Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Bateman AC. Hyperplastic polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumorhyperplastic.html. Accessed December 21st, 2024.
Definition / general
- Very common type of polyp in the colon and rectum
- Often numerous, particularly within the rectum
- Usually small (5 mm or less)
- Associated with no significant risk of malignant progression
Essential features
- Can occur throughout the large intestine but is most common in the sigmoid colon and rectum
- Associated with no significant risk of malignant progression
- Serrated architecture with a sawtooth appearance, with serrations generally limited to the upper half of the crypts
- Main differential diagnosis is with sessile serrated lesions (SSLs)
- Microvesicular variant not uncommonly contains a BRAF gene mutation
Terminology
- These lesions used to be termed metaplastic polyps
- Microvesicular and goblet cell rich variants exist
- Goblet cell poor variant no longer recognized
ICD coding
- ICD-10: K63.5 - polyp of colon
Epidemiology
- Common lesions and the most common type of serrated colorectal polyp (80%) (Scand J Gastroenterol 2017;52:654)
- Identified most often in adulthood
- M > F (Cancer 1982;49:819)
- Little or no associated risk of colorectal cancer development
Sites
- Large intestine
- Can occur throughout the large intestine but is most common in the sigmoid colon and rectum
- Commonly multiple within the rectum
- Reference: Histopathology 2021;78:780
Pathophysiology
- Unknown
Etiology
- Shares lifestyle risk factors with colorectal adenoma and colorectal cancer; e.g. low dietary fiber content, raised body mass index, increased alcohol consumption and cigarette smoking are all associated with an increased risk of hyperplastic polyp development (Gastroenterology 1997;113:423)
Clinical features
- Almost always asymptomatic
- May be present as part of a spectrum of lesions that also includes sessile serrated lesions, in serrated polyposis (Am J Gastroenterol 2012;107:1315)
Diagnosis
- Diagnosis is made on histological examination
Case reports
- 23 year old woman with juvenile polyposis (Cancer 1979;43:1906)
- 44 year old man with traditional serrated adenoma originating from a goblet cell hyperplastic polyp (Anal Quant Cytopathol Histpathol 2014;36:351)
- 61 year old man with serrated polyposis syndrome (Cureus 2020;12:e9198)
Treatment
- Endoscopic biopsy or removal is often performed to confirm the diagnosis
- No further treatment is required unless the patient is thought to have serrated polyposis, in which case endoscopic surveillance may be warranted
Gross description
- These are small mucosal lesions, typically less than 5 mm in size
- Appear as slightly elevated and pale lesions at endoscopy but lack the mucin cap that is commonly seen with sessile serrated lesions (World J Gastroenterol 2018;24:3250)
Microscopic (histologic) description
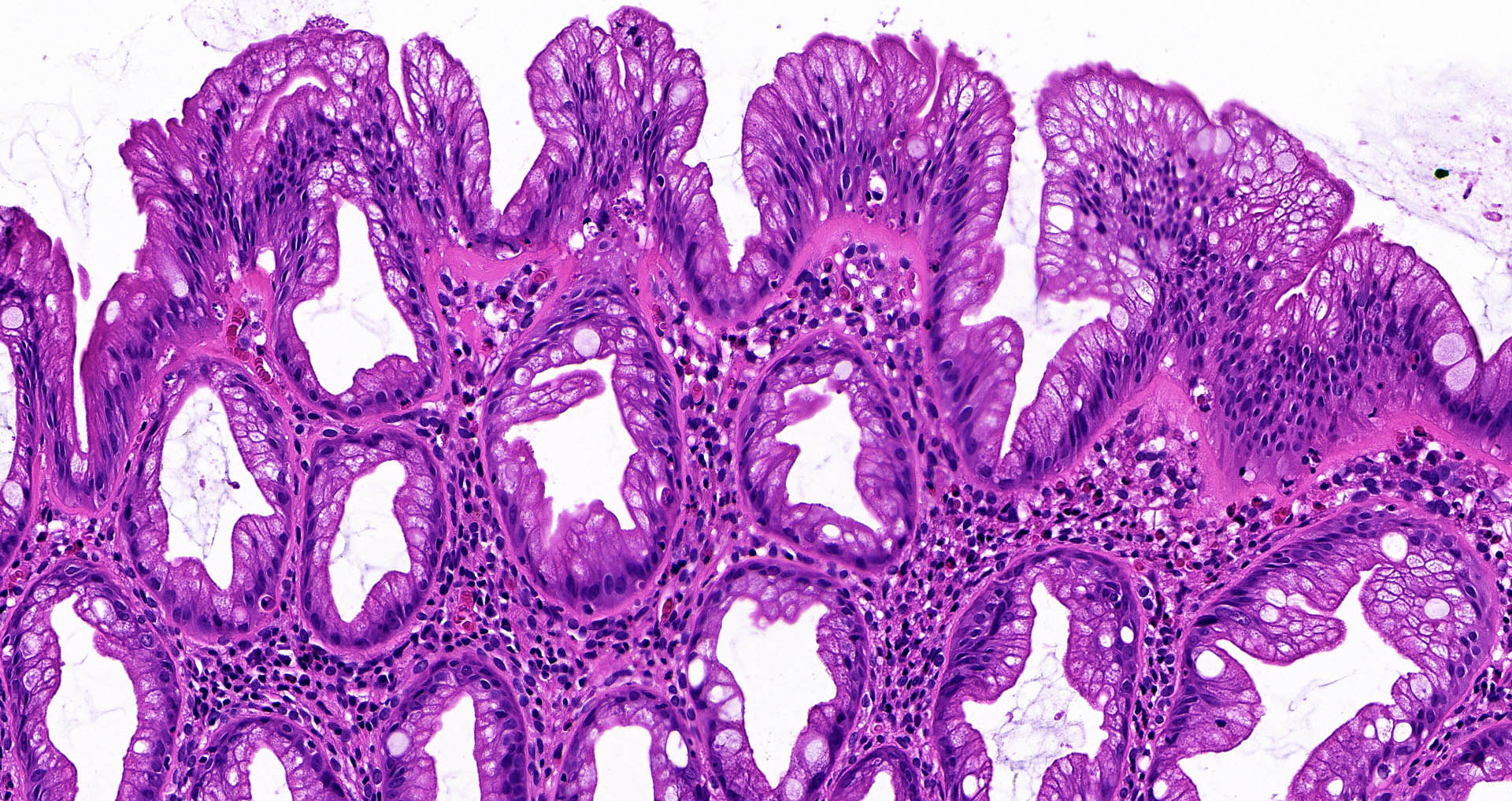
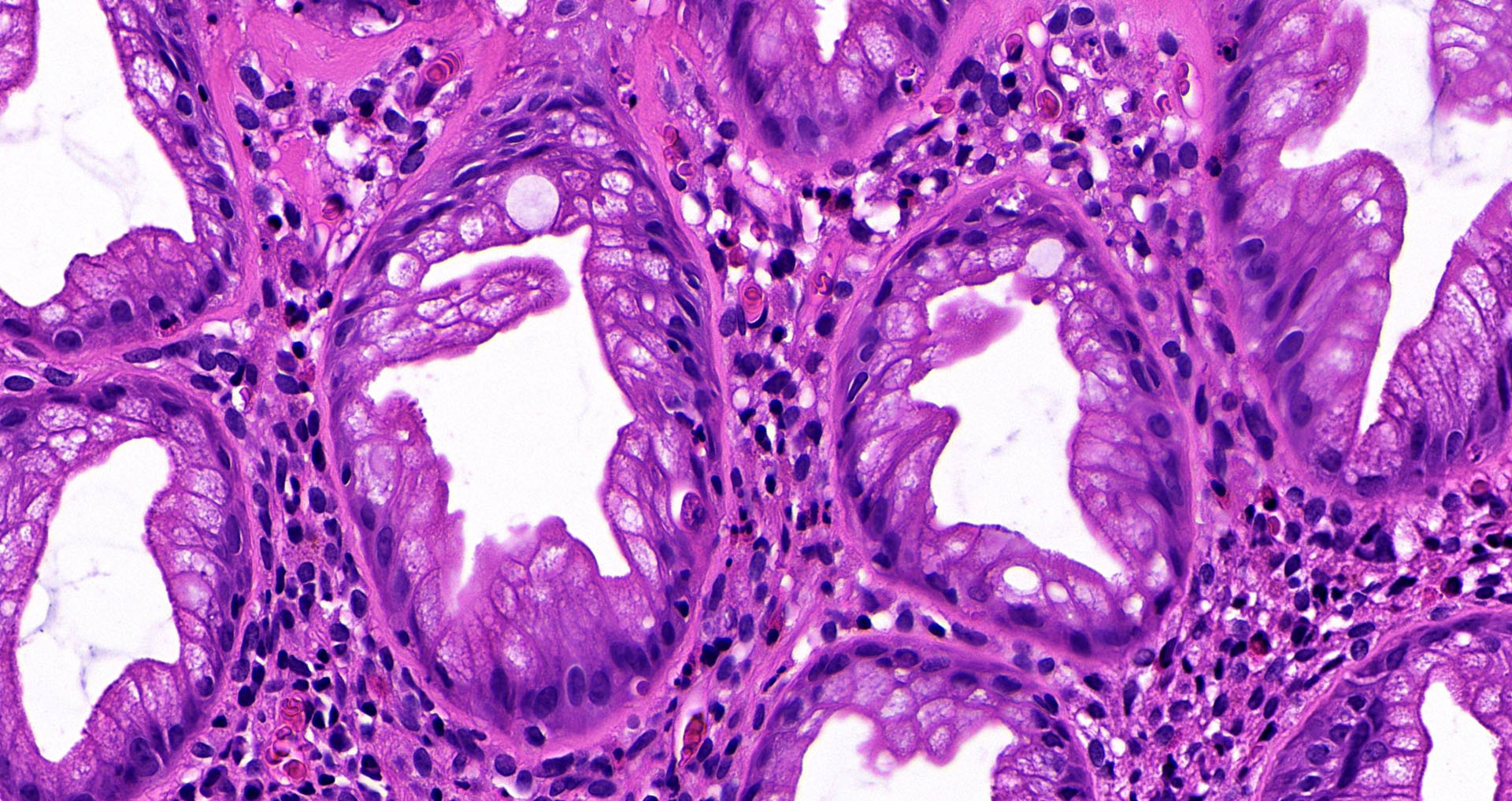
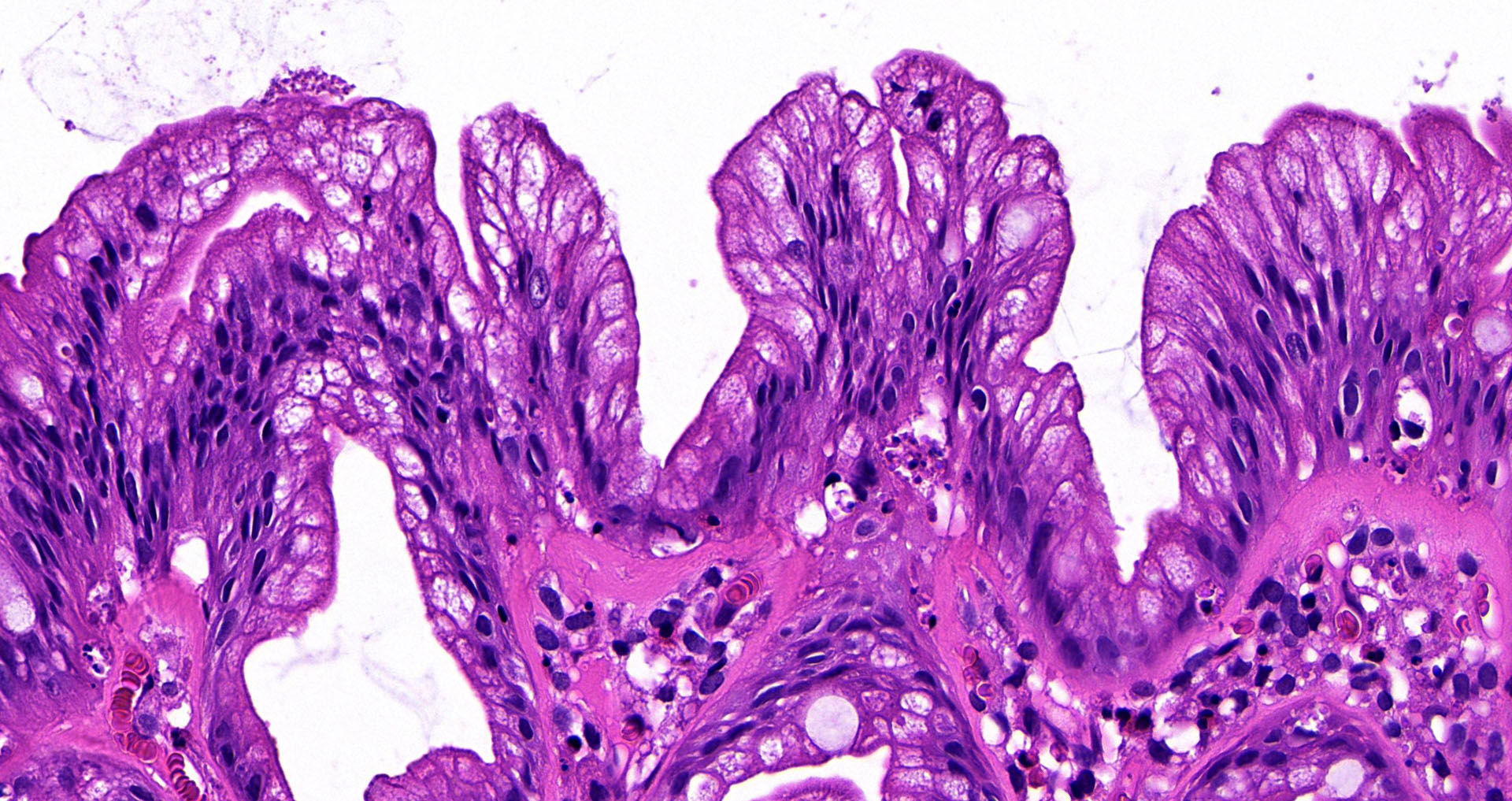
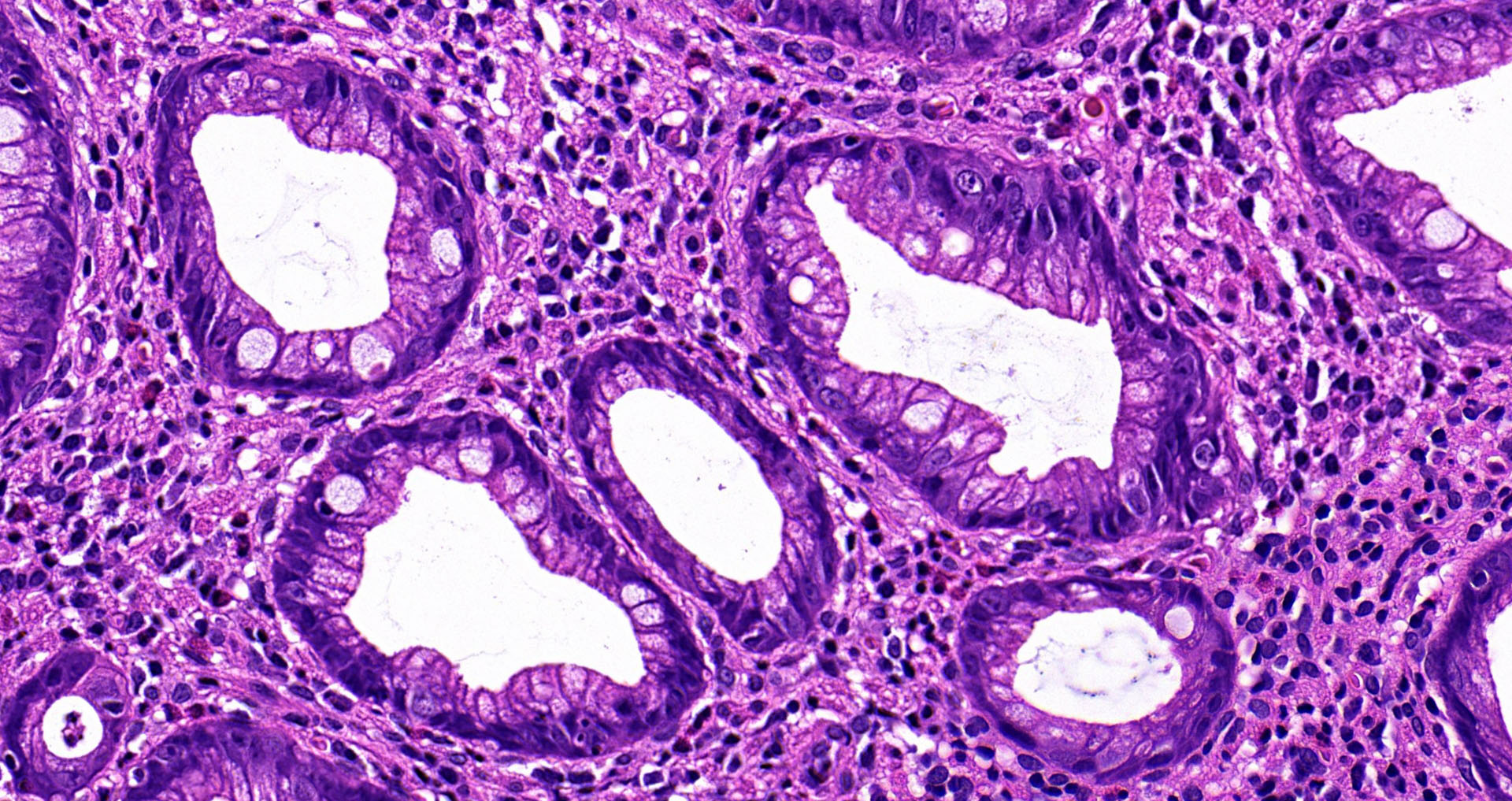
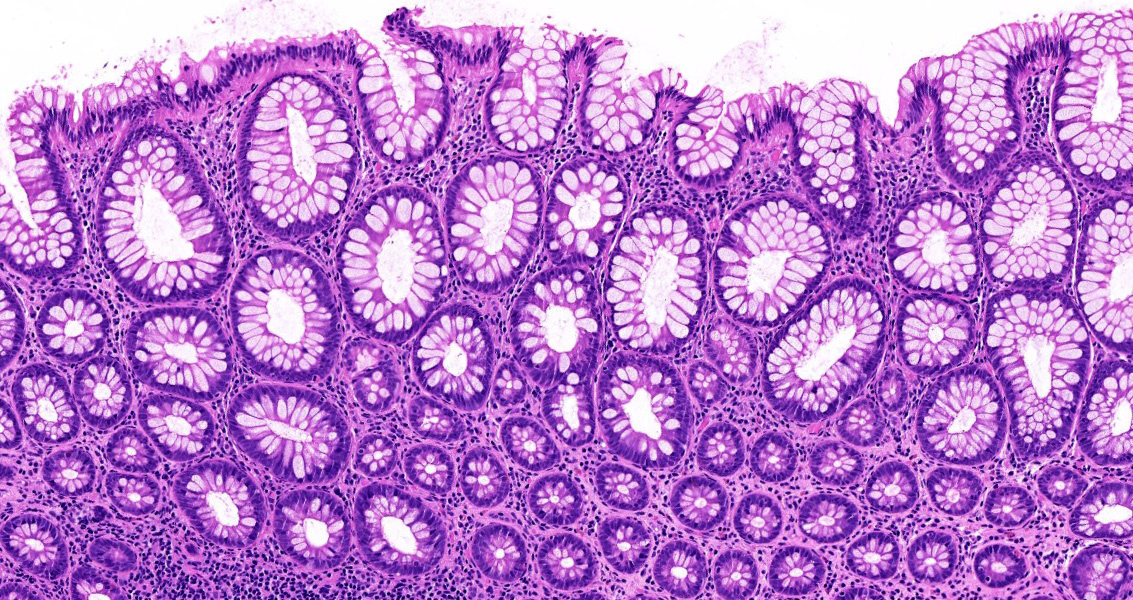
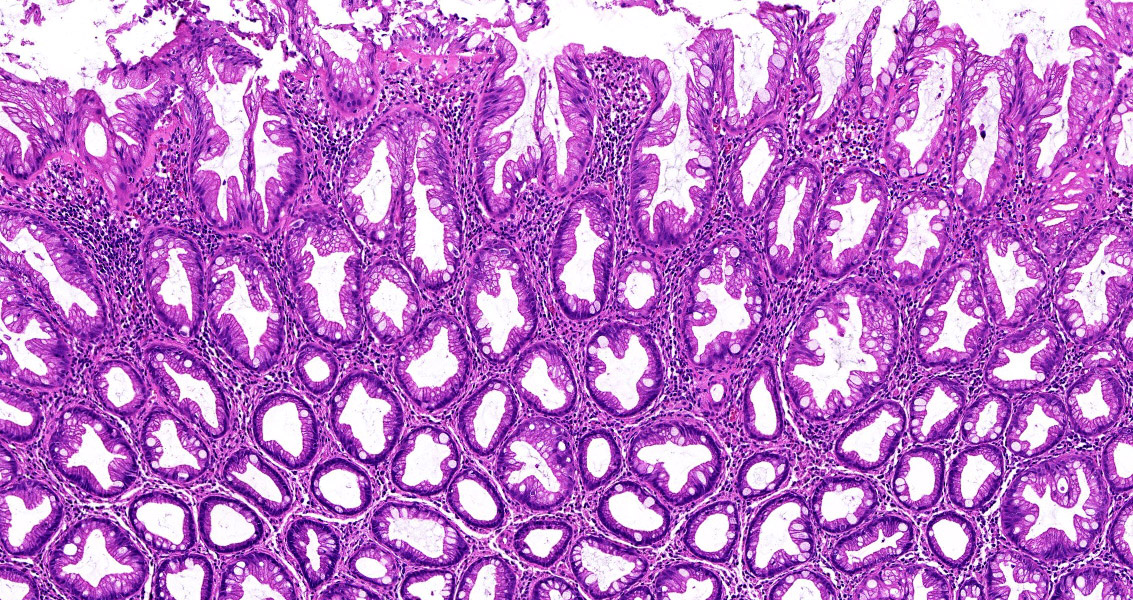
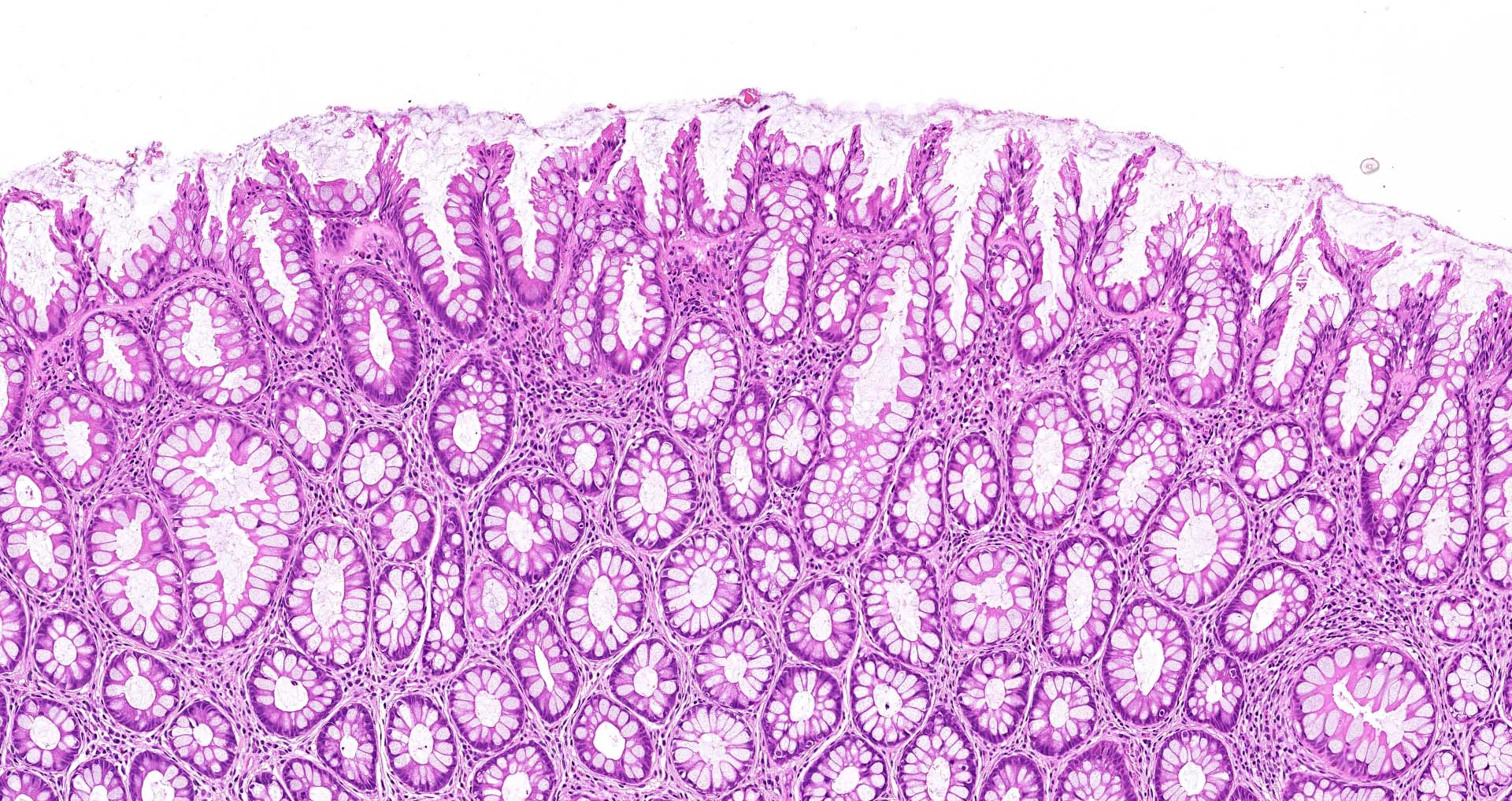
- Serrated architecture with a sawtooth appearance, with serrations generally limited to the upper half of the crypts
- Mild nuclear enlargement, stratification and hyperchromasia, limited to the crypt bases
- No dilated, branched or horizontally spreading crypts
- No evidence of conventional dysplasia, e.g. as is seen in colorectal adenomas
- Microvesicular variant is more common and comprises epithelial cells with small mucin vacuoles
- Goblet cell rich variant is less common and contains prominent goblet cells
- Comparison with adjacent nonlesional large intestinal mucosa may facilitate the recognition of goblet cell rich variant and reduce the risk of underdiagnosis, since the serrations are more subtle than in the microvesicular type (Histopathology 2021;78:634)
Microscopic (histologic) images
Positive stains
- Ki67 immunohistochemistry shows proliferation confined to the lower portions of the polyp, mirroring the morphological evidence of maturation towards the surface
Molecular / cytogenetics description
- Microvesicular variant not uncommonly contains a BRAF gene mutation (J Clin Pathol 2009;62:516)
- Goblet cell rich variant may contain a KRAS gene mutation (J Gastroenterol Hepatol 2017;32:358)
Sample pathology report
- Rectum, cold biopsy excision of 4 mm polyp:
- Hyperplastic polyp
Differential diagnosis
- Sessile serrated lesions (SSLs):
- Prominent serration extending into the lower half of the crypts
- Branched, dilated or laterally spreading crypts with little or no intervening lamia propria
- Herniation into the superficial submucosa
- May show conventional dysplasia
- Traditional serrated adenomas:
- Larger size
- Villiform architecture
- Eosinophilic cytoplasm
- Pencillate nuclei
- Ectopic crypts (Histopathology 2021;78:634)
Board review style question #1
Which of the following is characteristic of hyperplastic polyps of the large intestine?
- Are rare lesions
- Different risk factors for development compared with those for adenomas
- Little or no association with an increased risk of colorectal cancer
- Not often multiple within the rectum
- Usually require treatment by bowel resection
Board review style answer #1
C. Hyperplastic polyps that occur outside of the context of polyposis syndrome are not associated with a significant risk of colorectal cancer, in contrast to sessile serrated lesions, which are associated with increased cancer risk.
Comment Here
Reference: Hyperplastic polyp
Comment Here
Reference: Hyperplastic polyp
Board review style question #2
Which of the following histological features is characteristic of a hyperplastic polyp of the large intestine?
- Branched crypts
- Conventional dysplasia
- Dilated glands with little or no intervening lamina propria
- Prominent glandular serration extending down to the crypt bases
- Sawtooth pattern glands within the superficial aspect of the lesion
Board review style answer #2
E. Hyperplastic polyps characteristically contain sawtooth pattern glands within the superficial aspect of the lesion. In contrast to sessile serrated lesions, hyperplastic polyps do not show serration to the crypt bases, branched crypts or dilated crypts.
Comment Here
Reference: Hyperplastic polyp
Comment Here
Reference: Hyperplastic polyp