Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Parra-Herran C. HPV associated adenocarcinoma (usual type and variants). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixhpvadenocarcinoma.html. Accessed December 22nd, 2024.
Definition / general
- Malignant neoplasm of the uterine cervix with a glandular phenotype
- 5 - 25% of invasive cervical carcinomas
Essential features
- Adenocarcinoma is the second most frequent cervical carcinoma, following squamous cell carcinoma (Curr Oncol Rep 2014;16:416)
- Adenocarcinomas of the uterine cervix associated with HPV infection represent 85 - 90% of all adenocarcinomas (Am J Surg Pathol 2018;42:214, Am J Surg Pathol 2019;43:75)
Terminology
- HPV associated adenocarcinomas are all described as a single group in the current World Health Organization of Tumours of Female Reproductive Organs (WHO Classification of Tumours Editorial Board: Female Genital Tumours, 5th Edition, 2020)
- Previously described types (usual, mucinous, etc.) are described as variants
- Usually associated with in situ adenocarcinoma
ICD coding
- ICD-O:
- 8140/3 - adenocarcinoma, usual type
- 8480/3 - mucinous carcinoma
- 8482/3 - mucinous adenocarcinoma, endocervical type
- 8144/3 - adenocarcinoma, intestinal type
- 8490/3 - mucinous carcinoma, signet ring cell type
- 8263/3 - villoglandular carcinoma
- 8574/3 - adenocarcinoma with neuroendocrine differentiation
- ICD-11: 2C77.1 - adenocarcinoma of cervix uteri
Epidemiology
- Adenocarcinoma is the second most frequent cervical carcinoma following squamous cell carcinoma (Curr Oncol Rep 2014;16:416)
- Incidence increasing in the U.S. and other developed countries from ~5% to ~20% between the 1960s and the 2000s (Cancer 2004;100:1035, Gynecol Oncol 2000;78:97)
- Cumulative incidence has also increased internationally (Int J Cancer 1998;75:536)
- Increased frequency in young women (Cancer 2004;100:1035)
Etiology
- Infection by high risk HPV (most commonly HPV types 18 and 16)
Clinical features
- Often vaginal bleeding or pelvic pain
- Abnormal cytology screening seen in ~88% of cases, either as glandular or squamous cell abnormalities (Cytojournal 2016;13:28)
- Often spreads to pelvic structures and regional lymph nodes
- Metastases most often to ovaries and fallopian tubes, less frequently to distant organs
- Stage is the most important prognostic factor; 5 year overall survival rates vary depending on stage: FIGO stage I - 79%, II - 37%, III / IV - less than 9% (see Staging)
Diagnosis
- Routine screening cervicovaginal cytology identifies many but not all cervical adenocarcinomas (J Low Gen Tract Dis 2017;21:91)
- Patients with abnormal cytology or symptoms (e.g. bleeding) are referred to examination by colposcopy (J Low Genit Tract Dis 2020;24:102)
- Adjunct imaging can be useful (pelvic ultrasound, MRI)
- Definitive diagnosis requires biopsy
Radiology description
- Mass occupying the canal or replacing the wall
- Nondiscrete thickening or distortion of the wall
Prognostic factors
- Poor prognostic factors:
- Advanced stage, which is largely determined by tumor size and depth of invasion (Int J Gynecol Cancer 2004;14:104)
- Lymphovascular space invasion
- Horizontal tumor extent (prognostically significant but no longer included in staging) (Gynecol Oncol 2020;158:266)
- Destructive pattern of stromal invasion (see Microscopic (histologic) description)
Case reports
- 34 year old woman with atypical glandular cells on Pap smear (Case #495)
- 50 year old woman with adenocarcinoma of the cervix involving the fallopian tube mucosa (Diagn Pathol 2016;11:77)
- 72 year old woman with intracranial metastases (Int J Gynecol Cancer 2005;15:561)
- Woman with ovarian recurrence after radical trachelectomy (Am J Obstet Gynecol 2005;193:1382)
- Woman with vaginal metastasis associated with traumatic vaginal tear (Gynecol Oncol 2005;96:857)
Treatment
- Early invasion (stage IA1 and IA2 without lymphovascular invasion) can be treated conservatively with cone (presuming negative margins) and no lymphadenectomy
- Patients with stage IA2 with lymphovascular invasion, IB1 and IB2 receive radical hysterectomy plus lymphadenectomy and consideration for adjuvant therapy (Int J Gynecol Pathol 2000;19:29, Int J Gynecol Cancer 2011;21:1640, Gynecol Oncol 2016;141:36, Int J Gynecol Pathol 2017;36:476)
- Advanced stage tumors (IB3, II - IV) receive neoadjuvant radiation therapy, cisplatin or other chemotherapy
- Less responsive to chemoradiotherapy than squamous cell carcinoma (Oncol Lett 2015;9:2791)
Gross description
- See Grossing
- When grossly visible (by definition, FIGO stage IB or greater), lesion can be exophytic, ulcerated or flat (Int J Gynaecol Obstet 2019;145:129, Int J Gynaecol Obstet 2019;147:279)
- On cut sectioning, there is variable growth into cervical wall
- Barrel shaped cervix with diffuse enlargement, if lesion is widely invasive
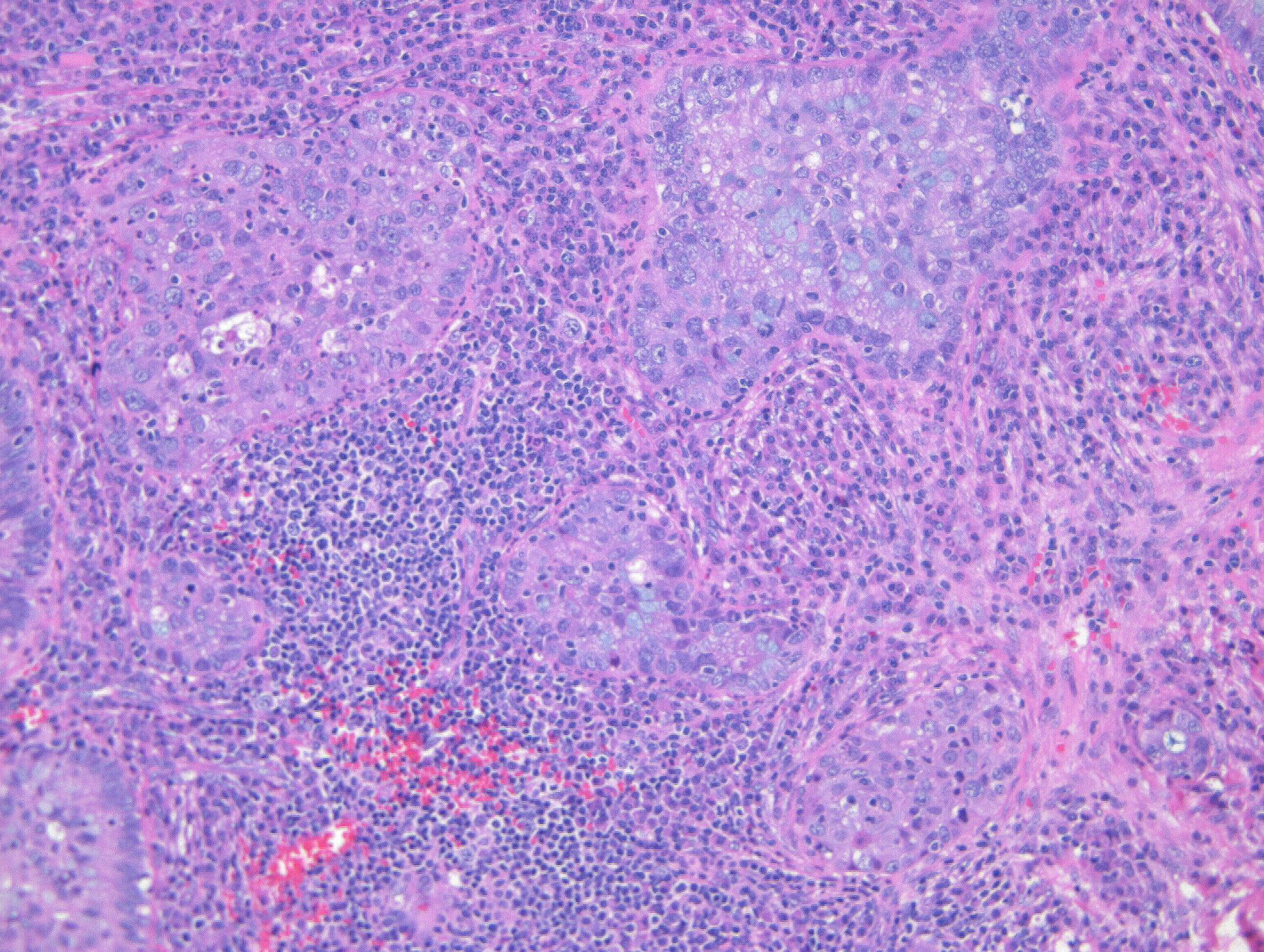
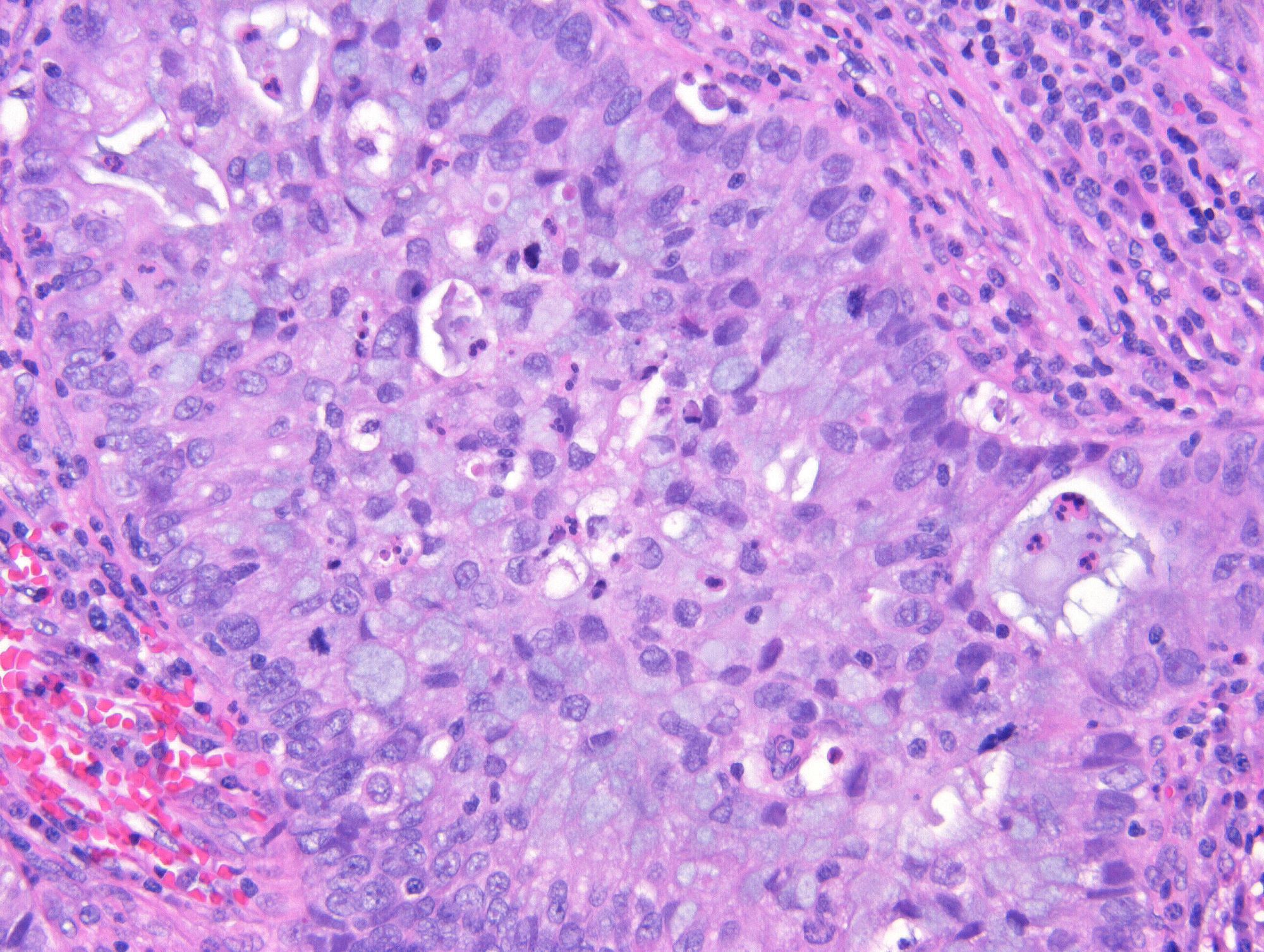
Microscopic (histologic) description
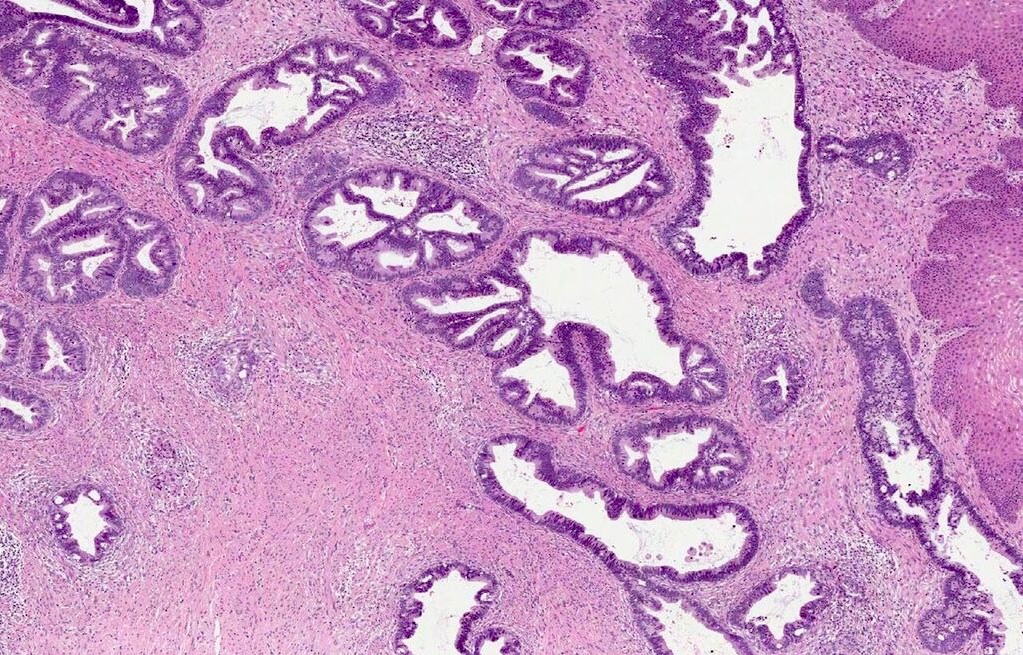
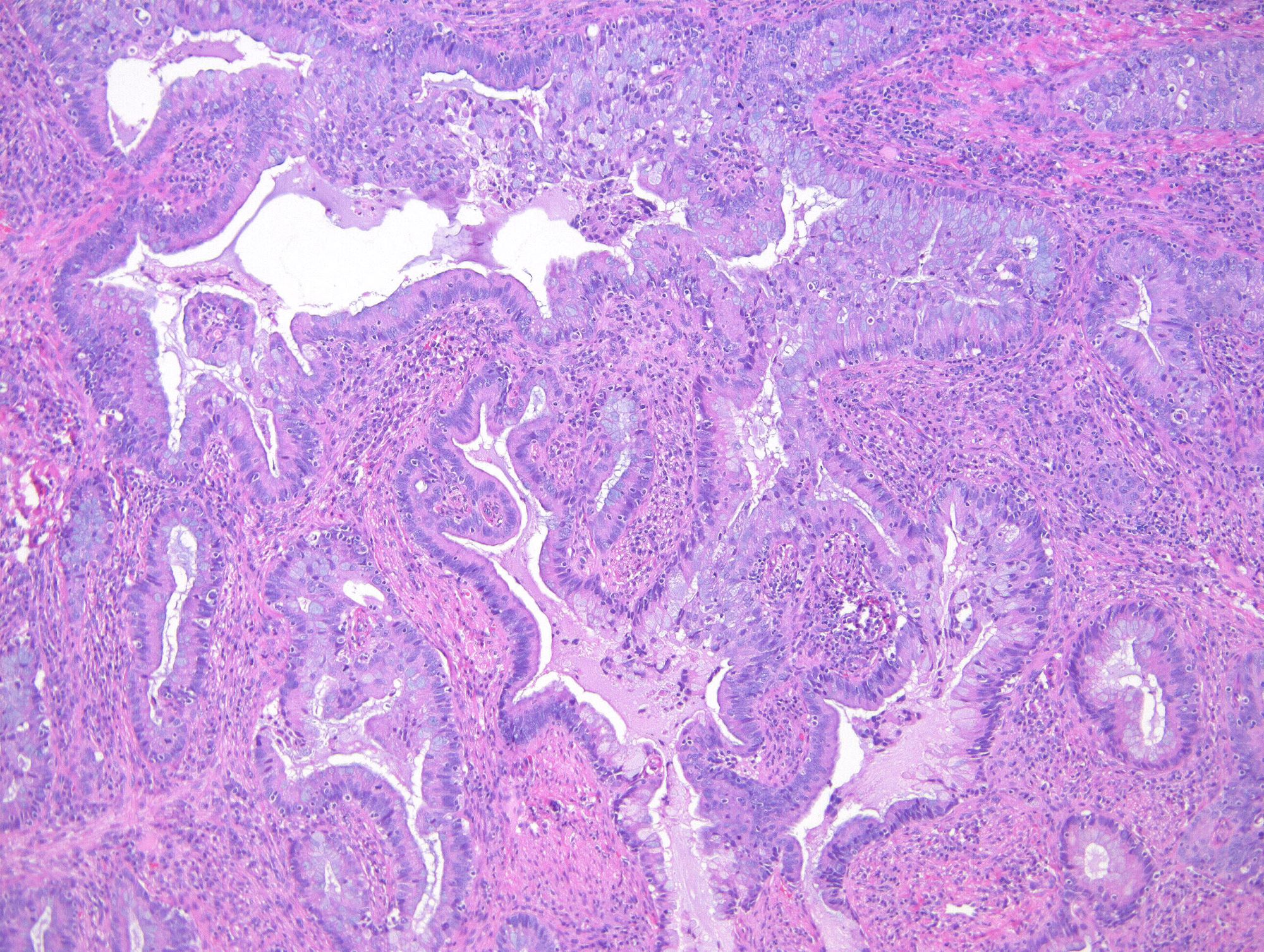
- Diagnosis of invasion by endocervical adenocarcinoma is based on the following features:
- Stromal infiltration in the form of:
- Marked glandular confluence with cribriform or microacinar architecture
- Irregularly shaped, angulated or fragmented glands with an adjacent desmoplastic stromal reaction
- Tumor cell clusters or individual cells
- Lymphovascular space invasion
- Increased number of glands with loss of a lobular arrangement and glandular density exceeding that of the normal cervix
- Glands are often close to thick walled vessels (Int J Gynecol Pathol 2005;24:125)
- Stromal infiltration in the form of:
- Superficially invasive carcinoma (FIGO stage IA1) is defined as a microscopic tumor with depth of 3 mm or less and negative resection margins (in partial samples)
Histologic types of HPV related endocervical adenocarcinoma
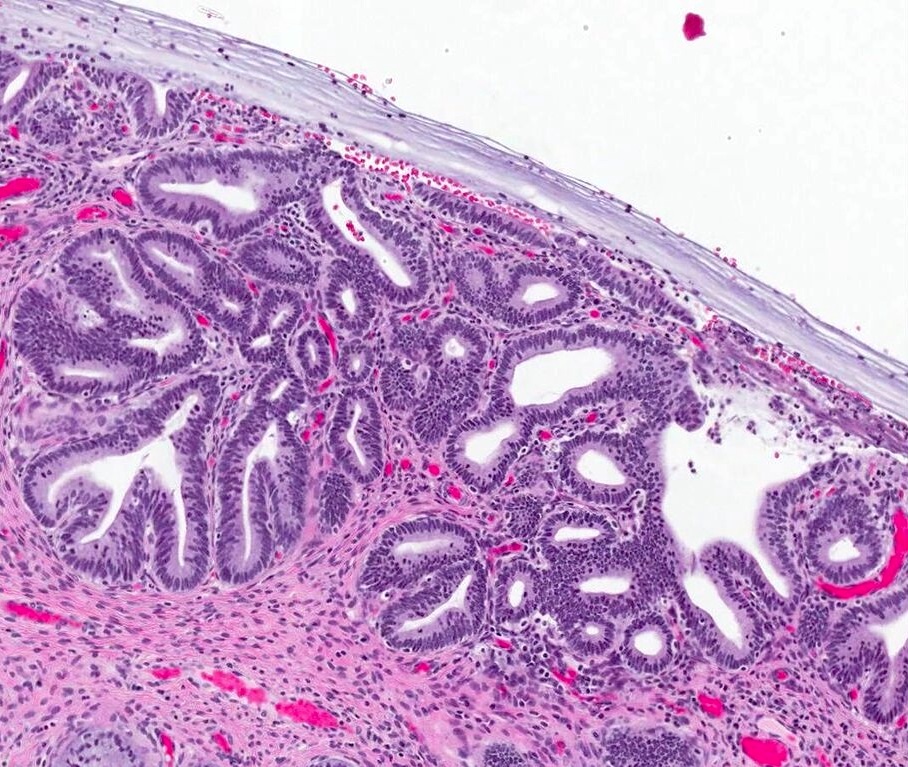
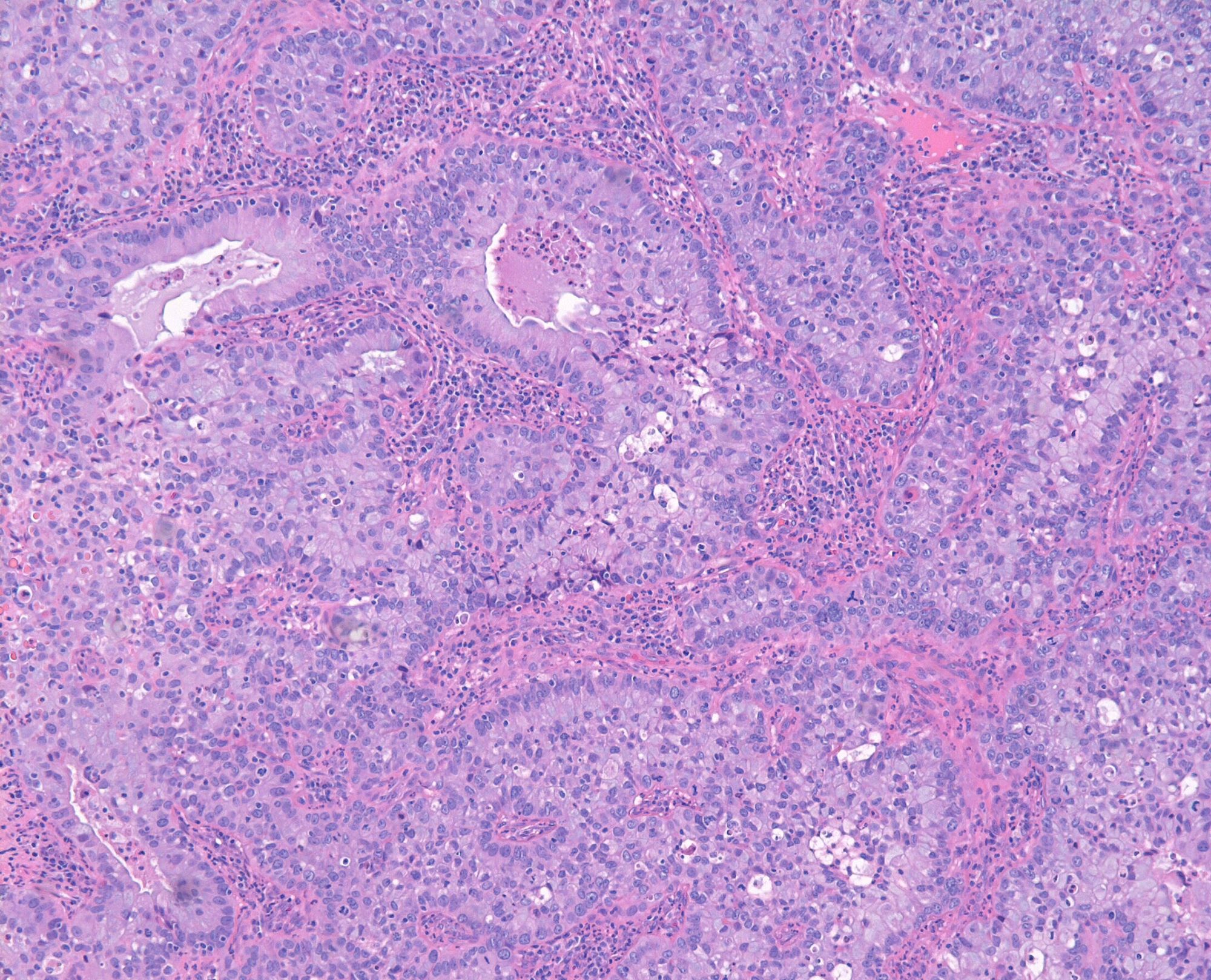
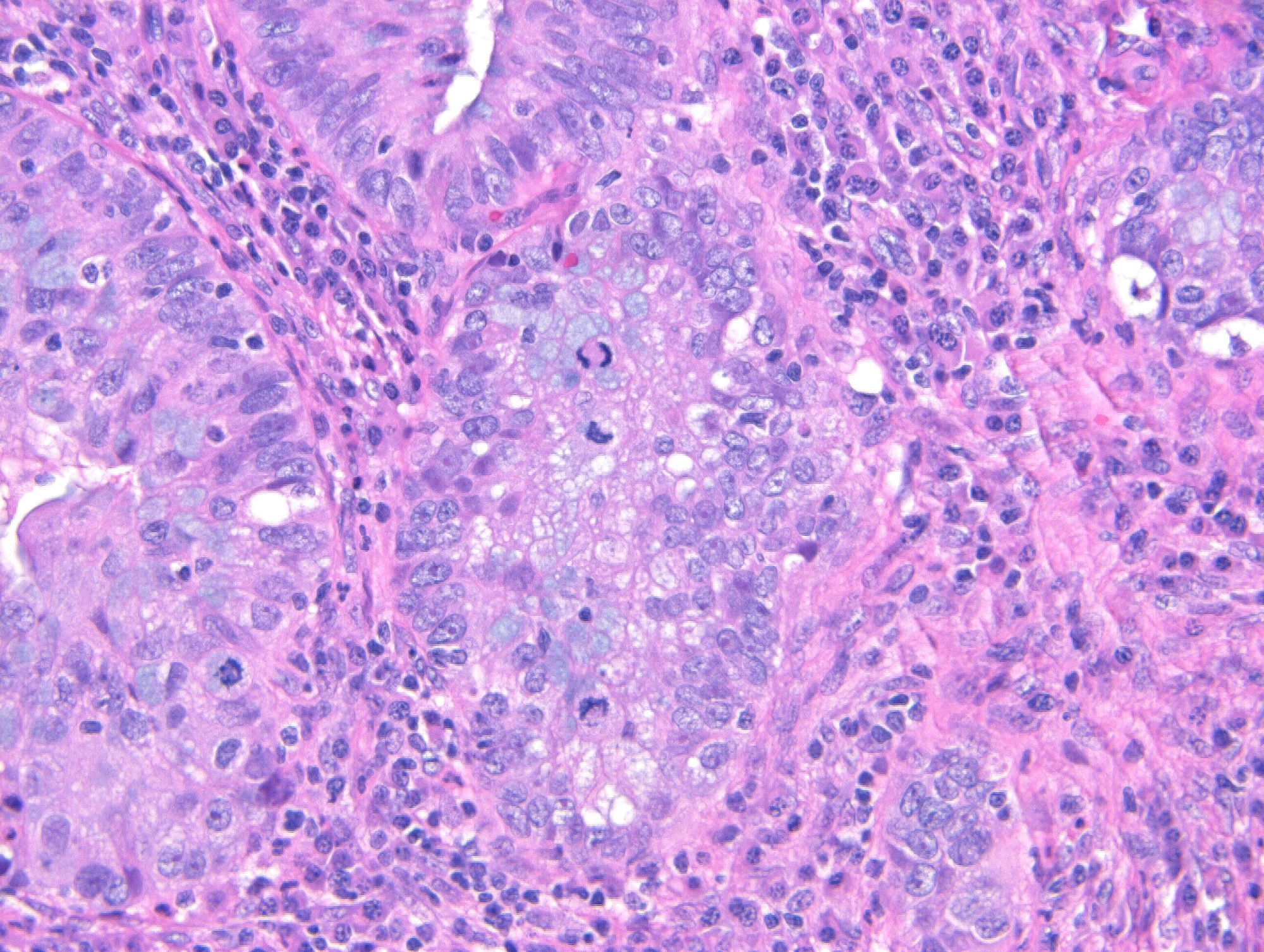
- Usual adenocarcinoma represents 70 - 90% of all endocervical adenocarcinomas and is characterized by:
- Mucin depleted epithelium, meaning mucinous cells comprise < 50% of the tumor volume; in turn, most of the population has columnar, nonmucinous indistinct cytoplasm
- Cells have columnar shape; nuclei are elongated, enlarged and hyperchromatic with coarse chromatin
- Loss of polarity and nuclear overlapping
- Brisk mitotic activity; mitotic figures are usually apical
- Mucinous adenocarcinoma is characterized by:
- Mucinous epithelium representing 50% or more of the tumor volume (usually represents the majority of the lesion)
- Mucinous epithelium can be of endocervical type, intestinal type or (rarely) with signet ring cells
- Intestinal adenocarcinomas show intestinal differentiation, goblet cells and (occasionally) Paneth cells (Arch Pathol Lab Med 1990;114:731)
- A novel variant, described as invasive stratified mucin producing carcinoma, is included in this subset; it is commonly associated with stratified mucin producing intraepithelial lesion (SMILE) and thought to represent an invasive manifestation of this type of growth (Am J Surg Pathol 2016;40:262, Am J Surg Pathol 2020;44:1374, Am J Surg Pathol 2020;44:873)
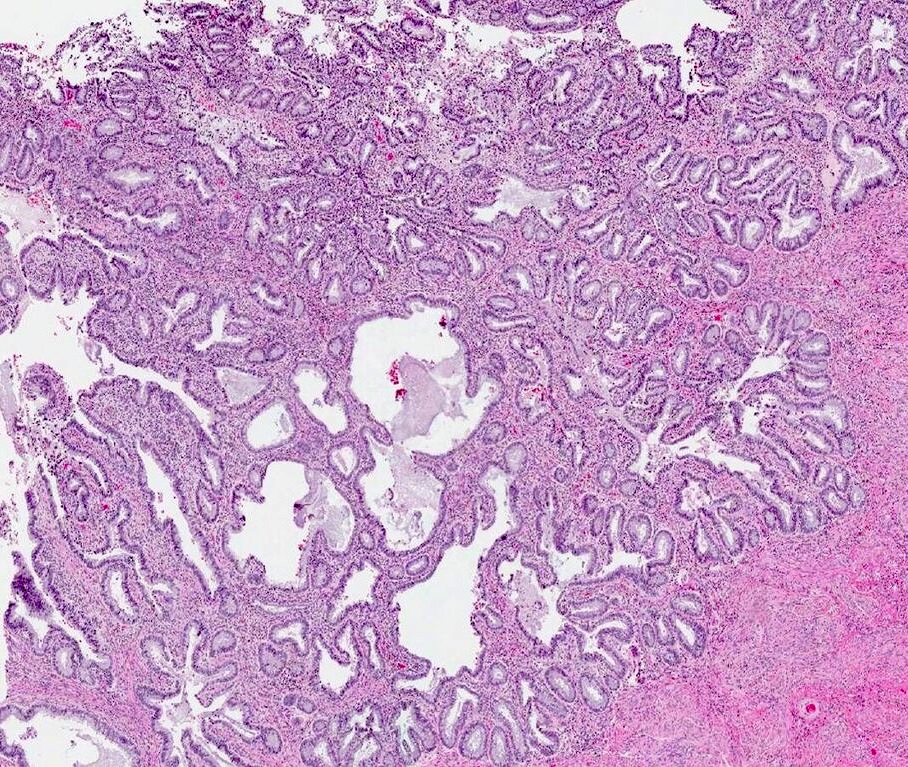
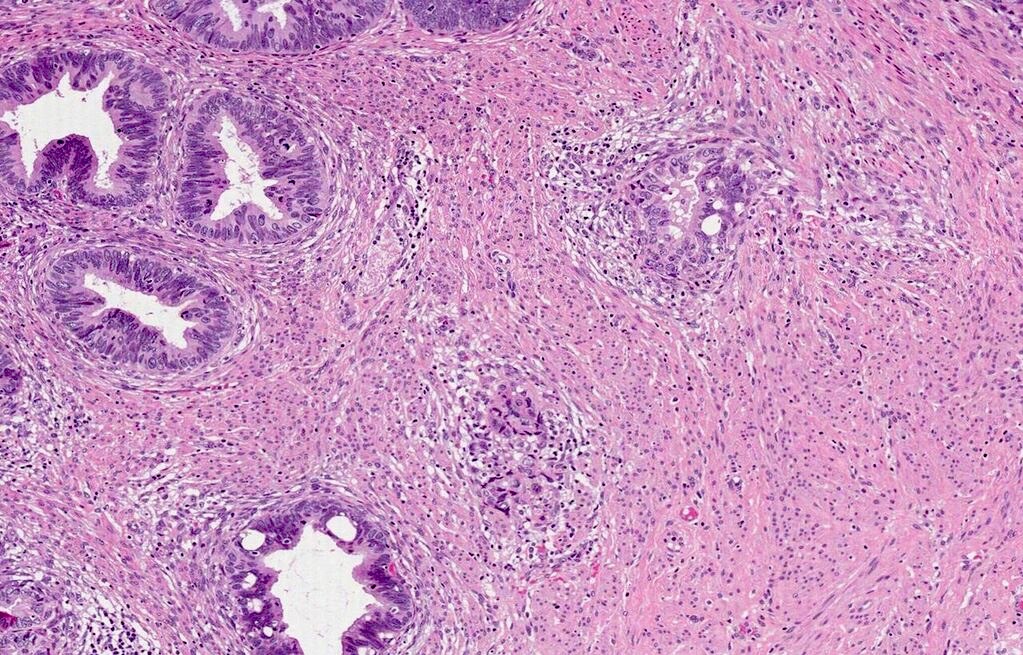
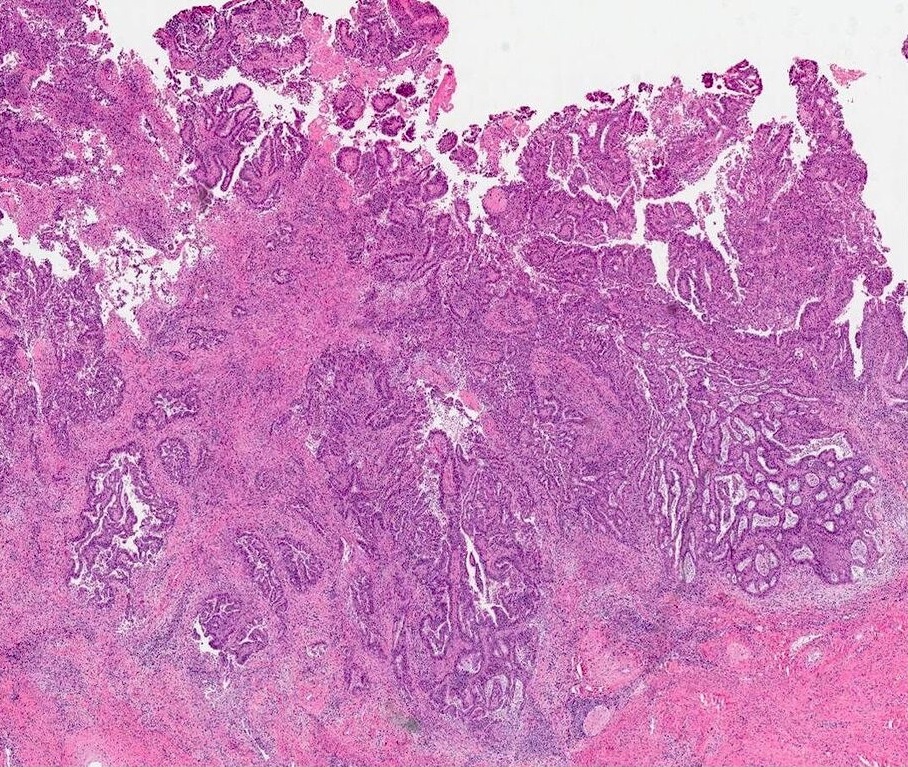
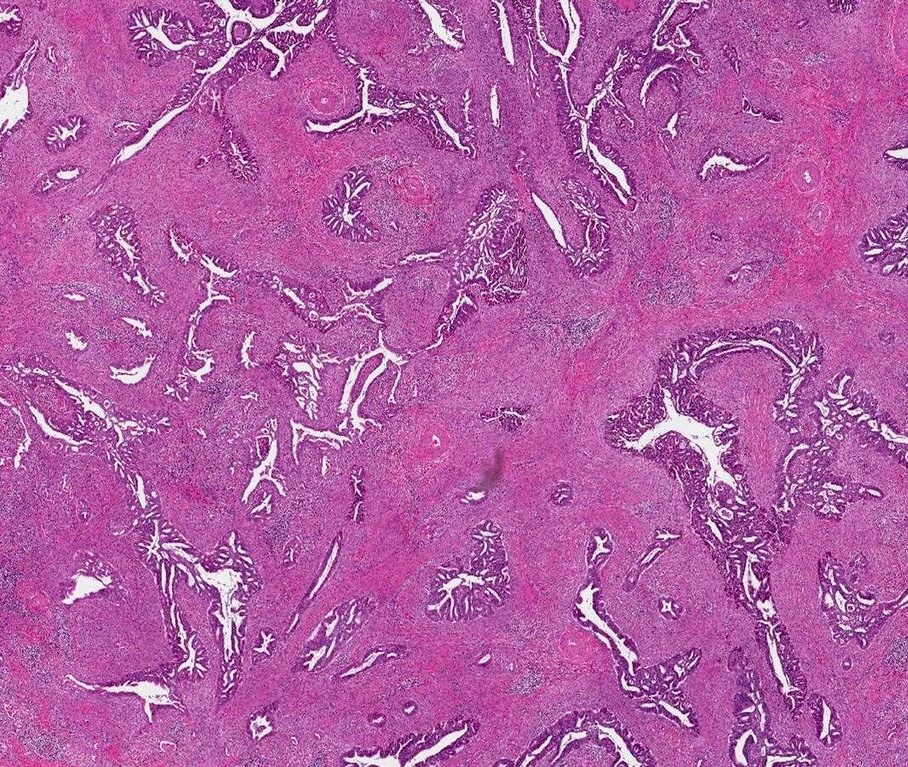
Pattern based classification (Silva system)
- Silva system classifies HPV associated adenocarcinomas based on growth pattern, rather than the size or grade of the invasive component (Int J Gynecol Pathol 2013;32:592, Am J Surg Pathol 2015;39:667)
- Tumors with a nondestructive pattern of invasion (pattern A) are associated with a 0% rate of lymph node metastases, whereas focally (B) and diffusely (C) destructive patterns have 4% and 23% rates of nodal involvement, respectively
- Similarly, pattern A tumors had 0% recurrence and 0% fatality rates, compared with pattern B tumors (1.2% and 0%, respectively) and pattern C tumors (22.1% and 8.8%, respectively)
- Multiple independent retrospective studies have validated the association between pattern of invasion and lymph node metastases, recurrence rates as well as survival
- However, there are reports of early, well differentiated, adenocarcinoma in situ (AIS)-like adenocarcinomas with ovarian metastases (Am J Surg Pathol 2008;32:1835)
Tumor classification based on pattern of stromal invasion (pattern based classification, Silva system)
- Classifies tumors into 3 categories as follows:
| Pattern A |
|
| Pattern B |
|
| Pattern C |
|
Tumor grade of adenocarcinoma
- For usual type adenocarcinoma, not variants; not universally accepted, not proven to be prognostically significant (Int J Gynecol Pathol 2021;40:S66)
- Grade 1:
- Well differentiated (10% or less solid growth)
- Tumor contains well formed regular glands with papillae
- Cells are elongated and columnar with uniform oval nuclei
- Minimal stratification (fewer than 3 cell layers in thickness)
- Infrequent mitotic figures
- Grade 2:
- Moderately differentiated (11 - 50% solid growth)
- Tumor contains complex glands with frequent bridging and cribriform formation
- Solid areas up to 50% of tumor
- Nuclei more rounded and irregular
- Small nucleoli present
- Mitoses more frequent
- Grade 3:
- Poorly differentiated (over 50% solid growth)
- Sheets of malignant cells
- Few glands are discernible
- Cells are large and irregular with pleomorphic nuclei
- Occasional signet cells are present
- Mitoses are abundant with abnormal forms
- Marked desmoplasia
- Necrosis is common
- Grade 1:
Microscopic (histologic) images
Cytology description
- Multilayering
- May form glandular structures with central lumina or acinar formations with peripheral nuclei
- Cells are pleomorphic, large or small with fluffy cytoplasm, cytoplasmic vacuolization, loss of nuclear polarity, true nuclear crowding, nuclei with clumped chromatin, marked variation of nucleoli, occasional mitotic figures
- Invasion is often characterized by heavy blood with abundant glandular epithelium, even without tumor diathesis or fully malignant nuclear criteria (Cancer 2002;96:5)
- May see morules (also seen with mesothelial cells, benign and malignant lesions)
- Endocervical adenocarcinoma: usually columnar with granular cytoplasm, rosettes, sheets with holes versus balls, round plump cells, molded groups
- Conventional smears that are false negative often have fewer and smaller abnormal cells, small nuclei, less atypia and less hyperchromasia (Arch Pathol Lab Med 2006;130:23)
Positive stains
- p16: overexpressed in > 95% of cases (diffuse, strong nuclear and cytoplasmic staining) (Int J Gynecol Pathol 2009;28:489)
- mCEA: 100% (any degree of staining)
- CK7
Negative stains
- ER and PR (weak staining in up to 20% of cases) (Int J Gynecol Pathol 2002;21:11)
- p53: normal staining pattern (not overexpressed or absent) (Am J Surg Pathol 2019;43:75)
- CD10 (positive only in mesonephric adenocarcinomas)
- p63 (Hum Pathol 2001;32:479)
- Vimentin (usually)
- CDX2, CK20
- Usually EBV negative (Arch Pathol Lab Med 1999;123:1098)
Molecular / cytogenetics description
- Associated with HPV 16 and HPV 18 in 85 - 95% of cases (Am J Clin Pathol 1996;106:52)
- Frequent KRAS and PIK3CA mutations, particularly in tumors with destructive stromal invasion (Mod Pathol 2017;30:1633, Gynecol Oncol 2018;151:196)
- HPV related adenocarcinomas have lower mutational burdens compared with HPV independent adenocarcinomas (Int J Gynecol Pathol 2020;39:578)
Sample pathology report
- Endocervical adenocarcinoma, HPV associated type (usual / mucinous)
- Macroscopic tumor size: __ cm
- Depth of invasion: __ mm (out of __ mm of cervical wall thickness)
- Pattern of invasion: A / B / C
- Lymphovascular space invasion: present / absent
- Resection margins (specify which): positive / negative; if negative, distance __ mm
- Stage: FIGO stage __, TNM stage __
Differential diagnosis
- Adenocarcinoma in situ:
- No histologic features of invasion as described above
- Reproducibility of the distinction between invasive and in situ adenocarcinoma is poor and distinction cannot be made in up to 20% of cases (Mod Pathol 2016;29:879, Int J Gynecol Pathol 2000;19:29)
- Endometrial endometrioid adenocarcinoma:
- No in situ cervical adenocarcinoma
- Continuity between cervix and endometrial tumors
- Usually myometrial invasion
- Bland squamous differentiation
- Stains may be helpful: negative or focal / superficial for CEA and mucin; positive for vimentin, ER and PR; p16 not overexpressed, negative for HPV by PCR or ISH (Am J Surg Pathol 2002;26:998)
- Gastric type adenocarcinoma:
- Clear cell adenocarcinoma:
- Mesonephric carcinoma:
- Deeply located tumor, heterogeneity of growth patterns including solid, cystic, spindle cell and mesonephric hyperplasia-like growth
- GATA3+++, calretinin+, TTF1++, CD10+
- Metastatic colorectal adenocarcinoma:
- Very rare; CDX2+, CK7-, CK20+ (Arch Pathol Lab Med 2003;127:1586, Jpn J Clin Oncol 1999;29:640)
- Metastatic adenocarcinoma (not colonic):
- Usually clinical evidence of widespread disease, angiolymphatic invasion, no surface involvement
- Mesonephric remnants:
- Deep, do not extend to surface, contain eosinophilic secretions, no mitotic activity, no atypia
- GATA3+++, calretinin+, TTF1++, CD10+
- Microglandular hyperplasia:
- Does not extend below deep margin of normal endocervical glands
- Usually young women taking oral contraceptives or pregnant
- Few mitotic figures
Board review style question #1
Board review style answer #1
C. Usual adenocarcinoma, the most common form adenocarcinoma of the cervix, is associated with HPV. Gastric type and clear cell carcinomas are known to be HPV independent. Endometrioid carcinoma is no longer a recognized subtype of HPV associated adenocarcinoma, as it leads to confusion with the usual type. True endometrioid carcinoma of the cervix is exceedingly rare and likely arises from cervical endometriosis. The term should be reserved to cases with definitive endometrioid morphology, negative p16 / HPV testing and absence of an endometrial primary.
Comment Here
Reference: HPV related adenocarcinoma (usual type and variants)
Comment Here
Reference: HPV related adenocarcinoma (usual type and variants)
Board review style question #2
Which of the following is a known adverse prognostic factor in patients with HPV associated endocervical adenocarcinoma?
- Pattern A invasion
- Lymphovascular space invasion
- Early stage
- Negative margin status
Board review style answer #2
B. Lymphovascular space invasion
Comment Here
Reference: HPV related adenocarcinoma (usual type and variants)
Comment Here
Reference: HPV related adenocarcinoma (usual type and variants)