Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mantilla JG, Ricciotti R. Osteochondroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/boneosteochondroma.html. Accessed January 11th, 2025.
Definition / general
- Benign bone surface tumor composed of mature bone with a cartilage cap
- May be solitary or occur as multiple hereditary exostoses (MHE)
Essential features
- Exophytic lesion of bone surface composed of a stalk of mature bone with a cartilaginous cap; the marrow space / cancellous bone of the stalk communicates with that of the underlying bone
Terminology
- Osteocartilaginous exostosis
ICD coding
- ICD-O: 9210/0 - Osteochondroma
- ICD-11: 2E83.Y & XH5Y87 - Other specified benign osteogenic tumors and osteochondroma
Epidemiology
- Common, approximately 35% of benign bone tumors and 10% of all bone tumors
- Predominance in men (M:F = 2:1)
- Most cases diagnosed in the first 2 decades of life
Sites
- Most common in the metaphysis of long bones: femur > humerus > tibia
- Involvement of flat bones (ilium, scapula) may occur
- Involvement of small bones of the hands and feet, ribs and vertebra is rare
Etiology
- Both solitary sporadic tumors and multiple hereditary exostoses (MHE) are associated with loss of function mutations in EXT1 (8q24) and EXT2 (11p11) genes (J Genet 2015;94:749)
- In solitary lesions, EXT gene inactivation is restricted to the cartilage cap and is somatic
- MHE shows autosomal dominant inheritance (Am J Hum Genet 1998;62:346); patients have heterozygous germline EXT1/EXT2 mutation, while their tumors usually show homozygous EXT mutation
Clinical features
- Often asymptomatic (J Bone Oncol 2017;8:23, In Vivo 2008;22:633)
- May cause symptoms due to fracture, growth or impingement of other structures (J Bone Oncol 2017;8:23, In Vivo 2008;22:633)
- Multiple lesions can occur in the setting of MHE (J Bone Oncol 2017;8:23, In Vivo 2008;22:633)
Diagnosis
- Radiologic pathologic correlation is often specific
- Secondary chondrosarcoma:
- Histologic features alone are usually not definitive for diagnosis
- Diagnosis of secondary chondrosarcoma arising in osteochondroma can be challenging and requires correlation with clinical and imaging findings (Mod Pathol 2012;25:1275, Radiology 2010;255:857, Oncogene 2012;31:1095)
- Tumor growth and thickening of the cartilage cap (usually > 2 cm) are suggestive of malignant transformation in skeletally mature patients
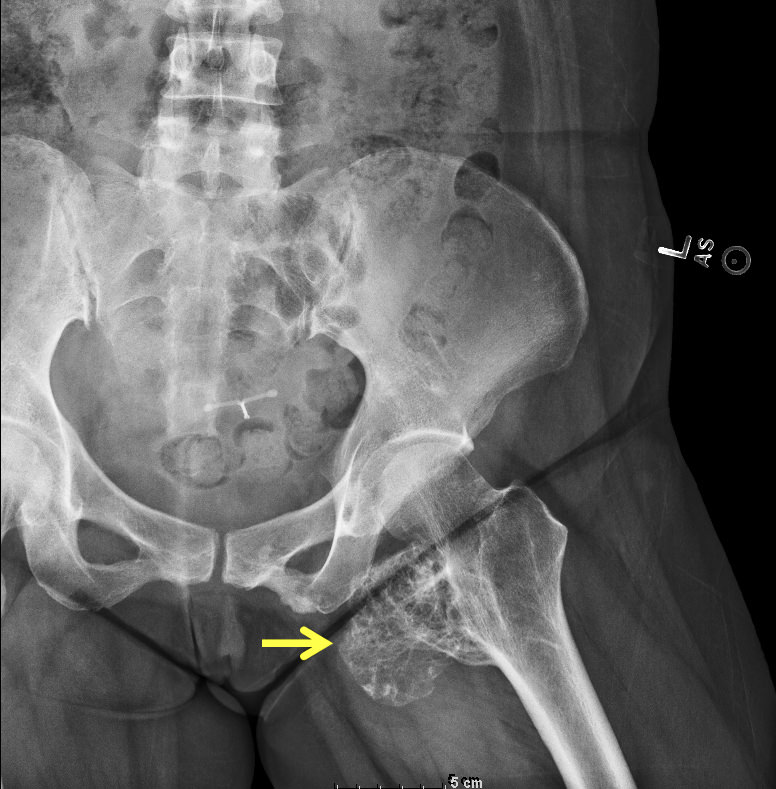
Radiology description
- Pedunculated or sessile
- Mature bony stalk continuous with the cortex; cancellous bone of stalk communicates with that of underlying bone
- Thin, lobulated cartilaginous cap, which may contain calcifications
- Growth perpendicular to the long axis of the bone
Radiology images
Prognostic factors
- Osteochondroma is a benign tumor (J Bone Oncol 2017;8:23, In Vivo 2008;22:633)
- Malignant transformation may occur as secondary chondrosarcoma and are usually a grade 1 to 2 conventional chondrosarcoma (J Bone Oncol 2017;8:23, In Vivo 2008;22:633)
- Solitary lesions have at most 1 - 2% risk of malignant transformation (J Bone Oncol 2017;8:23, In Vivo 2008;22:633)
- Multiple osteochondromas in the setting of MHE have a higher risk of malignant transformation (5 - 25% overall) (J Bone Oncol 2017;8:23, In Vivo 2008;22:633, Orphanet J Rare Dis 2008;3:3)
- Secondary chondrosarcomas are usually grade 1 - 2 conventional chondrosarcoma (J Bone Oncol 2017;8:23, In Vivo 2008;22:633)
Case reports
- 12 year old girl with minute mesenchymal chondrosarcoma within osteochondroma (Hum Pathol 2018;81:255)
- 15 year old boy with painless lump in the arm (radiology) (BMJ 2016;354:i4503)
Treatment
- Growth often stops after skeletal maturity and may spontaneously regress
- Excision is typically curative in solitary lesions, with rare local recurrence
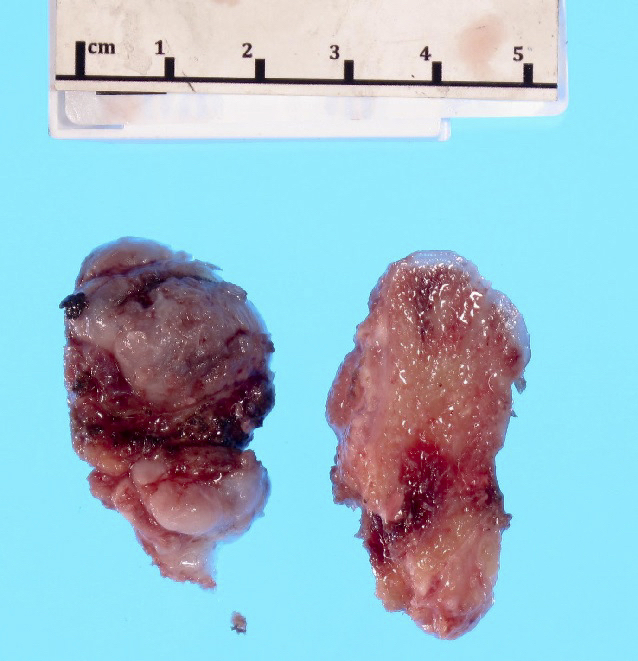
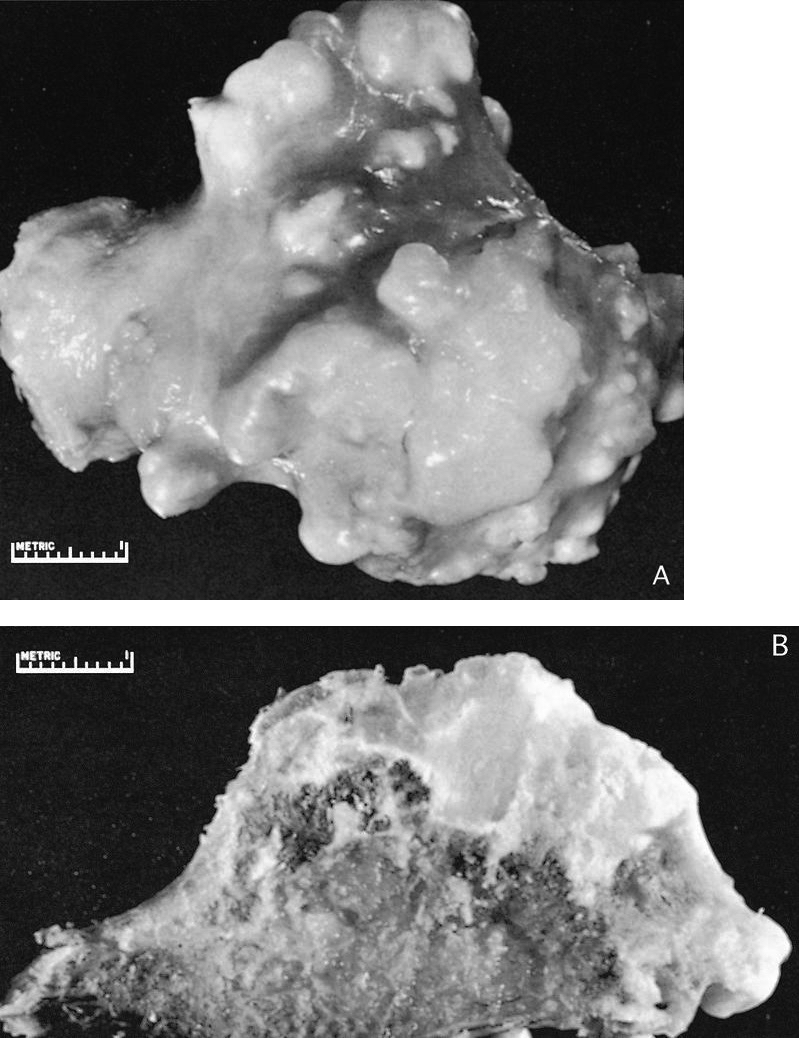
Gross description
- Pedunculated or sessile bony lesion with hyaline cartilage cap
Gross images
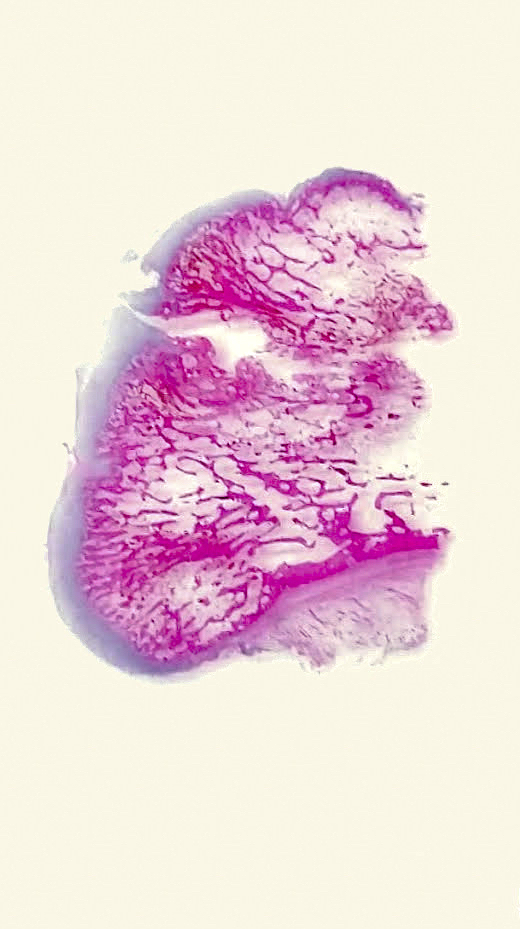
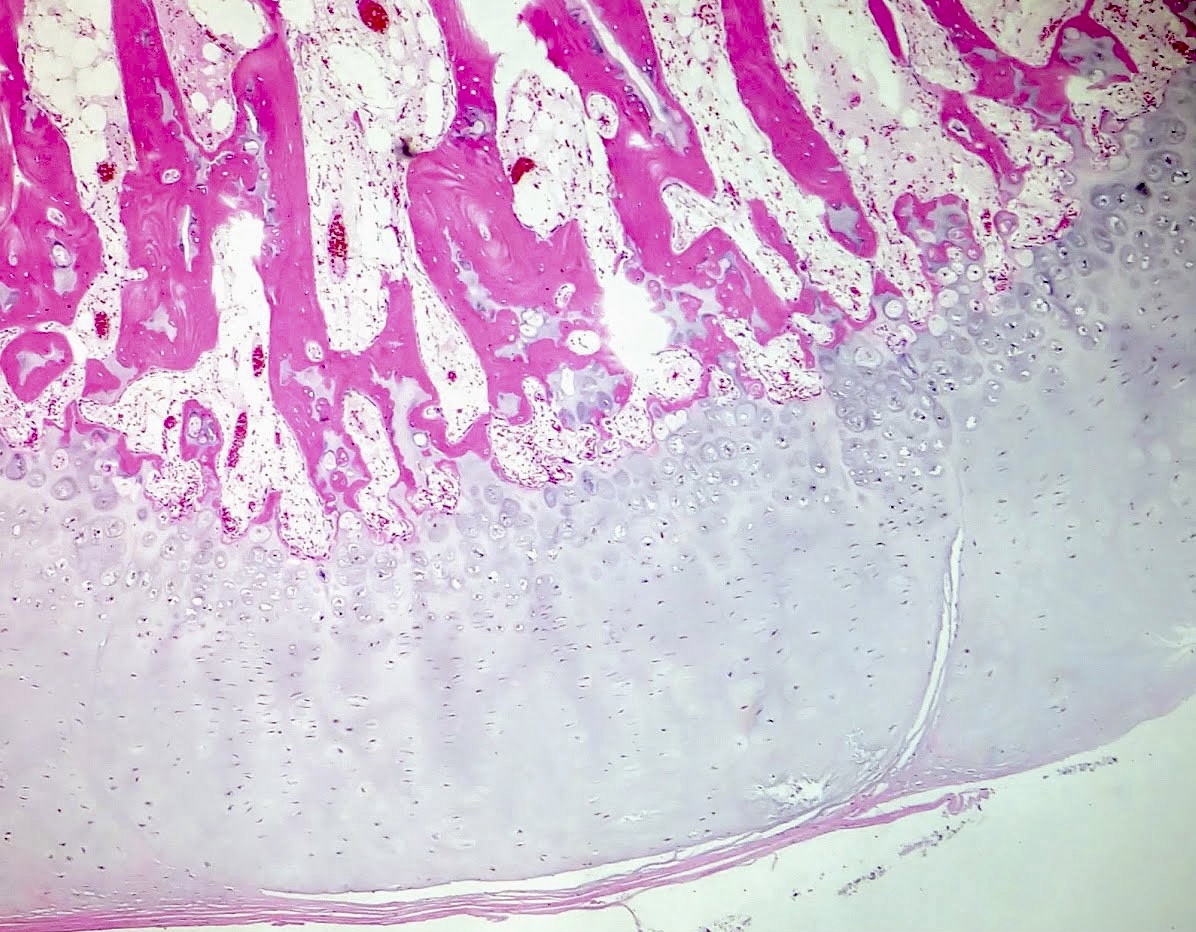
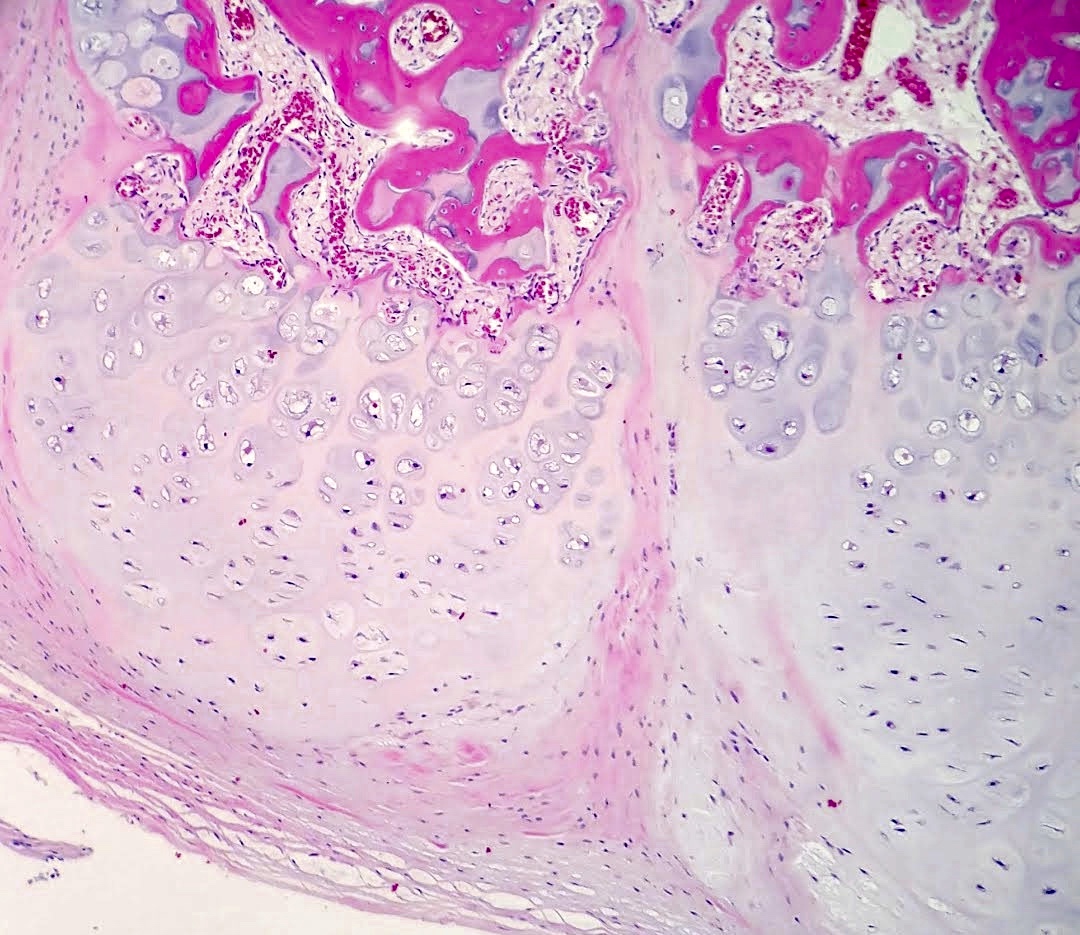
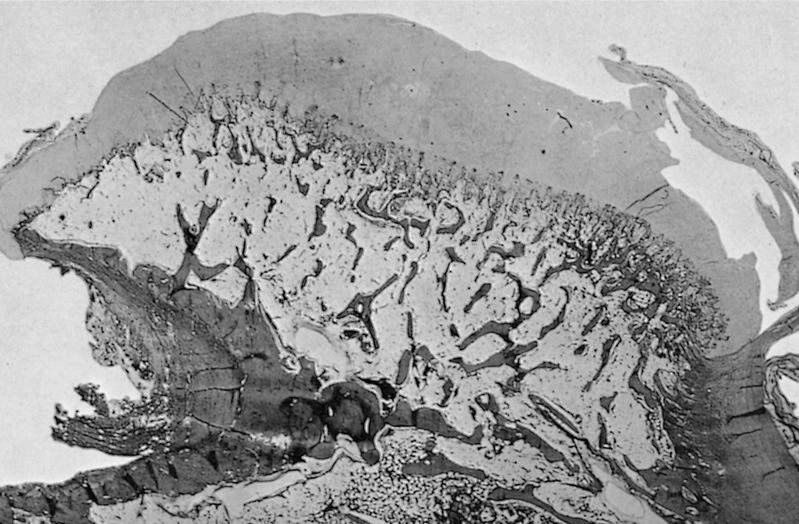
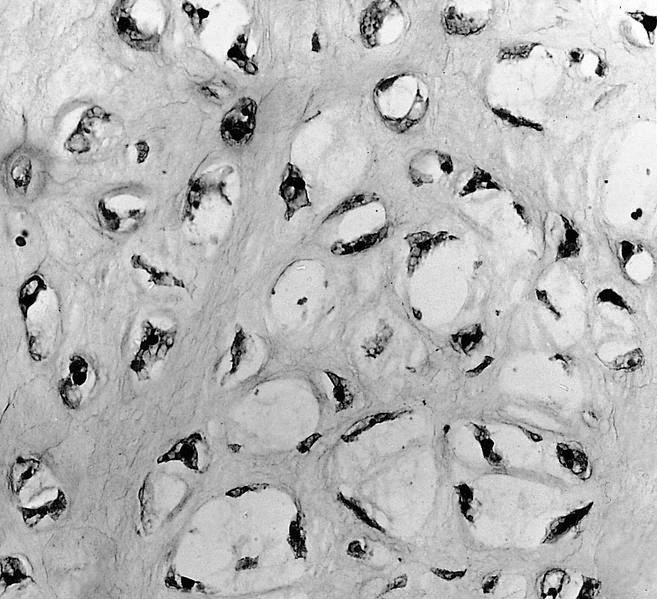
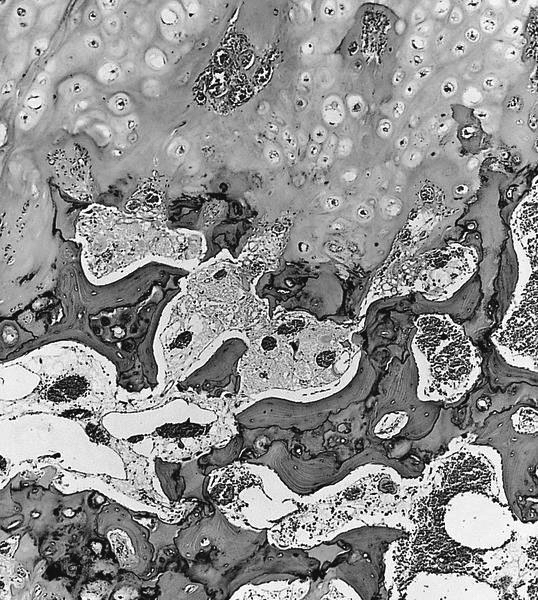
Microscopic (histologic) description
- Cap composed of mature hyaline cartilage with overlying fibrous perichondrium
- In young patients, transition between bone and cartilage cap resembles growth plate, showing endochondral ossification into mature bone; cartilage cap diminishes and may essentially be absent in older adults
- Marrow elements may be present within bony stalk; marrow space / cancellous bone contiguous with that of the native bone
Microscopic (histologic) images
Molecular / cytogenetics description
- Solitary osteochondroma and MHE associated with EXT1 and EXT2 mutations
Sample pathology report
- Knee mass, excision:
- Osteochondroma
Differential diagnosis
- Bizarre parosteal osteochondromatous proliferation (Nora lesion):
- Disorganized growth of bone and cartilage with characteristic blue bone
- Typically located in the distal extremities (J Orthop 2018;15:138)
- Florid reactive periostitis:
- Mixture of reactive woven bone and fibrous tissue without zonation
- Typically arises in the periosteum of fingers
- Parosteal osteosarcoma:
- Similar location and age group
- More aggressive growth areas of neoplastic woven bone formation and fibroblastic areas
- Can have a cartilage cap in up to 25% of cases
- Secondary chondrosarcoma:
- Infiltrative growth with permeation of bone or extension into soft tissue
- Usually well differentiated but with invasion into surrounding tissue
Board review style question #1
Which of the following is true about the epidemiology of osteochondromas?
- Congenital lesions are relatively common
- Female predominance
- Most lesions arise in long bones
- Most common in the elderly
- Multiple lesions are more common
Board review style answer #1
Board review style question #2
Which of the following is true regarding secondary chondrosarcoma?
- Most common subtype is clear cell chondrosarcoma
- Patients with multiple osteochondromas have a higher overall risk of developing chondrosarcoma
- Risk of malignancy in patients with multiple hereditary exostosis is near 50%
- Risk of malignancy in solitary osteochondromas is high
Board review style answer #2
B. Patients with multiple osteochondromas have a higher overall risk of developing chondrosarcoma
Comment Here
Reference: Osteochondroma
Comment Here
Reference: Osteochondroma