Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Turashvili G. Microglandular hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixMGH.html. Accessed March 31st, 2025.
Definition / general
- Benign, nonneoplastic endocervical glandular proliferation
Essential features
- Benign lesion not requiring treatment
- Usually incidental microscopic finding in reproductive women
- Associated with hormonal exposure (pregnancy, postpartum, oral contraceptive pills, hormone replacement therapy)
- May mimic cervical and endometrial adenocarcinomas
Terminology
- Microglandular adenosis
- Microglandular change
Epidemiology
- Common in reproductive age women, rarely postmenopausal
- Typically incidental
Sites
- Cervix
Etiology
- Most likely due to hormonal exposure (pregnancy, postpartum, progestogen therapy) (J Low Genit Tract Dis 2016;20:162)
Clinical features
- Usually asymptomatic
- May present with contact bleeding
- May form solitary or multiple polypoid masses (Arch Pathol Lab Med 2010;134:393)
- May involve an endocervical polyp
Diagnosis
- Microscopic examination
Prognostic factors
- Excellent prognosis
Case reports
- 19 year old woman with atypical endocervical microglandular hyperplasia and ligneous cervicitis associated with plasminogen deficiency (Int J Gynecol Pathol 2013;32:329)
- 30 year old woman with atypical endocervical microglandular hyperplasia associated with plasminogen deficiency (Int J Gynecol Pathol 2021;40:224)
Treatment
- Not required
Gross description
- Most often unremarkable
- May be multifocal
- Rarely, polypoid and ulcerated (Arch Pathol Lab Med 2010;134:393)
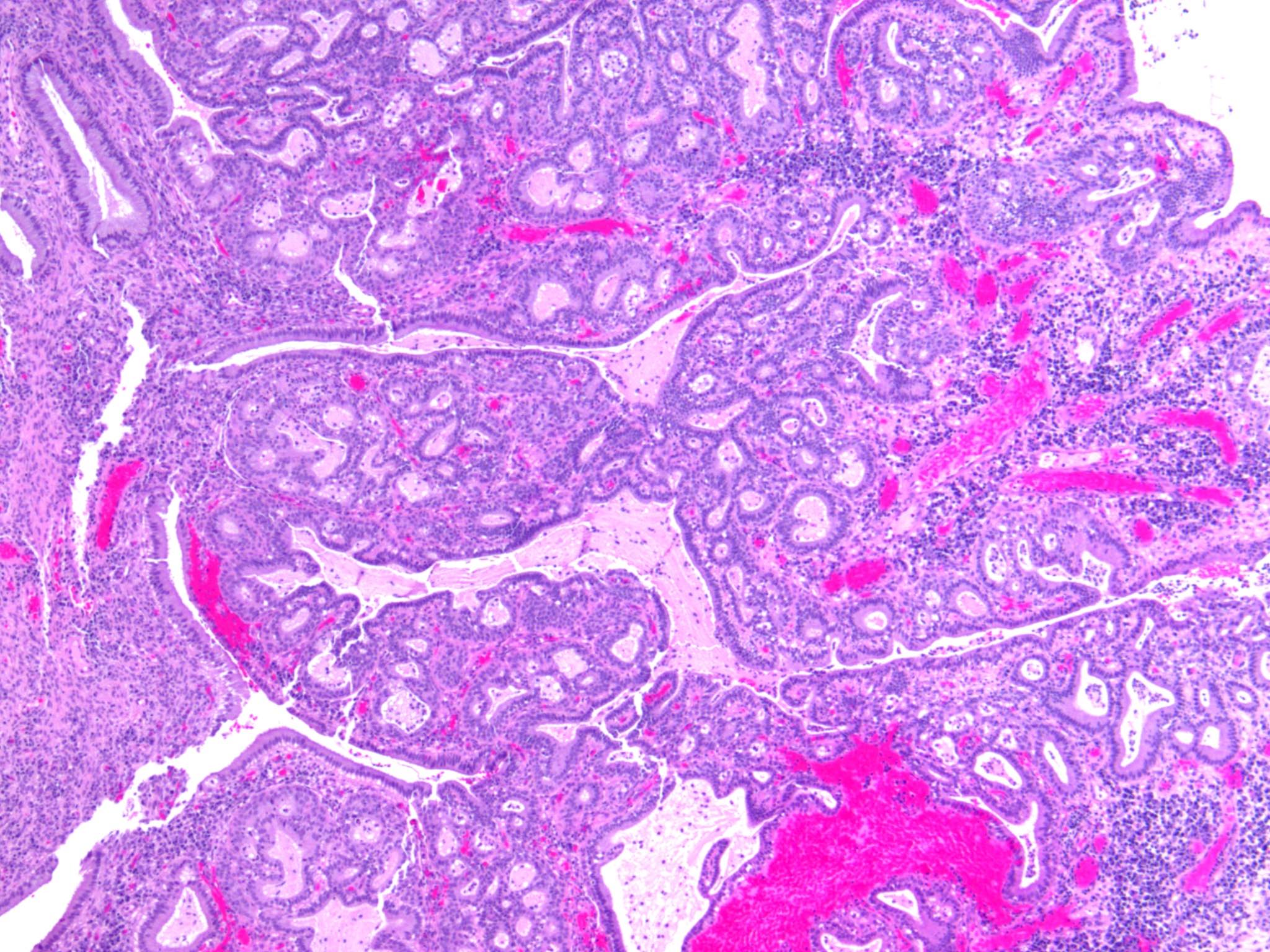
Microscopic (histologic) description
- Solitary or multiple polypoid lesions
- Often superficial location
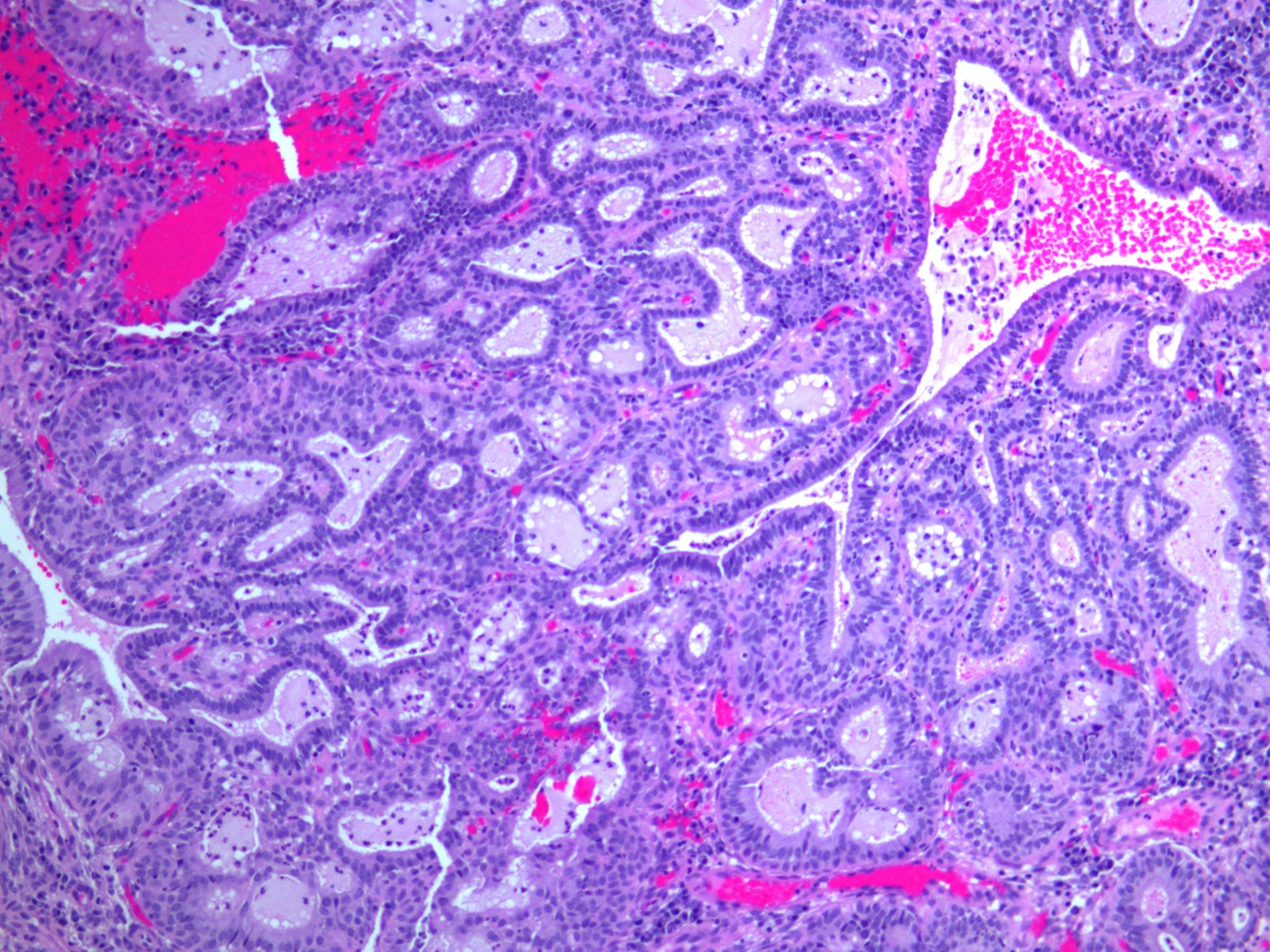
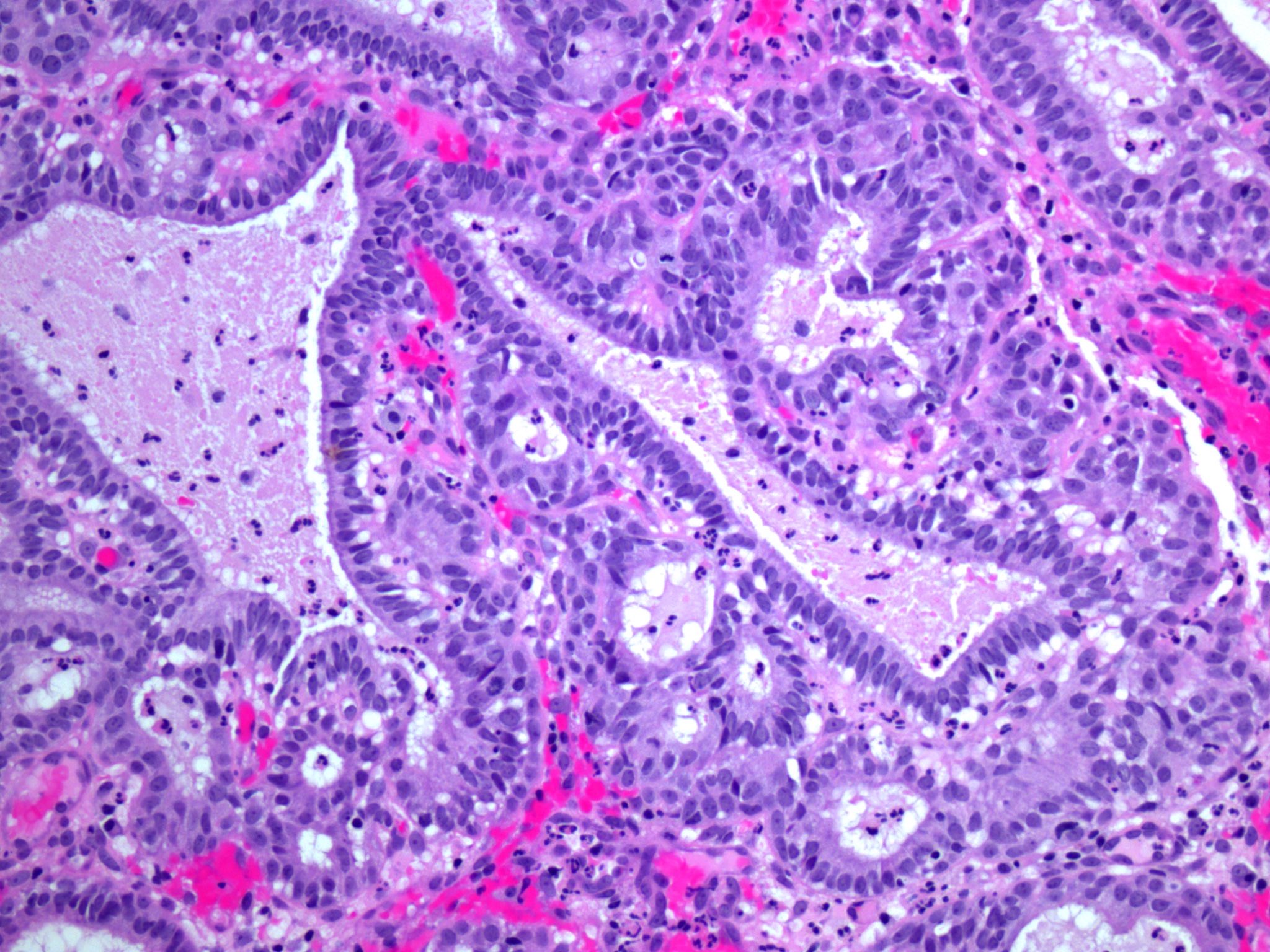
- Complex proliferation of back to back tubular or cystically dilated glands with scant intervening stroma
- Intraluminal mucin with acute inflammation
- Mixed stromal inflammatory infiltrate
- May be associated with immature or mature squamous metaplasia
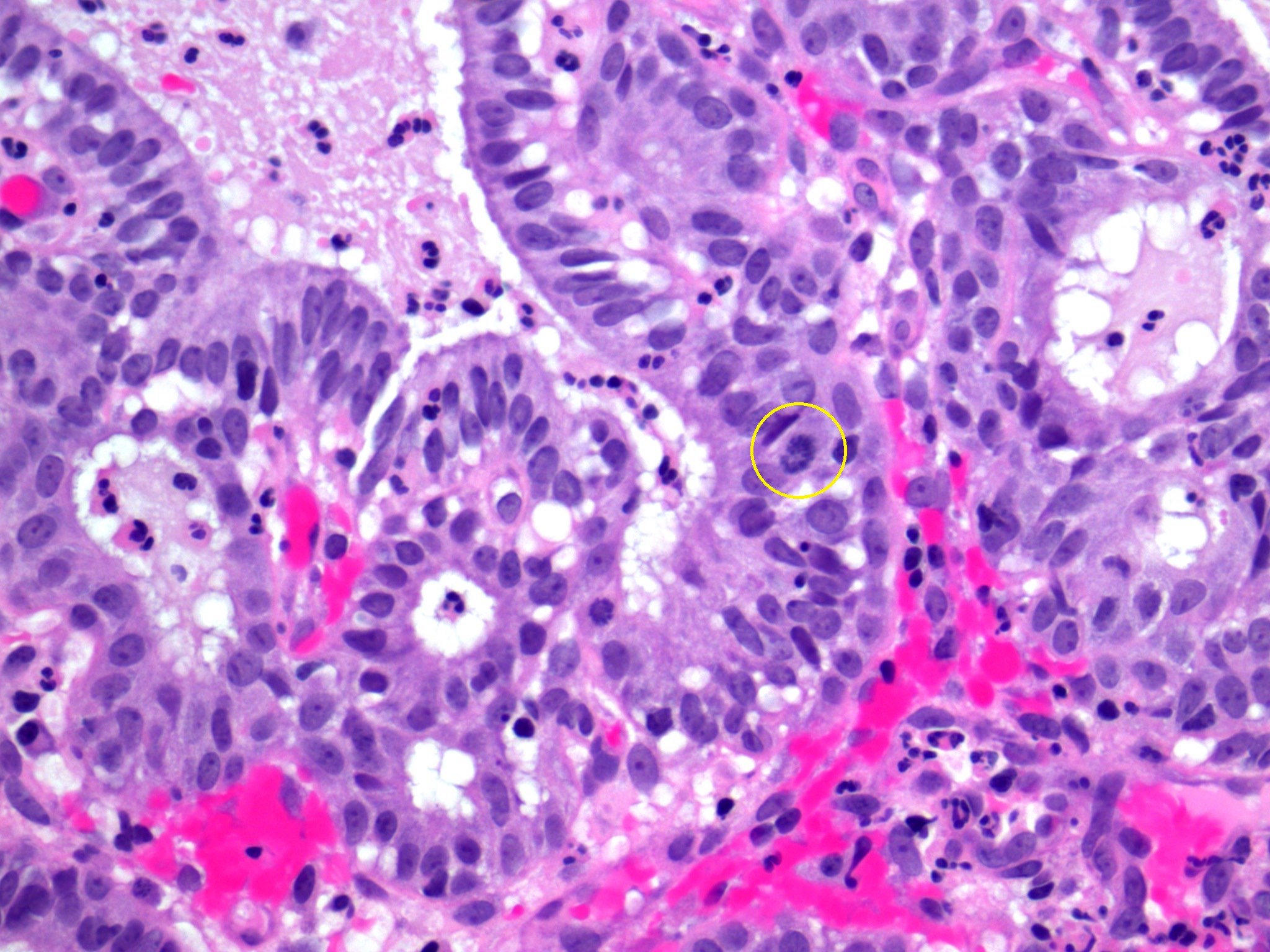
- Glands are lined by bland cuboidal, columnar or flattened cells with subnuclear and supranuclear vacuoles (may not be well developed in some cases), indistinct nucleoli, absent or rare (≤ 3 per 10 high power fields) mitoses (Int J Gynecol Pathol 2003;22:261)
- Variable reserve cells or immature squamous cells beneath endocervical cells
- Rare unusual features (atypical microglandular hyperplasia):
- Solid, reticular, trabecular or pseudoinfiltrative growth (Am J Surg Pathol 1989;13:50)
- Abundant myxoid or hyalinized stroma and mucin pools
- Signet ring or hobnail cells (Am J Surg Pathol 1989;13:50)
- Cytologic atypia with nuclear enlargement and prominent nucleoli (Int J Gynecol Pathol 2021;40:224, Am J Surg Pathol 1989;13:50)
- Increased mitoses (Int J Gynecol Pathol 2014;33:524, Am J Surg Pathol 1989;13:50)
Microscopic (histologic) images
Cytology description
- Nonspecific changes
- Spectrum of benign appearing to bi or tridimensional clusters of cuboidal or columnar glandular cells with vacuolated cytoplasm, microlumina or fenestration (Acta Cytol 1999;43:110)
- Admixture of cells with immature squamous metaplasia and reserve cells with scant cytoplasm and small, round nuclei (Diagn Cytopathol 2004;30:57, Acta Cytol 1999;43:110)
- Inflammatory cells
- Glandular cells may show cytologic atypia with enlarged, hyperchromatic, crowded nuclei, smooth nuclear contours, fine chromatin, sometimes multiple nucleoli, mitoses, apoptotic bodies and watery diathesis, mimicking high grade squamous intraepithelial lesion (Diagn Cytopathol 1994;10:326, Acta Cytol 2000;44:661)
Positive stains
- ER
- PR
- PAX2 (Int J Gynecol Pathol 2015;34:90)
- Cyclin D1 (Int J Gynecol Pathol 2015;34:90)
- p63: reserve cells (Hum Pathol 2005;36:154, Adv Anat Pathol 2009;16:316)
- CK17: reserve cells (Am J Clin Pathol 2017;148:264)
- Mucin (vacuoles and lumina)
Negative stains
- p16: usually negative, may be positive (Int J Gynecol Pathol 2009;28:107)
- Vimentin (Int J Gynecol Pathol 2003;22:261)
- CEA (Int J Gynecol Pathol 2003;22:261)
- Ki67: low proliferation index
Sample pathology report
- Endocervix, curettings:
- Fragments of benign endocervical tissue
- (Microglandular hyperplasia need not be reported; may be included in microscopic description)
Differential diagnosis
- Endometrioid adenocarcinoma, microglandular pattern (microglandular hyperplasia-like endometrioid adenocarcinoma):
- Usually postmenopausal women
- At least some cytologic atypia and mitotic activity, stromal foamy macrophages, luminal mature squamous metaplasia
- Positive for vimentin, loss of PAX2, high Ki67 index in some studies (Am J Surg Pathol 1992;16:1092, Int J Gynecol Pathol 2003;22:261, Ann Diagn Pathol 2003;7:180, Int J Gynecol Pathol 2015;34:90)
- Clear cell carcinoma:
- Endocervical adenocarcinoma, usual type:
- Endocervical adenocarcinoma in situ:
Additional references
Board review style question #1
Which of the following entities is the closest mimic of microglandular hyperplasia?
- Endometrial serous carcinoma
- Nabothian cysts
- Clear cell carcinoma
- Minimal deviation adenocarcinoma
- Endometrial endometrioid carcinoma, microglandular pattern (microglandular hyperplasia-like endometrioid adenocarcinoma)
Board review style answer #1
E. Endometrial endometrioid carcinoma, microglandular pattern (microglandular hyperplasia-like endometrioid adenocarcinoma)
Comment Here
Reference: Microglandular hyperplasia
Comment Here
Reference: Microglandular hyperplasia
Board review style question #2
Which of the following statements is true for microglandular hyperplasia?
- Microglandular hyperplasia is a nonobligate precursor of usual type endocervical adenocarcinoma
- Microglandular hyperplasia is often seen in patients with Cowden syndrome
- Microglandular hyperplasia is associated with increased risk of clear cell carcinoma
- Microglandular hyperplasia is often associated with endometrial endometrioid adenocarcinoma, microglandular pattern
- Microglandular hyperplasia is usually an incidental finding in women of reproductive age
Board review style answer #2
E. Microglandular hyperplasia is usually an incidental finding in women of reproductive age
Comment Here
Reference: Microglandular hyperplasia
Comment Here
Reference: Microglandular hyperplasia