Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Parakh R, Tretiakova M. Squamous metaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdersquamousmetaplasia.html. Accessed April 1st, 2025.
Definition / general
- Replacement of urothelium with stratified squamous epithelium
- 2 subtypes: nonkeratinizing and keratinizing
Essential features
- Presence of squamous epithelium
- May show glycogenation (clearing of cytoplasm)
- Nonneoplastic cytology: normally maturing squamous epithelium from basal to superficial
- Hyperkeratosis and parakeratosis with presence of granular layer might be seen
- Absence of koilocytosis
Terminology
- Keratinizing subtype is also called leukoplakia (clinical term)
ICD coding
- ICD-10: N32.89 - other specified disorders of bladder
Epidemiology
- All ages
- Normally seen in the trigone of the bladder in women of reproductive age
Sites
- Bladder (most commonly), ureter and renal pelvis
- In trigone of women, it is normal variation and not metaplasia
Pathophysiology
- Chronic irritation, inflammation, catheters, stones, infection (Urol Int 2008;81:247)
- Reversible if the irritating or inciting factor is removed
- With continued insult, can progress to preneoplastic / premalignant (in situ) and invasive squamous cell carcinoma (Histopathology 2019;74:68)
Etiology
- Urinary tract infections: Escherichia coli, Proteus and Streptococcus faecalis
- Schistosomiasis is commonly associated, due to chronicity (J Cell Biol 2005;171:835)
- Urinary tract irritants: indwelling catheters, urinary calculi, urinary outflow obstruction, fistula, tumors (J Urol 1999;161:1106)
- Bladder exstrophy
- Neurogenic bladder, previous bladder surgery
- Vitamin A deficiency
Clinical features
- Vaginal (nonkeratinizing) subtype:
- Also called pseudomembranous trigonitis; common in trigone
- Normal finding in females
- Rarely occurs in children (Urol Int 2006;77:46)
- Keratinizing subtype:
- Also called leukoplakia
- More common in males
- Associated with chronic irritation (catheters, stones, parasite eggs)
- Rule out atypia
- Risk factor for squamous cell carcinoma (Urol Int 2008;81:247, Eur Urol 2002;42:469)
Diagnosis
- Cystoscopy: flaky, white, plaque-like lesions, mucosal irregularity (BMJ Case Rep 2018;2018:bcr2018225303)
Prognostic factors
- Keratinizing squamous metaplasia may transform to squamous dysplasia / carcinoma (Urol Int 2008;81:247)
- Important to report extent of involvement
- Sampling of all lesional tissue is important to rule out dysplastic in situ or invasive squamous lesion in the vicinity
- Requires close follow up
Case reports
- 22 year old man with leukoplakia of the urinary bladder (BMJ Case Rep 2018;2018:bcr2018227019)
- 34 year old woman presenting with bladder mulberry-like fibroepithelial polyp with calcification and squamous cell metaplasia mimicking bladder carcinoma (J Int Med Res 2020;48:300060519896911)
- 54 year old man with tetraplegia, keratinizing squamous metaplasia and prophylactic cystectomy (J Spinal Cord Med 2007;30:389)
- 62 year old man with keratinizing squamous metaplasia of the bladder (BMJ Case Rep 2018;2018:bcr2018225303)
- 3 women in one family with no bladder pathology (J Urol 1987;137:979)
Treatment
- Spontaneous resolution in some
- Careful follow up of keratinizing squamous metaplasia, particularly if atypical, to detect dysplasia or carcinoma (Urol Int 2008;81:247, Am J Surg Pathol 2006;30:883)
- Transurethral resection and fulguration
- Prophylactic cystectomy is reserved for extensive disease (Eur Urol 2002;42:469)
- Possibly sodium pentosan polysulfate (used for painful bladder syndrome / interstitial cystitis) (Drugs 2006;66:821)
Clinical images
Gross description
- Epithelial lining appears paler or thicker than normal with irregular borders and a surrounding zone of erythema
- Sometimes presents with subtle changes
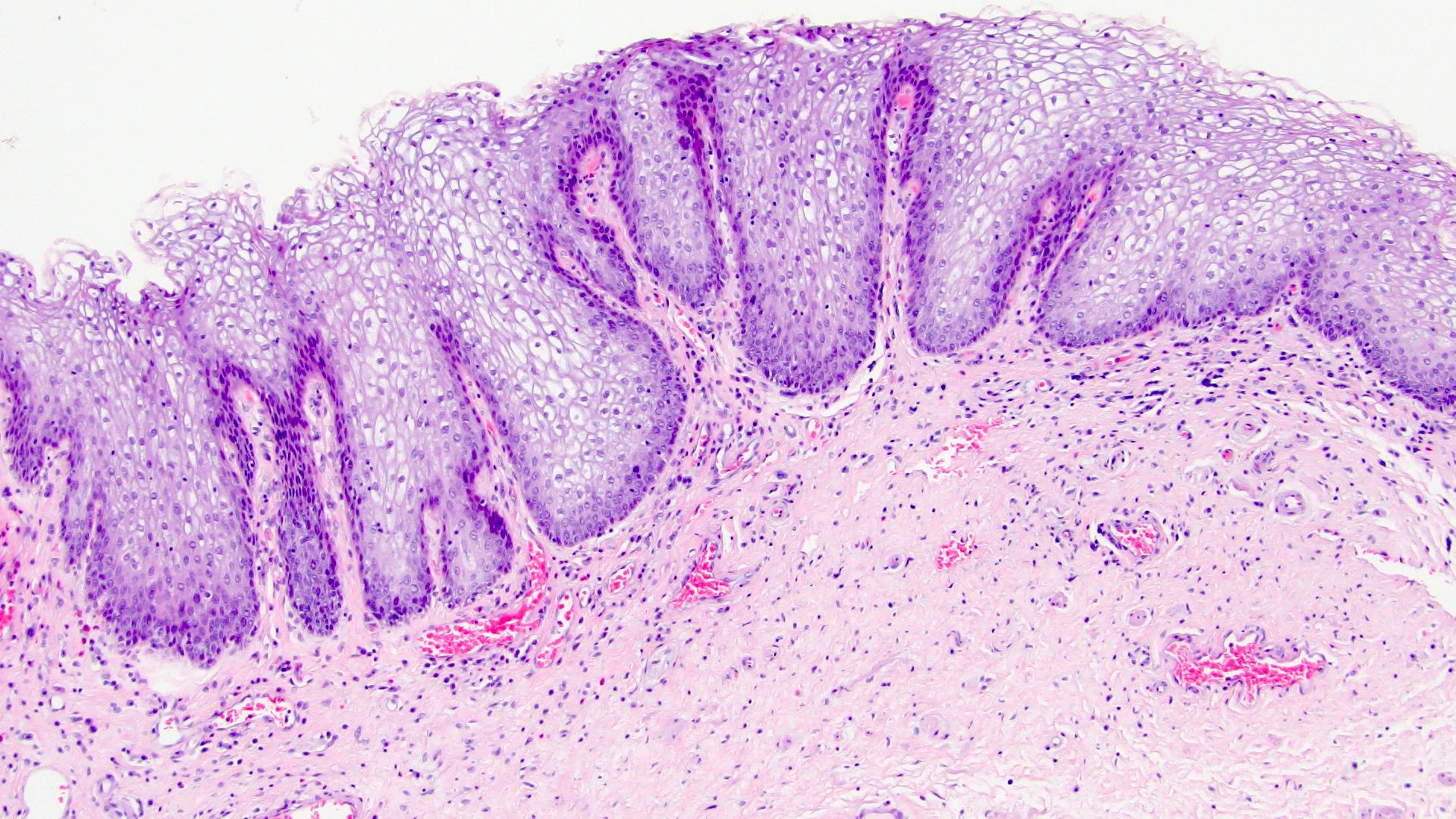
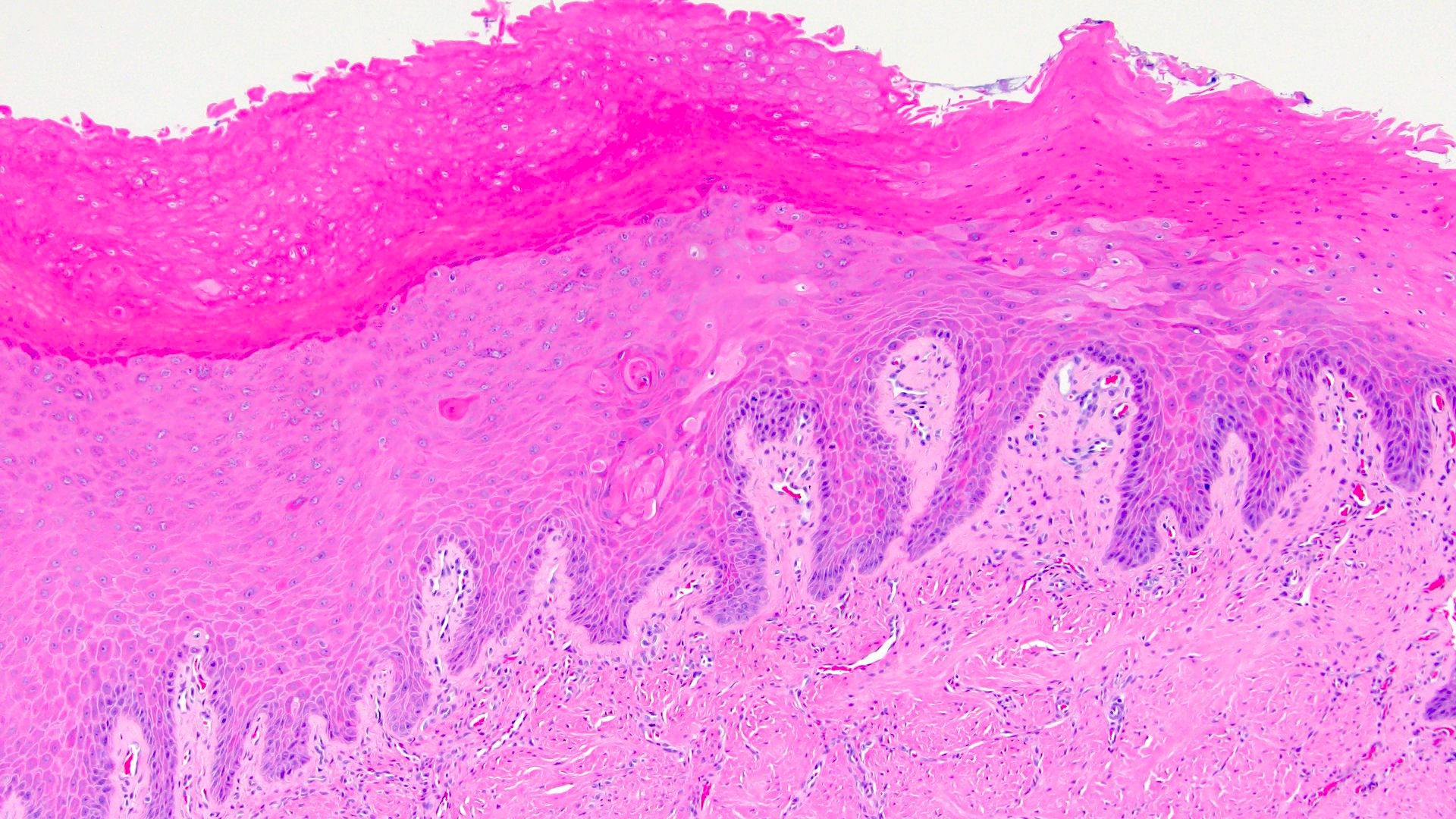
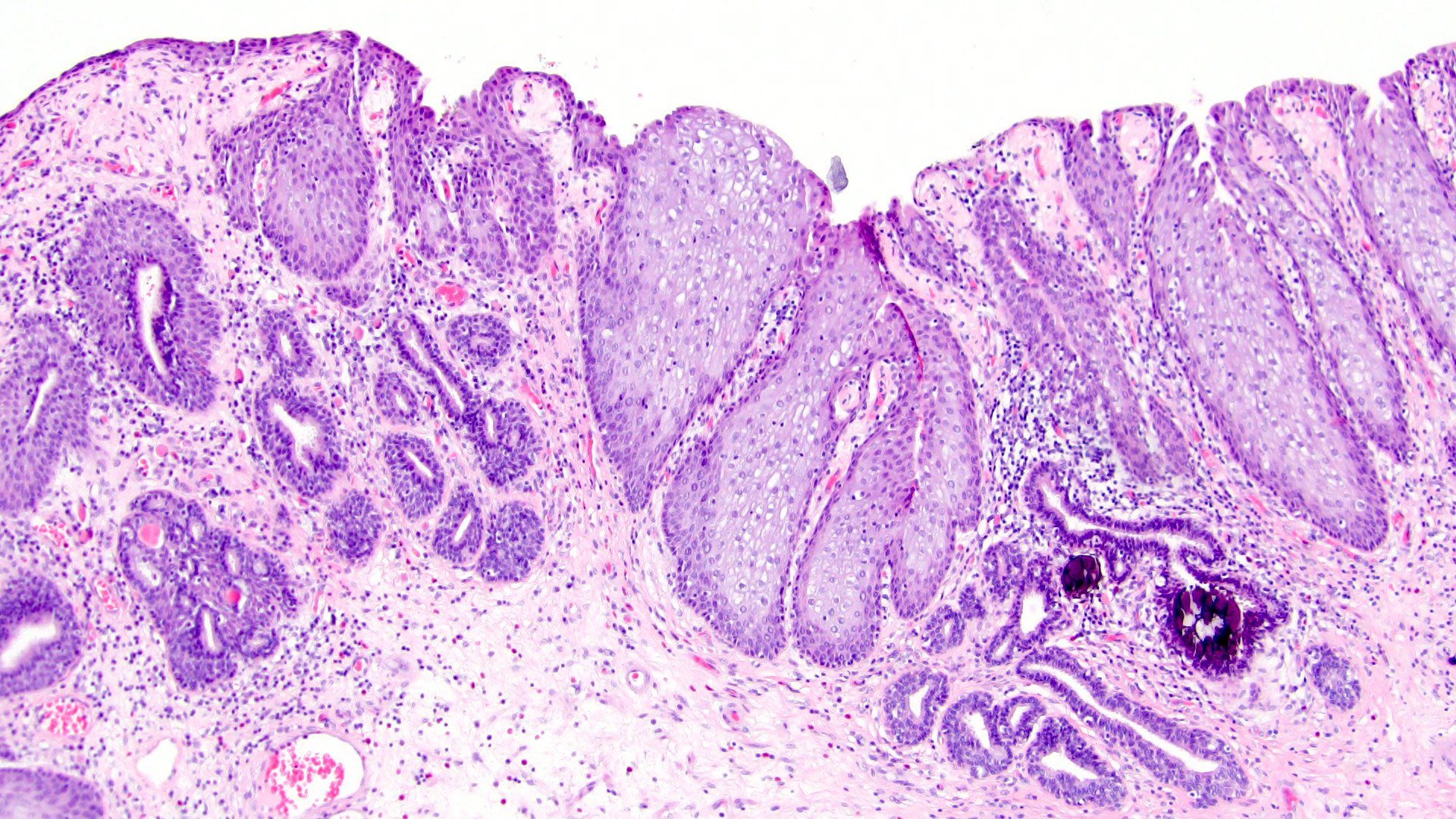
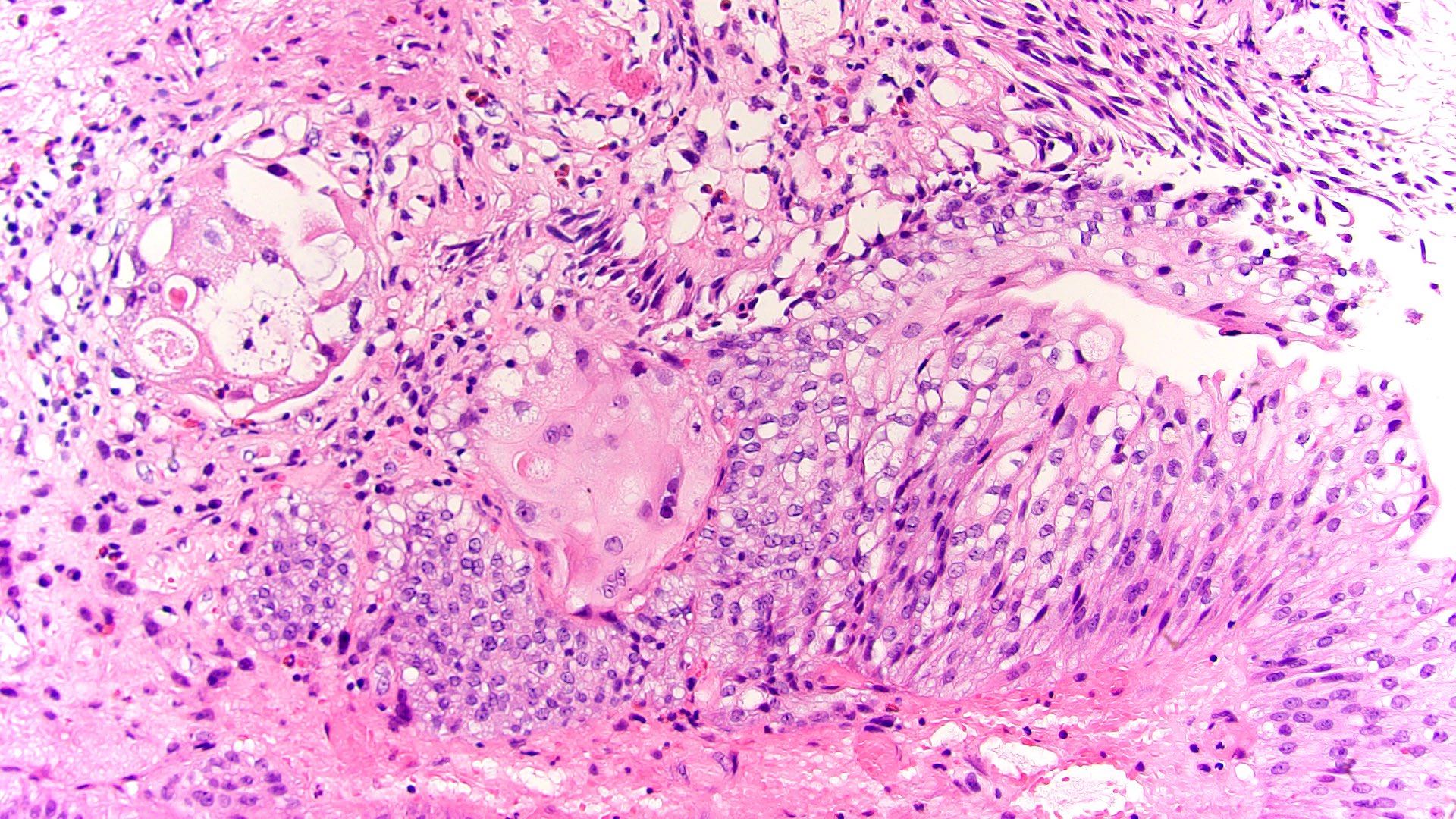
Microscopic (histologic) description
- Nonkeratinized squamous metaplasia:
- Epithelium has abundant intracytoplasmic glycogen, like vaginal or cervical epithelium
- Trigone in women may have glycogenated nonkeratinizing squamous mucosa and is considered as a normal histologic variant with no significantly increased risk for squamous carcinoma
- May not be reported if lacking associated dysplastic changes
- Keratinizing squamous metaplasia:
- Hyperkeratotic squamous epithelium with or without parakeratosis (Urol Int 2008;81:247)
- Presence and extent of keratinizing squamous metaplasia should be reported
Microscopic (histologic) images
Cytology description
- Benign squamous cells
Positive stains
- Important to rule out premalignant or invasive changes in squamous differentiation (p53 variable, wild type expression)
- Squamous cell markers: p63, p40, CK5/6, CK14 (Spinal Cord 2003;41:432)
- Increased EGFR expression and frequent loss of FOXA1 (Am J Surg Pathol 2006;30:883)
Negative stains
- Uroplakin II, CK7, CK20 (loss of umbrella cells), GATA3 (only basal)
- HPV ISH
Molecular / cytogenetics description
- Molecular drivers of keratinizing squamous metaplasia are poorly studied but at least 1 human tissue regeneration model implicates PPARy and PTEN in its development (Am J Pathol 2013;182:449)
Sample pathology report
- Bladder, biopsy:
- Keratinizing squamous metaplasia; ~20% in submitted sample (see comment)
- Comment: Entire tissue received was submitted to rule out premalignant or invasive lesions. If clinical concern remains on close clinical follow up, sampling of multiple areas is recommended.
Differential diagnosis
- Radiation atypia:
- Degenerative type epithelial changes, pseudocarcinomatous hyperplasia, multinucleation, fibrin thrombi
- Squamous papilloma:
- Exophytic papillary fibrovascular cores lined by benign squamous epithelium
- Lack of inflammation or koilocytosis
- Squamous dysplasia:
- Atypia, lack of maturation, increased mitoses, high N/C ratio
- If full thickness, qualifies for in situ squamous cell carcinoma
- Urothelial carcinoma in situ (CIS):
- Marked full thickness urothelial atypia
- No keratinization or intercellular bridges
- Squamous cell carcinoma (renal pelvis, ureter and bladder):
- Marked atypia, hemorrhage, necrosis, invasion into lamina propria
- Rule out more common urothelial carcinoma with variable amount of squamous differentiation
- Verrucous hyperplasia:
- Church spire-like multilayering, benign cytology
- Verrucous carcinoma:
- Large size
- Well differentiated tumor with broad based invasive front, lymphocytic inflammation at the base
- Condyloma acuminatum:
- Exophytic proliferation of nonkeratinizing squamous changes with viral cytopathic effect exhibited by koilocytosis (perinuclear clearing with nuclear membrane irregularity), binucleation
- No deep extension into lamina propria
- Associated with urethral changes in immunosuppressed
Additional references
Board review style question #1
Board review style answer #1
A. Extent of disease. More extensive squamous metaplasia is associated with increased risk of in situ and invasive squamous cell carcinoma. The cut off percentage is not established but the patient will be recommended for frequent follow ups.
Comment Here
Reference: Squamous metaplasia
Comment Here
Reference: Squamous metaplasia
Board review style question #2
A 45 year old woman with a history of lupus erythematosus has urgency, frequency and irritation during micturition for 6 months. She undergoes cystoscopy with irregularity in bladder mucosa. A bladder biopsy reveals vaginal type mucosa without any dysplasia. The biopsy is most likely taken from which of the following areas?
- Anterior bladder wall
- Bladder neck
- Near ureteral orifices
- Trigone of bladder
Board review style answer #2
D. Trigone of bladder. Trigone of bladder may have vaginal type or glycogenated nonkeratinizing mucosa without any associated abnormality in females. In this patient, the biopsy was done to rule out flat carcinoma in situ, which may clinically mimic interstitial cystitis. Interstitial cystitis is a condition of unknown etiology, with some cases associated with autoimmune disorders, such as lupus erythematosus.
Comment Here
Reference: Squamous metaplasia
Comment Here
Reference: Squamous metaplasia