Table of Contents
Definition / general | Essential features | Epidemiology | Pathophysiology | Clinical features | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Whole mount images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Tretter EM, Schoenfield LR. Melanoma-uvea. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyeuveamelanoma.html. Accessed December 28th, 2024.
Definition / general
- Malignant neoplasm of melanocytes within uveal tract, including iris, ciliary body and choroid
Essential features
- Tumor center located in iris, ciliary body or choroid (Methods Mol Biol 2014;1102:397)
- Approximately half metastasize, almost exclusively to liver (Methods Mol Biol 2014;1102:397)
- Tumor size, location and cell type are the most important histopathologic prognostic factors but molecular testing plays an increasing clinical role in prognostication
Epidemiology
- Most common primary intraocular malignancy in adults (PDQ Cancer Information Summaries: Intraocular (Uveal) Melanoma Treatment [Accessed 7 August 2018])
- Incidence is 5.1 new cases per million people in United States, which is low compared to other countries (Ophthalmol Clin North Am 2005;18:75)
- Mean age at diagnosis is 61 years (Br J Ophthalmol 2015;99:1550)
- Risk factors include light skin, Caucasian race, light eye color, inability to tan; weak association with sunlight exposure (Cancer Causes Control 2003;14:251, Ophthalmol Clin North Am 2005;18:75)
Pathophysiology
- May arise from preexisting uveal nevi or de novo (Arch Ophthalmol 2009;127:981)
Clinical features
- Half of cases are asymptomatic and discovered on exam; half present with visual disturbance
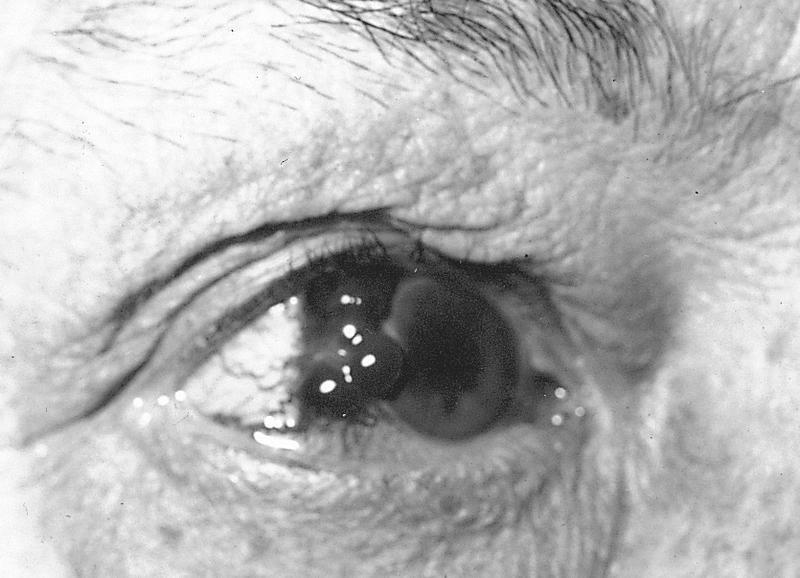
- Melanoma of iris: presents as elevated mass with variable pigmentation, often with distortion of pupil and prominent vessels
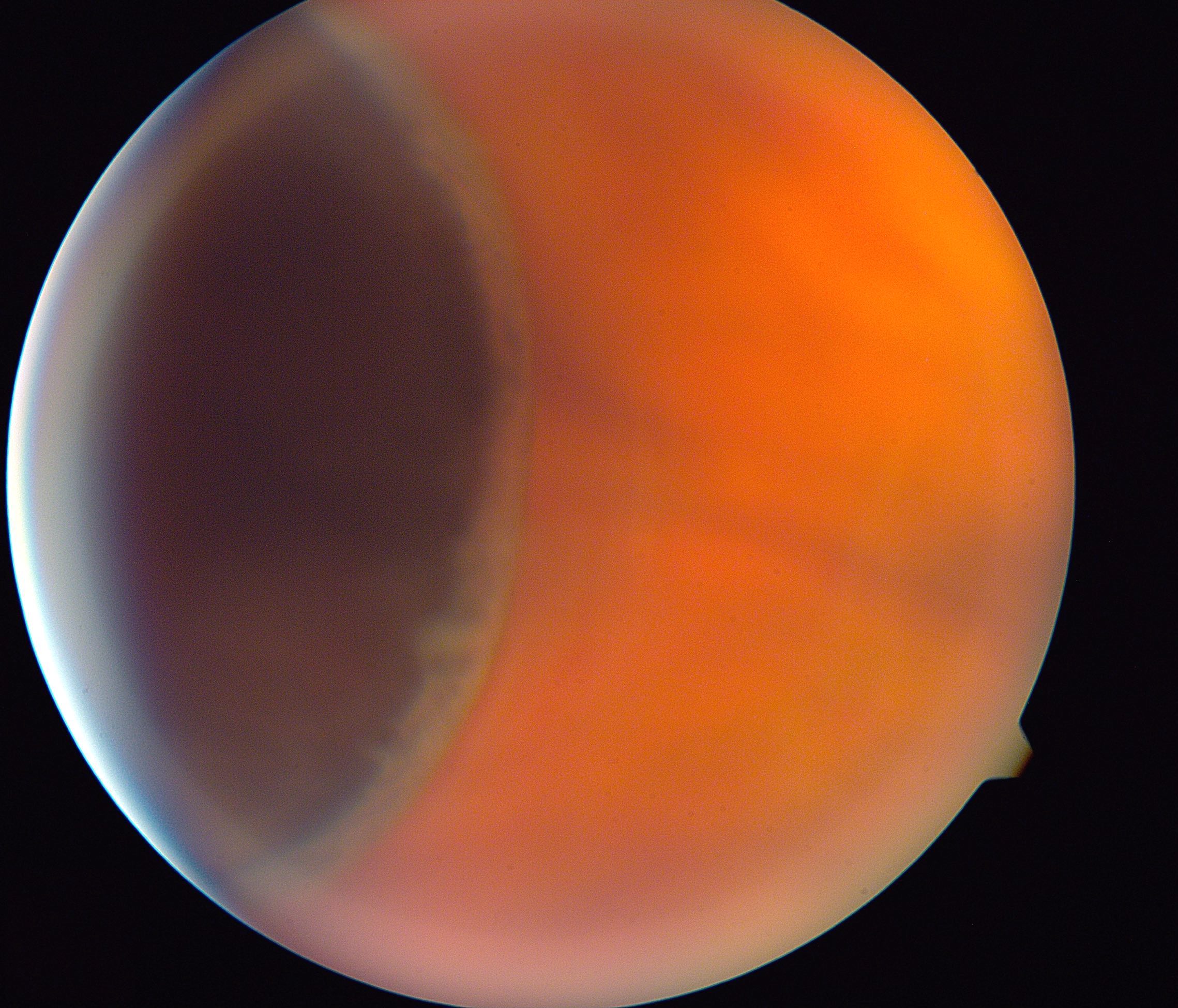
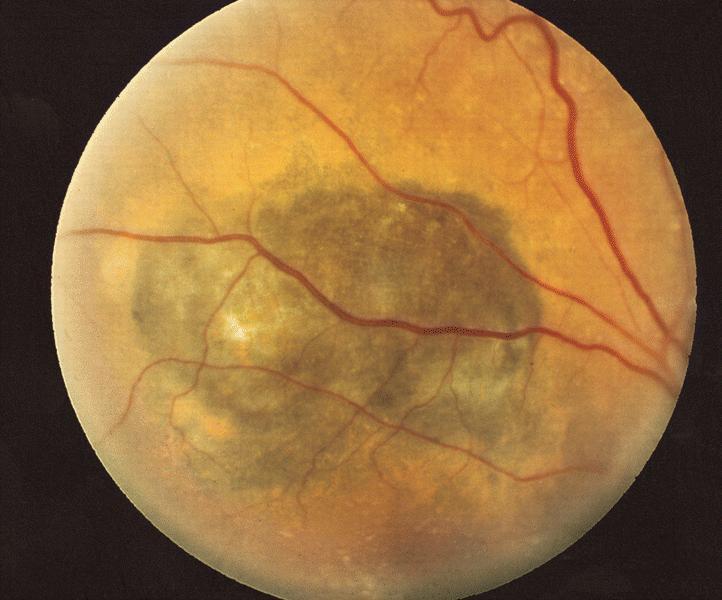
- Melanoma of choroid: irregular, slate gray, solid, choroidal tumor that may extend through Bruch membrane into retina and vitreous producing retinal detachment, macular edema, choroidal hemorrhage; occasionally spreads along scleral canals into orbit, rarely invades optic nerve
- Melanoma of ciliary body: may interfere with accommodation or cause localized cataract
- Tends to spread through scleral emissary canal
- Up to half of cases metastasize
- Distant metastases nearly exclusively to liver (95%), sometimes to lung and bone (Methods Mol Biol 2014;1102:397)
- Lymphatic spread uncommon due to lack of lymphatic channels in eye
Prognostic factors
- Size of tumor
- Ciliary body involvement
- Extension outside of orbit, metastasis and recurrence have very poor prognosis (Ophthalmology 1991;98:383)
- Cytogenetic abnormalities, particularly monosomy 3 and gain of 8q (Cancer Control 2016;23:93)
- Gene expression profiling (class 1A, 1B and 2) (Ophthalmology 2012;119:1596, Clin Cancer Res 2007;13:1466, Ophthalmology 2014;121:1281, JAMA Ophthalmol 2016;134:734)
- Histologic features: mitoses, cell type (spindle B versus epithelioid), extravascular matrix loops, tumor infiltrating lymphocytes and macrophages (PDQ Cancer Information Summaries: Intraocular (Uveal) Melanoma Treatment [Accessed 7 August 2018])
Case reports
- 19 year old man with melanoma of anterior chamber presenting as pigmentary glaucoma (Surv Ophthalmol 2017;62:670)
- 60 year old woman with sudden ocular pain (Indian J Ophthalmol 2018;66:1059)
- 63 year old woman with extension of choroidal melanoma after brachytherapy (Ophthalmology 2017;124:1503)
- 74 year old man with metastases treated with ipilimumab and nivolumab (Pigment Cell Melanoma Res 2017;30:558)
Treatment
- Episcleral brachytherapy utilizing radioactive seeds is the mainstay of eye sparing treatment and yields equivalent survival rates to enucleation (Arch Ophthalmol 2001;119:969, Clin Ophthalmol 2018;12:925)
- Location and size of tumor affect ability to use this mode of treatment (Brachytherapy 2014;13:1)
- Local resection for select tumors of the iris and ciliary body
- Enucleation reserved for large tumors (PDQ Cancer Information Summaries: Intraocular (Uveal) Melanoma Treatment [Accessed 7 August 2018])
- Rarely evisceration is necessary
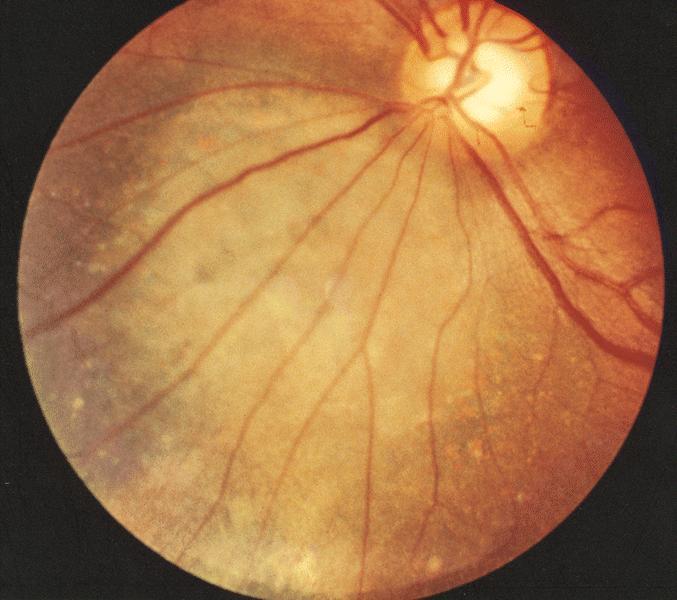
Clinical images
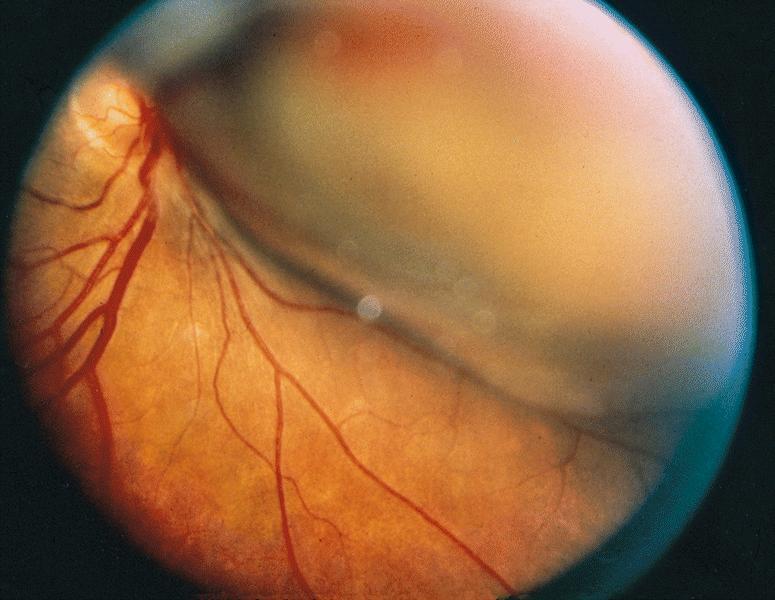
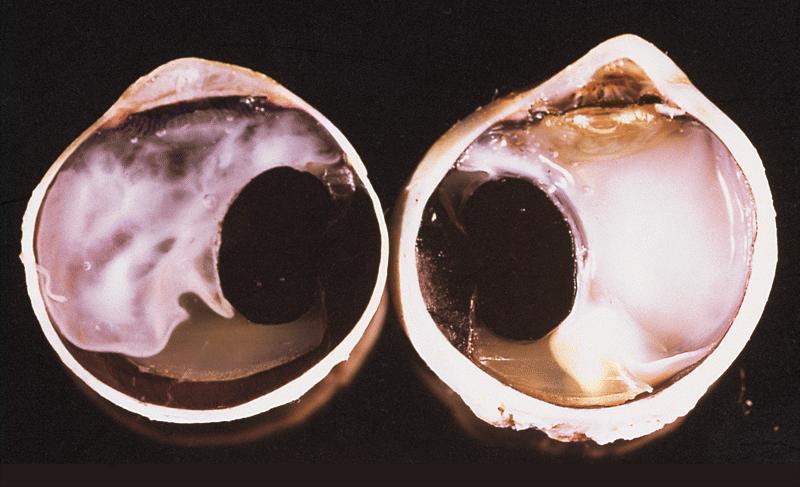
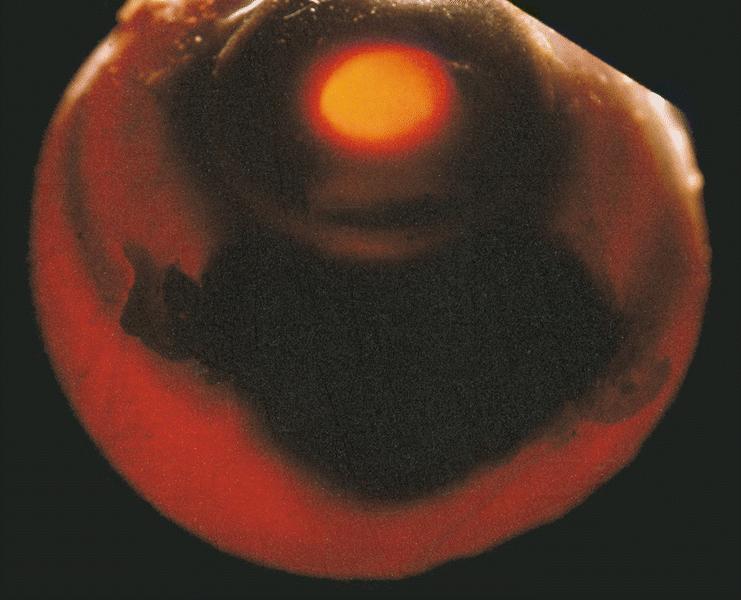
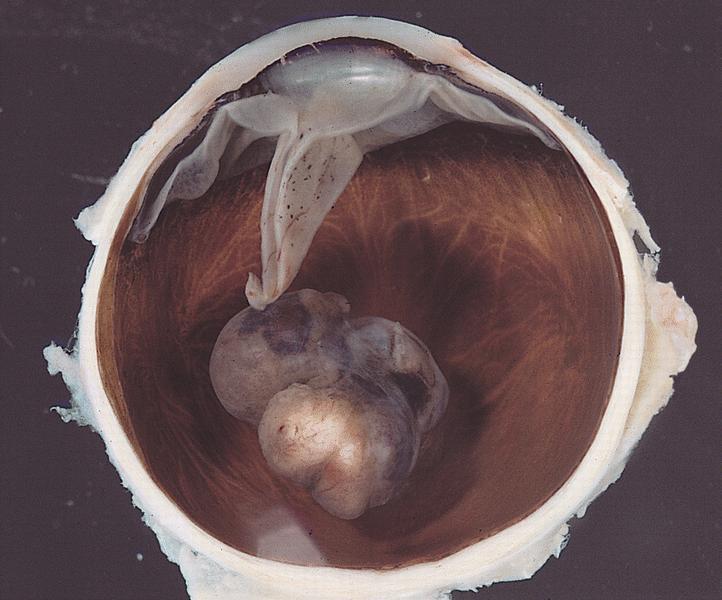
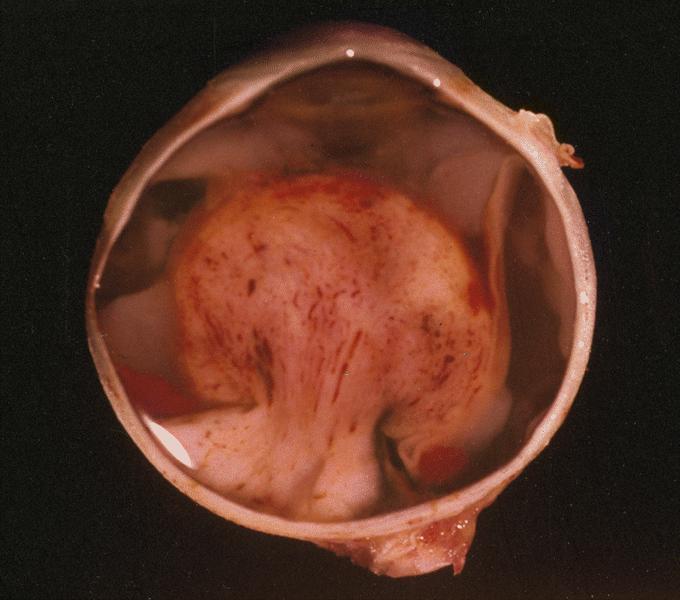
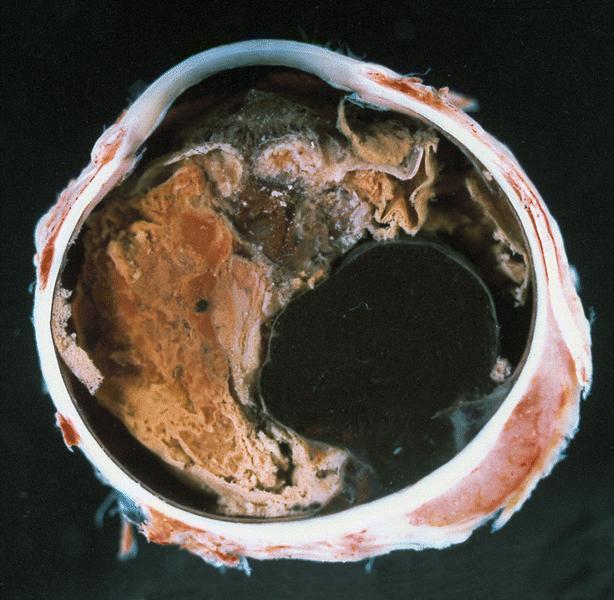
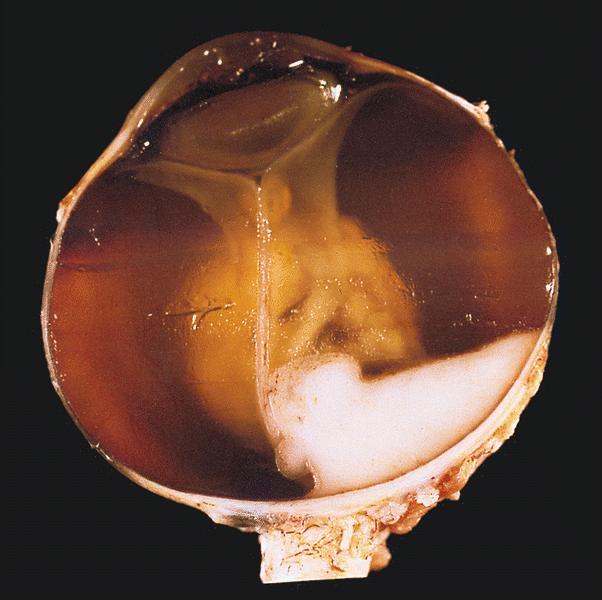
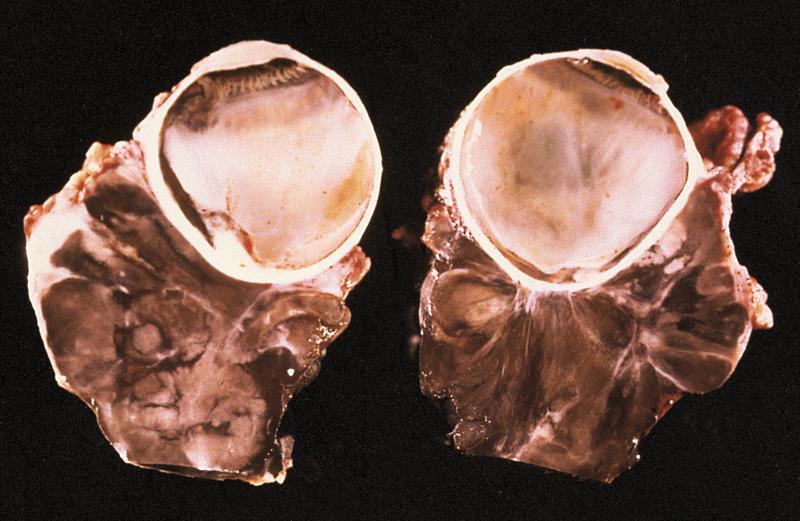
Gross description
- Small uveal melanomas may be difficult to distinguish from a nevus clinically; size criteria are used
- Gross findings suspicious for melanoma include:
- Orange pigment
- Subretinal fluid
- Tumor thickness > 2 mm
- Low internal reflectivity on ultrasound examination
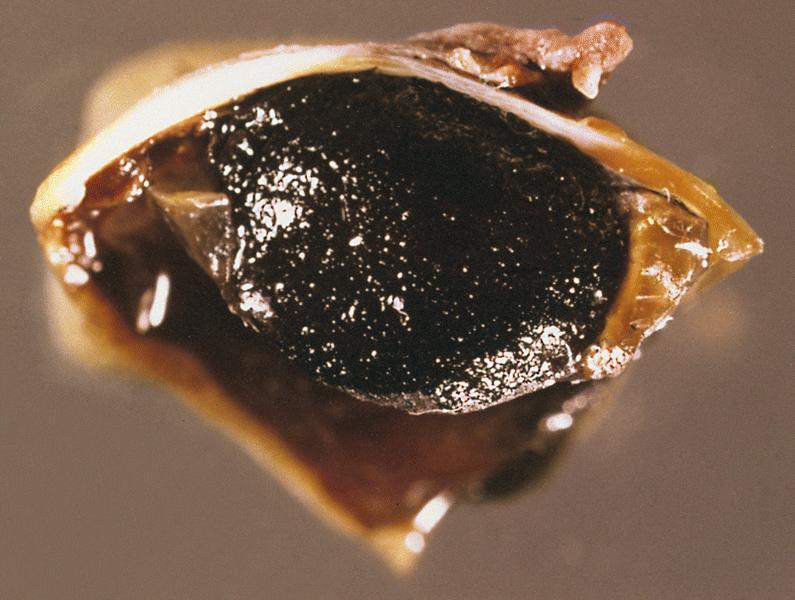
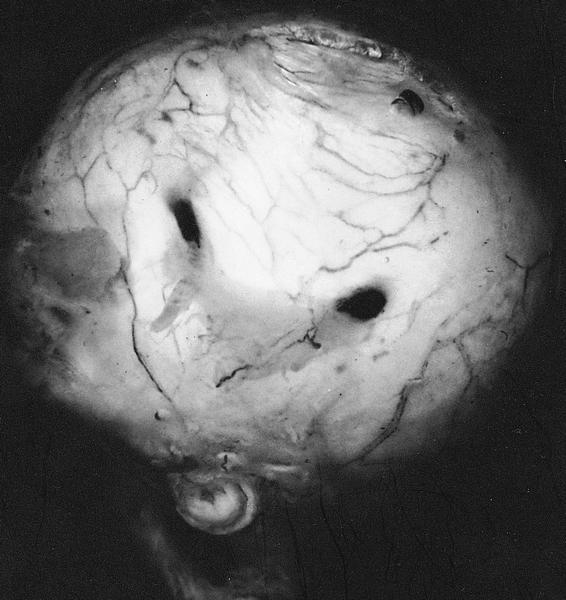
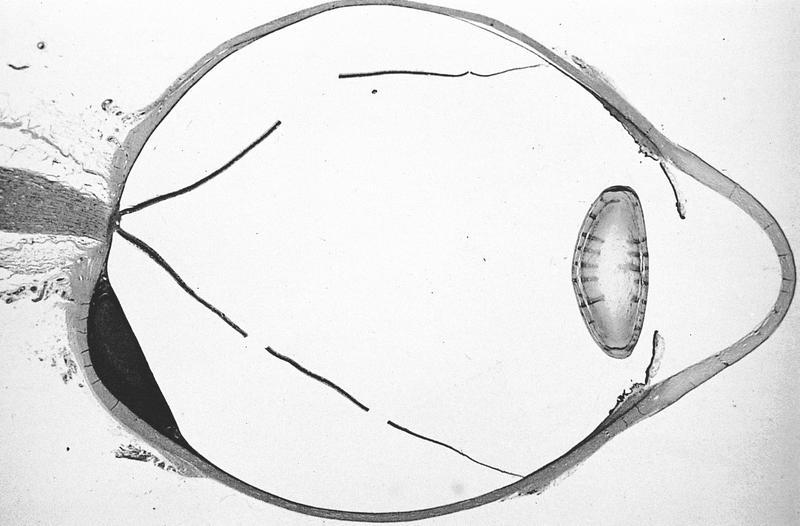
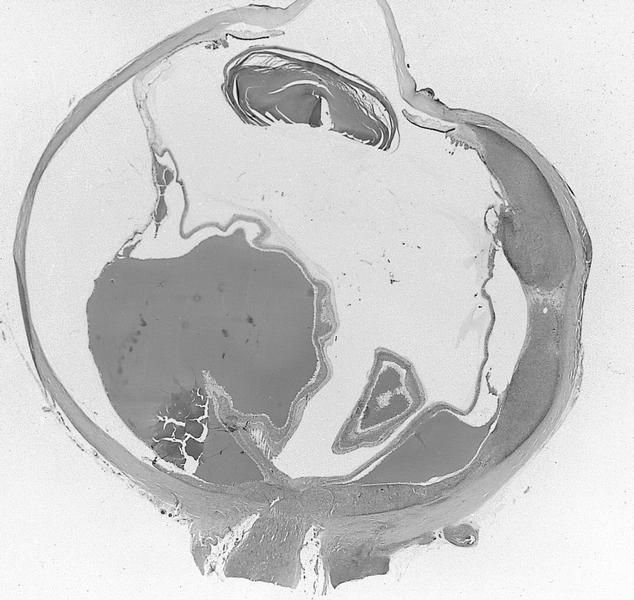
Gross images
Contributed by Lynn R. Schoenfield, M.D. and AFIP images
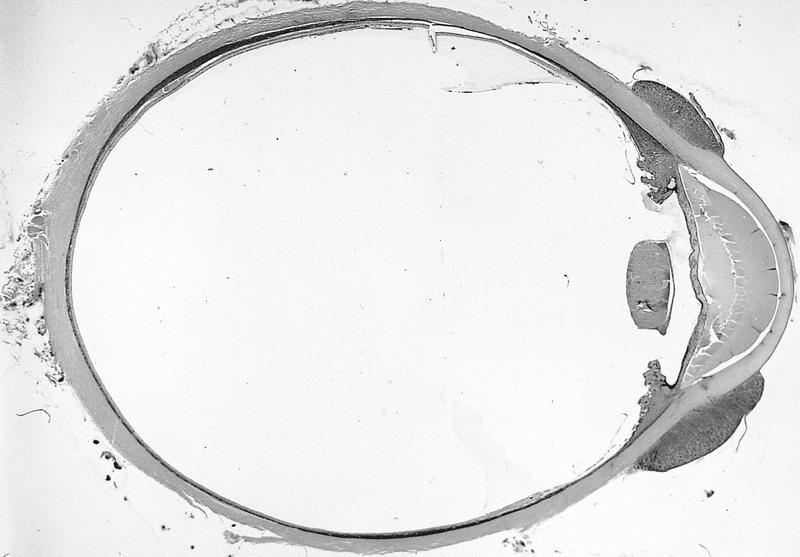
Whole mount images
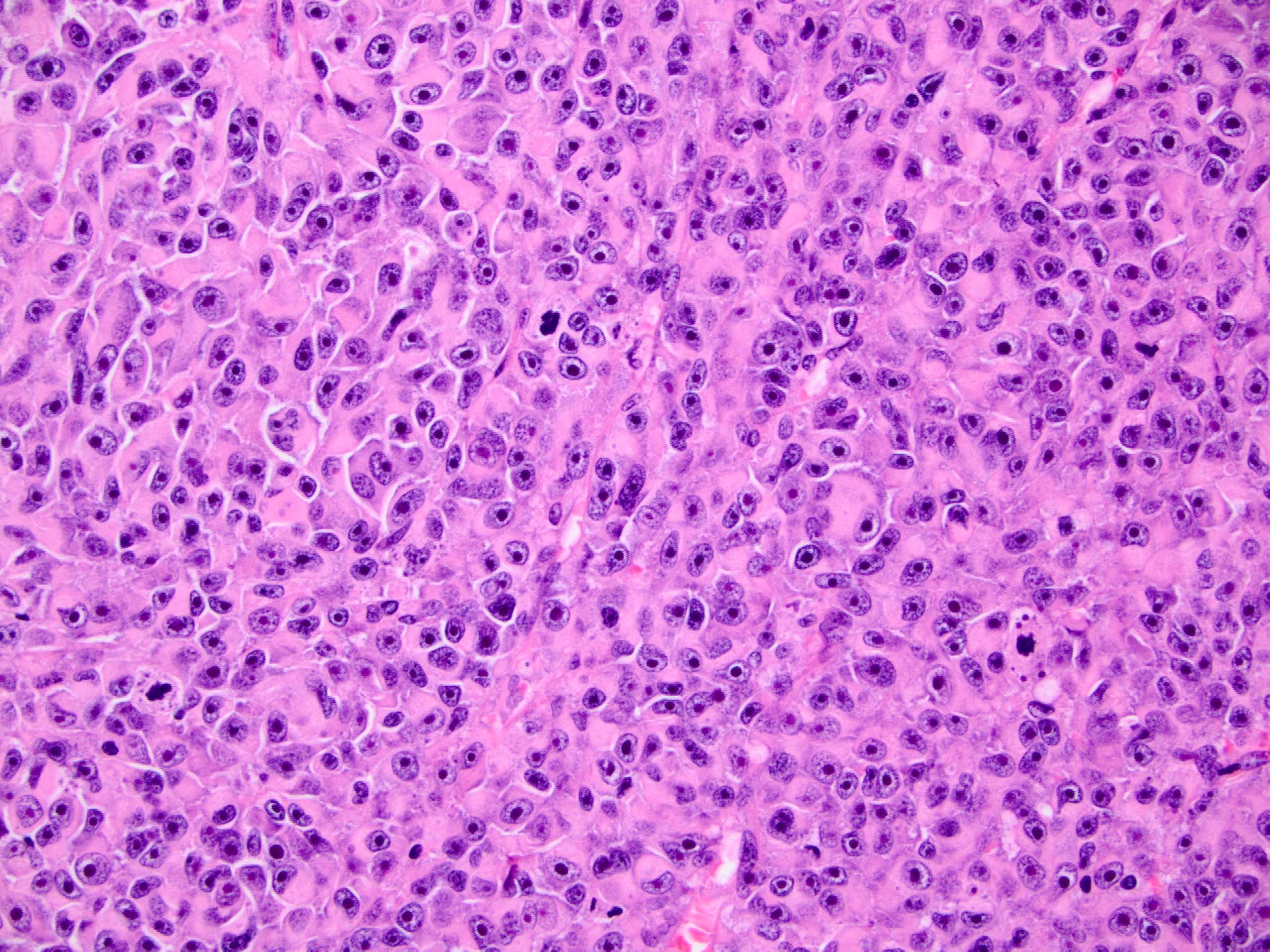
Microscopic (histologic) description
- There are 2 distinct cell types and most tumors contain a combination of the 2:
- Spindle B cells: spindle shaped cells with large oval nuclei and distinct nucleoli
- Epithelioid cells: large polygonal cells with atypical nuclei, 1 or more prominent nucleoli and sometimes intranuclear pseudoinclusions
- Note that spindle A cells also exist, which are spindle shaped cells with slender nuclei that lack visible nucleoli; these are typically benign and are the melanocytes of uveal nevi
Microscopic (histologic) images
Positive stains
- HMB45: specific and sensitive
- S100: sensitive
- Vimentin, MelanA, MITF1 (Arch Pathol Lab Med 1996;120:497, Invest Ophthalmol Vis Sci 2002;43:2533, Methods Mol Biol 2014;1102:397)
- SOX10: highly sensitive for melanocytic proliferation
- Ki67 and pHH3: used to estimate proliferation rate but not for clinical management
Negative stains
- Cytokeratin markers should be negative but may sometimes stain focally
Molecular / cytogenetics description
- Monosomy 3, 8q gain and expression profiling (Invest Ophthalmol Vis Sci 2001;42:313, Clin Cancer Res 2007;13:1466)
Differential diagnosis
- Metastatic carcinoma (especially if amelanotic):
- Nevi:
- Small uveal melanomas may be difficult to distinguish from a nevus clinically; size criteria are used
- Clinical findings suspicious for melanoma include:
- Orange pigment
- Subretinal fluid
- Tumor thickness > 2 mm
- Low internal reflectivity on ultrasound examination
Board review style question #1
Which feature is suspicious for uveal melanoma as opposed to choroidal nevus?
- High internal reflectivity on ultrasound examination
- Lack of subretinal fluid
- Orange pigment
- Tumor thickness of 1.5 mm
Board review style answer #1
Board review style question #2
Board review style answer #2