Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zoroquiain P. Chalazion. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyechalazion.html. Accessed April 26th, 2024.
Definition / general
- Very common, inflammatory eyelid lesion, characterized by granulomatous inflammation with lipogranulomas
- All specimens with tissue should be submitted to rule out malignant neoplasms and other masquerading conditions; most of the time they are not submitted
Essential features
- Very frequent inflammatory eyelid lesion
- More frequent in the upper eyelid
- Broad histopathological spectrum from acute to more chronic findings
- Lipogranulomas, suppurated granulomas, granulation tissue and fibrosing inflammation
- Can masquerade as neoplastic process
ICD coding
- ICD-10: H00.19 - chalazion unspecified eye, unspecified eyelid
Epidemiology
- More common in younger adults than in children, uncommon in late life
Sites
- Eyelid
Pathophysiology
- Probably due to obstruction or nonspecific inflammation (blepharitis) surrounding sebaceous gland ducts, leading to discharge of sebaceous material into surrounding tissue and resulting in intense foreign body granulomatous inflammatory reaction
- Superficial chalazion from Zeis gland
- Deep chalazion from Meibomian gland
- May erupt through conjunctival surface of eyelid (internal chalazion)
Etiology
- More significant: history of chalazion and blepharitis
- Less significant: rosacea, gastritis, anxiety and smoking (Cornea 2011;30:1376)
- There is no evidence that cosmetics in the eyelid causes, aggravates or protects from this condition
Clinical features
- Upper eyelid > lower eyelid
- Slowly growing mass with variability in size on a day to day basis
- Solitary, nontender nodule; eversion helps to identify the lesion
- Clinically may masquerade as sebaceous carcinoma and other neoplasms (Eye (Lond) 2004;18:135)
Diagnosis
- Typically suspected upon clinical examination
- Histologic examination of resected tissue can confirm the diagnosis
Treatment
- Medical treatment includes applying of heat and massage at least twice a day
- No benefit with antibacterial topical preparations except when infected (hordoleum) (BMJ 2010; 341 :c4044)
- Surgical management using incision and curettage is a second line of treatment
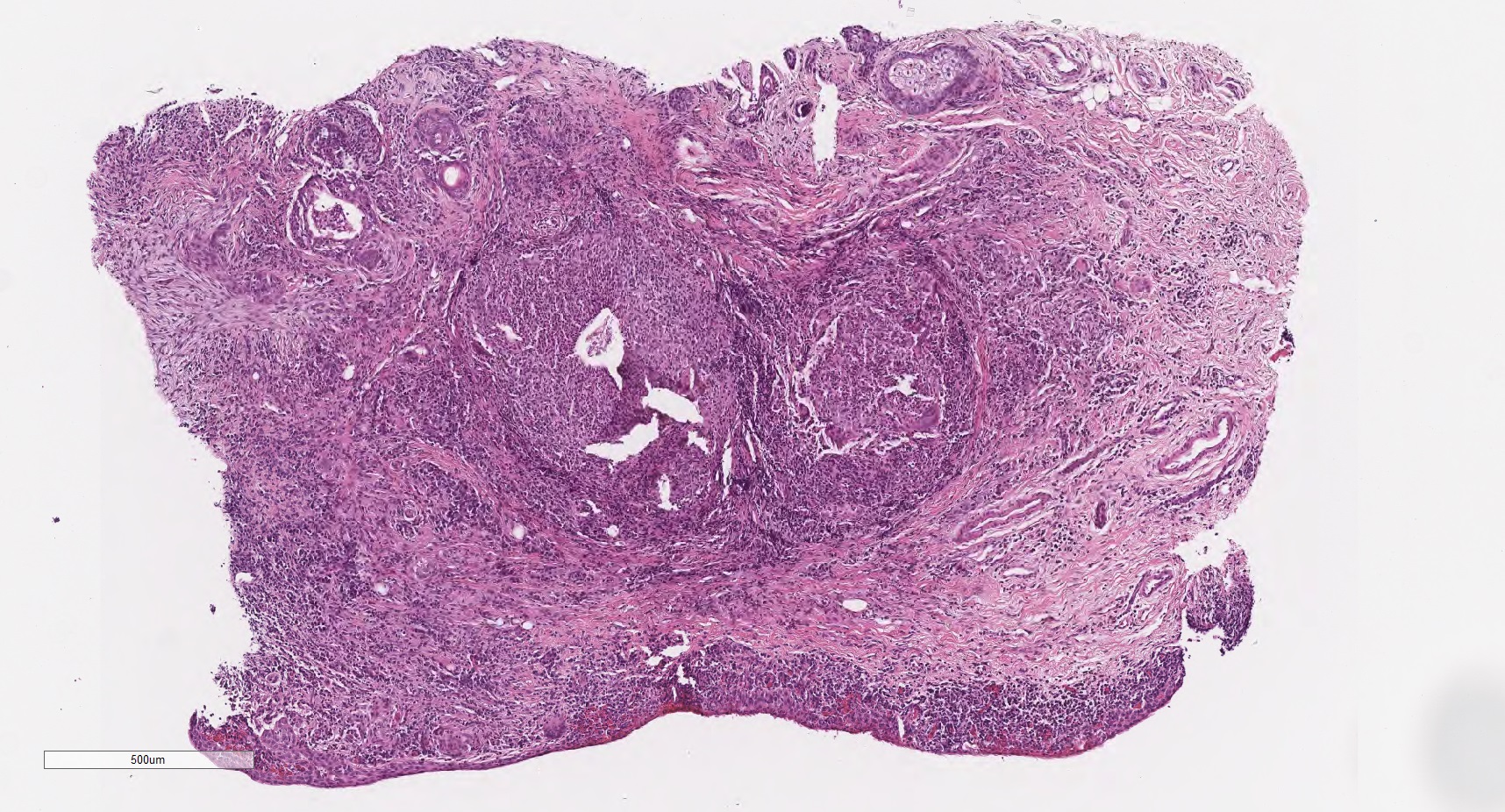
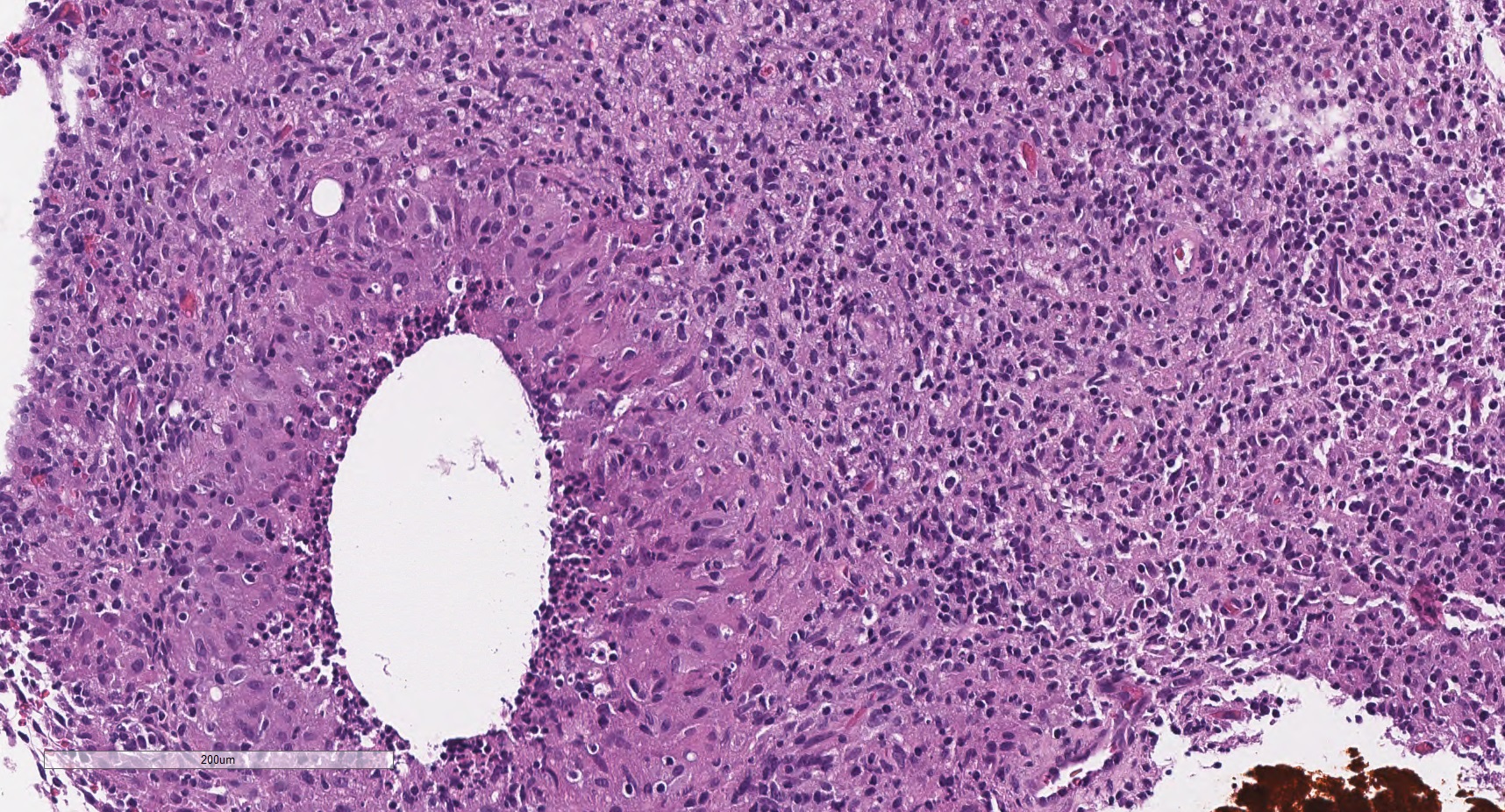
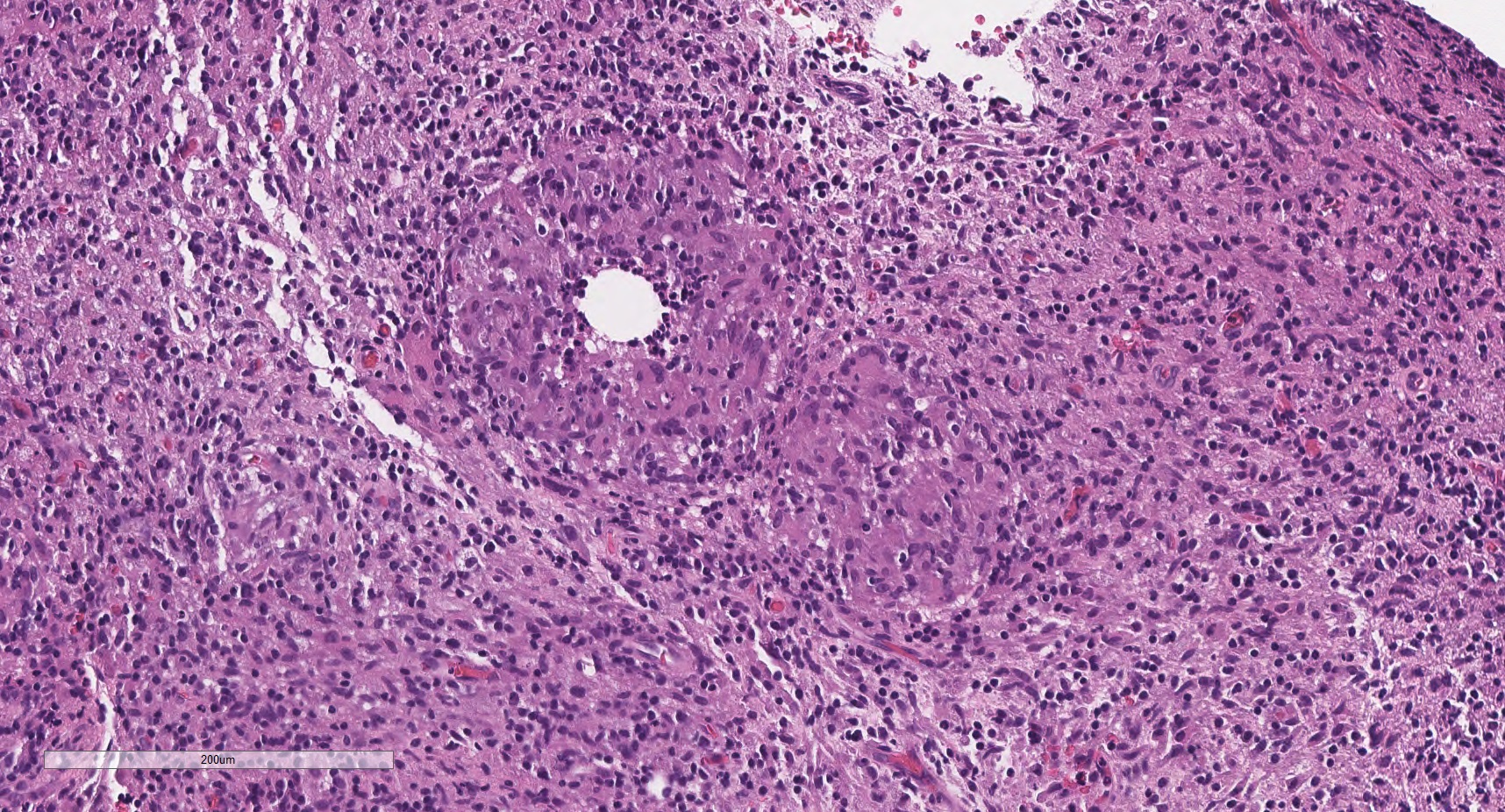
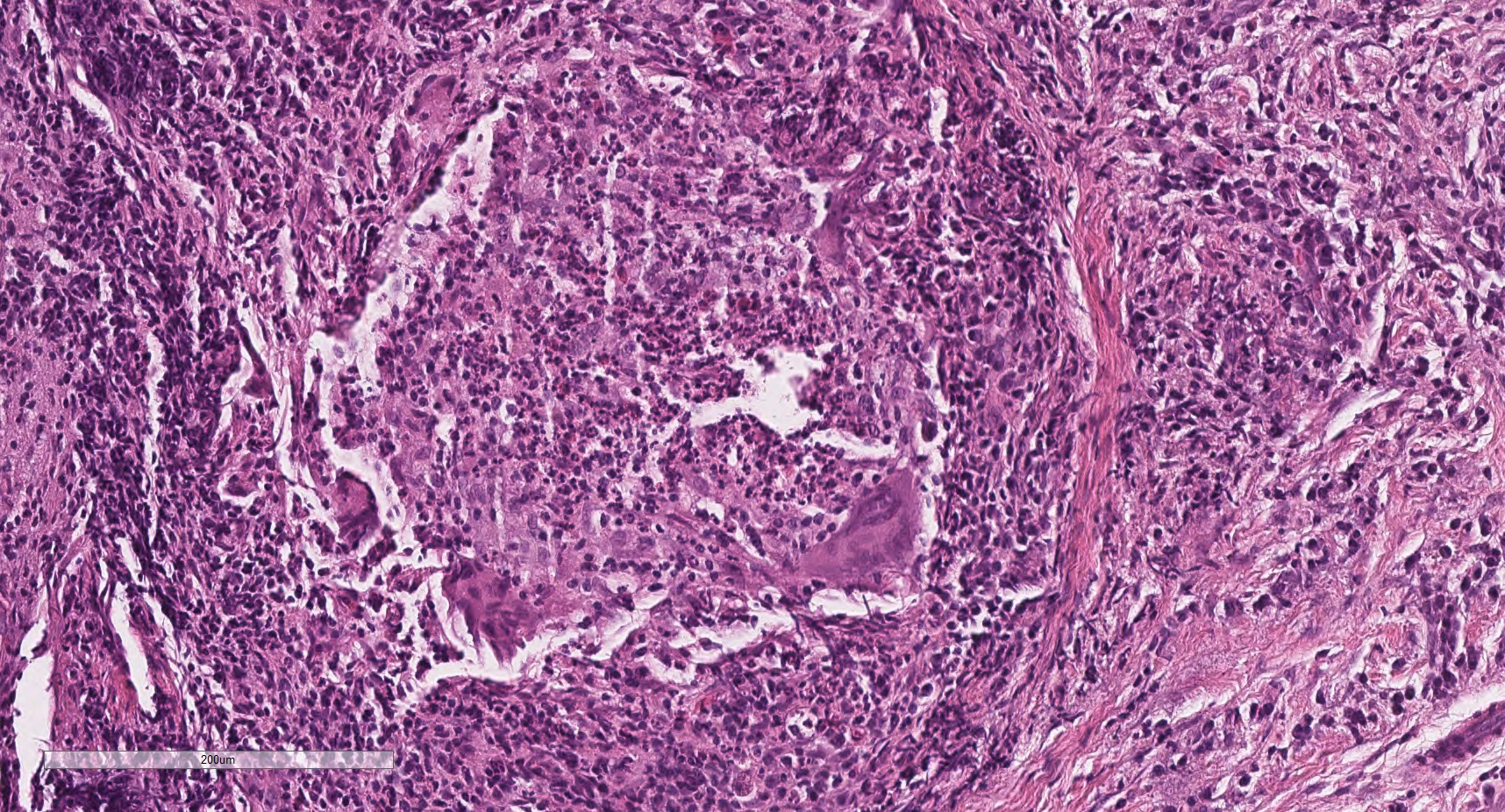
Microscopic (histologic) description
- Lipogranuloma (empty spaces surrounded by epithelioid and foamy histiocytes with multinucleated foreign body and or Touton type giant cells)
- Some lesions have granulation tissue, fibrosis or suppurative inflammation
- Early lesions can have necrotizing (neutrophilic) granulomas
- Conchoidal bodies and asteroid bodies can be observed
Microscopic (histologic) images
Positive stains
- Oil Red O: positive in the lipid droplets (central clearings)
Negative stains
- Grocott methenamine stain (GMS) and Ziehl-Neelsen could be helpful to rule out microorganisms when suspected
Sample pathology report
- Right eyelid, nodule, excision:
- Chalazion (lipogranulomas) (see comment)
- Comment: There is no sign of malignancy.
Differential diagnosis
- Steatocystoma:
- Cystic lesion lined by pluristratified epithelium without granular stratum wavy keratin
- Some sebaceous gland can be present attached to the cyst
- Sebaceous carcinoma:
- Basal cell carcinoma:
- Basaloid neoplasm with palisades and stromal clefts
- IHC: EMA-
- Hematolymphoid neoplasms:
- Myeloid sarcoma:
- Large cells with large cytoplasm and blastoid nucleus
- IHC: lysozyme+
- Histiocytic neoplasm (Langerhans and non-Langerhans):
- Neoplastic process of large cells with reniform nuclei (non-Langerhans) or grooved nuclei (Langerhans)
- Lymphoma:
- Myeloid sarcoma:
- Infectious granulomas:
- Necrotizing or caseiform granulomas
- Ziehl-Neelsen or Kinyoun+ when mycobacteria present
- GMS+ for fungal granulomas
- Autoimmune inflammation:
- Granulomatosis with polyangiitis:
- Necrosis, granulomas and angeitis present
- IgG4 related disease:
- Lymphoplasmacytic infiltrate with storiform fibrosis
- Lymphoid aggregates
- Obliterative phlebitis
- IgG4/IgGt ratio higher than 60%
- Granulomatosis with polyangiitis:
Board review style question #1
Board review style answer #1
C. Lipogranulomas. This is the key morphological finding in chalazion. The granulomas are usually nonnecrotizing. All the other changes such as lymphoplasmacytic chronic inflammation of the tarsal plate, exuberant granulation tissue and fibrosing chronic inflammation could be present but are nonspecific.
Comment Here
Reference: Chalazion of eyelid
Comment Here
Reference: Chalazion of eyelid
Board review style question #2
What is the most common location of a chalazion?
- External canthus
- Inner canthus
- Lower eyelid
- Upper eyelid
Board review style answer #2
D. Upper eyelid. The most common site of a chalazion is the upper eyelid, followed by the lower eyelid. Canthal location is rare.
Comment Here
Reference: Chalazion of eyelid
Comment Here
Reference: Chalazion of eyelid