Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3 | Board review style question #4 | Board review style answer #4Cite this page: Bansal N, Weisenberg E. Salmonella (typhoid and nontyphoidal). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonsalmonella.html. Accessed April 19th, 2024.
Definition / general
- Disease caused by Salmonella species infection
- While overlap exists, species causing typhoid fever and nontyphoidal species are often categorized separately
- Salmonellosis is a food borne disease caused mainly by Salmonella typhi serotype, although Salmonella paratyphi A, B, C can cause similar disease
- Salmonella penetrate the small bowel epithelium after ingestion, enter lymphoid tissue and disseminates via the lymphatic or hematogenous route
- Typhoid fever is characterized by severe systemic illness with fever, relative bradycardia and considerable constitutional symptoms including abdominal pain (Med J Armed Forces India 2003;59:130)
- Causes intestinal bleeding due to ulcers in distal ileum or proximal colon (Dig Liver Dis 2004;36:141)
- Bleeding may be massive (Dis Colon Rectum 1986;29:511)
Essential features
- Salmonellosis is considered a food borne disease
- Typhoid fever:
- Sometimes known as enteric fever, is a life threatening illness caused by Salmonella typhi sometimes called Salmonella enterica serotype Typhi or S. paratyphi
- Infects from 20 to 30 million people a year, mostly in the developing world
- In industrialized countries, it is usually encountered in travelers
- Nontyphoid species:
- Usually cause acute, self limited gastroenteritis
- The Centers for Disease Control and Prevention (CDC) estimates that one million cases, 19,000 hospitalizations, and 450 deaths occur each year in the United States
- Tens of millions of cases occur worldwide each year causing an estimated 100,000 deaths
- Disease is spread through ingestion of contaminated food or water, most often in a sporadic fashion but sometimes through foodborne outbreaks that often are associated with suboptimal sanitary practices or food preparation
- Typhoid colitis is caused by Salmonella enterica organisms, mainly S. typhi
- S. typhi occurs only in humans
- Salmonellosis is a food borne disease caused by ingestion of contaminated food
- Salmonella penetrate the small bowel epithelium after ingestion, enter the lymphoid tissue and disseminates via the lymphatic or hematogenous route
- Typhoid fever is characterized by severe systemic illness with fever, relative bradycardia and considerable constitutional symptoms including abdominal pain (Med J Armed Forces India 2003;59:130)
- Salmonella typhi affects mainly the proximal colon causing ulceration and rarely massive bleeding (Dig Liver Dis 2004;36:141, Dis Colon Rectum 1986;29:511)
Terminology
- Typhoid fever
- Enteric fever
- Salmonella is named after the veterinarian Elmer Daniel Salmon
- Salmonella are gram negative rods
- Salmonella species bacteria are serotyped based on the chemical content of the O antigens found on the surface and the protein content of part of the flagella known as the H antigen
- Over 2500 serotypes have been described; however, under 100 are known to be associated with human disease
- Serotyping is currently done by molecular methods
- S. typhi and S. paratyphi are associated with typhoid fever
- Some of the more common nontyphoidal species are:
- S. enteritidis
- S. typhimurium
- S. muenchen
- S. adnatum and S. give
- S. paratyphi may also cause nontyphoidal disease
ICD coding
- ICD-10: A01.09 - typhoid fever with other complications
Epidemiology
- Worldwide over 20 million cases of typhoid fever occur each year, mostly in the developing world
- Approximately 1800 cases of typhoid fever occur in the United States annually, mostly in travelers
- From 1.0 to 1.2 million cases of nontyphoidal illness occur in the United States each year, causing about 19,000 hospitalizations and 450 deaths
- Tens of millions of nontyphoidal illness occur worldwide, causing over 100,000 deaths each year
- Disease occurs from ingestion of bacteria, usually in food or water, eggs, milk, meat, poultry
- Vegetables contaminated with animal feces are commonly implicated
- Food borne outbreaks, often associated with less than sanitary conditions, are common sources of disease
- However, in the United States approximately 60% of cases occur sporadically
- Fecal oral transmission may occur; disease after contact with infected animals is another source
- Salmonellosis is a common cause of traveler diarrhea
- All serotypes at least in theory may cause human disease
- Serotypes may or may not be host specific
- When serotypes specific to other species infect humans. severe disease may result
- S. typhi is restricted to humans
- Risk factors for infection include:
- Lack of access to clean water
- Poor sanitation. especially regarding food handling
- Flooding
- Ingestion of plants fertilized with sewage
- Urban environments
- Sexual transmission has been reported
- Both typhoidal and nontyphoidal salmonellosis may occur in health care workers when proper hand hygiene is not practiced
- Travelers to the developing world are often infected with S. paratyphi; vaccination against S. typhi is common prior to travel
- Spreads through the oral-fecal route, mostly waterborne or via food infected by carriers, rarely through oral-anal sexual contact (Clin Infect Dis 2003;37:141)
- More common in children and young adults
- Most prevalent in developing countries and overcrowded areas with poor sanitation
- High incidence (more than 100 cases per 100,000 person years) in South central Asia, Southeast Asia, southern Africa (Bull World Health Organ 2004;82:346, J Glob Health 2012;2:010401)
- In developed countries, disease is usually limited to travelers to countries where typhoid fever is endemic (Lancet Infect Dis 2005;5:623)
- The Vi polysaccharide typhoid vaccine is ineffective against most S. paratyphi, which lack the Vi antigen targeted by the vaccine (Lancet Infect Dis 2005;5:623)
Sites
- Most common is terminal ileum (100%), followed by ileocecal valve (57%), ascending colon (43%), transverse colon (29%) (Dig Liver Dis 2004;36:141)
- Nontyphoidal Salmonella infects the small and large bowel
- S. typhi typically spreads to the liver, spleen, bone marrow and lymph nodes
- Extraintestinal spread is uncommon in nontyphoidal Salmonella but may occur with severe disease
Pathophysiology
- Salmonella possess cellular mechanisms enabling bacterial proteins to be transferred to enterocytes and M cells with subsequent growth within endosomes
- Subsequent events include an inflammatory response with neutrophil recruitment and mucosal damage
- The host immune response typically controls nontyphoidal infection; however, the very young, elderly, debilitated and immunosuppressed may lack the response necessary to control infection
- S. typhi more commonly invades M cells
- Bacteria are phagocytosed by histiocytes in underlying lymphoid tissue
- The bacteria proliferate and widely disseminate through blood vessels and lymphatic channels
- S. typhi is a gram negative bacillus typically transmitted via the fecal-oral route
- Entry of S. typhi into the small bowel epithelium after ingestion appears to be mediated by the cystic fibrosis transmembrane conductance regulator (CFTR)
- S. typhi proliferates intracellularly in the submucosa, initially in the second part of the Peyer patches, leading to hypertrophy via recruitment of mononuclear cells and lymphocytes
- Over the next 7 - 21 days, further proliferation occurs in these organs, then organisms are released into the bile and reinfect the ileal lymphoid tissue, then organisms disseminate to the liver, spleen and reticuloendothelial system via the lymphatic system and bloodstream (Clin Exp Gastroenterol 2012;5:213)
- Replication within the reticuloendothelial system is a hallmark of enteric fever and is responsible for the clinical findings of prostration, generalized sepsis and hepatosplenomegaly
- An effective vaccine for S. typhi exists
Etiology
- Salmonella are gram negative bacilli
- S. typhi is found only in humans
- Nontyphoidal species are found in humans, domestic and wild animals
- In general, infection occurs through ingestion of contaminated food or water or the fecal-oral route
- Nontyphoidal Salmonella are commonly found in food and companion animals including poultry, cattle, swine, parrots, cats, dogs and turtles
- Eggs, milk, meat, poultry and contaminated vegetables are commonly implicated
- Direct person to person transmission as well as transmission from pets may occur
- In this setting, the source of the transmission may not appear ill
Clinical features
- Symptoms of nontyphoidal salmonellosis generally start 12 - 36 hours after ingestion of bacteria but may occur after 6 - 72 hours
- Ingestion of very few organisms may cause disease
- Typically patients suffer self limited illness characterized by diarrhea, abdominal pain, fever, nausea and occasionally vomiting that is unpleasant but rarely life threatening
- May be life threatening In infants, elderly, immunocompromised or debilitated patients, due to dehydration or dissemination of bacteria
- Very rarely, toxic megacolon may complicate infection
- Individuals with achlorhydria or hypochlorhydria from drugs, chronic Helicobacter pylori infection or other causes are at higher risk of infection
- Some patients develop a reactive arthritis that may last for months and lead to chronic arthritis
- Typhoid fever causes symptoms shortly after bacteria are ingested
- Patients suffer from severe abdominal pain, bloody diarrhea, bloating, anorexia, nausea, vomiting, headache
- A brief asymptomatic period is followed by bacteremia with fever and flu-like illness
- Blood cultures are almost always positive at this time and antibiotic therapy may be lifesaving
- With disease progression in untreated patients, high fever and abdominal pain occurs that may mimic appendicitis; lasts for about two weeks
- If patients survive, symptoms slowly abate
- Possible extraintestinal complications include CNS disease, endocarditis, myocarditis, pneumonia, cholecystitis, osteomyelitis (patients with sickle cell disease are particularly prone to osteomyelitis)
- Disease relapses may occur
- First week of illness: rising ("stepwise") fever associated with chills, although frank rigors are rare
- Also relative bradycardia or pulse-temperature dissociation is common
- Second week of illness: abdominal pain develops and "rose spots" (faint salmon colored macules on the trunk and abdomen) may be seen
- Third week of illness: hepatosplenomegaly, intestinal bleeding and perforation
due to ileocecal lymphatic hyperplasia of the Peyer patches may occur,
together with secondary bacteremia and peritonitis (Lancet Infect Dis 2005;5:623)
- Perforation is four times more common in males than females (Am J Epidemiol 2004;160:46)
- Chronic Salmonella carriage is defined as excretion of the organism in stool or urine >12 months after acute infection
Diagnosis
- Nontyphoidal salmonellosis traditionally has been diagnosed by stool culture although many patients do not seek medical attention
- Recently a PCR based assay has been introduced that, in addition to Salmonella species bacteria, also detects Camplyobacter group, Shigella species, Vibrio group, Yersinia enterocolitica, Shiga toxin 1 and 2, Norovirus G1 / GII, Rotavirus A and Aeromonas species
- Serotyping is done to characterize disease outbreaks
- Typhoid fever is diagnosed by blood or stool culture
- In the developing world where laboratory facilities may not be readily available, disease may be treated empirically
- Bone marrow culture is the most sensitive test available, as it remains positive even after 5 days of antibiotic therapy (Lancet 1975; 1:1211)
Laboratory
- CBC shows leukopenia and thrombocytopenia
- Cultures can be from blood, stool, urine, rose spots, the blood mononuclear cell platelet fraction, bone marrow, gastric or intestinal secretions
- A positive culture for S. typhi or S. paratyphi is obtained in more than 90% of patients if blood, bone marrow and intestinal secretions are all performed
- Because almost all S. typhi organisms in blood are associated with the mononuclear cell platelet fraction, centrifugation of blood and culture of this fraction can reduce the time for isolation of the organism but does not increase the sensitivity
- Children also have a higher incidence of positive stool cultures than adults (60% versus 27%)
- The duodenal string test is useful for sampling the upper GI tract (J Infect Dis 1984;149:157)
Radiology description
- Most common colonoscopic finding is multiple variably sized punched out ulcers with slightly elevated margins
- Also edematous hyperemic mucosal patches with hemorrhagic spots or shallow erosions
Prognostic factors
- Nontyphoidal salmonellosis is almost always a self limited infection, except in infants, the elderly, immunocompromised and debilitated patients
- Antibiotic therapy is usually efficacious in these patients, although antibiotic resistance is a growing problem
- Without treatment, typhoid fever may be lethal even in healthy individuals but the prognosis is worse in infants, the elderly, immunocompromised and debilitated patients
- Prompt initiation of antibiotic therapy greatly improves patient outcome; although again, antibiotic resistance is a growing problem
Case reports
- Nontyphoidal Salmonella:
- Infant with large bowel obstruction as presentation of salmonella enterocolitis (Pediatr Surg Int 2000;16:525)
- 37 week old infant boy with Salmonella berta meningitis (J Perinatol 2014;34:798)
- 51 year old man with Salmonella dublin infection (Eur J Gastroenterol Hepatol 2001;13:587)
- 57 year old man with endovascular infection with Salmonella group C (Germs 2015;5:99)
- 62 year old man with toxic megacolon due to Salmonella (Int J Colorectal Dis 2002;17:275)
- Family outbreaks of nontyphoidal salmonellosis (Case Rep Infect Dis 2015;2015:864640)
- Toxic megacolon in Salmonella colitis (Acta Paediatr Taiwan 2000;41:43)
- Typhoidal Salmonella:
- 10 year old child with Salmonella typhi coinfection with dengue fever (J Infect Dev Ctries 2015;9:1033)
- 18 year old man with acute scrotal ulcers in typhoid fever (Trop Med Health 2015;43:69)
- 30 year old man with gastrointestinal bleeding from paratyphoid A fever (World J Gastroenterol 2015;21:1040)
- Breast abscess by Salmonella paratyphi (J Clin Diagn Res 2015;9:DD03)
Treatment
- Nontyphoidal Salmonella usually:
- Only requires supportive care, particularly hydration
- Antibiotics are indicated for severe disease and vulnerable patients
- Ceftriaxone and ciprofloxacin are currently recommended by the CDC
- Antibiotic resistance is a growing problem
- Antibiotic therapy for typhoid fever is obligatory and should not be delayed for confirmatory laboratory testing
- Prolonged course of antimicrobials and supportive care with transfusions
- Antibiotic therapy for typhoid fever is obligatory and should not be delayed for confirmatory laboratory testing
- Ceftriaxone and ciprofloxacin are currently recommended by the CDC (CDC: Typhoid Fever and Paratyphoid Fever [Accessed 28 November 2017], Lancet Infect Dis 2005;5:623)
- Third generation fluoroquinolones are also recommended but resistance has been reported
- In the past, chloramphenicol, trimethoprim-sulfamethoxazole, cephalosporins and first generation fluoroquinolones were used but antibiotic resistance developed
- Surgery may be necessary for intestinal perforation or gallbladder disease
- Selective angiography and platinum coil embolization is used for severe, life threatening lower gastrointestinal hemorrhage
- WHO recommendations for the public and travelers include:
- Ensure food is properly cooked and hot when served
- Avoid raw milk and products made from raw milk
- Avoid ice unless made from safe water
- Use disinfecting tablets for water unless its purity is certain
- Wash hands thoroughly with soap and water after contact with pets or farm animals and after using the toilet
- Wash fruits and vegetables thoroughly and if possible, peel fruits and vegetables unless optimal sanitary practices are known to have taken place
- Recommendations for food handlers and producers include:
- Maintain a clean workspace
- Separate raw and cooked food
- Cook food thoroughly
- Keep food at safe temperatures
- Use safe water and raw materials
- Practice good personal hygiene
- Do not work if have fever, diarrhea, vomiting or infected skin lesions
- Protect fields from animal contamination
Gross description
- Colonoscopy in patients with mild nontyphoidal salmonellosis shows nonspecific findings including edema and petechial hemorrhage; more severe disease is associated with friability and ulceration
- Typhoid fever causes marked enlargement of Peyer patches and lymphoid tissue in the appendix and ascending colon leading to mucosal elevation along the axis of the ileum
- Perforation may occur
- Small gray, soft nodules (typhoid nodules) may be present in the liver
- There is splenomegaly and lymphadenopathy
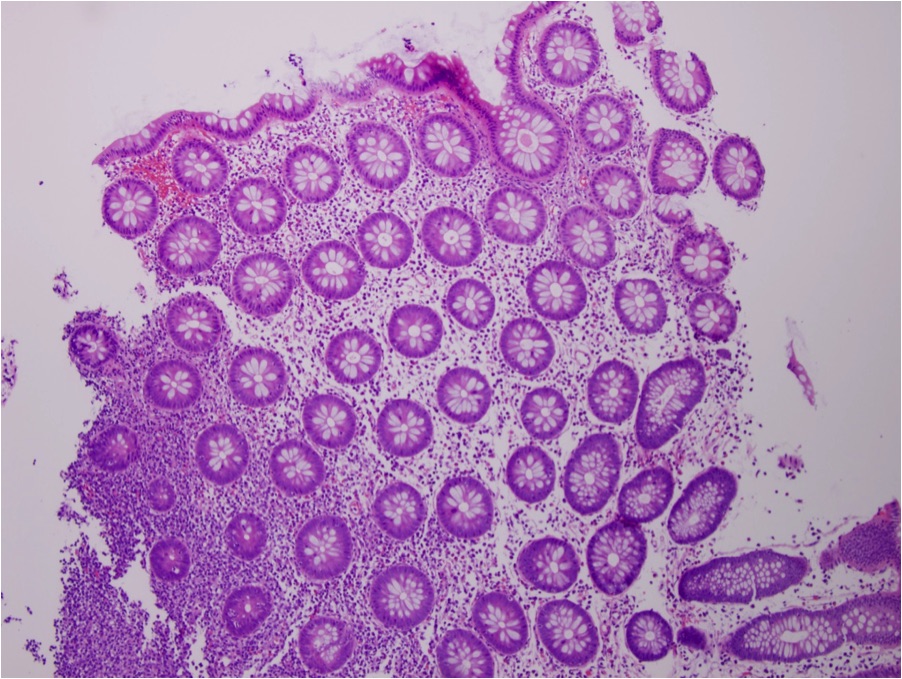
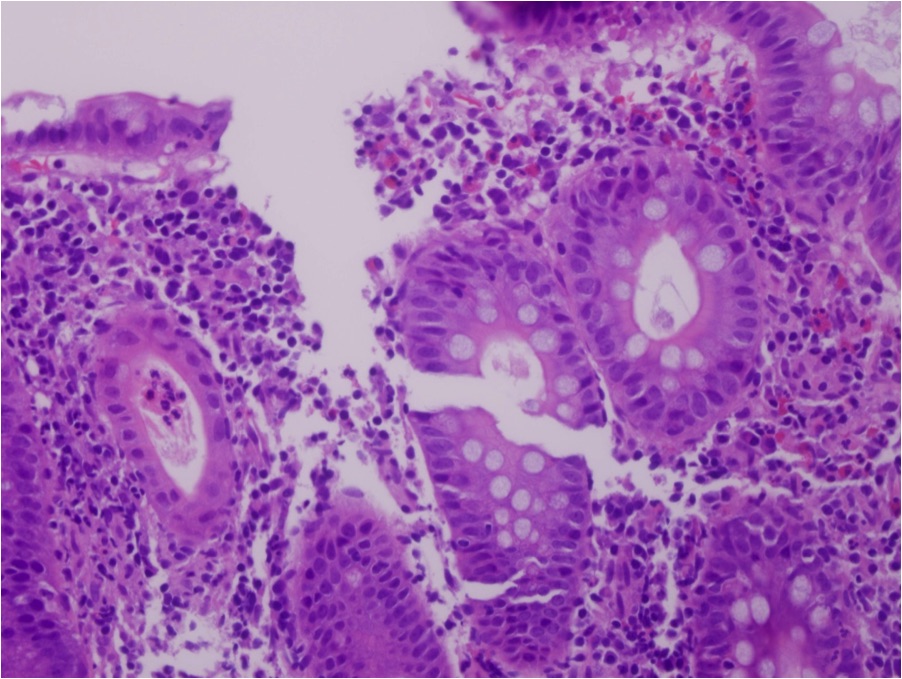
Microscopic (histologic) description
- Nontyphoidal salmonellosis is rarely biopsied
- The findings are a non-specific acute self limited colitis
- The crypt architecture is maintained, there are increased mixed inflammatory cells within the lamina propria in a patchy distribution with foci of cryptitis and possible crypt abscesses
- Long standing cases may demonstrate architectural distortion raising the spectre of idiopathic inflammatory bowel disease
- This is also true of S. typhimurium infection
- Knowledge of culture results is necessary to render a specific diagnosis
- S. typhi shows neutrophils, histiocytes with cytoplasmic bacteria, nuclear debris and hemorrhage within the lamina propria associated with a lymphoplasmacytic infiltrate
- The spleen and lymph nodes show sinus histiocytosis that distorts the normal architecture
- Typhoid nodules in the liver show aggregates of histiocytes with necrotic debris
- Typhoid nodules may also be found in bone marrow and lymph nodes
Microscopic (histologic) images
Differential diagnosis
- The differential diagnosis of nontyphoidal salmonellosis includes other enteric pathogens that cause acute self limited colitis including Shigella and Campylobacter
- Long standing cases may mimic idiopathic inflammatory bowel disease
Additional references
- Kumar: Robbins & Cotran Pathologic Basis of Disease, 9th Edition, Bennett: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 8th Edition, 2014, Odze: Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas, 1st Edition, Kradin: Diagnostic Pathology of Infectious Disease, 1st Edition, 2010, WHO - Salmonella, WHO - Typhoid fever, CDC - Salmonella, CDC - Typhoid Fever, CDC - Multidrug Resistant Salmonella
Board review style question #1
Which of the following are common sources of infection for Salmonella?
- Food borne
- Food borne and water borne
- Sexual transmission
- Water borne
Board review style answer #1
Board review style question #2
Which serotype of Salmonella occurs only in humans?
- S. choleraesuis
- S. typhi
- S. typhimurium
- None of the above
Board review style answer #2
Board review style question #3
Which site is most commonly involved by Salmonella?
- Colon
- Gall bladder
- Ileum
- Stomach
Board review style answer #3
Board review style question #4
Which is the most common site of localization of S. typhi in humans?
- Gastric epithelium
- Interstitial cell of Cajal
- Neurons
- Peyer patches
Board review style answer #4