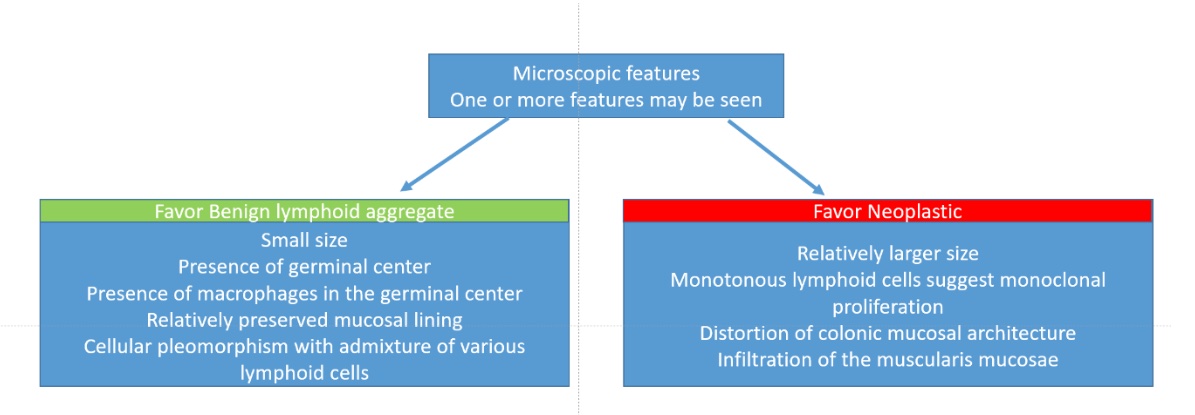
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kantu T, Rishi A. Lymphoid polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anuslymphoidpolyp.html. Accessed December 26th, 2024.
Definition / general
- Benign lesion that may endoscopically resemble a mucosal polyp
- Predominantly asymptomatic and incidental
Essential features
- Endoscopically, these lesions may appear as small nodules (Case Rep Gastrointest Med 2018;2018:5758689)
- Frequently sampled as a polyp biopsy or polypectomy
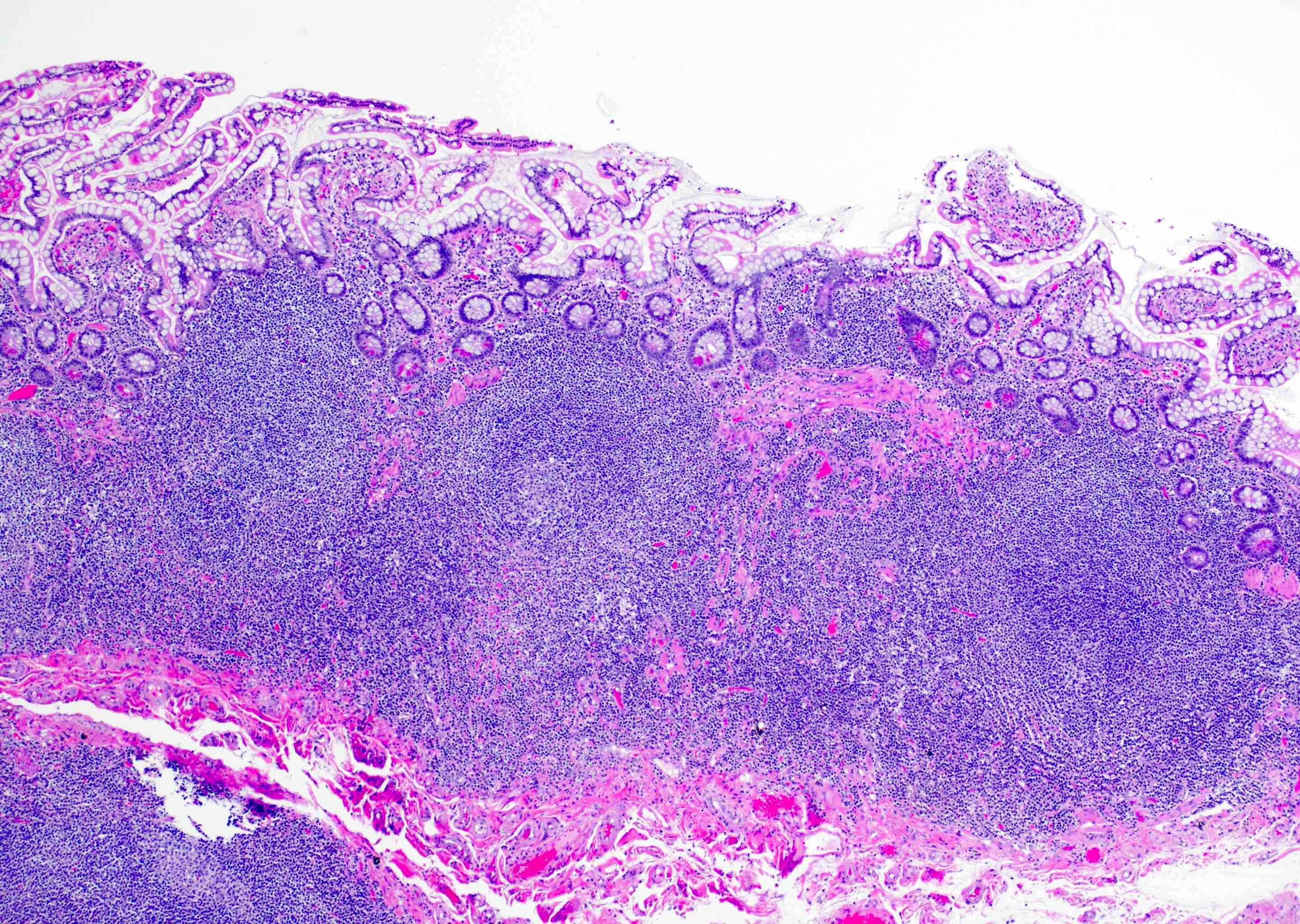
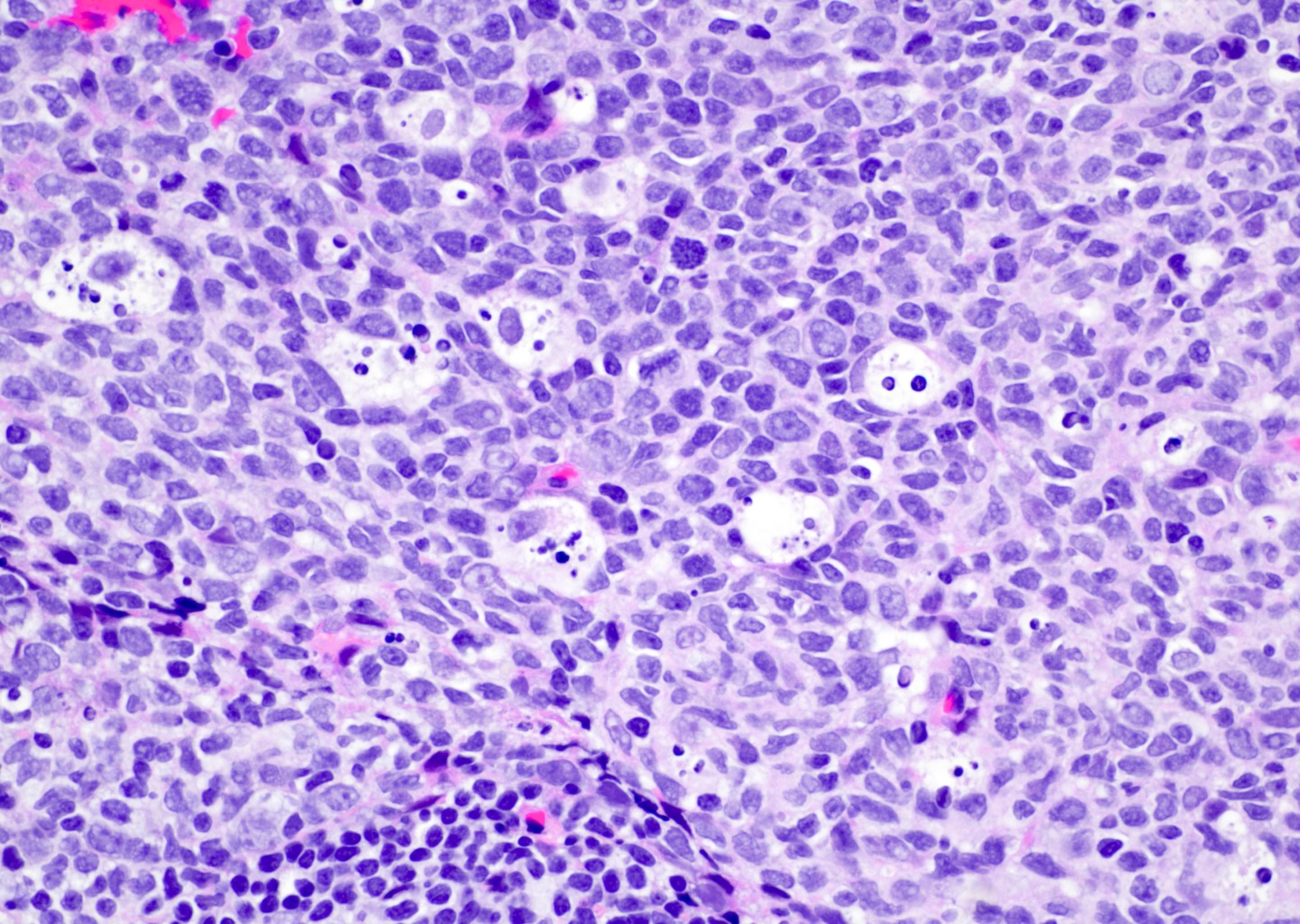
- Consideration of a neoplastic hematolymphoid process is suggested when the lymphoid aggregate appears monotonous and without an obvious germinal center; very small nonneoplastic lymphoid follicles may not develop germinal centers
Terminology
- Also called nodular lymphoid hyperplasia, lymphoid aggregate, rectal tonsil
- The term pseudolymphoma is not recommended
- Various terminologies may be used to report the findings of lymphoid polyp on a pathology report
- May be reported as reactive lymphoid aggregate if there is a prominent germinal center with polymorphous population of cells and tingible body macrophages
- Other reporting terminology may be colonic mucosa with prominent lymphoid aggregate; otherwise with no significant histopathological changes
- The latter may be used when there is no other associated lesion in addition to the colonic lymphoid polyp
- Note: there are instances when certain lesions, such as hyperplastic polyp or sessile serrated lesions / polyp, may occur alongside lymphoid polyp (see Microscopic (histologic) images)
Epidemiology
- More frequent in younger population and in children
- Nodular lymphoid hyperplasia, normally between 2 and 10 mm, may occur as a normal physiology (World J Gastrointest Endosc 2014;6:534)
- Certain immunodeficiency disorders and infections are associated with prominent lymphoid aggregates and may appear polypoid on endoscopic examination
- Examples include common variable immunodeficiency (CVID), selective IgA deficiency, Giardia infection, human immunodeficiency virus infection (uncommon), celiac disease and Helicobacter pylori infection
Sites
- Widely distributed throughout the stomach, small intestine and large bowel
- Polypoid endoscopic findings are more frequent in the colon and particularly in the ileocecal region because of prominent Peyer patches
Pathophysiology
- Lymphoid follicles may occur as the normal component of intestinal or gut associated mucosal lymphoid tissue (Ann N Y Acad Sci 2010;1207:E86)
- Gut associated lymphoid tissue (GALT) contains a significant percentage of immune cells (up to 70%)
- Mucosa overlying the lymphoid follicles is specialized follicle associated epithelium that is rich in macrophages and specialized antigen presenting cells (Biomedicines 2022;10:226)
- Average diameter of lymphoid aggregates ranges from 0.1 to 0.7 mm
- Reactive hyperplasia of GALT due to various infections can occur and lead to the appearance of polypoid or granular mucosa
- Associated with adenovirus infection, immunodeficiency (low IgA and IgM)
- EBV associated with immunosuppression may cause progression of the benign lymphoid follicle to lymphoma (Am J Surg Pathol 2019;43:1253)
Etiology
- No specific etiology has been associated and such lesions are frequently seen
- Certain specific conditions have an association; before considering a strong association be reported on pathology diagnosis, it is recommended to have more clinical information
- ~20% of adults with CVID may have nodular lymphoid hyperplasia or have more frequent lymphoid polyps; diffuse nodular hyperplasia may occur more frequently in the proximal small bowel (Indian J Pathol Microbiol 2009;52:530)
Clinical features
- Usually localized but may show diffuse involvement of mucosa when the portion of colon is diverted from the fecal stream (see Colon-Diversion colitis)
- Rectal lymphoid polyps are usually asymptomatic but colonic lymphoid polyps may present with gastrointestinal bleeding
- Children: multiple lesions; larger lymphoid polyps may cause intestinal obstruction and intussusception
- Adults: usually an isolated lesion
- Subtypes: idiopathic (most common), reactive, hypogammaglobulinemia associated
- Awareness of associated conditions such as CVID or IgA deficiency can be helpful to correlate clinical findings with histology
- Such systemic associations are more common with lymphoid aggregates in the small bowel and with increased numbers of lymphoid aggregates at an unusual mucosal site
- Frequent physiological lymphoid aggregates normally occur as Peyer patches in the ileocecal region and should generally not raise concern
- Nodular lymphoid hyperplasia is associated with some other conditions, such as common variable immunodeficiency, selective IgA deficiency, Giardia infection, human immunodeficiency virus infection, celiac disease and Helicobacter pylori infection, etc. (Arch Pathol Lab Med 2013;137:83)
- Associated conditions are due to the antigenic stimulation of lymphoglandular complexes
- A study done on lymphoid aggregates suggests prediction of chronic diarrhea in a subset of patients
- References: Case Rep Surg 2019;2019:9017863, Int J Colorectal Dis 1991;6:165, Indian J Pathol Microbiol 2009;52:530, Endoscopy 2013;45:320, Toxicol Pathol 2006;34:599
Diagnosis
- Diagnosis is made on light microscopy on routine H&E stain
- Special stains are usually not required except when the lymphoid aggregate appears neoplastic on the H&E stain
Prognostic factors
- Overall favorable outcome with no follow up required for benign lymphoid aggregates
Case reports
- 47 year old man with a history of left colon cancer, left colon resection for 12 years and rectal bleeding (Case Rep Pathol 2015;2015:646270)
- 64 year old woman with change in bowel habit and anemia (Case Rep Gastrointest Med 2018;2018:5758689)
- 11 cases of GALT associated pseudoinvasion / epithelial misplacement (J Pathol Transl Med 2020;54:135)
Treatment
- Polypectomy
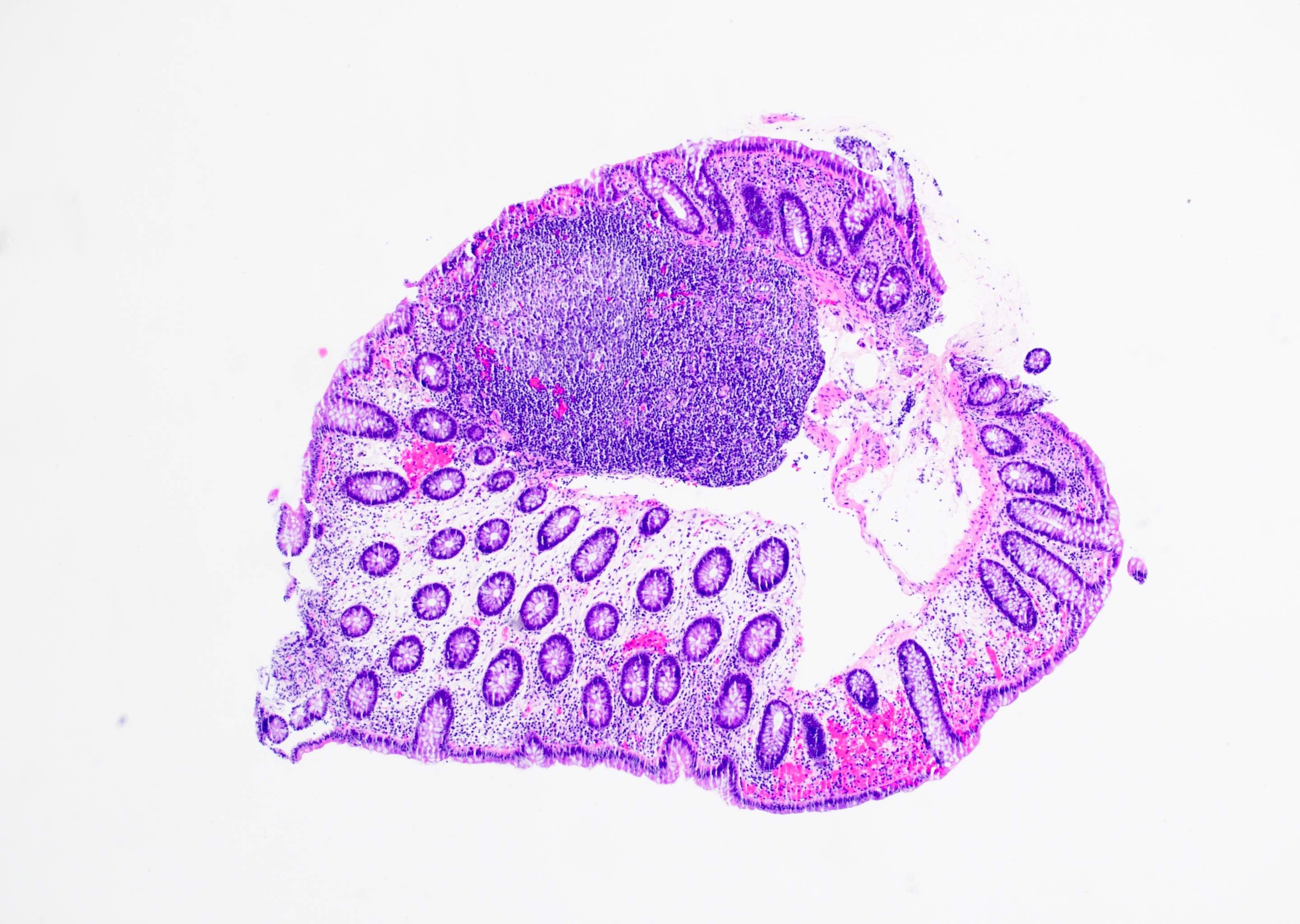
Gross description
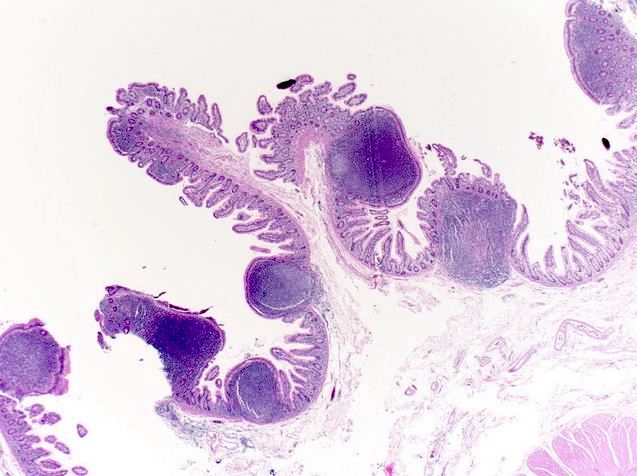
- Small polypoid or raised lesions, which generally are sessile or may have broad stalk
- Surface erosions with acute inflammation over the lymphoid polyp / follicle clinically and endoscopically may appear as an aphthoid ulceration, which may indicate possibility of Crohn's colitis but is not diagnostic
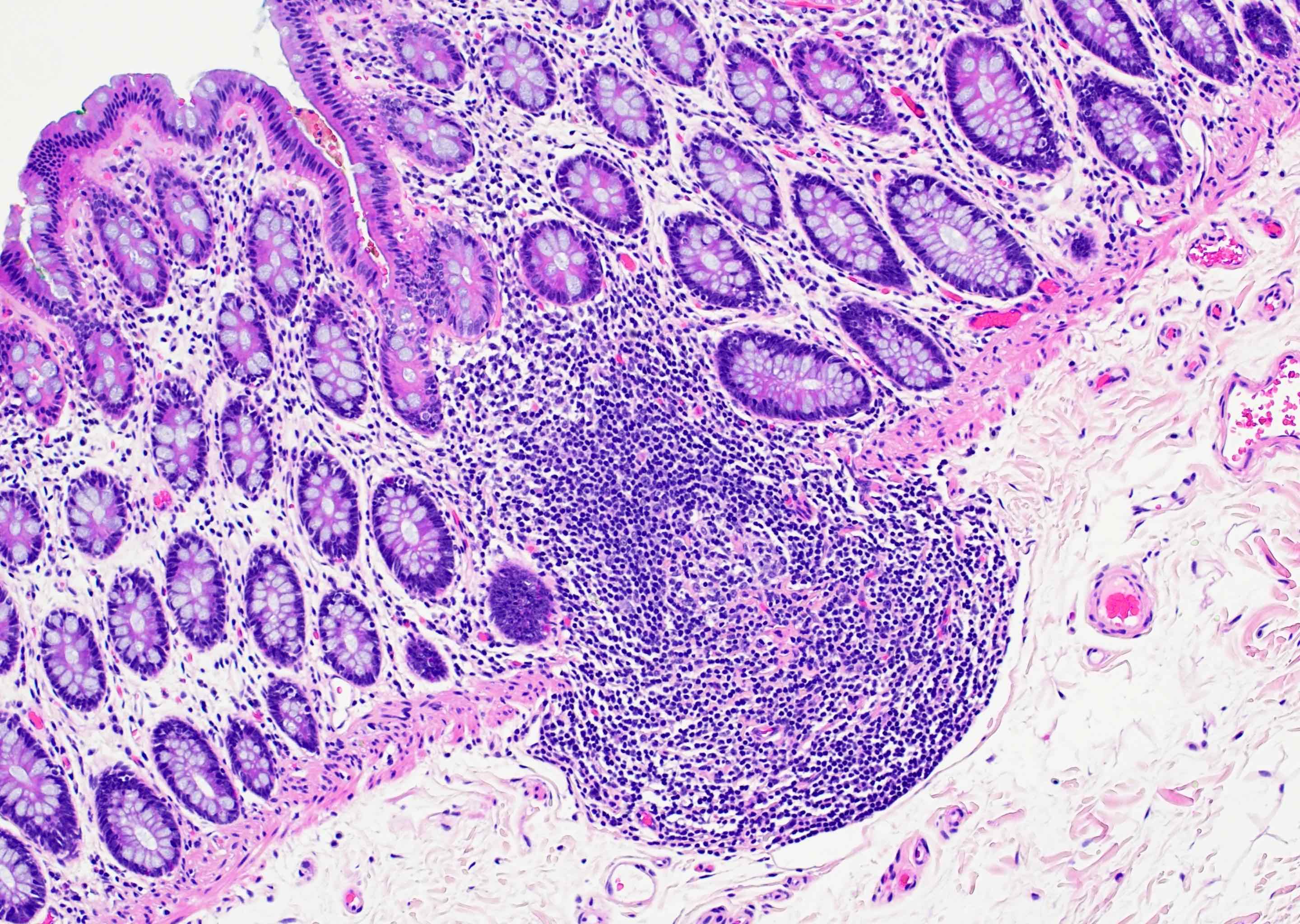
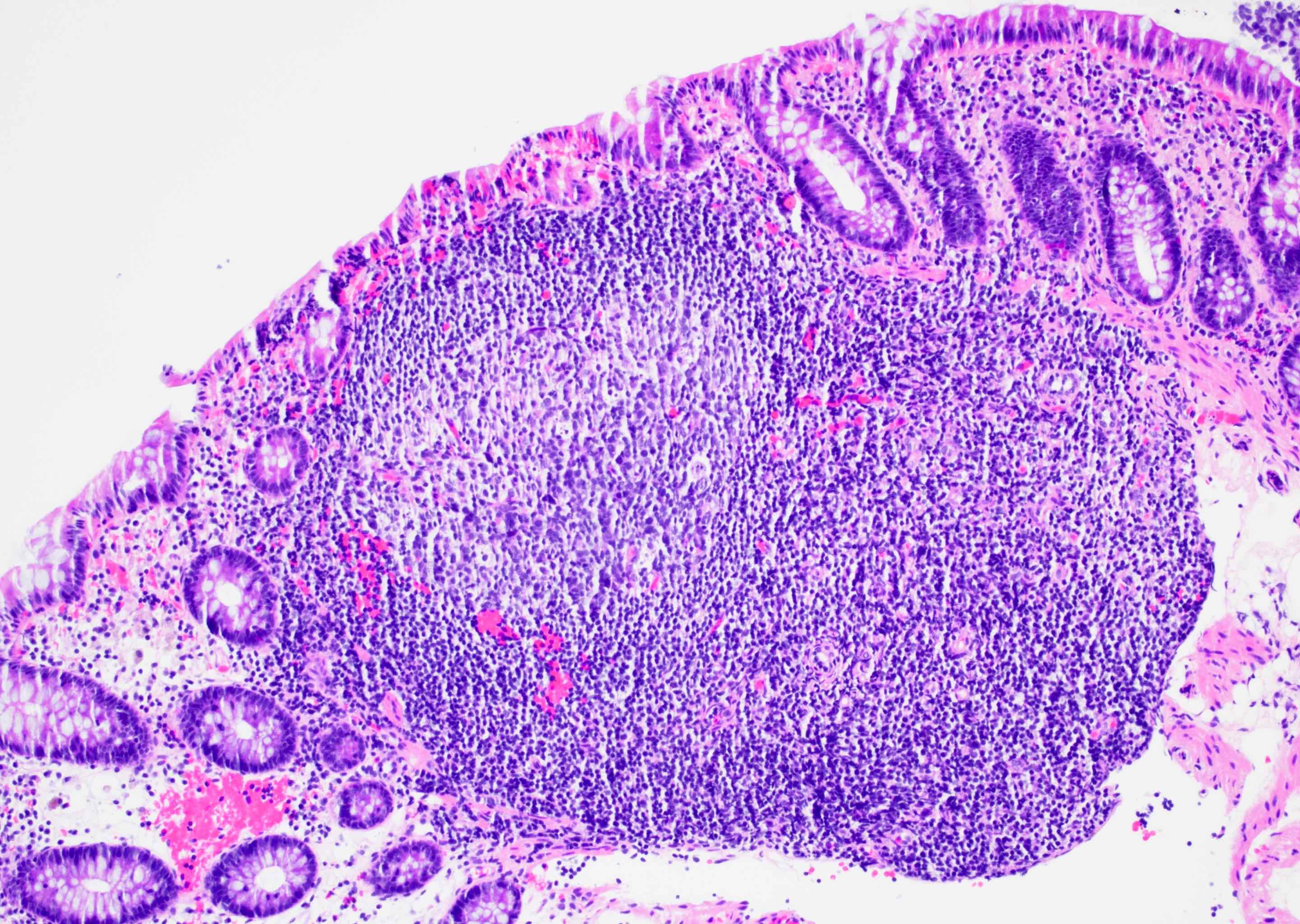
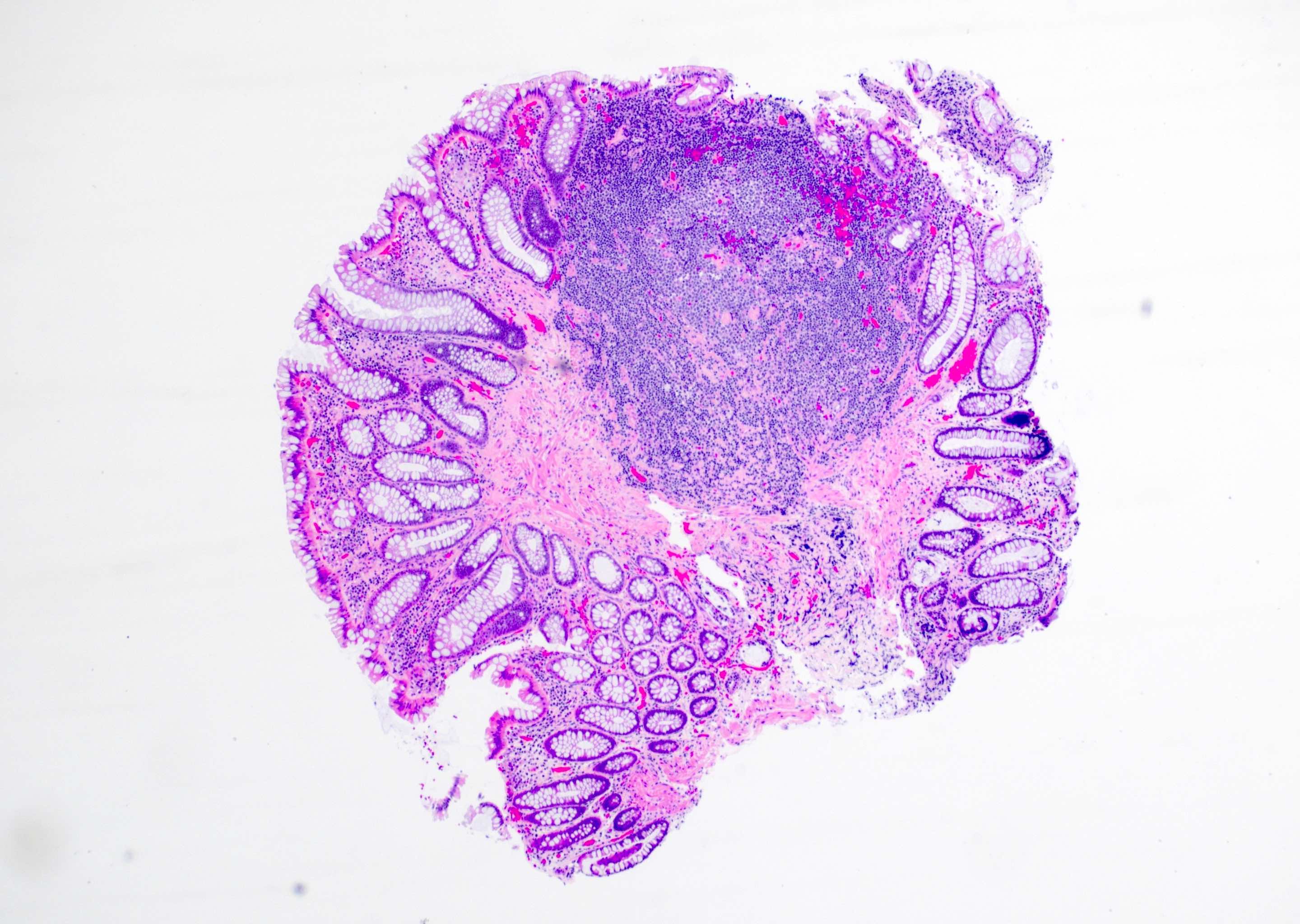
Microscopic (histologic) description
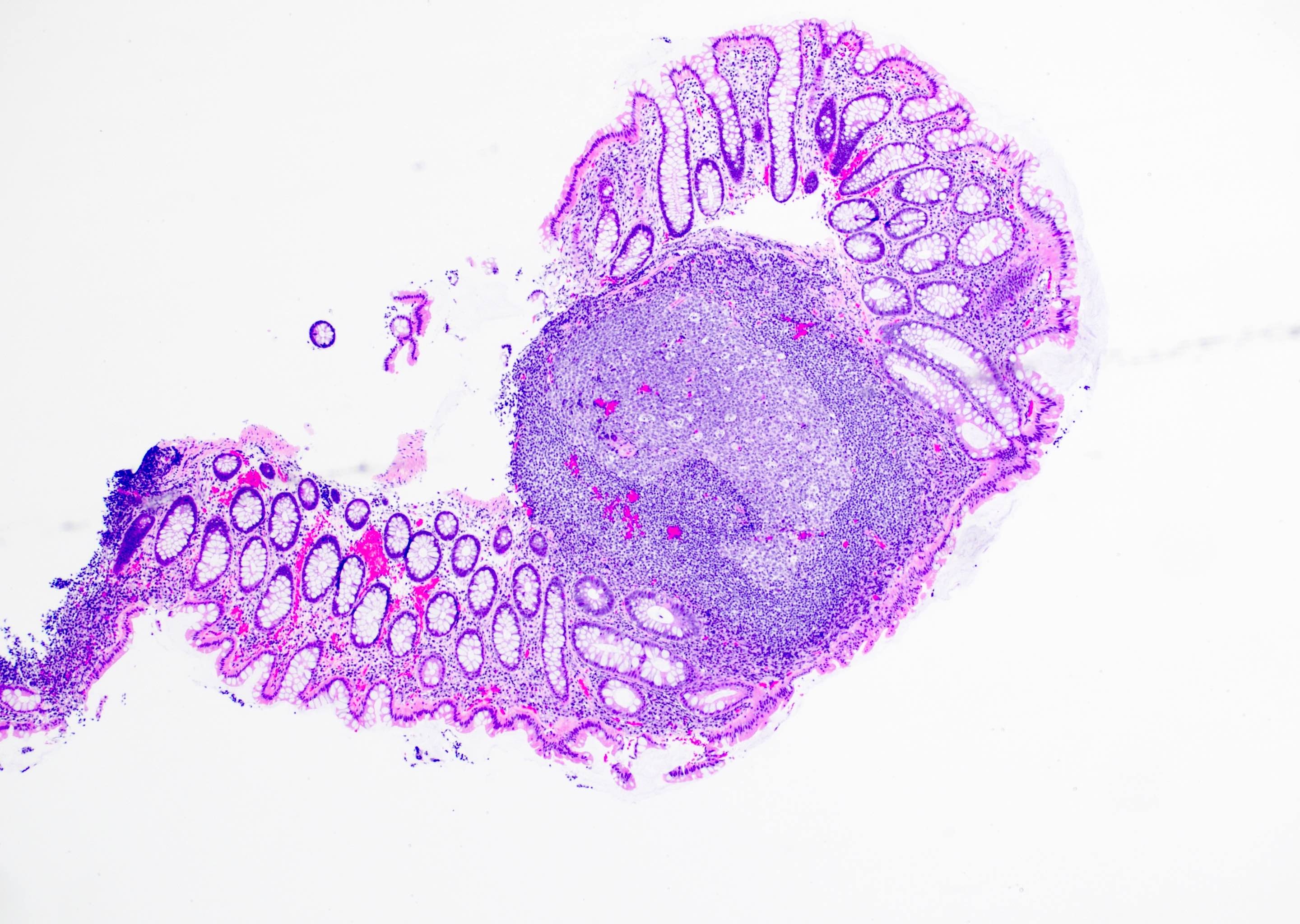
- Intestinal mucosal associated lymphoid tissue (MALT) is distributed throughout the large intestinal tract as lymphoglandular complexes (World J Gastrointest Oncol 2019;11:59)
- They may be located within the lamina propria or extend to the deeper layers within muscularis mucosae or submucosa
- Antigenic stimulation of lymphoglandular complex leads to prominent lymphoid aggregates, thereby forming lymphoid polyp
- Benign lymphoid follicles covered by columnar (colonic mucosa) or transitional epithelium (anorectal mucosa)
- Surface epithelium is usually flat but may have reactive epithelial changes in the form of surface hyperplasia in the distal rectum
- Germinal centers may be seen in larger lymphoid polyps
- Reactive lymphoid follicles may also be present in the lamina propria (more commonly) or submucosa
- Intraepithelial lymphocytes are commonly present over a lymphoid polyp and should not be considered pathologic
- Intraepithelial neutrophils over a lymphoid follicle is a pathologic finding and should be reported in the final diagnosis as focal acute inflammation
- It is discouraged to use the term colitis if the acute inflammation is identified in focal areas; this is to prevent the patient from falsely being clinically labeled with chronic inflammatory bowel disease
- Presence or absence of dysplasia in the surface epithelium of the lymphoid polyp is not dependent on the nature of underlying lymphoid follicle
- Herniation of normal colonic epithelium or dysplastic epithelium (tubular adenoma) may occur and could pose a diagnostic challenge to evaluate for invasion
- This could be further challenging if the herniated epithelium has high grade dysplasia (Am J Surg Pathol 2018;42:1083)
Positive stains
- Admixture of CD20 positive B cells and CD3 positive T cells
- Kappa and lambda stains show polyclonal cells
- Ki67 proliferation index is low
- Reference: Toxicol Pathol 2006;34:599
Negative stains
- BCL2 is negative in germinal centers (only scattered T cells in germinal centers stain positive)
Sample pathology report
- Colon, polyp, polypectomy:
- Colonic mucosa with lymphoid aggregate; otherwise, with no significant histopathologic findings (see comment)
- Comment: The mucosal lymphoid tissue shows polymorphous population of lymphoid tissue. There is an admixture of CD20 positive B cells and CD3 positive T cells. CD45 stain shows no aberrant expression in the regions stained by CD20.
- Note: Immunohistochemical stains are not required for the majority of cases. Comment may be added for cases where there are immunohistochemical stains performed based on morphologic (H&E) concern. In routine cases without immunohistochemistry, comment is not required.
Differential diagnosis
- MALT lymphoma and follicular lymphoma:
- More uniform appearance of small to medium sized type B lymphocytes with histological overlap with MALT lymphoma
- Translocation t(14;18)(q32;q21) is a characteristic finding for follicular lymphoma
- Lymphoma immunohistochemical panel workup is essential for the subclassification of neoplastic hematolymphoid process
- Inverted lymphoglandular polyp (Case Rep Pathol 2015:2015:646270):
- In some instances, the dysplastic colonic epithelium may herniate or extend into the prominent mucosal or submucosal lymphoid aggregates
- Although the location of dysplastic epithelium may raise a concern for an invasive malignancy, the herniated tissue still retains the mucosal morphology with intact lamina propria and without any desmoplastic reaction
- Smooth muscle markers such as desmin immunohistochemistry may be misleading in cases where herniation of dysplastic epithelium extends into submucosal lymphoid aggregates
- On the contrary, invasive adenocarcinoma extending to the lymphoid aggregate will lack lamina propria and may have angulated pattern of arrangement of malignant glands
- Frequently, fibrous stroma or desmoplastic reaction will accompany invasive malignancy extending to the lymphoid aggregates
Board review style question #1
A 14 year old boy presented with small sessile polypoid areas in the terminal ileum. A wide mucosal biopsy was performed with concern for inflammatory bowel disease. There was no clinical history of failure to thrive or frequent infections. Which of the following is the most likely diagnosis?
- IgA deficiency
- MALT lymphoma
- Mucosa associated lymphoid tissue (Peyer patches)
- Small bowel follicular lymphoma
Board review style answer #1
C. Mucosa associated lymphoid tissue (Peyer patches). Mucosa associated lymphoid tissue is the most likely diagnosis because of the age of the patient and presence of reactive germinal centers and lymphoid follicles, which do not show a fused pattern. Answer A is incorrect because IgA deficiency disease will present with numerous lymphoid follicles in the upper gastrointestinal tract and higher propensity to infections. Answers B and D are incorrect because lymphomas will appear to have monotonous small to medium sized lymphocytes and generally lack lymphoid aggregate.
Comment Here
Reference: Lymphoid polyp
Comment Here
Reference: Lymphoid polyp
Board review style question #2
Board review style answer #2
C. Polymorphous population of lymphocytes in the germinal centers. Nonneoplastic germinal center will have admixture of cells of variable sizes. Answer B is incorrect because a neoplastic hematolymphoid process will have a monotonous appearance of small to medium sized lymphocytes with high Ki67 proliferation index. Answer A is incorrect because benign follicles frequently show germinal center and presence of tingible body macrophages. Answer D is incorrect because BCL2 should be negative in germinal centers of benign mucosal lymphoid aggregate.
Comment Here
Reference: Lymphoid polyp
Comment Here
Reference: Lymphoid polyp