Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis / laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesCite this page: Weisenberg E. Yersiniosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonyersinia.html. Accessed April 16th, 2024.
Definition / general
- Infection by Yersinia enterocolitica and less commonly Y. pseudotuberculosis, pleomorphic, facultative gram negative bacilli from the family Enterobacteriaceae
Essential features
- Zoonotic infection whose reservoir consists of a variety of domestic and wild animals
- Infection is usually acquired by ingesting the microorganisms; disease rarely occurs after blood transfusion
- Vast majority of cases occur after ingestion of contaminated food or water; infection rarely occurs subsequent to contact with animals or patients
- Most common in childhood
- Most common manifestation is enterocolitis lasting one to three weeks with fever, diarrhea and abdominal pain; other patients present with mesenteric lymphadenitis or terminal ileitis with symptomatology mimicking acute appendicitis that includes right lower quadrant pain and tenderness with leukocytosis; involvement of the appendix may occur
- Associated suppurative pharyngitis is not uncommon and may occur in the absence of gastrointestinal illness
- Most cases are self limiting but on occasion, mesenteric vein thrombosis, bowel rupture or sepsis may occur, especially in patients with comorbidities
- Noninfectious complications that occur in a minority of patients include reactive polyarthritis and polyarteritis nodosa
- Relatively common in parts of northern Europe
- Uncommon in the U.S., it is NOT an important cause of tropical diarrhea
ICD coding
Epidemiology
- Y. enterocolitica is widely distributed
- Animal reservoir includes pigs, rodents, birds, cattle, horses, sheep, goats, foxes, porcupines, dogs and cats
- Uncommon in U.S., the CDC estimates it causes 117,000 illnesses, 640 hospitalizations and 35 deaths in U.S. annually (CDC - Yersiniosis) with an incidence of 0.28 cases per 100,000 population in 2014 (CDC - Yersiniosis)
- More common in parts of Northern Europe including Germany, Denmark and Finland
- Does occur in the tropics but it is not considered an important cause of tropical diarrhea
- Has over 60 serotypes based on O and H antigens and 6 biotypes
- Most pathologic strains are serotypes O:3, O:5.27, O:8 and O:9 and biotypes 2, 3 and 4
- Serotypes O:3 and O:9 cause most disease in Europe, serotypes O:3 and O:8 cause most disease in U.S. and Canada
- Y. pseudotuberculosis has a separate system; there are 6 serotypes and 4 subtypes
- Infection is usually fecal-oral and occurs after ingestion of contaminated food or water; however, occurs less commonly after contact with an infected animal or carcass
- Butchers and workers in slaughterhouses are at increased risk
- Disease has occurred after contact with feces from household pets and from environmental surfaces
- Yersinia can grow at 4°C and infections have occurred after blood transfusion
- Outbreaks have been linked to contaminated milk (pasteurized and unpasteurized), raw vegetables and chitterlings (raw pork intestines)
- Rarely, transmission from a mother to her newborn has occurred
- Y. enterocolitica has been cultured from lakes, streams and drinking water; however, this is only a rare cause of disease
- Infections in the northern hemisphere are more common in November through January
- Children especially under 4 years are affected more commonly than adults
- Y. pseudotuberculosis is widely distributed and is widespread in nature; most reports of disease are from Europe
- Animal reservoir includes rodents, deer, birds and farm animals
- More common in winter
- Outbreaks have been linked to contaminated milk and produce
- Patients are usually 5 to 14 years old and males are affected three times more frequently than females
- A chronic carrier state for Yersinia is not described but patients may shed bacteria for weeks to months after yersiniosis
Sites
- Most disease in children under 4 is associated with an enterocolitis affecting the terminal ileum and proximal colon
- Disease in older patients generally involves the terminal ileum and mesenteric lymph nodes and may affect the appendix
- A minority of patients have suppurative pharyngitis, rarely without gastrointestinal illness
- A reactive polyarthritis occurs in 15% of patients, especially those with HLA B27
- Polyarteritis nodosa is an uncommon complication
- In septic patients, involvement of the lungs, liver, spleen and central nervous system has been reported
Pathophysiology
- An inoculum of 109 organisms is believed necessary to cause disease that occurs after a 4 to 7 day incubation period
- Microorganisms invade the intestine via M cells, which are involved in antigen presentation and are prominent over Peyer patches and prefer sites dense with lymphoid tissue, accounting for predilection for the terminal ileum, proximal colon and occasionally the pharynx
- Invasive proteins and enterotoxin are produced
- Plasmid mediated virulence factors include resistance to phagocytosis by neutrophils, interference with platelet aggregation, interference with complement activation and suppression of tumor necrosis factor α which causes enterocytes to undergo apoptosis
- Invasion of the mucosa leads to active, chronic or granulomatous inflammation with necrosis and ulceration that varies in extent depending on the severity of the disease
- Yersiniae are unable to chelate iron and rely on siderophores produced by other bacteria
- Iron overload as seen in chronic hemolytic states greatly increases the pathogenicity of Yersinia infections and patients being treated with deferoxamine are at particularly high risk
- Reactive polyarthritis is likely related to molecular mimicry and is especially common in those with HLA B27
Clinical features
- Necrotizing enterocolitis has been described in infants
- Children under 4 usually suffer an acute self limited enterocolitis lasting 1 to 3 weeks associated with fever, diarrhea, nausea and vomiting in 15 to 40% of cases
- In severe cases, bloody diarrhea or (rarely) ileal perforation may occur
- In older patients. the terminal ileum and mesenteric lymph nodes are involved, causing right lower quadrant pain and tenderness with leukocytosis that mimics acute appendicitis that in many cases has led to appendectomies
- The appendix may be uninvolved or show variable inflammatory changes, including granulomatous appendicitis
- Exudative pharyngitis occurs in up to 8% of patients, sometimes without gastrointestinal disease
- A reactive polyarthritis occurs in approximately 15% of patients and is especially common in patients with HLA B27; it may last for months but eventually resolves
- Polyarteritis nodosa occurs in up to 30% of cases, especially in women; it generally resolves within one month
- It is unusual for yersiniosis to last longer than a month but chronic infections occur
- In severe cases, mesenteric vessel thrombosis with intestinal necrosis and hemorrhage may occur
- Septicemia is more common in patients with comorbidities such as immunosuppression, underlying malignancy, old age or chronic hemolysis, especially with deferoxamine therapy and may involve the liver, spleen, lungs or central nervous system
- Yersinia sepsis is often fatal even with antibiotic treatment
- Y. pseudotuberculosis usually causes mesenteric lymphadenitis; it has been linked to a scarlet fever-like illness. and there are reports linking it to Kawasaki disease
Diagnosis / laboratory
- PCR based testing or isolation of the organism from stool (the CDC recommends cefsulodin-irgasan-novobiocin (CIN) agar and incubation at 25°C), lymph nodes, bile, pharyngeal exudate, blood, abscesses or peritoneal fluid
- Serologic testing is available but generally not indicated in the clinical setting
Radiology description
- Imaging studies may show thickening of the terminal ileum and ascending colon with mesenteric lymphadenopathy
- Severe disease may lead to bowel perforation with peritonitis and free air under the diaphragm
Prognostic factors
- Most patients suffer mild symptoms that are self limiting
- Disease is more severe in immunocompromised patients, debilitated patients and patients with iron overload, especially with deferoxamine therapy
Case reports
- 17 year old boy with Yersinia enterocolitica infection mimicking appendicitis (BMJ Case Rep 2015;2015:bcr2015211861 )
- 36 year old woman dies after blood transfusion (Blood Transfus 2015;13:528)
- 41 year old woman with massive rectal bleeding (J Med Case Rep 2016;10:6)
- 49 year old man with ascitic fluid infection and bacteremia due to Y. pseudotuberculosis three years post liver transplant (Int J Infect Dis 2015;34:122)
- 70 year old woman with cellulitis and skin abscesses (Medicine (Baltimore) 2016;95:e3988)
Treatment
- Self limited infections are usually not treated
- Patients with persistent infection or sepsis usually receive aminoglycosides, sulfamethoxazole / trimethoprim, doxycycline or ciprofloxacin
- Patients with persistent infection or sepsis due to Y. pseudotuberculosis are usually treated with ampicillin, tetracycline or an aminoglycoside
- Patients with reactive arthritis usually are treated with NSAIDs, intra-articular corticosteroid injections and physical therapy
Gross description
- In uncomplicated cases, the bowel wall is thickened and edematous and demonstrates ulcers over Peyer patches or lymphoid aggregates
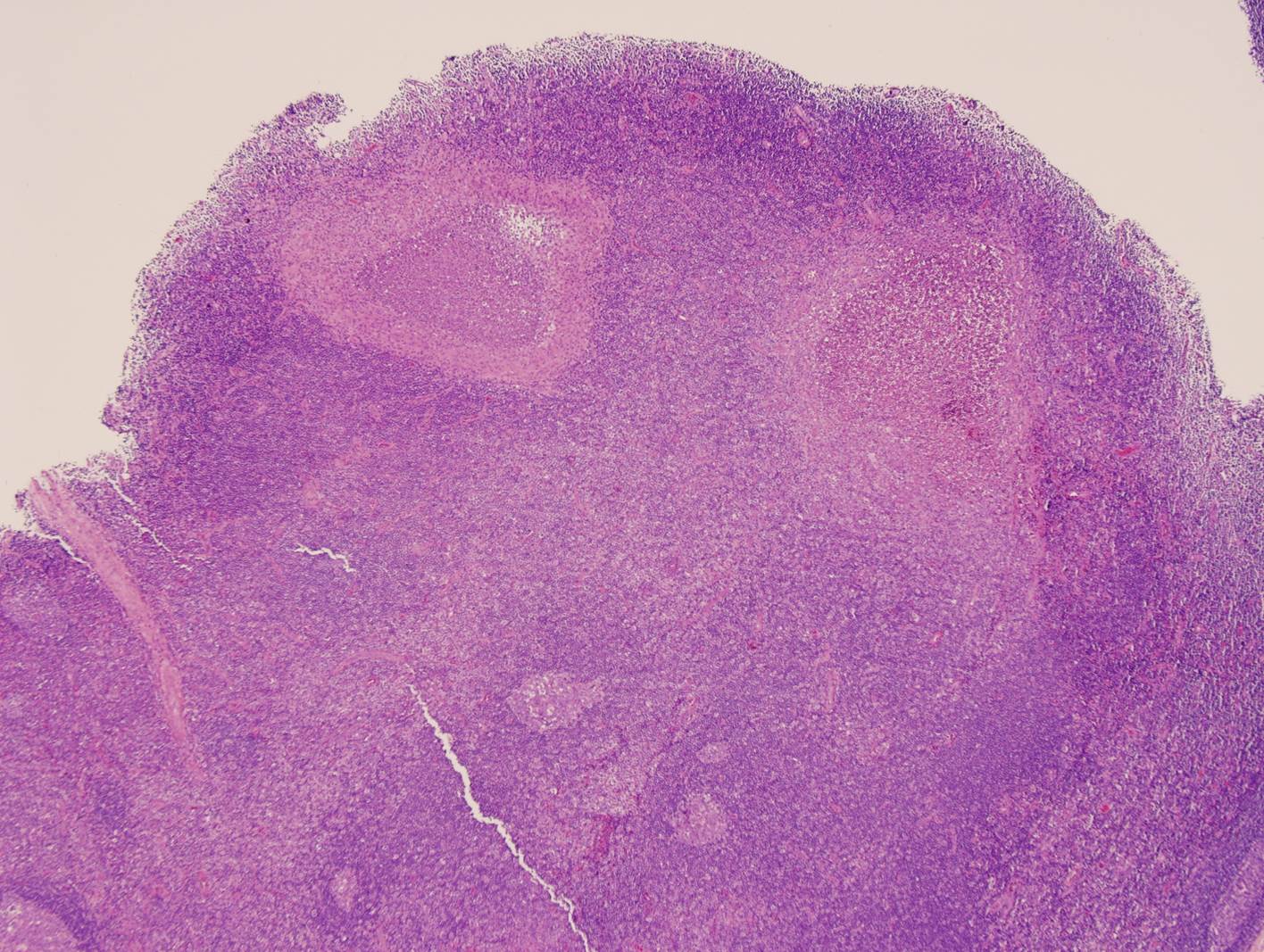
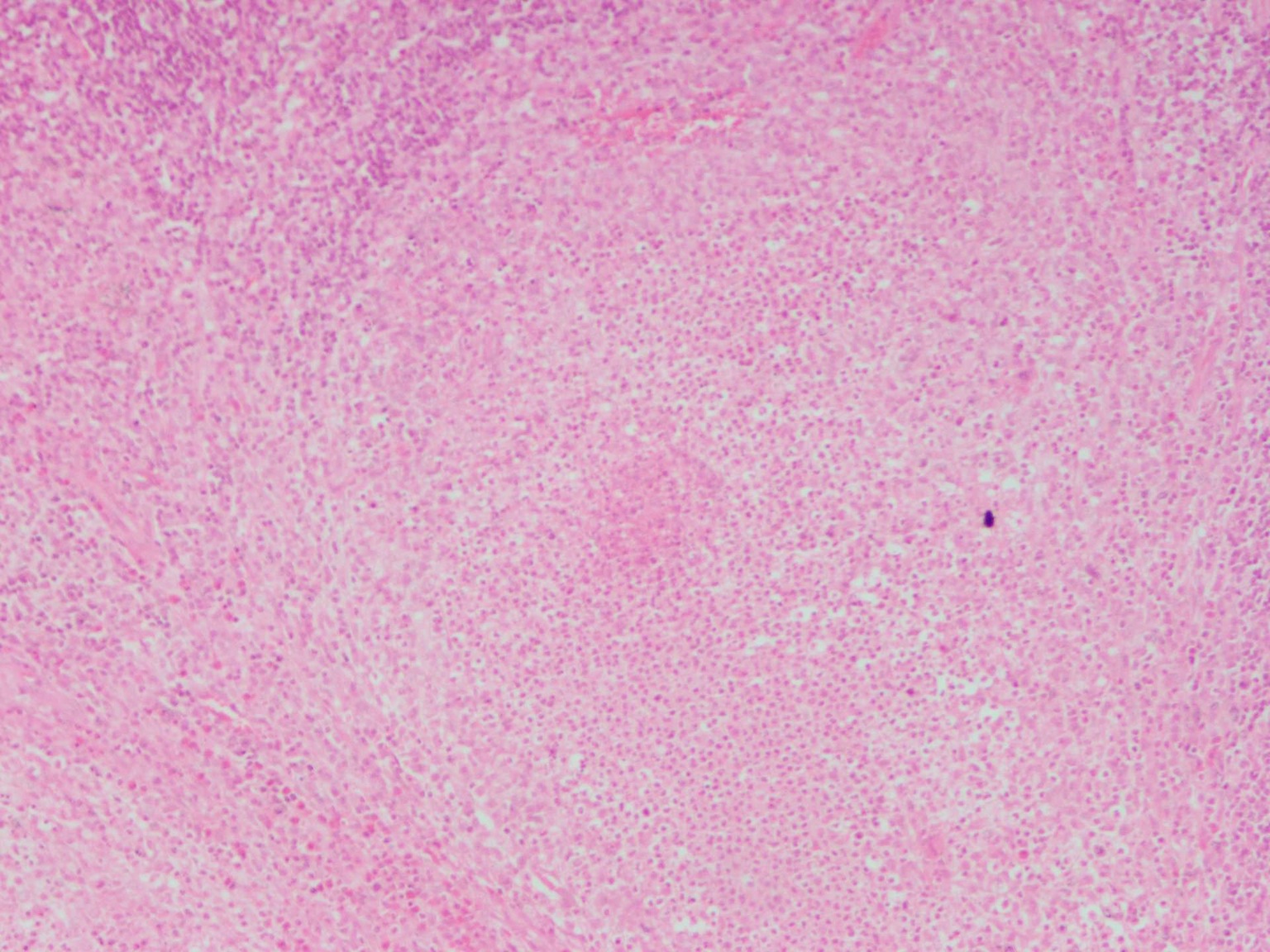
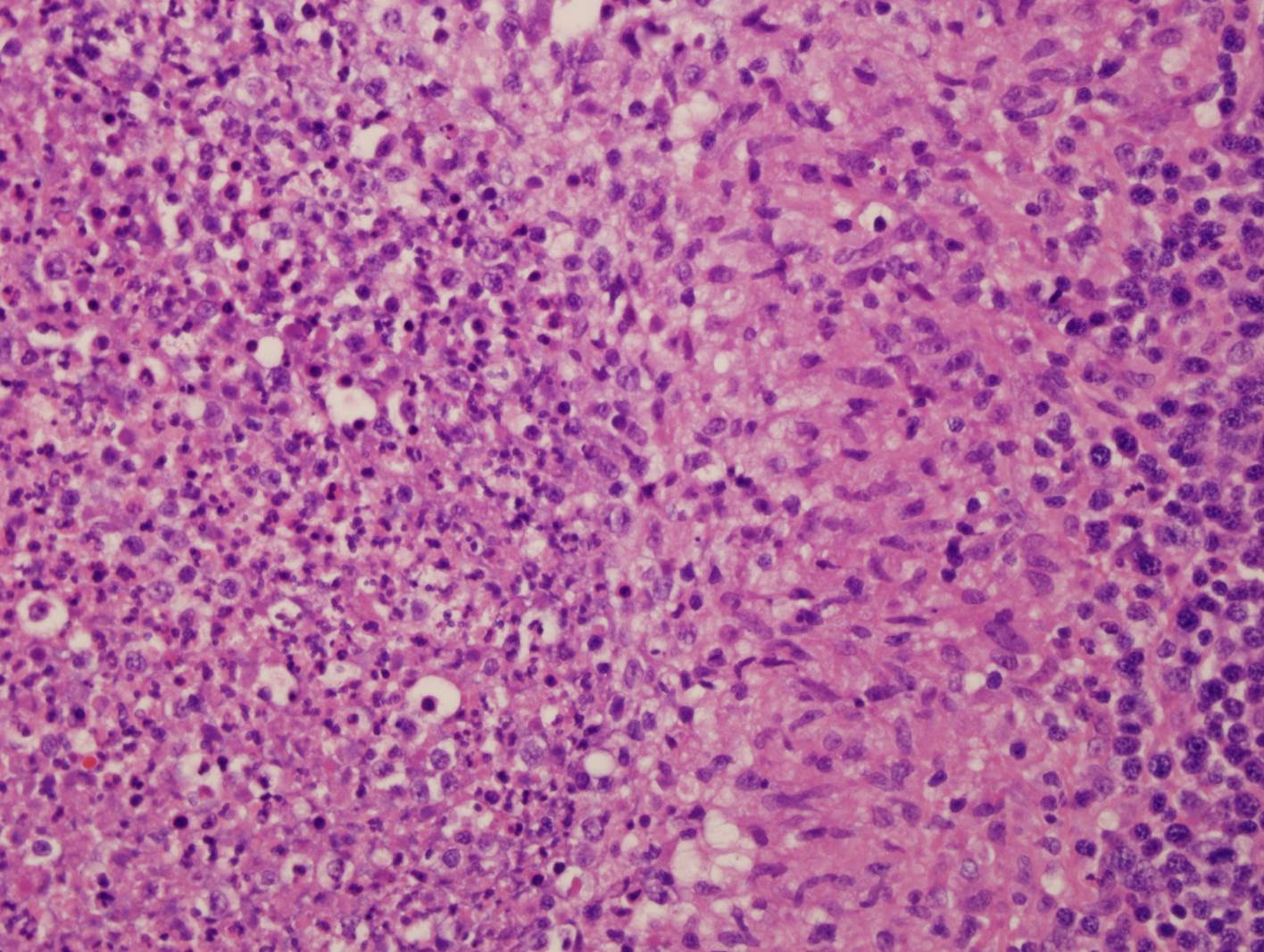
Microscopic (histologic) description
- Affected mucosa variably demonstrates lymphoid hyperplasia, cryptitis and crypt abscesses, generally without significant architectural changes typical of acute self limited colitis and granulomas with central abscess formation (suppurative granulomas)
- Chronic infection may be associated with architectural changes
- Lymphoid hyperplasia, neutrophilic infiltrates and suppurative granulomas may involve mesenteric lymph nodes
Microscopic (histologic) images
Differential diagnosis
- Crohn's disease, other agents of acute self limited colitis, acute appendicitis
- In lymph nodes: cat scratch disease, lymphogranuloma venereum