Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Immunofluorescence description | Immunofluorescence images | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Larqué A. Pauci-immune complex crescentic glomerulonephritis / ANCA associated vasculitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyANCArelatedgngen.html. Accessed November 26th, 2024.
Definition / general
- Pauci-immune necrotizing crescentic glomerulonephritis related to or caused by antineutrophil cytoplasmic antibody (ANCA)
Essential features
- Pauci-immune necrotizing crescentic glomerulonephritis (renal biopsy: gold standard)
- Rapidly progressive glomerulonephritis with hematuria and proteinuria
- Small vessel necrotizing vasculitis associated with ANCAs that can be renal limited or with systemic vasculitis: granulomatous with polyangiitis, microscopic polyangiitis, eosinophlic granulomatous with polyangiitis or renal limited vasculitis (J Am Soc Nephrol 2010;21:1628)
Terminology
- Pauci-immune glomerulonephritis
- Pauci-immune crescentic glomerulonephritis
- ANCA associated vasculitis
ICD coding
- ICD10: NO1.7 - rapidly progressive nephritic syndrome with diffuse crescentic glomerulonephritis
Epidemiology
- By far the most common cause of rapidly progressive glomerulonephritis in adults (Kidney Int 2003;63:1164)
- 80% of pauci-immune crescentic glomerulonephritis is associated with ANCA (Kidney Int 2003;63:1164)
- Crescentic glomerulonephritis occurs in 75 - 80% of patients with granulomatosis with polyangiitis, 80 - 100% of microscopic polyangiitis and 25 - 40% of eosinophilic granulomatosis with polyangiitis (Semin Arthritis Rheum 2005;35:95, Clin Rheumatol 2017;36:1949)
- Age: > 60 years (53%); 21 - 60 years (39%); < 20 years (8%) (Kidney Int 2003;63:1164)
- No gender predilection
- Geographic variation of antimyeloperoxidase and proteinase 3 (PR3) ANCA (Mod Rheumatol 2010;20:54)
Sites
- Kidney glomeruli
Pathophysiology
- ANCA is a primary pathogenic factor, mainly by augmenting leukocyte endothelial interactions (Mod Rheumatol 2010;20:54)
- In vitro evidence:
- ANCA IgG can activate cytokine primed neutrophils by interacting with myeloperoxidase (MPO) or PR3 at the surface of the cells
- Endothelial injury by ANCA activated neutrophils and disruption of glomerular capillary walls
- Alternative complement pathway activation by ANCA activated neutrophils (Nat Rev Rheumatol 2014;10:463)
Etiology
- Trigger for ANCA production generally unknown
- Presumed immune dysregulation (Th17 / Treg) (Eur J Immunol 2017;47:724)
- Microbial factors and molecular mimicry (J Immunol Res 2015;2015:858027, Nat Med 2008;14:1088)
- Can be precipitated by drugs: propylthiouracil, hydralazine, minocycline, levamisole adulterated cocaine (Curr Opin Rheumatol 2014;26:42, Curr Opin Rheumatol 2013;25:50)
- Suggested risk factors
- Distinct HLA class II associations for MPO and PR3 ANCA (Am J Kidney Dis 2013;62:1176)
- Leptin receptor gene (LEPR) polymorphism (Rheumatology (Oxford) 2010;49:907)
- CTLA4 and PTPN22 (single nucleotide polymorphisms) (BMC Med Genet 2009;10:121)
- Epigenetic control of MPO and PR3 expression, both neutrophil cytoplasmic enzymes (J Clin Invest 2010;120:3209, Presse Med 2015;44:e223)
Clinical features
- Rapid deterioration of renal function
- Oliguria, hematuria and proteinuria (usually nonnephrotic range)
- Flu-like syndrome common at onset (fever, arthralgia, myalgia)
- Signs of extrarenal vasculitis in ~ 75% (Mod Rheumatol 2010;20:54, Semin Arthritis Rheum 2005;35:95)
- Microscopic polyangiitis: renal involvement (90%), lung usually affected, also skin, ear, nose, throat, musculoskeletal, nervous system, gastrointestinal
- Granulomatosis with polyangiitis: kidney, upper airway and lung involvement in 90% of cases
- Eosinophilic granulomatosis with polyangiitis: four phases - allergic, eosinophilic, vasculitic, postvasculitic (Colvin: Diagnostic Pathology - Kidney Diseases, 2nd Edition, 2015)
Diagnosis
- Rapidly progressive glomerulonephritis clinically
- Pauci-immune crescentic glomerulonephritis pathologically
- Positivity for ANCA (Clin Rheumatol 2017;36:1949)
- Extrarenal clinical manifestations in systemic vasculitis
Laboratory
- Positive ANCA test by indirect immunofluorescence plus enzyme linked immunosorbent assays in serum
- Sensitivity of 80% and specificity of 96% for pauci-immune glomerulonephritis
- Negative ANCA in ~ 20% of pauci-immune glomerulonephritis
- Type of ANCA does not permit specific diagnosis
- MPO ANCA most common in pauci-immune glomerulonephritis, microscopic polyangiitis and eosinophilic granulomatosis with polyangiitis (50 - 60%)
- PR3 ANCA most common in granulomatosis with polyangiitis (~ 75%)
- Other (atypical) ANCA specificities described
- React with lactoferrin, elastase and P-cathepsin-G in serum
- Found in variety of conditions with chronic inflammation or infection
- Negative ANCA associated with absence of disease activity
- Normal complement levels in serum
- Peripheral eosinophilia in 10 - 20% of microscopic polyangiitis
- References: Kidney Int 2000;57:846, Clin Rev Allergy Immunol 2013;45:109
Prognostic factors
- ~ 75% achieve remission
- ~ 30% relapse, frequently with PR3 ANCA
- 60 - 75% 5 year patient and kidney survival
- Risk factors for early death
- Higher serum creatinine or dialysis dependence at onset
- Female gender
- Age > 65 years (J Am Soc Nephrol 2006;17:1224, Clin Exp Rheumatol 2004;22:S94, J Am Soc Nephrol 2010;21:1628)
- Pathological prognostic features
- Number of normal glomeruli (strong predictor of renal function)
- Active lesions are associated with renal recovery: active glomerular necrosis and crescents, higher in granulomatosis with polyangiitis
- Chronic lesions are associated with poor renal prognosis: glomerulosclerosis higher in microscopic polyangiitis or MPO ANCA than in granulomatosis with polyangiitis or PR3 ANCA patients (Clin Rheumatol 2017;36:1949, Nephrol Dial Transplant 2005;20:96)
Case reports
- 19 year old woman with PR3 vasculitis presenting with symptomatic renal wedge infarction (BMC Nephrol 2019;20:84)
- 55 year old man with MPO ANCA associated necrotizing glomerulonephritis in rheumatoid arthritis (J Nephropathol 2017;6:58)
- 59 year old man with myeloperoxidase ANCA negative microscopic polyangiitis with pulmonary hemorrhage and IgA nephropathy (Case Rep Dermatol 2011;3:22)
- 66 year old woman with de novo ANCA associated vasculitis after renal transplantation (BMC Nephrol 2018;19:270)
- 67 year old woman with giant cell arteritis and granulomatosis with polyangiitis (Am J Case Rep 2018;19:651)
- 78 year old woman with ANCA associated necrotizing glomerulonephritis overlapping with mesangial proliferative lupus nephritis (Case Rep Rheumatol 2018;2018:3076806)
Treatment
- Cyclophosphamide and prednisolone to induce remission
- Maintenance therapy with less toxic drugs such as mycophenolate mofetil, azathioprine
- Plasmapheresis or plasma exchange in refractory cases
- Rituximab (anti-CD20) for induction or relapses (Nat Rev Rheumatol 2014;10:484)
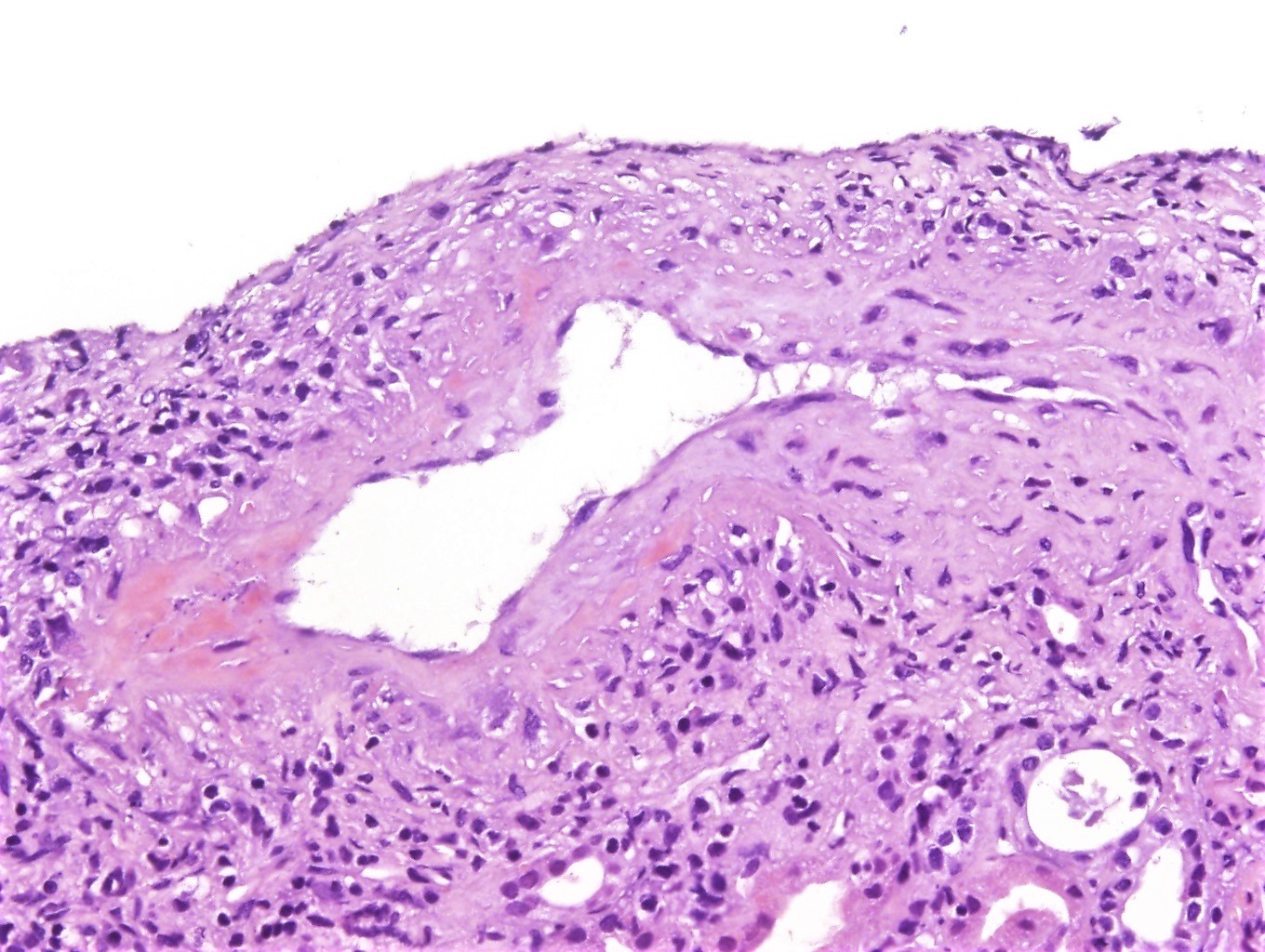
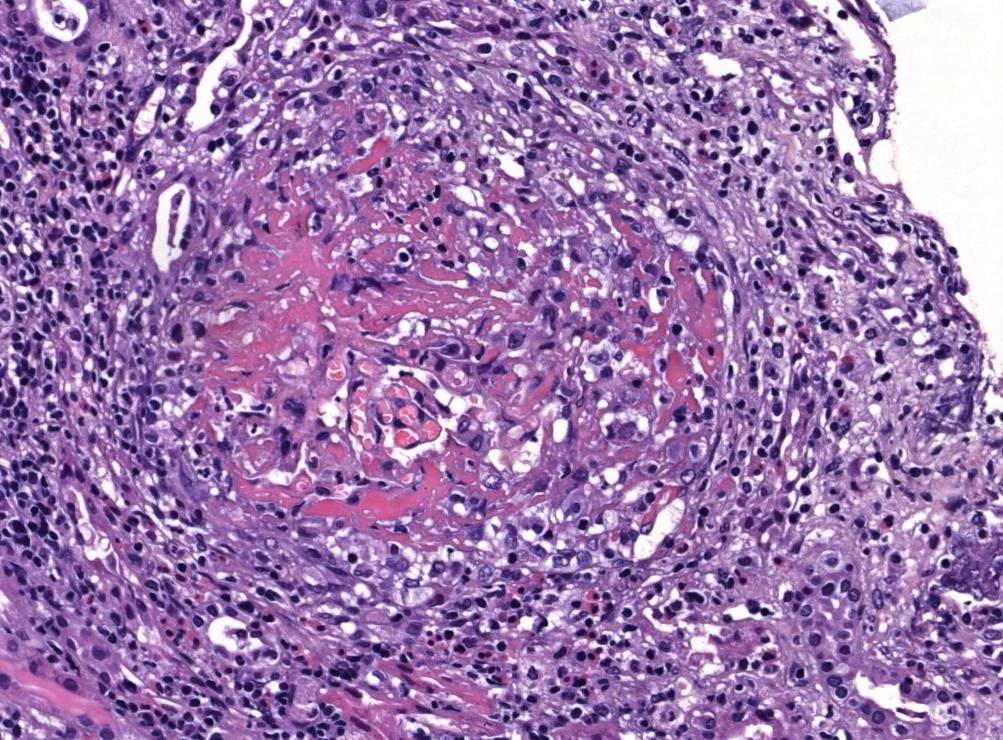
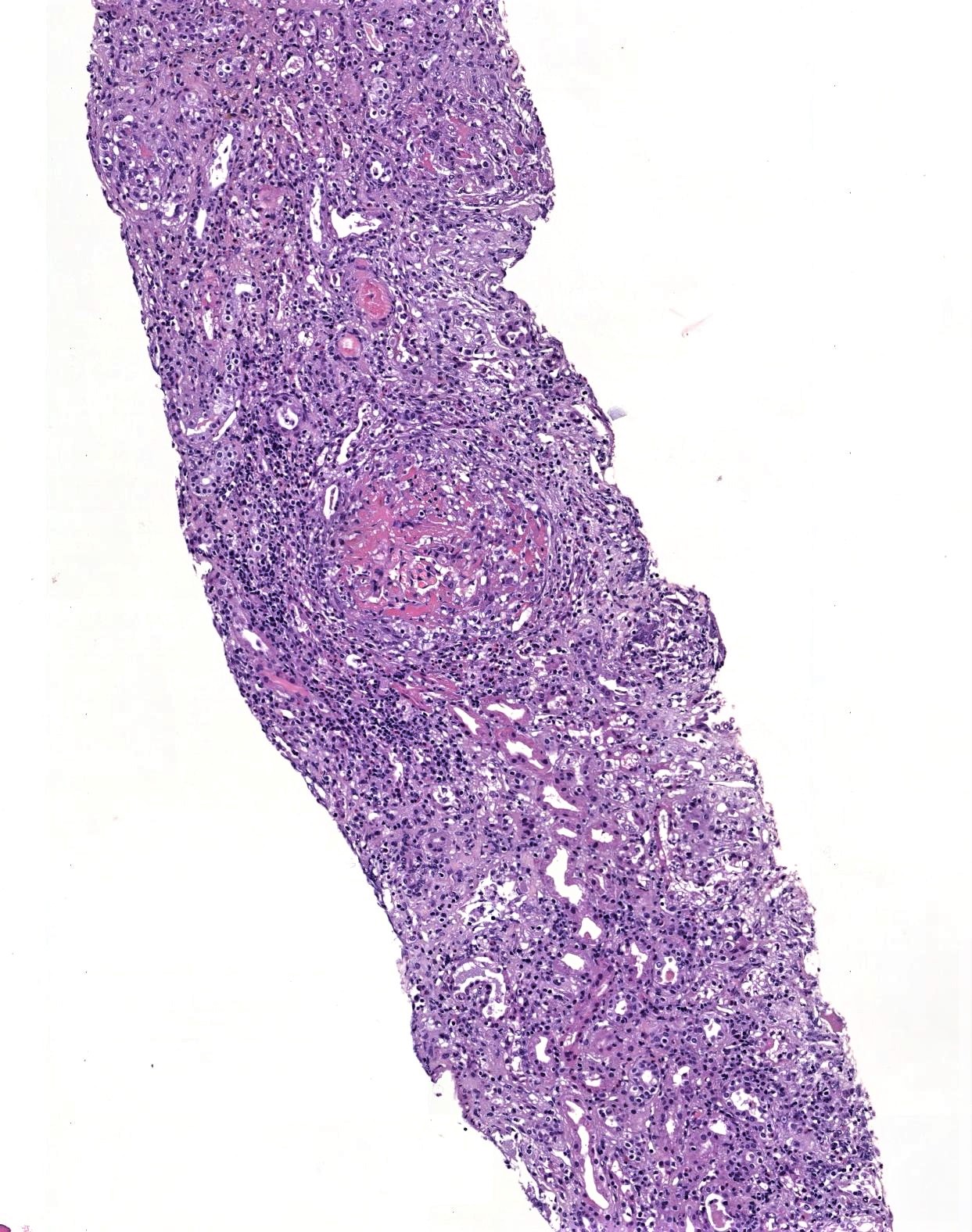
Microscopic (histologic) description
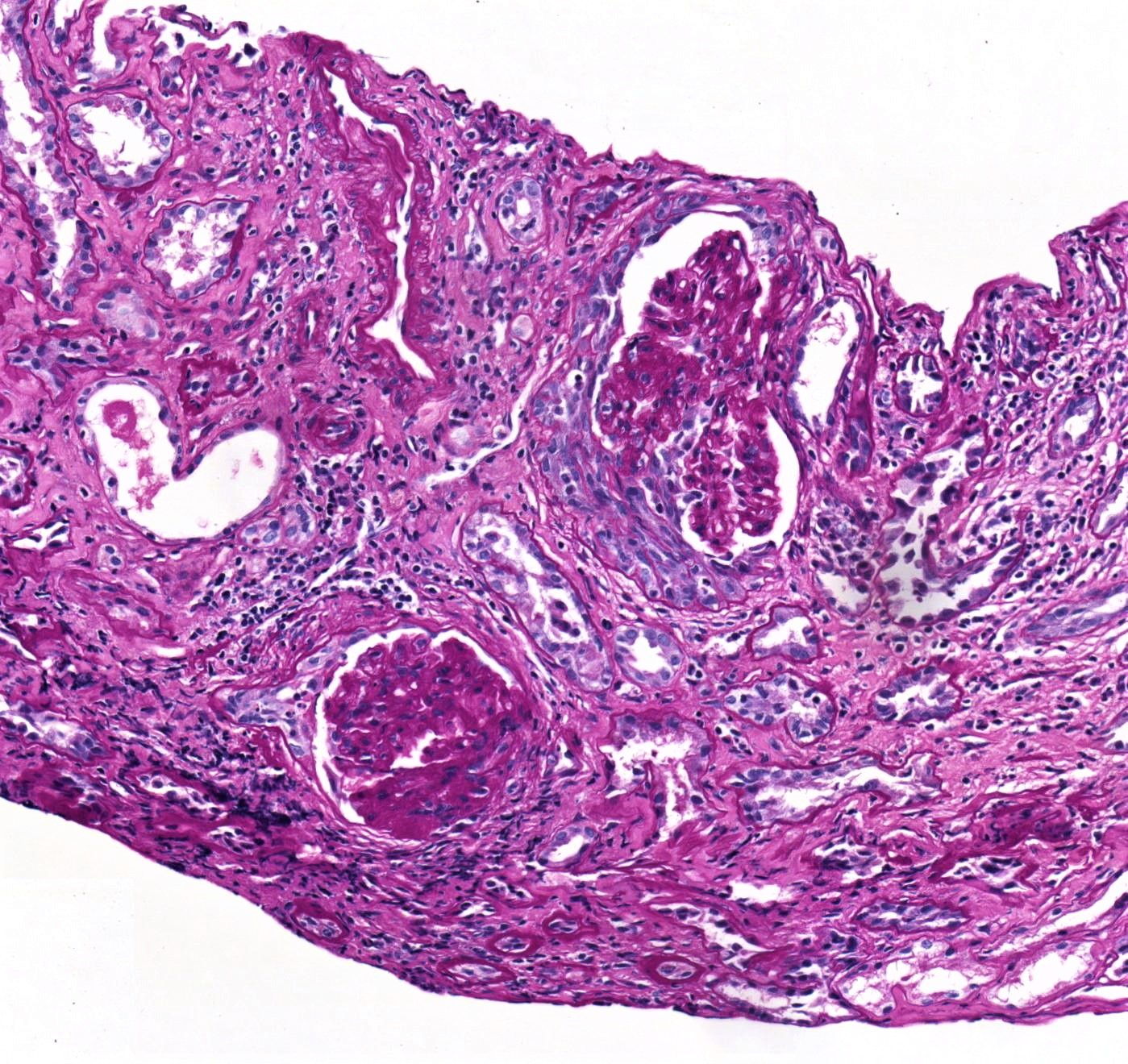
- Pathological classification (J Am Soc Nephrol 2010;21:1628)
- Focal (> 50% normal glomeruli)
- Crescentic (> 50% cellular or fibrocellular crescents):
- Crescents containing > 10% cellularity included
- Fibrous crescents not counted
- Mixed (heterogeneous glomerular lesions, none predominating as > 50%)
- Sclerotic (> 50% global glomerulosclerosis, defined as > 80% of capillary tuft sclerosed)
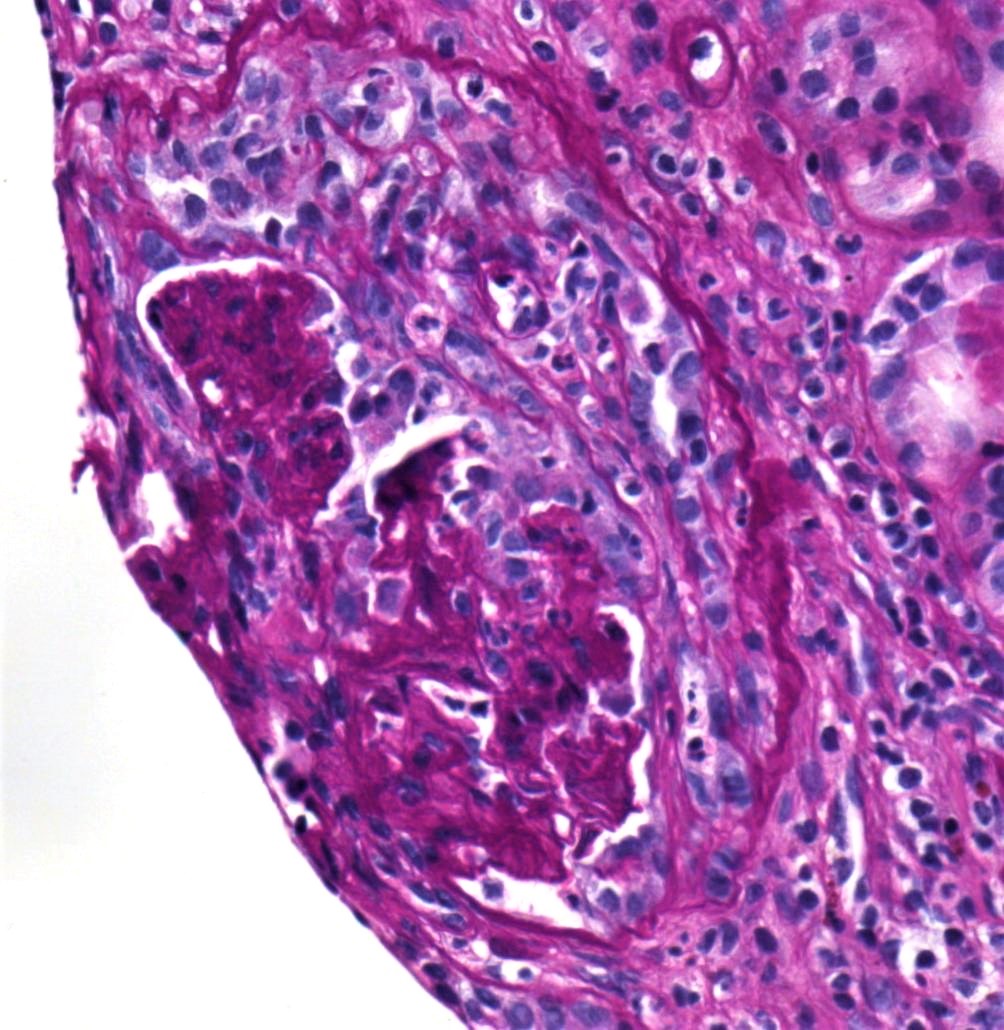
- Focal segmental fibrinoid necrosis (glomerular basement membrane is disrupted in areas of necrosis)
- Extracapillary proliferation with the accumulation of macrophages and epithelial cells in Bowman space (age of crescents: cellular, fibrocellular, fibrous)
- Karyorrhectic debris and fibrin thrombi are frequently seen within the affected glomerular capillary lumens
- Active periglomerular inflammation and rupture of Bowman capsule
- Sometimes periglomerular granulomatous inflammation
- Normal glomeruli usually present
- Endocapillary hypercellularity, typical of immune complex mediated glomerulonephritides, is lacking
- Variable inflammation, predominantly composed of lymphocytes, histiocytes, plasma cells and sometimes brisk number of eosinophils
- Granulomas suggest the possibility of underlying granulomatous with polyangiitis or eosinophilic granulomatous with polyangiitis
- Note that an apparent interstitial granuloma adjacent to a disrupted Bowman capsule does not carry the same connotation
- Vasculitis 5 - 35%; involves small arteries, arterioles, capillaries, venules
- Interlobular arteries usually site affected in systemic vasculitis
- Leukocytoclastic vasculitis pattern (neutrophils, fibrinoid necrosis)
- Necrotizing, leukocytoclastic angiitis of the medullary vasa recta (frequently associated with interstitial hemorrhage and the presence of neutrophilic tubulitis and neutrophils within tubular lumens) (Colvin: Diagnostic Pathology: Kidney Diseases, 2nd Edition, 2015, Zhou: Silva's Diagnostic Renal Pathology, 2nd Edition, 2017)
Microscopic (histologic) images
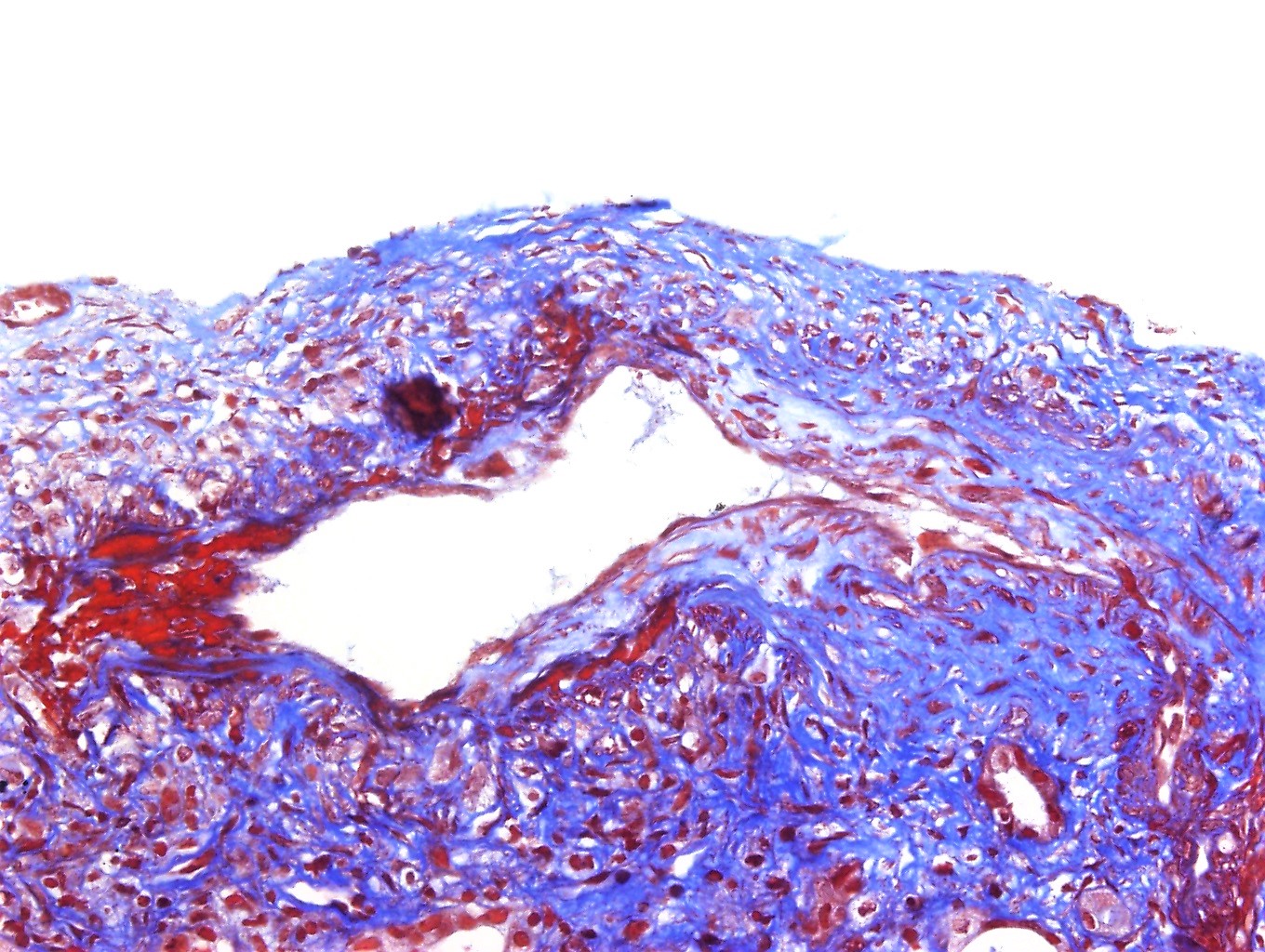
Immunohistochemistry & special stains
- Immunohistochemistry not used for diagnosis
- PAS, Jones silver and trichrome are used to evaluate morphology but are not specific for the type of glomerular disease
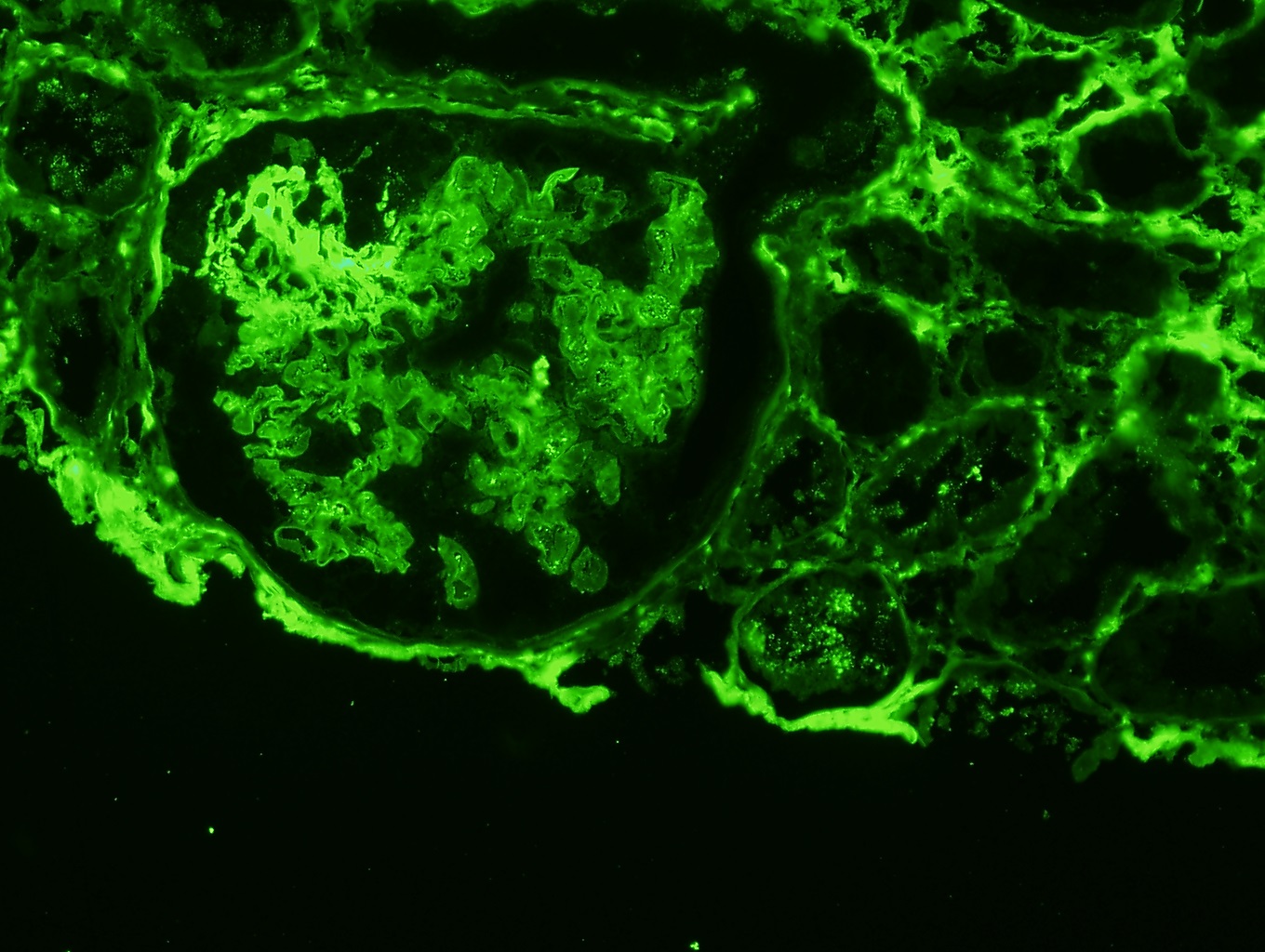
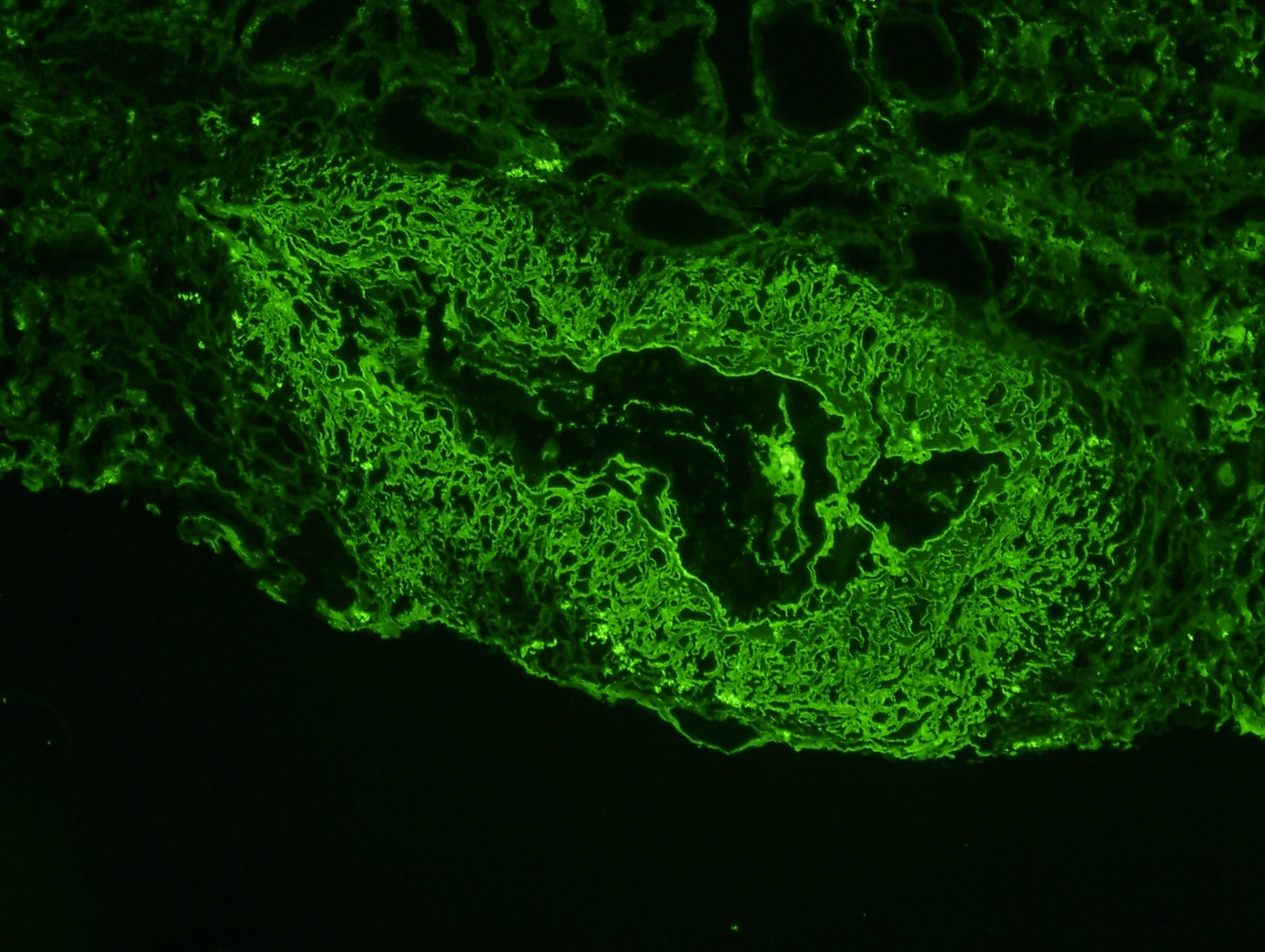
Immunofluorescence description
- Pauci-immune glomerular pattern (weak ≤ 1+) granular staining for IgG, IgM, IgA, C3 and C1q
- There is no evidence of glomerular immunodeposits
- Active crescents and fibrinoid necrosis stain for fibrin
- Reference: Am J Pathol 1989;135:921
Immunofluorescence images
Electron microscopy description
- Electron microscopy generally contributes little, mainly recapitulating the changes seen on light microscopy
- Subendothelial edema, microthrombosis and degranulation of neutrophils are present but immune deposits are absent (J Am Soc Nephrol 2010;21:1628)
Sample pathology report
- Left kidney, biopsy:
- Focal necrotizing and crescentic ANCA glomerulonephritis
- Adequacy: adequate (cortex 80%, medulla 20%)
- Microscopic description: 13 glomeruli, 5 of these exhibited crescents (one with fibrinoid necrosis), including 2 cellular crescents and 3 fibrocellular crescents. Fibrosis occupying 30% of the interstitium with minimal lymphoplasmacytic infiltrate. There was no evidence of extraglomerular arteritis.
- Immunofluorescence microscopy: Number of glomeruli: 3. There were no deposits of IgA, IgM, IgG, C3, C1q or fibrin.
- Focal necrotizing and crescentic ANCA glomerulonephritis
Differential diagnosis
- ANCA negative crescentic glomerulonephritis:
- Serologic testing for ANCA negative
- Antiglomerular basement membrane disease (anti-GBM):
- Bright, linear staining of glomerular basement membranes for IgG
- Vasculitis absent
- Immune complex mediated crescentic glomerulonephritis:
- 2+ or greater of Ig and complement
- Some due to specific diseases such as lupus, cryoglobulinemia, IgA nephropathy, membranoproliferative glomerulonephritis
- ANCA superimposed on other diseases:
- Membranous glomerulonephritis, IgA nephropathy, lupus nephritis may have crescents and necrosis due to superimposed ANCA glomerulonephritis
- Drug induced pauci-immune crescentic glomerulonephritis (CEN Case Rep 2016;5:188)
- Thrombotic microangiopathies:
- Subendothelial widening along the glomerular capillaries with endothelial cell swelling and loss of fenestration by ultrastructural examination
Board review style question #1
Board review style answer #1
D. Pauci-immune necrotizing and crescentic glomerulonephritis, ANCA associated
Comment Here
Reference: Pauci-immune complex crescentic glomerulonephritis / ANCA associated vasculitis
Comment Here
Reference: Pauci-immune complex crescentic glomerulonephritis / ANCA associated vasculitis
Board review style question #2
- Which of the following signs and symptoms are common in ANCA related glomerulonephritis?
- Edema
- Lipiduria
- Nephrotic range proteinuria
- Rapidly progressive renal failure
Board review style answer #2
D. Rapidly progressive renal failure
Comment Here
Reference: Pauci-immune complex crescentic glomerulonephritis / ANCA associated vasculitis
Comment Here
Reference: Pauci-immune complex crescentic glomerulonephritis / ANCA associated vasculitis