Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3 | Board review style question #4 | Board review style answer #4Cite this page: Tozbikian G. Fibroadenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastfibroadenoma.html. Accessed March 28th, 2025.
Definition / general
- Benign biphasic tumor composed of a proliferation of both glandular epithelial and stromal components of the terminal duct lobular unit
Essential features
- Most common breast tumor in adolescent and young women
- Benign biphasic tumor comprised of glandular epithelium and specialized interlobular stroma of the terminal ductal lobular unit (Pathol Annu 1994;29:1)
- Can show a spectrum of histologic appearances; generally uniform in stromal cellularity and distribution of glandular and stromal elements within a given lesion (an important distinction from phyllodes tumor)
- Fibroadenomas with hypercellular stroma and prominent intracanalicular pattern can show morphologic overlap with benign phyllodes tumors, especially in needle biopsy specimens
Terminology
- Fibroadenoma, usual type fibroadenoma, adult type fibroadenoma
- Myxoid fibroadenoma
- Juvenile fibroadenoma
- Complex fibroadenoma
ICD coding
- ICD-10: D24 - benign neoplasm of breast
Epidemiology
- Most common benign tumor of the female breast
- Most common breast tumor in adolescent and young women
- Can occur at any age, median age of 25 years (J R Coll Surg Edinb 1988;33:16)
- Juvenile fibroadenoma generally occurs in younger and adolescent patients < 20 years; reported in children at a very young age (Am J Surg Pathol 1985;9:730, Jpn J Clin Oncol 2011;41:260)
- Complex fibroadenoma reported in older patients with median age between 35 - 47 years (Am J Clin Pathol 2001;115:736, AJR Am J Roentgenol 2008;190:214)
- Myxoid fibroadenoma is associated with Carney complex (Am J Surg Pathol 1991;15:713)
- Increased relative risk (1.5 - 2.0) of subsequent breast cancer; relative risk is higher (3.1) in complex fibroadenomas; no increased risk for juvenile fibroadenoma (N Engl J Med 1994;331:10, Int J Cancer 1994;57:681, Breast J 2017;23:182)
Sites
- Breast
- Can occur in axilla accessory breast tissue
Etiology
- Increased risk associated with cyclosporine immunosuppression (Clin Nephrol 2004;61:151)
Clinical features
- Often presents as painless, firm, mobile, slow growing mass
- Usually solitary, can be multiple and bilateral
- Usually less than 3 cm in diameter but may grow to large size (AJR Am J Roentgenol 2008;190:214)
Diagnosis
- Histologic examination of involved tissue
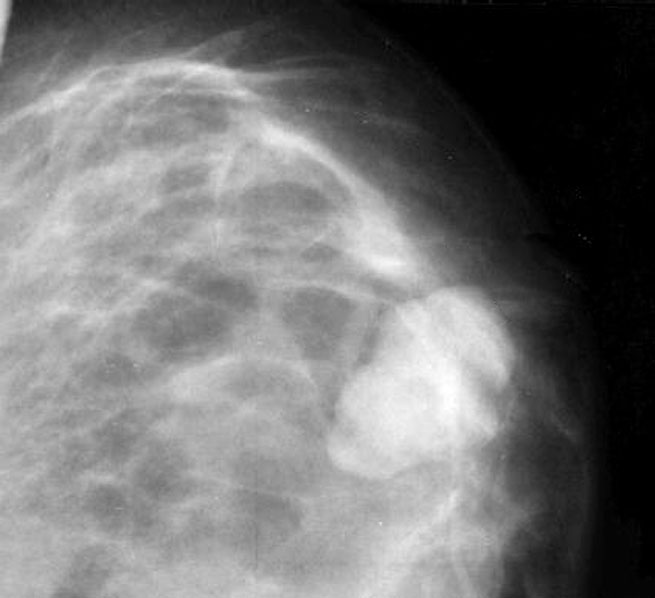
Radiology description
- Sonographically seen usually as a round or oval mass, smooth margins with hypo or isoechoic features (Radiology 1989;172:671, Invest Radiol 1986;21:34, AJR Am J Roentgenol 1983;140:369)
- Can be associated with calcifications, especially in postmenopausal patients
Radiology images
Contributed by Mark R. Wick, M.D., Azadeh Khayyat, M.D. and Julie M. Jorns, M.D. (Case #533)
Images hosted on other servers:
Case reports
- 12 year old girl with breast mass (Int J Surg Case Rep 2017;41:427)
- 16 year old girl with 28 cm left breast mass (BMJ Case Rep 2019;12:e227277)
- 17 year old girl with recurrent juvenile fibroadenoma (Medicine (Baltimore) 2018;97:e10765)
- 18 year old woman with mass in axilla accessory breast tissue (BMJ Case Rep 2015;2015:bcr2015209535)
- 35 year old woman with left breast mass (Breast Dis 2015;35:49)
- 37 year old woman with increased uptake of breast mass on PET scan (Clin Nucl Med 2017;42:145)
- 44 year old woman with bilateral breast masses (Oncol Lett 2015;10:1397)
- Premenopausal woman with family history of breast cancer was found to have a subcentimeter mass with calcifications on mammogram (Case of the month #533)
Treatment
- Management depends on patient risk factors and patient preference
- Conservative management with close clinical followup, especially if concordant radiology findings (Br J Surg 1987;74:857)
- Local surgical excision, especially if symptomatic (Am J Surg Pathol 1985;9:730)
- If atypia / neoplasia is found within a fibroadenoma, the surgical and systemic therapeutic management is specific and appropriate to the primary atypical / neoplastic lesion
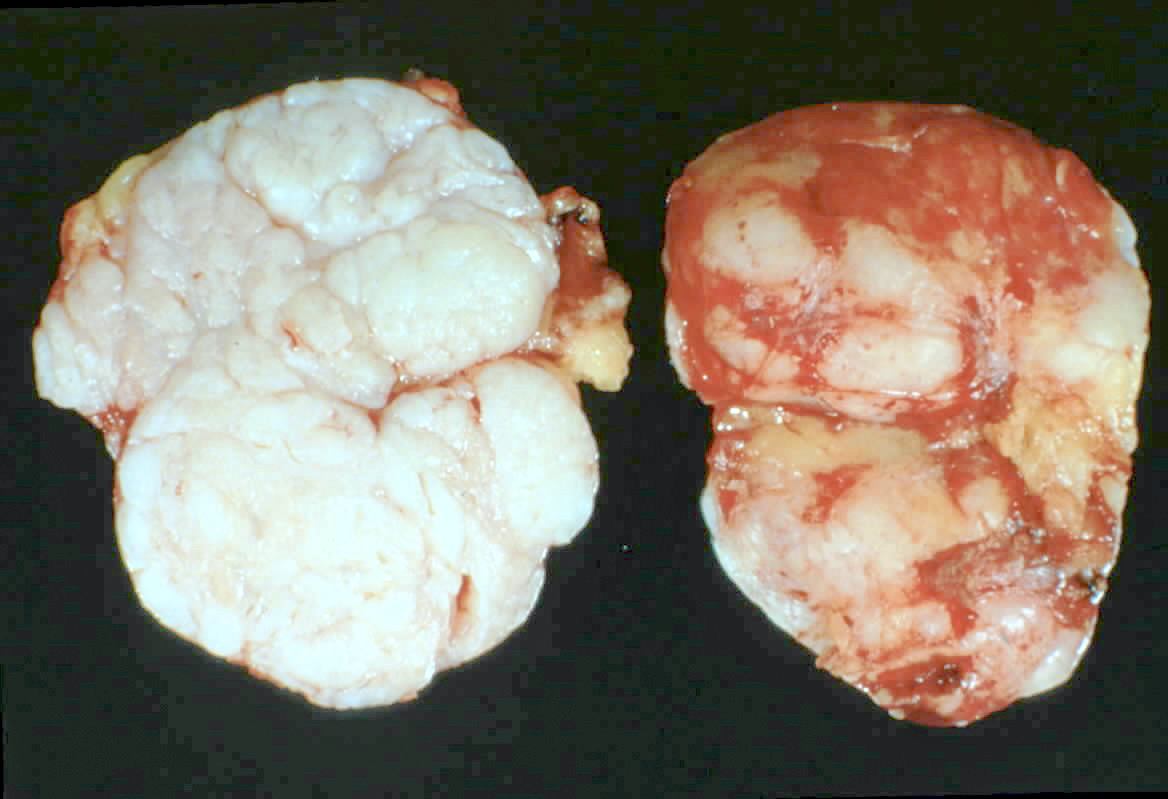
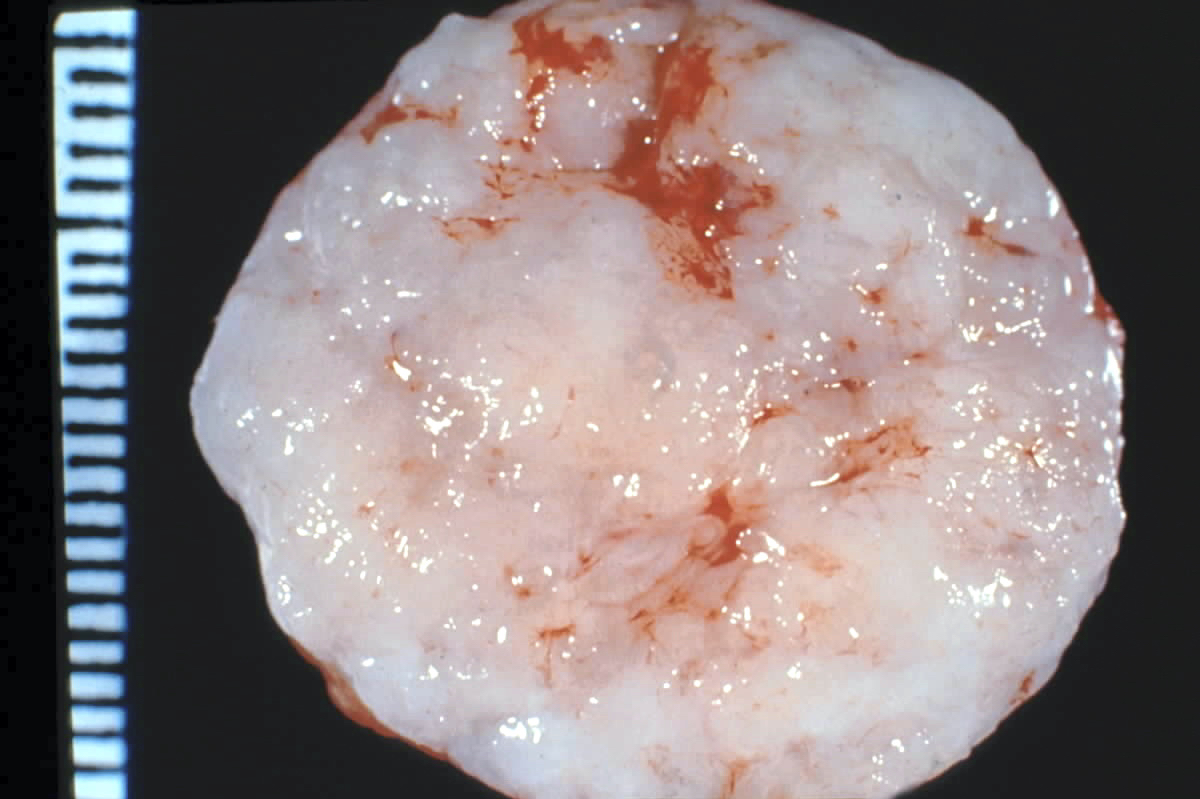
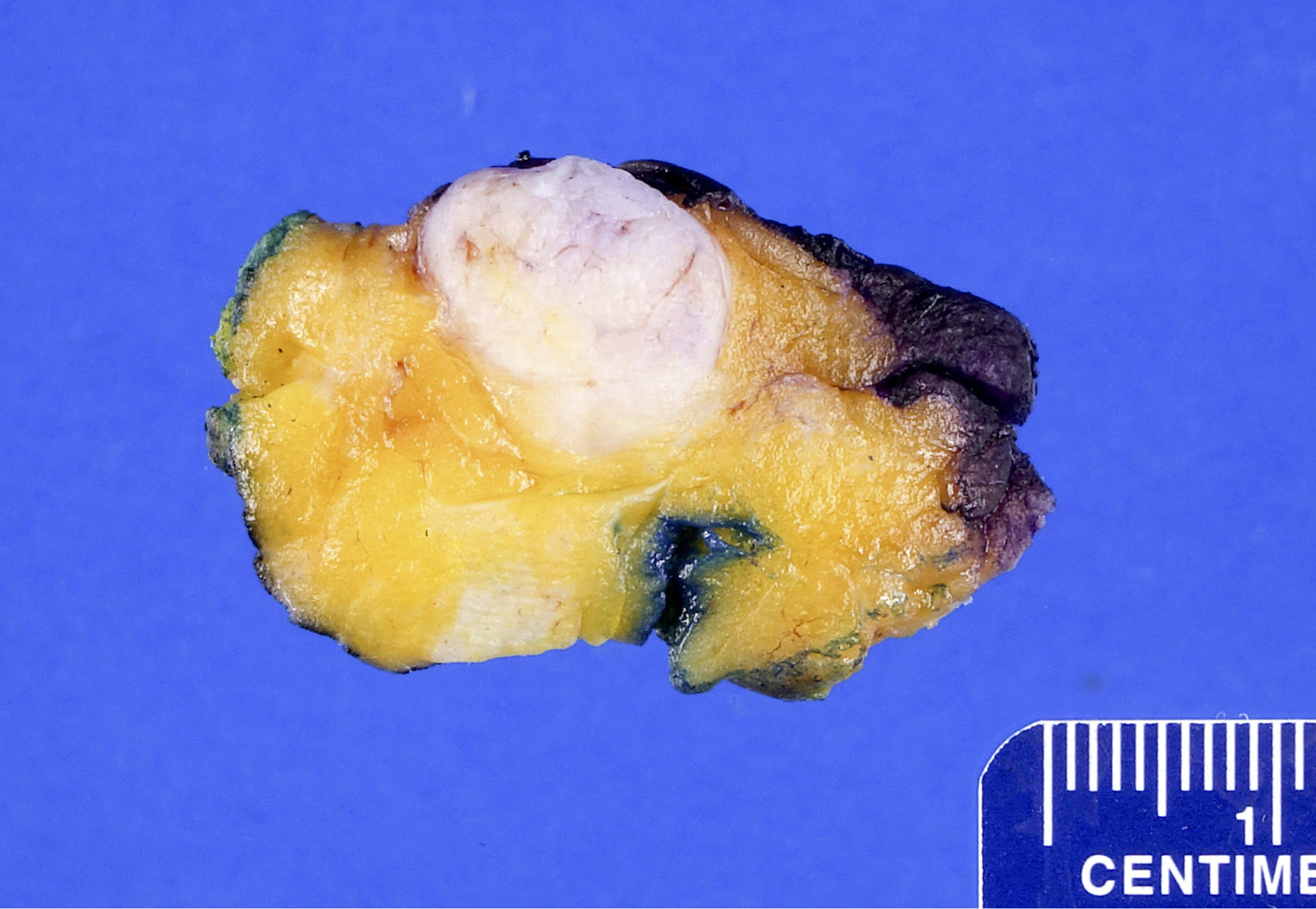
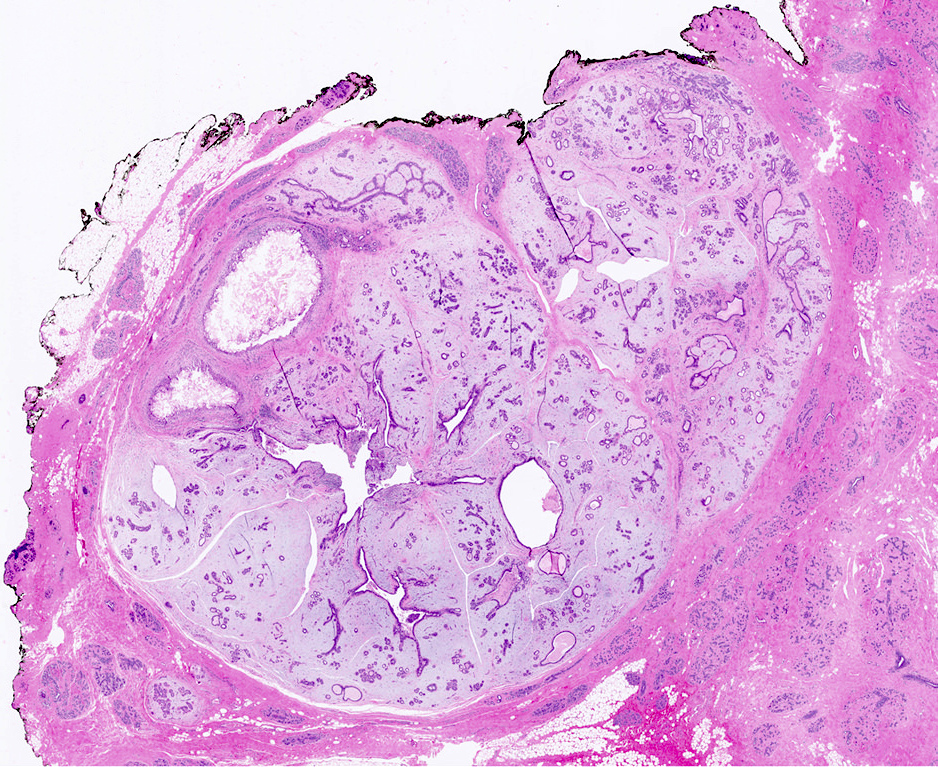
Gross description
- Firm, well circumscribed, ovoid mass with bosselated surface, lobulations bulge above the cut surface, slit-like spaces
- May have mucoid or fibrotic appearance; can be calcified
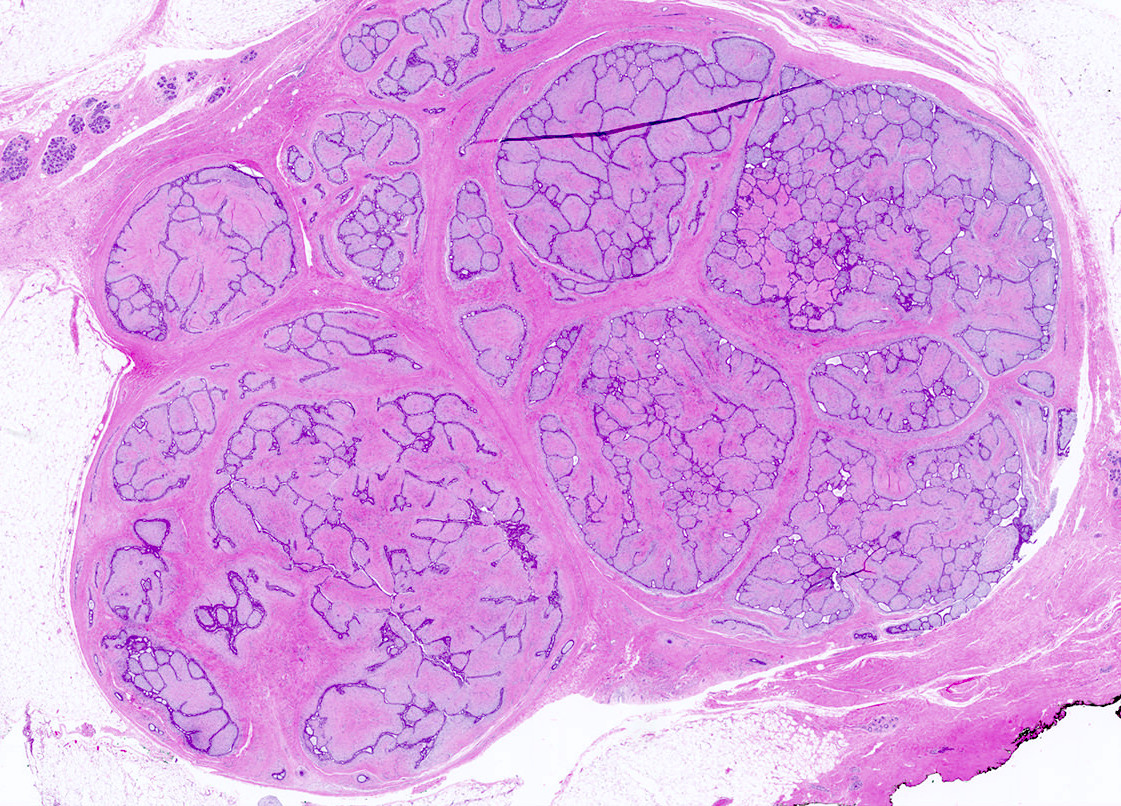
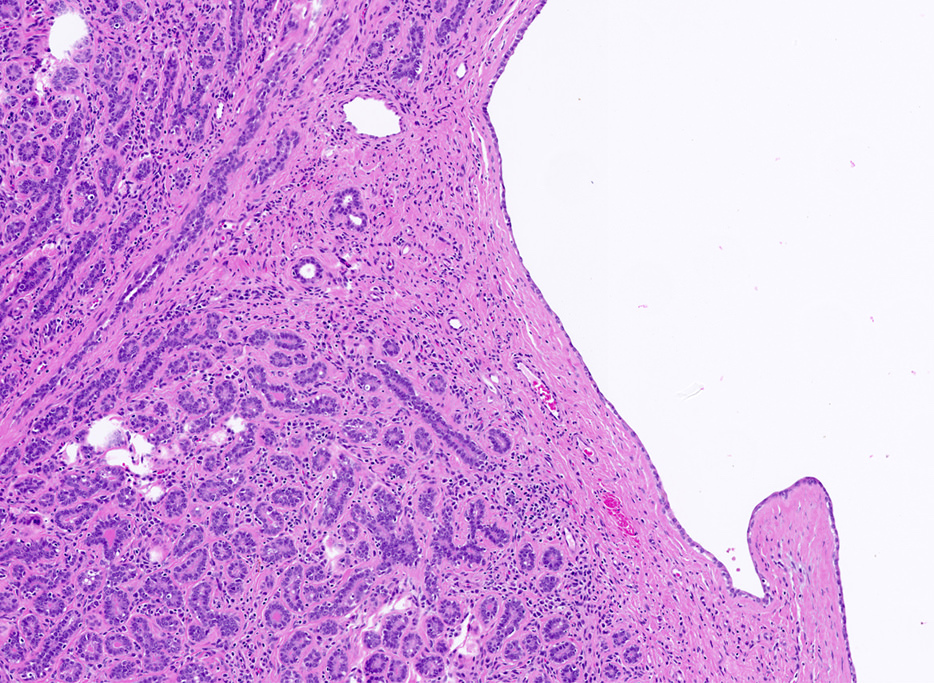
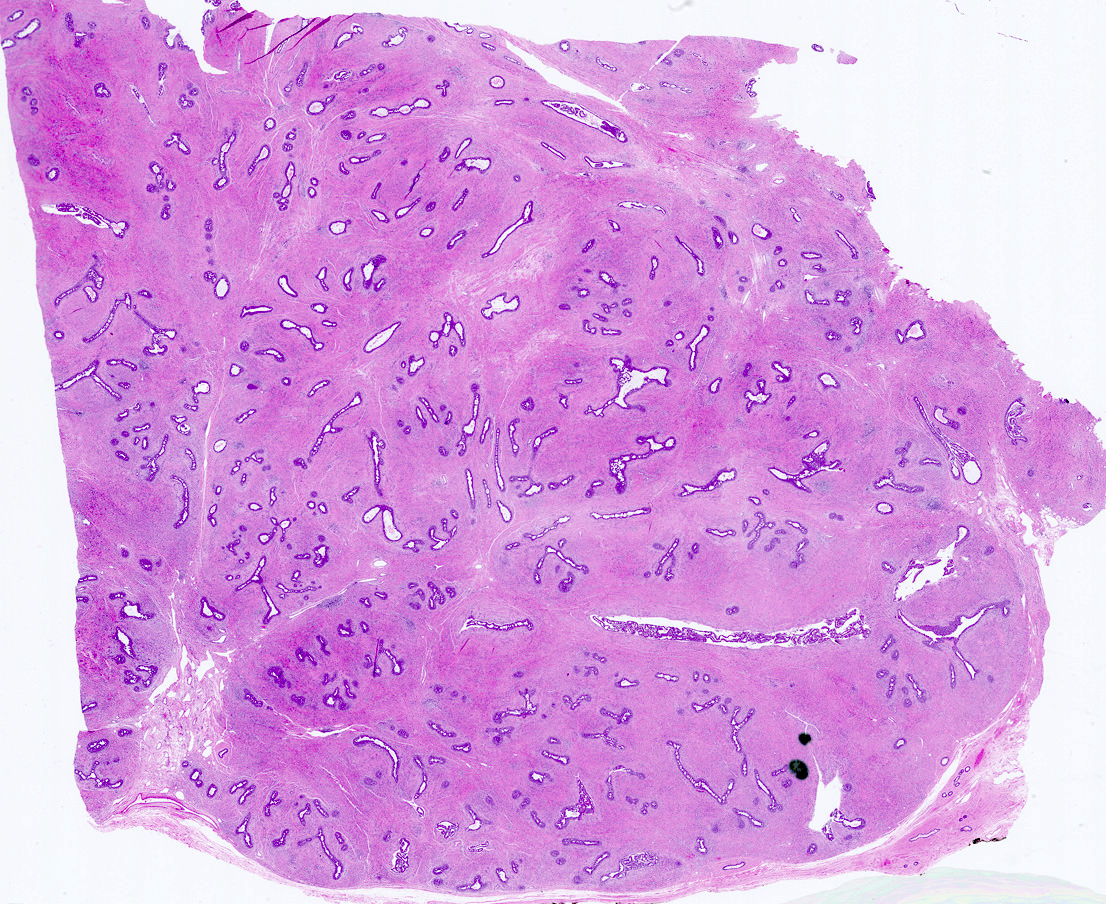
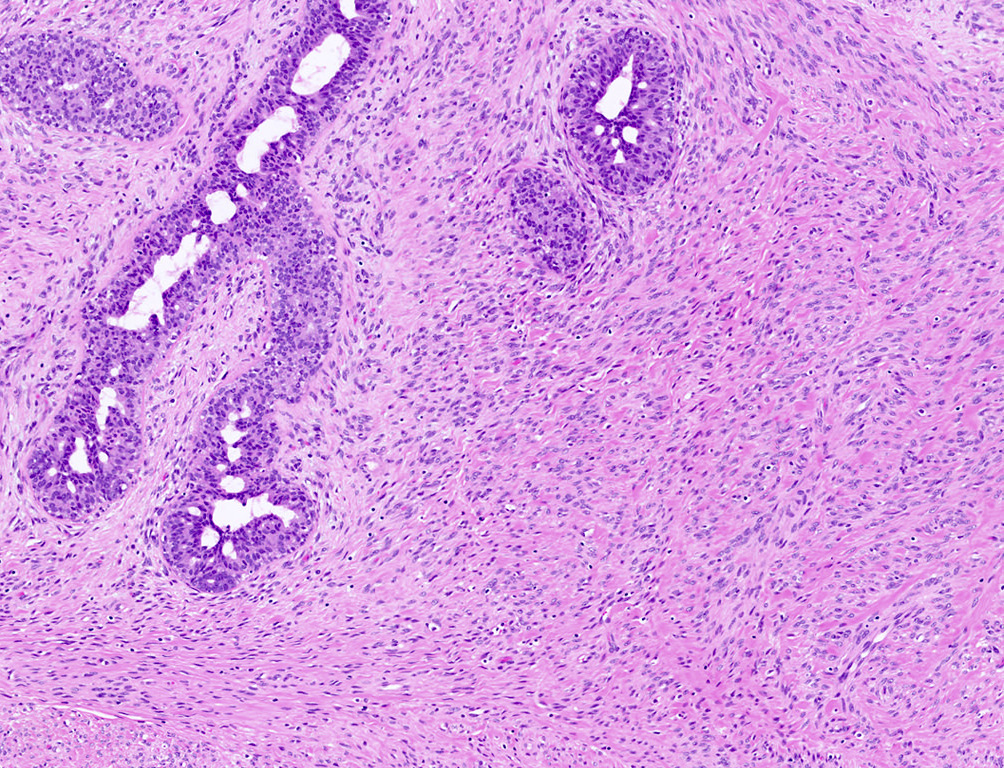
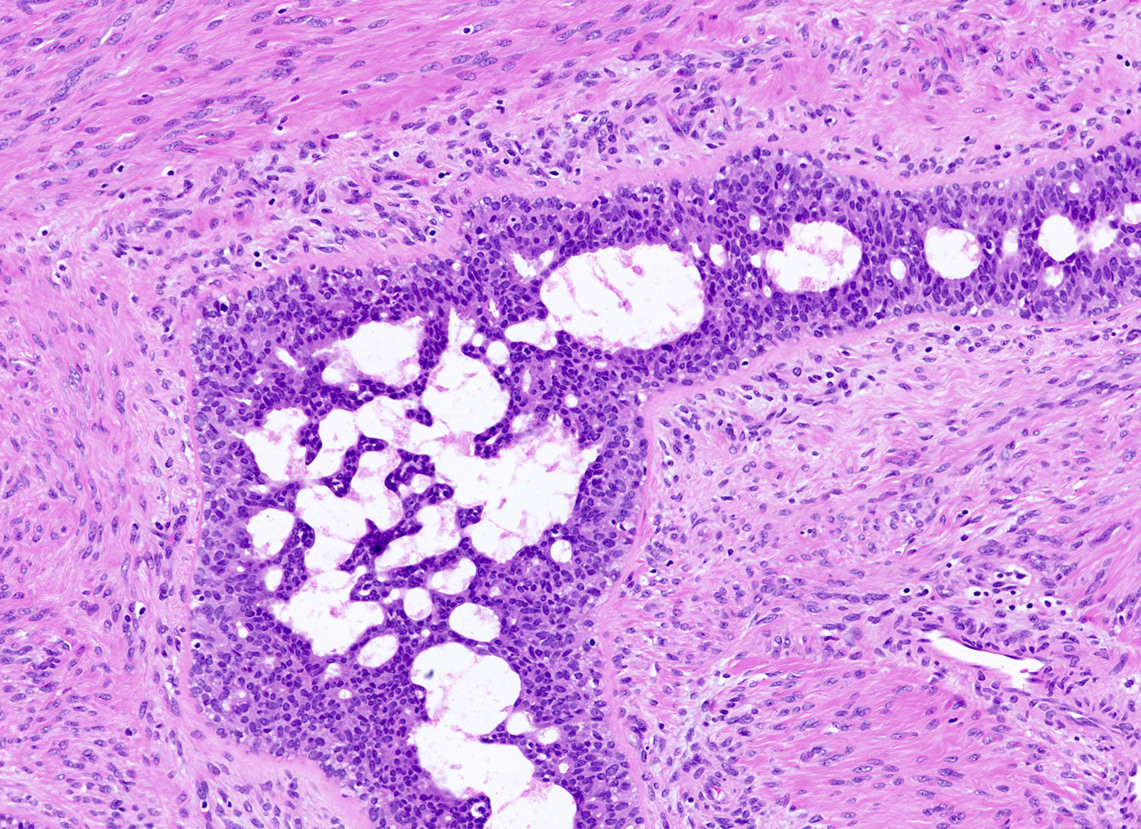
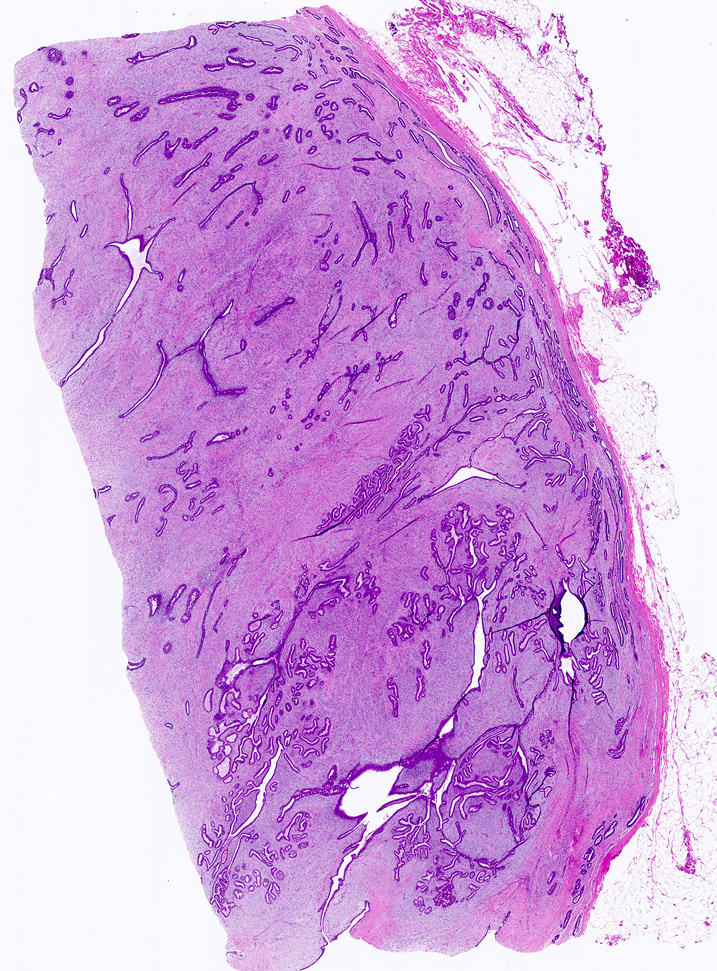
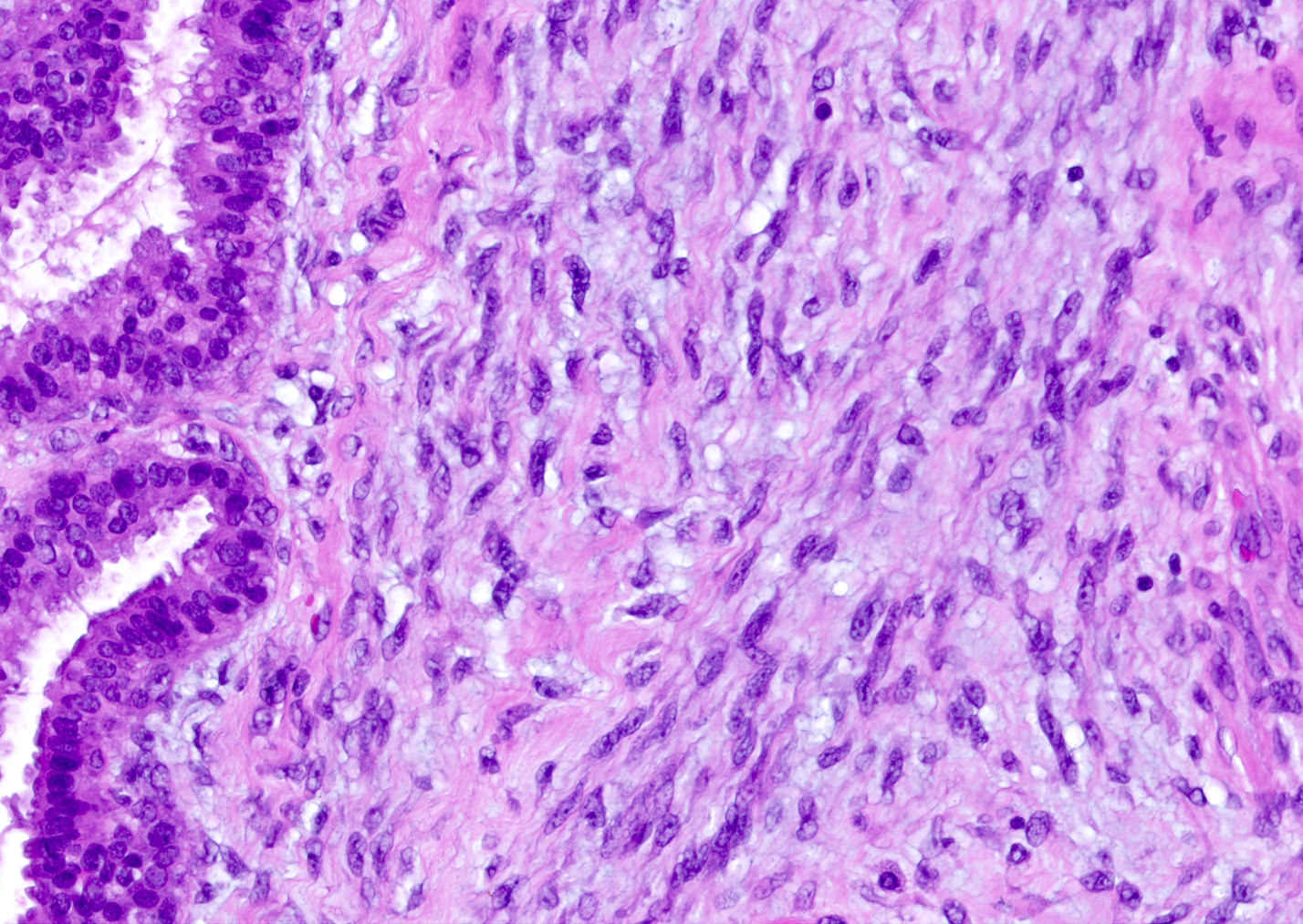
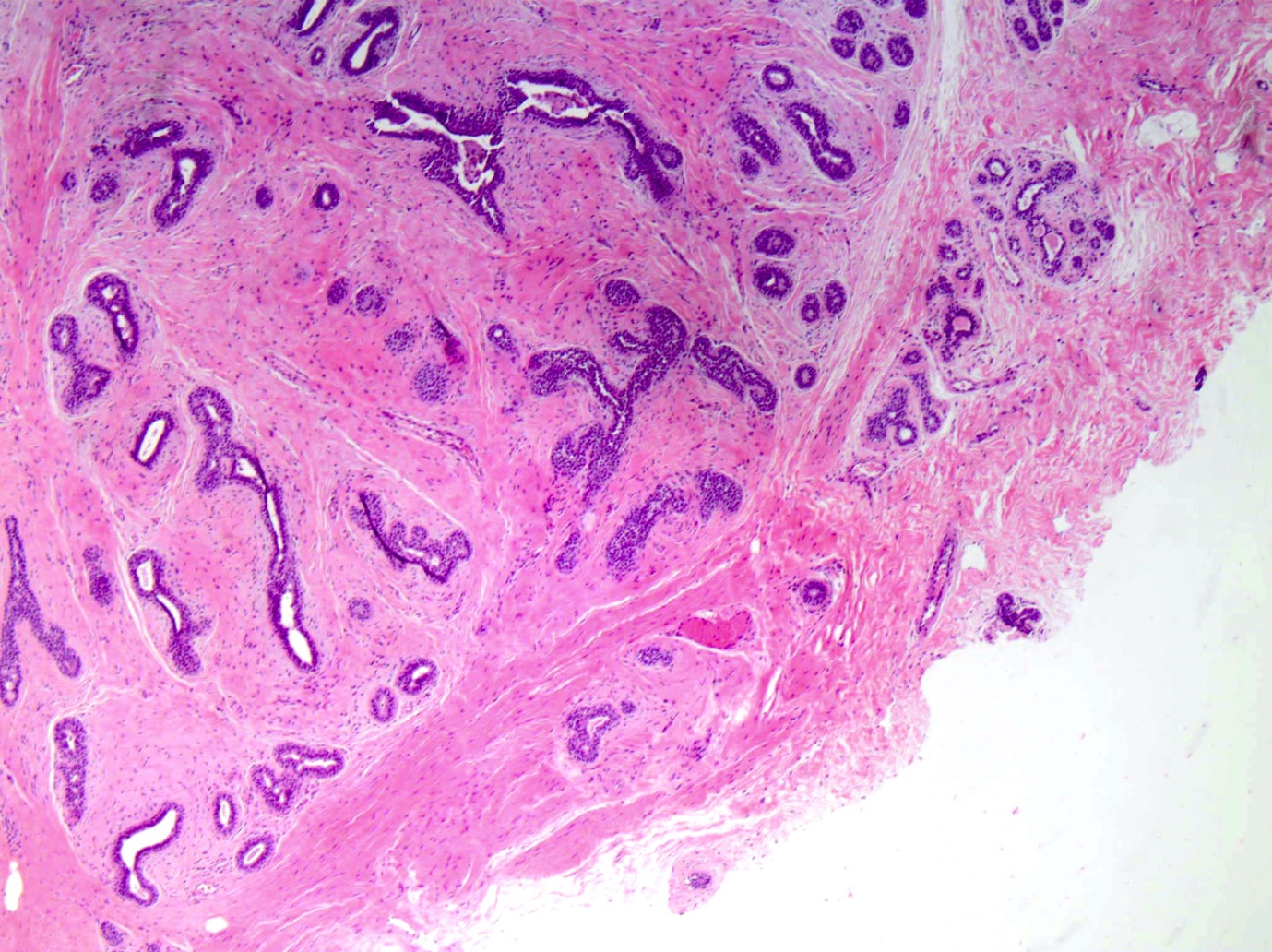
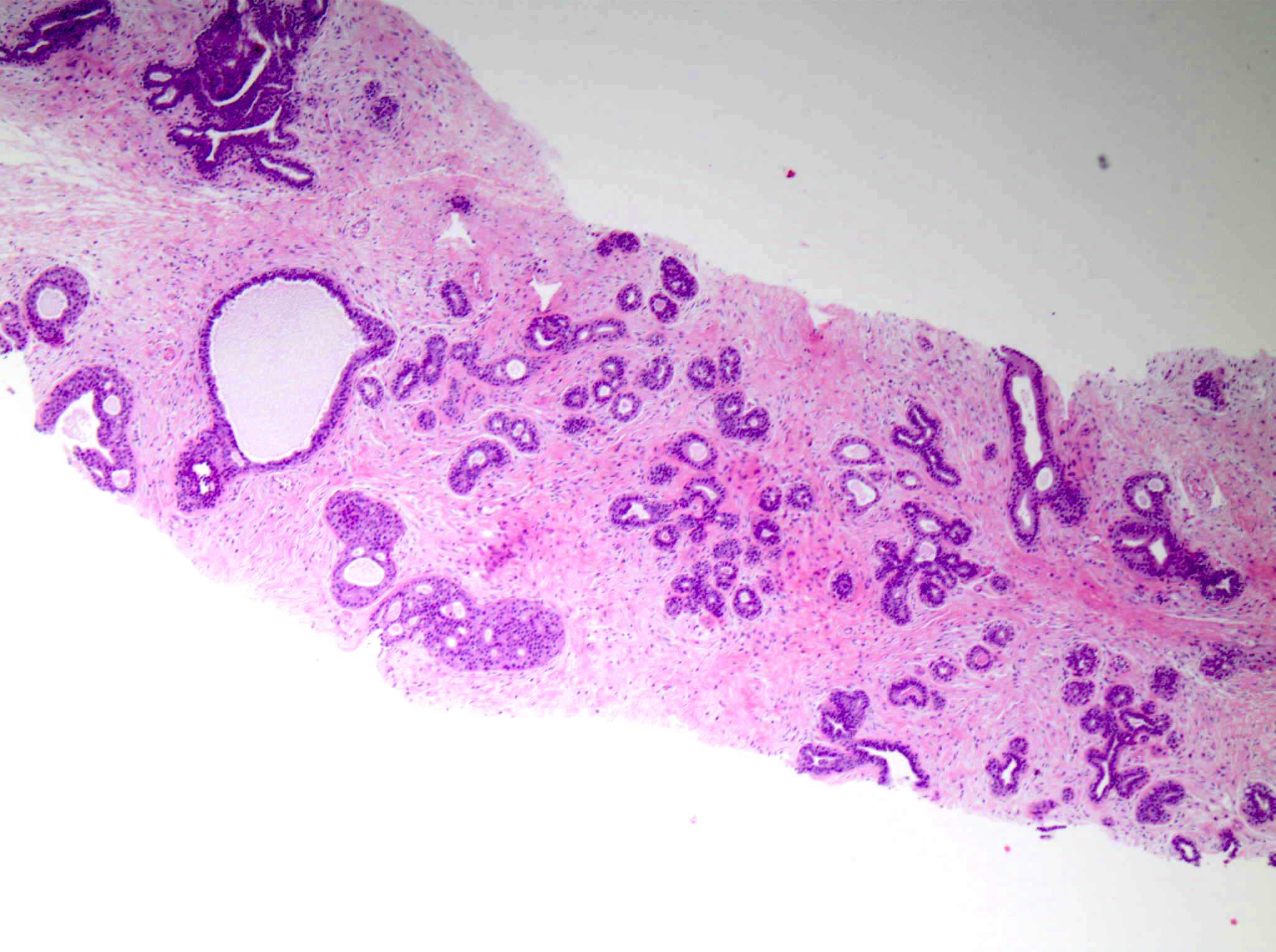
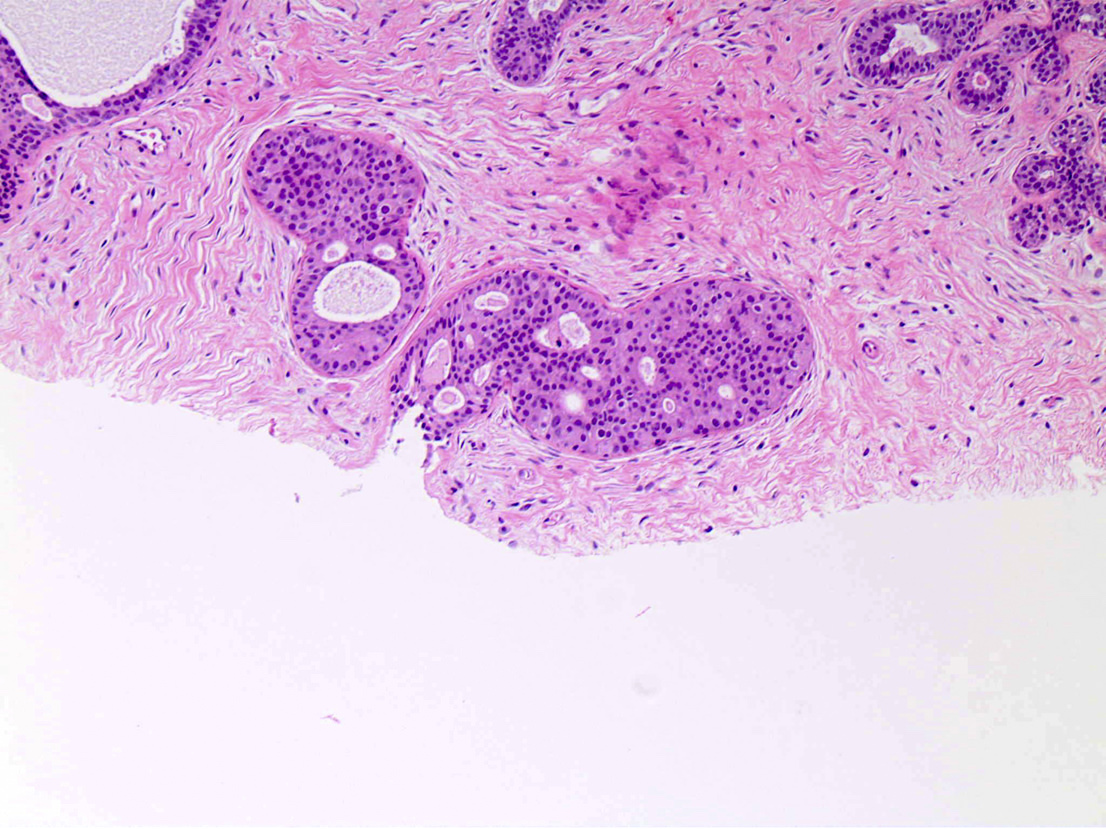
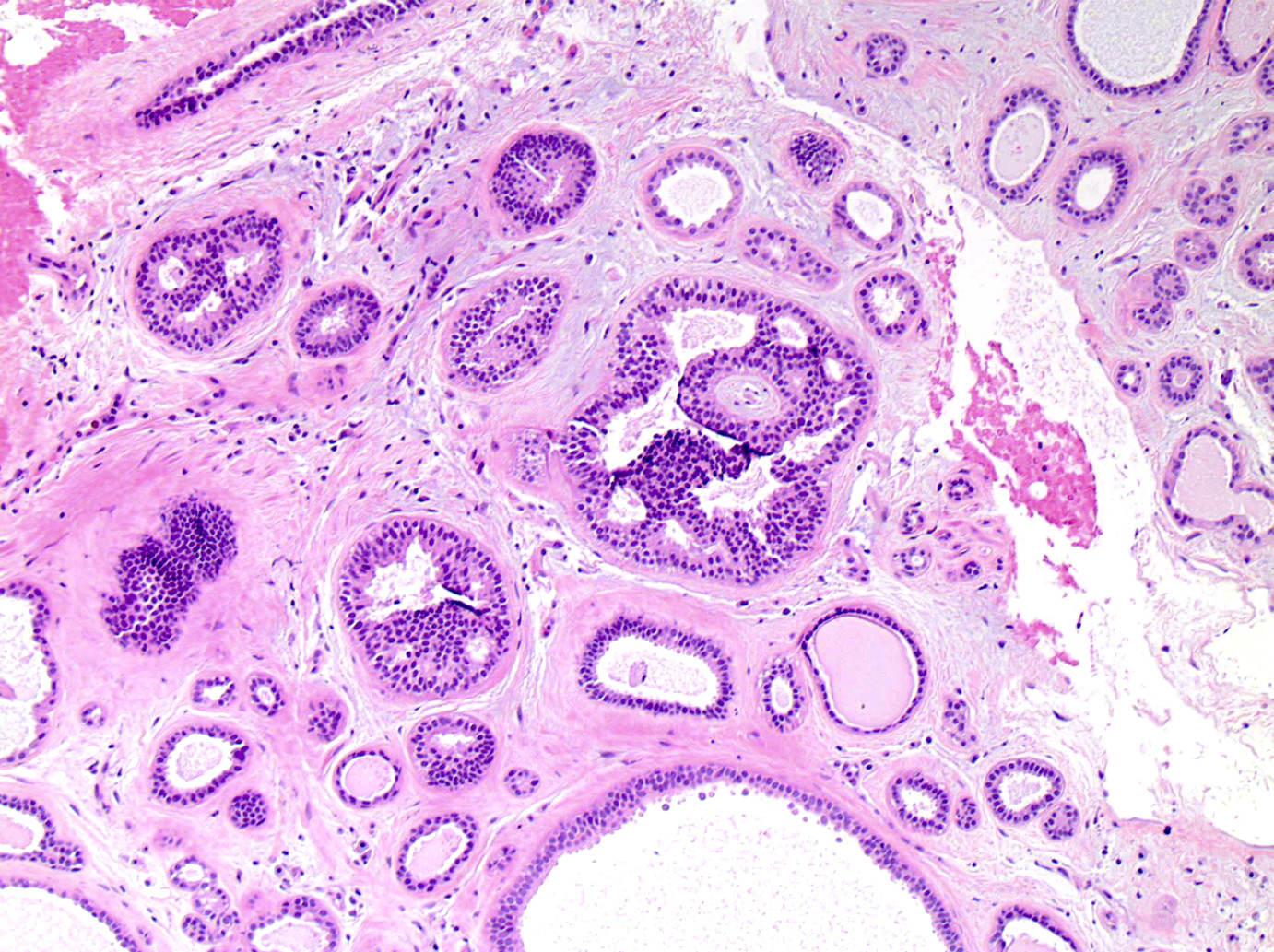
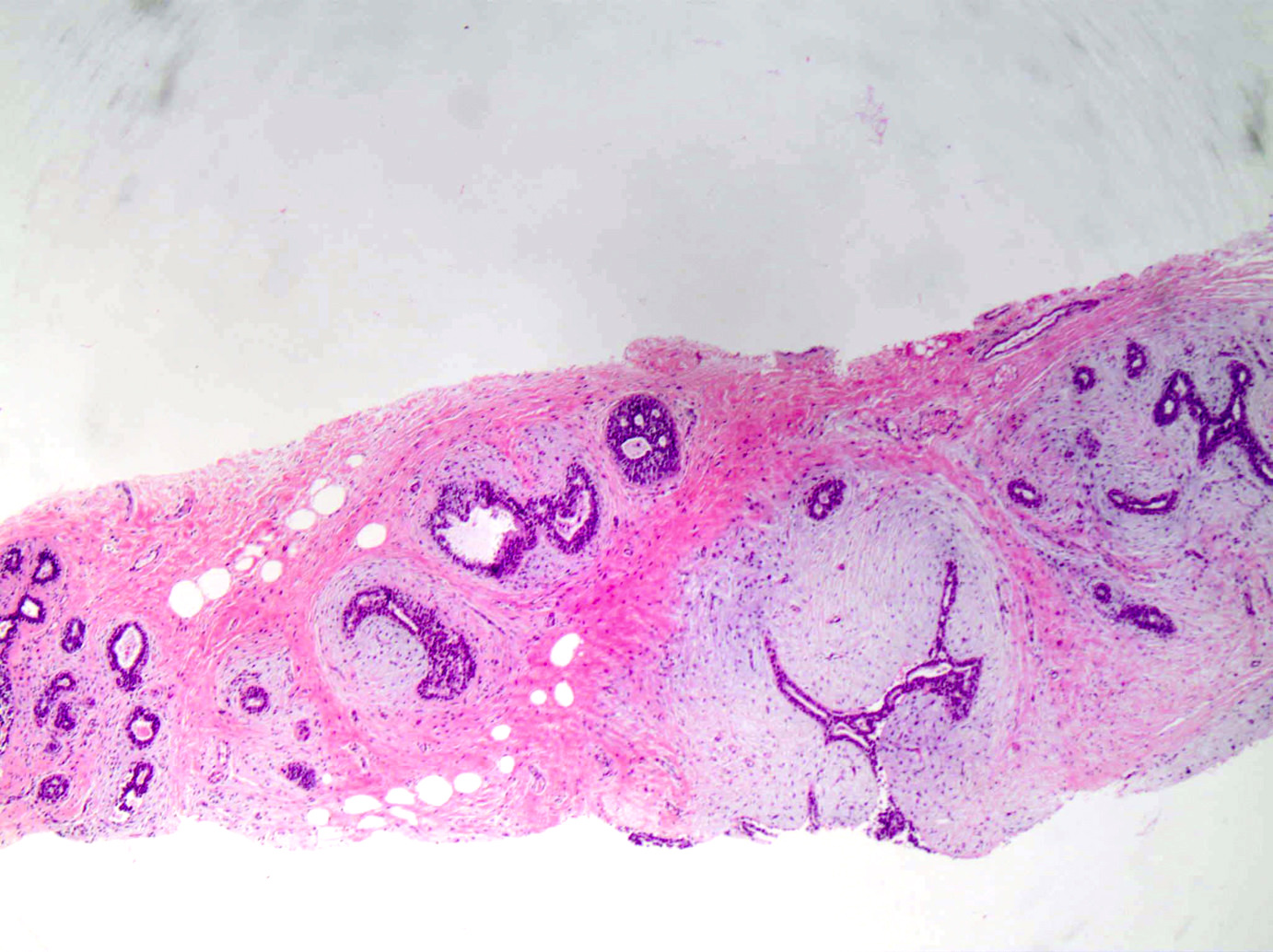
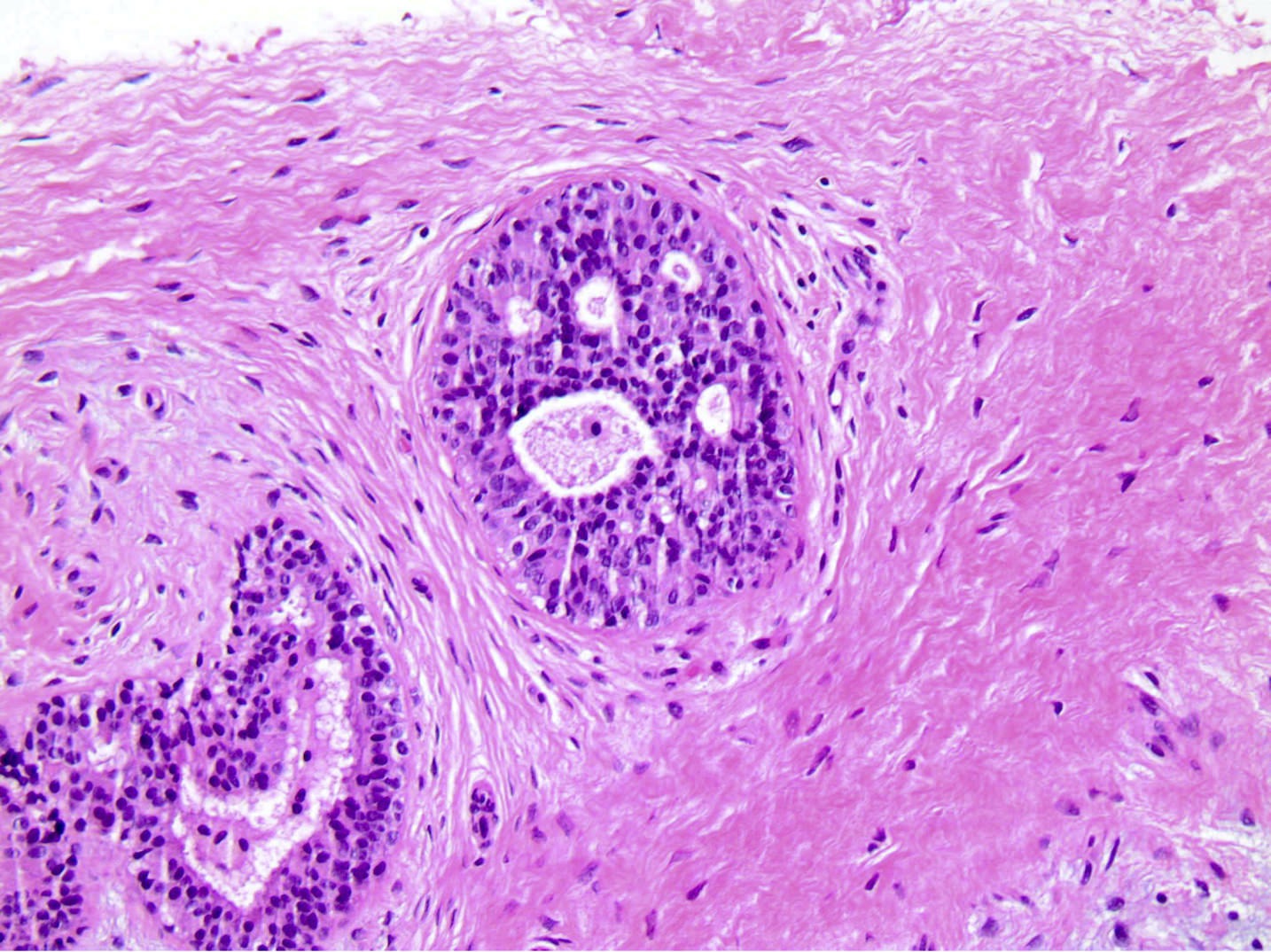
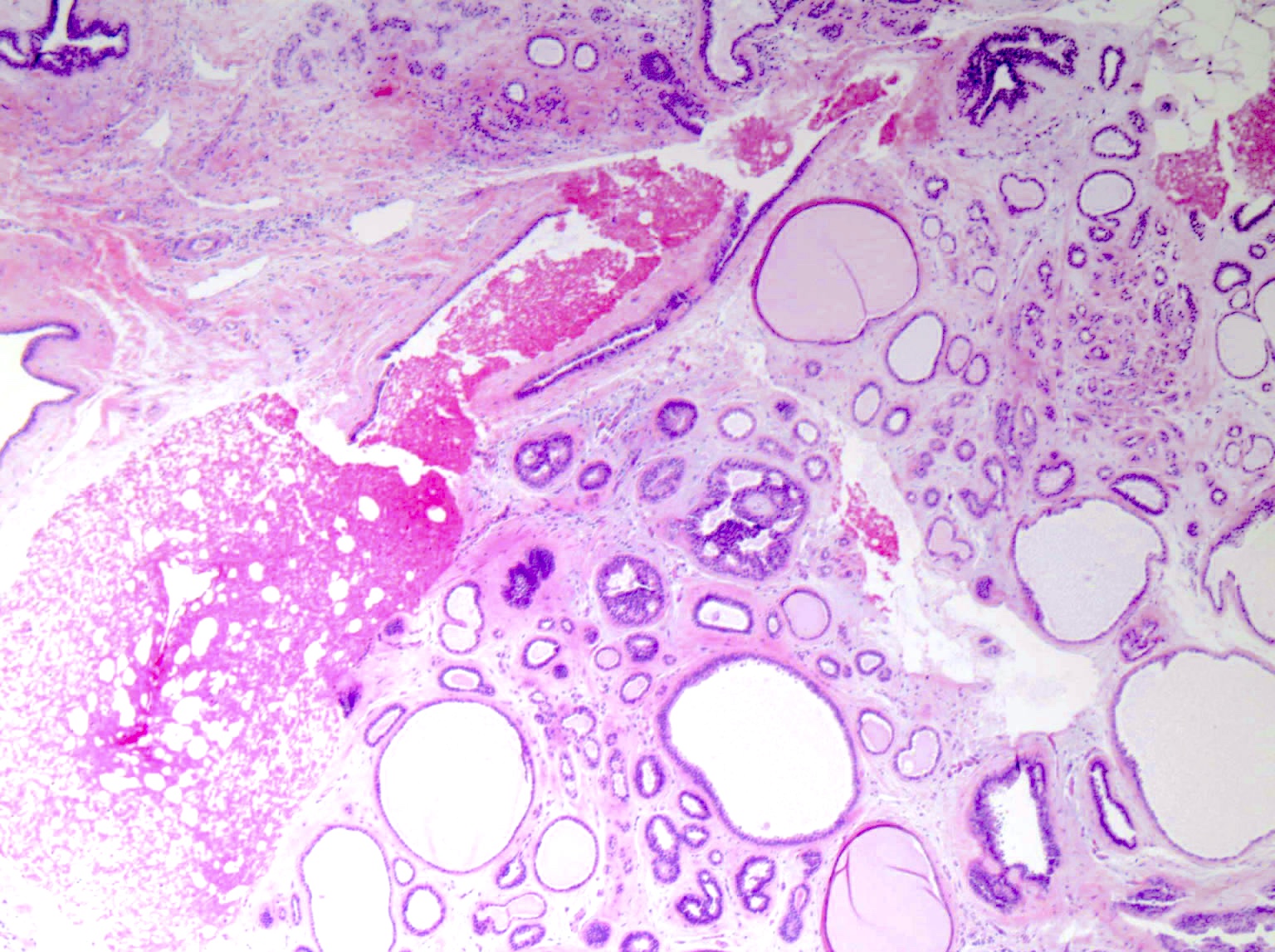
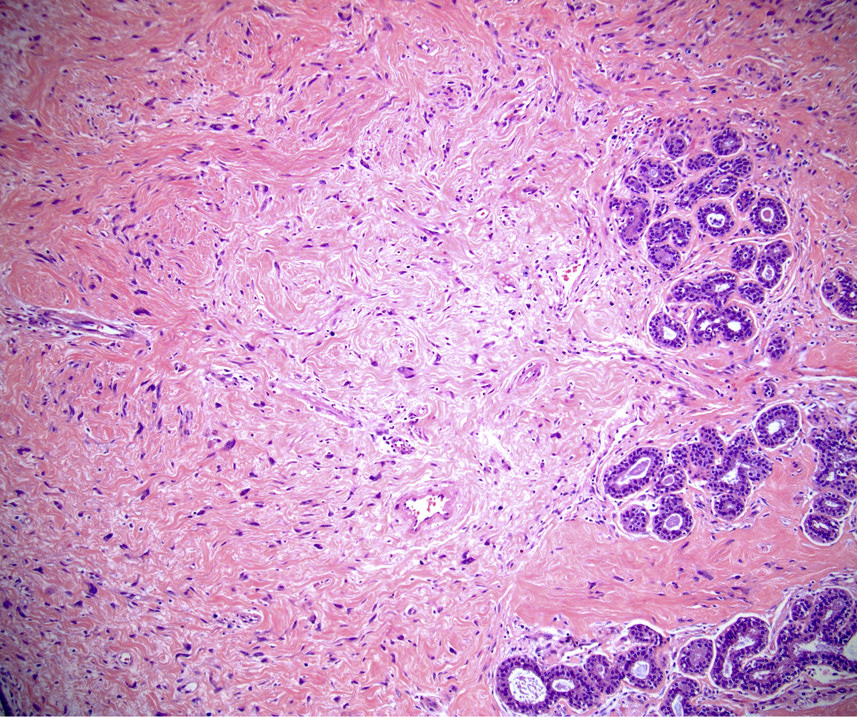
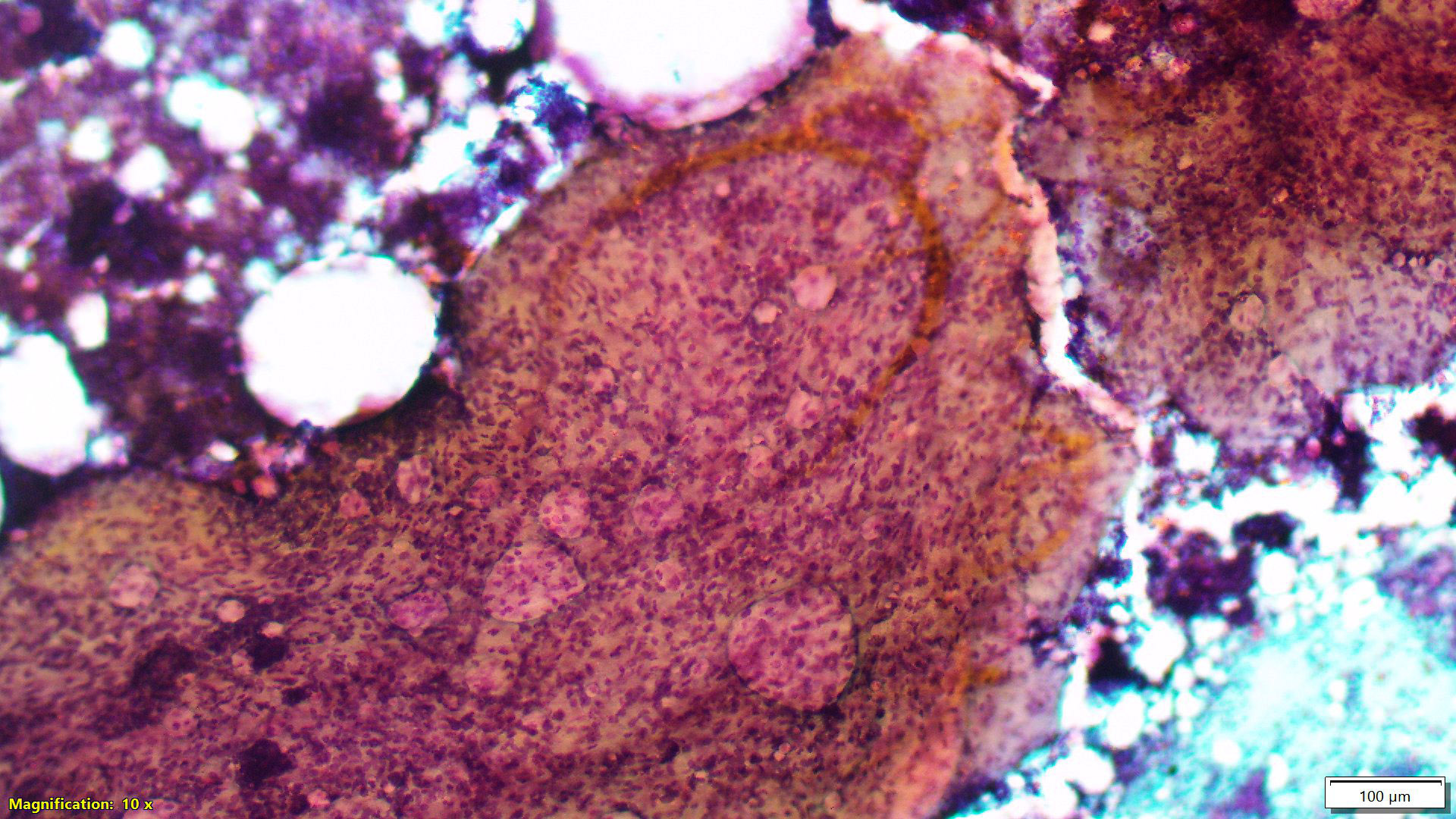
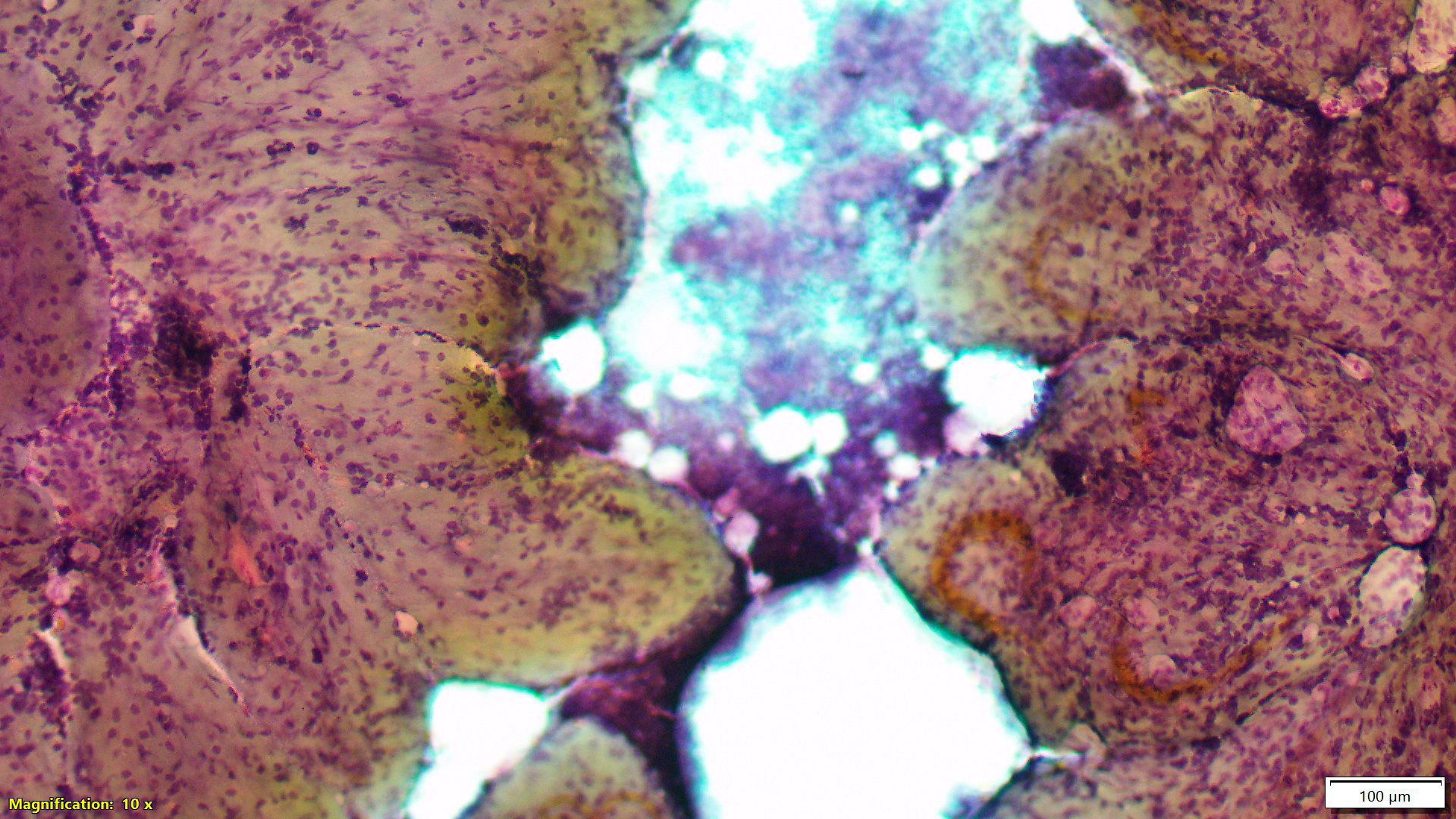
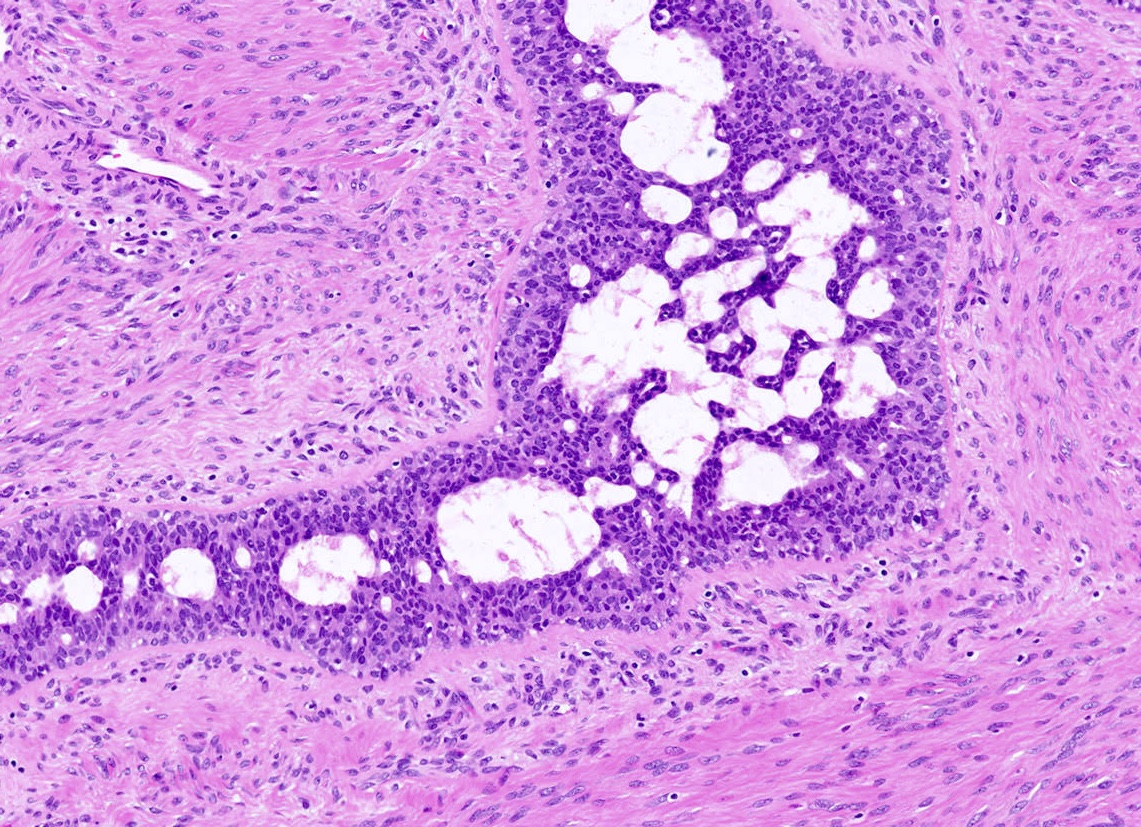
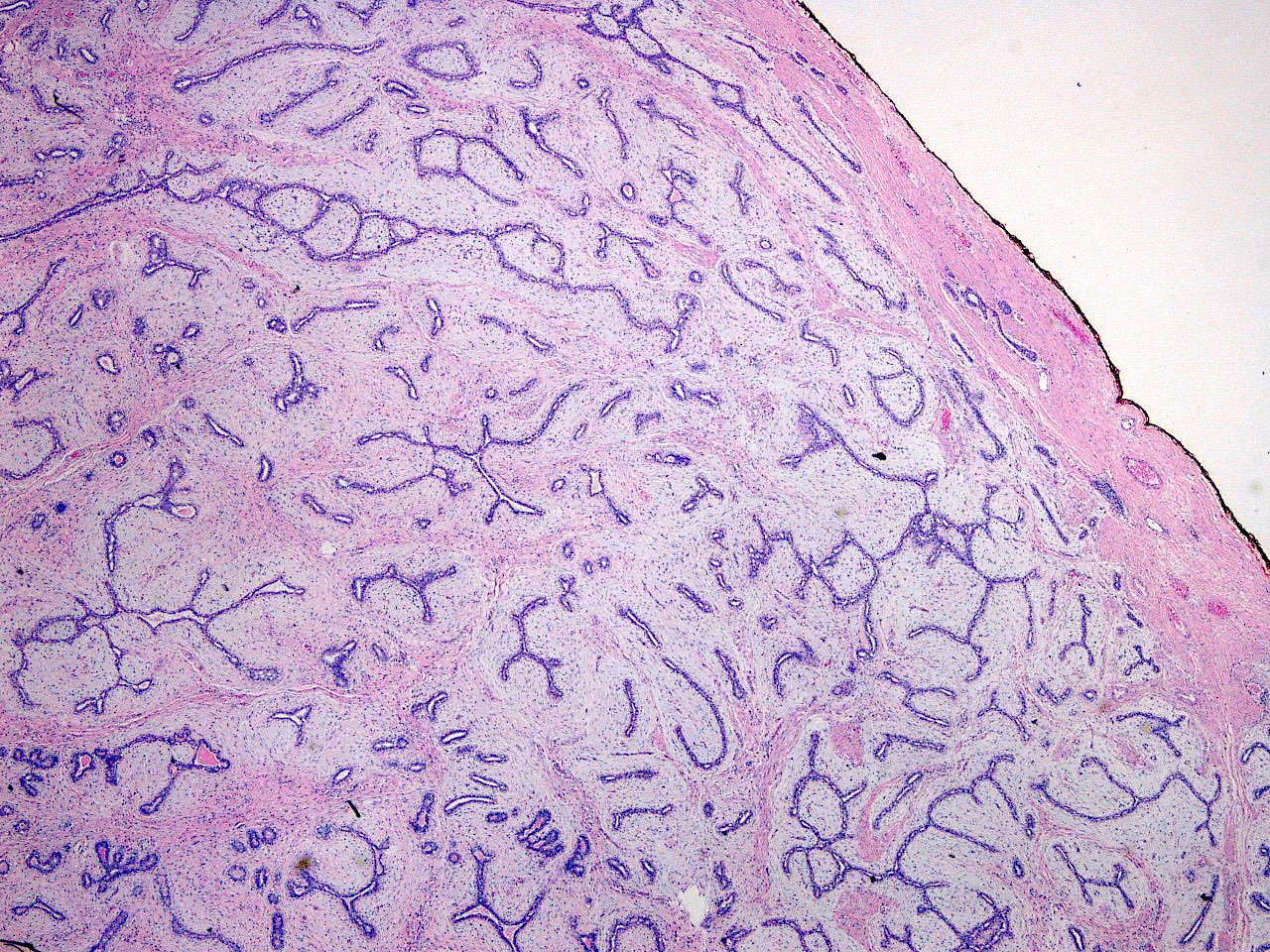
Microscopic (histologic) description
- Well circumscribed, unencapsulated
- Biphasic tumor, proliferation of both glandular and stromal elements
- Glandular component
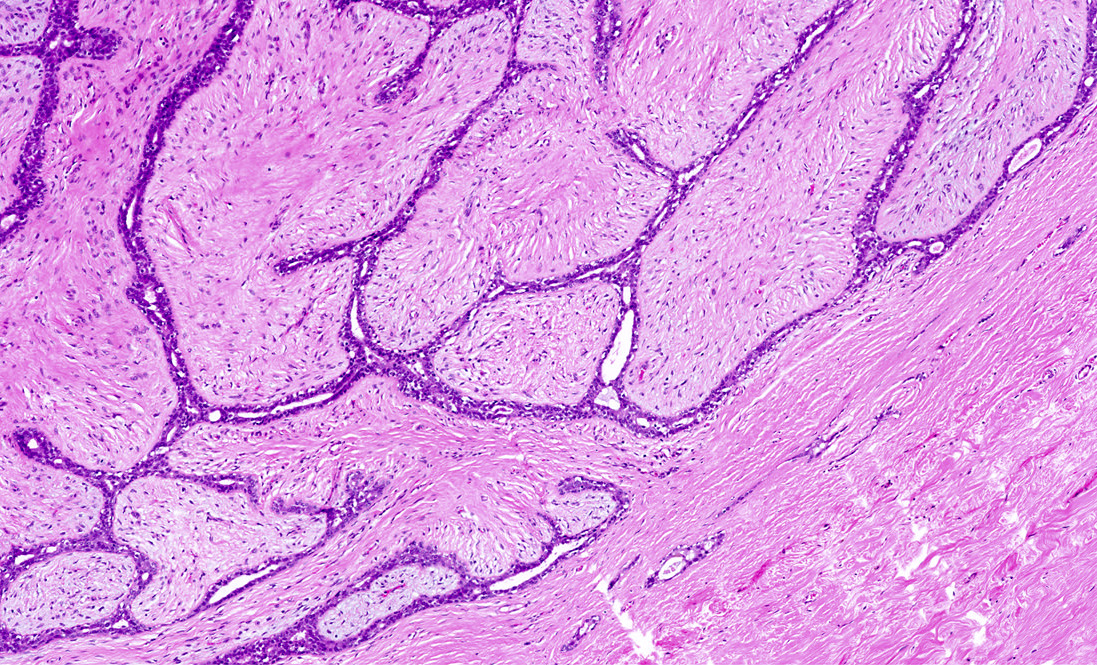
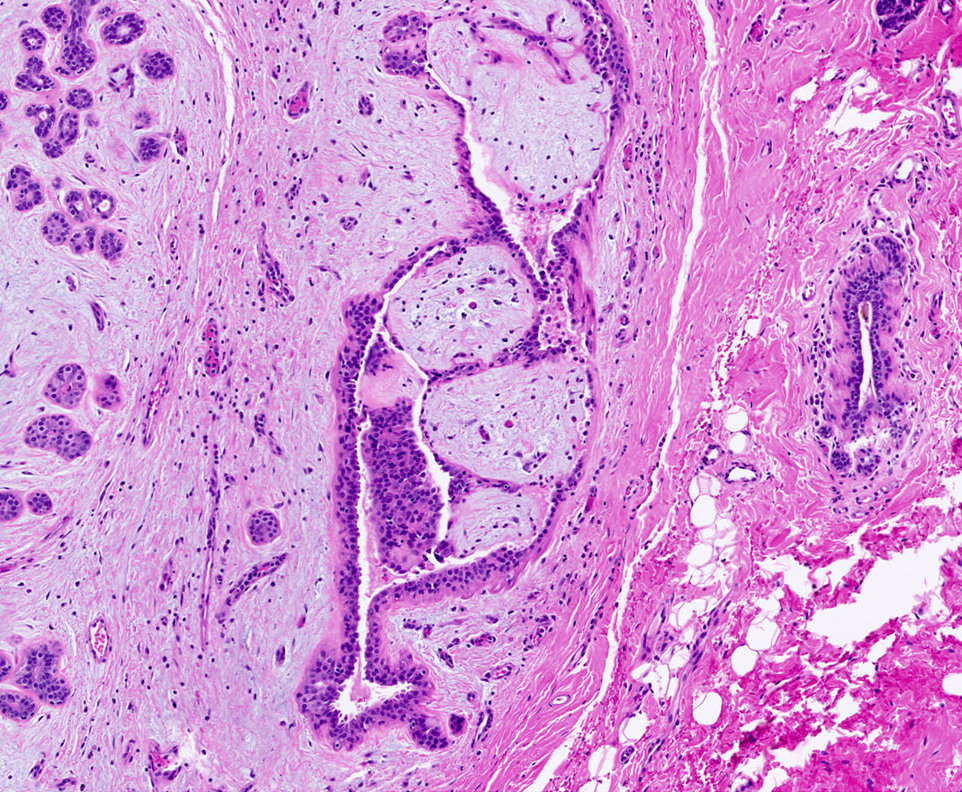
- 2 recognized growth patterns (of no clinical significance, both patterns may occur within a single lesion)
- Intracanalicular: glands are compressed into linear branching structures by proliferating stroma
- Pericanalicular: glands retain open lumens but are separated by expanded stroma
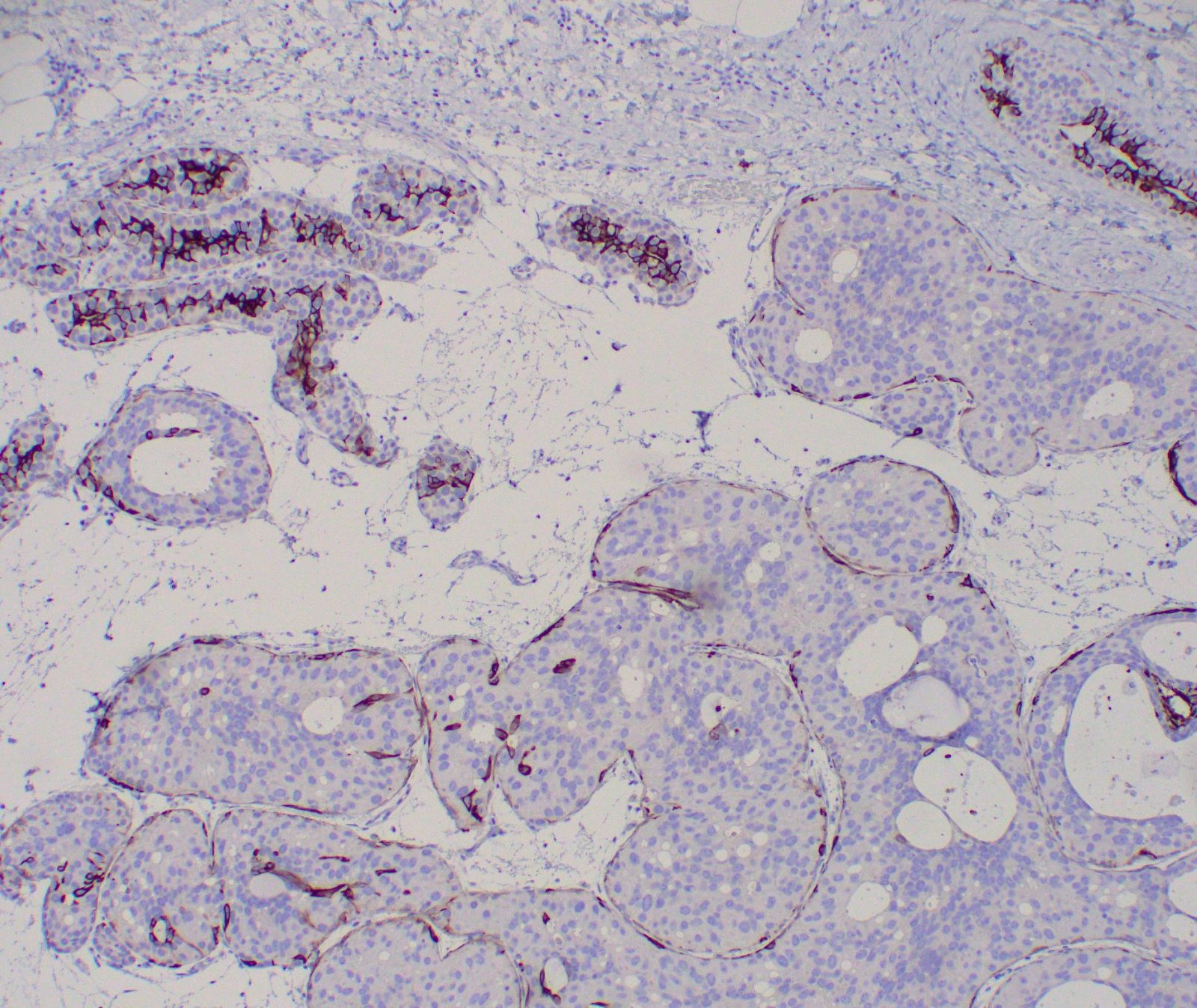
- Glandular elements have intact myoepithelial cell layer
- Often associated with usual type ductal hyperplasia, apocrine metaplasia, cyst formation or squamous metaplasia
- Rare mitotic activity can be observed in the glandular component, has no clinical significance
- 2 recognized growth patterns (of no clinical significance, both patterns may occur within a single lesion)
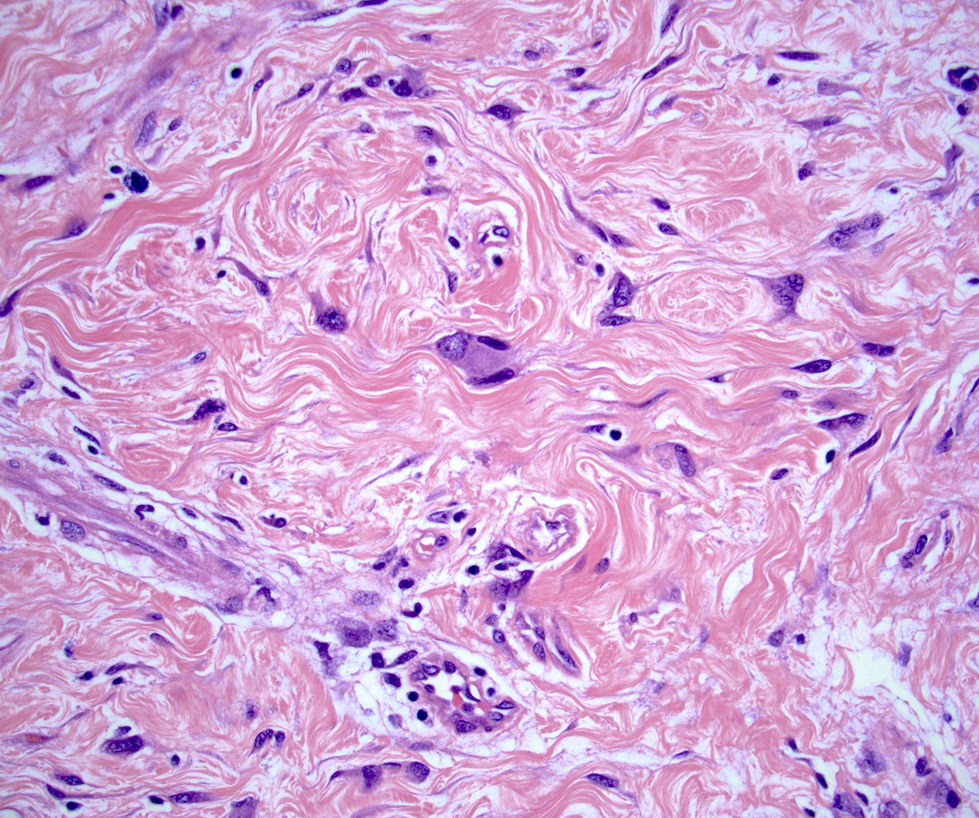
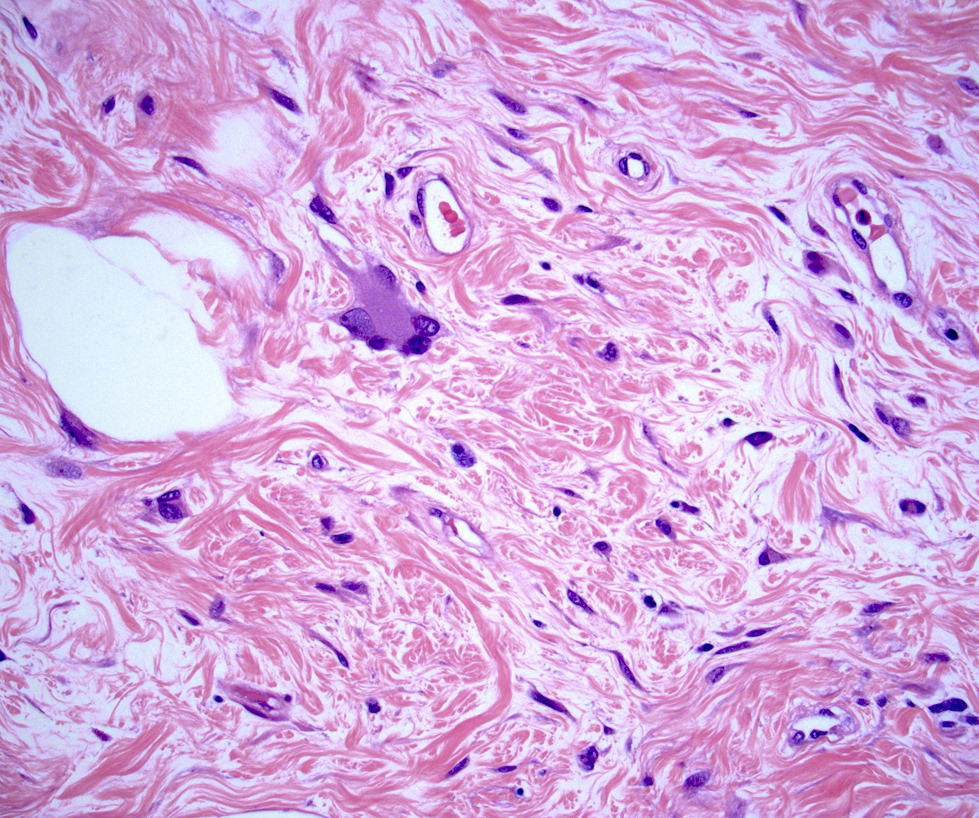
- Stromal component
- Generally uniform cellularity within a given lesion
- Collagen and bland spindle shaped stromal cells with ovoid or elongated nuclei
- Usually no mitotic activity; rare mitotic activity may be present in young or pregnant patients (Breast J 2017;23:182)
- No stromal atypia
- Stroma may show myxoid change or hyalinization
- May show multinucleated giants cells (Am J Surg Pathol 1986;10:823, Arch Pathol Lab Med 1994;118:912)
- Rarely benign heterologous stromal elements (adipose, smooth muscle, osteochondroid metaplasia)
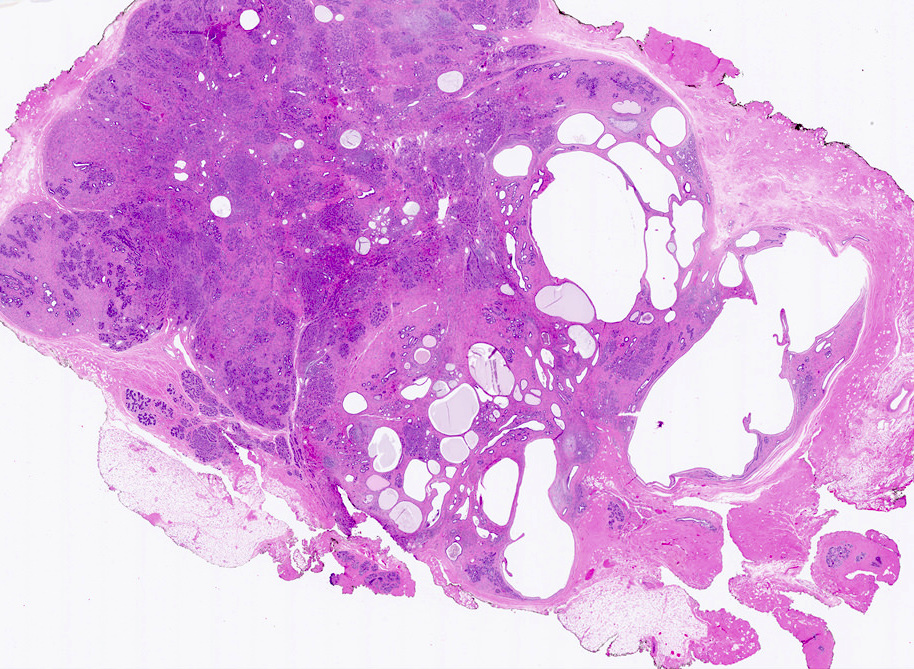
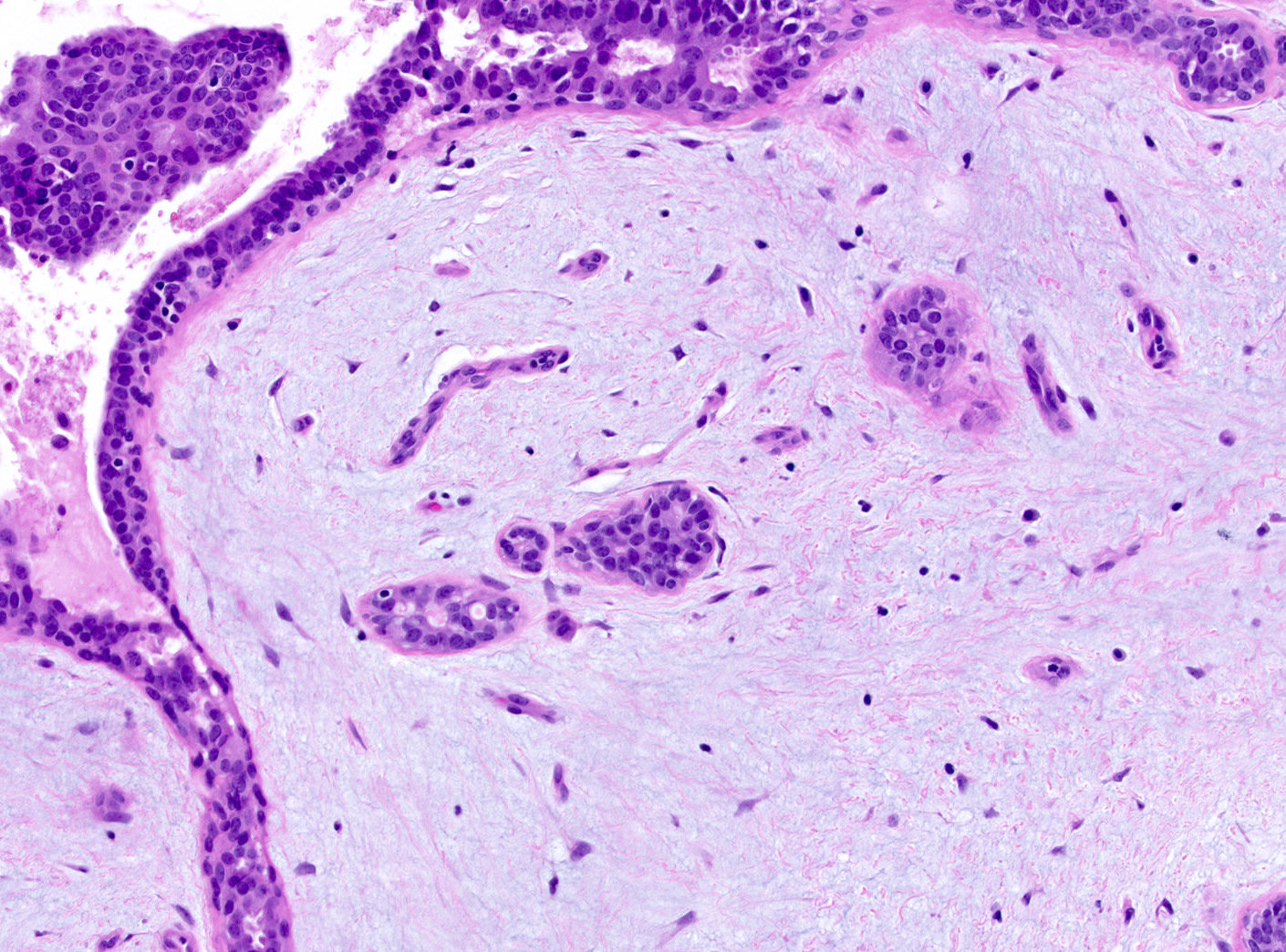
- Fibroadenomas may be involved by mammary neoplasia (e.g. invasive breast carcinoma, ductal carcinoma in situ, lobular carcinoma in situ) and atypical epithelial proliferations (e.g. atypical ductal hyperplasia, atypical lobular hyperplasia) often as a result of spread from an adjacent lesion
- Variants
- Myxoid fibroadenoma
- Similar structure but with prominent myxoid stromal change composed of abundant pale, blue-gray extracellular matrix material
- Complex fibroadenoma
- Cysts > 3 mm, sclerosing adenosis, epithelial microcalcifications or papillary apocrine metaplasia (N Engl J Med 1994;331:10)
- Cellular fibroadenoma
- Diffuse stromal hypercellularity
- Juvenile fibroadenoma
- Increased stromal cellularity
- Increased epithelial hyperplasia with gynecomastoid-like micropapillary projections
- Fascicular stromal arrangement
- Pericanalicular growth pattern
- May show rapid growth and large size (Am J Surg Pathol 1985;9:730)
- Myxoid fibroadenoma
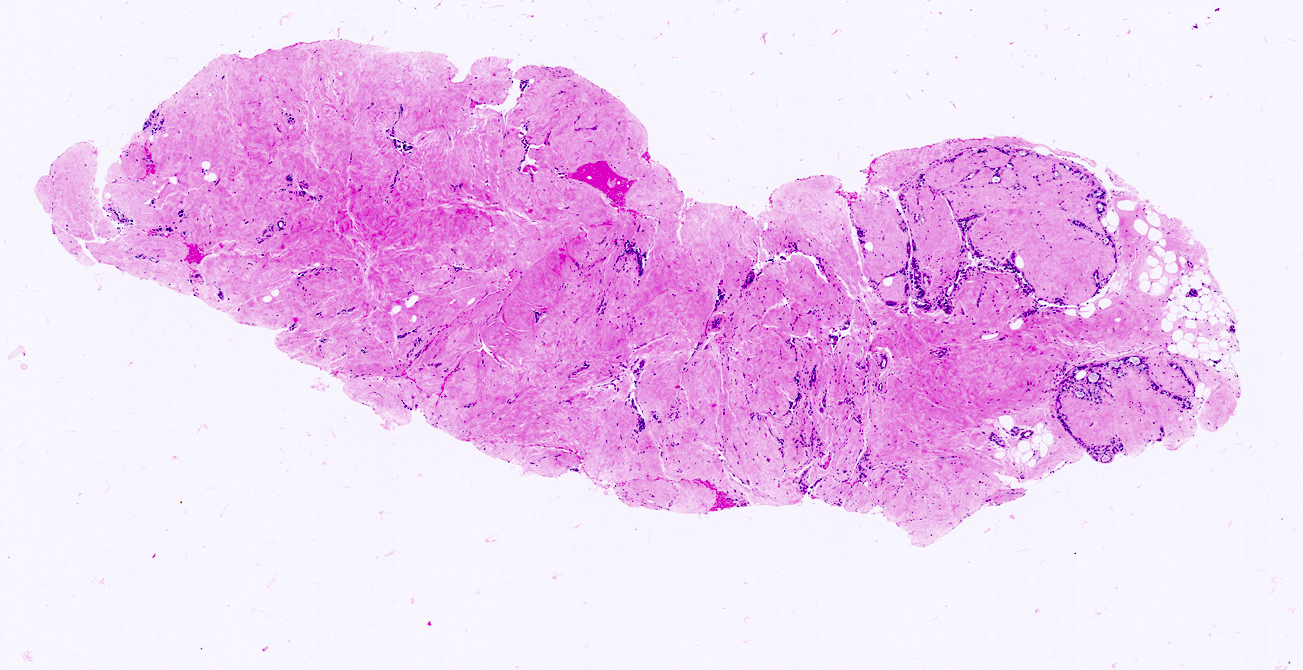
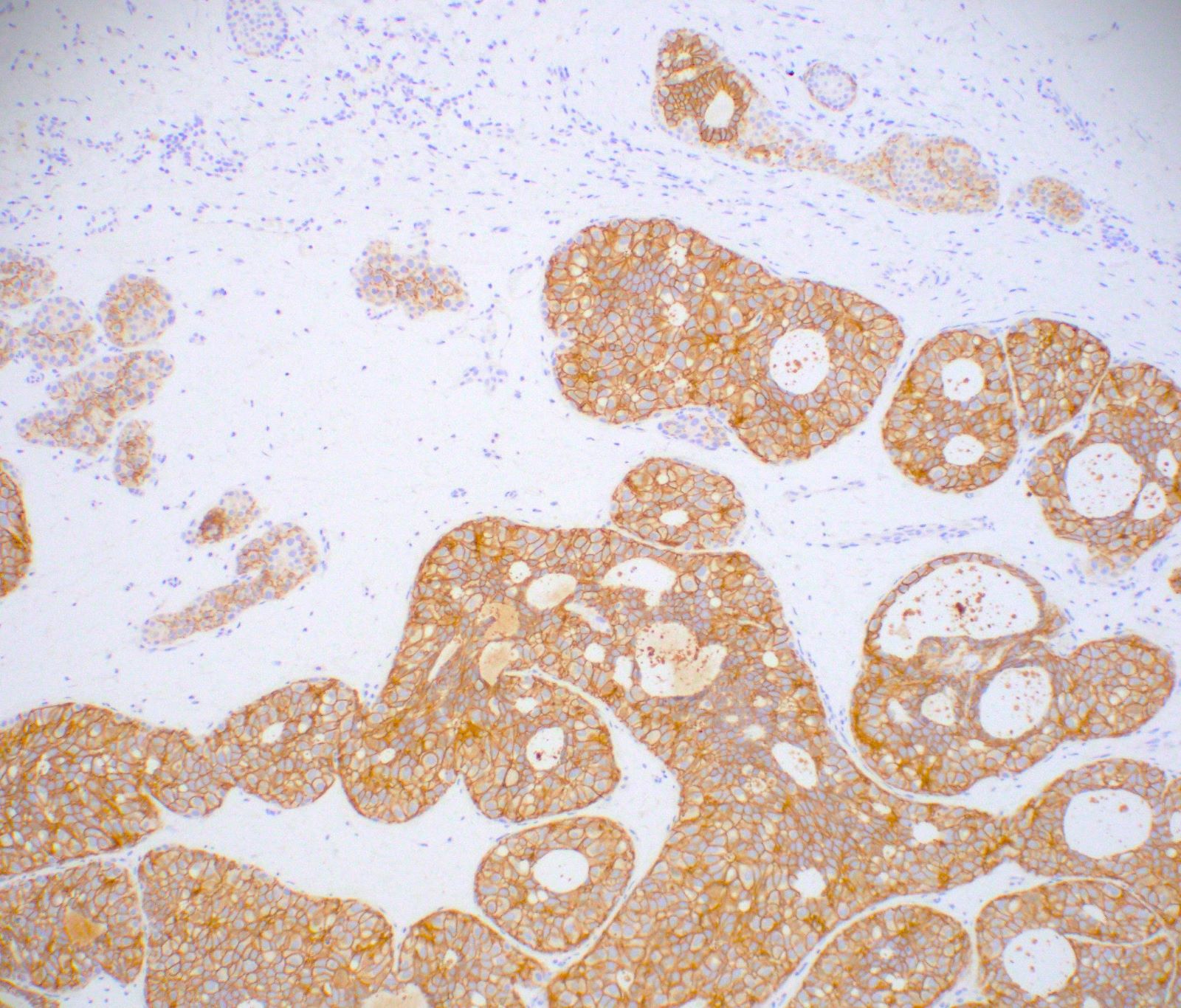
Microscopic (histologic) images
Contributed by Gary Tozbikian, M.D., Debra Zynger, M.D., Azadeh Khayyat, M.D. and Julie M. Jorns, M.D. (Case #533)
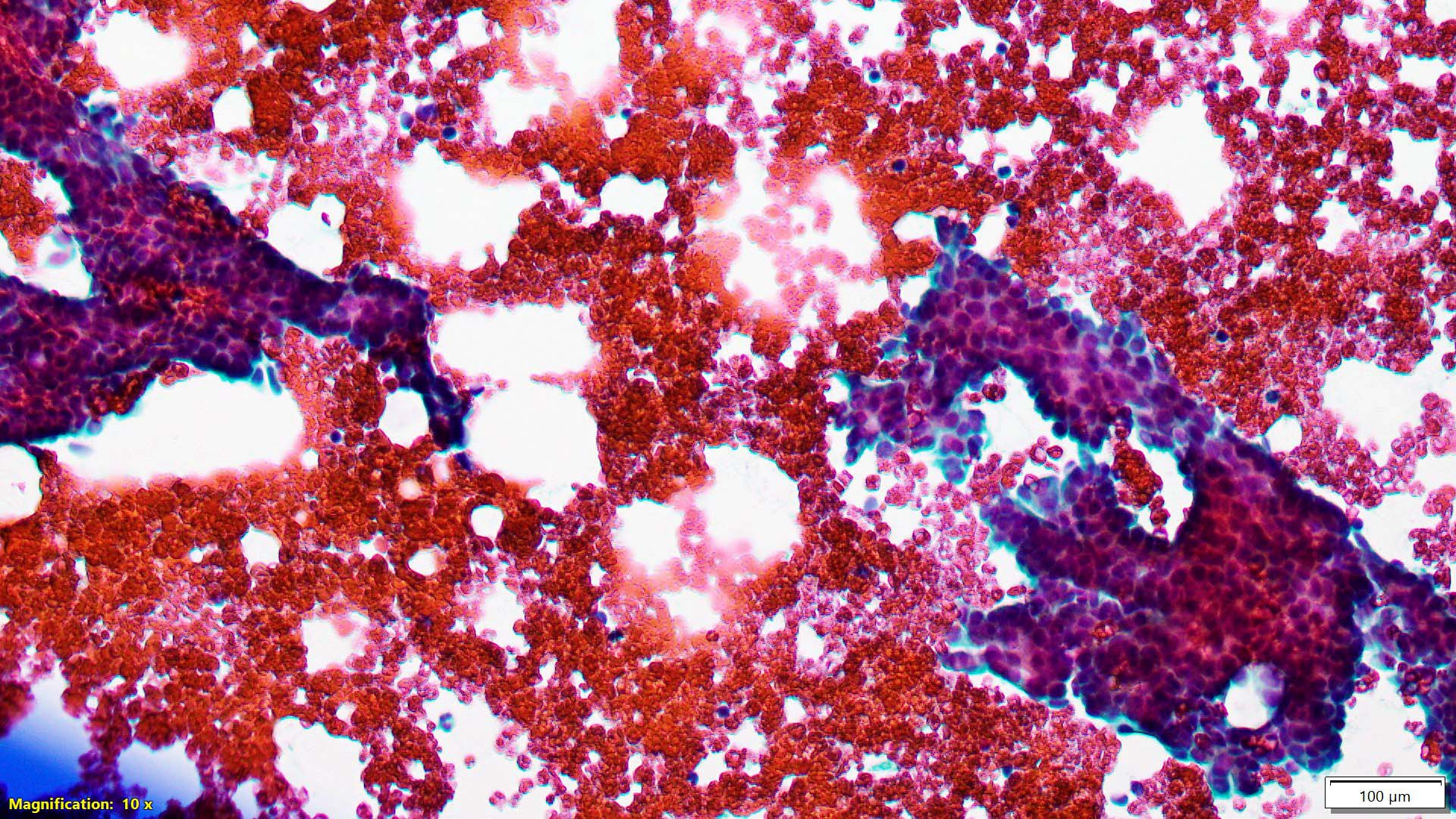
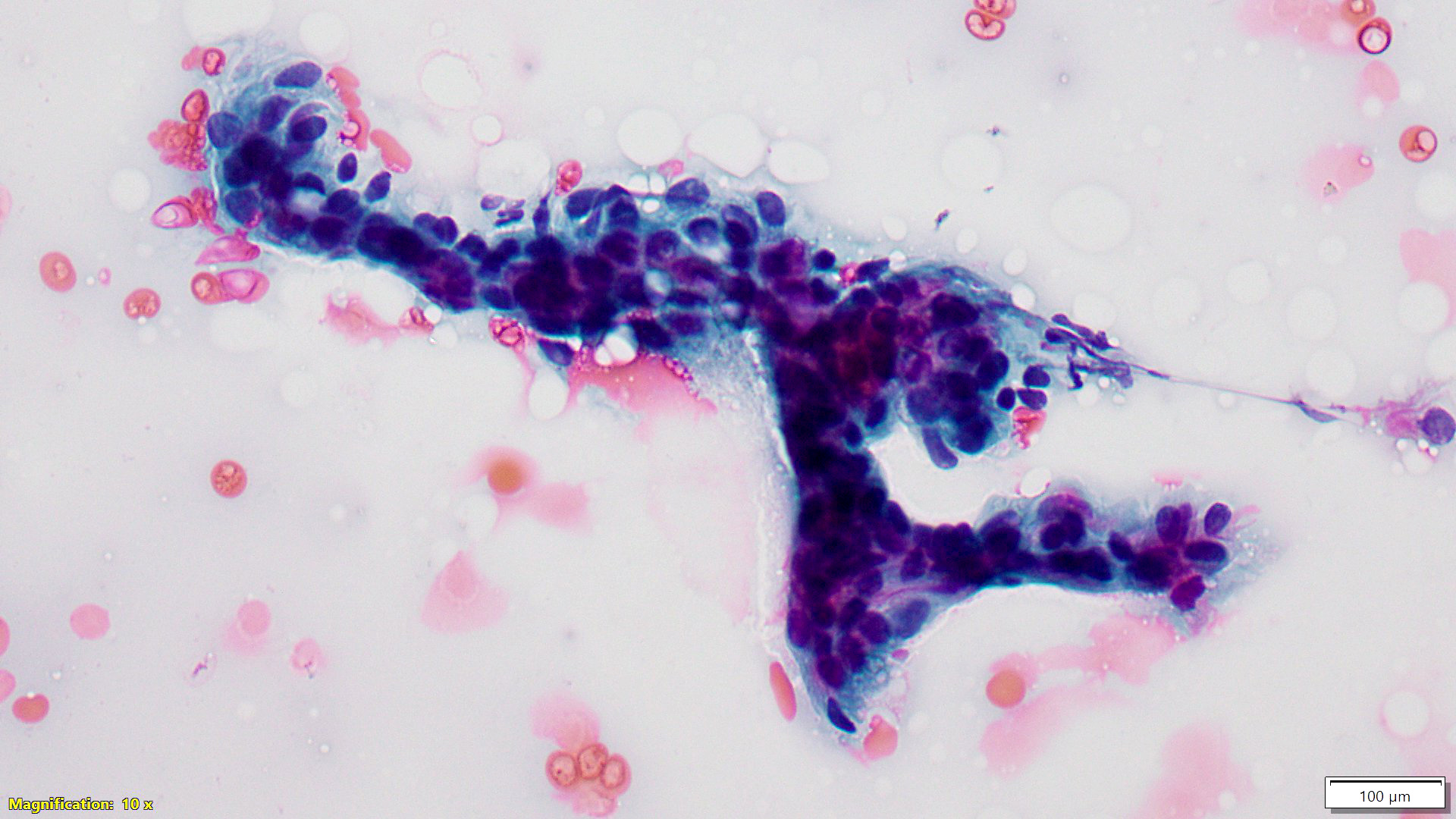
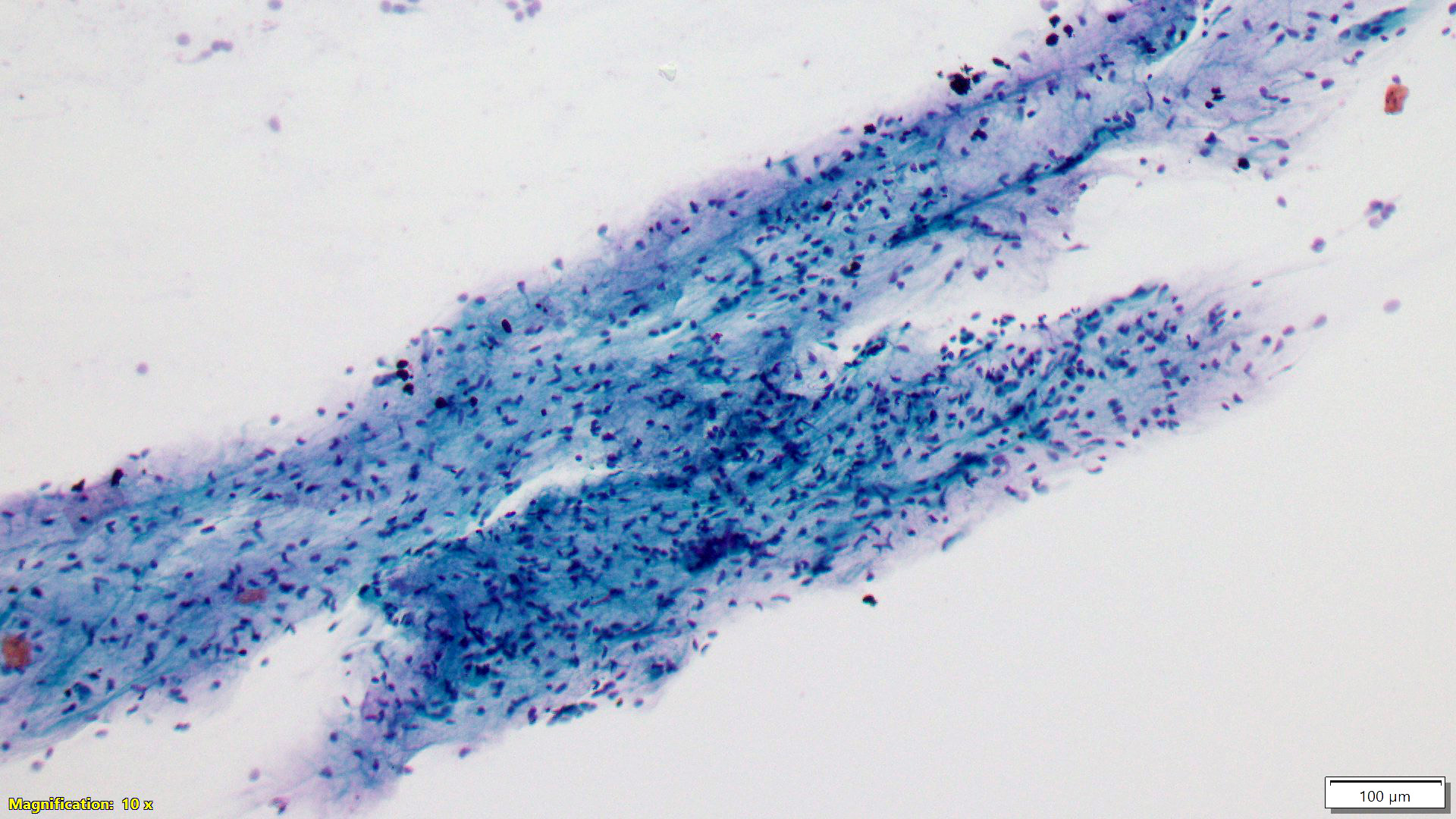
Cytology description
- Usual (adult type) fibroadenoma: biphasic population composed of abundant spindle stromal cells and naked nuclei, epithelium arranged in antler horn clusters or fenestrated honeycomb sheets (Am J Clin Pathol 1988;89:707, Acta Cytol 1991;35:695)
- Myxoid fibroadenoma: high cellularity with stroma and epithelium embedded in myxoid background (Diagn Cytopathol 2001;25:278, Am J Clin Pathol 2003;120:194)
Cytology images
Positive stains
- Stromal cells
- Epithelial cells
Negative stains
- Stromal cells
- Cytokeratins
- Ki67 proliferation index is lower compared with phyllodes tumors but some overlap with benign phyllodes tumor (Am J Clin Pathol 2005;124:342, Histopathology 2010;57:220, Int J Surg Pathol 2008;16:137, Pathol Res Pract 1998;194:97)
Molecular / cytogenetics description
- MED12 exon 2 mutations in usual (adult type) fibroadenoma; likely a driver genetic event (NPJ Breast Cancer 2016;2:16035, Nat Genet 2014;46:877, Histopathology 2015;67:719)
- Myxoid fibroadenomas lack MED12 mutations (Histopathology 2017;71:626)
- RARA mutations (Nat Genet 2015;47:1341, J Pathol 2016;238:508)
- Cellular variant of fibroadenoma shows higher rates of mutation in PIK3CA and MAP3KI (Mod Pathol 2021;34:1320)
- Fewer mutations (e.g. MED12, TERT promoter, RB1, EGFR) compared with benign phyllodes tumor (Mod Pathol 2021;34:1320)
Videos
Fibroadenoma
Sample pathology report
- Breast, right, 2:00 zone 2, ultrasound guided core biopsy:
- Fibroadenoma
Differential diagnosis
- Phyllodes tumor:
- Well developed leaf-like architecture, with accompanied increased stromal cellularity
- Prominent mitotic activity ≥ 3/10 high power fields or the finding of 3 or more characteristic histologic features (stromal overgrowth, fat infiltration, stromal fragmentation, subepithelial stromal condensation, stromal nuclear pleomorphism) is predictive of phyllodes tumor (versus fibroadenoma) in core biopsy specimens (Am J Clin Pathol 2014;142:362)
- Hamartoma of breast:
- Integral adipose component
- Disordered but morphologically normal appearing ducts and lobules
- Tubular adenoma:
- Prominent pericanalicular adenosis-like epithelial proliferation with little intervening stroma
- Fibroadenomatoid changes (sclerosing lobular hyperplasia, fibroadenomatoid mastopathy):
- Generally does not form a clinically dominant mass
- Individual lobule or few groups of lobules with collagenized interlobular stroma and loss of interlobular stromal mucopolysaccharides (Hum Pathol 1984;15:336, Pathology 1987;19:393, Malays J Pathol 1991;13:101)
- Myxoma:
- Lacks glandular elements (versus myxoid fibroadenoma)
Board review style question #1
A 13 year old girl presents with a firm, palpable 3.5 cm breast mass. She undergoes an ultrasound guided biopsy and subsequent local excision showing a fibroepithelial lesion with circumscribed borders, uniformly increased stromal cellularity, glandular proliferation with pericanalicular growth pattern and prominent gynecomastoid-like usual type ductal hyperplasia. Rare mitotic activity (< 1/10 high power fields) is identified. Stromal cytologic atypia is not present. What is the correct diagnosis?
- Fibroadenoma
- Juvenile fibroadenoma
- Myxoid fibroadenoma
- Phyllodes tumor (benign)
- Phyllodes tumor (borderline)
Board review style answer #1
B. Juvenile fibroadenoma. The clinical presentation and histologic features are characteristic of a juvenile fibroadenoma.
Comment Here
Reference: Fibroadenoma
Comment Here
Reference: Fibroadenoma
Board review style question #2
A 25 year old woman presents with a 3 cm breast mass. An ultrasound guided biopsy shows a fibroepithelial lesion. Which histologic feature is consistent with a diagnosis of fibroadenoma?
- Circumscribed borders
- Marked stromal cytologic atypia
- Stromal condensation around glandular structures
- Stromal mitotic activity (7 - 8/10 high power fields)
- Stromal overgrowth
Board review style answer #2
A. Circumscribed borders. Fibroadenomas generally show noninfiltrative, circumscribed borders. The histologic features in answer choices B, C, D and E are observed in phyllodes tumors.
Comment Here
Reference: Fibroadenoma
Comment Here
Reference: Fibroadenoma
Board review style question #3
Board review style answer #3
B. Most common benign tumor arising in the breast. This is a fibroadenoma.
Comment Here
Reference: Fibroadenoma
Comment Here
Reference: Fibroadenoma
Board review style question #4
Fibroadenomas harbor epithelial atypia or malignancy at approximately what rate?
- 0.2%
- 2%
- 20%
- 50%
Board review style answer #4
B. 2%. The classification and behavior of fibroepithelial tumors of the breast including fibroadenoma and phyllodes tumor is driven by the stroma. However, epithelial changes may be seen and are thought to occur by chance or are driven by unrelated risk factor(s). Thus, epithelial atypia and malignancy is uncommon, with a recent large study by Krishnamurthy et al. showing a rate of ~2% (Breast Dis 2019;38:97). See Case #533 for more information.
Comment Here
Reference: Fibroadenoma
Comment Here
Reference: Fibroadenoma