Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Challa B, Esnakula AK. Histoplasmosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonhistoplasmosis.html. Accessed April 2nd, 2025.
Definition / general
- Histoplasmosis is an invasive mycosis caused by inhalation of the spores of dimorphic fungi Histoplasma capsulatum (Int J Surg Pathol 2017;25:592)
- The most common endemic mycoses in the United States and in certain areas of Mexico, Central America and South America (Infect Dis Clin North Am 2016;30:207)
Essential features
- Invasive mycosis caused by inhalation of the spores of dimorphic fungi Histoplasma capsulatum
- Distal ileum and cecum are most commonly affected, followed by the rectum and descending colon
- Tissue culture and histopathology remain the gold standard for the diagnosis of colonic histoplasmosis
- Small, round to ovoid, narrow based budding yeast cells measuring 2 - 5 micrometers
- Stains positive for Gomori methenamine silver (GMS) stain and periodic acid-Schiff (PAS); negative for mucicarmine and Fontana-Masson silver stain
Terminology
- Also called Cave disease, Darling disease, Ohio Valley disease, reticuloendotheliosis, Spelunker lung and Caver disease (BMJ Case Rep 2016;2016:bcr2016216423)
ICD coding
Epidemiology
- Occurs widely but is highly endemic in Ohio, Mississippi river valleys and Latin America
- Also endemic in Asia, Southeast Asia and India
- Centers for Disease Control records estimate 50,000 infections yearly (Infect Dis Clin North Am 2016;30:207)
- Gastrointestinal (GI) infection by Histoplasma is common and a manifestation of disseminated disease
- Gastrointestinal tract is involved in 50 - 70% of disseminated cases
- Occurs in 0.05% cases in immunocompetent hosts
- Symptoms occur in 3 - 12% of patients (Gastrointest Endosc 2020;91:951, Int J Surg Pathol 2017;25:592)
- At autopsy, about 70% of patients with disseminated histoplasmosis have GI involvement (South Med J 2004;97:172)
Sites
- Distal ileum and cecum are most commonly affected, followed by the rectum and descending colon
- Colon is among the most frequently affected sites in GI (Gastrointest Endosc 2020;91:951)
Pathophysiology
- Dimorphic fungus exists as a mold in the environment
- Once inhaled, it enters the lung and transforms into yeast form at 35 - 37 °C
- Alveolar macrophages phagocytose these yeast forms, which multiply intracellularly until the advent of immune response
- Primary infection is usually asymptomatic and becomes reactivated in immunocompromised states
- Usually manifests as acute or chronic pulmonary disease
- Severe cases: disseminated to the skin, adrenal gland, central nervous system, lymph nodes, spleen, bone marrow and GI tract (Int J Surg Pathol 2017;25:592)
- In most healthy individuals, nonviable organisms persist in granulomas
Etiology
- Risk factors: HIV / AIDS, autoimmune disease, old age, organ transplant, hepatitis C virus infection, hematologic malignancies, corticosteroid use, tumor necrosis factor antagonists, primary immunodeficiency syndromes (ACG Case Rep J 2021;8:e00598, BMC Infect Dis 2013;13:143)
- Most commonly linked to farming, exposure to chicken coops or caves, remodeling or demolition of old buildings and cutting down trees or clearing brush from sites in which blackbirds have roosted (Infect Dis Clin North Am 2016;30:207)
Clinical features
- Symptoms: fever, diarrhea, altered bowel habits, GI bleeding (ACG Case Rep J 2021;8:e00598)
Diagnosis
- Multifaceted approach: history, clinical features, radiographic / endoscopic findings, blood, stool, tissue culture, antigen and antibody testing and molecular testing
- The European Organization for Research and Treatment of Cancer / Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC / MSG) criteria for the diagnosis of invasive fungal infections:
- Proven diagnosis: confirmation by either histopathology or culture
- Probable diagnosis: the presence of an appropriate clinical presentation, a predisposing condition and mycological evidence, such as the presence of antigenuria (J Clin Microbiol 2017;55:1612)
- Tissue culture and histopathology remain the gold standard for the diagnosis of colonic histoplasmosis (Case Rep Med 2018;2018:2723489, J Fungi (Basel) 2020;7:12)
- Slow, takes 4 - 6 weeks
Laboratory
- Culture and microbiology stains:
- Histoplasma capsulatum stains poorly for Gram stain
- Calcuflour white binds to chitin in fungal cell walls and helps in identification
- Colonies show septate hyphae followed by smooth or less commonly spiny microconidia (2 - 5 micrometers in size) and characteristic tuberculate macroconidia (7 - 15 micrometers)
- Small, round to oval, narrow based budding yeast forms at 37 °C
- Antigen detection:
- Galactomannan antigen testing in body fluids: rapid test (Infect Dis Clin North Am 2016;30:207)
- Sensitivity of enzyme immunoassay (EIA) is high in patients with disseminated disease (95%)
- Urine antigen detection: more sensitive than serum
- EIA's quantitative nature also allows for sequential monitoring of antigen clearance
- Crossreactivity can be seen with Blastomyces dermatitidis, Paracoccidioides brasiliensis, T. marneffei and less commonly, Coccidioides immitis and Coccidioides posadasii
- Antibody detection:
- Antibodies detectable after 4 - 8 weeks
- More suitable for diagnosis of subacute or chronic histoplasmosis
- A titer of ≥ 1:32 or 4 fold rise in antibody titers from acute to convalescent phase is strongly suggestive of acute infection
- Antibodies detectable after 4 - 8 weeks
- Molecular methods: polymerase chain reaction (PCR) assays
- Role uncertain
- Variable sensitivities reported in published studies (J Clin Microbiol 2017;55:1612)
Radiology description
- Bowel wall thickening, mass lesions, signs suggesting bowel obstruction, free peritoneal air (J Med Microbiol 2010;59:610)
- Other findings of disseminated disease: hepatosplenomegaly, pulmonary infiltrates, generalized lymphadenopathy
Prognostic factors
- Prognosis is good after early and aggressive treatment; the disease is fatal if remains untreated (Int J Surg Pathol 2017;25:592)
- Improvements in both antiretroviral and antifungal therapies appear to have contributed to a lower prevalence and may favorably impact the prognosis of this disease (Diagn Microbiol Infect Dis 2006;55:195)
Case reports
- 30 year old cachectic woman with a history of HIV and poor compliance with highly active antiretroviral therapy (HAART) presents with diffuse abdominal pain and fever (Cureus 2020;12:e7775)
- 39 year old man with HIV presents with severe pain in the abdomen (Case Rep Med 2018;2018:8923972)
- 57 year old asymptomatic man with a history of orthotopic liver transplant was found to have sessile polyps on elective surveillance colonoscopy (ACG Case Rep J 2021;8:e00598)
- 60 year old woman presents with recurrent diarrhea and abdominal discomfort (Cureus 2018;10:e2951)
- 60 year old man presents with 75 pound weight loss and dysphagia, and was found to have idiopathic Cd4 T lymphocytopenia (Cureus 2021;13:e19748)
Treatment
- According to the Infectious Diseases Society of America, clinical guidelines for the treatment of GI histoplasmosis without CNS involvement: amphotericin B (300 mg/kg daily) for 1 - 2 weeks followed by oral itraconazole (200 mg 3 times daily for 3 days and then 200 mg twice a day for a total of at least 12 months) (Infect Dis Clin North Am 2016;30:207)
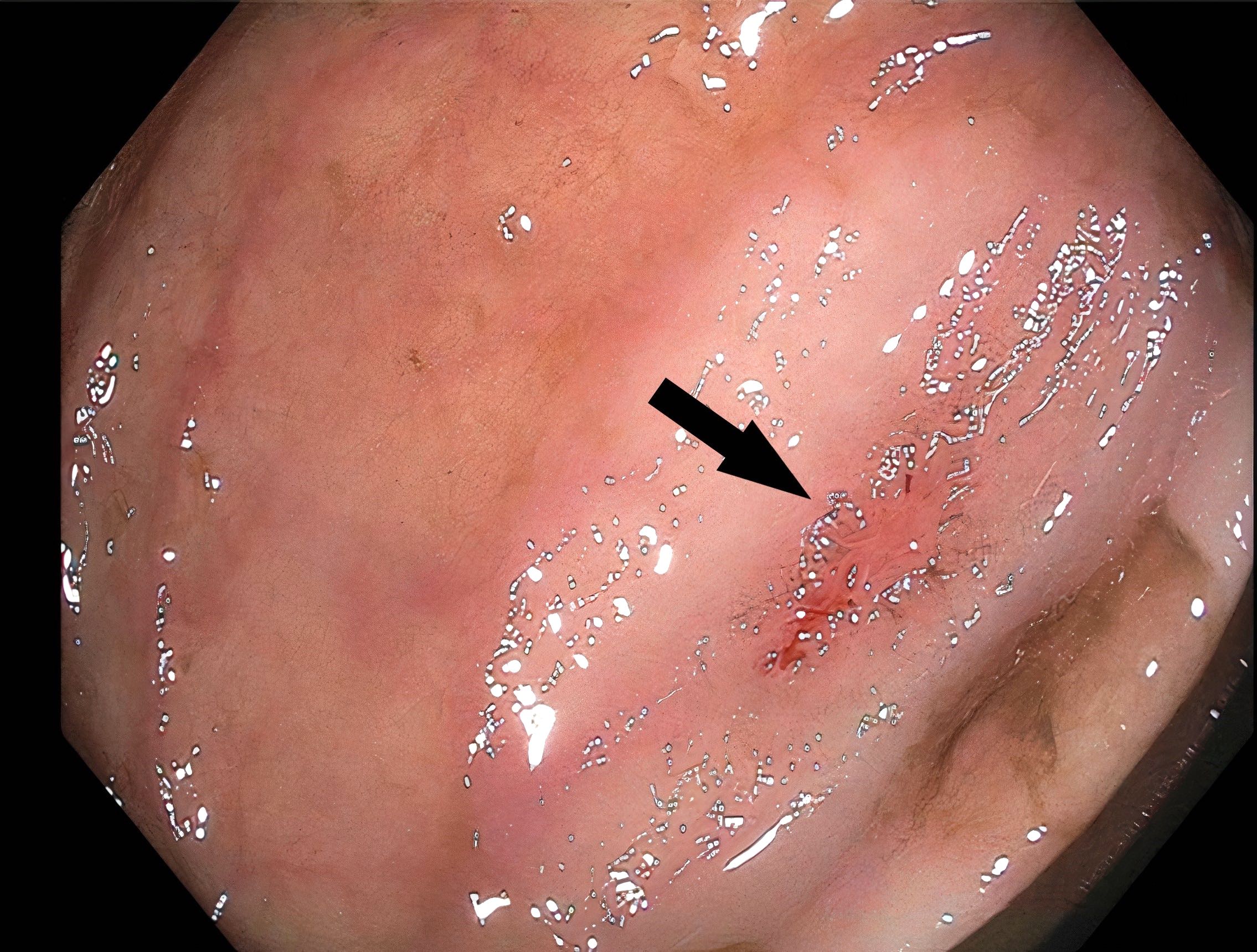
Clinical images
Gross description
- Focal / multiple mucosal ulcerations, polypoid lesions, strictures, obstruction due to circumferential thickening (Gig Sanit 1986:39)
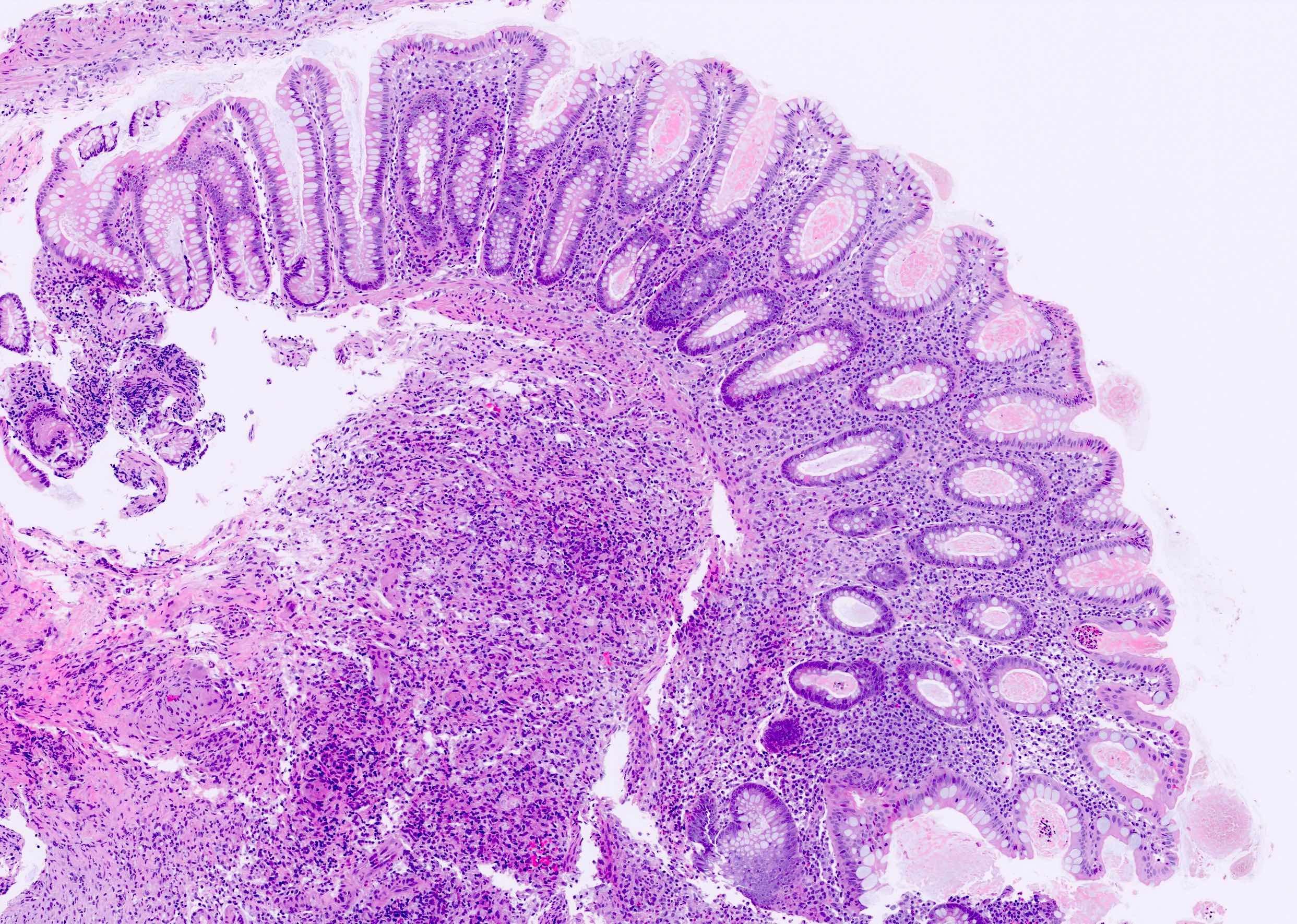
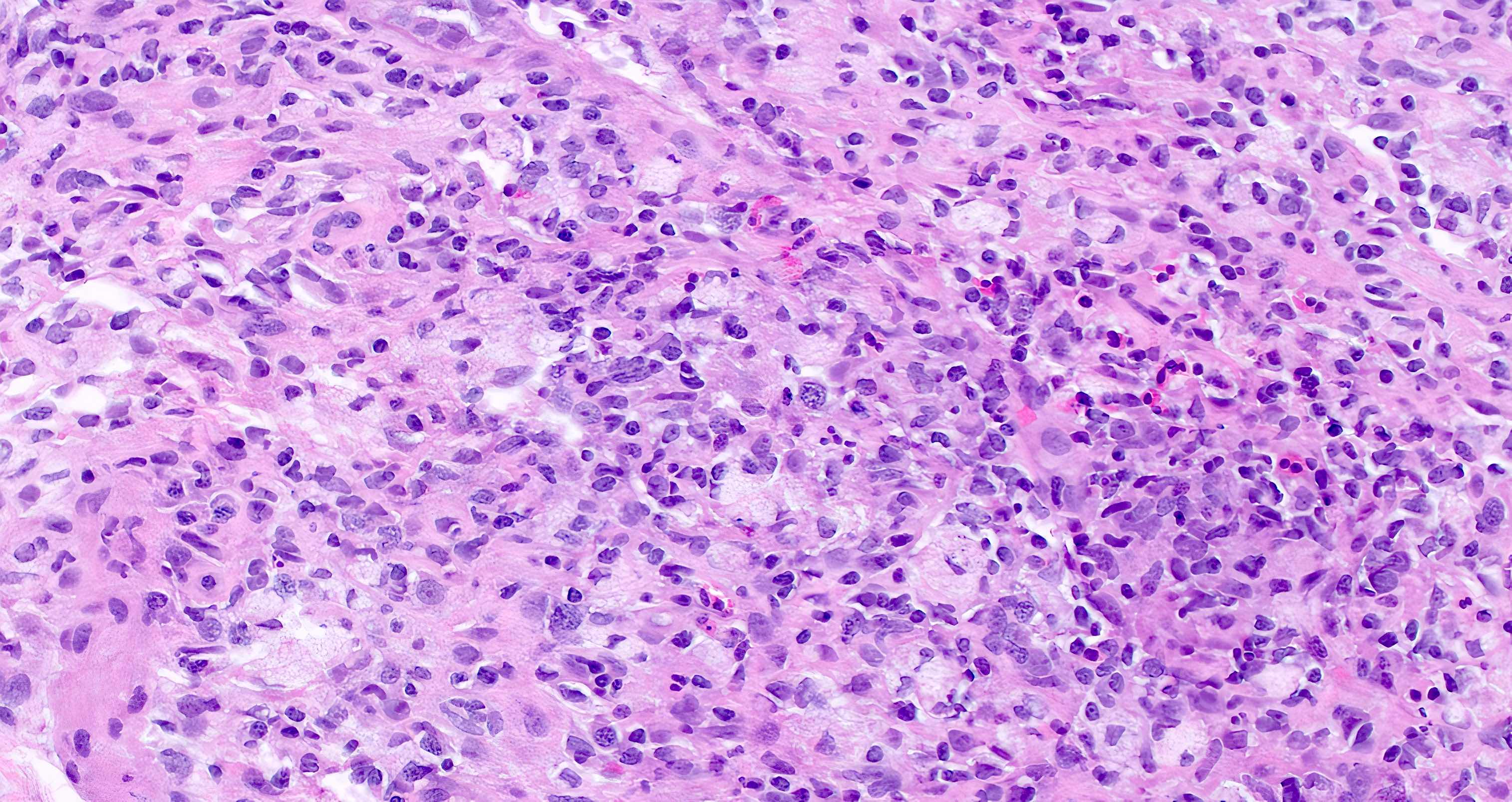
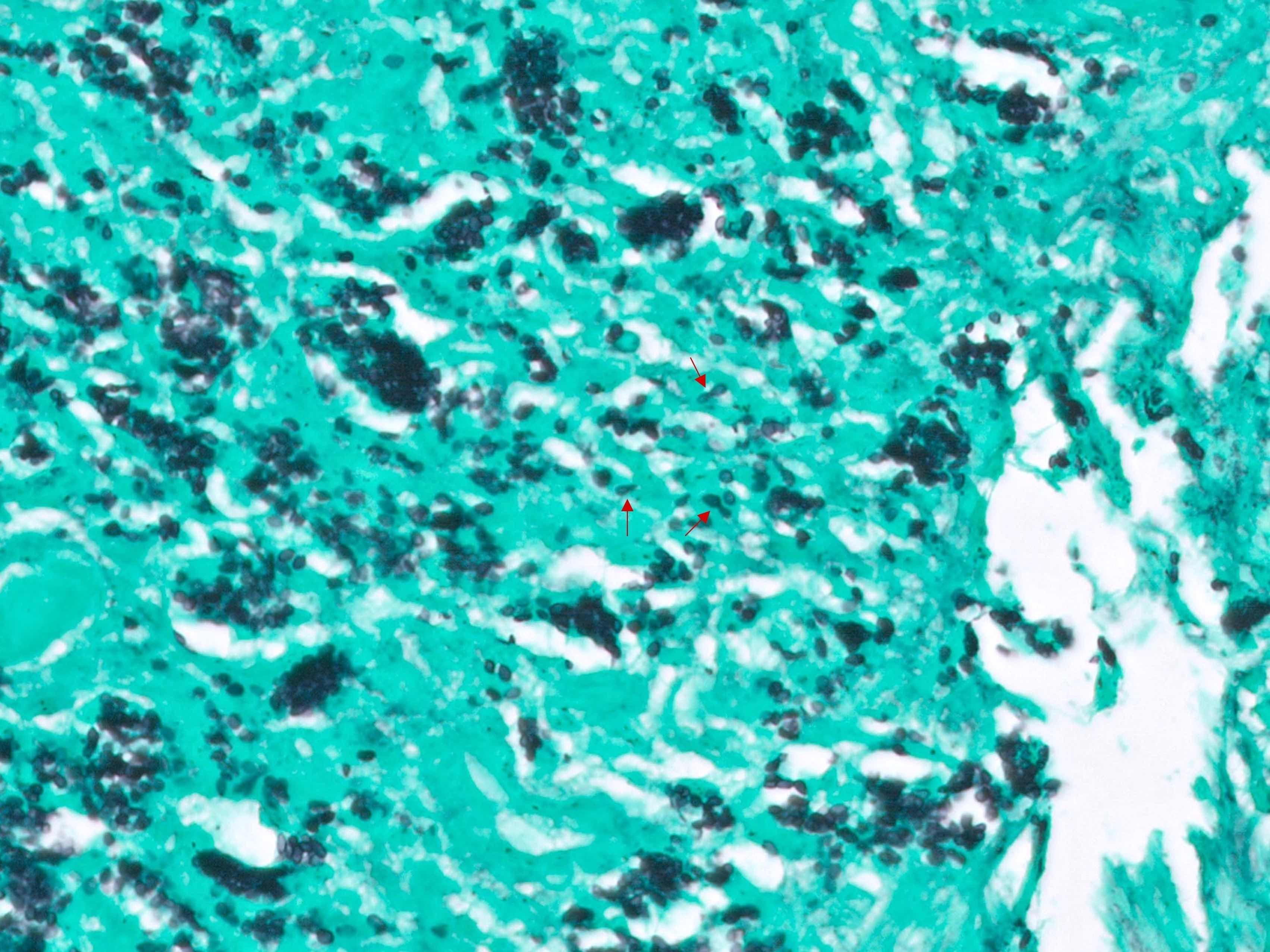
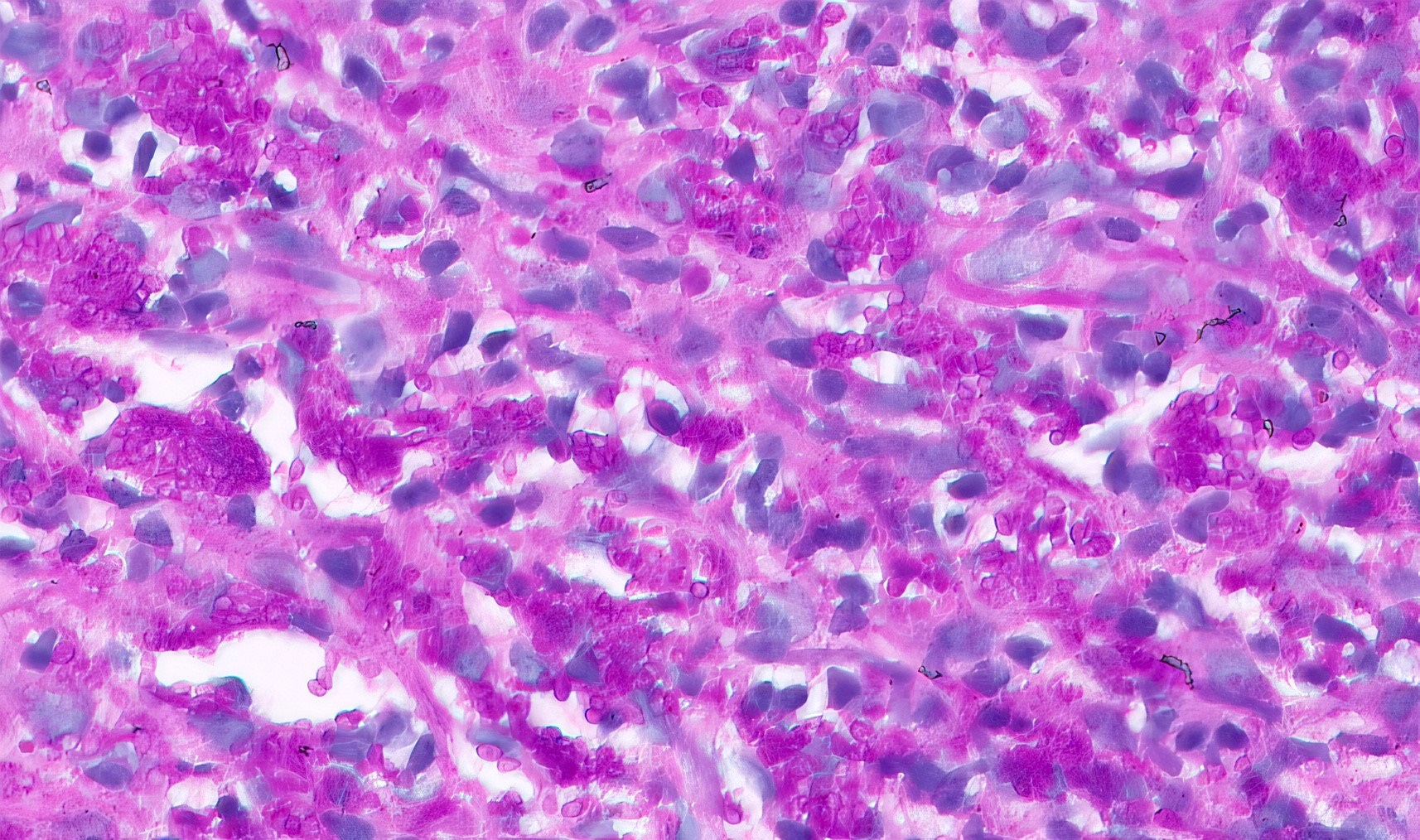
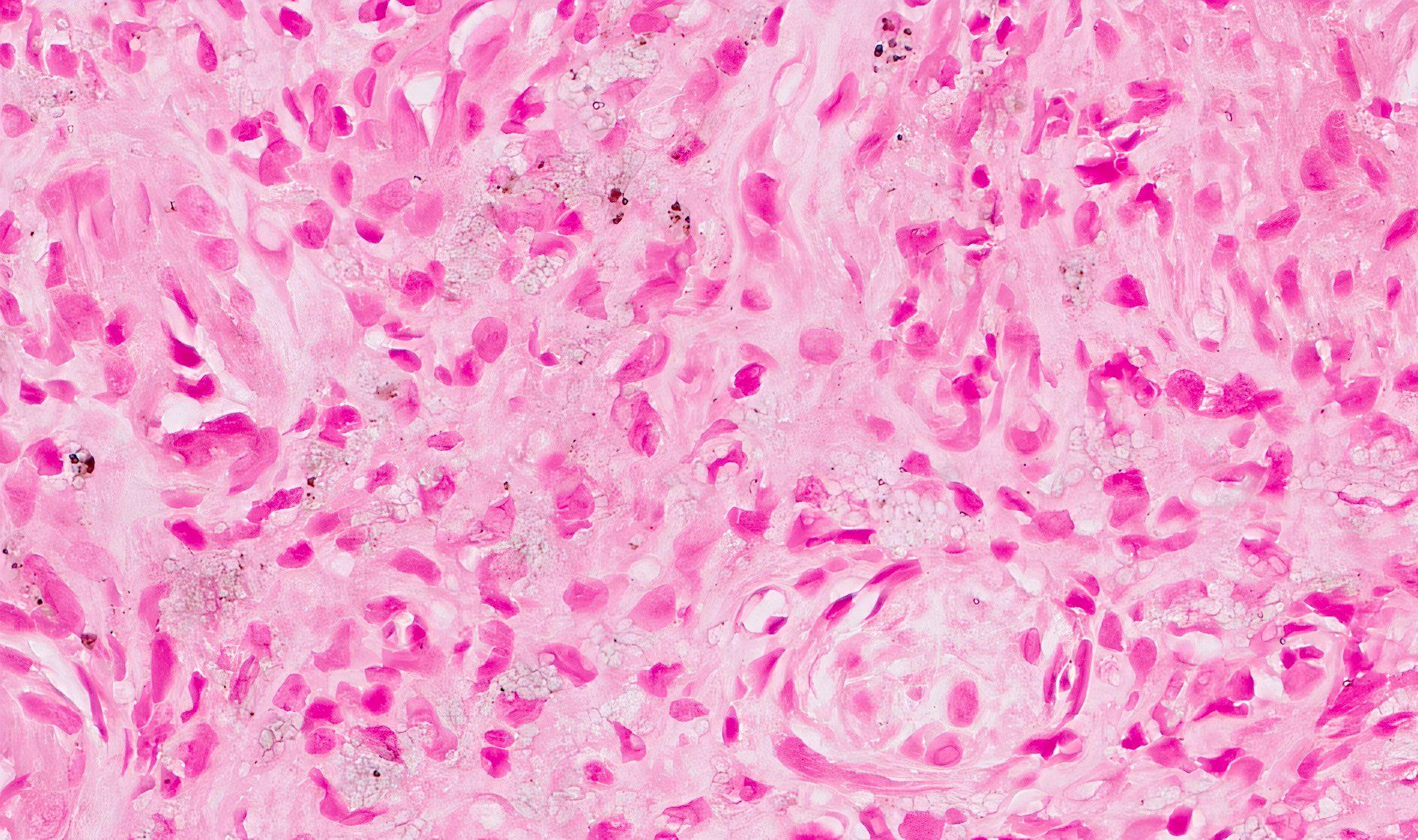
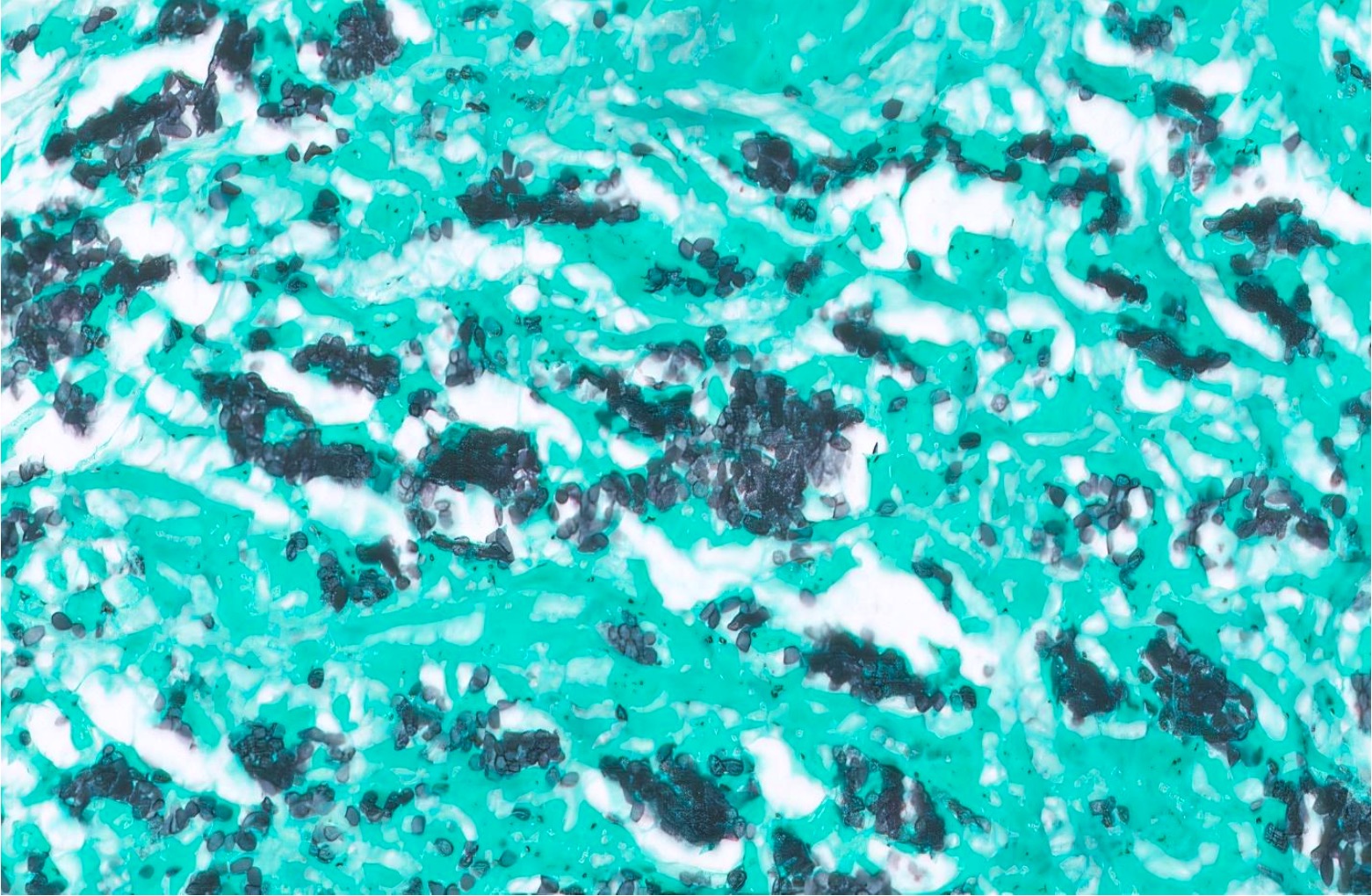
Microscopic (histologic) description
- Colonic tissue shows diffuse expansion of lamina propria and submucosa by foamy histiocytes associated with lymphocytes and eosinophils; mucosal ulceration can be seen frequently (Clin Chest Med 2009;30:217)
- Granulomas are less frequently observed
- Organisms are usually intracellular within histiocytes, rarely extracellular mixed with ulcer debris (Am J Clin Pathol 2000;113:64)
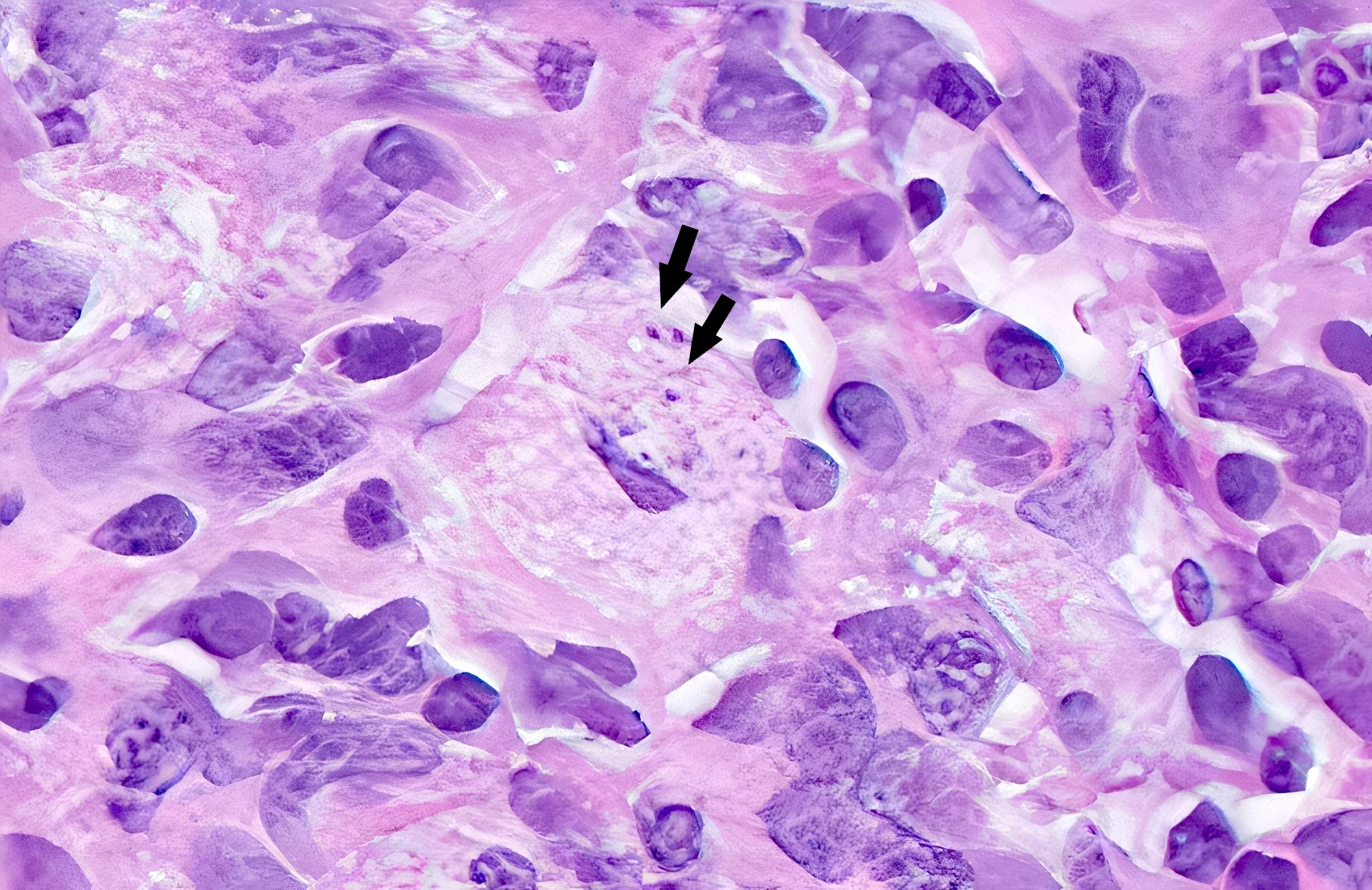
- Protoplasm of the organisms retracts during fixation, resulting in a pseudocapsule on routine H&E (Pathologe 2022;43:16)
- GMS and PAS special stains highlight the yeast cell wall and are helpful for characterization of the organisms
- Romanowsky type stains, such as the Wright-Giemsa stain, impart a dark blue hue to the fungal nuclear compartment
- Yeast forms can also pick up Ziehl-Neelsen stain (J Pathol Transl Med 2017;51:482)
- H. capsulatum var. capsulatum: small, round to ovoid, narrow based budding yeast forms measuring 2 - 5 micrometers
- H. capsulatum var. duboisii are larger and measure 6 - 12 micrometers (Infect Dis Clin North Am 2016;30:207)
Microscopic (histologic) images
Virtual slides
Negative stains
Videos
Histoplasmosis colitis
Colonoscopy in histoplasmosis
Sample pathology report
- Colon, cecum, ulcer, biopsy:
- Mucosal and submucosal histiocytic inflammation containing numerous yeasts, morphologically compatible with Histoplasmosis capsulatum (positive GMS and PAS stains, negative mucicarmine and Fontana-Masson stains)
Differential diagnosis
- Infections mimicking histoplasmosis:
- Candida, Pneumocystis, Talaromyces, Cryptococcus, Blastomyces and leishmaniasis:
- Candida glabrata resembles Histoplasma but shows variably sized yeast cells and more frequent budding, lacks halos, is Gram stain positive and is usually extracellular
- Pneumocystis jiroveci and Talaromyces marneffei also resemble Histoplasma but rarely involve colon (Pathologe 2022;43:16)
- Pneumocystis can show GMS and PAS positivity but cysts are larger (5 - 8 micrometers), do not show budding and are predominantly extracellular
- Mucicarmine stains Cryptococcus capsule (3 - 8 micrometers) and produces characteristic halos
- Unencapsulated forms of Cryptococcus: Fontana-Masson stain can be used to stain cryptococcal melanin
- Blastomyces are larger (up to 15 micrometers) and show broad based budding and thick walls and can stain positive for Congo red (J Clin Microbiol 2017;55:1612, J Cutan Pathol 2008;35:27)
- Leishmaniasis shows small (2 - 4 micrometers) round to oval organisms with bar shaped kinetoplast and stains negative on GMS, positive on Giemsa and is usually extracellular (Am J Trop Med Hyg 2010;83:209)
- Candida, Pneumocystis, Talaromyces, Cryptococcus, Blastomyces and leishmaniasis:
- Granulomatous / IBD colitis:
- No fungal organisms
- Malakoplakia:
Additional references
Board review style question #1
A 45 year old man with a history of HIV presents with abdominal pain and diarrhea. Colonoscopy showed erythematous mucosal ulceration in the cecum. Biopsy from the ulcer showed numerous foamy histiocytes. GMS stain highlights numerous intracellular small, round to oval organisms as shown in the above image. Organisms stain positive with PAS and negative with mucicarmine. What is the diagnosis?
- Candidiasis
- Cryptococcosis
- Histoplasmosis
- Leishmaniasis
Board review style answer #1
C. Histoplasmosis. GMS stain highlights numerous intracellular round to oval yeast forms showing narrow based budding, morphologically consistent with histoplasmosis.
Comment Here
Reference: Histoplasmosis
Comment Here
Reference: Histoplasmosis
Board review style question #2
The organisms shown in this image stain positive for GMS and PAS and negative for mucicarmine. What is the gold standard for diagnosis of the tissue invasive disease caused by these organisms?
- Clinical history and imaging findings
- Imaging findings and serology testing
- Serology testing and histopathological examination
- Tissue culture and histopathological examination
Board review style answer #2
D. Tissue culture and histopathological diagnosis. The diagnosis is histoplasmosis. Clinical history and imaging findings can be nonspecific in histoplasmosis, while serology testing can be false negative or show crossreactivity with other organisms. Tissue culture isolates the organisms and histopathological examination with H&E and special stains help in definitive diagnosis.
Comment Here
Reference: Histoplasmosis
Comment Here
Reference: Histoplasmosis