Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Patel P, Yeaney G. Acanthamoeba keratitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyecorneaacanthamoeba.html. Accessed April 19th, 2024.
Definition / general
- Rare, serious parasitic infection of the cornea occurring mostly in contact lens wearers
- Acanthamoeba are free living, ubiquitous protozoa found in soil and freshwater (tap water, hot tubs, swimming pools)
Essential features
- Clinically has a waxing and waning course and may be difficult to diagnose and treat
- Direct correlation with contact lens wearing or corneal trauma with exposure to soil or contaminated water (Parasite 2015:22:10)
- Microscopic features include ulceration, necrosis, heavy neutrophilic and macrophage infiltrates
- Encysted forms may be highlighted with PAS or GMS stains (Hum Pathol 2013;44:918)
Terminology
- Amebic keratitis
Epidemiology
- 85% of cases occur in contact lens wearers (CDC: Sources of Infection and Risk Factors [Accessed 17 November 2023])
- Risk factors include poor contact lens hygiene (e.g., wearing lenses overnight or during swimming / showering) and orthokeratology (specially fitted lenses) (J Clin Med 2021;10:942)
Sites
- Cornea, typically unilateral but can be bilateral (Am J Ophthalmol 2008;145:193)
- Sclera or conjunctiva
- In prolonged cases, chorioretinitis
Pathophysiology
- Breaching of the surface epithelium
- Keratocyte depletion by the invading trophozoites
- Neutrophilic inflammatory response
- Stromal necrosis (leukocytoclastic) (Br J Ophthalmol 1993;77:366, Pathogens 2021;10:323)
Etiology
- Direct correlation with contact lens wearing (Parasite 2015:22:10)
- Corneal trauma with exposure to soil or contaminated water (Parasite 2015:22:10, Folia Parasitol (Praha) 2003;50:97, J Infect Public Health 2023;16:841)
- Most common infectious species are Acanthamoeba castellani and Acanthamoeba polyphaga (Pathogens 2021;10:323)
Clinical features
- Waxing and waning course
- Classically severe pain disproportionate to the clinical picture (Br J Ophthalmol 1995;79:1078)
- However, can also be painless, leading to diagnostic uncertainties (Diagnostics (Basel) 2023;13:2655)
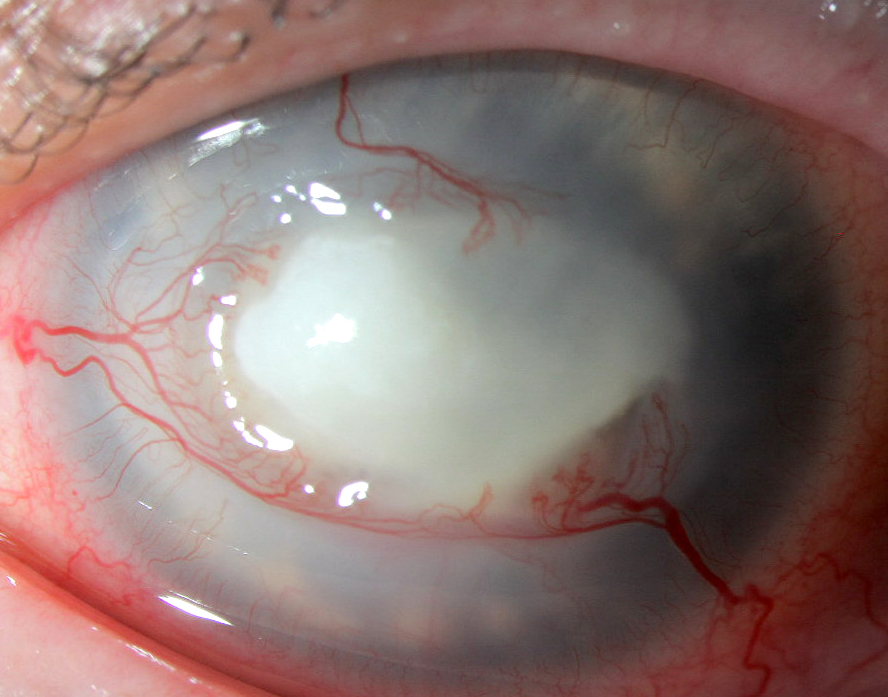
- Pattern of radial perineural infiltrates on ophthalmic exam (may lead to misdiagnosis as herpes simplex keratitis) (Br J Ophthalmol 1995;79:1078)
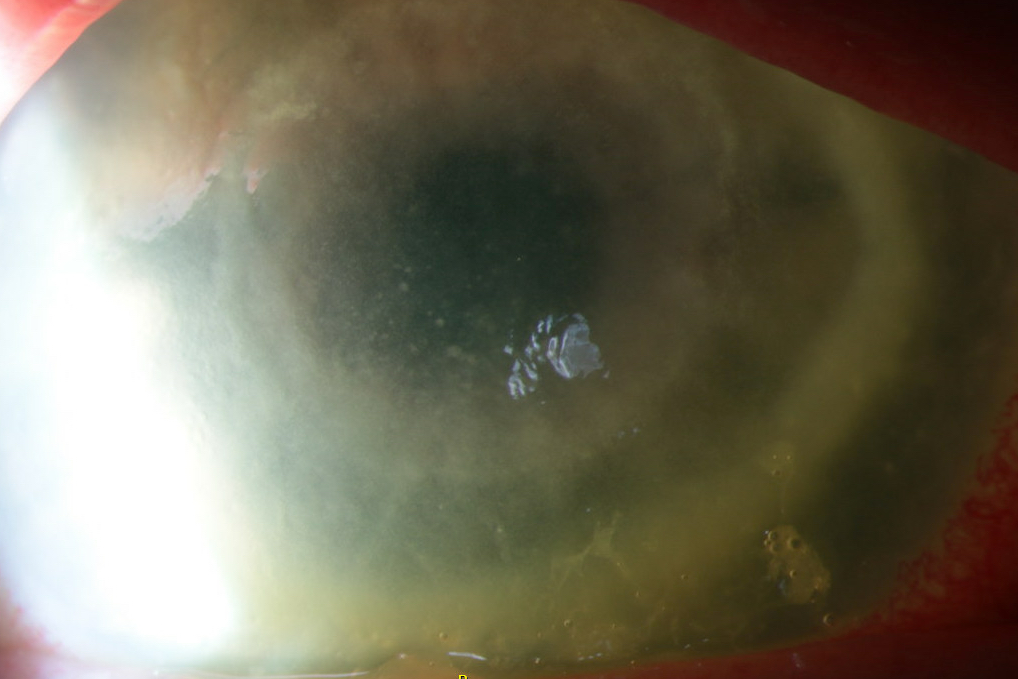
- Late: ring shaped stromal infiltrate and central ulcer on slit lamp exam (Diagnostics (Basel) 2023;13:2655)
Diagnosis
- Slit lamp examination with or without fluorescein application (Parasite 2015:22:10, J Infect Public Health 2023;16:841)
- Anterior segment optical coherence tomography (Diagnostics (Basel) 2023;13:2655)
- Corneal scraping for microbiological culture and PCR
- Note: culture may require up to 10 days of incubation, which can delay the diagnosis and treatment (Diagnostics (Basel) 2023;13:2655)
- Corneal biopsy following negative scrape
Laboratory
- Amoebic cyst walls identified by direct microscopy on calcofluor white (CFW) and potassium hydroxide (KOH) wet mount (Diagnostics (Basel) 2023;13:2655, J Infect Public Health 2023;16:841)
Prognostic factors
- Poor outcomes associated with both delayed diagnosis and the use of corticosteroids before therapy (Br J Ophthalmol 2018;102:1431)
- Older age is associated with worse outcome (Br J Ophthalmol 2018;102:1431)
Case reports
- 20 year old man with orthokeratology contact lenses, right eye pain and redness for 2 days and dendrite-like anterior stromal keratitis coinfected with Acanthamoeba and Pseudomonas (Taiwan J Ophthalmol 2019;9:131)
- 26 year old woman with history of immunocompetence and contact lens use presented with severe pain, photophobia, tearing and decreased visual acuity of her left eye for 2 months (Parasitol Res 2021;120:1121)
- 53 year old woman with contact lens use and a 2 month history of a persistent left corneal ulcer (Hum Pathol 2013;44:918)
- 65 year old man presented with a 10 year history of bilateral uveitis, scleritis and eventual complete loss of vision and severe pain in both eyes (bilateral enucleation) (Am J Ophthalmol Case Rep 2020:20:100970)
- 74 year old woman with history of extended soft contact lens use and intense painful ring corneal ulcer refractory to conventional antibiotics (Pathogens 2021;10:323)
- 76 year old man with rigid gas permeable lens use in the setting of keratoconus presented after a 4 month history of corneal ulcer of the left eye (BMJ Case Rep 2021;14:e241864)
Treatment
- Acanthamoeba trophozoite form is susceptible but the cystic form is highly drug resistant and may persist for months
- Principal initial treatment is topical biguanide, such as polyhexamethylene biguanide (PHMB) 0.02 - 0.08% or chlorhexidine 0.02 - 0.06% (J Clin Med 2021;10:942)
- PHMB 0.08% monotherapy (Ophthalmology 2023 Oct 4 [Epub ahead of print])
- In severe cases, therapeutic keratoplasty
Clinical images
Gross description
- Transparent to opacified / cloudy disc shaped tissue
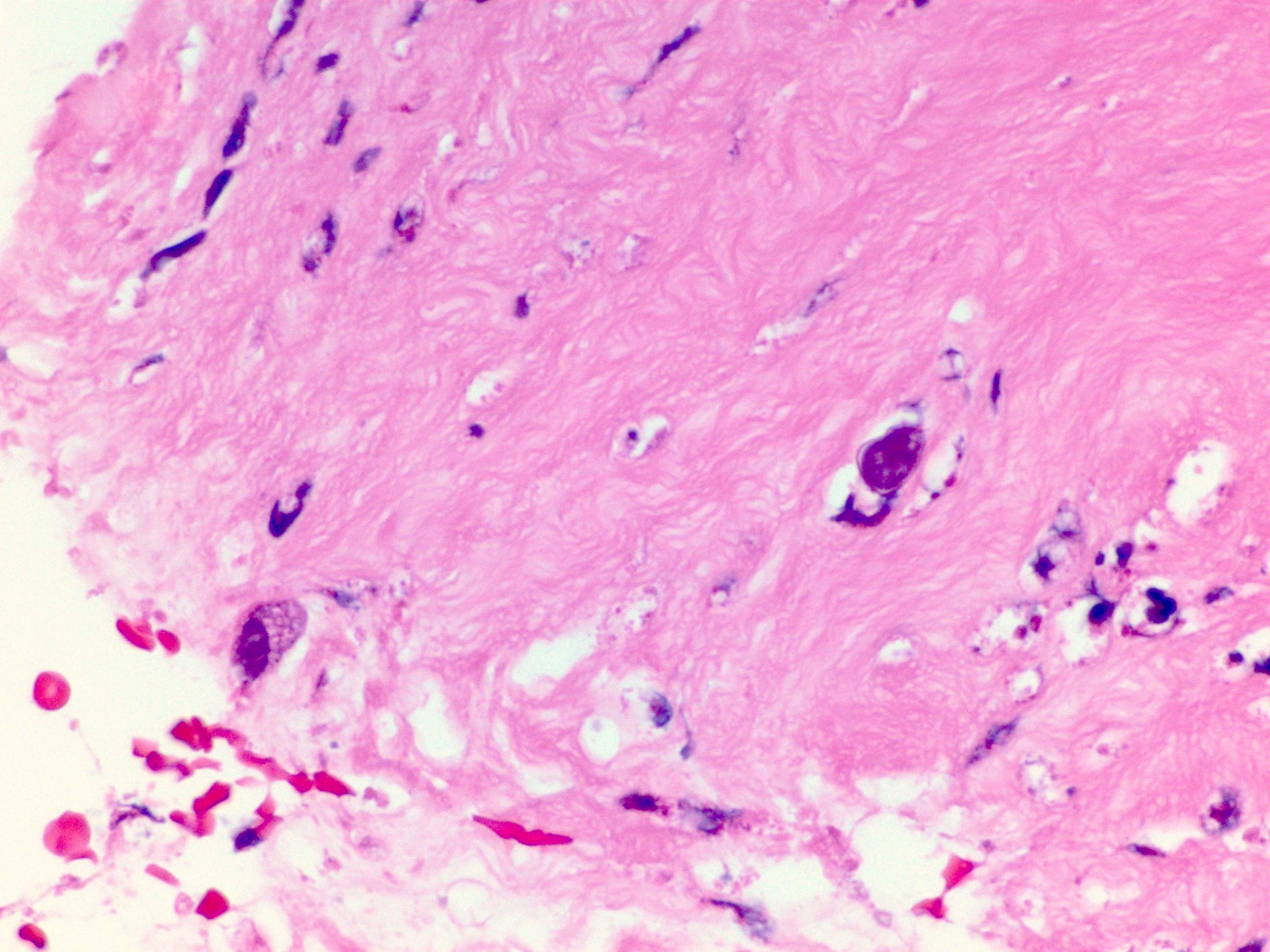
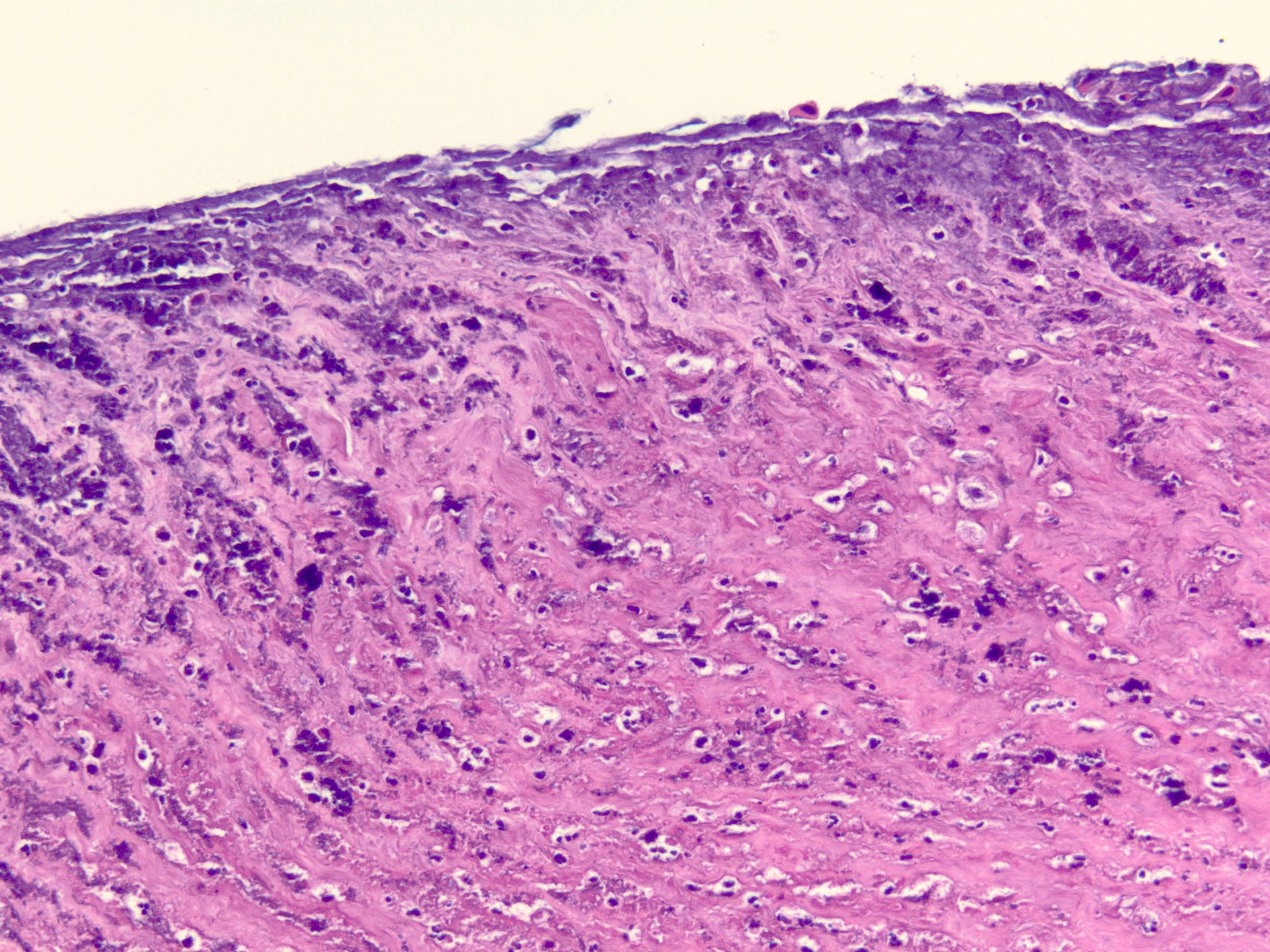
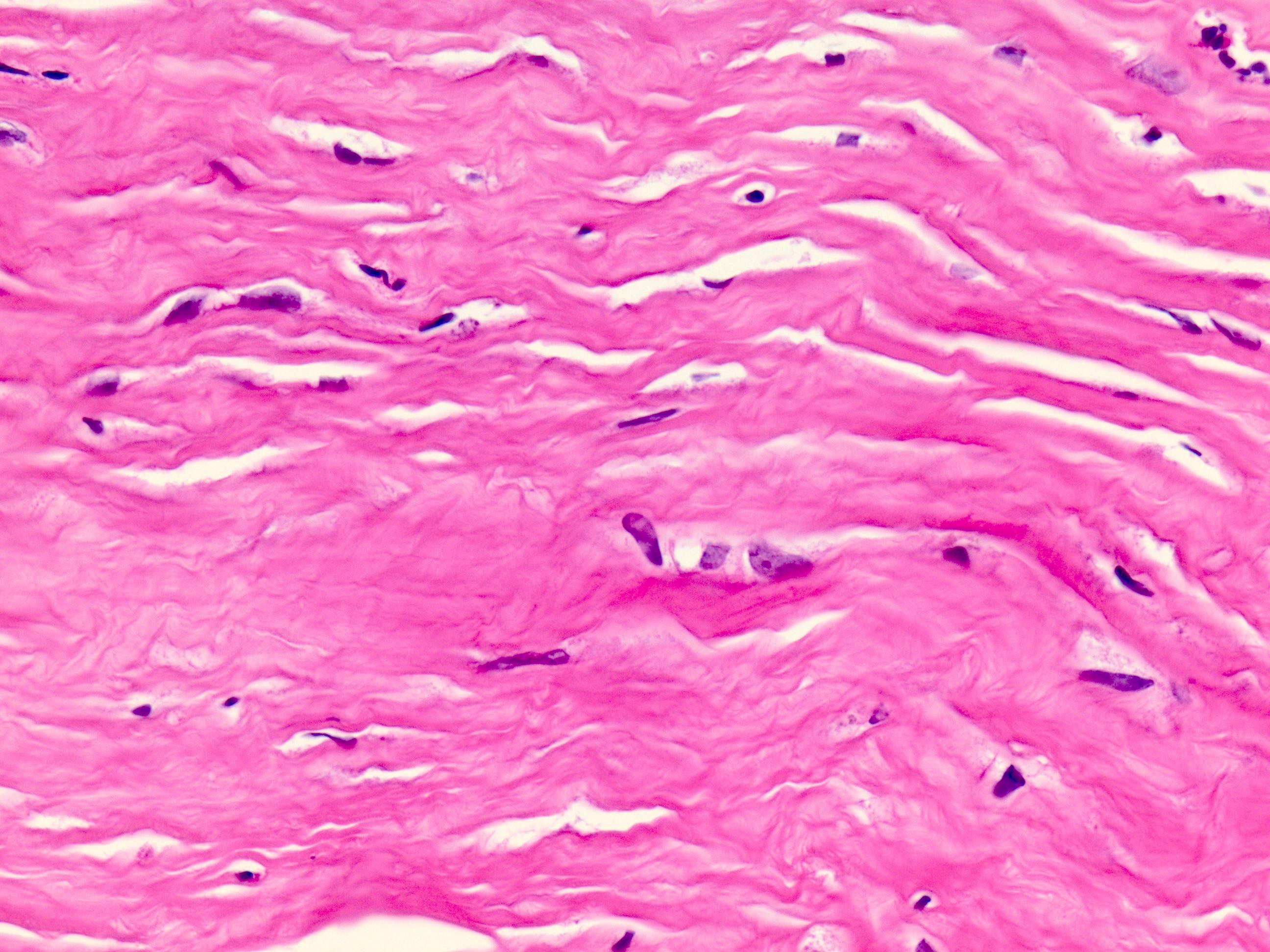
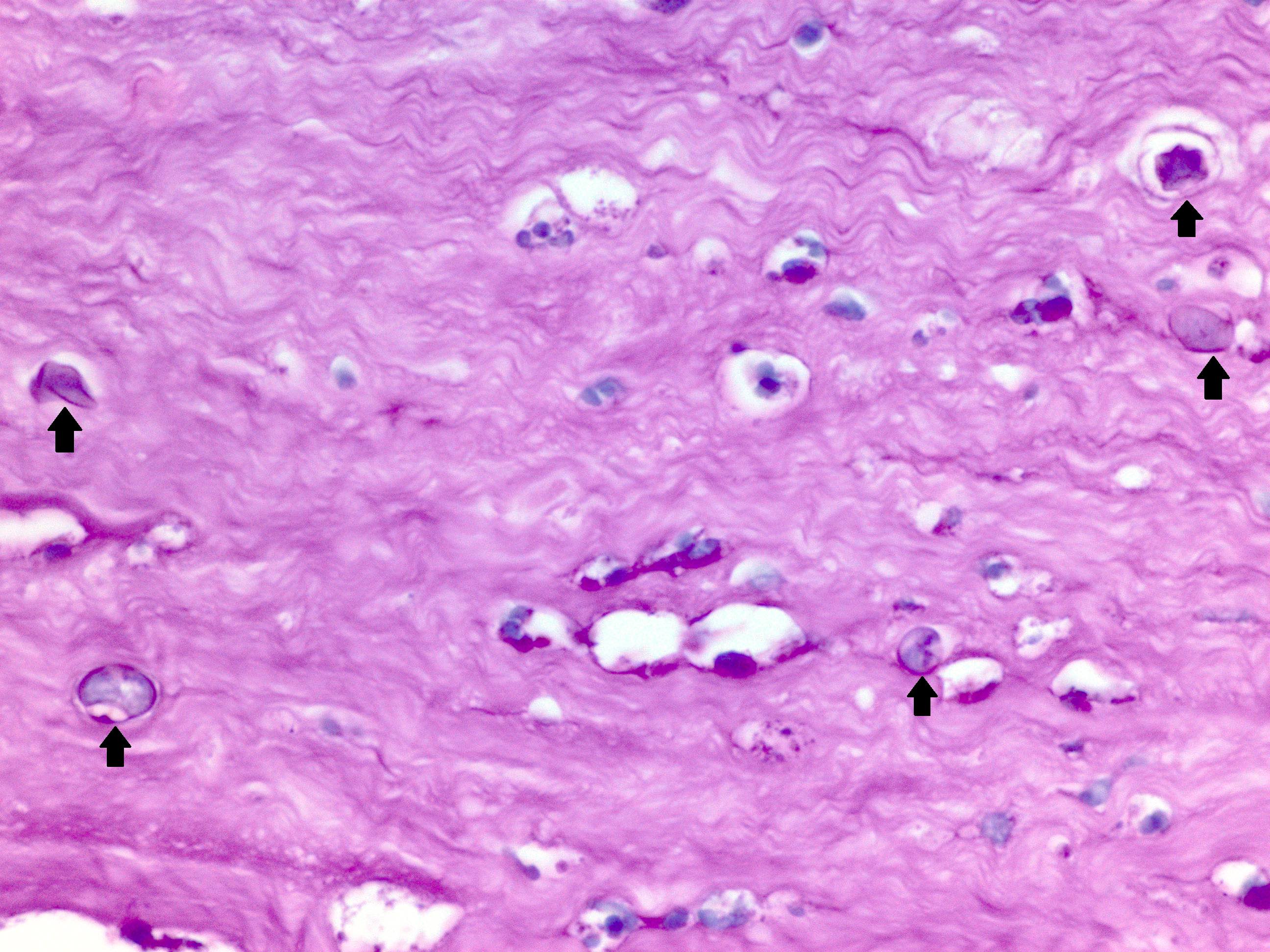
Microscopic (histologic) description
- Ulceration, necrosis, heavy neutrophil and macrophage infiltrates
- May have granulomatous inflammation
- Encysted forms
- Typically, absence of lymphocytes (Hum Pathol 2013;44:918)
Microscopic (histologic) images
Cytology description
- Impression cytology with double walled Acanthamoeba cysts and occasional trophozoites scattered among corneal epithelia (Pathogens 2021;10:323)
- Acanthamoeba cysts identified as unstained, hollow structures on Diff-Quik stain (Diagn Cytopathol 2023;51:98)
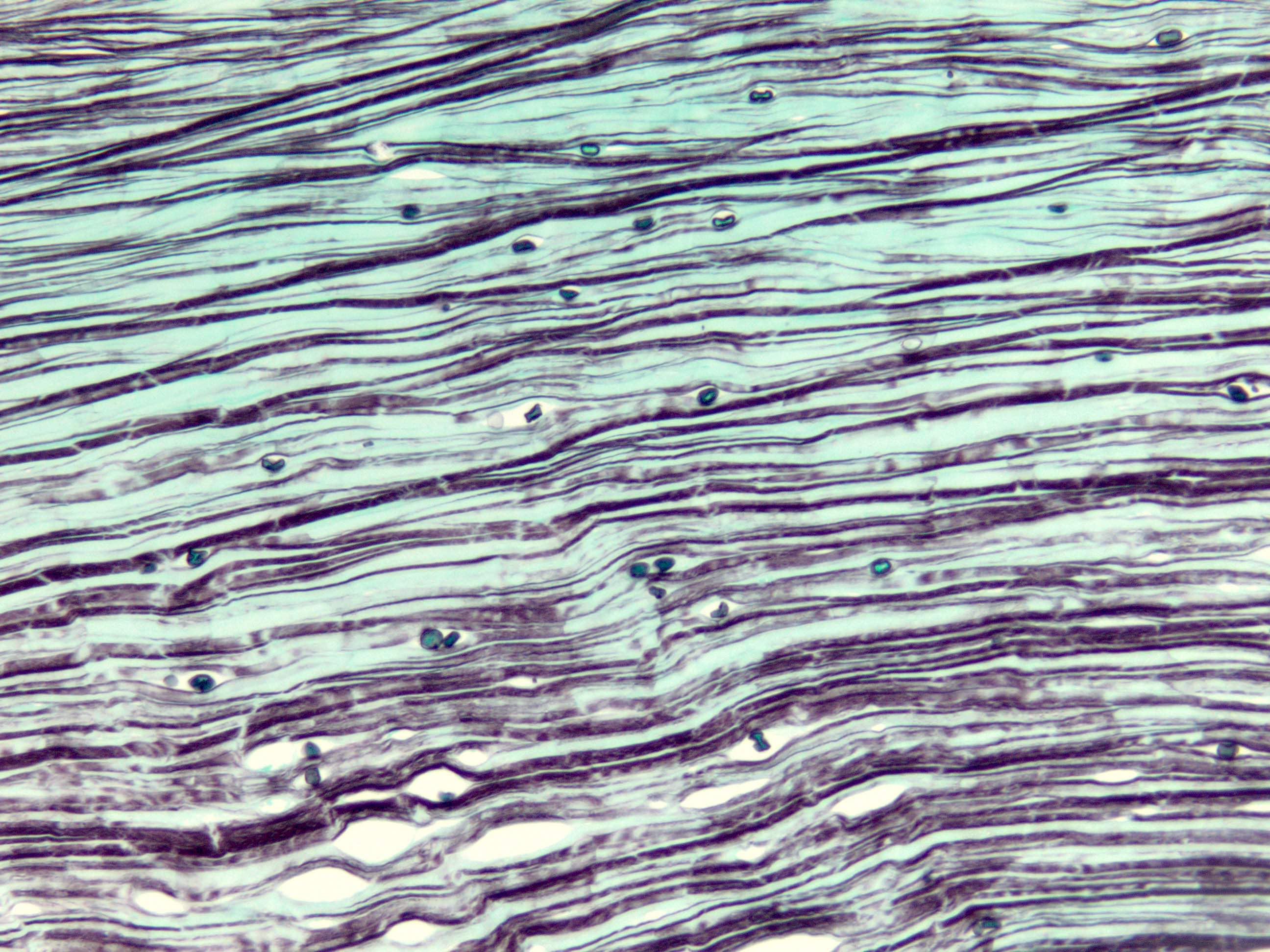
Positive stains
- GMS highlights walls of amoebic cysts (silver / black)
- PAS highlights walls of amoebic cysts
- Immunohistochemical stains for Acanthamoeba spp. exist but are not readily available in most clinical settings (Mod Pathol 2007;20:1230)
Negative stains
Electron microscopy description
- Typically for education / research rather than diagnosis: transmission electron micrograph showing an encysted Acanthamoeba organism with outer ectocyst layer, mitochondria, lipid vacuoles and lysosomes; adjacent neutrophils (Am J Ophthalmol 1987;103:626)
Videos
Clinical presentation of Acanthamoeba keratitis
Sample pathology report
- Eye, (side) cornea, biopsy or keratoplasty:
- Acanthamoeba keratitis (see comment)
- Comment: The cornea is ulcerated with necrosis and neutrophils. PAS and GMS stains highlight amoebic forms. PAS also highlights the Descemet membrane.
Differential diagnosis
- Herpetic keratitis:
- Ulceration, may or may not have Cowdry A intranuclear inclusions in corneal epithelium at edge of ulcer (may be IHC HSV1 / HSV2 positive)
- Lymphocytes, plasma cells, vascularization
- Multinucleated giant cells around Descemet membrane
- Mycotic (fungal) keratitis:
Board review style question #1
A 25 year old man with orthokeratology (specially fitted lenses) presents with severe pain in his left eye. The slit lamp examination shows a pattern of radial perineural and ring infiltrate in cornea. Corneal biopsy following negative direct smear examination on corneal scrapes shows focal ulceration of the surface with loss of epithelium; infiltrate of inflammatory cells, mainly polymorphonuclear cells and macrophages, are shown in the image above. What is the most likely diagnosis?
- Acanthamoeba keratitis
- Bacterial keratitis
- Herpetic keratitis
- Mycotic (fungal) keratitis
Board review style answer #1
A. Acanthamoeba keratitis. H&E sections at high power show several Acanthamoeba infiltrating corneal stroma in varying states of degeneration. Microscopic features on corneal biopsy also include ulceration, necrosis, neutrophilic and macrophage infiltrates; may show nonnecrotizing granulomatous inflammation. Encysted forms may be highlighted with PAS or GMS stains. Answer C is incorrect because a corneal biopsy for herpetic keratitis shows inflammatory infiltrates of mainly lymphocytes, plasma cells with stromal vascularization on H&E sections. Multinucleated giant cells around Descemet membrane are also identified. Answer D is incorrect because a corneal biopsy for mycotic (fungal) keratitis shows granulomatous, chronic nongranulomatous or rarely purulent inflammation on H&E sections; PAS or GMS positive for yeast or hyphal forms. Answer B is incorrect because microscopic findings of infiltration of the stroma by polymorphonuclear leukocytes occur in acute bacterial keratitis. The endothelium is often damaged and may have associated hypopyon and corneal perforation. Gram stain often shows bacteria in the stroma bordering the inflammatory infiltrate.
Comment Here
Reference: Acanthamoeba keratitis
Comment Here
Reference: Acanthamoeba keratitis
Board review style question #2
A 52 year old man who is a soft contact lens wearer presents with left eye pain and vision changes. Ophthalmic exam shows a ring shaped corneal stromal defect. Corneal biopsy reveals necrosis, neutrophilic infiltrates as shown in the image above. Which of the following is the best choice of stain to confirm the diagnosis?
- AFB Fite
- AFB Ziehl-Neelsen
- GMS
- Gram
- Mucicarmine
Board review style answer #2
C. GMS. GMS staining will highlight the encysted forms of amoeba in this description of Acanthamoeba keratitis. Answer A is incorrect because AFB Fite is used for Nocardia and would not stain amoebic forms. Answer B is incorrect because AFB Ziehl-Neelsen identifies acid fast organisms such as tuberculosis but would not stain amoebic forms. Answer D is incorrect because Gram stain is typically for bacterial organisms and would not be helpful in amoebic keratitis. Answer E is incorrect because mucicarmine is a stain for mucin and highlights cryptococcal forms, for example but is not helpful in this case of Acanthamoeba keratitis.
Comment Here
Reference: Acanthamoeba keratitis
Comment Here
Reference: Acanthamoeba keratitis