- pTX: primary tumor cannot be assessed
- pT0: no evidence of primary tumor
- pT1 (I): tumor confined to corpus uteri
- pT1a (IA): tumor limited to endometrium or invades < 50% of the myometrium
- pT1b (IB): tumor invades ≥ 50% of the myometrium
- pT2 (II): tumor invades stromal connective tissue of the cervix but does not extend beyond uterus
- pT3 (III): tumor involving serosa, adnexa, vagina or parametrium
- pT3a (IIIA): tumor involves serosa or adnexa (direct extension or metastasis)
- pT3b (IIIB): vaginal involvement (direct extension or metastasis) or parametrial involvement
- pT4 (IVA): tumor invades bladder mucosa or bowel mucosa (bullous edema is not sufficient to classify a tumor as pT4)
Notes:
- Endocervical glandular involvement only should be considered as stage I and not stage II
- pTis is no longer a staging category
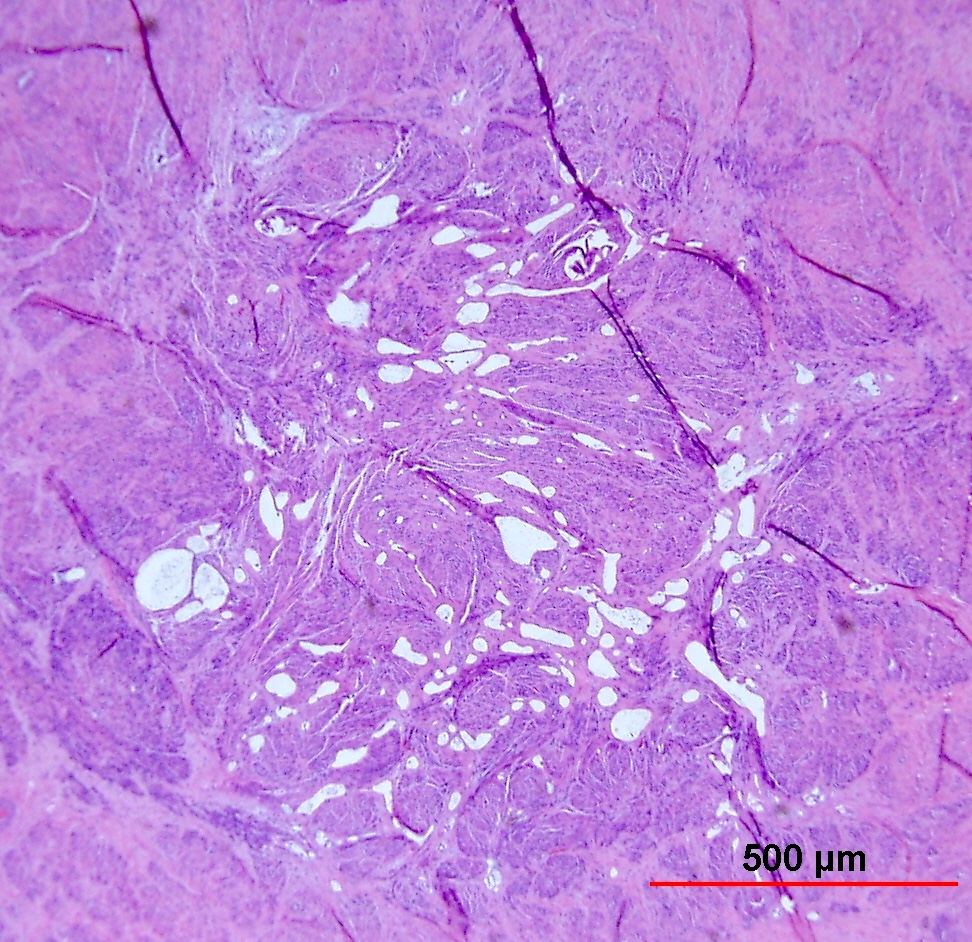
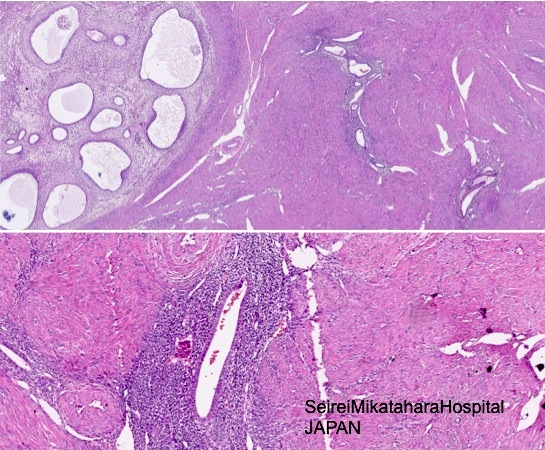
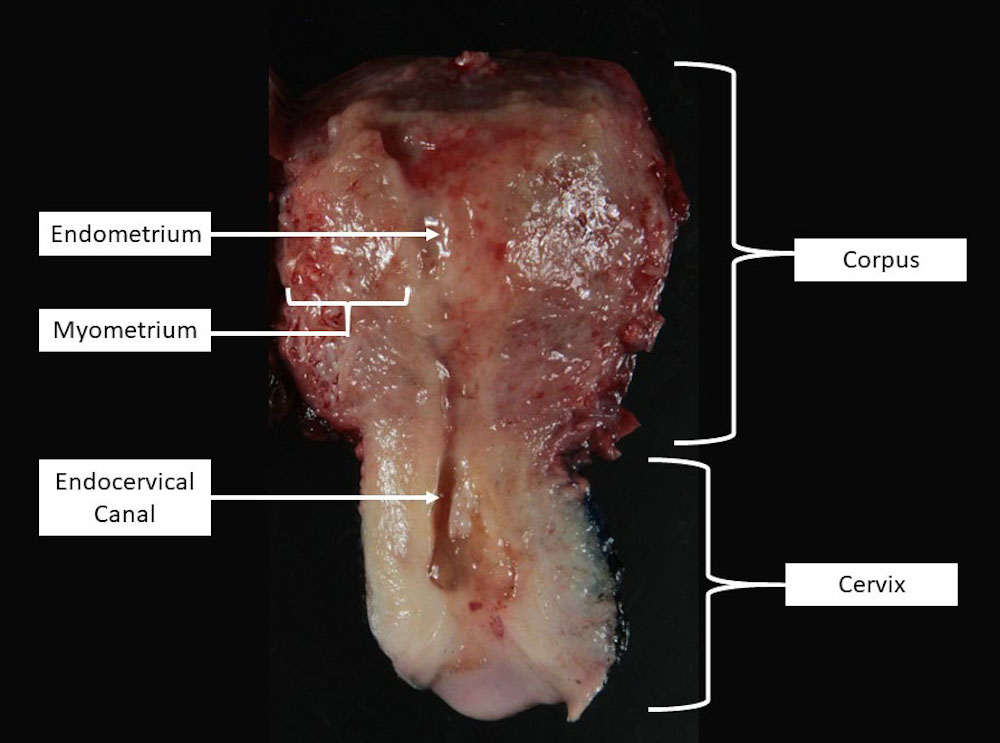
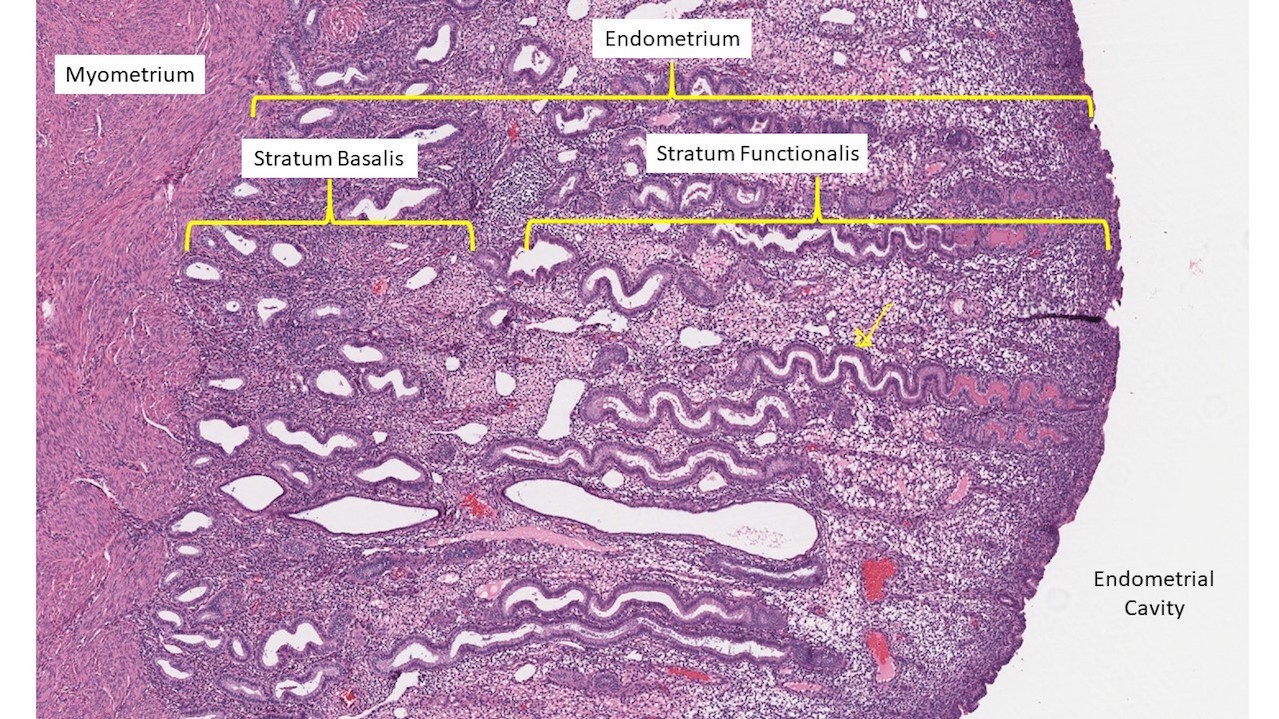
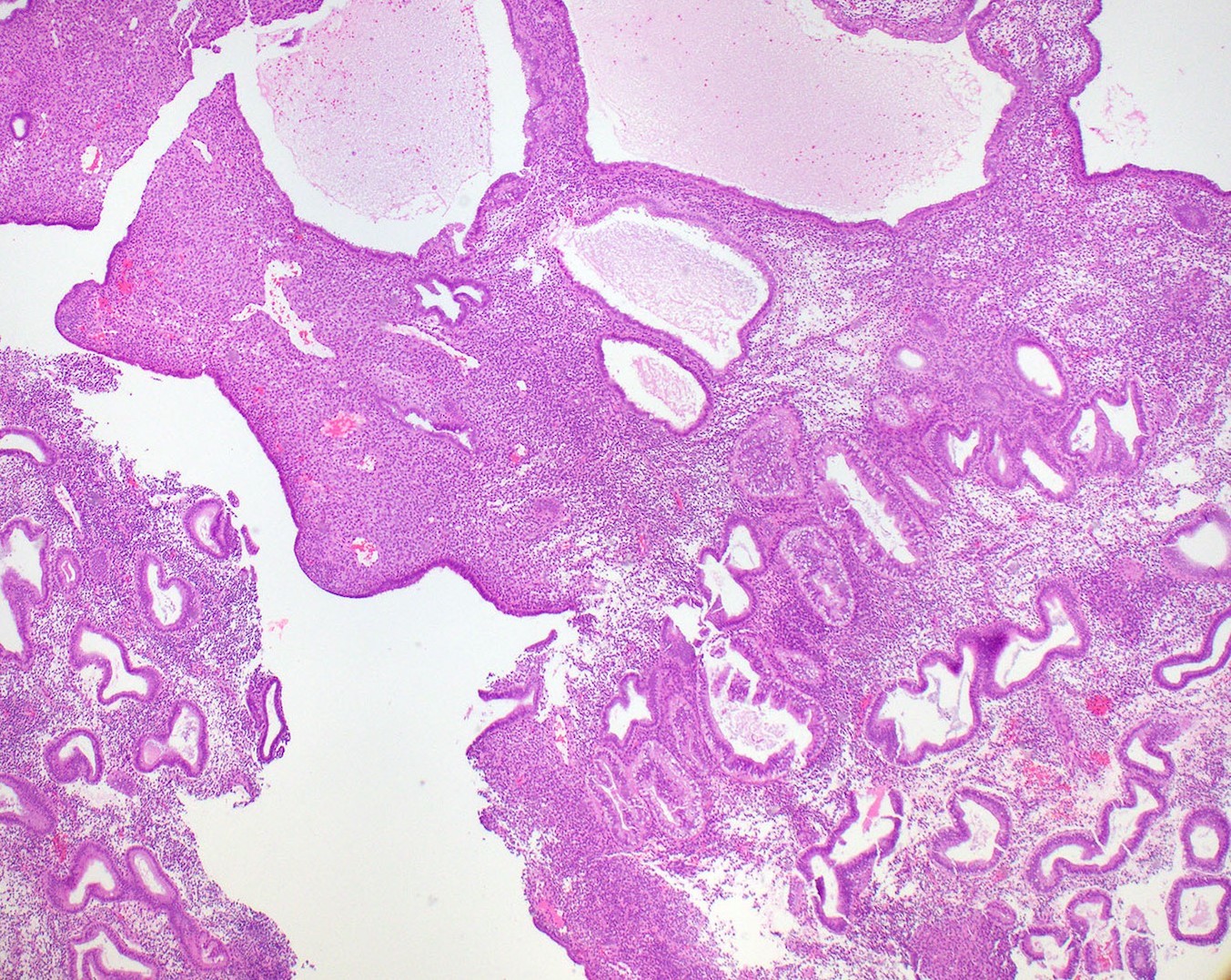
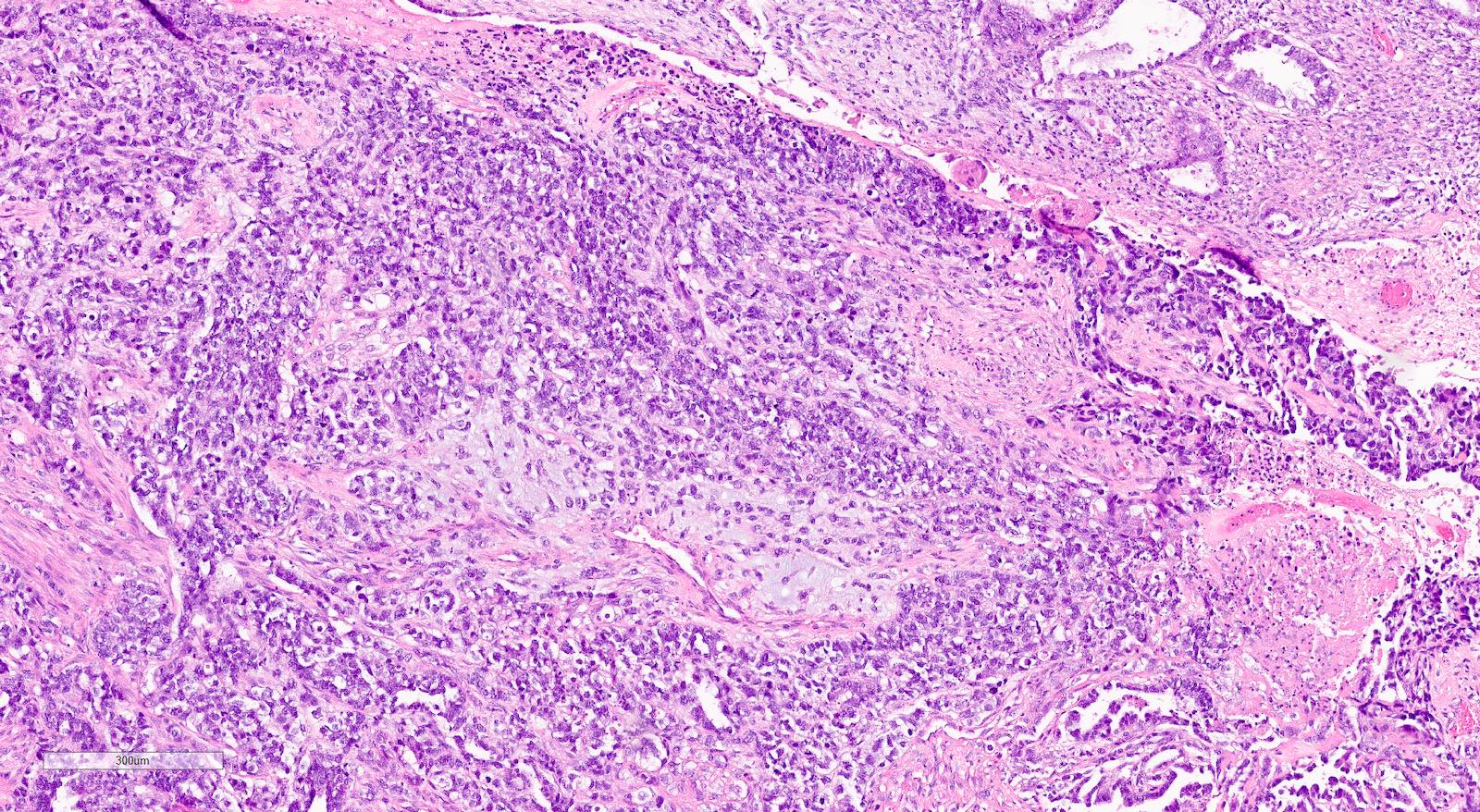
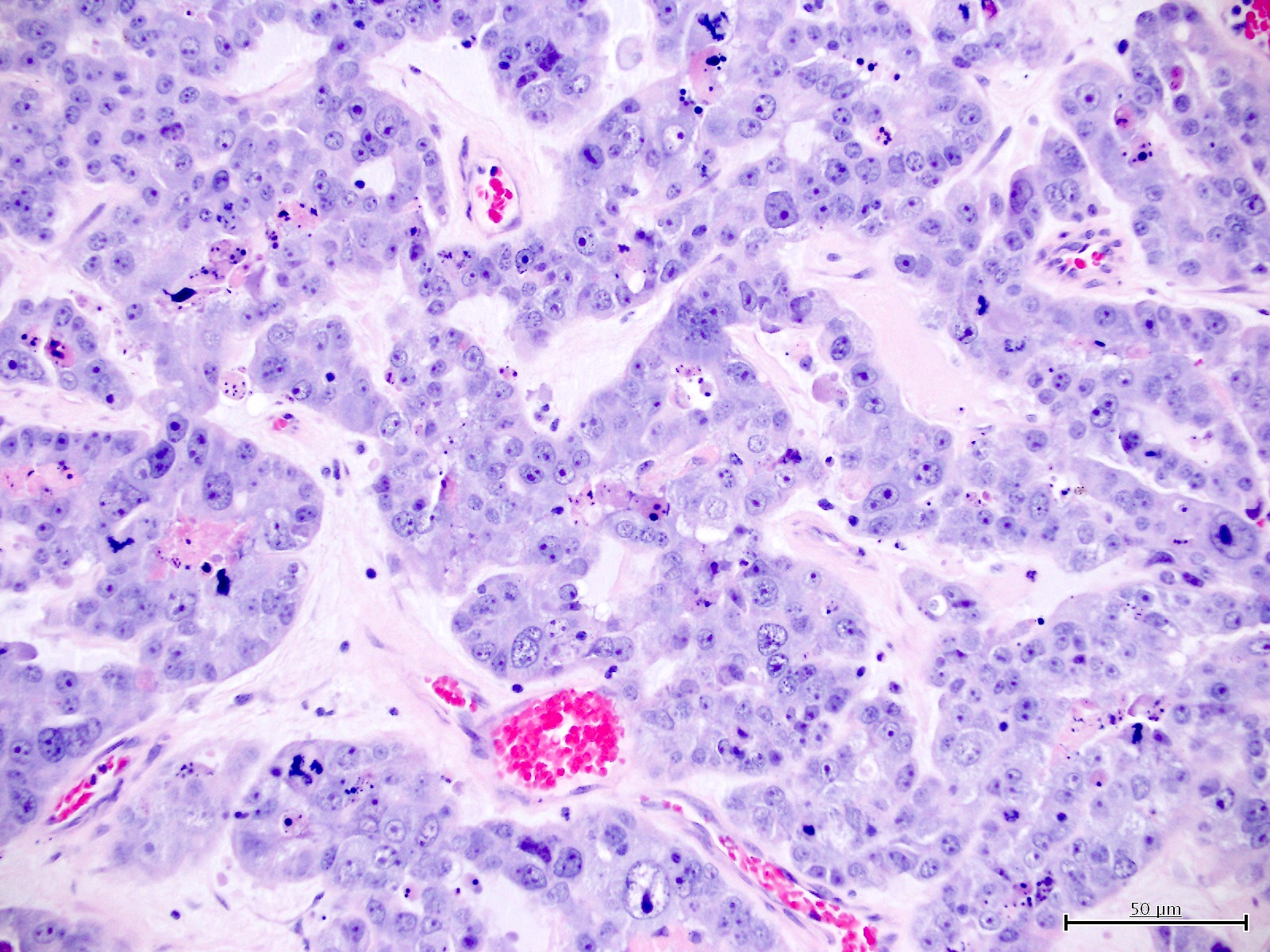
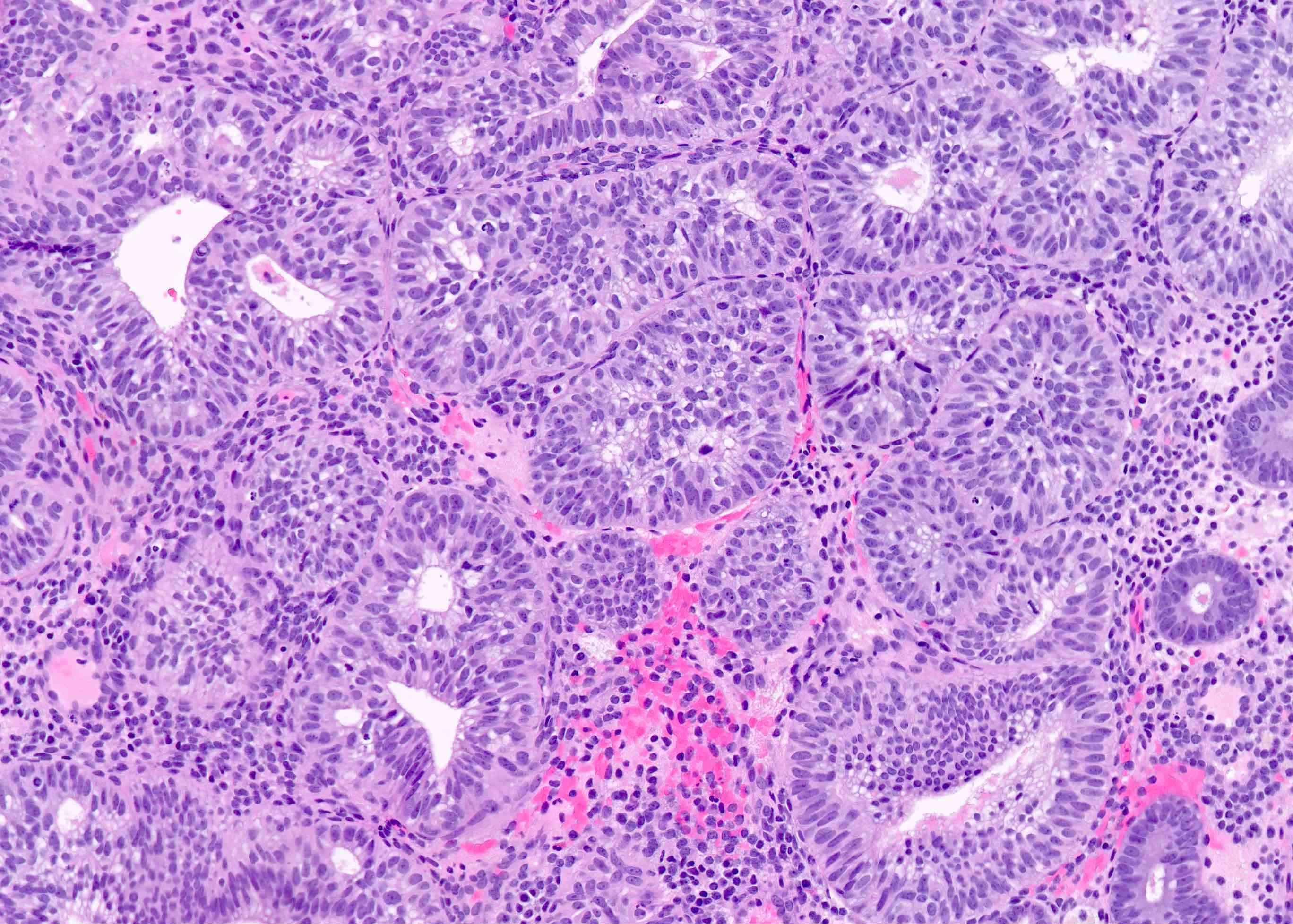
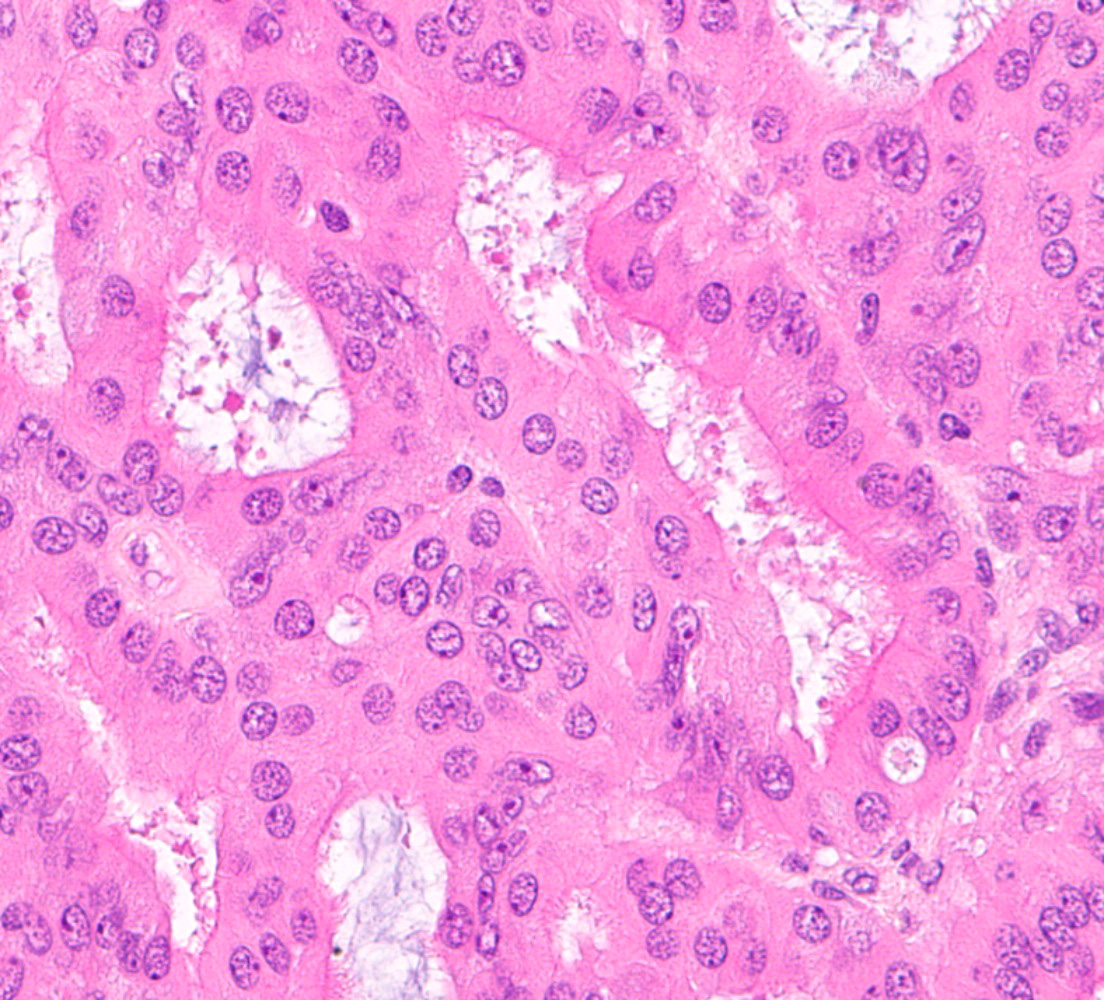
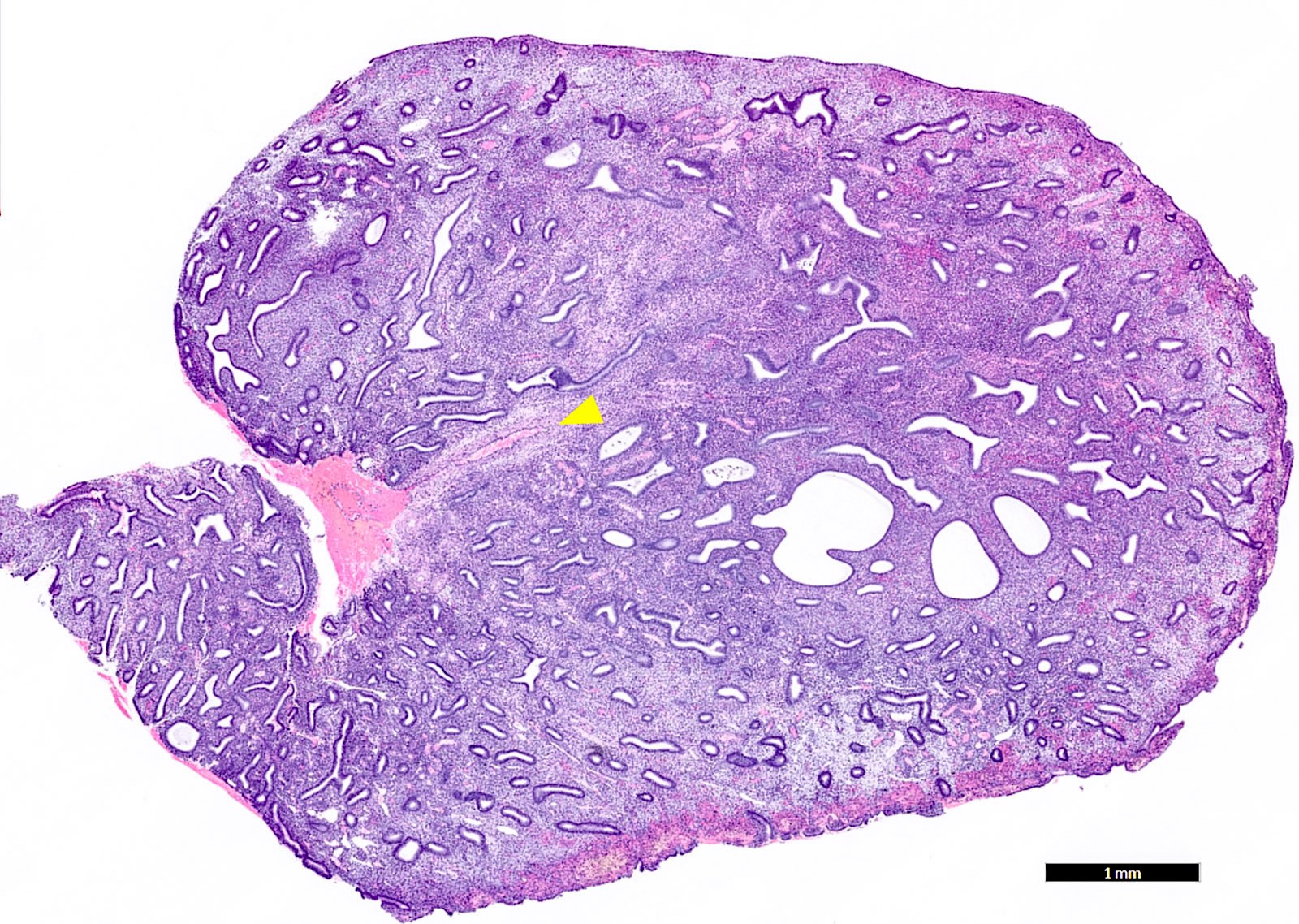
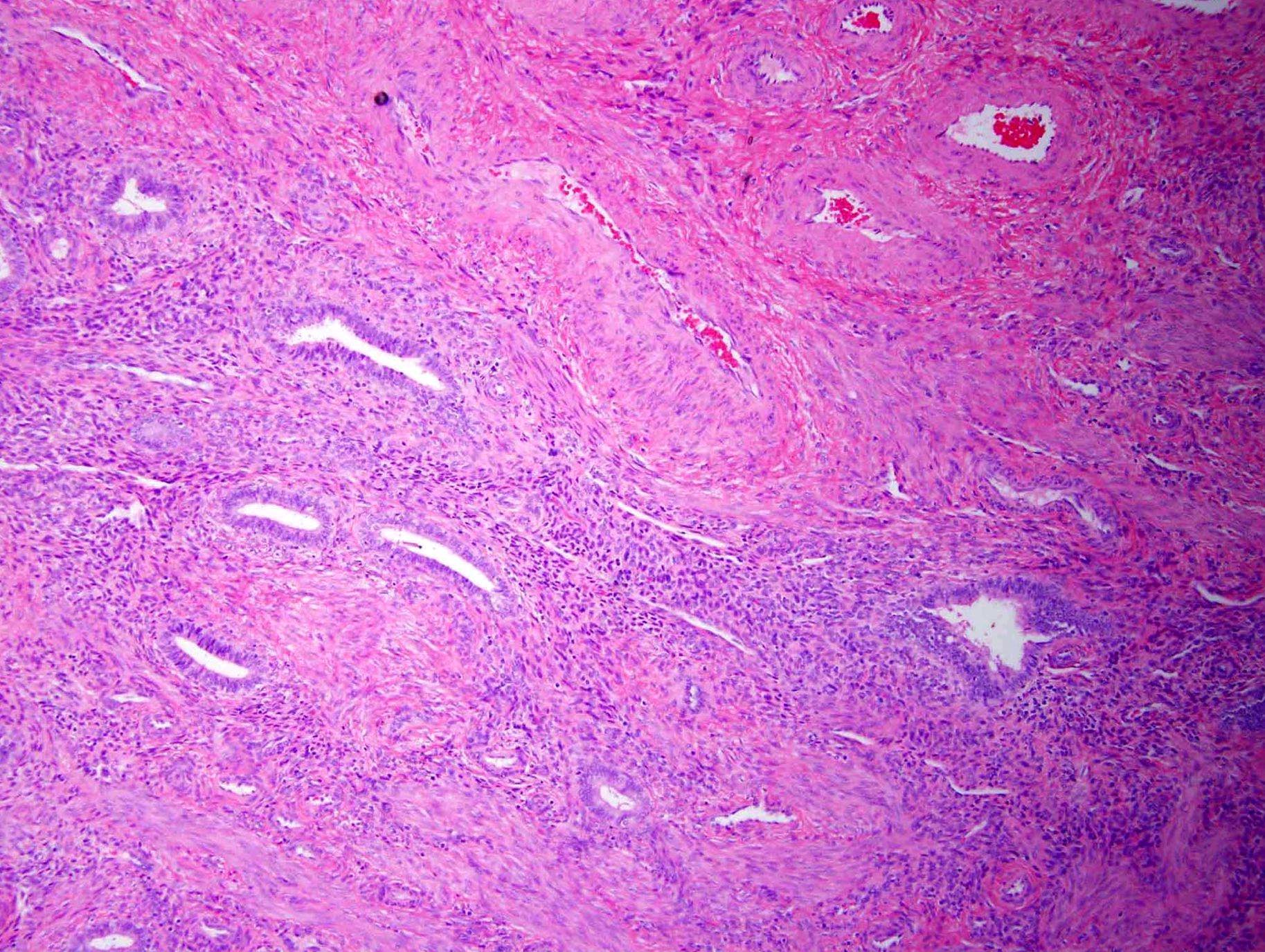
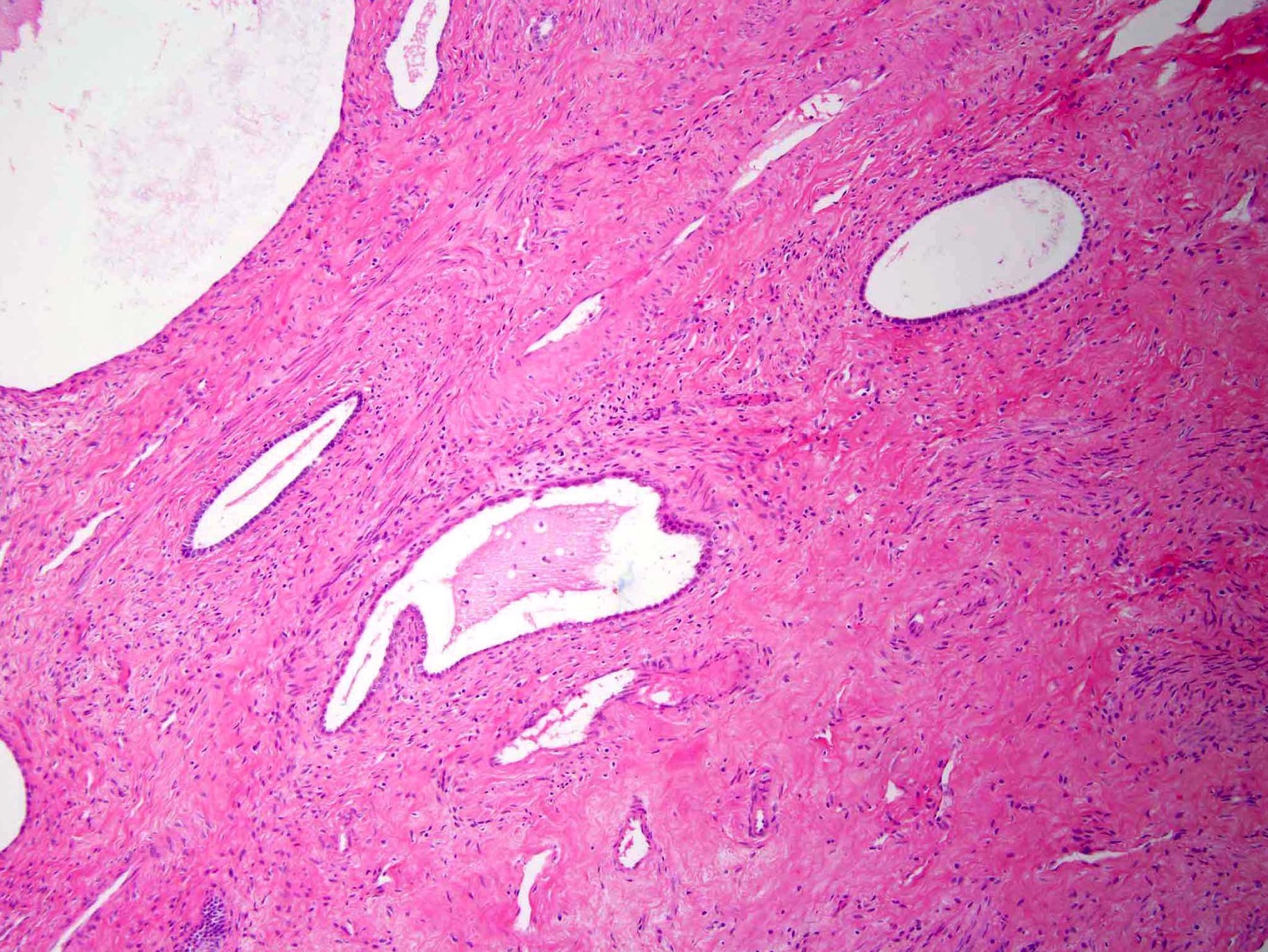
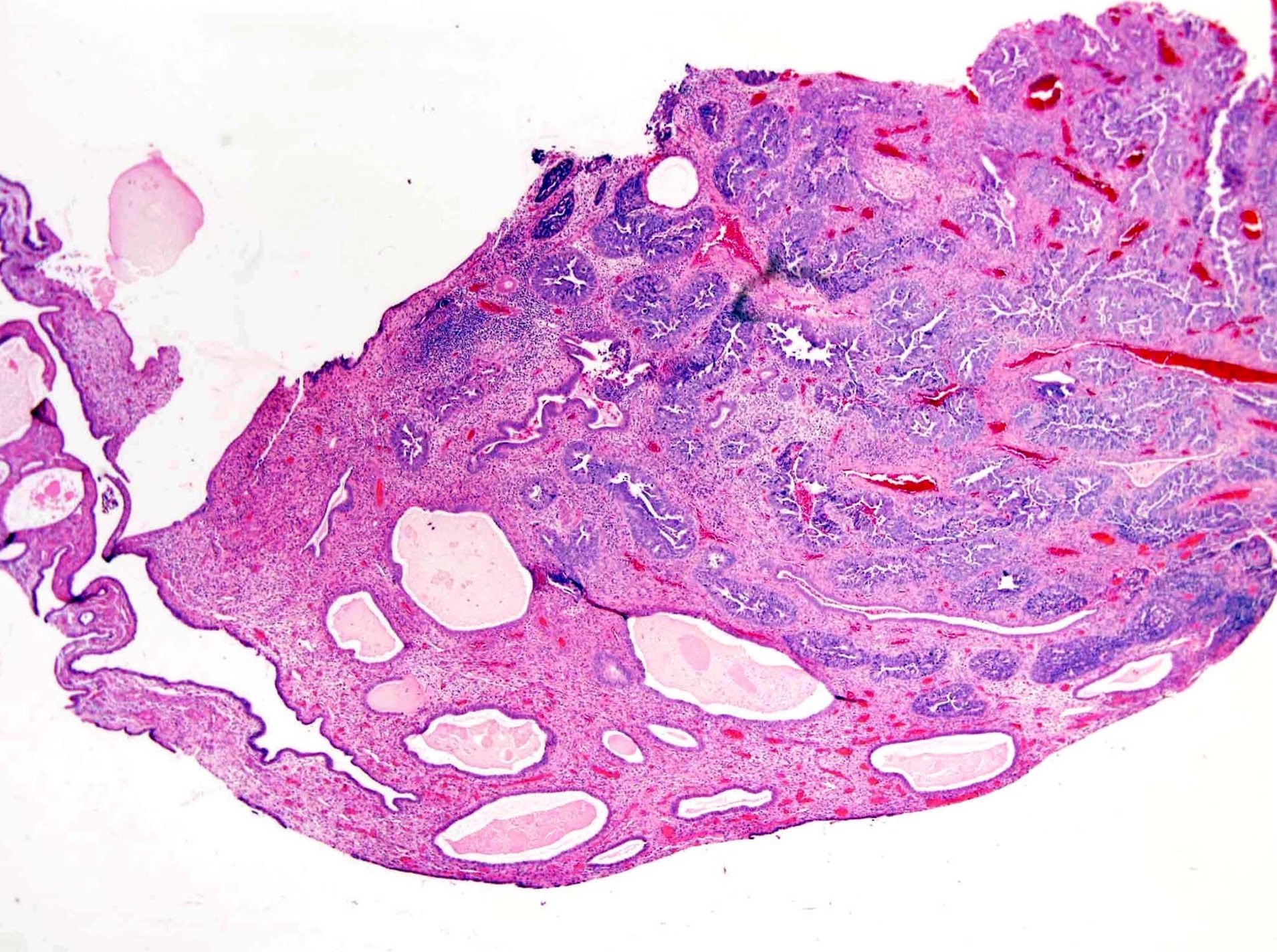
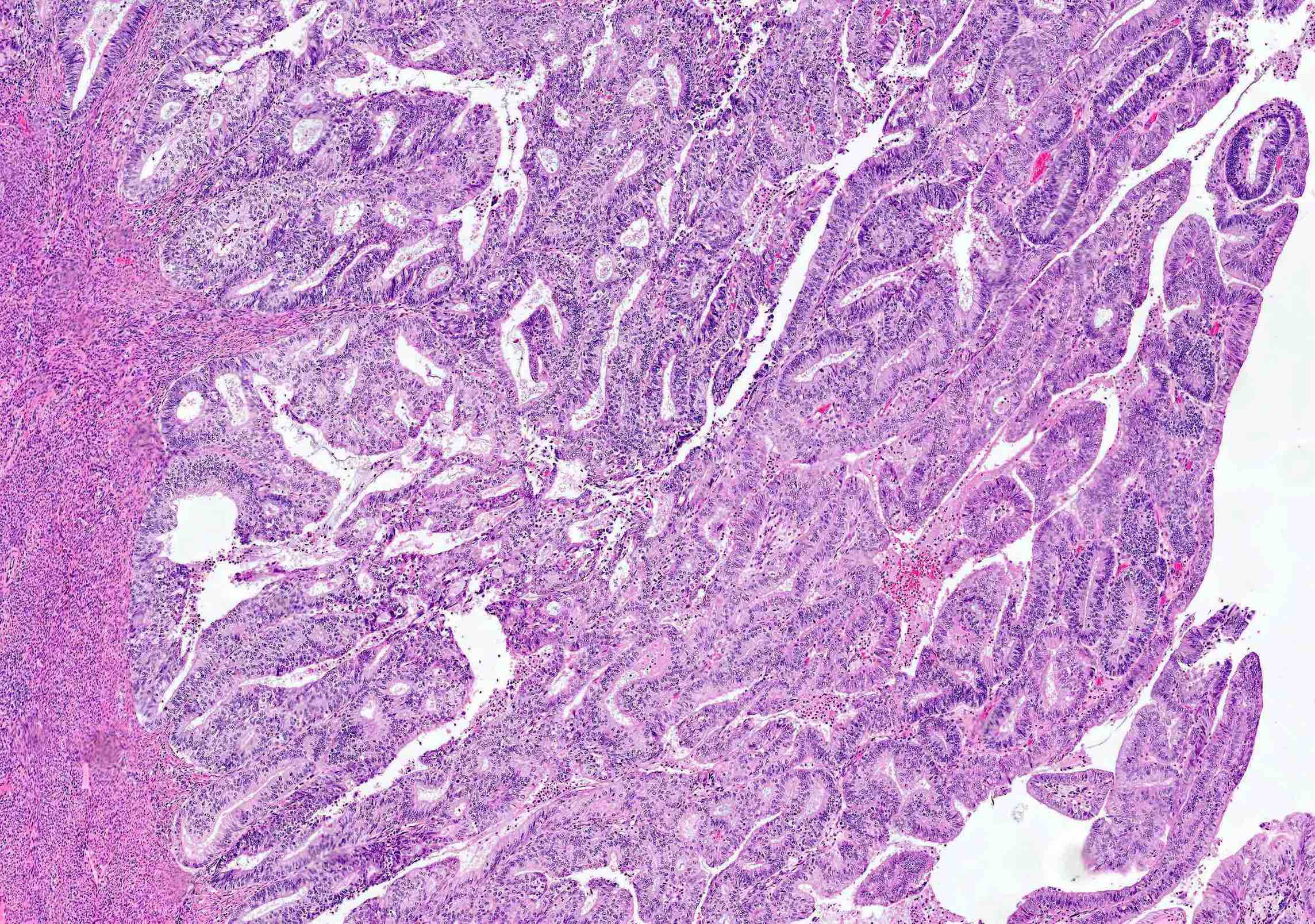
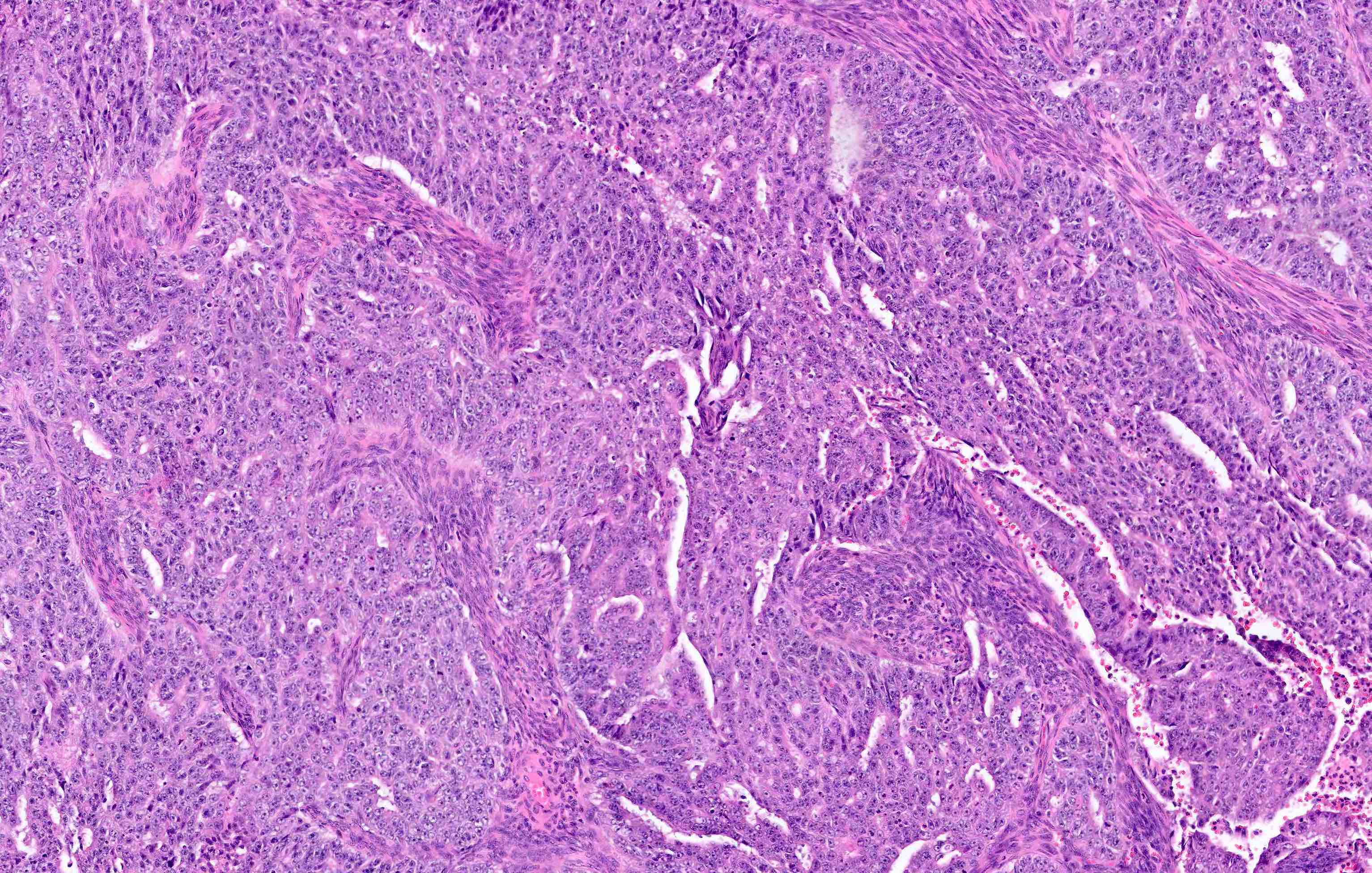
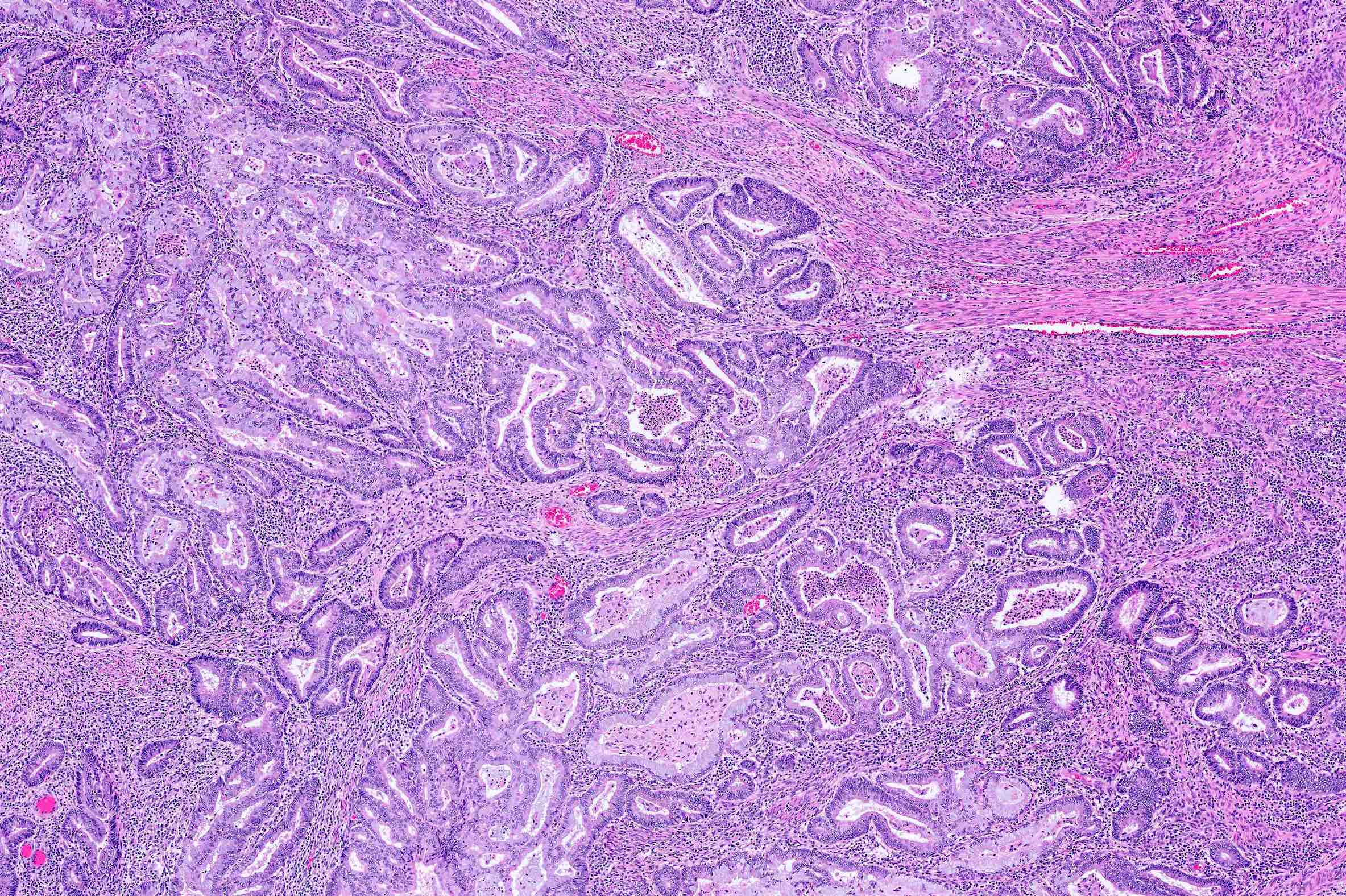
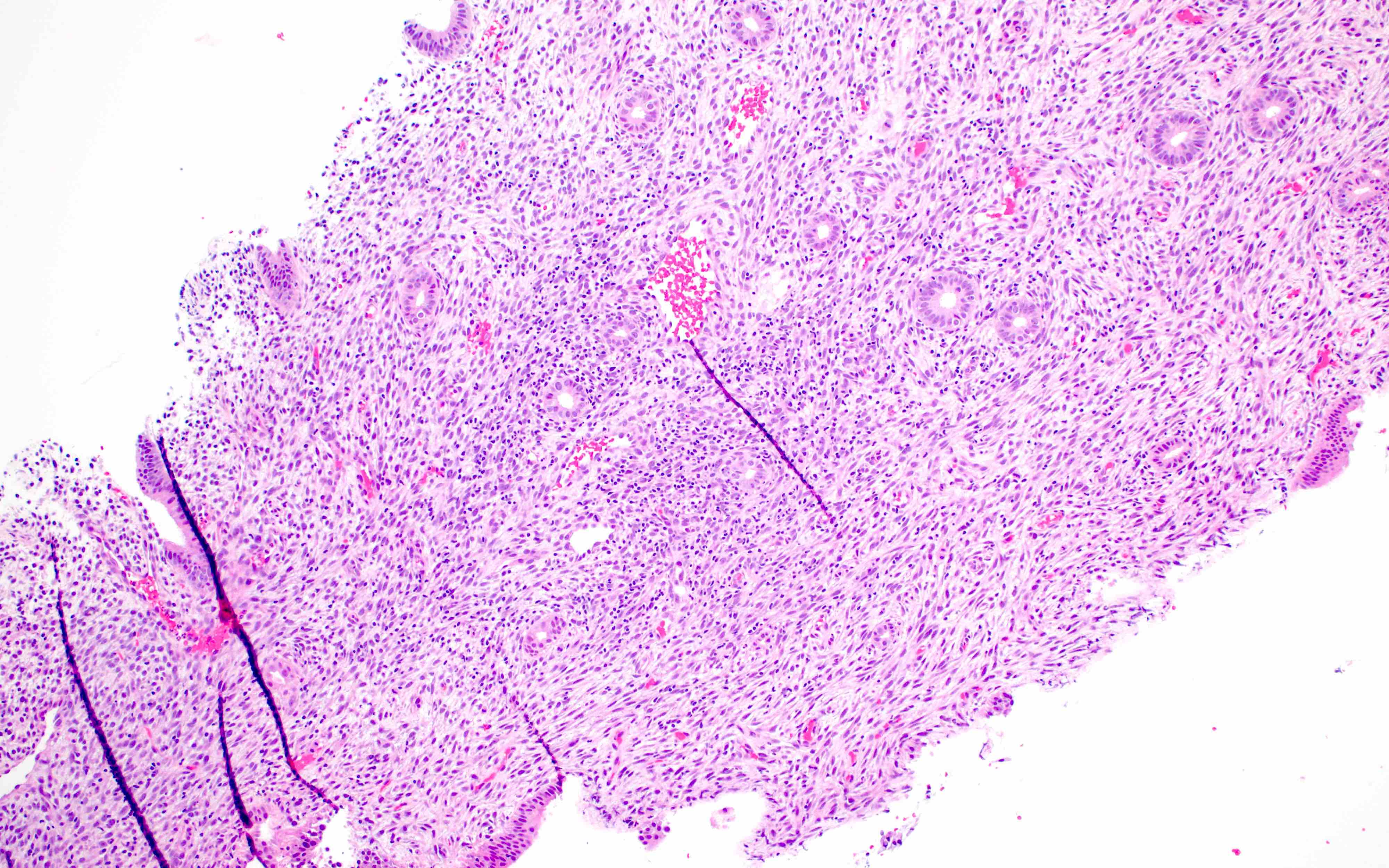
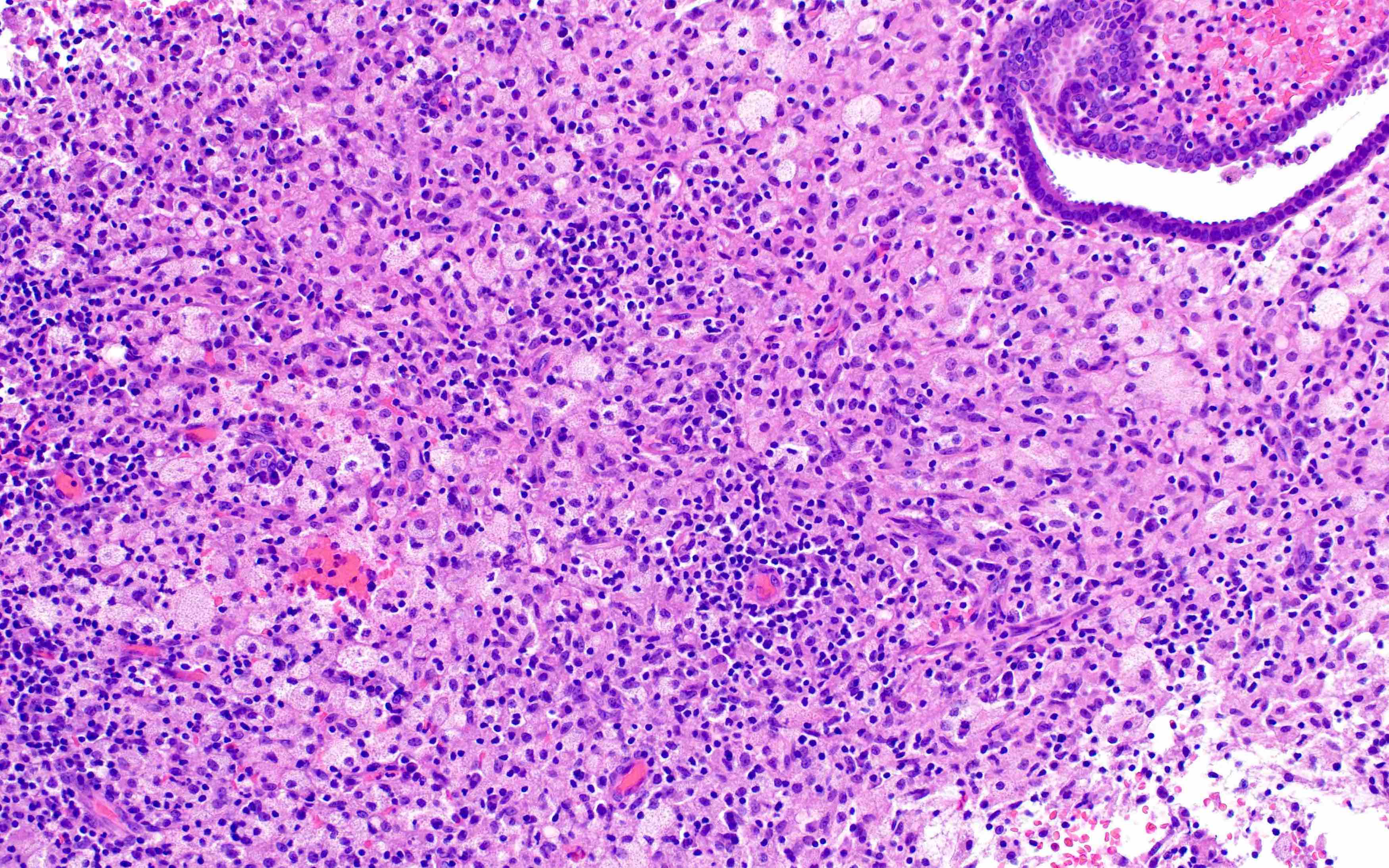
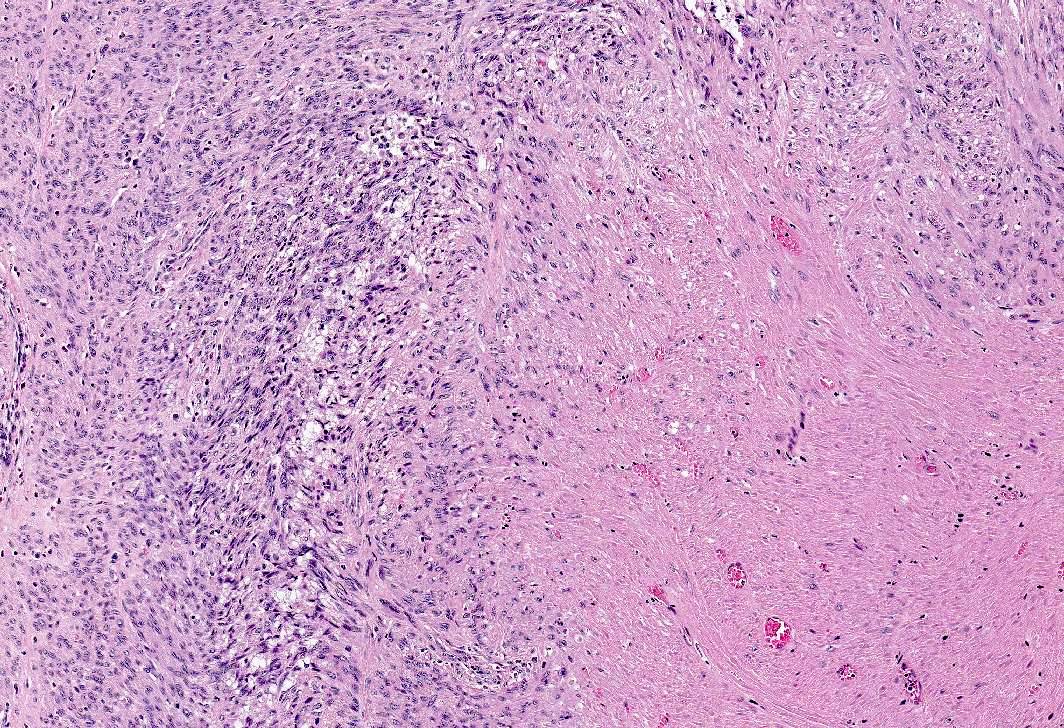
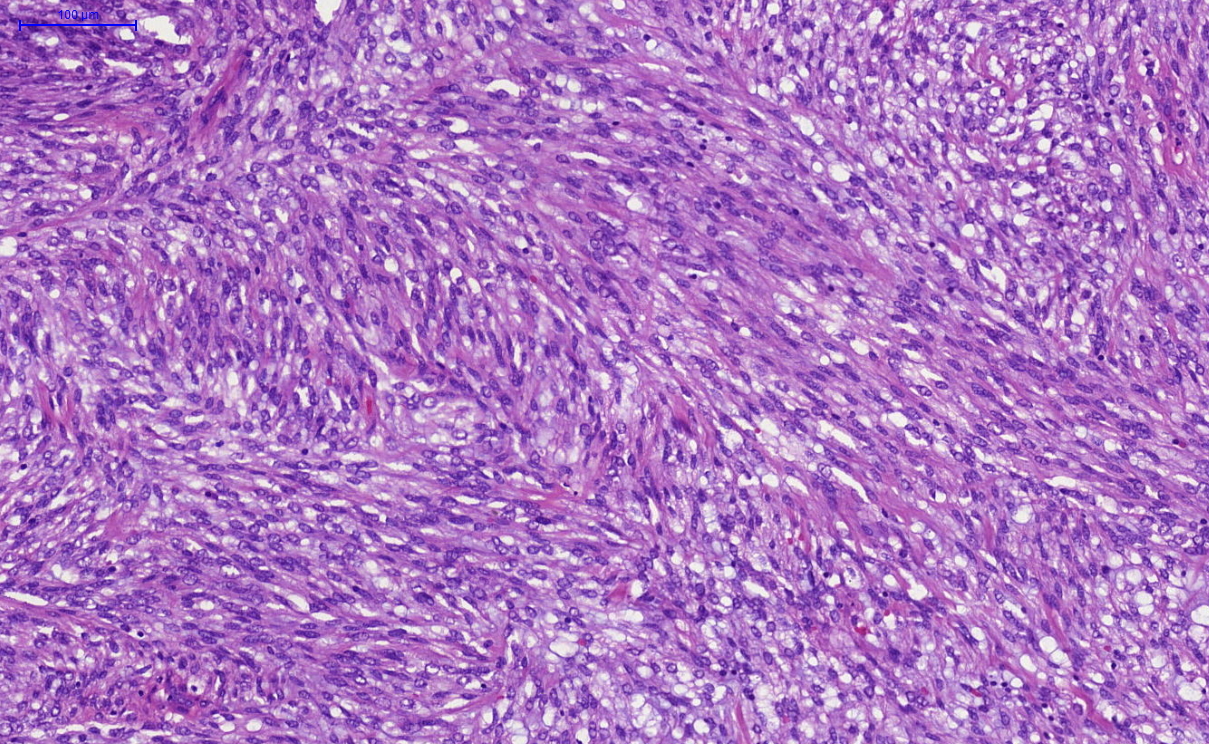
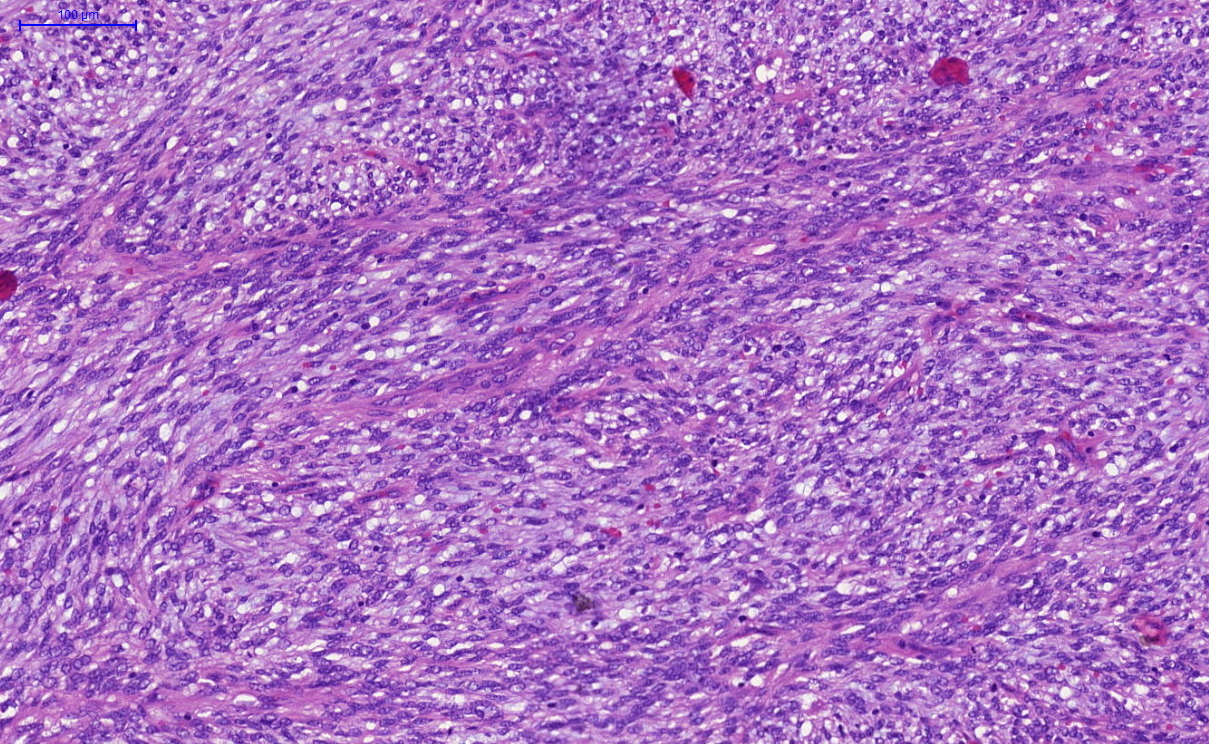
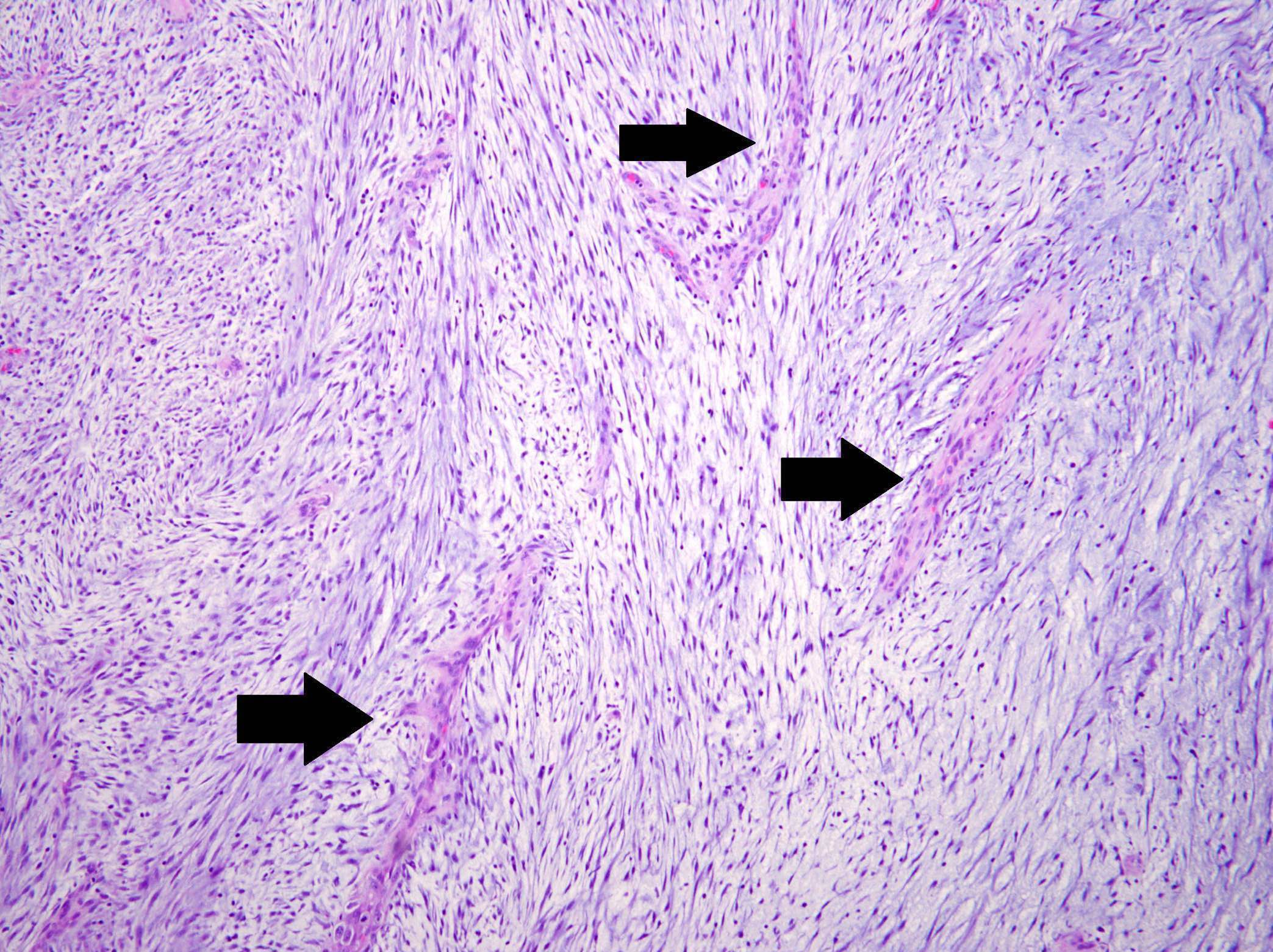
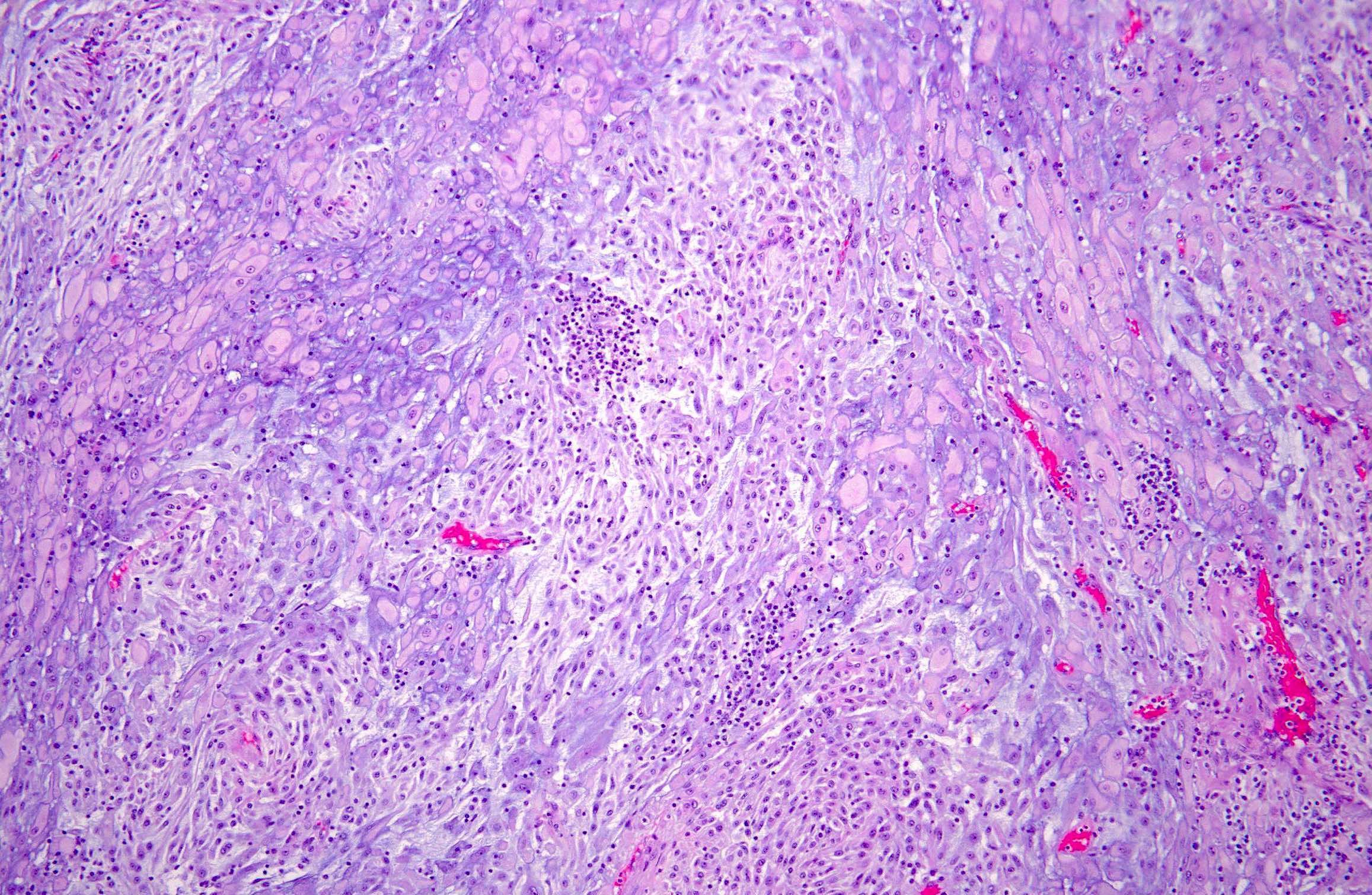
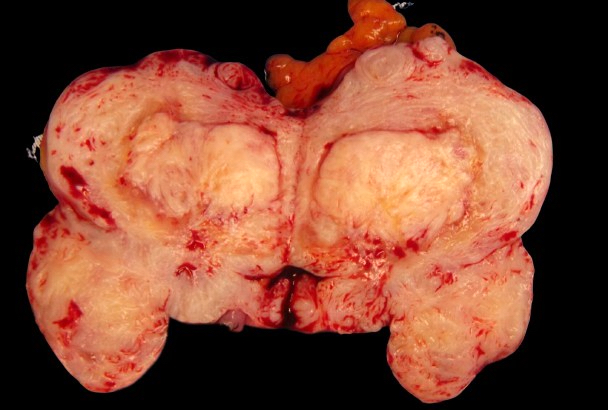
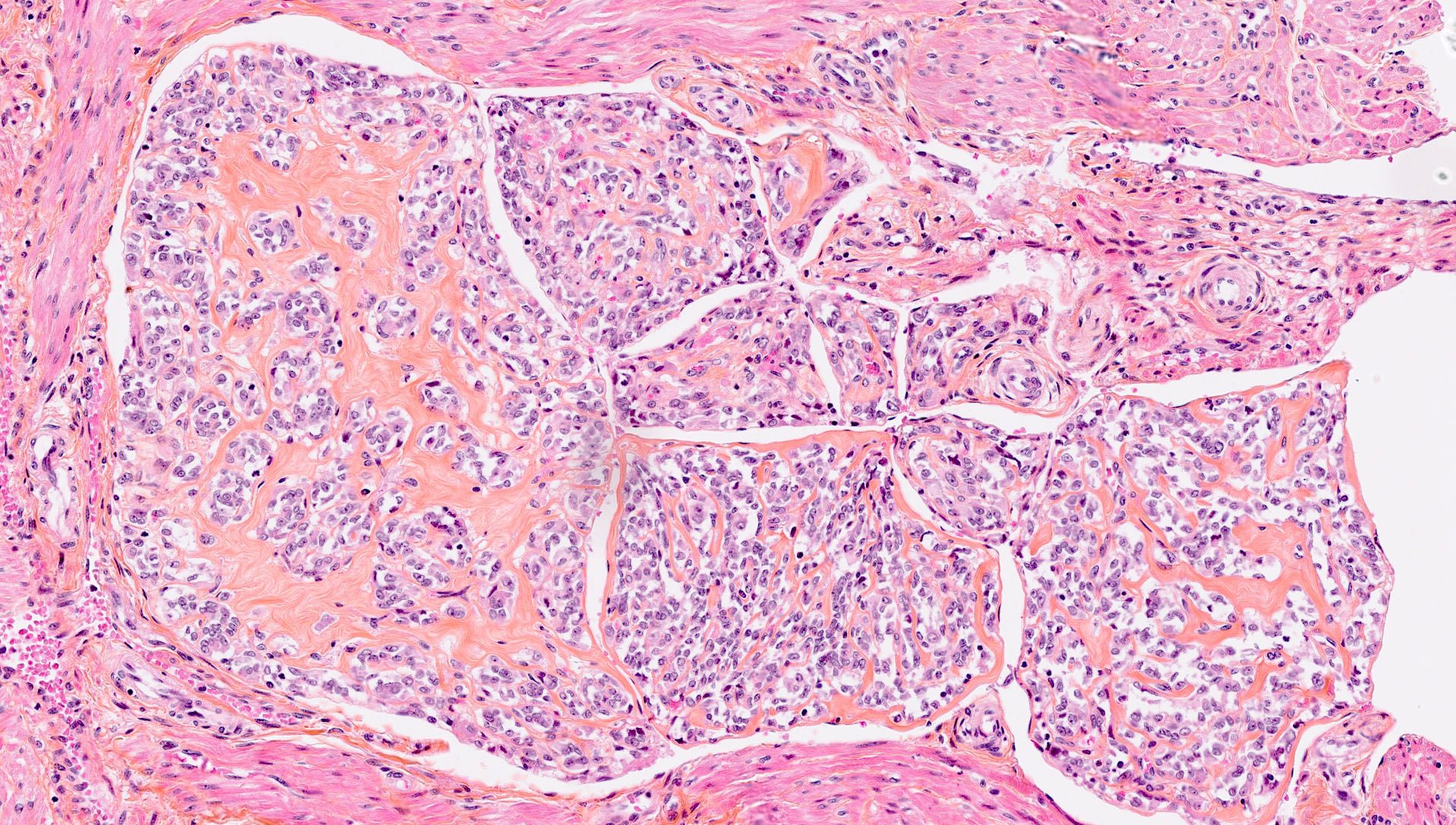
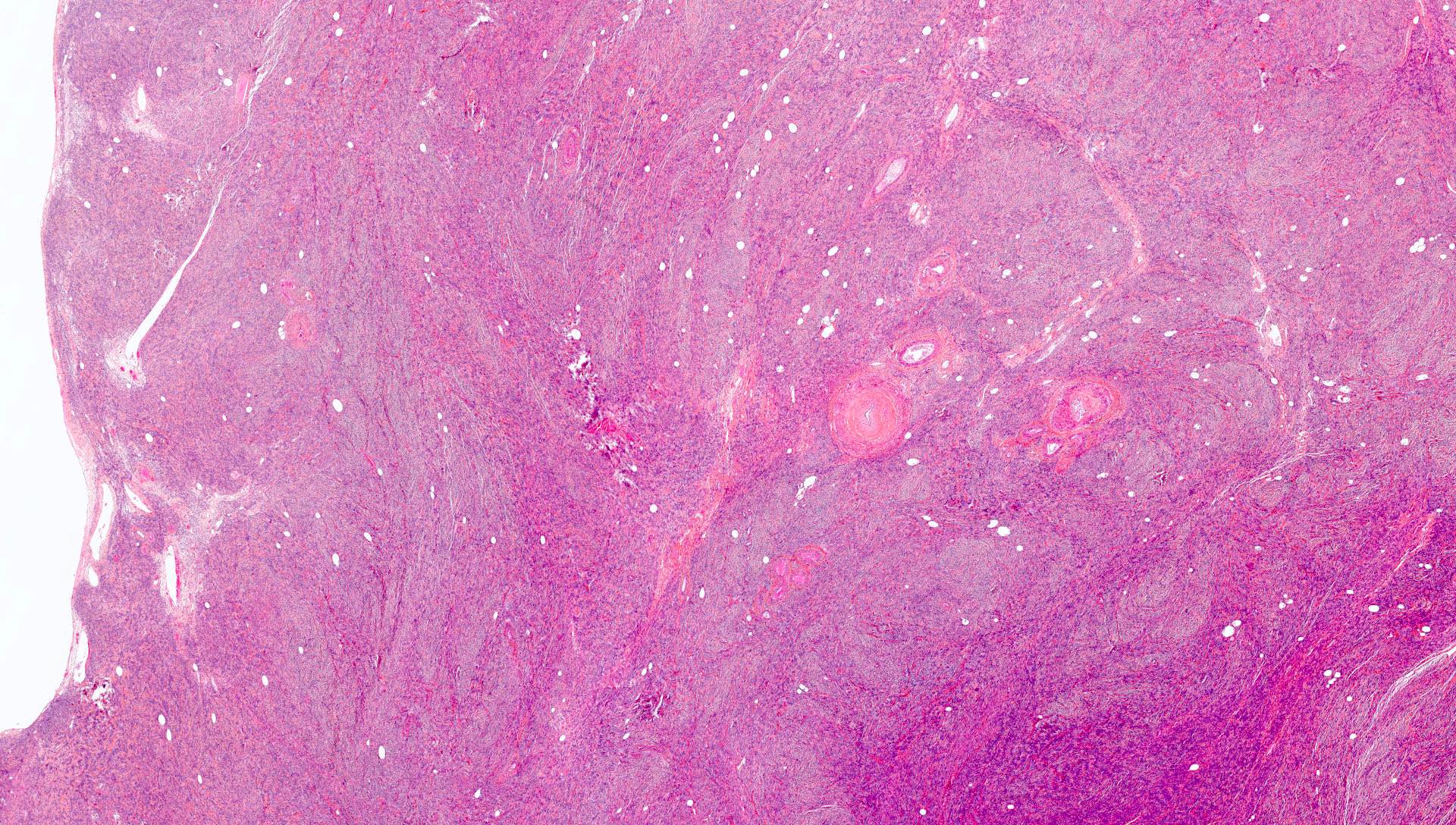
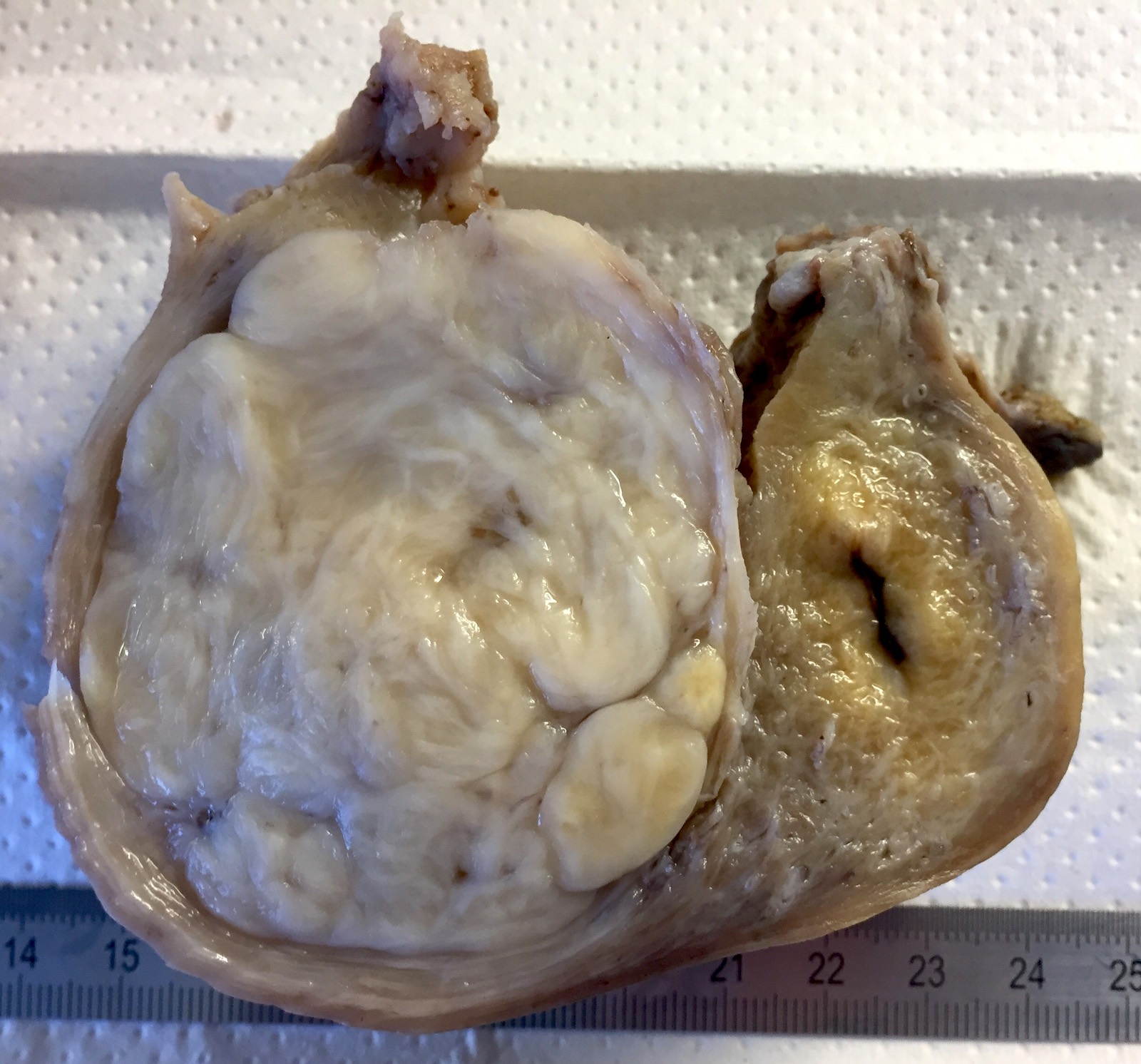
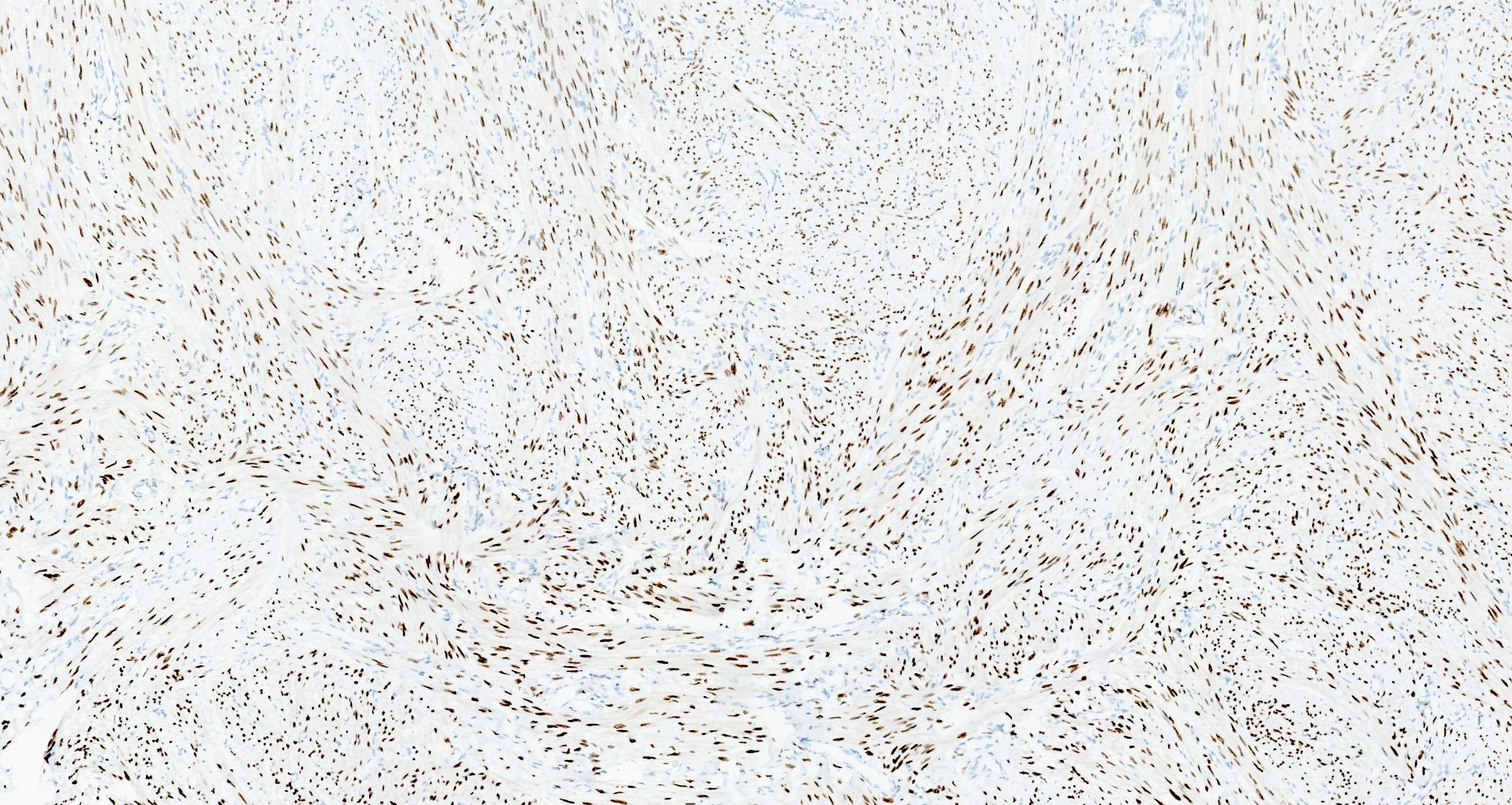
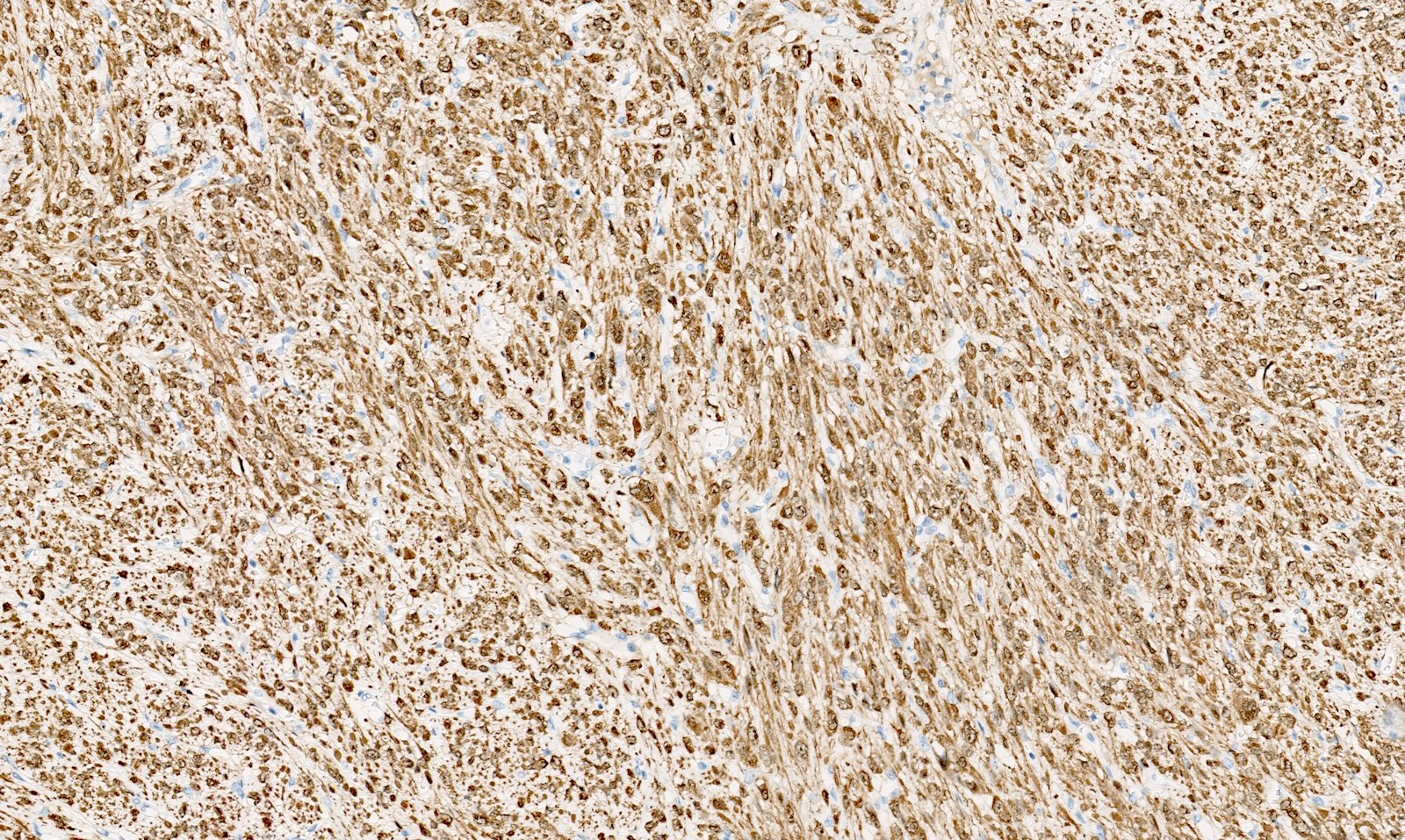
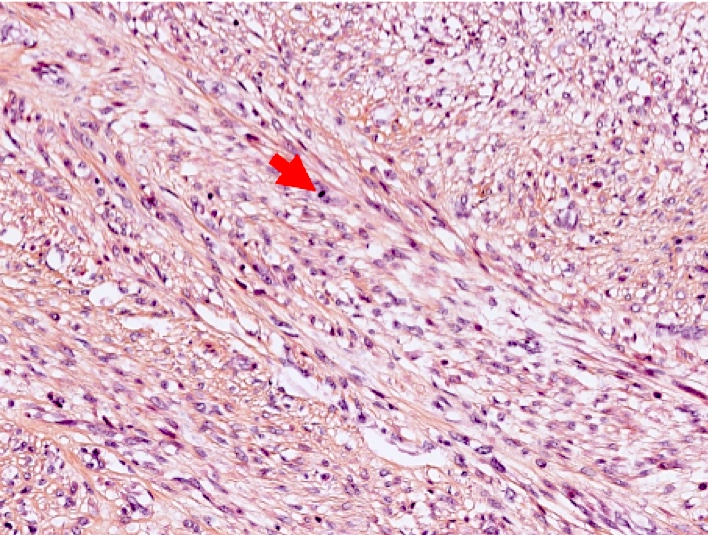
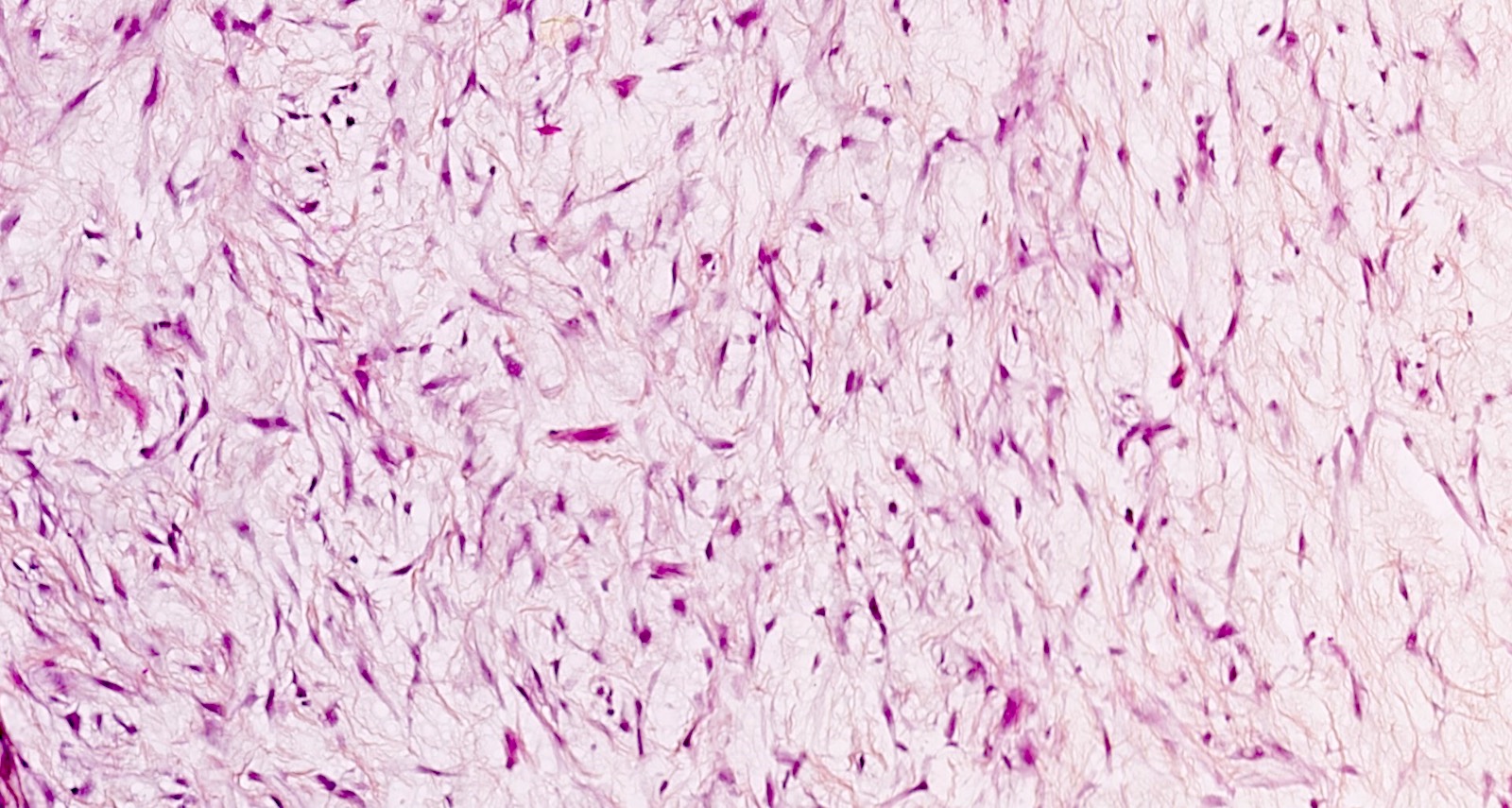
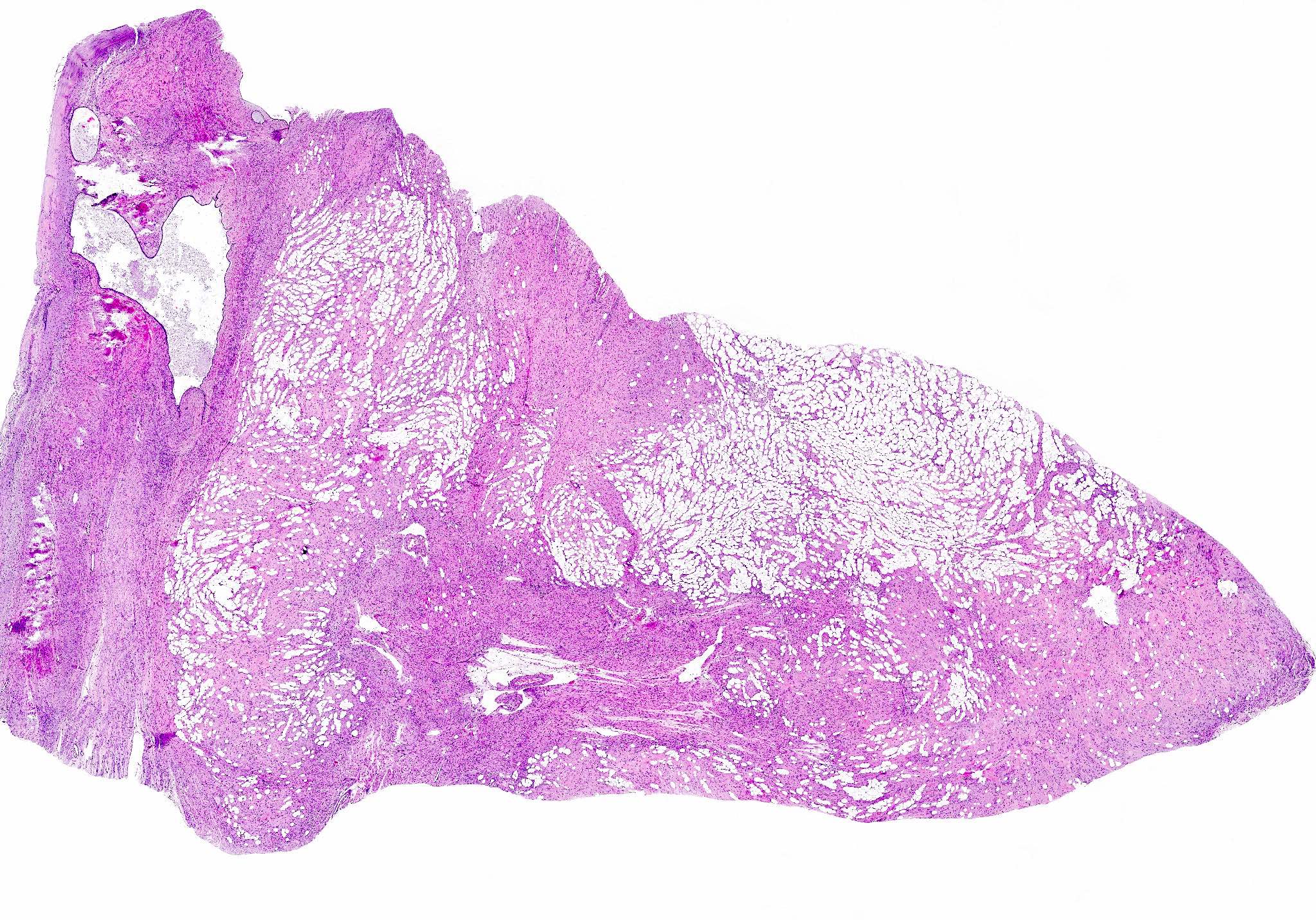
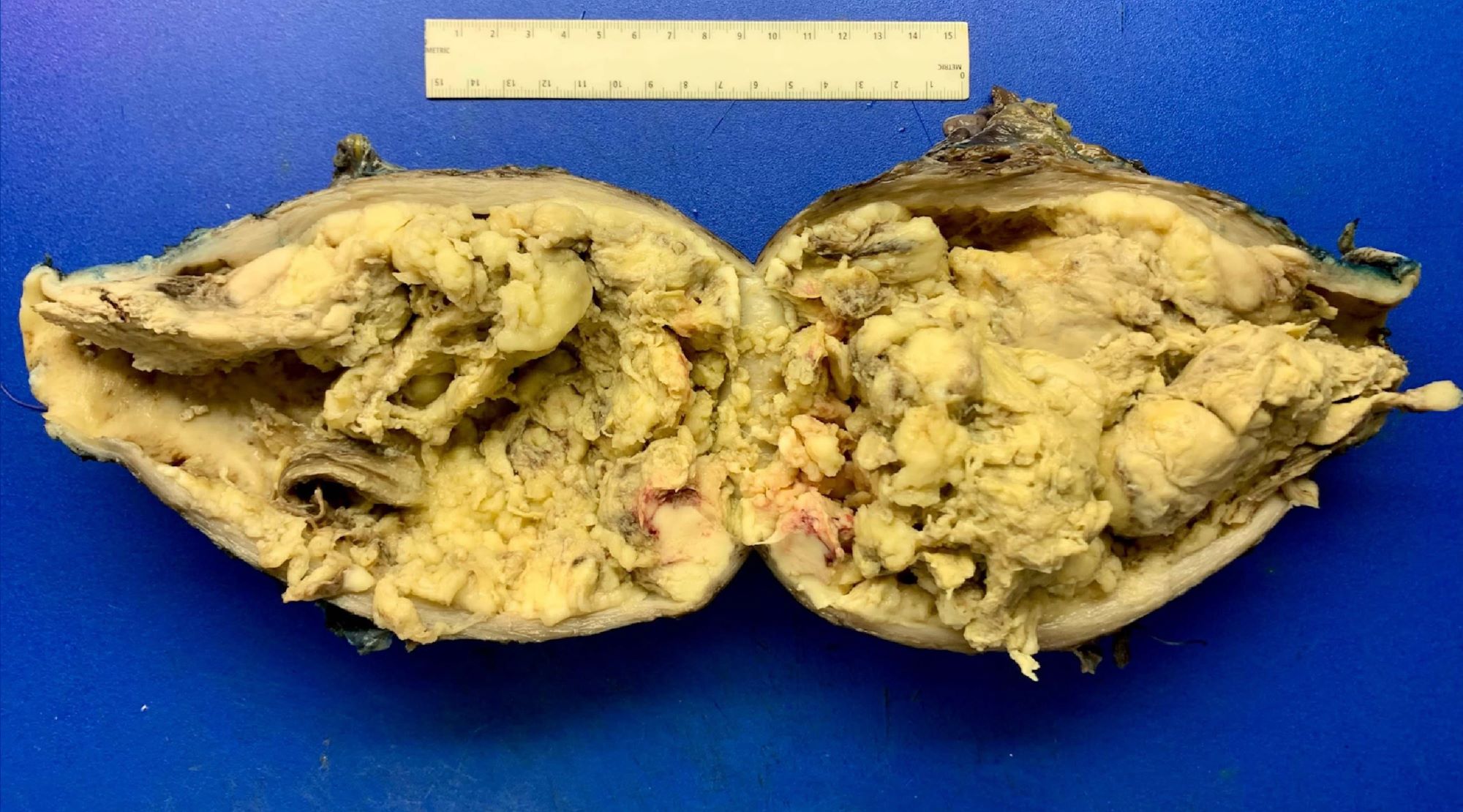
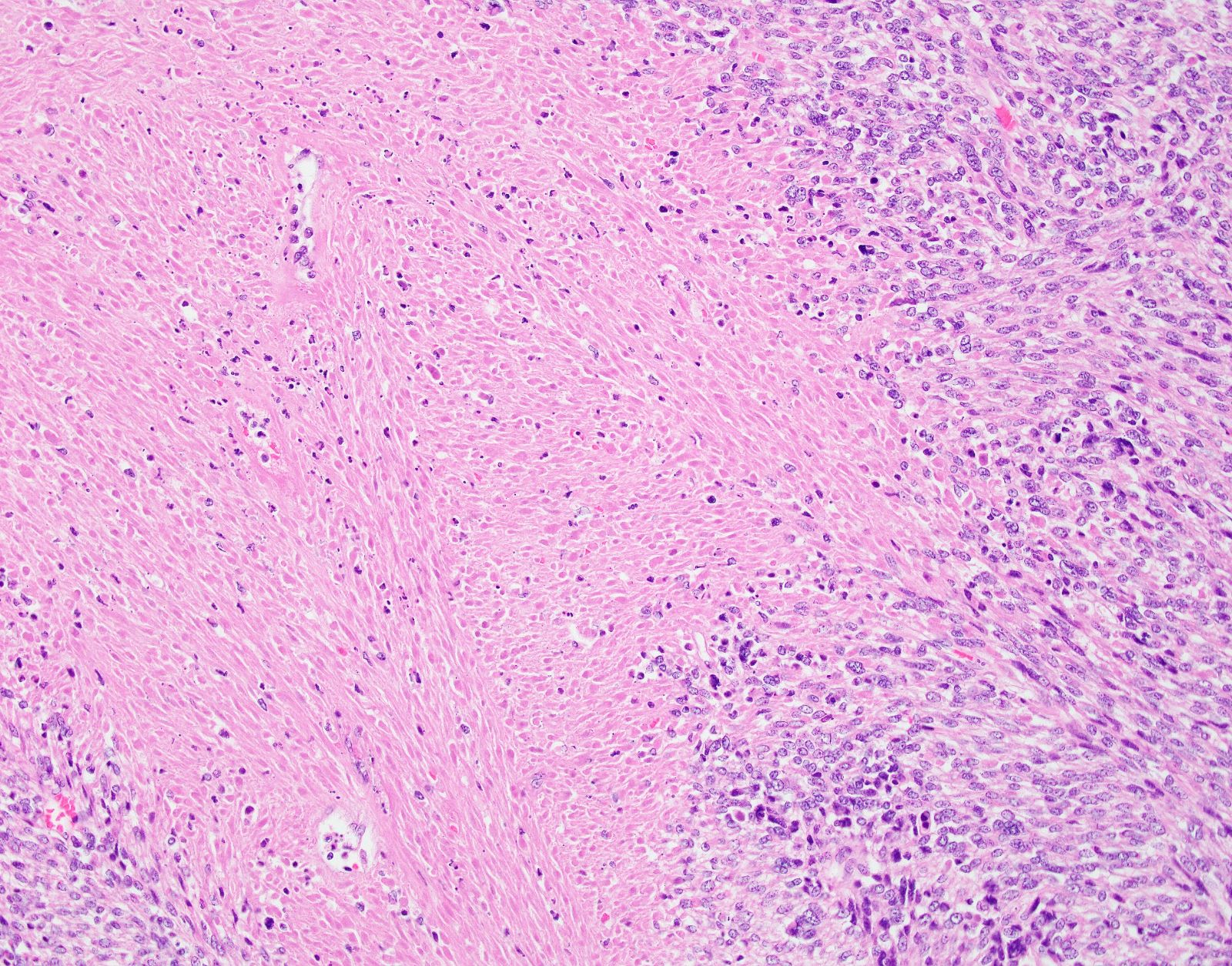
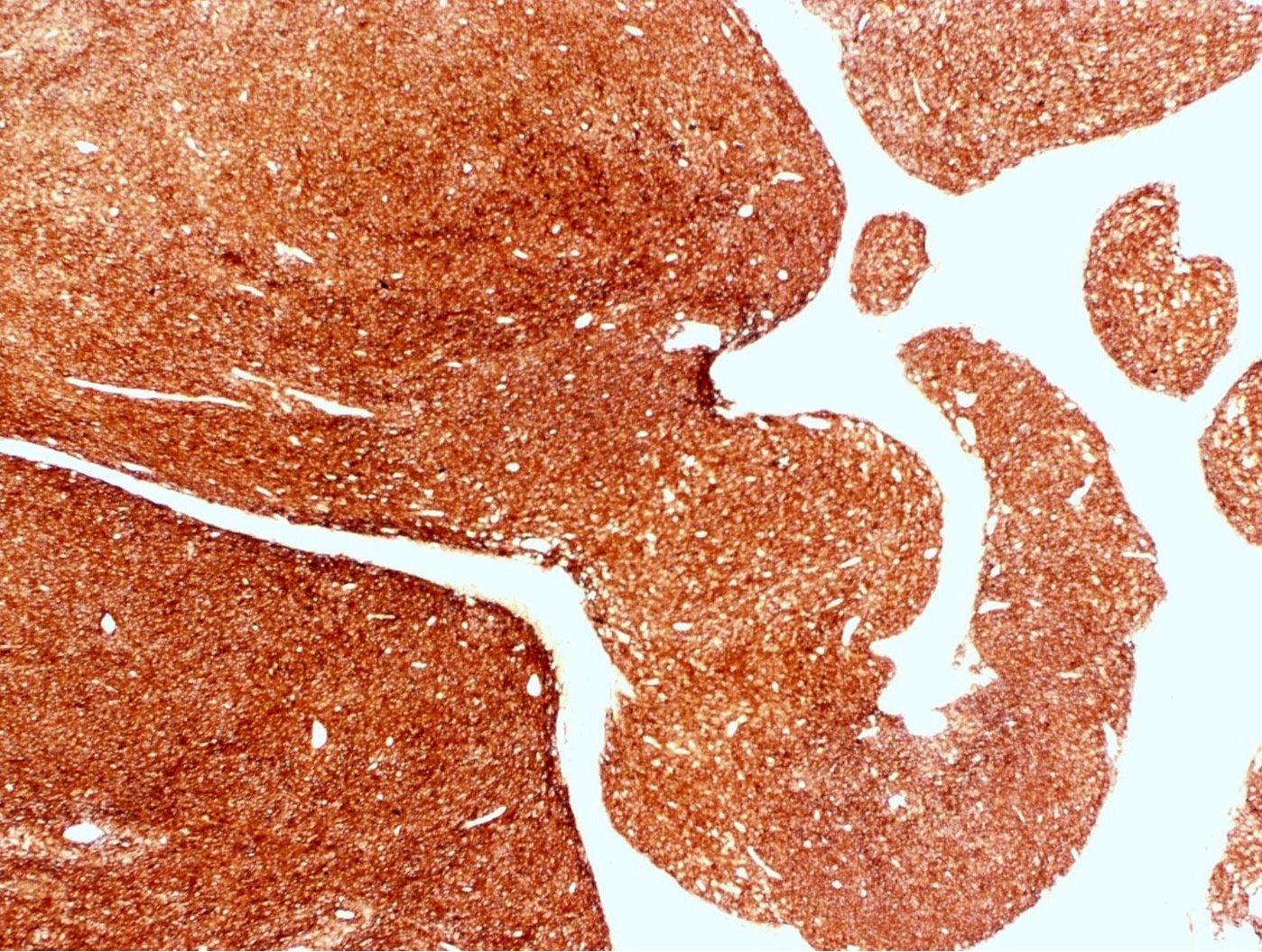
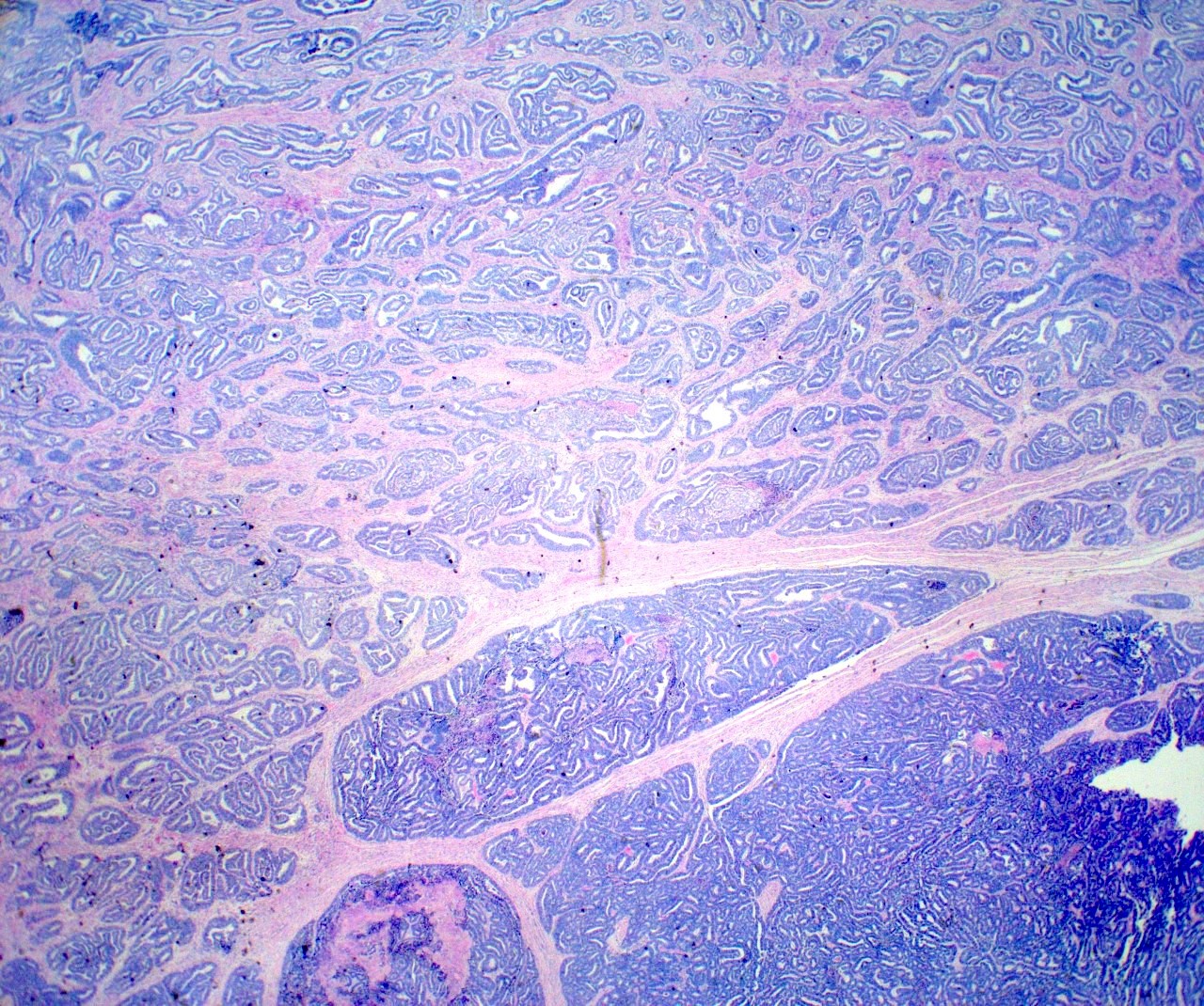
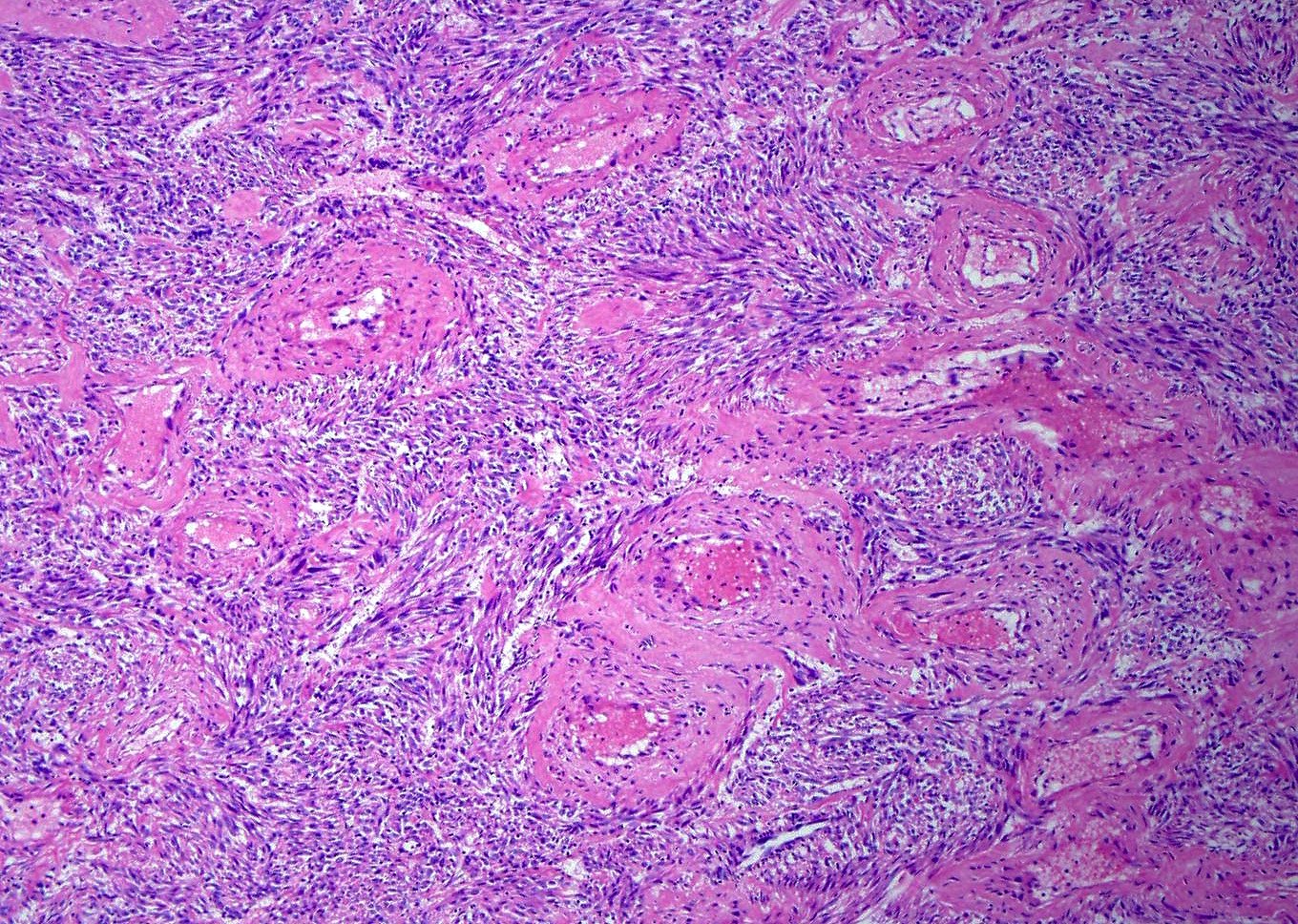
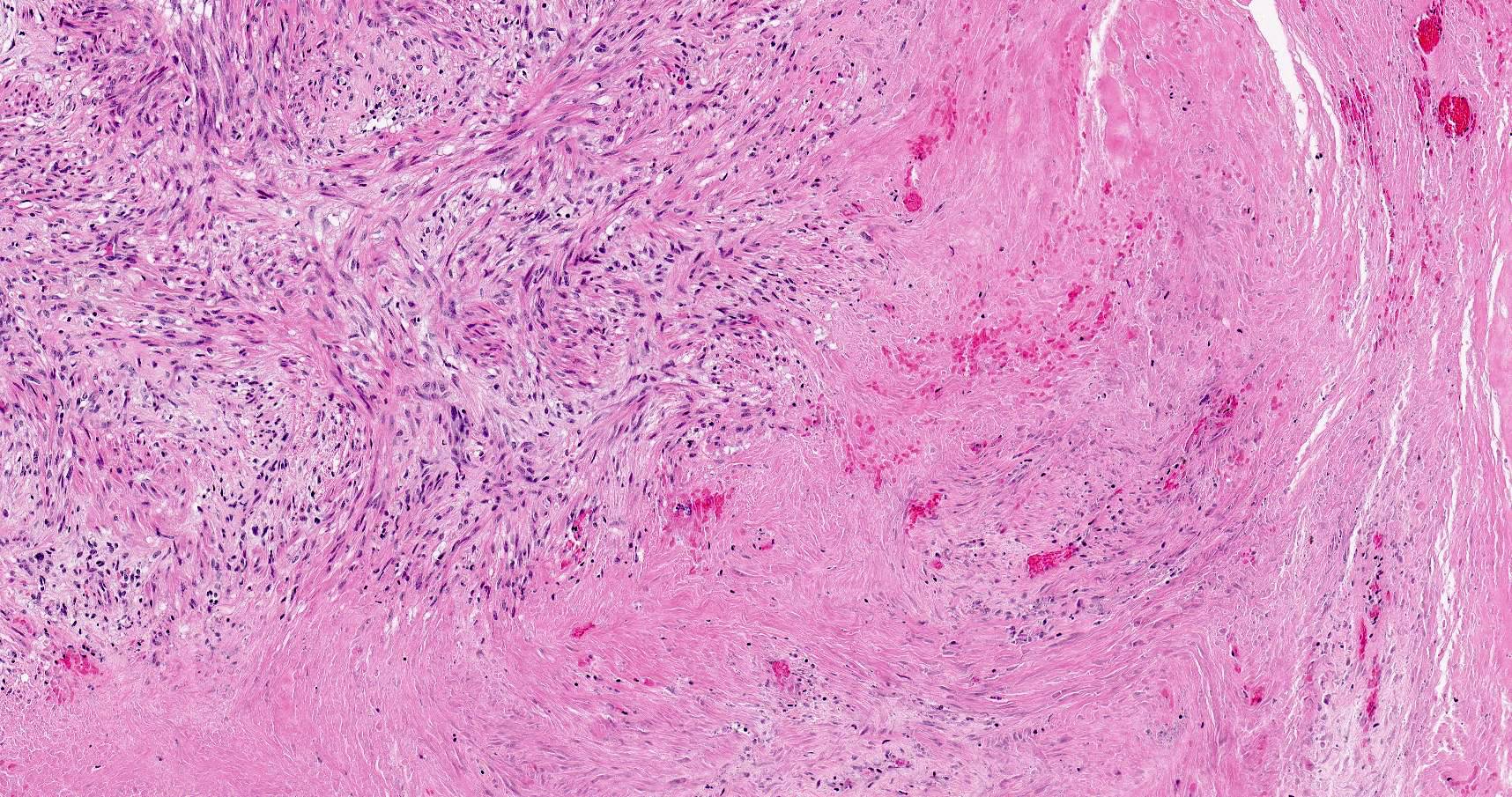
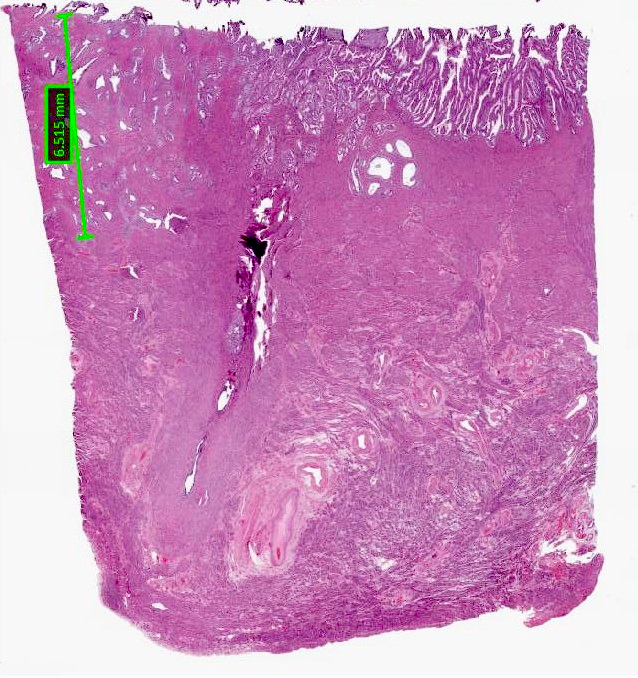
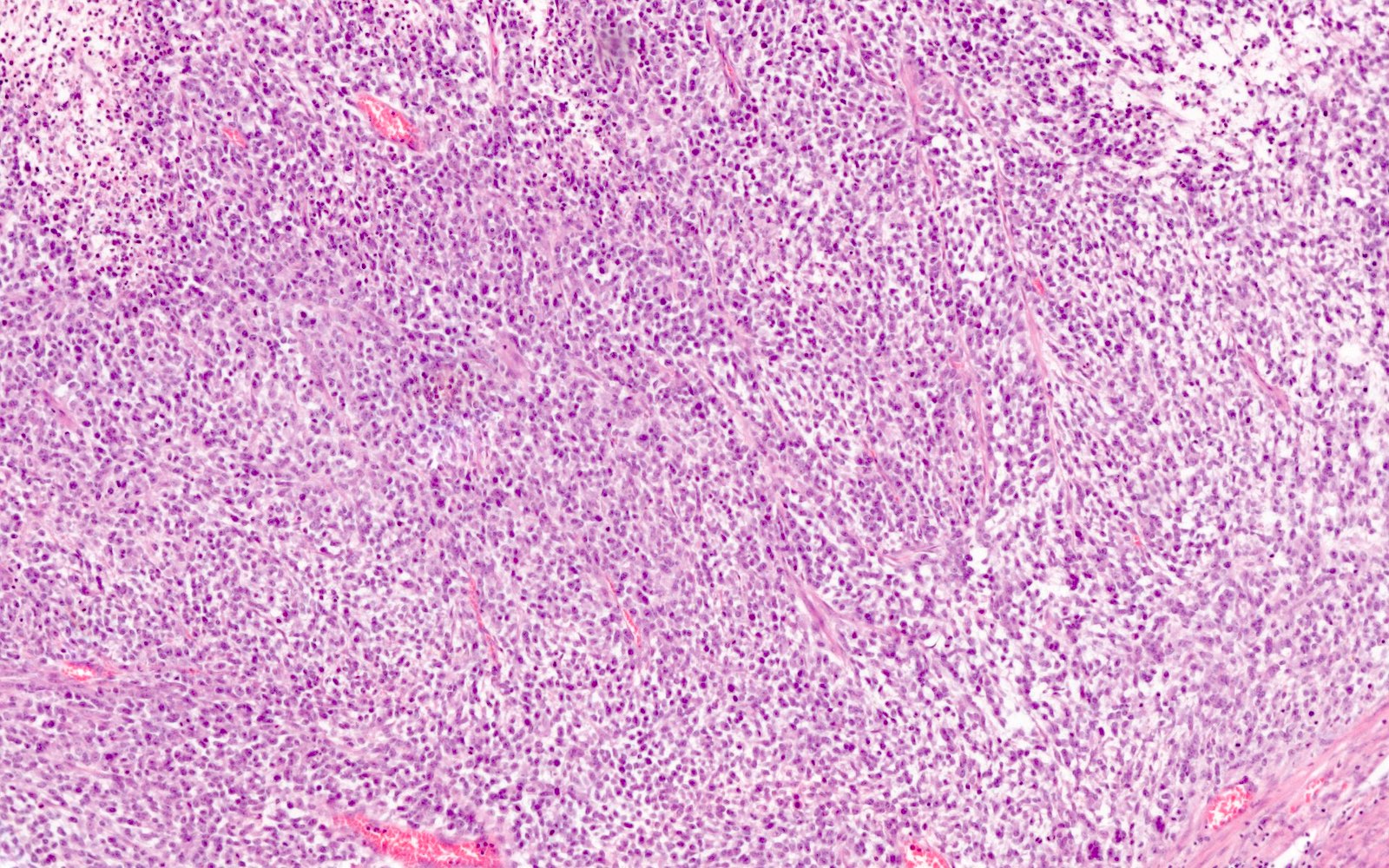
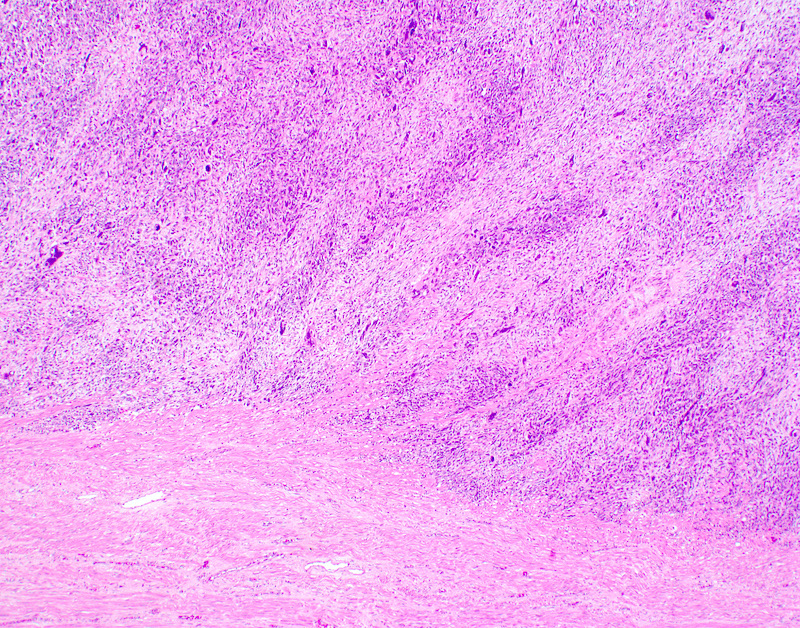
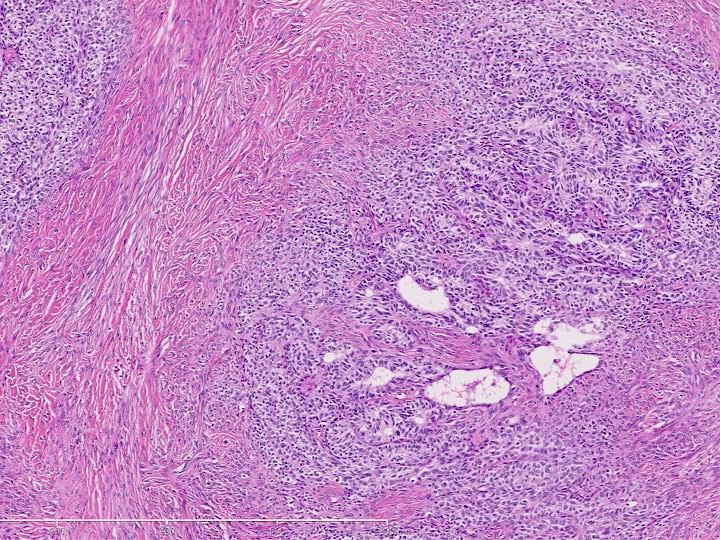
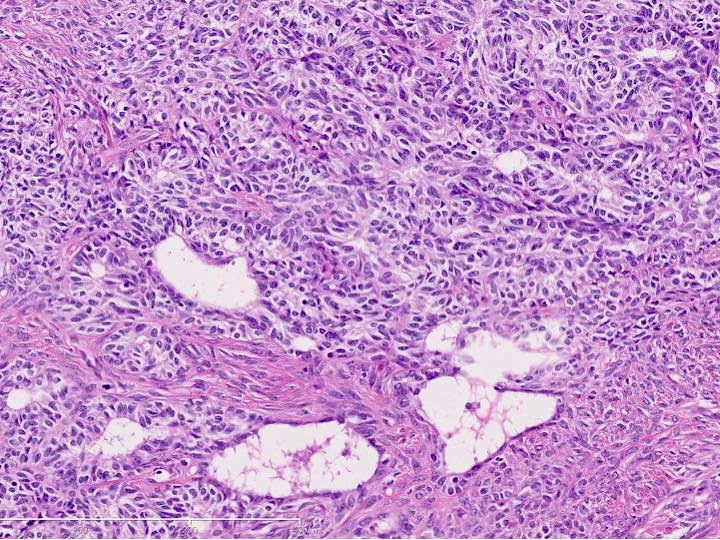
- Myometrial invasion:
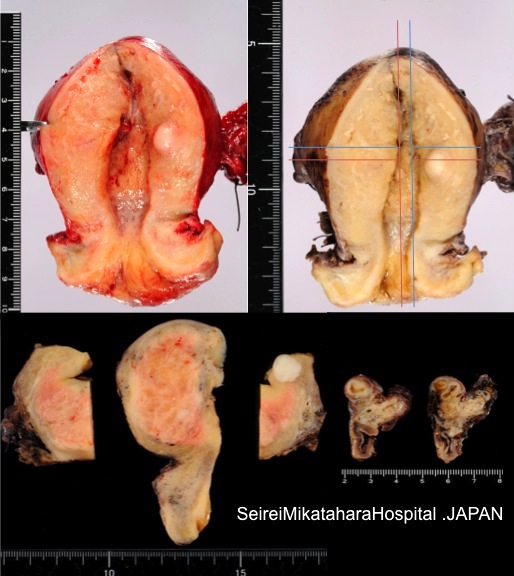
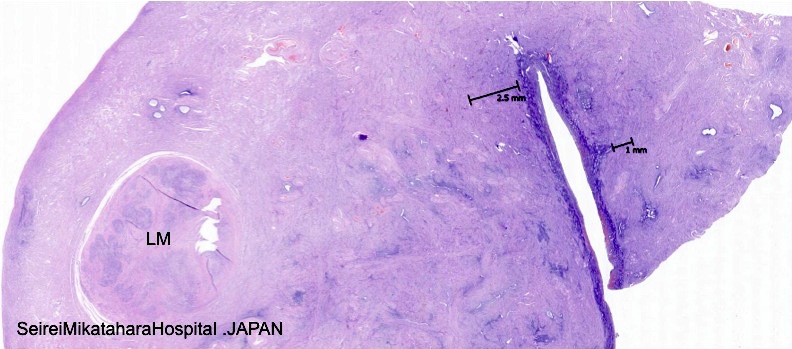
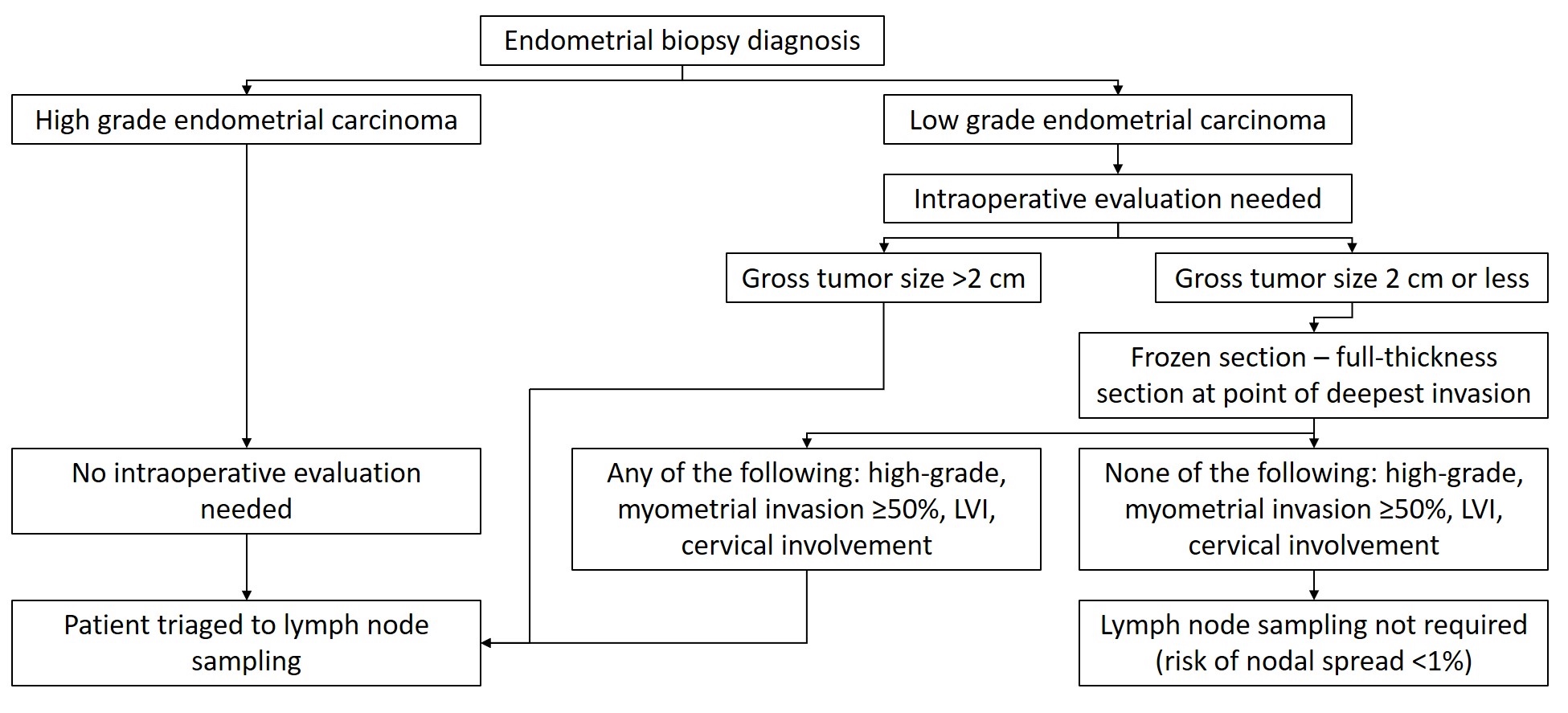
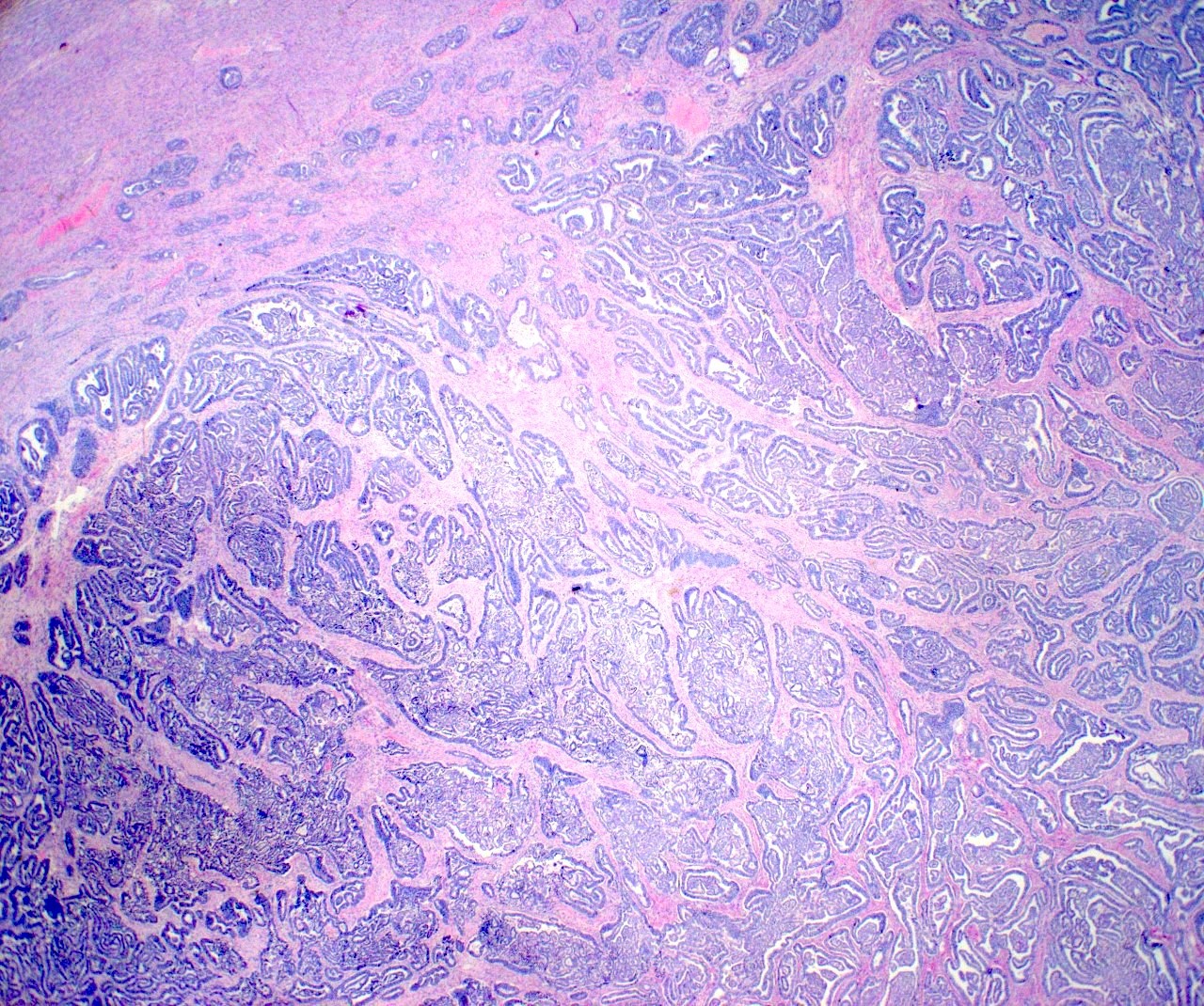
- According to the ISGYP recommendations, this variable should be reported as none or less than half (< 50%) or half or more (≥ 50%) of the myometrial wall thickness
- This approach is relatively easy and obviates in most cases the need to locate the endomyometrial junction (which is difficult when the junction is completely obliterated or not sampled in the sections)
- In addition, other variables than can be reported include myoinvasion in terms of absolute numbers (invasive carcinoma depth in mm / myometrial thickness in mm) and the percentage of myometrial wall involved by tumor (a derivative of the absolute measurements in mm)
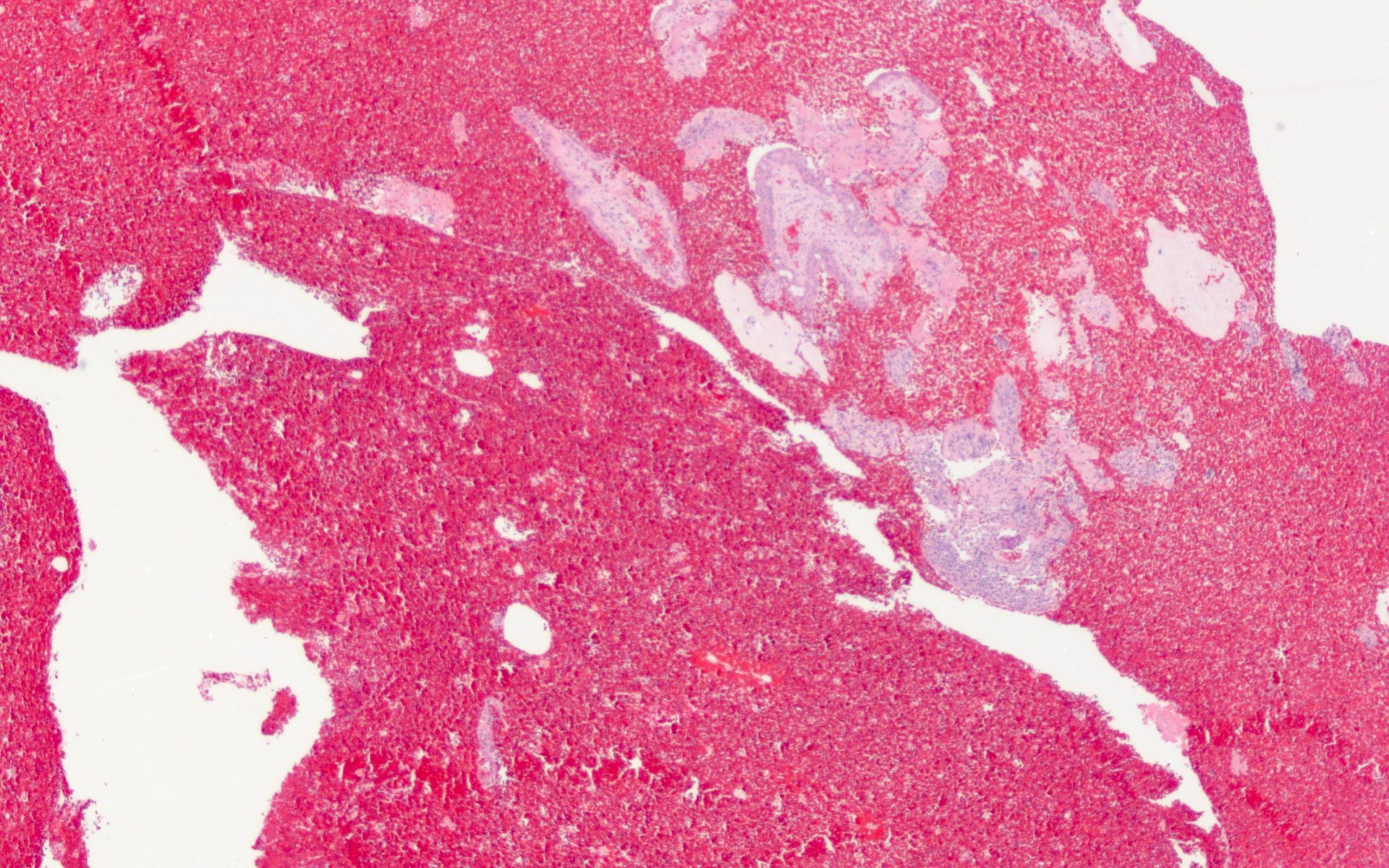
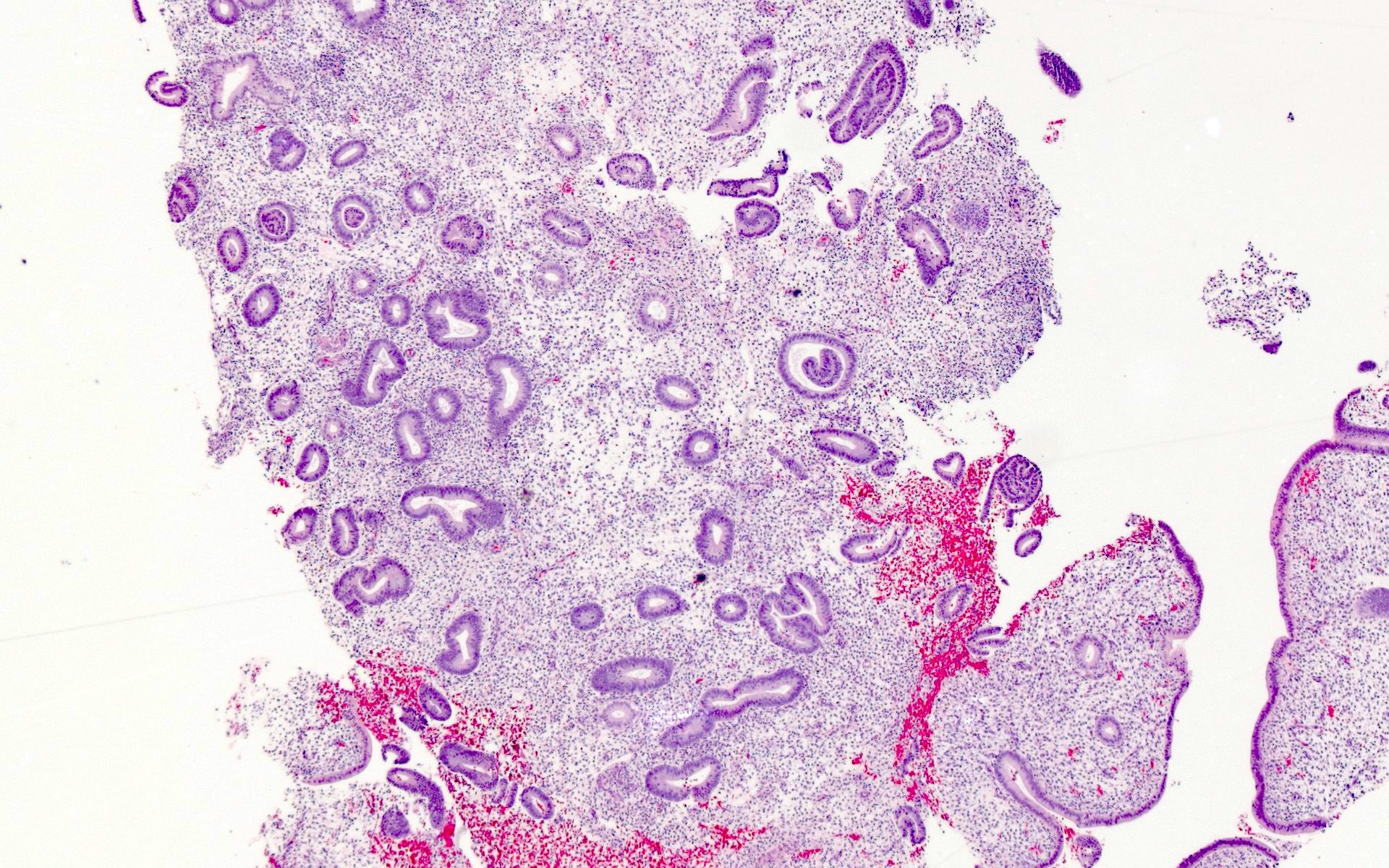
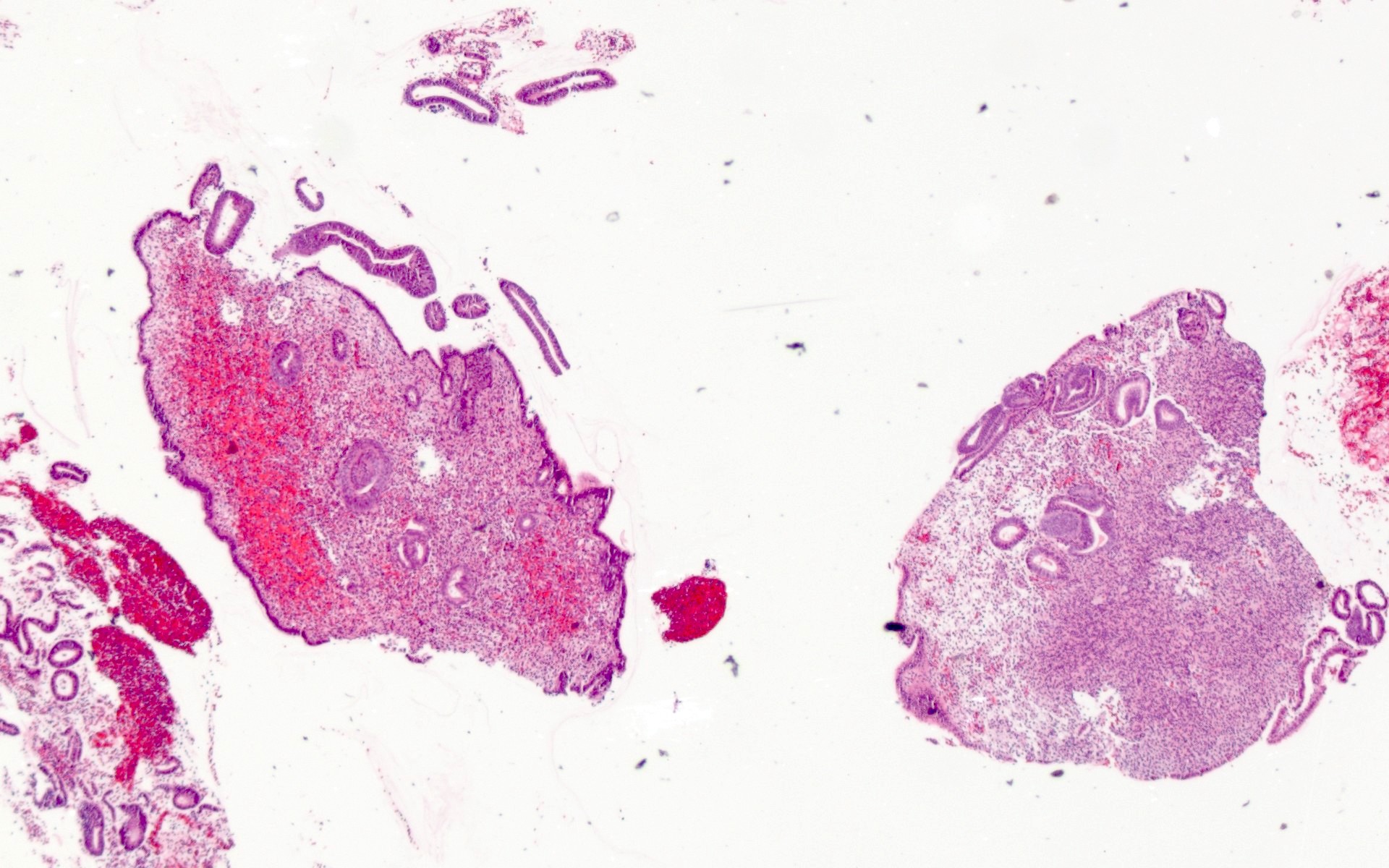
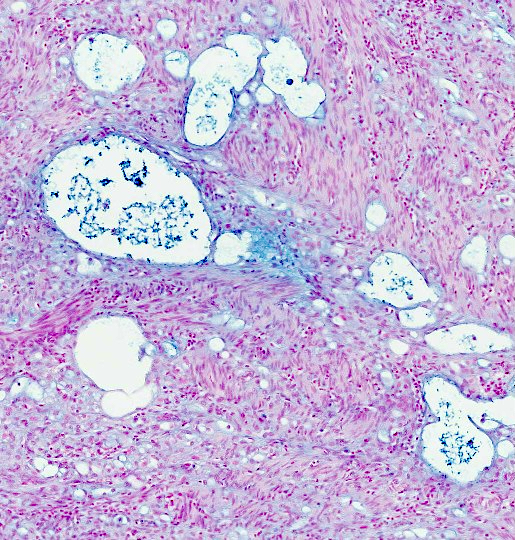
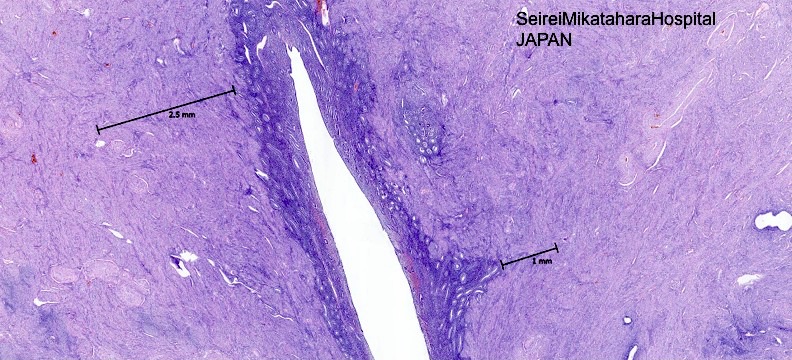
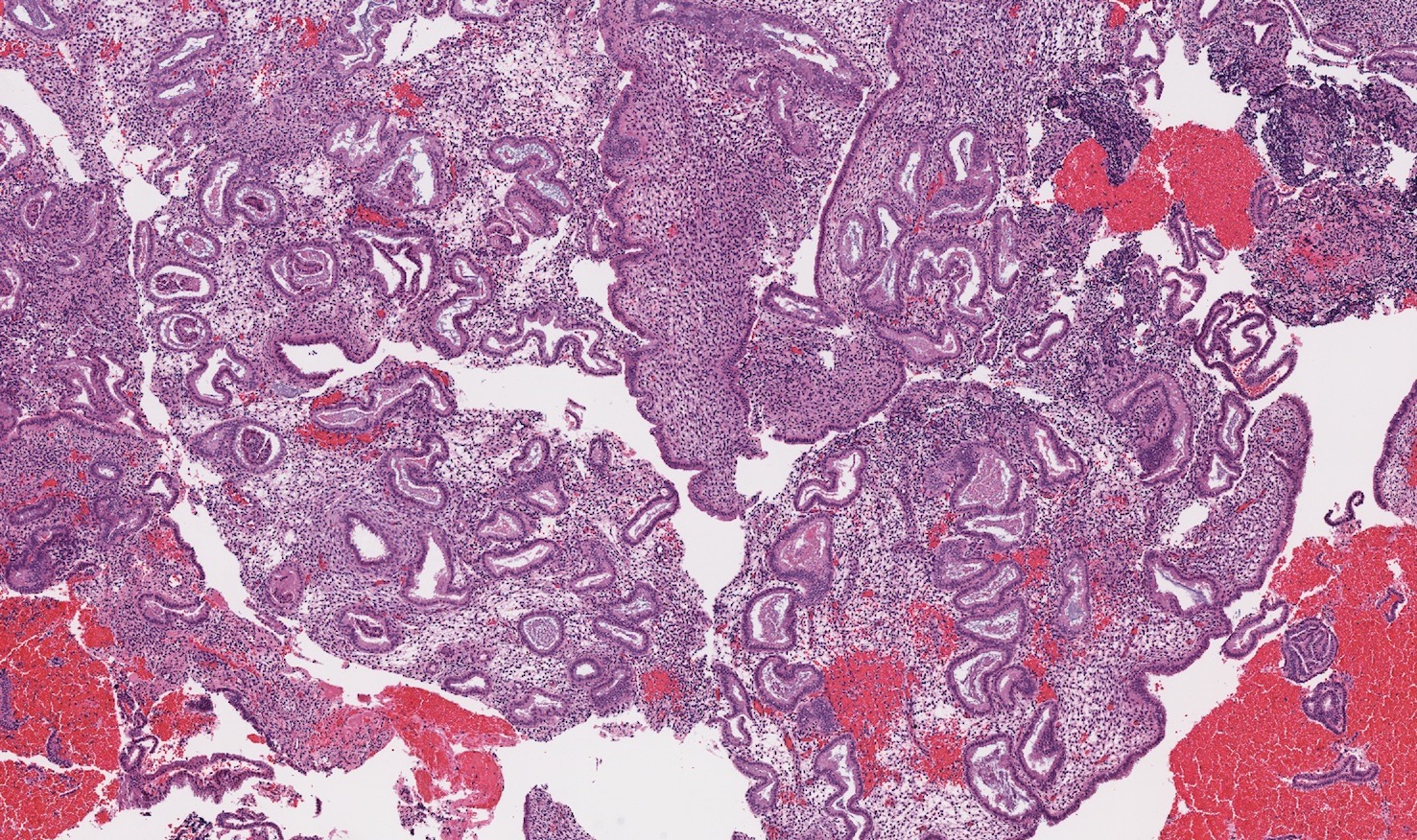
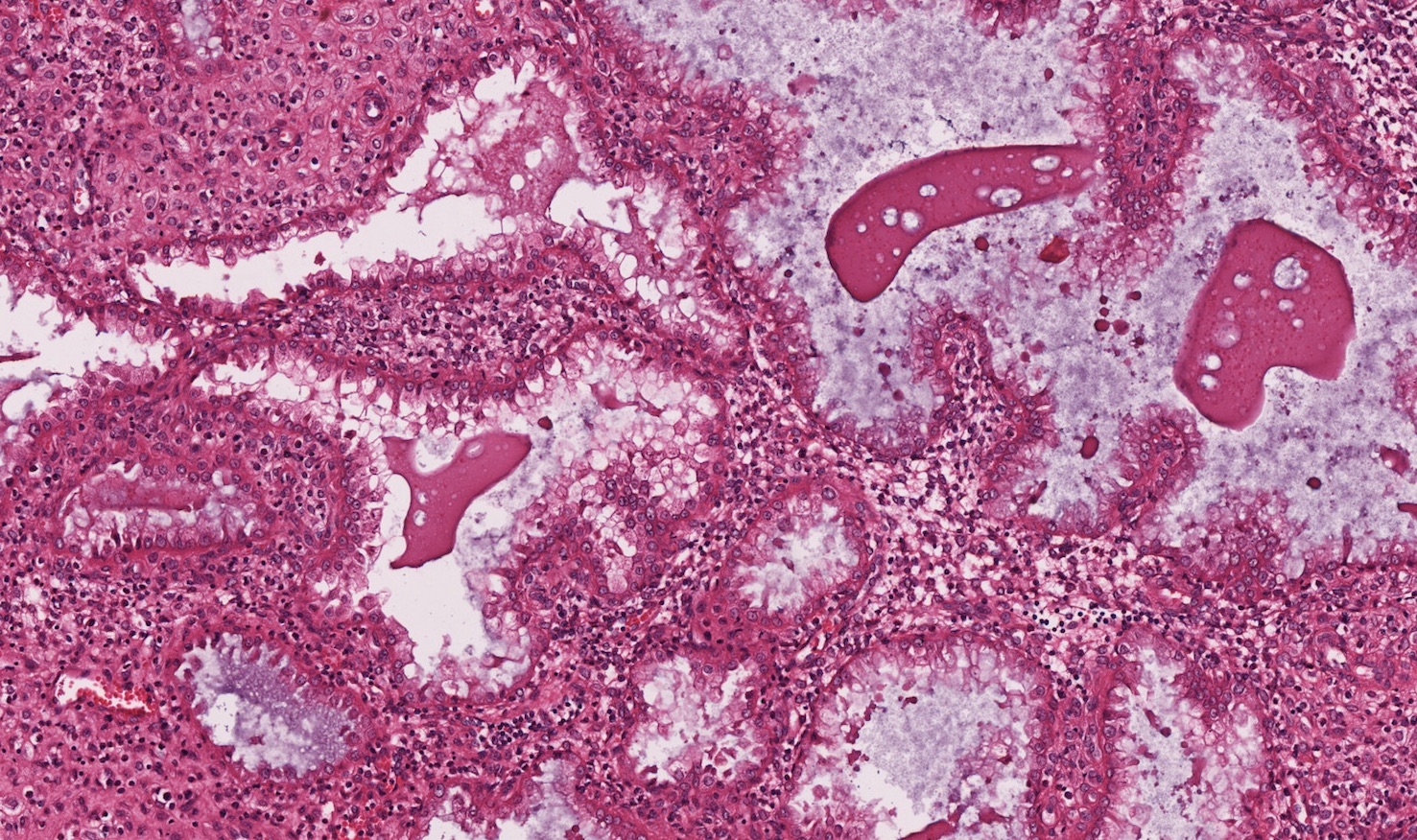
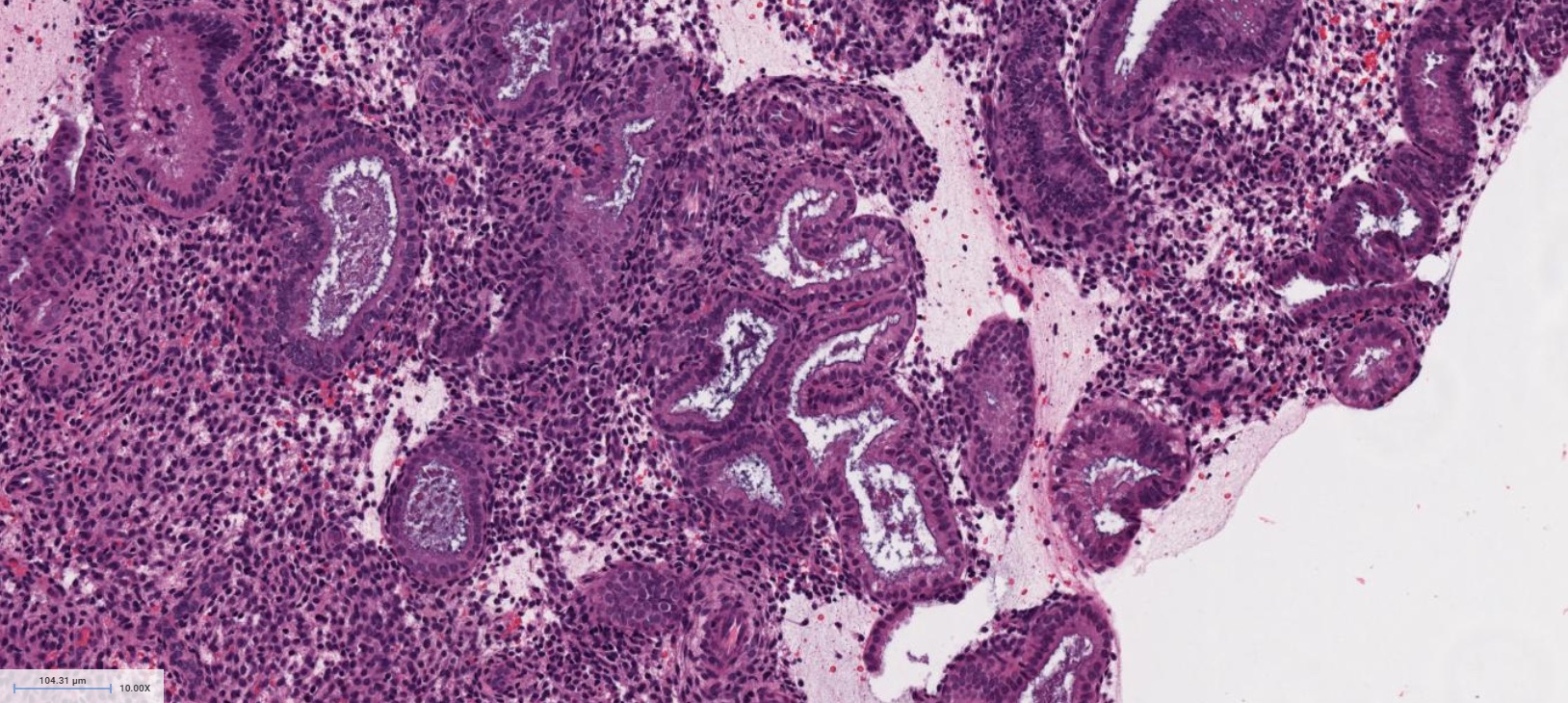
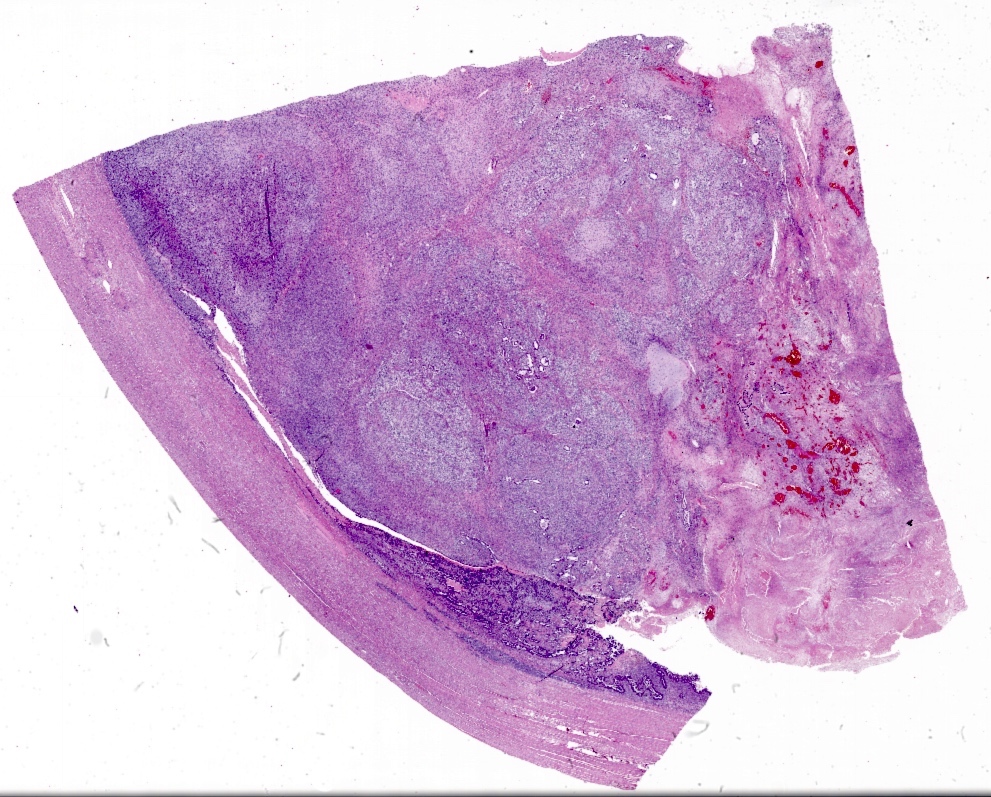
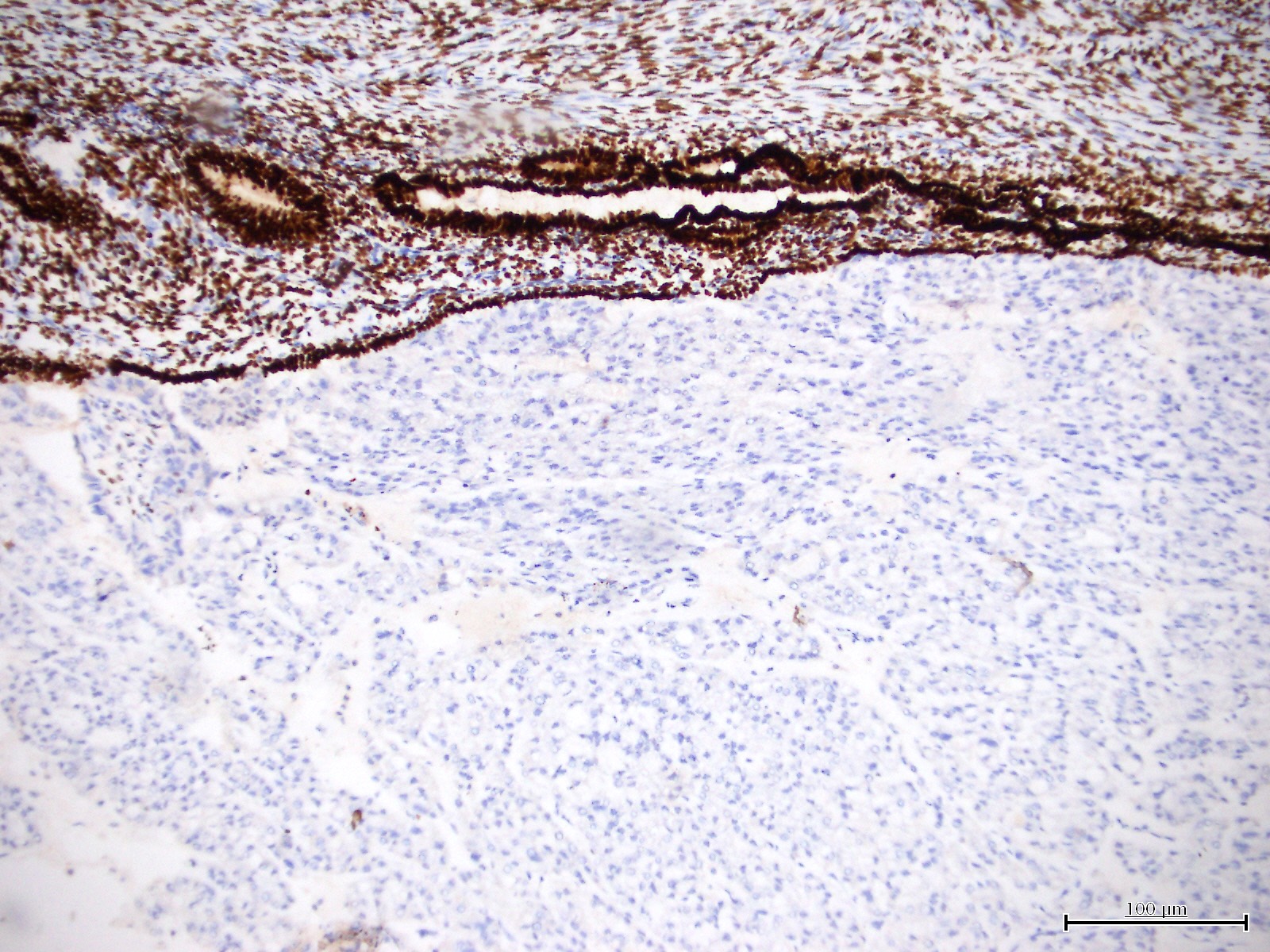
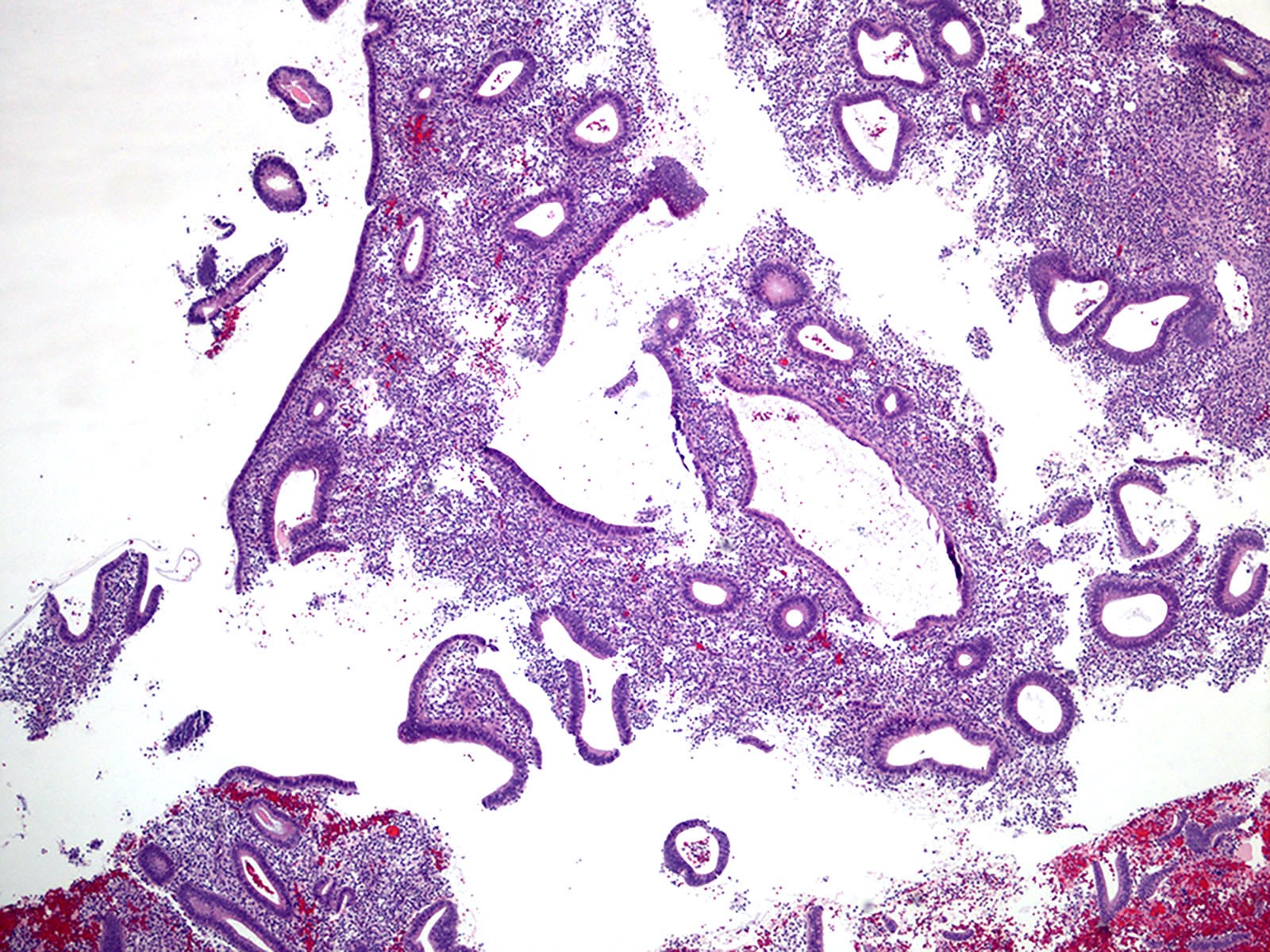
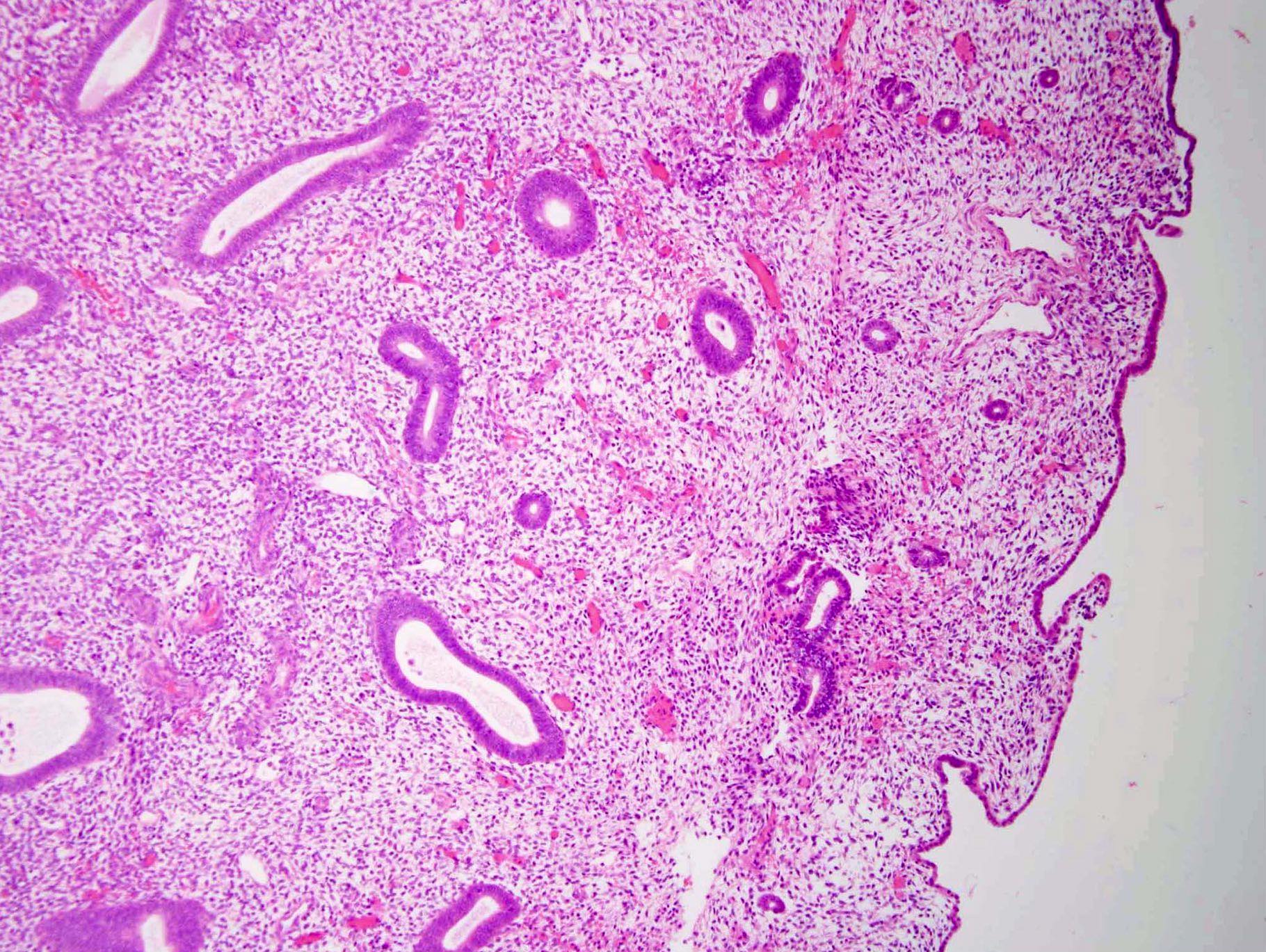
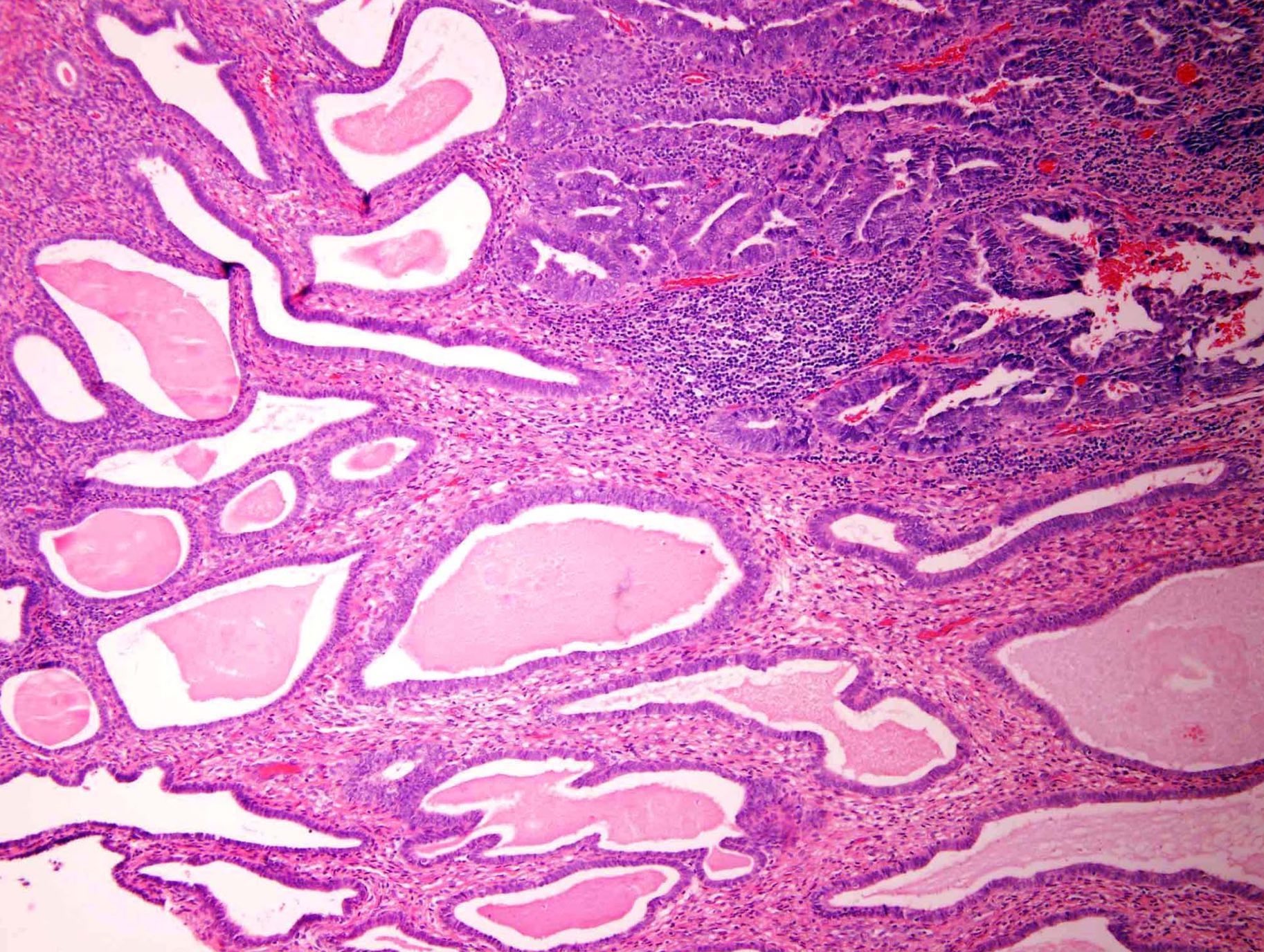
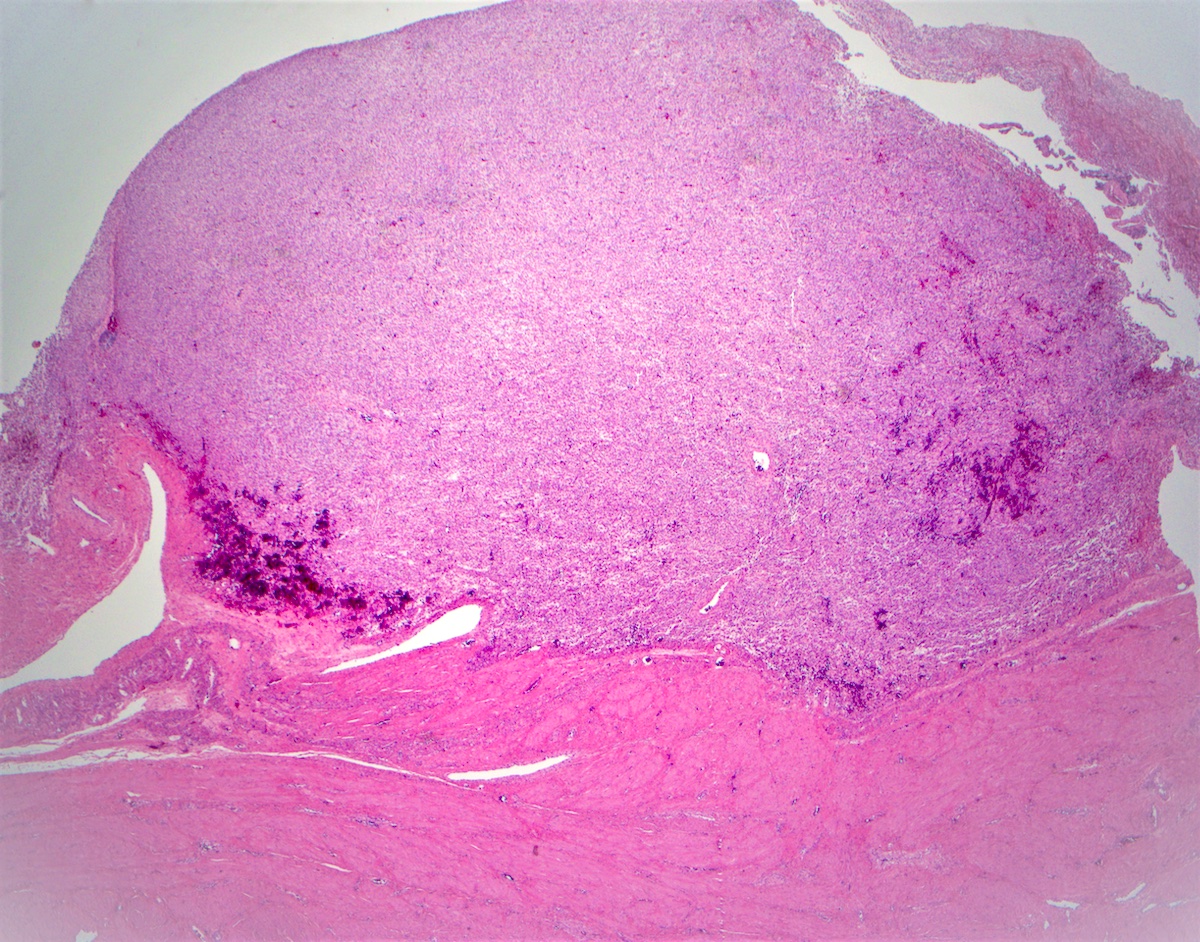
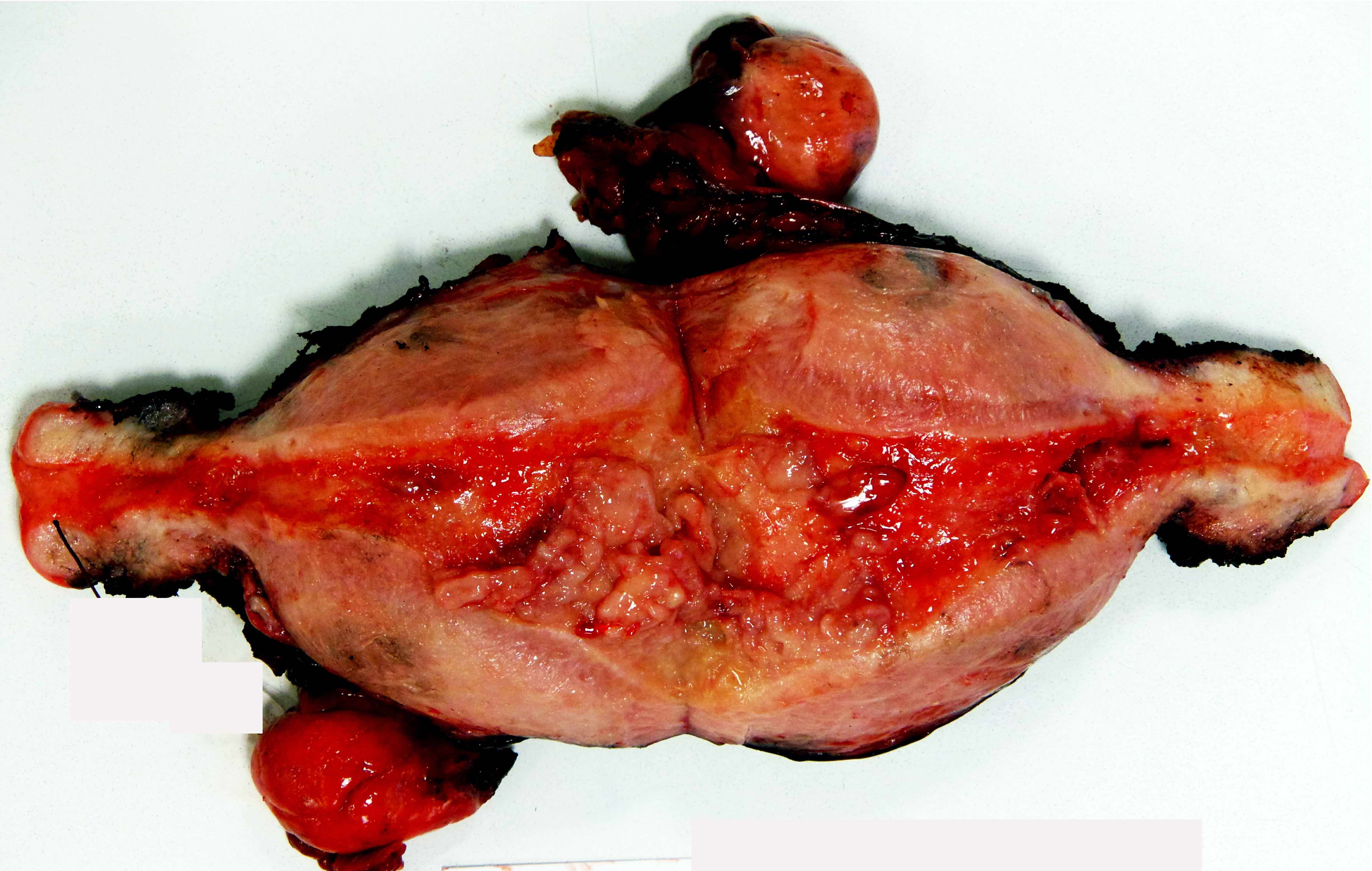
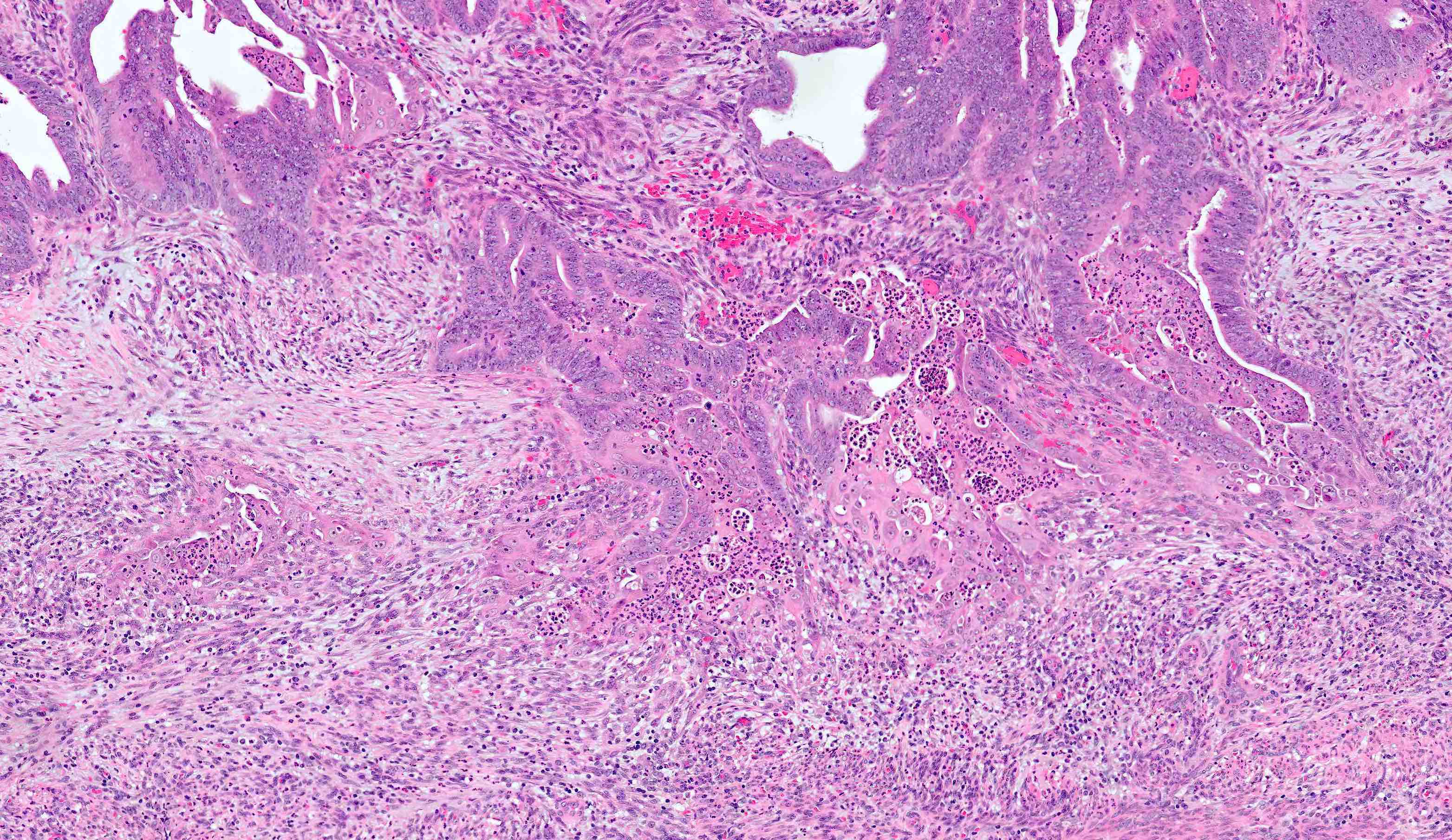
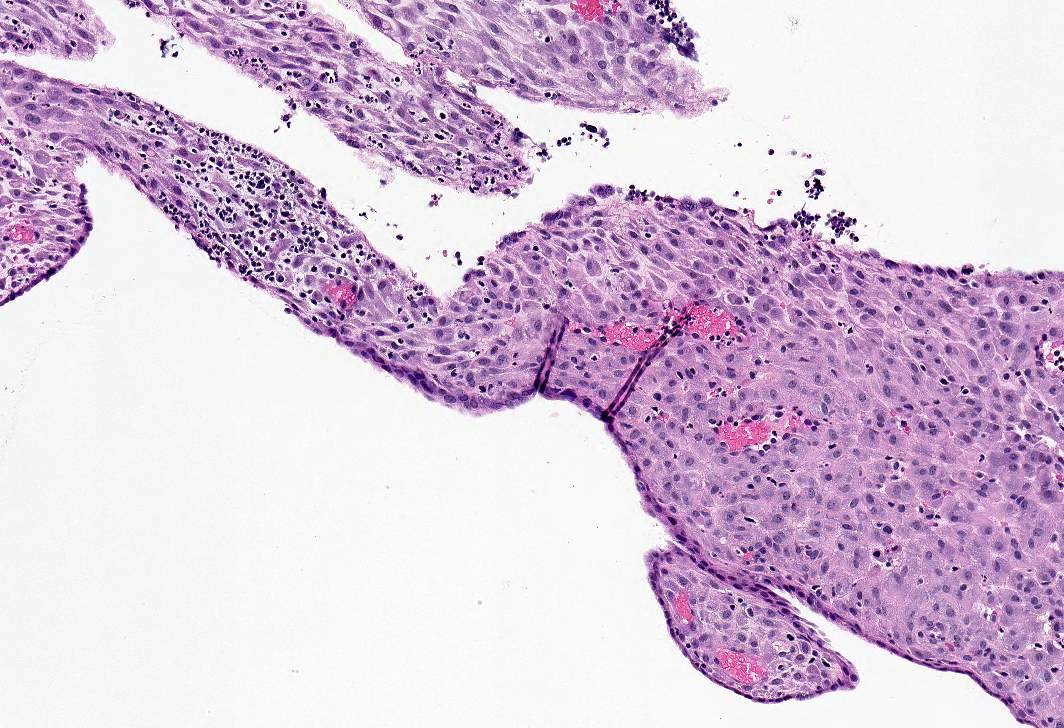
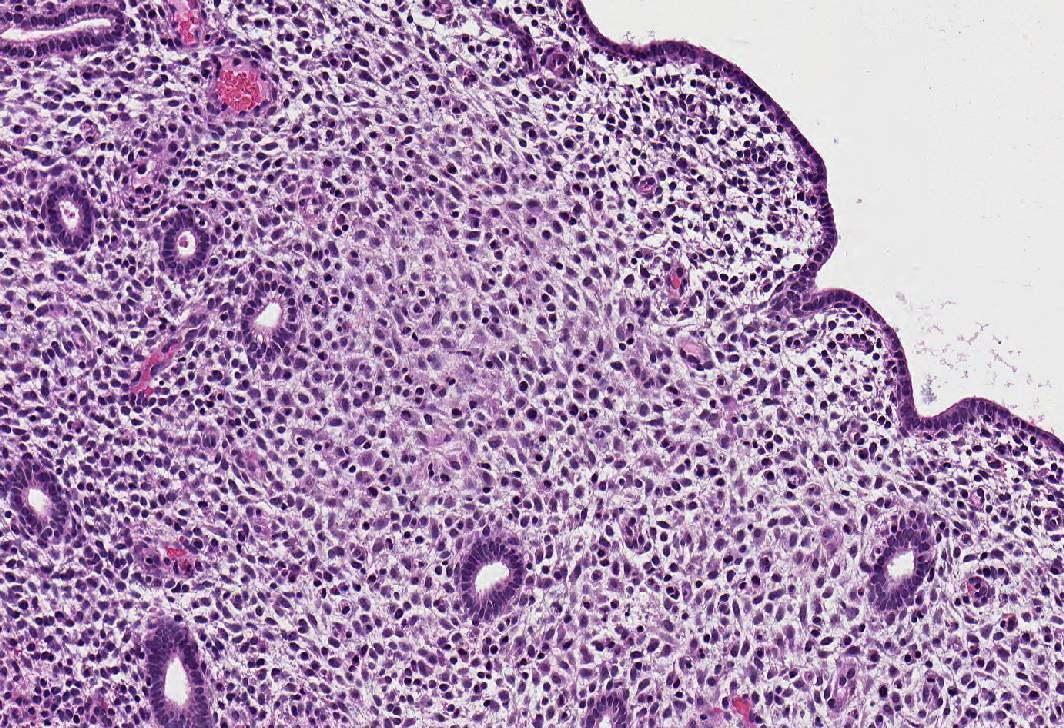
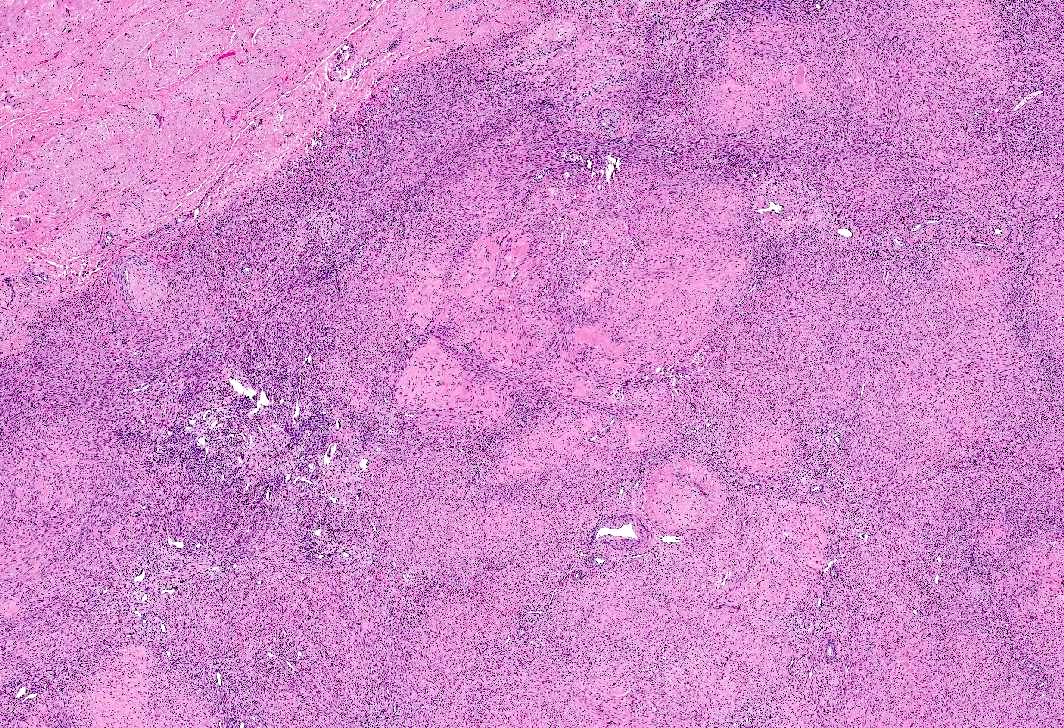
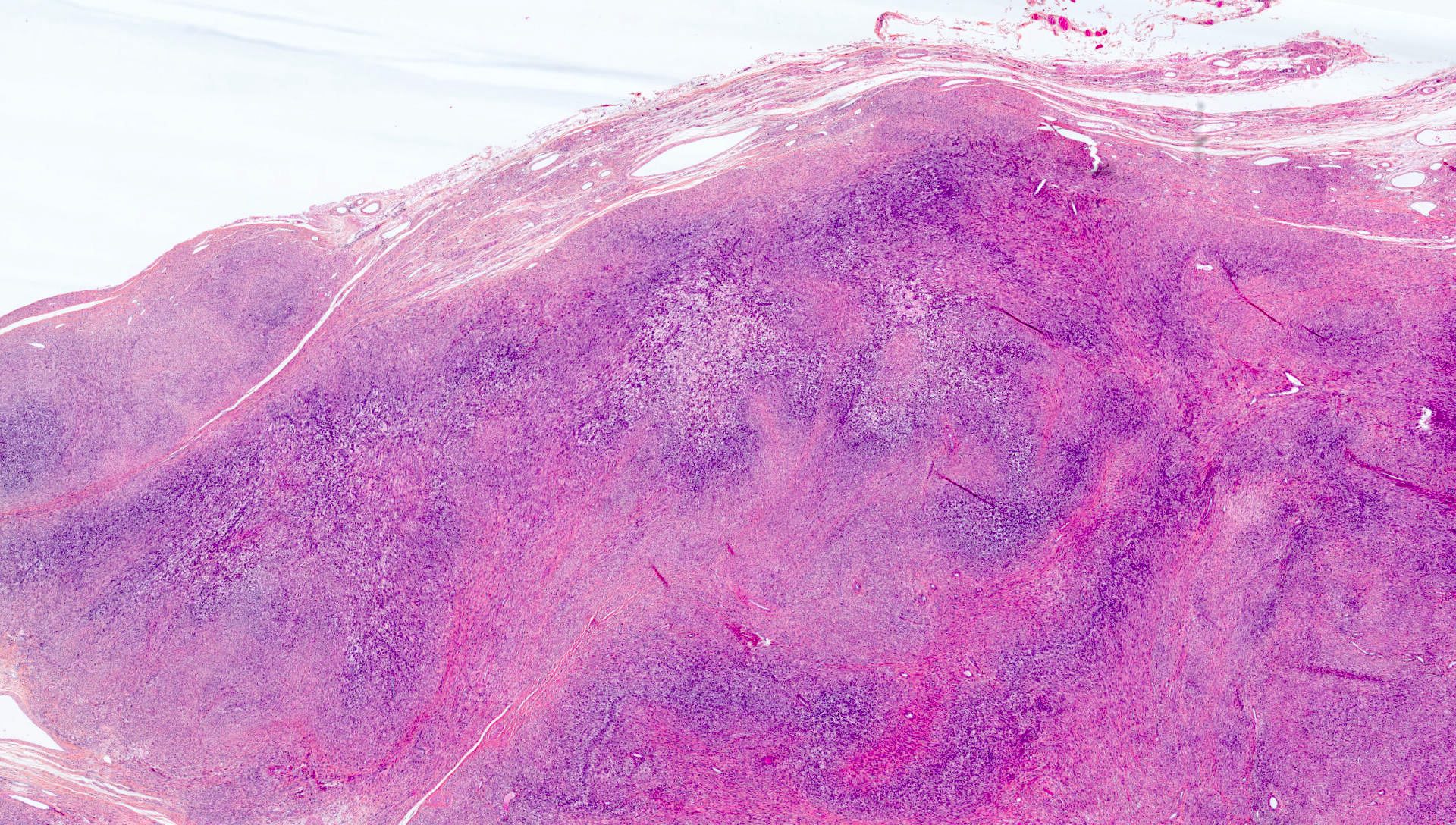
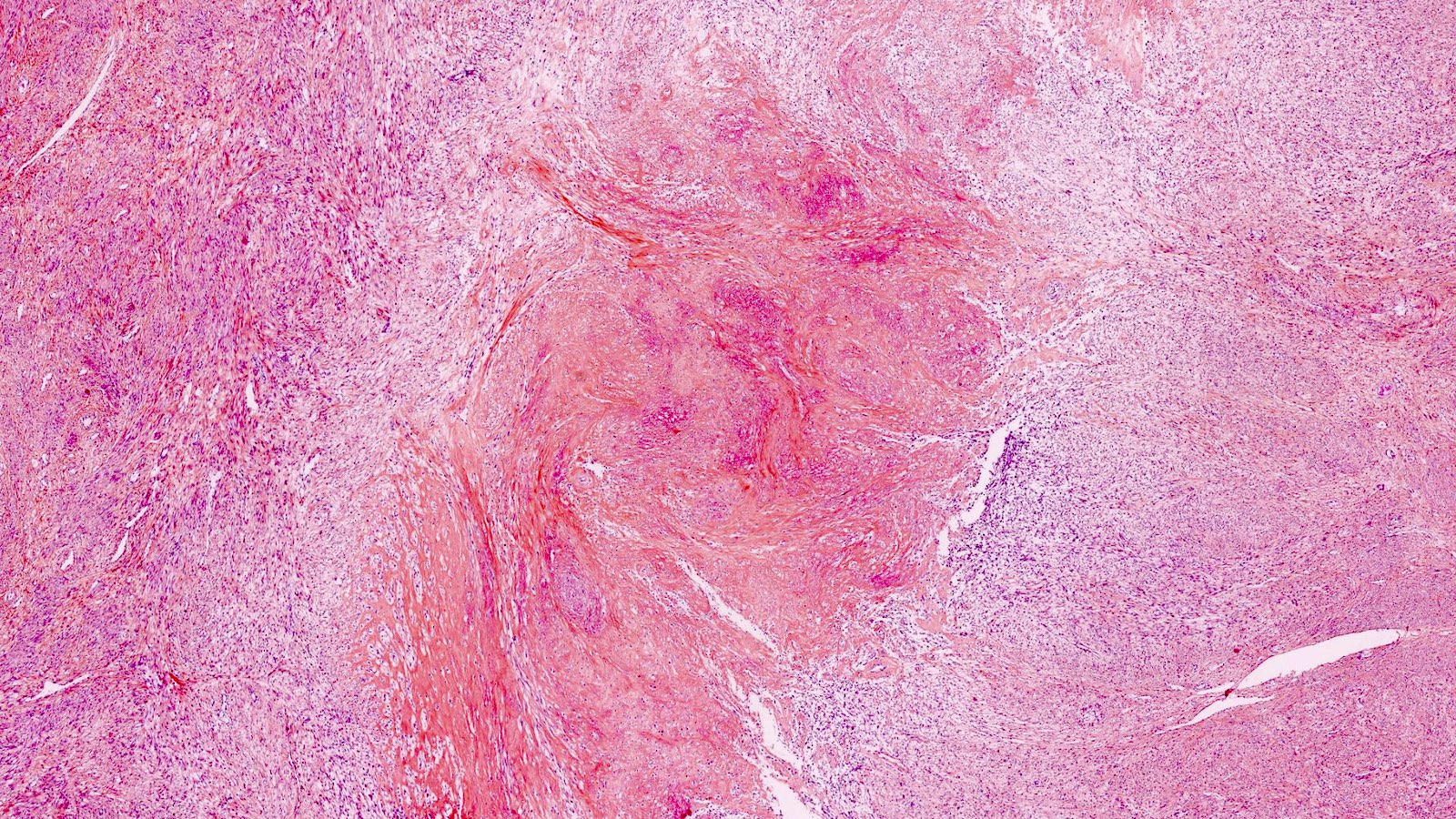
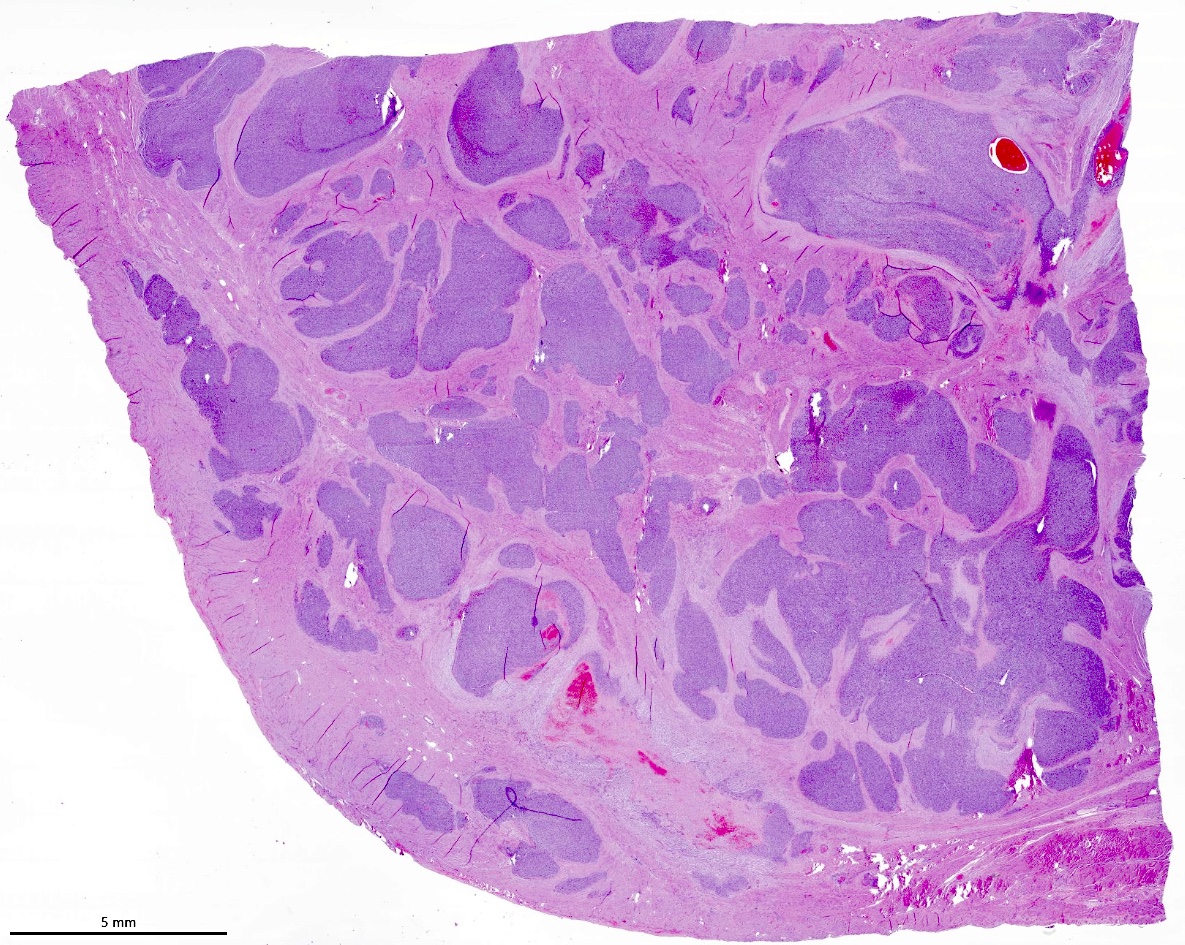
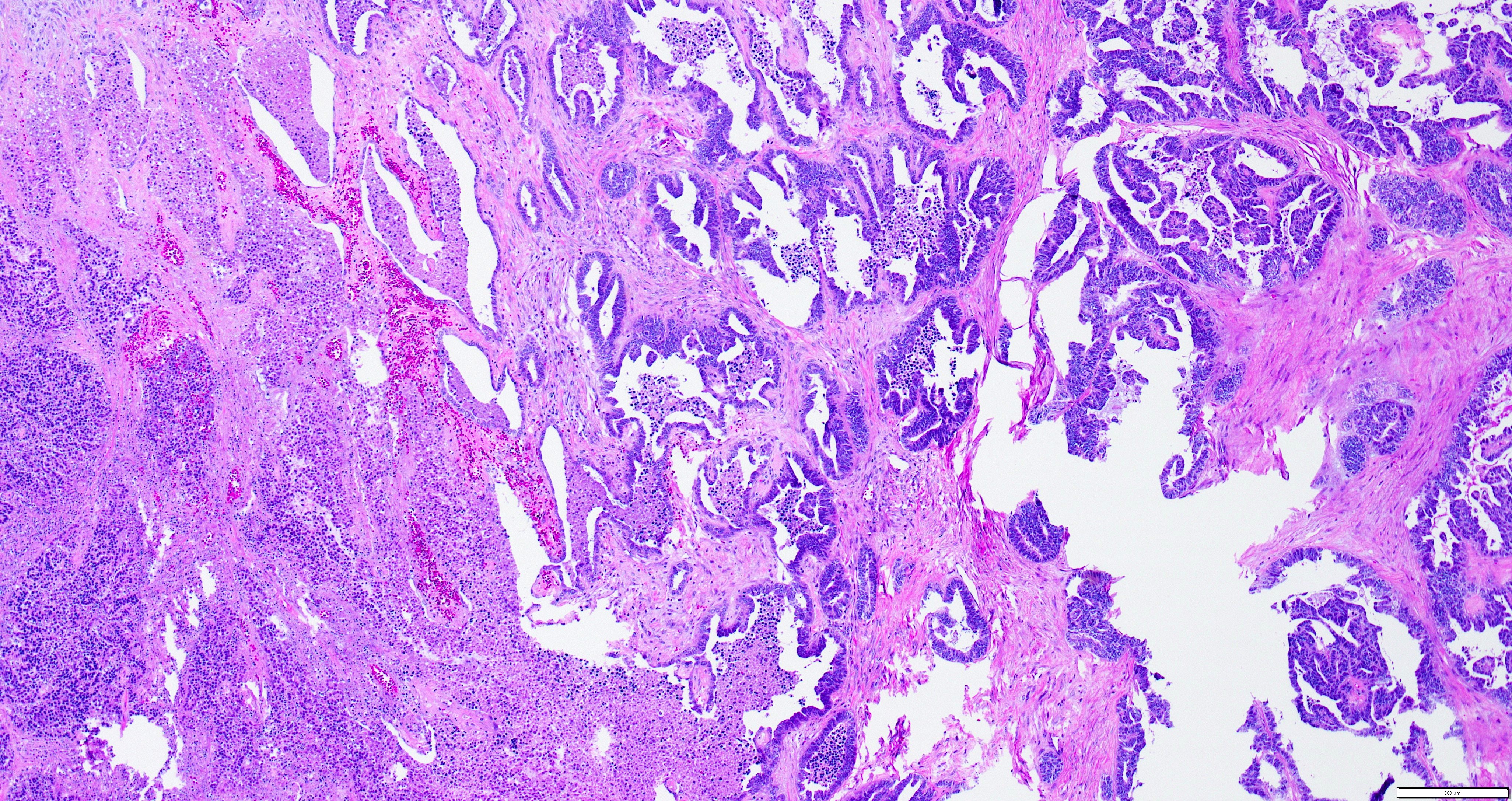
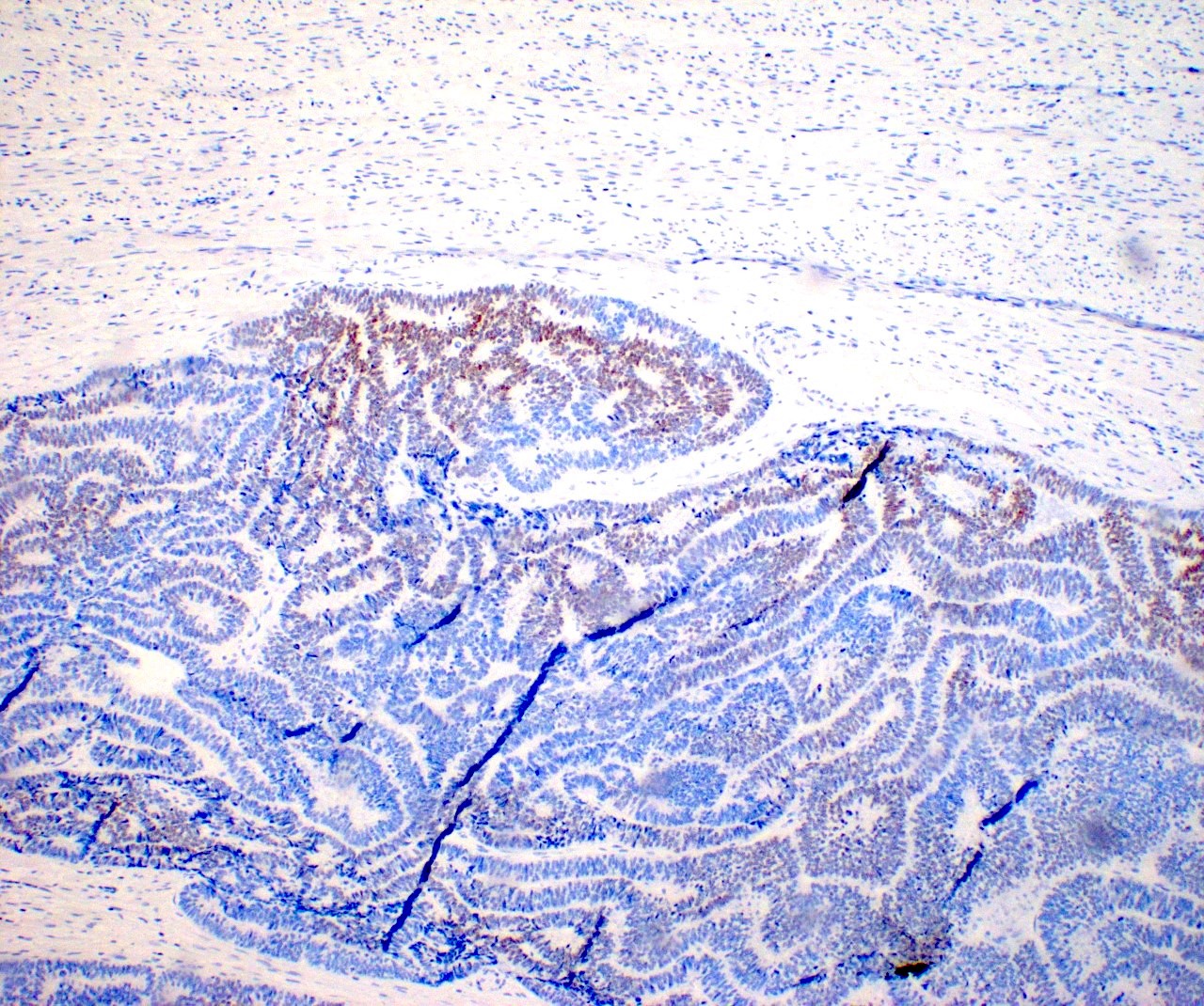
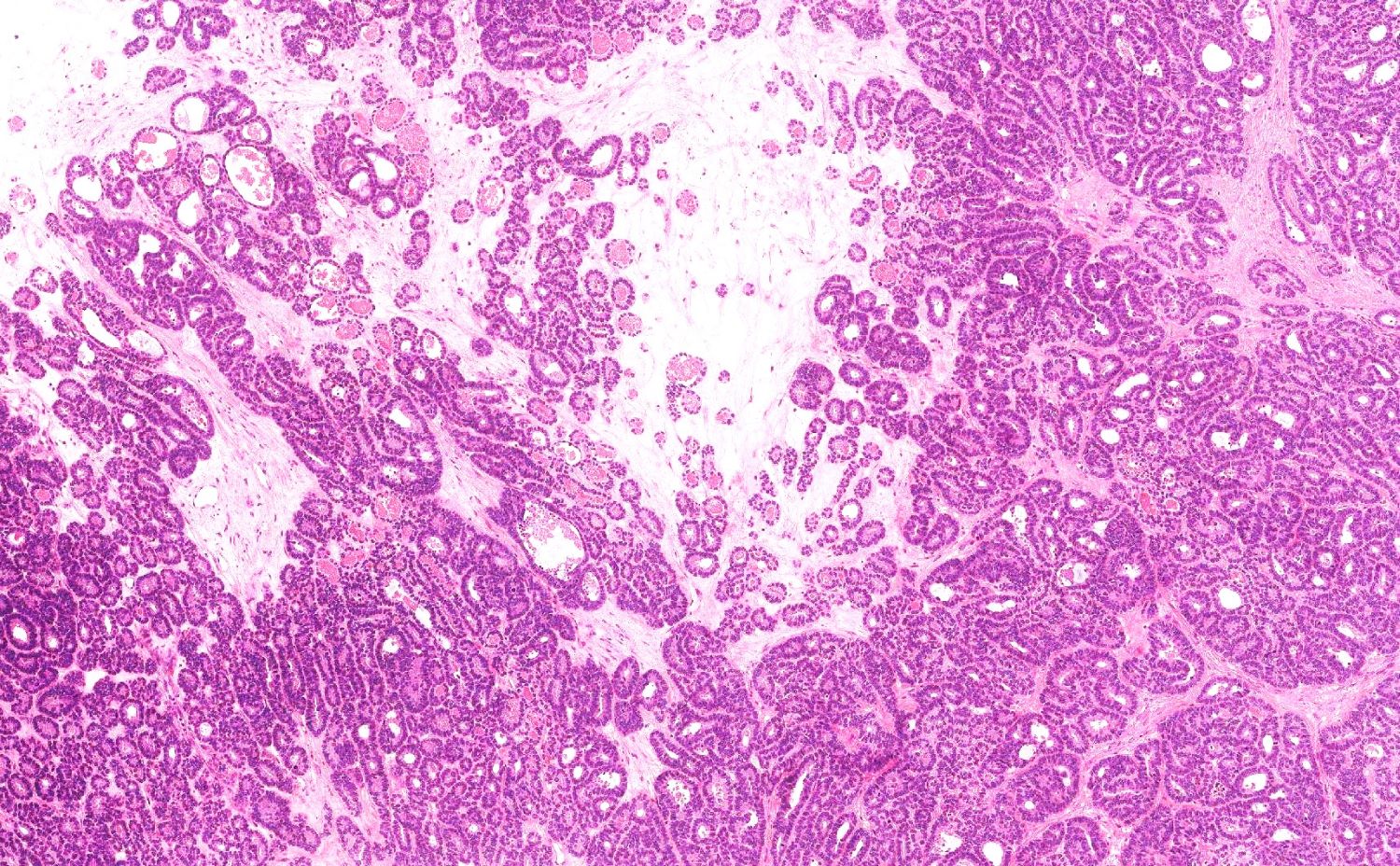
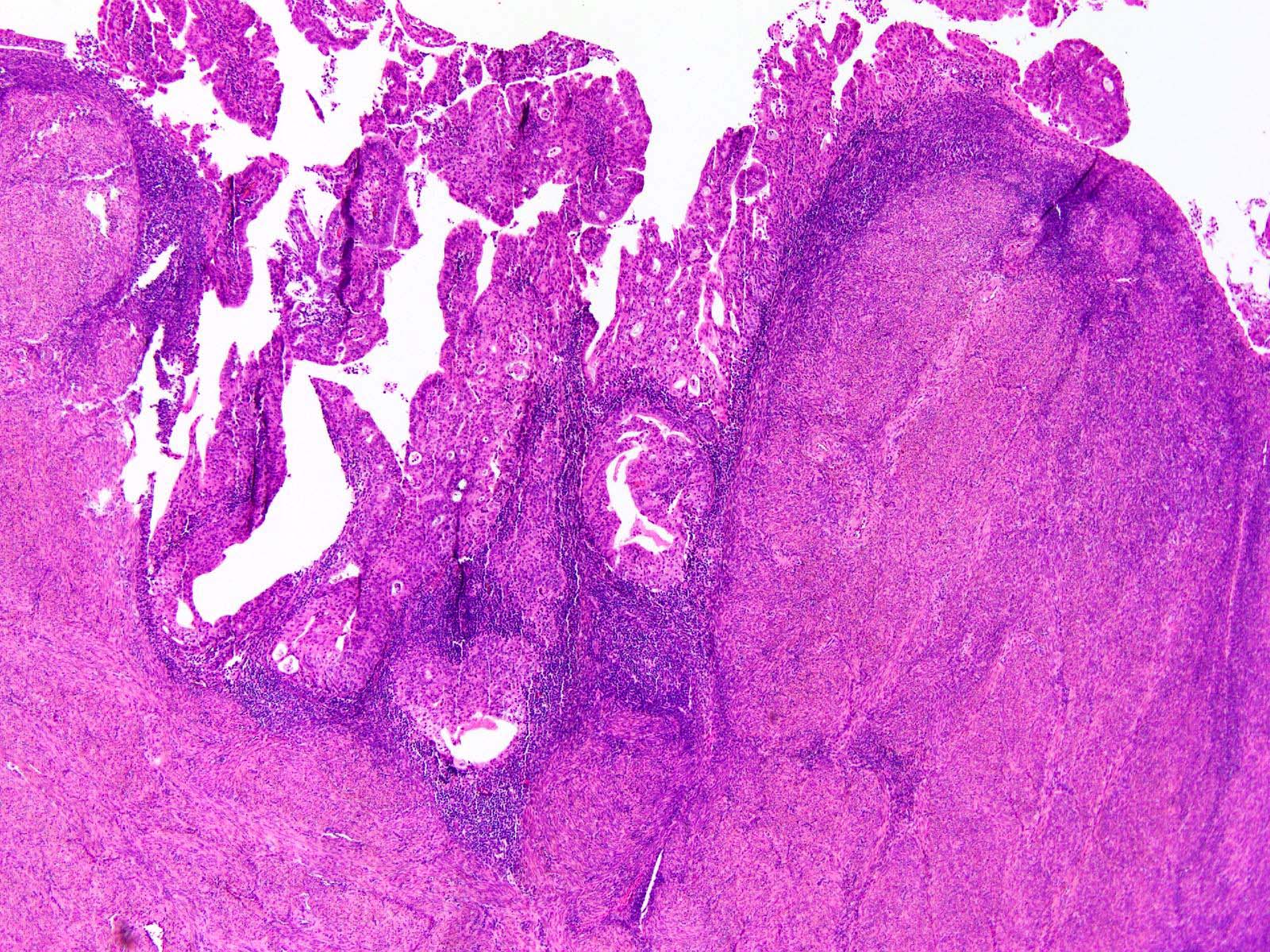
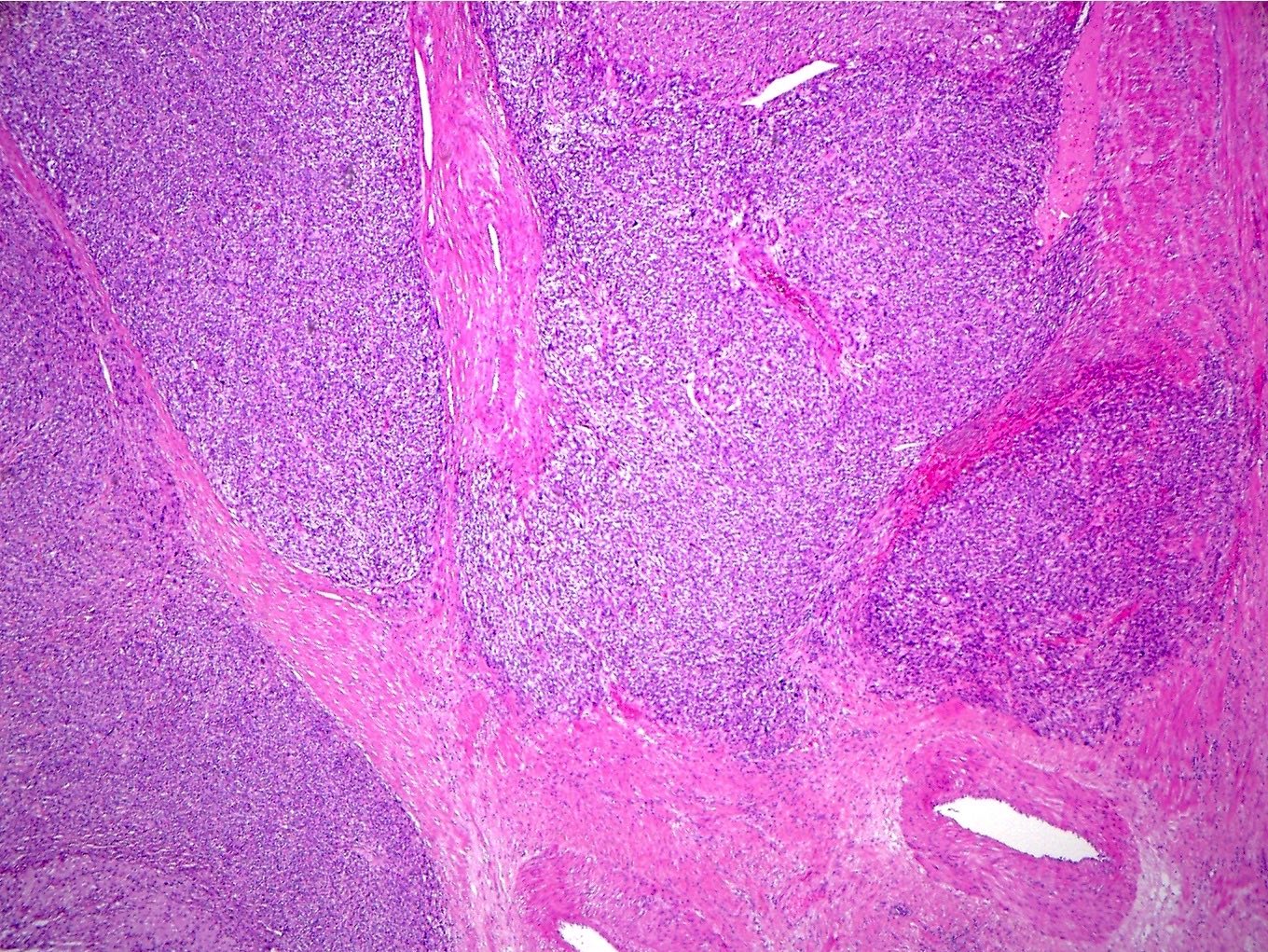
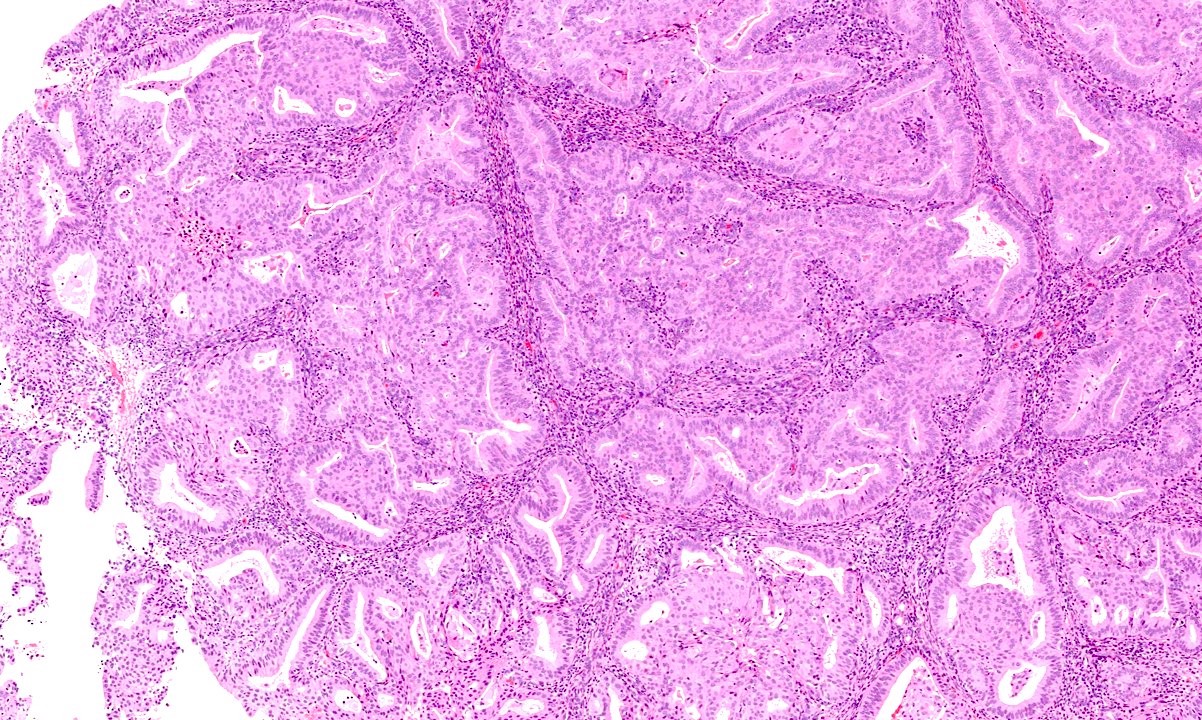
- Assessment should be performed at the deepest point of tumor invasion on a full thickness section of the wall spanning from mucosal surface to serosa (Figure 1)
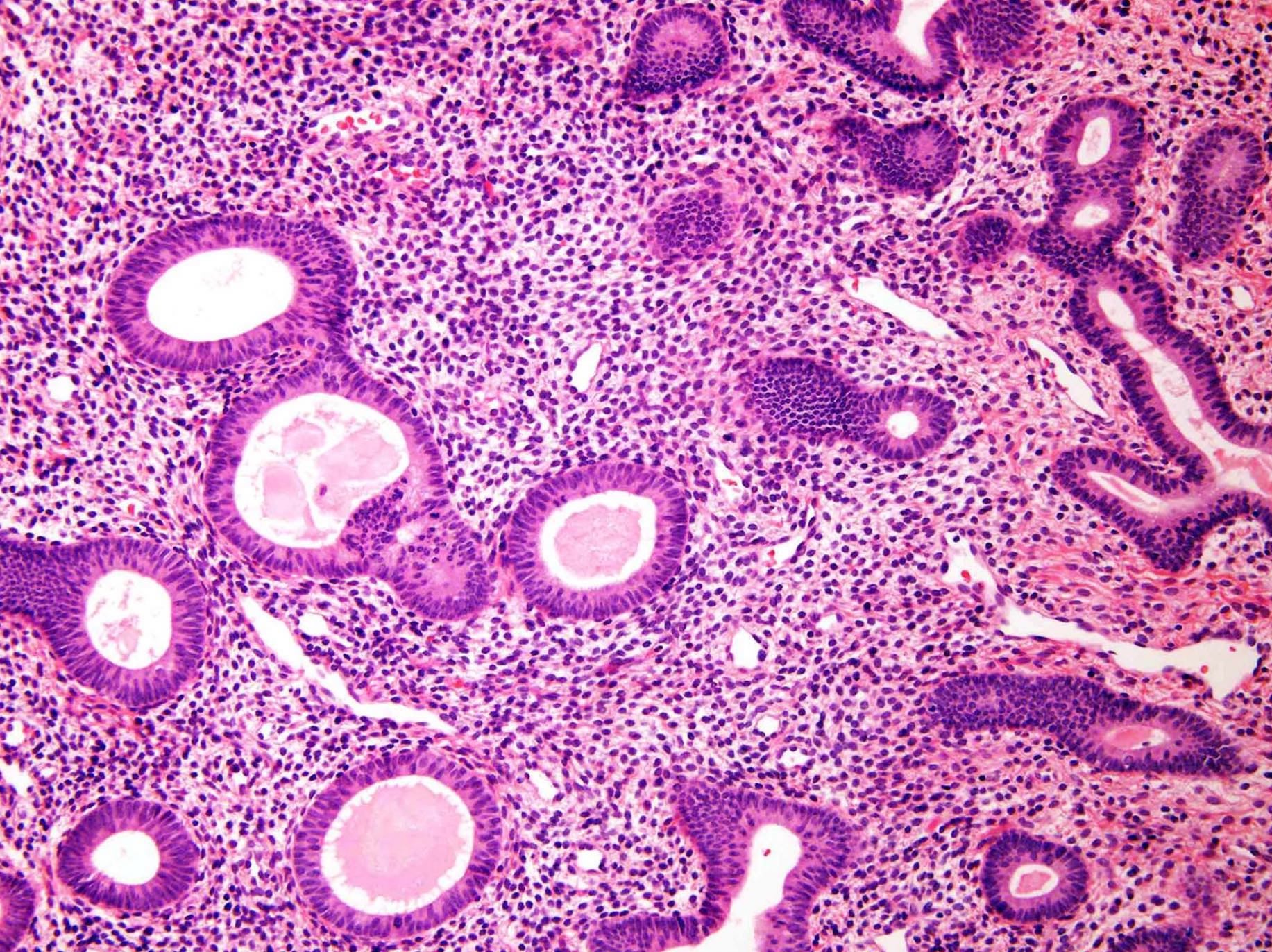
- Involvement of adenomyosis by carcinoma does not by itself portend a worse prognosis
- These cases behave similarly to stage IA tumors (Gynecol Oncol 1990;37:401, Int J Gynecol Pathol 2010;29:445)
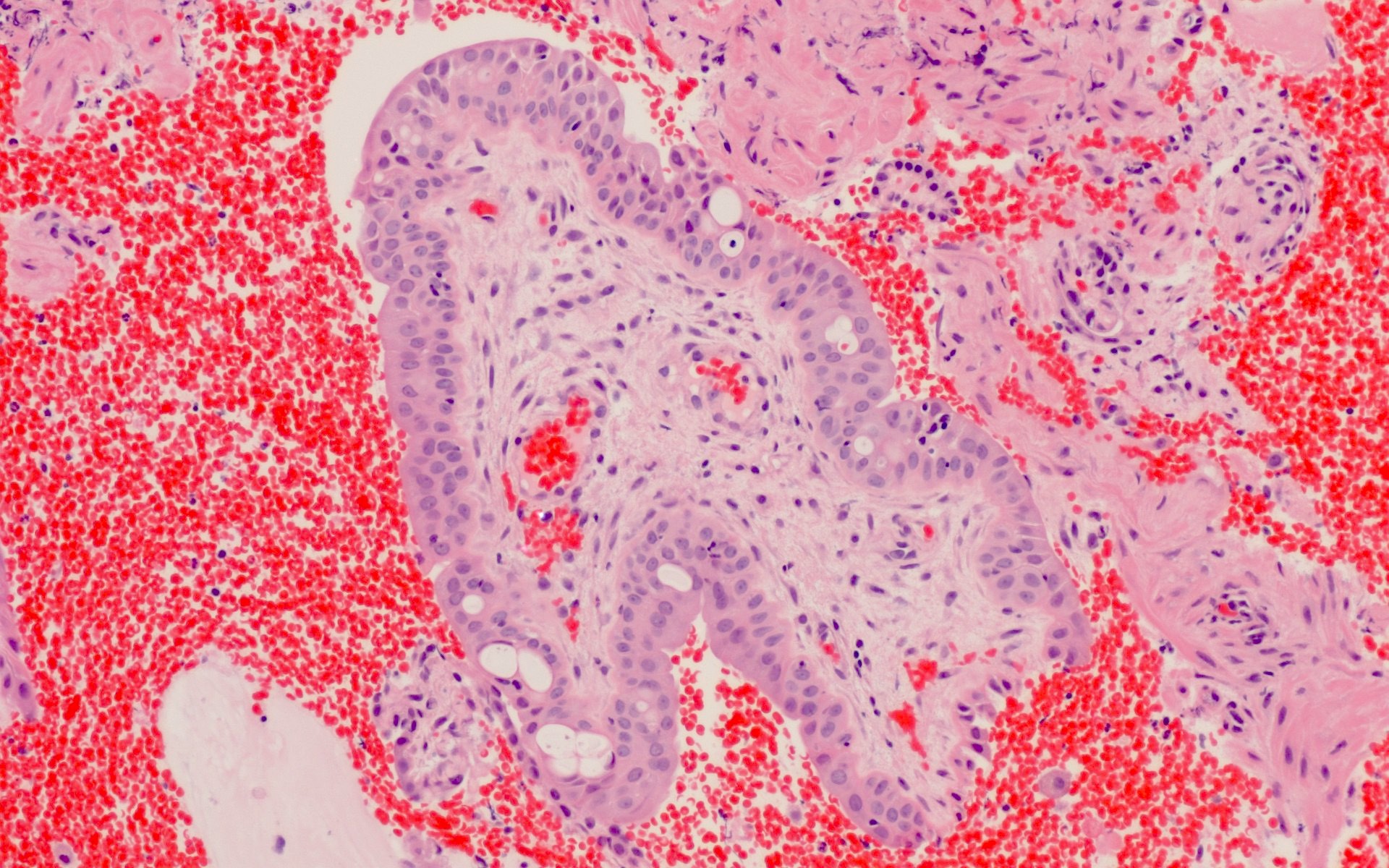
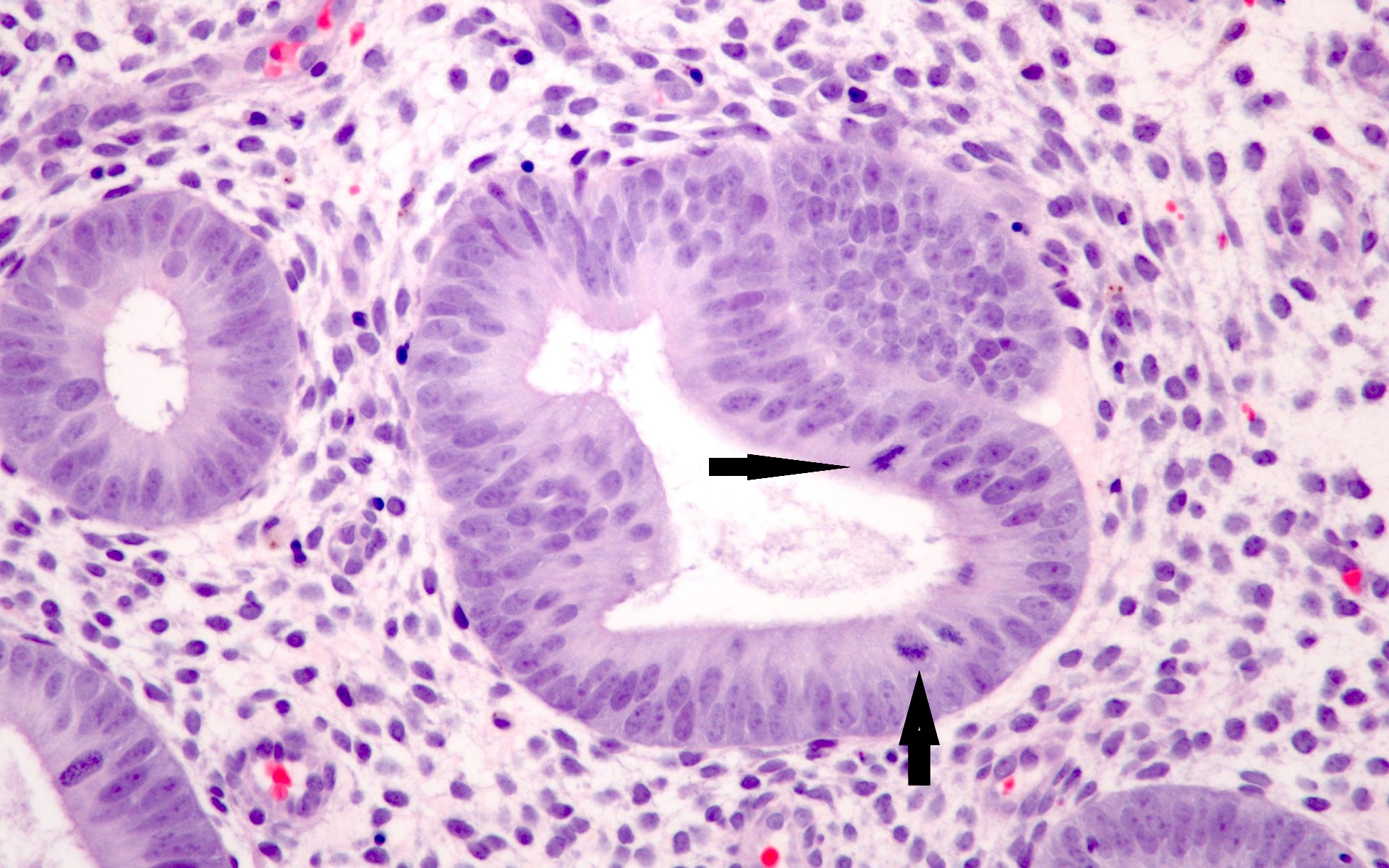
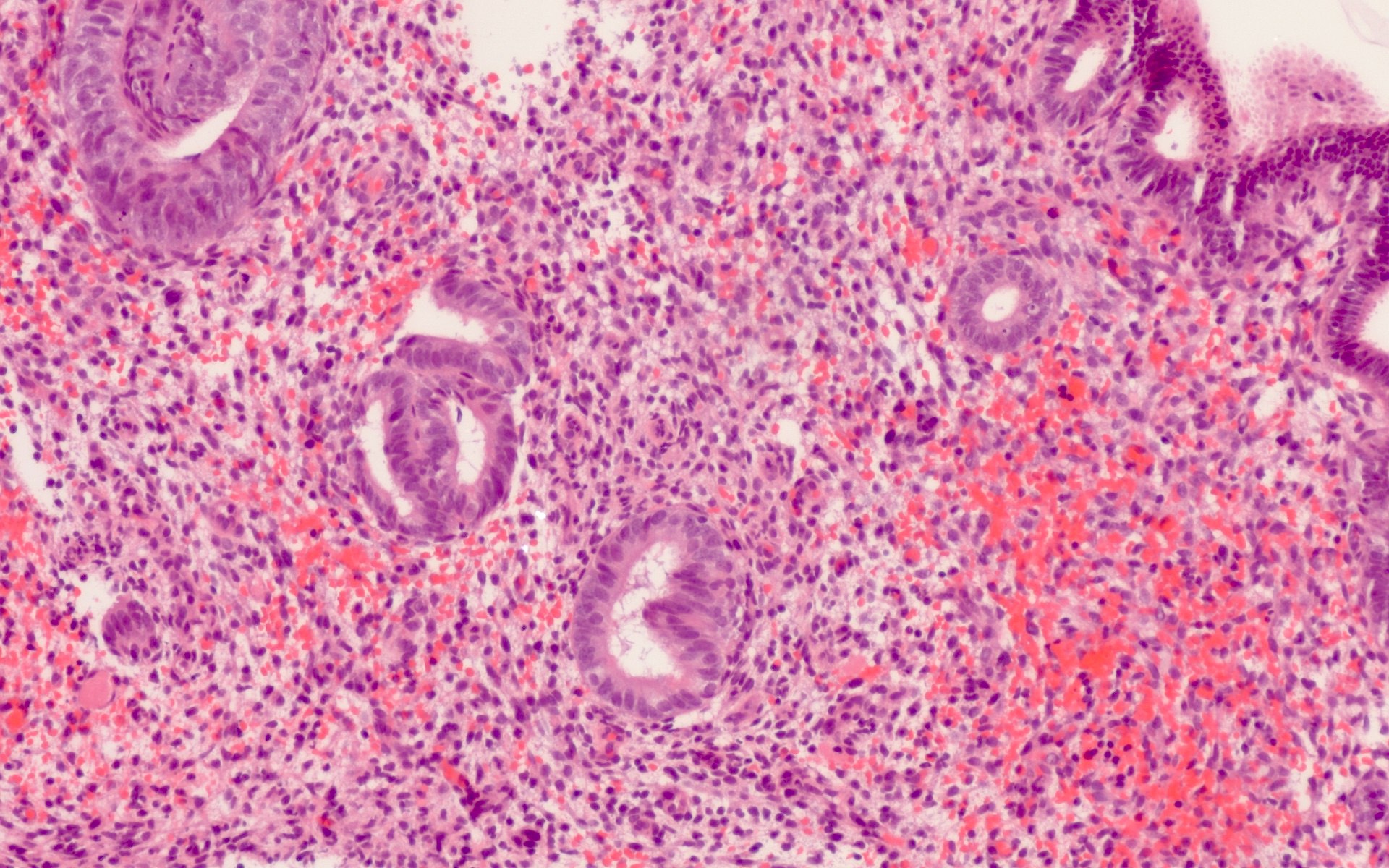
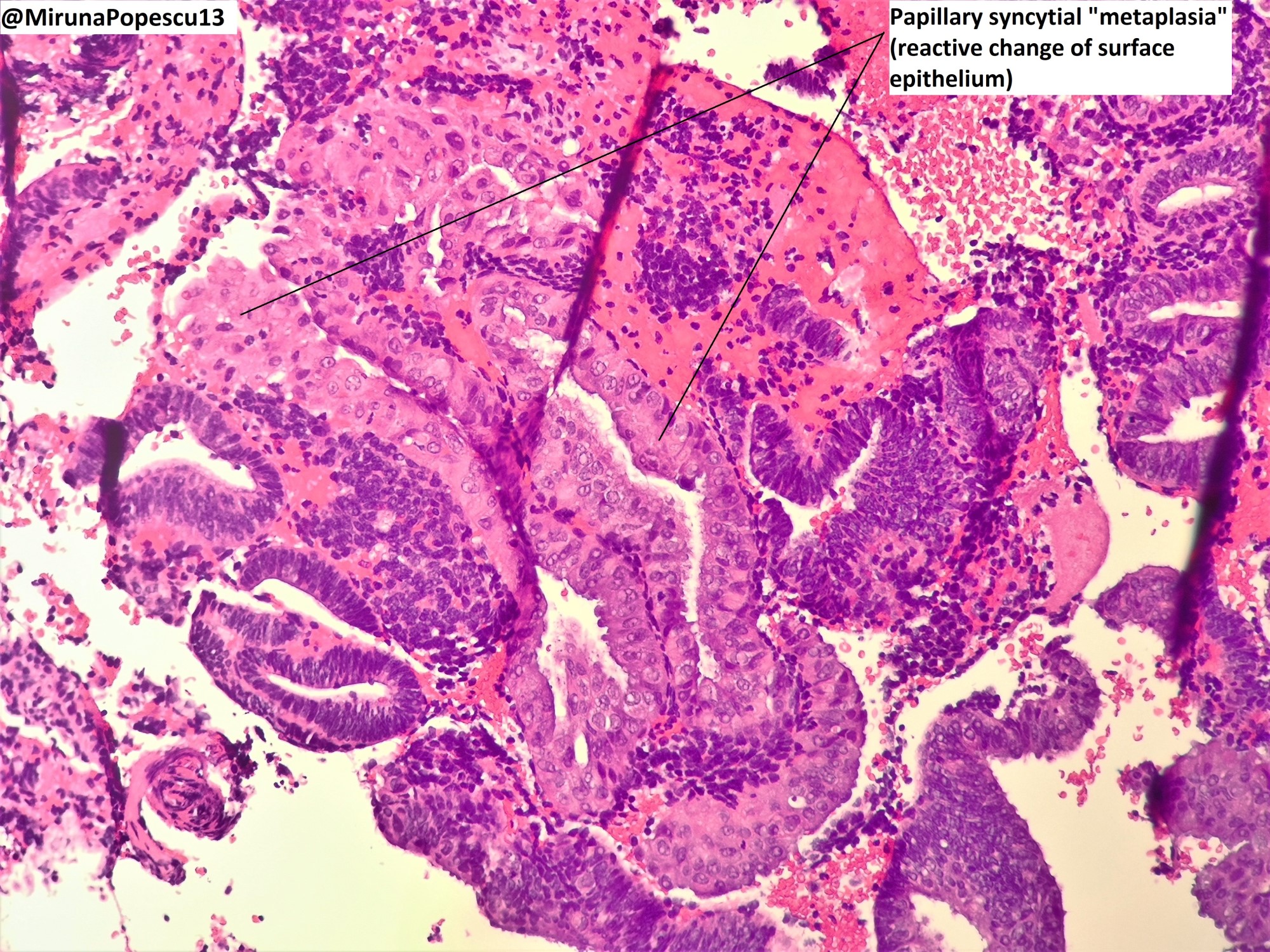
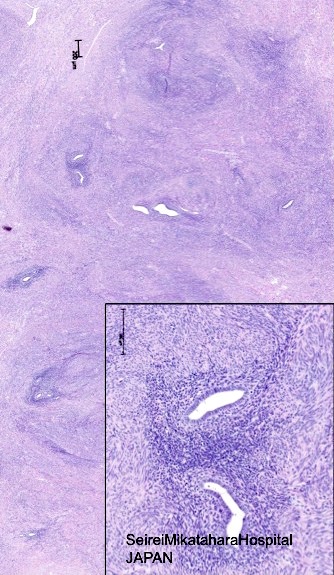
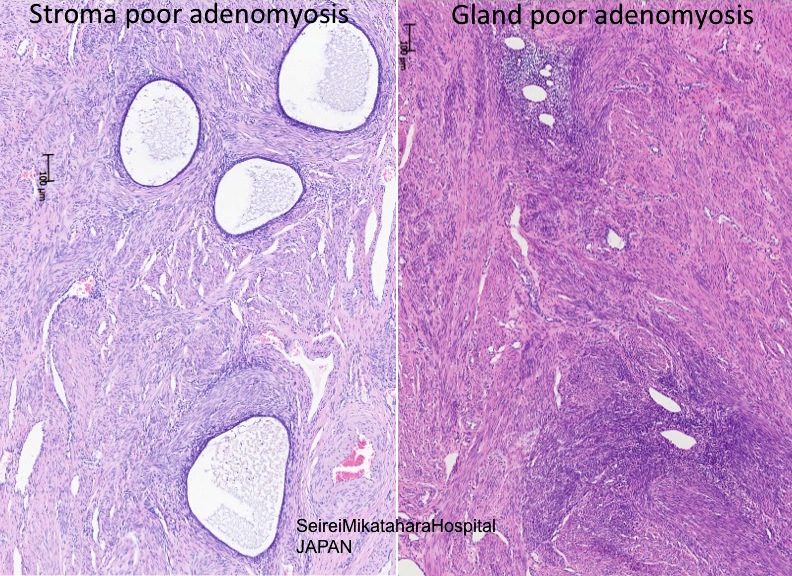
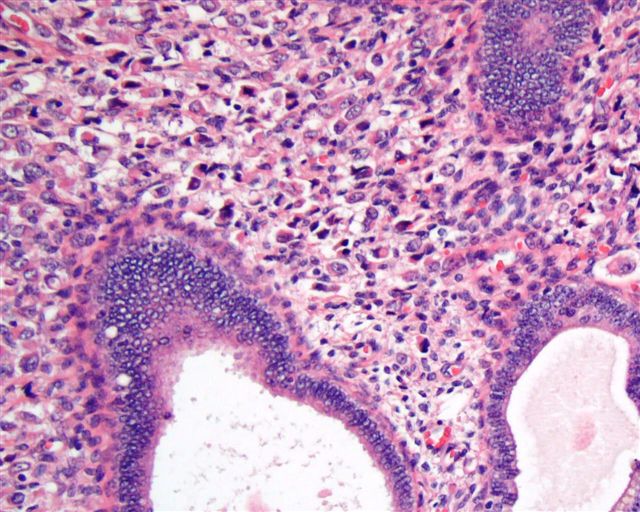
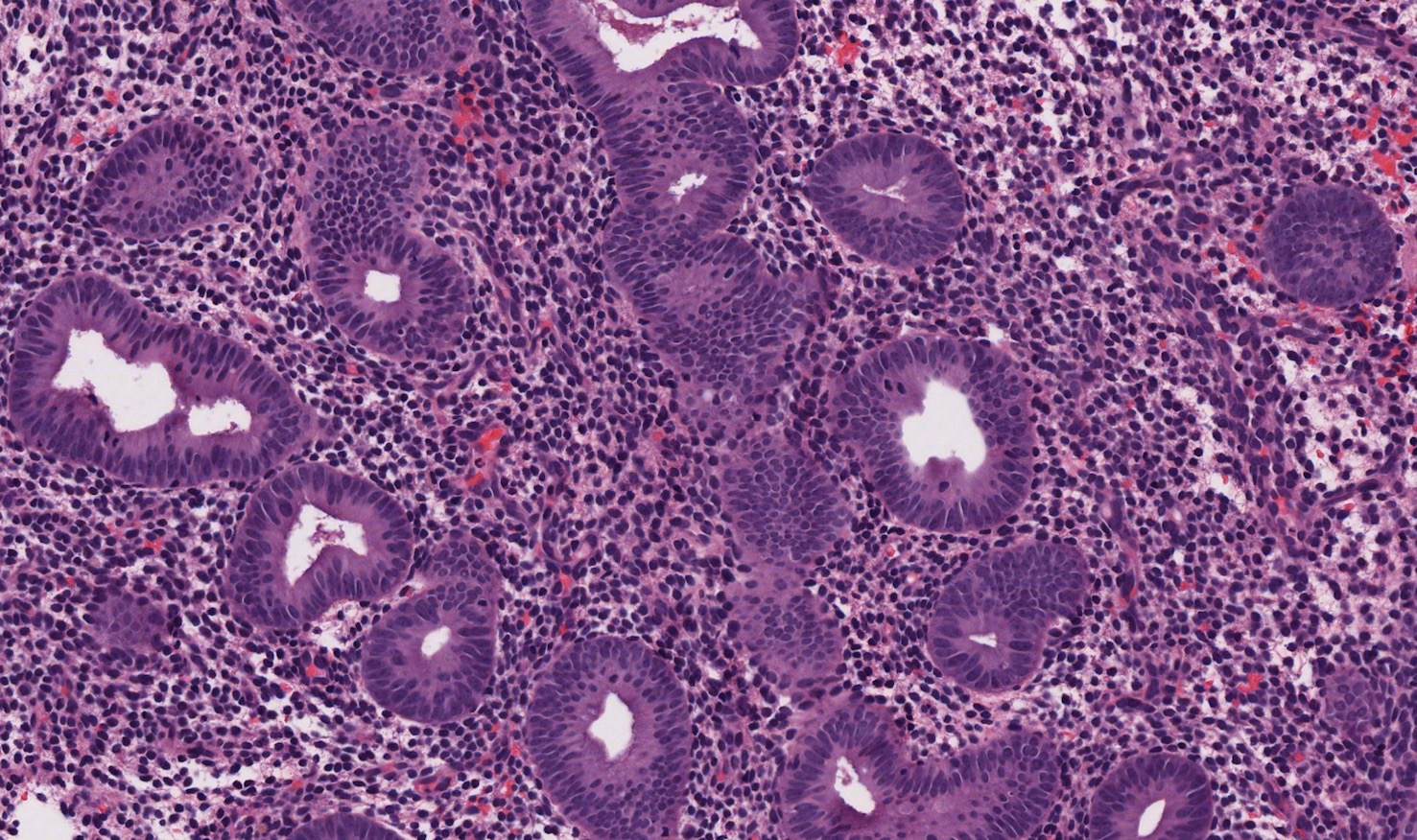
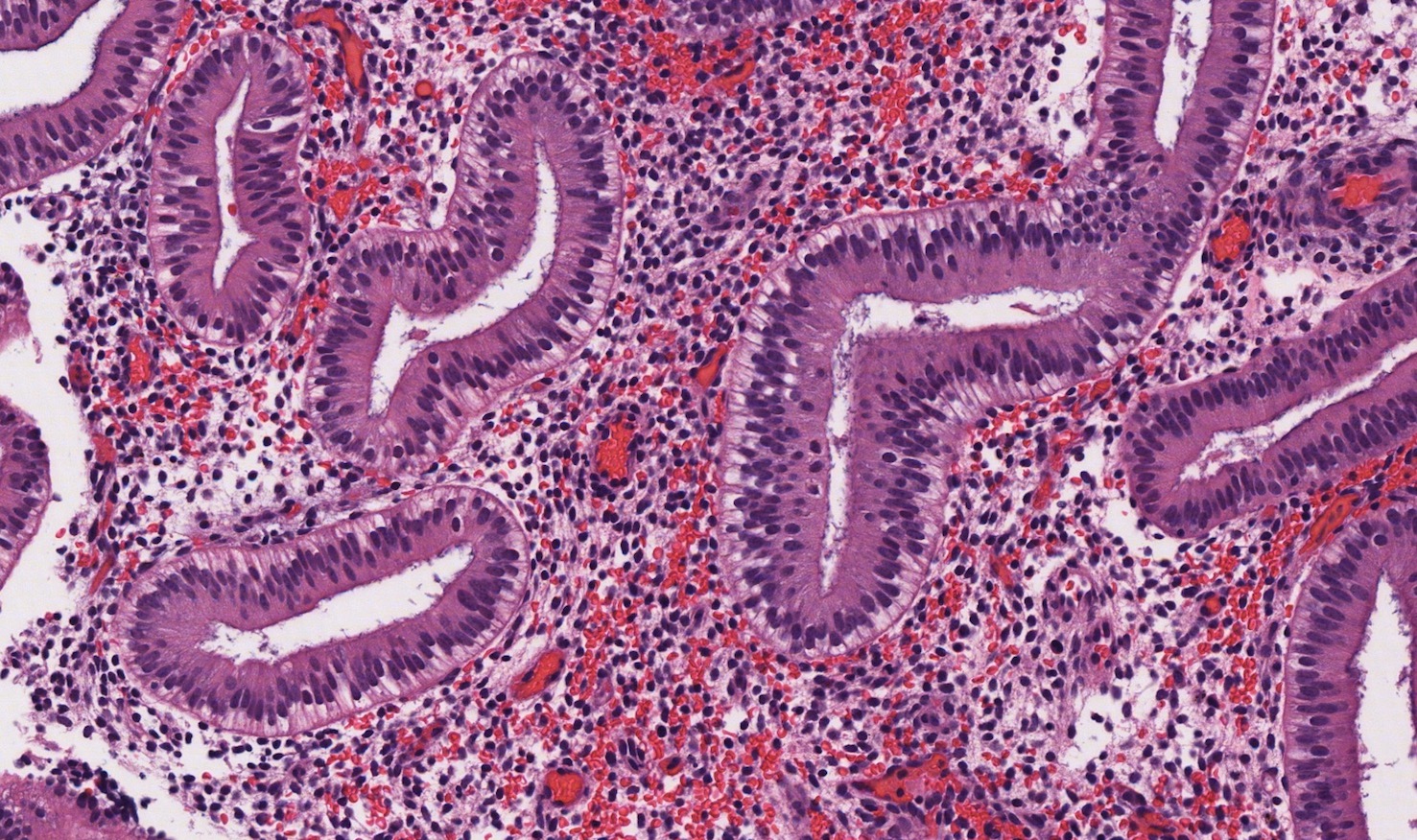
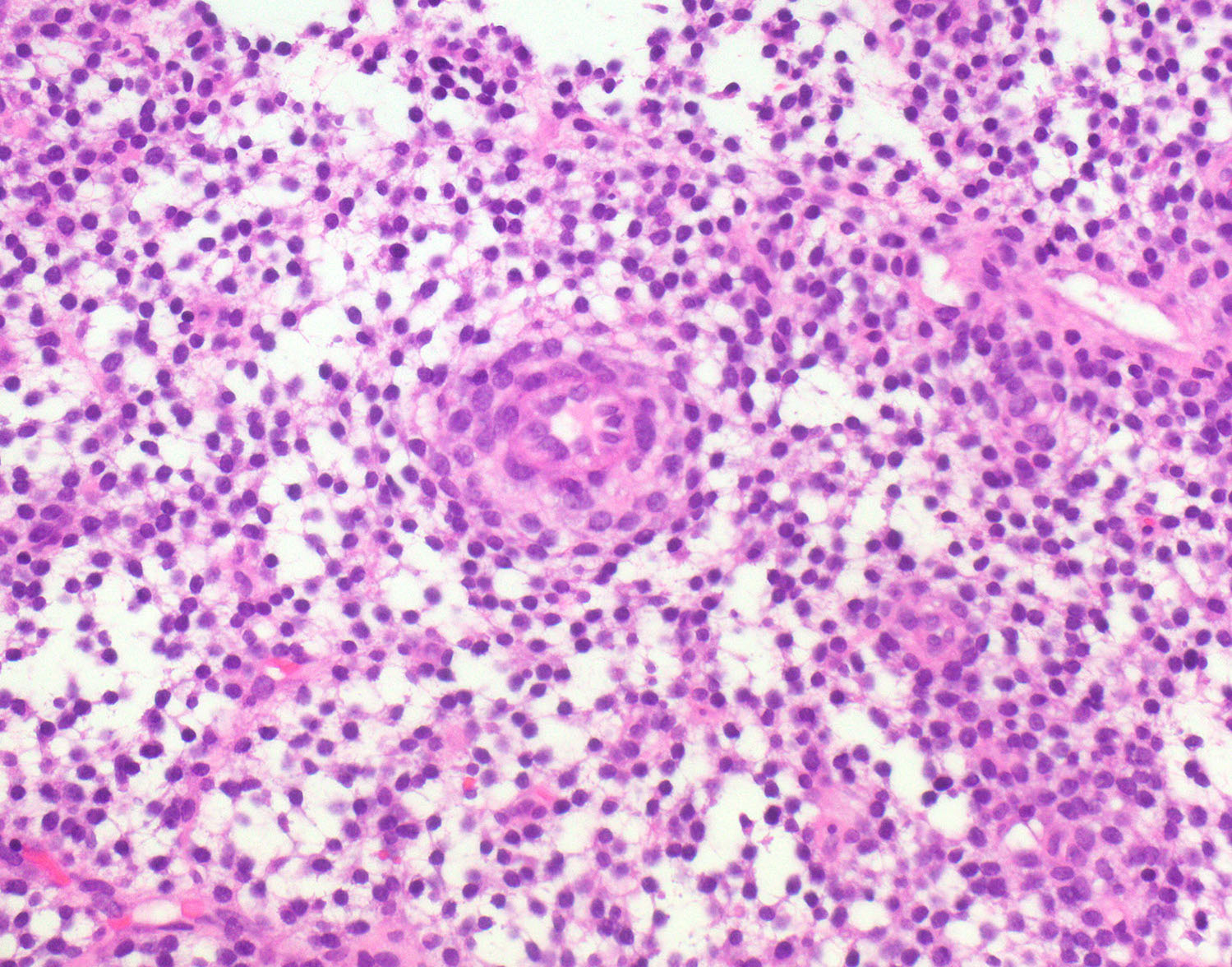
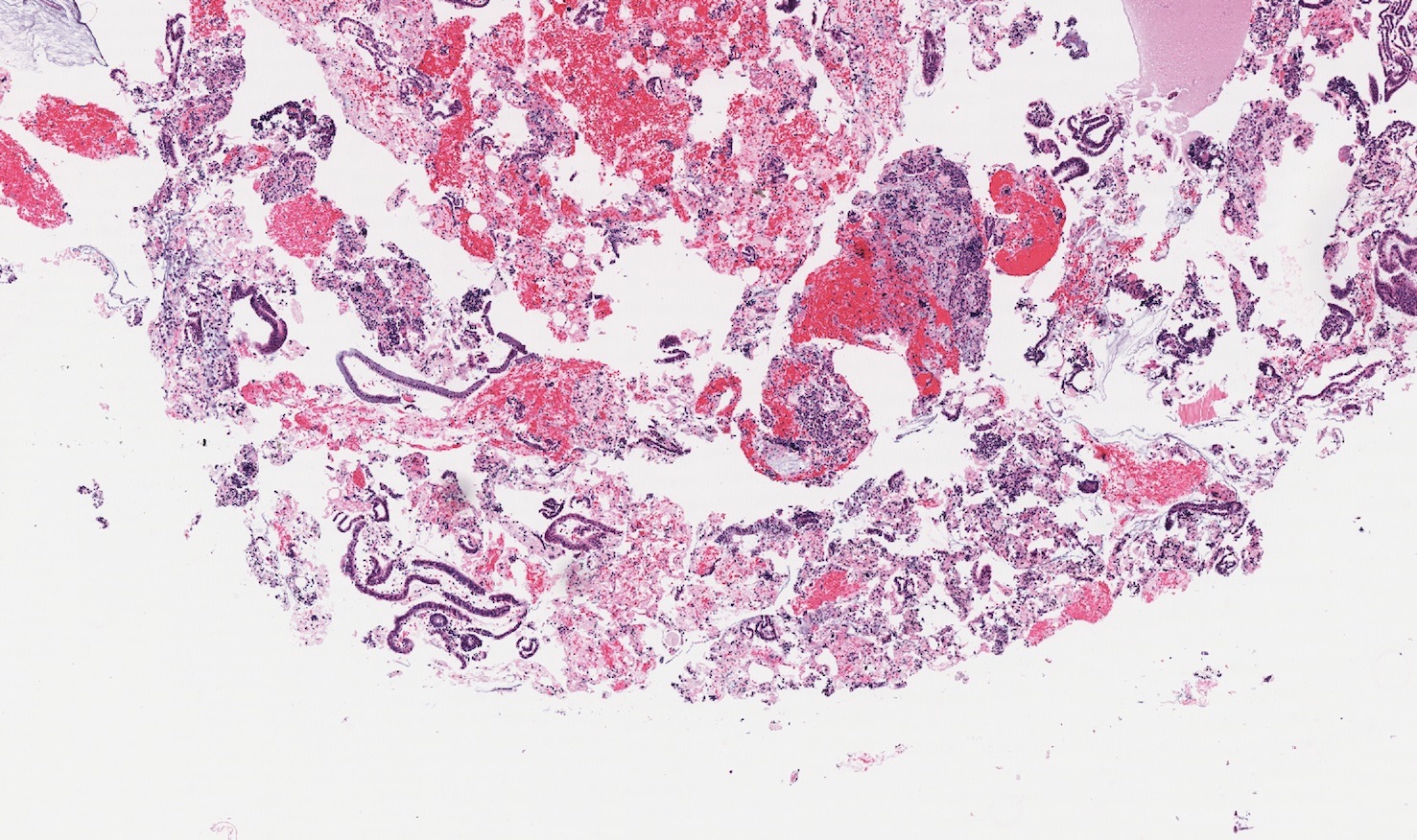
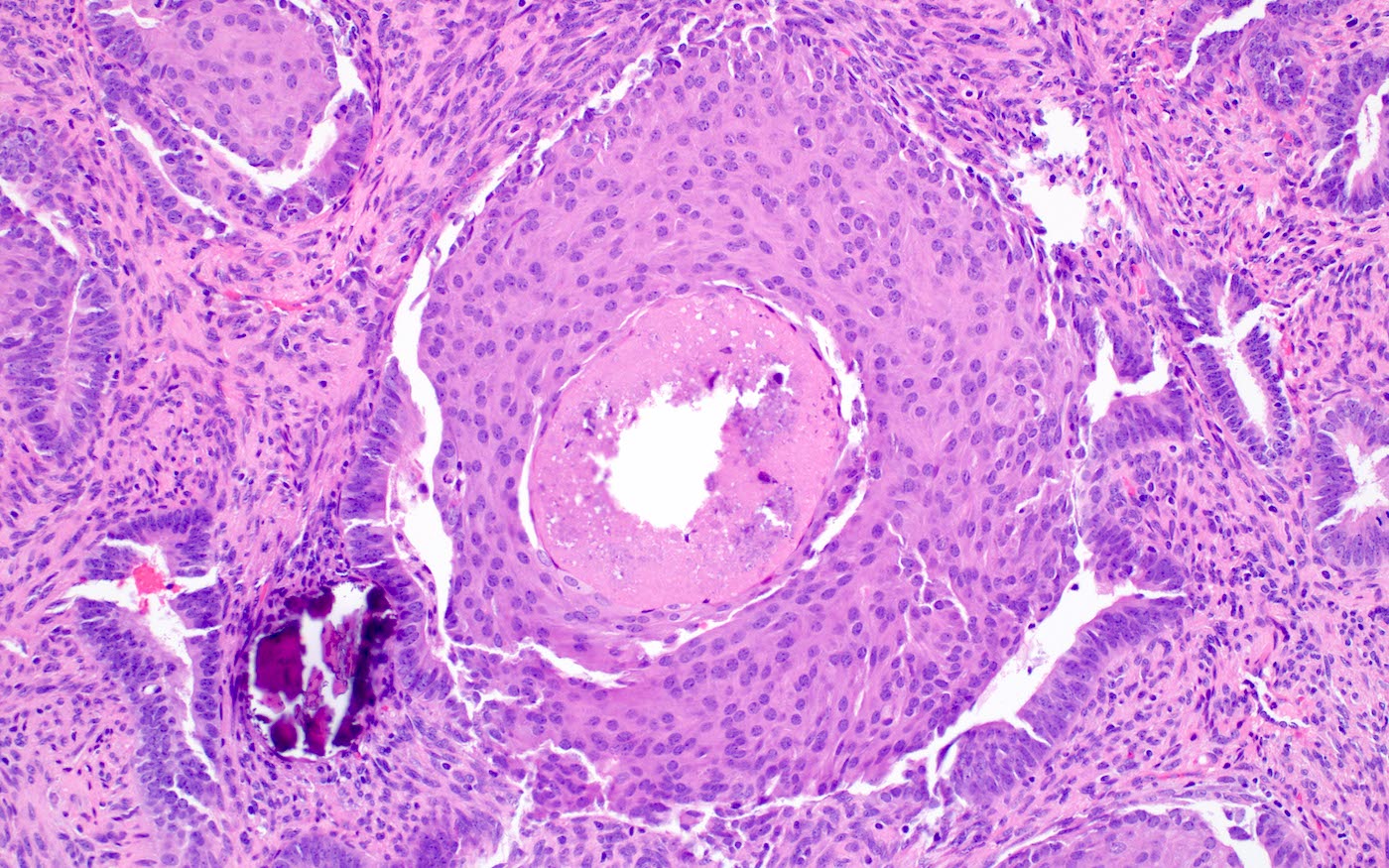
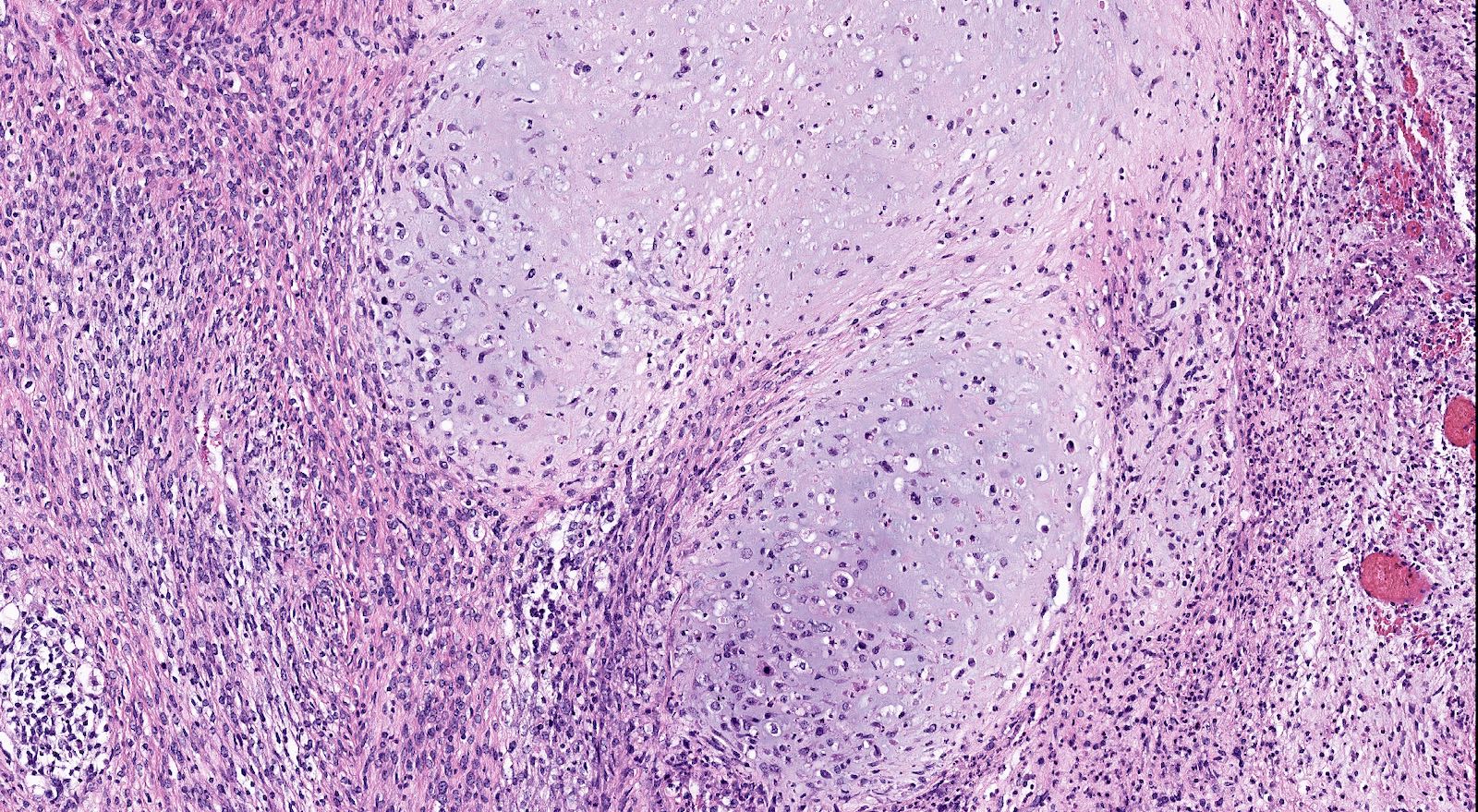
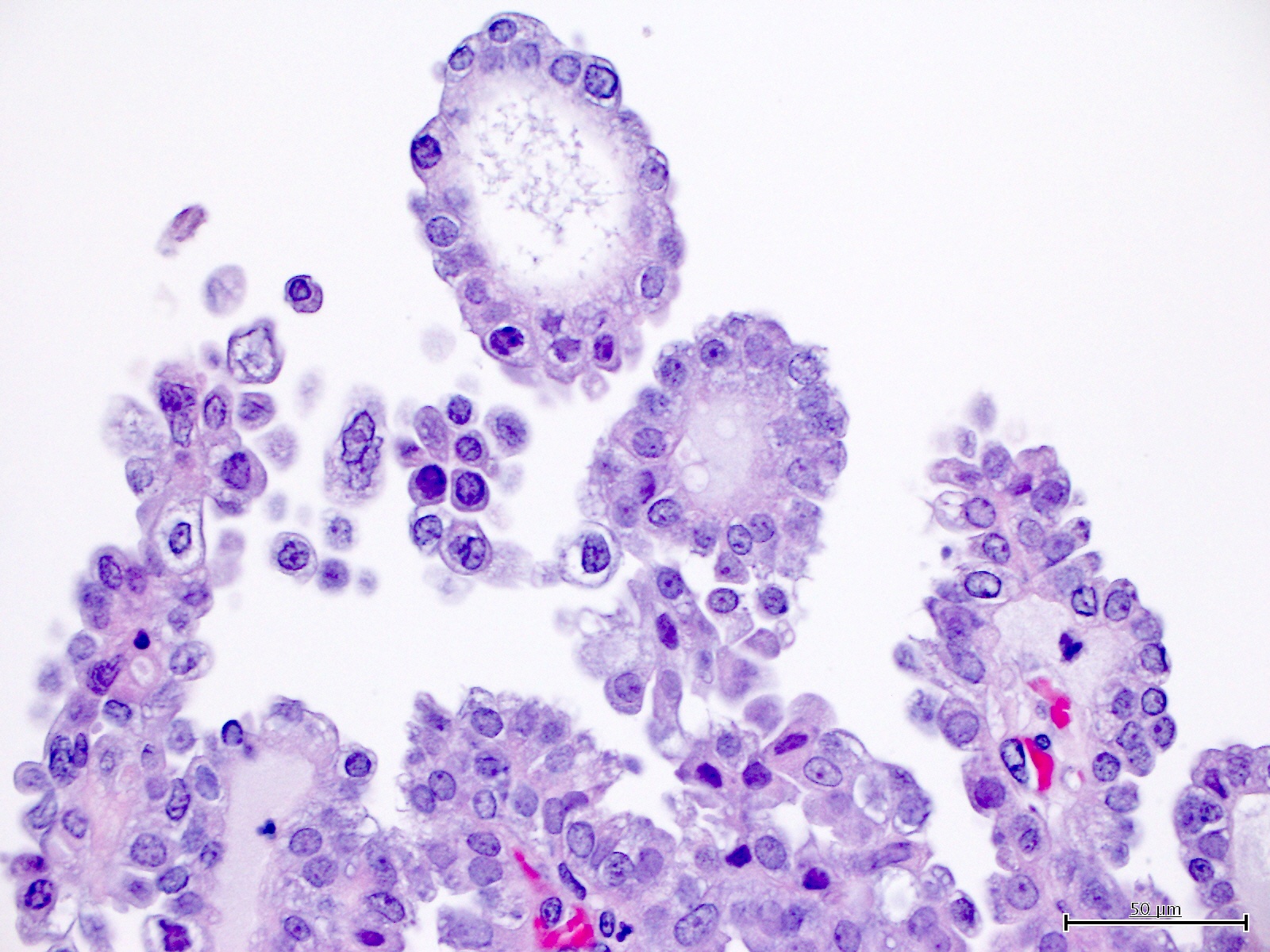
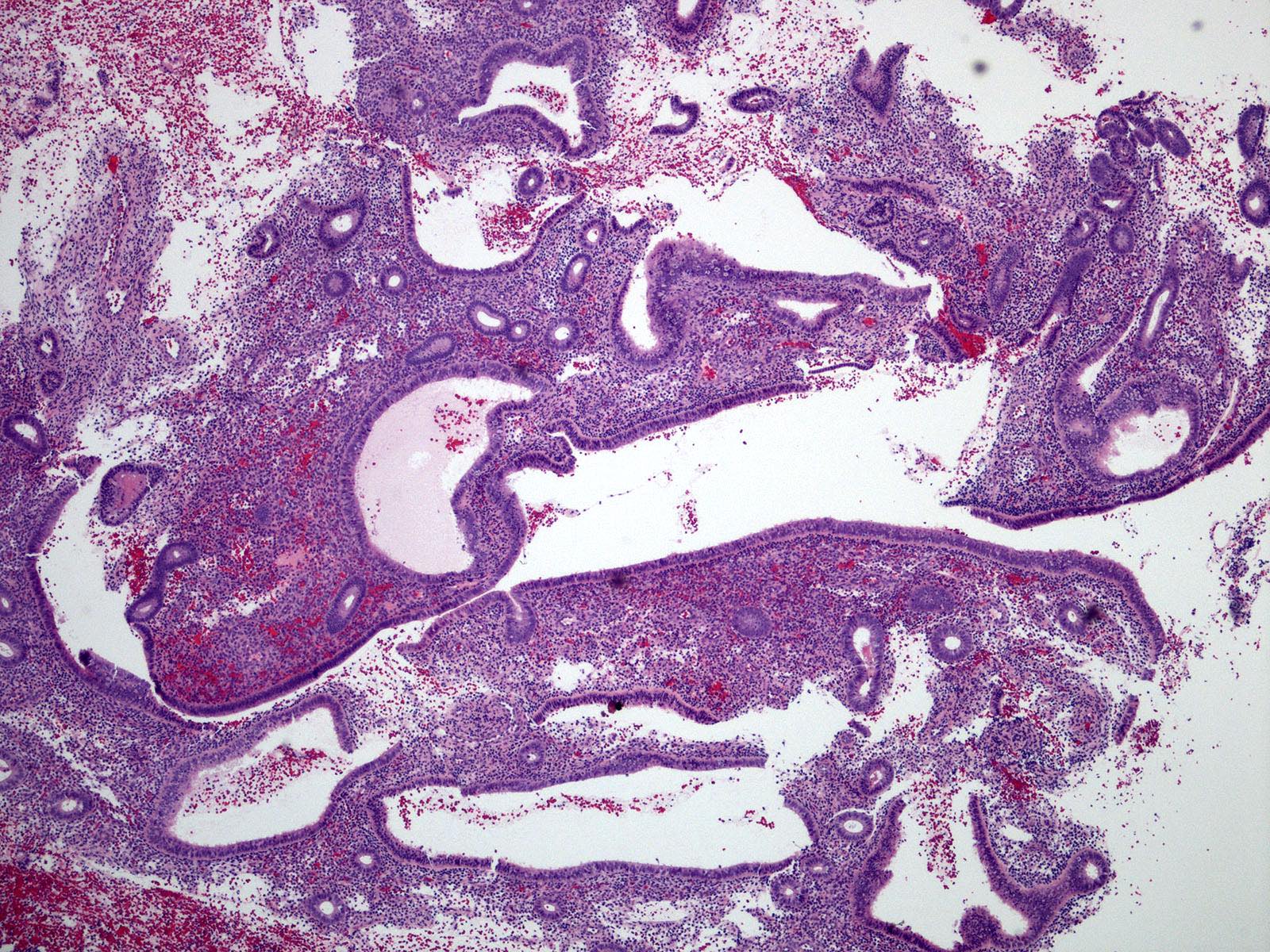
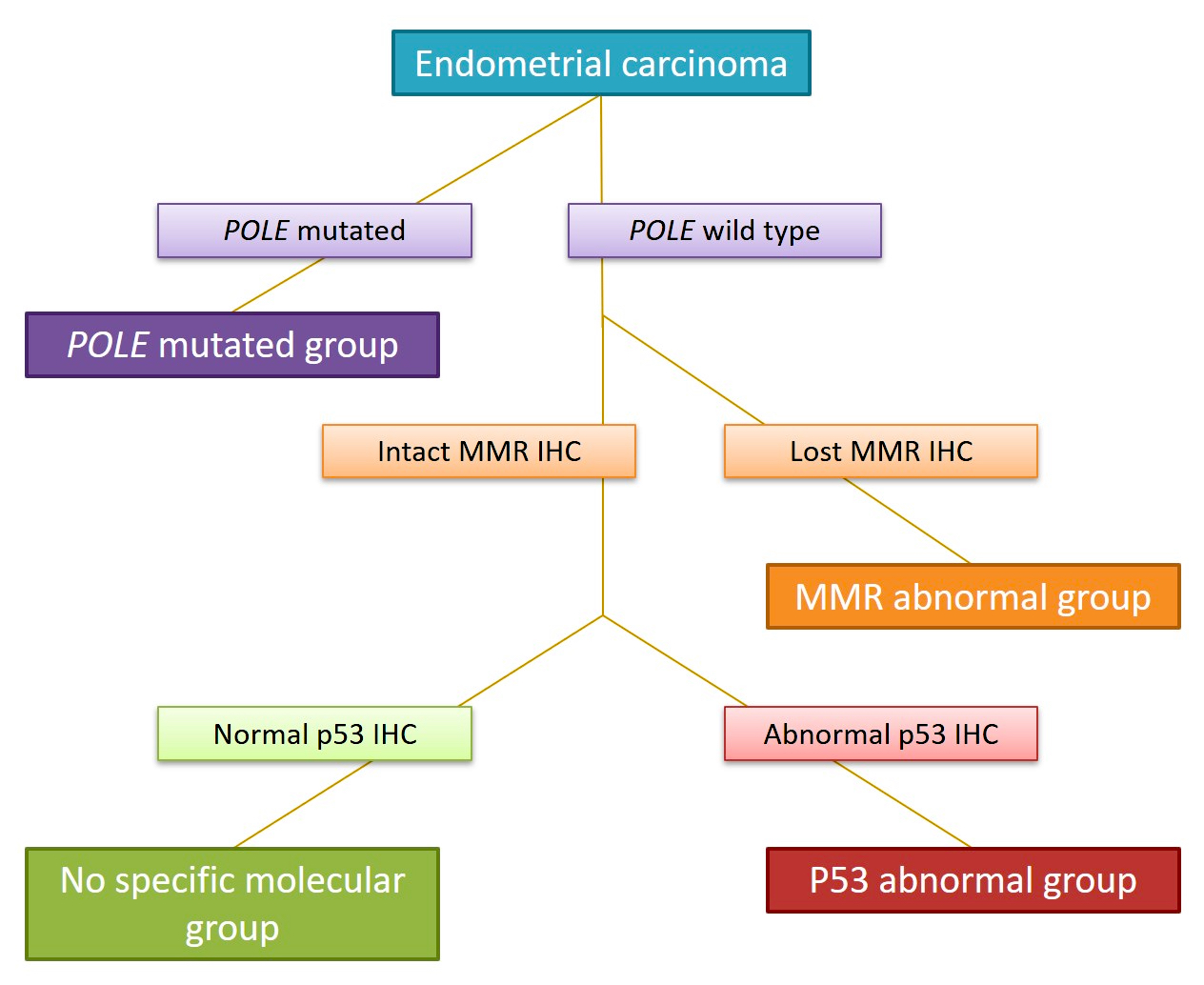
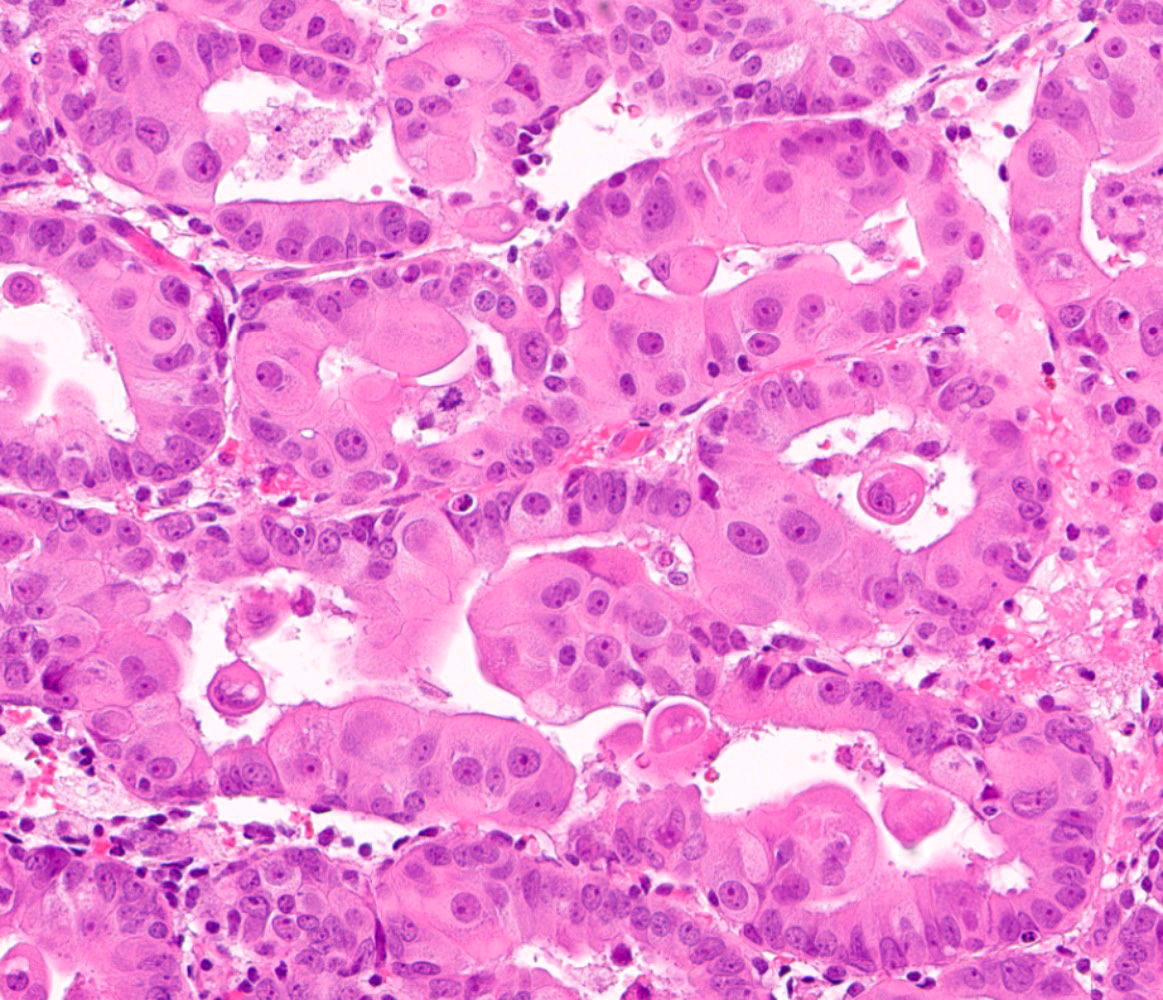
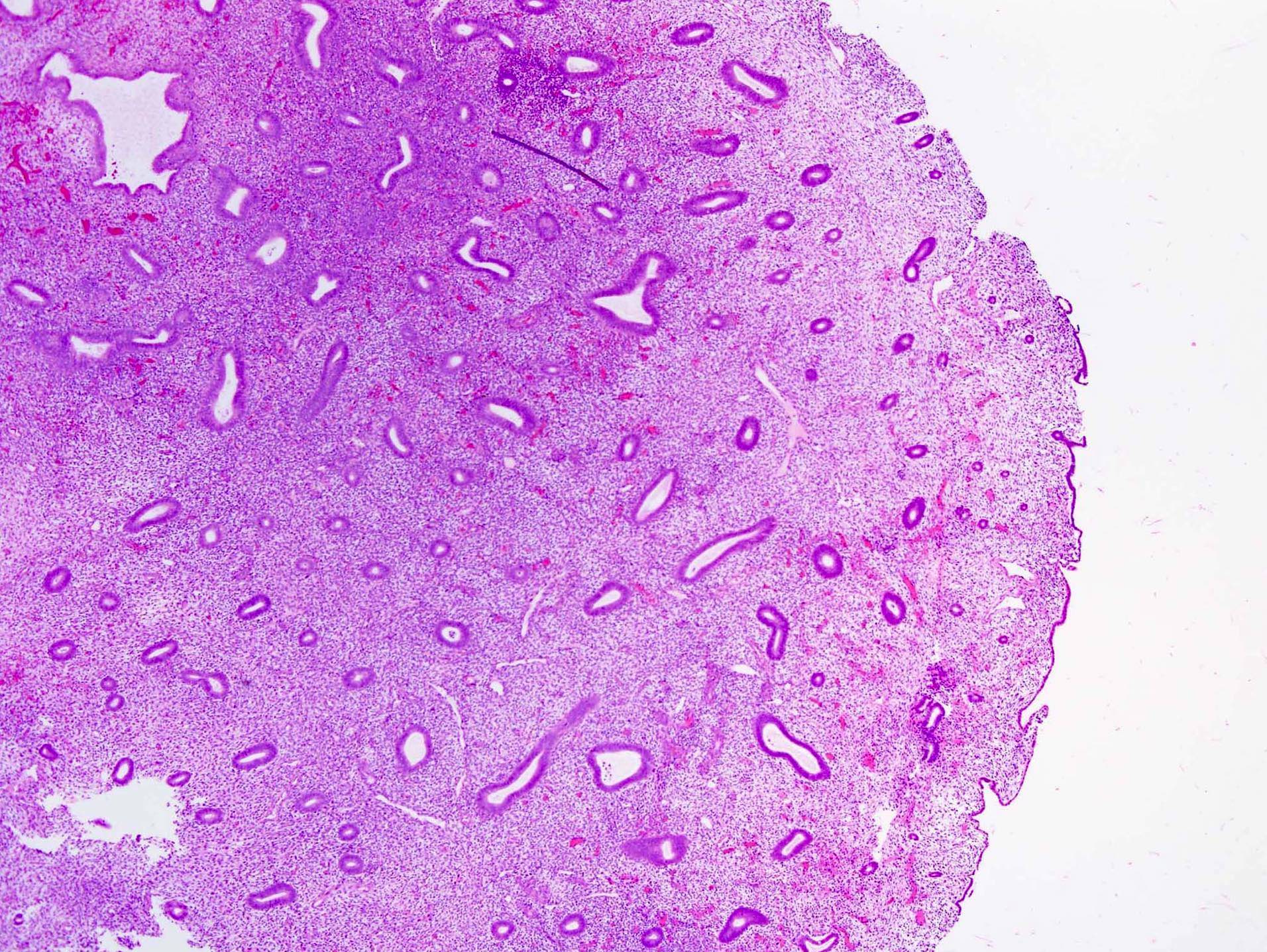
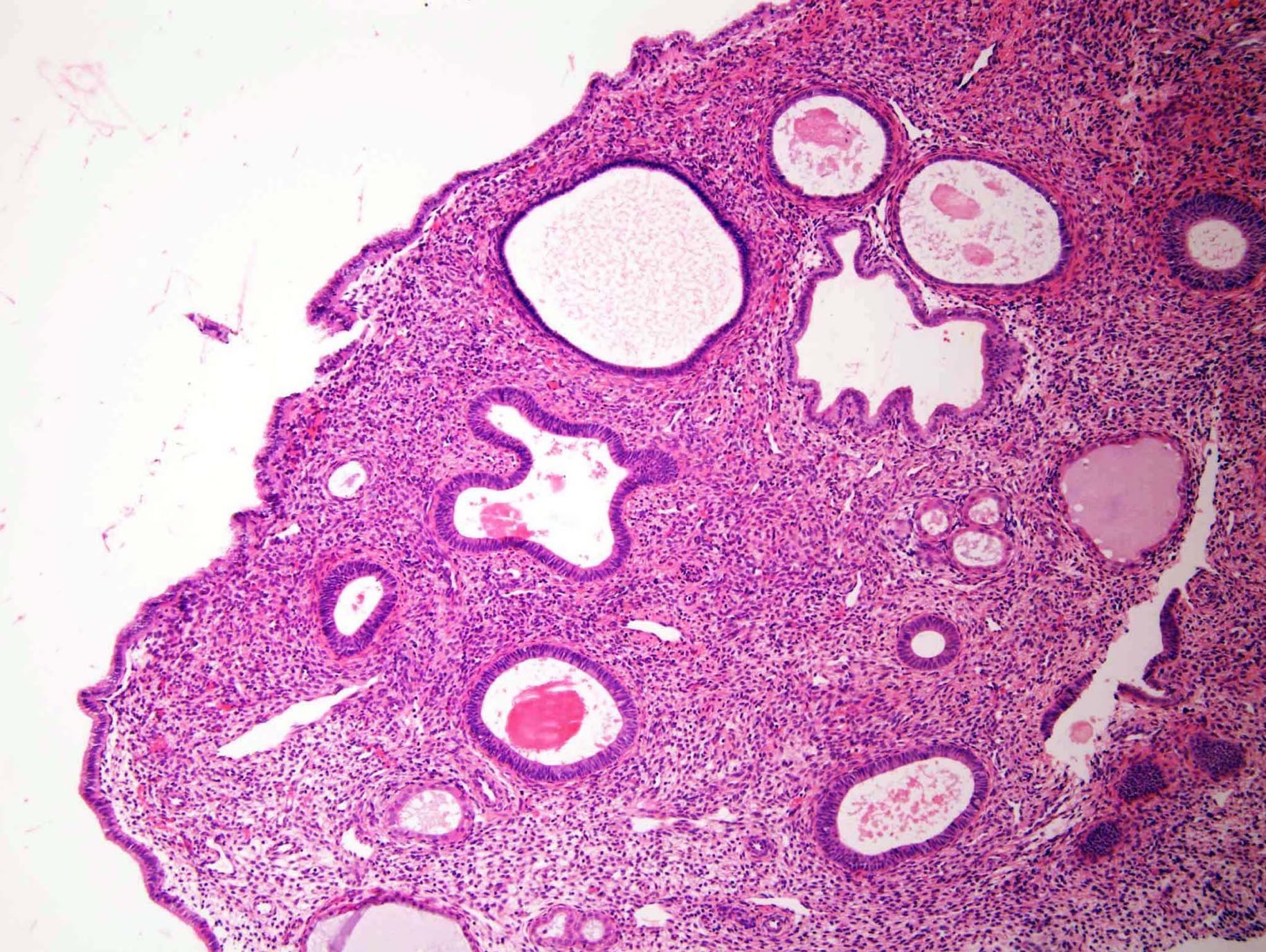
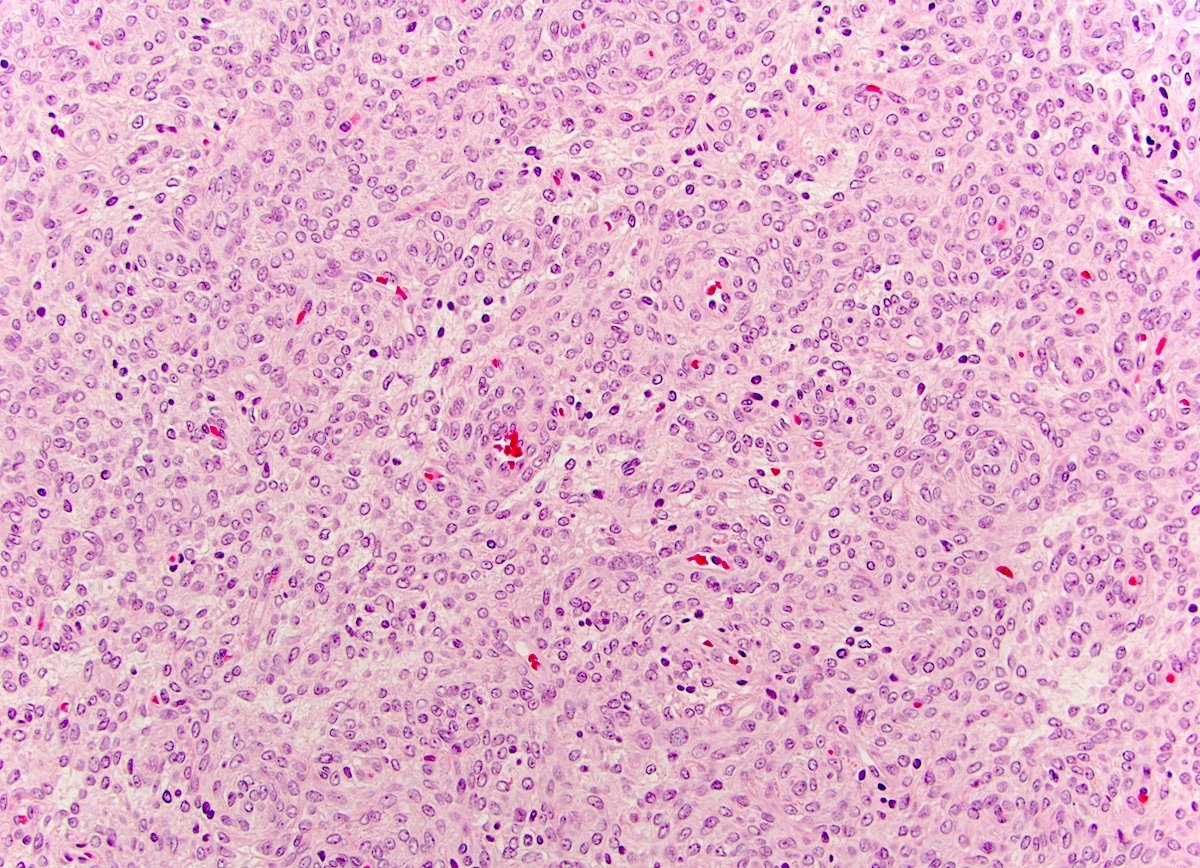
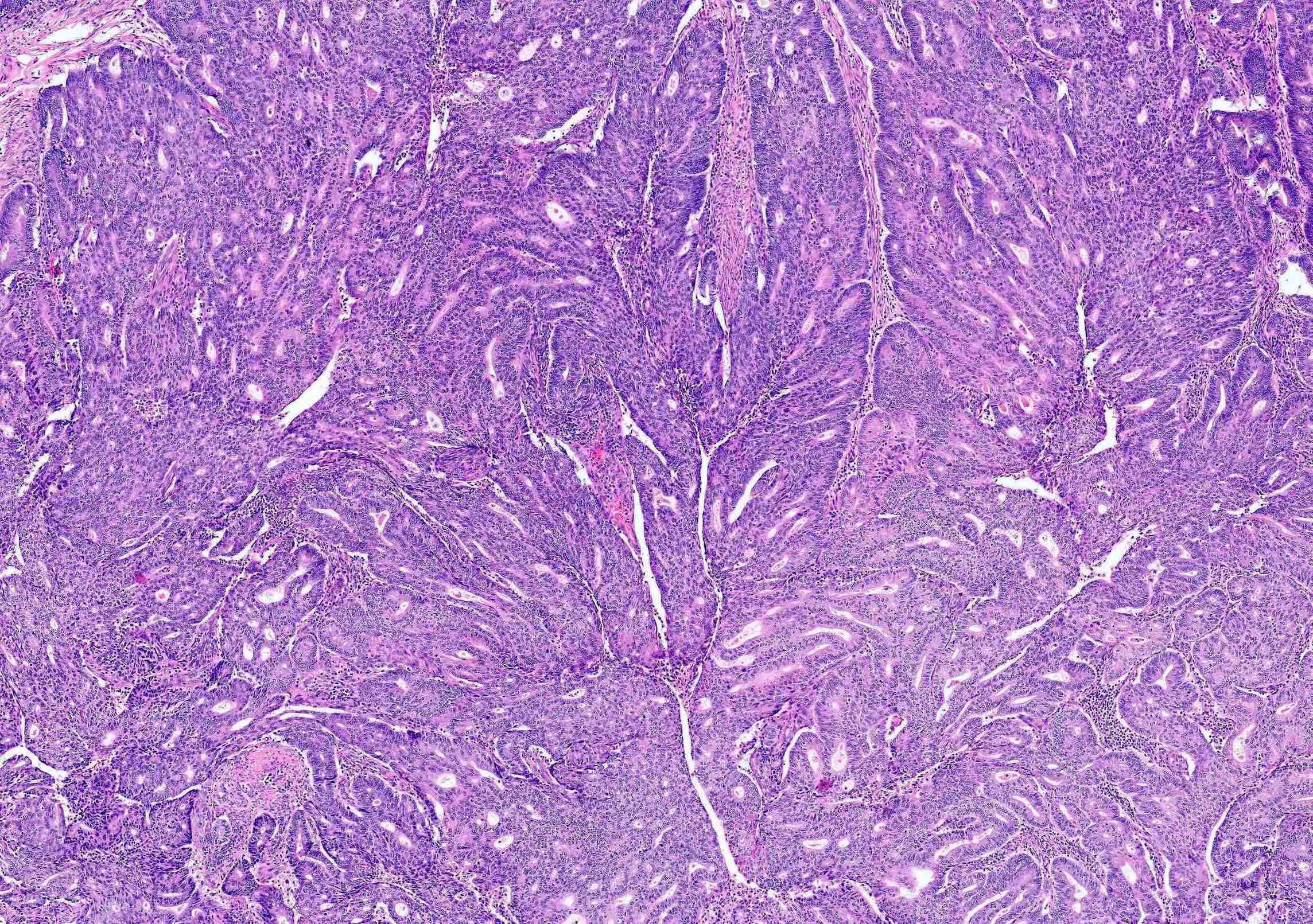
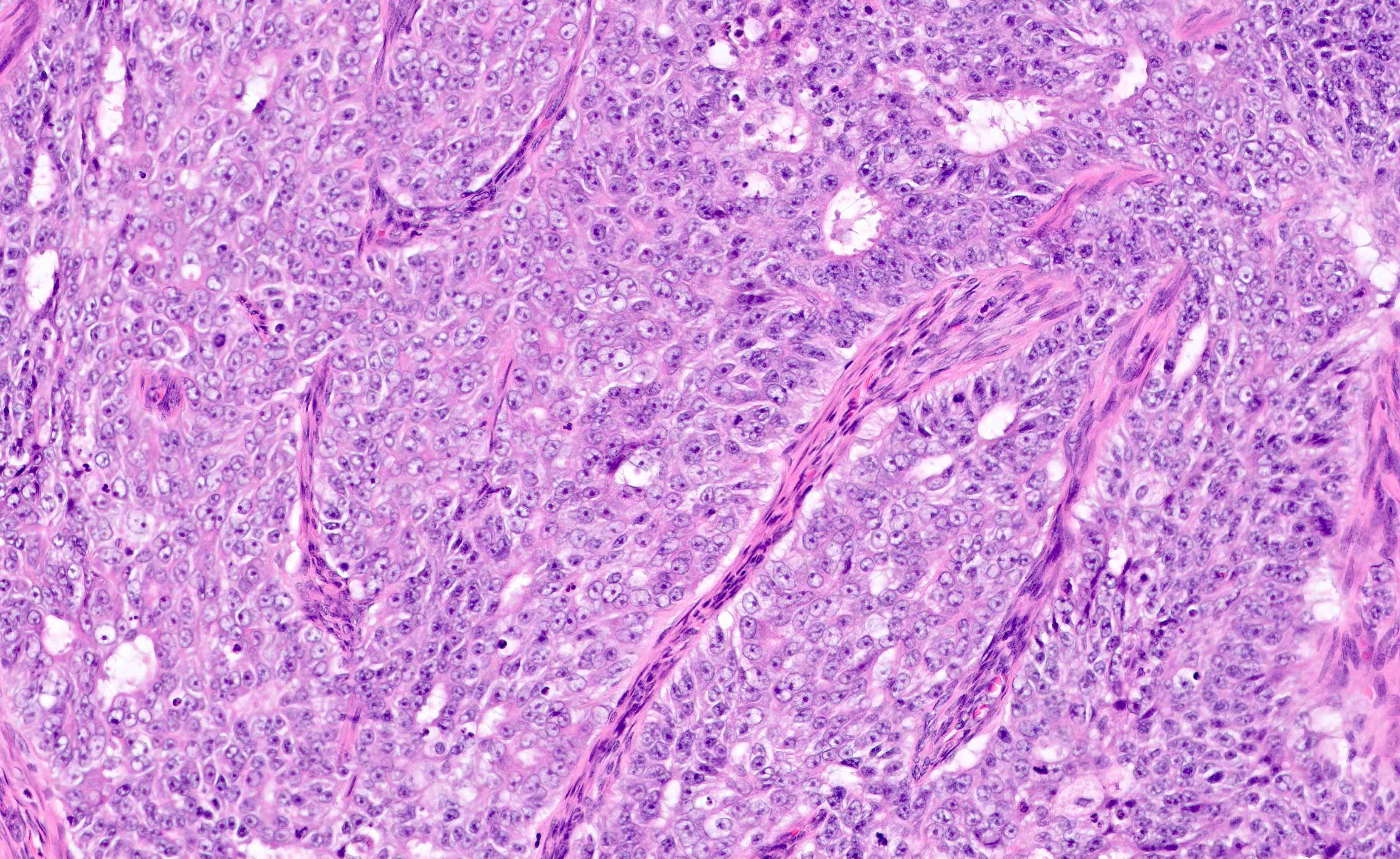
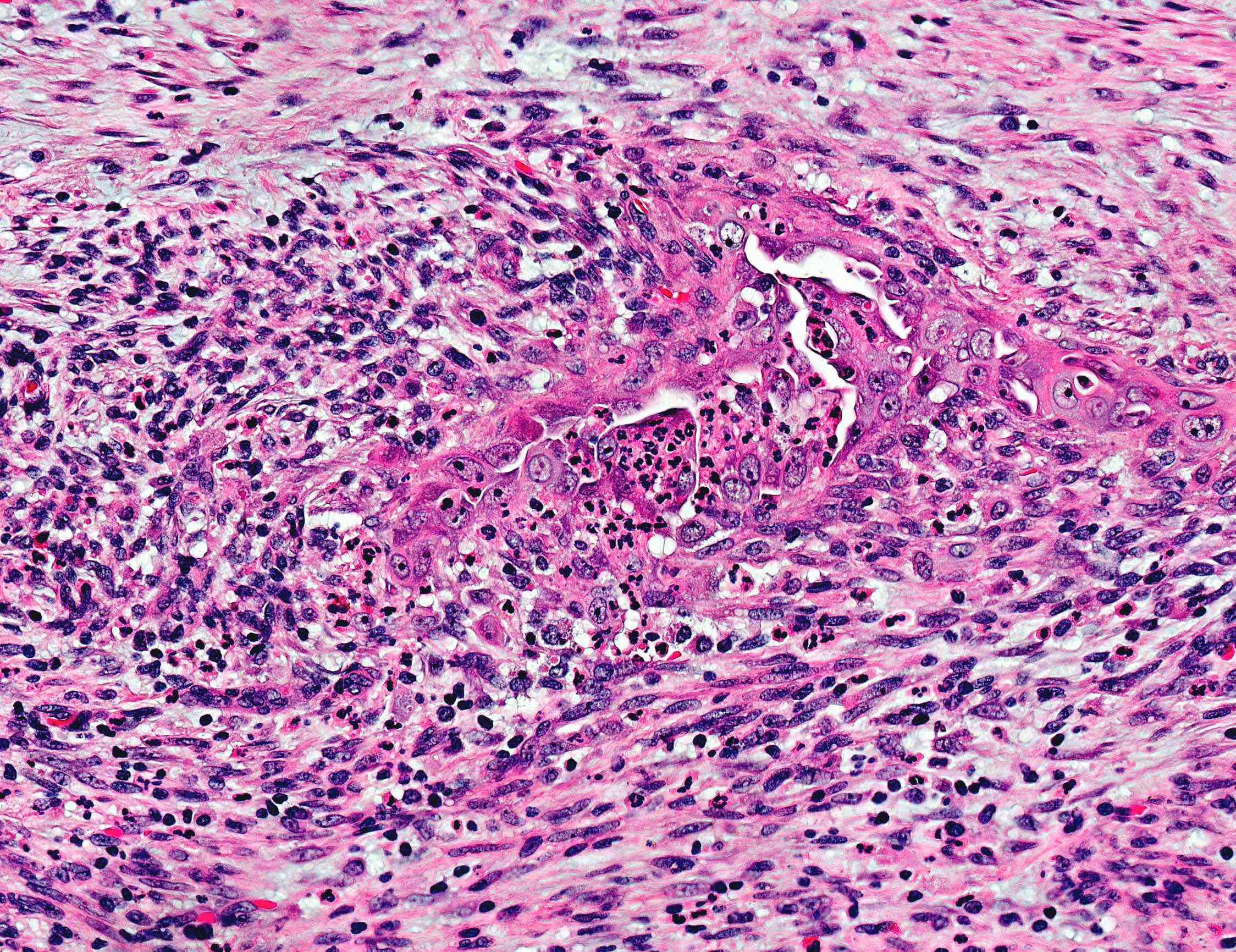
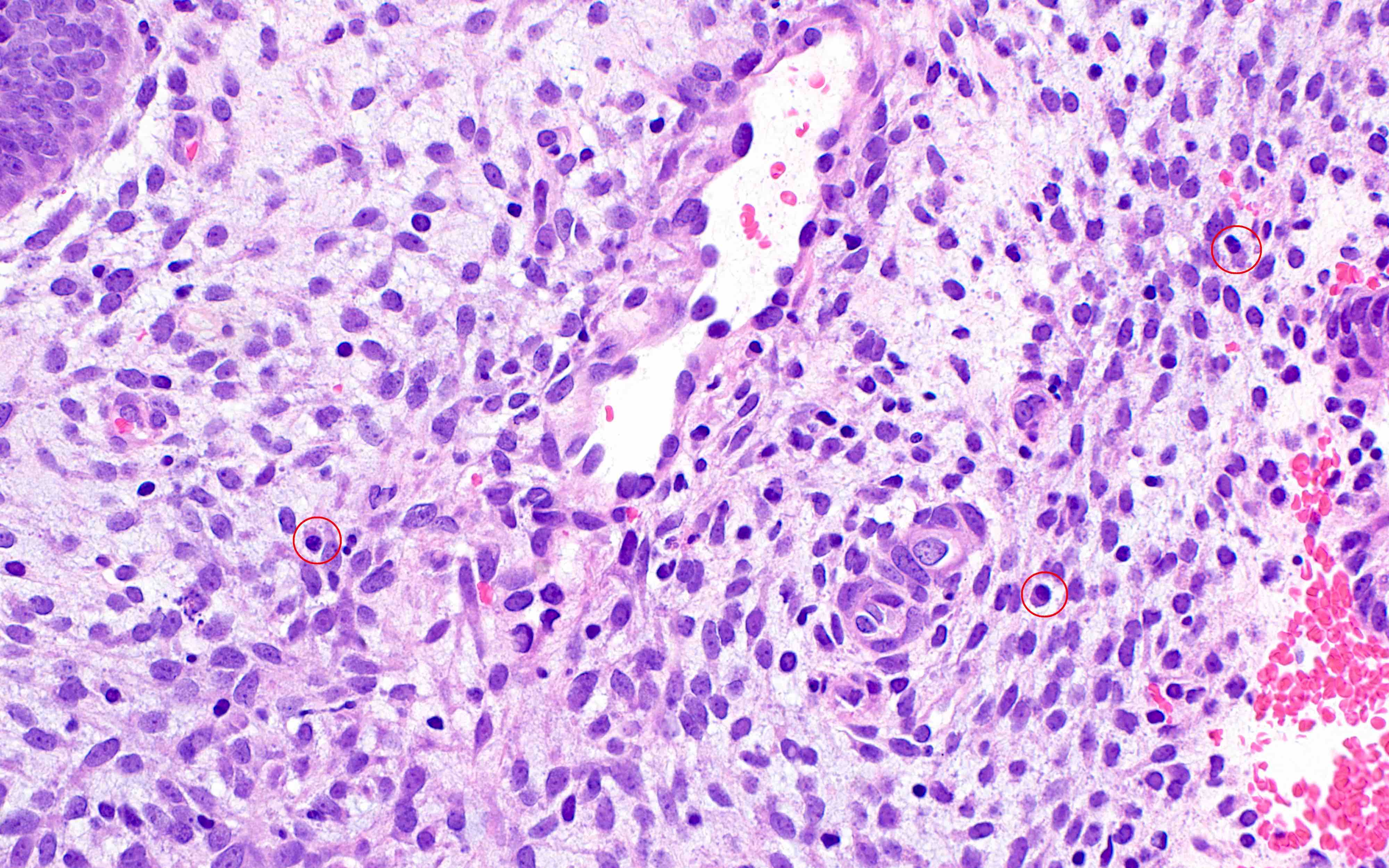
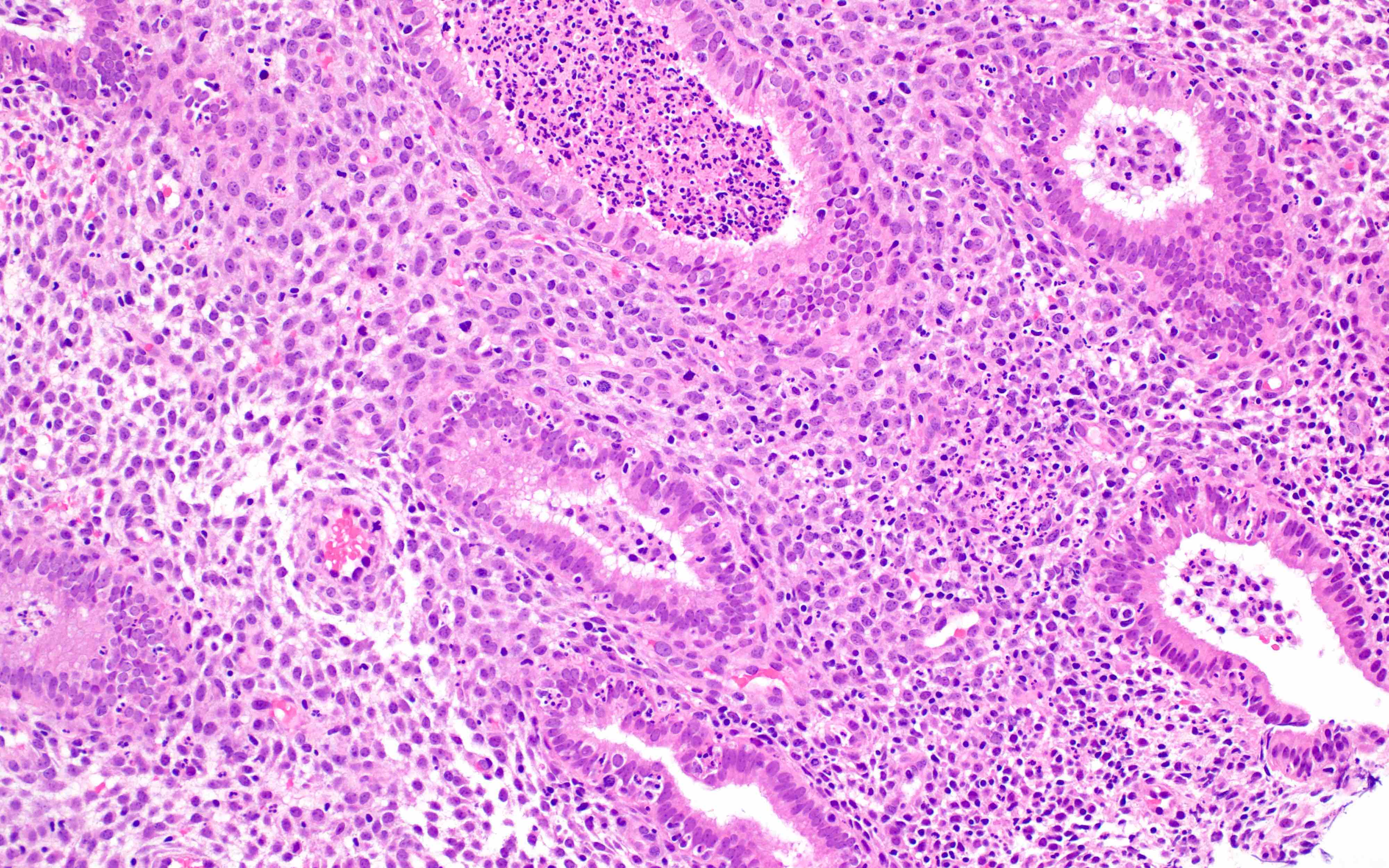
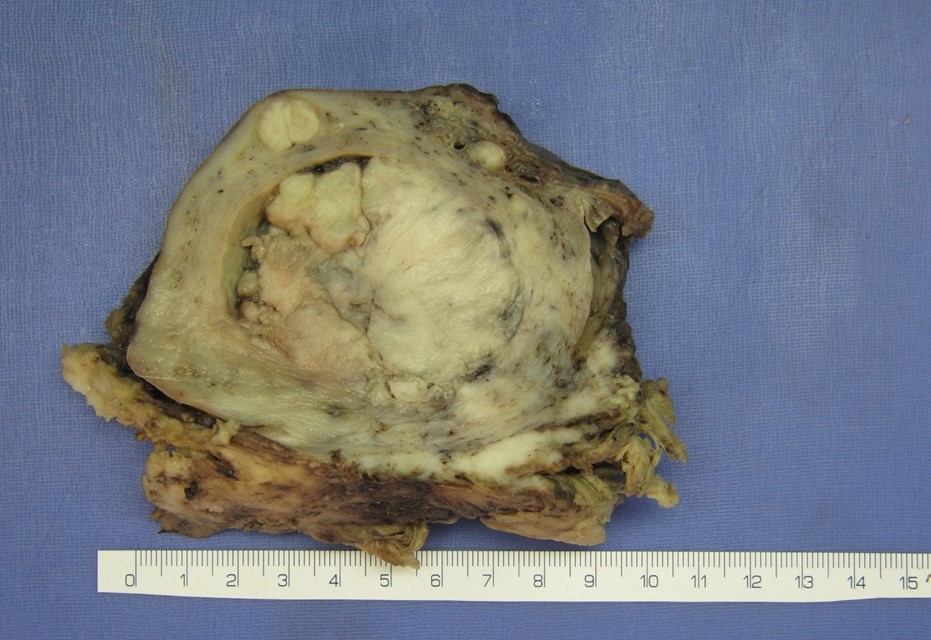
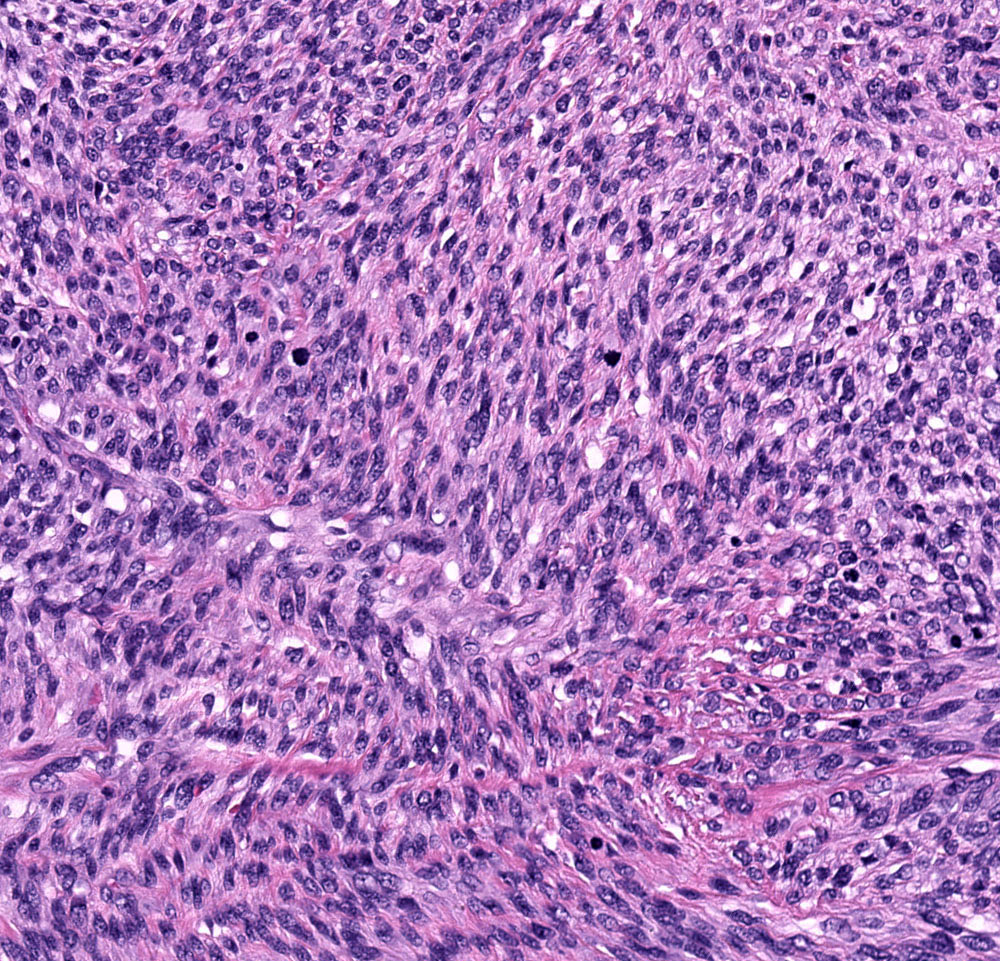
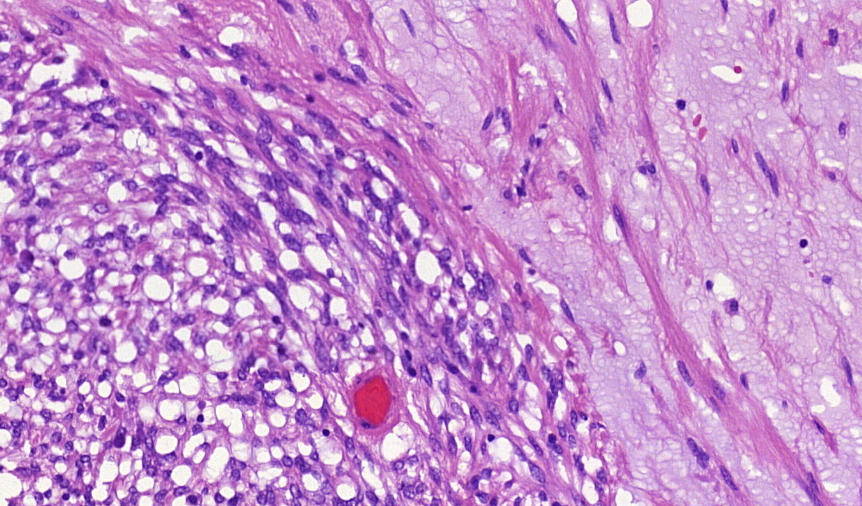
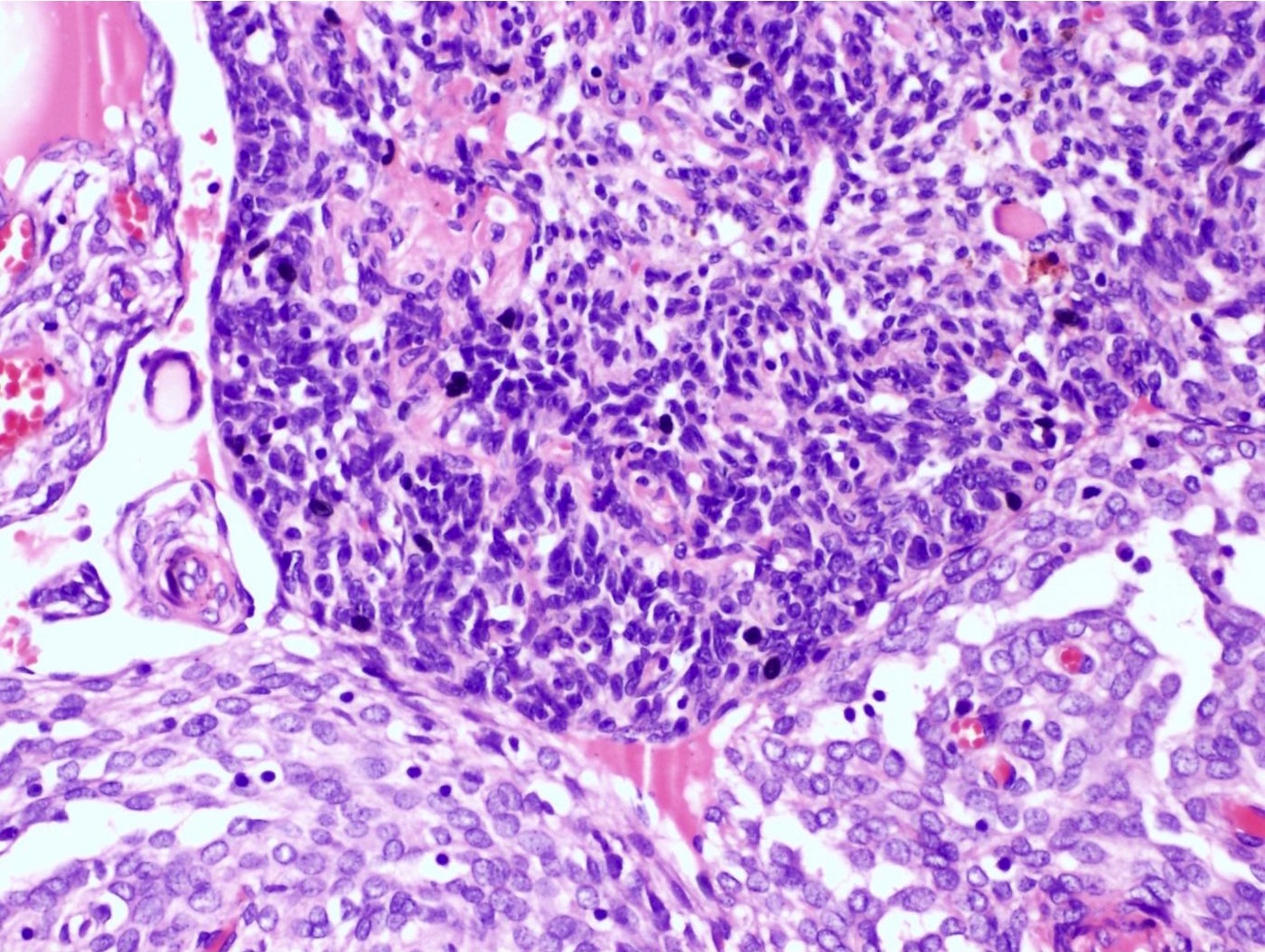
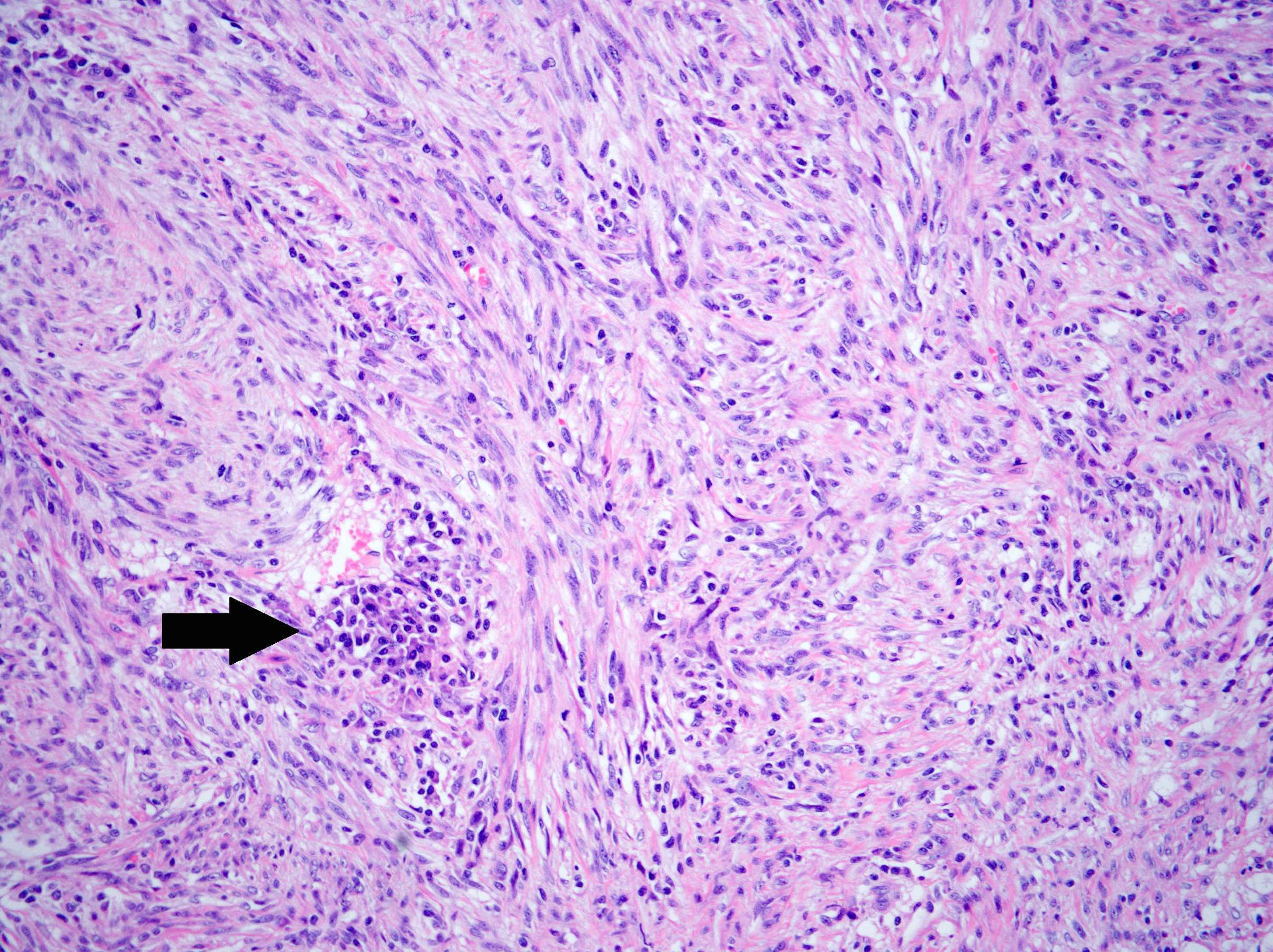
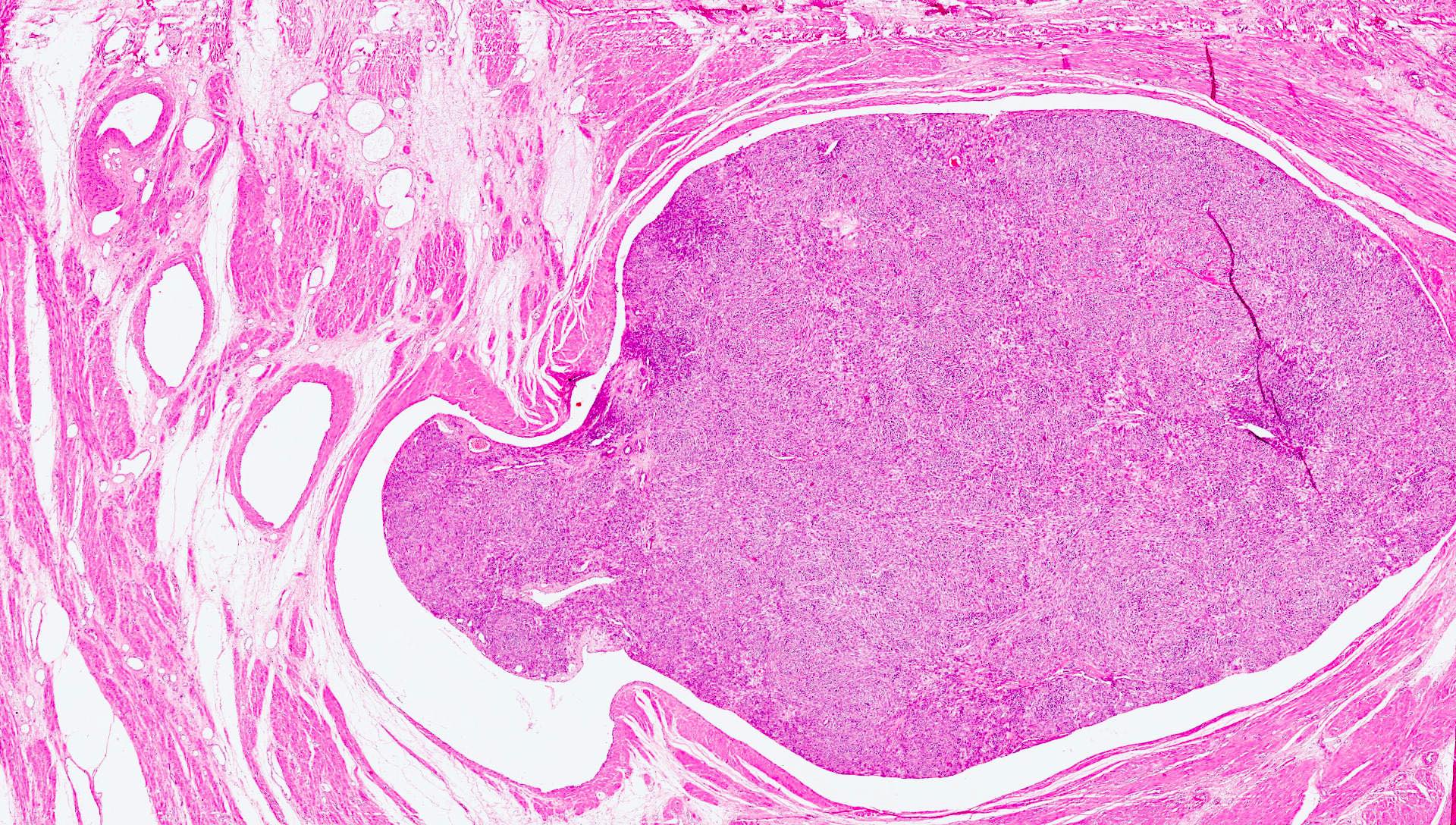
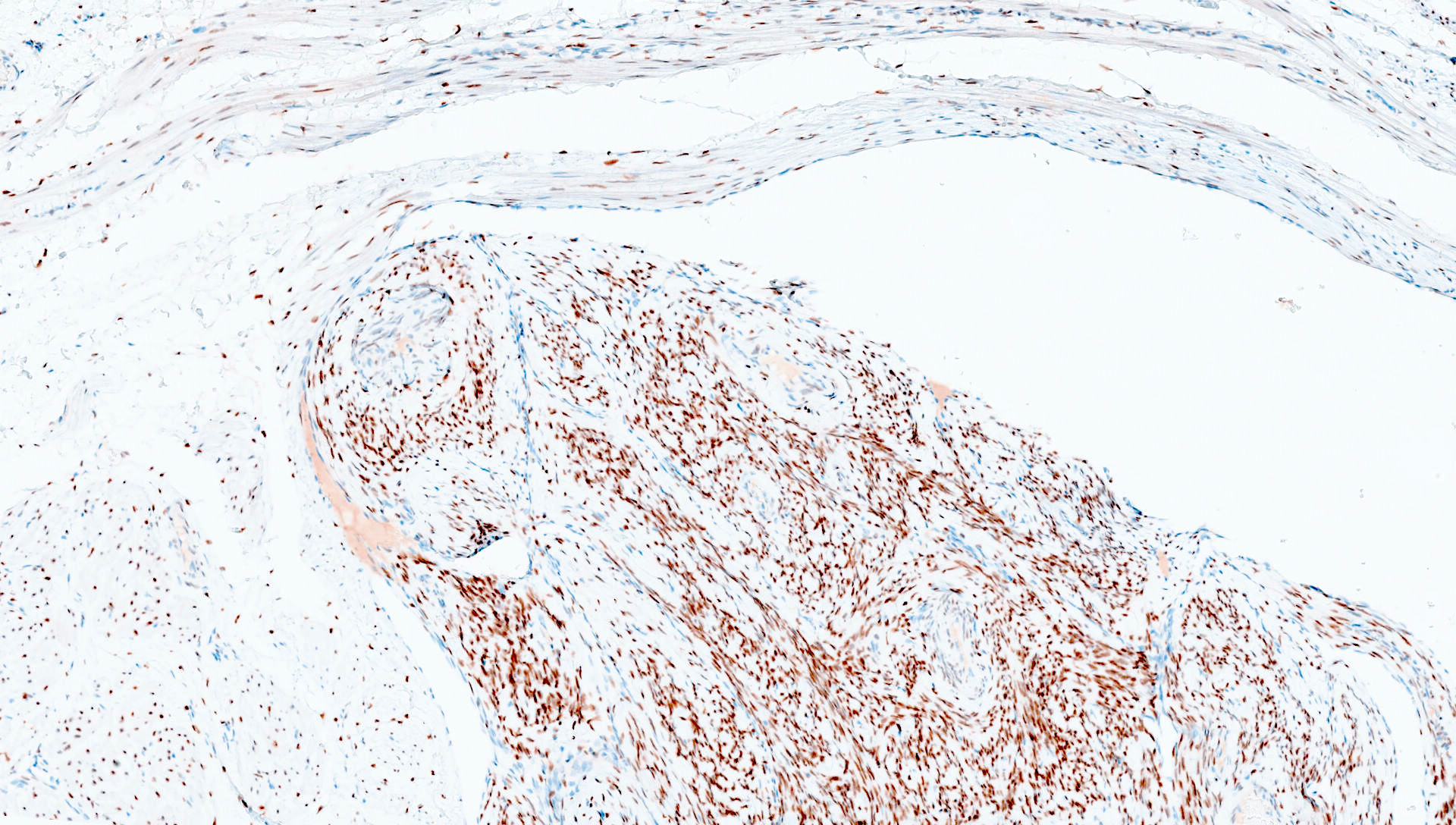
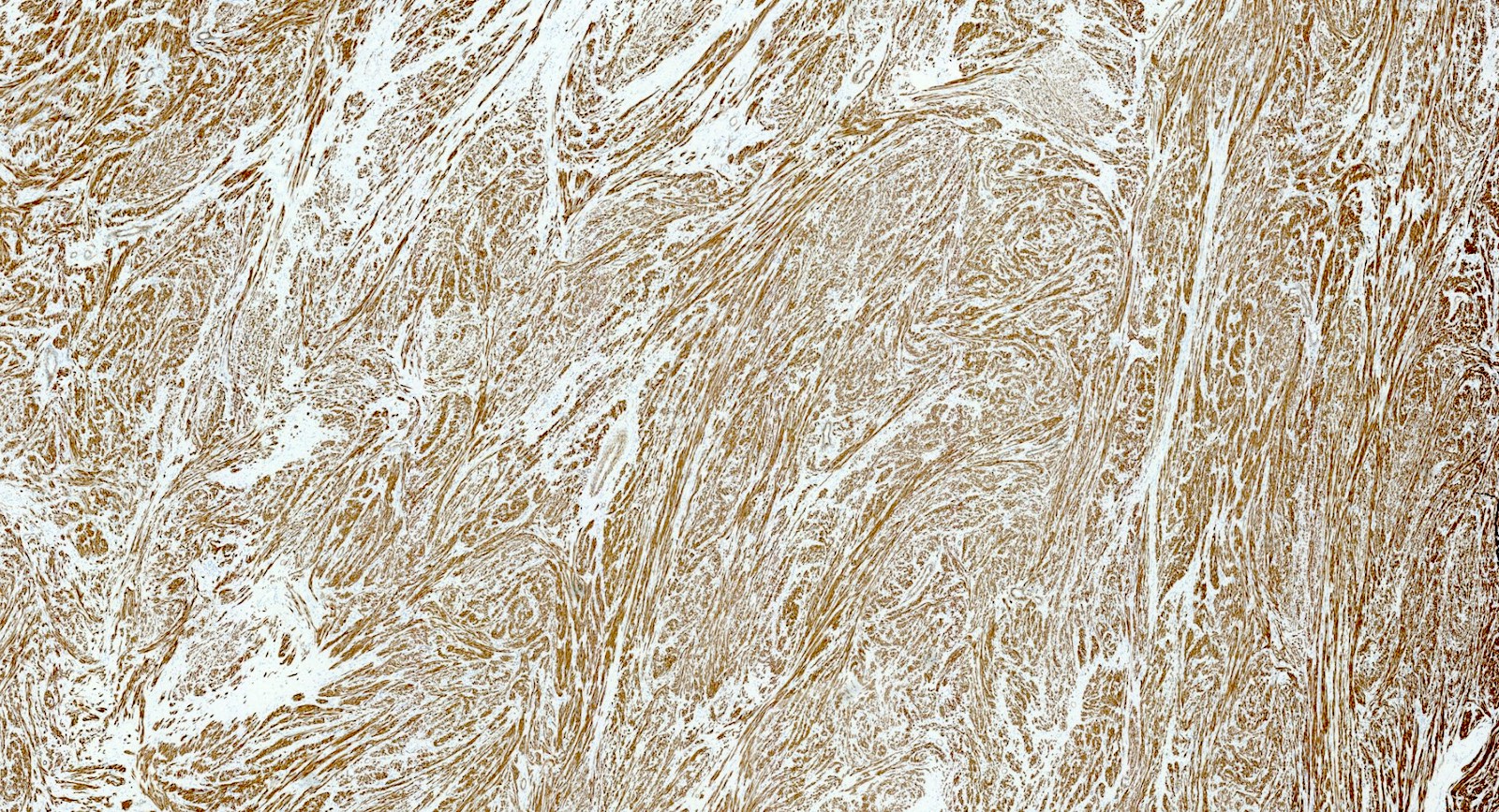
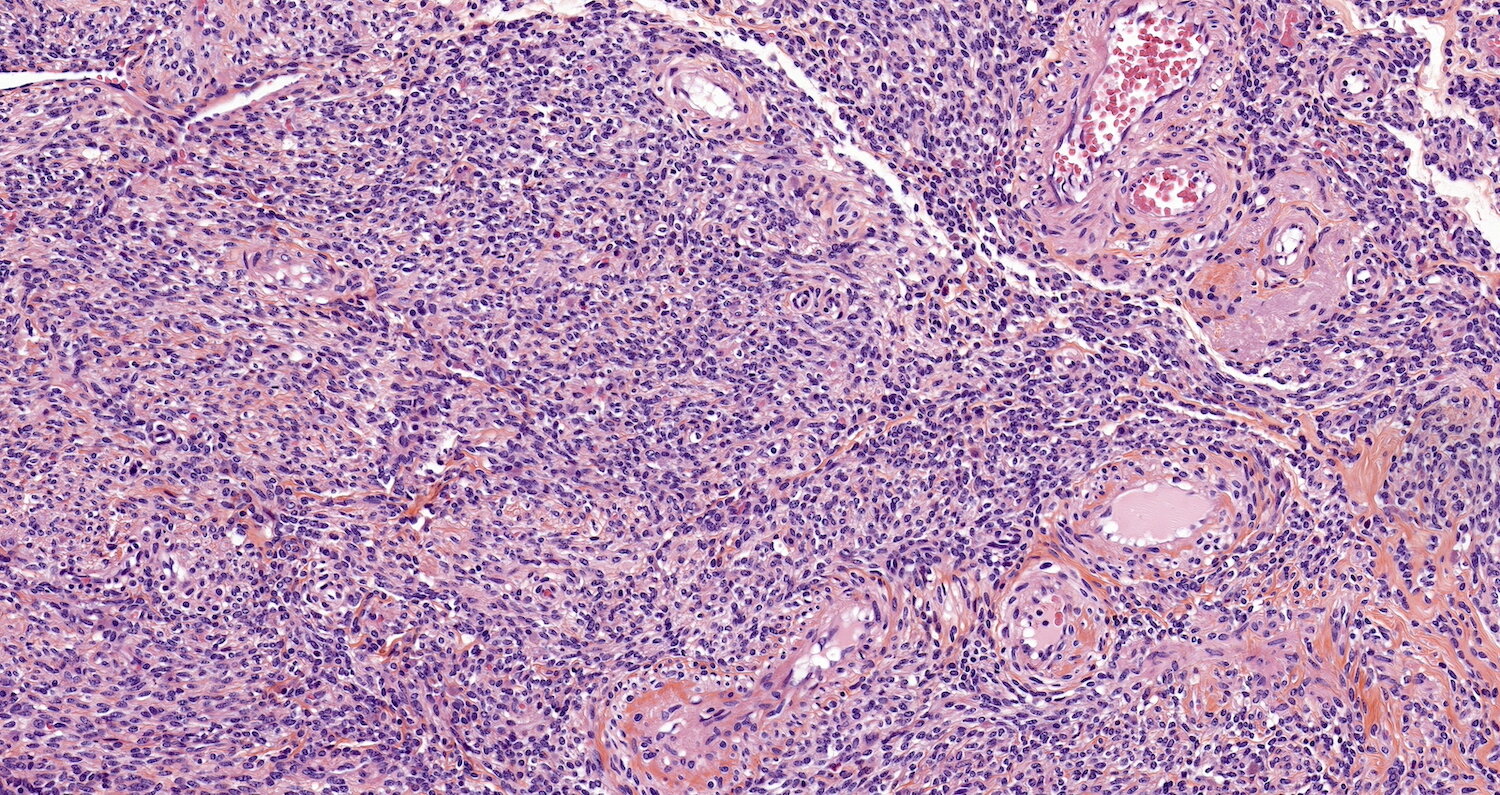
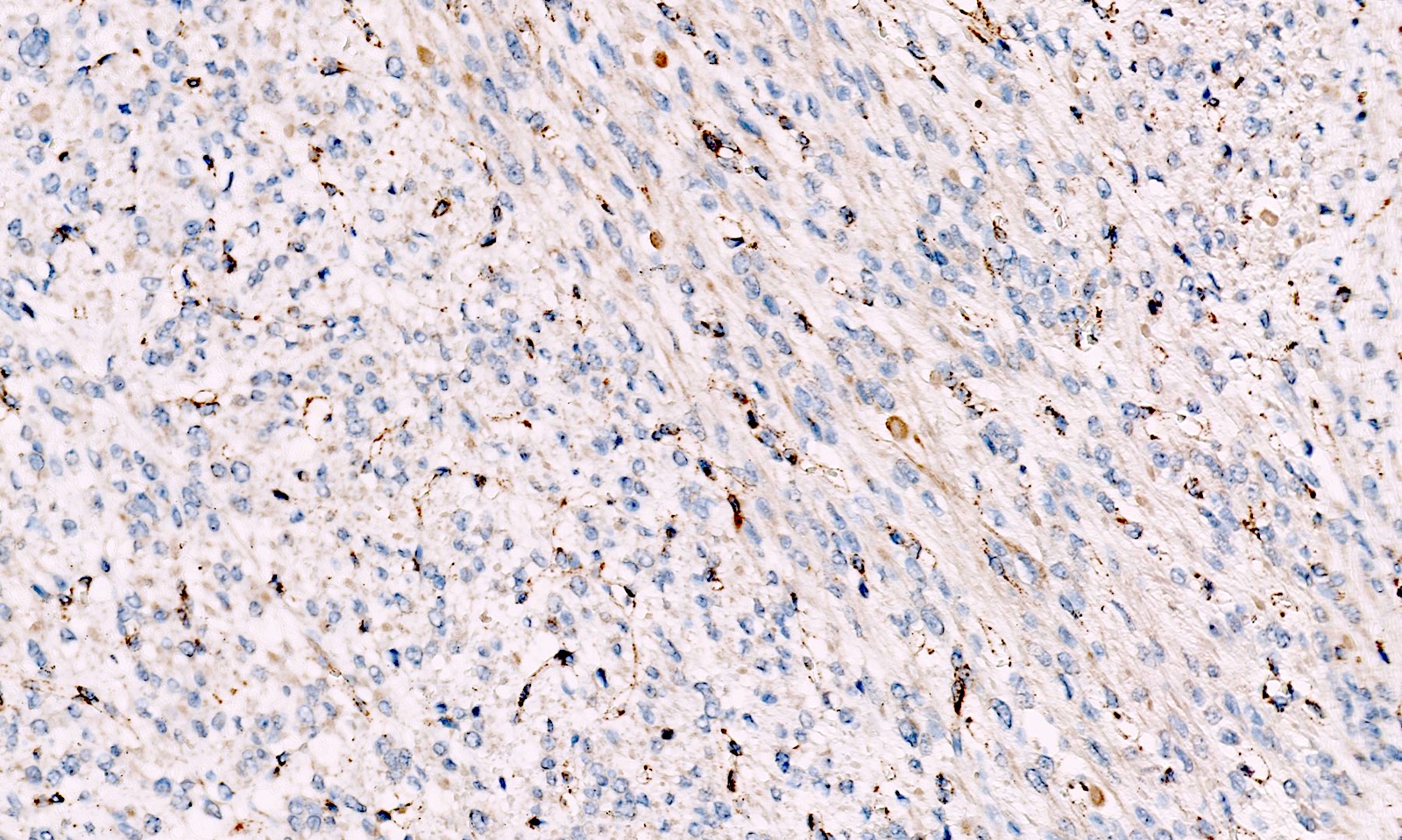
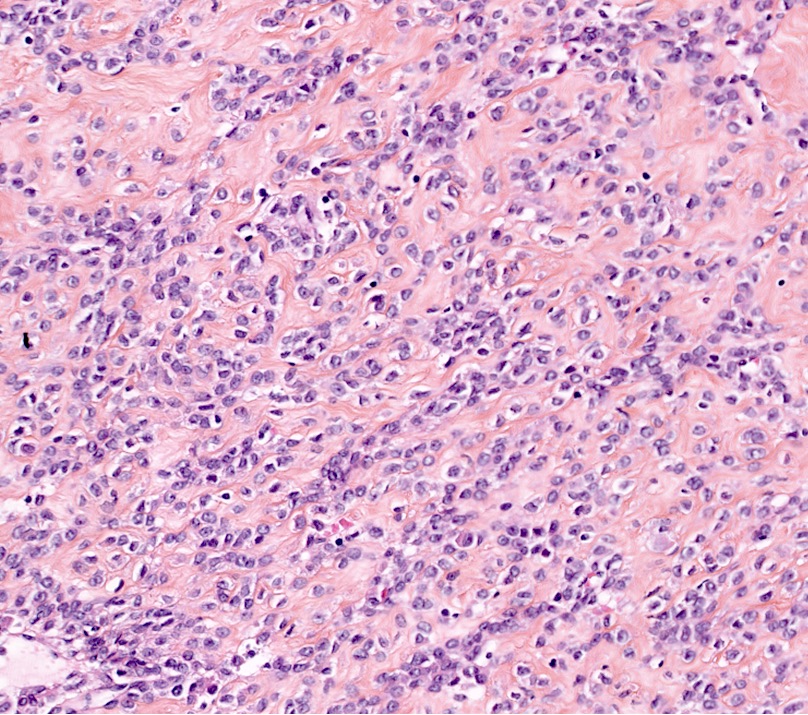
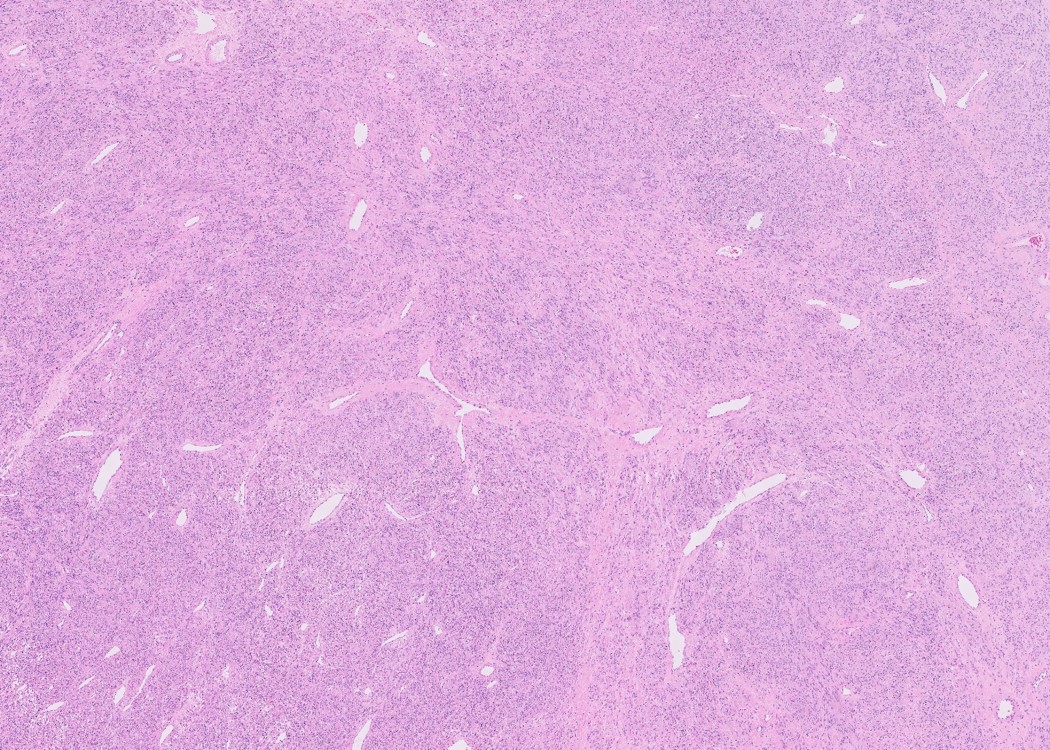
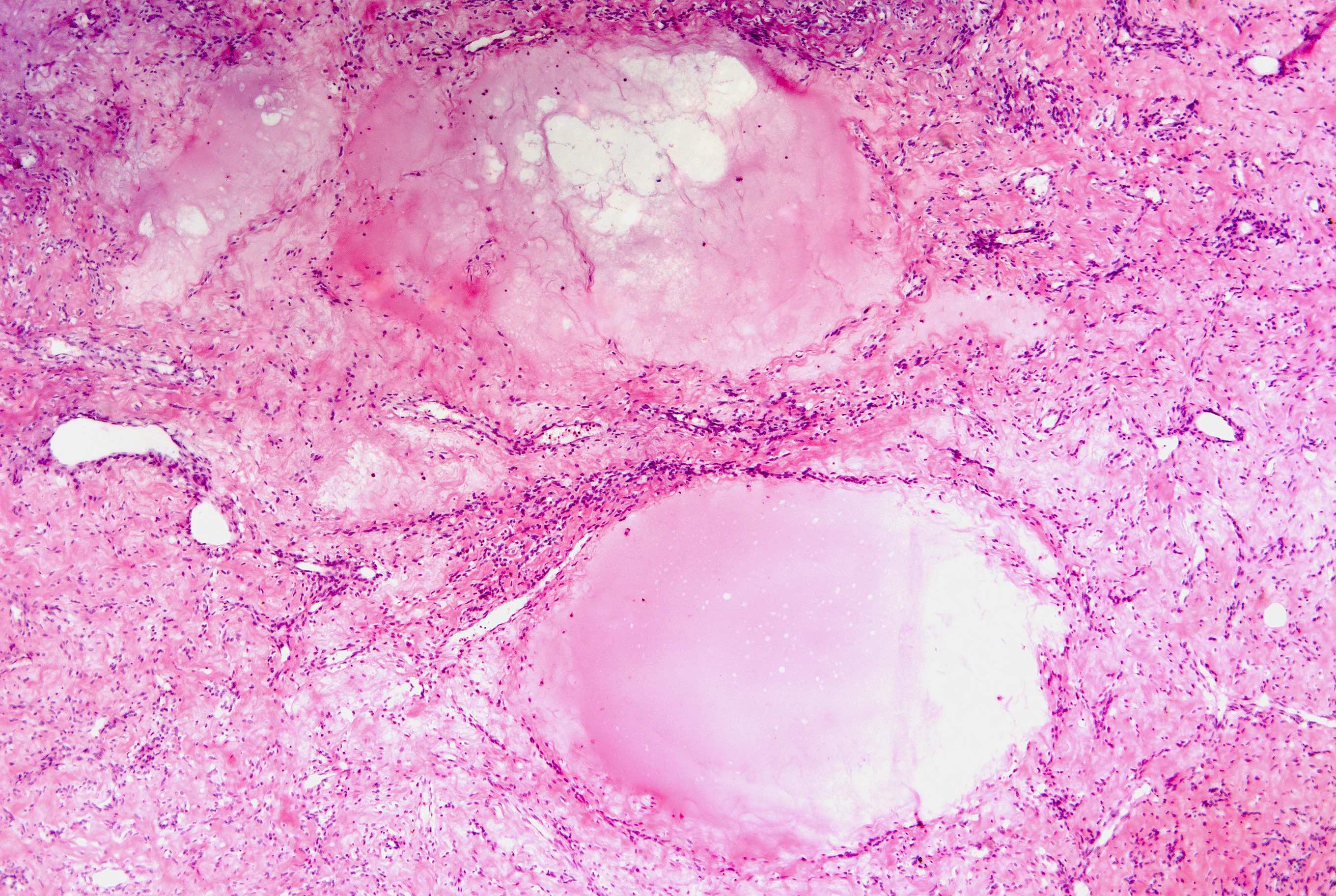
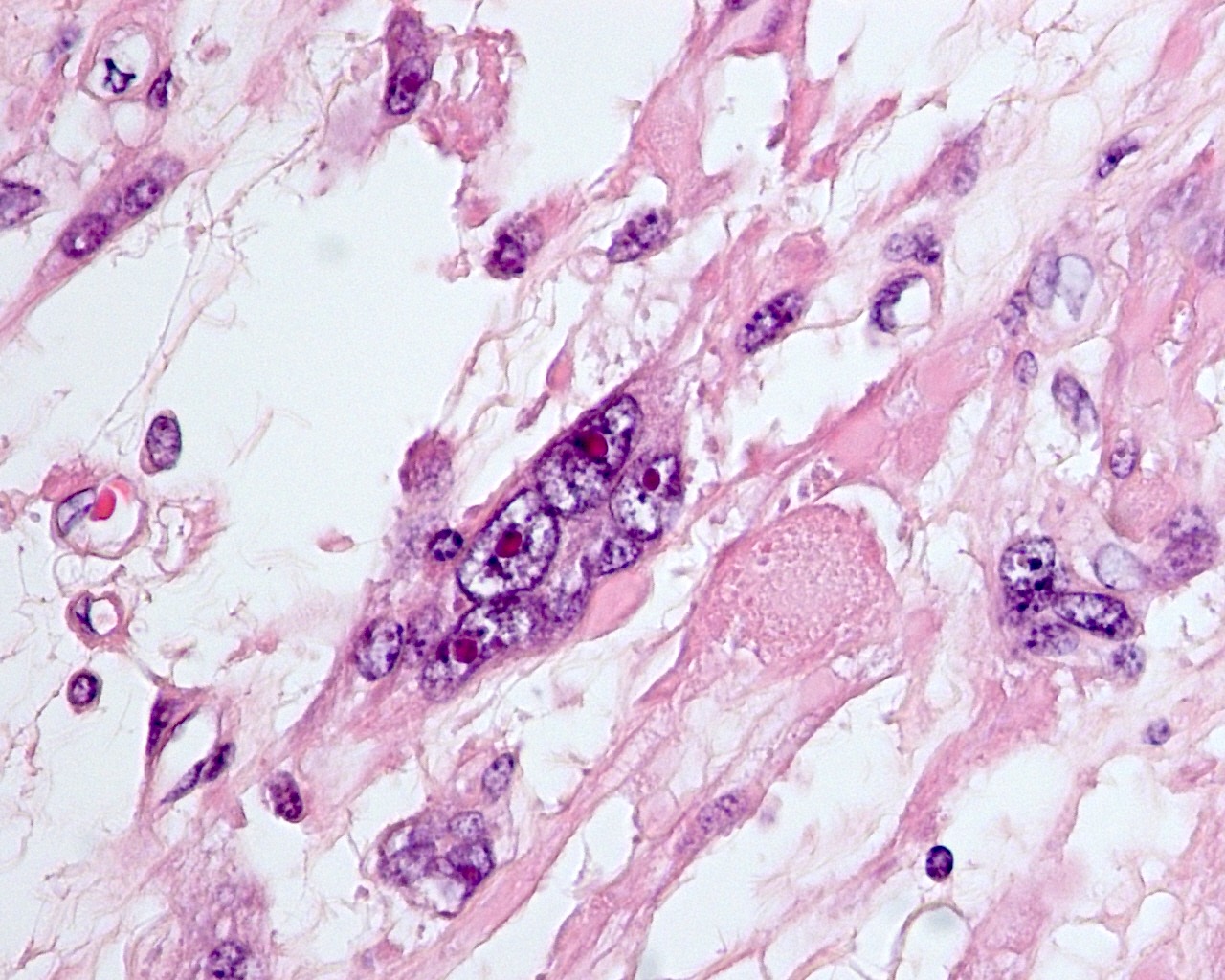
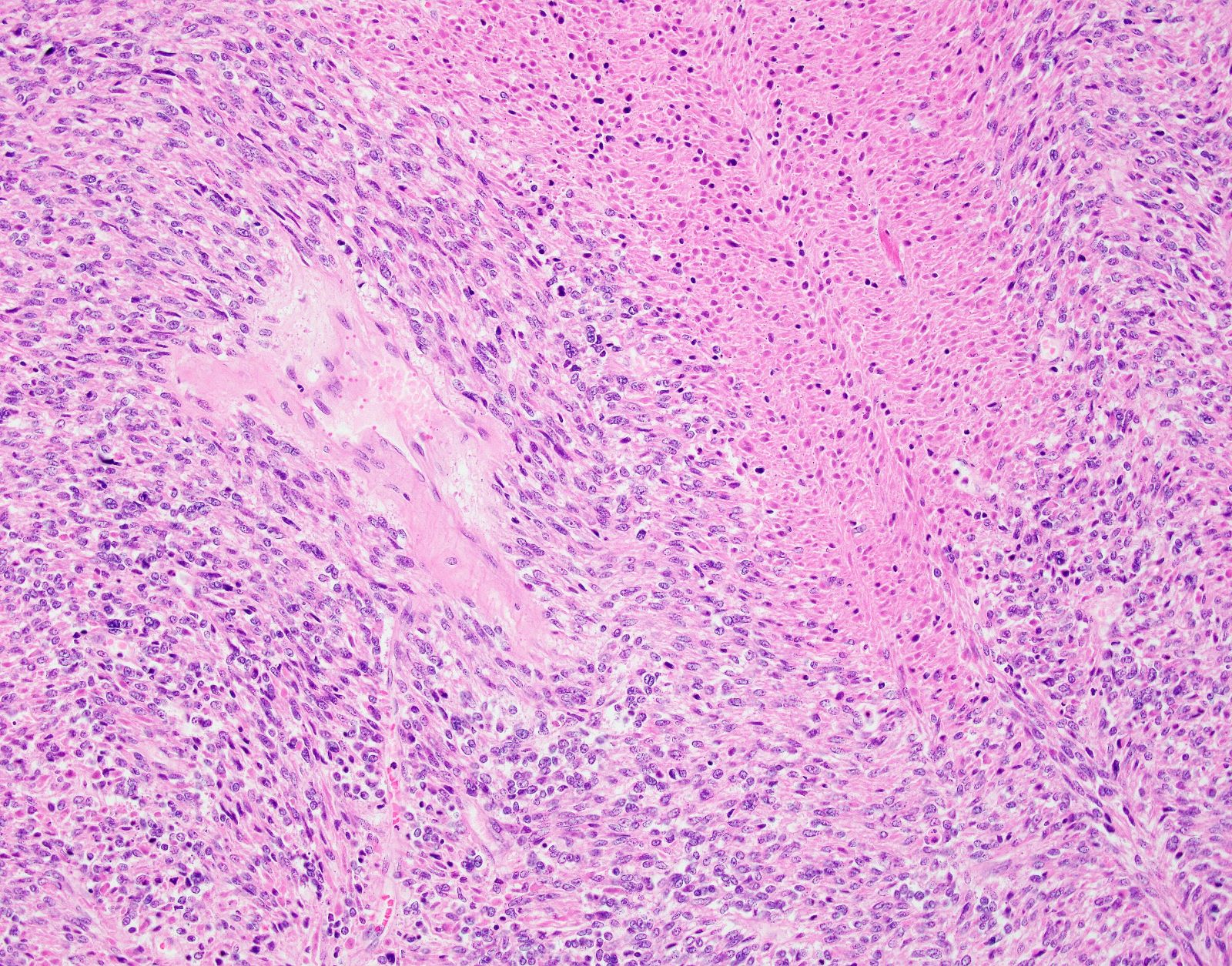
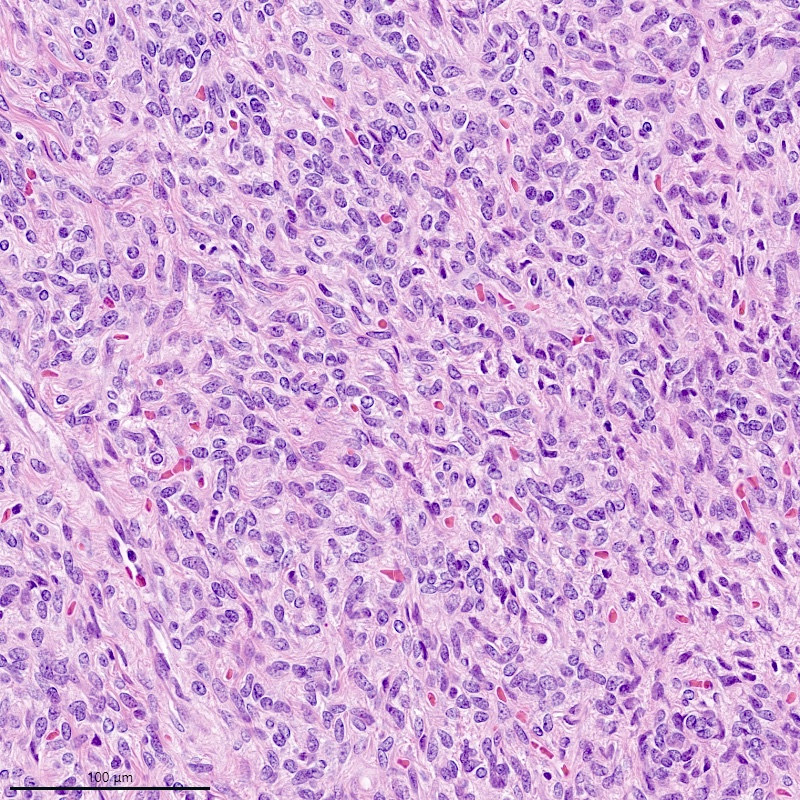
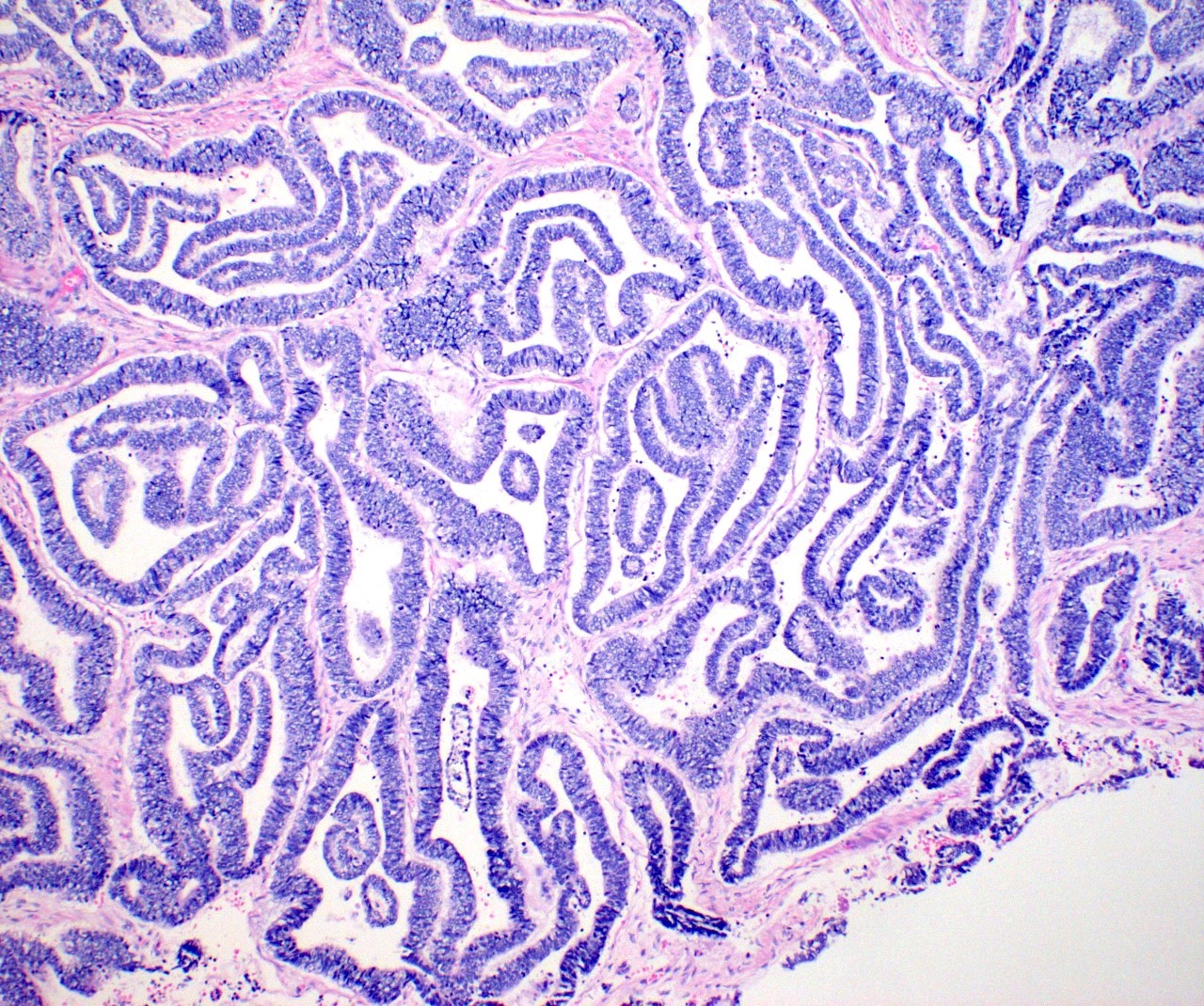
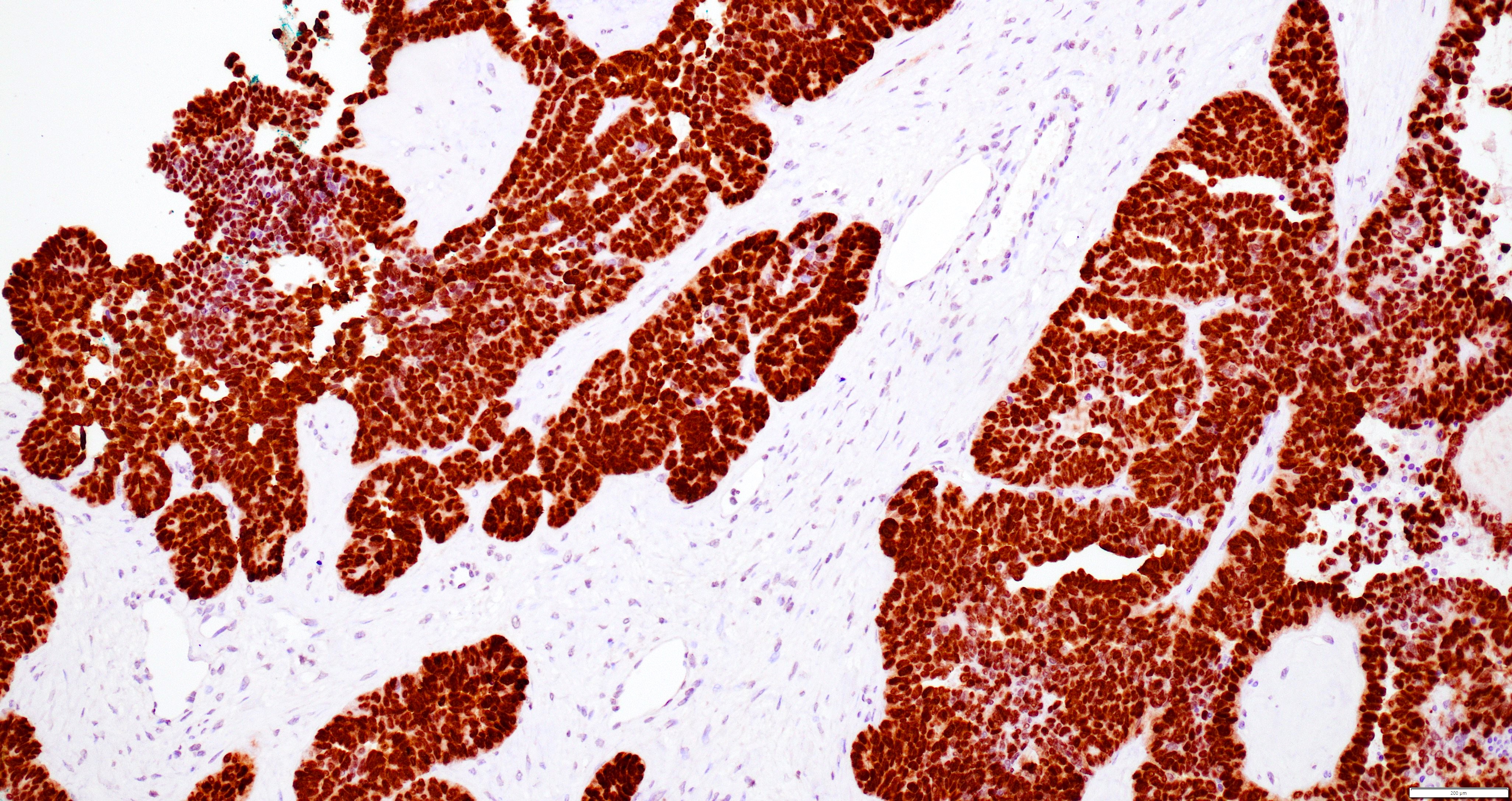
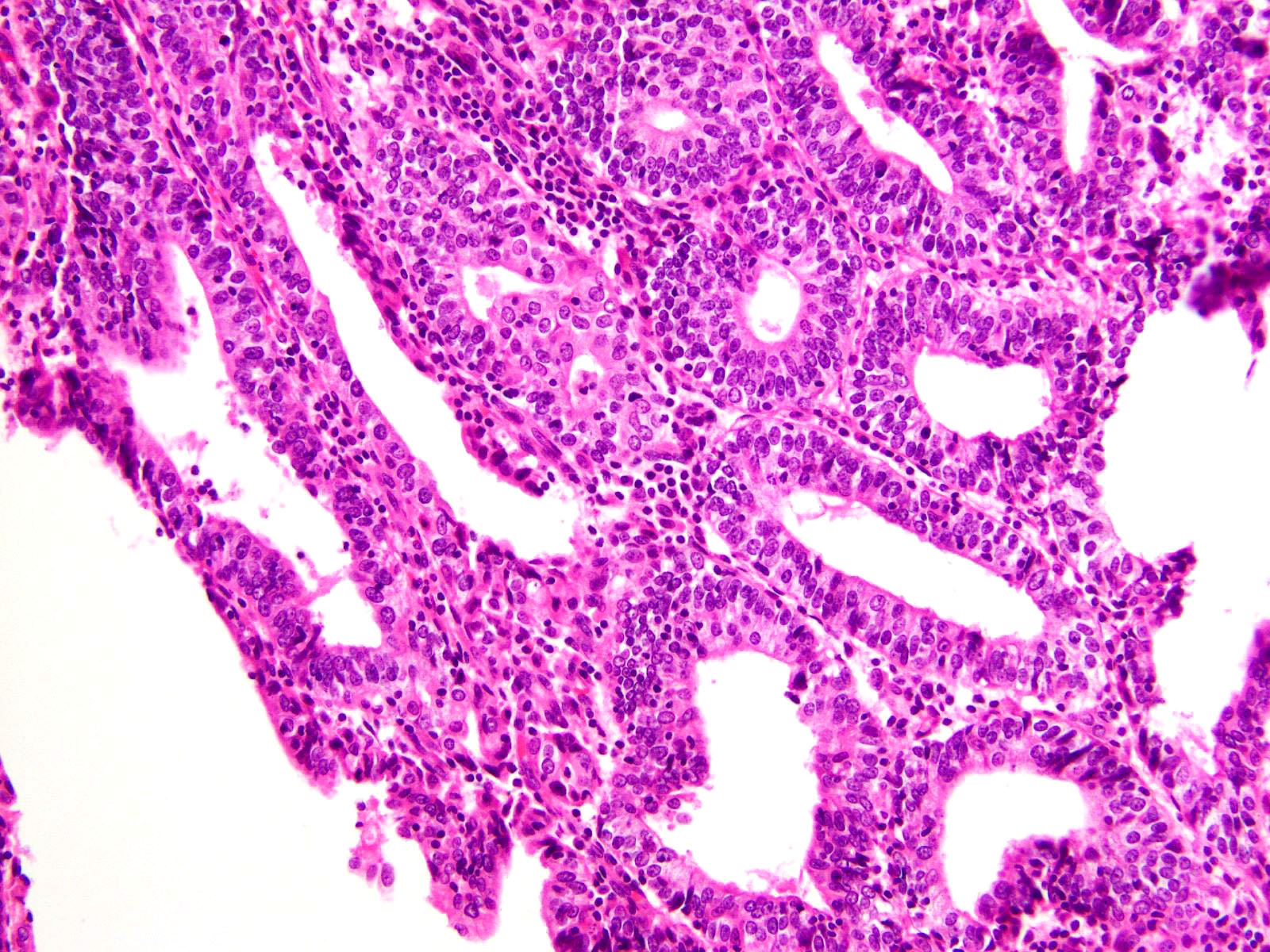
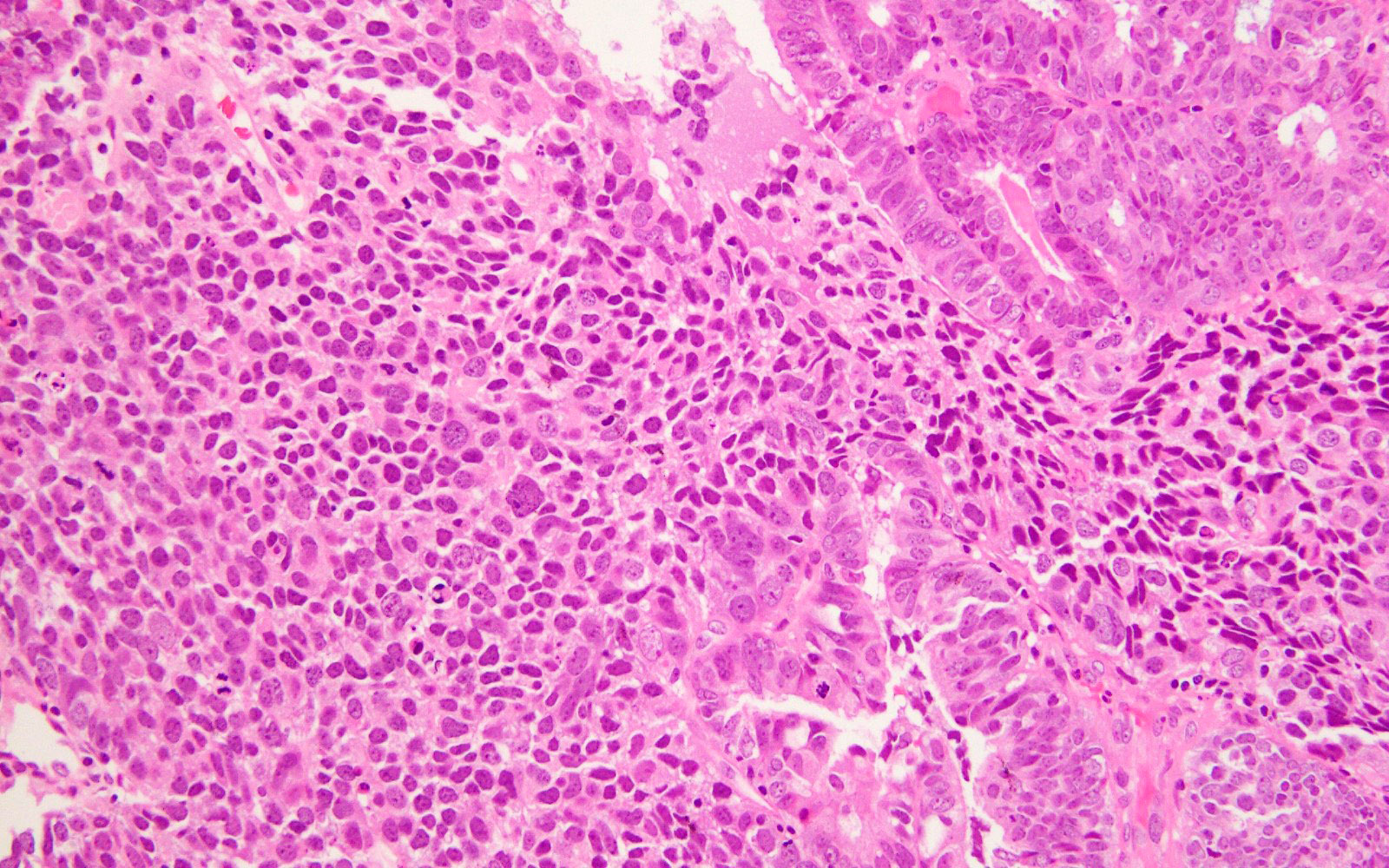
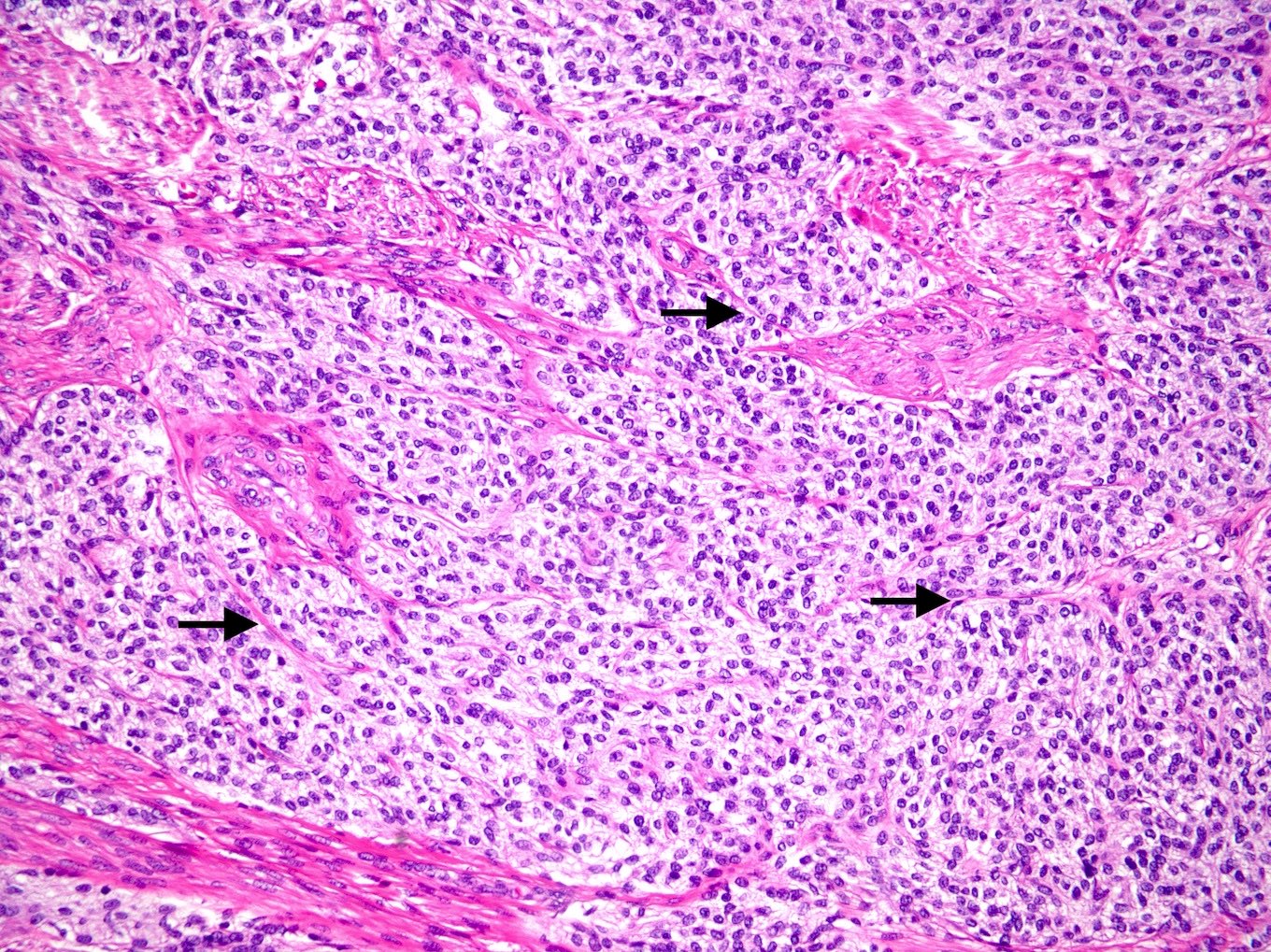
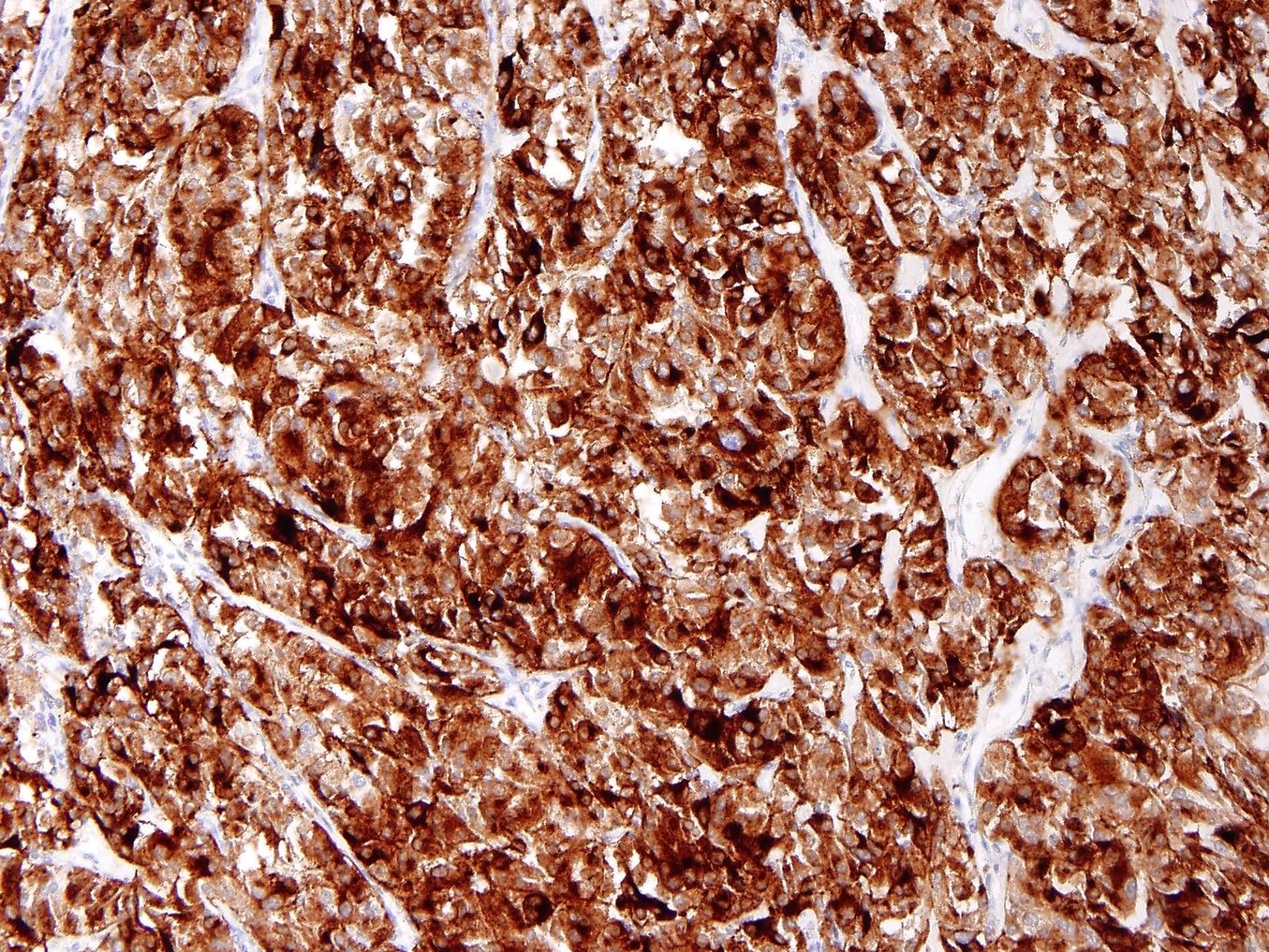
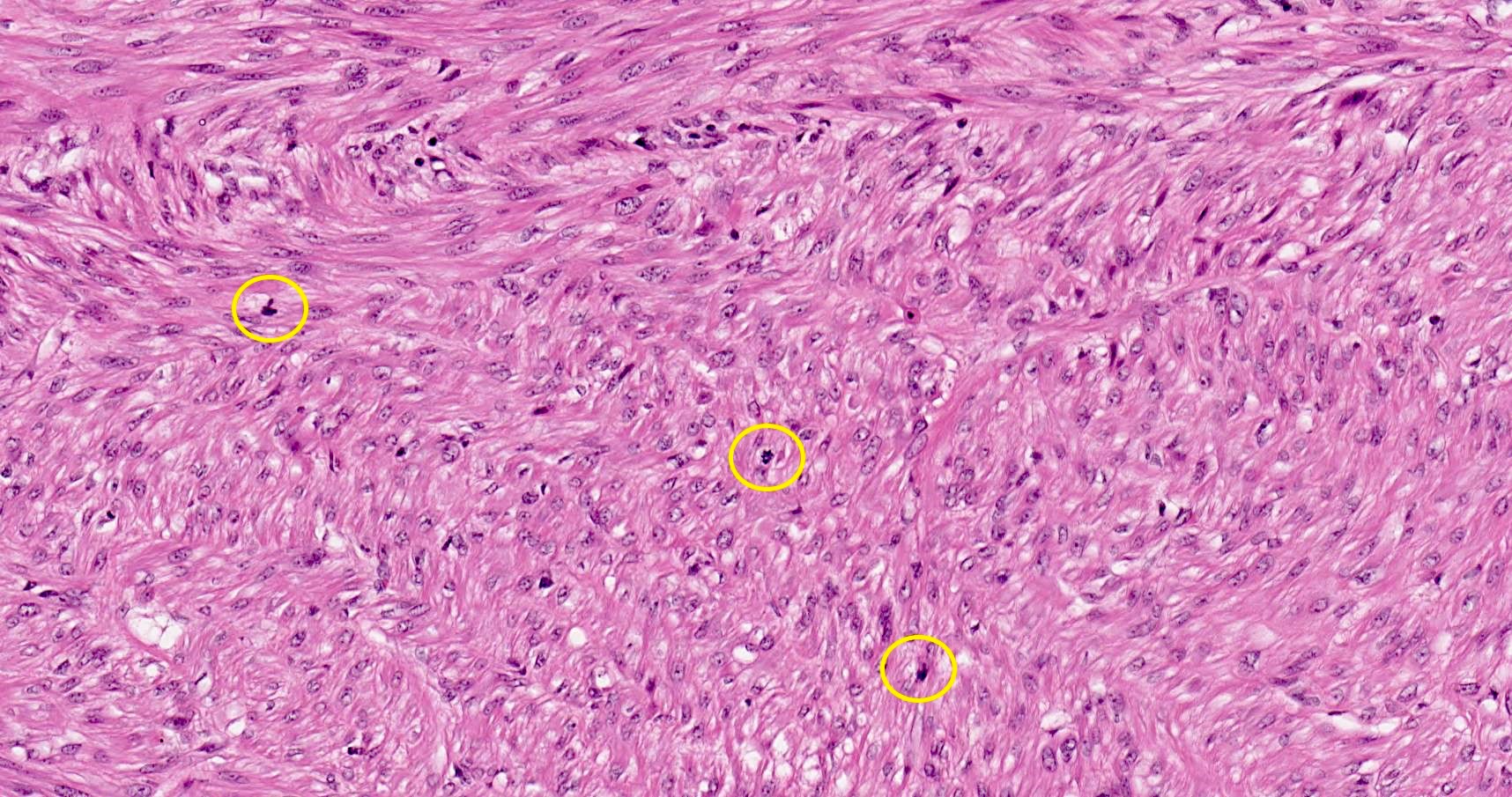
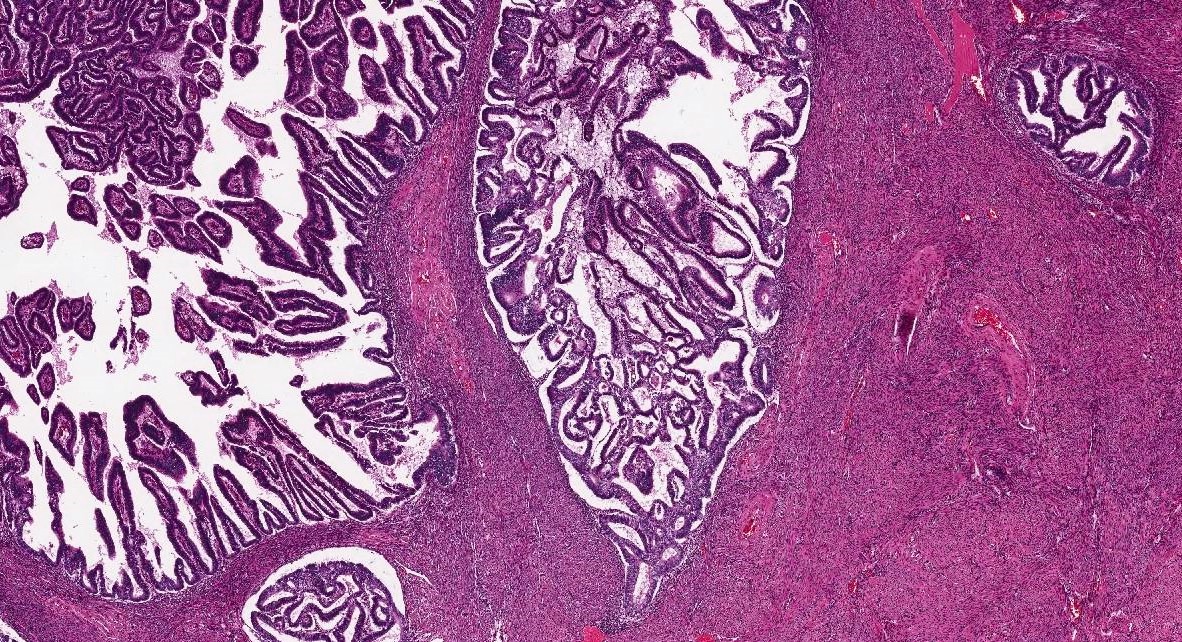
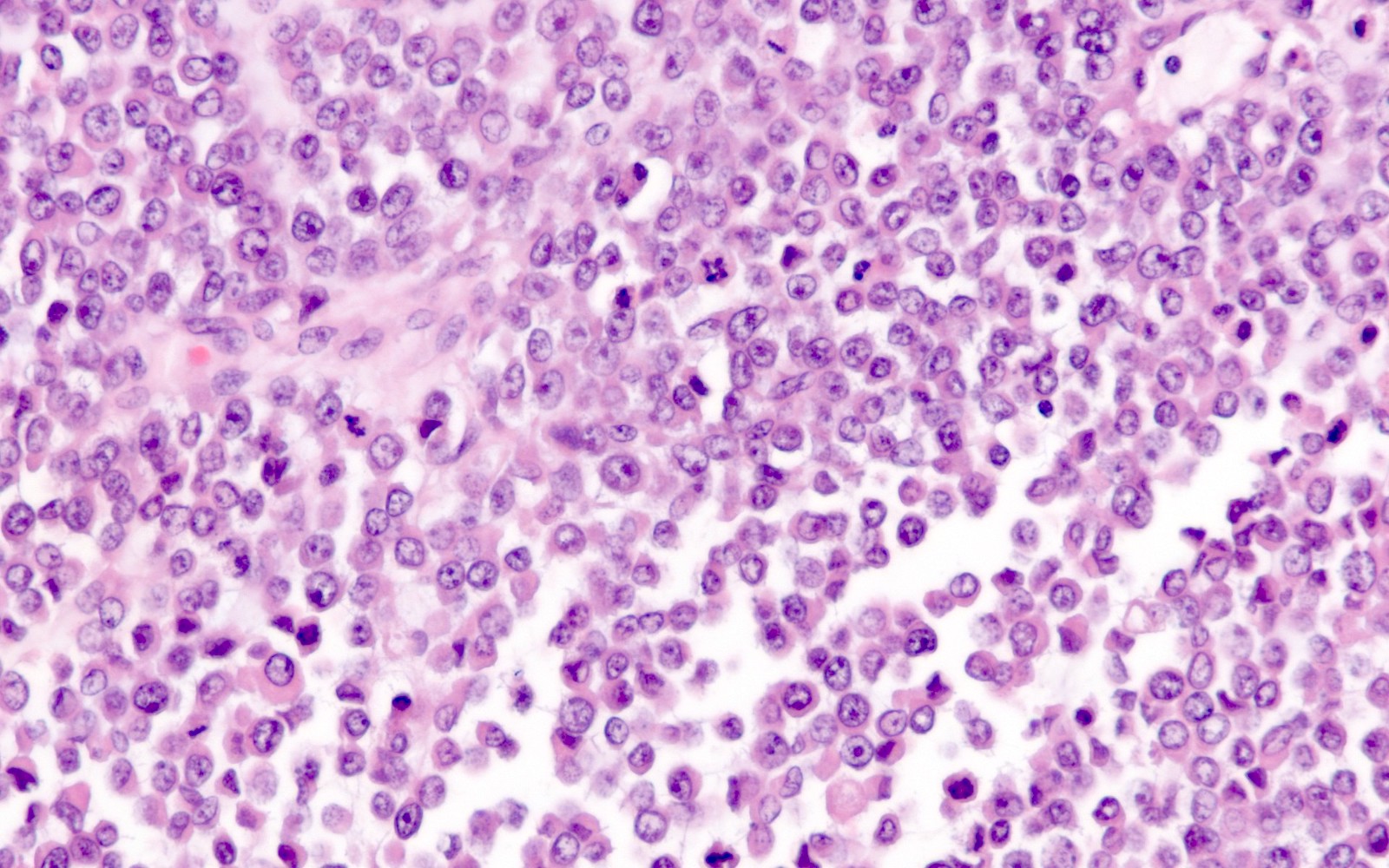
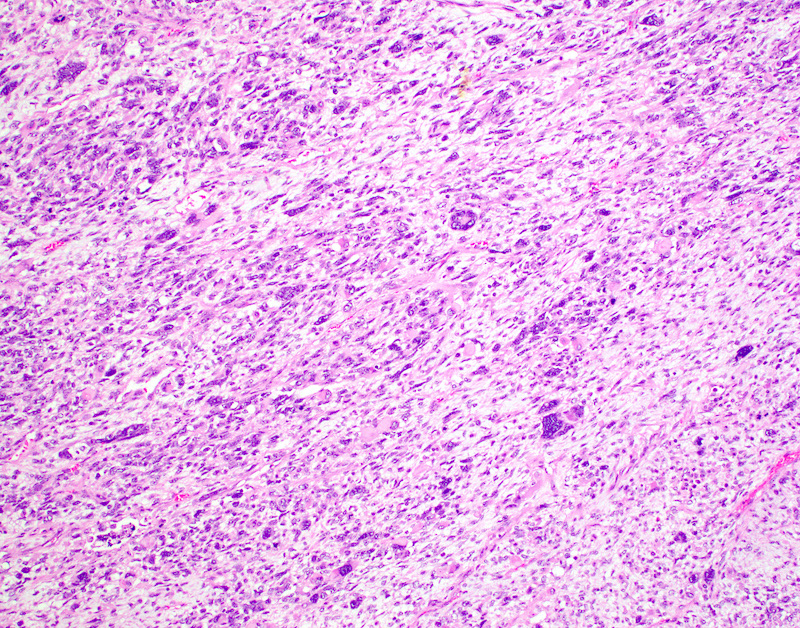
- Carcinoma is confined to the endometrium / adenomyosis when:
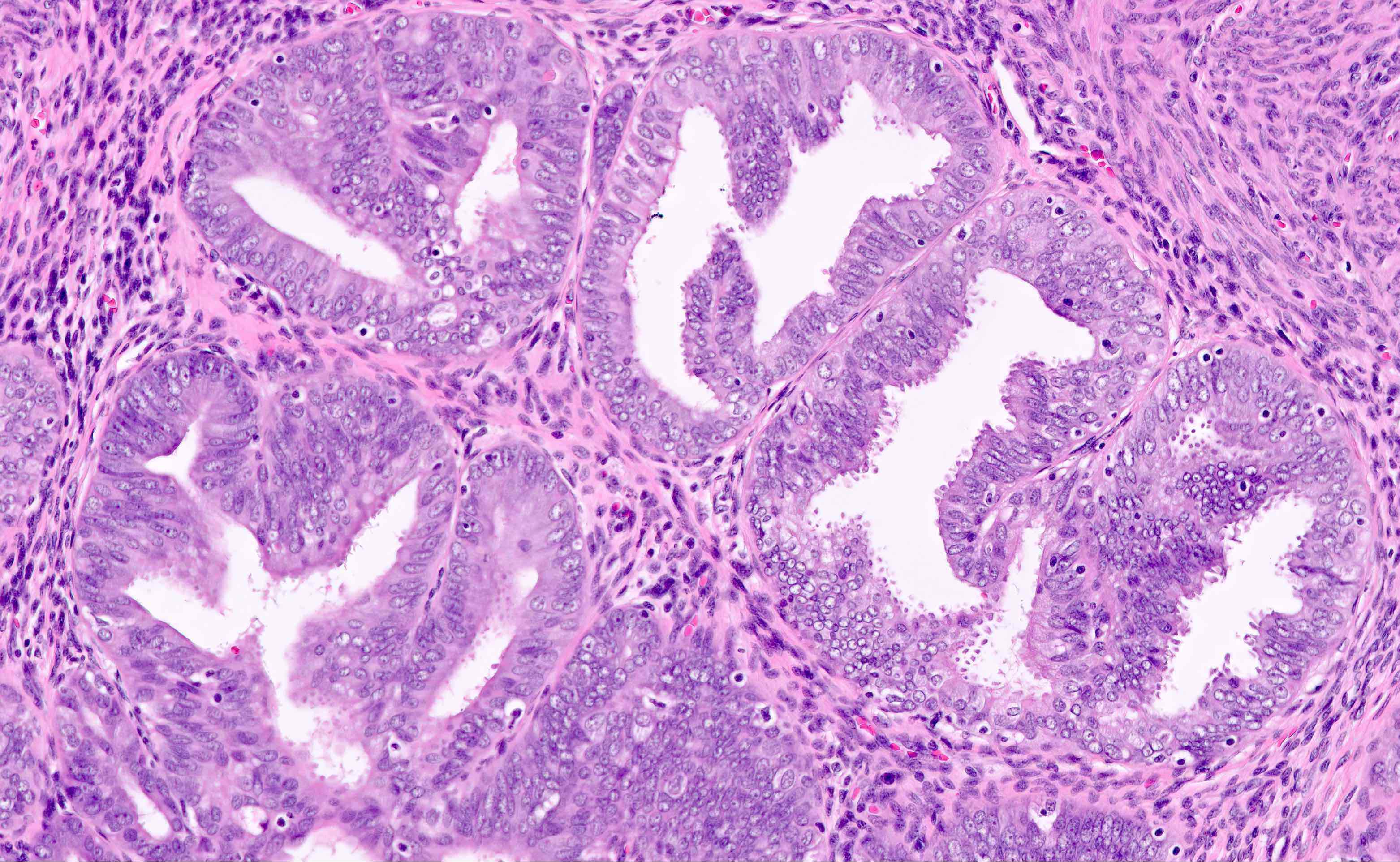
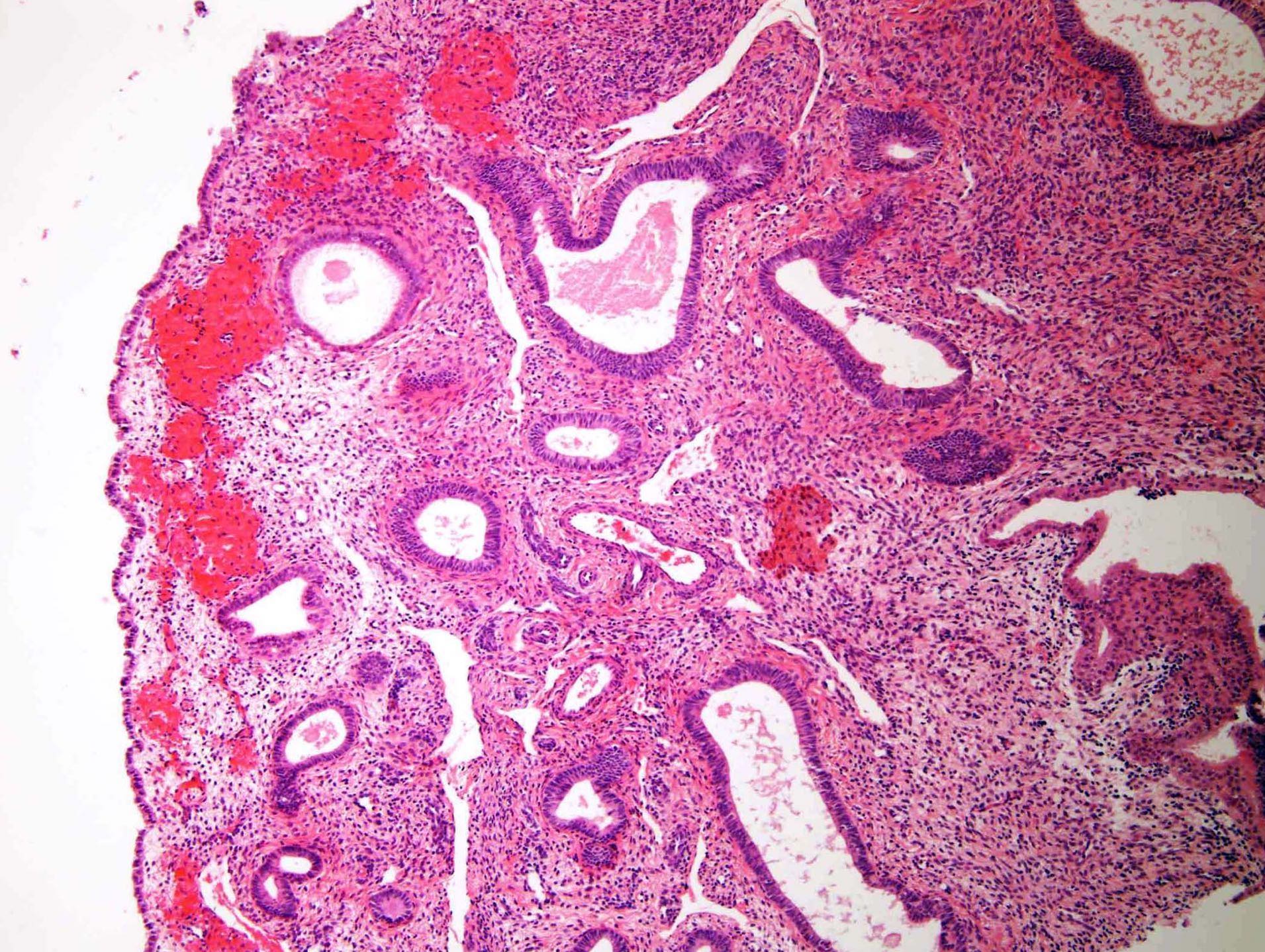
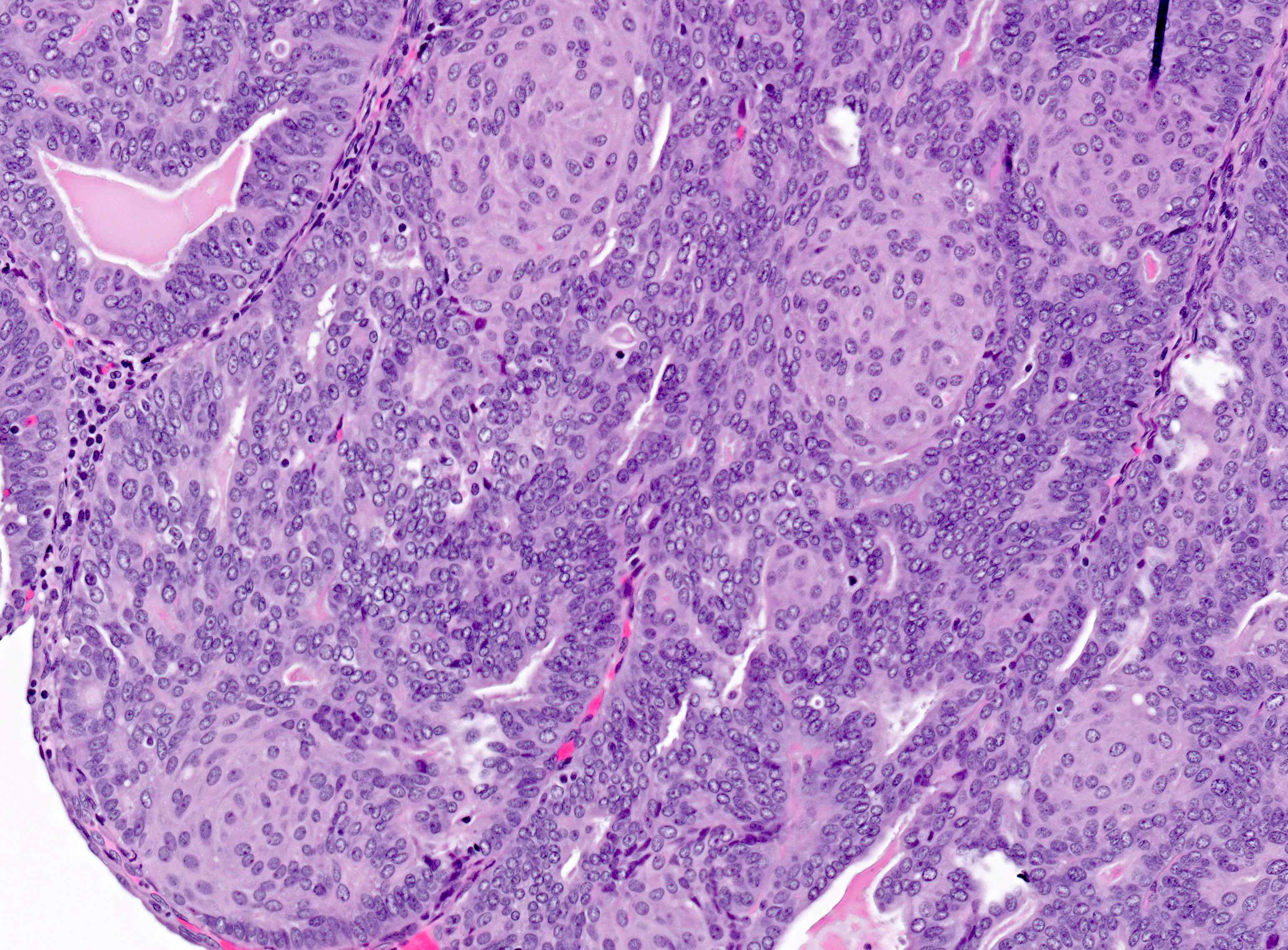
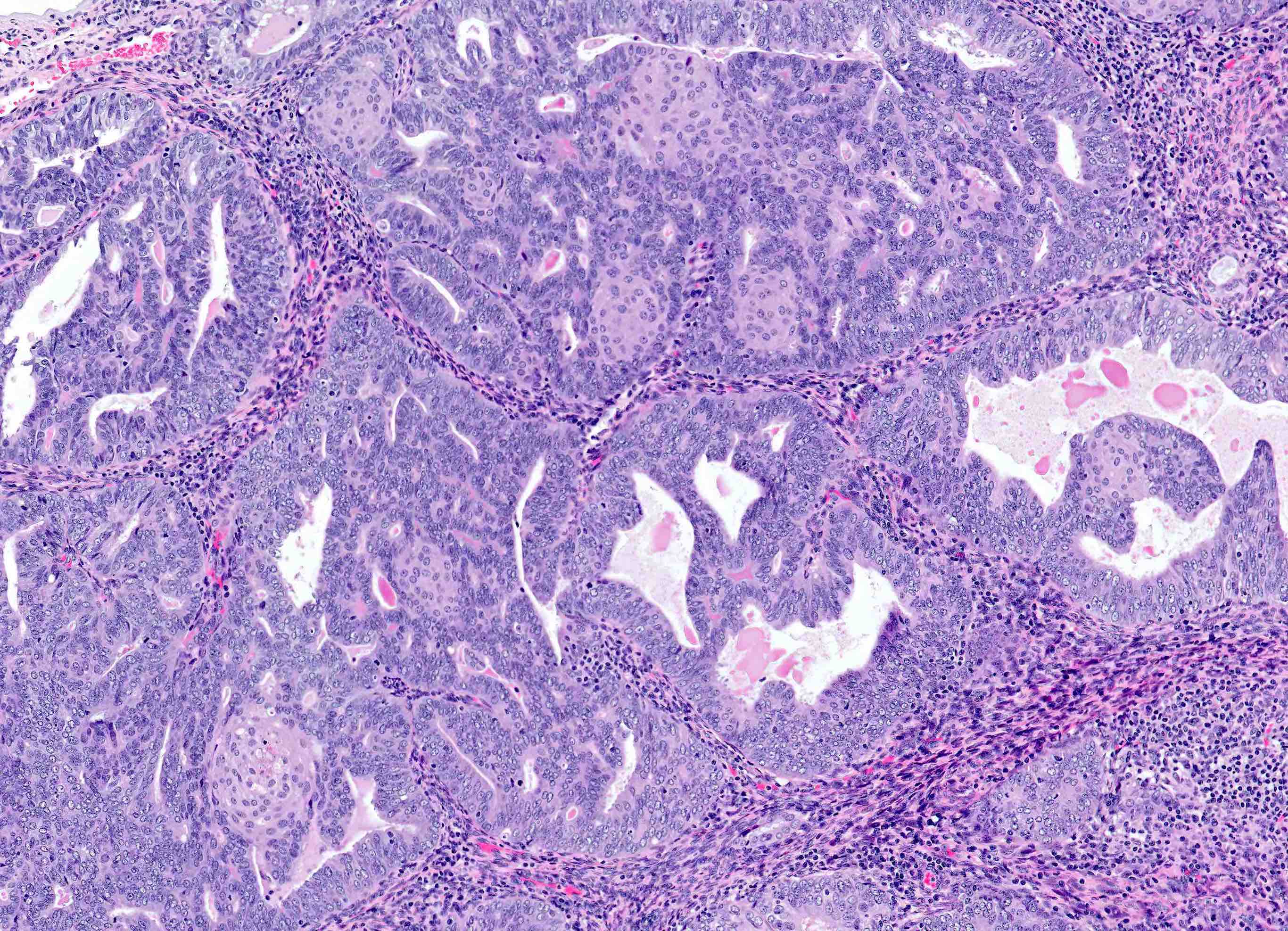
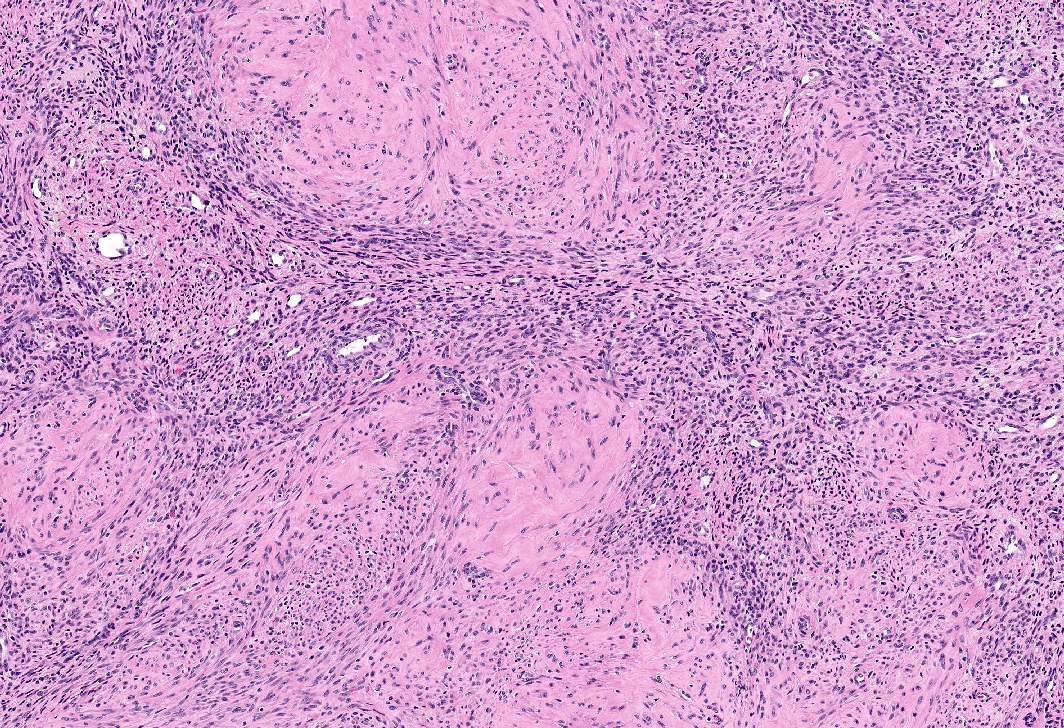
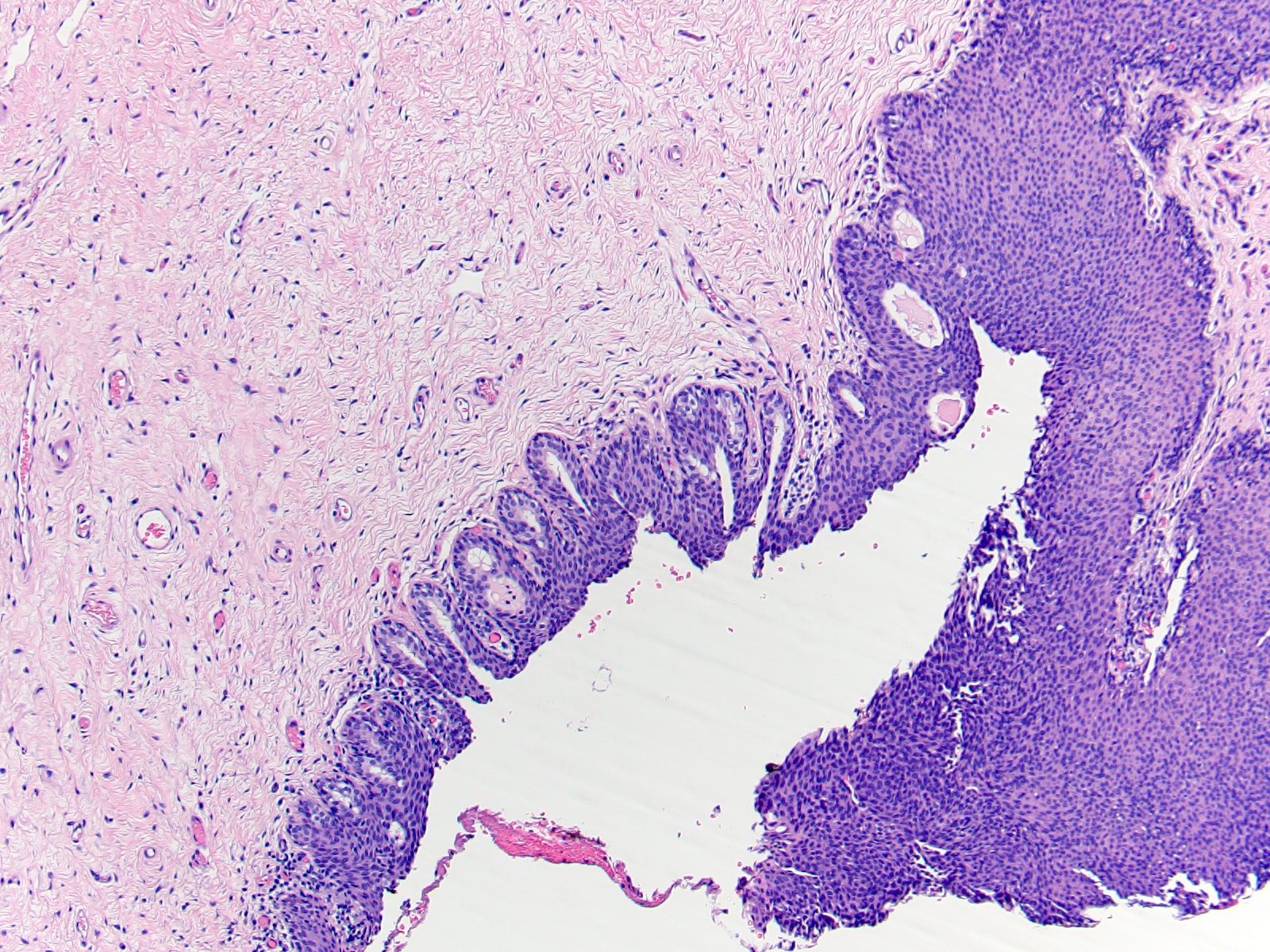
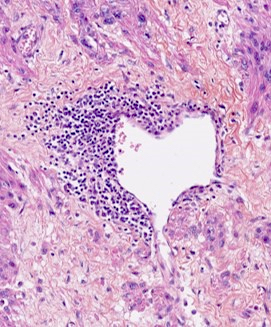
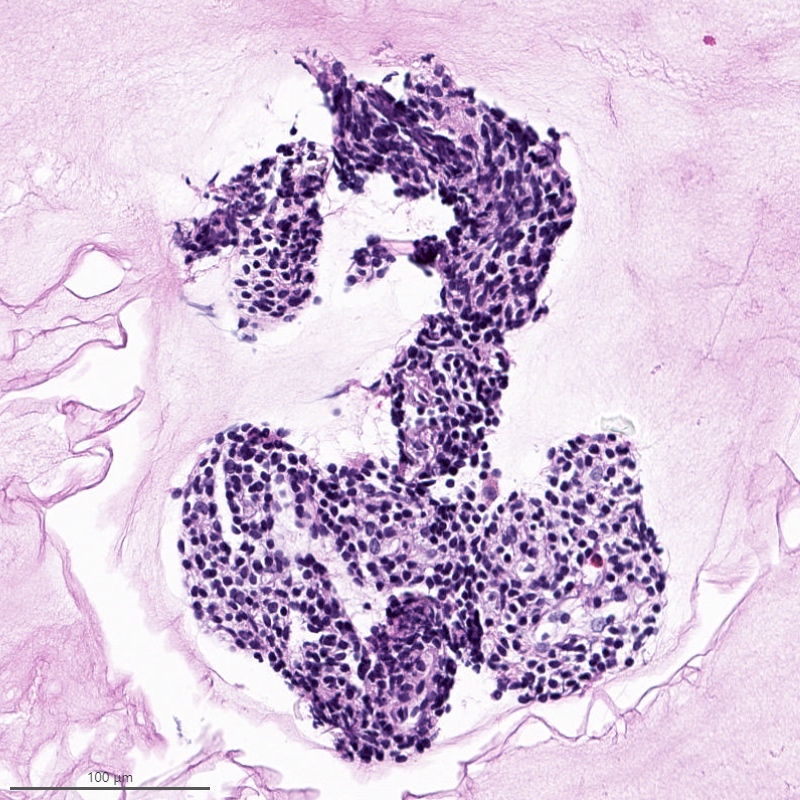
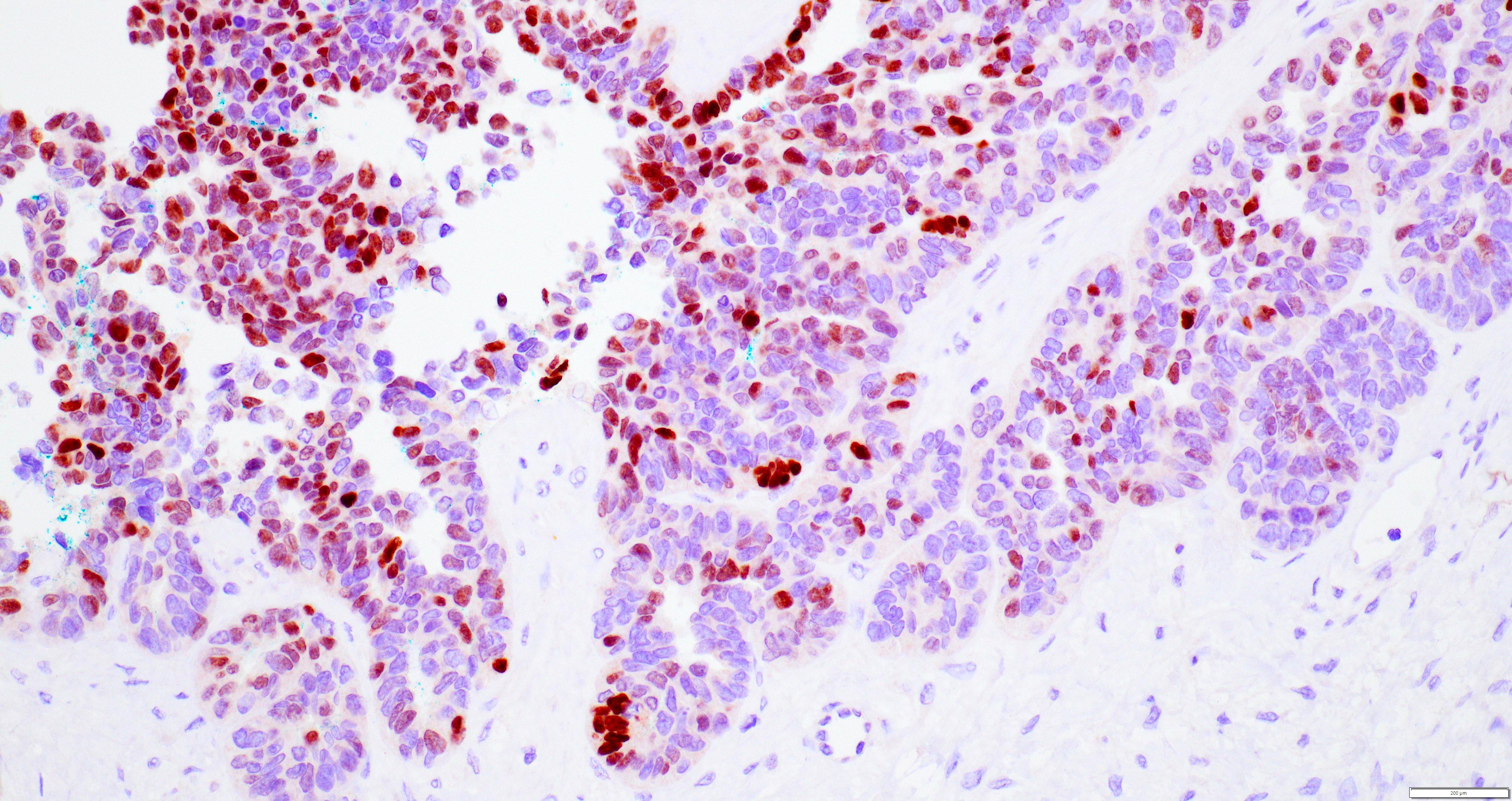
- Focus of carcinoma has a round or ovoid shape with a smooth and convex outer contour (regardless of its size) (Figure 2)
- Outer contour smoothly continues with adjacent uninvolved endomyometrial interface
- Residual endometrial type stroma or benign endometrial glands are present in the periphery or within the focus
- There is no significant desmoplastic reaction
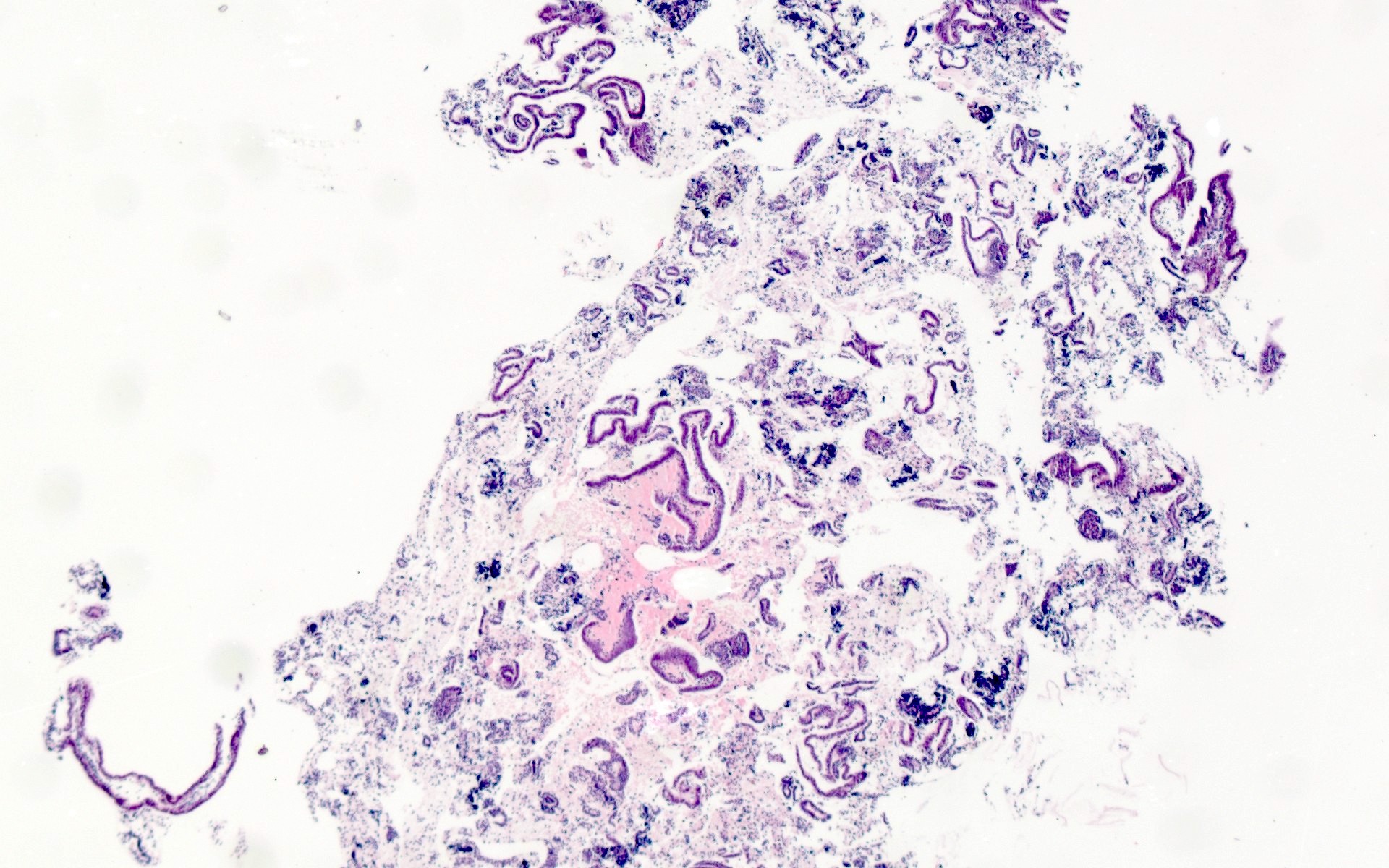
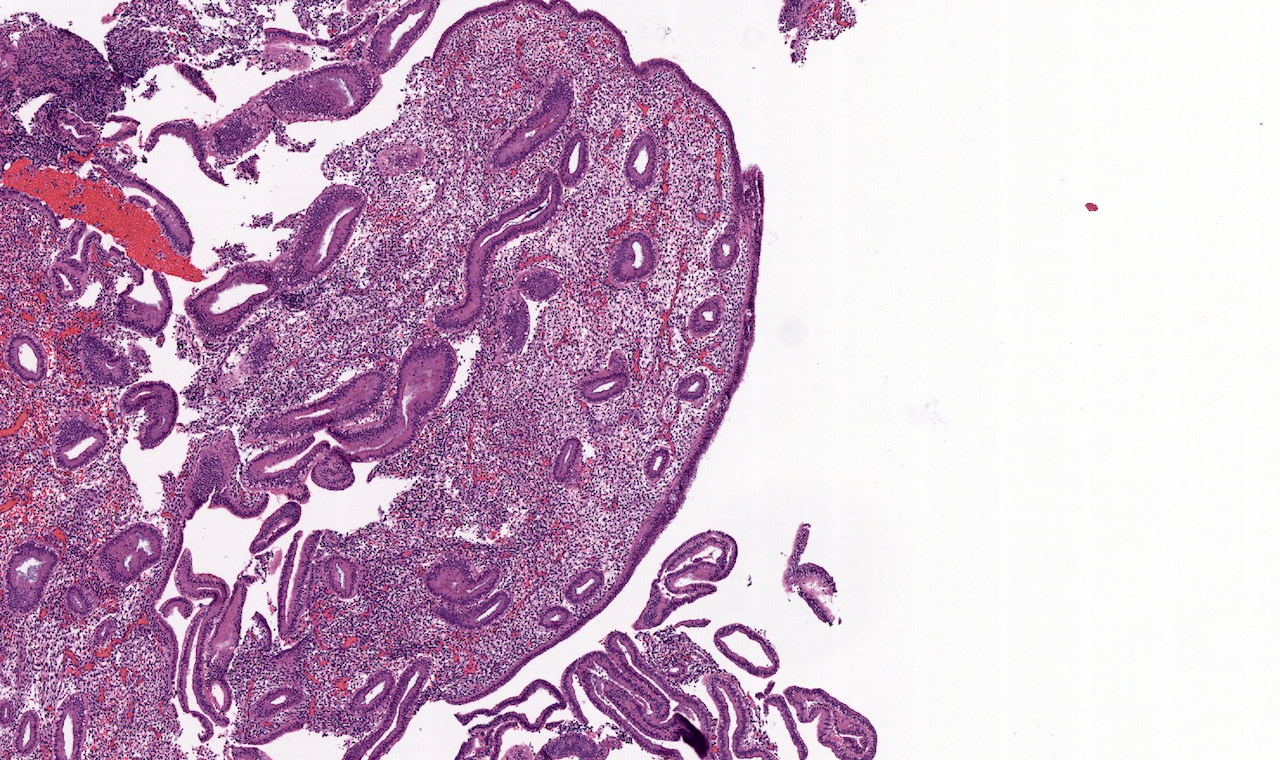
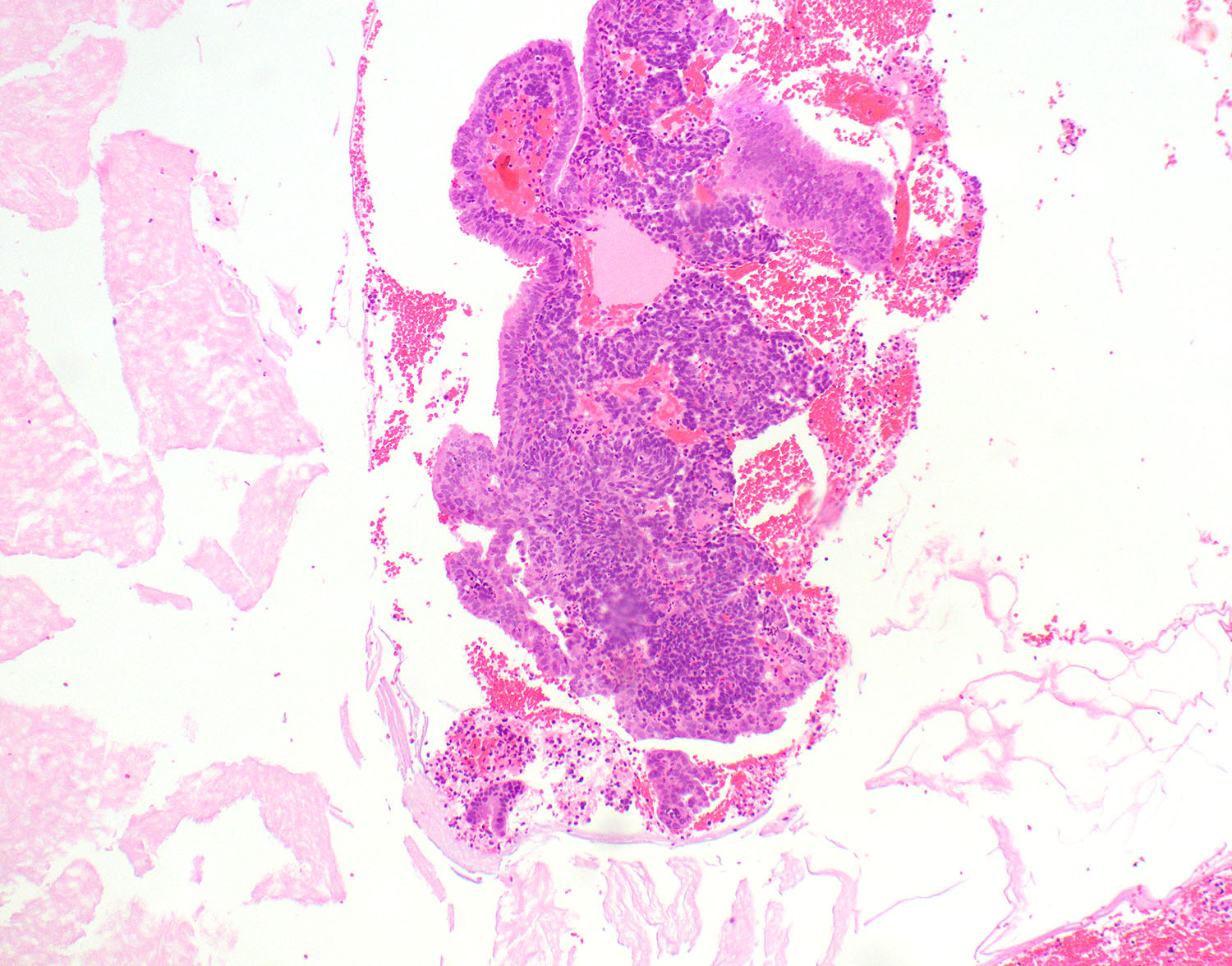
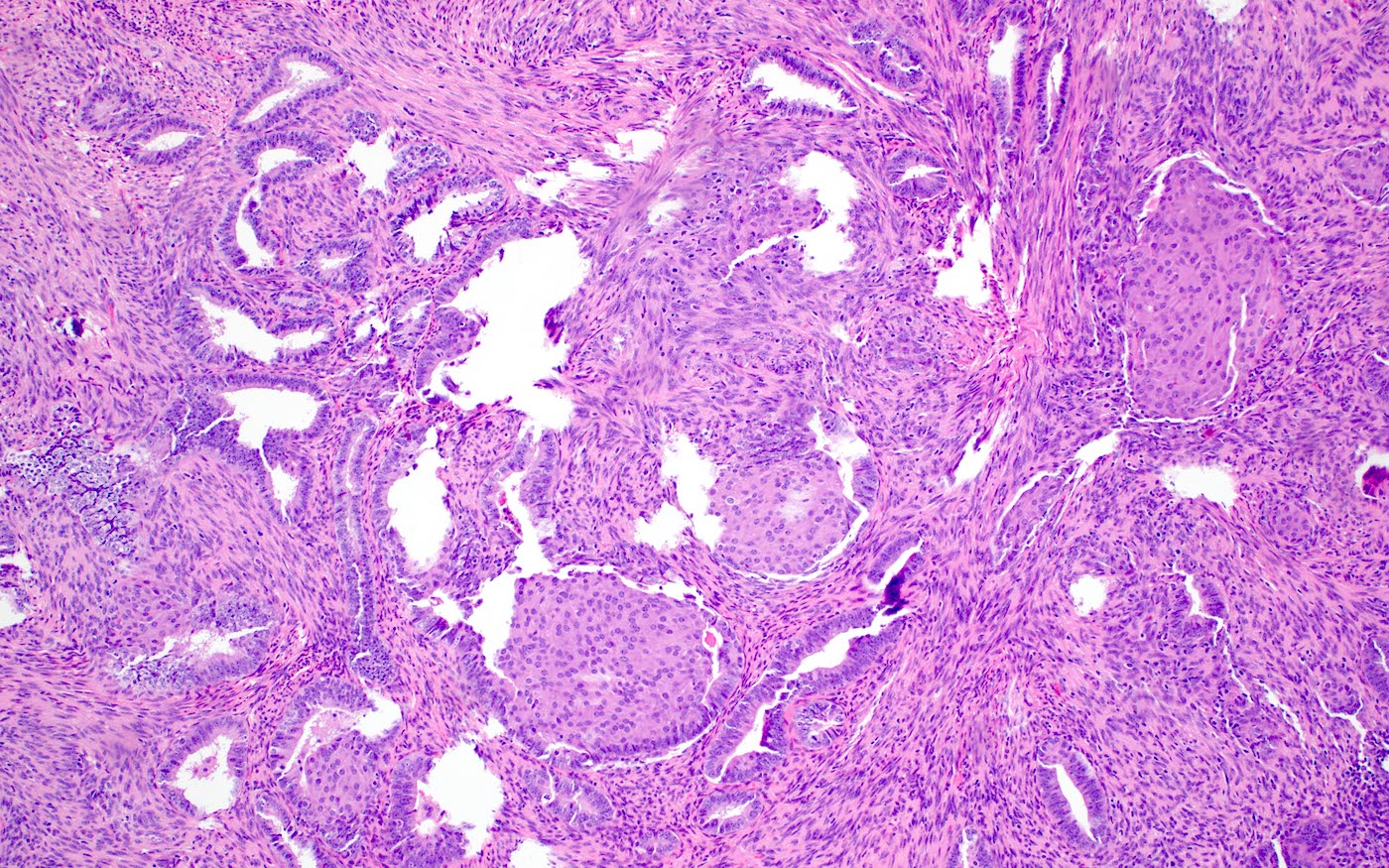
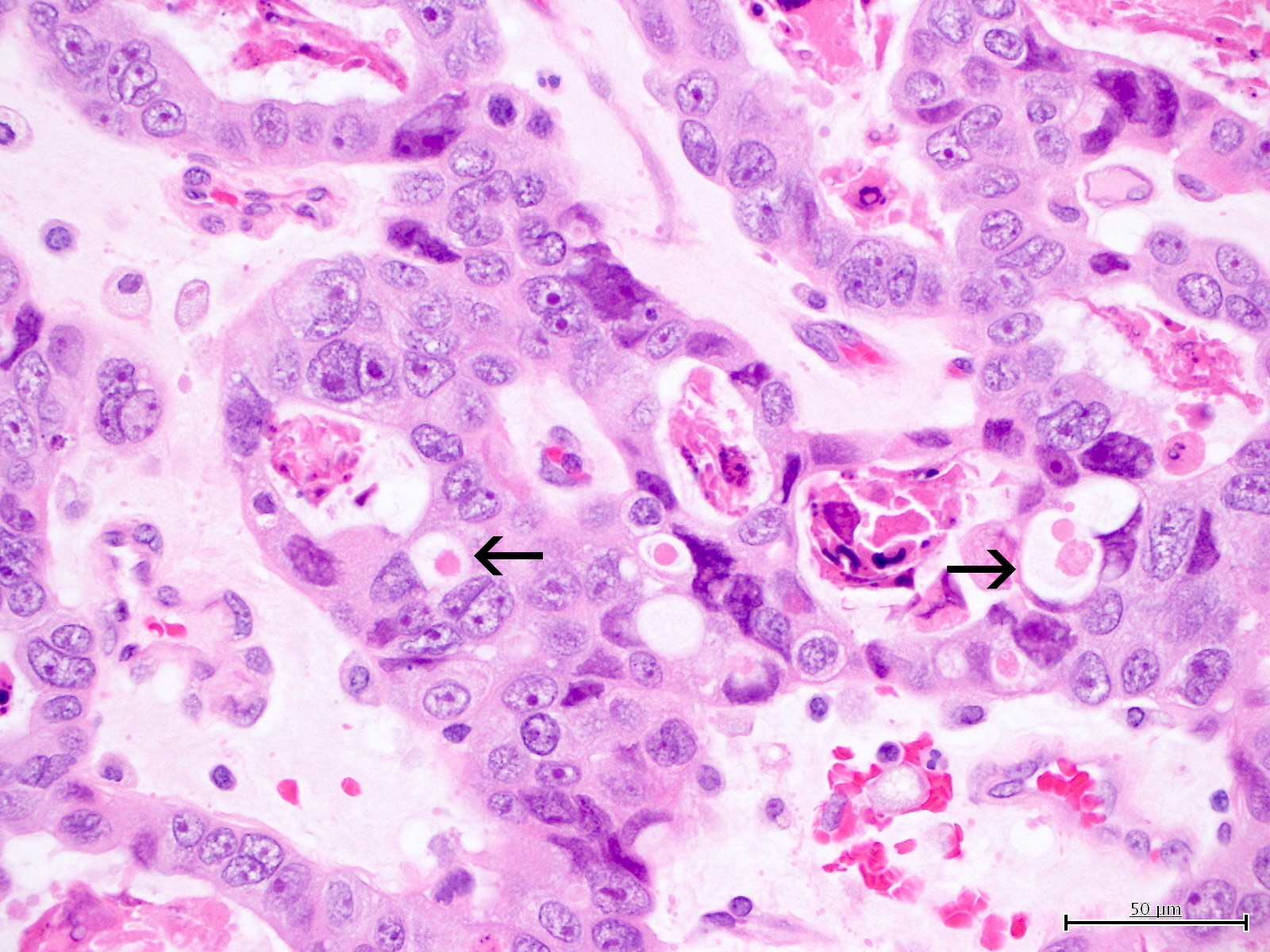
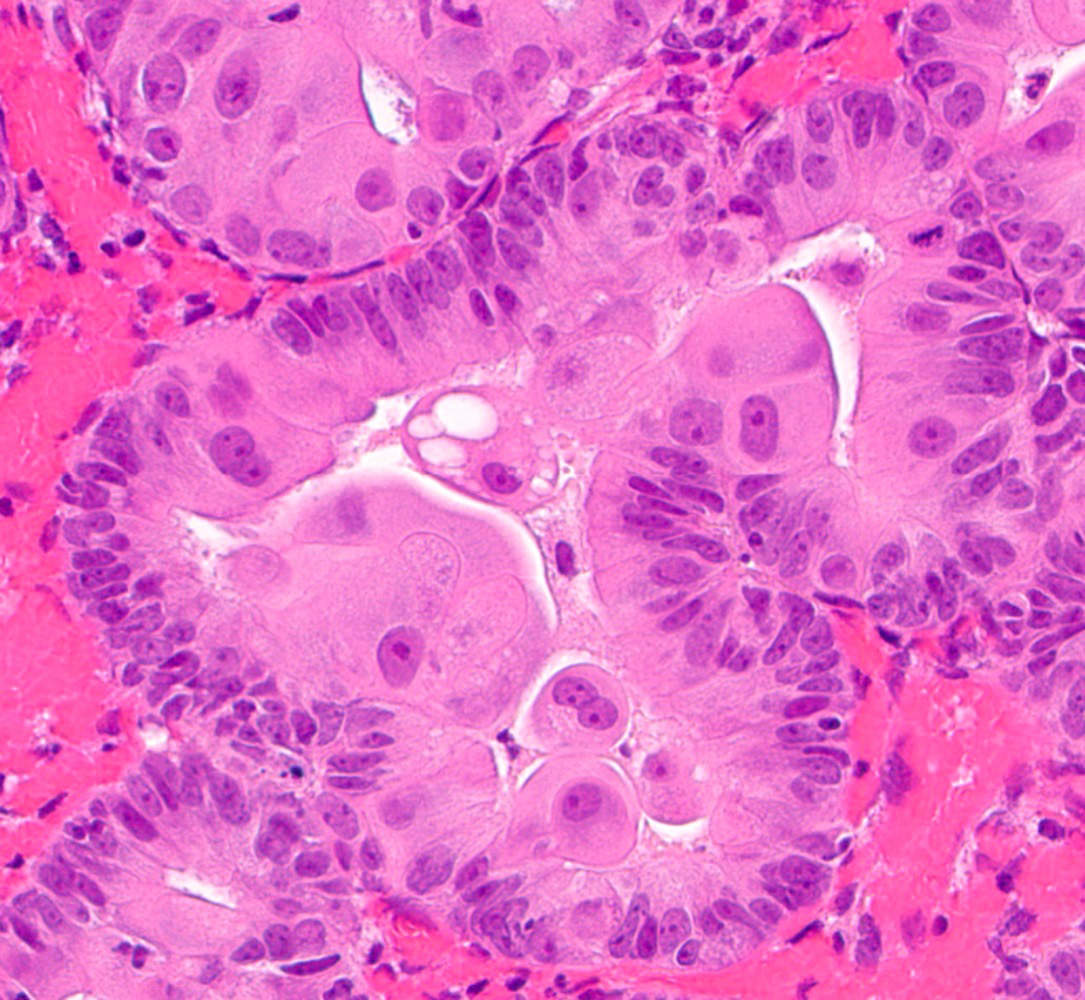
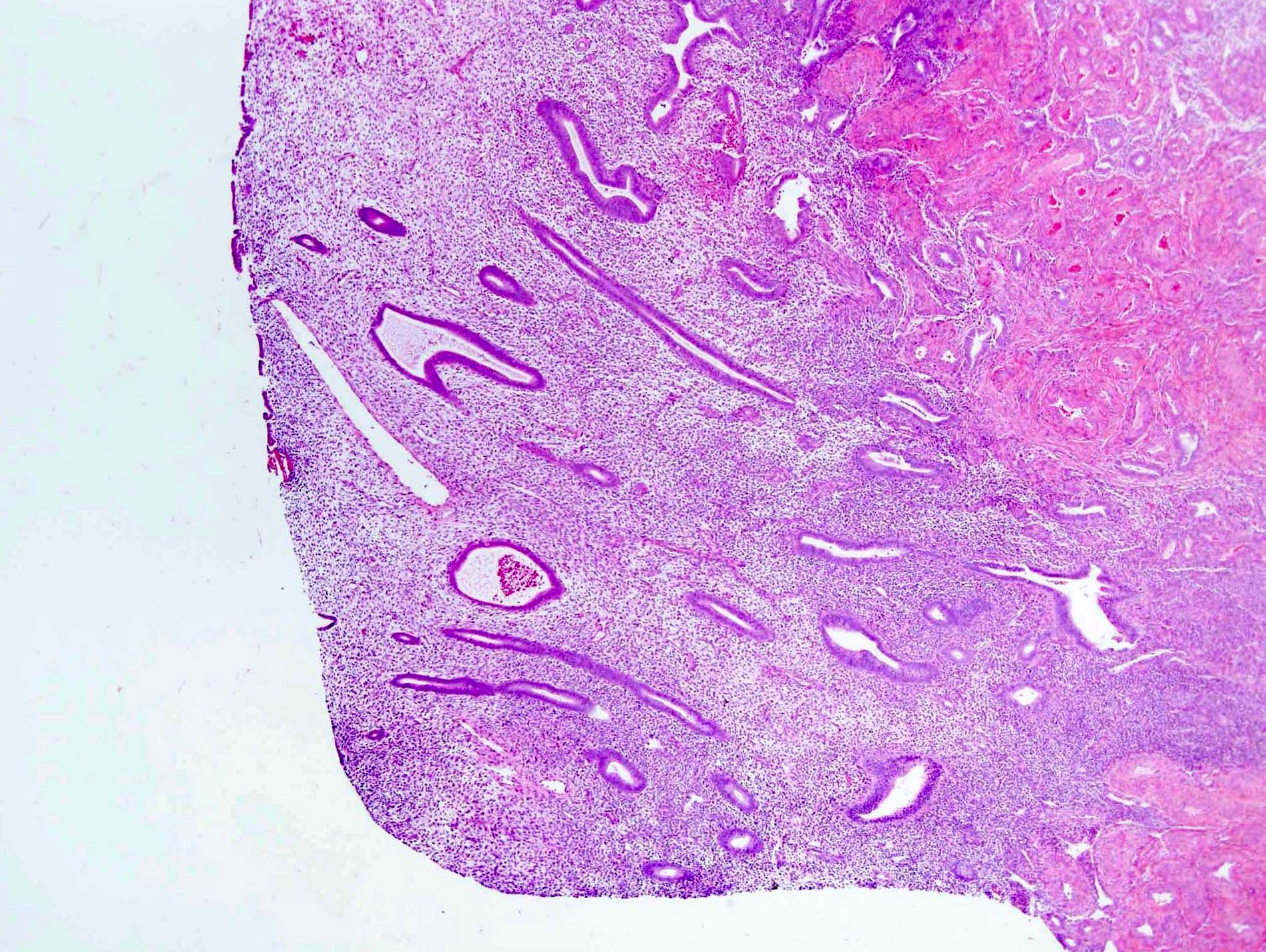
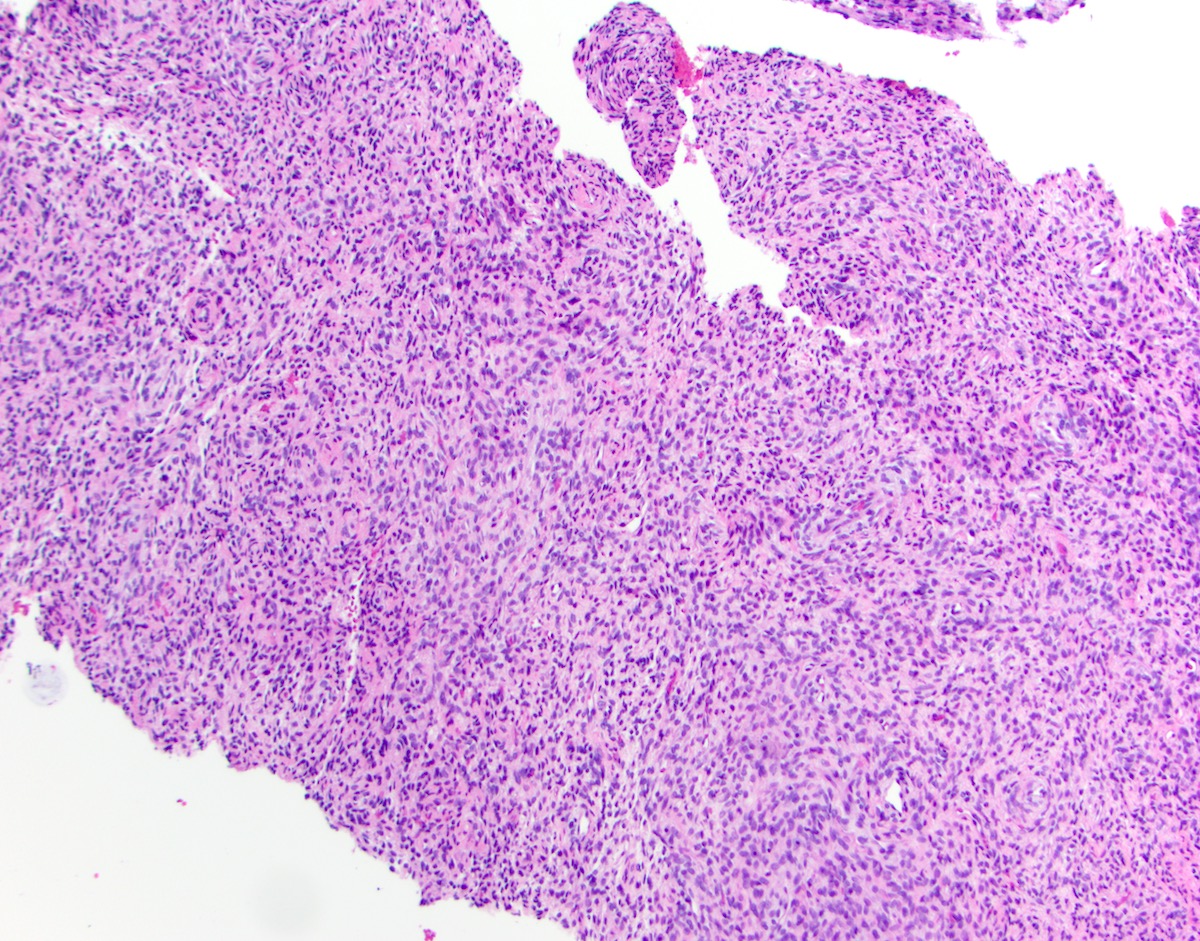
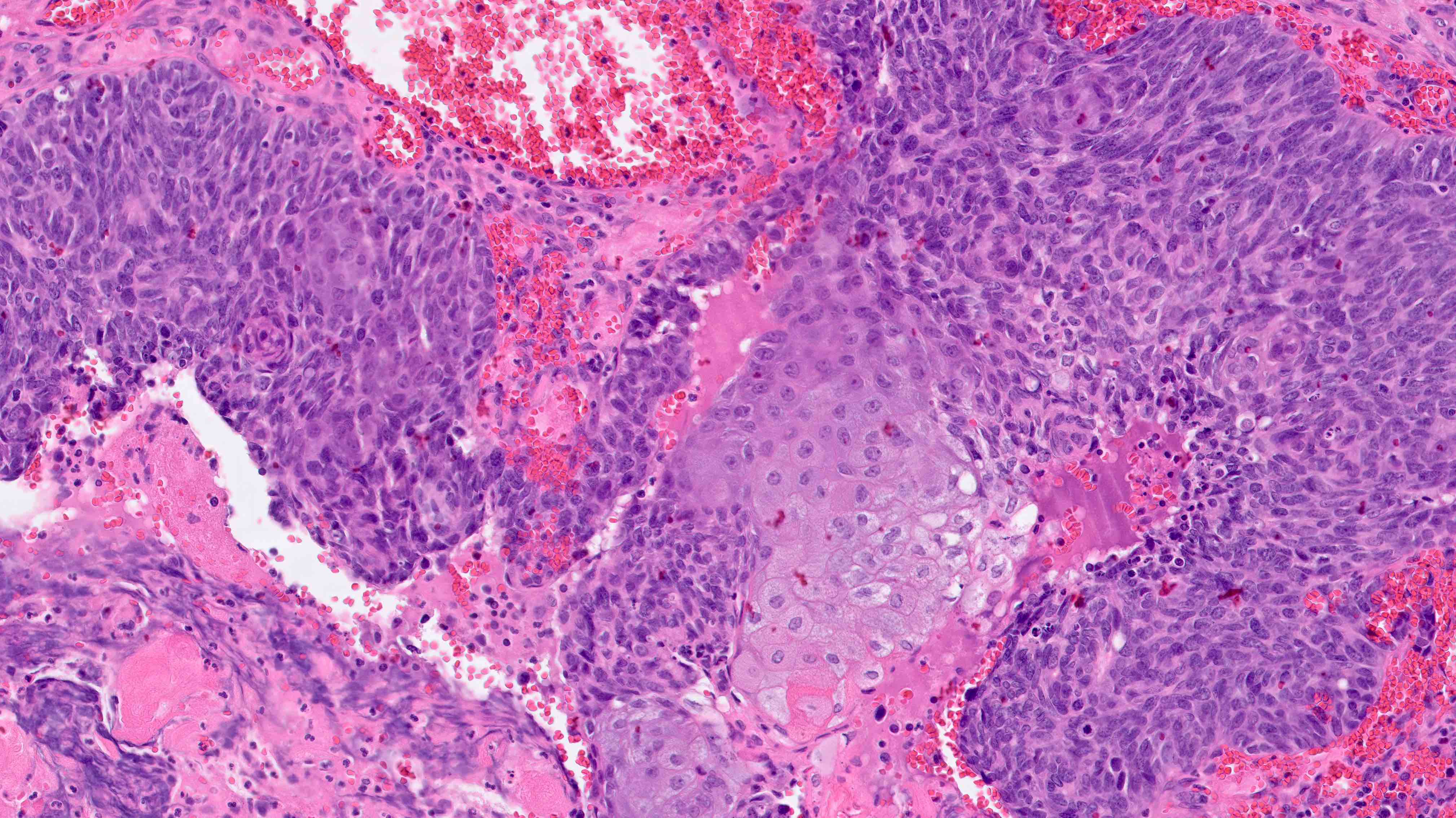
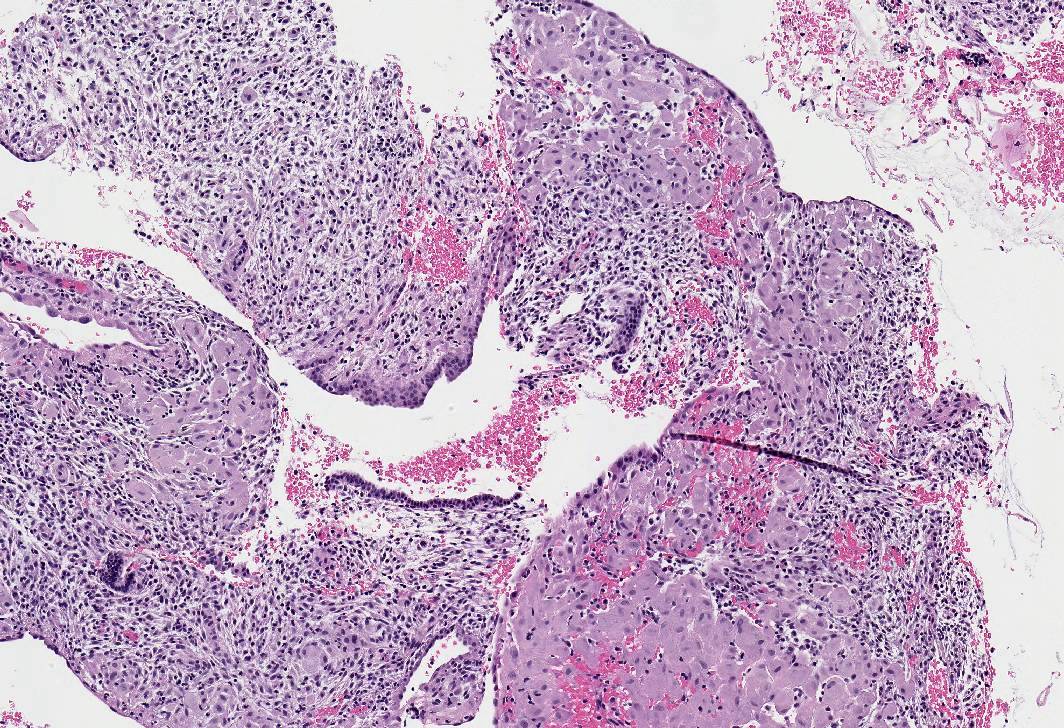
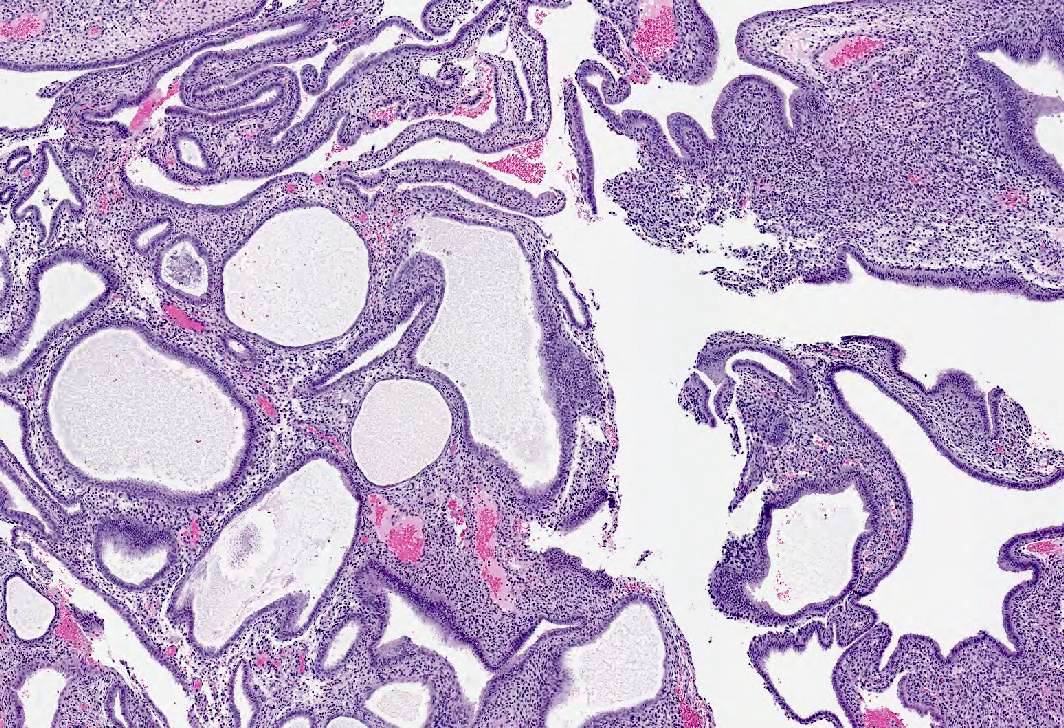
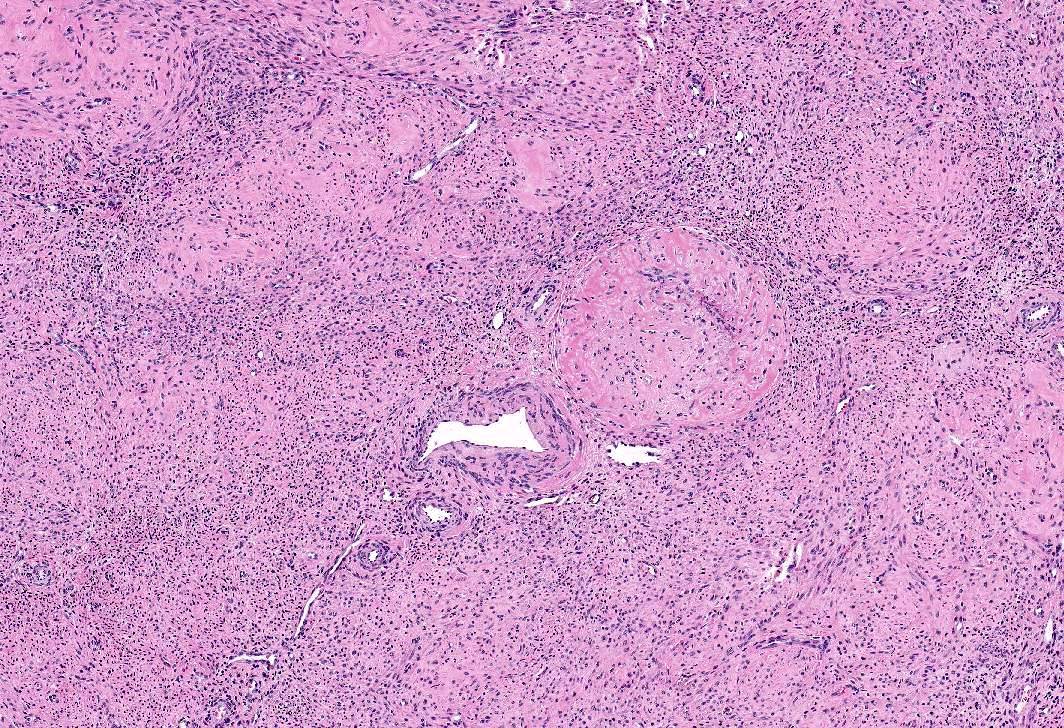
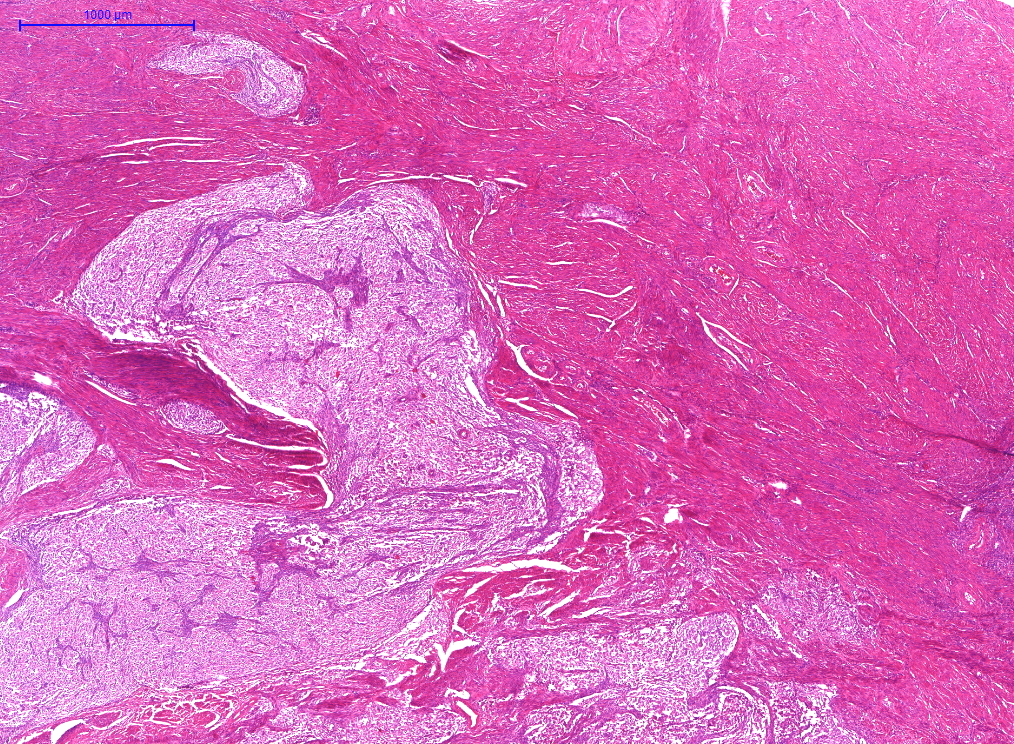
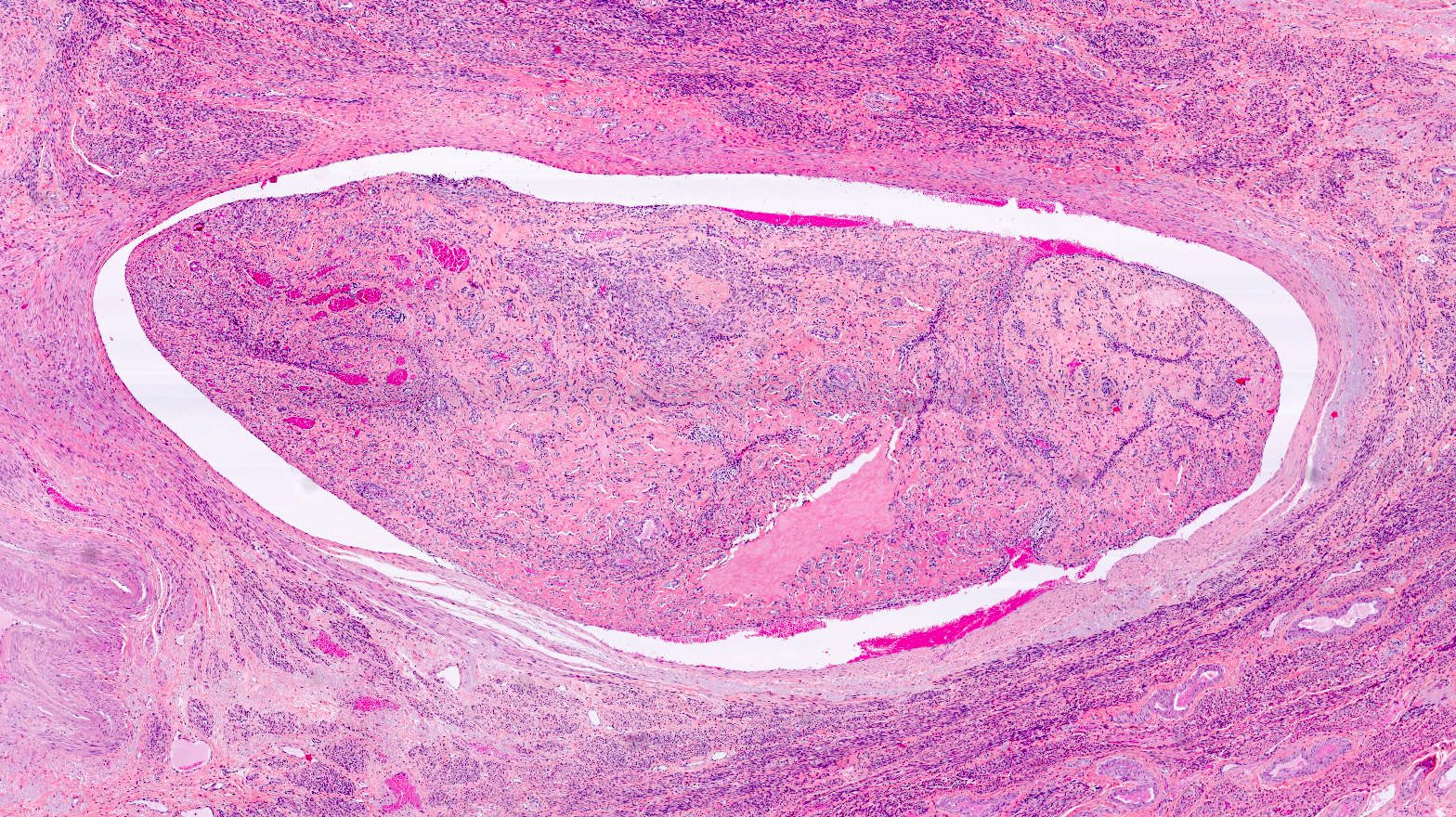
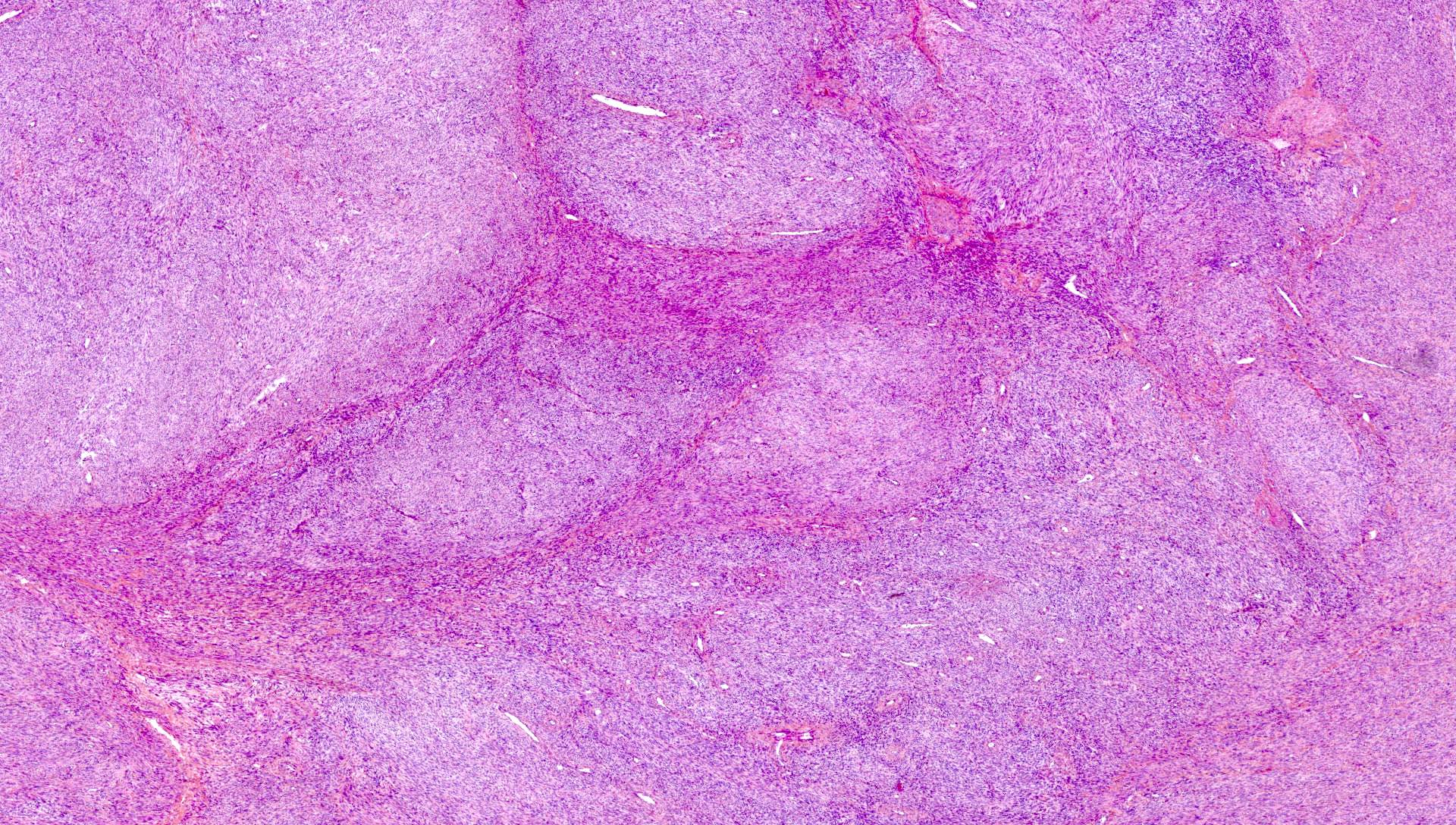
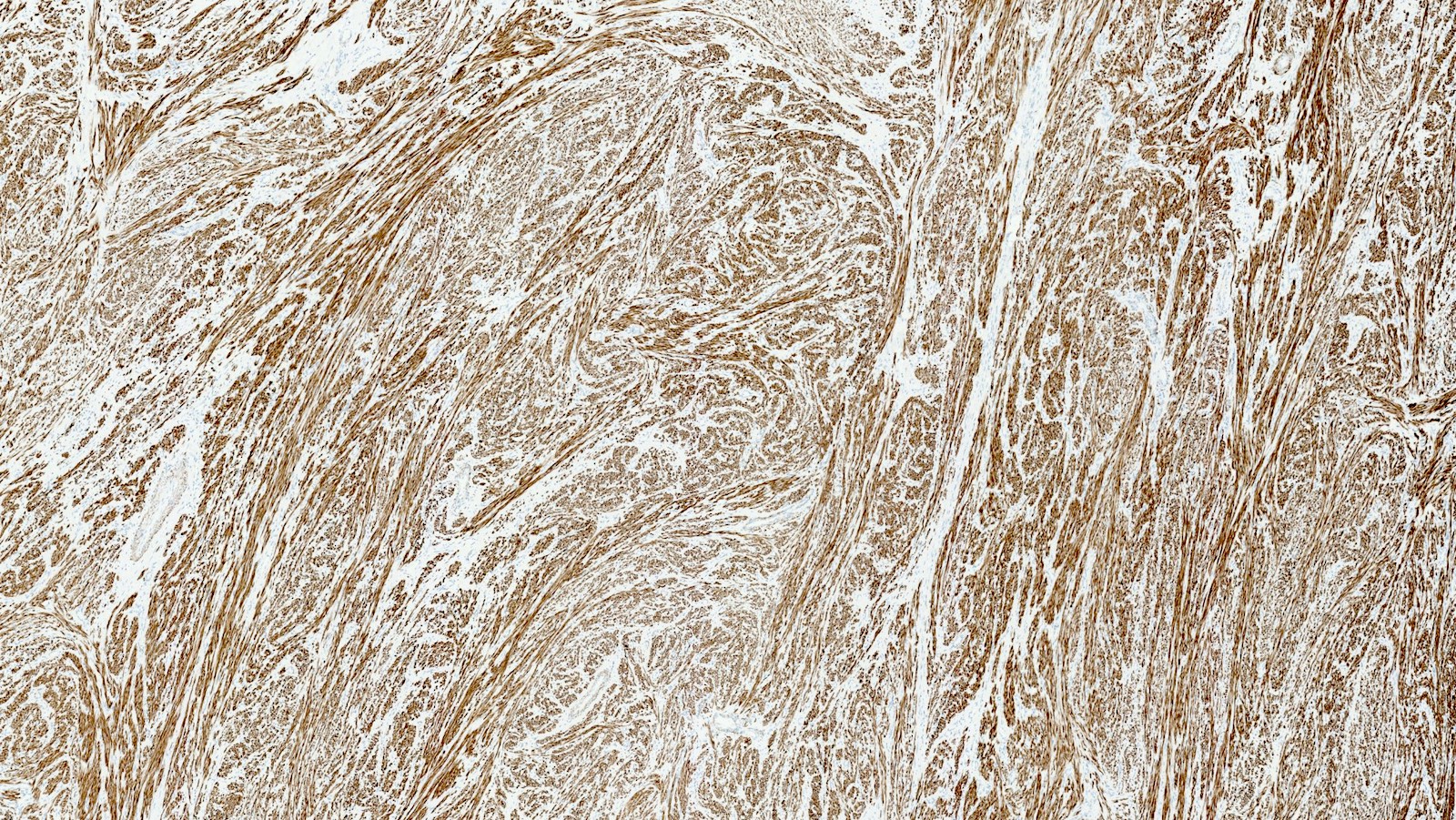
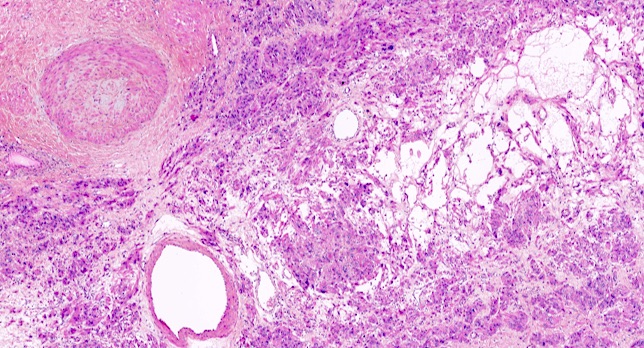
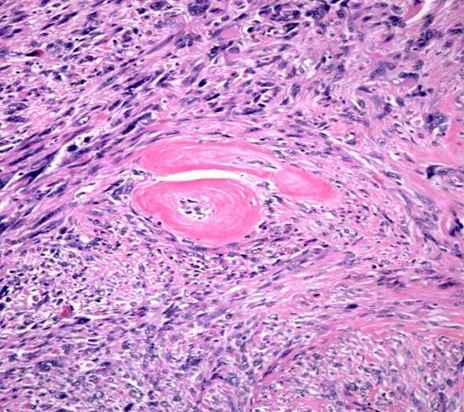
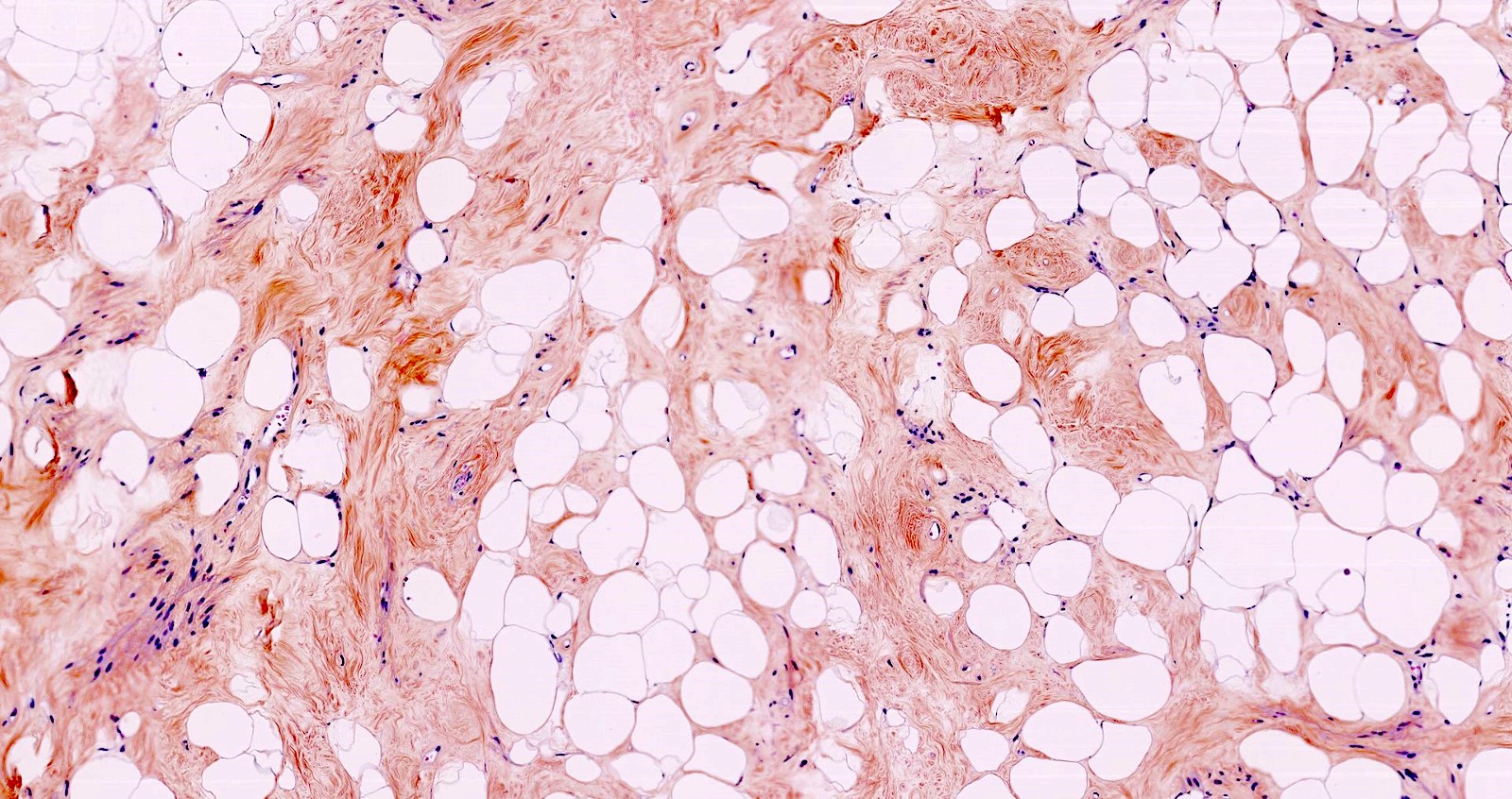
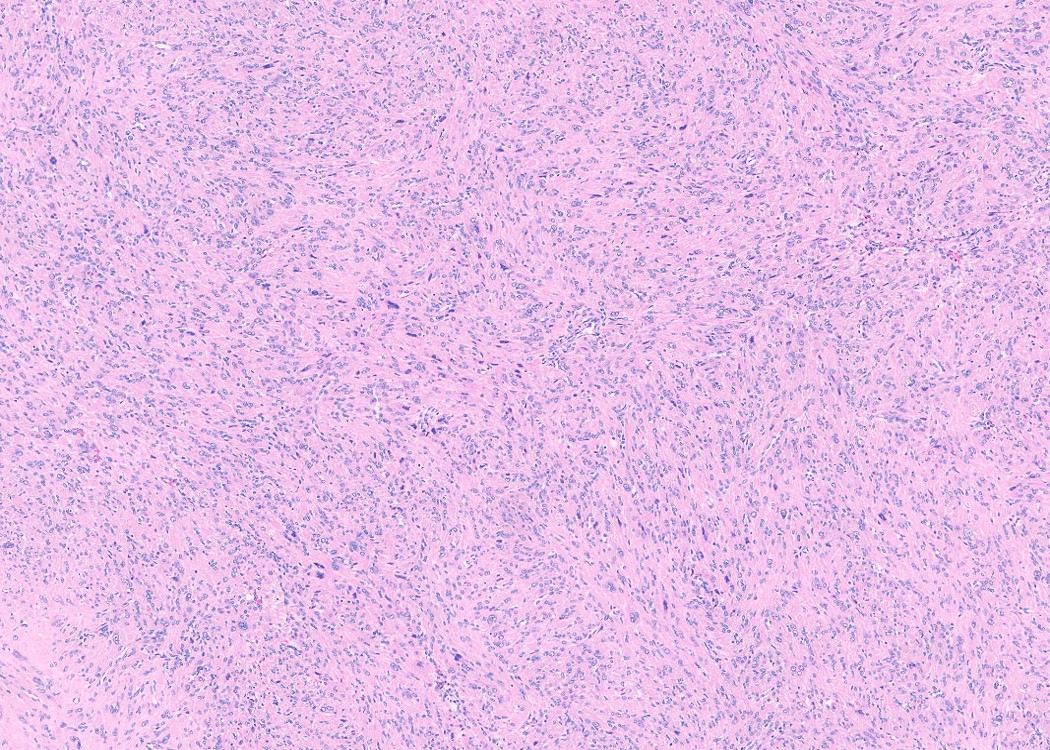
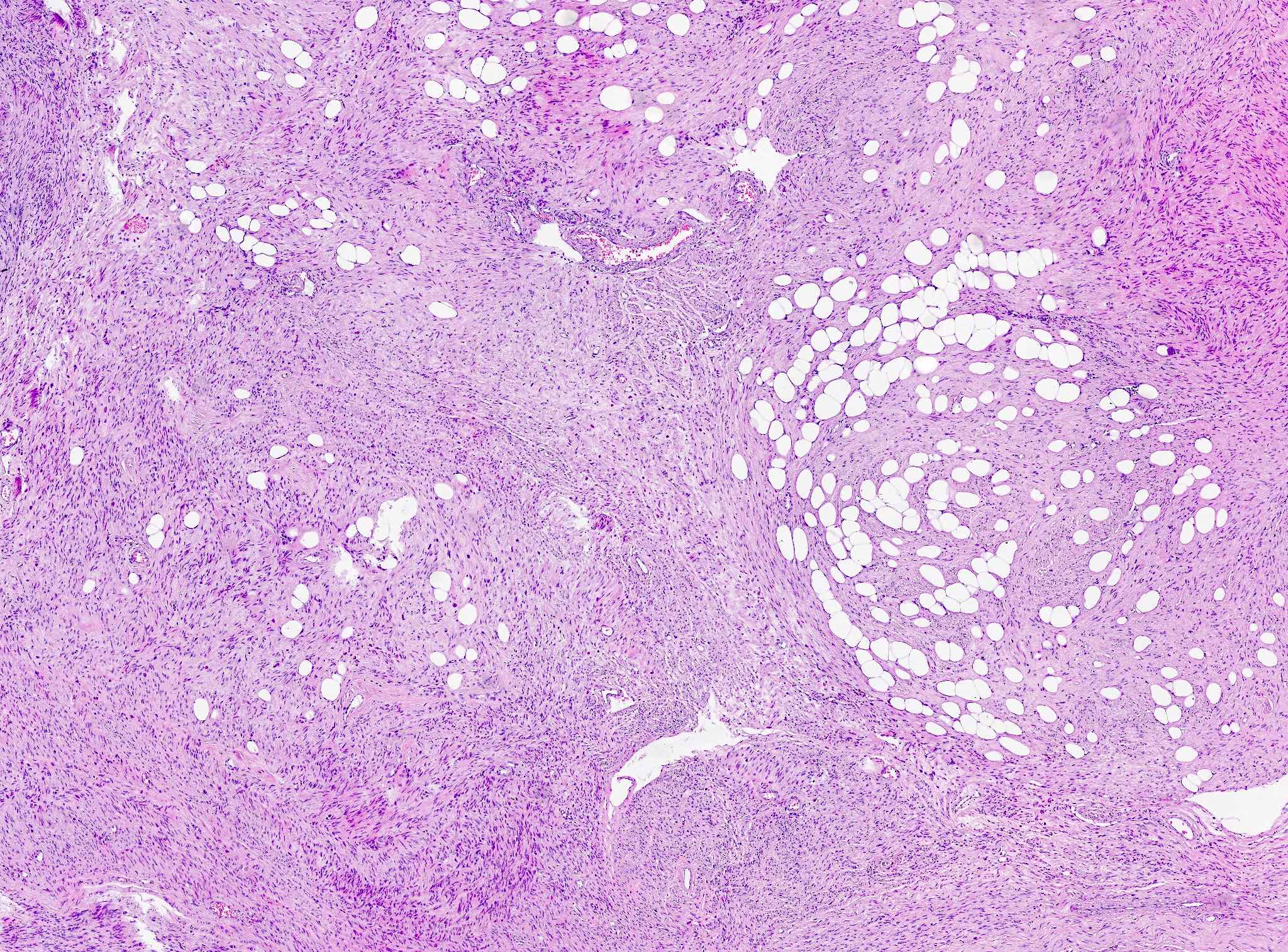
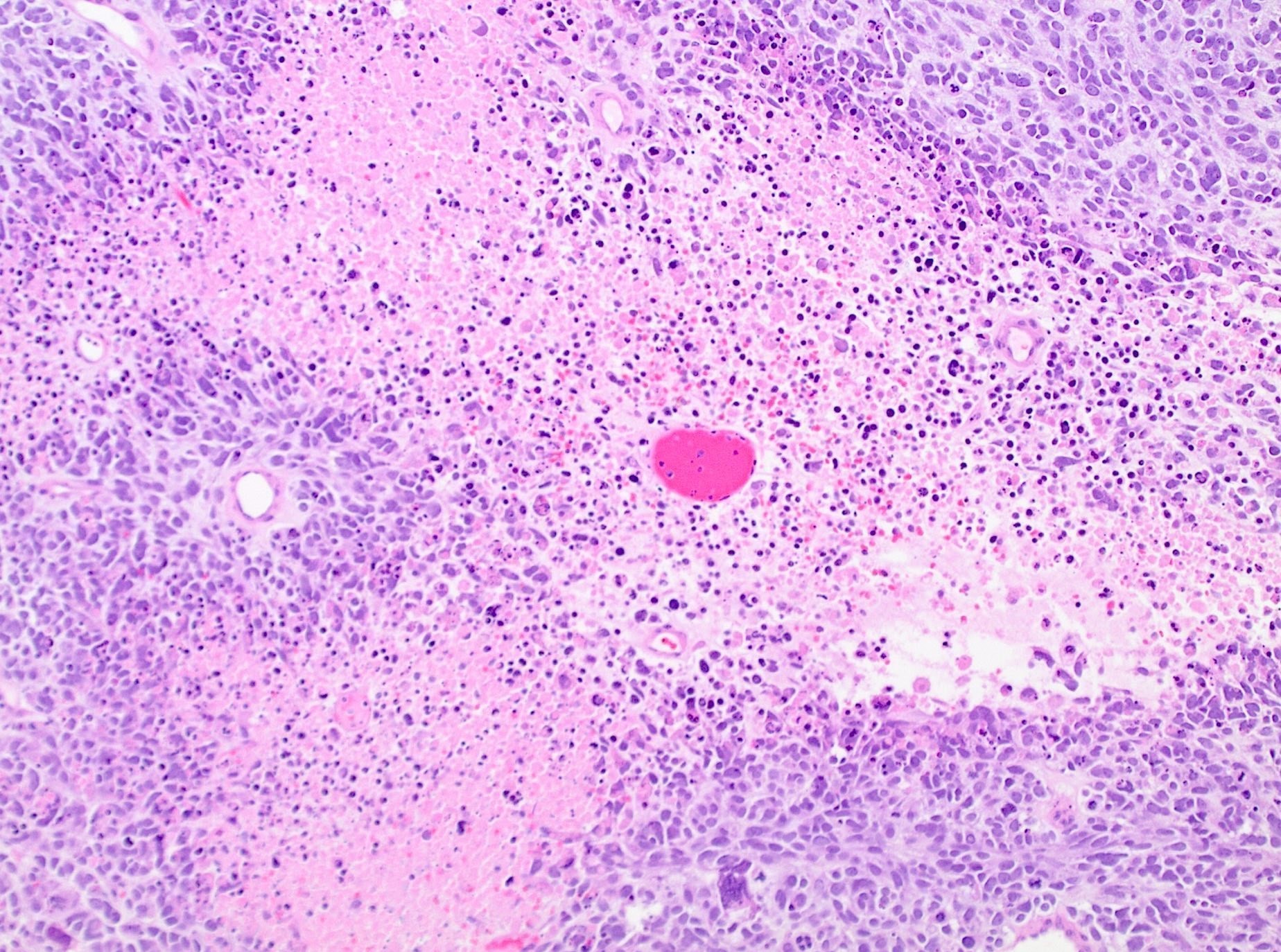
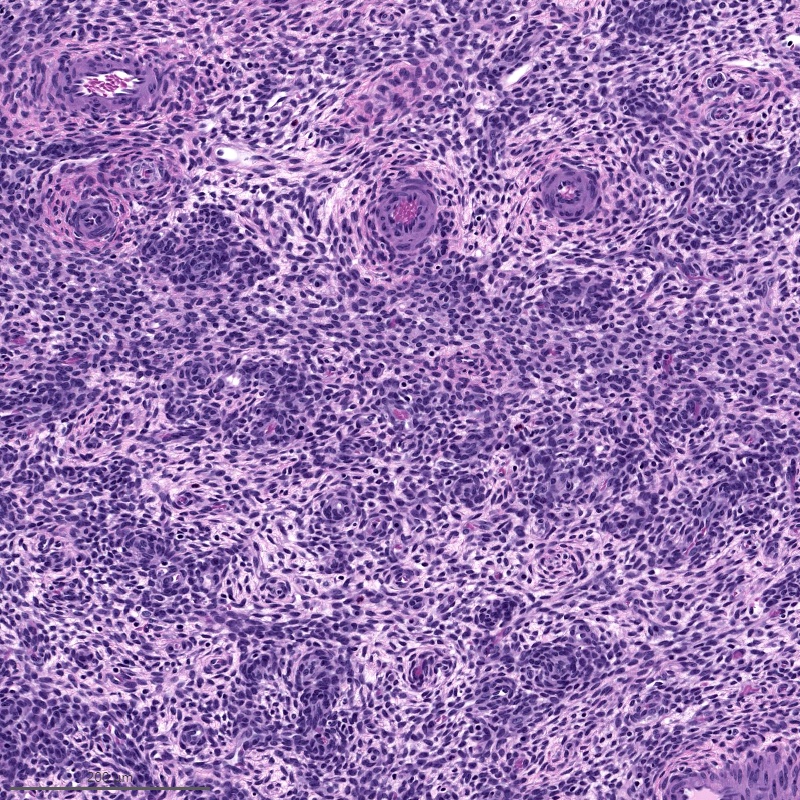
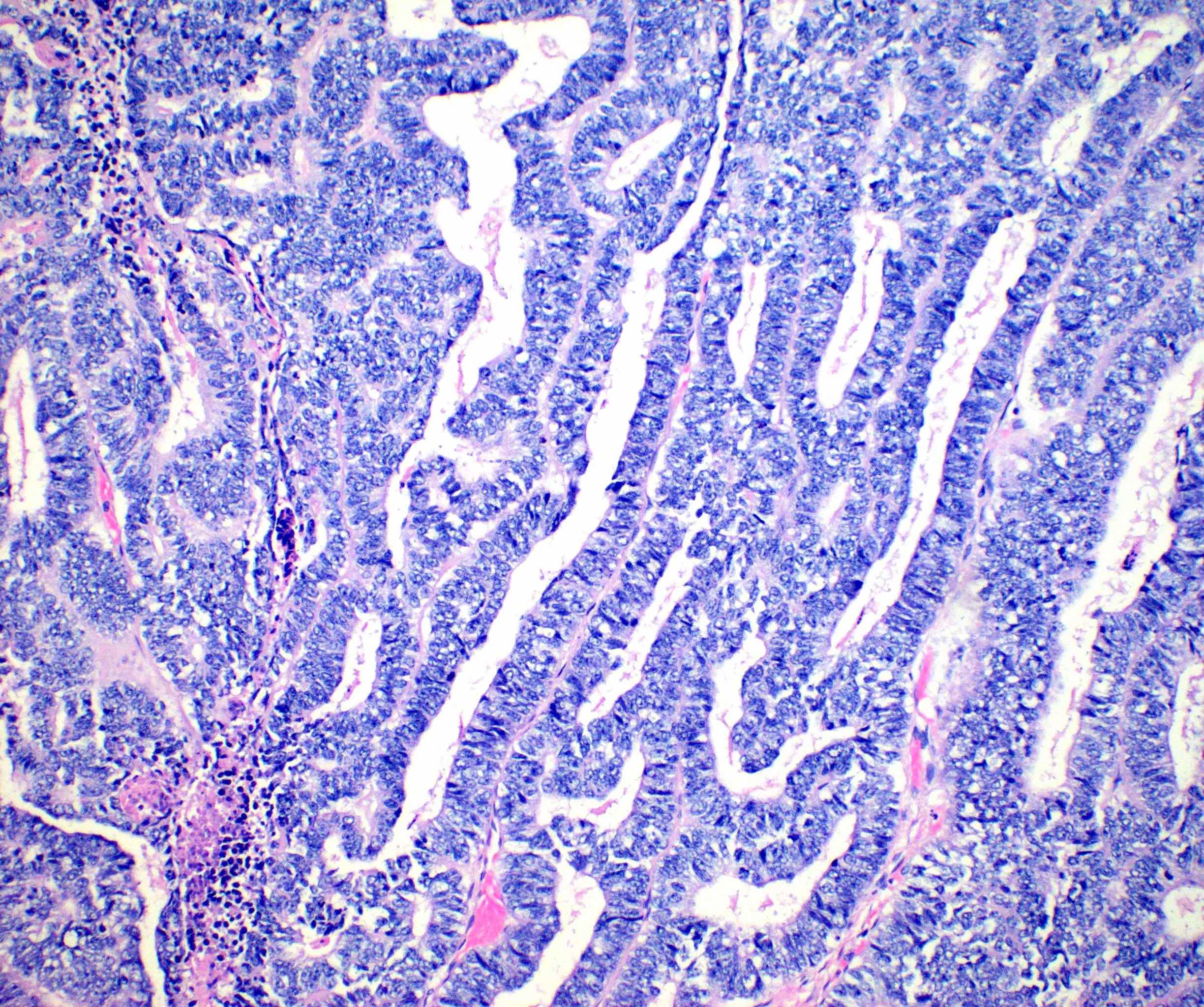
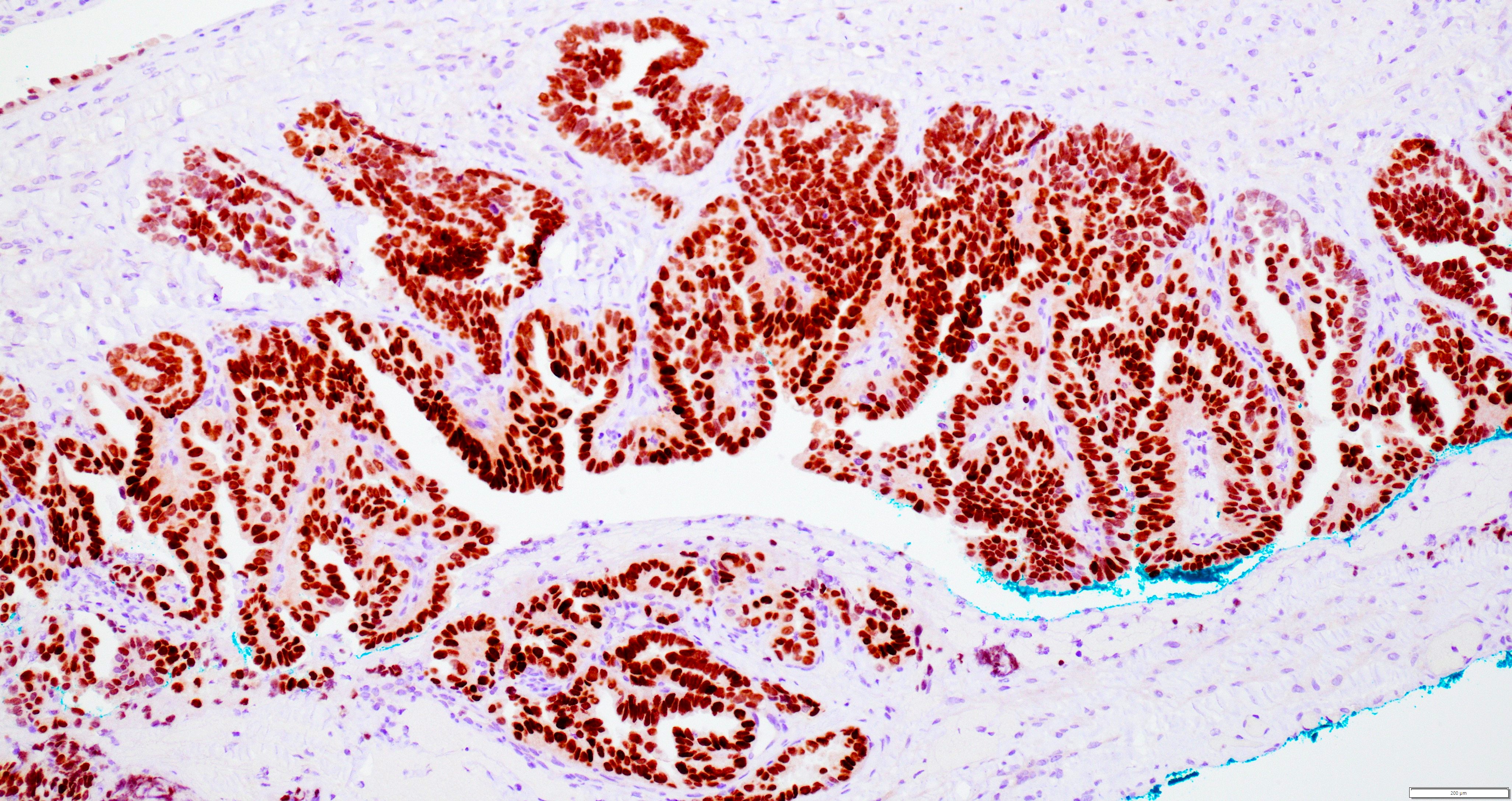
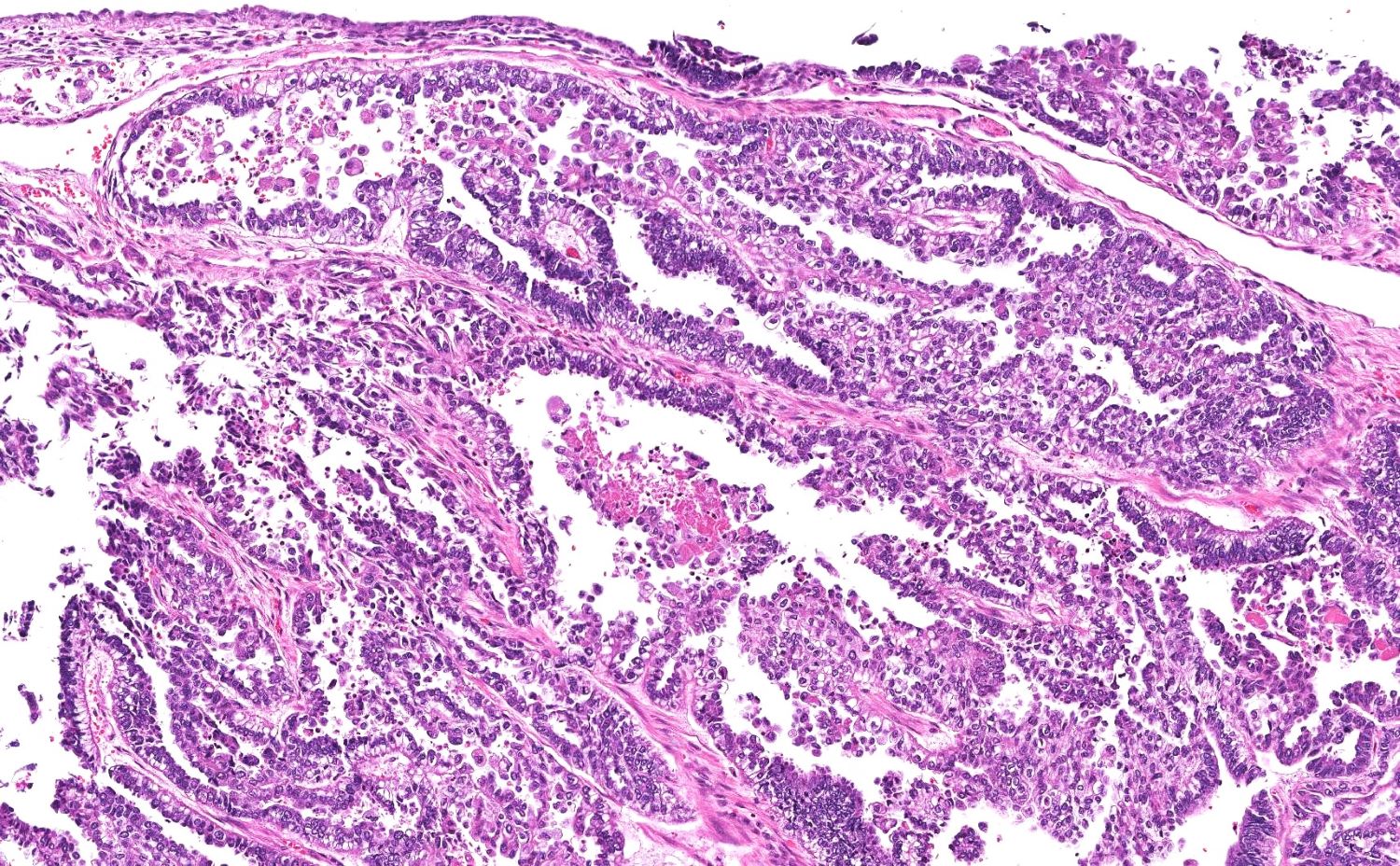
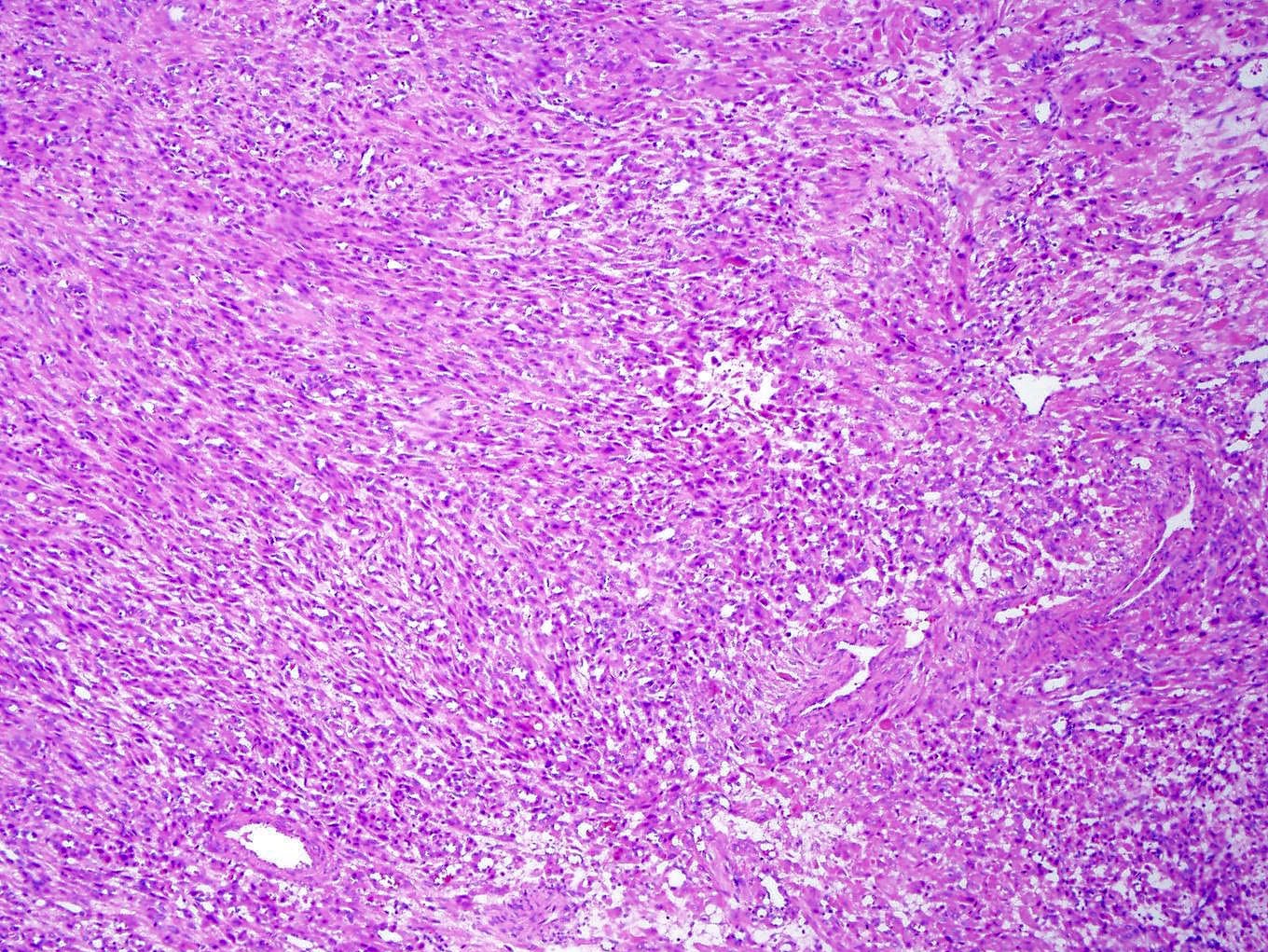
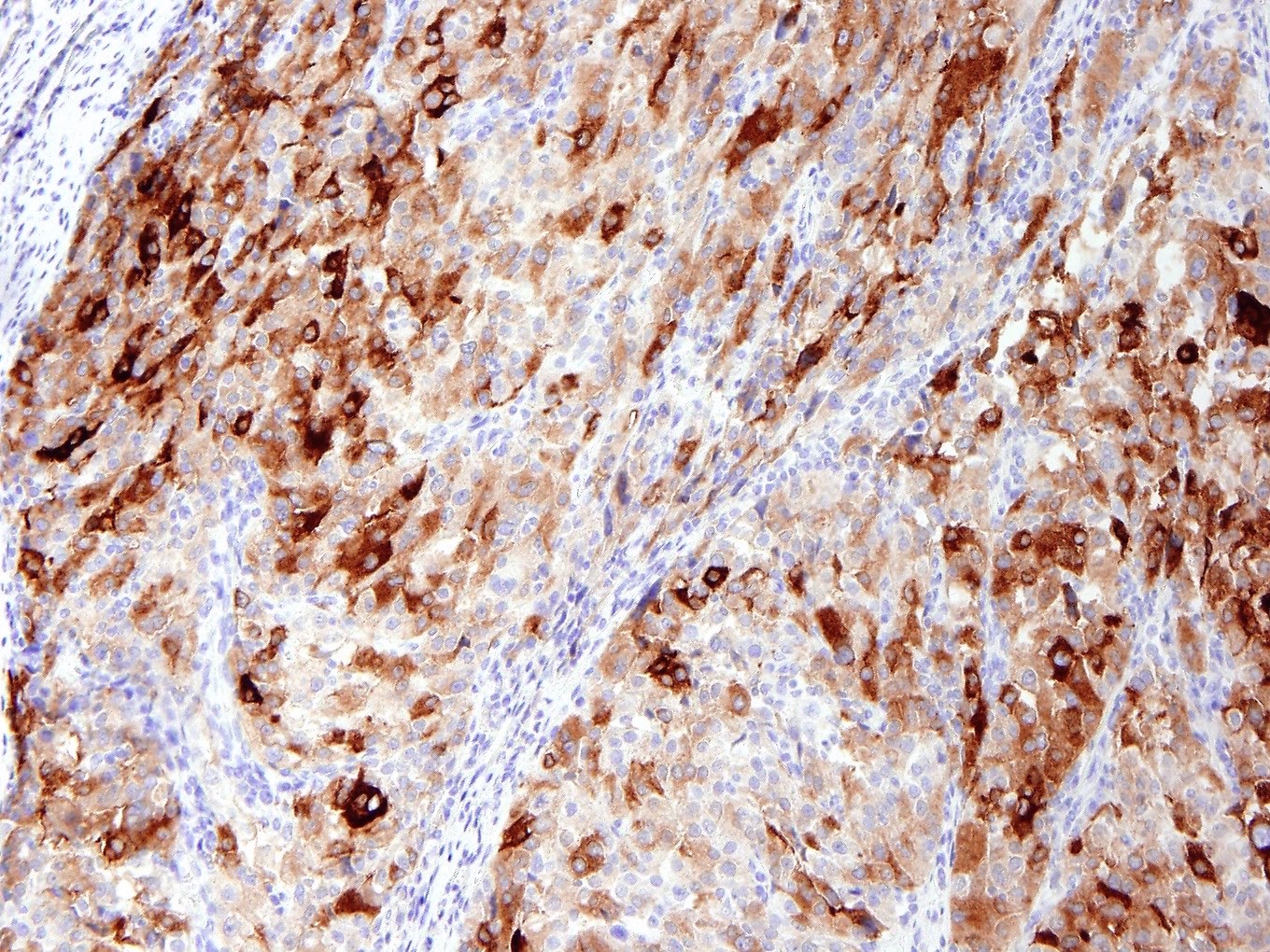
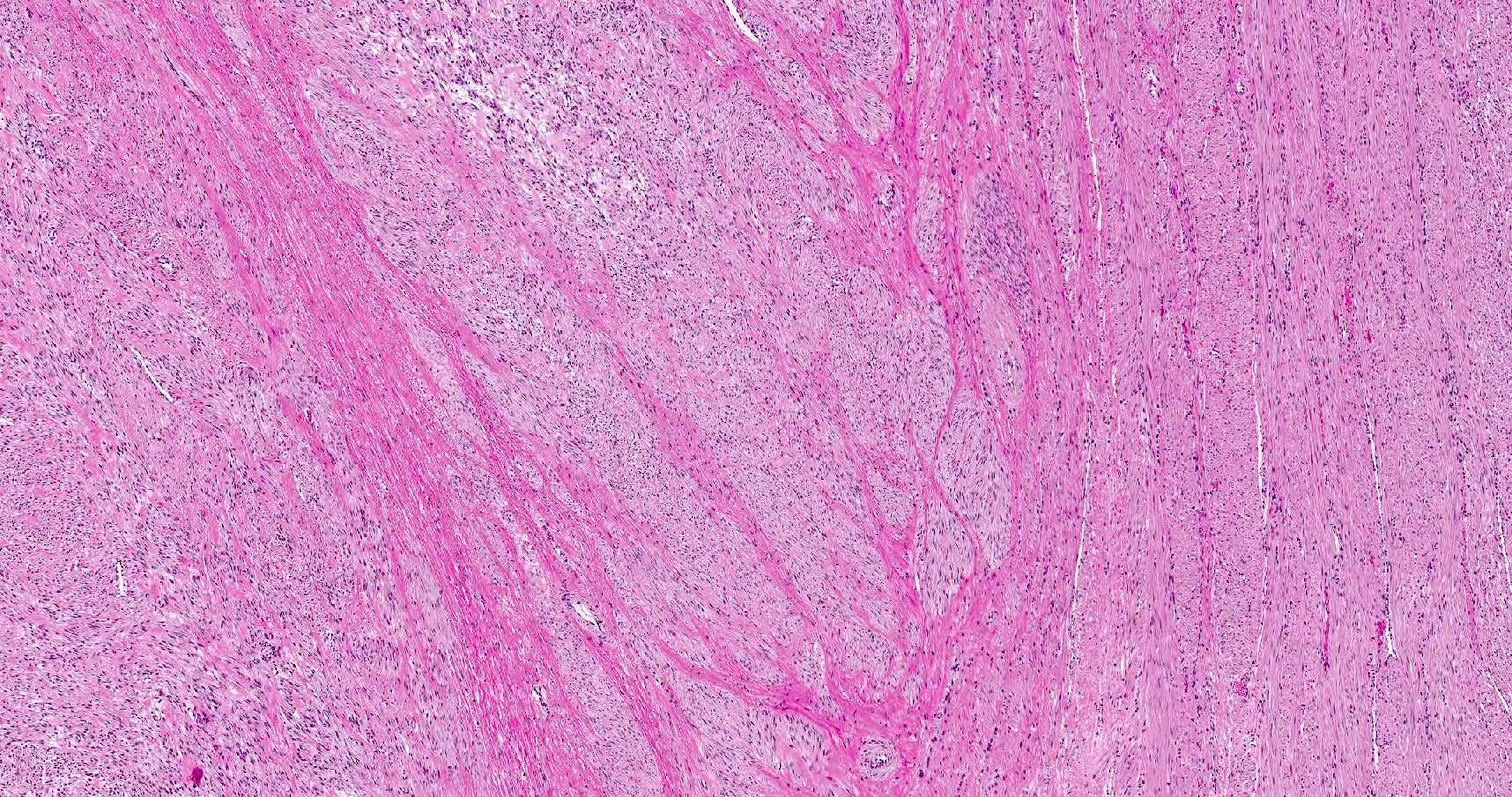
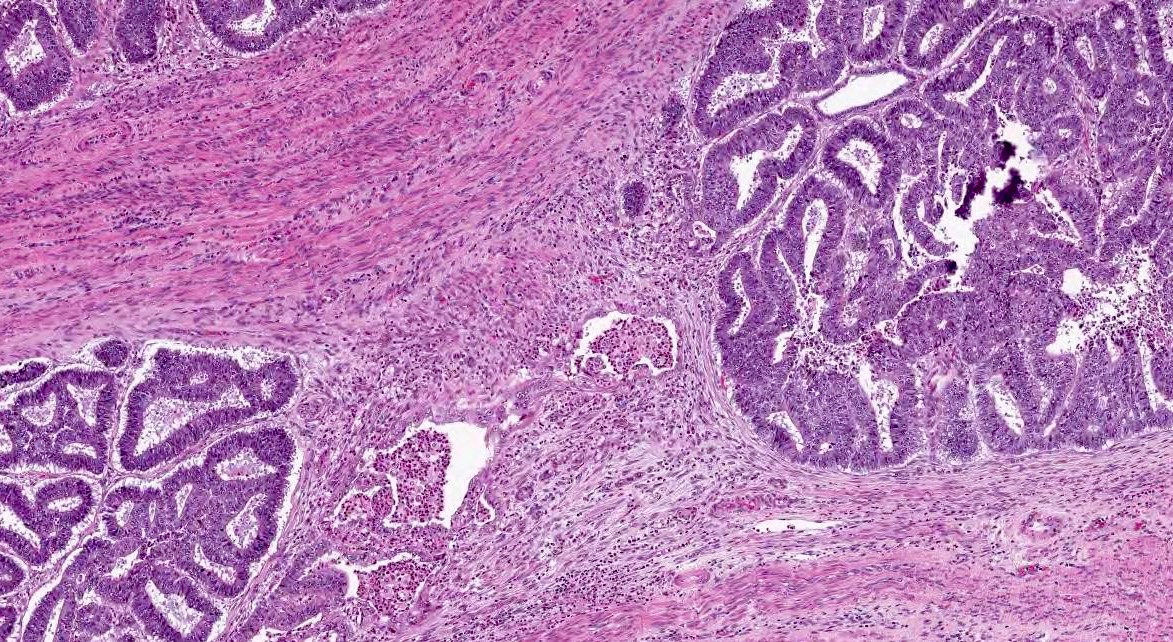
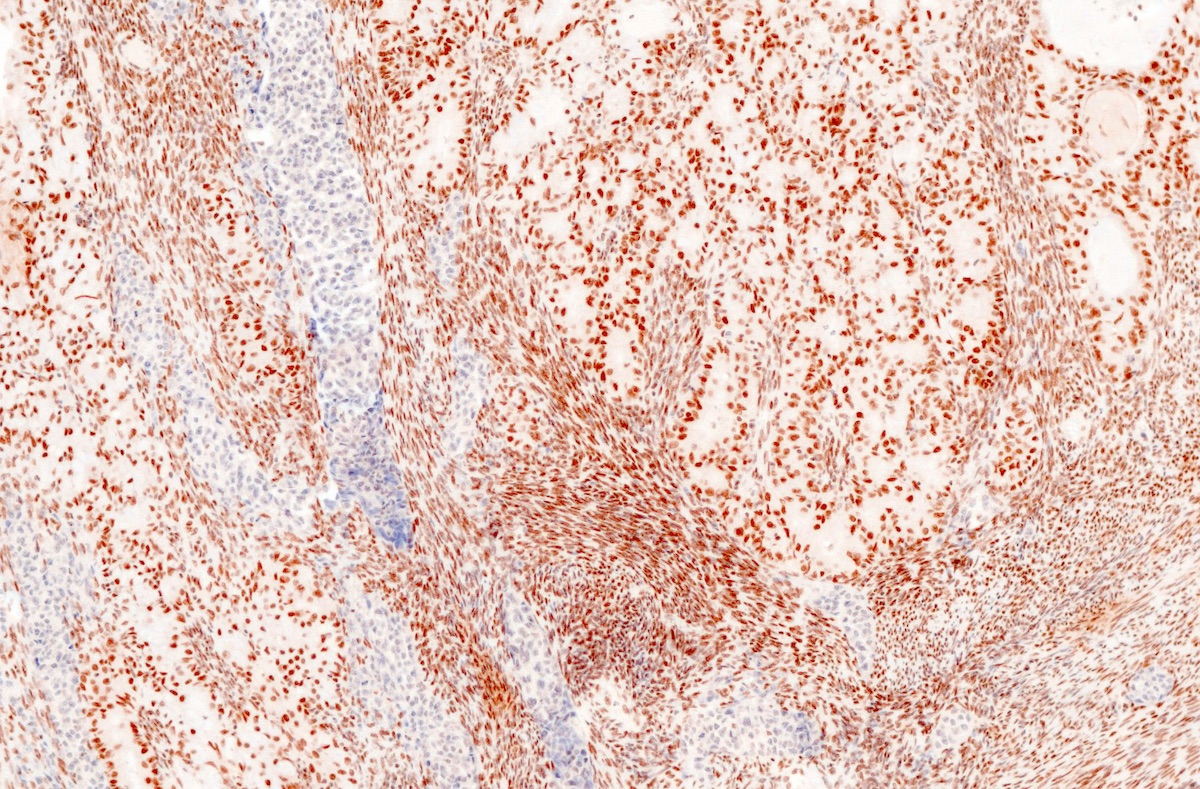
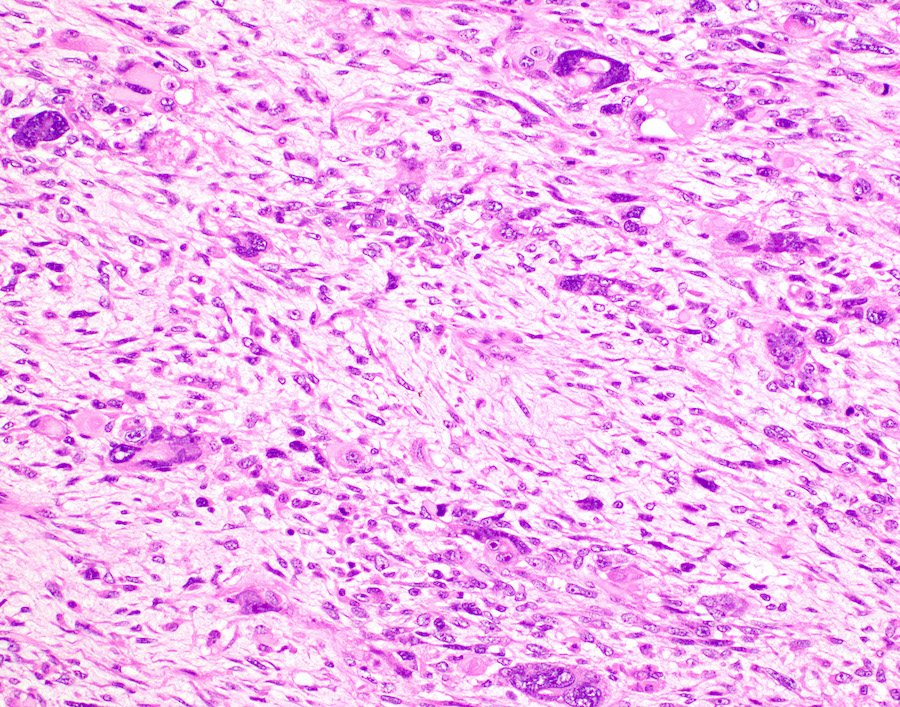
- If myometrial invasion arises from areas of adenomyosis, the location of the deepest myoinvasive point with respect to the entire uterine wall should be recorded (inner versus outer wall) (Figure 3)
- There is controversy in whether to assign stage IA or IB to a carcinoma with foci of invasion in the outer wall arising from adenomyosis; the ISGyP endometrial carcinoma consensus recommends:
- If the foci are few and clearly arising from deep adenomyosis, it is advisable to categorize these lesions as stage IA; there is emerging evidence showing that these lesions behave more indolently, similar to stage IA tumors (Int J Gynecol Pathol 2019;38:S93, Mod Pathol 2019;32:1)
- If, on the other hand, myoinvasive carcinoma from adenomyosis is rather extensive and seen throughout the wall, it is prudent to classify the tumor as stage IB (Int J Gynecol Pathol 2019;38:S93)
- There is controversy in whether to assign stage IA or IB to a carcinoma with foci of invasion in the outer wall arising from adenomyosis; the ISGyP endometrial carcinoma consensus recommends:
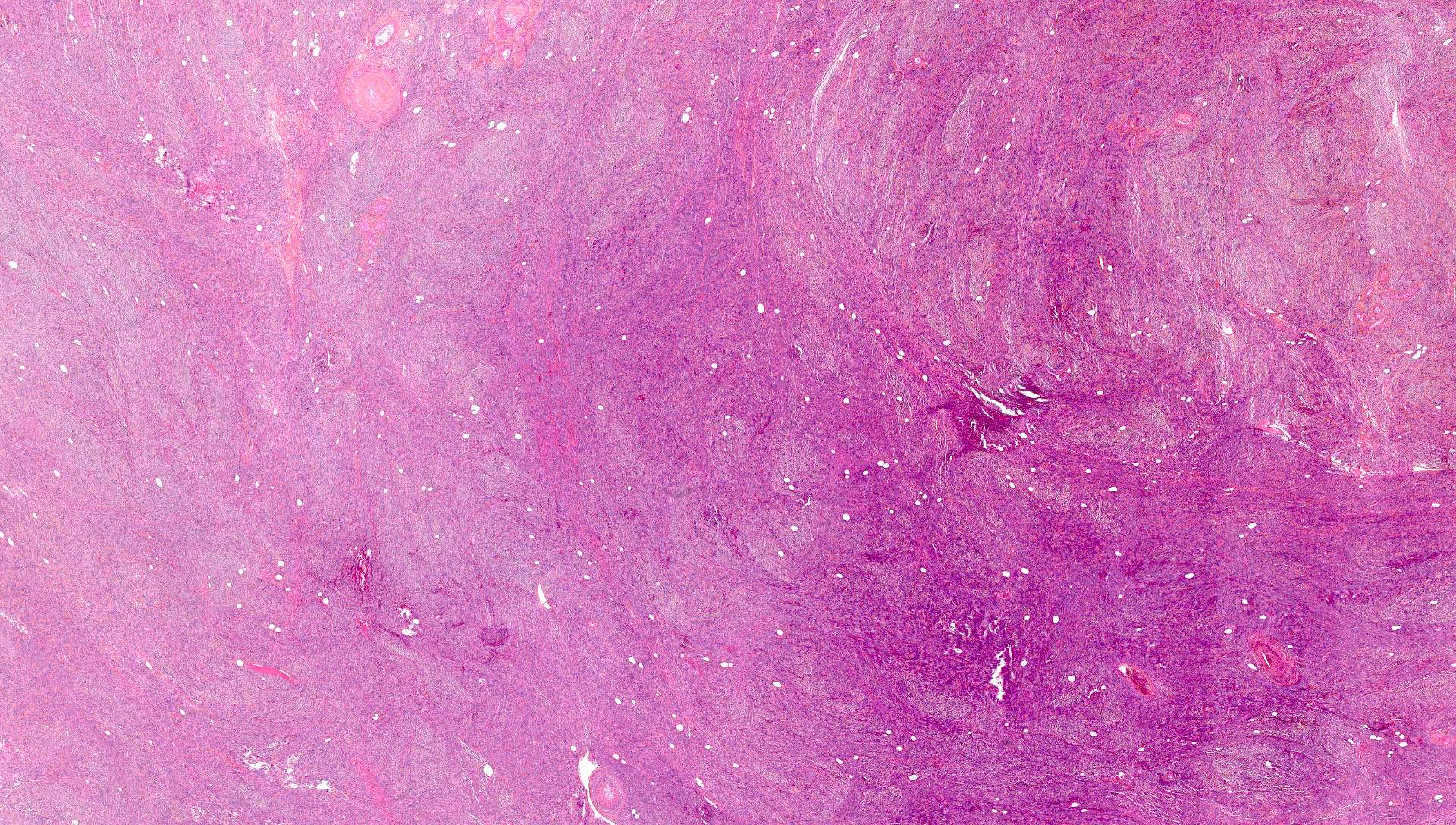
- If the tumor is exophytic at the point of deepest myometrial invasion, the nearest endomyometrial junction should be identified and depth should be measured from that point
- Same recommendation applies to tumors arising from or involving an endometrial polyp
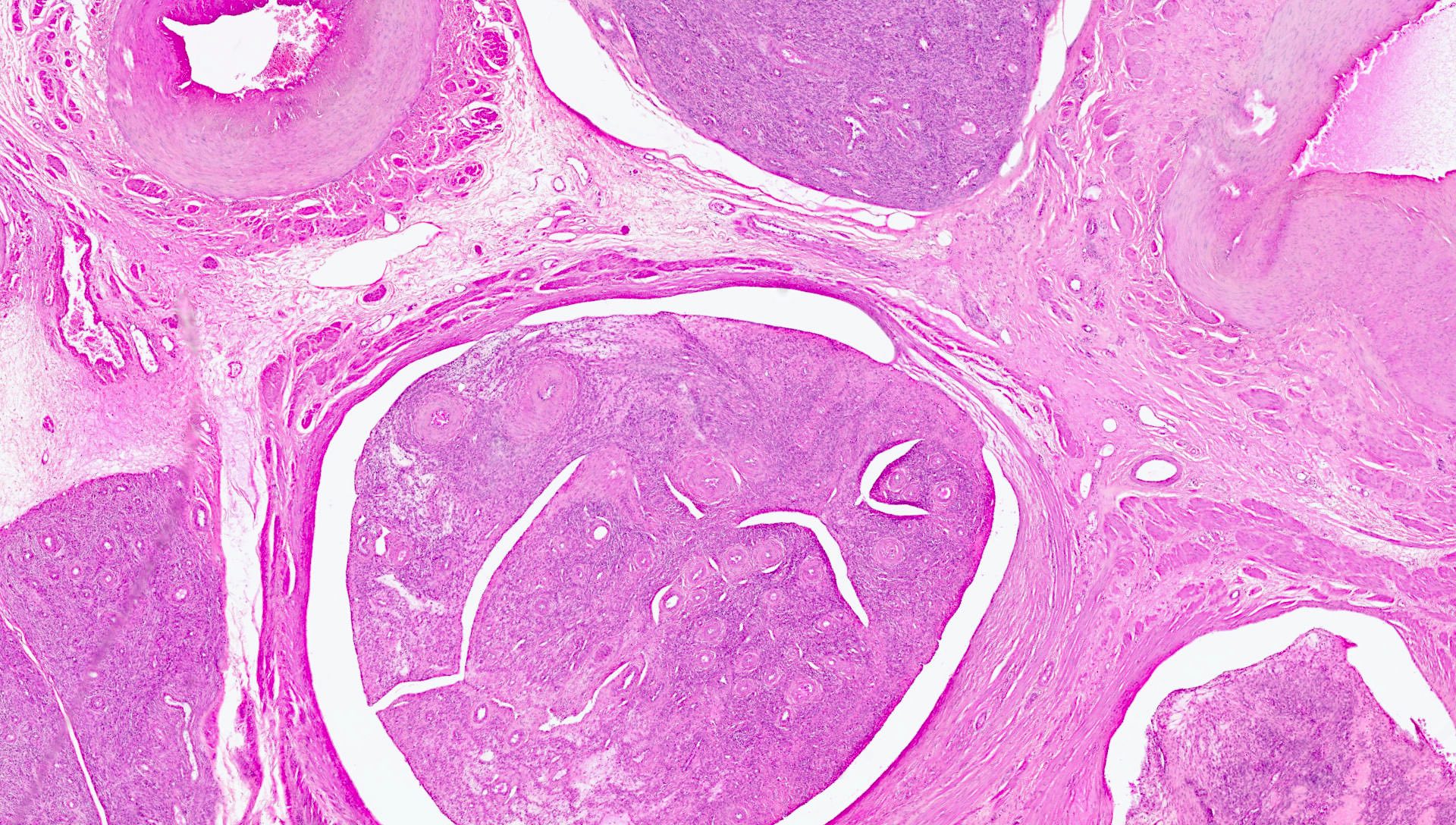
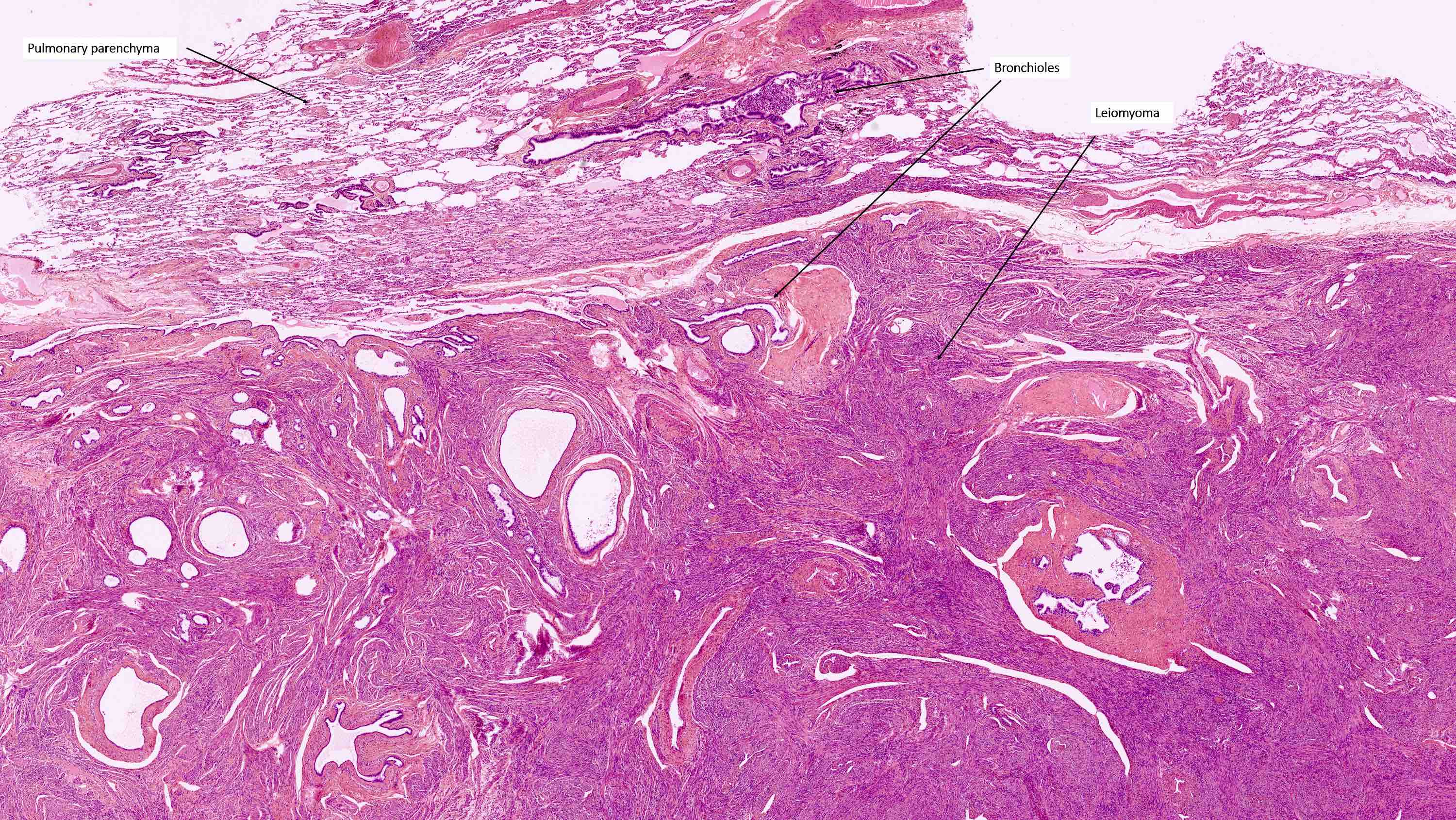
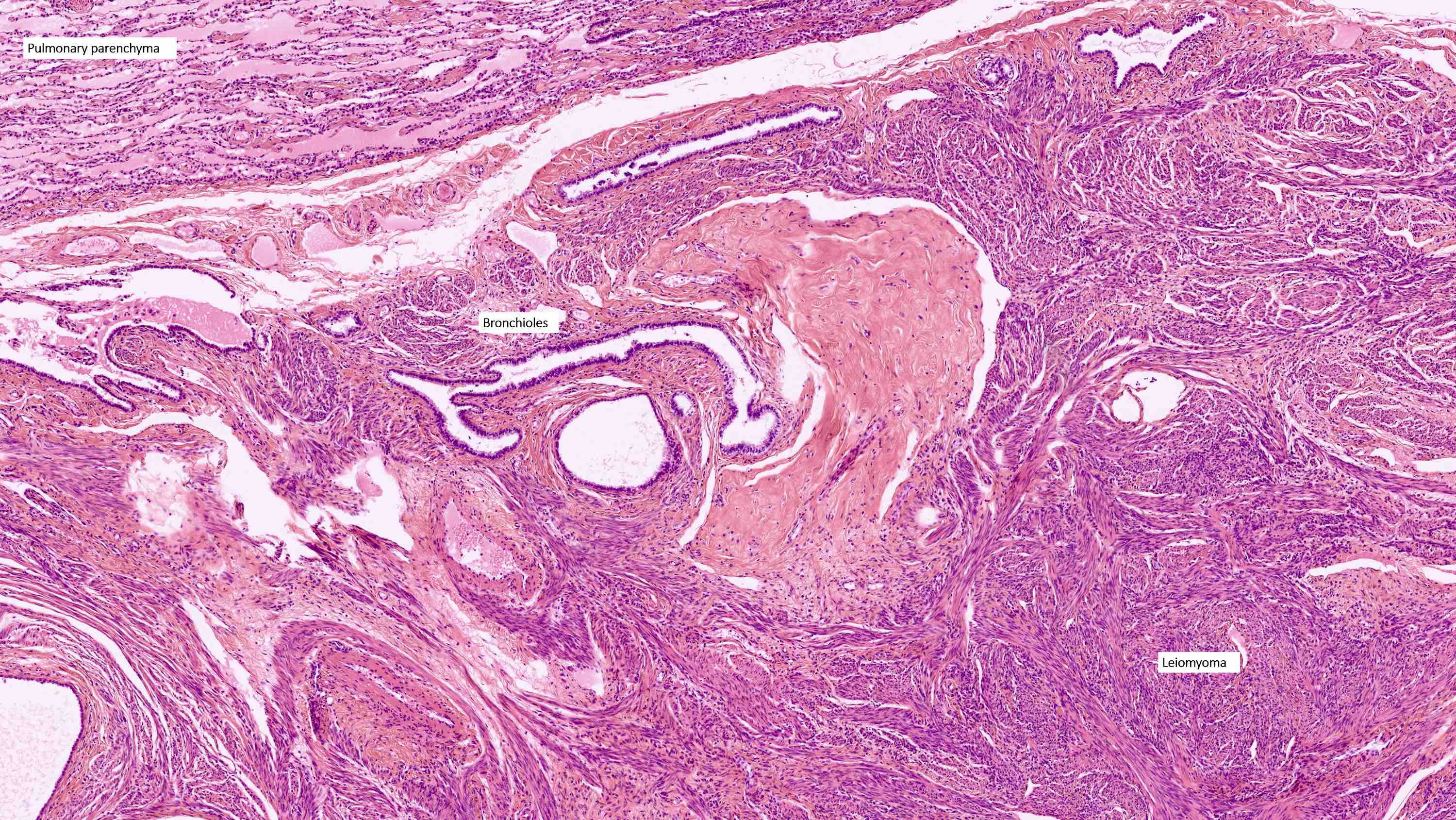
- If the carcinoma at the point of deepest invasion involves a leiomyoma, the myometrial thickness should include the leiomyoma (Int J Gynecol Pathol 2019;38:S93)
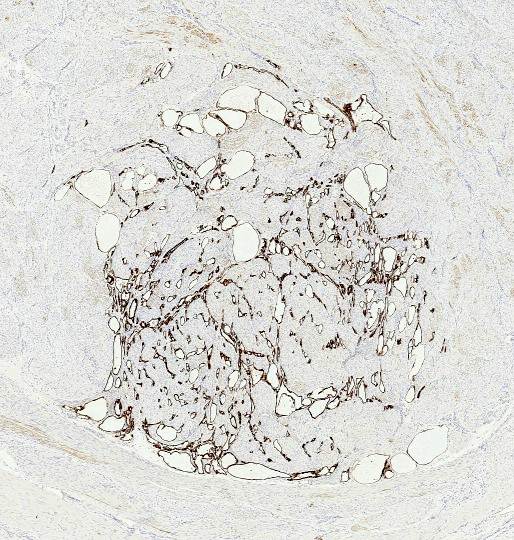
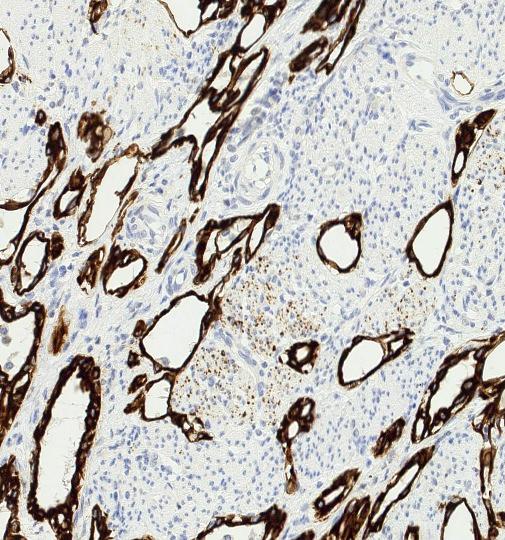
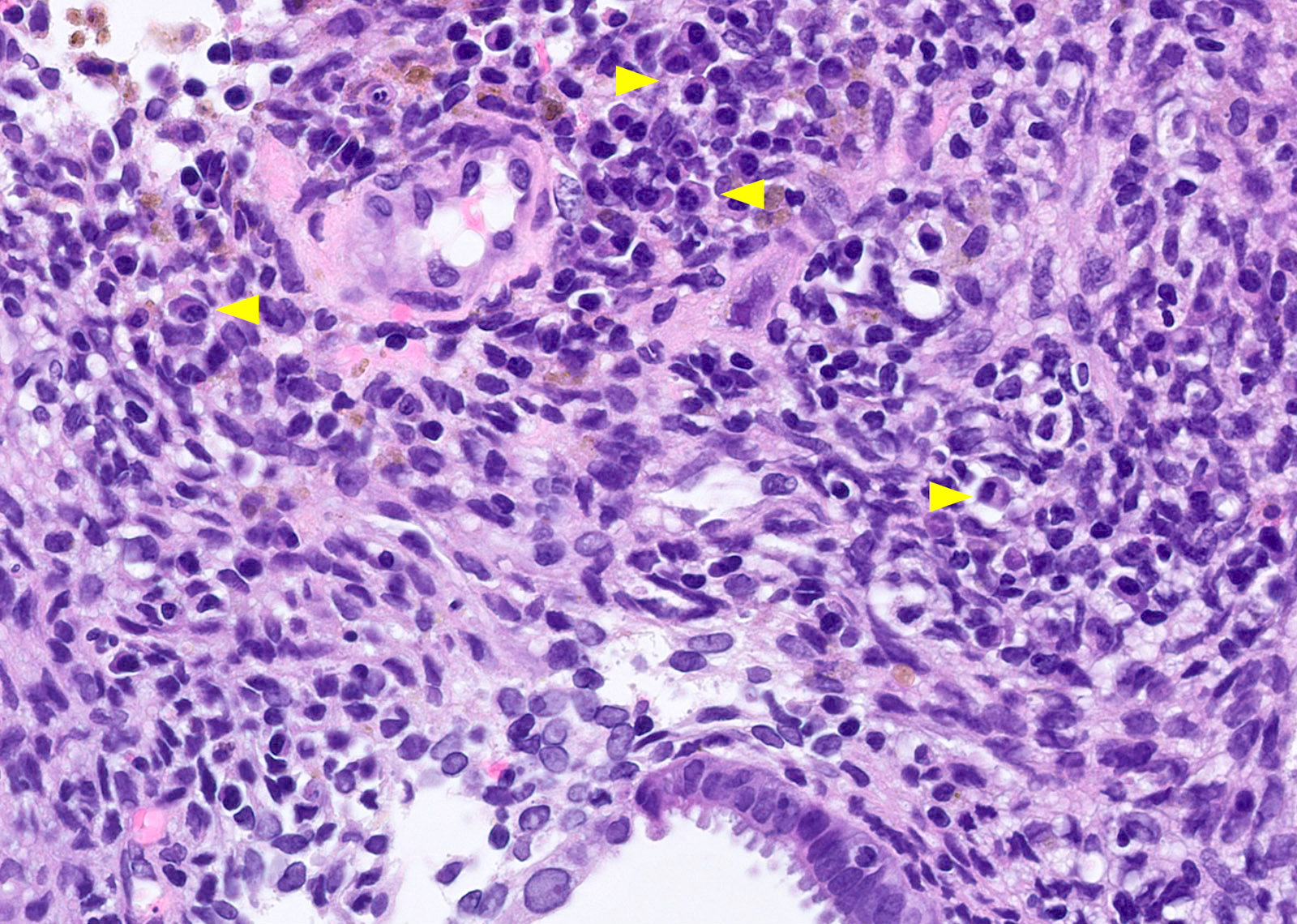
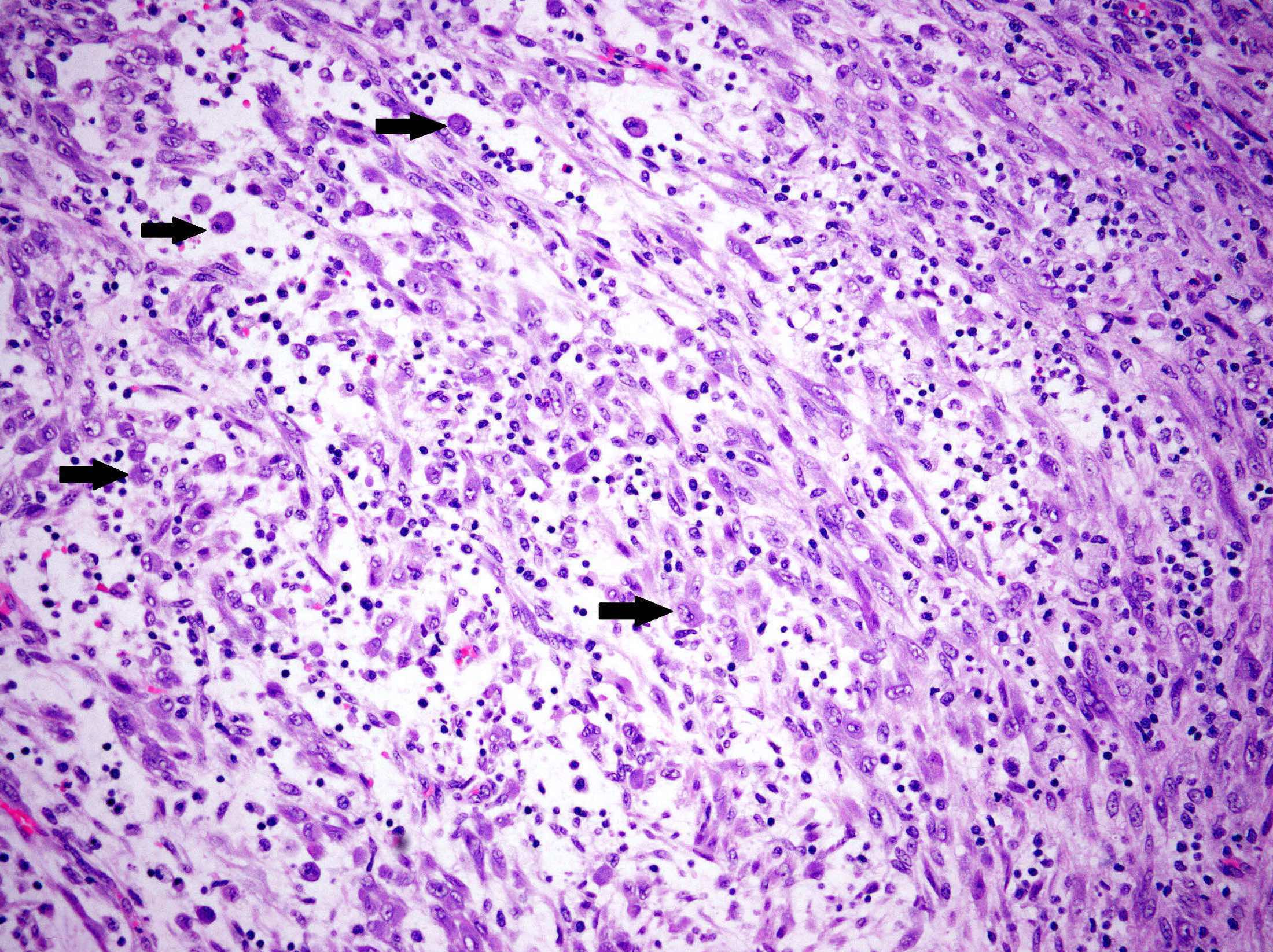
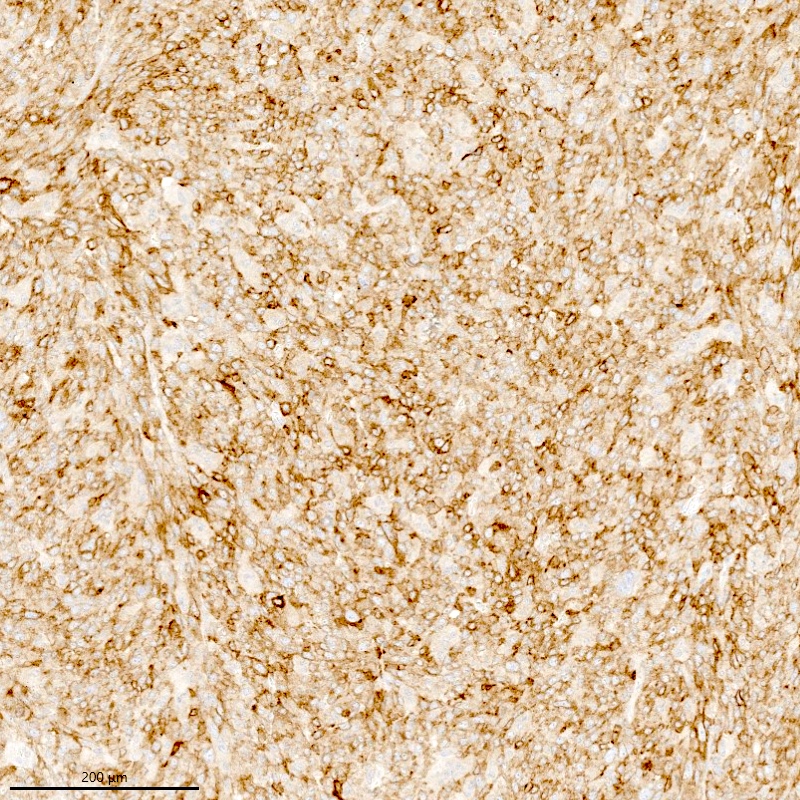
- Lymphovascular space invasion (LVI) should not be included in the assessment of myometrial invasion
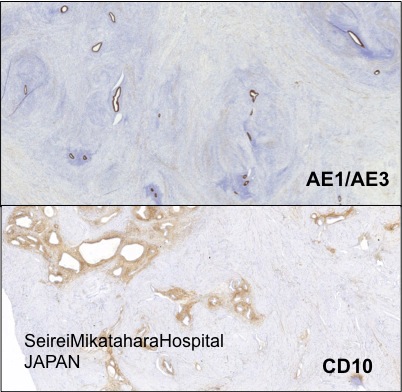
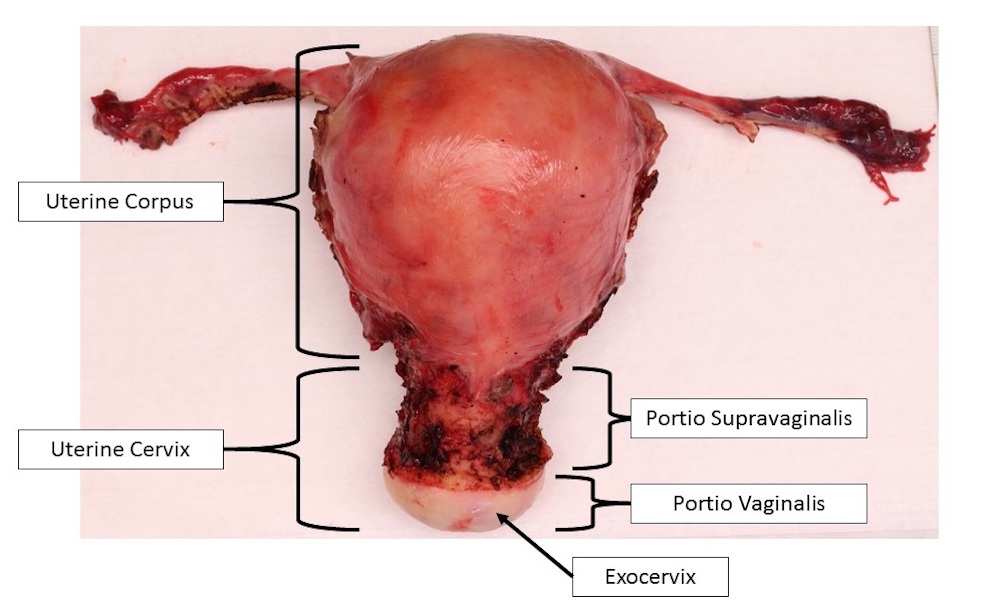
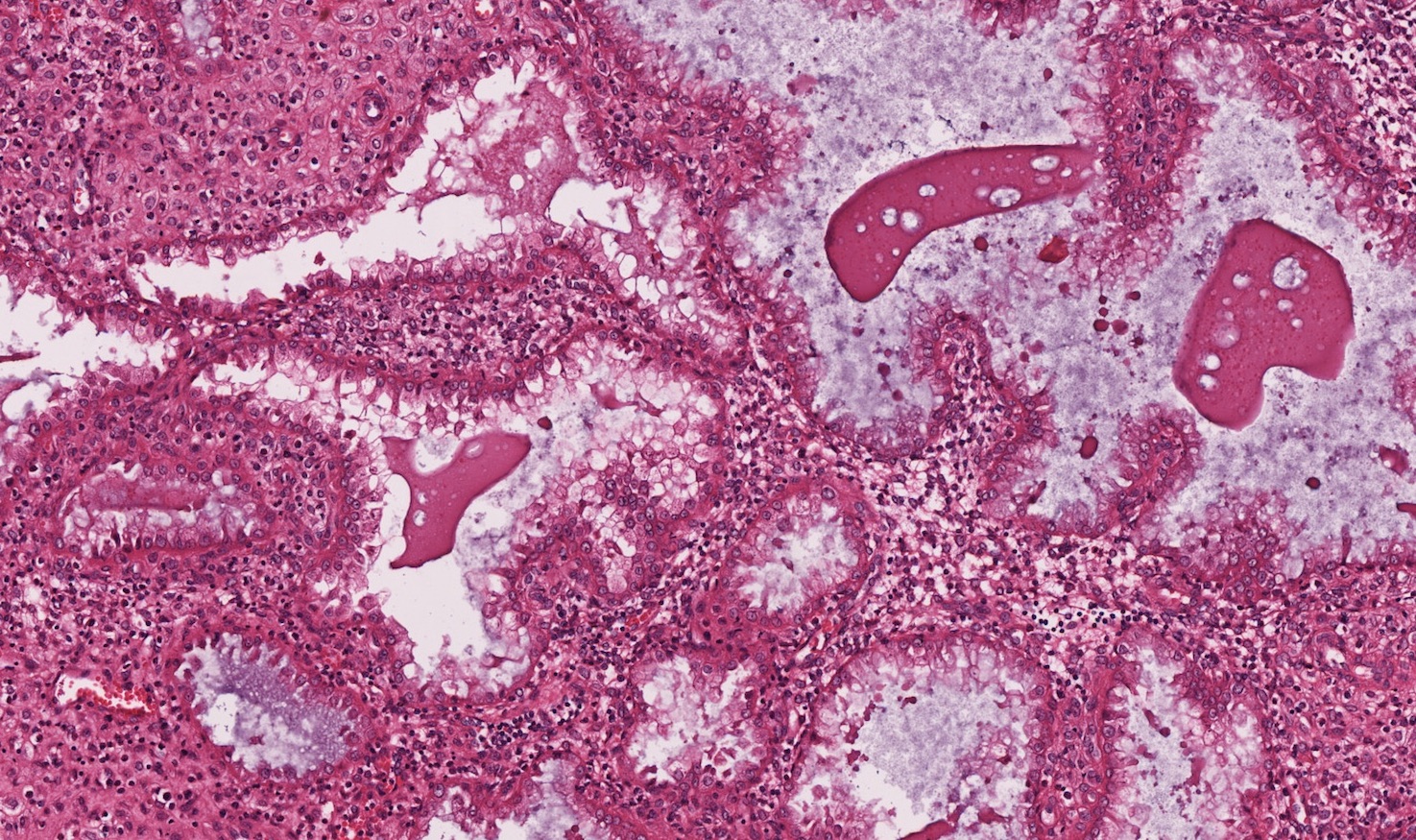
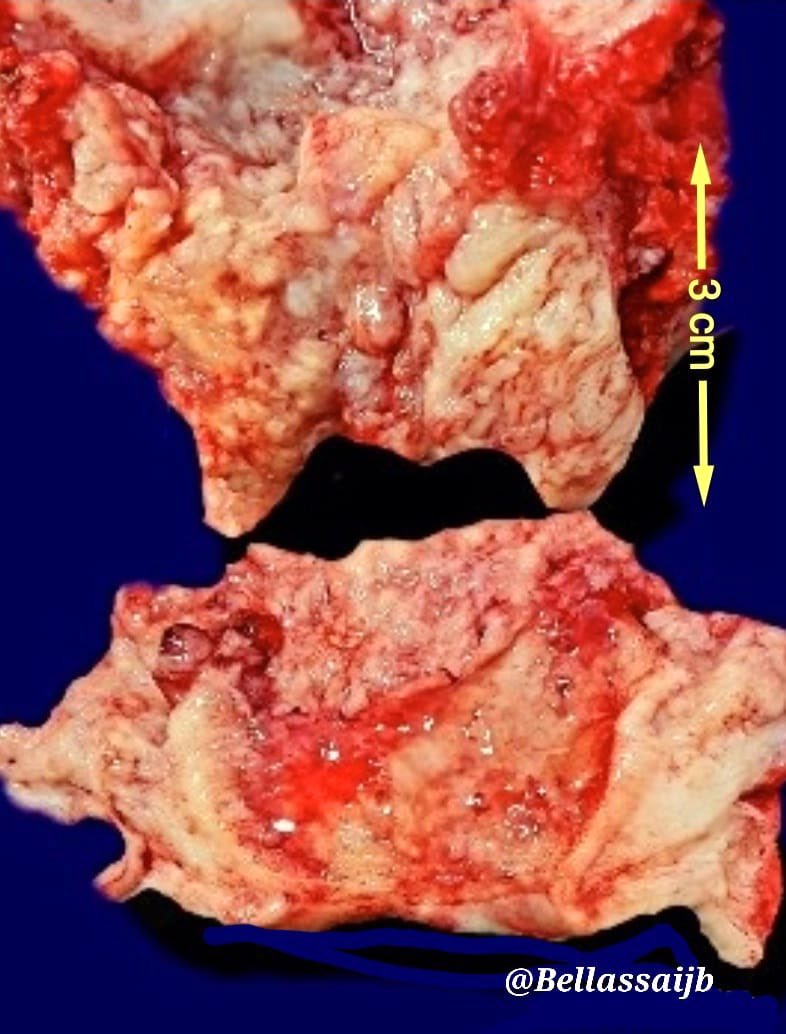
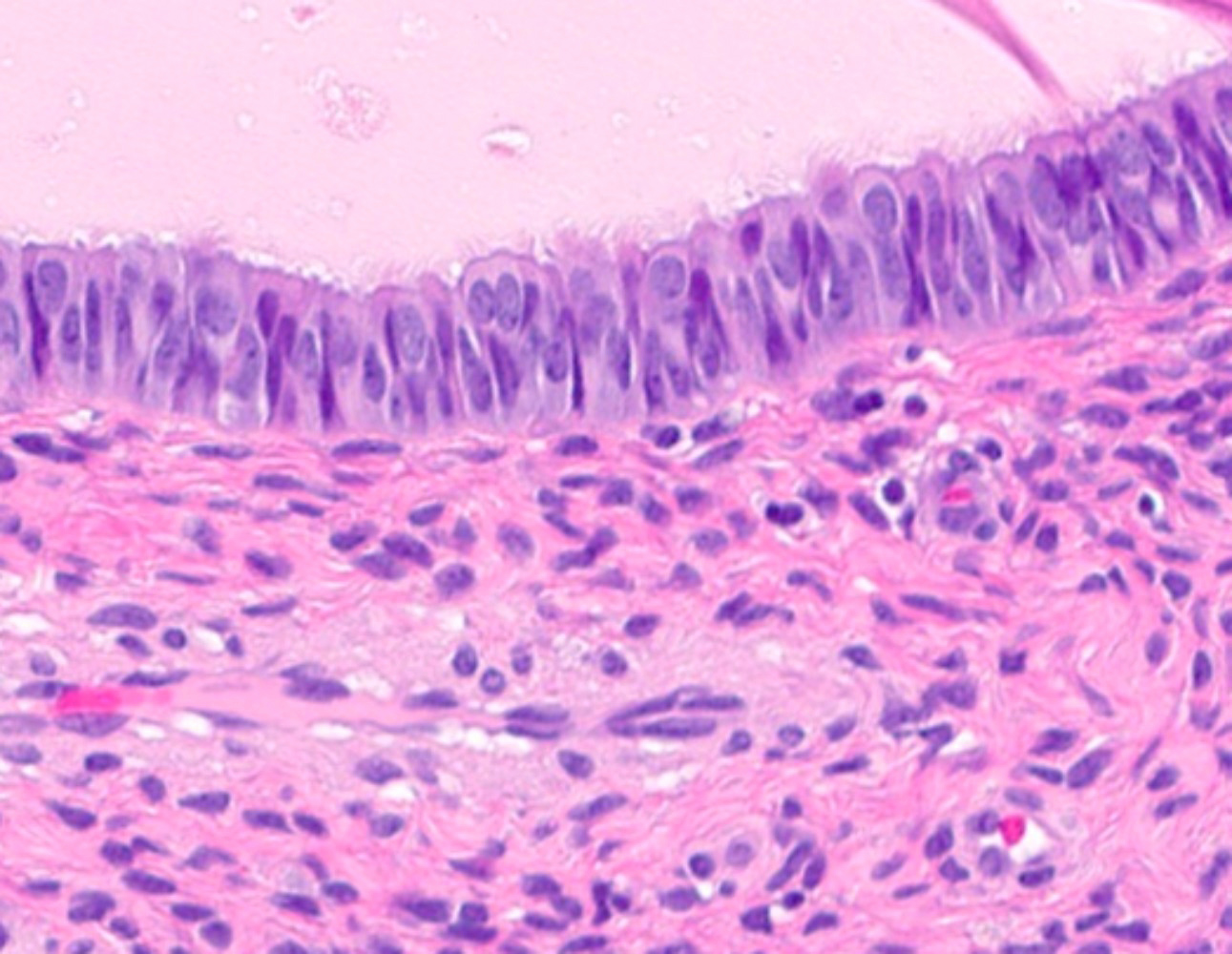
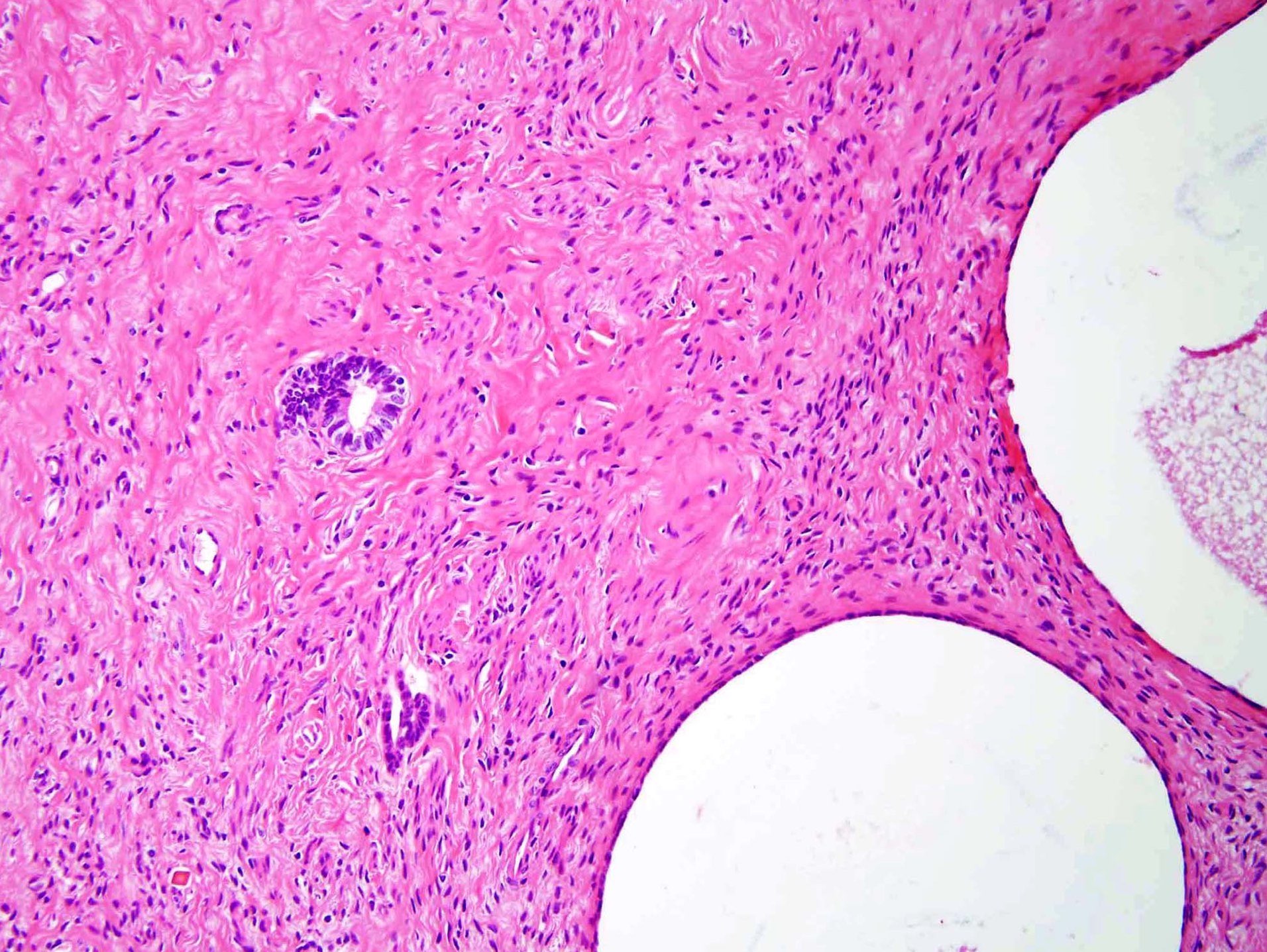
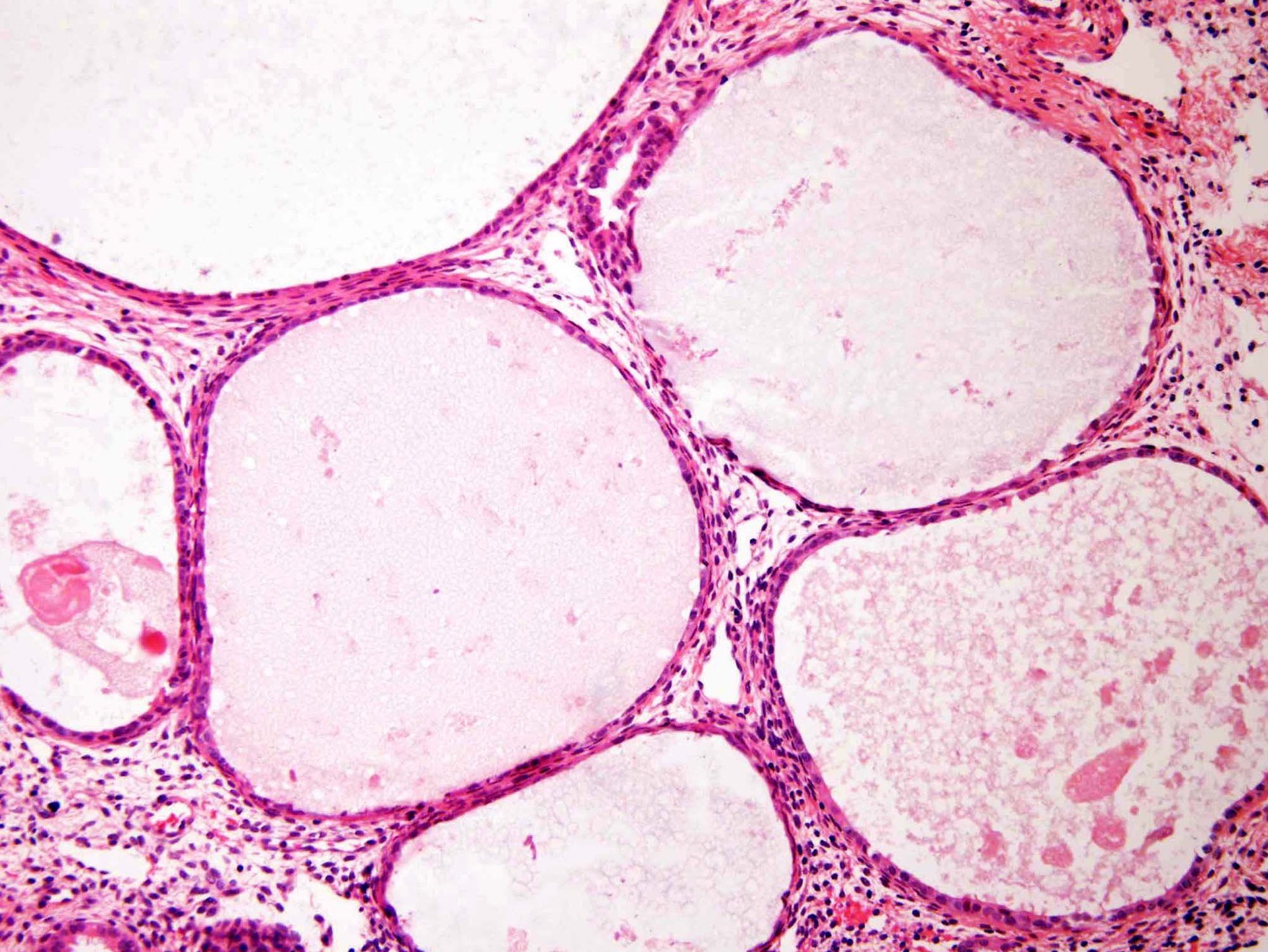
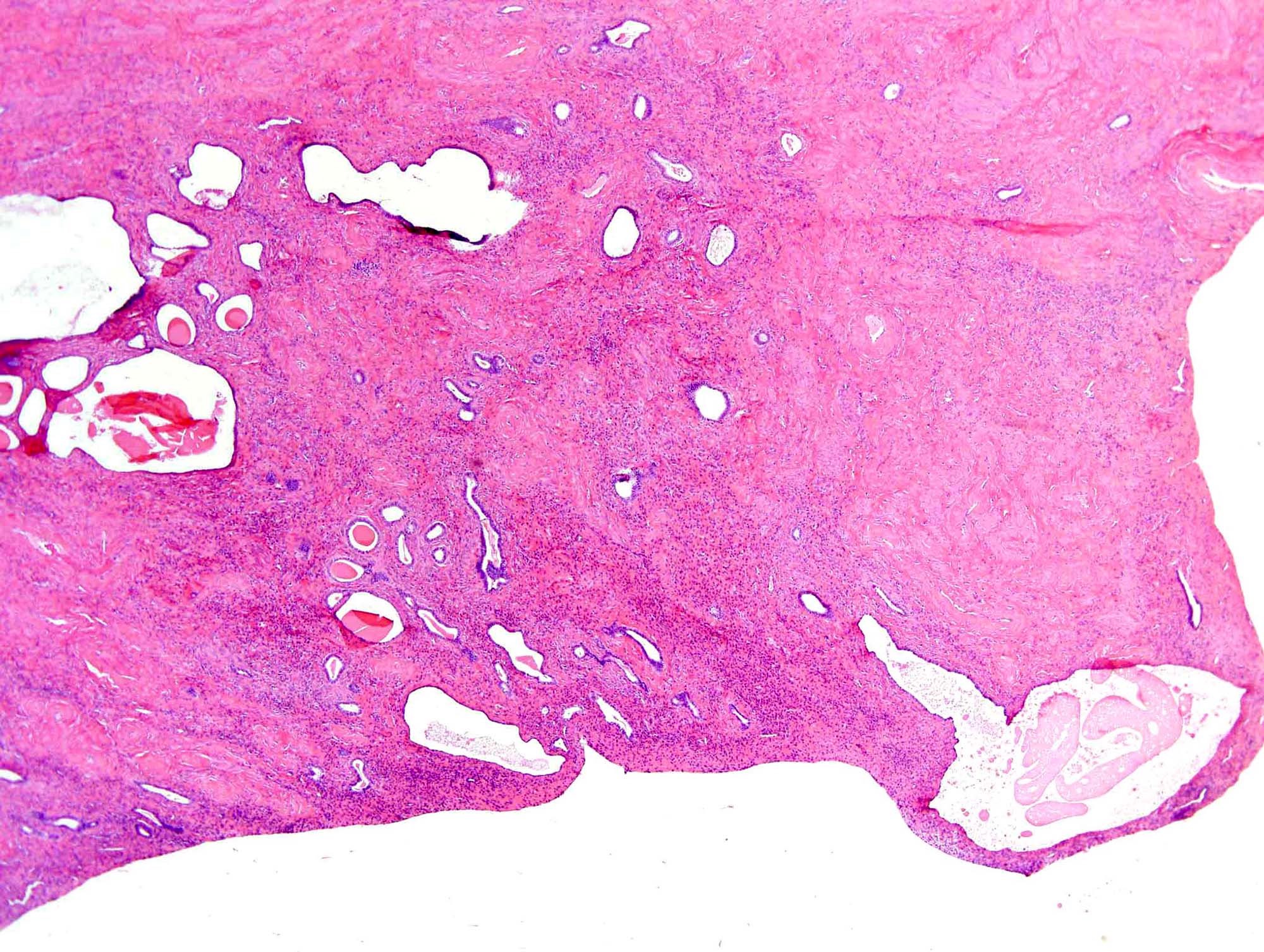
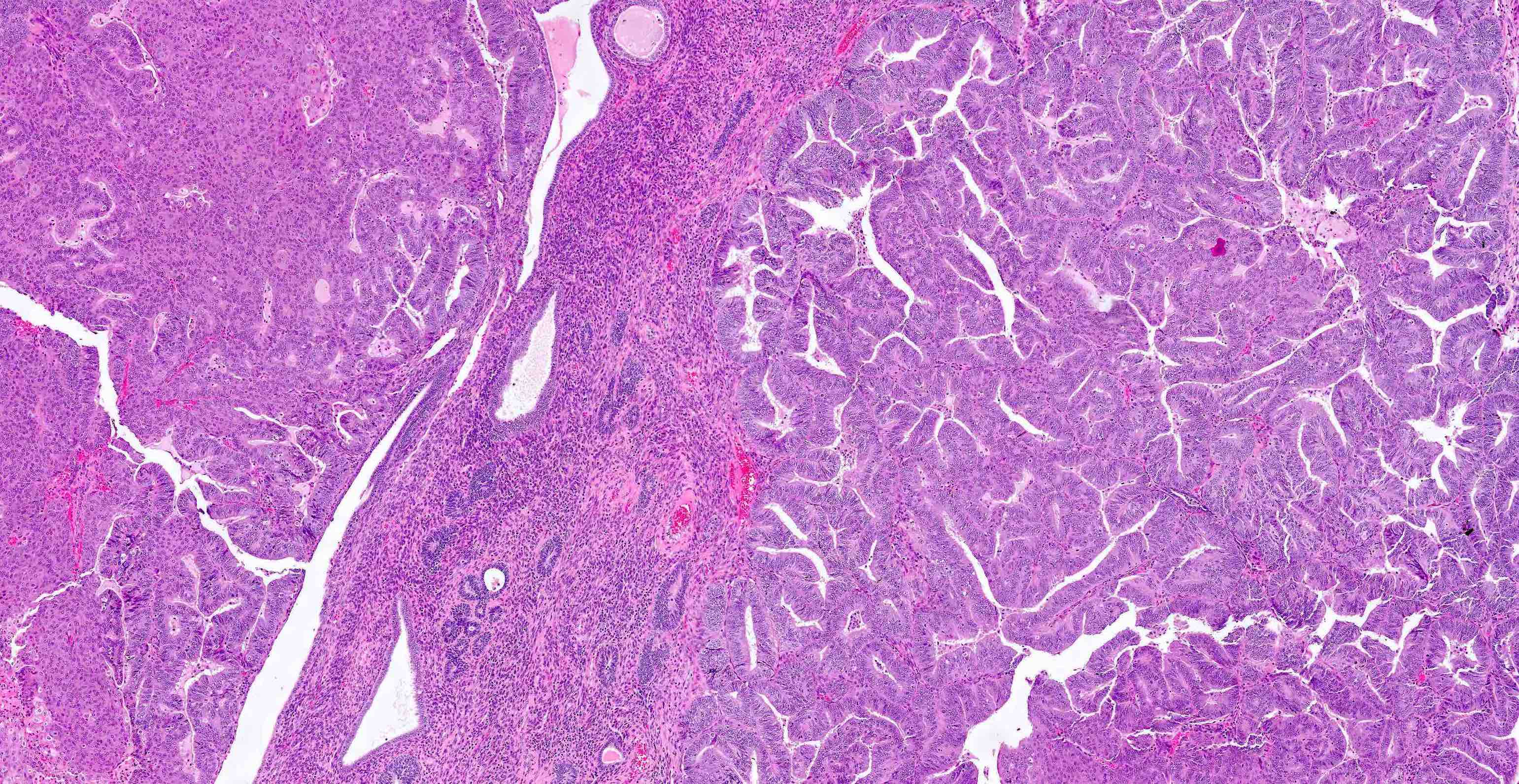
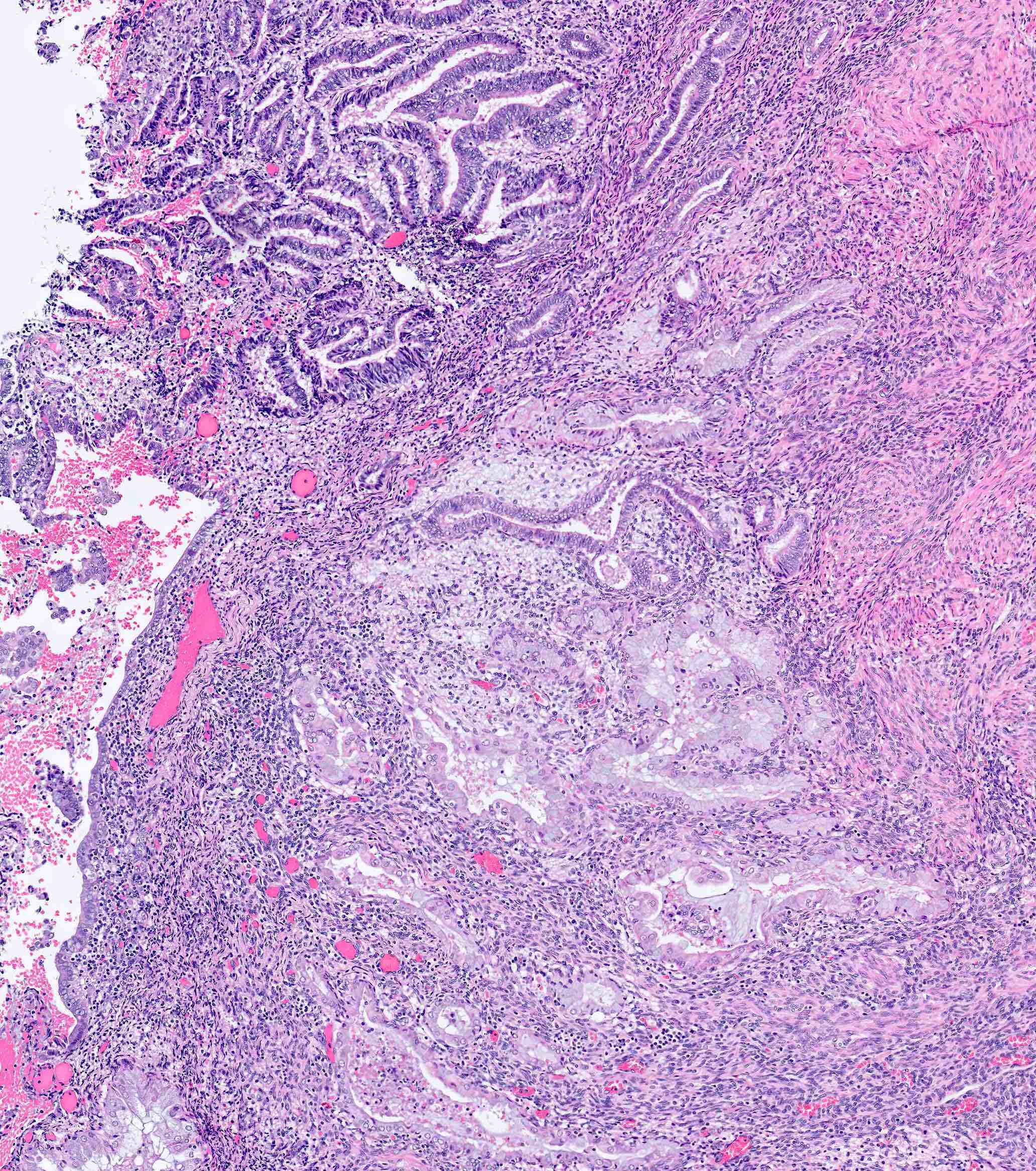
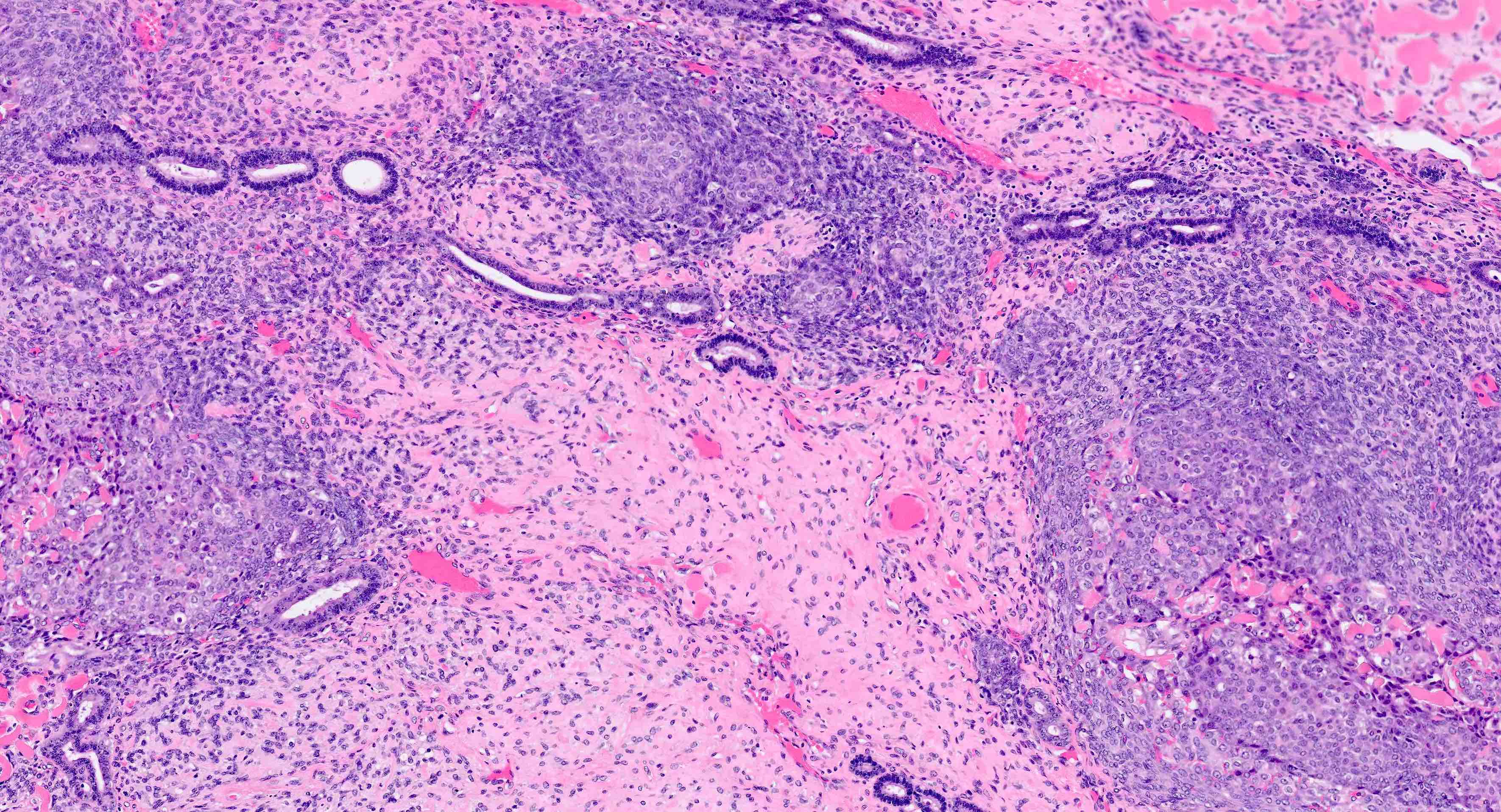
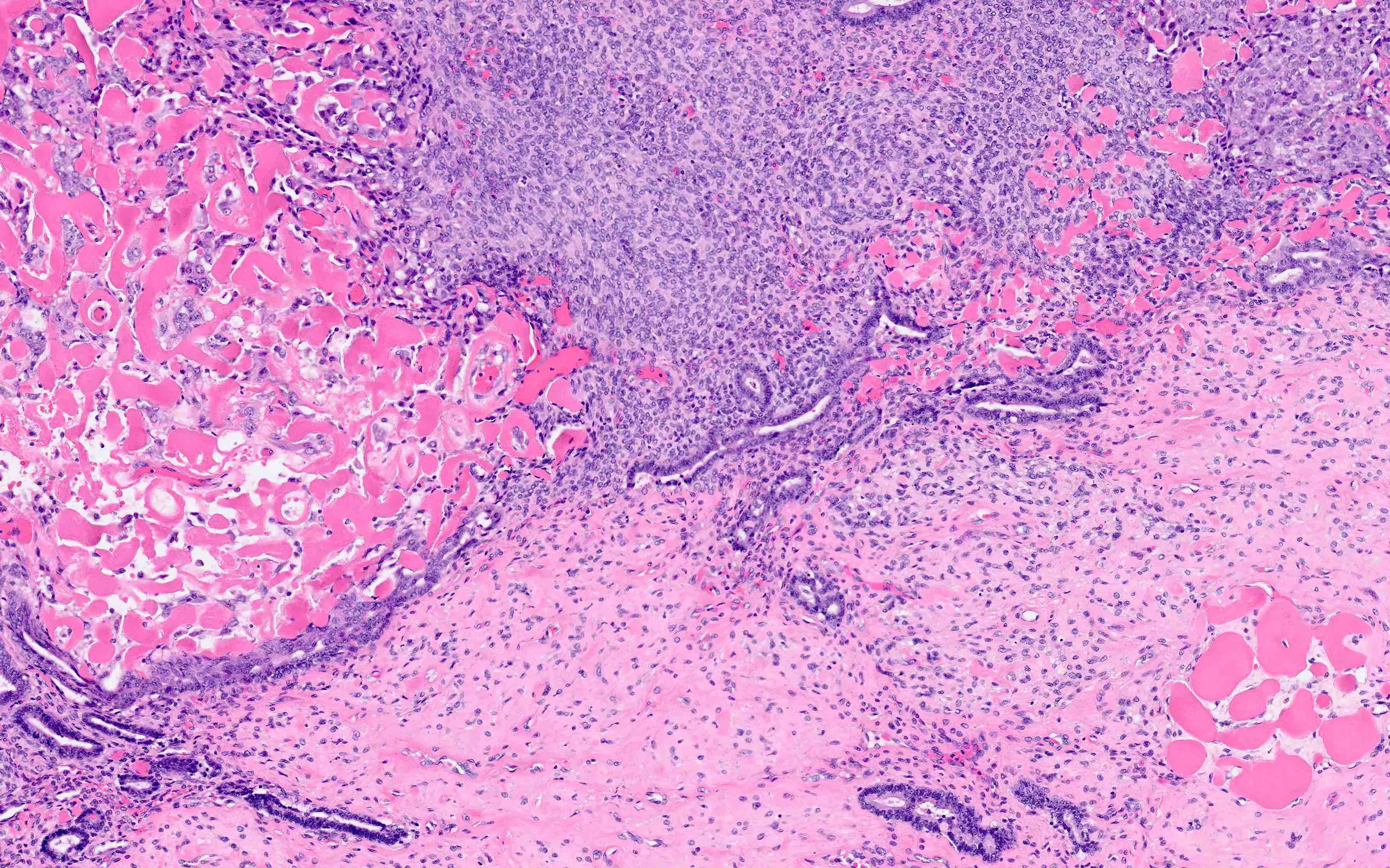
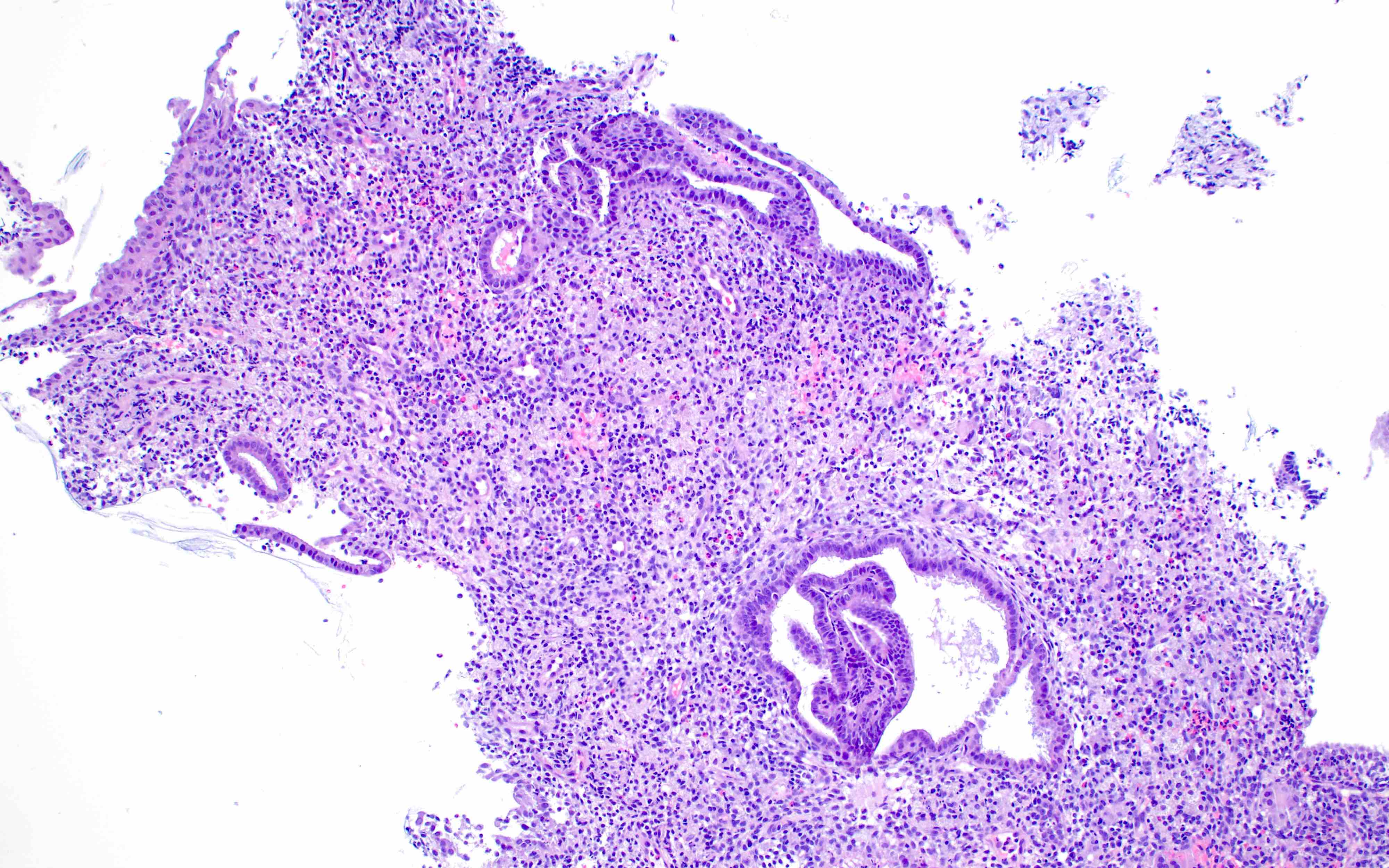
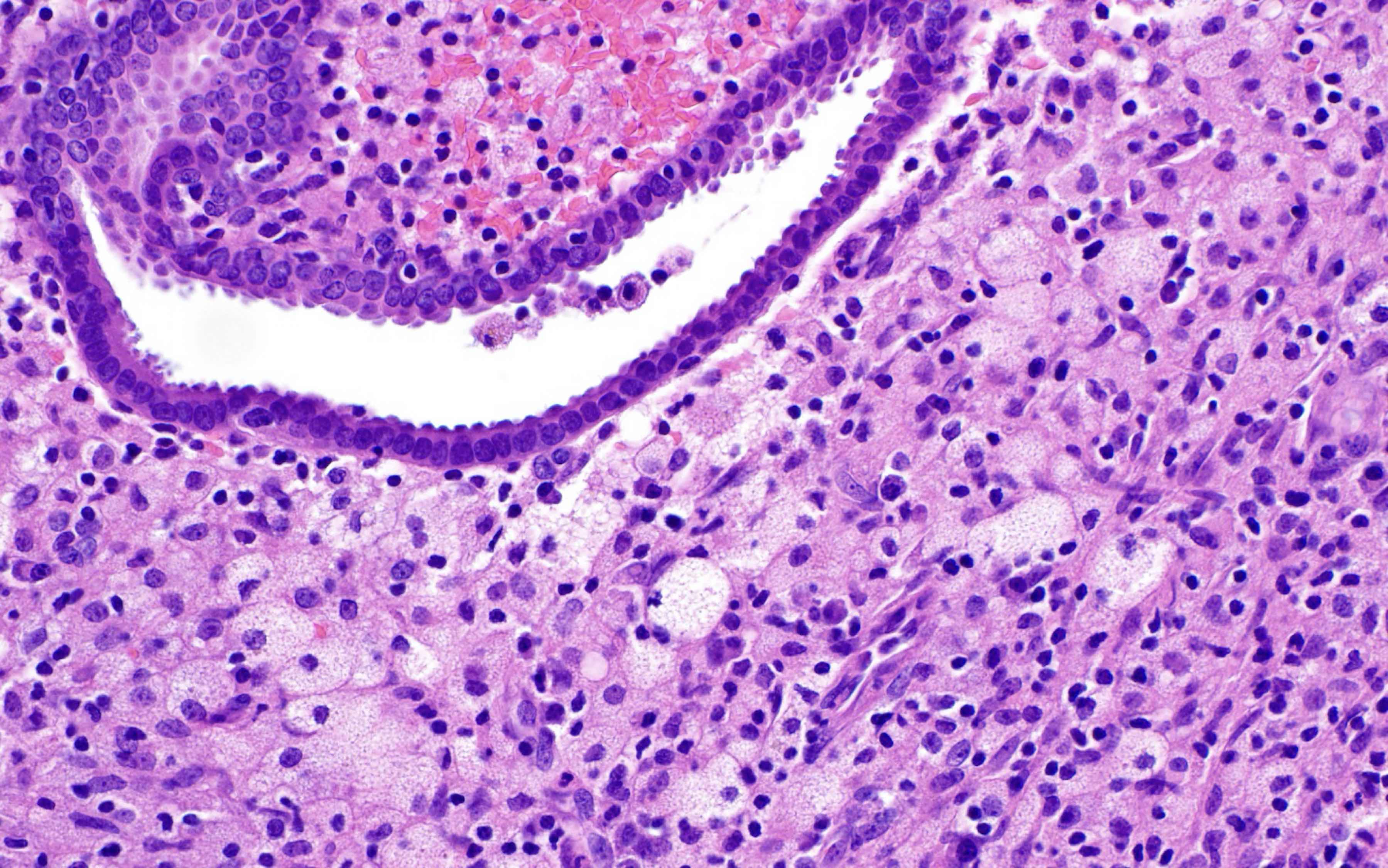
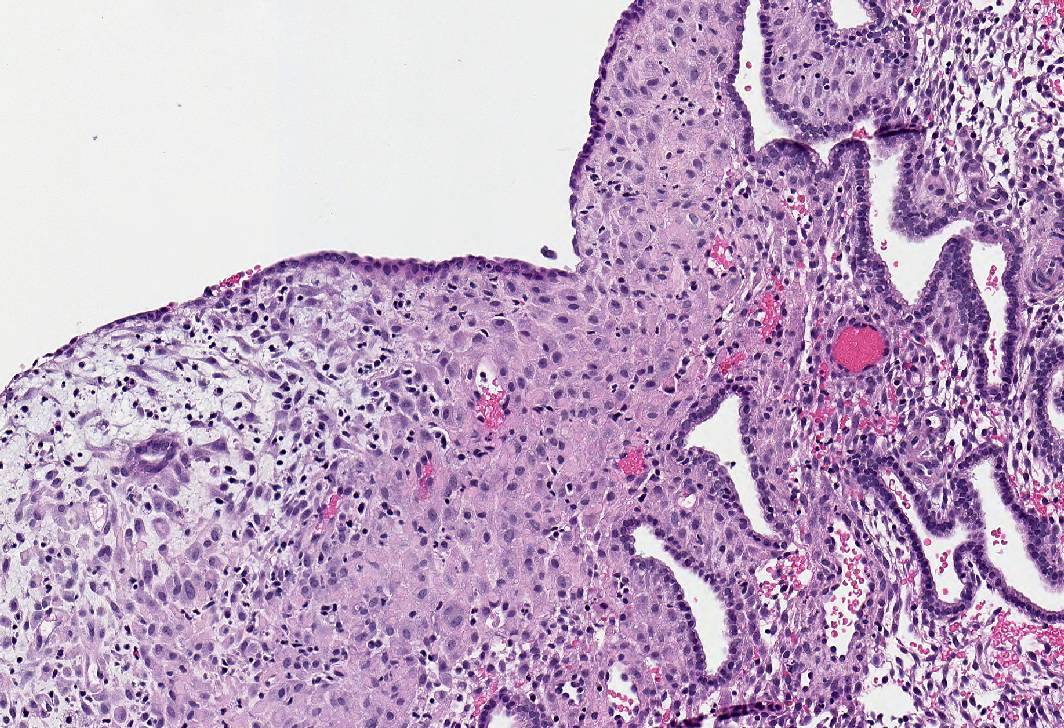
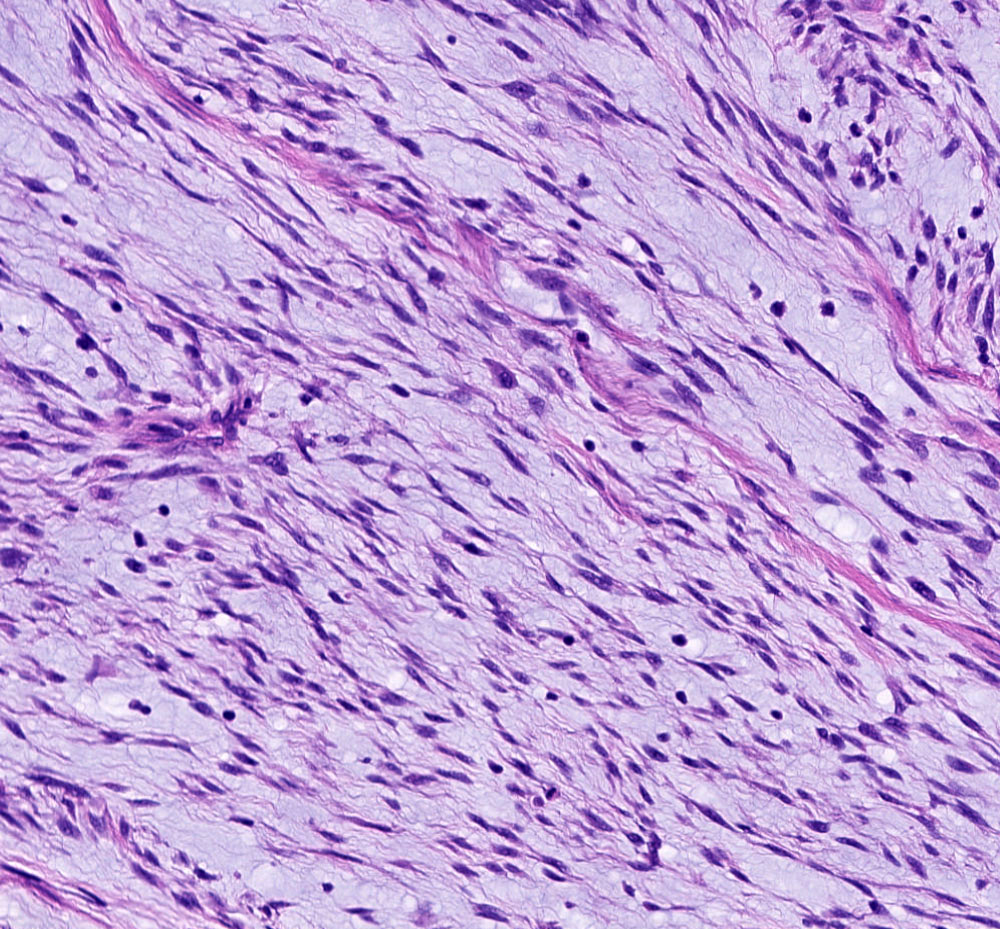
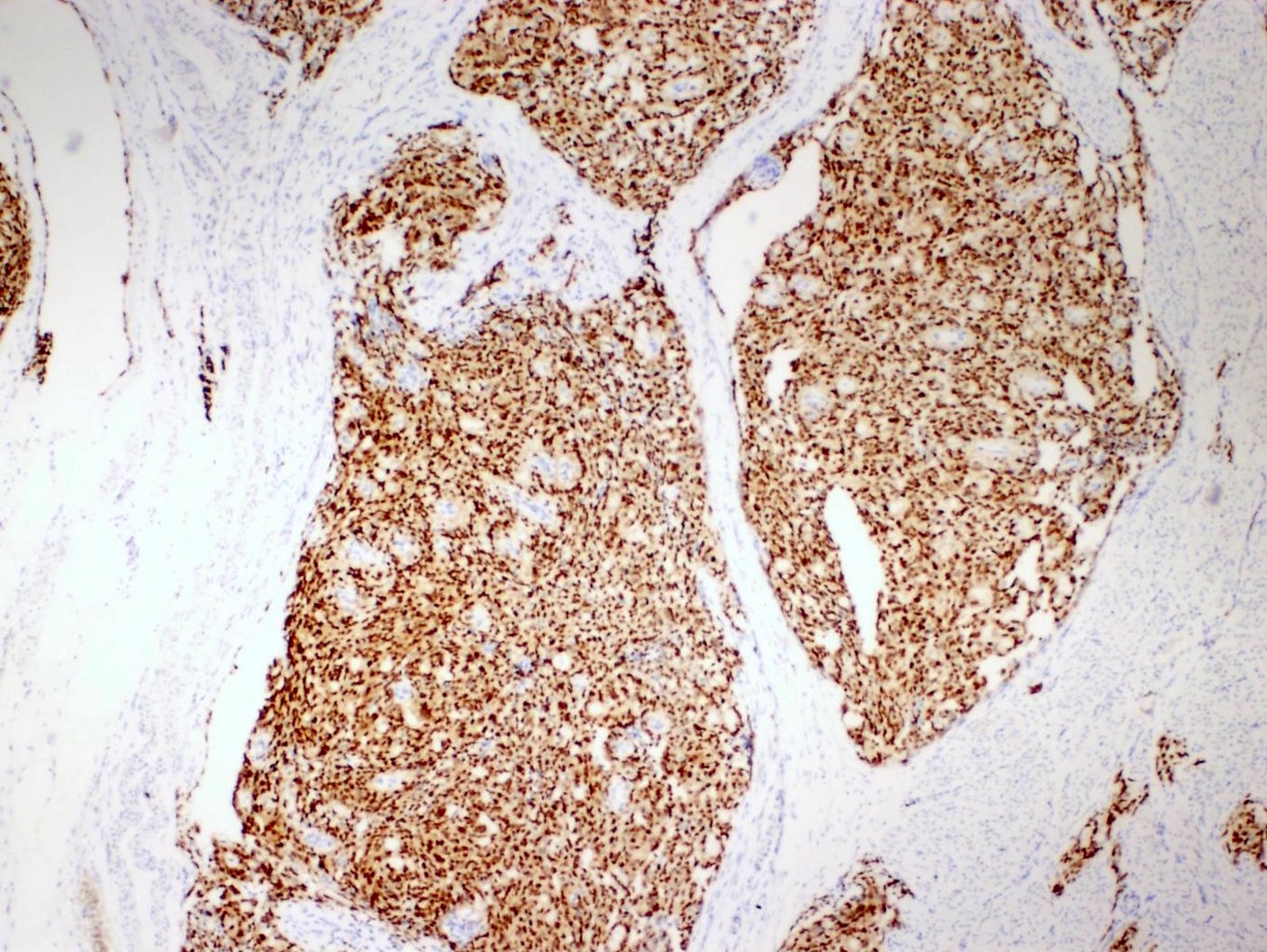
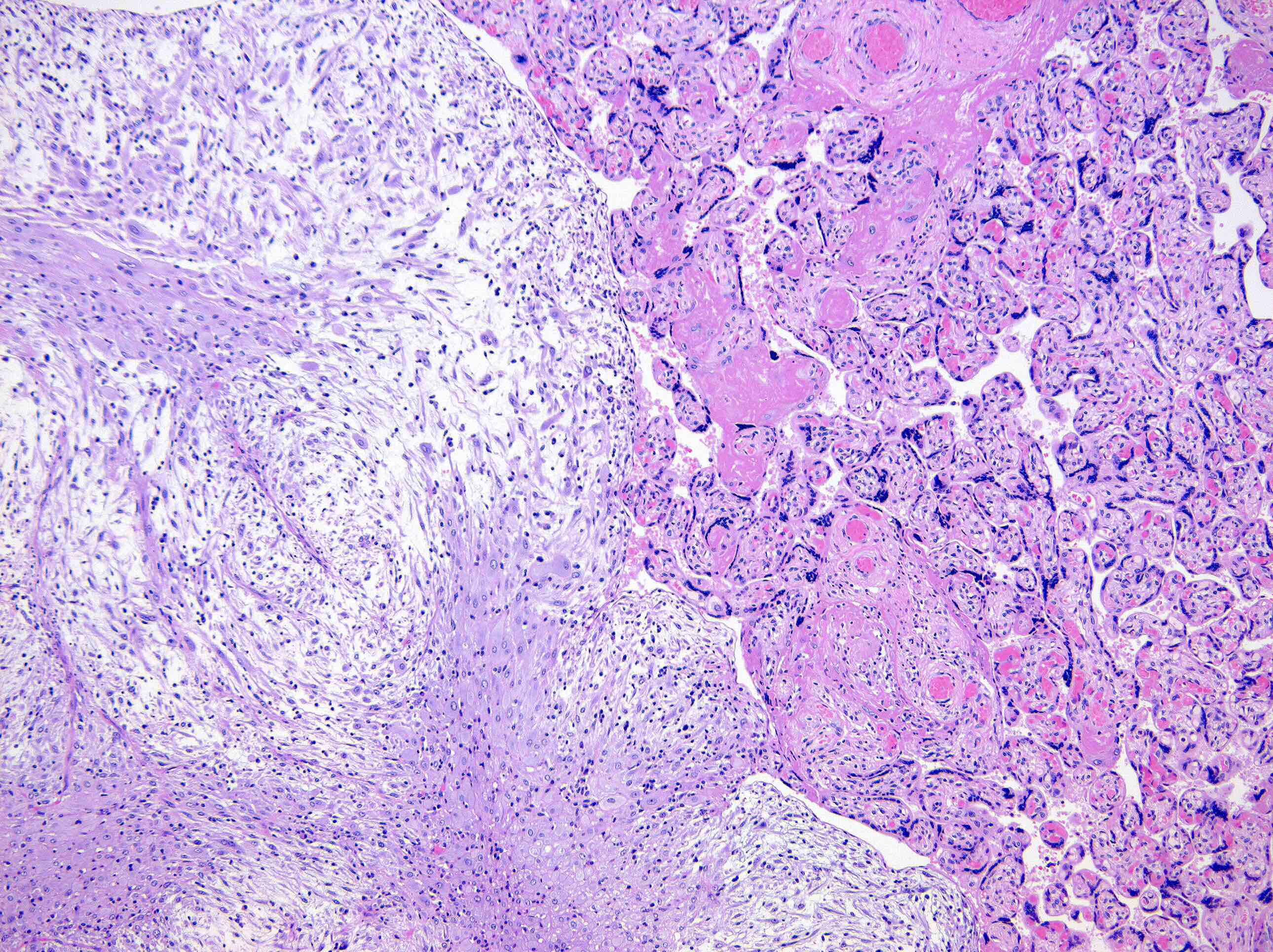
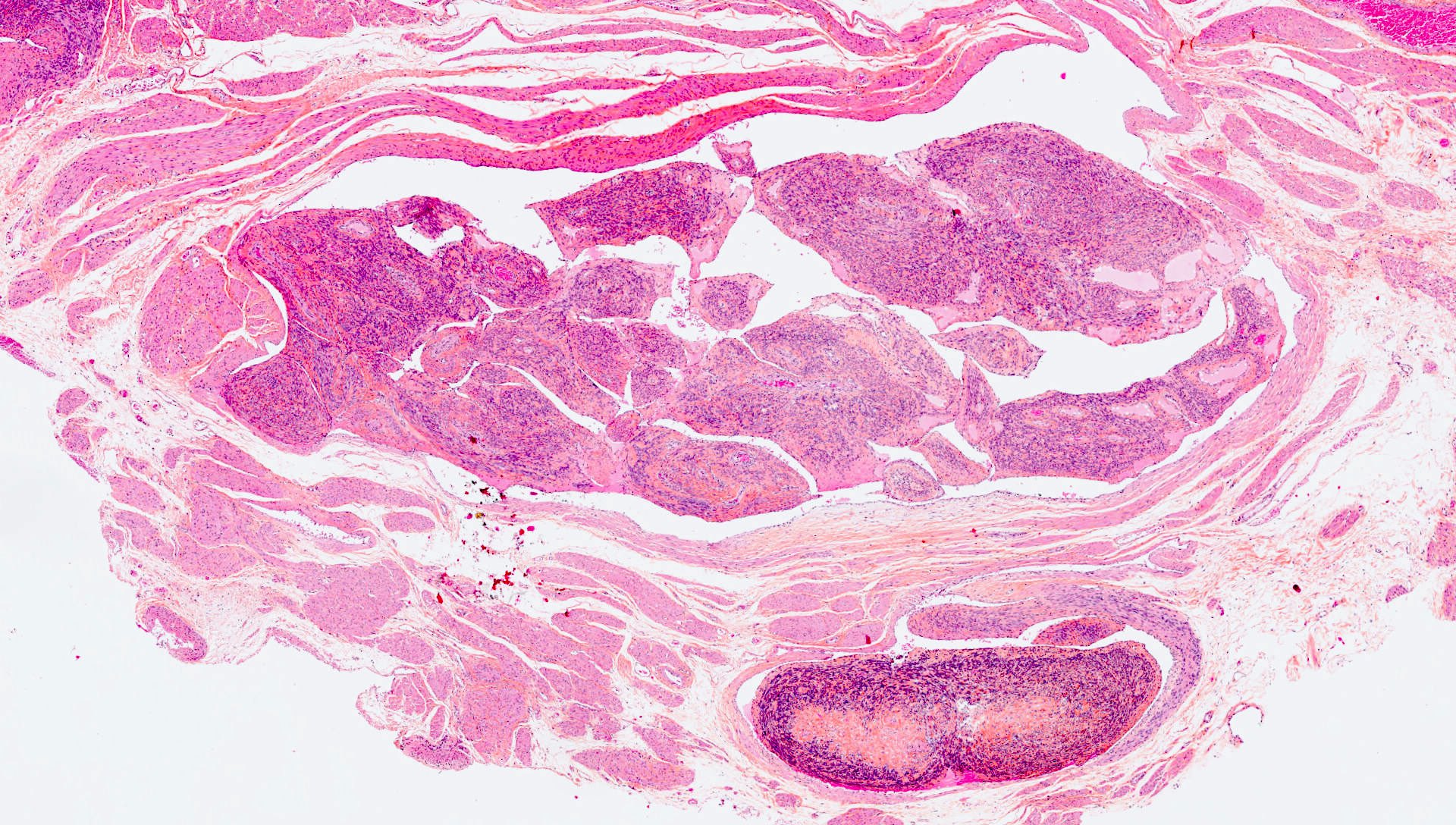
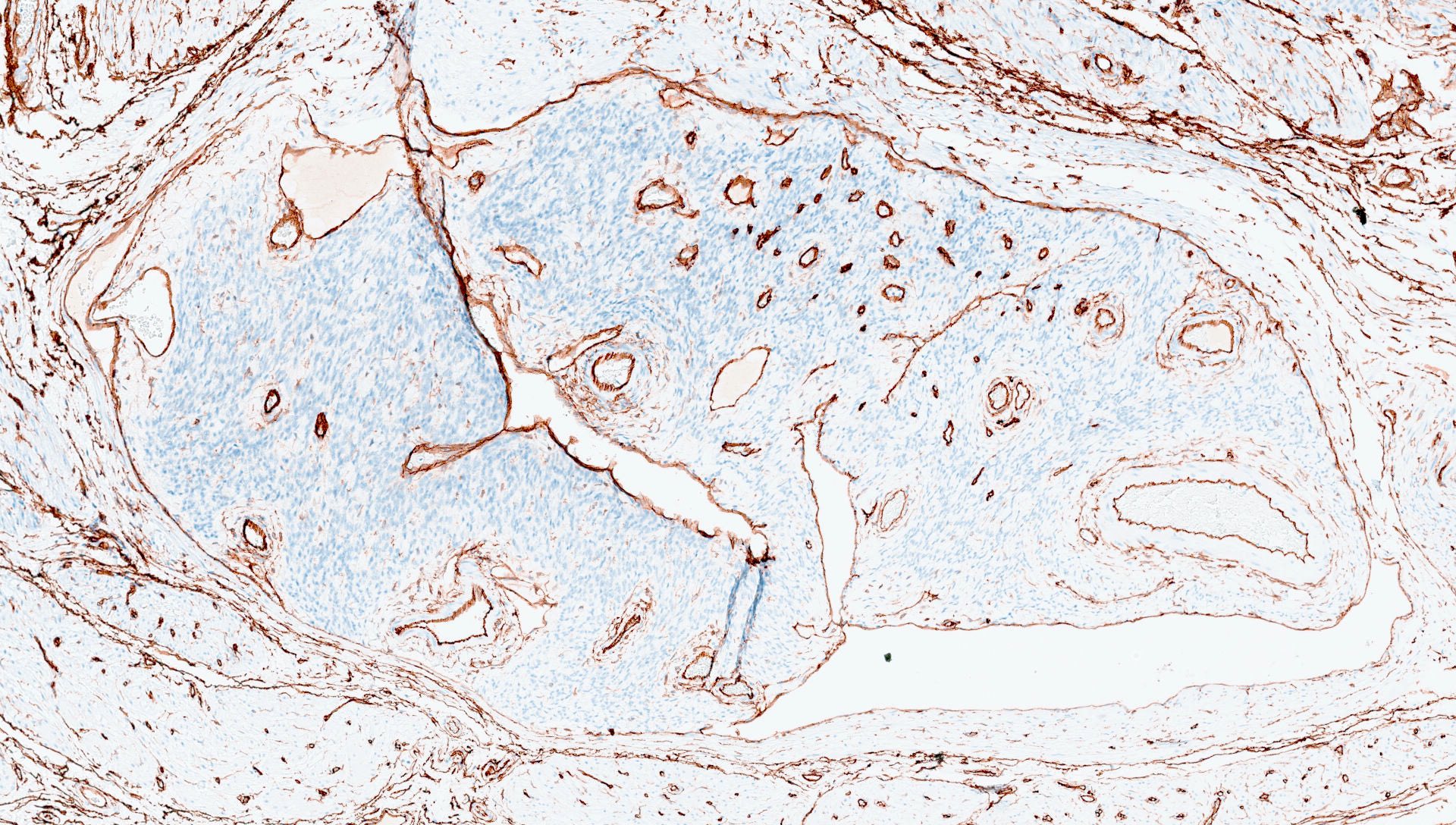
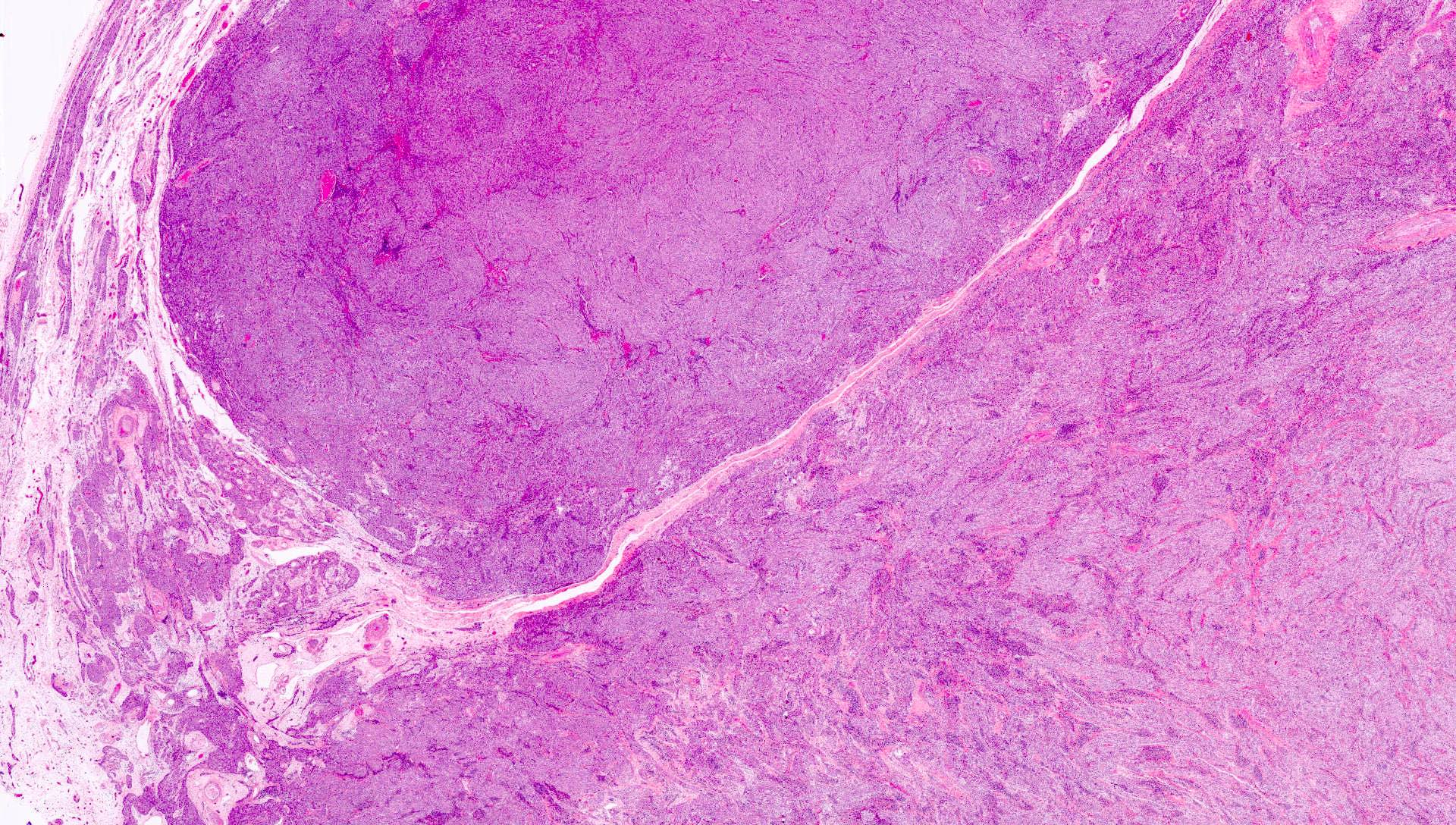
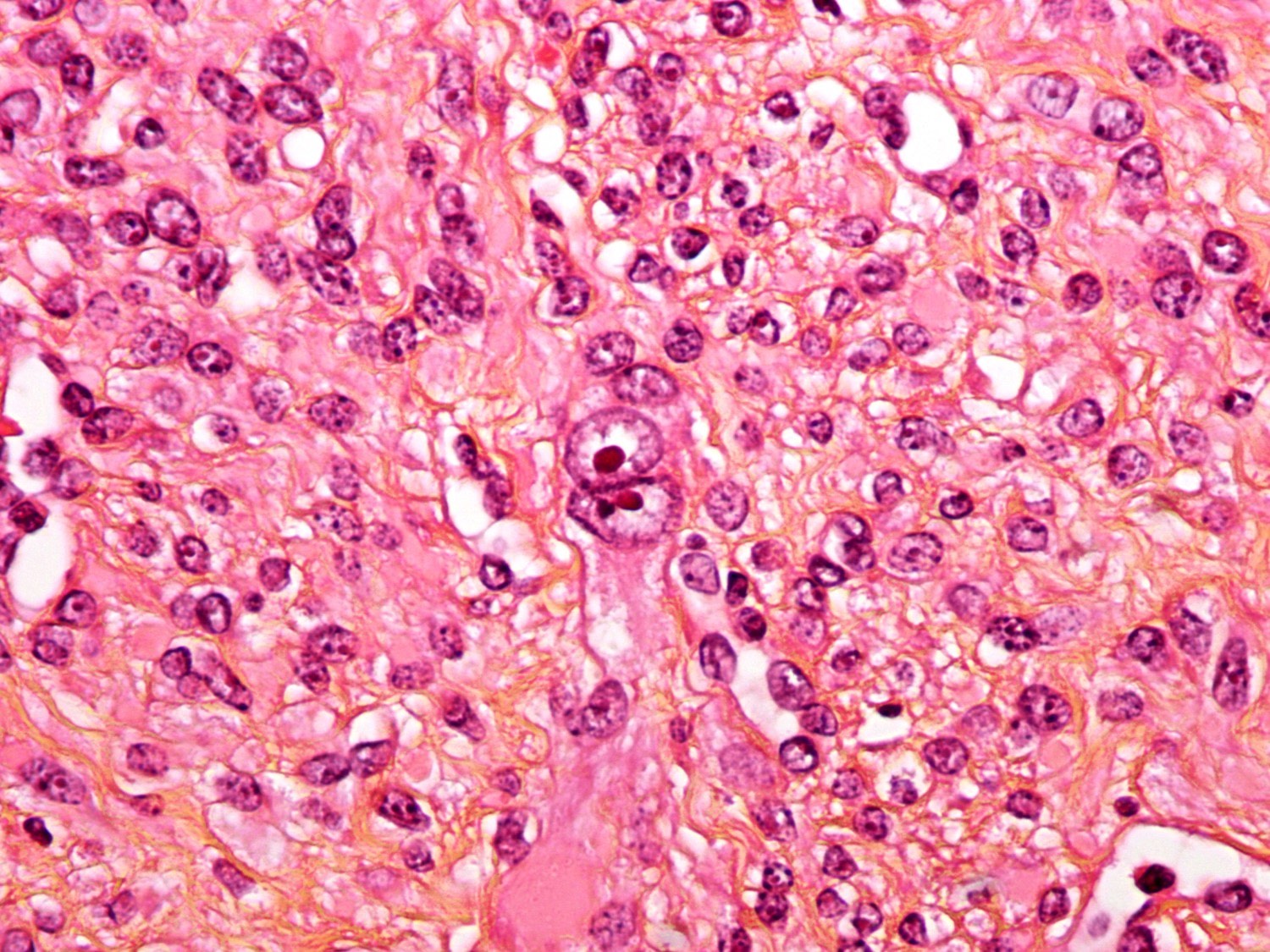
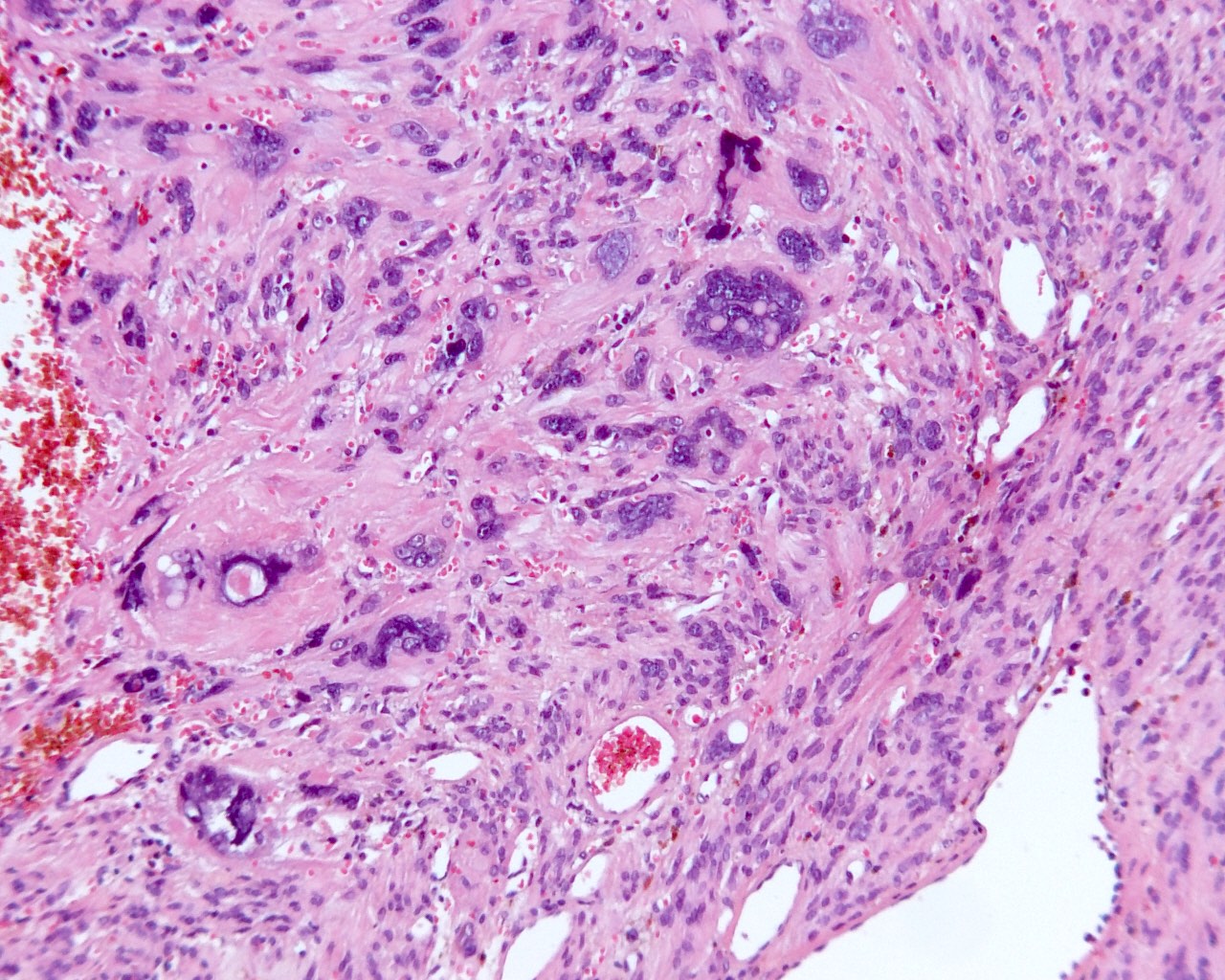
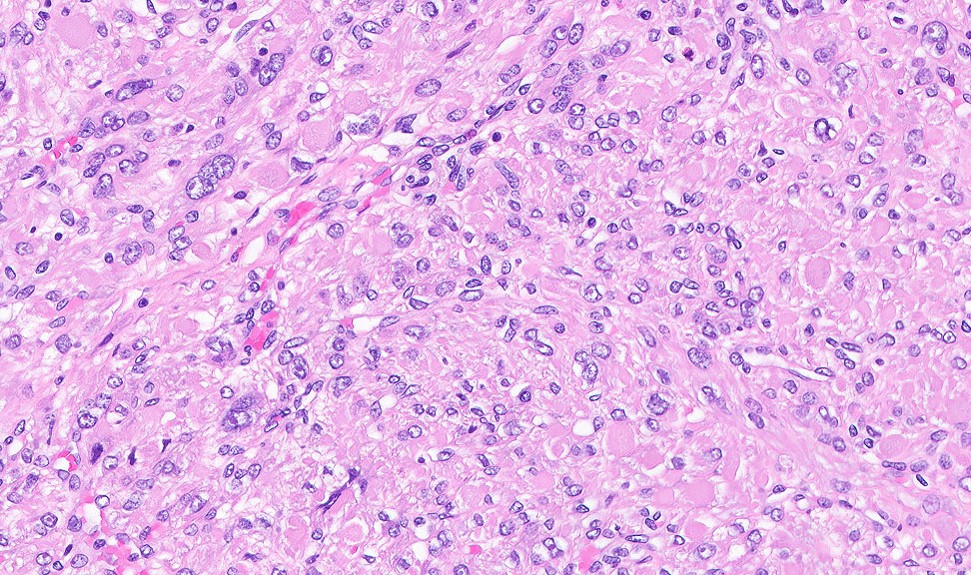
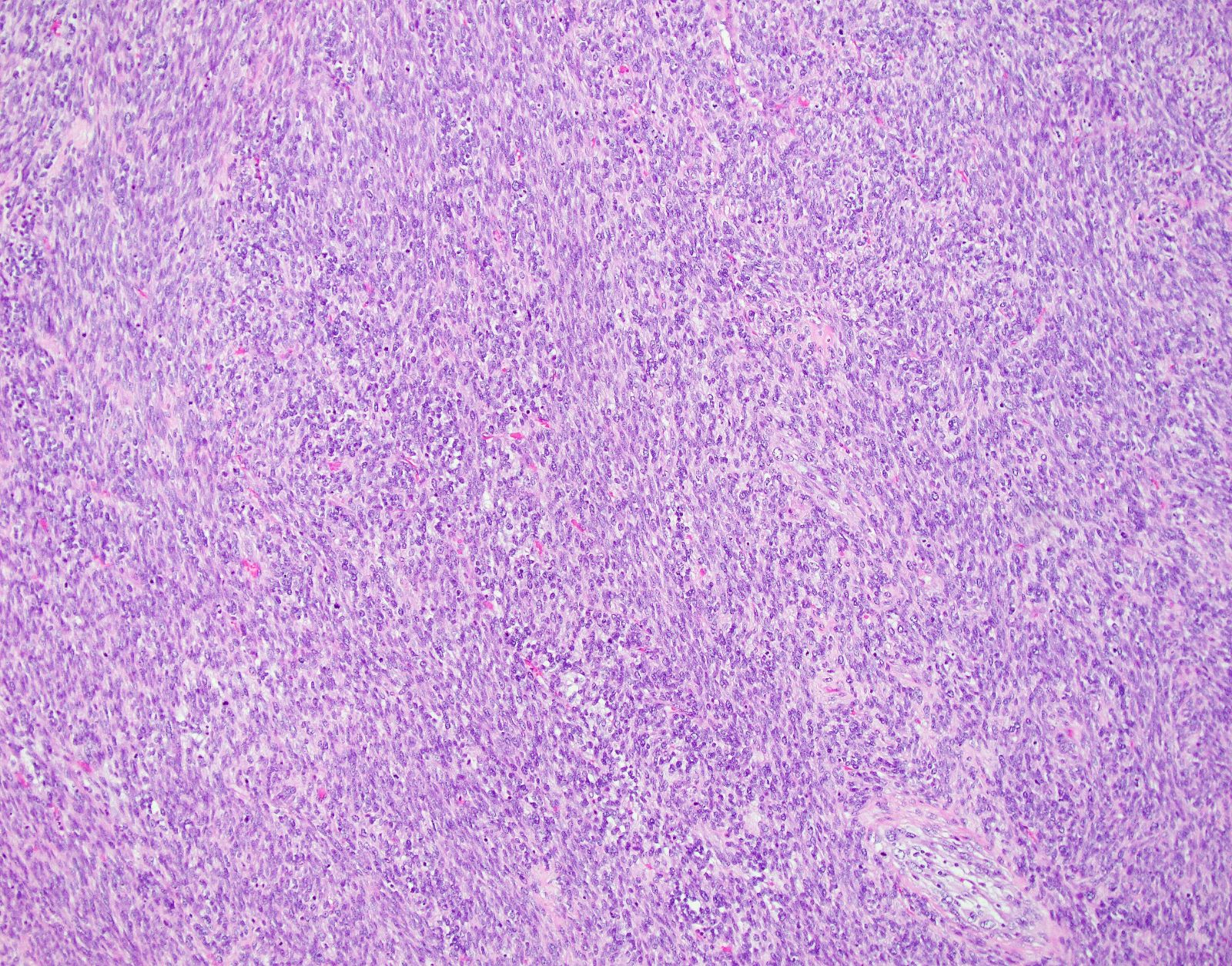
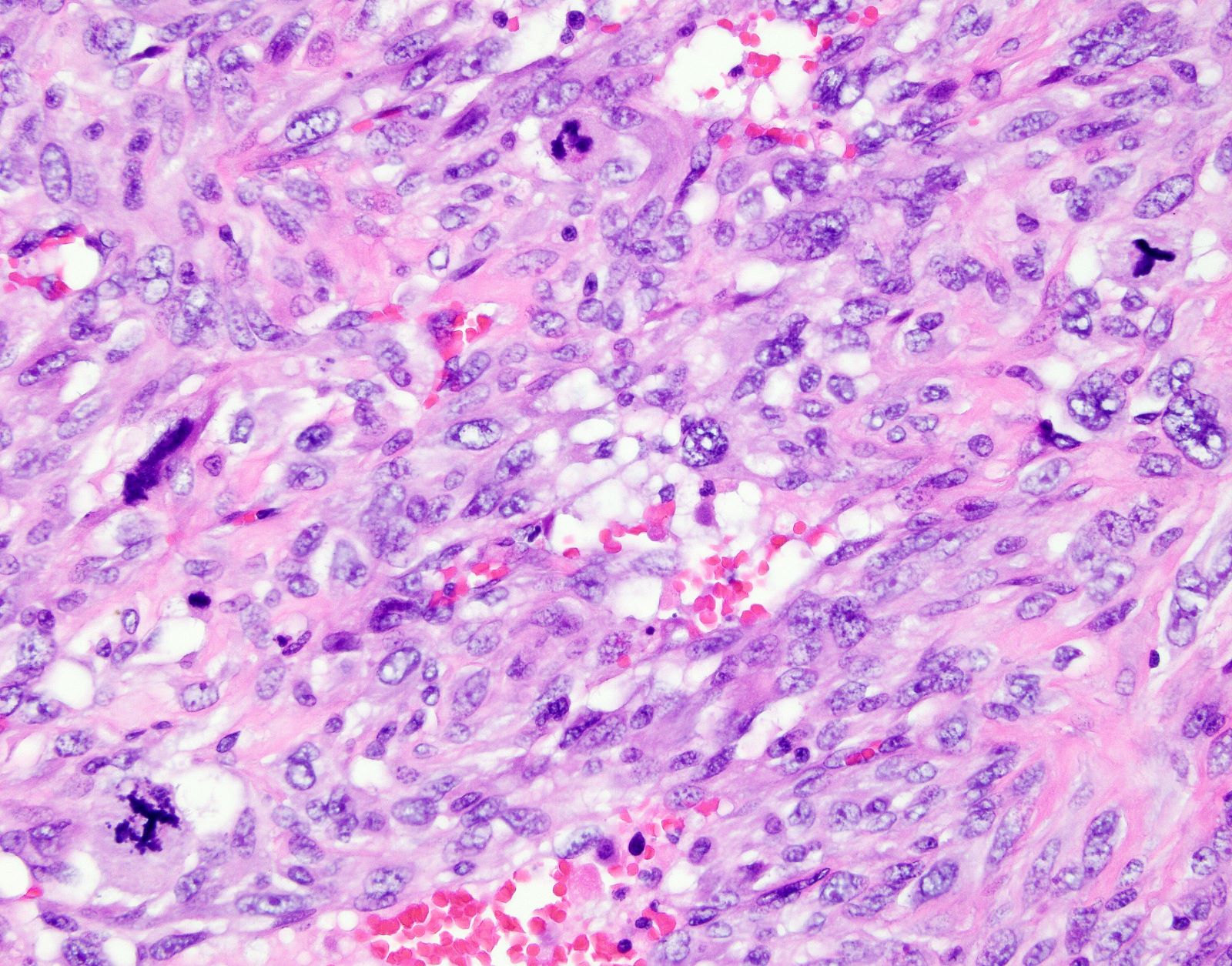
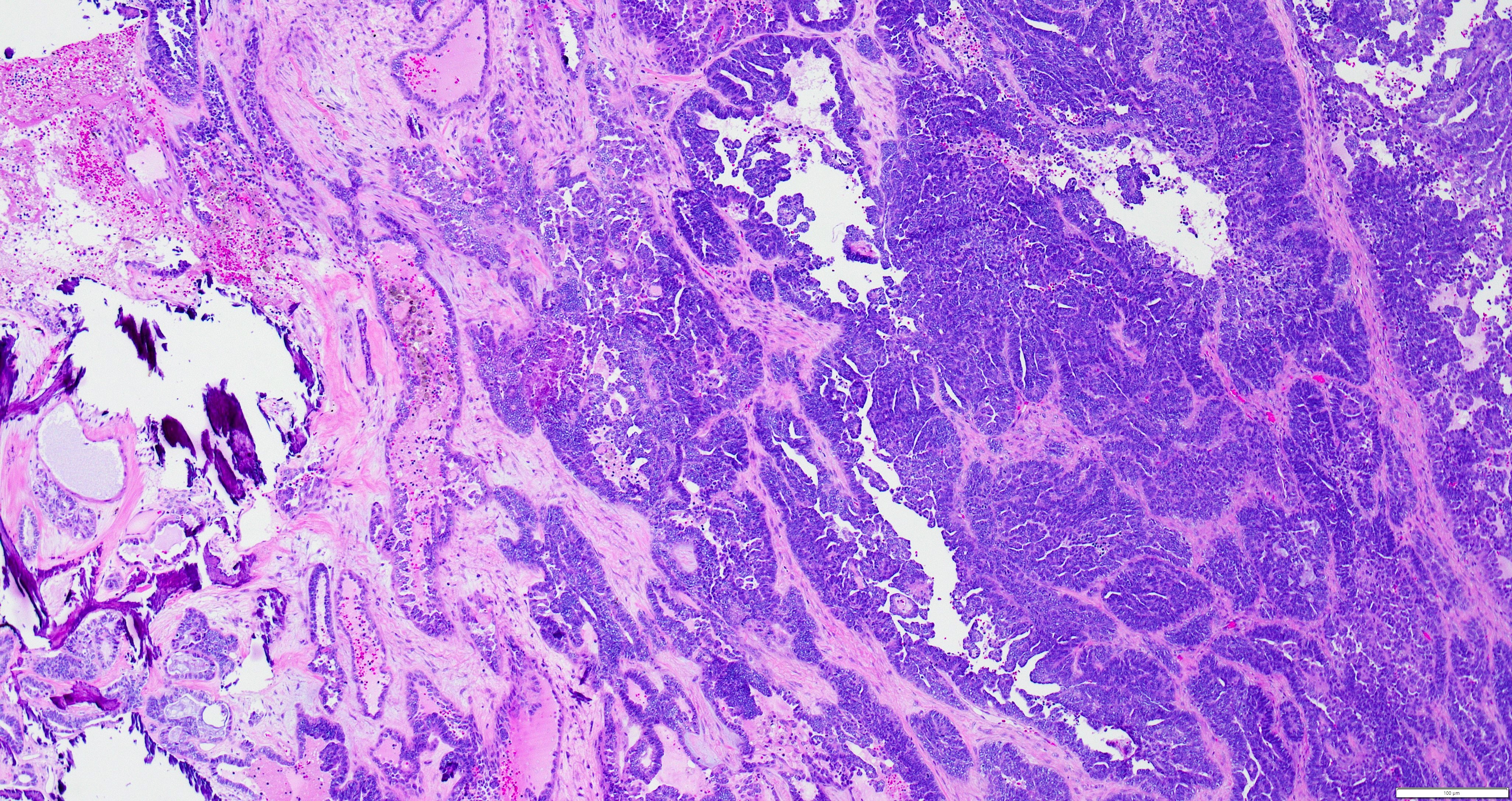
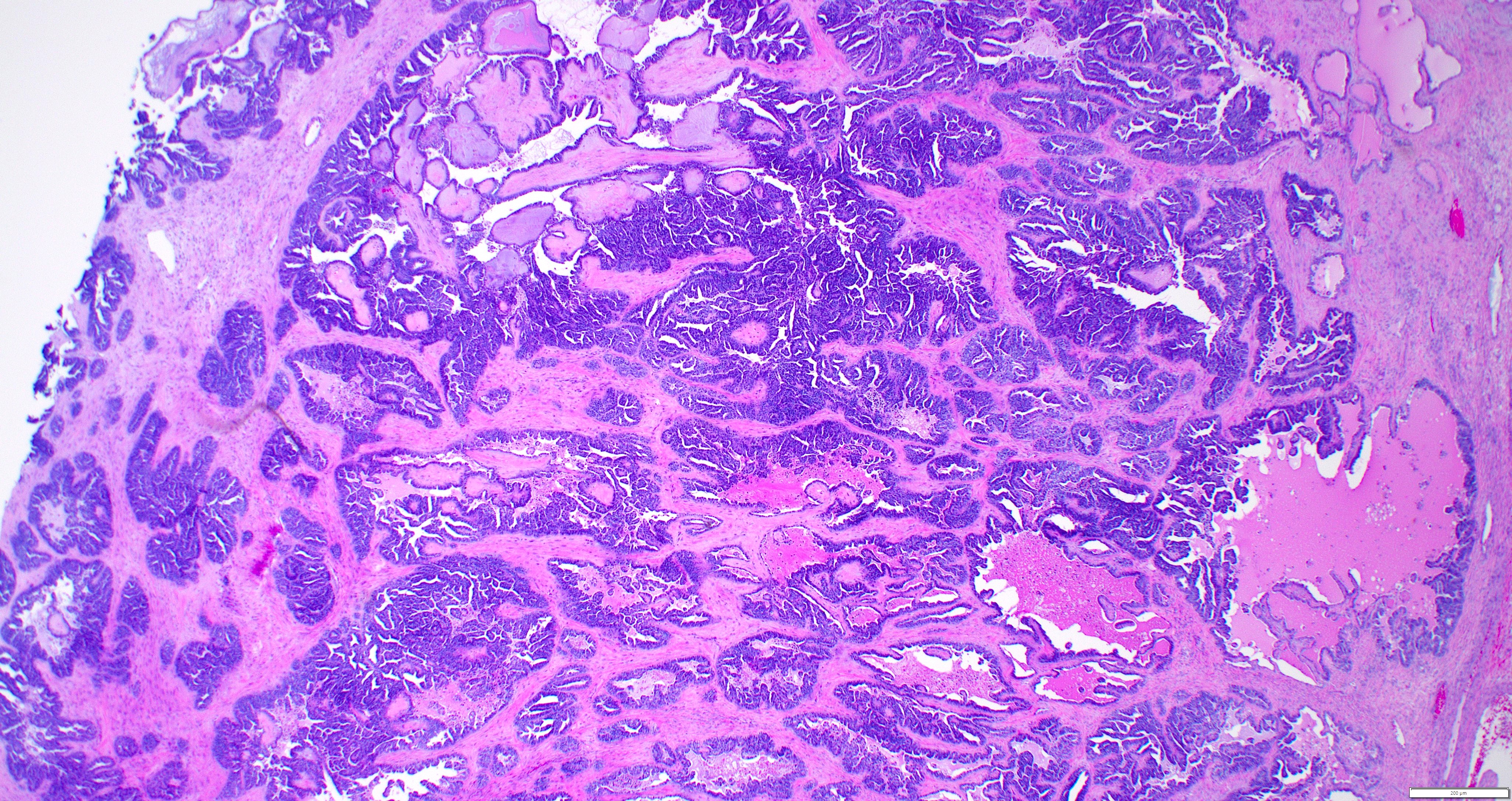
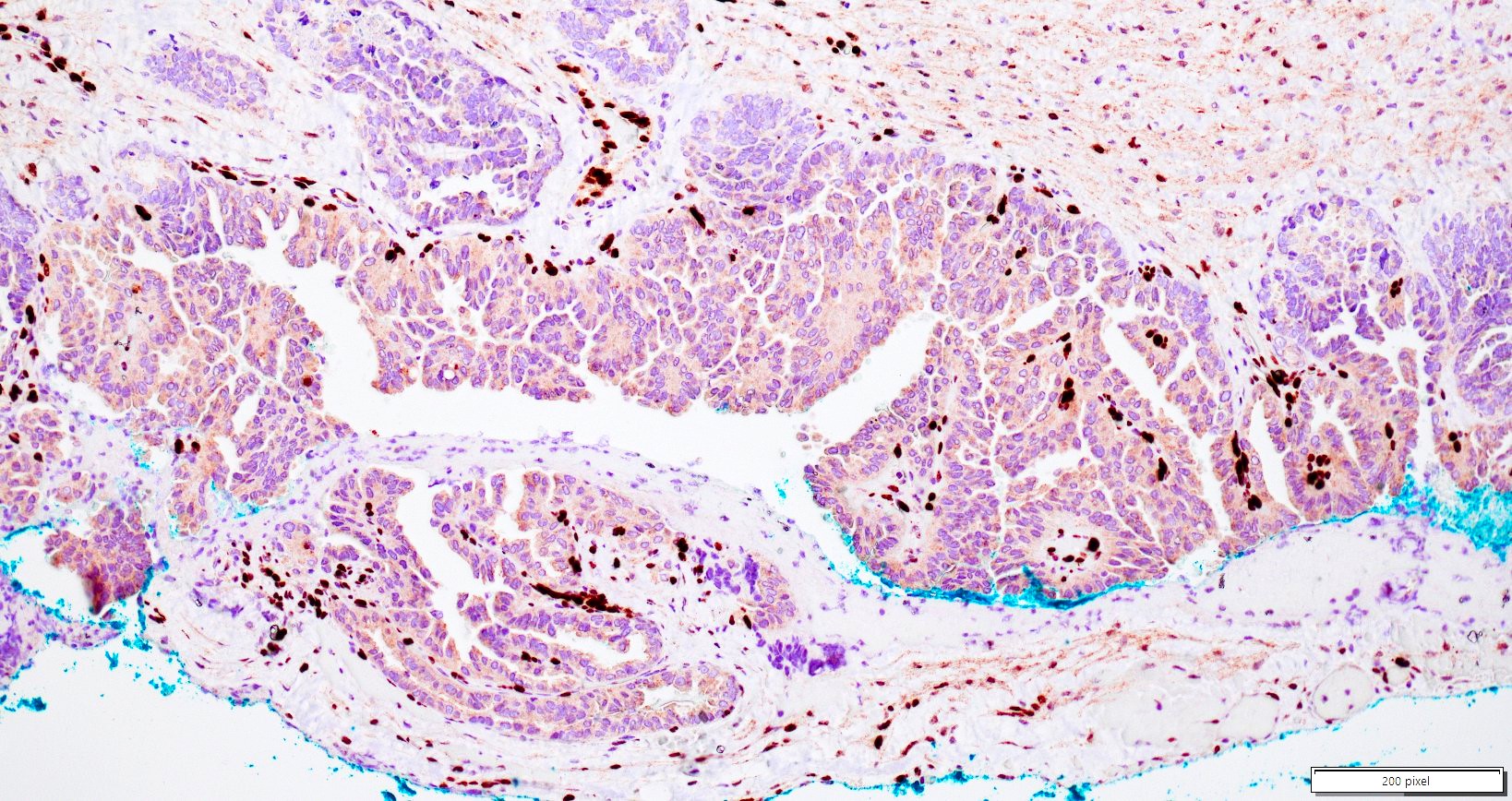
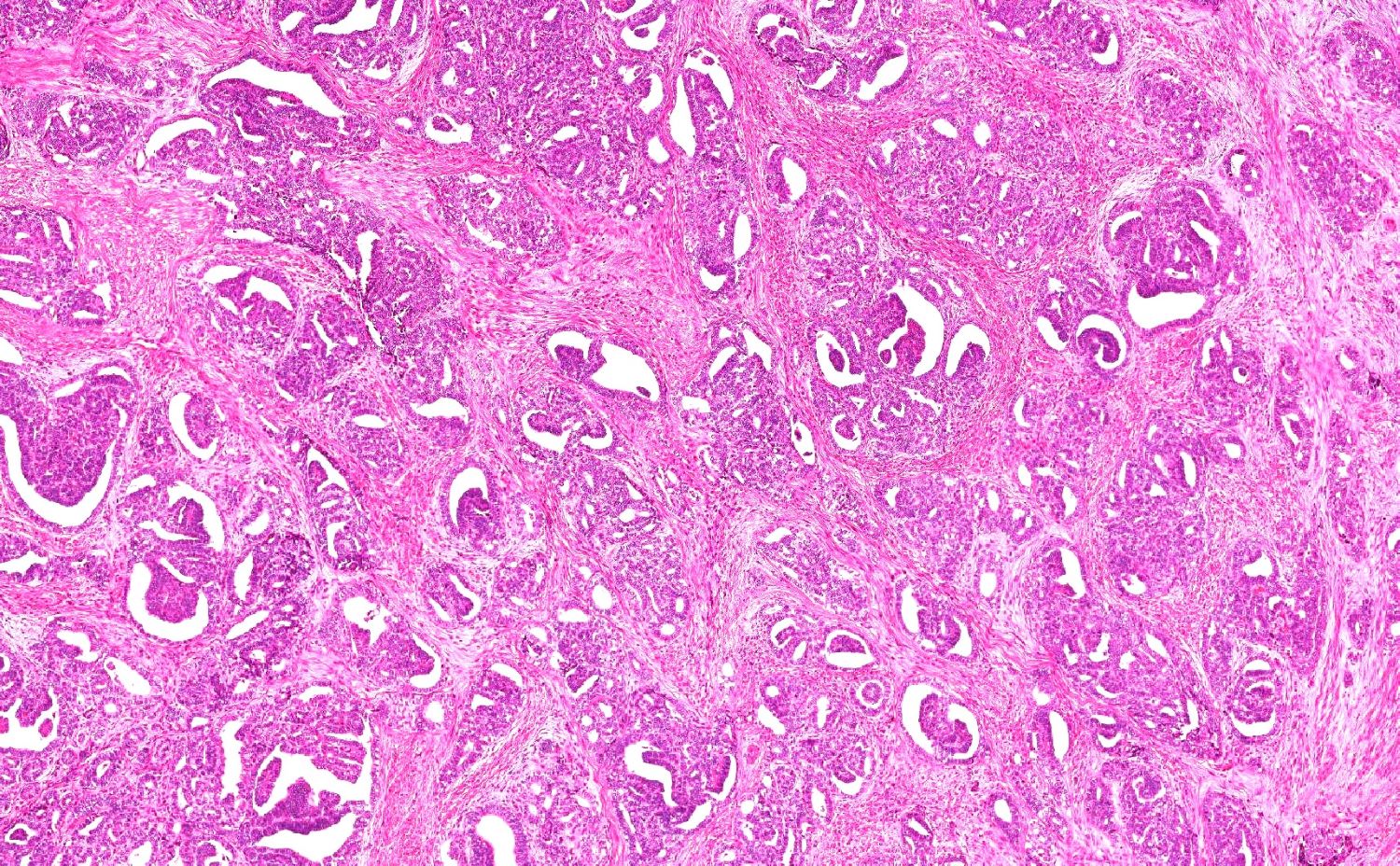
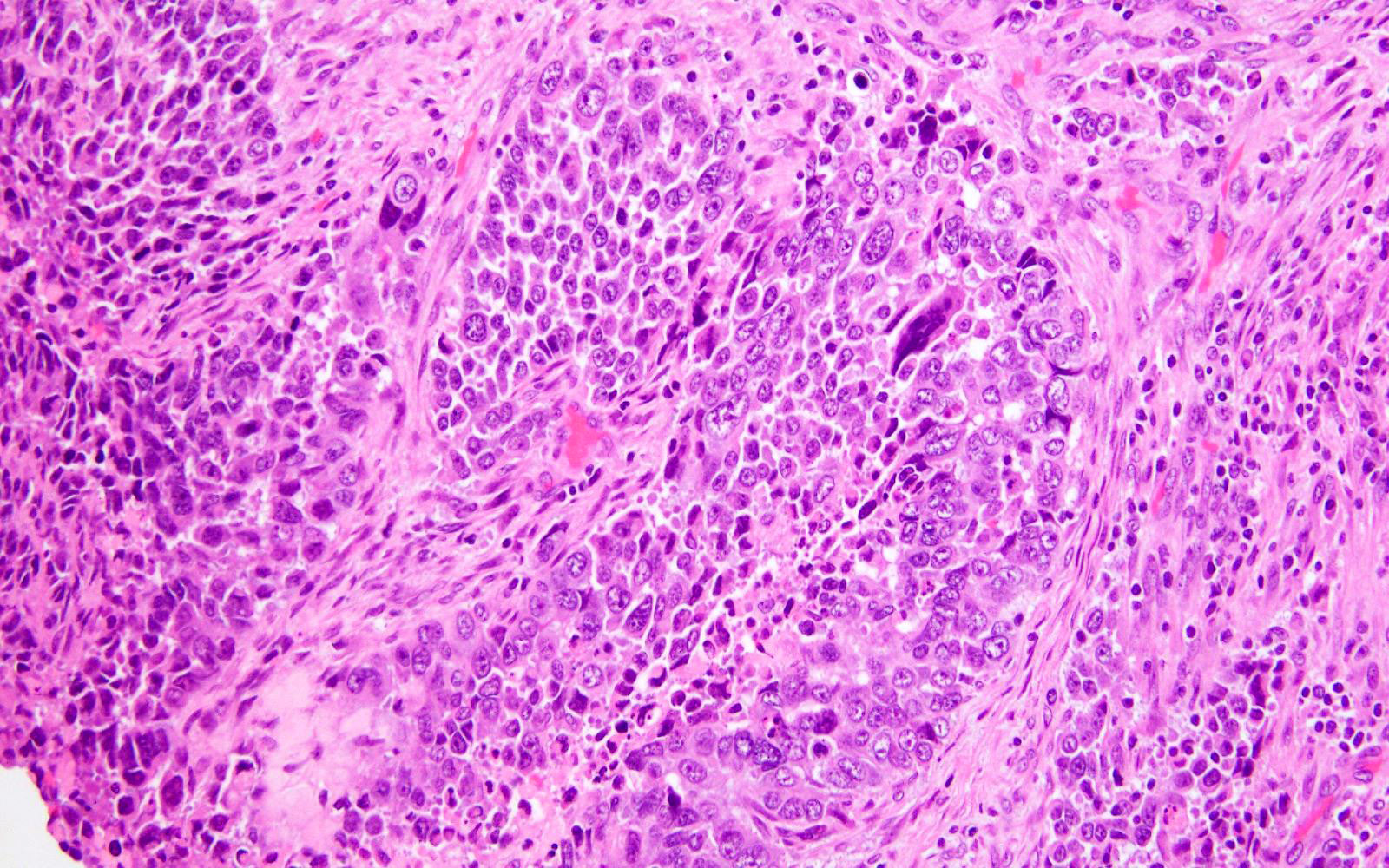
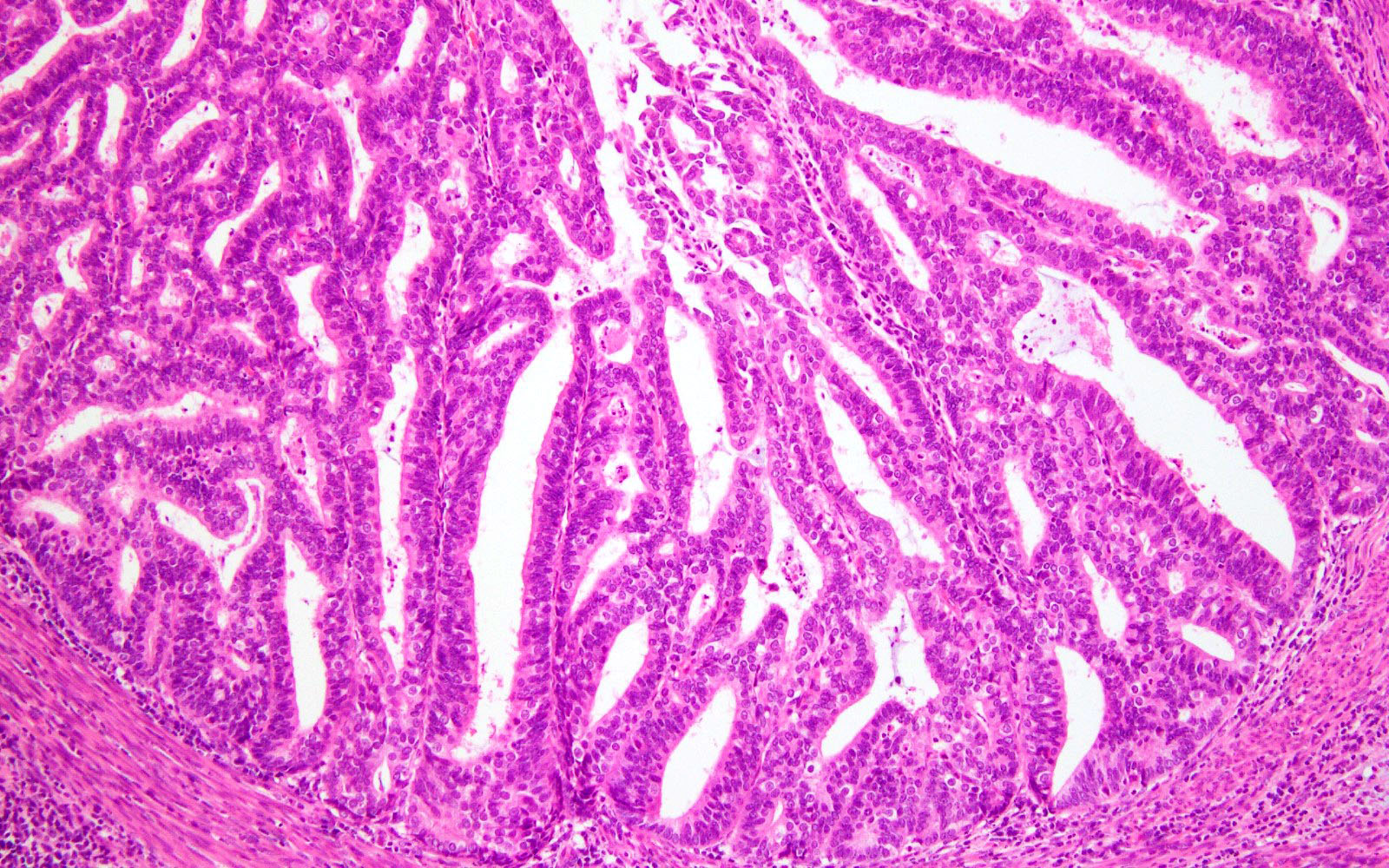
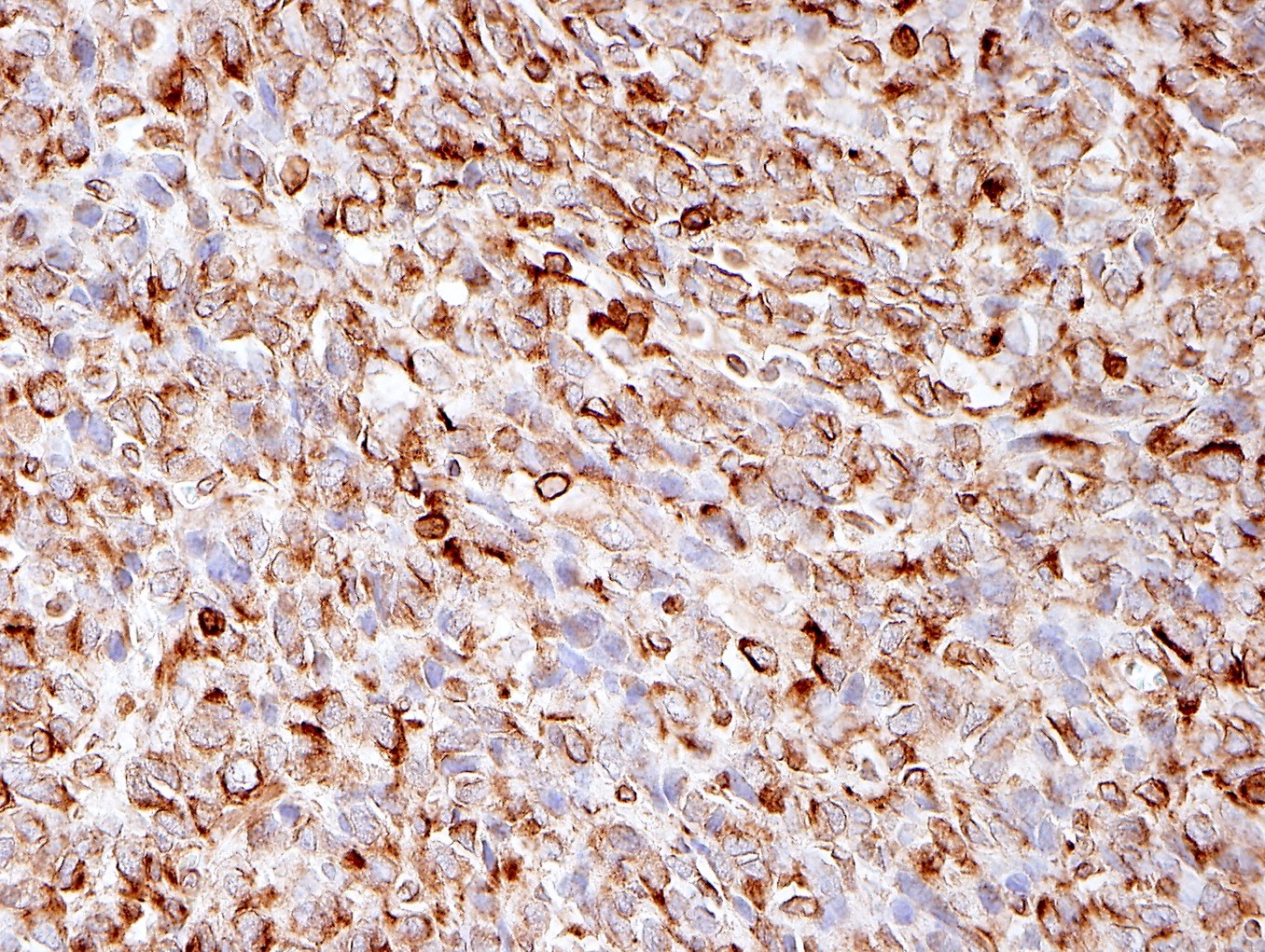
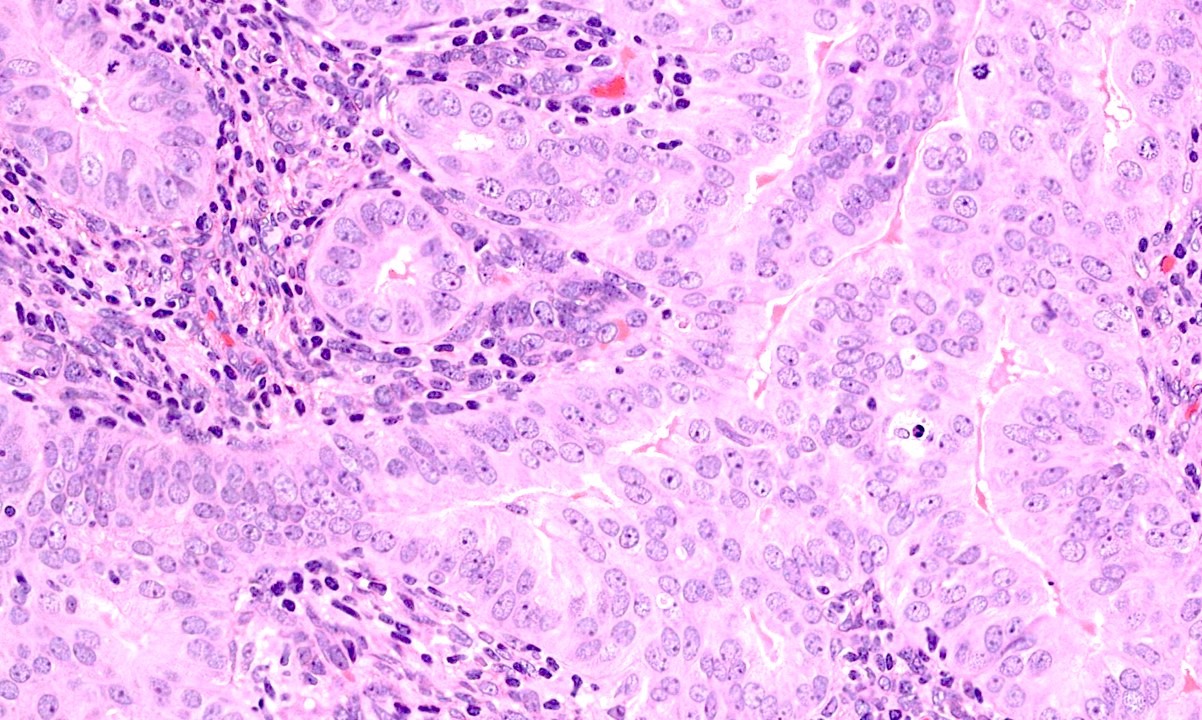
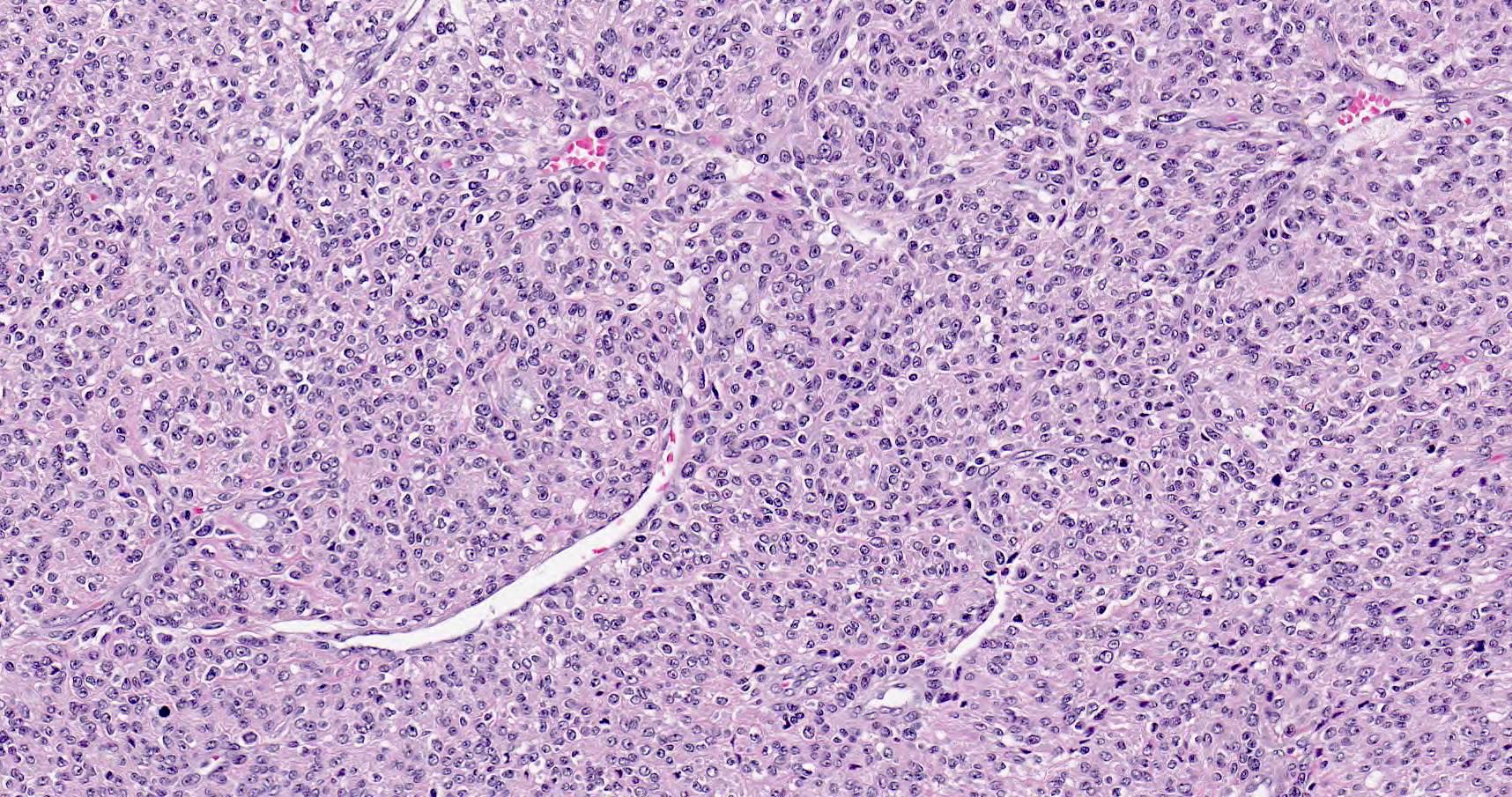
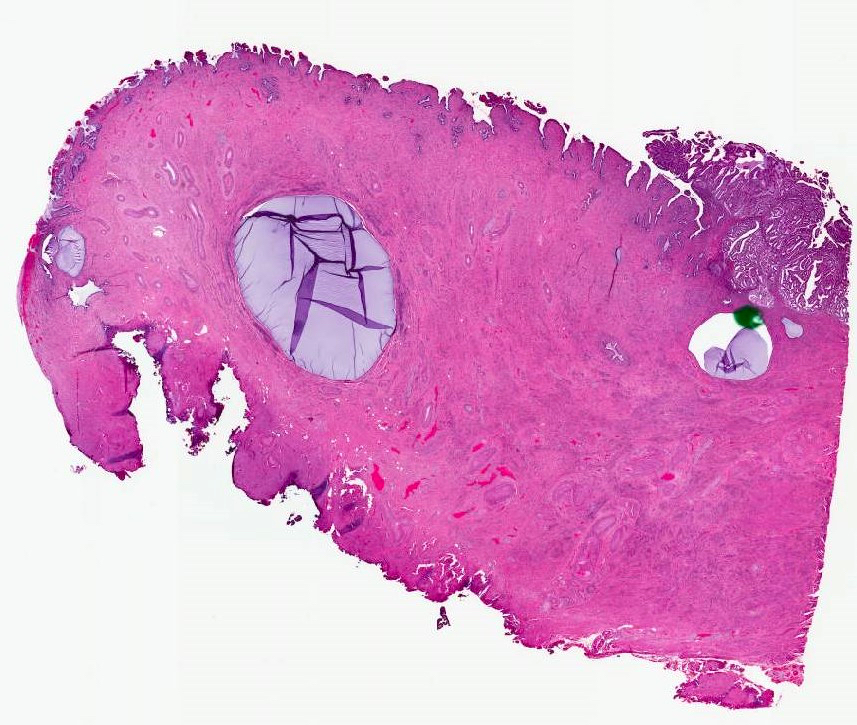
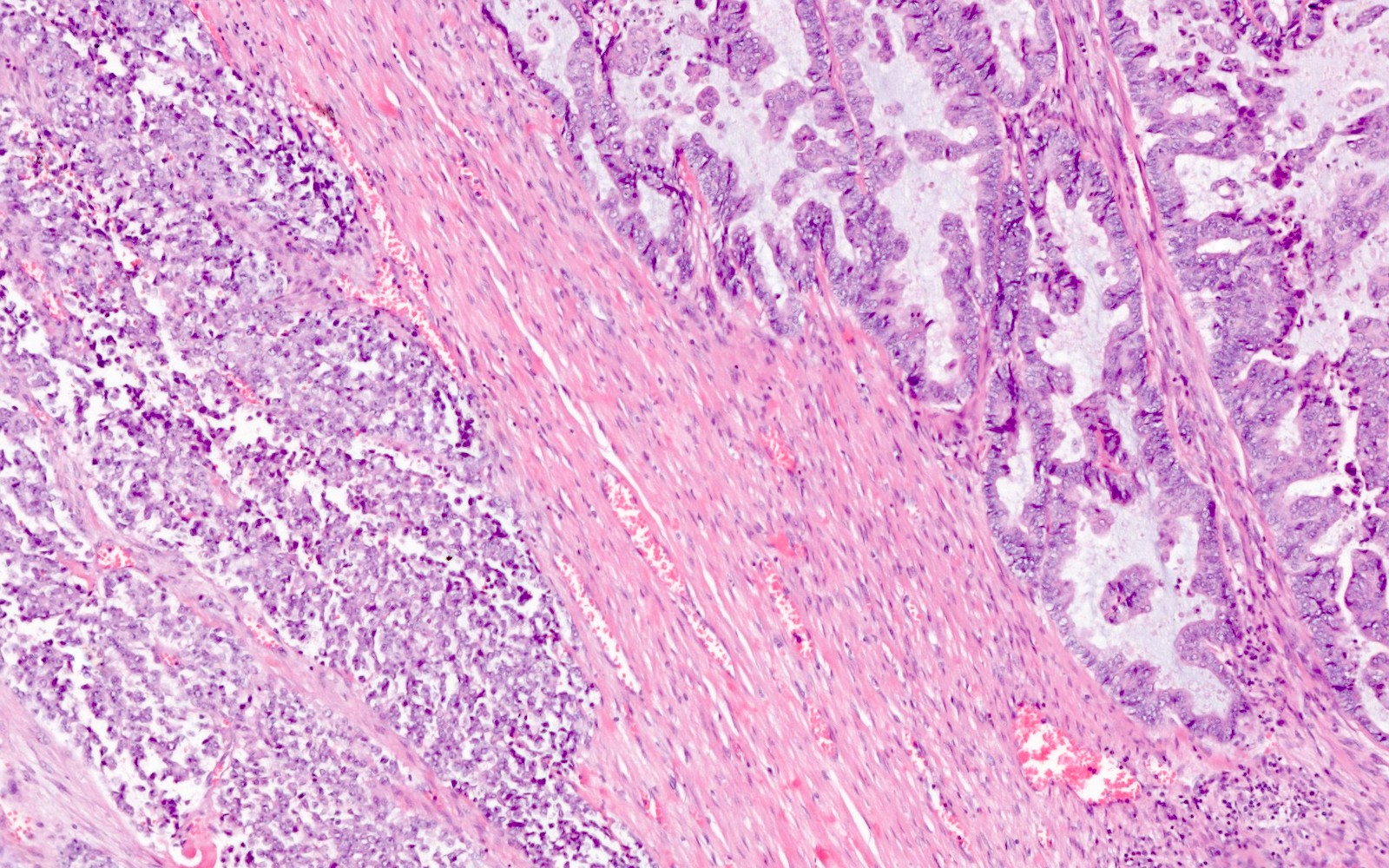
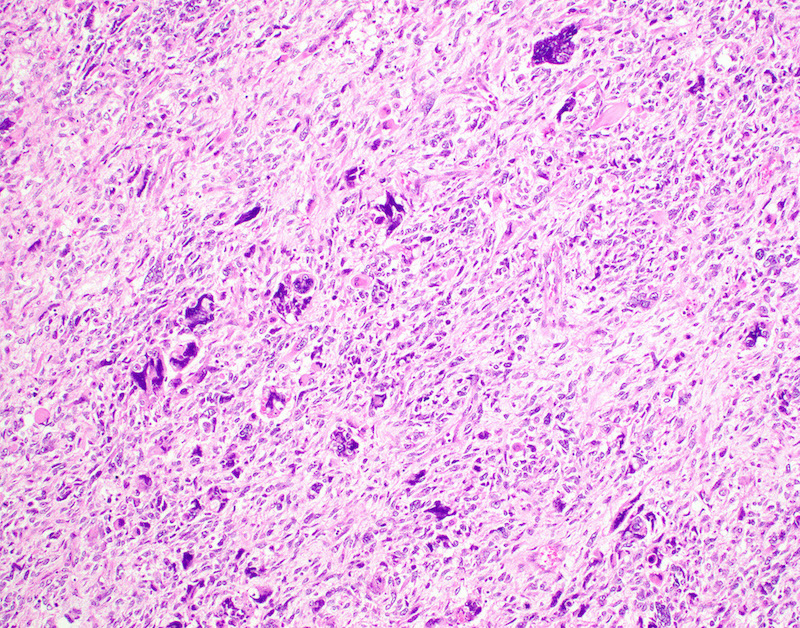
- Cervical stromal involvement:
- Presence of cervical stromal involvement defines stage II
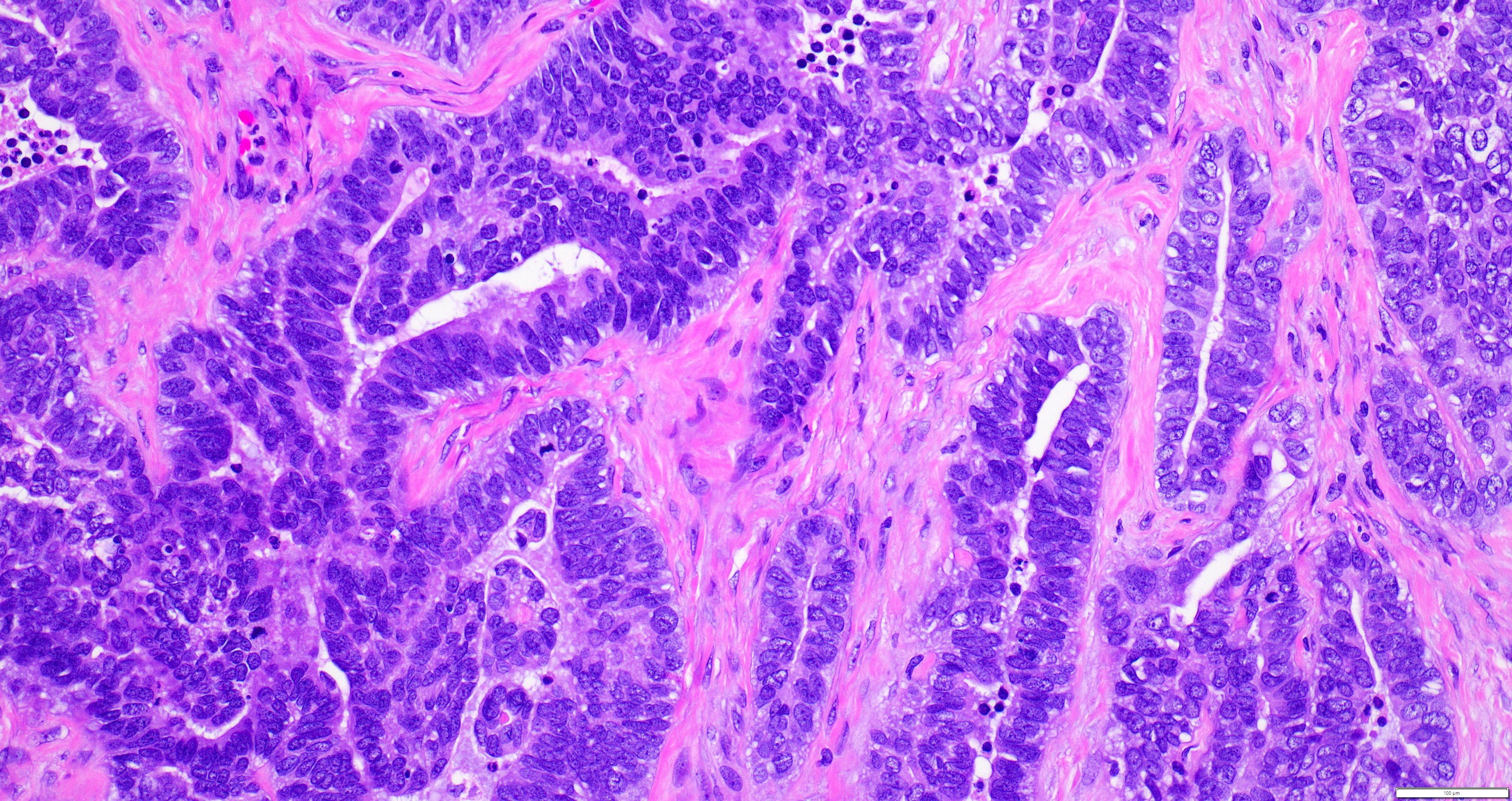
- Depth of invasion into the cervical stroma and margin status should be reported, as it may influence adjuvant radiation treatment (Brachytherapy 2019;18:606)
- Assessment of cervical involvement is inconsistent between gynecologic pathologists (Am J Surg Pathol 2011;35:289)
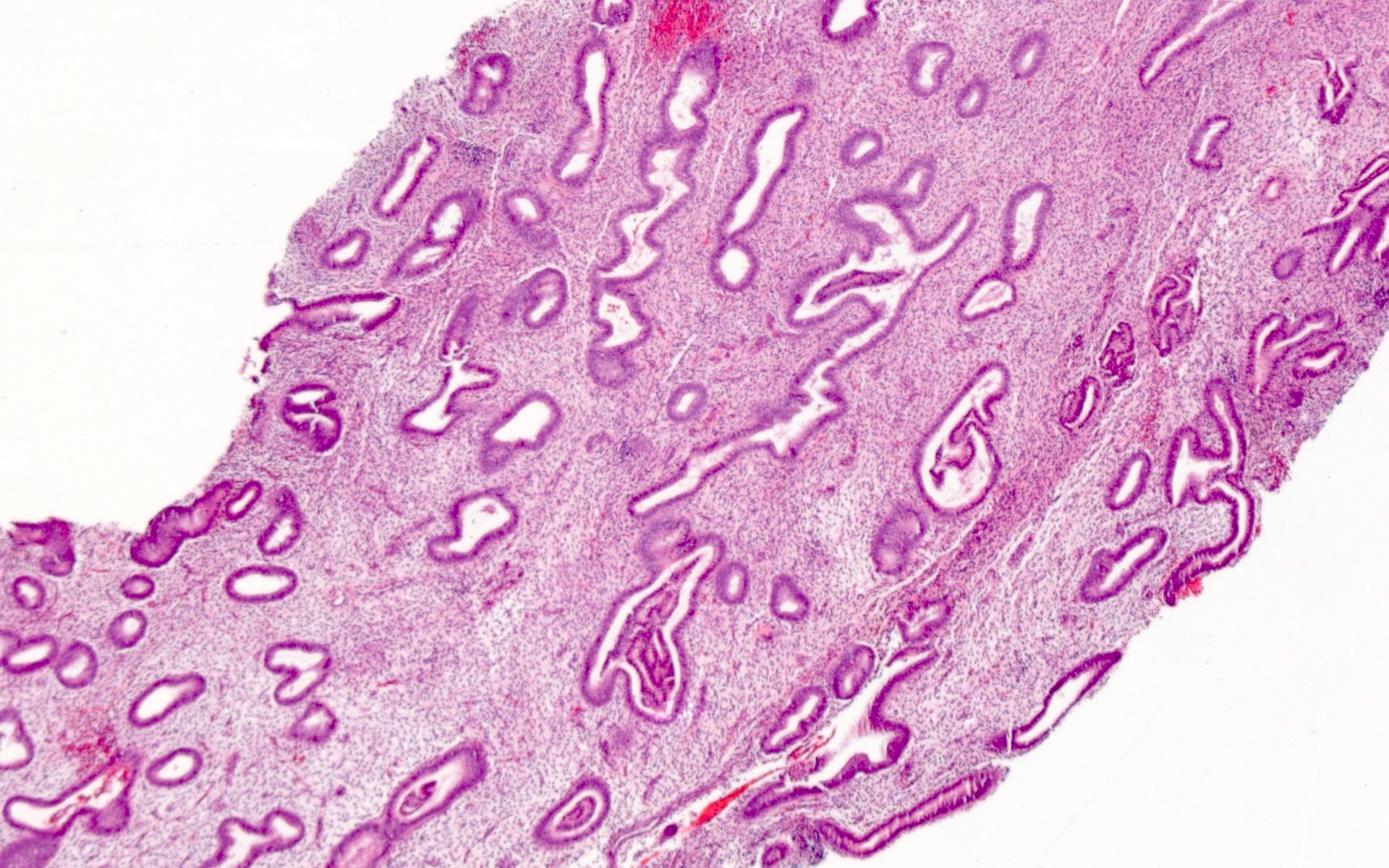
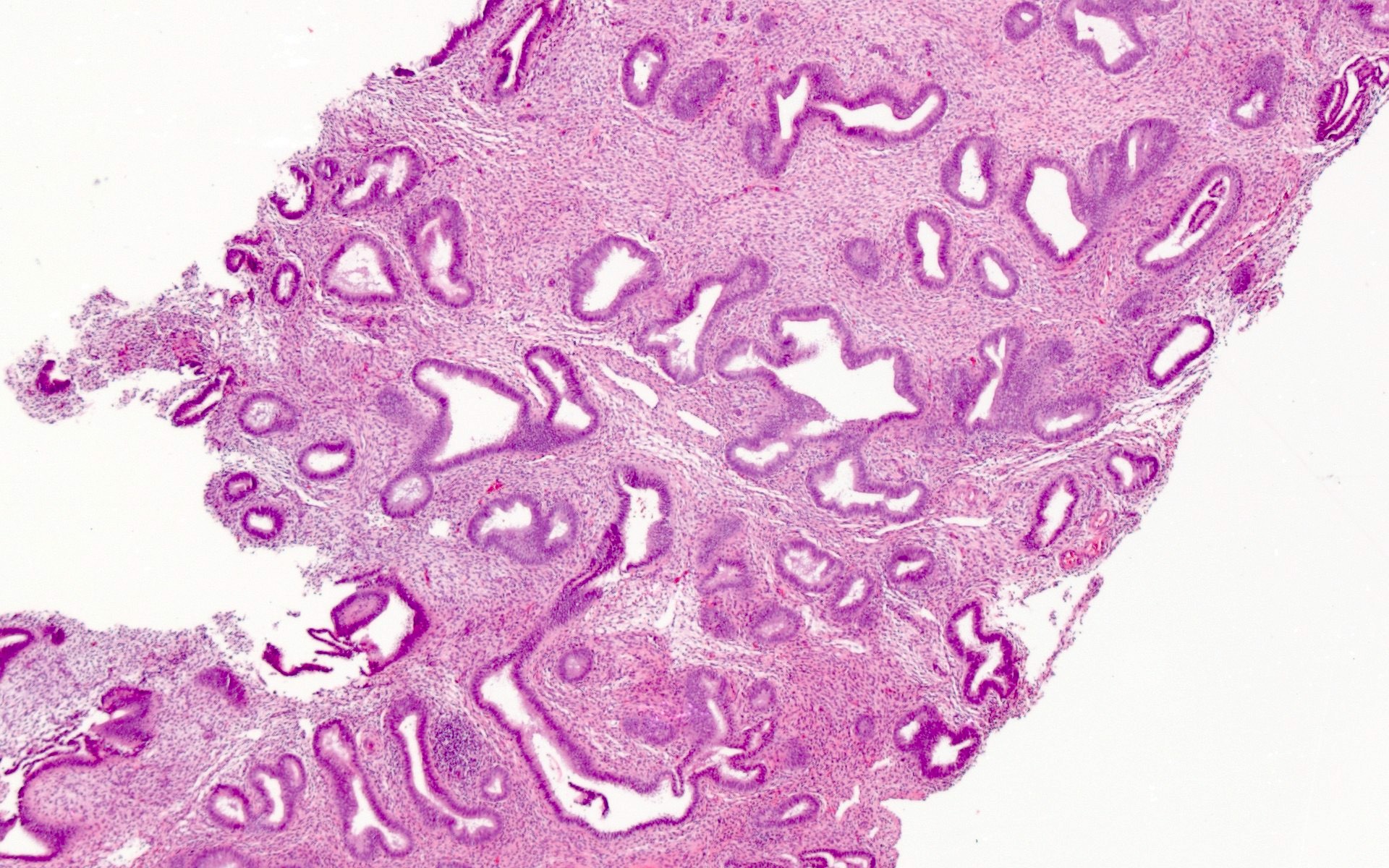
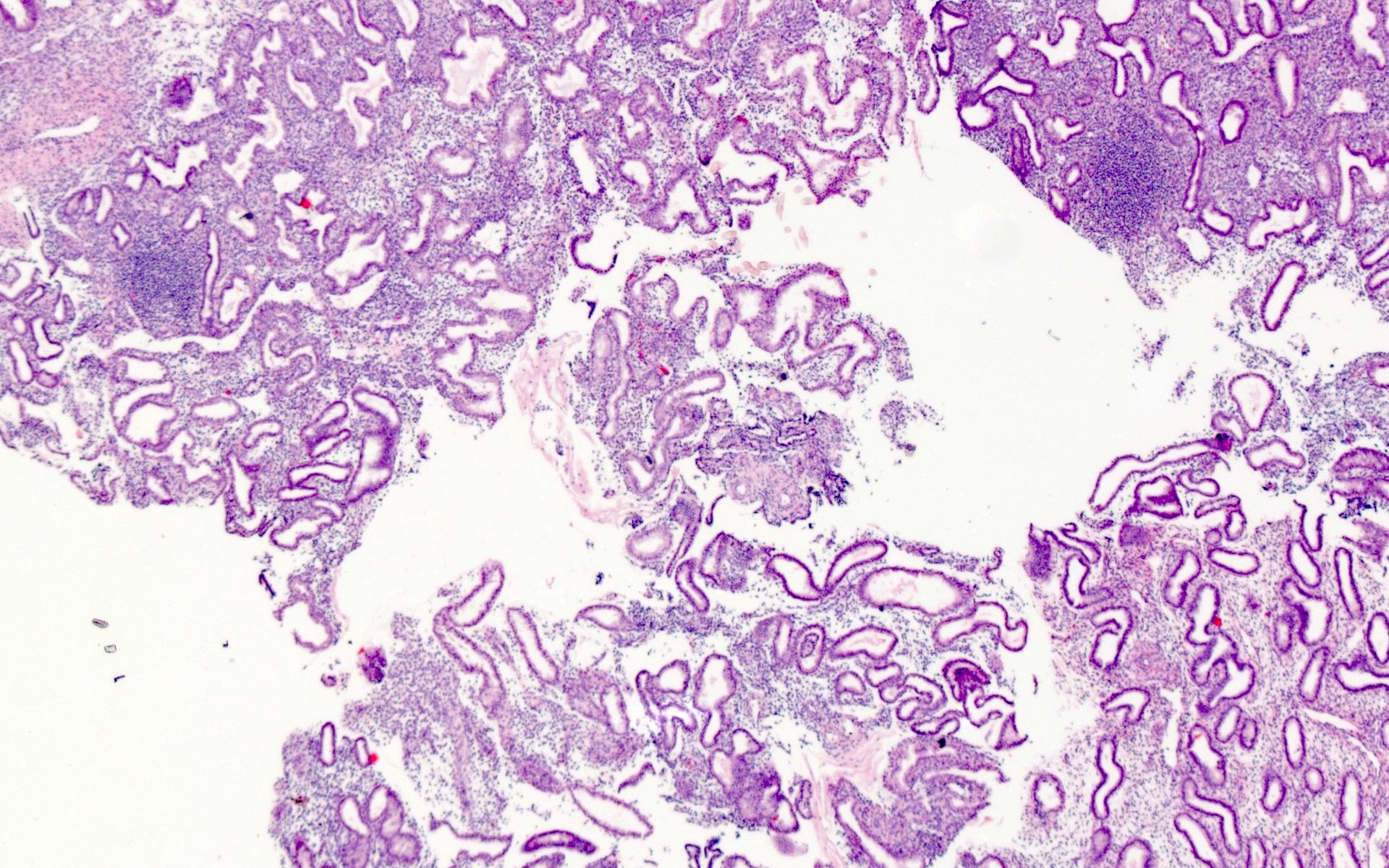
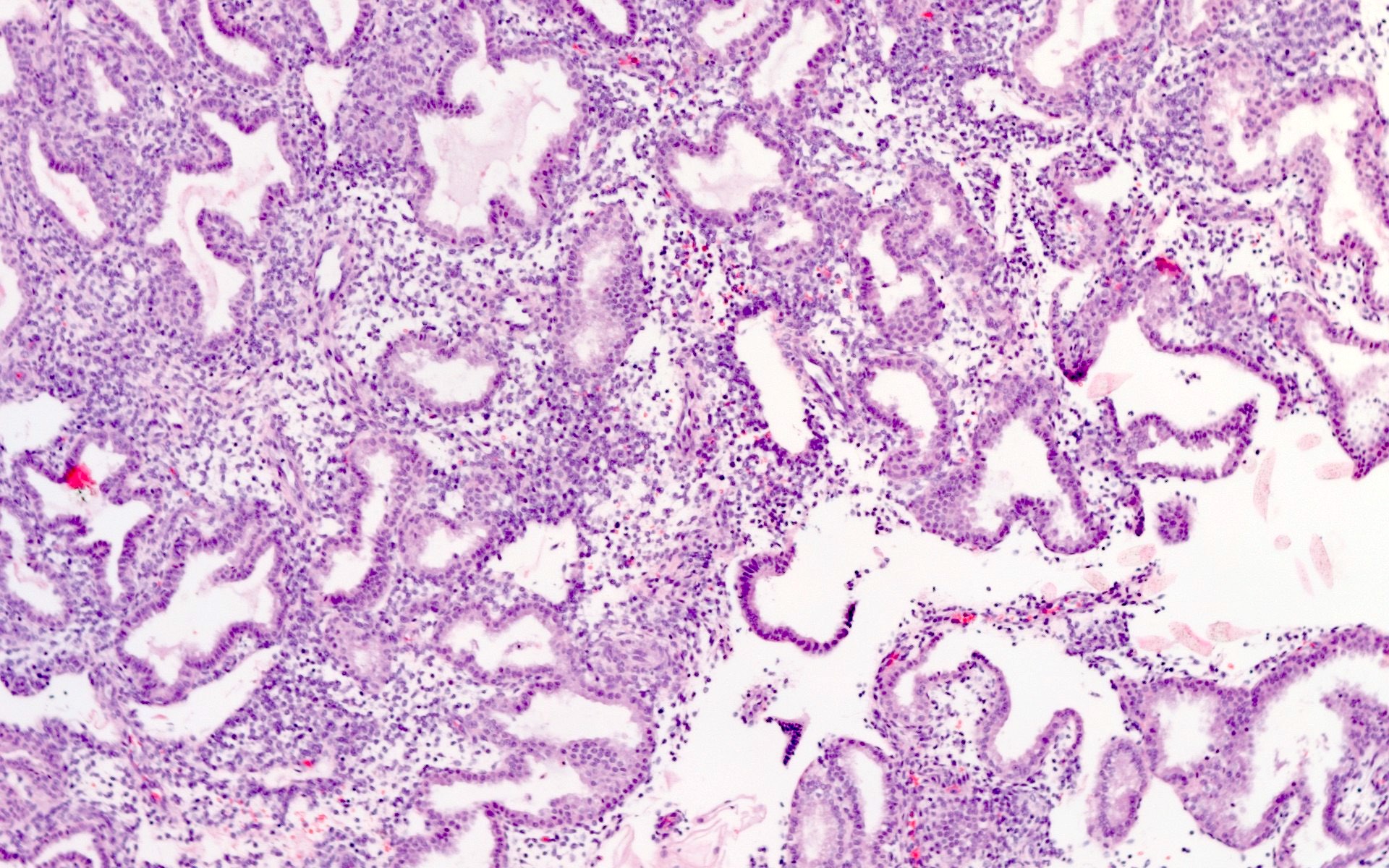
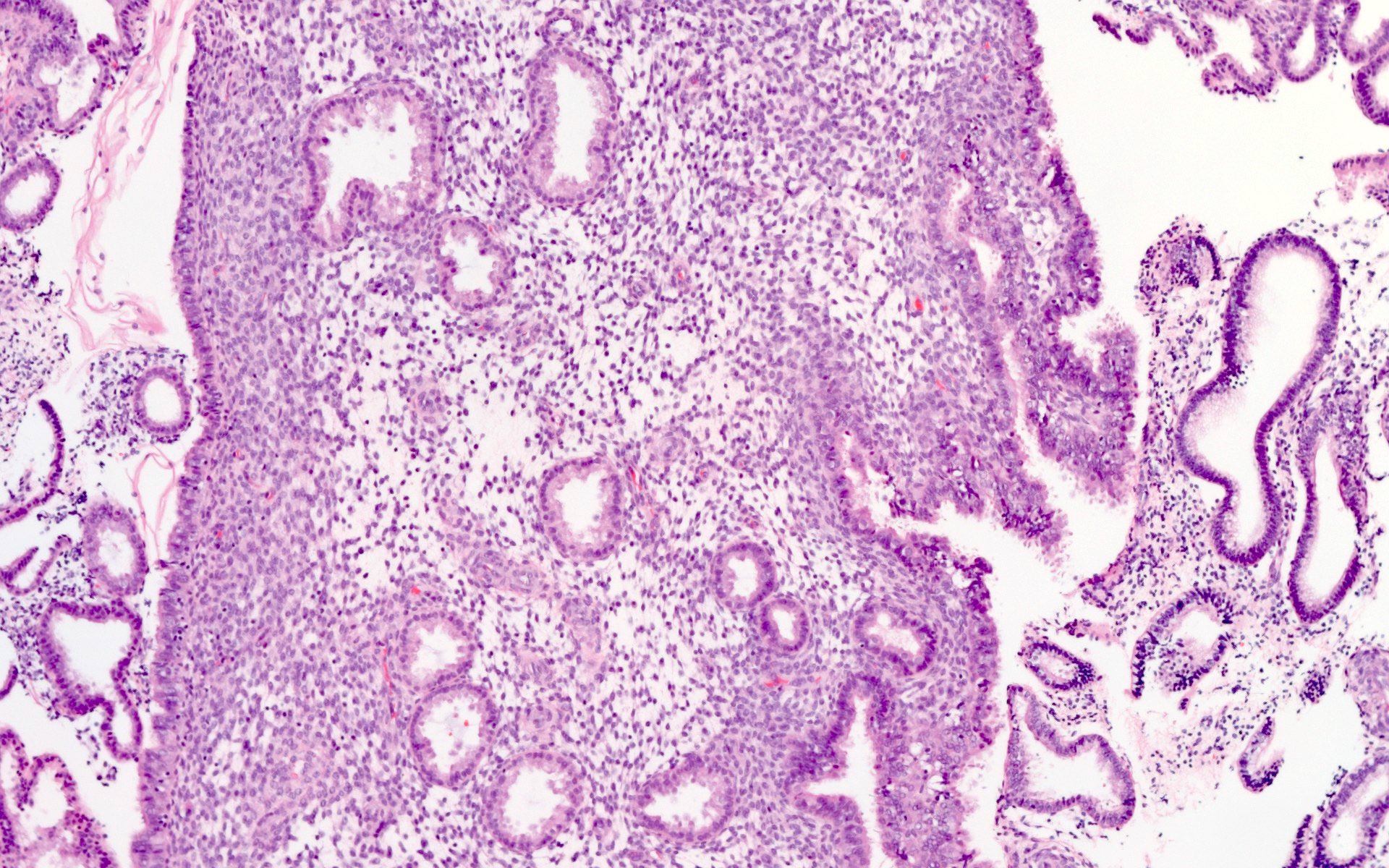
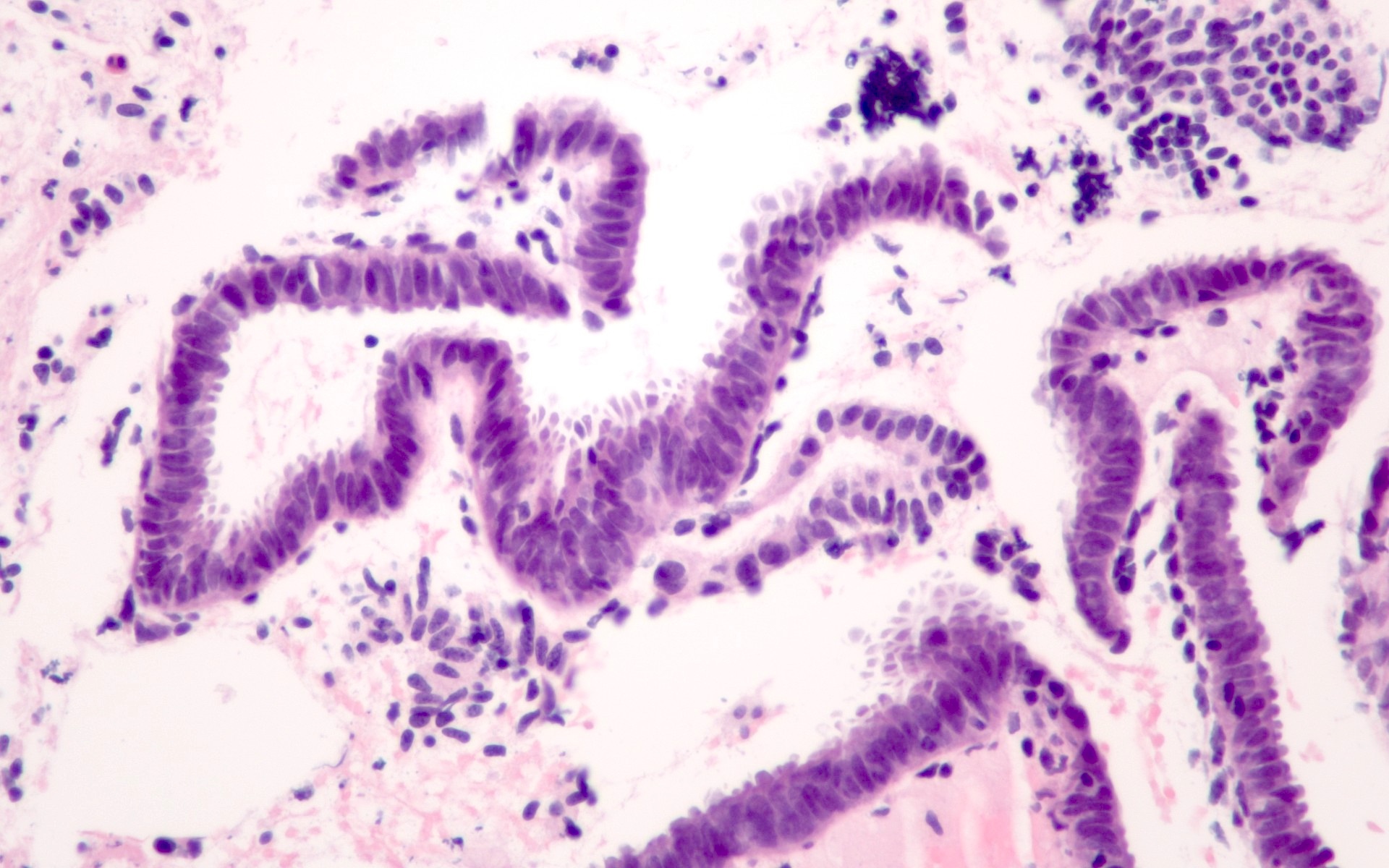
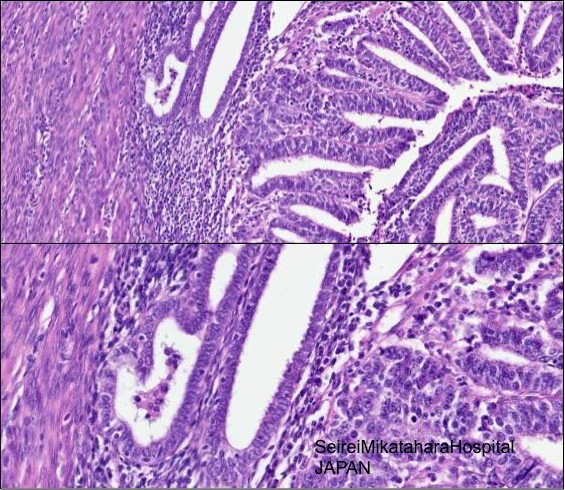
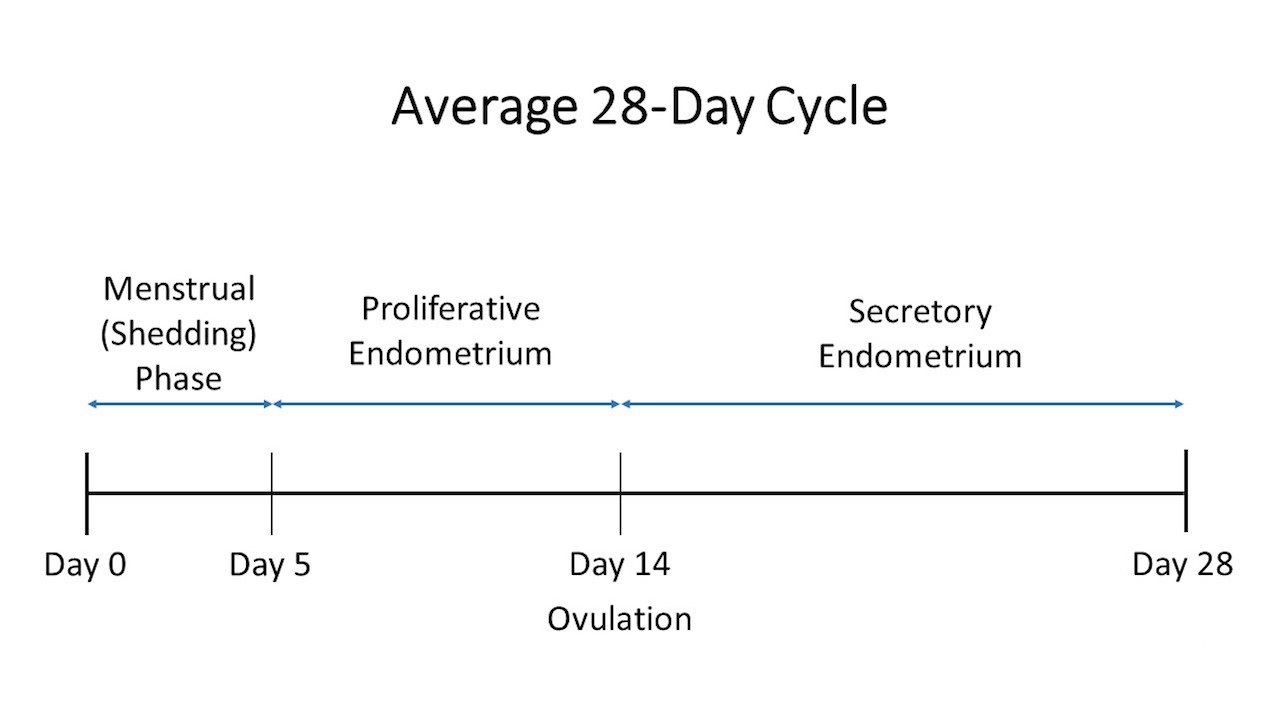
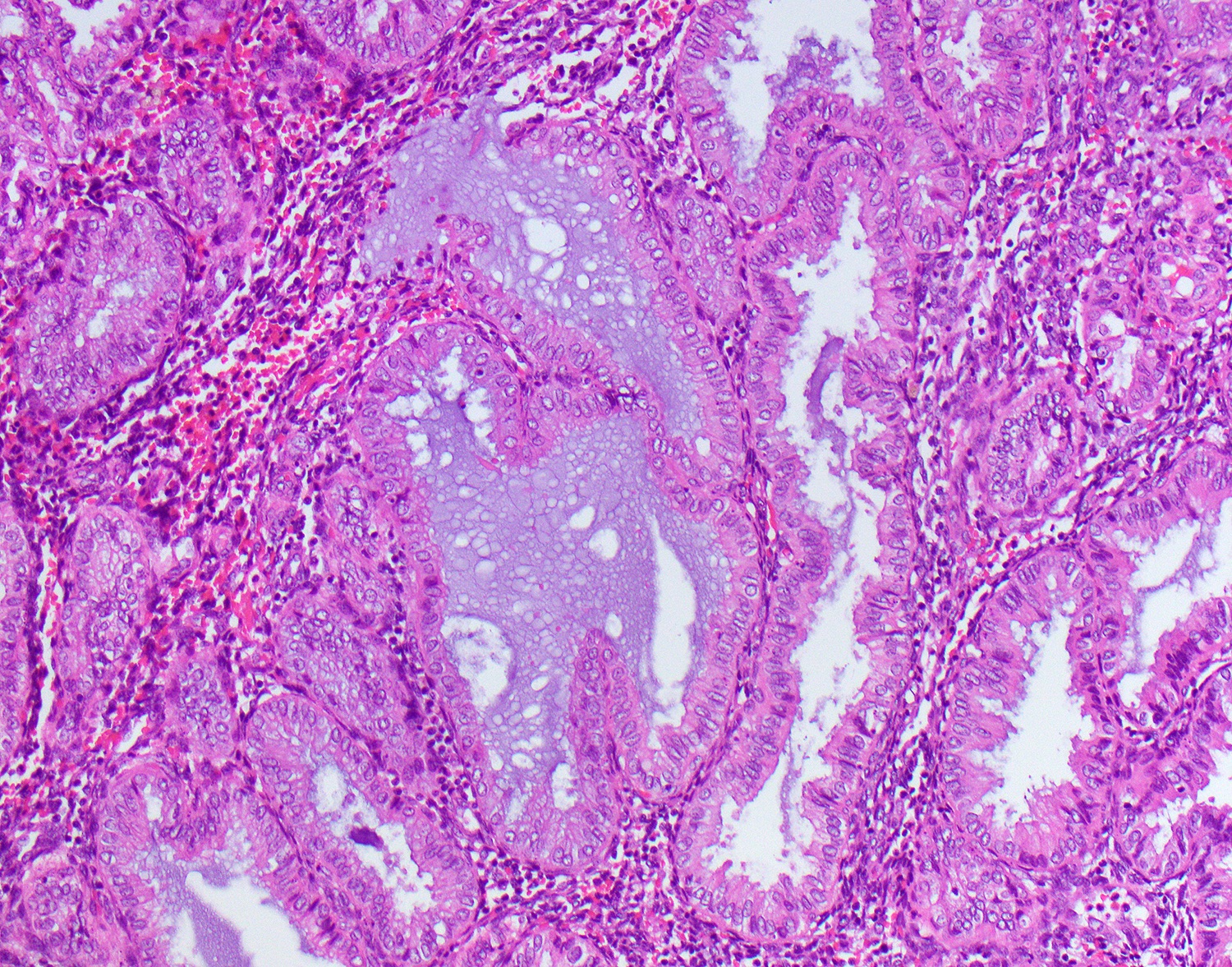
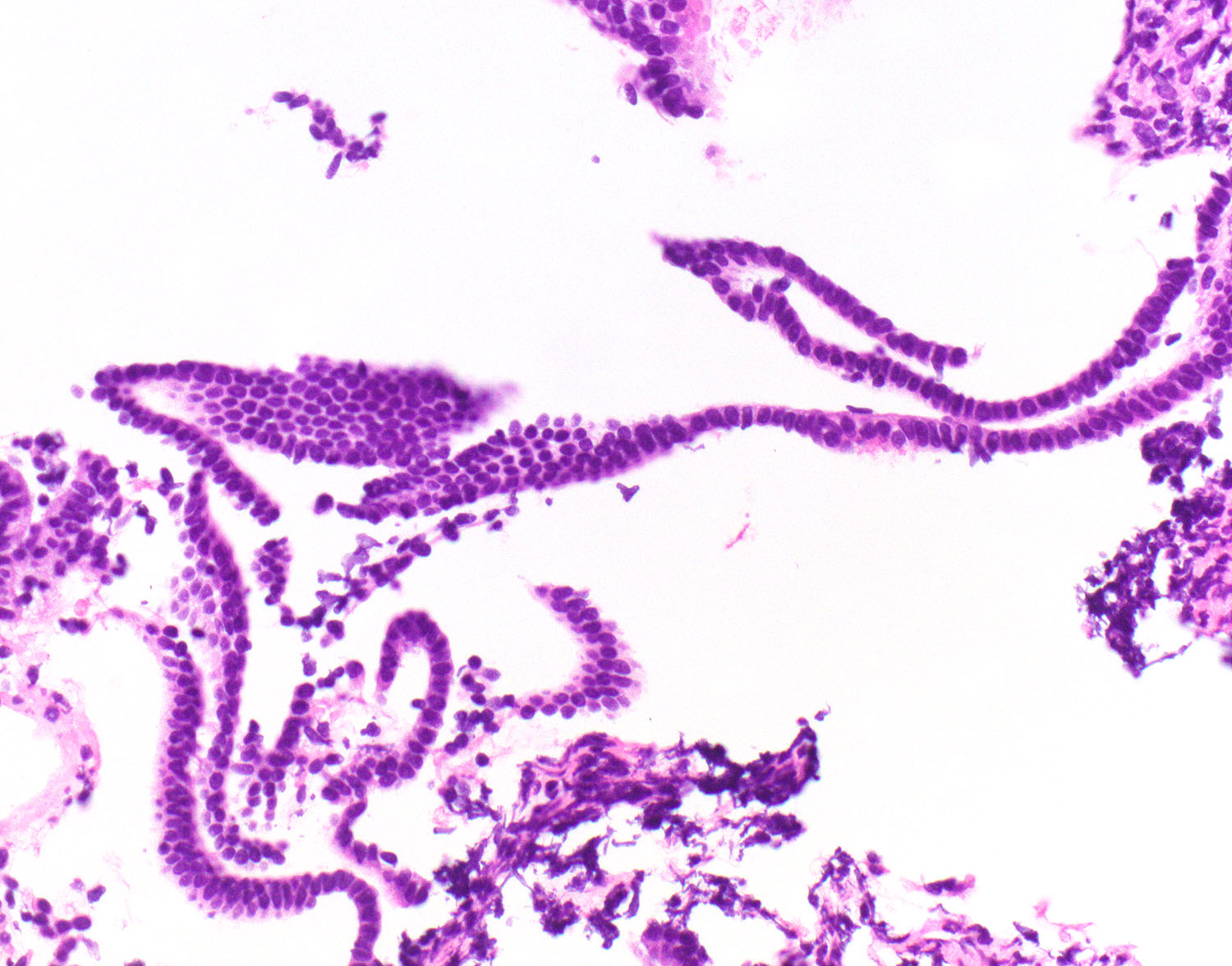
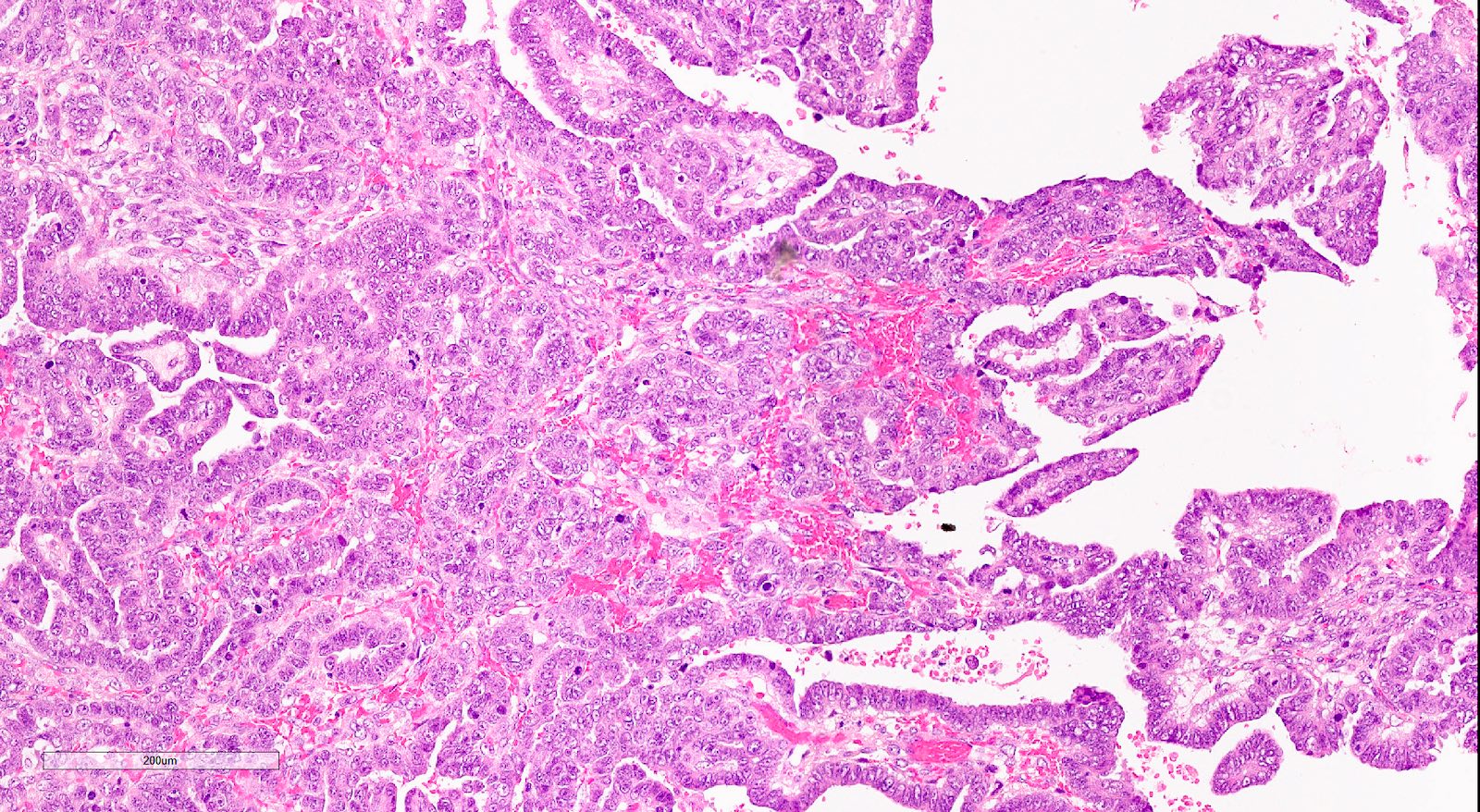
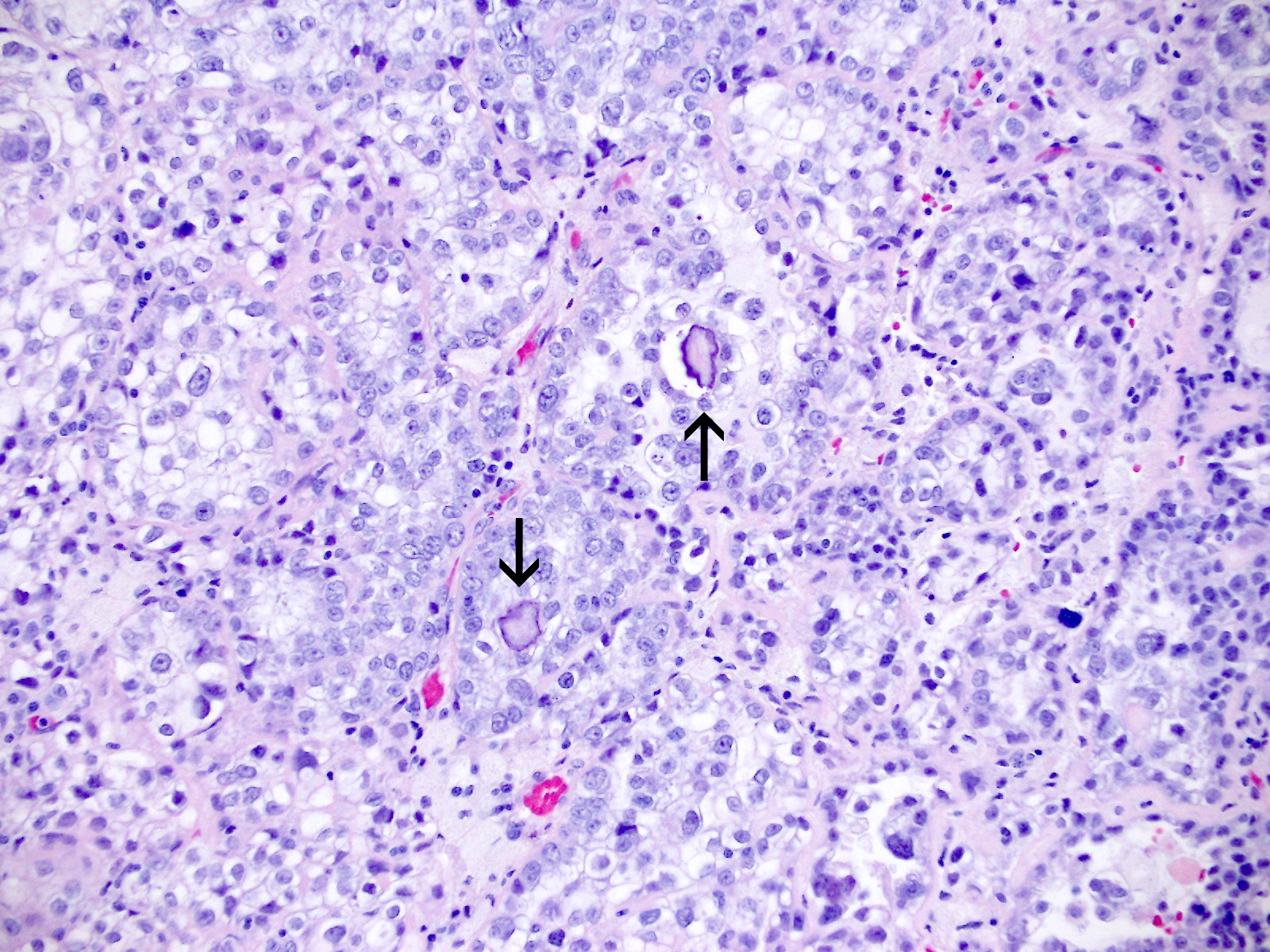
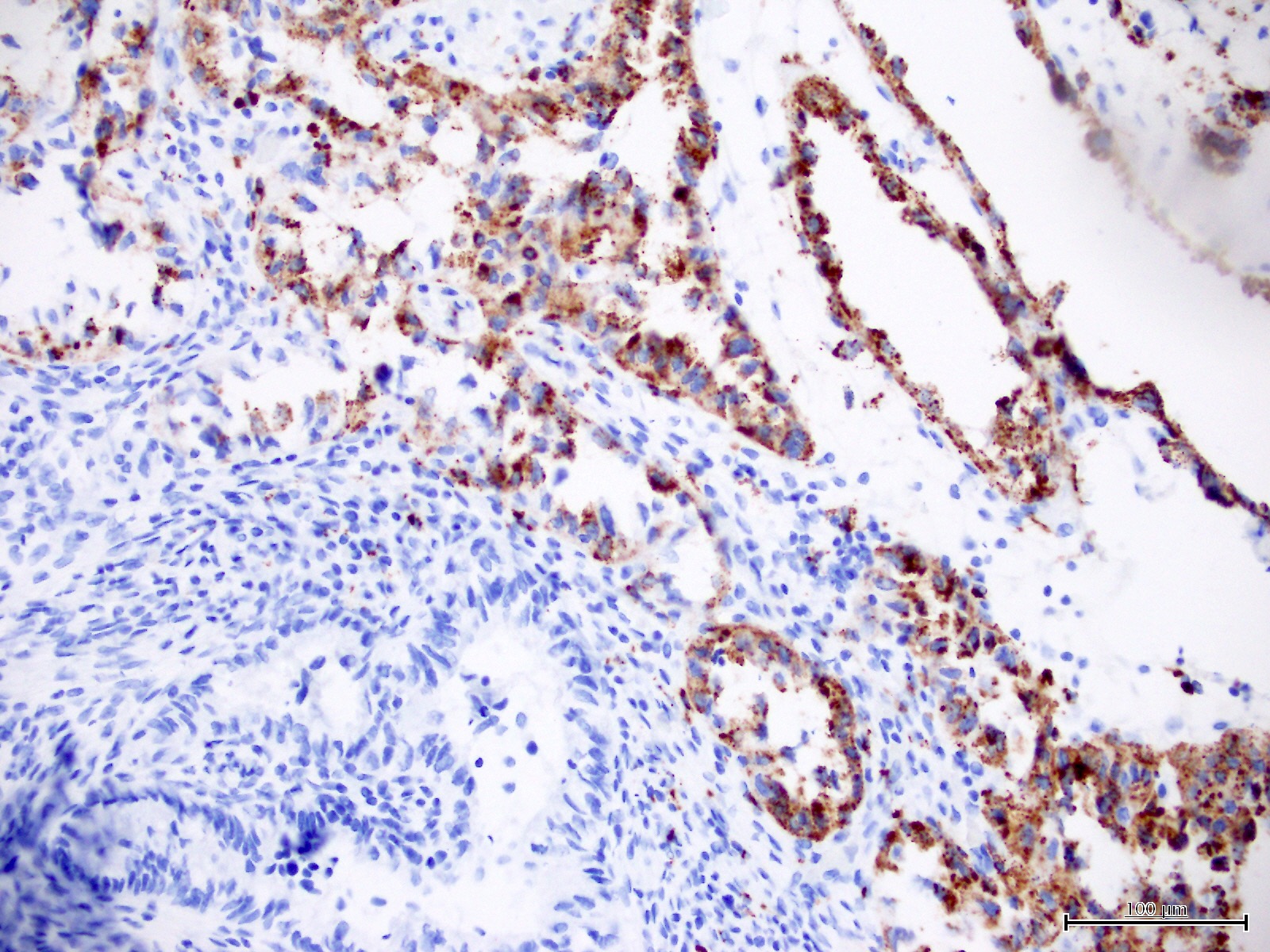
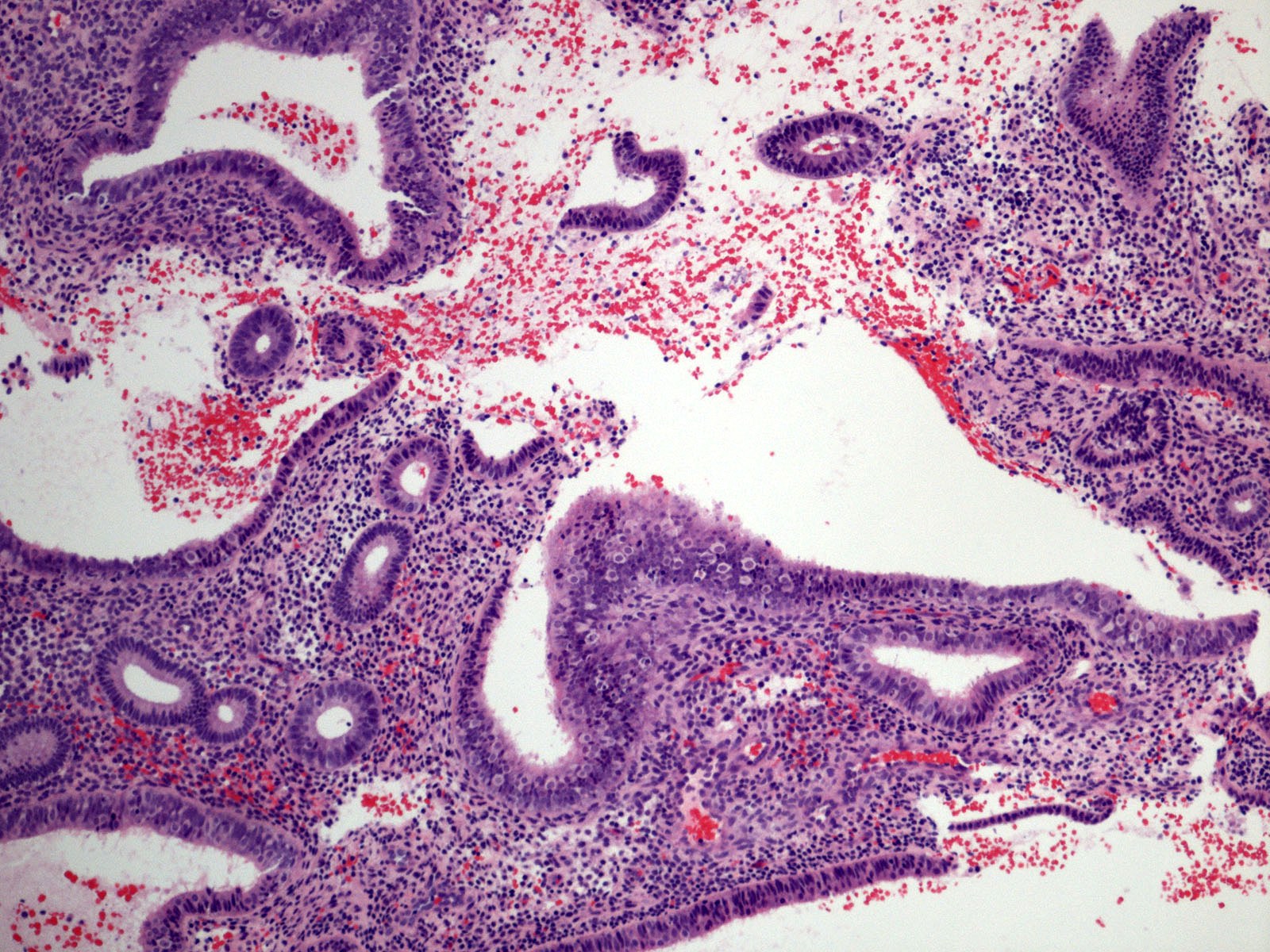
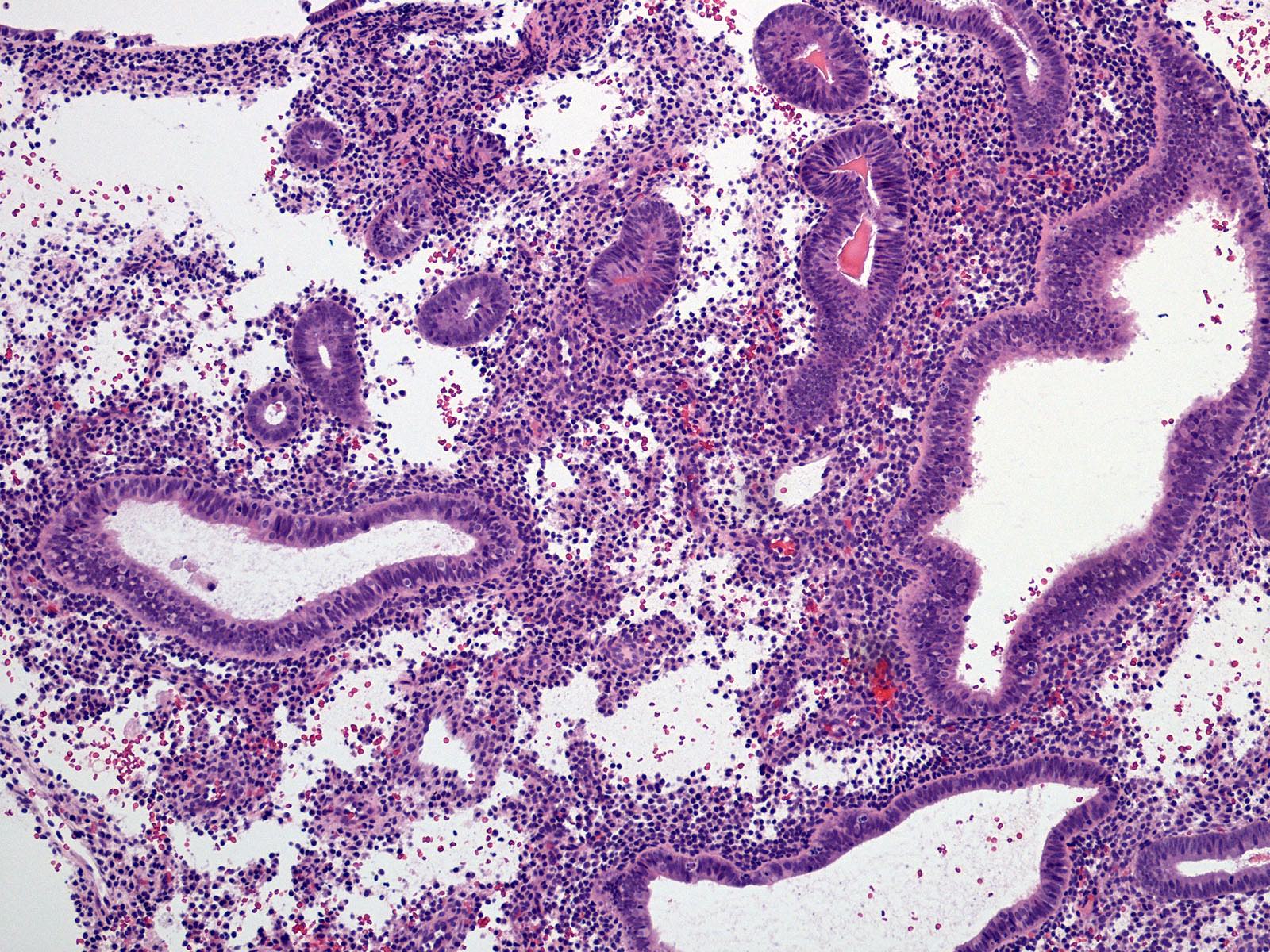
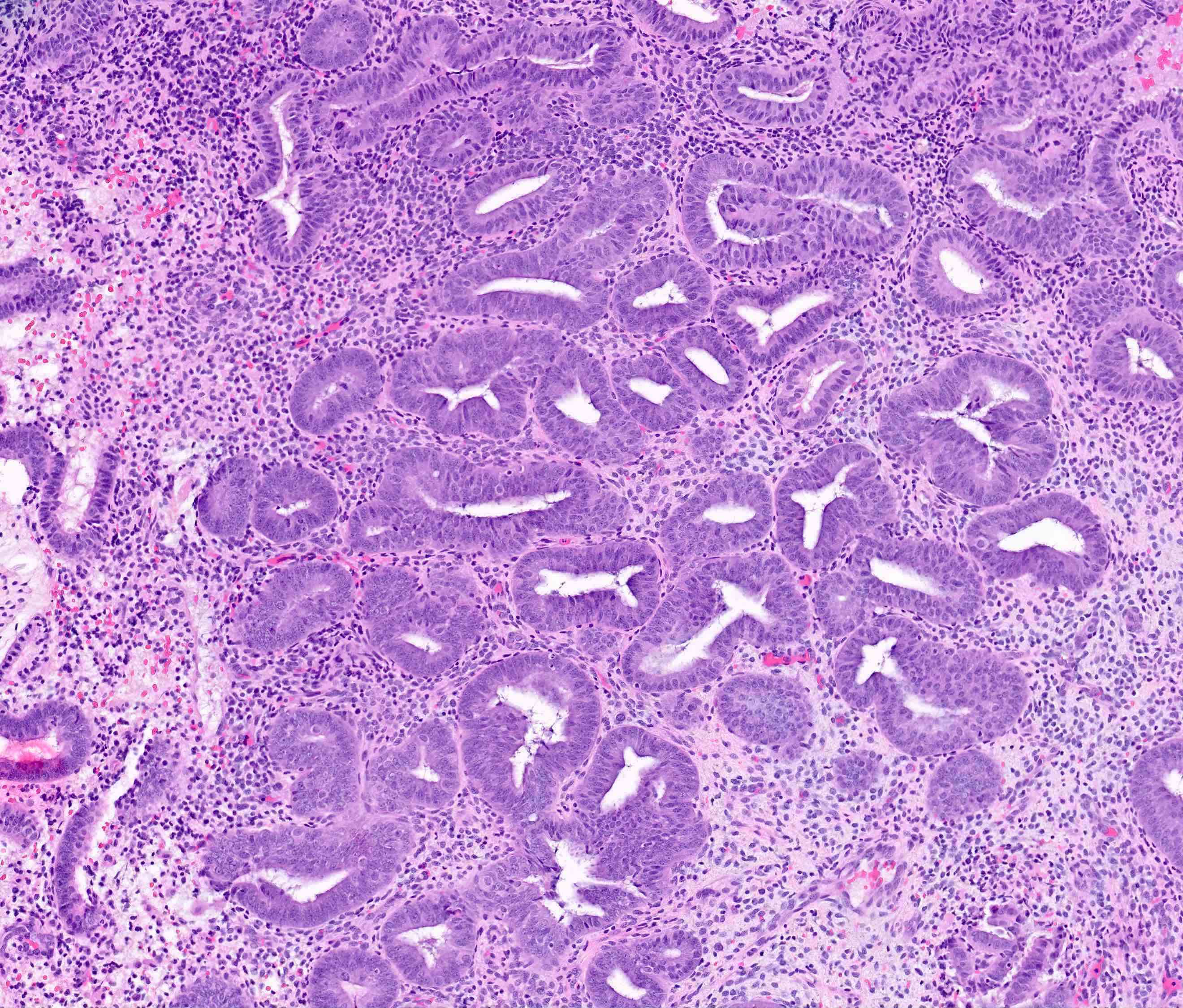
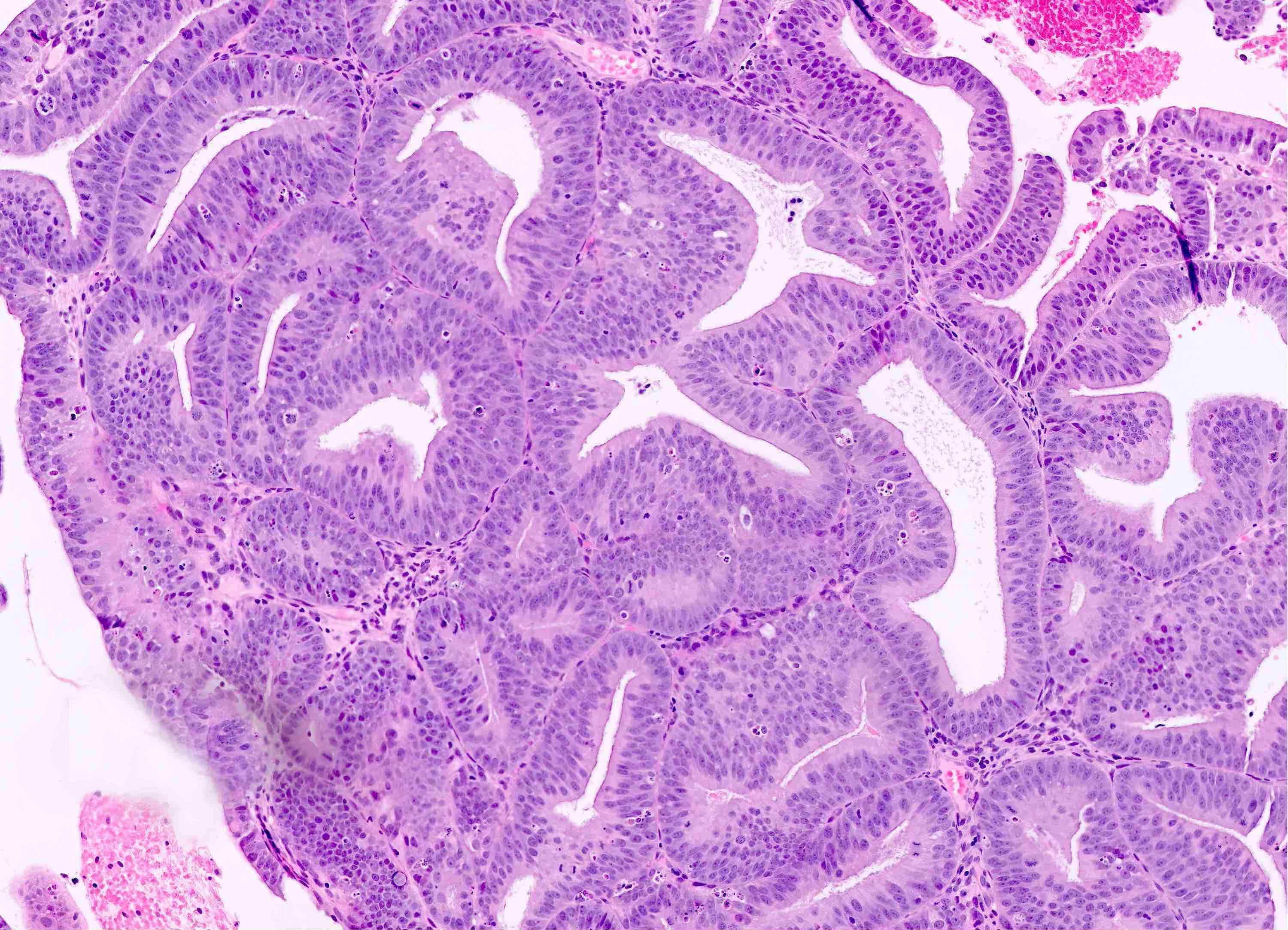
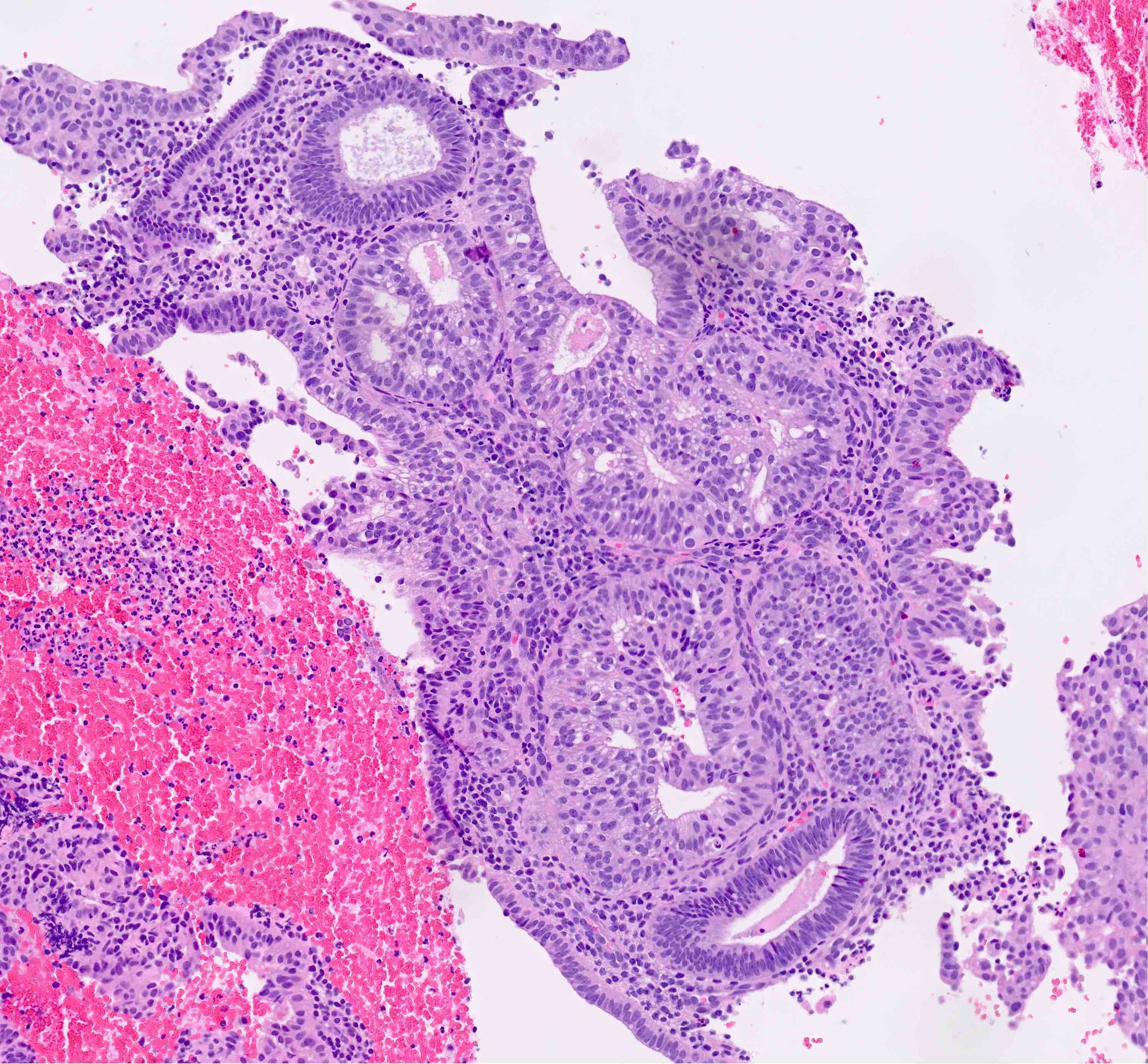
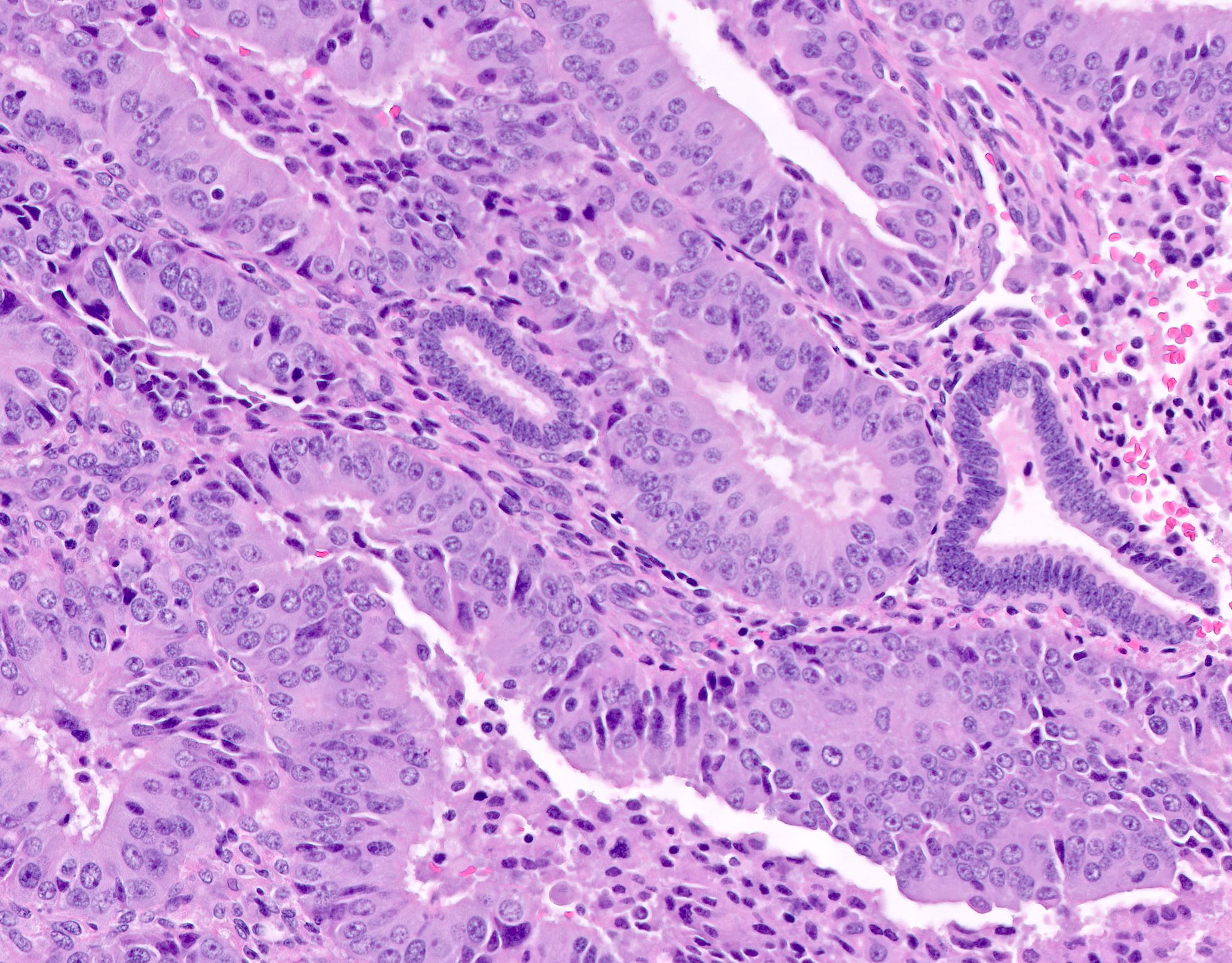
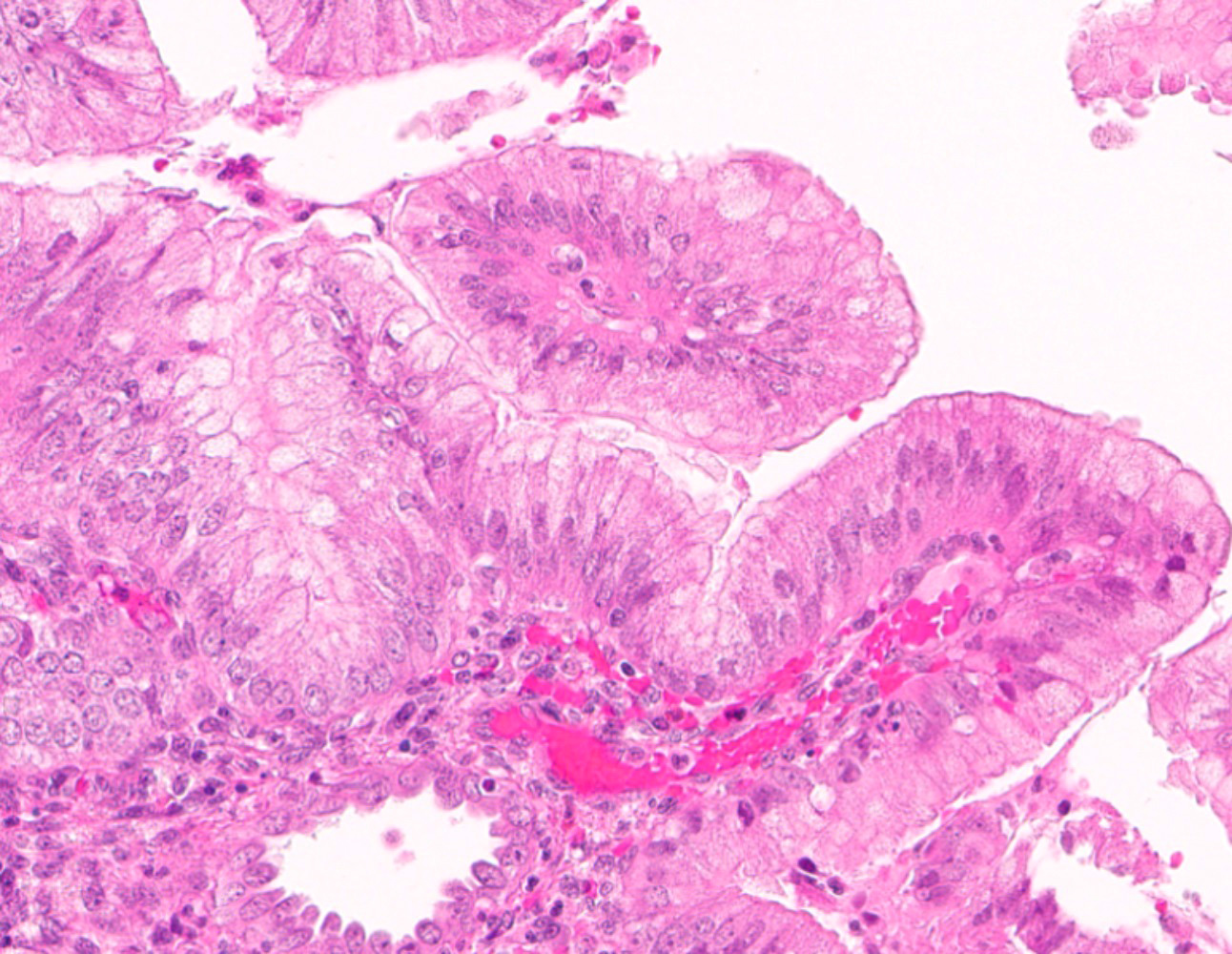
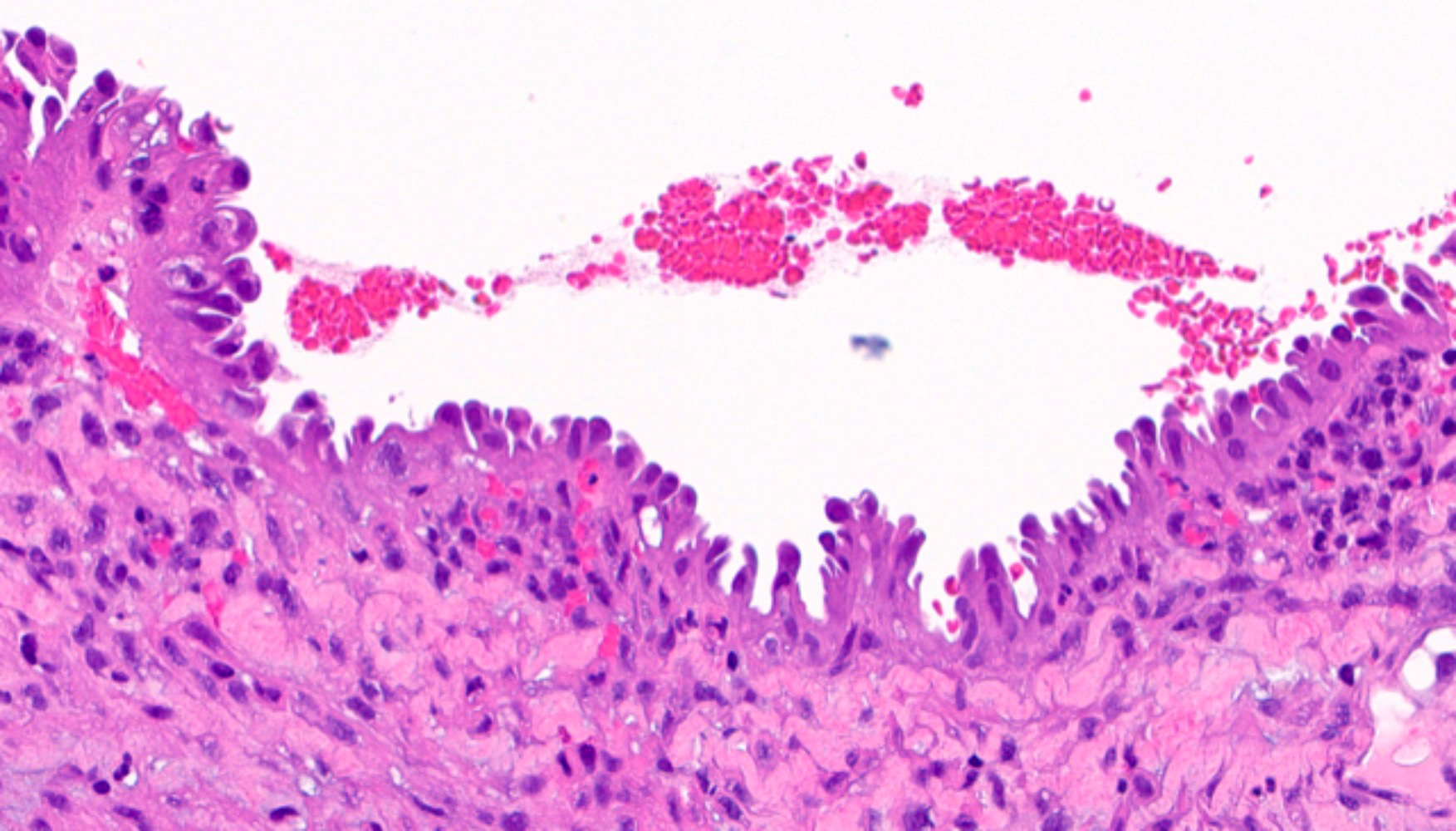
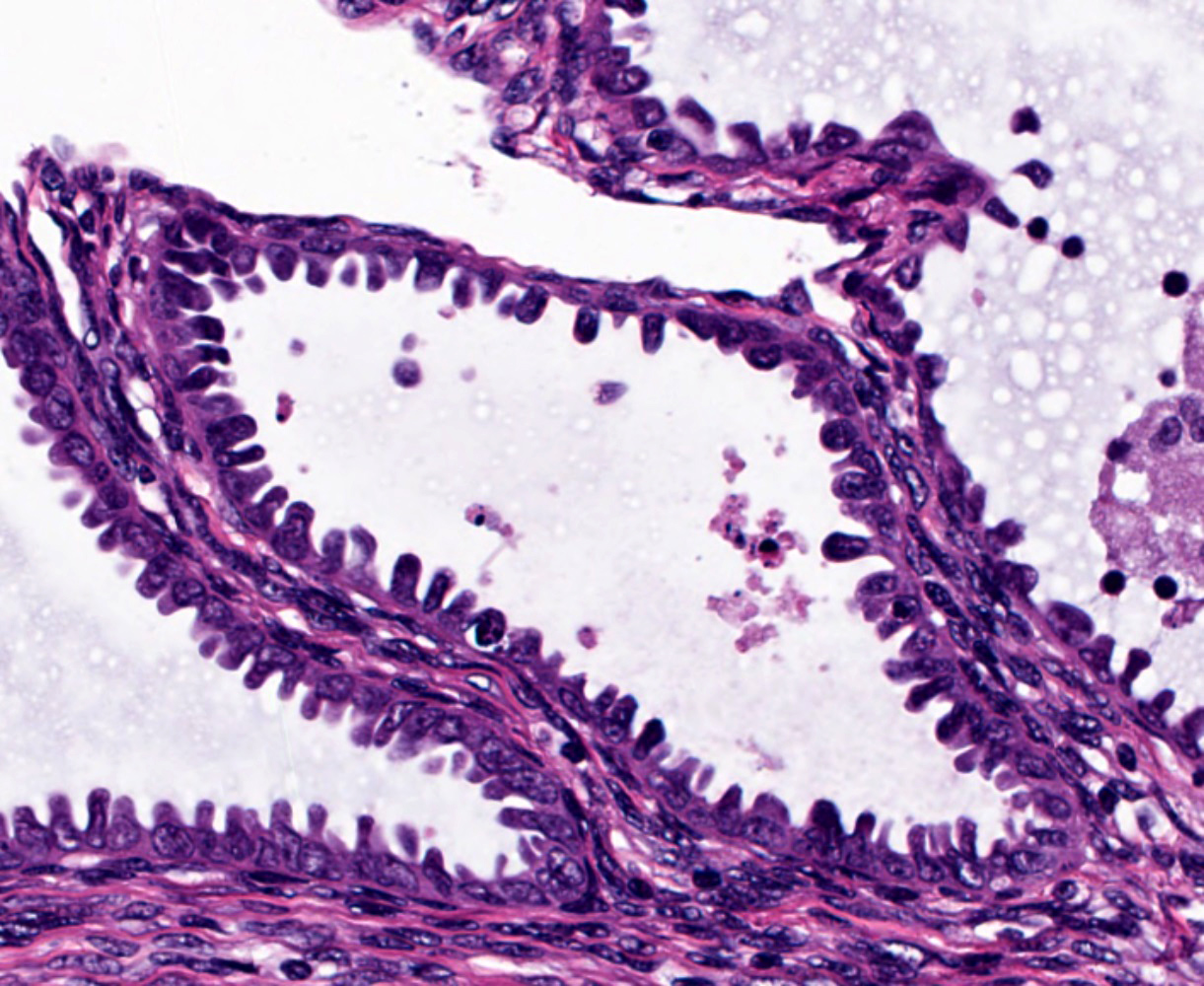
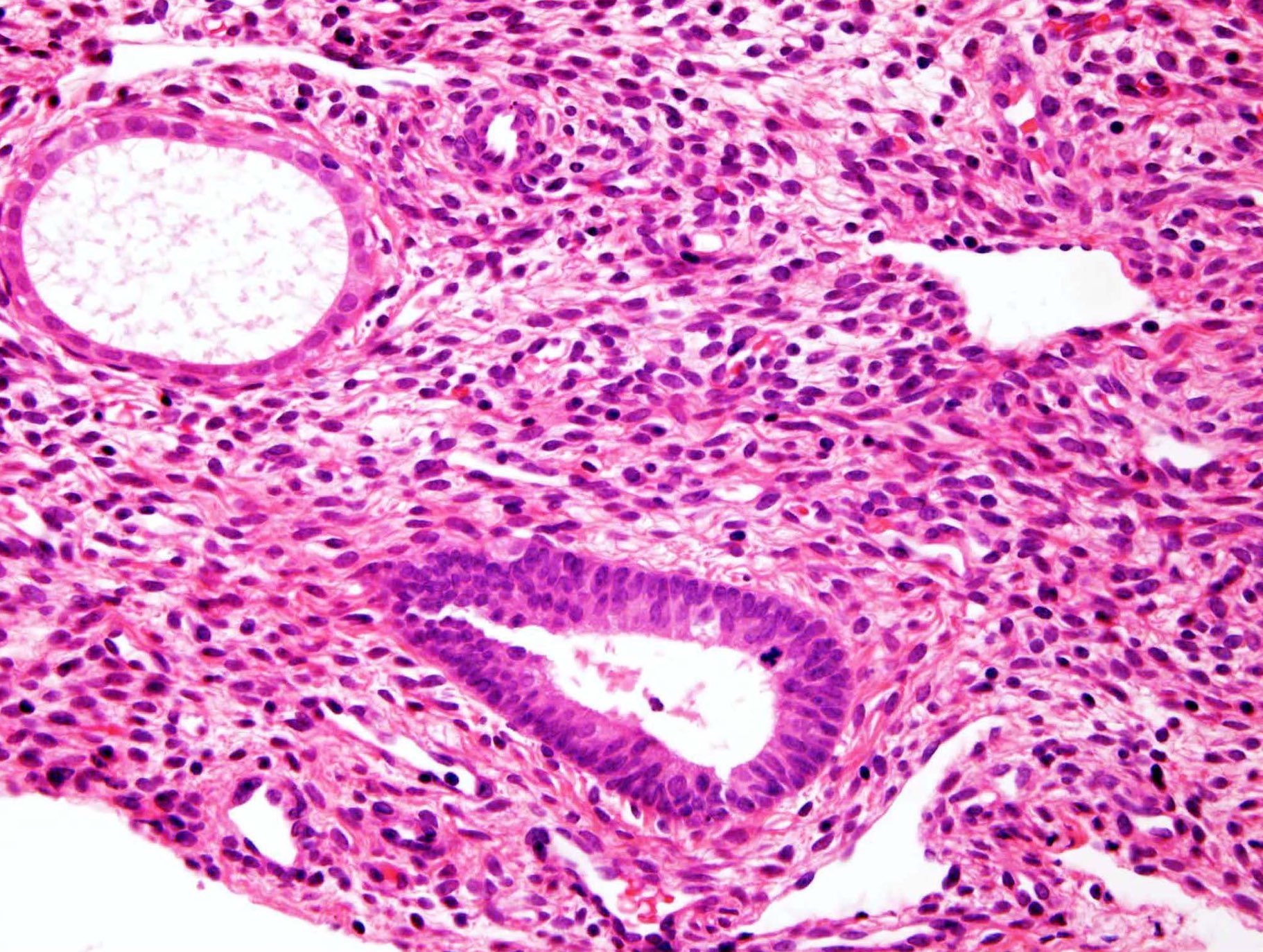
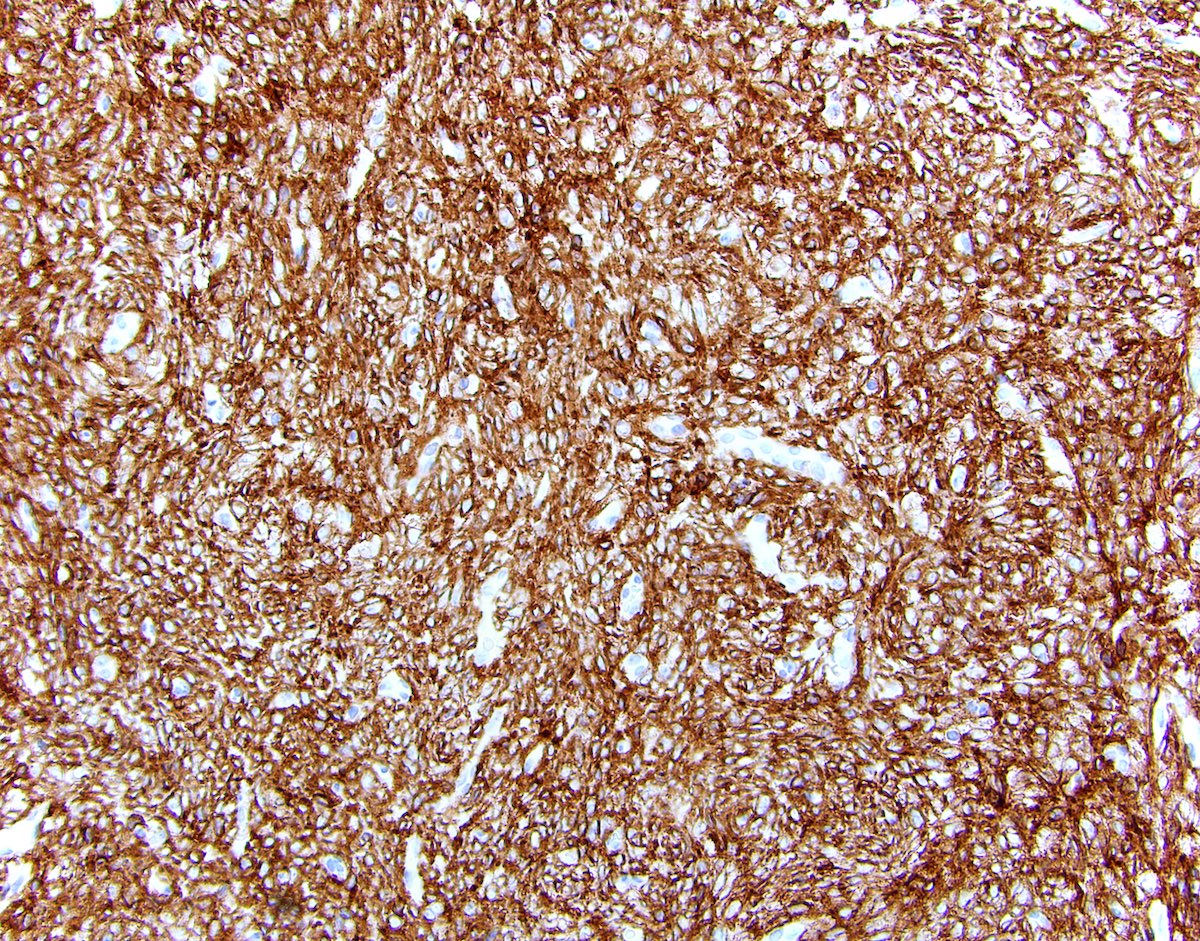
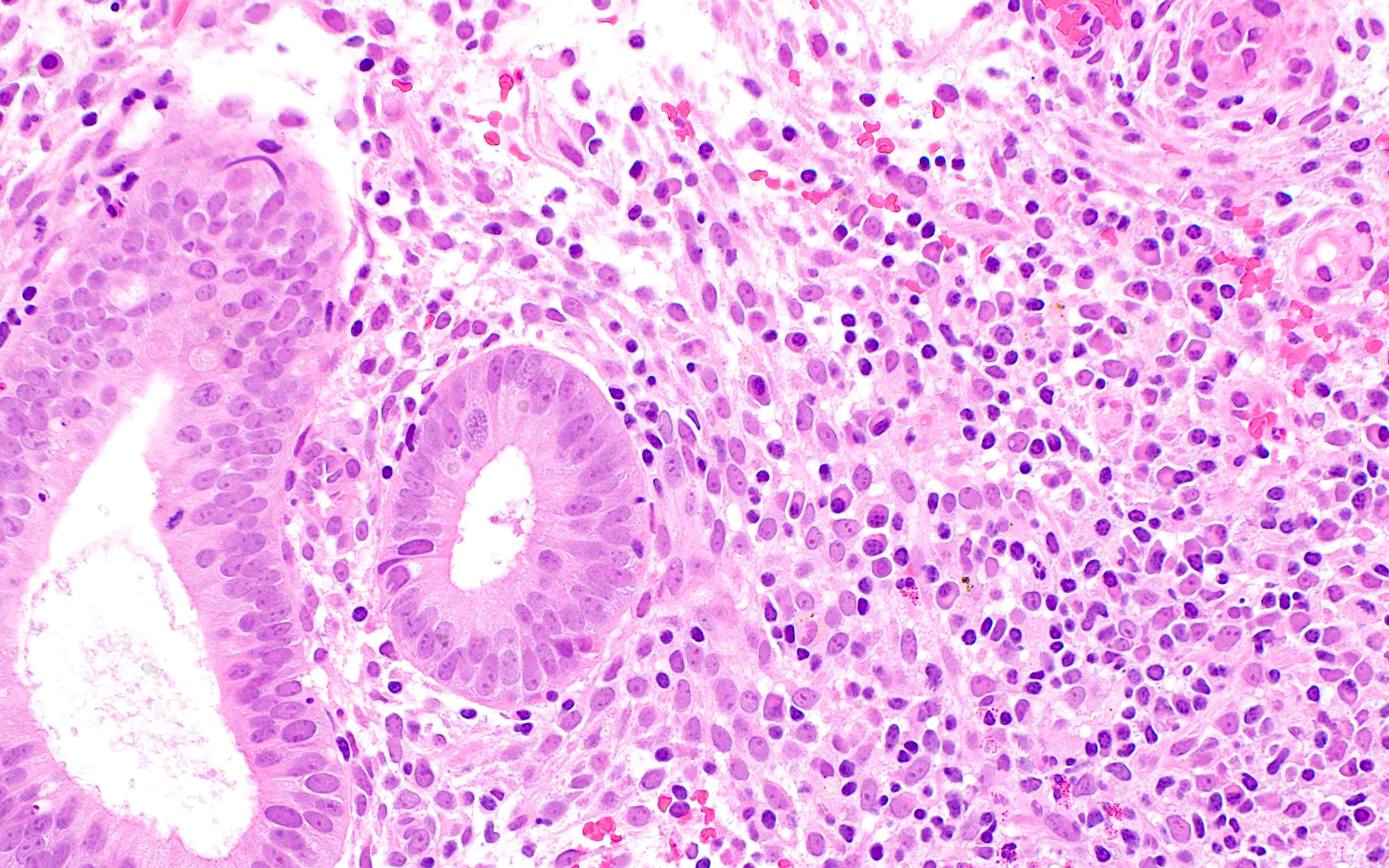
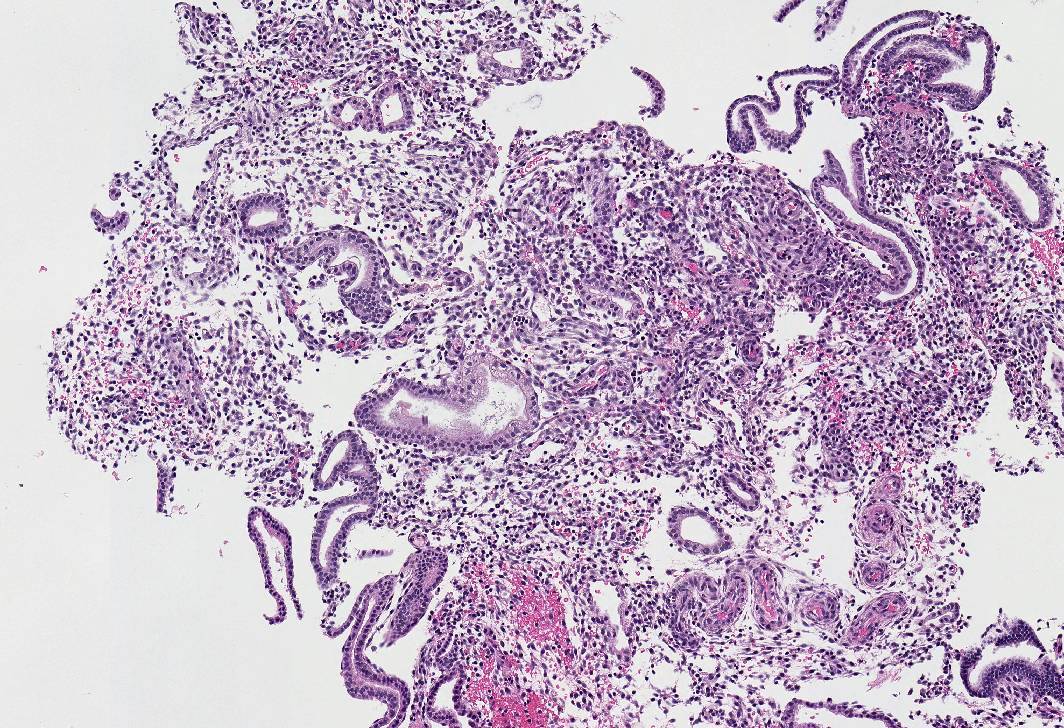
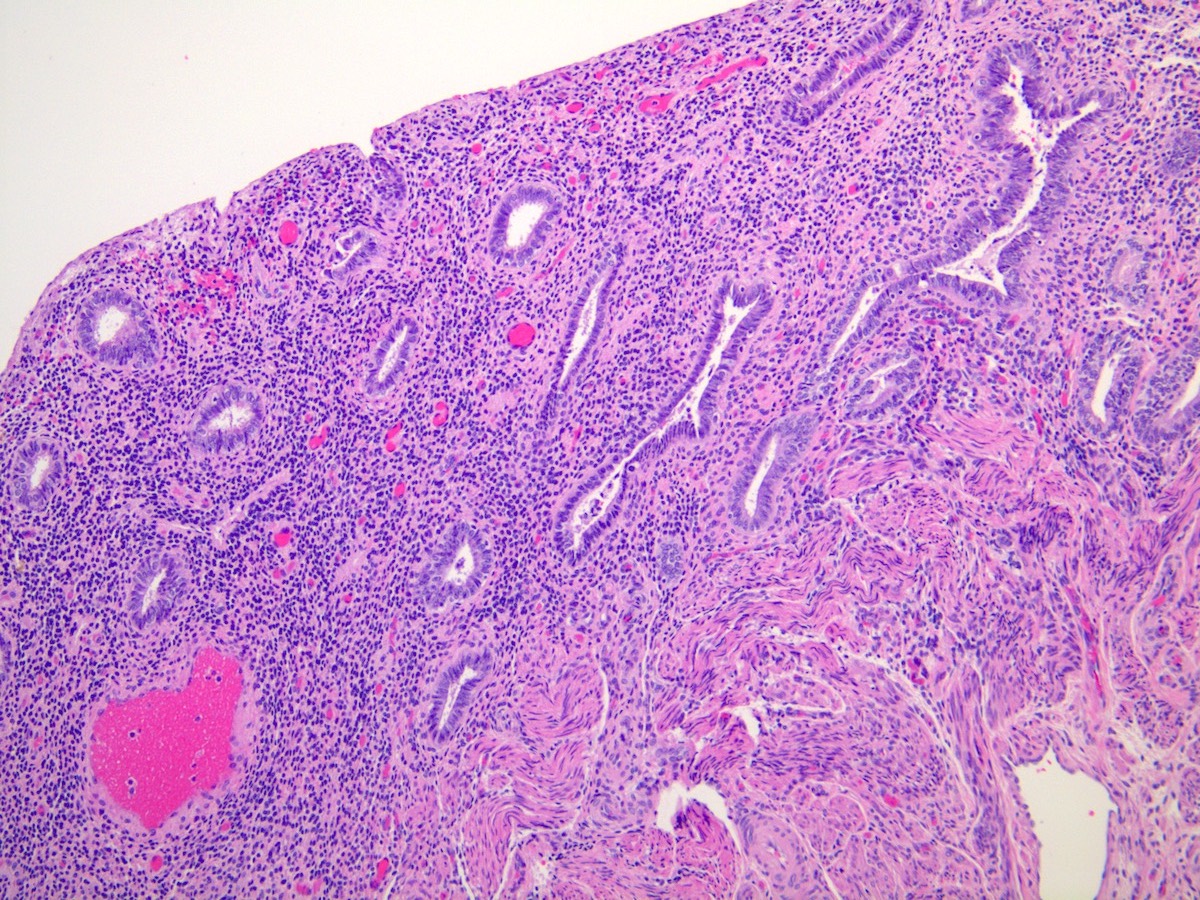
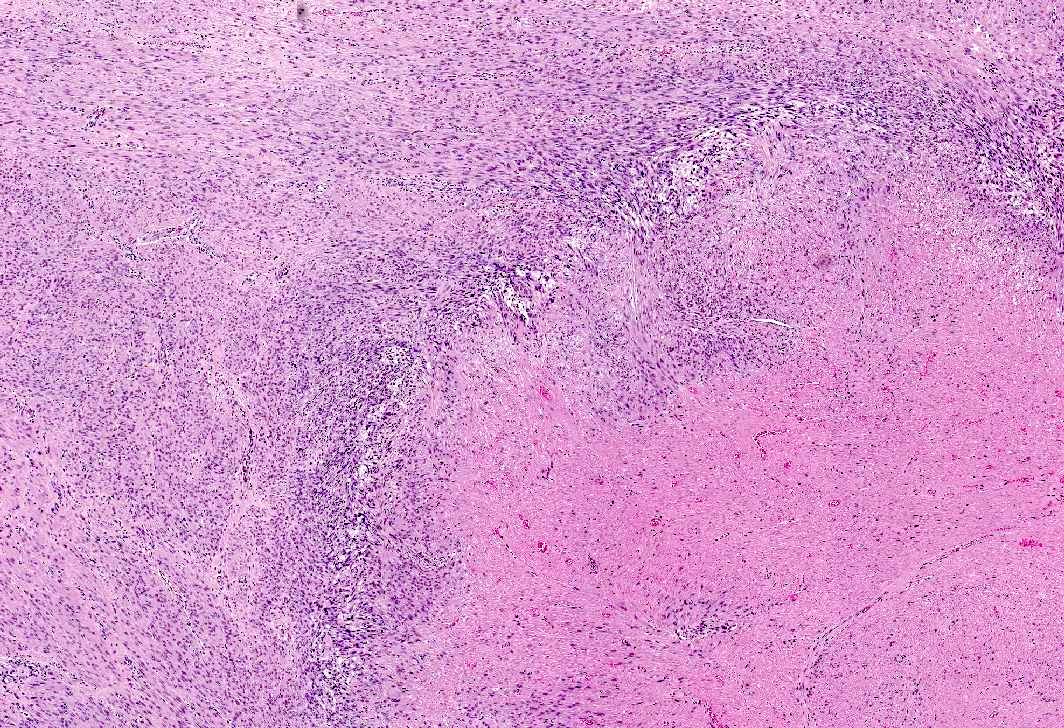
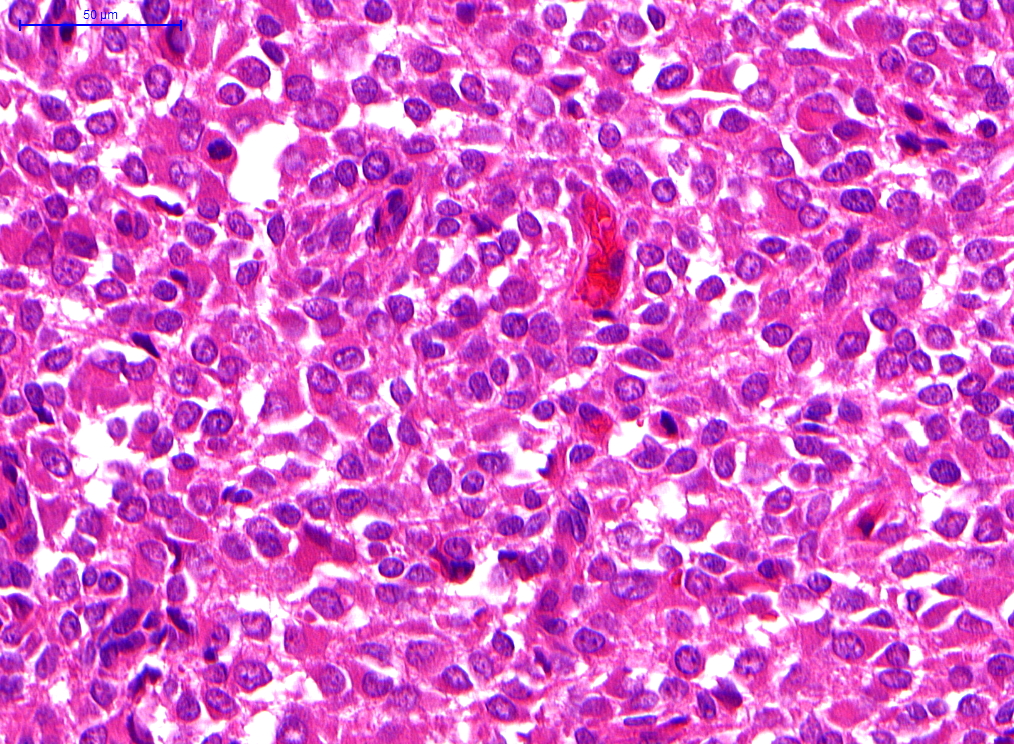
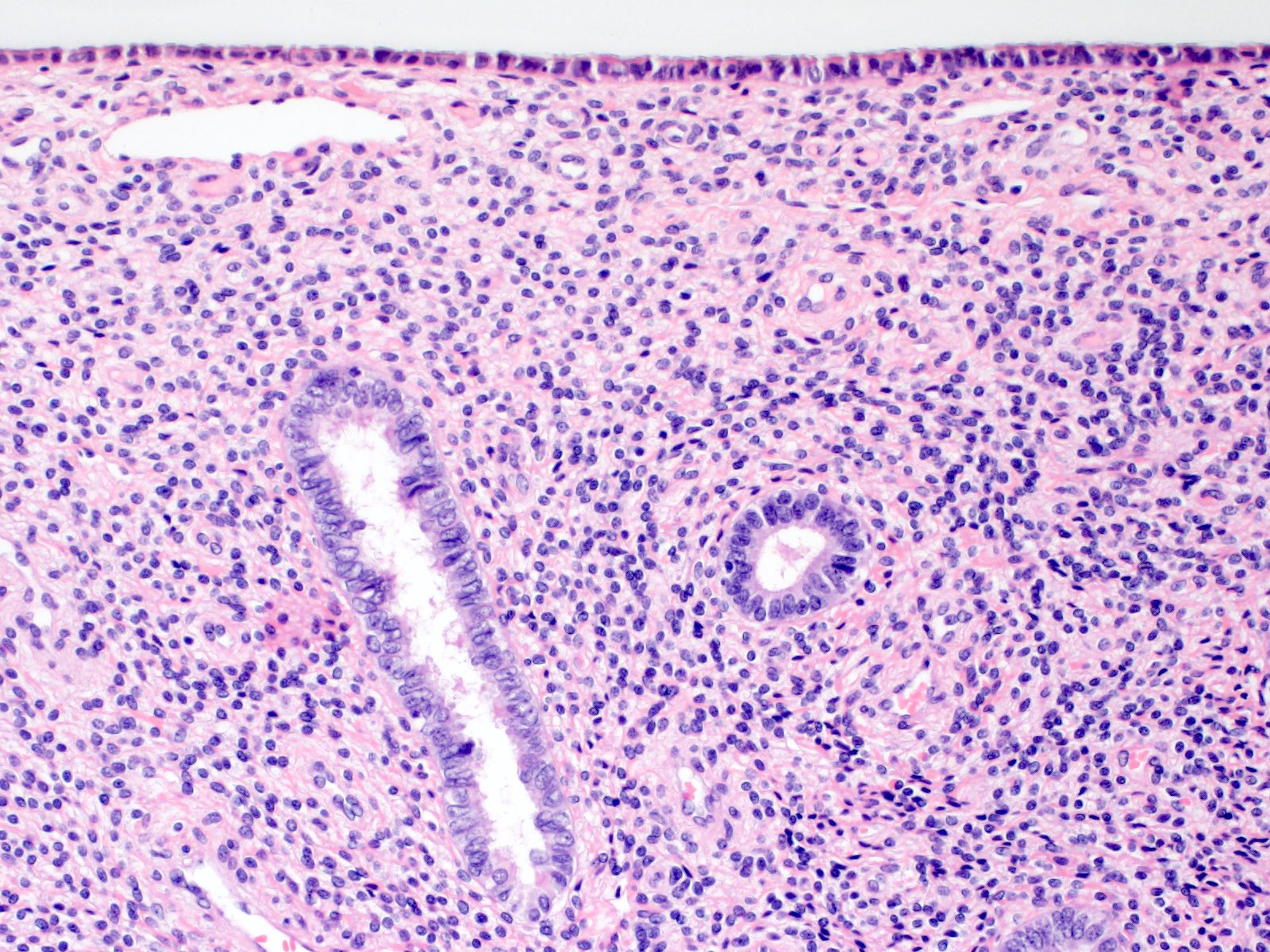
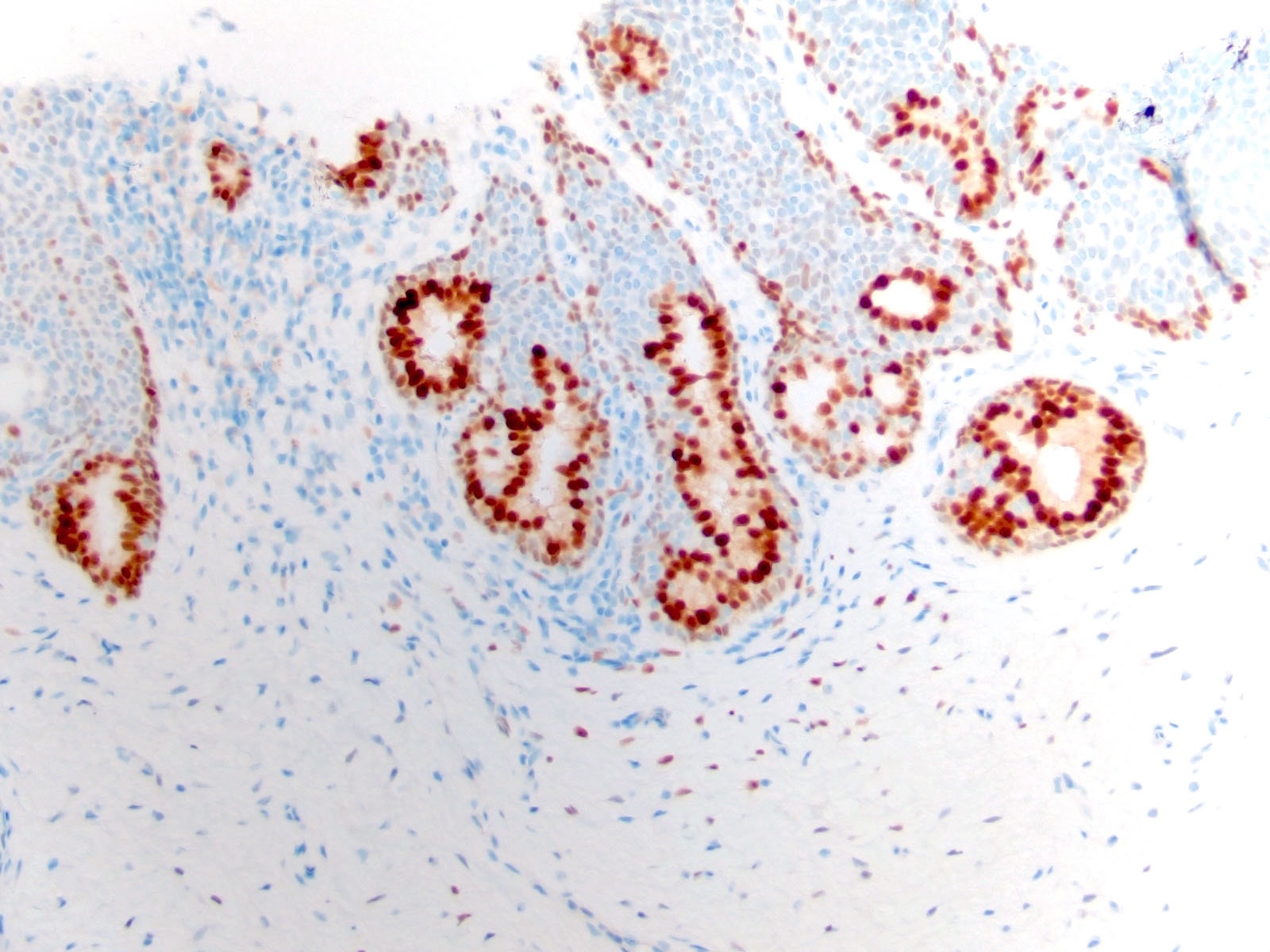
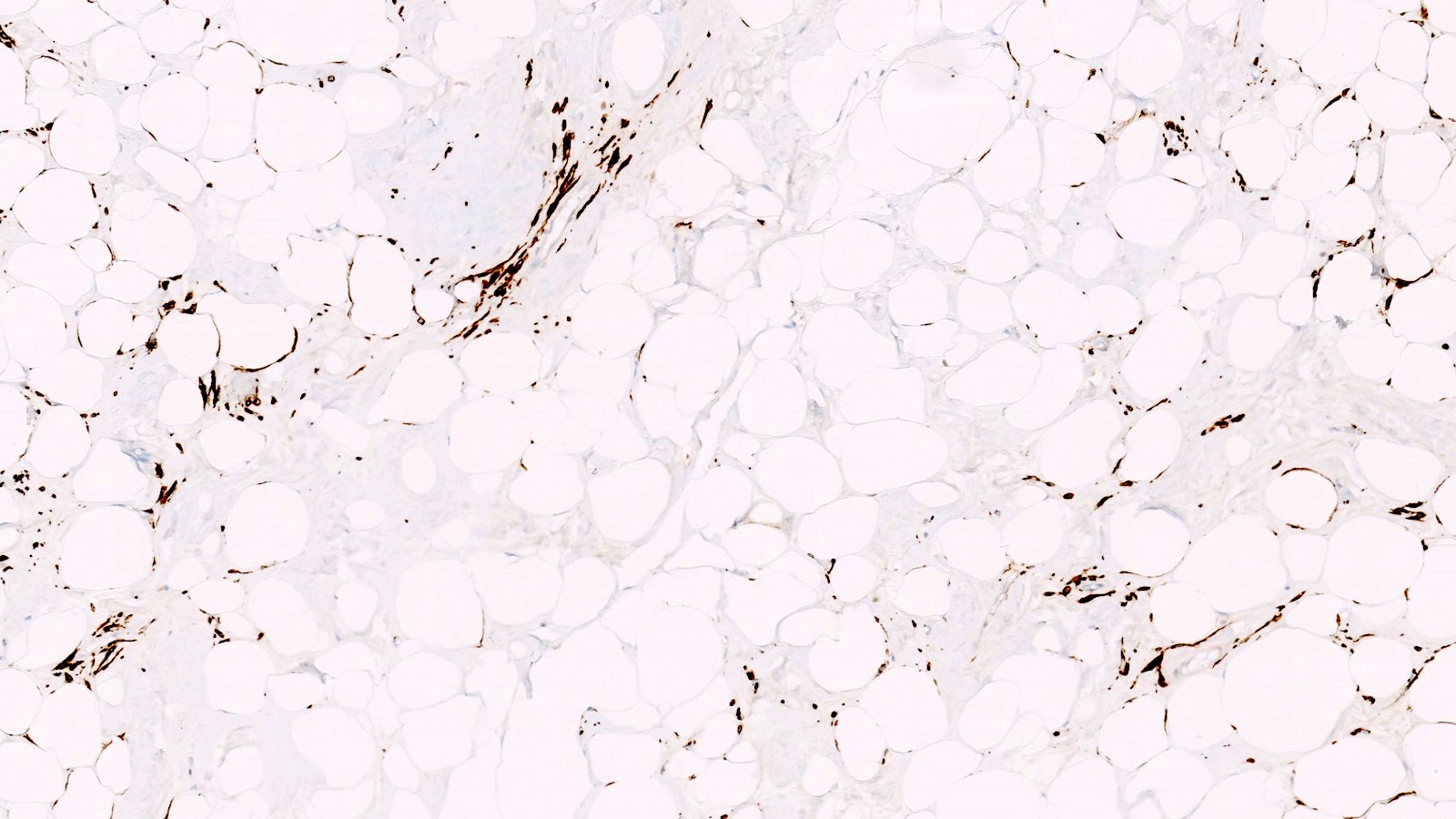
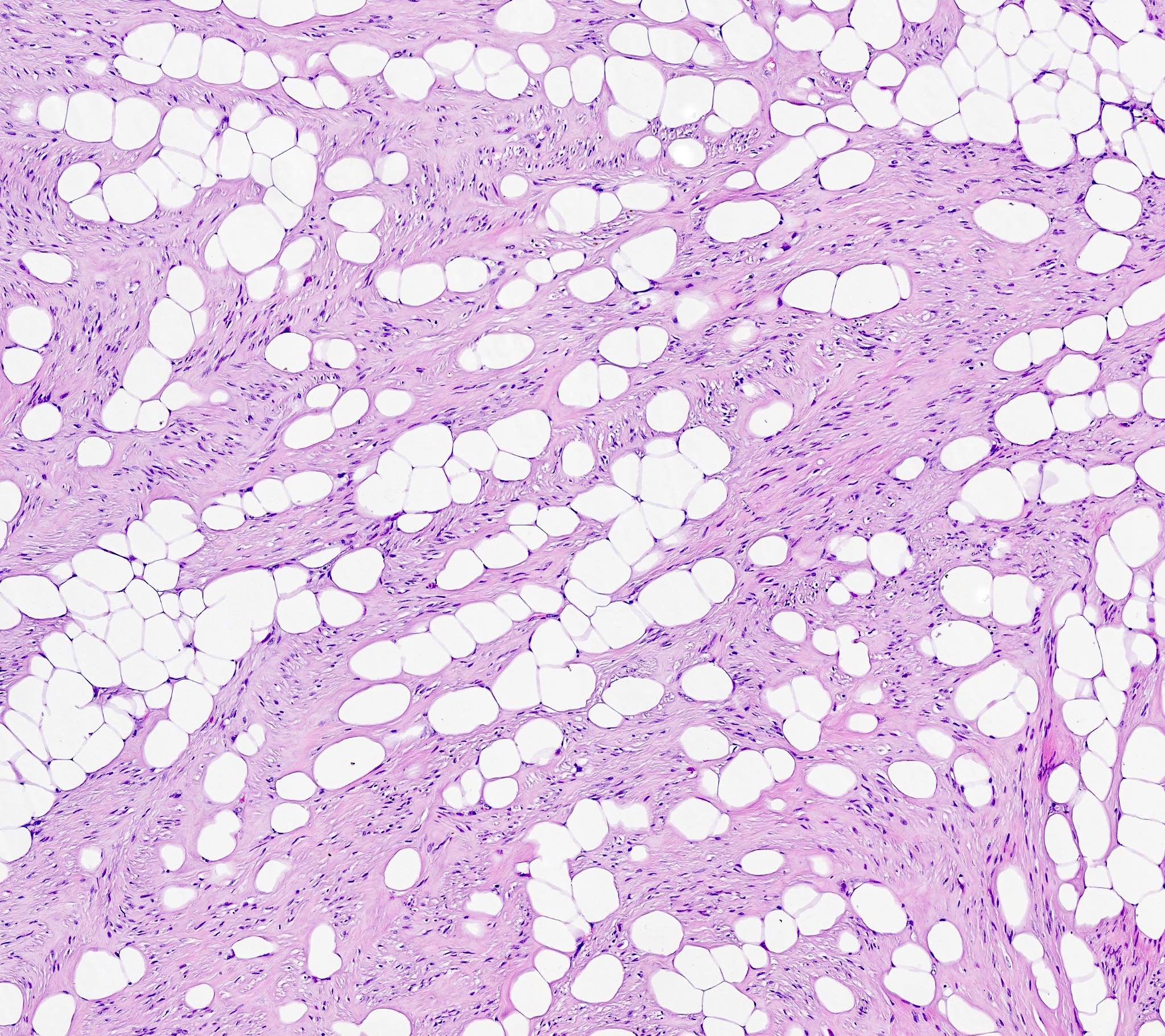
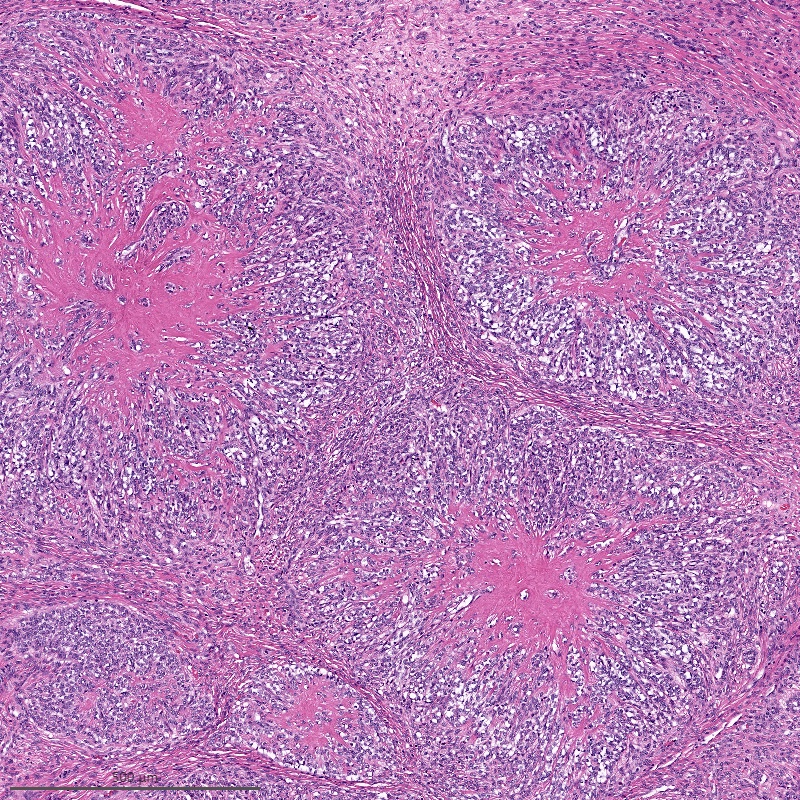
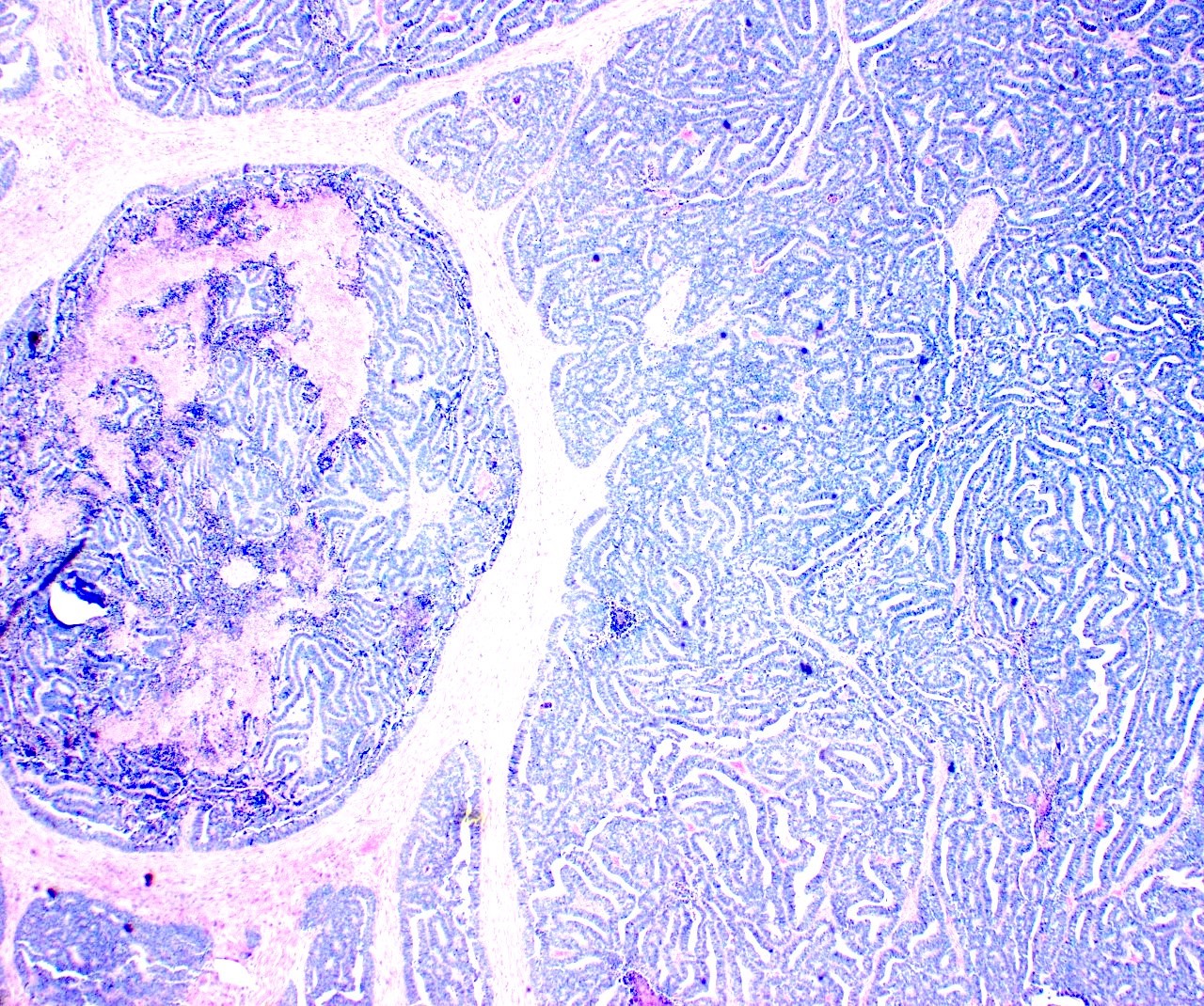
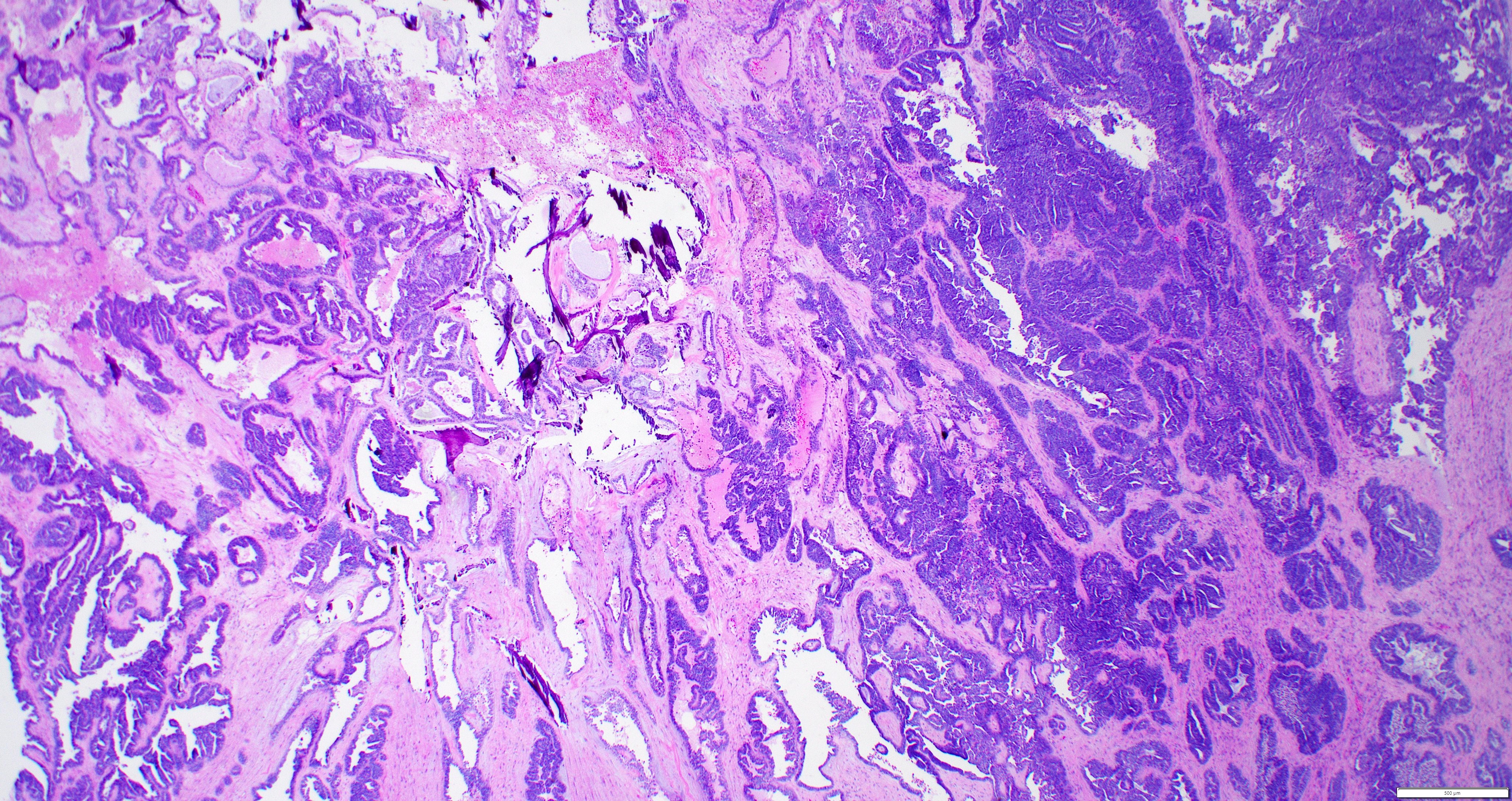
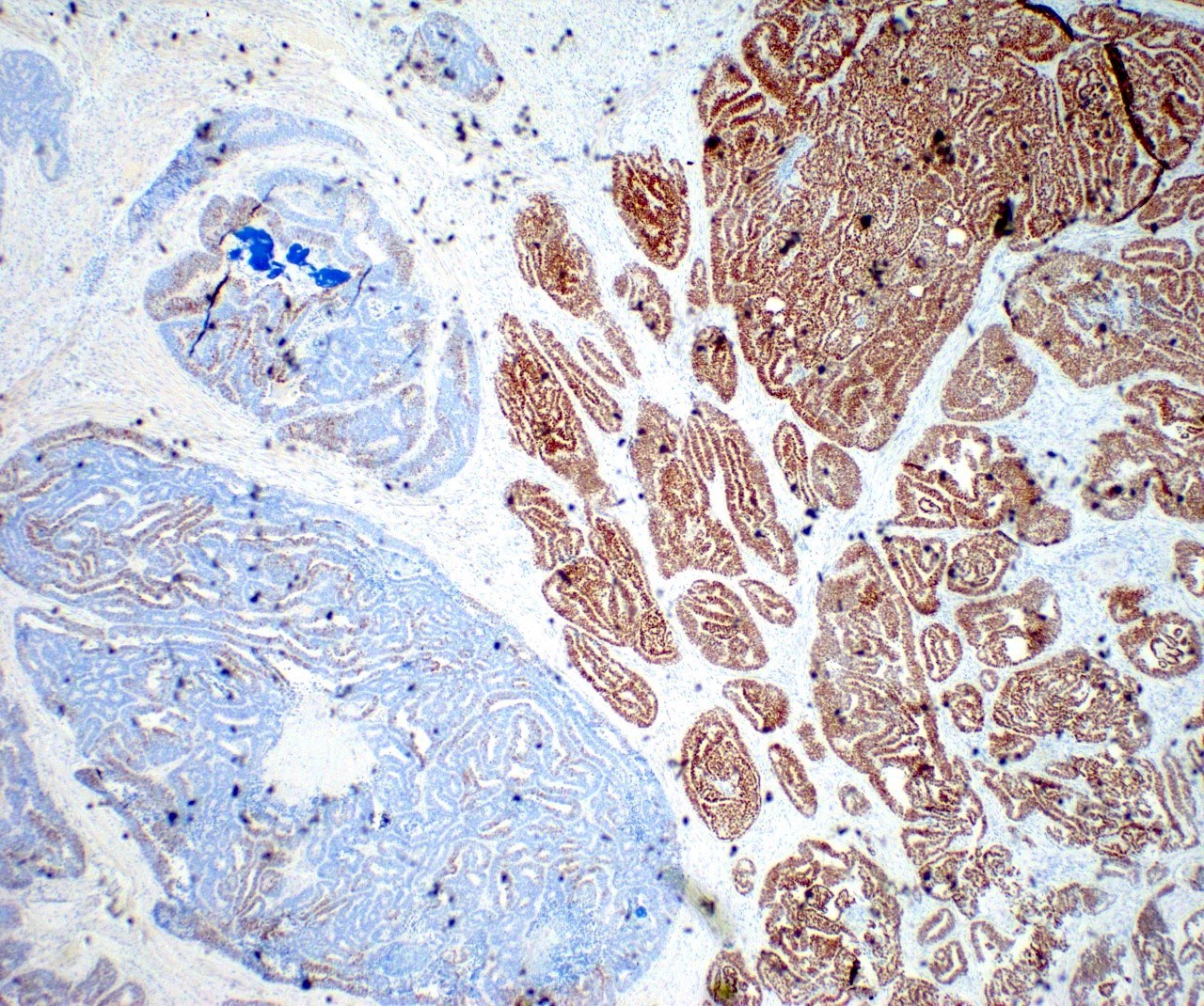
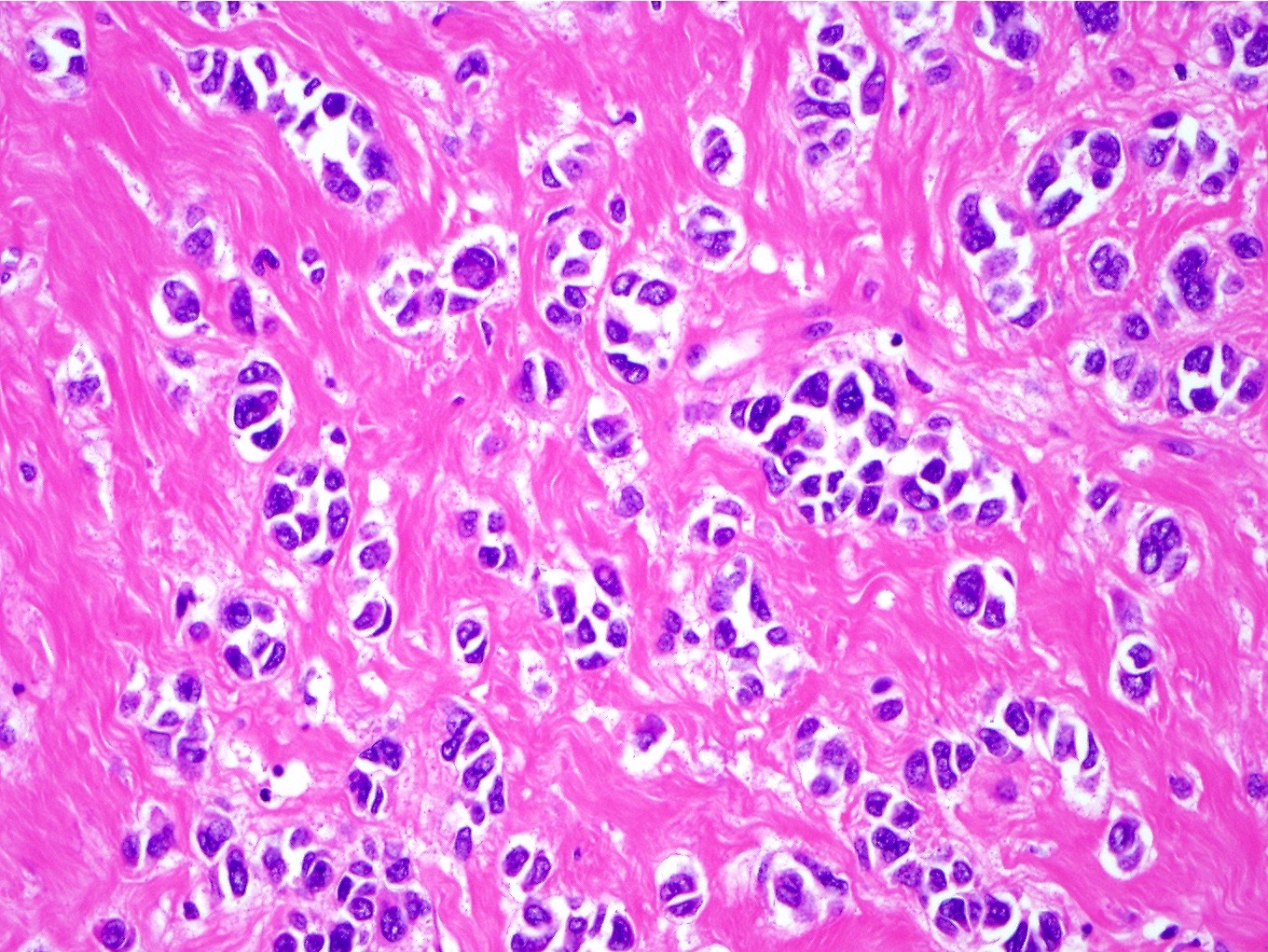
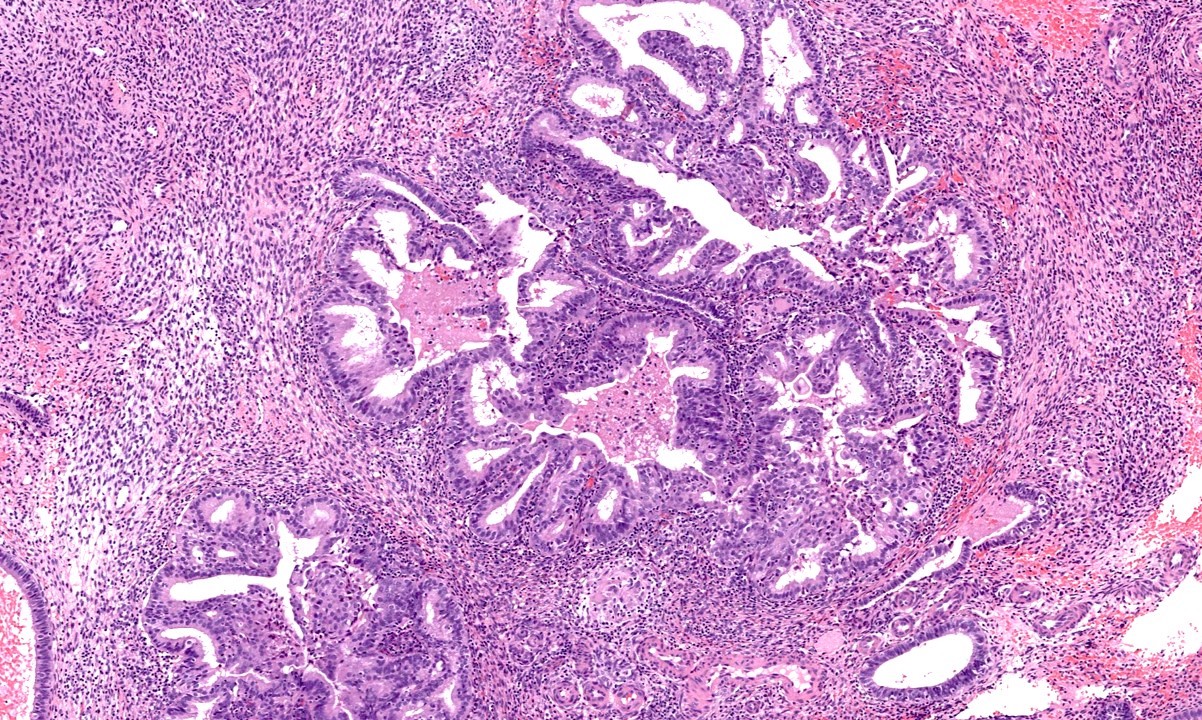
- Uppermost endocervical mucinous gland in the section should be considered as the upper limit of the endocervix (Adv Anat Pathol 2018;25:71)
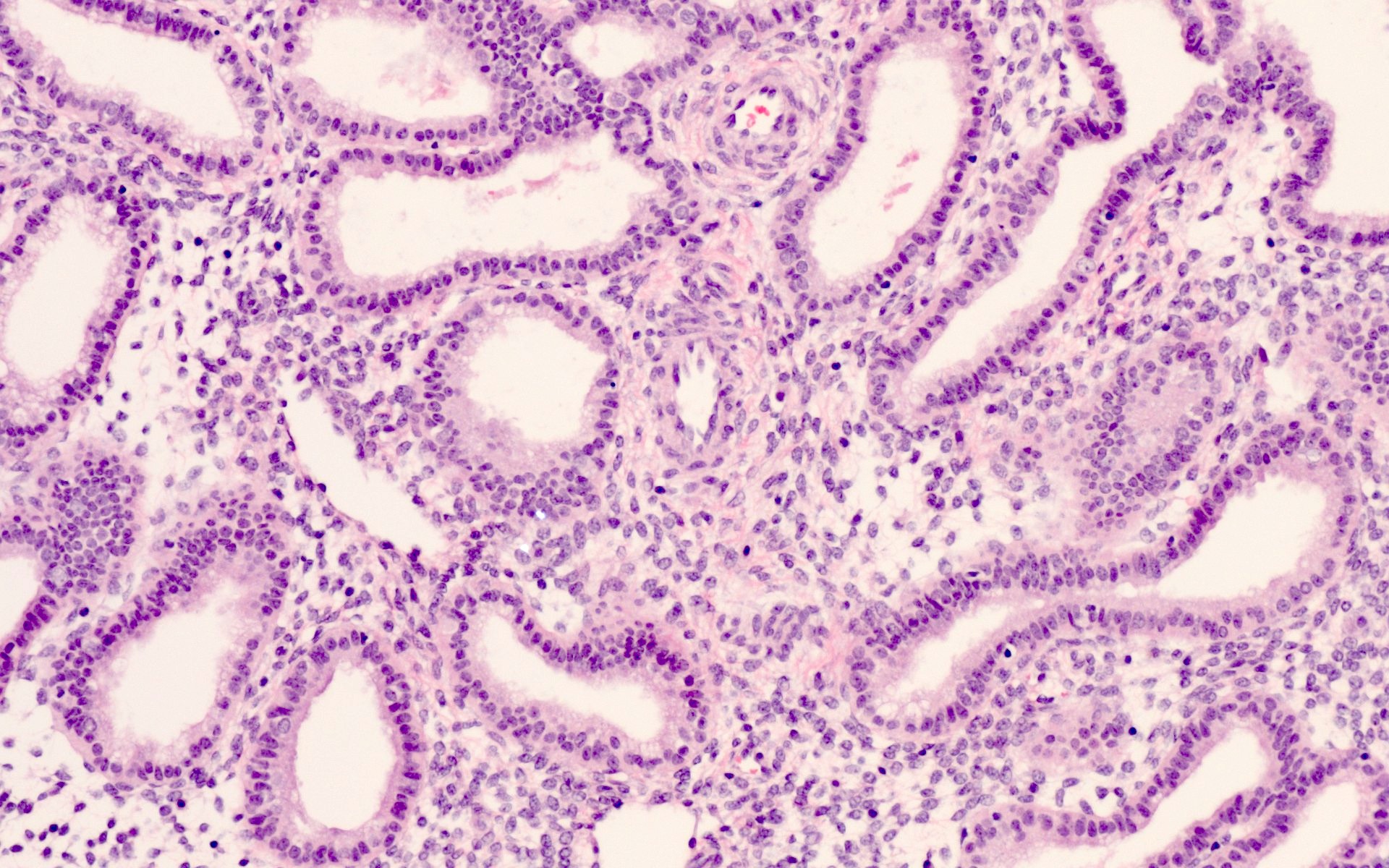
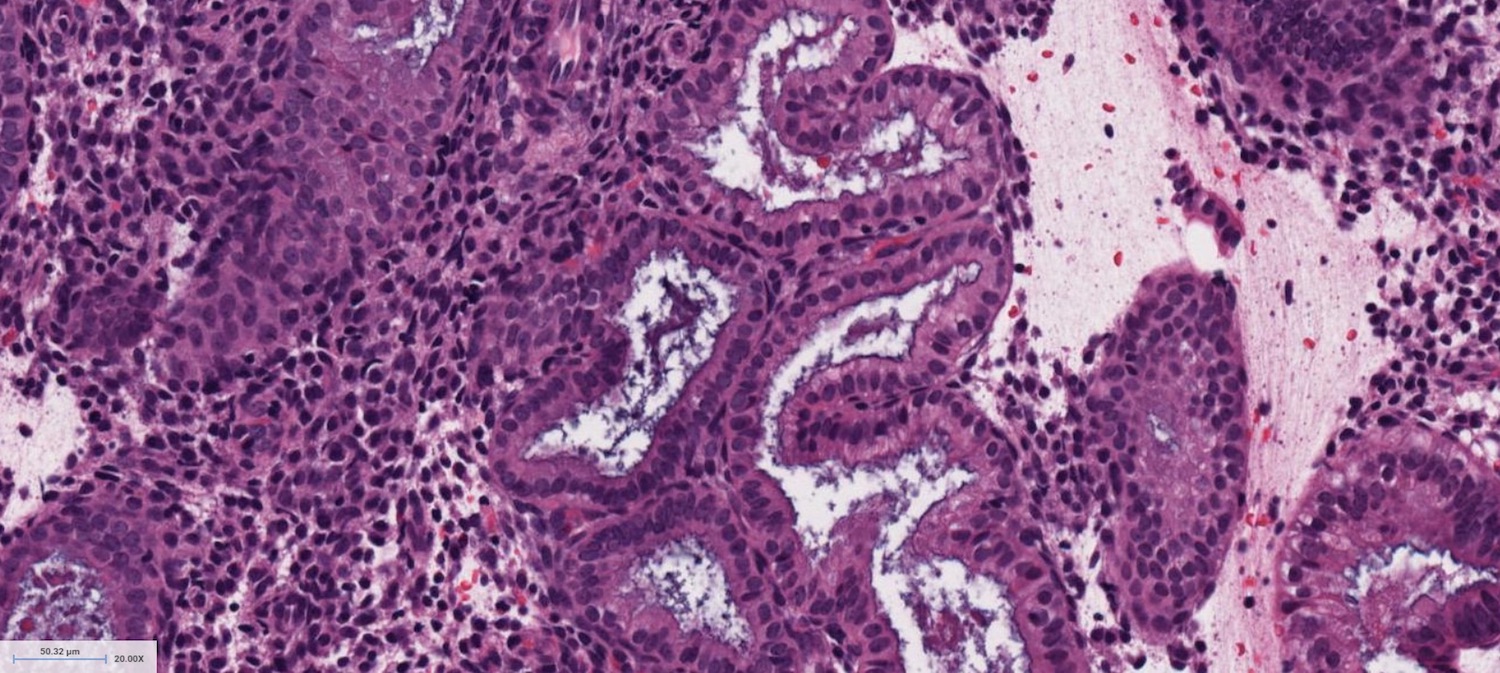
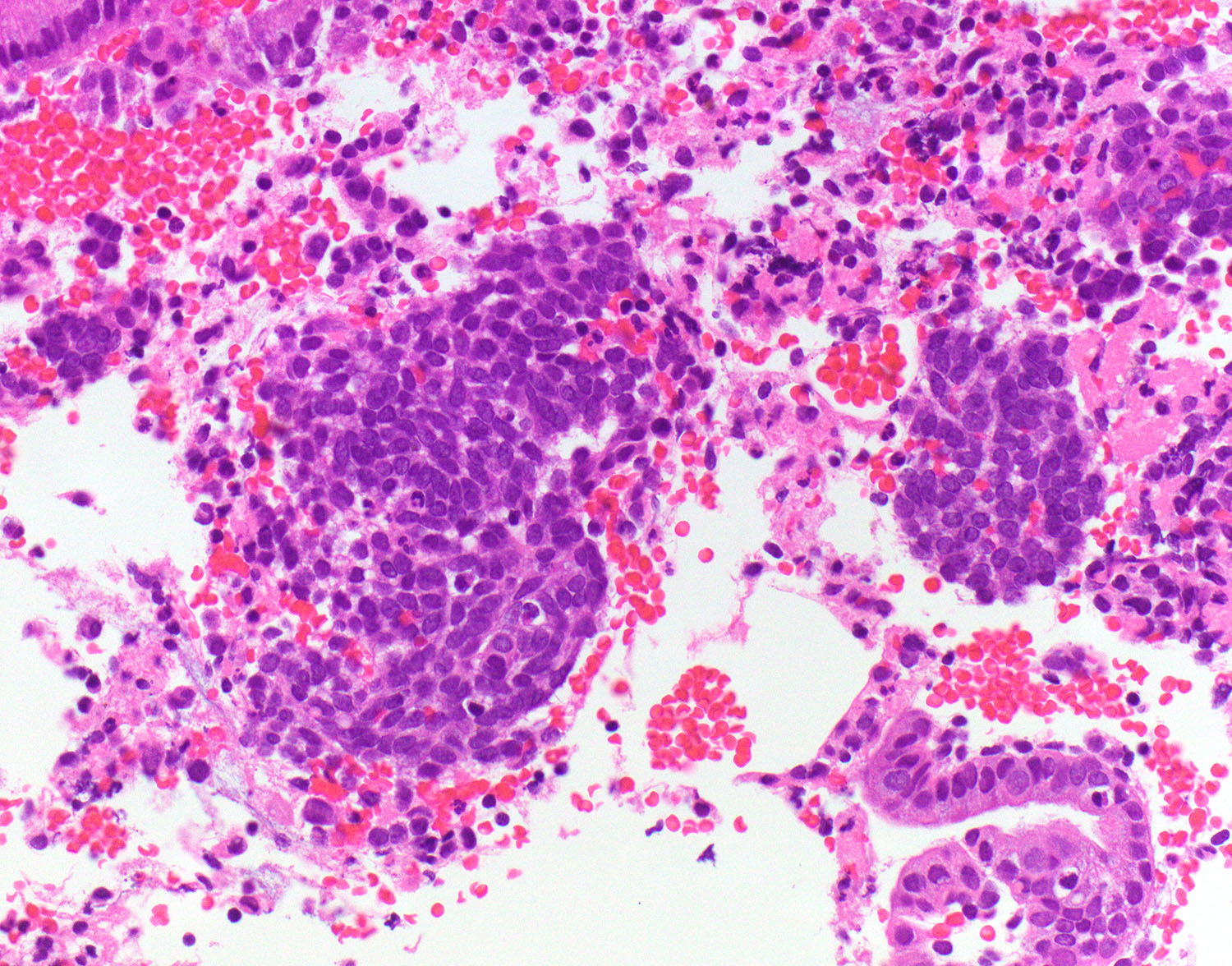
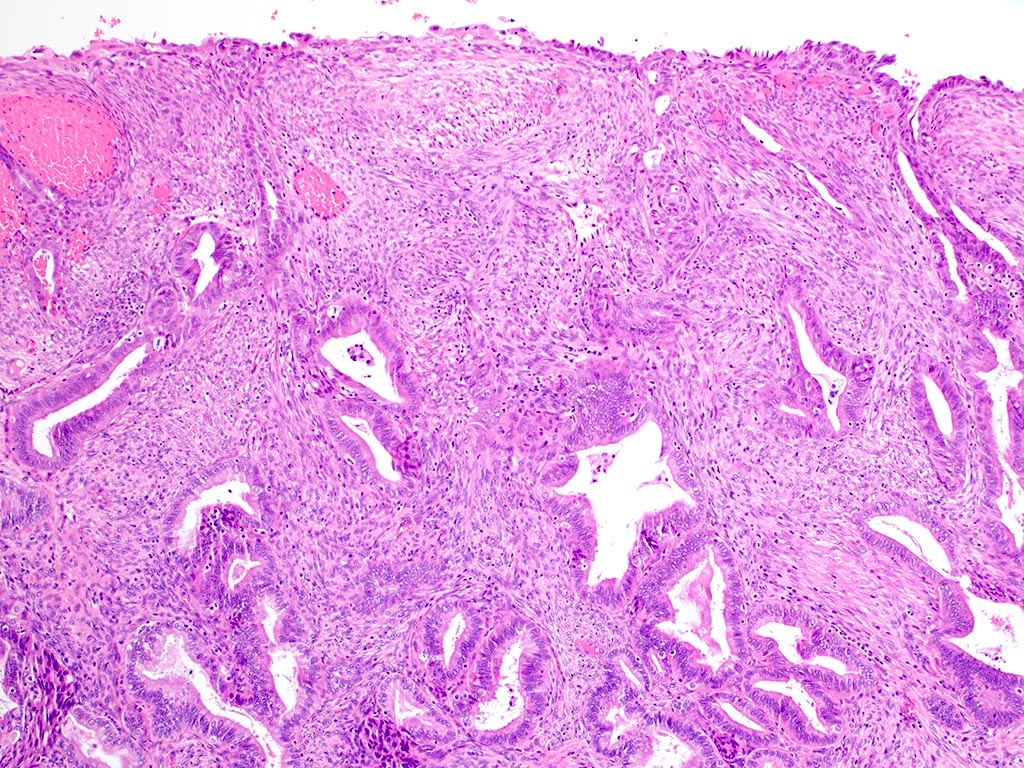
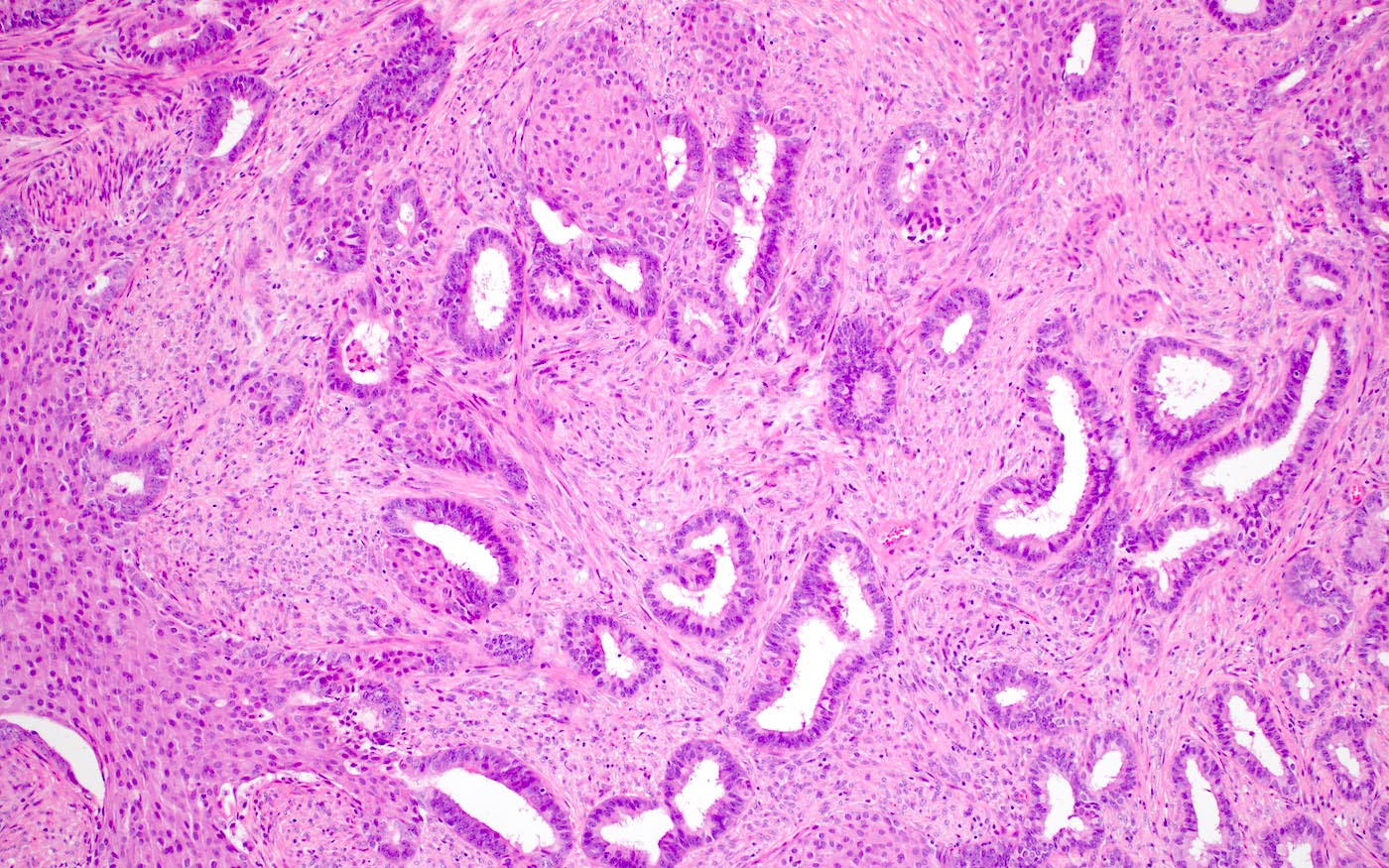
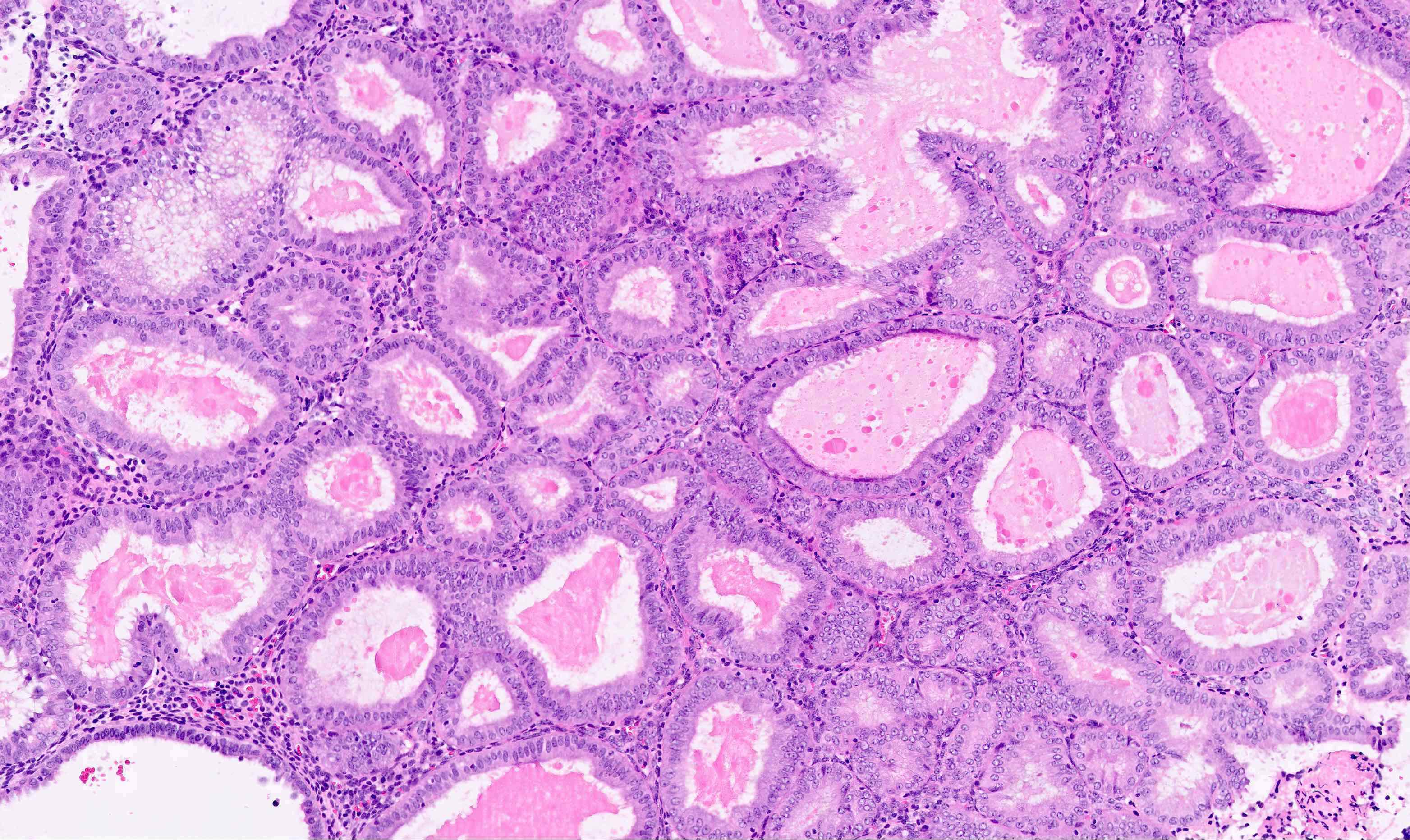
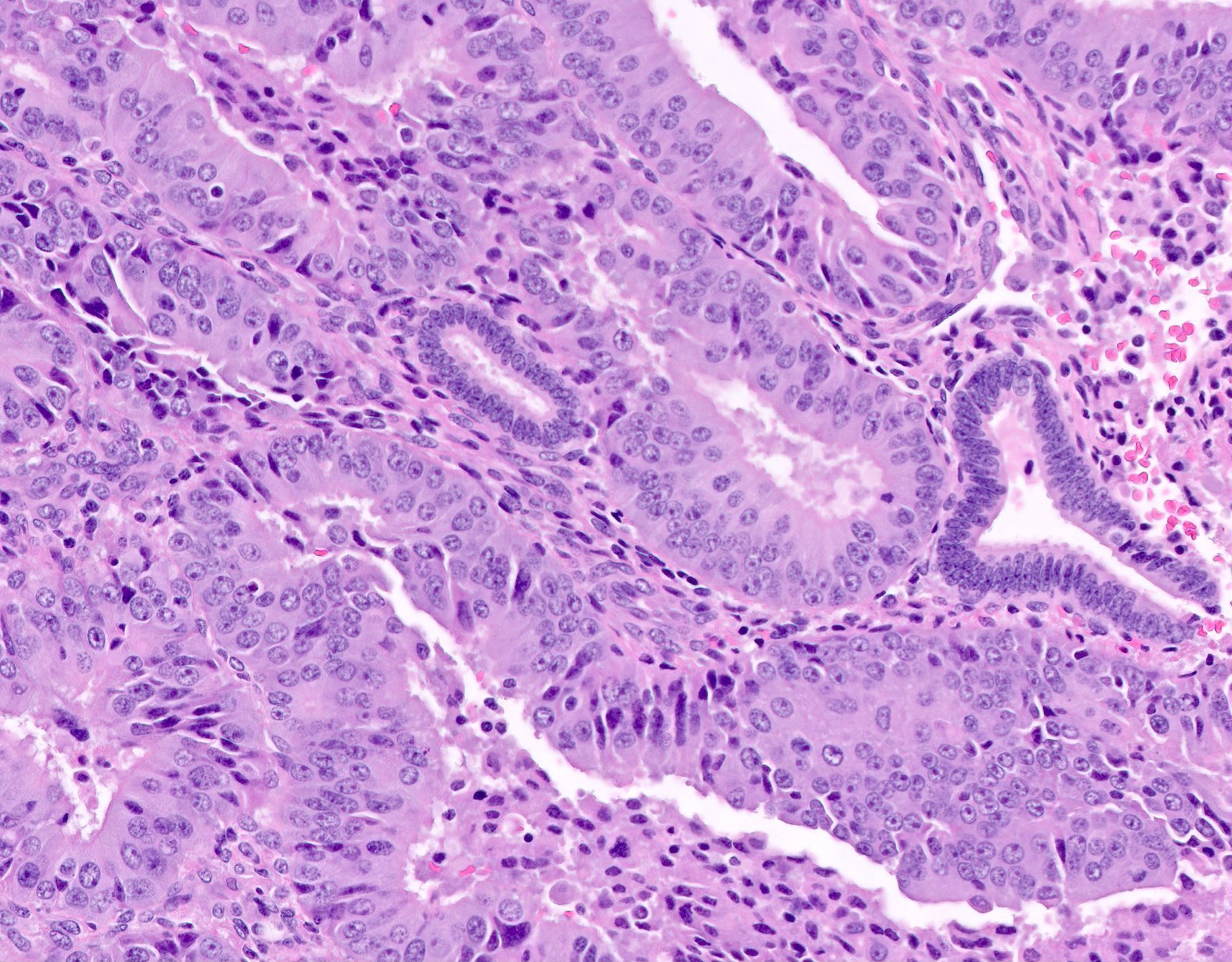
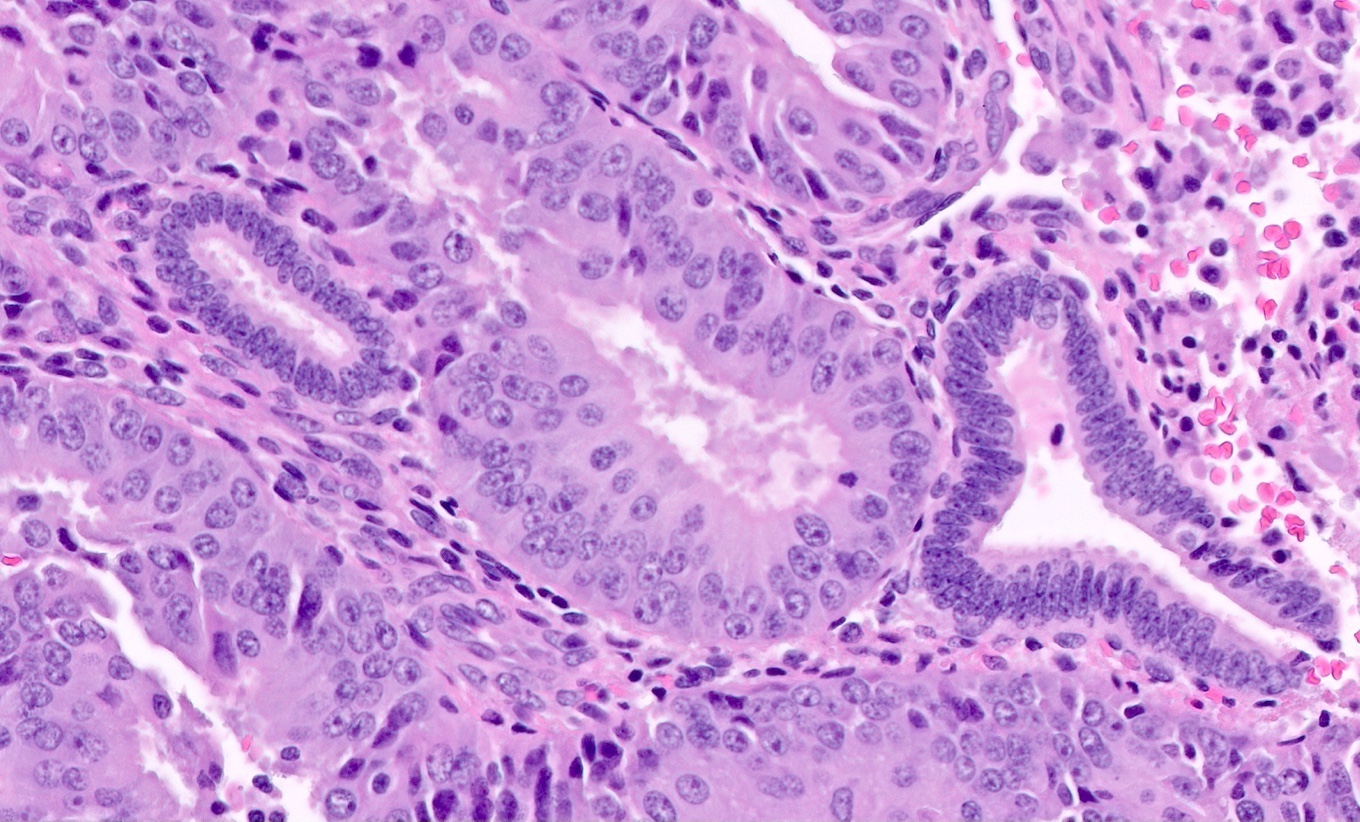
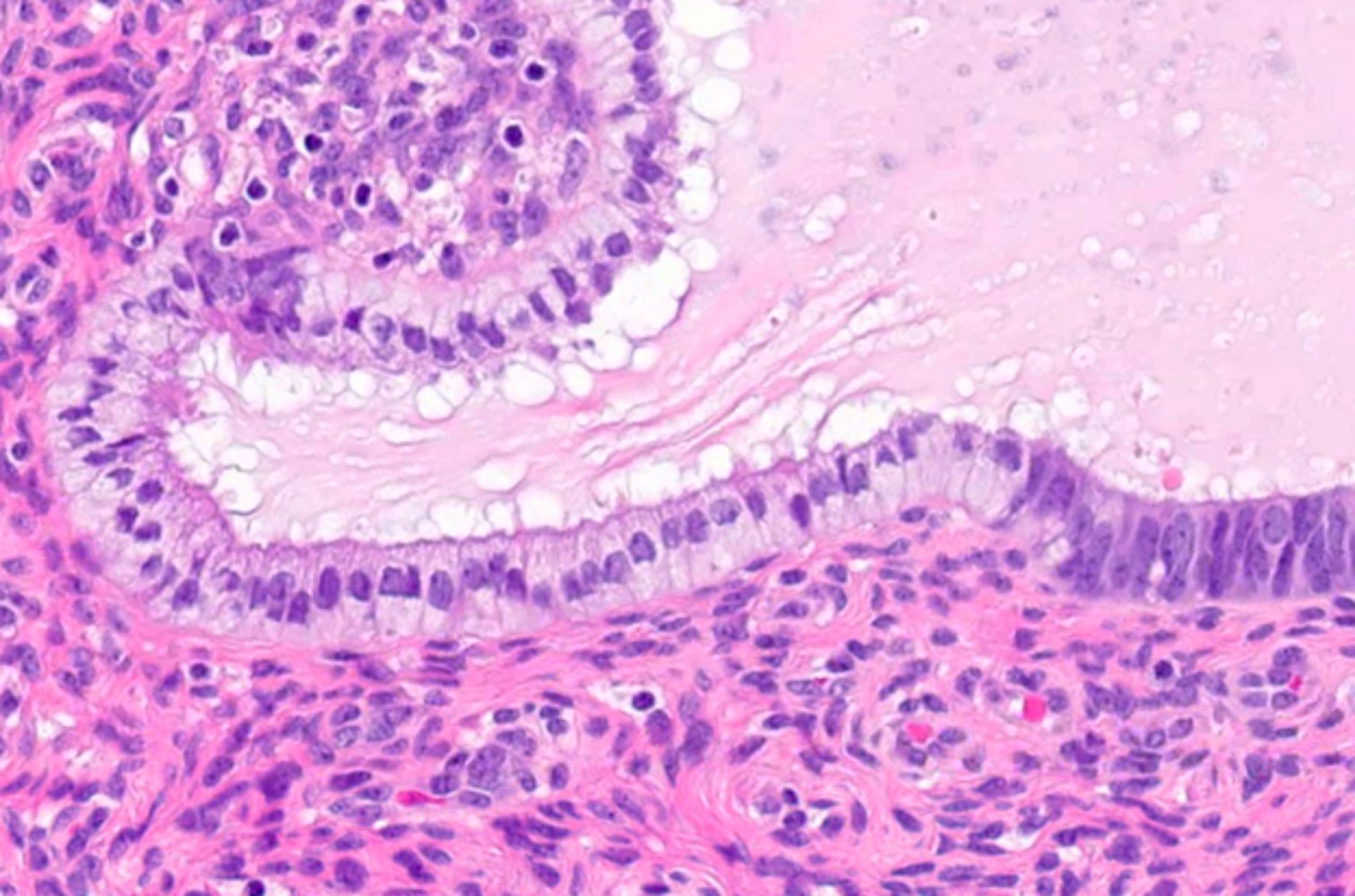
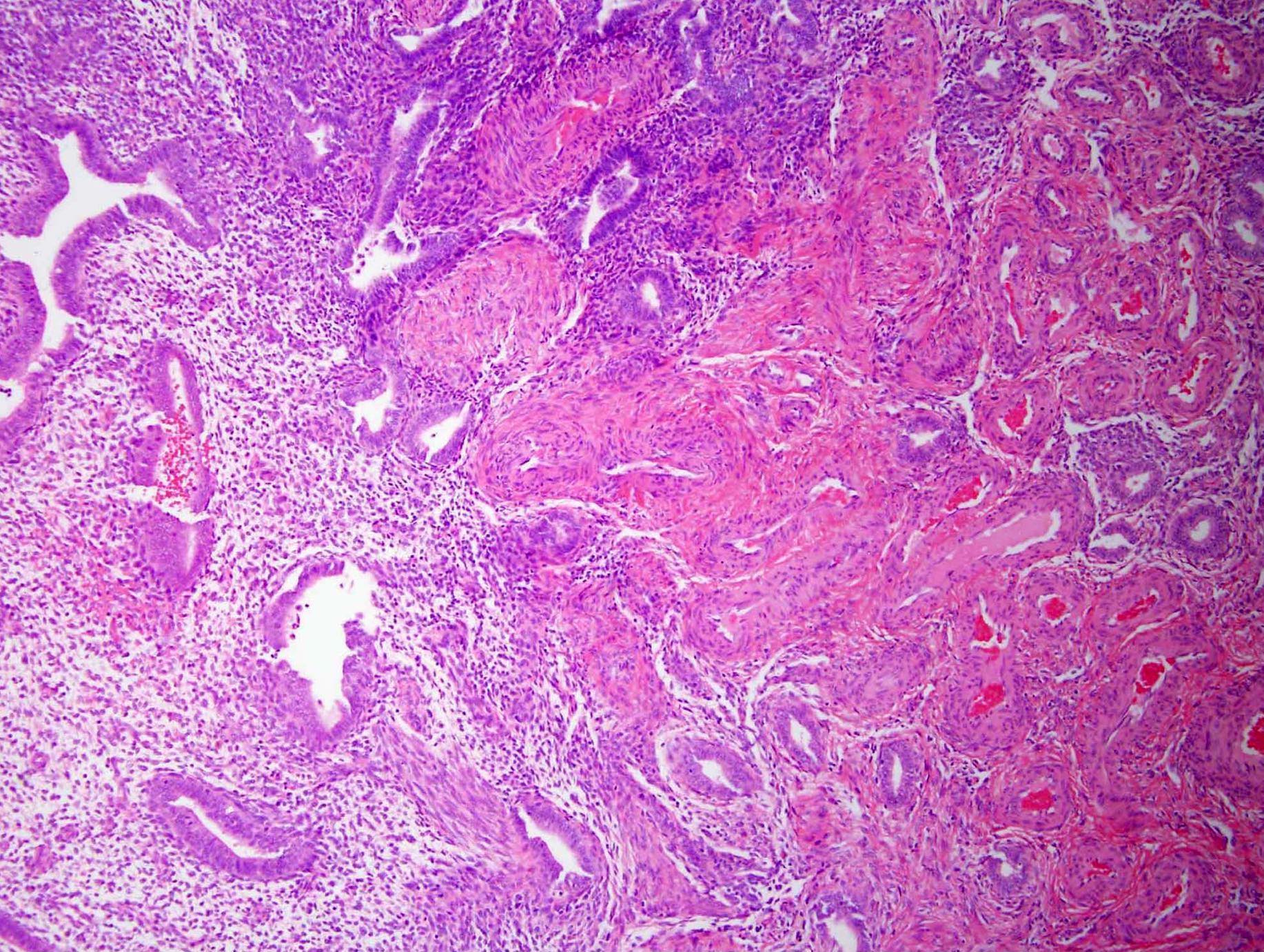
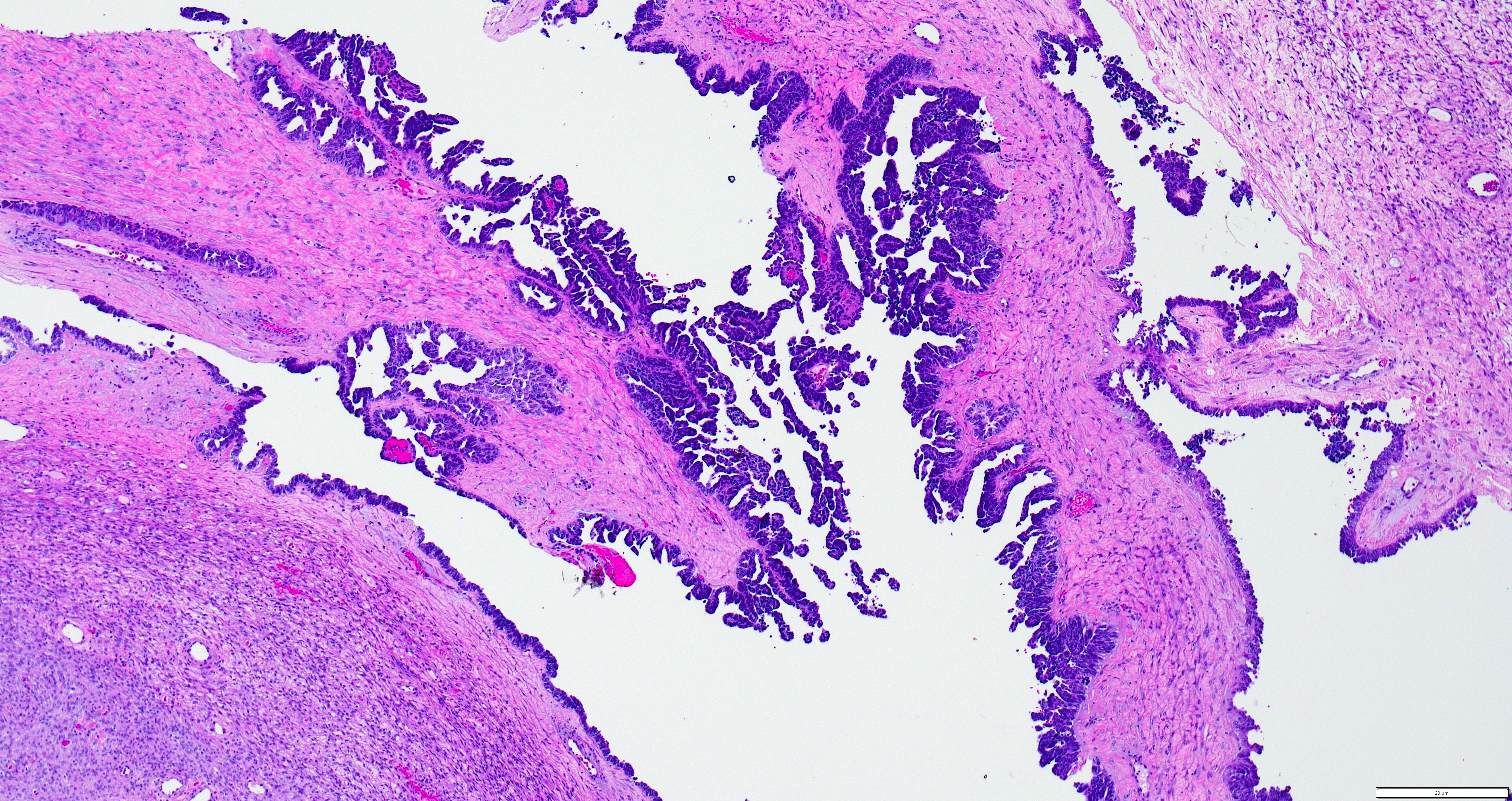
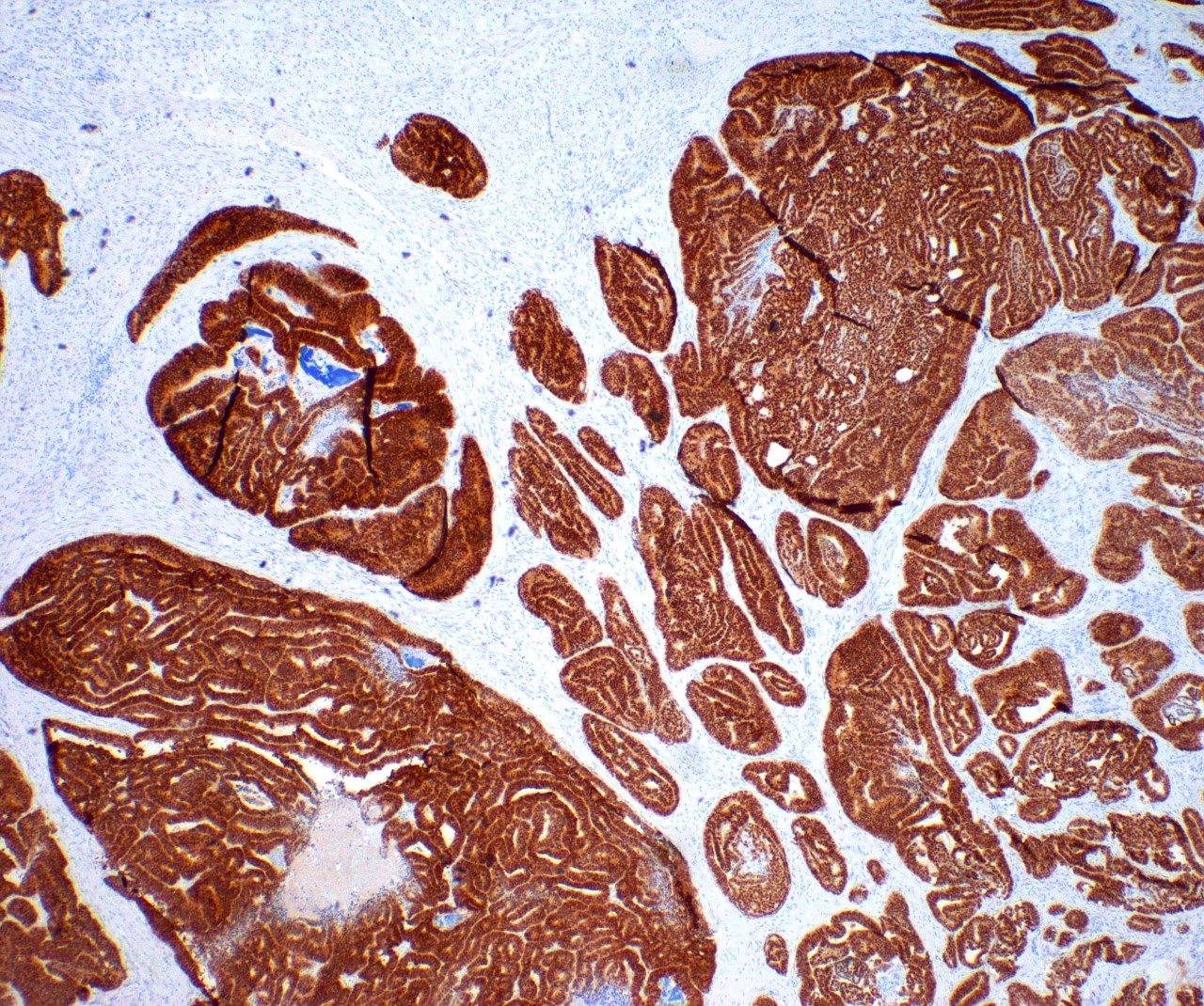
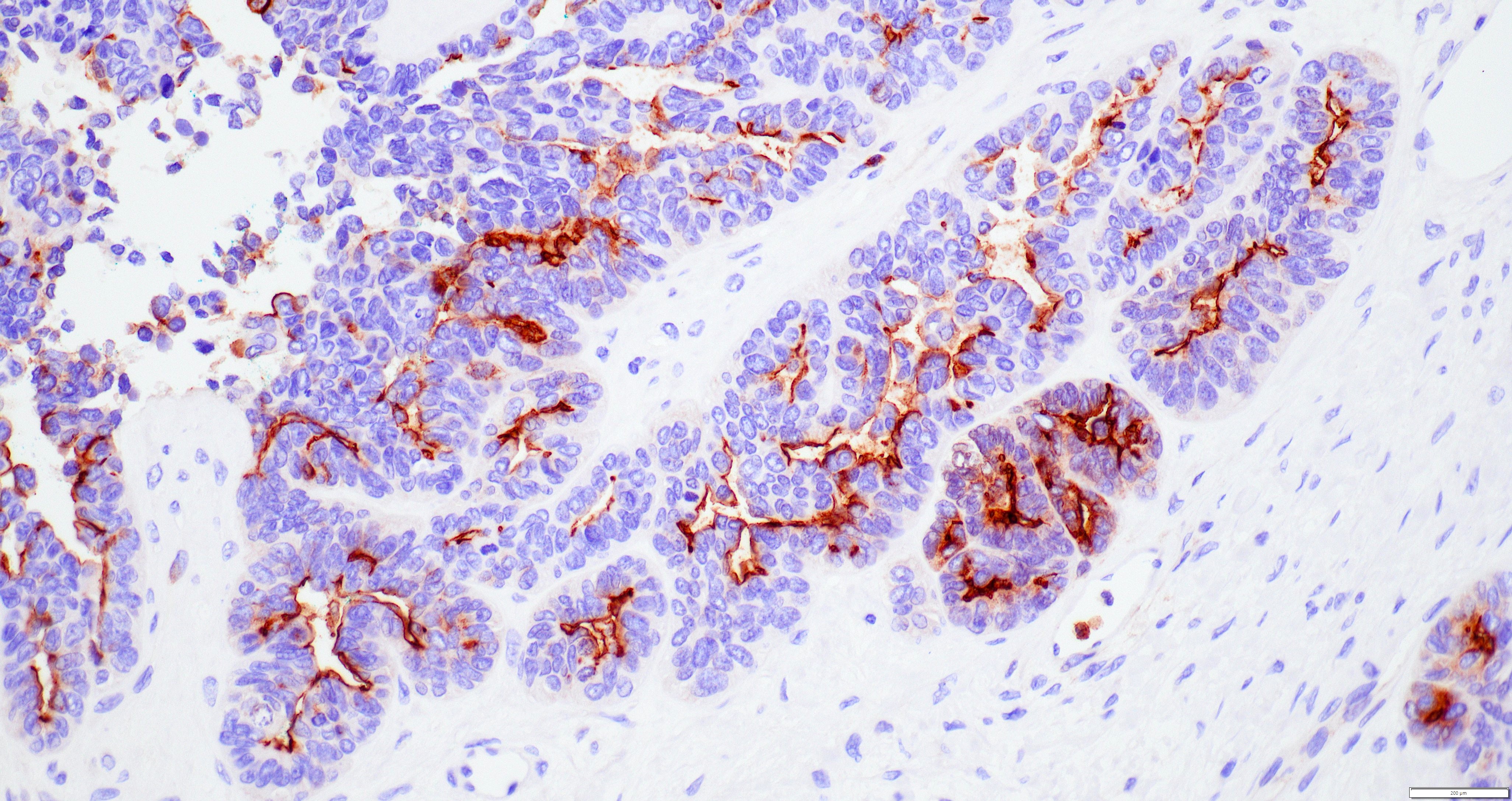
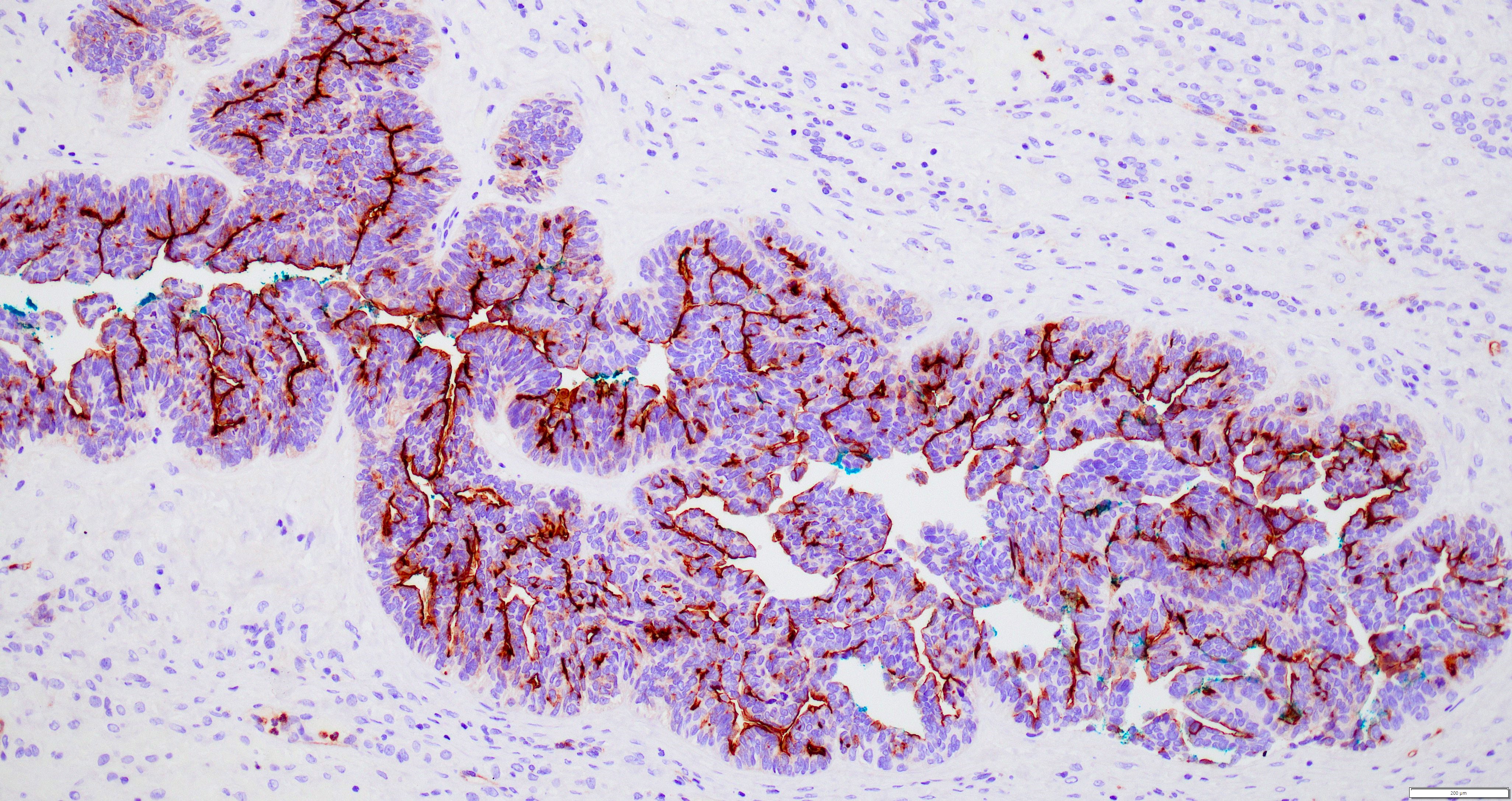
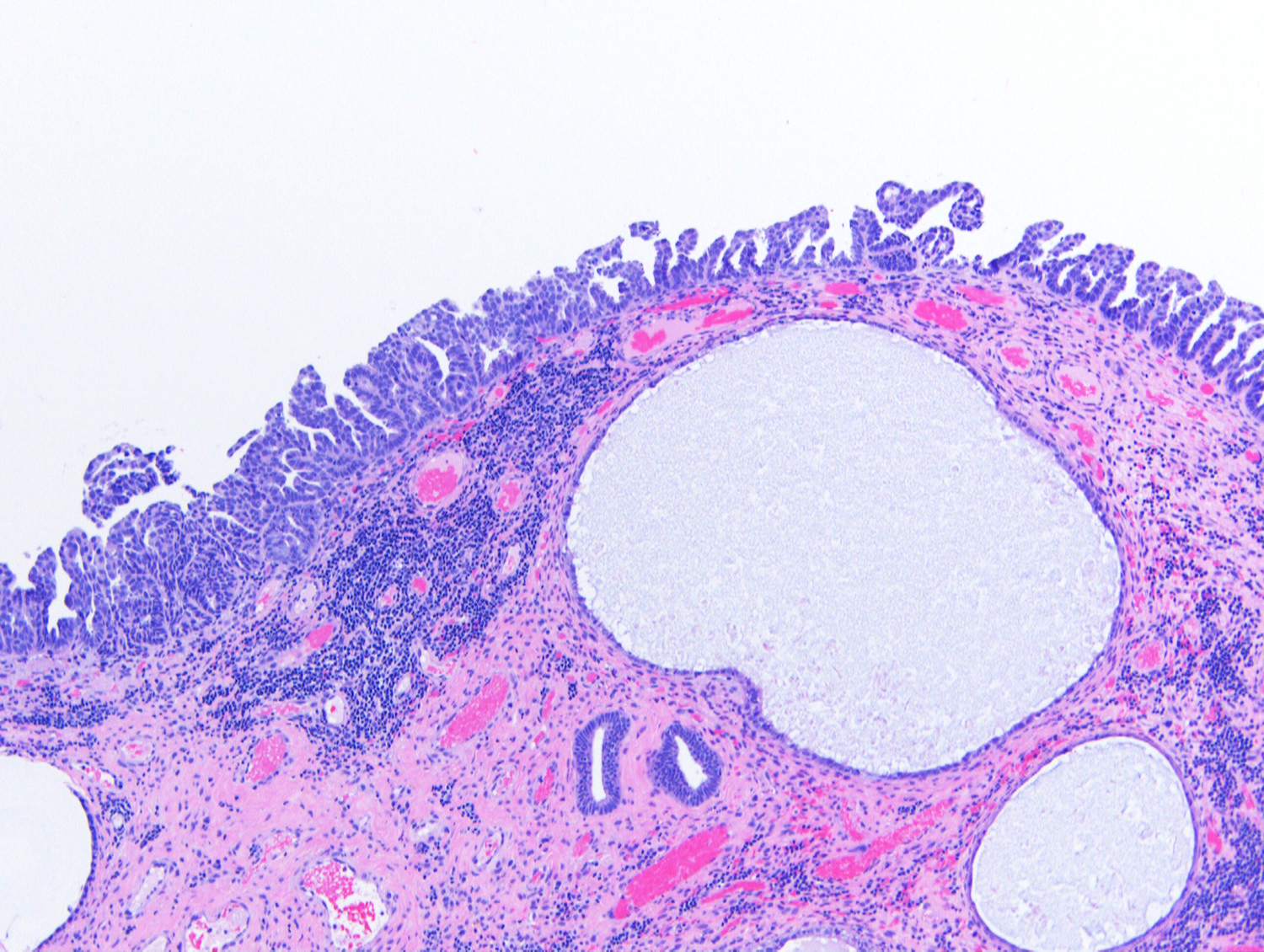
- If unsure whether tumor is in the cervix or lower uterine segment, identify the most proximal endocervical mucinous gland, which will define the boundary between these anatomic locations (Figures 4 and 5)
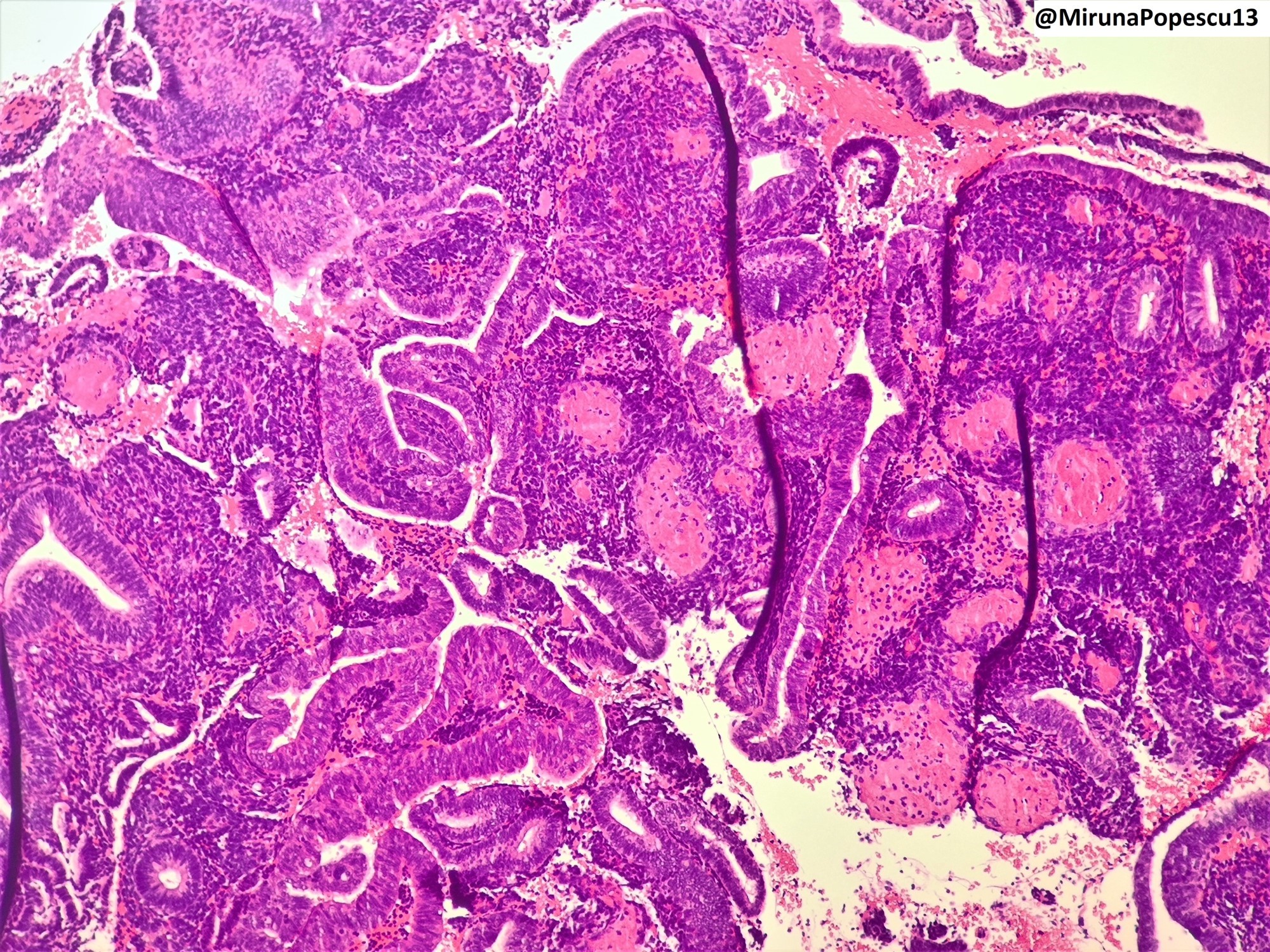
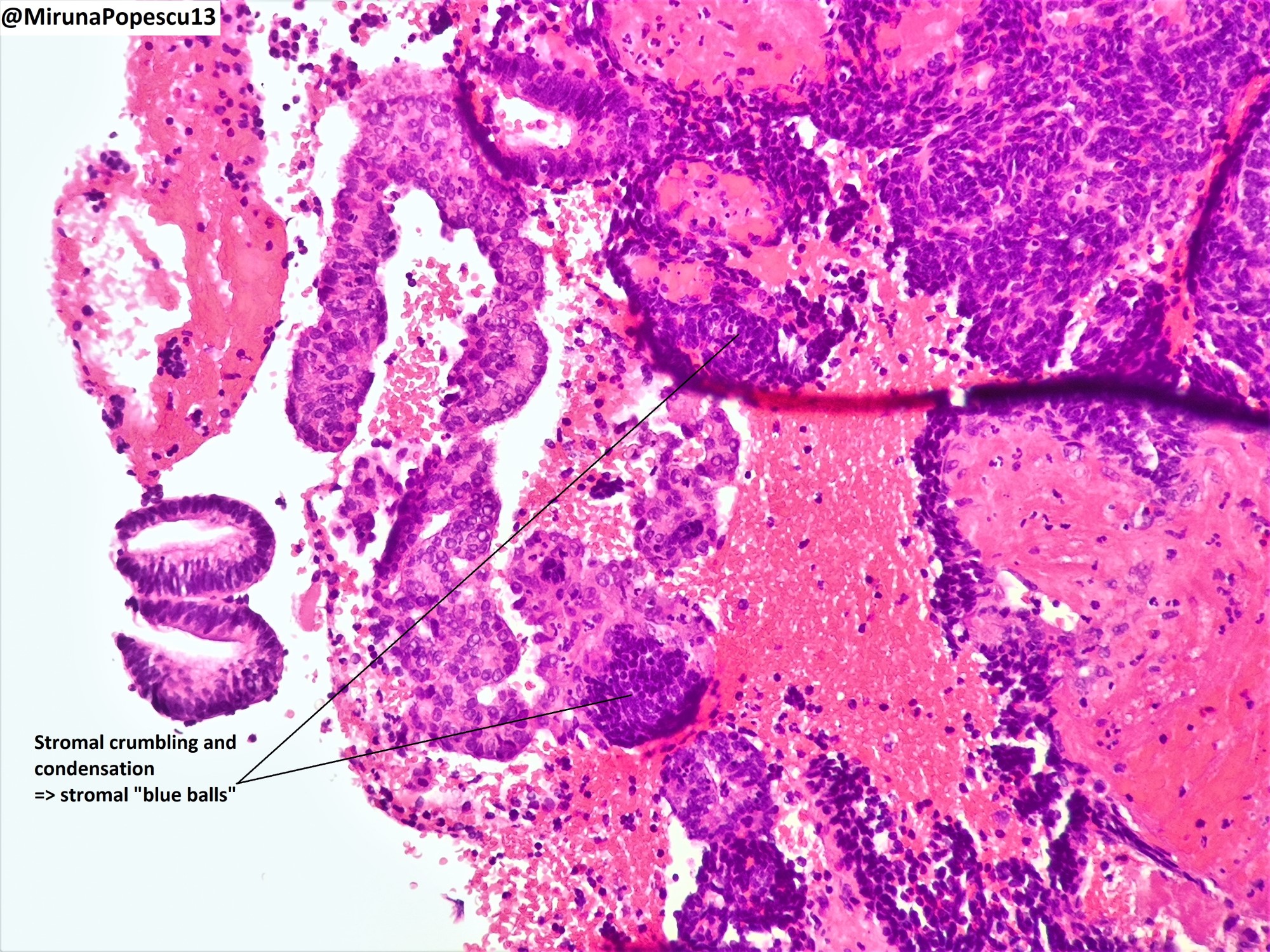
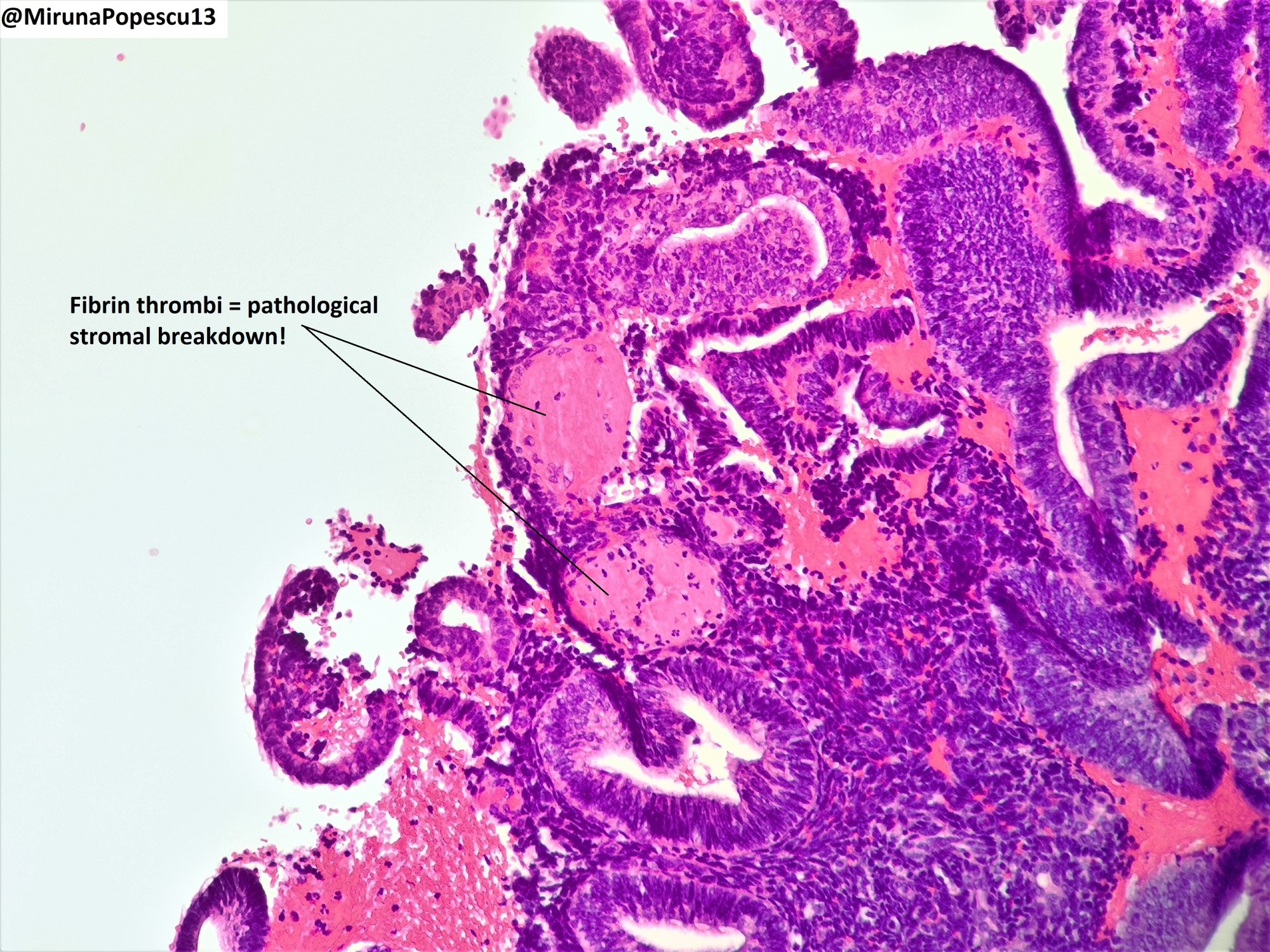
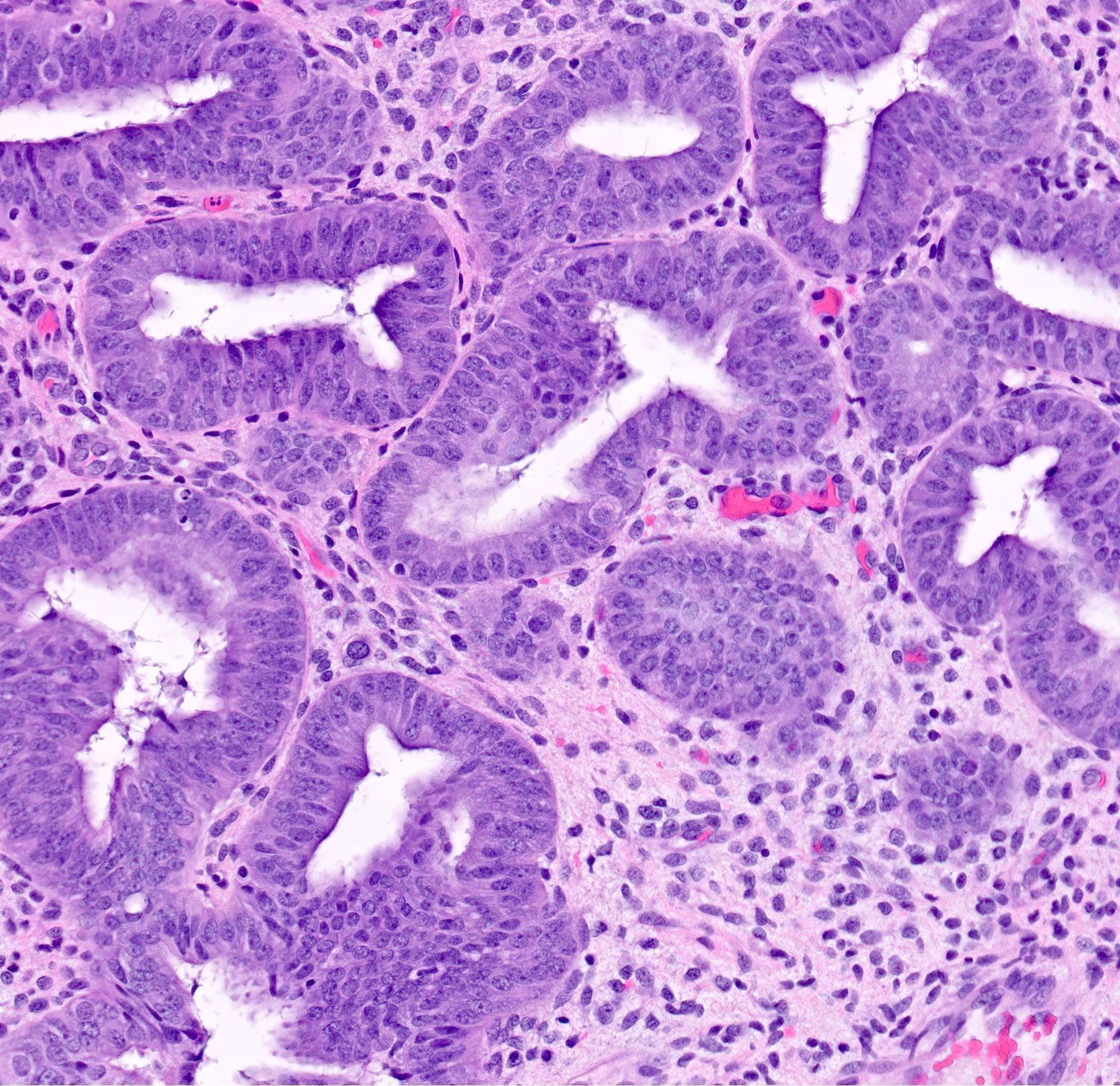
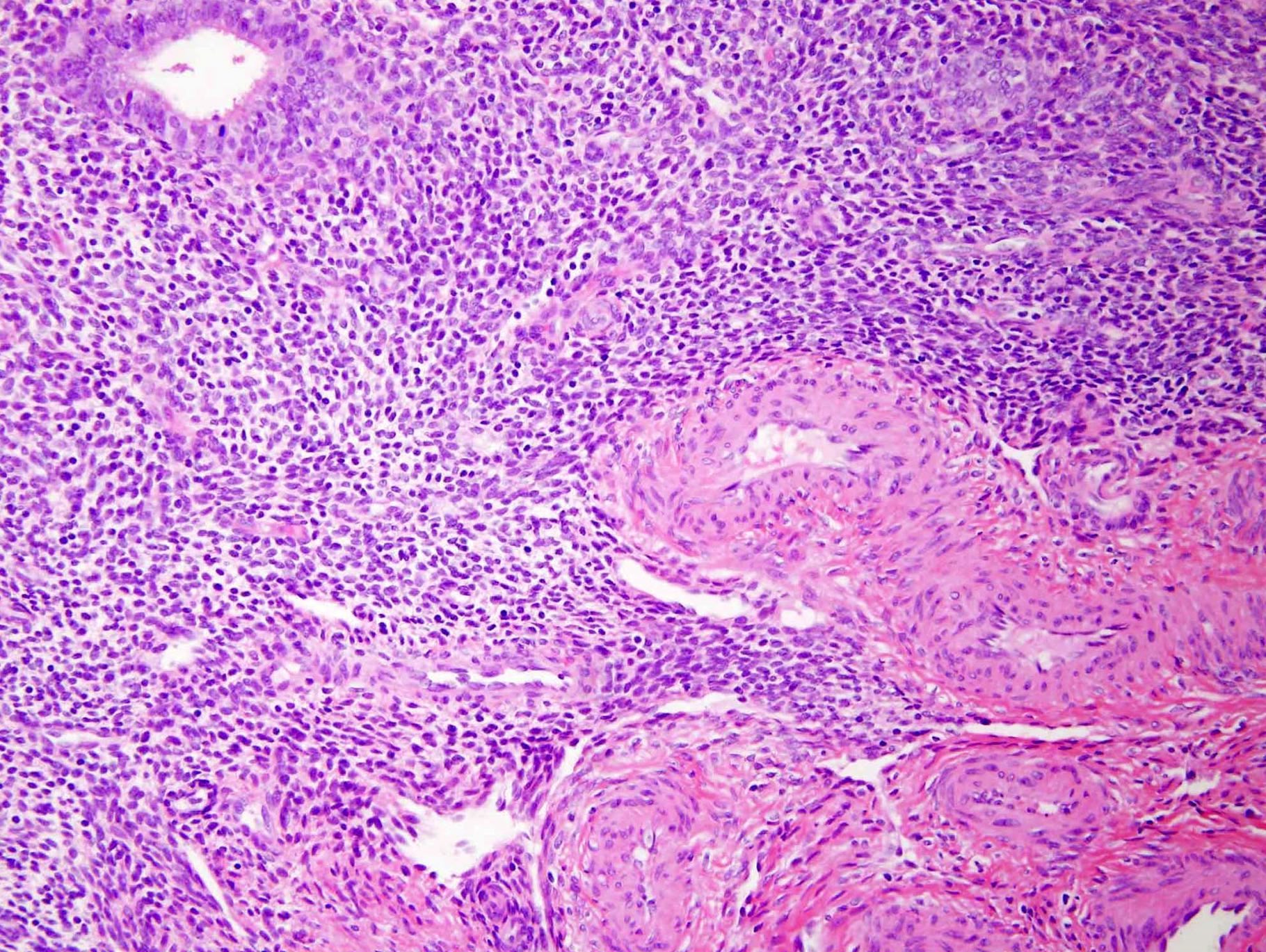
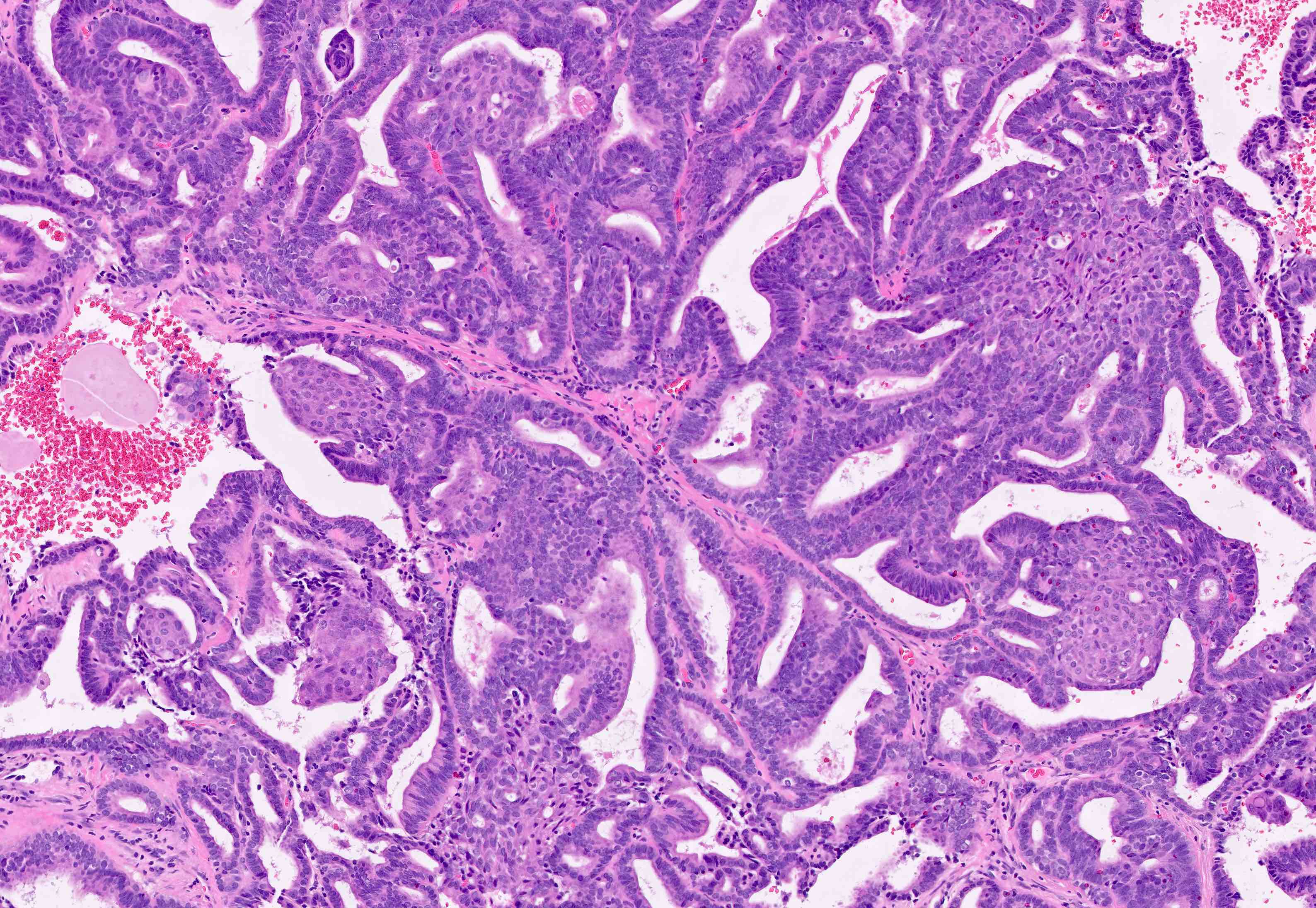
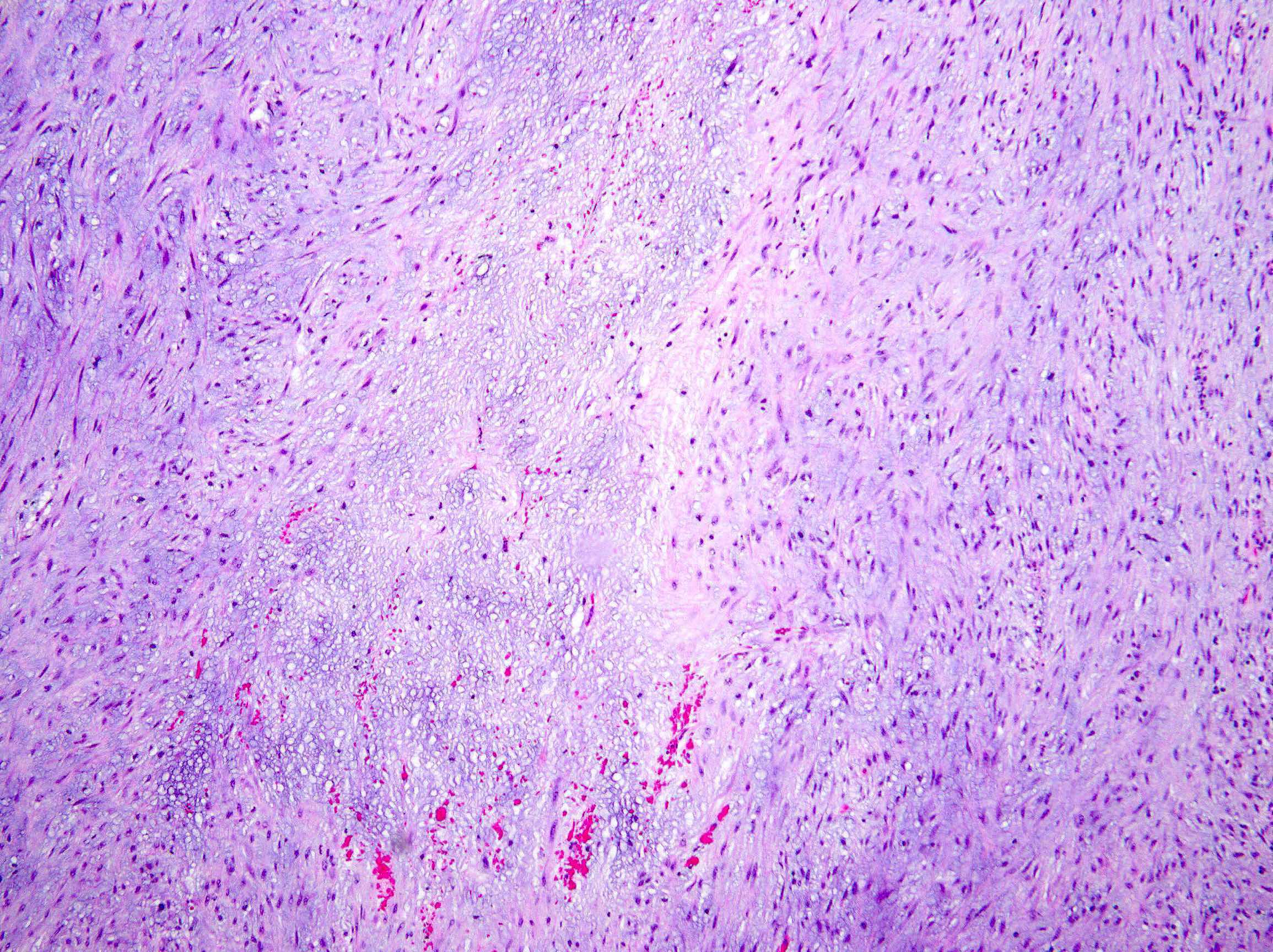
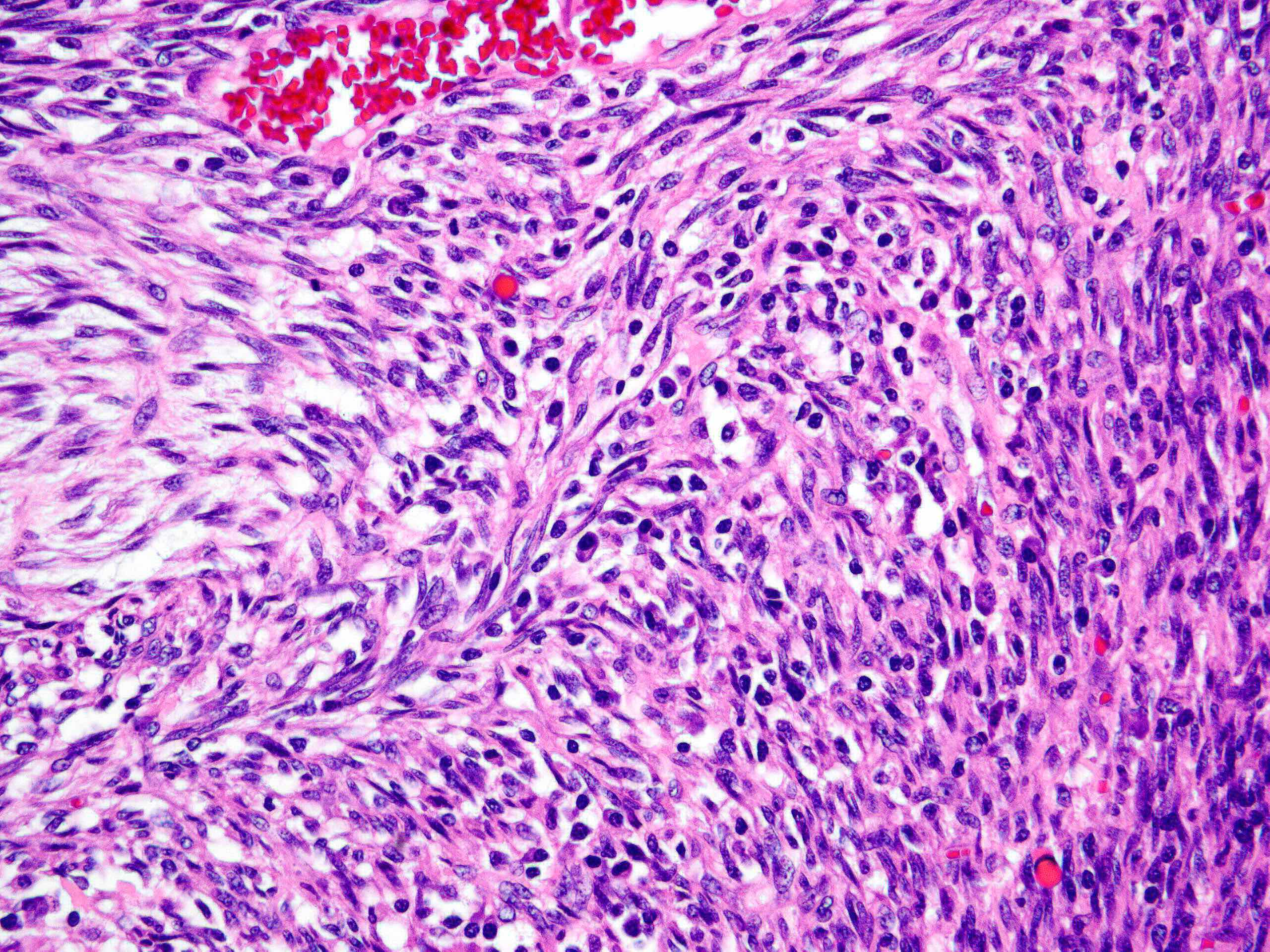
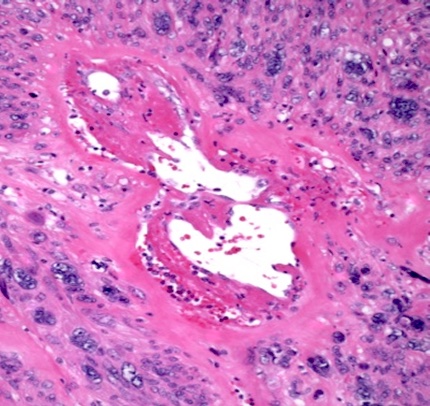
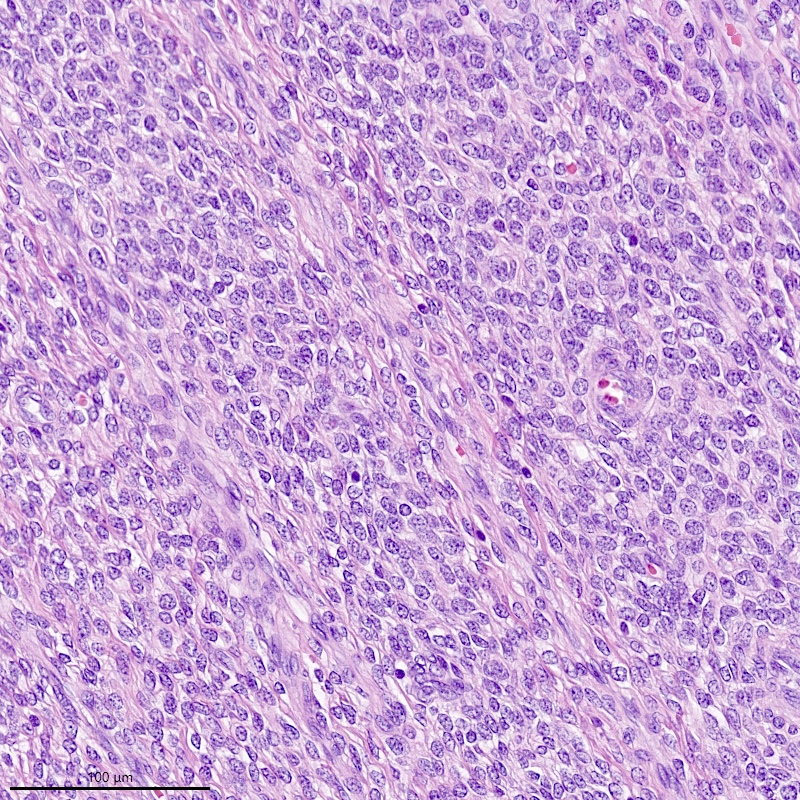
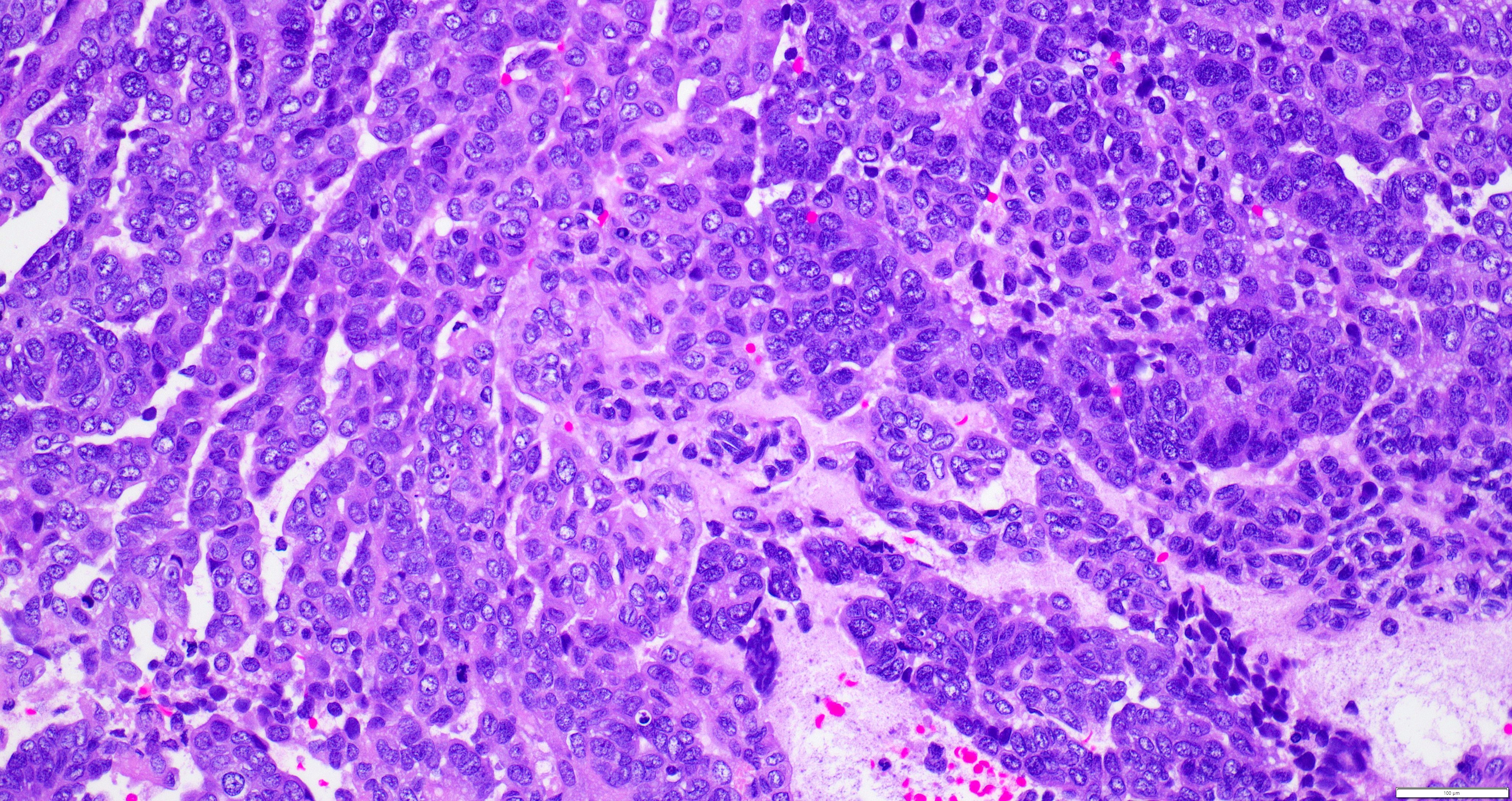
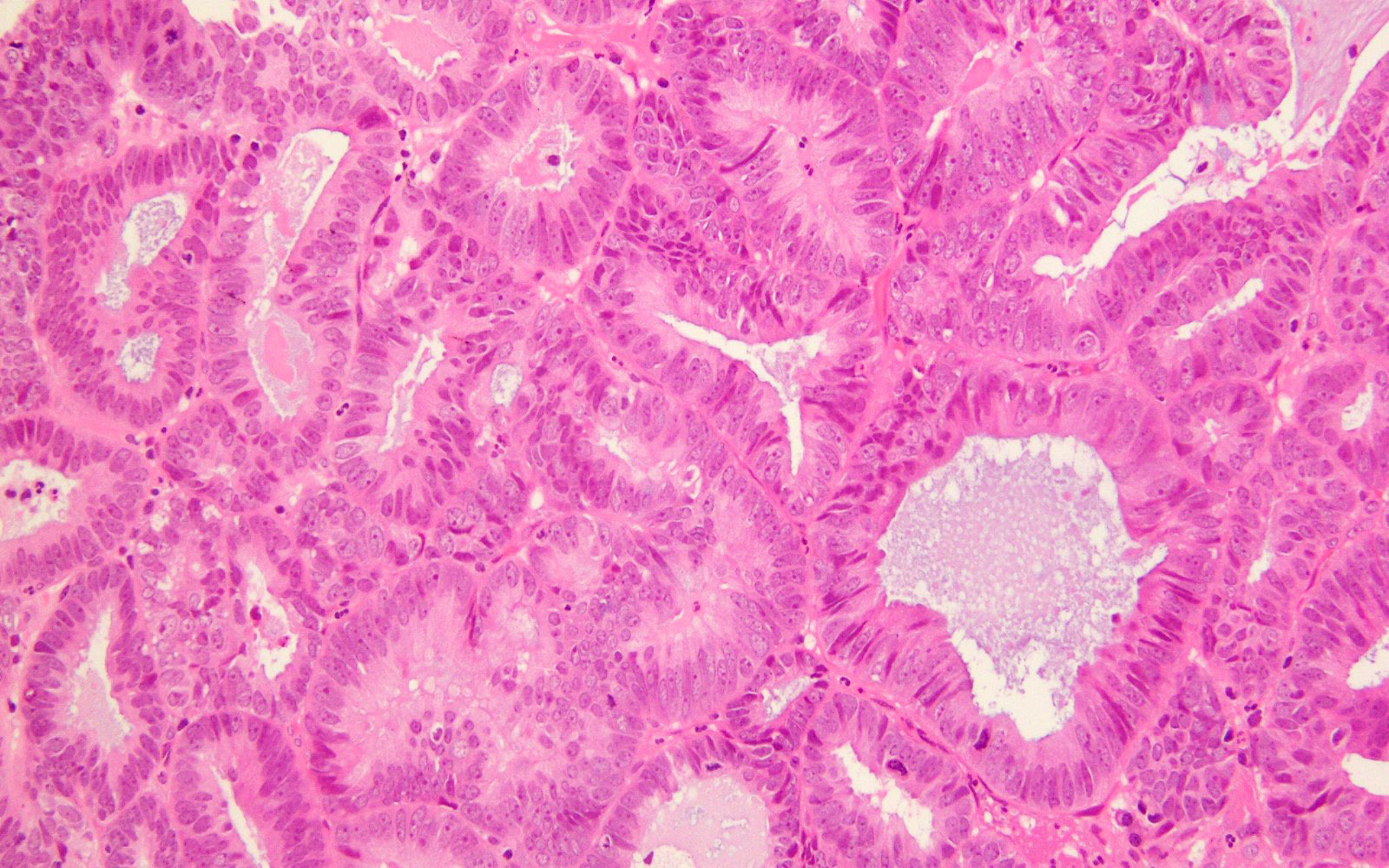
- Stromal invasion can be seen as obviously infiltrative glands or cells with desmoplasia or as complex architecture relative to the normal endocervical glandular compartment
- Carcinoma confined to the surface or to endocervical glands can be reported but does not modify stage or impact prognosis
- Reporting the depth of cervical stromal invasion by endometrial carcinoma is optional
- The National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology Uterine Neoplasms lists deep cervical stromal invasion as an adverse risk factor in patients with stage II endometrial carcinoma (NCCN: Uterine Neoplasms [Accessed 9 February 2023])
- Estimation of depth of cervical wall invasion may be used to determine the type of adjuvant radiation (Brachytherapy 2019;18:606)
- Depth of invasion into the cervix can be measured in mm, providing the thickness of the cervical wall at that level in mm as well
- Alternatively, it can be reported in terms of invasion confined to 33% of the wall, 66% of the wall or extending to the outer third of the wall
- It is recommended to measure the distance between tumor and margin: distal cervical / vaginal mucosa and parametrial margins
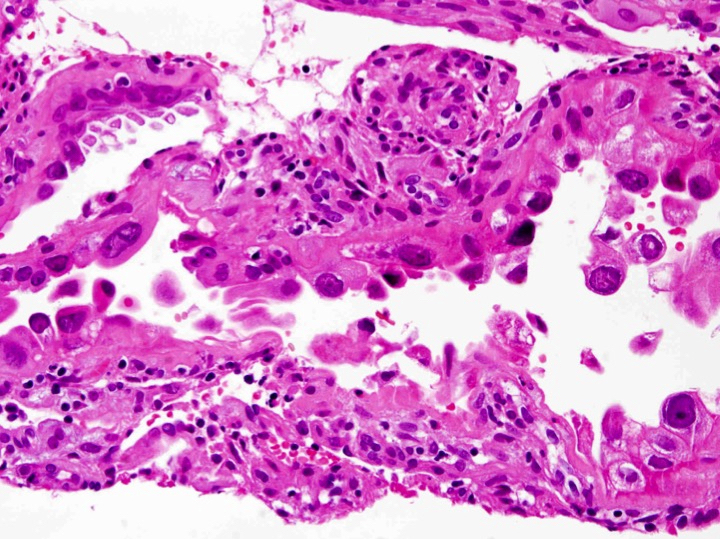
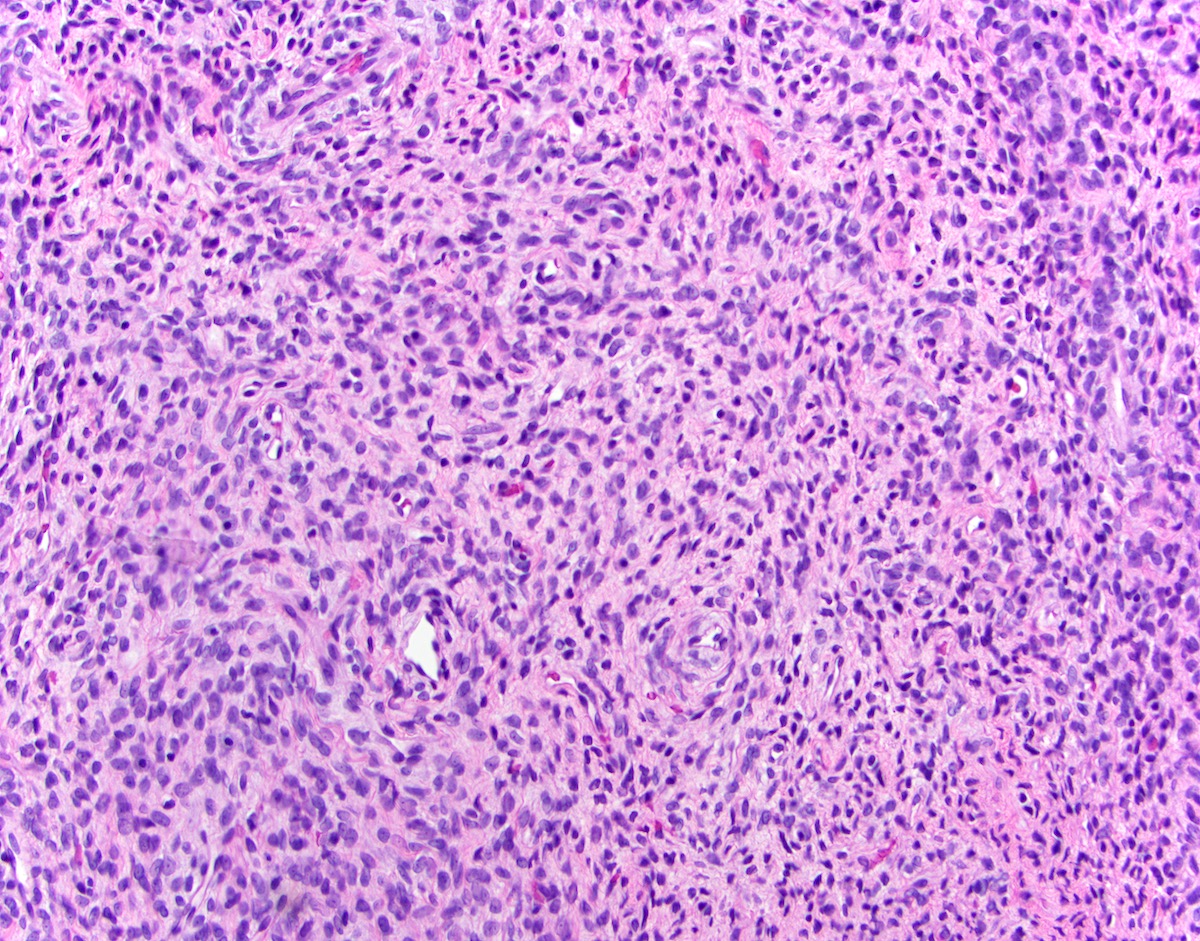
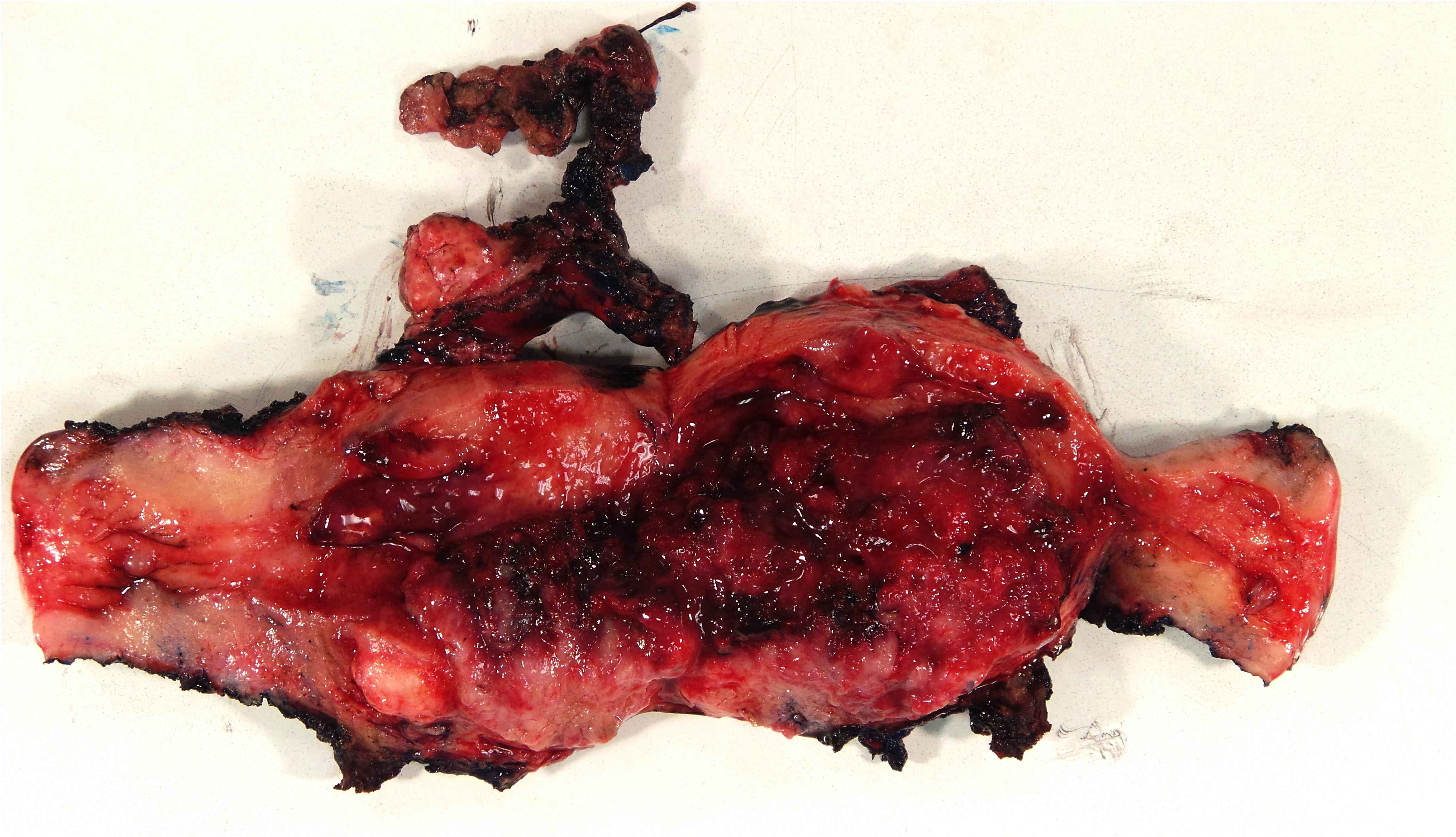
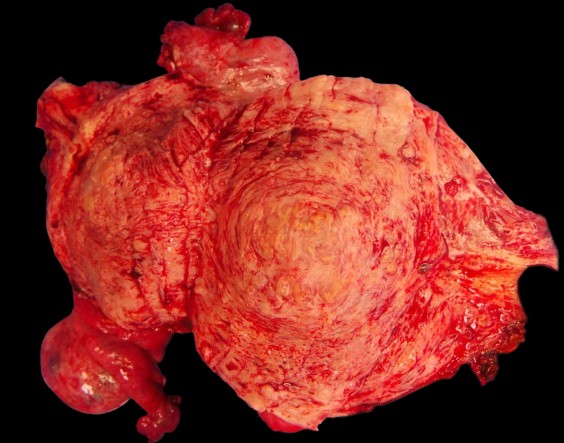
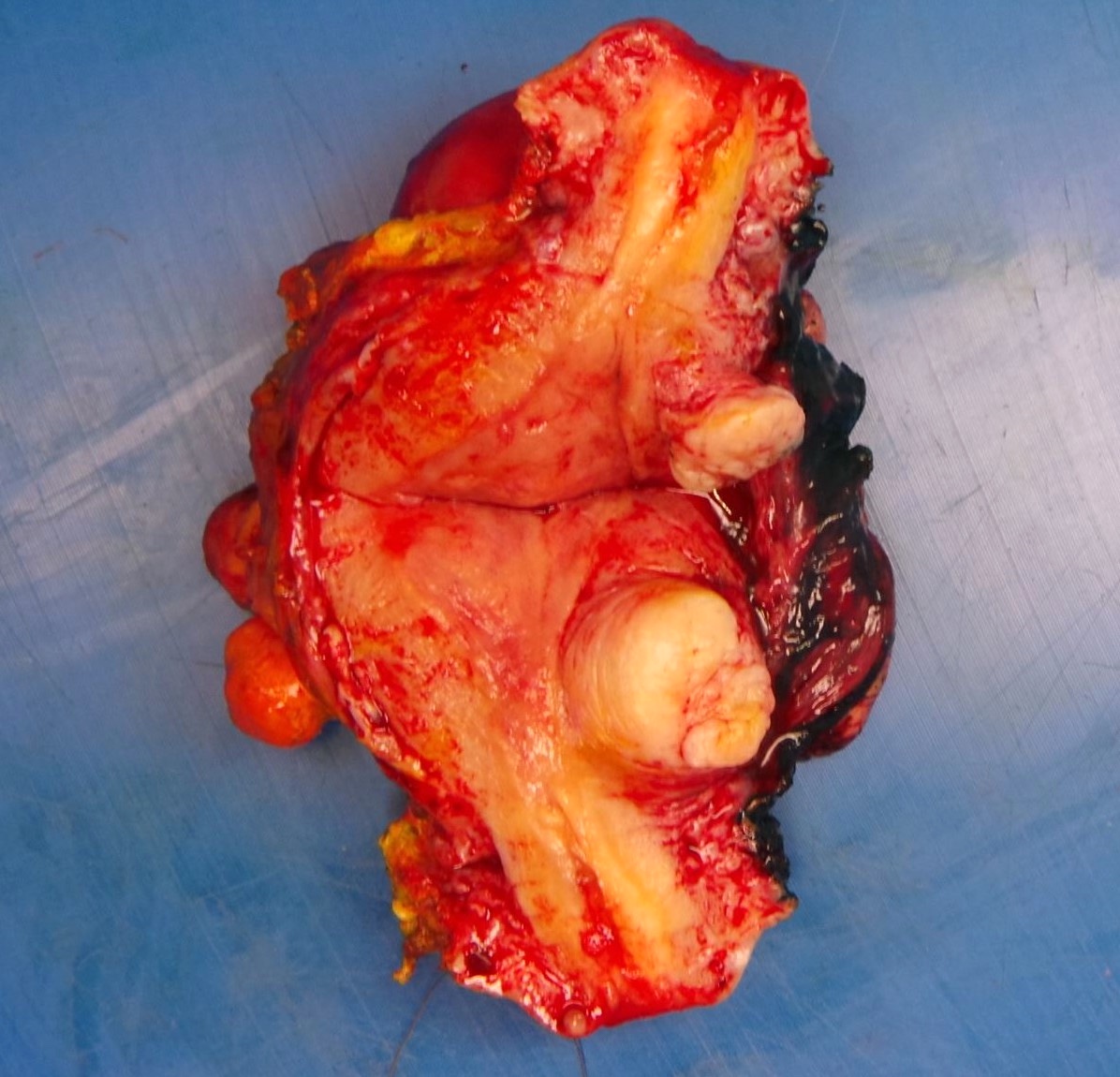
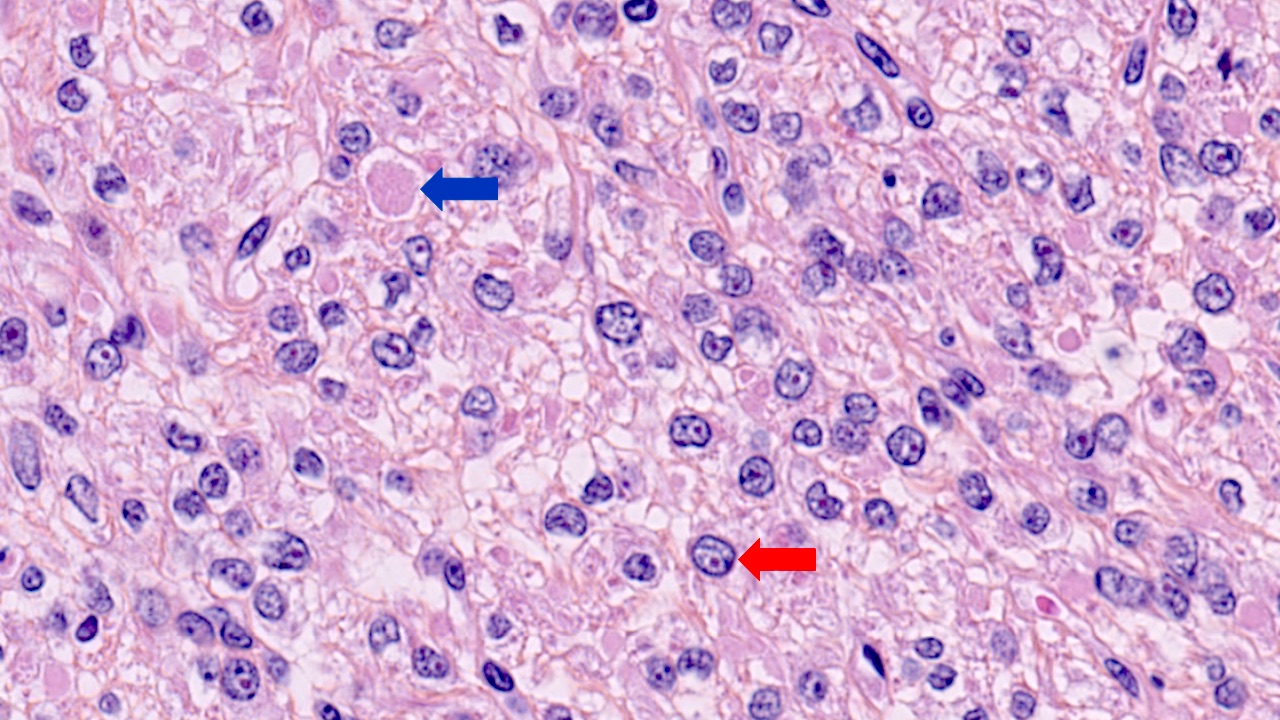
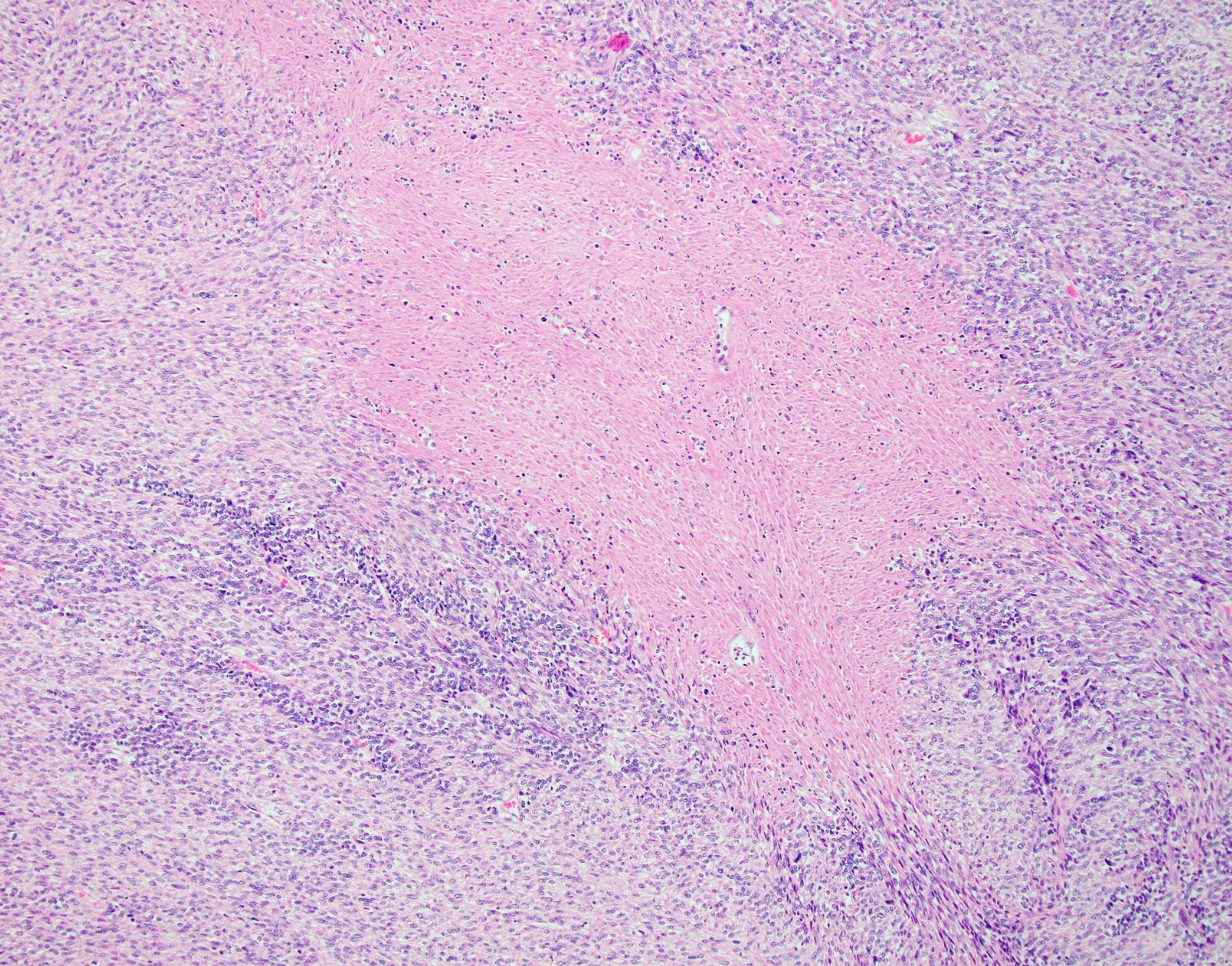
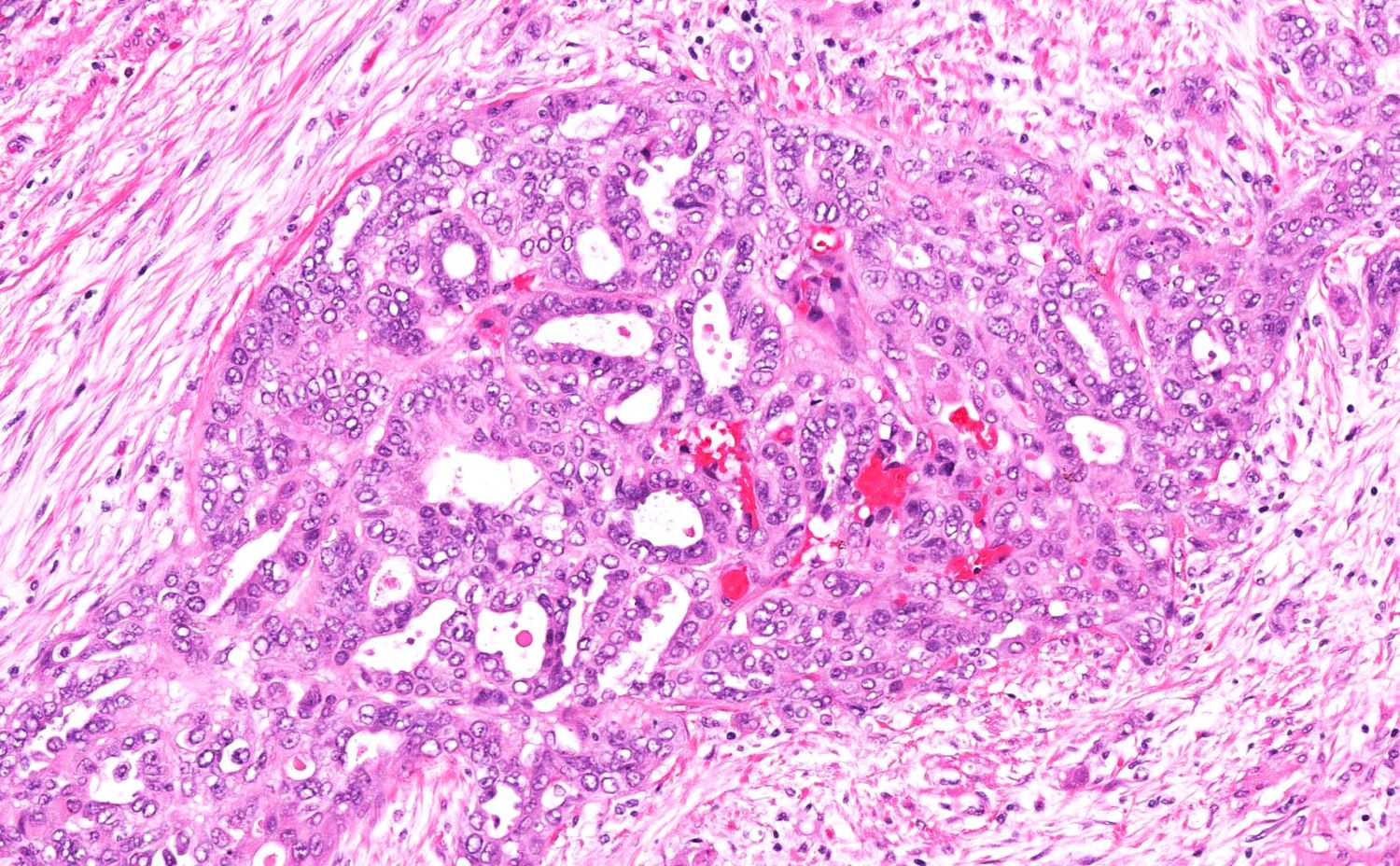
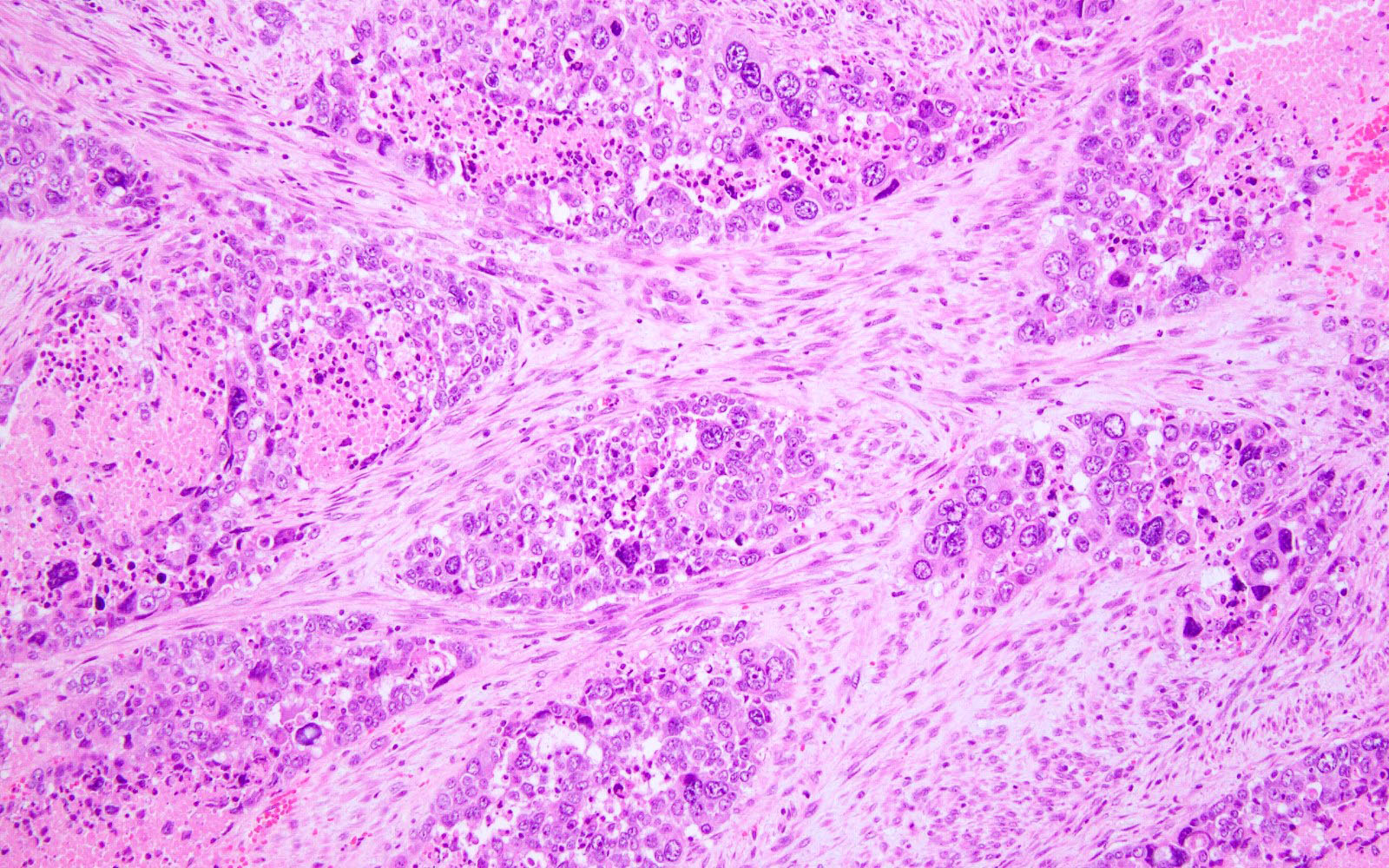
- Serosal involvement:
- Involvement of the uterine serosa is an adverse prognostic factor and warrants a stage IIIA
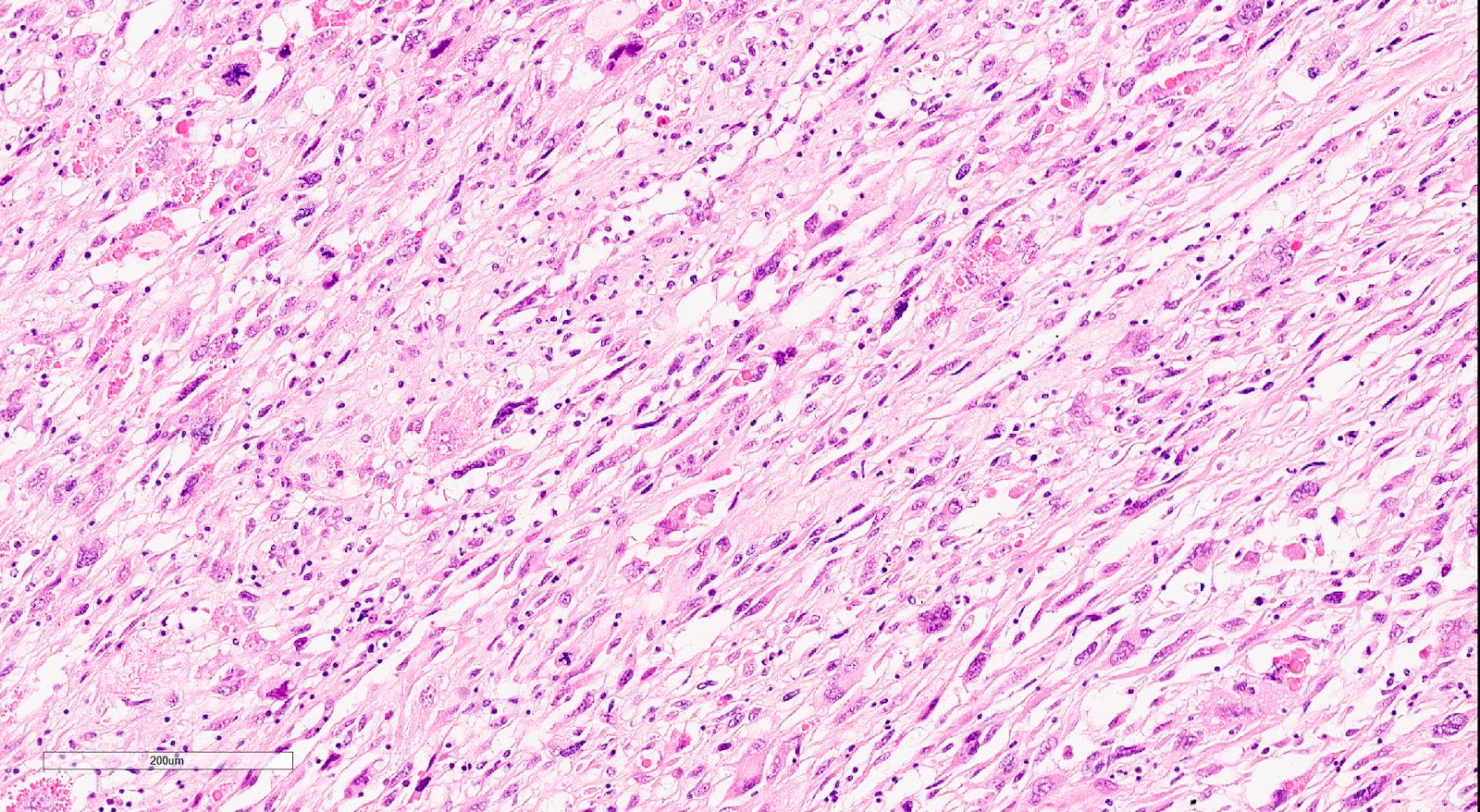
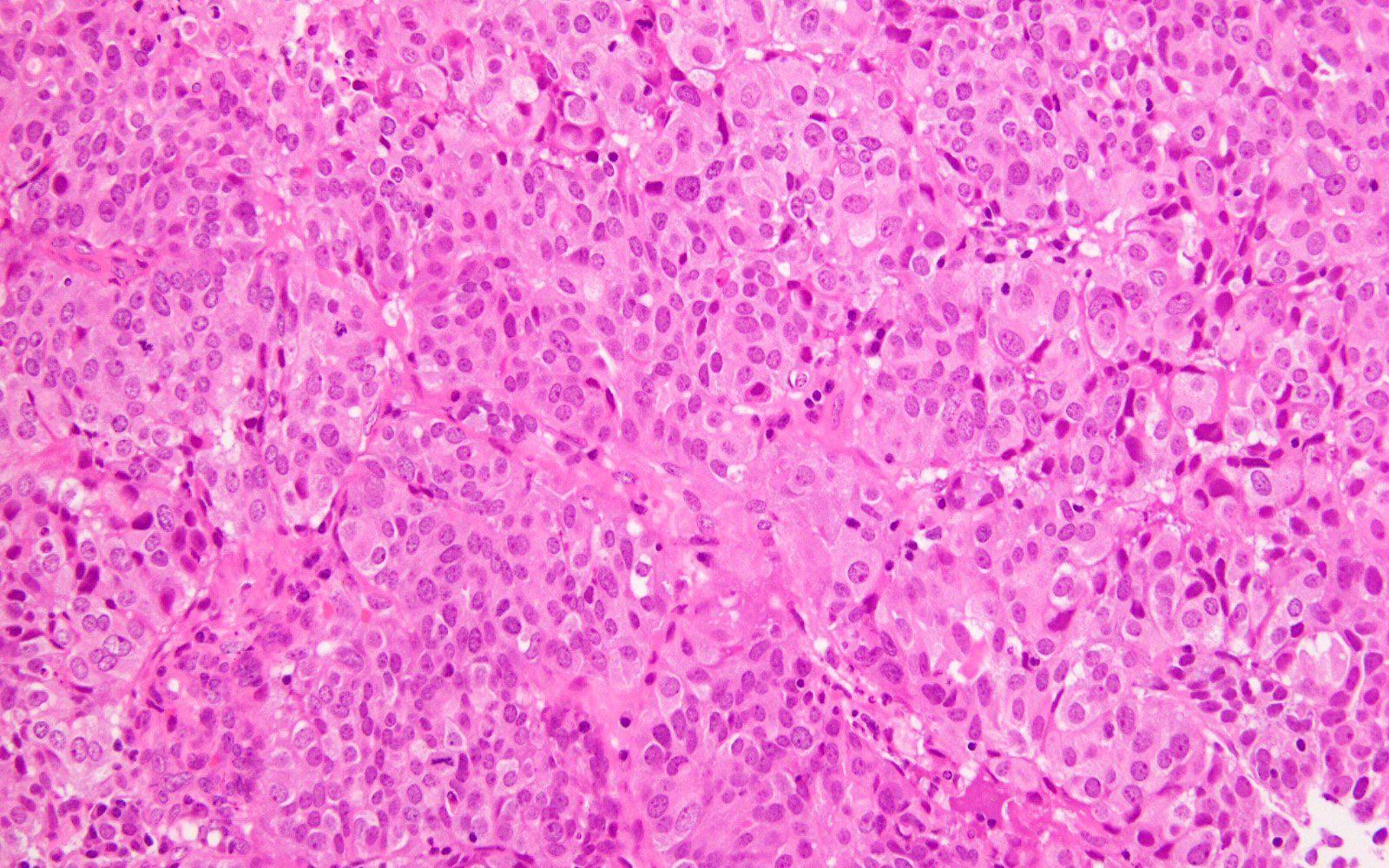
- Involvement of the serosa is diagnosed when the tumor perforates through the mesothelium lined outer surface of the uterus; this is seen as an area of disruption of the serosa with tumor involvement, sometimes with soft tissue or other structures attached to it
- Sometimes a desmoplastic stromal reaction is present
- Locating the serosal plane flanking the area in question and extending the plane through the area of desmoplasia can be helpful; serosal involvement is considered present if there is disruption of that plane or carcinoma extends beyond the plane (Int J Gynecol Pathol 2022;41:S90)
- According to ISGYP guidelines, tumor that infiltrates the entire myometrial thickness and reaches submesothelial fibroconnective tissue should also be reported as serosal involvement (Int J Gynecol Pathol 2019;38:S93)
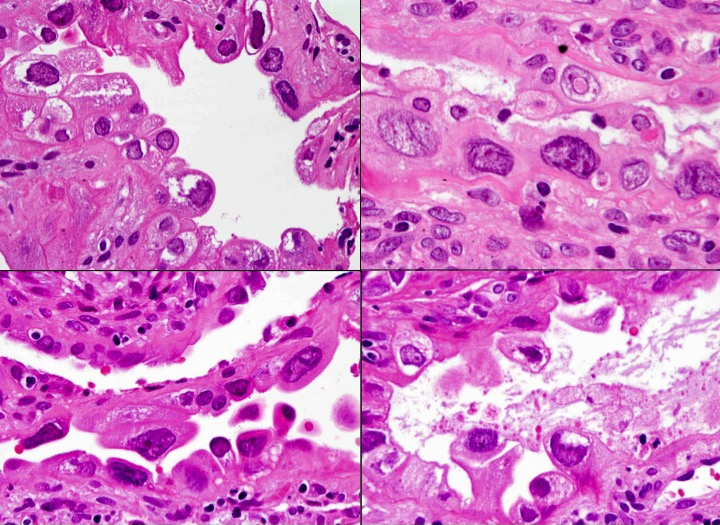
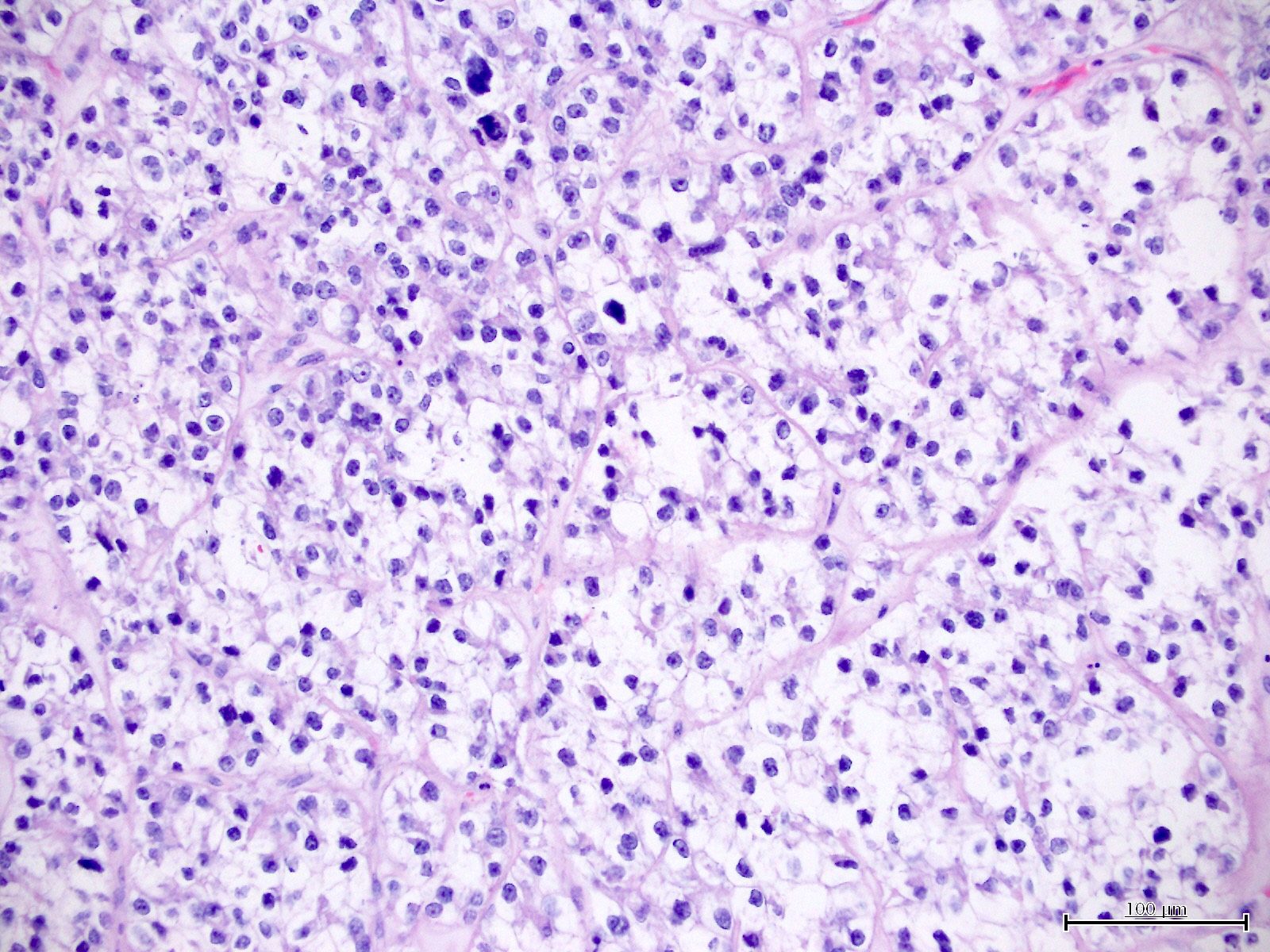
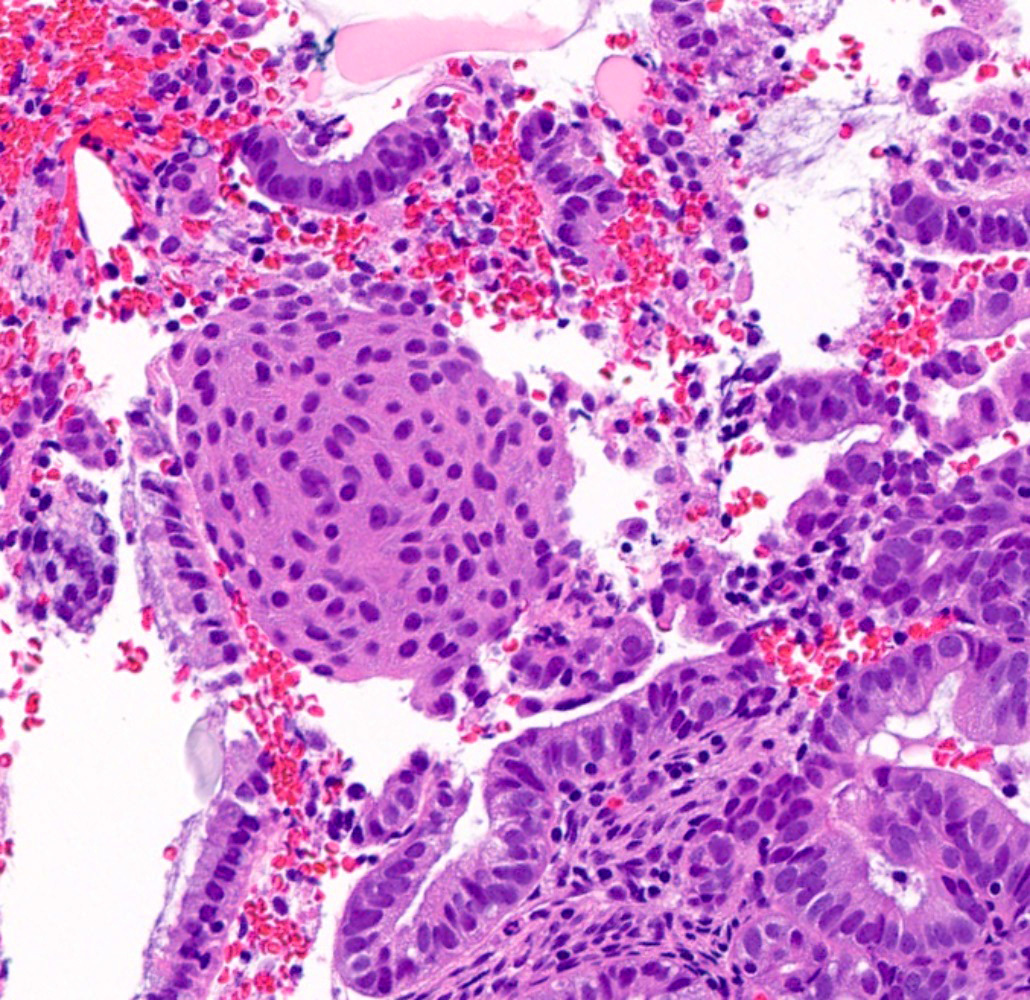
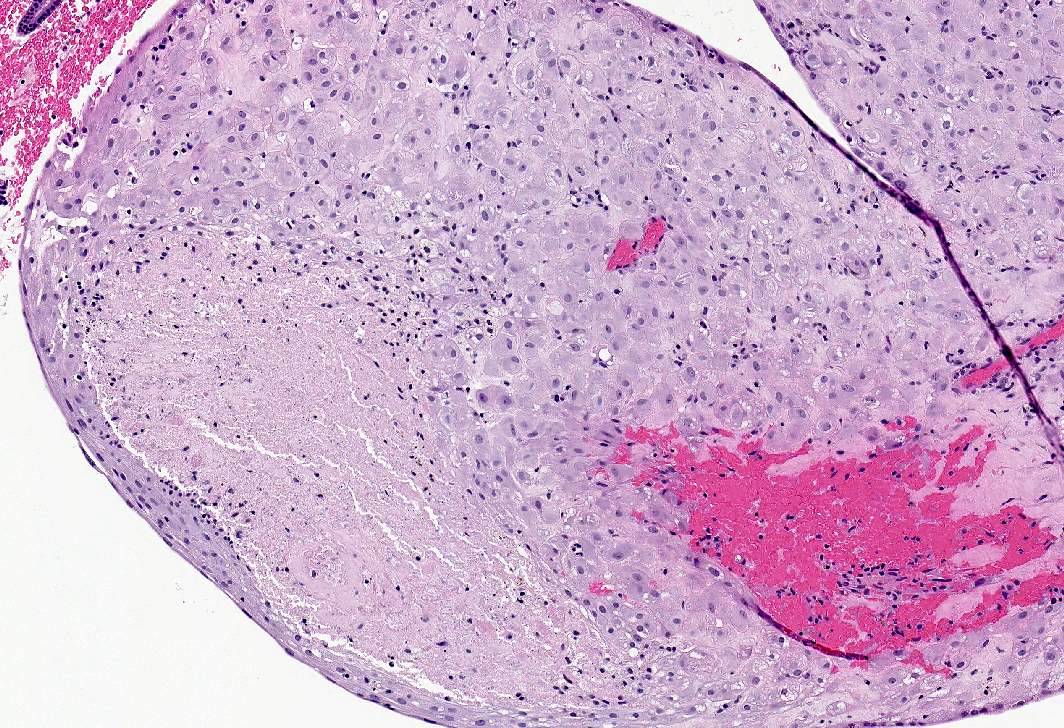
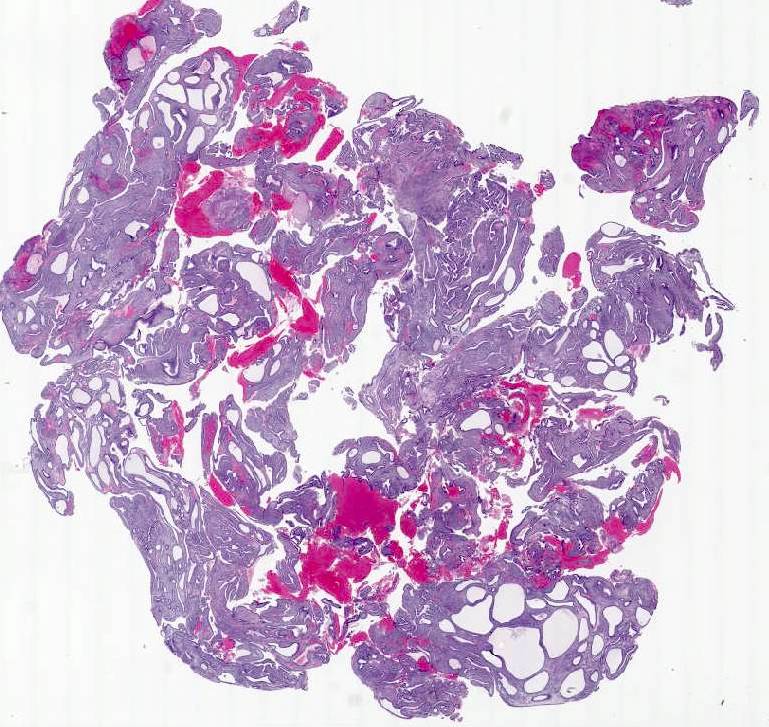
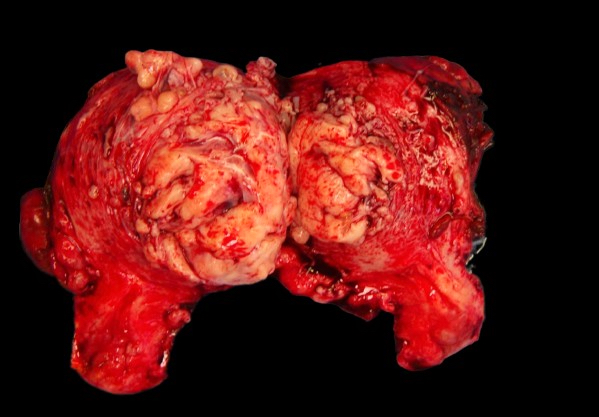
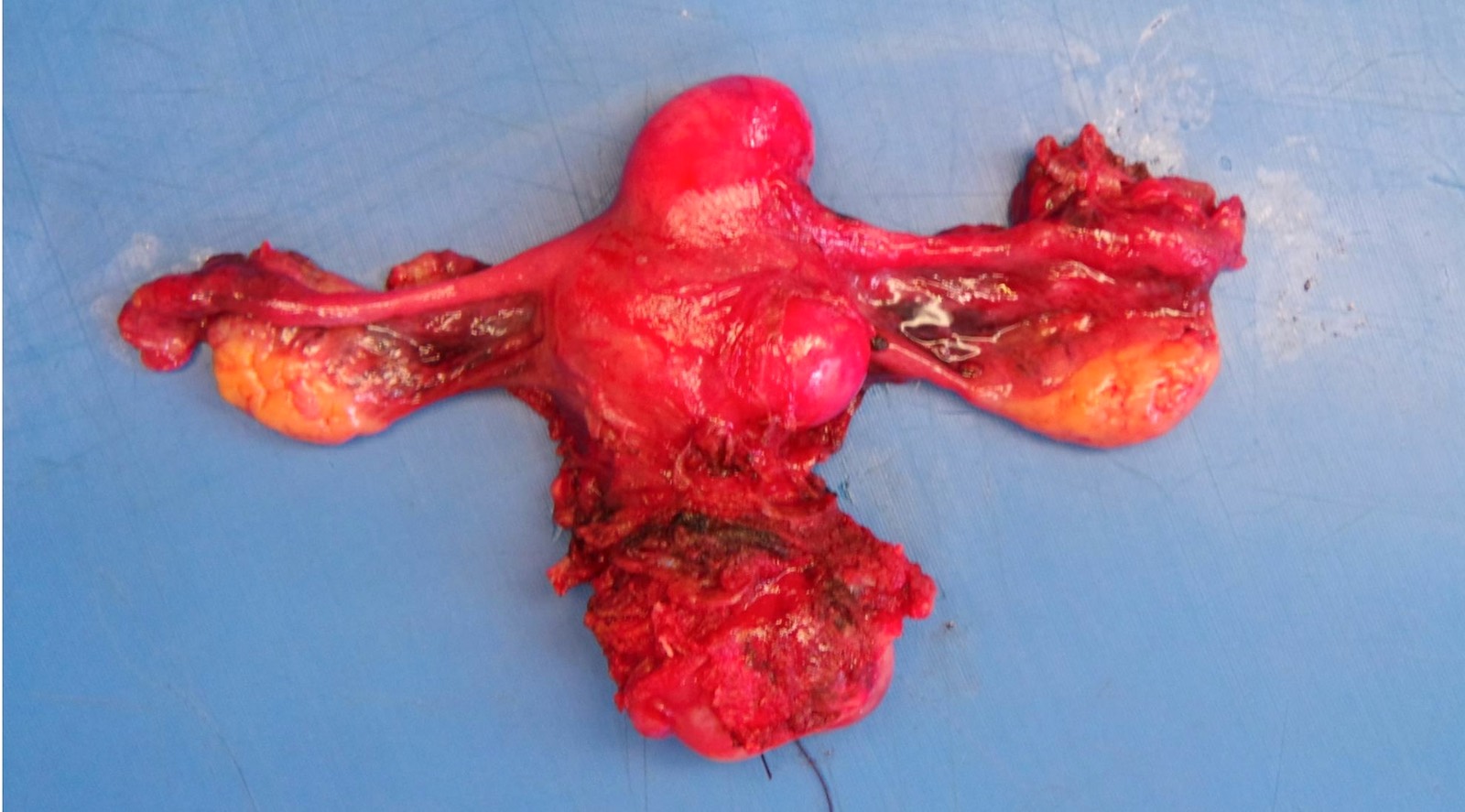
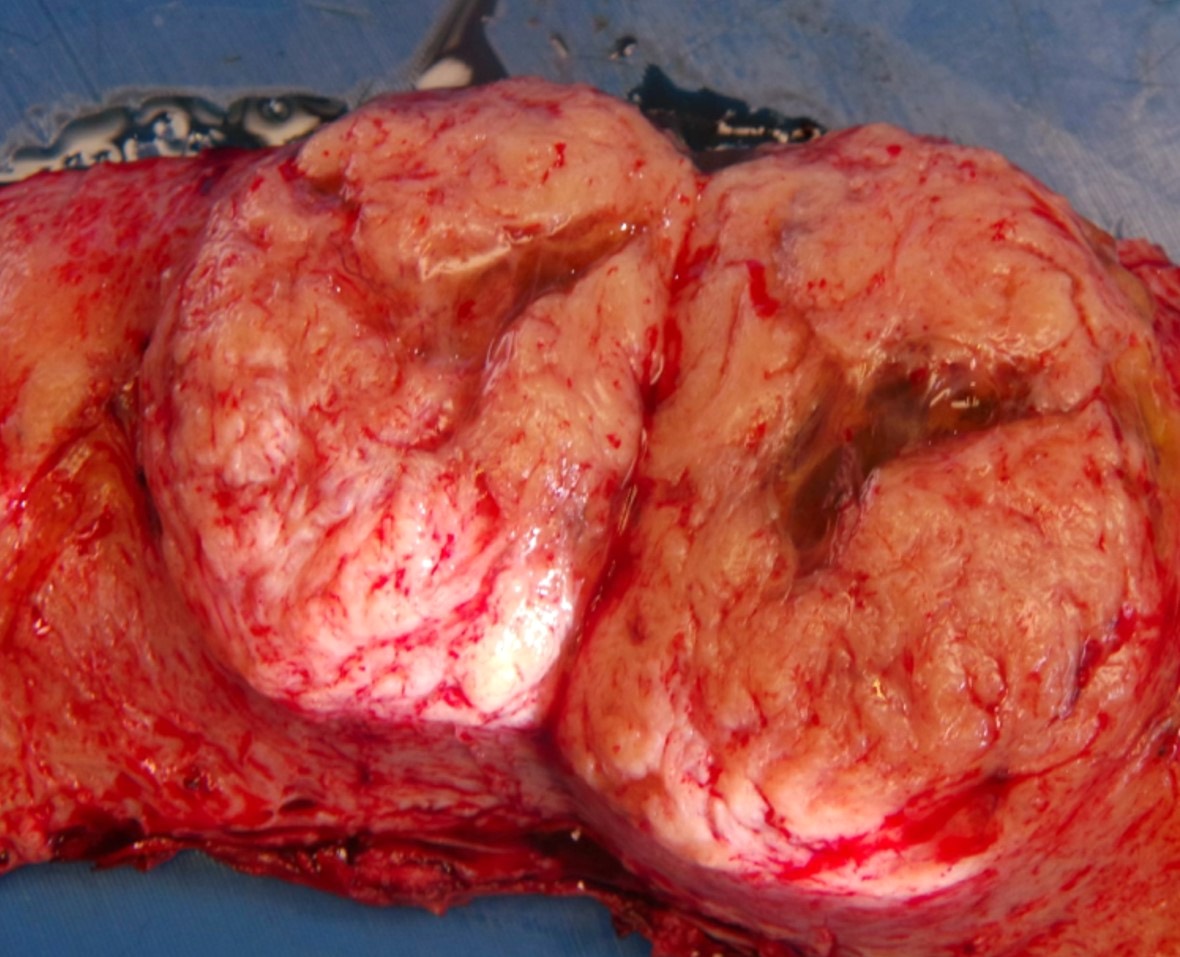
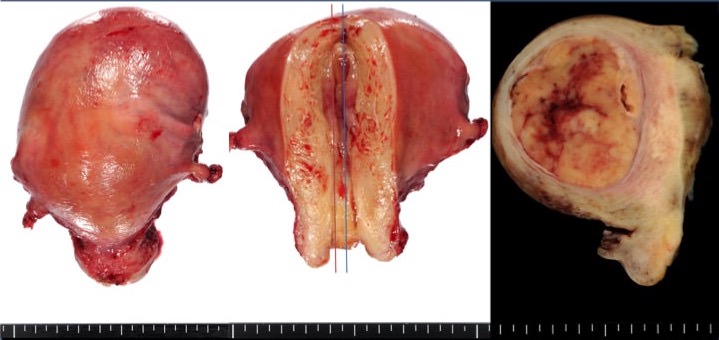
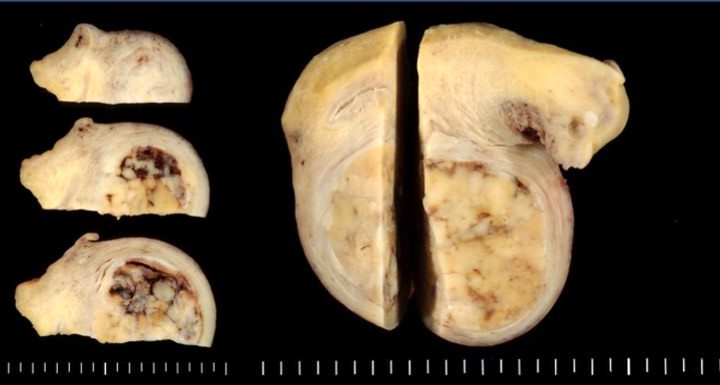
- Adnexal involvement (versus synchronous ovarian carcinoma):
- Distinguishing between the following is relevant for staging and treatment:
- Synchronous ovarian and endometrial tumors
- Primary endometrial with metastatic ovarian involvement
- Primary ovarian with metastatic endometrial involvement
- However, it is often difficult to separate these scenarios on pathologic examination and one may only suggest one possibility over the others
- Synchronous ovarian carcinoma is present in up to 30% of reproductive age women with endometrial cancer (Int J Womens Health 2014;6:691, Obstet Gynecol 2005;106:693)
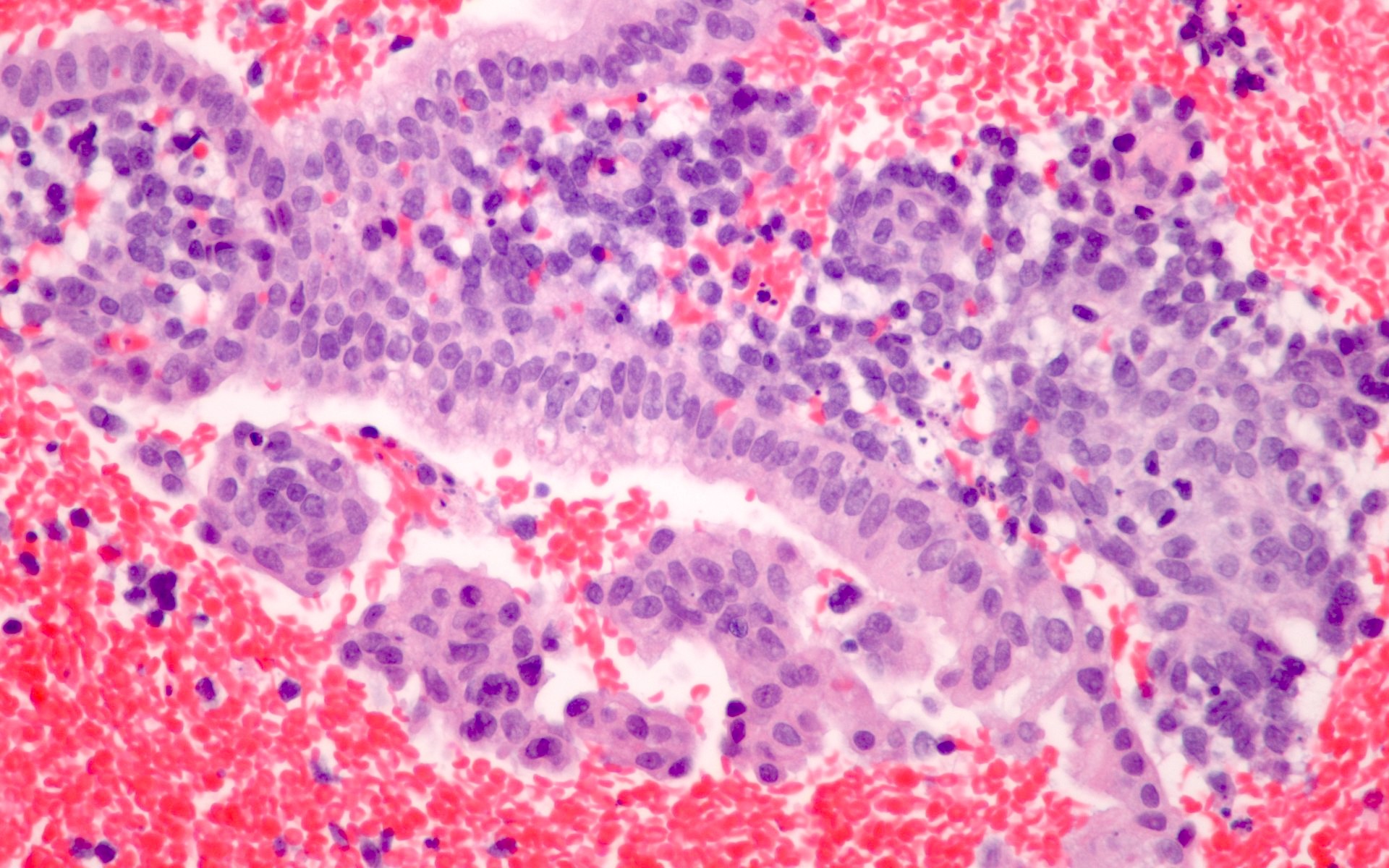
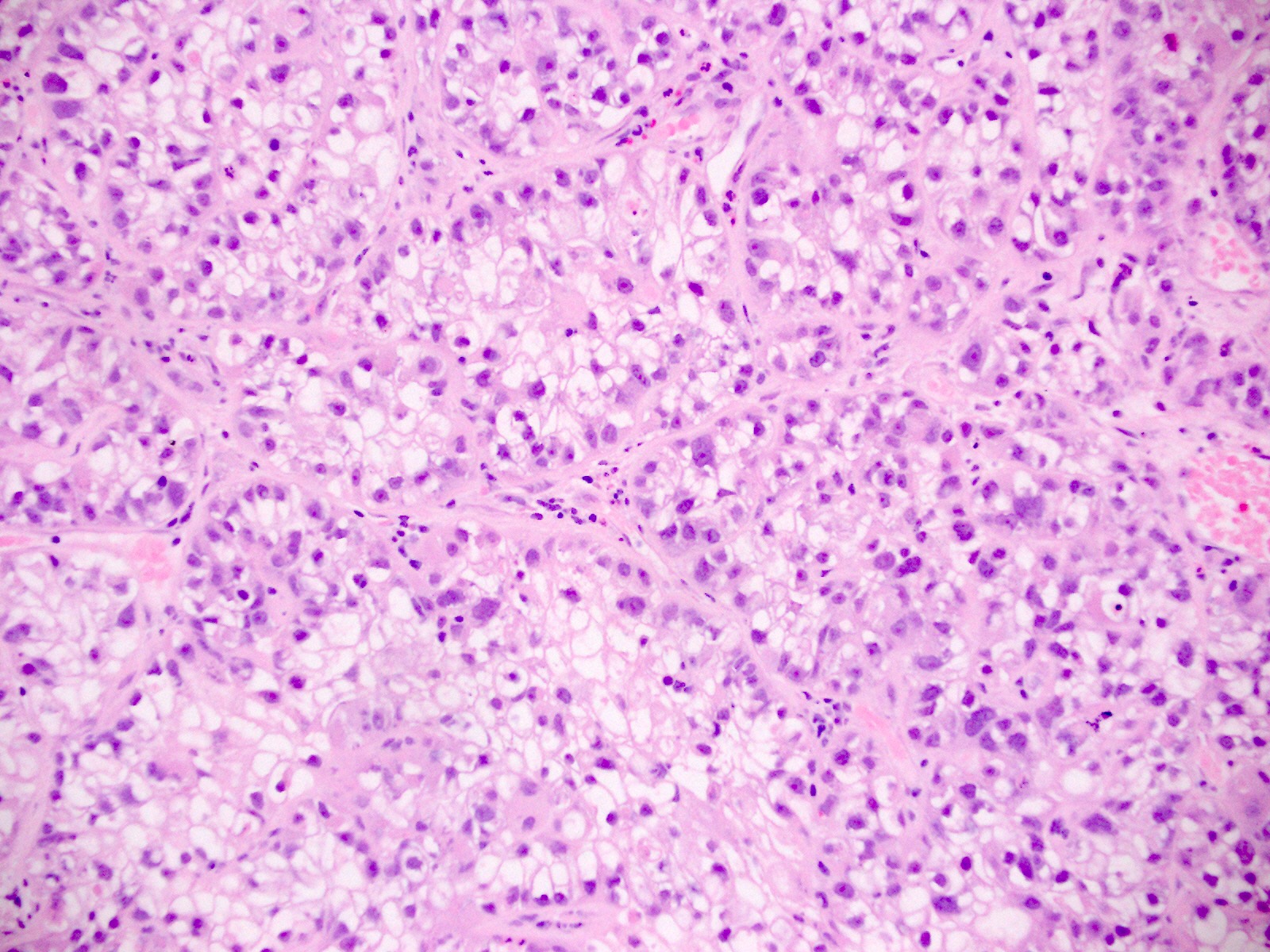
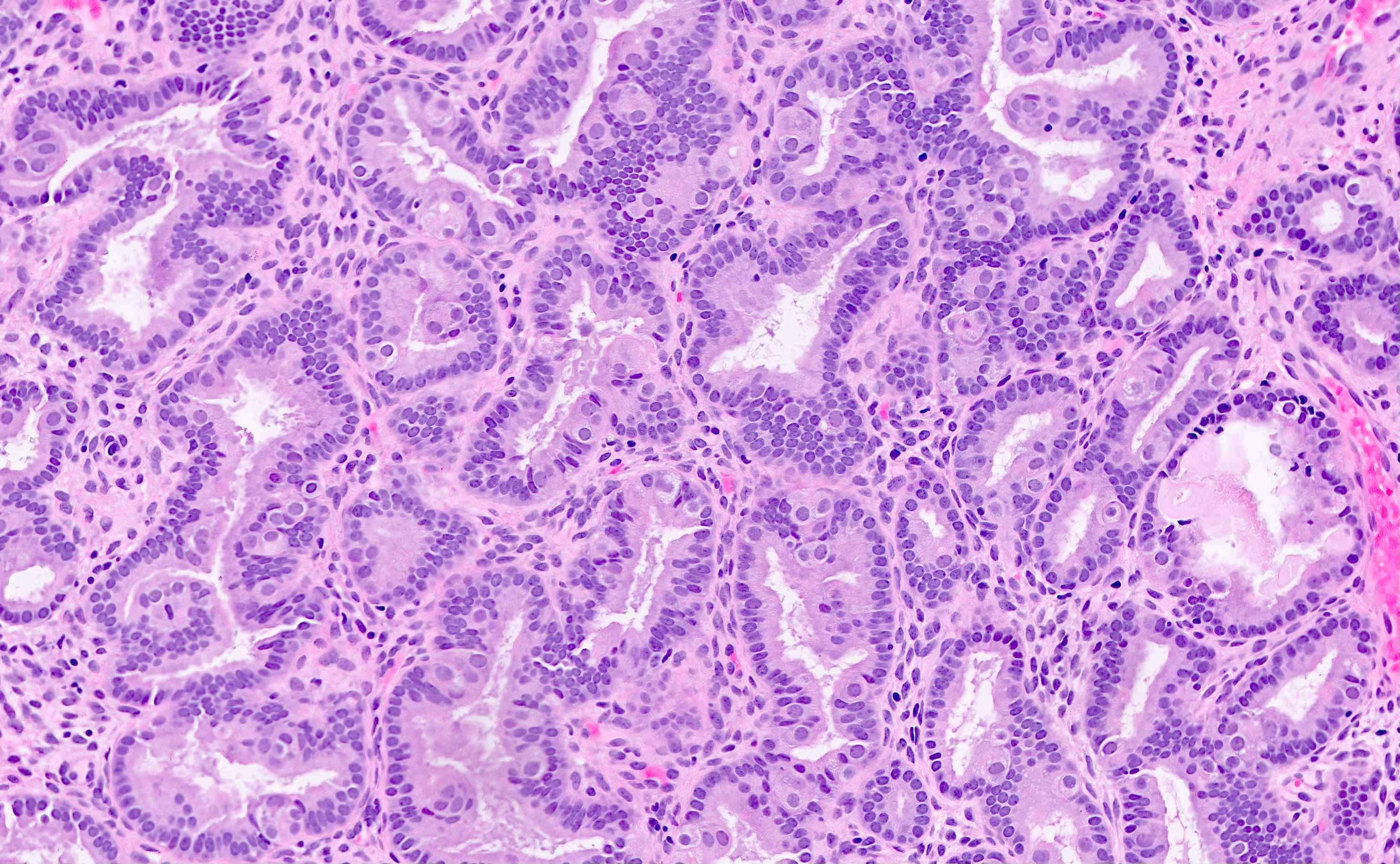
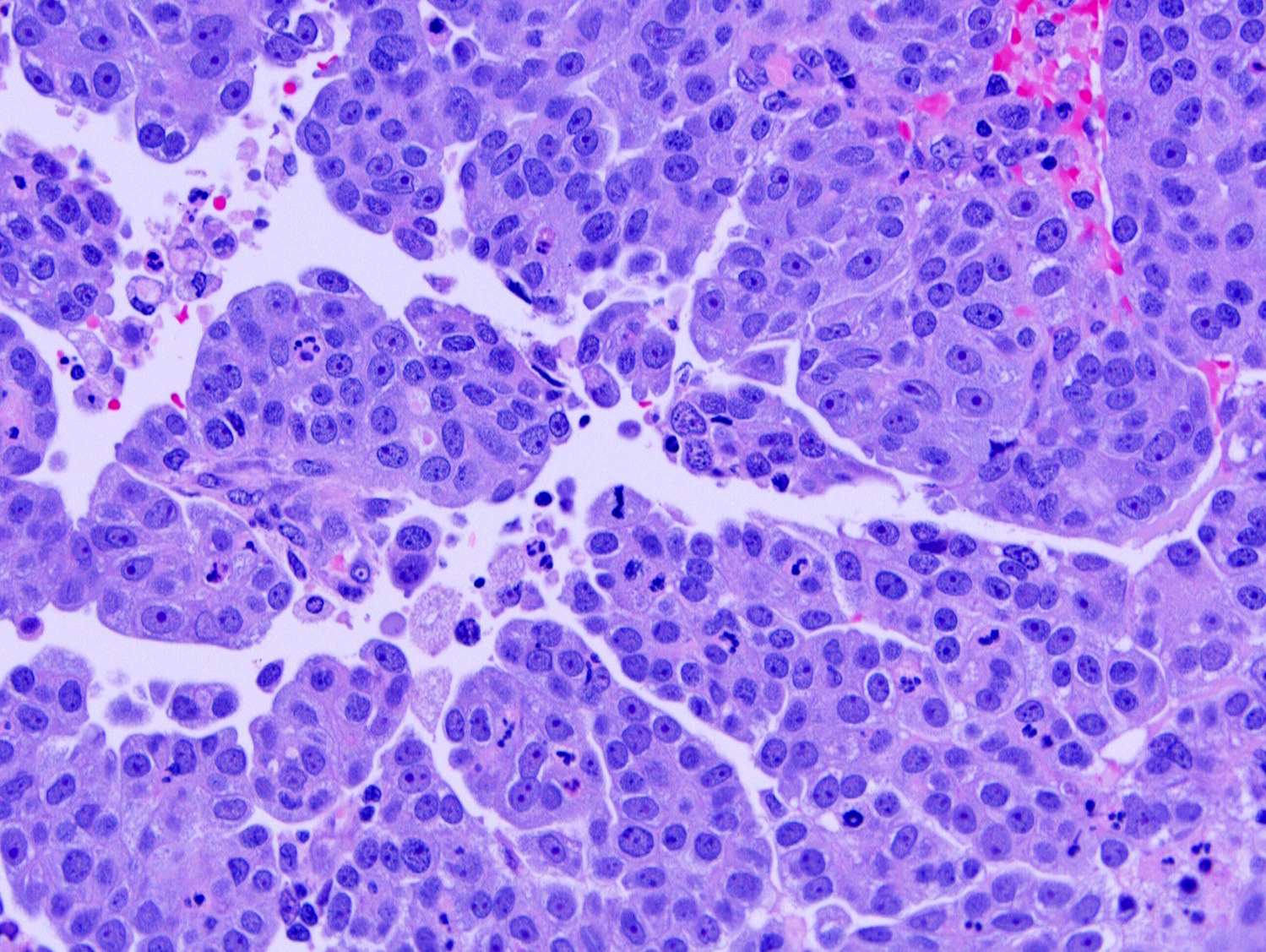
- When present, synchronous ovarian and endometrial carcinomas usually have the same histologic type (vast majority are low grade endometrioid)
- Synchronous endometrial and ovarian endometrioid carcinoma have good prognosis, similar to those with only endometrial or only ovarian stage I cancer (Int J Gynecol Cancer 2014;24:54, Clin Cancer Res 2008;14:5840)
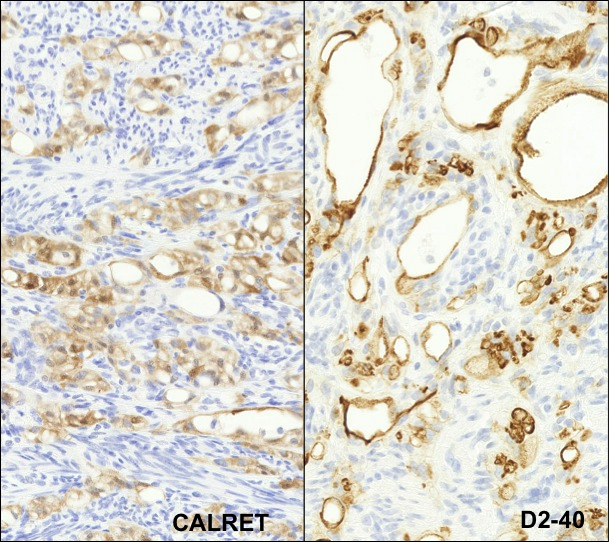
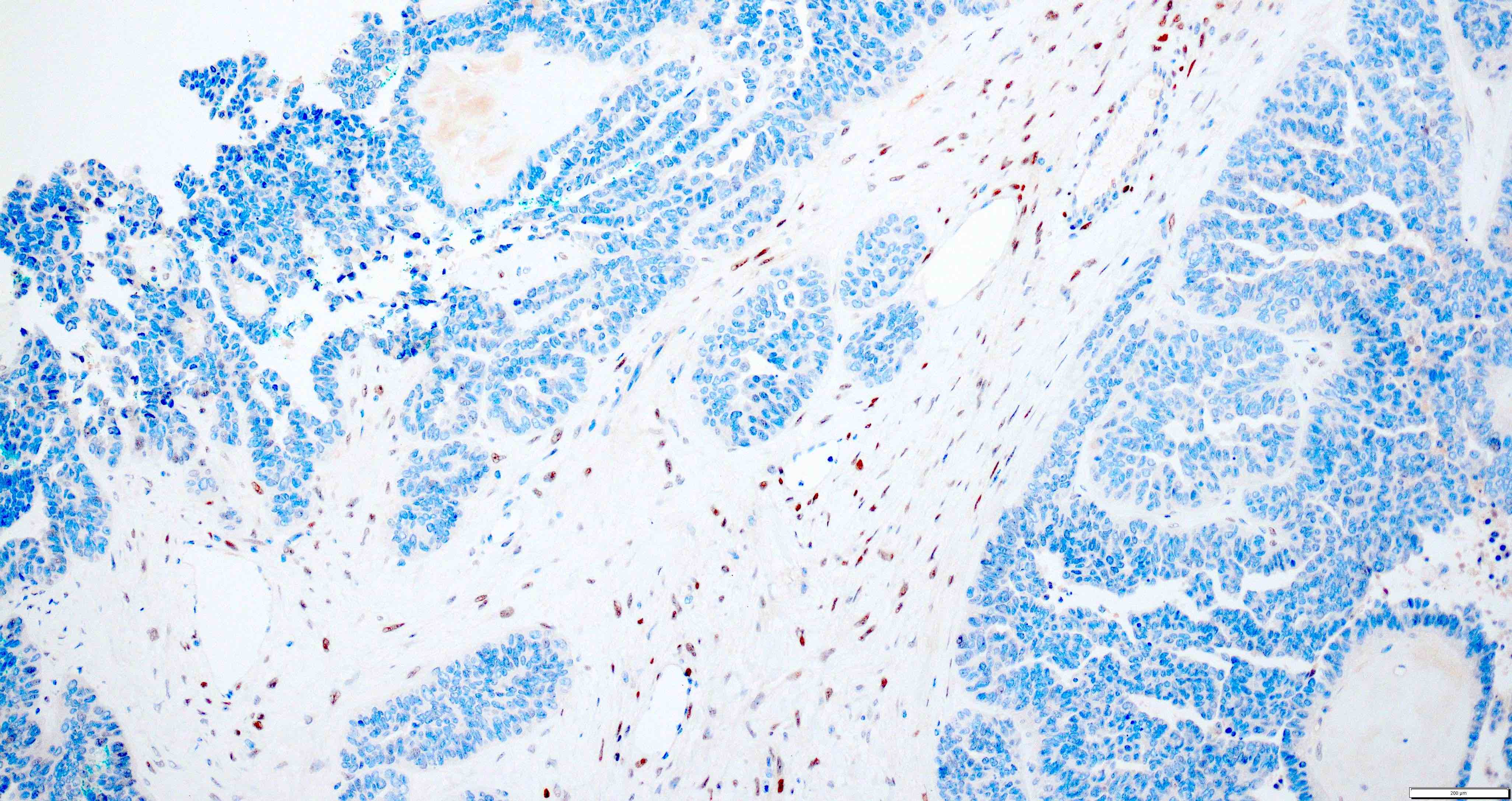
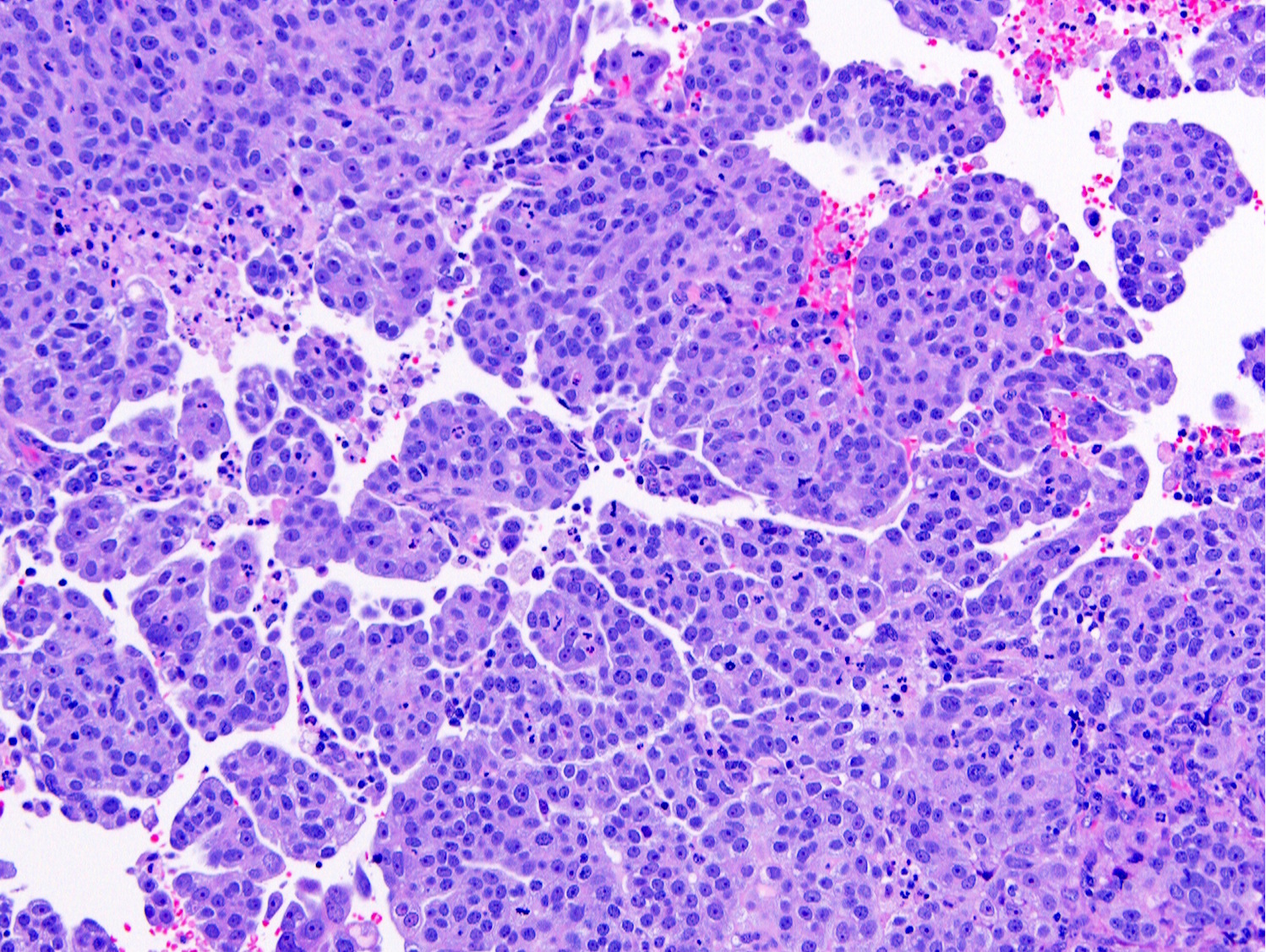
- Features that support 2 synchronous carcinomas include:
- Different histologic types or tumor grades
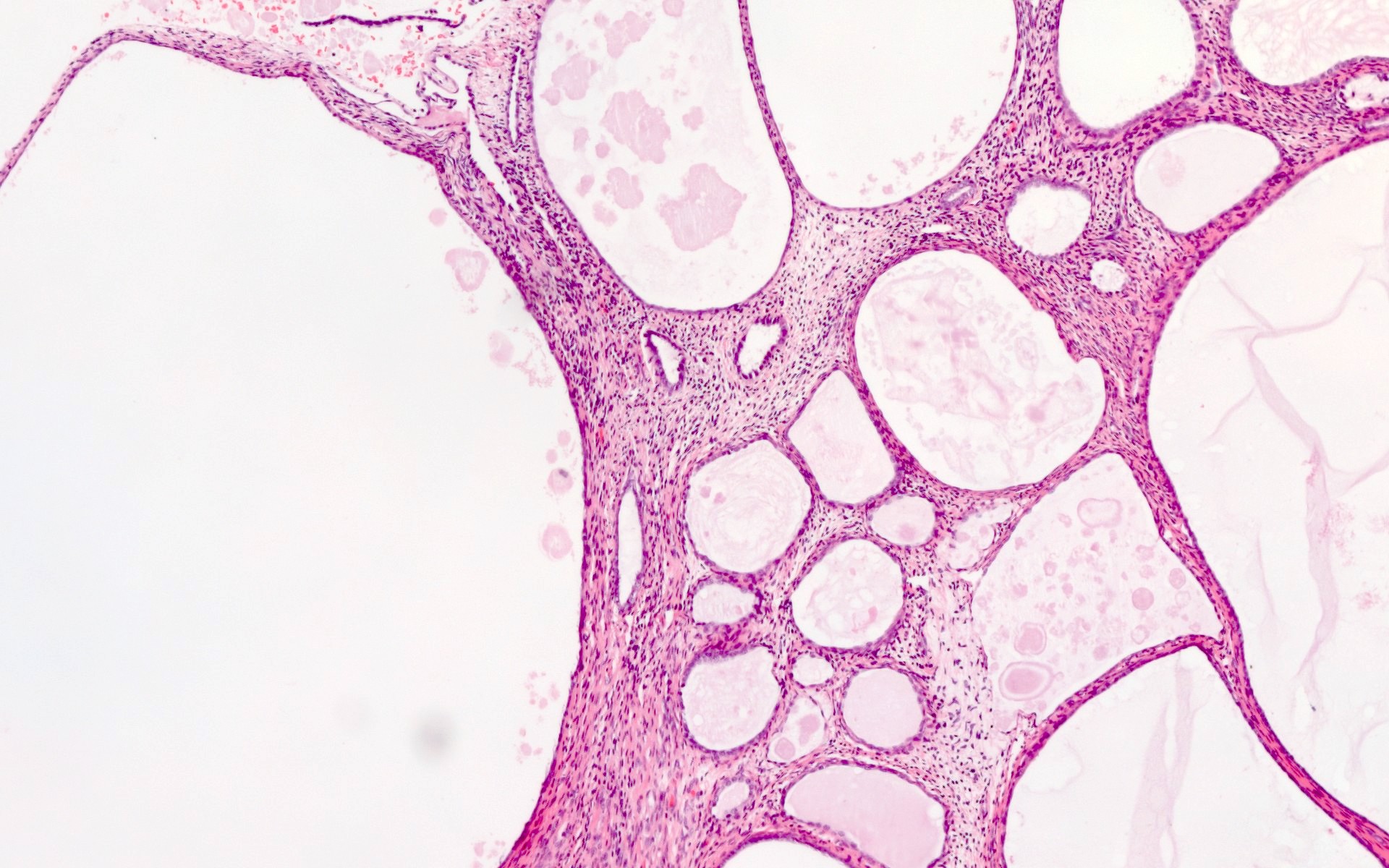
- Endometrial carcinoma has absent or only superficial myometrial invasion
- Ovarian carcinoma is confined to the ovary
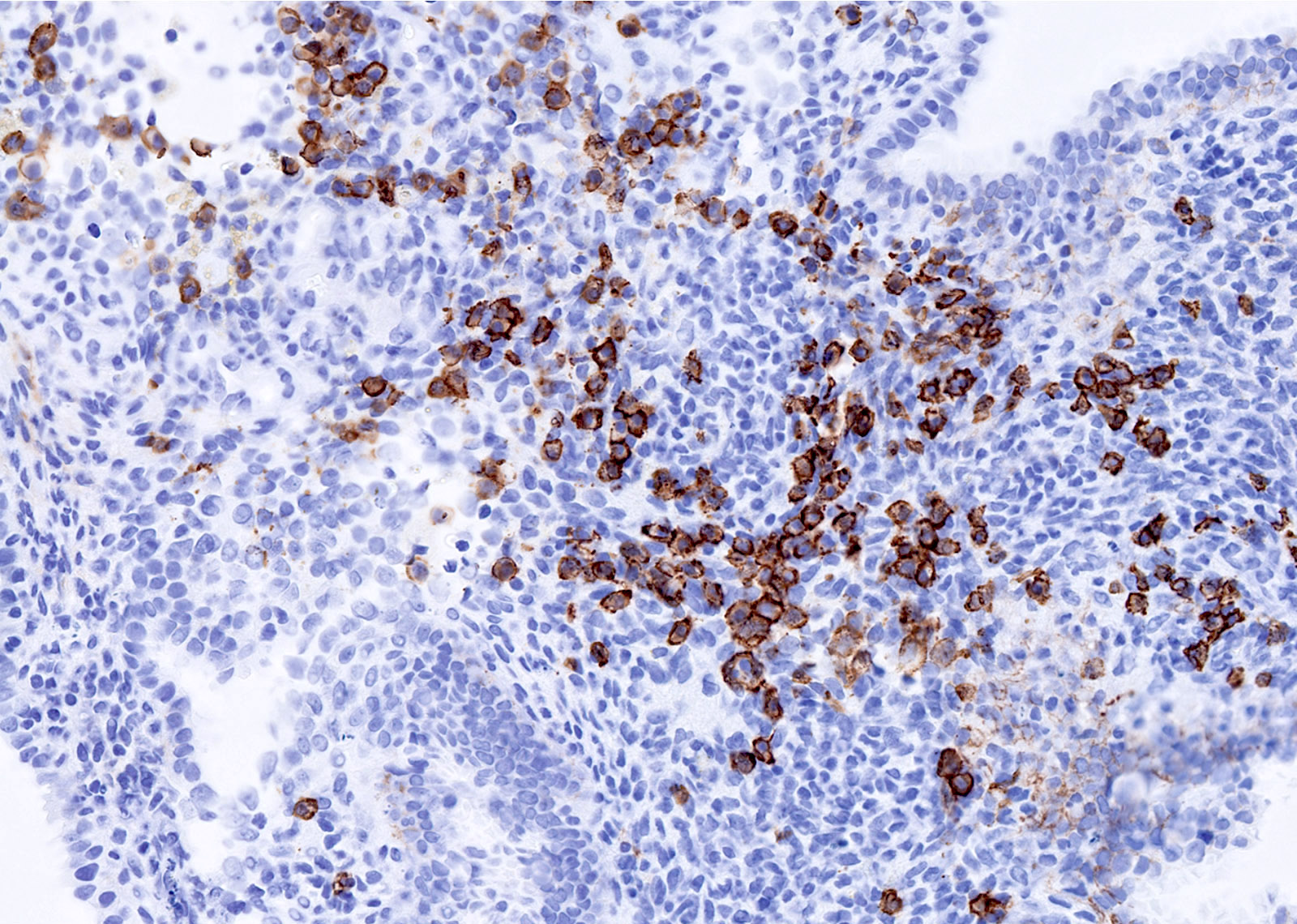
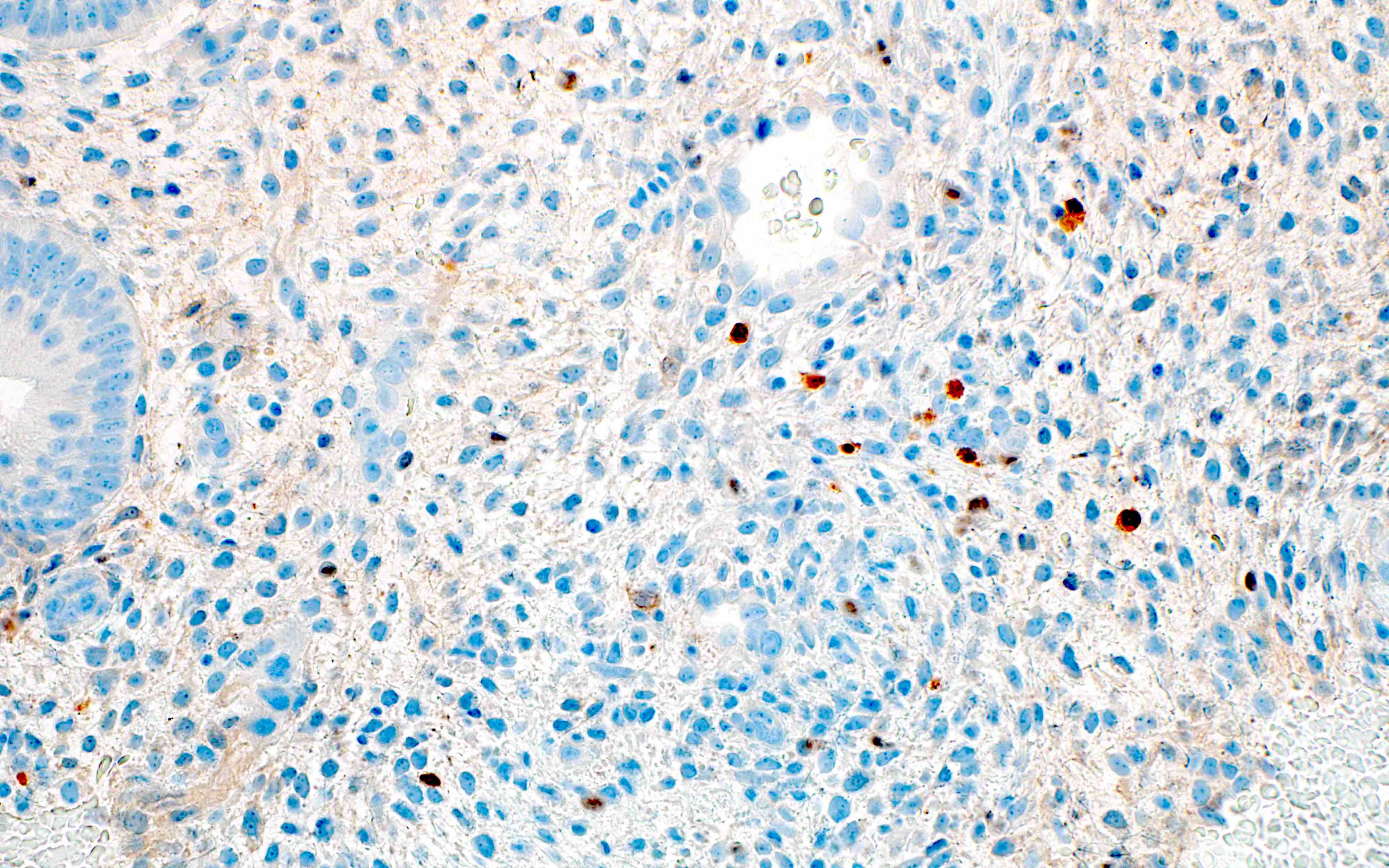
- Absence of lymphovascular space invasion
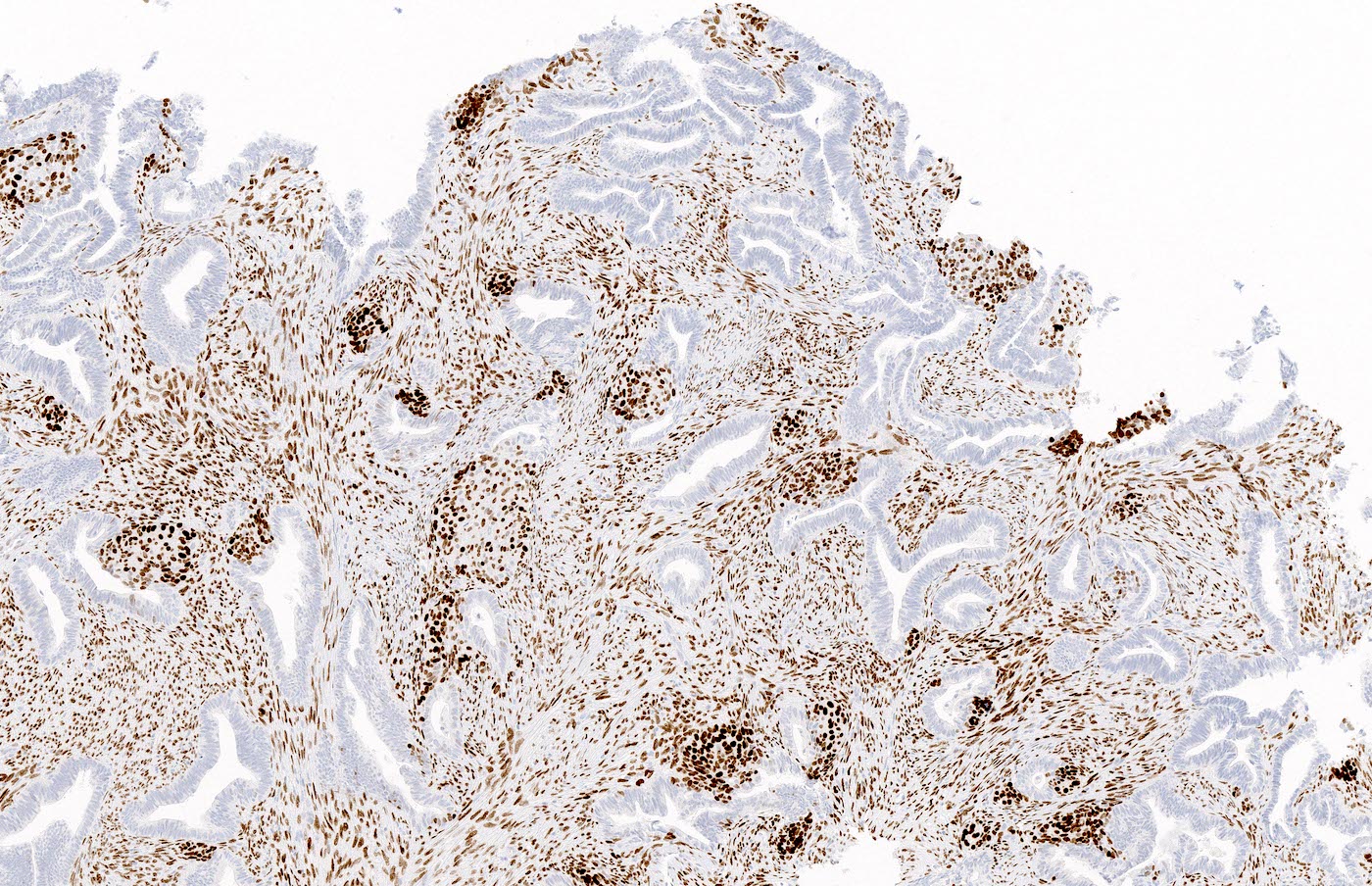
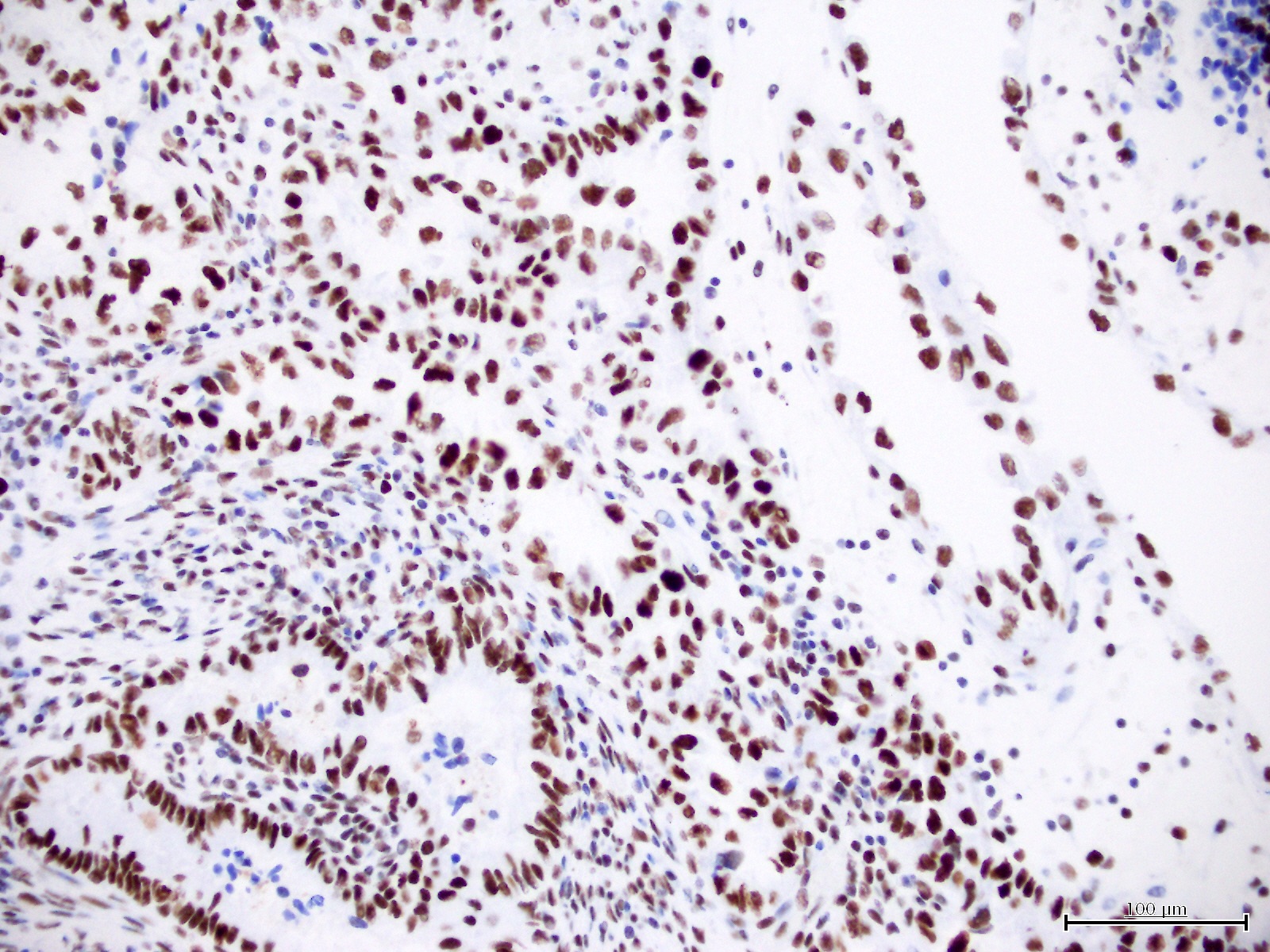
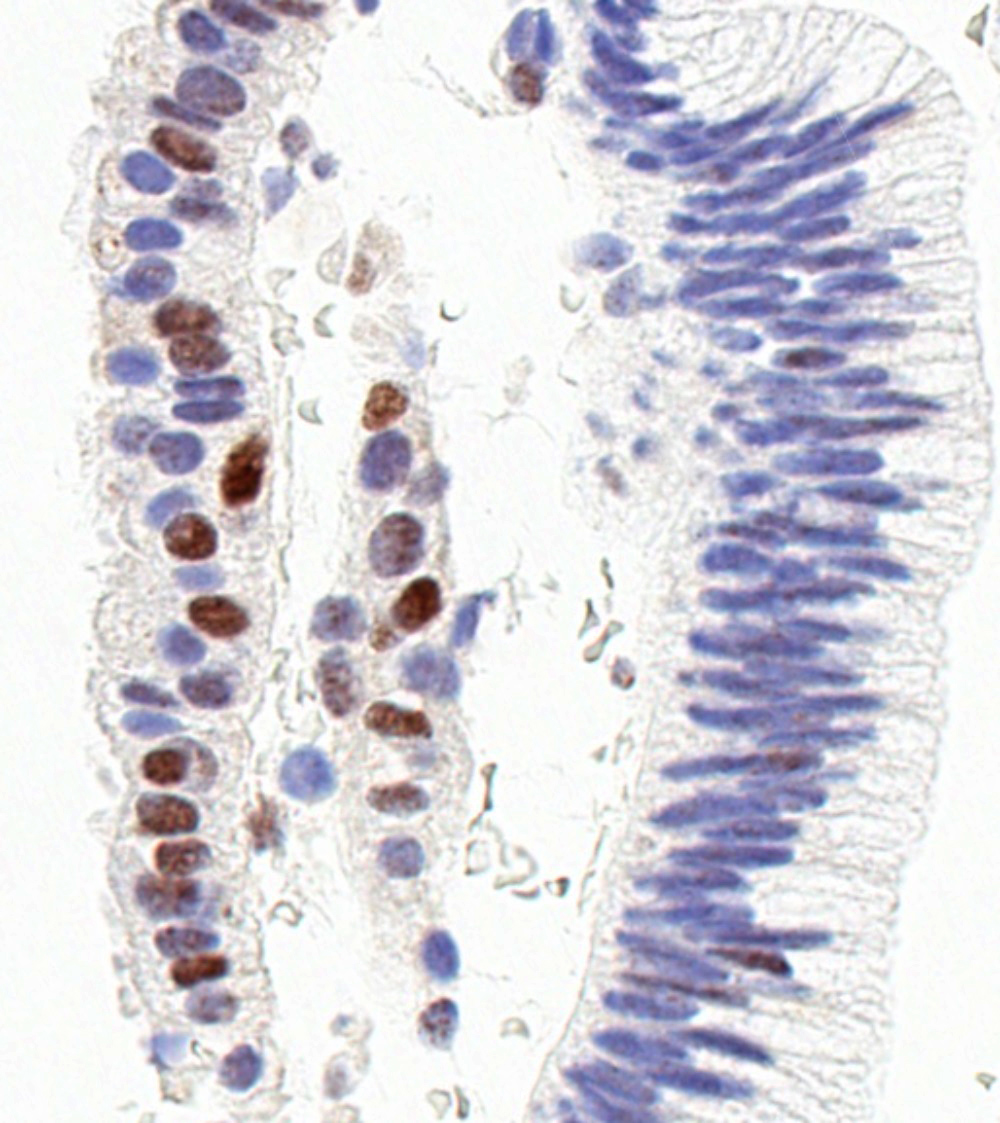
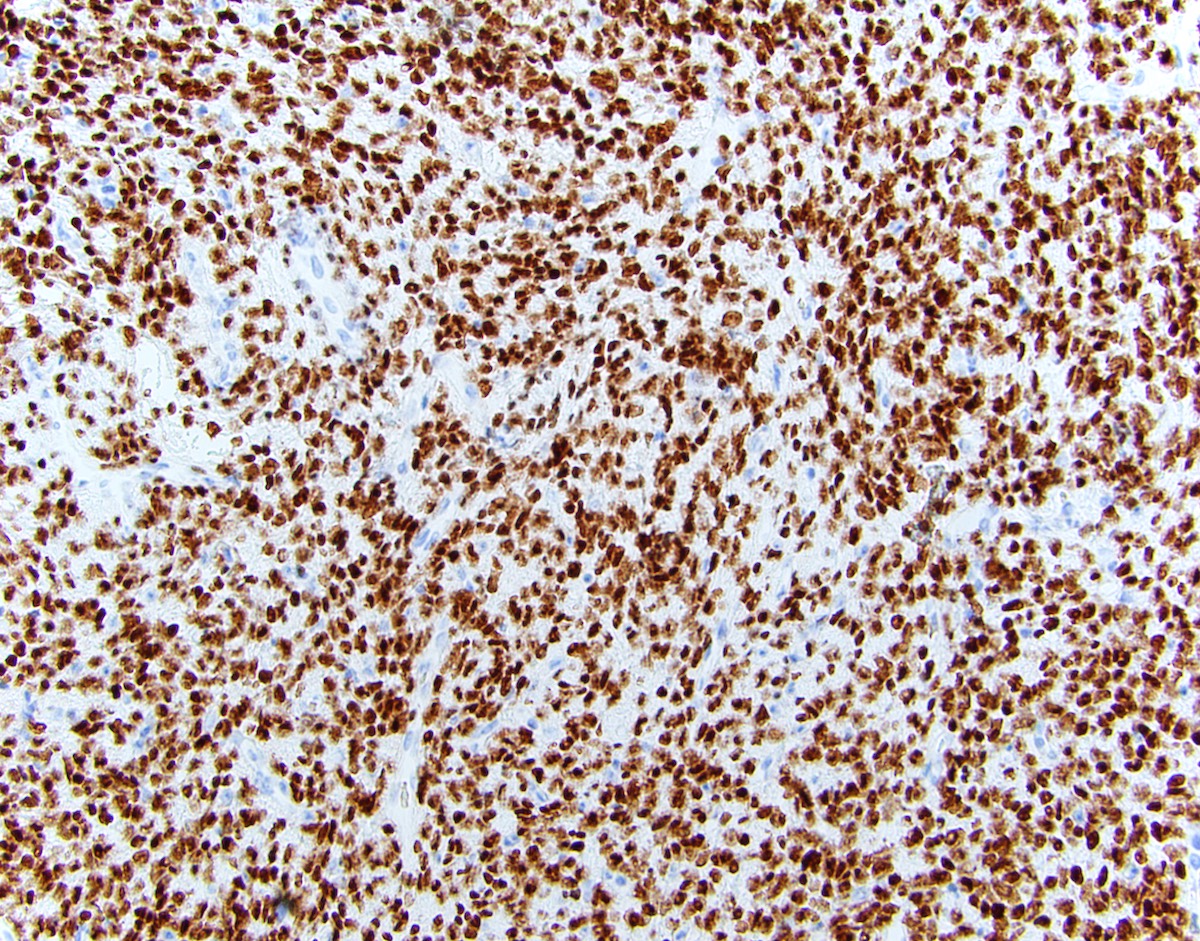
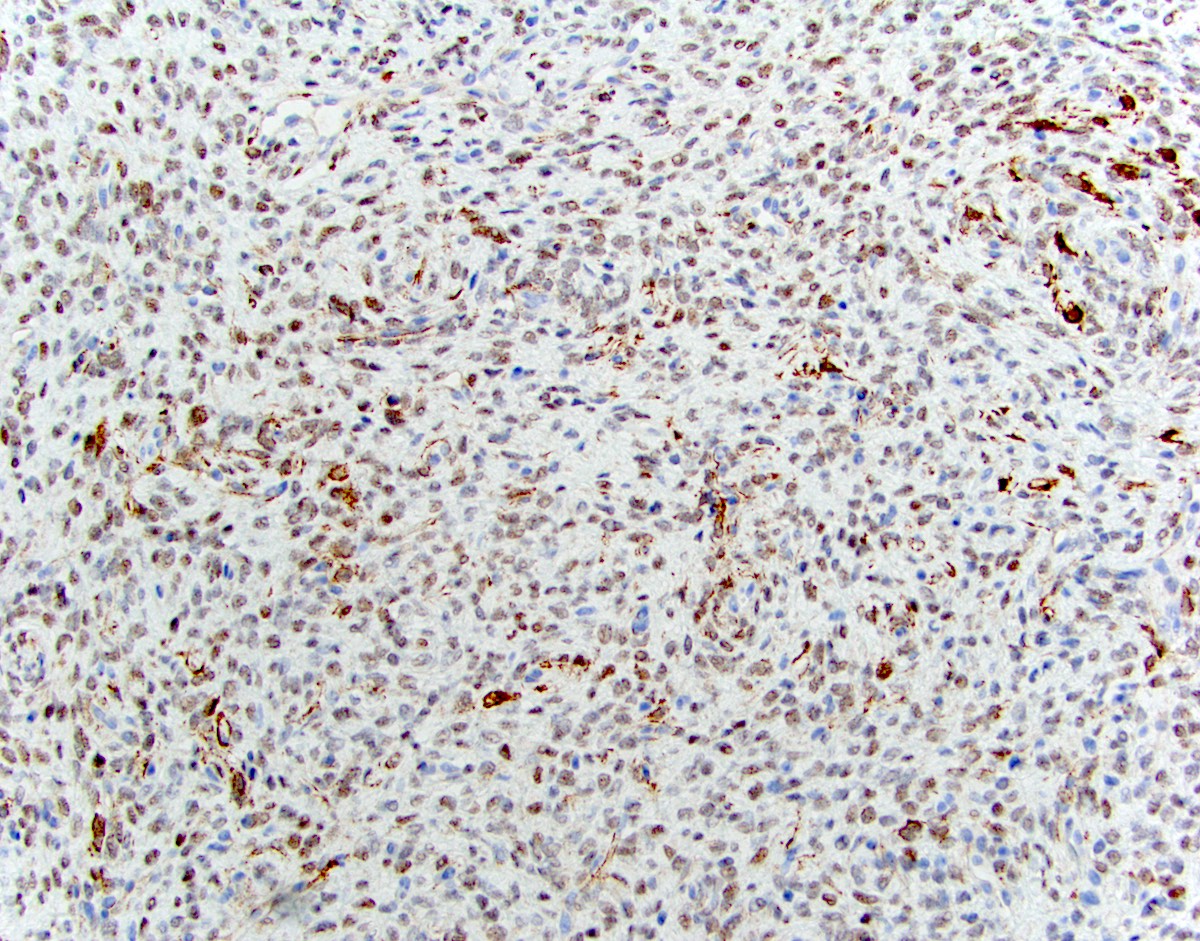
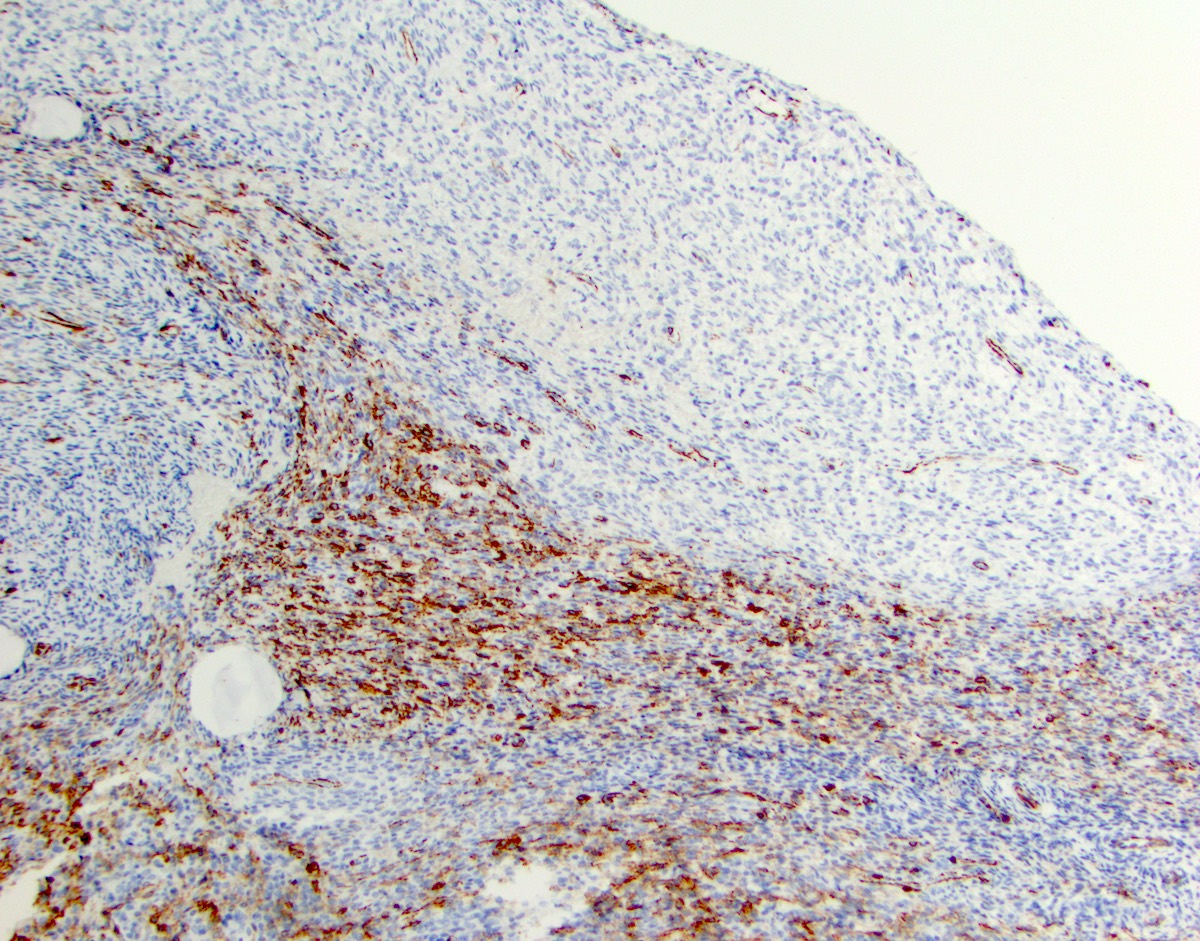
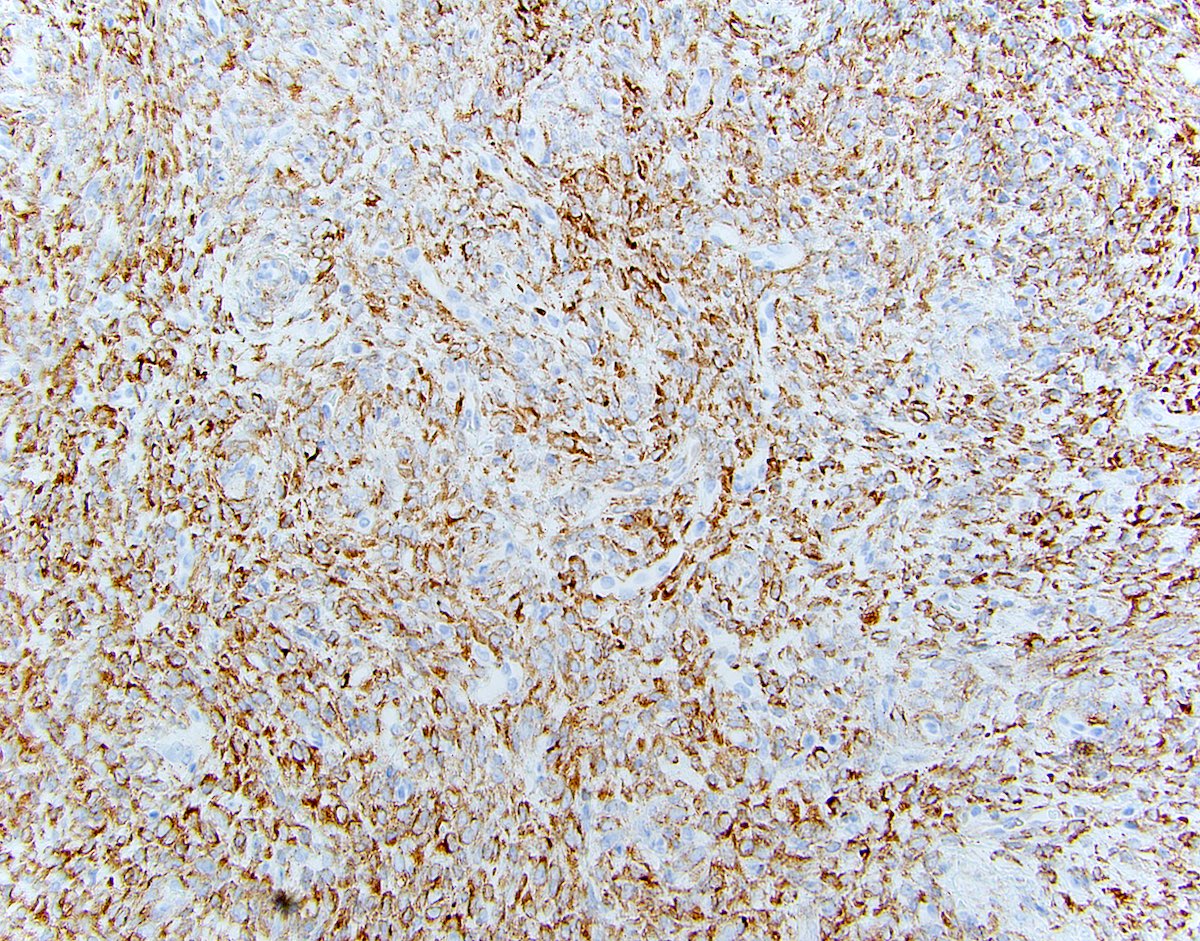
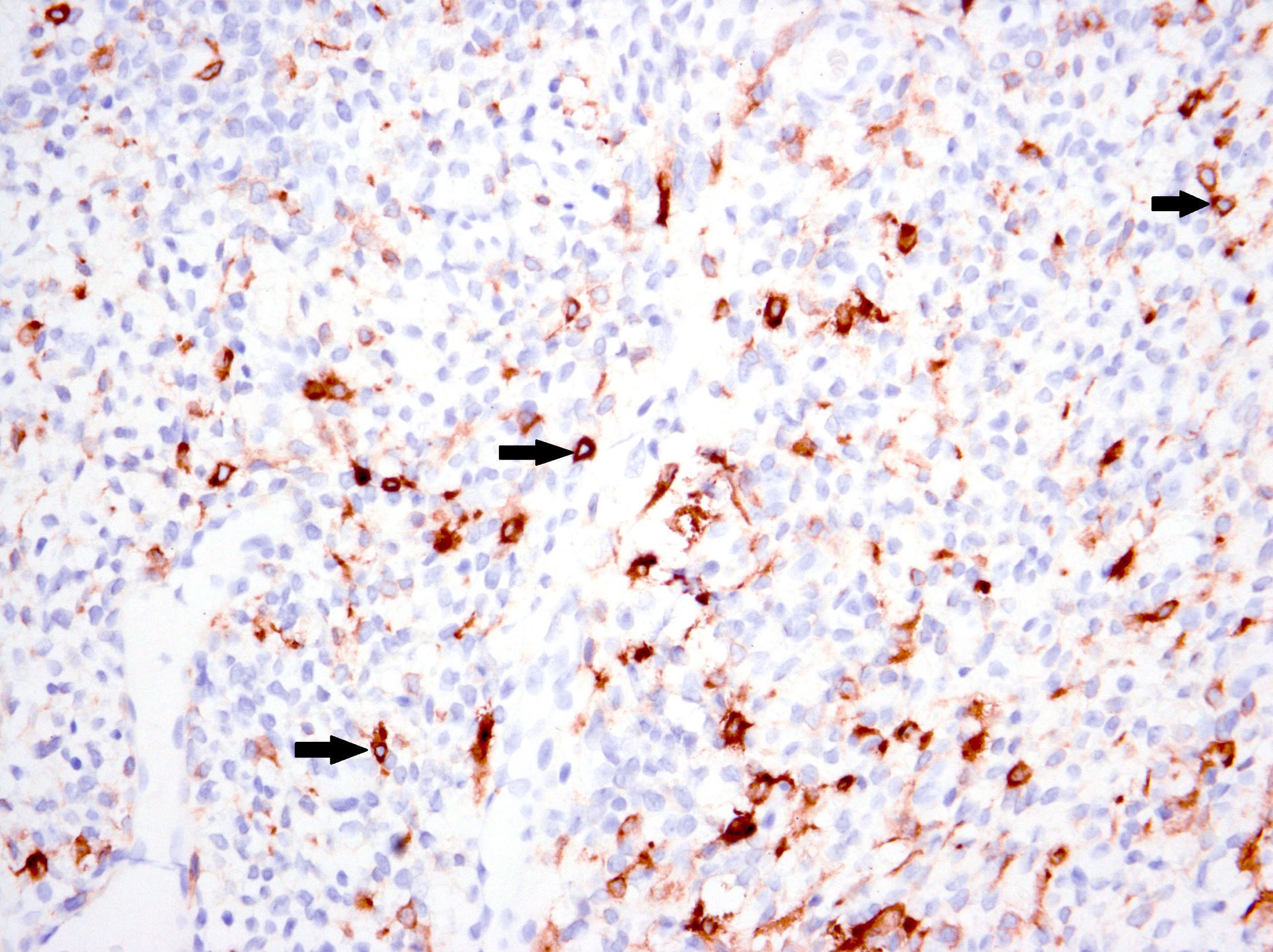
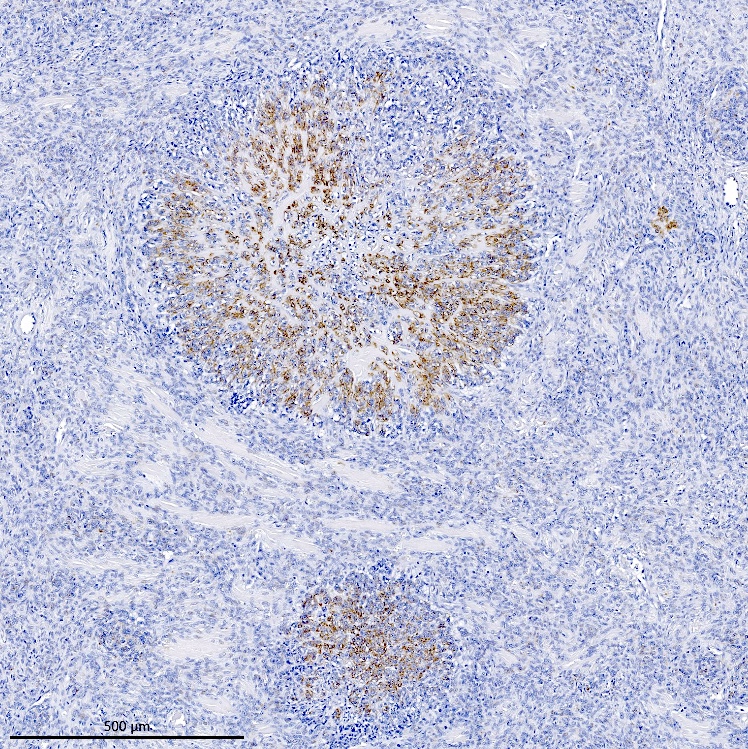
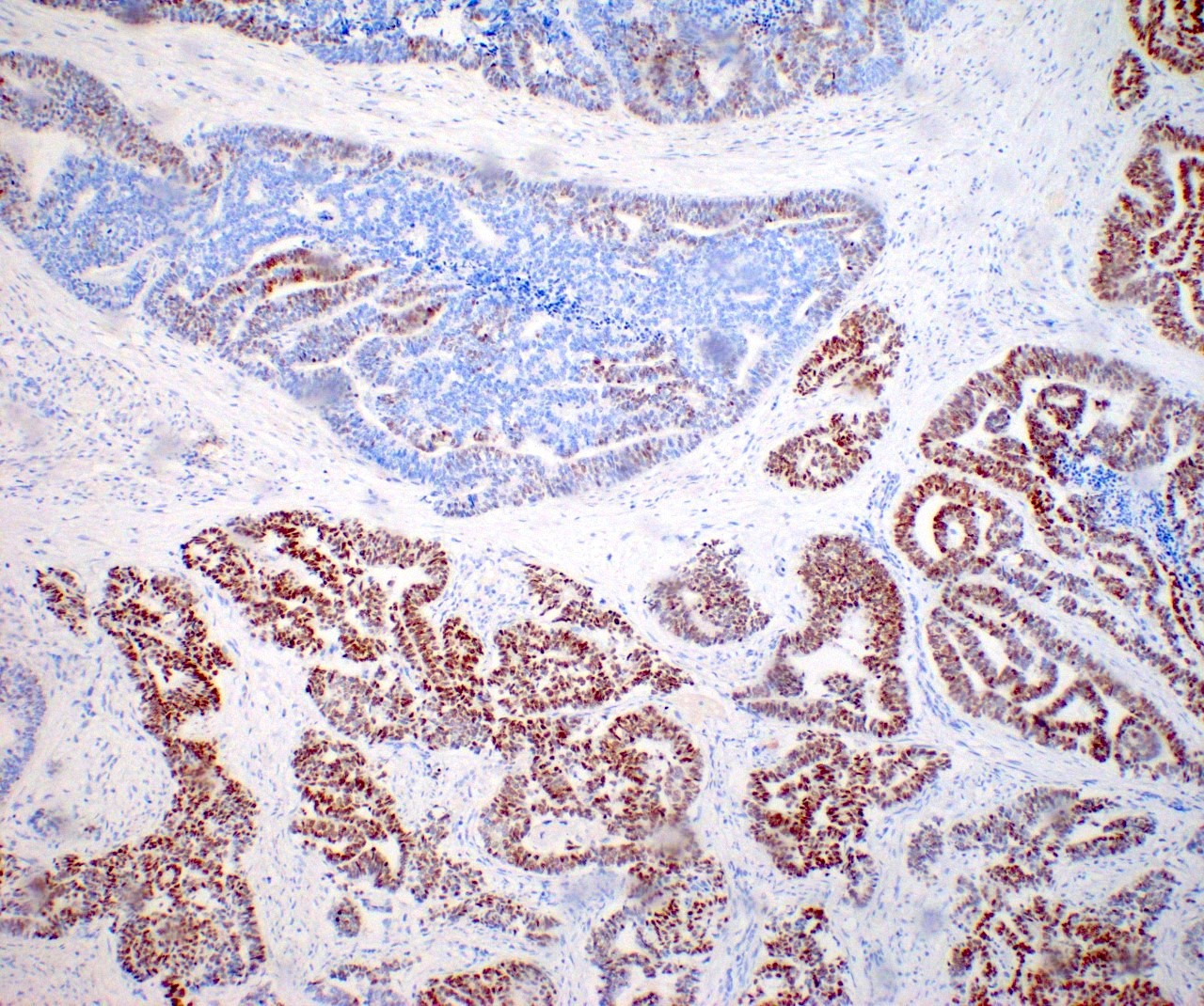
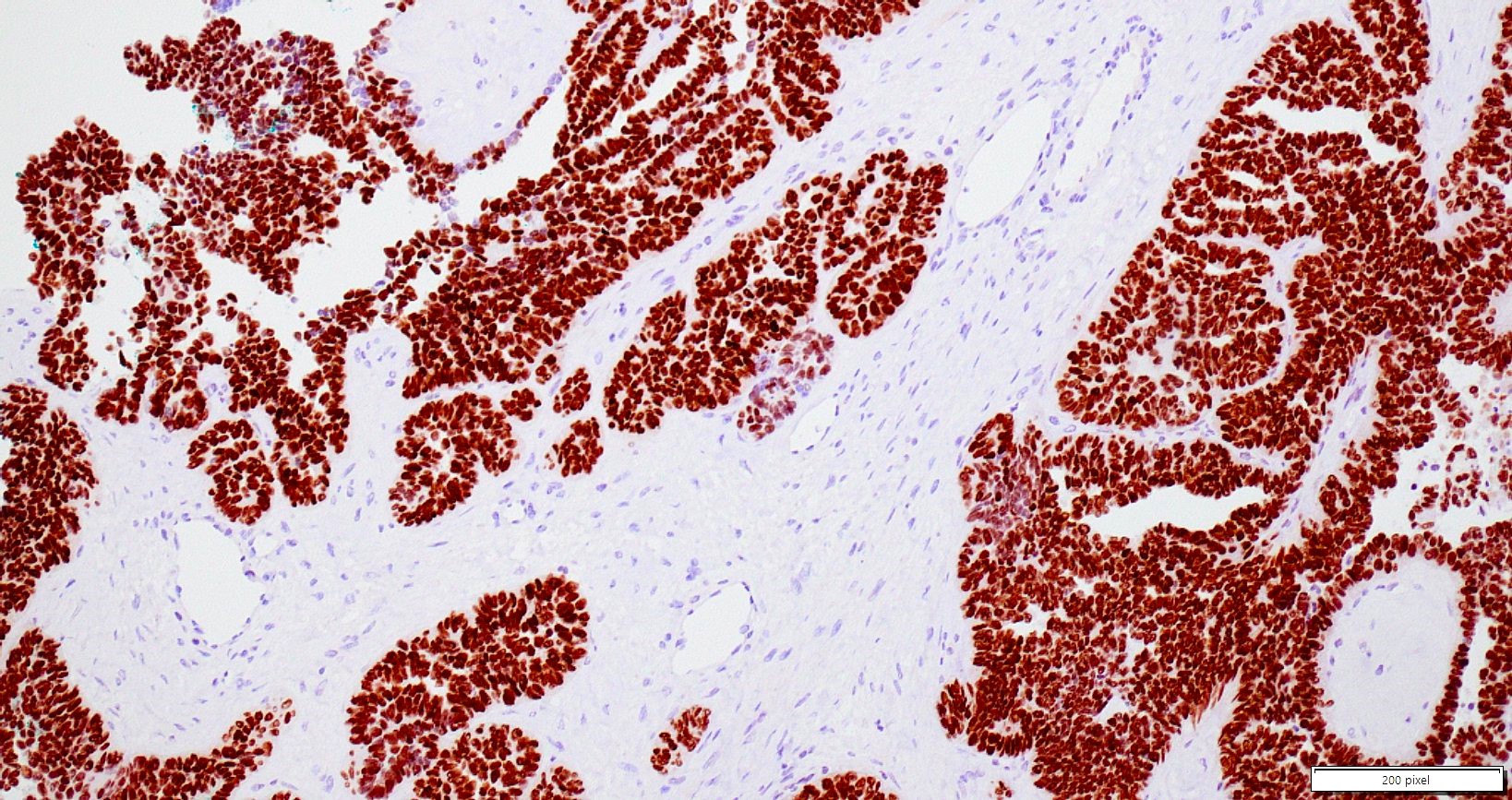
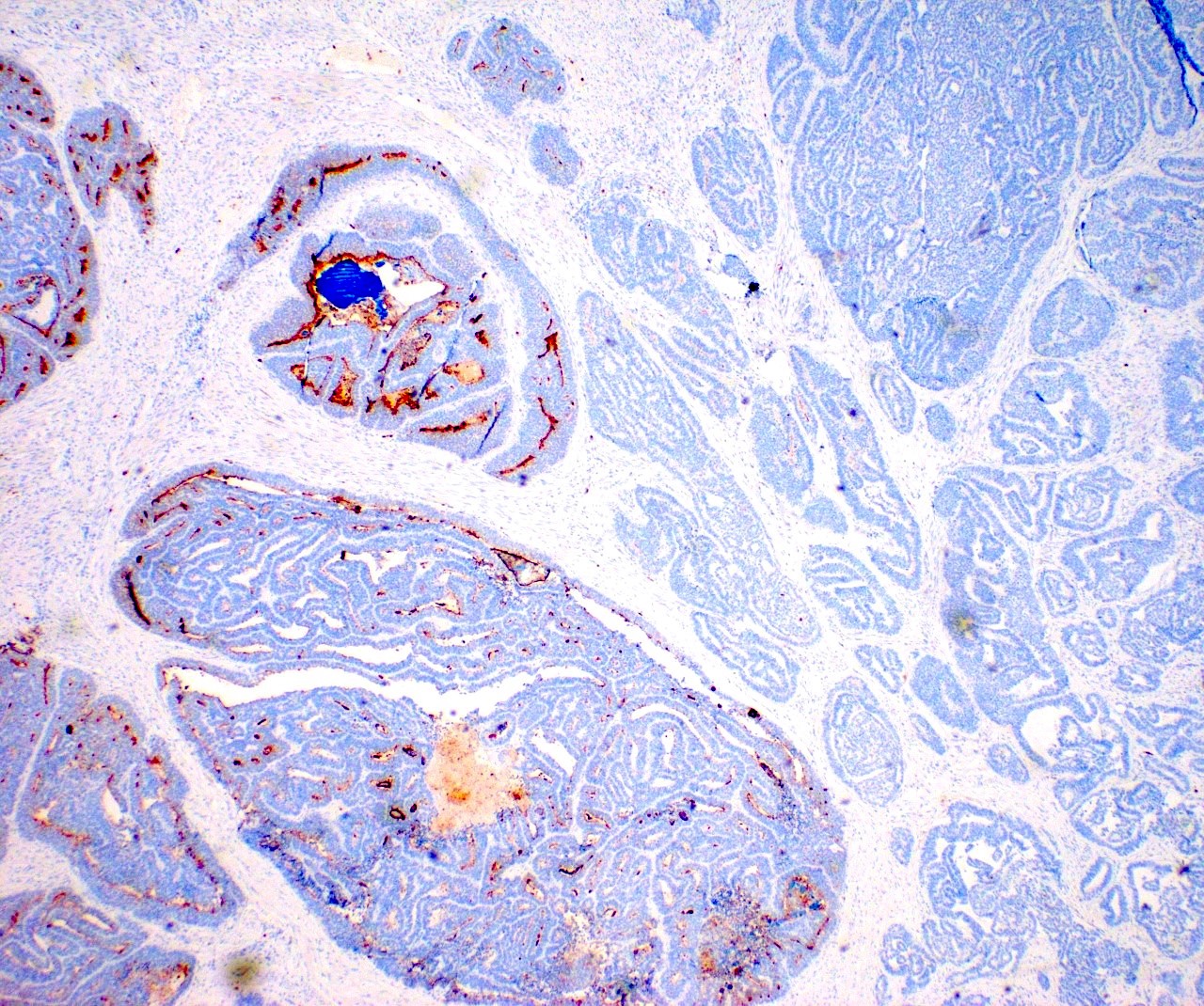
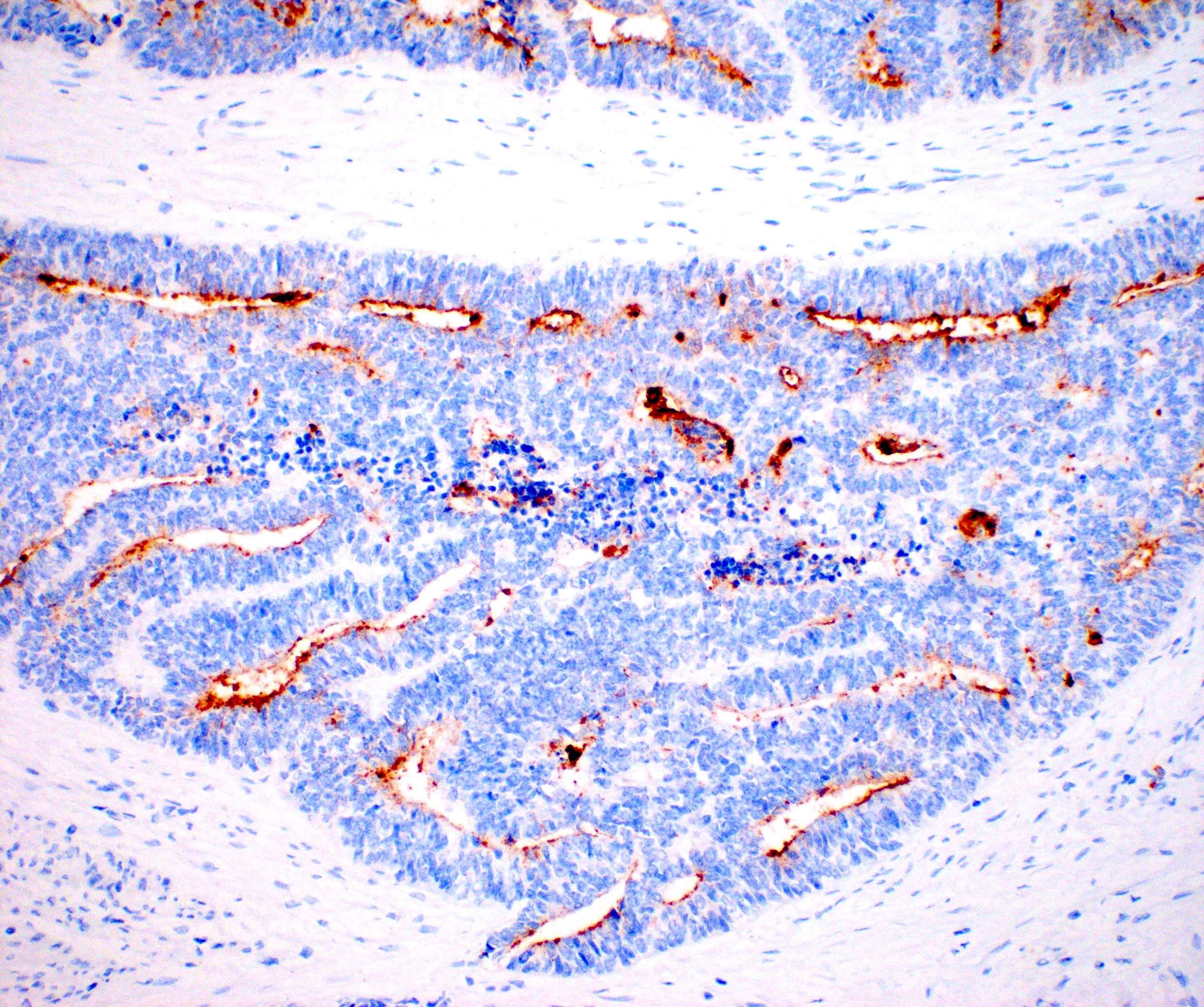
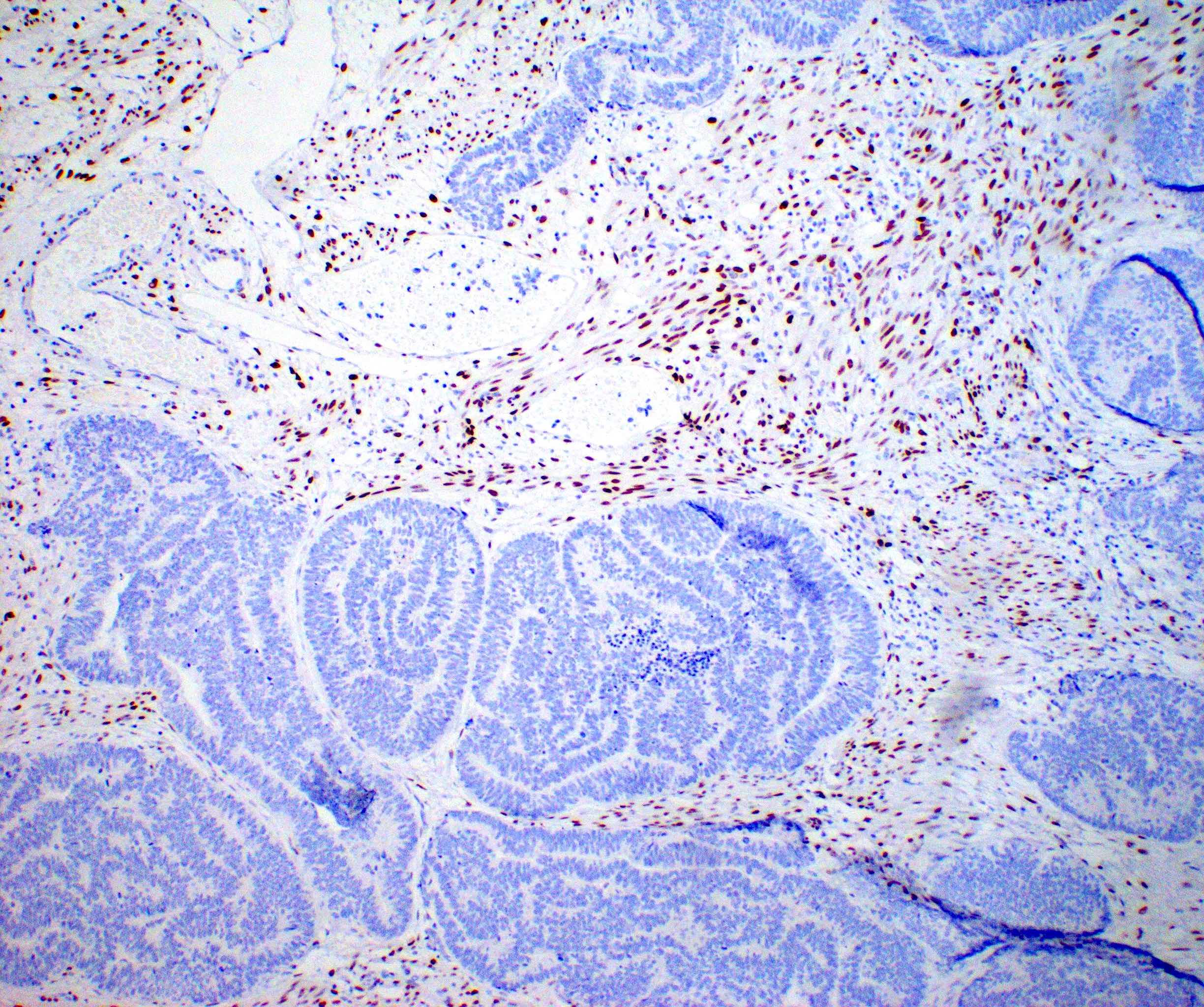
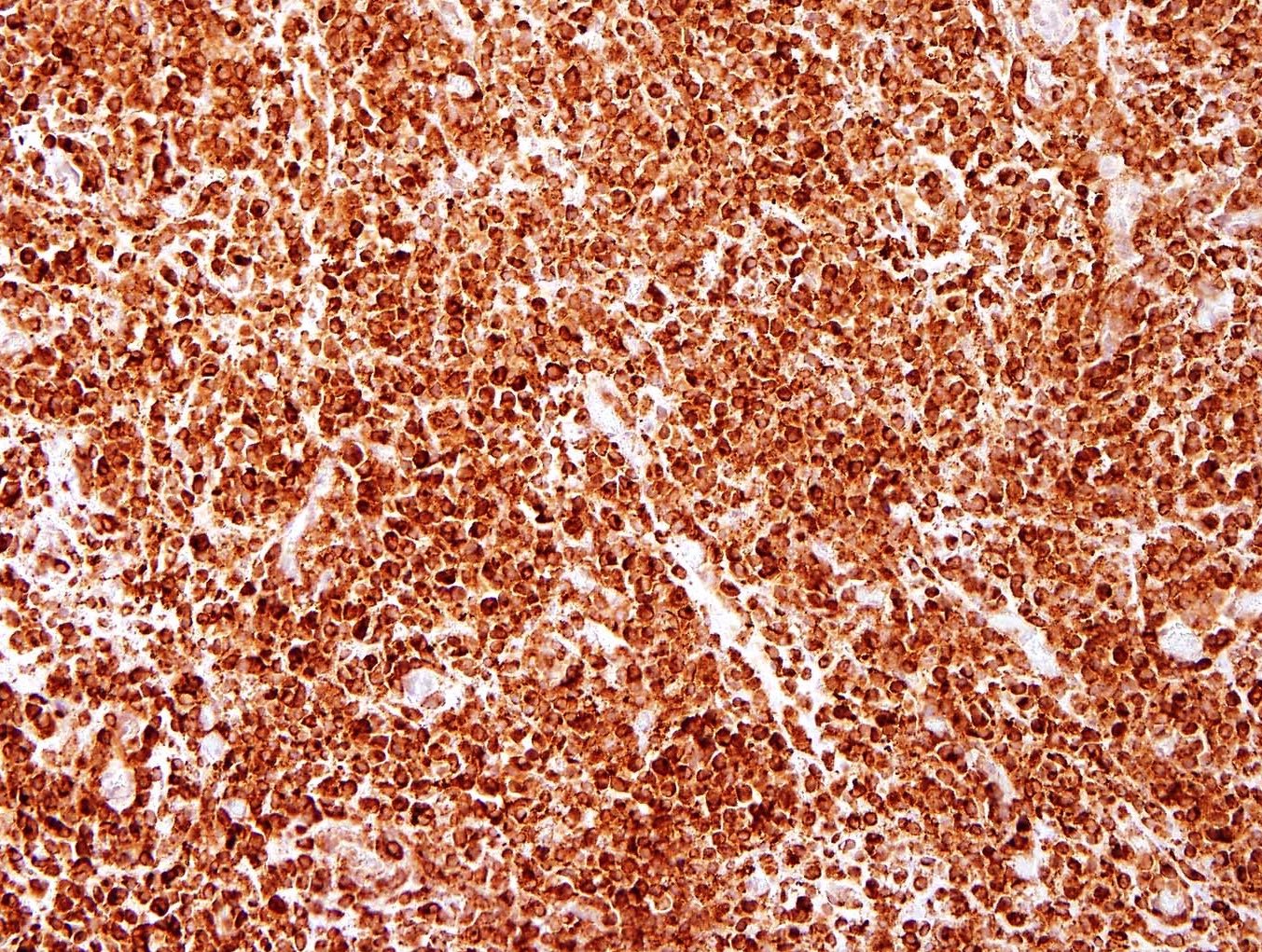
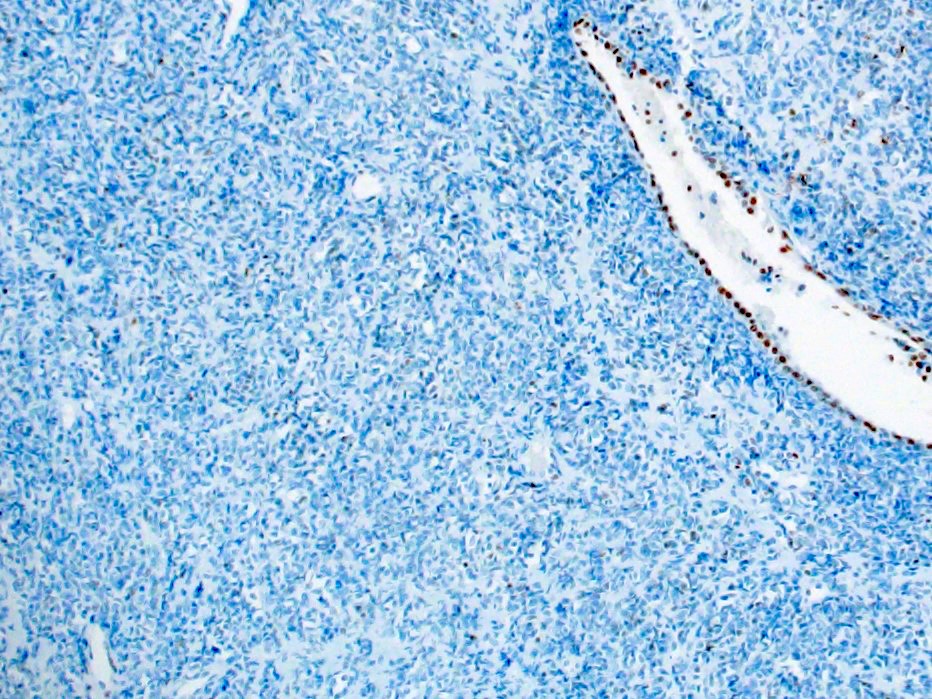
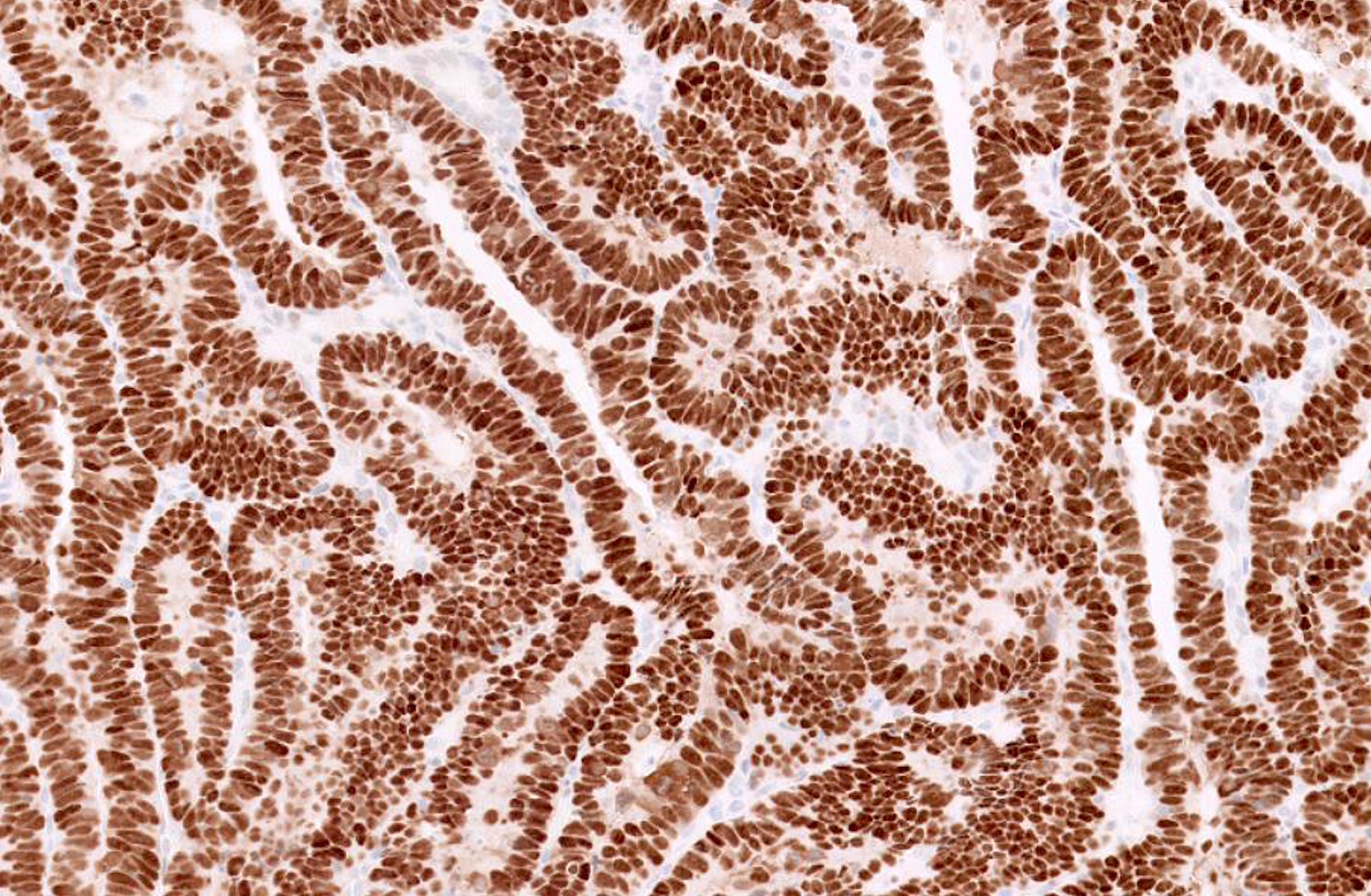
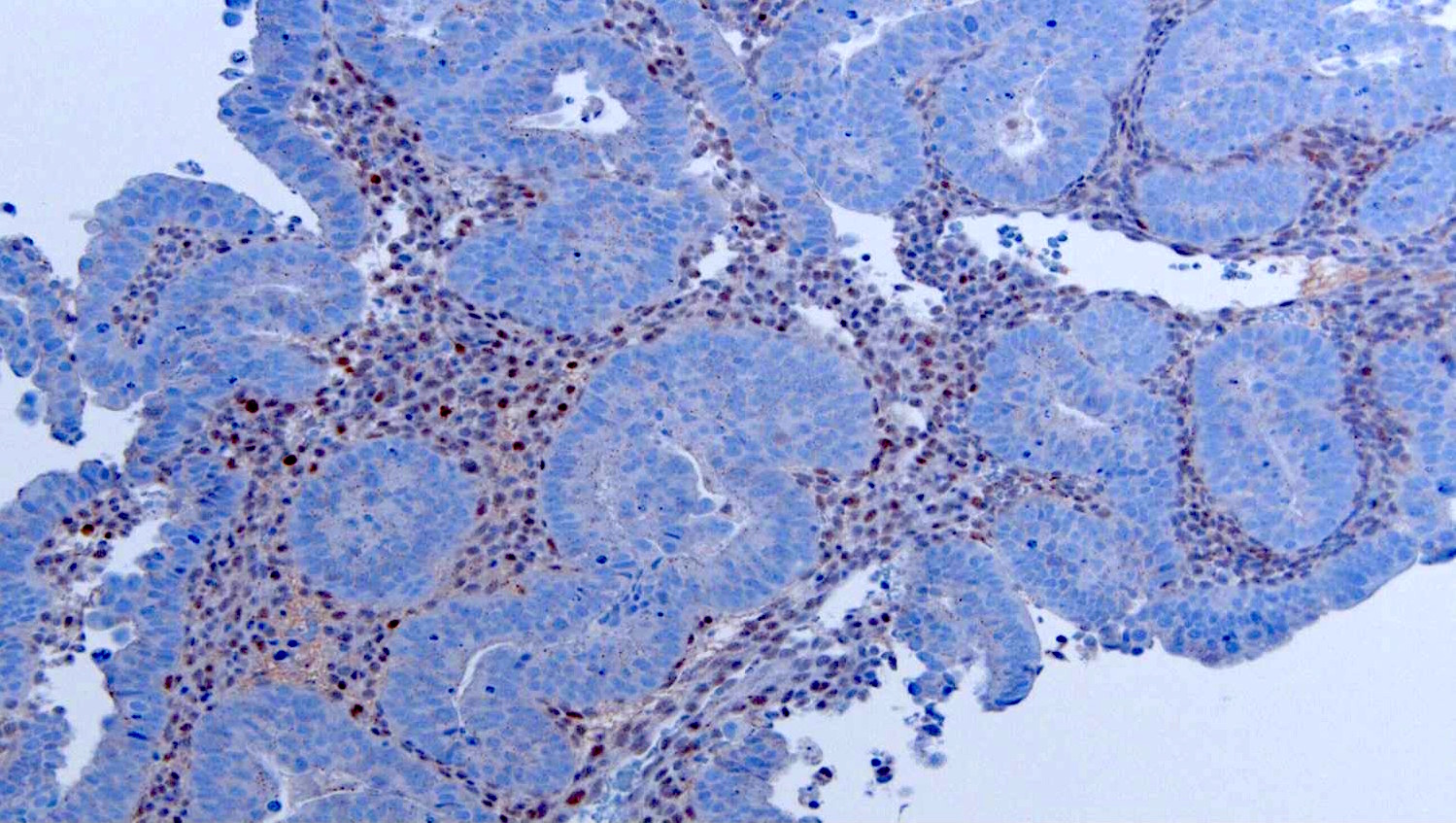
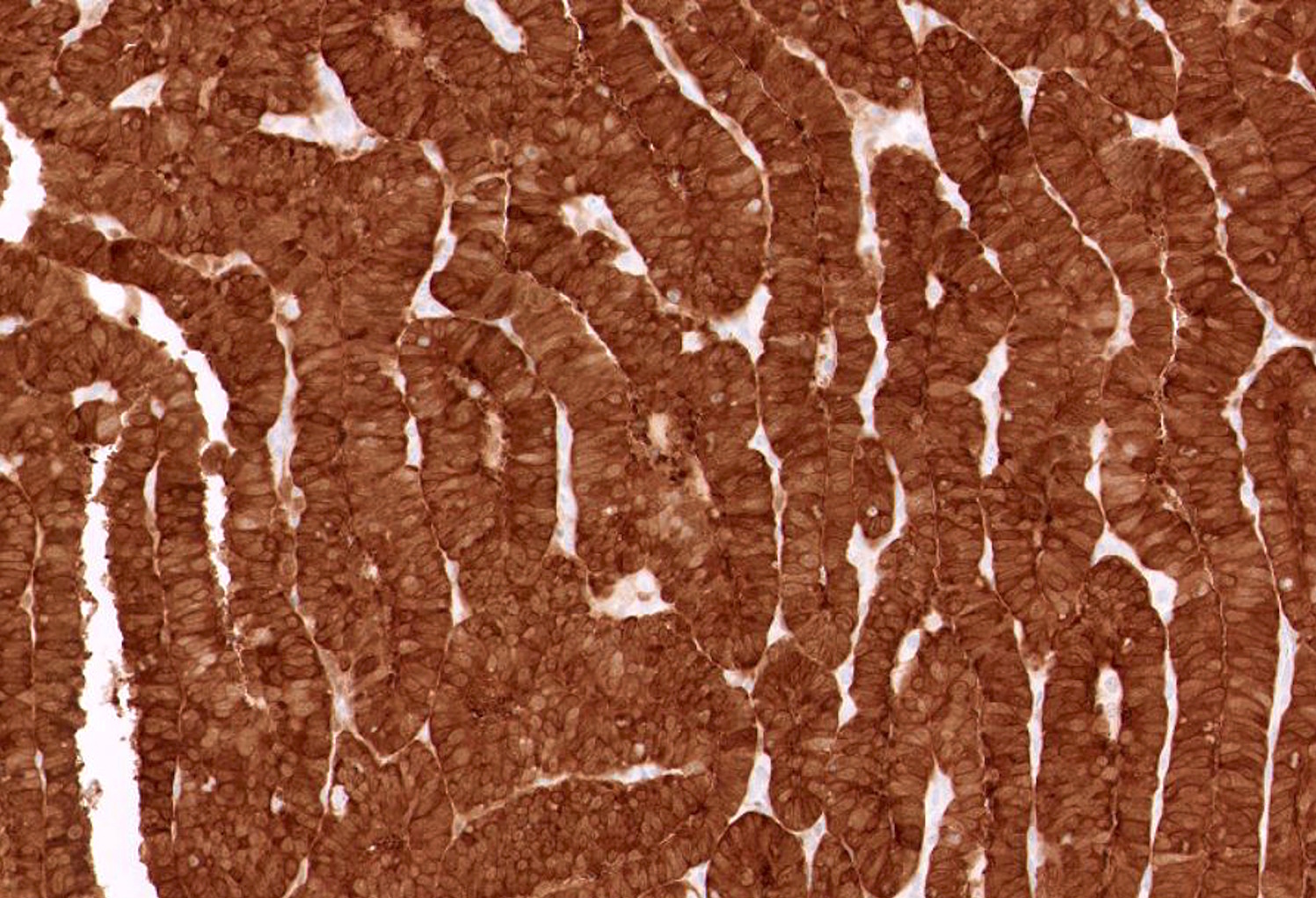
- Different patterns of mismatch repair (MMR) or hormone receptor expression by IHC
- Conversely, secondary ovarian involvement by a primary endometrial tumor should be considered when:
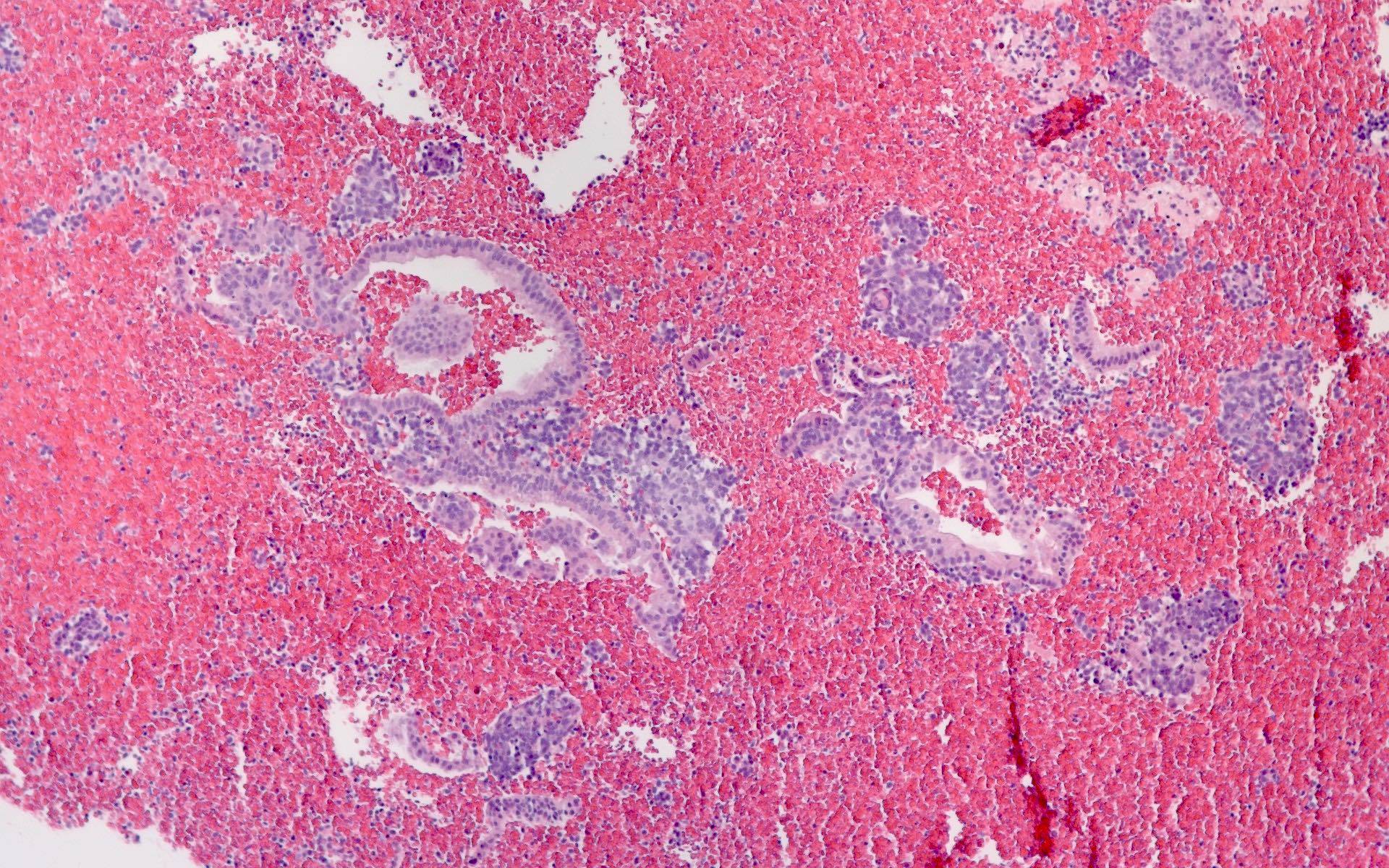
- Endometrial tumor has deep myometrial invasion, lymphovascular space invasion, serosal or parametrial involvement
- Bilateral ovarian involvement
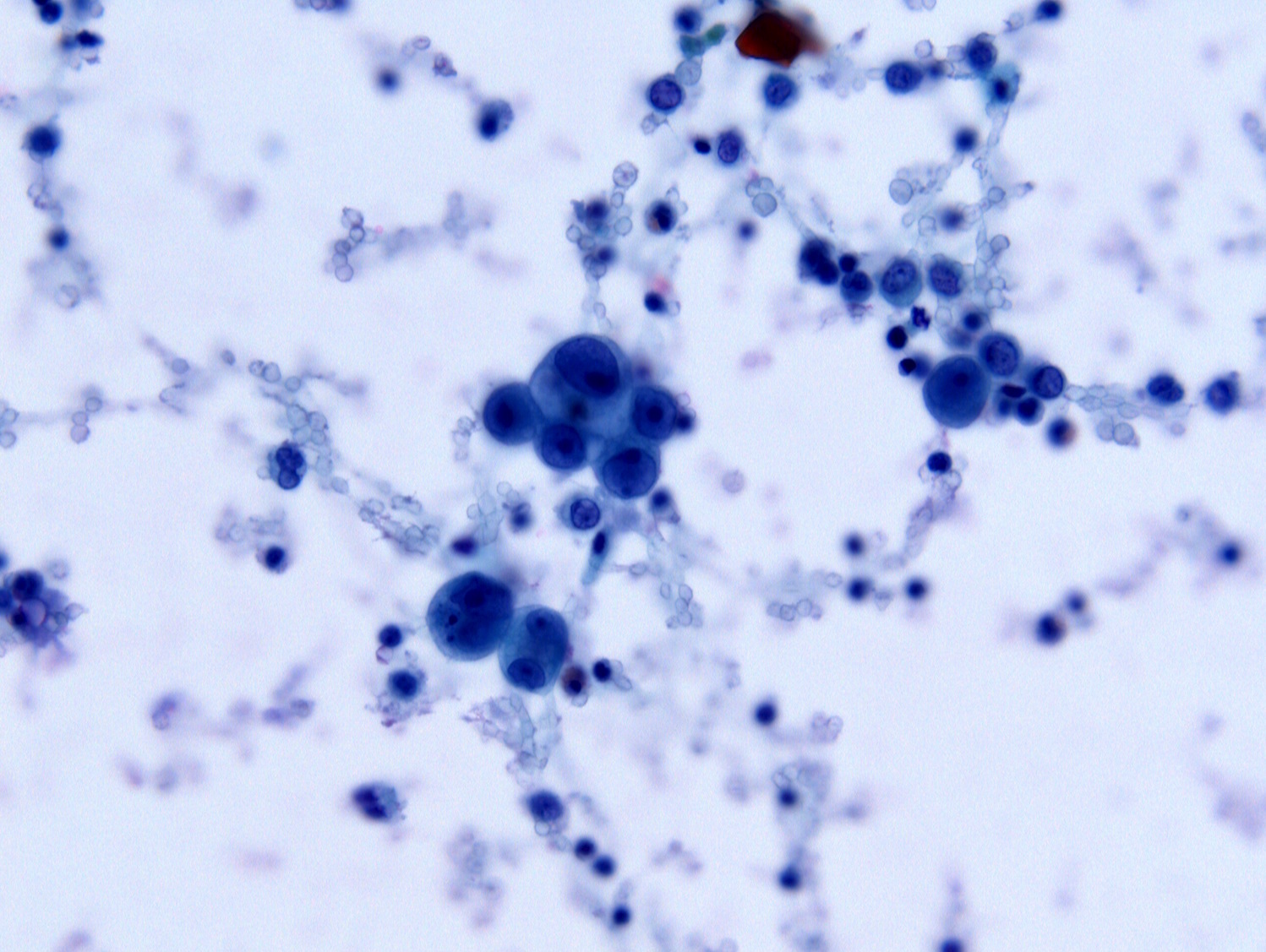
- Ovarian tumor involves surface and has extensive lymphovascular space invasion
- Both tumors show similar MMR and hormone receptor expression by IHC
- Distinguishing between the following is relevant for staging and treatment: