Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Abels E, He J. Fat necrosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastfatnecrosis.html. Accessed March 30th, 2025.
Definition / general
- Nonneoplastic inflammatory breast lesion characterized by necrotic adipose tissue with foamy histiocytes, chronic inflammatory cells and multinucleated giant cells
Essential features
- Nonneoplastic inflammatory reaction that is commonly secondary to adipose tissue injury
- May simulate carcinoma both clinically and radiologically
- There are different radiographical and histological stages which vary based on time from inciting event
Epidemiology
- 0.6% of breast excisions
- Age range: 37 - 68 years (mean age: ~50 years) (Breast 2006;15:313)
- Most described in perimenopausal women after trauma, surgery or biopsy
Sites
- Any part of the breast may be affected
- After trauma, typically occurs at site of injury and is commonly detected in periareolar and subareolar region; it is often superficial in location since these sites are most vulnerable to trauma (Lipids Health Dis 2019;18:158)
- In patients with no history of trauma, lesion is most often seen in upper outer quadrant of breast
Pathophysiology
- Many cases are due to previous biopsy procedures (such as fine needle aspiration or needle core biopsy), surgical procedure or radiation therapy (Plast Reconstr Surg 2014;134:1202)
- May result from incidental trauma
Etiology
- Trauma:
- Blunt trauma to breast (e.g., seat belt injury after motor vehicle accident) (J Plast Reconstr Aesthet Surg 2015;68:382)
- Iatrogenic injury:
- Fine needle aspiration, core needle biopsy, mastectomy or lumpectomy of breast, autologous fat injection, reduction mammoplasty, breast implants (Breast Cancer 2019;26:125)
- Radiation therapy:
- Due to postradiation vascular damage with subsequent ischemia, including external beam, MammoSite, iridium implantation, intraoperative radiation
- Other rare causes:
- Anticoagulant treatment (warfarin [Coumadin]), polyarteritis nodosa, Weber-Christian disease, granulomatous angiopanniculitis, lupus mastitis, injection of methylene blue dye
- Unknown cause in ~50% of patients
Clinical features
- Typically present with a painless superficial solitary mass which may mimic cancer, especially in patients who have undergone breast conserving surgery and radiation therapy (Lipids Health Dis 2019;18:139)
- Firm and relatively circumscribed on palpation, may span 2 cm in diameter (average)
- Occasionally can be associated with skin changes: bruising and tenderness, tethering or dimpling of the overlying skin if the lesion is superficially located, nipple retraction
Diagnosis
- Palpation of breast mass, radiographical findings and correlation with clinical history of trauma or breast procedures (Lipids Health Dis 2019;18:139)
- Core needle biopsy is frequently performed if there are masses or calcifications
- Tissue diagnosis needs to correlate with imaging findings and must be used to distinguish from fat necrosis next to another lesion
Radiology description
- Many cases can be identified by radiographic appearance (e.g., forming mammographic masses or mammographic calcifications)
- Manifestations on mammography, ultrasonography and MRI depend upon its stage of evolution; features can be variable and may be indistinguishable from carcinoma (Radiol Res Pract 2015:613139)
- Time from inciting event may be useful in correlating radiographic findings (Br J Radiol 2018;91:20180213)
- Mammography usually reveals ill defined irregular mass with or without calcifications or focal asymmetries around central area of necrotic adipose tissue
- May contain punctate, irregular or coarse pleomorphic calcifications
- Sonography demonstrates a discrete mass which may be well circumscribed or ill defined
- Sonographic appearance is variable and is usually associated with distortion of the parenchymal architecture
- Less frequently, the lesion may appear as a lipid (oil) cyst which consists of a circumscribed, round or oval radiolucent oil filled cyst that is partly calcified
- Oil cysts typically show posterior acoustic shadowing by sonography
- Eggshell calcifications are late findings with characteristic appearance around central area of necrotic adipose tissue
- MRI demonstrates a wide spectrum of findings
- Necrotic fat usually shows low signal intensity on T1 weighted MRI
- Fibrosis may be seen as architectural distortion
Radiology images
Prognostic factors
- Should resolve or regress over time (Br J Radiol 2018;91:20180213)
- Degenerated fat may persist for years within a fibrotic scar
Case reports
- 40 year old woman with breast pain for 3 months (Pan Afr Med J 2016;25:235)
- 63 year old woman was found to have a left breast mass after quadrantectomy and radiation (Magn Reson Imaging 2004;22:285)
- 66 year old woman with palpable breast masses one month after a car accident (Eur J Ultrasound 2000;11:213)
- 71 year old woman with painful bilateral breast masses and overlying skin changes (Dermatol Online J 2018;24:13030)
- Case series of fat necrosis after breast conserving oncoplastic surgery (Breast Cancer 2019;26:125)
Treatment
- Biopsy the lesion to confirm the diagnosis if clinical / radiological features can not distinguish from cancer
- Follow up with imaging and clinical examination to detect occult carcinoma that might be masked by coexisting fat necrosis
- Surgical excision is usually not necessary after the diagnosis has been established, only for painful or aesthetically undesirable lesions (StatPearls: Breast Fat Necrosis [Accessed 1 May 2020])
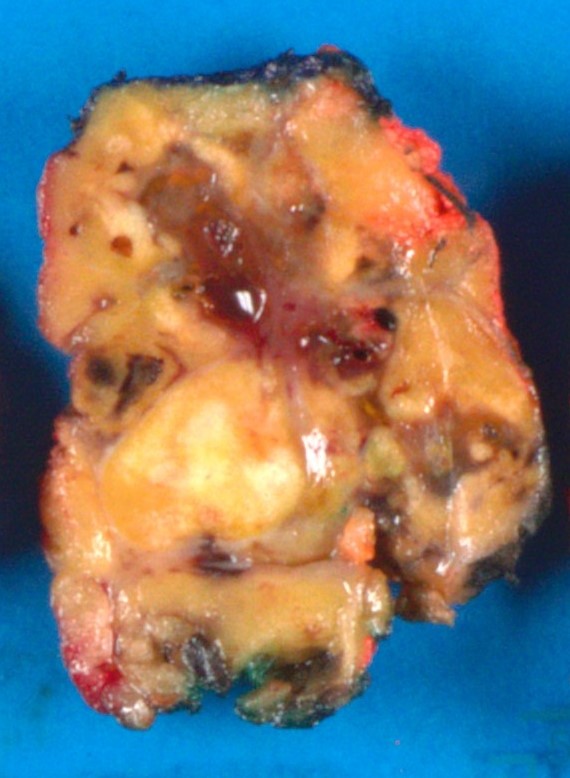
Gross description
- Varies based on time from injury
- Early lesion has the appearance of hemorrhage in indurated fat (Radiol Res Pract 2015:613139)
- Cut surface of the lesion has a variegated, yellow-gray appearance with focally reddish color
- After several weeks, it appears as a firm yellow-gray nodule / mass with a demarcated border
- Mass may retract surrounding parenchyma, cystic degeneration may develop in the center, showing a cavity containing oily fluid secondary to necrotic fat with calcification in the cystic walls
- At a later stage, the lesion may show a dense scar that may appear like a mass
- Early lesion has the appearance of hemorrhage in indurated fat (Radiol Res Pract 2015:613139)
Frozen section description
- Frozen sections are difficult to obtain due to high fat content of specimen
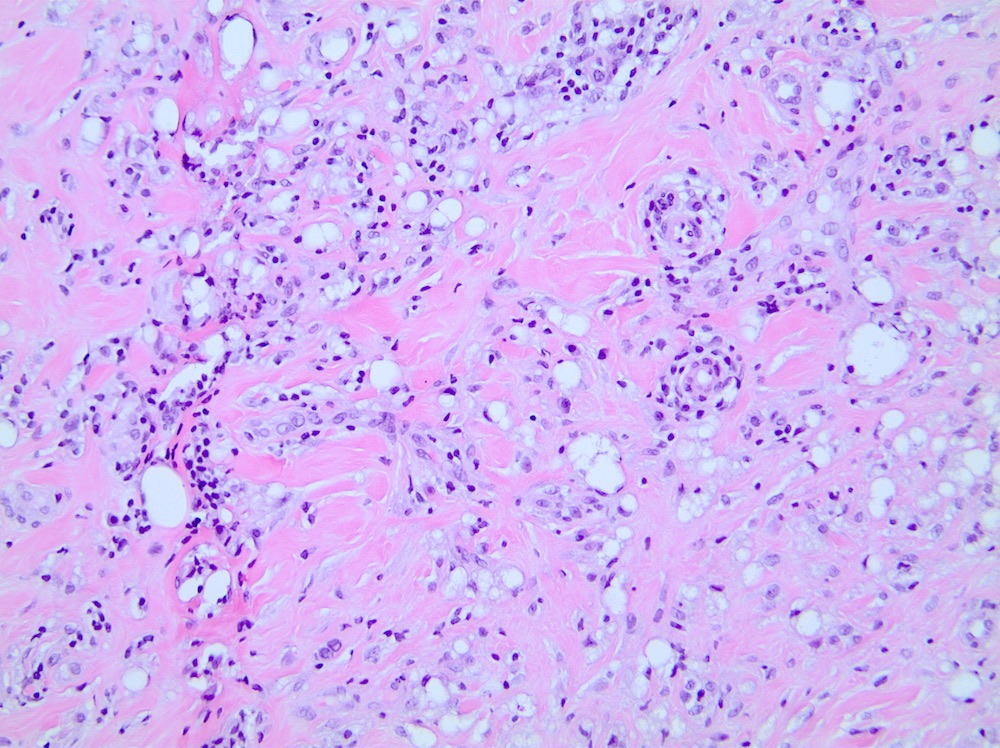
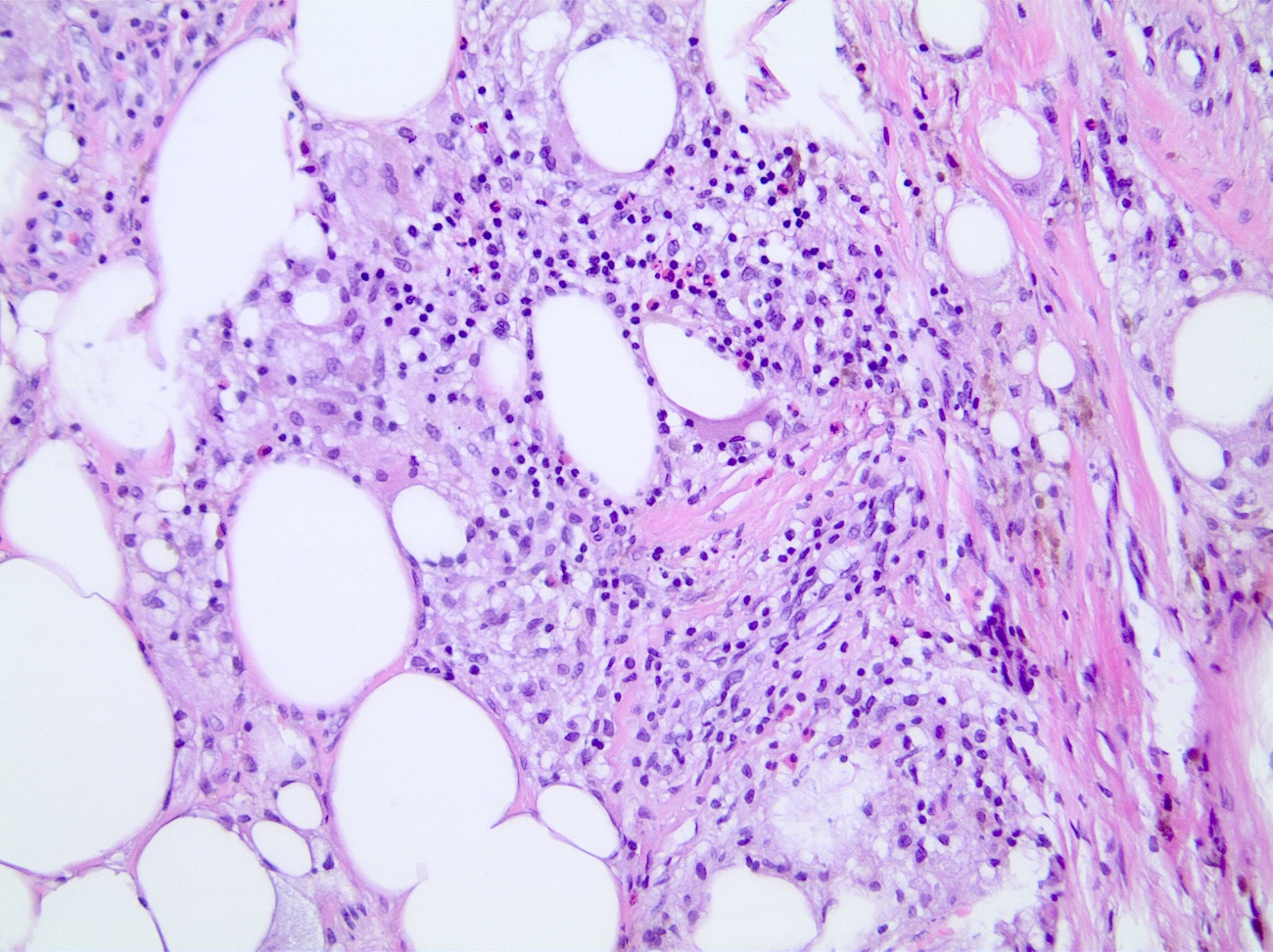
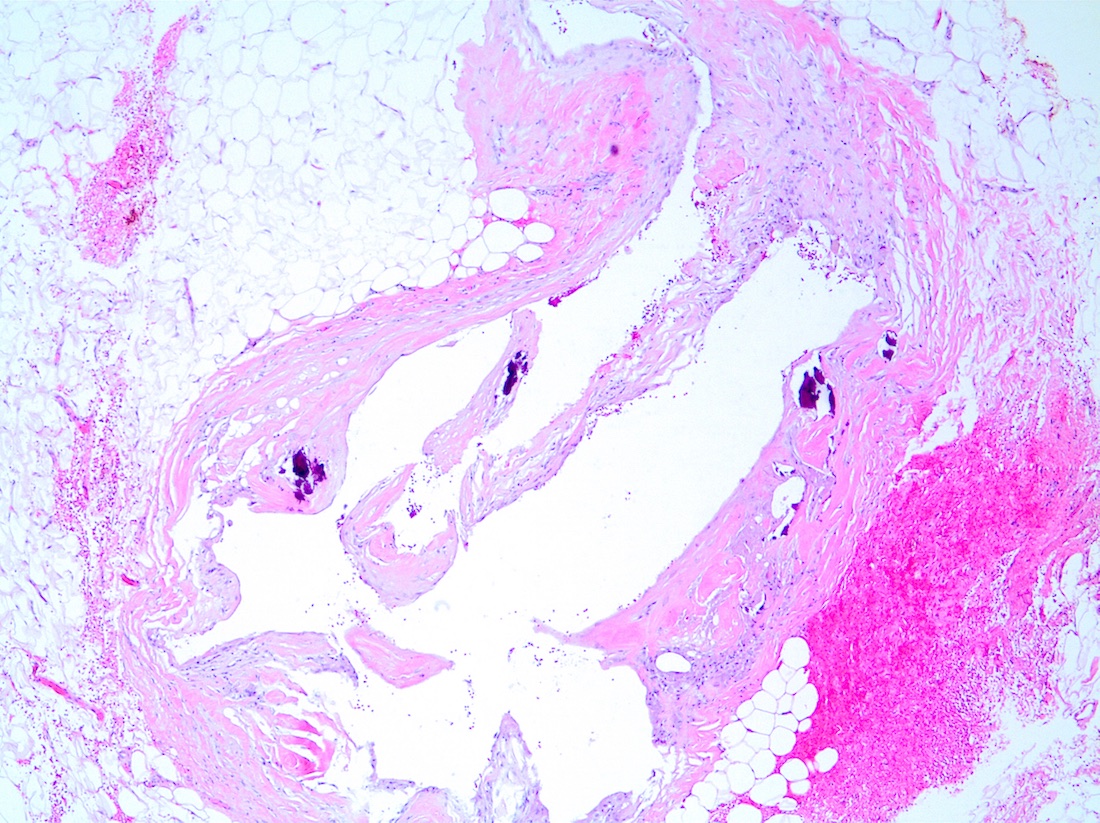
Microscopic (histologic) description
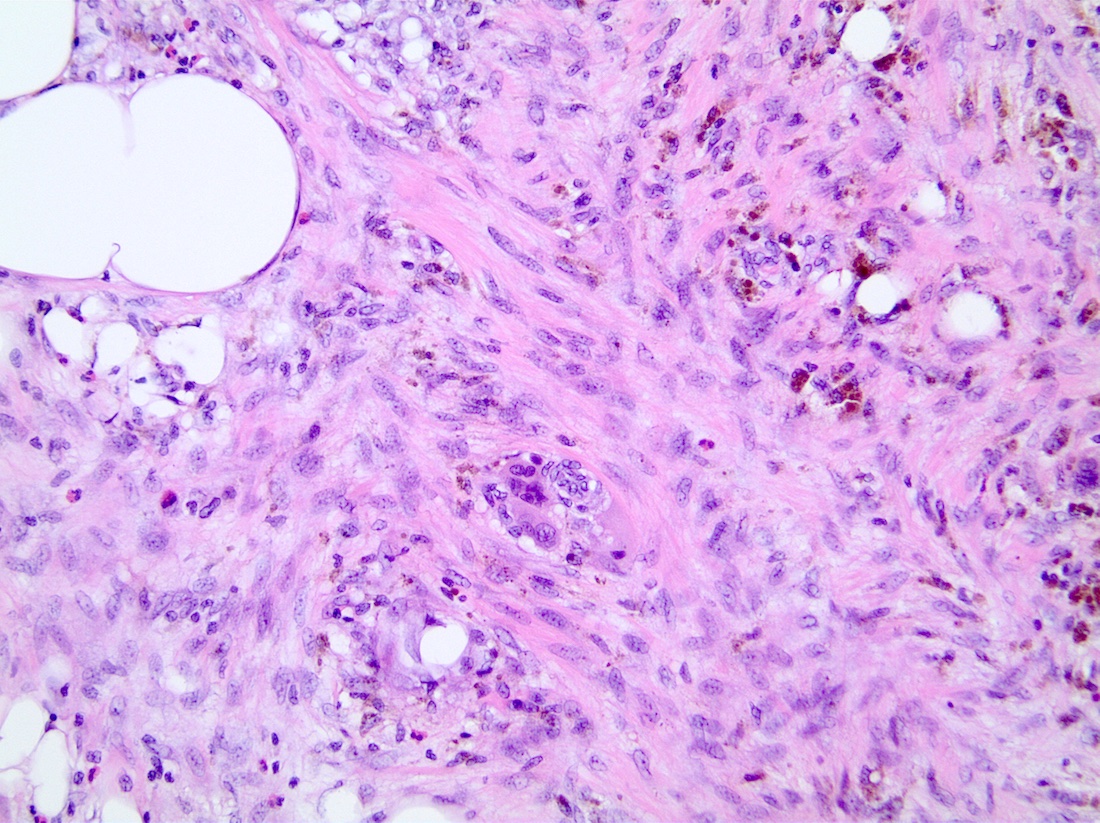
- Histiocytes are relatively uniform in size with round nuclei, fine intracytoplasmic vacuoles and no indentation of the nucleus
- Varies based on time from injury
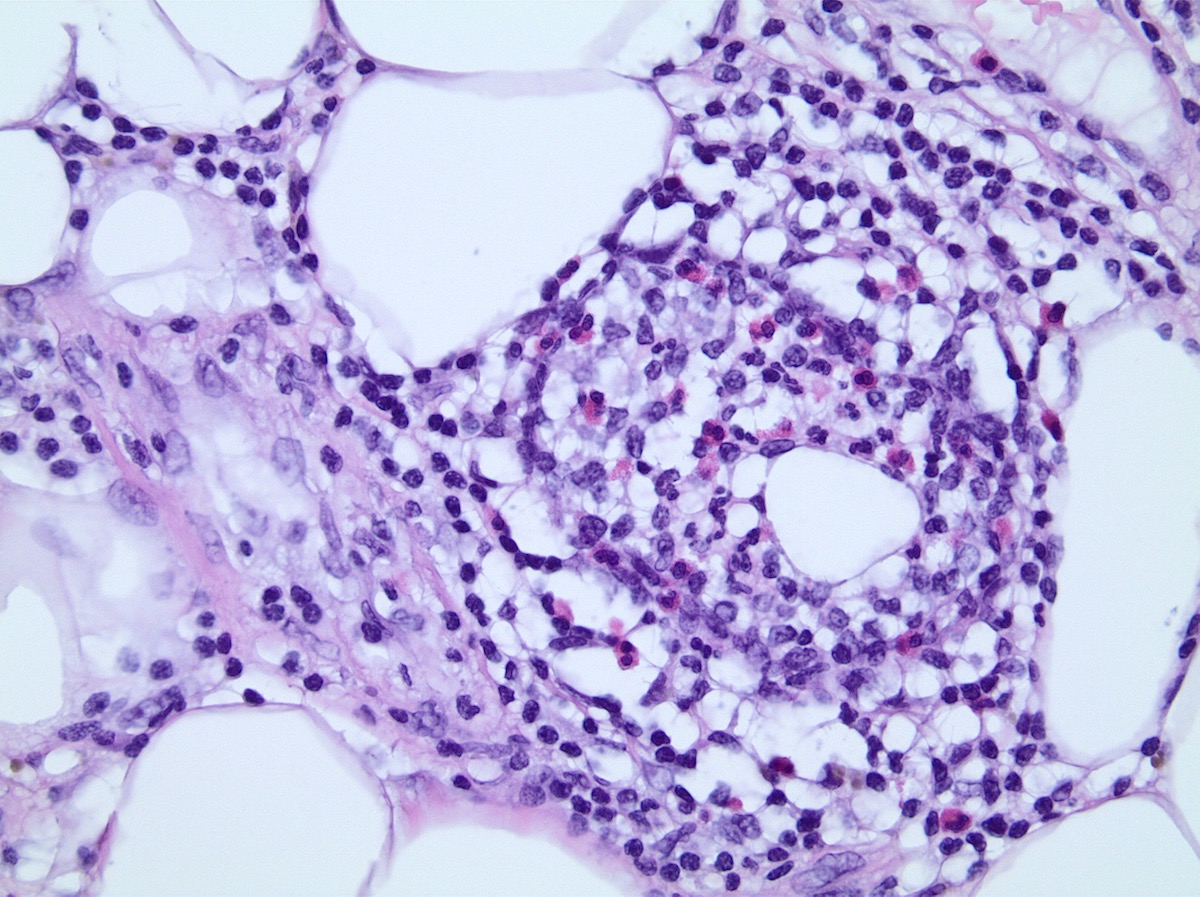
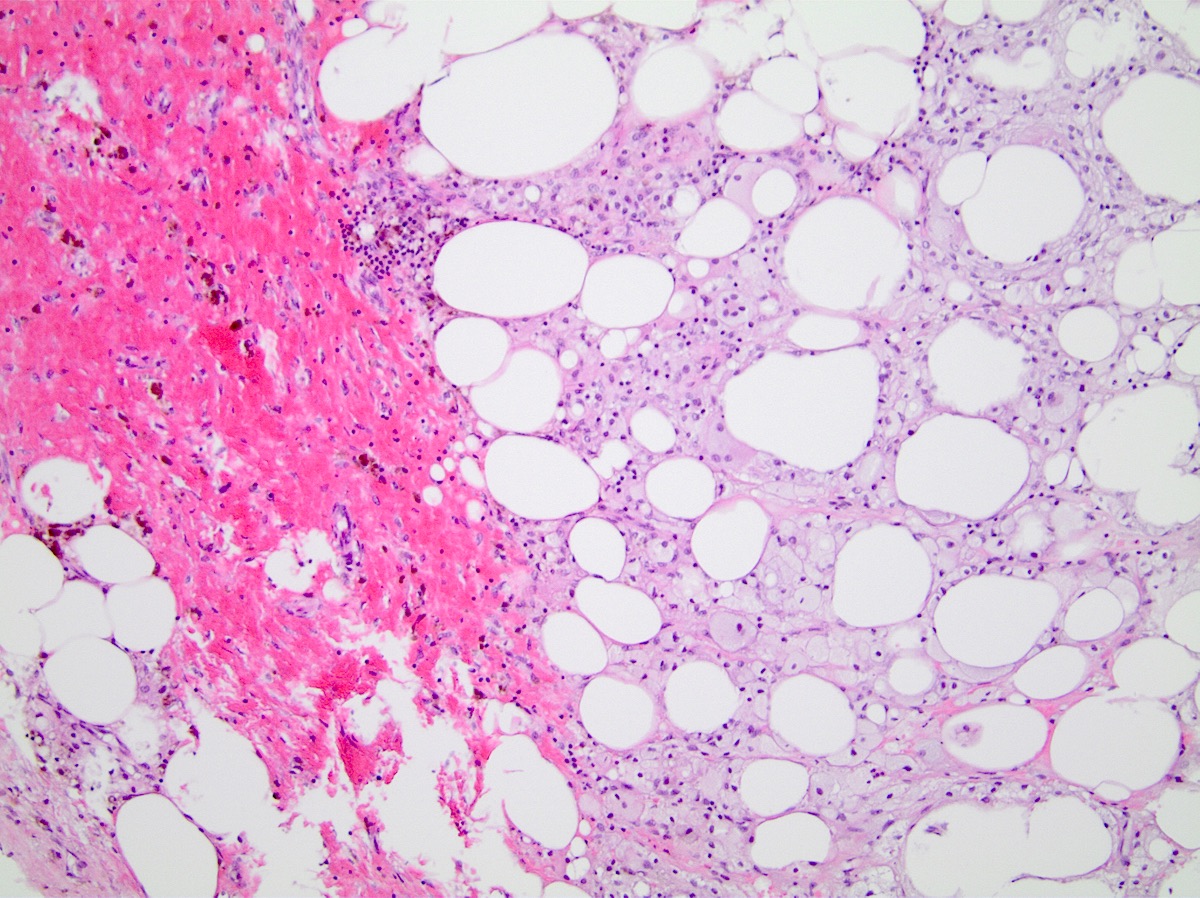
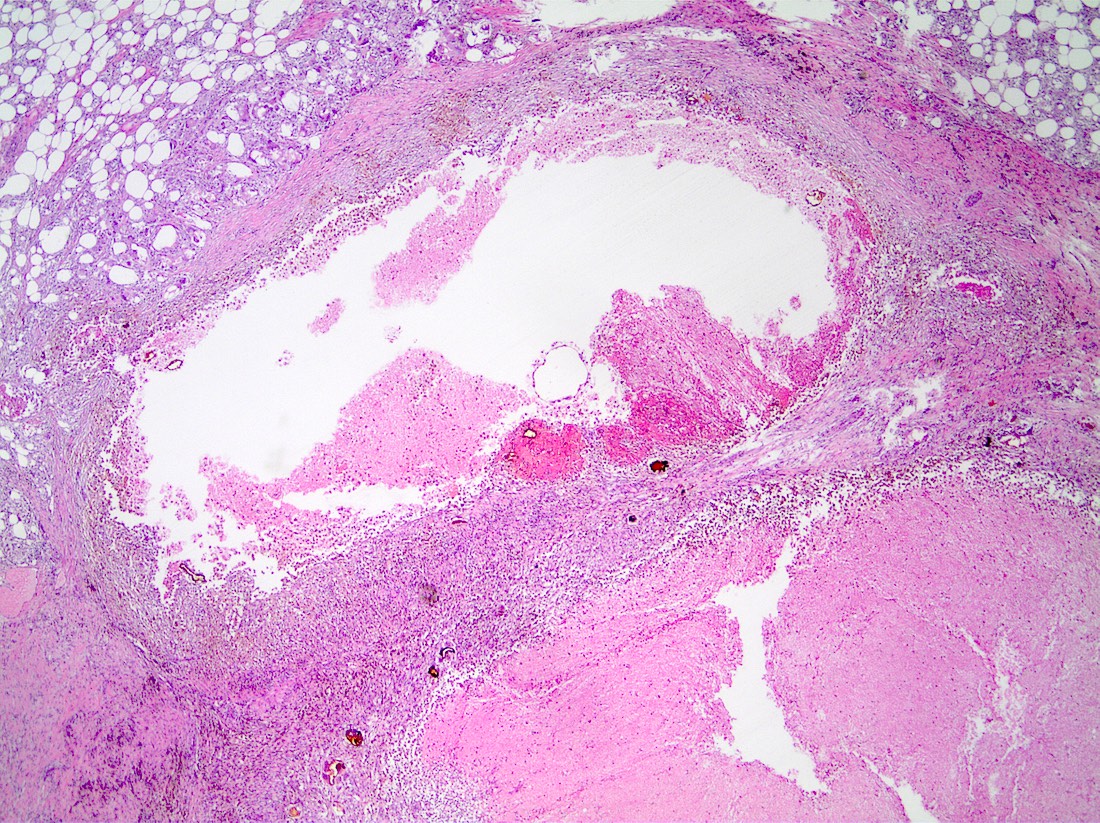
- Early stage:
- Necrosis of adipocytes (fine vacuolization, diminished size and dropout)
- Focal hemorrhage in fat (AJR Am J Roentgenol 2009;192:815)
- Cystic degeneration may result in cavity with or without calcifications in cyst walls
- Formation of demarcated distinct yellow-gray and focally reddish mass over several weeks
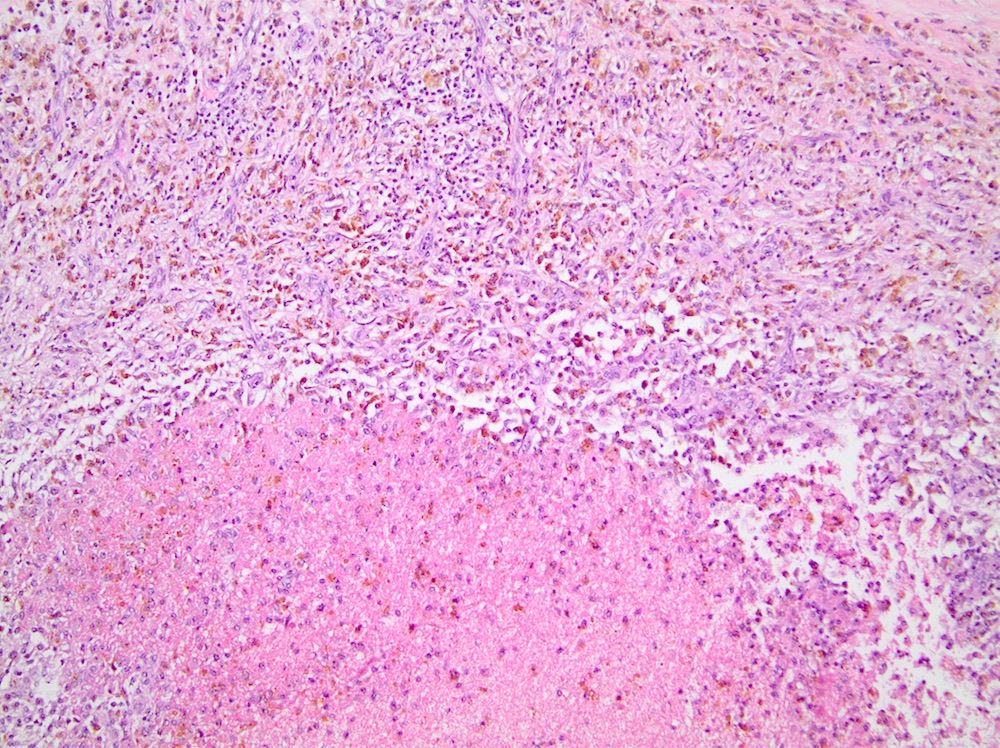
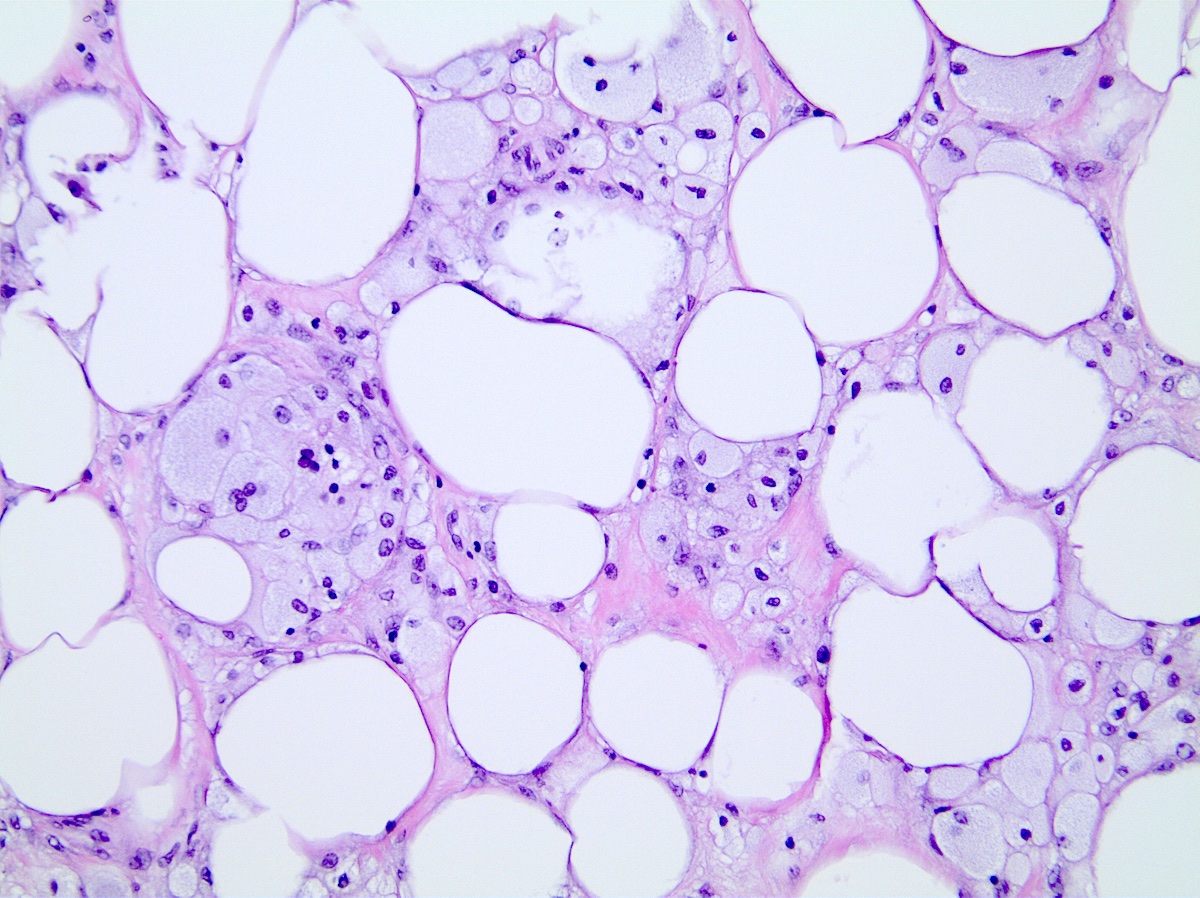
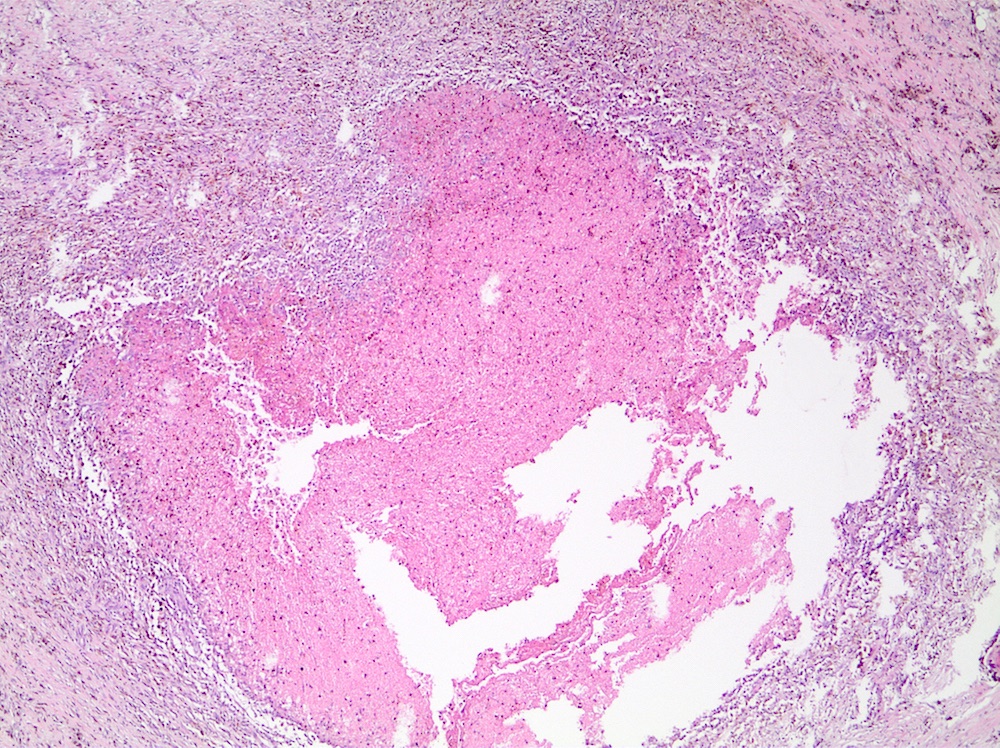
- Intermediate stage:
- Mixed inflammatory cell infiltrate of histiocytes, lymphocytes, plasma cells, sometimes with eosinophils
- Lipid laden foamy histiocytes and multinucleated foreign body type giant cells are due to phagocytosis of necrotic adipocytes
- Hemosiderin deposition
- Early fibrosis with hypercellular areas of fibroblastic proliferation
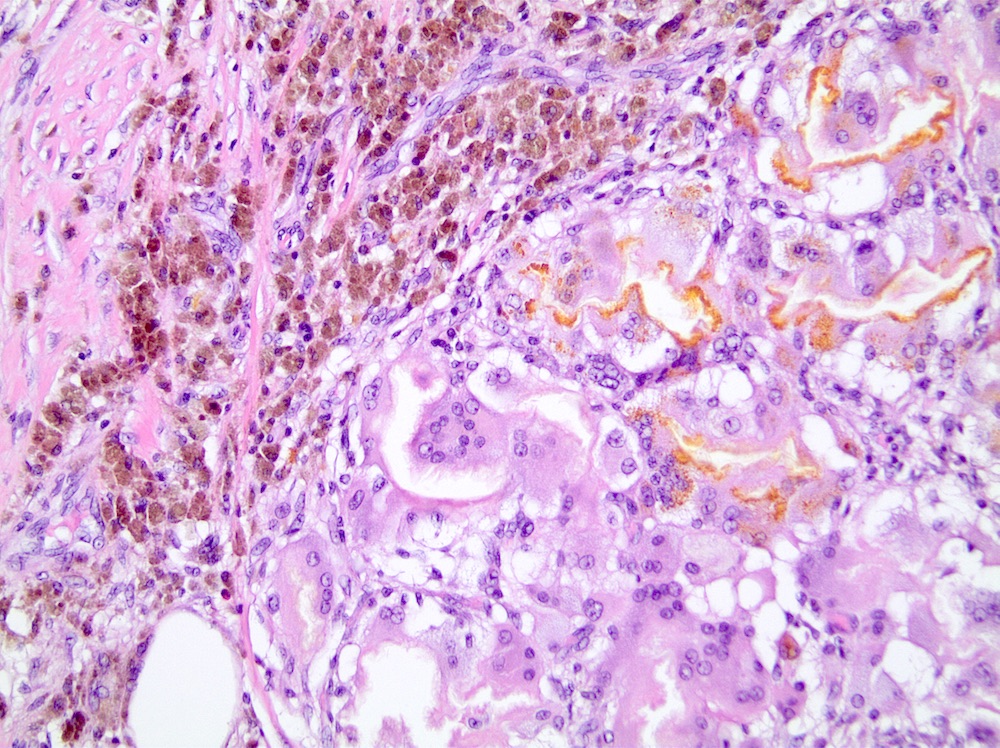
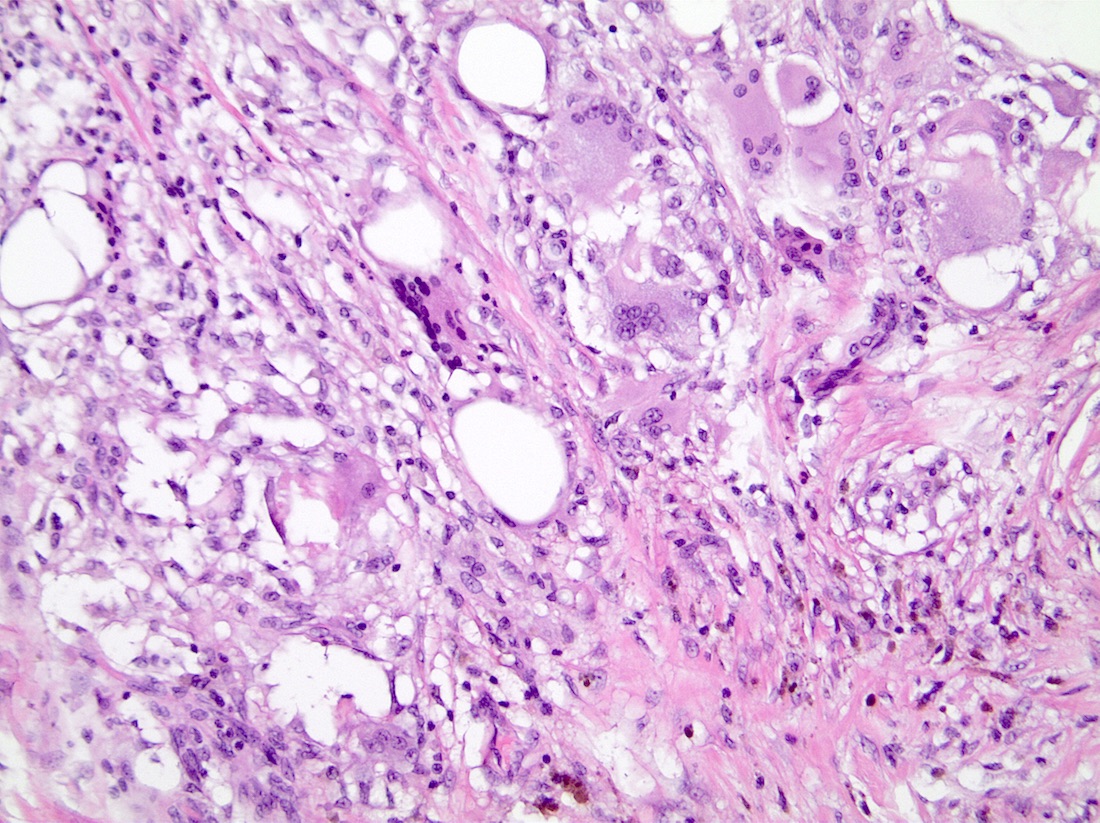
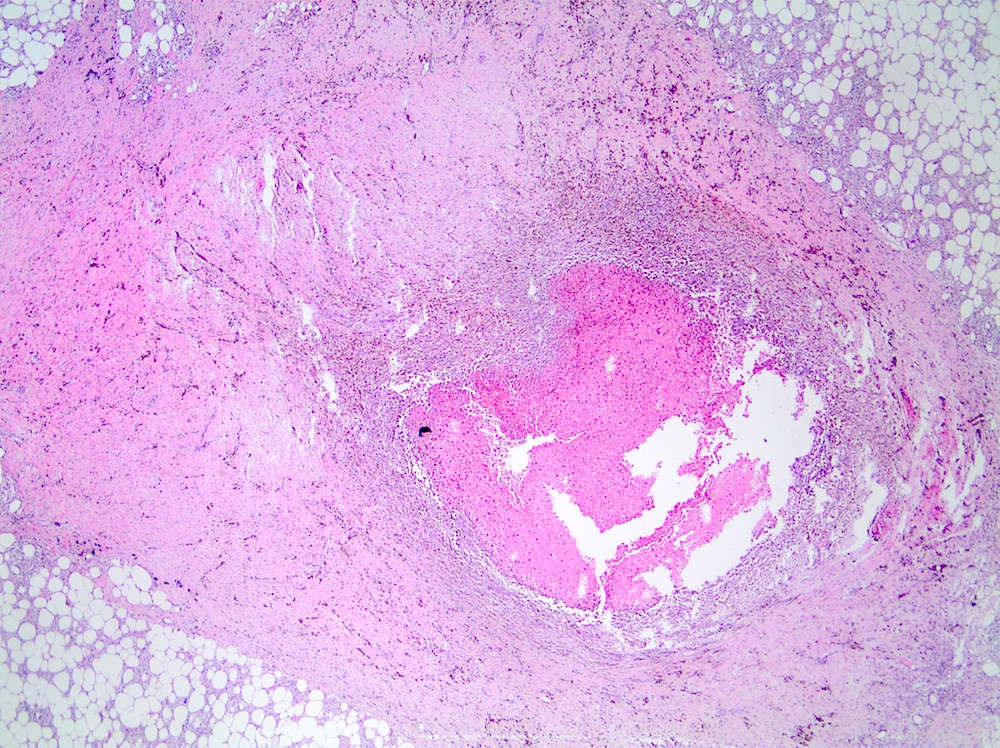
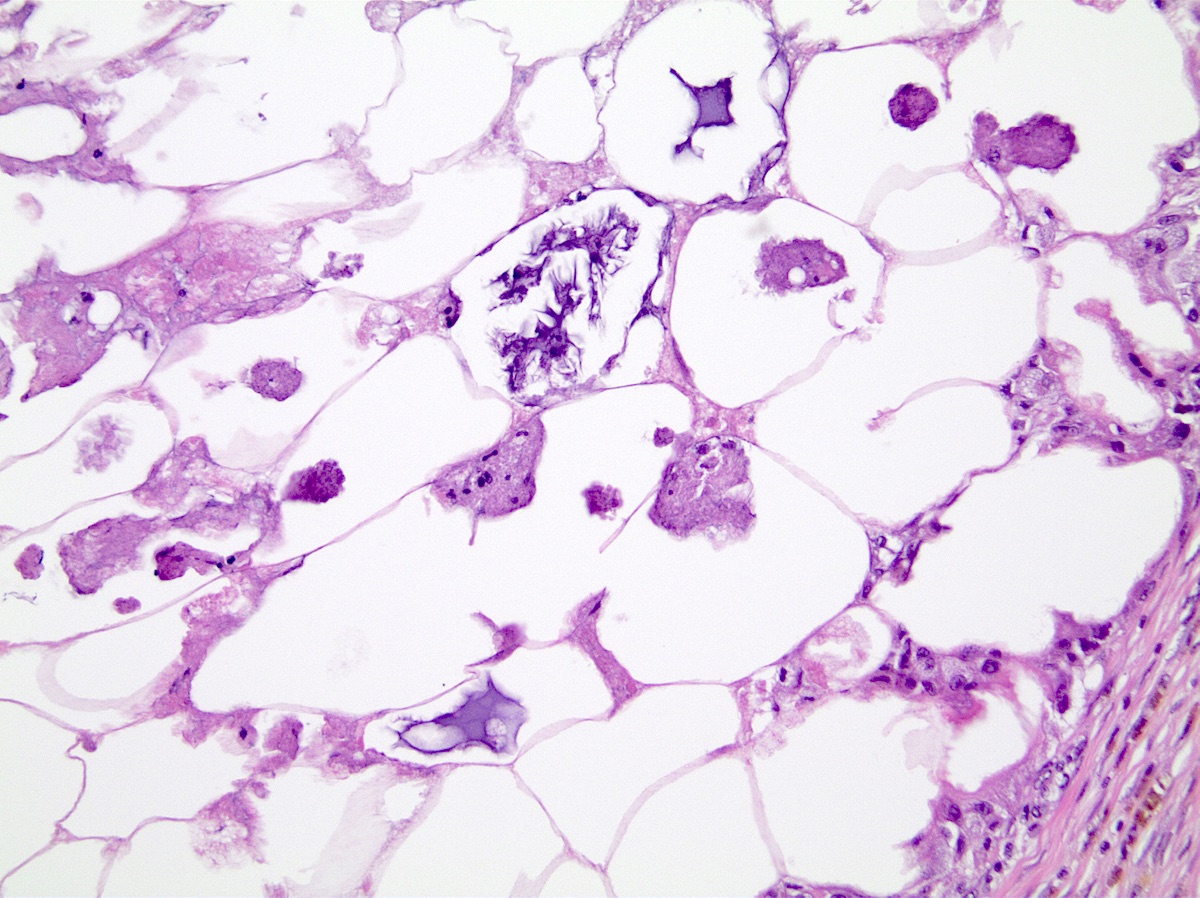
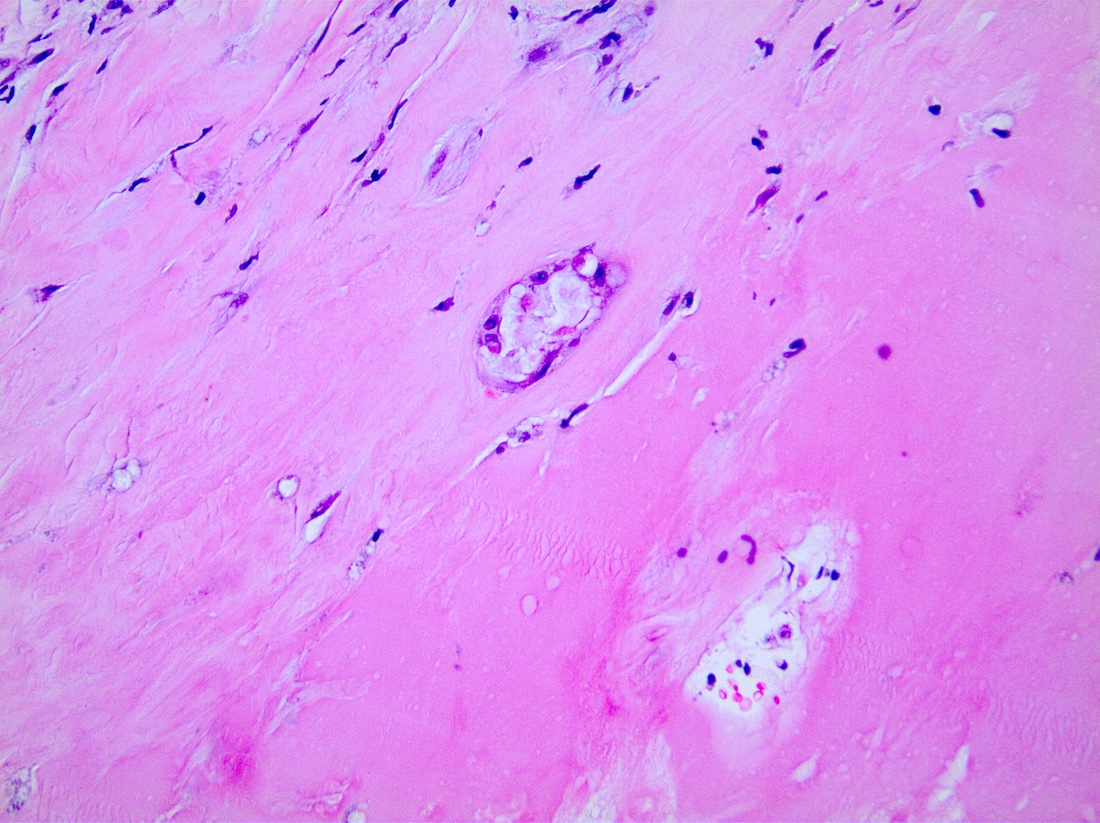
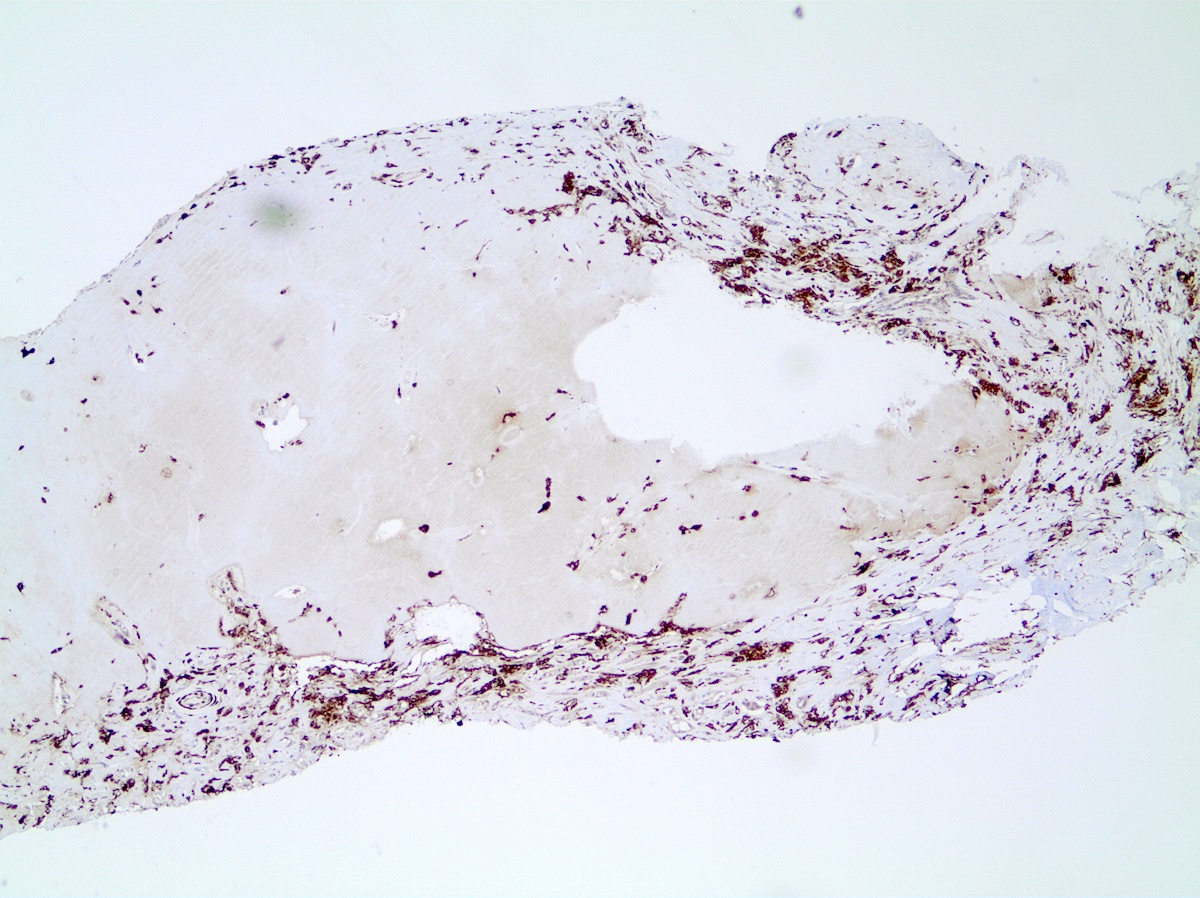
- Late stage:
- Varying degrees of fibrosis and calcifications may remain for years
- Fibrosis contract into a scar and may result in irregular mass
- Loculated necrotic fat within a cyst surrounded by dense fibrous tissue (oil cyst) with dense calcification in the walls of cysts (eggshell calcifications)
- Reactive squamous metaplasia may develop in the epithelium of ducts and lobules in the area of lesion
- Early stage:
Microscopic (histologic) images
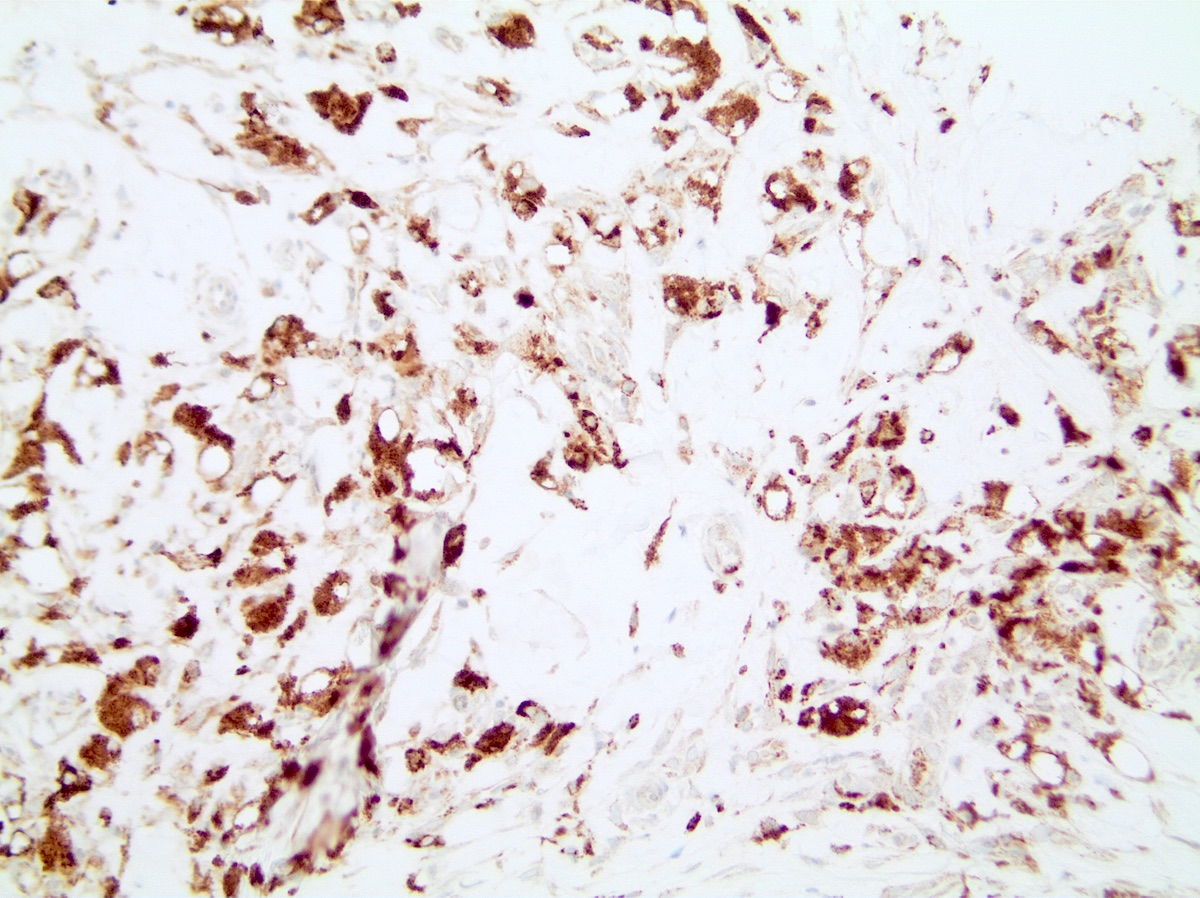
Contributed by Jing He, M.D.
Cytology description
- Characterized by lipid laden histiocytes (lipophages), multinucleated giant cells and degenerating adipocytes (AJR Am J Roentgenol 2009;192:815)
- Lipid laden macrophages demonstrate abundant foamy cytoplasm with variably sized clear lipid vacuoles and small, bland nuclei
- Histiocytes are relatively uniform in size with round nuclei, fine intracytoplasmic vacuoles and no indentation of the nucleus
- Degenerating adipocytes are characterized by aggregates of adipocytes that have lost their nuclei and have finely granular cytoplasm instead of the clear cytoplasm that is characteristic of lipid
- Reactive and reparative changes involving fibroblasts and histiocytes can result in cells with large pleomorphic nuclei and prominent nucleoli
- Background may show scattered inflammatory cells, hemosiderin laden macrophages, globules and acellular lipid
- Scant clusters of ductal epithelial cells are usually cytologically bland but may exhibit cytologic atypia with pleomorphic nuclei and prominent nucleoli
Positive stains
Videos
Breast traumatic fat necrosis
Breast inflammatory conditions
Sample pathology report
- Breast, right, retroareolar, core biopsy:
- Fat necrosis
Differential diagnosis
- Breast carcinoma:
- May have abundant foamy cytoplasm and small bland nuclei that can mimic histiocytes
- Usually demonstrates more nuclear atypia
- Cytokeratin+, CD68-
- Lipomatous neoplasm:
- Granular cell tumor:
- Amyloidosis (Pathol Res Pract 2019;215:152699):
- Can present as mass or calcifications with amyloid surrounding adipocytes
- Usually associated with systemic amyloidosis and hematologic disorder such as plasmacytoma
- No chronic inflammatory cell infiltrate
- Amyloid deposits within blood vessel walls and causes thickening of basement membranes and vascular walls
- Congo red apple green birefringence under polarized microscopy
- Erdheim-Chester disease:
- Infrequent xanthomatous form of non Langerhans cell histiocytosis
- Usually synchronous nonmammary subcutaneous nodules, osseous and orbital lesions
- Infiltration of foamy histiocytes, Touton type giant cells, plasma cells and epithelioid granuloma
- CD68+, factor XIIIa (strong)+, S100 variable, CD1a-
Board review style question #1
- A 65 year old woman has a clinical history of right breast carcinoma treated with local resection and radiation therapy. Her mammogram showed an ill defined irregular mass with calcifications within the right breast. A stereotactic core biopsy shows microcalcifications within the lesion. Which of the following is true about this lesion?
- Continue routine surveillance for this patient
- Negative CD68 and positive AE1 / AE3 are characteristic of this lesion
- The patient has recurrent breast carcinoma
- The patient requires surgical excision of this lesion followed by chemotherapy
Board review style answer #1
A. Continue routine surveillance for this patient. Fat necrosis of the breast is a possible sequela of breast tissue trauma or surgical procedure. This patient likely developed fat necrosis after her initial resection and radiation therapy. When the diagnosis is unclear from radiology, biopsy is necessary to rule out cancer. The biopsy section shows foamy lipid laden histiocytes, mixed inflammatory cells infiltrate and disruption of adipocytes, associated with microcalcification. Positive CD68 and negative AE1 / AE3 can help to distinguish fat necrosis from recurrent carcinoma of breast. Fat necrosis is a nonneoplastic inflammatory process and usually surgical treatment is not required.
Comment Here
Reference: Fat necrosis of breast
Comment Here
Reference: Fat necrosis of breast
Board review style question #2
- A 45 year old woman developed a palpable mass in the subareolar area of the left breast. Mammogram shows a cystic lesion with eggshell calcifications in the cyst wall. She reports a recent history of a car accident in which she had minor injuries and was wearing her seatbelt. Which of the following is the most likely sequela of the lesion?
- The cyst will often become infected and require surgical drainage
- The lesion will be replaced by varying degrees of fibrosis
- The lesion will eventually progress to invasive carcinoma if left untreated
- The lesion will grow and compress surrounding tissue
Board review style answer #2
B. The lesion will be replaced by varying degrees of fibrosis. Fat necrosis has three stages of evolution. The first stage is characterized by disruption of adipocytes following an inciting event. This can lead to local cyst formation with or without calcifications. In the intermediate stage, inflammatory cells phagocytose the necrotic adipocytes and fibroblasts proliferate. Eventually the fibroblasts replace the necrotic areas with varying degrees of fibrosis. Fat necrosis is a nonneoplastic inflammatory lesion that usually resolve or regress over time.
Comment Here
Reference: Fat necrosis of breast
Comment Here
Reference: Fat necrosis of breast