Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Murshed KA, Taha NM, Akhtar M. Diabetic kidney disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneydiabetes.html. Accessed December 17th, 2024.
Definition / general
- Diabetic kidney disease is a morphologic structural change in the kidney induced by longstanding hyperglycemia manifested as relentless matrix expansion
Essential features
- Diabetic kidney disease is a morphological structural change in the glomeruli that occurs due to longstanding hyperglycemia (Contrib Nephrol 2011;170:36)
- Characterized by mesangial matrix expansion and diffuse thickening of glomerular, tubular and Bowman capsule basement membranes
- Mesangial matrix expansion can be diffuse, nodular or both
- Additional insudative lesions due to deposition of lipohyaline involving blood vessels (vascular hyalinosis), glomerular capillaries (hyaline caps) and Bowman capsule (capsular drop)
- Immunofluorescent microscopy usually reveals diffuse linear staining for immunoglobulin IgG along glomerular capillaries and tubular basement membranes; intensity usually 1+
Terminology
- Diabetic nephropathy
- Diabetic glomerulosclerosis (nodular or diffuse)
- Kimmelstiel-Wilson lesion
- Intercapillary glomerulosclerosis
ICD coding
Epidemiology
- Occurrence of diabetes is worldwide; incidence is rising in developing countries (Adv Anat Pathol 2020;27:87)
- Highly susceptible ethnic groups: Black, Native American, Hispanic (Kidney Dial 2022;2:433)
Sites
- Renal cortical glomeruli
Pathophysiology
- Hyperglycemia is the main initiator
- Interaction between high intracellular sugar levels and the free amino groups on proteins, lipids and nucleic acids results in the formation of advanced glycation end products
- These compounds induce excess extracellular matrix production and reduce matrix degradation by matrix metalloproteinases (J Diabetes Investig 2011;2:243)
- Increase in type IV collagen and a decrease in laminin and heparan sulfate proteoglycan resulting in loss of anionic charge leading to increased glomerular filtration of albumin
- Hyperglycemia may also lead to podocyte damage and progressive loss resulting in focal denudation of glomerular basement membrane (GBM)
- Denuded GBM attaches to the parietal epithelial cells and the Bowman capsule, resulting in segmental glomerulosclerosis (Kidney Int Suppl 2007;72:S36)
Etiology
- Usually presents after 15 years of having diabetes mellitus (Adv Anat Pathol 2020;27:87)
- Type 1 diabetes mellitus
- 10% of cases
- Develops in 30% of patients
- Associated with loss of insulin producing cells
- Generally seen in younger patients (< 30 years)
- Type 2 diabetes mellitus
- 90% of cases
- Develops in 50% of patients
- Due to less than adequate insulin production and insulin resistance
- Generally seen in older patients
- Usually have additional comorbidities (hypertension, cardiovascular disease)
Clinical features
- Severity is related to diabetes duration, degree of glycemic control and genetic factors (Nat Rev Dis Primers 2015;1:15018)
- Begins with microalbuminuria, defined as loss of small amounts of albumin into the urine (30 - 300 mg/d)
- Later, larger amounts of albumin are lost in the urine macroalbuminuria, detectable by dipstick urinalysis (> 300 mg/d)
- With disease progression, gradual decline in kidney function occurs, ultimately leading to end stage renal disease
Diagnosis
- Diagnosis is usually established on kidney biopsy
Laboratory
- Proteinuria
- Hyperglycemia
- Glycosuria
- Hemoglobin A1C
Prognostic factors
- Type 1 diabetes: end stage renal disease in 50% with overt nephropathy within 10 years and in > 75% by 20 years
- Type 2 diabetes: end stage renal disease is faster due to the presence of several comorbidities that affect the kidney, such as hypertension and atherosclerosis (Ren Fail 2022;44:1309)
Case reports
- 56 year old man with collapsing glomerulopathy superimposed on diabetic nephropathy (Indian J Nephrol 2019;29:207)
- 58 year old nondiabetic man with diabetic nephropathy (Pathol Res Pract 2016;212:1199)
- 59 year old woman with diabetic nephropathy aggravating the progression and prognosis of COVID-19 associated acute limb ischemia (F1000Res 2021;10:584)
- 62 year old Chinese man with advanced diabetic kidney disease complicated by acute interstitial nephritis (World Acad Sci J 2021;3:37)
- 70 year old man with diabetes mellitus for 26 years combined with IgA nephropathy (Front Endocrinol (Lausanne) 2022;13:992933)
Treatment
- Strict glycemic control is the mainstay of therapy for both type 1 and type 2 diabetes mellitus
- Long term glycemic control may halt progression and possibly reverse some matrix expansion over many years (Nat Rev Dis Primers 2015;1:15018)
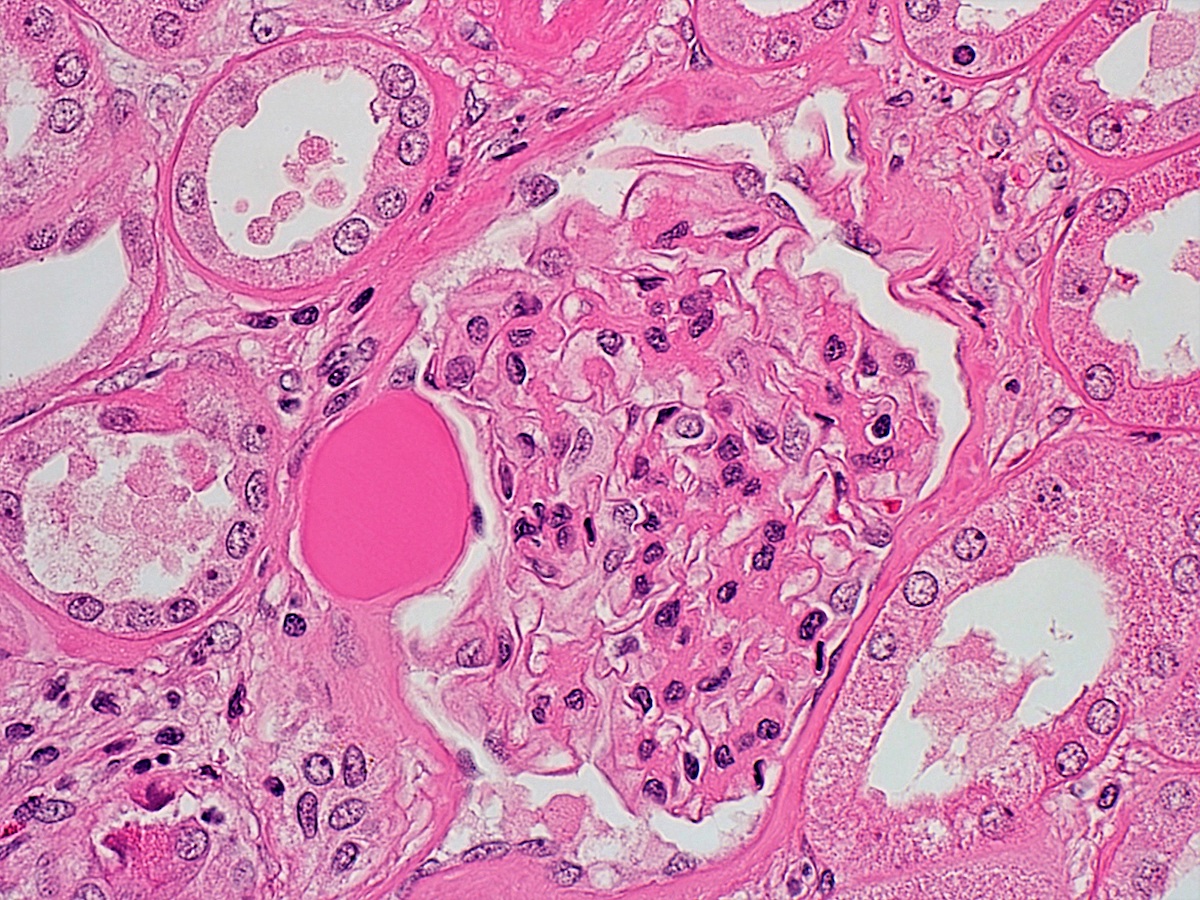
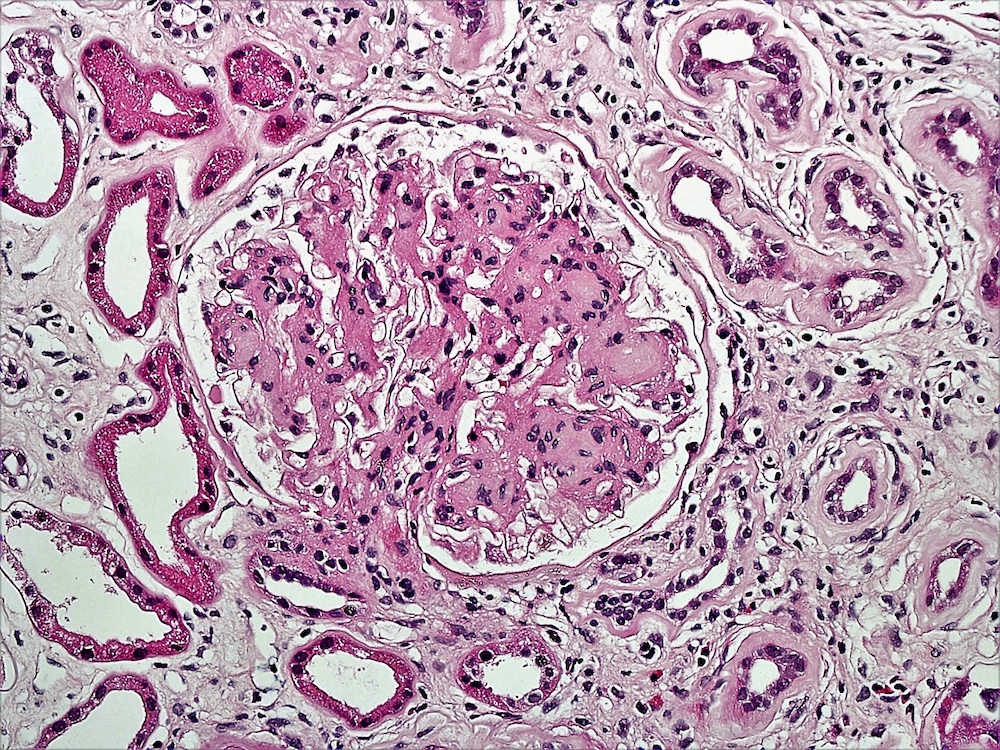
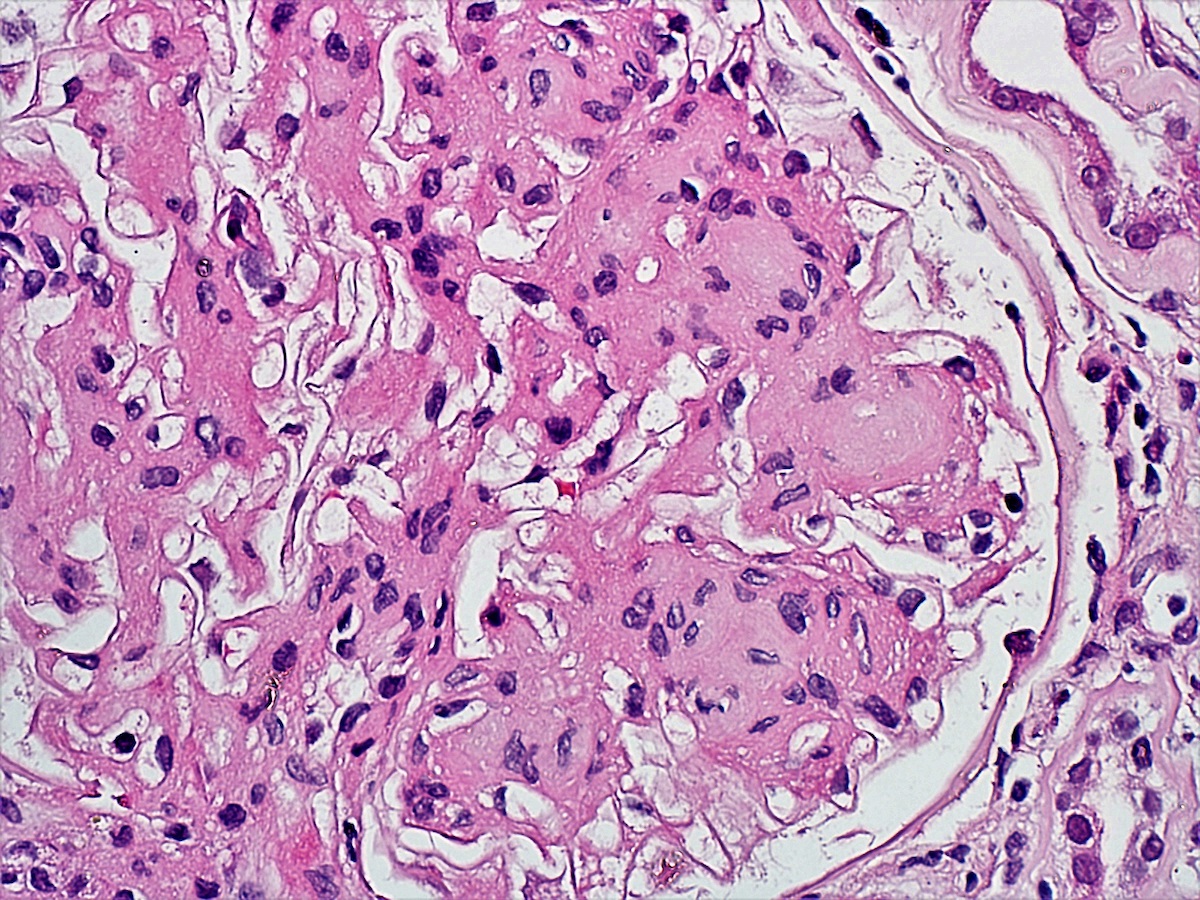
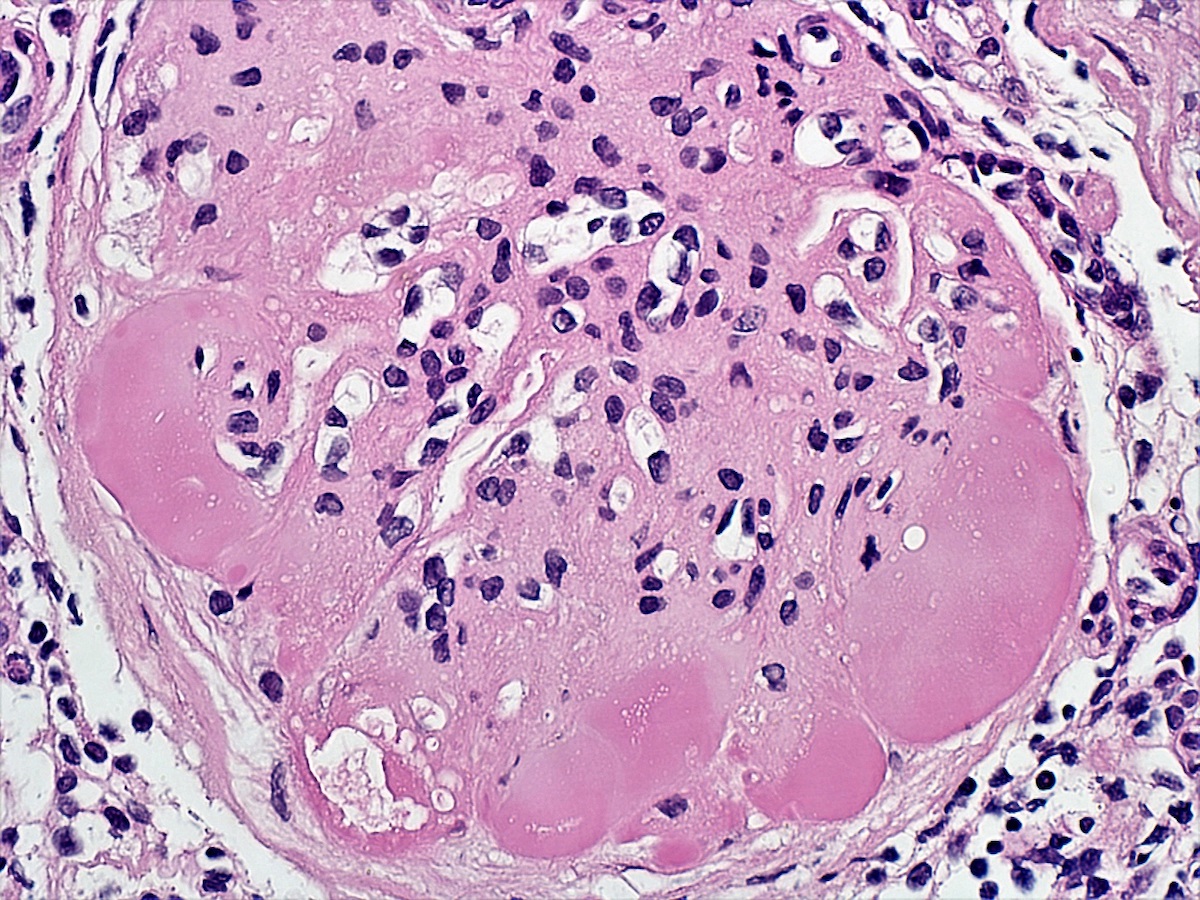
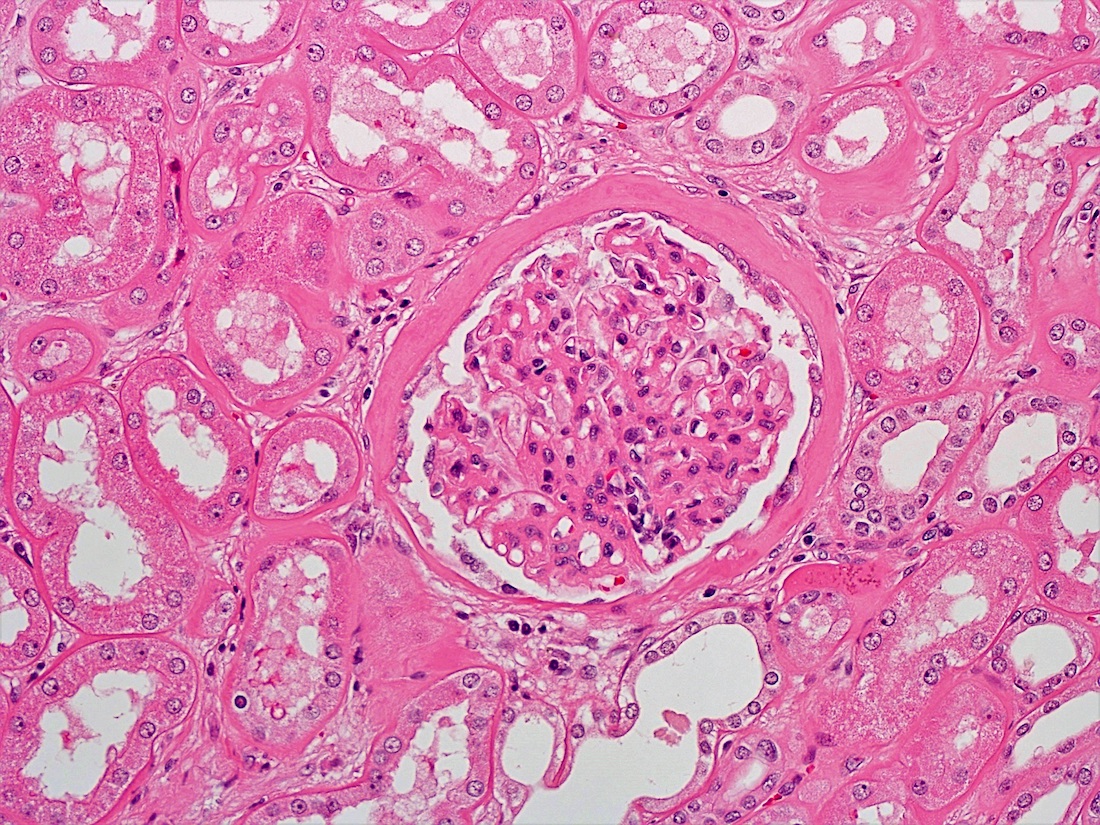
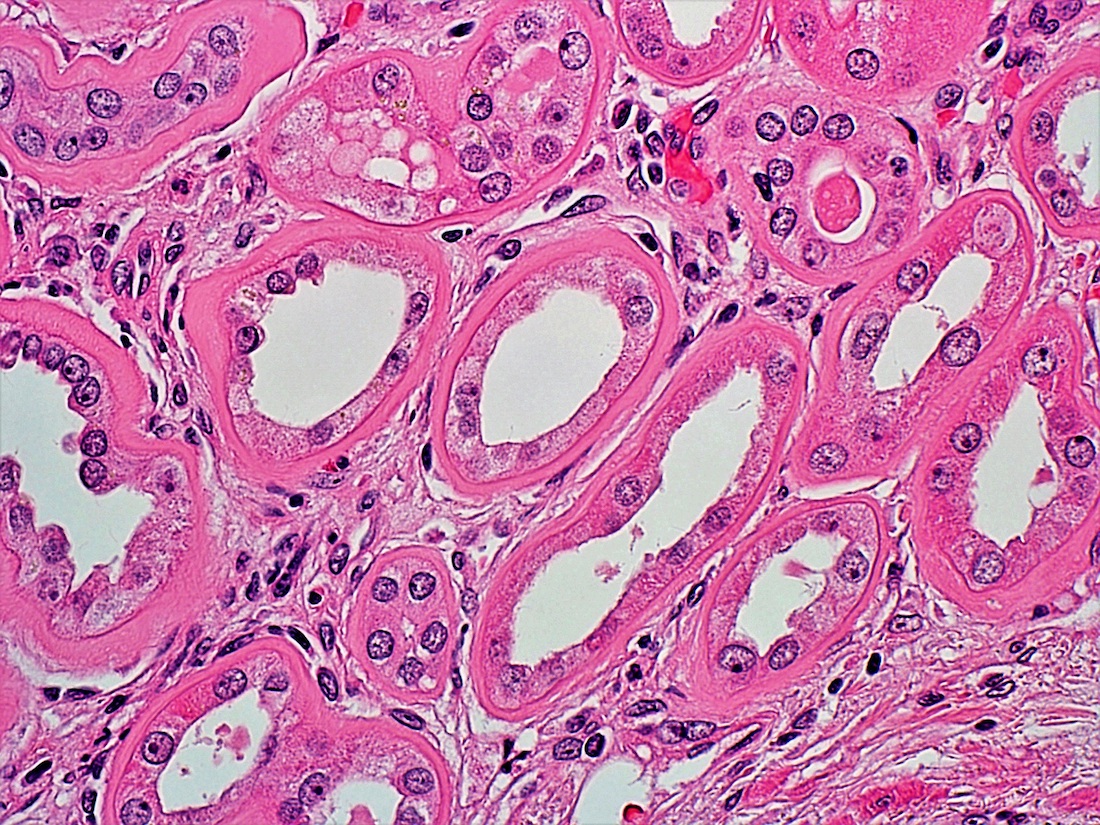
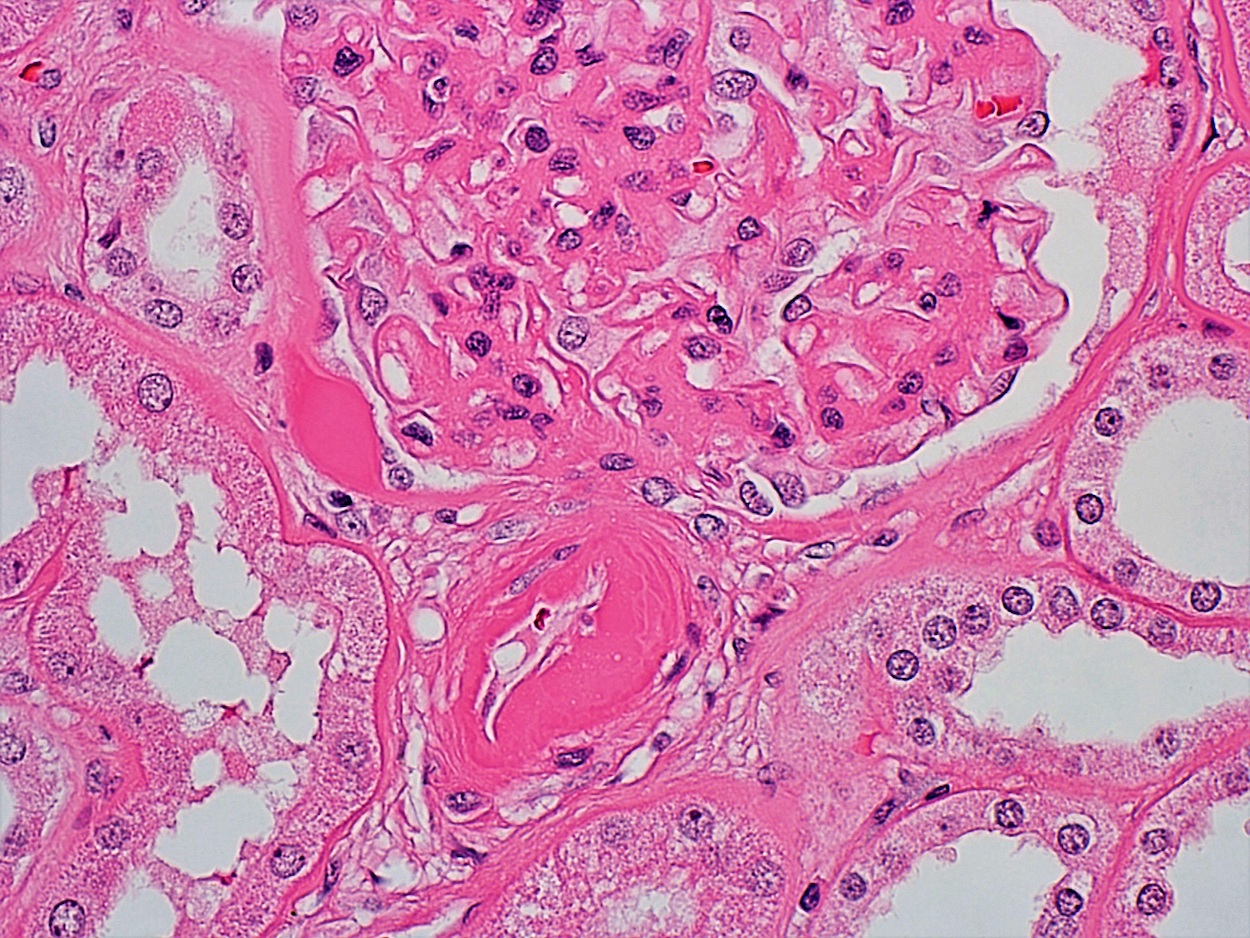
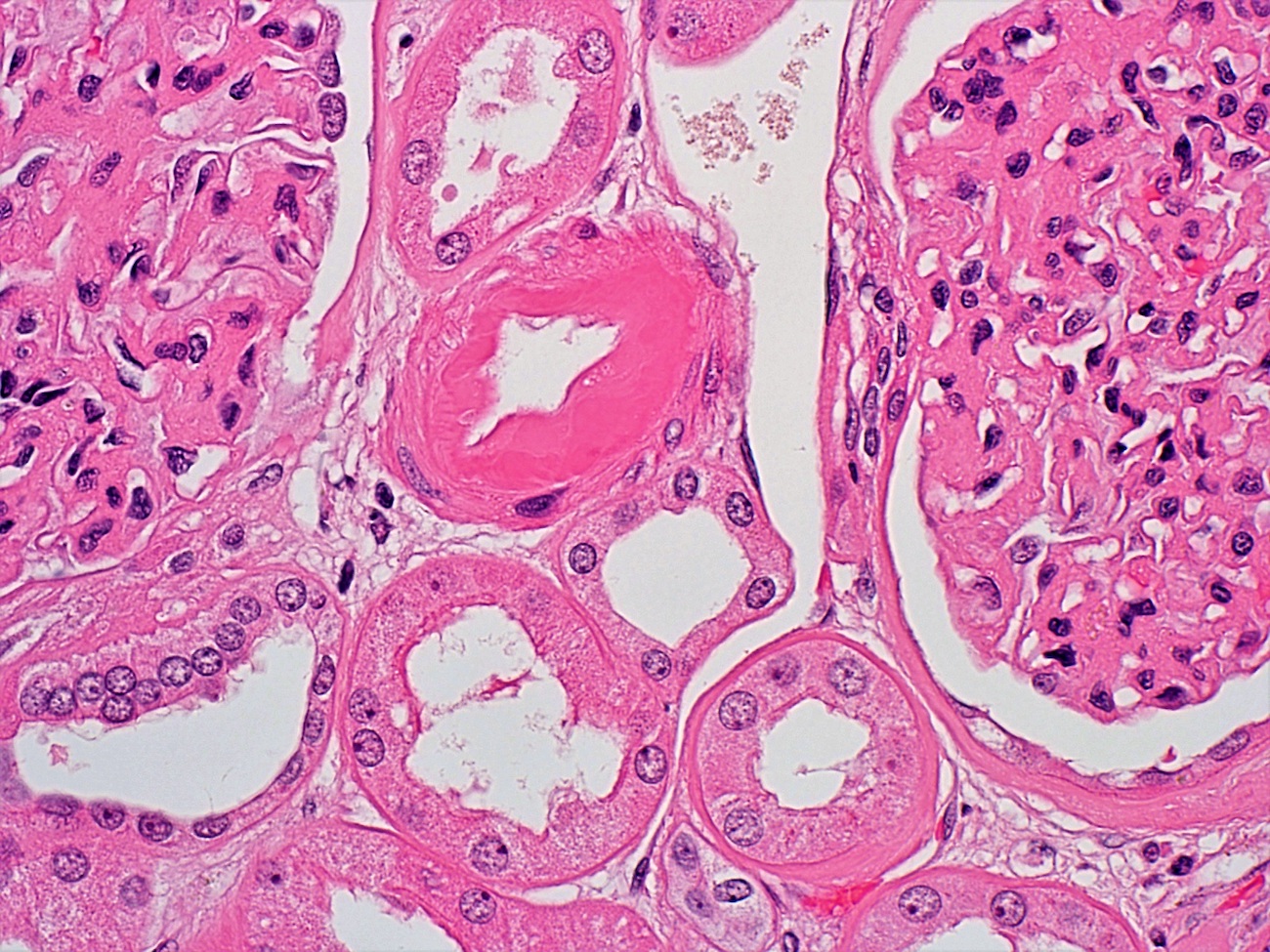
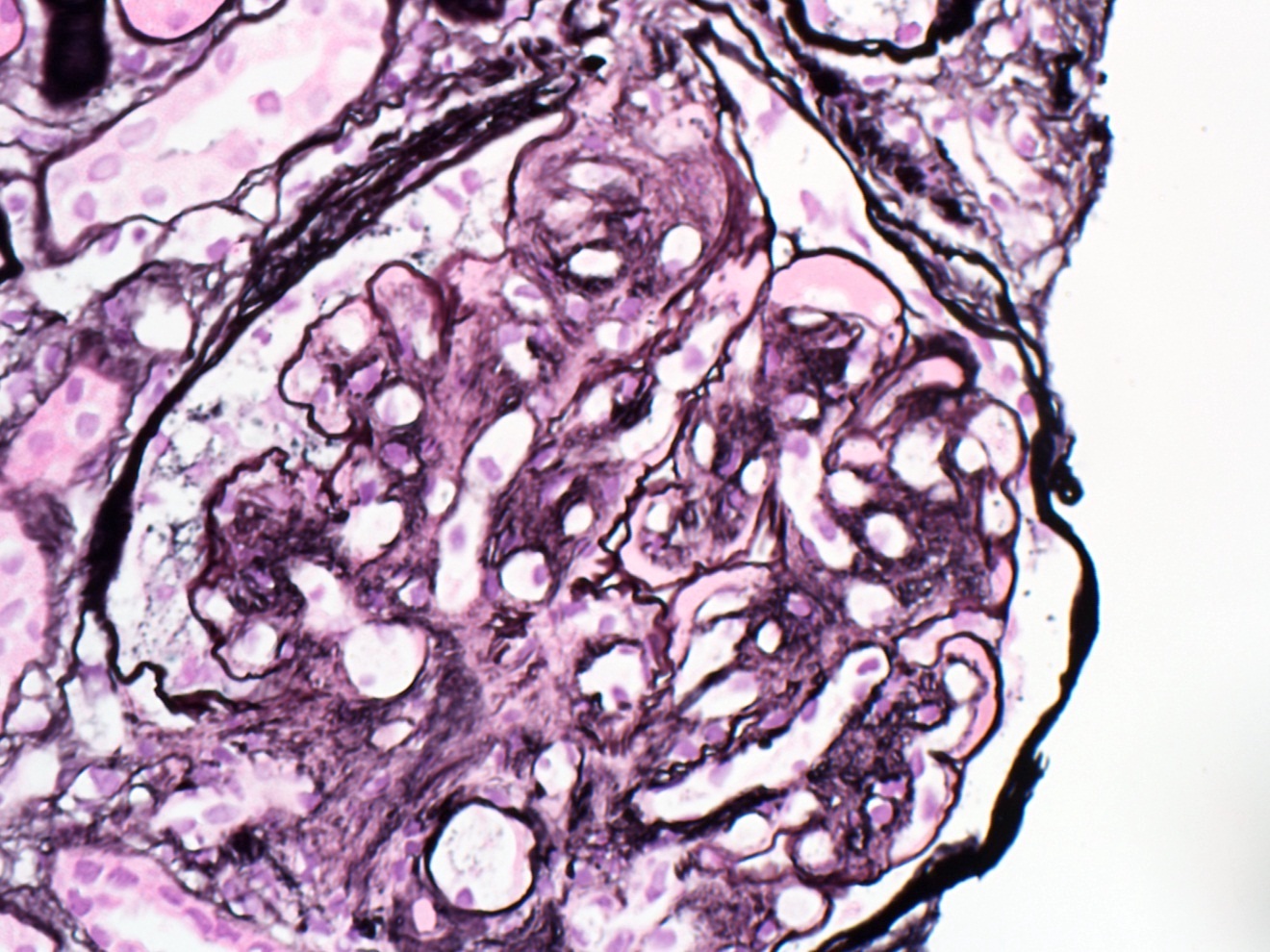
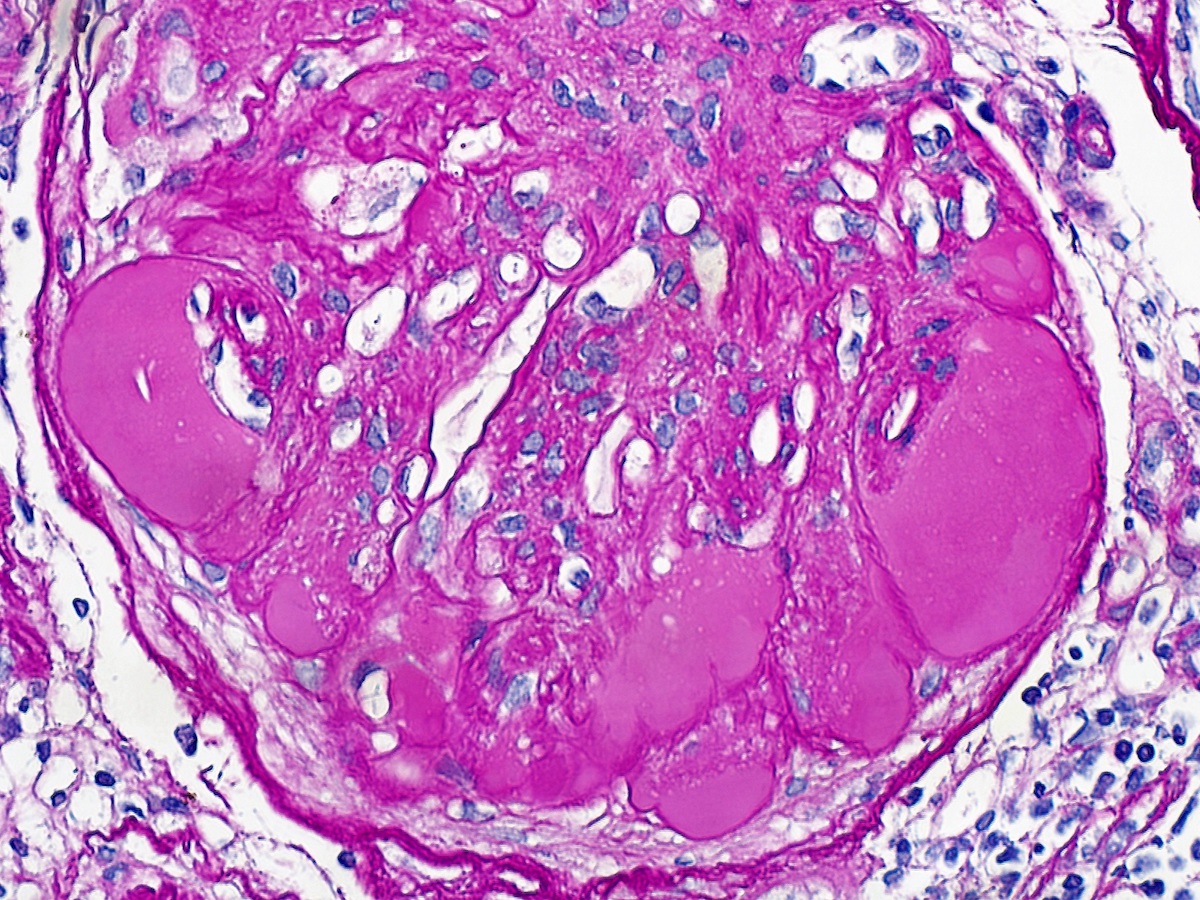
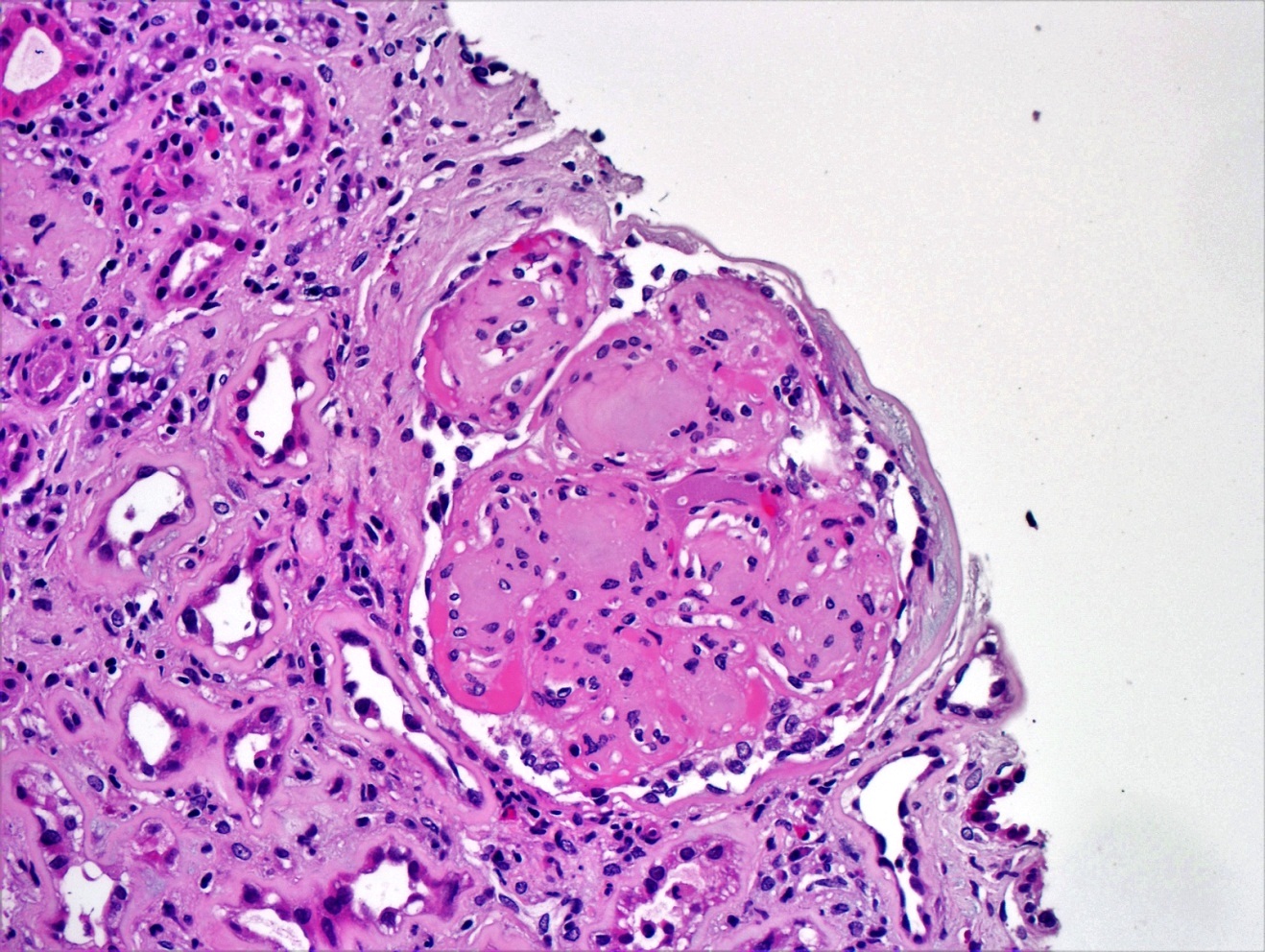
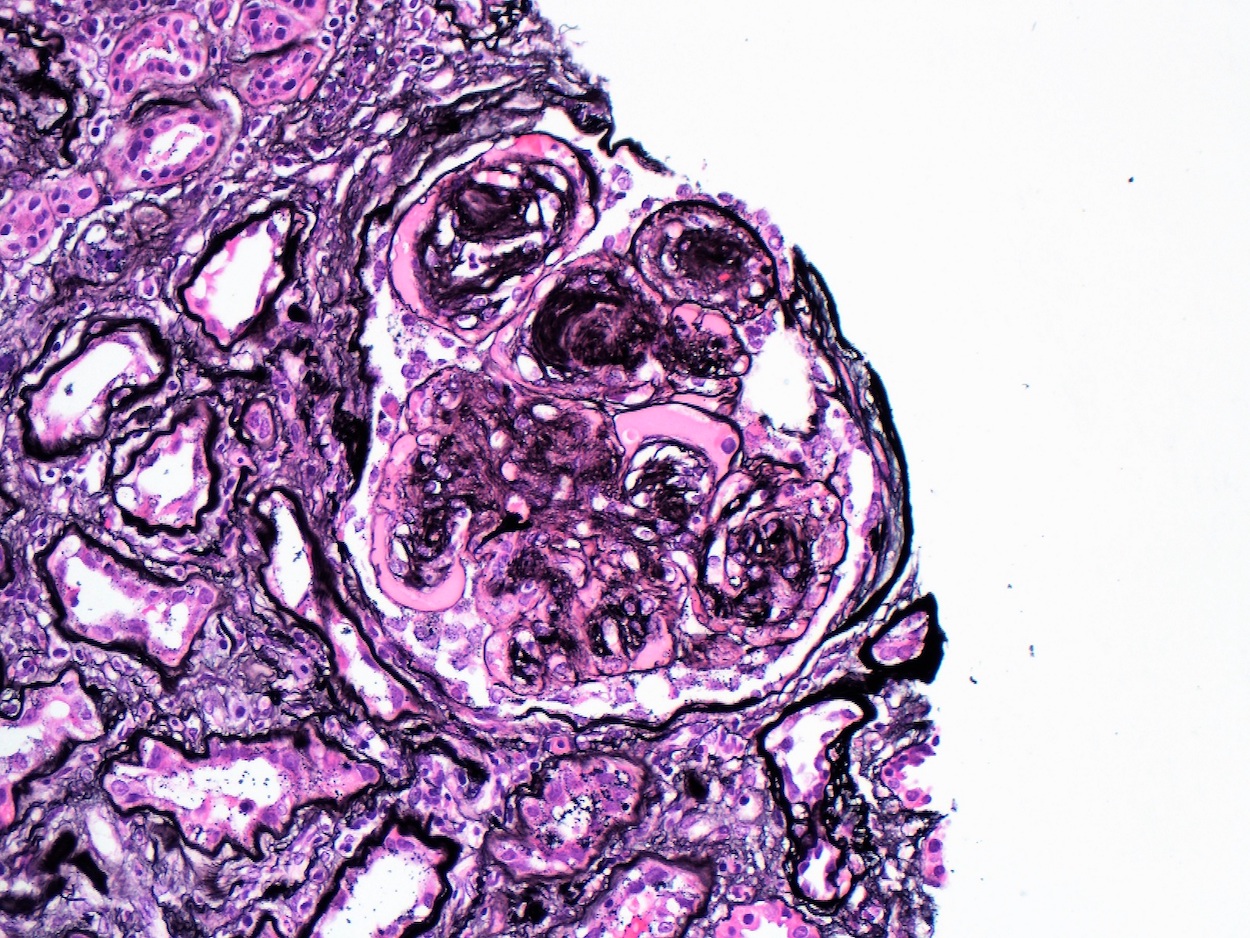
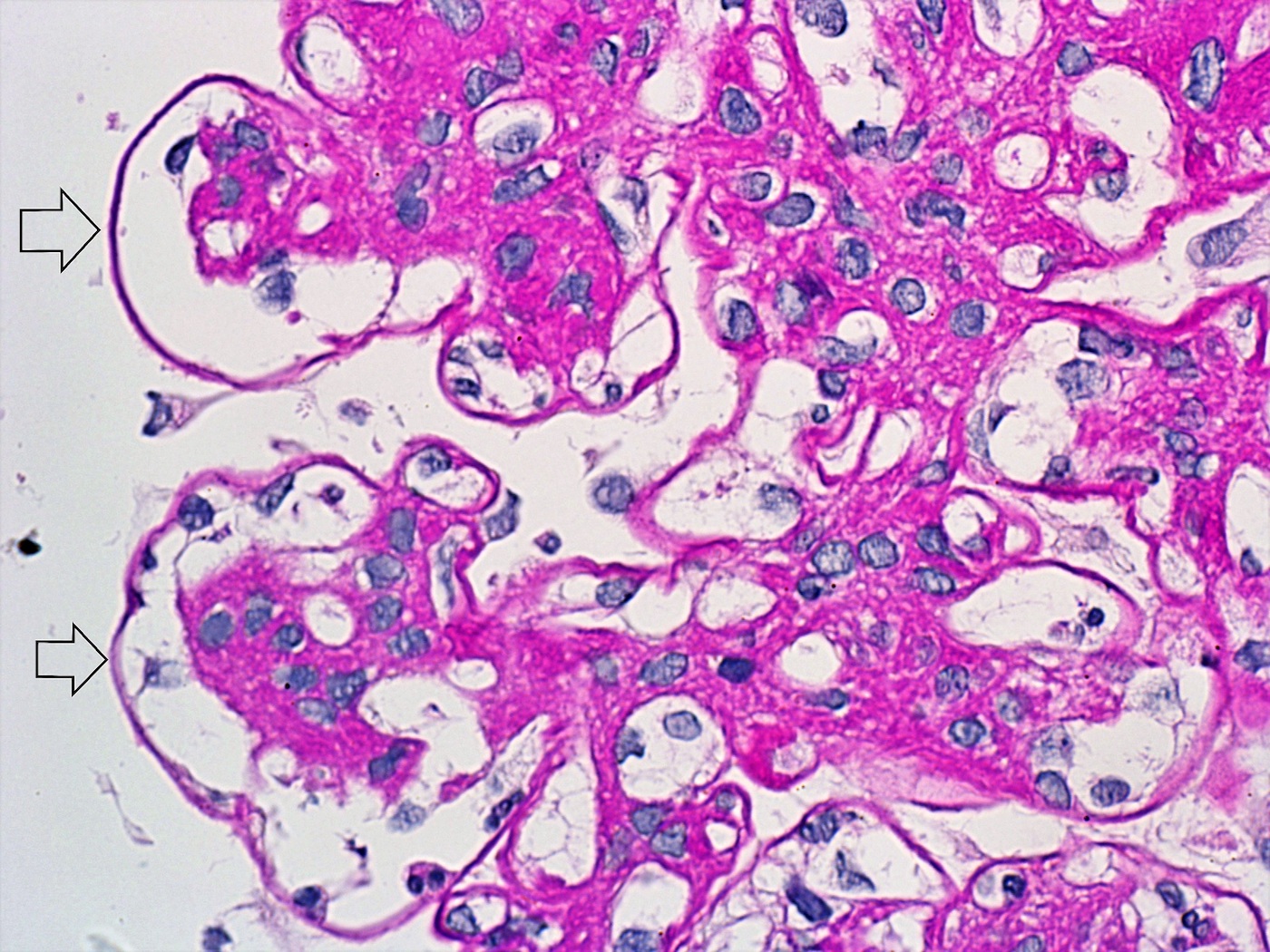
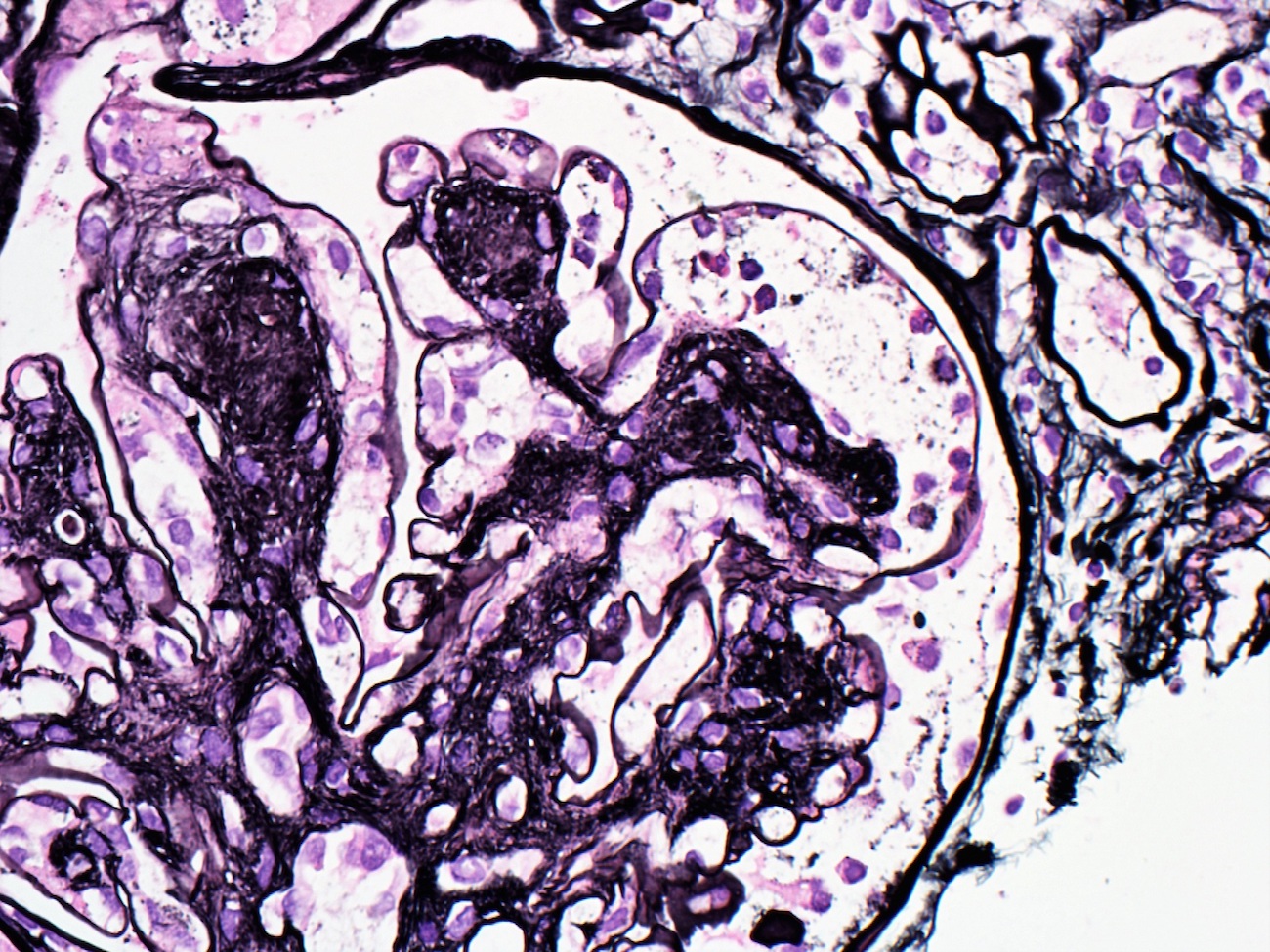
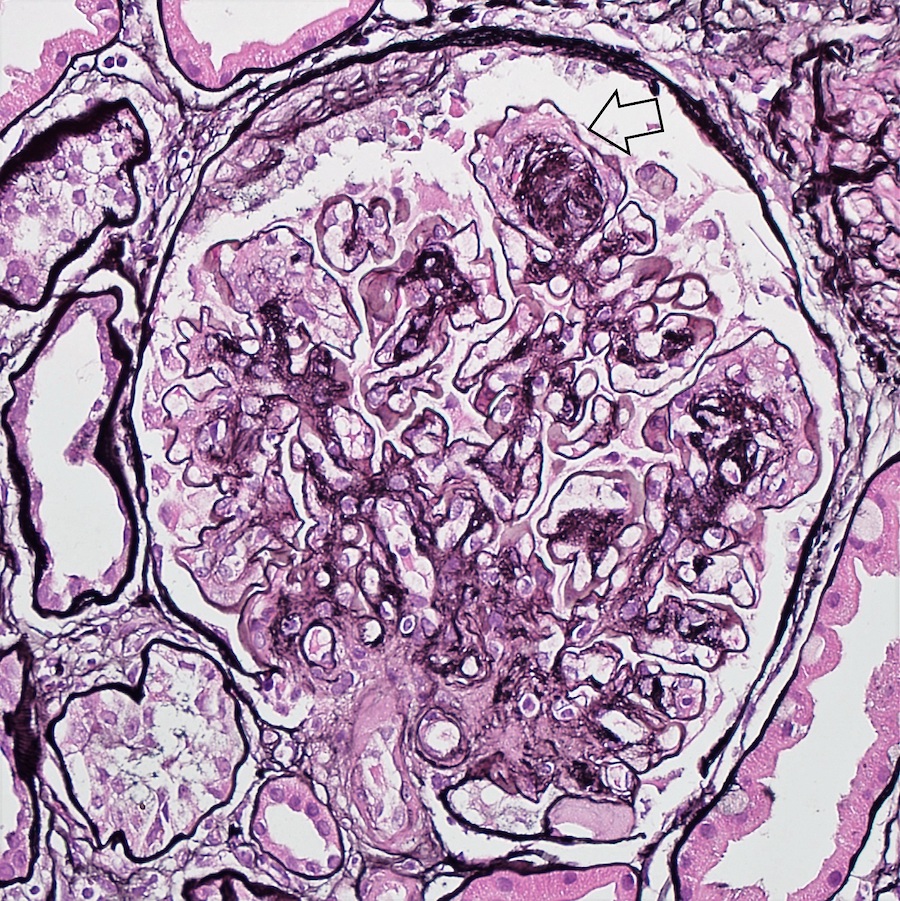
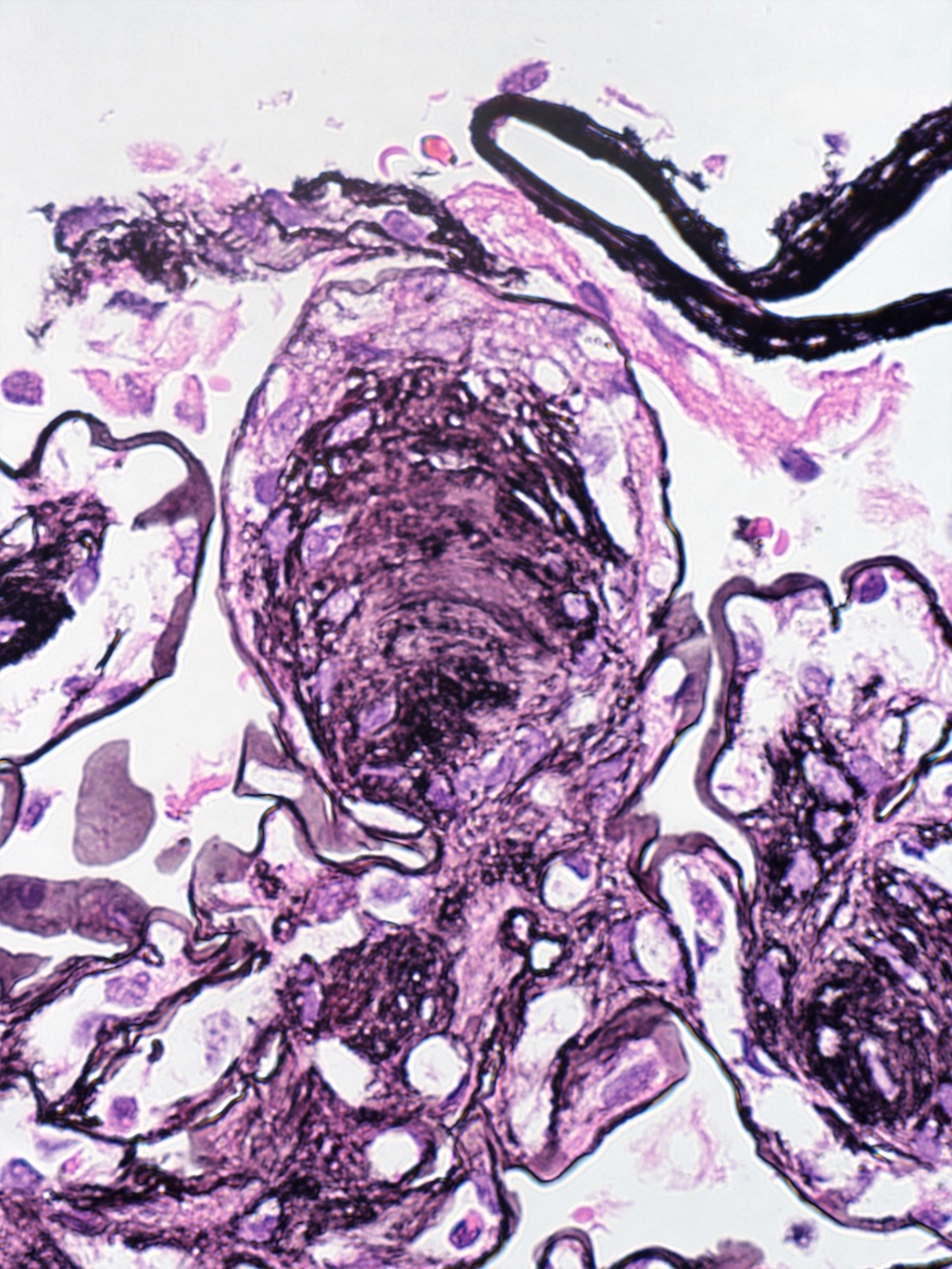
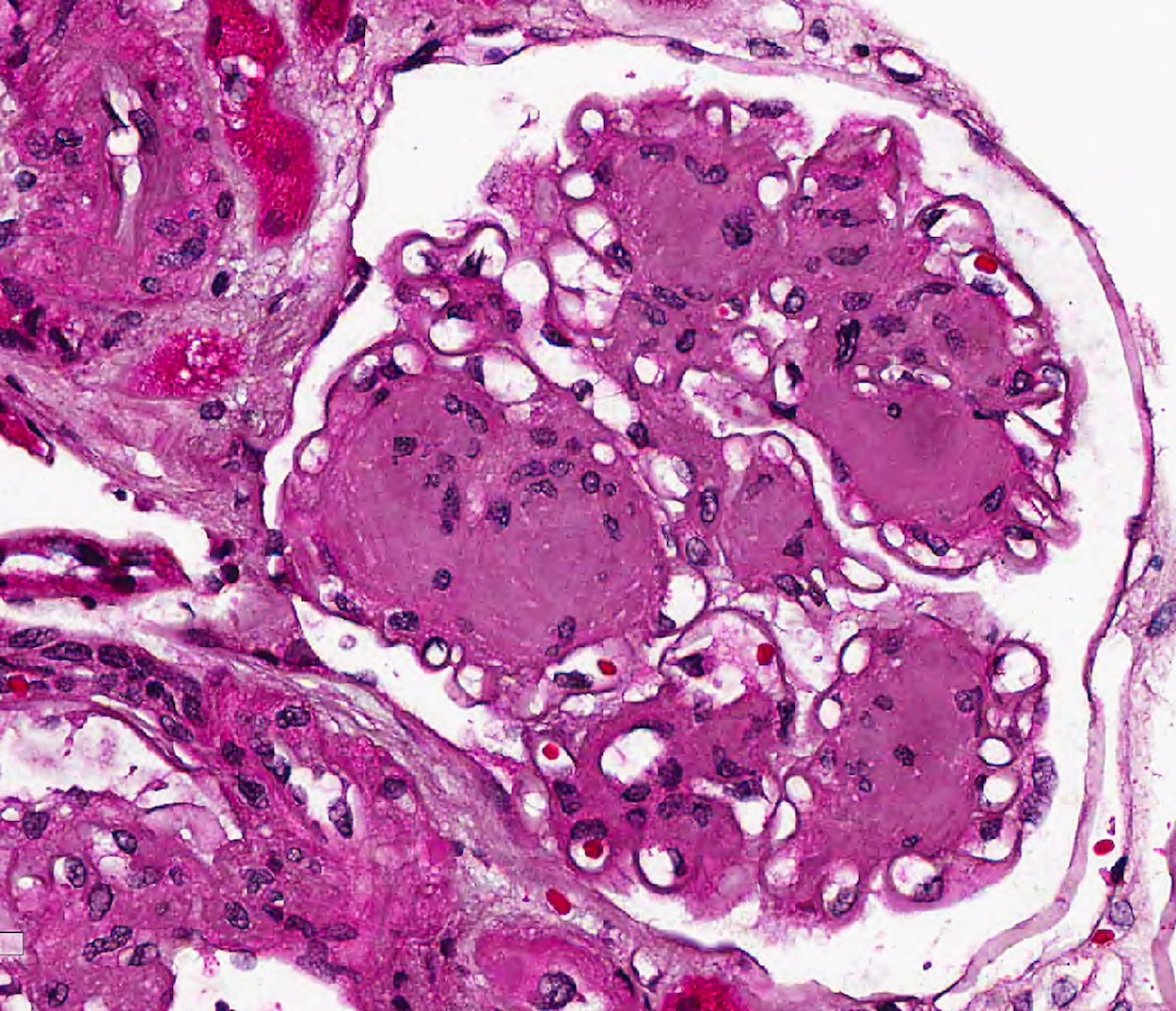
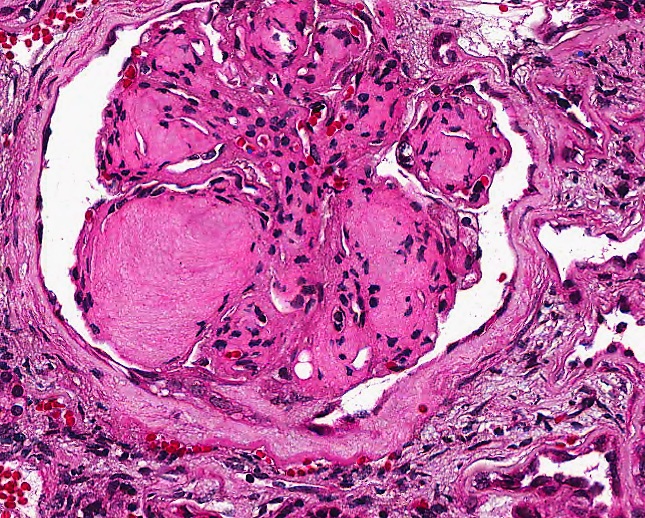
Microscopic (histologic) description
- Diffuse uniform thickening of glomerular basement membrane (GBM)
- Matrix expansion encroaching on the capillary lumina may be diffuse, nodular or both
- Nodular lesions are also called Kimmelsteil-Wilson lesions (Contrib Nephrol 2011;170:36)
- Microaneurysms of glomerular capillaries develop due to mesangiolysis
- These later give rise to large solitary nodules, which may reveal a laminated architecture on Jones silver stain
- Vascular hyalinosis is a common finding
- Hyalinosis of afferent and efferent arterioles usually seen but rare in other diseases
- Large subendothelial lipohyaline deposits may be present at the periphery of the glomerular tuft (hyaline caps)
- Similar deposits along the Bowman capsule capsular drops, which are specific
- In later stages, segmental glomerulosclerosis, especially at the tubular outlet tip lesion, is common
- Tubular atrophy, chronic interstitial inflammation and fibrosis, thickening of the tubular basement membranes
- Interstitial eosinophilic inflammatory cell infiltrate can sometimes be seen (Nephrol Dial Transplant 2015;30:1370)
- Papillary necrosis characterized by necrosis and sloughing off of renal papillae
- Renal Pathology Society histologic classification system for diabetic nephropathy proposed in 2010 (J Am Soc Nephrol 2010;21:556)
- Class I: mild or nonspecific changes on light microscopy and confirmed GBM thickening proven by electron microscopy
- > 395 nm in women and > 430 nm in men
- Class II: diffuse mesangial expansion
- IIa: mild mesangial expansion in > 25% of the observed mesangium
- Area of mesangial expansion < area of the capillary cavity
- IIb: severe mesangial expansion in > 25% of the observed mesangium
- Area of mesangial expansion > area of the capillary cavity
- IIa: mild mesangial expansion in > 25% of the observed mesangium
- Class III: nodular sclerosis (Kimmelstiel-Wilson lesions)
- At least 1 Kimmelstiel-Wilson lesion and none of the changes described in class IV, without > 50% globally sclerosed glomeruli on biopsy
- Class IV: advanced diabetic glomerulosclerosis
- > 50% globally sclerosed glomeruli on biopsy with clinical or pathologic evidence indicating that the sclerosis stems from diabetic nephropathy
- Class I: mild or nonspecific changes on light microscopy and confirmed GBM thickening proven by electron microscopy
Microscopic (histologic) images
Contributed by Khaled A. Murshed, M.D., Noheir M. Taha, M.B.B.Ch., M.D. and Mohammed Akhtar, M.D.
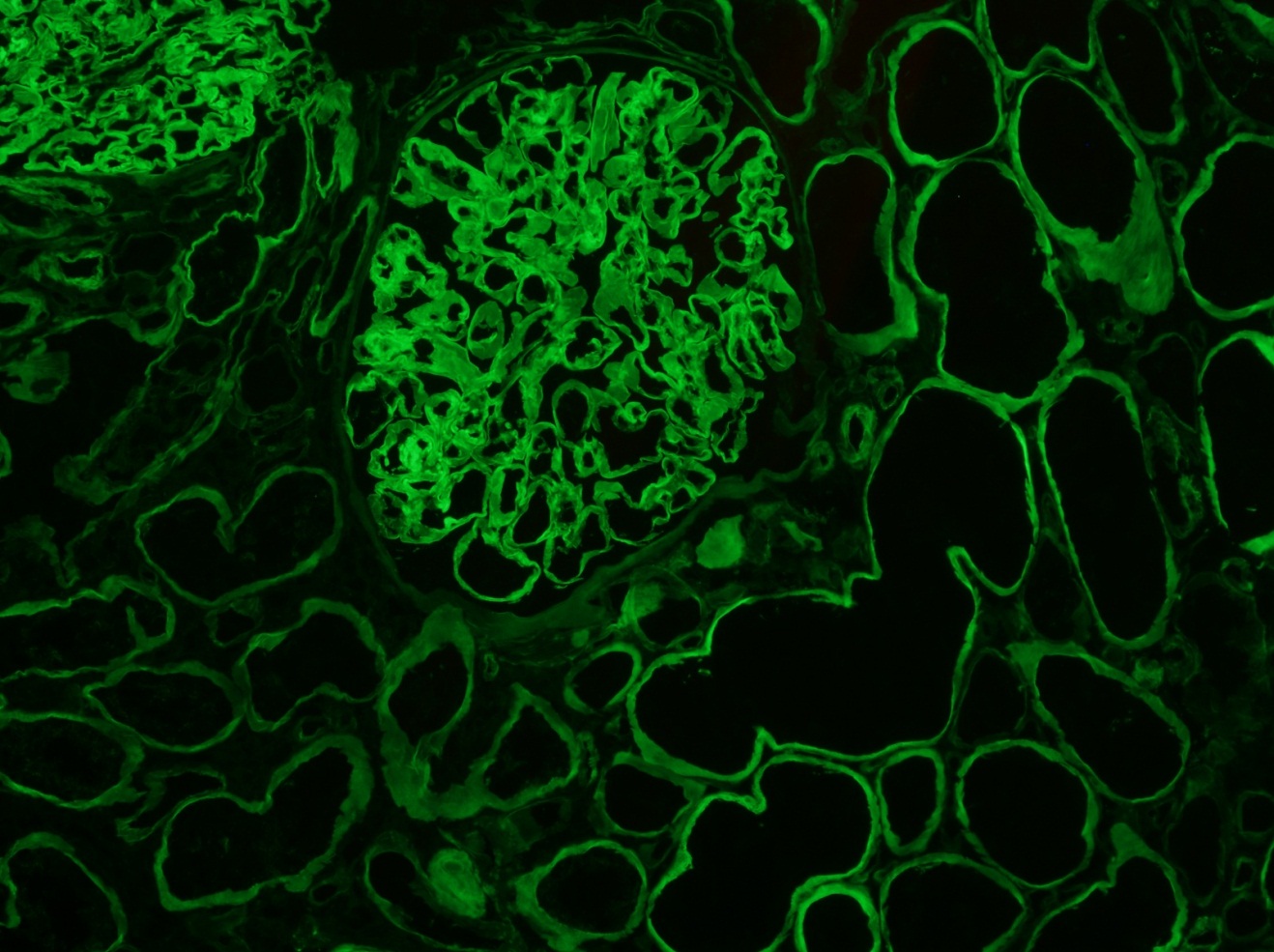
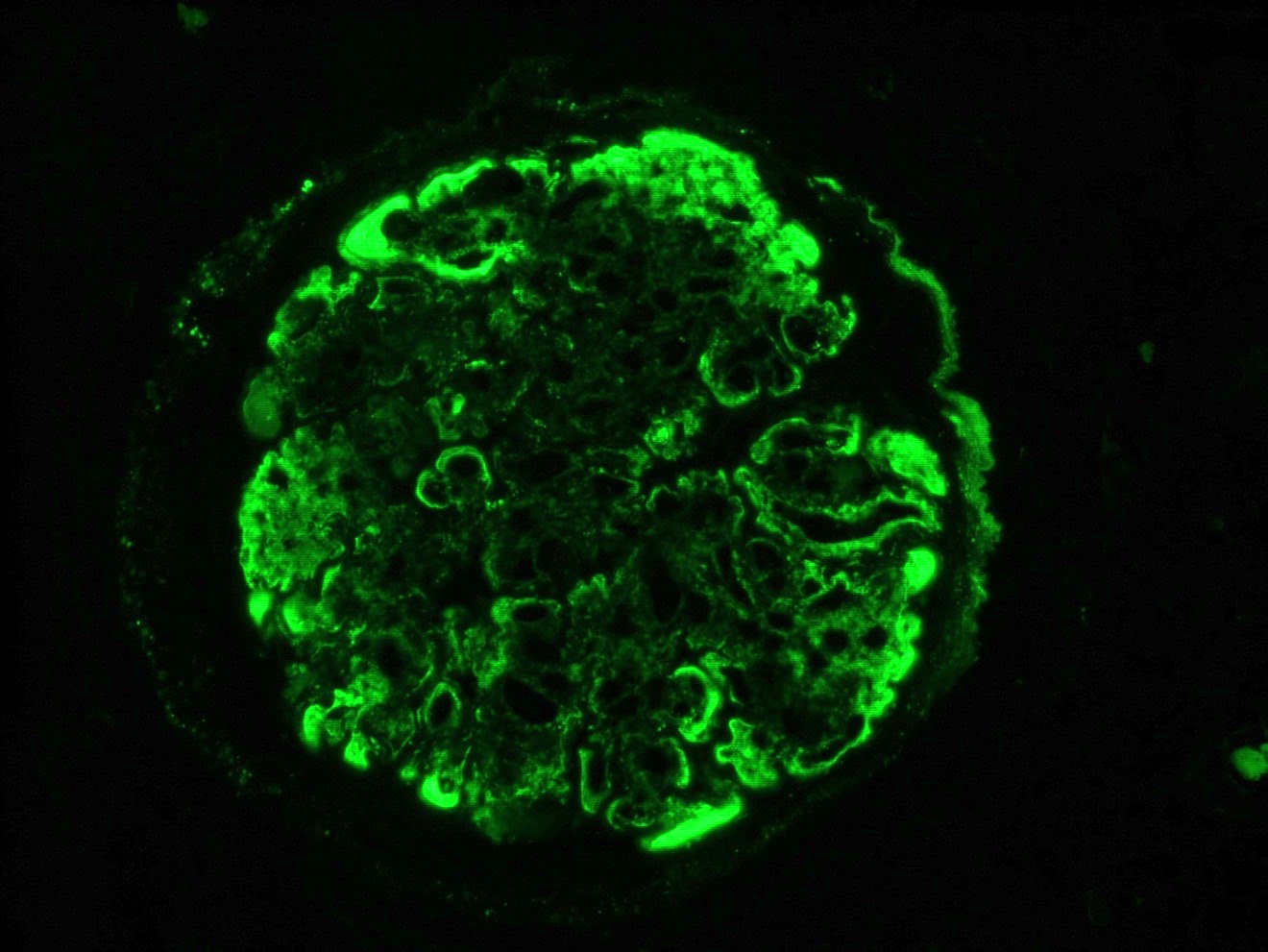
Immunofluorescence description
- Diffuse linear accentuation of the glomerular basement membrane (GBM) and tubular basement membrane (TBM) with IgG, kappa and lambda light chains and albumin
- 33% of cases may show similar staining for IgM and C3 with lesser intensity
- Faint staining of the mesangial areas and mesangial nodules may be seen
- Lipohyaline caps at the periphery of the glomerulus usually show positivity for IgM, C3 and C1q
- This should not be interpreted as indication of immune complex deposition (Contrib Nephrol 2011;170:36)
Immunofluorescence images
Positive stains
- Expanded mesangium is positive for periodic acid-Schiff (PAS), Jones methenamine silver, trichrome
Negative stains
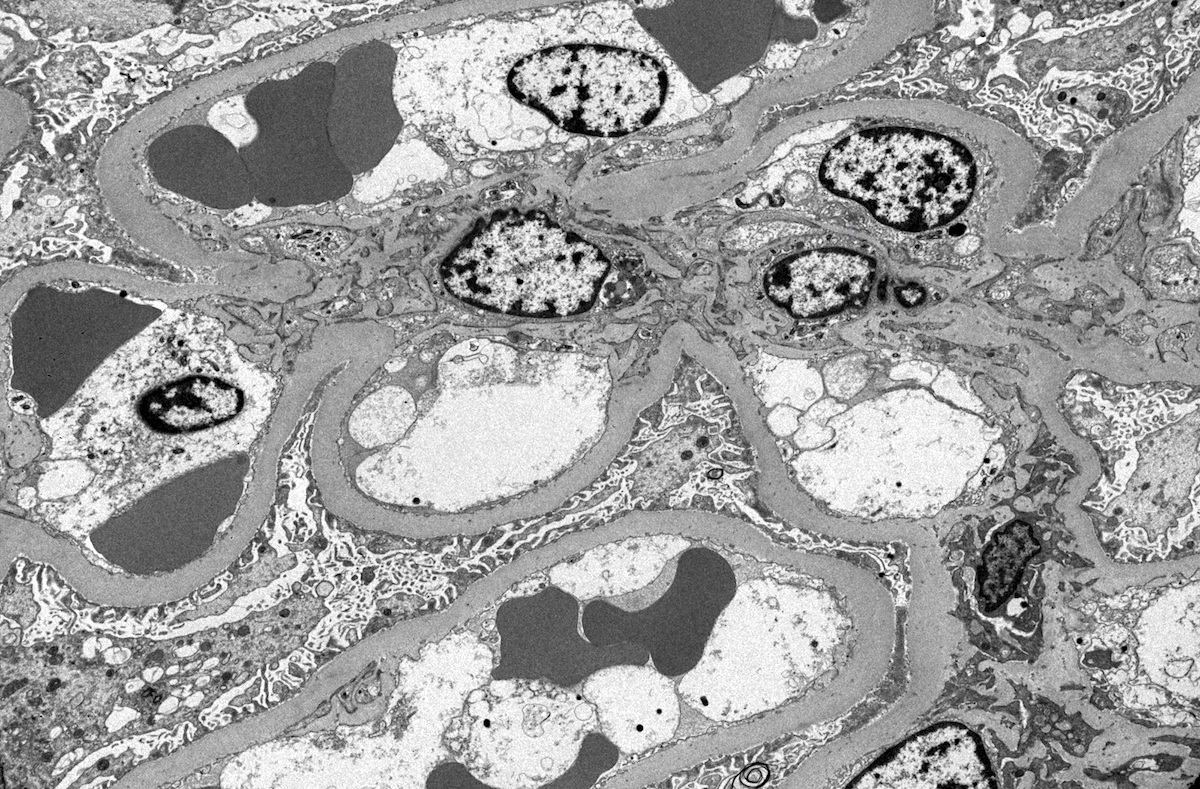
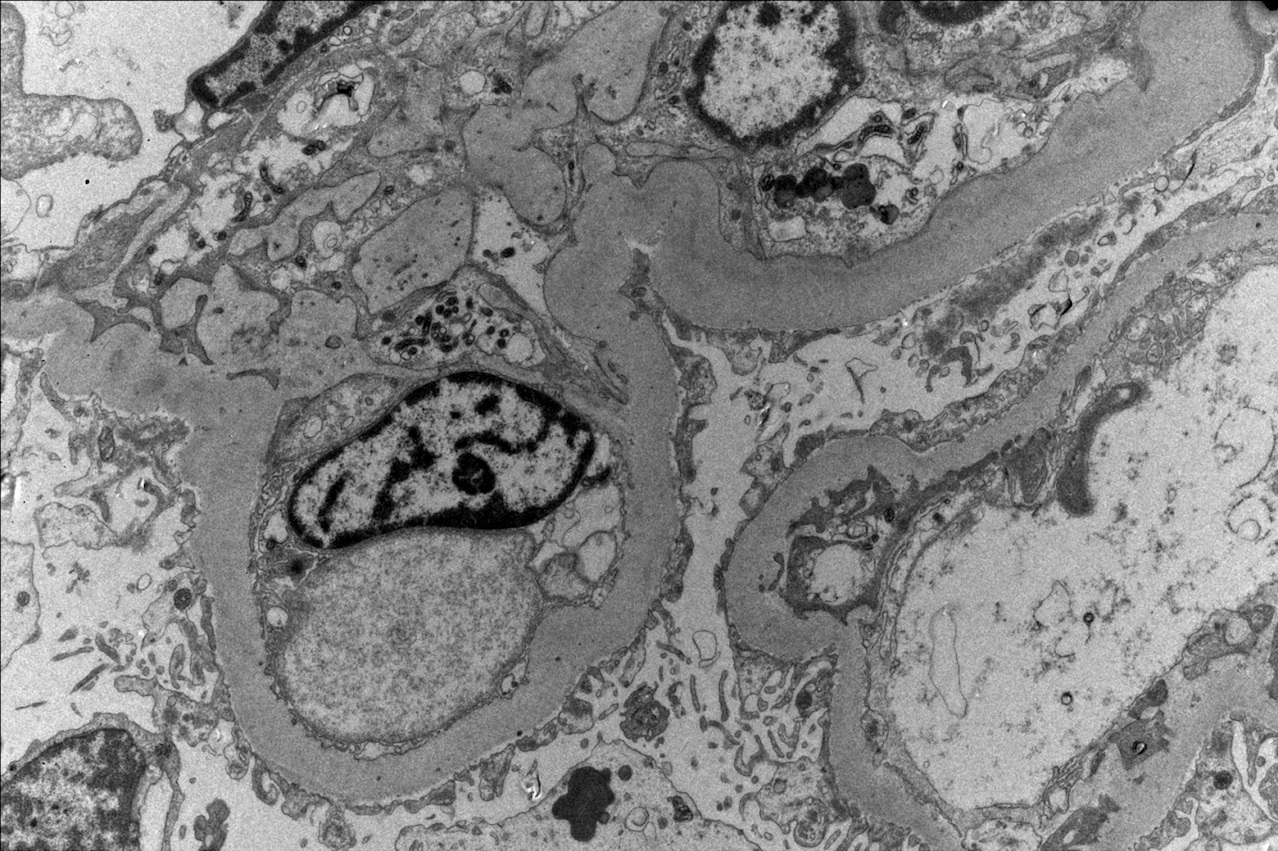
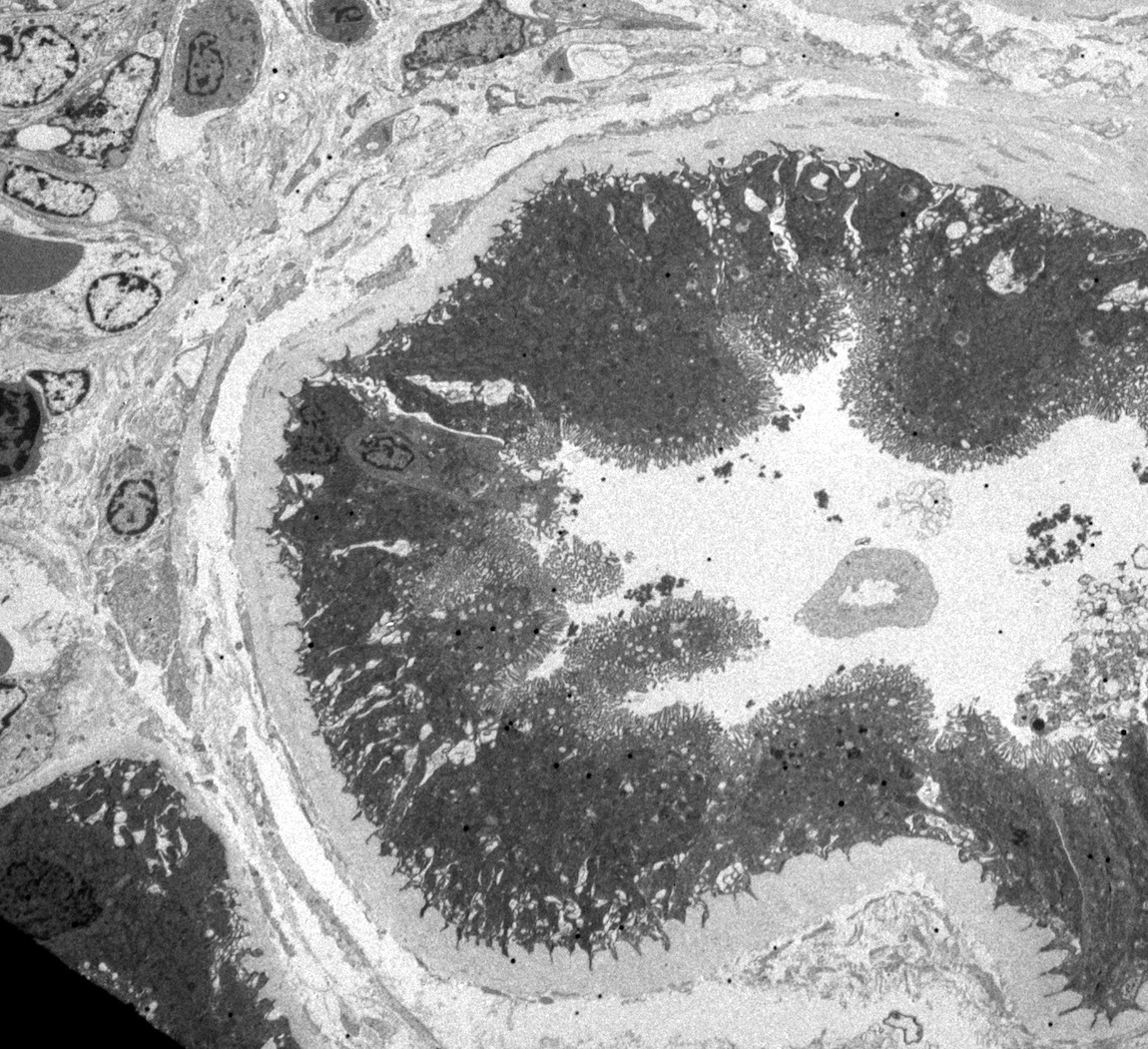
Electron microscopy description
- Diffuse thickening of the glomerular basement membrane is the earliest structural change demonstrable in almost all diabetic patients, with or without nephropathy (Contrib Nephrol 2011;170:36)
- Mesangial regions are expanded due to increased mesangial matrix limiting the capillary luminal space
- No immune complex deposits
- Variable foot process effacement and podocyte loss
Electron microscopy images
Videos
Diabetic nephropathy
Sample pathology report
- Left kidney, ultrasound guided needle biopsy:
- Diabetic kidney disease, diffuse and nodular type (class III) (see comment)
- Global glomerulosclerosis (6/15), focal segmental glomerulosclerosis (1/15)
- Tubular atrophy and interstitial fibrosis, moderate
- Hyaline arteriolosclerosis, moderate to severe
- Comment: Biopsy reveals changes of moderately advanced diabetic kidney disease. There is no evidence of any superimposed immune complex mediated glomerulonephritis. The proteinuria in this patient is probably due to the diabetic kidney disease complicated by secondary focal and segmental glomerulosclerosis (FSGS). Clinicopathologic correlation is suggested.
Differential diagnosis
- Renal amyloidosis:
- Mesangial nodules are Congo red positive with apple green birefringence under polarized light (Adv Anat Pathol 2020;27:87)
- IgA nephropathy:
- IgA dominant immunofluorescent pattern
- Renal monoclonal immunoglobulin light chain deposition disease or monoclonal immunoglobulin heavy chain deposition disease:
- Immunofluorescence reveals diffuse linear staining of the glomerular basement membrane with monoclonal immunoglobulin light or heavy chains
- Electron microscopy shows a continuous band of electron dense granular powdery deposits within the mesangial nodules, subendothelial space and along external side of the tubular basement membranes
- Membranoproliferative glomerulonephritis (MPGN):
- Marked endocapillary proliferation with double contouring of the peripheral capillary loops identified on PAS and Jones methenamine silver stains
- Immunofluorescence shows diffuse granular glomerular capillary loop and mesangial deposition of C3 with variable immunoglobulin deposition
- Electron microscopy shows mesangial and subendothelial electron dense deposits
- Dense deposit disease:
- Light microscopic features may resemble MPGN, immunofluorescence reveals deposition of C3 only
- Ultrastructurally characterized by large intramembranous nonimmune complex type electron dense deposits
- Fibrillar glomerulonephritis:
- Deposition of usually polyclonal IgG by immunofluorescence, corresponding haphazardly arranged fibrils measuring 12 - 24 nm diameter by electron microscopy and DNAJB9 positivity by immunohistochemistry
- Immunotactoid glomerulonephritis:
- Deposition of usually monotypic IgG by immunofluorescence and corresponding haphazard to parallel arranged fibrils with hollow core measuring ≥ 30 nm diameter by electron microscopy
- Fibronectin glomerulopathy:
- Glomerular nodules are PAS positive but silver and Congo red stains are negative
- Electron microscopy shows electron dense deposits in the mesangium that are finely granular or have a fibrillary substructure with randomly arranged 12 - 16 nm fibrils
- Diagnosis confirmed by intense immunohistochemical staining for fibronectin in the mesangium and along the glomerular capillaries
Board review style question #1
A 57 year old woman was found to have proteinuria. A renal biopsy showed the findings in the image above (PAS). Which of the following conditions is the most important differential diagnosis?
- Lupus nephritis
- Membranous glomerulonephritis
- Minimal change disease
- Postinfectious glomerulonephritis
- Renal amyloidosis
Board review style answer #1
E. Renal amyloidosis. The image shows diabetic kidney disease. In renal amyloidosis, mesangial nodules similar to those seen in diabetic kidney disease can occur. Answer A is incorrect because although lupus nephritis can have a wide morphological spectrum, mesangial nodules are very uncommon. Answer B is incorrect because in membranous glomerulonephritis, there will be mainly thickening of glomerular basement membranes. Answer C is incorrect because in minimal change disease, mesangial nodules do not occur. Answer D is incorrect because the main histologic change in postinfectious glomerulonephritis is endocapillary hypercellularity.
Comment Here
Reference: Diabetic kidney disease
Comment Here
Reference: Diabetic kidney disease
Board review style question #2
On immunofluorescent microscopy, what is the usual finding in diabetic kidney disease?
- Diffuse coarse granular staining of C3 along the glomerular capillaries and mesangium
- Diffuse coarse granular staining of IgG along the glomerular capillaries
- Diffuse mesangial staining for IgA
- Dull linear staining of glomerular and tubular basement membranes for IgG
- Immunofluorescent microscopy is typically negative
Board review style answer #2
D. Dull linear staining of glomerular and tubular basement membranes for IgG.
In diabetic kidney disease, there will usually be linear staining along glomerular and tubular basement membranes of IgG. Answer C is incorrect because mesangial staining for IgA is seen in IgA nephropathy. Answer A is incorrect because coarse granular mesangial and capillary staining of C3 is seen in C3 glomerulonephritis. Answer B is incorrect because granular staining of IgG along the capillary walls is seen in membranous glomerulonephritis. Answer E is incorrect because immunofluorescence studies are negative in minimal change disease.
Comment Here
Reference: Diabetic kidney disease
Comment Here
Reference: Diabetic kidney disease
Board review style question #3
In a patient suspected to have diabetic kidney disease, what is the earliest structural change in a kidney biopsy recognized by electron microscopy?
- Deposits of randomly oriented nonbranching fibrils in the mesangium
- Diffuse effacement of podocyte foot processes
- Diffuse thickening of the glomerular basement membrane
- Electron dense subepithelial deposits
- Expansion of the mesangial regions
Board review style answer #3
C. Diffuse thickening of the glomerular basement membrane.
In patients with diabetic kidney disease, the earliest ultrastructural change seen is thickening of glomerular basement membrane, which precedes other morphological changes. Answer A is incorrect because deposits of nonbranching fibrils are seen in amyloidosis. Answer B is incorrect because effacement of podocyte foot processes is seen in minimal change disease and focal and segmental glomerulosclerosis. Answer D is incorrect because electron dense subepithelial deposits are seen in membranous glomerulonephritis. Answer E is incorrect because although expansion of mesangial region occurs in diabetic kidney disease, it develops later.
Comment Here
Reference: Diabetic kidney disease
Comment Here
Reference: Diabetic kidney disease