Table of Contents
Definition / general | Essential features | Physiology | Diagrams / tables | Clinical features | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Devins K, Schwartz L. Histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixnormalhistology.html. Accessed April 25th, 2024.
Definition / general
- Lower portion of the uterus which connects the uterine corpus to the vaginal canal
Essential features
- Exocervix is lined by stratified squamous epithelium
- Endocervix is lined by columnar mucinous epithelium
- Transformation zone is the hormonally responsive zone of metaplasia between the exocervix and endocervix
- Squamocolumnar junction is the precise histologic transition between squamous and glandular epithelium
- Transformation zone is usual site of persistent infection with high risk subtypes of human papillomavirus (HPV), the most common cause of cervical carcinoma
Physiology
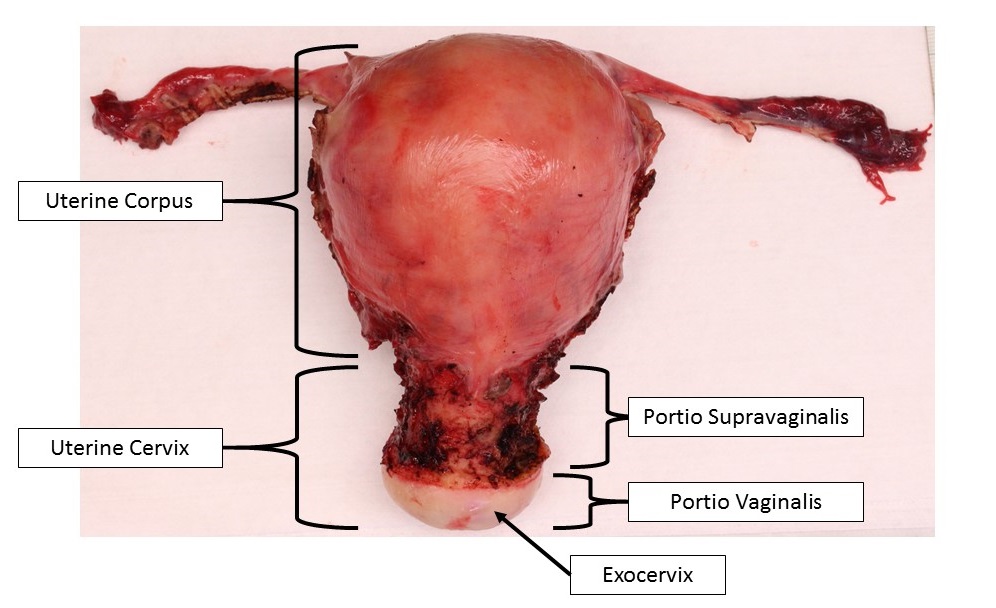
- 2 anatomic portions:
- Portio vaginalis: anatomic portion of cervix inferior to vaginal reflection and within vaginal canal
- Portio supravaginalis: anatomic portion of cervix superior to vaginal reflection
- Ectocervix (exocervix): external mucosal surface of portio vaginalis
- Normally lined by nonkeratinizing stratified squamous epithelium
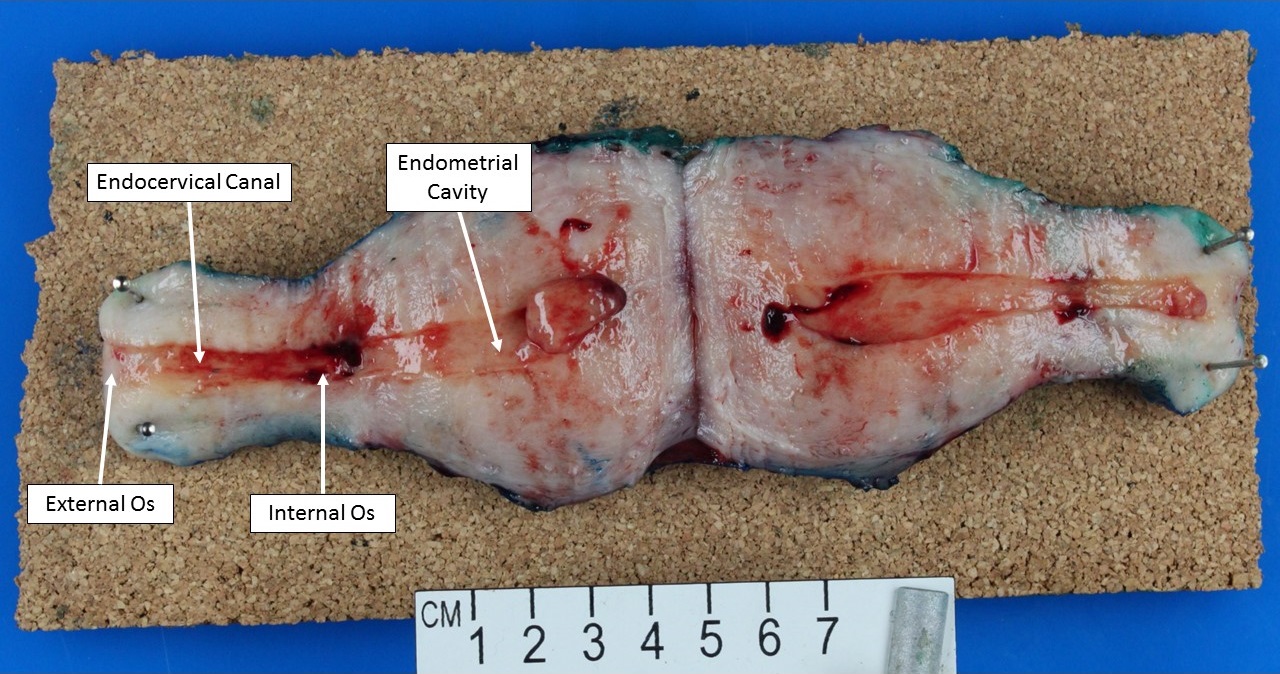
- Endocervix (endocervical canal): mucosa lined cylindrical canal leading from ectocervix to uterine cavity
- Normally lined by single layer of mucinous columnar epithelium
- External os: anatomic opening of the endocervical canal onto the ectocervix
- Represents the inferior limit of the endocervix
- Internal os: anatomic widening of the endocervical canal as it opens and gradually transitions into the uterine cavity
- Represents the superior limit of the endocervix and distal aspect of the lower uterine segment
- Squamocolumnar junction: histologic junction between squamous epithelium of ectocervix and columnar glandular epithelium of endocervix; location changes throughout life in response to hormonal status and age
- Squamocolumnar junction is located on outer surface of portio vaginalis at birth due to effect of maternal hormones; rapidly recedes into endocervical canal until menarche (J Reprod Med 1976;16:221)
- In early adolescence, squamocolumnar junction migrates distally from the external os onto the exocervix in response to pubertal hormones, forming the ectropion
- Ectropion: physiologic ectopic columnar epithelium present on exocervix beginning at adolescence
- Ectropion is gradually replaced by squamous metaplasia throughout reproductive years and the functional squamocolumnar junction slowly recedes towards the external os
- Transformation zone: the physiologic area of metaplastic squamous epithelium between the exocervix and the endocervix; it begins distally at the original squamocolumnar junction present at adolescence and extends proximally to the current functional squamocolumnar junction
- Squamocolumnar junction often recedes within external os following menopause
Diagrams / tables
Clinical features
- Transformation zone is the usual site of persistent infection with high risk subtypes of human papillomavirus (HPV), the most common cause of cervical carcinoma (J Clin Pathol 2002;55:244)
Gross description
- Cylindrical structure forming lower ~ third of uterus, connecting uterine corpus to vaginal canal
- Anatomic position within the pelvic cavity between the urinary bladder (anterior) and rectum (posterior)
- Anterior portion can be identified by a higher peritoneal reflection, due to location of the bladder in vivo (J Clin Pathol 1993;46:388)
Microscopic (histologic) description
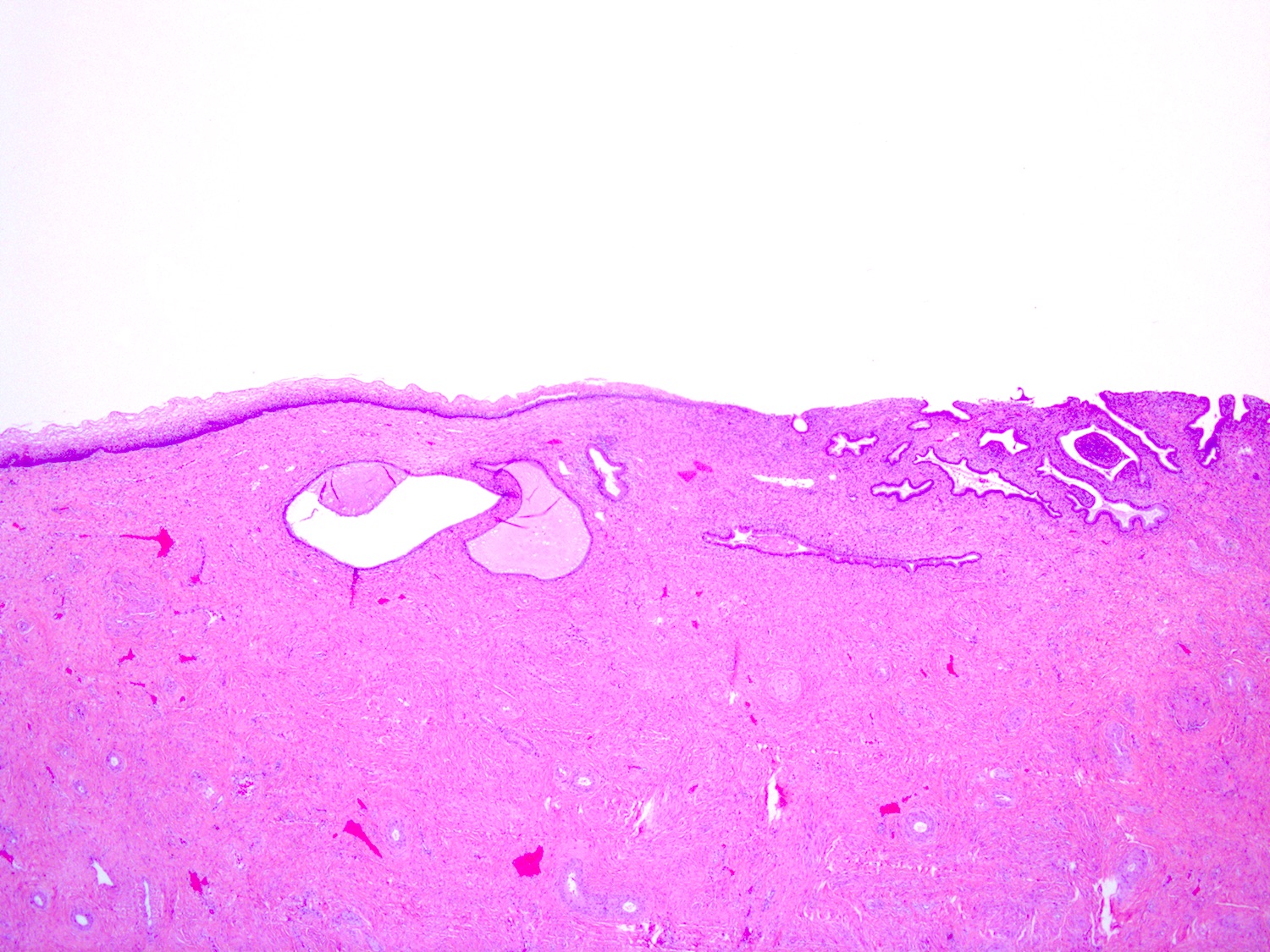
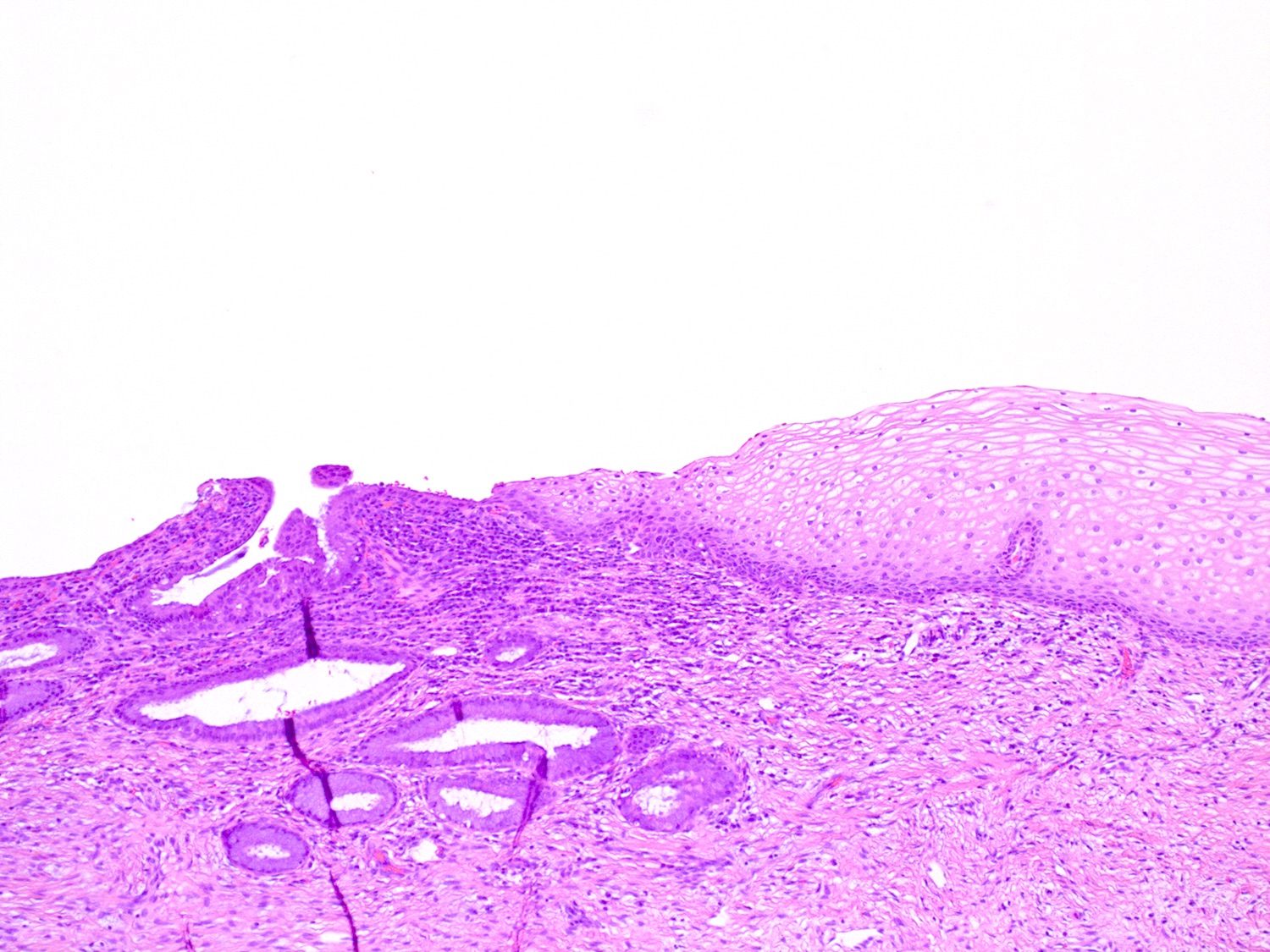
- Ectocervix
- Stratified nonkeratinizing squamous epithelium
- Basal cells: deepest layer; dense nuclear chromatin, uniform oval nuclei oriented perpendicular to basement membrane, scant cytoplasm
- Parabasal cells: located just above the basal cell layer; slightly more cytoplasm than basal cells; may be multiple cell layers thick
- Intermediate cells: abundant cytoplasm which may be pink or clear due to glycogen accumulation
- Superficial cells: small, round nuclei; abundant pink or clear cytoplasm; cells flatten and are oriented parallel to basement membrane
- Hormone responsive
- Superficial cells predominate in early cycle due to estrogen
- Intermediate cells predominate in late cycle due to progestins
- Loss of intermediate and superficial cells (atrophy) occurs postmenopause
- Rare melanocytes, Langerhans cells and endocrine cells have been identified (Br J Obstet Gynaecol 1983;90:400, Virchows Arch A Pathol Anat Histopathol 1987;411:293)
- Stratified nonkeratinizing squamous epithelium
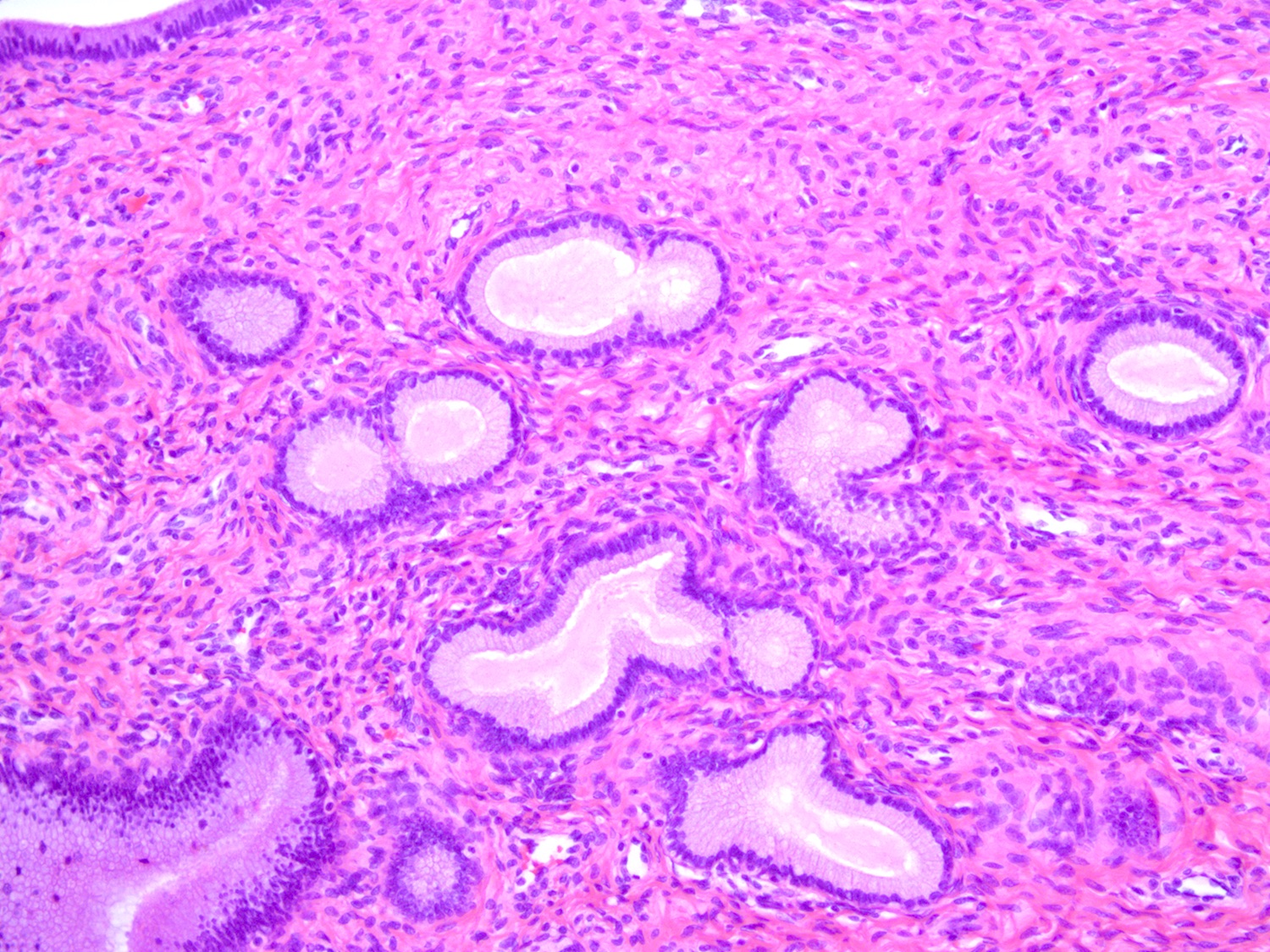
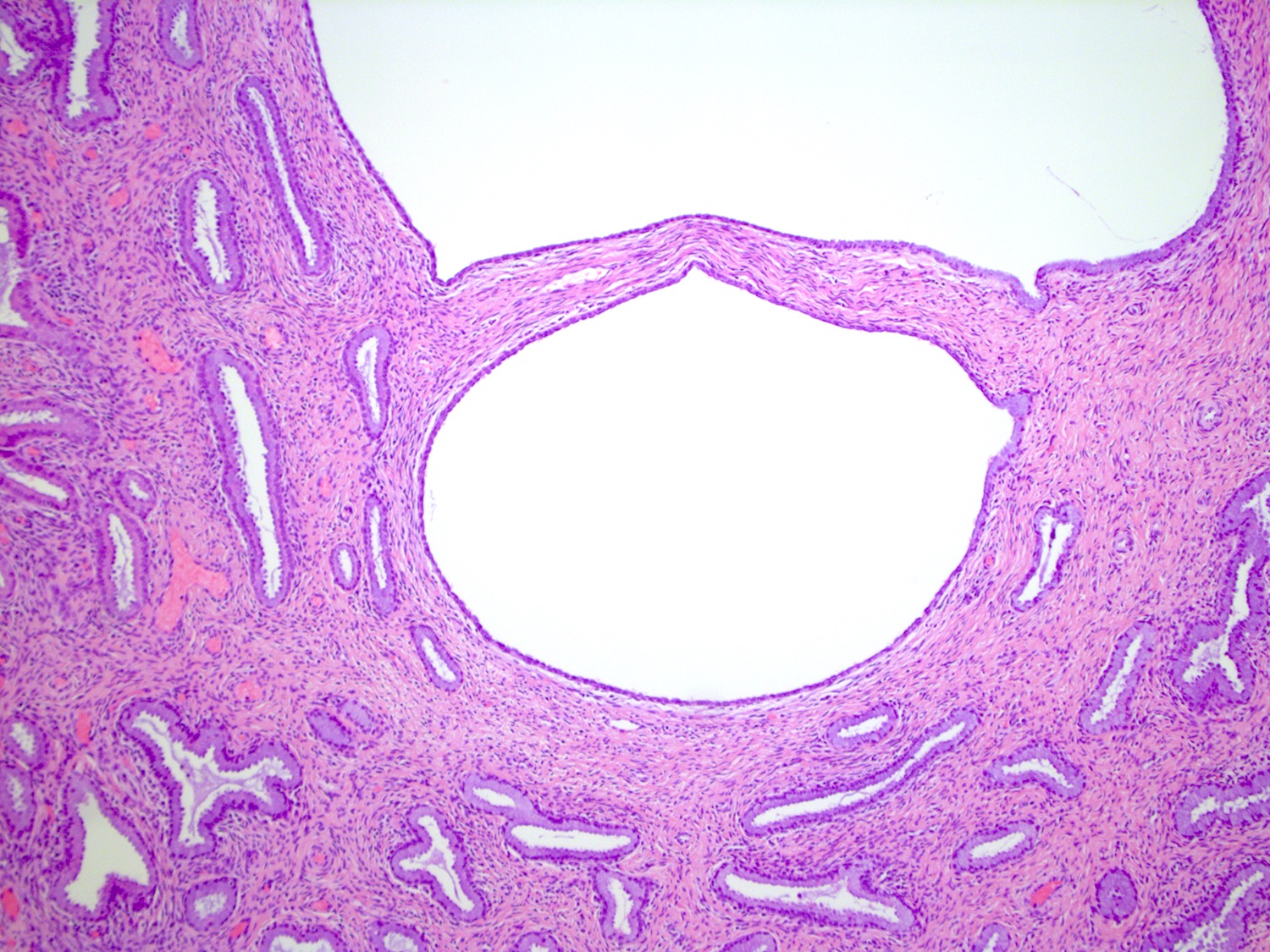
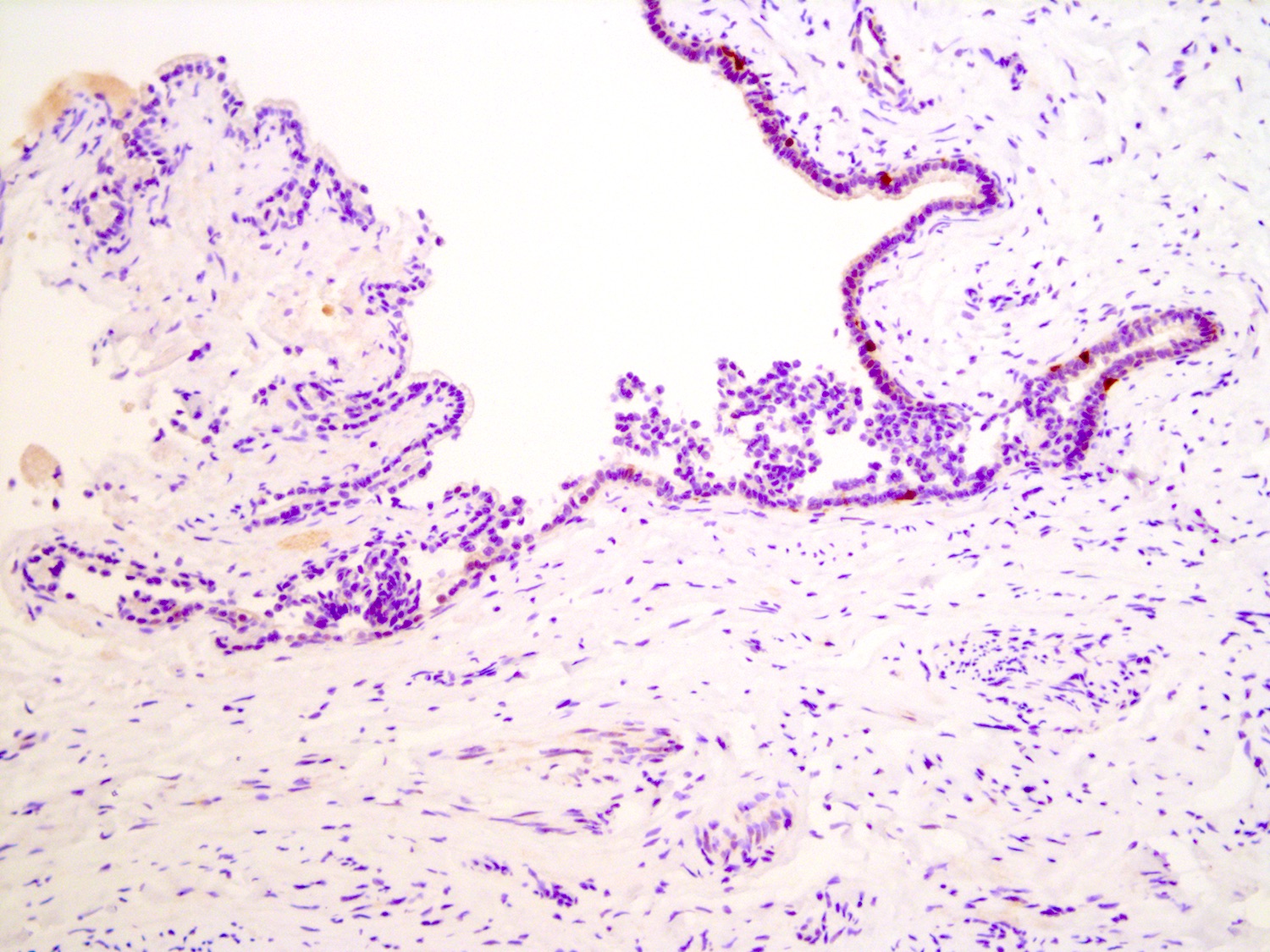
- Endocervix
- Single layer of mucinous columnar cells with dense, uniform, oval, basally oriented nuclei and apical mucin
- Mucin has a pale bluish appearance in H&E preparations; with PAS-Alcian blue stain, apical mucin stains intense blue / purple (due to the presence of acid type mucin)
- Ciliated cells can be found (usually in the context of tuboendometrioid metaplasia)
- Inconspicuous underlying reserve cell layer
- Forms infoldings, clefts and glands of variable shape
- Transformation zone
- Metaplastic cells: formed by endocervical reserve cells differentiating toward squamous lineage
- Located at transition between glandular and squamous epithelia
- Similar appearance to parabasal cells with relatively scant cytoplasm and dense nuclei
- Endocervical epithelium may overlie metaplastic cells
- Variable nonspecific inflammatory infiltrate consisting of lymphocytes, plasma cells and even neutrophils is common and is not necessarily associated with infection
- Metaplastic cells: formed by endocervical reserve cells differentiating toward squamous lineage
- Cervical stroma
- Mostly fibrous tissue with some haphazard smooth muscle fibers
- Blood vessels often numerous and prominent
- Mesonephric rests / remnants
- Remnants of involuted embryologic mesonephric (Wolffian) ducts
- Present in lateral cervical wall in ~33% of women
- Microscopic clusters of tubules lined by single layer of cuboidal cells with eosinophilic luminal secretions (Am J Surg Pathol 1990;14:1100)
Microscopic (histologic) images
Cytology description
Positive stains
Negative stains
- p16: negative or patchy (Adv Anat Pathol 2006;13:8)
Additional references
Board review style question #1
Which of the following is true about the squamocolumnar junction of the cervix, shown in the image?
- Relatively static and does not undergo significant histologic changes after birth
- Inflammatory infiltrate at the squamocolumnar junction is abnormal and indicates infection
- Migrates distally from the external os during menopause
- Migrates distally from the external os in response to estrogens during adolescence
Board review style answer #1
D. The squamocolumnar junction and transformation zone are hormonally responsive. The squamocolumnar junction actively migrates distally onto the exocervix in response to estrogens at puberty.
Comment Here
Reference: Cervix - histology
Comment Here
Reference: Cervix - histology
Board review style question #2
Which of the following best describes the appearance of normal endocervical epithelium?
- Columnar cells with basally located nuclei, apical mucin and occasional cilia
- Tall pseudostratified nuclei with conspicuous apoptotic bodies and apical mitotic figures
- Stratified cuboidal cells with scattered mucocytes
- Stratified nonkeratinizing squamous epithelium
Board review style answer #2
A. Normal endocervical epithelium consists of columnar cells with round, basally oriented nuclei and pink apical cytoplasm. Ciliated cells can be found.
Comment Here
Reference: Cervix - histology
Comment Here
Reference: Cervix - histology