Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Muller, KE. Acute mastitis / abscess. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastacutemastitis.html. Accessed April 2nd, 2025.
Definition / general
- Infection or inflammation of breast tissue, usually bacterial, often seen in association with lactation
- If untreated, may form abscess and fistulous tracts
Essential features
- Infection or inflammation of breast tissue, usually bacterial, often seen in association with lactation
- If untreated, may form abscess and fistulous tracts
- Staphylococcus aureus most common organism
- Microscopic examination reveals a mixed dense inflammatory infiltrate, predominantly neutrophils, in breast tissue
Terminology
- Puerperal mastitis
ICD coding
- ICD-10:
- ICD-11:
Epidemiology
- Incidence in 2 - 33% of lactating women (Am J Epidemiol 2002;155:103, Med Microbiol Immunol 2018;207:83)
- 3% with mastitis have an abscess (BJOG 2004;111:1378)
- Risk factors: age (21 - 35 years old), mastitis with previous child, cracked or sore nipples, use of ointments, incorrect breastfeeding practices, peripartum antibiotic therapy (Med Microbiol Immunol 2018;207:83)
Sites
- Subareolar (nonpuerperal)
Pathophysiology
- Infection via the mammary duct system; typically occurs within 2 - 3 weeks after the start of lactation (Breastfeed Med 2014;9:239)
- Staphylococcus aureus is most common organism transmitted from skin or infant (Breastfeed Med 2014;9:239)
- Accumulation of inadequately drained milk in ducts and lobules creates a microenvironment that fosters bacterial growth (Hoda: Rosen’s Breast Pathology, 4th Edition, 2014)
- Infrequent complication is abscess formation (localized collection of purulent material)
- Milk samples show loss of bacterial diversity (J Hum Lact 2015;31:406)
- Subareolar or nonpuerperal abscesses most often a consequence of squamous metaplasia of lactiferous ducts (SMOLD) (J Pathol Transl Med 2015;49:279)
Etiology
- Associated with lactation and cracks in nipple
- Common scenarios: infrequent feeding, oversupply of milk, rapid weaning, illness in mother or child, clogged duct (J Hum Lact 1998;14:101)
- Also associated with eczema, nipple dermatoses and postreduction mammoplasty
- Bacteria often not isolated from culture
- Pregnancy related infections are usually due to Staphylococcus
- Usually unilateral, often methicillin resistant Staphylococcus aureus (MRSA) (Arch Surg 2007;142:881, Asian J Surg 2009;32:55)
- Also Staphylococcus epidermidis (BMC Microbiol 2009;9:82, J Hum Lact 2015;31:406)
- Streptococcus usually causes diffuse infections leading to scarring but is uncommon today (J Hum Lact 2020;890334420965147)
- Tuberculosis may occur in endemic areas (Med Princ Pract 2009;18:245, Int J Infect Dis 2019;87:135)
- Nonpregnancy related infections may be polymicrobial or associated with diabetes (Am J Med Sci 2009;338:123)
Clinical features
- Erythema, swelling, firmness, breast pain, fever, malaise, decreased milk outflow
- Abscess: well circumscribed fluctuant mass in addition to above features
- African Americans may have higher risk of abscess formation (World J Surg 2009;33:2582)
- Obesity (BMI > 30) and smoking risk factors for abscess (World J Surg 2009;33:2582)
- Zuska disease (periductal mastitis): clinical scenario of recurring subareolar abscesses and sinus formation (Am J Surg 1951;81:312)
- Fungal mastitis: rare
- Actinomycosis may develop in nipple and form a sinus tract
- Candida infection may interfere with breast feeding but Candida albicans is not present in milk ducts in women with clinical symptoms of ductal candidiasis (Breastfeed Med 2009;4:57)
Diagnosis
- Based on history and clinical findings
- Ultrasound preferred imagining modality (Radiol Bras 2020;53:405)
- Biopsy may be warranted for suspected abscess, atypical presentation, recurrent infection or treatment failure; Gram stain and culture (aerobic and anaerobic) with sensitivities to guide antibiotic selection (rarely needed)
- FNA can be used to drain (Am Fam Physician 2008;78:727)
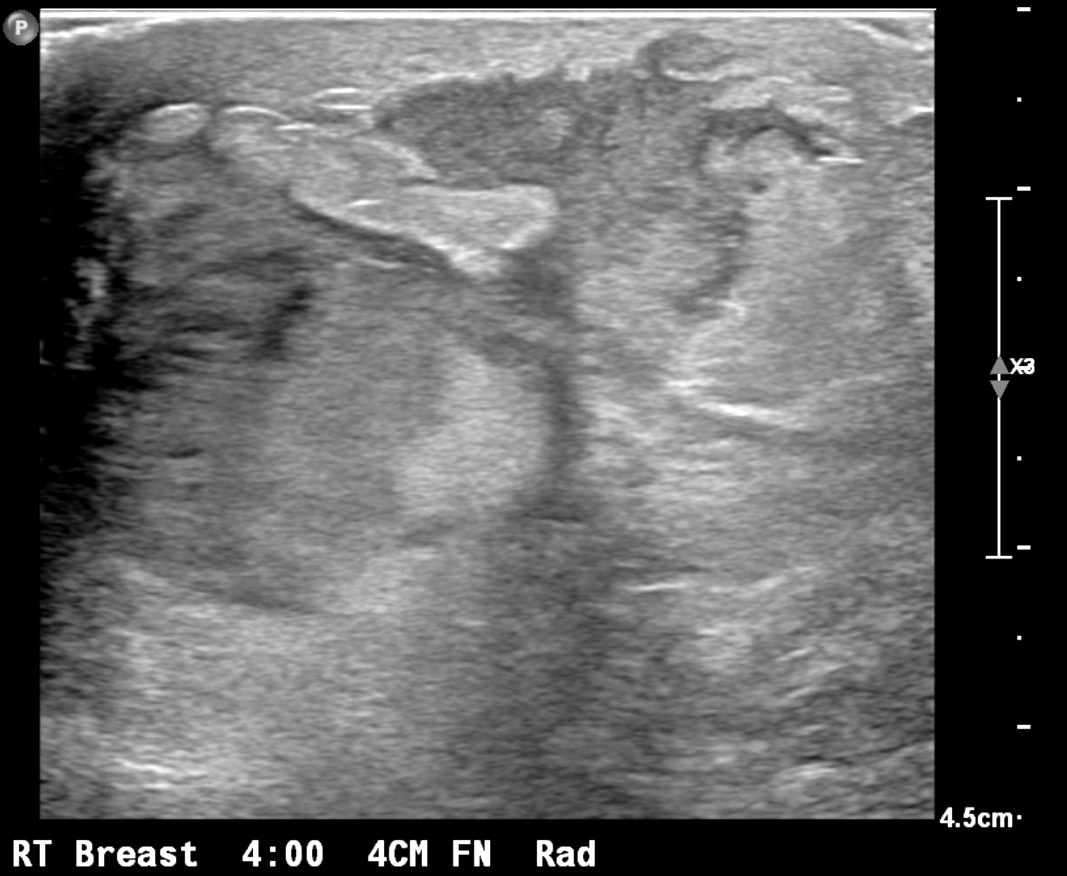
Radiology description
- Ultrasound (preferred modality): abscess shows hypoechoic lesion of purulent material, well circumscribed, macrolobulated, irregular or ill defined with septa and thick echogenic rim (Radiographics 2011;31:1683, Radiographics 2007;27 Suppl 1:S101)
- Mammography of limited value due to nonspecific findings
Radiology images
Prognostic factors
- Recurrent breast abscesses are more likely to be smokers and have mixed bacterial and anaerobic infections (World J Surg 2009;33:2582)
Case reports
- 16 year old girl with MRSA abscess and toxic shock syndrome (Oxf Med Case Reports 2019;2019:omz054)
- 21 year old lactating woman with Listeria breast abscess (Cureus 2017;9:e1006)
- 22 year old woman with endogenous endophthalmitis secondary to mastitis (Indian J Ophthalmol 2020;68:2595)
- 30 year old woman with Mycobacterium fortuitum abscess following breast nipple piercing (IDCases 2020;21:e00847)
- 31 year old woman with tubercular mastitis mimicking malignancy (Prague Med Rep 2020;121:267)
- 32 year old nonlactating woman with Neisseria gonorrhoeae mastitis and abscess (IDCases 2019;18:e00620)
- 36 year old woman with Histoplasma capsulatum causing granulomatous mastitis (Arch Pathol Lab Med 2006;130:e1)
- 39 year old woman with nonpuerperal breast abscess due to Prevotella bivia (Clin Case Rep 2020;8:1399)
- 48 year old woman with Salmonella enteritidis breast abscess (BMJ Case Rep 2018;2018:bcr2018226075)
- 52 year old man with Trichophyton rubrum causing bilateral male breast enlargement (Breast 2006;15:263)
- 55 year old diabetic woman with Fusarium (Indian J Med Microbiol 2005;23:198)
- Report of saline filled breast implants contaminated with Curvularia in 5 patients (J Infect Dis 2005;192:170)
- Immunosuppressed patient with breast nodule due to coccidiomycosis (Arch Pathol Lab Med 1991;115:1064)
- Cryptococcus in HIV+ patient (J Infect 2008;57:82)
- 2 cases of Histoplasma capsulatum causing granulomatous mastitis (Hum Pathol 1989;20:47)
- Young woman who had nipples pierced, presented with right breast pain, erythema and drainage (Case of the Month #515)
Treatment
- Symptomatic treatment: effective milk removal via breastfeeding, pumping or hand expressing to fully empty breasts, analgesia, warm compress (Am Fam Physician 2008;78:727)
- Kneading and dispersing manipulation for early stage disease (Zhong Xi Yi Jie He Xue Bao 2009;7:1130)
- Antibiotics targeting Staphylococcus species are mainstay of treatment, although effectiveness is debated (J Hum Lact 2008;24:311, Cochrane Database Syst Rev 2013:CD005458)
- Aspiration or incision and drainage; now considered last resort for abscess management (Radiographics 2011;31:1683, Expert Rev Anti Infect Ther 2014;12:753)
- Urokinase irrigation may be useful for large abscesses (J Ultrasound Med 2009;28:449)
- Ultrasound guided drainage (Radiology 2004;232:904, Br J Radiol 2005;78:186)
- Probiotics (Benef Microbes 2014;5:169, Appl Environ Microbiol 2008;74:4650, Clin Infect Dis 2010;50:1551)
Clinical images
Contributed by Ayesha Farooq, M.B.B.S. and Julie Jorns, M.D. (Case #515)
Images hosted on other servers:
Gross description
- Excisions rare; specimens usually from incision and drainage procedures and typically received in fragments
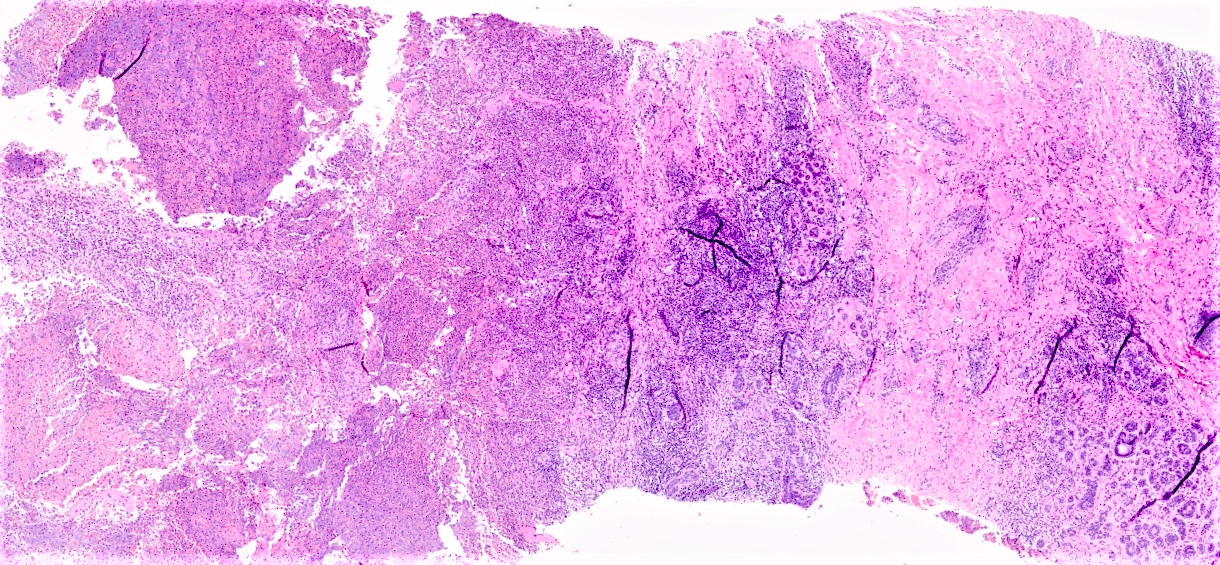
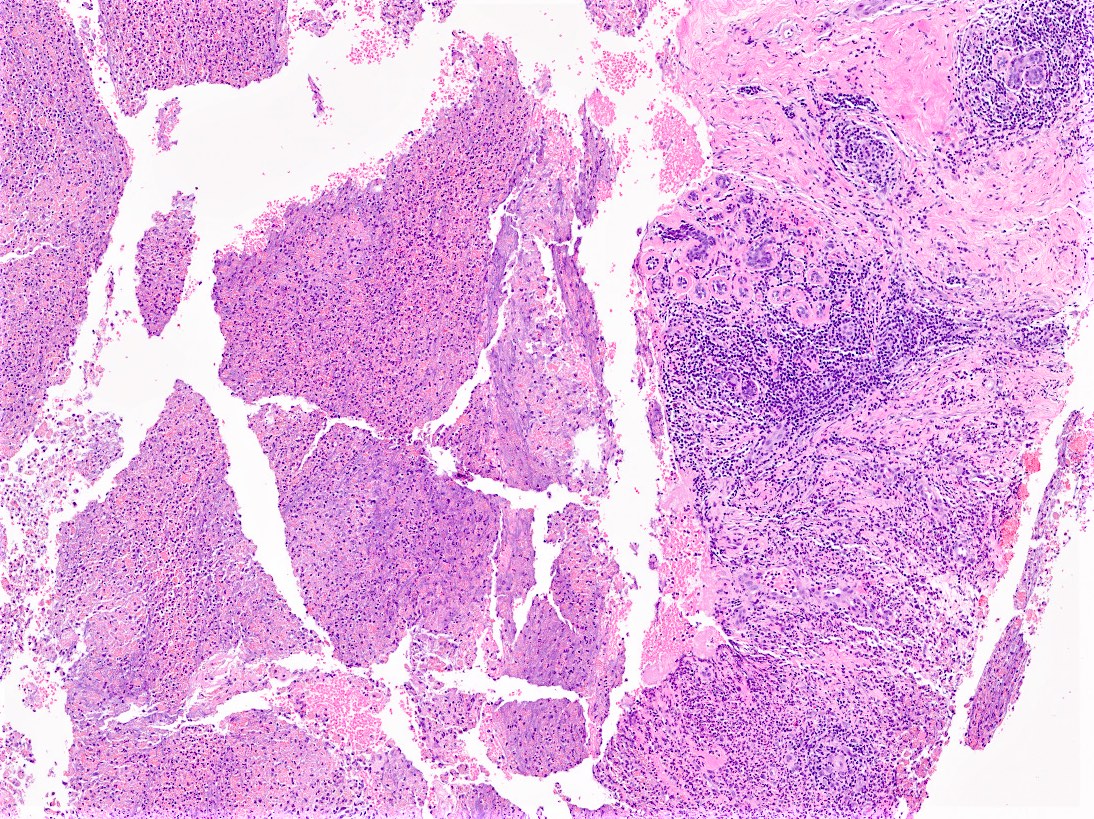
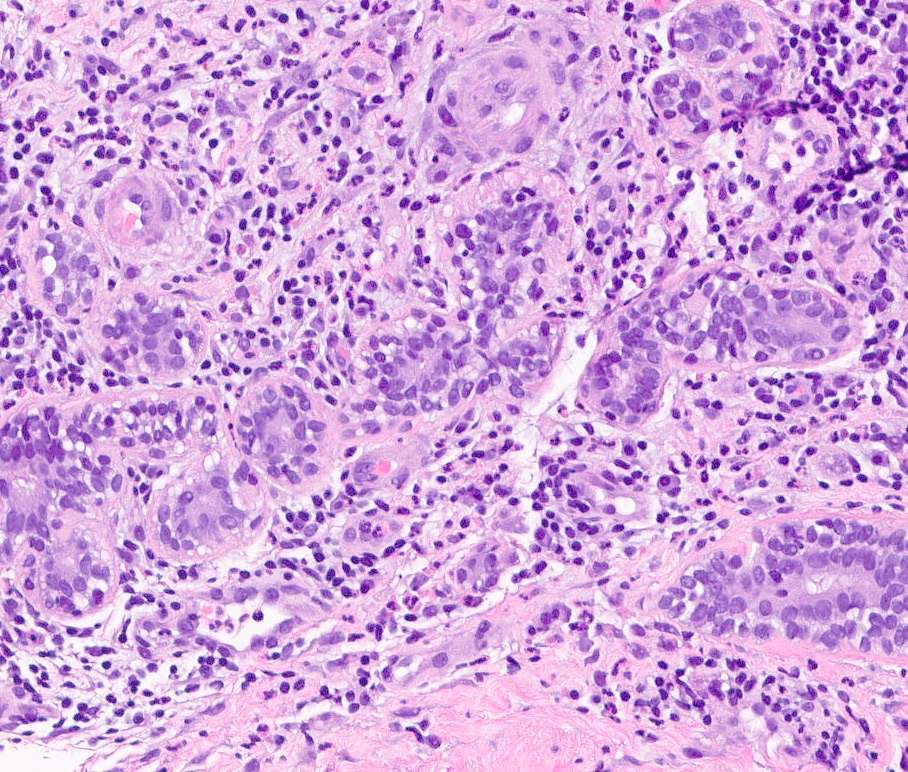
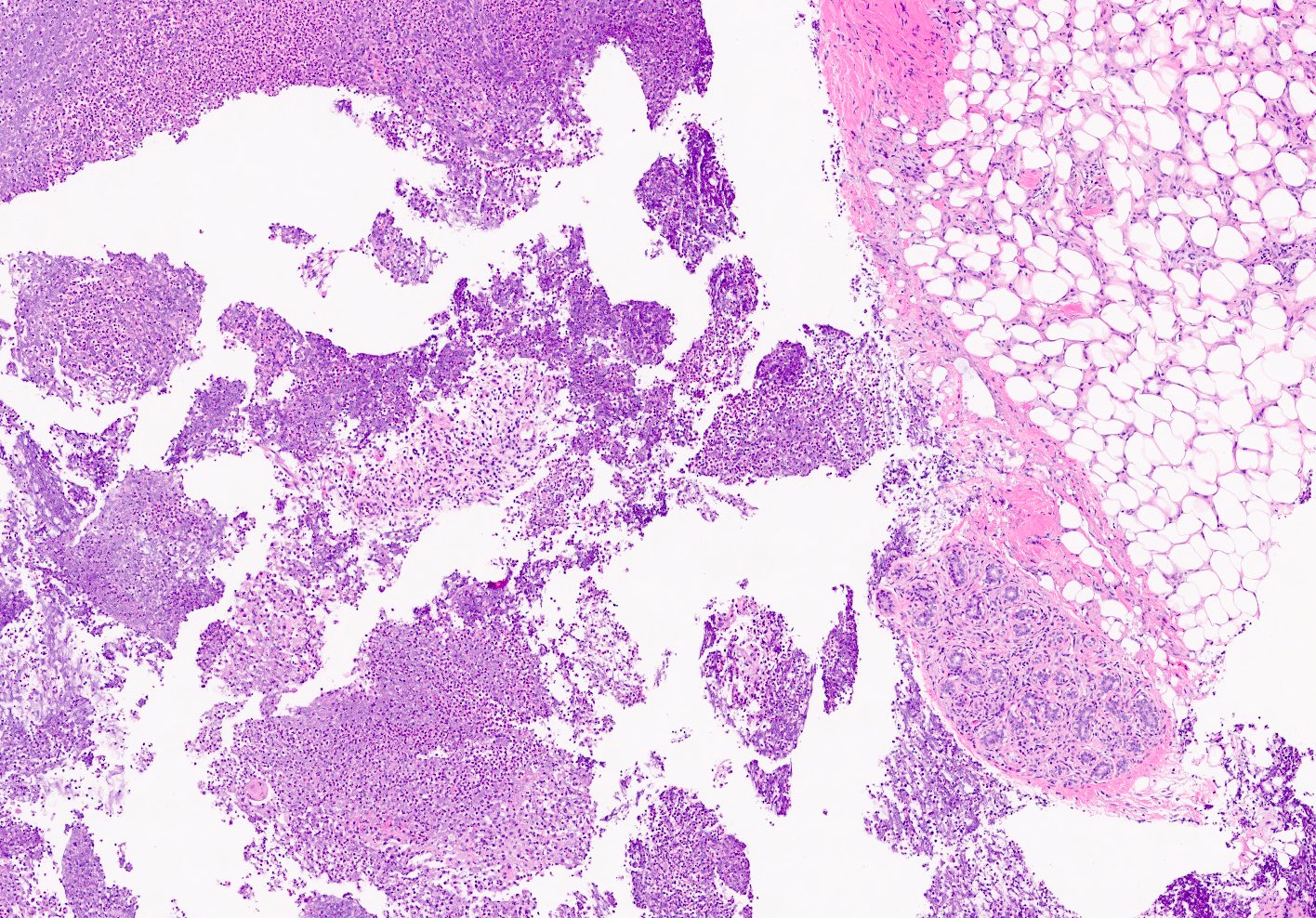
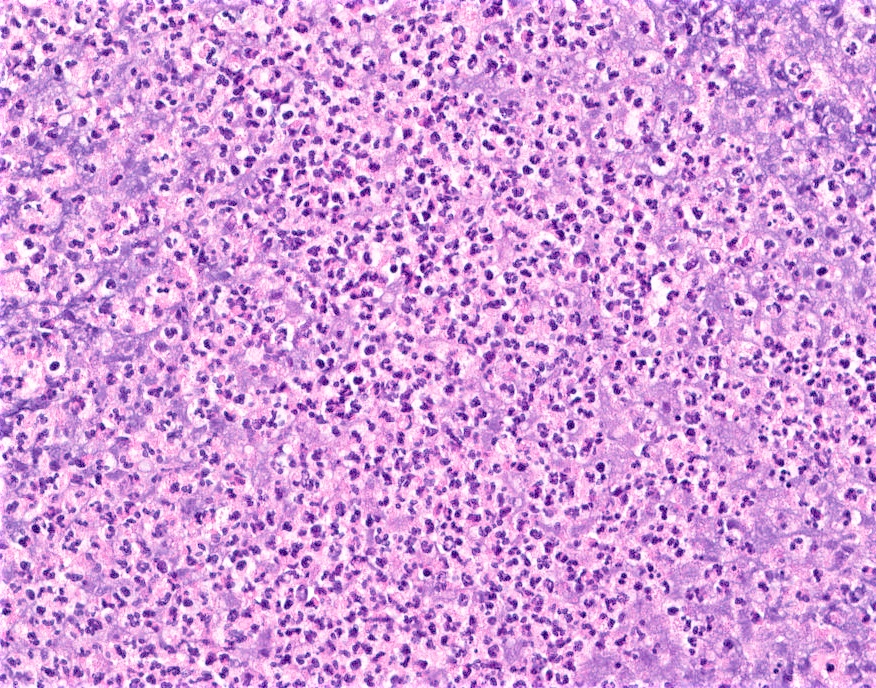
Microscopic (histologic) description
- Mixed dense inflammatory infiltrate, predominantly neutrophils, in breast tissue
- May obscure underlying normal breast tissue
- Tissue necrosis may be present
- Gram stain for microorganisms may reveal bacterial forms (gram positive cocci) associated with neutrophilic infiltrate
- Granulation tissue and chronic inflammation with resolution
- Lymphocytes, giant cells and granulomas are not typical (J Pathol Transl Med 2015;49:279)
Microscopic (histologic) images
Contributed by Kristen E. Muller, D.O.
Contributed by Ayesha Farooq, M.B.B.S. and Julie Jorns, M.D. (Case #515)
Cytology description
- Background of acute inflammation and necrotic debris (Cytopathology 1992;3:281)
Positive stains
- Gram stain may highlight Gram positive bacterial forms
Sample pathology report
- Right breast, core needle biopsy:
- Breast tissue with abundant acute inflammation and bacterial forms identified on Gram stain (see comment)
- Comment: The histologic findings are compatible with acute mastitis and abscess formation in the appropriate clinical context. Clinical correlation and correlation with microbiology studies (if performed) is recommended.
Differential diagnosis
- Squamous metaplasia of lactiferous ducts (SMOLD):
- Subareolar location
- Lactiferous ducts with squamous metaplasia
- Multinucleated giant cells associated with keratin debris
- Strong association with smoking
- Fat necrosis:
- Infarcted adipocytes, lipid laden macrophages, foreign body giant cell reaction
- Initially acute inflammatory infiltrate may be present, chronic inflammation predominates in older lesions
- History of surgery, prior biopsy, radiation, trauma
- Idiopathic granulomatous mastitis:
- Granulomatous inflammation (lymphocytes, plasma cells, histiocytes, multinucleated giant cells)
- Lobulocentric pattern, may obliterate lobules
- May have neutrophils forming microabscesses surrounding empty microcysts; features overlap with cystic neutrophilic granulomatous mastitis, which may have gram positive bacilli within microcysts (Corynebacterium)
- Duct ectasia:
- Foamy histiocytes within lumen and within wall and epithelium of ducts, periductal fibrosis
- Inflammatory cells typically chronic; acute inflammatory infiltrate rarely present
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2
A. Abscess may form as a complication if left untreated
Comment Here
Reference: Acute mastitis / abscess
Comment Here
Reference: Acute mastitis / abscess
Board review style question #3
What is a common causative microorganism associated with nipple piercing related infection?
- Salmonella
- Shigella
- Staphylococcus
- Stenotrophomonas
Board review style answer #3