Table of Contents
Definition / general | Epidemiology | Sites | Etiology | Clinical features | Oncocytoid renal cell carcinoma after neuroblastoma | Diagnosis | Laboratory | Radiology description | Radiology images | Classification | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Perrino C, Zynger DL, Tretiakova M. Neuroblastoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/adrenalneuroblastoma.html. Accessed January 8th, 2025.
Definition / general
- Primitive neoplasm of neuroectodermal origin
- Composed of immature neuroblasts
Epidemiology
- 4th most common malignant tumor in childhood
- Median age at presentation 23 months, peak 0-4 years (J Paediatr Child Health 2012;22:103)
- Slightly more common in boys (1.2:1) (J Paediatr Child Health 2012;22:103)
- Rarely diagnosed prenatally (most often in 3rd trimester) on ultrasound (Ultrasound Obstet Gynecol 1999;13:446, Ultrasound Obstet Gynecol 1999;13:351, Ultrasound Obstet Gynecol 1997;10:68)
Sites
- Occurs anywhere in distribution of sympathoadrenal neuroendocrine system
- Most in adrenal gland (~40%), followed by connective / subcutaneous / soft tissue (~20%), retroperitoneum (~15%), mediastinum (~10%) (SEER Program: NIH Pub No 99-4649; Bethesda, MD, 1999)
Etiology
- Clonal proliferation of immature cells of neural crest origin
- Definitive risk factors not established
Clinical features
- Clinical features depend on location / extent of tumor
- Severe ill health, malnourishment, pain all suggest metastatic disease
- Abdominal mass
- Watery diarrhea syndrome (6%)
- Opsoclonus-myoclonus-ataxia syndrome: rapid eye movements, ataxia, irregular muscle movements
- Heterochromia iridis: cervical, mediastinal neuroblastoma (prenatal / postnatal interruption of sympathetic tracts that mediate pigmentation of iris)
- Horner's syndrome (damage to sympathetic trunk resulting in miosis, ptosis, enophthalmos, anhidrosis): head, neck, thorax tumors
- Paralysis: paraspinal tumors
- Skin bruising associated with metastases to skin
- Raccoon eyes associated with metastases to orbit cause bruising and proptosis
- References: J Paediatr Child Health 2012;22:103, Lack: Tumors of the Adrenal Glands and Extraadrenal Paraganglia, AFIP 2007)
Oncocytoid renal cell carcinoma after neuroblastoma
- Renal neoplasms occurring in patients with a history of neuroblastoma (NB) do not represent a single entity but a heterogenous group of renal cell carcinomas (RCCs) (Am J Surg Pathol 2016;40:989)
- This RCC subtype is no longer listed as an independent WHO entity due to lack of distinctive immunohistochemical and molecular markers, however it remains a provisional RCC entity in the 2016 WHO classification
- Originally described in 1999 (Am J Surg Pathol 1999;23:772), see also Urology 2007;70:178.e13
- Patients with NB have a well documented increased risk of RCC compared with the general population but tumors that arise in these patients demonstrate diverse morphologic features, including:
- Oncocytoid appearance
- Appearance similar to the classic morphology of Xp11 or t(6;11) translocation RCC
- Features of hybrid oncocytic / chromophobe tumor
- Papillary RCC-like histology (Arch Pathol Lab Med 2016;140:1026, Am J Surg Pathol 2016;40:989)
Diagnosis
- Abdominal imaging (J Paediatr Child Health 2012;22:103) and laboratory markers (see below) are useful
Laboratory
- Urine biochemistry for catecholamines or their metabolites (dopamine, vanillylmandelic acid, homovanillic acid)
- Nonspecific markers: thrombocytosis, increased ferritin, neuron-specific enolase, lactate dehydrogenase (J Paediatr Child Health 2012;22:103)
Radiology description
- Irregularly shaped, lobulated, +/- calcification / necrosis / hemorrhage, usually heterogeneous on contrast-enhanced CT (Endocr Relat Cancer 2007;14:587)
Classification
Histologic classification systems
Staging
- Shimada Classification (J Natl Cancer Inst 1984;73:405)
- Histologic classification system first proposed in 1984 with prognostic implications
- International Neuroblastoma Pathology Classification System (INPC) (Cancer 1999;86:349)
- Original Shimada classification system was modified and renamed in 1999
- New system also shown to have prognostic implications (Cancer 1999;86:364)
- 3 subtypes of neuroblastoma: undifferentiated, poorly differentiated, differentiating
Subtype Description Undifferentiated - Tumor cells small to medium, indiscernible to small amount of cytoplasm, vague cytoplasmic borders
- Nuclei round to elongated, salt and pepper chromatin, distinct nucleoli
- No background neuropil
- Need ancillary studies to establish diagnosis
Poorly differentiated - Background neuropil present
- ≤ 5% of tumor cells are differentiating neuroblasts
Differentiating - Abundant background neuropil
- ≥ 5% of tumor cells are differentiating neuroblasts
- % of differentiating neuroblasts is more important criteria than amount of neuropil
- If present, Schwannian stromal development with mature / maturing ganglion cells <50% of tumor with a continuous transition zone to neuroblastomatous areas
- NOTE: undifferentiated and poorly differentiated neuroblastoma may have focal / diffuse areas with large, spindled, anaplastic, pleomorphic or even rhabdoid undifferentiated cells
Staging
- 2 main staging systems:
- International Neuroblastoma Staging System (INSS) (J Clin Oncol 1993;11:1466)
- Based on extent of surgical resection
- Must be applied after surgery for most accurate stage assignment
Stage Description 1 - Localized tumor with complete gross excision, with / without microscopic residual disease
- Ipsilateral lymph nodes negative for tumor microscopically
- Lymph nodes attached to and removed with primary tumor may be positive
2A - Localized tumor with incomplete gross excision
- Ipsilateral lymph nodes negative for tumor microscopically
2B - Localized tumor with / without complete gross excision
- Ipsilateral, nonadherent lymph nodes positive for tumor
- Enlarged contralateral lymph nodes must be negative for tumor microscopically
3 - Unresectable unilateral tumor infiltrating across the midline (midline is defined as the vertebral column)
- with / without regional lymph node involvement
OR - Localized unilateral tumor
- With contralateral regional lymph node involvement
OR - Midline tumor
- With bilateral extension by infiltration (unresectable) or by lymph node involvement
4 - Disseminated tumor to distant lymph nodes, bone, bone marrow, liver, skin and/or other organs (except as defined for stage 4S)
4S - Localized primary tumor (as defined for stage 1, 2A, or 2B) with dissemination limited to skin, liver and/or bone marrow (<10% of nucleated cells)
- Only in infants <1 year in age
- International Neuroblastoma Risk Group (INRG) Staging System (J Clin Oncol 2009;27:289, J Clin Oncol 2009;27:298)
- More recent
- Pre-surgical risk assessment tool
- Based on clinical features and imaging studies
Stage Description L1 - Localized tumor not involving vital structures as defined by list of image-defined risk factors (IDRF)
- Confined to one body compartment
L2 - Locoregional tumor
- One / more IDRF
M - Distant metastases (except stage MS)
MS - Children <18 months of age
- Metastases confined to skin, liver and/or bone marrow
- International Neuroblastoma Staging System (INSS) (J Clin Oncol 1993;11:1466)
Prognostic factors
- 2 staging systems (INSS, INRG) are incorporated into different risk stratification systems:
- Children's Oncology Group (Pediatr Blood Cancer 2013;60:985)
- Uses INSS stage, age, MYCN status, DNA ploidy, INPC histology
- Assigns one of three prognostic groups (low, intermediate, or high risk)
- INRG Criteria (J Clin Oncol 2009;27:289)
- Uses INRG stage, with age, histologic category, grade of differentiation, MYCN status, 11q status, ploidy
- Assigns one of four risk stratification groups (very low, low, intermediate, high)
- Children's Oncology Group (Pediatr Blood Cancer 2013;60:985)
- Many prognostic factors have been proposed, most robust of which include: histologic subtype, grade of tumor differentiation, stage, age at diagnosis, MYCN status (Pediatr Clin North Am 2015;62:225, J Clin Oncol 2009;27:289)
- Some additional favorable prognostic factors:
- Abundant lymphoid infiltrates
- Location in neck, thorax, pelvis
- Some additional unfavorable prognostic factors:
- MYC-N amplification (>10 copies/cell)
- ALK amplification (Nat Rev Cancer 2013;13:397)
- Chromosome 1p36.3 or 11q23 deletion
- Near-diploid DNA content (patients <18 months with metastatic disease)
- Increasing age
Case reports
- Neuroblastoma and adrenal morphologic features in anencephalic infants (Arch Pathol Lab Med 1979;103:119)
- Prenatal diagnosis of adrenal neuroblastoma by ultrasound (Ultrasound Obstet Gynecol 1999;13:446)
- 2 day old girl with bilateral neuroblastoma in situ (J Korean Med Sci 1993;8:99)
- 2 day old boy with congenital neuroblastoma with multiple metastases (J Korean Med Sci 2003;18:618)
- 9 month old girl with isolated enophthalmos (BMC Pediatr 2014;14:237)
- 11 month old girl with neuroblastoma and pathologic femur fracture (Acta Orthop Traumatol Turc 2013;47:60)
- 3 year old boy with raccoon eyes in a case of metastatic neuroblastoma (Indian J Dermatol Venereol Leprol 2012;78:740)
- 3 year old boy with abdominal neuroblastoma and inferior vena cava anomaly (Singapore Med J 2013;54:e201)
- 3 year old boy with pediatric bladder neuroblastoma (Can Urol Assoc J 2013;7:E609)
- 18 year old presenting with primary ovarian tumor and abdominal metastases (Am J Surg Pathol 1982;6:283)
- 30 year old man with solid mass of the right adrenal gland (Case Rep Oncol Med 2013;2013:393128)
- 38 year old woman with adult neuroblastoma of the ovary (J Cancer Res Ther 2010;6:367)
- 47 year old man with adrenal neuroblastoma (J Cancer Res Ther 2013;9:96)
- 61 year old man with metastatic composite paraganglioma with neuroblastoma (J Med Case Rep 2010;4:374)
- Chromaffin cell differentiation of a neuroblastoma after chemotherapy and radiotherapy (Am J Surg Pathol 2004;28:548)
Treatment
- Observation (J Paediatr Child Health 2012;22:103)
- Antenatal diagnosis, age <1 year, stage 4S tumor
- Surgery (J Paediatr Child Health 2012;22:103)
- Localized tumor with favorable biological characteristics
- Chemotherapy (J Paediatr Child Health 2012;22:103)
- Low risk, stage 4S disease with life-/organ-threatening symptoms
- Surgery and chemotherapy (J Paediatr Child Health 2012;22:103)
- High risk or unresectable stage III tumors (induction chemotherapy)
- Intermediate risk that is primarily unresectable (moderate chemotherapy)
- High risk metastatic disease (induction +/- postoperative myeloablative chemotherapy followed by autologous stem cell rescue)
- Radiotherapy (J Paediatr Child Health 2012;22:103)
- High risk disease
- Immunotherapy (Nat Rev Cancer 2013;13:397)
- High-risk patients with neuroblastoma can be maintained in continual remission with anti-GD2-specific monoclonal antibody therapy combined with GM-CSF with / without IL-2
- Future directions (Nat Rev Cancer 2013;13:397)
- ALK-targeted therapy is being explored
Gross description
- Variable, circumscribed, ovoid mass to multilobated tumor
- Hemorrhagic with vague, bulging lobules
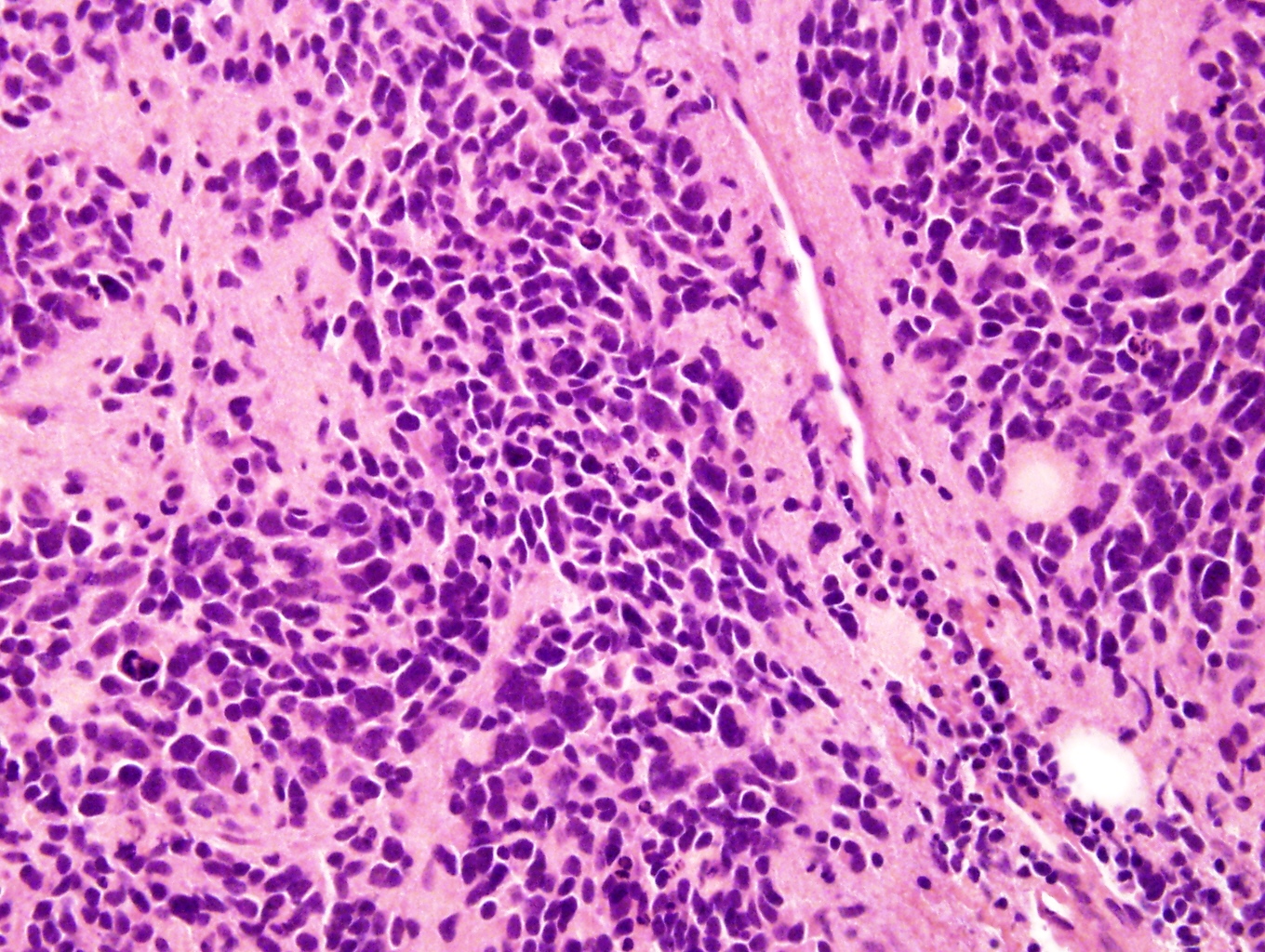
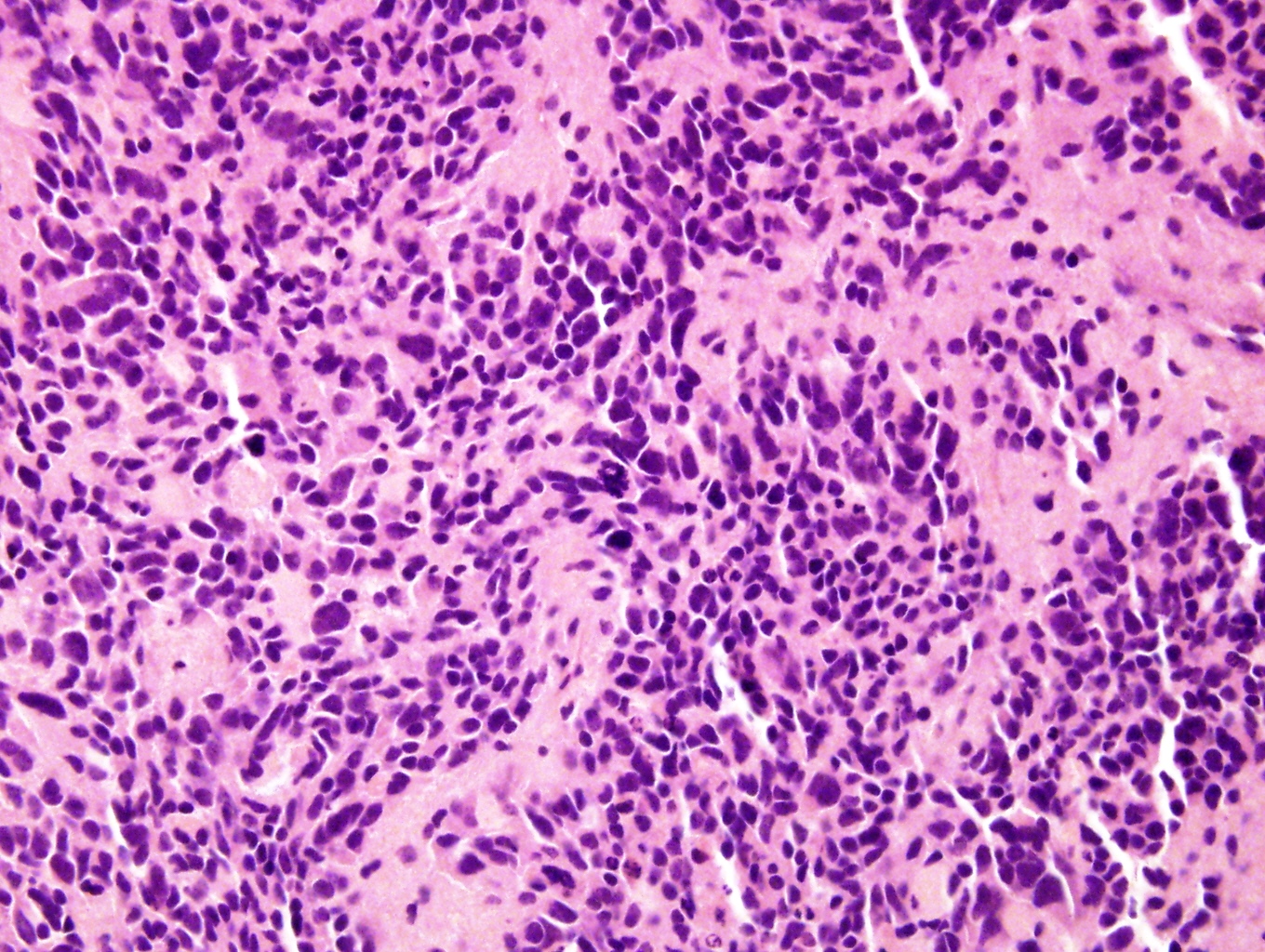
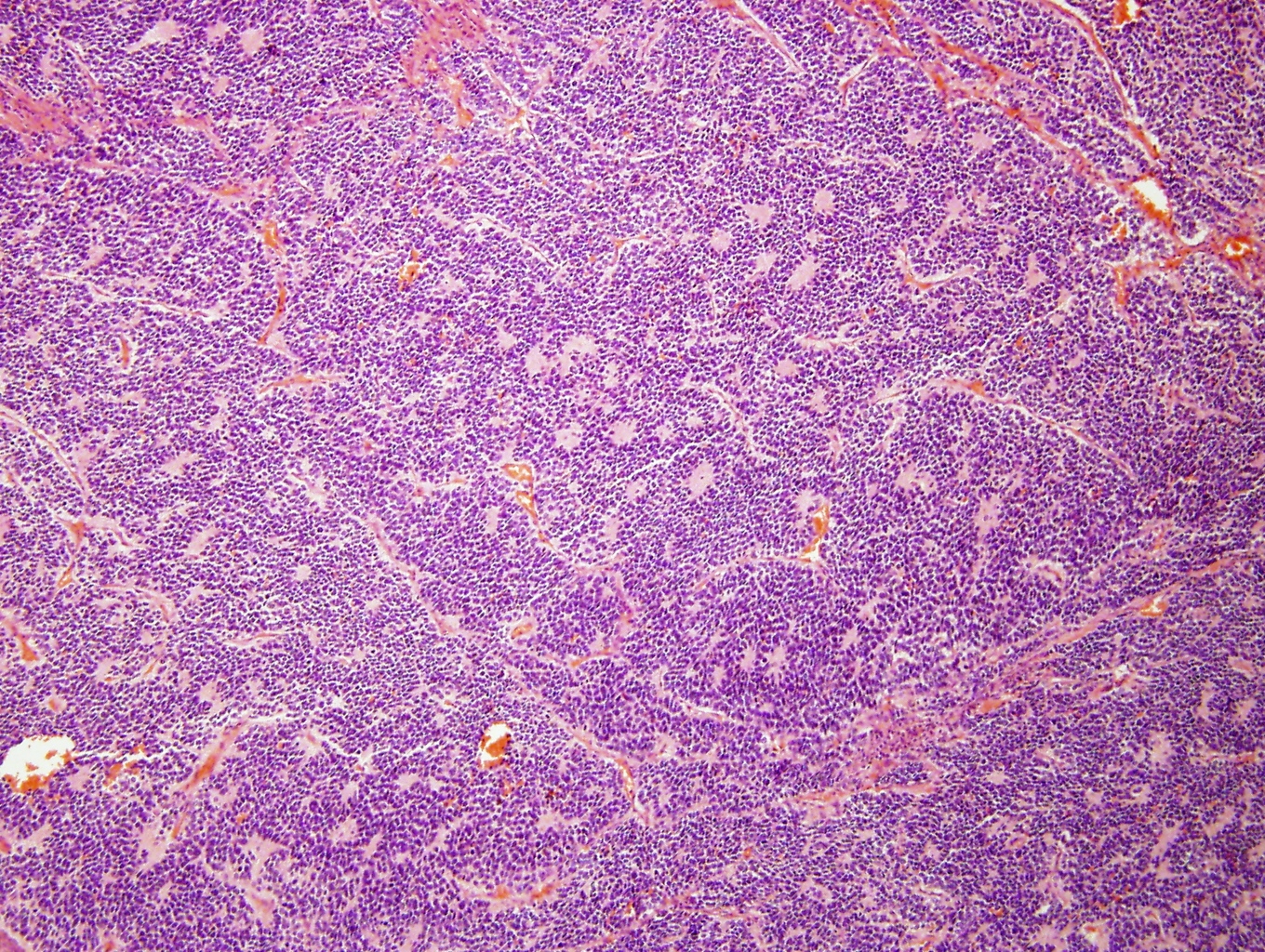
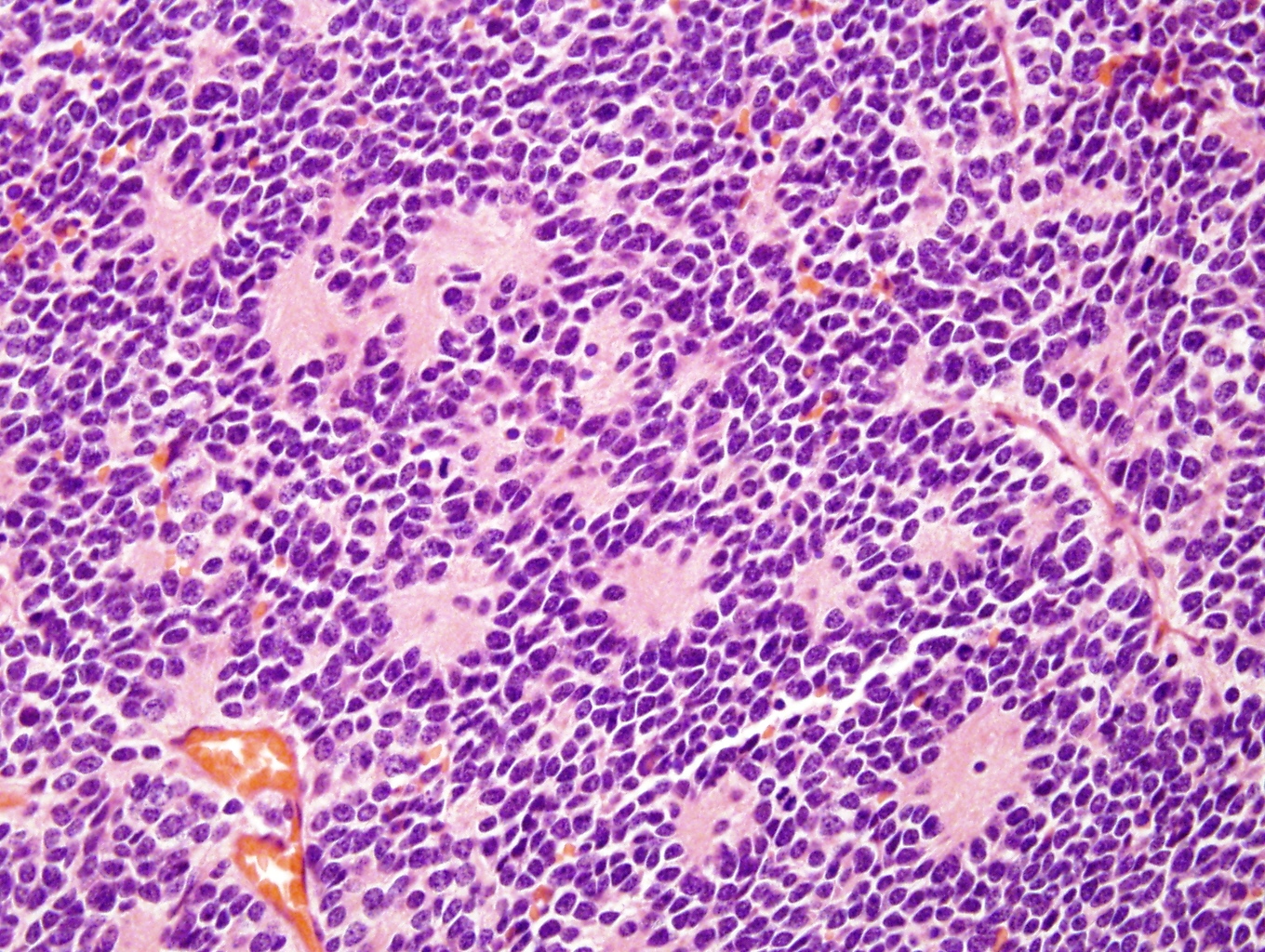
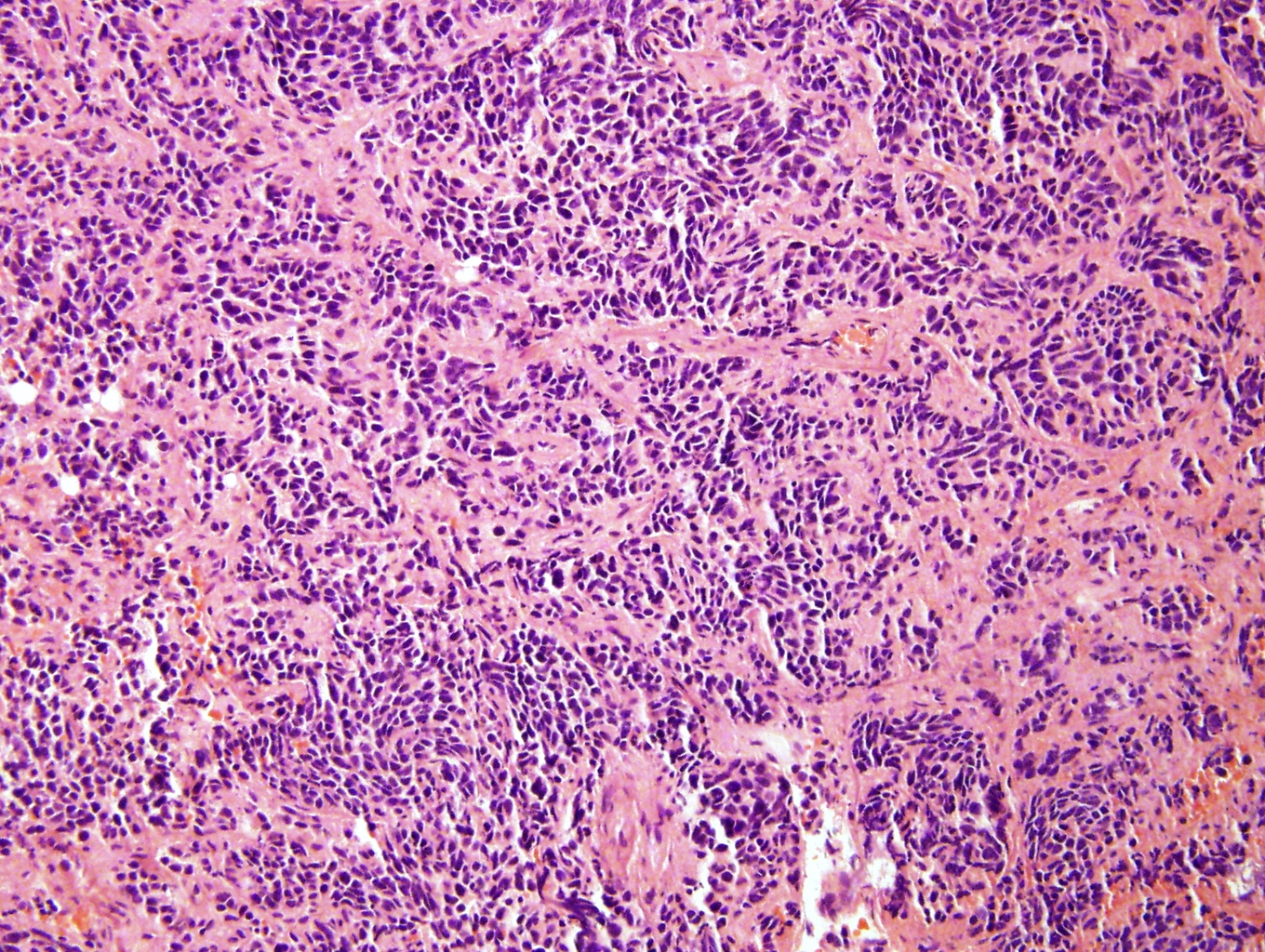
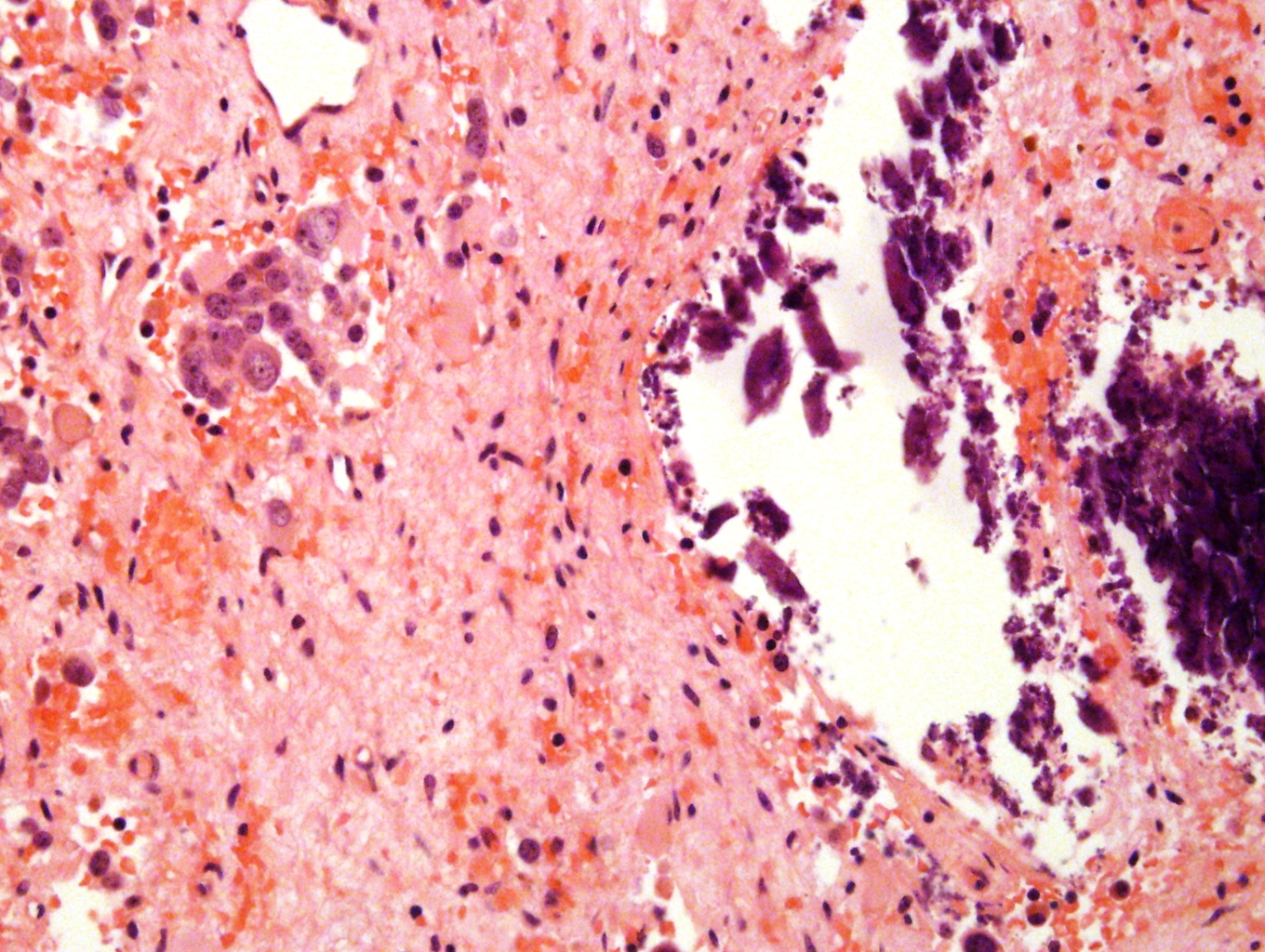
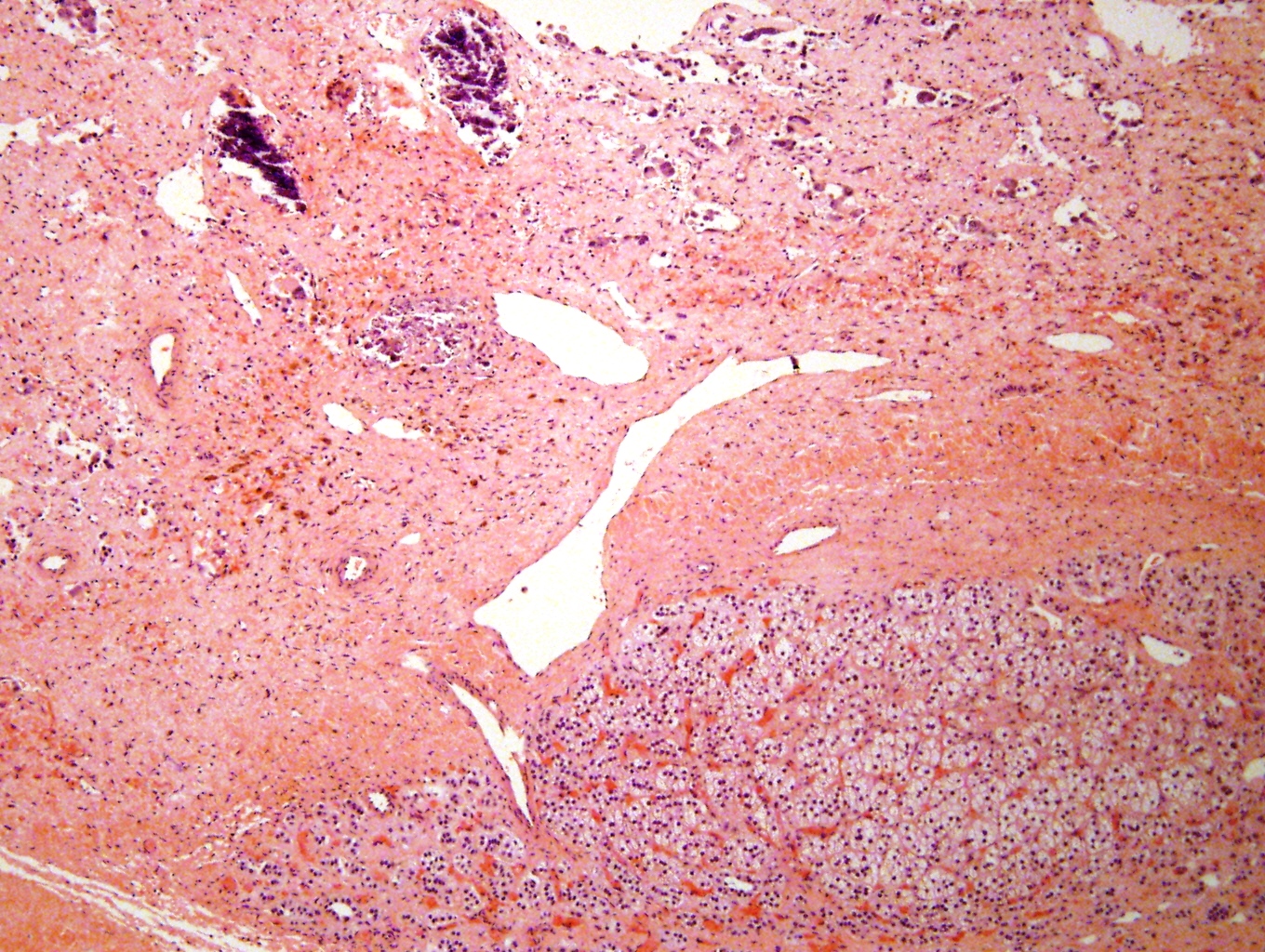
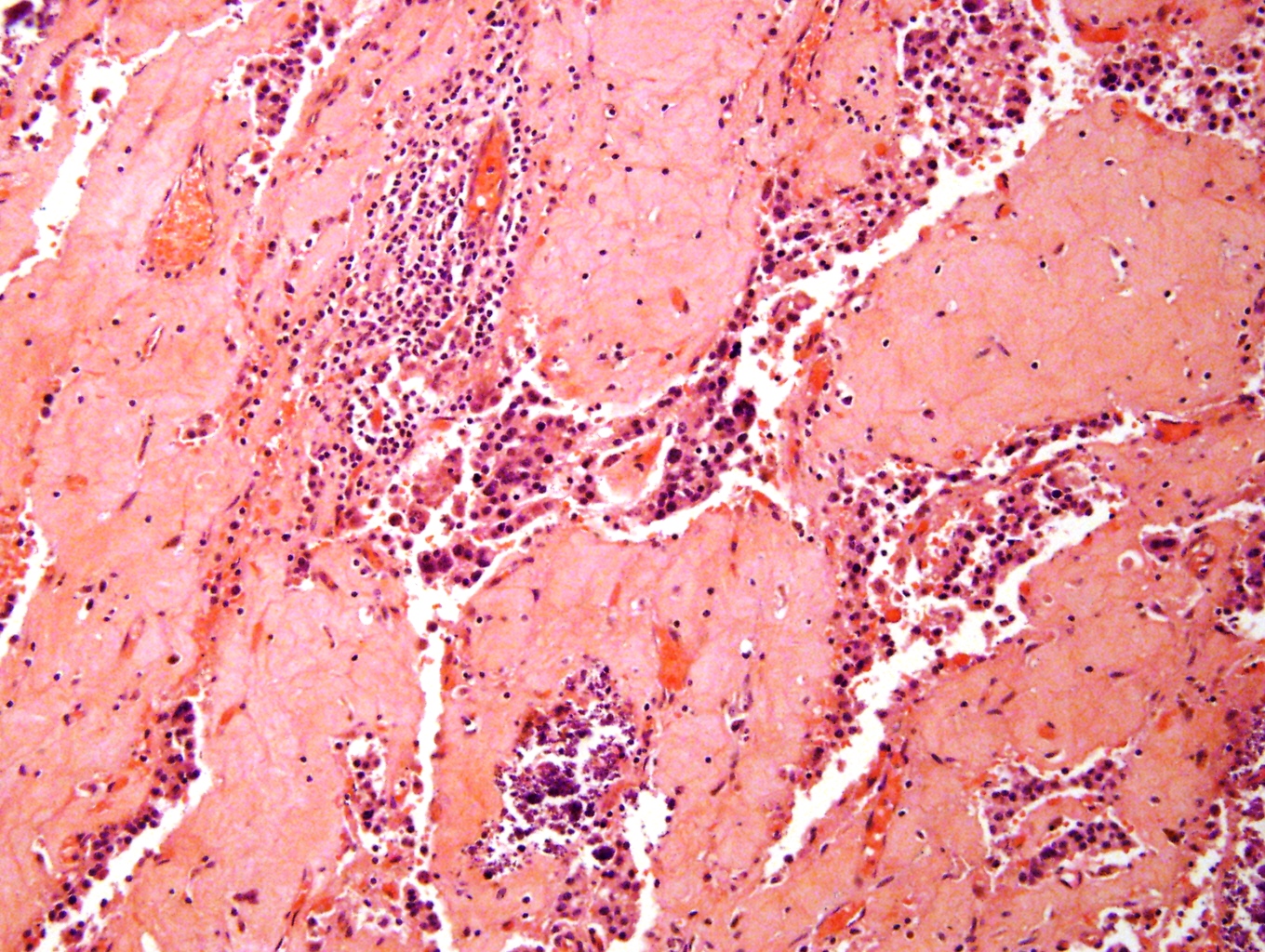
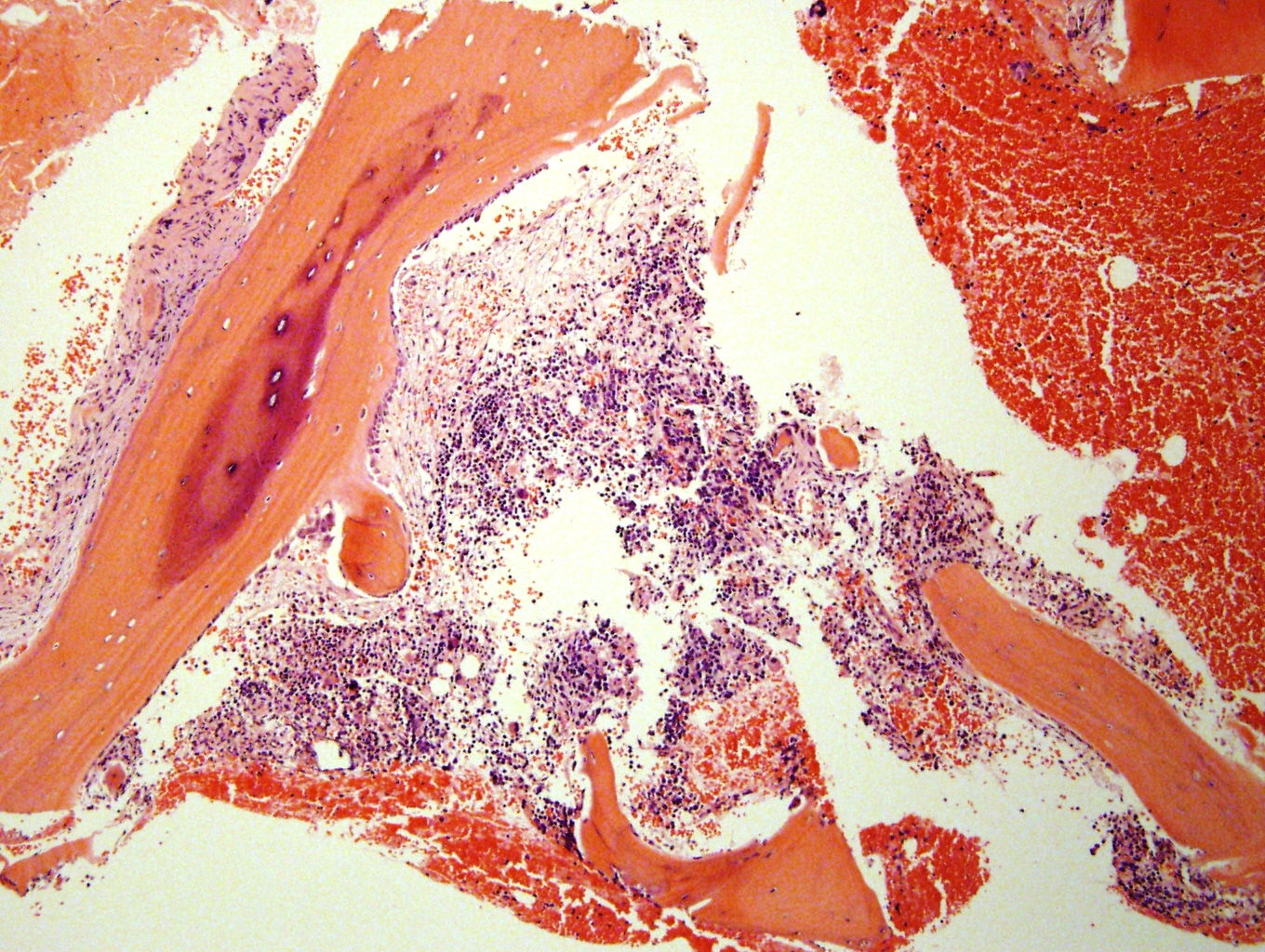
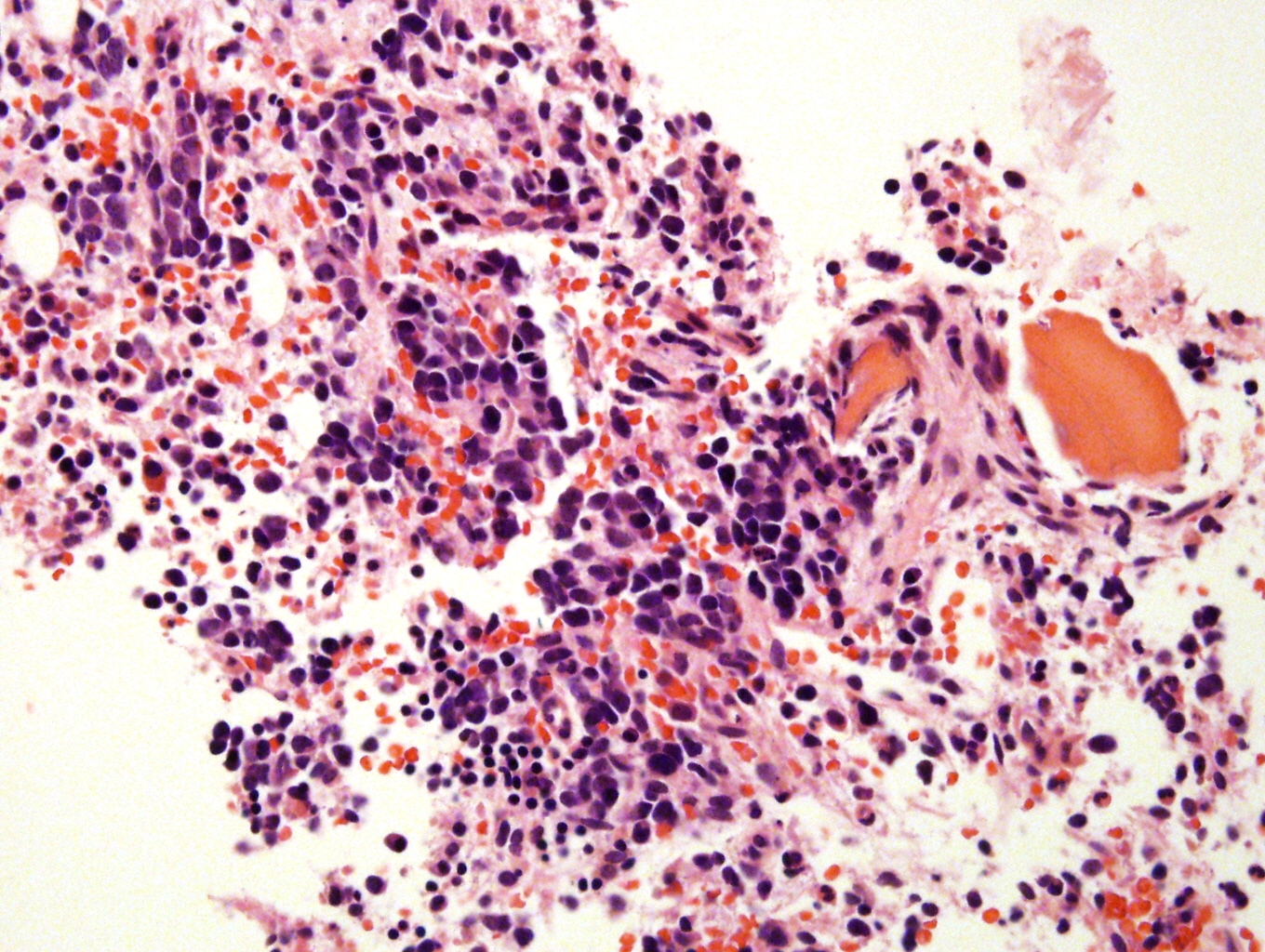
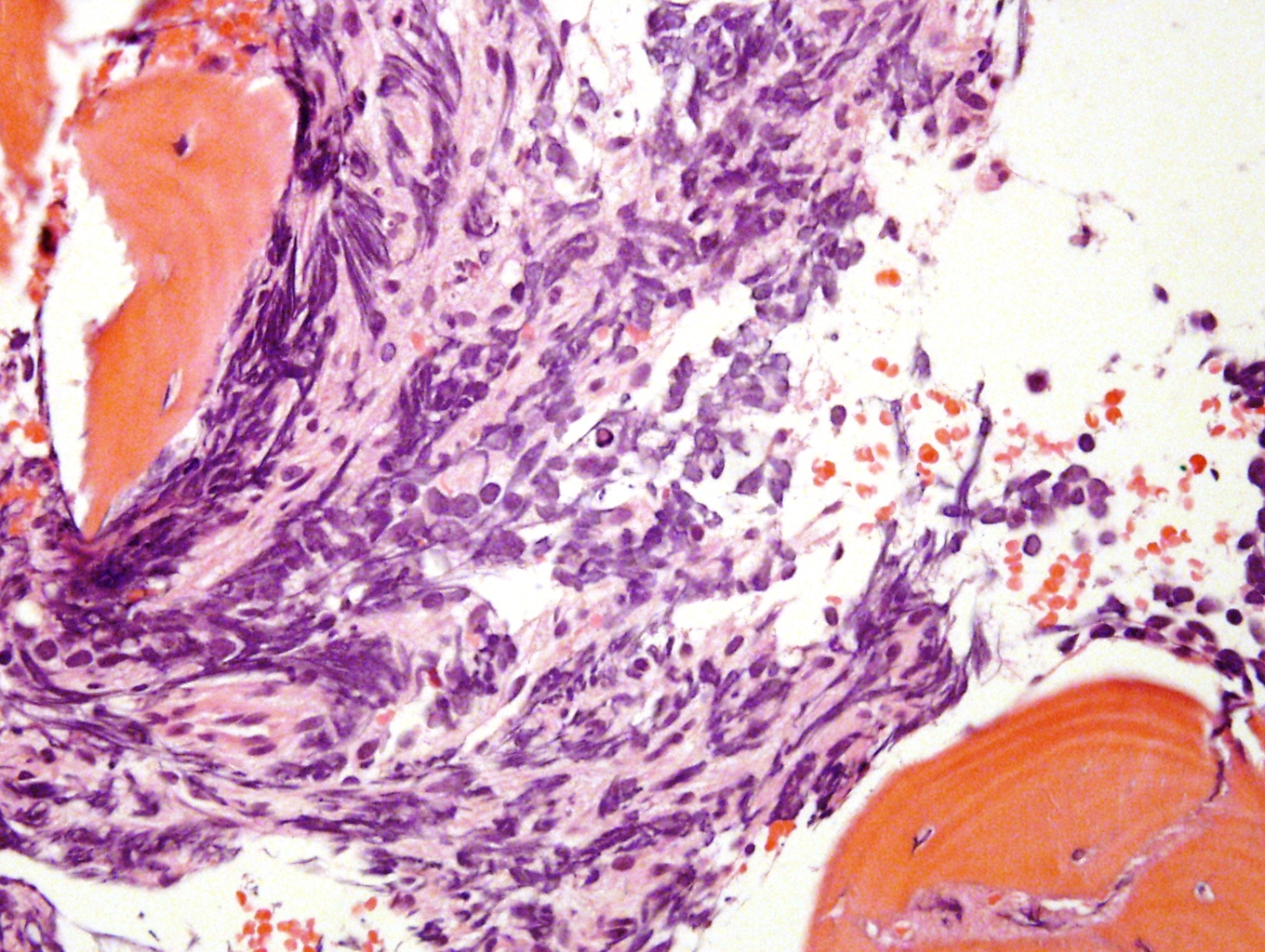
Microscopic (histologic) description
- Small round blue cell tumor
- Neuroblasts (Cancer 1999;86:349)
- Undifferentiated: small to medium, salt and pepper chromatin, elongated shape, may contain distinct nucleoli, indiscernible / small amount of cytoplasm, vague cytoplasmic borders
- Differentiating (toward ganglion cells): synchronous differentiation of nucleus (enlarged, eccentric nucleus with vesicular chromatin and single prominent nucleolus) and abundant, eosinophilic / amphophilic cytoplasm
- May have anaplastic, pleomorphic, spindled, rhabdoid variants
- May form Homer-Wright pseudorosettes surrounding delicate, eosinophilic neuropil
- Coagulation necrosis, fibrin, or collagen may be present (Cancer 1999;86:349)
- In poorly differentiated or differentiating subtypes, Schwann cells and differentiated / differentiating ganglion cells may be found (especially at tumor periphery) (Cancer 1999;86:349)
Neuroblastoma in situ
- Usually incidental finding at autopsy in 0.4 to 2.5% of infants less than 3 months
- May not be neoplastic or may mature into ganglioneuroma
- Clusters of immature neuroblasts, from 0.7 to 9.5 mm, with frequent cystic change
Treatment effect
- Cannot grade tumors as favorable or unfavorab
- Extensive fibrosis and calcification may obscure margin involvement
- Also necrosis and chronic inflammation
Microscopic (histologic) images
Contributed by Carmen Perrino, M.D.
Images hosted on other servers:
Virtual slides
Cytology description
- Neuroblasts: uniform, small, blue cells with hyperchromatic to vesicular chromatin and scant, eosinophilic, fibrillary cytoplasm, may form Homer-Wright rosettes
Positive stains
- Neuron specific enolase (NSE), CD57, CD56, protein gene product 9.5 (PGP 9.5), Leu-7, GD2, NB84, synaptophysin, chromogranin, neurofilament protein, ALK-1 (>90%), PHOX2B, glial fibrillary acidic protein (GFAP) (variable) (Am J Pathol 2012;180:1223, Am J Surg Pathol 2012;36:1141, Dabbs: Diagnostic Immunohistochemistry, 4th Edition, 2013)
Negative stains
Electron microscopy description
- Most characteristic features are arrays of neuritic processes containing microtubules, diffuse intermediate filaments, and sparse dense-core neurosecretory granules (average diameter 100 nm) (Ultrastruct Pathol 1994;18:149)
Electron microscopy images
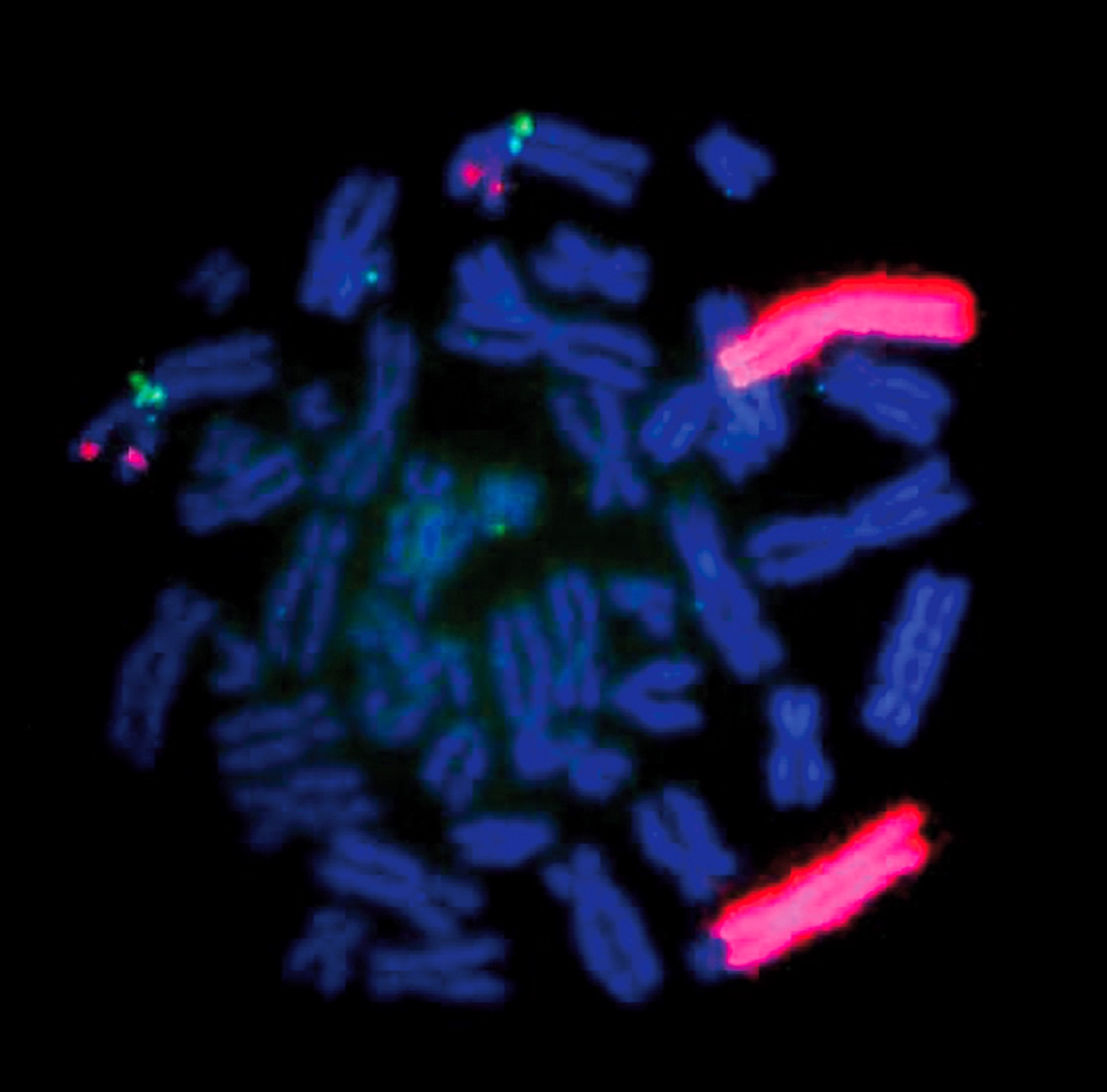
Molecular / cytogenetics description
- Familial neuroblastoma (Nat Rev Cancer 2013;13:397)
- Rare (<2%), due to mutations in genes (PHOX2B, ALK) involved in signaling pathways important for development of sympathoadrenal lineage
- Genome-wide association studies have revealed several single nucleotide polymorphisms (SNPs) which give rise to and/or contribute to progression of neuroblastoma: LINC00340 and LOC729177 (FLJ44180), BARD1, LMO1, DUSP12, HSD17B12, DDX4-IL31RA, HACE1, LIN28B
- Sporadic neuroblastoma (Nat Rev Cancer 2013;13:397)
- ALK amplification associated with poor prognosis
- 6-10% of neuroblastomas have somatic ALK mutations
- 3-4% of neuroblastomas have high risk ALK amplifications
- MYCN amplification (≥ 10 copies for diploid genome or >4 fold signal relative to chromosome 2) associated with poor prognosis
- Occurs in ~22% of tumors
- ATRX mutations among most common in sporadic neuroblastomas, but not sufficient for tumorigenesis
- Association with age at diagnosis
- No ATRX mutations in very young children (<18 months) with stage 4 disease and better prognosis
- ATRX mutations occur in 17% of children 18 months to 12 years with stage 4 disease, and in 44% of patients >12 years, all with very poor prognosis
- Association with age at diagnosis
- Frequent mutations in Rac/Rho pathway and ARID1A and ARRID1B genes identified by whole genome sequencing, significance of each yet to be elucidated (Nat Rev Cancer 2013;13:397)
- ALK amplification associated with poor prognosis
Differential diagnosis
- Adrenal hemorrhage (versus cystic neuroblastoma)
- Desmoplastic small round cell tumor
- Ewing's sarcoma/primitive neuroectodermal tumor (PNET)
- Ganglioneuroblastoma: especially nodular variant
- Ganglioneuroma
- Lymphoma
- Malignant rhabdoid tumor
- Melanoma
- Schwannoma / neurilemmoma with neuroblastoma-like features
Board review style question #1
The image shown above is a Wright-Giemsa stained bone marrow aspirate smear from a 6 month old child who presented with a 5 cm abdominal mass. Which of the following answer choices, if present, would result in an improved prognosis for the patient?
- FISH shows loss of chromosome 1p
- FISH shows loss of chromosome 11q
- Molecular diagnostic testing shows N-myc amplification
- The child is less than 1 year old
- The child is male
Board review style answer #1
D. The child is less than 1 year old. The bone marrow aspirate shows clusters of small, round, blue cells with smudged chromatin and nuclear molding; given the history of a child with an abdominal mass, this is consistent with metastatic neuroblastoma in the bone marrow. If the patient is less than 1 year old and has metastatic disease limited to skin, liver and bone marrow, the tumor would be staged as 4S, which has a good prognosis. In contrast, N-myc amplification and loss of chromosomes 1p and 11q are associated with a worse prognosis.
Comment Here
Reference: Neuroblastoma
Comment Here
Reference: Neuroblastoma