Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Whole mount images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lochner R, Couce M. Retinoblastoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyeretinaretinoblastoma.html. Accessed January 1st, 2025.
Definition / general
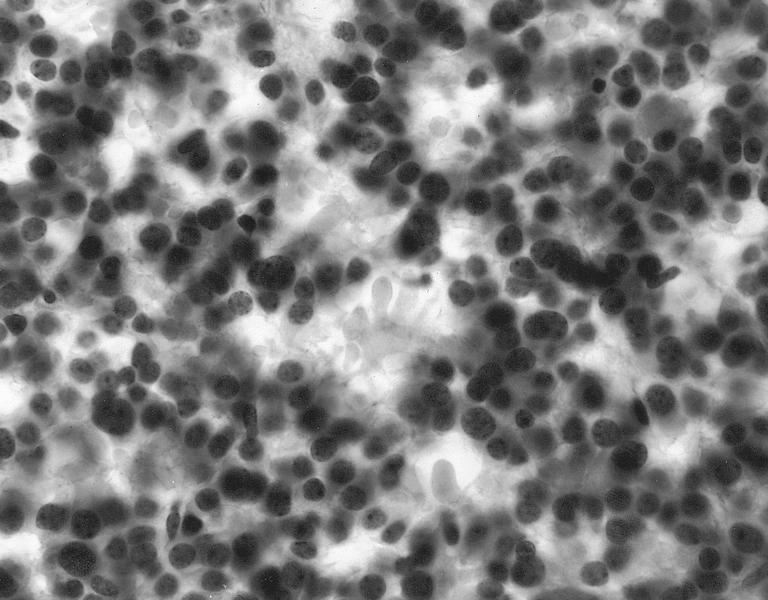
- Retinoblastoma is the most common intraocular malignancy in children characterized by hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests and trabeculae
- Prognosis dependent on many factors; histopathological evaluation determines metastatic risk, including tumor invasion into anterior chamber, significant invasion into choroid (at least 3 mm) and postlaminar optic nerve invasion
- Retinoma / retinocytoma is the benign form of retinoblastoma
Essential features
- Most common intraocular malignancy of childhood (1 in 16,000 - 18,000 births) (Nat Rev Dis Primers 2015;1:15021)
- Often due to loss or inactivation of both alleles of the retinoblastoma 1 gene (RB1) (Knudson 2 hit hypothesis)
- Hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests and trabeculae, often with calcifications and necrosis
- Most often has presurgical diagnosis by radiological and clinical features
- Localized chemotherapy is first line treatment, followed by systemic therapy and surgery
ICD coding
Epidemiology
- Most common intraocular malignancy of childhood (1 in 16,000 - 18,000 births) (Nat Rev Dis Primers 2015;1:15021)
- > 40% of cases are located in 6 countries in Asia-Pacific region (Eye (Lond) 2019;33:87)
- Approximately 90% in middle and low income countries (Nat Rev Dis Primers 2015;1:15021)
Sites
- Sporadic retinoblastoma usually unilateral eye
- Inherited retinoblastoma often bilateral eyes
- Can be trilateral (pineoblastoma) or very rarely quadrilateral (pineoblastoma and suprasellar primitive neuroectodermal tumor) (Pediatr Blood Cancer 2010;55:570)
Pathophysiology
- Loss or inactivation of both alleles of the retinoblastoma 1 gene (RB1)
- Tumor suppressor gene located at 13q14.2 locus
- Encodes RB1 protein
- Knudson 2 hit hypothesis
- Results from 2 separate mutations:
- First mutation is somatic or germline
- Second mutation is somatic
- Results from 2 separate mutations:
- Germline mutations in RB1 lead to inherited / familial retinoblastoma
- Earlier age of onset (J Neurosci Res 2019;97:29)
- Often bilateral involvement but can be trilateral or quadrilateral (Pediatr Blood Cancer 2010;55:570)
- Predisposes to development of other malignancies including osteosarcoma and melanoma (Pneumologie 1990;44:327)
- Reference: Annu Rev Pathol 2015;10:547
Etiology
- Inherited germline mutation of RB1
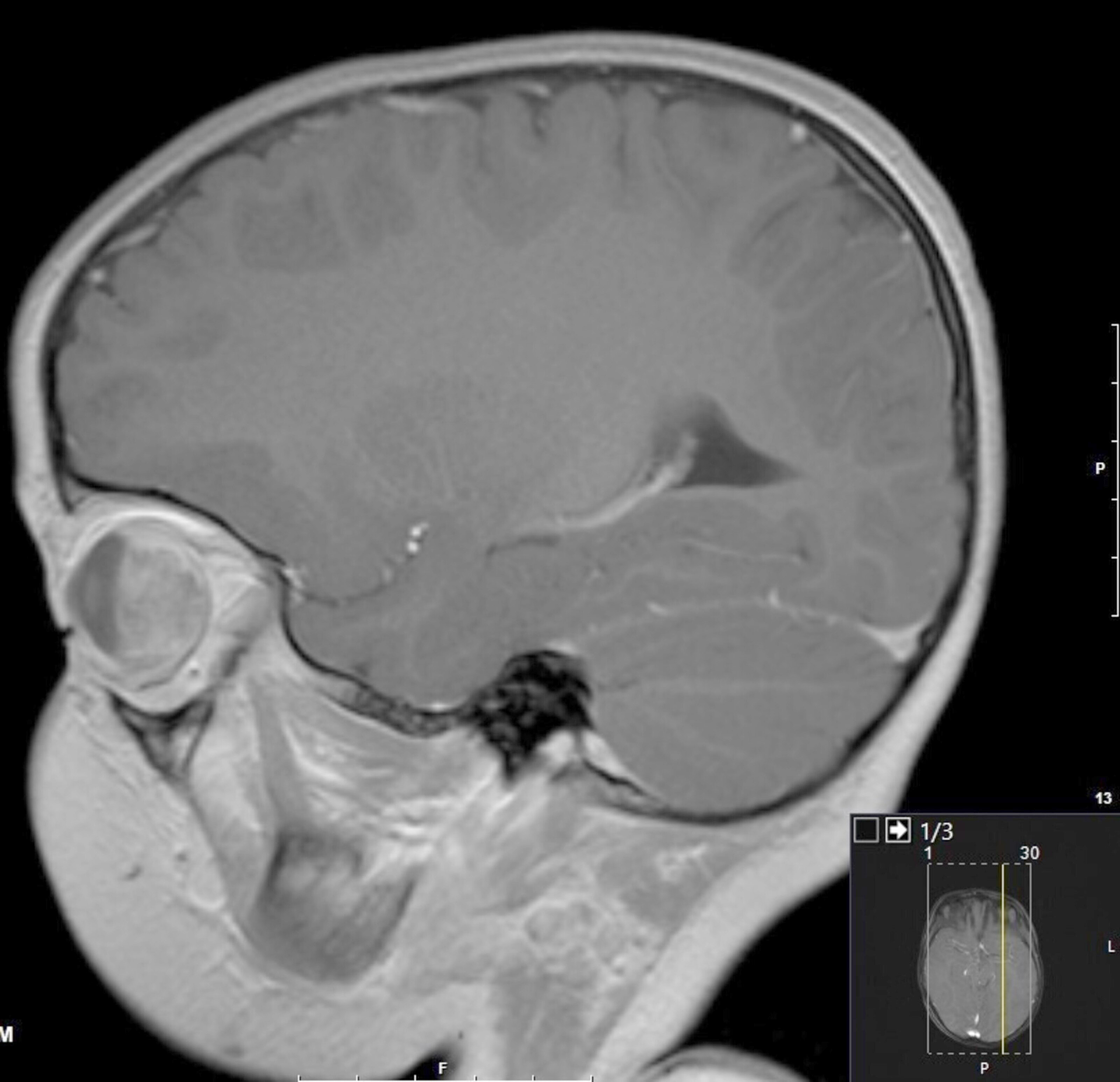
Clinical features
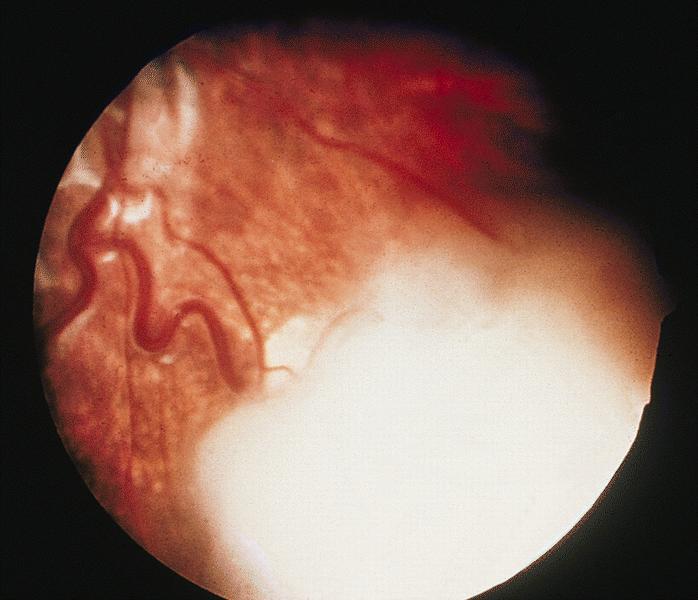
- Leukocoria (white reflex) of affected eye (late presenting sign) (J Neurosci Res 2019;97:29, J Ophthalmol 2020;2020:9315784)
- Glaucoma
- Strabismus (second most common sign)
- Eye pain
- Decreased visual acuity
- Retinal detachment
Diagnosis
- Diagnosis is almost always made clinically and radiologically
- High resolution MRI used for preoperative planning
- Can reliably detect optic nerve invasion, choroid and extrascleral invasion (Egypt J Radiol Nucl Med 2020;51:28)
- Can be diagnosed histopathologically post surgery
- Controversial use of FNA / cytology with concern for tumor seeding
- Can be done safely in select cases where imaging is not definitive (Int J Ophthalmol 2016;9:1233)
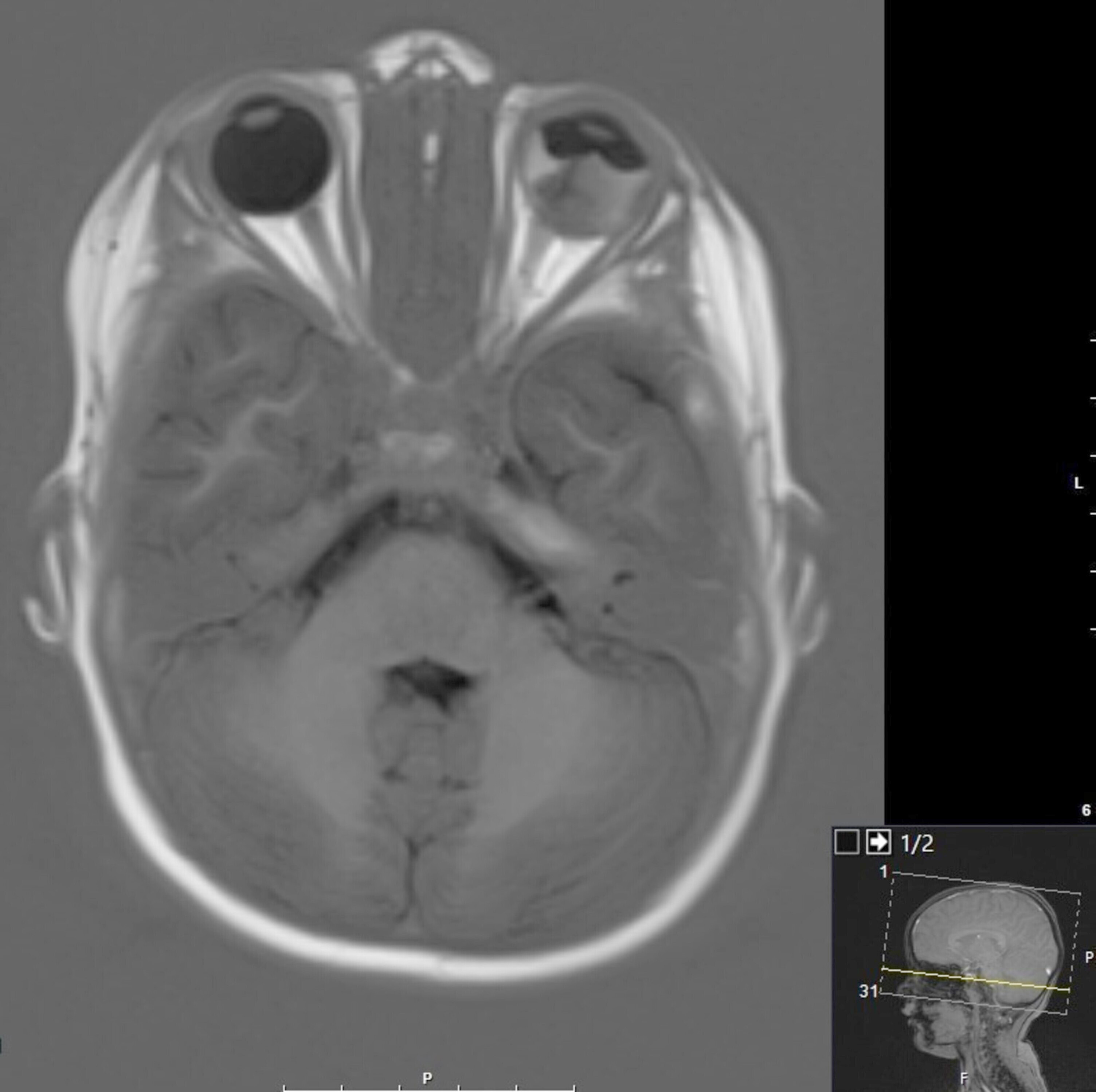
Radiology description
- Most often diagnosed via imaging
- Ultrasound:
- Does not require sedation or exposure to radiation
- Can visualize tumor calcification (J Neurosci Res 2019;97:29)
- Variably heterogeneous, echogenic soft tissue mass (AJR Am J Roentgenol 2000;175:495)
- Helps monitor tumor in treatment
- MRI:
- Modality of choice for pretreatment staging and surgical planning
- Helps correlate calcifications on ultrasound to confirm diagnosis
- T2 hypointense compared with surrounding vitreous
- Variable sensitivity for detecting high risk features (Ophthalmology 2014;121:1109)
- Optic nerve (59%), choroidal (74%) and scleral invasion (88%)
- CT:
- Exposure to radiation not preferred, especially in patients with RB1 germline predisposed to a second malignancy
- Contrast enhancing retrolental mass with calcifications
Radiology images
Prognostic factors
- > 95% survival in high income countries and ~30% survival in low income countries (Nat Rev Dis Primers 2015;1:15021, Cancer Lett 2014;351:59, Can J Ophthalmol 2009;44:S1)
- Risk of metastatic spread evaluated by histology post enucleation
- High risk histopathological features
- Involvement of optic nerve, choroid or anterior ocular structures (Oncogene 2018;37:1551, Arch Ophthalmol 2011;129:1422)
- High risk histopathological features
- International Intraocular Retinoblastoma Classification
- Classifies tumors into 5 groups based on clinical and radiological features:
- Group A (tumor ≤ 3 mm away from the fovea and disk)
- Group B (larger tumor without dissemination)
- Group C (local tumor dissemination)
- Group D (diffuse tumor dissemination)
- Group E (unsalvageable eye)
- Classifies tumors into 5 groups based on clinical and radiological features:
Case reports
- 23 year old man treated with primary intra-arterial and intravitreal chemotherapy (Oman J Ophthalmol 2019;12:119)
- 55 year old woman with late stage intraocular mass, diagnosed with FNA (J Cytol 2018;35:120)
- 3 sets of twins with retinoblastoma discordance (Indian J Ophthalmol 2019;67:436)
Treatment
- Evolved significantly from enucleation to vision sparing, localized chemotherapy
- Intraophthalmic artery / nerve chemotherapy
- Increased concentration within eye with less systemic effect
- Cured 85% of group D high risk cases in one trial (PLoS One 2016;11:e0151343)
- Systemic chemotherapy
- Second choice following targeted chemotherapy
- Increased systemic side effects and less effective
- Adjuvant in very high risk cases treats any micrometastases
- Role for primary enucleation in some high risk and all very high risk cases and in low income countries (Br J Ophthalmol 2018;102:265, Oncogene 2018;37:1551)
- Single curative procedure with low recurrence
Clinical images
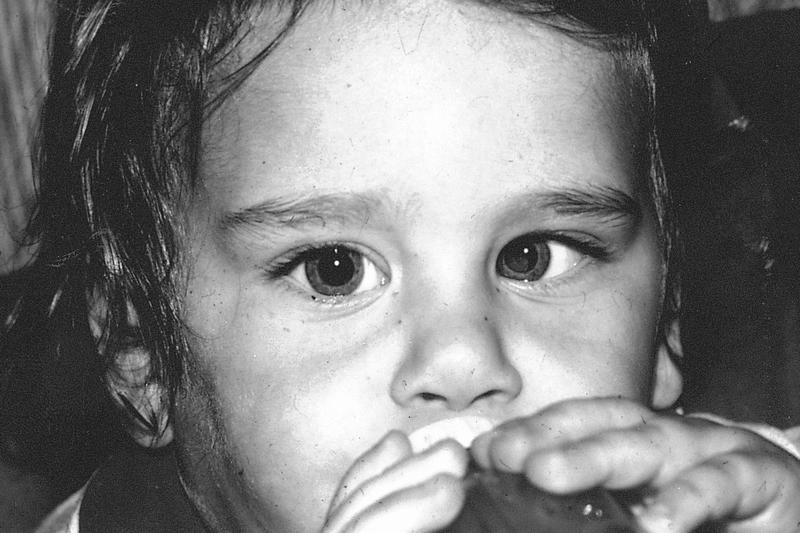
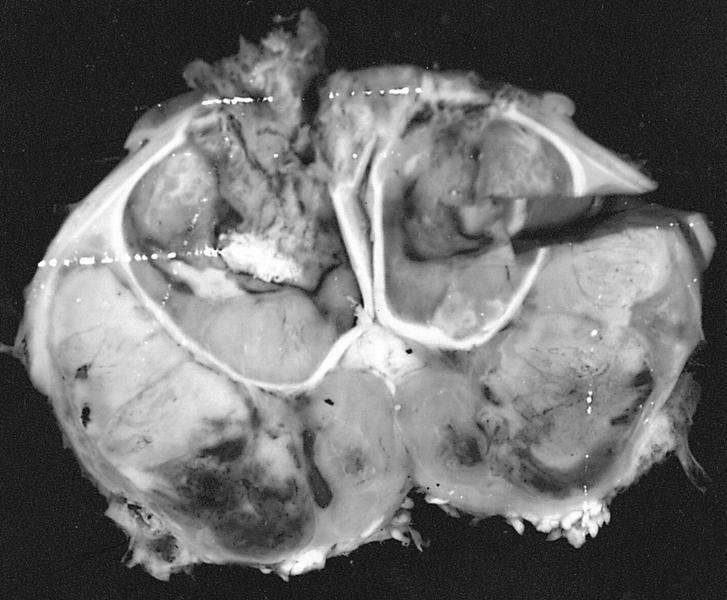
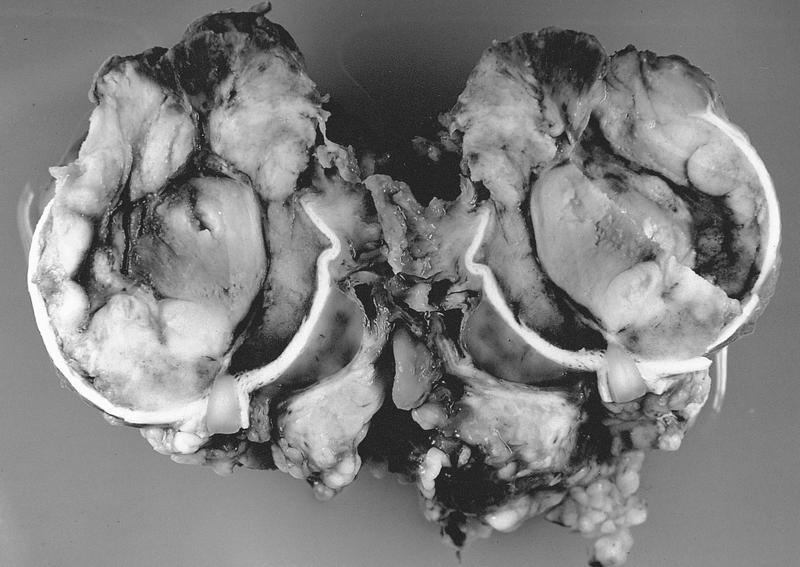
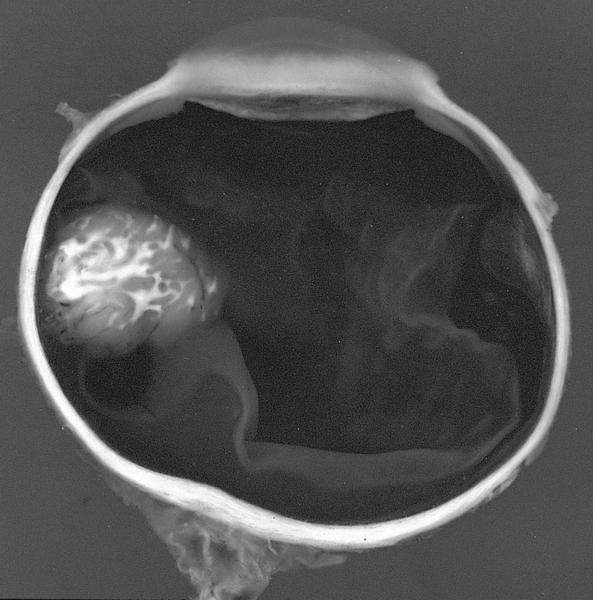
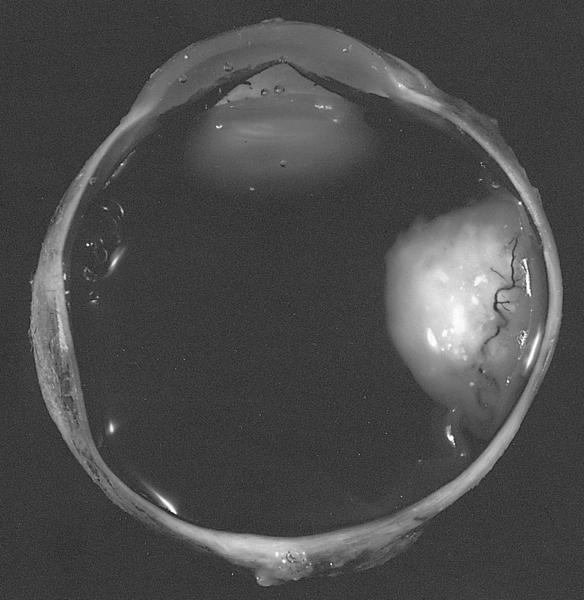
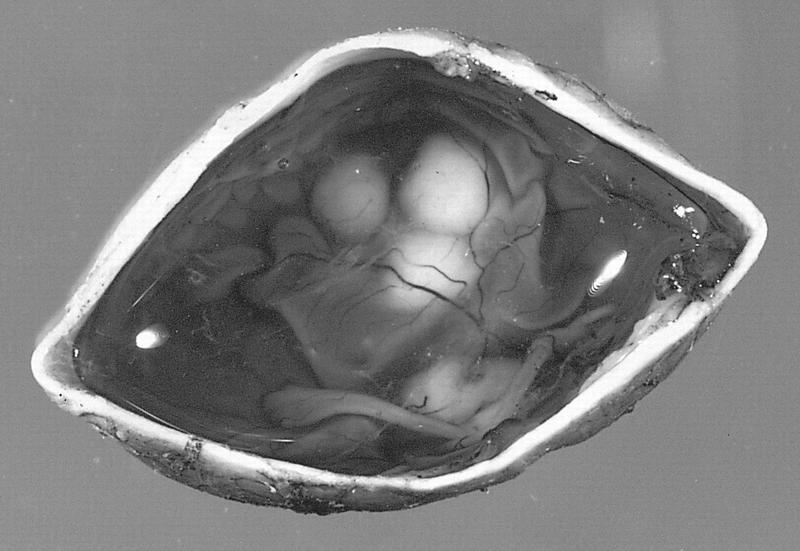
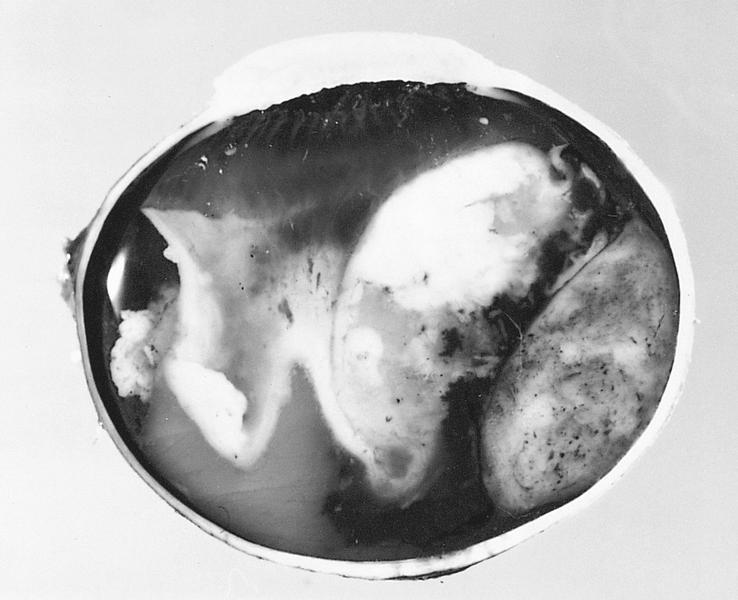
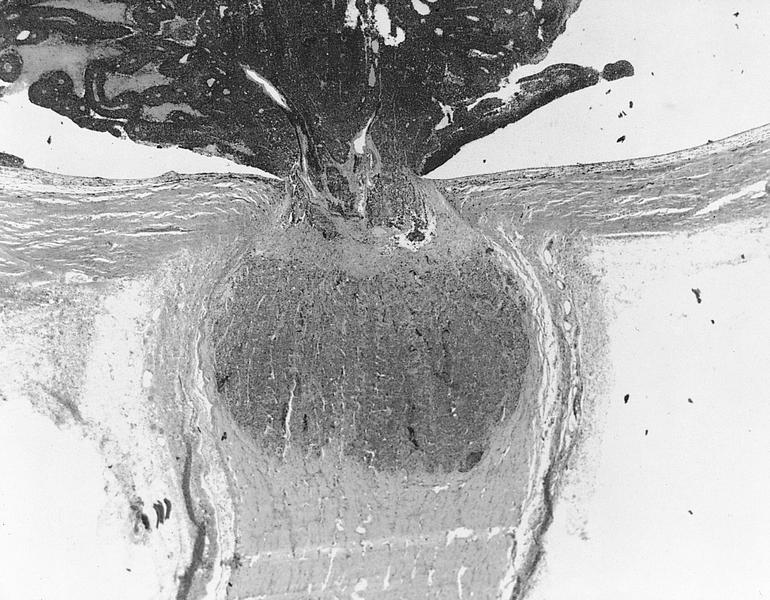
Gross description
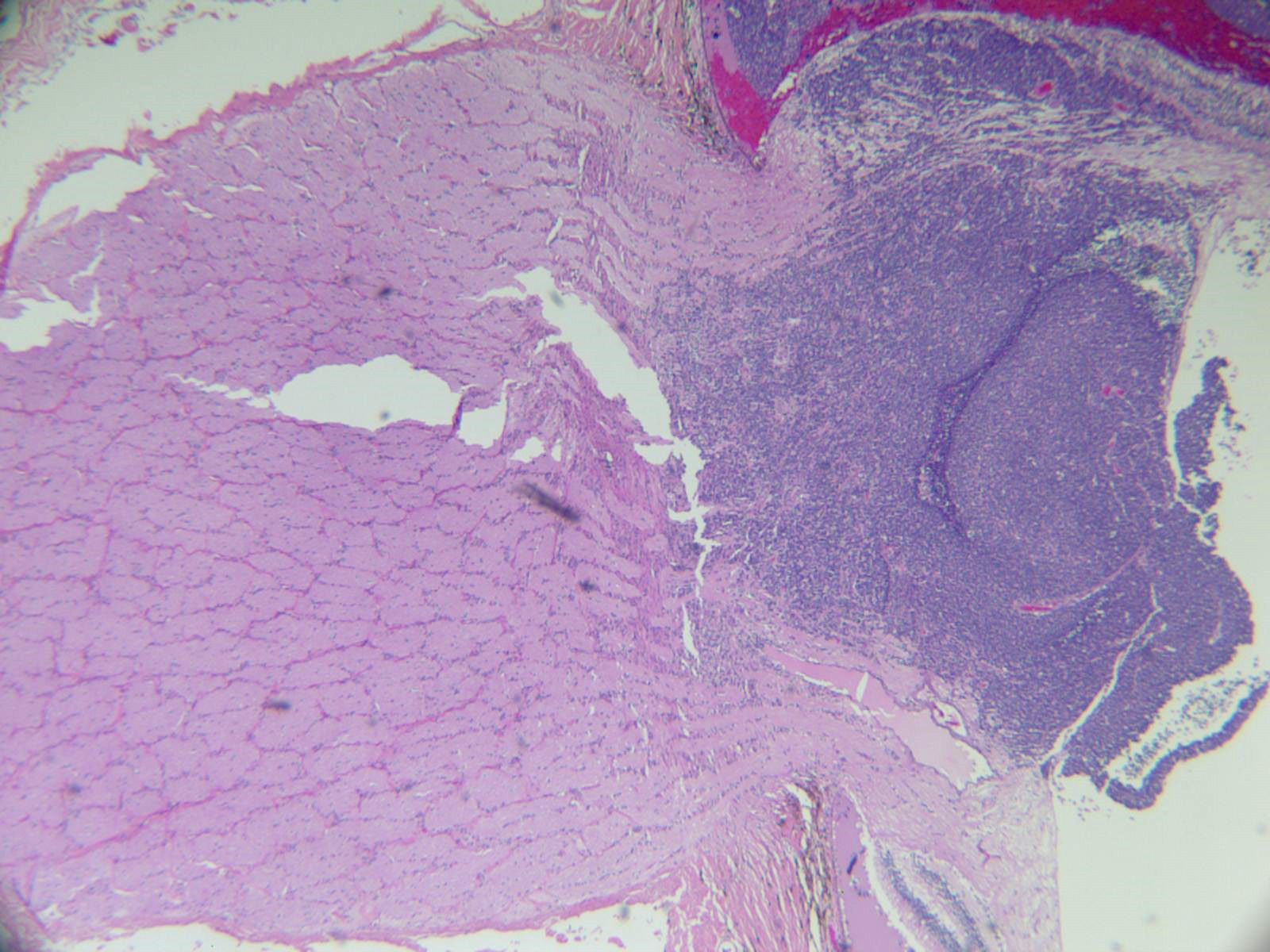
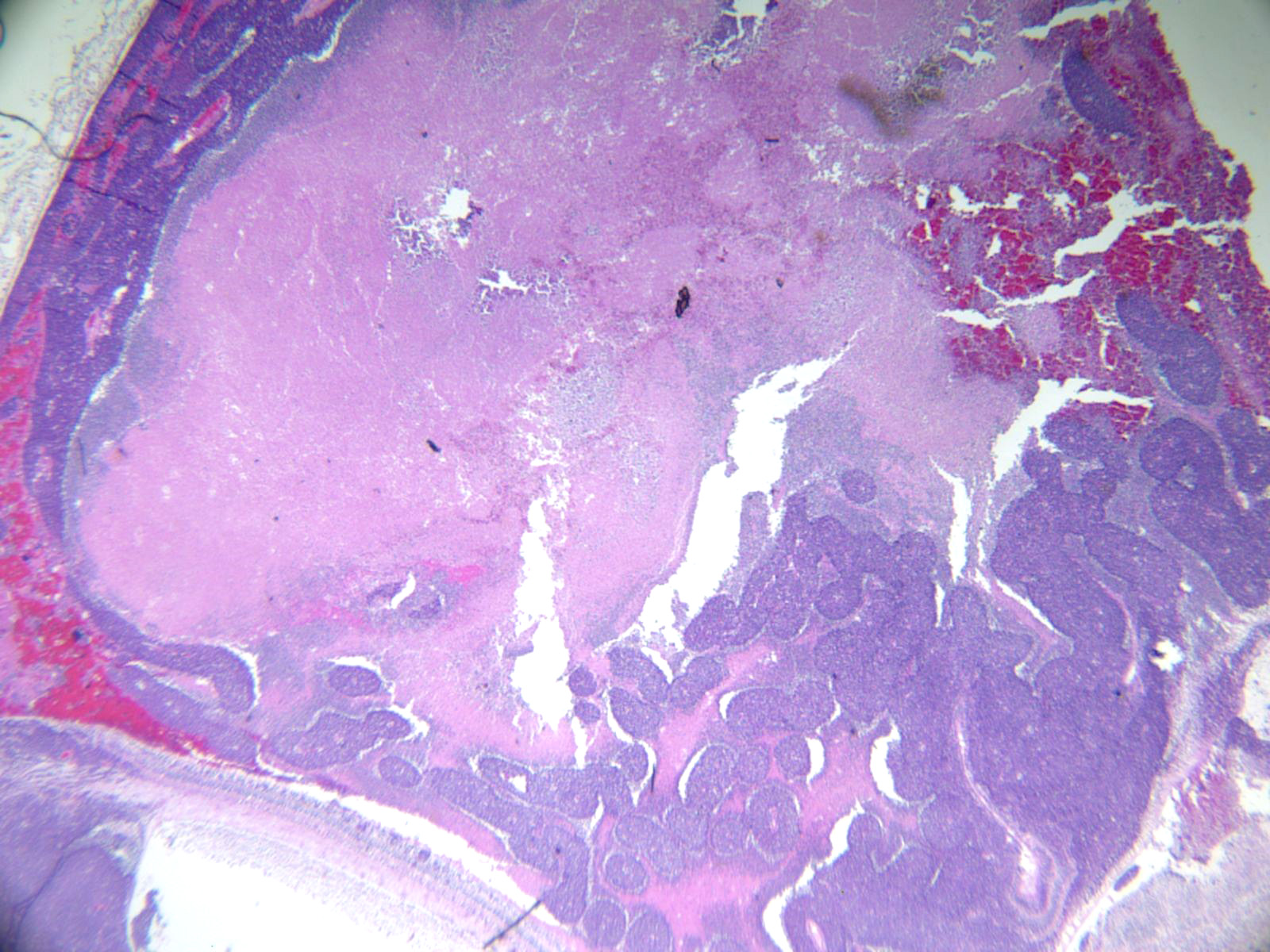
- Creamy white with chalky areas of calcification and yellow necrotic areas
- May grow inward (endophytic) or outward toward choroid (exophytic)
- Rarely are diffusely infiltrative; typically seeds intraocularly
- References: Int J Ophthalmol 2018;11:2011, Turk Patoloji Derg 2015;31:45
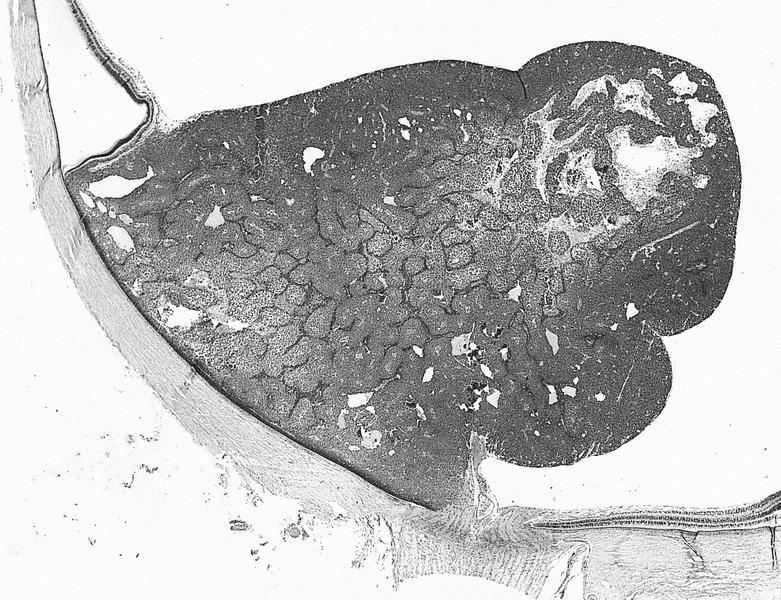
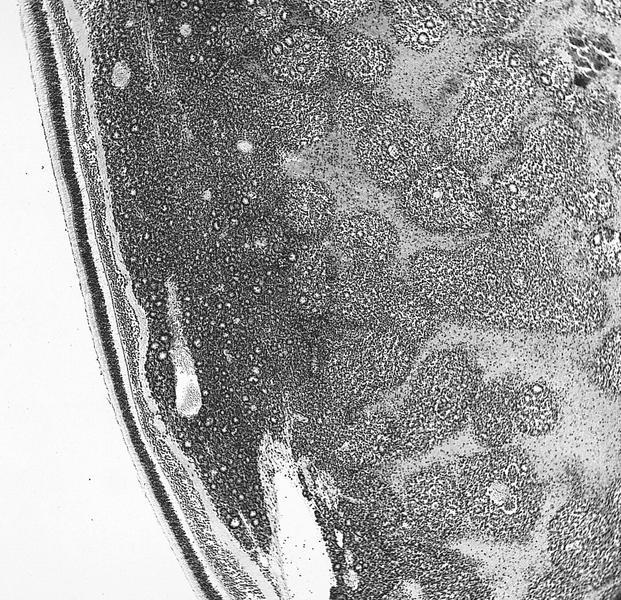
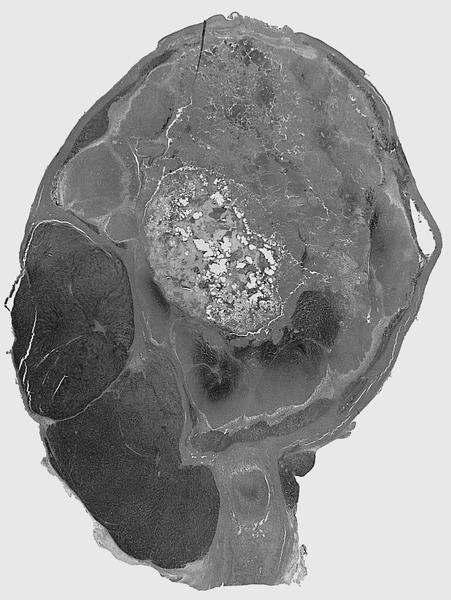
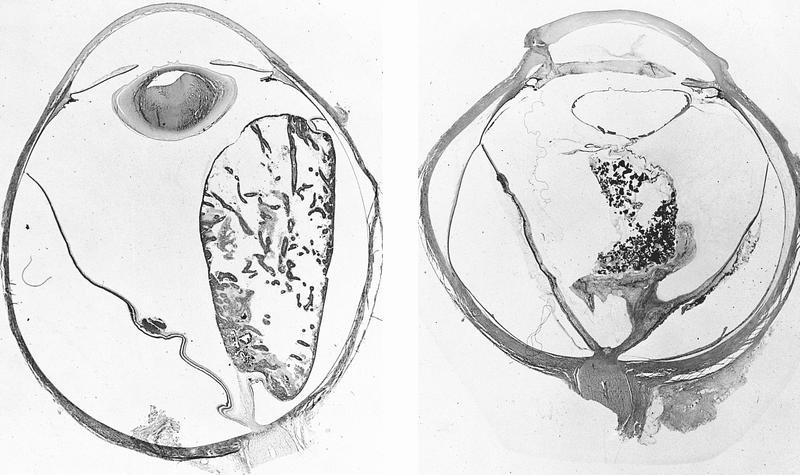
Gross images
Contributed by Marta Couce, M.D., Ph.D. and AFIP images
Frozen section description
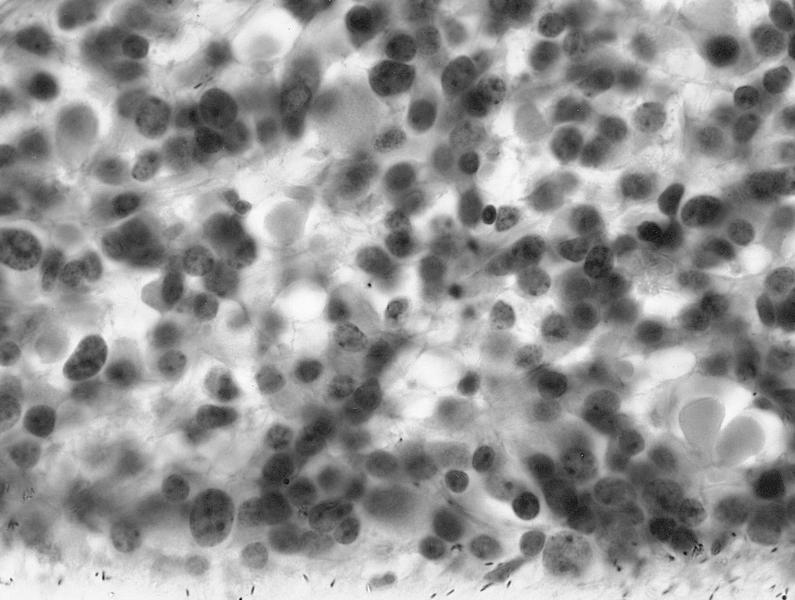
- Cluster of partially crushed, small round blue cells
- Touch prep helpful in evaluating optic nerve margin
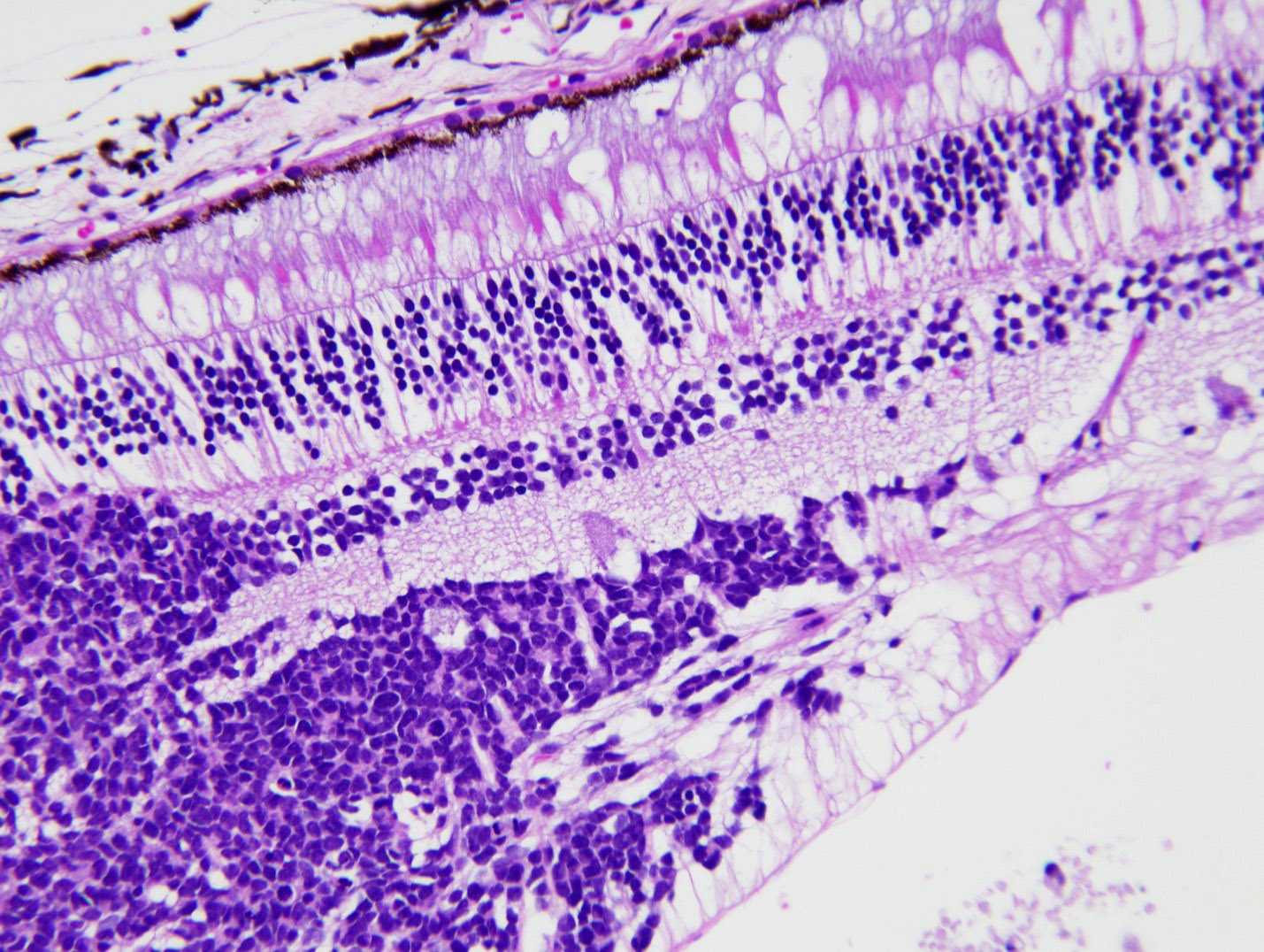
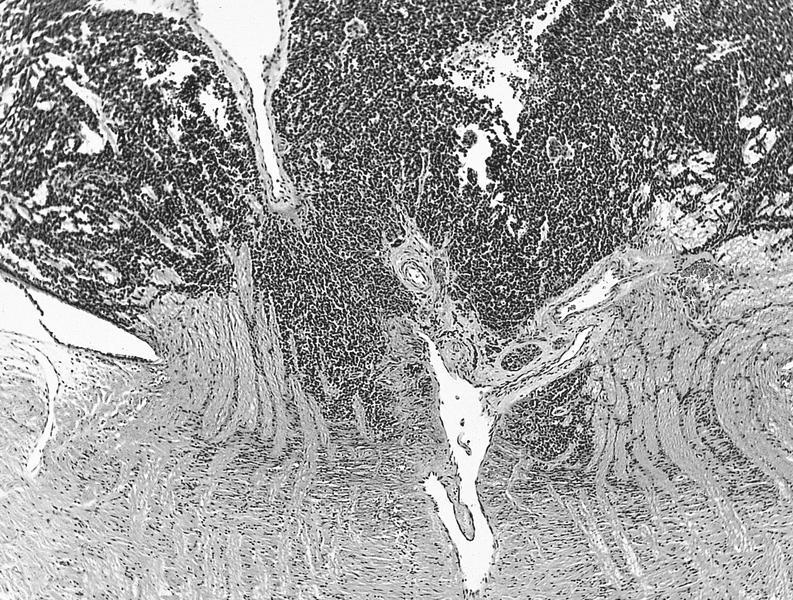
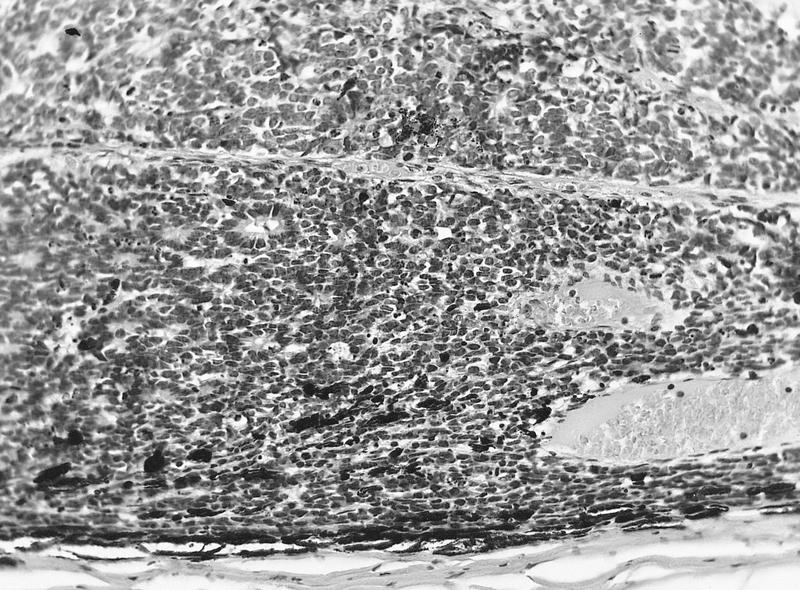
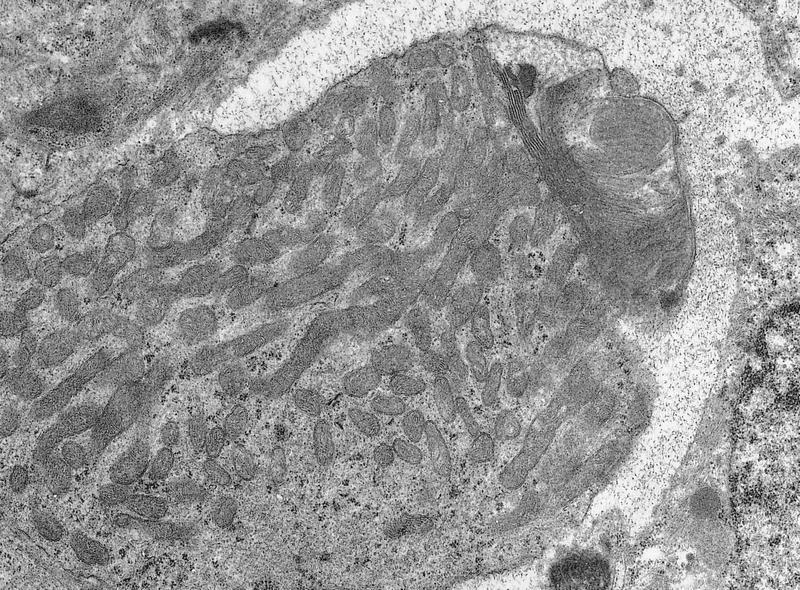
Microscopic (histologic) description
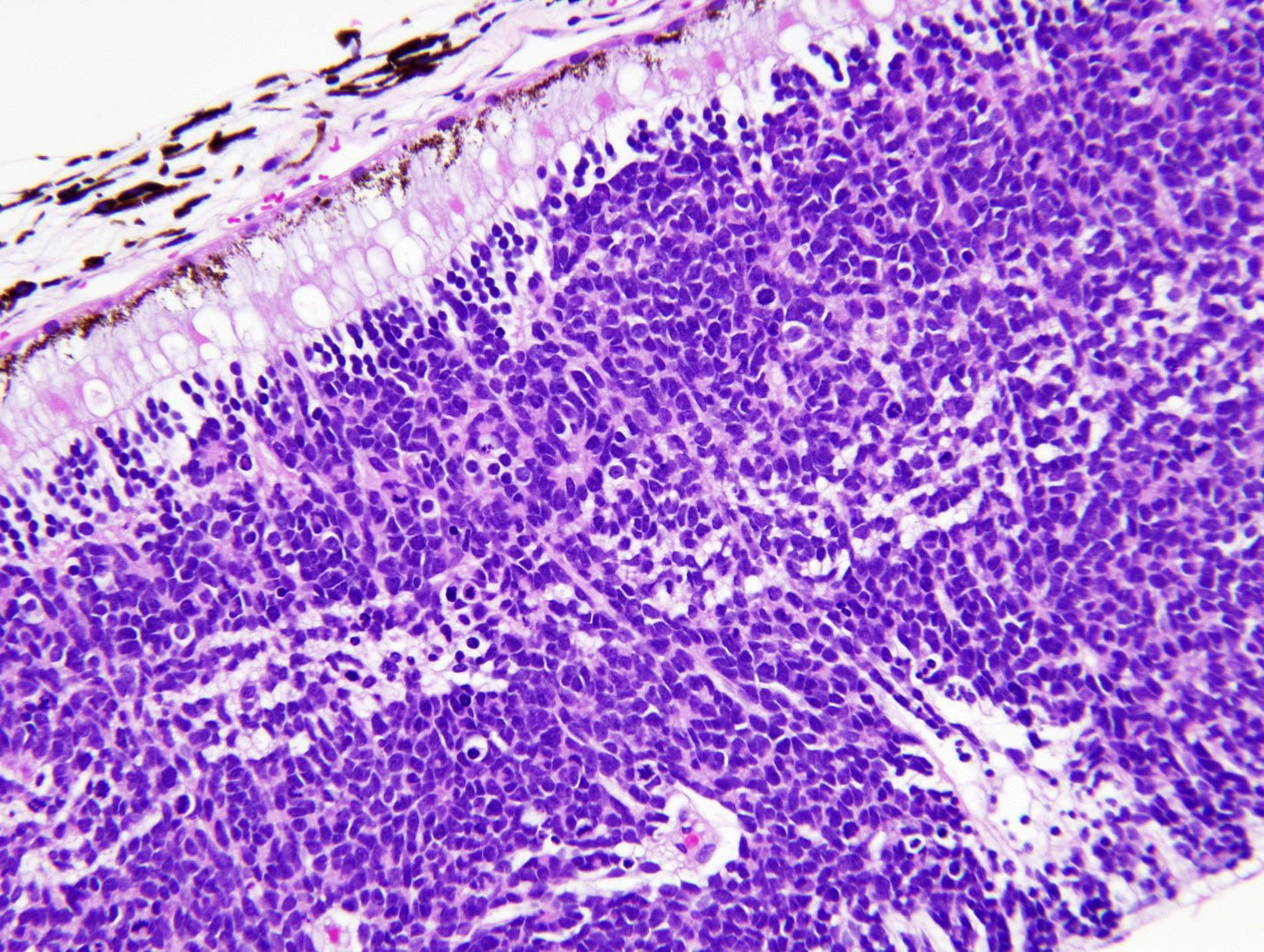
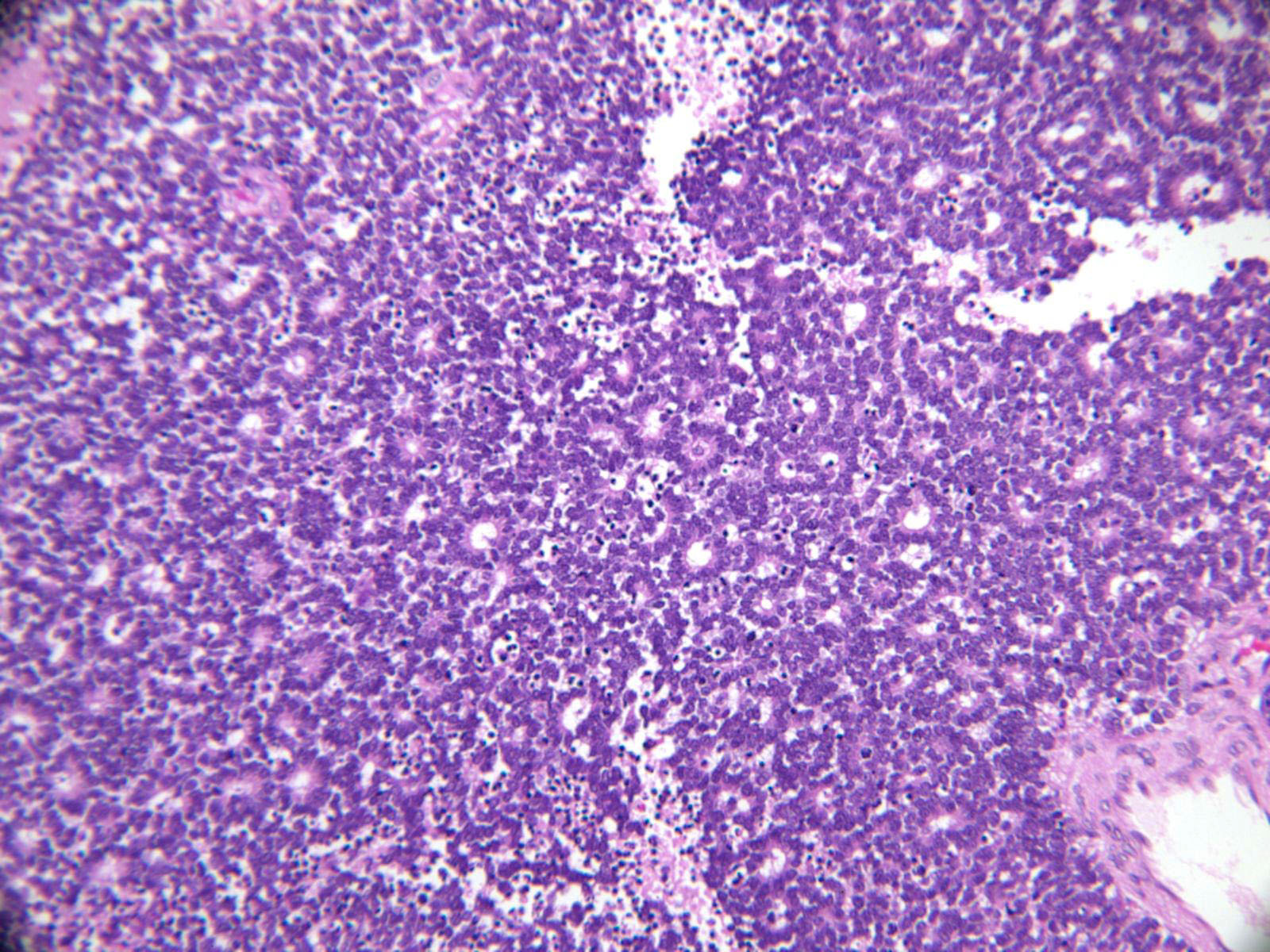
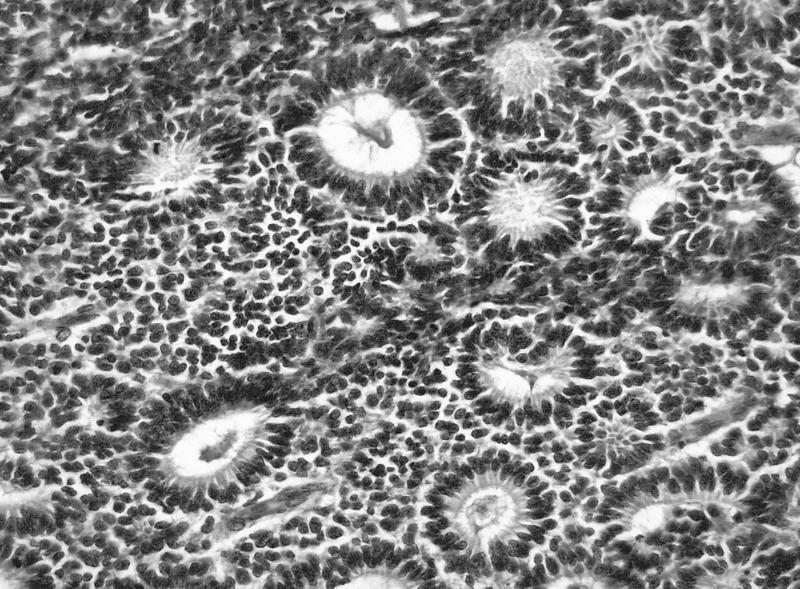
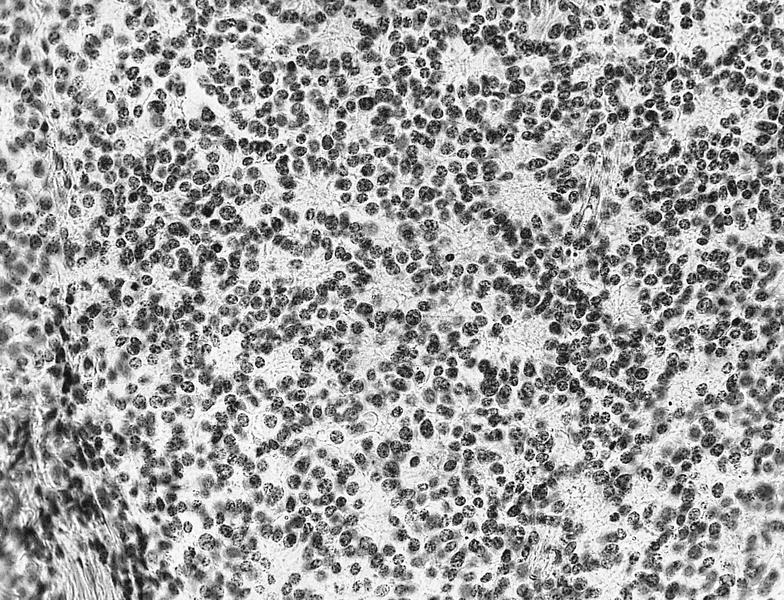
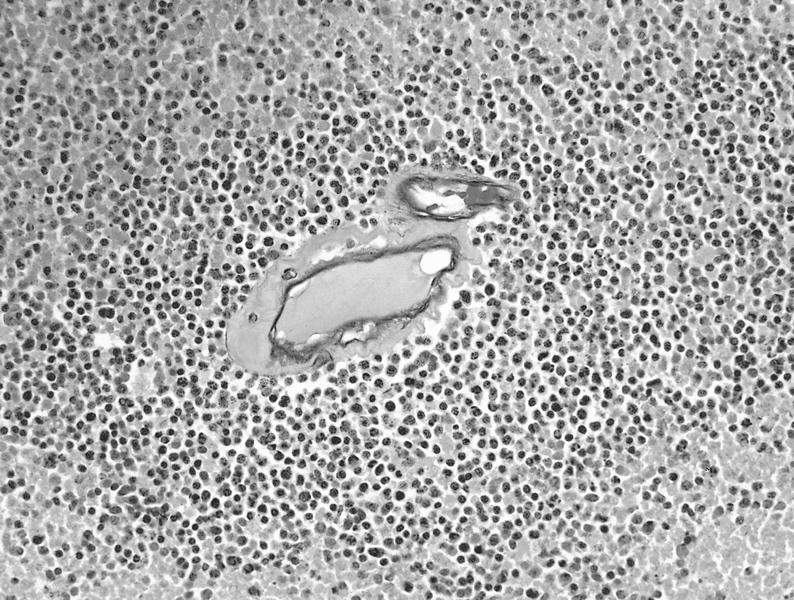
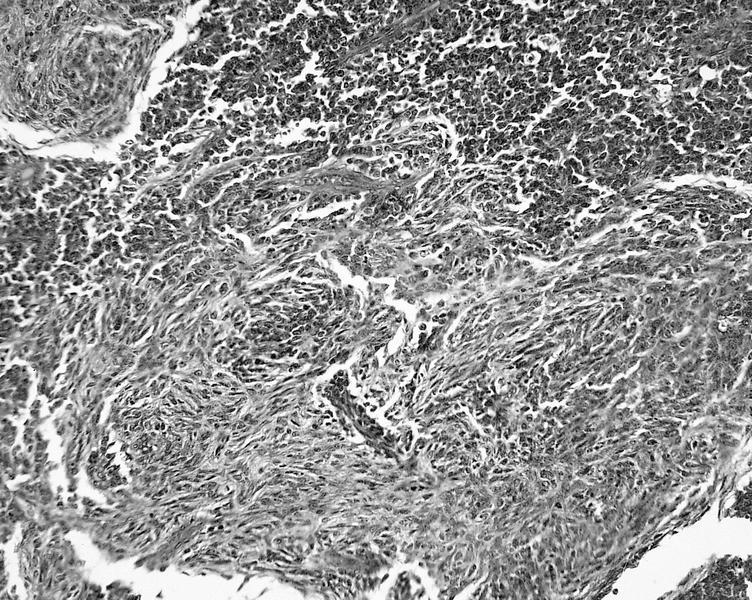
- Hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests and trabeculae (Ophthalmology 2012;119:850)
- Variable differentiation
- Calcification and perivascular ischemic necrosis common
- Flexner-Wintersteiner rosettes (most common)
- Central lumen with basally located nuclei
- Analogous to outer limiting membrane of normal retina
- Homer Wright rosettes (less common in retinoblastoma)
- Lack of central lumen
- Tumor nuclei displaced away from eosinophilic center
- Fleurettes
- Tumor cells arranged side by side with central lumen
- Resembles fleur de lis
- Tumor cells arranged side by side with central lumen
- Photoreceptor differentiation
- Histological high risk features (tumor involving any of the following structures) (Community Eye Health 2018;31:17)
- Anterior chamber
- Iris
- Trabecular meshwork
- Schlemm canal
- Ciliary body
- Choroid
- Sclera
- Extraocular structures
- Retrolaminar optic nerve
- Histologic grade:
- G1: tumor with areas of retinocytoma (fleurettes or neuronal differentiation accounting for more than half of tumor)
- G2: tumor with many rosettes, Flexner-Wintersteiner or Homer Wright rosettes accounting for more than half of tumor
- G3: tumor with occasional rosettes, Flexner-Wintersteiner or Homer Wright rosettes accounting for less than half of tumor
- G4: tumor with poorly differentiated cells without rosettes or with extensive areas of anaplasia
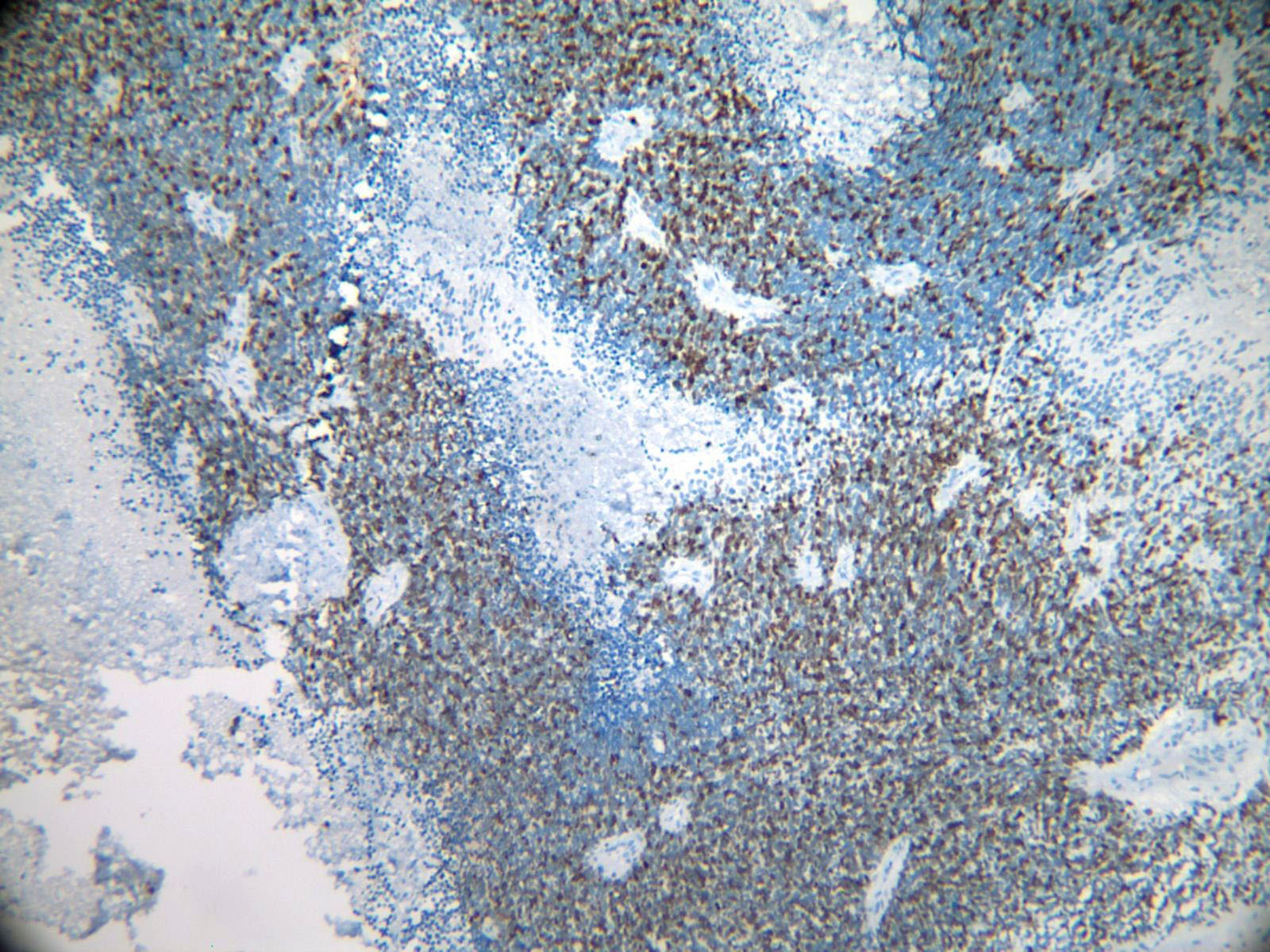
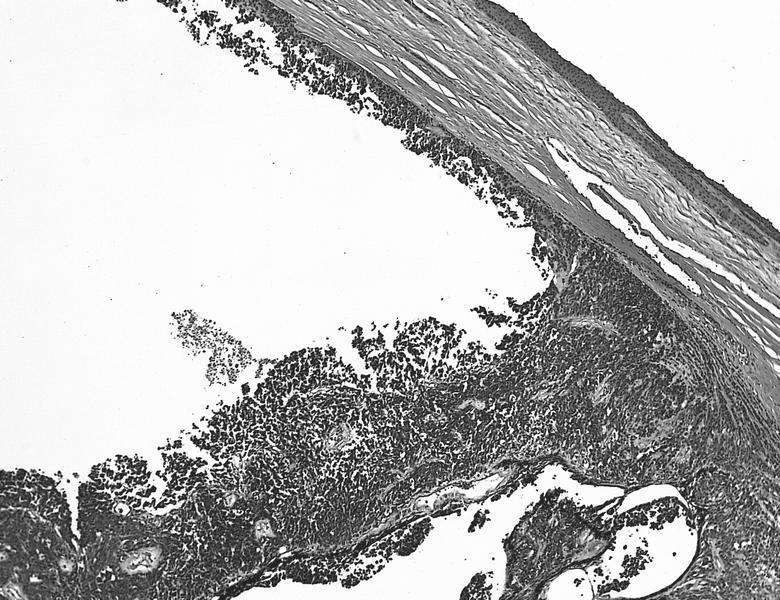
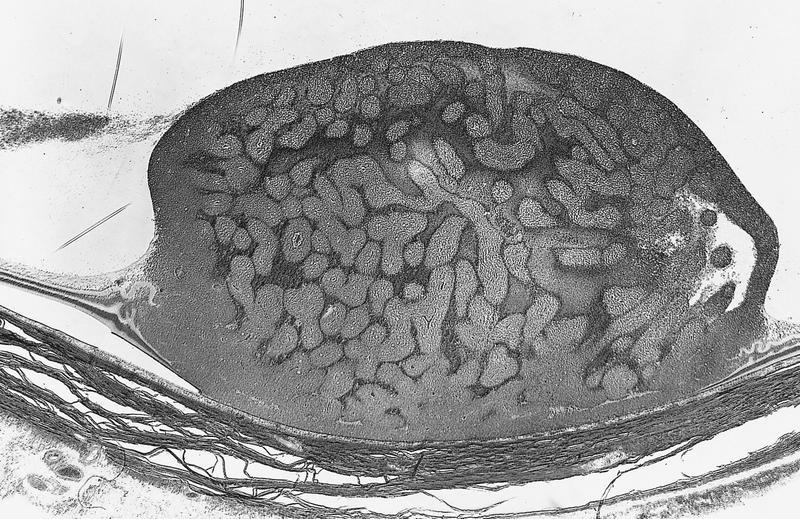
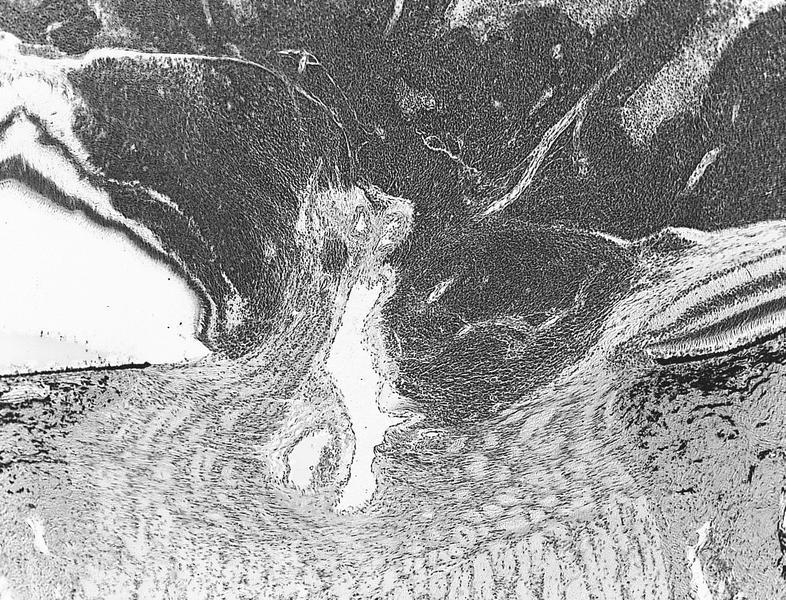
Microscopic (histologic) images
Contributed by Marta Couce, M.D., Ph.D.
AFIP images
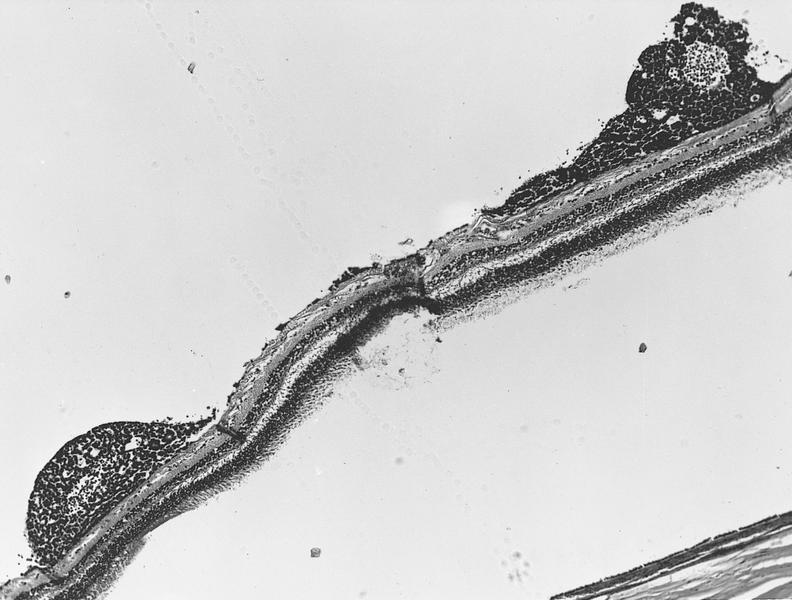
Whole mount images
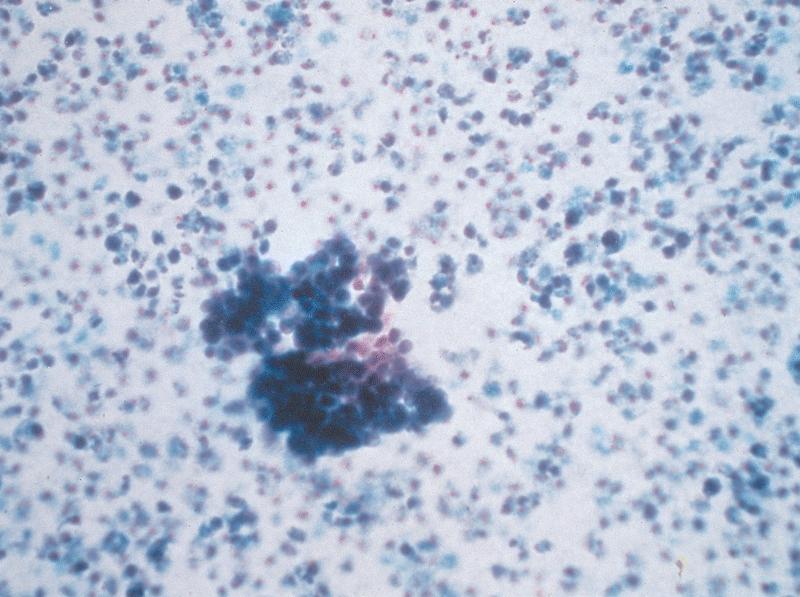
Cytology description
- Variably cellular
- Small round cells with scant cytoplasm
- Clusters and rosettes
- PAS positive granules
- Must have mitosis and apoptosis
- Reference: J Cytol 2018;35:120
Cytology images
Positive stains
Negative stains
Molecular / cytogenetics description
- Recurrent chromosomal abnormalities (Annu Rev Pathol 2015;10:547)
- Isochromosome 6p (45%)
- E2F3 and DEK genes
- Gain of regions of chromosome 1q (44%)
- zsKIF14 and MDM4 genes
- Monosomy 16 (18%)
- CDH11 gene
- Gain of 1p (13%)
- Less common - loss of sex chromosomes and alterations in 17 and 19
- Isochromosome 6p (45%)
- Whole genome sequencing revealed recurrent BCOR mutations in 13% of retinoblastomas (Nature 2012;481:329)
- Sonic hedgehog signaling proteins (J Clin Pathol 2015;68:6)
- SHH (98.7%), GLI1 (85.9%) and GLI2 (92.2%) frequently expressed in retinoblastoma
- 26.6% of 79 cases had strong SHH expression
- High SHH expression closely related to advanced disease
- SHH (98.7%), GLI1 (85.9%) and GLI2 (92.2%) frequently expressed in retinoblastoma
- Non-RB1 mutated retinoblastomas (2.7%)
- Vast majority MYCN mutated
- Also has role in controlled E2F1, E2F2 and E2F3 genes
- Frequent gain of 19p, 17p/q and 2p and telomeric end of 9q
- Very small percentage have RB1 inactivated by chromothriptic event in chromosome 13
- Vast majority MYCN mutated
Sample pathology report
- Eye, right, enucleation:
- Retinoblastoma (follow College of American Pathologists: Protocol for the Examination of Specimens From Patients With Retinoblastoma [Accessed 11 October 2021])
- Case summary: retinoblastoma
- AJCC-UICC 8
- Case summary report
- No known preoperative therapy
- Procedure
- Enucleation
- Total length of optic nerve
- Less than 1 mm
- Tumor sampling for molecular studies
- Yes
- Specimen laterality
- Right
- Tumor
- Tumor site (macroscopic examination / transillumination)
- Superotemporal quadrant of globe
- Tumor site after sectioning
- Superotemporal
- Tumor size after sectioning
- Greatest basal diameter of tumor
- Exact measurement: 6 mm
- Basal diameter at cut edge of tumor
- Exact measurement: 2 mm
- Greatest thickness of tumor
- Exact measurement: 3 mm
- Percentage of vitreous cavity occupied by tumor
- Specify percentage: 15%
- Distance from anterior edge of tumor to limbus at cut edge
- Exact distance: 7 mm
- Distance from posterior margin of tumor base to edge of optic disc
- Exact distance: 6 mm
- Greatest basal diameter of tumor
- Tumor growth pattern
- Exophytic
- Histologic grade
- G2 (tumor with many rosettes [Flexner-Wintersteiner or Homer Wright rosettes accounting for more than half of tumor])
- Anaplasia grade
- Mild
- Histopathologic features suggesting MYCN amplification
- Not identified
- Extent of optic nerve invasion
- None identified
- Tumor site (macroscopic examination / transillumination)
- Margins
- Margin status (select all that apply)
- All margins negative for tumor
- Margin status (select all that apply)
- Regional lymph nodes
- Regional lymph node status
- Not applicable (no regional lymph nodes submitted or found)
- Regional lymph node status
- Pathologic stage classification (pTNM, AJCC 8th edition)
- TNM descriptors (select all that apply)
- Not applicable
- pT category
- pT1: intraocular tumor without any local invasion, focal choroidal invasion or prelaminar or intralaminar involvement of the optic nerve head
- pN category
- pN not assigned (no nodes submitted or found)
- pM category (required only if confirmed pathologically)
- Not applicable - pM cannot be determined from the submitted specimen(s)
- TNM descriptors (select all that apply)
Differential diagnosis
- Astrocytoma:
- Generally not small, round blue cell pattern
- GFAP positive
- Leukemia / lymphoma:
- Massive retinal gliosis:
- No rosettes or fleurettes
- No necrosis or calcifications
Board review style question #1
An 8 year old girl had an enucleation that showed a white, chalky intraocular tumor. A histologic image is shown above. Which of the following statements is true regarding this entity?
- Enucleation remains the best initial treatment
- Involvement of the optic nerve is not considered a significant prognostic factor
- Majority of these tumors have MYCN mutations
- Recommended initial treatment paradigm is chemoreduction
- Strabismus is never seen in patients with this tumor
Board review style answer #1
Board review style question #2
Retinoblastomas can occur both in sporadic and familial forms. Which of the following features is more indicative of a sporadic tumor?
- Bilateral retinoblastomas
- Development of subsequent melanoma or osteosarcoma
- Early age of onset
- Germline mutation of Rb gene
- Late age of onset
Board review style answer #2
E. Late age of onset. Familial tumors result from germline mutations in the Rb gene and are more likely to be bilateral or trilateral. They have an early age of onset and are prone to the development of other malignancies, including osteosarcoma, melanoma, sarcoma and breast cancer.
Comment Here
Reference: Retinoblastoma
Comment Here
Reference: Retinoblastoma