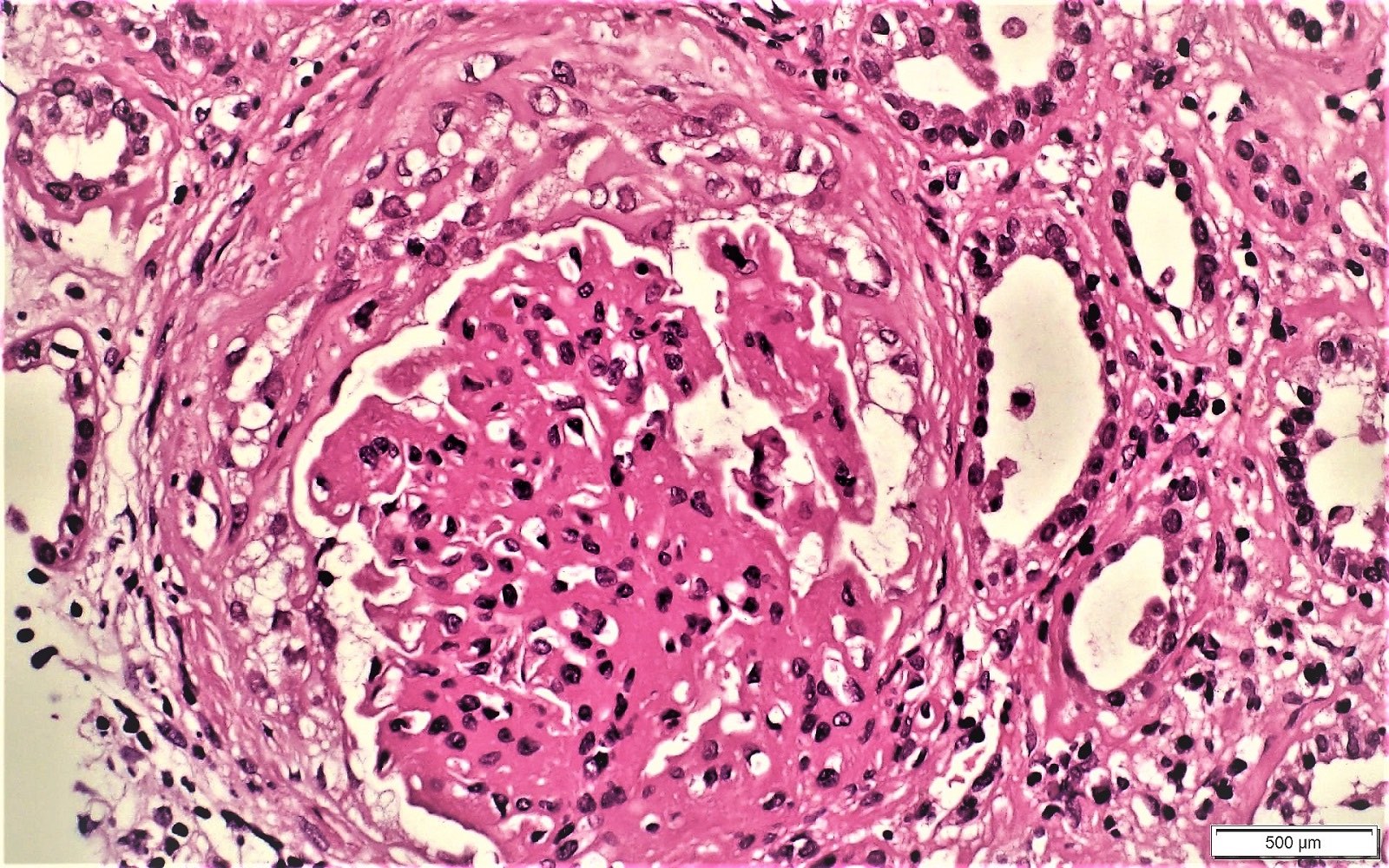
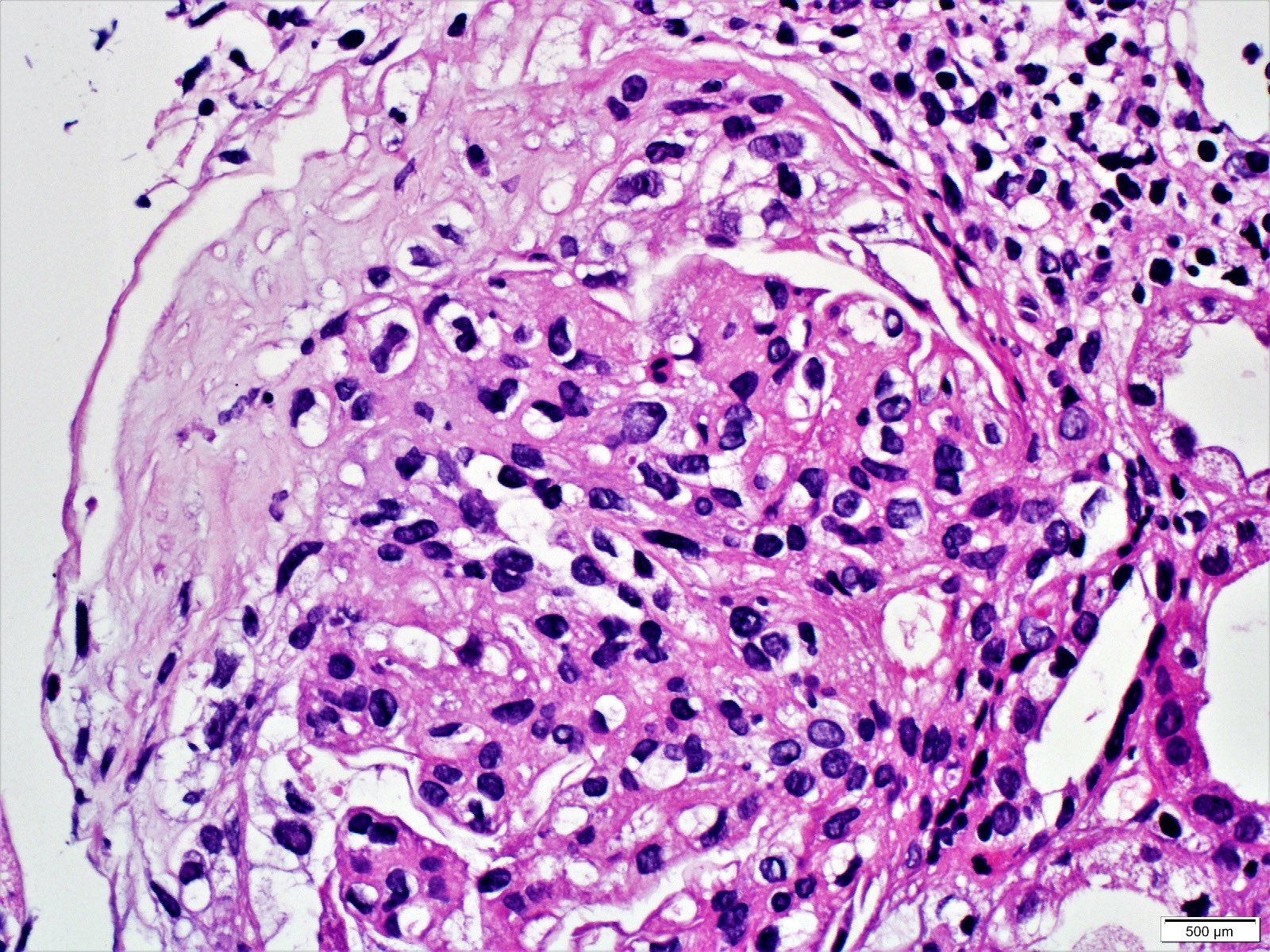
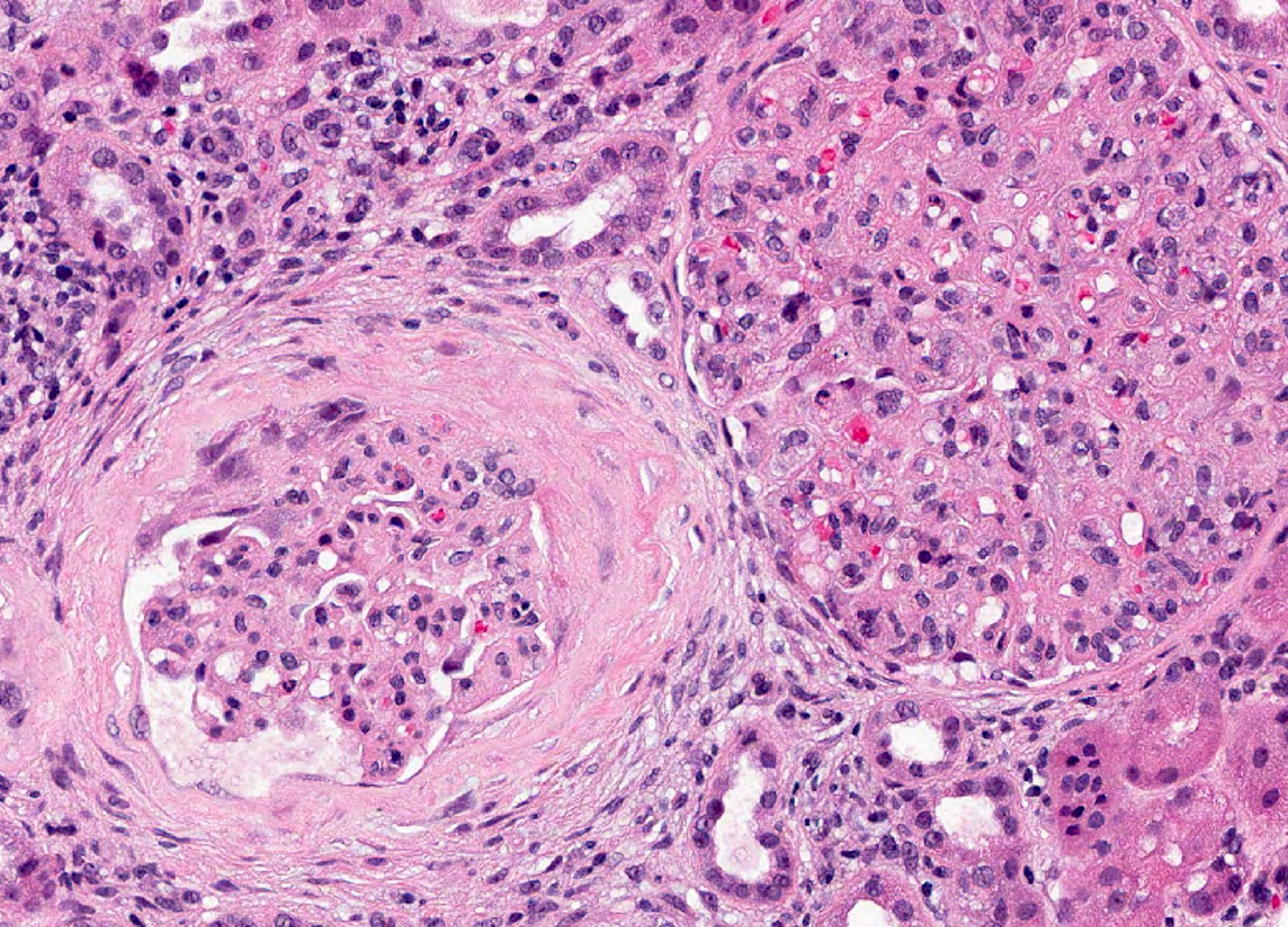
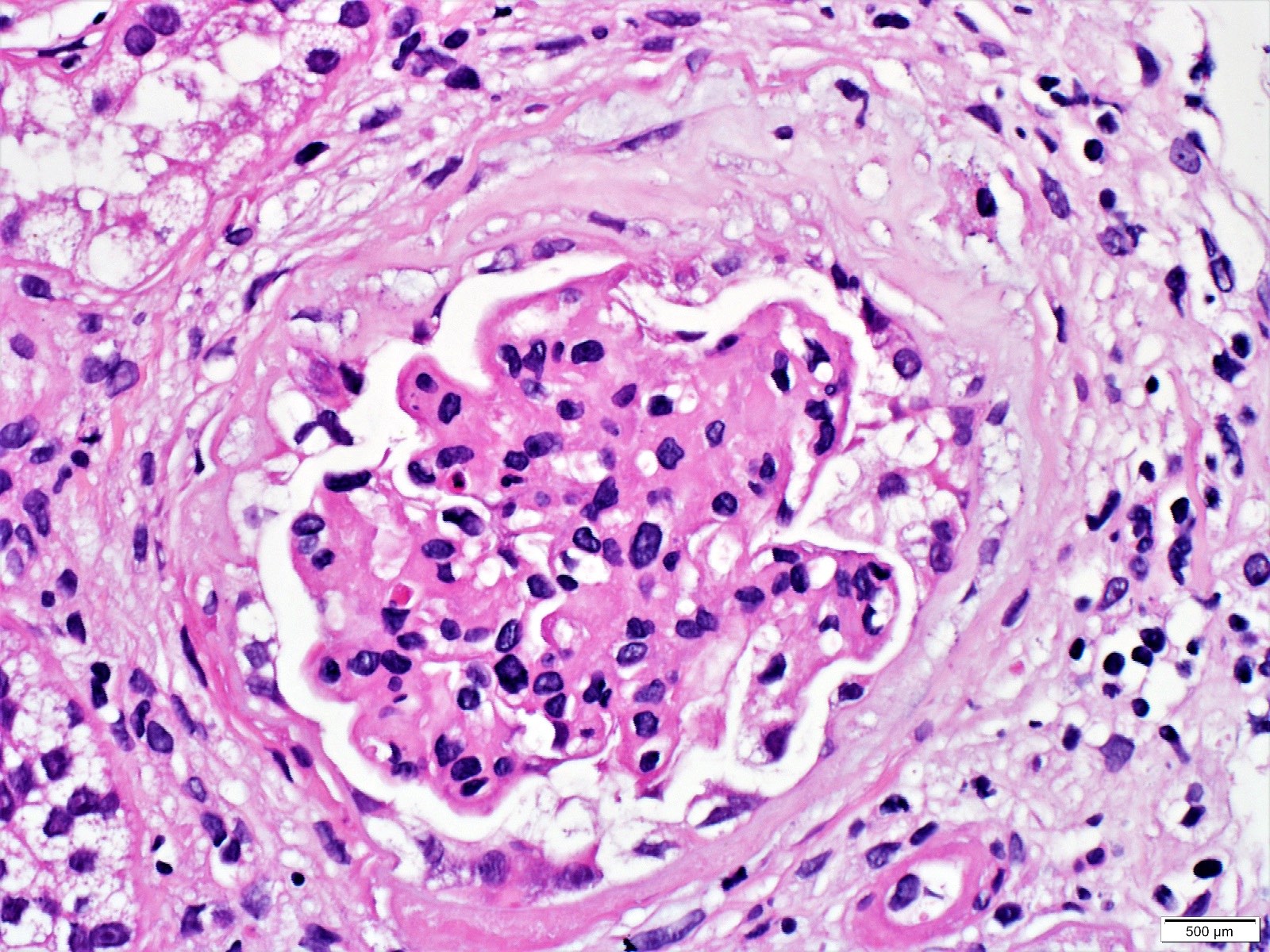
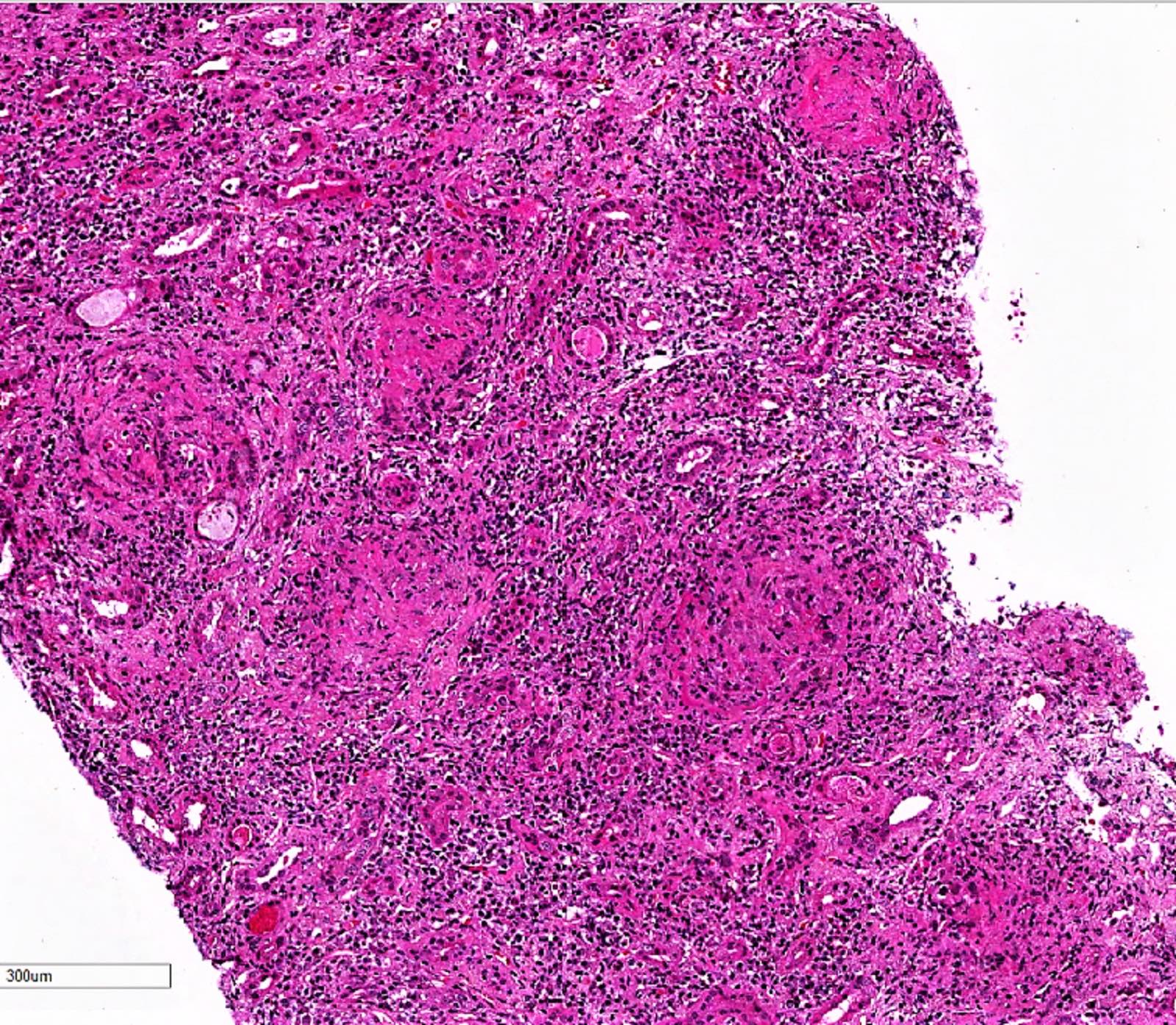
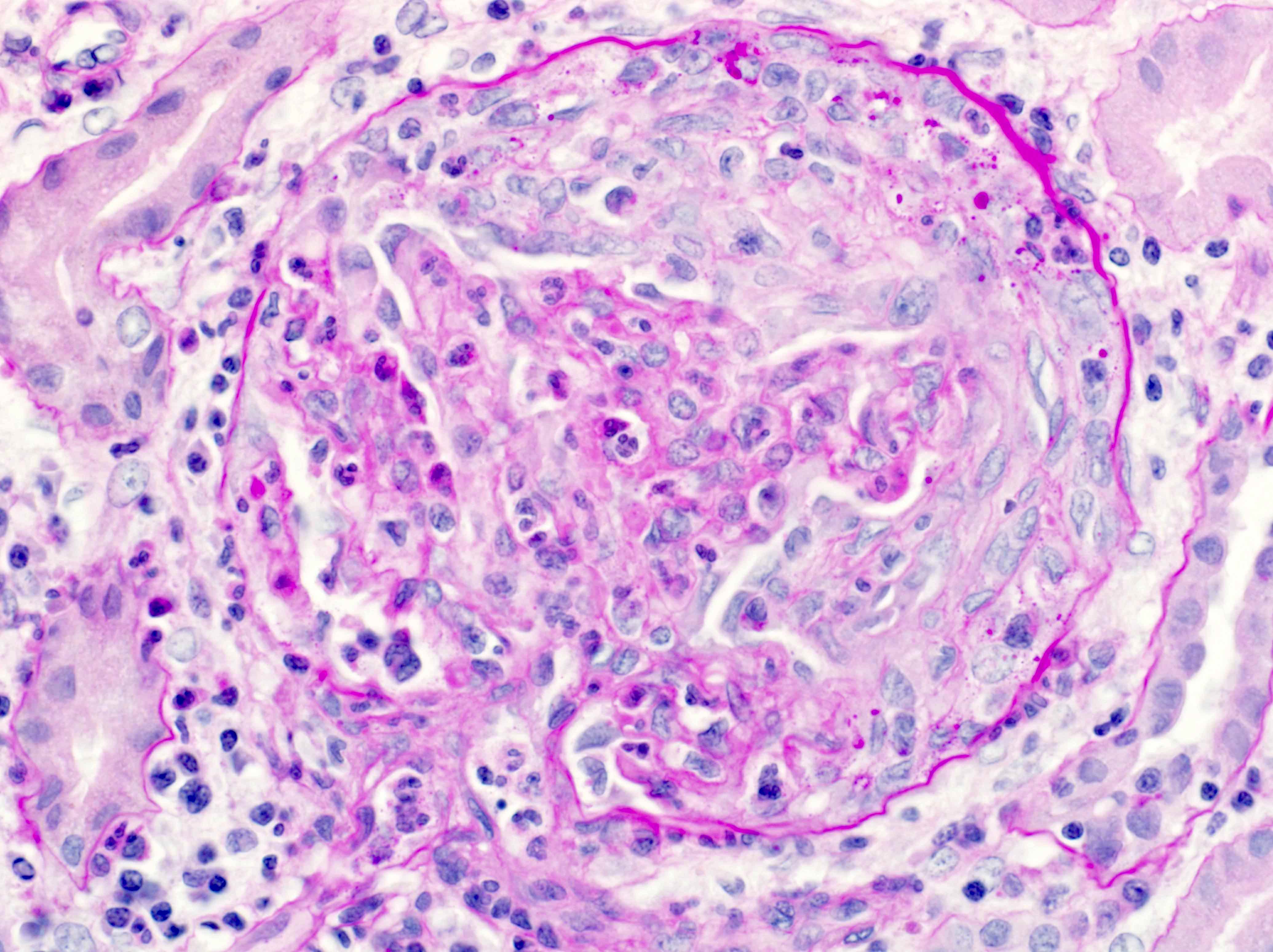
Microscopic (histologic) description
- Extracapillary cellular proliferation (crescents) composed of parietal epithelial cells, macrophages and fibrin
- Segmental fibrinoid necrosis of the glomerular tufts
- Active periglomerular inflammation in cases with rupture of Bowman capsule
- In anti-GBM disease, crescents are uniform and temporally homogeneous, showing the same stage of activity and chronicity (Adv Anat Pathol 2021;28:59)
- In pauci-immune complex crescentic GN, crescents are heterogeneous at variable ages with mixture of cellular, fibrocellular and fibrous crescents; the underlying glomerular architecture is generally normal (Adv Anat Pathol 2021;28:59)
- In immune complex mediated crescentic GN, there are often underlying glomerular architectural changes including esangial or endocapillary proliferation (systemic lupus erythematosus, IgAN)
- Small vessel vasculitis is a feature for pauci-immune complex crescentic glomerulonephritis CGN
- Crescents are classified based on their composition and age into: (J Am Soc Nephrol 2016;27:1278)
- Cellular crescent: extracapillary cell proliferation of more than 2 cell layers, involving at least 10% of glomerular circumference with > 50% of the lesion occupied by cells
- Fibrocellular crescent: extracapillary lesion comprising cells and extracellular matrix with < 50% cells and < 90% matrix
- Fibrous crescent: extracapillary crescents with > 90% matrix
Microscopic (histologic) images
Contributed by Khaled A. Murshed, M.D., Noheir M. Taha, M.B.B.Ch., M.D. and Mohammed Akhtar, M.D.
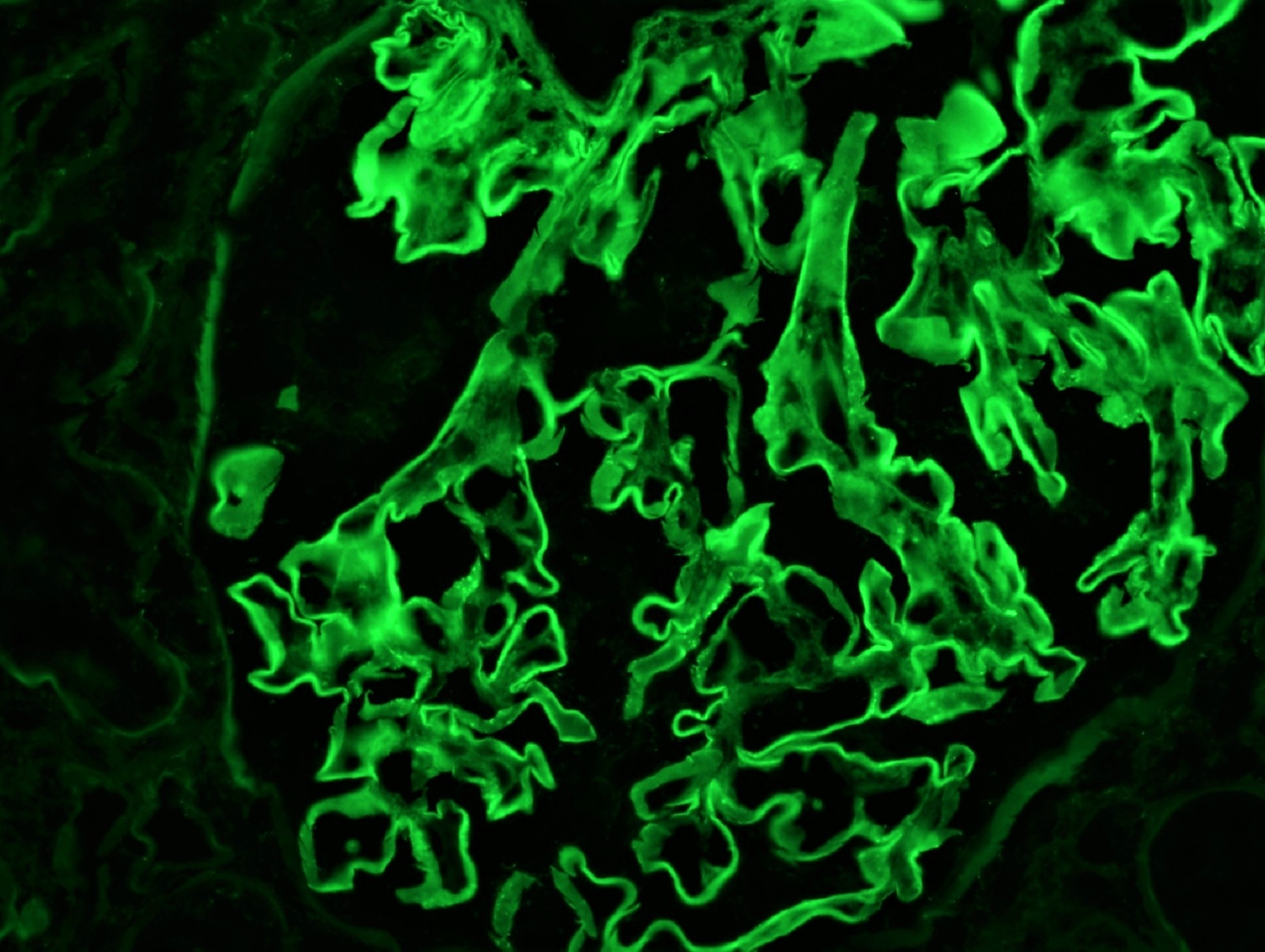
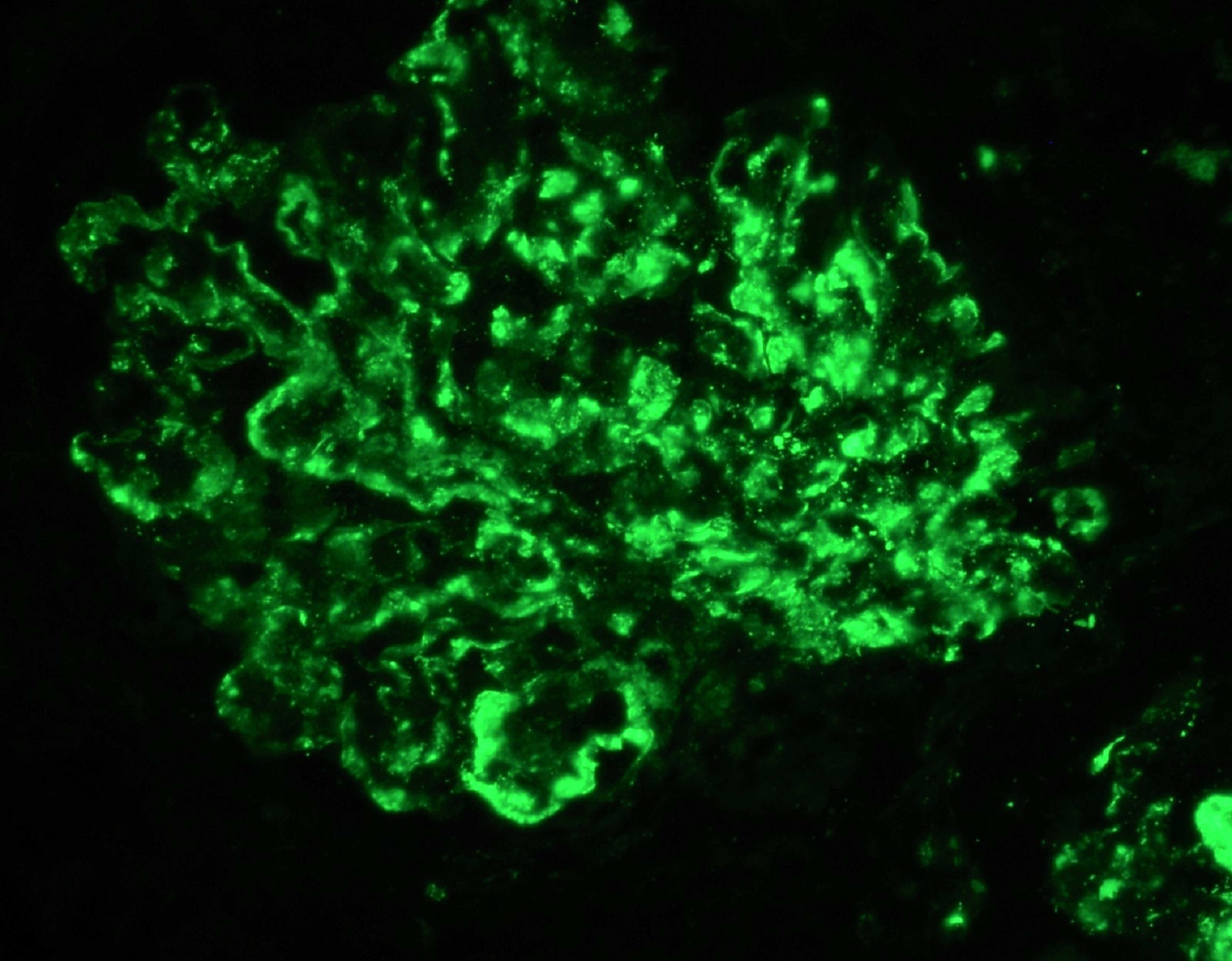
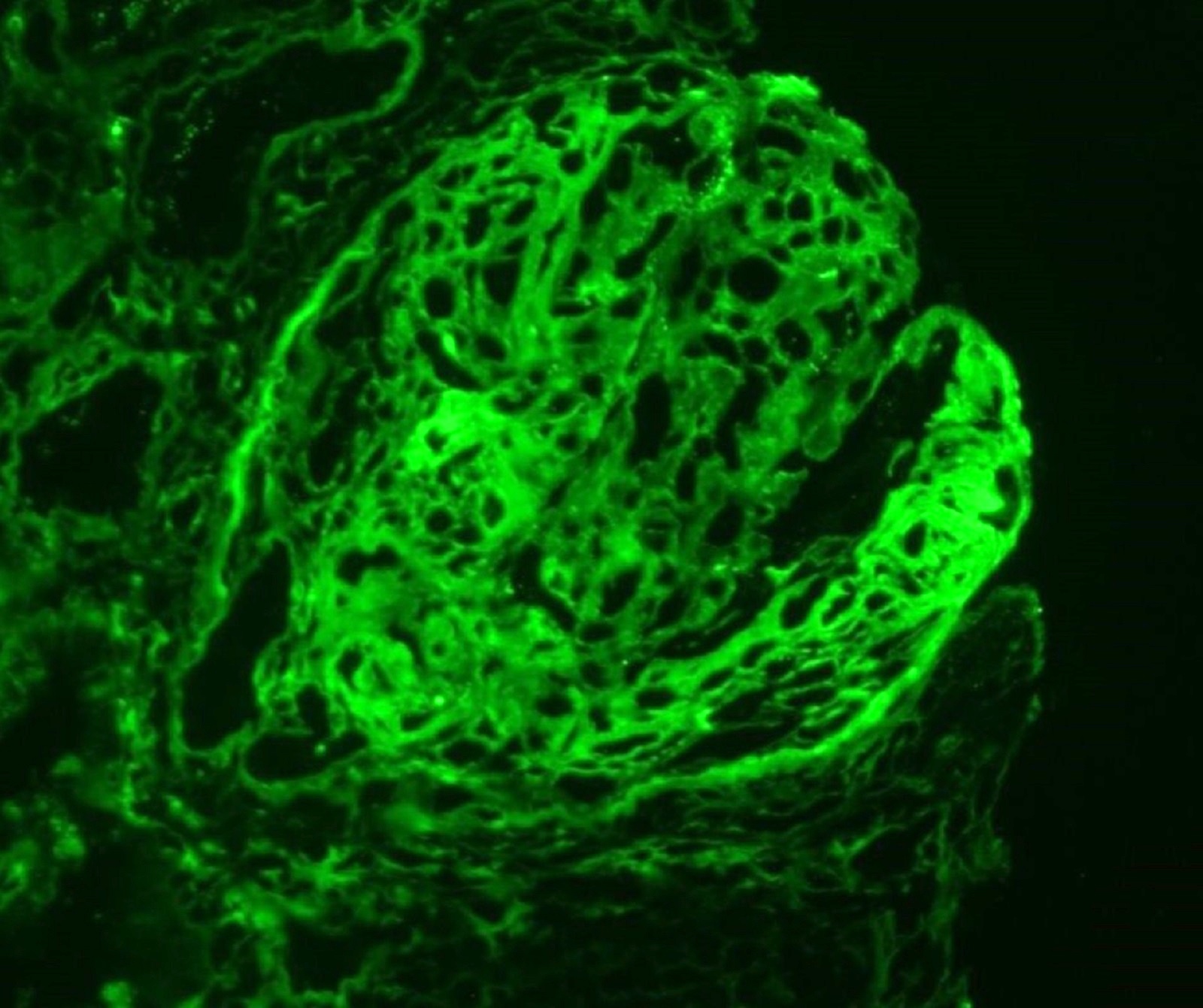
Immunofluorescence description
- Anti-GBM disease: strong linear staining of IgG and frequently C3 along GBM (Adv Anat Pathol 2021;28:59)
- Similar pattern along tubular basement membranes in some cases
- Immune complex mediated crescentic GN: granular deposits of Ig and complement; their type and location (subepithelial, subendothelial, mesangial) depend on the underlying etiology
- Pauci-immune complex crescentic GN: negative or weak (≤ 1+) staining of Ig and complement (pauci-immune pattern)
- Fibrin deposition in cellular crescents and foci of fibrinoid necrosis
Immunofluorescence images
Positive stains
- PAS, Jones methenamine silver and trichrome are used to evaluate the morphology
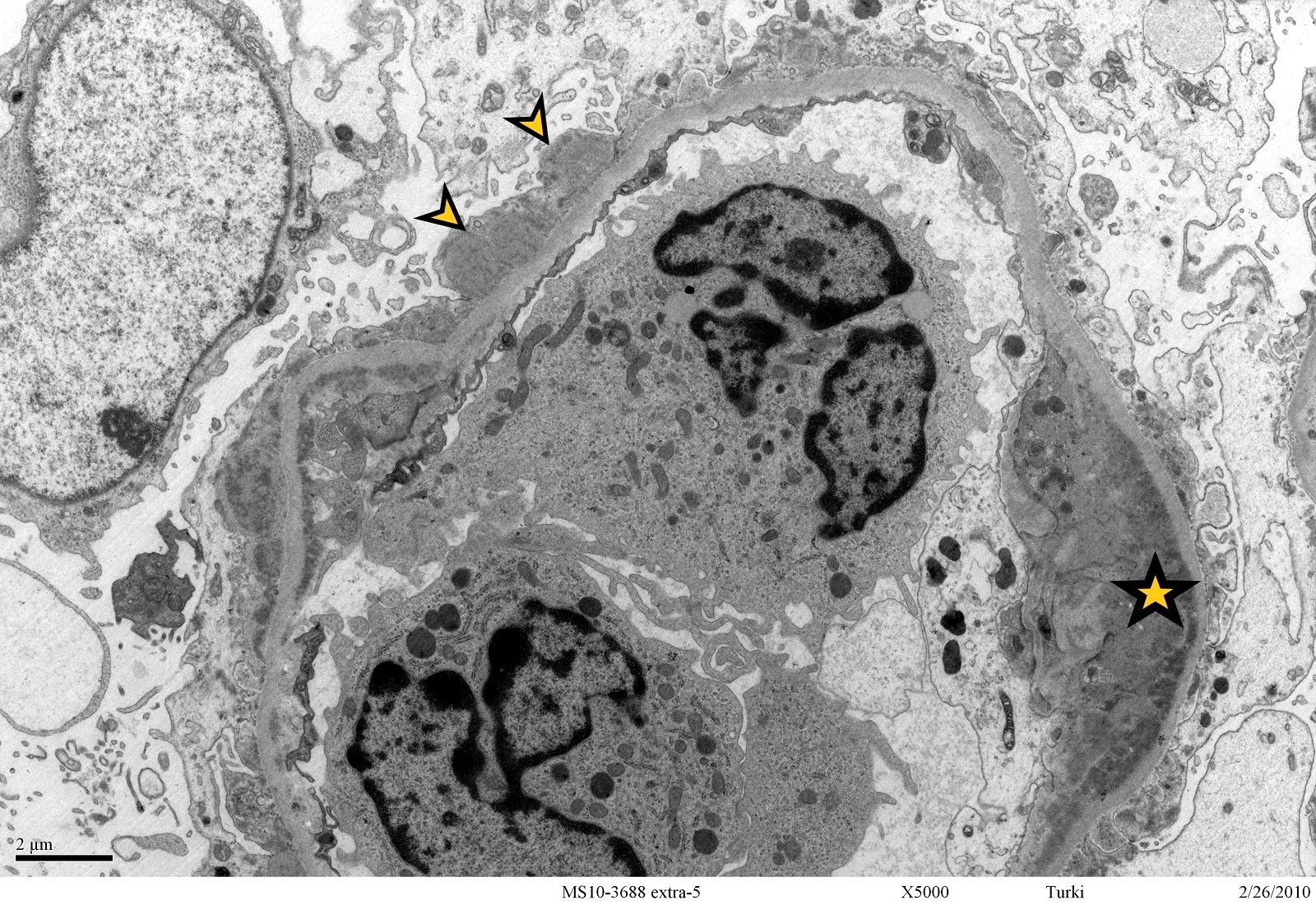
Electron microscopy description
- Anti-GBM disease: no electron dense deposits
- Immune complex mediated crescentic GN: electron dense deposits are present within glomeruli; their location depends on the underlying etiology (J Am Soc Nephrol 2016;27:1278)
- Pauci-immune complex crescentic GN: no electron dense deposits
- Breaks and rupture of GBM
Electron microscopy images
Sample pathology report
- Left kidney, needle core biopsy:
- Crescentic glomerulonephritis secondary to anti-GBM disease (see comment)
- Cellular crescent (9/13), fibrocellular / fibrous crescents (0/13)
- Global glomerulosclerosis (0/13), segmental glomerulosclerosis (0/13)
- Interstitial inflammation, moderate
- Tubular atrophy and interstitial fibrosis, mild
- Arteriosclerosis, moderate
- Comment: Indirect immunofluorescence studies show diffuse linear staining of IgG (2+) and C3 (2+) along the GBM and tubular basement membrane with negative staining for IgA, IgM and C1q. The findings are consistent with anti-GBM disease.
Differential diagnosis
- RPGN is a clinical diagnosis, not a pathology diagnosis so the differential is most important to nephrologists, not pathologists; the usual pathology correlate is a crescentic glomerulonephritis due to different etiologies
Board review style question #1
Which of the following is true about the glomerular disease depicted in the image?
- It presents clinically as a slowly progressive disease
- Immune complex mediated crescentic glomerulonephritis (type 2) is associated with linear staining of IgG along glomerular basement membrane
- Anti-GBM disease (type 1) is associated with granular staining of IgG along glomerular basement membrane
- In pauci-immune complex crescentic GN (type 3), electron dense deposits are commonly present
- Pauci-immune complex crescentic GN (type 3) is the most common subtype of crescentic glomerulonephritis
Board review style answer #1
E. Pauci-immune complex crescentic GN (type 3) is the most common subtype of crescentic glomerulonephritis
Comment Here
Reference: Crescentic glomerulonephritis overview
Comment Here
Reference: Crescentic glomerulonephritis overview
Board review style question #2
Regarding the pathogenesis of crescentic glomerulonephritis, which of the following is the first and most crucial event that leads to crescent formation?
- Podocyte injury
- Epithelial mesenchymal transition
- Podocyte effacement
- Endothelial cell injury
- Parietal cell damage
Board review style answer #2