Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jin Y, Zhang L. Granulomatous inflammation. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonemarrowgranulomatousinflammation.html. Accessed January 2nd, 2025.
Definition / general
- Granuloma is formed by aggregates of histiocytes / macrophages, admixed with variable inflammatory cells, with or without giant cells
- An infrequent histopathologic finding, 0.3 - 3% of bone marrow biopsy, related to various conditions, infectious or noninfectious
- Identification of underlying etiologies is the key to treatment and prognosis
Essential features
- An infrequent histopathologic finding related to various conditions
- Underlying etiologies include infections, sarcoidosis, hematologic and nonhematologic malignancies, drug reaction, autoimmune diseases and other disorders
- 2 common histologic findings: caseating or noncaseating
- Morphologic features only are not reliable to differentiate between causes; it is necessary to combine morphology with microbiologic, serologic, molecular and clinical findings for full interpretation
Terminology
- Bone marrow granulomas
- Granulomatous bone marrow disease
- Granulomatous lesion in bone marrow
- Granulomatous bone marrow inflammation
ICD coding
- ICD-10: L92.9 - granulomatous disorder of the skin and subcutaneous tissue, unspecified
Epidemiology
- Broad age range, mainly aged > 40 years
- Slight male predominance
- Mainly in patients with immune deficiency (HIV), hematologic malignancy and sarcoidosis
- Higher risk in patients with fever of unknown origin (15 times more likely than when biopsied for other reasons) (Hematol Pathol 1988;2:43)
Sites
- Bone marrow
- Can be seen in other body sites
- Bone marrow involvement is usually associated with disseminated disease
- Reference: Medicine (Baltimore) 2018;97:e9726
Pathophysiology
- Unknown at this time
Etiology
- Infections:
- Bacteria: M. tuberculosis, M. avium, M. pneumoniae, brucellosis, typhoid fever, Q fever, Rocky Mountain spotted fever, Bartonella
- Fungi: histoplasmosis, cryptococcosis, aspergillosis, Candida, Talaromyces marneffei
- Virus: EBV, CMV
- Protozoa: leishmaniasis
- Hematologic disorders:
- Non-Hodgkin lymphoma, mostly T / NK cell origin (e.g., angioimmunoblastic T cell lymphoma)
- Acute lymphoblastic leukemia (ALL)
- Chronic lymphocytic lymphoma (CLL)
- Multiple myeloma (MM)
- Monoclonal gammopathy of undetermined significance (MGUS)
- Acute myeloid leukemia (AML)
- Hodgkin lymphoma
- Myelodysplastic / myeloproliferative neoplasm (MDS / MPN)
- Sarcoidosis
- Drug reaction:
- Anti-inflammatory agents (ibuprofen, indomethacin)
- Antiarrhymthics (amiodarone, procainamide, tocainide)
- Sulfanamide
- Interferon β, interferon α2b
- BCGitis
- Autoimmune disease:
- Lupus
- Sjögren syndrome
- Antineutrophil cytoplasmic antibodies (ANCA) associated vasculitis
- Mixed connective tissue disease
- Rheumatoid arthritis
- Primary biliary cirrhosis
- Behçet disease
- Nonhematologic malignancy:
- Renal cell carcinoma
- Breast cancer
- Ovary cancer
- Bladder cancer
- Hepatic sarcoma
- Other diseases:
- Silicosis
- Various collagen vascular diseases
- Gouty tophi
- Foreign bodies
- Unknown etiology
- References: Medicine (Baltimore) 2018;97:e9726, Int J Lab Hematol 2018;40:123, E J Intern Med 2013;24:468, Hematol Pathol 1988;2:43, Medicine 1983;62:372, J Hematol 2020;9:37, Am J Med Case Rep 2021;9:83
Clinical features
- Fever
- Fatigue and weakness
- Dyspnea and cough
- Lymphadenopathy / hepatosplenomegaly
- Reference: Medicine (Baltimore) 2018;97:e9726
Diagnosis
- Diagnosis is based on histological examination of bone marrow biopsy and a series of ancillary tests upon clinical setting
Laboratory
- Anemia, thrombocytopenia, lymphopenia
- Positive or negative for microorganisms
- Serological changes related to infectious or autoimmune etiology
- Reference: Medicine (Baltimore) 2018;97:e9726
Prognostic factors
- Prognosis varies according to underlying causes
- Good prognosis for those caused by drug reaction (e.g., BCGitis) and for those without definitive underlying causes (West J Med 1996;164:510, E J Intern Med 2013;24:468)
Case reports
- 9.5 year old Indian girl who presented with bleeding manifestation, skin rash, uveitis and arthritis (Eur J Rheumatol 2020;7:190)
- 46 year old man with fever, shortness of breath, myalgia and general malaise (Am J Med Case Rep 2021;9:83)
- 53 year old woman presented with fever, chills and rigors associated with occipital headache (Blood 2019;133:2730)
- 54 year old woman with history of weight loss and low grade fever (J Ayub Med Coll Abbottabad 2018;30:S671)
- 69 year old woman suffered from cervical pain due to lymphadenopathy (Cancer Radiother 2021;25:51)
Treatment
- Treatment varies for specific underlying causes
- Steroids for sarcoidosis
- Cytoreductive therapy for hematologic malignancies
- Immunomodulators for autoimmune disorders
- Drug discontinuation for drug reaction
- Reference: Medicine (Baltimore) 2018;97:e9726
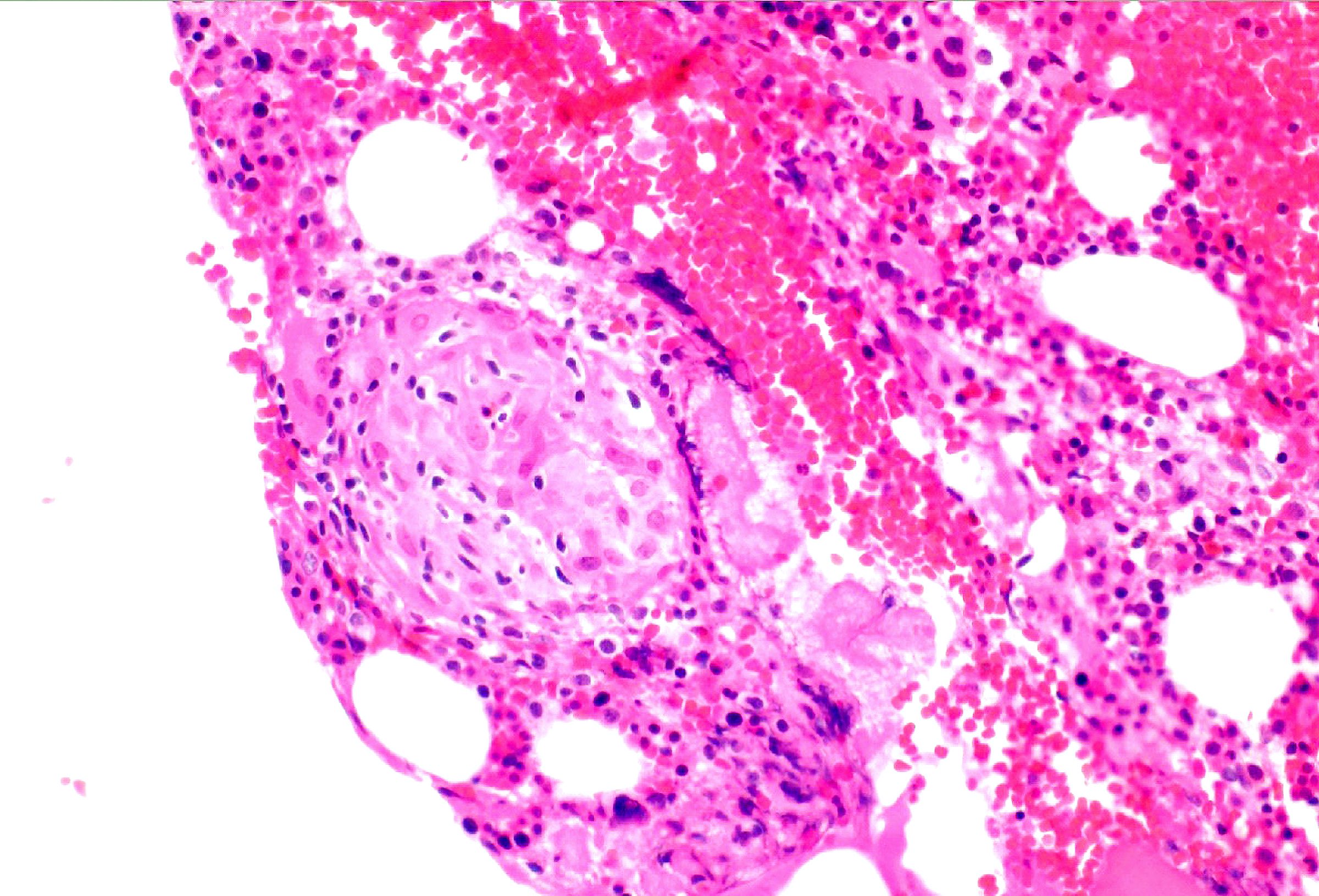
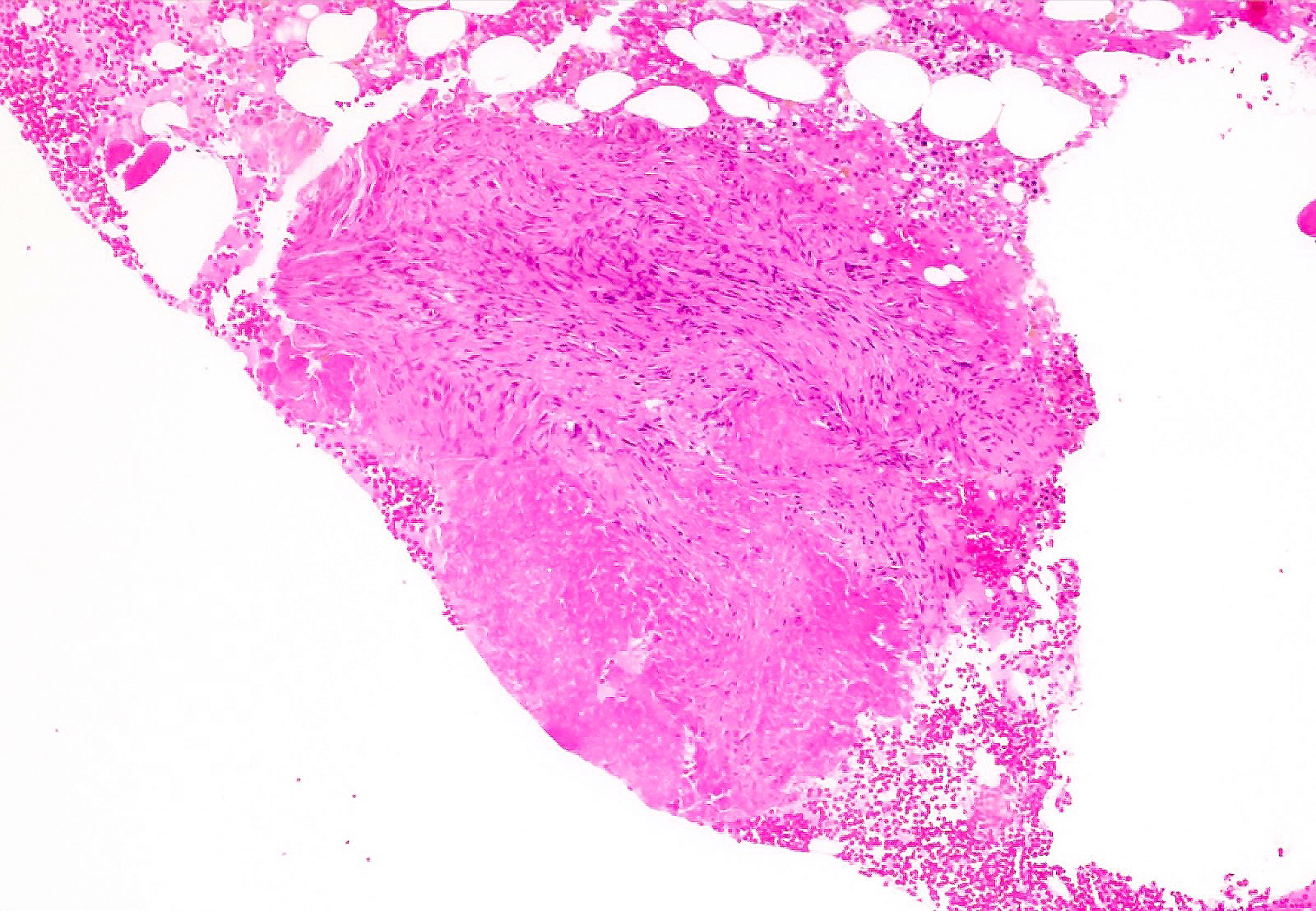
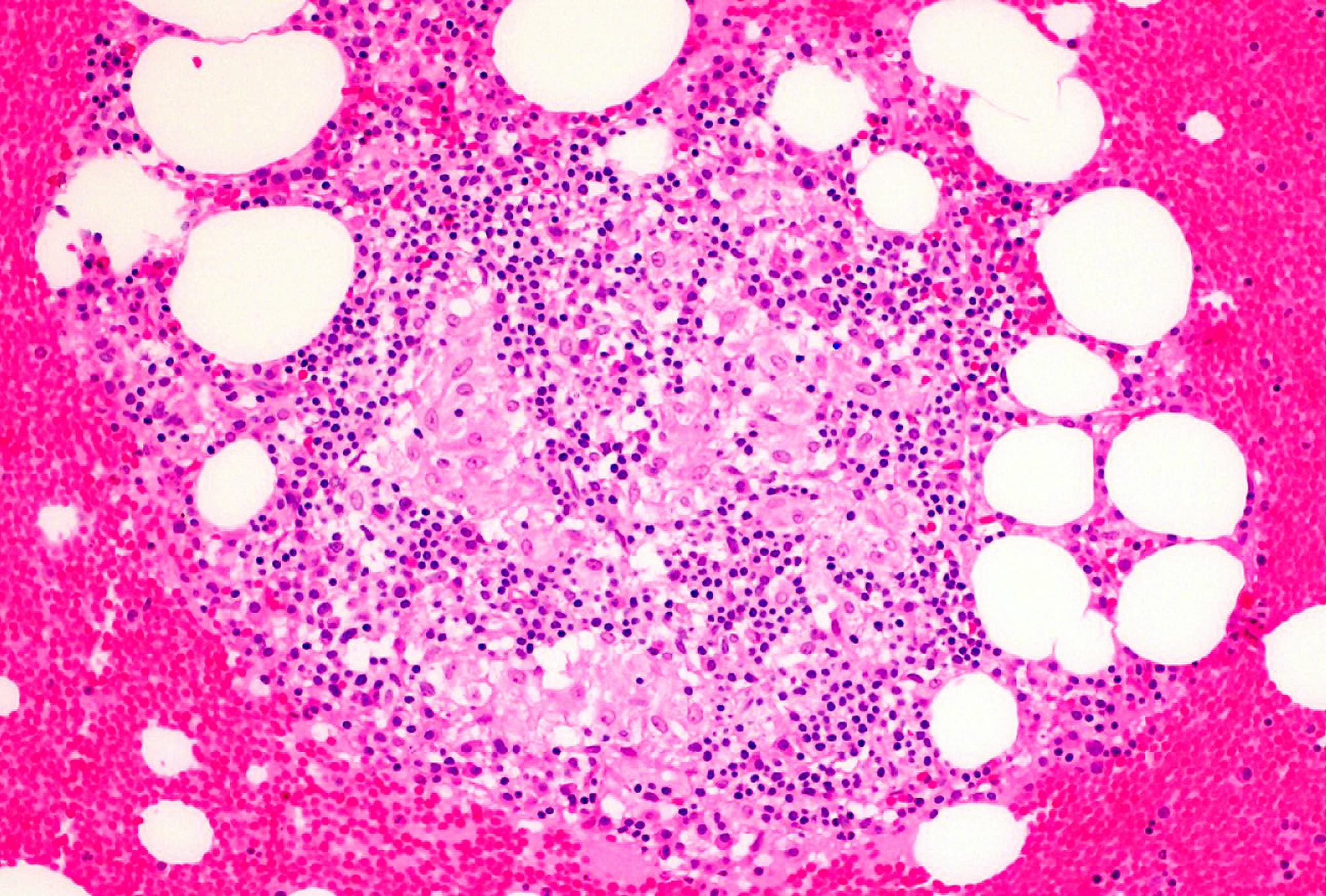
Microscopic (histologic) description
- Major types: lipogranuloma (insignificant), epithelioid granuloma (caseating, noncaseating)
- Lipogranuloma: prominent aggregates of histiocytes with variably sized lipid vacuoles; most common type
- Epithelioid granuloma: loose or discrete aggregates of eosinophilic histiocytes / macrophages with variable giant cell formation and variable central caseation / necrosis; usually small, focal and nonnecrotic; often paratrabecularly located; many subtypes; characteristic features for certain causes but not specific
- Caseating / necrotizing granuloma: containing a central area of necrosis (caseation), are significant and usually indicate infection (tuberculosis, Brucella, Rickettsia, fungi)
- Noncaseating granuloma:
- Ring or doughnut granuloma: fibrin and inflammatory cells arranged around a central clear space; associated with Q fever but not specific, can also be seen in Brucella, typhoid, rare viral infections
- Foreign body granuloma: multinucleated giant cell's response to exogenous material, often visible by polarized light
- Sarcoid type granuloma: multiple noncaseating granulomas, occasional fibrinoid necrosis in active cases
- Mycobacterium avium complex related granuloma: clusters of histiocytes with needle-like inclusions in cytoplasm resembling Gaucher cells
- Chronic granulomatous disease: usually nonspecific, presence of active chronic inflammation and pigmented macrophages should raise suspicion (Histopathology 2005;47:508)
- Nonspecific: small and rare epithelioid granulomas may also be clinically insignificant
Microscopic (histologic) images
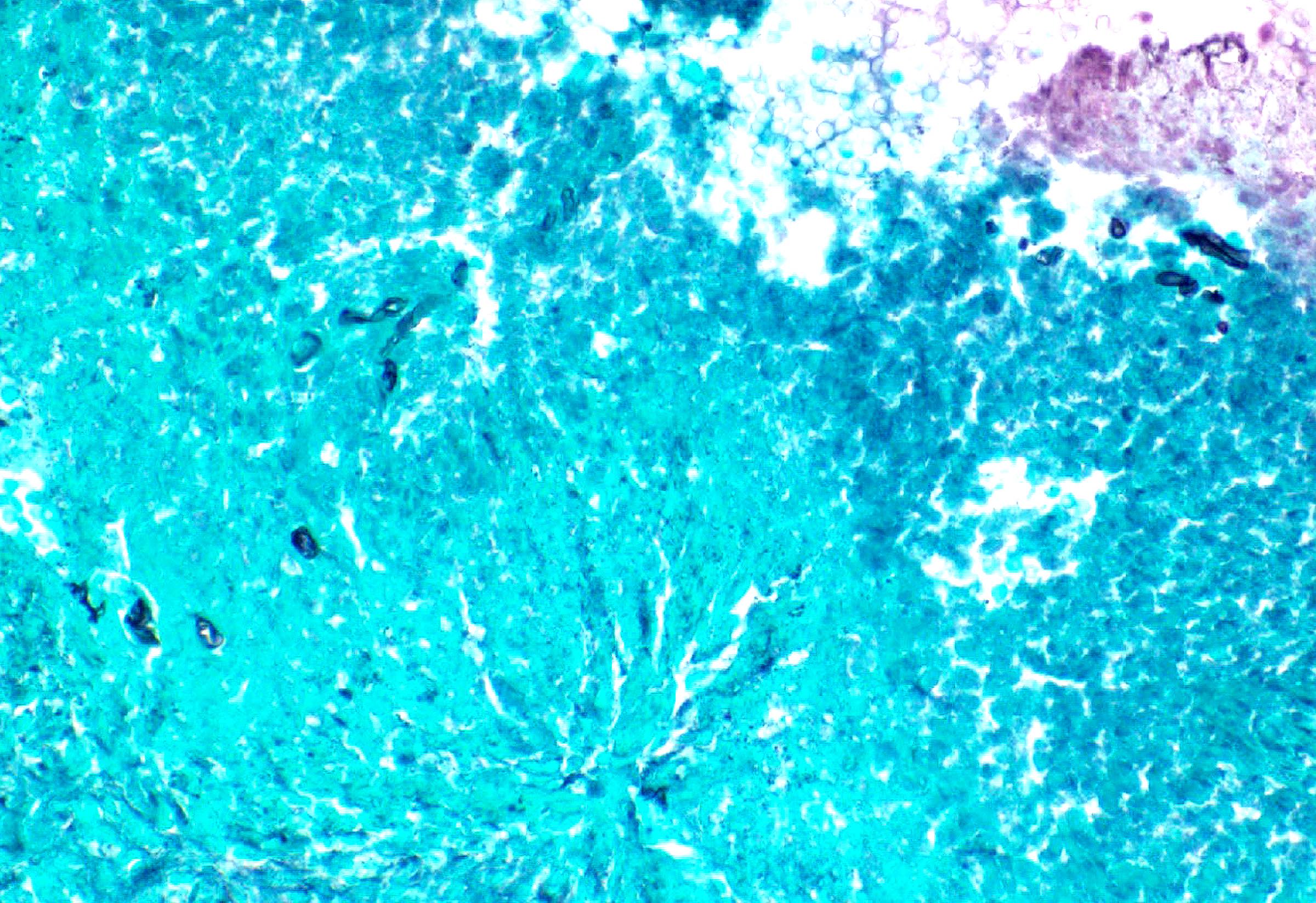
Positive stains
- CD68, CD163: highlight the cluster of histiocytes
- Acid fast bacilli (AFB): positive for mycobacterial infection
- Grocott methenamine silver (GMS): positive for fungal infection (J Clin Tuberc Other Mycobact Dis 2017;7:1)
Negative stains
Flow cytometry description
- Can be applied for diagnosis of non-Hodgkin lymphoma if lymphoma is suspected clinically in a setting of granulomatous inflammation
Molecular / cytogenetics description
- Genetic testing for chronic granulomatous disease (CGD): these 5 genes (CYBA, CYBB, NCF1, NCF2 or NCF4) are frequently mutated
Sample pathology report
- Bone marrow, right posterior iliac crest, core biopsy, clot section:
- Necrotizing granuloma with fungal hyphae (see comment)
- Clinical history: Acute myelogenous leukemia. Status postchemotherapy was in complete remission. Rule out relapse.
- No evidence of residual leukemia
- Comment: The marrow is hypocellular with left shifted granulopoiesis and erythroid predominance. There is no morphologic, immunophenotypic or flow cytometric evidence of residual leukemia. The fungal hyphae identified are poorly preserved, precluding further characterization.
- CBC: WBC: 2.3 k/mm³, Hgb: 10.1 g/dL, MCV: 89.0 fL, Platelets: 56 k/mm³. Differential count (%): Neutrophils: 17, Bands: 40, Lymphocytes: 38, Monocytes: 3, Eosinophils: 1.
- Peripheral smear: Manual review of the peripheral blood shows normocytic / normochromic anemia, thrombocytopenia and moderate leukopenia. RBCs: Normocytic / normochromic red blood cells, mild anisocytosis, mild polychromasia. WBC: Moderate leukopenia. Granulocytes with left shift and toxic changes. Blasts are not increased. Platelets: Moderate thrombocytopenia. Large platelets are noted.
- Bone marrow biopsy: Quality: adequate. Cellularity: hypocellular (5 - 10%). Hematopoiesis: Erythropoiesis is increased. Granulopoiesis is decreased. Megakaryocytes are decreased with normal morphology. No significant changes in medullary bone are noted. Single necrotizing granuloma is identified. Special stains: Reticulin (1+): reticulin fibrosis is present. Iron: stainable iron is increased (3+). PAS: stains appropriately, fungal hyphae are identified. GMS: fungal hyphae are identified. CD34: no increase in blasts. CD117: no increase in mononuclear cells. CD68: positive in histiocytic cells.
- Bone marrow clot section: Quality: adequate. Cellularity: 5 - 10% morphologic features are similar to those observed in the core biopsy.
Differential diagnosis
- Hodgkin lymphoma:
- Histiocytic cell neoplasms (Ann Hematol 2018;97:2117):
- Langerhans cell histiocytosis:
- Often associated with variable numbers of eosinophils
- Expresses CD1a, CD207 (langerin), BCL1 and S100
- Hemophagocytic lymphohistiocytosis:
- Increased histiocytes exhibiting hemophagocytosis of mostly erythrocytes
- Usually presents with very severe clinical symptoms (hepatosplenomegaly) and significant abnormal lab tests (cytopenia, liver function, high ferritin levels, elevated triglyceride level and or soluble IL25 level)
- Histiocytic sarcoma:
- Rosai-Dorfman disease:
- Erdheim-Chester disease:
- Langerhans cell histiocytosis:
- Storage diseases:
- Gaucher disease:
- Niemann-Pick disease:
- Foamy macrophage with round lipid inclusion
- Molecular mutations in SMPD1, NPC1 or NPC2
- Infection:
- Whipple disease:
- Infiltration of foamy macrophage
- Strongly PAS+
- Bacilliform inclusions
- Whipple disease:
Board review style question #1
A 64 year old patient with acute myeloid leukemia (AML), status postinduction chemotherapy, had a bone marrow biopsy for disease monitoring. The morphologic findings are shown in the hematoxylin and eosin (H&E) slide (see above image). By immunohistochemistry, the aggregated histiocytic cells are positive for CD64 and negative for CD30, CD1a, langerin, S100, PAS, AFB and GMS. What is the most accurate diagnosis?
- Bone marrow granuloma
- Hodgkin lymphoma
- Langerhans cell histiocytosis
- Whipple Disease
Board review style answer #1
A. Bone marrow granuloma. Morphologically, it shows pure noncaseating granuloma without Reed-Sternberg cells, Touton giant cells or sheets of blasts. Negativity for above stains (CD30, CD1a, langerin, S100, PAS, AFB, GMS) excludes a diagnosis of Hodgkin lymphoma (CD30+), Langerhans histiocytosis (langerin+, CD1a+, S100 variable) and Whipple disease (PAS+).
Comment Here
Reference: Granulomatous inflammation
Comment Here
Reference: Granulomatous inflammation
Board review style question #2
Among the following descriptions about bone marrow granulomas, which one is true?
- Detection of bone marrow granulomas can exclude an underlying malignant process
- Different morphologic subtypes of granuloma are diagnostic of specific etiologic conditions
- It is necessary to combine morphology with microbiologic, serologic, molecular and clinical findings to have a full interpretation of underlying etiologies
- They are a frequent histopathologic finding that points to an autoimmune disorder
Board review style answer #2
C. It is necessary to combine morphology with microbiologic, serologic, molecular and clinical findings to have a full interpretation of underlying etiologies
Comment Here
Reference: Granulomatous inflammation
Comment Here
Reference: Granulomatous inflammation