Table of Contents
Definition / general | Essential features | Epidemiology | Diagrams / tables | Prognostic factors | Microscopic (histologic) images | Videos | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jain PV, Jorns JM. Histologic grading. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignanthistologic.html. Accessed April 23rd, 2024.
Definition / general
- Most commonly used system is the Nottingham combined histologic grade (Elston-Ellis modification of Scarff-Bloom-Richardson grading system) based on (a) tubule and gland formation, (b) nuclear pleomorphism, (c) number of mitotic figures in most active areas (Histopathology 1991;19:403, Br J Cancer 1957;11:359)
- Tumor should be graded based on representative portion of tumor (Arch Pathol Lab Med 1983;107:411)
Essential features
- Nottingham modification of Bloom-Richardson system, based on (a) tumor tubule formation, (b) nuclear pleomorphism and (c) number of mitotic figures in most active areas, with each given a score of 1, 2 or 3
- Scoring is done as follows
- 3 - 5 points: well differentiated (grade I)
- 6 - 7 points: moderately differentiated (grade II)
- 8 - 9 points: poorly differentiated (grade III)
- Histologic grade is a strong predictor of survival
Tumor tubule or gland formation
- 1 point: > 75% of tumor
- 2 points: 10 - 75% of tumor
- 3 points: < 10% of tumor
- Notes
- Overall appearance of the tumor must be taken into consideration in scoring tubule formation
- Tubules must have clear central lumina to be counted
Nuclear pleomorphism
- 1 point: minimal nuclear variation in size and shape (< 1.5 times the size of benign epithelial cell nuclei), even chromatin, inapparent to inconspicuous nucleoli
- 2 points: moderate nuclear variation in size and shape (1.5 - 2 times the size of benign epithelial cell nuclei), typically visible but small nucleoli
- 3 points: marked nuclear variation in size and shape (> 2 times the size of benign epithelial cell nuclei), often prominent nucleoli
- Notes
- Evaluate areas with greatest atypia
- For infiltrating lobular carcinoma, more emphasis has been placed on nuclear pleomorphism since tubule formation and mitotic activity show little variation, with proposal of a 2 tiered (nuclear grade 1 versus 2 / 3) system by some (Ann Diagn Pathol 2009;13:223)
Number of mitotic figures in most active area, counting 10 high power fields
| (a) | (b) | (c) | |
| 1 point | 0 - 5 | 0 - 9 | 0 - 11 |
| 2 points | 6 - 11 | 10 - 19 | 12 - 22 |
| 3 points | 11+ | 20+ | 23+ |
- (a) Nikon or Labophot 40x objective or comparable with field diameter of 0.44 mm
- (b) Leitz or Ortholux 25x objective or comparable with field diameter of 0.59 mm
- (c) Leitz or Diaplan 40x objective or comparable with field diameter of 0.63 mm
- Notes
- Count mitotic figures at peripheral leading edge of the tumor in most mitotically active area; count 10 high power fields in the same area but not necessarily contiguous; select fields with as much tumor as possible; avoid poorly preserved areas
- Hyperchromatic, karyorrhectic or apoptotic nuclei should be excluded; only clearly identifiable mitotic figures should be counted
- Quick scan mitotic impression is less accurate (Hum Pathol 2008;39:584)
Scoring
- 3 - 5 points: well differentiated (grade I)
- 6 - 7 points: moderately differentiated (grade II)
- 8 - 9 points: poorly differentiated (grade III)
| Feature | Subcategory | Score | |
| 1 | Tumor tubule or gland formation | > 75% of tumor | 1 |
| 10 - 75% of tumor | 2 | ||
| < 10% of tumor | 3 | ||
| 2 | Nuclear pleomorphism | Minimal variation in nuclear size and shape | 1 |
| Moderate variation in nuclear size and shape | 2 | ||
| Marked variation in nuclear size and shape | 3 | ||
| 3 | Mitotic count (per 10 high power fields) | See table above (dependent on microscope field area) | 1 |
| 2 | |||
| 3 | |||
| Total score | Grade I (well differentiated) | 3 - 5 | |
| Grade II (moderately differentiated) | 6 or 7 | ||
| Grade III (poorly differentiated) | 8 or 9 |
Epidemiology
- In the U.S., Black people overall have higher grade tumors than White people (Cancer 2003;98:908)
Prognostic factors
- Histologic grade is an independent predictor of both breast cancer specific survival (BCSS) and disease free survival (DFS) in operable breast cancer (Mod Pathol 2005;18:1067)
Criticisms of Nottingham-Bloom-Richardson grading system
- Grading has been criticized for low reproducibility (Mod Pathol 2005;18:1067, Virchows Arch 2007;450:627)
- Reproducibility is highest at the ends of the spectrum of grade, with highest interobserver agreement for tubule formation versus other components (Mod Pathol 2021;34:701, Am J Clin Pathol 1995;103:195, Mod Pathol 2005;18:1067)
- Concept of a moderately differentiated category has been criticized (Pathobiology 2008;75:104, J Natl Cancer Inst 2006;98:262)
- Grade components are given equal weight but have different predictive value, with tubule formation being least predictive and nuclear pleomorphism and mitotic index having higher predictive value (Cancer 1989;64:1914)
Challenges of Nottingham-Bloom-Richardson grading system
- Small foci of carcinoma and crush or other artifacts on core biopsy may not allow adequate assessment of mitotic activity
- Spot count (number of mitoses in a single high power field) has been suggested as a surrogate and may be the only way to estimate mitotic activity in cases with limited tumor (Cancer 1989;64:1914)
- Tumors with 3 + 3 + 1 pattern (i.e., < 10% tubules, marked nuclear pleomorphism but few mitotic figures) may have low mitotic count due to failure to fix tumor immediately after excision, which allows tumor cells to complete cell division and leads to reduction in observed mitotic figures; Ki67 may serve as surrogate for mitotic figure counting in these cases (Oncologist 2008;13:477)
Possible steps to overcome limitations
- Interobserver reproducibility of histologic grade can be improved by better distinction between various categories for nuclear pleomorphism (Am J Clin Pathol 1995;103:195)
- Correlation with a proliferation marker such as Ki67 can help facilitate reproducibility and add complementary information to the modified Bloom-Richardson grading system; it can be used to further categorize grade II tumors into 2 prognostic subgroups with prognosis equivalent to grades I and III, respectively (J Cancer Res Ther 2018;14:537, Mod Pathol 2005;18:1067)
- Counting 20 - 30 rather than 10 high power fields to generate the mitotic score has been suggested to allow for lowering the cutoffs for mitotic index (Mod Pathol 2005;18:1067)
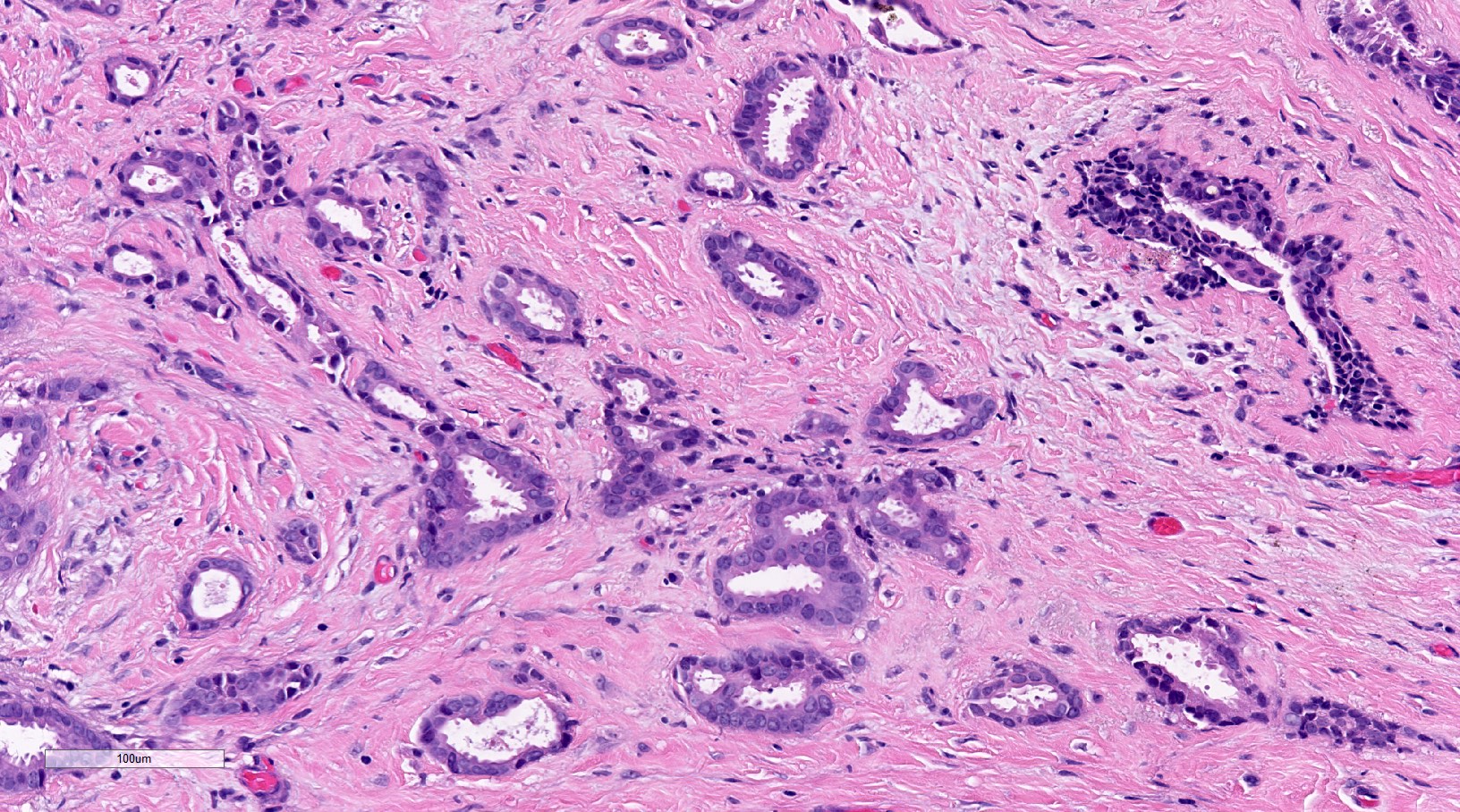
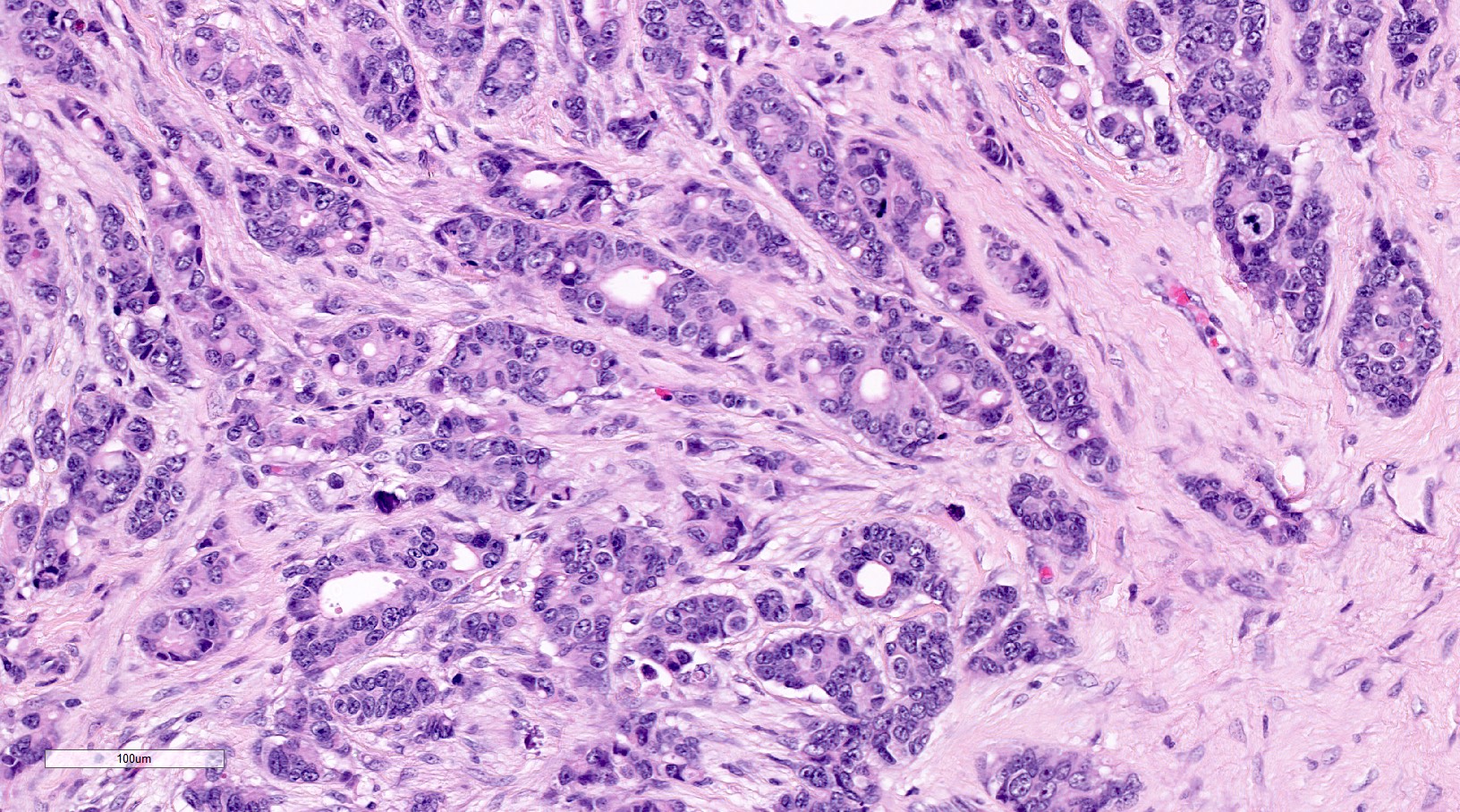
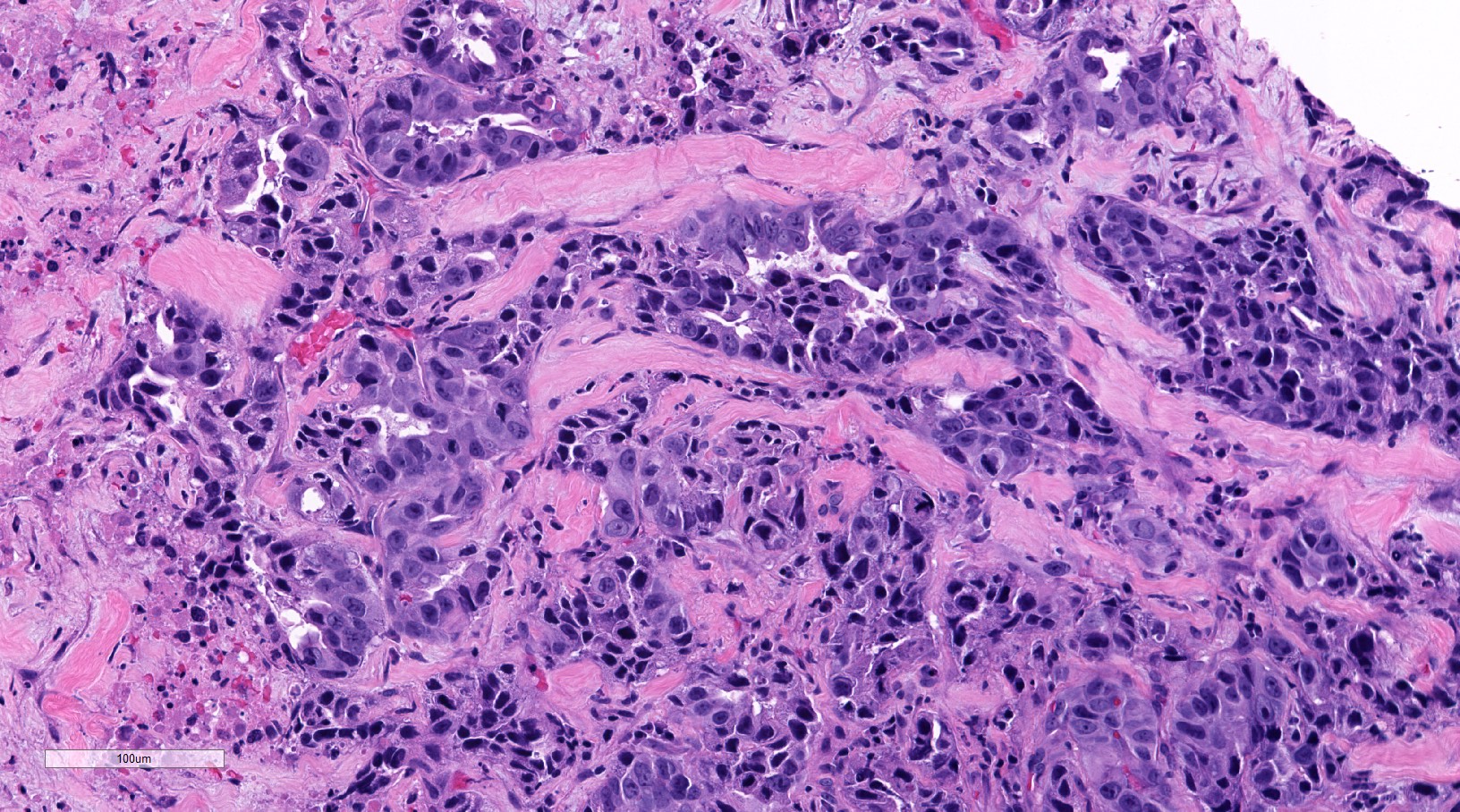
Microscopic (histologic) images
Videos
Breast ductal carcinoma (breast cancer)
Breast cancer grading and staging
Sample pathology report
- Right breast, core biopsy:
- Invasive ductal carcinoma, preliminary Nottingham (modified Bloom-Richardson) grade 1 (tubules - 1, nuclear pleomorphism - 2, mitotic activity - 1)
Additional references
Board review style question #1
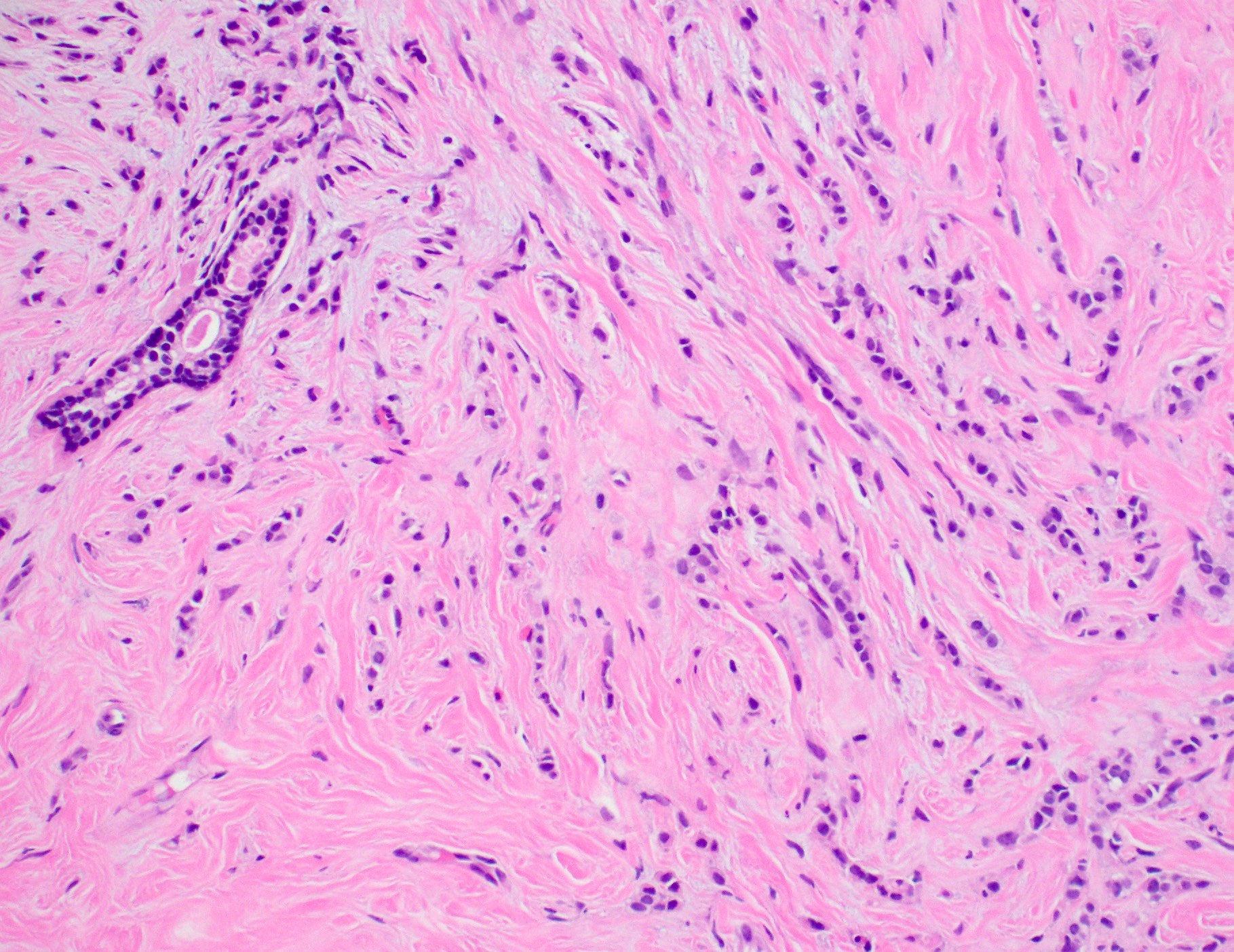
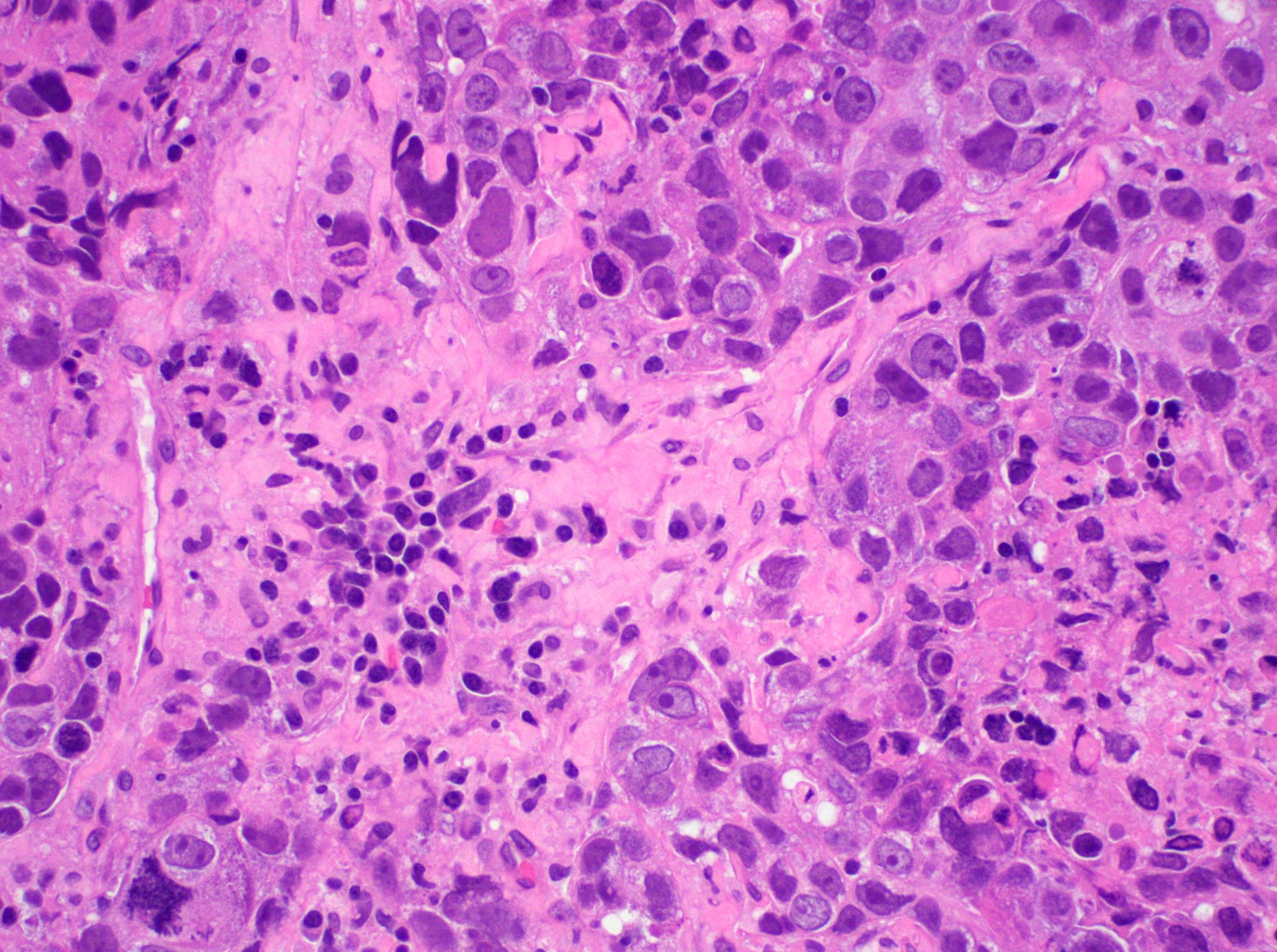
A 52 year old woman has a breast biopsy showing the histology pictured above (H&E, 20x). A subsequent resection shows similar histology throughout the tumor. What is the Nottingham grade of this invasive breast carcinoma?
- Grade 1 (tubules - 1, nuclear pleomorphism - 1, mitotic activity - 1)
- Grade 1 (tubules - 1, nuclear pleomorphism - 2, mitotic activity - 1)
- Grade 1 (tubules - 3, nuclear pleomorphism - 1, mitotic activity - 1)
- Grade 2 (tubules - 3, nuclear pleomorphism - 2, mitotic activity - 1)
- Grade 2 (tubules - 3, nuclear pleomorphism - 2, mitotic activity - 2)
Board review style answer #1
C. Grade 1 (tubules - 3, nuclear pleomorphism - 1, mitotic activity - 1). The tumor is an invasive lobular carcinoma, which consists of infiltrative small cells (score 1 - similar in size to adjacent benign glandular epithelial cells) with minimal pleomorphism (score 1) arranged in linear files with no tubule formation (score 3), resulting in a Nottingham combined score of 5, for overall grade of 1 or a well differentiated carcinoma. Invasive lobular carcinomas have little variation in tubule formation (there is typically none but tubules may occasionally be seen) and mitotic activity, which is usually low. Thus, the Nottingham grade is often reliant on the degree of nuclear pleomorphism, which is typically minimal (score 1), resulting in an overall grade of 1 or moderate (score 2), resulting in an overall grade of 2. The other answers are incorrect as the tumor does not show any significant tubule formation (indicated in answers A and B), pleomorphism (answers B, D and E) or mitotic activity (answer E).
Comment Here
Reference: Breast - Histologic grading
Comment Here
Reference: Breast - Histologic grading
Board review style question #2
When evaluating Nottingham grade of invasive breast carcinoma, what is typically the best area of the tumor to assess mitotic score?
- Central portion
- Entire tumor
- Peripheral leading edge
- Region with greatest tubules
Board review style answer #2
C. Peripheral leading edge.
Answer B is incorrect because while the entire tumor should be examined for histologic features, the peripheral leading edge is typically most mitotically active and this area should be focused on while generating the mitotic score component in Nottingham grading. Answer A is incorrect because the central portion of a breast cancer may have central fibrosis or necrosis and may be less well preserved in resection specimens, potentially resulting in falsely lower mitotic activity than indicative of the tumor biology. Answer D is incorrect because areas with higher tubule formation are more likely to be well differentiated areas of a heterogeneous tumor with lower mitotic activity and not representative of the most aggressive portion of the tumor.
Comment Here
Reference: Breast - Histologic grading
Comment Here
Reference: Breast - Histologic grading