Superpage
Superpage Topics
CD80-89
ABCC2
Acid fast / Auramine-rhodamine
Acid phosphatase
ACTH (pending)
Actin - general / cardiac
Actin - muscle specific
Actin, alpha smooth muscle type
Adenovirus
Adipophilin (pending)
Albumin
Alcian blue
ALK
Alkaline phosphatase
Alpha fetoprotein (AFP)
Alpha-1 antitrypsin
Alpha-1-antichymotrypsin
Alpha-synuclein
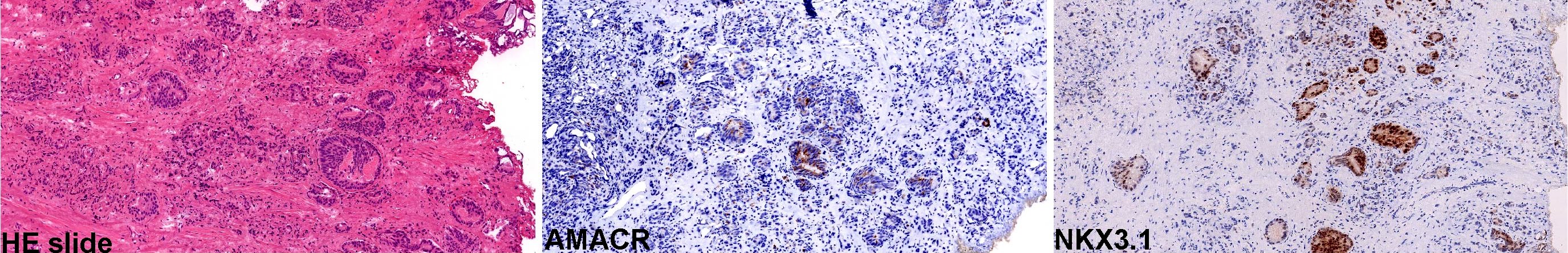
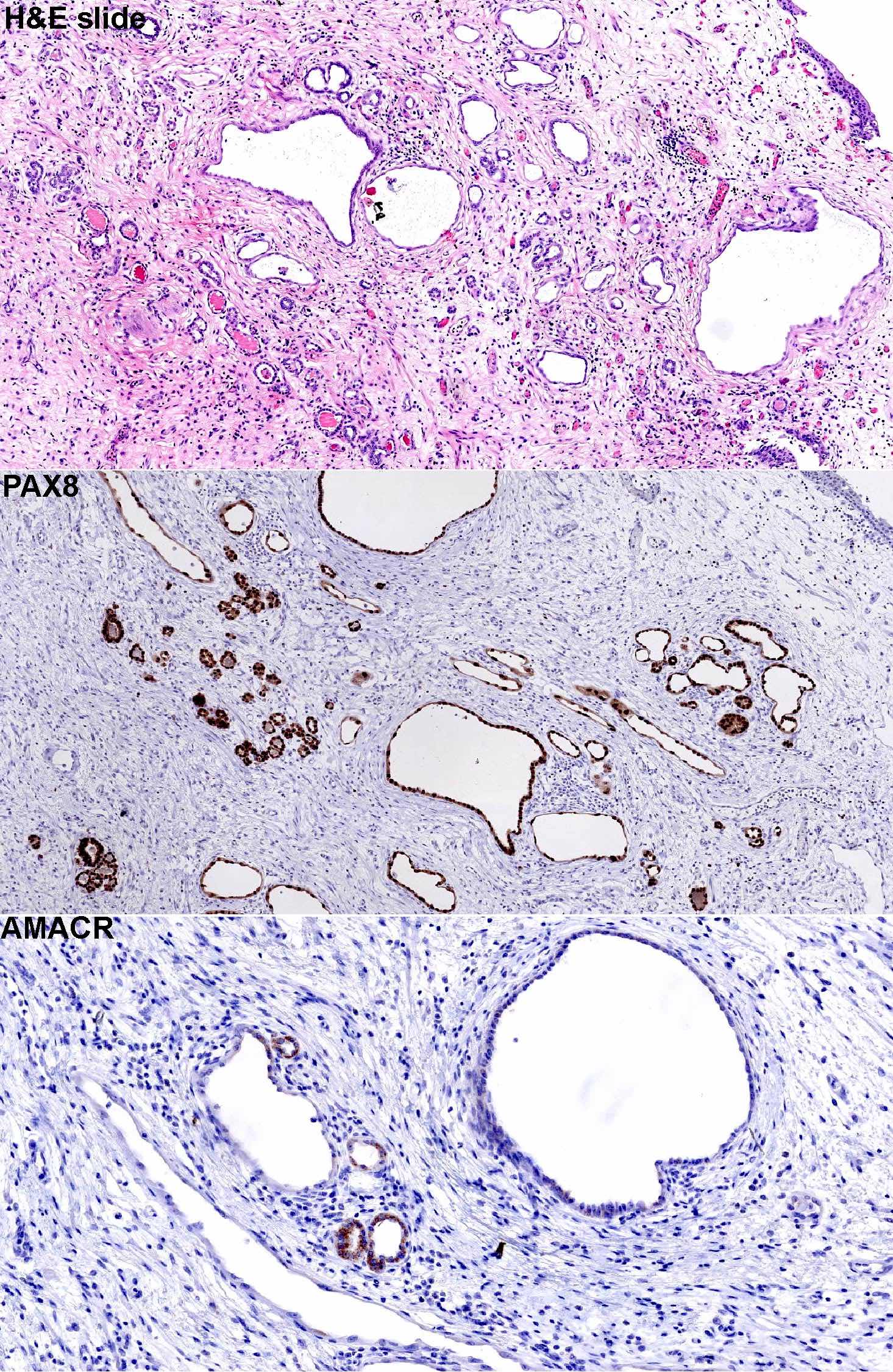
AMACR
Amyloid beta and amyloid beta precursor protein
Androgen receptor (AR)
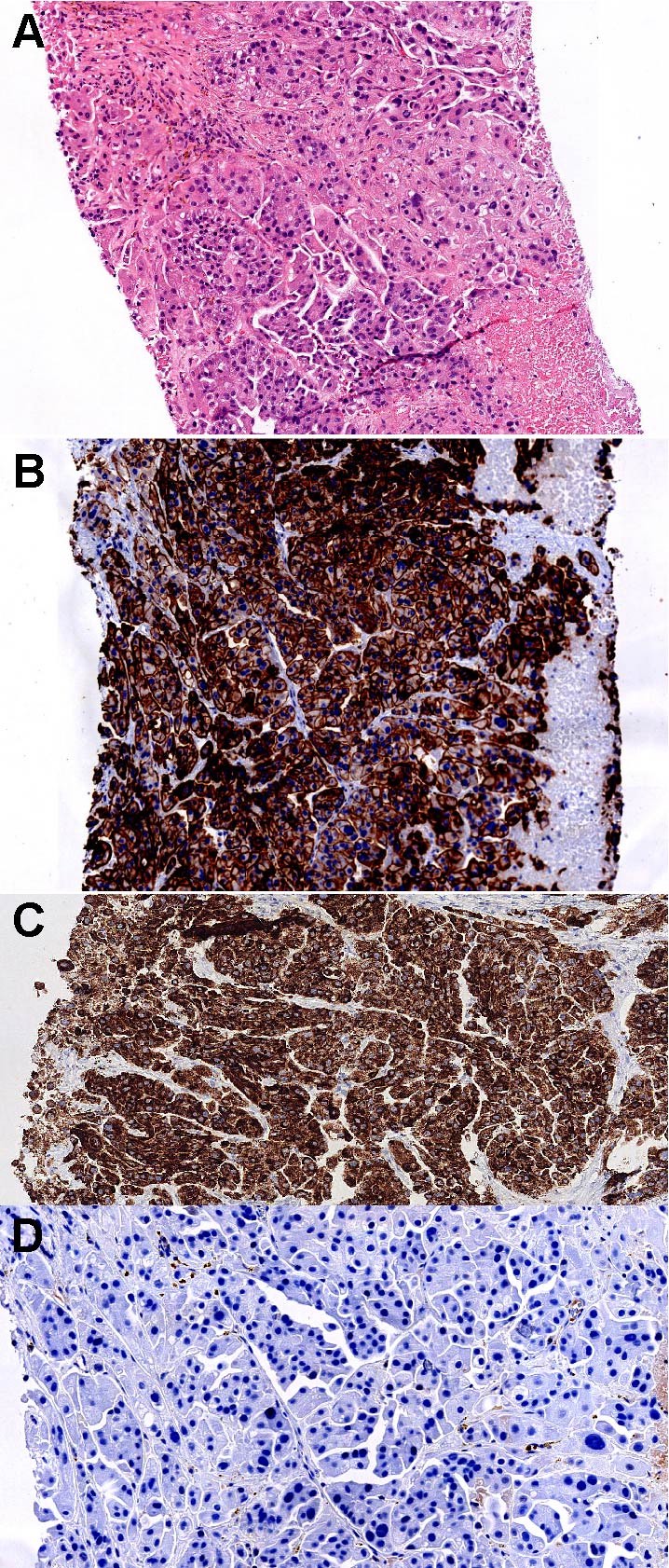
Arginase1
ARID1A
AT8 (pending)
ATDX (ATRX)
ATM
B72.3
BAP1
BCL10 (pending)
BCL2
BCL6
BCOR
BerEP4 / EpCAM
Beta catenin
Beta catenin
BOB1
Brachyury
BRAF V600E
BRAF-melanoma
BSEP (pending)
C4d (pending)
CA 19-9
CA125
Calcitonin
Calcium
Caldesmon
Calponin
Calretinin
CAMTA1
Carbonic anhydrase IX
Carcinoma of unknown primary
Cathepsin K
CCNB3 (pending)
CD markers - 190-199
CD Markers - General
CD markers - other
CD1-9
CD10
CD10-19
CD100-109
CD103
CD105
CD110-119
CD117
CD120-129
CD123
CD13
CD130-139
CD138
CD140-149
CD15
CD150-159
CD160-169
CD170-179
CD180-189
CD19
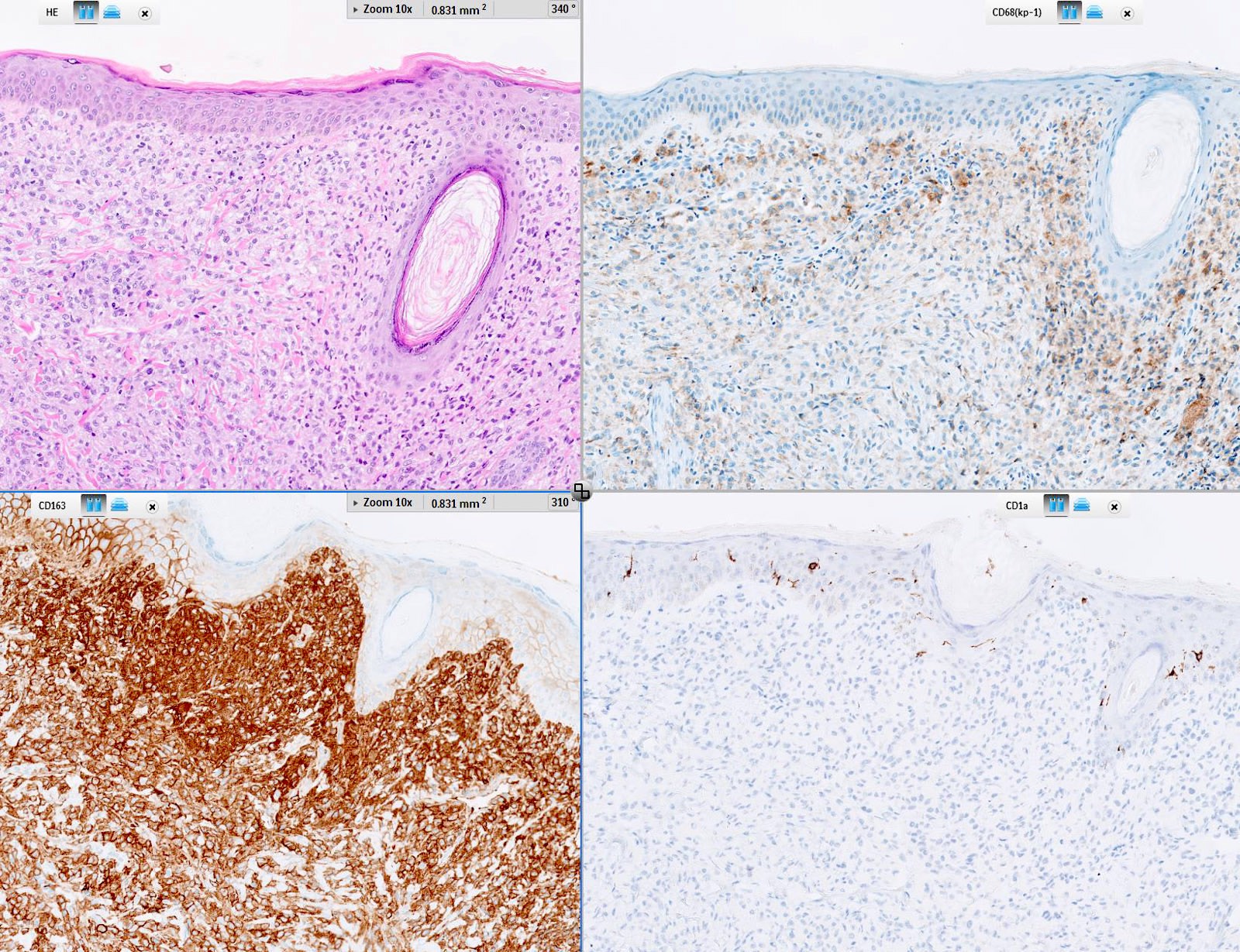
CD1a
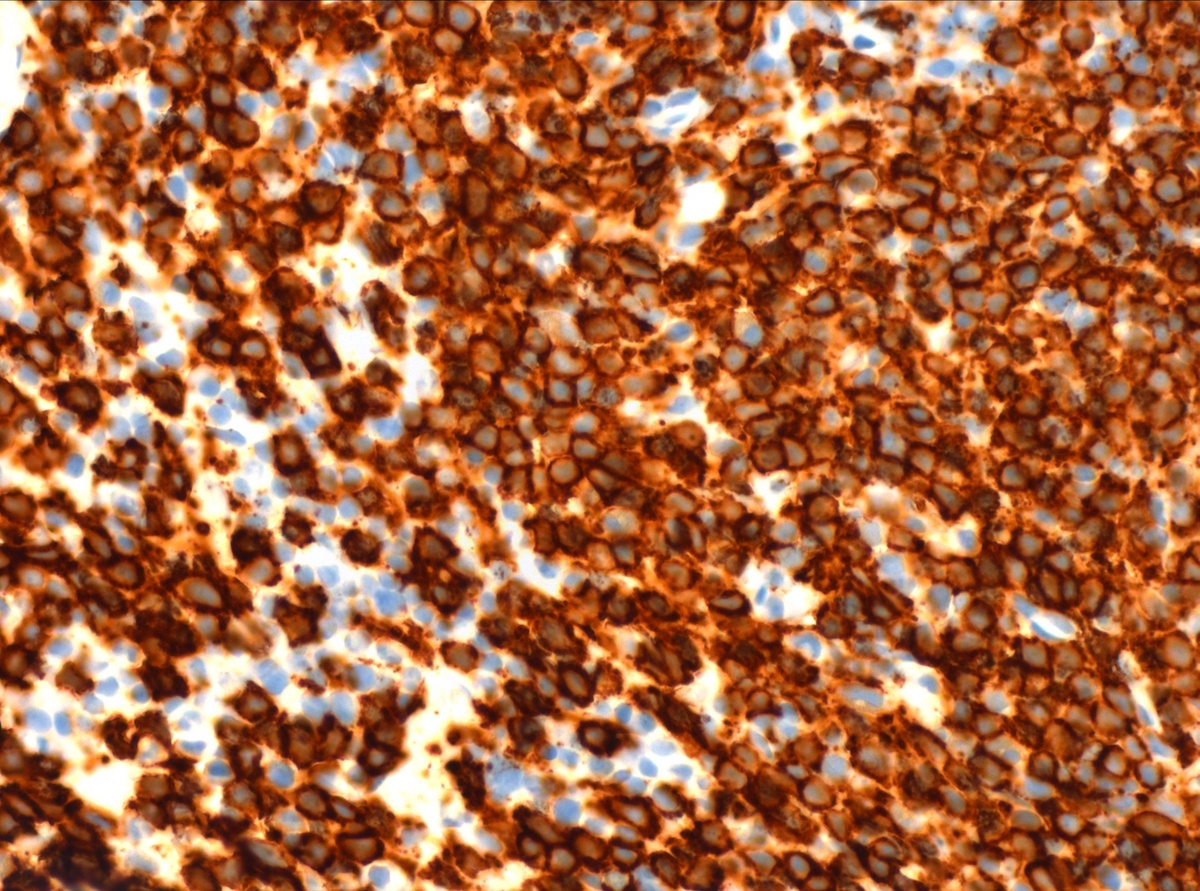
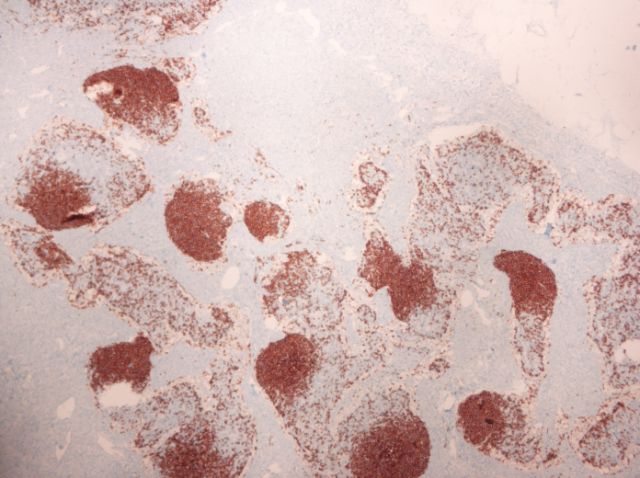
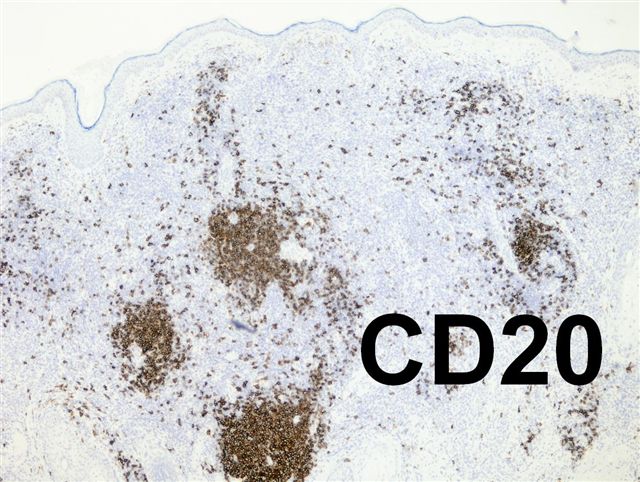
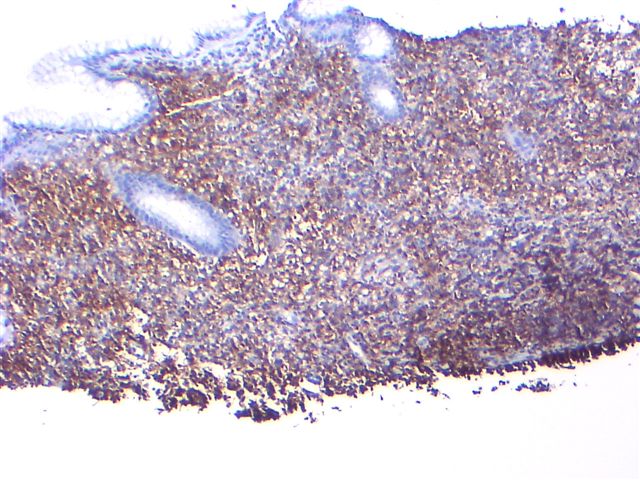
CD20
CD20-29
CD200-209
CD21
CD220-229
CD23
CD230-239
CD240-249
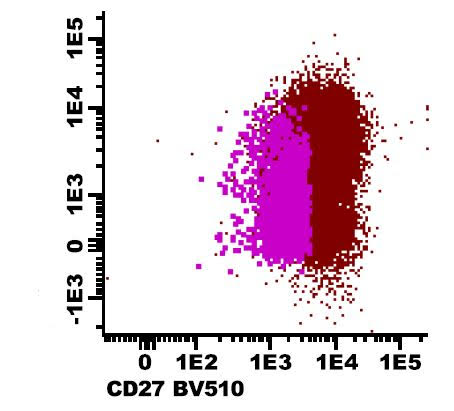
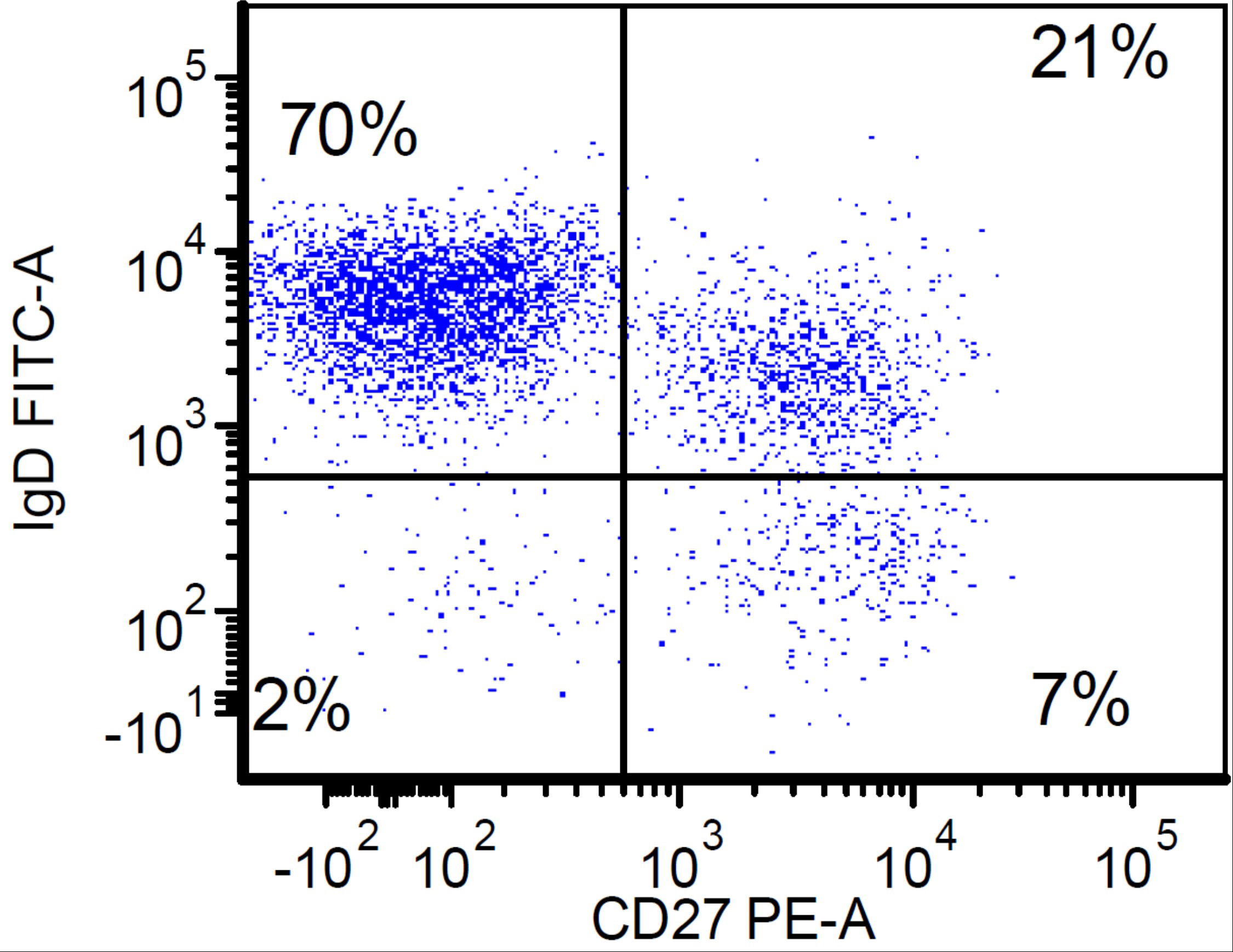
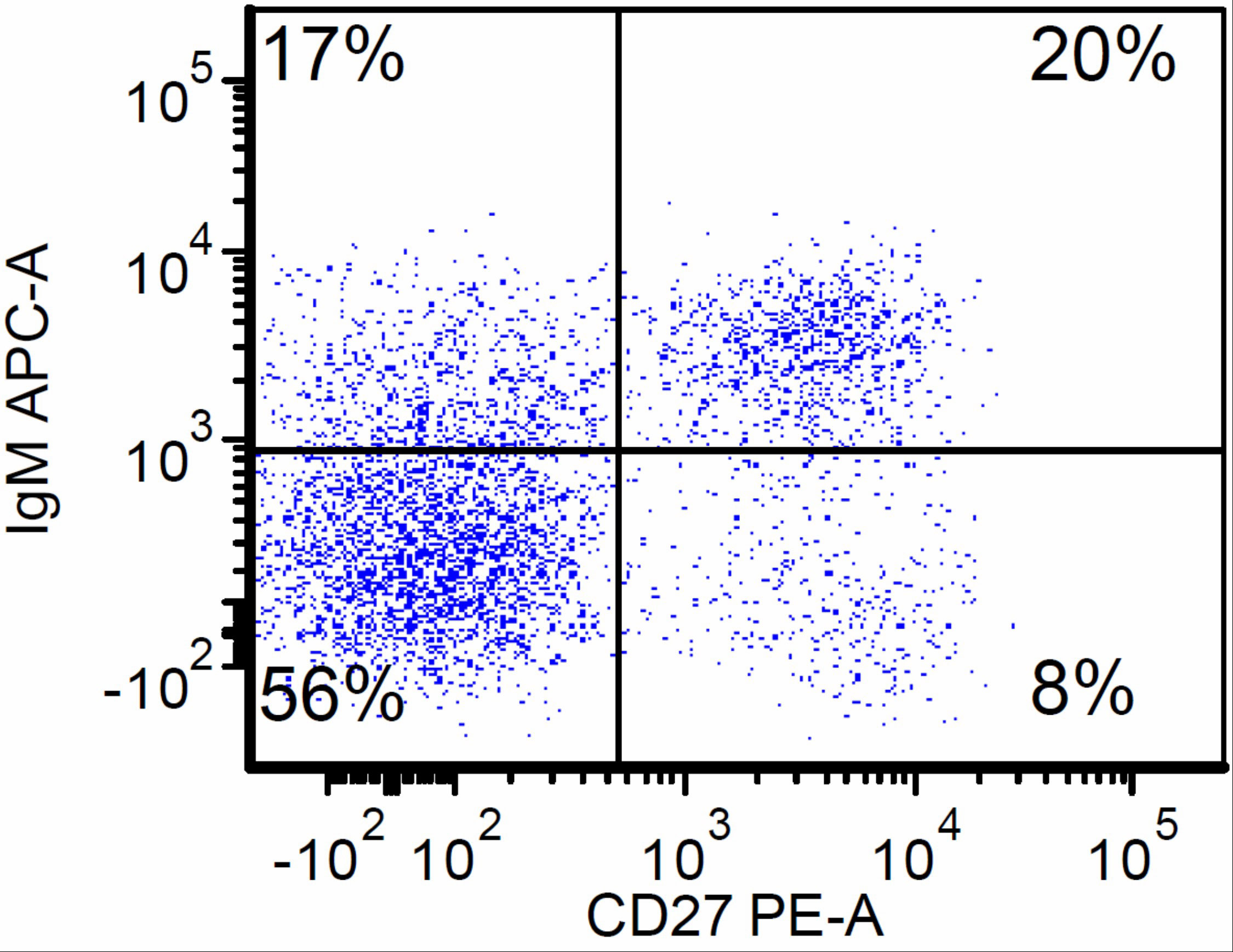
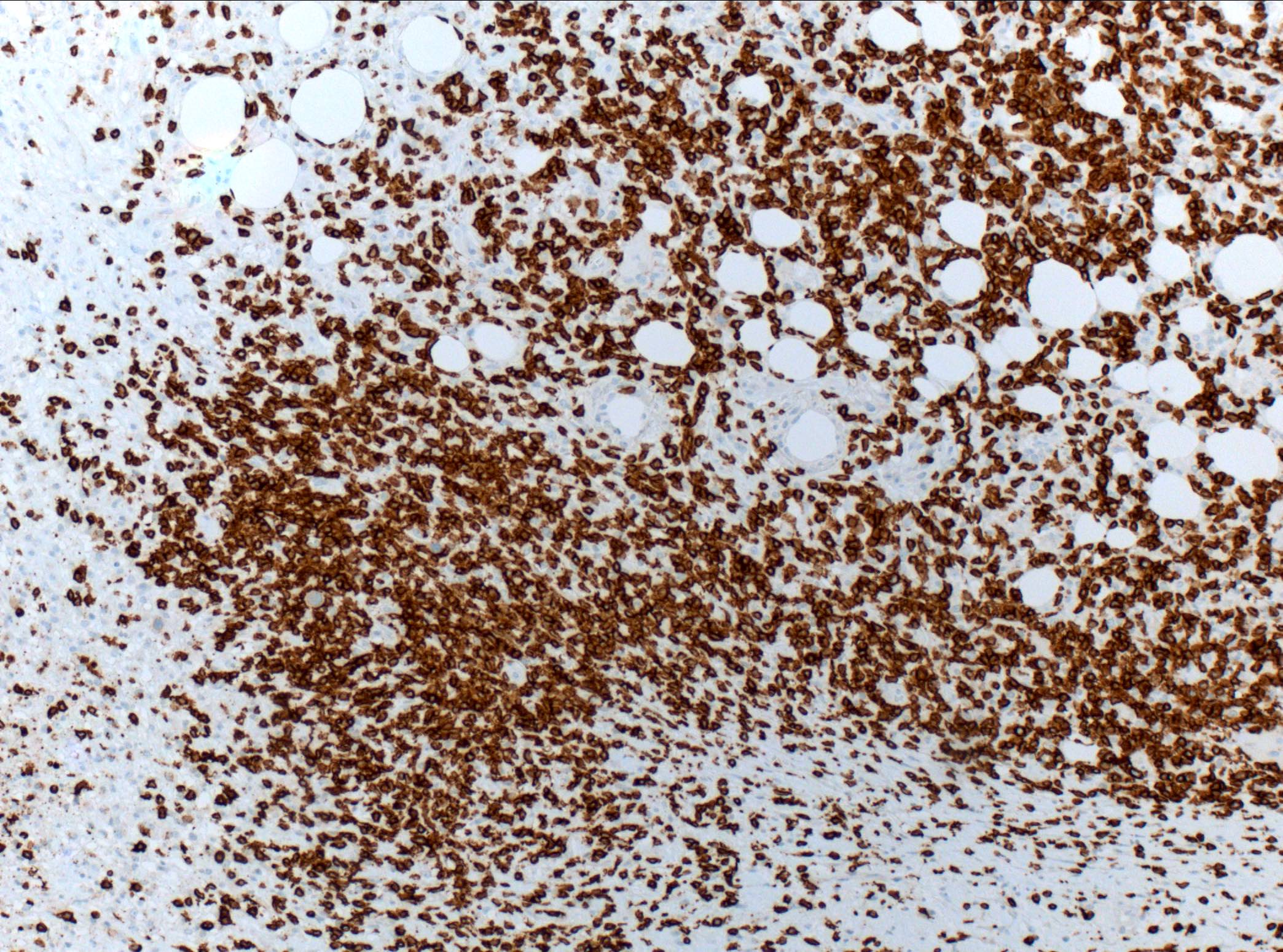
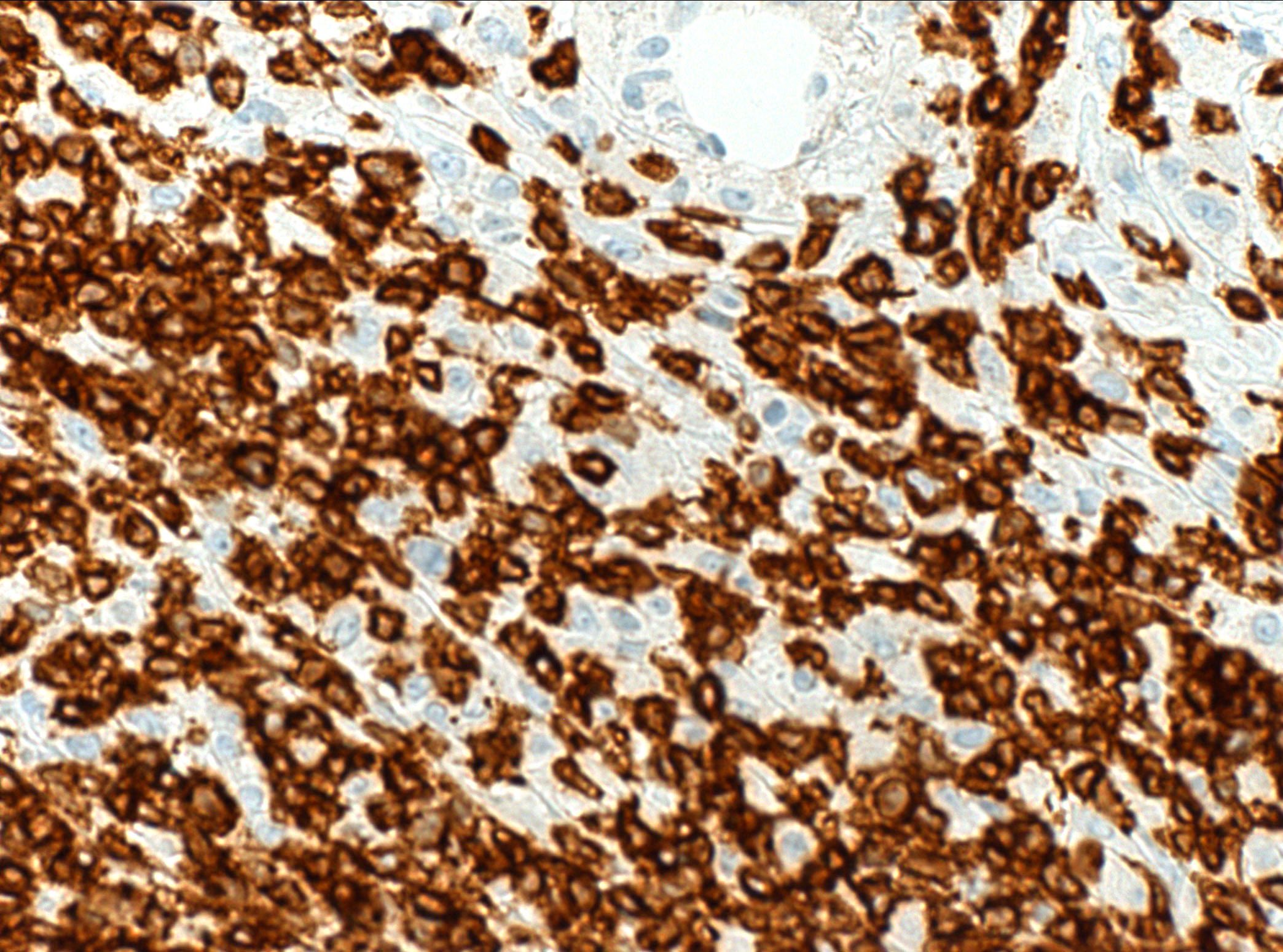
CD27
CD270-279
CD278 / ICOS (pending)
CD280-289
CD3
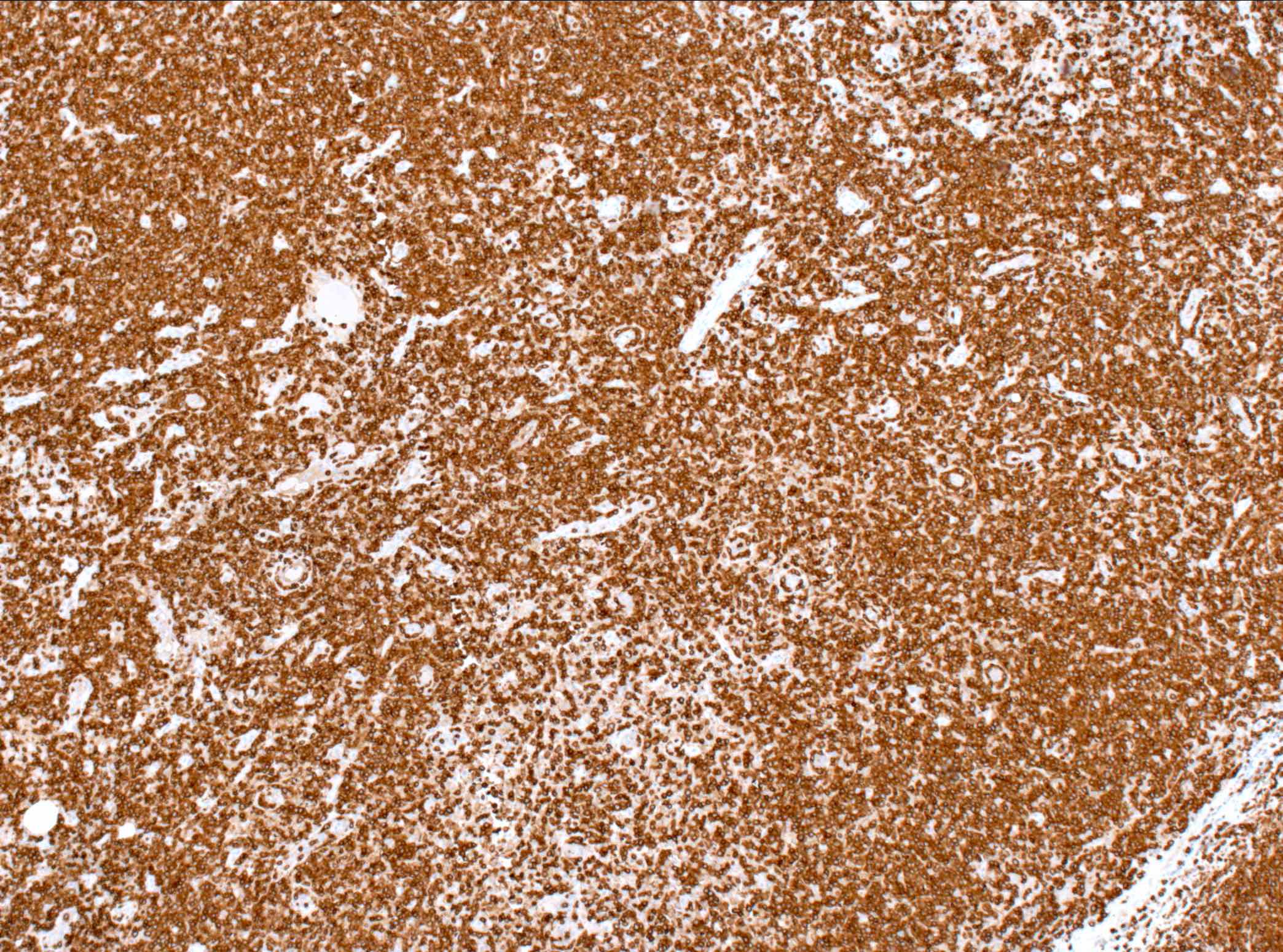
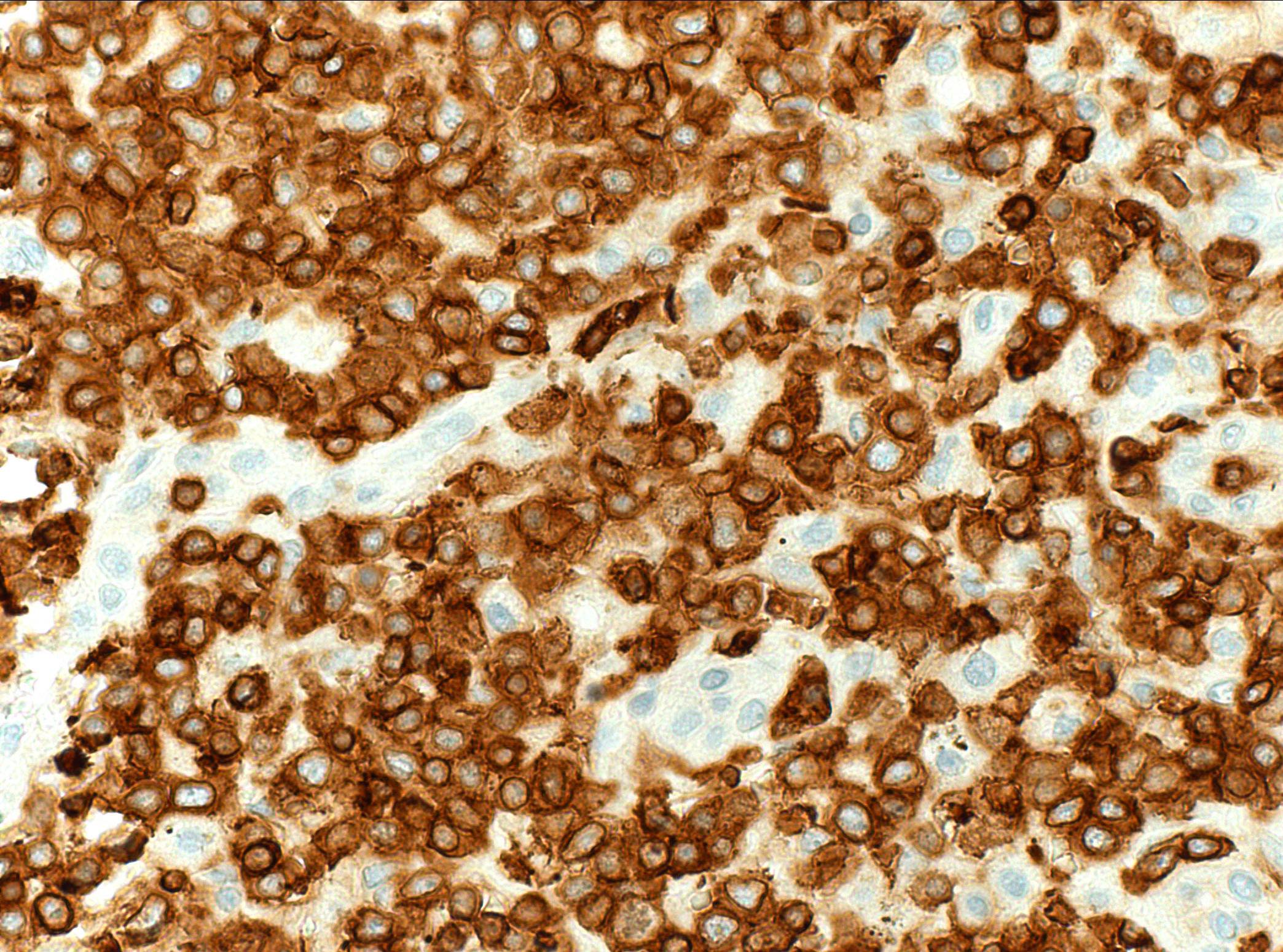
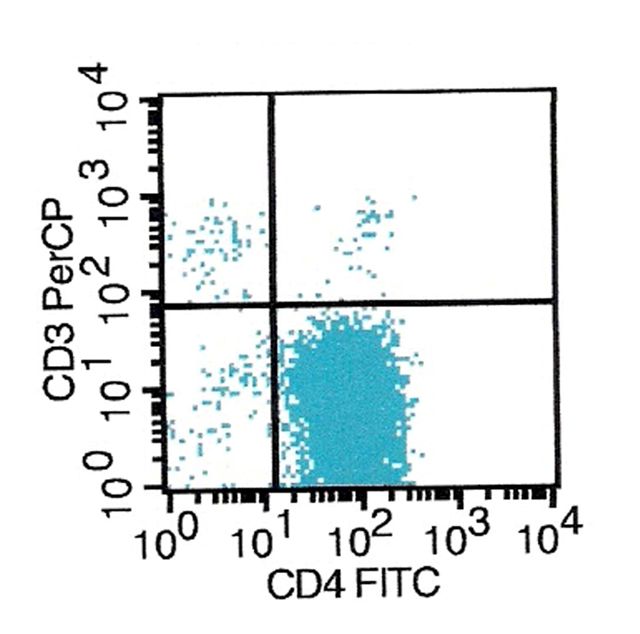
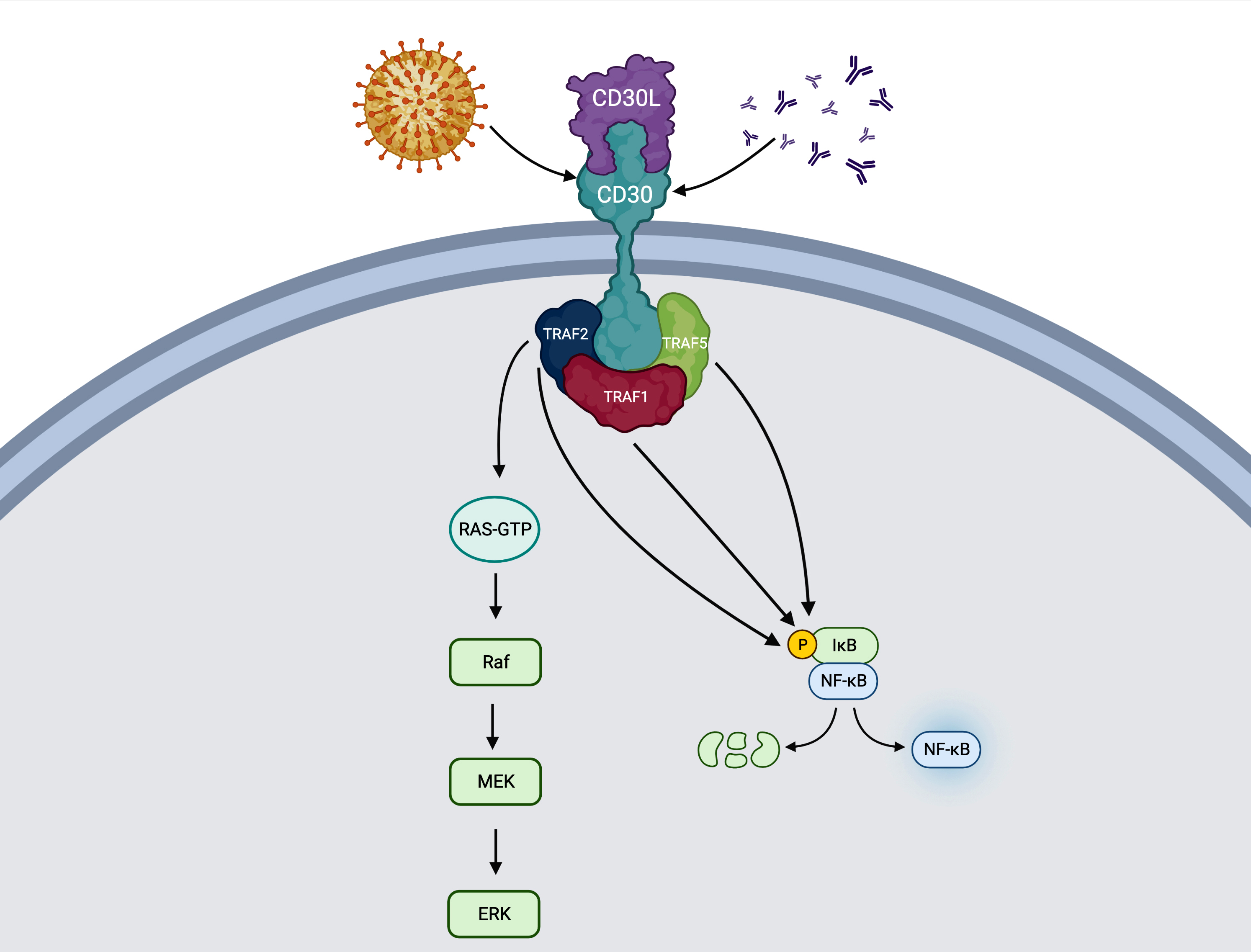
CD30
CD30-39
CD31
CD33
CD34
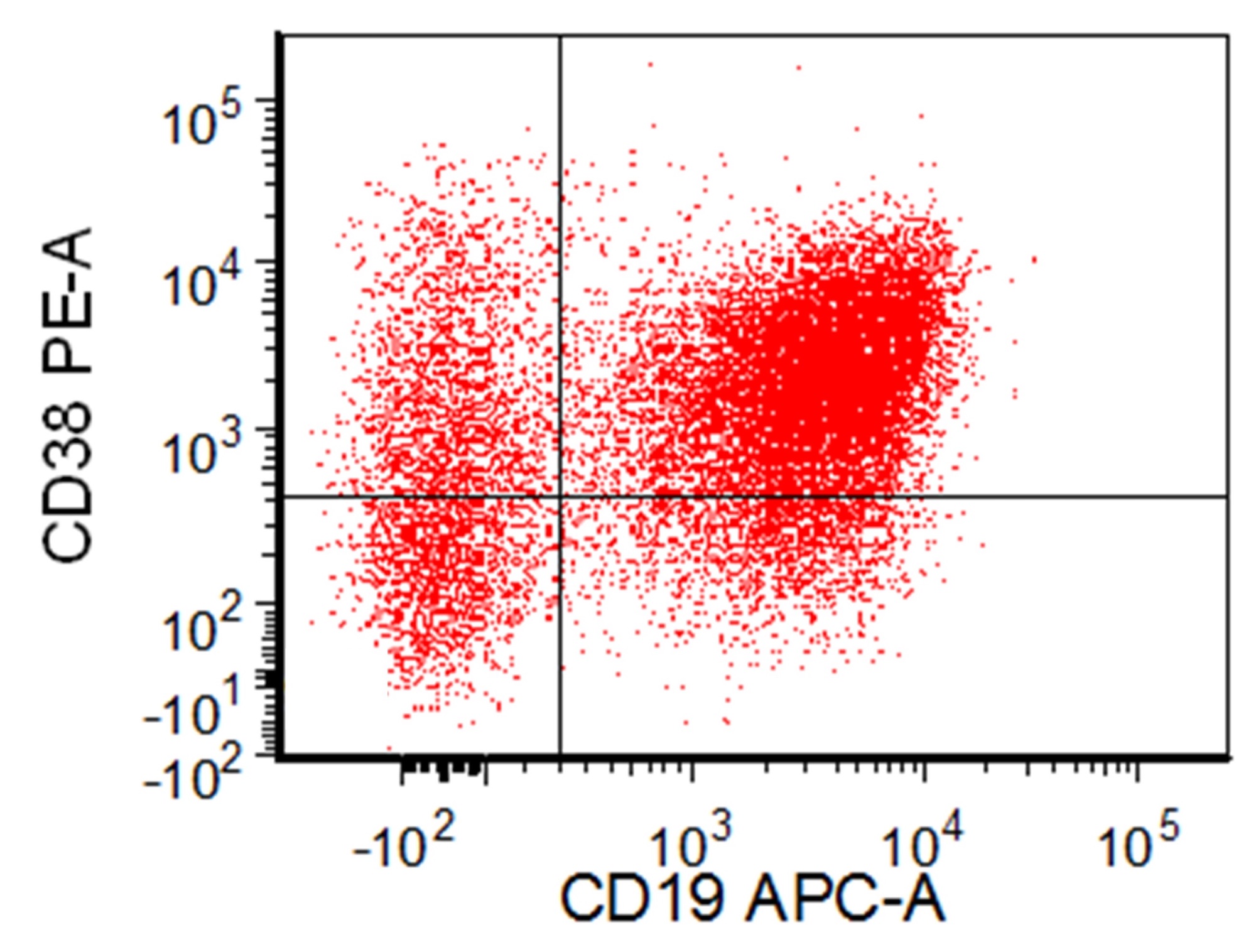
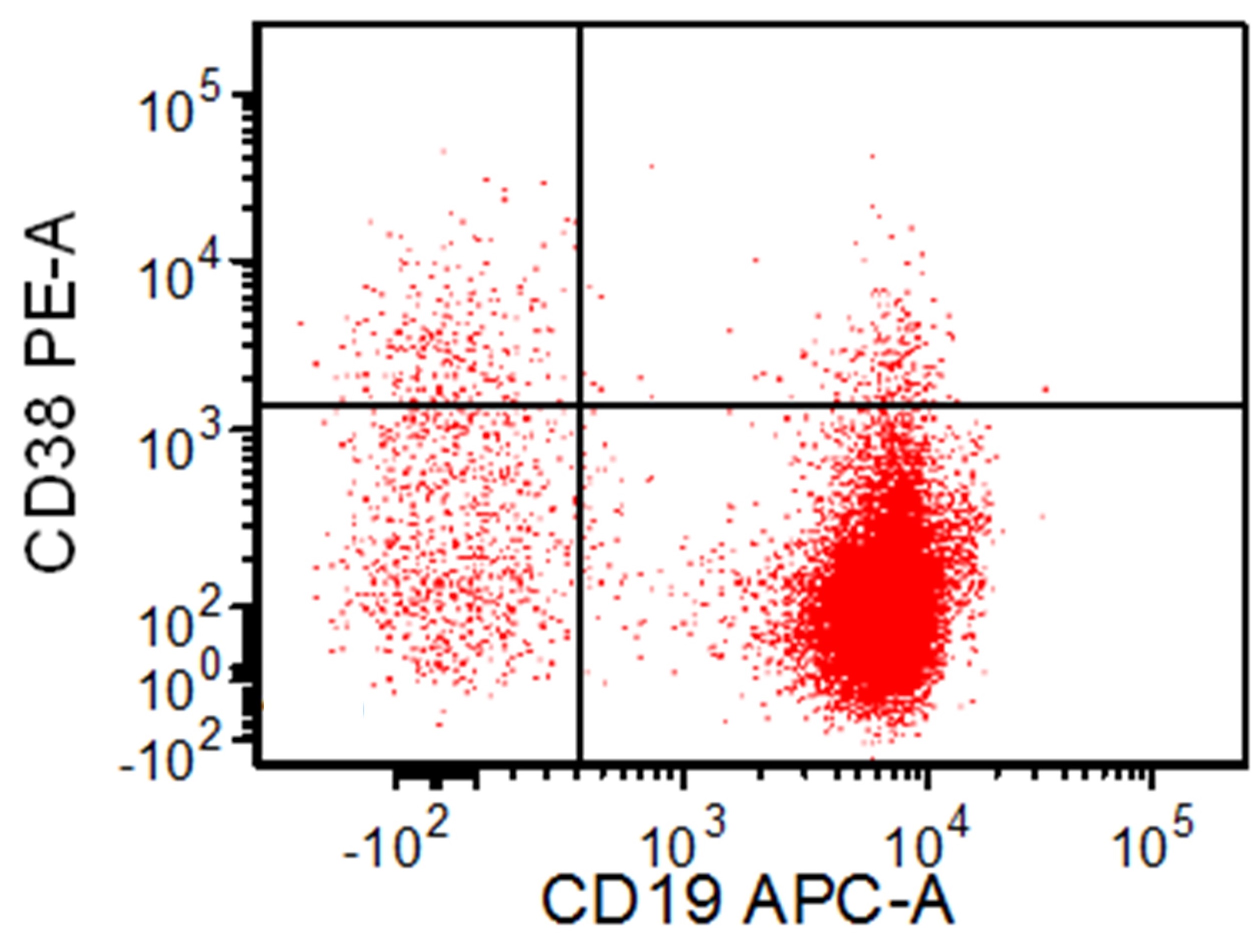
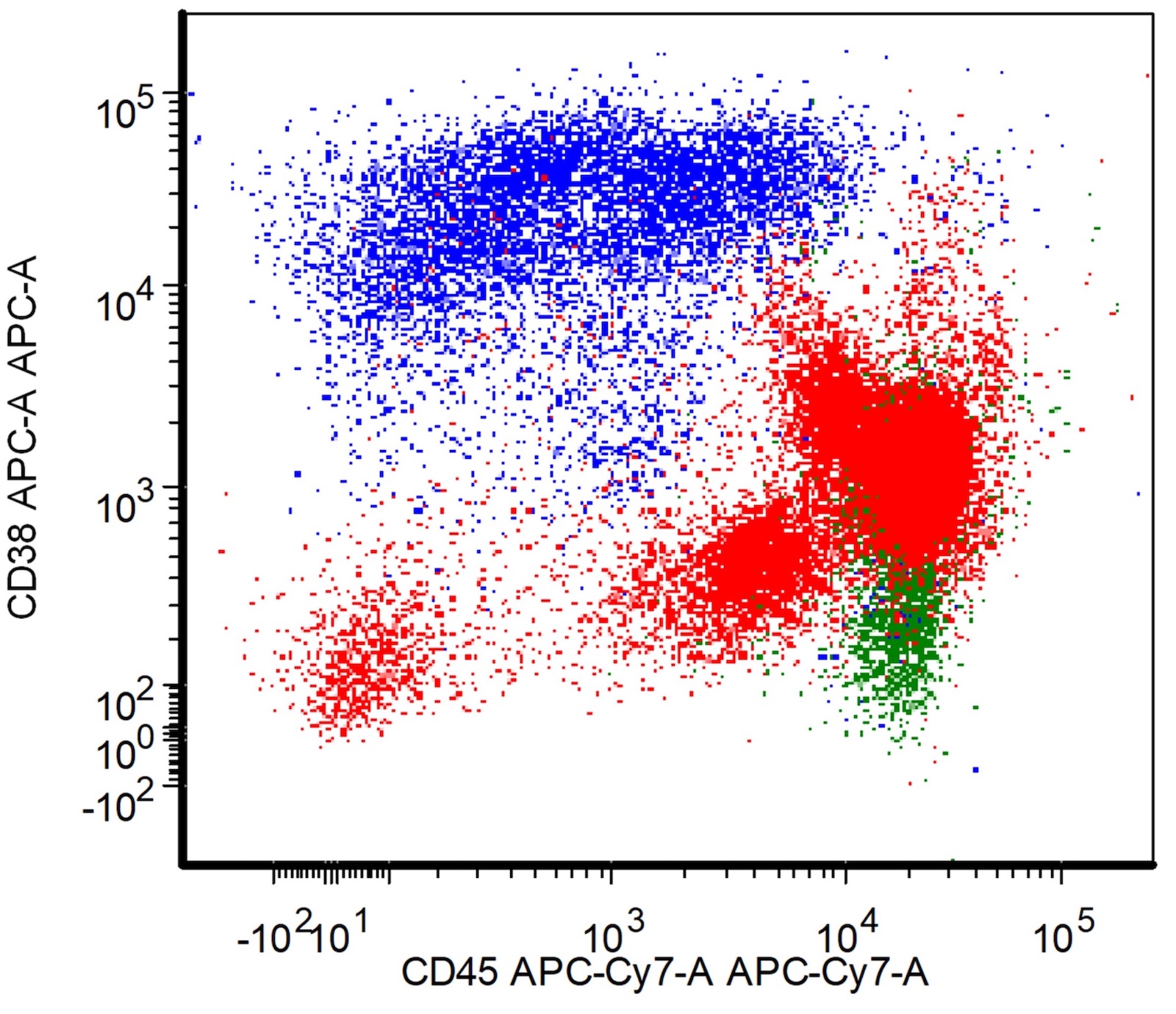
CD38
CD4
CD40-49
CD43
CD44
CD45 (LCA)
CD45RA
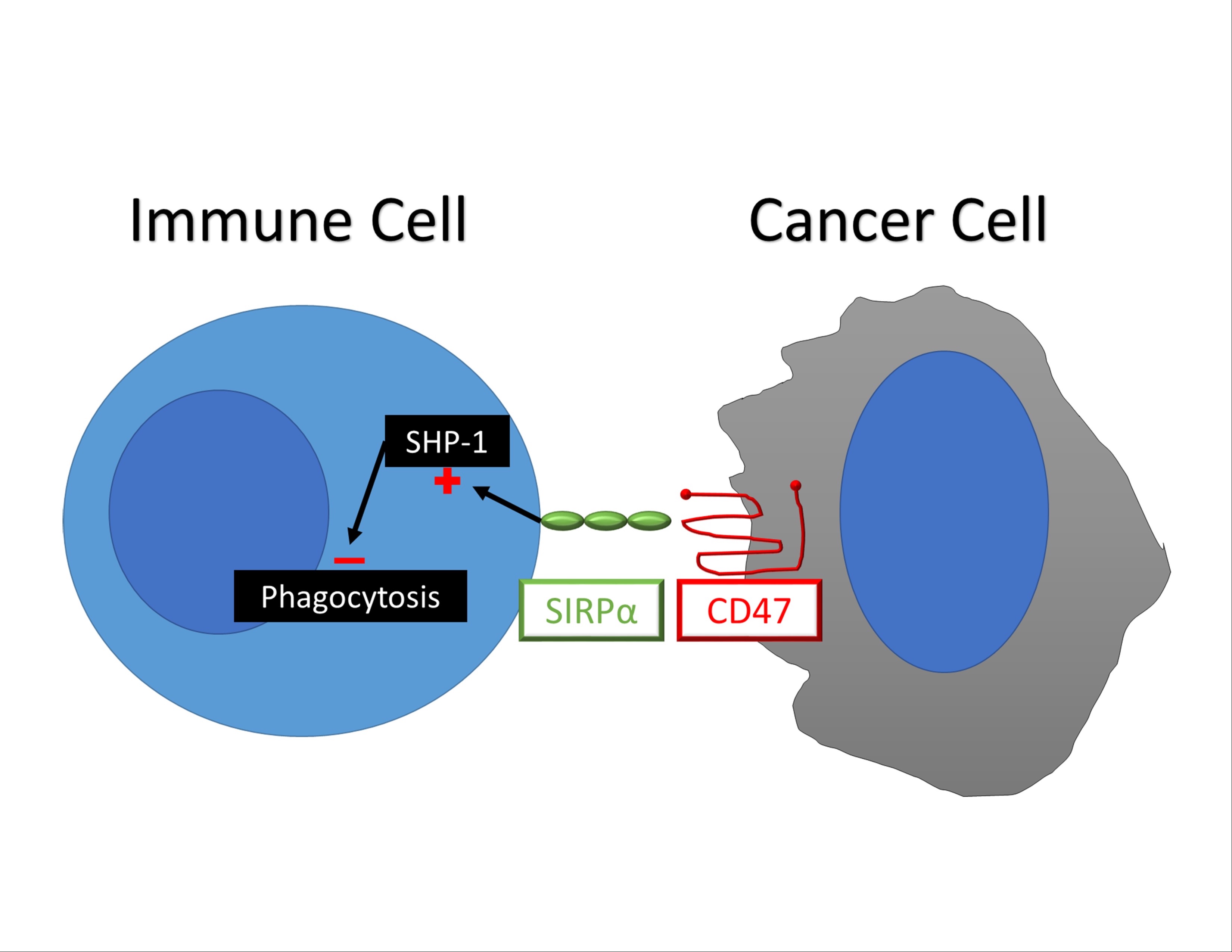
CD47
CD49
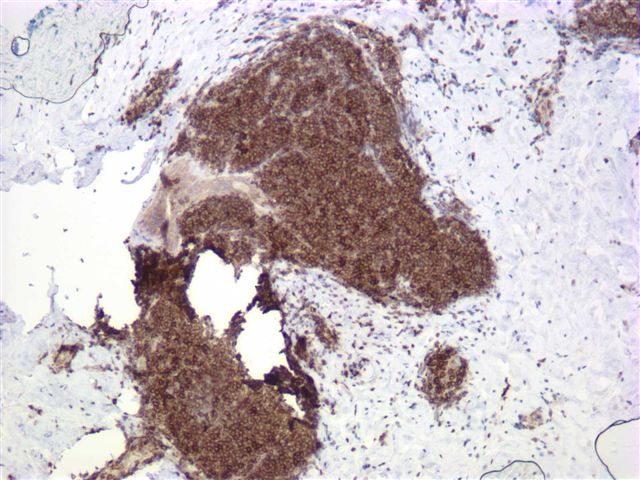
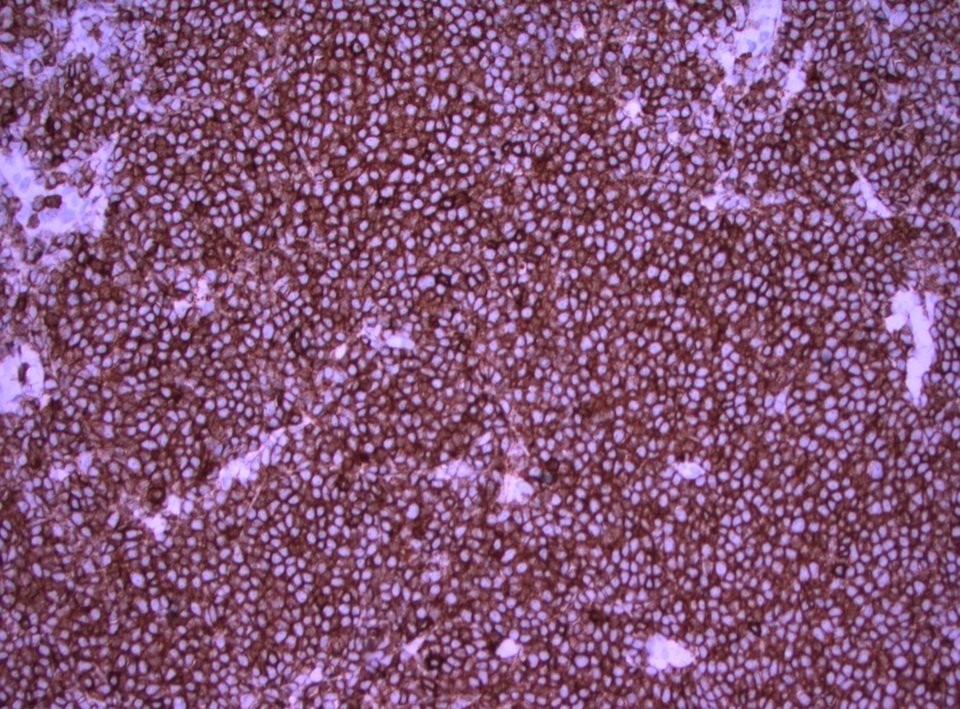
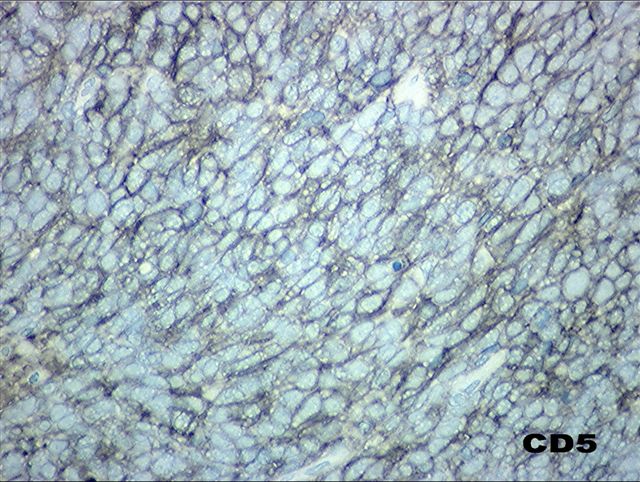
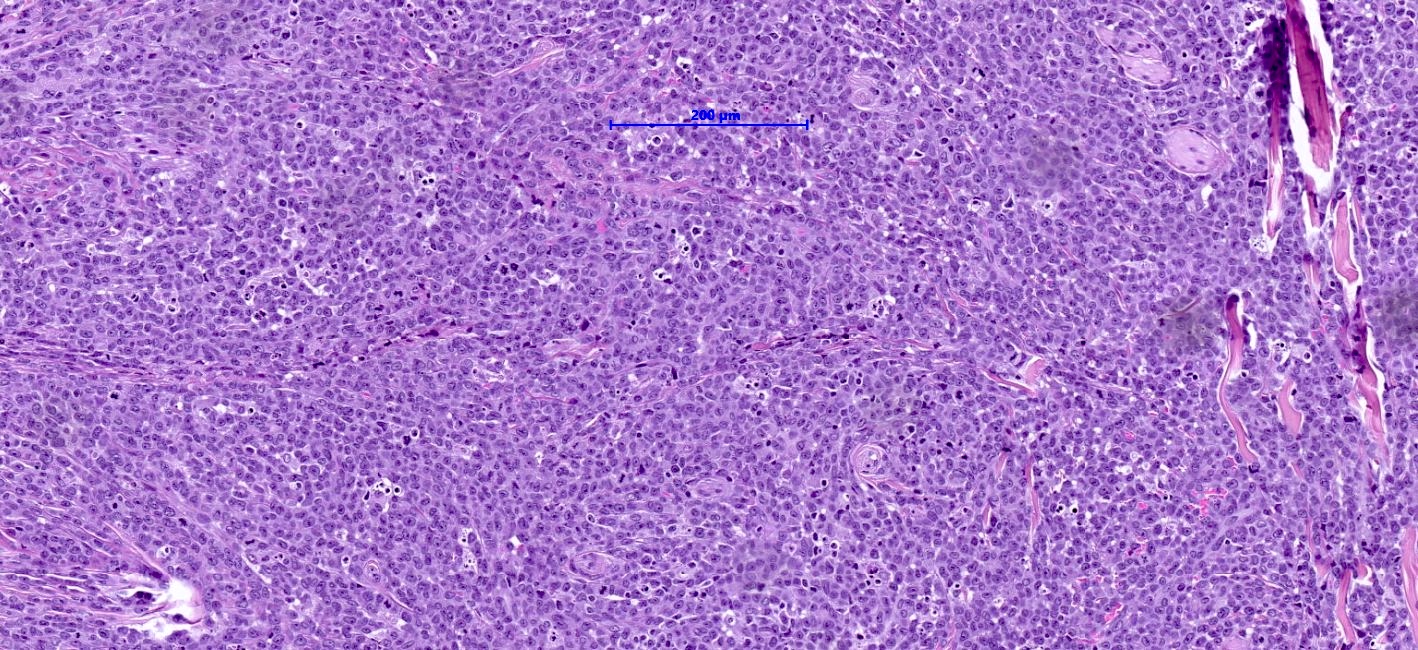
CD5
CD50-59
CD56
CD57
CD60-69
CD61
CD63
CD68
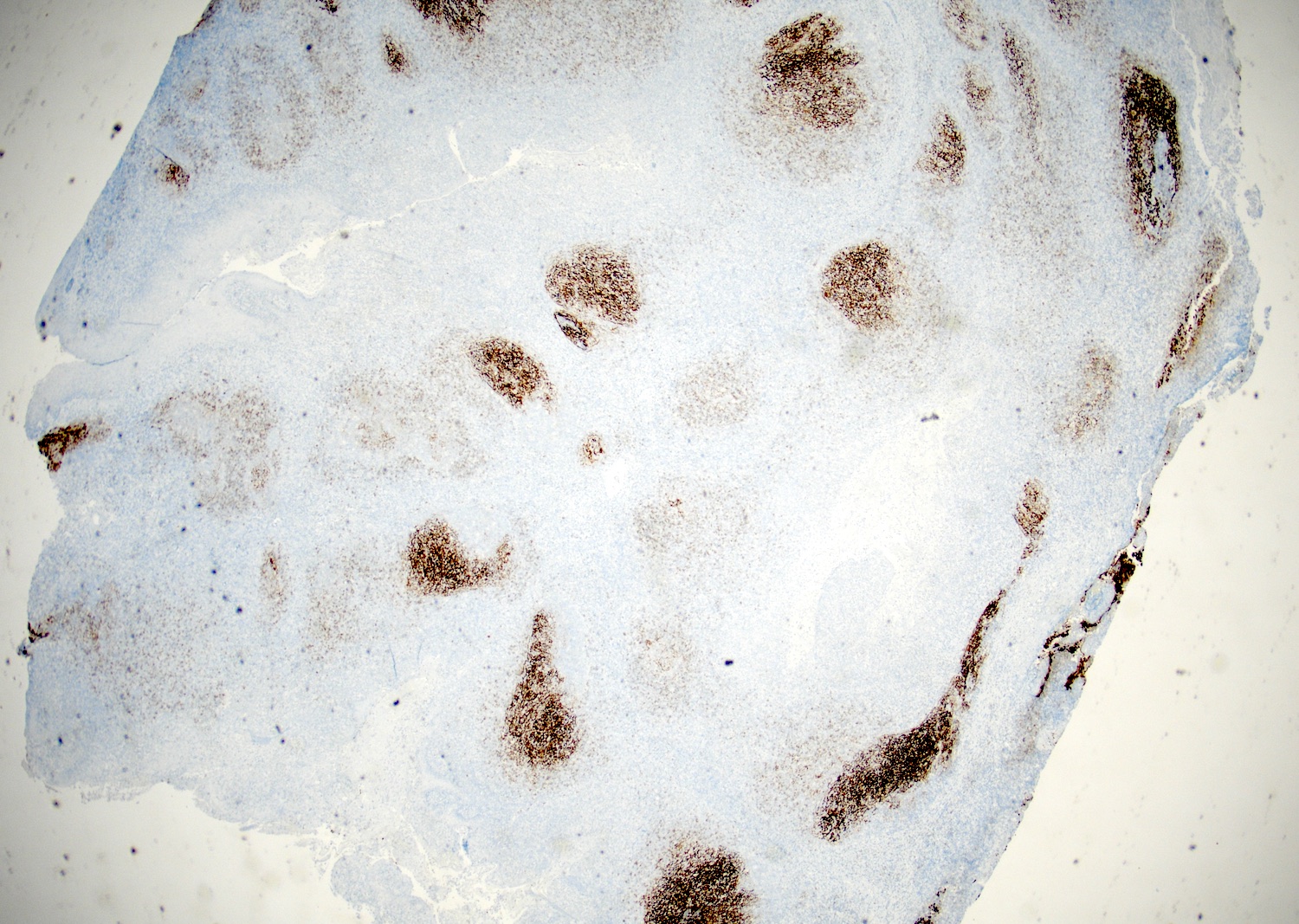
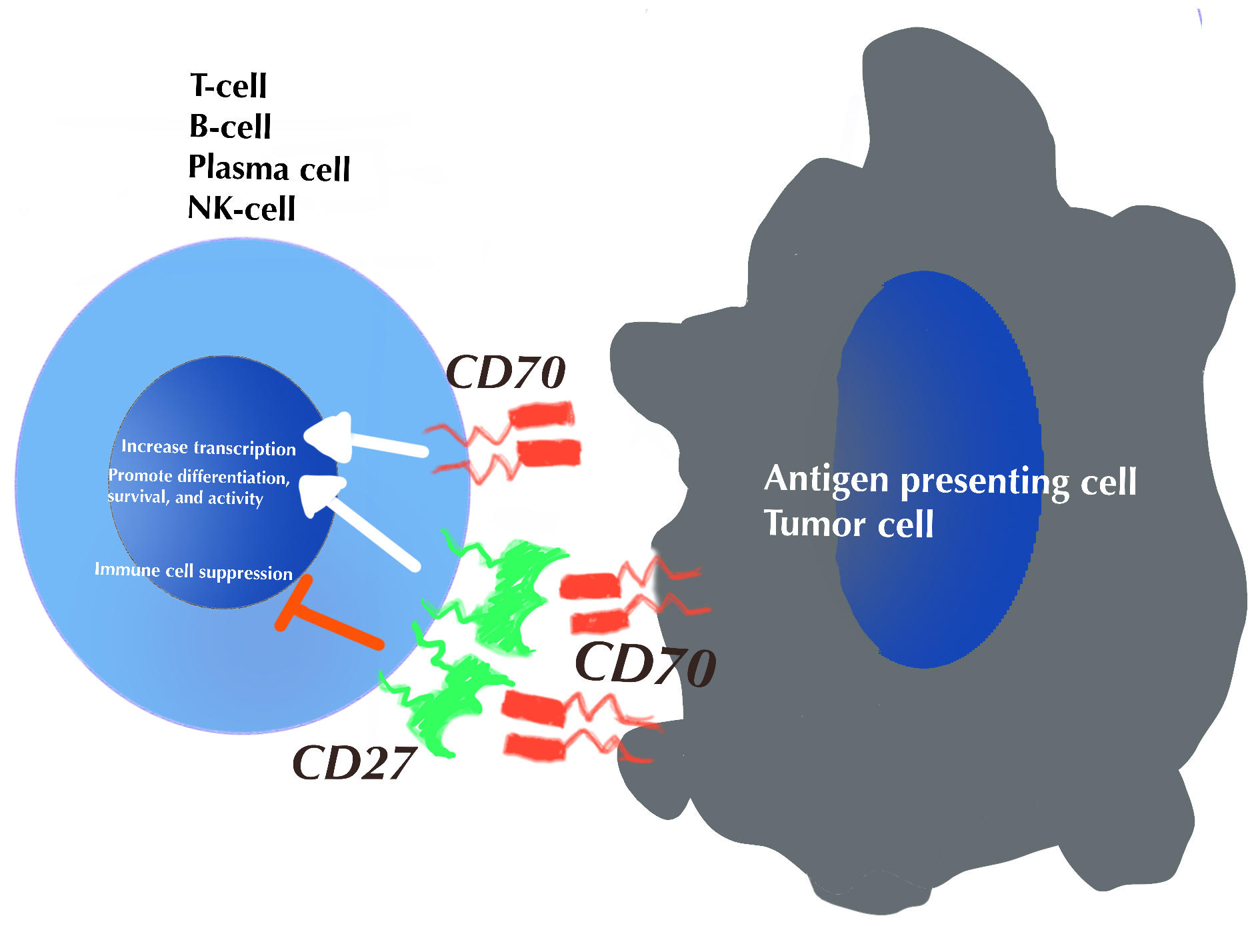
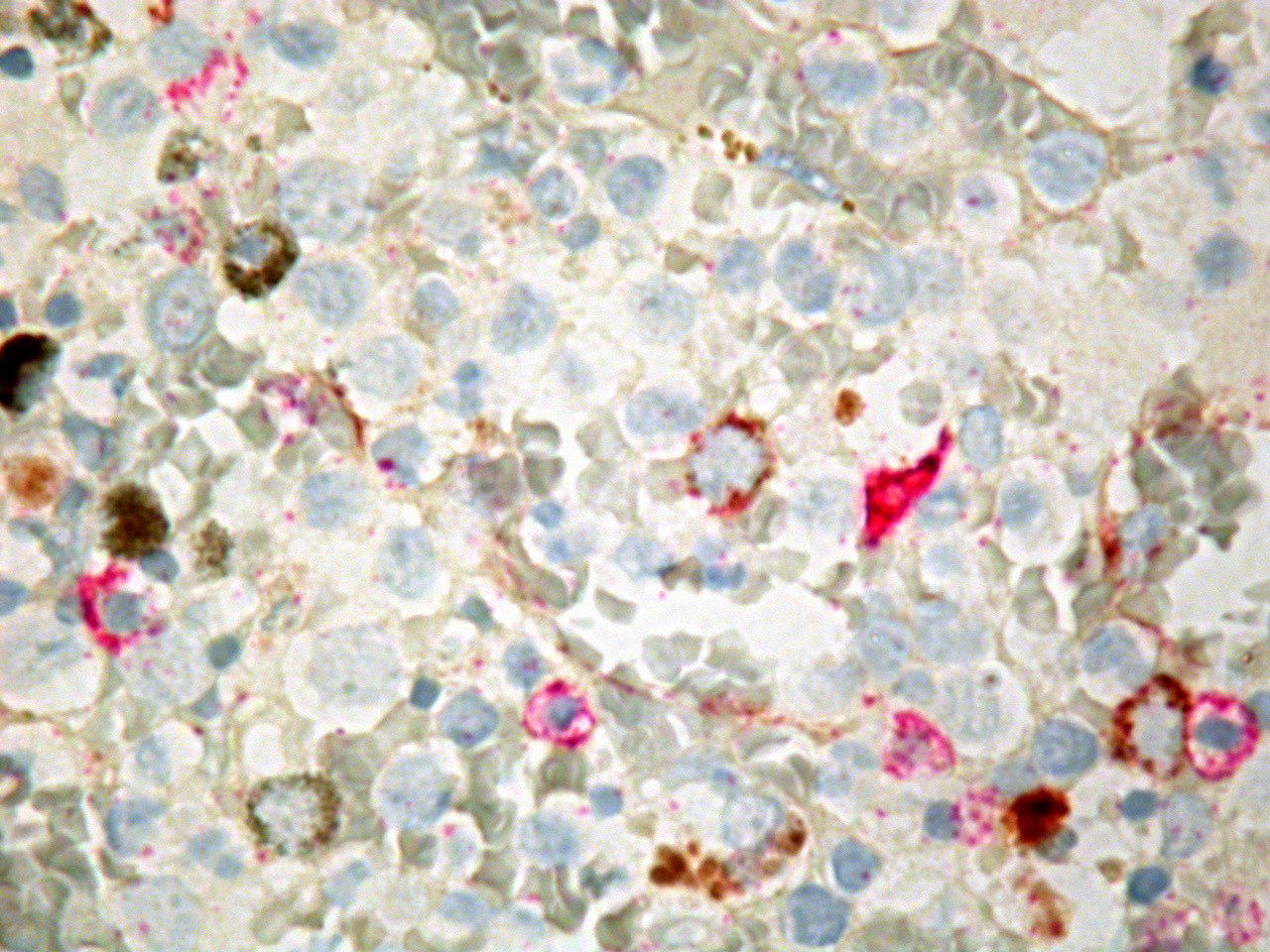
CD70
CD70-79
CD71
CD79a
CD79b
CD8
CD9
CD90-99
CD95
CD99
CDK4
CDw210-219
CDX2
CEA / CD66e
Chloroacetate esterase
Chromogranin
CK 8/18 (pending)
Claudins
Collagen type IV
Colon cancer biomarker testing (including MSI / Lynch)
Congo red
Copper
CXCL13 (pending)
Cyclin D1
Cyclooxygenase 2 (COX2)
Cytochrome c oxidase (COX)
Cytokeratin 10 (CK10, K10)
Cytokeratin 14 (CK14, K14)
Cytokeratin 17 (CK17, K17)
Cytokeratin 18 (CK18, K18)
Cytokeratin 19 (CK19, K19)
Cytokeratin 20 (CK20, K20)
Cytokeratin 34 beta E12
Cytokeratin 35 beta H11
Cytokeratin 5/6 and CK5
Cytokeratin 7 (CK7, K7)
Cytokeratin 8 (CK8, K8)
Cytokeratin AE1 / AE3
Cytokeratin CAM 5.2
Cytokeratin MNF 116
Cytokeratins (CK) - general
Cytokeratins - uncommon
Cytomegalovirus (CMV)
D2-40 (Podoplanin)
DBA-44
DDIT3 (pending)
Desmin
Dicer
DNAJB9 (pending)
DOG1
DUX4
E-cadherin
EBER1 and EBER2
EBNA2 (pending)
EGFR mutation specific antibodies
Elastic fibers
Enzyme cytochemistry
Epithelial membrane antigen (EMA)
ERG
Estrogen receptor
Estrogen receptor
EWSR1
EZH2
Factor VIII related antigen
Factor XIIIa
Fascin
Filaggrin
FLI1
FMC7
FN1 (pending)
Follicular dendritic cell secreted protein (FDCSP) (pending)
Fontana-Masson
FOS (pending)
FOSB (pending)
FOXL2
FOXP3
Fumarate Hydratase (FH), S-(2-succino) cysteine (2SC)
Galectin3
Gastrin (pending)
GATA3
GCET (pending)
GD2 (pending)
Giemsa / Helicobacter pylori
Glial fibrillary acidic protein (GFAP)
GLUT1
Glutamine synthetase (pending)
Glypican 3
GMS
Gram stain
Granzyme B
GRM1 (pending)
Gross cystic disease fluid protein 15 (GCDFP-15)
H3.3 G34W (H3F3A)
H3K27M (pending)
H3K27me3
H3K36M (pending)
Hansel stain
HBME
hCG
HepPar1
HER2 (c-erbB2) breast
HER2 colon
HER2 stomach/GE junction
HGAL
HHV8 / KSHV
HIK1083
HLA-DR
HMB45
HMGA2 (pending)
HNF-1B
HPV (Human papillomavirus)
HSP70 (pending)
HSV (pending)
Human placental lactogen
IDH1 (R132H)
IFITM1
IgA IgD IgG IgM (pending)
IgG4
IHC procedure
IMP3
Inhibin
INI1 / SMARCB1
INSM1
Iron
Islet 1 (Isl1) (pending)
Jones methenamine silver
Kappa & lambda light chains
Ki67
KIT
L1-CAM (pending)
Leder stain
LEF1
LFABP (pending)
Lipochrome (lipofuscin) pigments
LMO2
Luxol fast blue
Lysozyme
Mammaglobin
Mast cell tryptase (MCT) (pending)
MCPyV (CM2B4)
MDM2
MDR / CD243
MDR3 (pending)
MEF2B
MelanA / MART1
Microphthalmia associated transcription factor (MITF)
MLH1
MLH3 (pending)
Movat pentachrome (pending)
MSH1
MSH2
MSH6
MUC2-MUC6
Mucins
Multigene products
MUM1 / IRF4
MYB
MYC
Myeloperoxidase (MPO)
Myogenin / myoglobin
NADH
Napsin A
NB84 (pending)
NCCT (pending)
NeuN
Neuron specific enolase (NSE)
NF1 / NF2
NFP / neurofilament
NGFR / p75 (pending)
NKX2.2 (pending)
NKX3.1
Nonspecific esterase
NPM1
NR4A3
NUTM1
OCT 3/4
OCT2
Oil red O
OLD Myeloperoxidase
Olig2
OSCAR cytokeratin
OTP (orthopedia) (pending)
p120 catenin
p16
p21
p27
p40
p53
p57 kip2
p62 (pending)
p63
Pan-TRK (EPR17341) [NTRK]
Parafibromin (CDC73)
PAS (Periodic acid-Schiff)
PAS Hematoxylin (PASH) (pending)
PAX2
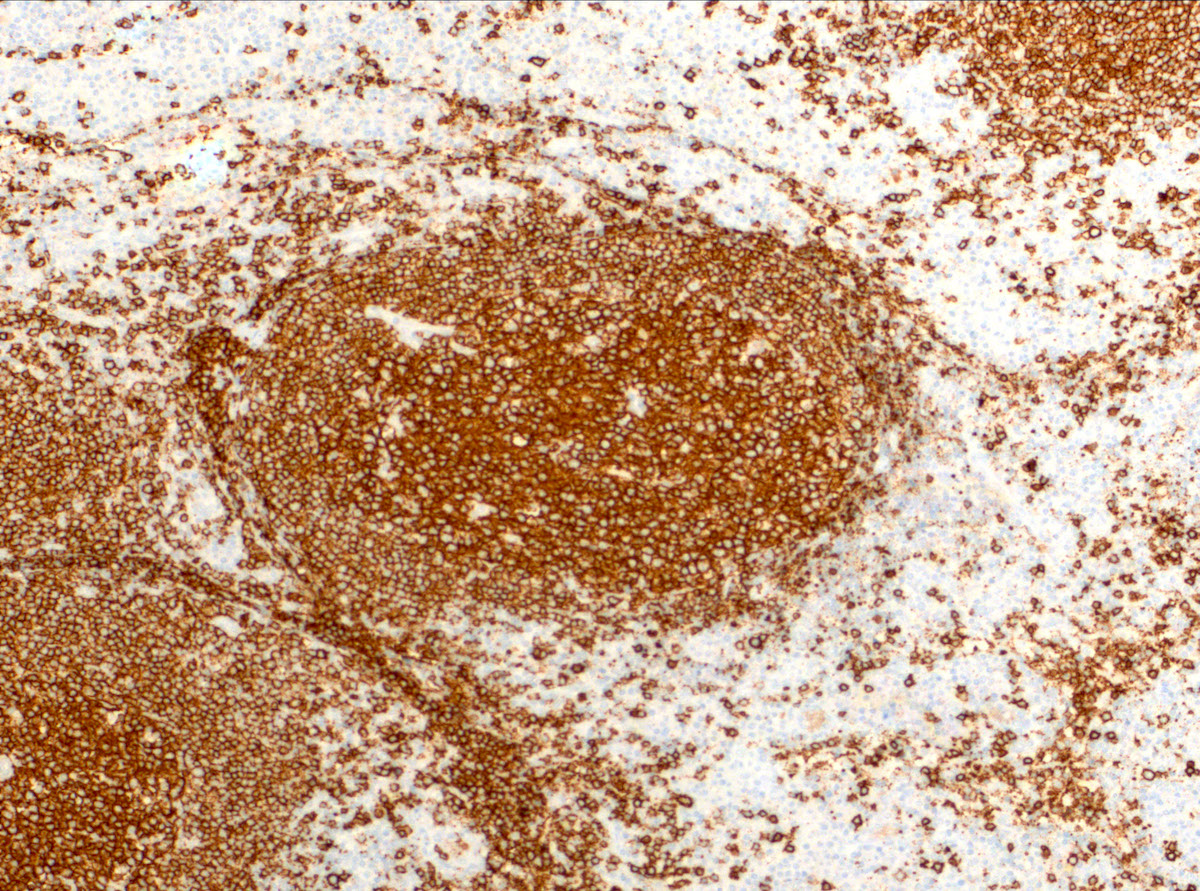
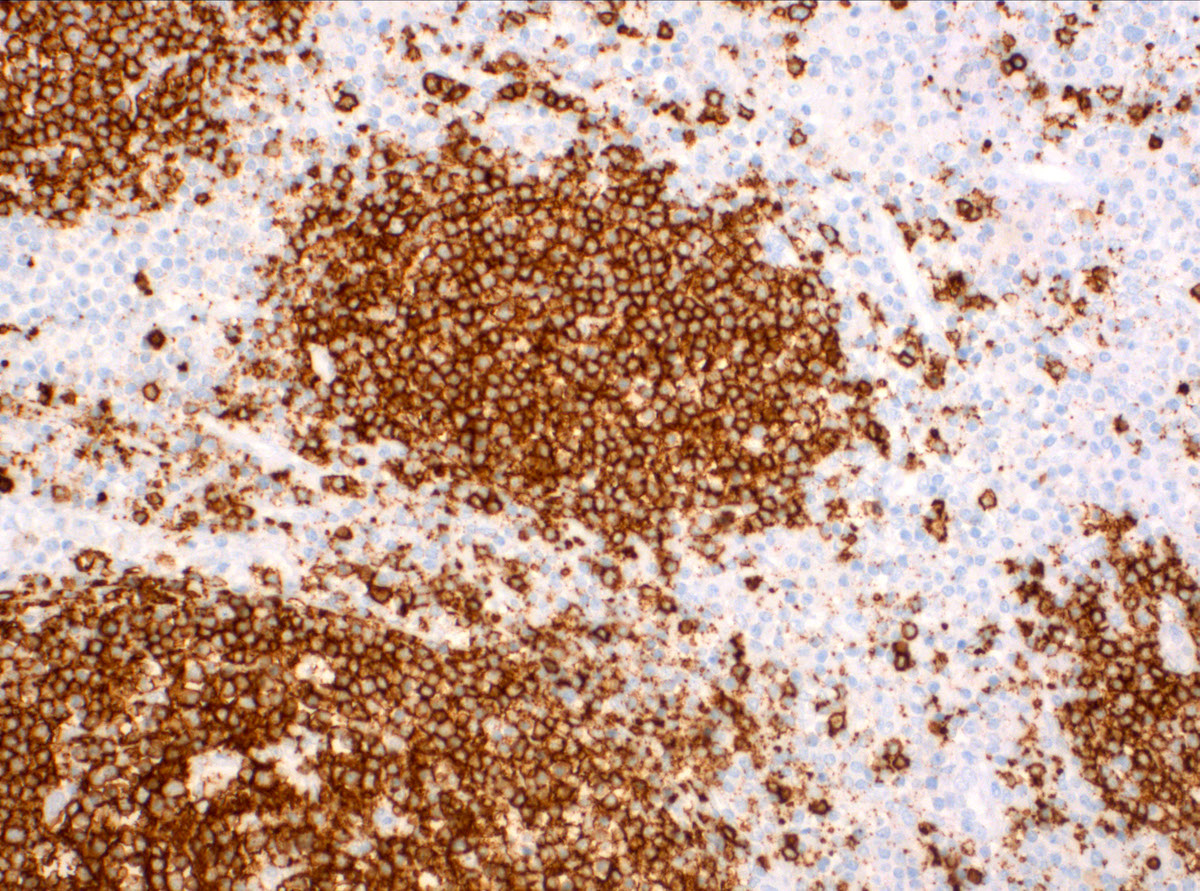
PAX5
PAX8
PCNA
PDGFRA
PDL1 22C3
PDL1 SP142
PDL1 SP263 (pending)
Perforin (pending)
PGP9.5 (pending)
PHLDA1 (pending)
Phosphohistone H3
Pit1
PLAG1
PLAP
PMS2
PRAME
PRAME
Prealbumin (pending)
Progesterone receptor
Programmed death-1 (PD-1)
Prostate specific antigen (PSA)
Prostate specific membrane antigen (PSMA)
Prostatic acid phosphatase (PAP)
Prostein / P501S
PROX1 (pending)
PTEN
PU.1
RB1
Renal cell carcinoma (RCC)
Reticulin
ROS1
S100
S100P
SALL4
SDH (pending)
SDHB (succinate dehydrogenase)
Selectins
Serum amyloid A (SAA)
SF1
SF1 (pending)
Sirius red
SMAD4 / DPC4
SMARCA4 / BRG1
Smooth muscle myosin heavy chain / SMMHC
Smoothelin
SOX10
SOX11
SOX17 (pending)
SOX2
SOX9
Special AT-rich sequence-binding protein 2 (SATB2)
SSTR2A
STAT6
Sudan Black B
SV40 (pending)
Synaptophysin
SYT / SSX (pending)
T cell leukemia / lymphoma protein 1 (TCL1)
TCR and variants (pending)
TDP-43 (pending)
TdT
TERT
TFE3
Thrombomodulin
Thyroglobulin
Tpit
Transducin-like enhancer of split 1 (TLE1)
TRAP (Tartrate resistant acid phosphatase)
Treponema pallidum IHC
Trichrome
TROP2 (pending)
TRPS1
Trypsin (pending)
TSC1 and TSC2
TSH (pending)
TTF1
Tyrosinase
Urates / uric acid
Uroplakin II
Uroplakin III
Villin
Vimentin
von Hippel Lindau (VHL)
von Willebrand factor (vWF)
Warthin-Starry silver stain
Wright-Giemsa stain
WT1
YAP1 CD80-89
Table of Contents
CD80 | CD81 | CD82 | CD83 | CD84 | CD85 | CD85A | CD85B | CD85C | CD85D | CD85E | CD85F | CD85G | CD85H | CD85I | CD85J | CD85K | CD85L | CD85M | CD86 | CD87 | CD88 | CD89 | Diagrams / tables | Microscopic (histologic) imagesCD80
- Also called B7-1, BB1
- T cells need 2 signals for activation; the first signal is antigen peptide presented on MHC class II through the T cell receptor
- The second (costimulatory) signal is delivered by CD80 or CD86, expressed on surface of antigen presenting cells, which interact with either CD28 or CD152 (CTLA-4)
- Has critical role in autoimmune, humoral and transplant responses
- Increased expression may cause excessive antigen presentation in fulminant hepatic failure, as an early step in its pathogenesis before the onset of tissue damage (Am J Pathol 1999;154:1711)
- Receptor for some adenovirus species (Virus Res 2006;122:144)
- No significant clinical use by pathologists
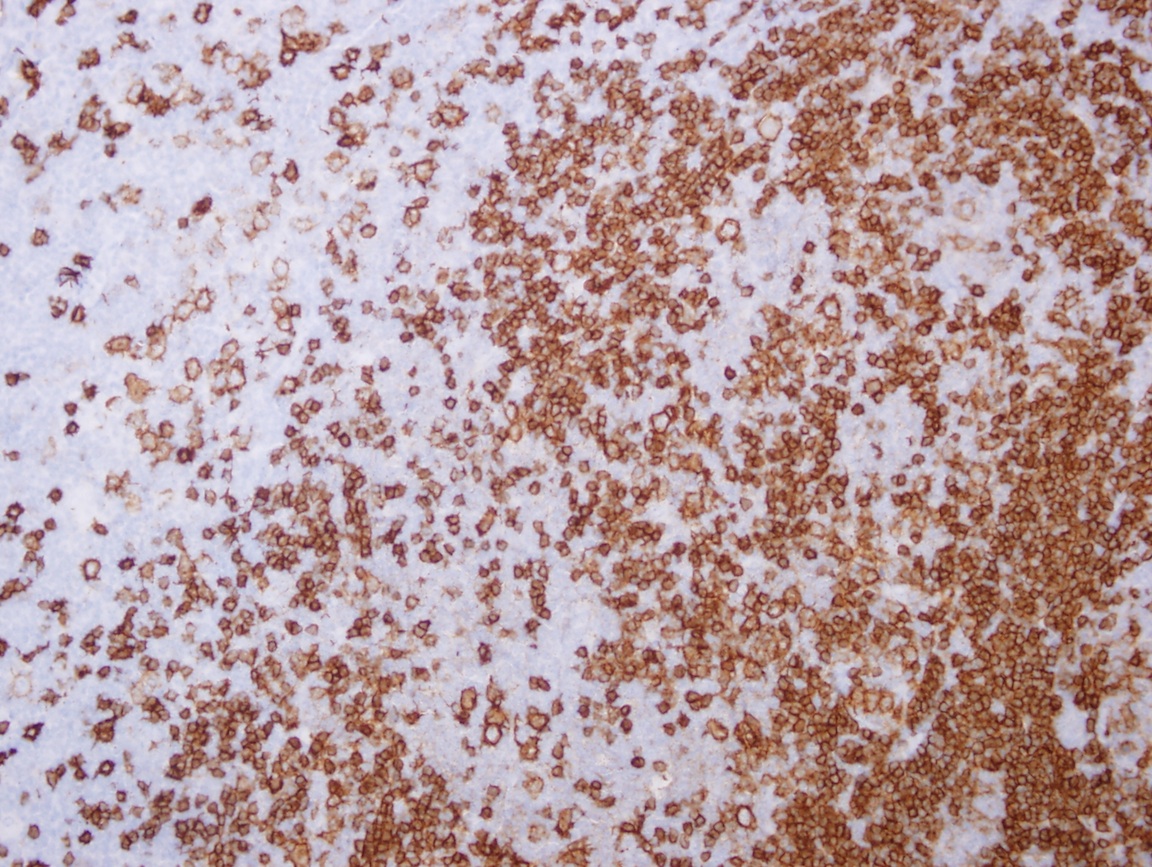
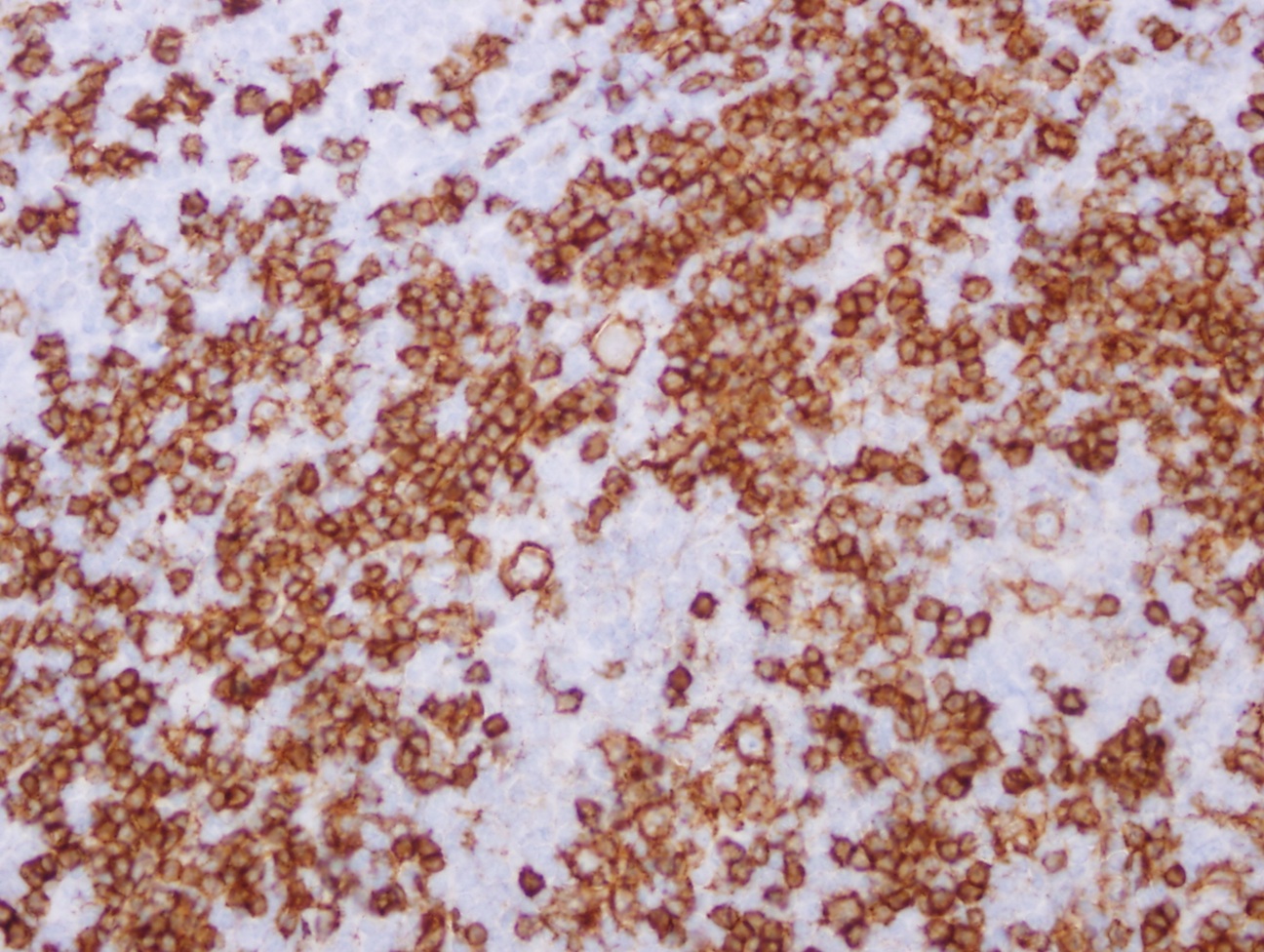
- Positive staining - normal: activated B cells, T cells, macrophages and dendritic cells
- Reference: OMIM: 112203 [Accessed 3 May 2021]
CD81
- Also called Target of an Anti-Proliferative Antibody (TAPA1)
- Receptor for Hepatitis C Virus E2 protein in B cells (J Virol 2006;80:8695)
- Also required for Plasmodium falciparum infectivity (Nat Med 2003;9:93)
- Upregulation on HIV1+ B cells may ultimately cause lymphoproliferative disorders (Clin Exp Immunol 2007;147:53)
- On B cells, is complexed with CD21, CD19 and Leu13; facilitates complement recognition
- Member of tetraspanin family; has close associations with major histocompatibility complex class I/II proteins
- Appears to promote muscle cell fusion and support myotube maintenance
- No significant clinical use by pathologists
- Positive staining - normal: lymphocytes, endothelial cells and epithelial cells
- Positive staining - tumors:
- HCV+ splenic diffuse large B cell lymphoma (Hum Pathol 2005;36:878)
- Burkitt’s lymphoma cell lines, neuroblastoma cell lines (J Pediatr Hematol Oncol 2000;22:20)
- Negative staining: erythrocytes, platelets and neutrophils
- Reference: OMIM: 186845 [Accessed 3 May 2021]
CD82
- Also called prostate cancer antimetastasis gene KAI1, kangai 1 (Chinese for anticancer)
- Metastasis suppressor gene
- Expression correlates with p53 expression
- Reduced expression of CD82 is associated with metastases / poor prognosis in carcinomas of:
- Bladder (Int J Urol 2004;11:74)
- Breast (Am J Pathol 1998;153:973, J Cancer Res Clin Oncol 2005;131:191)
- Colon (World J Gastroenterol 2004;10:2245)
- Endometrium (Clin Cancer Res 2003;9:1393)
- Larynx (Lin Chuang Er Bi Yan Hou Ke Za Zhi 2005;19:1065)
- Oral cavity (Clin Cancer Res 2002;8:828)
- Thyroid (Int J Mol Med 2004;14:517, Pathol Res Pract 2003;199:79)
- Expression reduces function of urokinase type plasminogen activator receptor (J Biol Chem 2005;280:14811)
- Uses by pathologists: possible use as prognostic marker (see above)
- Positive staining - normal: activated / differentiated hematopoietic cells, endothelial cells and epithelium
- Negative staining: erythrocytes
- Reference: OMIM: 600623 [Accessed 3 May 2021]
CD83
- Also called HB15
- May assist in antigen presentation or cellular interactions that follow lymphocyte activation
- Soluble form inhibits dendritic cell maturation and inhibits dendritic cell-mediated T cell proliferation (J Med Dent Sci 2006;53:85)
- Elevated serum levels seen in mantle cell lymphoma and CLL (Leuk Res 2004;28:237)
- Higher number of activated dendritic cells may be good prognostic factor for breast carcinoma (Int J Cancer 2003;104:92), cholangiocarcinoma (Hum Pathol 2004;35:881), colorectal liver metastases (Hum Pathol 2004;35:1392), gallbladder carcinoma (Oncol Rep 2005;14:353), gastric carcinoma-EBV+ (Am J Surg Pathol 2006;30:59) and advanced (Oncol Rep 2005;14:369)
- Uses by pathologists: marker for activated dendritic cells
- Positive staining - normal:
- Activated (mature) dendritic cells, activated T and B lymphocytes, monocytes / macrophages (transient) (Biochem J 2005;385:85)
- Langerhans cells, thymic epithelial cells, neutrophils during acute bacterial infection (Clin Exp Immunol 2002;130:501)
- Decidua (Am J Pathol 2000;157:159)
- Positive staining - disease:
- Infantile hemangioma endothelium (Am J Pathol 2006;168:621)
- Reed-Sternberg cells (Pathology 1997;29:294)
- Churg-Strauss syndrome myocarditis in inflammatory infiltrates (Arch Pathol Lab Med 2003;127:98)
- Reference: OMIM: 604534 [Accessed 3 May 2021]
CD84
- Also called Signaling Lymphocytic Activation Molecule 5 (SLAM5)
- Adhesion molecule that increases proliferative responses of activated T cells (J Immunol 2003;171:2485)
- Mediates platelet aggregation (Blood 2005;106:3028)
- No significant clinical use by pathologists
- Positive staining - normal:
- B cells, thymocytes (J Immunol 2001;167:3668)
- Mature T cells, memory T cells (high) (Tissue Antigens 2004;64:132)
- Monocytes / macrophages, platelets, dendritic cells, granulocytes and CD34+ hematopoietic progenitor cells (Exp Hematol 2003;31:798)
- Reference: OMIM: 604513 [Accessed 3 May 2021]
CD85
- Previously entire Immunoglobulin-like Transcript (ILT) family was clustered as CD85; now subclassified as CD85a to CD85m
- Also called Leukocyte Immunoglobulin-like Receptors (LIR) and Monocyte / Macrophage Immunoglobulin-like Receptors (MIR)
- CD85 itself is now called CD85J
- Family of immunoreceptors expressed on monocytes and B cells; lower levels on dendritic cells and NK cells
- Prevents NK / T cell killing and inhibits B cells by negative signaling receptors
- Note: some family members have activating functions (see specific family members below)
- References: Nat Immunol 2001;2:661, J Biol Chem 2006;281:19536
CD85A
- Also called ILT5, LIR3, LILRB3 (leukocyte immunoglobulin-like receptor subfamily, member 3), HL9
- Involved in NK mediated cytotoxicity
- An inhibitory receptor for MHC class I molecules
- No significant clinical use by pathologists
- Positive staining: myeloid cells, monocytes / macrophages, B cells, T cells (some), NK cells, basophils, eosinophils, dendritic cells (weak) (Blood 2004;104:2832, Proc Natl Acad Sci USA 2003;100:1174)
- Reference: OMIM: 604820 [Accessed 3 May 2021]
CD85B
CD85C
- Also called LIR8, LILRB5
- May act as receptor for class I MHC antigens
- No significant clinical use by pathologists
- Positive staining: NK cells
- Reference: OMIM: 604814 [Accessed 3 May 2021]
CD85D
- Also called ILT4, LIR2, MIR10, LILRB2
- Down regulates the immune response; involved in the development of tolerance
- Upregulated by HLA-G in antigen-presenting cells, NK cells and T cells (FASEB J 2005;19:662)
- Interacts with human leukocyte antigen A, B and G molecules and transmits negative signals that interfere with the activation of monocytes and dendritic cells (Hum Immunol 2004;65:700)
- Also competes with CD8A for binding to class I MHC antigens
- IL-10 renders dendritic cells hypostimulatory by upregulating cell surface CD85D and by inhibiting soluble CD85D in vitro; similar effect on endothelial cells (Eur J Immunol 2004;34:74, Eur J Immunol 2006;37:177)
- No significant clinical use by pathologists
- Positive staining: NK cells, T cells, monocytes / macrophages, dendritic cells, eosinophils (Proc Natl Acad Sci USA 2003;100:1174)
- Reference: OMIM: 604815 [Accessed 3 May 2021]
CD85E
- Also called ILT6, LIR4, LILRA3
- May act as soluble receptor for class I MHC antigens
- Homozygous deletions associated with multiple sclerosis (7% vs 4% of normals) (Genes Immun 2005;6:445)
- 85% of Japanese lack functional CD85E alleles (Hum Genet 2006;119:436)
- No significant clinical use by pathologists
- Positive staining: B cells, NK cells, peripheral blood monocytes, lung
- Reference: OMIM: 604818 [Accessed 3 May 2021]
CD85F
- Also called ILT11, LILRB7, LIR9
- May play a role in triggering innate immune responses (Blood 2003;101:1484)
- Membrane bound and secreted
- No significant clinical use by pathologists
- Positive staining: neutrophils, monocytes
- Negative staining: B cells, T cells, NK cells
- Reference: OMIM: 606047 [Accessed 3 May 2021]
CD85G
- Also called ILT7, LILRA4
- May act as receptor for class I MHC antigens
- No significant clinical use by pathologists
- Positive staining: plasmacytoid dendritic cells (J Exp Med 2006;203:1399)
- Negative staining: myeloid dendritic cells, other white blood cells
CD85H
- Also called ILT1, LIR7, LILRA2
- May act as receptor for class I MHC antigens
- Activating receptor for eosinophils (Proc Natl Acad Sci USA 2003;100:1174)
- No significant clinical use by pathologists
- Positive staining: basophils, myeloid and plasmacytoid dendritic cells (Blood 2004;104:2832)
- Negative staining: monocytes, T cells, B cells, NK cells
- Reference: OMIM: 604812 [Accessed 3 May 2021]
CD85I
- Also called LIR6, CD85i
- Note: since some biologists use lower case, CD85l [CD85L] may be confused with CD85i
- No significant clinical use by pathologists
- Positive staining: B cells, monocytes
- Negative staining: dendritic cells, NK cells, T cells
- References: OMIM: 604810 [Accessed 3 May 2021], J Immunol 2003;171:3056
CD85J
- Also called CD85, LIR1, ILT2, MIR7, LILRB1
- Transduces negative signals that prevent killing of MHC class I expressing cells
- Binds classical (HLA-A and HLA-B) and non-classical (HLA-G, HLA-E and HLA-F) MHC class I molecules
- Upregulated by HLA-G in antigen presenting cells, NK cells and T cells (FASEB J 2005;19:662)
- Receptor for CMV UL18 protein, which resembles MHC class I molecules (J Virol 2005;79:2251)
- No significant clinical use by pathologists
- Positive staining: B cells, monocytes, dendritic cells (low), T cells (some), NK cells (some)
- Reference: OMIM: 604811 [Accessed 3 May 2021]
CD85K
- Also called ILT3, LIR5, HM18, LILRB4
- Upregulated by HLA-G in antigen-presenting cells, NK cells and T cells (FASEB J 2005;19:662)
- Receptor for class I MHC antigens
- Recognizes broad spectrum of HLA-A, HLA-B, HLA-C and HLA-G alleles
- Involved in downregulation of immune response and development of tolerance, including transplants (Int Immunol 2004;16:1055)
- Aspirin use is associated with upregulation (Am J Transplant 2006;6:2046)
- No significant clinical use by pathologists
- Positive staining: dendritic cells (various), monocytes / macrophages, endothelial cells (Gene 2004;331:159, J Exp Med 1997;185:1743, Transplantation 2006;82:S30)
- Reference: OMIM: 604821 [Accessed 3 May 2021]
CD85L
- Also called ILT9, LILRA6P, LILRP1
- No significant clinical use by pathologists
- Reference: Eur J Immunol 1998;28:3959
CD85M
- Also called ILT10, LILRA5
- No significant clinical use by pathologists
- Positive staining: T cell subsets, monocytes, macrophages, neutrophils, dendritic cells and B lymphocytes (Washington State University)
CD86
- Also called B7-2
- T cells need 2 signals for activation: the first signal is antigen peptide presented on MHC class II through the T cell receptor
- The second (costimulatory) signal is delivered by CD80 or CD86, expressed on surface of antigen presenting cells, which interact with either CD28 or CD152 (CTLA-4)
- CD80 and CD86 appear to have opposing functions on regulatory T cells (J Immunol 2004;172:2778)
- Polymorphisms are associated with:
- Liver transplant acceptance (Transpl Immunol 2005;15:69)
- Systemic sclerosis (Int J Immunogenet 2006;33:155)
- Increased expression may cause excessive antigen presentation in fulminant hepatic failure as an early step in its pathogenesis before the onset of tissue damage (Am J Pathol 1999;154:1711)
- High circulating soluble levels are poor prognostic factor in myeloma (Br J Haematol 2006;133:165)
- Associated with severe asthma (Thorax 2004;59:870)
- Receptor for some adenovirus species (Virus Res 2006;122:144)
- Associated with H. pylori dependent early stage high grade MALT lymphoma of stomach (World J Gastroenterol 2005;11:4357)
- No significant clinical use by pathologists
- Positive staining - normal:
- B cells, thymocytes (J Immunol 2001;167:3668)
- Mature T cells, memory T cells (high, Tissue Antigens 2004;64:132)
- Monocytes / macrophages, platelets, dendritic cells, granulocytes and CD34+ hematopoietic progenitor cells (Exp Hematol 2003;31:798)
- Interdigitating dendritic cells in T zones of secondary lymphoid organs, Langerhans cells, peripheral blood dendritic cells, memory B cells, germinal center B cells, monocytes, endothelial cells, activated T cells
- Positive staining - disease:
- AML (29%) (Clin Cancer Res 2005;11:5708)
- Ulcerative colitis (100%) (Dig Dis Sci 2004;49:1738)
- Negative staining: immature dendritic cells
- Reference: OMIM: 601020 [Accessed 3 May 2021]
CD87
- Also called urokinase plasminogen activator receptor (uPA-R), PLAUR
- Membrane protein responsible for plasmin expression on cells
- Binds both the proprotein and mature forms of urokinase plasminogen activator
- Subject to negative feedback regulation by uPA, which cleaves it to an inactive form
- Implicated in metastasis - receptors for uPA and plasmin are found at leading edge of tumor cells; plasmin causes hydrolysis of extra-cellular matrix proteins in the path of cellular invasion
- Plasma levels of different soluble receptors are increased and predict mortality in HIV patients (J Acquir Immune Defic Syndr 2005;39:23)
- Pre-storage leukofiltration reduces transfusion reactions, perhaps due to reduction in soluble CD87 (Transfus Med 2004;14:305)
- Hypoxia and glucose deprivation may induce tumor invasion and metastases by upregulating CD87 (Exp Mol Med 2004;36:57, Exp Cell Res 2006;312:1685)
- Upregulated by dialysis and associated with clinical findings (Blood Purif 2006;24:236)
- Receptor for Group A Streptococcus (J Mol Biol 2005;350:27)
- No significant clinical use by pathologists
- Positive staining. - normal:
- T cells, NK cells, monocytes / macrophages, bands and neutrophils (Cytometry B Clin Cytom 2003;51:9)
- Endothelial cells, fibroblasts, basophils (J Immunol 2004;173:5739)
- Smooth muscle cells, keratinocytes, placental trophoblasts, hepatocytes
- Positive staining - tumors:
- Carcinomas of breast (Am J Pathol 2000;157:1219)
- Colon and prostate; prostatic nodal metastases (Hum Pathol 2006;37:1442)
- Melanoma, malignant and benign primary CNS tumors (Appl Immunohistochem Mol Morphol 2005;13:184)
- Negative staining: normal prostate, B / T cells and Hodgkin lymphoma (Am J Clin Pathol 1994;102:835)
- References: OMIM: 173391 [Accessed 3 May 2021], Wikipedia: Urokinase receptor [Accessed 3 May 2021]
CD88
- Also called C5R1, C5aR
- Receptor for C5a, the chemotactic and inflammatory peptide anaphylatoxin
- Stimulates chemotaxis, granule enzyme release and superoxide anion production
- May potentiate leukotriene production in lung and contribute to inflammation in asthma (Microbiol Immunol 2005;49:981)
- But also protects against airway hyperresponsiveness (J Clin Invest 2006;116:783)
- May also be involved in pathogenesis of COPD (Am J Respir Cell Mol Biol 2004;31:216)
- CD87 may mediate upregulation of CD88 in glomerular mesangial cells (J Cell Sci 2005;118:2743, Nephrol Dial Transplant 2000;15:1888)
- Reduced levels on neutrophils in HIV patients (J Infect Dis 2001;183:662)
- CD88 antagonists may be useful for treating complement mediated disorders (J Biomed Biotechnol 2006;2006:28945, J Immunol 2005;174:783)
- No significant clinical use by pathologists
- Positive staining - normal:
- Granulocytes, macrophages / monocytes, dendritic cells, mast cells (variable) (J Allergy Clin Immunol 2005;115:1162)
- Eosinophils (Eur J Immunol 1996;26:1560)
- Endothelial cells, hepatocytes, reactive astrocytes and microglia (Am J Pathol 1997;150:31)
- Keratinocytes in inflamed skin (Am J Pathol 1999;154:495)
- Positive staining - disease:
- Synoviocytes in arthritis (Chin Med J (Engl) 2003;116:1408)
- Mast cell sarcoma (Am J Surg Pathol 2003;27:1013)
- Reference: OMIM: 113995 [Accessed 3 May 2021]
CD89
- Also called FCAR, FCalphaR
- IgA Fc receptor, binds IgA and eliminates IgA coated targets
- Induces phagocytosis, degranulation, respiratory burst and killing of microorganisms
- Pathogenic group A and group B streptococci produce virulence factors that block the binding of IgA to CD89, inhibiting IgA-mediated immunity (J Biol Chem 2006;281:1389)
- No significant clinical use by pathologists
- Positive staining - normal: neutrophils, monocytes / macrophages, activated eosinophils, alveolar and splenic macrophages, interstitial dendritic cells
- Negative staining: mesangial cells (J Am Soc Nephrol 2000;11:241)
- Reference: OMIM: 147045 [Accessed 3 May 2021]
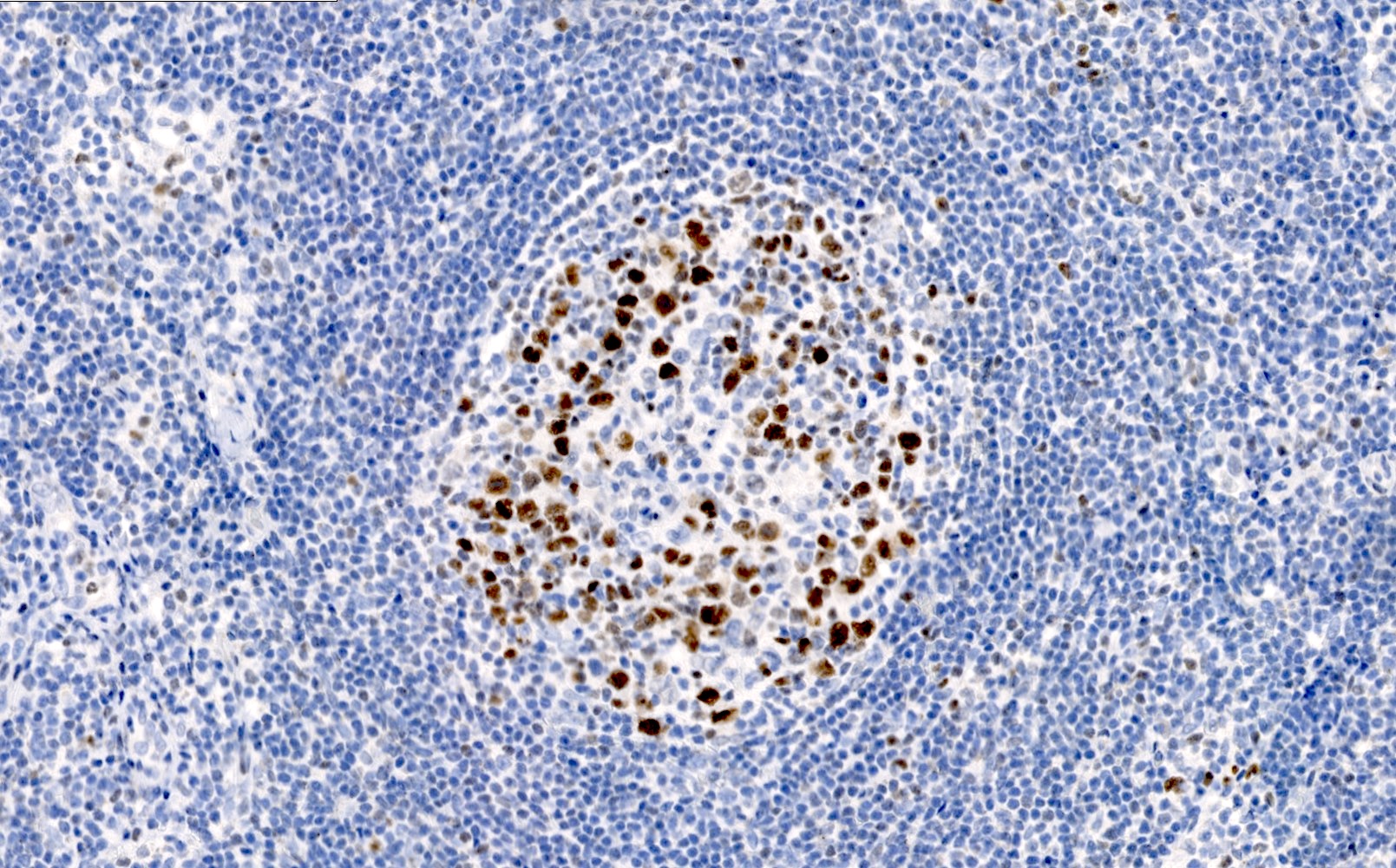
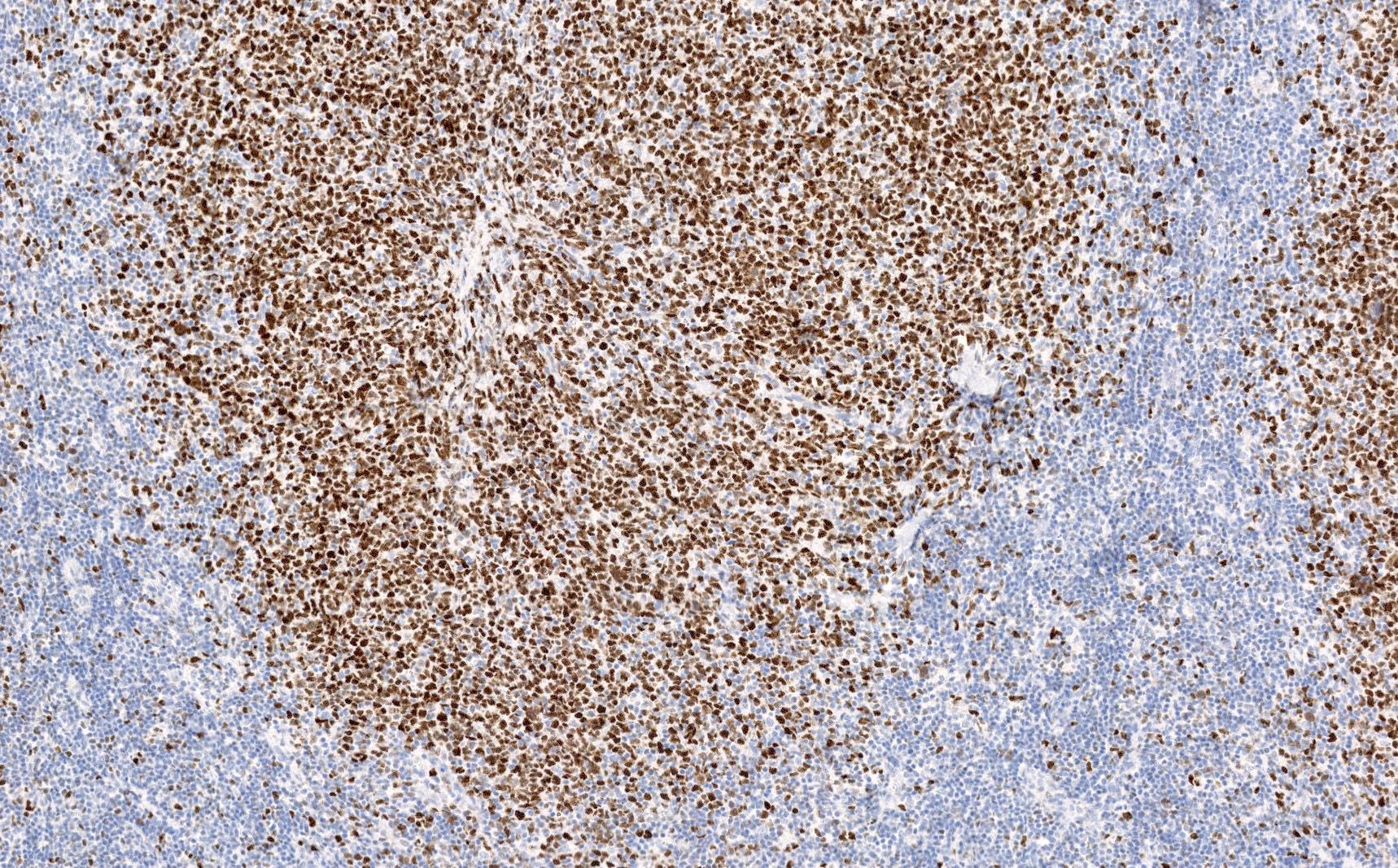
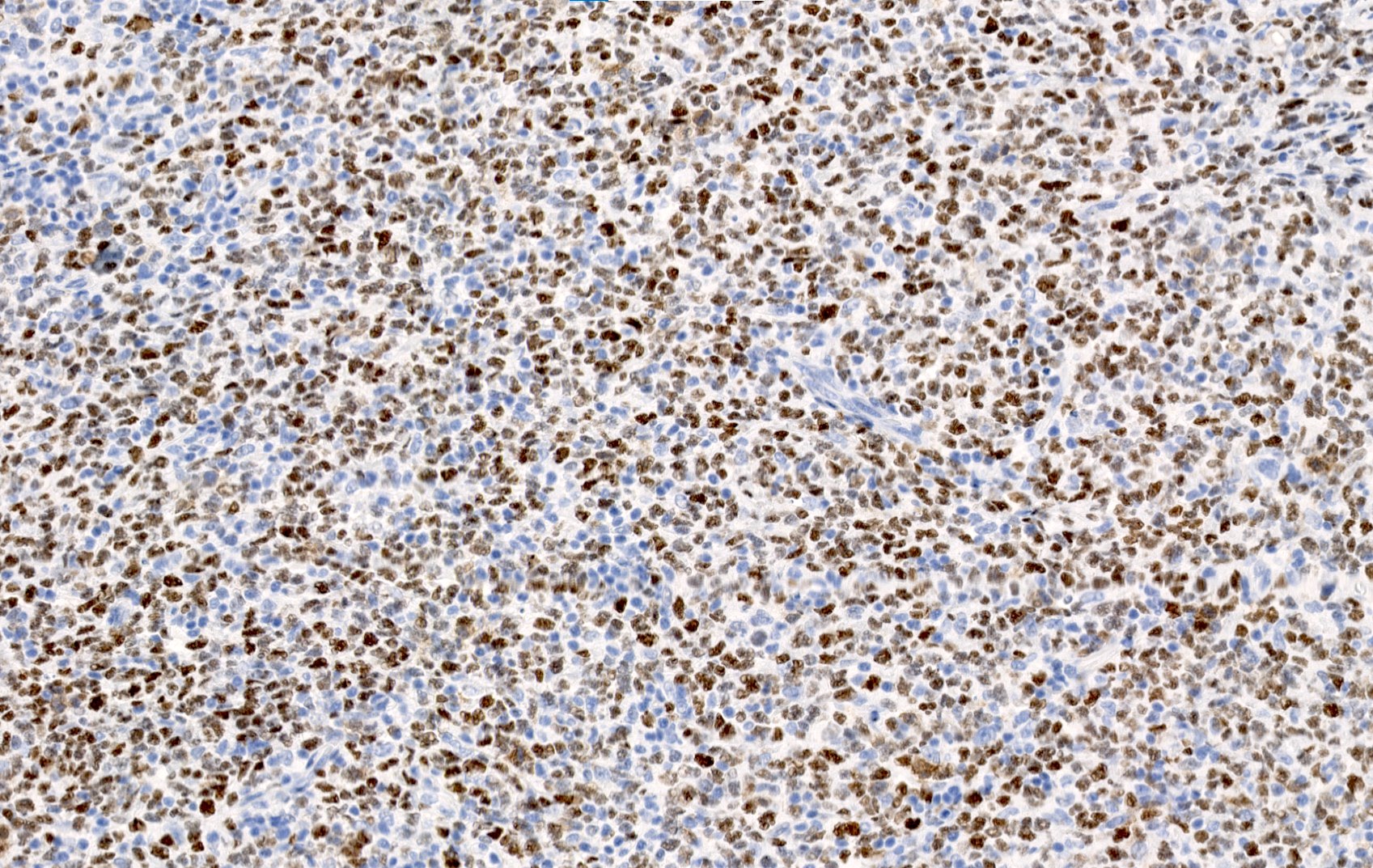
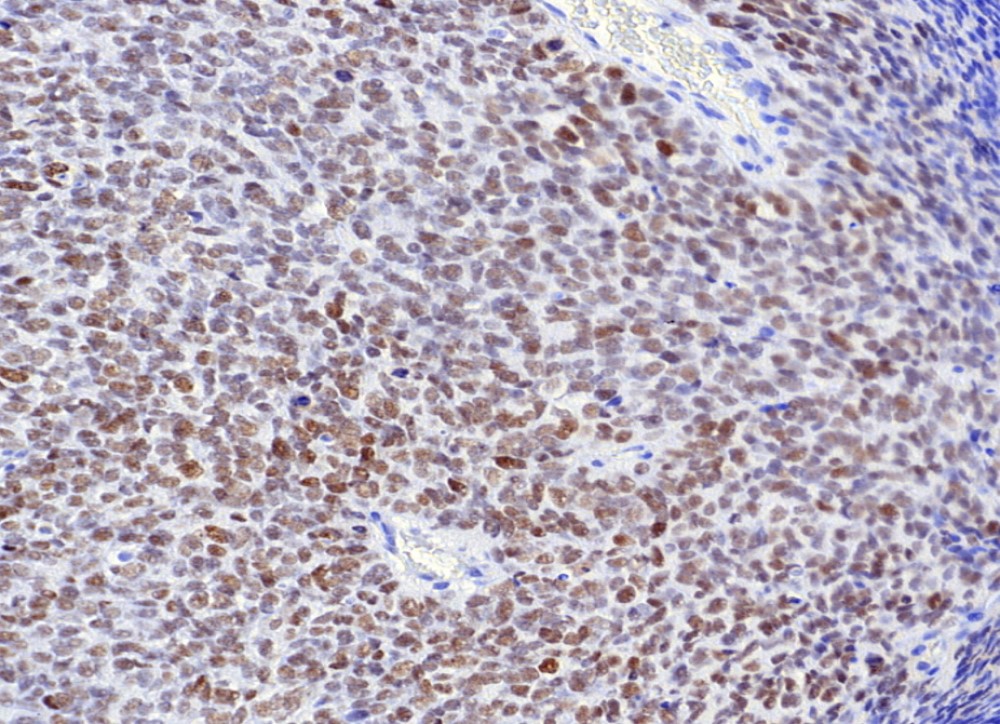
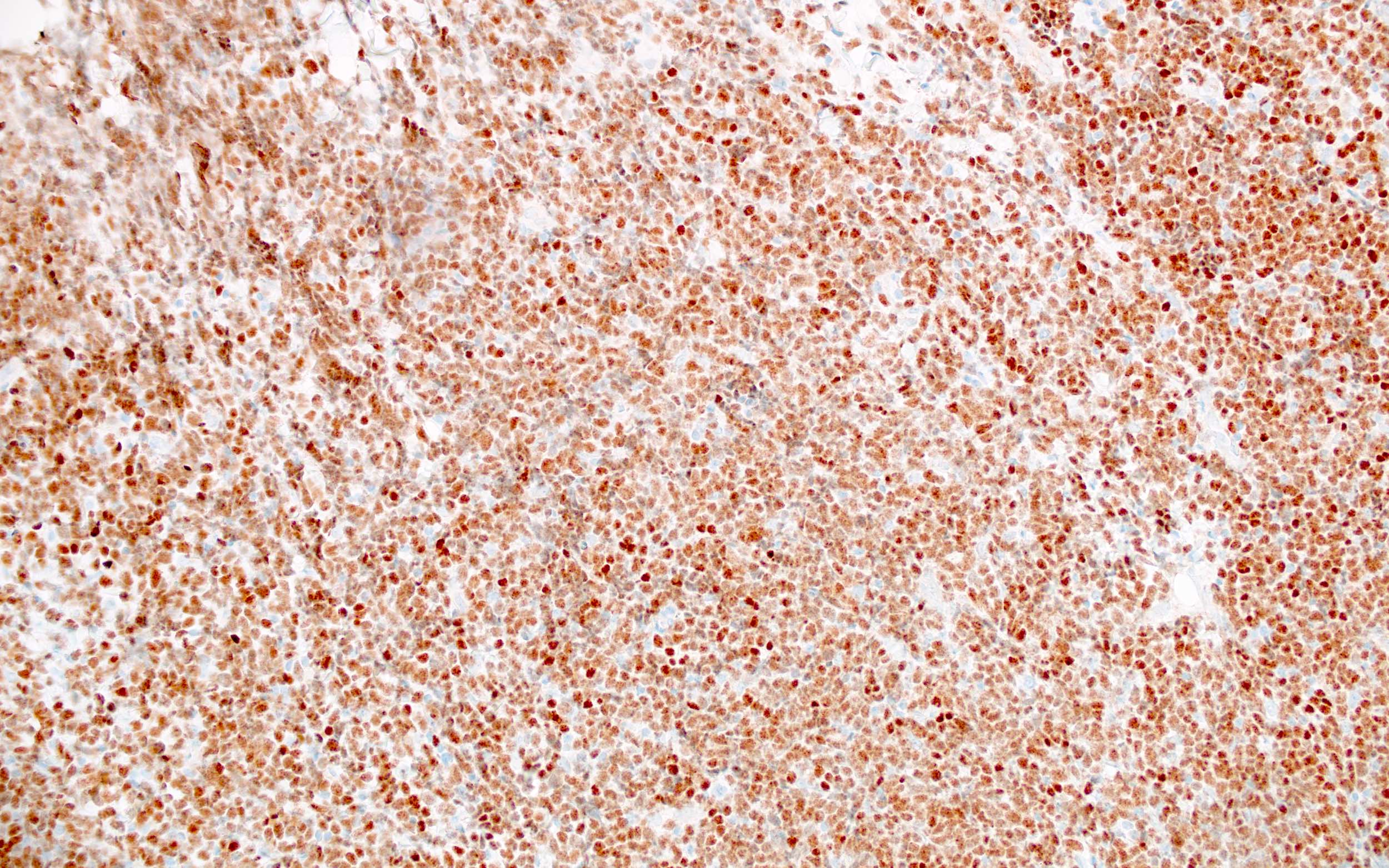
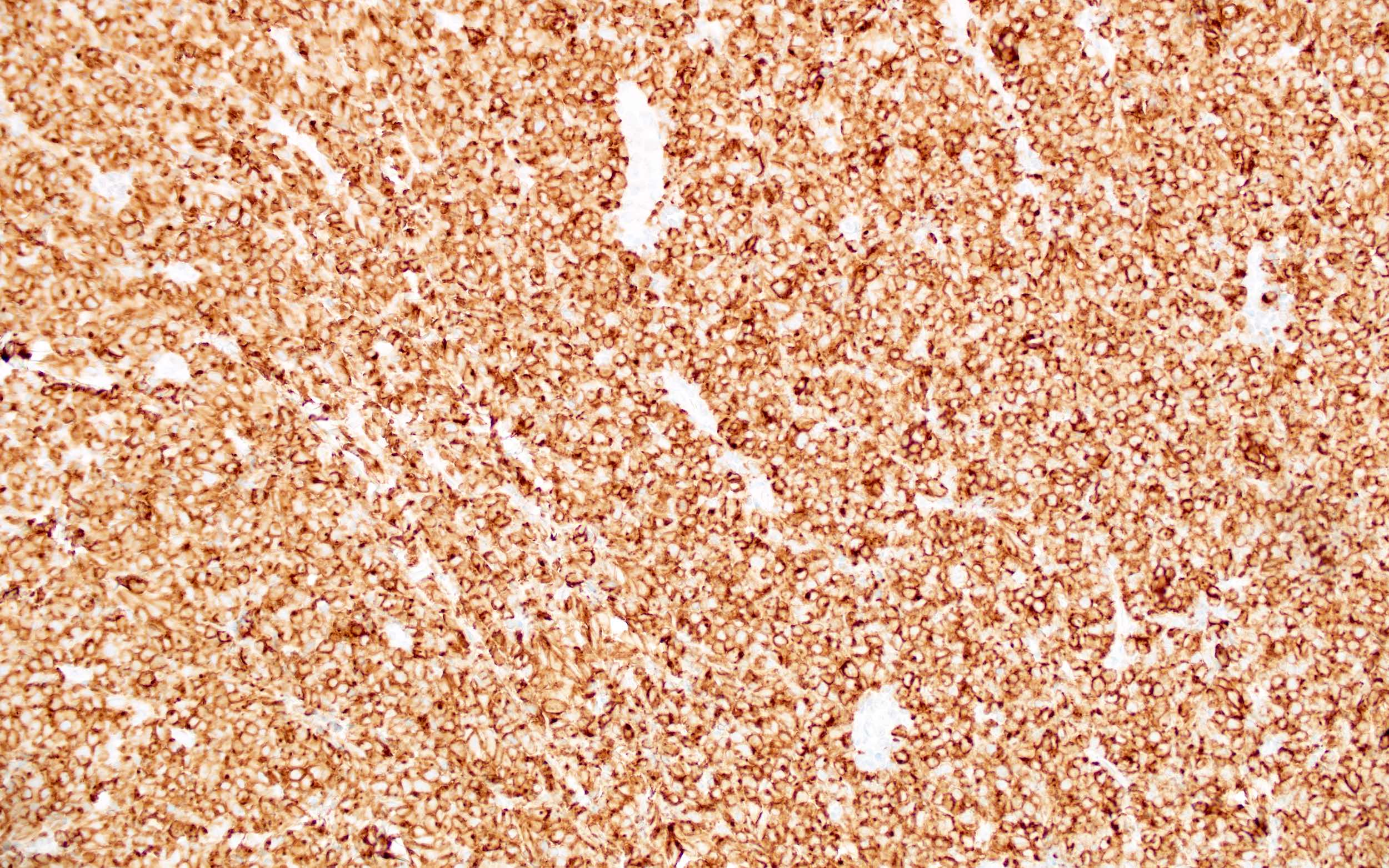
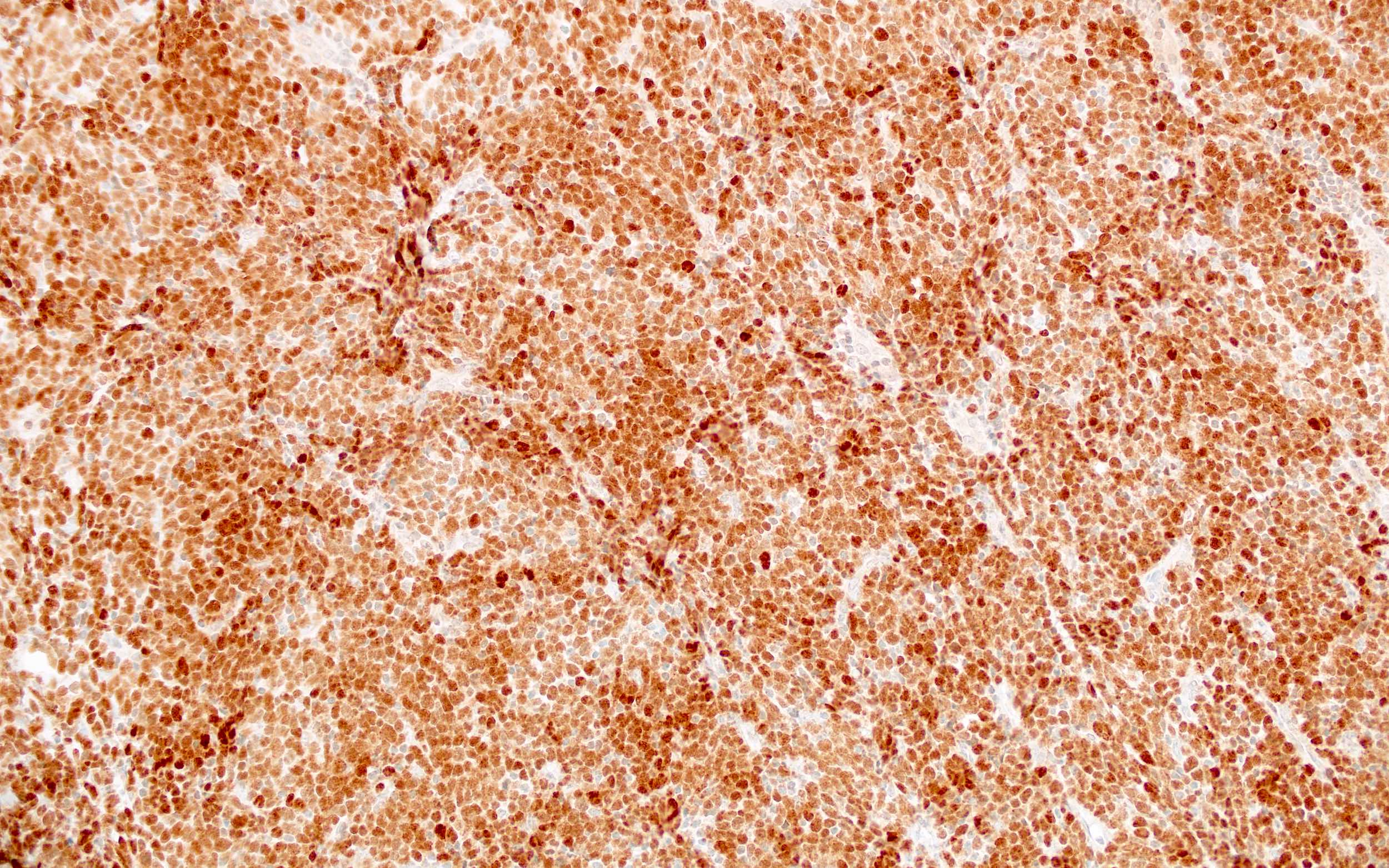
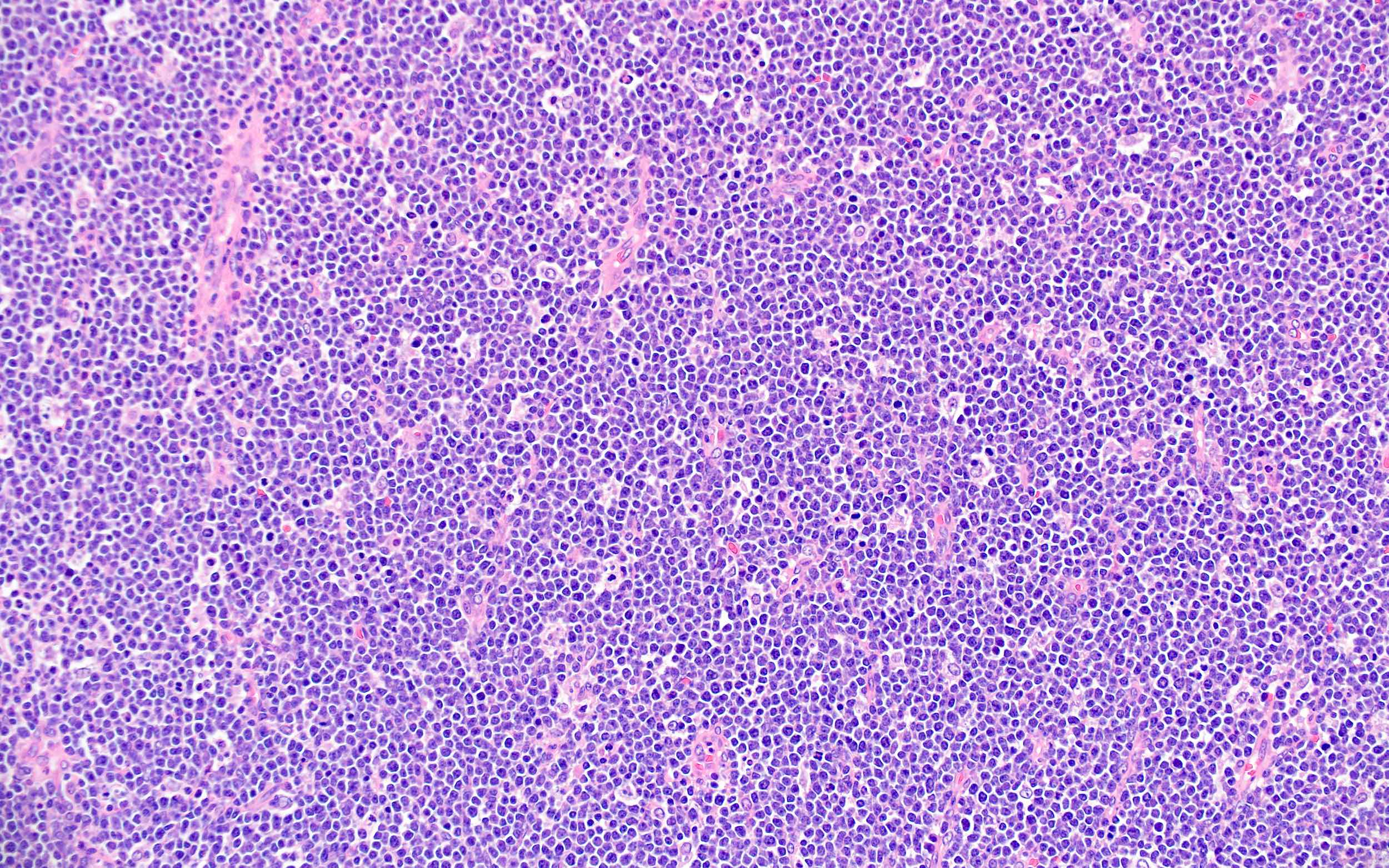
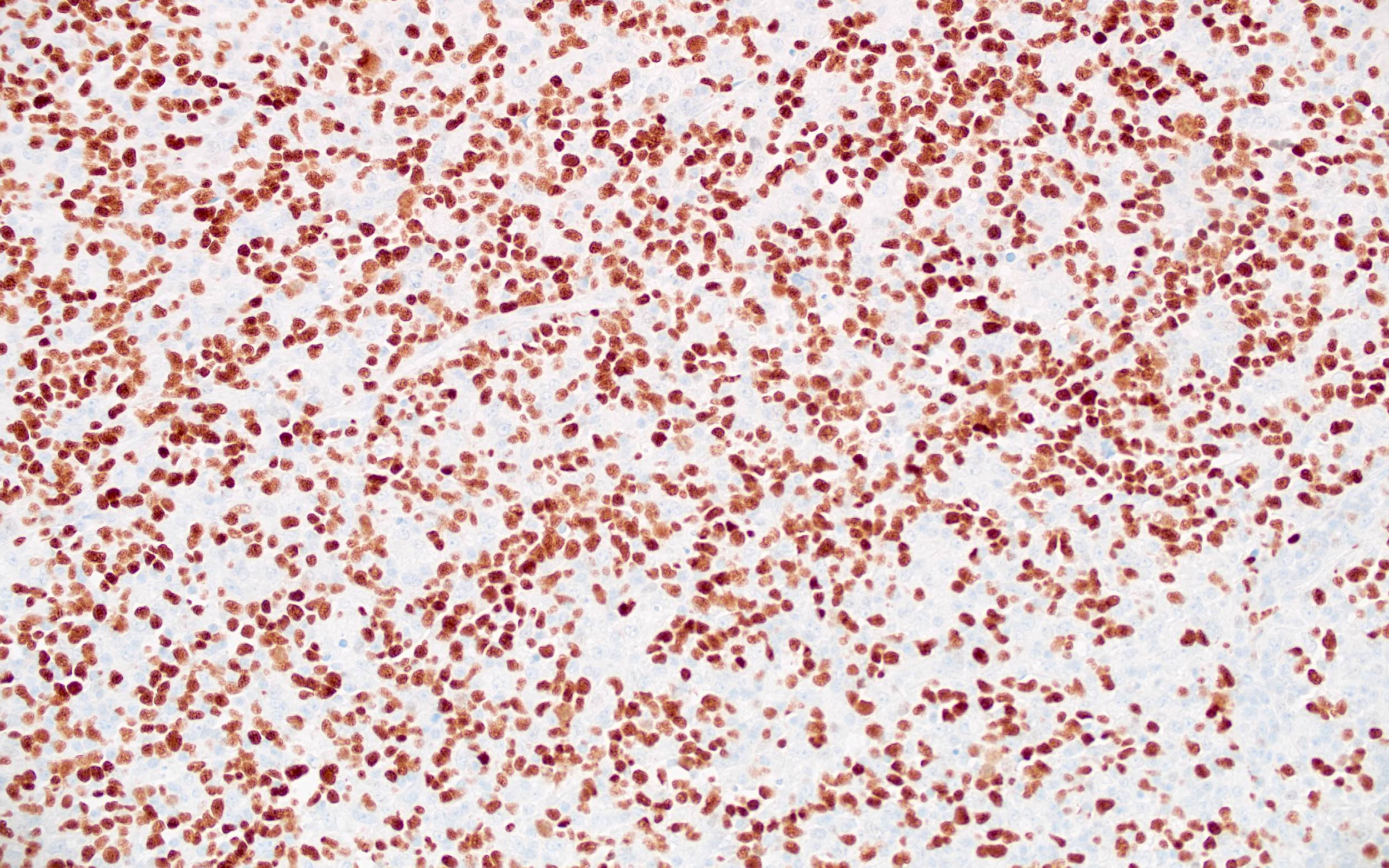
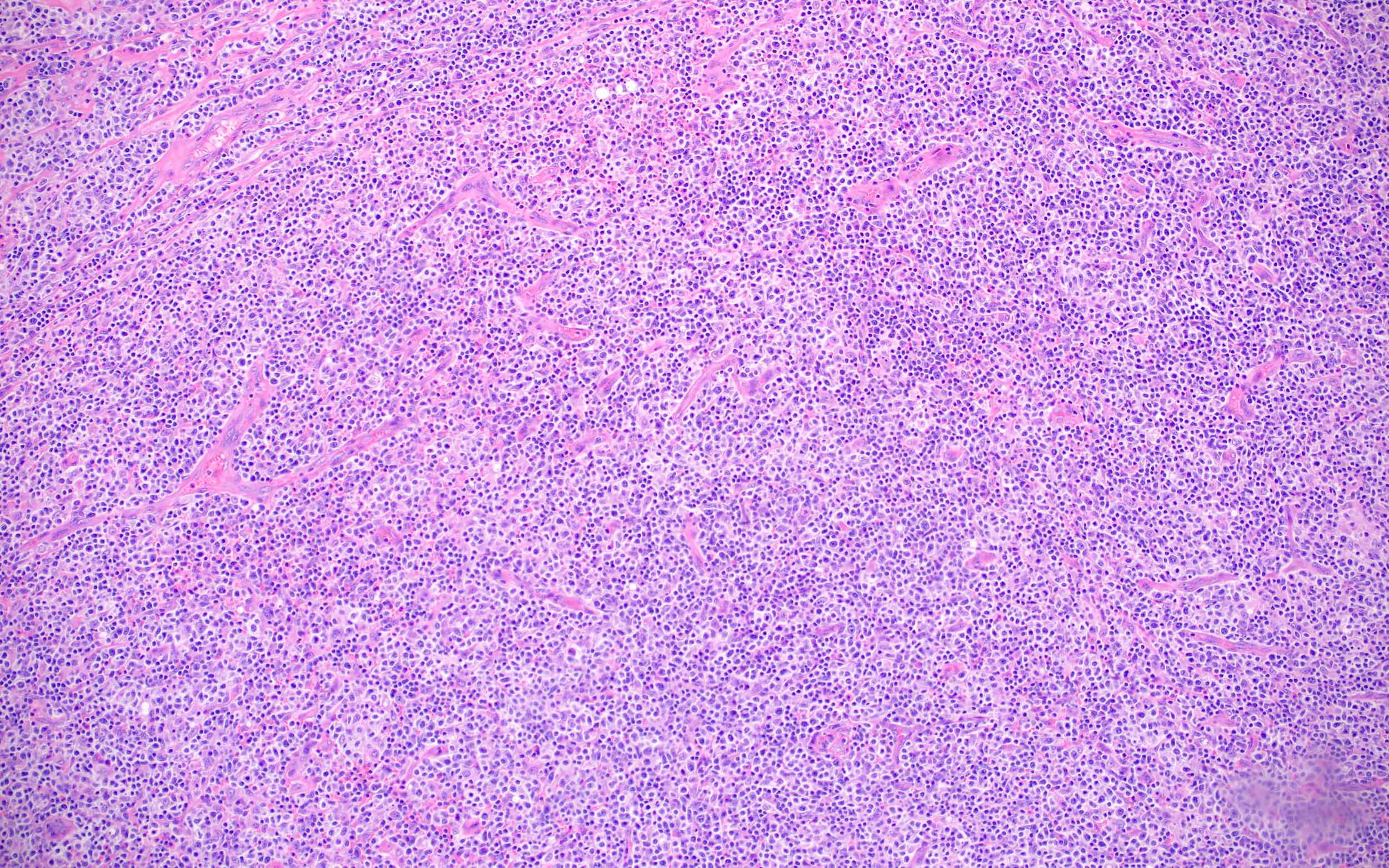
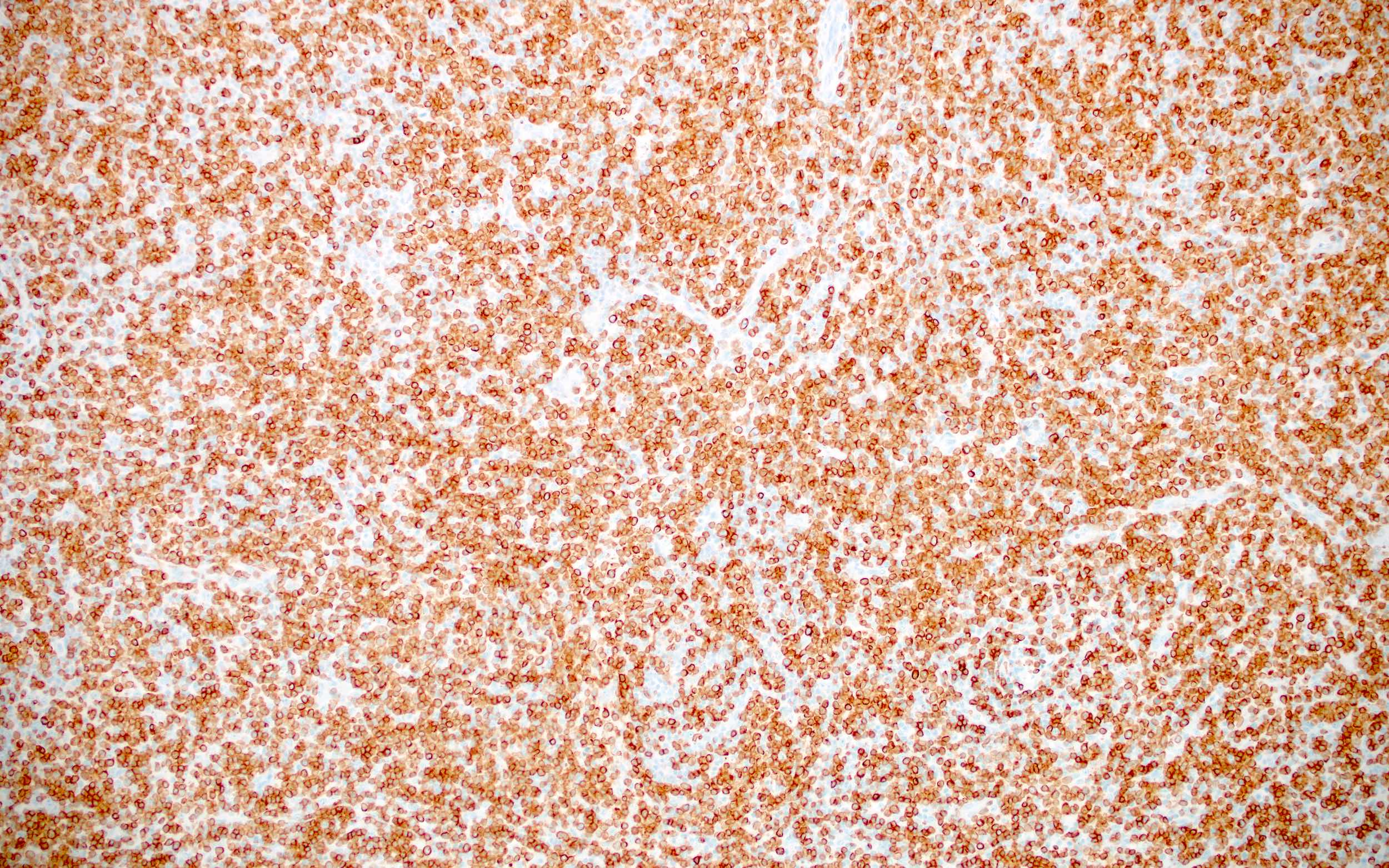
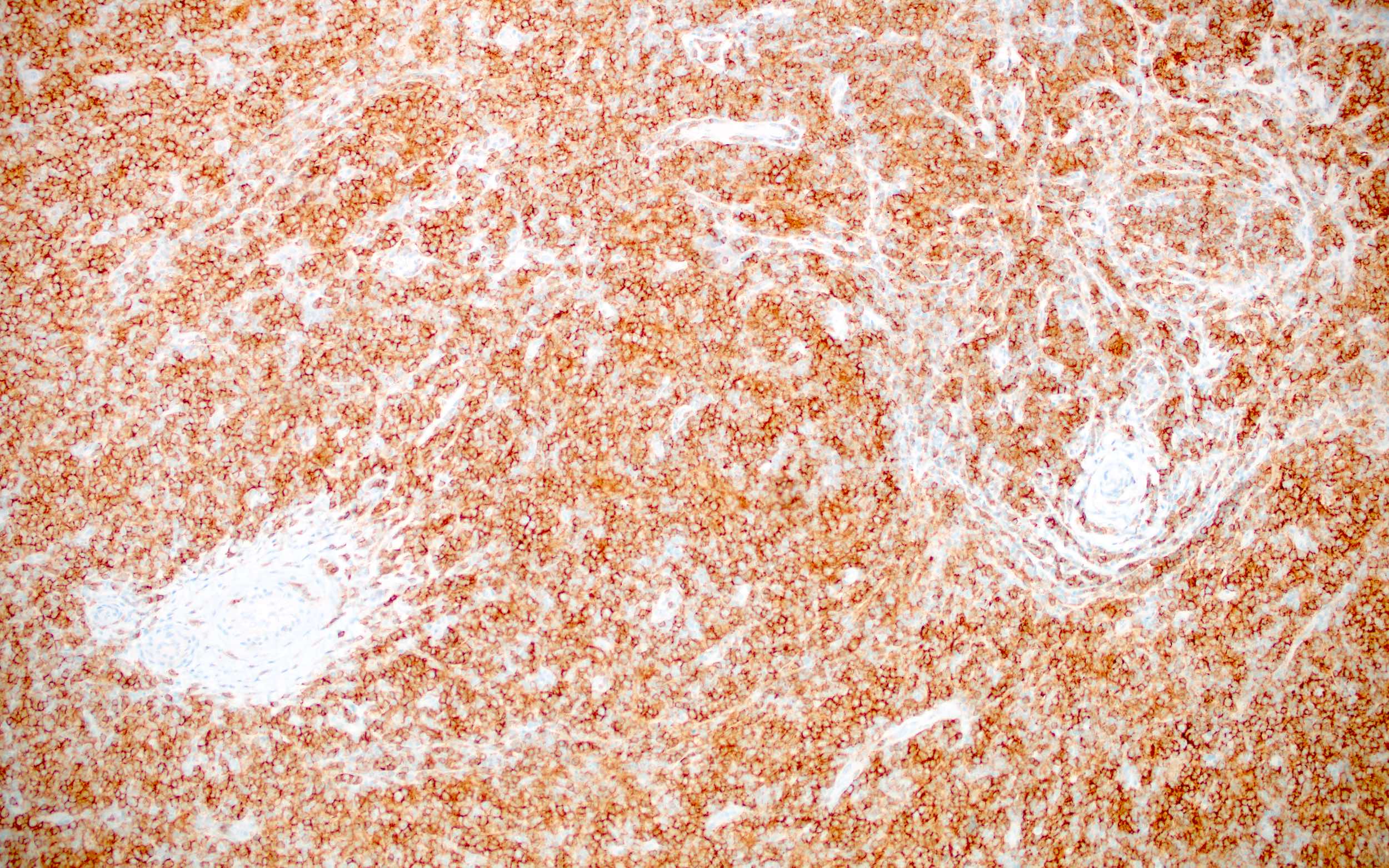
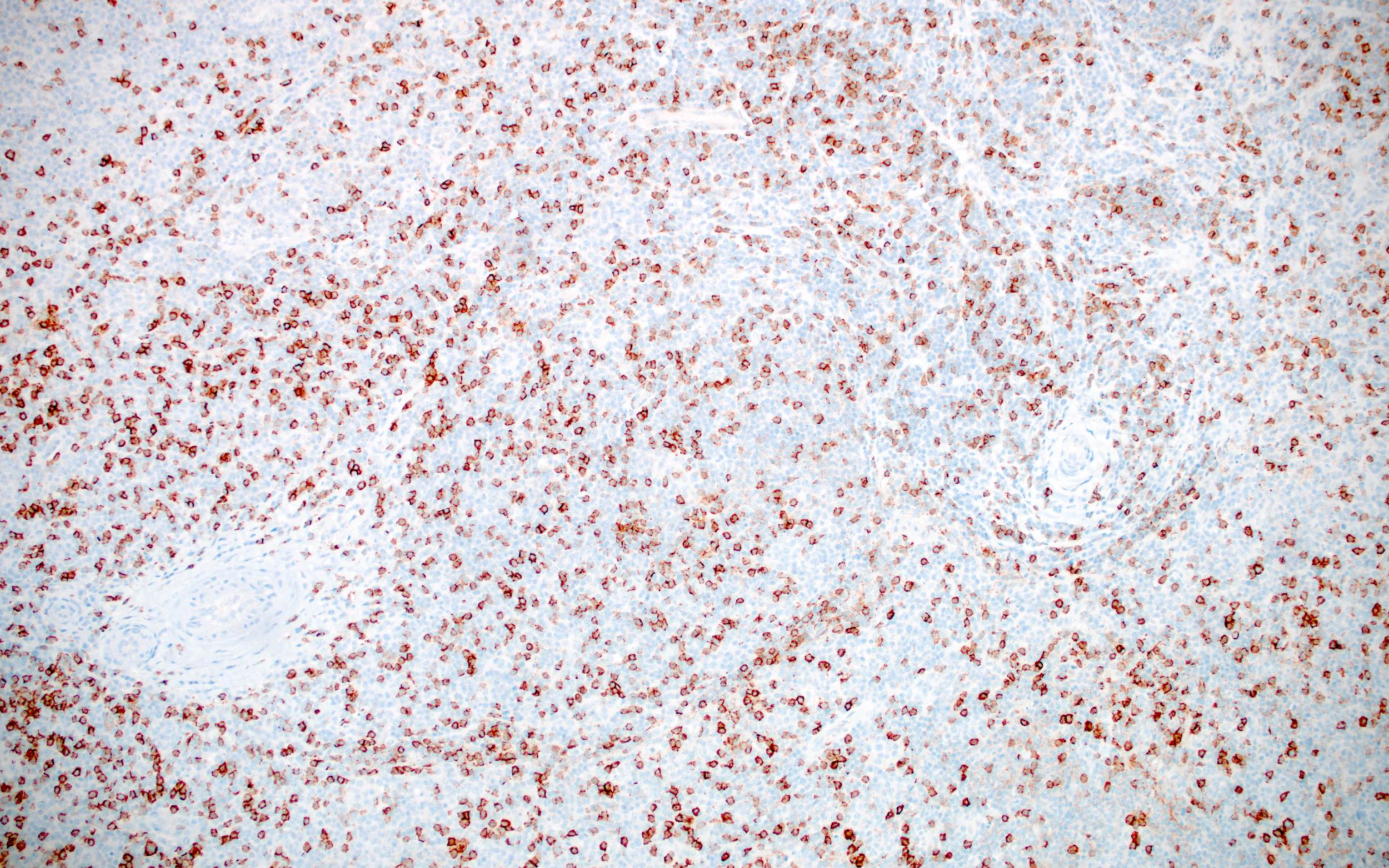
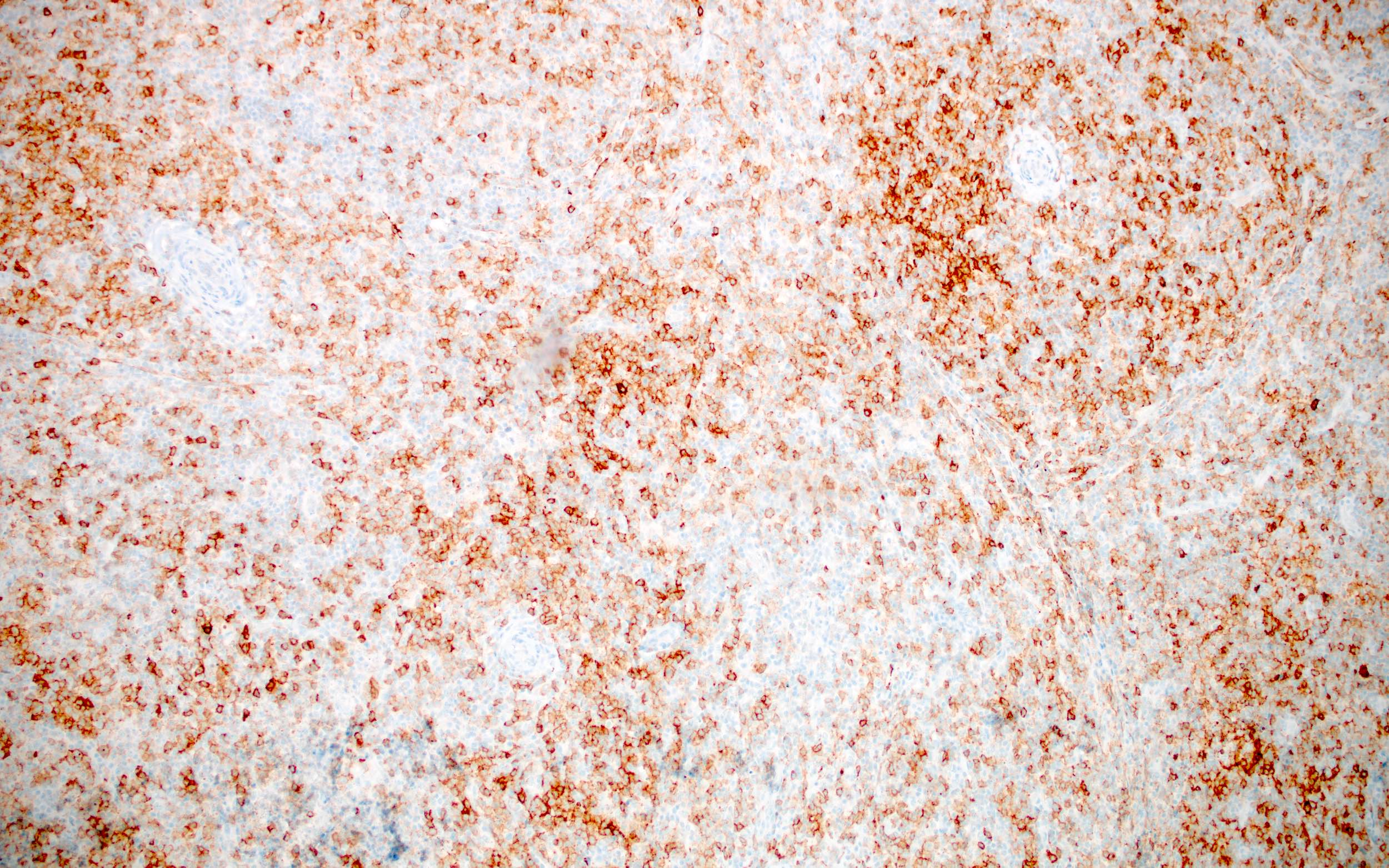
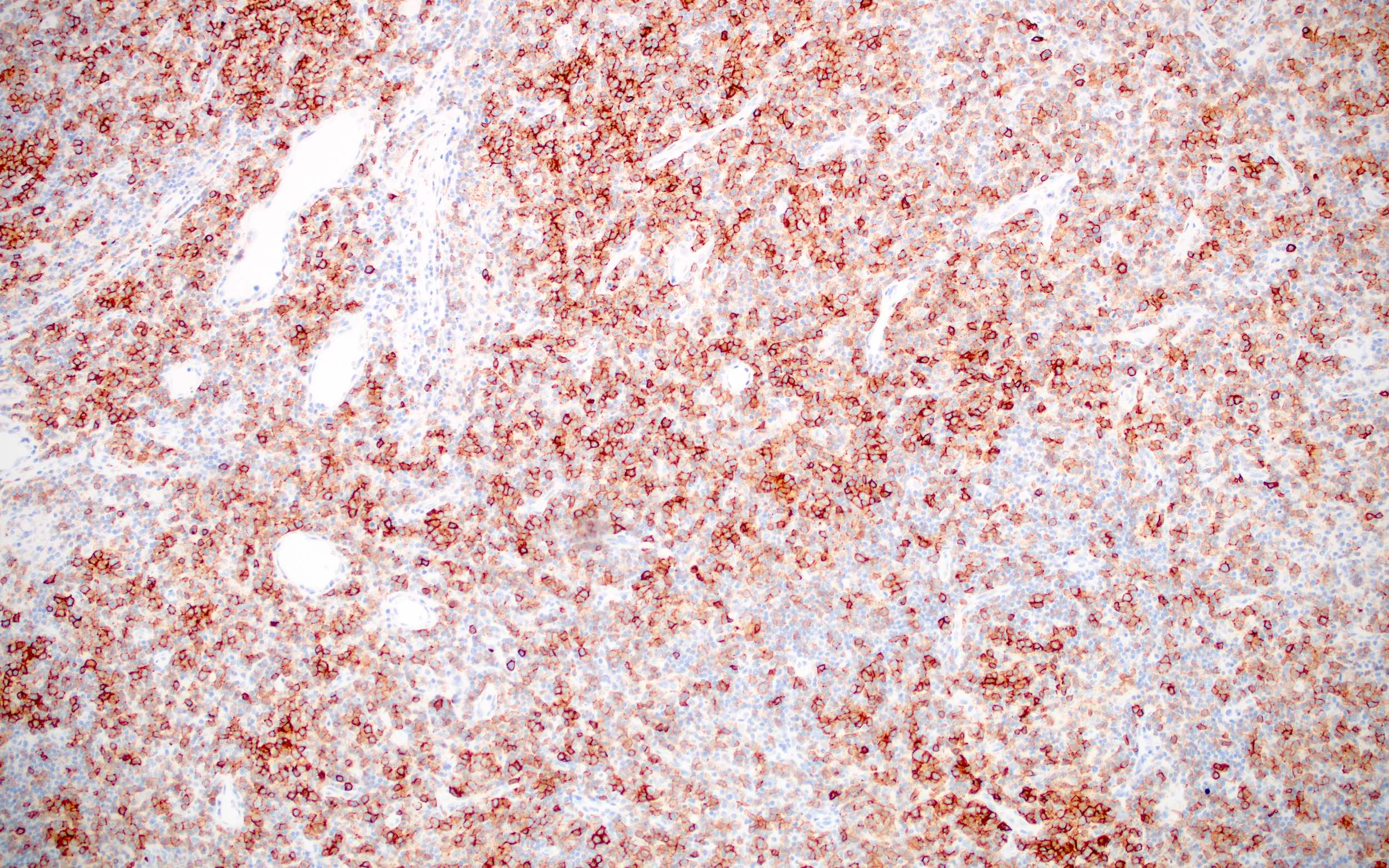
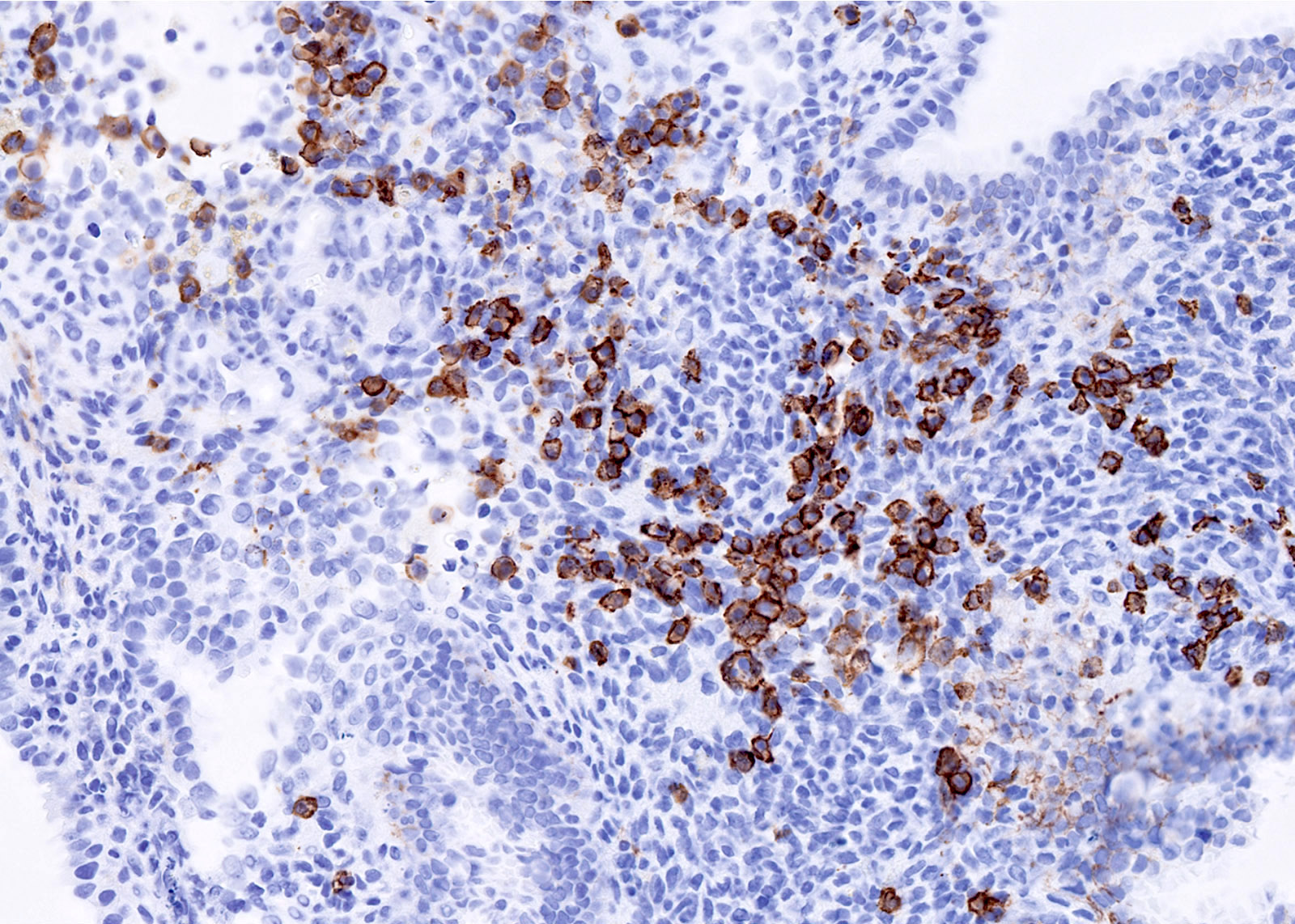
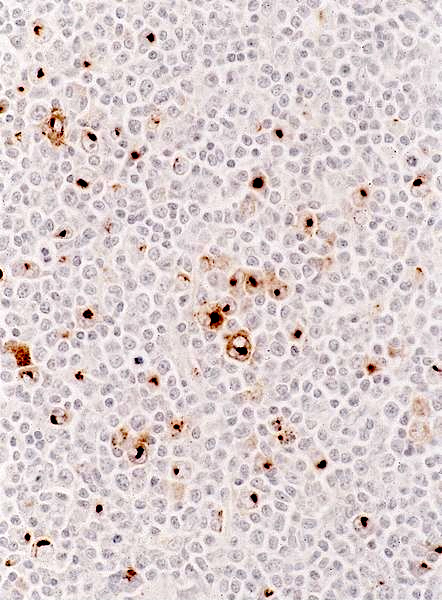
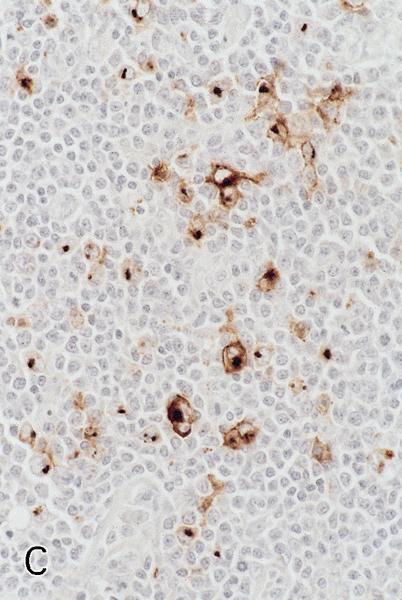
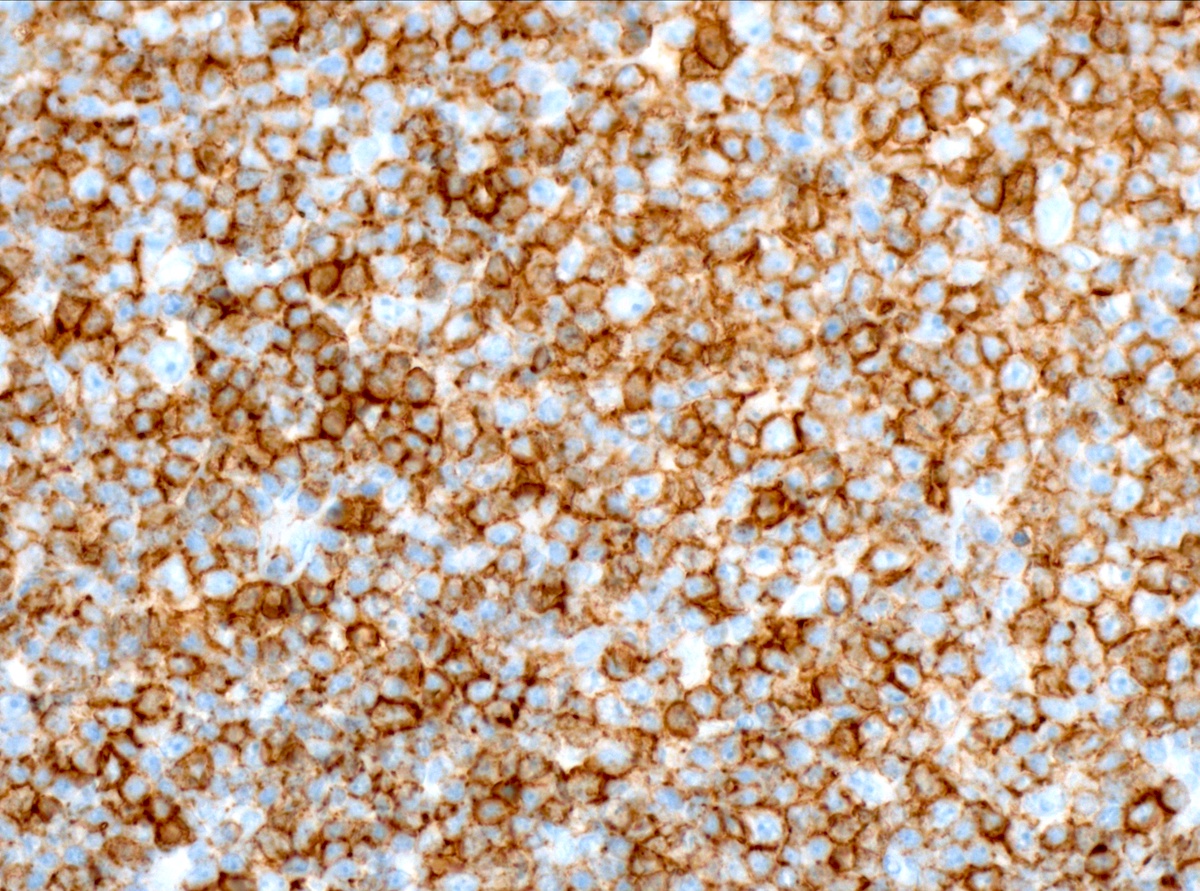
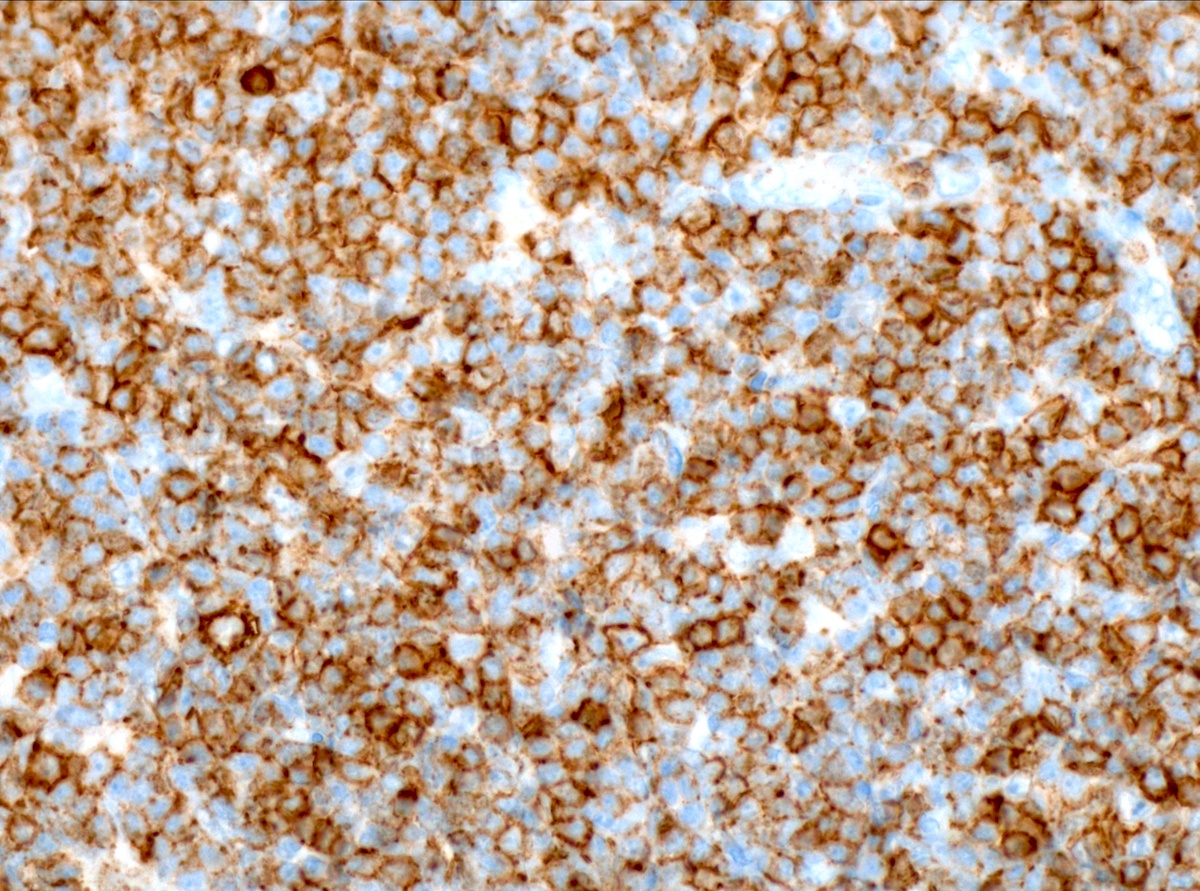
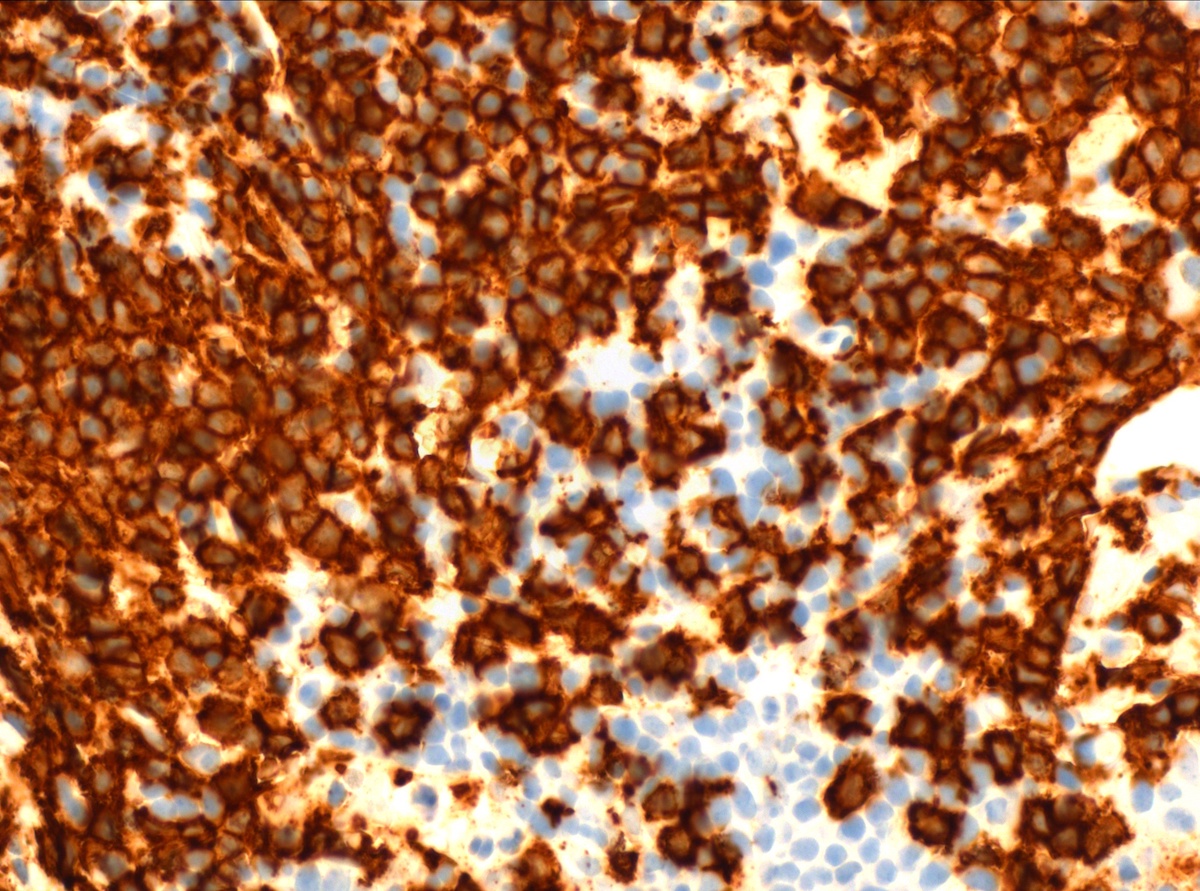
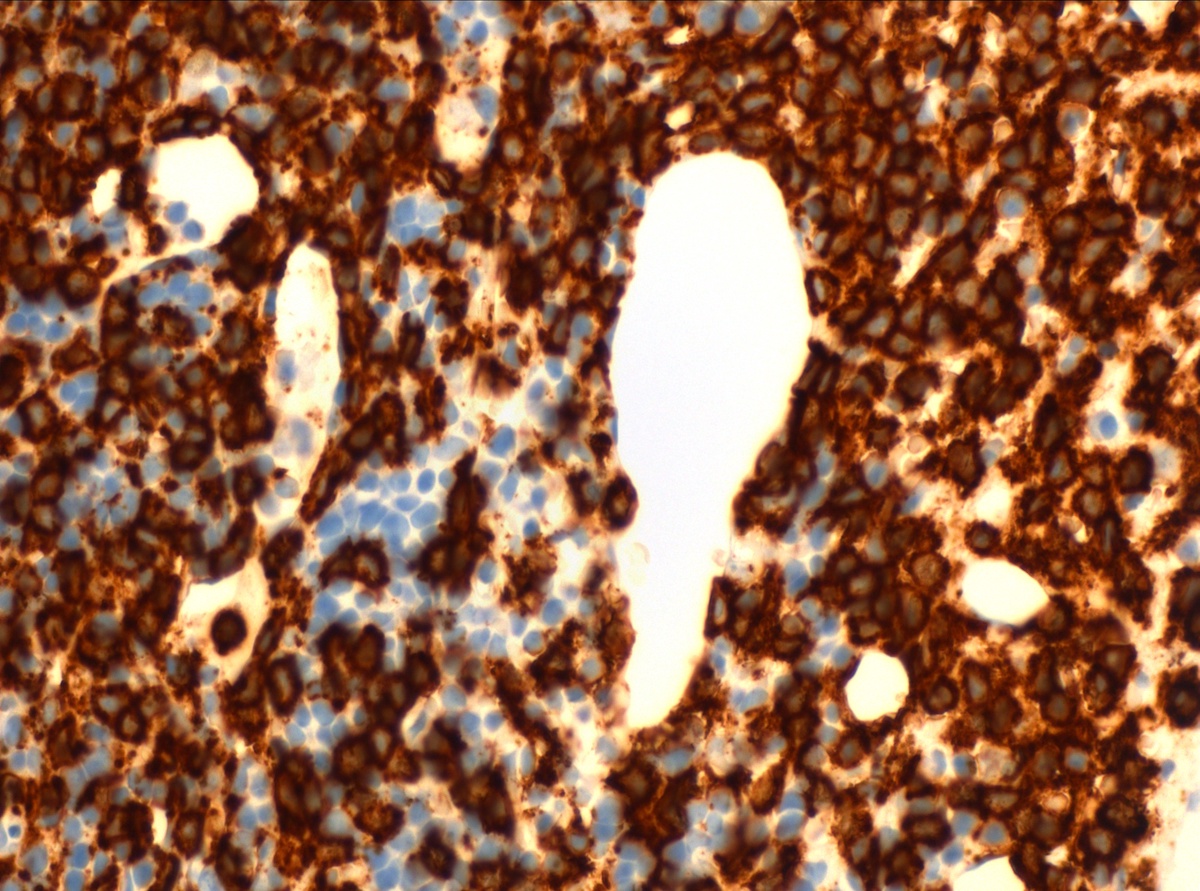
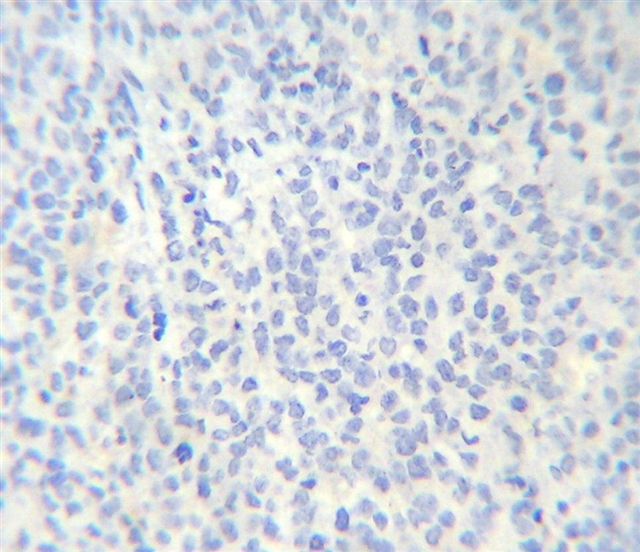
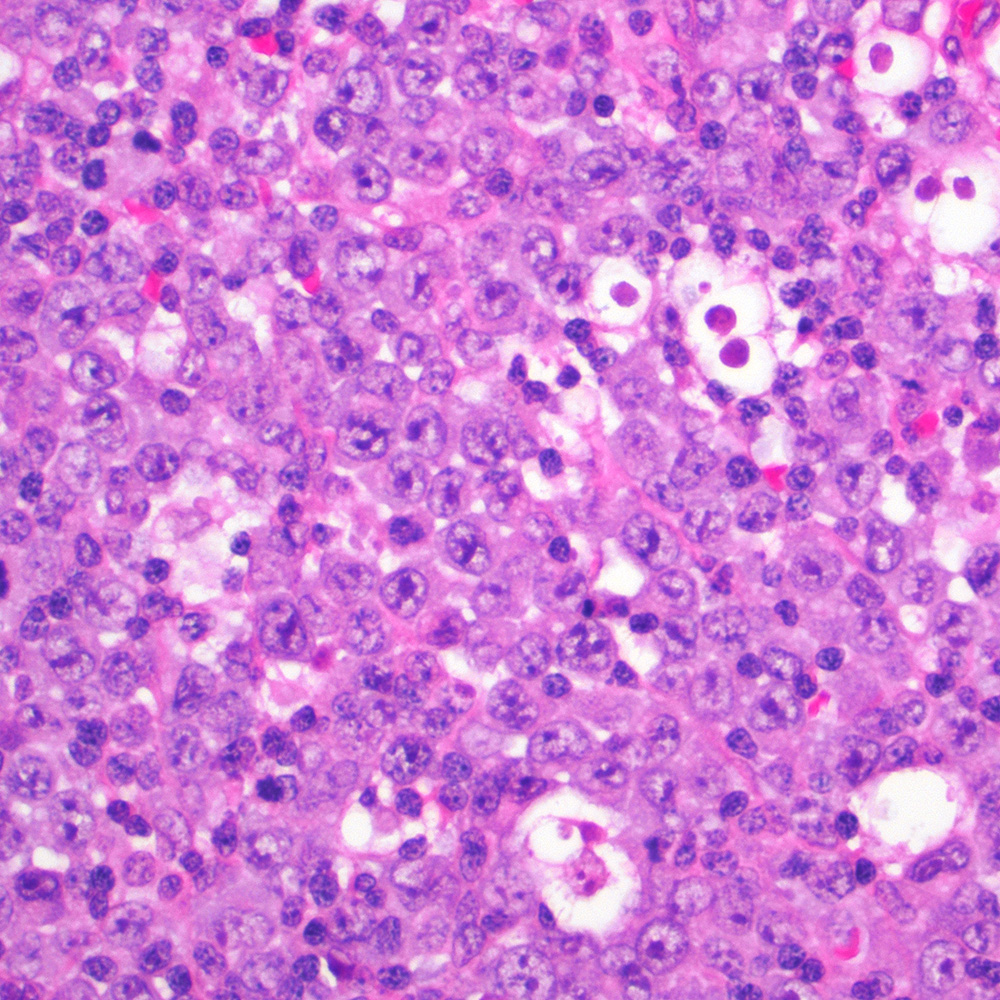
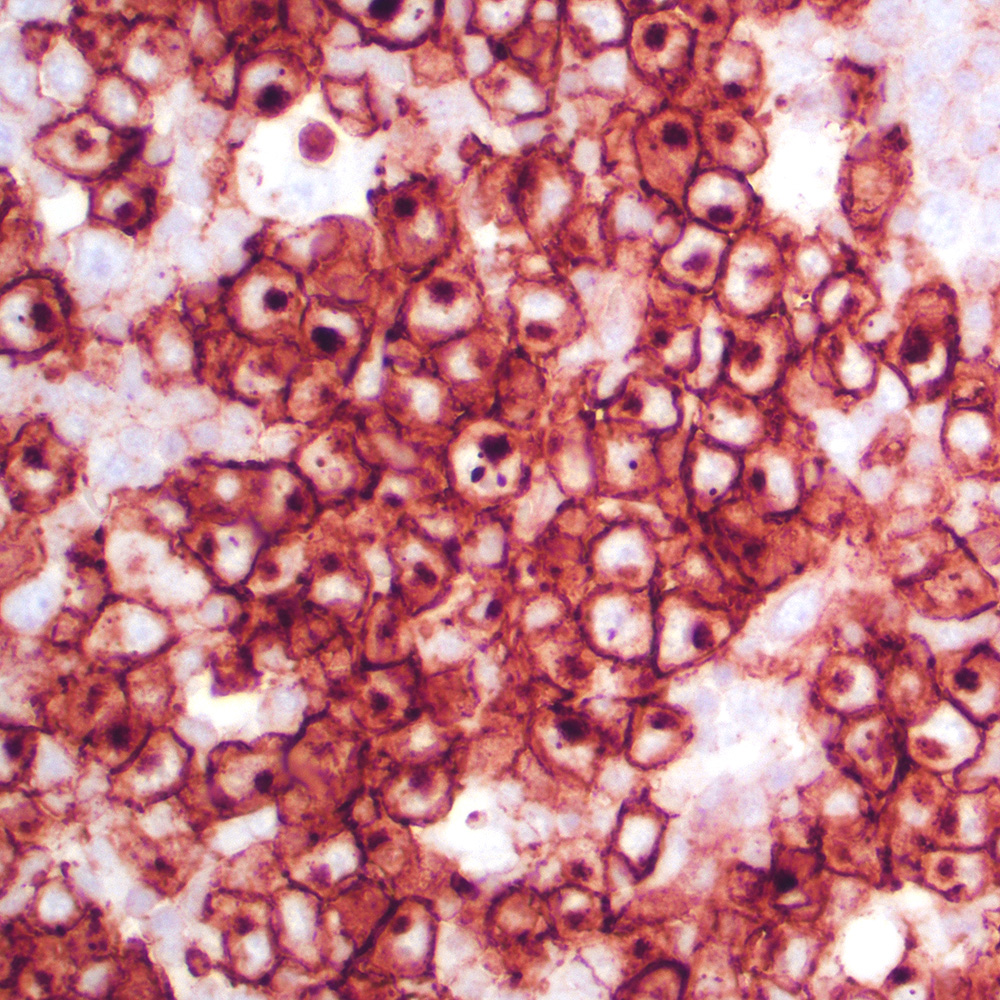
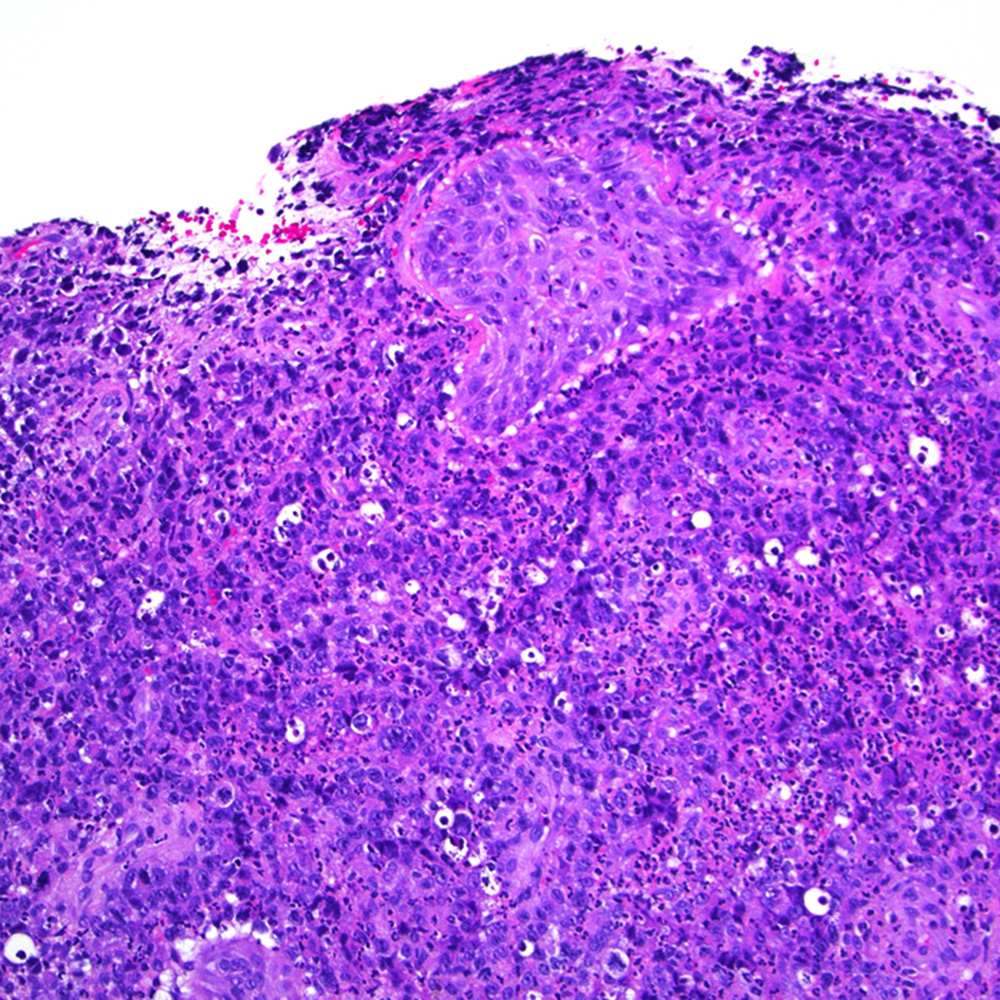
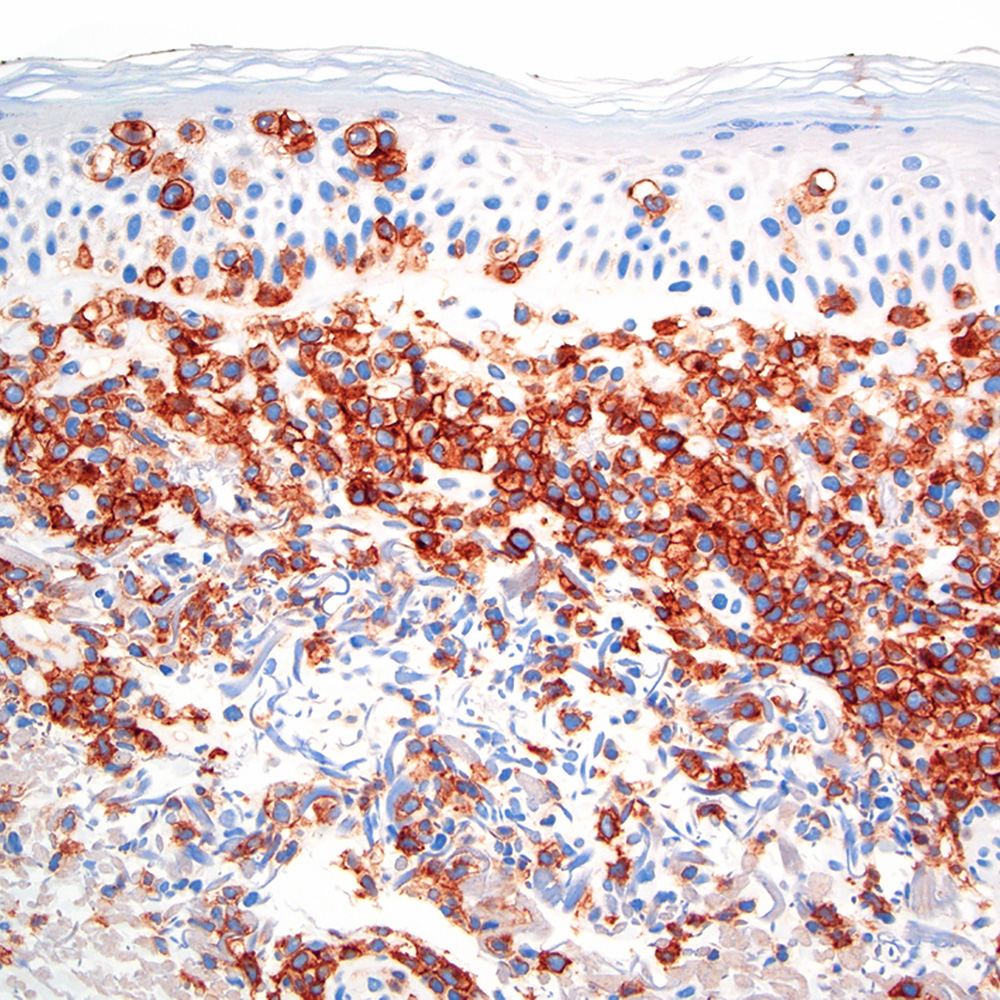
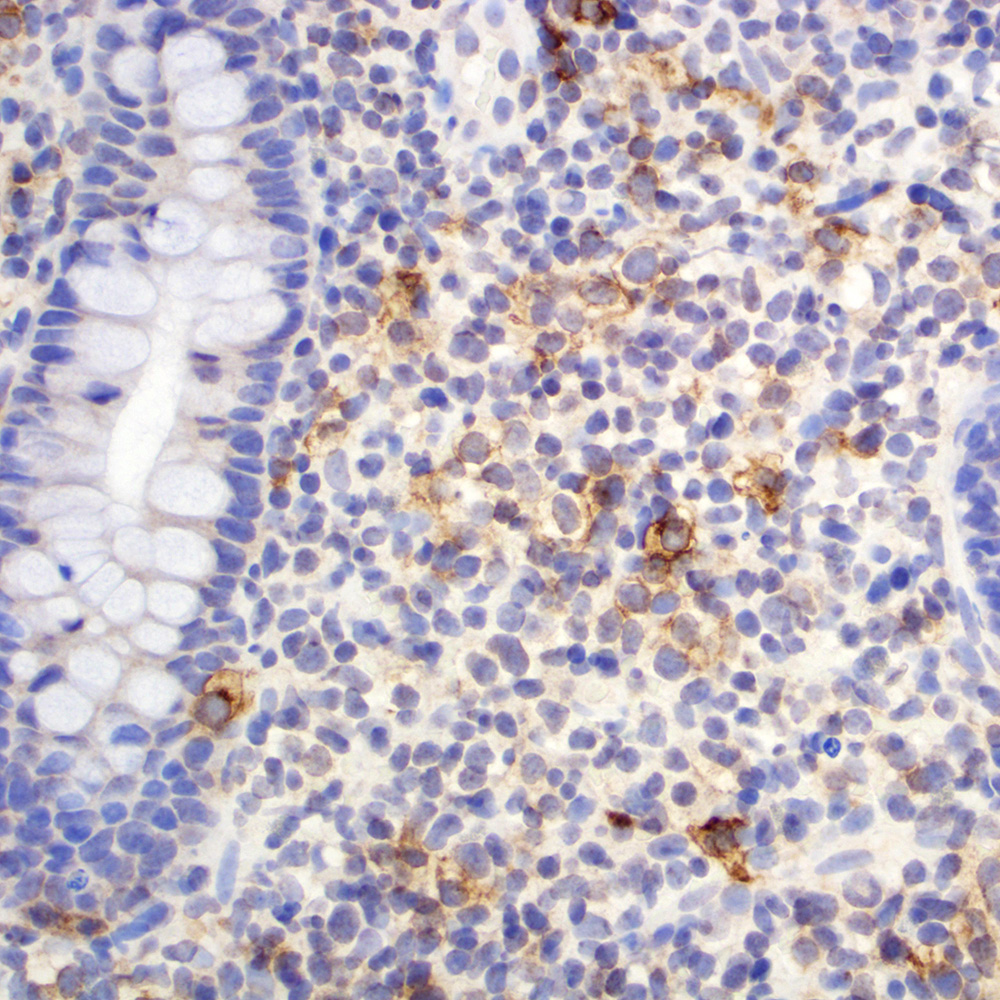
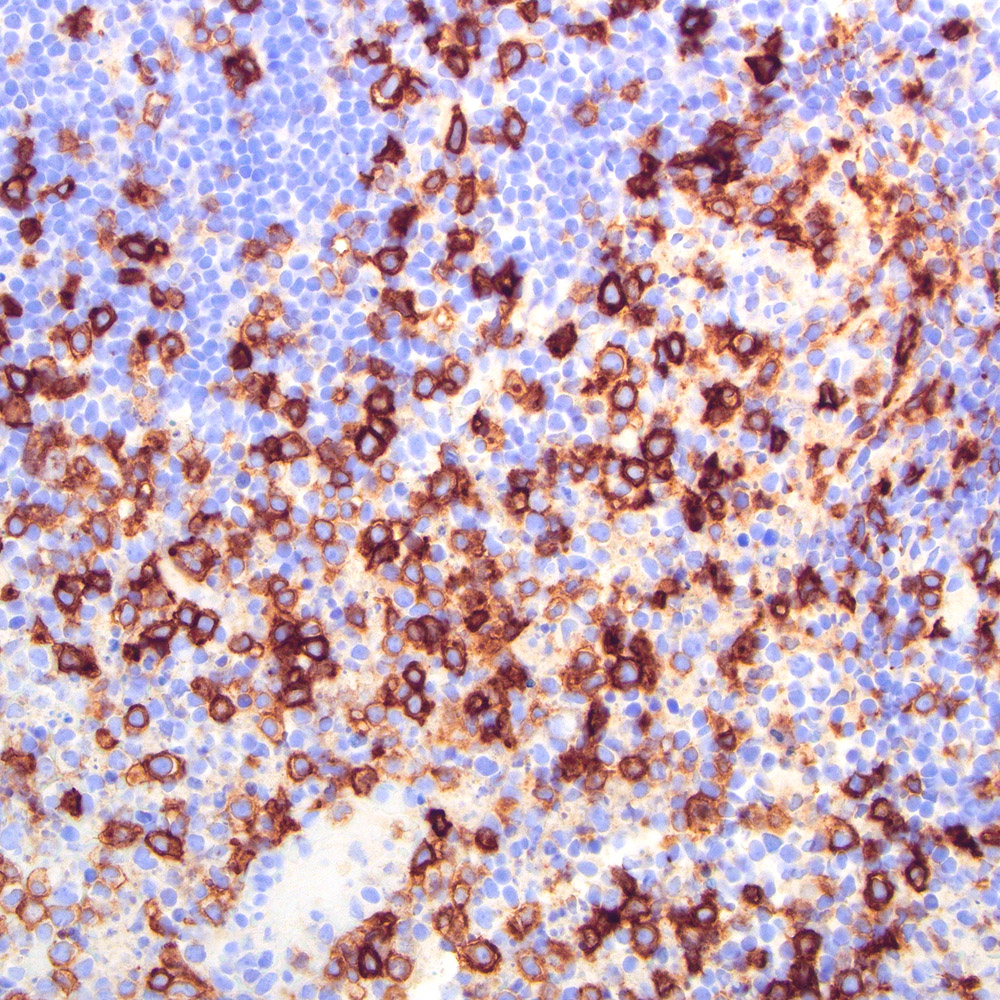
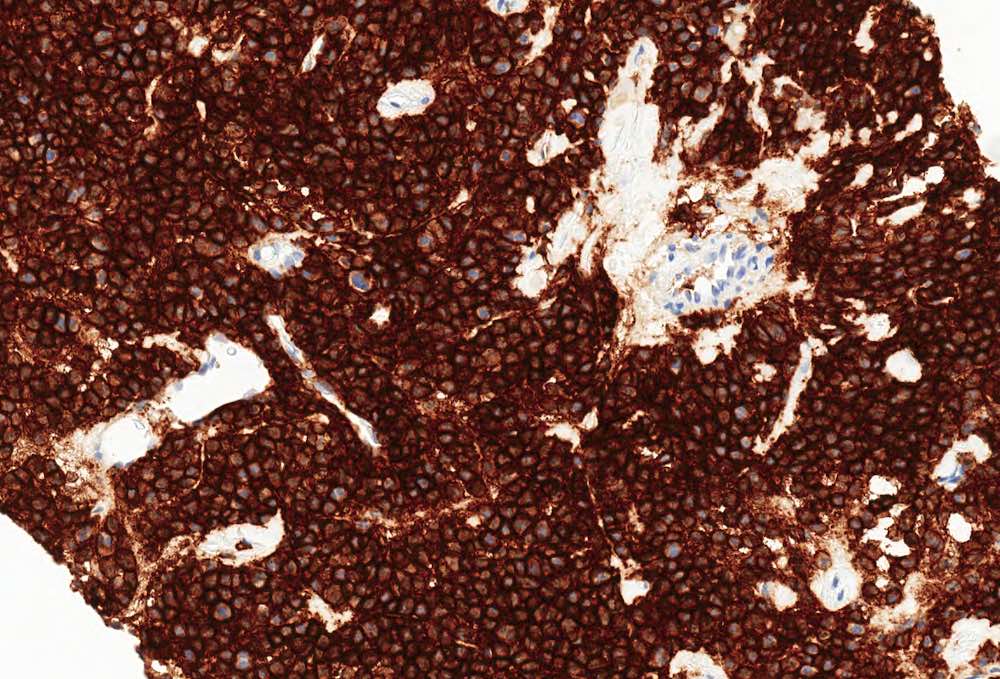
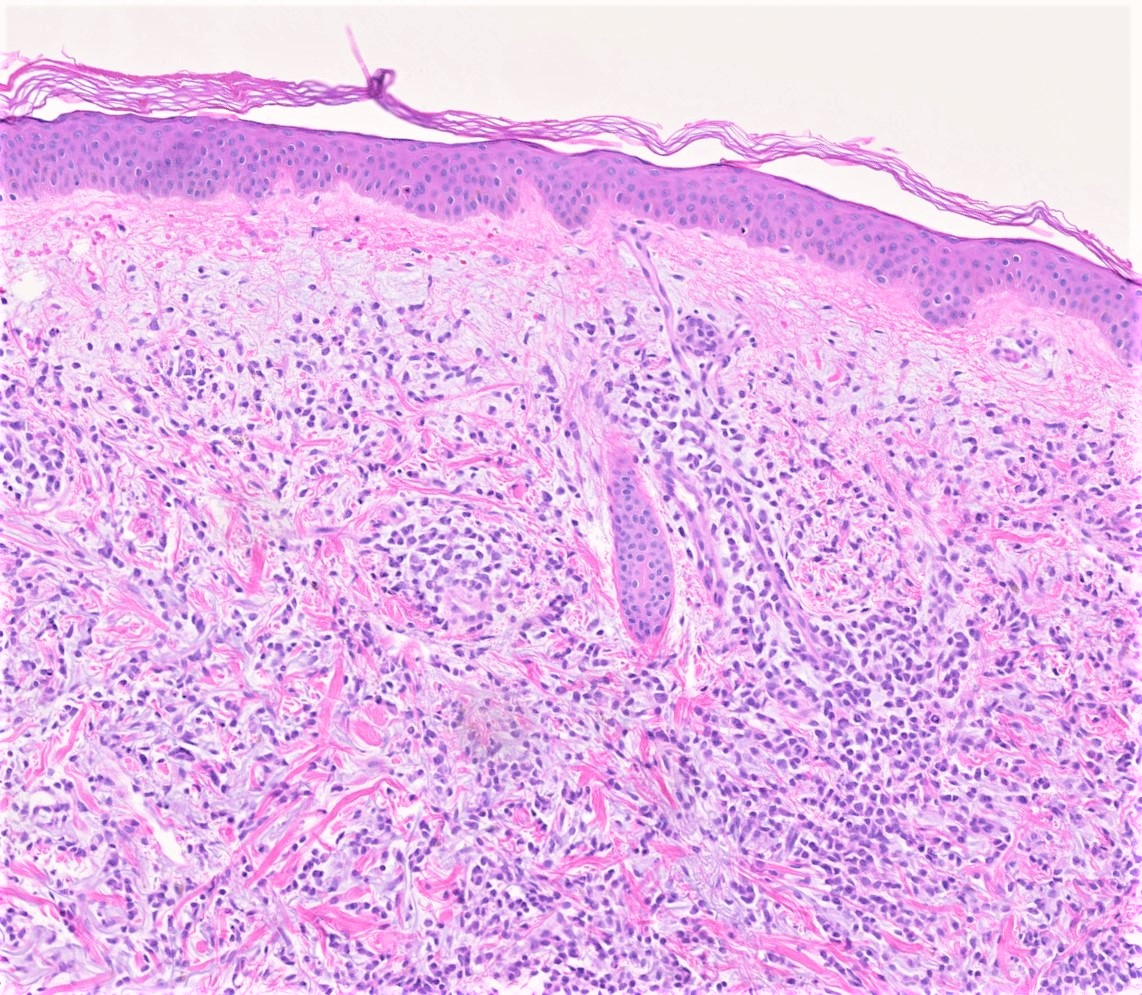
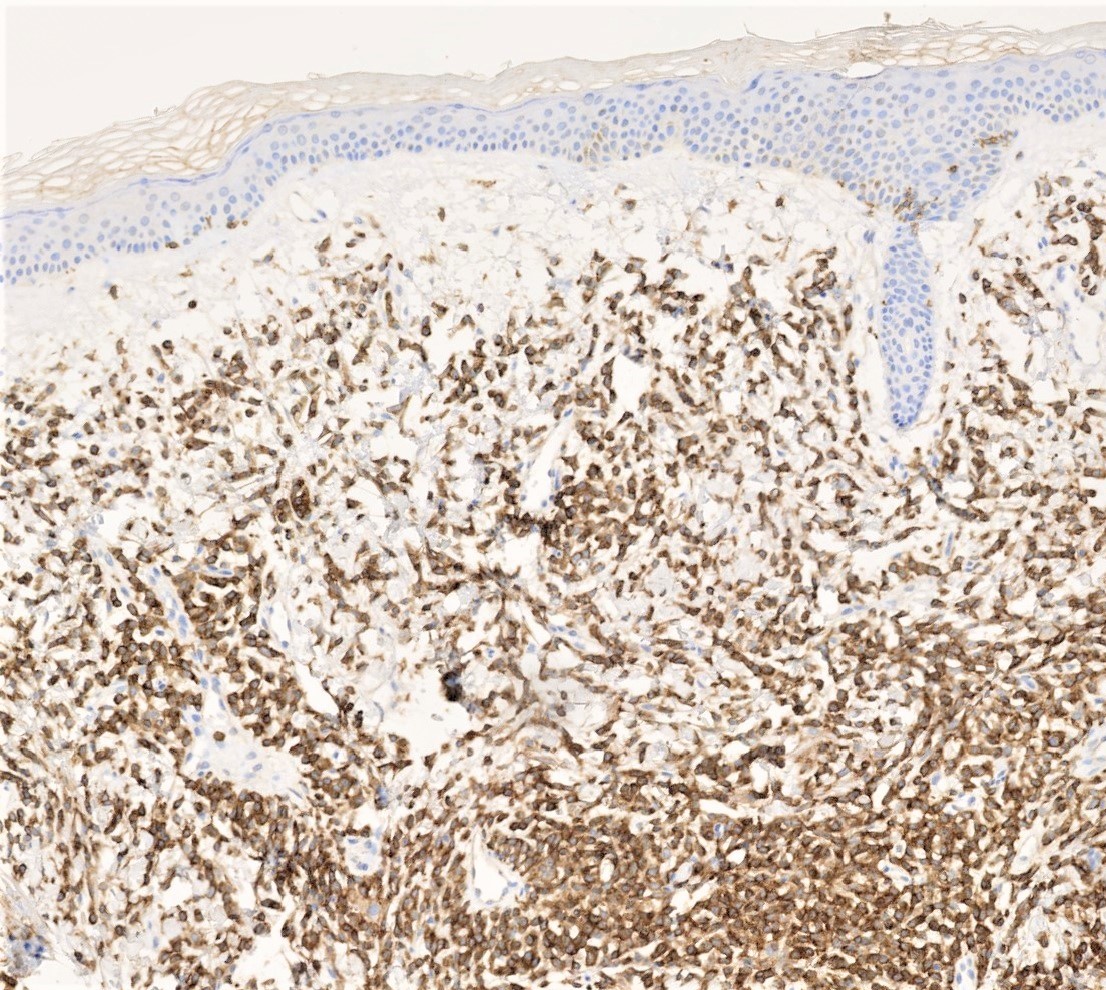
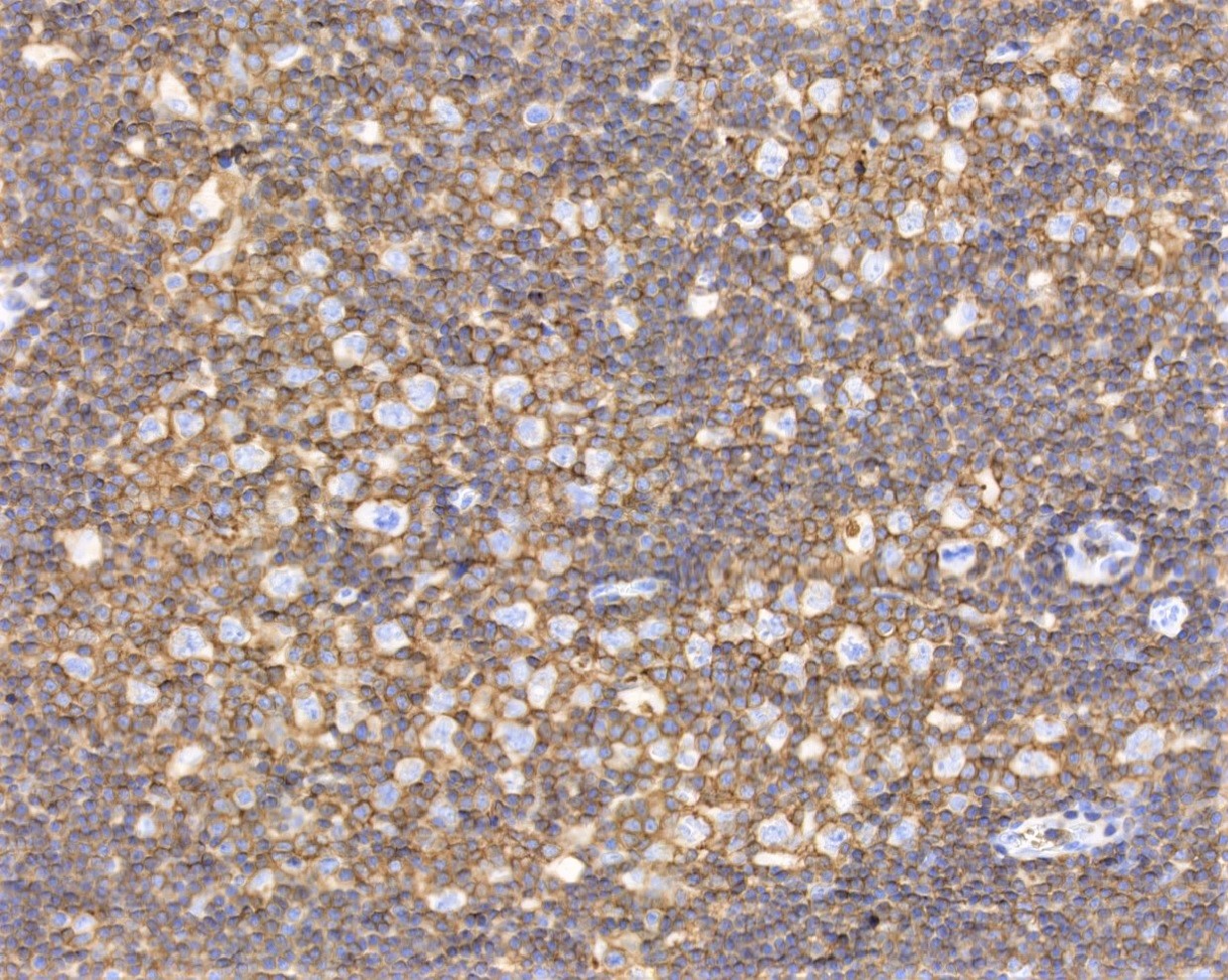
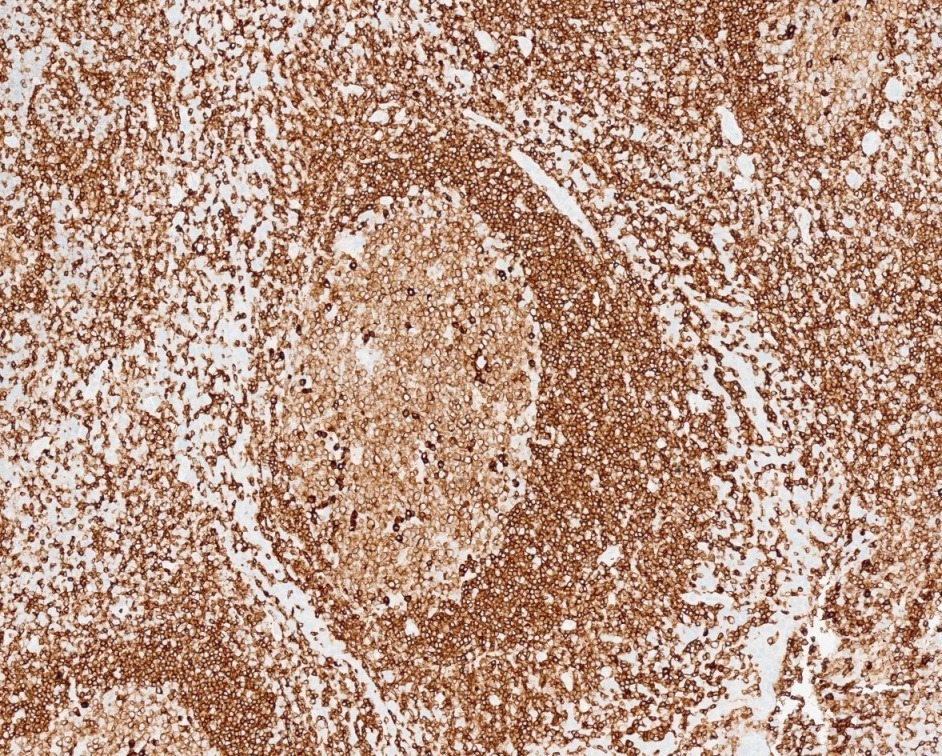
Microscopic (histologic) images
Images hosted on other servers:
ABCC2
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Adenosine triphosphate (ATP) binding cassette subfamily C member 2 (ABCC2) belongs to the C subfamily of the ABC transmembrane protein transporters
- It is located on chromosome 10 (Nat Rev Cancer 2010;10:147)
- ABCC transporters are involved in active drug transportation
- Contributes to chemotherapy resistance in some tumors by what is thought to be drug efflux mechanisms
- Recent publications show that ATP transporters contribute to cancer aggressiveness beyond the drug efflux effect (Cancer Biol Med 2020;17:253)
- Also called multidrug resistant protein 2 (MRP2)
Essential features
- ABCC2 staining patterns could potentially be used as prognostic biomarkers in papillary renal cell carcinomas (PRCC); the brush border staining pattern was shown to predict disease progression on both univariate and multivariate disease free survival analysis (Hum Pathol 2022;120:57, Mod Pathol 2022;35:657)
- ABCC2 has prognostic significance in some tumors, particularly papillary renal cell carcinoma, as well as breast, colon, pancreas, ovary and fallopian tube
- Might have predictive significance as it has been implicated in chemotherapy resistance
Terminology
- Adenosine triphosphate (ATP) binding cassette subfamily C member 2 (ABCC2)
- Multidrug resistance associated protein 2 (MRP2)
- Canalicular multispecific organic anion transporter 1 (CMOAT1)
- Canalicular multidrug resistance protein (cMRP)
- ABC30
- Dubin-Johnson syndrome (DJS)
Pathophysiology
- ABC transporters have 7 subfamilies
- In mammals, ABC transporters are expressed in liver, intestine, blood brain barrier, placenta and kidney, with 49 ABC genes in the human genome (Hum Genomics 2009;3:281)
- ABCC2 belongs to the C subfamily, also known as multidrug resistance protein family (Nat Rev Cancer 2010;10:147)
- They are involved in active drug transportation
- ABCC2 itself is only expressed in proximal renal tubules, bile canaliculi and placenta (Drug Metab Rev 2010;42:402)
- ABCC2 contributes to chemotherapy resistance through active ATP dependent efflux of drugs (Nat Rev Cancer 2010;10:147)
- Some studies indicate that ABC transporters play a role in tumor biology beyond the efflux properties (Nat Rev Cancer 2010;10:147, Cancer Biol Med 2020;17:253)
- Transporters are ATP dependent
- Cells enriched in ABC transporters are reported to be larger than average and hold numerous mitochondria to compensate for the high energy demand of the transporter
- This could contribute to the oncocytic nature of some of the reported ABCC2 high tumors (Curr Cancer Drug Targets 2005;5:457)
- Renal drug transporters, including ABCC2, are upregulated downstream to the NRF2-ARE pathway, which is enriched in high grade papillary renal cell carcinoma (old type 2) (N Engl J Med 2016;374:135, Toxicol In Vitro 2015;29:884)
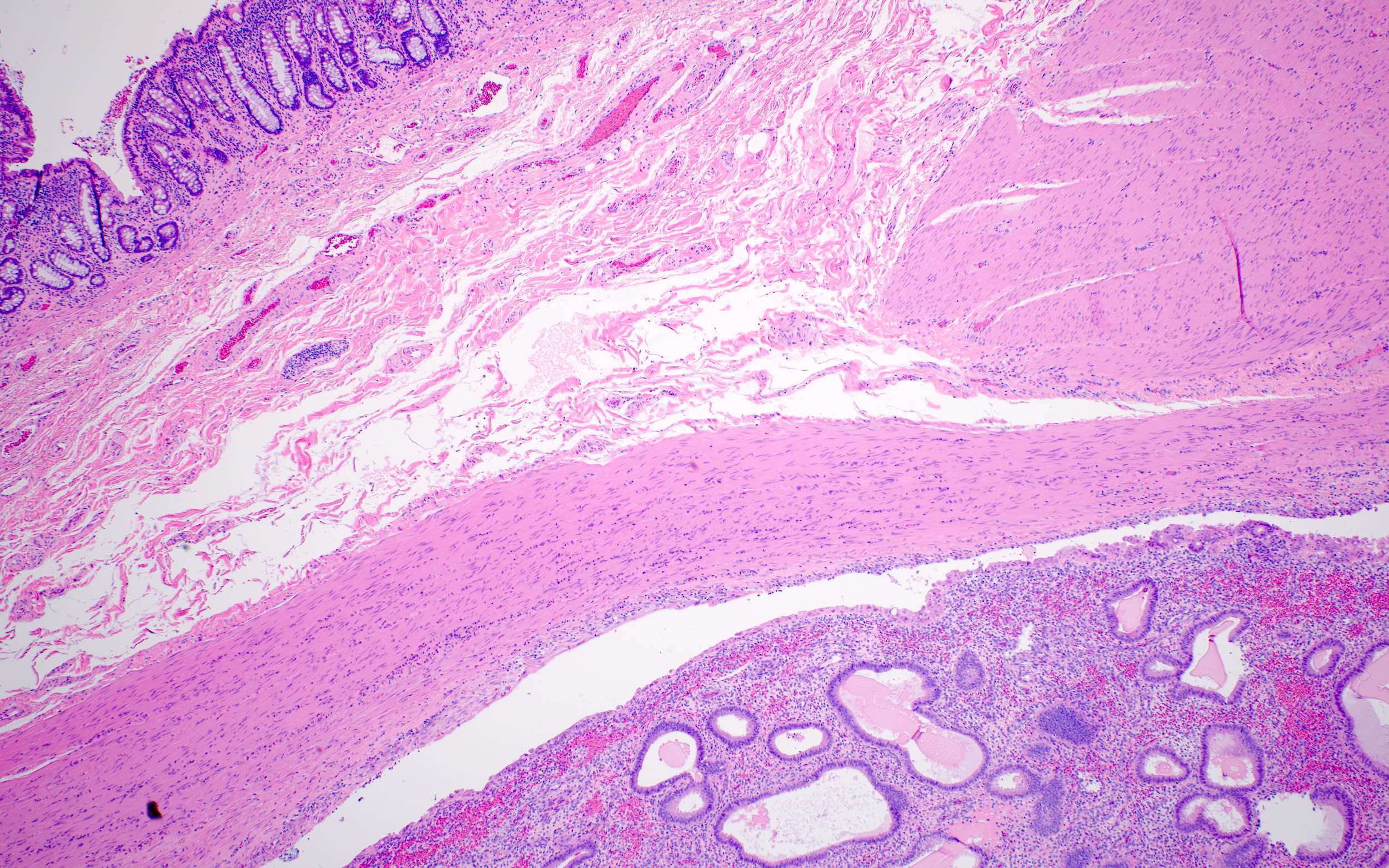
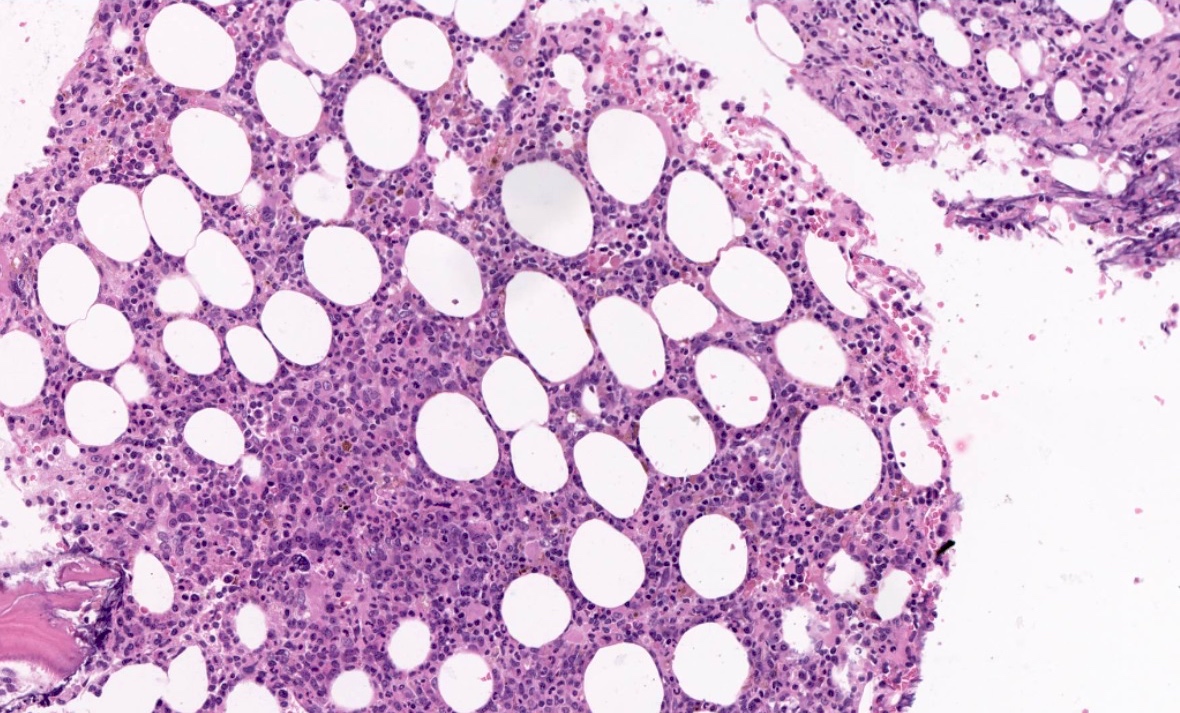
Clinical features
- Germline mutations in ABCC2 are associated with autosomal recessive Dubin-Johnson syndrome
- It is characterized by impaired secretion of conjugated bilirubin by hepatocytes
- Grossly, the liver is black in appearance
- Microscopically, there is accumulation of dark, PASD positive, coarsely granular pigment in the centrilobular zone
- Electron microscopy shows the pigment accumulating in lysosomes
- These patients are usually asymptomatic, with incidental detection of hyperbilirubinemia (StatPearls: Dubin Johnson Syndrome [Accessed 25 July 2023])
Interpretation
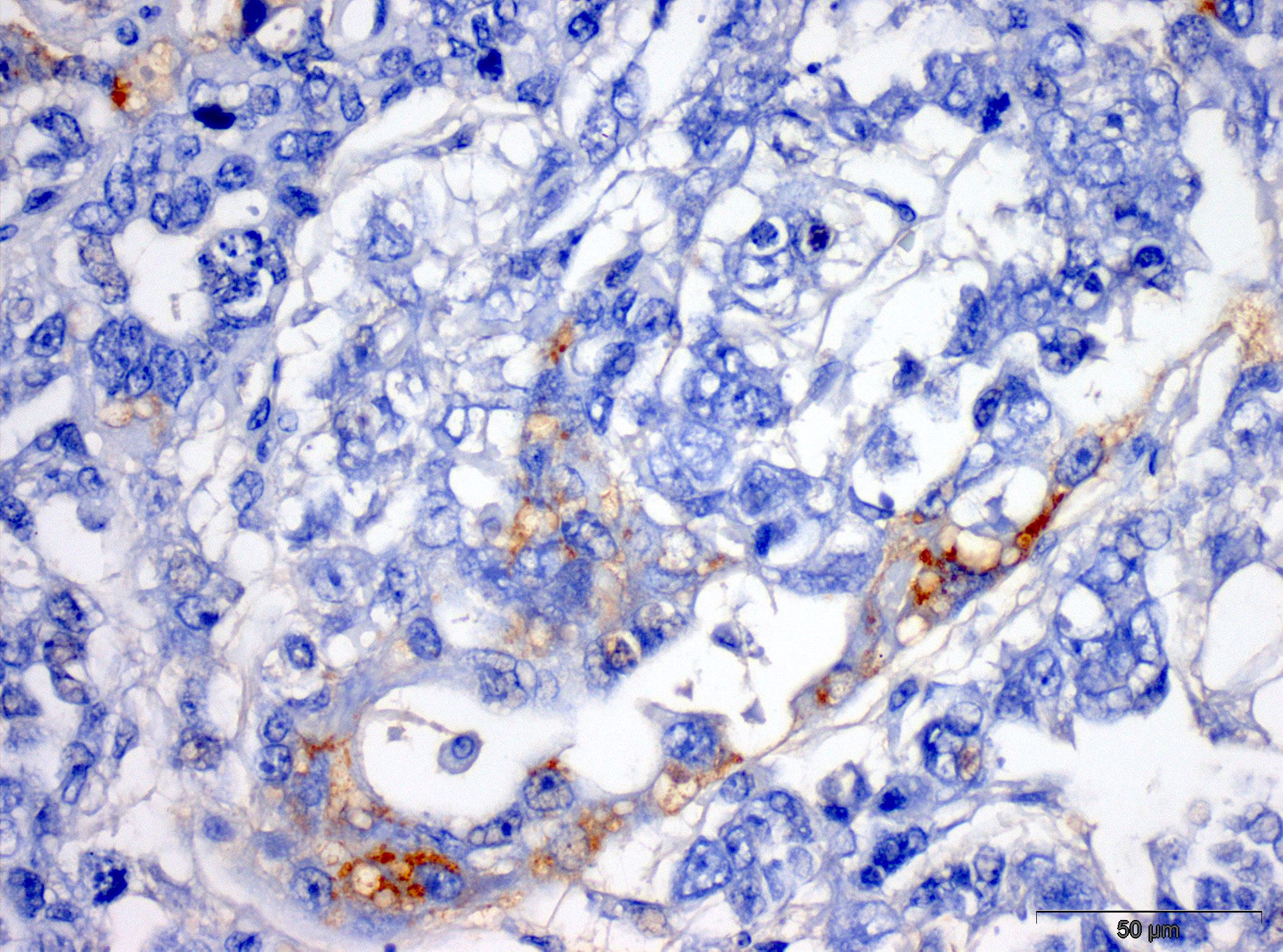
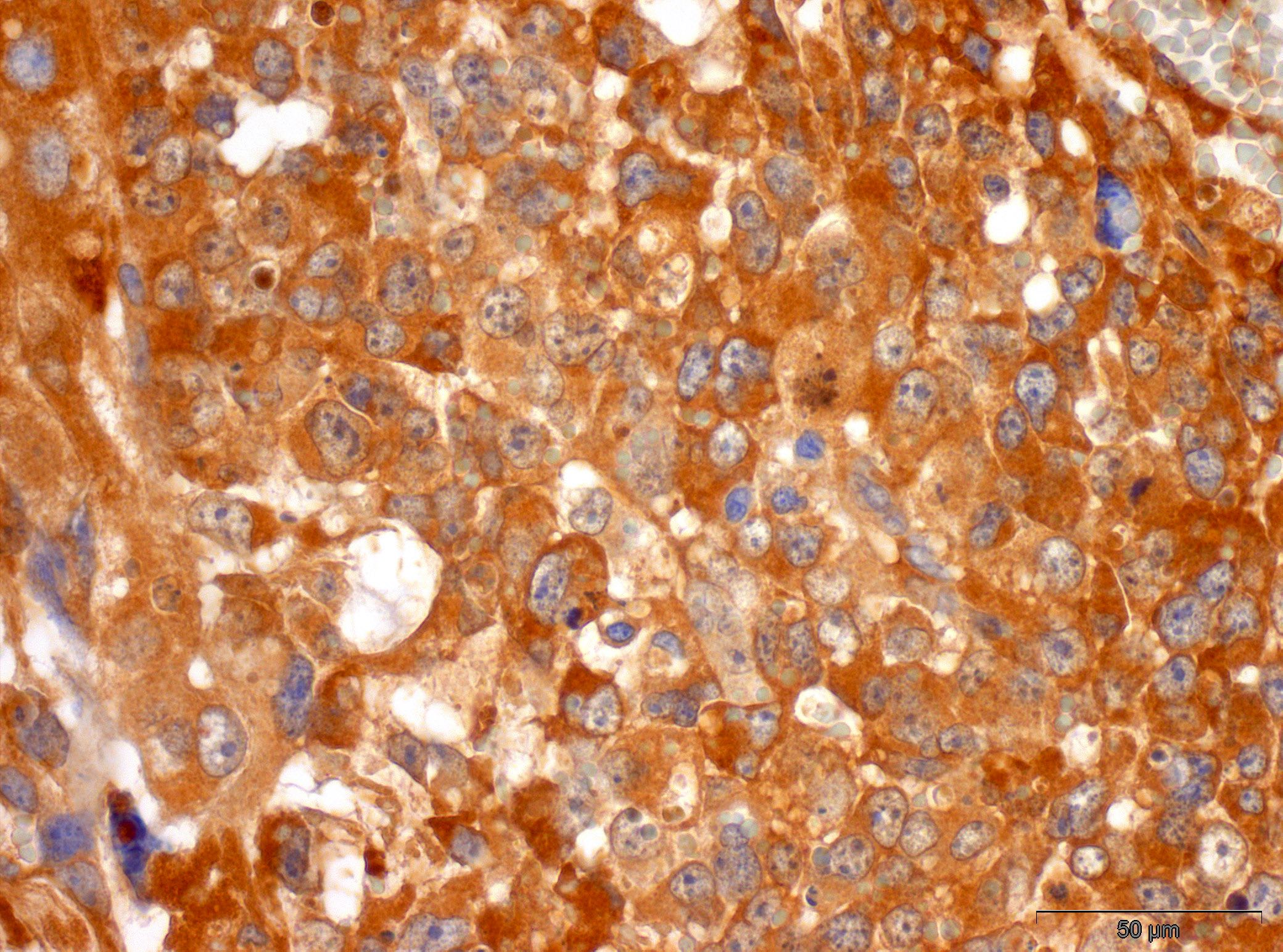
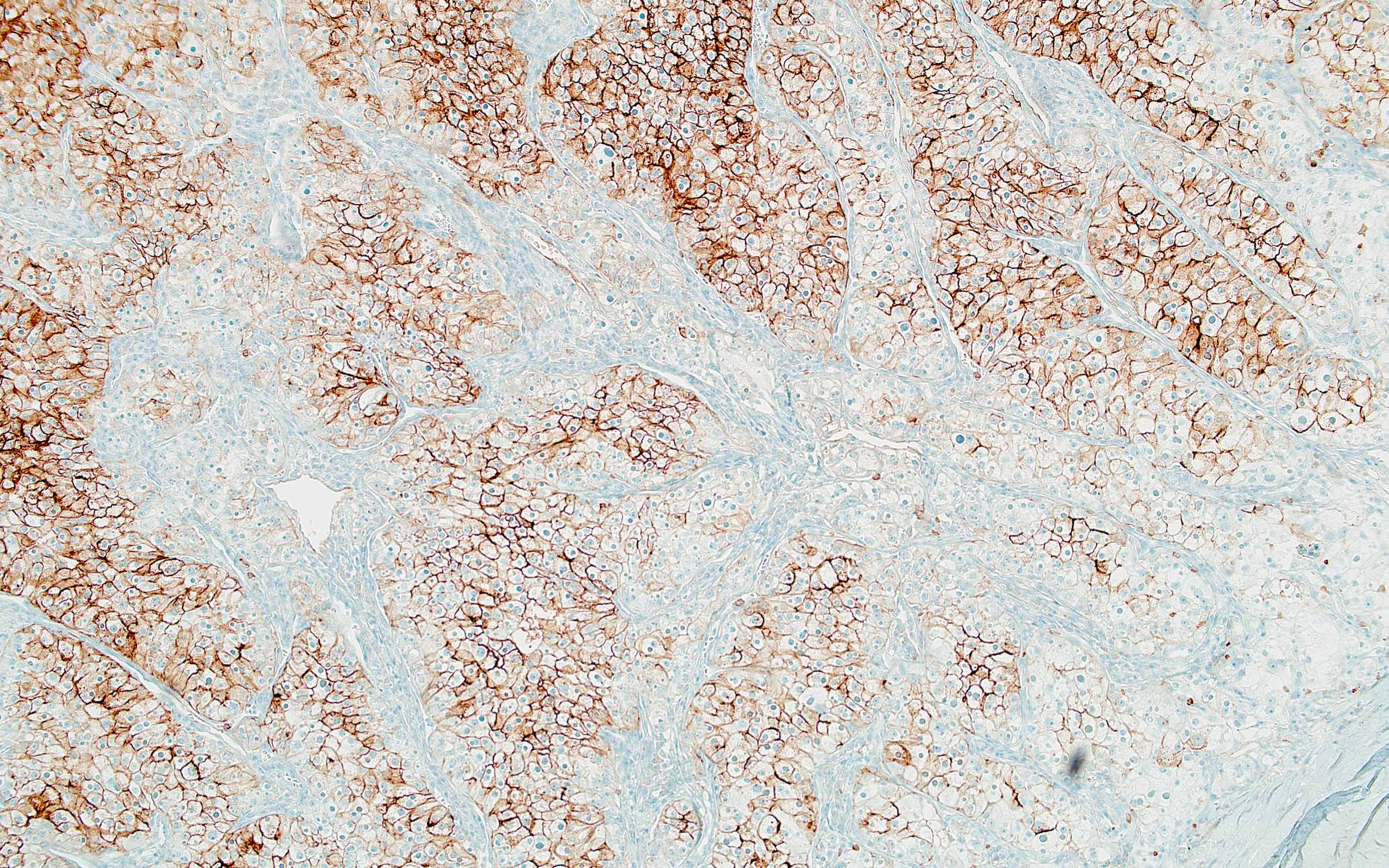
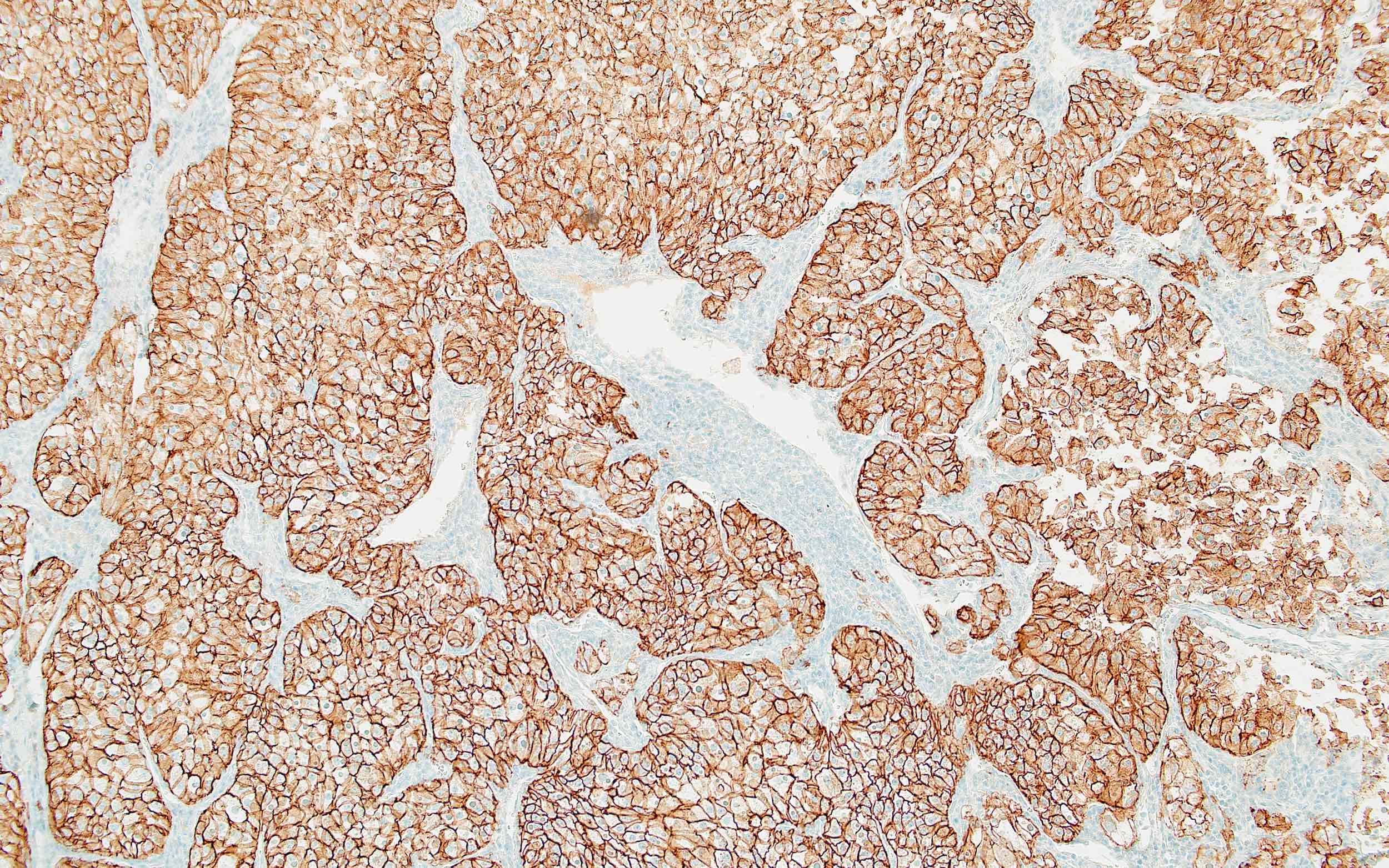
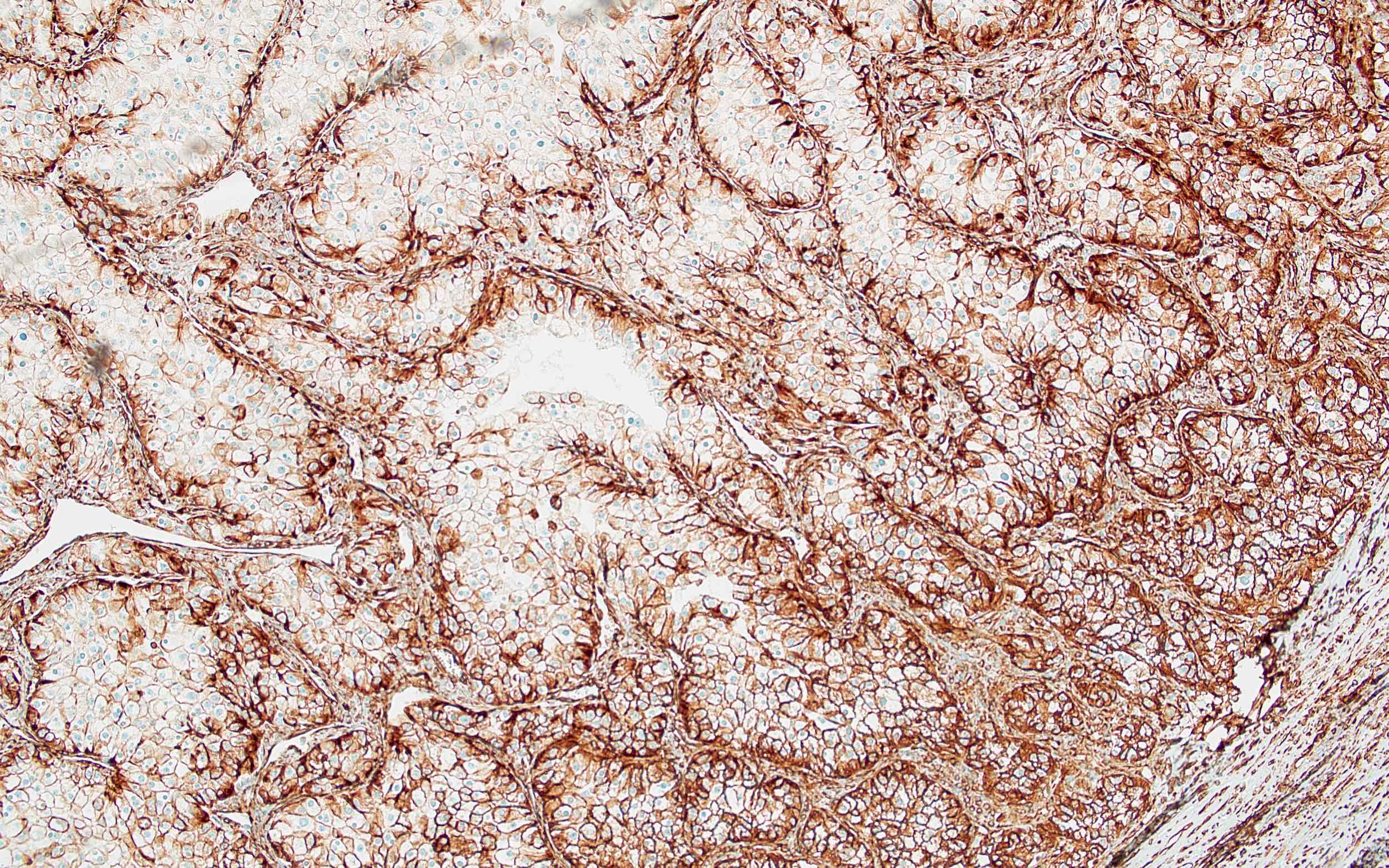
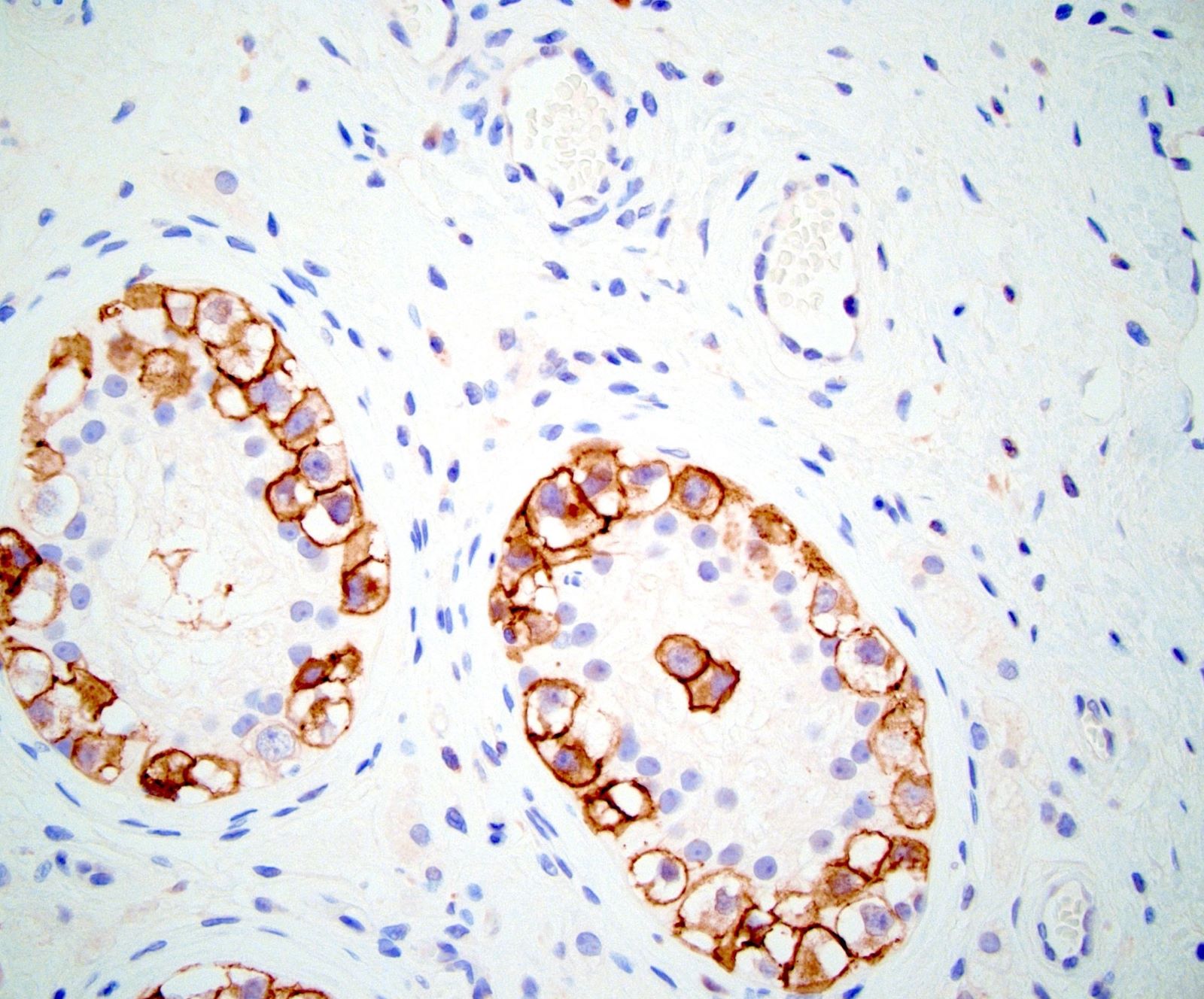
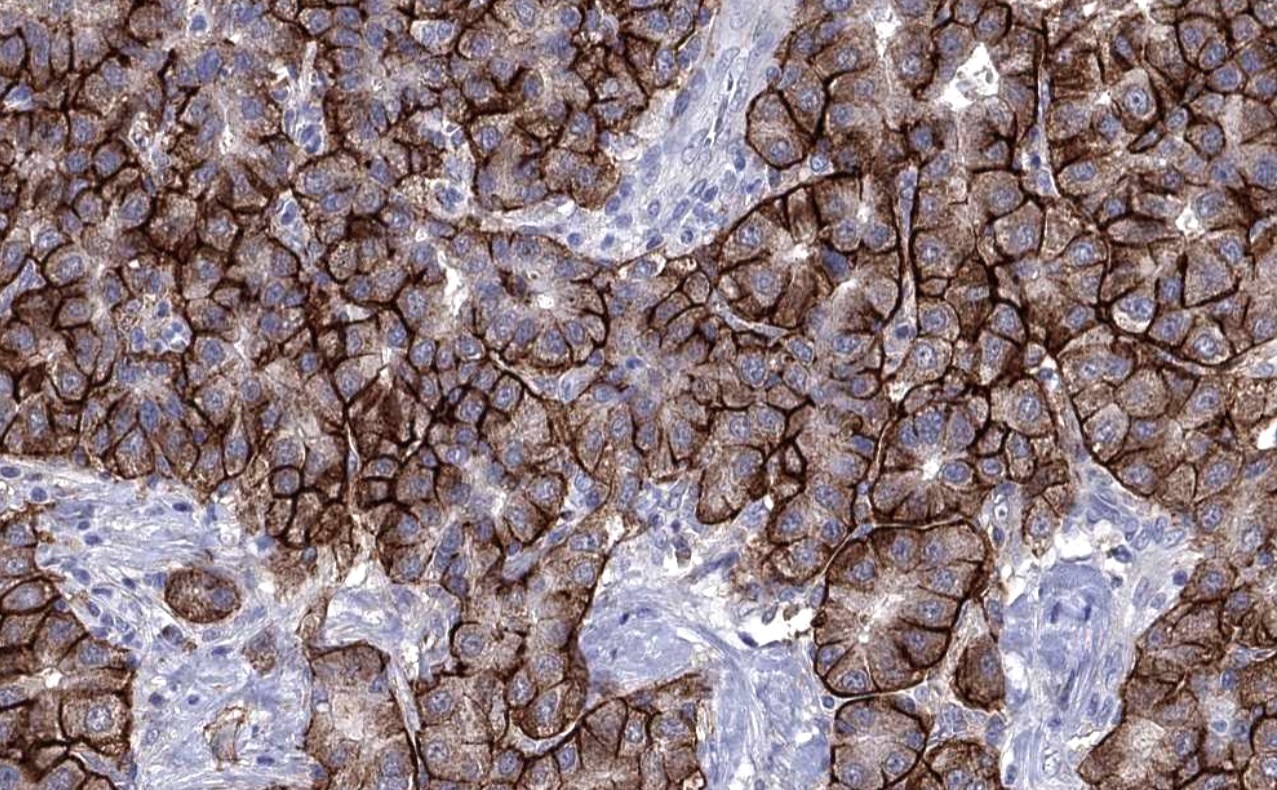
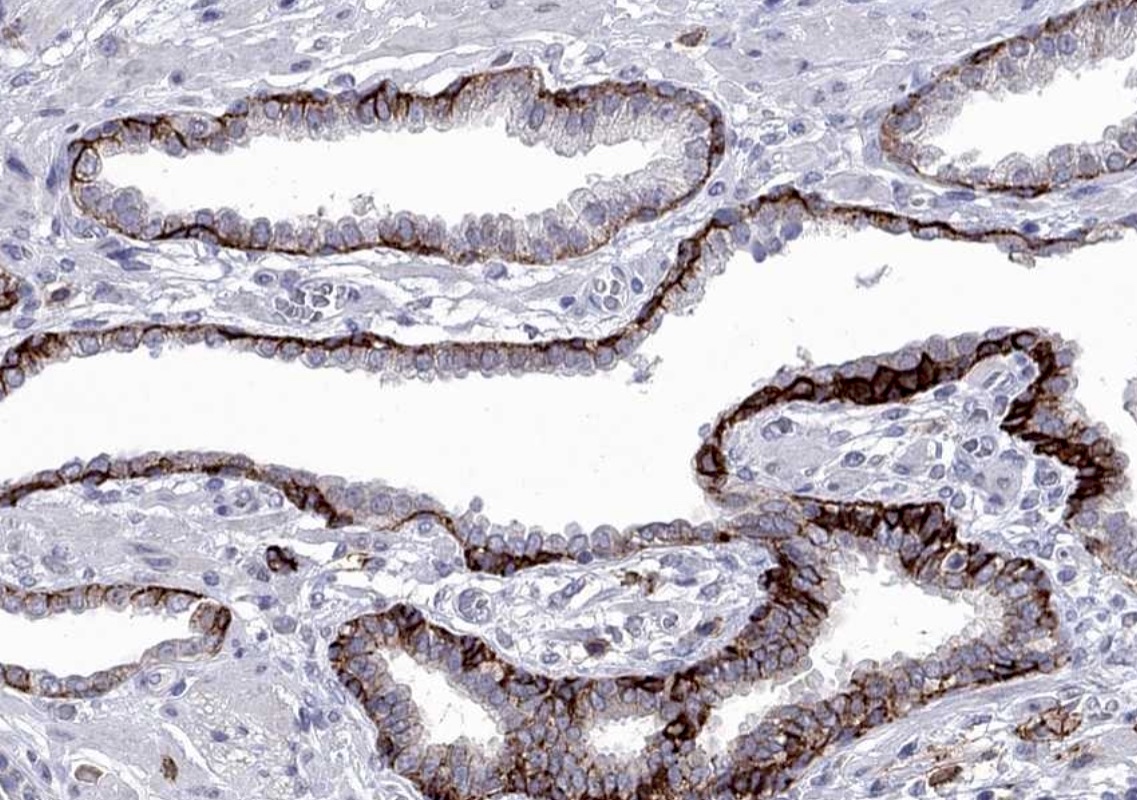
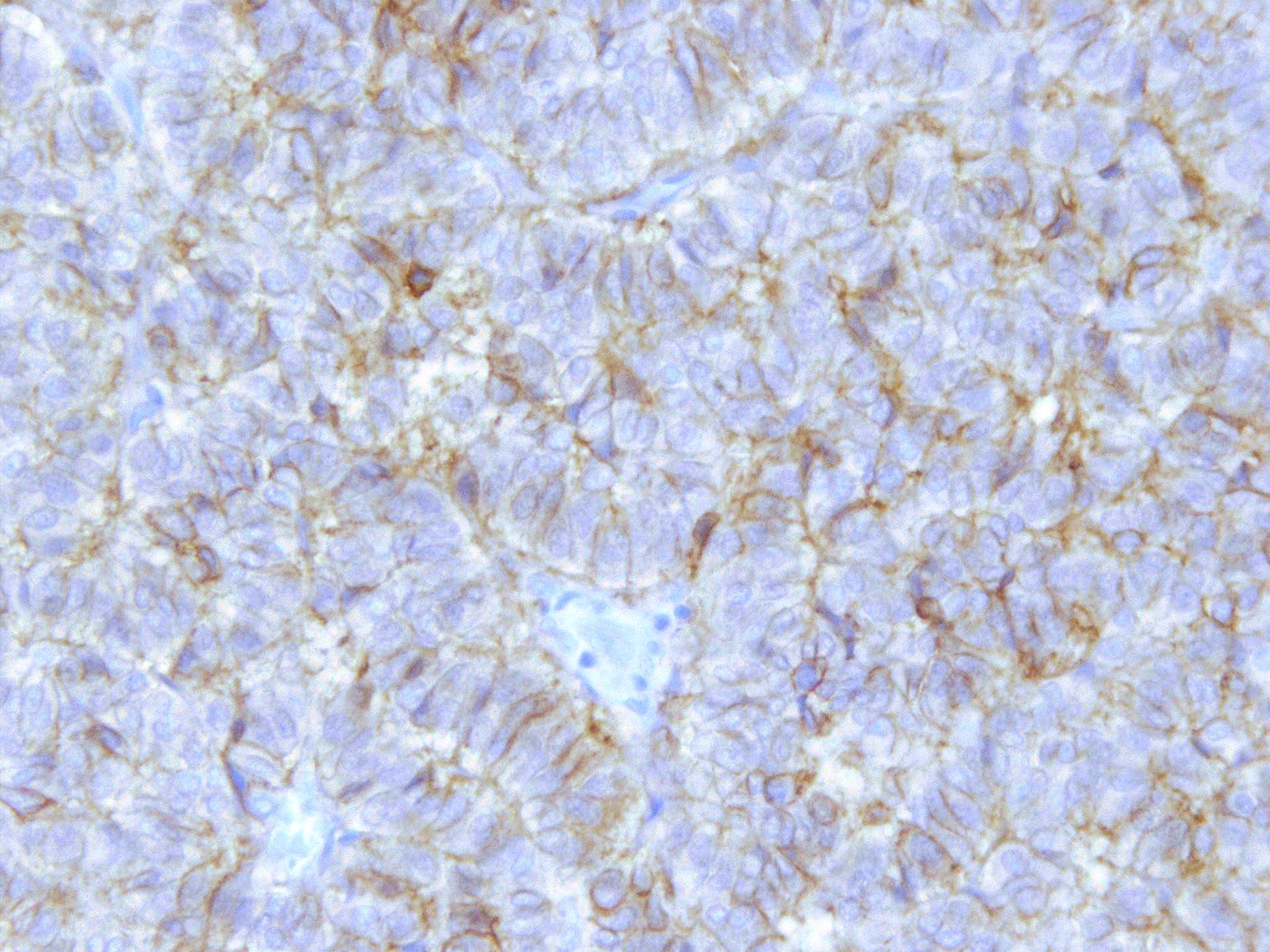
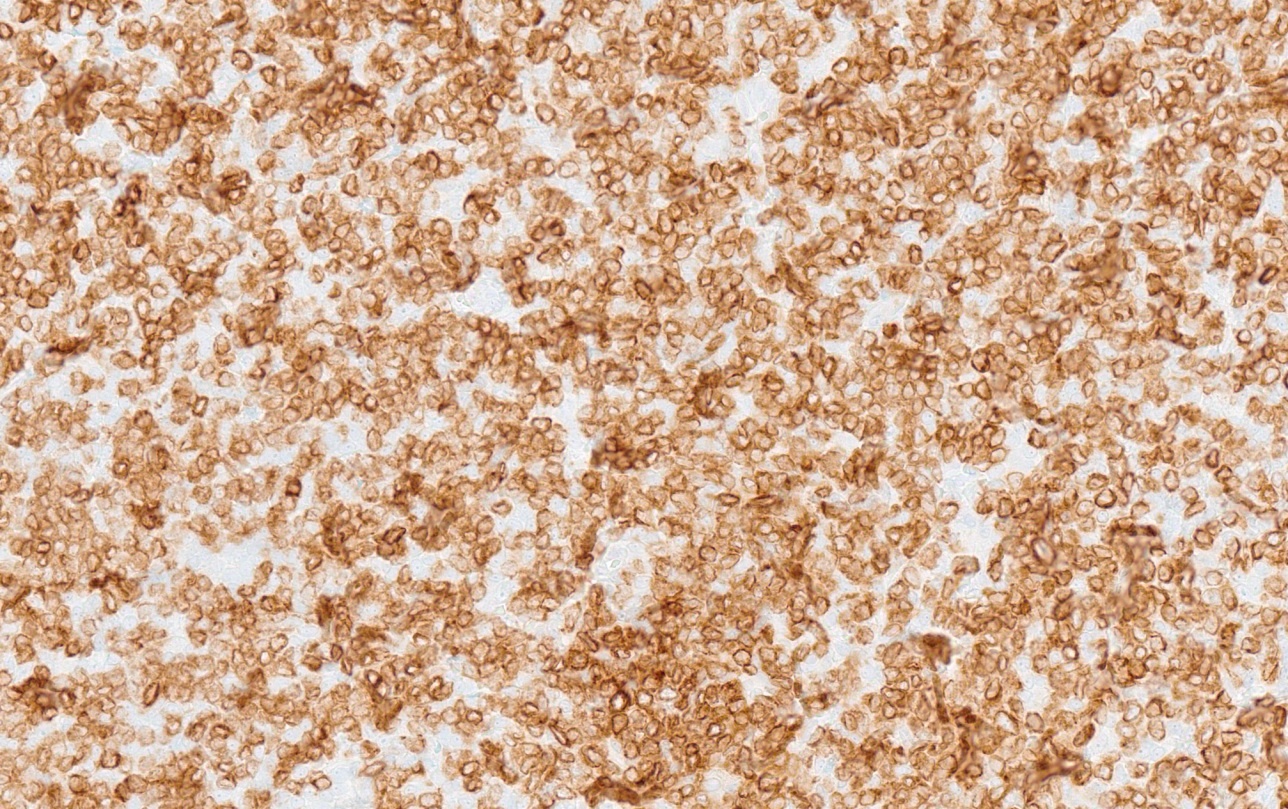
- Normally expressed in the proximal renal tubules and bile canaliculi; it is expressed predominantly as a brush border pattern in proximal renal tubules, accompanied often with some weak / blush granular cytoplasmic staining
- Cytoplasmic and brush border expression using ABCC2 knock out validated monoclonal antibody in papillary renal carcinoma (Hum Pathol 2022;120:57)
- Quantity of brush border staining is shown to be significant in predicting survival (USCAP 2023 Abstracts: Genitourinary Pathology (Including Renal Tumors) [Accessed 25 July 2023])
- Additional nuclear staining reported in breast, ovary and fallopian tube (Pathol Oncol Res 2012;18:331, Clin Cancer Res 2006;12:7149, Arch Gynecol Obstet 2013;287:563)
Uses by pathologists
- Papillary renal cell carcinoma: pattern of ABCC2 expression provides prognostic stratification
- Latest evidence shows that only brush border expression predicts disease progression in papillary renal cell carcinoma (Am J Surg Pathol 2017;41:1618, Hum Pathol 2022;120:57, USCAP 2023 Abstracts: Genitourinary Pathology (Including Renal Tumors) [Accessed 25 July 2023])
- There is some evidence that ABCC2 expression might have predictive value in papillary renal cell carcinoma (Mol Oncol 2018;12:1673)
- Dubin-Johnson syndrome related cholestasis: loss of MRP2 / ABCC2 in canalicular membranes of hepatocytes
Prognostic factors
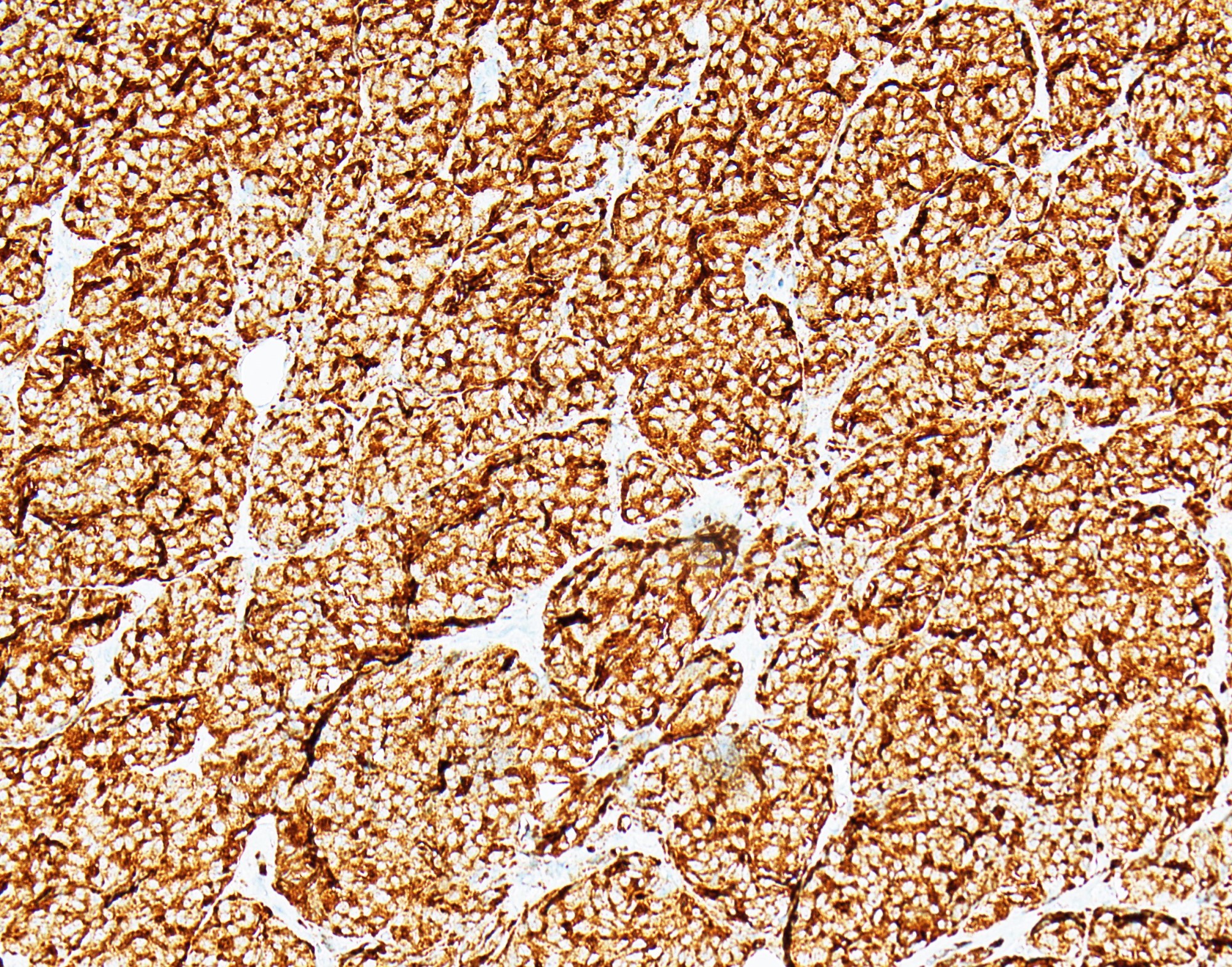
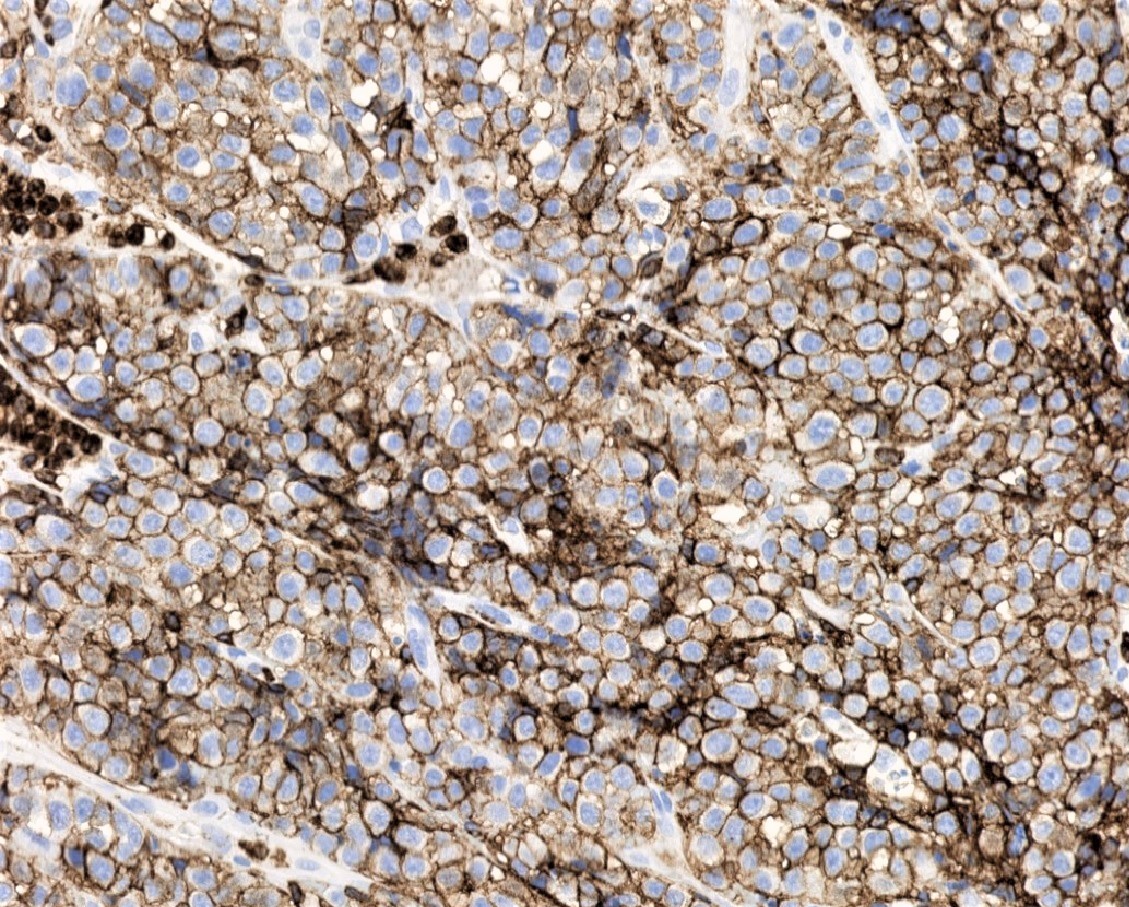
- Papillary renal cell carcinoma can be prognostically stratified using monoclonal knock out validated ABCC2 IHC (Am J Surg Pathol 2017;41:1618, Eur Urol Focus 2018;4:740, Hum Pathol 2022;120:57, USCAP 2023 Abstracts: Genitourinary Pathology (Including Renal Tumors) [Accessed 25 July 2023])
- Negative and cytoplasmic staining showing favorable survival outcomes
- Brush border expression associated with poor prognosis
- Prognostic and predictive marker for other tumors
- ABCC2 immunohistochemistry is reported to have prognostic value and potential predictive value (associated with chemotherapy resistance) in colon carcinoma, pancreatic carcinoma, ovarian carcinoma, fallopian tube carcinoma and breast carcinoma (Gynecol Oncol 2006;100:239, Clin Cancer Res 2000;6:2401, Clin Cancer Res 2006;12:7149, Pathol Oncol Res 2012;18:331, Arch Gynecol Obstet 2013;287:563, Sci Rep 2019;9:19782)
- Possible predictive value in metastatic papillary renal cell carcinoma (Mol Oncol 2018;12:1673)
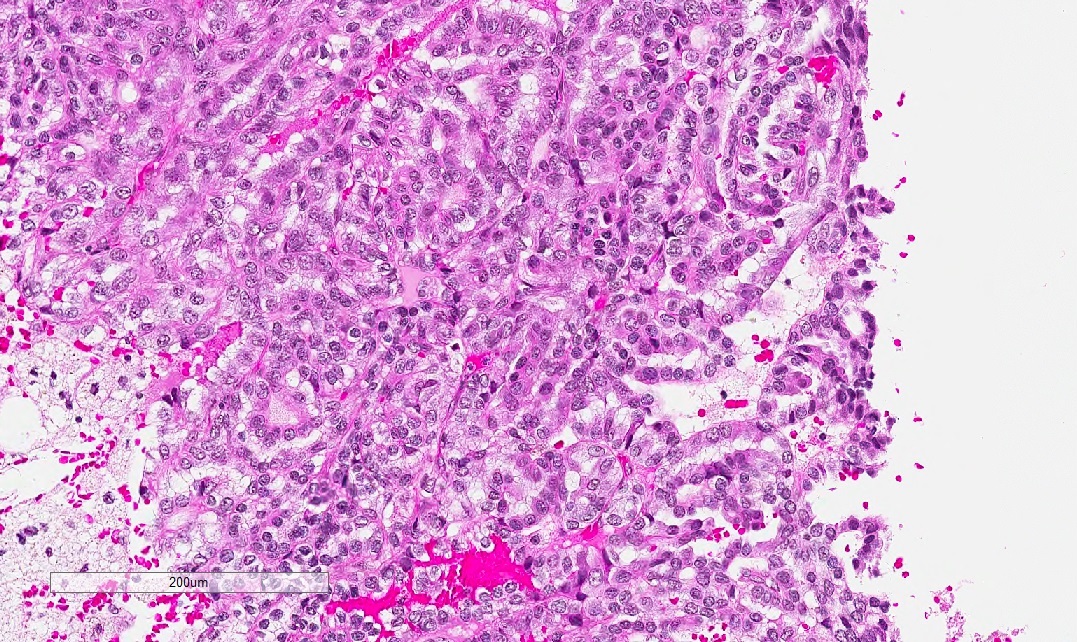
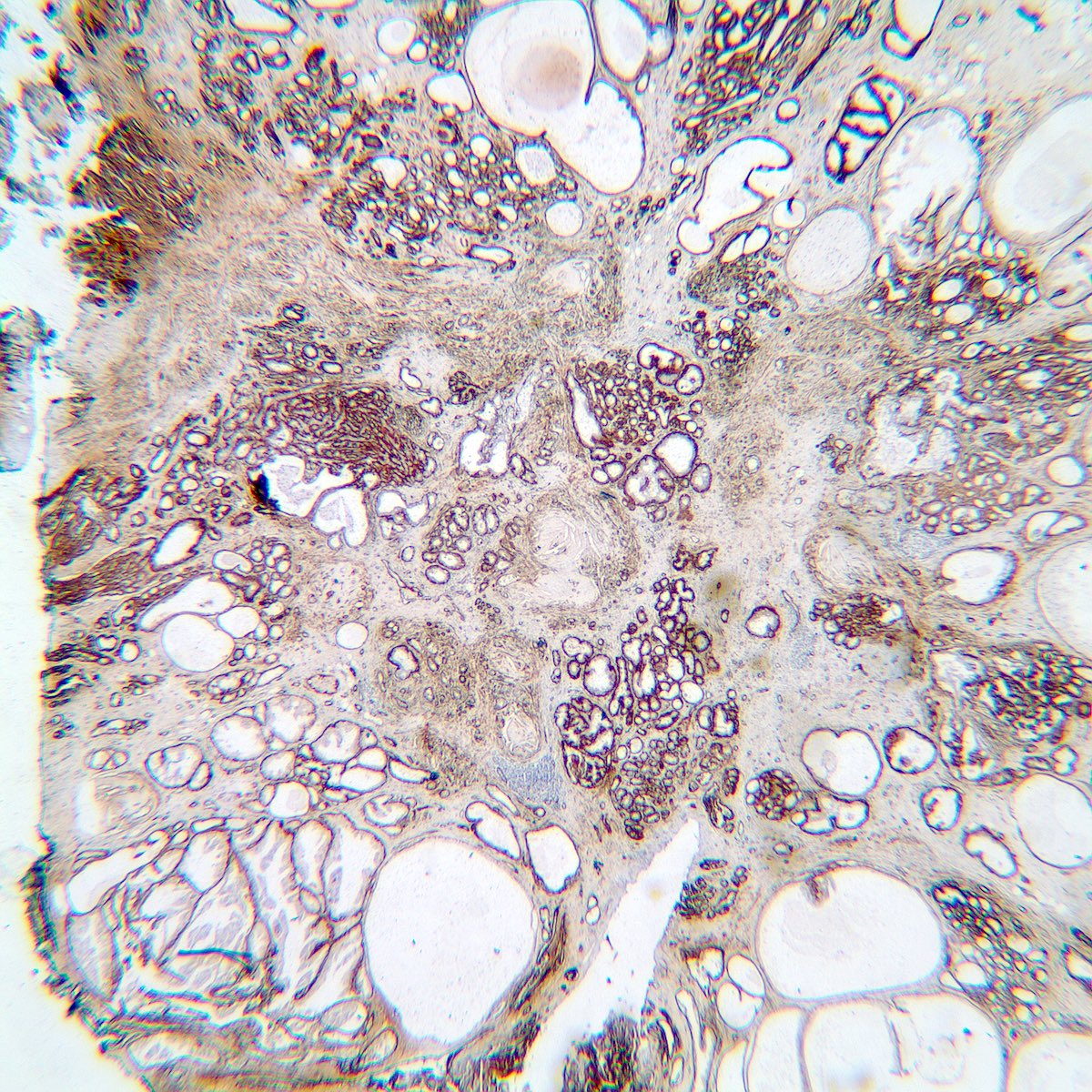
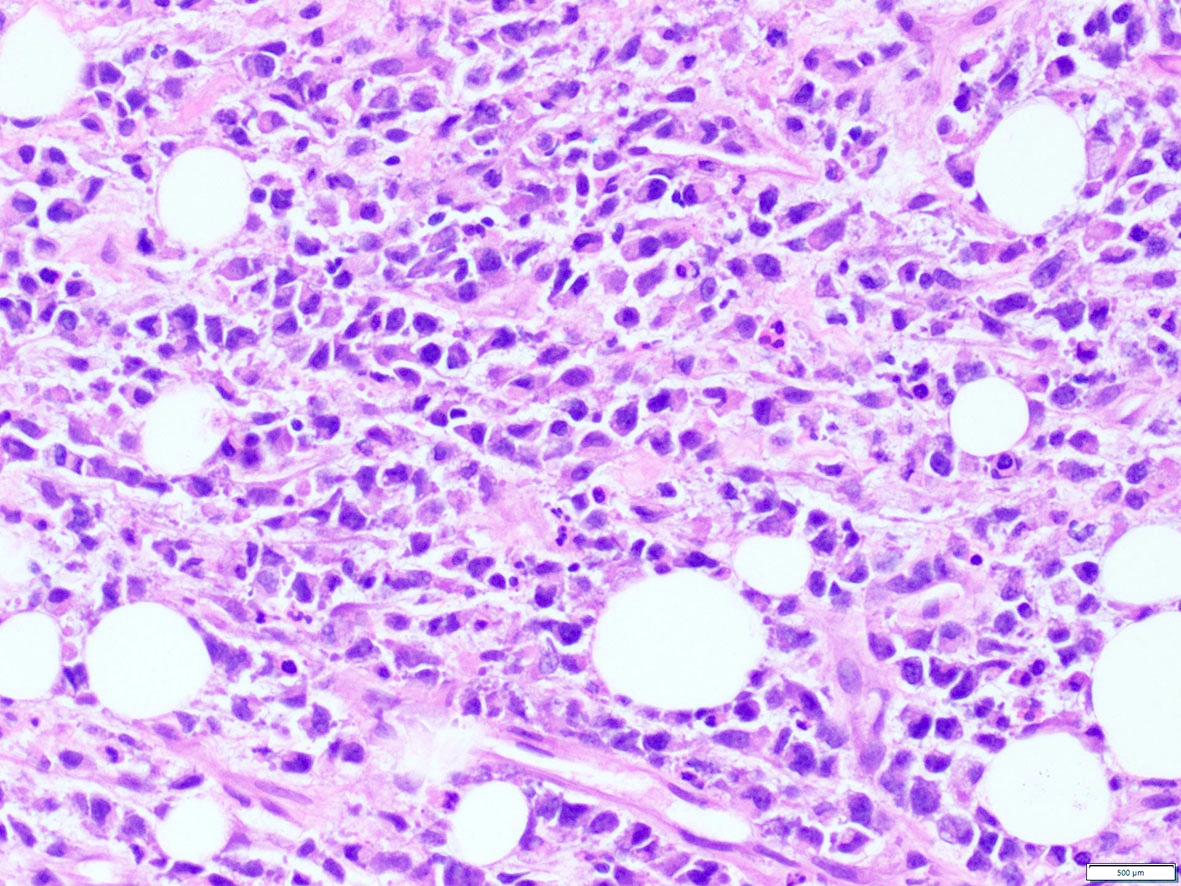
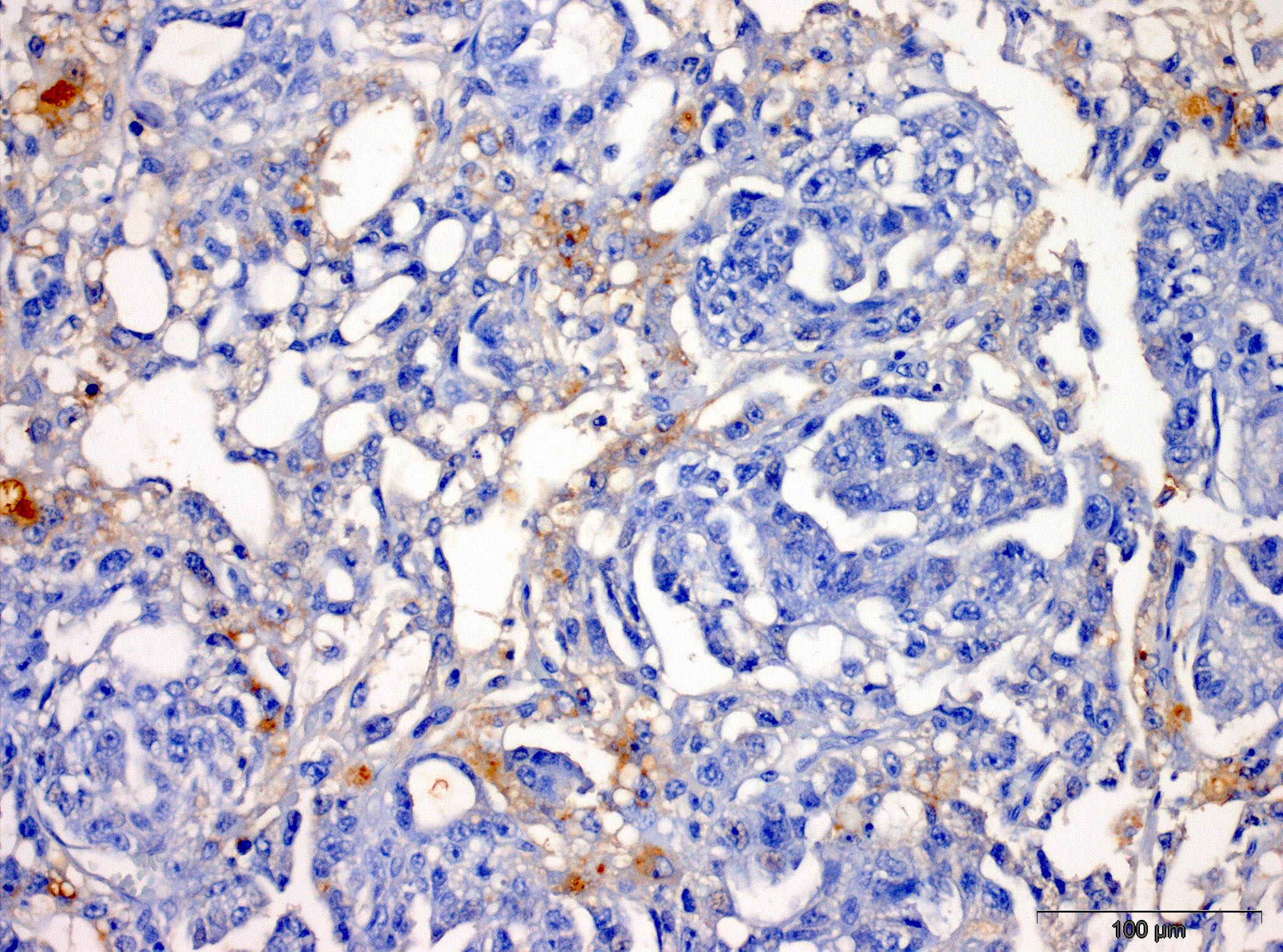
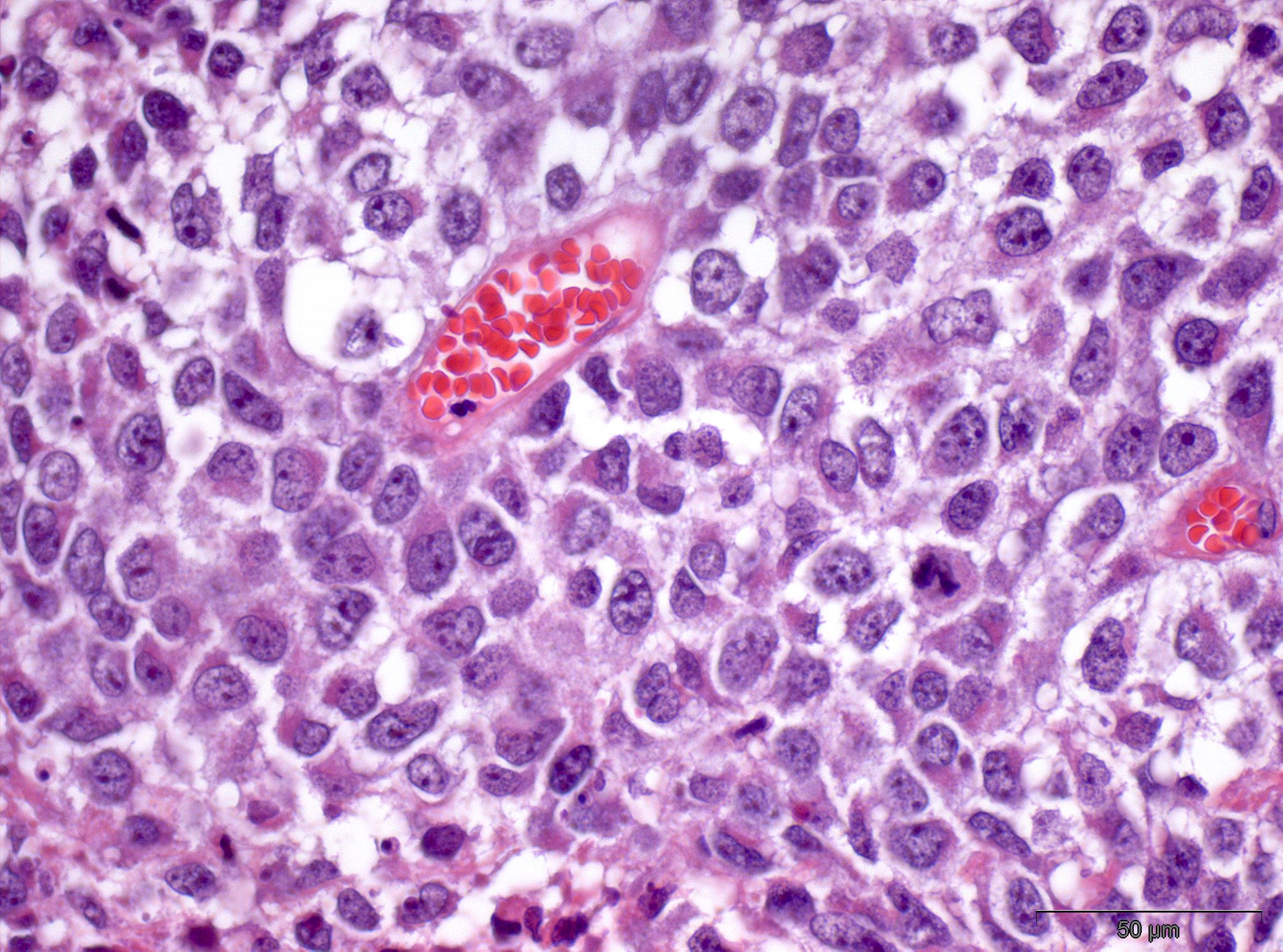
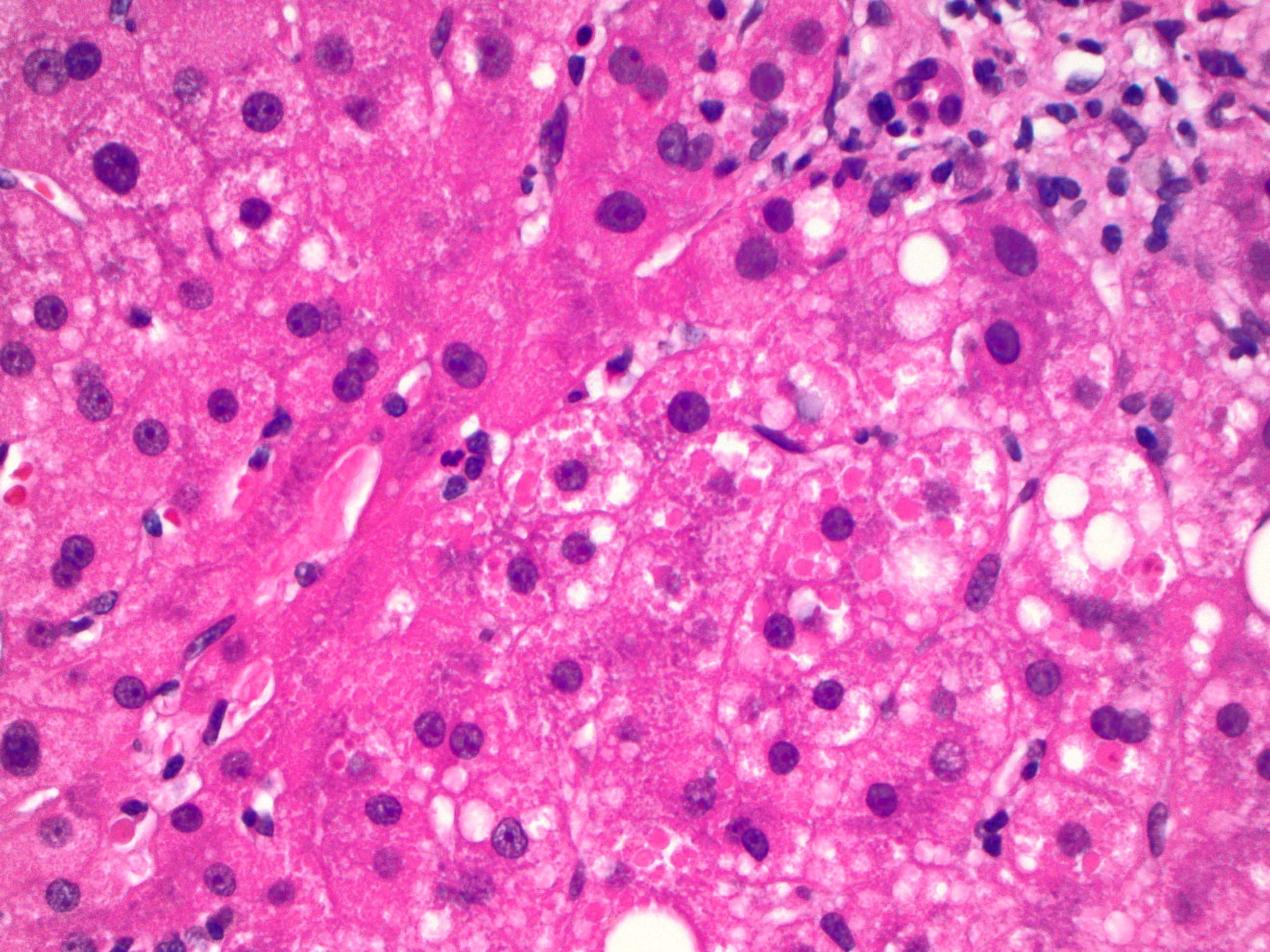
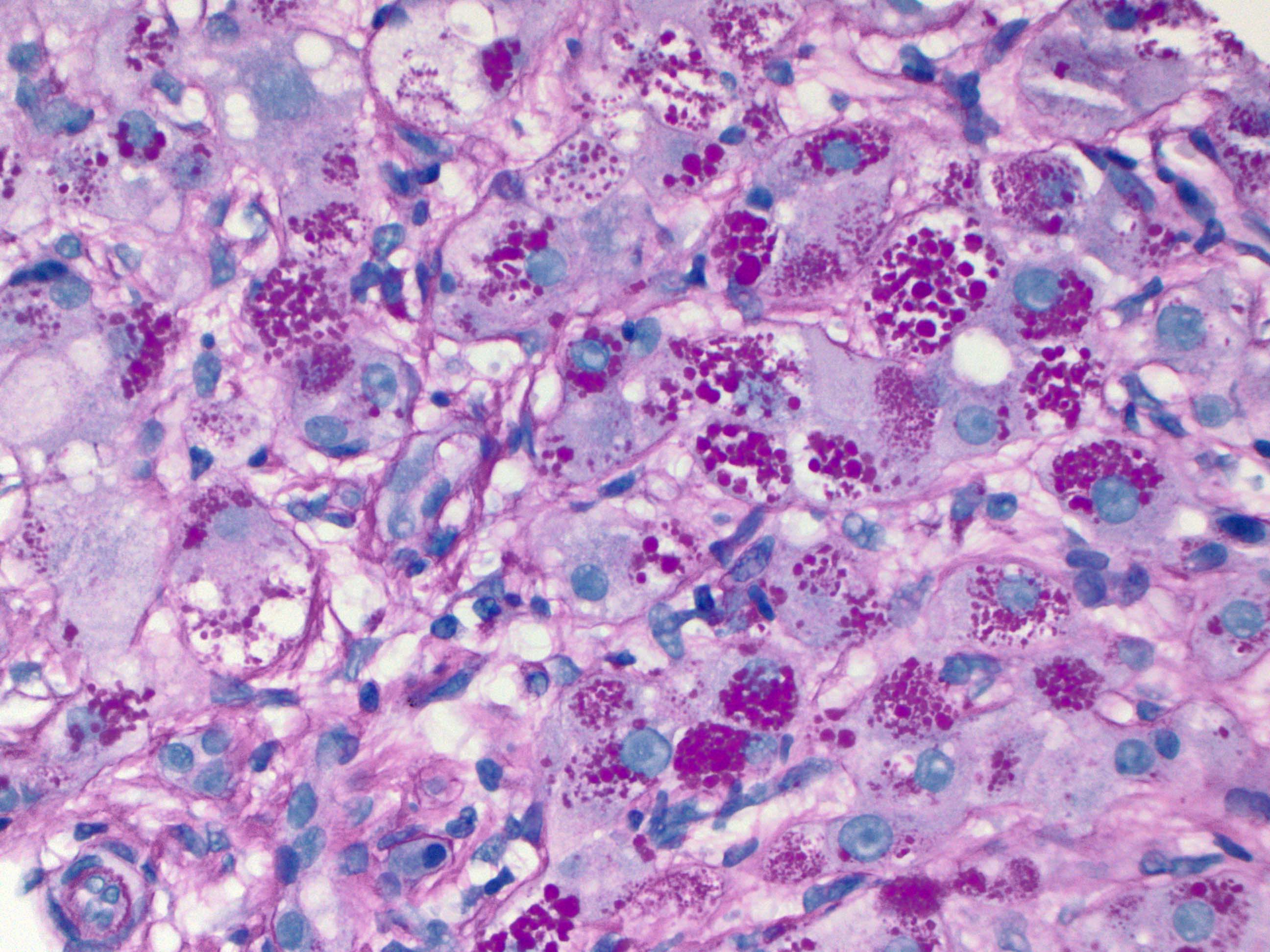
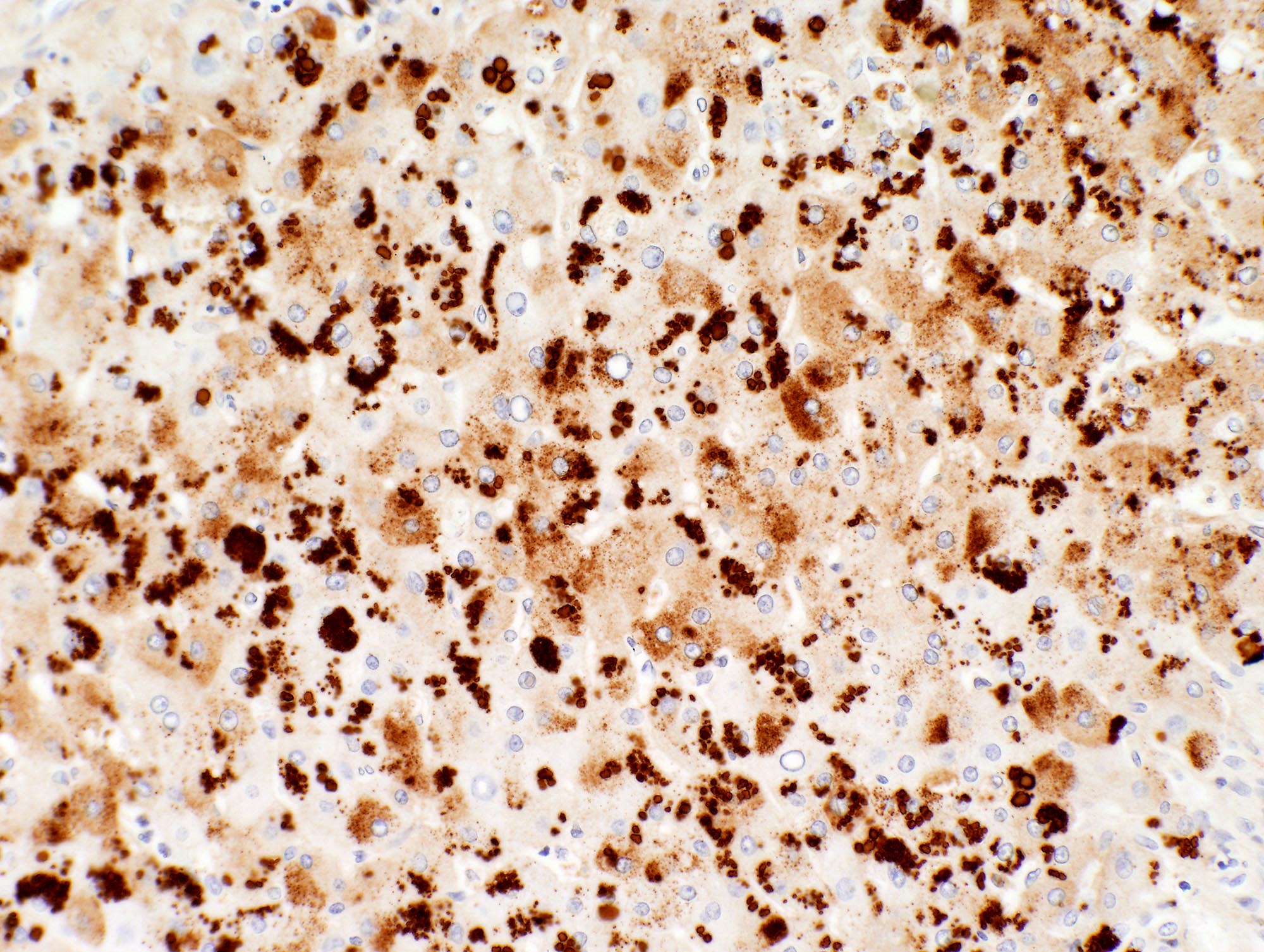
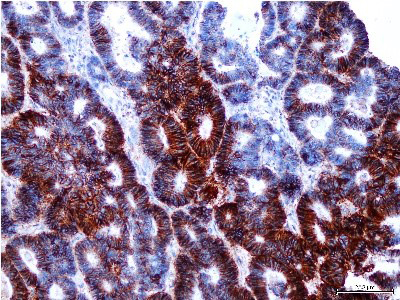
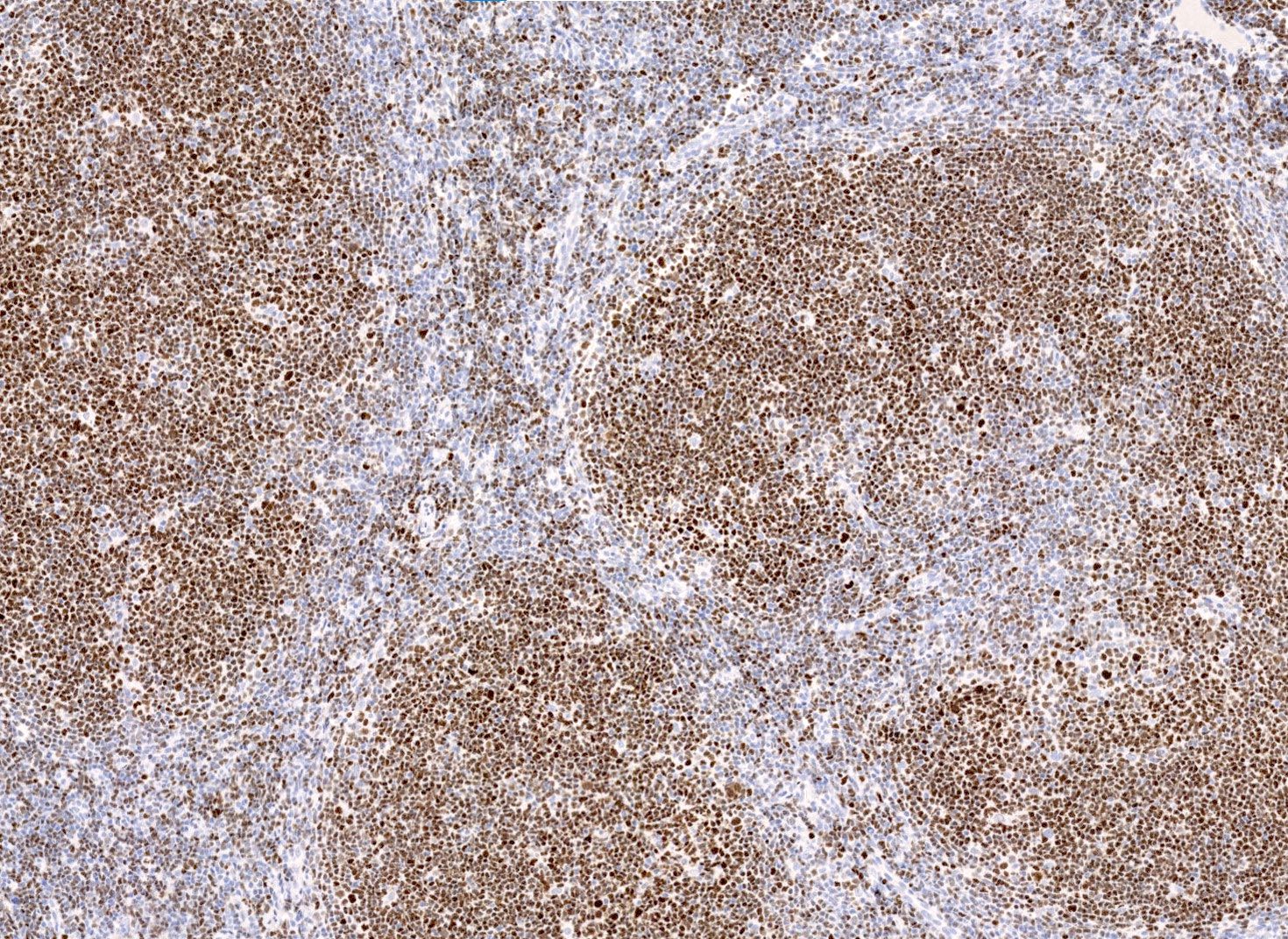
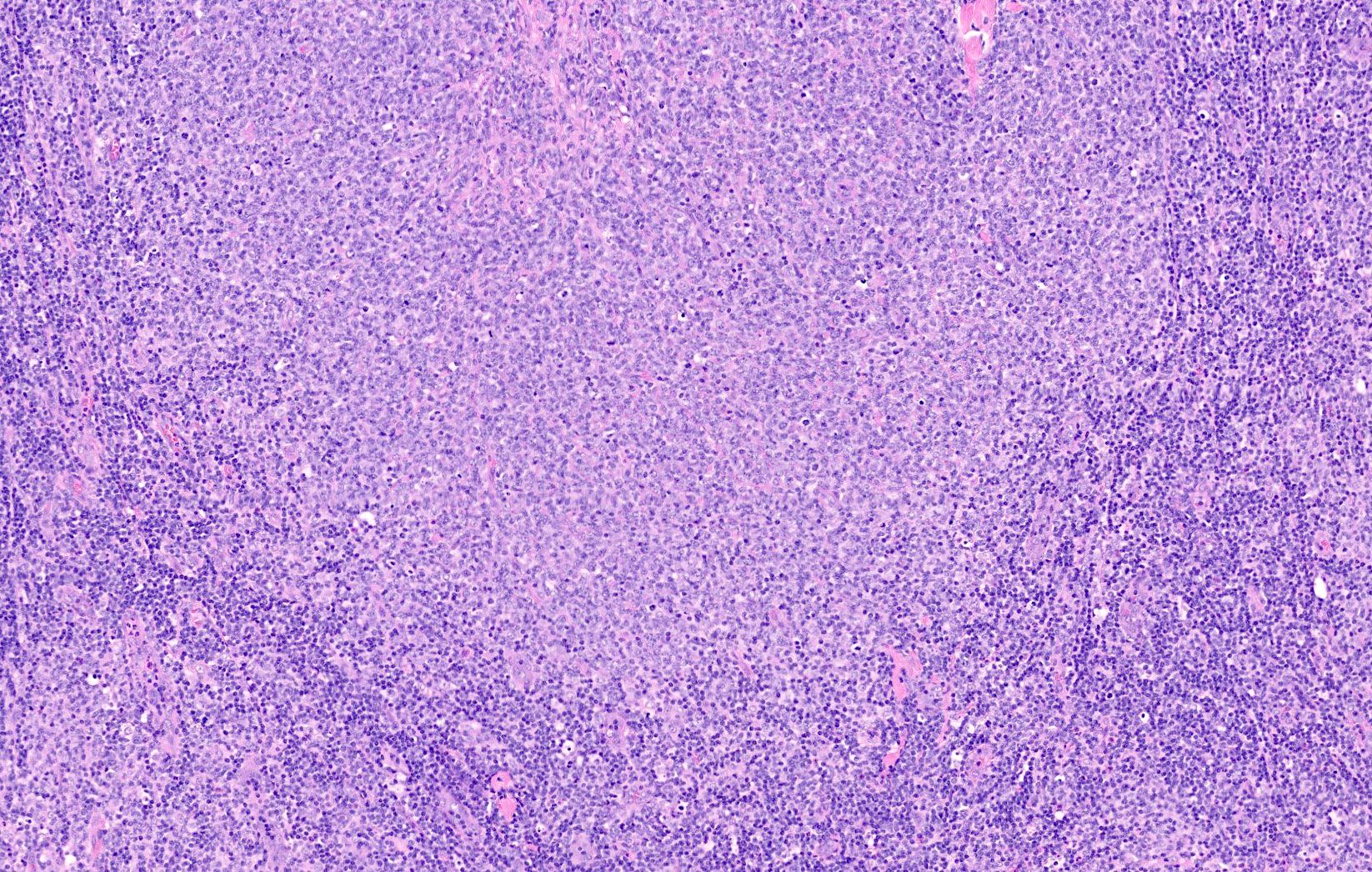
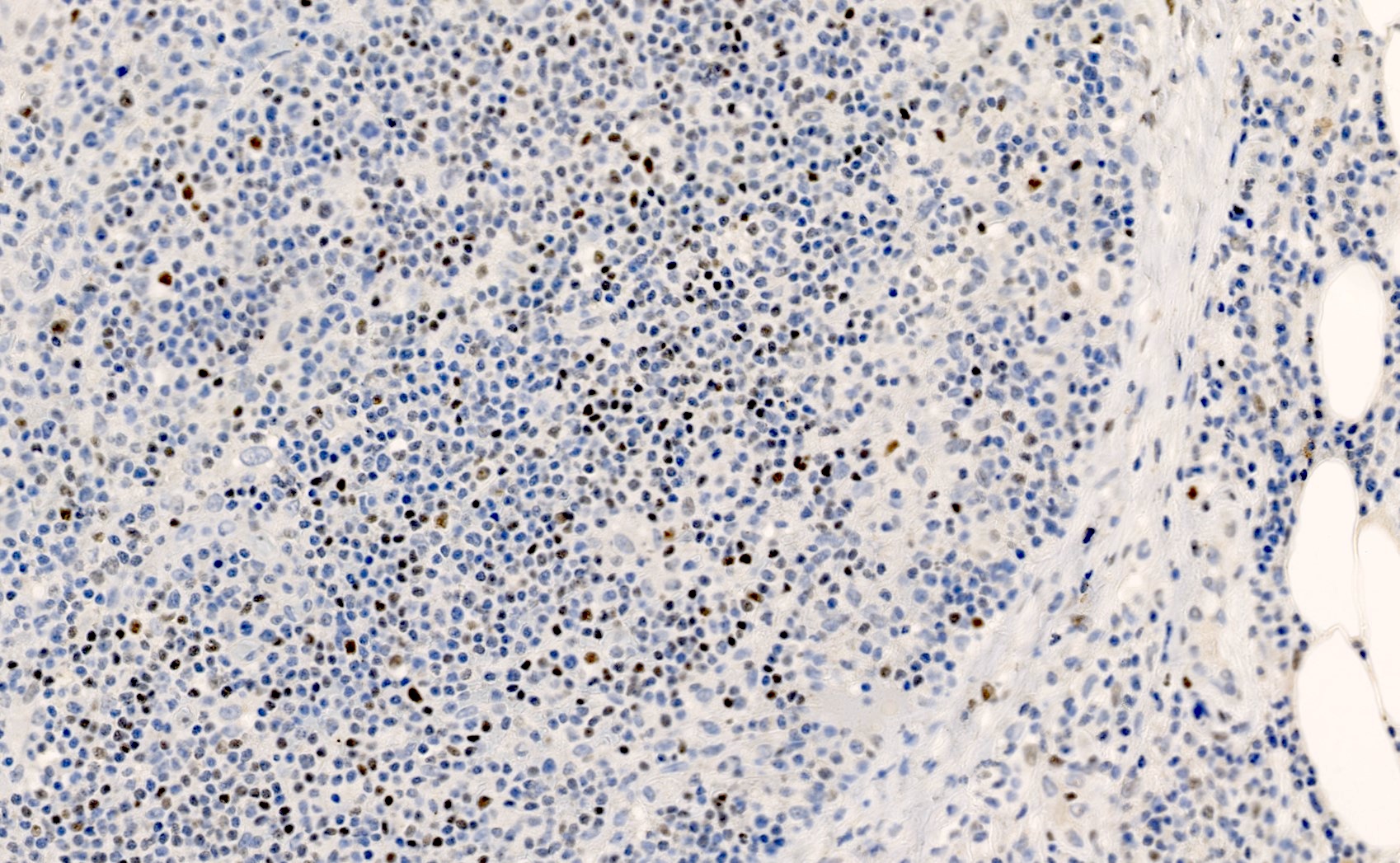
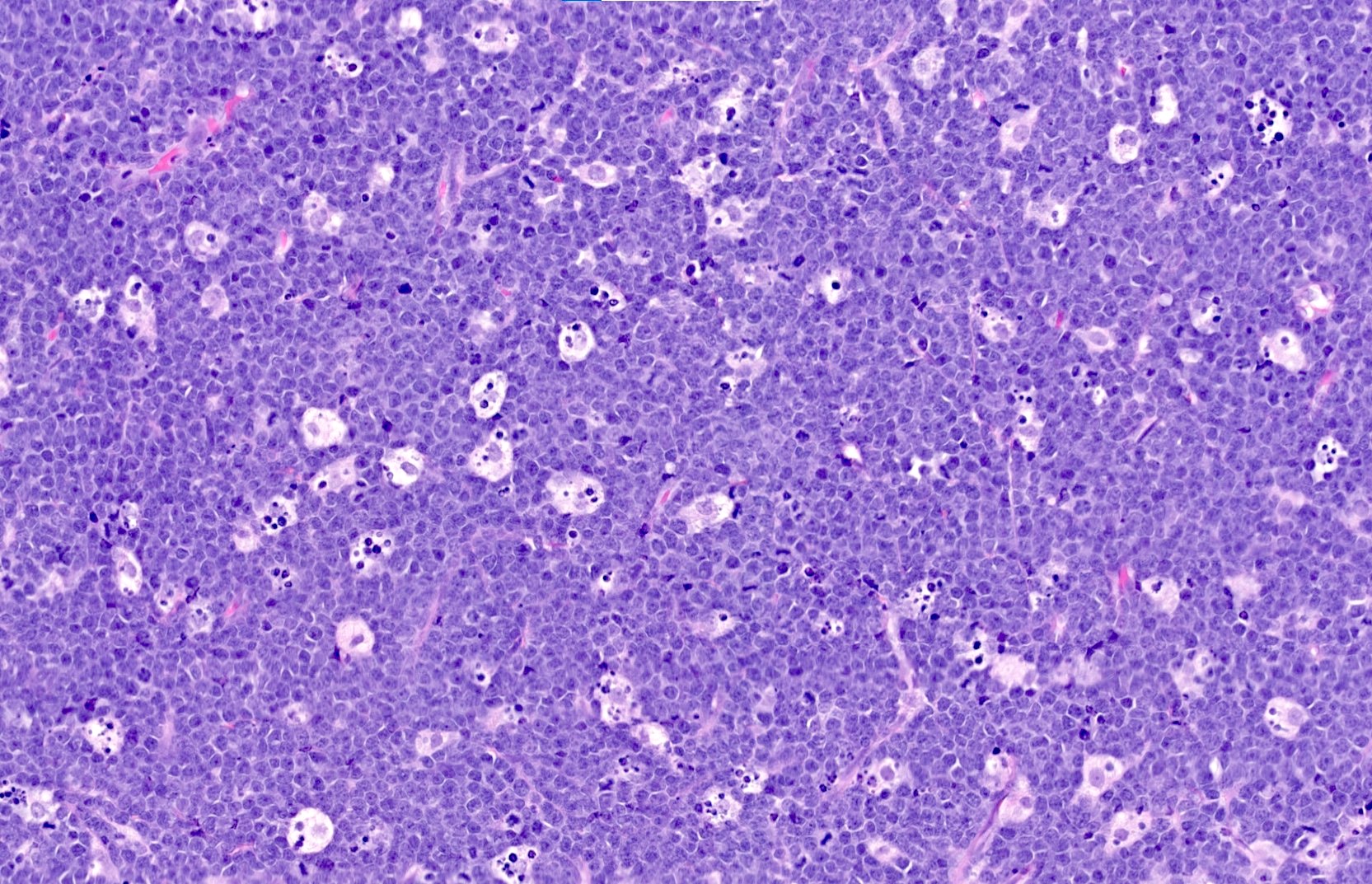
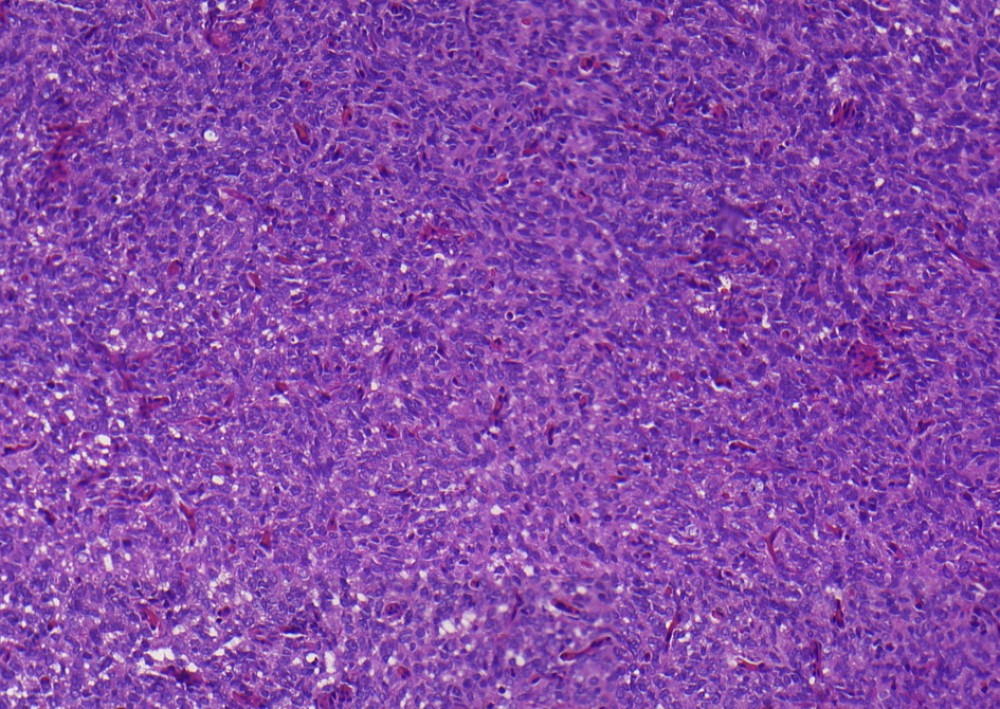
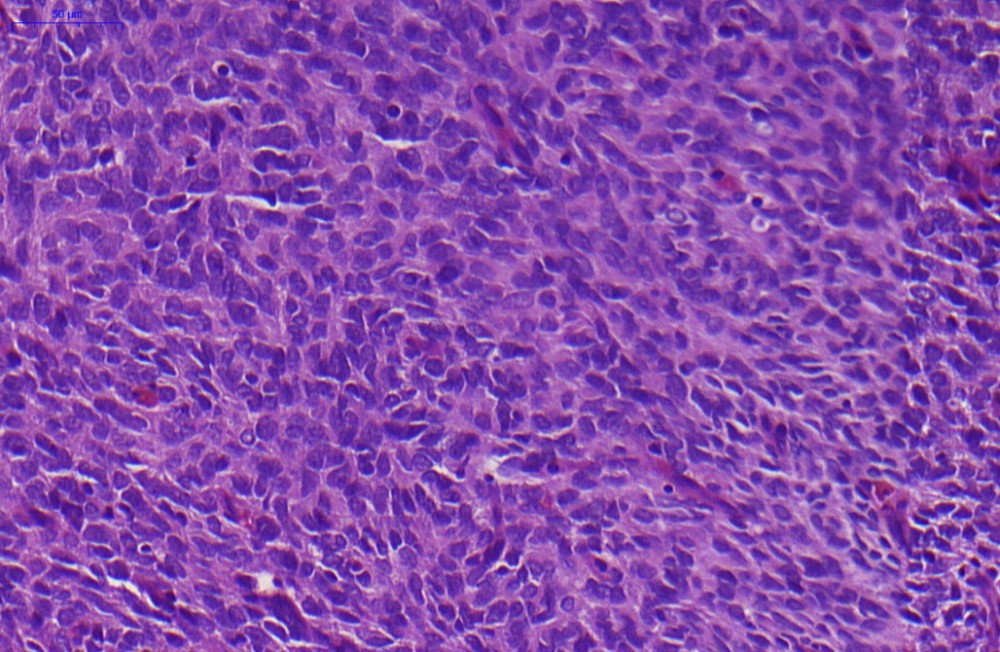
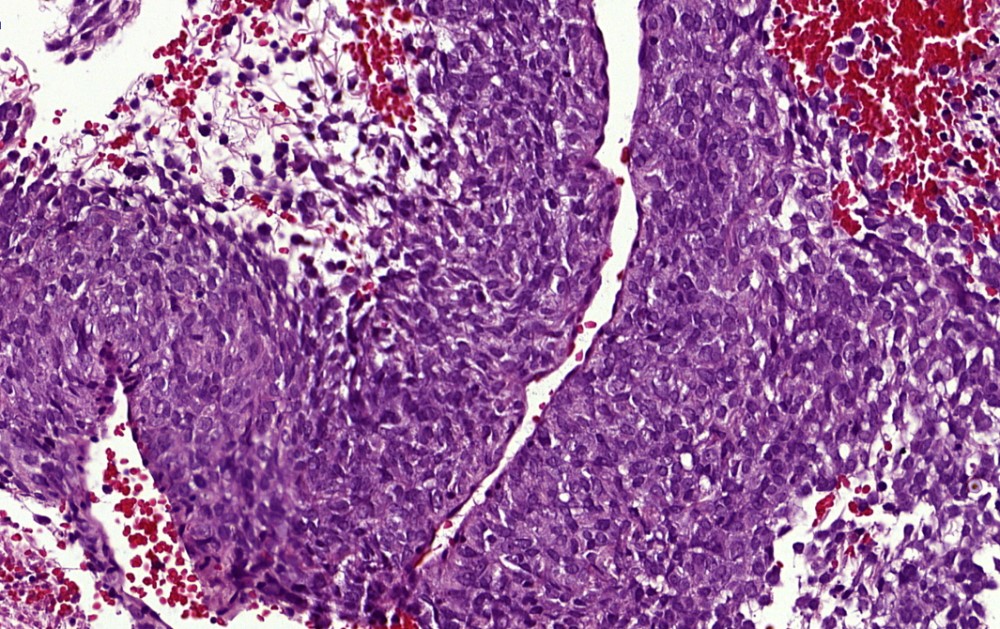
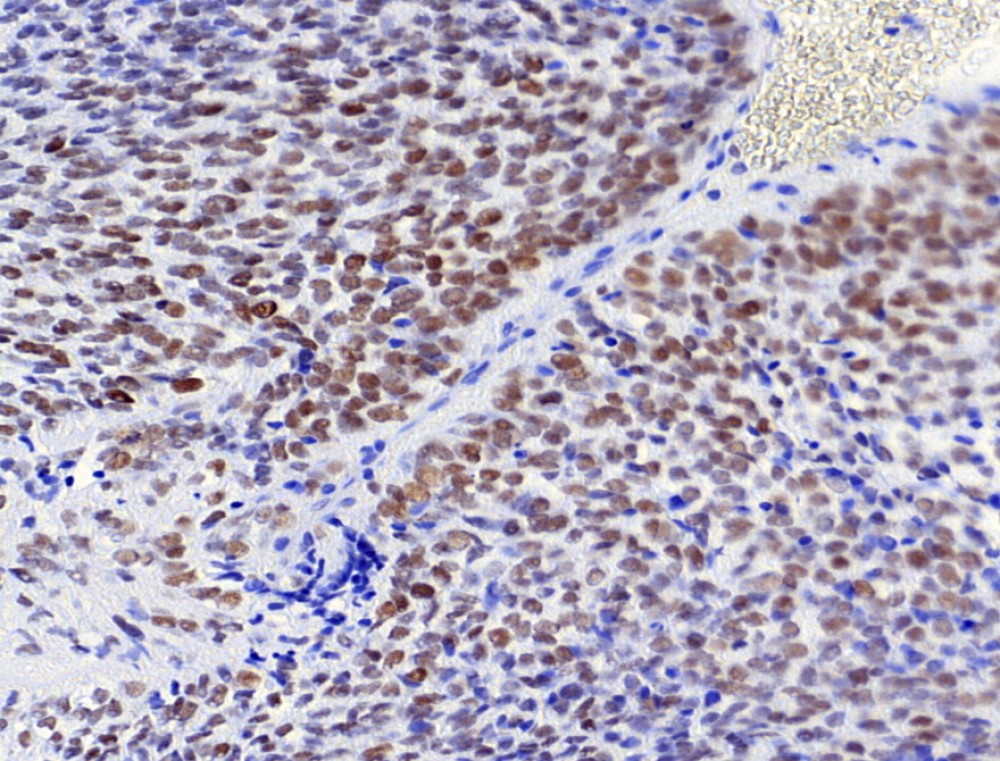
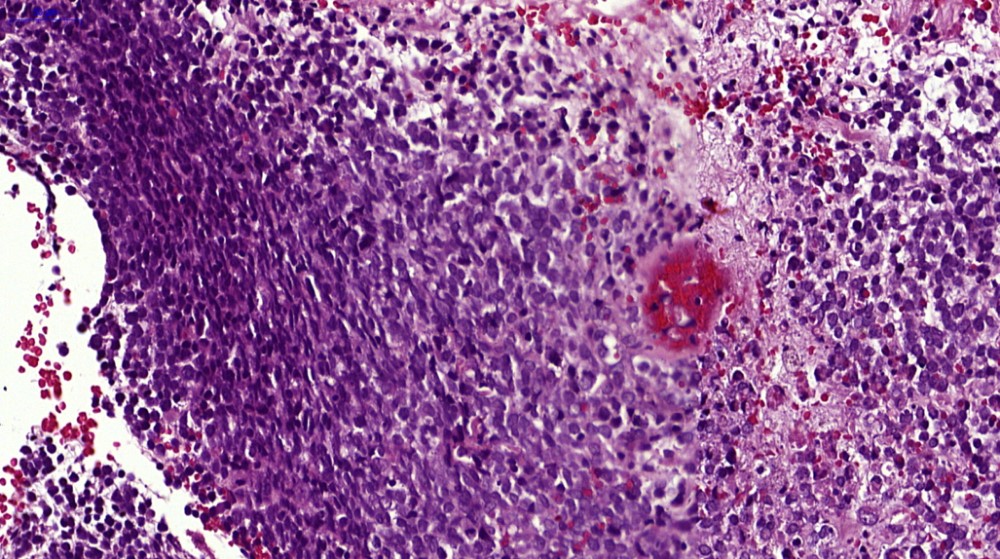
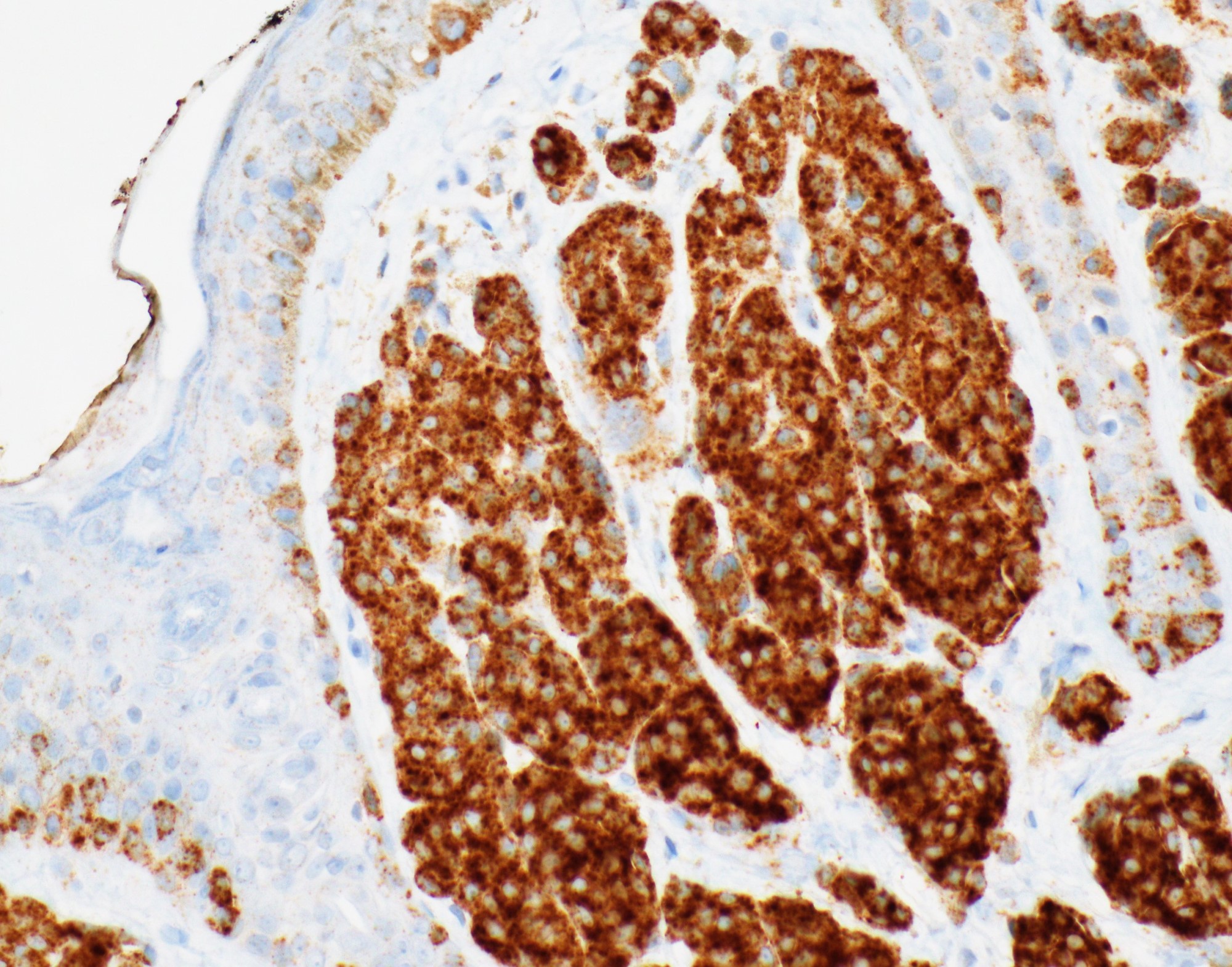
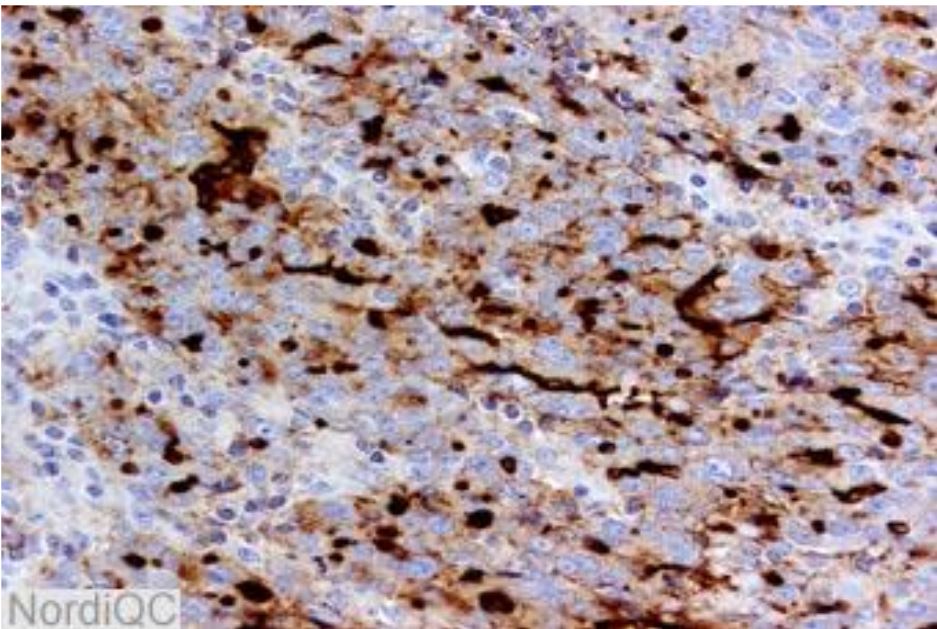
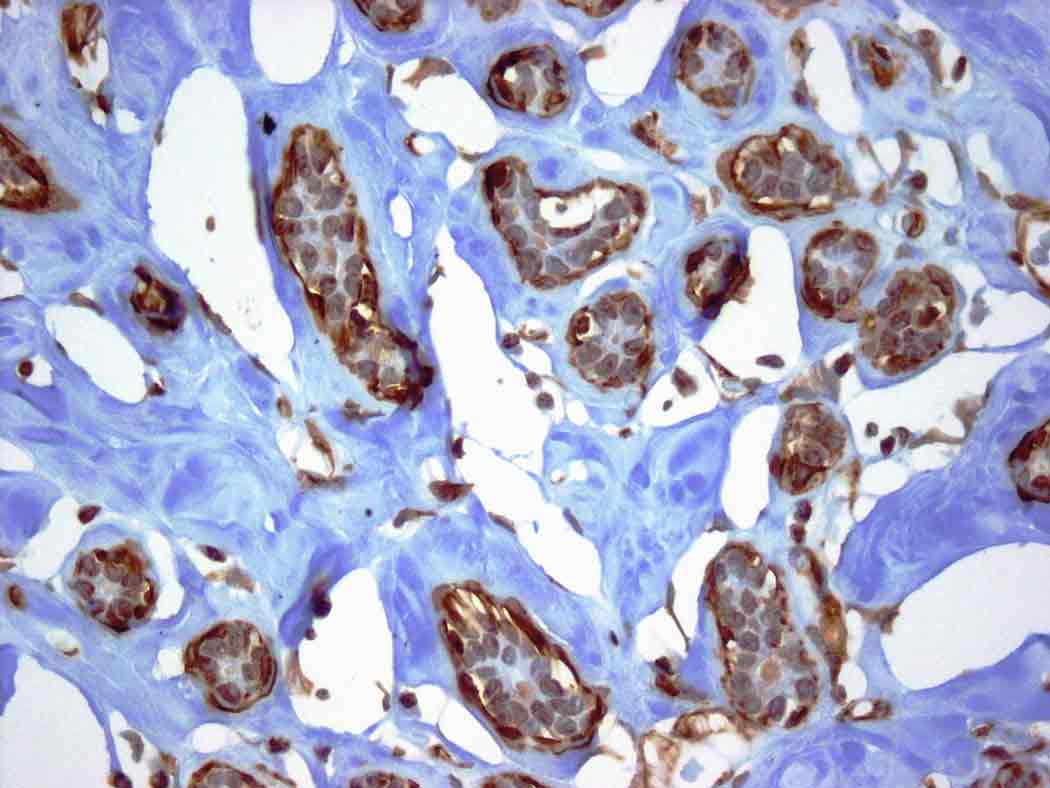
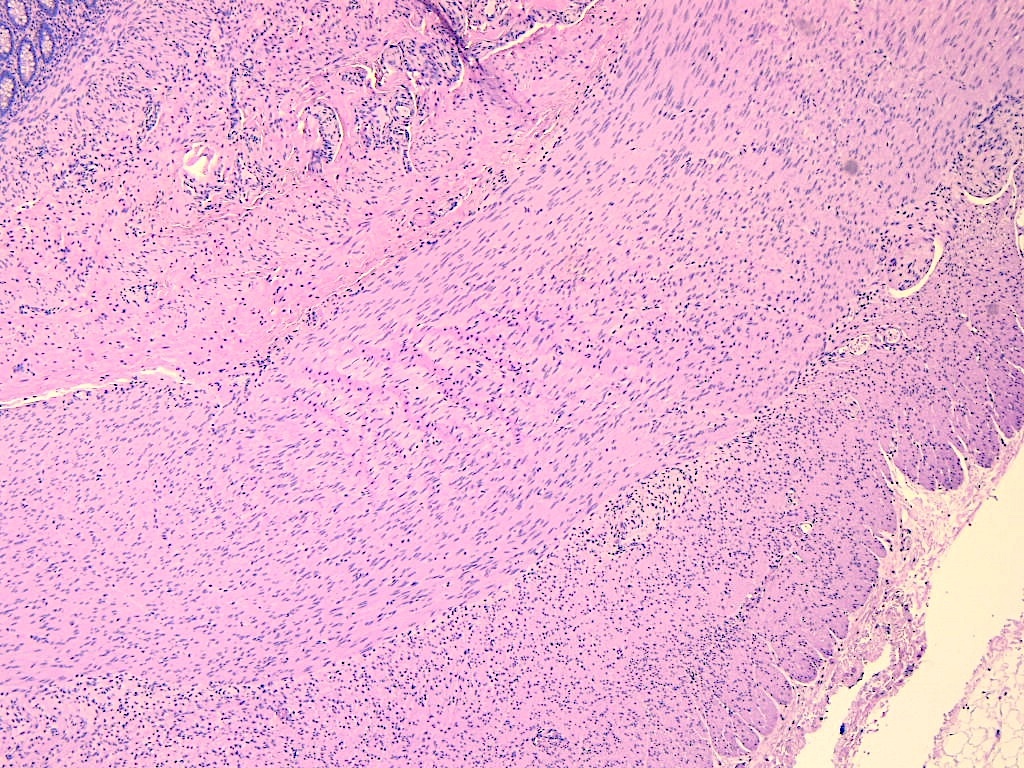
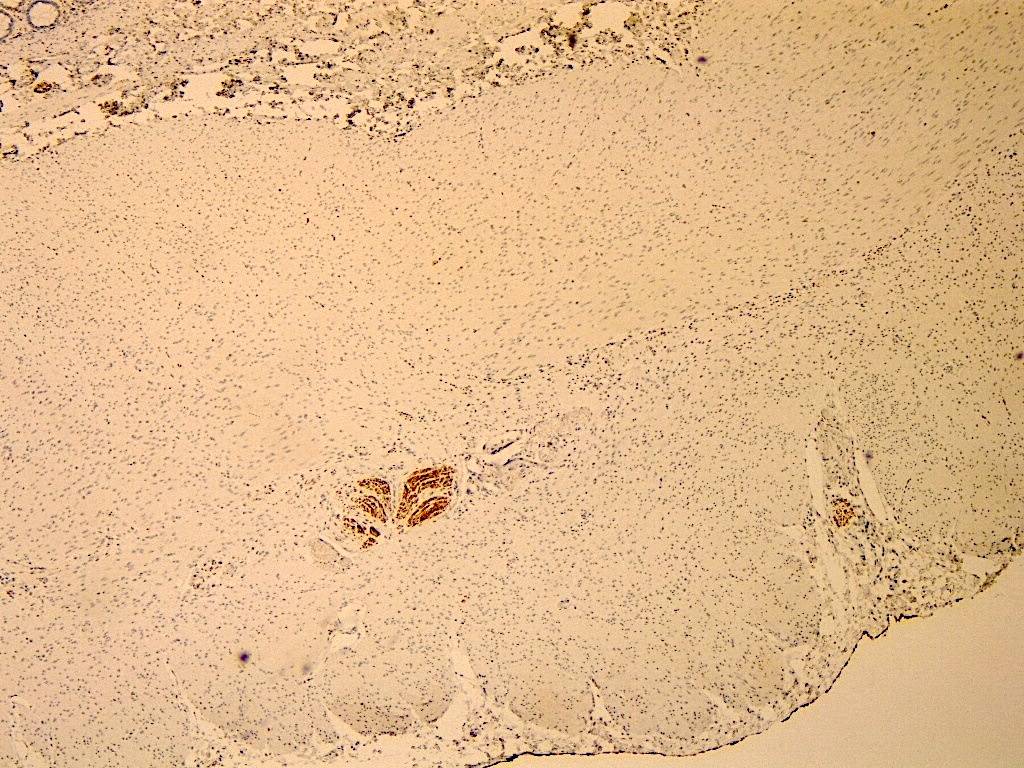
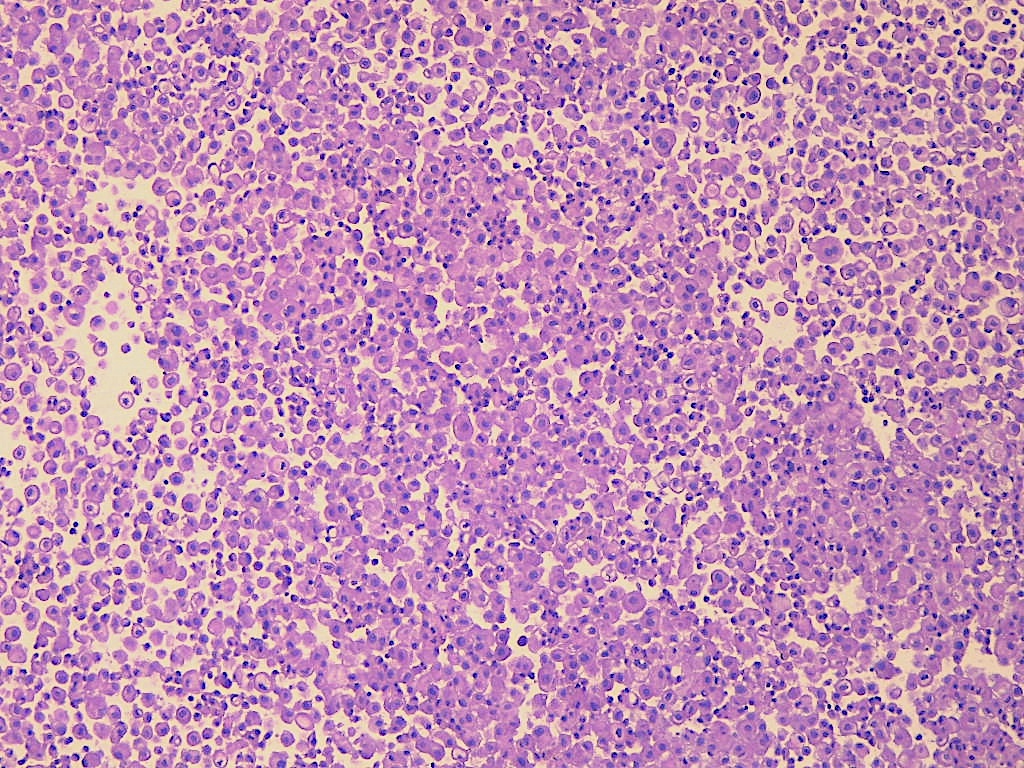
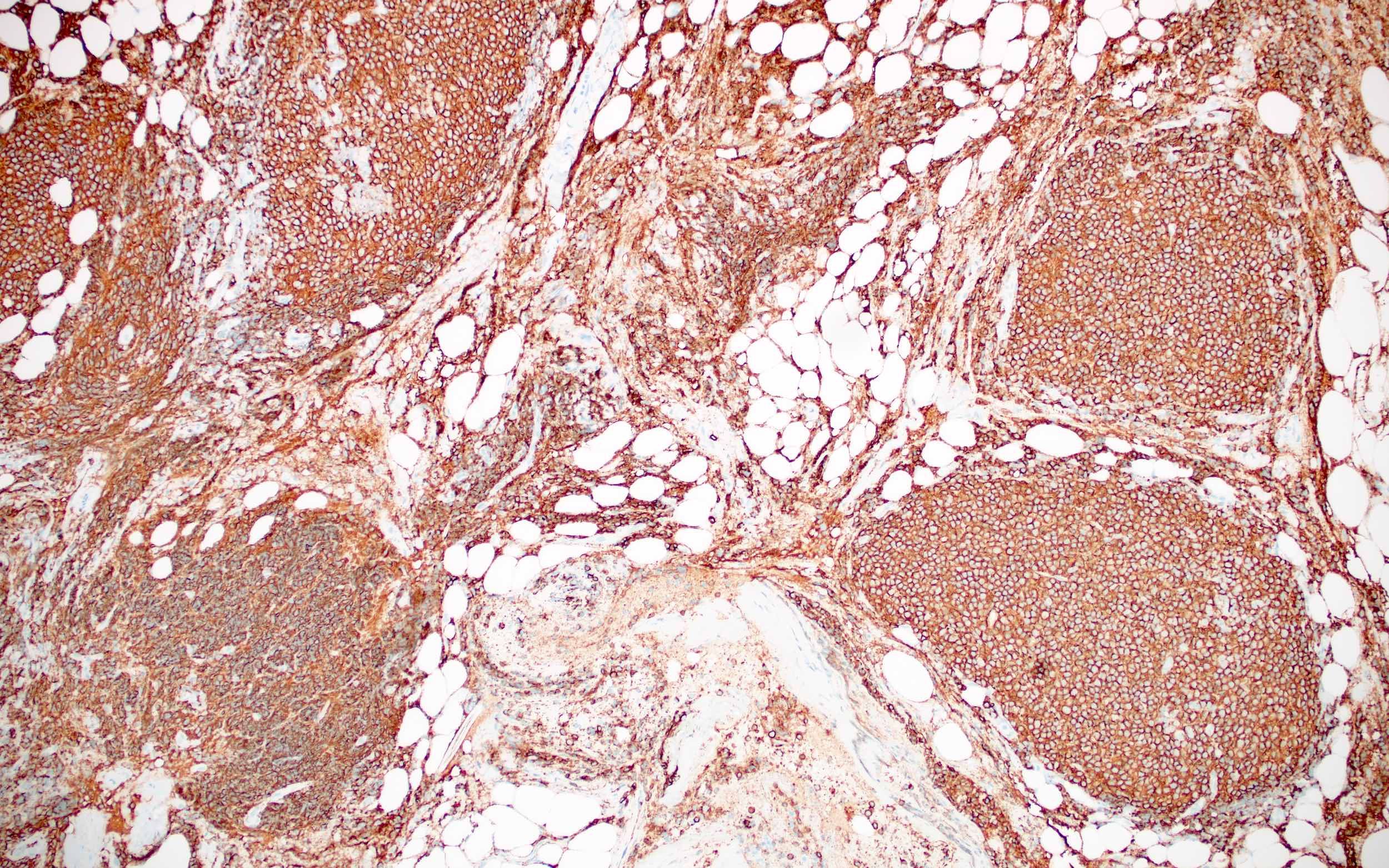
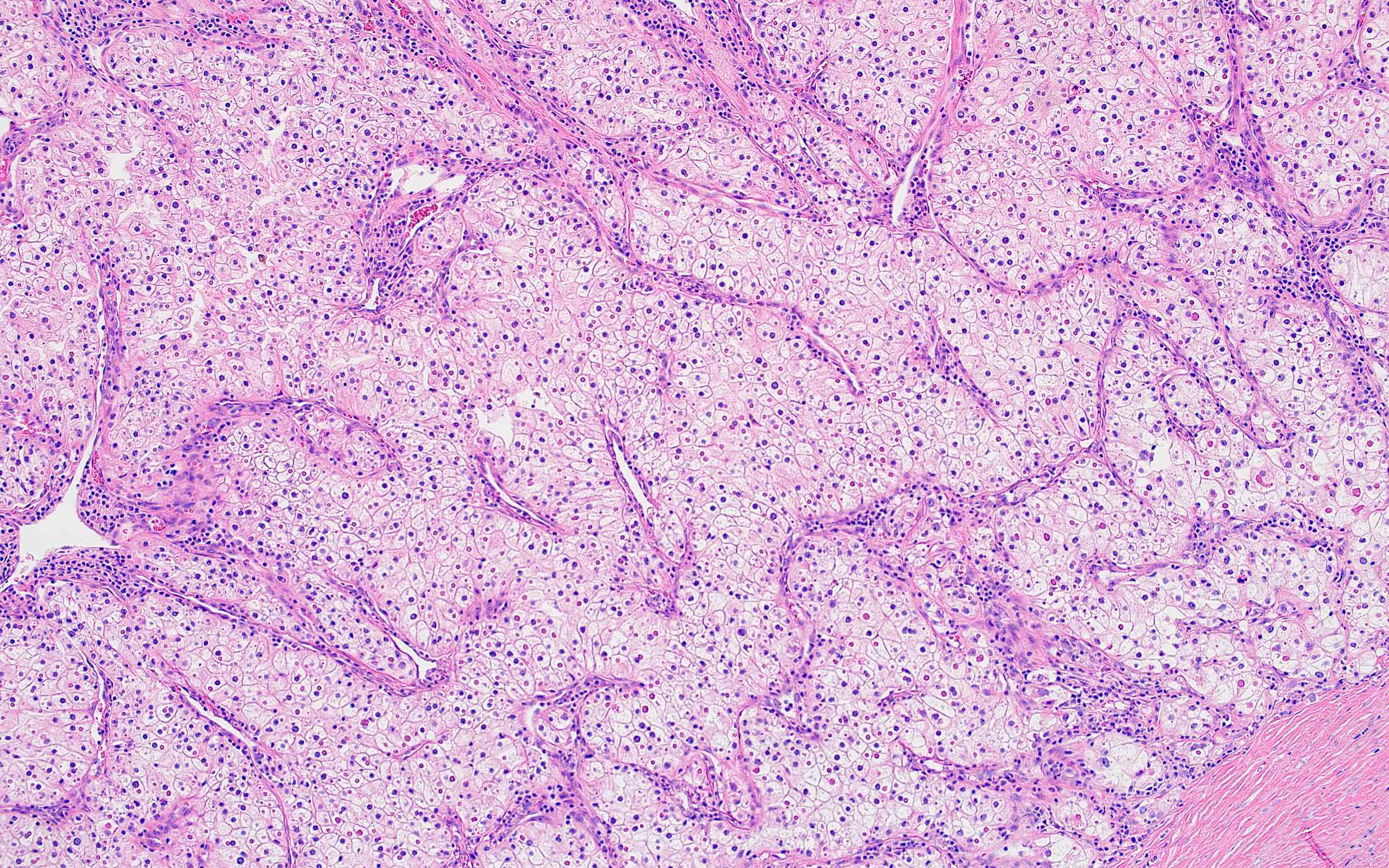
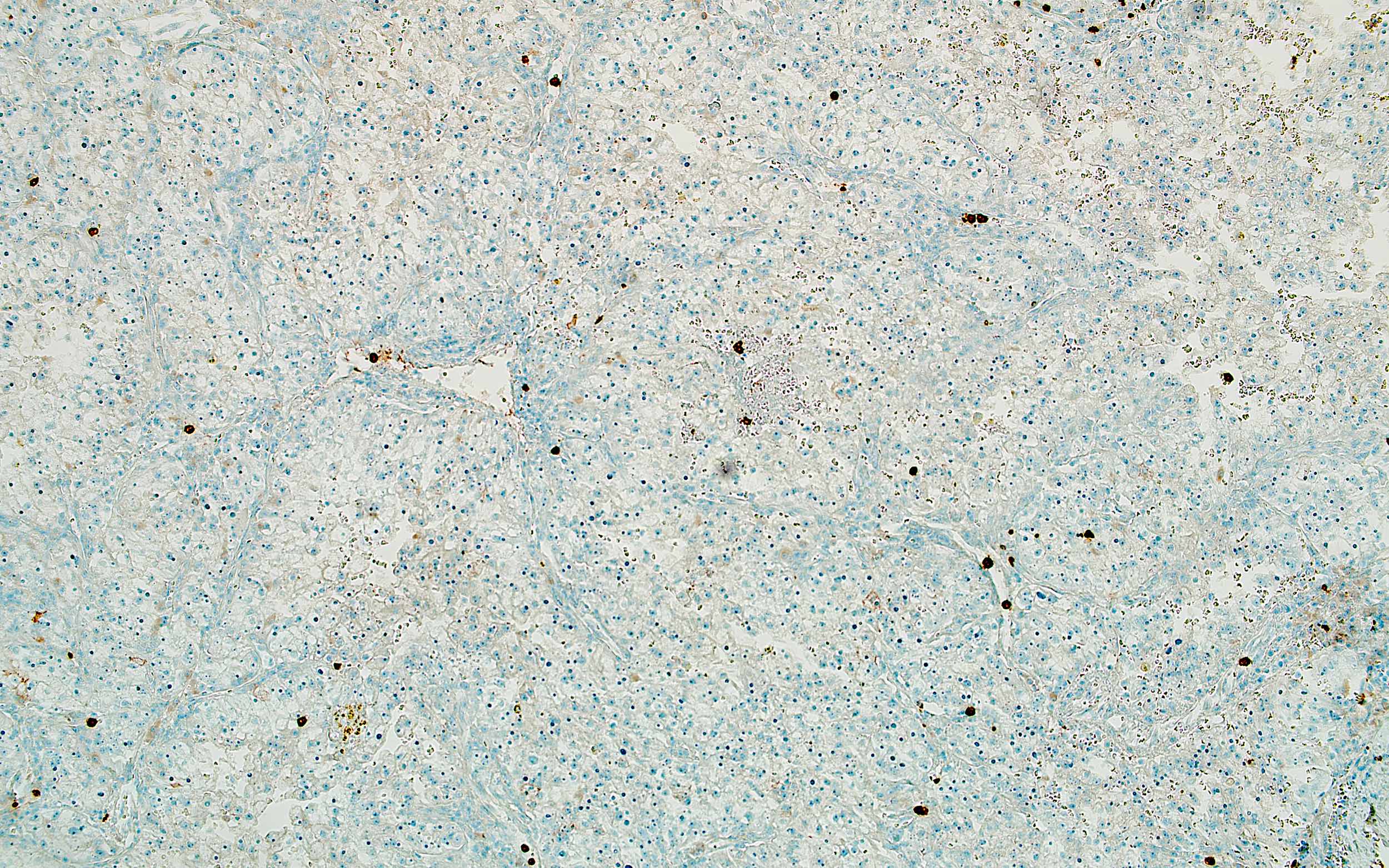
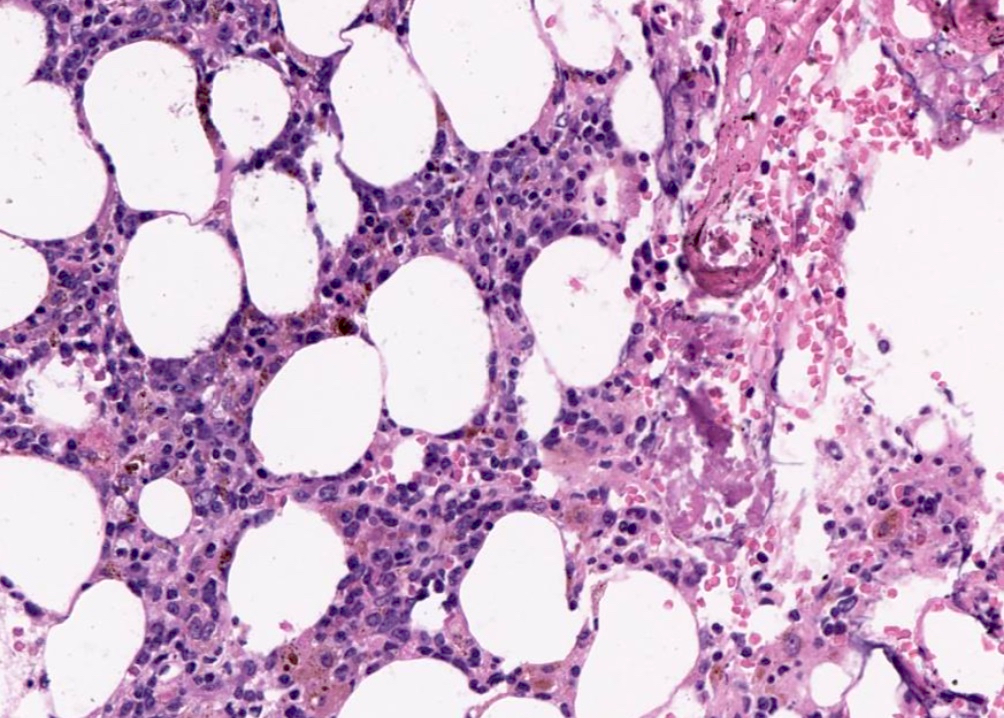
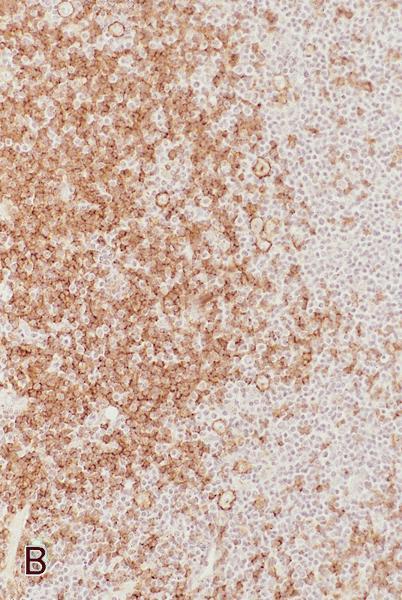
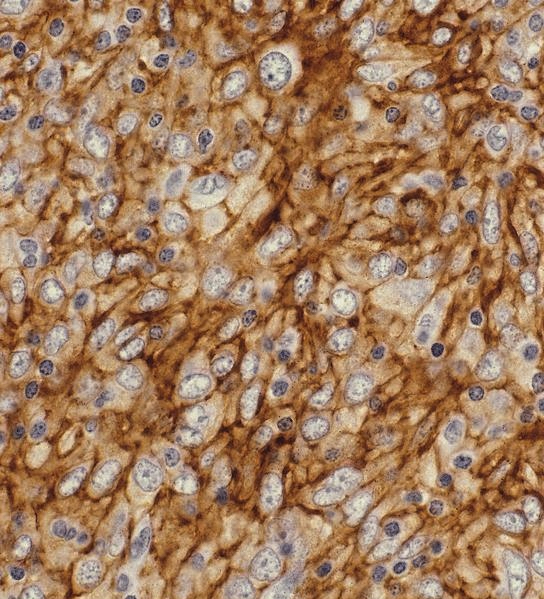
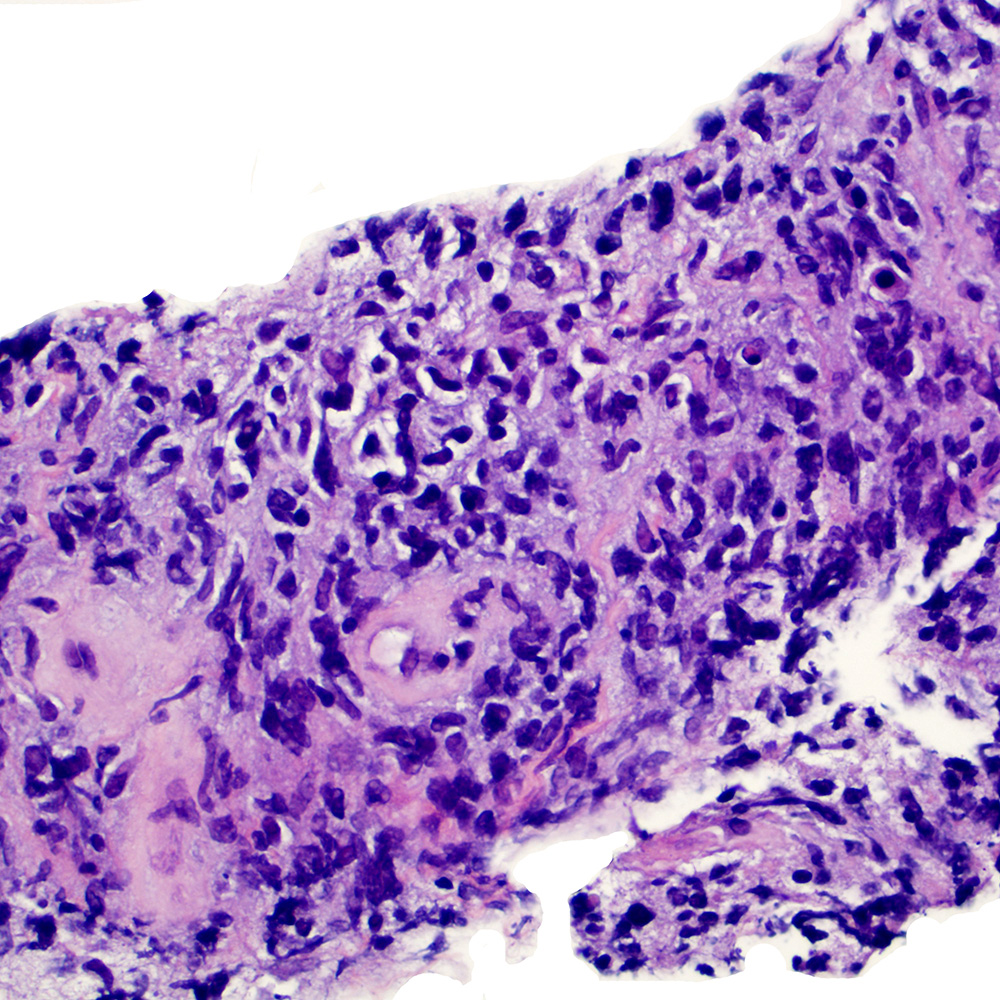
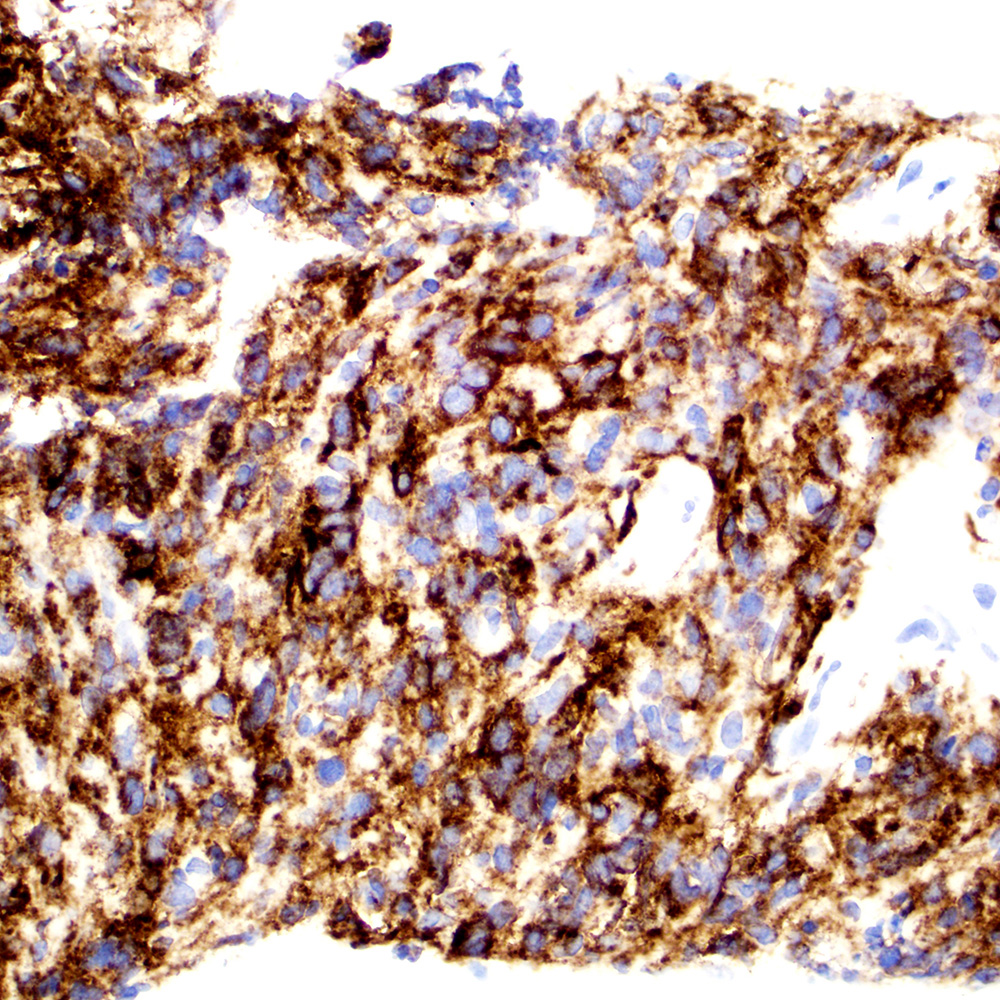
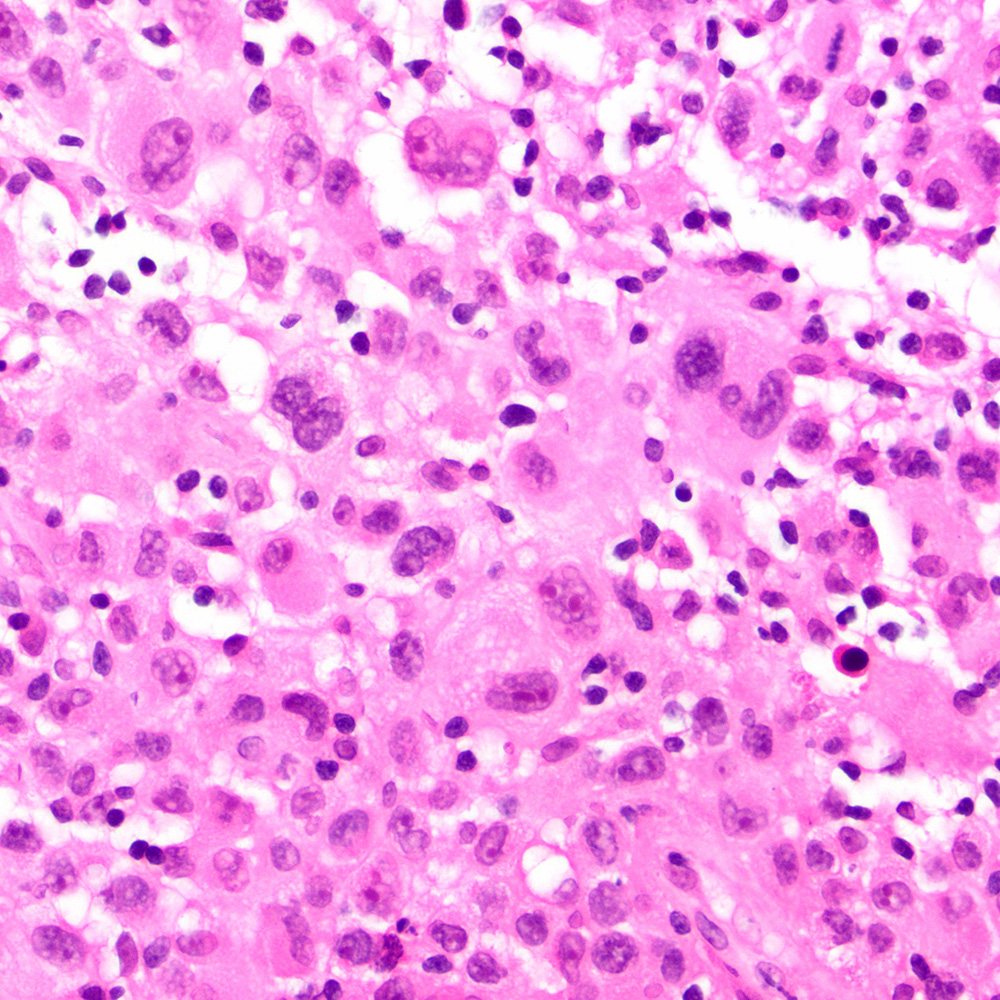
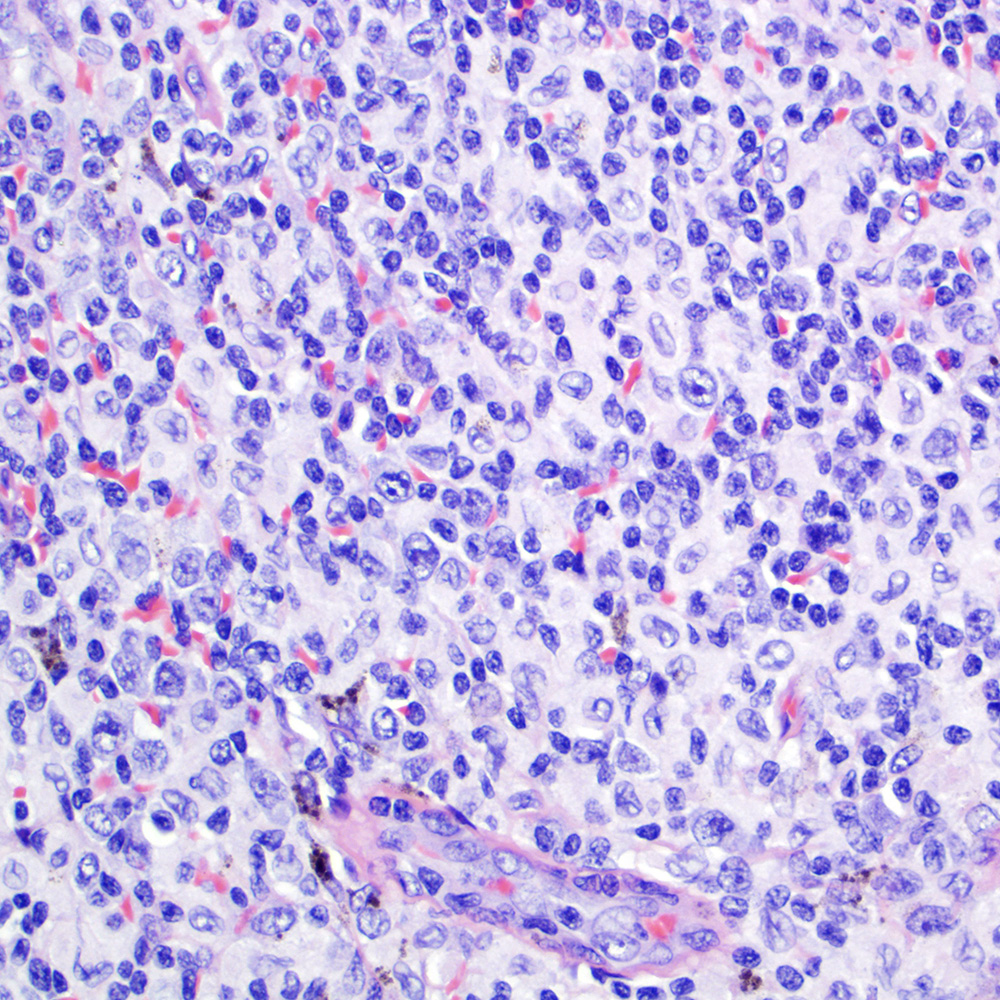
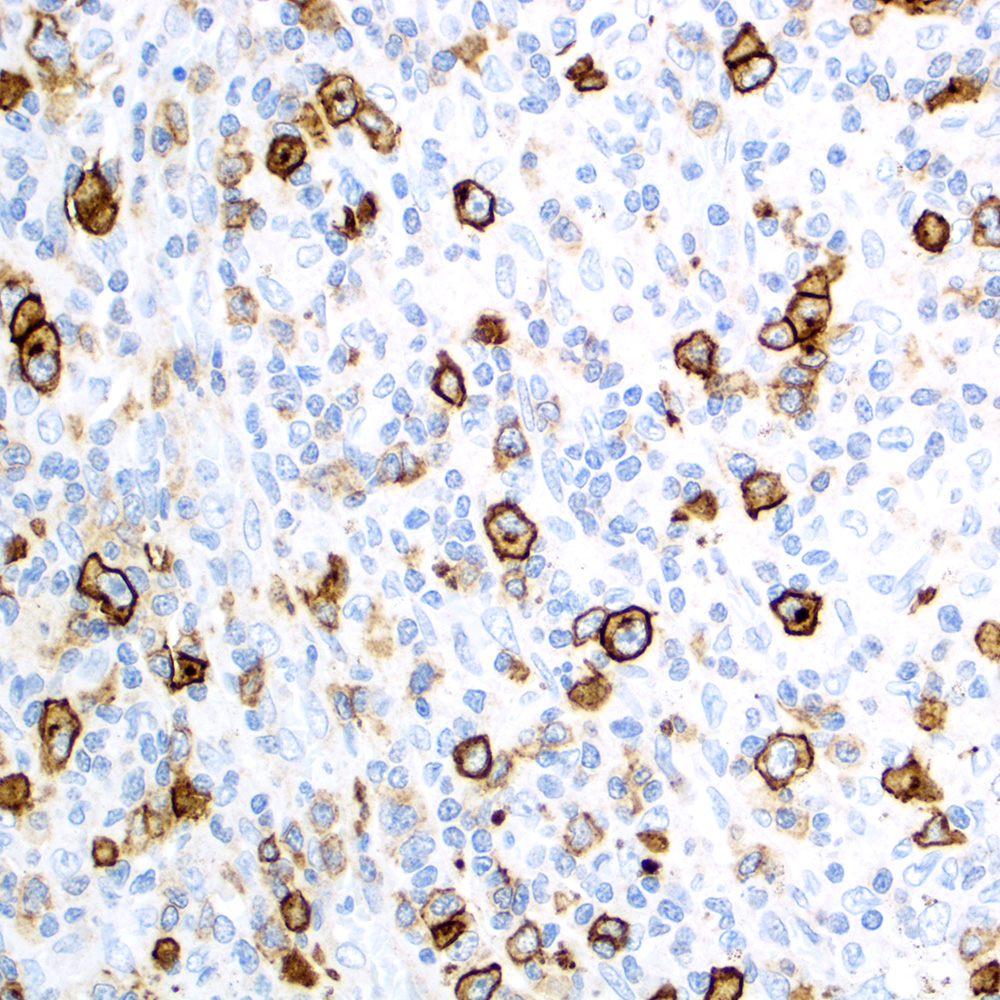
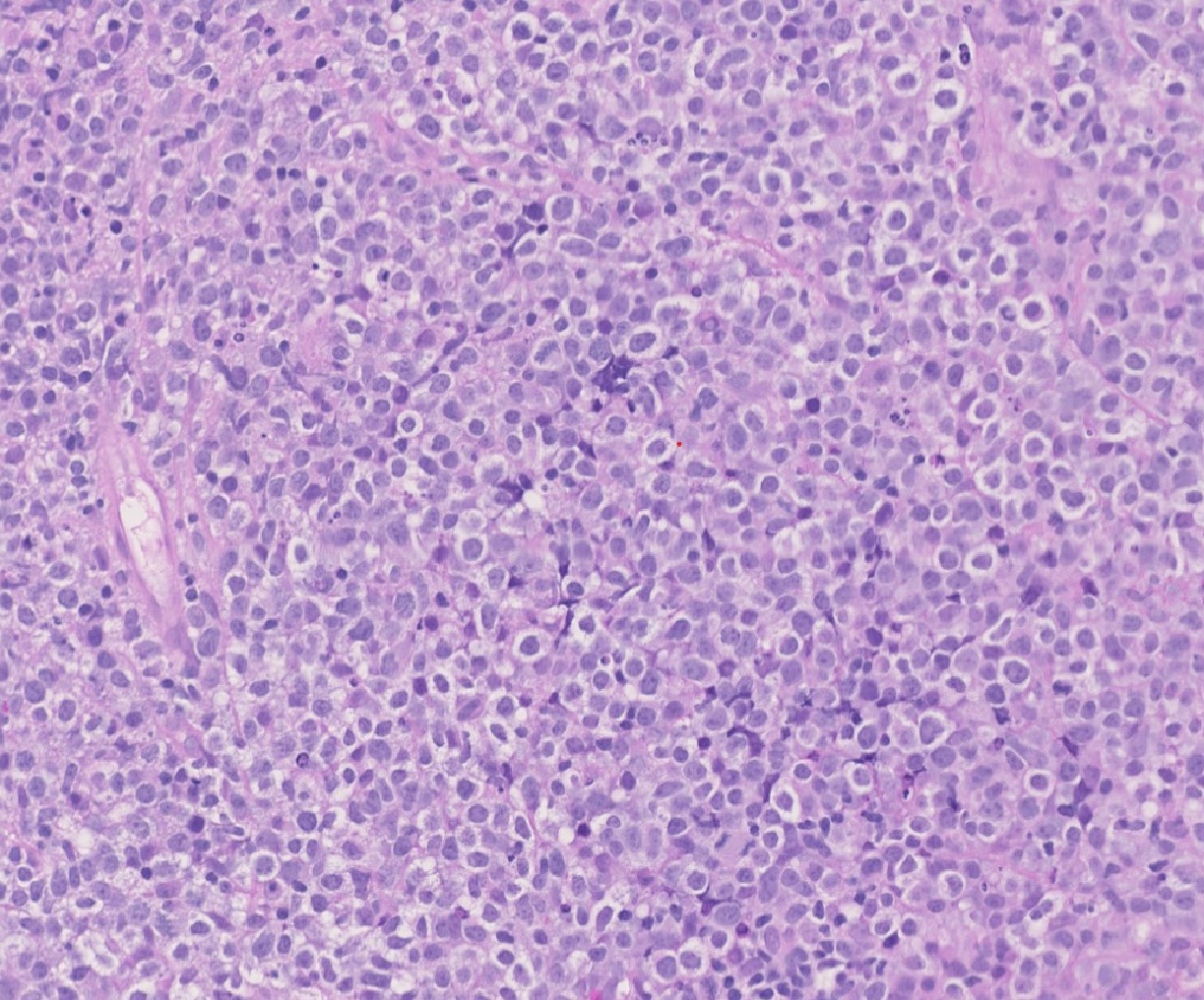
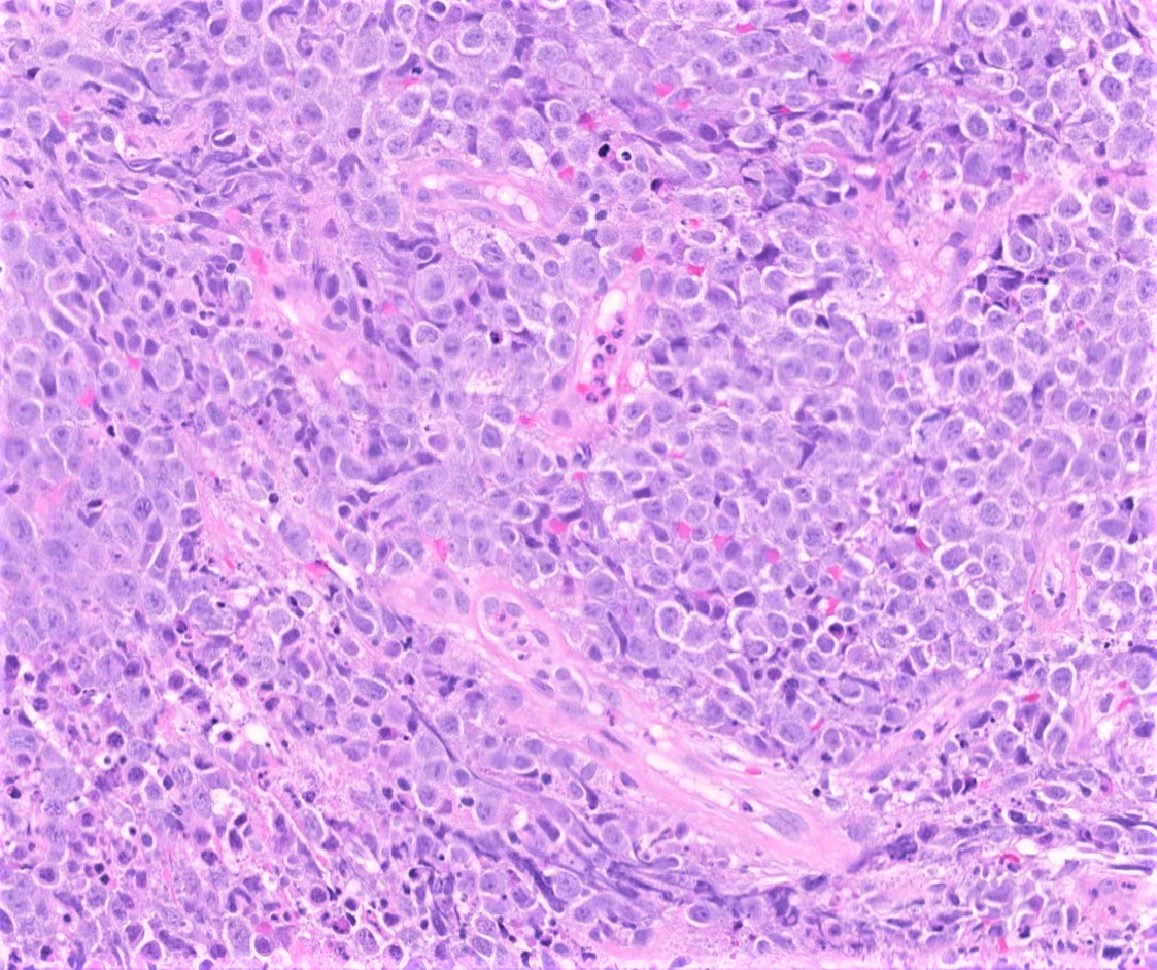
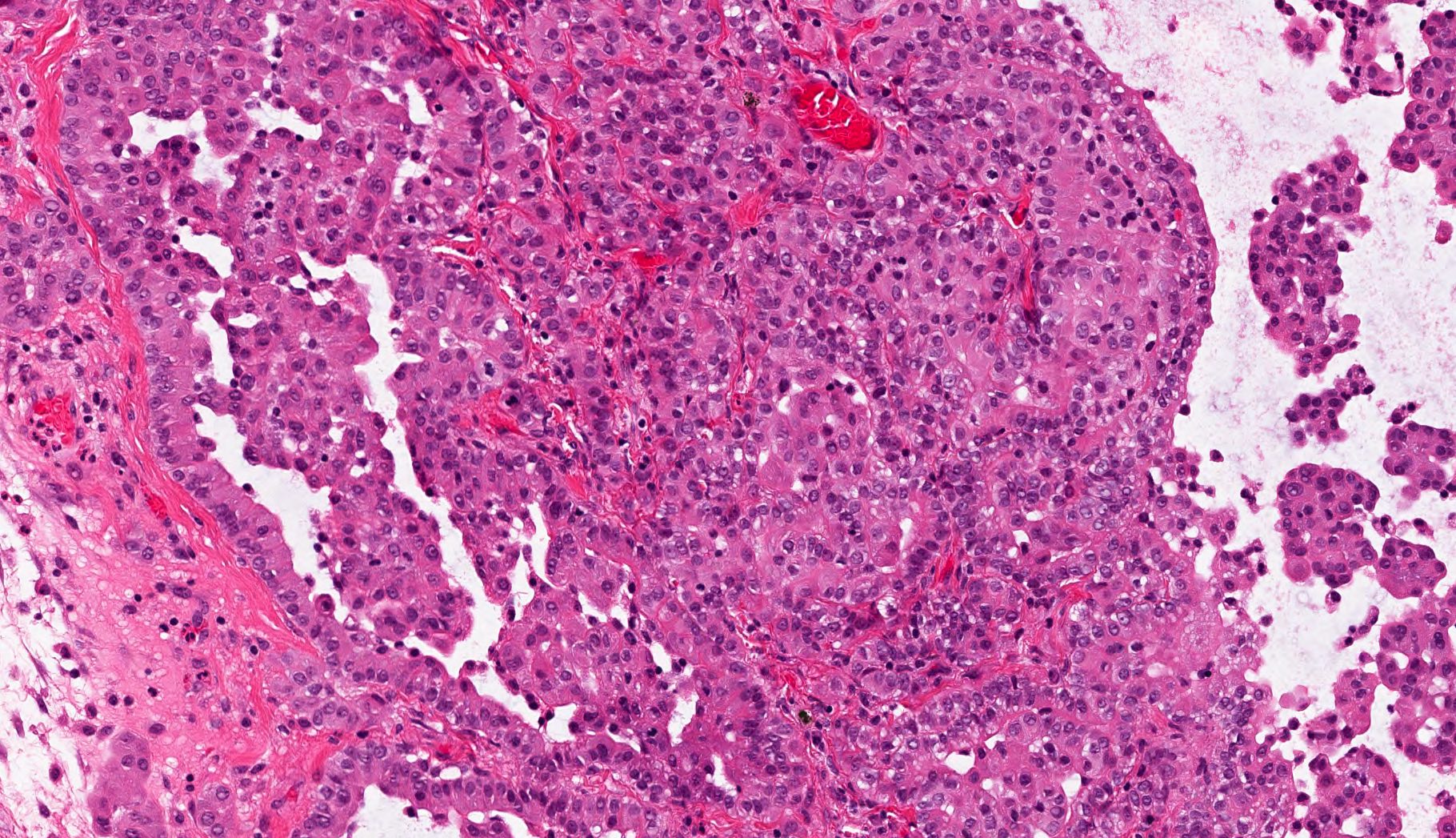
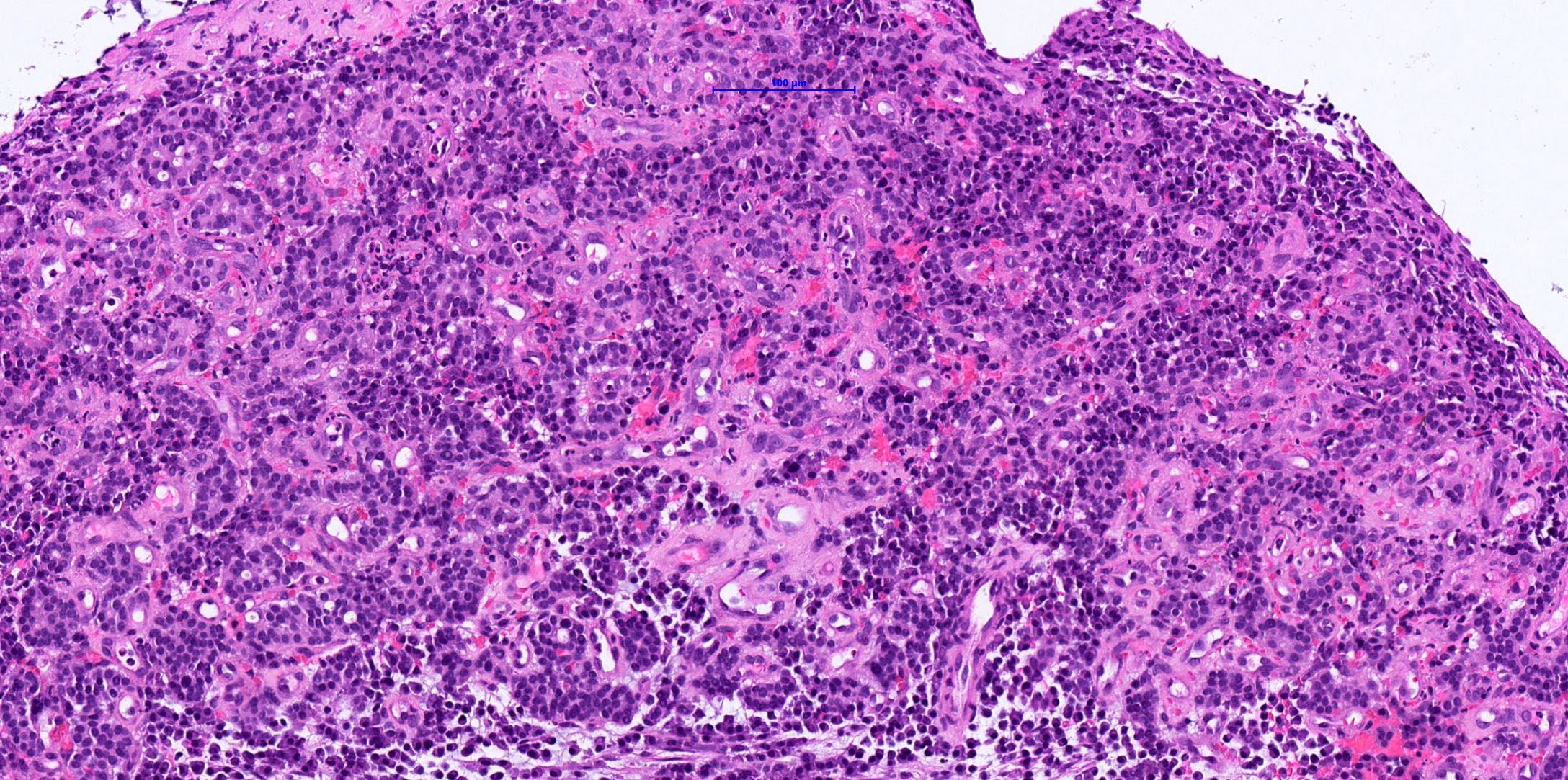
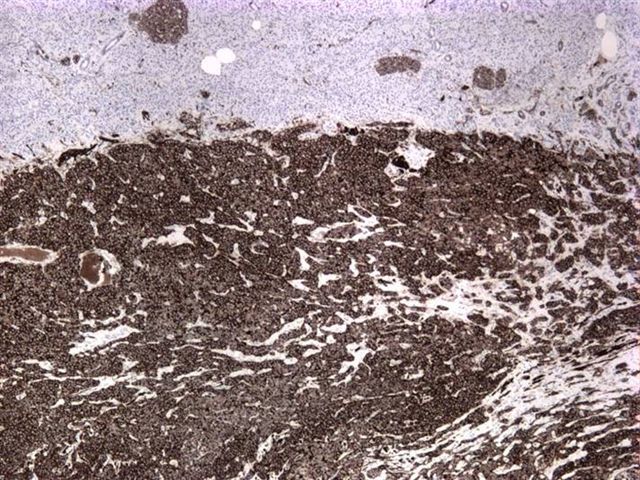
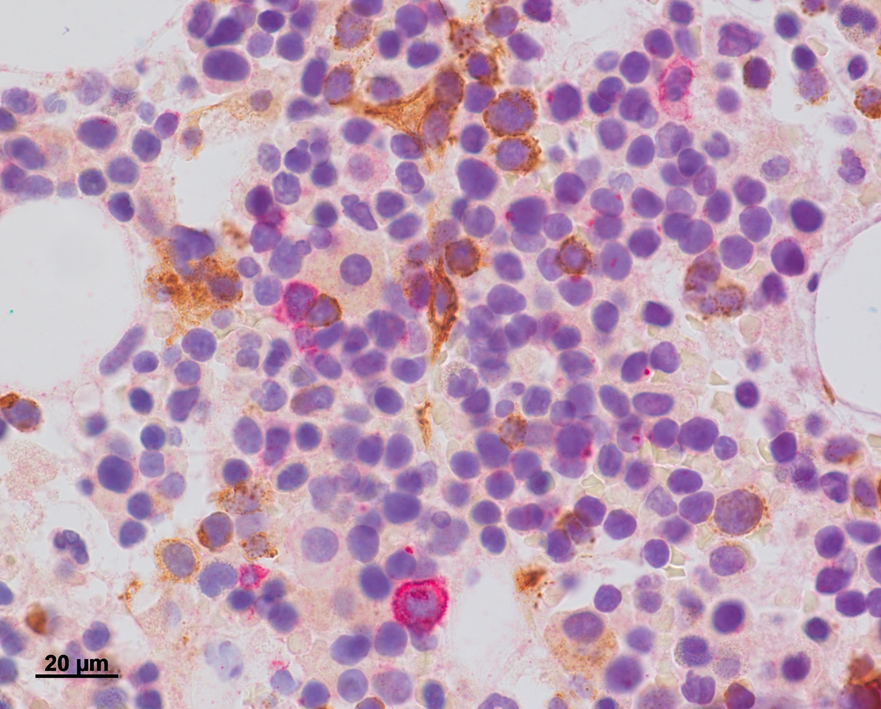
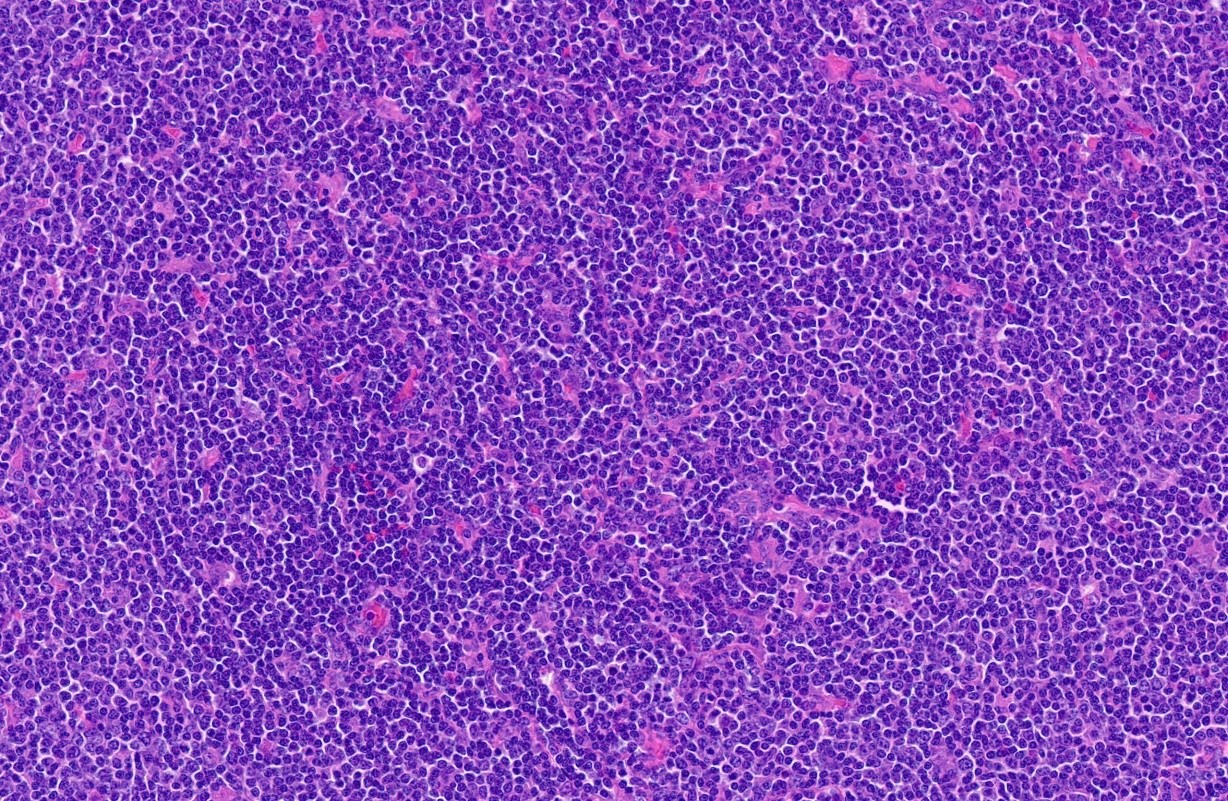
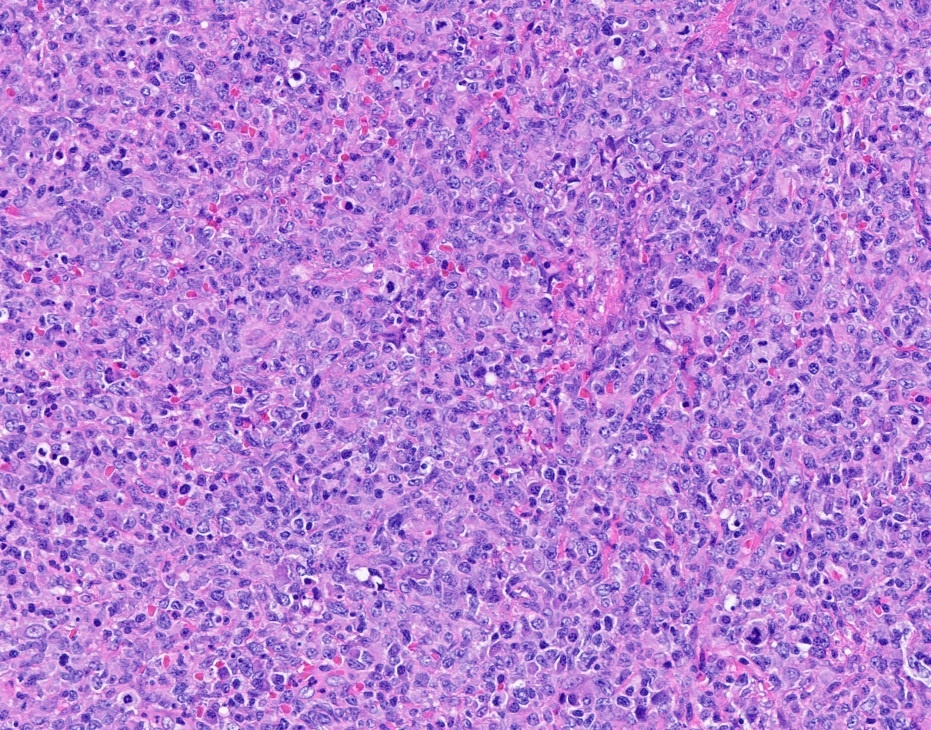
Microscopic (histologic) description
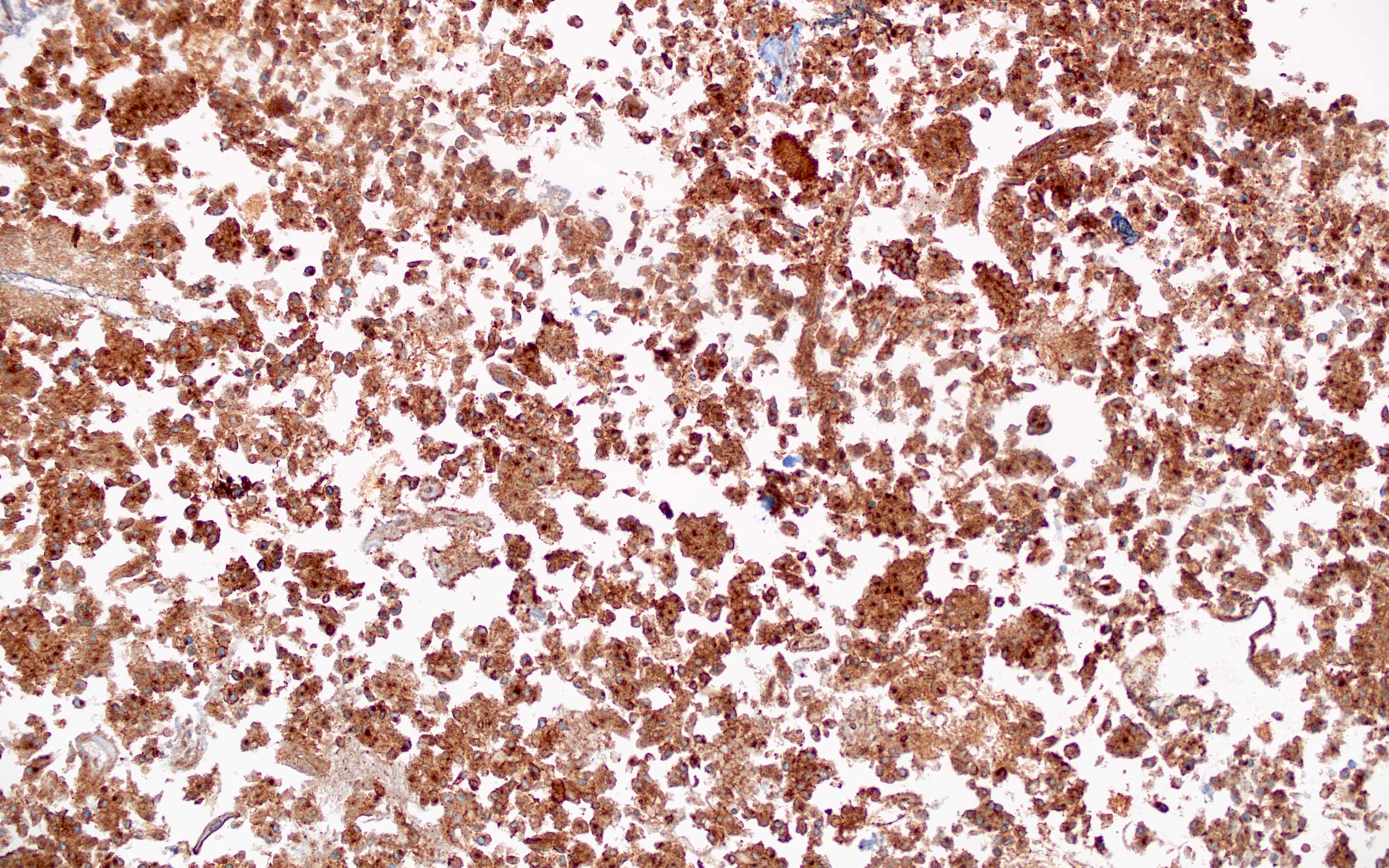
- Papillary renal cell carcinoma (Am J Surg Pathol 2017;41:1618, Hum Pathol 2022;120:57, USCAP 2023 Abstracts: Genitourinary Pathology (Including Renal Tumors) [Accessed 25 July 2023])
- Negative: shows complete absence of ABCC2 staining
- Cytoplasmic: weak (blush) granular cytoplasmic staining equal to the background proximal renal tubules
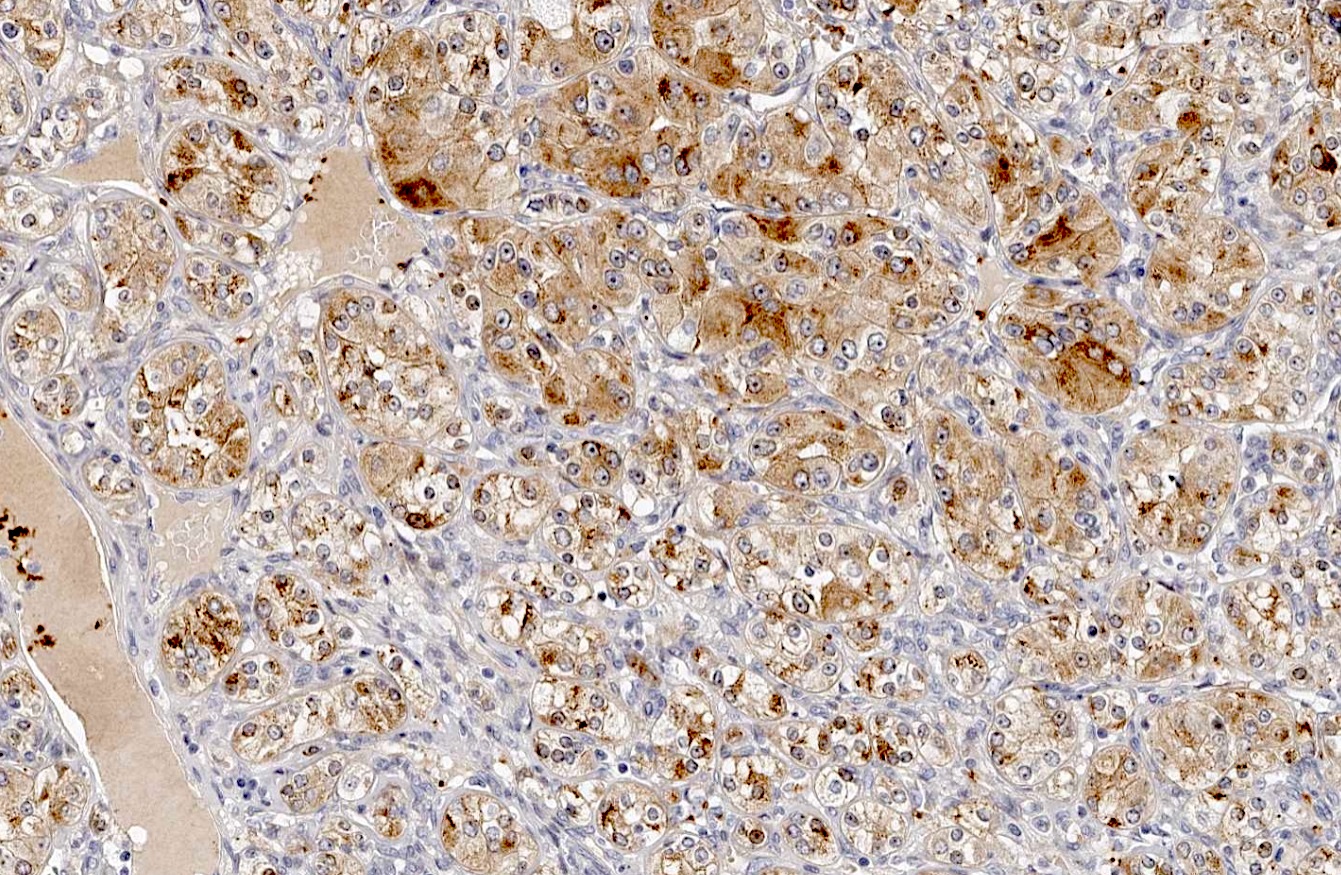
- < 50% brush border: patchy or focal brush border ABCC2 staining in < 50% of the tumor; internal control for brush border expression is the proximal renal tubules
- ≥ 50% brush border: strong or diffuse brush border staining involving ≥ 50% of the tumor
- May help to distinguish some oncocytic / eosinophilic papillary renal cell carcinomas (Am J Surg Pathol 2019;43:1099, USCAP 2023 Abstracts: Genitourinary Pathology (Including Renal Tumors) [Accessed 25 July 2023])
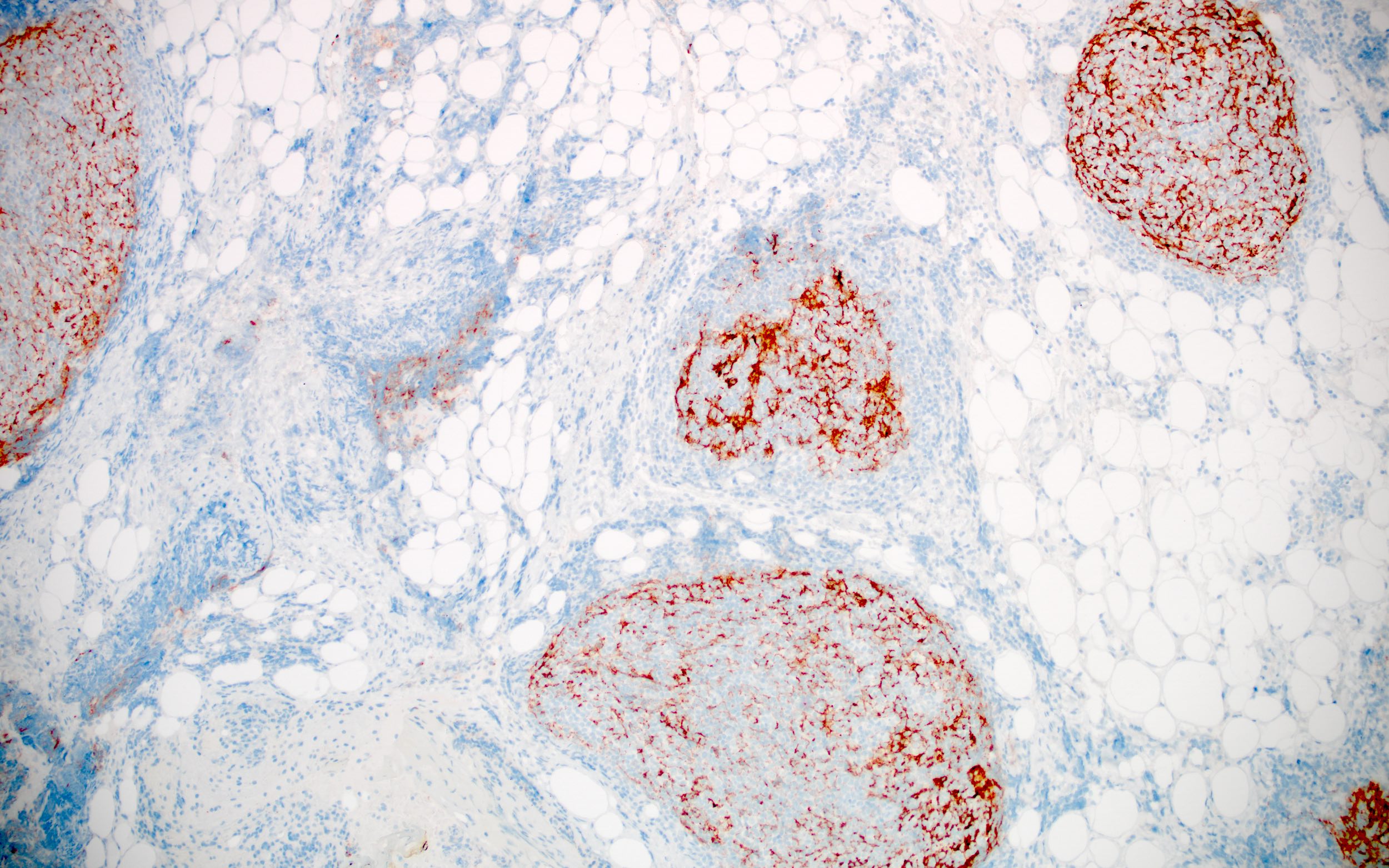
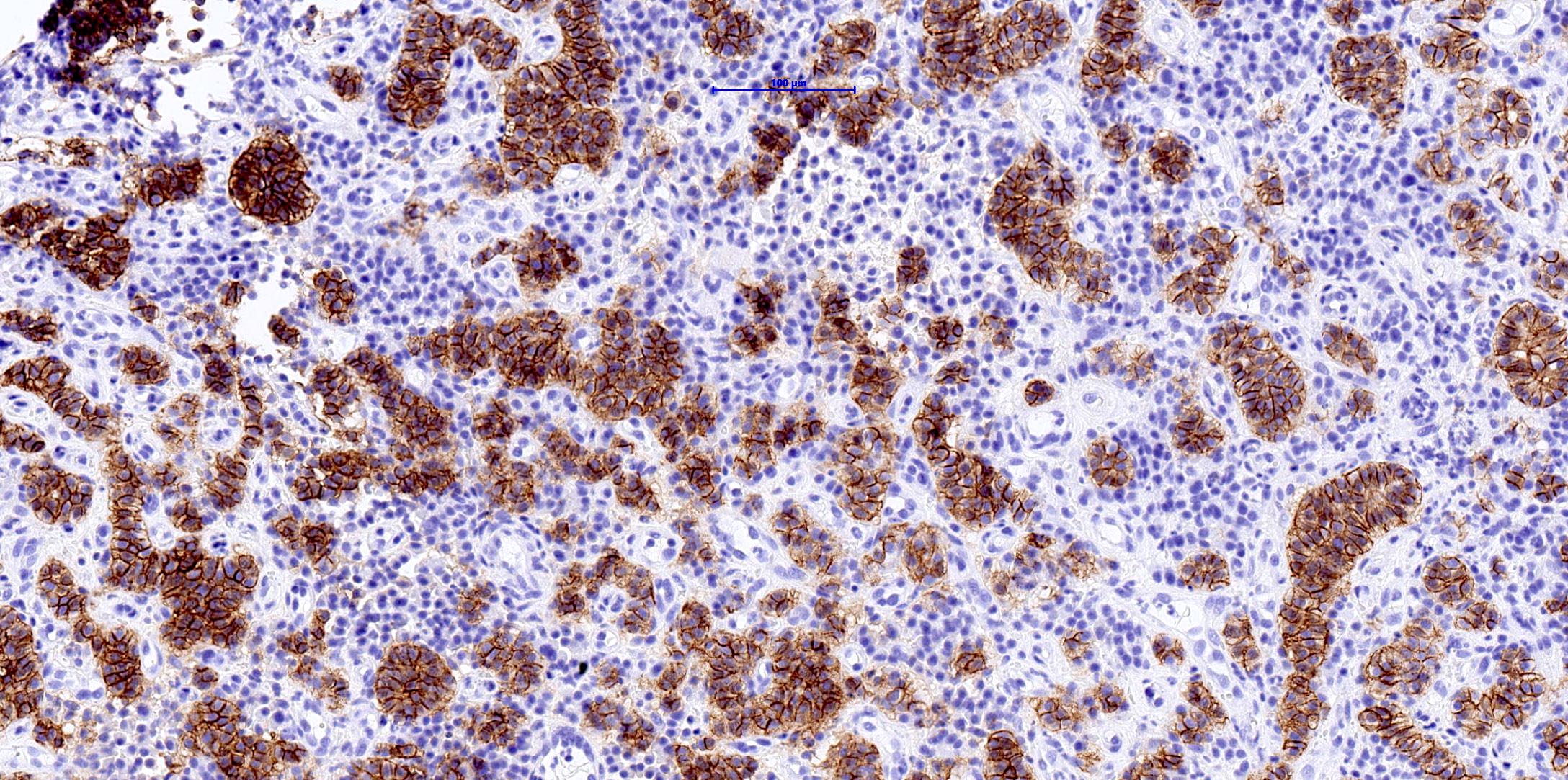
- Papillary renal neoplasm with reverse polarity: weak cytoplasmic staining of ABCC2 and negative for brush border expression, which corresponds to no or minimal RNA ISH transcripts; they harbor GATA3+ nuclear staining
- Eosinophilic papillary renal cell carcinoma: brush border ABCC2 expression, with corresponding high RNA ISH transcript level
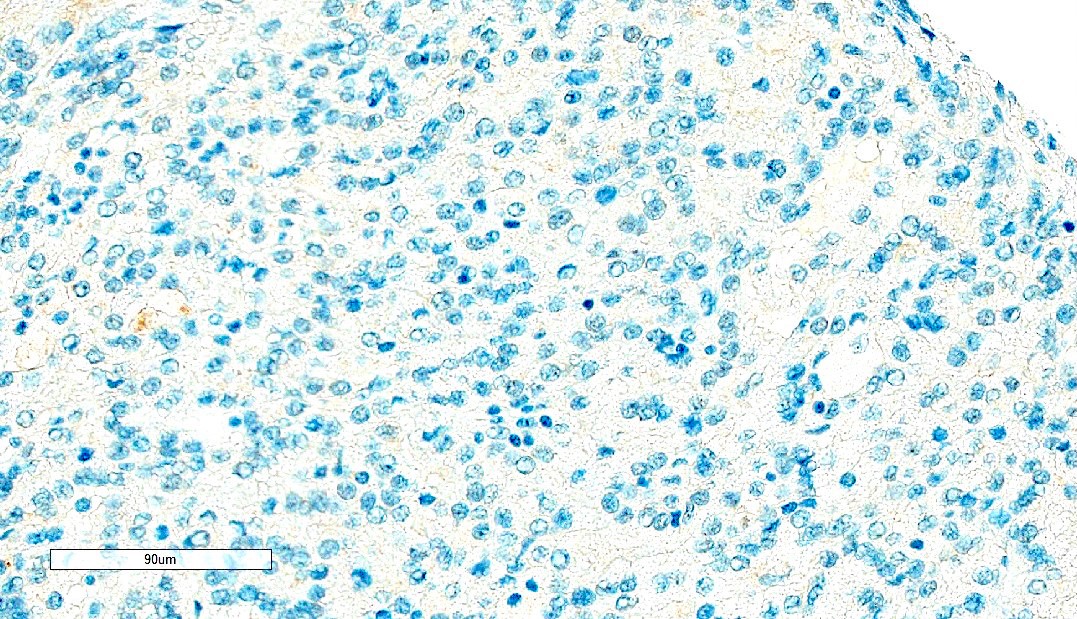
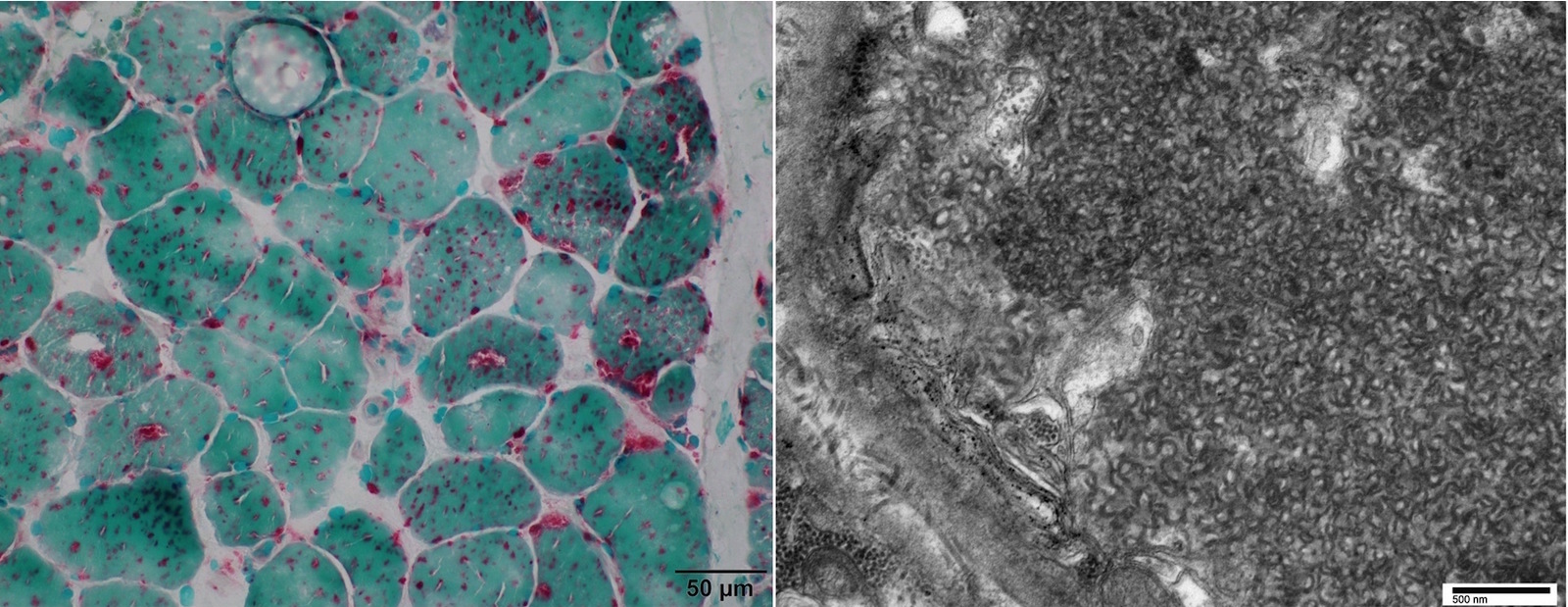
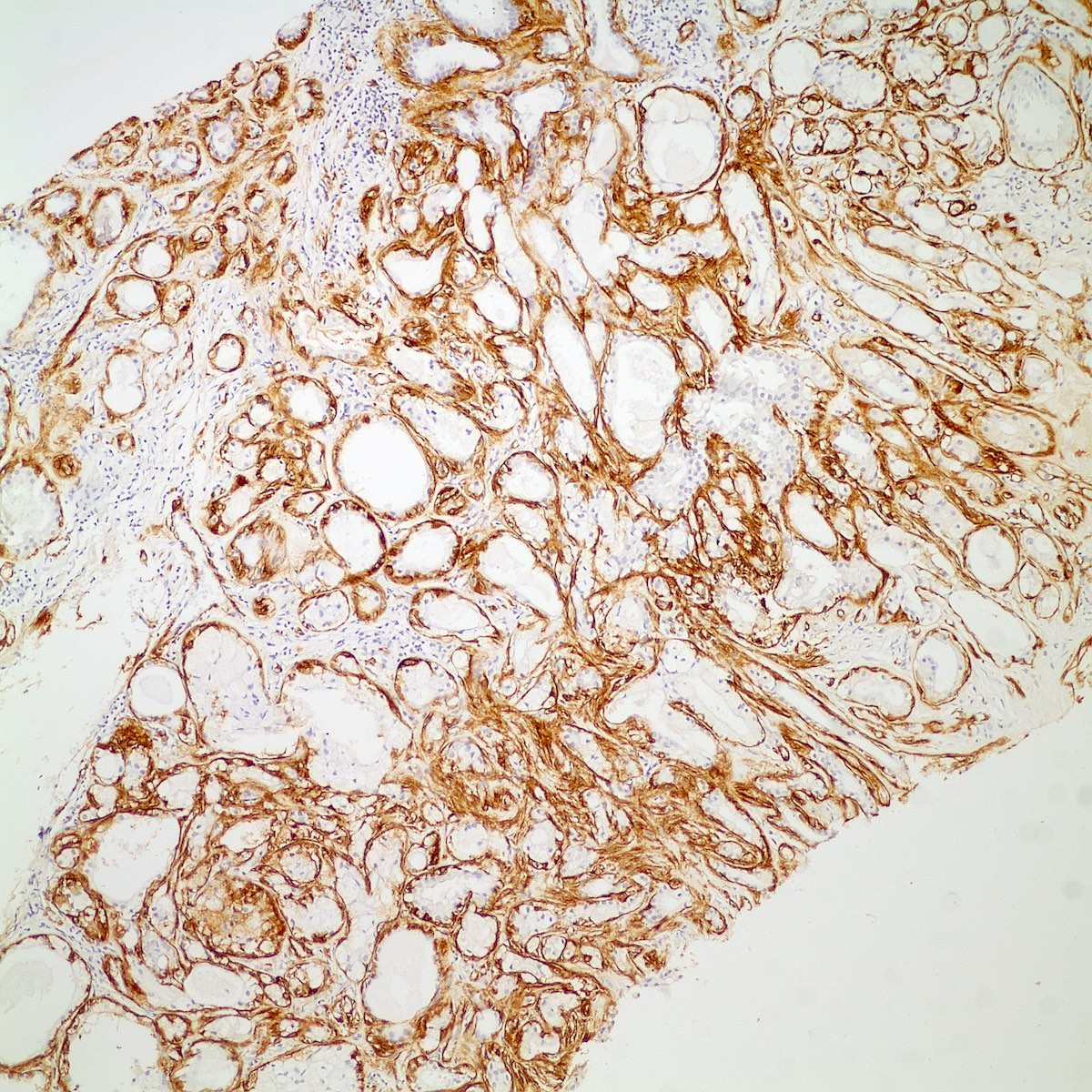
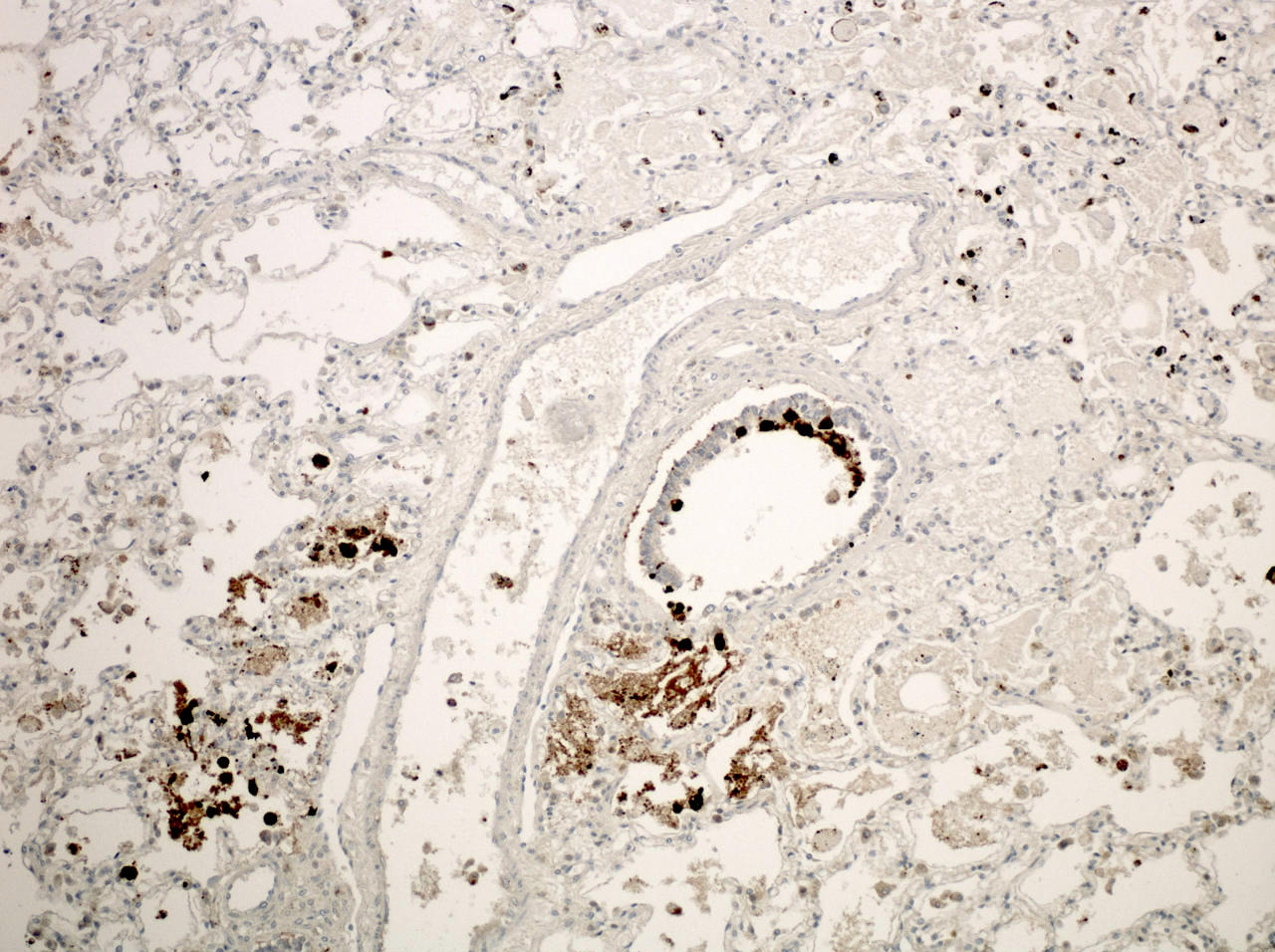
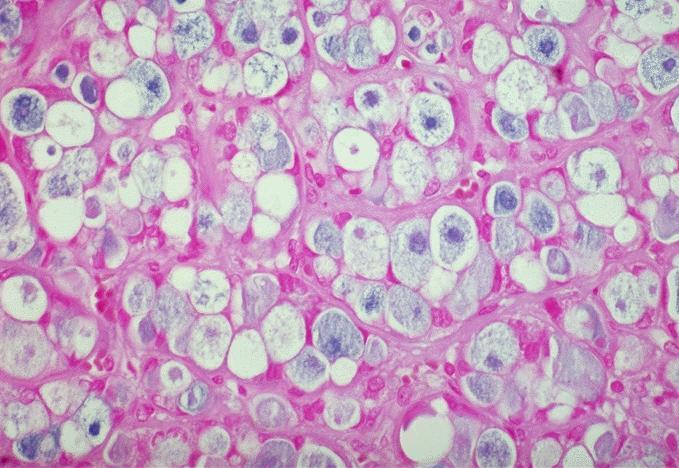
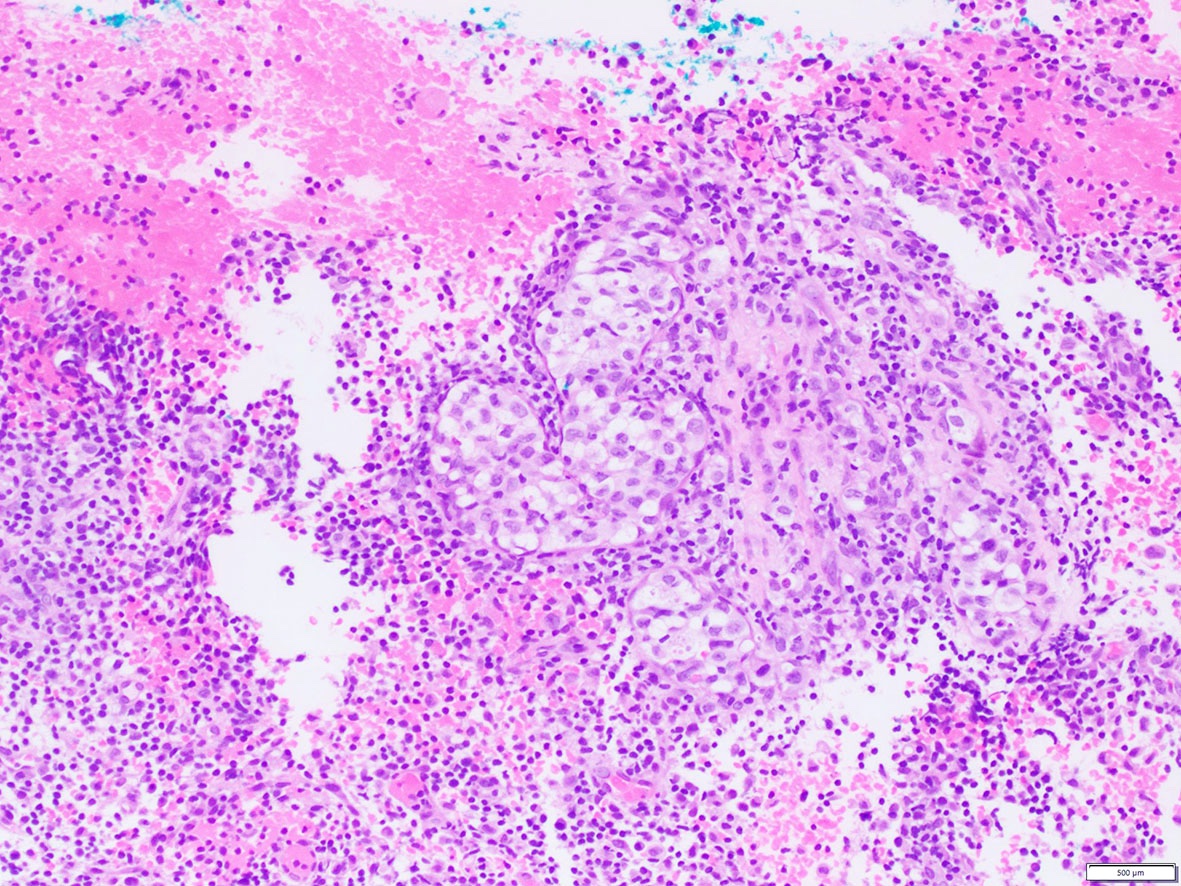
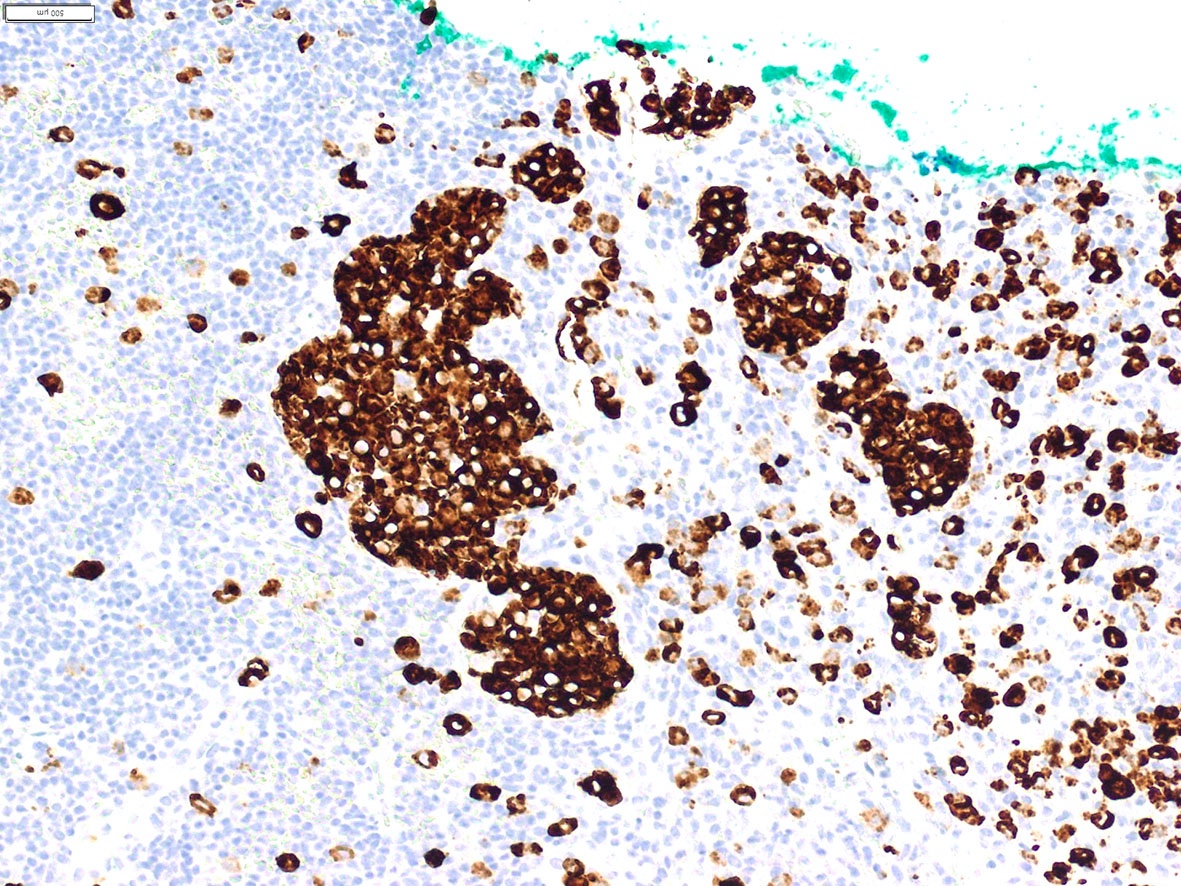
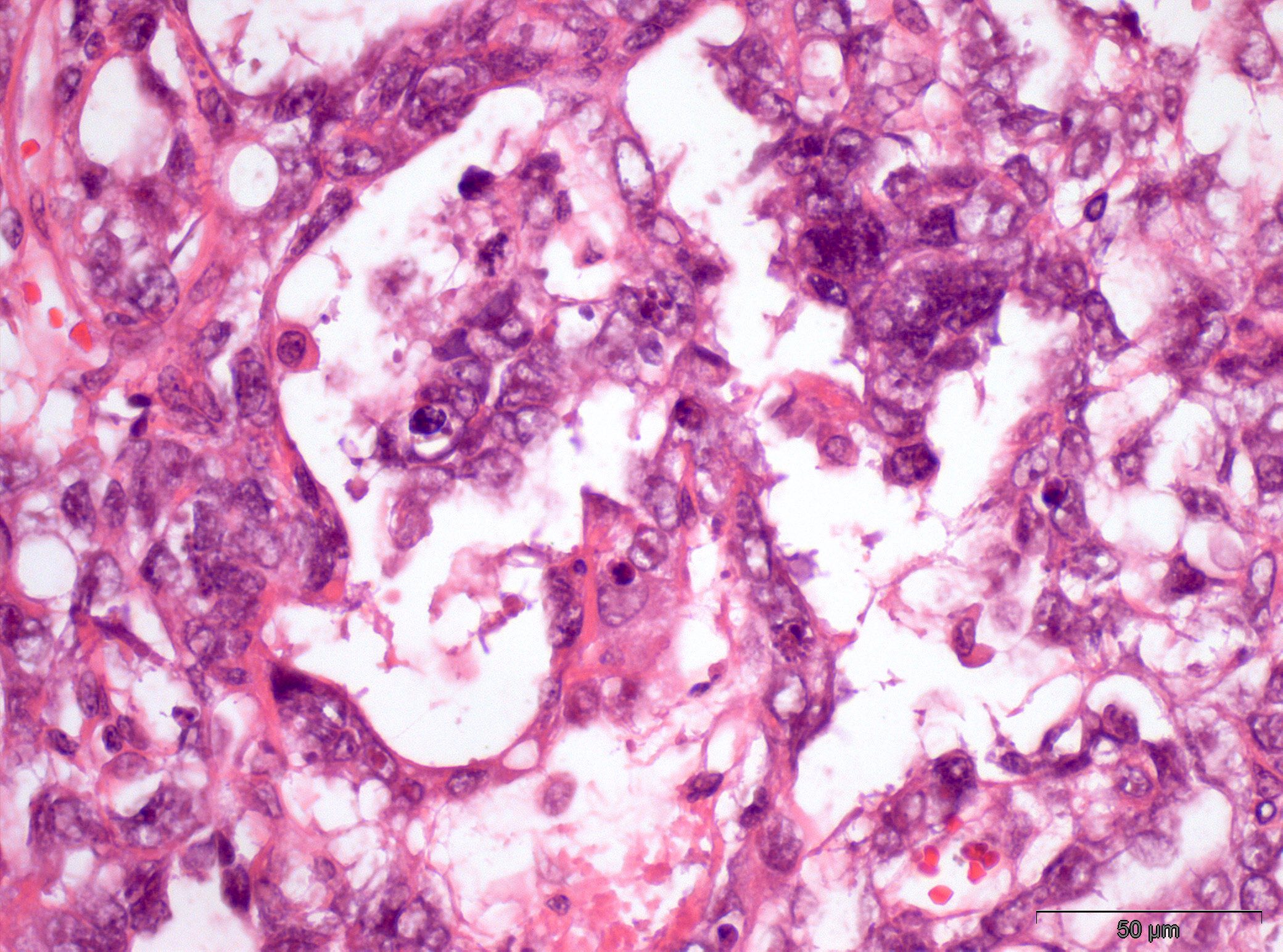
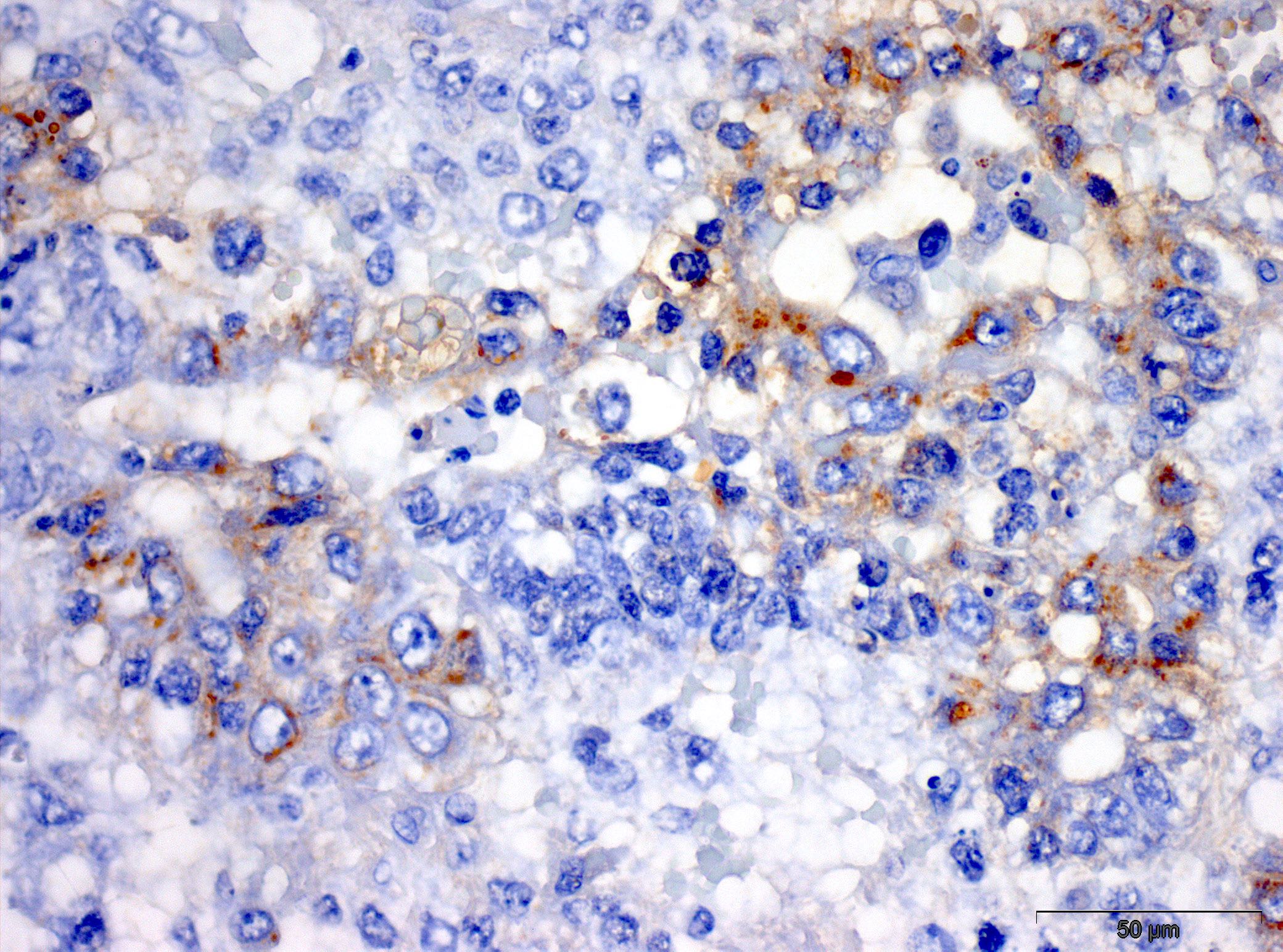
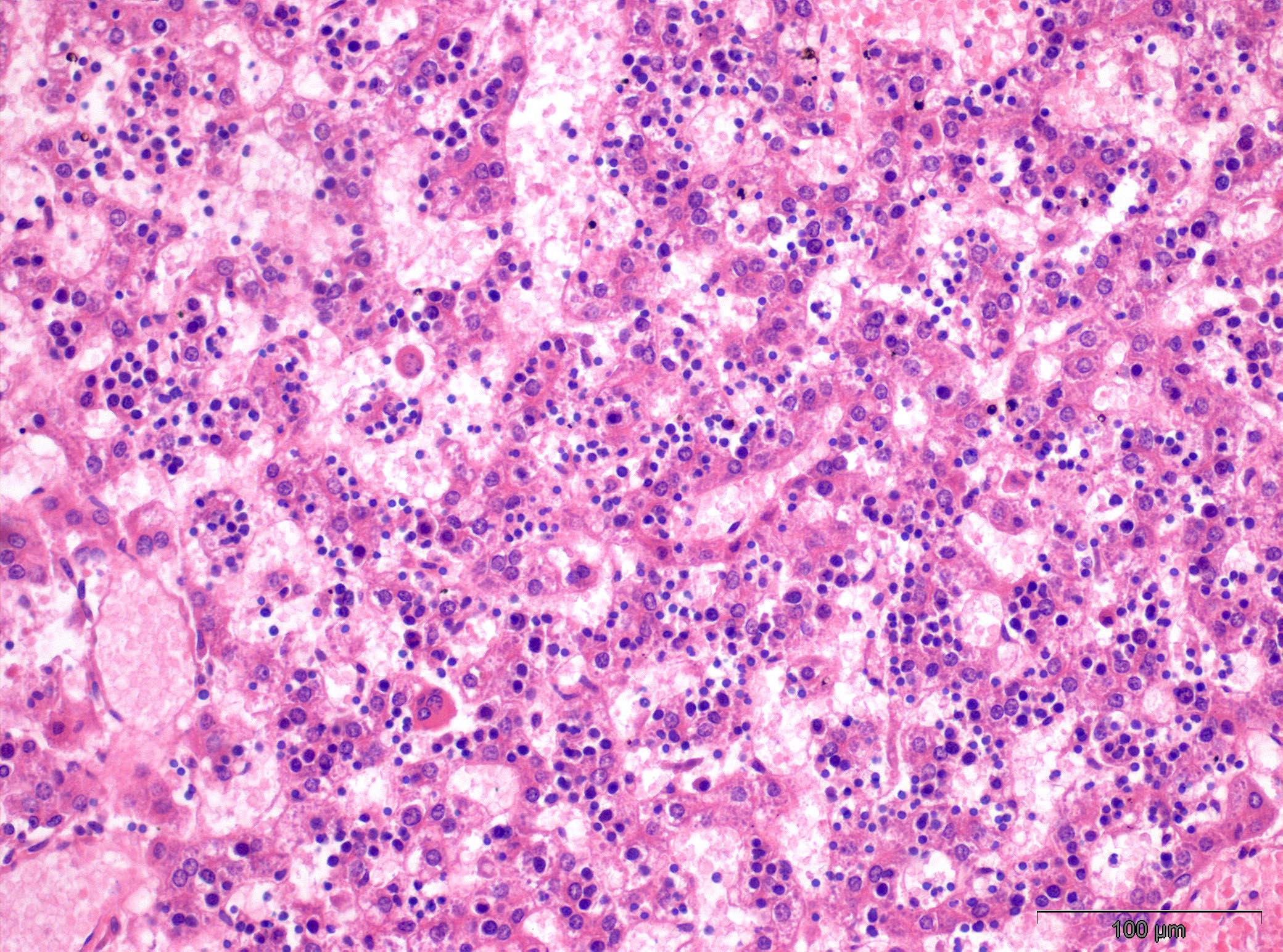
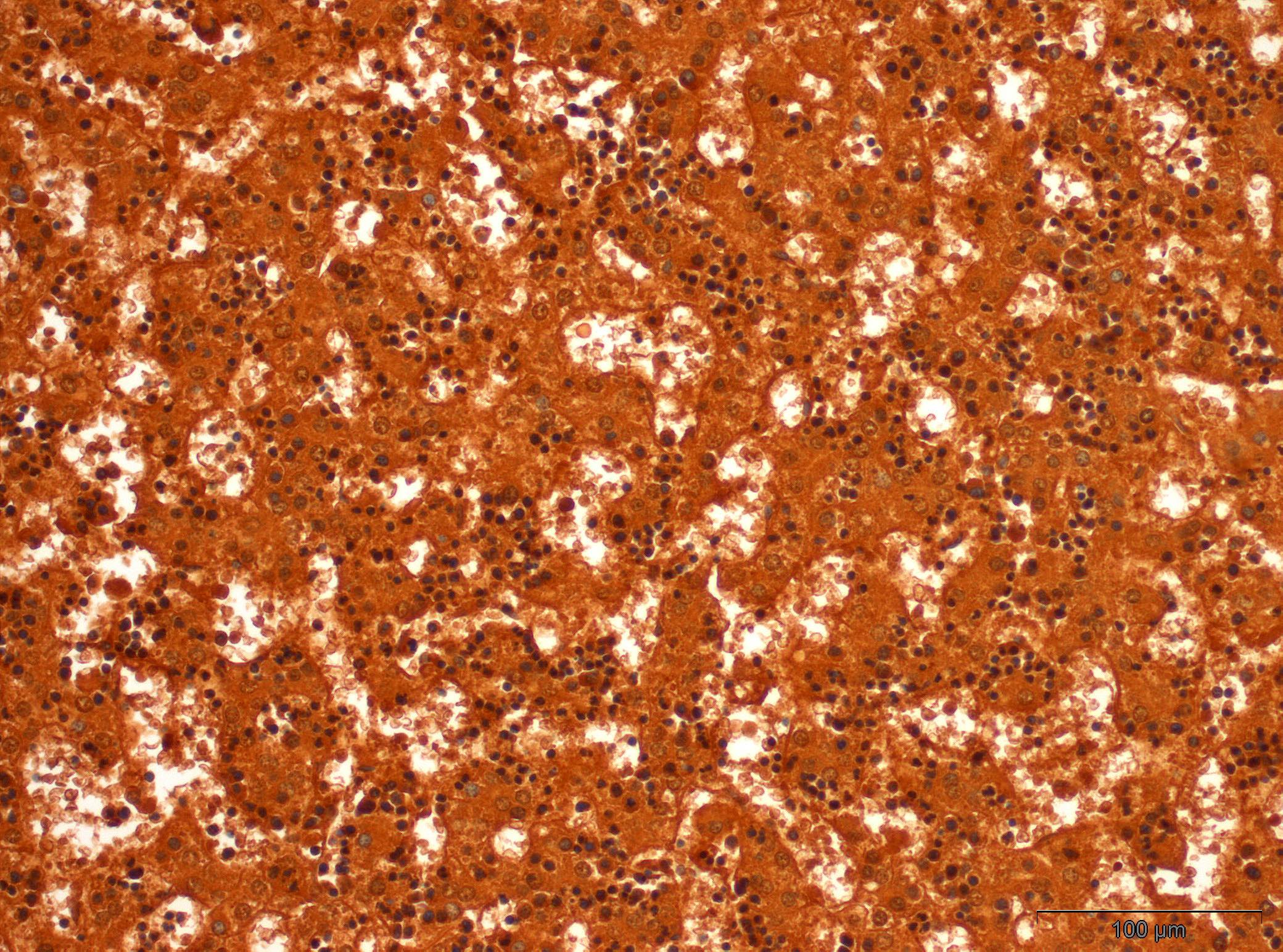
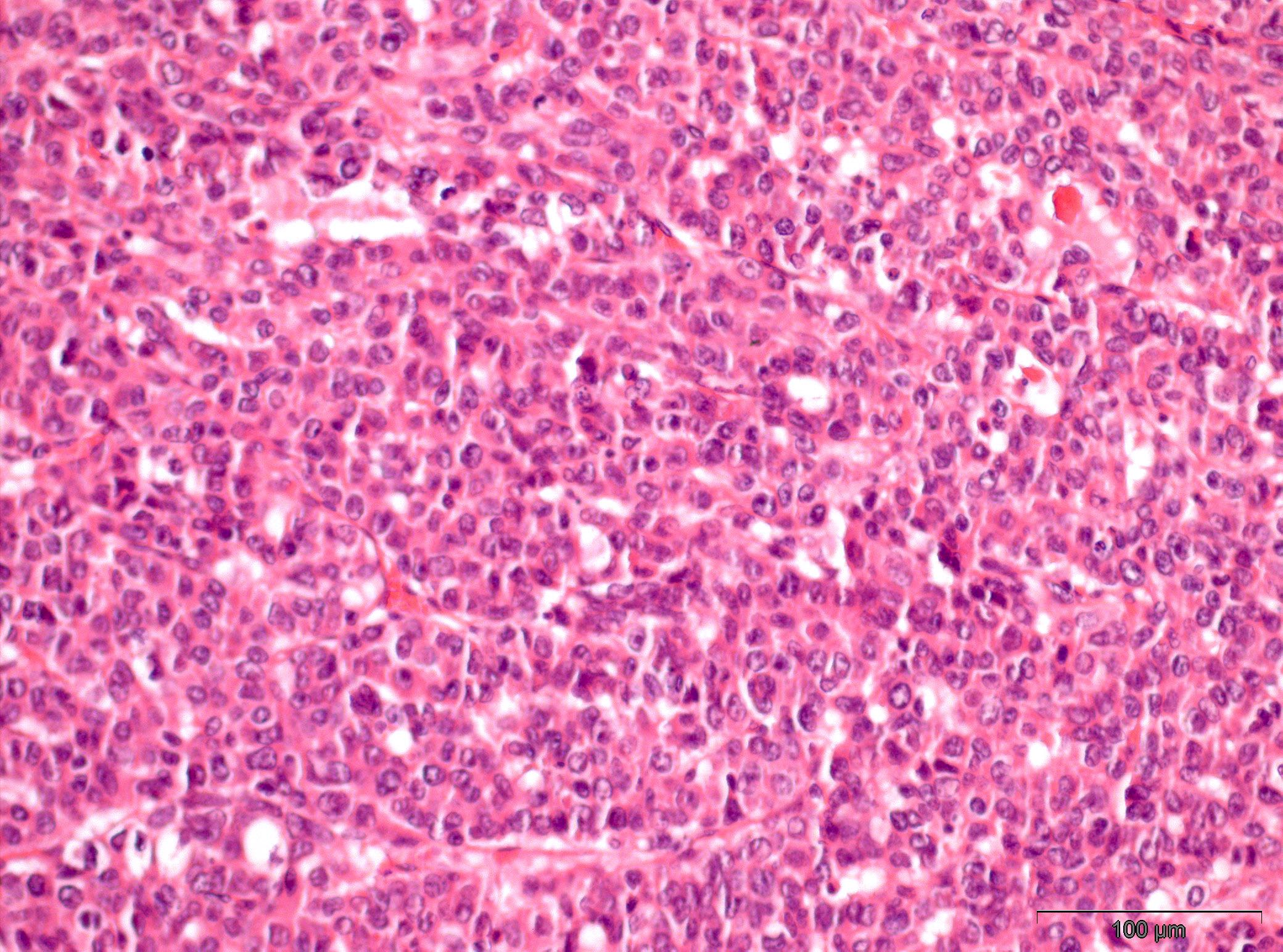
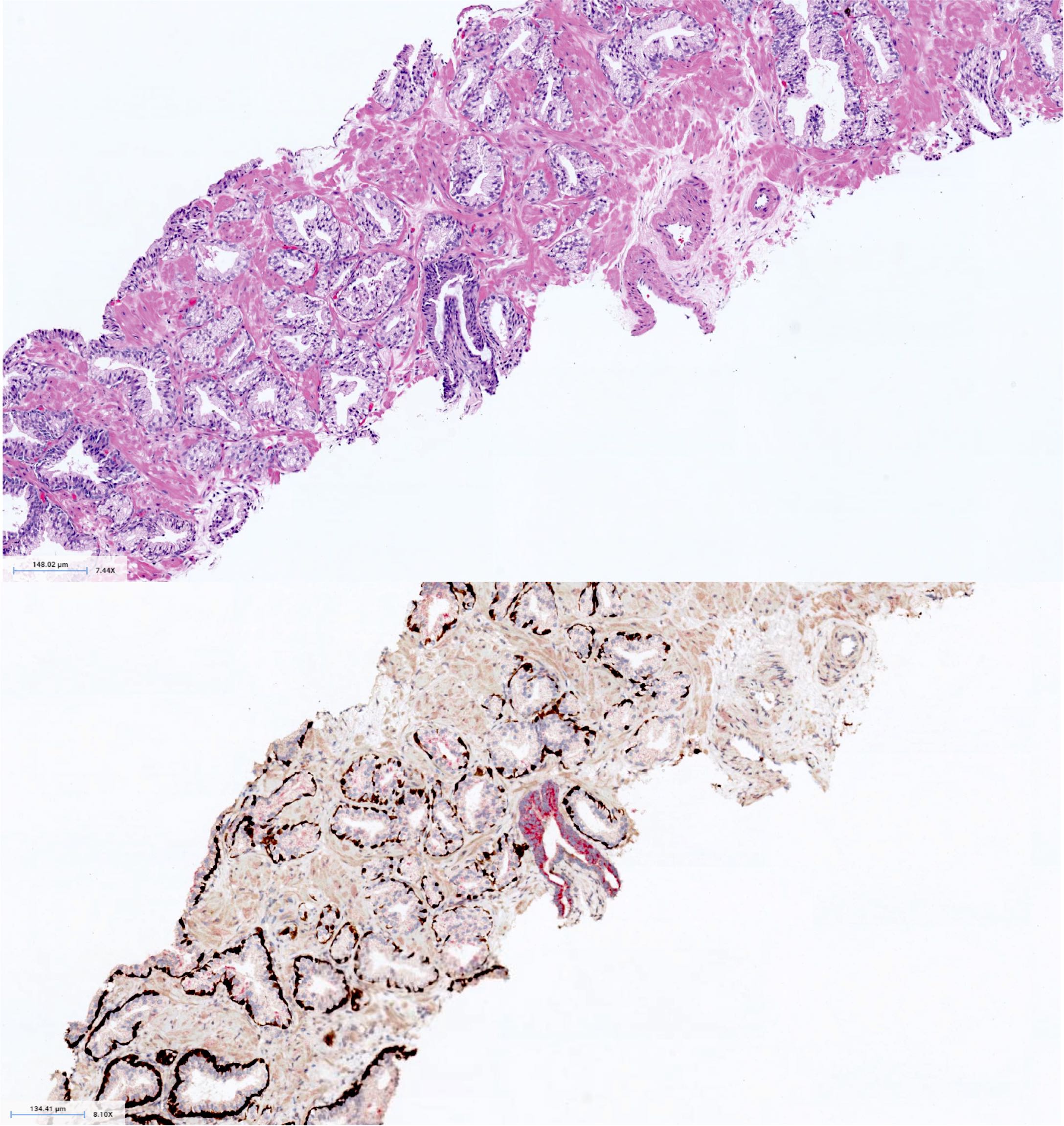
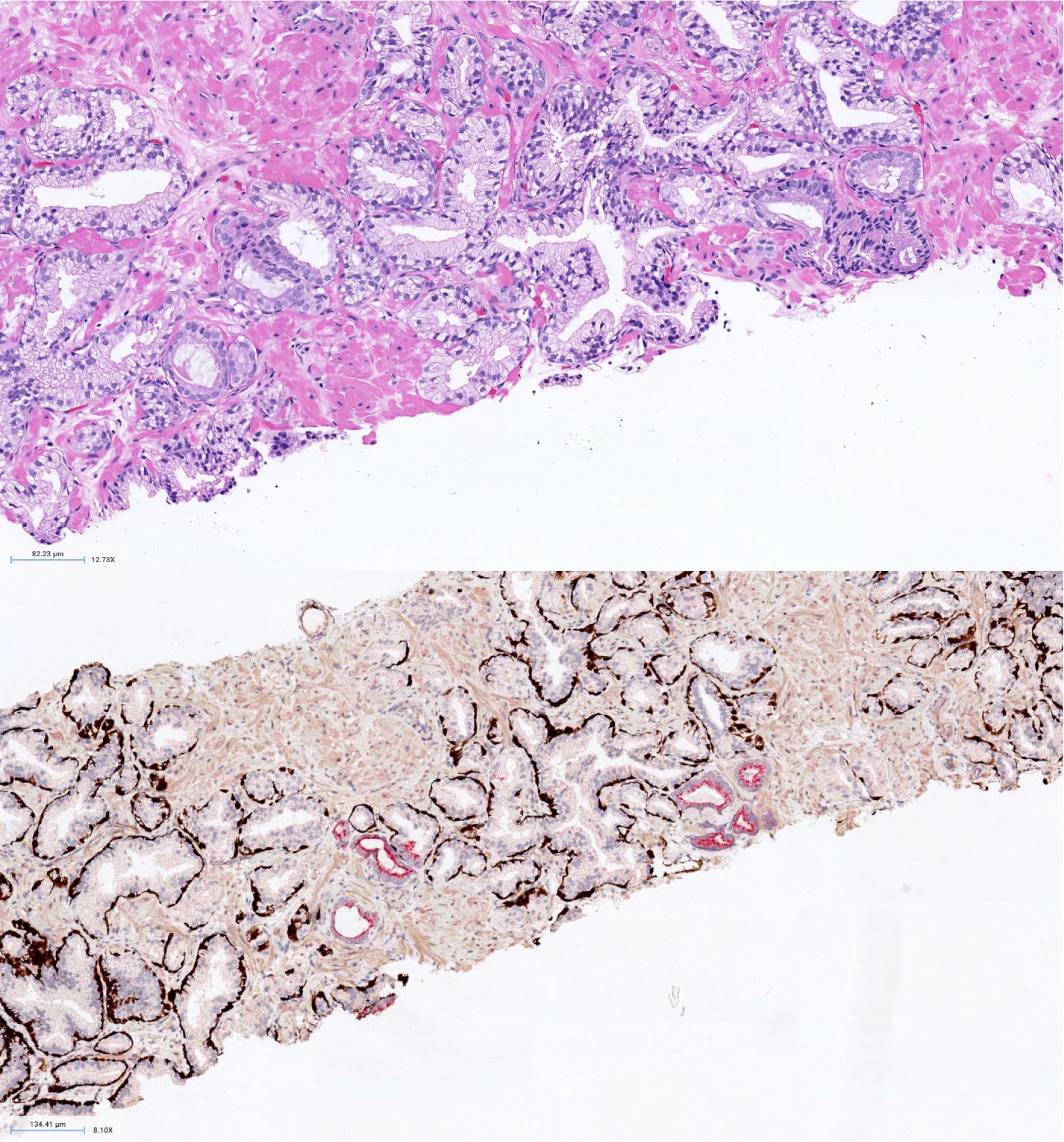
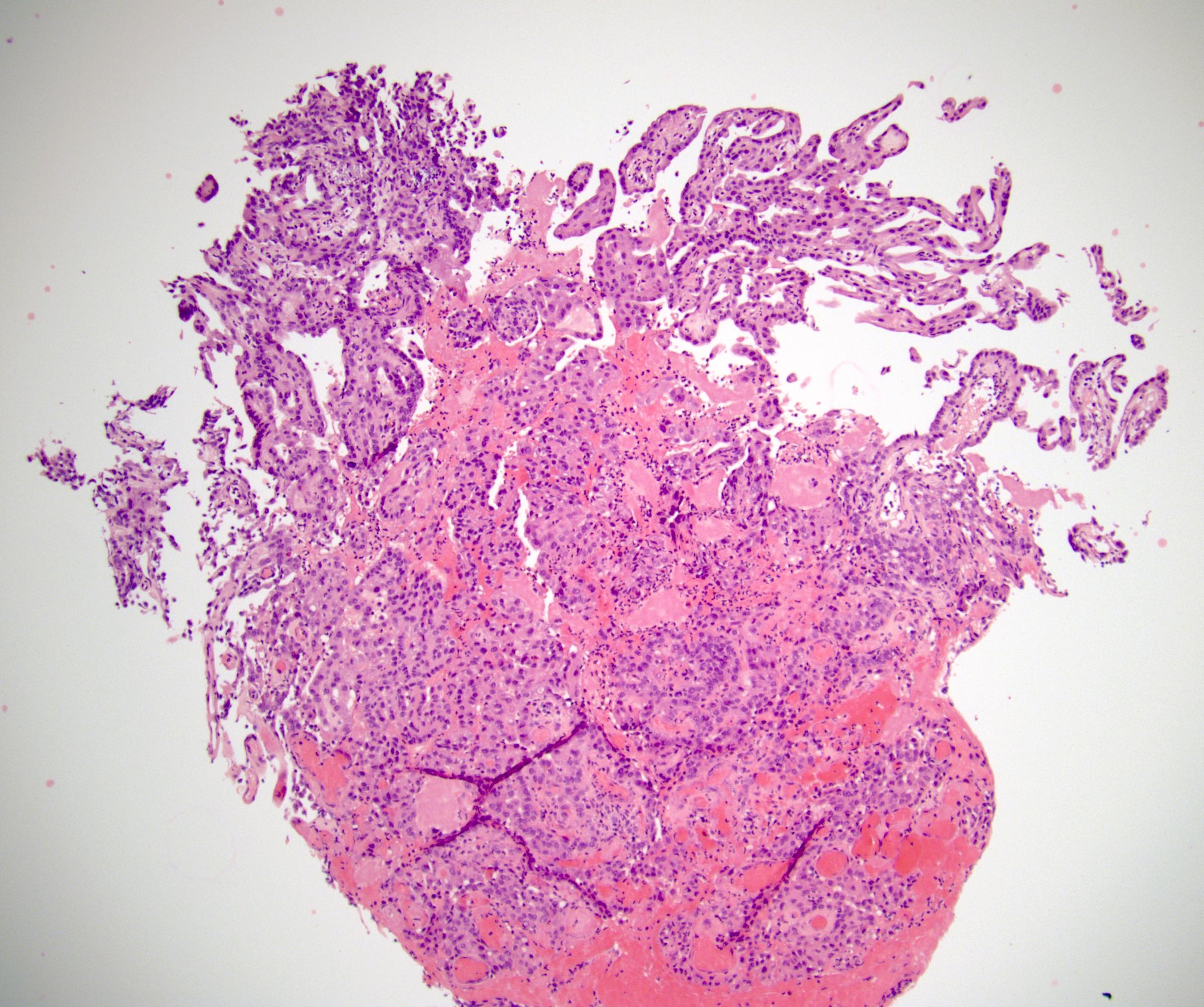
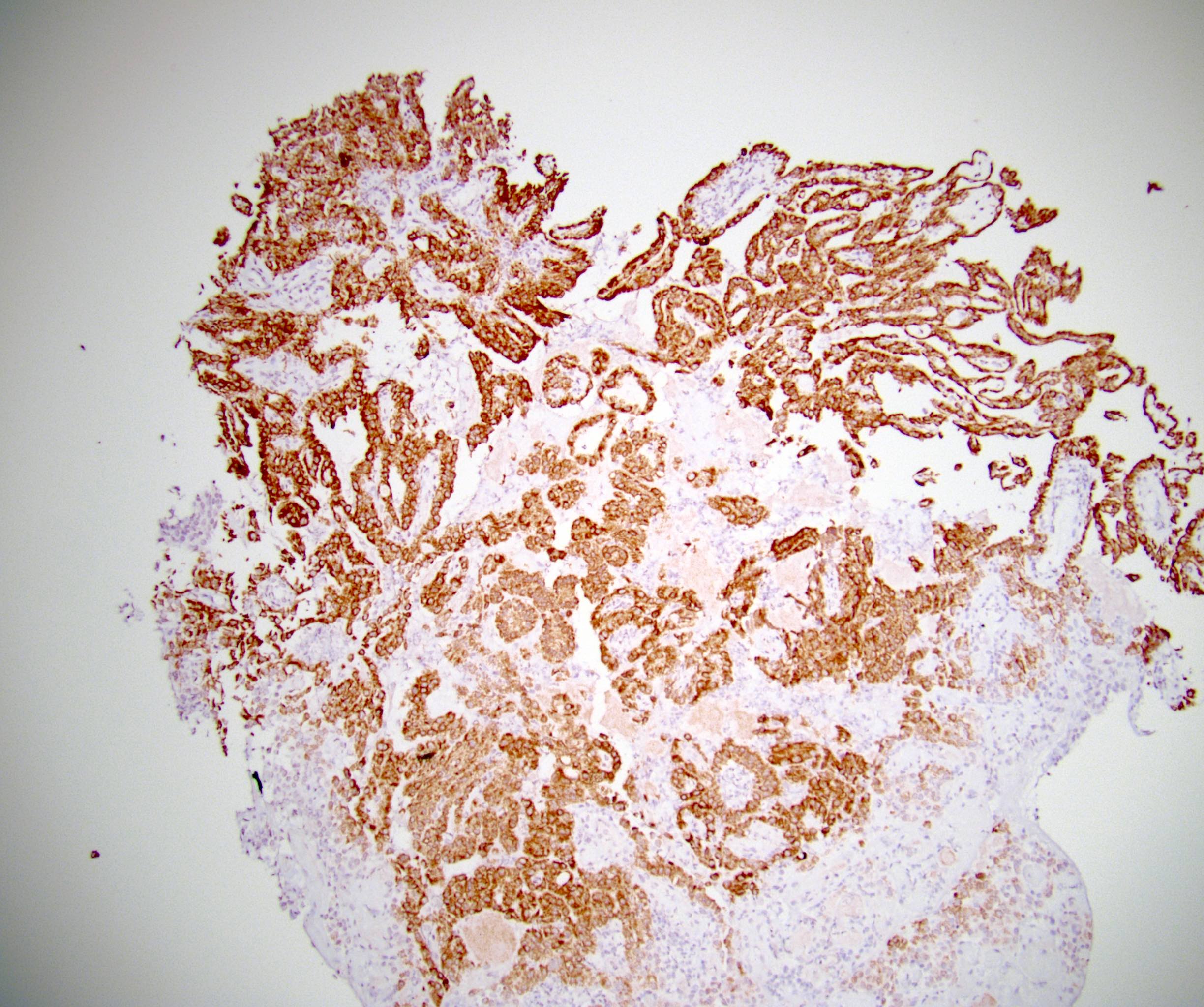
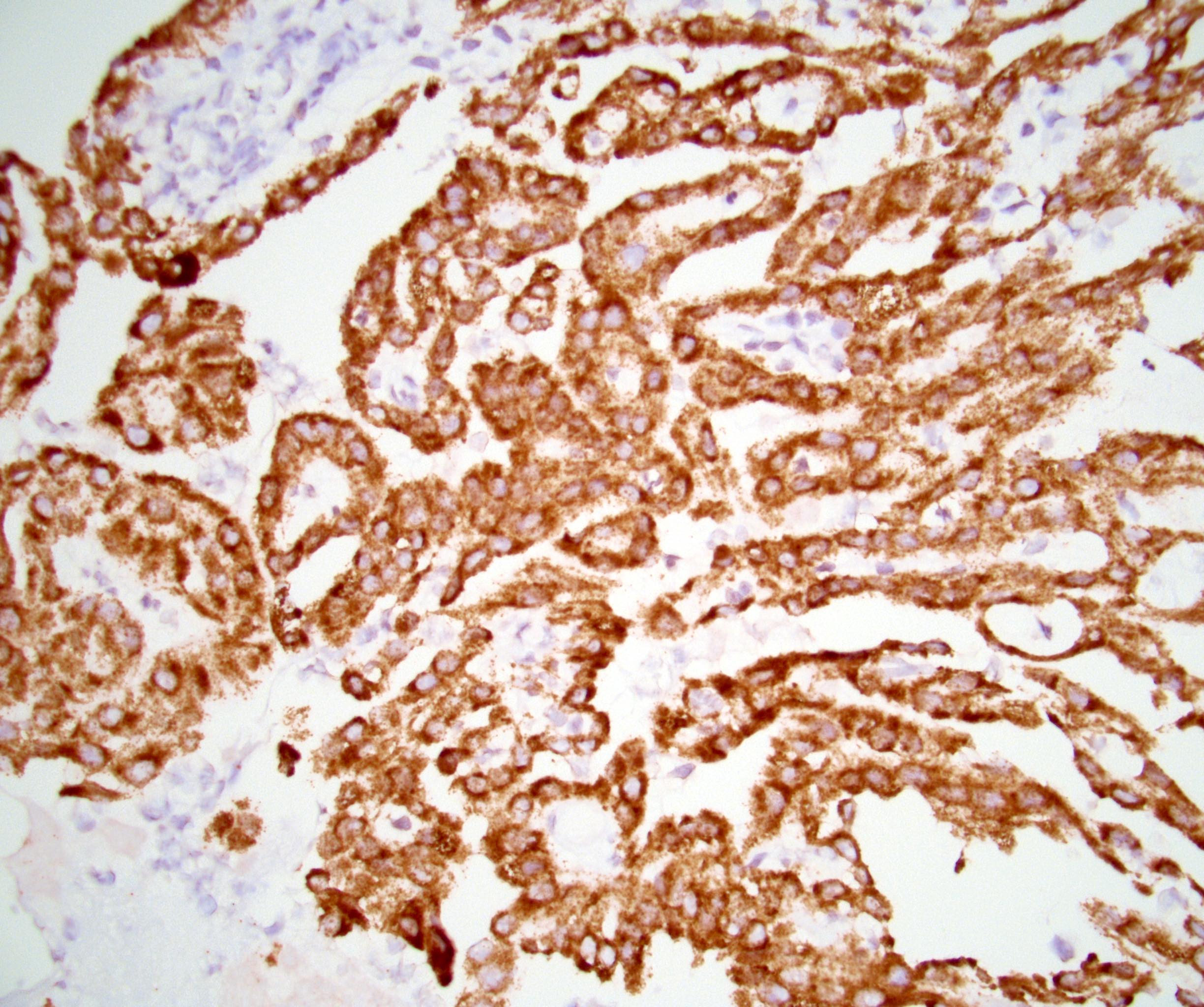
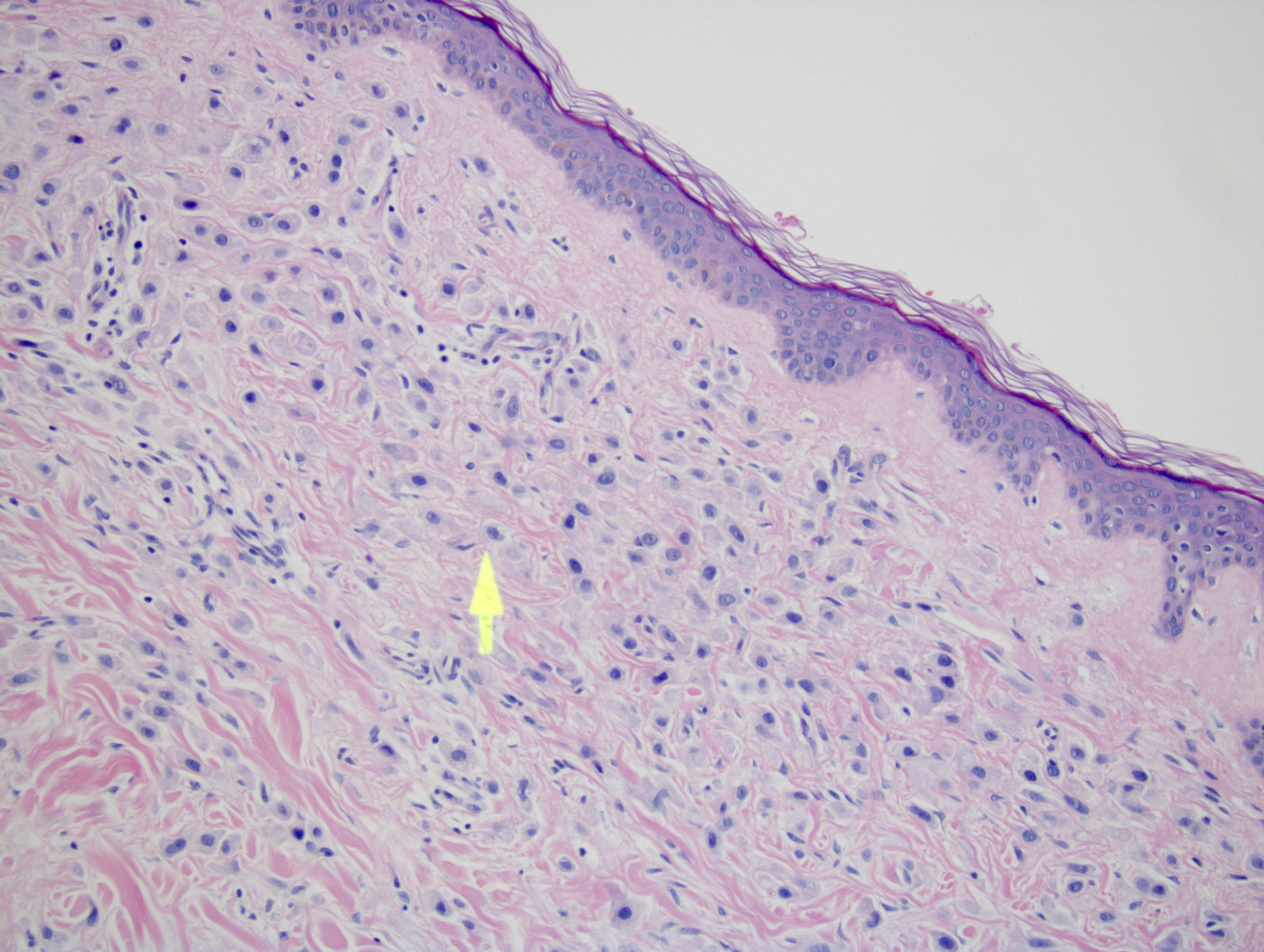
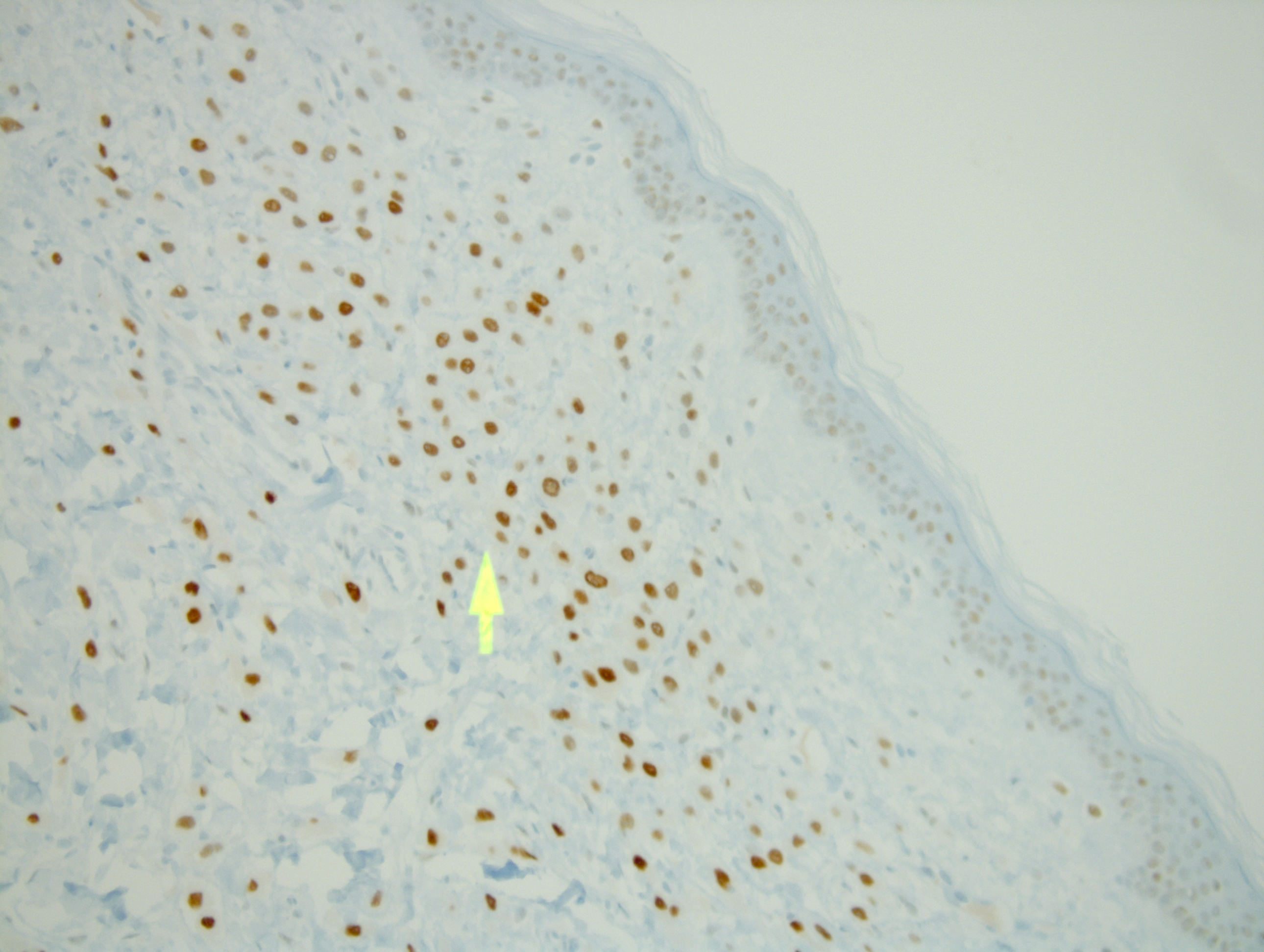
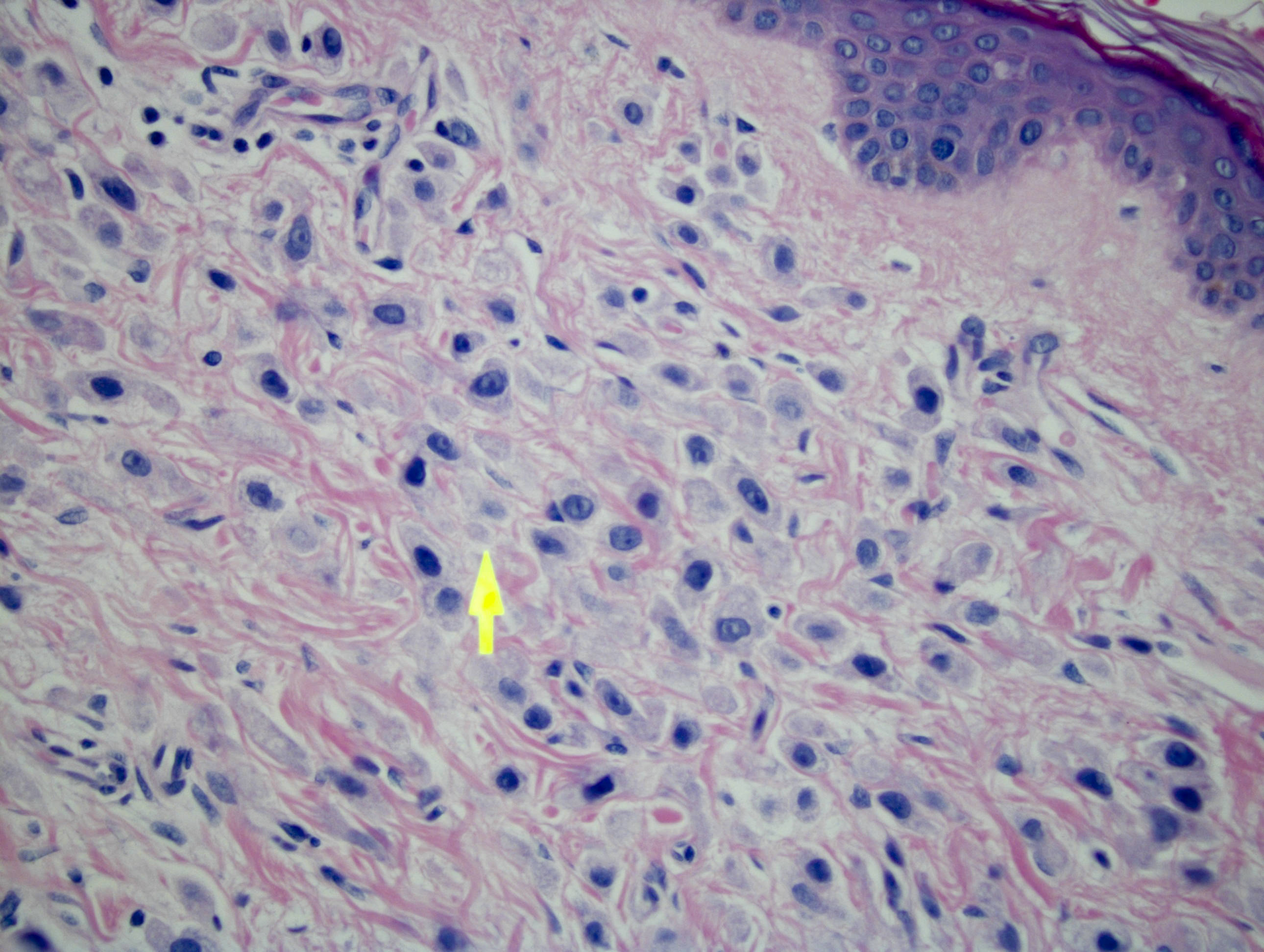
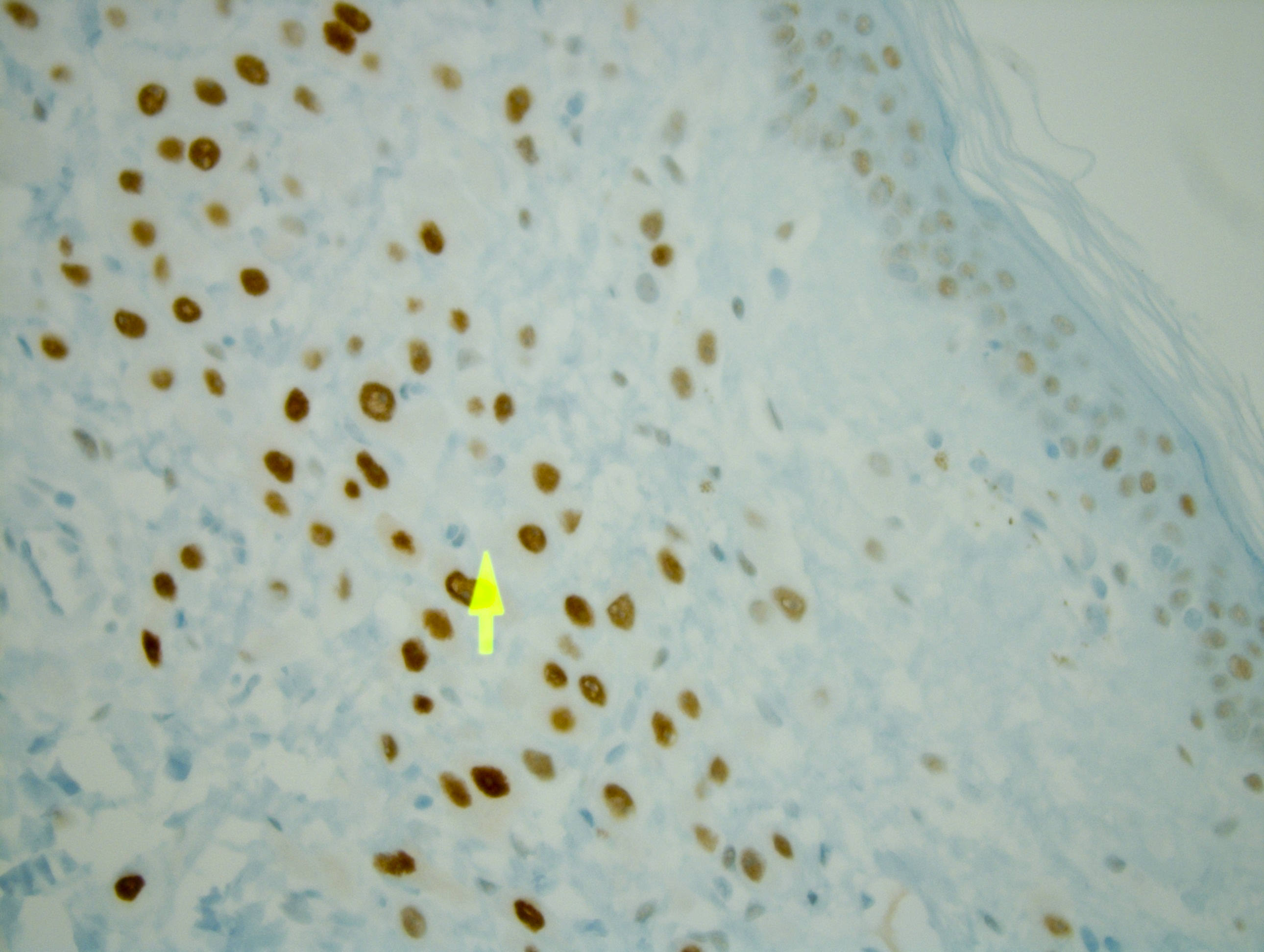
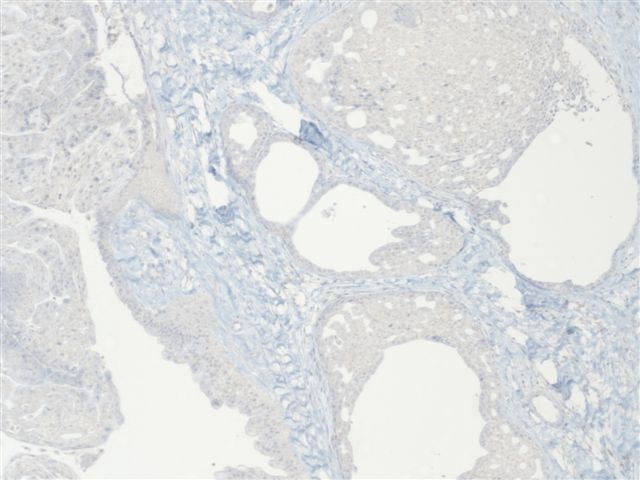
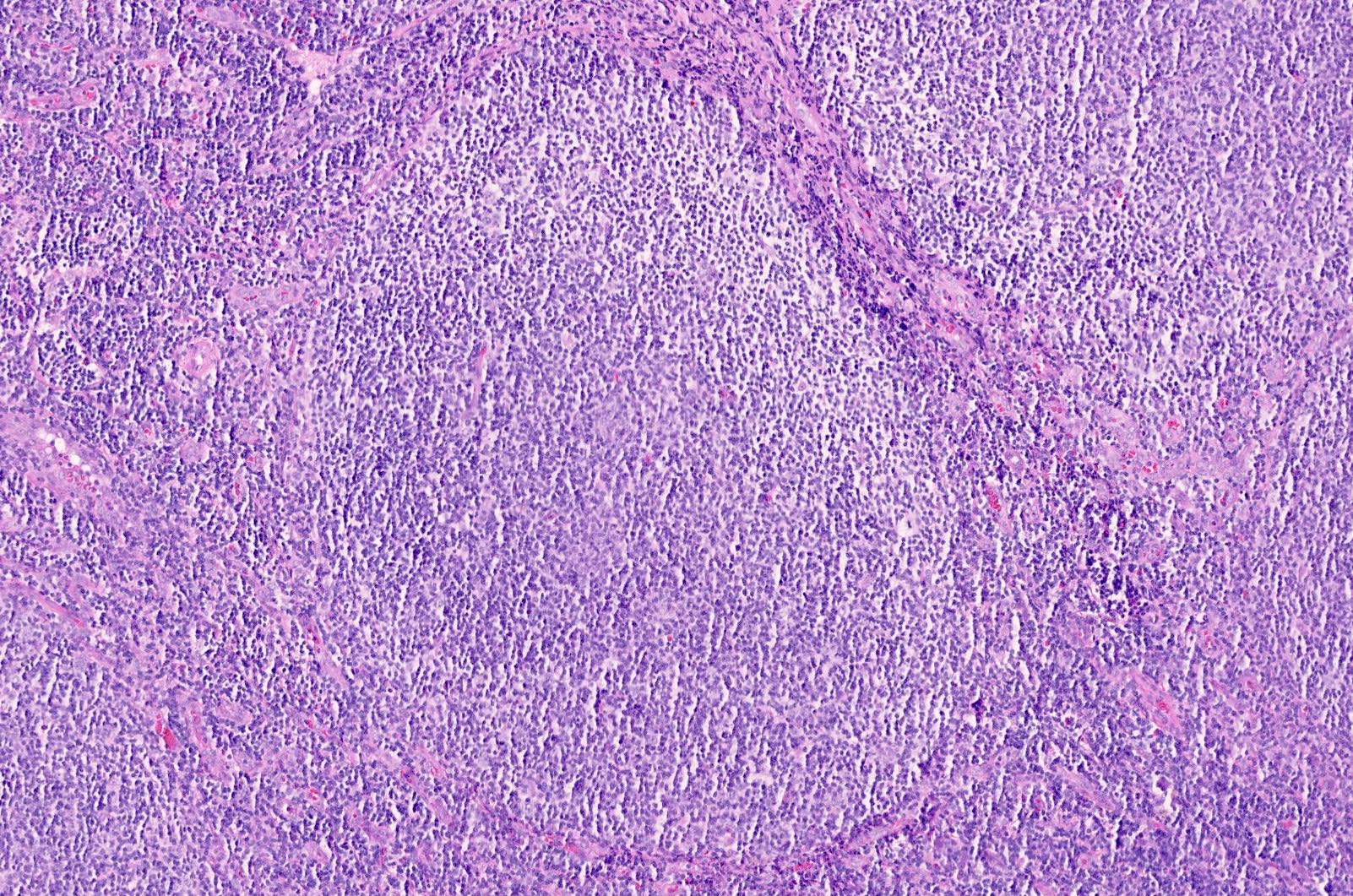
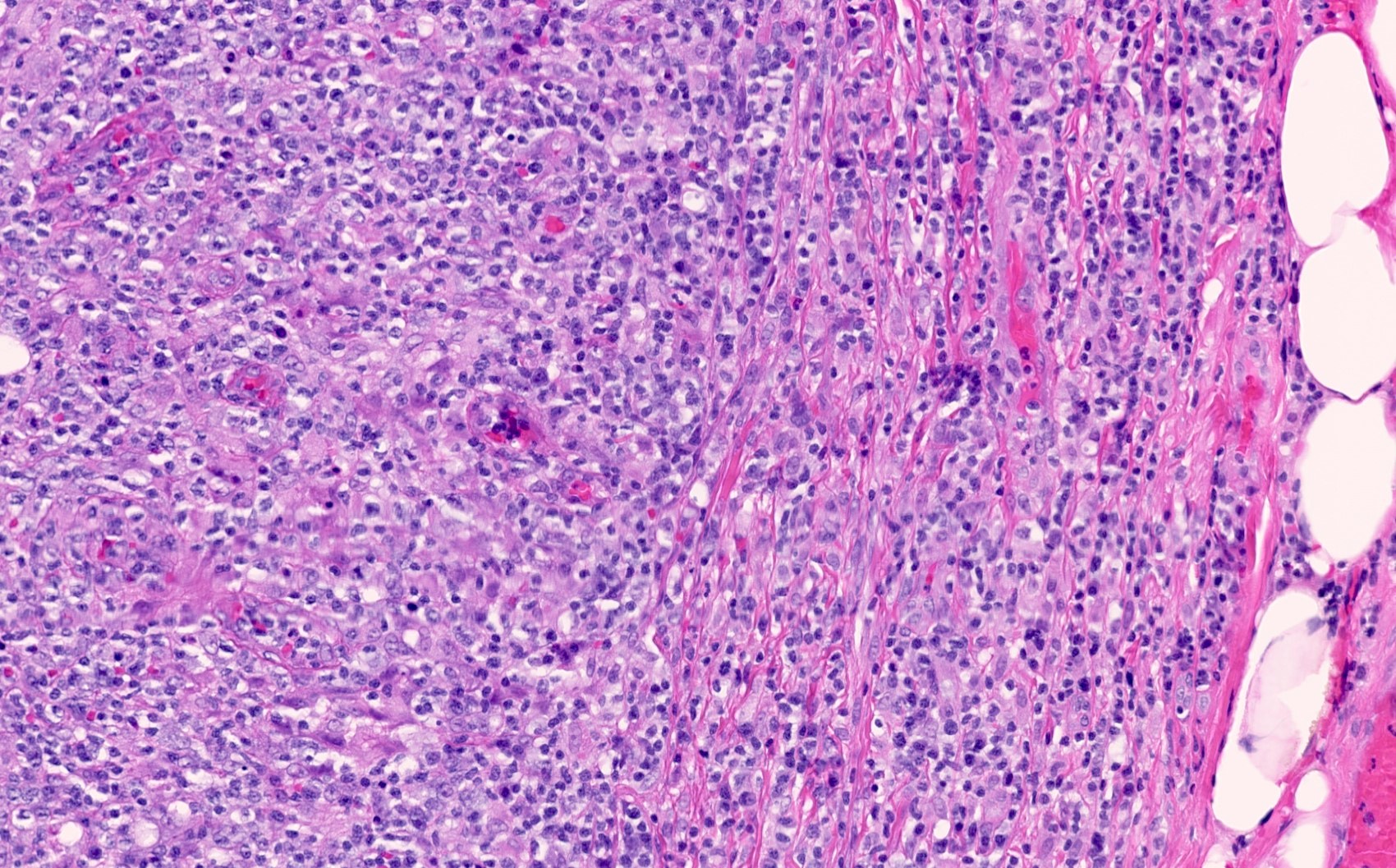
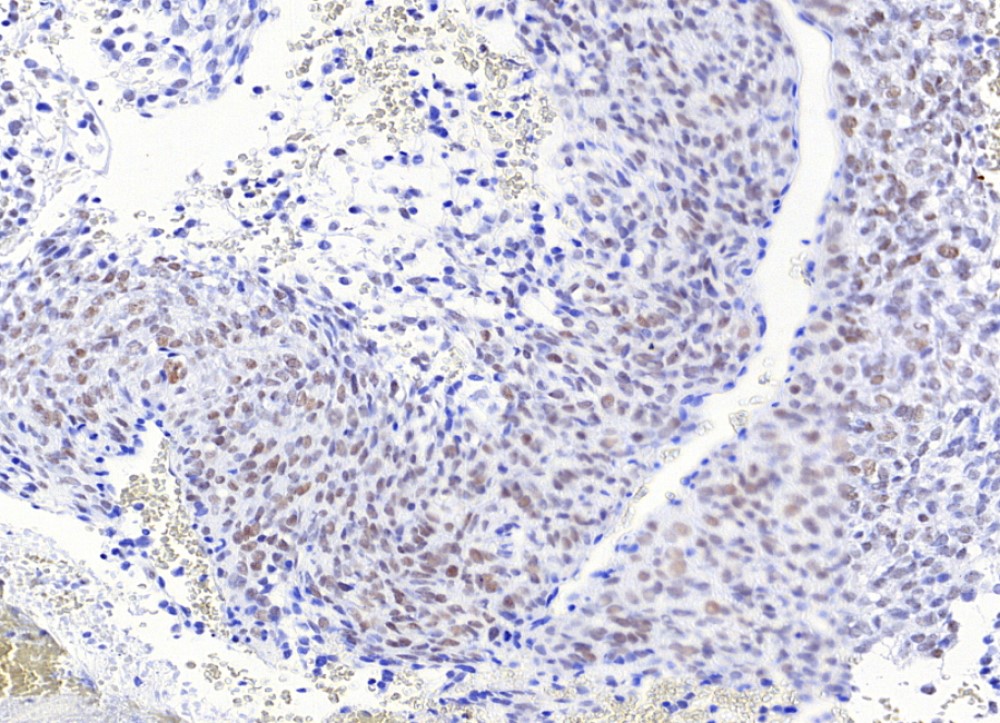
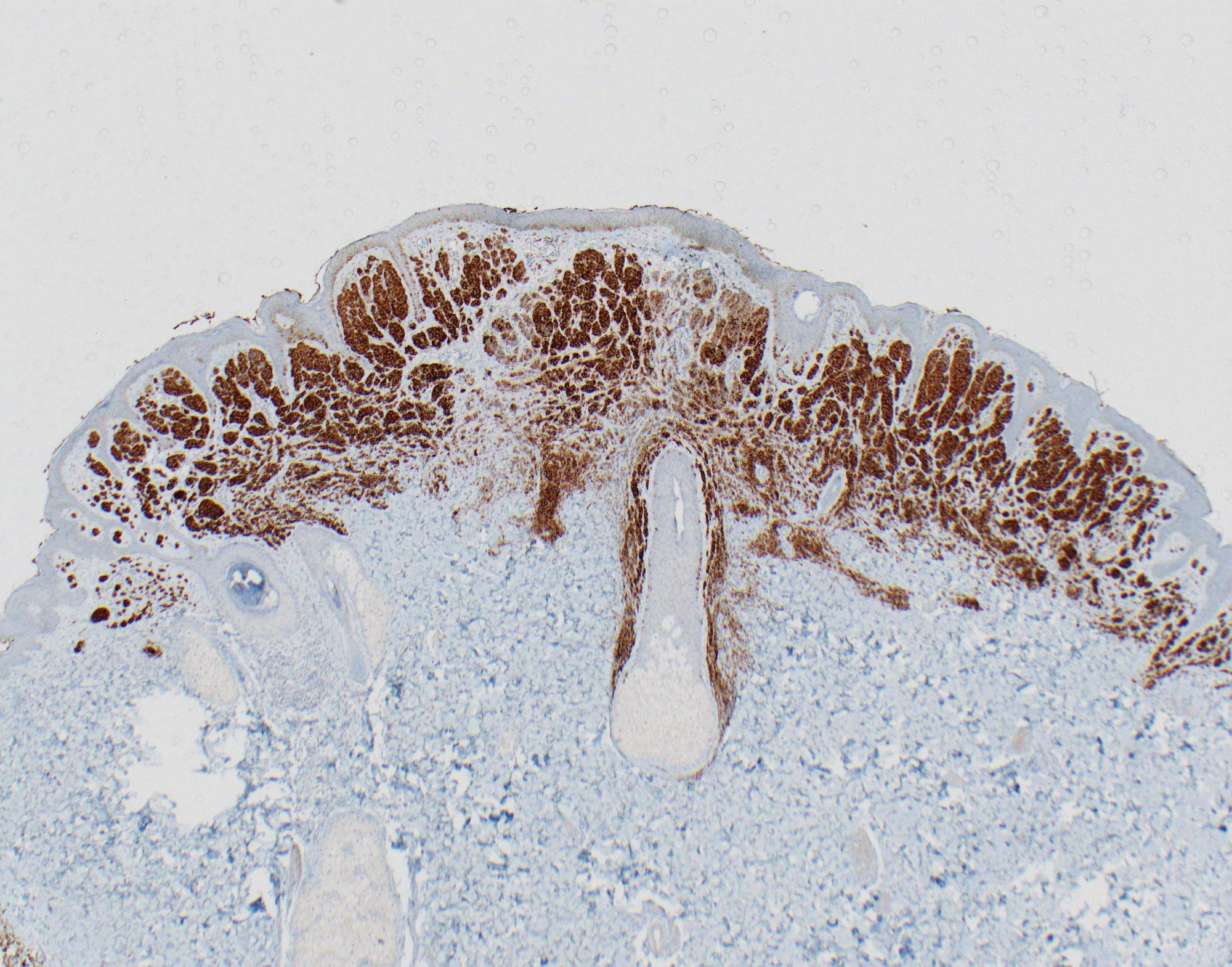
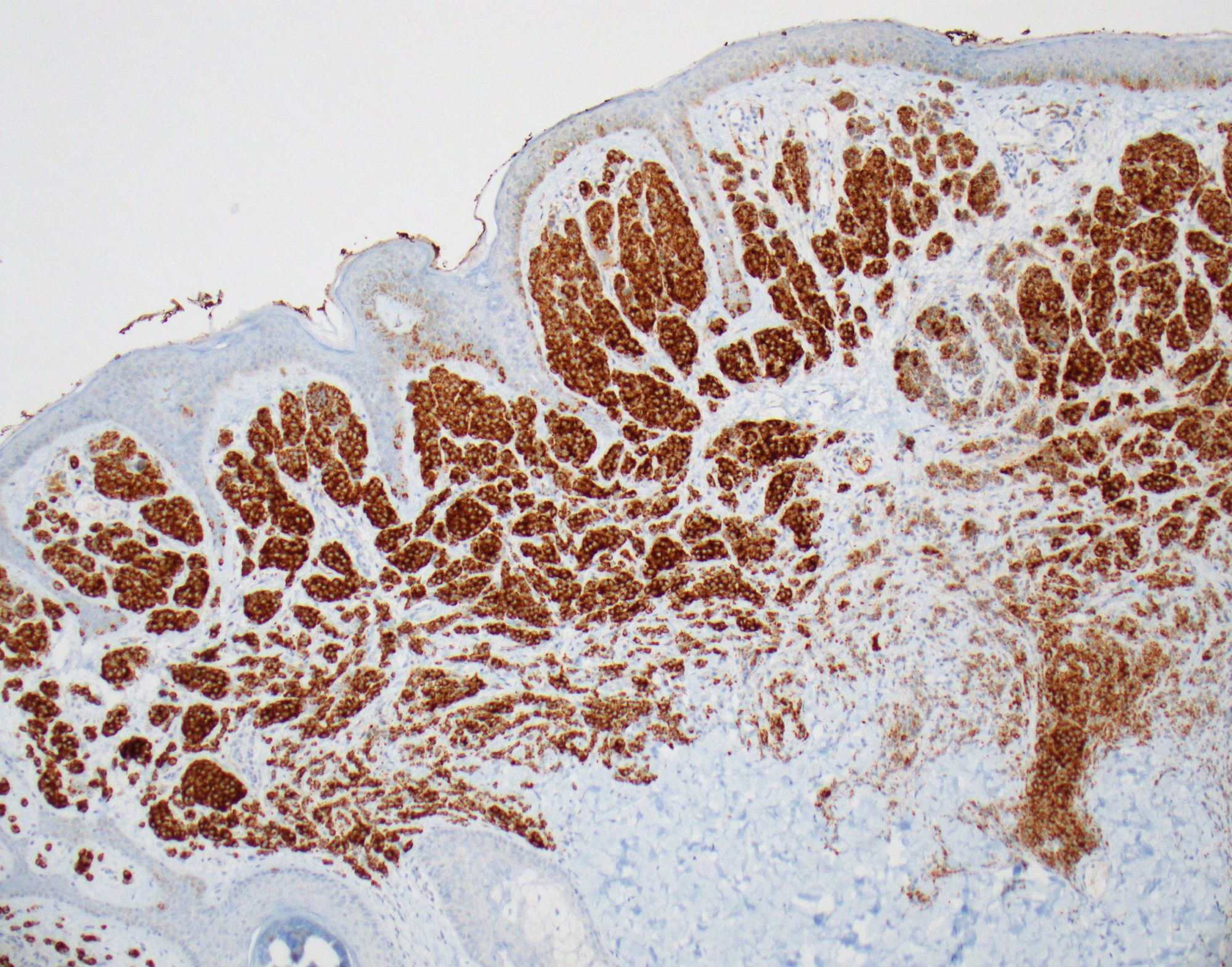
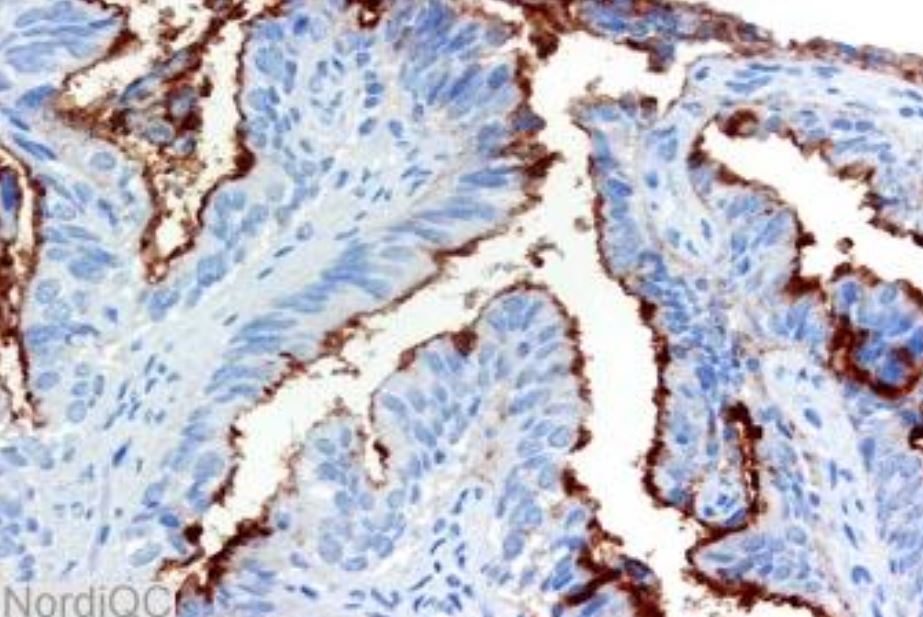
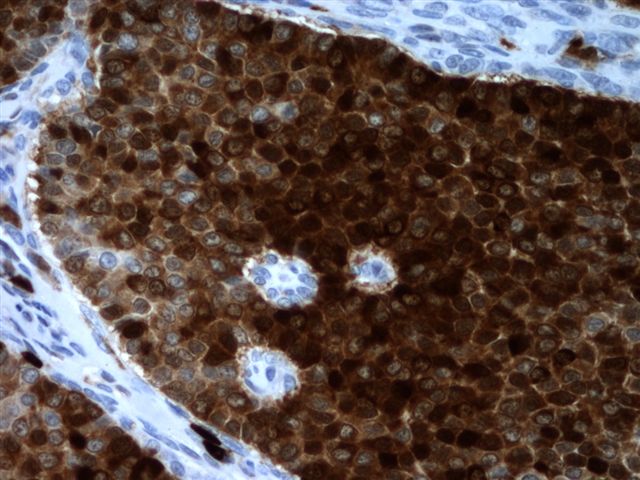
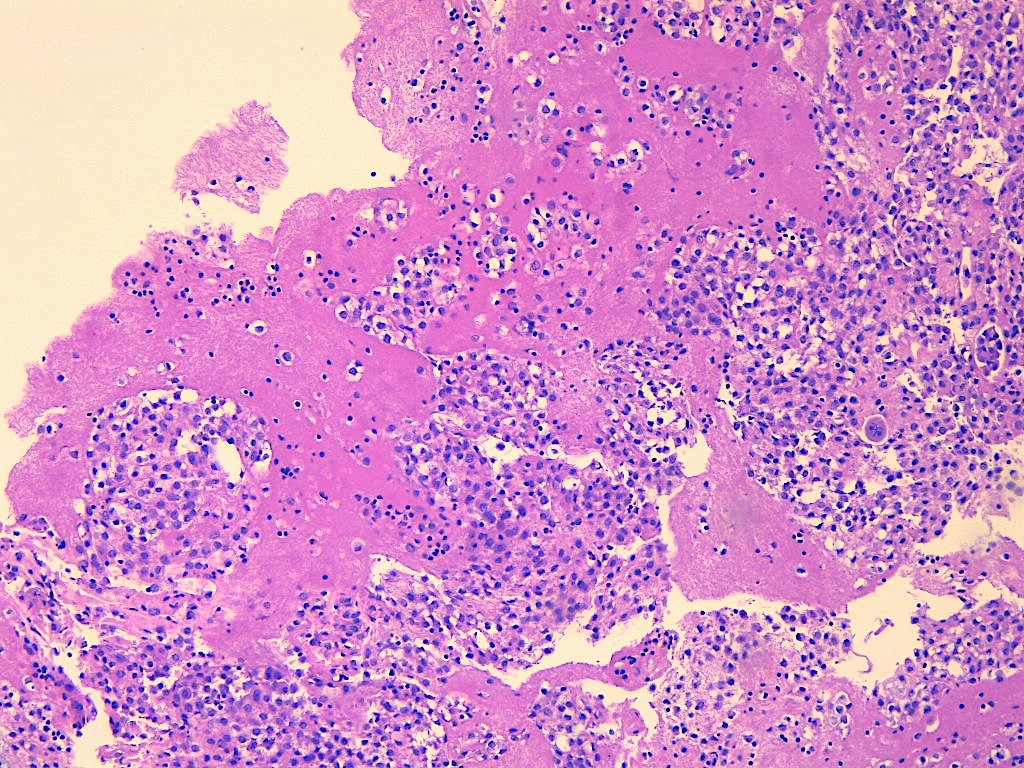
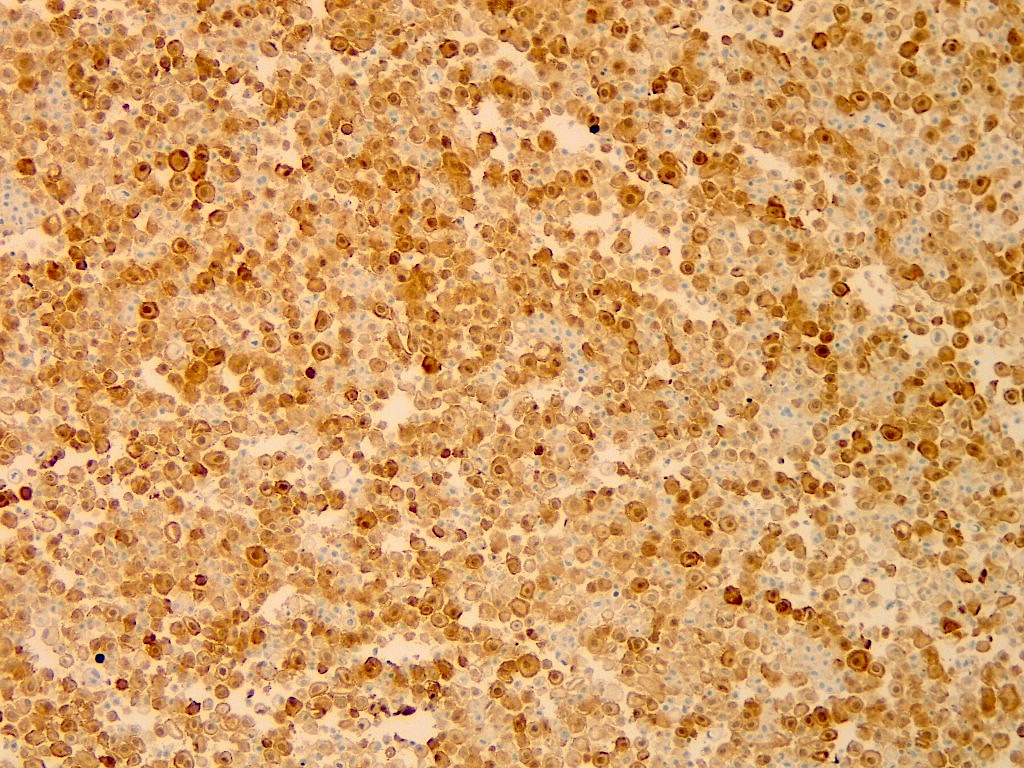
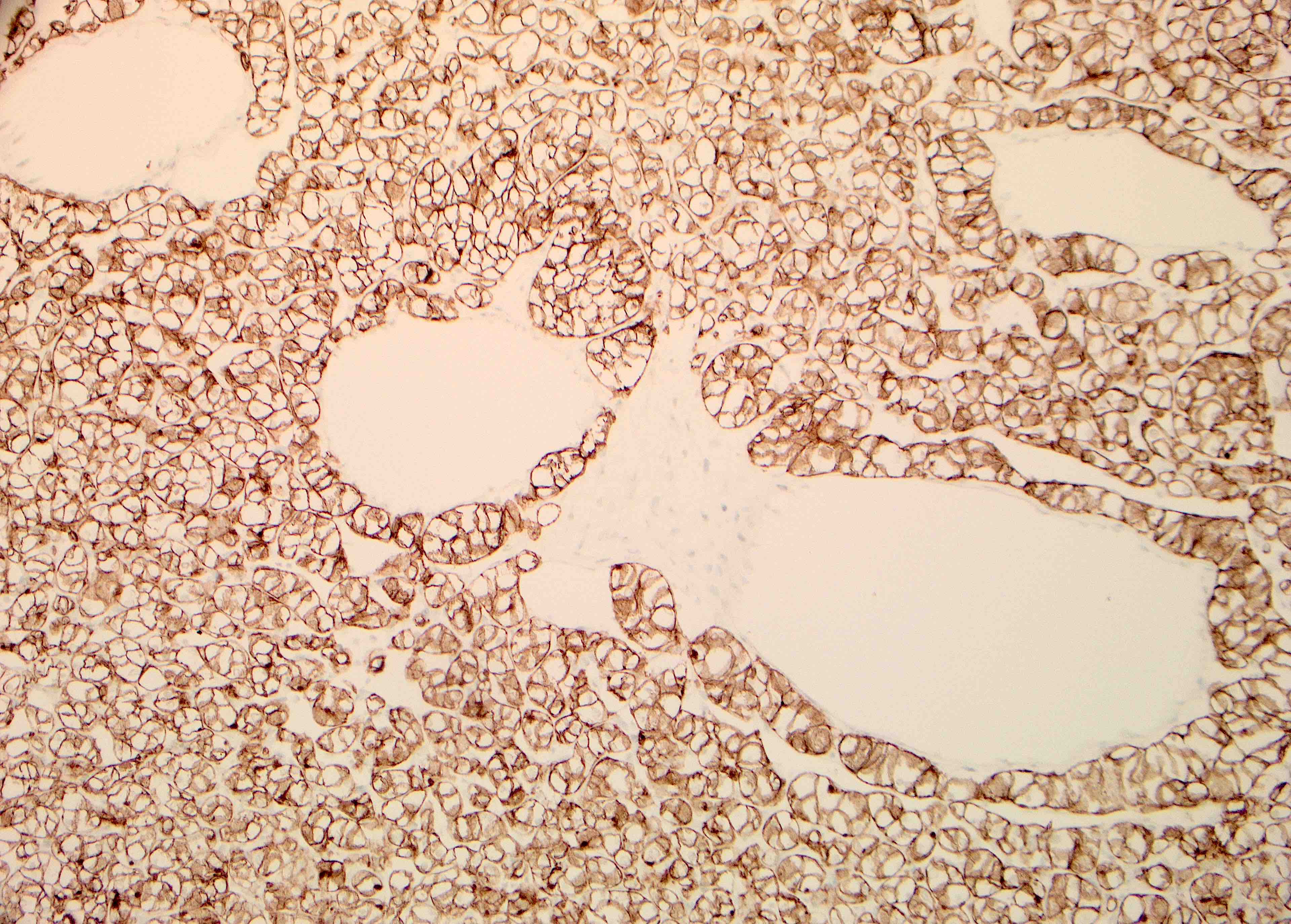
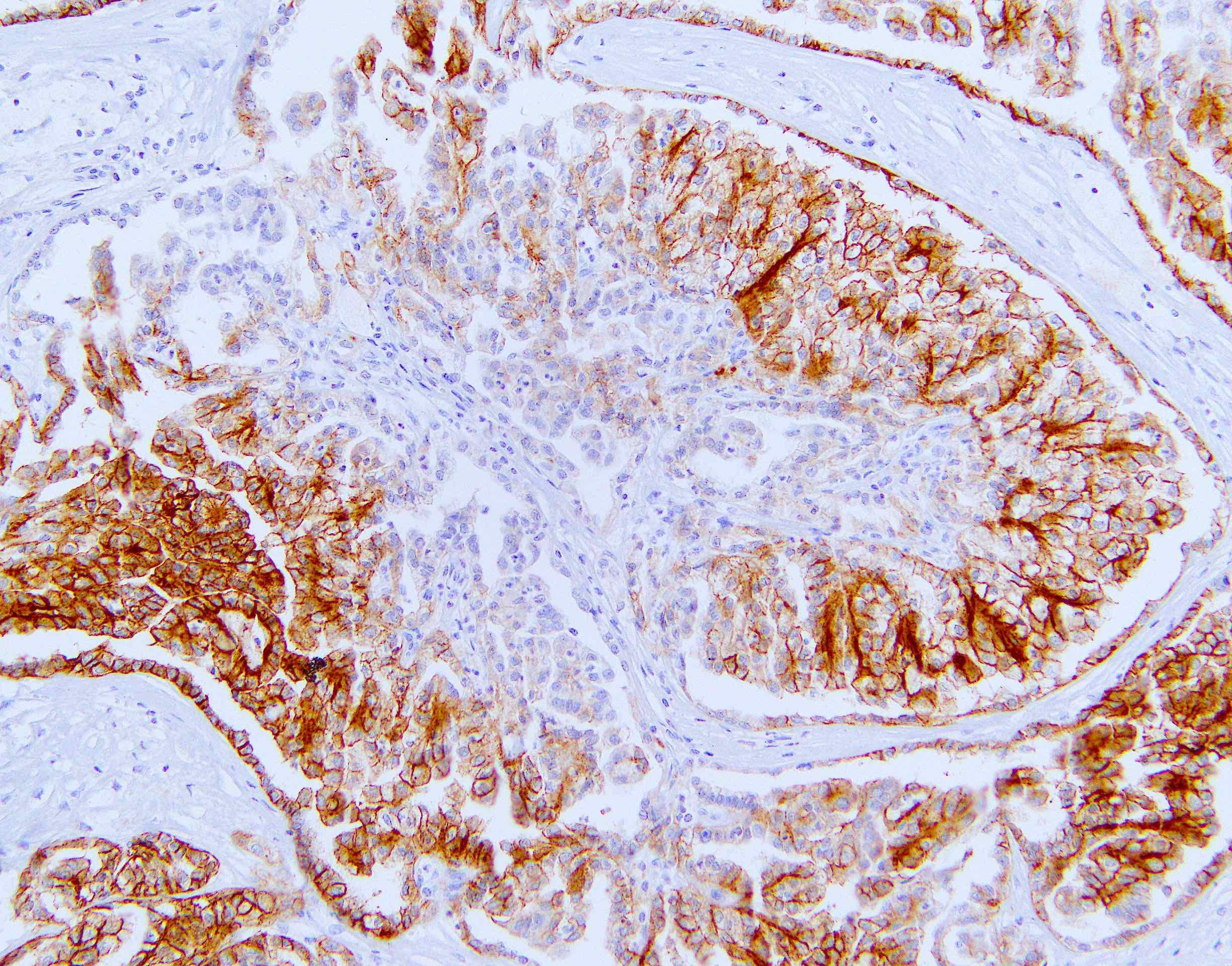
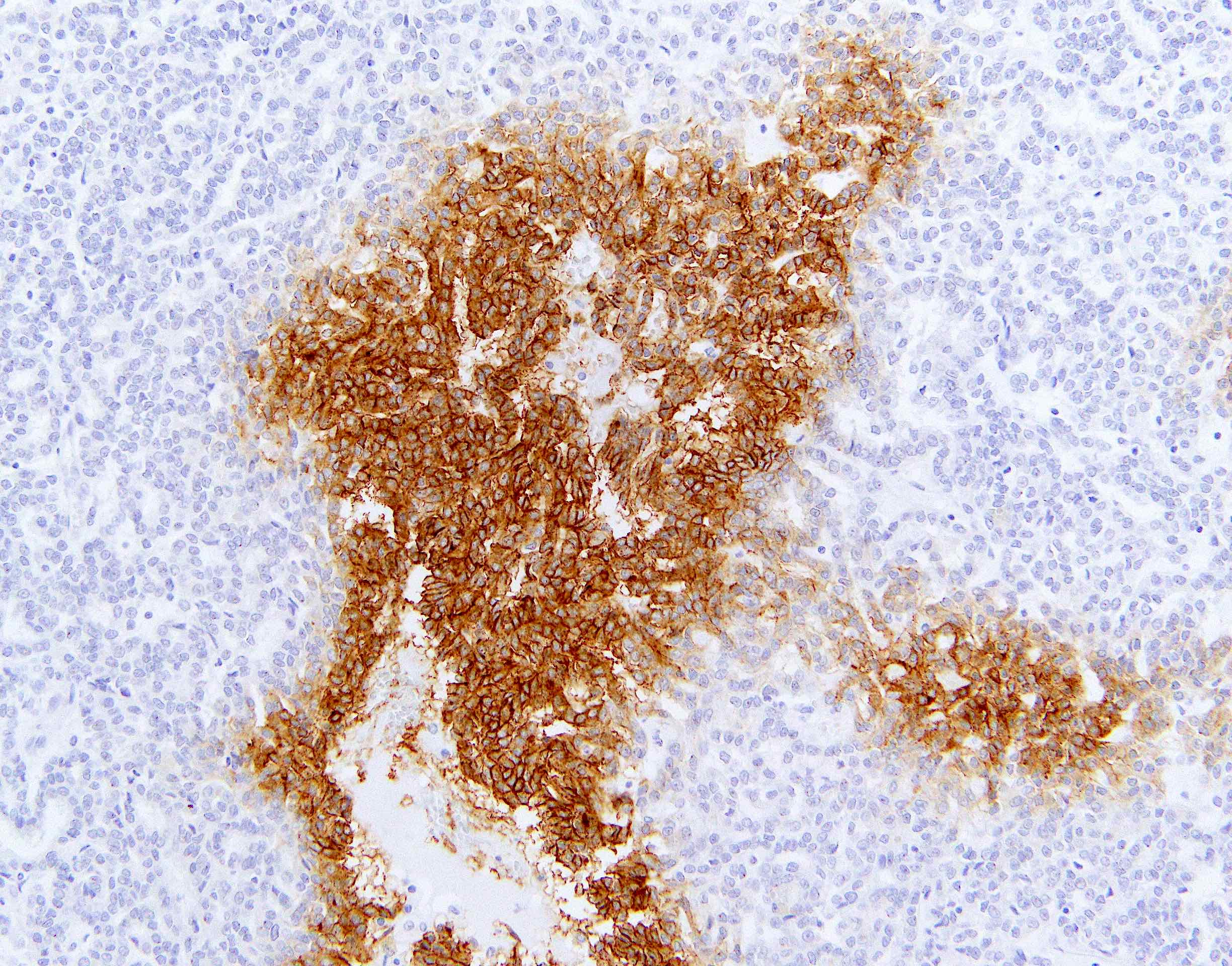
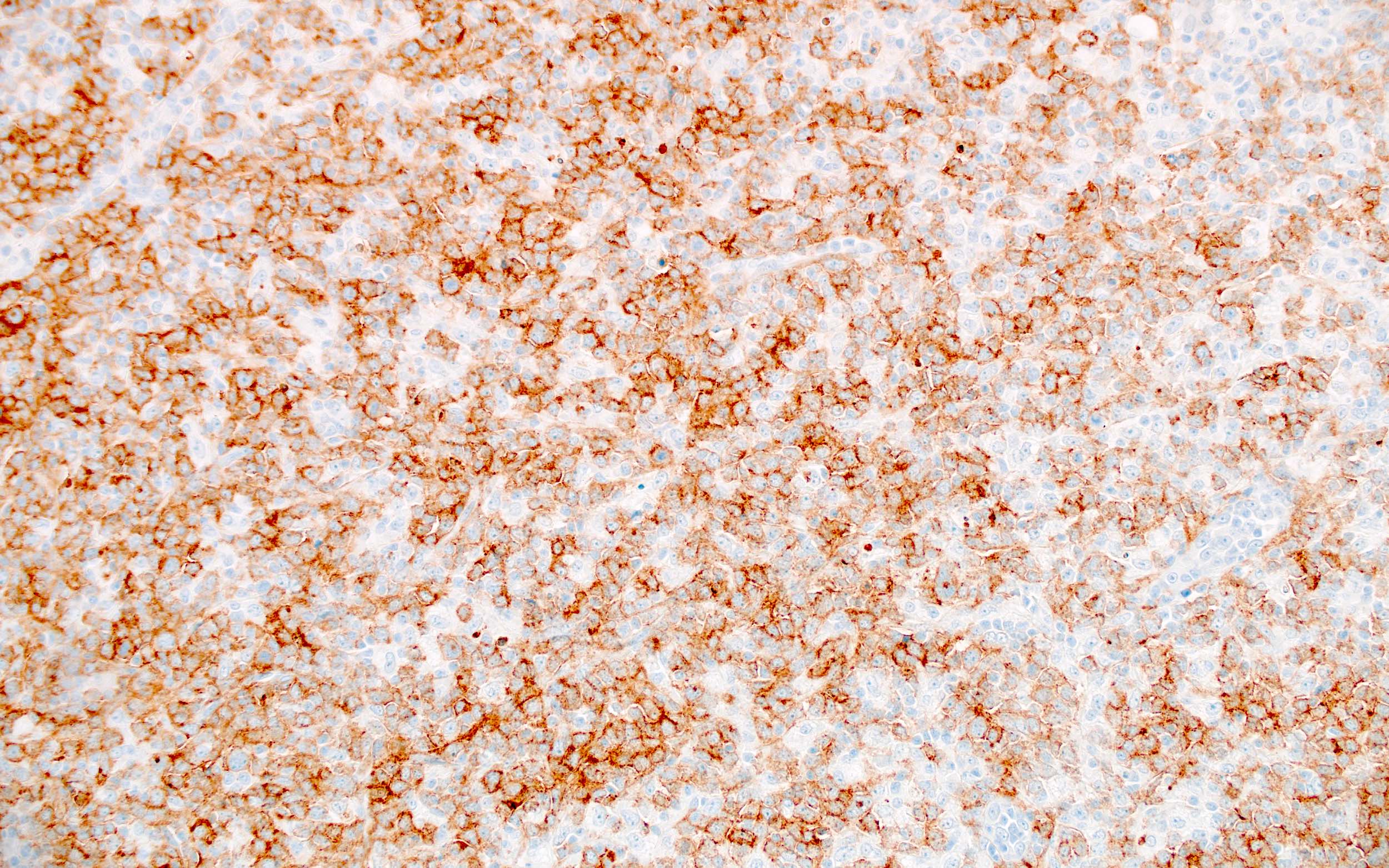
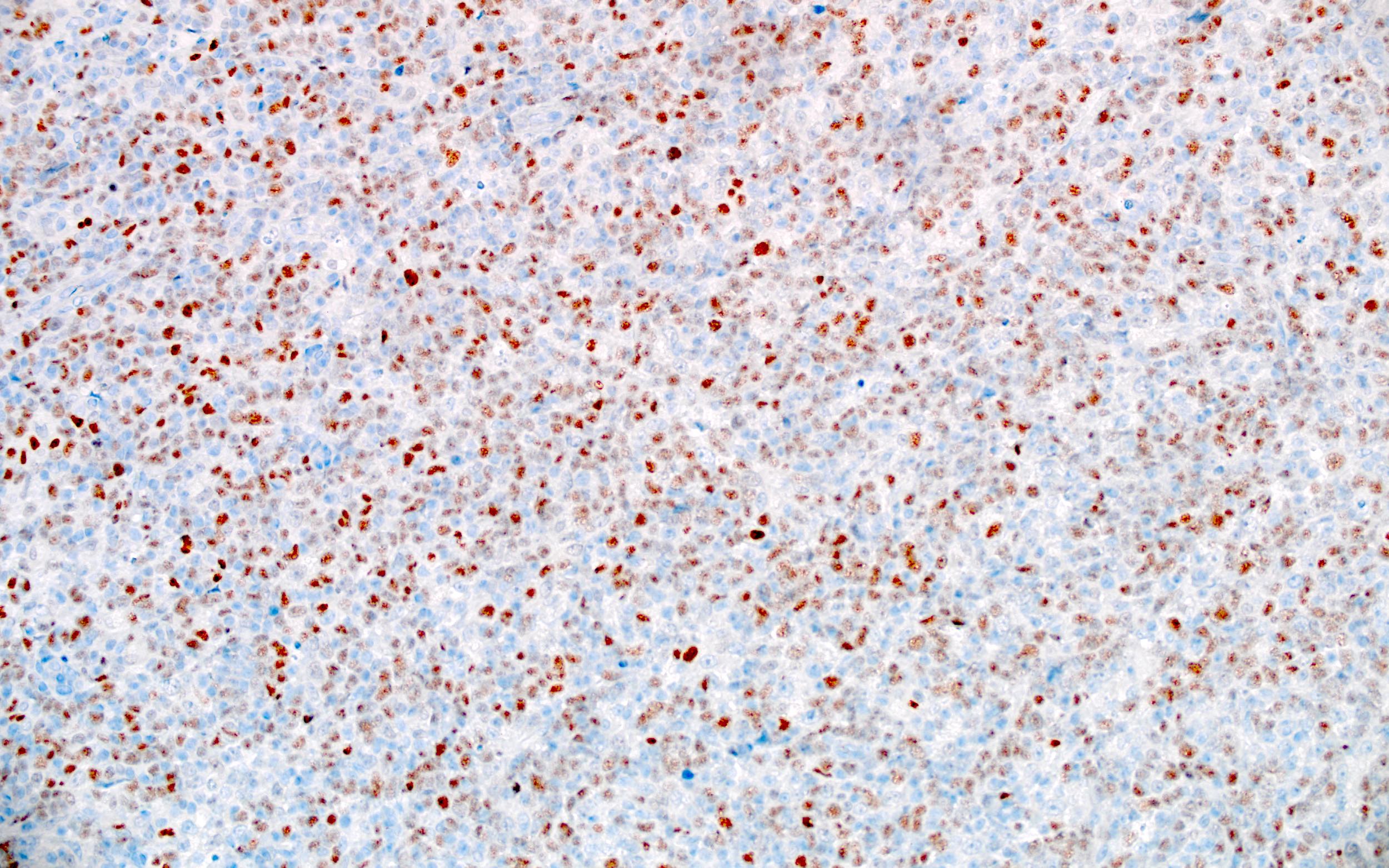
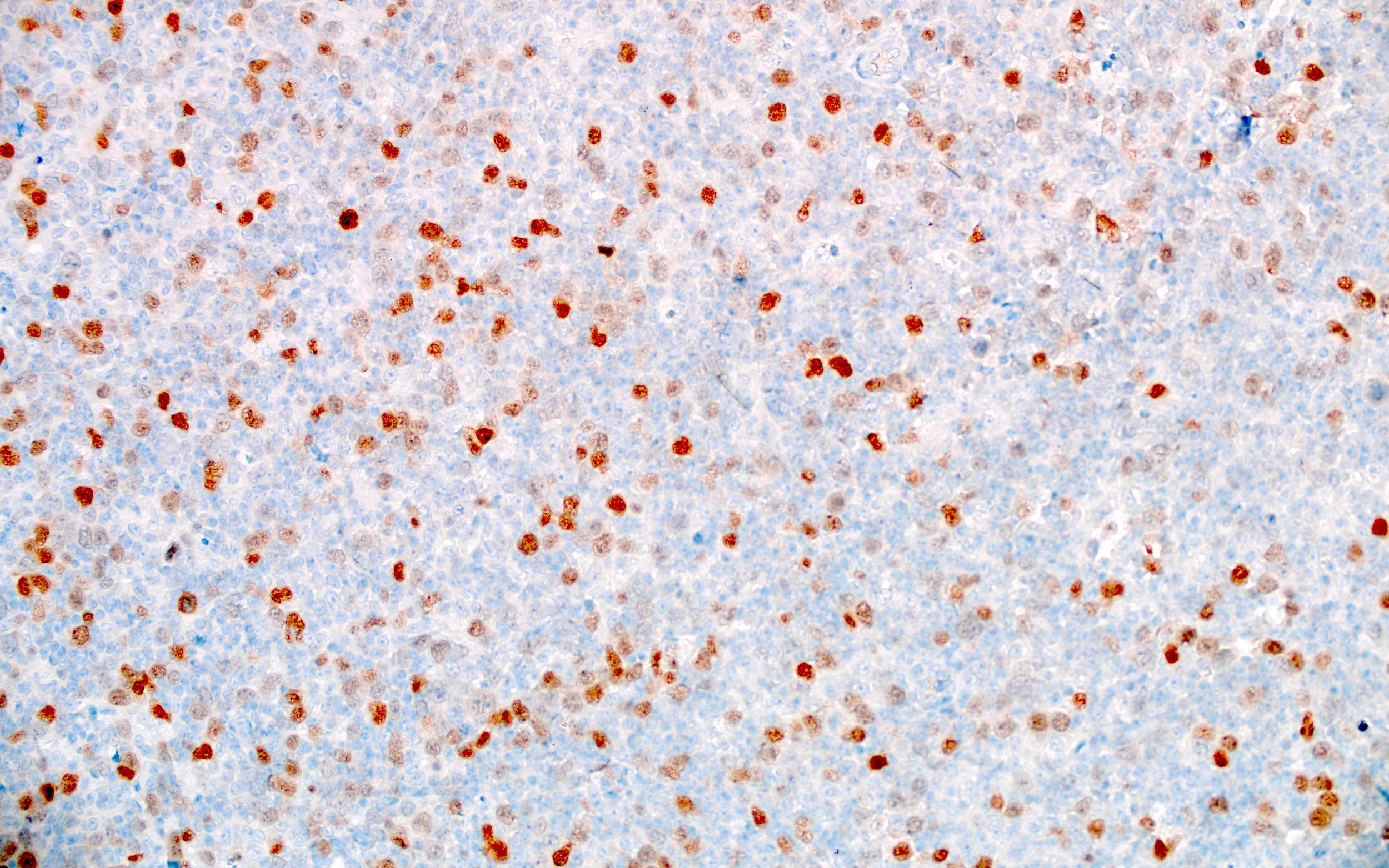
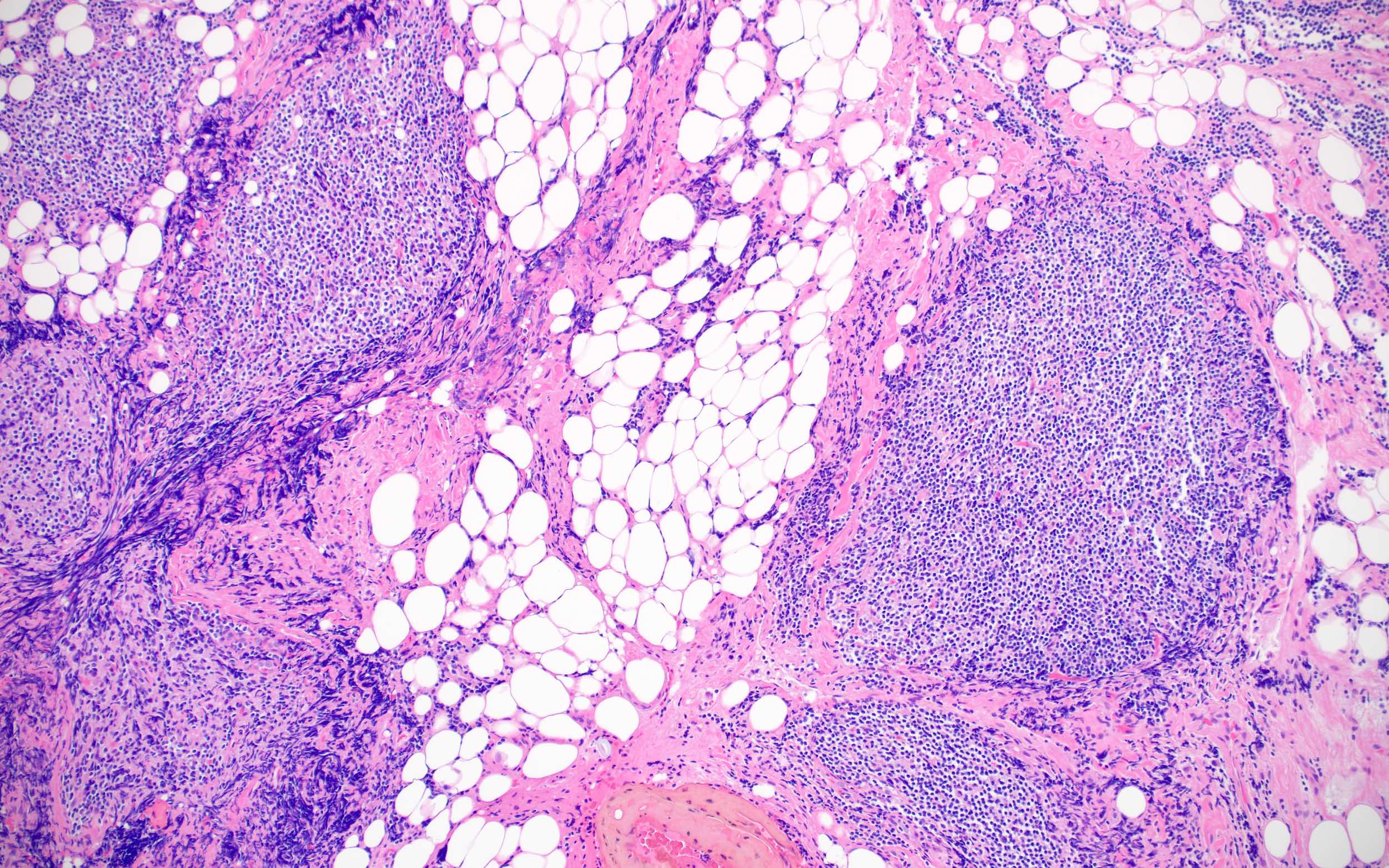
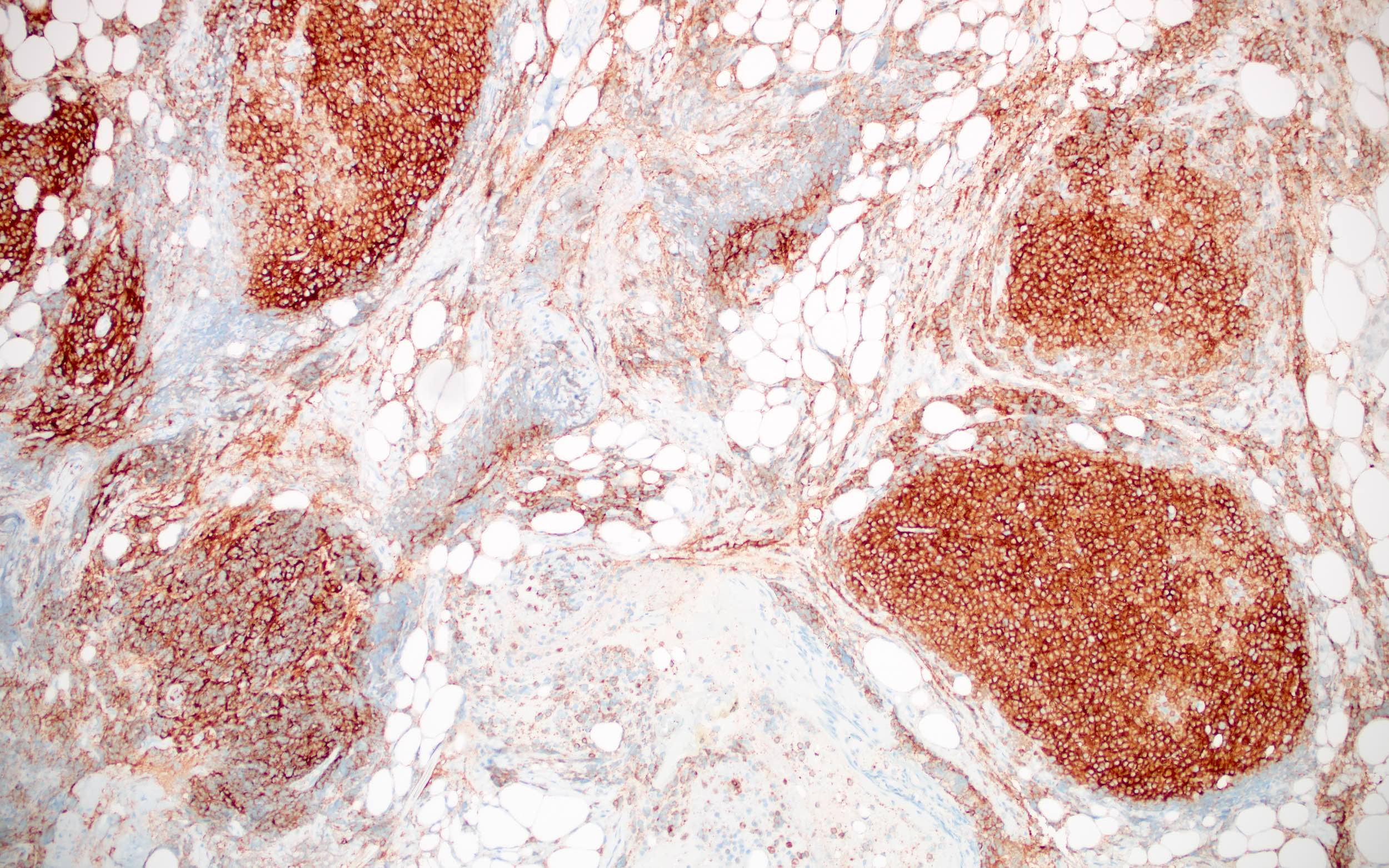
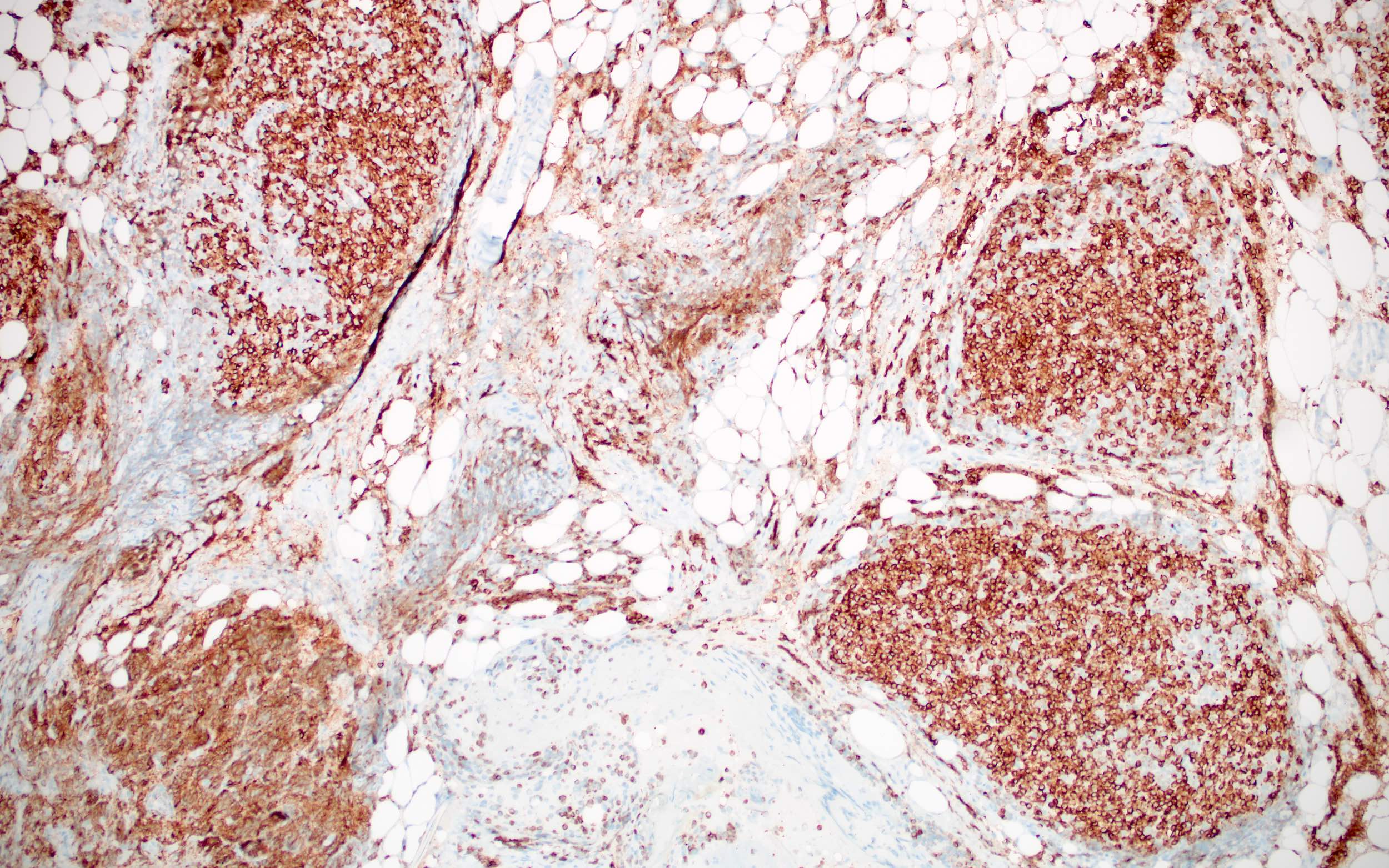
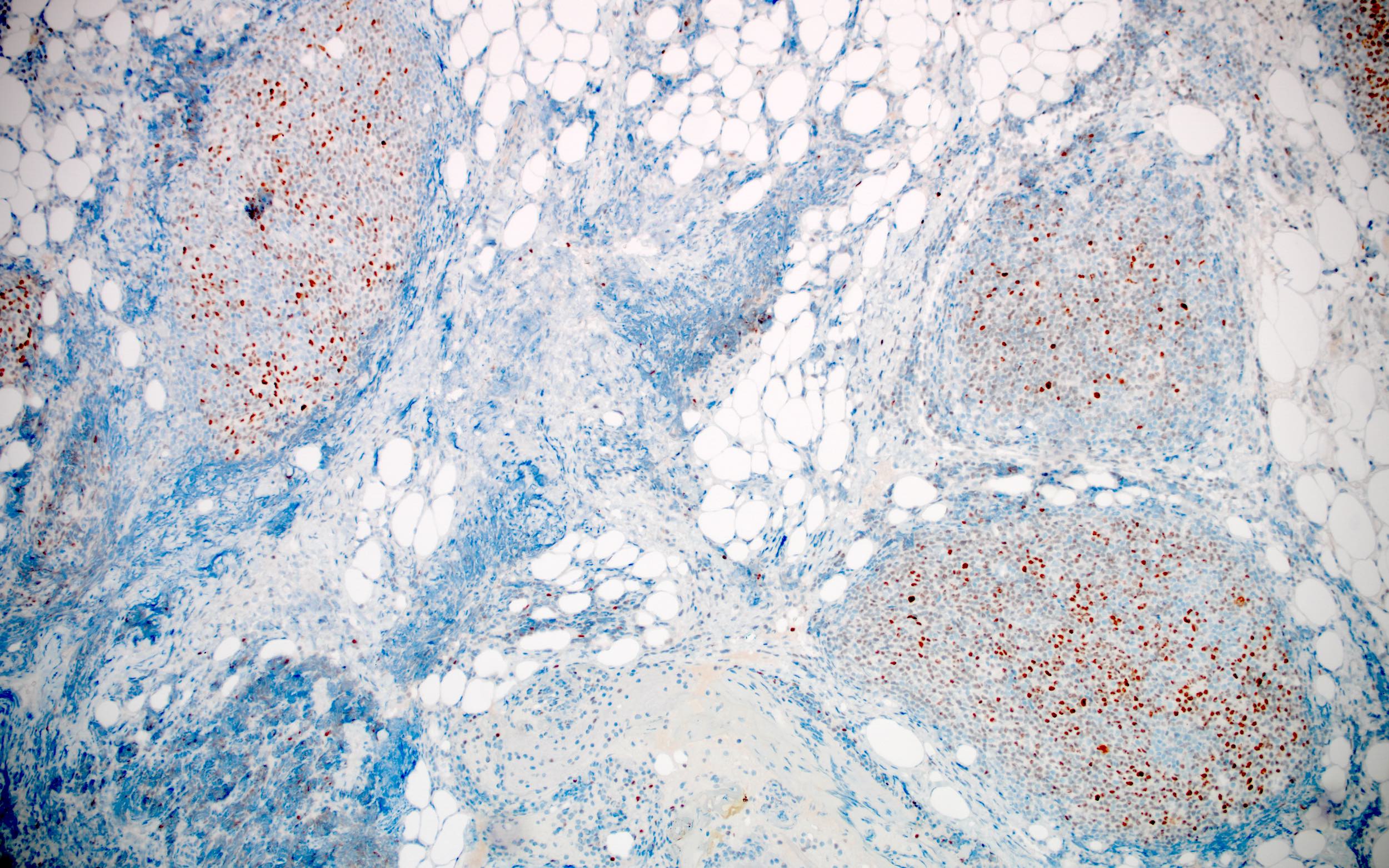
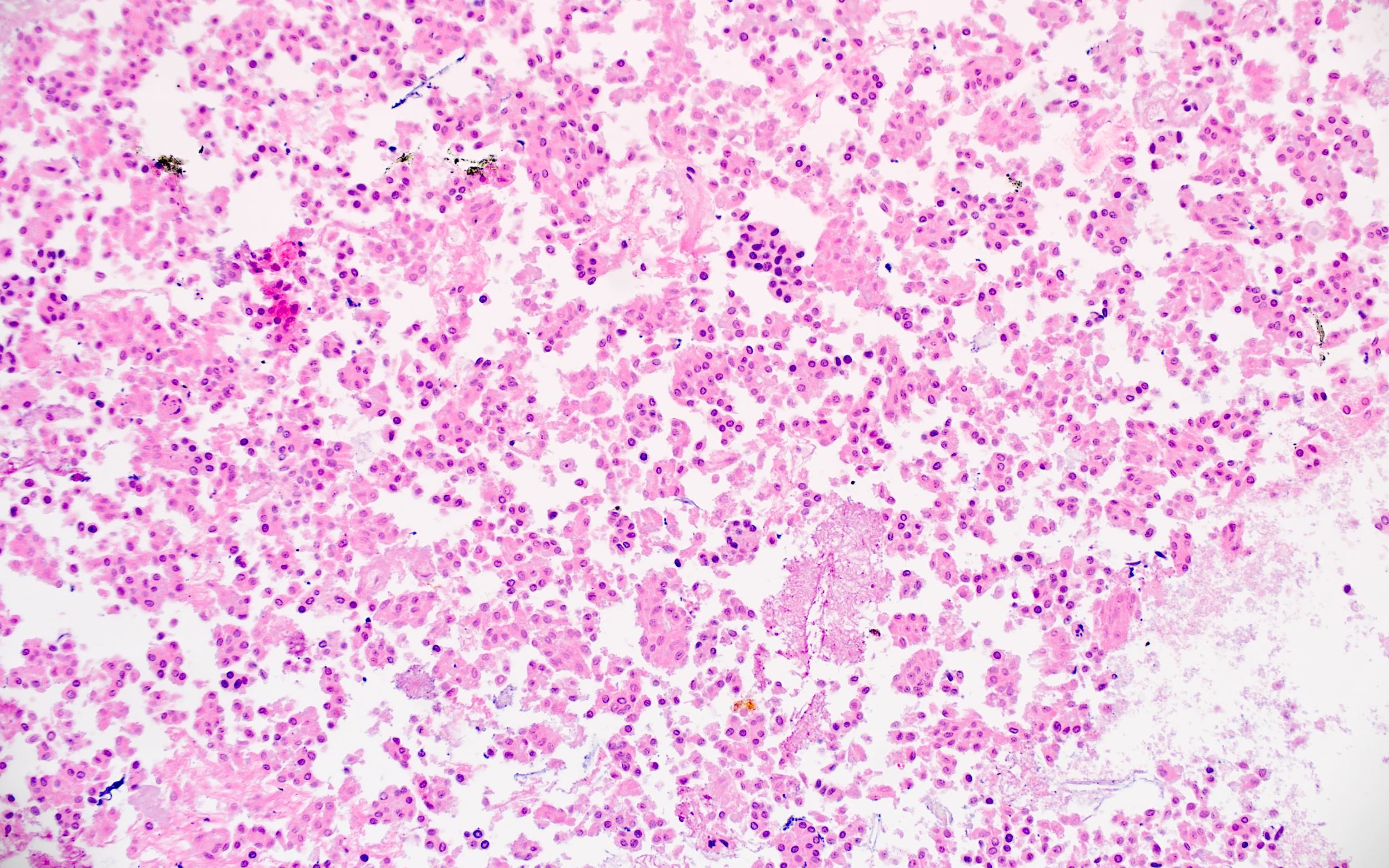
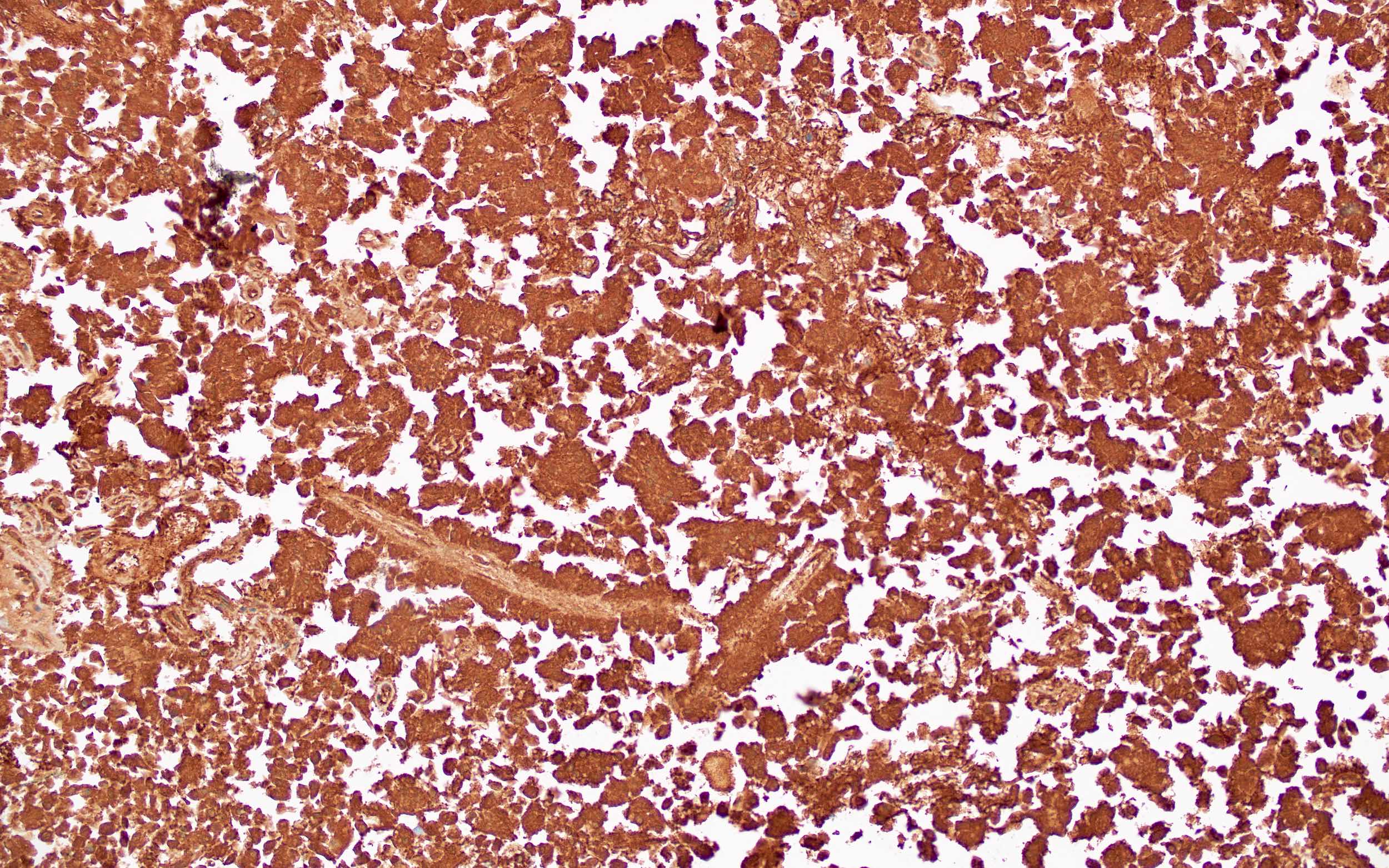
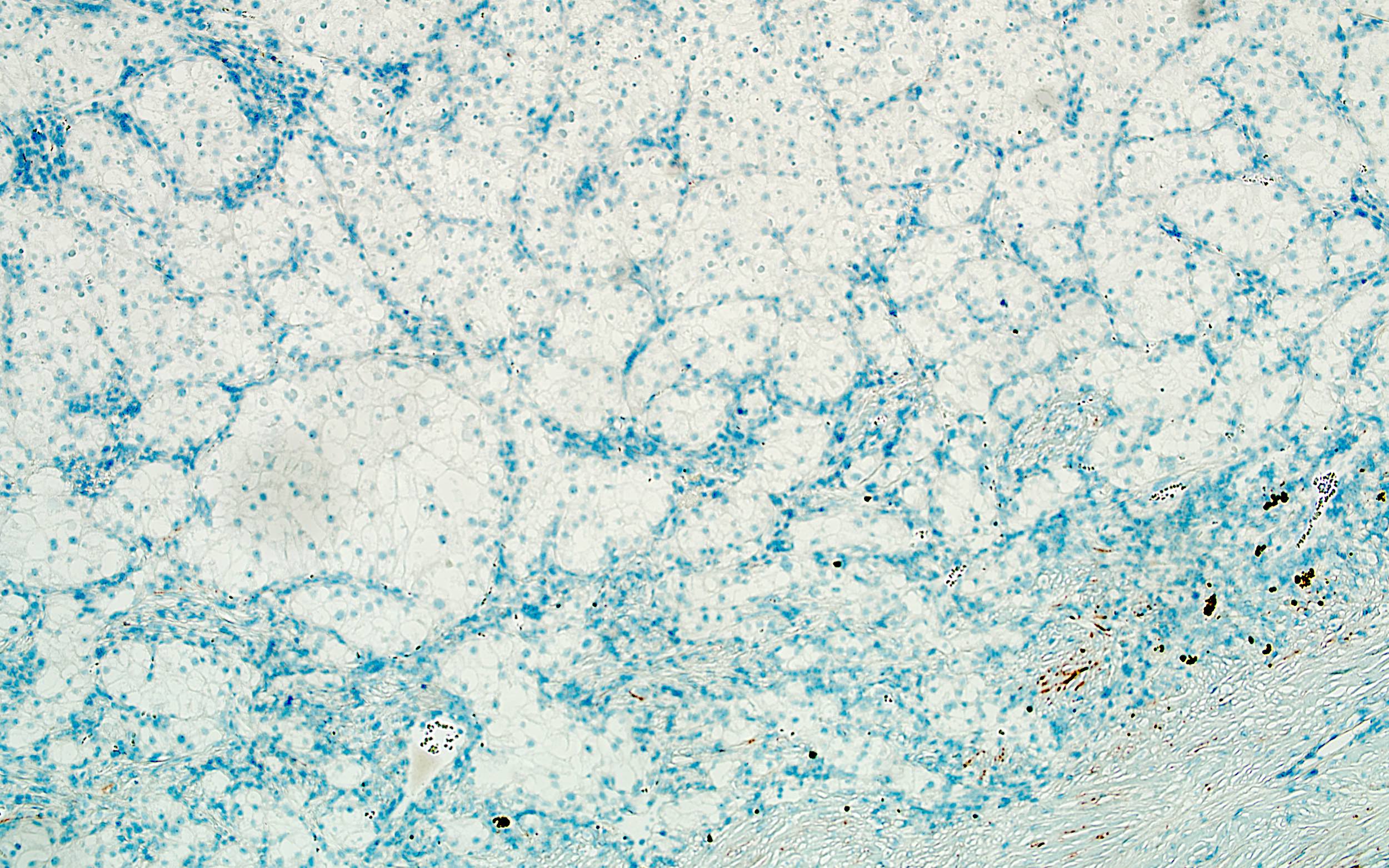
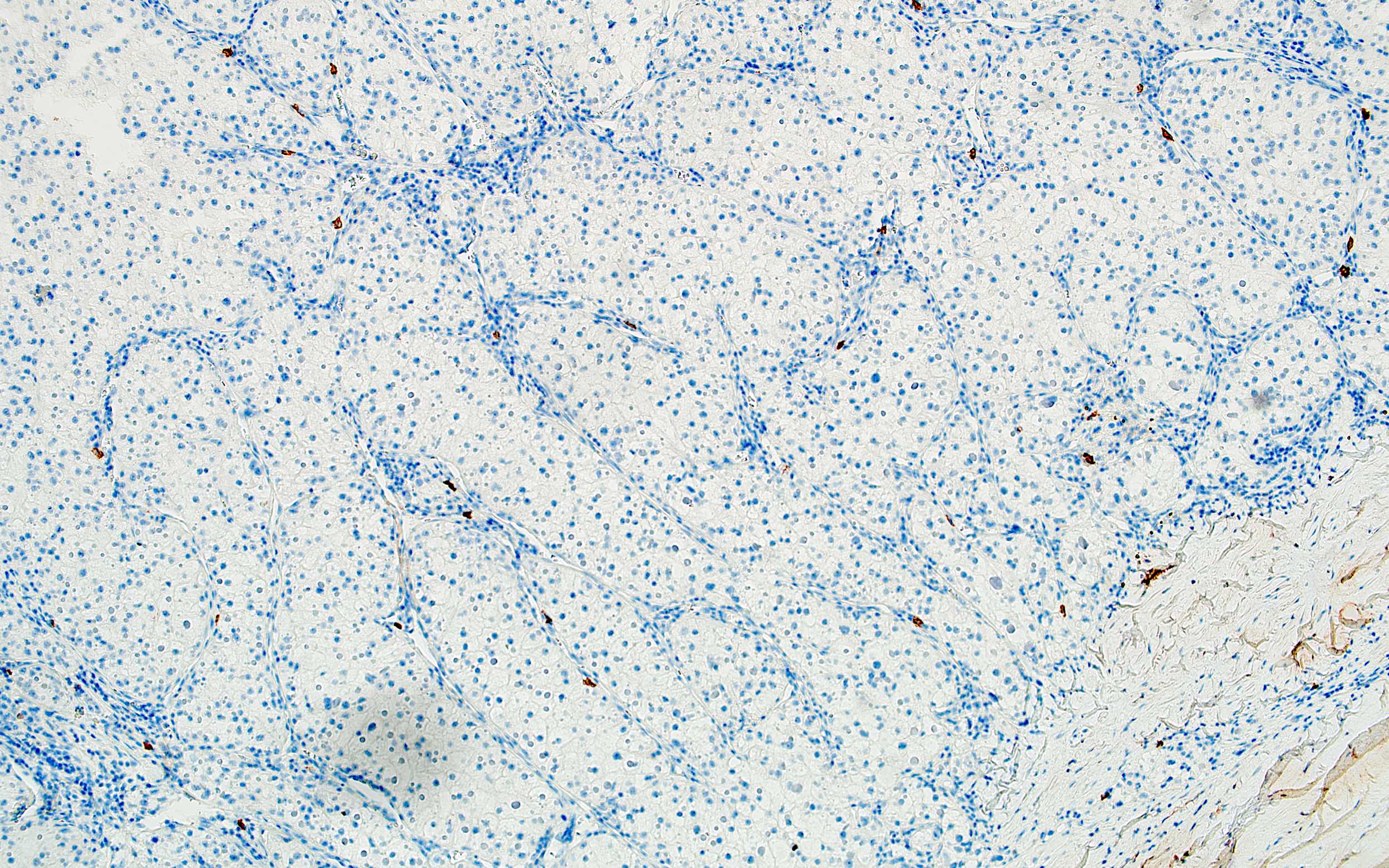
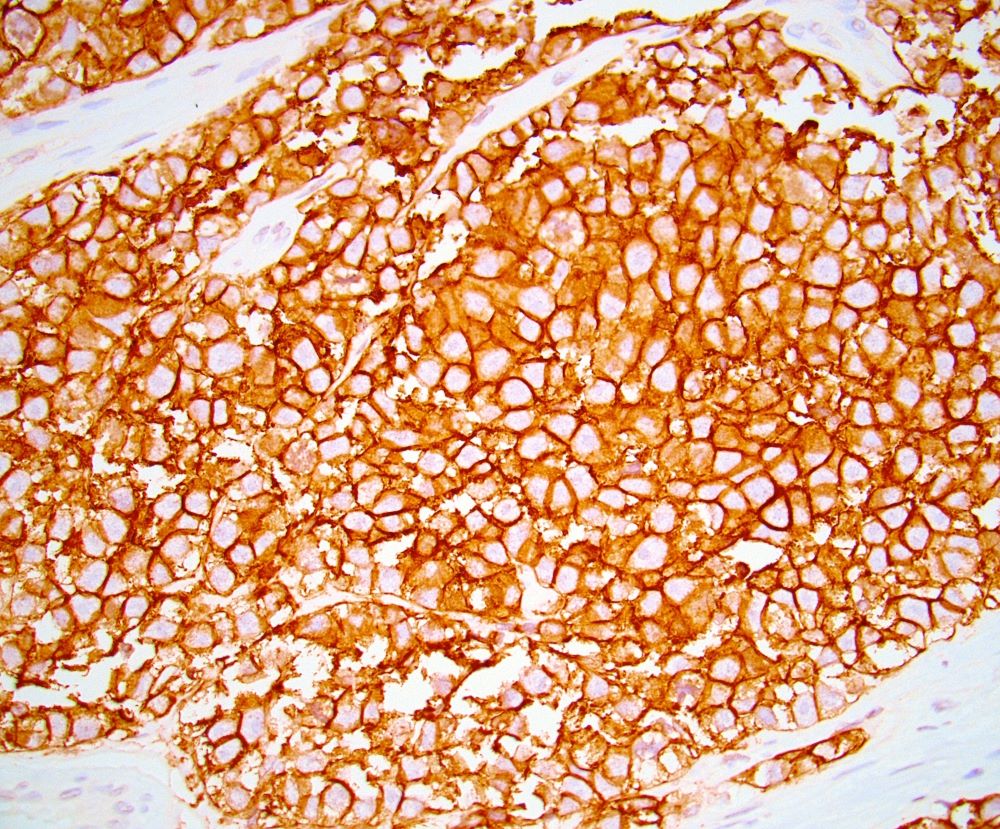
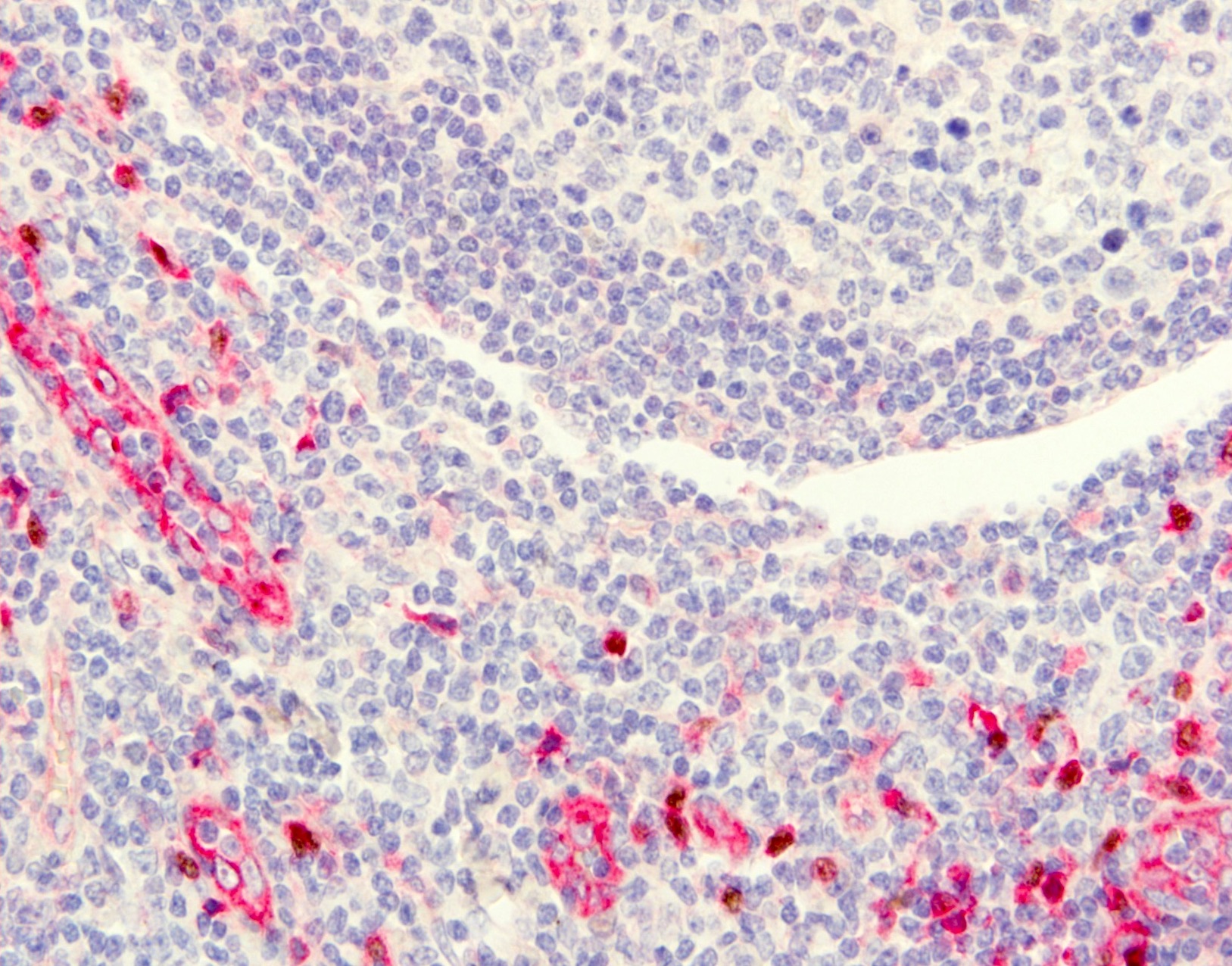
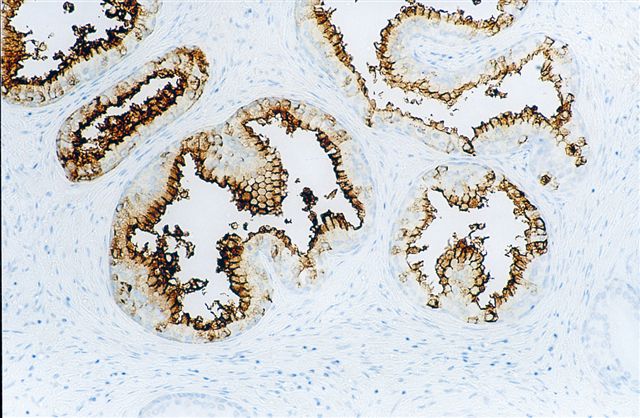
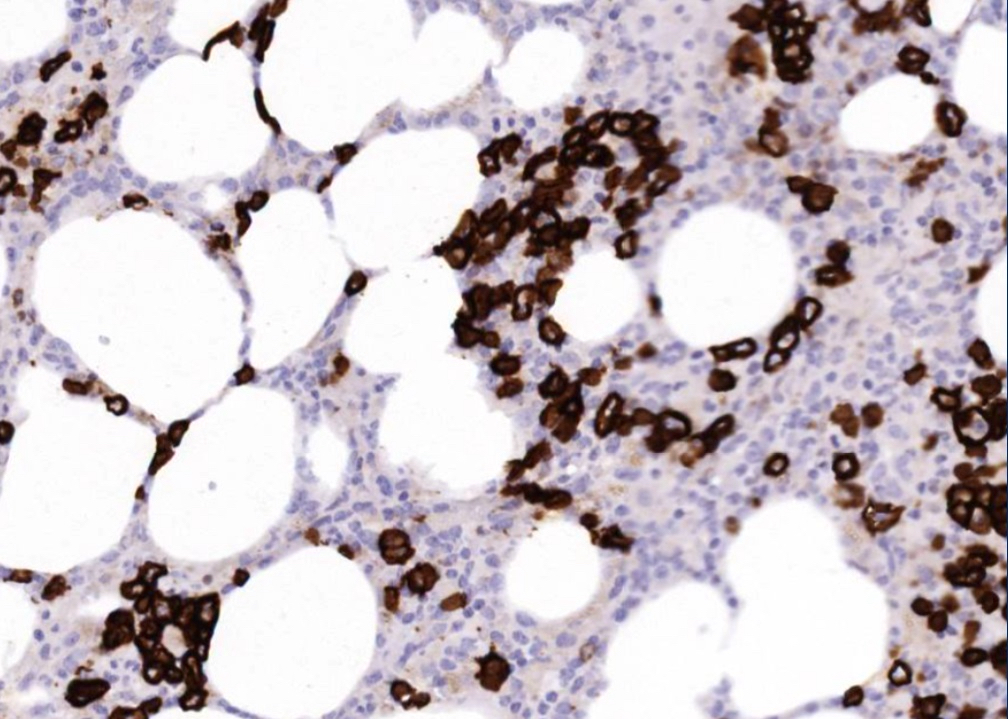
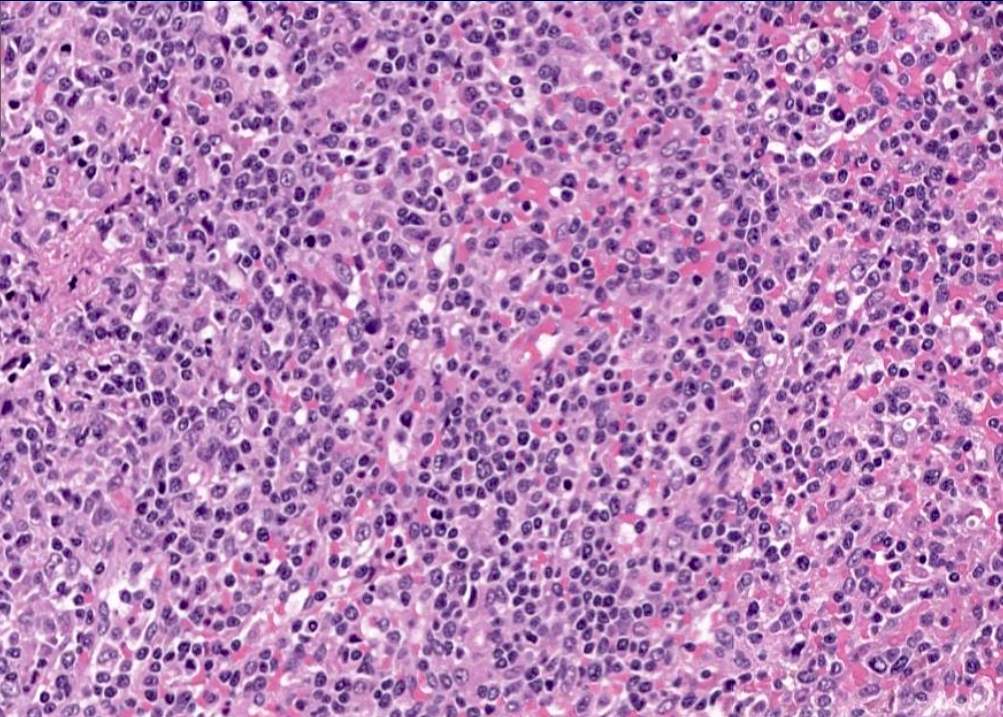
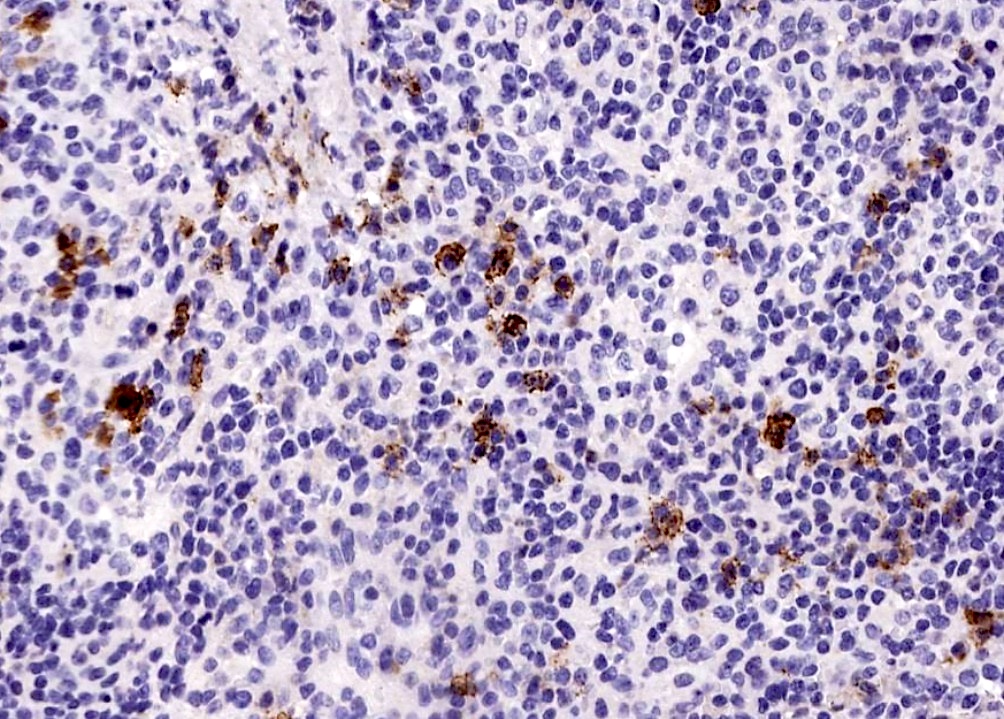
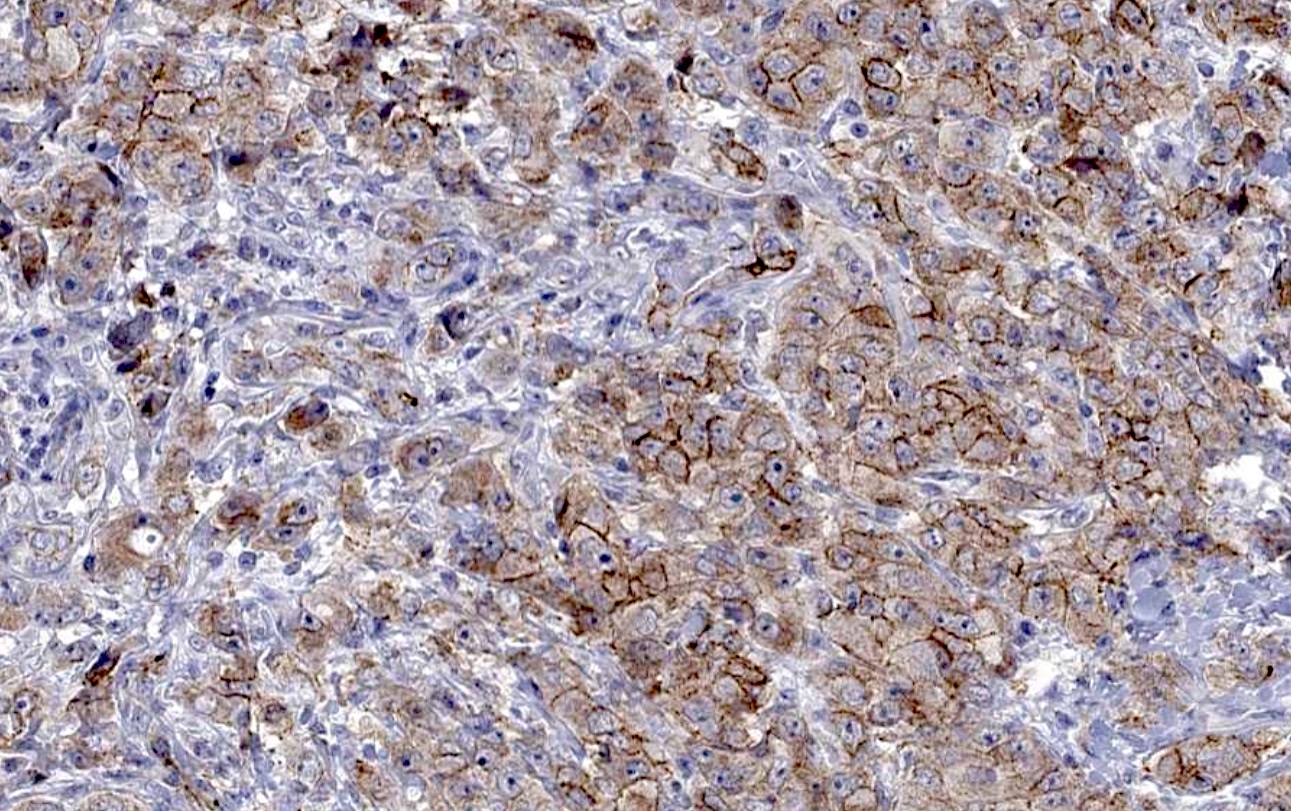
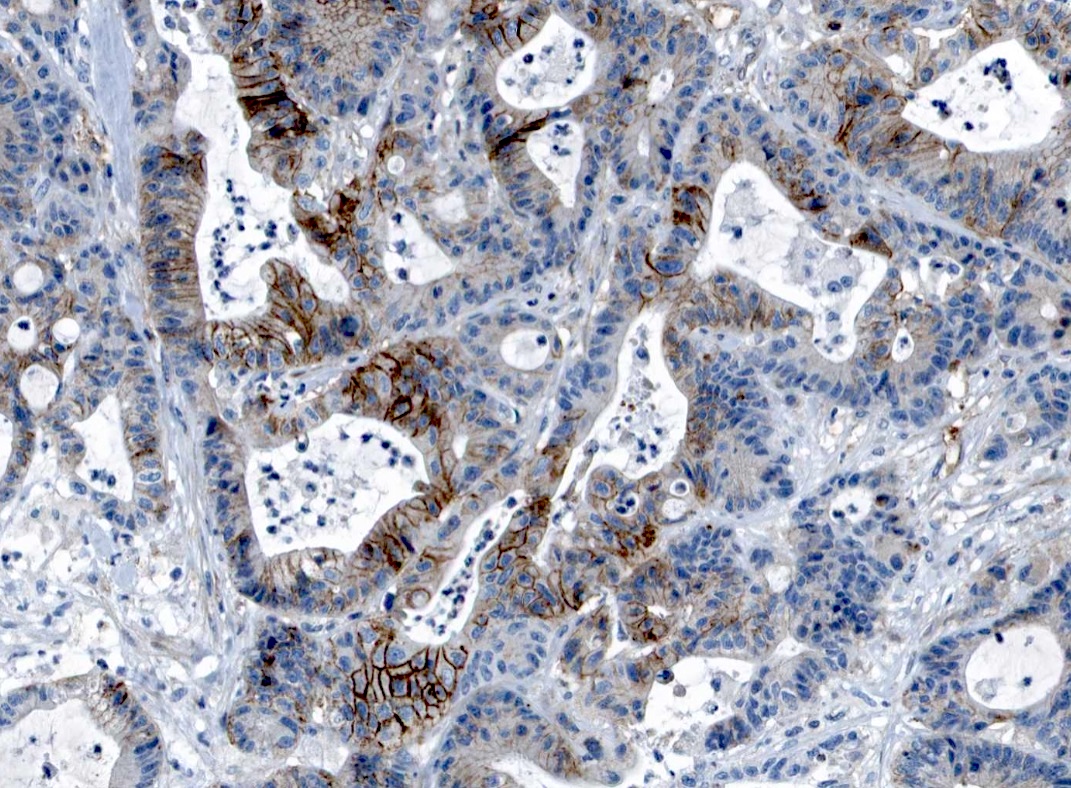
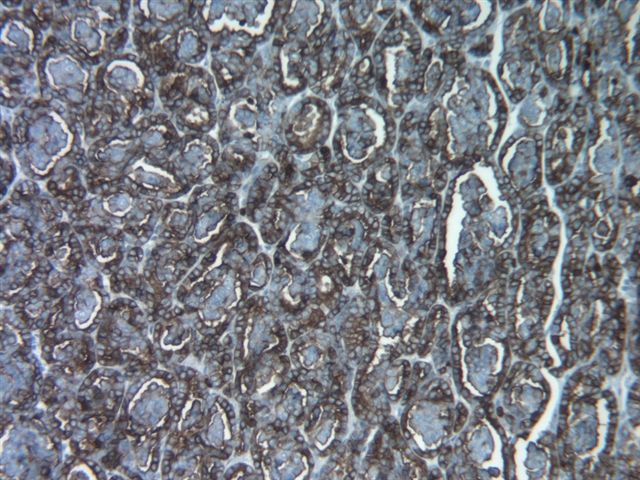
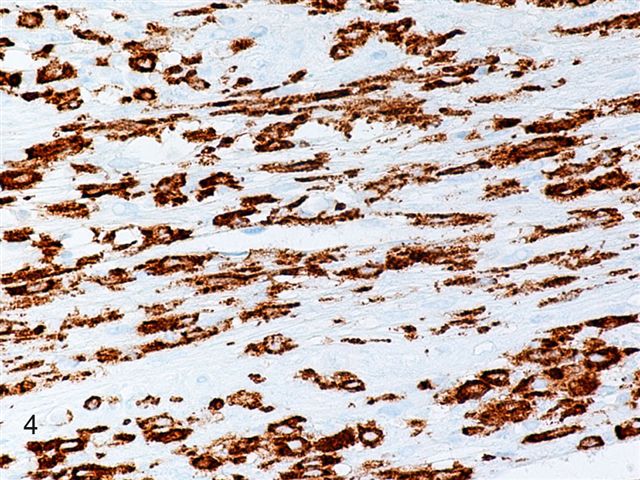
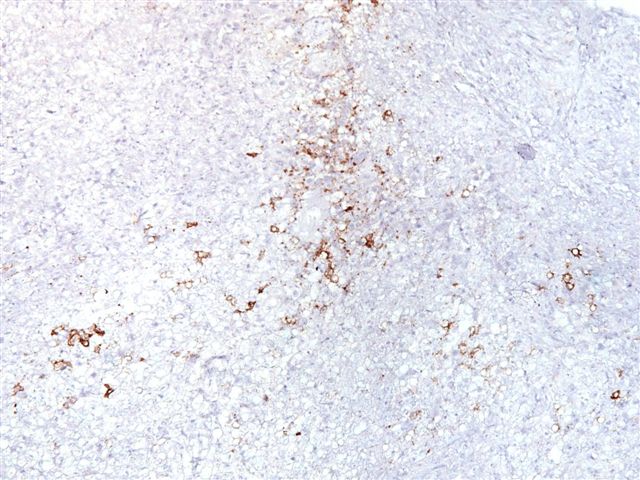
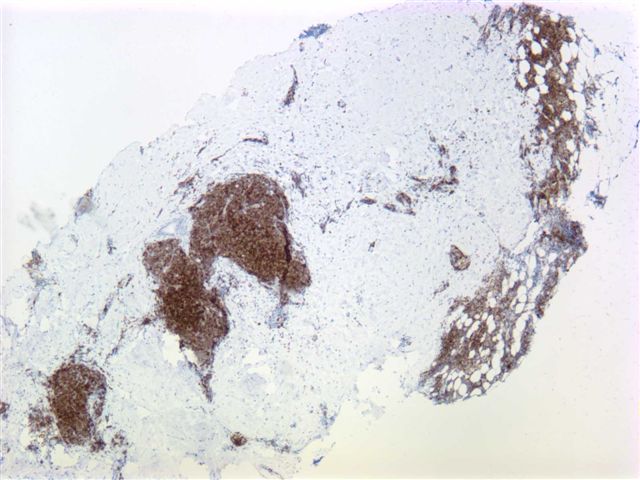
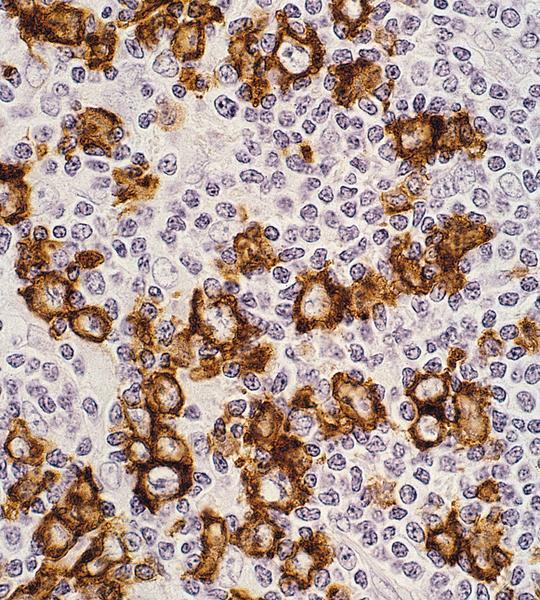
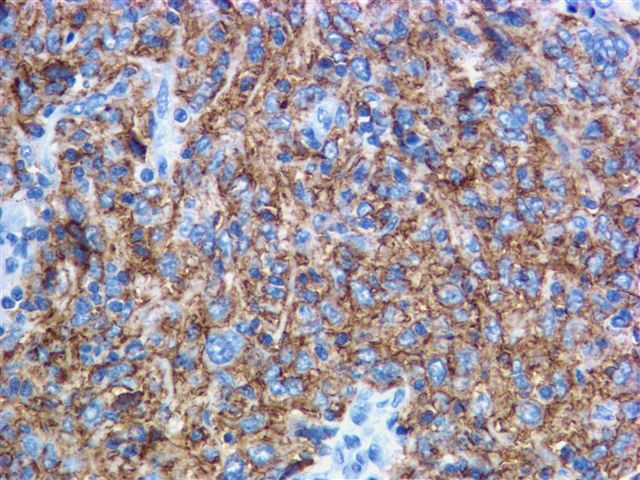
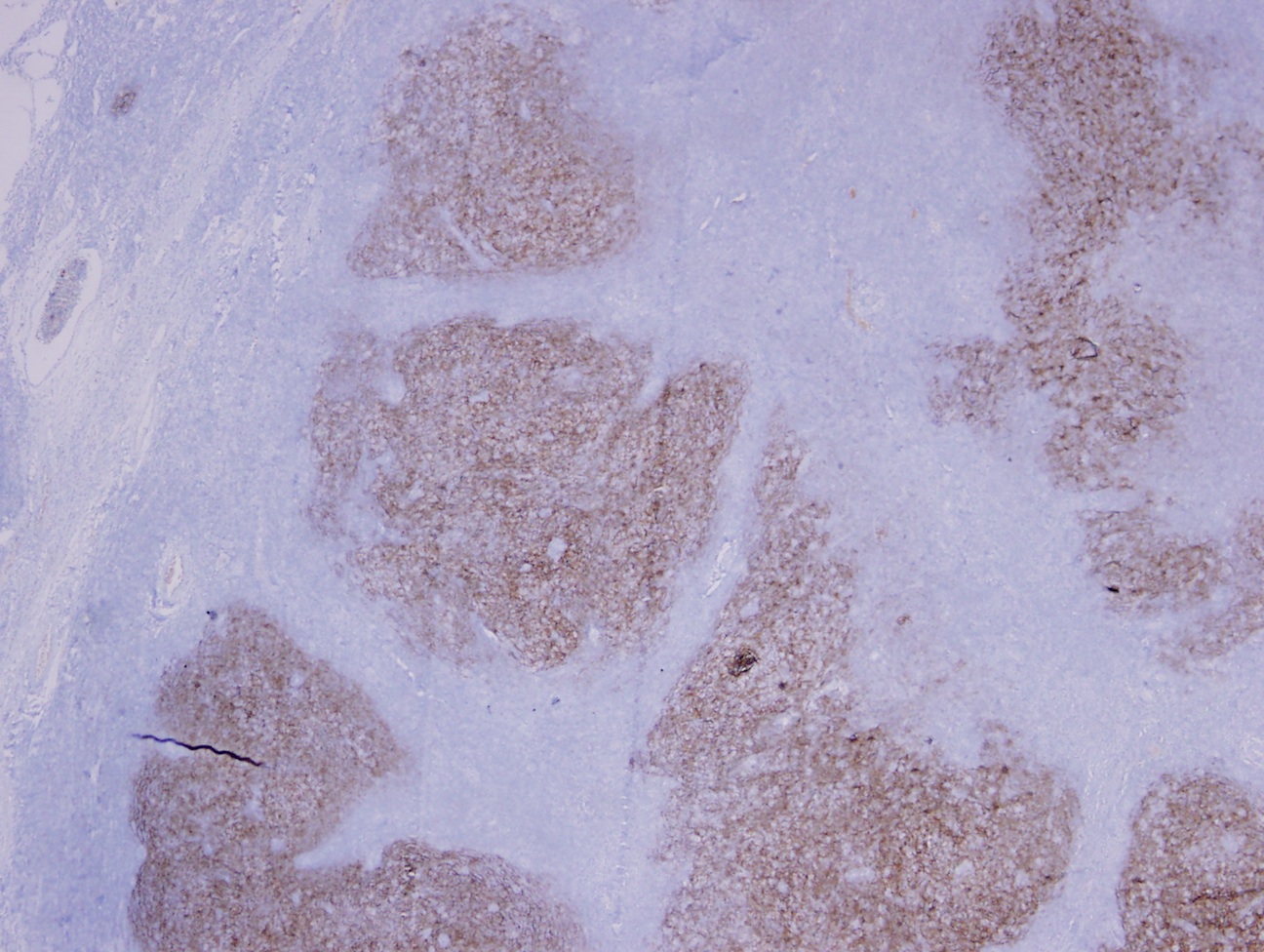
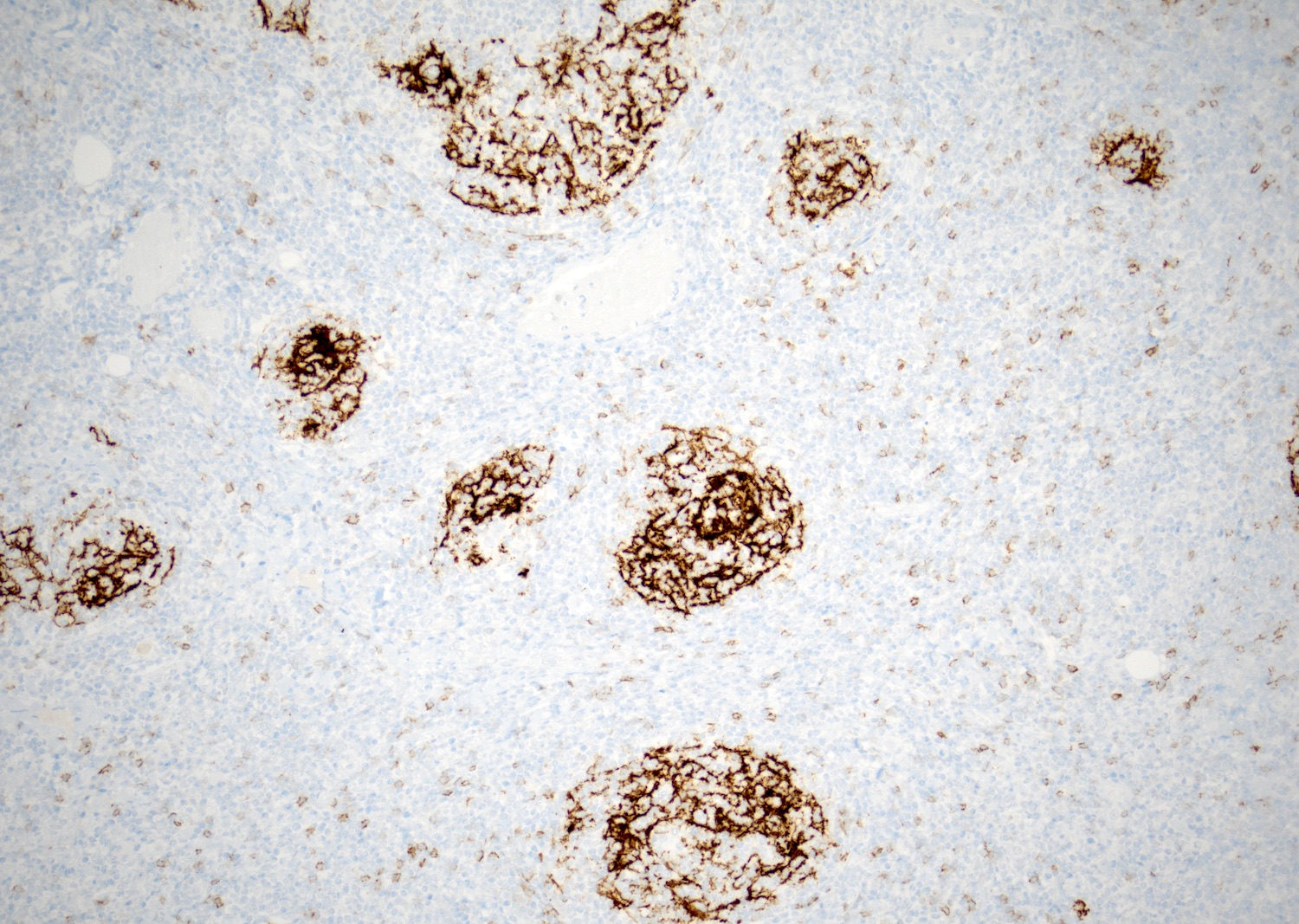
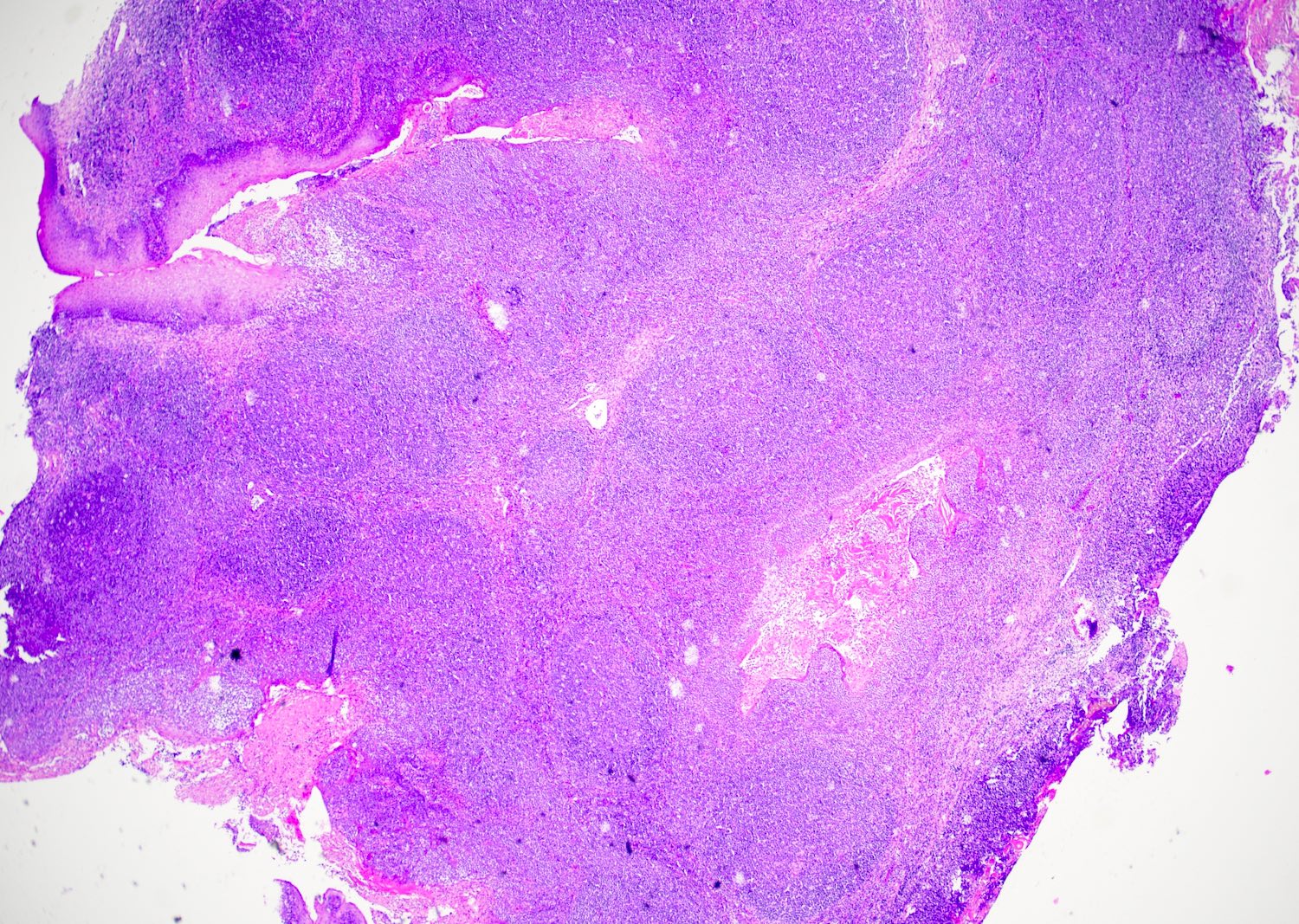
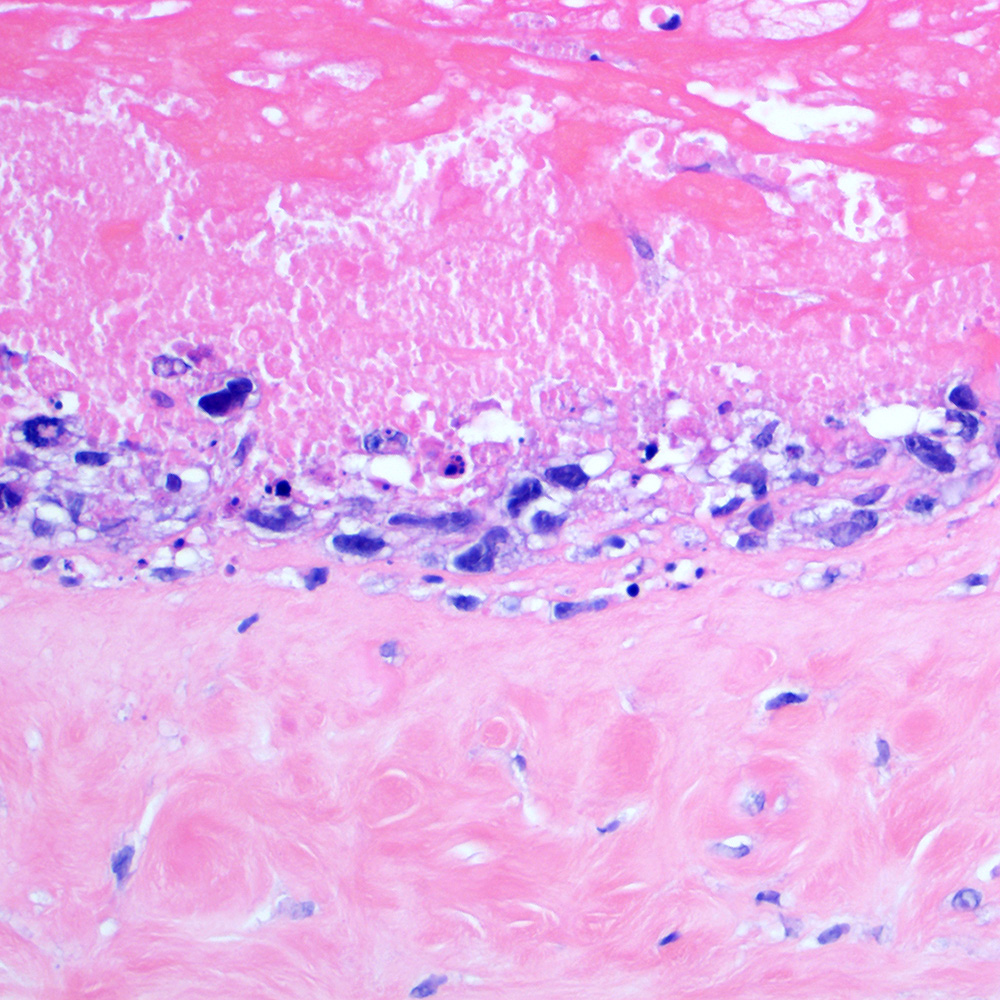
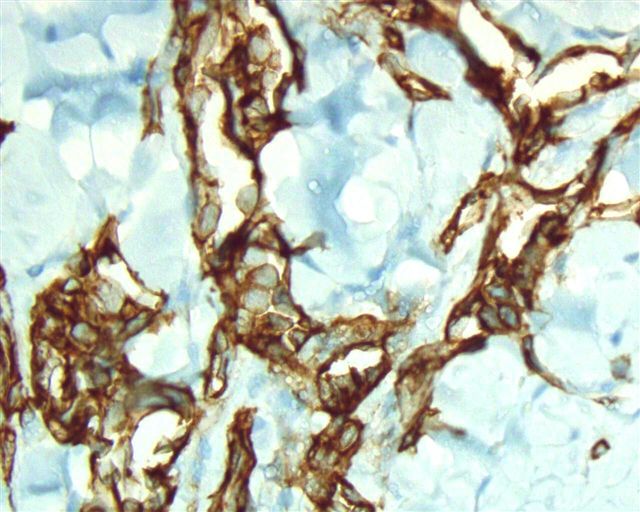
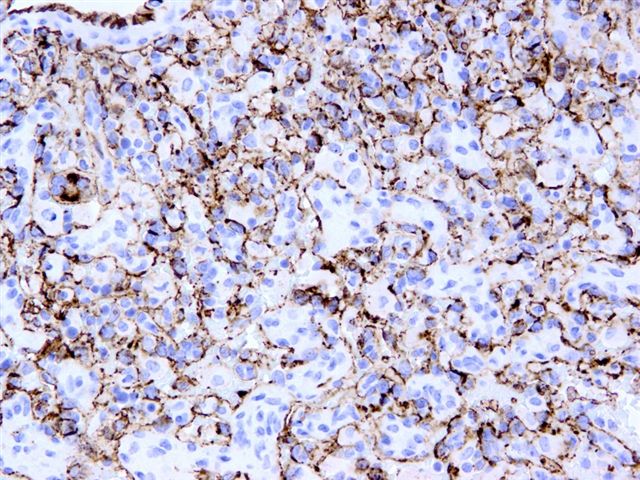
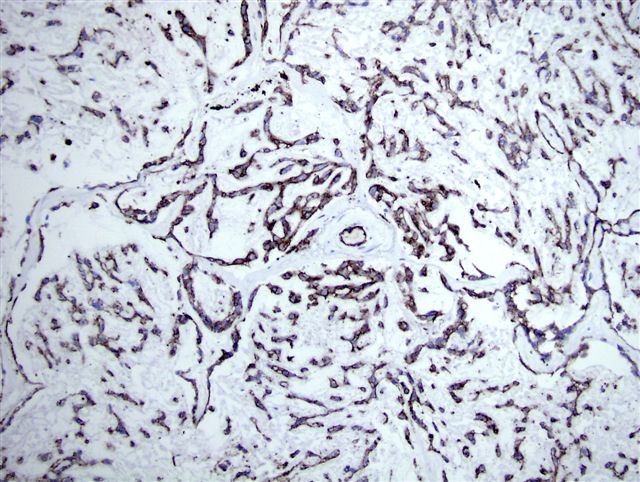
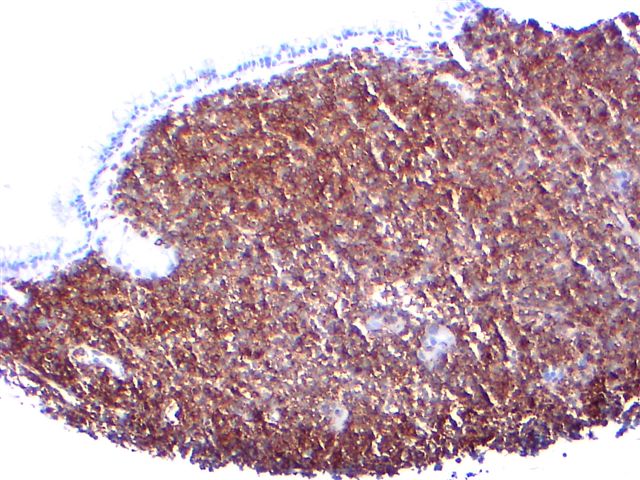
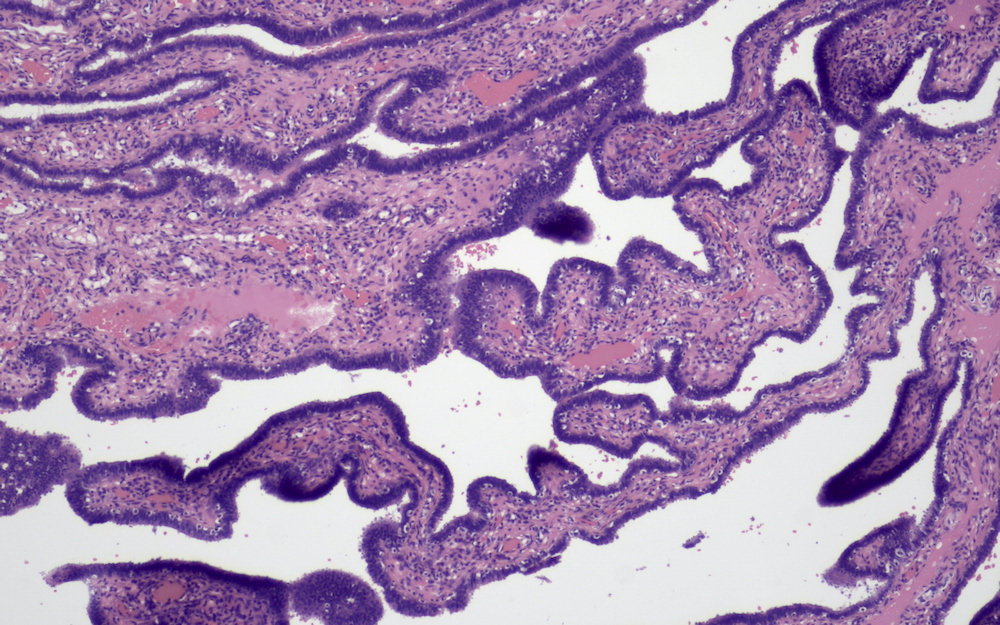
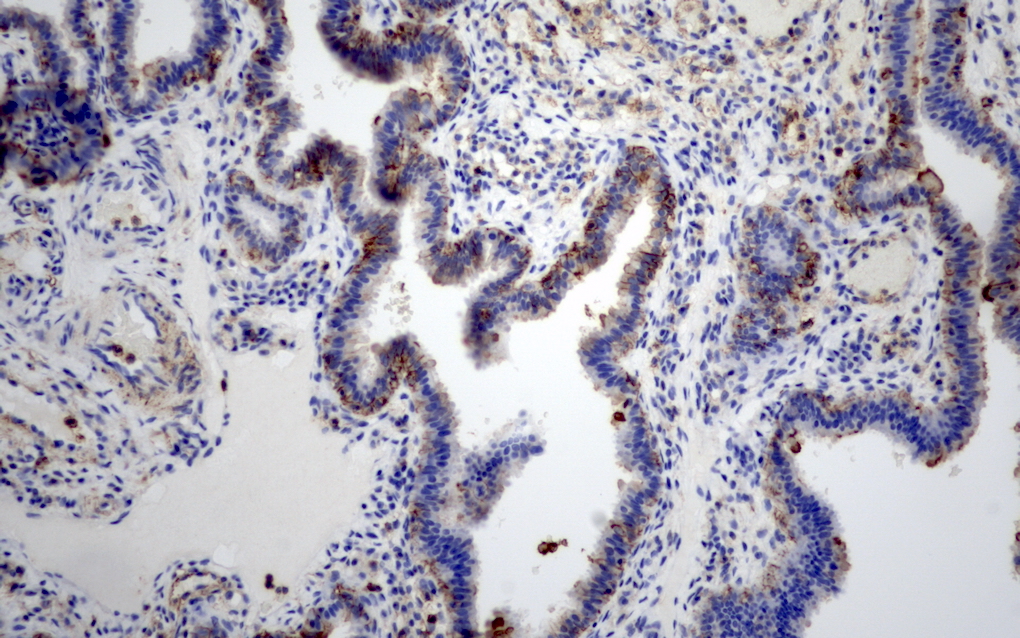
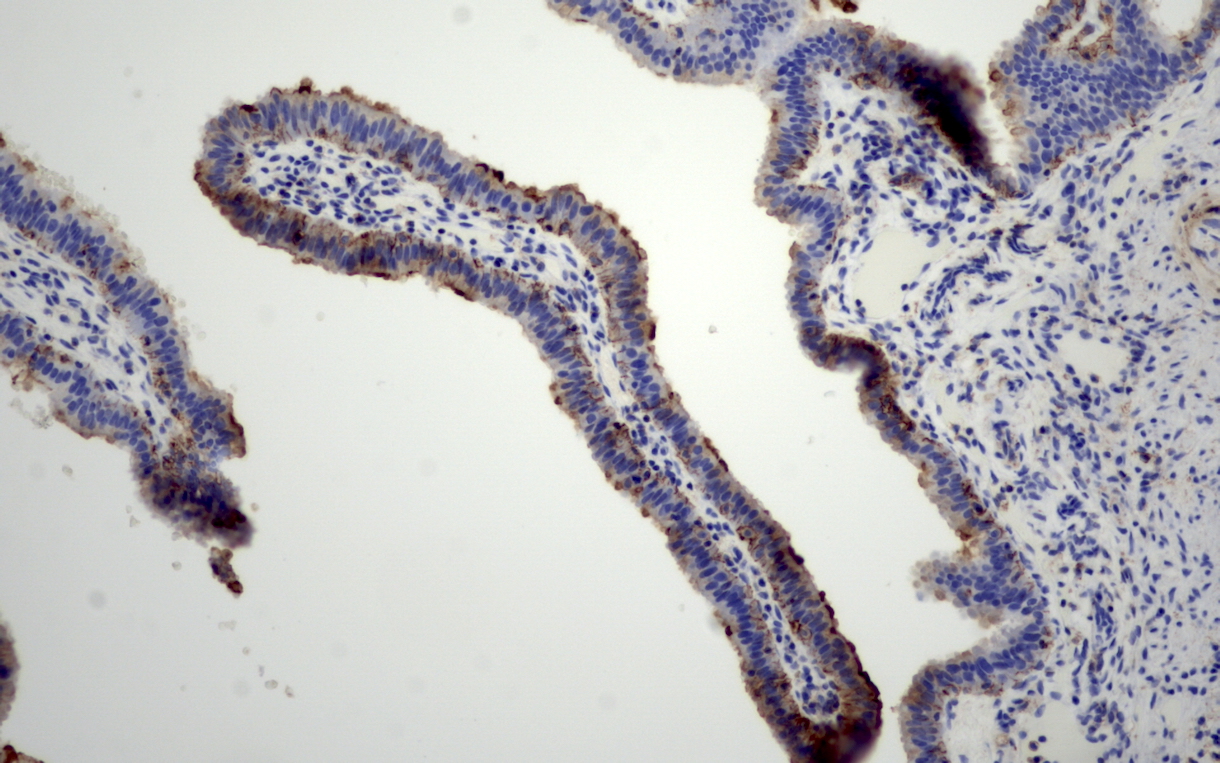
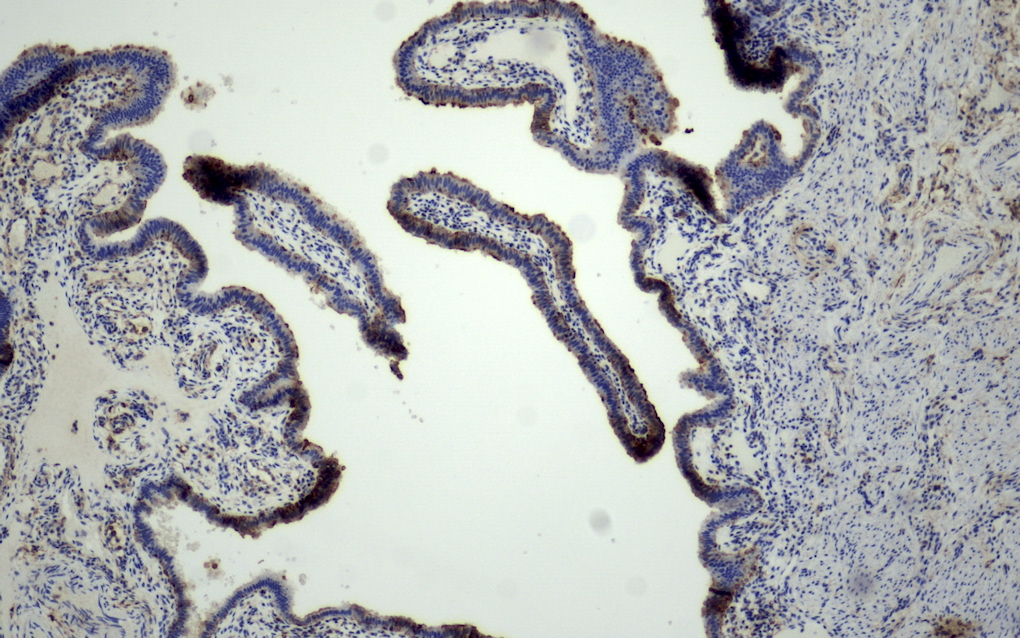
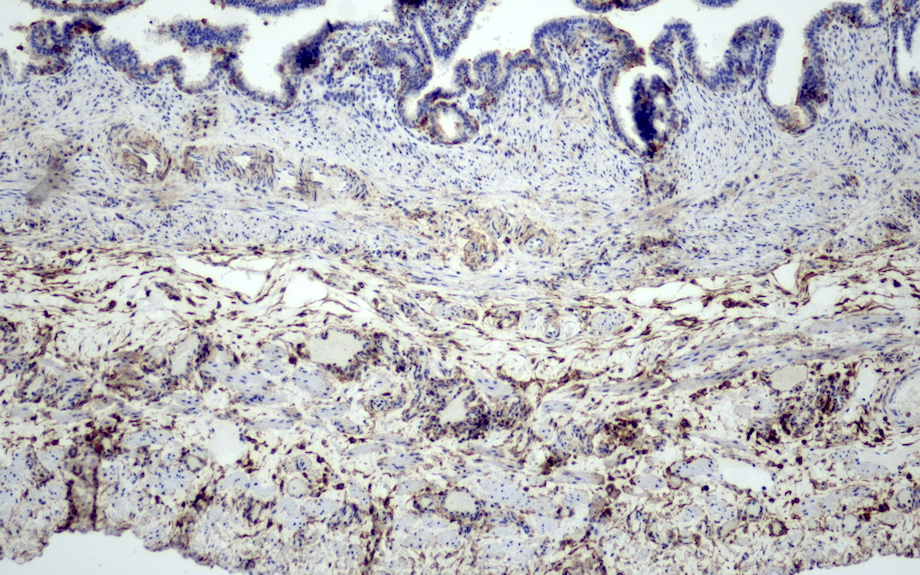
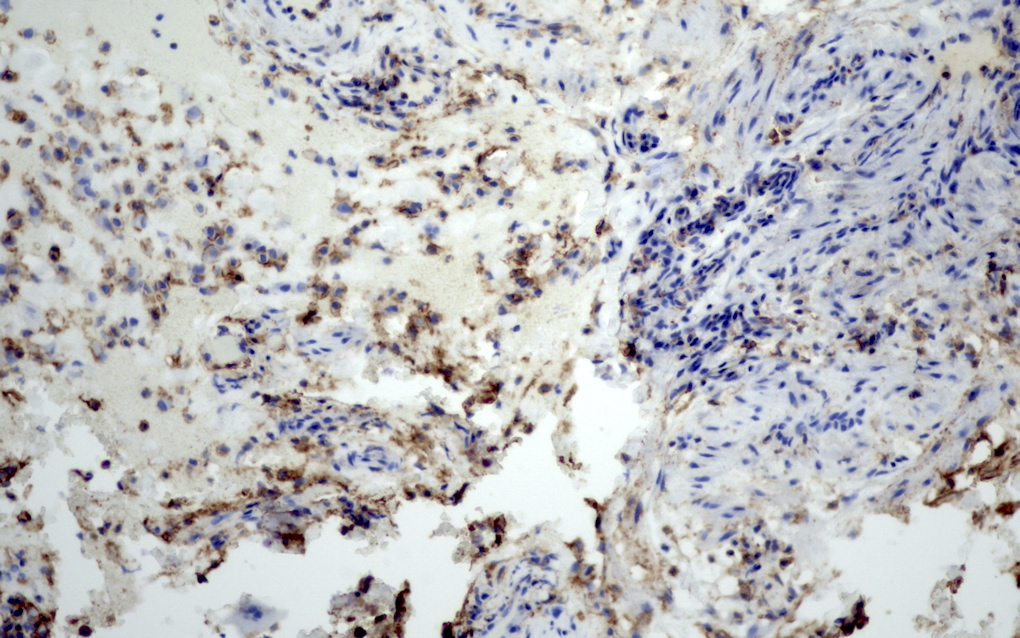
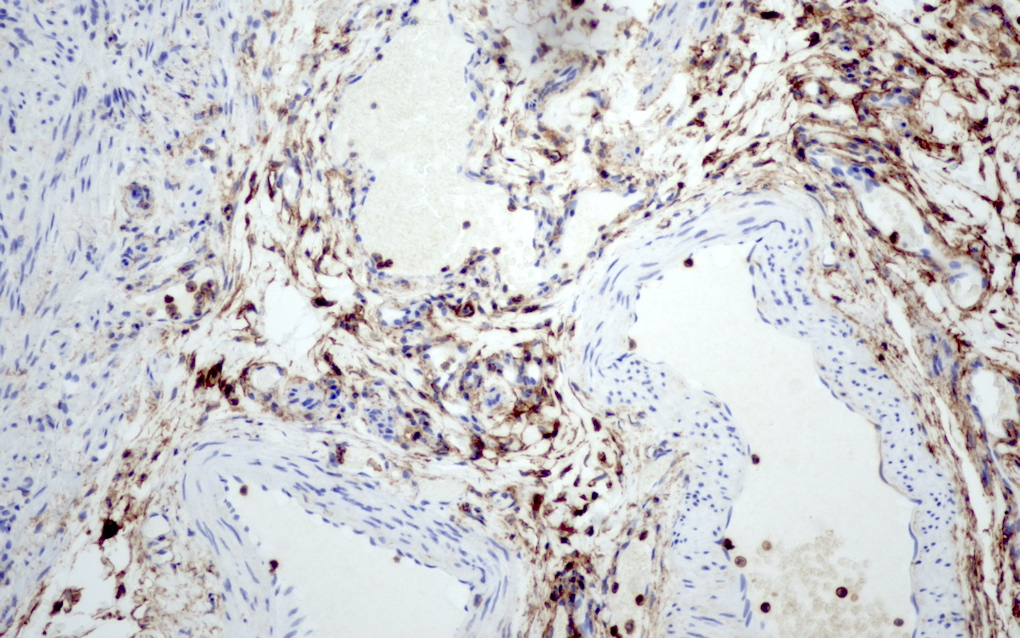
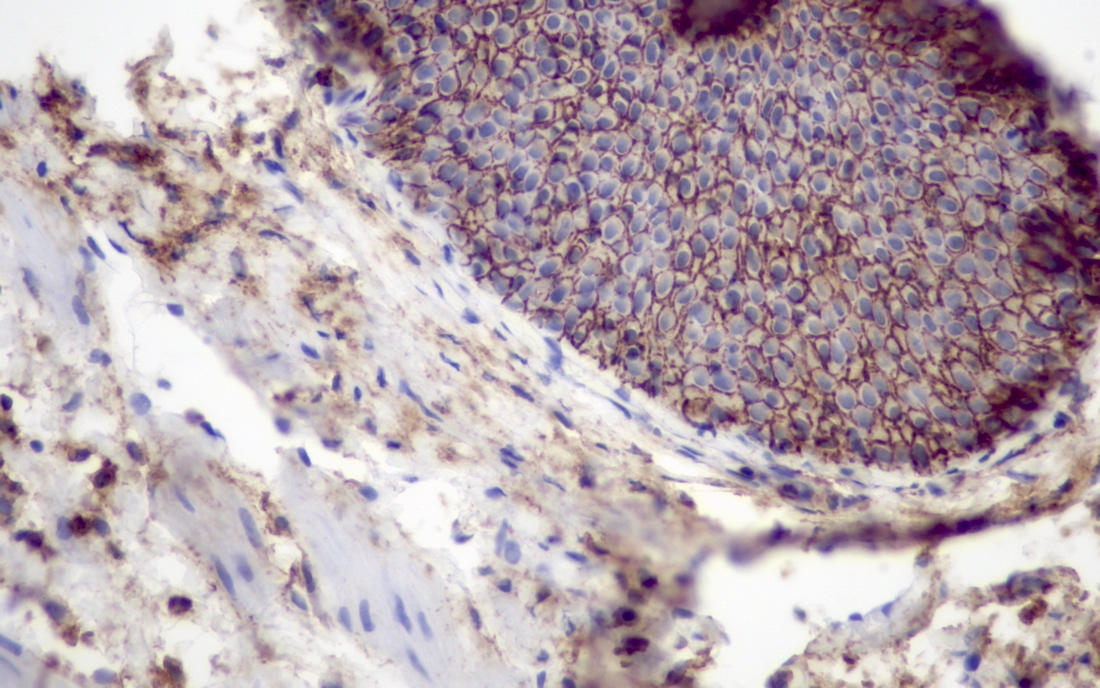
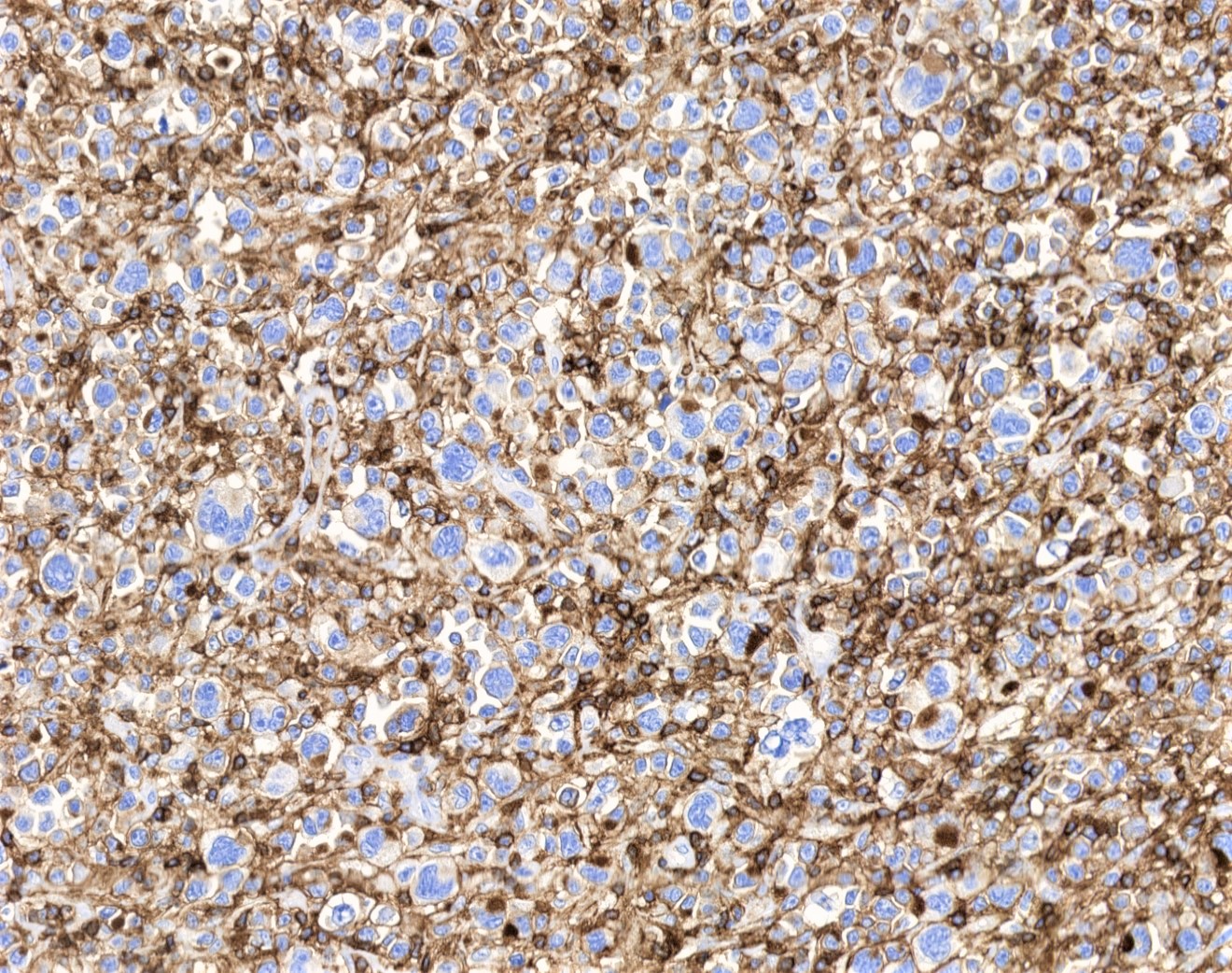
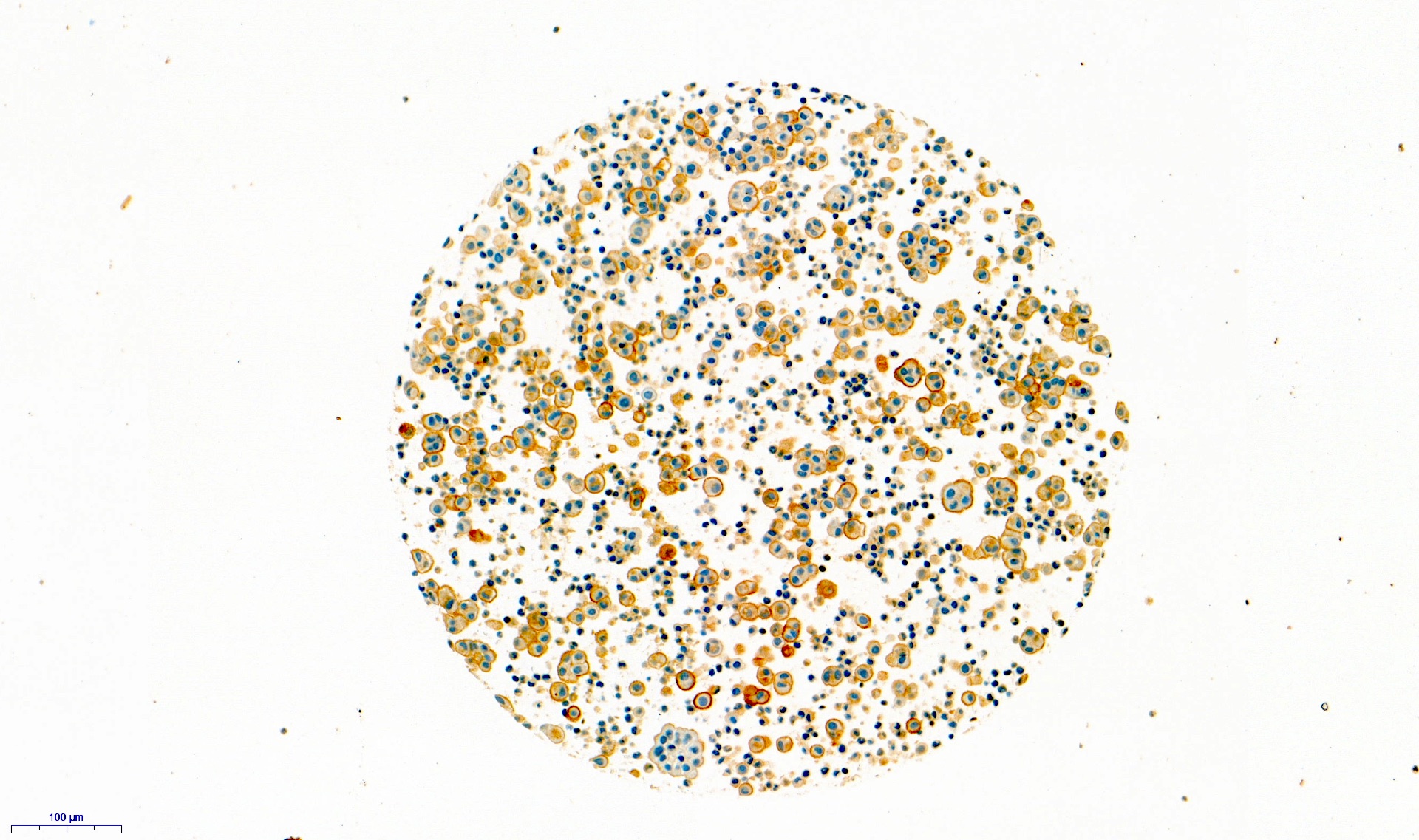
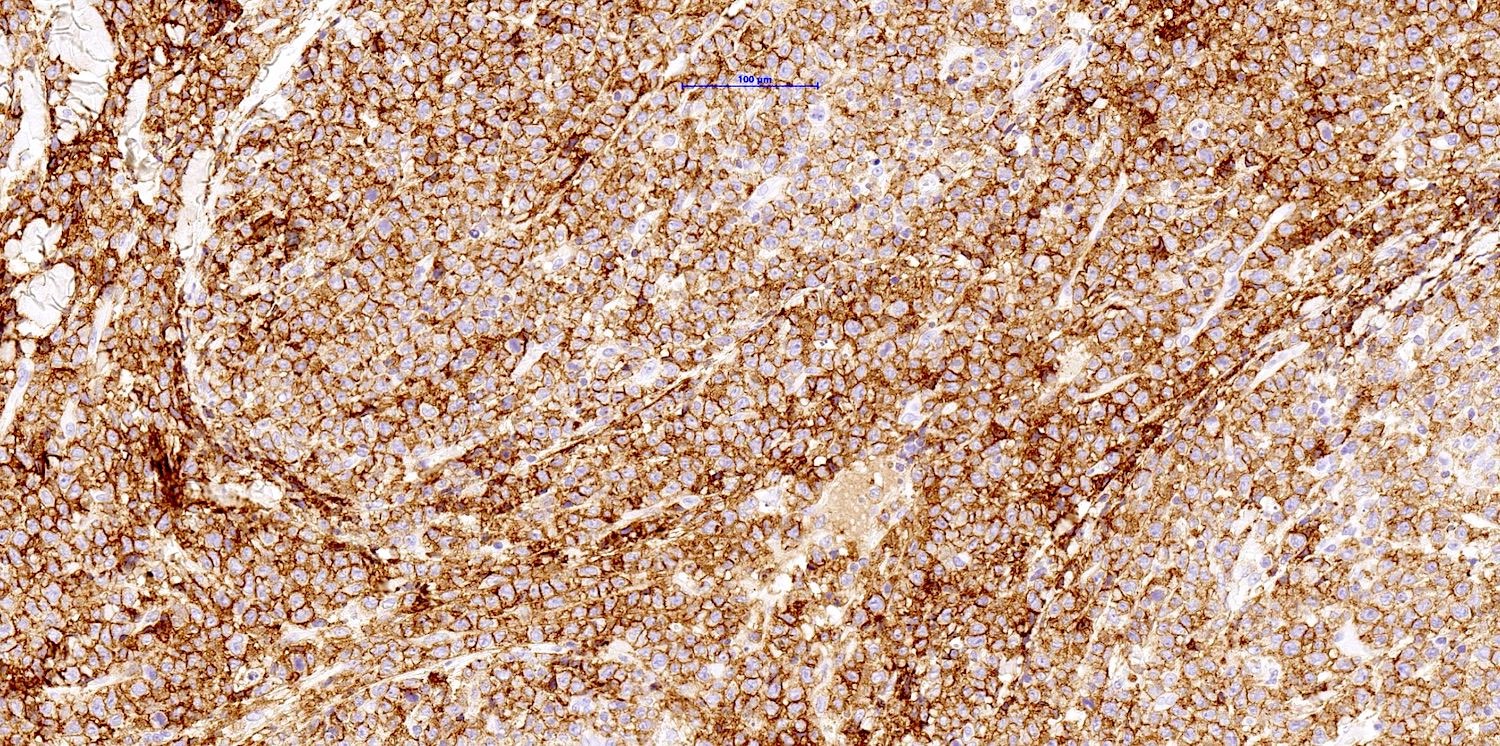
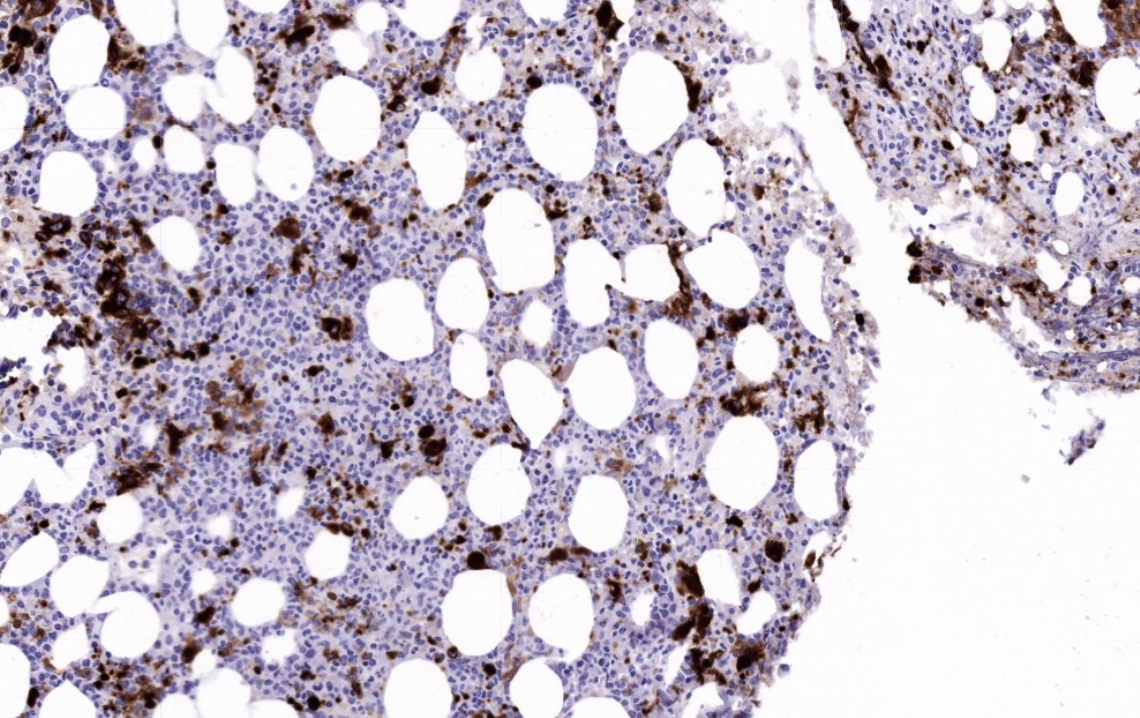
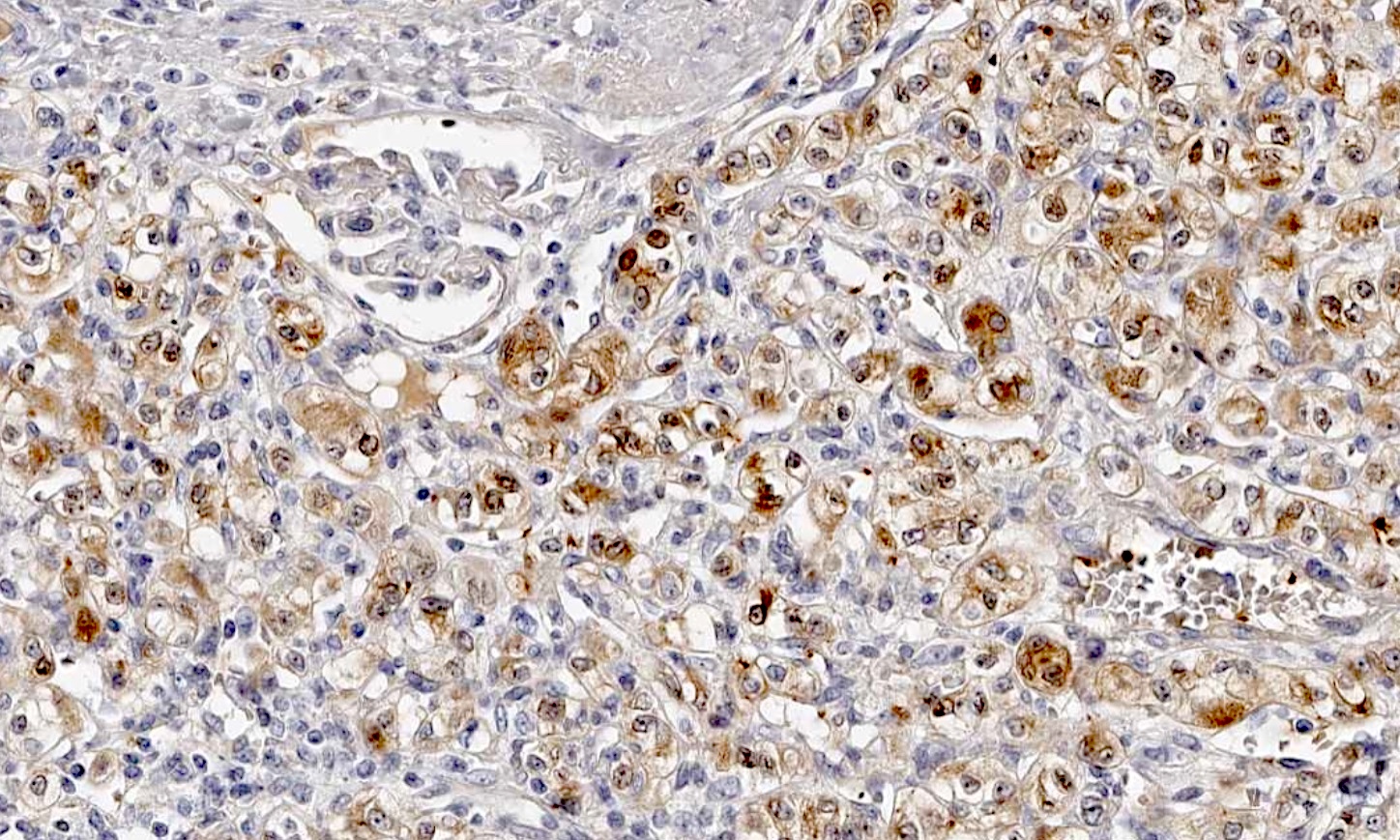
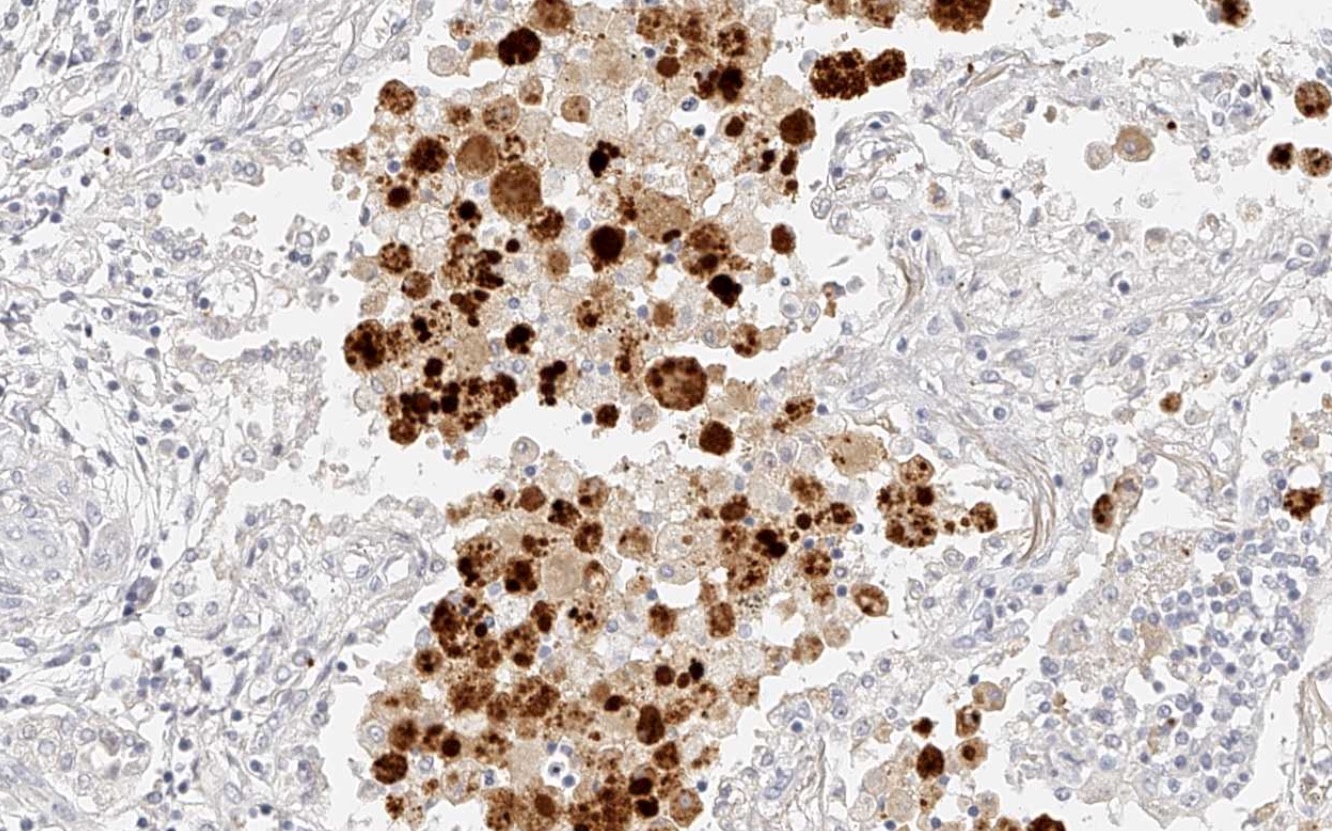
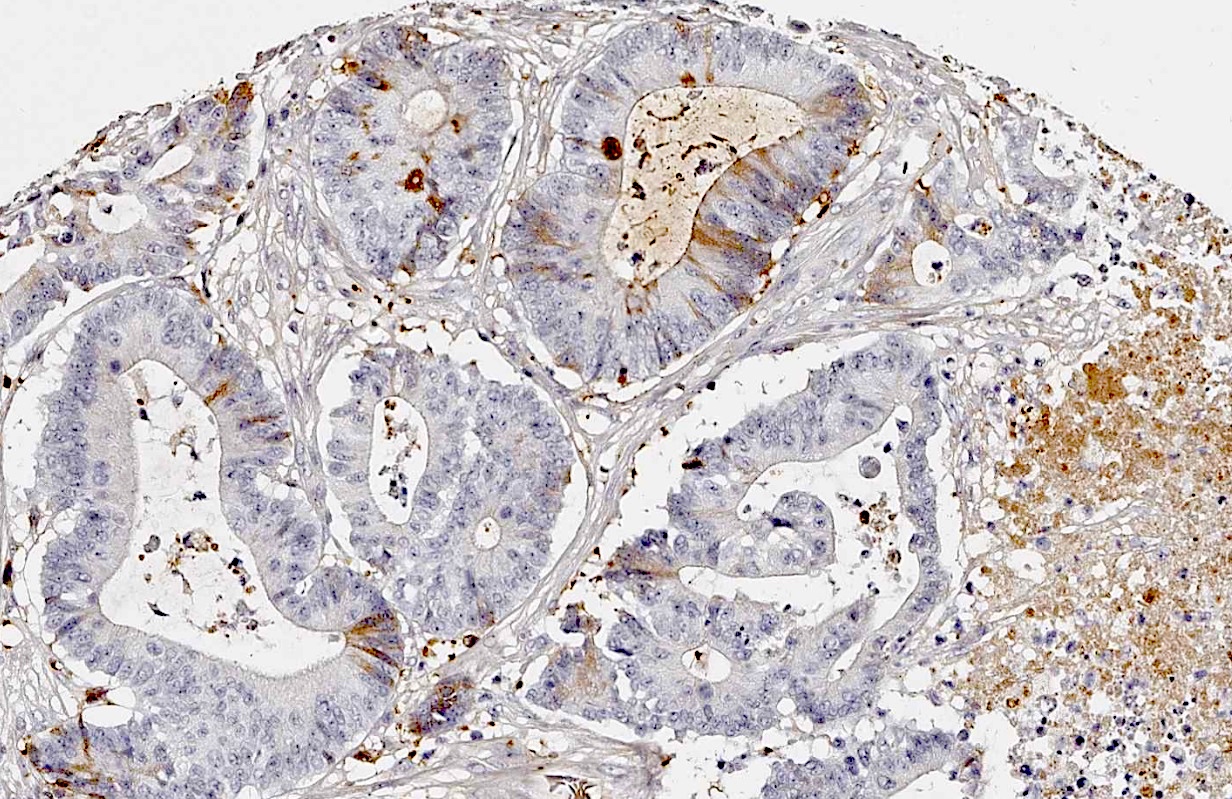
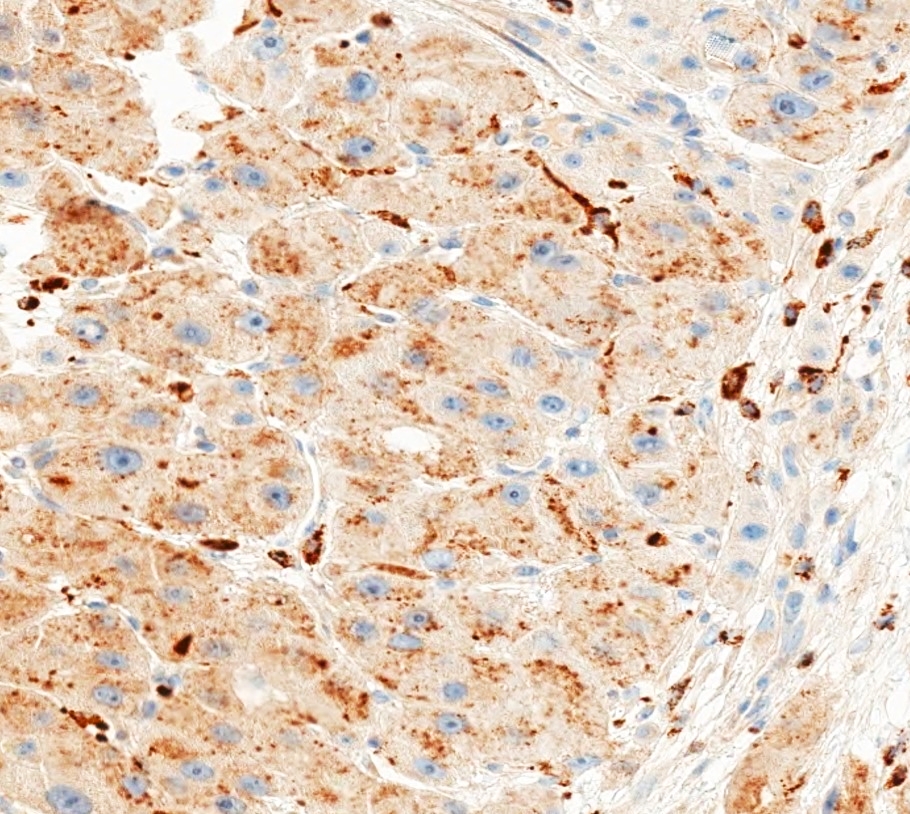
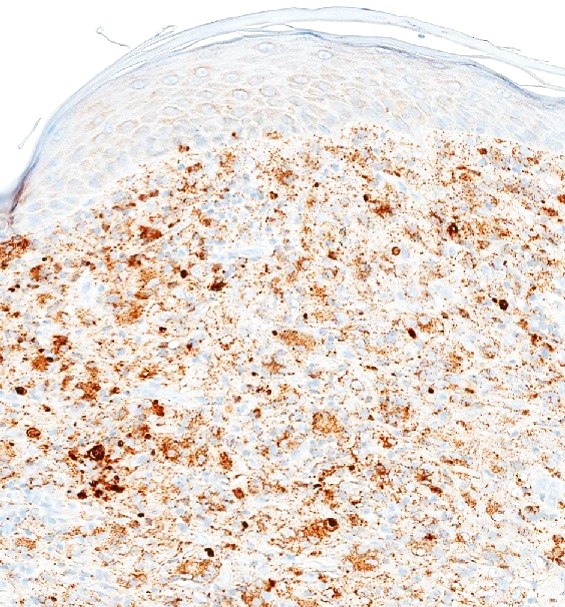
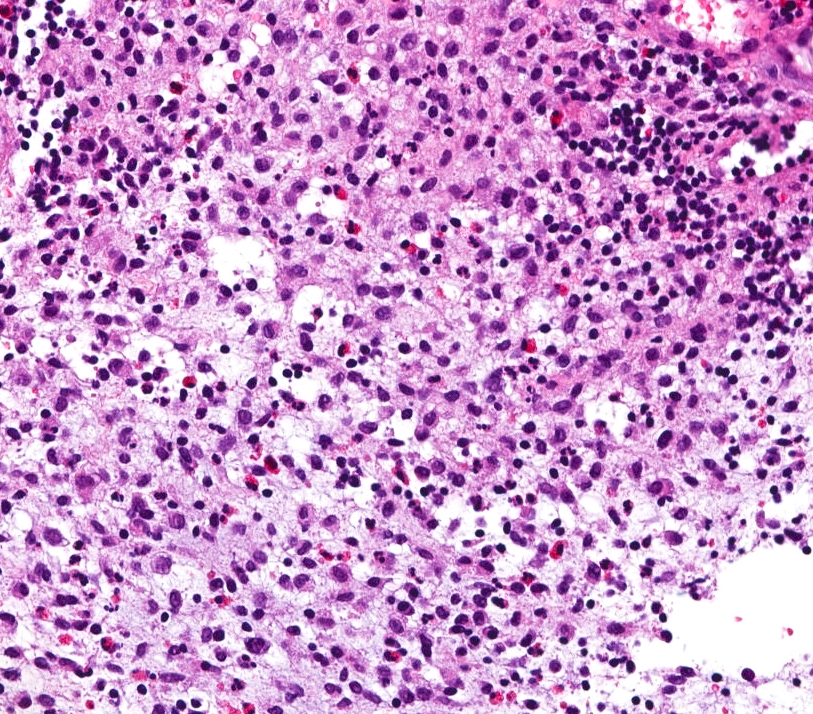
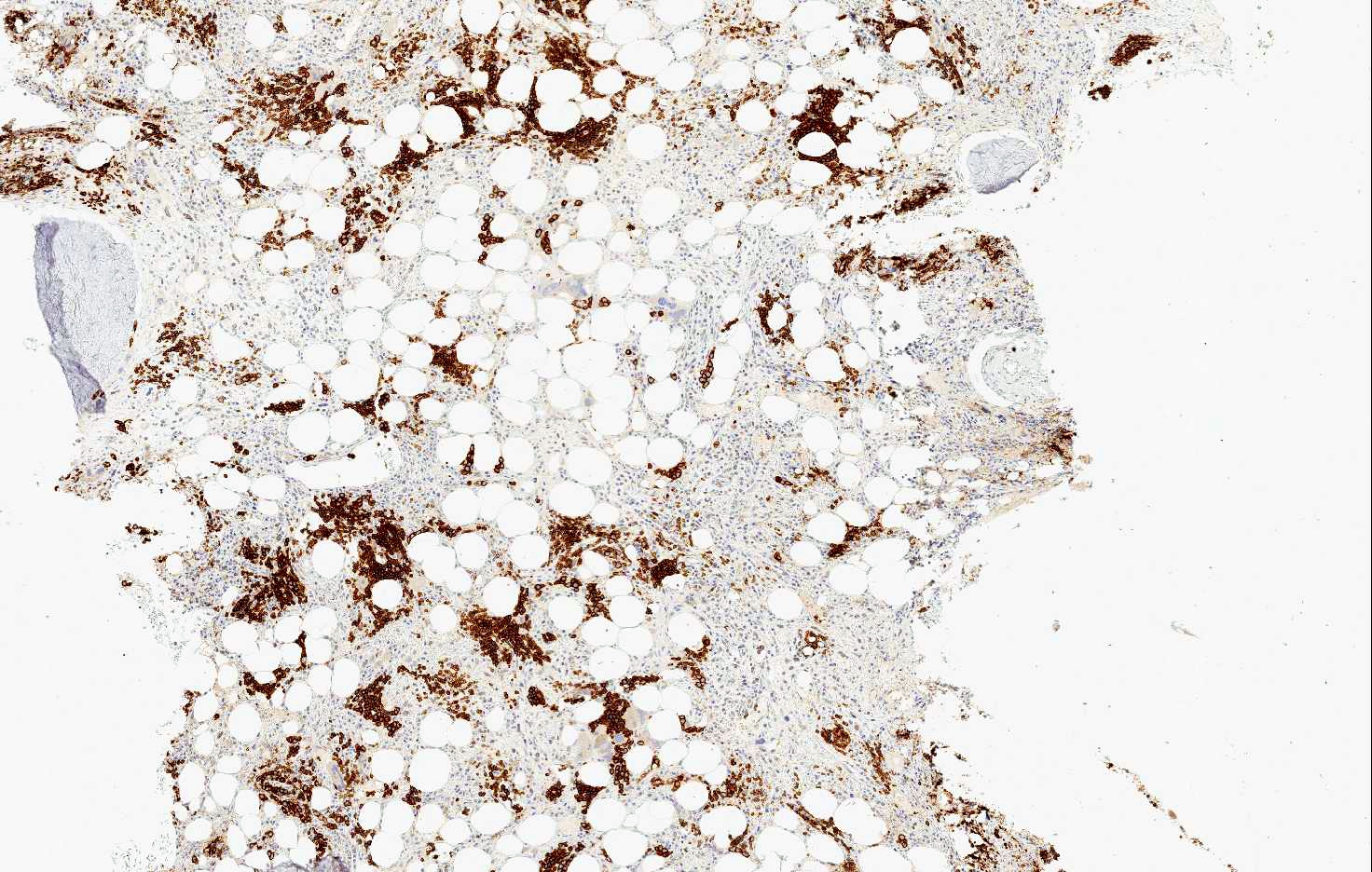
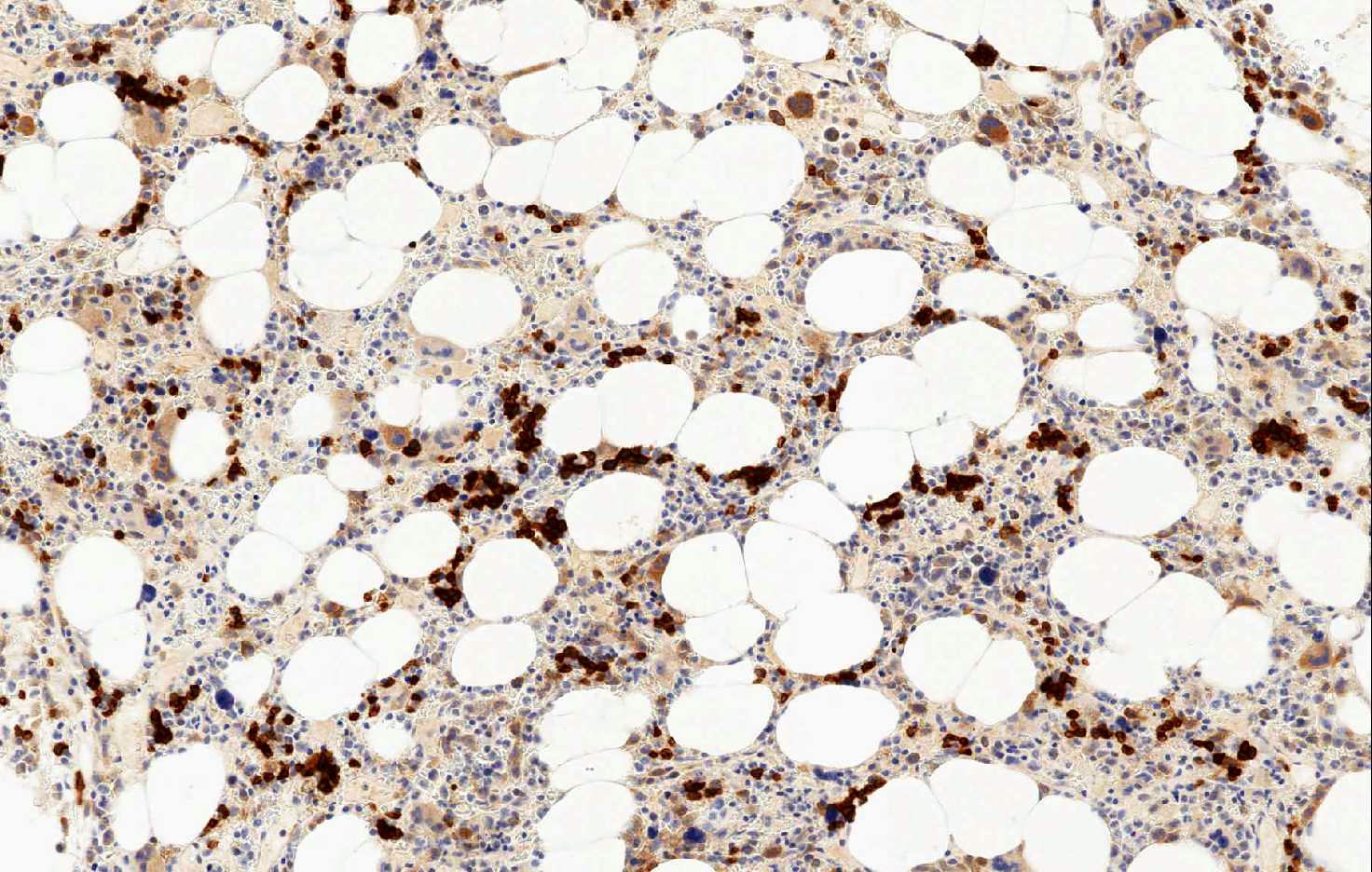
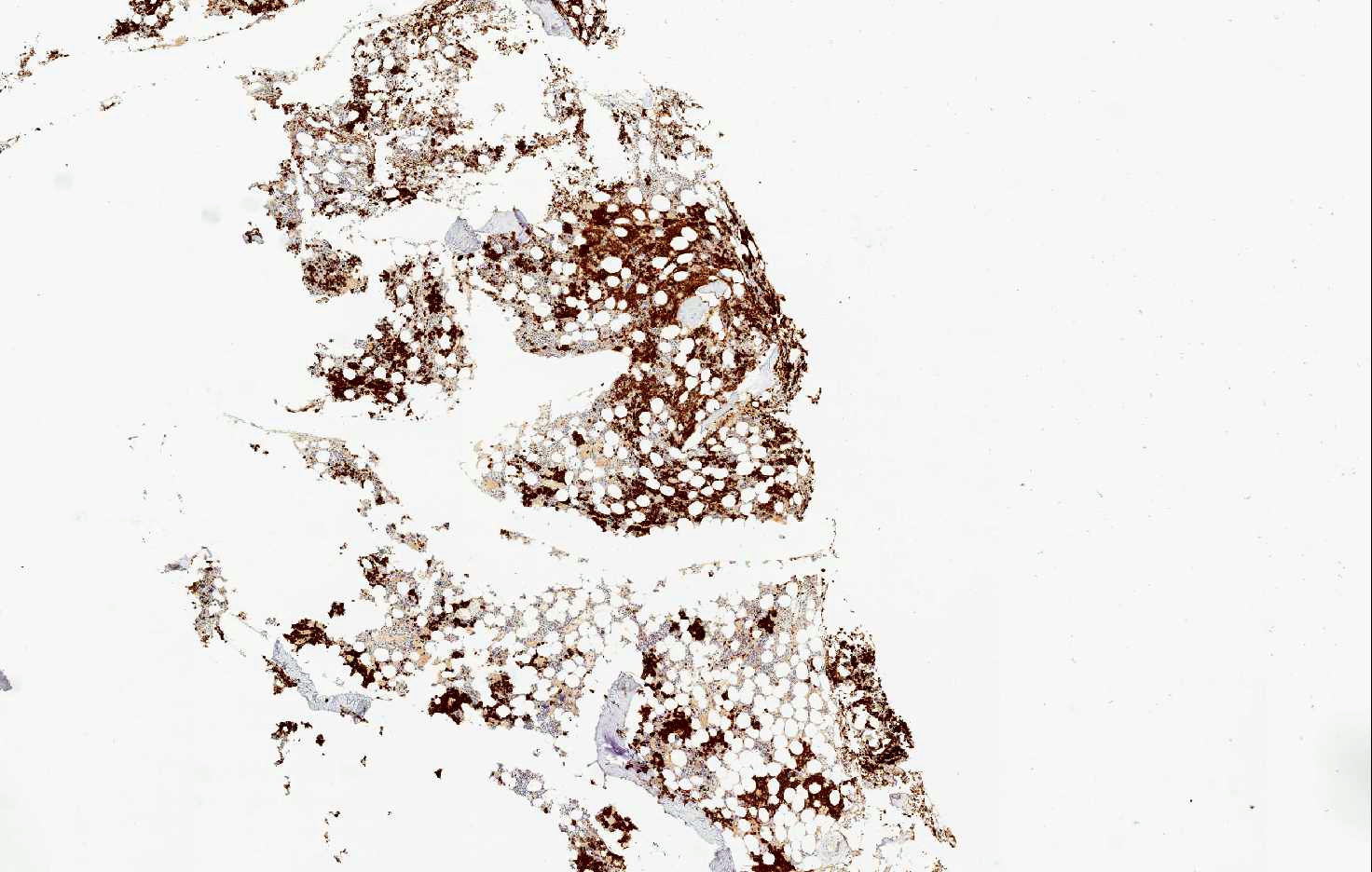
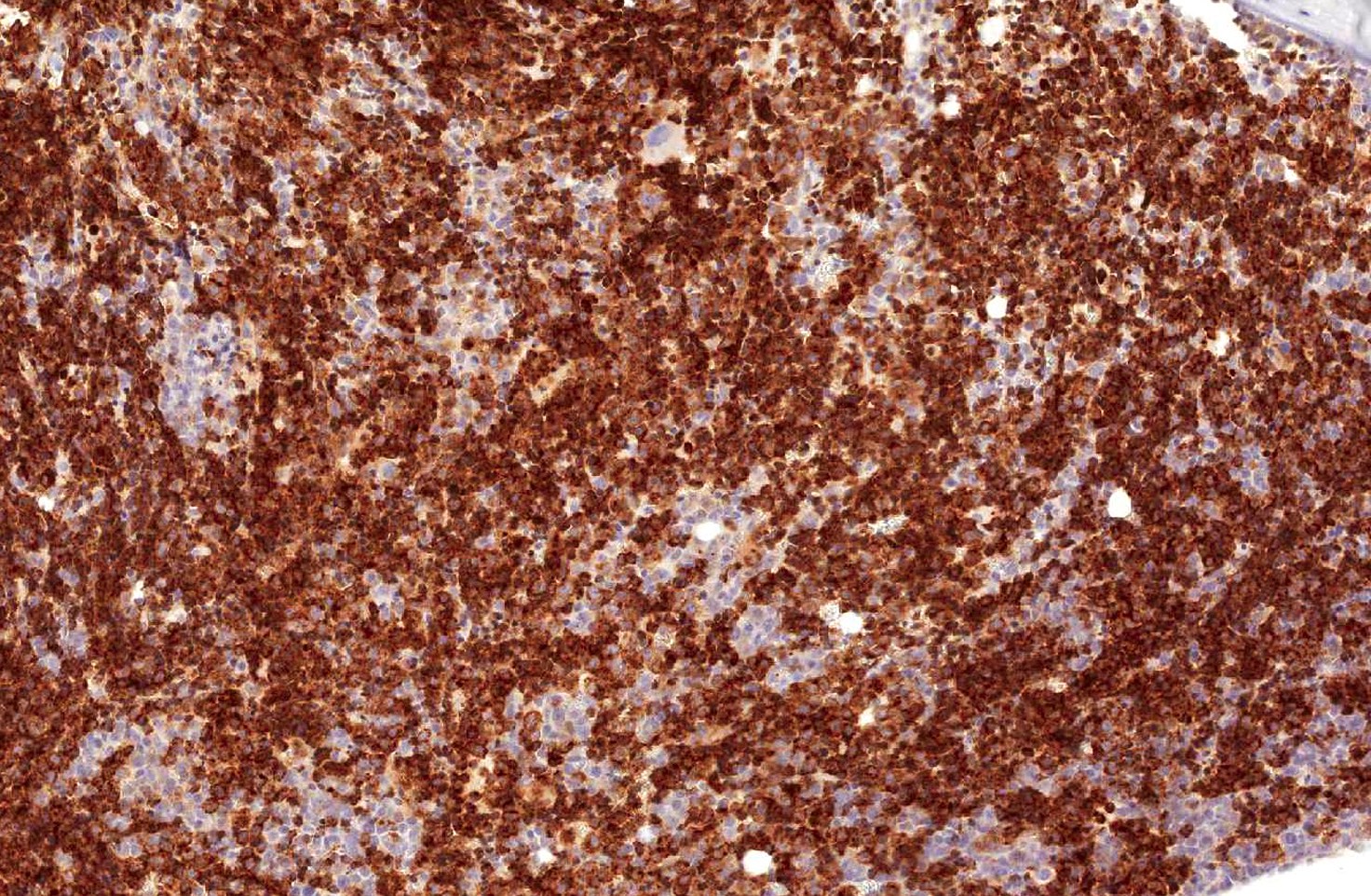
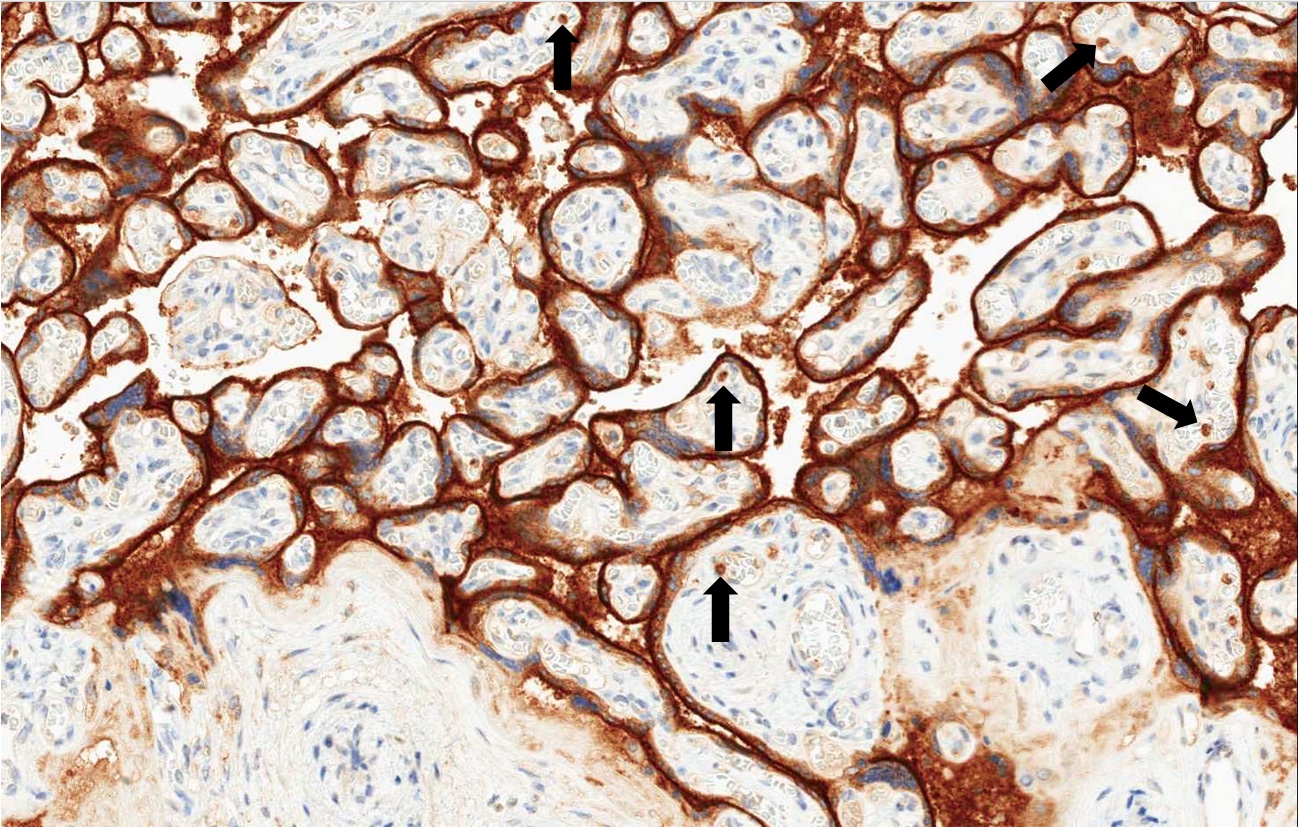
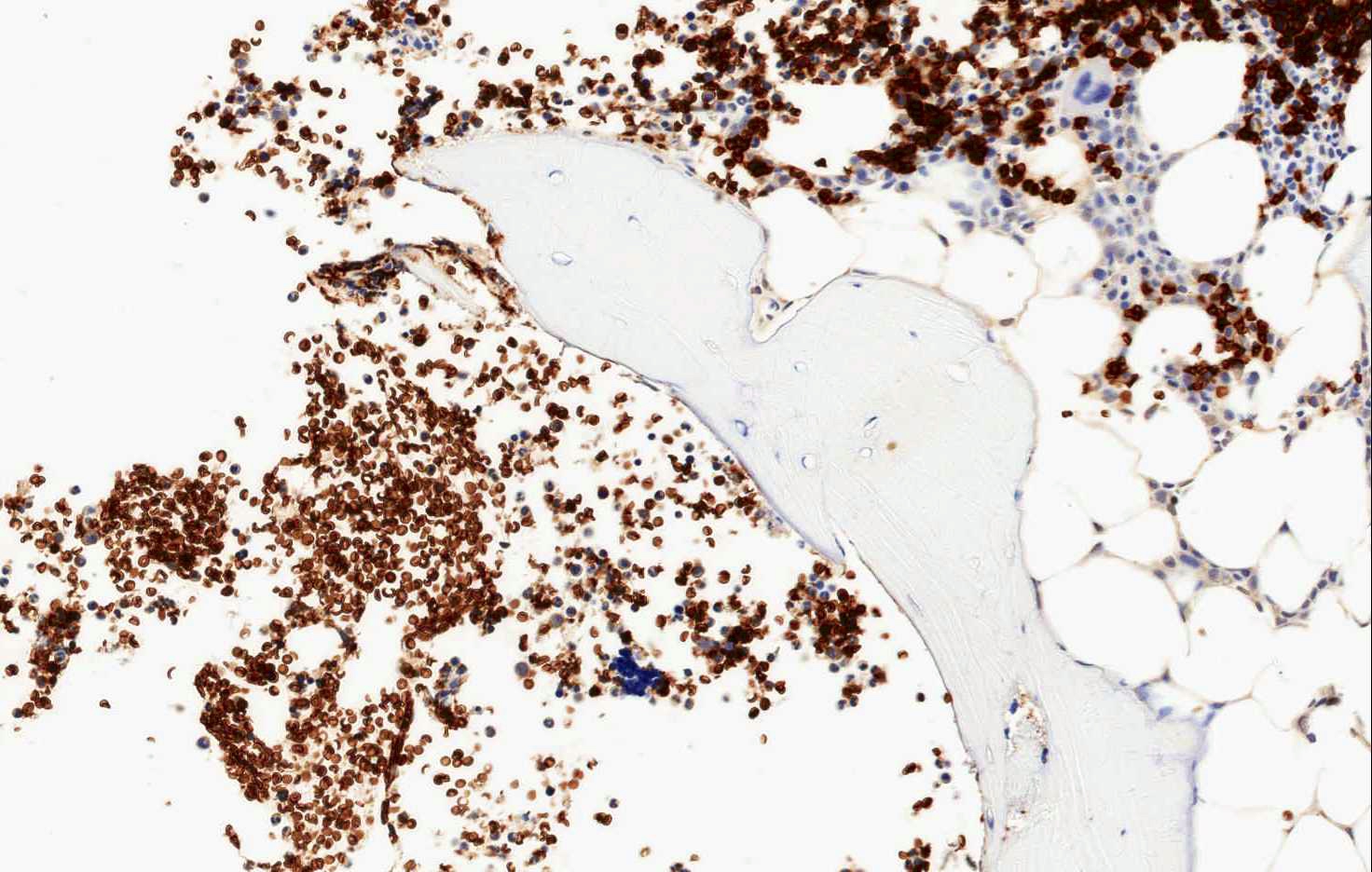
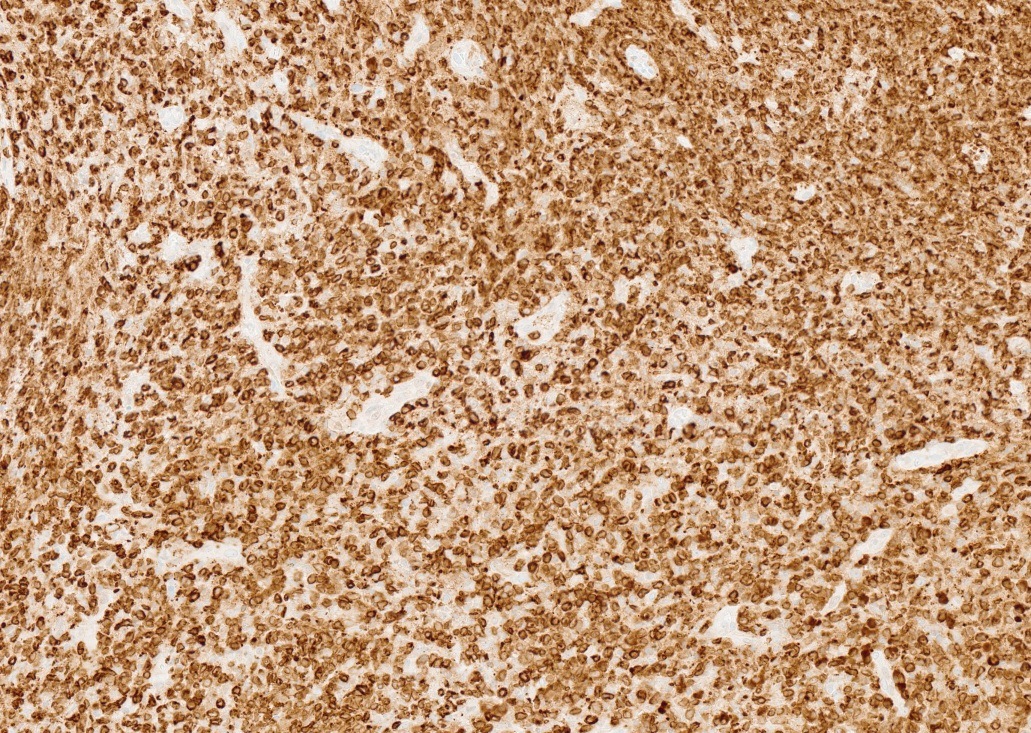
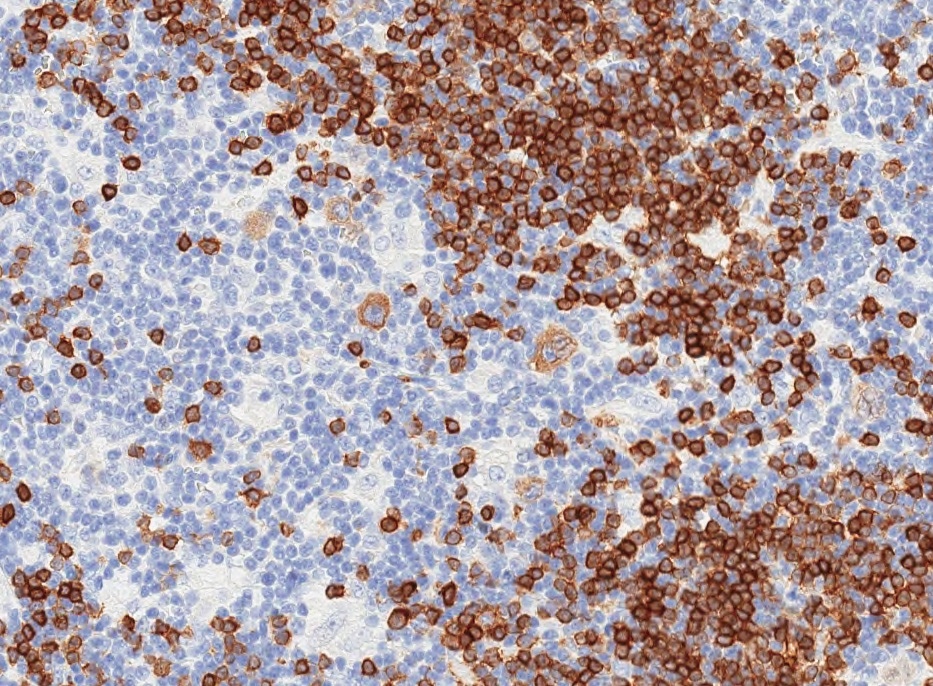
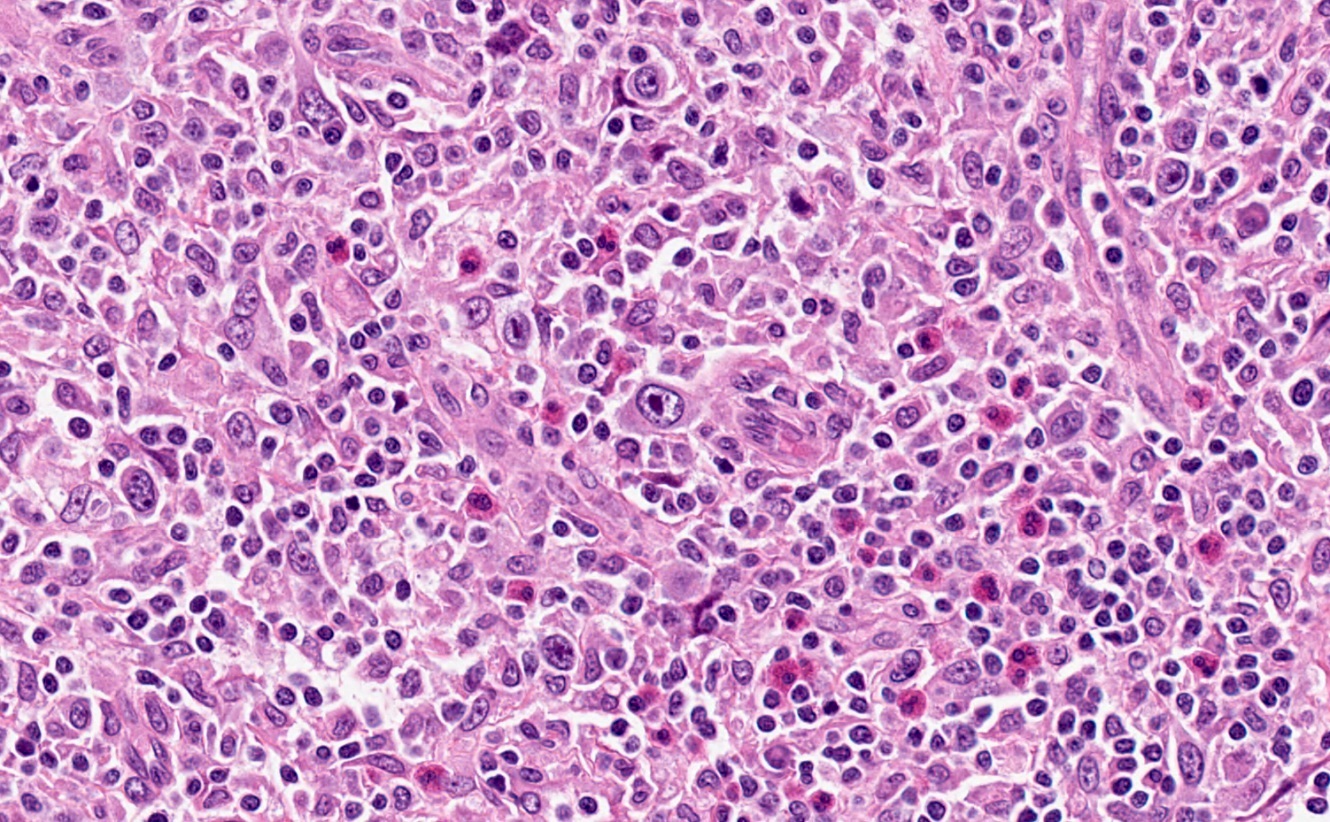
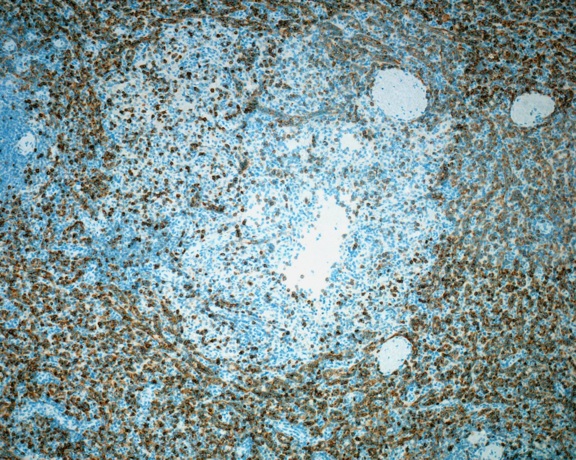
Microscopic (histologic) images
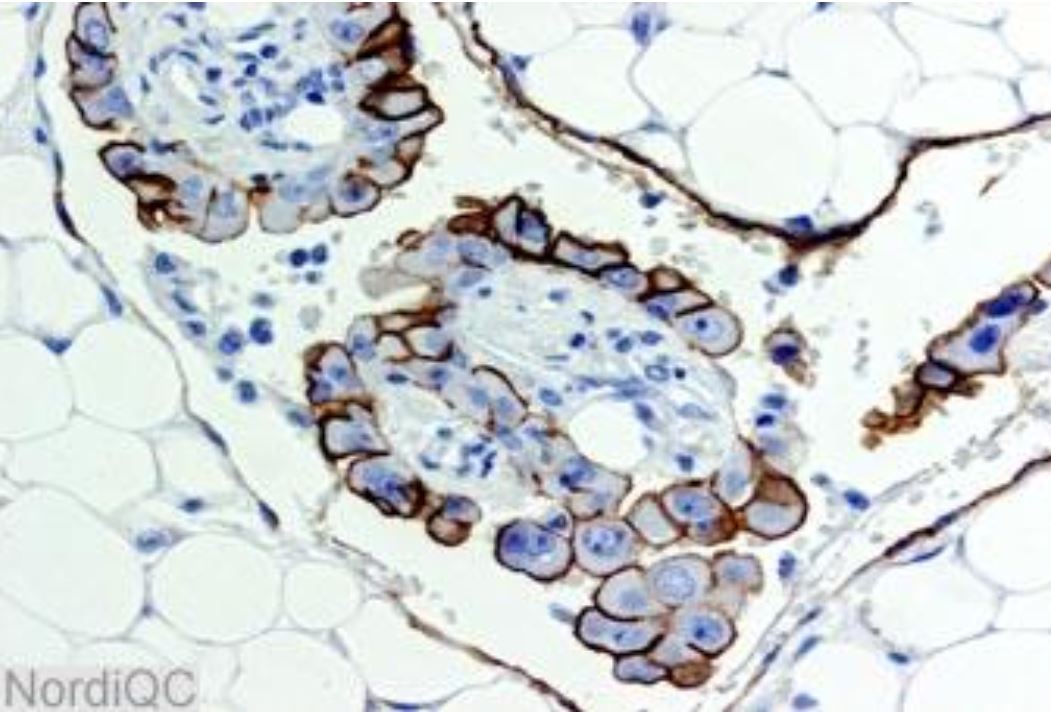
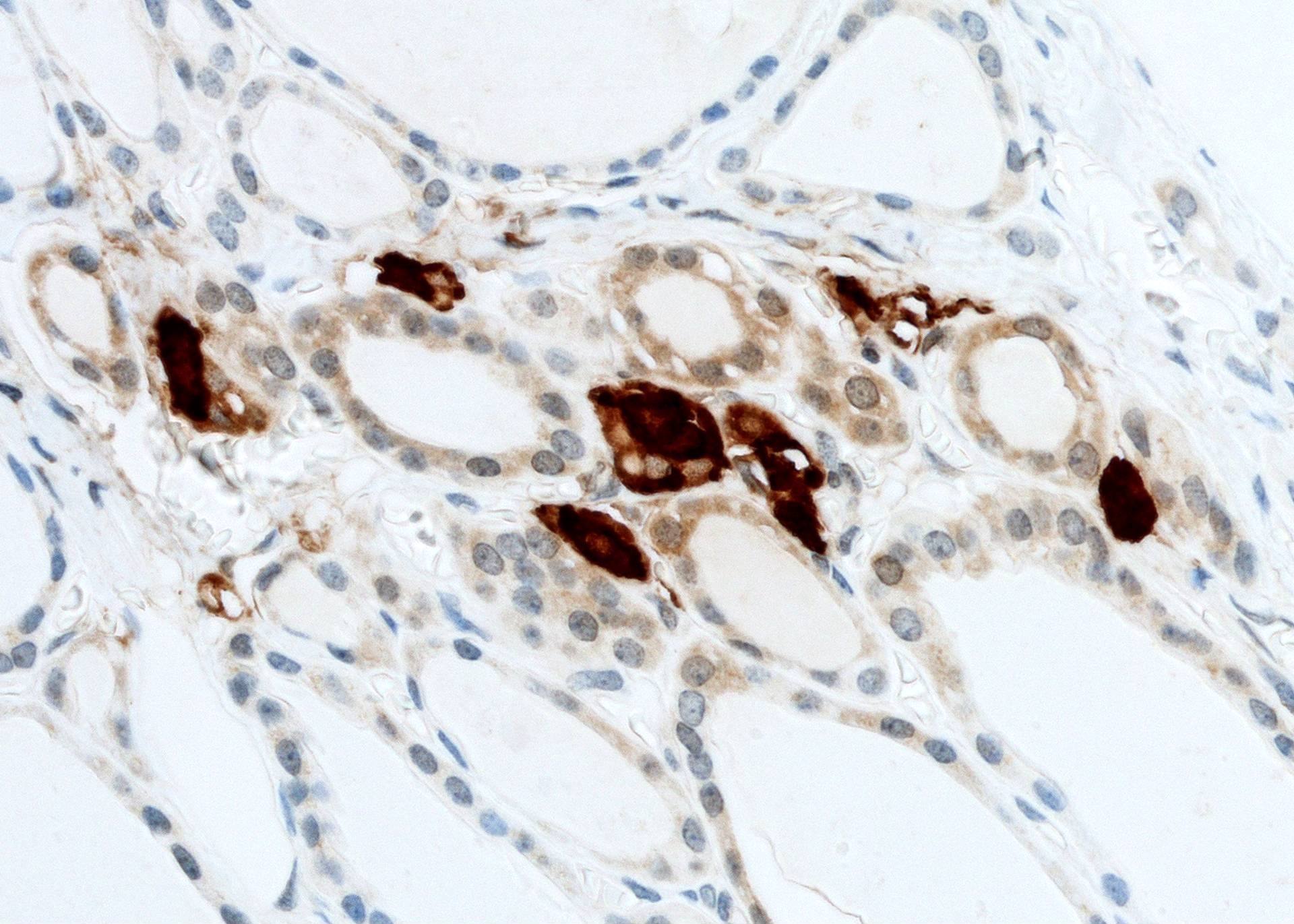
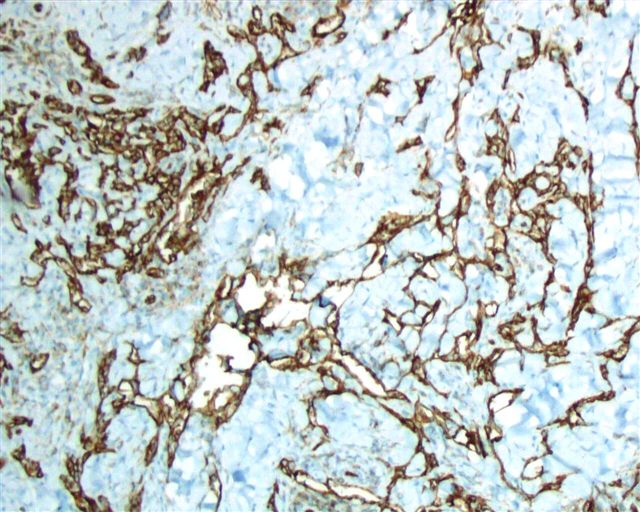
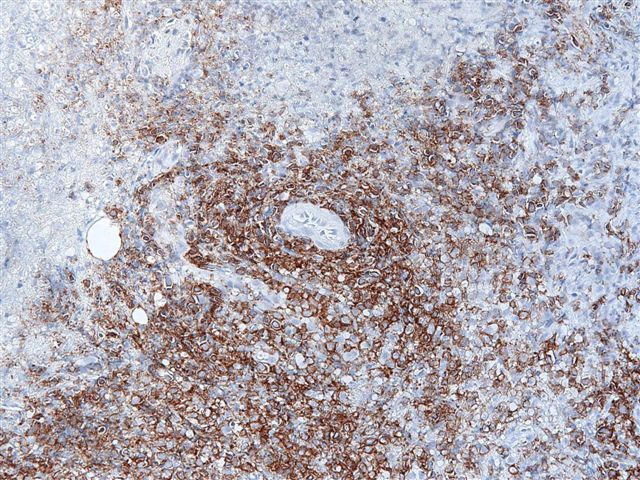
Positive staining - normal
- Renal tubules (weak blush cytoplasmic and brush border; monoclonal antibody) (Hum Pathol 2022;120:57)
- Liver bile canaliculi (bile canaliculi expression, brush border expression; monoclonal antibody) (J Tissue Eng Regen Med 2018;12:2287)
- Endocrine pancreas - membranous (Histopathology 2002;41:65)
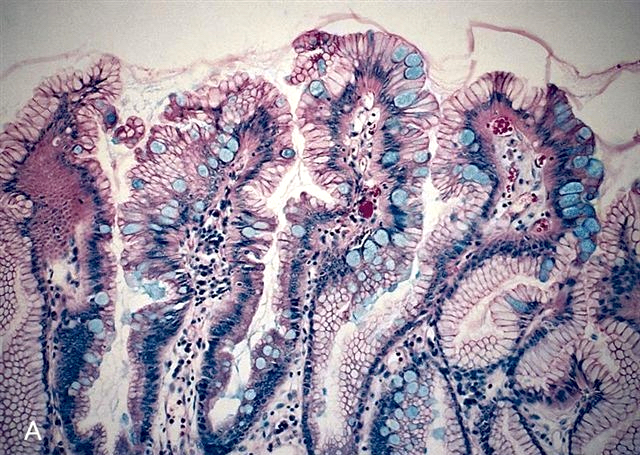
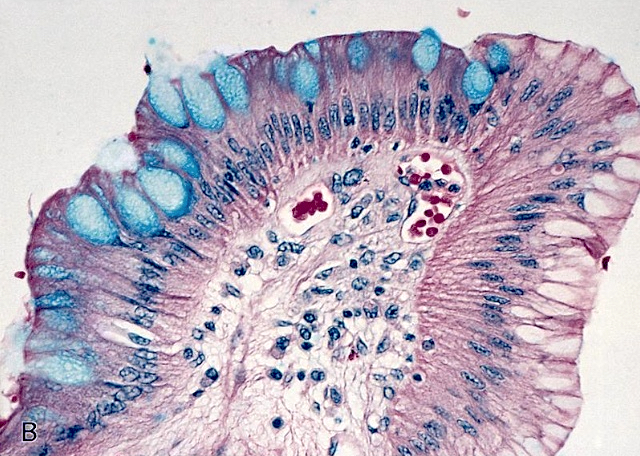
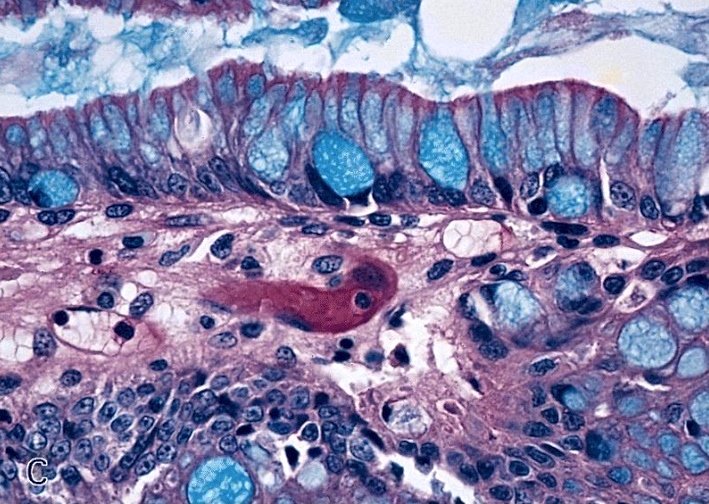
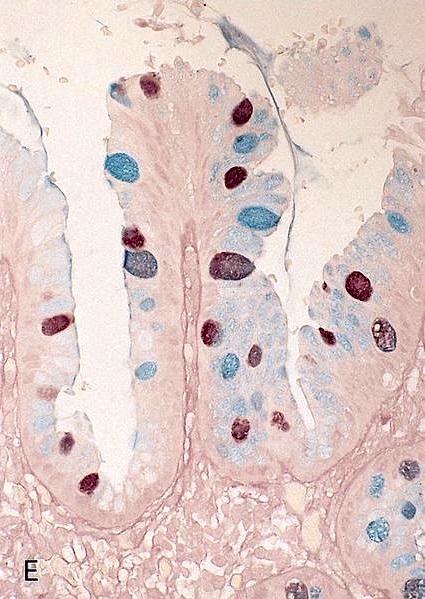
- Small intestine / colon (Histopathology 2002;41:65)
Positive staining - disease
- Papillary renal cell carcinoma (weak blush cytoplasmic and brush border) (Hum Pathol 2022;120:57)
- Colon adenocarcinoma (cytoplasmic) (Clin Cancer Res 2000;6:2401)
- Pancreatic adenocarcinoma - brush border (Sci Rep 2019;9:19782)
- Ovarian cancer (cytoplasmic and nuclear) (Gynecol Oncol 2006;100:239, Clin Cancer Res 2006;12:7149)
- Breast carcinoma (cytoplasmic and nuclear) (Pathol Oncol Res 2012;18:331)
- Fallopian tube carcinoma (cytoplasmic and nuclear) (Arch Gynecol Obstet 2013;287:563)
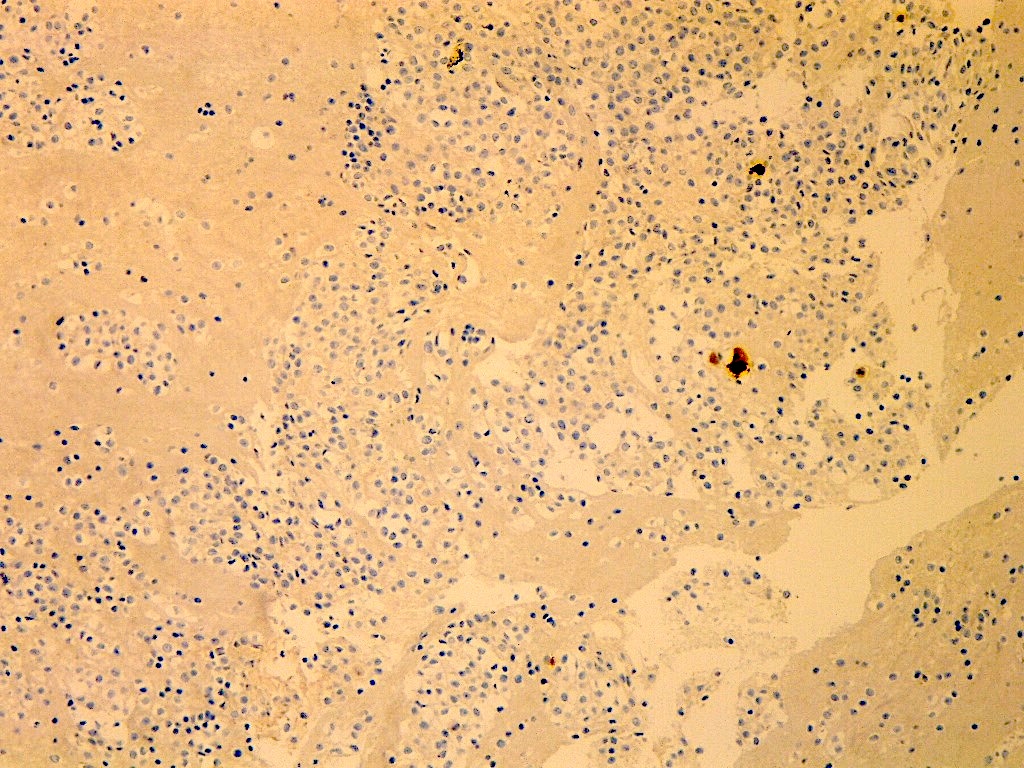
Negative staining
- Papillary renal cell carcinoma (low risk group) (Hum Pathol 2022;120:57)
- Glomeruli (Hum Pathol 2022;120:57)
- Brain (J Pharmacol Exp Ther 2004;311:449)
- Lymph nodes (Histopathology 2002;41:65)
- Endocrine pancreas (Histopathology 2002;41:65)
Molecular / cytogenetics description
- Molecular analysis of papillary renal cell carcinoma showed statistically significant very high ABCC2 gene expression by RNA sequencing platform in papillary renal cell carcinoma formerly classified as type 2
- Data was based on The Cancer Genome Atlas papillary cohort (Eur Urol Focus 2018;4:740)
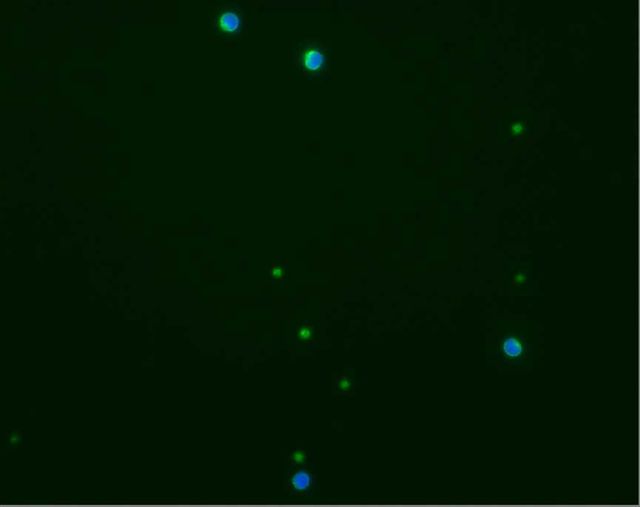
- ABCC2 RNA transcripts can be quantitatively assessed by ISH (USCAP 2023 Abstracts: Genitourinary Pathology (Including Renal Tumors) [Accessed 25 July 2023])
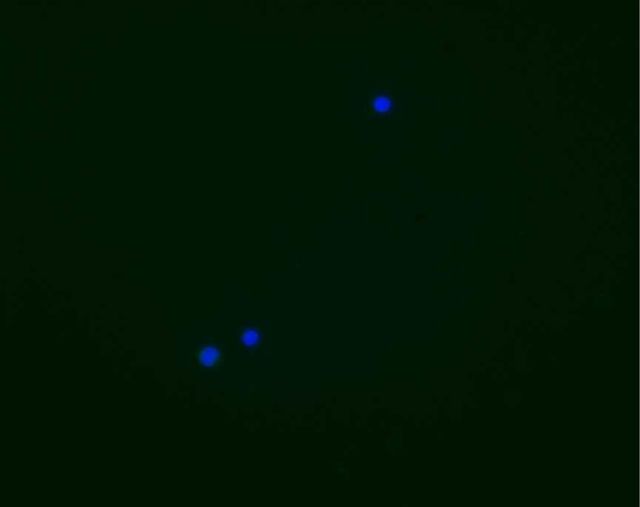
- Negative: complete absence of RNA signals
- Cytoplasmic blush: focal cytoplasmic RNA ISH signals
- Brush border < 50%: scattered punctate RNA ISH signals
- Brush border ≥ 50%: dense, numerous RNA ISH signals
- Studies on colon cancer, breast carcinoma, fallopian tube carcinoma and ovarian carcinoma showed correlation between ABCC2 gene expression by polymerase chain reaction and clinical outcomes, as well as chemotherapy resistance (Gynecol Oncol 2006;100:239, Clin Cancer Res 2000;6:2401, Clin Cancer Res 2006;12:7149, Pathol Oncol Res 2012;18:331, Arch Gynecol Obstet 2013;287:563)
Sample pathology report
- Kidney, mass, nephrectomy:
- Papillary renal cell carcinoma (see comment)
- Comment: ABCC2 brush border staining pattern > 50% shown by immunohistochemistry.
Board review style question #1
A 56 year old man has an incidentally discovered renal mass, 4 cm in size. He was treated with partial nephrectomy. Microscopic examination shows a papillary renal cell carcinoma (PRCC). An immunopanel including ABCC2 IHC stain is ordered. Which pattern of staining may predict a poor clinical outcome?
- Brush border staining in ≥ 50% of the PRCC cells
- Complete absence of ABCC2 staining in the tumor with preserved staining in renal tubules
- Concurrent ABCC2 and GATA3 expression in PRCC cells
- Weak patchy cytoplasmic ABCC2 staining in the PRCC cells
Board review style answer #1
A. Brush border staining in ≥ 50% of the PRCC cells. Brush border ABCC2 staining in the tumor is shown to be a poor prognostic feature in papillary renal cell carcinoma ≤ 4 cm in size. Brush border pattern also correlates with higher ABCC2 RNA transcript by ISH. Answers B and D are incorrect because completely negative or cytoplasmic expression shows a relatively better prognosis. Answer C is incorrect because GATA3 positive papillary renal cell carcinoma is known as the entity of papillary renal neoplasm of reverse polarity which is quite indolent.
Comment Here
Reference: ABCC2
Comment Here
Reference: ABCC2
Acid fast / Auramine-rhodamine
Definition / general
- Acid fast refers to microorganisms whose cell wall has a high lipid content of mycolic acids and long chain fatty acids, which traditionally is considered to cause them to bind and retain the complex basic dye carbol-fuchsin even after strong decolorization with acid-alcohol (thus "acid-fast") (Wikipedia)
- Hänscheid et. al. believe auramine O actually binds to nucleic acids, not to the cell wall (see Lancet Infect Dis 2007;7:236, J Microbiol Methods 2008;74:119)
- Partially acid fast organisms exhibit both acid fast and non-acid fast bacilli and filaments in a single strain
- Standardization recommended for interpretation (Hum Pathol 2012;43:1845)
- Sputum smears may misidentify acid-fast bacilli as Mycobacterium tuberculosis in HIV+ patients (J Acquir Immune Defic Syndr 2013;63:168)
- Acid fast organisms include Mycobacteria, oocysts of Cryptosporidium parvum, Cyclospora, Isospora; also hooklets of cysticerci
- Partially acid fast organisms include Actinomyces: Dietzia (Int J Syst Evol Microbiol 2006;56:1667), Gordonia (Emerg Infect Dis 2000;6:382), Nocardiae (Surg Infect (Larchmt) 2012;13:163), Rhodococcus (South Med J 1991;84:1217), Tsukamurella (J Med Case Rep 2008;2:207); also rarely Mycobacterium peregrinum (J Clin Microbiol 2005;43:2015)
- Note: nucleic acid based tests can rapidly detect and speciate mycobacteria (Arch Pathol Lab Med 2008;132:1333, Thorax 2008;63:317)
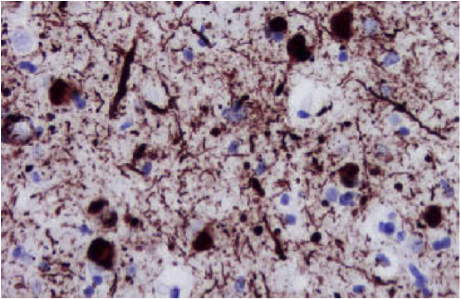
Methods
- Ziehl-Neelsen (classic): common method; bacteria stain bright red due to retention of carbol-fuchsin dye; background is methylene blue counterstain; procedure involves heat (#1, #2)
- Ziehl-Neelsen (modified bleach): may be more sensitive than classic stain (Acta Cytol 2008;52:325,J Cytol 2012;29:165)
- Ziehl-Neelsen (modified for stool specimens): does not require heating (Centers for Disease Control)
- Kinyoun: common method; uses more concentrated fuchsin dye and lipid solvent, but no heat; bacteria stain bright red against green background (#1, #2)
- Fite: to detect M. leprae (leprosy) and Rhodococcus (Diagn Cytopathol 2001;24:244); combines peanut / vegetable oil with xylene to minimize exposure of bacteria cell wall to organic solvents and protect precarious acid-fastness of organism (#1, #2)
- Ellis and Zabrowarny: protocol excludes phenol; procedure (J Clin Pathol 1993;46:559)
- Auramine-rhodamine: mixture of Auramine O and Rhodamine B dyes, auramine binds to mycolic acid in cell wall; detection requires a fluorescence microscope (mercury vapor lamp or LED), but is most sensitive stain for mycobacteria (Hum Pathol 1984;15:1085, PLoS One 2011;6:e22495); saves time in searching for microorganisms (Clin Infect Dis 2008;47:203); procedure
- Water filters are recommended to reduce false positives due to non-TB mycobacteria (Appl Environ Microbiol 2007;73:6296)
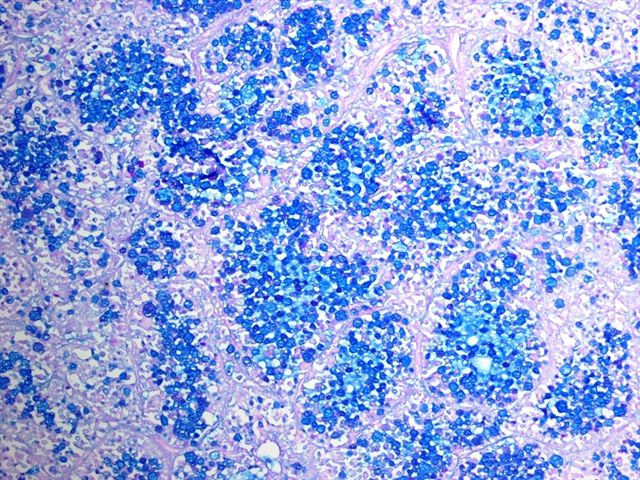
Microscopic (histologic) images
Images hosted on other servers:
Cryptosporidium:
Videos
Acid fast stain
Acid phosphatase
Table of Contents
Definition / general | Essential features | Terminology | Interpretation | Uses by pathologists | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Definition / general
- Acid phosphatase is not a single enzyme but rather a group of enzymes that hydrolyze and release phosphate group from different substrates
- By definition, they function best in an acidic environment and are normally localized in the lysosomes (Mol Pathol 2002;55:65)
- In muscle biopsies, the acid phosphatase stain is an enzyme histochemical stain that relies on endogenous acid phosphatase activity in the muscle specimen to hydrolyze the artificial naphthol AS-B1 phosphate substrate into naphthol, producing a brick red reaction product (Dubowitz: Muscle Biopsy: A Practical Approach, 4th Edition, 2013)
- Therefore, the acid phosphatase stain must be performed on cryosections of snap-frozen fresh muscle tissue
- Acid phosphatase should be differentiated from the antibody based immunohistochemical stains Prostatic Acid Phosphatase (PAP or PSAP) and Tartrate Resistant Acid Phosphatase (TRAP)
- PAP is a marker for prostate cancer (Biochem Mol Biol Int 1994;33:567)
- TRAP is a marker for osteoclasts (Calcif Tissue Int 1982;34:285)
Essential features
- In muscle biopsies, acid phosphatase stain is mainly used to highlight macrophages, red rimmed vacuoles in inclusion body myositis, lysosome storage disorders and other hereditary or acquired vacuolar myopathies associated with abnormal lysosomal activity
Terminology
- Nonspecific acid phosphatase(s)
Interpretation
- Lysosomes
Uses by pathologists
- Highlights degenerating fibers and macrophages (Dubowitz: Muscle Biopsy: A Practical Approach, 4th Edition, 2013)
- Detects muscle disorders with lysosomal abnormalities, including lysosomal storage diseases and variable hereditary or acquired vacuolar myopathies associated with lysosomal dysfunction or excessive autophagic activity; see disease specific references under Positive staining - disease section
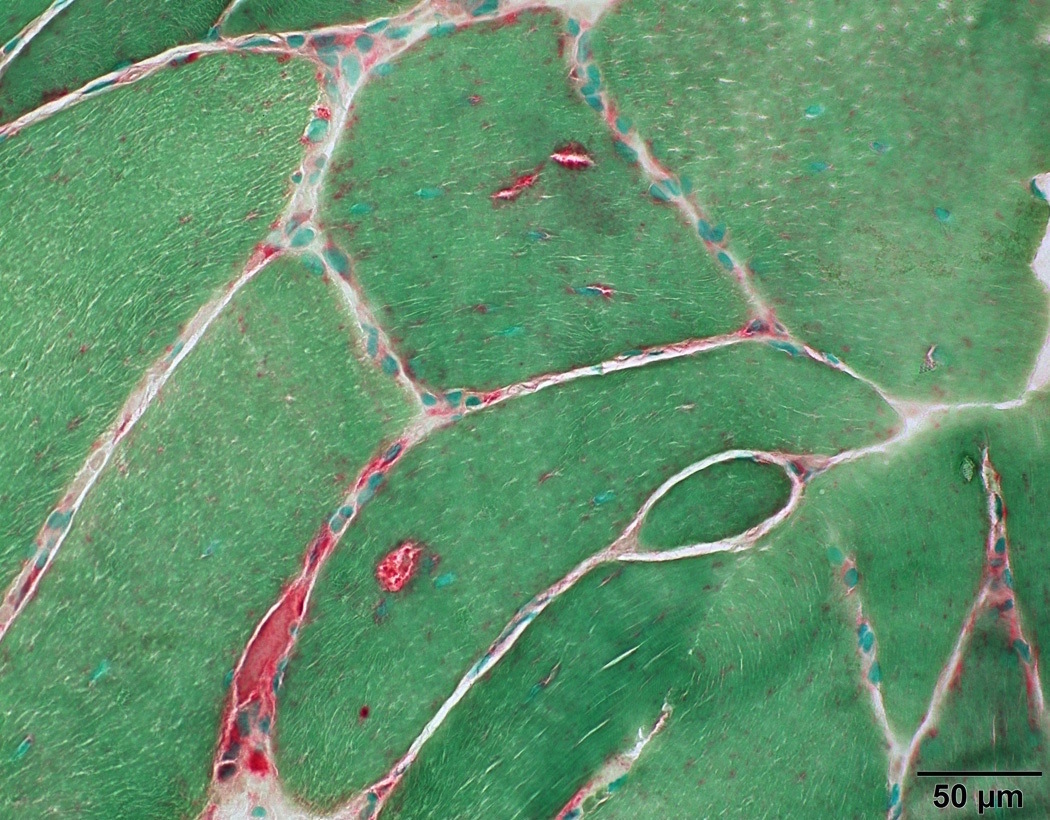
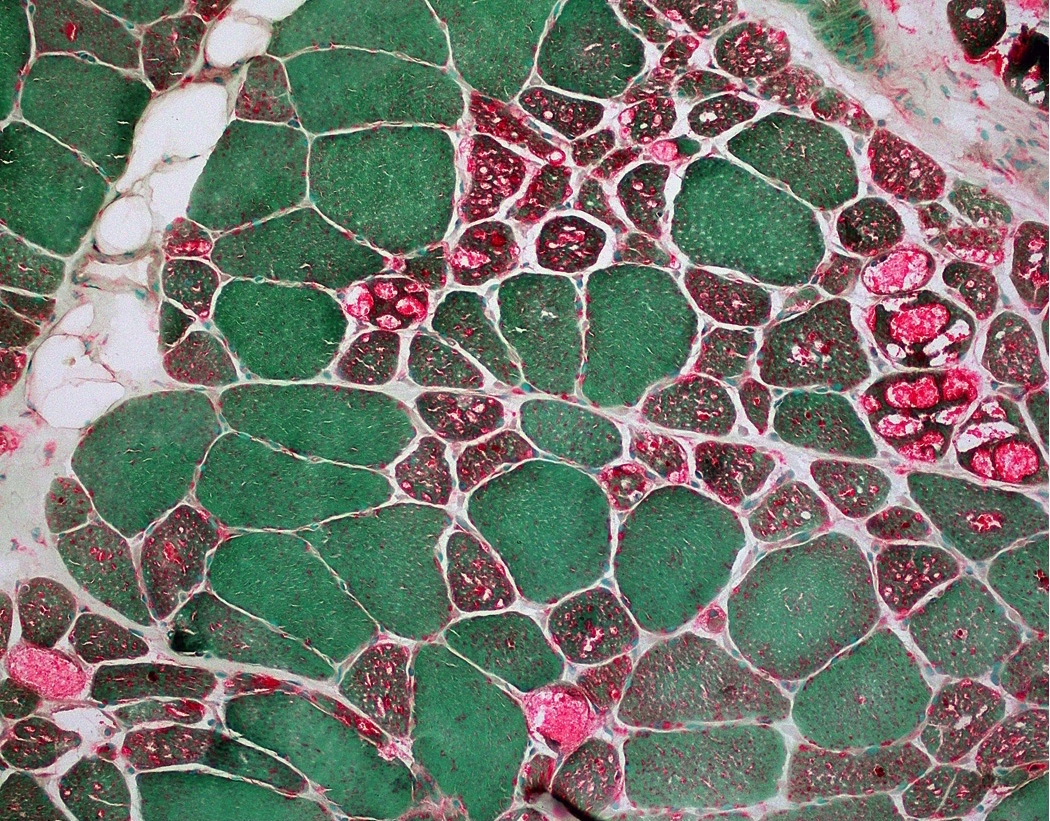
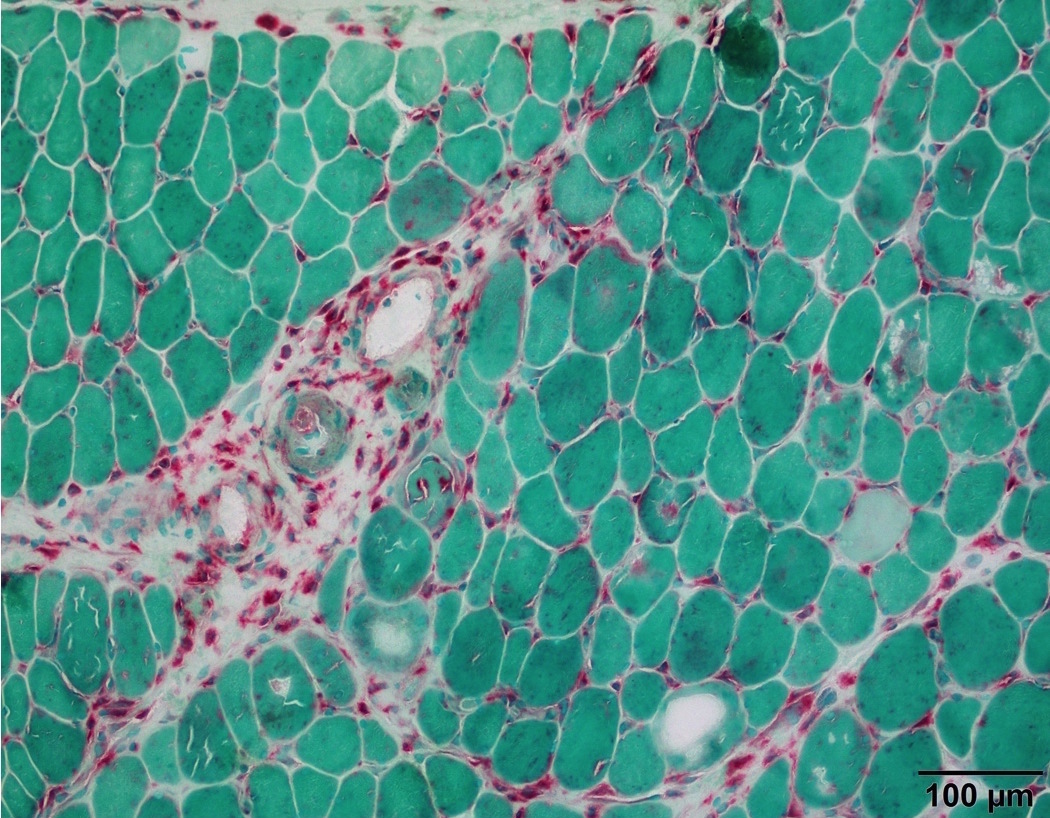
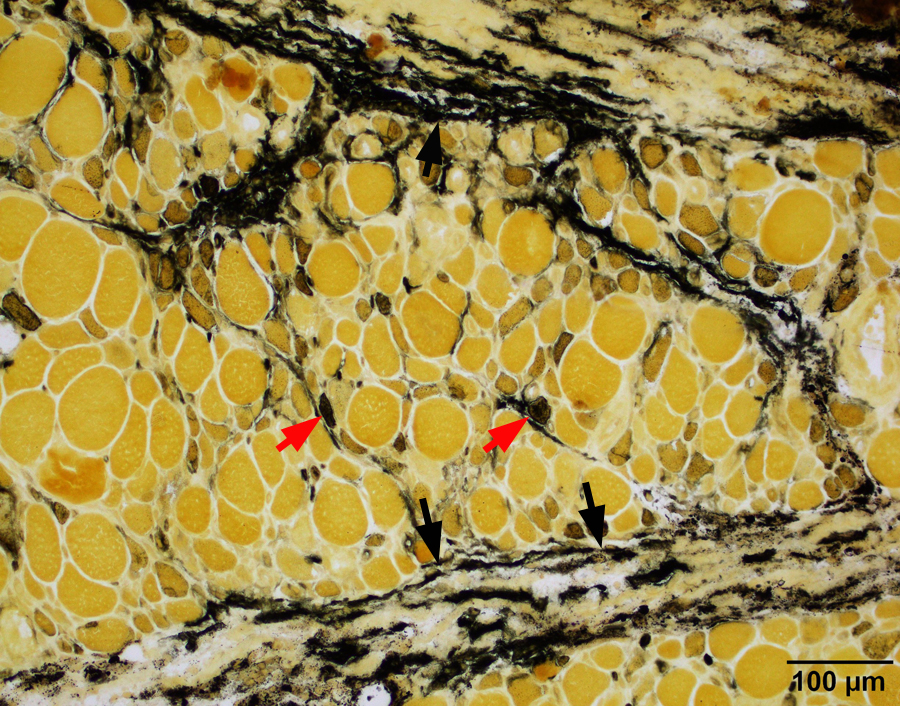
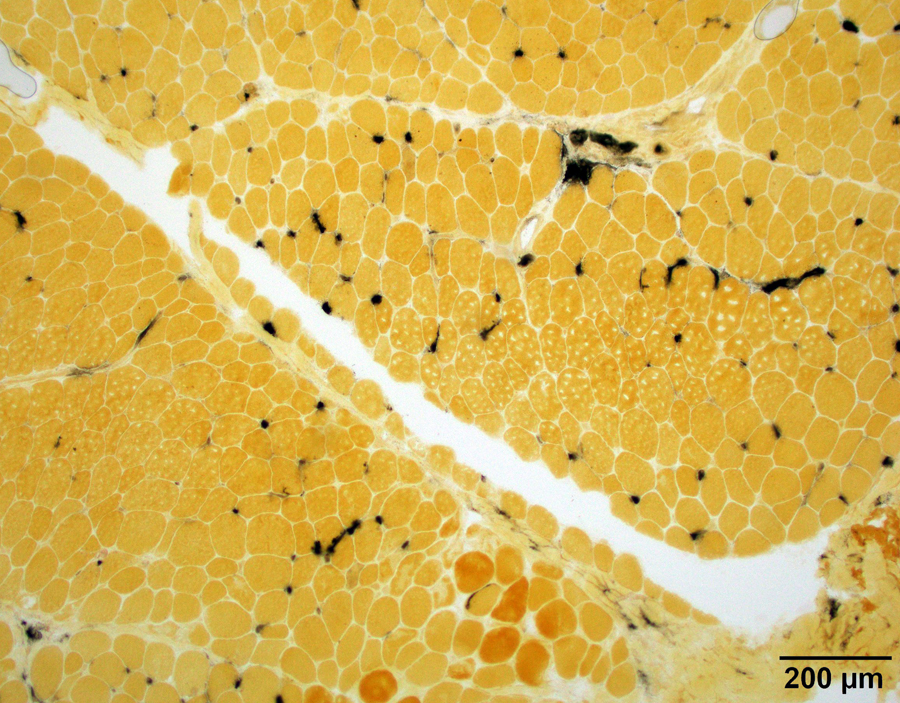
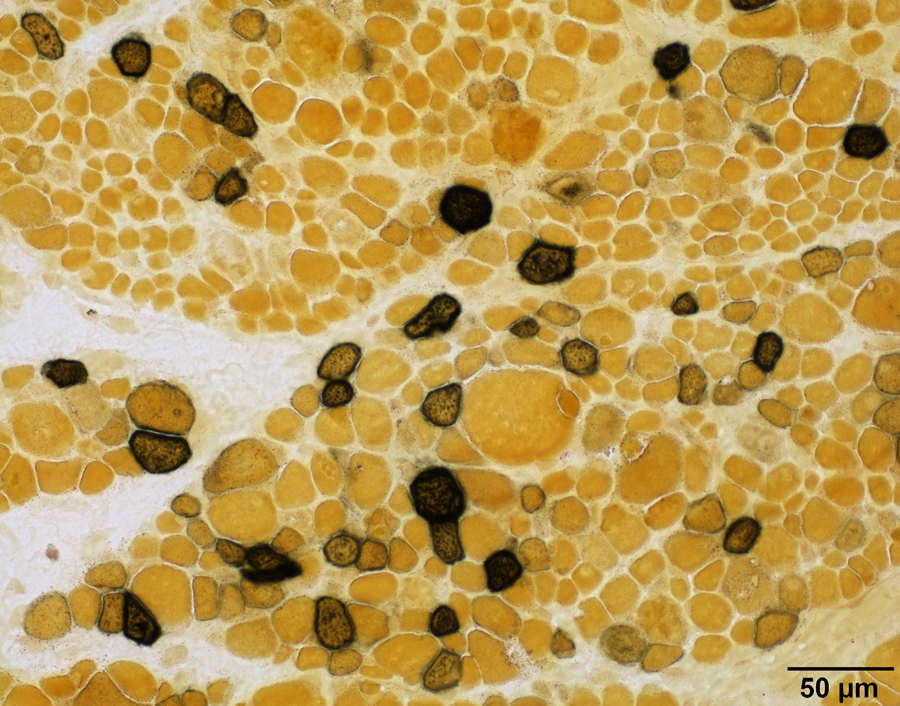
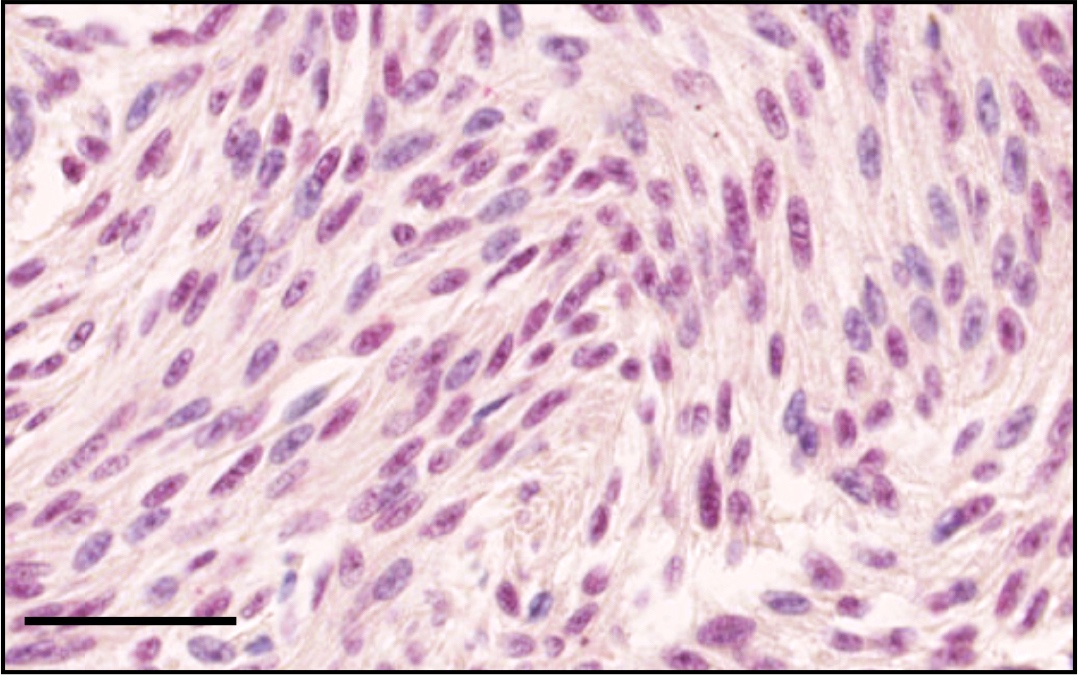
Microscopic (histologic) description
- Staining of lipofuscin in myofiber is punctate granular, predominantly subsarcolemmal (Dubowitz: Muscle Biopsy: A Practical Approach, 4th Edition, 2013)
- Staining of lysosomes or lysosomal vacuoles in myofiber is punctate and predominantly sarcoplasmic; see disease specific references under Positive staining - disease section
- Staining of degenerating myofibers and paraspinal myofibers is a weak diffuse blush in the sarcoplasm
- Staining of macrophages is strong cytoplasmic
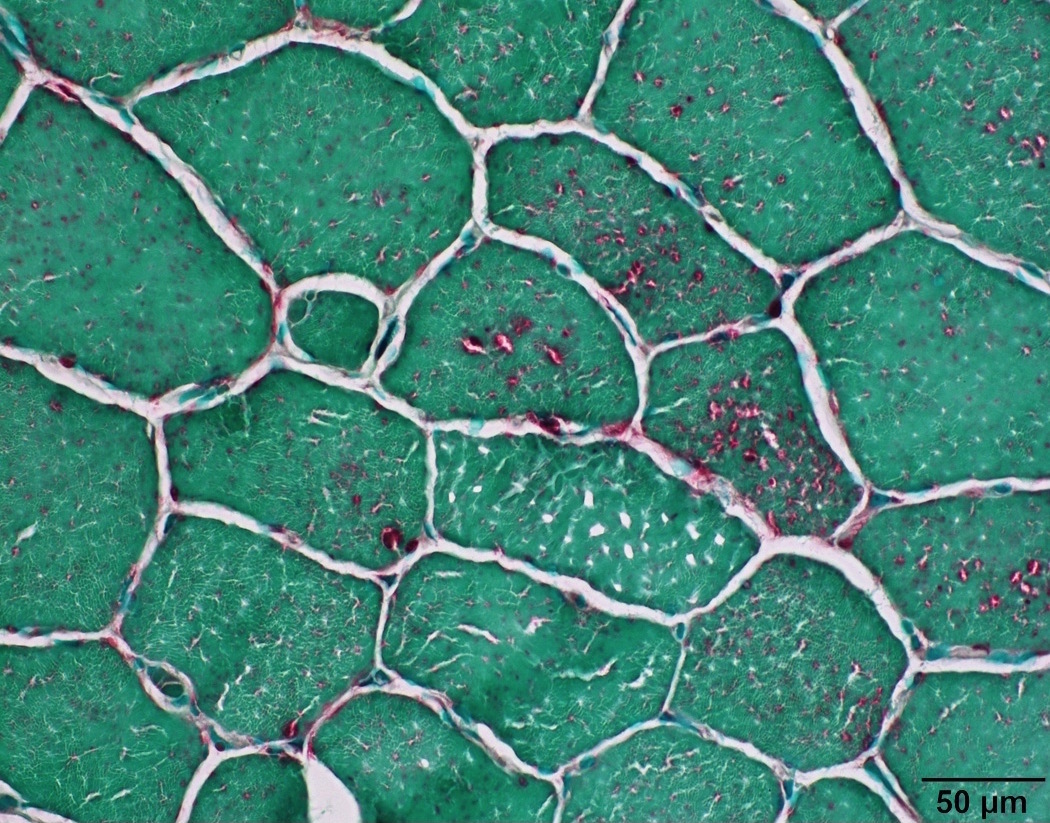
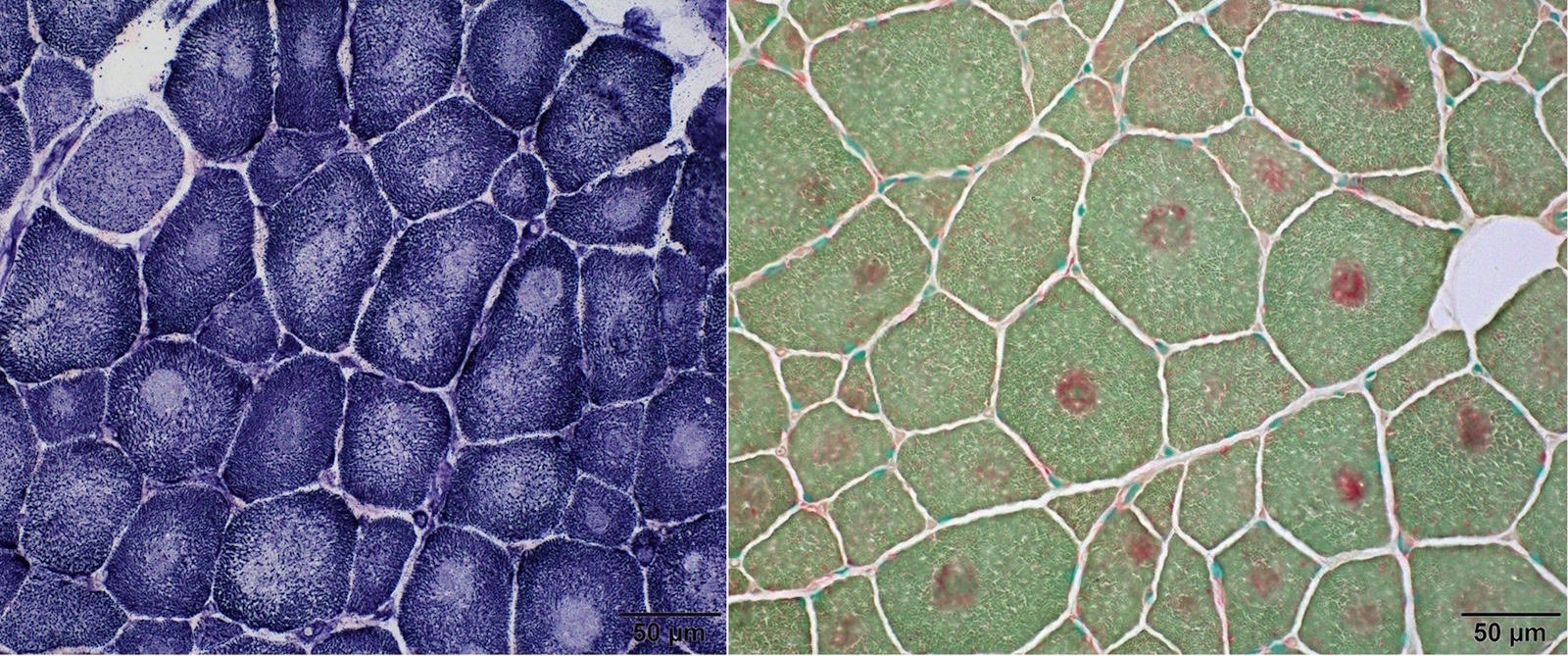
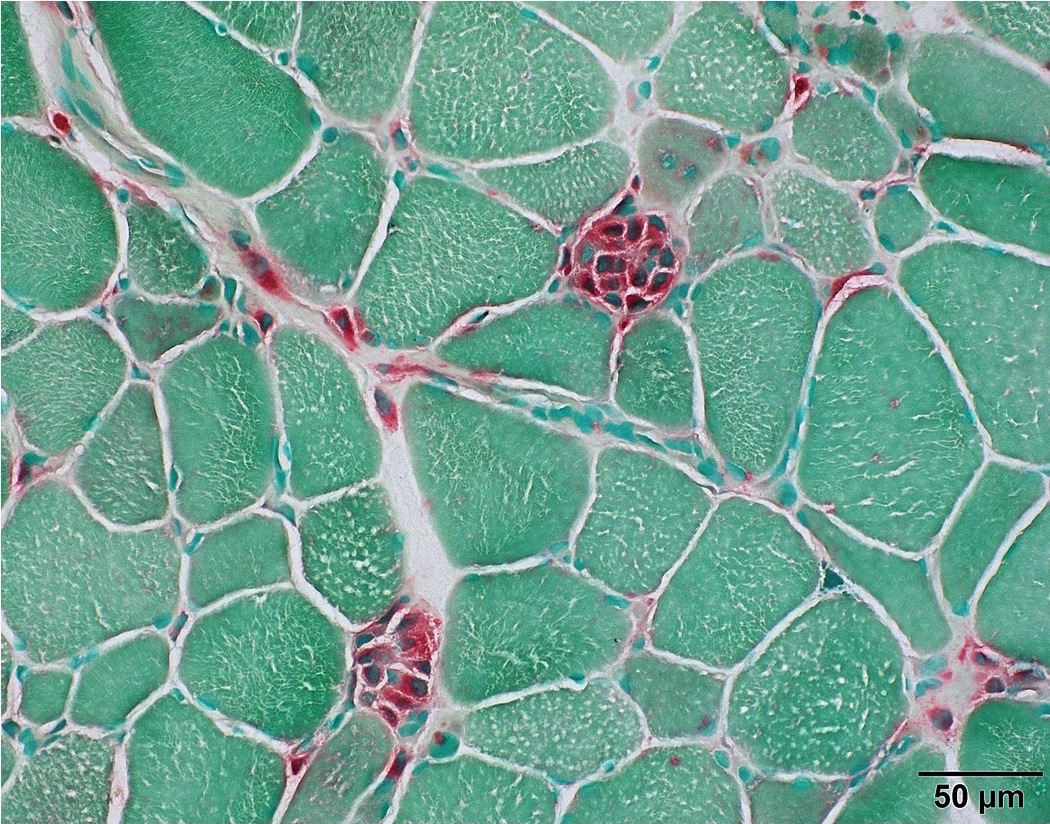
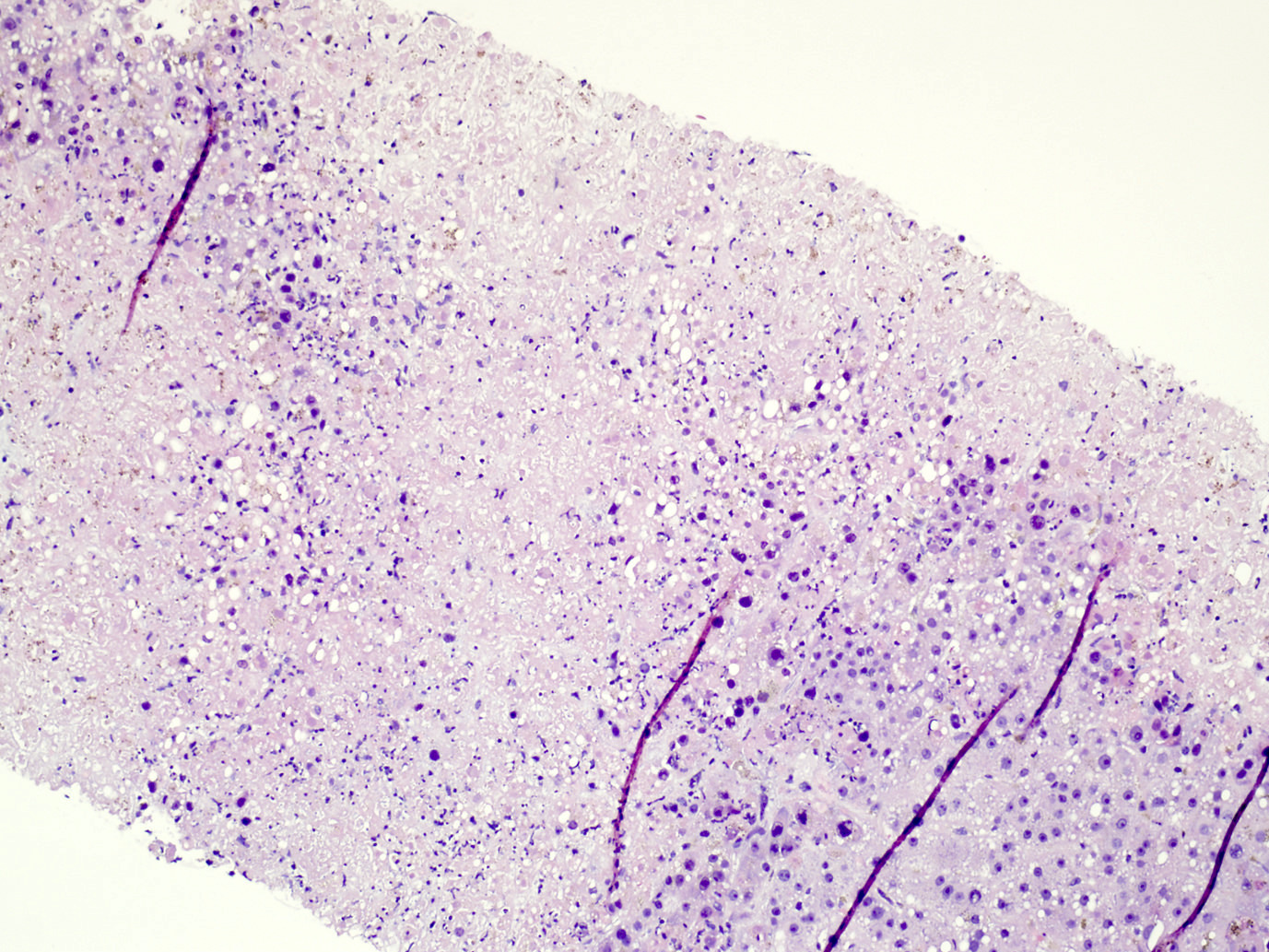
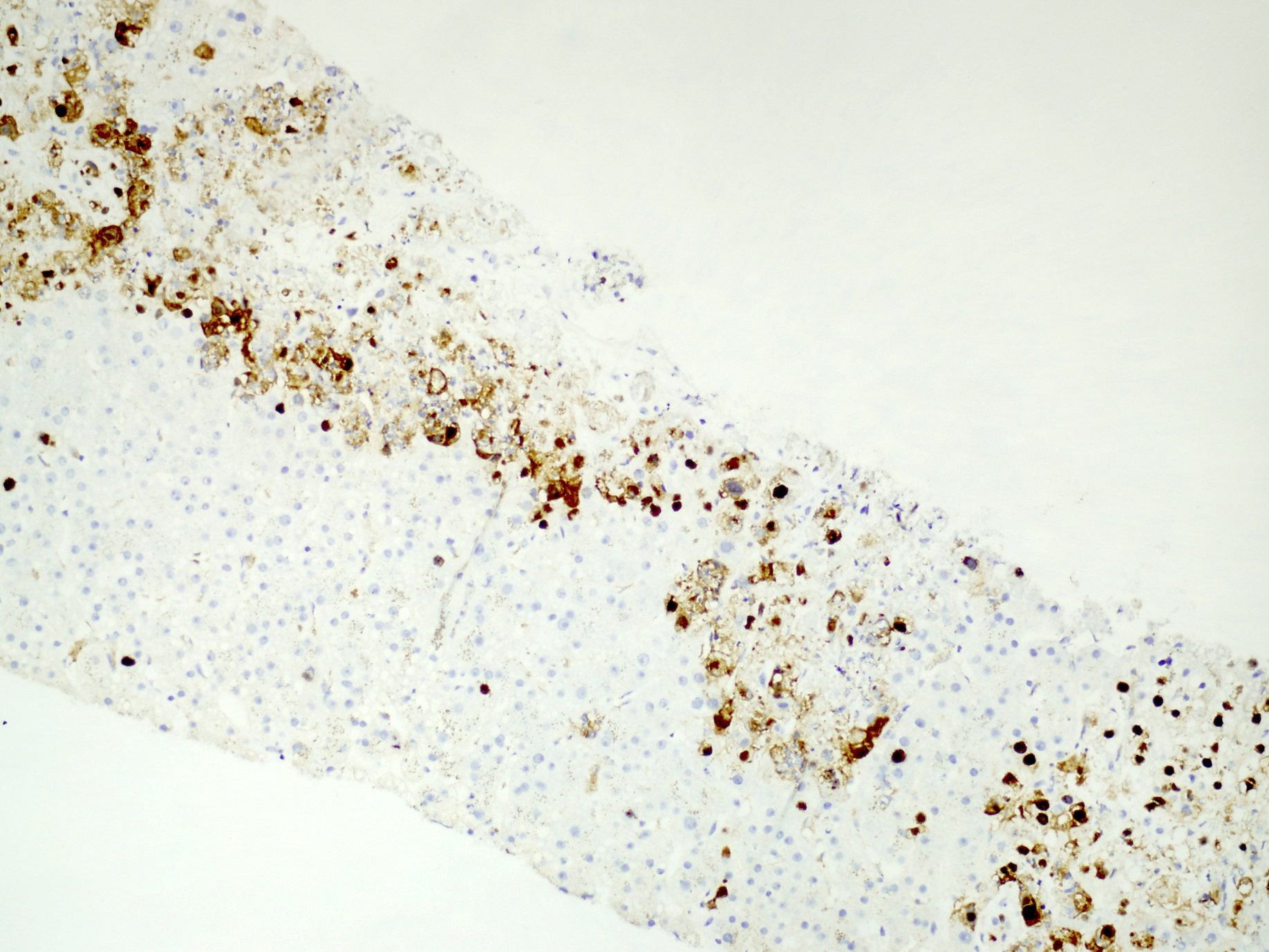
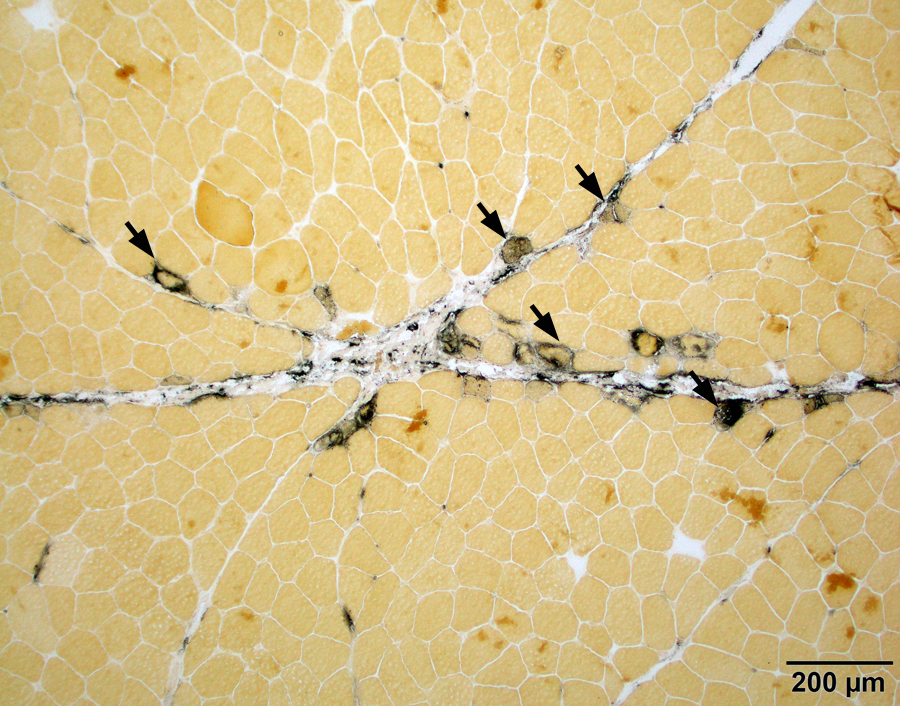
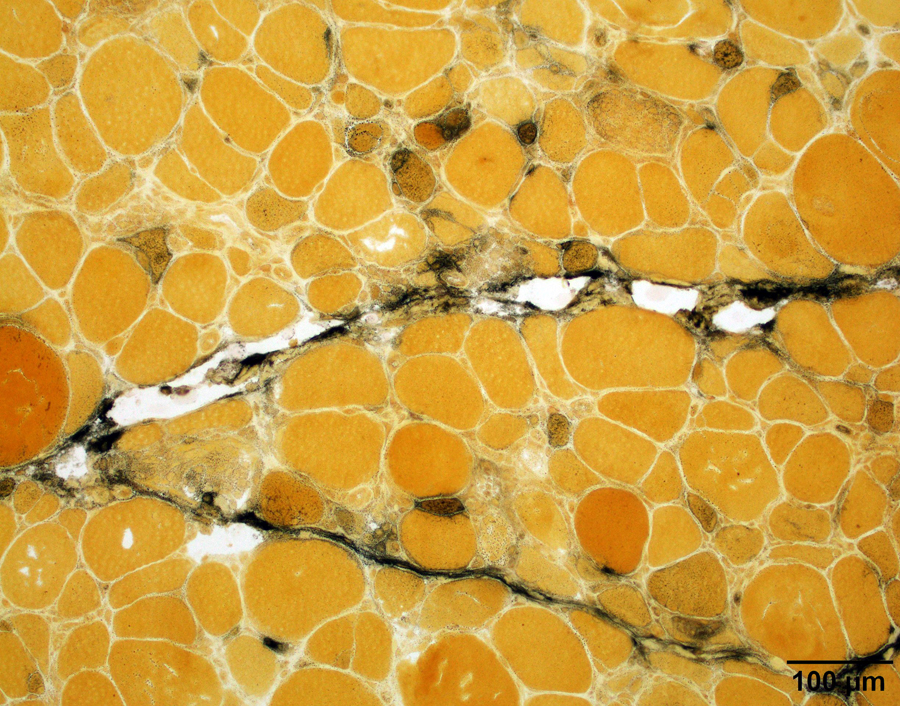
Microscopic (histologic) images
Positive staining - normal
- Stains lysosomes in myofibers, which are inconspicuous in normal fibers
- Stains lipofuscin in muscle fibers, which are usually subsarcolemmally located and increase with age
- Increased in paraspinal muscles (Muscle Nerve 2015;52:45)
Positive staining - disease
- Degenerating and regenerating myofibers (J Neurol Sci 1977;33:95)
- Macrophages (Muscle Nerve 1995;18:242)
- Rimmed vacuoles in inclusion body myositis (Ann Neurol 1988;23:258)
- Acid maltase deficiency/Pompe disease/Glycogen storage disease type II (Acta Neuropathol Commun 2014;2:2)
- Vacuoles in cystinosis distal vacuolar myopathy (Ann Neurol 1994;35:181)
- Vacuoles in X-linked myopathy with excessive autophagy (XMEA) (Biomed Res Int 2018;2018:5069042)
- Vacuoles in Danon disease (J Neuropathol Exp Neurol 2005;64:513)
- Chloroquine and hydroxychloroquine induced myopathy (Am J Med 1987;82:447)
- Colchicine induced myopathy (Acta Neuropathol 2002;103:100)
- Chronic vitamin E deficiency (Ann N Y Acad Sci 1982;393:84)
Negative staining
- Other types of glycogen storage diseases besides acid maltase deficiency (GSD II) (J Clin Neurosci 2015;22:1674)
Board review style question #1
- Which of the following components in muscle fiber stains acid phosphatase?
- Lipid droplet
- Lysosome
- Mitochondria
- Myosin filament
- Sarcoplasmic reticulum
Board review style answer #1
ACTH (pending)
[Pending]
Actin - general / cardiac
Table of Contents
Definition / general | Pathophysiology | Clinical features | Alpha cardiac actin | Diagrams / tables | Microscopic (histologic) imagesDefinition / general
- Globular protein that forms microfilaments; found in all eukaryotic cells except nematode sperm (Wikipedia)
- Highly conserved, differs by at most 20% between algae and humans
- Participates in more protein-protein interactions than any known protein
Pathophysiology
- The monomeric subunit of microfilaments, one of 3 major components of cytoskeleton (also microtubules and intermediate filaments); also a component of thin filaments (part of contractile apparatus of muscle cells)
- Can transition between monomeric (G-actin) and filamentous (F-actin) states under control of nucleotide hydrolysis, ions, and actin-binding proteins (Annu Rev Biophys 2011;40:169)
- Mammalian muscle cells contain alpha and gamma smooth muscle actin, alpha cardiac actin and alpha skeletal actin
- Mammalian nonmuscle cells contain beta cytoplasmic actin and gamma cytoplasmic actin
- Functions in all cells:
- Forms part of cytoskeleton, which gives mechanical support to cell and is part of signal transduction
- Assists with motility and phagocytosis
- Helps myosins transport organelles and other substances through cell
- Actin cytoskeleton may act as sensor and mediator of apoptosis (Bioarchitecture 2012;2:75)
- Function in muscle cells: contraction
- Actin cap: recently characterized cytoskeletal organelle composed of thick and highly contractile acto-myosin filaments anchored to apical surface of interphase nucleus (Soft Matter 2013;9:5516)
Clinical features
- Persistence of high titers of anti-actin serum antibodies is associated with disease activity in autoimmune hepatitis (Hepatology 2013;59:592)
Alpha cardiac actin
- Also called ACTC1
- Two types of alpha sarcomeric / striated actin: alpha cardiac type and alpha skeletal muscle type; both are expressed in cardiac and skeletal muscle, but the proportions vary at different developmental periods (J Biol Chem 1994;269:12212) or with disease (Rapid Commun Mass Spectrom 2003;17:1467)
- Existence of two actin isoforms and their conformational differences may be part of tuning regulatory mechanism, by which the cardiac muscle cells can maintain their biological function under pathological conditions (Biochem Biophys Res Commun 2008;368:696)
- Mutations in alpha cardiac actin may cause dilated or hypertrophic cardiomyopathy (J Mol Cell Cardiol 2000;32:1687, J Biol Chem 2006;281:16777); location of mutations correlate with type of functional change (PLoS One 2012;7:e36821)
- Mutations may cause familial atrial septal defects (Hum Mol Genet 2008;17:256) due to reduced ACTC1 expression inducing cardiomyocyte apoptosis (Circ J 2010;74:2410)
Diagrams / tables
Actin - muscle specific
Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Discovered in 1987 (Am J Pathol 1987;126:51); also called HHF35, MSA
- Recognizes all alpha actins (skeletal, smooth, cardiac) and gamma smooth muscle actin; but not beta cytoplasmic or gamma cytoplasmic actin (the latter is also called non-muscle actin)
- Recognizes actin expressed in all cells with muscle differentiation (cardiac, smooth and skeletal muscle), myoepithelial cells, myofibroblasts, pericytes and myogenic tumors (Am J Clin Pathol 1991;96:32)
Uses by pathologists
- Identify skeletal muscle (Tumori 2007;93:198, J Cutan Pathol 2007;34:352) and smooth muscle cells (Eur Respir J 2001;17:316) in normal tissue or various disease entities
- Classify tumors with smooth or skeletal muscle, pericytes, myofibroblasts (Cardiovasc Pathol 2006;15:91) or myoepithelial cells
- Differentiate leiomyosarcoma (MSA+, keratin-) from spindle cell carcinoma (MSA-, keratin+, Am J Otolaryngol 2005;26:201)
Microscopic (histologic) images
Positive staining - normal
- Cardiac muscle, decidua, myoepithelial cells (although calponin and vimentin may be better, Braz Dent J 2007;18:192), myofibroblasts, pericytes, skeletal muscle, smooth muscle and vascular smooth muscle
Positive staining - disease
- Adenoid cystic carcinoma-myoepithelial component (J Oral Maxillofac Surg 2006;64:415)
- Angiomyolipoma
- Cardiac rhabdomyoma
- Chondroblastoma (35%, Hum Pathol 1997;28:316)
- Endometriosis-smooth muscle (Hum Reprod 2000;15:767)
- Fibromatosis (Acta Cytol 1991;35:403)
- Giant cell tumor of bone (Ultrastruct Pathol 2013;37:183)
- Glioblastoma multiforme (occasional)
- Glomus tumor (Hum Pathol 1999;30:1259)
- Inflammatory myofibroblastic tumor (Mod Pathol 2001;14:784)
- Leiomyoma (Int J Gynecol Pathol 1995;14:134)
- Leiomyosarcoma (80-100%, J Pak Med Assoc 2005;55:138, APMIS 1997;105:793, Histopathology 2013;63:194)
- Malignant fibrous histiocytoma (30%, J Clin Pathol 2003;56:666)
- Mucinous cystic neoplasm (ovarian type stroma, Saudi Med J 2013;34:80), although most studies report smooth muscle actin (Am J Surg Pathol 1999;23:1)
- Myoepithelioma (Zhonghua Bing Li Xue Za Zhi 2005;34:211)
- Myofibroblastic sarcoma (Chin Med J (Engl) 2007;120:363, Hum Pathol 2008;39:846)
- Myofibroblastoma (variable)
- Myofibroma (Histopathology 2012;60:E1)
- Myopericytoma (Hum Pathol 2010;41:1500)
- Osteosarcoma (Am J Clin Pathol 2000;113:663)
- Perivascular epithelioid cell tumors (Diagn Pathol 2012;7:183), although most studies report smooth muscle actin
- Pleomorphic adenoma (Hum Pathol 1991;22:1206)
- Rhabdomyosarcoma (but MyoD1 and myogenin are more specific / sensitive, Am J Surg Pathol 2006;30:962)
- Sinonasal-type hemangiopericytoma (Head Neck 2005;27:124, Am J Surg Pathol 2003;27:737)
- Solitary fibrous tumor (variable staining, Mod Pathol 1997;10:443)
Negative staining
- Angiomyofibroblastoma (Pathol Int 1995;45:487), mesothelioma-epithelioid (Am J Surg Pathol 2006;30:463)
Actin, alpha smooth muscle type
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Actin is a 43000 kDa ubiquitous protein found in all cells
- Actins are involved in cell motility (alpha, smooth muscle) and the maintenance of the cytoskeleton (beta and gamma, all cells)
- Antibodies to alpha smooth muscle actin do not detect the other actin isoforms
Essential features
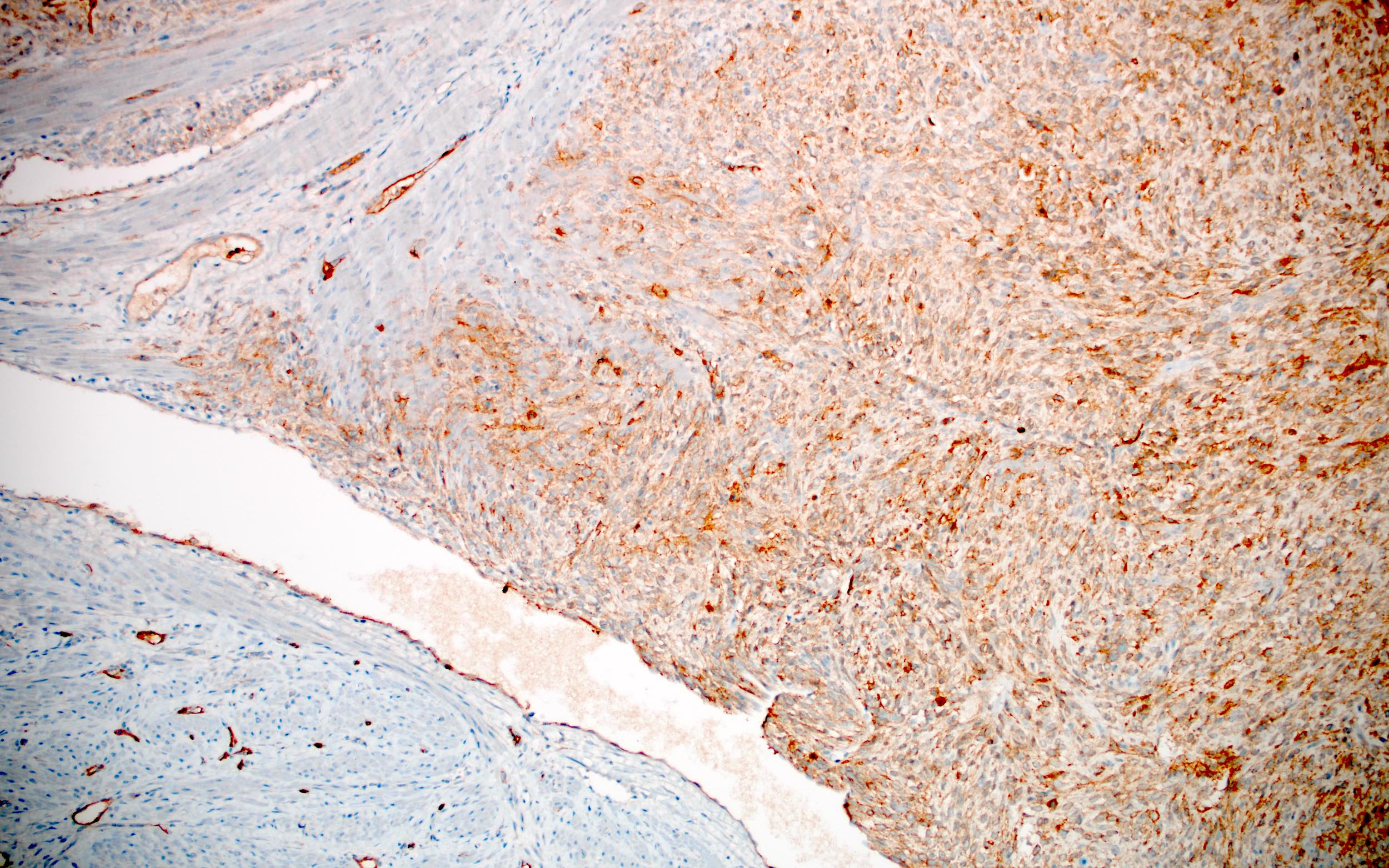
- Involved in cell motility
- Identifies pericytes, myoepithelial cells, smooth muscle cells and myofibroblasts in normal, reactive or neoplastic tissue
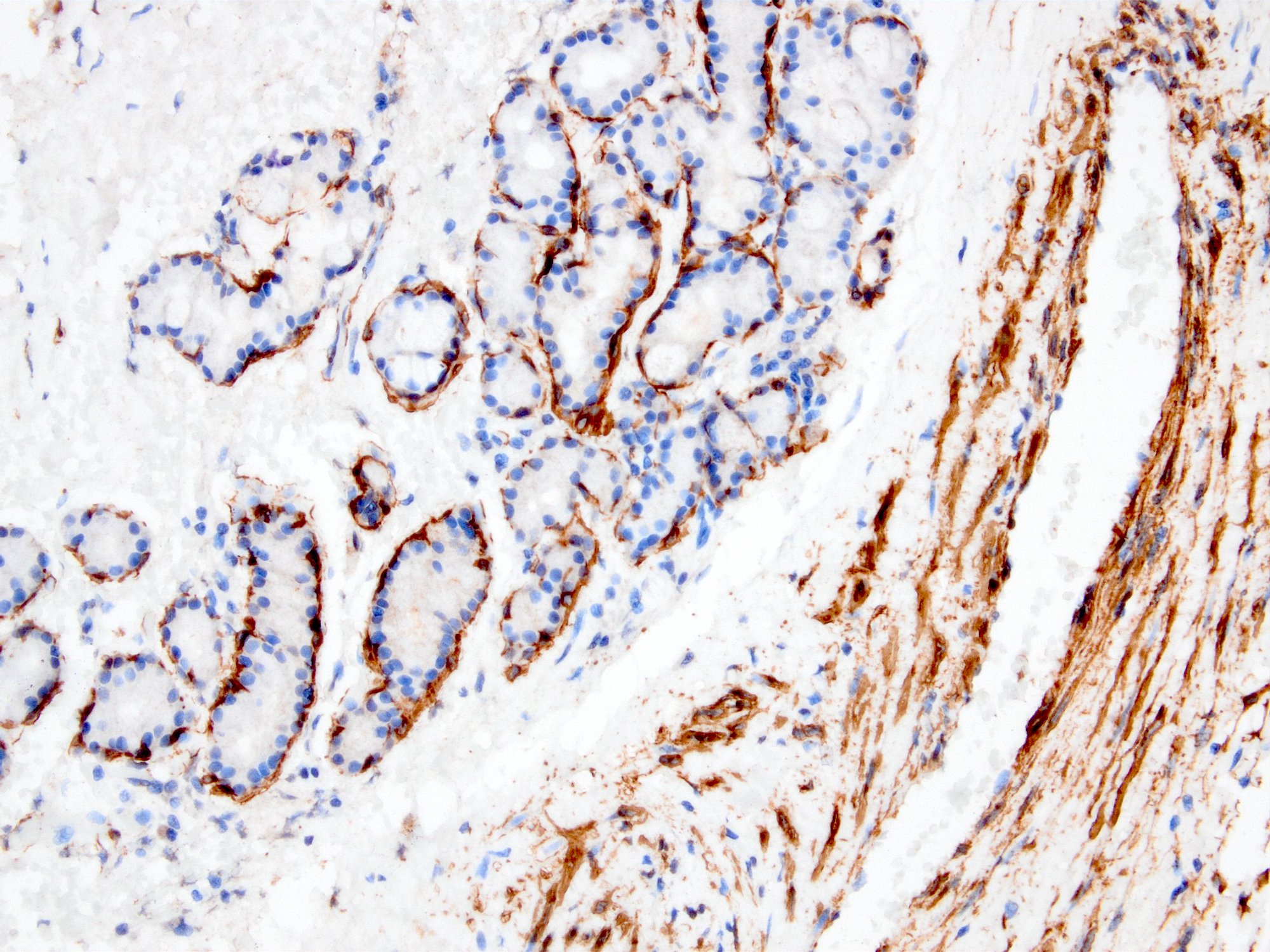
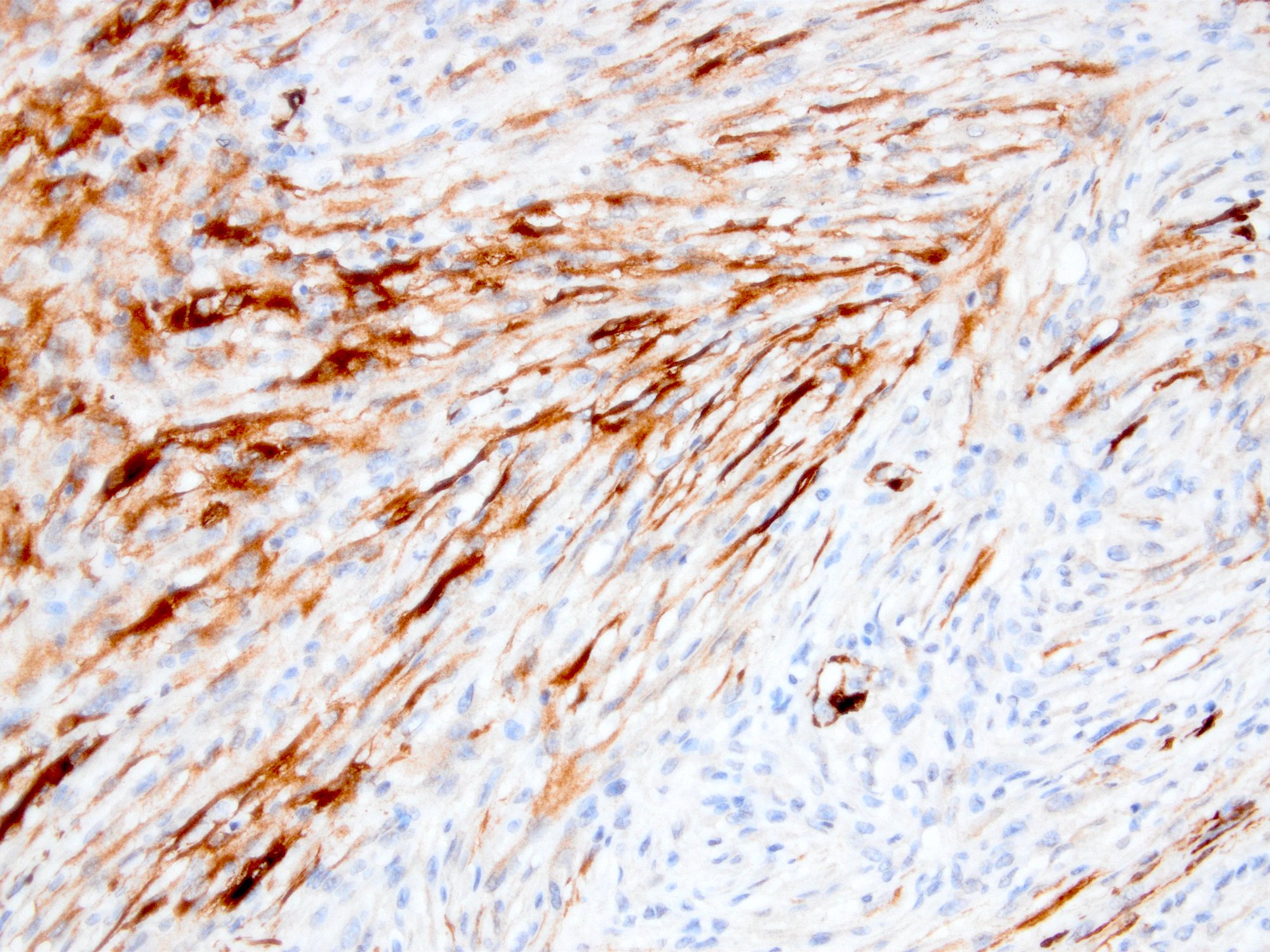
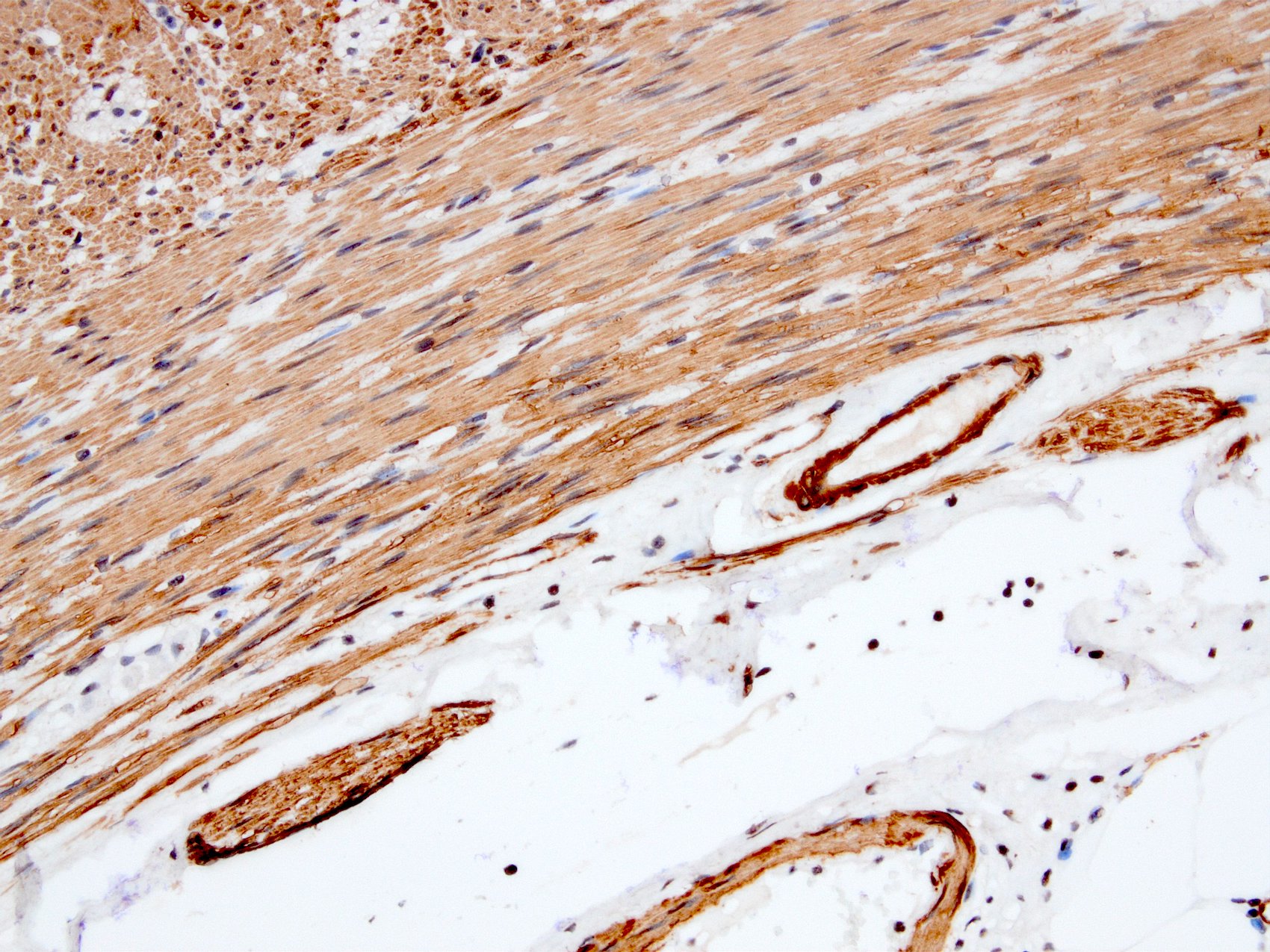
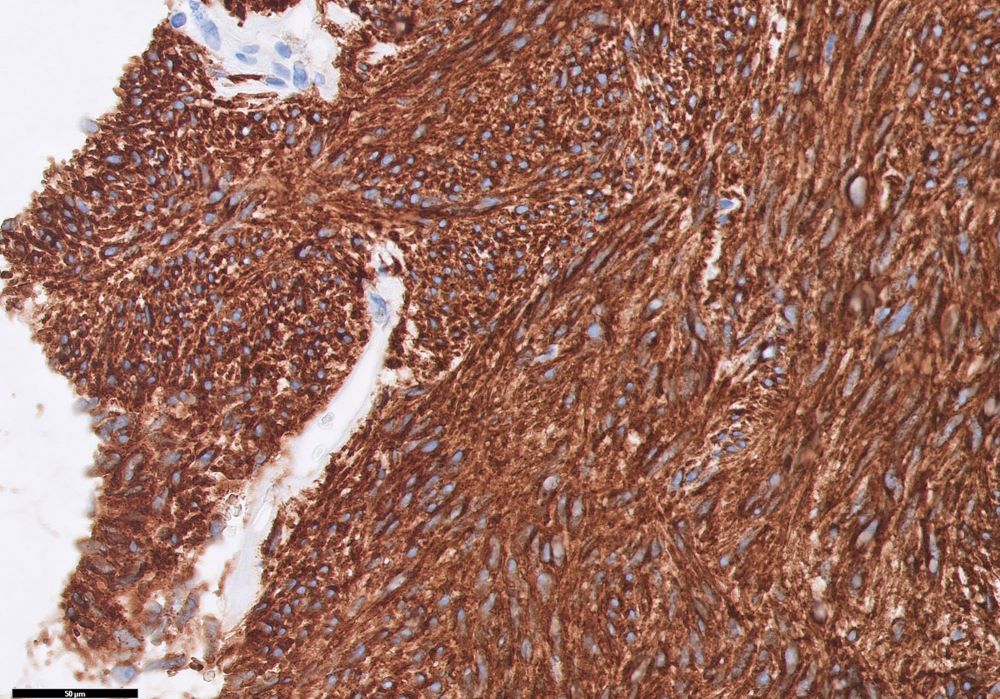
- Myofibroblastic staining (tram track) versus smooth muscle staining (block cytoplasmic)
Terminology
- Also called smooth muscle actin, SMA; clone ASM1 / 1A4 or sm 1
Pathophysiology
- 3 types: alpha, beta and gamma
- Alpha actins are found in muscle tissues and required for contraction, whereas the beta and gamma actins function as components of the cytoskeleton in many cells
- Expression correlates with the activation of myofibroblasts (Mol Cell Biochem 2008;308:201)
- May play a role in epithelial mesenchymal transition of carcinomas (Rom J Morphol Embryol 2014;55:1383)
Clinical features
- Controversial results on deficiency in intestinal pseudoobstruction (J Clin Pathol 2004;57:1168, Pediatr Surg Int 2008;24:1191, Gut 2004;53:1583)
- Immunoexpression may predict aggressive behavior in cutaneous basal cell carcinoma (Hum Pathol 2010;41:1128)
- Potential prognostic factor in idiopathic pulmonary fibrosis (Clinics (Sao Paulo) 2012;67:1039)
Interpretation
- Membranous or cytoplasmic staining
Uses by pathologists
- Identify smooth muscle cells and myofibroblasts in normal, reactive or neoplastic tissue (Am J Respir Cell Mol Biol 1999;20:582, Am J Dermatopathol 2006;28:105)
- Identify myoepithelial cells in normal, neoplastic or diseased breast, salivary glands or sweat glands
- May be helpful to rule out invasion
- May be particularly important in cytology specimens
- Reference: Anticancer Res 2003;23:4175
- Identify pericytes to correlate with hematogenous metastasis and prognosis (Oncology 2005;69:159)
- Help distinguish pleuropulmonary desmoid tumors (SMA+) from solitary fibrous tumor (SMA-) (Arch Pathol Lab Med 2006;130:1503)
- Note: in breast papillary lesions, p63 is more sensitive and specific because smooth muscle actin also stains myofibroblasts / stromal cells (J Clin Pathol 2007;60:315)
Prognostic factors
- Myogenic differentiation (either only SMA or SMA+ desmin) in dedifferentiated liposarcoma significantly decreases 5 year disease free survival (Am J Surg Pathol 2020;44:799)
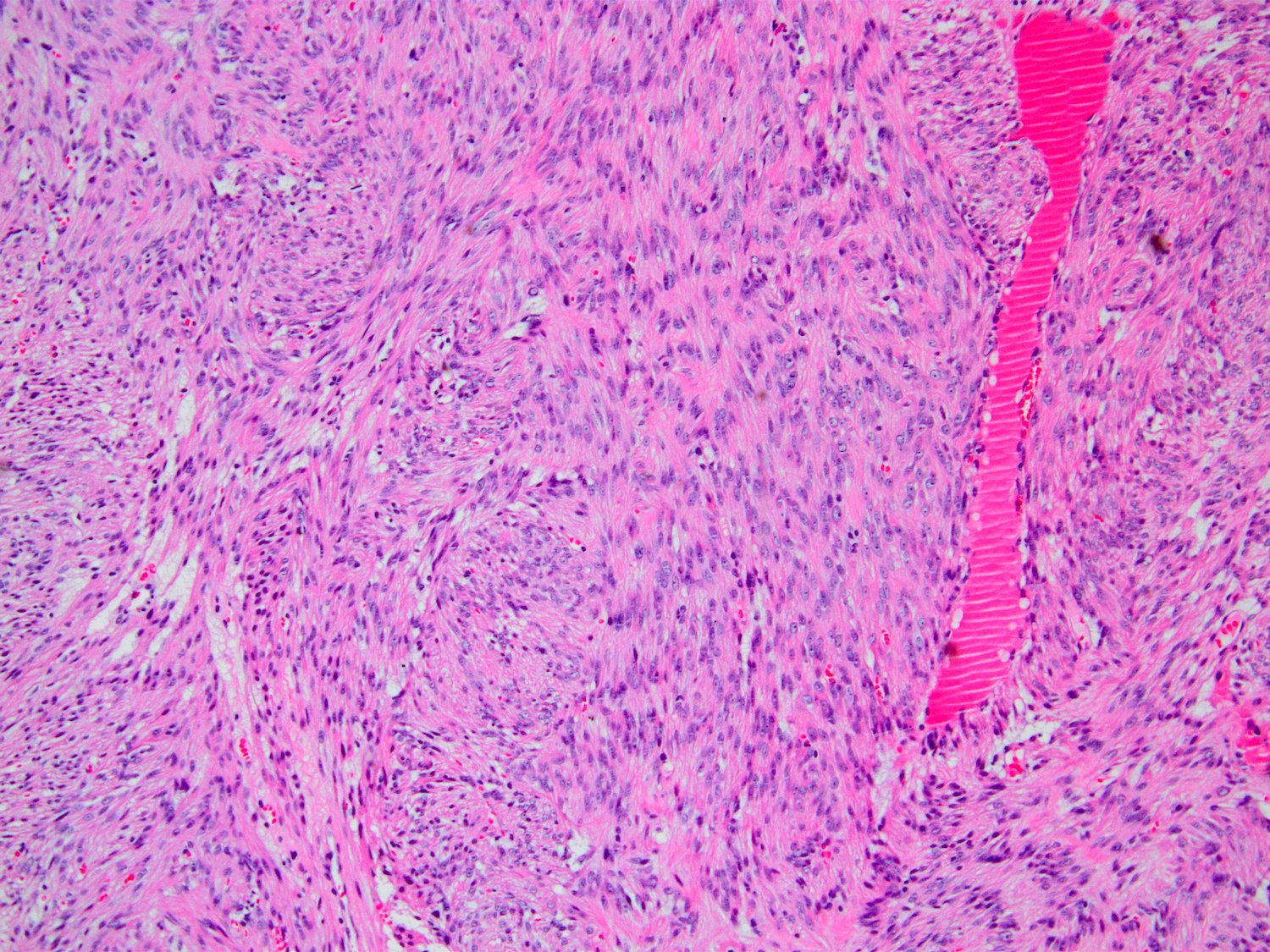
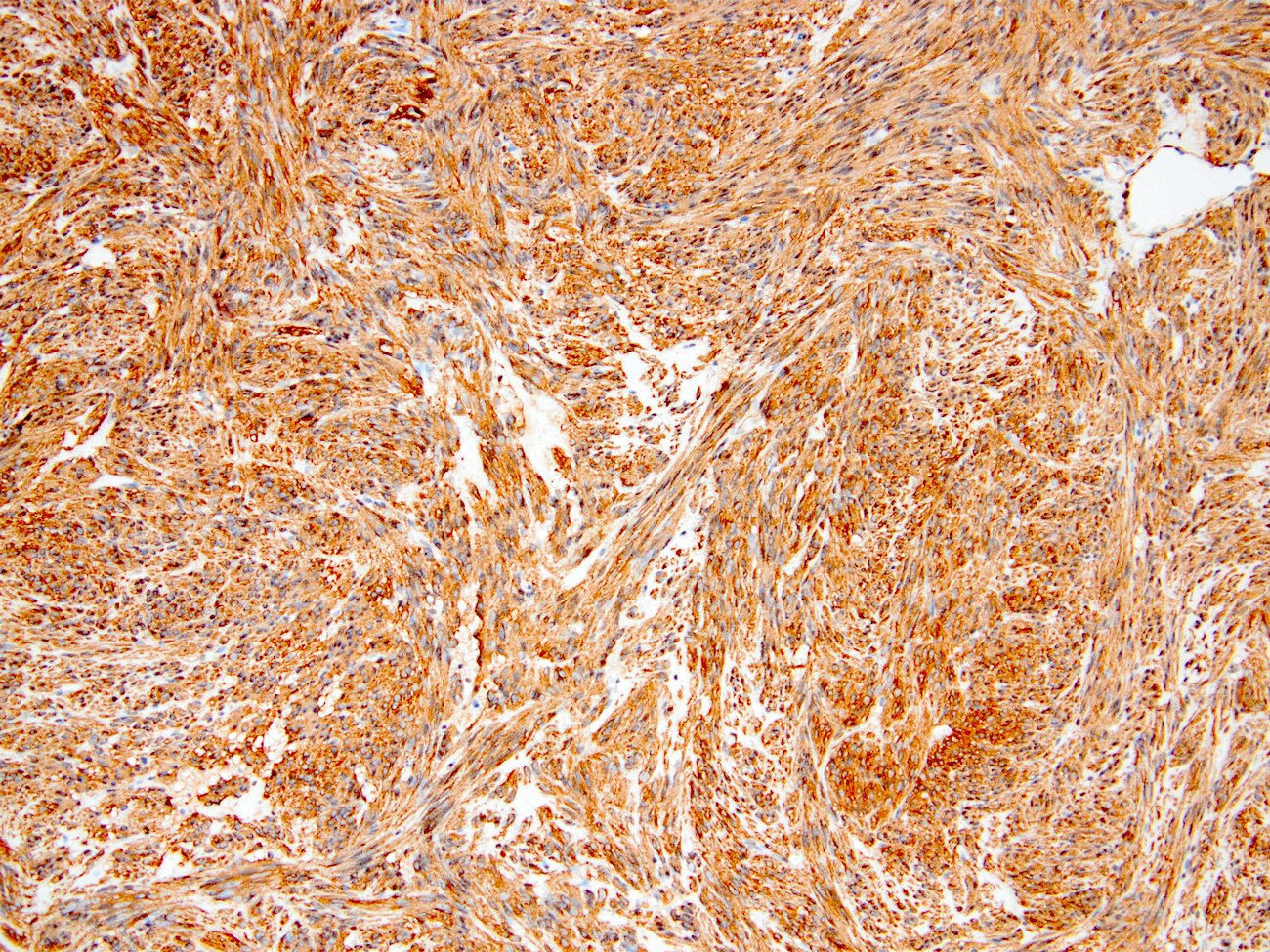
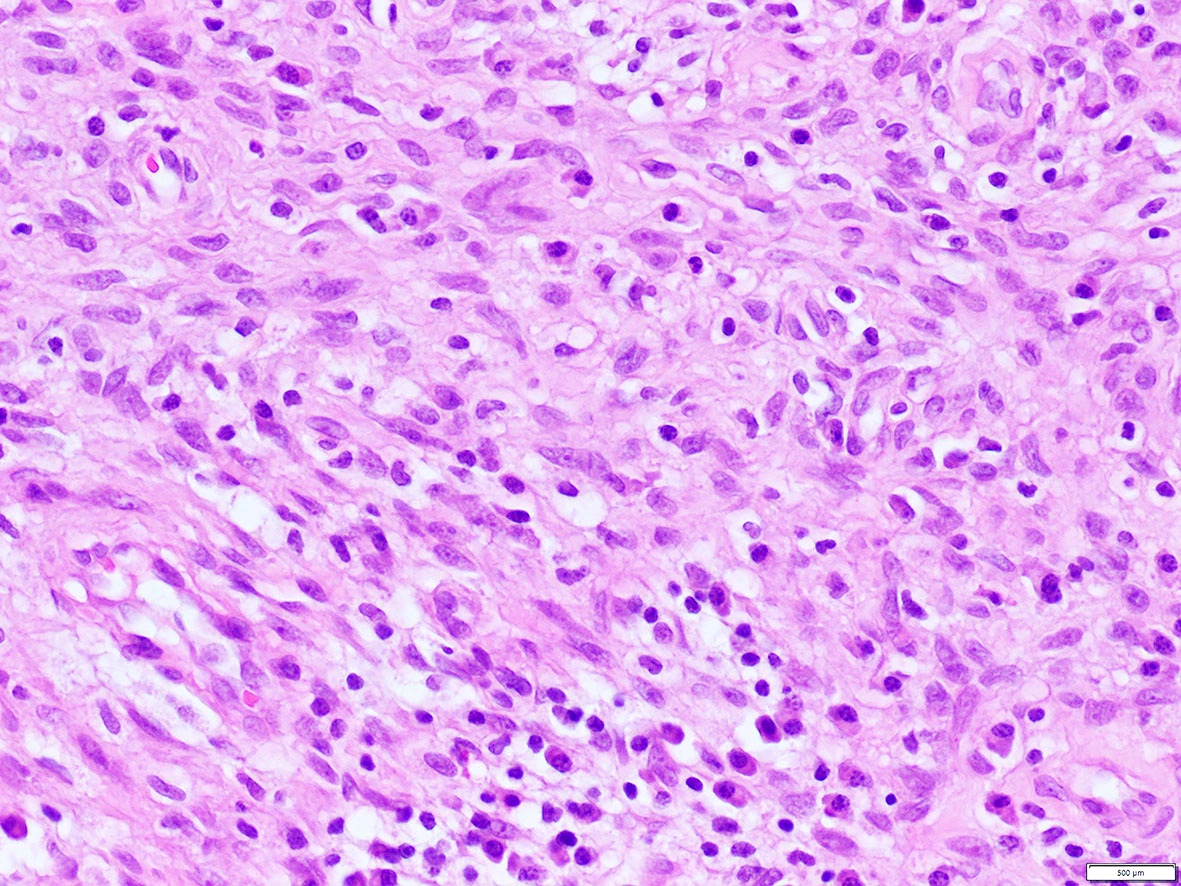
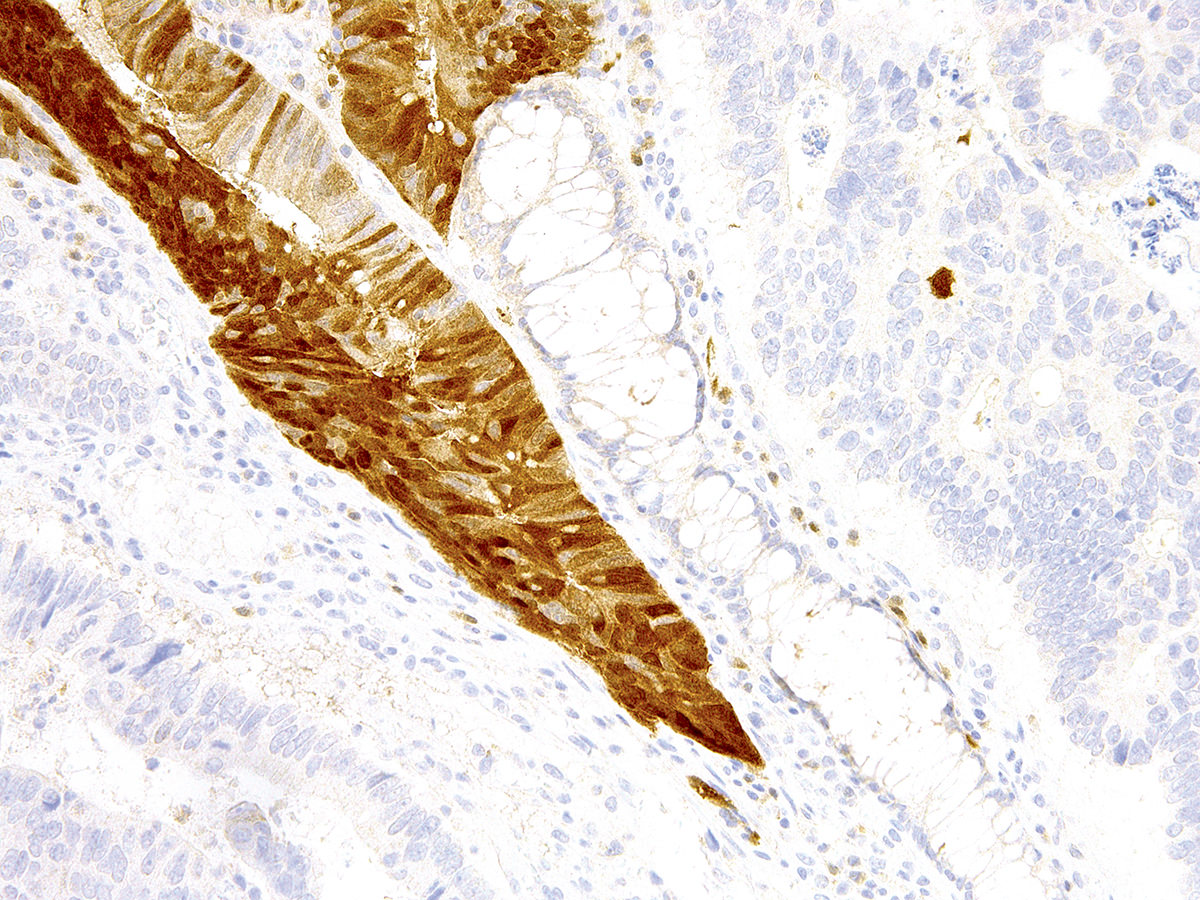
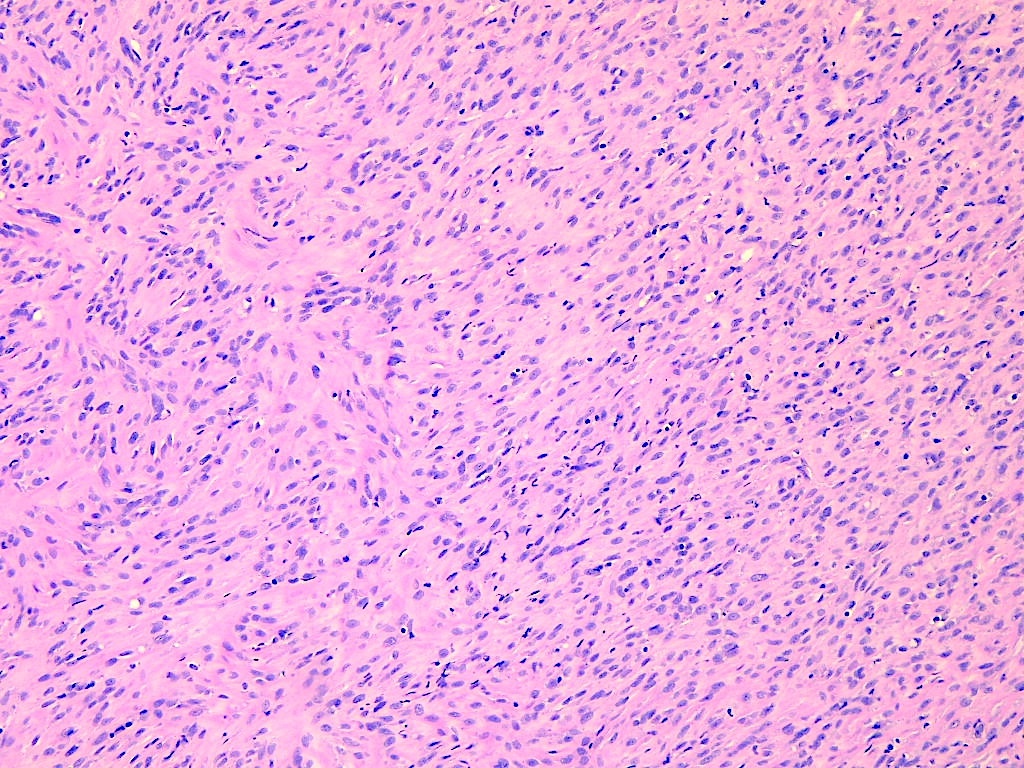
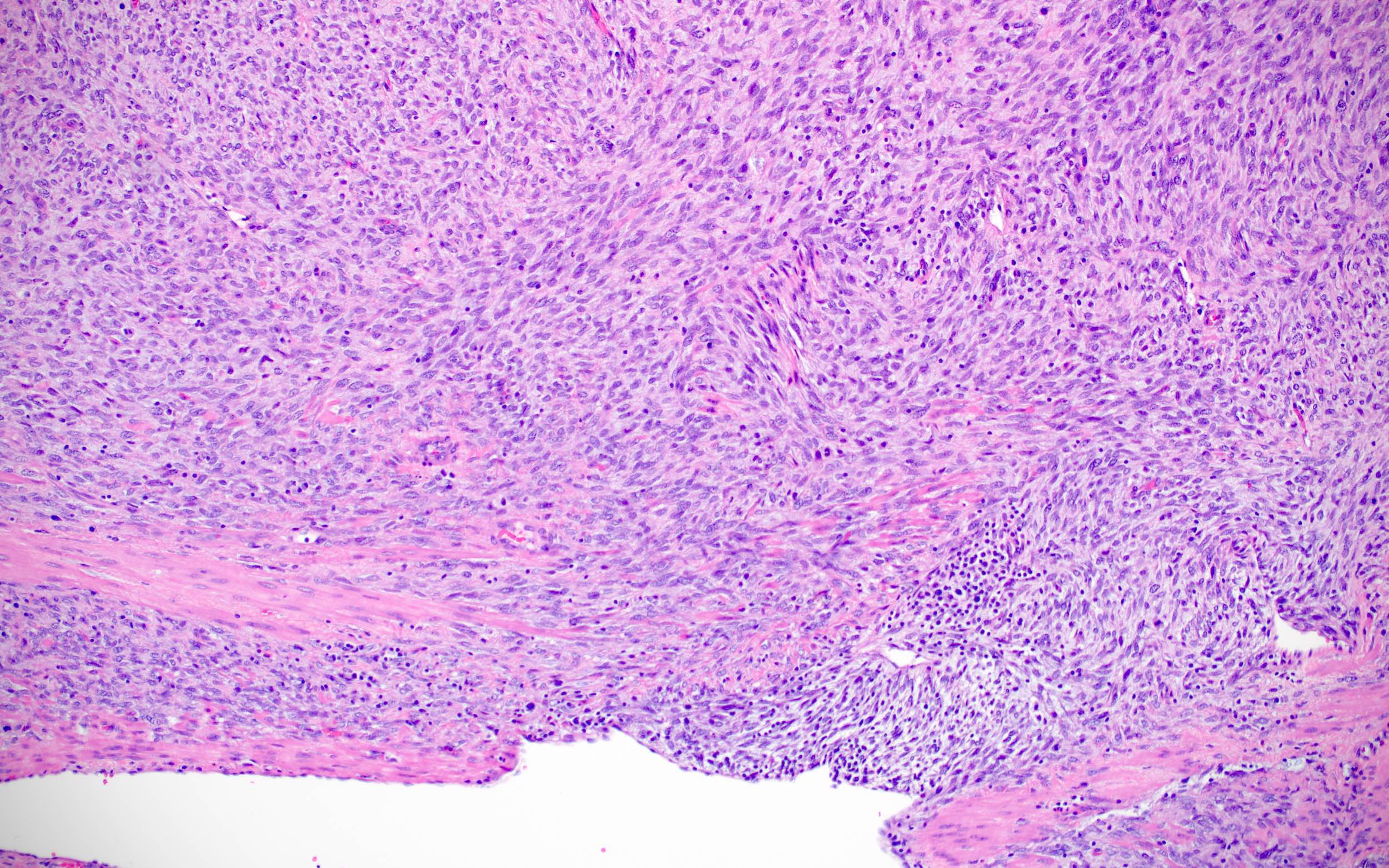
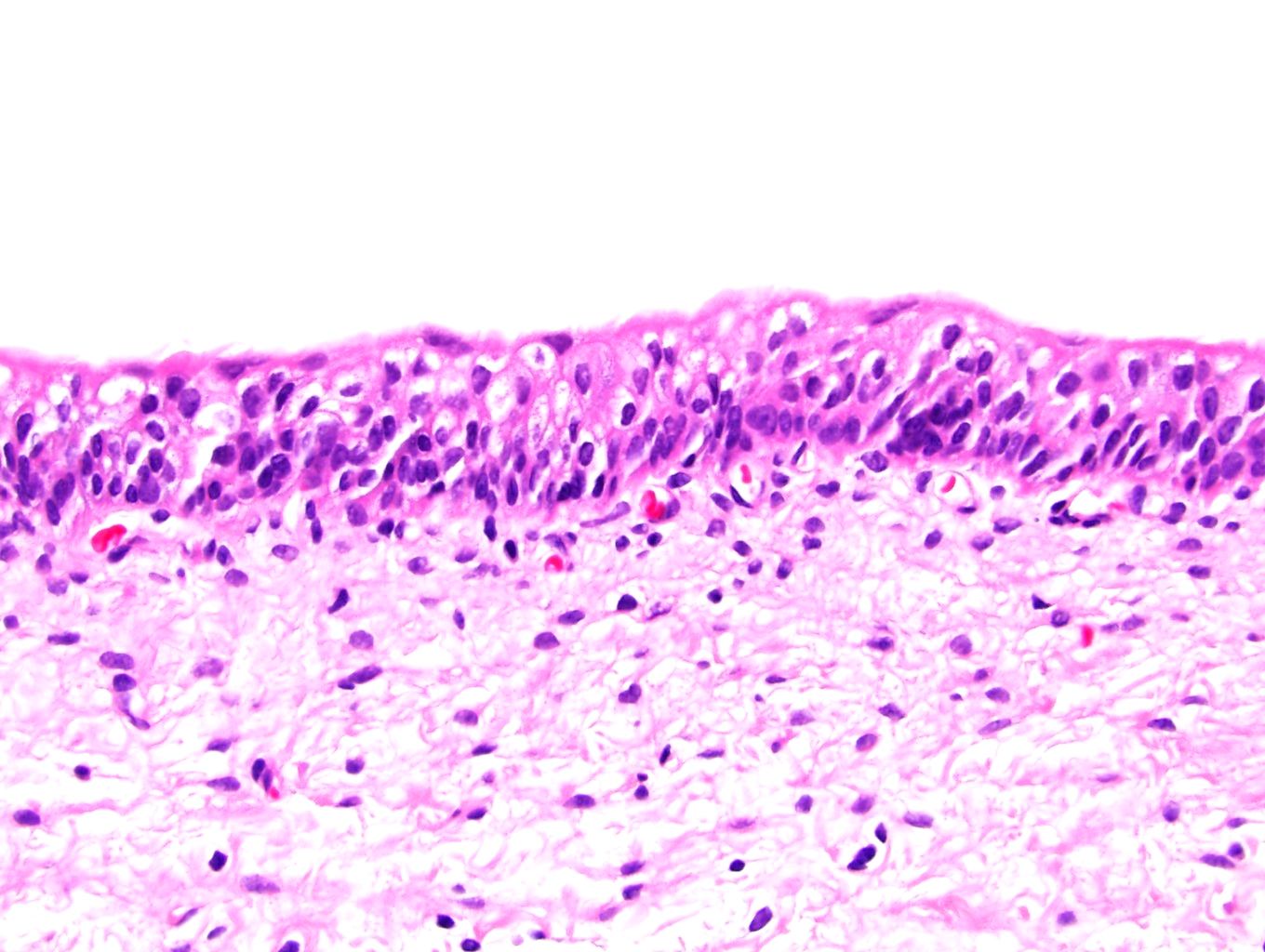
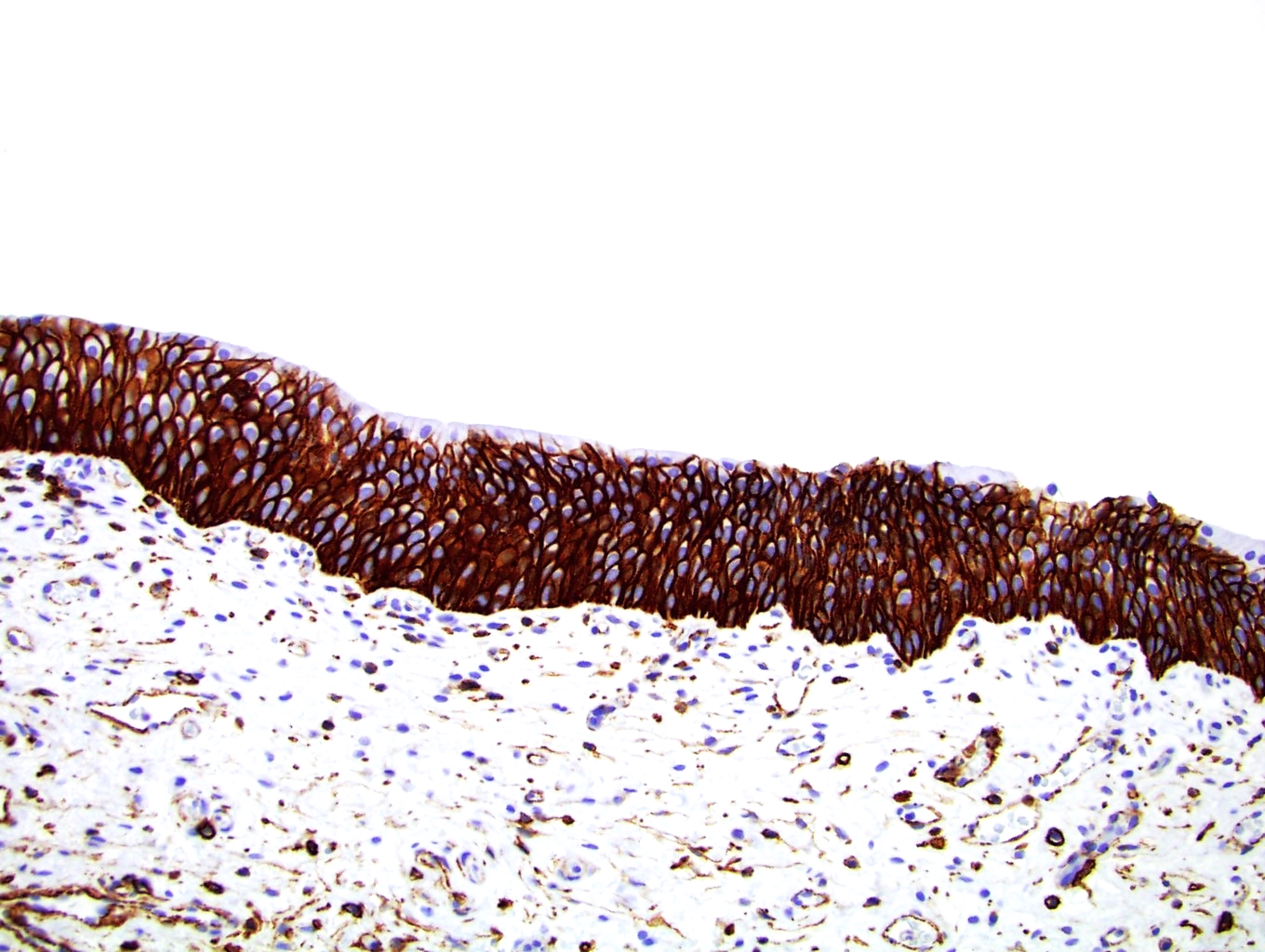
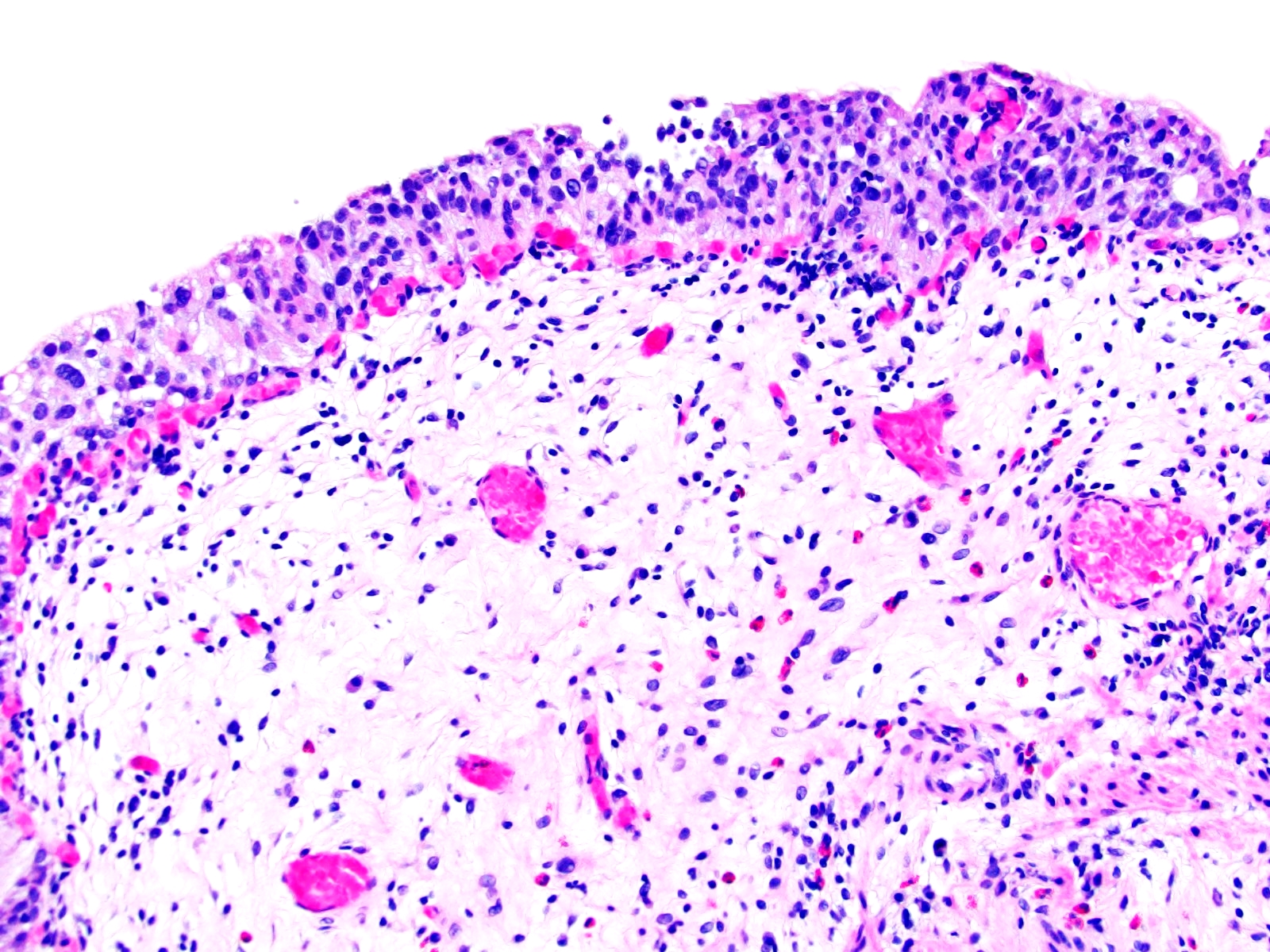
Microscopic (histologic) description
- Myofibroblastic staining (tram track) versus smooth muscle staining (block cytoplasmic)
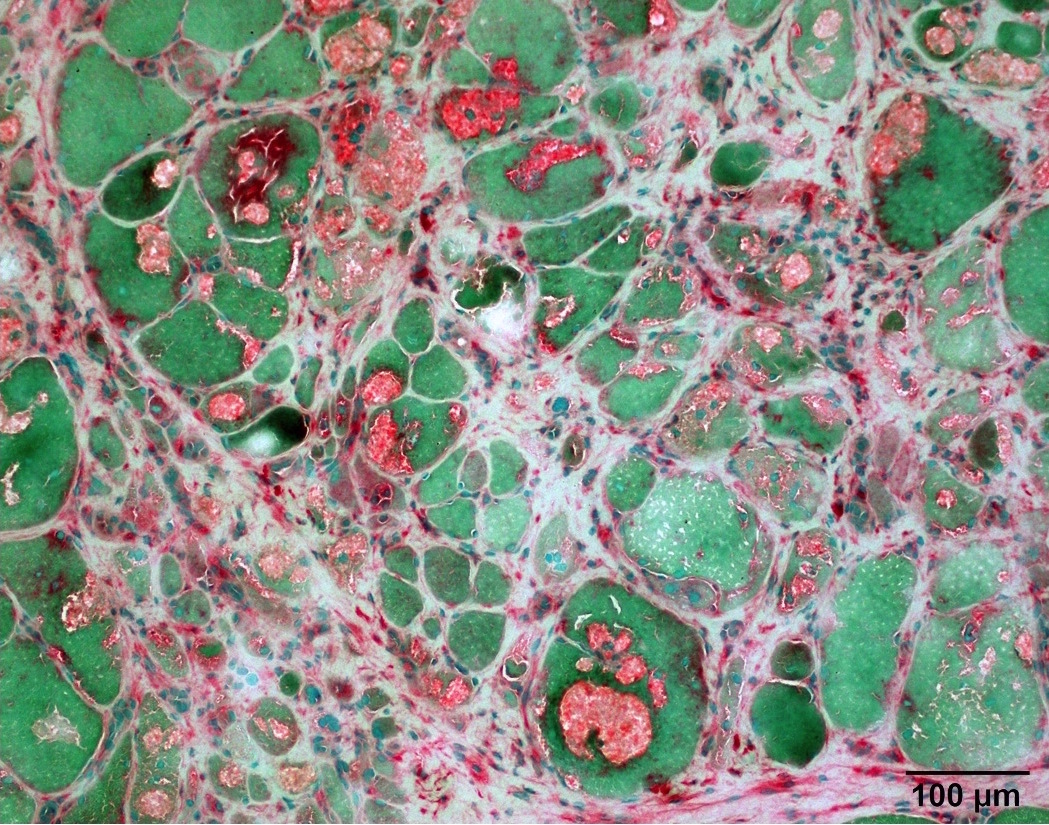
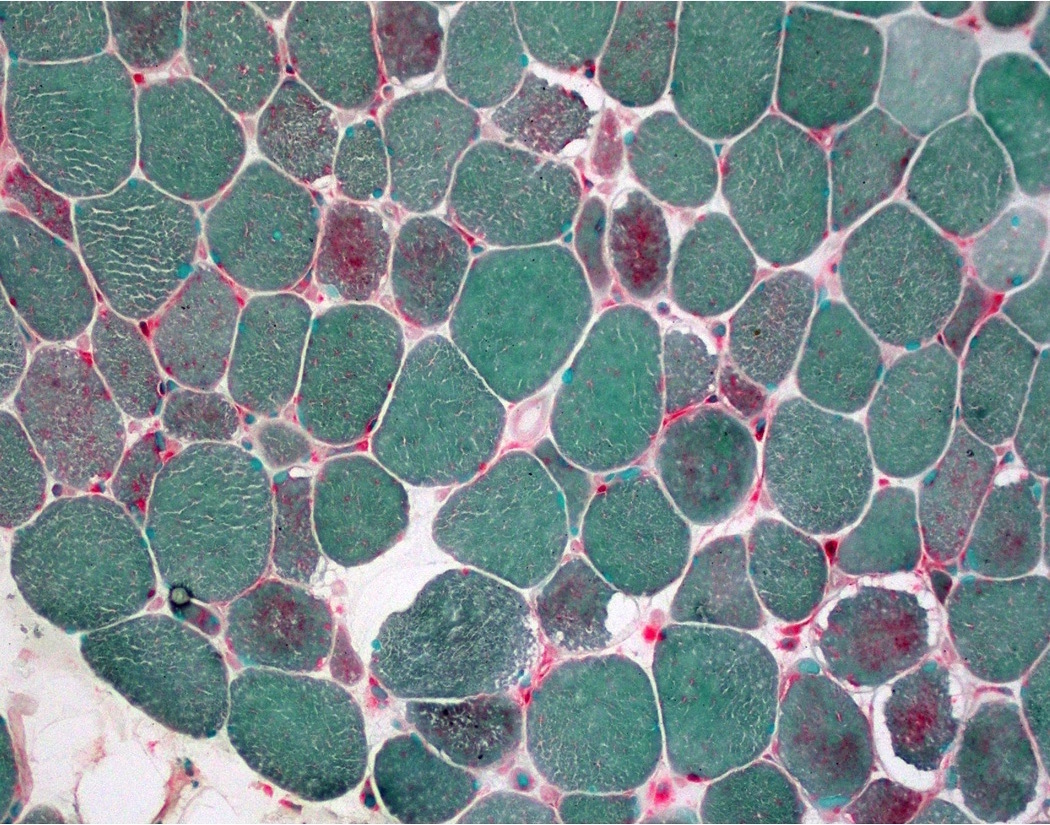
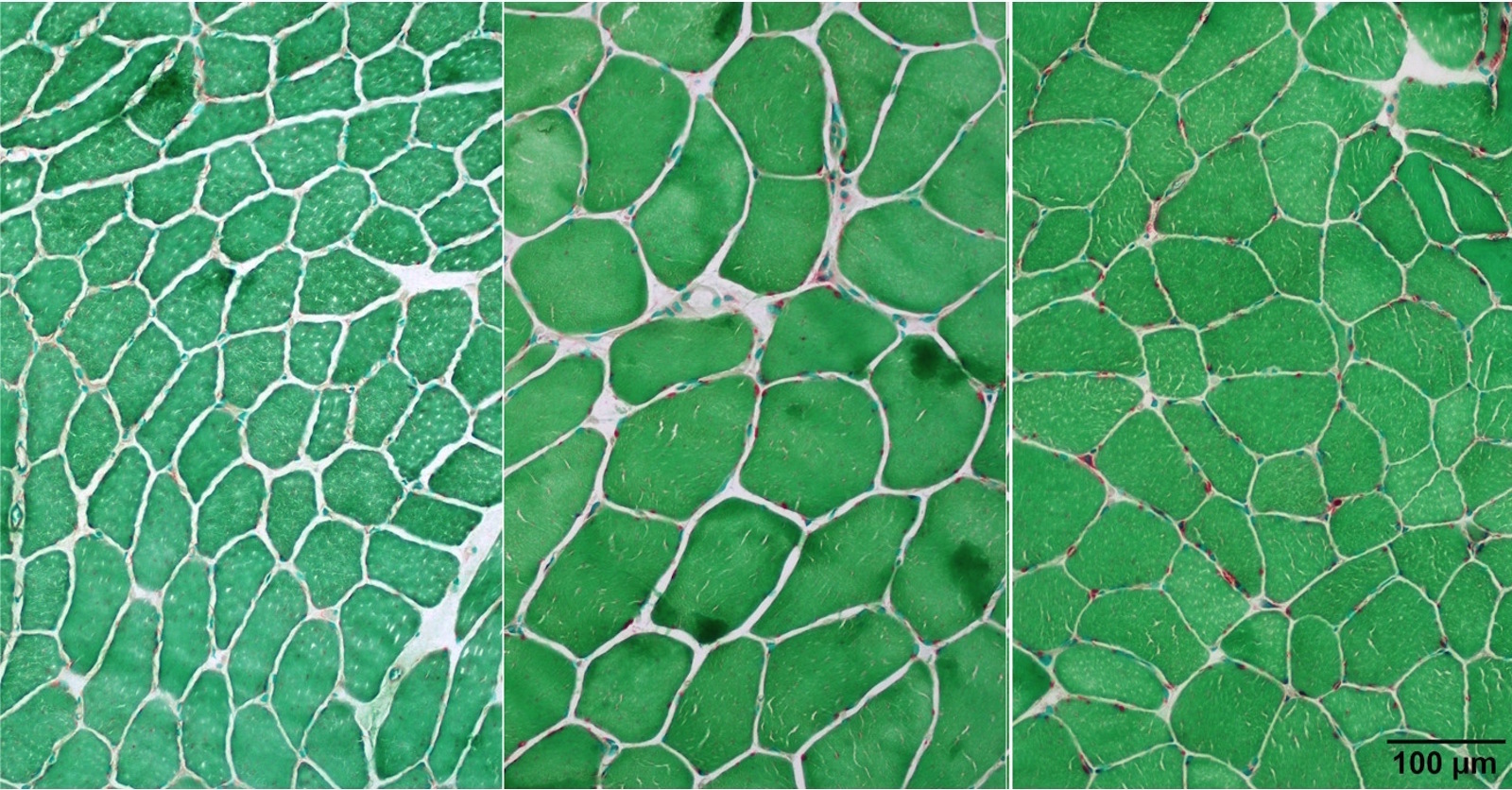
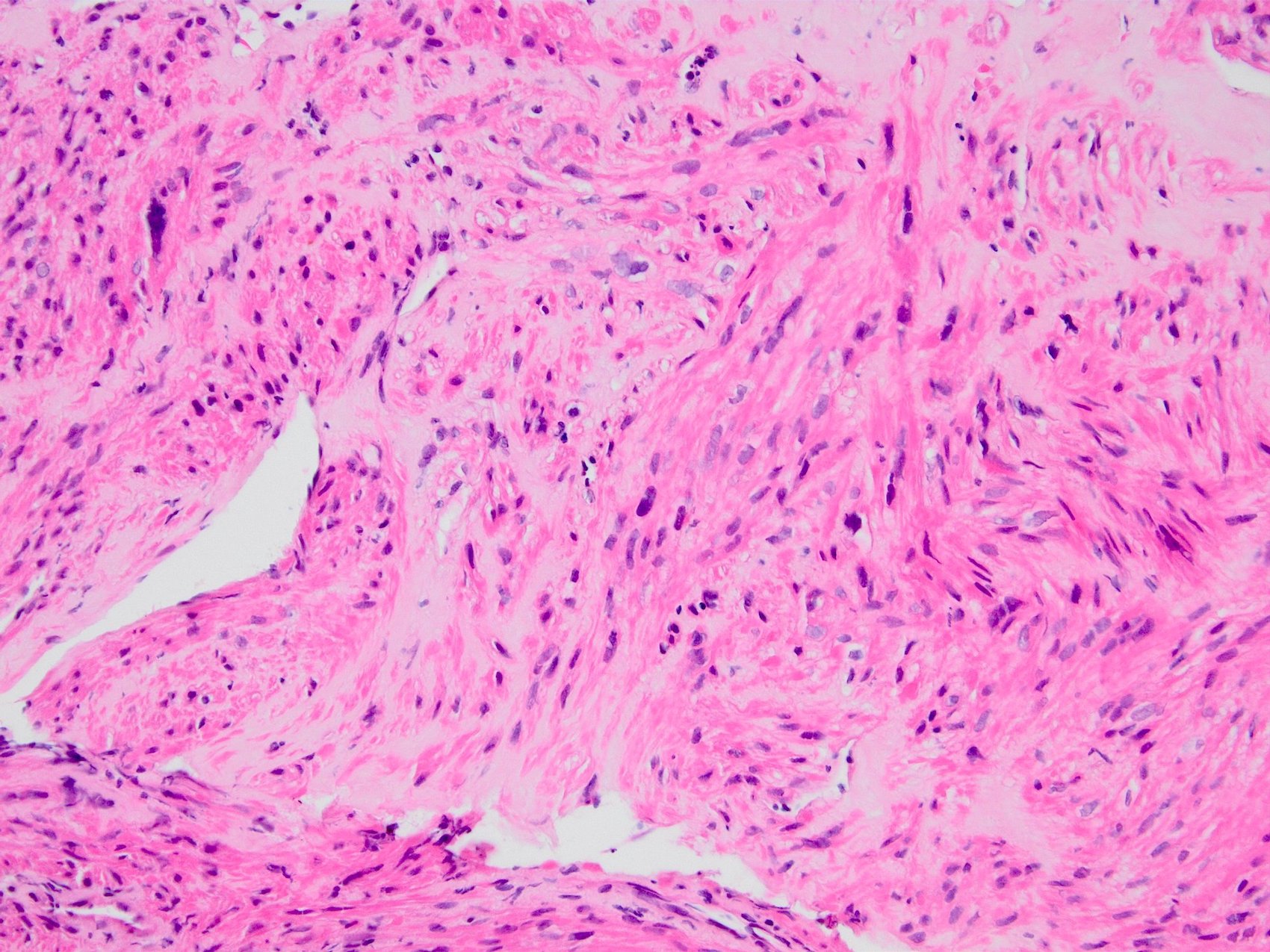
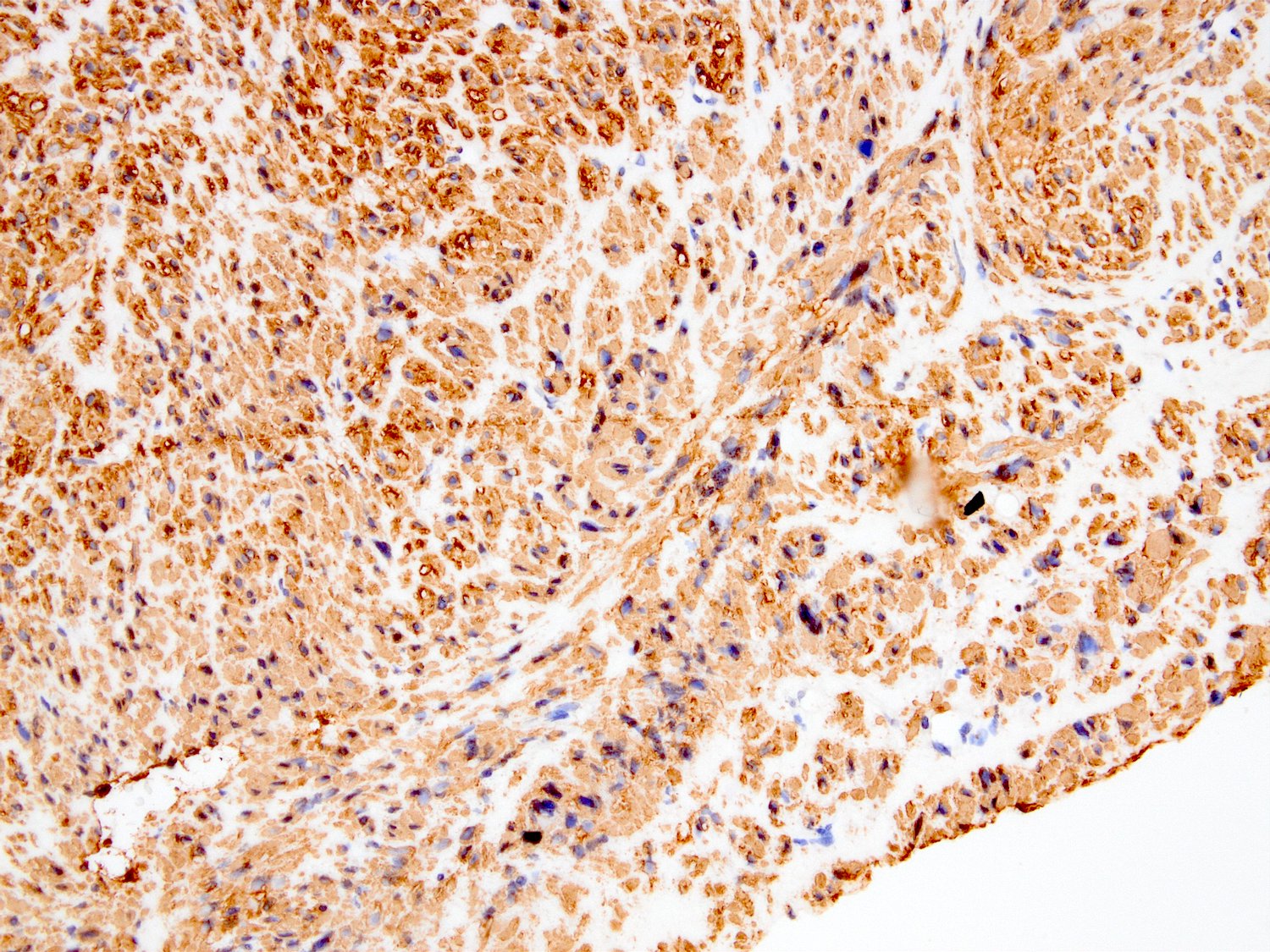
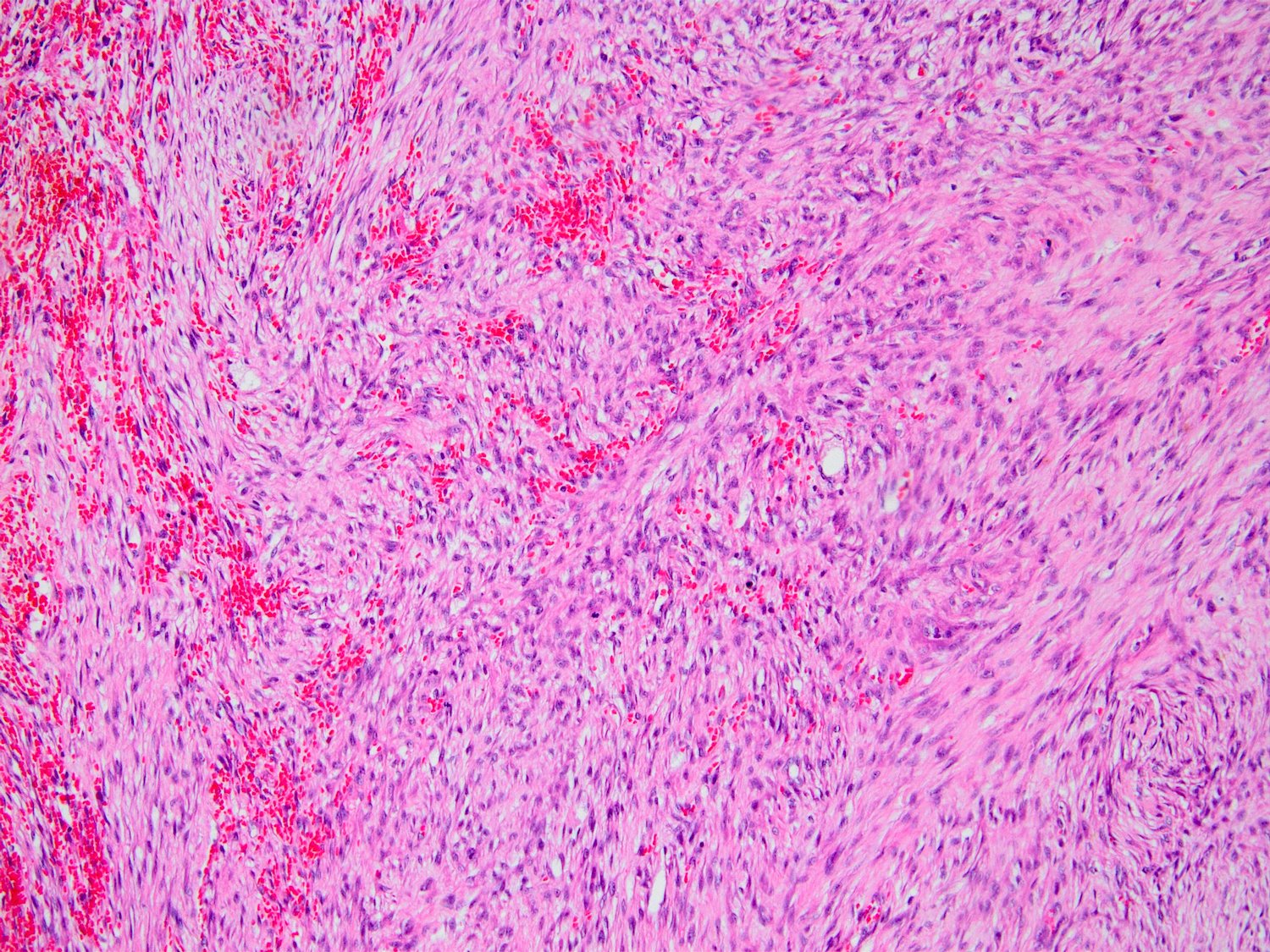
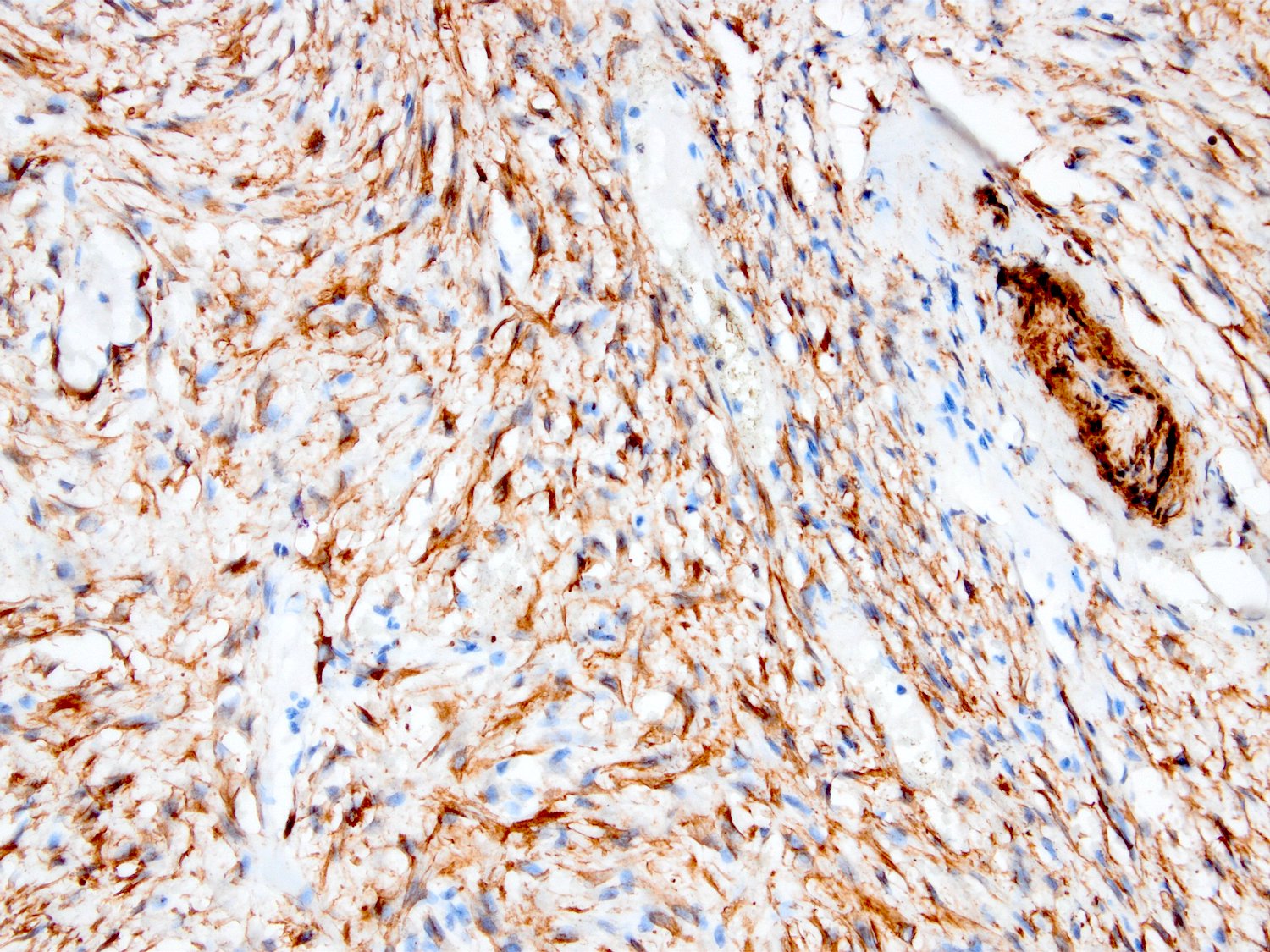
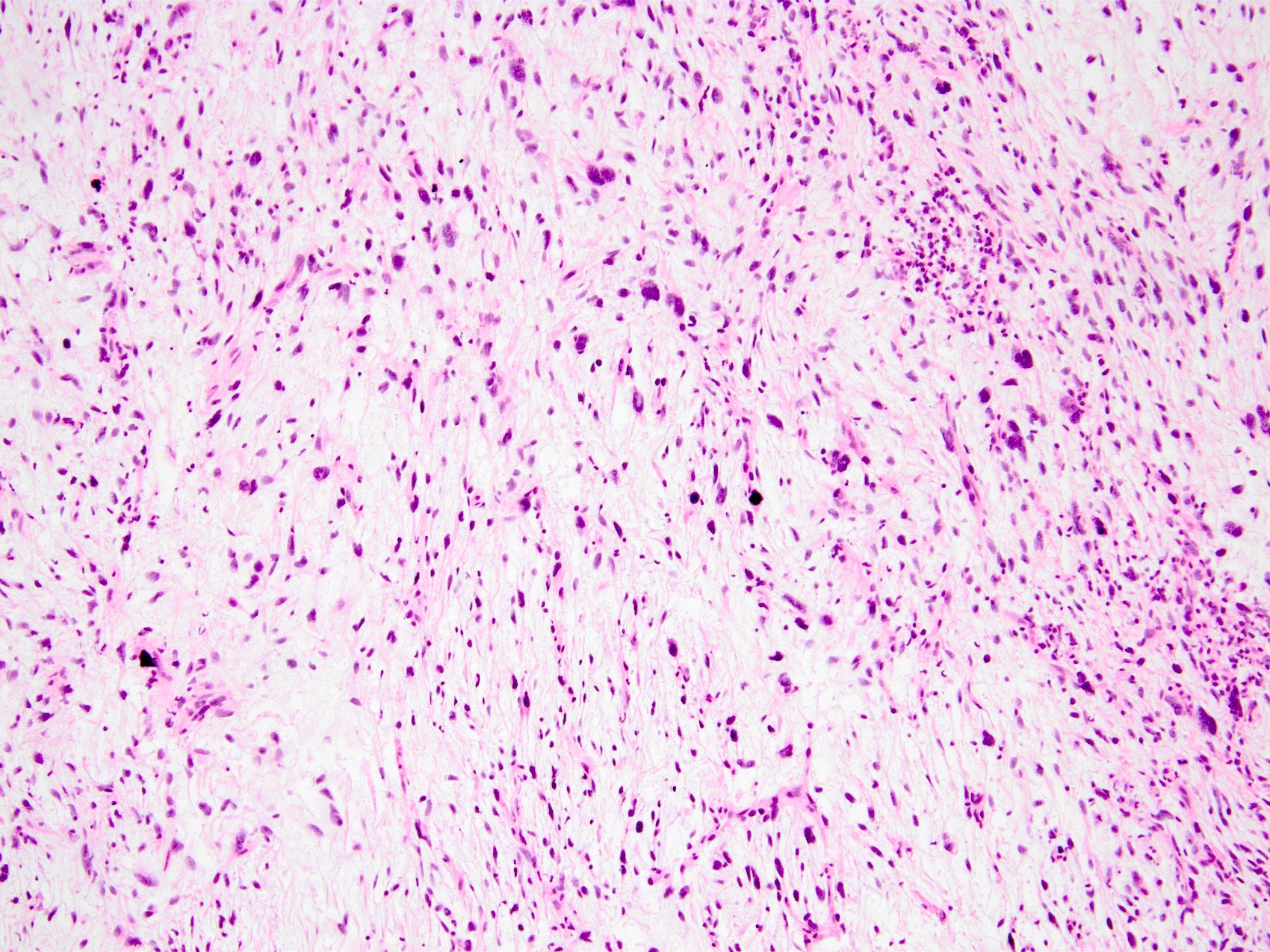
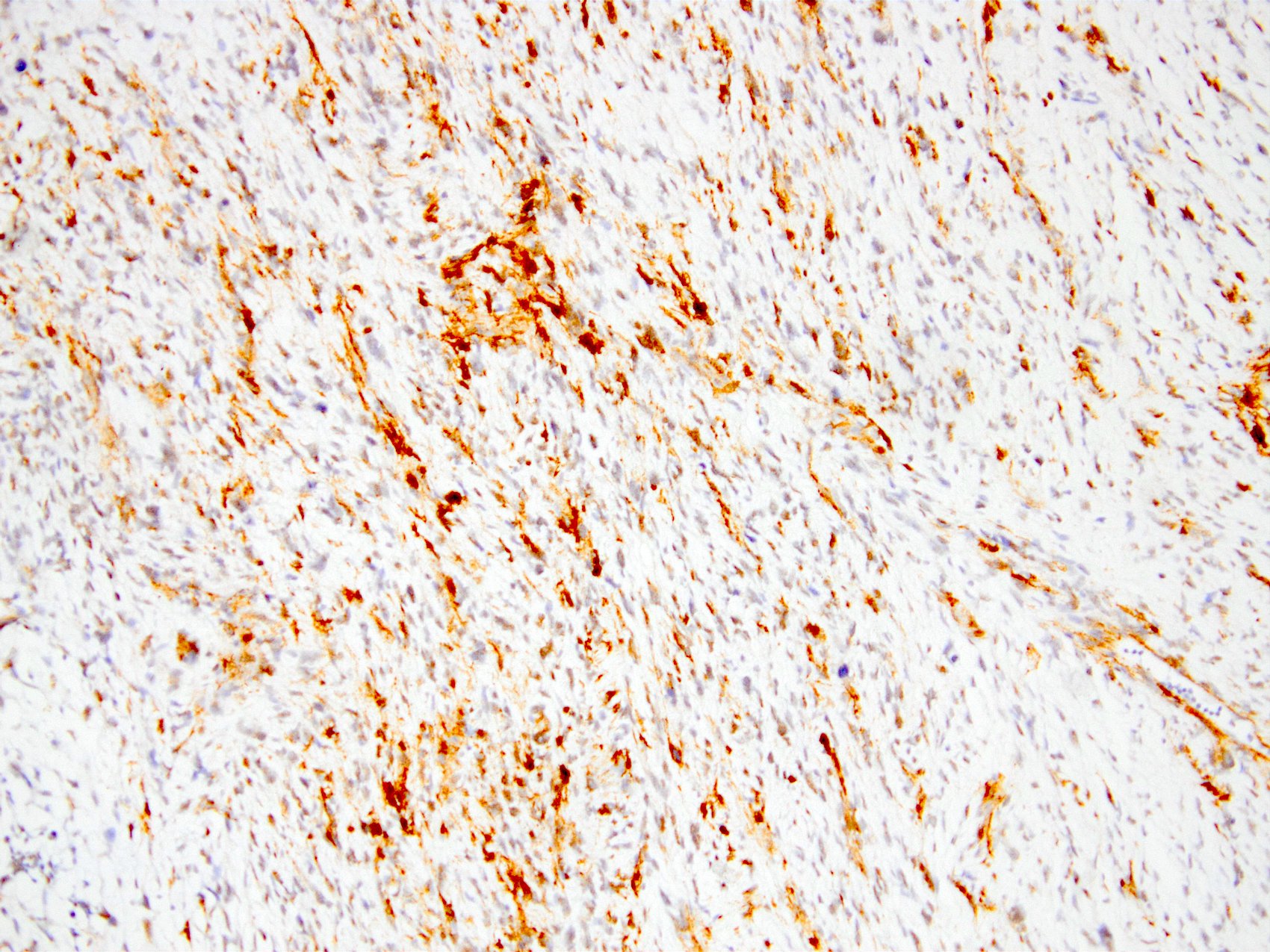
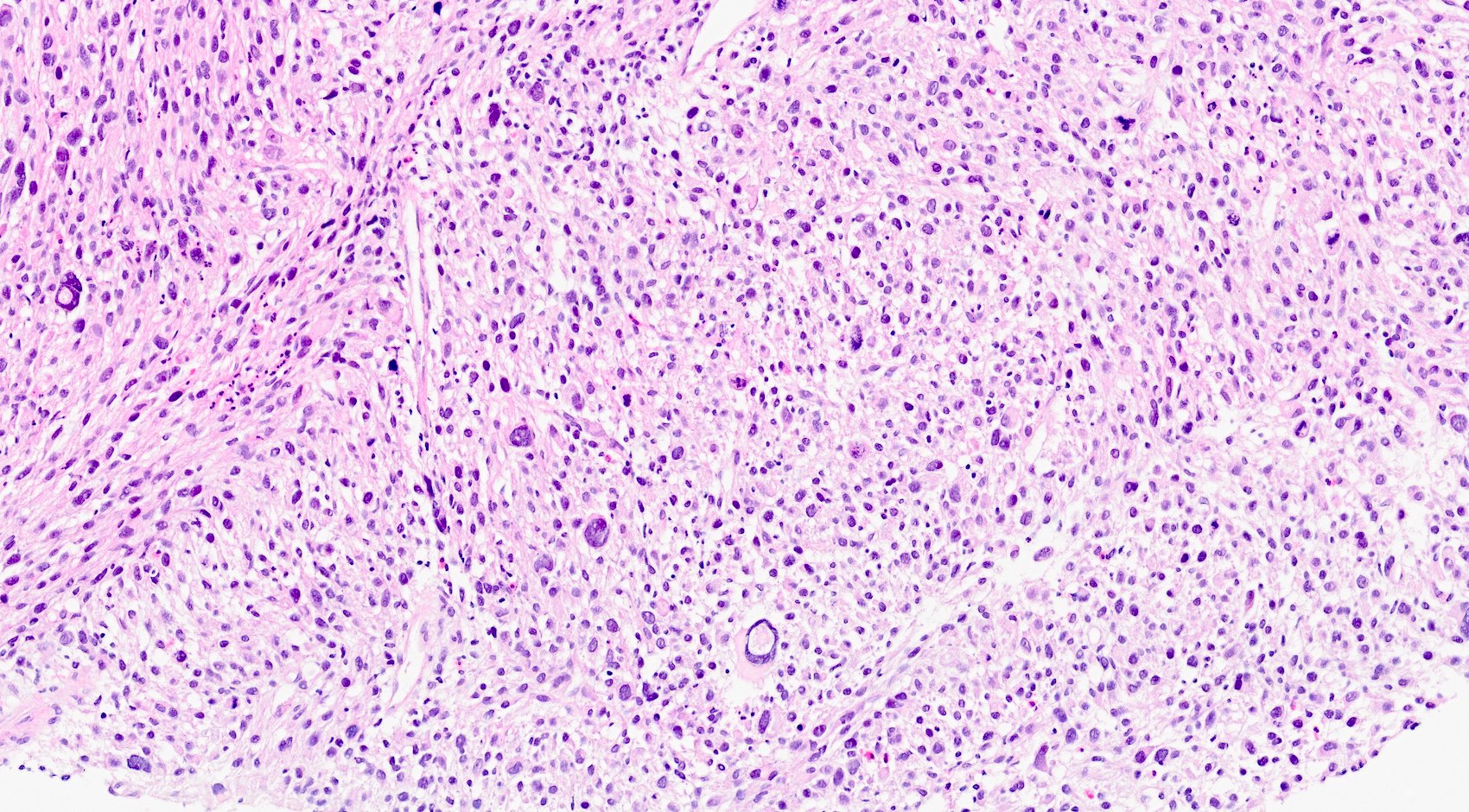
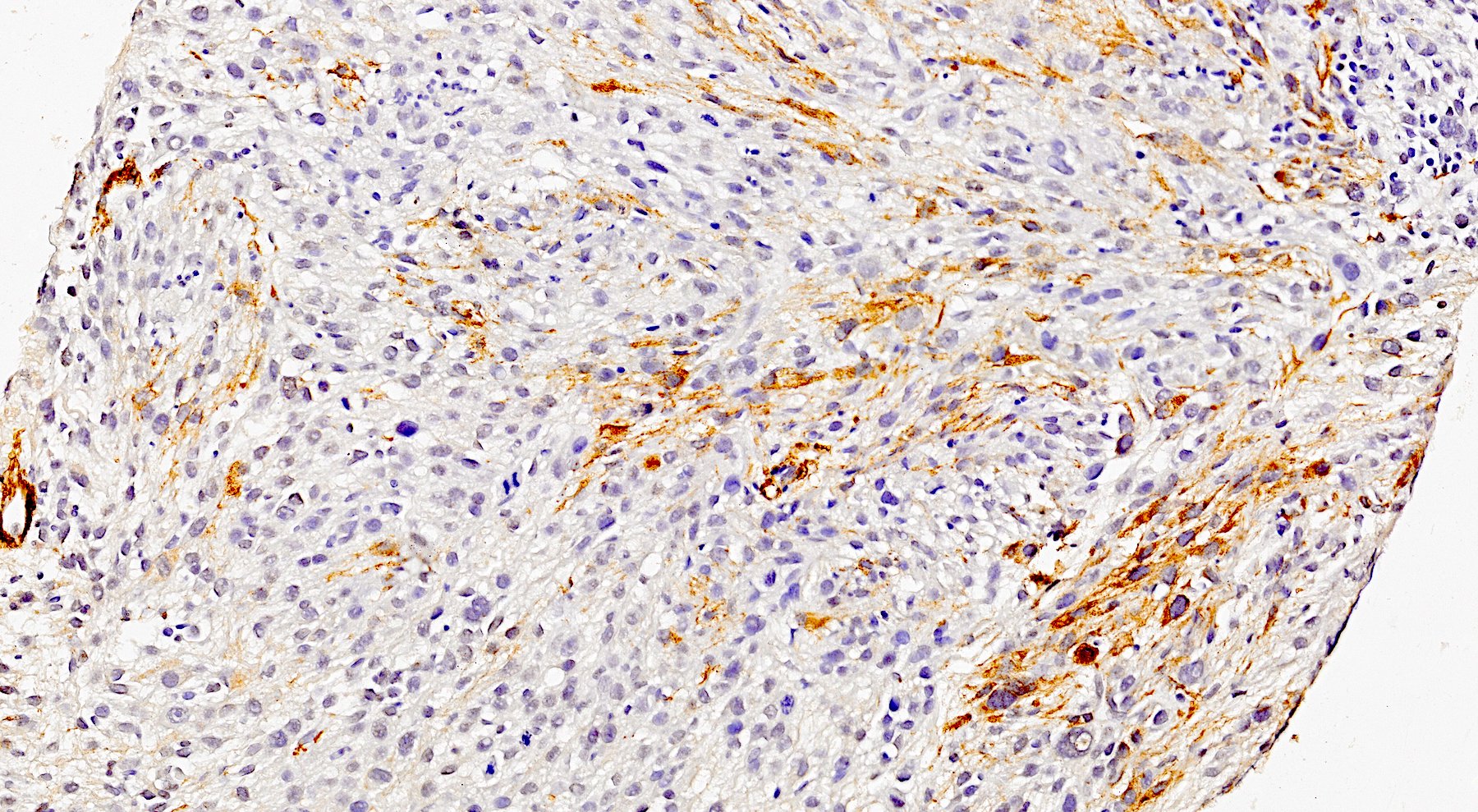
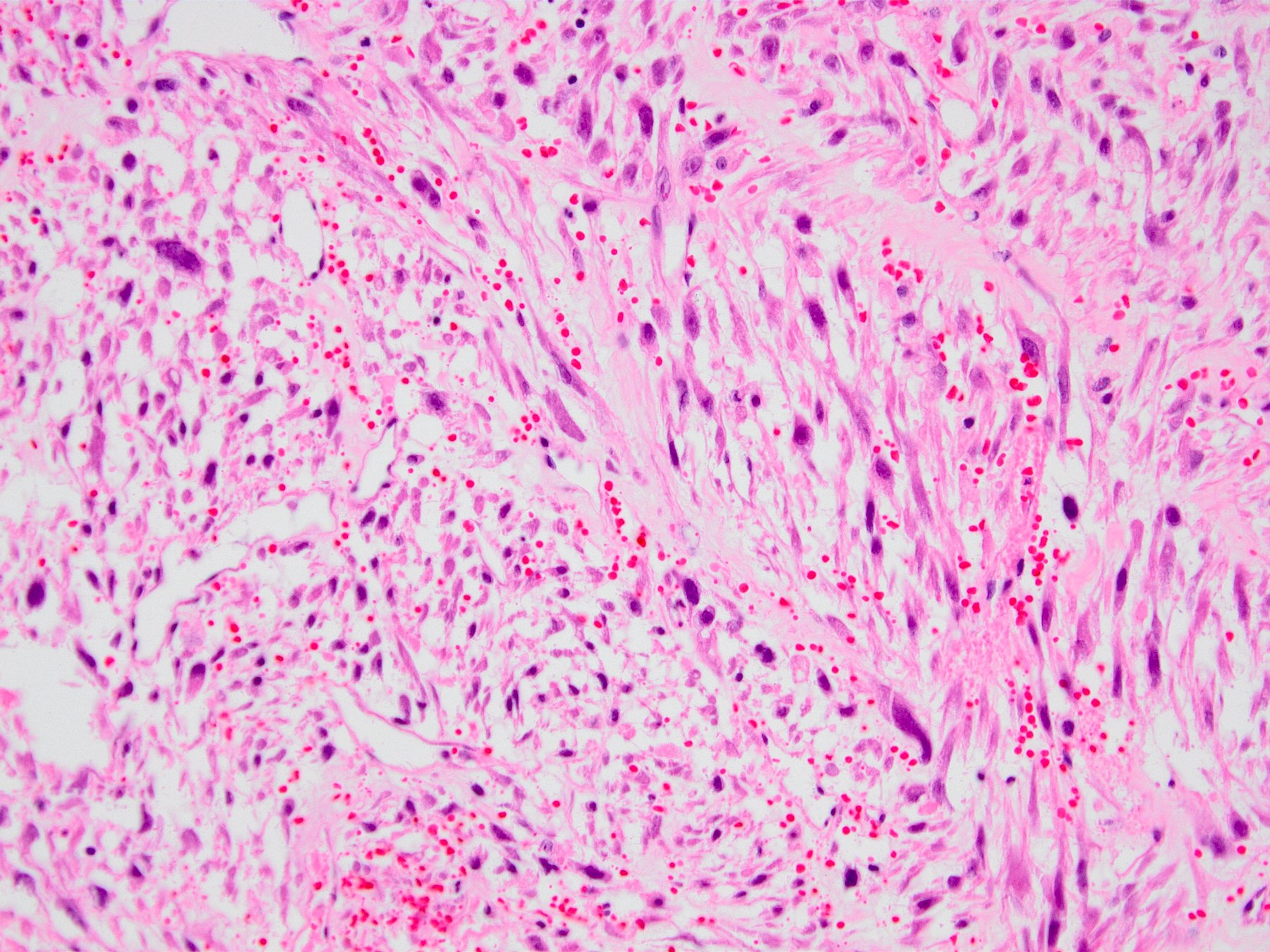
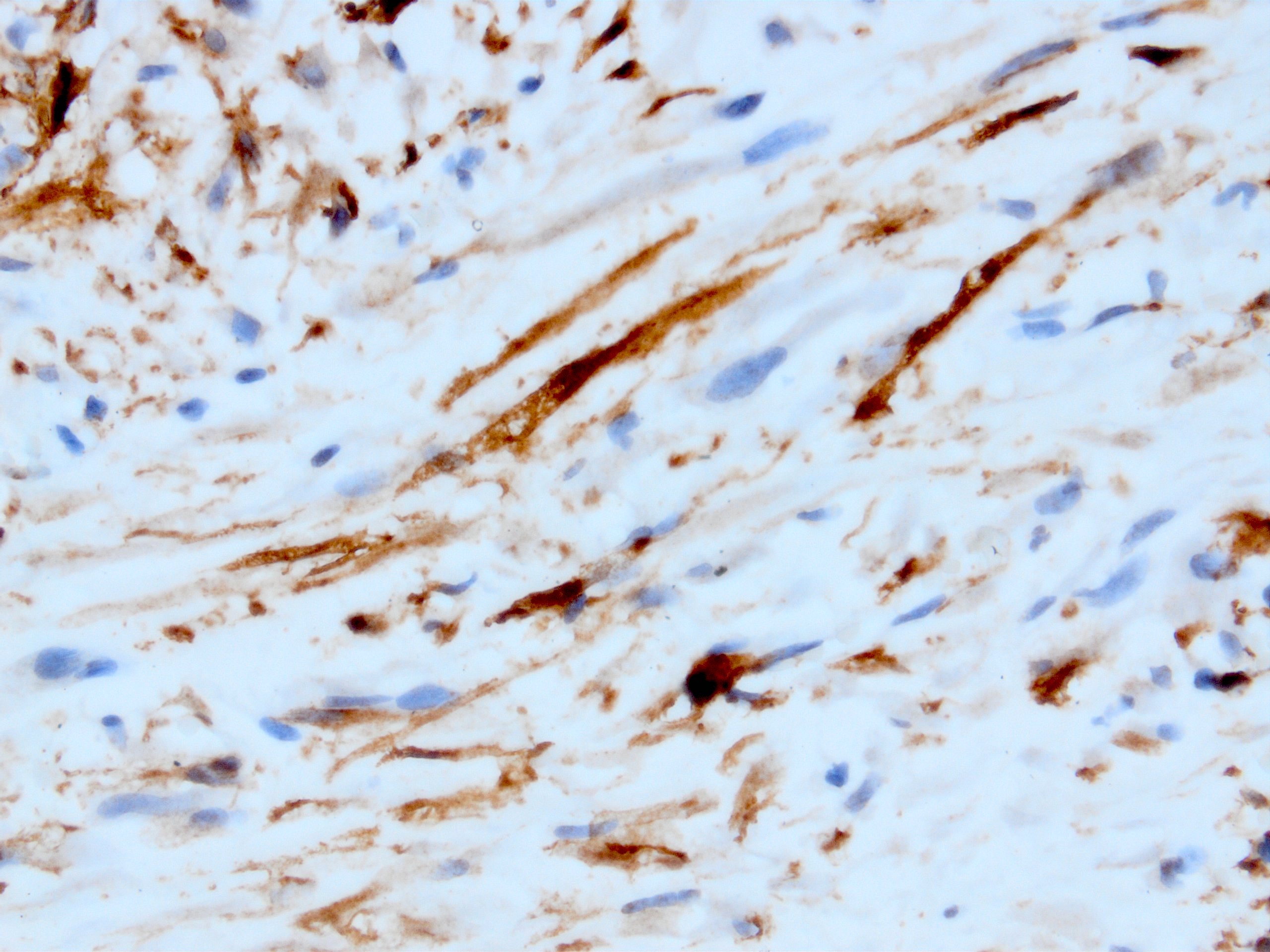
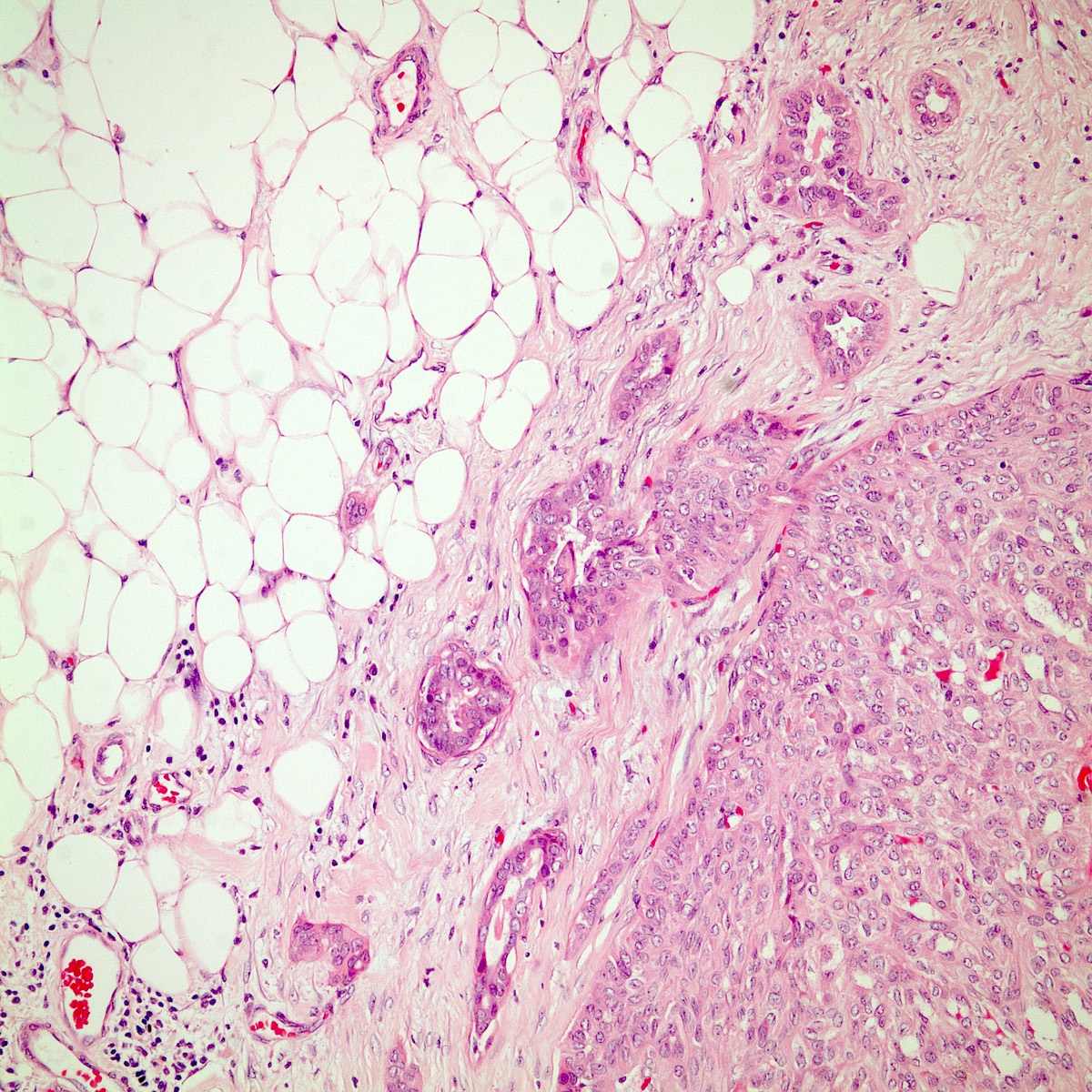
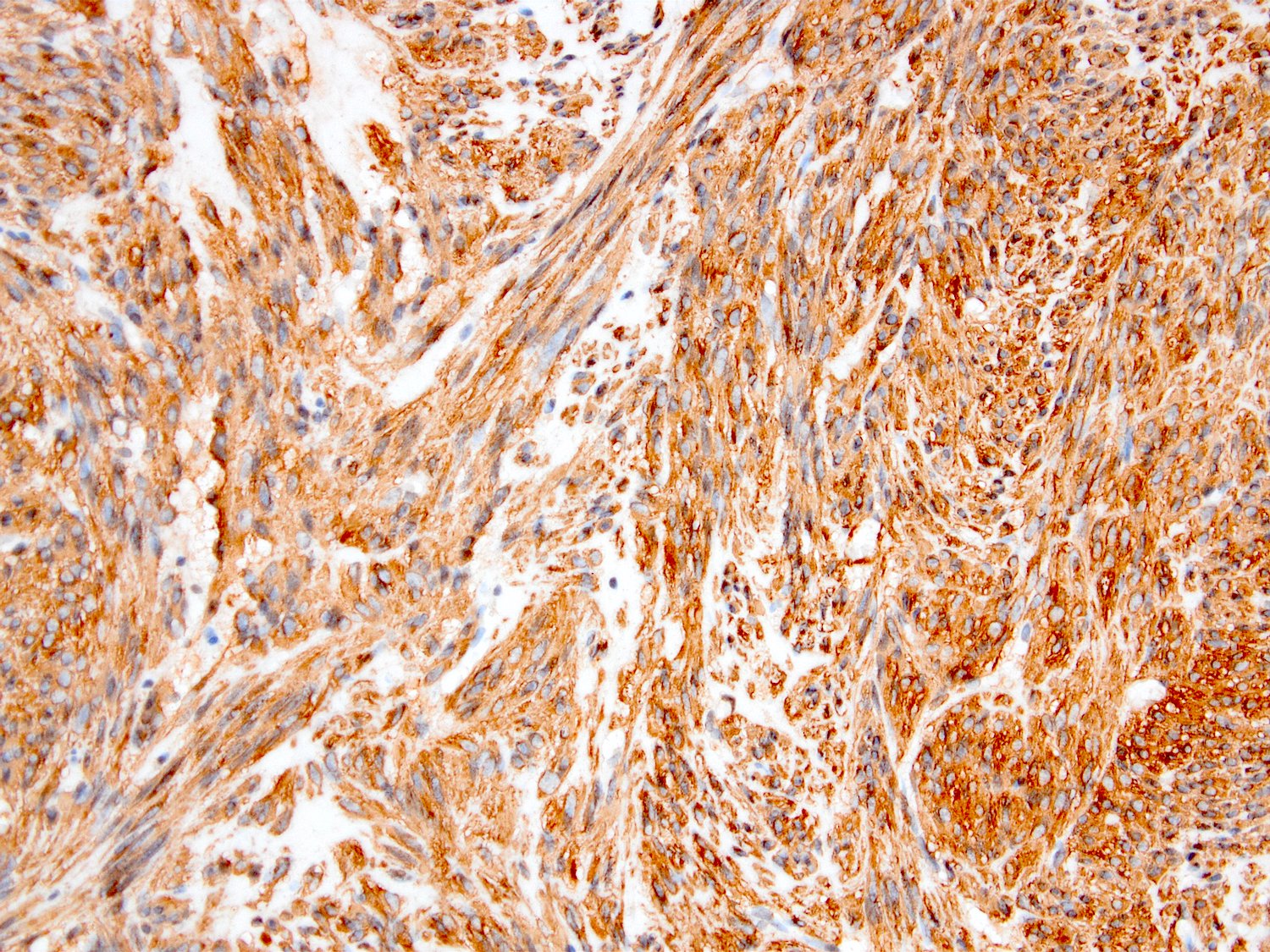
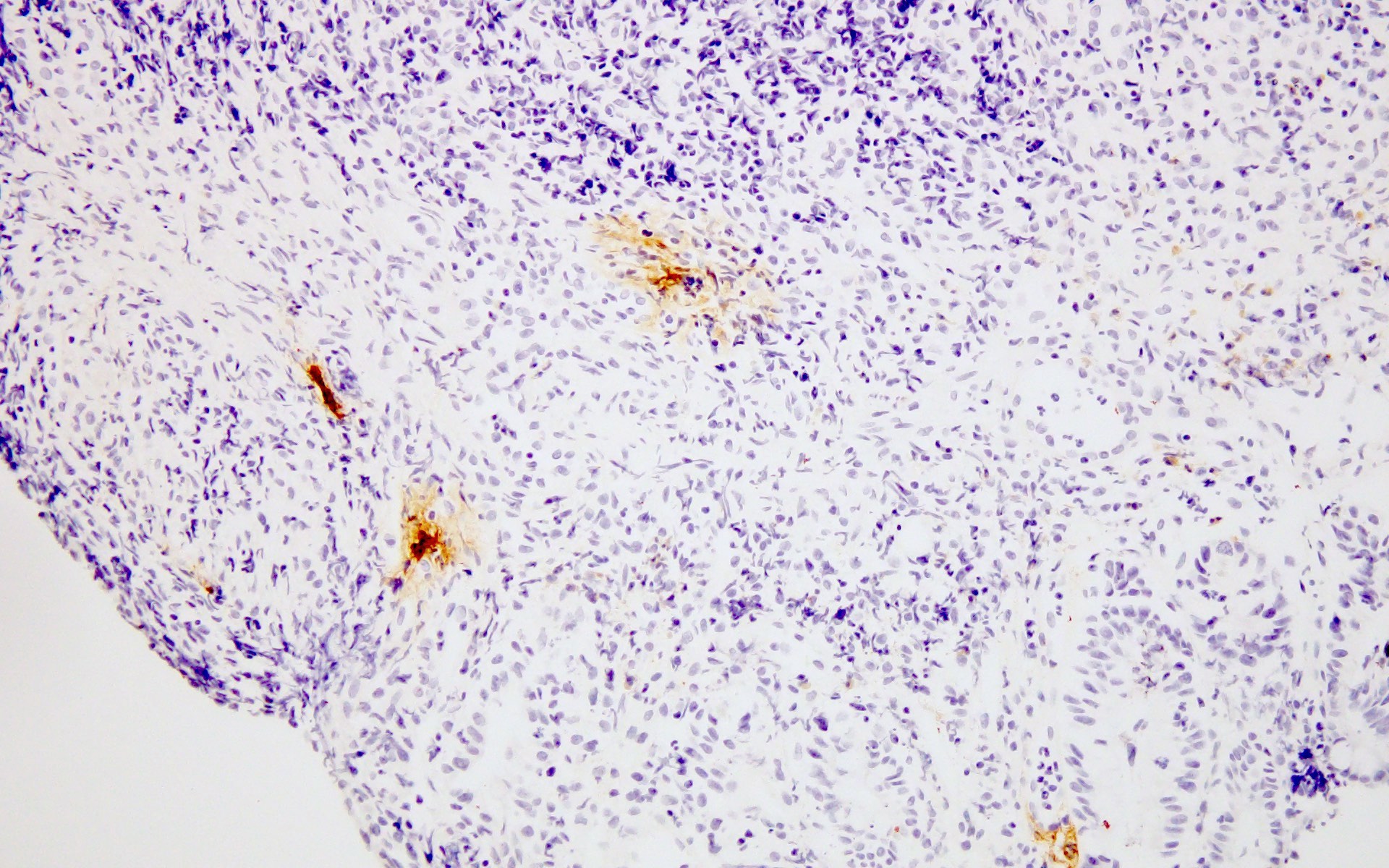
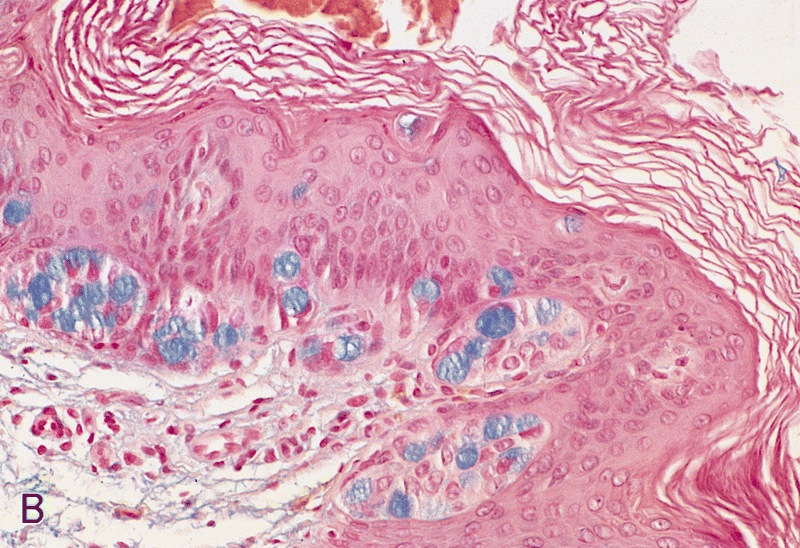
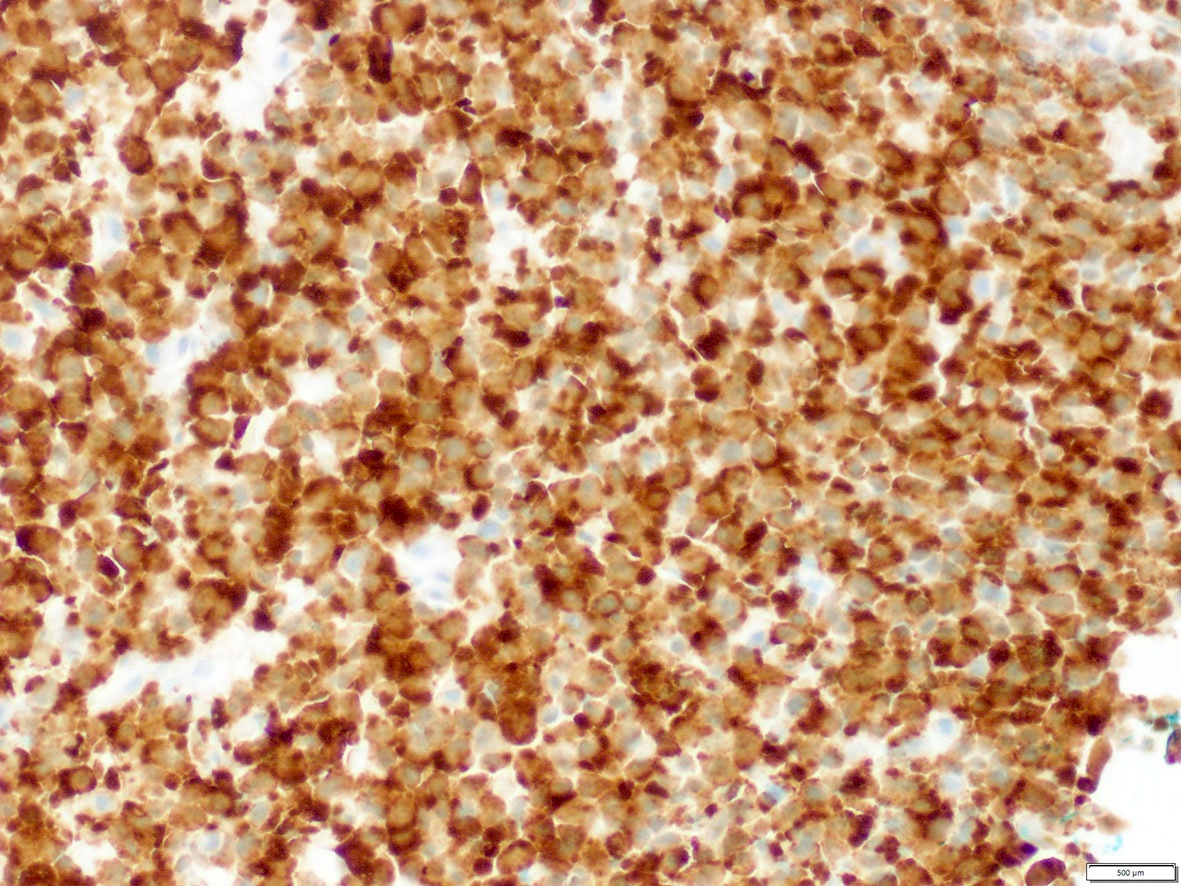
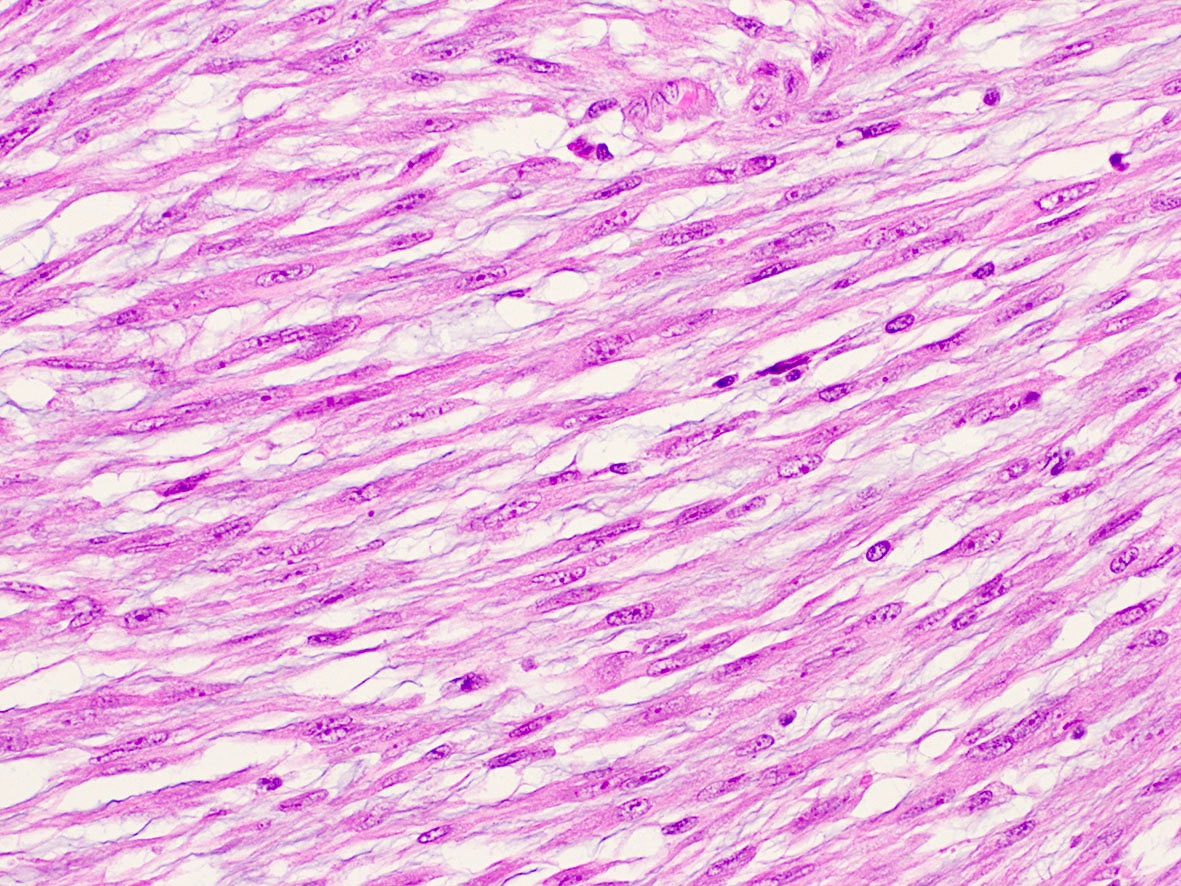
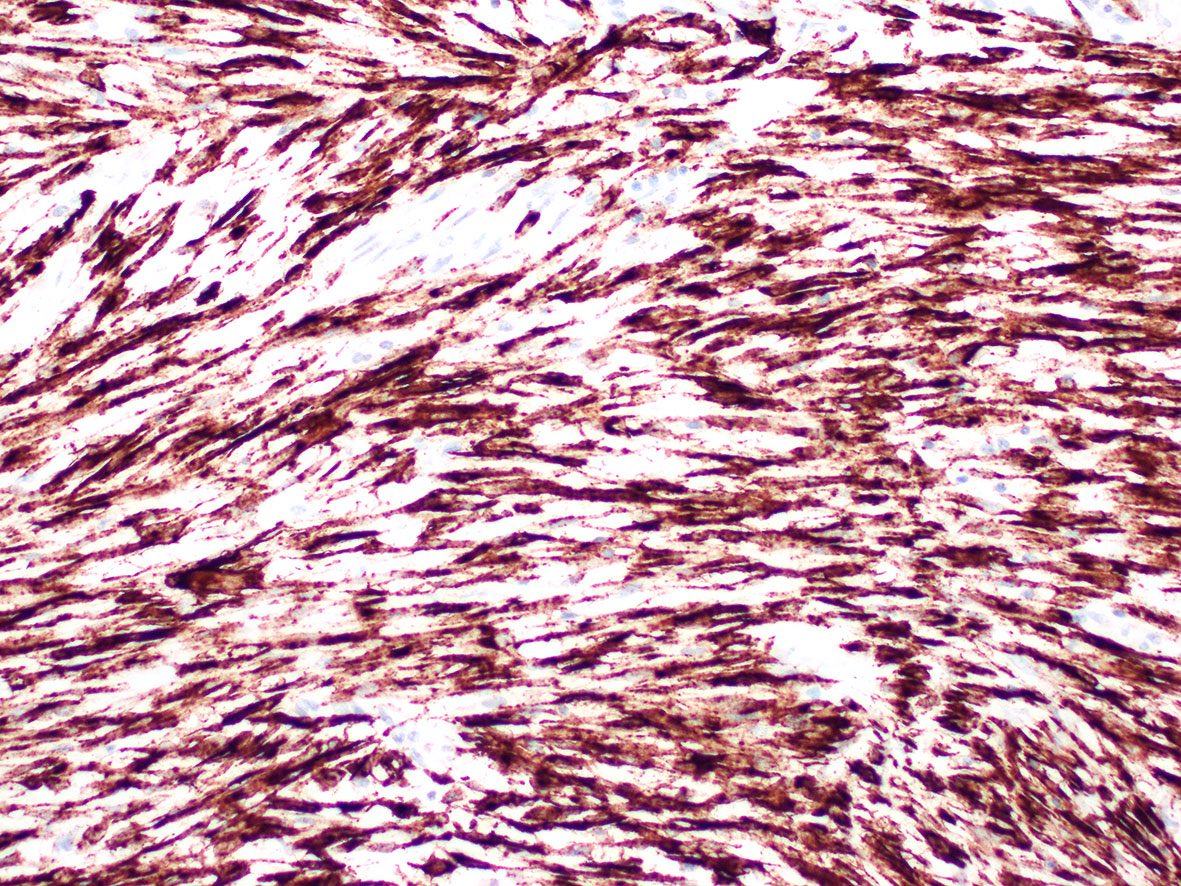
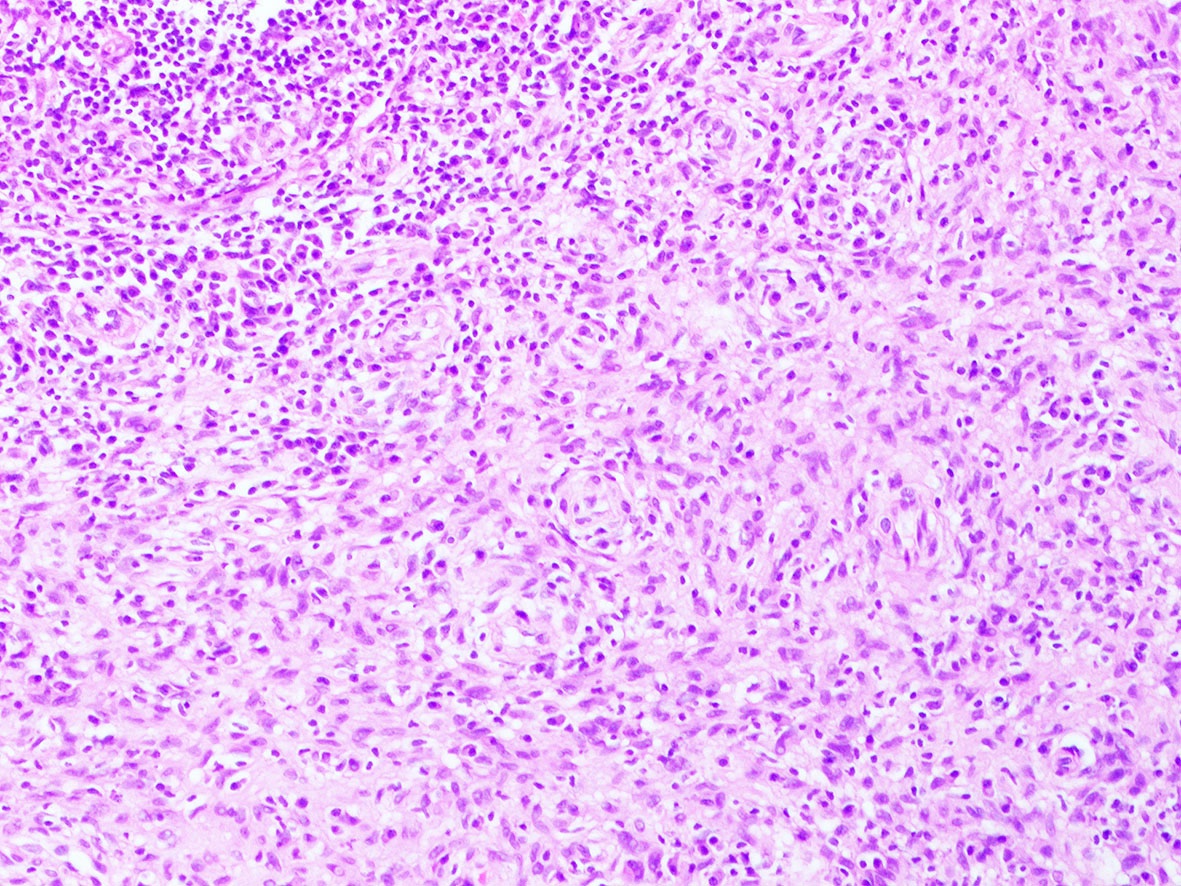
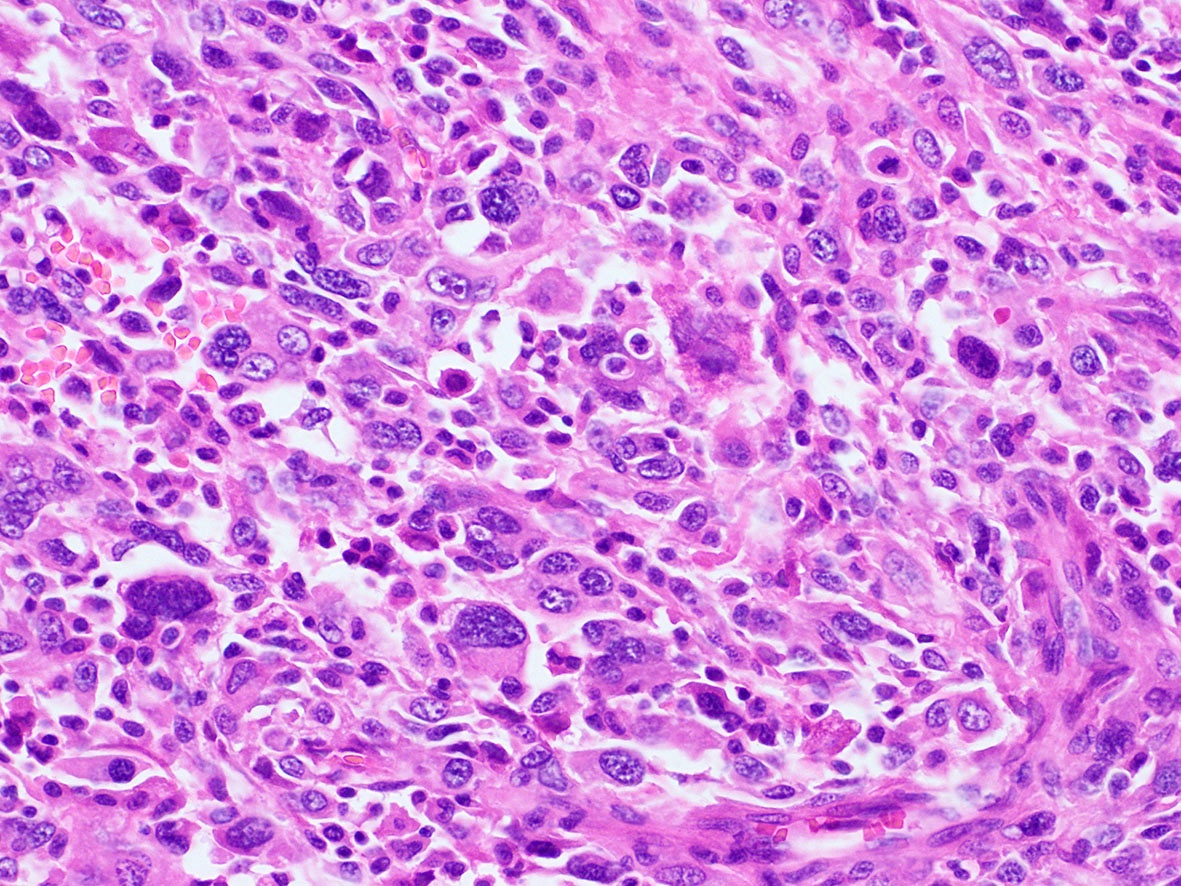
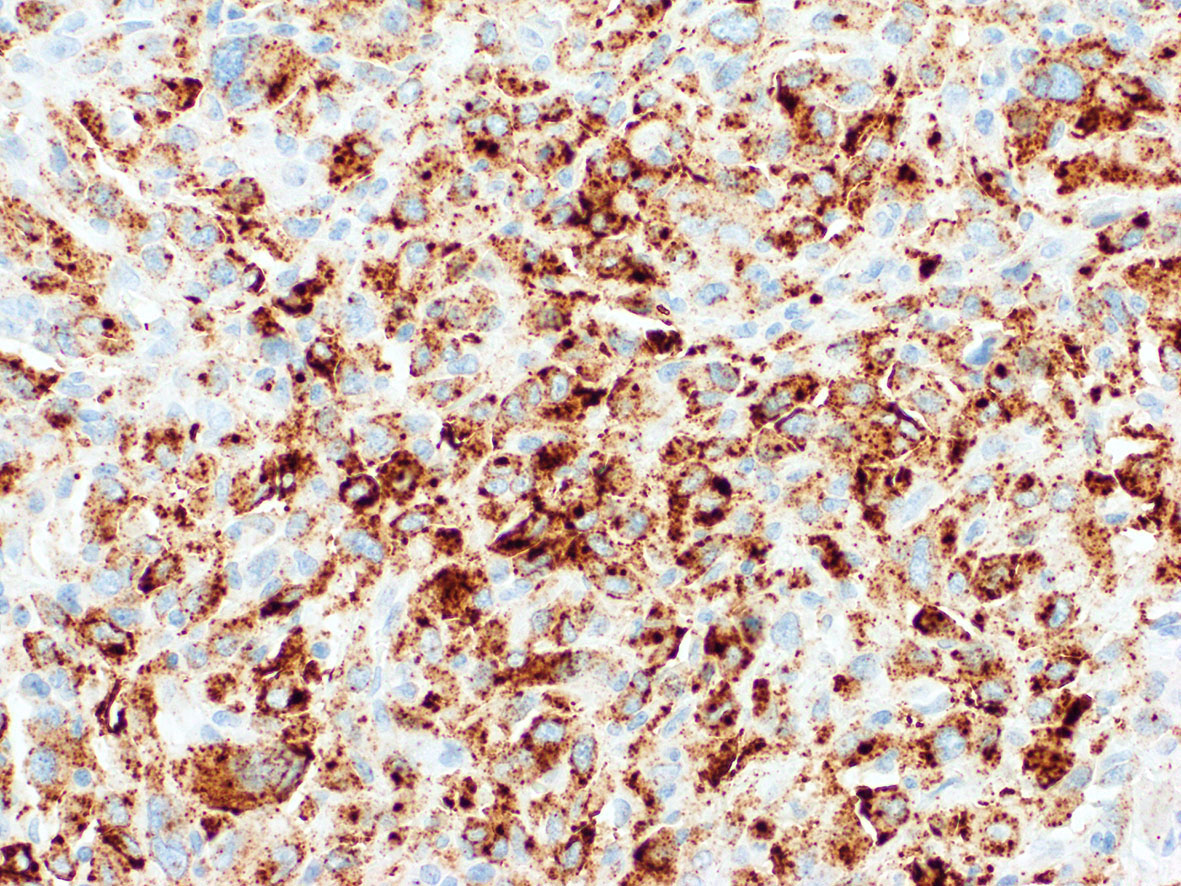
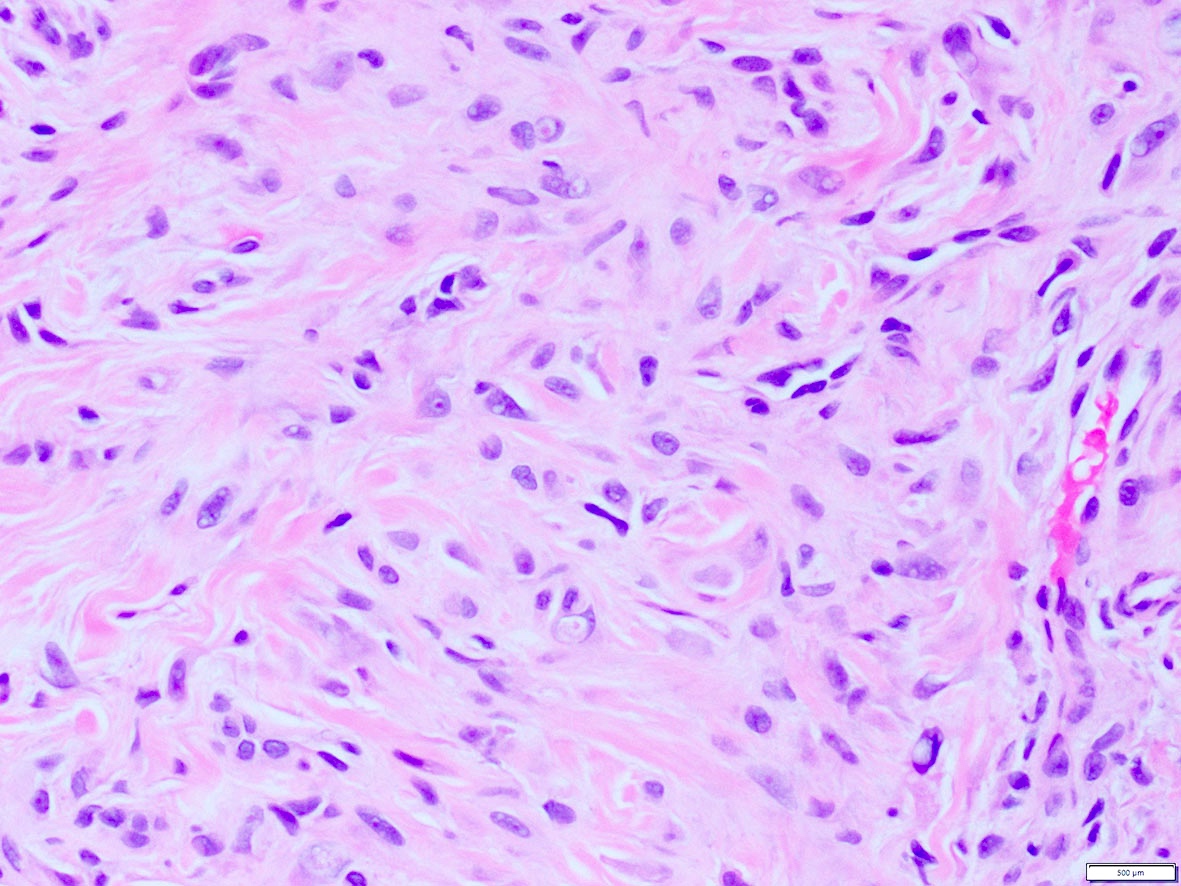
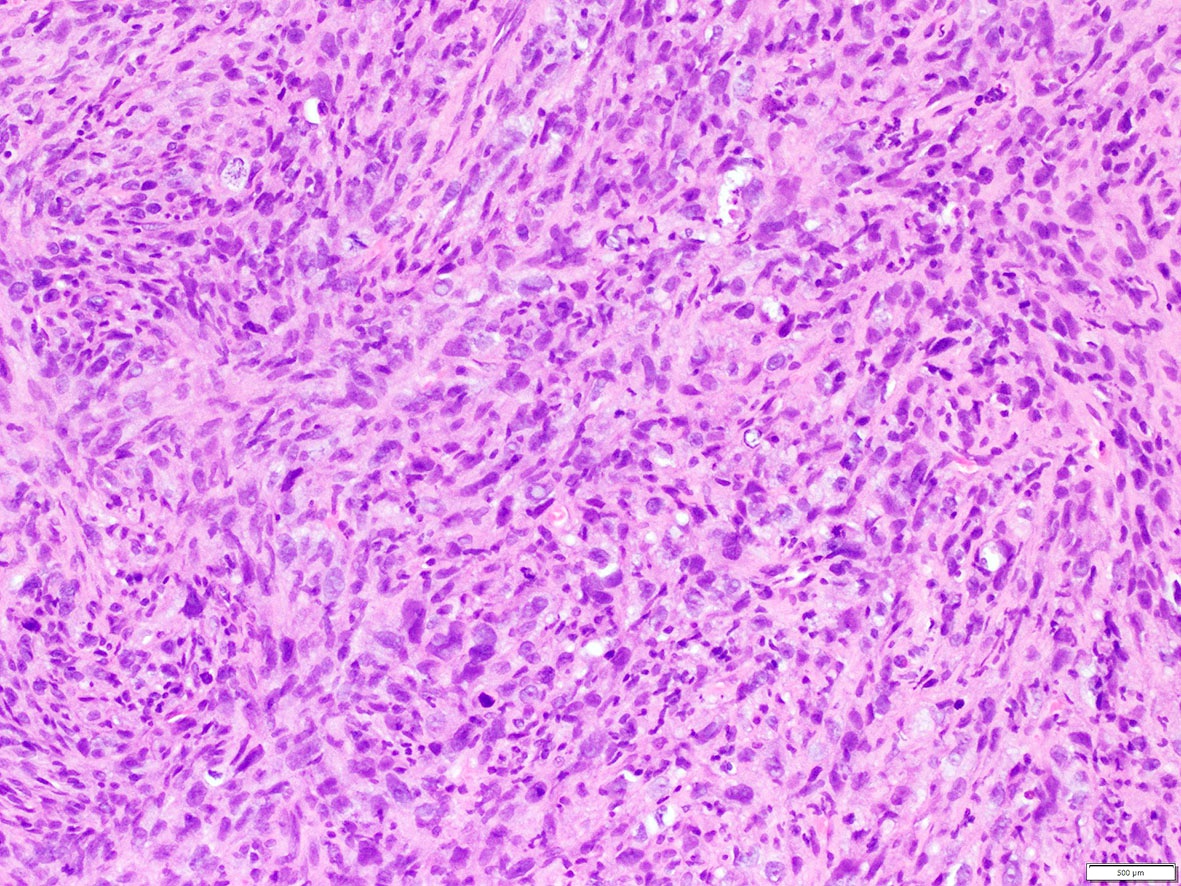
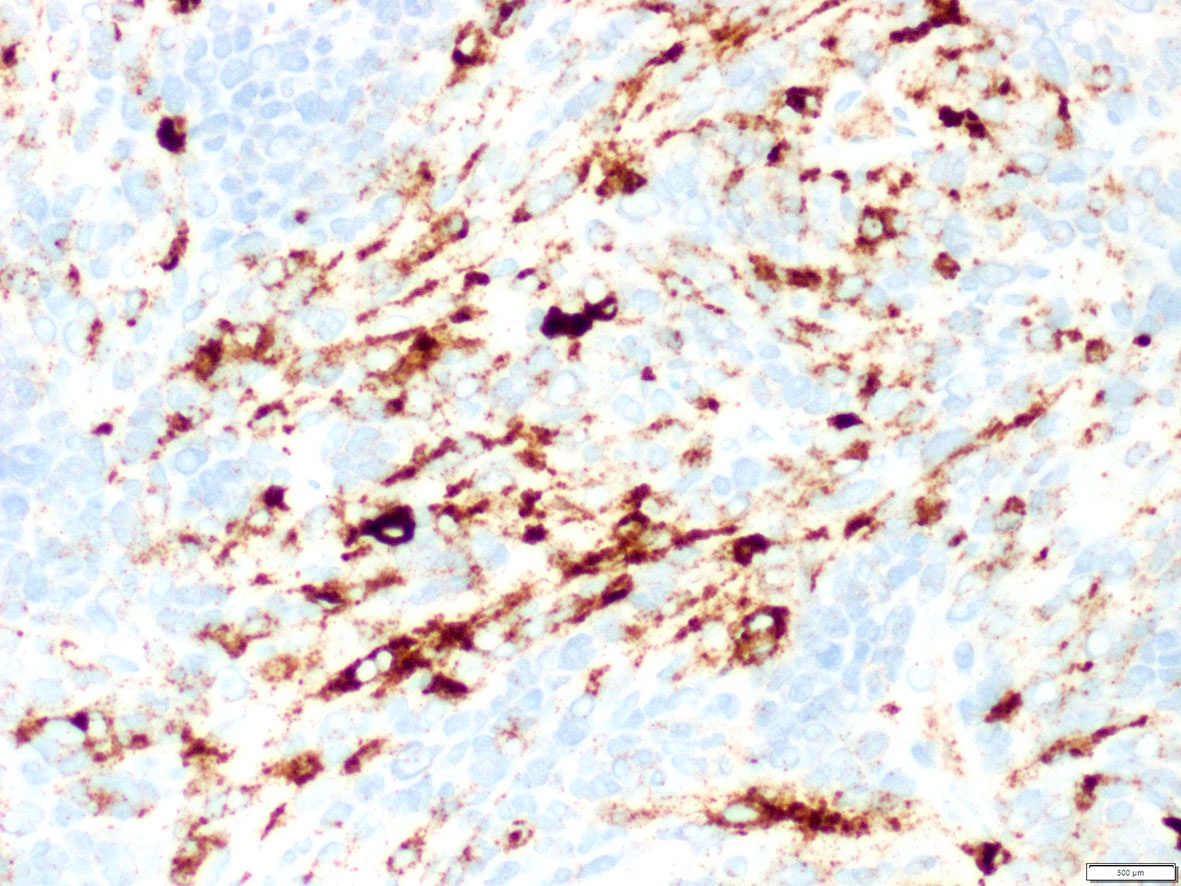
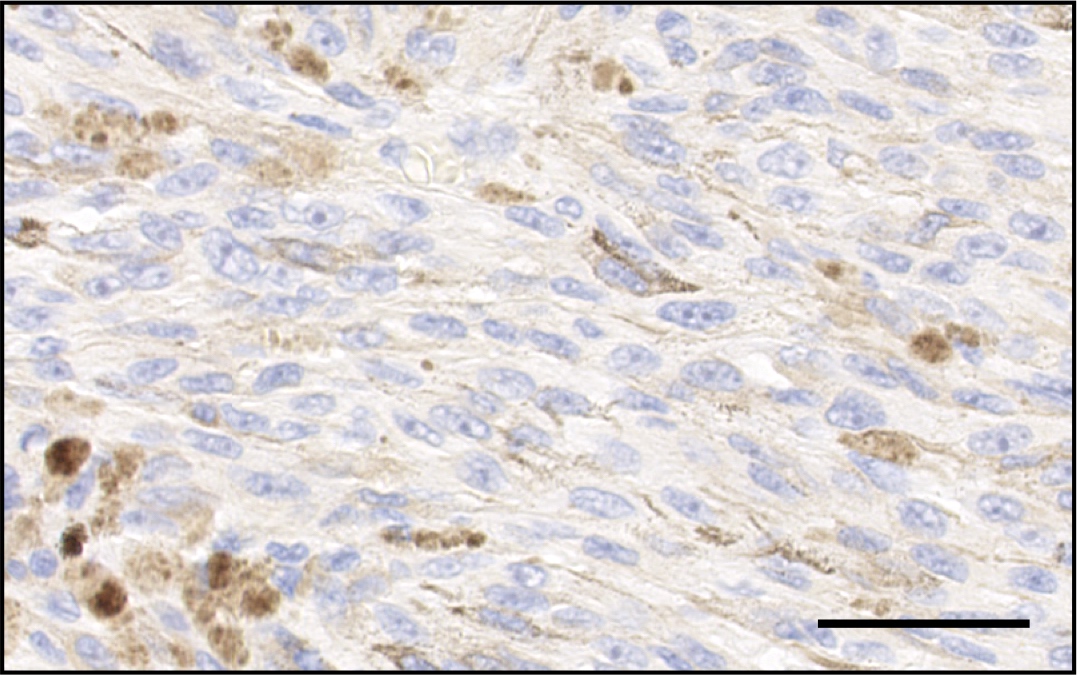
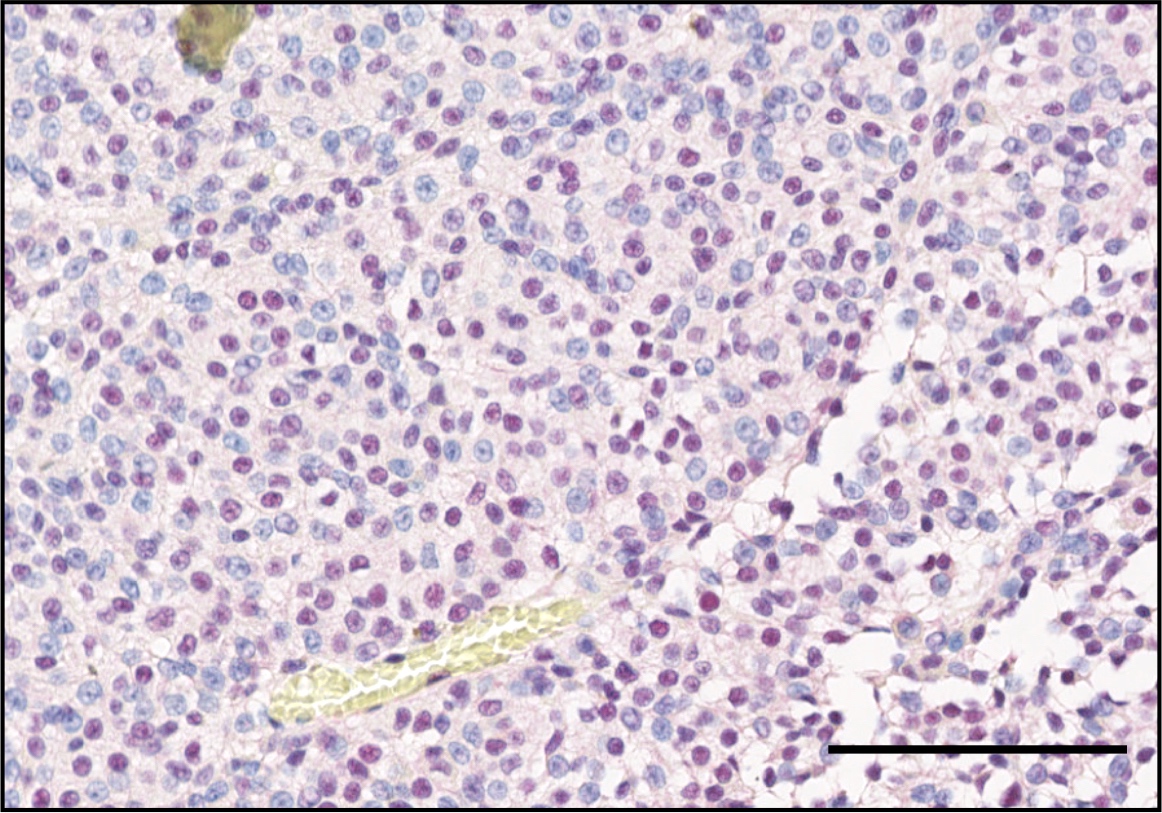
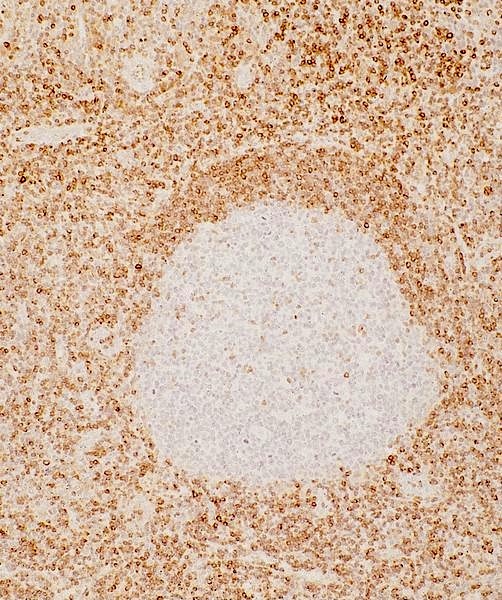
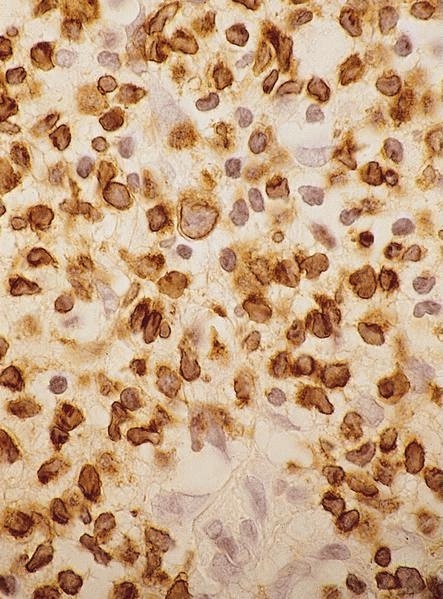
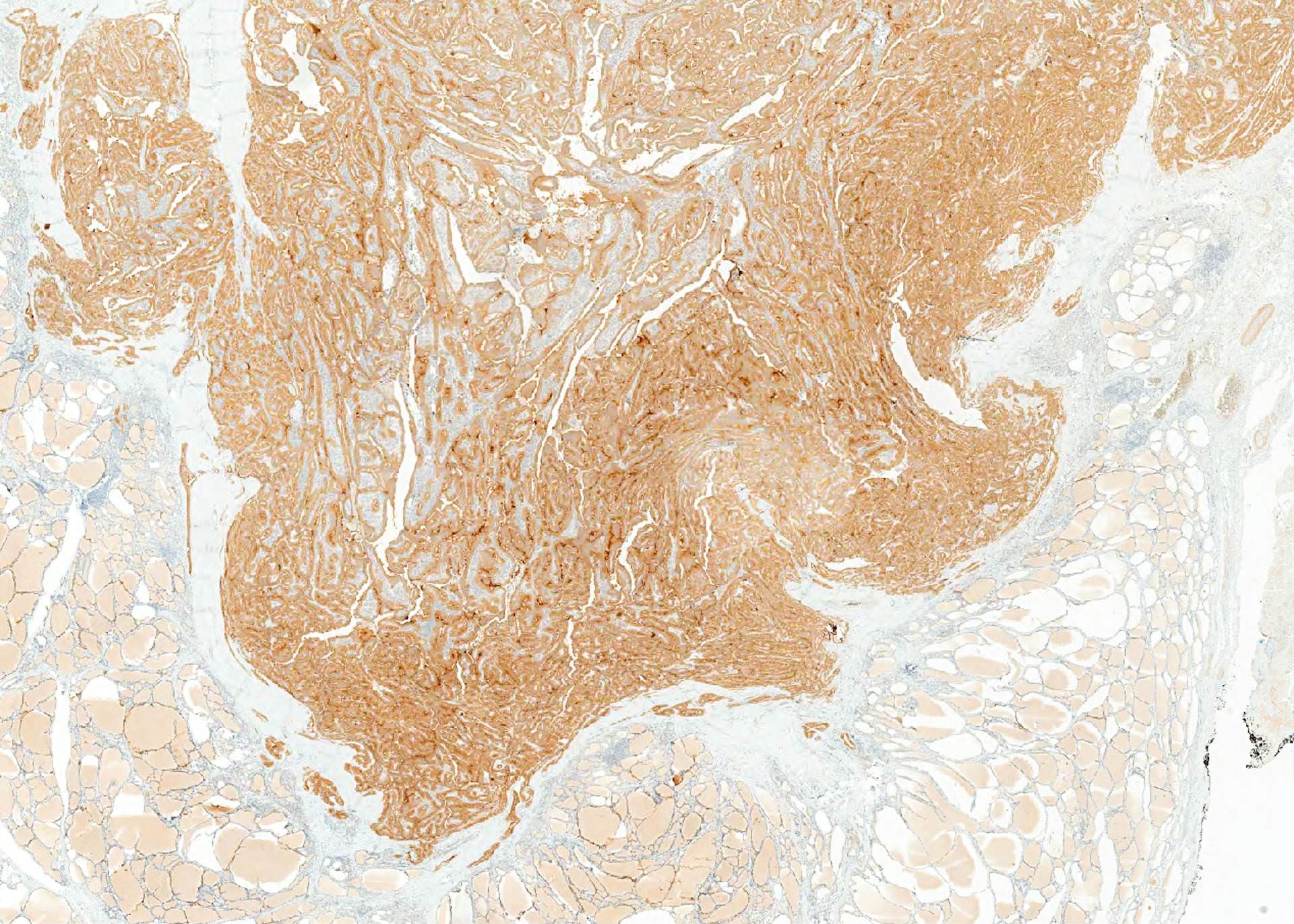
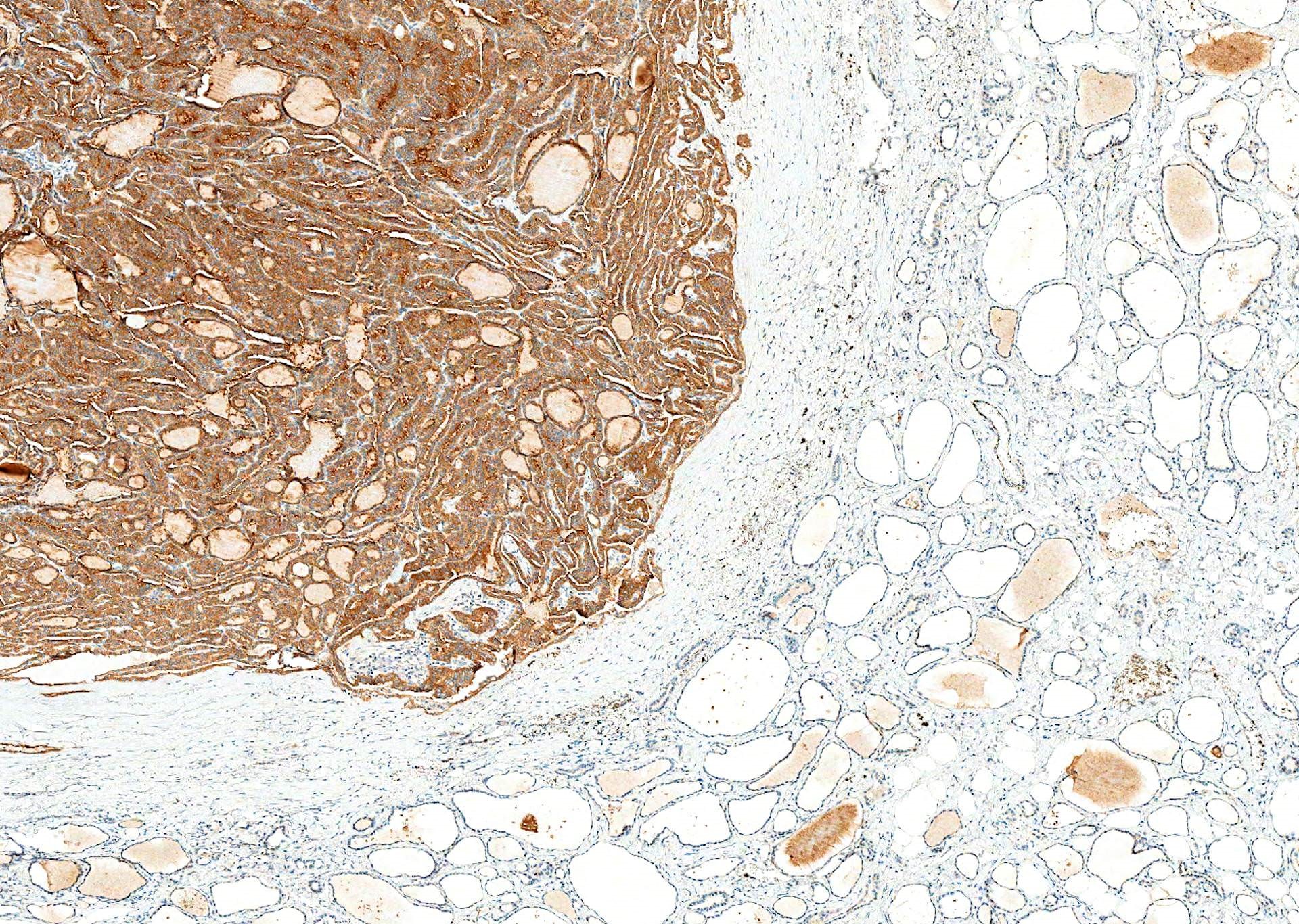
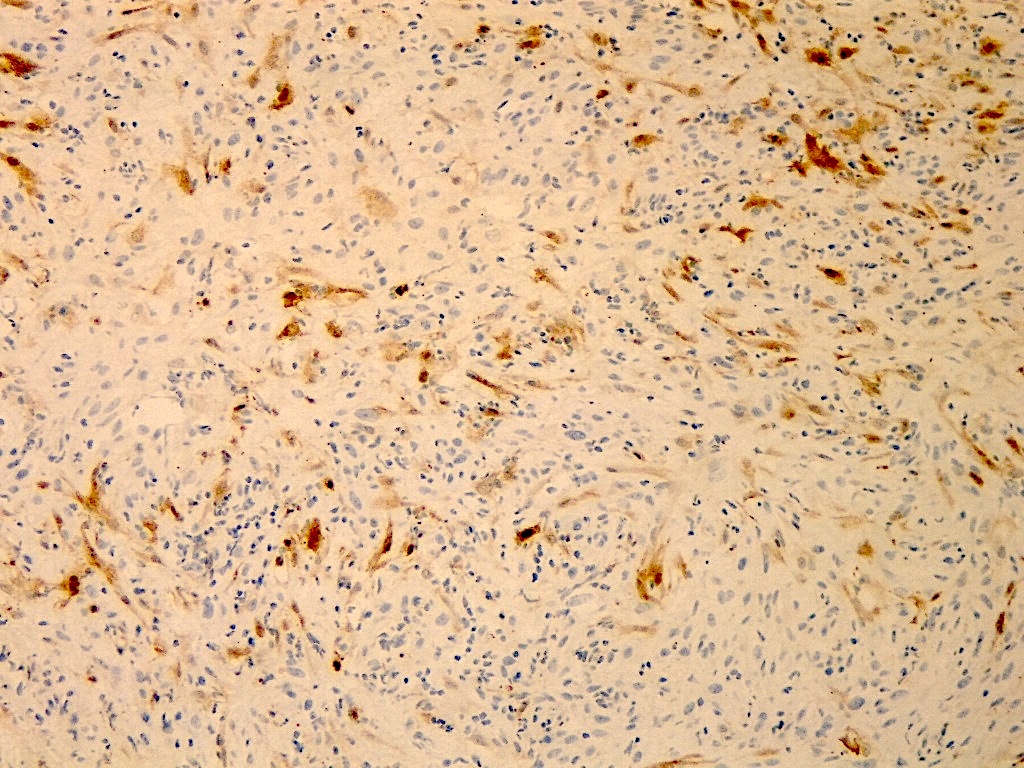
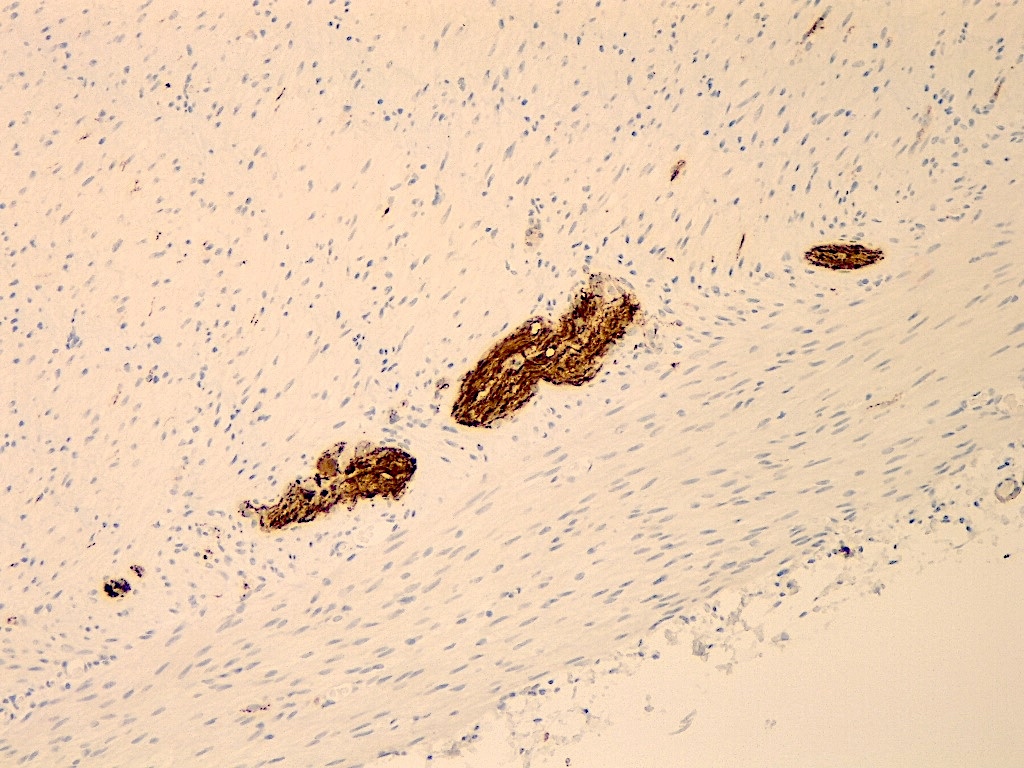
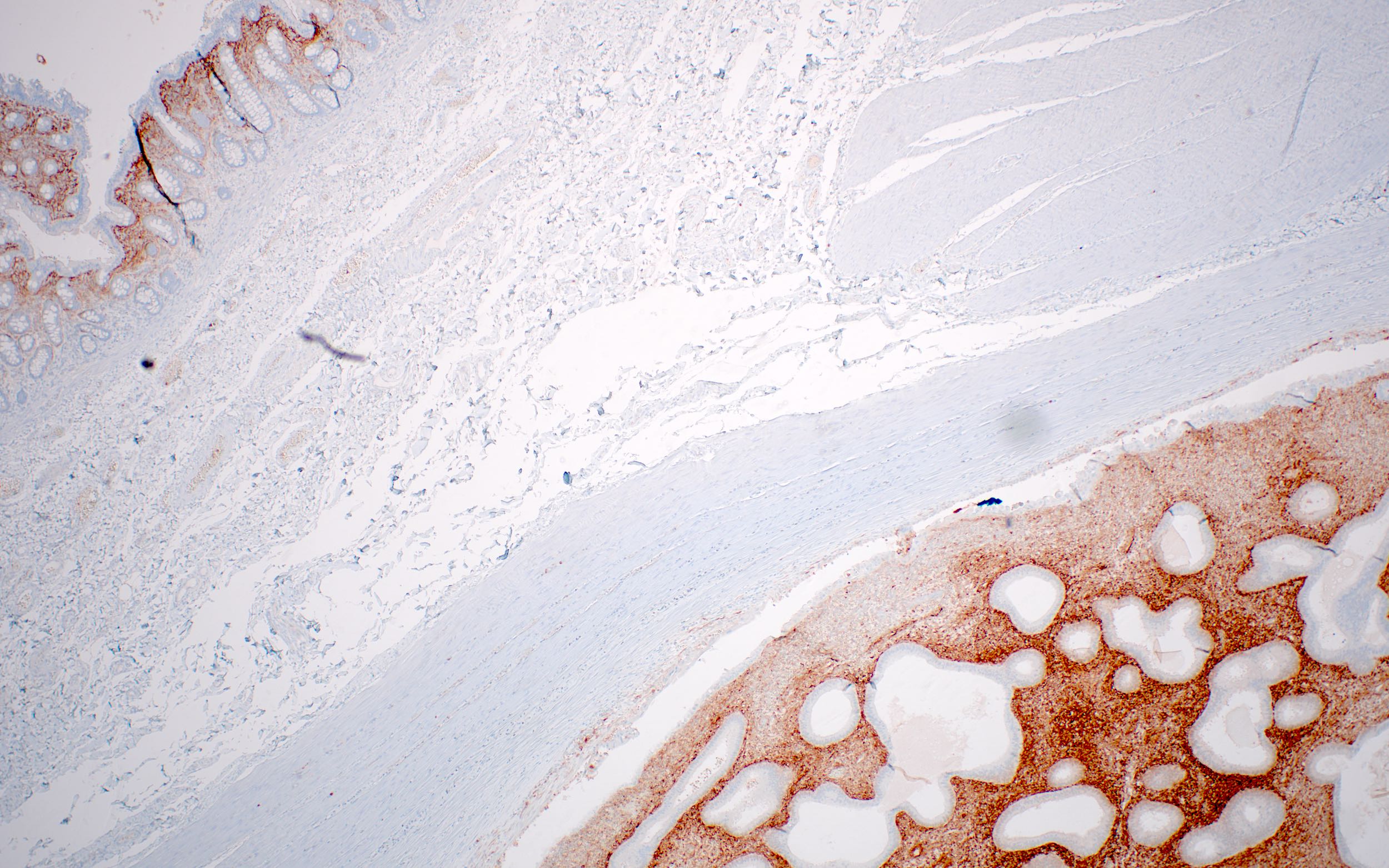
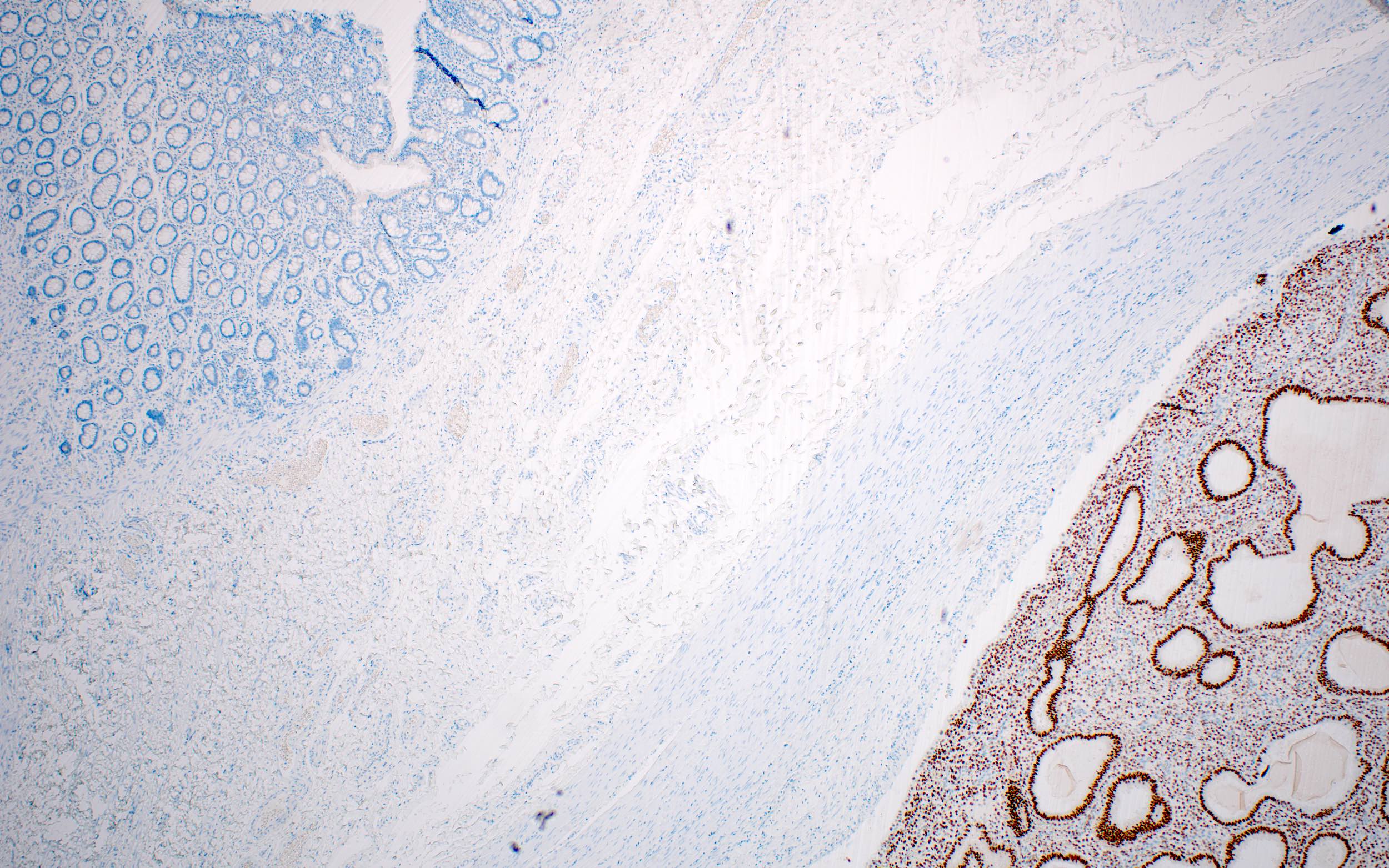
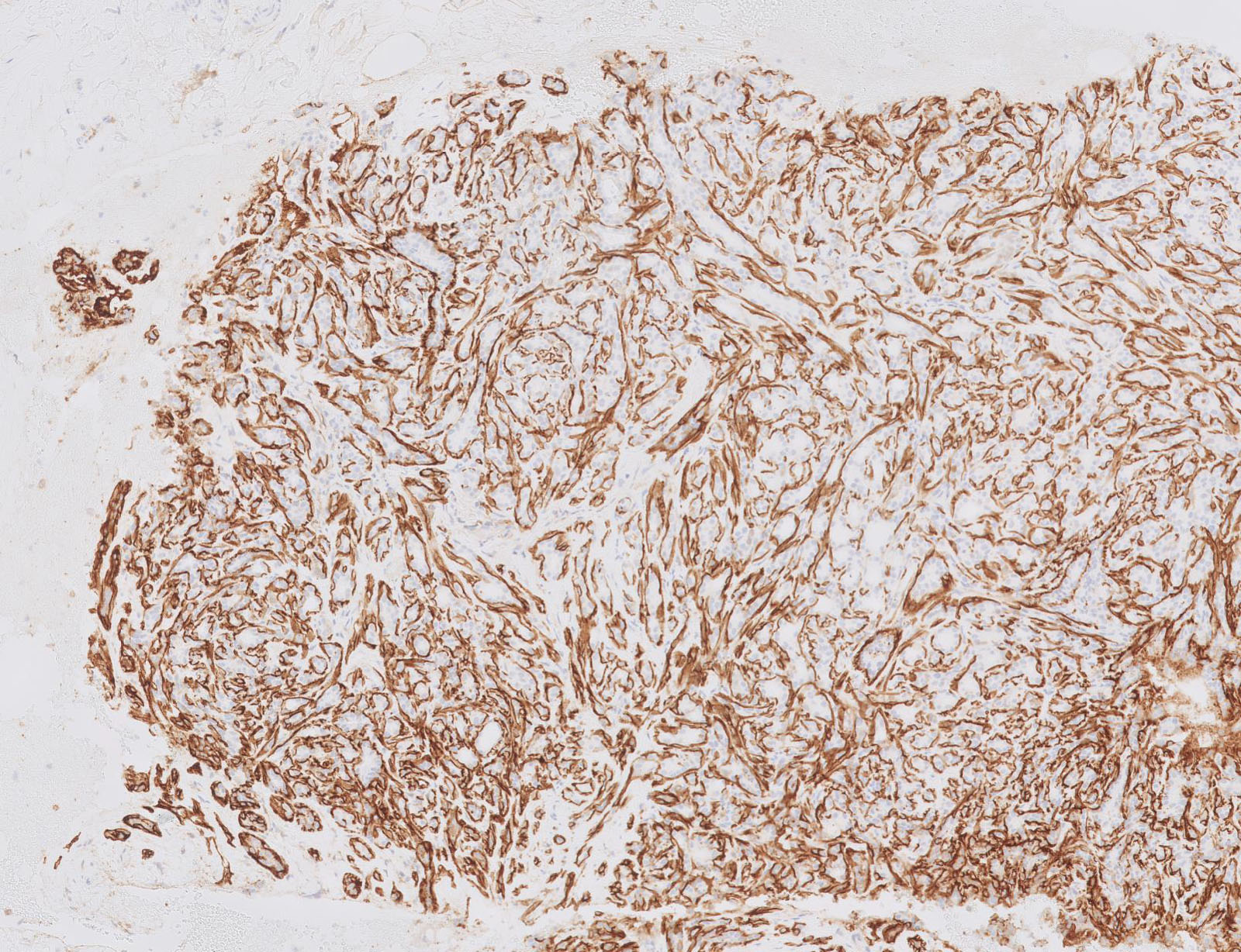
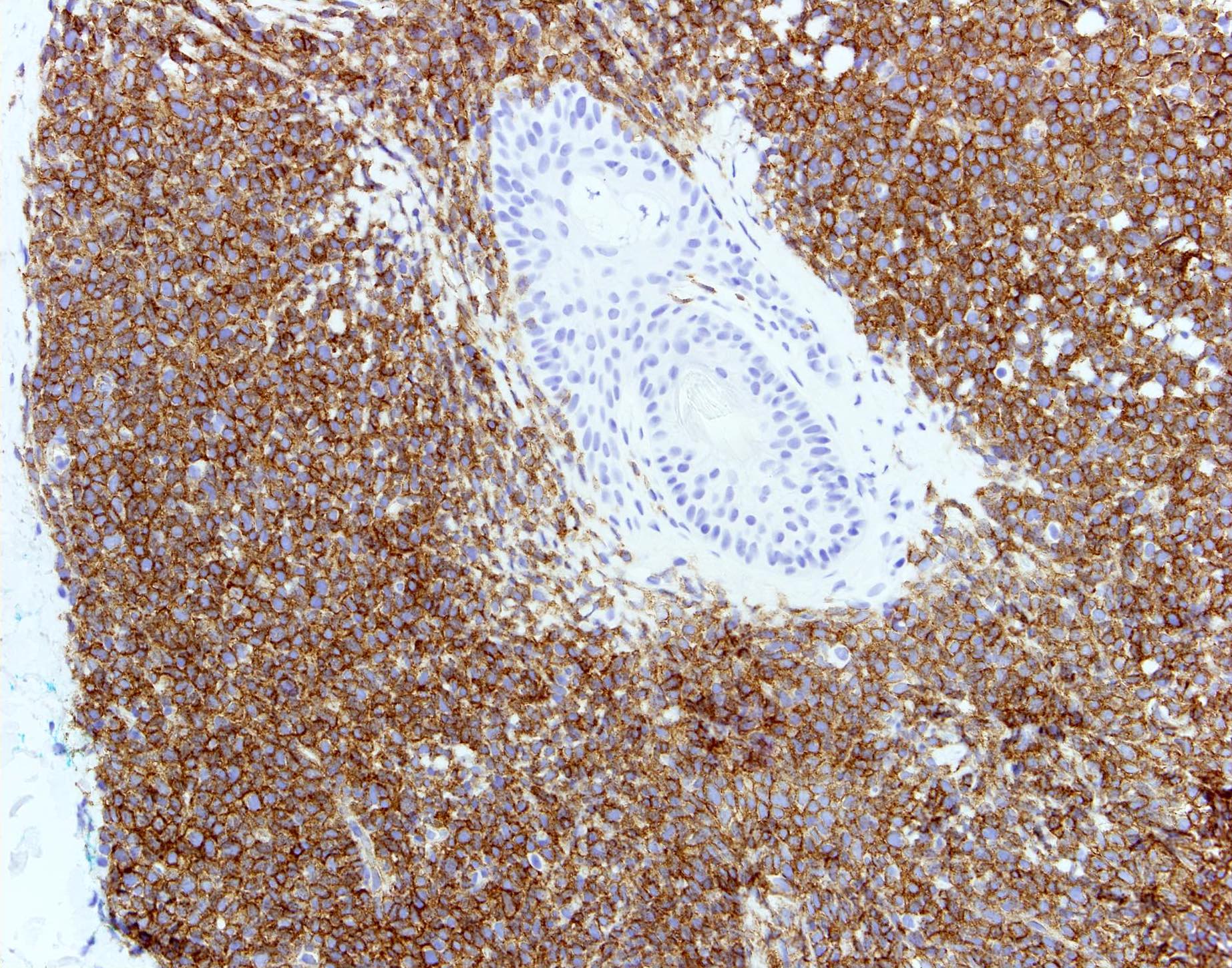
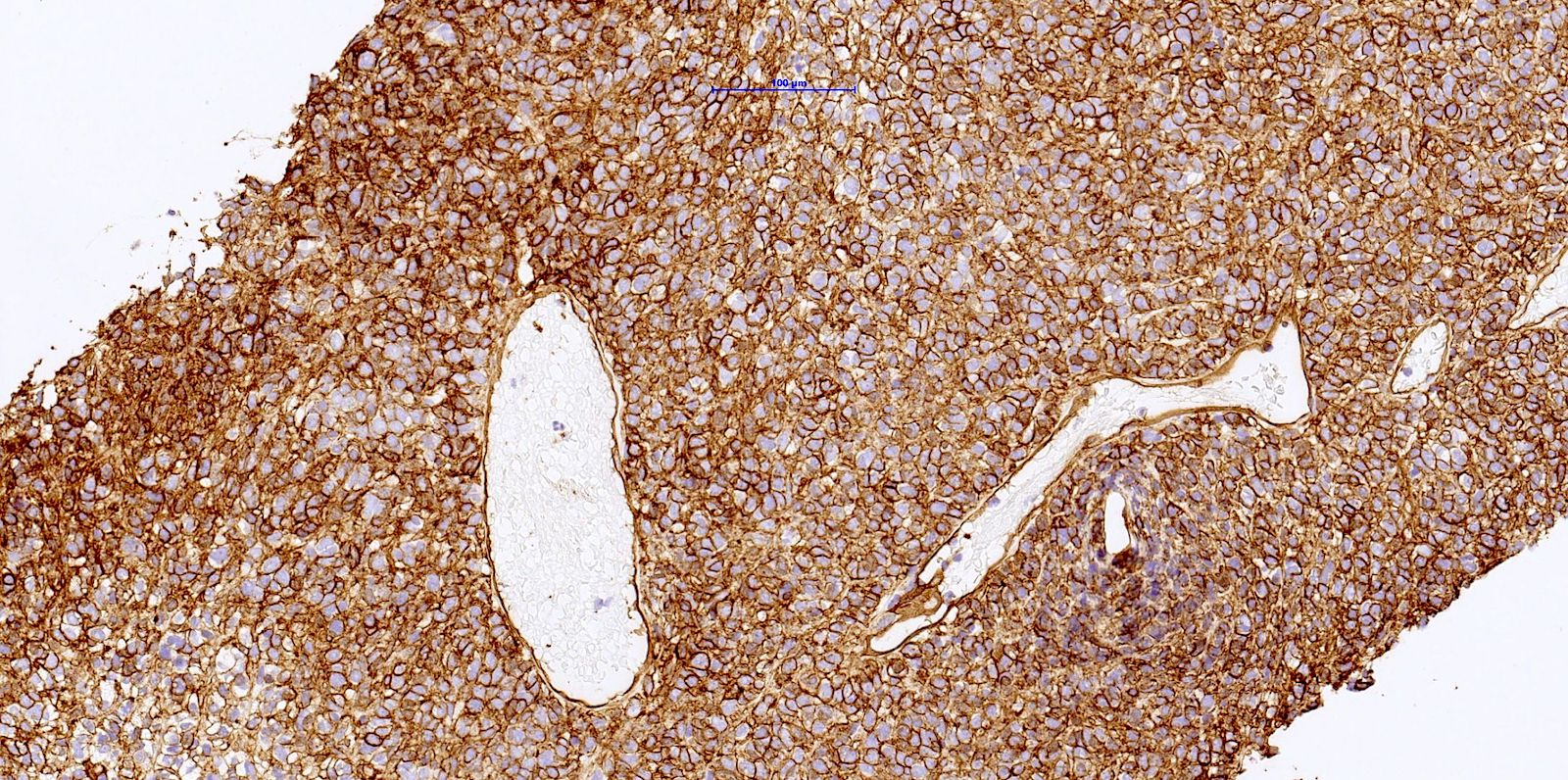
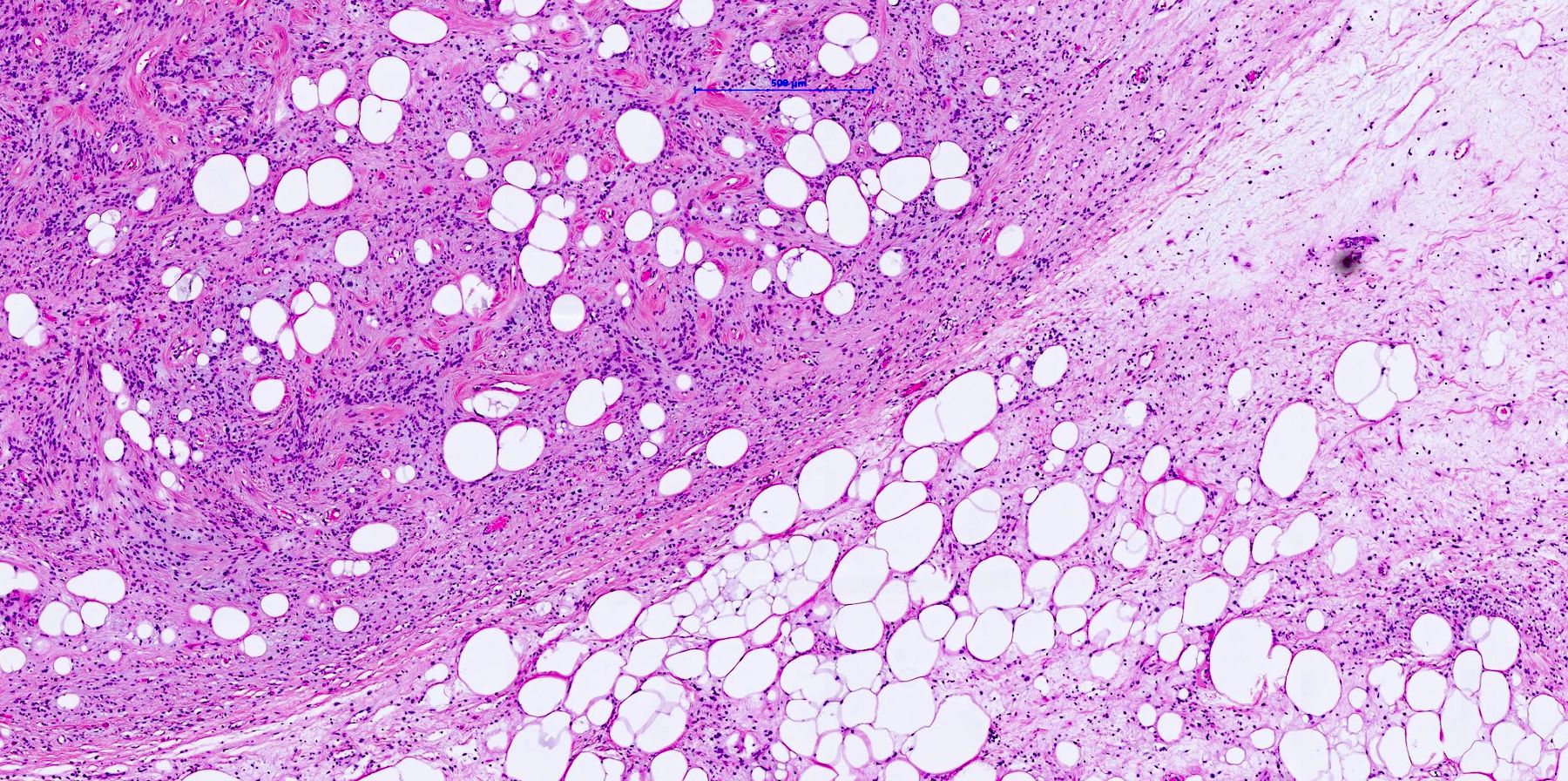
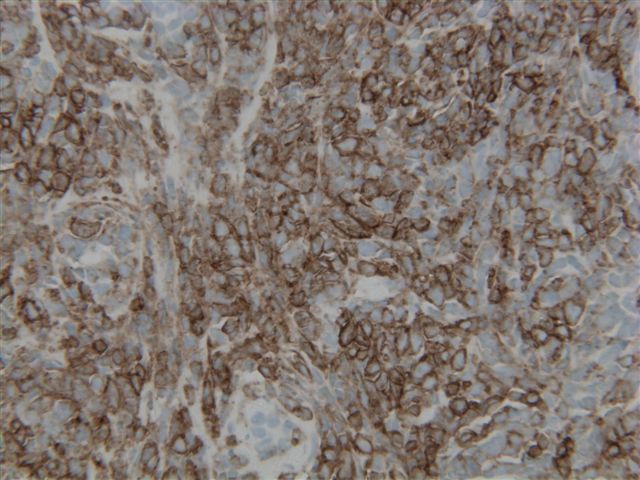
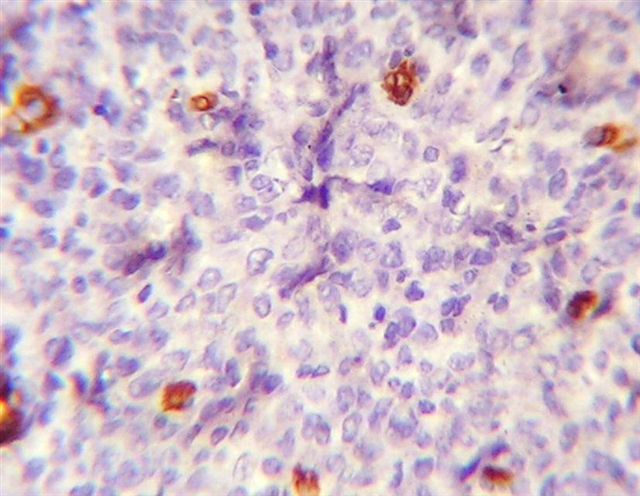
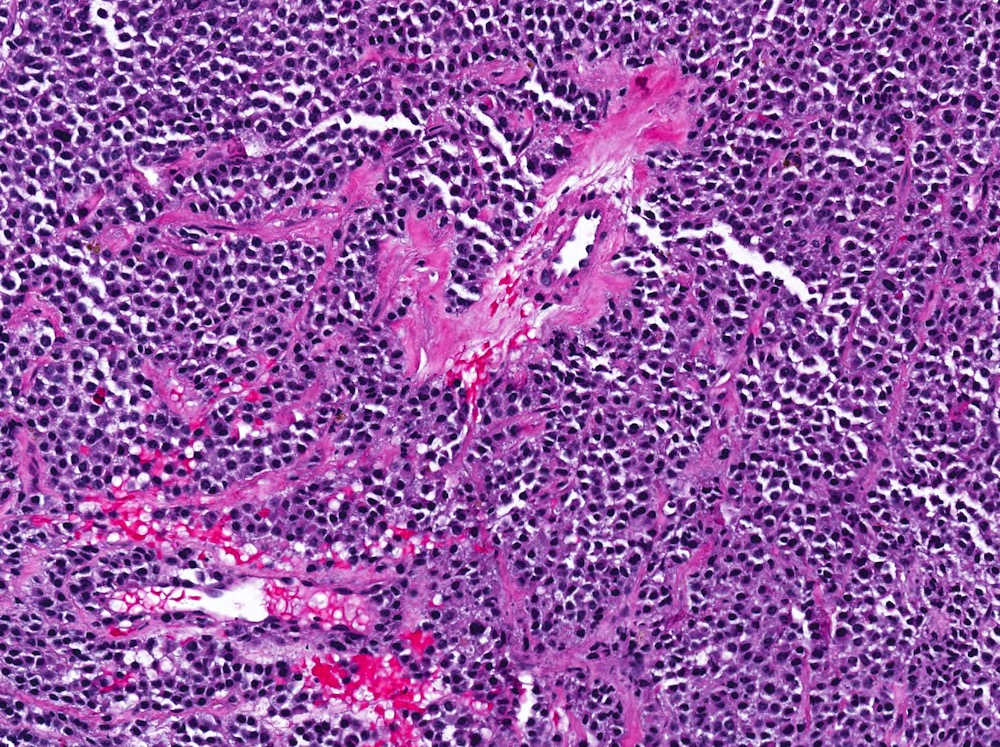
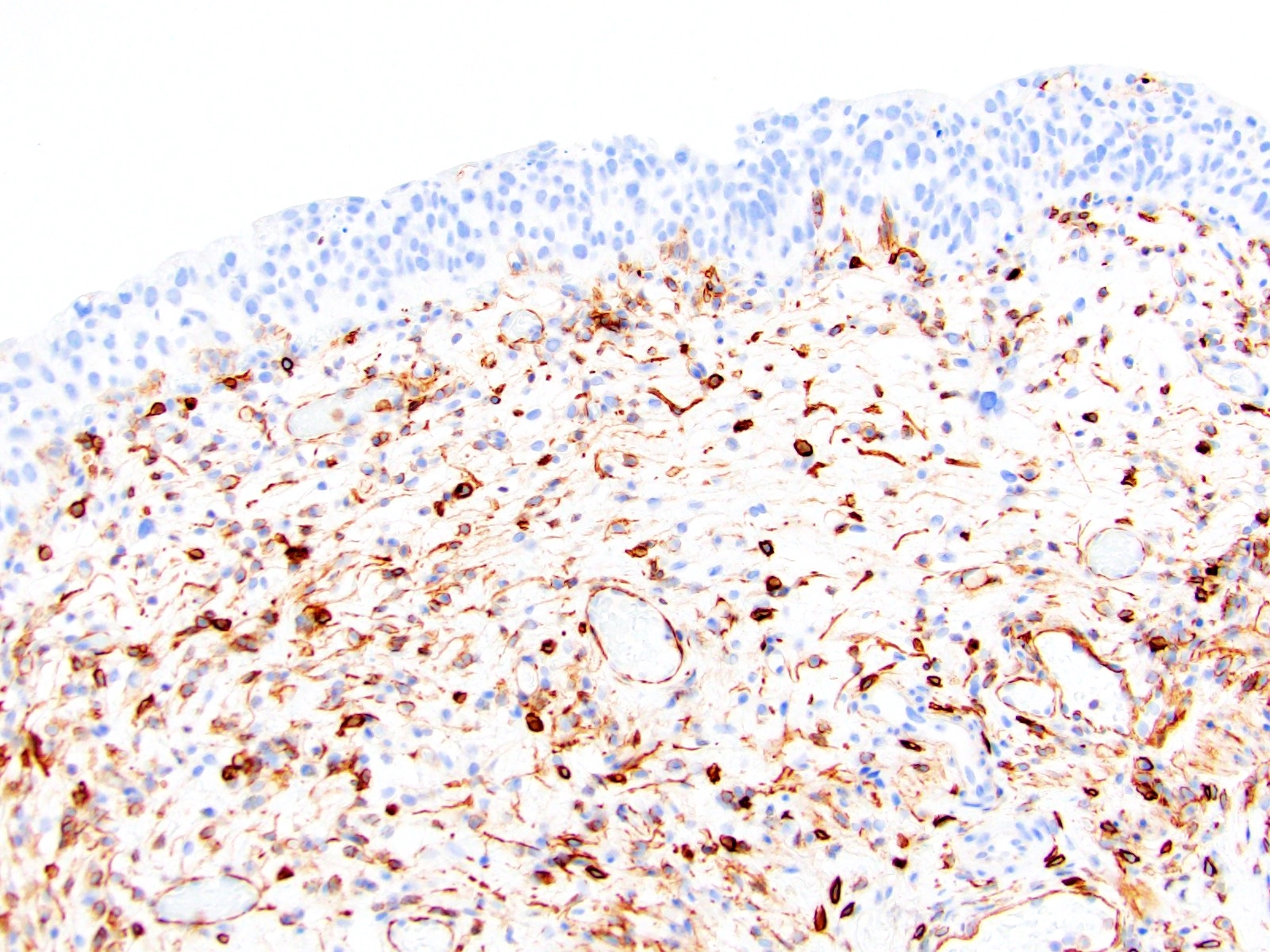
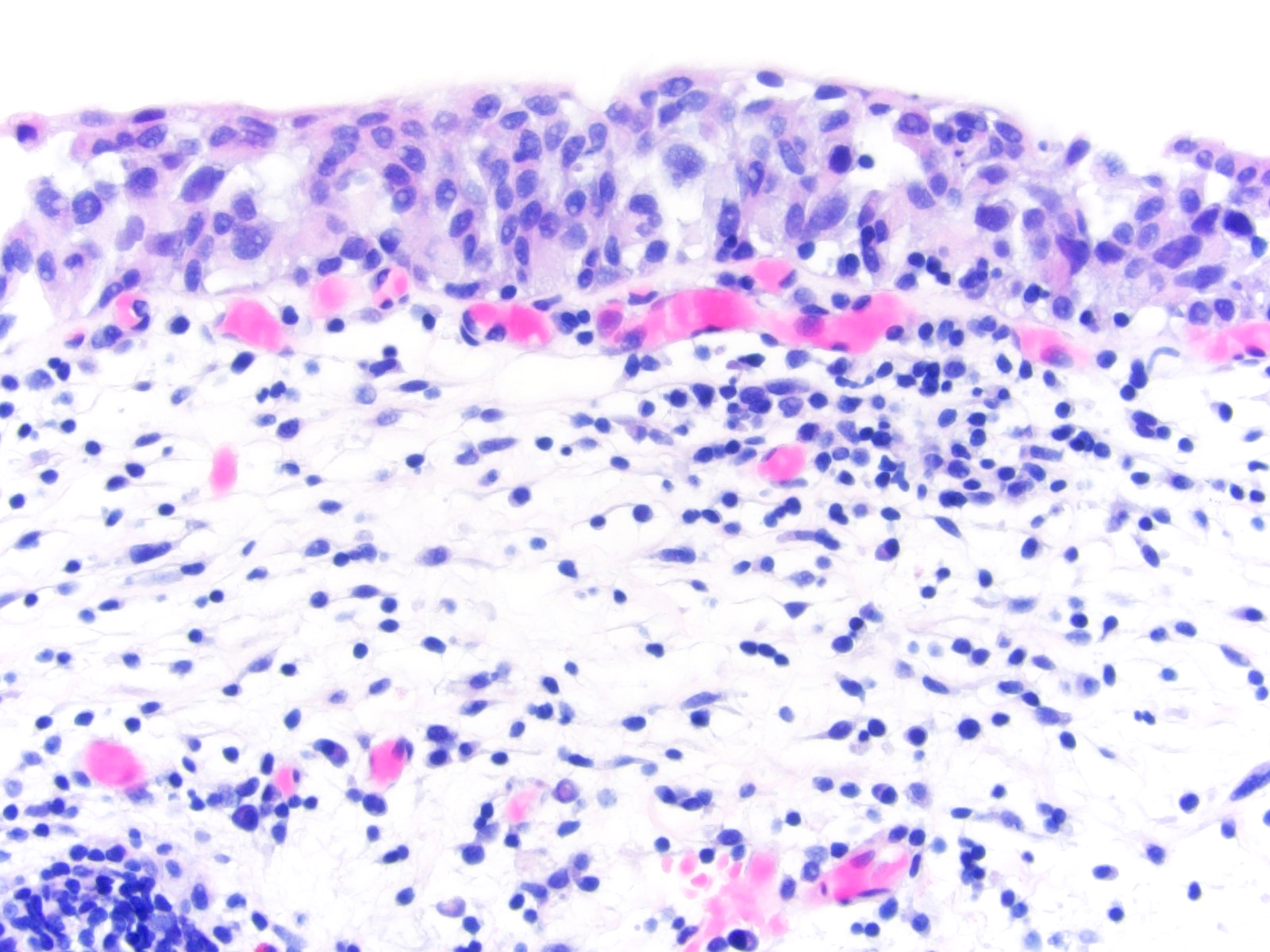
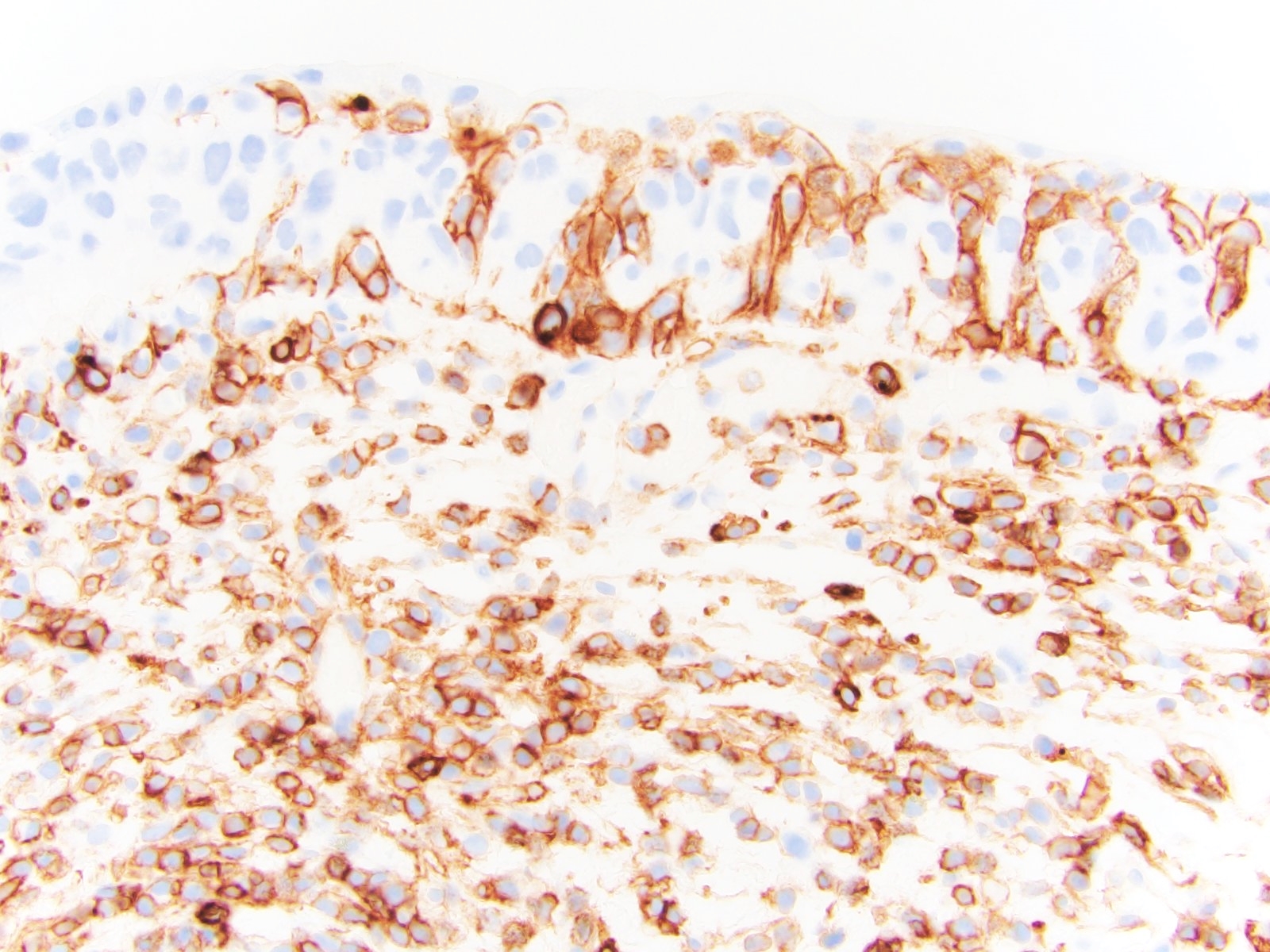
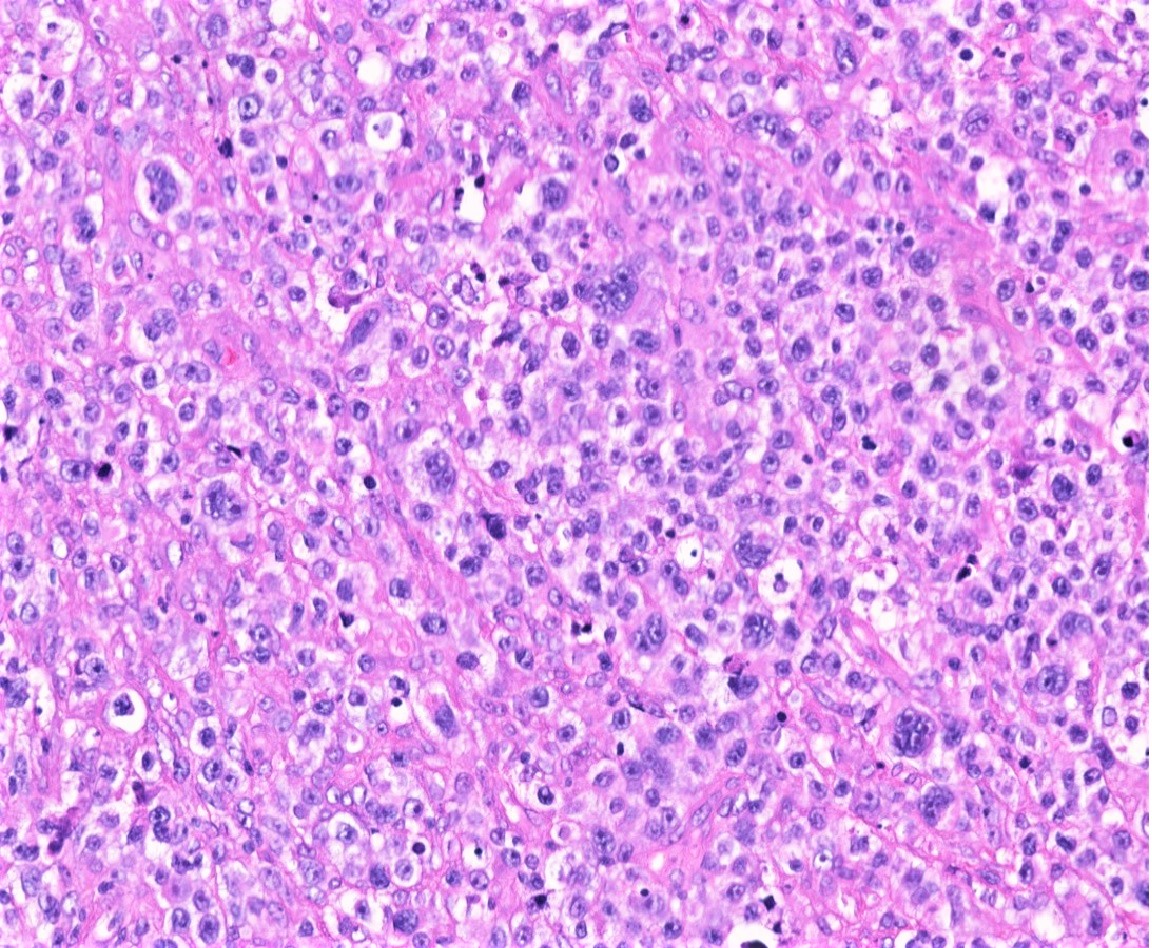
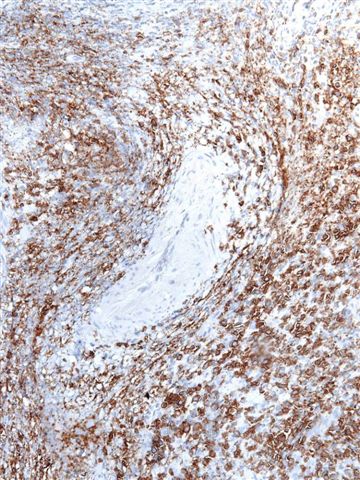
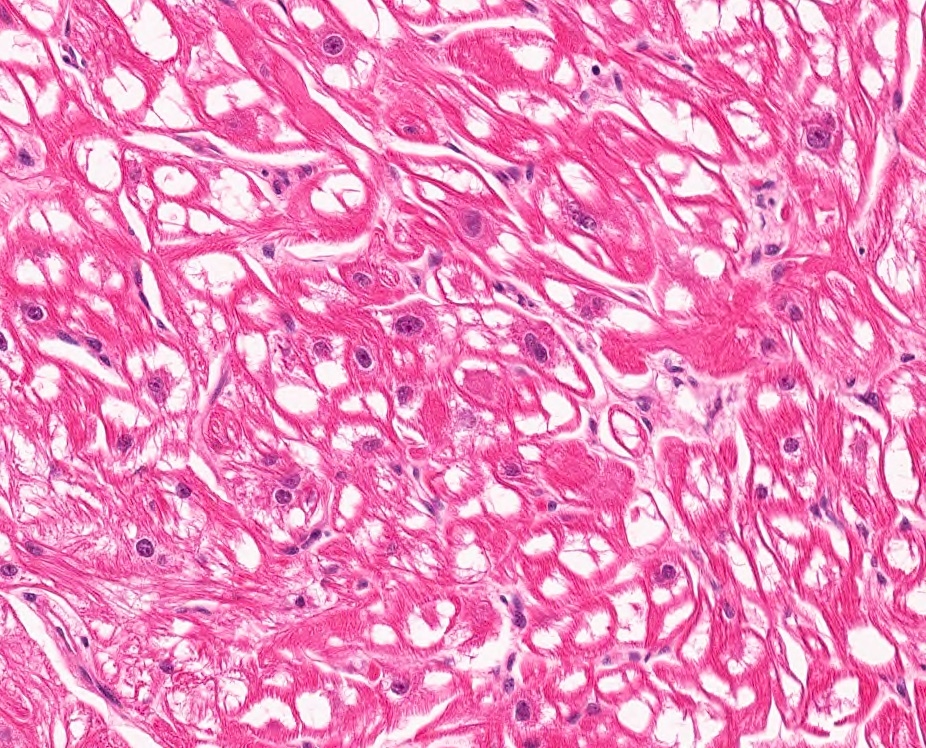
Microscopic (histologic) images
Contributed by Kemal Kösemehmetoğlu, M.D.
Virtual slides
Positive staining - normal
- Breast myoepithelial cells (most) (Breast Cancer Res 2003;5:R151, Proc Natl Acad Sci U S A 1993;90:999)
- Chondrocytes, choroidal nonvascular smooth muscle cells (Folia Biol (Praha) 2006;52:167, J Anat 2005;207:381)
- Decidual stromal cells, fibroblastic reticulum cells (Hum Reprod 1999;14:1599, J Cancer Res Clin Oncol 1981;101:149)
- Glomus coccygeum, hepatic stellate cells (Arch Pathol Lab Med 1999;123:905, Virchows Arch 1997;430:195)
- Myofibroblasts (except alveolar and some granulation tissue / scars) (J Histochem Cytochem 1992;40:1955, Lab Invest 1989;60:275, Int J Legal Med 1992;105:99)
- Osteoblasts (J Orthop Res 2002;20:622)
- Pericytes (J Histochem Cytochem 1989;37:315)
- Salivary glands (APMIS 1991;99:405)
- Smooth muscle and vascular smooth muscle (Proc Natl Acad Sci U S A 1981;78:298)
- Sweat glands and tracheobronchial glands (J Histochem Cytochem 1988;36:659)
Positive staining - disease
- Adenoid cystic carcinoma (Arch Pathol Lab Med 1999;123:801)
- Atypical teratoid / rhabdoid tumor (J Neurosurg 1996;85:56, Brain Tumor Pathol 2008;25:79)
- Benign fibrous histiocytoma (in deep form 38%) (Am J Surg Pathol 2008;32:354)
- Biphenotypic sinonasal sarcoma (Am J Surg Pathol 2012;36:517)
- Cellular angiofibroma (focal, 41%) (Mod Pathol 2011;24:82)
- Cellular neurothekeoma (at least focal in 57%) (Am J Surg Pathol 2007;31:329)
- Collagenous spherulosis (Mod Pathol 2006;19:1351)
- Chronic obstructive pulmonary disease (COPD): large airways have increased expression of SMA (Respir Res 2011;12:48)
- Epstein-Barr virus associated smooth muscle tumour (EBV SMT) (Am J Surg Pathol 2006;30:75)
- Endometrial stromal sarcoma (65%) (Gynecol Oncol 2004;92:71)
- Epithelial myoepithelial carcinoma (Am J Surg Pathol 2007;31:44)
- Fibromatosis (56%) (Am J Surg Pathol 2002;26:1296)
- Gastrointestinal stromal tumor (GIST) (45%) (Am J Surg Pathol 2002;26:1296, Am J Pathol 1990;136:771)
- Glomus tumor (Hum Pathol 1999;30:1259, Am J Pathol 1990;136:771)
- Granulosa cell tumors of ovary, both adult and juvenile (variable) (Mod Pathol 1995;8:25)
- Inflammatory myofibroblastic tumor (Am J Surg Pathol 1991;15:1146, Ann Diagn Pathol 2001;5:335, Am J Surg Pathol 1992;16:896, Turk J Gastroenterol 2012;23:399)
- Leiomyoma (Am J Dermatopathol 2006;28:105, Am J Pathol 1987;128:91)
- Leiomyosarcoma (Int J Gynecol Pathol 2011;30:236, Anticancer Res 2005;25:1559)
- Liposarcoma, pleomorphic (focal in 40 - 50%), dedifferentiated (50%), well differentiated (in the form of pericytic mimicry) (Am J Surg Pathol 2002;26:601, Am J Surg Pathol 2004;28:1257, Am J Surg Pathol 2020;44:799, Hum Pathol 2016;54:92)
- Melanoma, desmoplastic / spindle cell (Am J Dermatopathol 1999;21:537, Am J Surg Pathol 2006;30:75, Am J Surg Pathol 1996;20:1489)
- Mesothelioma, sarcomatoid (60%) (Histopathology 2003;42:270)
- Myoepithelioma (Hum Pathol 2004;35:14, Am J Surg Pathol 2003;27:1183)
- Myofibroma / myopericytoma (Am J Pathol 1987;128:91)
- Myofibroblastic sarcoma (Chin Med J (Engl) 2007;120:363, Int J Oral Sci 2012;4:170, Am J Dermatopathol 2006;28:105)
- Neurothekeoma (40% focal) (Am J Pathol 1987;128:91)
- Nodular fasciitis (Ann Diagn Pathol 2002;6:94, Am J Dermatopathol 2006;28:105)
- PEComas (angiomyolipoma, pulmonary lymphangioleiomyomatosis) (J Egypt Natl Canc Inst 2013;25:125, J Clin Pathol 1993;46:479, Tohoku J Exp Med 2003;199:119)
- Plexiform fibrohistiocytic tumor (Am J Surg Pathol 1994;18:668, Histopathology 1991;19:503)
- Plexiform fibromyxoma (Am J Surg Pathol 2009;33:1624)
- Renal mixed epithelial and stromal tumor (Arch Pathol Lab Med 2006;130:80, Beijing Da Xue Xue Bao 2008;40:415)
- Rhabdomyoma (focal / rare) (Hum Pathol 1993;24:754, Hum Pathol 1993;24:608)
- Rhabdomyosarcoma embryonal, alveolar and sclerosing / spindle cell (Pediatr Dev Pathol 2005;8:427, Korean J Ophthalmol 2006;20:70, Virchows Arch 2006;449:554)
- Soft tissue perineurioma (21%) (Am J Surg Pathol 2005;29:845)
- Synovial sarcoma (25%) Mod Pathol 2007;20:760)
- Undifferentiated pleomorphic sarcoma (focal) (J Clin Pathol 2003;56:666, Histopathology 2006;48:453)
Negative staining
- Normal tissue:
- Cardiac muscle (positive during development) (J Cell Sci 2007;120:229)
- Skeletal muscle (J Cell Biol 1985;100:807)
- Basal cells of prostate glands (Am J Surg Pathol 1996;20:1489)
- Disease:
- Angiomyofibroblastoma (rarely focal) (Hum Pathol 1997;28:1046)
- Carcinomas (usually)
- Cellular benign fibrous histiocytoma (Am J Surg Pathol 1994;18:668)
- Clear cell sarcoma (J Clin Pathol 2010;63:416)
- Epithelioid sarcoma proximal type (15 - 33%) (Am J Surg Pathol 1997;21:130, Mod Pathol 2001;14:655)
- Fibrosarcoma, infantile and adult type (rare / focal; expression does not exclude diagnosis) (Am J Clin Pathol 2001;115:348)
- Hemosiderotic fibrolipomatous tumor (Histopathology 2006;48:453)
- Liposarcoma, myxoid type (rarely focal) (Am J Clin Pathol 1995;103:20)
- Low grade fibromyxoid sarcoma (LGFMS) (rare / focal) (Lab Invest 2005;85:408)
- Myofibroblastoma (occasionally focally positive) (Pathology 2005;37:144, Am J Surg Pathol 2001;25:1022)
- Ossifying fibromyxoid tumor (weak); 6% (J Laryngol Otol 1993;107:75, Am J Surg Pathol 2011;35:1615)
- Thecoma / fibrothecoma (Mod Pathol 1995;8:25)
- Schwannoma, solitary fibrous tumor (Arch Pathol Lab Med 2006;130:1503, Diagn Pathol 2021;16:32)
- Sclerosing epithelioid fibrosarcoma (Am J Surg Pathol 1995;19:979)
Sample pathology report
- Right 3rd intercostal space, wide excision:
- Leiomyosarcoma, grade 3 (see comment)
- Comment: Immunohistochemically, neoplastic cells showed diffuse strong cytoplasmic staining for SMA, desmin and h-caldesmon.
- Right thigh, excisional biopsy:
- Nodular fasciitis (see comment)
- Comment: Immunohistochemically, neoplastic cells were positive for SMA in myofibroblastic pattern (tram track staining) and negative for desmin.
Board review style question #1
Board review style answer #1
B. Demonstrates smooth muscle type of SMA staining
Comment Here
Reference: Actin, alpha smooth muscle type
Comment Here
Reference: Actin, alpha smooth muscle type
Adenovirus
Table of Contents
Definition / general | Essential features | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - disease | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Antiadenovirus is a cocktail of mouse monoclonal antibodies derived from cell culture supernatant
- Though there are numerous genera within the Adenoviridae family, the antigen targeted (group specific hexon antigen) in commercially available antiadenovirus cocktails has been selected to detect all known, clinically important adenovirus serotypes
Essential features
- Antiadenovirus is a cocktail of mouse monoclonal antibodies with nuclear and cytoplasmic staining pattern developed to detect all known serotypes of adenovirus
- False positives are extremely uncommon
- Most false negatives (cases with positive viral cytopathic effect and negative IHC) result from exhaustion of the diagnostic tissue
Pathophysiology
- Double stranded, nonenveloped DNA viruses with a single, nonsegmented linear genome capped by covalently bound terminal proteins at either end of the genome
- Adenovirus produces nuclear inclusions without cytomegaly
- Virus binds to coxsackie adenovirus receptor, CD46 (complement regulatory protein), desmoglein 2 or sialic acid (primary receptor used depends on the viral serogroup), followed by viral internalization (Rev Med Virol 2009;19:165, Nat Med 2011;17:96)
- Viral replication cycle takes ~32 - 36 hours and up to 10,000 virions can be produced; new virions remain in the cell until it degenerates and lyses (Tille: Bailey & Scott's Diagnostic Microbiology, 13th Edition, 2013)
Clinical features
- Adenoviruses are spread via aerosols, in fecal matter or through close contact
- Adenovirus infection is especially common in military barracks and college dormitories
- Children under 14 and immunocompromised patients (including transplant recipients) are especially vulnerable
- Though certain viral subclasses exhibit seasonality, adenovirus infections occur all year round
- Reference: Trends Mol Med 2023;29:4
Interpretation
- Nuclear and cytoplasmic
- False positives are extremely uncommon
- Most false negatives (cases with positive viral cytopathic effect and negative IHC) result from exhaustion of the diagnostic tissue (Am J Clin Pathol 2017;147:96)
- Other limitations of this and other IHC tests are fixation time of tissues, dilution factor of antibody, retrieval method utilized and incubation time; optimal performance should be established through positive and negative controls
Uses by pathologists
- Various commercially available antibodies used for immunohistochemistry may not provide complete coverage against all 51 serotypes of adenovirus; diagnosis needs to be confirmed by polymerase chain reaction or electron microscopy
- Allograft infection in solid organ transplant recipients (Virchows Arch 2015;467:603)
- Adenovirus interstitial nephritis in renal allograft recipients (Kidney Int 2023;103;378, Clin J Am Soc Nephrol 2012;7:1884)
- Adenoviral enteropathy in small bowel transplantation recipients (Clin Transplant 2016;30:1433, Arch Pathol Lab Med 2008;132:703)
- Adenovirus hepatitis in the adult allograft liver (Transplantation 1997;64:1483)
- Detection of adenovirus in hematopoietic stem cell transplant patients (Leuk Lymphoma 2004;45:873)
- Similar antibodies used to detect adenoviruses on tissue section are commercially available for laboratory use in enzyme immunoassays
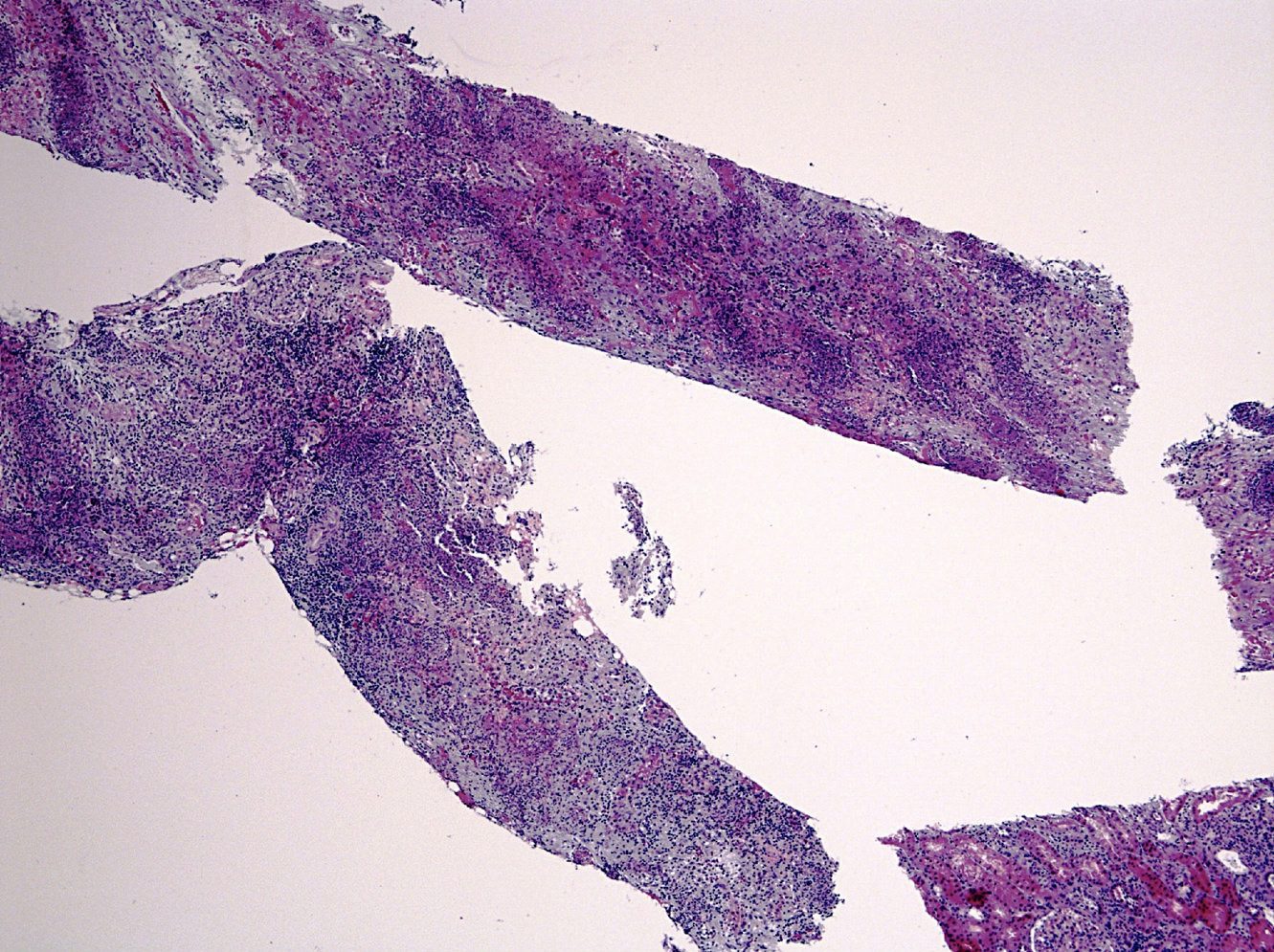
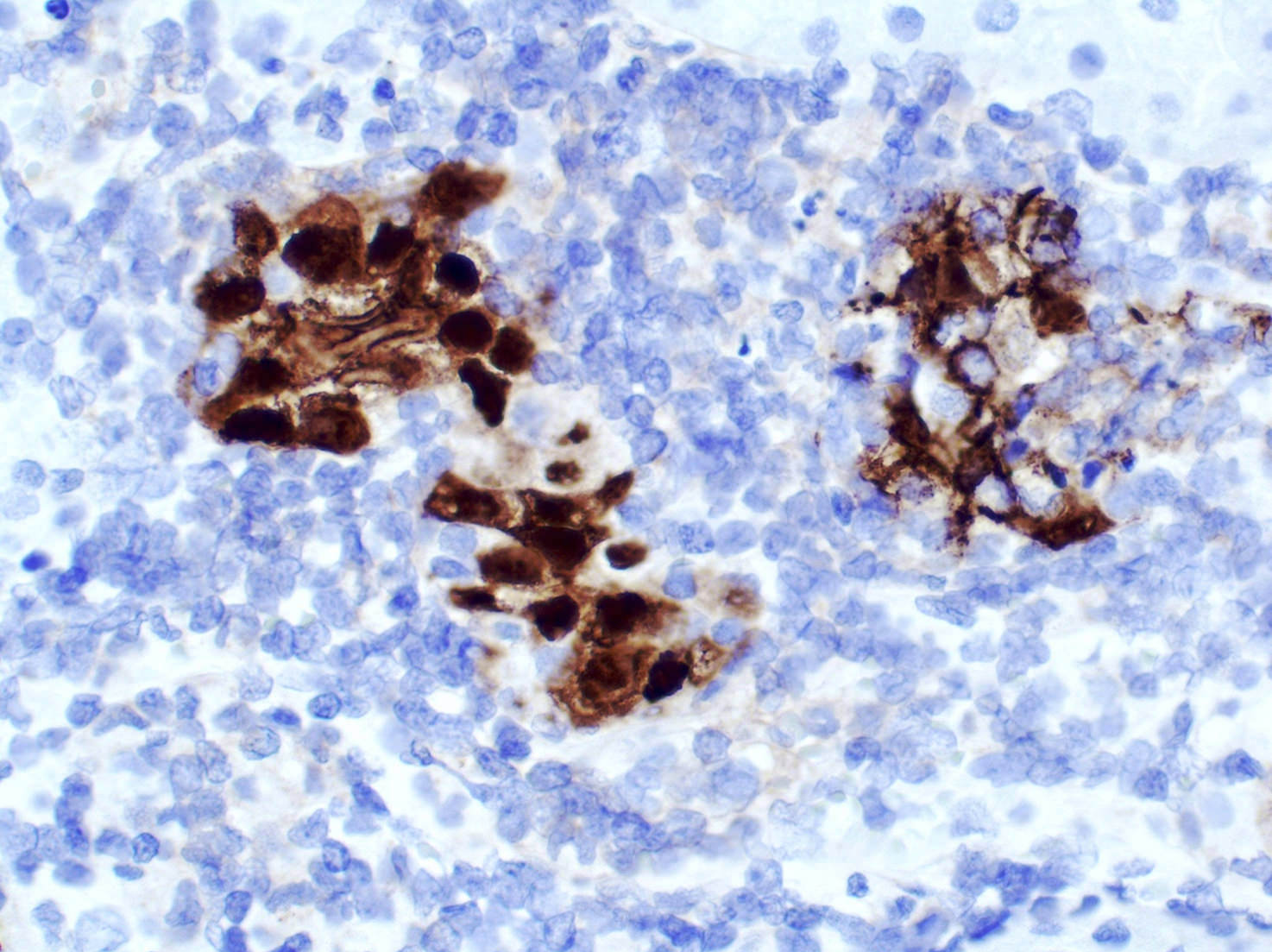
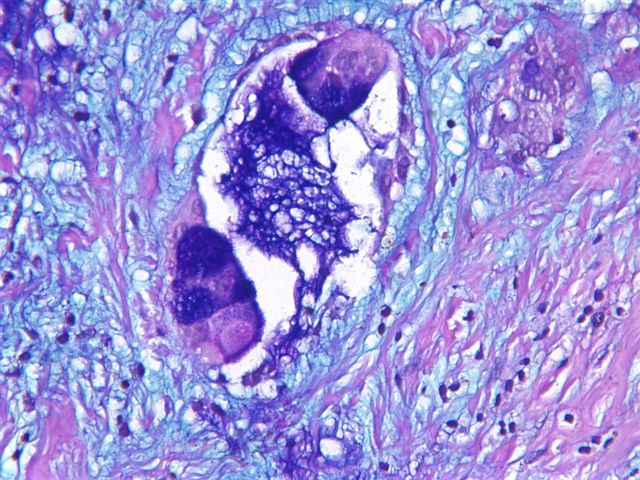
Microscopic (histologic) images
Positive staining - disease
- Adenovirus infection in pediatric solid organ and hematopoietic stem cell transplantation (Curr Infect Dis Rep 2012;14:658)
Molecular / cytogenetics description
- Gene amplification or DNA in situ hybridization can be used for identification
Sample pathology report
- Kidney, needle core biopsy:
- Adenovirus nephritis (see comment)
- Comment: Renal parenchyma with necrotizing tubulointerstitial nephritis is consistent with adenovirus nephritis. Immunohistochemical stain for adenovirus shows nuclear and cytoplasmic expression in affected cells.
- Liver, needle core biopsy:
- Adenovirus hepatitis (see comment)
- Comment: Liver parenchyma with necrotizing hepatitis is consistent with adenovirus hepatitis. Immunohistochemical stain for adenovirus shows nuclear and cytoplasmic expression in affected cells.
Additional references
Board review style question #1
Board review style answer #1
D. Nuclear and cytoplasmic. Of the choices listed, nuclear and cytoplasmic staining is seen in IHC for adenovirus. However, a virus specific diagnosis cannot be made based on the pattern of stain alone, as other stains can show nuclear and cytoplasmic staining. For example, diffuse and strong nuclear or nuclear and cytoplasmic staining involving the basal and parabasal layers of squamous epithelium is seen in p16 testing for HPV (block-like staining). Thus, the diagnosis is based on the antibody specificity while the pattern of stain is helpful. Moreover, the type of infected cell can be helpful in the differential diagnosis (e.g., CMV typically infects endothelium while adenovirus infects epithelial cells, as illustrated in this topic). Cytoplasmic stain is typically seen in IHC for several keratins or other intracytoplasmic proteins; stain for CK20 in Merkel cell carcinoma is an exception. Dot-like stain is typically seen for CK20 in Merkel cell carcinoma. Nuclear stain is positive in IHC for polyoma virus.
Comment Here
Reference: Adenovirus
Comment Here
Reference: Adenovirus
Adipophilin (pending)
[Pending]
Albumin
Definition / general
- Most common serum protein
- 65K protein produced by ALB gene on #4, by liver (Wikipedia)
- 50% of total plasma protein content; usual serum concentration of 40 g/L
- Binds to water, bilirubin, calcium, fatty acids, hormones (acts as carrier protein), potassium, sodium, and various drugs
- Main function of serum albumin is to regulate blood colloidal osmotic pressure
- Bovine serum albumin (BSA): plasma protein from cows that maintains osmotic pressure in blood plasma for proper distribution of body fluids between intravascular compartments and body tissues
- Rarely used as IHC marker for liver
Clinical features
- Laboratory:
- For serum albumin measure, most instrument systems do NOT have satisfactory total-error performance (Arch Pathol Lab Med 2013;137:912)
- Serum albumin may be a low cost diagnostic marker for tuberculosis in HIV+ patients eligible for antiretroviral therapy (Bioimpacts 2013;3:123)
- In type 2 diabetes patients with stable angina and chronic total coronary occlusion, increased serum glycated albumin levels are associated with impaired coronary collateral growth (Cardiovasc Diabetol 2013;12:165)
- Deficiency causes familial dysalbuminemic hyperthyroxinemia (MIM:103600)
- Surgical pathology
- Useful to differentiate cholangiocarcinoma (positive) from metastatic adenocarcinoma (usually negative, Ann Surg Oncol 2016;23:290, Am J Clin Pathol 2019;152:190, Am J Surg Pathol 2002;26:989) as well as intrahepatic from extrahepatic cholangiocarcinoma
Microscopic (histologic) images
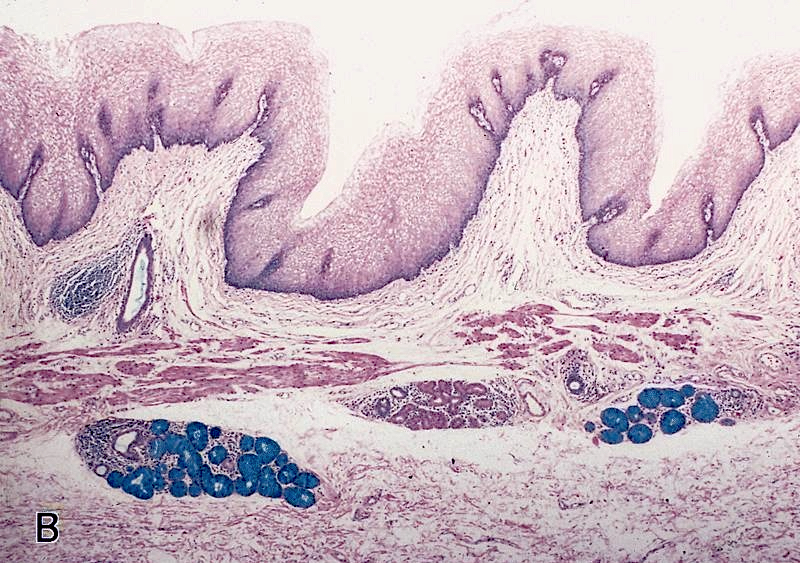
Alcian blue
Table of Contents
Definition / general | Uses by pathologists | Clinical features | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Common "routine" stain (not an immunohistochemical stain) to detect mucins (Wikipedia: Alcian Blue Stain [Accessed 8 August 2018])
- At pH 2.5, detects acidic mucins
- At pH 1.0, detects highly acidic mucins
- Stained parts are blue to bluish green
- Note: all references below are to pH 2.5 unless otherwise indicated
Uses by pathologists
- Stains acid-simple, nonsulfated and acid-simple mesenchymal mucins at pH 2.5, acid-complex sulfated mucins at pH 1.0 and acid-complex connective tissue mucins at pH 0.5; does NOT stain neutral mucins
- PAS-Alcian blue may be best pan mucin combination; PAS also stains glycogen, but predigestion with diastase will remove the glycogen
- Alcian blue-high iron diamine detects sulfomucins (brown) and sialomucins (blue)
Clinical features
- Procedure (University of Utah)
- May be useful in FNA diagnosis of salivary gland pleomorphic adenoma (J Cytol 2012;29:221)
- Stains glycosaminoglycan deposits in macular corneal dystrophy (Korean J Ophthalmol 2013;27:454)
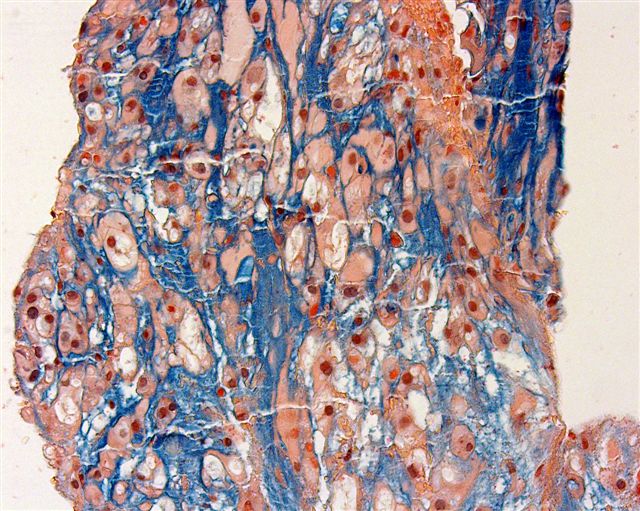
Microscopic (histologic) images
AFIP images and Cases #78, 94 and 110
Images hosted other servers:
Positive staining - normal
- Colloid of thyroid gland, goblet cells and mucous glands
Positive staining - disease
- Adenocarcinoma, adenosquamous carcinoma, mast cell leukemia (Acta Med Croatica 2013;67:61)
- Mucinous tumors, myxedema (dermal mucin), myxoma (mucoid matrix), nodular mucinosis (breast, other) and Paget disease of scrotum
Negative staining
- Lipids / lipid entities (lipoma, liposarcoma), Paget disease of esophagus, squamous cell carcinoma (acantholytic variant-breast & other sites, pseudoglandular variant-penis & other sites), xanthelasma
ALK
Table of Contents
Definition / general | Essential features | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Anaplastic lymphoma kinase gene is at 2p23; protein is called ALK1, CD246
- Membrane spanning tyrosine kinase receptor, member of insulin receptor family
- First discovered in anaplastic large cell lymphoma (ALCL) with t (2;5) being the first ALK fusion identified to NPM (nucleophosmin protein)
- References: OMIM: 105590 [Accessed 25 June 2021], Science 1994;263:1281, Genes Chromosomes Cancer 2002;34:354
Essential features
- ALK overexpression occurs as a result of diverse alterations, including translocation, mutation and amplification / polysomy, among others
- Tumors harboring ALK translocations are potentially sensitive to ALK inhibitors
- Pathologists should be aware of the frequency of ALK overexpression and translocations according to tumor type to maximize ALK screening in the appropriate clinical setting
- Understanding the limitations of testing methodologies is important to avoid pitfalls in interpretation
- ALK expression in itself is a defining feature of specific entities, which when present, enables tumor classification and subtyping in routine pathology practice.
Pathophysiology
- Activation of ALK receptor requires ligand binding, which triggers homodimerization and transphosphorylation of its tyrosine kinase inhibitor (TKI) domain
- ALK is an orphan receptor with no known ligand; heparin is one of the known activating ligands, which promotes ALK signaling through heparin sulfation, leading to ALK dimerization (Science Signaling 2015;8:ra6)
- Downstream signaling pathways triggered by ALK include STAT3, ERK1 / ERK2, PLC and PI3K / AKT, which upon activation lead to cell proliferation and survival
- In the inactive state, the ALK receptor promotes apoptosis via caspase 3 activation, leading to kinase inactivation
- In ALK chromosomal rearrangements, the 3' portion of ALK, which contains the TKI domain, fuses with the 5' of a partner gene that provides the N-terminus with the dimerization domain
- Fusion chimeric oncoproteins result in constitutive autophosphorylation of the ALK kinase, leading to uncontrolled cell proliferation and survival
- References: Oncol Lett 2019;17:2020, Cancers (Basel) 2019;11:275
Clinical features
- Large group of unrelated malignant and benign tumors express ALK; its expression is not a marker of malignant phenotype
- Prognostic significance of ALK expression depends on tumor type, the underlying molecular mechanism of ALK expression and sensitivity to ALK inhibitors
- ALK rearrangement predicts response to ALK inhibitors
- Testing for ALK rearrangements is recommended in all patients with lung adenocarcinomas to guide therapy
- ALK inhibitors are offered to any ALK rearranged tumor in the advanced or metastatic setting
- Therapeutic inhibition of ALK fusion oncoproteins is achieved through small molecule TKI, with crizotinib being the first ALK TKI approved by the FDA
- ALK driven resistance occurs due to secondary mutations in the kinase domain or gene amplification
- Second (i.e. ceritinib and alectinib) and third (i.e. lorlatinib) generation TKI are used to overcome resistance, including emerging new targets of the ALK signaling pathway (i.e. STAT3, PI3K or ERK / MEK)
- References: Cancers (Basel) 2019;11:275, Oncol Lett 2019;17:2020
Interpretation
- Detection of ALK gene alterations by current technology
- Immunohistochemistry
- Strong granular cytoplasmic expression for ALK with or without membranous or nuclear expression is predictive of ALK rearrangement and response to ALK TKI
- Positive IHC correlates with tumor response to ALK inhibitors even in ALK FISH negative cases (J Clin Pathol 2021 [Epub ahead of print], Arch Pathol Lab Med 2018;142:321)
- Absence of ALK protein expression indicates that a tumor is unlikely to harbor ALK rearrangement or to respond to ALK inhibitors
- Different clones available: D5F3, 5A4, 1A4 and ALK1 (J Clin Pathol 2021 [Epub ahead of print], Arch Pathol Lab Med 2018;142:321)
- 5A4 and D5F3 are equivalent alternatives to ALK FISH testing; in particular, the Ventana ALK D5F3 CDx Assay is an FDA approved companion diagnostic assay to determine eligibility for ALK inhibitors (J Clin Pathol 2021 [Epub ahead of print], Arch Pathol Lab Med 2018;142:321)
- Clone ALK1 is currently mostly limited to ALCL and not recommended for screening rearrangements in solid tumors due to poor sensitivity (67 - 100%) (Arch Pathol Lab Med 2018;142:321)
- Pattern of ALK staining varies, depending on the gene fusion partner:
- Nuclear and cytoplasmic expression: NPM1-ALK and RANBP2-ALK fusions and the ALKATI isoform (Am J Surg Pathol 2017;41:25, Am J Surg Pathol 2011;35:135, Am J Surg Pathol 2016;40:786)
- Membranous and cytoplasmic expression: TPM3-ALK fusions (Semin Diagn Pathol 2020;37:57)
- Diffuse cytoplasmic expression: identified with the following fusion partners: EML4, ATIC, TFG, TPM4, MYH9, ALO17, TRAF1, PABPC1, EEF1G; CLTC-ALK fusion shows cytoplasmic granular / dotted pattern (Semin Diagn Pathol 2020;37:57, Am J Surg Pathol 2017;41:25)
- Pitfalls in ALK IHC:
- Faint cytoplasmic labelling for ALK should be designated as equivocal, as this can occur in the absence of specific targeted alterations
- False positive stain in neuroendocrine cells
- Nonspecific background staining in mucin
- False negative stain in cells with signet ring cell morphology due to nuclear displacement by mucin (J Clin Pathol 2021 [Epub ahead of print])
- Immunohistochemistry
- Reference: Tsao: IASLC Atlas of ALK and ROS1 Testing in Lung Cancer, 2nd Edition, 2016
Uses by pathologists
- ALK immunohistochemistry (IHC) is used as a predictive biomarker of an underlying ALK translocation (or other gene alteration), to identify patients who can potentially benefit from ALK inhibitors
- Presence of ALK positivity by IHC in the context of specific histological features allows tumor classification in routine pathology practice
- References: J Clin Pathol 2021 Apr 19 [Epub ahead of print], Arch Pathol Lab Med 2018;142:321
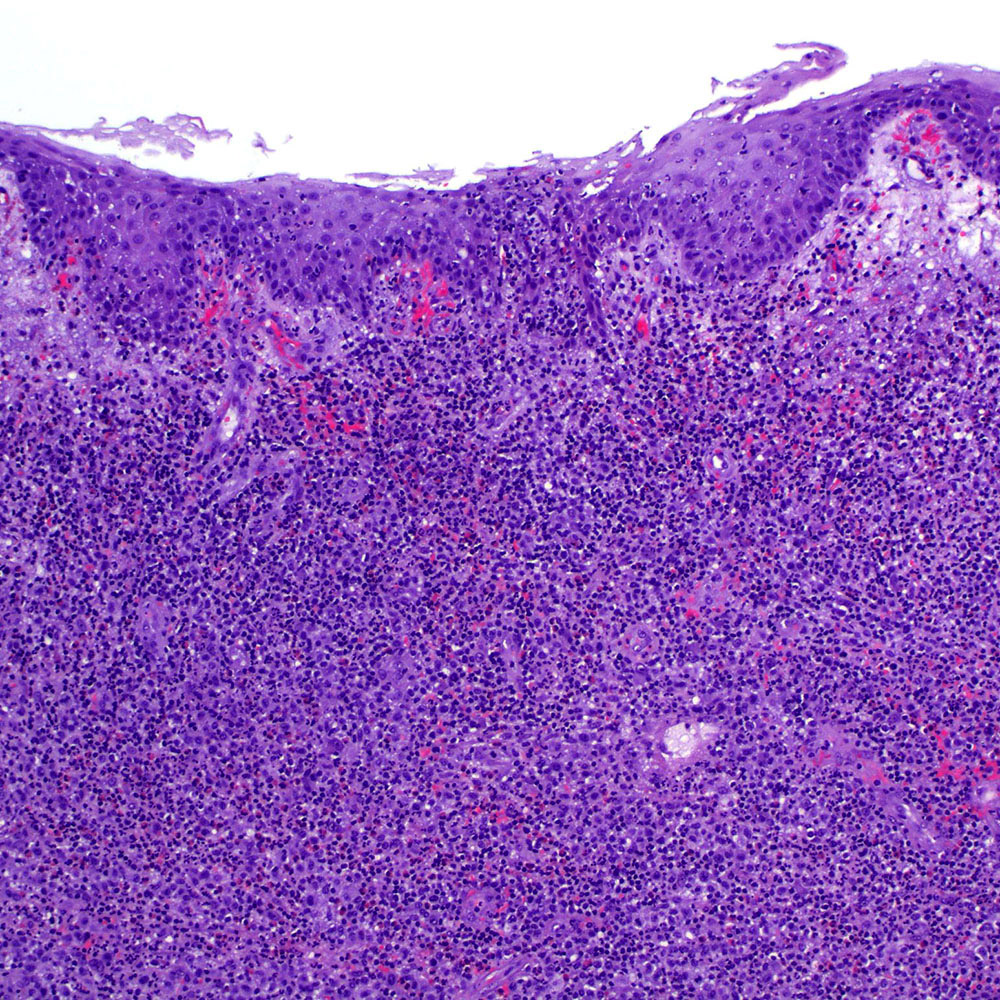
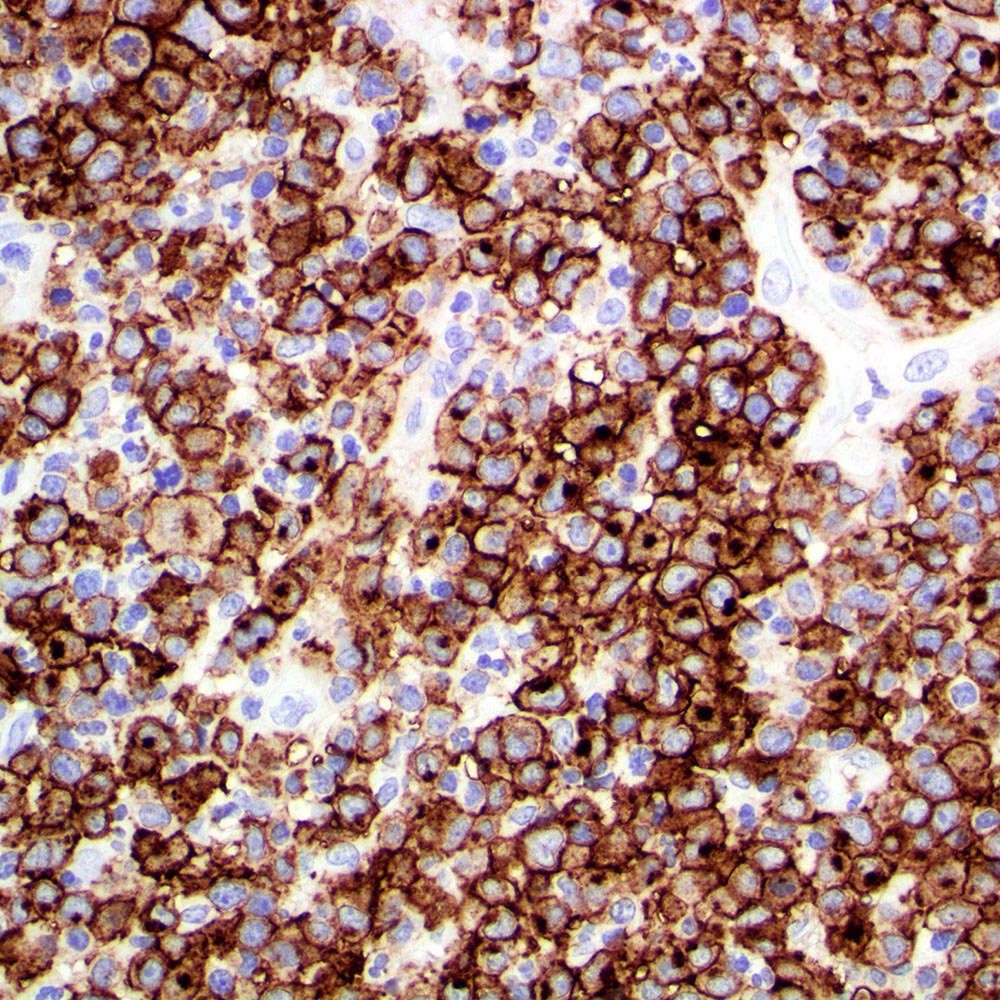
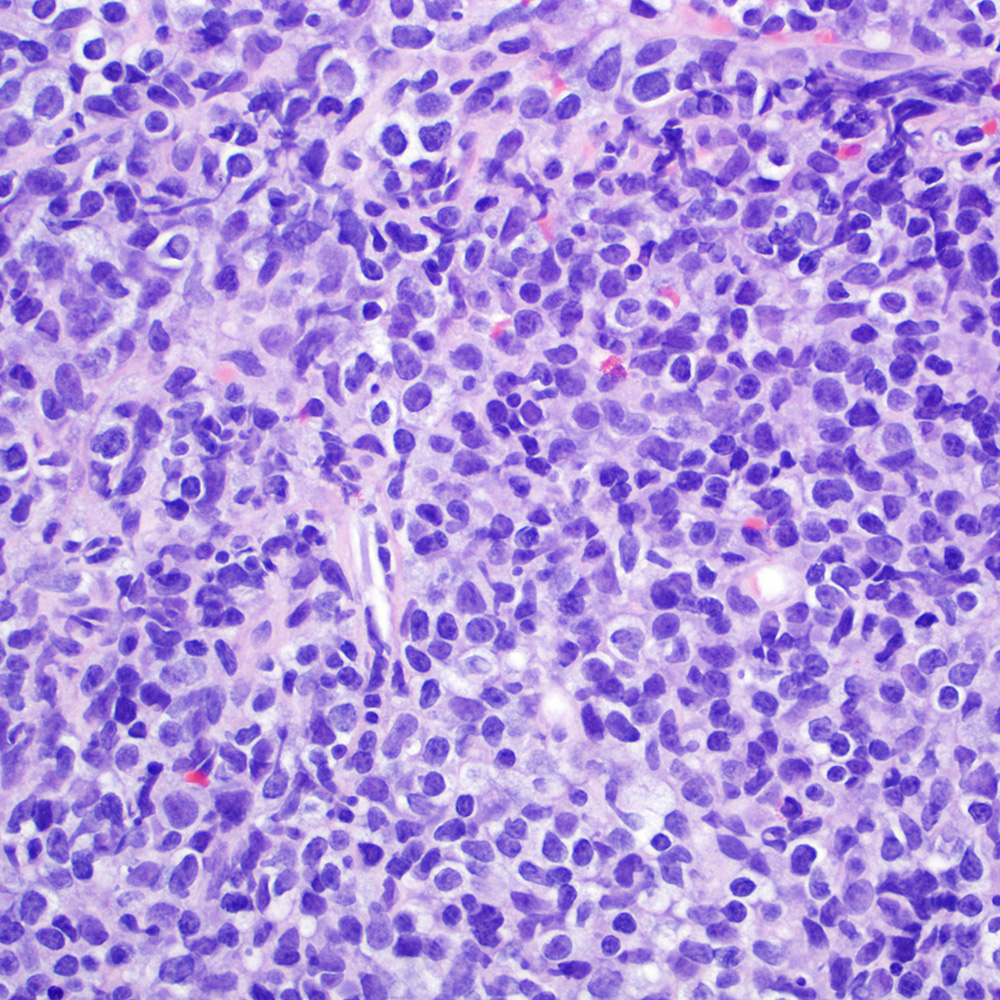
Microscopic (histologic) images
Contributed by A. Cristina Vargas, M.B.B.S., Ph.D., Patricia Guzman, M.D., Fiona Bonar, M.B.B.Ch., Alison Cheah, M.B.B.S. and Martin Jones, M.B.B.S.
Positive staining - normal
- ALK expression in normal tissue is limited to restricted zones of the brain, peripheral nervous system and testis
Positive staining - disease
- ALK overexpression as a result of gene translocations / fusions:
- ALK+ anaplastic large cell lymphoma (ALCL) (Science 1994;263:1281, Semin Diagn Pathol 2020;37:57)
- Approximately 4% of lung adenocarcinomas, which show an association with mucinous cribriform and solid signet ring cell patterns and usually lack significant pleomorphism (J Clin Pathol 2021 [Epub ahead of print], Am J Surg Pathol 2011;35:1226)
- 50% of inflammatory myofibroblastic tumors (IMT) (Am J Surg Pathol 2015;39:957)
- Including the aggressive variant, epithelioid inflammatory myofibroblastic sarcoma (Am J Surg Pathol 2011;35:135)
- Thyroid carcinomas, predominantly papillary (in particular the follicular variant), poorly differentiated and anaplastic (Am J Surg Pathol 2015;39:652, Endocr Relat Cancer 2019;26:803)
- 10% of Spitz tumors, including nevi, atypical Spitz tumors and Spitzoid melanomas (Am J Surg Pathol 2015;39:581)
- ALK+ large B cell lymphoma, a variant of diffuse large B cell lymphoma (DLBCL) (Am J Surg Pathol 2017;41:25)
- Distinct subgroup of renal cell carcinomas, usually in the pediatric population (Genes Chromosomes Cancer 2016;55:442)
- Rare salivary gland carcinomas, including myoepithelial carcinoma, secretory carcinoma, intraductal carcinoma and salivary duct carcinoma (Virchows Arch 2021;478:933, Am J Surg Pathol 2020;44:962)
- ALK+ histiocytosis, which can present as localized disease or systemic involvement at a wide age range (Mod Pathol 2019;32:598)
- Including presentation as breast masses (Am J Surg Pathol 2021;45:347)
- Rare cases (0.1%) of colorectal carcinomas, usually DNA mismatch repair deficient and pancreatic adenocarcinoma (Am J Surg Pathol 2020;44:1224, J Natl Compr Canc Netw 2017;15:555)
- Subset (3%) of peritoneal mesotheliomas, including pediatric cases but not in the pleural counterpart (JAMA Oncol 2018;4:235, Am J Surg Pathol 2021;45:653)
- Unrelated cutaneous neoplasms:
- Epithelioid fibrous histiocytoma (> 80%) (Mod Pathol 2015;28:904)
- Non neural granular cell tumor (NNGCT) (Am J Surg Pathol 2018;42:1133)
- Primary ALK+ cutaneous ALCL (2%) (Am J Surg Pathol 2020;44:776)
- Other soft tissue tumors:
- 2.4% of leiomyosarcoma (Mol Cancer Res 2019;17:676)
- And a group of mesenchymal spindle cell neoplasms with a specific phenotype (S100+ / SOX10- / CD34+) (Genes Chromosomes Cancer 2021;60:282, Genes Chromosomes Cancer 2018;57:611)
Table: ALK gene fusion partners according to tumor entity
| Tumor type | Most common ALK gene fusion partners | References |
| Lung adenocarcinoma | EML4 (80%), NPM1, CLTC, TPM3, RANBP2, STRN, ATIC, KIF5B, TPM4, TFG, HIP1, SQSTM1, A2M, KLC1, TPR | J Clin Pathol 2021 [Epub ahead of print], Am J Surg Pathol 2011;35:1226, Oncol Lett 2019;17:2020 |
| Anaplastic large cell lymphoma (ALCL) | NPM1 (80%), TPM3, ATIC, TFG, CLTC, MSN, TPM4, MYH9, ALO17, TRAF1, EEF1G, PAPBC1, SQSTM1 | Science 1994;263:1281, Semin Diagn Pathol 2020;37:57, Oncol Lett 2019;17:2020 |
| ALK+ primary cutaneous ALCL | NPM1, TRAF1, ATIC, TPM3 | Am J Surg Pathol 2020;44:776 |
| Inflammatory myofibroblastic tumor (IMT) | TPM3, TPM4, RANBP2, TFG, CARS, ATIC LMNA, PRKAR1A, CLTC, FN1, SEC31A, EML4, DCTN1, PPFIBP1, FN1 | Am J Surg Pathol 2015;39:957, Oncol Lett 2019;17:2020 |
| Epithelioid IMT | RANBP2 | Am J Surg Pathol 2011;35:135 |
| Spitz tumors | DCTN1, TPM3, NPM1, TPR | Am J Surg Pathol 2015;39:581 |
| Thyroid carcinoma | STRN, EML4, TFG, GTF2IRD1, CCDC149, ITSN2, CTSB, PPP1R21, DCTN1 | Am J Surg Pathol 2015;39:652, Endocr Relat Cancer 2019;26:803, Oncol Lett 2019;17:2020 |
| Renal cell carcinomas | TPM3, EML4 , STRN, VCL | Genes Chromosomes Cancer 2016;55:442, Oncol Lett 2019;17:2020 |
| Peritoneal mesothelioma | STRN, ATG16L1, TPM1 | JAMA Oncol 2018;4:235, Am J Surg Pathol 2021;45:653 |
| ALK+ histiocytosis | TPM3, KIF5B | Mod Pathol 2019;32:598, Am J Surg Pathol 2021;45:347 |
| Salivary gland carcinomas | MSN (myoepithelial), CTNNA1 (secretory), STRN, MYO18A (intraductal), HNRNPH3, EML4 (salivary duct) | Virchows Arch 2021;478:933, Am J Surg Pathol 2020;44:962 |
| Colorectal adenocarcinoma | EML4, TPM4, CAD, SPTBN1, SLMAP, DIAPH2, LOC101929227, DIAPH2, STRN | Am J Surg Pathol 2020;44:1224, Oncol Lett 2019;17:2020 |
| Pancreatic adenocarcinoma | EML4, STRN | J Natl Compr Canc Netw 2017;15:555 |
| Leiomyosarcoma | STK32B, IGFBP5, ACTG2, TNS1, KANK2 | Mol Cancer Res 2019;17:676 |
| Mesenchymal spindle cell tumors (S100+ / SOX10- / CD34+) | EML4, PPP1CB, CLIP1 | Genes Chromosomes Cancer 2021;60:282, Genes Chromosomes Cancer 2018;57:611 |
| Non neural granular cell tumor (NNGCT) | DCTN1, SQSTM1 | Am J Surg Pathol 2018;42:1133 |
| Epithelioid fibrous histiocytoma | VCL, SQSTM1 | Mod Pathol 2015;28:904 |
| ALK+ large B cell lymphoma | CLTC, NPM1, SEC31A, SQSTM1, RANBP2, IGL | Am J Surg Pathol 2017;41:25 |
- ALK overexpression as a result of mutations or other gene alterations
- Medulloblastomas can harbor ALK somatic or germline mutations (e.g. p.M1199L, c.3605delG), amplification or increased mRNA expression (Am J Surg Pathol 2017;41:781)
- Subset of acral melanoma harbors the so called ALKATI isoform, arising from an alternative transcription initiation (Am J Surg Pathol 2016;40:786)
- ALK overexpression not associated with gene fusions or well characterized gene alterations
- Rhabdomyosarcomas (RMS) of embryonal and alveolar types including the recently described group FET-TFCP2 rearranged (RMS) (Mod Pathol 2020;33:404)
- Proportion of breast cancers with overexpression due to gene amplification (Breast Cancer Res 2015;17:127)
- Angiomatoid fibrous histiocytoma (Am J Surg Pathol 2019;43:93)
- Merkel cell carcinoma (Cancers (Basel) 2017;9:123)
- Small subset of salivary gland carcinomas (Virchows Arch 2021;478:933)
Molecular / cytogenetics description
- Fluorescent in situ hybridization (FISH)
- FISH using break apart (BA) probes is the most widely available technology for detection of ALK gene rearrangements in routine clinical practice
- Currently, the Vysis ALK Break Apart FISH Probe Kit (Abbott Molecular, Des Plaines, Illinois, USA) is the only approved companion diagnostic tool for crizotinib based treatment eligibility
- FISH BA positive result is established using a threshold of 15% tumor cells showing either signals separated by at least 2 probe diameters or 3’ isolated red signals (due to deletion of the 5' probe)
- Isolated 3’ red signal pattern and other atypical signal patterns (5’ green signals or red doublet) can result in false positive and negative results when compared with detection by next generation sequencing
- Polysomy including increased copy number or amplification detected by FISH does not predict response to therapy with targeted ALK inhibitors
- Issues associated with discordant IHC and FISH or false negative FISH: complex deletions / rearrangements, cryptic insertions, alterations of ALK promoter and gene amplification
- Next generation sequencing and mutation testing
- There is a good degree of concordance among FISH, next generation sequencing and IHC but discordant cases occur due to rare fusions or complex rearrangements only detected by next generation sequencing
- RNA sequencing or other next generation sequencing based technology is recommended to elucidate cases with atypical / isolated signal FISH patterns
- Routine somatic testing to identify secondary ALK mutations arising in the setting of acquired resistance to ALK inhibitors is currently not recommended in the routine setting
- ALK germline mutation testing should be targeted in specific clinical settings
- References: Clin Lung Cancer 2019;20:e421, Lung Cancer 2019;131:62, Arch Pathol Lab Med 2018;142:321, J Clin Pathol 2021 [Epub ahead of print], Tsao: IASLC Atlas of ALK and ROS1 Testing in Lung Cancer, 2nd Edition, 2016
Molecular / cytogenetics images
Sample pathology report
- ALK should be reported following the guidelines established for lung adenocarcinoma (e.g. template for biomarker testing established by the College of American Pathologists: Lungbiomarker v1.3.0.2). An example report following this template includes the following:
- ALK rearrangement by molecular methods
- Rearrangement identified
- EML4-ALK
- Rearrangement identified
- Polysomy:
- Absent
- ALK by immunohistochemistry
- Positive: cytoplasmic and nuclear expression (Clone D5F3)
- ALK rearrangement testing method(s)
- In situ hybridization (fluorescence [FISH])
- Immunohistochemistry
- Ventana ALK (D5F3) immunohistochemistry (IHC) assay
- ALK rearrangement by molecular methods
- Full template of report (College of American Pathologists: Lungbiomarker v1.3.0.2) available in CAP: Cancer Protocol Templates [Accessed 30 June 2021]
Board review style question #1
What is the expected diagnosis for a uterine spindle cell tumor with this histological appearance? The tumor displayed focal smooth muscle expression, strong ALK overexpression on IHC and an ALK translocation was confirmed by FISH.
- Endometrial stromal sarcoma
- Epitheliod myofibroblastic sarcoma
- Inflammatory myofibroblastic tumor
- Leiomyoma
- Spindle cell tumor (S100+ / SOX10- / CD34+) with ALK translocations
Board review style answer #1
Board review style question #2
What are the most common tumors harboring ALK translocations?
- Anaplastic large cell lymphoma, Spitz tumors, thyroid carcinomas and renal cell carcinomas
- Colorectal adenocarcinoma, inflammatory myofibroblastic tumors, anaplastic large cell lymphoma and Merkel cell carcinoma
- Lung adenocarcinoma, breast cancer, inflammatory myofibroblastic tumors, rhabdomyosarcoma and Spitz tumors
- Lung adenocarcinoma, inflammatory myofibroblastic tumors, anaplastic large cell lymphoma and Spitz tumors
- Melanoma, lung adenocarcinoma, inflammatory myofibroblastic tumors and diffuse large B cell lymphoma
Board review style answer #2
D. Lung adenocarcinoma, inflammatory myofibroblastic tumors, anaplastic large cell lymphoma and Spitz tumors
Comment Here
Reference: ALK
Comment Here
Reference: ALK
Alkaline phosphatase
Table of Contents
Definition / general | Essential features | Terminology | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Definition / general
- An enzyme histochemical stain that relies on endogenous alkaline phosphatase activity to hydrolyze exogenous alpha naphthyl acid phosphate substrate to form naphthol, which in turn reacts with fast blue RR salt to form a black reaction product (Zhou: A Case-Based Guide to Neuromuscular Pathology, 1st Edition, 2020)
- Alkaline phosphatase reaction generates air bubbles if the section is cover slipped prematurely; to minimize this, it is advisable to wait at least 45 minutes before placing the coverslip over the stained section
Essential features
- In skeletal muscle, alkaline phosphatase is normally only present in the endothelium of arterioles but not in capillaries, myofibers or connective tissue (Nature 1962;195:611, J Histochem Cytochem 1970;18:55, Arch Histol Cytol 1998;61:215)
- The main use in a skeletal muscle biopsy is to highlight regenerating myofibers and connective tissue injury (Zhou: A Case-Based Guide to Neuromuscular Pathology, 1st Edition, 2020)
- Immune myopathies with perimysial pathology (IMPP), highlighted by alkaline phosphatase, are more commonly associated with antisynthetase syndrome associated autoantibodies, particularly Jo1 autoantibody; these patients are more likely to have interstitial lung disease, arthritis, Raynaud phenomenon, mechanic hands and excellent response to immune modulation therapy (Brain 2015;138:2485, Neurol Neuroimmunol Neuroinflamm 2018;5:e434)
- Elsewhere in the body, alkaline phosphatase enzyme activity is also widely present in bone, cartilage, biliary tract, kidney, intestine and a variety of human tumors (Burstone: Enzyme Histochemistry and Its Application in the Study of Neoplasms, 1st Edition, 1962)
Terminology
- Other names: Gomori alkaline phosphatase stain, nonspecific alkaline phosphatases
Interpretation
- Assess for black reaction product
Uses by pathologists
- In muscle biopsies:
- Identify regenerating myofibers of all causes (not limited to inflammatory myopathies) (J Histochem Cytochem 1970;18:55, Dubowitz: Muscle Biopsy - A Practical Approach, 4th Edition, 2013, Zhou: A Case-Based Guide to Neuromuscular Pathology, 1st Edition, 2020)
- Identify connective tissue injury in immune myopathies with perimysial pathology (IMPP) (Brain 2015;138:2485, Neurol Neuroimmunol Neuroinflamm 2018;5:e434)
- Increased endomysial capillary alkaline phosphatase reactivity is seen in a subset of myositis with poor response to steroids (Am J Pathol 1980;101:159)
Prognostic factors
- Immune myopathies with perimysial pathology (IMPP) are associated with excellent response to immune modulation therapy (Neurol Neuroimmunol Neuroinflamm 2018;5:e434)
- Inflammatory myopathies with high endomysial capillary alkaline phosphatase reactivity responded poorly to steroids (Am J Pathol 1980;101:159)
Microscopic (histologic) description
- Staining pattern varies depending on structure highlighted:
- Regenerating fibers: sarcoplasmic (J Histochem Cytochem 1970;18:55)
- Arterioles and capillaries: endothelium cytoplasmic (Nature 1962;195:611)
- Perimysial connective tissue: connective tissue / collagen (Neurol Neuroimmunol Neuroinflamm 2018;5:e434)
- Denervated myofibers: sarcoplasmic (J Histochem Cytochem 1970;18:55)
Microscopic (histologic) images
Positive staining - normal
- Endothelium of arterioles of skeletal muscle (Nature 1962;195:611, J Histochem Cytochem 1970;18:55, Arch Histol Cytol 1998;61:215)
Positive staining - disease
- Connective tissue reactivity:
- Perimysial connective tissue in antisynthetase syndrome associate myositis, necrotizing myopathy with anti-HMGCR autoantibody and a subset of dermatomyositis (Brain 2015;138:2485, Neurol Neuroimmunol Neuroinflamm 2018;5:e434, Neurol Neuroimmunol Neuroinflamm 2015;2:e124)
- Myofiber reactivity:
- Regenerating fibers of all causes (not limited to inflammatory myopathies) (J Histochem Cytochem 1970;18:55)
- Can be seen in a small subset of denervated myofibers in adults with amyotrophic lateral sclerosis or peripheral neuropathies or young children with infantile spinal muscular atrophy (J Histochem Cytochem 1970;18:55)
- Capillary reactivity:
- Endomysial capillary reactivity is increased in a subset of dermatomyositis (Am J Pathol 1980;101:159)
Negative staining
- Myofibers undergoing active necrosis or phagocytosis
- Duchene muscular dystrophy, limb girdle muscular dystrophy or experimental ischemic myopathy do not show perimysial connective tissue reactivity (Am J Pathol 1980;101:159)
Board review style question #1
Board review style answer #1
Alpha fetoprotein (AFP)
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Definition / general
- Alpha fetoprotein is a marker related to embryonic development (yolk sac), mainly used for diagnosing germ cell tumors and liver tumors
- Overall specific but not sensitive marker
Essential features
- Positive immunostaining in a subset of hepatocellular carcinomas and hepatoblastomas but also found to be positive in other liver diseases
- Positive immunostaining can be found in the various patterns of yolk sac tumor but also can be positive in teratoma
- Positive in various tumors with hepatoid differentiation
Terminology
- Alpha fetoprotein (AFP)
- First detected in high concentrations in human embryonal and fetal serum, named alpha-1 globulin (Scand J Clin Lab Invest 1956;8:174)
Pathophysiology
- Part of the albuminoid gene superfamily, gene mapped on chromosome 4 (4q11-q22) (Nucleic Acids Res 1985;13:8007)
- Major protein in serum of early mammalian embryos, synthesized at the site of embryonal hematopoiesis: the yolk sac (J Clin Invest 1967;46:1010)
- Function: transport and binding of ligands, growth regulator during embryonic development, immune regulatory functions (Exp Biol Med (Maywood) 2001;226:377, Annu Rev Med 1977;28:453)
Clinical features
- High serum levels in several conditions:
- Pregnancy
- Hepatic disorders
- Malignancies (hepatocellular carcinomas, germ cell tumors - especially with yolk sac tumor components, neoplasms of endodermal origin - lung, gastric, colon - especially if associated hepatoid foci, liver metastases, pediatric tumors such as pancreatoblastoma)
- History of gastrointestinal / hepatic surgery
- Hereditary ataxia telangiectasia, in cases of liver damage by chemotherapy or anesthetics (Annu Rev Med 1977;28:453, Hum Pathol 2008;39:1115, Gastroenterology 1979;77:787, Nat Rev Urol 2016;13:715, JOP 2007;8:55)
- Specific serum isoforms: L1, in nonneoplastic liver disease; L2, in yolk sac tumor; L3, in liver cancer
- Both L2 and L3 can be elevated in pediatric yolk sac tumor, reflecting both yolk sac and hepatic differentiation (J Pediatr Surg 1989;24:350)
- Elevations in maternal serum and amniotic fluid may indicate fetal abnormalities, including neural tube defects (Am J Obstet Gynecol 2006;195:1623)
- Serum levels drop after birth (still elevated until around 6 months of age, needing care in interpretation); small amounts still produced in adults (Annu Rev Med 1977;28:453)
- Serum AFP increases in 50 - 70% of patients with nonseminoma germ cell tumors; half life is 5 to 7 days; prominent elevations in pure seminomas usually indicate yolk sac differentiation in metastatic locations; patients should be treated as having mixed germ cell tumor (Nat Rev Urol 2020;17:201)
Interpretation
- Membranous or cytoplasmic staining is expected; granular
Uses by pathologists
- Supporting the diagnosis of germ cell tumors (testicular, ovarian or extragonadal), especially those with identifiable yolk sac tumor foci (Mod Pathol 2005;18:S61)
- Supporting the diagnosis of hepatocellular disease (including nonneoplastic diseases such as chronic hepatitis, and neoplastic diseases such as hepatocellular carcinoma and hepatoblastoma) (World J Gastroenterol 2005;11:5015)
- Confirming suspected hepatoid foci within other neoplasms or confirming that tumor cells produce AFP in case of remarkable elevations of this marker in patient serum (Mod Pathol 1997;10:686)
Prognostic factors
- Preoperative levels are prognostic for hepatocellular carcinoma (World J Surg Oncol 2013;11:212)
- Normal AFP hepatocellular carcinoma patients were significantly older, had fewer chronic liver conditions such as viral hepatitis or cirrhosis and had better survival; tumors were smaller, less vascular and well differentiated (J Clin Med 2019;8:E1736)
- Part of staging and prognostic grouping in germ cell tumors, correlation with response to treatment, both in testis and ovary (Biomed Res Int 2019;2019:5030349, Mol Clin Oncol 2015;3:125)
Microscopic (histologic) images
Contributed by João Lobo, M.D., Rui Henrique, M.D., Ph.D.
Virtual slides
Positive staining - normal
- Well fixed and nonautolyzed embryonal liver is a reliable positive control
- Early gut, yolk sac; nonspecific background reaction frequent in necrotic and cystic areas, since it is a protein secreted in serum (Int J Dev Biol 2012;56:755)
- Low expression in normal adult liver (EBioMedicine 2018;33:57)
Positive staining - disease
- Yolk sac tumor (62%)
- Specific marker but less sensitive than glypican 3 (glypican 3 stains 97% of solid yolk sac tumors, which can mimic seminoma) (Pathology 2018;50:88)
- In primitive patterns, usually with a strong granular cytoplasmic positivity, especially in intracellular lumina; can be positive in hyaline globules, although this is not frequent (Hum Pathol 1988;19:995)
- In classical patterns, staining may be heterogeneous but is consistent
- In somatic glandular patterns, staining is incomplete, more focal or absent, difficult to identify at low power (Histopathology 2014;65:51)
- Positive foci within embryoid bodies or embryonal carcinoma reflect differentiation into yolk sac tumor (Acta Pathol Microbiol Immunol Scand A 1983;91:165)
- Hepatocellular carcinoma (2 - 62%)
- Specific but not a sensitive marker (Hum Pathol 2002;33:1175)
- Infantile hemangioendothelioma can show expression (Hum Pathol 2010;41:763)
- Cirrhosis, chronic hepatitis B and other liver diseases can show low level expression in liver (EBioMedicine 2018;33:57)
- Reports of positivity in multiple tumors with hepatoid or enteric differentiation or of pediatric origin, such as enteroblastic gastric carcinoma, lung carcinoma, gallbladder carcinoma, colon carcinoma, sex cord stromal tumors like Sertoli-Leydig tumors, among others (Case Rep Pathol 2018;2018:3620293, Respir Med 2016;119:175, JOP 2007;8:55, summarized in World J Gastroenterol 2013;19:321)
Negative staining
- Germ cell neoplasia in situ (GCNIS)
- Seminoma
- Embryonal carcinoma
- Choriocarcinoma
- Gonadoblastoma
- Spermatocytic tumor
- Teratoma: can be positive in some epithelial components (20%) (Acta Pathol Microbiol Immunol Scand A 1983;91:165)
- Hepatoblastoma (15%): not significantly associated with subtype (Eur J Cancer 2012;48:1853)
- Cholangiocarcinoma
- Metastatic adenocarcinomas to the liver (5%)
Board review style question #1
Which of the following is true about the immunohistochemical expression of AFP?
- It can be positive in other liver diseases besides hepatocellular carcinoma and hepatoblastoma
- It is more sensitive than glypican 3 for diagnosing yolk sac tumor
- Nuclear staining is expected
- Seminomas are typically positive
- Teratomas are invariably negative
Board review style answer #1
A. It can be positive in other liver diseases besides hepatocellular carcinoma and hepatoblastoma. It is a specific marker but less sensitive than glypican 3. Seminomas are typically negative. Cytoplasmic or membrane staining is expected. Teratomas may show positivity in certain epithelial elements. Other liver diseases and liver tumors can show positive immunostaining, including metastatic disease to the liver.
Comment Here
Reference: Alpha fetoprotein (AFP)
Comment Here
Reference: Alpha fetoprotein (AFP)
Alpha-1 antitrypsin
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Acute phase plasma protein
- Inhibits neutrophil elastase, which causes tissue damage and maintains protease / antiprotease balance in the lung (J Proteome Res 2014;13:3131)
- Most abundant circulating serine protease inhibitor predominantly derived from hepatocytes (J Proteome Res 2014;13:3131)
- Member of serpin superfamily; homologous to alpha-1 antichymotrypsin (Biochem Soc Trans 2002;30:93)
Essential features
- Intracytoplasmic globules in hepatocytes, preferentially in zone 1 near the portal tracts; can be patchy
- Alpha-1 antitrypsin positive globules will also be highlighted by periodic acid-Schiff diastase (PASD) stain
- Presence of alpha-1 antitrypsin globules does not differentiate between homozygous versus heterozygous deficiency states (J Hepatol 2000;32:406)
- Expressed in a variety of tumors and pathologic processes, though not commonly used for diagnostic purposes in such entities
Terminology
- Sometimes abbreviated AAT or A1AT
Pathophysiology
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
Clinical features
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
- AAT deficiency is highly underdiagnosed
- Due to overlap of clinical symptoms, testing should be performed in individuals with chronic obstructive pulmonary disease (COPD), liver disease, poorly responsive asthma, cANCA vasculitis, panniculitis or bronchiectasis, in addition to first degree relatives of people with AAT deficiency (N Engl J Med 2020;382:1443)
Interpretation
- Intracytoplasmic globules in hepatocytes (Clin Liver Dis 2018;22:643)
- May be difficult to visualize in neonates, who may show finely granular cytoplasmic staining (Clin Liver Dis 2018;22:643)
Uses by pathologists
- To diagnose alpha-1 antitrypsin deficiency in the appropriate clinical context
- Initial laboratory test is serum AAT, which is decreased in AAT deficiency (< 1.1 g/L)
- Correlation with enzyme phenotype (e.g., PiMZ or PiZZ) is recommended to confirm the diagnosis and determine heterozygous versus homozygous deficiency state
- Note: there is no direct correlation between the serum AAT value, the Pi phenotype and the presence or absence of immunoreactive periportal AAT granules; thus, IHC alone cannot confirm or exclude AAT deficiency (J Clin Pathol 1986;39:58)
- Can be used to study AAT protein expression within the human liver or exogenous AAT that is delivered through gene therapy (Methods Mol Biol 2017;1639:139)
Prognostic factors
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
Microscopic (histologic) images
Positive staining - normal
- In addition to hepatocytes, A1AT is secreted from monocytes and macrophages, small intestinal enterocytes and bronchial epithelial cells (Clin Immunol Immunopathol 1980;16:84, J Clin Invest 1993;92:2022, J Clin Invest 1986;77:1952, J Biol Chem 1997;272:8250)
Positive staining - disease
- A1AT globules seen in the livers of patients with alpha-1 antitrypsin deficiency (Clin Gastroenterol Hepatol 2012;10:575)
- Pitfall: globules can sometimes also be seen in cirrhotic livers of any etiology
- Various tumor types have been shown to have positive AAT staining; however, such immunohistochemistry is currently not used for diagnosis of specific tumor types
Negative staining
- Similar appearing globules that are negative for AAT IHC are present in other diseases, such as alpha-1 antichymotrypsin deficiency, antithrombin III deficiency and fibrinogen storage disorders (Gonzalez: Non-Neoplastic Liver Pathology - A Pathologist's Survival Guide, 1st Edition, 2016)
Molecular / cytogenetics description
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
- SERPINA1 gene
- Allele: Glu342Lys is most common SERPINA1 point mutation (J Hepatol 2016;65:413)
Sample pathology report
- Liver, random, ultrasound guided needle core biopsy:
- Alpha-1 antitrypsin deficiency (see comment)
- Comment: Scattered hepatocytes with PAS diastase positive intracytoplasmic globules, highlighted by immunohistochemistry for alpha-1 antitrypsin, suggestive of alpha-1 antitrypsin deficiency. Correlation with laboratory testing for serum levels and alpha-1 antitrypsin phenotype is recommended.
Board review style question #1
A 38 year old man with clinical concern for early onset liver fibrosis has longstanding mild to moderate elevation in transaminases. Viral hepatitis serology is negative and there is no recent history of medication changes or herbal supplement use. A liver biopsy was performed and showed mild portal inflammation with no significant interface activity. A trichrome stain showed bridging fibrosis. Many hepatocytes showed periodic acid-Schiff diastase (PASD) positive cytoplasmic globules. What is the likely etiology of the patient's liver disease and the confirmatory immunohistochemistry that would aid with diagnosis?
- Alcohol; glutamine synthetase
- Alpha-1 antitrypsin deficiency; alpha-1 antitrypsin
- Autoimmune hepatitis; CD138
- Steatohepatitis; heat shock protein
- Viral hepatitis; hepatitis B surface antigen
Board review style answer #1
B. Alpha-1 antitrypsin deficiency; alpha-1 antitrypsin. Answers A, C, D and E are incorrect because although liver fibrosis has a variety of etiologies, intracytoplasmic globules that express alpha-1 antitrypsin in hepatocytes are compatible with alpha-1 antitrypsin deficiency.
Comment Here
Reference: Alpha-1 antitrypsin
Comment Here
Reference: Alpha-1 antitrypsin
Alpha-1-antichymotrypsin
Table of Contents
Definition / general | Clinical features | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - tumorsDefinition / general
- Also called α1-ACT
- Acute phase protein / plasma protease inhibitor, mainly produced by liver in response to cytokines such as oncostatin M
- May limit tissue damage produced by excessive inflammation associated proteolysis
- Also localizes to nuclei of hepatic cells to control chromatin condensation and proliferation (Gastroenterology 2013;144:818)
- Homologous to alpha-1-antitrypsin
- Chymotrypsin is digestive enzyme produced by pancreas
Clinical features
- Heart: has role in pathophysiology of heart failure (Circ Heart Fail 2013;6:853)
- Kidney: part of plasma molecular profile associated with acute cellular renal allograft rejection (Transplantation 2011;92:388)
- Skin: has role in skin repair (J Biol Chem 2011;286:28889)
- Umbilical cord: may help differentiate between stillborns and liveborns (Pathol Res Pract 2009;205:534)
Uses by pathologists
- Marker for acinic / acinar cell carcinoma in breast (Case Rep Oncol Med 2013;2013:372947), pancreas, salivary gland
Microscopic (histologic) images
Positive staining - normal
- Histiocytes, reticulum cells
Positive staining - tumors
- Acinic / acinar cell carcinomas of breast, pancreas, salivary gland tumors
- Hepatoid adenocarcinoma of stomach (World J Gastroenterol 2013;19:4437)
- Solid-pseudopapillay neoplasm of pancreas
Alpha-synuclein
Table of Contents
Definition / general | Uses by pathologists | Clinical features | Microscopic (histologic) images | Positive stains | Additional referencesDefinition / general
- Member of the synuclein family of soluble proteins (alpha-synuclein, beta-synuclein and gamma-synuclein) that are commonly present in CNS of vertebrates
- Expressed in the neocortex, hippocampus, substantia niagra, thalamus and cerebellum
- Main location is within the presynaptic terminals of neurons in both membrane-bound and cytosolic free forms
- Can be seen in neuroglial cells and melanocytic cells; highly expressed in the neuronal mitochondria of the olfactory bulb, hippocampus, striatum and thalamus
- Three isoforms have been isolated by alternative splicing
- Most research is the full length isoform with 140 amino acids
- Others are alpha-synuclein-112 and alpha-synuclein-126 (Wikipedia)
Uses by pathologists
- Diagnosis of (a) Parkinson disease (PD) / brainstem predominant type of Lewy body disease, and (b) dementia with Lewy bodies (DLB), the two most frequent synucleinopathies.
- These neurodegenerative multisystem disorders have widespread occurrence of α-synuclein containing deposits in the central, peripheral, and autonomic systems. For both, staging/classification systems are based on semiquantitative assessment of the distribution and progression pattern of α-synuclein pathology, which are considered to be linked to clinical dysfunction (Biochimica et Biophysica Acta;2009:1792;730, Int J Clin Exp Pathol 2014;7:1714, Mov Disord 2016;31:193
Clinical features
- Forms insoluble aggregates in the group of pathological disorders known as synucleopathies, characterized by:
- Formation of neuronal Lewy bodies and Lewy neurites in idiopathic Parkinson disease and dementia with Lewy bodies
- Oligodendroglial cytoplasmic inclusions in multiple system atrophy
- Large axonal spheroids in several rarer neuroaxonal dystrophies
- Both the sporadic and the familial form of Alzheimer disease also demonstrate alpha-synuclein protein
- In recent years, several studies have shown that alpha-synuclein aggregation can also be detected outside the central nervous system, particularly in the enteric nervous system of the gastrointestinal tract of PD patients using immunohistochemistry
- This has the potential to enable an early diagnosis of the disease as well as enhance the neuroprotective effects of the available therapeutic modalities
Microscopic (histologic) images
Positive stains
- Brain tissue: neocortex, hippocampus, substantia niagra, thalamus and cerebellum (within the presynaptic terminals of neurons in both membrane bound and cytosolic free forms)
- Olfactory bulb, hippocampus, striatum and thalamus (highly expressed in mitochondria)
- Also neuroglial cells, melanocytic cells
Additional references
AMACR
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3 | Board review style question #4 | Board review style answer #4Definition / general
- Alpha methylacyl CoA racemase (AMACR) is a mitochondrial and peroxisomal enzyme, a 382 amino acid protein essential in lipid metabolism, encoded by a 1621 bp sequence gene, located on chromosome 5p13 (J Clin Pathol 2003;56:892)
- One of the most widely used markers of prostate carcinoma, because this protein is upregulated in prostate carcinoma and not found in benign prostate tissue (J Clin Pathol 2003;56:892, Am J Surg Pathol 2014;38:e6)
Essential features
- Cytoplasmic expression is seen in prostate adenocarcinoma (80%), colon adenocarcinoma (90%) and in many other cancers, including ovarian, lung cancers, lymphoma and melanoma (Am J Surg Pathol 2002;26:926)
Terminology
- P504S (antibody against AMACR)
Pathophysiology
- AMACR catalyzes the racemization of alpha methyl branched carboxylic coenzyme A thioesters and this enzyme is essential in the oxidation of bile acid intermediates and branched chain fatty acids (J Clin Pathol 2003;56:892)
- Phytanic acid, present in red meat and dairy products, is one of the primary substrates of AMACR and has been found to be elevated in prostate adenocarcinoma (Prostate 2011;71:498)
- AMACR is important in the pharmacological activation of ibuprofen and related drugs (Bioorg Chem 2019;92:103264)
Clinical features
- Adult onset sensory motor neuropathy is developed due to mutations in the AMACR gene, associated with reduced enzyme activity (J Clin Pathol 2003;56:892)
- Diets rich in dairy products and red meat increases the risk for developing prostate cancer, because dairy products and red meat are the major dietary sources of the branched chain fatty acid substrates of AMACR / P504S (J Clin Pathol 2003;56:892)
- AMACR gene polymorphisms (D175G and M9V polymorphisms) are thought to affect the expression of the enzyme and might be risk factors for prostate cancer (Asian Pac J Cancer Prev 2015;16:1857, Prostate 2008;68:1373)
Interpretation
- Cytoplasmic granular staining pattern
Uses by pathologists
- Used to aid in the diagnosis of prostatic adenocarcinoma with a strong granular cytoplasmic staining in luminal cells; however, can be positive in benign mimics (J Clin Pathol 2003;56:892, Am J Surg Pathol 2014;38:e6)
- Overexpression of AMACR in combination with absence of basal cell markers (p63 or high molecular weight cytokeratin [HMWCK]) is typical of prostatic adenocarcinoma (Am J Surg Pathol 2007;31:889)
- A triple stain cocktail using a brown chromogen for basal cell markers (both p63 and HMWCK) and a red chromogen for AMACR is shown to be better than basal cell markers by themselves and supports rational usage of tissue (Am J Surg Pathol 2014;38:e6)
Prognostic factors
- It has been shown that high expression of AMACR might represent an adverse prognostic factor in different types of tumors, such as gastric adenocarcinoma, hepatocellular carcinoma, gallbladder carcinoma, nasopharyngeal carcinoma, gastrointestinal stromal tumor and myxofibrosarcoma (Int J Med Sci 2018;15:638, Tumour Biol 2014;35:7983, J Clin Pathol 2014;67:974)
Microscopic (histologic) images
Positive staining - normal
- Kidney:
- Epithelial cells of the proximal tubules show strong and distinct granular cytoplasmic staining (The Human Protein Atlas: AMACR [Accessed 21 April 2020])
- Epithelial cells of the distal tubules show a weak granular cytoplasmic staining reaction
- GI / liver:
- Hepatocytes and epithelium of the gastrointestinal tract show moderate cytoplasmic staining
Positive staining - disease
- Prostate:
- Prostatic adenocarcinoma: majority are positive with sensitivity from 82% to 100% (Am J Surg Pathol 2014;38:e6, Am J Surg Pathol 2007;31:889, Am J Surg Pathol 2003;27:772)
- High grade prostatic intraepithelial neoplasia (HGPIN) (J Urol 2006;175:820, Int J Clin Exp Pathol 2009;2:327)
- Partial atrophy: can also lack basal cell expression (Am J Surg Pathol 2008;32:851)
- Adenosis and other small glandular proliferations: on needle biopsy 64% of cases of crowded glands are positive and most had patchy or patchy / negative basal cells (Am J Surg Pathol 2005;29:874)
- Kidney:
- Papillary renal cell carcinoma (Am J Surg Pathol 2014;38:e35)
- MiTF-TFE translocation associated renal cell carcinoma (Am J Surg Pathol 2014;38:e35)
- Urothelial tract:
- Urothelial carcinoma in situ (sensitivity 73% and specificity 97%) (Diagn Pathol 2019;14:91)
- Nephrogenic adenoma: can also be negative for basal cell markers (Ann Diagn Pathol 2019;38:11, Hum Pathol 2019;94:11)
- Clear cell adenocarcinoma
- Skene gland adenocarcinoma (Am J Surg Pathol 2018;42:1513)
- Gynecologic:
- Mesonephric carcinoma
- Clear cell carcinoma (Appl Immunohistochem Mol Morphol 2019 Jul 29 [Epub ahead of print])
- GI / liver:
- Barrett esophagus, ulcerative colitis, Crohn's disease: marker of dysplasia and carcinoma (Am J Surg Pathol 2006;30:871, J Clin Diagn Res 2017;11:EC35, Twitter: Andres Matoso [Accessed 21 April 2020])
- Gastric adenocarcinoma
- Colonic adenocarcinoma (J Clin Diagn Res 2016;10:EC10)
- Melanoma / dysplastic nevi: might distinguish from conventional melanocytic nevi (Tumour Biol 2014;35:12015)
Negative staining
- Kidney:
- Clear cell renal cell carcinoma
- Clear cell papillary renal cell carcinoma
- Chromophobe renal cell carcinoma
- Metanephric adenoma
- Wilms tumor
- Prostate:
- Nonneoplastic prostatic tissue (Int J Clin Exp Pathol 2009;2:327, Am J Surg Pathol 2014;38:e6, Am J Surg Pathol 2007;31:889, Am J Surg Pathol 2003;27:772)
- Urothelial tract:
- Nonneoplastic urothelium
- Papillary cystadenoma of the epididymis and broad ligament: 20% may weakly express (Am J Surg Pathol 2014;38:713)
Additional references
Board review style question #1
Biopsy of a lymph node shows metastasis of an unknown tumor. Which immunohistochemical panel is consistent with primary prostate carcinoma?
- AE1 / AE3-, S100+, MelanA+, AMACR+
- AMACR+, CDX2+, CK20+
- AMACR+, p63-, HMWCK-, NKX3.1+
- AMACR+, p63+, HMWCK+, NKX3.1-
Board review style answer #1
Board review style question #2
Transurethral resection of the urinary bladder reveals a neoplastic proliferation, composed of small glandular structures, which are positive for AMACR and NKX3.1. What is the diagnosis?
- Adenocarcinoma of the urinary bladder, intestinal type
- Clear cell adenocarcinoma urinary bladder
- Invasive urothelial carcinoma
- Prostate adenocarcinoma (metastatic or direct invasion)
Board review style answer #2
Board review style question #3
Biopsy of the paraaortal lymph node of a 60 year old man shows metastatic tumor (figure A), which is positive for 34 beta E12 (figure B) and AMACR (figure C) but negative for NKX3.1 (figure D). The tumor is also positive for GATA and CK7 (not shown) but negative for CDX2 (not shown). What is the diagnosis?
- Metastatic colorectal adenocarcinoma
- Metastatic prostate adenocarcinoma
- Metastatic squamous cell carcinoma
- Metastatic urothelial cell carcinoma
Board review style answer #3
Board review style question #4
In the resection specimen of the urinary bladder of a 60 year old man with known invasive high grade urothelial cell carcinoma and multifocal carcinoma in situ, a glandular and cystic lesion was found under the urothelial lining (see image). The lesion is positive for PAX8 and AMACR. What is the diagnosis?
- Invasive urothelial cell carcinoma
- Metastatic colorectal adenocarcinoma
- Metastatic prostate adenocarcinoma
- Nephrogenic adenoma
Board review style answer #4
Amyloid beta and amyloid beta precursor protein
Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Flow cytometry description | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosis | Additional referencesDefinition / general
- Amyloid beta (A4) precursor protein (APP) is part of the type 1 transmembrane protein family
- The APP gene is located on chromosome 21 and encodes for a cell surface receptor and transmembrane precursor protein
- There are three homologs of APP: APP, APLP1 and APLP2 (Mol Neurodegener 2011;6:27)
- Cleavage of APP sequentially by beta secretase (rate limiting step) and gamma secretase produces beta amyloid (amyloid beta, A4, Abeta) peptides of 40 - 43 amino acids, as well as other peptides that have transcriptional, antimicrobial, or antifungal activities (Curr Opin Neurol 2000;13:377)
- The beta amyloid sequence is unique to APP and is not present in APLP1 or APLP2
- Cleavage of the precursor protein by gamma secretase is not precise and thus generates different forms of beta amyloid with Abeta40 being the most abundant, accounting for 80 - 90% of the beta amyloid that is produced (J Alzheimers Dis 2010;19:311)
- Beta amyloid peptides polymerize to form oligomers that then form fibrils or plaques
- Oligomers and fibrils of beta amyloid are deposited in the brain and in the cerebrovascular system; these deposits lead to the development of Alzheimer disease and cerebral amyloid angiopathy
- The Abeta42 form accounts for 5 - 10% of the amyloid beta peptides but is more hydrophilic and prone to fibril formation; it is the main form that is deposited in the brain
- Beta amyloid oligomers are also seen in inclusion body myositis and lewy body dementia
- Mutations in the APP gene lead to autosomal dominant / familial Alzheimer disease type 1, that accounts for less than 5% of Alzheimer cases and comprises 10 - 15% of early onset familial Alzheimer disease (Eur Neurol 1995;35:8, Am J Hum Genet 1999;65:664, Genet Med 2011;13:597)
- Mutations in APP also lead to autosomal dominant hereditary cerebral hemorrhage with amyloidosis-Dutch type (Neuropathology 2005;25:288)
Essential features
- Amyloid beta precursor protein is cleaved into several peptides with different functions, including beta amyloid
- There are several forms of beta amyloid peptides that aggregate to form oligomers and fibrils that are deposited in the brain and cerebral vasculature causing disease
- Studies suggest that beta amyloid oligomers, not the fibrils, are the neurotoxic form (J Neurosci 1999;19:8876, Nature 2002;418:291, PNAS 1998;95:6448)
- Mutations in APP lead to autosomal dominant Alzheimer disease and hereditary cerebral hemorrhage with amyloidosis-Dutch type, a type of cerebral amyloid angiopathy
- The association of beta amyloid deposits to the degree of dementia is weak at best
- Beta amyloid deposits in the brain and vasculature can be found in healthy, cognitively normal people
Terminology
- Amyloid beta precursor protein is also known as APP, AAA, AD1, PN2, ABPP, APPI, CVAP, ABETA, PN-II, CTFgamma
- Beta amyloid is also referred to as amyloid beta, Abeta, or A4
Epidemiology
- The prevalence of beta amyloid deposits in the brain ranges between 0 and 47% in cognitively normal elderly people and between 68 and 100% in those with Alzheimer disease (Neurology 2009;73:754, Alzheimers Dement 2010;6:221, Neurology 2012;79:1636, J Nucl Med 2009;50:878)
- Vascular beta amyloid has been detected in 27% of cognitively normal controls and 78% of patients with cerebral amyloid angiopathy (Mov Disord 2003;18:81, Folia Neuropathol 2013;51:120)
Sites
- The amyloid beta precursor protein is expressed in central nervous system as well as other normal tissues
- Beta amyloid oligomers and fibrils are generally found in the central nervous system and cerebral vasculature
Pathophysiology
- Beta amyloid peptides produced by cleavage of APP polymerize to form oligomers and then fibrils or plaques
- The accumulation of beta amyloid plaques in the brain (extracellular) and in the media and adventitia of medium and small arteries of the cerebral cortex and leptomeninges contributes to the development and progression of Alzheimer disease and cerebral amyloid angiopathy (Curr Med Chem 2009;16:2498)
- Recent studies have suggested that the oligomeric form of beta amyloid is the neurotoxic form that contributes to the pathology of beta amyloid
- The apolipoprotein E E4 allele is speculated to prevent the suppression of amyloid production or the clearance of amyloid
Etiology
- Some beta amyloid peptides are unstable in free form and thus polymerize to form fibrils and plaques
- Accumulation of amyloid plaques in the brain is dependent on the rate of production and clearance out of the brain
- Neurotoxicity of beta amyloid and Tau (a microtubule-associated protein) deposits are thought to contribute significantly to Alzheimer disease, but the etiology of Alzheimer disease and cerebral amyloid angiopathy is not known
Clinical features
- Alzheimer disease: progressive memory loss and cognitive impairment, mood and personality changes, depression, anxiety – in part due to the accumulation of beta amyloid deposits in the brain
- Cerebral amyloid angiopathy: dementia, intracranial hemorrhage – due to beta amyloid deposits in the vasculature
Diagnosis
- Beta amyloid can be detected using Congo red staining, immunohistochemical staining or PET imaging
- Alzheimer disease: the presence of beta amyloid plaques and neurofibrillary tangles is essential for the diagnosis of Alzheimer disease (Alzheimer Dementia 2012;8:1) but is not pathognomonic for the disease – beta amyloid plaques may be seen in normal aging and neurofibrillary tangles can be present in other neurodegenerative disorders
- Cerebral amyloid angiopathy: clinical and MRI evidence of hemorrhage or hematomas with cortical biopsy demonstrating vascular amyloid deposition (Ann Neruol 2004;55:250)
- Histologic evaluation of vessels is required for definitive diagnosis
Laboratory
- Levels of beta amyloid are generally low in the cerebrospinal fluid of Alzheimer patients and cerebral amyloid angiopathic patients
Radiology description
- Guidelines for the use of PET imaging in differentiating Alzheimer disease from other types of dementia are set by the Amyloid Imaging Taskforce
- PET imaging uses 3 FDA approved beta amyloid tracers (florbetapir F 18, flutemetamol F18 and florbetaben F18) to detect beta amyloid deposits in the brain (Arch Neurol 2011;68:1404, JAMA 2011;305:275, Alzheimer Dis Assoc Disord 2012;26:8)
Prognostic factors
- Mutations in APP that lead to early onset Alzheimer disease result in a more aggressive disease and rapid course
- Cerebral amyloid angiopathy:
- Lobar intracranial hemorrhages have a better prognosis than hypertensive deep ganglionic bleeds
- 25 - 40% recurrence rate, which are associated with increased mortality (up to 40%); patients are at highest risk in the first year
Case reports
- Cerebral amyloid angiopathy-related inflammation (Case Rep Neurol Med 2015;2015:483020)
- Misdiagnosis of inclusion body myositis (J Med Case Rep 2015;9:169)
- Sporadic cerebral amyloid angiopathy with giant cell reaction (Acta Neuropathol 1990;81:95)
Treatment
- There are no effective therapies for APP or the accumulation of beta amyloid
- Symptomatic treatment of Alzheimer disease include drugs that modulate neurotransmitters (Ach and NMDA) and psychotropic medications
- Treatment of cerebral amyloid angiopathy includes standard therapy for intracranial hemorrhage, steroids and immunosuppressants for patients with co-existing vasculitis
Microscopic (histologic) description
- Beta amyloid:
- Extracellular cortical deposits
- Pink amorphous extracellular material surrounded by a halo
- May also be surrounded by dystrophic / degenerating neurites and reactive glia, cotton wool plaques, amyloid lakes, subpial bands
- Homogenous, eosinophilic substance in vessel wall, may have a smudged appearance; fibrinoid necrosis in amyloid-laden vessels
- Yellow-green birefringence with Congo red stain and polarization
- Immunohistochemical staining for APP is cytoplasmic
- Subcellular localization in golgi apparatus of APP seen in human cell line U-2 OS
Microscopic (histologic) images
Virtual slides
Positive stains
- Weak to moderate APP staining in neuronal cells
- Weak positive APP staining has also been noted in other normal tissues such as the GI tract and male reproductive system
- Weak to moderate cytoplasmic APP staining is seen in many malignant tissues with strong staining noted in some testicular and urothelial cancer tissues
Negative stains
- APP: normal liver and skeletal tissue
Flow cytometry description
- Currently experimental for the detection of beta amyloid oligomers (J Alzheimers Dis 2007;11:117)
Electron microscopy description
- Beta amyloid plaques on EM appear as a dense core of star-like beta amyloid fibril bundles surrounded by dystrophic neurites, activated microglia and reactive astrocytes (Tosoni A., Barbiano di Belgiojoso G. and Nebuloni M.: Electron Microscopy in the Diagnosis of Amyloidosis, 2011)
Molecular / cytogenetics description
- Pathogenic mutations in APP are generally missense or nonsense mutations (but can also include deletions, insertions and splice site mutations) and mainly occur in exons 16 and 17
- Clinical sequence analysis or mutation scanning may be performed for the entire gene or restricted to exons 16 and 17 only
- Duplication mutations of APP are detected by FISH analysis and account for less than 1% of the pathogenic mutations in APP (Nat Genet 2006;38:24)
Differential diagnosis
Additional references
Androgen receptor (AR)
Table of Contents
Definition / general | Essential features | Pathophysiology | Diagnosis | Clinical features | Uses by pathologists | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Androgen receptor (AR) is a member of the superfamily of ligand responsive transcription regulators
- It functions in the nucleus where it is believed to act as a transcriptional regulator mediating the action of androgens
- 918 amino acid protein encoded by a single copy gene on X q11 - q12
Essential features
- Expressed variably by both ER / PR+ as well as ER / PR- breast cancers
- Most useful for triple negative breast cancer, luminal androgen subtype
- Detected by IHC or gene classifier (molecular testing)
- Predicts favorable prognosis in early stage disease based on current studies, some controversy exists
- Ongoing trials to study the effect of androgen receptor targeted therapy in
- AR+ triple negative breast cancer
- Hormone receptor positive metastatic breast cancer
- HER2+ metastatic breast cancer
Pathophysiology
- Expressed in two types of mammary epithelial cells:
- Metaplastic apocrine cells (lack ER / PR)
- Luminal epithelial cells (5 - 30%) (co-expressed with ER / PR)
Diagnosis
- May be detected by gene classifier or IHC
- Any nuclear IHC staining in tumor cells is considered as positive result but further subdivided into subgroups with 1 - 10% and > 10% positive staining
Clinical features
- Expressed variably depending on tumor subtype:
- ER+ breast tumors: 67 - 88%
- All molecular apocrine tumors
- 12 - 50% of ER- classic invasive ductal carcinoma
- Triple negative breast tumors: 6.6 - 75%; range due to variable cutoffs, source of antibody and methodologies, highest expression in luminal androgen receptor subtype (Breast Cancer Res Treat 2011;130:477, Clin Cancer Res 2011;17:1867, Clin Cancer Res 2013;19:5505, Clin Adv Hematol Oncol 2016;14:186)
- Predicts favorable prognosis based on some studies, however controversy exists
Uses by pathologists
- Apocrine marker
- Breast carcinoma marker helpful in determining primary site of metastases
- Paget disease marker
- Sebaceous carcinoma marker; may help differentiate from squamous cell and basal cell carcinomas (Am J Clin Pathol 2010;134:22)
Treatment
- In addition to neoadjuvant chemotherapy, patients with AR+ tumors may benefit from AR targeted therapies such as bicalutamide (AR antagonist) or enzalutamide (AR inhibitor) (ascopost: Targeting the Androgen Receptor in Breast Cancer [Accessed 8 May, 2018])
- Newer therapies are underway
Microscopic (histologic) description
- Nuclear stain in tumor cells is quantified
Microscopic (histologic) images
Contributed by Monika Roychowdhury, M.D.
Case #214
Images hosted on other servers:
Positive staining - normal
- Skin apocrine and sebaceous glands (J Invest Dermatol 1991;97:264), prostate basal cells (J Steroid Biochem Mol Biol 1992;41:693)
- Early male and female fetal gonads (Hum Reprod 2004;19:1659)
- Also oral mucosa
Positive staining - disease
- Breast: apocrine metaplasia (100%, J Clin Pathol 1999;52:838) apocrine DCIS (J Clin Pathol 2002;55:14) apocrine carcinoma (Jpn J Clin Oncol 2012;42:375, Case Rep Pathol 2013;2013:170918), cystic hypersecretory DCIS (Histopathology 2005;46:43), high grade DCIS, high grade invasive breast carcinoma (primary and metastatic), mammary and extramammary Paget disease (Mod Pathol 2005;18:1283), PASH spindle cells (Int J Clin Exp Pathol 2009;3:87), sebaceous carcinoma, tall cell-like tumors (Int J Surg Pathol 2006;14:79)
- Associated with better prognosis in all types of breast cancer, and better overall survival in ER+ tumors (PLoS One 2013;8:e82650)
- Nasal cavity: nasopharyngeal angiofibroma (75%, Mod Pathol 1998;11:1122, stromal cells in 38% Am J Clin Pathol 2006;125:832)
- Ovary: serous tumors (50%), Sertoli-Leydig tumor (Hum Pathol 1997;28:1206), ovarian surface epithelium (higher AR staining in patients with cervical squamous cell carcinoma, J Ovarian Res 2013;6:85)
- Salivary glands: giant cell tumor, salivary duct carcinomas (Am J Clin Pathol 2003;119:801)
- Skin: Paget disease, sebaceous carcinoma (Am J Clin Pathol 2010;134:22)
- Soft tissue: desmoid tumor (53%, Tohoku J Exp Med 2006;210:189), spindle cell lipoma in men and most women (Arch Pathol Lab Med 2008;132:81)
- Uterus: adenosarcoma (35%), endometrial polyp with atypical features, endometrial stromal nodule, endometrium in polycystic ovarian syndrome. (Biol Reprod 2002;66:297), leiomyosarcoma (variable, Cancer 2004;101:1455, Tumour Biol 2011;32:451)
Negative staining
- Neuroendocrine cells
- Adenomatoid tumor, BRCA1 breast carcinoma, breast fibromatosis (Arch Pathol Lab Med 2000;124:276)
Additional references
Board review style question #1
Androgen receptor testing is most useful in:
- ER+, PR+, HER2+ breast tumor
- ER+, PR+, HER2- breast tumor
- ER-, PR-, HER2+ breast tumor
- ER-, PR-, HER2- breast tumor
Board review style answer #1
Arginase1
Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining - diseaseDefinition / general
- Binuclear manganese metalloenzyme that catalyzes hydrolysis of arginine to ornithine and urea (Wikipedia: Arginase [Accessed 3 August 2023)
- Also called liver arginase
- Critical regulator of nitric oxide synthesis and vascular function
- Defects cause vascular disease, pulmonary disease, infectious disease, immune cell function or cancer
- Argininemia: rare autosomal recessive disorder of urea cycle due to mutations in arginase gene; arginine is elevated in blood and cerebrospinal fluid, causes periodic hyperammonemia, associated with developmental delay, seizures, intellectual disability, hypotonia, ataxia and progressive spastic quadriplegia (OMIM: 207800 [Accessed 3 August 2023])
Uses by pathologists
- Sensitive and specific marker of benign and malignant hepatocytes (Am J Surg Pathol 2010;34:1147)
- Helps distinguish hepatocellular carcinoma from metastatic carcinoma (Diagn Pathol 2012;7:149, Am J Clin Pathol 2012;138:203)
- But also stains some intrahepatic cholangiocarcinomas (Oncol Lett 2011;2:1046)
Microscopic (histologic) images
Contributed by GenomeMe and Cell Marque Corporation
Images hosted on other servers:
Positive staining - normal
- Hepatocytes
Positive staining - disease
- Hepatocellular carcinoma
- Granuloma associated macrophages; lung: type II pneumocytes (FEMS Immunol Med Microbiol 2012;66:265)
- Pancreatic adenocarcinoma (13%) (Cancer Cytopathol 2012;120:230)
Negative staining - disease
- Most cholangiocarcinomas, although intrahepatic cholangiocarcinomas may be positive (Hepat Mon 2015;15:e30336, Oncol Lett 2011;2:1046)
ARID1A
Table of Contents
Definition / general | Clinical features | Diagrams / tables | Microscopic (histologic) images | Positive staining - normal | Negative stainsDefinition / general
- AT Rich Interactive Domain 1A (SWI-like) tumor suppressor gene at 1p36.11 encodes BAF250A, a member of the SWI/SNF ATP-dependent chromatin-remodeling complexes (J Gynecol Oncol 2013;24:376)
- Involved in tissue development and cellular differentiation
- Inactivation of components of chromatin-remodeling complex are associated with malignancy
- Most ARID1A somatic mutations are frame-shift or nonsense mutations that contribute to mRNA decay and loss of protein expression
- 5% of ARID1A mutations are in-frame insertions or deletions (indels) that involve only a small stretch of peptides (Neoplasia 2012;14:986)
Clinical features
- Bladder: mutations associated with poor prognosis urothelial carcinomas (PLoS One 2013;8:e62483)
- Breast: loss of expression associated with carcinoma (
Tumour Biol 2014;35:4813)
- May be due to promoter hypermethylation (PLoS One 2013;8:e53931)
- Cervix: loss of expression a poor prognostic factor (Hum Pathol 2013;44:1365)
- Loss in 31% of adenocarcinoma / adenosquamous carcinoma (Int J Gynecol Cancer 2012;22:208)
- Endocervical-type mucinous borderline tumors may be related to endometrioid tumors based on mutation and loss of expression of ARID1A (Int J Gynecol Pathol 2012;31:297)
- Colorectum: mutated in 39% of microsatellite instability (MSI) cancers (Int J Cancer 2014;135:611 Dec 31)
- Esophagus: mutated in 15% of Barrett's related high grade dysplasia or esophageal adenocarcinoma (Oncogene 2014;33:347)
- Loss of expression in 12-16% of Barrett's related dysplasia / esophageal adenocarcinoma
- Kidney: loss of expression a poor prognostic factor in clear cell carcinoma (Am J Pathol 2013;182:1163)
- Neuroblastoma: mutations of ARID1A or ARID1B in 11%; poor prognostic factor (Nat Genet 2013;45:12)
- Ovary: loss of expression in 52% of clear cell carcinoma (Mod Pathol 2014;27:983)
- Loss of expression may be early event in endometriosis-associated ovarian carcinoma (Int J Mol Sci 2013;14:18824, Int J Clin Exp Pathol 2012;5:642, Int J Gynecol Cancer 2012;22:1310)
- Stomach: loss of expression in gastric carcinoma associated with poor prognosis (PLoS One 2012;7:e40364, Virchows Arch 2012;461:367)
- Uterus: loss of expression may play important role in tumor progression of endometrioid carcinoma (Am J Surg Pathol 2013;37:1342)
- Loss of expression in 46% of high grade endometrioid carcinomas; associated with mismatch repair deficiency and normal p53 expression (Mod Pathol 2014;27:255, Mod Pathol 2013;26:1525)
- Loss of expression in 20% of endometrial clear cell carcinomas, does not predict prognosis (Mod Pathol 2013;26:1101)
Microscopic (histologic) images
Positive staining - normal
- Normal tissue shows ARID1A staining
Negative stains
- Various tumors (see above) show loss of ARID1A staining
AT8 (pending)
[Pending]
ATDX (ATRX)
Table of Contents
Definition / general | Terminology | Clinical features | Uses by pathologists | Microscopic (histologic) imagesDefinition / general
- Alpha-Thalassemia/intellectual Disability syndrome X-linked
- Chromatin remodelling protein important in DNA replication, telomere stability, gene transcription, chromosome congression and cohesion during cell division (Epigenetics 2013;8:3)
- Member of SWI/SNF protein family of DNA dependent ATPases
- Is recruited to site of DNA damage; required for efficient checkpoint activation and faithful replication restart (J Biol Chem 2013;288:6342)
- Death domain-associated protein (Daxx) cooperates with ATRX
- Have essential roles in adenovirus gene expression; illustrates importance of early viral proteins to counteract cellular chromatin remodelling (Nucleic Acids Res 2013;41:3532)
- HSV also represses ATRX (J Virol 2012;86:10093)
Terminology
- Previously termed Alpha Thalassemia / Mental Retardation syndrome
Clinical features
- Associated with rare genetic disorder ATDX (ATRX) syndrome, which includes developmental delay, cognitive impairment, various skeletal deformities (PLoS One 2013;8:e85526, Nat Struct Mol Biol 2011;18:769, J Hum Genet 2012;57:73, Eur J Hum Genet 2011;19:717)
- Acquired α-thalassemia myelodysplastic syndrome (ATMDS): rare acquired syndrome characterized by somatic point mutation in ATRX gene in patients with chronic myeloid disorders (Hemoglobin 2012;36:581)
- CNS: loss of ATRX expression in 45% of anaplastic astrocytomas, 27% of anaplastic oligoastrocytomas, 10% of anaplastic oligodendrogliomas (Acta Neuropathol 2013;126:443)
- Occurs in pediatric and adult high grade astrocytoma (Mod Pathol 2013;26:1425)
- Alternative Lengthening of Telomeres (ALT) is a non-telomerase mechanism of telomere lengthening that occurs in ~10% of cancers overall and is particularly common in astrocytic brain tumors; ATRX may be a repressor of ALT (PLoS One 2012;7:e50062, Oncotarget 2012;3:1194)
- Genetic signatures, including ATRX, may refine classification of gliomas (Oncotarget 2012;3:709)
- Pancreas: loss of ATRX is associated with chromosomal instability in pancreatic endocrine tumors and shorter survival (Gastroenterology 2014;146:453, Horm Cancer 2013;4:165, Mod Pathol 2012;25:1033, Science 2011;333:425)
Uses by pathologists
- See clinical features above
Microscopic (histologic) images
ATM
Table of Contents
Definition / general | Essential features | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Molecular / cytogenetics descriptionDefinition / general
- Ataxia telangiectasia mutated (ATM), on chromosome 11q22-23, was discovered in 1995 as the single gene, which when mutated causes ataxia telangiectasia (Science 1995;268:1749)
- Early integral component of the DNA damage response pathway, which is recruited to the site of genetic damage and affects cell cycle arrest (Trends Biochem Sci 2006;31:402)
Essential features
- Gene mutation responsible for ataxia telangiectasia
- Integral early component of DNA damage response pathway, without which cells are prone to accumulating mutations and genetic instability
- Apart from ataxia telangiectasia, also manifests clinically as sensitivity to radiation induced DNA damage and susceptibility to a number of cancers in heterozygote carriers as well as homozygotes
- Immunostaining for ATM currently restricted to research, though publications have shown relationship to prognosis and treatment response in a number of cancer types
Pathophysiology
- Loss of function mutations lead to inability to repair DNA damage that accumulates endogenously with metabolic processes, replication errors during cell division or with exposure to exogenous agents (EMBO J 2008;27:589)
- Subsequent genetic instability, defective reparative response to DNA double strand breaks from ionizing radiation and telomeric shortening with premature cellular senescence contributes to the 2 main clinical manifestations: ataxia telangiectasia and predisposition to cancers (Orphanet J Rare Dis 2016;11:159)
Clinical features
- Ataxia telangiectasia: autosomal recessive inherited condition with cerebellar ataxia, telangiectatic vessels, immunodeficiency, radiation sensitivity and susceptibility to cancers (Orphanet J Rare Dis 2016;11:159)
- Malignancies typically associated with ataxia telangiectasia include mainly lymphomas and leukemias, especially in childhood and additionally breast, gastric and liver cancers in adulthood (J Clin Oncol 2015;33:202)
- Increased risk for cancer also seen in ATM mutation carriers, mainly breast and gastrointestinal tract cancers (Clin Genet 2016;90:105)
Interpretation
- Both nuclear and cytoplasmic staining patterns have been reported
Uses by pathologists
- No current routine clinical use
Prognostic factors
- Factors below are reported in research publications without current routine clinical application
- ATM mutation found in subset of chronic lymphocytic leukemia and may relate to inferior outcome and influence chemotherapy response (Haematologica 2013;98:112)
- May determine susceptibility to blast crisis in chronic myeloid leukemia (DNA Repair (Amst) 2013;12:500)
- May determine radiation resistance in glioma stem cells (Oncol Rep 2013;30:1793)
- ATM mutation suggested as prognostic or predictive marker to immunotherapy response in a number of other tumors, including endometrial cancer, metastatic colorectal cancer, melanoma and bladder cancer (Pathol Res Pract 2020;216:153032, Sci Rep 2019;9:285, PLoS One 2015;10:e0134678, Front Genet 2020;11:933)
- Together with its upstream protein complex MRE11 in the DNA damage response pathway, may be predictive of radiotherapy response and prognosis in rectal cancer (PLoS One 2016;11:e0167675)
Positive staining - normal
- Most normal tissues expected to show some level of staining; for instance, large bowel mucosal epithelium both adjacent to and away from rectal adenocarcinoma (PLoS One 2016;11:e0167675)
Positive staining - disease
- Overexpression seen in prostate cancers compared with normal prostate tissue (Am J Clin Pathol 2004;121:231)
Molecular / cytogenetics description
- Loss of ATM found in genomic analysis of nodal, splenic marginal zone and lymphoplasmacytic lymphomas (Mod Pathol 2012;25:651)
B72.3
Table of Contents
Definition / general | Interpretation | Uses by pathologists | Positive staining - normal | Positive staining - malignant | Negative stains | Microscopic (histologic) imagesDefinition / general
- Definition: monoclonal antibody that recognizes tumor-associated glyocoprotein 72 (TAG-72), a mucin-like sugar and protein complex on the surface of many cancer cells
- Antibody is directed against the Sialyl-Tn blood group antigen
Interpretation
- Cytoplasmic staining
Uses by pathologists
- Distinguish pulmonary adenocarcinoma (positive) from mesothelioma (negative) as part of a panel (Diagn Cytopathol 1997;17:115)
- Distinguish carcinoma in cytology specimens (positive) from benign effusions (usually negative, but may have focal staining, J Clin Pathol 1990;43:1026, Acta Cytol 1987;31:537, Diagn Cytopathol 2007;35:300)
- Confirm diagnosis of breast apocrine carcinoma (APMIS 2006;114:712)
Positive staining - normal
- Colonic mucosa (Hum Pathol 1989;20:994), endometrium-secretory, endometriosis (J Clin Endocrinol Metab 1993;76:1075), gastric/duodenal goblet cells-coarsely granular, gastric/duodenal epithelium-finely granular (Diagn Cytopathol 2005;33:381)
Positive staining - malignant
- Angiosarcoma-epithelioid, breast apocrine carcinoma (92%), breast ductal carcinoma, colonic adenocarcinoma, endometrial carcinoma, esophageal squamous cell carcinoma, lung adenocarcinoma, ovarian serous tumors and implants, pancreatic ductal adenocarcinoma and intraductal oncocytic papillary neoplasm, prostatic adenocarcinoma, salivary gland carcinoma including duct carcinoma, mucoepidermoid carcinoma (Laryngoscope 1994;104:304) and malignant mixed tumor; testicular ovarian surface epithelial-like tumor, testicular serous papillary carcinoma, vulvar Paget’s disease
Negative stains
Normal tissue:
- Mesothelial cells, most benign cells except colon, duodenum, endometrium, gastric
Disease:
- Adrenocortical adenoma, adrenocortical carcinoma, anaplastic meningioma, lung small cell carcinoma, mesothelial cell inclusions in lymph nodes, mesothelial cysts in the kidney, mesothelioma, ovarian adnexal tumor of probable wolffian origin, ovarian primary retroperitoneal mucinous cystadenoma, ovarian small cell carcinoma-hypercalcemic type
Microscopic (histologic) images
BAP1
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- BAP1: BRCA1 Associated Protein-1, located on chromosome 3p21.1
- Loss of BAP1 expression in tumor nuclei is associated with poor patient prognosis in several cancers
- Loss of BAP1 expression can be used to differentiate certain malignant lesions from benign proliferations
Essential features
- BAP1 is functionally a tumor suppressor (Proc Natl Acad Sci USA 2014;111:285)
- BAP1 is a deubiquitinase that associates with multiprotein complexes that regulate key cellular pathways, including the cell cycle, cellular differentiation, cell death, gluconeogenesis and the DNA damage response (Nat Rev Cancer 2013;13:153)
- Used by pathologists for:
- Prognostication of uveal melanoma
- Differentiation of metastatic uveal melanoma (at least 77% negative) from metastatic skin melanoma (5% negative) (Br J Cancer 2014;111:1373, Nat Genet 2011;43:1018)
- Differentiation of mesothelioma from benign mesothelial proliferation
Terminology
- BAP1
- UCHL2
- Hucep-6
- HUCEP-13
Pathophysiology
- Ubiquitin tag promotes breakdown of certain proteins
- BAP1 removes ubiquitin tags, thereby inhibiting protein breakdown, which affects diverse cellular processes
- BAP1 is thought to help inhibit cell proliferation and promote apoptosis of damaged cells
- BAP1 protein is normally localized in the cell nucleus due to the presence of a nuclear localization sequence (NLS)
- In the presence of a ubiquitin conjugating enzyme (UBE20), NLS will be covered with ubiquitin localizing the BAP1 protein in the cytoplasm
- Wild type BAP1 protein has the capability to remove the ubiquitin and hence is able to enter back into the nucleus
- Mutated BAP1 protein loses its autodeubiquitination property and remains in the cytoplasm (Ocul Oncol Pathol 2020;6:129)
- BAP1 cytogenetic location: 3p21.1
- Molecular location: base pairs 52,401,004 to 52,410,030 on chromosome 3
Clinical features
- Lack of nuclear BAP1 expression has been associated with aggressive disease and worse survival in uveal melanoma and breast cancer (Transl Vis Sci Technol 2019;8:11, Br J Ophthalmol 2021;105:582, PLoS ONE 2019;14:e0211507)
- Loss of nuclear BAP1 expression can be used to differentiate mesothelioma from reactive mesothelial proliferations (Mod Pathol 2015;28:1043)
- Germline BAP1 mutations have been associated with:
- Familial melanoma (J Natl Cancer Inst 2018;110:1328)
- Meningioma (Neuro Oncol 2017;19:1447)
- Lung adenocarcinoma (J Med Genet 2011;48:856)
- Renal cell carcinoma (Am J Hum Genet 2013;92:974)
- Basal cell carcinoma (Clin Genet 2015;88:273)
- Squamous cell carcinoma (Pathology 2017;49:539)
- A cancer syndrome characterized by early onset of benign melanocytic skin tumors and later in life by a high incidence of mesothelioma, uveal melanoma, cutaneous melanoma and possibly additional cancers (Nat Rev Cancer 2013;13:153)
Interpretation
- Nuclear staining: any visible nuclear staining above background is sufficient for positive classification
- Degree of cytoplasmic staining is prognostically irrelevant but has shown some correlation with gene expression class 2 in uveal melanoma (associated with poor prognosis) (Ocul Oncol Pathol 2020;6:129)
Uses by pathologists
- For prognostication of uveal melanoma: lack of BAP1 expression in tumor nuclei associated with significantly shorter metastasis free survival (Ophthalmology 2018;125:203)
- For differentiation of metastatic uveal melanoma (at least 77% negative) from metastatic skin melanoma (5% negative) (Br J Cancer 2014;111:1373, Nat Genet 2011;43:1018)
- For differentiation of mesothelioma from benign mesothelial proliferation: in biopsies initially interpreted as reactive mesothelial proliferation, BAP1 loss was 100% predictive of malignancy (Mod Pathol 2015;28:1043)
Prognostic factors
- Nuclear staining in < 33% of tumor cell nuclei associated with significantly shorter metastasis free survival and a hazard ratio of > 20 for uveal melanoma metastasis (Transl Vis Sci Technol 2019;8:11, Ocul Oncol Pathol 2020;6:129)
Microscopic (histologic) description
- Recommended method for BAP1 scoring of uveal melanoma:
- Make sure the stain works in both external controls (e.g. skin or BAP1 positive uveal melanoma tissue from previous cases) and internal controls (e.g. ganglion layer of retina, normal melanocytes in choroid or iris or optic nerve nuclei)
- Under low magnification (40x), select the tumor area with most intense BAP1 staining
- Within this area, use higher magnification to assess the percentage of tumor cells with nuclear stain
- Count at least 100 cells in each of 3 high power fields (200x - 400x)
- Use the mean score for classification:
- If < 33% of tumor nuclei are positive, classify as BAP1 low
- If ≥ 33% are positive, classify as BAP1 high
- Some pathologists would argue that uveal melanomas usually have either complete absence of staining (0% positive tumor nuclei) or fully retained expression (100% positive tumor nuclei) and that mixed tumors (1 - 99% positive tumor nuclei) are exceptions (J Pathol Clin Res 2018;4:26)
- Regarding melanocytic nevi:
- Benign melanocytic nevi associated with BAP1 germline mutations are often spitzoid or epitheliod
- These melanocytic tumors may have overlapping features with melanoma
- Spitzoid tumors often lack epidermal hyperplasia, Kamino bodies, clefting
- Many lesions are highly cellular, pleomorphic and can contain molecular aberrations occasionally identified in melanoma (Nat Genet 2011;43:1018)
- Benign melanocytic nevi associated with BAP1 germline mutations are often spitzoid or epitheliod
Microscopic (histologic) images
Positive staining - normal
- BAP1 is expressed in most normal tissues
- Recommendable positive controls are pancreas, skin, ganglion layer of retina, normal melanocytes or optic nerve nuclei (J Pathol Clin Res 2018;4:26, Br J Ophthalmol 2021;105:582)
Positive staining - disease
- Metastatic skin melanoma (95% positive) (Br J Cancer 2014;111:1373, Nat Genet 2011;43:1018)
Negative staining
- Uveal melanoma: 37 - 63% of tumors negative (Br J Ophthalmol 2021;105:582, Ocul Oncol Pathol 2020;6:129)
- Mesothelioma: 66% of tumors negative (Mod Pathol 2015;28:1043)
Molecular / cytogenetics description
- Multiplatform analysis has identified 4 molecularly distinct subtypes of uveal melanoma, of which 2 are associated with poor prognosis monosomy 3 and 2 with disomy 3 (Cancer Cell 2017;32:204)
- Disomy 3 is associated with mutations in EIF1AX and SF3B1 (Cancer Cell 2017;32:204)
- Monosomy 3 is associated with aberrant BAP1 (Cancer Cell 2017;32:204)
- In a quarter of BAP1 negative uveal melanomas, no BAP1 mutation is identified (J Pathol Clin Res 2018;4:26)
Sample pathology report
- Eye with uveal melanoma, enucleation:
- BAP1 IHC: low expression (tumor proportion score 10%)
- BAP1 IHC is a prognostic test in uveal melanoma. Classification is as follows: if < 33% of tumor nuclei are positive, classify as low. If ≥ 33% are positive, classify as high. The tumor proportion score is estimated by manual quantification or digital image analysis.
Board review style question #1
Board review style answer #1
C. Loss of nuclear expression of BAP1 is associated with a poor prognosis
Comment Here
Reference: BAP1
Comment Here
Reference: BAP1
BCL10 (pending)
Table of Contents
Definition / generalDefinition / general
[Pending]
BCL2
Table of Contents
Definition / general | Pathophysiology | Diagrams / tables | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Definition / general
- "b cell lymphoma #2"
- Proto-oncogene at 18q21.3
- Encodes 25 kDa protein, mainly localized to inner mitochondrial membrane; also endoplasmic reticulum and nuclear envelope
Pathophysiology
- Prevents cells from undergoing apoptosis
- BCL2 overexpression increase lifespan of B cells; may maintain memory B cells, plasma cells and neurons by prolonging life span without cell division
- May participate in ion channel formation and alteration of membrane permeability, necessary for initiation of apoptosis
- Non-phosphorylated BCL2 inhibits apoptosis, and Bax homodimers normally cause apoptosis; Bax can bind to and inhibit non-phosphorylated BCL2, promoting apoptosis
- Epstein-Barr virus latent membrane protein-1 (LMP-1) interacts with BCL2 promoter, leading to prolonged lifespan for B cells
- Surprisingly, BCL2 overexpression in osteoblasts causes osteocyte apoptosis (PLoS One 2011;6:e27487)
Diagrams / tables
Interpretation
- Nuclear and cytoplasmic staining
Uses by pathologists
- (1) Distinguish follicular hyperplasia of lymph node (germinal centers are BCL2 negative) from follicular lymphoma (germinal centers are BCL2+); BCL2 usually overexpressed in follicular lymphoma due to t(14,18)(q32;q21), which brings BCL2 gene adjacent to active immunoglobulin heavy chain (IgH) gene; however, some follicular lymphomas are BCL2 negative (Am J Surg Pathol 2011;35:1691, Am J Surg Pathol 2009;33:591)
- (2) Detect immature enteric ganglion cells in pediatric intestinal pseudo-obstruction (Am J Surg Pathol 2005;29:1017)
- (3) Diffuse large cell lymphoma: adverse prognostic factor in some studies (Mod Pathol 2005;18:1113, Clin Cancer Res 2011;15:7785)
- (4) Myelodysplastic syndrome: increased expression associated with progression
- (5) May have prognostic value in early stage breast cancer (Br J Cancer 2010;103:668)
Microscopic (histologic) images
Positive staining - normal
- Lymph node: small B lymphocytes in mantle zone and cells within T cell areas
- Adrenal cortex, melanocyties, thymus-medullary cells, thyroid gland solid cell nests
- Immature (but not mature) small ganglion cells
Positive staining - disease
- Hematopoietic: follicular lymphoma (germinal centers stain); also acute lymphoblastic leukemia, angiotropic / intravascular lymphoma, Burkitt lymphoma (occasionally, Indian J Pathol Microbiol 2011;54:290), diffuse large B cell lymphoma (variable), extranodal NK/T-cell lymphoma, nasal-type: 39% (Am J Clin Pathol 2008;130:343), Hodgkin lymphoma (classical): 27% (Hum Pathol 2007;38:103), mantle cell lymphoma, marginal zone lymphoma (variable), persistent polyclonal lymphocytosis, plasmablastic lymphoma, SLL
- Other: adrenal cortical adenoma and carcinoma (Mod Pathol 1998;11:716), atrioventricular node tumor of heart, basal cell carcinoma (skin and prostate, Am J Surg Pathol 2007;31:697), breast-benign stromal spindle cell tumor, breast-columnar cell lesions, breast-micropapillary carcinoma, breast-phyllodes tumor (stromal cells), cervix-mesonephric remnants / rests, cervix-tuboendometrial metaplasia, collecting duct carcinoma-kidney, colorectal adenomas / carcinomas, dermatofibrosarcoma protuberans
- Giant cell angiofibroma, hemangiopericytoma, large cell neuroendocrine carcinoma (salivary glands), low grade fibromyxoid sarcoma of soft tissue, lymphoepithelioma-like carcinoma, melanoma (uvea, Arch Pathol Lab Med 1996;120:497), myofibroblastoma, pheochromocytoma (variable)
- Sclerosing epithelioid fibrosarcoma, small cell carcinoma (breast), solitary fibrous tumor, spindle cell epithelioma of vagina (Arch Pathol Lab Med 2001;125:547), squamous cell carcinoma (uterus), squamous papilloma (conjunctiva, Ann NY Acad Sci 2004;1030:419), synovial sarcoma (Hum Pathol 1996;27:1060), thyroid gland-CASTLE
Negative staining
- Anaplastic lymphoma, apocrine benign / malignant lesions, benign fibrous histiocytoma, lymphoid hyperplasia (marginal zone cells in hyperplastic areas are BCL2+, germinal centers are BCL2-), lymphoplasmayctic lymphoma
Board review style question #1
The translocation that puts the IgH locus on chromosome 14 and the BCL2 locus on chromosome 18 together, is a trademark of which disease?
- Anaplastic large cell lymphoma
- Burkitt lymphoma
- Follicular lymphoma
- Splenic marginal cell leukemia
- Hodgkin lymphoma
Board review style answer #1
C. Follicular lymphoma; more than 90% of FL is associated with t(14;18).
Citation: Kumar: Robbins & Cotran Pathologic Basis of Disease, Eighth Edition, 2009, McPherson: Henry's Clinical Diagnosis and Management by Laboratory Methods, Twenty Second Edition, 2011 (Chapter 33)
Source: BoardVitals, 2/5/2014
- Incorrect: anaplastic large cell lymphoma is primarily associated with t(2;5).
- Incorrect: Burkitt lymphoma is primarily associated with t(8;14), also t(2;8) and t(8;22)
- Incorrect: Hodgkin lymphoma is not associated with a specific translocation (although BCL6 translocations may be seen in L&H cells).
- Incorrect: splenic marginal cell leukemia is not associated with a specific translocation.
Citation: Kumar: Robbins & Cotran Pathologic Basis of Disease, Eighth Edition, 2009, McPherson: Henry's Clinical Diagnosis and Management by Laboratory Methods, Twenty Second Edition, 2011 (Chapter 33)
Source: BoardVitals, 2/5/2014
BCL6
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Transcription factor located at 3q27 that is required for germinal center B cell formation and follicular helper T cell (TFH) differentiation (Immunol Rev 2019;288:214, Trends Immunol 2021;42:336)
- Protects germinal center B cells against DNA damage induced apoptosis during somatic hypermutation and class switch recombination (Trends Mol Med 2014;20:343)
- Translocations help define double or triple hit lymphomas if paired with translocations in MYC or BCL2 (J Clin Pathol 2020;73:126)
Essential features
- Proto-oncogenic transcription factor that is involved in regulating B cell response to DNA damage (Trends Immunol 2021;42:336)
- Marker of germinal center differentiation (Immunol Rev 2019;288:214)
- Responsible for transcriptional regulation and lineage differentiation of follicular helper T cells (Trends Immunol 2021;42:336)
Terminology
- B cell lymphoma 6
Pathophysiology
- Proto-oncogene: normally inhibits germinal center lymphocytes' response to DNA damage to allow for immunoglobulin somatic hypermutation by repressing tumor suppressor TP53 and CDKN1A, ATR and CHEK1 (Blood Cells Mol Dis 2008;41:95)
- Suppresses the expression of antiapoptotic BCL2 (Front Cell Dev Biol 2019;7:272)
Interpretation
- Nuclear staining
Uses by pathologists
- Marker of germinal center differentiation (also CD10) (Immunol Rev 2019;288:214)
- Can be used together with BCL2 and other stains to distinguish follicular lymphoma from other small B cell lymphomas (World J Gastroenterol 2016;22:1674)
- Used along with CD10 and MUM1 to classify diffuse large B cell lymphoma (DLBCL) as germinal center or nongerminal center derived (Blood 2004;103:275)
- Can be used in the diagnosis of Burkitt lymphoma (Mod Pathol 2010;23:909)
- Coexpression of BCL6 and BCL2 by immunohistochemistry is abnormal and can help distinguish follicular lymphoma (85 - 90% in grade 1 - 2, < 50% in grade 3) from reactive follicular hyperplasia (Histopathology 2013;62:860, Am J Hematol 2020;95:316)
- Marker of TFH cells used in the diagnosis of angioimmunoblastic T cell lymphoma (AITL) and other T cell lymphomas of TFH phenotype (also CD10, PD-1, ICOS and CXCL13) (Blood 2017;129:1095)
Prognostic factors
- Large cell lymphomas with rearrangements of MYC, BCL2 or BCL6 (double or triple hit lymphomas) are classified as high grade B cell lymphomas and carry a poor prognosis (Diagn Pathol 2019;14:81)
- DLBCL with a germinal center B cell-like phenotype have better prognosis compared to those that are nongerminal center type (Blood 2004;103:275)
Microscopic (histologic) images
Contributed by Elena M. Fenu, M.D.
Virtual slides
Positive staining - normal
- Germinal center B cells, follicular helper T cells (Immunol Rev 2019;288:214, Trends Immunol 2021;42:336)
Positive staining - disease
- Follicular lymphoma (including cutaneous follicle center lymphoma) and germinal center subtype DLBCL (Am J Surg Pathol 2001;25:732, J Cancer 2020;11:190)
- Burkitt lymphoma (Mod Pathol 2010;23:909)
- Angioimmunoblastic T cell lymphoma, nodal follicular T cell lymphoma and nodal peripheral T cell lymphoma with follicular helper phenotype and follicular helper T cell derived cutaneous T cell lymphomas (Blood 2017;129:1095, Pathology 2020;52:78, Blood 2019;133:1703)
- Nodular lymphocyte predominant Hodgkin lymphoma (Case Rep Pathol 2014;2014:956217)
- BCL6 expression may occasionally be seen in solid tumors, including neuroblastoma and mesenchymal tumors (Transl Oncol 2009;2:128, J Clin Pathol 2011;64:866)
Negative staining
- Late germinal center or postgerminal center B cells or plasma cells
- Nongerminal center subtype DLBCL (J Cancer 2020;11:190)
- MALT lymphoma / nodal marginal zone lymphoma (although colonized follicles have BCL6 positive cells), mantle cell lymphoma (usually) (Am J Clin Pathol 2009;132:39, Appl Immunohistochem Mol Morphol 2010;18:103)
- Reed-Sternberg cells of classic Hodgkin lymphoma (usually, ~15% may be positive) (Haematologica 2007;92:1343)
Molecular / cytogenetics description
- Diagnosis of double or triple hit DLBCL is based on break apart FISH of MYC, BCL2 and BCL6 (Ann Lab Med 2020;40:361)
Sample pathology report
- Lymph node, left inguinal, excision:
- Diffuse large B cell lymphoma, germinal center B cell subtype (see comment)
- Comment: There is total replacement of the nodal architecture by diffuse sheets of large lymphocytes with irregular nuclear contours, open chromatin and distinct nucleoli. The tumor cells are immunoreactive for CD20, CD10, BCL6 and BCL2 and negative for MUM1, MYC and CD30, which confirms the diagnosis. The Ki67 proliferation rate is approximately 60 - 70%.
Board review style question #1
A lymph node biopsy morphologically demonstrates involvement by a large cell lymphoma. The neoplastic cells stain positive for CD20, BCL6, BCL2, MUM1 and MYC and negative for CD3, CD10, CD30 and CD138. What is the diagnosis?
- Anaplastic large cell lymphoma (ALCL)
- Diffuse large B cell lymphoma (DLBCL), germinal center subtype
- Diffuse large B cell lymphoma (DLBCL), nongerminal center subtype
- Plasmablastic lymphoma
- T cell / histiocyte rich large B cell lymphoma
Board review style answer #1
C. DLBCL, nongerminal center subtype. The neoplastic cells are positive for CD20, denoting a B cell origin. Following the Hans algorithm, a DLBCL that is negative for CD10 and positive for both BCL6 and MUM1 is nongerminal center subtype. ALCL is a T cell lymphoma and typically positive for CD30. Plasmablastic lymphoma expresses markers of plasmacytic differentiation like CD138 and is negative or only weakly positive for CD20.
Comment Here
Reference: BCL6
Comment Here
Reference: BCL6
BCOR
Table of Contents
Definition / general | Essential features | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Definition / general
- BCL6 transcriptional corepressor (BCOR) is located at Xp11.4 locus (Genes Dev 2000;14:1810, J Clin Pathol 2020;73:314)
- Encodes a protein which is involved in transcriptional repression in association with BCL6 and epigenetic silencing through polycomb repressive complex 1 (PRC1) (Epigenomics 2019;11:835)
Essential features
- BCOR immunohistochemistry can be used diagnostically to separate tumors with BCOR gene alteration (rearrangement or internal tandem duplication) from their histological mimics (mainly the group of small / ovoid round cell sarcomas) (Pediatr Blood Cancer 2014;61:2191, Histopathology 2020;76:509)
Pathophysiology
- BCOR is a corepressor when bound to BCL6 (Genes Dev 2000;14:1810)
- BCOR forms part of the polycomb repressive complex 1 which ubiquitinates H2AK119 causing epigenetic silencing (Biochem Soc Trans 2017;45:193)
- Involved in early embryonic development and the differentiation of embryonic stem cells into ectoderm, mesoderm and hematopoietic lineages (PLoS One 2008;3:e2814)
- BCOR-CCNB3 fusion results from an X chromosomal paracentric inversion linking the BCOR sequence to exon 5 of CCNB3 (Histopathology 2018;72:320)
Clinical features
- Associated with cancer of several locations and oculofaciocardiodental syndrome (Nat Genet 2004;36:411)
- Soft tissue / bone, kidney, uterus and brain are the most common tumor locations (Am J Surg Pathol 2018;42:1128, Histopathology 2018;72:320, Pediatr Blood Cancer 2014;61:2191, Am J Surg Pathol 2016;40:1670, Am J Surg Pathol 2017;41:1713, Nat Genet 2012;44:461, Histopathology 2020;76:509, Am J Surg Pathol 2008;32:1228, Am J Surg Pathol 2018;42:335, Histopathology 2020;76:64, Expert Rev Mol Diagn 2020;20:293)
- BCOR rearranged sarcomas show a striking male predominance and mainly occur in children / adolescents, although the uterine form can occur in the adult population (Pediatr Blood Cancer 2014;61:2191, Mod Pathol 2017;30:1251)
Interpretation
- Distinct diffuse nuclear staining (Am J Surg Pathol 2016;40:1670, Am J Surg Pathol 2016;40:1009, Histopathology 2020;76:509)
Uses by pathologists
- Specific marker for BCOR associated tumors
- Cannot distinguish BCOR rearranged sarcomas from other round cell sarcomas with BCOR overexpression (Am J Surg Pathol 2016;40:1670, Am J Surg Pathol 2016;40:1009, Histopathology 2020;76:509)
Microscopic (histologic) images
Positive staining - normal
- Spermatogonia (Am J Surg Pathol 2016;40:1670)
Positive staining - disease
- Undifferentiated small round cell sarcomas with BCOR rearrangements in bone, soft tissue, abdominal / pelvic and visceral location:
- BCOR-CCNB3 gene fusion (Am J Surg Pathol 2018;42:604), (Histopathology 2020;76:509)
- BCOR-MAML3 gene fusion (Am J Surg Pathol 2016;40:1670)
- ZC3H7B-BCOR gene fusion (chest wall) (Histopathology 2020;76:509)
- BCOR-KMT2D gene fusion (Am J Surg Pathol 2018;42:604)
- BCOR internal tandem duplication (Am J Surg Pathol 2016;40:1670, Am J Surg Pathol 2018;42:1128, Histopathology 2018;72:320, Nat Commun 2015;6:8891)
Negative staining
- Desmoplastic small round cell tumor (Am J Surg Pathol 2016;40:1670)
- Myxofibrosarcoma (Am J Surg Pathol 2016;40:1670)
- Ossifying fibromyxoid tumor (Am J Surg Pathol 2016;40:1670, Genes Chromosomes Cancer 2014;53:183)
- Angiosarcoma (Am J Surg Pathol 2016;40:1670)
- Chondrosarcoma (Am J Surg Pathol 2016;40:1670)
- Low grade fibromyxoid sarcoma (Am J Surg Pathol 2016;40:1670)
Board review style question #1
Board review style answer #1
BerEP4 / EpCAM
Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Cytology images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Antibody to cell membrane glycoproteins expressed on healthy epithelia and in various carcinomas
- Also known as epithelial cell adhesion molecule, BerEp4 (Ber-EP4, J Clin Pathol 1990;43:213), MOC31 (MOC-31, Acta Neuropathol 1991;83:46), CD326, TACSTD1 protein
- MOC31 and BerEP4 are both anti-EpCAM antibodies, MOC31 appears to be superior (Appl Immunohistochem Mol Morphol 2009;17:202)
- Anti-EpCam antibodies are in clinical trials for patients with cancer (Br J Cancer 2007;96:417)
Uses by pathologists
- Membranous staining
- Sensitive and specific for lung adenocarcinoma (positive) vs. mesothelioma (negative, Am J Surg Pathol 2001;25:43)
- May help distinguish, as part of a panel, hepatocellular carcinoma (usually negative) from metastatic adenocarcinoma to liver or cholangiocarcinoma (usually positive, Mod Pathol 2002;15:1279)
- Immunoexpression may predict poor survival in carcinomas of breast, gallbladder (Am J Clin Pathol 2008;129:424), ovary, pancreas
Microscopic (histologic) images
Cytology images
Positive staining - normal
- Basolateral surface of epithelial cells
Positive staining - disease
- Most carcinomas (Hum Pathol 2004;35:122, J Clin Pathol 2011;64:415)
- Barrett metaplasia (J Clin Pathol 2006;59:260)
- Chromophobe renal cell carcinoma (75%), papillary renal cell carcinoma (55%), clear cell renal carcinoma (18%), metastatic renal cell carcinoma (14%, Am J Surg Pathol 2005;29:83)
- Synovial sarcoma (Am J Surg Pathol 2001;25:610)
Negative staining
- Epidermal keratinocytes, gastric parietal cells, hepatocytes, myoepithelial cells, squamous epithelia, thymic cortical epithelium (Front Biosci 2008;13:3096)
- Lymphoma, mesothelioma, most soft tissue sarcomas
- Adenomatoid tumor; renal oncocytoma
Beta catenin
Table of Contents
Definition / general | Pathophysiology | Clinical features | Diagrams / tables | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Protein encoded by CTNNB1 gene, coordinates cell-cell adhesion and gene transcription (Wikipedia: Beta Catenin [Accessed 18 December 2018])
Pathophysiology
- Part of Wnt signalling pathway, highly conserved pathway with critical role in embryologic development (Dev Cell 2009;17:9), carcinogenesis and epithelial-to-mesenchymal transition
- Upon Wnt activation, β catenin is translocated from membrane (where it interacts with E-cadherin) to cytoplasm and nucleus, where it interacts with transcriptional activators
Clinical features
- Mutations and overexpression of β catenin are associated with various carcinomas
- Colon: plays a critical role in tumorigenesis (mutations in APC or β catenin present in 90% of colon cancers)
- Thyroid: pathway important for anaplastic and possibly papillary thyroid carciomas (Front Endocrinol (Lausanne) 2012;3:31)
- Uterus: endometrioid endometrial carcinoma is associated with β catenin mutations
Diagrams / tables
Uses by pathologists
- Interpretation: nuclear staining is significant in fibroblasts; nuclear or cytoplasmic staining is significant in epithelial cells
- Classify hepatocellular adenoma subtypes and distinguish from focal nodular hyperplasia (Am J Surg Pathol 2012;36:1691, Int J Hepatol 2013;2013:268625, Hum Pathol 2013;44:750)
- Positive / mutated in fibromatosis (Mod Pathol 2012;25:1551)
- Distinguish mesenteric fibromatosis (positive with nuclear staining due to mutations in APC / β catenin pathway causing nuclear accumulation) from GIST tumors (negative) and sclerosing mesenteritis (negative, Am J Surg Pathol 2002;26:1296)
- Distinguish fibromatosis (diffuse or rarely focal nuclear staining for deep tumors) from low grade fibromyxoid sarcoma and other myofibroblastic, or fibroblastic tumors / sarcomas (negative for nuclear staining, Am J Surg Pathol 2005;29:653)
- Identify isolated tumor cells in neuroblastoma (Am J Clin Pathol 2009;131:49)
- Poor prognostic factor for nasopharyngeal carcinoma (Hum Pathol 2013;44:1357)
Microscopic (histologic) images
Positive staining - normal
- Fibroblasts and endothelial cells (cytoplasmic-membranous staining)
Positive staining - disease
- Breast: fibromatosis, phyllodes tumors (spindle cell component), metaplastic carcinoma (23%, Mod Pathol 2010;23:1438)
- Colon serrated adenomas (particularly with dysplasia, Am J Surg Pathol 2009;33:1823)
- Colon neoplasms with Paneth cell differentiation (Hum Pathol 2009;40:872)
- Desmoid-type fibromatosis
- Endometrioid carcinoma of endometrium and ovary, particularly squamous morules (Hum Pathol 2005;36:605)
- Liver: hepatoblastoma and possibly nested stromal epithelial tumor (Hum Pathol 2012;43:1815)
- Neuroblastoma (Am J Clin Pathol 2009;131:49)
- Ovarian microcystic stromal tumor (Am J Surg Pathol 2011;35:1429)
- PNET, rhabdomyosarcoma, Wilm tumor (childhood, Am J Clin Pathol 2009;131:49)
- Pancreas: solid papillary neoplasm (Am J Clin Pathol 2009;132:831)
- Pulmonary lymphangioleiomyomatosis (Am J Clin Pathol 2011;135:776)
- Renal angioleiomyoma (Am J Clin Pathol 2011;135:776)
- Solitary fibrous tumors (nuclear staining in 33%, remainder had membranous or membranous / cytoplasmic staining, Arch Pathol Lab Med 2005;129:776)
Negative staining
- GIST, sclerosing mesenteritis, low grade fibromyxoid sarcoma, myofibroblastic or fibroblastic tumors
Beta catenin
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Protein encoded by the CTNNB1 gene with dual functions in cell adhesion and Wnt signaling (Am J Clin Pathol 2019;151:529)
Essential features
- Responsible for maintaining structural integrity of many epithelial tissues
- Mutations in CTNNB1 relevant to certain types of cancer
- In the nucleus, beta catenin can act as cofactor in the upregulation of oncogenes like cyclin D1 and c-Myc
- Increase in protein expression is considered a hallmark of Wnt driven cancers (J Hematol Oncol 2020;13:165)
- Belongs to armadillo protein family
- Discovered in late 1980s as an E-cadherin associated protein (Biol Res 2020;53:33)
Terminology
- Beta catenin (β catenin)
- CTNNB1
- Catenin (cadherin associated protein), beta 1
Pathophysiology
- In normal tissues, beta catenin levels are regulated (targeted and degraded) by a complex of cytoplasmic proteins including adenomatous polyposis coli (APC), glycogen synthase kinase 3 (GSK3) and casein kinase 1 (CK1) (Cold Spring Harb Perspect Biol 2013;5:a007898)
- Without activation of the Wnt pathway, most beta catenin localizes at the cellular membrane
- Upon Wnt activation, β catenin is translocated from the cell membrane (where it interacts with E-cadherin) to the cytoplasm and then nucleus, where it interacts with transcriptional activators, leading to cellular proliferation (Dev Cell 2009;17:9)
- Alterations in either beta catenin or APC can result in the accumulation of beta catenin within the nucleus
- Nuclear localization of beta catenin is known to associate with malignant transformation in many cancers (Oncotarget 2017;8:33972)
Diagrams / tables
Clinical features
- Loss of beta catenin membrane expression with overexpression in the cytoplasm and nucleus is associated with various carcinomas including breast, colon and pancreas
- Breast
- Nuclear and cytoplasmic accumulation in basal-like breast cancers
- Reduced membrane expression observed with tumor progression (Am J Pathol 2010;176:2911)
- Colon
- Beta catenin plays a critical role in tumorigenesis (activating Wnt signaling mutations present in 90% of colon cancers) (Sci Rep 2020;10:2957)
- Membrane expression in normal colorectal epithelium
- Staining pattern shifts to cytoplasmic / nuclear in tumor tissue (World J Gastroenterol 2008;14:3866)
- Thyroid
- Wnt pathway important for anaplastic and possibly papillary thyroid carcinomas
- Shifts from membrane location to cytoplasmic in malignant tumors (Front Endocrinol (Lausanne) 2012;3:31)
- Uterus
- Endometrial carcinoma is associated with beta catenin mutations (exon 3 in CTNNB1) (Front Oncol 2022;12:1009345)
- Liver
- Beta catenin expression is membranous for normal hepatocytes
- Mutations in CTNNB1 occur in about a third of human hepatocellular carcinomas (HCC) (J Clin Invest 2022;132:e154515)
- Pancreas
- Strong membrane staining in primary tumors of pancreatic neuroendocrine tumors (PanNETs); nuclear staining present in advanced stages including metastasis (World J Gastrointest Oncol 2016;8:615)
- Low grade sinonasal adenocarcinoma (nuclear localization) (Case Rep Pathol 2018;2018:8741017)
- Lung
- Reduced membrane expression of beta catenin with increased expression in cytoplasm and nucleus for non-small cell lung cancer (NSCLC) (Transl Lung Cancer Res 2017;6:97)
- Skin (melanoma)
- Loss of membrane expression as melanoma progresses from primary to metastatic
- Low frequency of CTNNB1 genetic mutations in melanomas, which does not correlate with nuclear expression (Mod Pathol 2002;15:454)
- Breast
Interpretation
- Membranous / cytoplasmic staining in normal tissues
- Increased cytoplasmic and nuclear expression in various cancers (see Clinical features)
- Weak nuclear expression of beta catenin may be observed in normal endometrium during proliferative phase
- Therefore, some authors only consider moderate levels of nuclear staining to be significant (Dev Cell 2009;17:9)
Uses by pathologists
- Beta catenin may be useful in the differential diagnosis of breast ductal carcinoma (membrane expression) versus lobular carcinoma (cytoplasmic expression)
- Nuclear beta catenin expression may be a helpful screening tool to distinguish ambiguous neoplasms like deep penetrating nevus (positive) from similar entities like blue melanocytic tumors, spitzoid tumors, nevoid and superficial spreading melanomas (all negative for nuclear expression) (Virchows Arch 2019;474:535)
- Increased nuclear expression of beta catenin may be useful as a diagnostic marker for desmoid type fibromatosis, as only a very limited subset (solitary fibrous tumor, synovial sarcoma and endometrial stromal sarcoma) of other mesenchymal neoplasms are positive for this marker (Mod Pathol 2005;18:68)
- Can help with classification of hepatocellular adenoma subtypes and identification of focal nodular hyperplasia (Am J Surg Pathol 2012;36:1691, Int J Hepatol 2013;2013:268625, Hum Pathol 2013;44:750)
- Beta catenin may be mutated or positive in fibromatosis (Mod Pathol 2012;25:1551)
- May help distinguish mesenteric fibromatosis (positive with nuclear staining due to mutations in APC / beta catenin pathway causing nuclear accumulation) from gastrointestinal stromal tumors (GISTs) (negative) and sclerosing mesenteritis (negative) (Am J Surg Pathol 2002;26:1296)
- Distinguish fibromatosis (diffuse or rarely focal nuclear staining for deep tumors) from low grade fibromyxoid sarcoma and other myofibroblastic or fibroblastic tumors / sarcomas (negative for nuclear staining) (Am J Surg Pathol 2005;29:653)
- Identify isolated tumor cells in neuroblastoma (Am J Clin Pathol 2009;131:49)
Prognostic factors
- Nuclear staining of beta catenin can indicate exon 3 mutations in CTNNB1, correlating with decreased survival in endometrial cancer (Am J Clin Pathol 2019;151:529)
- Reduced or negative membranous staining in gastric tumors associated with advanced stage and shorter survival (Br J Cancer 1999;81:1392, Int J Clin Exp Pathol 2017;10:8980)
- Poor prognostic factor for nasopharyngeal carcinoma (Hum Pathol 2013;44:1357)
- Reduced membrane expression and increased cytoplasmic / nuclear immunohistochemical staining in NSCLC is correlated with poor prognosis (Transl Lung Cancer Res 2017;6:97)
Microscopic (histologic) description
No information provided
Microscopic (histologic) images
Virtual slides
None
Positive staining - normal
- Membrane expression of beta catenin can be found in many normal tissues and some benign tumors (Med Pharm Rep 2019;92:246, J Hepatocell Carcinoma 2018;5:61)
- Fibroblasts and endothelial cells (cytoplasmic or membranous staining)
Positive staining - disease
- Gastric cancer
- Nuclear expression (58%) (Int J Clin Exp Pathol 2010;3:782)
- Most gastric cancers show reduced or weak membrane expression (51.7%) (Int J Clin Exp Pathol 2017;10:8980, Br J Cancer 1999;81:1392)
- Invasive ductal carcinoma of the breast
- Membrane expression (70%) (Asian Pac J Cancer Prev 2021;22:3493)
- In basal-like breast cancer, nuclear (72%) and cytoplasmic (88%) expression is increased; membrane expression may also be present (Am J Pathol 2010;176:2911)
- Liver cancer
- Reduced membrane expression with an increase in cytoplasmic and nuclear expression in cirrhosis and hepatocellular carcinoma (73%) (J Hepatocell Carcinoma 2018;5:61)
- Bone cancer
- Osteoid producing primary tumors of bone exhibit cytoplasmic or membrane expression of beta catenin (73%) (Virchows Arch 2021;479:529)
- Endometrioid carcinoma of endometrium and ovary, particularly squamous morules (Hum Pathol 2005;36:605)
- Neuroblastoma (Am J Clin Pathol 2009;131:49)
- Ovarian microcystic stromal tumor (Am J Surg Pathol 2011;35:1429)
- Primitive neuroectodermal tumors (PNET), rhabdomyosarcoma, Wilms tumor (Am J Clin Pathol 2009;131:49)
- Pancreas: solid papillary neoplasm (Am J Clin Pathol 2009;132:831)
- Pulmonary lymphangioleiomyomatosis (Am J Clin Pathol 2011;135:776)
- Renal angioleiomyoma (Am J Clin Pathol 2011;135:776)
- Solitary fibrous tumors (nuclear staining in 33%, remainder had membranous or membranous / cytoplasmic staining) (Arch Pathol Lab Med 2005;129:776)
- Desmoid fibromatosis: 80% nuclear beta catenin staining (PLoS One 2021;16:e0250619)
Negative staining
- GIST, sclerosing mesenteritis, low grade fibromyxoid sarcoma, myofibroblastic or fibroblastic tumors (low grades may show some nuclear staining) (Mod Pathol 2014;27:S47)
Molecular / cytogenetics description
- Mutations in CTNNB1 (exon 3) have been detected in 30% of intestinal and diffuse type gastric cancers (World J Exp Med 2015;5:84)
- Deletions or missense mutations in exon 3 of CTNNB1 are the most common genetic abnormality leading to hepatocellular carcinoma (J Hepatocell Carcinoma 2018;5:61)
Molecular / cytogenetics images
None
Sample pathology report
- Pancreas, distal pancreatectomy:
- Solid pseudopapillary neoplasm (SPPN) (see comment)
- Comment: A 28 year old female presents with abdominal pain and fever without jaundice, change in stool color or diarrhea. CT and ultrasound imaging of the abdomen exhibited a solid and cystic tumor measuring 8 cm near the tail of the pancreas. Tumor cells were positive for beta catenin, CD10, CD56, CD117 and cyclin D1. Beta catenin was expressed in the nucleus of tumor cells.
Additional references
None
Board review style question #1
Which exon mutation in beta catenin is most commonly detected in endometrial carcinomas, resulting in increased nuclear expression?
- Exon 3
- Exon 7
- Exon 8
- Exon 13
Board review style answer #1
A. Exon 3. Studies have demonstrated that 30 - 60% of endometrial carcinoma cases exhibit nuclear accumulation of beta catenin in tumor cells because of mutations in exon 3 of CTNNB1. Answers B and C and are incorrect because these mutations are not commonly found in endometrial carcinoma and only weakly activate beta catenin in some other cancers like hepatocellular carcinomas. Answer D is incorrect because mutations in exon 13 are not associated with endometrial carcinomas but are more consistent with CTNNB1 syndrome with symptoms of cognitive and motor impairment.
Comment Here
Reference: Beta catenin
Comment Here
Reference: Beta catenin
Board review style question #2
Which of the following staining patterns for beta catenin would be most common in pancreatic tissue?
- Increased membranous expression of beta catenin in stages III - IV of pancreatic tumors
- Loss of membrane expression in ductal cells of normal pancreatic tissue
- Increased nuclear expression of beta catenin in solid pseudopapillary neoplasm
- Normal pancreatic tissue with increased nuclear beta catenin expression
Board review style answer #2
C. Increased nuclear expression of beta catenin in solid pseudopapillary neoplasm. Solid pseudopapillary neoplasms of the pancreas frequently harbor genetic mutations within the beta catenin gene, resulting in aberrant nuclear expression of the protein by IHC. Answer B is incorrect because beta catenin is predominantly located and positively expressed on the membrane of ductal cells in normal pancreatic tissue. Answer A is incorrect because beta catenin expression on the membrane is lost in later stages of pancreatic tumors. Answer D is incorrect because nuclear expression of beta catenin is associated with more advanced stages of pancreatic tumors.
Comment Here
Reference: Beta catenin
Comment Here
Reference: Beta catenin
BOB1
Table of Contents
Definition / general | Pathophysiology / etiology | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- B cell specific Octamer Binding protein-1
Pathophysiology / etiology
- B cell transcription factor
- Coactivator of OCT-2
- Appears to mediate antigen-dependent germinal center formation
Uses by pathologists
- Identify B cells in germinal centers, mantle cells and lymphomas
- Determine lineage of CD20 negative B cell neoplasms (Am J Clin Pathol 2006;126:534)
- Help differentiate classical Hodgkin's lymphoma (BOB1 negative) from primary mediastinal large B-cell lymphoma (positive, Histopathology 2010;56:217)
Microscopic (histologic) images
Positive staining - normal
- B cells, normal hematopoietic elements (weak staining, Am J Clin Pathol 2006;126:916)
Positive staining - disease
- B cell lymphoma (germinal center derived, Am J Pathol 2000;156:501), lymphocyte predominant Hodgkin lymphoma (Mod Pathol 2006;19:1010), T cell lymphoma, AML (~ 48%)
Negative staining
- Classic Hodgkin lymphoma (may have weak staining, Mod Pathol 2004;17:1531, but see Diagn Pathol 2007;2:10)
Brachyury
Table of Contents
Definition / general | Pathophysiology | Interpretation | Uses by pathologists | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Transcription factor essential for notochordal cell differentiation, elongation of axis and specification of posterior mesodermal elements (Mod Pathol 2009;22:996)
Pathophysiology
- Brachyury (T) is founding member of T box (Tbx) family
- Transcriptional activator expressed throughout the nascent mesoderm, tailbud and notochord
- Involved in the induction and regional specification of mesoderm
- Brachyury deficient embryos lack tail and trunk structures and die shortly after gastrulation (PLoS One 2011;6:e28394)
- In tumor cells, induces epithelial-mesenchymal transition, an important step in progression toward metastasis (J Clin Invest 2010;120:533)
Interpretation
- Nuclear staining
Uses by pathologists
- Distinguish chordoma from histologic mimics, including clear cell renal cell carcinoma, chondrosarcoma, chordoid meningioma (Am J Surg Pathol 2009;33:669, Mod Pathol 2011;24:425)
Positive staining - normal
- Spermatogonia
Positive staining - disease
- Benign notochordal cell tumor of extraosseous origin (Am J Surg Pathol 2011;35:1158), chordoma (90%+ sensitive, Am J Surg Pathol 2009;33:669, Arch Pathol Lab Med 2010;134:1181), hemangioblastoma (Am J Surg Pathol 2008;32:572)
Negative staining
- Carcinomas, lymphomas, sarcomas
- Invasive urothelial carcinoma with chordoid features (Am J Surg Pathol 2009;33:1213)
BRAF V600E
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- BRAF is a serine / threonine kinase, part of the MAPK signaling pathway
- Abbreviation for v-raf murine sarcoma viral oncogene homolog B1
- BRAF V600E (Val600Glu) is an activating somatic mutation
Essential features
- BRAF V600E mutations can be reliably detected using immunohistochemistry
- BRAF V600E status is important therapeutically in melanoma
- Interpretation can be difficult due to melanin pigment
Terminology
- BRAF VE1 (antibody)
- BRAF V599E (older designation of mutation)
Pathophysiology
- Majority due to thymine to adenine transversion at position 1799 in exon 15 of BRAF
- Minority are due to an insertion deletion of 2 adenines at positions 1798 and 1799 in exon 15 of BRAF (V600E2)
- Both mutations result in an identical BRAF V600E protein, which is detected by the antibody
Interpretation
- Cytoplasmic stain
- Melanin pigment and hemosiderin can mimic brown chromogen, making interpretation of heavily pigmented lesions very difficult (if not impossible)
- Variation in staining can be due to cautery, necrosis, storage time in archive and previous frozen section (Acta Neuropathol 2011;122:11)
Uses by pathologists
- BRAF V600E immunohistochemistry is sensitive and specific for BRAF V600E mutations in colorectal carcinoma, papillary thyroid carcinoma and melanoma (Am J Surg Pathol 2014;38:1418, Virchows Arch 2015;467:155, Am J Surg Pathol 2013;37:61)
- Melanoma: identify those melanomas sensitive to BRAF inhibitors, such as vemurafenib and dabrafenib (N Engl J Med 2011;364:2507)
- Melanoma: differentiate Spitz tumors from Spitzoid melanomas (Mod Pathol 2017;30:640)
- Colorectal carcinoma: differentiate Lynch syndrome (BRAF negative) from sporadic MSI tumors (BRAF mutation in 40 - 50%); prognostic (Am J Surg Pathol 2013;37:1592, Mod Pathol 2014;27:644)
- Thyroid: BRAF V600E mutation associated with high risk features in papillary thyroid cancer (J Clin Endocrinol Metab 2005;90:6373)
- Neuropathology: distinguishing papillary craniopharyngiomas (95% positive for BRAF V600E) from adamantinomatous craniopharyngiomas (0% positive for BRAF V600E)
- Neuropathology: distinguishing glioblastoma from pleomorphic xanthoastrocytomas
Microscopic (histologic) images
Positive staining - normal
- Nil
Positive staining - disease
- Melanocytic lesions
- ~50 - 80% of melanocytic nevi (Nat Genet 2003;33:19, PLoS One 2013;8:e69639)
- ~50% of lymph node capsular nevi (Hum Pathol 2017;59:48)
- ~40 - 60% of cutaneous nonacral melanomas (Nature 2002;417:949, Cell 2015;161:1681, PLoS One 2013;8:e69639)
- Neuropathology
- ~60% of pleomorphic xanthoastrocytomas (PLoS One 2011;6:e17948)
- 20 - 60% of gangliogliomas (Acta Neuropathol 2011;121:397)
- 10% of pilocytic astrocytomas (Acta Neuropathol 2011;121:397)
- 95% of papillary craniopharyngioma (Nat Genet 2014;46:161)
- Thyroid
- 40 - 50% of papillary thyroid carcinomas, enriched in tall cell variant (over 80%) (Virchows Arch 2015;467:155, Endocr Relat Cancer 2005;12:245)
- ~15% of poorly differentiated thyroid carcinomas (J Clin Endocrinol Metab 2013;98:E1414)
- 20 - 60% of anaplastic thyroid carcinomas (J Clin Endocrinol Metab 2013;98:E1414, Hum Mol Genet 2015;24:2318, Thyroid 2017;27:682)
- Colorectal
- > 90% of sessile serrated lesions (Cancer Res 2003;63:4878, Am J Surg Pathol 2007;31:1452)
- ~10% of colorectal adenocarcinomas
- ~70% of borderline serous ovarian tumors and 10 - 20% of low grade serous carcinoma (Hum Pathol 2013;44:329)
- Hematopathology
- Hairy cell leukemia (N Engl J Med 2011;364:2305)
- Langerhans cell histiocytosis: BRAF V600E in up to 65% of cases
- Erdheim-Chester disease: BRAF V600E in about 50% of cases
- 60% of ameloblastoma (J Pathol 2014;232:492)
- Metanephric adenoma
- Papillary craniopharyngeoma
Negative staining
- Does not stain other BRAF mutations (both non-V600E and V600-non-E), including potentially actionable mutations (Am J Surg Pathol 2013;37:61)
- Clear cell sarcoma (melanoma of soft parts) (N Engl J Med 2005;353:2135)
- Rare in acral and mucosal melanoma (N Engl J Med 2005;353:2135)
Sample pathology report
- Soft tissue, perinephric, biopsy:
- Histiocytic neoplasm with BRAF V600E mutation by immunohistochemistry, consistent with Erdheim-Chester disease in the appropriate clinical context (see comment)
- Comment: The histologic sections demonstrate adipose tissue with an infiltrate of foamy histiocytes admixed with scattered Touton giant cells. There is extensive fibrosis present. Immunoperoxidase studies were performed on paraffin embedded sections using antibodies directed against the following antigens: CD1a, CD68, CD163, factor XIIIa, IgG, IgG4, langerin, S100 and BRAF V600E. The foamy histiocytes are positive for CD68, CD163 and factor XIIIa and are negative for S100, CD1a and langerin. The lesional histiocytes are positive for BRAF V600E mutation by immunohistochemistry. There is no increase in number of IgG4 positive plasma cells or an abnormal IgG4/IgG ratio.
Board review style question #1
Board review style answer #1
C. Adamantinomatous craniopharyngiomas do not show BRAF V600E mutations (these tumors show WNT pathway activation with beta catenin mutations).
Comment Here
Reference: BRAF V600E
Comment Here
Reference: BRAF V600E
BRAF-melanoma
Table of Contents
Definition / general | Diagrams / tables | Mutations | Associated findings | Associated histological findings | Detection methods | Inhibitor therapy | Mechanisms of resistance | Emerging combination therapiesDefinition / general
- BRAF is the gene encoding the B-Raf enzyme, a serine / threonine kinase involved in cell replication within the MAP kinase pathway (J Transl Med 2012;10:85)
- BRAF may either form a heterodimer or homodimer for activation
- BRAF activation is enhanced by RAS
- Inhibition normally comes from ERK
- MEK is the only known substrate of BRAF and is activated through phosphorylation
Mutations
- BRAF mutations are found in ~50% of all melanomas (N Engl J Med 2005;353:2135)
- The most common mutation is V600E, accounting for ~80 - 90% of all BRAF mutations identified
- Less common mutations include V600K (10 - 20%), V600R (up to 5%), K601E (< 1%), G469A (< 1%), D594G (< 1%), V600M (< 1%), V600 'E2' (< 1%), L597V (< 1%)
- BRAF appears to be nearly mutually exclusive with NRAS and KIT mutations
- Overall survival does not appear to be affected by different types of BRAF mutations
Associated findings
- Age < 55 years has been the #1 predictor of BRAF mutations (PLoS Med 2008;5:e120, Clin Cancer Res 2012;18:3242)
- Melanomas arising on nonchronically sun damaged skin, acquired nevi and nodal nevi also have an association with BRAF mutations
- Older age, melanomas arising from chronically sun damaged skin, melanomas arising in an acral or mucosal site and congenital nevi are NOT associated with BRAF mutations
Associated histological findings
- Larger, rounder and more pigmented melanocytes (PLoS Med 2008;5:e120)
- Pagetoid scatter
- Nest formation
- Sharp demarcation from uninvolved adjacent epidermis / dermis
- Thickened epidermis
- Ulceration, tumor thickness and mitotic count have NOT been associated with BRAF mutations
Detection methods
- Historically detected using Sanger sequencing (numerous truncated strands secondary to dideoxynucleoside truncation are run on a gel and sequence is determined by speed and fluorescent labeling)
- Cobas 4800 (Roche) testing is touted as a superior method of detection for V600E mutations but only detects ~50% V600K mutations and even lower detection for lower frequency mutations (Arch Pathol Lab Med 2012;136:1385)
- PCR kit (Qiagen) detects V600E, Ec, K, D and R
- PCR and DNA melting curve analysis
Inhibitor therapy
- All patients with unresectable stage III and IV are recommended to undergo BRAF mutation analysis
- Vemurafenib and dabrafenib are ATP competitive and selective BRAF inhibitors which have a high affinity for mutated BRAF enzymes and a much lower affinity for wild type enzymes
- BRAF inhibitors significantly improve both progression free survival and overall survival in patients with BRAF mutations (N Engl J Med 2012;366:707, N Engl J Med 2011;364:2507)
- Approximately 50% of patients respond (only 5% of patients on dacarbazine respond, the only chemotherapeutic drug approved by the FDA)
- Both a reduction in tumor size and a marked increase in tumor infiltrating CD4+ and CD8+ lymphocytes are seen (Clin Cancer Res 2012;18:1386)
- No impact on overall immune response has been noted
- Approximately 1/4 of patients on inhibitors develop classic cutaneous squamous cell carcinoma and squamous cell carcinoma, keratoacathoma type, thought to be due to paradoxical activation of RAS mutations within keratinocytes
- Trametinib, a MEK inhibitor, has been shown to improve progression free survival and overall survival as well (N Engl J Med 2012;367:107)
Mechanisms of resistance
- After drug treatment, there is a high rate of resistance over time
- Mechanisms of resistance involve both the MAPK pathway and AKT pathway
- In the MAPK pathway, changes in NRAS, CRAF, MEK, ERK and COT have been described (Cancer Res 2008;68:4853, Nature 2010;468:973, J Clin Oncol 2011;29:3085)
- In the AKT pathway, changes in PDGFRβ and IGF1 have been described (Nature 2010;468:973, Cancer Cell 2010;18:683)
- One alternate splicing variant designated p61BRAF has also been described
Emerging combination therapies
- New combination therapies are being evaluated for preventing or overcoming BRAF inhibitor resistance (Proc Natl Acad Sci USA 2013;110:4015)
- Both BRAF and MEK inhibitors as well as BRAF and mTOR inhibitors have been shown to overcome resistance in vitro
- Cross resistance between BRAF and MEK inhibition has also been described and may be secondary to the specific form of resistance employed (J Invest Dermatol 2012;132:1850)
BSEP (pending)
[Pending]
C4d (pending)
Table of Contents
Definition / generalDefinition / general
[Pending]
CA 19-9
Table of Contents
Definition / general | Terminology | Pathophysiology | Prognostic factors | Clinical features | Microscopic (histologic) images | Positive staining - normalDefinition / general
- Modified Lewis(a) blood group antigen secreted by or expressed on the surface of cancer cells
- Used primarily as a serum tumor marker to screen for pancreatic cancer and to monitor effectiveness of therapy
- However, only 50 - 75% sensitive for initial screening of pancreatic cancer and relatively nonspecific
Terminology
- Carbohydrate Antigen 19-9
Pathophysiology
- Synthesis strongly depends on tissue specific and epigenetically regulated expression of B3GALT5 and ST3GAL (Biochim Biophys Acta 2017;1861:3210)
- Acquires tumor marker properties in pancreas due to its reabsorption into vessels and elevation in serum
- May play an active role in metastatic spread of cancer by facilitating the adhesion of cancer cells to platelets, endothelium and leukocytes (Pathol Res Pract 2000;196:259, Acta Biochim Pol 2002;49:303, J Biol Chem 2008;283:15647)
Prognostic factors
- Negative staining may be favorable in medullary thyroid cancer (Endocr Pract 2015;21:590)
- High preoperative serum levels are a poor prognostic factor for pancreatic cancer (Hepatogastroenterology 1998;45:253)
Clinical features
- Used primarily as a serum biomarker
- As a serum screening test for pancreatic cancer, is more sensitive than CEA but less sensitive than CXCL8 (Pol Arch Intern Med 2018 Jul 27 [Epub ahead of print])
- Used to screen for pancreatic cancer but has limited sensitivity and specificity
- May also be elevated in patients with cholangiocarcinoma or colon cancer
- Serum levels also elevated in cirrhosis, cholestasis and pancreatitis but values are usually below 1,000 U/mL.
- Note: individuals that are Lewis negative (5 - 7% of population) do not express CA 19-9 due to the lack of the enzyme fucosyltransferase needed for CA 19-9 production; as a result, a low or undetectable serum CA 19-9 concentration is not informative regarding cancer recurrence (Mayo Clinic: CA19 [Accessed 10 September 2018])
- Medullary thyroid carcinoma:
- Serum testing is routinely used in diagnosis and followup (J Clin Endocrinol Metab 2005;90:6077, Eur J Endocrinol 2008;158:239)
- Detected in 6% of pathologic specimens (Endocr Pract 2015;21:590)
- Lung adenocarcinoma associated malignant pleural effusions:
- Highly specific (98%) to differentiate from benign effusions but only 55% sensitive (Pathology 2015;47:123)
Positive staining - normal
- Placenta (Eur J Gynaecol Oncol 2012;33:281)
CA125
Table of Contents
Definition / general | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Cancer antigen 125 (CA-125) is a protein encoded by MUC16 gene, used as a tumor marker, because it is 79% sensitive for ovarian cancer
- Not specific, because elevated in other tumors and in inflammatory conditions
Terminology
- Also known as MUC16
Pathophysiology
- High molecular weight membrane associated mucin found in cornea and conjunctiva, in respiratory tract and female reproductive tract epithelium
- As a mucin, forms lubricating barrier against foreign particles and infectious agents
Clinical features
- Elevated in carcinomas of breast, cervix (Asian Pac J Cancer Prev 2010;11:1745), endometrium, fallopian tubes, GI, lung, ovary; also endometriosis, pregnancy, inflammatory disorders
Interpretation
- Strong membranous staining, fallopian tube is good control
Uses by pathologists
- (1) For ovarian carcinomas, use serum levels to follow response to treatment and predict prognosis (Ann Oncol 2008;19:327)
- (2) In UK, recommended to use serum levels to screen women with symptoms of ovarian cancer (National Health Service Press Release)
- (3) Serial measurements may be more specific for ovarian cancer
- (4) Useful in immunohistochemistry to confirm ovarian origin of tumor (Am J Surg Pathol 2005;29:1482)
- (5) Serum levels may have role in assessing heart failure (Clin Cardiol 2011;34:244, Eur Heart J 2010;31:1752)
- High serum CA-125 levels are due to serosal fluids and serosal involvement of various diseases of ovarian or non-ovarian origin (Gynecol Oncol 2002;85:108)
- Serum levels not recommended for general low-risk ovarian cancer screening due to lack of sensitivity, particularly for low stage tumors (only 50% sensitive for stage I)
Microscopic (histologic) images
Positive staining - normal
- Fetus: amnion, coelomic and Müllerian epithelium (Asia Oceania J Obstet Gynaecol 1990;16:379)
- Adults: mesothelial cells and luminal surface of epithelial cells of endocervix, endometrium, fallopian tube; also in small amounts in epithelium of apocrine sweat glands, biliary tract, colon, mammary gland, pancreas, stomach
Positive staining - disease
- Carcinomas of biliary tree, breast, cervix, endometrium, fallopian tubes, liver, lung, ovary (serous, usually not mucinous), pancreas; ovarian sex cord tumors
- Alveolar rhabdomyosarcoma of uterus, desmoplastic small round cell tumor of pelvic peritoneum, epithelioid sarcoma (Arch Pathol Lab Med 2006;130:871, Jpn J Clin Oncol 2004;34:149), intralobar pulmonary sequestration (Intern Med 2002;41:875), leiomyoma of ileal mesentery, mesothelioma, seminal vessel adenocarcinoma
- Endometriosis (Hum Pathol 2008;39:954), inflammatory disorderes, leiomyomas of ileal mesentery, pregnancy
Negative staining
- Normal ovary, squamous cells
Calcitonin
Table of Contents
Definition / general | Case reports | Uses by pathologists | Microscopic (histologic) images | Additional referencesDefinition / general
- Calcitonin (thyrocalcitonin) is a 32 amino acid linear polypeptide hormone (molecular weight 3,421Kd) that participates in calcium and phosphorus metabolism
- It is formed by the proteolytic cleavage of a larger pre-propeptide, which is a product of the CALC1 gene (CALC)
- In humans, it is primarily produced by the parafollicular cells (C cells) of the thyroid
- Other tissues such as the lungs and intestinal tract can also synthesize calcitonin
- The calcitonin receptor protein has been shown to be a member of the seven transmembrane G protein coupled receptor family, which is coupled by G5 to adenylate cyclase and thereby to the generation of CAMP in target cells
Case reports
- 43 year old woman with medullary thyroid carcinoma, small cell variant (Acta Cytol 2010;54:911)
- 57 year old woman with mixed medullary - papillary carcinoma thyroid (J Lab Physicians 2014;6:133)
- Prognostic value of calcitonin immunostaining in medullary carcinoma of the thyroid (J Clin Endocrinol Metab 1984;59:850)
- Diagnosis and management of medullary thyroid carcinoma (Diagn Cytopathol 2007;35:285)
- Profiling of the calcitonin-calcitonin receptor axis in primary prostate cancer (Oncol Rep 2013;30:1265)
- Hypercalcitoninemia in a patient with a recurrent goiter and insulinoma (Exp Clin Endocrinol Diabetes 2006;114:217)
Uses by pathologists
- As a marker for medullary thyroid carcinoma (MTC), especially when facing histologic subtypes such as the follicular, papillary or encapsulated variants that can pose diagnostic difficulties with follicular cell–derived carcinomas and paraganglioma (Arch Pathol Lab Med 2008;132:359)
- Although highly specific, calcitonin staining may be patchy in medullary carcinomas and 5% of these tumors may be negative for this marker
- In tumors with no staining and still suspected to be MTC, calcitonin and calcitonin gene–related peptide mRNA can be demonstrated by in situ hybridization (Arch Pathol Lab Med 2010;134:207)
- To evaluate for C cell hyperplasia associated with familial MTC
- High grade neuroendocrine tumors can also stain with calcitonin, and metastatic lesions can be misinterpreted as having arisen in the thyroid (Adv Anat Pathol 2004;11:202)
- Immunoreactive calcitonin along with calmodulin has been stained and quantitated in solitary endocrine cells which are increased in number and staining intensity in cystic fibrosis lung when compared to COPD and normal lungs
- The calcitonin and calmodulin may be associated with increased calcium in pulmonary secretions leading to selective colonization of the lung by a limited number of pathogenic bacteria and enhanced pulmonary infection (Chest 1986;89:327)
Microscopic (histologic) images
Additional references
Calcium
Definition / general
- With routine staining, calcium forms a blue-black lake with hematoxylin, usually with sharp edges
- von Kossa method: silver is substituted for calcium in calcium salts; light or a photographic developer turns the silver black; only stains calcium bound to an anion such as phosphate or carbonate; most useful when large amounts of phosphates and carbonates are present, as with bone
- Alizarin red S forms an orange-red lake with calcium at a pH of 4.2; works best with small amounts of calcium such as in Michaelis-Gutman bodies; this method is used on Dupont ACA analyzer to measure serum calcium photometrically
- Azan stain used to distinguish osteoid from mineralized bone.
Microscopic (histologic) images
Caldesmon
Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining - normal | Negative staining - diseaseDefinition / general
- Caldesmon binds calcium, calmodulin, tropomyosin and actin and regulates smooth muscle contraction (Int J Biochem Cell Biol 1997;29:1047)
- Regulates smooth muscle contraction and relaxation
- May play a role in preventing unwanted contractions (Am J Physiol Heart Circ Physiol 2009;297:H1930)
- Interpretation: cytoplasmic staining
- h-caldesmon is high molecular weight isoform, found in smooth muscle cells; l-caldesmon isoform is distributed in non-muscle cells (J Biol Chem 1991;266:355)
Uses by pathologists
- Very useful to distinguish smooth muscle cells / lesions (positive) from myofibroblastic cells / lesions (negative or only a few cells positive, Am J Clin Pathol 2000;114:746, Am J Dermatopathol 2006;28:105)
- Distinguish uterine leiomyoma or leiomyosarcoma (positive) from endometrial stromal tumors (negative, Am J Surg Pathol 2001;25:455), but endometrial stromal tumors may have focal smooth muscle differentiation (Am J Surg Pathol 2002;26:1142)
- Sensitive and specific for epithelioid peritoneal mesothelioma (positive) versus ovarian serous carcinoma (negative, Am J Surg Pathol 2007;31:1139) and epithelioid pleural mesothelioma (positive) versus pulmonary adenocarcinoma (negative, Am J Surg Pathol 2006;30:463)
Microscopic (histologic) images
Positive staining - normal
- Smooth muscle cells (vascular, visceral)
Positive staining - disease
- Angioleiomyoma (Hum Pathol 2007;38:645), gastrointestinal stomal tumor (61%, Pathol Oncol Res 2005;11:11), glomus tumor (Hum Pathol 1999;30:392), inflammatory myofibroblastic tumor (focal, Am J Surg Pathol 2006;30:1502)
- Leiomyoma / leiomyomatosis (Eur J Gynaecol Oncol 2004;25:481), leiomyosarcoma (Am J Surg Pathol 2004;28:178, Am J Surg Pathol 2001;25:455, but see Appl Immunohistochem Mol Morphol 2001;9:302)
- Myopericytoma (Am J Surg Pathol 2006;30:104), perivascular epithelioid cell tumors (Int J Gynecol Pathol 2005;24:341), sclerosing PEComa (92%, Am J Surg Pathol 2008;32:493)
Negative staining - normal
- Endometrium, endometrial stroma, myofibroblasts (J Submicrosc Cytol Pathol 2005;37:231), pericytes
Negative staining - disease
- Cellular angiofibroma (Mod Pathol 2011;24:82), dermatomyofibroma (J Cutan Pathol 2011;38:967), endometrial stromal tumor (references above), fibromatosis, inflammatory myofibroblastic sarcoma-epithelioid (Am J Surg Pathol 2011;35:135)
- Mesothelial tumors of peritoneum, myofibroblastoma (Pathology 2005;37:144), myofibroblastic lesions (Int J Surg Pathol 2005;13:57)
- Nodular fasciitis, ovarian serous tumors, PEComa-primary cutaneous (Am J Surg Pathol 2008;32:608) pleural malignant mesotheliomas (96%, Am J Surg Pathol 2010;34:627)
- Rhabdomyosarcoma (Am J Surg Pathol 2005;29:1106), synovial sarcoma (Am J Surg Pathol 2002;26:1434)
Calponin
Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Actin filament associated regulatory protein
- h1 (basic) isoform is smooth muscle specific, but a late stage smooth muscle marker; described below
- h2 isoform is found in smooth muscle and non muscle cells; not described below
Uses by pathologists
- Identify myoepithelial cells in breast lesions (Histopathology 2005;47:202)
- Help differentiate breast collagenous spherulosis (positive) from adenoid cystic carcinoma (negative, Mod Pathol 2006;19:1351), although adenoid cystic carcinoma is calponin positive in salivary gland tumors (Arch Pathol Lab Med 1999;123:801)
Microscopic (histologic) images
Positive staining - normal
- Smooth muscle, myoepithelial cells (most but not all, Breast Cancer Res 2003;5:R151), myofibroblasts (Am J Surg Pathol 2003;27:82, Proc Natl Acad Sci U S A 1993;90:999); also keratinocytes and nerve fibers (Virchows Arch 2000;437:58), choroidal non-vascular smooth muscle cells (J Anat 2005;207:381)
Positive staining - disease
- Atypical fibroxanthoma (30%, Virchows Arch 2002;440:404), benign fibrous histiocytoma (65%), collagenous spherulosis (Mod Pathol 2006;19:1351), DFSP (40%), fibromatosis (Am J Dermatopathol 2006;28:105), fibrosarcoma (60%), glomus tumor (Am J Surg Pathol 2002;26:301), leiomyoma, leiomyosarcoma, MFH of bone (47%, J Clin Pathol 2002;55:853), MPNST (40%), myoepithelioma-skin, myofibroblastic lesions, myofibroblasts in desmoplastic stroma of carcinomas, nodular fasciitis, solitary fibrous tumor (70%), synovial sarcoma (Histopathology 2003;42:588)
Negative staining
- Adenoid cystic carcinoma
Calretinin
Table of Contents
Definition / general | Essential features | Pathophysiology | Interpretation | Uses by pathologists | Microscopic (histologic) images | Virtual slides | Cytology images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Calcium binding protein (Hum Pathol 2003;34:994)
Essential features
- Nuclear and cytoplasmic staining
- Used primarily in the diagnosis of Hirschsprung disease and to confirm sex cord stromal or mesothelial lineage
- Also positive in adrenal cortical lesions, mesonephric carcinoma, female adnexal tumor of probable Wolffian origin (FATWO) and STK11 adnexal tumor
Pathophysiology
- 29 kilodalton calcium binding protein of the calmodulin superfamily (Hum Pathol 2003;34:994)
- Function is not clearly understood but it is thought to act as a buffer or sensor of intracellular calcium ions (Hum Pathol 2006;37:312, Hum Pathol 2003;34:994)
Interpretation
- Nuclear and cytoplasmic (Mod Pathol 2007;20:248)
Uses by pathologists
- Differentiate (as part of a panel) pleural mesothelioma (positive) from lung adenocarcinoma (negative) (Mod Pathol 2007;20:248, Indian J Pathol Microbiol 2021;64:655, Am J Surg Pathol 2003;27:150, Arch Pathol Lab Med 2018;142:89)
- Differentiate (as part of a panel) peritoneal mesothelioma (positive) from ovarian serous carcinoma (negative); however, calretinin can stain a significant minority of serous carcinomas (Am J Surg Pathol 2007;31:1139, Am J Surg Pathol 1998;22:1203)
- Confirm mesothelial origin in pleural or peritoneal specimens (Hum Pathol 2003;34:994)
- Diagnosis of Hirschsprung disease (showing an absence of mucosal innervation) (Pediatr Dev Pathol 2021;24:19, Mod Pathol 2009;22:1379)
- Differentiate (as part of a panel) adrenal cortical lesions (positive) from metastatic renal cell carcinoma (negative) (Am J Surg Pathol 2011;35:678)
- Differentiate (as part of a panel) adrenal cortical lesions (positive) from pheochromocytoma (negative) (Am J Surg Pathol 2010;34:423)
- Diagnosing (as part of panel) sex cord stromal tumors (ovarian and testis) (Hum Pathol 2003;34:994, Am J Surg Pathol 2021;45:1303, Hum Pathol 2005;36:195)
- Used as part of a panel in diagnosing cervical mesonephric carcinoma (Am J Surg Pathol 2018;42:1596, Am J Surg Pathol 2001;25:379)
- Used as part of a panel in the diagnosis of STK11 adnexal tumors and FATWO (Am J Surg Pathol 2021;45:1061, Mod Pathol 2020;33:734)
- Differentiate schwannoma (positive) from neurofibroma (negative or focal) (Am J Clin Pathol 2004;122:552)
Microscopic (histologic) images
Virtual slides
Positive staining - normal
- Mesothelial cells (Hum Pathol 2003;34:994)
- CNS (neurons, granular cells, astrocytes, Purkinje cells) (Hum Pathol 2003;34:994, Hum Pathol 2006;37:312)
- Leydig cells (Hum Pathol 2003;34:994)
- Ovary (theca cells, granulosa cells) (Hum Pathol 2003;34:994)
- Endometrial stromal cells (Hum Pathol 2003;34:994)
- Breast luminal cells (weak) (Hum Pathol 2003;34:994)
- Adrenal cortical cells and sustentacular cells (Hum Pathol 2003;34:994, Appl Immunohistochem Mol Morphol 2010;18:414)
- Salivary gland serous cells (weak) (Hum Pathol 2003;34:994)
- Colonic ganglion cells (Pediatr Dev Pathol 2021;24:19)
- Adipocytes (Hum Pathol 2006;37:312)
Positive staining - disease
- Mesothelioma (81 - 100%; 57% sarcomatoid) (Hum Pathol 2003;34:994, Mod Pathol 2007;20:248, Sci Rep 2021;11:12554, Indian J Pathol Microbiol 2021;64:655, Am J Clin Pathol 2008;130:771, Am J Surg Pathol 2007;31:1139, Hum Pathol 2019;92:48)
- Adrenal cortical lesions:
- Adenoma (100%) (Hum Pathol 2003;34:994, Appl Immunohistochem Mol Morphol 2010;18:414)
- Carcinoma (50 - 80%) (Hum Pathol 2003;34:994, Am J Surg Pathol 2011;35:678)
- Testicular sex cord stromal tumors:
- Leydig cell tumor (79 - 100%) (Hum Pathol 2003;34:994, Am J Surg Pathol 2021;45:1303)
- Juvenile granulosa cell tumors (86%) (Am J Surg Pathol 2021;45:1303)
- Large cell calcifying Sertoli cell tumors (50%) (Am J Surg Pathol 2021;45:1303)
- Adult granulosa cell tumors (50%) (Am J Surg Pathol 2021;45:1303)
- Sertoli cell tumors (44%) (Am J Surg Pathol 2021;45:1303)
- Ovarian sex cord stromal tumors:
- Adult granulosa cell tumor (90%) (Hum Pathol 2005;36:195)
- Sertoli-Leydig cell tumor (57%) (Hum Pathol 2005;36:195)
- Female adnexal tumor of probable Wolffian origin (40 - 57%) (Mod Pathol 2020;33:734, Arch Pathol Lab Med 2022;146:166)
- STK11 adnexal tumor (100%) (Am J Surg Pathol 2021;45:1061)
- Cervical mesonephric adenocarcinoma (50 - 88%) (Am J Surg Pathol 2018;42:1596, Am J Surg Pathol 2001;25:379)
- Adenomatoid tumors (100%) (Appl Immunohistochem Mol Morphol 2012;20:173)
- Ameloblastoma (90 - 94%) (Histopathology 2000;37:27, Appl Immunohistochem Mol Morphol 2014;22:762)
- Keratocystic odontogenic tumor (80%) (Appl Immunohistochem Mol Morphol 2014;22:762)
- Lipoma (96%) (Hum Pathol 2006;37:312)
- Liposarcoma (97%) (Hum Pathol 2006;37:312)
- Cardiac myxoma (74%) (Histol Histopathol 2001;16:1031)
- Colonic medullary carcinoma (73%) (Hum Pathol 2009;40:398)
- Schwannoma (96%) (Am J Clin Pathol 2004;122:552)
Negative staining
- Note: calretinin is usually negative in the below entities, with variable, generally rare, positive cases (see percentages below)
- Derm:
- Squamous cell carcinoma (19%) (Hum Pathol 2003;34:994)
- Malignant melanoma (14%) (Hum Pathol 2003;34:994)
- Head and neck:
- Laryngeal squamous cell carcinoma (23%) (Hum Pathol 2003;34:994)
- Oral cavity, squamous cell carcinoma (22%) (Hum Pathol 2003;34:994)
- Adenomatoid odontogenic tumor (0%) (Appl Immunohistochem Mol Morphol 2014;22:762)
- Thoracic:
- Lung small cell carcinoma (41 - 49%) (Hum Pathol 2003;34:994, Am J Surg Pathol 2003;27:150)
- Lung squamous cell carcinoma (22 - 34%) (Hum Pathol 2003;34:994, Am J Surg Pathol 2003;27:150)
- Lung adenocarcinoma (0 - 11%) (Am J Surg Pathol 2003;27:150, Hum Pathol 2003;34:1155)
- Thymic carcinoma (36%) (Hum Pathol 2003;34:1155)
- Thymoma (3%) (Hum Pathol 2003;34:1155)
- Breast:
- Invasive mammary carcinoma of no special type (ductal carcinoma) (4%) (Hum Pathol 2003;34:994)
- Medullary carcinoma (44%) (Hum Pathol 2003;34:994)
- Mucinous carcinoma (11%) (Hum Pathol 2003;34:994)
- Papillary carcinoma (14%) (Hum Pathol 2003;34:994)
- Phyllodes tumor (23%) (Hum Pathol 2003;34:994)
- Gynecologic:
- Ovarian endometrioid carcinoma (18 - 36%) (Hum Pathol 2003;34:994, Hum Pathol 2005;36:195)
- Ovarian serous carcinoma (10 - 45%) (Hum Pathol 2003;34:994, Am J Clin Pathol 2008;130:771, Am J Surg Pathol 2007;31:1139, Am J Surg Pathol 1998;22:1203)
- Ovarian microcystic stromal tumor (6%) (Am J Surg Pathol 2009;33:367)
- Ovarian fibroma - thecoma (14 - 33%) (Hum Pathol 2005;36:195)
- Squamous cell carcinoma (cervix, vulva, vagina) (10 - 18%) (Hum Pathol 2003;34:994)
- Endocervical adenocarcinoma (0%) (Am J Surg Pathol 2018;42:1596)
- Endometrial mesonephric-like carcinoma (0%) (Am J Surg Pathol 2018;42:1596)
- Endometrial endometrioid adenocarcinoma (7%) (Am J Surg Pathol 2018;42:1596)
- Endometrial serous carcinoma (9%) (Am J Surg Pathol 2018;42:1596)
- Endometrial clear cell carcinoma (14%) (Am J Surg Pathol 2018;42:1596)
- Endometrial carcinosarcoma (26%) (Am J Surg Pathol 2018;42:1596)
- Gastrointestinal:
- Hepatocellular carcinoma (2%) (Hum Pathol 2003;34:994)
- Pancreatic adenocarcinoma (5%) (Hum Pathol 2003;34:994)
- Gastric adenocarcinoma (6%) (Hum Pathol 2003;34:994)
- Small intestine, adenocarcinoma (11%) (Hum Pathol 2003;34:994)
- Colonic adenocarcinoma (5 - 6%) (Hum Pathol 2003;34:994, Pathol Oncol Res 2016;22:725)
- Genitourinary:
- Prostatic adenocarcinoma (7%) (Hum Pathol 2003;34:994)
- Renal cell carcinoma, clear cell type (3 - 10%) (Hum Pathol 2003;34:994, Appl Immunohistochem Mol Morphol 2010;18:414, Am J Surg Pathol 2011;35:678)
- Renal cell carcinoma, papillary type (10%) (Hum Pathol 2003;34:994)
- Urothelial carcinoma (5%) (Hum Pathol 2003;34:994)
- Testicular seminoma (9%) (Hum Pathol 2003;34:994)
- Testicular fibroma - thecoma (25%) (Am J Surg Pathol 2021;45:1303)
- Testicular myoid gonadal stromal tumor (0%) (Am J Surg Pathol 2021;45:1303)
- Rete testis adenocarcinoma (40%) (Am J Surg Pathol 2019;43:670)
- Neuroendocrine:
- Paraganglioma (16 - 27%) (Hum Pathol 2003;34:994, Appl Immunohistochem Mol Morphol 2010;18:414)
- Pheochromocytoma (3%) (Hum Pathol 2003;34:994)
- Thyroid medullary carcinoma (30%) (Hum Pathol 2003;34:994)
- CNS:
- Astrocytoma (28%) (Hum Pathol 2003;34:994)
- Ependymoma (7%) (Hum Pathol 2003;34:994)
- Glioblastoma multiforme (16%) (Hum Pathol 2003;34:994)
- Oligodendroglioma (17%) (Hum Pathol 2003;34:994)
- Other:
- Desmoplastic small round cell tumor (19%) (Mod Pathol 2003;16:229)
- Neurofibroma (7%) (Am J Clin Pathol 2004;122:552)
Sample pathology report
- Right pleura, core needle biopsy:
- Mesothelioma
- Immunohistochemistry performed shows the following staining profile in the lesional cells:
- Positive: calretinin, WT1
- Negative: TTF1, Claudin4
Board review style question #1
A pleural fluid specimen consists of abundant clusters of atypical cells. Pancytokeratin and WT1 stains are positive, while Claudin4 and BerEp4 are negative. The figure above shows a calretinin stain. What is the most appropriate statement?
- The biomarker result is noncontributory due to a lack of specificity
- The biomarker result is supportive of a lung adenocarcinoma
- The biomarker result is supportive of a lung squamous cell carcinoma
- The biomarker result is supportive of malignant mesothelioma
Board review style answer #1
CAMTA1
Table of Contents
Definition / general | Clinical features | Uses by pathologists | Positive stains | Negative stains | Additional referencesDefinition / general
- Calmodulin binding transcription activator 1 (CAMTA1)
- Putative tumor suppressor transcription activator
- Interacts with calmodulin
- Functions as calcium sensitive regulator of gene expression
Clinical features
- CAMTA1 shows deletion in classic oligodendroglial tumors with 1p LOH (Clin Cancer Res 2005;11:1119)
- Deletion from the nervous system of mutant mice results in loss of Purkinje cells, cerebellar atrophy and ataxia (Proc Natl Acad Sci U S A. 2014;111:11521)
Uses by pathologists
- Highly specific and sensitive marker for epitheliod hemangioendothelioma (Histopathology 2015;67:827)
- Most epithelioid hemangioendotheliomas have translocation involving 1p36.3 and 3q25, resulting in WWTR1 - CAMTA1 gene fusion (Sci Transl Med 2011;3:98ra82, Genes Chromosomes Cancer 2011;50:644, Am J Surg Pathol 2001;25:684)
- FISH for WWTR1 - CAMTA1 is a helpful diagnostic tool for epithelioid hemangioendothelioma in small biopsies (Am J Surg Pathol 2015;39:132)
- CAMTA1 IHC differentiates epithelioid hemangioendothelioma from other tumors with epithelioid morphology (Am J Surg Pathol 2016;40:94)
Positive stains
- Staining localization:
- Nuclear
- Normal:
- Higher levels of expression seen in cerebellar granular cell layer
- Expressed also in midbrain, pons, and medulla (Proc Natl Acad Sci U S A 2014;111:11521)
- Disease:
- Epithelioid hemangioendothelioma
- 1 of 37 invasive ductal carcinomas showed CAMTA1 positivity
Negative stains
- Negative in epithelial tumors of bile duct, breast (lobular), endometrium, kidney, liver, lung, ovary, prostate, stomach, thyroid
- Negative in anaplastic large cell lymphoma, angiosarcoma, epithelioid hemangioma, GIST, melanoma, MPNST, myoepithelioma, PEComa, schwannoma, squamous cell carcinoma, synovial sarcoma, urothelial carcinoma
Additional references
Carbonic anhydrase IX
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Member of zinc metalloenzyme family, which accelerates the rate of conversion between carbon dioxide (CO2) and bicarbonate (HCO3) (Am J Clin Pathol 2014;141:219)
- Transmembrane protein that is regulated by hypoxia (Cancer Res 2000;60:7075, SpringerLink: Carbonic Anhydrase - Mechanism, Regulation, Links to Disease, and Industrial Applications [Accessed 17 February 2021])
- Roles in cell proliferation and migration, cell adhesion, tumorigenesis and pH control (Cancer Res 2004;64:6160, Oncogene 2010;29:6509)
Essential features
- Carbonic anhydrase IX (CAIX / CA9) is a transmembrane protein (membranous expression) (Am J Clin Pathol 2014;141:219)
- Primarily used in differentiating kidney tumors but not specific to renal primary tumors
- Diffusely positive in clear cell renal cell carcinoma (box-like) and clear cell papillary renal cell carcinoma (cup-like) (Histopathology 2020;77:659)
- Strong membranous staining in mesothelioma, mesothelial lesions and mesothelium (Virchows Arch 2012;460:89, Am J Clin Pathol 2014;142:82)
- Upregulated in hypoxic environments, including around necrosis (Cancer Res 2000;60:7075)
Terminology
- Carbonic anhydrase IX / CA9 (NCBI: CA9 Carbonic Anhydrase 9 [Accessed 11 December 2020])
- MN / G250 (NCBI: CA9 Carbonic Anhydrase 9 [Accessed 11 December 2020])
Pathophysiology
- CAIX is under control of the hypoxia inducible factor 1 (HIF1) and is predominantly located in chronically hypoxic tumor regions (Semin Cancer Biol 2015;31:52, Cancer Res 2000;60:7075)
- CAIX protein is attached to the plasma membrane with a single transmembrane domain (Br J Cancer 2020;122:157)
- CAIX catalyzes the reversible hydration of CO2 at the plasma membrane (Br J Cancer 2020;122:157)
- By facilitating CO2 excretion, CAIX maintains a more intracellular alkaline pH and more acidic extracellular space, facilitating invasion (J Biol Chem 2008;283:20473, J Biol Chem 2009;284:20299, Oncotarget 2012;3:84)
- CAIX also drives cell migration and invasion by both catalytic and noncatalytic mechanisms (J Biol Chem 2012;287:3392, Front Physiol 2013;4:271, Cancer Res 2009;69:358)
- CAIX expression also promotes cell cancer cell migration by competing with E-cadherin for binding to β catenin, inactivation of Rho kinase and induction of epithelial - mesenchymal transition (Exp Cell Res 2003;290:332, J Cell Sci 2011;124:1077)
Clinical features
- CAIX is overexpressed in hypoxia; hypoxia inducible factor is controlled by the VHL gene (Nature 1999;399:271)
Interpretation
- Membranous staining (box-like or cup-like [negative luminal border])
- Disregard cytoplasmic staining
Uses by pathologists
- Primarily used in differentiating renal cell carcinoma (RCC) subtypes
- Clear cell RCC (diffuse) versus papillary RCC (focal, very often < 50%) (Histopathology 2020;77:659, Am J Clin Pathol 2014;141:219)
- Clear cell RCC (diffuse, box-like) versus clear cell papillary RCC (diffuse, cup-like) (Histopathology 2020;77:659)
- Clear cell RCC (diffuse) versus chromophobe RCC (negative) (Histopathology 2020;77:659, Am J Clin Pathol 2014;141:219)
- Clear cell RCC (diffuse) versus Xp11 translocation RCC (negative or focal) (Histopathology 2020;77:659, Am J Surg Pathol 2010;34:1295)
- Supports clear cell RCC subtype in metastatic tumor consistent with RCC primary
- Potential in discriminating select meningioma subtypes (negative in clear cell versus positive in microcystic and angiomatous (J Neuropathol Exp Neurol 2019;78:1081)
Prognostic factors
- Prognostic role under investigation in multiple organ systems
- May be associated with worse outcome in clear cell renal cell carcinoma and papillary renal cell carcinoma (Urol Oncol 2018;36:531.e19, Eur J Surg Oncol 2020;46:209)
- Expression may be a negative prognostic marker in:
- Hepatocellular carcinoma (Int J Oncol 2017;51:1179)
- Breast carcinoma; may also be associated with better treatment response in breast carcinoma (Histol Histopathol 2011;26:1279, Cancer Res 2011;71:3364, BMC Cancer 2019;19:1173)
- Gastric adenocarcinoma (J Environ Pathol Toxicol Oncol 2016;35:207)
- Pancreatic ductal adenocarcinoma (Pathol Oncol Res 2018;24:899)
- Oral squamous cell carcinoma (Int J Mol Sci 2019;20:375, Oncotarget 2017;8:83088, Oral Oncol 2012;48:615)
Microscopic (histologic) images
Positive staining - normal
- Liver bile ducts (Am J Clin Pathol 2014;141:219)
- Gastric (body and antrum) (Am J Clin Pathol 2014;141:219)
- Duodenum (Am J Clin Pathol 2014;141:219)
- Mesothelium (Virchows Arch 2012;460:89)
Positive staining - disease
- Clear cell renal cell carcinoma (> 90%, diffuse, box-like) (Histopathology 2020;77:659)
- Clear cell papillary renal cell carcinoma (100%, diffuse, cup-like) (Histopathology 2020;77:659)
- Papillary renal cell carcinoma (30 - 82%, focal only) (Histopathology 2020;77:659, Am J Clin Pathol 2014;141:219, Histopathology 2011;59:1229)
- Malignant mesothelioma (100%, diffuse, box-like) (Virchows Arch 2012;460:89)
- Adenomatoid tumor (100%, diffuse, box-like) (Virchows Arch 2012;460:89)
- Endolymphatic sac tumors (100%) (Head Neck Pathol 2019;13:355)
- Epididymal papillary cystadenoma (100%) (Urology 2018;112:172)
- Clear cell adenocarcinoma of the urothelial tract (Histopathology 2011;59:1229)
- Pancreatic serous cystadenoma (100%) (Pancreatology 2009;9:182)
- Intrahepatic cholangiocarcinoma (90%) (Am J Clin Pathol 2014;141:219)
- Other tumors may be positive but staining is less diffuse and often concentrated in areas of necrosis:
- Urothelial carcinoma (35 - 100%) (Am J Clin Pathol 2014;141:219, Histopathology 2011;59:1229)
- Endocervical adenocarcinoma (> 60%) (Am J Clin Pathol 2014;141:219)
- Pancreatic adenocarcinoma (> 50%) (Am J Clin Pathol 2014;141:219)
- Squamous cell carcinoma (> 50%) (Am J Clin Pathol 2014;141:219)
- Gastric adenocarcinoma (42 - 57%) (J Environ Pathol Toxicol Oncol 2016;35:207, Am J Clin Pathol 2014;141:219)
- Colonic adenocarcinoma (> 50%) (Am J Clin Pathol 2014;141:219)
- Endometrial endometrioid adenocarcinoma (> 50%) (Am J Clin Pathol 2014;141:219)
Negative staining
- Chromophobe renal cell carcinoma (Histopathology 2020;77:659, Am J Clin Pathol 2014;141:219)
- Oncocytoma (Histopathology 2020;77:659, Am J Clin Pathol 2014;141:219)
- Translocation renal cell carcinoma (5 - 37%) (Am J Surg Pathol 2020;44:1450, Histopathology 2020;77:659, Am J Surg Pathol 2010;34:1295)
- Hepatocellular carcinoma (15%) (Am J Clin Pathol 2014;141:219)
- Seminoma (0 - 7%) (Histopathology 2011;59:1229, Am J Clin Pathol 2014;141:219)
- Yolk sac tumor (Histopathology 2011;59:1229)
- Choriocarcinoma (Histopathology 2011;59:1229)
- Leydig cell tumor (Histopathology 2011;59:1229)
- Pheochromocytoma (Histopathology 2011;59:1229)
- Adrenal cortical adenoma (Histopathology 2011;59:1229)
- Breast invasive carcinoma of no special type (ductal) (0 - 15%, higher with increasing grade) (Am J Clin Pathol 2014;141:219)
- Prostate adenocarcinoma (Histopathology 2011;59:1229, Am J Clin Pathol 2014;141:219)
- Thyroid papillary carcinoma (Am J Clin Pathol 2014;141:219)
- Renal cortex tubules and glomeruli
Board review style question #1
A 68 year old man was found to have a 2.5 cm cystic kidney mass. The mass was positive for CK7 while negative for CD10 and AMACR. CAIX showed the staining pattern in the picture above. What is the diagnosis?
- Clear cell renal cell carcinoma
- Clear cell papillary renal cell carcinoma
- Multilocular cystic renal neoplasm of low malignant potential
- Papillary renal cell carcinoma
Board review style answer #1
Board review style question #2
Board review style answer #2
Carcinoma of unknown primary
Definition / general
- 3-5% of cancer diagnoses
- Choice of marker depends on what tumors are logically within the differential diagnosis
- Molecular products must be validated to show adequate performance characteristics for clinical use (Arch Pathol Lab Med 2010;134:216)
- Analysis may be affected by tumor heterogeneity (Genome Med 2013;5:29)
- Tumors of unknown primaries, even when accurately classified by molecular methods, may harbour molecular/genetic traits distinct from tumors of known primaries, and have poorer response to treatment (Cancer Treat Rev 2009;35:221)
- Immunohistochemistry profiles:
- Carcinoma of unknown primary, 18 markers (MD Anderson): table, Gastrointest Cancer Res 2007;1:229
- Adenocarcinoma, 12 markers + PCR (Turin, Italy): algorithm, J Transl Med 2012;10:12
- Adenocarcinoma, 15 markers (Tokyo, Japan): algorithm, PLoS One 2012;7:e31181
- Gene expression assays:
- Measures expression of up to thousands of genes simultaneously to identify those whose expression has changed compared to baseline (normal) levels
- Adenocarcinoma (Amsterdam): J Clin Oncol 2008;26:4435
- Carcinoma of unknown primary determined using Pathwork Tissue of Origin Test: Am J Surg Pathol 2013;37:1067, Diagn Pathol 2010;5:26
- Test also works on body fluid specimens: Cancer Cytopathol 2012;120:62
- Test may soon be offered by Response Genetics
- Poorly differentiated / undifferentiated tumors-1550 gene expression profile (The Methodist Hospital): J Clin Oncol 2009;27:2503
- Carcinoma of unknown primary determined using microarray reference database (Helsinki, Finland): Genome Med 2011;3:63
- Hybrid using IHC and gene expression assays:
- Carcinoma of unknown primary (Moffitt Cancer Center): J Mol Diagn 2010;12:476
- RT-PCR:
- RT-PCR (bioTheranostics): Oncologist 2010;15:500, J Clin Oncol 2013;31:217
- Computational:
- Computational strategy using high-throughput sequencing (ISOLATE): Bioinformatics 2009;25:2882
- MicroRNA based PCR methods:
- Rosetta Genomics: Oncologist 2012;17:801, Mol Cancer 2013;12:57
- CNS metastases (Heidelberg, Germany): Oncologist 2011;16:165
- 47 miRNA signature (Ferrara, Italy): J Pathol 2011;225:43
- 48 miRNA signature (MD Anderson) Clin Cancer Res 2011;17:4063
Recommended IHC markers
- Epithelial markers: low molecular weight keratin (CAM 5.2), AE1-AE3 cytokeratin cocktail, CK7, CK20, CEA and EMA
- Alternative epithelial markers on sarcomatoid carcinoma include p63, MOC-31 and TTF1 (Mod Pathol 2005;18:1471)
- Melanocytic markers: S100 (also a mesenchymal marker), HMB45, MelanA / Mart1
- Lymphoid markers: CD3 (T cells), CD20 (B cells), CD15 (Hodgkin), CD30 (Hodgkin & other) and various others
- Histiocytic markers: CD68, lysozyme, CD1a (Langerhans cells)
- Neuroendocrine markers: neuron specific enolase, chromogranin, synaptophysin, CD56 and CD57
- Mesenchymal markers: vimentin (non-specific), factor XIIIa (fibrous histiocytoma), factor VIII (vessels), CD31 (vessels), CD34 (vessels), D2-40 (lymphatics), HHF35 (actin), smooth muscle actin and desmin
- Cell proliferation / apoptosis markers: Ki-67, bcl2
Cathepsin K
Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Lysosomal, papain-like cysteine protease with high matrix-degrading activity; expression is driven by microphthalmia transcription factor (MITF) in osteoclasts
- Responsible for bone resorption and remodeling
- Germline mutations cause sclerosing osteochondrodysplasia pycnodysostosis, a rare autosomal recessive skeletal dysplasia characterized by abnormal bone and tooth development
Uses by pathologists
- Diagnosis of renal angiomyolipoma and other renal erivascular epithelioid cell tumors (Mod Pathol 2012;25:100)
Microscopic (histologic) images
Positive staining - normal
- Fibroblasts (skin, lung, J Am Acad Dermatol 2012;66:e89), osteoclasts
- Intervertebral disc (Arthritis Res Ther 2011;13:R140)
- Skin: stratum corneum, mature sebaceous cells, outer root sheath of hair follicles (J Eur Acad Dermatol Venereol 2013;27:e128)
Positive staining - disease
- Alveolar soft parts sarcoma (Mod Pathol 2011;24:1313)
- Basal cell carcinoma (J Eur Acad Dermatol Venereol 2013;27:e128)
- Cholesteatoma (Mod Pathol 2001;14:1226), chordoma (Hum Pathol 2000;31:834)
- Granular cell tumor, histiocytic lesions, melanoma (Am J Clin Pathol 2013;139:151)
- Kidney: perivascular epithelioid cell tumor (diffuse, Mod Pathol 2012;25:100), PRCC-TFE3 carcinomas (Mod Pathol 2011;24:1313)
- Lung: lymphangioleiomyomatosis (Mod Pathol 2009;22:161)
- Osteoclastic giant cells
- Melanoma, osteoclastoma
Negative staining
- Endothelium
- Most carcinomas (Am J Clin Pathol 2013;139:151)
CCNB3 (pending)
[Pending]
CD markers - 190-199
Table of Contents
CD190 | CCR1 (CD191) | CCR2 (CD192) | CCR3 (CD193) | CCR4 (CD194) | CCR5 (CD195) | CCR6 (CD196) | CCR7 (CD197) | CCR8 (CD198) | CCR9 (CD199) | Diagrams / tables | Microscopic (histologic) images | Virtual slidesCCR1 (CD191)
- Member of beta chemokine receptor family; its major ligands are CCL3/MIP-1α, CCL5/RANTES and CCL7/MCP-3 (PLoS One 2011;6:e21772)
- Also called chemokine C-C motif receptor 1, CD191
- Note: maize protein cinnamoyl-CoA reductase 1 is also called CCR1 (J Exp Bot 2011;62:3837)
- Clinical features:
- Participates in pathogenesis of several renal diseases by orchestrating myeloid cell kidney infiltration (Am J Pathol 2012;180:1040)
- May play an important role in multiple myeloma (Future Med Chem 2011;3:1889)
- Antagonists are being developed for use in rheumatoid arthritis (Clin Pharmacol Ther 2011;89:726)
- Positive stains: monocytes/macrophages, neutrophils, lymphocytes, eosinophils, dendritic cells, basophils (Allergy 2006;61:1054)
CCR2 (CD192)
- Receptor for MCP1, MCP3, MCP4 chemokines; alternative coreceptor with CD4 for HIV1
- Abbreviation for chemokine C-C motif ligand 2 (CCL2)-chemokine C-C motif receptor 2
- Also known as CD192, but most publications use CCR2
- Inflammatory cytokine with 374 amino acids that mediates biologic effects of CCL2, also known as monocyte chemoattractant protein 1 (MCP1); CCL2-CCR2 may be involved in neuroinflammation and chronic pain (J Neuroinflammation 2012;9:136)
- In astrocytes, CCL2 binding may be CCR2 independent (Brain Res 2012;1437:115)
- During chemotaxis, may act as scavenger consuming the chemokine (PLoS One 2012;7:e37208)
- Clinical features:
- Reduced levels in peripheral blood mononuclear cells in patients with amyotrophic lateral sclerosis (PLoS One 2012;7:e38382)
- Mutations associated with reduced risk for:
- Severe coronary artery disease (Intern Med 2011;50:2457)
- Delay in progression of HIV to AIDS (AIDS 2000;14:483)
- Mutations associated with increased risk for:
- Osteoporosis and osteopenia (Genet Test Mol Biomarkers 2012;16:229)
- Chronic renal failure (Intern Med 2011;502457:649)
- Oral cancer (Oral Oncol 2011;47:577)
- Uses by pathologists: none
- Positive staining: neurons, monocytes; controversial if expressed on microglia, or due to infiltrating monocytes
CCR3 (CD193)
- C-C chemokine receptor type 3; also known as CD193
- G protein-coupled receptor for eotaxins
- Marker for Th2 cells (type 2 helper T cells, which promote humoral immune system)
- Constitutively expressed at high levels in eosinophils; primary chemokine receptor responsible for eosinophil recruitment to inflamed tissues (Exp Mol Med 2012;44:268)
- Clinical features:
- May play an integral role in pathogenesis of allergic diseases including asthma, allergic dermatitis, allergic rhinitis (Respir Res 2010;11:17)
- Important drug target for inflammatory diseases
- May also play a role in:
- Neovascular age-related macular degeneration (Invest Ophthalmol Vis Sci 2011;52:8271, J Mol Cell Biol 2009;1:17)
- Ulcerative colitis (Clin Exp Immunol 2010;162:337)
- CCR3 expression on peripheral blood lymphocytes is associated with EBV related infectious mononucleosis (Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi 2010;24:355)
- CCR3 gene polymorphisms may contribute to aspirin exacerbated respiratory disease (Respir Med 2010;104:626)
- May play an integral role in pathogenesis of allergic diseases including asthma, allergic dermatitis, allergic rhinitis (Respir Res 2010;11:17)
- Uses by pathologists: possible basophil selection marker for flow cytometry (Allergy 2011;66:85, Cytometry A 2011;79:102)
- Positive staining - normal:
- Bronchial smooth muscle and epithelium (Clin Exp Allergy 2012;42:1040)
- Eosinophils, basophils, mast cells
- Th2 helper cells
- Epidermal keratinocytes and dermal fibroblasts
- Positive staining - disease:
- Cutaneous melanoma and squamous cell carcinoma (Ann Dermatol 2010;22:412)
- Cutaneous T cell lymphoma (J Invest Dermatol 2010;130:2304)
CCR4 (CD194)
- CC chemokine receptor 4
- Seven-transmembrane G-protein coupled receptor, selectively expressed on Th2 cells and regulatory T cells
- CCR4-NOT deadenylase complex is key eukaryotic regulator of gene transcription and cytoplasmic mRNA degradation (Protein Cell 2011;2:755, FEBS Lett 2011;585:2182)
- Catalyzes removal of mRNA poly(A) tails, repressing translation and committing mRNA to degradation (RNA Biol 2013;10(2):228)
- Receptor for CCL2 (MCP-1), CCL4 (MIP-1), CCL5 (RANTES), CCL17 (TARC), CCL22 (Macrophage-derived chemokine) (Wikipedia-CCR4)
- Clinical features:
- Tumor cells may function as Treg cells with CCR4 expression, contributing to tumor survival by downregulating host immunity; tumor cells also produce CCR4 ligands which attract other CCR4+ Treg cells to tumor site (Cancer Sci 2011;102:44)
- Humanized anti-CCR4 monoclonal antibody, mogamulizumab (KW-0761), is being studied to treat peripheral T cell lymphoma (Curr Hematol Malig Rep 2012;7:235)
- Uses by pathologists: none
- Positive staining - normal: Th2 cells and regulatory T cells
- Positive staining - disease:
- Carcinomas of breast and stomach (Breast Cancer Res Treat 2012;131:837, Cancer Sci 2011;102:1264)
- Lymphoma:
- Anaplastic large cell lymphoma (60% of nodal ALK tumors) (Mod Pathol 2002;15:838)
- CLL in peripheral blood (low levels) (Eur J Haematol 2011;87:80)
- Peripheral T cell lymphoma, including adult T cell leukemia / lymphoma (Am J Surg Pathol 2007;31:216)
- Dermis based lymphomas (Am J Surg Pathol 2006;30:1111)
CCR5 (CD195)
- Chemokine (C-C motif) receptor 5; also known as CD195
- Surface receptor and attachment site for HIV and SIV into CD4+ cells, along with CXCR4 (CD184) (Exp Biol Med (Maywood) 2011;236:637)
- Those with CCR5-Δ32 mutation may have HIV resistance (Wikipedia)
- Receptor for CD8 chemokines RANTES, MIP 1-alpha, MIP 1-beta, monocyte chemoattractant protein 2 (MCP-2)
- Also receptor for Staphylococcus aureus leukotoxin ED (Nature 2013;493:51)
- Uses by pathologists: none
- Positive staining - normal: T cells, macrophages
CCR6 (CD196)
- C-C chemokine receptor type 6 gene
- Note: also refers to Clostridium difficile isolate
- Member of G protein-coupled receptor superfamily at 6q27, 374 amino acids (MW 42K Da, Wikipedia)
- Binds only a single ligand, CCL20 / macrophage inflammatory protein 3 alpha / MIP-3 alpha (Exp Cell Res 2011;317:613)
- Important for B lineage maturation, antigen driven B cell differentiation
- Mediates recruitment of T cells to inflamed sites (Arthritis Res Ther 2012;14:R73, J Dermatol 2012;39:838)
- CCL20-CCR6 axis mediates migration of circulating regulatory T cells into tumor microenvironment; may cause tumor progression in colon, liver, lung, prostatic carcinomas (PLoS One 2011;6:e24856, PLoS One 2011;6:e24671)
- Clinical features:
- CCR6 polymorphisms are risk factor for rheumatoid arthritis in Asian females but a protective factor in males (DNA Cell Biol 2012;31:607)
- Associated with chronic GVHD and invasive fungal disease (Biol Blood Marrow Transplant 2011;17:1443)
- May be favorable prognostic factor in lung adenocarcinoma (Tumour Biol 2011;32:197)
- Some statins may help treat psoriasis by inhibiting CCL20 / CCR6 interaction (Exp Dermatol 2011;20:855)
- Memory CCR6+ CD4+ T cells are preferential targets for productive HIV1 infection (J Immunol 2011;186:4618)
- CCR6 polymorphisms are risk factor for rheumatoid arthritis in Asian females but a protective factor in males (DNA Cell Biol 2012;31:607)
- Uses by pathologists: none
- Positive staining - normal:
- Immature dendritic cells, memory T cells that produce IL17 or IL22 (Th17 or Th22) (J Exp Med 2011;208:1875)
- Lymphoid tissue in GI tract
- Positive staining - disease:
- Gastric carcinoma (Pathol Int 2011;61:645)
- Lymphoma: mantle cell, marginal zone, MALT (Hum Pathol 2002;33:1227)
CCR7 (CD197)
- C-C chemokine receptor type 7
- Ligands are CCL19 and CCL21 (Wikipedia-C-C chemokine receptor type 7)
- Chemokine receptor that is 7 transmembrane domain G protein-coupled receptor
- Facilitates T cell migration to and compartmentation within secondary lymph nodes (J Immunol 2011;187:5645, PLoS One 2011;6:e18183)
- Promotes cell proliferation via extracellular signal-regulated kinase (ERK) pathway; may prevent apoptosis by upregulating bcl2 and downregulating bax and caspase3 (PLoS One 2012;7:e33262)
- Clinical features:
- Aberrant CCR7 expression in various malignancies has been linked to pro-survival, invasive and metastatic pathways (J Biol Chem 2012;287:3581)
- CCR7-CCL21 pathway may have role in rheumatoid arthritis angiogenesis (Arthritis Rheum 2012;64:2471)
- Macrophages participate in lymphangiogenesis in idiopathic diffuse alveolar damage through CCL19-CCR7 signal (Hum Pathol 2009;40:1553)
- 85 year old man with primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma which transformed from indolent to aggressive phase in association with CCR7+ conversion (Dermatol Online J 2012;18:5)
- Uses by pathologists: tumor infiltration by CCR7+ T cells may be favorable prognostic marker in advanced colorectal carcinoma (Clin Cancer Res 2012;18:850)
- Positive staining - normal:
- Dendritic cells (Mediators Inflamm 2012;2012:320953)
- Macrophages (some)
- T lymphocytes (some) (Oncoimmunology 2012;1:531, Am J Clin Pathol 2010;133:281)
- Positive staining - disease:
- Various carcinomas including:
- Breast (J Cell Physiol 2013;228:341)
- Esophagus (Ann Surg Oncol 2012;19:3606)
- Head and neck: squamous cell (J Biol Chem 2012;287:3581)
- Lung (PLoS One 2012;7:e33262)
- Melanoma (Microcirculation 2011;18:172, Hum Pathol 2007;38:768)
- MALT lymphoma and some diffuse large B cell lymphomas (Mod Pathol 2013;26:182)
- Various carcinomas including:
CCR8 (CD198)
- Chemokine (C-C motif) receptor 8; also known as CDw198
- Chemokine receptor associated with asthma / allergic diseases via Th2 pathway
- Ligand is CCL1 (Wikipedia)
- Antagonists may have efficacy against asthma
- May play a role in macrophage recruitment and activation in:
- Type 1 diabetes (J Immunol 2007;179:5760)
- COPD (Clin Vaccine Immunol 2011;18:2050)
- Endometriosis (Fertil Steril 2007;88:317)
- May be alternate coreceptor for HIV1 and HIV2 (Virology 2010;408:174)
- Uses by pathologists: no uses at this time
- Positive staining - normal:
- Dendritic cells (Biochem Pharmacol 2012;83:778)
- Eosinophils
- T cells (particularly Th2) (Biochem Biophys Res Commun 2011;407:764)
- Thymus
CCR9 (CD199)
- Also known as CDw199, GPR28, CC chemokine receptor 9
- Chemokine receptor; mediates chemotaxis in response to thymus-expressed chemokine (TECK) selectively expressed in thymus and small intestine
- Clinical features:
- Abnormal regulation of chemokine TECK and its receptor CCR9 in endometriotic milieu is involved in pathogenesis of endometriosis (Cell Mol Immunol 2010;7:51)
- Has role in inflammatory bowel disease (Expert Opin Ther Targets 2009;13:297)
- CCR9 and its ligand CCL25 have important role in breast cancer cell survival and resistance to cisplatin (World J Surg Oncol 2011;9:46)
- Plays pivotal role in drug resistance and invasion in T-ALL, ovarian cancer (World J Surg Oncol 2010;8:62, J Ovarian Res 2010;3:15)
- Uses by pathologists: none at this time
Diagrams / tables
Microscopic (histologic) images
Images hosted on other servers:
CCR3:
CCR4:
CCR6:
CCR7:
CCR9:
Virtual slides
CD Markers - General
Definition / general
- CD: cluster designation or cluster of differentiation; a protocol to identify and investigate cell surface molecules
- Nomenclature proposed in 1982 at First International Workshop and Conference on Human Leukocyte Differentiation Antigens (HLDA)
- A classification system for monoclonal antibodies generated by laboratories worldwide against cell surface molecules, initially on leukocytes, but now also from other cell types
- Data is collated and analyzed by cluster analysis based on pattern of binding to leukocytes or other cell types
- Must be at least two monoclonal antibodies for each antigen
- "w" indicates that the CD is not well characterized or is represented by only one monoclonal antibody
- Current CD markers range from CD1 to CD371
- Interpretation should be based on cellular distribution of staining (i.e. membranous, cytoplasmic, nuclear), proportion of positively stained cells, staining intensity and cutoff levels
Physiology
- CD molecules have various functions, including receptors or ligands; also cell adhesion, antigen presentation
- Although commonly used by pathologists to characterize cells, they most likely also have an important (although sometimes unknown) function in cell physiology
Uses by pathologists
- Used in immunohistochemistry and flow cytometry to characterize unknown cell types or to better understand known cell types
Additional references
- Lists of CD markers: UniProt - Swiss-Prot Protein Knowledgebase, HCDM website
- Information on each HLDA workshop:
- First workshop: Presse Med 1984;13:2311, Bernard: Leucocyte Typing: Human Leucocyte Differentiation Antigens Detected by Monoclonal Antibodies (Springer 1984)
- Second workshop: Reinherz: Leukocyte Typing II (Springer 1985)
- Third workshop: Leukemia 1987;1:231, McMichael: Leukocyte Typing III (Oxford University Press 1987)
- Fourth workshop: Blood 1989;74:1448, Am J Pathol 1989;135:420, Knapp: Leukocyte Typing IV (Oxford University Press 1990)
- Fifth workshop: J Immunol 1994;152:1, Schlossman: Leukocyte Typing V (Oxford University Press 1995)
- Sixth workshop: Bull World Health Organ 1997;75:385, Kishimoto: Leukocyte Typing VI (Oxford University Press 1998)
- Seventh workshop: J Immunol Methods 2003;275:1, Tissue Antigens 2001;58:425, J Leukoc Biol 2001;70:685, Mason: Leukocyte Typing VII (Oxford University Press 2002)
- Eighth workshop: Blood 2005;106:3123
- Ninth workshop: Immunol Lett 2011;134:104
- Tenth workshop: Clin Transl Immunology 2015;4:e47
CD markers - other
Table of Contents
CD150 | CD151 | CD152 | CD153 | CD154 | CD155 | CD156a | CD156b | CD156c | CD157 | CD158 | CD158a | CD158b | CD159a | CD159c | CD170 | CD171 | CD172a | CD173 | CD174 | CD175 | CD176 | CD177 | CD178 | CD179 | CD180 | CD181 / CD128 | CD182 / CXCR2 | CD183 / CXCR3 | CD184 | CD185 | CD186 | CD187 | CD188 | CD189 | CD190 | CD191 / CCR1 | CD192 / CCR2 | CD193 / CCR3 | CD194 / CCR4 | CD195 / CCR5 | CD196 / CCR6 | CD197 / CCR7 | CD198 / CCR8 | CD199 / CCR9 | CDw210 | CD211 | CD212 | CD213 | CD214 | CD215 | CD216 | CDw217 | CD218 | CD219 | CD220 | CD221 | CD222 | CD223 | CD224 | CD225 | CD226 | CD227 | CD228 | CD229 | CD240CE | CD240D | CD240DCE | CD241 | CD242 | CD243 | CD244 | CD245 | CD246 | CD247 | CD248 | CD249 | CD281 | CD282 | CD283 | CD284 | CD289 | CD303 | CD333 | CD351 | CD352 | CD353 | CD354 | CD355 | CD357 | CD358 | CD360 | CD361 | CD365 | CD366 | CD367 | CD368 | CD369 | CD370 | CD371 | Diagrams / tables | Microscopic (histologic) images | Virtual slides | Peripheral smear imagesCD150
CD151
CD152
- Also known as cytotoxic T lymphocyte associated protein 4, CTLA4
- Negative regulator of T cell activation
- CTLA4 restriction fragment length polymorphisms are linked to various autoimmune disorders
- Shares sequence homology with CD28; also shares ligands CD80 and CD86 with CD28
- Positive staining - normal: activated but not resting T cells, activated B cells
- Reference: OMIM CD152
CD154
- Also known as CD40 ligand, CD40L, TNF related activation protein (TRAP)
- Regulates B cell function by engaging CD40
- Defective gene prevents immunoglobulin class switch and is associated with hyper IgM syndrome, autoimmune hematologic disorders, disorganized nodal follicular architecture and PAS positive plasmacytoid cells containing IgM, lymph nodes without germinal centers, shortened lifespan, often with gastrointestinal cancers (cholangiocarcinoma, hepatocellular carcinoma and adenocarcinoma) and Cryptosporidium parvum infection
- Positive staining - normal: T cells
CD155
CD156a
CD156b
CD156c
- Also known as ADAM10
- Protein belonging to a superfamily of metalloproteases (Anal Cell Pathol (Amst) 2015;2015:975436)
CD157
CD158
- Member of KIR (killer cell immunoglobulin like receptor) family, also called killer cell inhibitory receptors
- Binding by HLA class I molecules causes inhibition of NK or T cell cytotoxic activity
- Melanoma specific cytotoxic T lymphocytes may express KIR and regulate their ability to kill these tumors
- Terminology:
- CD158c: KIR2DS6 / KIRX
- CD158d: KIR2DL4
- CD158e1: KIR3DL1 / p70
- CD158e2: KIR3DS1 / p70
- CD158f: KIR2DL5 (Front Immunol 2017;7:698)
- CD158g: KIR2DS5
- CD158h: KIR2DS1 / p50.1
- CD158i: KIR2DS4 / p50.3
- CD158j: KIR2DS2 / p50.2
- CD158k: KIR3DL2 / p140
- CD158z: KIR3DL7 / KIRC1
- Positive staining - normal: natural killer cells (NK cells), some T cells
CD158a
CD158b
CD159a
CD159c
- Plays a role as a receptor for the recognition of MHC class I HLA-E molecules by natural killer cells and some cytotoxic T cells (Front Immunol 2018;9:686)
- Also known as NKG2C, KLRC2
- Positive staining - normal: natural killer cells and CD8+ T cells
CD170
CD171
- Aka L1
- Adhesion molecule required for normal neurohistogenesis
- Mutations cause CRASH (Corpus callosum hypoplasia / agenesis, Retardation, Aphasia, Spastic paraplegia / shuffling gait and Hydrocephalus due to stenosis of aqueduct of Sylvius), an X linked neurologic disorder
- May mediate kidney branching morphogenesis, maintenance of lymph node architecture during immune response, costimulation of T cell activation in vitro
- Positive staining - normal: postmitotic neurons, glia, epithelial cells (some), lymphoid cells (some), myeloid (some), monocytes
CD173
CD174
CD175
CD176
CD177
CD178
- Aka CD95 ligand, Fas ligand (FasL)
- Important role in T cell mediated cytotoxicity; induces apoptosis in Fas expressing target cells
- Cells in immune privileged sites (testis, anterior chamber of eye, placenta) constitutively express FasL, which induces apoptosis in Fas expressing infiltrating T cells, minimizing inflammatory responses that might damage important physiologic functions at these sites
- May influence interaction of tumor cells with host immune system; theory is that FasL+ tumor cells induce apoptosis in infiltrating Fas+ mononuclear cells
- Fas-FasL binding triggers apoptosis in lymphocytes
- Mutations may be related to some cases of Systemic Lupus Erythematosis (SLE)
- Processed by metalloproteases which cause shedding of extracellular portion into blood (sFas L)
- Positive staining - normal: activated and cytotoxic T cells, testis, anterior chamber of eye, placenta; also Sertoli cells, neurons, thyroid epithelial cells
- Positive staining - tumors: Reed-Sternberg cells of Hodgkin’s lymphoma (nodular sclerosis and mixed cellularity) (Am J Surg Pathol 2001;25:388)
CD179
- CD179a:
- Aka VpreB1
- Associates noncovalently with CD179b to form surrogate light chain as component of preB cell receptor, which plays a critical role in early B cell differentiation
- CD179b:
- Aka lambda 5
- Associates noncovalently with CD179a to form surrogate light chain as component of preB cell receptor, which plays a critical role in early B cell differentiation
- Mutations impair B cell development and cause agammaglobulinemia
- Positive staining - normal: preB cells
CD180
- Also called RP105
- Regulates B cell recognition of lipopolysaccharide, a membrane constituent of gram-negative bacteria
- Positive staining - normal: mantle zone and marginal zone B cells (strong), other B cells (weak / negative); peripheral blood monocytes, dendritic cells
CD181 / CD128
- Also called CXCR1, IL8Ralpha; previously called CDw128A
- Chemokine receptor, powerful neutrophil chemotactic factor
- Positive staining - normal: neutrophils, basophils, T cell subset, monocytes, keratinocytes
- Positive staining - disease: T cells in allergic rhinitis (J Immunol 2004;172:268)
CD182 / CXCR2
- Also called CXCR2; formerly called CD128b
- Interleukin 8 receptor beta subunit (IL8RB); binds multiple CXC chemokines including IL8 (CXCL8)
- Chemokine receptor, powerful neutrophil chemotactic factor, particularly to sites of inflammation
- Interpretation: cytoplasmic staining
- Uses by pathologists: no significant uses by pathologists
- Positive staining - normal: mature granulocytes, keratinocytes, neuroendocrine cells, projection neurons (Arch Pathol Lab Med 2000;124:520)
- Positive staining - disease: carcinoid tumor (classic, atypical, metastatic), pituitary adenoma, pheochromocytoma, medullary carcinoma
- Negative staining: parathyroid cells; small cell carcinoma of lung / cervix, large cell lung neuroendocrine carcinoma, Merkel cell carcinoma, neuroblastoma, melanoma
- See Diagrams / tables
- See Microscopic (histologic) images
CD183 / CXCR3
- Also called CXCR3
- Receptor for some chemokines; binding of chemokines to CD183 induces integrin activation, cytoskeletal changes and chemotactic migration in inflammation associated effector T cells
- CD183+ T cells detected in inflamed tissues of patients with juvenile rheumatoid arthritis, multiple sclerosis, sarcoidosis, hepatitis C
- Positive staining - normal: T cells in inflamed tissue, eosinophils, plasmacytoid dendritic cells, hematopoietic progenitors
- Negative staining: naïve T cells in peripheral blood
CD184
- Also called CXCR4, stromal cell derived factor 1 (SDF1)
- Receptor for the CXC chemokine SDF1
- Also major HIV / SIV coreceptor (with CCR5 / CD195)
- Involved in B cell development, myelopoiesis, cardiac ventricular septum formation, blood vessel formation in GI tract, cerebellar granular cell development
- Positive staining - normal: all mature blood cells, blood progenitor cells, endothelial and epithelial cells, astrocytes, neurons
CD185
- Multipass membrane protein of CXC chemokine receptor family
- Also called CXCR5, BLR1 (Burkitt lymphoma receptor 1)
- Pathophysiology:
- Binds to B Lymphocyte Chemoattractant (BLC / CXCL13) (J Exp Med 1998;187:655)
- Involved in B cell migration into B cell follicles of spleen and Peyer patches (J Immunol 2009;182:2610)
- Critical for function of follicular helper T (TFH) cells
- May have role in survival and maintainance of cardiac structure upon pressure overload by regulating proteoglycans essential for correct collagen assembly (PLoS One 2011;6:e18668)
- May be important for ectopic mucosa associated lymphoid tissue neogenesis in chronic Helicobacter pylori induced inflammation (J Mol Med (Berl) 2010;88:1169)
- During HIV1 infection, altered expression of CXCR5 / CXCL13 may cause B cell dysfunction (Blood 2008;112:4401)
- Upregulated in rheumatoid arthritis synovial tissue and expressed in various cell types (Arthritis Res Ther 2005;7:R217)
- Interpretation: cytoplasmic staining
- Uses by pathologists: no significant uses by pathologists
- Positive staining - normal: mature B cells
- Positive staining - disease: Burkitt's lymphoma, mantle cell lymphoma; AIDS related non-Hodgkin lymphoma (Blood 2009;113:4604, AIDS Res Treat 2010;2010:164586)
- See Microscopic (histologic) images
CD191 / CCR1
- Member of beta chemokine receptor family; its major ligands are CCL3 / MIP1ɑ, CCL5 / RANTES and CCL7 / MCP3 (PLoS One 2011;6:e21772)
- Also called chemokine C-C motif receptor 1, CD191
- Note: maize protein cinnamoyl-CoA reductase 1 is also called CCR1 (J Exp Bot 2011;62:3837)
- Clinical features:
- Participates in pathogenesis of several renal diseases by orchestrating myeloid cell kidney infiltration (Am J Pathol 2012;180:1040)
- May play an important role in multiple myeloma (Future Med Chem 2011;3:1889)
- Antagonists are being developed for use in rheumatoid arthritis (Clin Pharmacol Ther 2011;89:726)
- Positive stains: monocytes / macrophages, neutrophils, lymphocytes, eosinophils, dendritic cells, basophils (Allergy 2006;61:1054)
CD192 / CCR2
- Receptor for MCP1, MCP3, MCP4 chemokines; alternative coreceptor with CD4 for HIV1
- Abbreviation for chemokine C-C motif ligand 2 (CCL2) chemokine C-C motif receptor 2
- Also known as CD192 but most publications use CCR2
- Inflammatory cytokine with 374 amino acids that mediates biologic effects of CCL2, also known as monocyte chemoattractant protein 1 (MCP1); CCL2-CCR2 may be involved in neuroinflammation and chronic pain (J Neuroinflammation 2012;9:136)
- In astrocytes, CCL2 binding may be CCR2 independent (Brain Res 2012;1437:115)
- During chemotaxis, may act as scavenger consuming the chemokine (PLoS One 2012;7:e37208)
- Clinical features:
- Reduced levels in peripheral blood mononuclear cells in patients with amyotrophic lateral sclerosis (PLoS One 2012;7:e37208)
- Mutations associated with reduced risk for:
- Severe coronary artery disease (Intern Med 2011;50:2457)
- Delay in progression of HIV to AIDS (AIDS 2000;14:483)
- Mutations associated with increased risk for:
- Osteoporosis and osteopenia (Genet Test Mol Biomarkers 2012;16:229)
- Chronic renal failure (Intern Med 2011;502457:649)
- Oral cancer (Oral Oncol 2011;47:577)
- Uses by pathologists: none
- Positive staining: neurons, monocytes; controversial if expressed on microglia or due to infiltrating monocytes
- See Diagrams / tables
CD193 / CCR3
- C-C chemokine receptor type 3; also known as CD193
- G protein coupled receptor for eotaxins
- Marker for Th2 cells (type 2 helper T cells, which promote humoral immune system)
- Constitutively expressed at high levels in eosinophils; primary chemokine receptor responsible for eosinophil recruitment to inflamed tissues (Exp Mol Med 2012;44:268)
- Clinical features:
- May play an integral role in pathogenesis of allergic diseases including asthma, allergic dermatitis, allergic rhinitis (Respir Res 2010;11:17)
- Important drug target for inflammatory diseases
- May also play a role in:
- Neovascular age related macular degeneration (Invest Ophthalmol Vis Sci 2011;52:8271, J Mol Cell Biol 2009;1:17)
- Ulcerative colitis (Clin Exp Immunol 2010;162:337)
- CCR3 expression on peripheral blood lymphocytes is associated with EBV related infectious mononucleosis (Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi 2010;24:355)
- CCR3 gene polymorphisms may contribute to aspirin exacerbated respiratory disease (Respir Med 2010;104:626)
- May play an integral role in pathogenesis of allergic diseases including asthma, allergic dermatitis, allergic rhinitis (Respir Res 2010;11:17)
- Uses by pathologists: possible basophil selection marker for flow cytometry (Allergy 2011;66:85, Cytometry A 2011;79:102)
- Positive staining - normal:
- Bronchial smooth muscle and epithelium (Clin Exp Allergy 2012;42:1040)
- Eosinophils, basophils, mast cells
- Th2 helper cells
- Epidermal keratinocytes and dermal fibroblasts
- Positive staining - disease:
- Cutaneous melanoma and squamous cell carcinoma (Ann Dermatol 2010;22:412)
- Cutaneous T cell lymphoma (J Invest Dermatol 2010;130:2304)
- See Diagrams / tables
CD194 / CCR4
- CC chemokine receptor 4
- Seven transmembrane G protein coupled receptor, selectively expressed on Th2 cells and regulatory T cells
- CCR4-NOT deadenylase complex is key eukaryotic regulator of gene transcription and cytoplasmic mRNA degradation (Protein Cell 2011;2:755, FEBS Lett 2011;585:2182)
- Catalyzes removal of mRNA poly(A) tails, repressing translation and committing mRNA to degradation (RNA Biol 2013;10:228)
- Receptor for CCL2 (MCP1), CCL4 (MIP1), CCL5 (RANTES), CCL17 (TARC), CCL22 (macrophage derived chemokine) (Wikipedia: CCR4 [Accessed 14 November 2022])
- Clinical features:
- Tumor cells may function as Treg cells with CCR4 expression, contributing to tumor survival by downregulating host immunity; tumor cells also produce CCR4 ligands which attract other CCR4+ Treg cells to tumor site (Cancer Sci 2011;102:44)
- Humanized anti-CCR4 monoclonal antibody, mogamulizumab (KW-0761), is being studied to treat peripheral T cell lymphoma (Curr Hematol Malig Rep 2012;7:235)
- Uses by pathologists: none
- Positive staining - normal: Th2 cells and regulatory T cells
- Positive staining - disease:
- Carcinomas of breast and stomach (Breast Cancer Res Treat 2012;131:837, Cancer Sci 2011;102:1264)
- Lymphoma:
- Anaplastic large cell lymphoma (60% of nodal ALK tumors) (Mod Pathol 2002;15:838)
- CLL in peripheral blood (low levels) (Eur J Haematol 2011;87:80)
- Peripheral T cell lymphoma, including adult T cell leukemia / lymphoma (Am J Surg Pathol 2007;31:216)
- Dermis based lymphomas (Am J Surg Pathol 2006;30:1111)
- See Diagrams / tables
CD195 / CCR5
- Chemokine (C-C motif) receptor 5; also known as CD195
- Surface receptor and attachment site for HIV and SIV into CD4+ cells, along with CXCR4 (CD184) (Exp Biol Med (Maywood) 2011;236:637)
- Those with CCR5-Δ32 mutation may have HIV resistance (Wikipedia: CCR5 [Accessed 14 November 2022])
- Receptor for CD8 chemokines RANTES, MIP 1 alpha, MIP 1 beta, monocyte chemoattractant protein 2 (MCP2)
- Also receptor for Staphylococcus aureus leukotoxin ED (Nature 2013;493:51)
- Uses by pathologists: none
- Positive staining - normal: T cells, macrophages
- See Diagrams / tables
CD196 / CCR6
- C-C chemokine receptor type 6 gene
- Note: also refers to Clostridium difficile isolate
- Member of G protein coupled receptor superfamily at 6q27, 374 amino acids (MW 42K Da) (Wikipedia: C-C Chemokine Receptor Type 6 [Accessed 14 November 2022])
- Binds only a single ligand, CCL20 / macrophage inflammatory protein 3 alpha / MIP3 alpha (Exp Cell Res 2011;317:613)
- Important for B lineage maturation, antigen driven B cell differentiation
- Mediates recruitment of T cells to inflamed sites (Arthritis Res Ther 2012;14:R73, J Dermatol 2012;39:838)
- CCL20-CCR6 axis mediates migration of circulating regulatory T cells into tumor microenvironment; may cause tumor progression in colon, liver, lung, prostatic carcinomas (PLoS One 2011;6:e24856, PLoS One 2011;6:e24671)
- Clinical features:
- CCR6 polymorphisms are risk factor for rheumatoid arthritis in Asian females but a protective factor in males (DNA Cell Biol 2012;31:607)
- Associated with chronic GVHD and invasive fungal disease (Biol Blood Marrow Transplant 2011;17:1443)
- May be favorable prognostic factor in lung adenocarcinoma (Tumour Biol 2011;32:197)
- Some statins may help treat psoriasis by inhibiting CCL20 / CCR6 interaction (Exp Dermatol 2011;20:855)
- Memory CCR6+ CD4+ T cells are preferential targets for productive HIV1 infection (J Immunol 2011;186:4618)
- CCR6 polymorphisms are risk factor for rheumatoid arthritis in Asian females but a protective factor in males (DNA Cell Biol 2012;31:607)
- Uses by pathologists: none
- Positive staining - normal:
- Immature dendritic cells, memory T cells that produce IL17 or IL22 (Th17 or Th22) (J Exp Med 2011;208:1875)
- Lymphoid tissue in GI tract
- Positive staining - disease:
- Gastric carcinoma (Pathol Int 2011;61:645)
- Lymphoma: mantle cell, marginal zone, MALT (Hum Pathol 2002;33:1227)
- See Diagrams / tables
CD197 / CCR7
- C-C chemokine receptor type 7
- Ligands are CCL19 and CCL21 (Wikipedia: C-C Chemokine Receptor Type 7 [Accessed 14 November 2022])
- Chemokine receptor that is 7 transmembrane domain G protein-coupled receptor
- Facilitates T cell migration to and compartmentation within secondary lymph nodes (J Immunol 2011;187:5645, PLoS One 2011;6:e18183)
- Promotes cell proliferation via extracellular signal regulated kinase (ERK) pathway; may prevent apoptosis by upregulating BCL2 and downregulating bax and caspase3 (PLoS One 2012;7:e33262)
- Clinical features:
- Aberrant CCR7 expression in various malignancies has been linked to prosurvival, invasive and metastatic pathways (J Biol Chem 2012;287:3581)
- CCR7-CCL21 pathway may have role in rheumatoid arthritis angiogenesis (Arthritis Rheum 2012;64:2471)
- Macrophages participate in lymphangiogenesis in idiopathic diffuse alveolar damage through CCL19-CCR7 signal (Hum Pathol 2009;40:1553)
- 85 year old man with primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma which transformed from indolent to aggressive phase in association with CCR7+ conversion (Dermatol Online J 2012;18:5)
- Uses by pathologists: tumor infiltration by CCR7+ T cells may be favorable prognostic marker in advanced colorectal carcinoma (Clin Cancer Res 2012;18:850)
- Positive staining - normal:
- Dendritic cells (Mediators Inflamm 2012;2012:320953)
- Macrophages (some)
- T lymphocytes (some) (Oncoimmunology 2012;1:531, Am J Clin Pathol 2010;133:281)
- Positive staining - disease:
- Various carcinomas including:
- Breast (J Cell Physiol 2013;228:341)
- Esophagus (Ann Surg Oncol 2012;19:3606)
- Head and neck: squamous cell (J Biol Chem 2012;287:3581)
- Lung (PLoS One 2012;7:e33262)
- Melanoma (Microcirculation 2011;18:172, Hum Pathol 2007;38:768)
- MALT lymphoma and some diffuse large B cell lymphomas (Mod Pathol 2013;26:182)
- Various carcinomas including:
- See Diagrams / tables
CD198 / CCR8
- Chemokine (C-C motif) receptor 8; also known as CDw198
- Chemokine receptor associated with asthma / allergic diseases via Th2 pathway
- Ligand is CCL1 (Wikipedia: CCR8 (gene) [Accessed 14 November 2022])
- Antagonists may have efficacy against asthma
- May play a role in macrophage recruitment and activation in:
- Type 1 diabetes (J Immunol 2007;179:5760)
- COPD (Clin Vaccine Immunol 2011;18:2050)
- Endometriosis (Fertil Steril 2007;88:317)
- May be alternate coreceptor for HIV1 and HIV2 (Virology 2010;408:174)
- Uses by pathologists: no uses at this time
- Positive staining - normal:
- Dendritic cells (Biochem Pharmacol 2012;83:778)
- Eosinophils
- T cells (particularly Th2) (Biochem Biophys Res Commun 2011;407:764)
- Thymus
CD199 / CCR9
- Also known as CDw199, GPR28, CC chemokine receptor 9
- Chemokine receptor; mediates chemotaxis in response to thymus expressed chemokine (TECK) selectively expressed in thymus and small intestine
- Clinical features:
- Abnormal regulation of chemokine TECK and its receptor CCR9 in endometriotic milieu is involved in pathogenesis of endometriosis (Cell Mol Immunol 2010;7:51)
- Has role in inflammatory bowel disease (Expert Opin Ther Targets 2009;13:297)
- CCR9 and its ligand CCL25 have important role in breast cancer cell survival and resistance to cisplatin (World J Surg Oncol 2011;9:46)
- Plays pivotal role in drug resistance and invasion in T-ALL, ovarian cancer (World J Surg Oncol 2010;8:62, J Ovarian Res 2010;3:15)
- Uses by pathologists: none at this time
- See Diagrams / tables
CDw210
- Aka IL10 receptor
- Interleukin 10 produced by B cells, T helper cells and monocyte / macrophages, exhibits diverse activities on different cell lines (OMIM 124092)
- IL10 inhibits macrophage activation by interferon gamma
- Positive staining - normal: monocytes, B and T cells, large granular lymphocytes, spleen, thymus, placenta, lung, liver
CD212
- Aka IL12 receptor
- Interleukin 12 promotes cell mediated immunity to intracellular pathogens by inducing type 1 helper T cell responses and interferon gamma production
- Lack of IL12 associated with severe, idiopathic mycobacterial and Salmonella infections, mature granulomas
- Positive staining - normal: T cells, NK cells
CD213
- CD213a1:
- Aka IL13 receptor, alpha 1
- Binds IL13 with low affinity
- With IL4r-alpha, can form a functional receptor for IL13
- Positive staining - normal: ubiquitous, B cells, T cells and endothelial cells, highest levels in heart, liver, skeletal muscle and ovary
- CD213a2:
- Aka IL13 receptor, alpha 2
- Inhibits binding of interleukin 13 to the IL13 cell surface receptor
- Positive staining - normal: placenta
CDw217
CD221
CD222
CD223
- Aka Lymphocyte-Activation Gene 3 (LAG3)
- Homologous to CD4
- Associates with MHC class II molecules on monocytes/dendritic cells, which are subsequently activated
- May help activated CD4+ and CD8+ T cells to fully activate monocytes and dendritic cells, leading to optimized MHC class I and class II T cell responses
- Positive staining - normal: activated T cells, activated NK cells
CD224
CD225
CD226
- Aka DNAM1, Platelet and T cell Activation antigen 1 (PTA1)
- Mediates adhesion to an unknown ligand
- T cell expression increased in some patients with autoimmune disease and viral infection
- Positive staining - normal: NK cells, platelets, monocytes, subset of B and T cells
- Negative staining: granulocytes, erythrocytes
CD227
- See EMA / MUC1
CD228
CD240CE
- Also called RH 30 CE, Rh blood group Cc and Ee blood group antigens; encodes RhC and RhE antigens on a single polypeptide
- On #1p36.11 adjacent to RH D gene
- Rh (rhesus) blood group system is second most clinically significant blood group after ABO; is most polymorphic blood group, with variations due to deletions, gene conversions and missense mutations
- Rh antigens are carried by an oligomer of two major erythroid specific polypeptides, the Rh (D and CcEe) proteins and the RhAG glycoprotein
- Rh proteins form a core complex critical to structure of erythrocyte membrane (Blood Rev 2006;20:93)
- May play a role in ammonia transport (J Biol Chem 2002;277:12499, Transfus Clin Biol 2006;13:132)
- Discrepant or doubtful serologic results can be resolved by sequence specific primer (PCR SSP) technique (Transfusion 2007;47:54S)
- Rarely causes hemolytic disease of newborn (Transfus Med 2000;10:305)
- Uses by pathologists: blood typing
- Positive staining - normal: erythroid cells
- References: Blood 2000;95:375, OMIM 111700
CD240D
- Also called RH30 D, Rh blood group D blood group antigen; is major antigen of the Rh system
- On #1p36.11 adjacent to RHCE gene
- Rh (rhesus) blood group system is second most clinically significant blood group after ABO; is most polymorphic blood group, with variations due to deletions, gene conversions and missense mutations
- Weak D, formerly called D(u), occurs in 0.2 to 1% of whites
- Exhibits reduced expression of D antigen (Blood 1999;93:385)
- Should not be labeled as Rh negative (Curr Opin Hematol 2006;13:476)
- Individuals are classified as Rh positive or negative based on presence or absence of highly immunogenic D antigen on red cell surface
- May have arisen historically by duplication of RHCE gene (Blood 2002;99:2272)
- Discrepant or doubtful serologic results can be resolved by sequence specific primer (PCR SSP) technique (Transfusion 2007;47:54S)
- Hemolytic disease of fetus and newborn: usually due to Rh negative woman whose partner is Rh+ or heterozygous and fetus is Rh+; woman has preexisting anti-RhD antibodies that cross placenta and harm fetus (Immunohematol 2006;22:188)
- Can use maternal plasma in alloimmunized pregnancies to determine fetal RhD status or for RHD and RHCE genotyping (Fetal Diagn Ther 2006;21:404, Prenat Diagn 2005;25:1079)
- Genotyping from amniotic fluid or chorionic villi sampling was performed in past but is more invasive (N Engl J Med 1998;339:1734, Clin Exp Med 2002;2:77)
- Rh positive mothers may rarely (0.15%) develop new antibodies (other than anti-RHD) in third trimester but no clinical significance (J Matern Fetal Neonatal Med 2007;20:59)
- Having Rh negative mother may be risk factor for autistic children, due to use of mercury containing Rho-immune globulin (J Matern Fetal Neonatal Med 2007;20:385)
- Uses by pathologists: blood typing
- Positive staining - normal: erythroid cells
- References: OMIM 111680, Wikipedia, eMedicine (Rh incompatibility)
CD240DCE
CD241
- Also called RH50 glycoprotein, RHAG, Rhesus blood group associated glycoprotein
- Located at #6p21.1 - p11
- Is a strictly required posttranscriptional factor regulating Rh membrane expression (Blood 2002;100:1038)
- Also appears to be an ammonium transporter and a CO2 channel (Proc Natl Acad Sci USA 2004;101:17222, FASEB J 2008;22:64)
- Defects cause Rh-null phenotype, associated with a chronic hemolytic anemia and spherostomatocytosis (OMIM 268150, J Biol Chem 1998;273:2207)
- Uses by pathologists: blood typing
- Positive staining - normal: erythroid cells
- Reference: OMIM 180297
CD242
- Also called intercellular adhesion molecule 4 (ICAM4), Landsteiner-Wiener (LW) blood group protein
- Discovered with antibody raised in guinea pigs injected with the cells of rhesus monkeys but Rh designation had already been taken
- Binds to CD11a / CD18, CD11b / CD18 and CD11c / CD18 (Blood 2007;109:802)
- May be critical in erythroblastic island formation, where erythroid progenitors differentiate (Blood 2006;108:2064)
- May be ligand for platelet activated alpha IIb beta 3 integrin (J Biol Chem 2003;278:4892)
- In sickle cell disease, contributes to red cell endothelial cell adhesion and vasoocclusion (Transfus Clin Biol 2006;13:44)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: erythroid cells
- References: OMIM 111250
CD243
- See Stains-MDR
CD244
- Also called Natural Killer cell receptor 2B4
- Regulates NK and T cell function in multiple ways (J Immunol 2005;175:2045)
- Coexpression of 2B4 and CD160 defines a CD8+ T lymphocyte subpopulation with high cytolytic effector activity (Eur J Immunol 2006;36:2359)
- Binds to CD48 (J Immunol 2006;176:4646)
- CD244 - CD48 interactions prevent NK cells from killing each other (Blood 2007;110:2020)
- Functional changes are associated with X linked lymphoproliferative disease (J Exp Med 2000;192:337, J Immunol 2000;165:2932)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal:
- NK cells
- CD8+ T cells
- Monocytes and basophils (Eur J Immunol 1999;29:1676)
- Eosinophils (J Immunol 2005;174:110)
- Spleen (Tissue Antigens 1999;54:27)
- Reference: OMIM 605554
CD245
- Also called p220 / 240
- Very little information is available for CD245 directly; appears to be identical to NPAT (nuclear protein, ataxia-telangiectasia locus)
- NPAT links S phase cyclin E / Cdk2 kinase activity to replication dependent histone gene transcription (Biochemistry 2006;45:15915, Mol Cell Biol 2005;25:6140)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: T cells (some), other white blood cells with varying intensity
CD246
- See Stains-ALK
CD247
- Also called T cell receptor zeta chain
- Forms T cell-CD3 receptor complex with TCR alpha / beta and gamma / delta heterodimers and CD3 (gamma, delta and epsilon) (Proc Natl Acad Sci USA 1988;85:9709)
- Couples antigen recognition to several intracellular signal transduction pathways; low expression causes impaired immune response
- Low expression in tumor infiltrating T cells in various disorders:
- Cancer of kidney (Cancer Invest 2004;22:871)
- Cancer of stomach (Cancer 2002;94:1437)
- Hodgkin’s lymphoma (Blood 1996;88:236)
- Active tuberculosis (J Infect Dis 2006;194:1385)
- Systemic lupus erythematosus (J Immunol 2002;169:6048, Adv Med Sci 2006;51:181)
- Normal pregnancy but not preeclampsia (Am J Obstet Gynecol 2003;189:843)
- Defects cause primary T cell immunodeficiency (OMIM 610163)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: T cells
- See Diagrams / tables
- See Microscopic (histologic) images
- Reference: OMIM 186780
CD248
- Also called endosialin, tumor endothelial marker 1 (TEM1)
- Cell surface glycoprotein associated with tumors: traditionally thought present in vascular endothelial cells (Proc Natl Acad Sci USA 1992;89:10832, J Biol Chem 2001;276:7408)
- May actually be marker of stromal fibroblasts (FEBS Lett 2005;579:2569)
- Not present (or weak) in nontumor associated endothelium
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal:
- Endometrium
- Embryos (Cancer Res 2001;61:6649)
- Fibroblasts and pericytes during lymphoid tissue development (FEBS Lett 2007;581:3550)
- RNA at low / moderate levels in many organs
- Positive staining - disease:
- MFH and other sarcomas, some capillaries and fibroblasts in carcinomas
- Endothelium of high grade brain tumors (J Neuropathol Exp Neurol 2004;63:1274)
- RNA at low / moderate levels in carcinomas (Cancer Immun 2005;5:10)
- See Microscopic (histologic) images
- Reference: OMIM 606064
CD249
- Also called ENPEP, glutamyl aminopeptidase, differentiation antigen gp160, aminopeptidase A
- Regulates blood pressure via renin-angiotensin system (J Biol Chem 2006;281:23503)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: kidney; also brain, heart, liver, lung, placenta, skeletal muscle, pancreas (Genomics 1993;17:657)
- Positive staining - disease:
- Cervical neoplasia (Lab Invest 2004;84:639)
- Renal cell carcinoma-some (Proc Natl Acad Sci USA 1993;90:7069)
- Reference: OMIM 138297
CD281
- TLR1_HUMAN (Q15399, OMIM 601194)
- TLR1, toll-like receptor 1 (toll / interleukin 1 receptor-like) (TIL)
CD282
- TLR2_HUMAN (O60603, OMIM 603028)
- TLR2, TIL4, toll-like receptor 2 (toll / interleukin 1 receptor-like protein 4)
CD283
- TLR3_HUMAN (O15455, OMIM 603029)
- TLR3, toll-like receptor 3
CD284
- TLR4_HUMAN (O00206, OMIM 603030)
- TLR4, toll-like receptor 4
CD289
- TLR9_HUMAN (Q9NR96, OMIM 605474)
- TLR9, toll-like receptor 9
CD333
- Also known as FGFR3
CD351
- Identified in 2011 at HLDA9 (Immunol Lett 2011;134:104)
- Also known as FCAMR, Fcα/μR
- Fc receptor for both IgA and IgM (Mol Immunol 2013;56:23, Mol Immunol 2011;48:1818, GeneCards: FCAMR Gene [Accessed 14 November 2022])
- Positive staining: intestinal lamina propria of appendix, small bowel, colorectum (macrophages, plasma cells, Paneth cells); follicular dendritic cells (Eur J Immunol 2007;37:3540) of germinal centers of some lymphoid follicles (Biochem Biophys Res Commun 2009;381:148)
CD352
- First described as CD352 at HLDA9 in 2011 (Immunol Lett 2011;134:104)
- Also known as Signaling lymphocytic activation molecule F6 (SLAMF6), Ly108 and NTBA
- Member of SLAM (CD150) family of receptors, which are leukocyte cell-surface glycoproteins involved in leukocyte activation; these molecules and their adaptor protein SAP contribute to germinal center formation, generation of plasma cells and memory B cells (Immunol Lett 2011;134:129)
- Costimulatory molecule with CD28 implicated in formation of Th17 lymphocytes and IL17A expression (J Biol Chem 2012;287:38168)
- One of several risk loci for Graves disease of thyroid (Hum Mol Genet 2013;22:3347)
- Increased expression on surface of T cells in system lupus erythematosus (J Immunol 2012;188:1206); this pathway may be defective in SLE T cells (Autoimmunity 2011;44:211)
- No usage for pathologists at this time
- Positive staining (normal): B cells, plasma cells (Immunol Lett 2011;134:122); also NK, T cells (Wikipedia)
CD353
- Also known as SLAMF8
- First described at HLAD9 in 2011 (Immunol Lett 2011;134:104)
- Member of CD2 family of cell surface proteins involved in lymphocyte activation (Wikipedia)
- Cell surface receptor expressed upon activation of macrophages by IFN-γ or bacteria
- Negatively regulates inflammatory responses via very high NADPH oxidase (Nox2) enzyme activity (J Immunol 2012;188:5829)
- Higher baseline expression in postmenopausal women with ER+ breast cancer is associated with poor antiproliferative response to neoadjuvant anastrozole (Clin Cancer Res 2013;19:2775)
- No uses by pathologists at this time
- Positive staining: lymphoid tissue (GeneCards: SLAMF8 Gene [Accessed 14 November 2022])
CD354
- Triggering REceptor on Myeloid cells; member of Ig superfamily
- sTREM1: soluble levels of TREM1
- Part of family of immune sensors which signal innate immune system and amplifies immune responses that promote pro-inflammatory cytokine production; neutrophils are major source of TREM1
- TREM1 is an activating receptor and requires association with transmembrane adapter molecule DAP12 (DNAX-associated protein 12) for cell signaling (PLoS One 2013;8:e82498, J Leukoc Biol 2013;93:209)
- TREM1 and MMPs orchestrate an "adaptive" form of innate immunity by modulating the monocyte response to endotoxin (J Leukoc Biol 2012;91:933)
- Dendritic cells: TREM1 induction by hypoxic microenvironment activates immature dendritic cells and regulates Th1 cell trafficking (Eur J Immunol 2013;43:949)
- Positive staining: Myeloid cells
- Acute bacterial infection: TREM1 mRNA levels inversely correlate with severity (Int J Med Sci 2014;11:215, Jpn J Infect Dis 2012;65:376)
- Asthma: elevated plasma levels of sTREM1 reflect its severity, state of exacerbation and presence of respiratory tract obstruction (Mediators Inflamm 2012;2012:628754)
- Hepatocellular carcinoma: TREM1 may be related to tumor's aggressive behavior (Cancer Sci 2012;103:984)
- Kidney injury: overlapping role with TLR2/4 and MyD88 signaling pathways in myeloid cell activation (PLoS One 2013;8:e68640)
- Labor: elevated sTREM1 levels in spontaneous term and preterm labor (PLoS One 2013;8:e56050); also in premature rupture of membranes and subclinical chorioamnionitis (Mol Med Rep 2012;5:663)
- Lung disease, non tuberculous mycobacterial: may be helpful in diagnosing and predicting outcome (Int J Tuberc Lung Dis 2011;15:1415)
- Obstructive sleep apnea: increased levels (Sleep 2013;36:923)
- Periodontitis: increased oral and systemic levels of sTREM1 (J Dent Res 2013;92:161, PLoS One 2013;8:e75784)
- Rheumatoid arthritis: correlates with disease activity and severity (J Rheumatol 2012;39:933)
- Sarcoidosis: increased TREM1 and TREM2 cell surface expression (Respirology 2013;18:455)
- Sepsis: sTREM1 is a marker of severe sepsis and a sepsis risk factor (Mediators Inflamm 2013;2013:969875); patients with E coli sepsis express TREM1 on blood neutrophils (Diagn Pathol 2013;8:24); also associated with myocardial dysfunction in patients with severe sepsis (Mediators Inflamm 2013;2013:819246)
CD355
- Class I MHC Restricted T cell Associated Molecule
- First identified at 9th Human Leukocyte Differentiation Antigens Workshop in 2011 / HLDA9 (Immunol Lett 2011;134:104)
- Expressed in epithelial cells along lateral membrane; important for early cell-cell contacts and cell-substrate interactions (J Cell Biochem 2010;111:111)
- Binds to cell adhesion molecule nectin-like 2 (Necl2) (Structure 2013;21:1430)
- Rapidly induced in NK, NKT and CD8+ T cells (Mol Immunol 2009;46:3379); may promote cytotoxic function of NK cells and lead to IFN-γ secretion by CD8+ T cells through interaction with Necl2 (J Immunol 2013;190:4868, Curr Opin Immunol 2012;24:246)
- 3 common variants of CRTAM gene are associated with an increased rate of asthma exacerbations based on a low circulating vitamin D level (J Allergy Clin Immunol 2012;129:368)
- No uses by pathologists at this time
- Positive staining: Epithelial cells; activated CD8+ and natural killer T cells
CD357
- Also called GITR / Glucocorticoid Induced Tumor necrosis factor Receptor family related protein
- Type I transmembrane protein belonging to the TNFR superfamily
- After activation, may influence effector and regulatory T cells (ScientificWorldJournal 2012;2012:308265, Wikipedia), causing autoimmune and inflammatory diseases such as rheumatoid arthritis and autoimmune thyroid disease (Clin Dev Immunol 2013;2013:340751)
- Ligand is GITRL
- Antibodies may serve as effective anti-tumor therapy (Curr Opin Immunol 2012;24:217)
- Polymorphisms are associated with Hashimoto thyroiditis prognosis (Clin Exp Immunol 2011;165:141)
- Inactivated during tumor progression in myeloma (PLoS One 2013;8:e66982)
- May have role in Sjogren syndrome (Reumatismo 2012;64:293)
- No significant uses by pathologists at this time
CD358
- Also called TNFRSF21, death receptor 6, DR6
- Member of tumor necrosis factor receptor superfamily
- First characterized at Ninth HLDA Workshop (HLDA9) (Immunol Lett 2011;134:104)
- Different from HLA-DR6 and protein product of direct repeat 6 (associated with HHV6A and HHV6B) (Int J Rheum Dis 2014;17:268, J Virol 2010;84:2648, Virology 2014;452:254)
- Induces apoptosis when overexpressed (FEBS Lett 1998;431:351)
- Highly expressed in brain
- Induces axon pruning and neuron death (J Neurodev Disord 2013;5:10); binds to amyloid precursor protein (APP); may be involved in development of Alzheimer's disease (J Mol Biol 2011;409:189, Proteins 2011;79:1376, Nature 2009;457:981)
- Regulates brain vascular development (Dev Cell 2012;22:403)
- May be involved in pathogenesis of endometriosis (Am J Reprod Immunol 2013;70:485)
- No specific uses by pathologists at this time
- Positive staining:
- Serum DR6 protein levels elevated in ovarian carcinoma (Cancer Biol Ther 2011;12:169)
- Also adult sarcoma, particularly synovial sarcoma (PLoS One 2012;7:e36525)
- Negative staining: serum DR6 levels not elevated in uterine carcinosarcoma, bladder, liver or pancreatic cancer
CD360
- Type I cytokine identified during 9th HLDA Workshop (Wikipedia: Type I Cytokine Receptor [Accessed 11 November 2022], Immunobiology 2009;214:41, Immunol Lett 2011;134:104)
- Produced when immune reaction reaches its peak by CD4+ T cells
- Regulates T cell, B cell, NK cell and myeloid cell functions (Biochem Biophys Res Commun 2010;392:171)
- Binds to a receptor complex of IL21R and the common gamma chain receptor subunit (CD132 / IL2R gamma)
- Also induces PD1 expression on T cells and plays a role in an immunologic cascade (Korean Circ J 2013;43:38)
- IL21 and IL21R gene polymorphisms may be associated with: Hashimoto thyroiditis, HBV infection (BMC Endocr Disord 2013;13:26, Hum Immunol 2013;74:567)
- Kawasaki disease (Korean Circ J 2013;43:38)
- Multiple sclerosis (Genes Immun 2010;11:279)
- Osteoporosis (J Bone Miner Res 2010;25:1042)
- Systemic lupus erythematosus (Arthritis Rheum 2009;60:2402)
- No specific uses for pathologists at this time
- Positive staining - normal: mature B cells, also T cells, NK cells, keratinocytes, some myeloid cells.
- Positive staining - disease: increased expression in systemic sclerosis; expressed in rheumatoid arthritis by synovial fibroblasts and synovial macrophages (Arthritis Rheum 2005;52:856, Arthritis Rheum 2004;50:1468)
- Reference: Int J Mol Med 2005;16:609
CD361
- Initially described at Ninth HLDA Workshop (Immunol Lett 2011;134:104, Immunol Lett 2011;134:145)
- Ecotropic Viral Integration site 2B (GeneCards: EVI2B Gene [Accessed 14 November 2022])
- Involved in melanocyte and keratinocyte differentiation
- Hemizygosity in neurofibromatosis type 1 (NF1), due to its codeletion with NF1 gene, may contribute to disease process (Am J Hum Genet 2001;69:516, Genomics 2000;66:93)
- Increased levels of EVI2B mRNA are present in fibroblast-like cells derived from neurofibroma (DNA Cell Biol 1999;18:345)
- Colorectal carcinoma: gene overexpression may predict relapse (DNA Cell Biol 2012;31:625)
- CLL: associated with 11q23 deletion (Leukemia 2001;15:1721)
- Melanoma: downregulated in melanoma cells by agouti signalling protein/ASIP (Pigment Cell Res 2003;16:65)
- No specific uses for pathologists at this time
CD365
- New CD marker designated at the Tenth Human Leukocyte Differentiation Antigen (HLDA10) Workshop (Clin Transl Immunology 2015;4:e47, Clin Transl Immunology 2016;5:e57, Clin Transl Immunology 2016;5:e61)
- Also known as hepatitis A virus cellular receptor 1 (HAVCR1)
- Antibodies 10-14 (clone FAB1750P) and 10-67 (clone 1D12) recognizing TIM1 (HAVCR1) were tested in the HLDA10 workshop (Clin Transl Immunology 2016;5:e57)
- TIM1 is a single pass type 1 membrane glycoprotein and a member of the Ig superfamily
- The antibodies bind to transfectants expressing TIM1 but show little reactivity to fresh healthy blood cells
- CD365 (HAVCR1) and mHavcr1 may be functional HAV receptors that mediate HAV infection (J Virol 2018;92:e02065, J Virol 2019;93:e01793, J Virol 2019;93:e02040)
CD366
- New CD marker designated at the Tenth Human Leukocyte Differentiation Antigen (HLDA10) Workshop (Clin Transl Immunology 2015;4:e47, Clin Transl Immunology 2016;5:e57, Clin Transl Immunology 2016;5:e61)
- Also known as HAVCR2, T cell Immunoglobulin and Mucin domain containing protein 3 / TIM3 (Clin Transl Immunology 2016;5:e57)
- Originally identified as a receptor on CD4+ and CD8+ T cells functioning as coinhibitory receptor
- Recent studies have shown that TIM3 is part of a module that contains multiple coinhibitory receptors (checkpoint receptors), which are coexpressed and coregulated on dysfunctional or 'exhausted' T cells in chronic viral infections and cancer
- Coblockade of TIM3 and programmed cell death 1 (PD1) can cause tumor regression in preclinical models and can improve anticancer T cell responses in patients with advanced cancers (Nat Rev Immunol 2020;20:173, J Immunother Cancer 2020;8:e000911)
- Presence on CD8+ T cells correlates with poor prognosis in renal cell carcinoma (J Vis Exp 2018;(132):56606)
- May be useful for detecting minimal residual disease (JCI Insight 2018;3:e98561)
CD367
- New CD marker designated at the Tenth Human Leukocyte Differentiation Antigen (HLDA10) Workshop (Clin Transl Immunology 2015;4:e47, Clin Transl Immunology 2016;5:e57, Clin Transl Immunology 2016;5:e61)
- Also known as CLEC4A, DCIR (Dendritic Cell Immunoreceptor), CLECSF6 (Clin Transl Immunology 2016;5:e57)
- A pattern recognition receptor expressed on dendritic cells, monocytes, macrophages, B cells and neutrophils ( BMC Immunol 2015 Oct 23;16:64)
- DCIR binds endogenous carbohydrates as well as pathogenic and viral antigens
- Antibodies 10-13 (clone 216110) and 10-71 (clone 111F8.04) bind to transient transfectants expressing DCIR (Clin Transl Immunology 2016;5:e57)
- Antibodies recognize a type II transmembrane protein that is a member of the C type lectin family
CD368
- New CD marker designated at the Tenth Human Leukocyte Differentiation Antigen (HLDA10) Workshop (Clin Transl Immunology 2015;4:e47, Clin Transl Immunology 2016;5:e57, Clin Transl Immunology 2016;5:e61)
- Also known as CLEC4D, MCL, CLECSF8, Dectin3 (Clin Transl Immunology 2016;5:e57)
- Strong binding to myeloid populations within peripheral blood mononuclear cells
- Antibodies recognize a type II transmembrane protein that is a member of the C type lectin family
- Key molecule in antimycobacterial host defense (Cell Host Microbe 2015;17:252)
CD369
- New CD marker designated at the Tenth Human Leukocyte Differentiation Antigen (HLDA10) Workshop (Clin Transl Immunology 2015;4:e47, Clin Transl Immunology 2016;5:e57, Clin Transl Immunology 2016;5:e61)
- Also known as CLEC7A, dectin1 (dendritic cell associated C type lectin 1), beta glucan receptor and C type lectin superfamily member 12 (Clin Transl Immunology 2016;5:e57)
- Pattern recognition receptor expressed primarily on cells of myeloid origin, including macrophages, dendritic cells and neutrophils (J Cell Sci 2020;133:jcs236166)
- Promotes wound healing by inducing early phase neutrophil accumulation (J Invest Dermatol 2021;141:164)
- Recognizes β-glucan on Candida albicans cell wall, leading to phagocytosis, oxidative burst, cytokine and chemokine production (J Cell Sci 2020;133:jcs236166)
- Variations may play a role in autism spectrum disorder due to genetic control of innate immune response (PLoS One;2015;10:e0137339)
CD370
- Designated at the Tenth Human Leukocyte Differentiation Antigen (HLDA10) Workshop (Clin Transl Immunology 2015;4:e47, Clin Transl Immunology 2016;5:e57, Clin Transl Immunology 2016;5:e61)
- Type II transmembrane glycoprotein member of the C type lectin family that functions as an endocytic receptor, particularly for the uptake and processing of dead cells through its ability to bind filamentous actin (Clin Transl Immunology 2016;5:e57)
- Also known as CLEC9A, DNGR, DNGR1 (Clin Transl Immunology 2016;5:e57)
- Links F-actin exposed by dying cells to favor cross presentation of dead cell associated antigens to CD8+ T cells; also exerts feedback to temper neutrophil recruitment and prevent additional tissue damage (Front Immunol 2020;11:251, Front Immunol 2020;10:3146)
- Binds thymic CD141+ dendritic cells in peripheral blood
- Part of an investigational anti-tumor vaccine due to its binding CD141+ dendritic cells and activating CD8+ T cells (Clin Transl Immunology 2020;9:e1141)
CD371
- Designated at the Tenth Human Leukocyte Differentiation Antigen (HLDA10) Workshop (Clin Transl Immunology 2015;4:e47, Clin Transl Immunology 2016;5:e57, Clin Transl Immunology 2016;5:e61)
- Also known as CLEC12A (C type lectin-like receptor), MICL (myeloid inhibitory C type lectin-like receptor), CLL , CLL1 (Clin Transl Immunology 2016;5:e57)
Diagrams / tables
Virtual slides
Peripheral smear images
CD1-9
Table of Contents
CD1 | CD1a | CD1b | CD1c | CD1d | CD1e | CD2 | CD2R | CD3 | CD4 | CD5 | CD6 | CD7 | CD8 | CD9 | Diagrams / tables | Microscopic (histologic) images | Electron microscopy imagesCD1
- Family of nonpolymorphic MHC class I-like glycoproteins on surface of various antigen presenting cells; member of immunoglobulin superfamily
- Mediate presentation of endogenous and foreign lipids (including bacterial lipid antigens) on cell surface for recognition by T cell receptors
- To sample a diverse antigen pool, CD1 proteins are repeatedly internalized and recycled; this may be assisted by lipid transfer proteins such as saposins (J Biol Chem 2013;288:19528, Proc Natl Acad Sci USA 2012;109:4357)
- May also mediate thymic T cell development
- Has 5 different subsets (CD1a, CD1b, CD1c, CD1d, CD1e), all noncovalently associated with beta 2 microglobulin, all on #1q22-23 (non MHC linked)
- Different CD1 forms bind to different types of lipid antigen based on differences in their antigen binding grooves (Nat Rev Immunol 2005;5:387)
- Separated into 2 groups based on sequence homology:
- Group 1 (CD1a, CD1b, CD1c) present in humans, some other mammals, not in mouse or rat
- Group 2 (CD1d) present in all mammals studied (Curr Pharm Des 2009;15:3311)
- CD1e is an intermediate form, expressed intracellularly (J Biol Chem 2000;275:37757)
- Pathophysiology:
- Cellular infection with Mycobacteria tuberculosis or exposure to mycobacterial cell wall products converts CD1- myeloid precursors into competent CD1+ antigen presenting cells (J Immunol 2005;175:1758)
- However M. tuberculosis possesses a successful tactic based, at least in part, on CD1 downregulation to evade CD1 dependent immunity (Clin Dev Immunol 2011;2011:790460)
- Pollen lipids are also recognized as antigens by T cells via CD1 dependent pathway (J Exp Med 2005;202:295)
- Cellular infection with Mycobacteria tuberculosis or exposure to mycobacterial cell wall products converts CD1- myeloid precursors into competent CD1+ antigen presenting cells (J Immunol 2005;175:1758)
- Clinical features:
- Inhibition of CD1 expression may be a mechanism of immune system evasion by:
- Metastatic melanoma (Am J Pathol 2004;165:1853)
- Leishmania donovani (Infect Immun 2004;72:589)
- Some mycobacteria (Infect Immun 2009;77:4947)
- Primary deficiency of microsomal triglyceride transfer protein in abetalipoproteinemia is associated with loss of CD1 function (J Clin Invest 2010;120:2889)
- Expression altered in multiple sclerosis (Clin Exp Immunol 2012;169:10)
- Inhibition of CD1 expression may be a mechanism of immune system evasion by:
- Uses by pathologists: CD1a is used to diagnose Langerhans cell histiocytosis and to exclude other entities that are CD1a negative
CD1a
- See CD1a
CD1b
- On chromosome 1q22-23 (not MHC linked); noncovalently associated with beta2 microglobulin
- Capable of binding ligands with greatly varying alkyl chain lengths (including Mycobacteria tuberculosis and Mycobacteria leprae) through a complex network of interconnected hydrophobic pockets (J Immunol 2004;172:2382, Proc Natl Acad Sci USA 2011;108:19335, OMIM: 188360 [Accessed 13 May 2021])
- Part of immune response to intracellular bacteria
- Human gammadelta T cells recognize Lipid A in a CD1b or CD1c restricted manner as a first response to gram negative bacteria (Biol Direct 2009;4:47)
- No significant clinical use by pathologists
- Positive staining - normal: cortical thymocytes, Langerhans cells (weaker staining than CD1a), myeloid dendritic cells, brain pyramidal cells and subpopulation of B cells
- Positive staining - disease:
- Dendritic cells in mycosis fungoides (J Cutan Pathol 1995;22:223)
- Myeloid leukemia, some B and T cell malignancies
- Monocytes of most sickle cell anemia patients (Hum Immunol 2004;65:1370)
- Negative staining: normal B cells
CD1c
- On chromosome 1q22-23 (not MHC linked); noncovalently associated with beta2 microglobulin
- Mediates the presentation of primarily lipid and glycolipid antigens of self or microbial origin to T cells (Immunity 2010;33:853)
- Has the capacity to present a wide repertoire of antigens to reactive T cells (Mol Immunol 2013;55:182, J Biol Chem 2011;286:37692)
- Expressed on a subset of myeloid dendritic cells; secrete IL10 in response to Escherichia coli (Eur J Immunol 2012;42:1512)
- Common CD1c antibody is BDCA1
- Clinical features:
- Assists with presentation of the phospholipid antigen mannosyl beta (1) phosphomycoketide (Clin Dev Immunol 2012;2012:981821)
- Produced by Mycobacteria tuberculosis and M. bovis Bacille-Calmette-Guerin (J Exp Med 2004;200:1559, Nature 2000;404:884)
- May activate intrathyroidal T cells in Hashimoto thyroiditis and Grave disease (J Immunol 2005;174:3773)
- May promote autoantibodies in systemic lupus erythematosus (J Immunol 2000;165:5338)
- No significant clinical use by pathologists
- Positive staining - normal:
- Cortical thymocytes, Langerhans cells (weaker staining than CD1a), immature myeloid dendritic cells (J Clin Invest 2007;117:2517)
- Subset of normal peripheral B cells, subset of activated T cells
- Positive staining - disease:
- Dendritic cells in mycosis fungoides (J Cutan Pathol 1995;22:223)
- Myeloid leukemia, some B and T cell malignancies and monocytes of most sickle cell anemia patients (Hum Immunol 2004;65:1370)
- Negative staining: normal B cells
- Electron microscopy description: present in early and late endosomes (J Exp Med 2000;192:281)
CD1d
- CD1d presents lipid antigens to natural killer T (NKT) cells; when activated, NKT cells rapidly produce Th1 and Th2 cytokines, typically represented by interferon gamma and IL4 (Wikipedia: CD1D [Accessed 31 July 2018], OMIM: 188410 [Accessed 31 July 2018])
- B cells also present lipid antigen to CD1d restricted invariant NKT cells, which contributes to maintaining tolerance in autoimmunity
- On chromosome 1q22-23 (not MHC linked)
- Also called R3G1
- Sole group 2 member of the CD1 family of MHC-like glycoproteins
- Clinical features:
- CD1d expression < 45% is predictive of CLL (Am J Clin Pathol 2011;136:400)
- Downregulated by B-CLL (Leukemia 2002;16:2429)
- Although the invariant natural killer T cell and CD1d axis is fundamentally intact in patients with early stage disease (Haematologica 2013;98:376)
- In paroxysmal nocturnal hemoglobinuria, a novel, autoreactive, CD1d restricted, glycosylphosphatidylinositol specific T cell population is expanded and may cause bone marrow failure (Blood 2013;121:2753)
- B cells are essential for iNKT cell expansion and activation in healthy donors but fail to exert a similar effect in SLE patients (Immunity 2012;36:477, J Exp Med 2010;207:943)
- May protect against lipid antigen rich infectious microbes on human scalp (J Clin Pathol 2005;58:1278)
- Downregulated by HPV and some other viruses (J Virol 2010;84:11614, Viruses 2012;4:2379)
- But not CMV (Biochem Biophys Res Commun 2011;413:616)
- Expressed in NKT cells active in autoimmune diabetes, tumor rejection and some microbial infections
- CD1d expression < 45% is predictive of CLL (Am J Clin Pathol 2011;136:400)
- Uses by pathologists: no significant clinical use by pathologists; may play a role in future vaccine development (Proc Natl Acad Sci U S A 2010;107:13010)
- Case reports: 6 year old boy with no apparent immunodeficiency who suffered severe life threatening infection with varicella vaccine virus, with low invariant natural killer T cells and diminished CD1d expression (J Infect Dis 2011;204:1893)
- Positive staining - normal:
- Dendritic cells, intestinal epithelial cells, B cell subset, NK T cell subset, low levels in thymus and monocytes (Immunol Lett 2005;100:42, J Immunol 2005;175:4416)
- Bronchial epithelium (PLoS One 2011;6:e22726)
- Scalp epidermis (basal and granular keratinocytes), pilosebaceous units and eccrine glands
- Testis: Leydig cell, Sertoli cells, spermatogonia; moderate expression in spermatocytes (Ultrastruct Pathol 2011;35:124)
- Positive staining - disease: some B and T cell malignancies; keratinocytes in psoriasis
- Negative staining: normal B cells
CD1e
- Participates in lipid antigen presentation without interacting with T cell receptor; binds lipids in lysosomes and facilitates processing of complex glycolipids, thus promoting editing of lipid antigens; may positively or negatively affect lipid presentation by CD1b, CD1c, CD1d (Proc Natl Acad Sci USA 2011;108:14228)
- Naturally occurring mutation in CD1e impairs lipid antigen presentation (J Immunol 2008;180:3642)
- Only CD1 protein existing in soluble form in late endosomes of dendritic cells; not expressed on cell surface
- On chromosome 1q22-23 (not MHC linked); noncovalently associated with beta2 microglobulin
- Clinical features:
- Processes mycobacterial antigen (instead of presenting antigen directly) and may help expand repertoire of glycolipid T cell antigens to optimize the immune response (Science 2005;310:1321, Proc Natl Acad Sci USA 2011;108:13230)
- Presentment is done by CD1b (J Biol Chem 2012;287:31494)
- Initially accumulates in Golgi of immature dendritic cells or transfected cells as a membrane associated form, then is transported to early and then late endosomes, then is cleaved into a soluble form, which facilitates the processing of glycolipids presented by other CD1 molecules transiting through the same compartments (Biochem J 2009;419:661)
- +6129 A/G gene polymorphisms are associated with multiple sclerosis (Immunol Invest 2010;39:874)
- Processes mycobacterial antigen (instead of presenting antigen directly) and may help expand repertoire of glycolipid T cell antigens to optimize the immune response (Science 2005;310:1321, Proc Natl Acad Sci USA 2011;108:13230)
- No significant clinical use by pathologists
- Positive staining - normal: dendritic cells
CD2
- Early T cell marker expressed on all peripheral blood T cells, 95% of thymocytes, NK cells but no B cells (OMIM: 186990 [Accessed 13 May 2021], J Biol Chem 2010;285:41755)
- Gene is at 1p13.1; protein is member of immunoglobulin superfamily
- Also called E rosette receptor because CD2 antibodies inhibit formation of rosettes with sheep erythrocytes
- Also called LFA2 (leukocyte function antigen), T11
- Pathophysiology:
- Binds CD58 (LFA3) on antigen presenting cells, which enables T cells to respond to lower concentrations of antigen (J Exp Med 1999;190:1383)
- Mediates adhesion between T cells and antigen presenting cells, induces costimulatory signals in T cells and T cell cytokine production, inhibits apoptosis of activated peripheral T cells (Immunology 2013;139:48)
- Regulates T cell anergy
- Regulates T and NK mediated cytolysis
- CD2 distinguishes 2 subsets of human plasmacytoid dendritic cells with distinct phenotype and functions (J Immunol 2009;182:6815)
- CD2 (low) plasmacytoid dendritic cells are depleted in HIV+ patients (Cell Mol Immunol 2011;8:441)
- CD2 promotes NK cell membrane nanotube formation (PLoS One 2012;7:e47664)
- Clinical features:
- Abnormal levels of CD2 expression by flow cytometry are frequently observed in mature T cell malignancies but clinical significance is unclear because of variability of CD2 expression in normal T cells (Cytometry B Clin Cytom 2010;78:169)
- Rare aberrant expression in B cell lymphomas (Appl Immunohistochem Mol Morphol 2011;19:579)
- High CD2 expression identifies latently infected resting memory CD4(+) T cells in vivo (J Virol 2013;87:9148)
- Siplizumab, an anti CD2 monoclonal antibody, was previously studied to treat plaque psoriasis; no current clinical trials as of last update (Int J Dermatol 2010;49:818)
- Uses by pathologists: T cell marker (membranous staining), although CD3 is more commonly used; marker of systemic mastocytosis
- Positive staining - normal:
- Thymocytes (95%), mature peripheral T cells (almost all), NK cells (80 - 90%), mast cells
- Variable thymic B cells (50%), Langerhans cells
- Positive staining - disease:
- T-ALL, other T cell lymphoma / leukemia, acute promyelocytic leukemia microgranular variant / FAB M3v (Leukemia 1995;9:1461)
- AML with pseudo-Chédiak-Higashi anomaly (Am J Clin Pathol 2006;125:791)
- Systemic mastocytosis (a minor criteria, Hum Pathol 2001;32:545)
- And other mast cell disease, thymoma (lymphocyte predominant)
- Variable:
- Acute myeloid lymphoma M0
- Rare:
- Pyothorax associated B cell lymphoma (Am J Surg Pathol 2002;26:724)
- Other non-Hodgkin B cell lymphomas, Reed-Sternberg / Hodgkins cells (Mod Pathol 2005;18:1542)
- Myeloma (Mod Pathol 1990;3:302)
- Myeloid leukemia
- Negative staining: B cells, basophils, nonhematopoietic neoplasms and mast cells in nonmastocytosis disorders (Am J Clin Pathol 2003;120:64)
CD2R
- CD2 epitope present on activated T cells, unmasked by conformational change of CD2 glycoprotein during activation
- No recent articles in literature
- No significant clinical use by pathologists
- Positive staining - normal: activated T cells
- Positive staining - disease: blood and synovial fluid T cells in rheumatoid arthritis; peripheral blood T cells in juvenile rheumatoid arthritis, SLE, ankylosing spondylitis and Lyme disease (Scand J Immunol 1991;34:351)
- Negative staining: resting T cells
CD3
- See CD3
CD4
- See CD4
CD5
- See CD5
CD6
- Adhesion molecule mediating binding of developing thymocytes with thymic epithelial cells (OMIM: 186720 [Accessed 13 May 2021])
- Belongs to ancient scavenger receptor superfamily; at #11q13
- Also called T cell differentiation antigen, T12
- Essential for stable contact between T cells and antigen presenting cells, which leads to T cell proliferation (Blood 2006;107:3212)
- Pathophysiology:
- Binds to CD166 (ALCAM)
- Monomeric 105 or 130kD membrane glycoprotein; size difference is due to differences in phosphorylation (Eur J Immunol 1995;25:2765)
- May be signaling attenuator whose expression alone is sufficient to restrain signaling in T cells (Eur J Immunol 2012;42:195)
- Clinical features:
- Antibodies to CD6 are used to deplete T cells from bone marrow transplants to prevent graft versus host disease (J Clin Oncol 2001;19:1152, Int J Hematol 1999;69:27, J Allergy Clin Immunol 2008;122:1185)
- Single nucleotide polymorphisms may be risk factor for multiple sclerosis (J Neuroimmunol 2010;223:100, PLoS One 2013;8:e62376)
- Due to altered proliferation of CD4+ T cells (J Immunol 2011;187:3286)
- No significant clinical use by pathologists
- Positive staining - normal:
- Mature T cells, B cell subset (B1 cells), NK cells (subset), CNS cells (J Innate Immun 2011;3:420)
- High levels on mature (medullary) thymocytes, low levels on immature (cortical) thymocytes
CD7
- T cell cell surface protein that plays important role in T cell B cell interaction in early lymphoid development
- Member of immunoglobulin superfamily at 17q25.2-25.3
- Membrane expression early during T cell development, before TCR rearrangement; persists until terminal stages of T cell development (OMIM: 186820 [Accessed 13 May 2021])
- Has costimulatory activity for T cells (Immunol Res 2001;24:31)
- Binds galectin 1 and is essential for galectin 1 mediated T cell death; loss of CD7 expression and altered cellular glycosylation may contribute to apoptosis resistance in mycosis fungoides (Mod Pathol 2003;16:543)
- Clinical features:
- Positive expression is a negative prognostic marker:
- Myeloid malignancies (Blood 2008;111:1067, Int J Hematol 2010;91:303)
- Epidermotropic CD8+ cytotoxic T cell lymphoma (Clin Exp Dermatol 2012;37:128)
- Loss of expression a negative prognostic marker:
- Acute myelogenous leukemia with FLT3 / ITD mutation (Am J Clin Pathol 2008;129:624)
- Adult T cell leukemia / lymphoma (Histopathology 2009;54:214)
- Aggressive NK cell lymphoma (Korean J Lab Med 2009;29:491)
- HTLV1 (PLoS One 2013;8:e53728)
- Downregulated in infectious mononucleosis (Am J Clin Pathol 2003;120:49)
- Positive expression is a negative prognostic marker:
- Uses by pathologists: marker for T-ALL; CD7 and CD33 may be useful to quantify lymphocyte subsets (Cytometry A 2013;83:316)
- Positive staining - normal:
- Thymocytes, mature T cells (85%), NK cells (majority) (Blood 2009;114:4823)
- Also monocytes, pluripotent hematopoietic progenitor cells, early myeloid cells, pre-B cells
- Positive staining - disease:
- T-ALL (very good marker) and other malignant immature T cells, CD7+ stem cell lymphoma (Am J Surg Pathol 2003;27:1366)
- NK lymphoma but expression lost in aggressive NK cell lymphoma (Korean J Lab Med 2009;29:491)
- Chronic myelogenous leukemia, Down syndrome associated transient myeloproliferative disorder and AML (Am J Clin Pathol 2001;116:204)
- AML (some), lymphocyte rich thymoma (Am J Clin Pathol 2004;121:268)
- Cholangiocarcinoma, epithelioid sarcoma, pancreatic ductal carcinoma (Am J Clin Pathol 2003;120:64)
- T cells in classical Hodgkin lymphoma (Cytometry B Clin Cytom 2009;76:169)
- Reed-Sternberg cells are negative (Mod Pathol 2005;18:1542)
- Rarely B cell lymphomas (Am J Clin Pathol 2001;115:396)
- Negative staining:
- Mature B cells, basophils, granulocytes
- B cell ALL, mycosis fungoides, adult T cell leukemia / lymphoma (Histopathology 2009;54:214)
CD8
- See CD8
CD9
- Cell surface protein that mediates adhesion, migration, signal transduction
- Also called tetraspanin CD9, motility related protein 1 (MRP1) (note: MRP is multidrug resistance associated protein)
- Antibodies are used to purge bone marrow in acute lymphoblastic leukemia prior to peripheral stem cell bone marrow transplant (Am J Pediatr Hematol Oncol 1993;15:162)
- Pathophysiology:
- Member of transmembrane 4 superfamily (tetraspanin family); tetraspanins have 4 hydrophobic domains, organize multimolecular complexes in plasma membrane; each tetraspanin associates specifically with integrins and other tetraspanins, forming primary complexes and leading to molecular network of interactions, the "tetraspanin web"
- Regulates cell motility, development, activation, growth and adhesion (Blood 2011;117:1840)
- Differentiation (OMIM: 143030 [Accessed 13 May 2021])
- Fertilization (oocyte CD9 is required for sperm egg fusion)
- Regulates paranodal junction formation (between neurons and glia)
- Required for microparticle release from coated platelets (Platelets 2009;20:361)
- Triggers platelet activation and aggregation
- Supports myotube maintenance and promotes muscle cell fusion
- Downregulation in ovarian carcinoma may promote tumor dissemination (Cancer Res 2005;65:2617)
- May suppress metastasis in small cell lung cancer by promoting apoptosis via calretinin expression (Cancer Res 2010;70:8025, FEBS Open Bio 2013;3:225)
- May mediate invasion by upregulating MMP9 (PLoS One 2013;8:e67766)
- Clinical features:
- Favorable prognostic marker for:
- Gallbladder carcinoma (World J Surg Oncol 2012;10:92)
- Gastric GIST (Cancer Sci 2011;102:883)
- Malignant mesothelioma (Oncol Rep 2013;29:21)
- Oral squamous cell carcinoma (Oral Oncol 2010;46:166)
- Poor prognosis factor in gastric carcinoma (Pathol Res Pract 2010;206:607)
- Favorable prognostic marker for:
- No significant clinical use by pathologists
- Positive staining - normal:
- Pre B cells, B cell subset, activated T cells, basophils, eosinophils (Am J Respir Cell Mol Biol 2012;46:188)
- Macrophages, megakaryocytes, plasma cells, plasma cell precursors in germinal centers (Biochem Biophys Res Commun 2013;431:41), platelets
- Brain, cardiac muscle, GI system, kidney (glomeruli, tubules and collective ducts), liver, lymphatic epithelium, ovarian surface epithelium, peripheral nerve, skin, spleen, thyroid, tonsil
- Positive staining - disease:
- Pre-B ALL, acute promyelocytic leukemia, astrocytoma, mast cell disease (J Histochem Cytochem 2002;50:1195)
- Vascular tumors: angiosarcoma, juvenile nasopharyngeal angiofibroma, Kaposi sarcoma (Mod Pathol 2003;16:1028)
- Negative staining: red blood cells, renal collecting duct carcinomas (almost all)
Diagrams / tables
Microscopic (histologic) images
Images hosted on other servers:
CD10
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Flow cytometry images | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Cell membrane zinc dependent metalloendopeptidase that is widely distributed in hematopoietic cells and hematopoietic neoplasms, normal kidney tissue and renal neoplasms, as well as a wide variety of additional tissues
- Important in diagnosis, subclassification and surveillance of B lymphoblastic leukemia (B ALL) (OMIM: Membrane Metalloendopeptidase; MME [Accessed 17 January 2023])
- Useful in diagnosis of other entities but must be used with caution, as staining is nonspecific
Essential features
- Membranous marker with extensive expression in normal tissues, complicating interpretation
- Critical for use in diagnosis and subclassification of leukemias (e.g., B lymphoblastic leukemia, mixed phenotype acute leukemia, etc.) and lymphomas (e.g., follicular lymphoma, Burkitt lymphoma, diffuse large B cell lymphoma, angioimmunoblastic T cell lymphoma)
- Additional uses in diagnosis of solid tumors (e.g., renal cell carcinoma, endometrial stromal sarcoma, solid pseudopapillary neoplasm of the pancreas, etc.)
Terminology
- Cluster of differentiation 10
- Also called common acute lymphoblastic leukemia antigen (CALLA), membrane metalloendopeptidase (MME), neutral endopeptidase, membrane associated (NEP), neutral endopeptidase 24.11, neprilysin, EC 3.4.24.11, enkephalinase, atriopeptidase
Pathophysiology
- Encoded by MME gene
- 85-110 kDa cell membrane metalloendopeptidase at 3q25.1-q25.2 that inactivates bioactive peptides, including atrial natriuretic factor, bombesin, β amyloid, endothelin 1, enkephalins, gastrin and substance P and through the cytoplasmic domain, directly interacts with ezrin / radixin / moesin proteins, Lyn kinase and the phosphatase and tensin homolog (PTEN) protein (J Pediatr Hematol Oncol 2010;32:2)
- In epithelial cells, CD10 loss from methylation leads to increased cell migration, cell growth and cell survival, contributing to neoplastic development and progression (J Pediatr Hematol Oncol 2010;32:2, Biochim Biophys Acta 2005;1751:52)
- In the central nervous system, CD10 knockout mice demonstrate increased levels of Aβ peptides in the brain and exhibit amyloid-like deposits with signs of neurodegeneration in the hippocampus and behavioral deficits (J Neurosci Res 2006;84:1871, Science 2001;292:1550)
- In the peripheral nervous system, CD10 decrease or loss resulting from MME gene loss of function mutations are associated with adult onset autosomal recessive Charcot-Marie-Tooth disease (AR-CMT) (Ann Neurol 2016;79:659)
Interpretation
- Cell membrane staining: general, classic staining pattern
- Apical surface staining only: well differentiated adenocarcinoma of colon, pancreas and prostate (Am J Clin Pathol 2000;113:374)
- Apical cytoplasmic staining: microvillus inclusion disease (intense apical cytoplasmic staining in small bowel enterocytes or focal apical cytoplasmic staining in absorptive colonocytes) versus linear brush border staining of enterocytes and negative colonic staining in normal tissue) (Am J Surg Pathol 2002;26:902, Orphanet J Rare Dis 2006;1:22, Am J Surg Pathol 2010;34:970)
- Canalicular staining: hepatocellular carcinoma (versus metastatic carcinomas) (Am J Surg Pathol 2001;25:1297, Am J Surg Pathol 2002;26:978)
- Diffuse cytoplasmic or membranous / Golgi staining pattern: poorly differentiated adenocarcinoma, endometrial stromal sarcoma, melanoma, renal cell carcinoma, urothelial carcinoma (Am J Clin Pathol 2000;113:374)
- Peritumoral stromal staining: trichoblastoma (versus epithelial staining in basal cell carcinoma and strong stromal staining in squamous cell carcinoma) (Int J Dermatol 2009;48:713, Iran J Med Sci 2013;38:100)
- Strong stromal staining: cutaneous squamous cell carcinoma (versus epithelial staining in basal cell carcinoma and peritumoral stromal staining in trichoblastoma) (Int J Dermatol 2009;48:713, Iran J Med Sci 2013;38:100)
Uses by pathologists
- B lymphoblastic leukemia (B ALL):
- One of first markers to identify leukemic cells in children, corresponding to name of common acute lymphoblastic leukemia antigen (CALLA)
- CD10 expression corresponds to the degree of differentiation of B lymphoblasts, differentiating early precursor B ALL / pro-B ALL (earliest stage) (CD10-) from common B ALL (intermediate stage) and pre-B ALL and transitional pre-B ALL (most mature stages) (CD10+)
- CD10- is associated with t(v;11q23.3); KMT2A (MLL) rearrangement, infantile (< 1 year of age) presentation and poor prognosis (Leukemia 2002;16:1233)
- May distinguish B lymphoblasts (aberrant overexpression or underexpression of CD10) from hematogones (CD10+) by minimal residual disease (MRD) flow cytometry (Leukemia 2001;15:1185)
- Bladder:
- Present in 40 - 50% of urothelial carcinoma and squamous cell carcinoma, with CD10 expression strongly correlated with high tumor grade and stage (Diagn Pathol 2009;4:38, Am J Clin Pathol 2005;124:371, J Environ Pathol Toxicol Oncol 2012;31:203, APMIS 2007;115:1206)
- Breast:
- Expression by myoepithelial cells (Mod Pathol 2002;15:397)
- Positive in mammary myofibroblastoma (Virchows Arch 2007;450:727)
- Rarely positive in:
- Invasive ductal carcinoma (Pathobiology 2015;82:259)
- Papilloma (J Clin Pathol 2007;60:958)
- Benign stroma (Virchows Arch 2006;448:871)
- Mammary sarcoma, NOS (Diagn Pathol 2013;8:14, Am J Surg Pathol 2006;30:450)
- Stromal expression is associated with increased biologic aggressiveness and poor prognosis in invasive ductal carcinoma (Mod Pathol 2007;20:84, Virchows Arch 2002;440:589)
- Stromal expression may change postchemotherapy and correlates with clinical response (Indian J Cancer 2013;50:46)
- Helps differentiate collagenous spherulosis (CD10+, HHF35+) from adenoid cystic carcinoma of the breast (CD10-, HHF35-) (Pathol Res Pract 2012;208:405)
- Ectopic prostatic tissue:
- Used with prostate specific antigen (PSA) and prostate specific alkaline phosphatase (PSAP) to confirm diagnosis in uterus and vagina (CD10+ in cytoplasm of basal cell layer) (Am J Surg Pathol 2006;30:209)
- Endometrial stromal tumors:
- Used with smooth muscle actin (SMA), muscle specific actin (MSA) and desmin to differentiate endometrial stromal tumors (CD10+) from uterine smooth muscle tumors (CD10-, with rare exceptions) (Mod Pathol 2001;14:465, Mod Pathol 2002;15:923)
- Endometriosis:
- May be useful in diagnosis, except in cervix (Adv Anat Pathol 2004;11:310)
- Gynecologic tumors:
- Mesonephric remnants (e.g., mesonephric remnants of the uterine cervix, epoophoron, rete ovarii) and tumors (e.g., mesonephric adenocarcinoma of the uterine cervix, tumors of wolffian origin of the broad ligament and ovary) are CD10+ (Am J Surg Pathol 2003;27:178)
- Trophoblast tissue of normal gestations, moles, choriocarcinoma and placental site trophoblastic tumors are CD10+ (Am J Surg Pathol 2003;27:178)
- Müllerian epithelium and tumors are CD10- (with the exception of squamous epithelium and tumors with squamous differentiation)
- CD10 differentiates primary clear cell carcinoma (CD10-) from metastatic renal cell carcinoma (CD10+) (Am J Surg Pathol 2003;27:178)
- Müllerian system derived mesenchymal neoplasms, including malignant Müllerian mixed tumor (MMMT) and Müllerian adenosarcoma without sarcomatous overgrowth (MA-NSO) are generally CD10+ (Mod Pathol 2001;14:465, Mod Pathol 2002;15:923, Am J Surg Pathol 2008;32:1013)
- Hepatocellular carcinoma:
- CD10+ is 52 - 82% sensitive and > 95% specific for differentiating hepatocellular carcinoma from metastatic carcinoma when exhibiting a canalicular pattern, though cannot differentiate benign hepatic tissue (Am J Surg Pathol 2001;25:1297, Am J Surg Pathol 2002;26:978, Diagn Cytopathol 2004;30:92)
- Another study recommends use of HepPar1, MOC31 and pCEA but not CD10 (Mod Pathol 2002;15:1279)
- Kidney tumors:
- Distinguish renal cell carcinoma, clear cell type, eosinophilic variant (CD10+) from chromophobe carcinoma, eosinophilic variant or oncocytoma (both CD10-) (Appl Immunohistochem Mol Morphol 2012;20:454)
- Liver:
- Support diagnosis of Alagille syndrome in pediatric patients (CD10+ canalicular surfaces in children > 24 months old; CD10- canalicular surfaces in children aged 2 months to 6 years of age) (Lab Invest 2007;87:1138)
- Lymphoma - angioimmunoblastic T cell (AITL) and other mature T cell lymphomas of T follicular helper (TFH) cell origin:
- Marker for T follicular helper cell phenotype (also BCL6, PD1, CXCL13, CXCR5, ICOS, SAP) in benign and malignant T cells (Mod Pathol 2003;16:879)
- Distinguish AITL and other mature T cell lymphomas of T follicular helper (TFH) cell origin (e.g., follicular T cell lymphoma and nodal peripheral T cell lymphoma with TFH phenotype) (CD10+) at nodal and extranodal sites from other T cell lymphomas (CD10-) (Mod Pathol 2011;24:993, Am J Surg Pathol 2004;28:54, Hum Pathol 2005;36:784)
- Lymphoma - Burkitt:
- CD10+ aids in diagnosis but must exclude CD10+ diffuse large B cell lymphoma, Burkitt-like lymphoma with 11q aberration, high grade B cell lymphoma with MYC and BCL2 / BCL6 rearrangement (double / triple hit lymphoma) (75 - 90% CD10+) and B lymphoblastic leukemia / lymphoma (B ALL / LBL) (Am J Clin Pathol 2012;137:665, Am J Clin Pathol 2010;133:718, Blood 2014;123:1187, Hematology Am Soc Hematol Educ Program 2014;2014:90)
- Lymphoma - diffuse large B cell (Mod Pathol 2005;18:1113, J Hematop 2009;2:187):
- Marker for germinal center phenotype (also HGAL, BCL6, CD38, LMO2, MEF2B), generally considered a favorable prognostic factor, secondary in part to association with cell of origin classification (germinal center B cell versus activated B cell) but see:
- Am J Clin Pathol 2001;116:183 (CD10+, BCL2+ tumors have poorer survival)
- Virchows Arch 2004;445:545 (no difference in survival)
- Sci Rep 2016;6:20465 (CD10+, MUM1+ tumors have similar survival to nongerminal center phenotype)
- Hans classification (Blood 2004;103:275, see diagram above)
- Marker for germinal center phenotype (also HGAL, BCL6, CD38, LMO2, MEF2B), generally considered a favorable prognostic factor, secondary in part to association with cell of origin classification (germinal center B cell versus activated B cell) but see:
- Lymphoma - follicular (Am J Clin Pathol 2002;117:291, Hum Pathol 2013;44:1328):
- CD10+ / strong (often stronger than normal germinal center B cells) aids in diagnosis of primary or secondary spread but:
- High grade follicular lymphomas and interfollicular infiltrates may be CD10- (Am J Clin Pathol 2001;115:862)
- Bone marrow involvement by follicular lymphoma may be CD10- (Am J Surg Pathol 2010;34:1266)
- Leukemic presentation by follicular lymphoma often CD10- (Am J Surg Pathol 2010;34:1266)
- Does not distinguish variants (diffuse, testicular, duodenal type follicular lymphoma), primary cutaneous follicle center lymphoma or pediatric type follicular lymphoma (all CD10+)
- Other lymphomas may be CD10+, including:
- Angioimmunoblastic T cell (see above)
- Burkitt (see above)
- Diffuse large B cell lymphoma (see above)
- Mantle cell (Appl Immunohistochem Mol Morphol 2010;18:103)
- Marginal zone (J Clin Pathol 1999;52:849)
- Hairy cell (Am J Clin Pathol 2003;120:228)
- Other rare CD5+, CD10+ lymphomas (Am J Clin Pathol 2003;119:218, Arch Pathol Lab Med 2001;125:951)
- CD10+ / strong (often stronger than normal germinal center B cells) aids in diagnosis of primary or secondary spread but:
- Microvillous inclusion disease:
- Intense CD10+ apical cytoplasmic staining in small bowel enterocytes or focal apical cytoplasmic staining in absorptive colonocytes (versus linear brush border staining of enterocytes and negative colonic staining in normal tissue) (Am J Surg Pathol 2002;26:902, Orphanet J Rare Dis 2006;1:22, Am J Surg Pathol 2010;34:970)
- Mixed phenotype acute leukemia (MPAL), B / myeloid:
- Component of evaluation for assignment of B cell lineage to a single blast population in cases of multiple lineage designation
- Strong CD19 with ≥ 1 of the following strongly expressed: CD10, CD79a, cytoplasmic CD22
- Or
- Weak CD19 with ≥ 2 of the following strongly expressed: CD10, CD79a, cytoplasmic CD22
- Strong CD19 with ≥ 1 of the following strongly expressed: CD10, CD79a, cytoplasmic CD22
- Myeloid lineage assignment requirements include
- MPO (by flow cytometry, immunohistochemistry or cytochemistry)
- Or
- Monocytic differentiation (≥ 2 of the following: nonspecific esterase, CD11c, CD14, CD64, lysozyme)
- MPO (by flow cytometry, immunohistochemistry or cytochemistry)
- Component of evaluation for assignment of B cell lineage to a single blast population in cases of multiple lineage designation
- Müllerian system derived neoplasms - MMMT and Müllerian adenosarcoma:
- CD10+ expression in Müllerian system derived mesenchymal neoplasms, including malignant Müllerian mixed tumor (MMMT) and Müllerian adenosarcoma without sarcomatous overgrowth (MA-NSO) (Mod Pathol 2001;14:465, Mod Pathol 2002;15:923, Am J Surg Pathol 2008;32:1013)
- Pancreas:
- Confirm diagnosis of solid pseudopapillary neoplasm (CD10+) (Am J Surg Pathol 2000;24:1361)
- Differentiates mucinous cystic neoplasms (CD10+ / CK20+) from intraductal papillary mucinous neoplasm of branch duct type (CD10- / CK20-) (Pancreas 2009;38:558)
- Skin tumors:
- CD10 staining patterns may aid in differentiation of basal cell carcinoma (epithelial staining), trichoblastoma (peritumoral stromal staining) and squamous cell carcinoma (strong stromal staining) (Int J Dermatol 2009;48:713, Iran J Med Sci 2013;38:100)
- Differentiates atypical fibroxanthoma (diffuse membranocytoplasmic staining) from spindle cell melanoma and sarcomatoid squamous cell carcinoma (CD10-) (J Cutan Pathol 2010;37:744)
- Membranous expression in majority of other xanthomatous skin lesions (xanthomas, xanthelasmas and xanthogranulomas) versus cytoplasmic expression in metastatic renal cell carcinomas, balloon cell nevi and nodular / clear cell hidradenomas (J Cutan Pathol 2005;32:348)
- Vascular tumors:
- Aids in differentiation of hemangioblastoma (usually CD10-, rarely focal staining) from metastatic renal cell carcinoma (CD10+) (Diagn Pathol 2012;7:39, Mod Pathol 2005;18:788)
- Epithelioid hemangioendothelioma can have strong / diffuse CD10+ (30%), mimicking metastatic renal cell carcinoma (Arch Pathol Lab Med 2009;133:1965)
Prognostic factors
- CD10- B lymphoblastic leukemia / lymphoma is associated with t(v;11q23.3); KMT2A (MLL) rearrangement, infantile (< 1 year of age) presentation and poor prognosis (Leukemia 2002;16:1233)
- CD10 in diffuse large B cell lymphoma is a marker for germinal center phenotype (also HGAL, BCL6, CD38, LMO2), generally considered a favorable prognostic factor, secondary in part to association with cell of origin classification (germinal center B cell versus activated B cell) (Mod Pathol 2005;18:1113, J Hematop 2009;2:187)
- Stromal expression in invasive breast carcinoma, no special type is associated with increased biologic aggressiveness and poor prognosis (Mod Pathol 2007;20:84, Virchows Arch 2002;440:589)
Microscopic (histologic) images
Contributed by Bradford Siegele, M.D., J.D.
Contributed by Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
Virtual slides
Positive staining - normal
- Hematopoietic cells:
- Hematogones, pre-T cells, T follicular helper cells, germinal center B cells, mature granulocytes
- Other cells:
- Adrenal cortex, choroid plexus,
- Endometrial stroma, endothelial cells (some), fibroblasts (Hypertension 1995;26:230)
- GU (male) epithelium, kidney (microvilli)
- Liver (bile canaliculi, biliary epithelium), mesonephric remnants, myoepithelial cells (breast) (Am J Surg Pathol 2003;27:178, Mod Pathol 2002;15:397, J Clin Pathol 2004;57:625)
- Ovary, placenta (cytotrophoblast, intermediate trophoblast, syncytiotrophoblast), prostate basal and secretory cells
- Small intestine (linear brush border staining, variable loss with active enteritis), Wolffian (but not Müllerian) type epithelium (Mod Pathol 2011;24:1627, Am J Surg Pathol 2003;27:178)
Positive staining - disease
- Leukemia / lymphoma:
- Angioimmunoblastic T cell and other nodal lymphomas of T follicular helper cell origin (T follicular helper cell, nodal peripheral T cell lymphoma with TFH phenotype)
- B lymphoblastic leukemia (B ALL / LBL) (75%), Burkitt, Burkitt-like with 11q aberration, chronic myeloid leukemia (CML) in B lymphoid blast crisis (90%) (Arch Pathol Lab Med 2000;124:704, Blood 2014;123:1187)
- Diffuse large B cell (variable; CD10+ is germinal center B cell defining by Hans criteria)
- Follicular lymphoma (70%) (diffuse, testicular and duodenal type variants, primary cutaneous follicle center lymphoma or pediatric type follicular lymphoma generally CD10+; high grade may be CD10-)
- High grade large B cell lymphoma with MYC and BCL2 / BCL6 rearrangements (double hit / triple hit lymphoma) (75 - 90% CD10+) (Hematology Am Soc Hematol Educ Program 2014;2014:90)
- Large B cell lymphoma with IRF4 rearrangement (66%) (Blood 2011;118:139)
- Mixed phenotype acute leukemia (B / T, B / myeloid)
- T lymphoblastic leukemia (T ALL / LBL) (63%) (Arch Pathol Lab Med 2000;124:704)
- Other:
- Breast cancer associated stroma, breast metaplastic carcinoma, breast myofibroblastoma, choriocarcinoma (Virchows Arch 2007;450:727)
- Colonic carcinoma and high grade dysplasia associated stroma, dermatofibroma, dermatofibrosarcoma (Hum Pathol 2002;33:806)
- Epithelioid hemangioendothelioma, Ewing sarcoma, female adnexal tumor of probable Wolffian origin (FATWO) (50 - 100%), gastric carcinoma associated stroma (Arch Pathol Lab Med 2009;133:1965, Jpn J Clin Oncol 2005;35:245)
- Hepatocellular carcinoma (canalicular pattern similar to polyclonal CEA) (Am J Pathol 2001;159:1415)
- Malignant mixed Müllerian tumors (MMMT)
- Malignant peripheral nerve sheath tumor (72%, usually focal) (Pathol Res Pract 2012;208:281)
- Mediastinal germ cell tumors
- Mesonephric tumors (Am J Surg Pathol 2001;25:1540)
- Mesothelioma (malignant) (Arch Pathol Lab Med 2006;130:823)
- Microvillous inclusion disease (strong cytoplasmic staining)
- Müllerian adenosarcoma
- Pancreatic adenocarcinoma (50%)
- Pancreatic solid pseudopapillary neoplasm
- Placental site trophoblastic tumor
- Prostatic adenocarcinoma (some Gleason pattern 4 and 5 cases)
- Renal cell carcinoma (most clear cell [94 - 100%], papillary [variable, 67 - 93%], chromophobe [variable, 0 - 72%], Xp11 translocation [100%]) (Am J Surg Pathol 2000;24:203, Mod Pathol 2005;18:535, Mod Pathol 2004;17:1455, Arch Pathol Lab Med 2011;135:92)
- Rhabdomyosarcoma (60%, particularly pleomorphic) and other sarcomas (variable)
- Seminoma / dysgerminoma (87 - 92%) (Int J Clin Exp Pathol 2013;6:498, Histol Histopathol 2014;29:101)
- Spindle cell lipoma (Virchows Arch 2007;450:727)
- Urothelial carcinoma (54%)
- Uterus: adenomyosis, cellular leiomyoma (50%), endometrial adenocarcinoma (may also be present in desmoplastic stroma), endometrial stromal tumor, leiomyosarcoma, other sarcomas (Am J Surg Pathol 2003;27:786)
- Yolk sac tumor
Negative staining
- Leukemia / lymphomas:
- Acute myeloid leukemia (AML), chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL), EBV+ lymphoproliferative disorders
- Lymphoplasmacytic (LPL) (usually), mantle cell, marginal zone (MALT, splenic, nodal) (usually), primary cutaneous diffuse large B cell, leg type, pyothorax associated
- Extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT lymphoma) (very rare) (Leuk Lymphoma 2012;53:1032)
- Hairy cell leukemia (10%) (Am J Clin Pathol 2003;120:228)
- Lymphoplasmacytic lymphoma (some), plasma cell myeloma (some), primary cutaneous diffuse large B cell (variable), plasmablastic (variable), primary mediastinal B cell (32%) (Am J Surg Pathol 2001;25:1277)
- Other:
- Atypical polypoid adenomyoma (stromal cells), clear cell carcinoma of female genital tract
- Colon (normal, diseased), erythroid and myeloid precursors, hemangioblastoma, high grade prostatic intraepithelial neoplasia (PIN) and basal cell hyperplasia, prostatic adenocarcinoma (all Gleason patterns 2 and 3, some 4 and 5) (Hum Pathol 2003;34:450)
- Melanoma (40%) (Mod Pathol 2004;17:1251)
- Schwannoma (45%)
Flow cytometry images
Sample pathology report
- Lymph node, right neck level 5, excision:
- Large B cell lymphoma (see comment)
- Morphology: diffuse large B cell type
- Hans criteria: germinal center B cell phenotype (CD10+, BCL6+, MUM1-)
- Double expressor status: double expressor phenotype (BCL2+, MYC+)
- Ki67 proliferation index: high (60 - 70%)
- EBER in situ hybridization studies: negative
- Comment: The findings are consistent with a diagnosis of a CD10+ large B cell lymphoma, with diffuse large B cell morphology. Ancillary studies, including fluorescence in situ hybridization studies to evaluate for MYC, BCL2 and BCL6 rearrangement status, are pending and will be reported in an addendum.
Board review style question #1
A 72 year old man presented for evaluation of a distal gastrointestinal tract adenocarcinoma, with staging computed tomography (CT) radiography that incidentally revealed bulky confluent mesenteric lymphadenopathy. Excision of mesenteric lymph nodes show effacement of nodal architecture as well as infiltration of mesenteric fat by a nodular infiltrate of small lymphoid cells with cleaved nuclei and condensed chromatin. The tumor cells are positive for CD45, CD20, CD10, BCL6 and BCL2. The images above show H&E, CD20, CD10 and BCL2 staining. The Ki67 proliferation index is ~5%. The tumor cells are negative for CD5 and CD23. What molecular / cytogenetic abnormality may be associated with this lymphoma?
- Deletion of 13q14.3
- MYD88 L265P mutation
- t(11;14)(q13;q32)
- t(11;18)(q21;q21)
- t(14;18)(q32;q21)
Board review style answer #1
E. t(14;18)(q32;q21). The morphologic appearance, including nodular infiltrates of small lymphoid cells with cleaved nuclei and condensed chromatin, in conjunction with the immunophenotype showing lymphoid cell positivity for CD20, CD10, BCL6 and BCL2, with a low Ki67 proliferation index, is compatible with a diagnosis of a low grade (grade 1 - 2) follicular lymphoma. The t(11;14)(q13;q32) translocation between the IGH and BCL2 genes is present in approximately 90% of grade 1 - 2 follicular lymphomas. Other small B cell lymphomas demonstrate different immunophenotypes and characteristic cytogenetic or molecular abnormalities, including chronic lymphocytic leukemia / small lymphocytic lymphoma (CD20+, CD10-, CD5+, CD23+; deletion of 13q14.3), lymphoplasmacytic lymphoma (CD20+, CD10-, CD5-; MYD88 L265P mutation) and extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT lymphoma) (CD20+, CD10-, CD5-, t(11;18)(q21;q21) [pulmonary and gastric] and t(14;18)(q32;q21) [thyroid, ocular adnexa, orbit and skin]), aiding in diagnostic differentiation.
Comment Here
Reference: CD10
Comment Here
Reference: CD10
CD10-19
Table of Contents
CD10 | CD11 | CD11a | CD11b | CD11c | CD11d | CDw12 | CD13 | CD14 | CD15 | CD15s | CD15u | CD16 / CD16a | CD16b | CD17 / CDw17 | CD18 | CD19 | Diagrams / tables | Microscopic (histologic) imagesCD10
- See CD10
CD11
- Alpha component of various integrins (CD11a, CD11b, CD11c, CD11d)
- Integrins are heterodimeric integral membrane proteins composed of an alpha chain and a beta chain
- Adhesion molecules of the beta2 integrin family (CD11 / CD18) plays an essential role in neutrophil recruitment and activation during inflammation
- Clinical features: deficiency of CD18 component (leukocyte adhesion deficiency) is a rare, inherited disorder, causing recurrent severe bacterial infections early in life, possibly fatal (OMIM: 116920 [Accessed 10 May 2021], Hematol Oncol Clin North Am 1988;2:13)
CD11a
- Alpha integrin chain at 16p11-13.1 that binds to CD18 and has various leukocyte functions (OMIM: 153370 [Accessed 10 May 2021])
- Also called integrin alpha L, ITGAL and LFA1 alpha chain (in complex with CD18)
- Pathophysiology:
- Alpha integrin chain which binds to CD18 and mediates leukocyte adhesion to endothelium, leukocyte trafficking through activated endothelium, lymphocyte blastogenesis, lymphocyte endothelial cell adhesion, lymphocyte recirculation through lymph nodes, cytotoxic T cell mediated killing and antibody dependent killing by neutrophils and monocytes
- Also mediates binding to unopsonized bacteria (e.g. E. coli) and fungi (e.g. Histoplasma capsulatum)
- With CD18, binds to ICAM1 (CD54), ICAM2 (CD102), ICAM3 (CD50) and ICAM4 (CD242)
- CD11a identifies effector and memory CD8+ T cells, independent of antigen specificity (Oncoimmunology 2013;2:e23972)
- Decreased levels in CD4+ T cells in infants with biliary atresia, due to hypermethylation of CD11a promoter region (Biochem Biophys Res Commun 2012;417:986)
- Increased levels in CD4+ T cells with immune thrombocytopenia (ITP) (J Clin Immunol 2011;31:632)
- Clinical features:
- Anti CD11a antibody therapy (efalizumab):
- Improves moderate / severe plaque psoriasis (J Cutan Med Surg 2003;7:198, Arch Dermatol 2002;138:591)
- Although may cause progressive multifocal leukoencephalopathy (Neurology 2012;78:458)
- Treatment of macular edema (Invest Ophthalmol Vis Sci 2011;52:6919)
- Treatment of moderate to severe Crohn disease (Dig Dis Sci 2011;56:1806)
- Phase I / II trials pending for immunosuppression in renal transplants (Am J Transplant 2007;7:1770)
- May act by promoting naïve T cell anergy (J Invest Dermatol 2008;128:2615)
- Improves moderate / severe plaque psoriasis (J Cutan Med Surg 2003;7:198, Arch Dermatol 2002;138:591)
- Uses by pathologists:
- CD11a deficiency during flow cytometry useful to diagnose acute promyelocytic leukemia (Am J Clin Pathol 2012;138:744)
- CD11a deficiency during flow cytometry useful to diagnose AML M7, Down syndrome related AML and transient myeloproliferative disease in children with and without Down syndrome (Cytometry B Clin Cytom 2013;84:370)
- Positive staining - normal: all leukocytes
- Positive staining - disease: acute promyelocytic leukemia post treatment (treatment induces expression (Leuk Res 2008;32:315)
- Negative staining: platelets, various intermediate and high grade lymphomas
- Anti CD11a antibody therapy (efalizumab):
CD11b
- Alpha component of an integrin at 16p11-13.1 that mediates adhesion (OMIM: 120980 [Accessed 10 May 2021])
- Also called integrin alpha M, Mac1 and CR3A
- Pathophysiology:
- Mediates monocyte / macrophage / granulocyte adhesion to substrates by opsonization with iC3b, leading to phagocytosis, neutrophil aggregation and chemotaxis
- Ligands include fibrinogen, Factor X, ICAM1, iC3b, Saccharomyces cerevisiae, Staphylococcus epidermidis and Histoplasma capsulatum
- Expression is associated with activation of T cells
- Clinical features:
- Gr1+ CD11b+ myeloid cells promote metastasis (Cancer Cell 2008;13:23)
- Poor prognostic factor in preB acute lymphoblastic leukemia, cytogenetically unfavorable AML (Blood 2010;115:3763, Leuk Res 2013;37:122)
- Documents maturation of tumor cells in acute promyelocytic leukemia patients receiving all trans retinoic acid therapy (cells become CD11b+, CD16+) or arsenic trioxide (CD11b+, CD33+) (Arch Pathol Lab Med 2003;127:e4, Mod Pathol 2000;13:954)
- Histoplasma capsulatum causes decreased cell surface CD11b expression and an antiapoptotic state on leukocytes (Scand J Immunol 2002;56:392)
- May be useful to diagnose aspirin induced asthma, due to upregulation of CD11b on eosinophils (Allergol Int 2013;62:367)
- rs1143679 variant is associated with systemic lupus erythematosus and impairs:
- CR3 monocyte functions (Ann Rheum Dis 2012;71:2028)
- Neutrophil functions (Arthritis Rheum 2013;65:2907)
- In Type 2 diabetes, hyperglycemia leads to increased CD11b on granulocytes and monocytes, exacerbating their inflammatory status (J Investig Med 2013;61:972)
- Uses by pathologists:
- Common myeloid marker and NK (natural killer cell) antigen
- Differentiates recovery from acute agranulocytosis (CD11b+, CD117-) from acute promyelocytic leukemia (CD11b-, CD117+) (Am J Clin Pathol 2002;118:31)
- Differentiates Down syndrome patients with AML (usually CD13+, CD11b+) from transient myeloproliferative disorder (usually CD13-, CD11b-) (Am J Clin Pathol 2001;116:204)
- May be useful for flow cytometry diagnosis of myelodysplastic syndrome as part of panel (Ann Clin Lab Sci 2012;42:271)
- Positive staining - normal:
- Granulocytes, macrophages
- Follicular dendritic cells, myeloid cells beginning with promyelocytes, NK cells, some B / T cells
- Positive staining - disease:
- Hairy cell leukemia (virtually all)
- Also acute myelogenous leukemia, lymphoma (various), sinus histiocytosis with massive lymphadenopathy (Am J Clin Pathol 2008;129:934, Hum Pathol 1992;23:647)
- Negative staining: Gaucher cells (Am J Clin Pathol 2004;122:359)
CD11c
- Integrin at 16p11-13.1 that acts as a fibrinogen receptor and is important in monocyte adhesion and chemotaxis (OMIM: 151510 [Accessed 10 May 2021])
- Also called integrin alpha X, CR4 and LeuM5
- Pathophysiology:
- Clears opsonized particles and immune complexes
- Also binds to fibrinogen and is involved in adhesion of monocytes and neutrophils to endothelium and chemotaxis
- CD11c+ CD206+ adipose tissue macrophages are associated with insulin resistance in human obesity (Diabetes 2010;59:1648)
- Clinical features:
- Associated with good prognosis in B-CLL
- High expression in polycystic ovary syndrome (Eur J Endocrinol 2012;167:705)
- Uses by pathologists: marker of histiocytes, NK cells; used to diagnose hairy cell leukemia (with other markers)
- Positive staining - normal:
- Granulocytes, macrophages, NK cells, dendritic cells (PLoS One 2012;7:e33556)
- 50% of activated CD4 / CD8+ T cells
- Positive staining - disease:
- Hairy cell leukemia (classic and variant) (Am J Clin Pathol 1991;96:100)
- AML M4 and M5 (50%), follicular lymphoma (some), Langerhans cell histiocytosis, lymphoplasmacytic lymphoma (81%) (Am J Clin Pathol 2005;124:414)
- Psoriatic skin lesions (Proc Natl Acad Sci USA 2005;102:19057)
- Sinus histiocytosis with massive lymphadenopathy (Hum Pathol 1992;23:647)
- Small lymphocytic lymphoma (Am J Clin Pathol 1998;110:582)
- Splenic lymphoma with villous lymphocytes (Am J Clin Pathol 1988;90:250)
- Negative staining:
- Mantle cell lymphoma (Am J Clin Pathol 2010;134:271)
- AML M3 (Am J Clin Pathol 1998;109:211)
- Splenic and nonsplenic marginal zone lymphoma (Am J Clin Pathol 1996;105:277)
CD11d
- Receptor for ICAM3 (CD50) and VCAM1 (CD106) at 16p11.2 (OMIM: 602453 [Accessed 10 May 2021])
- Also called integrin alpha D
- No significant clinical use by pathologists
- Positive staining - not malignant: macrophage foam cells within atherosclerotic plaques
- Negative staining: B cells, follicular dendritic cells
CDw12
- Has been deleted
- In mice, includes Wdr59 antibody
- Only 4 PubMed citations, most recently in 1998 (Leuk Res 1998;22:537)
- No significant clinical use by pathologists
- Positive staining - normal: granulocytes, monocytes, NK cells and platelets
- Negative staining: basophils, bone marrow precursors and AML
- References: Blood 1987;70:1872, Blood 1990;75:198, Folia Biol (Praha) 1993;39:124, GeneCards: CDW12 [Accessed 10 May 2021]
CD13
- See CD13
CD14
- Pattern recognition receptor that detects antigenic molecules on the surface of various microorganisms
- Also called lipopolysaccharide (LPS) receptor, monocyte differentiation antigen
- Mutations can prevent adequate inflammatory response to infection, leading to systemic infections
- Pathophysiology:
- GPI linked pattern recognition receptor that detects antigenic molecules on the surface of bacteria (lipoteichoic acid on gram positive, lipopolysaccharides on gram negative), myobacteria (glycolipids) and fungi (mannans), as part of the innate (nonadaptive) immune system (adaptive immune system refers to lymphocytes recognizing microorganism proteins via T cell receptors and antibodies) (Wikipedia: Innate Immune System [Accessed 10 May 2021]
- Soluble form of CD14 is secreted by liver and monocytes; in low concentrations it confers LPS responsiveness to cells which are otherwise CD14 negative
- Macrophages with a multiprotein complex of CD14, MD2 and TLR4 bind to LPS, causing macrophage activation and release of cytokines (Mol Immunol 2014;57:210)
- Overstimulation may cause toxic shock syndrome (Nature 1998;392:505)
- Detection of lipopolysaccharide induces IL12 production (mediated by CD14), producing interferon gamma, which steers immune system away from allergy driven Th2 phenotype, associated with IgE production
- Important for clearance of apoptotic cells (Nature 1998;392:505, PLoS One 2013;8:e70691)
- Early promonocytes express MY4 epitope; mature monocytes express MO2 epitope; neoplastic monocytes also often express MY4 but not MO2 (Am J Clin Pathol 2005;124:930)
- Clinical features:
- May regulate gastric cancer cell epithelial-mesenchymal transition and invasion (Oncol Rep 2013;30:2725)
- CD14-159C/T polymorphism:
- Contributes to TB susceptibility, particularly in Asians (Int J Tuberc Lung Dis 2013;17:1472)
- May be risk factor for chronic lung disease in India (Indian J Hum Genet 2013;19:188)
- Uses by pathologists: identify mature monocytes / macrophages
- Positive staining - normal: macrophages / monocytes (90%), Langerhans cells, dendritic cells, B cells and granulocytes (weak, 30%)
- Positive staining - disease: AML M4 / M5 (50 - 90%), chronic myelomonocytic leukemia and histiocytic sarcoma (Am J Clin Pathol 2011;135:720)
- Negative staining:
- Myeloid progenitors, AML M0 - M2 (usually), M3, M6 and M7
- Sinusoidal histiocytes with phagocytic properties (erythrophagocytosis, anthracosis, tingible body macrophages) (Hum Pathol 2006;37:68)
- Gaucher macrophages (Hum Pathol 1992;23:1410)
- Most epithelial and endothelial cells
- Reference: OMIM: 158120 [Accessed 10 May 2021]
CD15
- See CD15
CD15s
- Biochemically similar to CD15 but with different functions
- Also known as sialyl Lewis X
- Important in leukocyte tethering and rolling (Wikipedia: Sialyl LewisX [Accessed 10 May 2021])
- Clinical features:
- May be associated with refractory Hodgkin lymphoma (J Cancer 2012;3:322)
- Deficiency causes Rambam-Hasharon syndrome (OMIM: 266265 [Accessed 10 May 2021])
- Also called leukocyte adhesion deficiency 2 (eMedicine: Leukocyte Adhesion Deficiency [Accessed 10 May 2021])
- Expression is correlated with susceptibility to human granulocytic ehrlichiosis (J Clin Invest 1999;103:407)
- Elevated serum levels in hospitalized infants with serious bacterial infections (Eur J Pediatr 2013;172:1363
- Exhibits reversed cell polarity in invasive micropapillary carcinoma of breast (Int J Surg Pathol 2010;18:193)
- Pathophysiology:
- Differs from CD15 by addition of a sialic acid; myeloid maturation is accompanied by relative loss of CD15s and gain of CD15 expression (Nat Chem Biol 2008;4:751)
- Mediates leukocyte rolling (Proc Natl Acad Sci USA 1997;94:3172)
- Ligand (receptor) for CD62P and CD62E
- May play a role in cluster formation in lymphoid follicles (Immunol Lett 2001;79:181)
- No significant clinical use by pathologists
- Positive staining - normal: granulocytes, macrophages; also some T cells, B cells and NK cells
- Positive staining - disease:
- Cirrhosis, metastatic carcinoma, fibrolamellar and other hepatocellular carcinoma (Arch Pathol Lab Med 1992;116:643)
- CD4+ CD56+ neoplasia (Leuk Lymphoma 2003;44:281)
- Sezary syndrome (J Am Acad Dermatol 2001;44:456)
- Negative staining: normal hepatocytes
CD15u
- Adhesion protein representing the sulfated form of CD15
- Also called sialyl 6-sulfo Lewis
- Major L selectin ligand on high endothelial venules of human peripheral lymph nodes (Biochem Biophys Res Commun 2000;278:90)
- No significant clinical use by pathologists
- Positive staining - normal:
- Neutrophils, basophils, mature granulocytes, monocytes, NK cells and T lymphocytes
- Also immature bone marrow cells, endothelial cells of high endothelium (HEV) of peripheral lymph nodes
- Expression on lymphocytes is variable depending on the antibodies used for detection
- Positive staining - disease: myelomonocytic leukemia cells, adenocarcinoma
CD16 / CD16a
- CD16 has been identified as IgG, Fc receptors FcγRIIIa (CD16a) and FcγRIIIb (CD16b), which participate in signal transduction
- Also known as Fc gamma receptor III A, FCGR3A, low affinity immunoglobulin gamma Fc region receptor III A
- CD14+ CD16+ monocytes have increased capacity to produce proinflammatory cytokines such as TNF alpha and are elevated in various inflammatory diseases, including coronary artery disease (Thromb Haemost 2004;92:419)
- CD16a polymorphisms influence:
- Severity but not the incidence of IgA nephropathy in Japanese patients (Nephrol Dial Transplant 2005;20:2439)
- Pathogenesis of coronary artery disease (Atherosclerosis 2005;180:277)
- Clinical response to rituximab and infliximab for Crohn disease (DNA Cell Biol 2012;31:1671, Br J Haematol 2011;154:223, Immunogenetics 2013;65:265)
- Can detect with real time PCR (Cancer Genet 2013;206:130)
- Loss of CD16a in children is associated with recurrent viral infections
- Pathophysiology:
- Gene is similar to that for CD16b
- Binds various IgG molecules, including rheumatoid factor
- Mediates antibody dependent cytotoxicity of foreign cells, phagocytosis and other antibody dependent responses but if target cell has class I MHC, the NK cell's killer cell inhibitory receptor (KIR) inhibits cytolysis
- Mediates platelet satellitism (Am J Clin Pathol 1995;103:740)
- Affinity to ligand is regulated by glycosylation (Immunology 2003;110:335)
- Uses by pathologists:
- NK cell and macrophage marker
- Used to subtype leukemia / lymphomas
- Note: preincubation with CD16 / CD32 antibodies is commonly used to prevent nonspecific binding
- Positive staining - normal: NK cells, granulocytes, monocytes / macrophages, T cells (reactive), immature thymocytes and placental trophoblast
- Positive staining - disease:
- NK proliferative disorders, hepatosplenic alpha beta and gamma delta T cell lymphomas (variable), T cell large granular lymphocyte leukemia (variable)
- CD16 expression, normally absent from eosinophils, is upregulated with allergic conditions (J Allergy Clin Immunol 2002;109:46)
- Or when stimulated in vitro with platelet activating factor or IFNgamma (Int Arch Allergy Immunol 2004;134:165)
- Negative staining: basophils; NK / T cell lymphoma nasal type
- Reference: OMIM: 146740 [Accessed 10 May 2021]
CD16b
- Most common receptor for the Fc domain of IgG on leukocytes
- Also known as Fc gamma receptor III B, low affinity immunoglobulin gamma Fc region receptor III-B
- Has allotypes that define the human neutrophil antigen 1 (HNA 1 and NA) system involved in major post transfusional reactions (Tissue Antigens 2004;64:119)
- Polymorphisms are associated with susceptibility to idiopathic pulmonary fibrosis (Lung 2010;188:475)
- Polymorphisms may be associated with malaria (PLoS One 2012;7:e46197, Hum Genet 2012;131:289)
- Low copy number is associated with glomerulonephritis in systemic lupus erythematosus (Nature 2006;439:851)
- CD16+ eosinophils are upregulated in allergic conditions (J Allergy Clin Immunol 2002;109:463)
- Pathophysiology:
- Highly homologous to CD16a
- Only Fc receptor linked to the plasma membrane by a GPI (glycosylphosphatidylinositol) anchor
- Occurs in 2 codominantly expressed allelic variants, NA1 and NA2, which exhibit different binding affinities for IgG1 and IgG3 subclasses
- No significant clinical use by pathologists
- Positive staining - normal: neutrophils, basophils (J Immunol 2009;182:2542)
CD17 / CDw17
- Most abundant glycosphingolipid in neutrophils; not a protein
- Also known as lactosylceramide
- CD17 is also a type of mutation in beta-thalassemia, unrelated to CD markers (Fetal Diagn Ther 2010;27:25)
- Pathophysiology:
- Defines successive stages in maturation of myeloid cell (Cell Mol Biol Lett 2003;8:911)
- Rapidly and extensively down modulated on activated granulocytes (J Immunol 1989;142:2784)
- Acts as a lipid second messenger in mediating TNF alpha, platelet derived growth factor and oxidized LDL induced phenotypic changes in cells of the vascular wall
- Acts as pattern recognition receptor in innate immunity (Arch Immunol Ther Exp (Warsz) 2013;61:217)
- Clinical features: elevated levels are present in plasma of patients with familial hypercholesterolemia and in plaque intima of aorta in patients who died of cardiovascular disease (Proc Natl Acad Sci U S A 2004;101:6490)
- No significant clinical use by pathologists
- Positive staining - normal: granulocytes, macrophages / monocytes, platelets, basophils, CD19+ B cells and tonsillar dendritic cells
CD18
- Integrin which forms the beta 2 chain of CD11a, CD11b, CD11c, CD11d to create a leukocyte adhesion molecule (OMIM: 600065 [Accessed 11 May 2021])
- Gene is designated ITGB2 (integrin beta 2)
- Combines with alpha L chain (CD11a) to form the integrin LFA1
- Combines with the alpha M chain (CD11b) to form the integrin Mac1 (macrophage antigen 1, complement receptor 3)
- Combines with the alpha X chain (CD11c) to form completement receptor 4
- Also combines with the alpha D chain (CD11d)
- Pathophysiology:
- Important for adhesion and signaling in the hematopoietic system (see CD11a, b, c)
- Also for phagocytosis (J Immunol 2002;169:2003)
- Clinical features:
- Deficiency of the CD18 component (leukocyte adhesion deficiency type 1) is a rare, inherited disorder, causing severe leukocytosis and recurrent severe bacterial infections early in life of skin and mucosal surfaces, possibly fatal, due to defective white blood cell adherence, chemotaxis, phagocytosis and bacterial killing (OMIM: 116920 [Accessed 11 May 2021], J Clin Immunol 2010;30:756)
- Note: leukocyte adhesion deficiency type 2 is due to a deficiency in CD15s
- Reduced expression also seen in Vogt-Koyanagi-Harada (VKH) syndrome (PLoS One 2011;6:e14616)
- CD11b / CD18 is receptor for Bordetella pertussis adhesin filamentous hemagglutinin (FHA) and for the adenylate cyclase toxin (ACT), which blocks neutrophil function (Infect Immun 2005;73:7317, J Exp Med 2001;193:1035)
- CD11b / CD18 induces neutrophilic response leading to killing of Steptococcus pyogenes (Eur J Immunol 2005;35:1472)
- May have role in development of diabetic retinopathy (Int J Ophthalmol 2012;5:202)
- No significant clinical use by pathologists
- Positive staining - normal: neutrophils, macrophages, monocytes, NK cells and basophils
- Negative staining - normal: often negative in acute promyelocytic leukemia (Am J Clin Pathol 2012;138:744)
CD19
- See CD19
Diagrams / tables
Microscopic (histologic) images
Images hosted on other servers:
CD100-109
Table of Contents
CD100 | CD101 | CD102 | CD103 | CD104 | CD105 | CD106 | CD107a | CD107b | CD108 | CD109 | Microscopic (histologic) imagesCD100
- Also called SEMA4D, semaphorin 4D
- Integral membrane protein and ligand for CD72 and plexin B1
- Functions:
- Regulates axonal growth cone guidance in the developing CNS through its receptor plexin B1, which may be related to its expression in invading islands of transformed epithelial cells (but not normal and noninvasive dysplastic epithelium) (Proc Natl Acad Sci USA 2006;103:9017)
- Evokes angiogenic responses from endothelial cells (Blood 2005;105:4321)
- Impairs monocyte migration
- After vascular injury, platelet associated CD100 binds to CD100 receptors on nearby platelets to promote thrombus formation (Proc Natl Acad Sci USA 2007;104:1621)
- Increases CD45 induced T cell adhesion
- Down regulates B cell expression of CD23
- Expression may have prognostic value in soft tissue sarcoma (Cancer 2007;110:164)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: most hematopoietic cells including platelets, increased expression after T cell activation
- Negative staining: immature bone marrow cells
- References: OMIM: 601866 [Accessed 30 April 2021], Wikipedia: Semaphorins [Accessed 30 April 2021]
CD101
- Also called immunoglobulin superfamily member 2 (IGSF2), V7
- Inhibits T cell activation induced by CD3 by:
- Inhibiting IL2RA expression on activated T cells and IL2 secretion (J Immunol 1998;161:209)
- Inducing IL10 production (Eur J Immunol 2000;30:3132)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: monocytes, granulocytes, dendritic cells, activated T lymphocytes in small intestine
- Positive staining - disease:
- CD4+ CD56+ blastic tumor cells (J Invest Dermatol 2005;124:668)
- Langerhans cell histiocytosis (Histopathology 2000;36:229)
- References: OMIM: 604516 [Accessed 30 April 2021], J Immunol 1998;161:2780
CD102
- Also called ICAM2
- Binds the leukocyte integrins LFA1 (CD11a / CD18) and Mac1 (CD11b / CD18)
- Provides costimulatory signal in immune response
- Important in lymphocyte recirculation (J Immunol 2003;171:2588)
- Endothelial ICAM2 mediates angiogenesis (Blood 2005;106:1636)
- Elevated serum levels in:
- Hemorrhagic fever with renal syndrome (Viral Immunol 2006;19:565)
- Idiopathic pulmonary fibrosis (Inflammation 2004;28:359)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: resting lymphocytes, monocytes, platelets, vascular endothelial cells
- Positive staining - disease: some lymphomas
- Negative staining: neutrophils
- Reference: OMIM: 146630 [Accessed 30 April 2021]
CD103
- See CD103
CD104
- Also called integrin beta 4 chain
- Tends to associate with alpha 6 subunit (CD49f)
- Adhesion receptor (for laminins) in normal epithelia that plays a critical role in structure of hemidesmosomes; associated with intermediate filaments
- May contribute to tumor progression via VEGF stimulation (Cancer Metastasis Rev 2005;24:413, J Cell Biol 2002;158:165)
- Overexpressed in pancreatic adenocarcinoma (J Histochem Cytochem 2005;53:799)
- Mutations are associated with epidermolysis bullosa with pyloric atresia (Exp Dermatol 2004;13:61)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: epithelium, thymocytes, Schwann cells
- Positive staining - disease: carcinomas (some)
- Reference: OMIM: 147557 [Accessed 30 April 2021]
CD105
- See CD105
CD106
- Also called VCAM1 (vascular cell adhesion molecule 1); alpha 4 beta 1 ligand
- Interacts with beta 1 integrin VLA4
- Adhesion molecular in activated endothelium; plays a role in migration of white blood cells (J Exp Med 2006;203:2763)
- May mediate endothelial progenitor cell recruitment to rheumatoid arthritis synovium (Arthritis Rheum 2007;56:1817)
- Associated with type II rheumatic disease (Cell Mol Biol (Noisy-le-grand) 2002;48:OL243)
- Important in initiation of atherosclerosis (J Clin Invest 2001;107:1255)
- Renal cell carcinoma may exploit VCAM1 overexpression for immune system escape (Cancer Res 2007;67:6003)
- On the other hand, down regulation in breast cancer is associated with nodal metastases (Pathol Oncol Res 2002;8:125)
- Increased expression: in placentas of women with pregnancy induced hypertension complicated by intrauterine growth restriction (Di Yi Jun Yi Da Xue Xue Bao 2002;22:1022)
- Increased plasma levels associated with:
- Breast cancer [high stage] with circulating cancer cells (Neoplasma 2006;53:538)
- Cancer (general): early stage or preclinical (Eur J Cancer 2005;41:2355)
- Dengue virus infection severity (J Med Virol 2004;72:445)
- Diabetes with poor control (high HbA1c) (Diabetes Care 2007;30:159)
- Arteriosclerosis obliterans (Clin Chim Acta 2007;377:198)
- Endometriosis: advanced (J Soc Gynecol Investig 2002;9:98)
- Sickle cell trait in athletes (J Appl Physiol 2007;102:169)
- Uses by pathologists: marker of endothelial damage (Endothelium 2006;13:335)
- Positive staining - normal: activated endothelial cells, lymphocytes, monocytes, neural cells, hematopoietic cells
- Positive staining - disease: renal cell carcinoma
- Reference: OMIM: 192225 [Accessed 30 April 2021]
CD107a
- Also called lysosome associated membrane protein 1 (LAMP1)
- Note: DC-LAMP is CD208
- Functions:
- Surface antigen transiently present on cell surface of CD8+ T cells after release of cytolytic granules (J Immunol Methods 2003;281:65)
- Basophil activation antigen (Cell Res 2005;15:325)
- Expression correlates with aggressiveness of melanocytic neoplasms (Melanoma Res 2006;16:235)
- Critical to phagosomes acquiring microbicidal capabilities (Cell Microbiol 2007;9:2153)
- Ligand to E-selectin mediated cell adhesion
- Uses by pathologists: defective CD107a surface expression discriminates between genetic subtypes of familial hemophagocytic lymphohistiocytosis (Blood 2006;108:2316)
- Positive staining - normal:
- Primarily endosome lysosome membranes, 1 - 2% on plasma membrane
- Degranulated platelets (Blood Coagul Fibrinolysis 2003;14:249)
- Activated neutrophils, T cells, endothelium
- Reference: OMIM: 153330 [Accessed 30 April 2021]
CD107b
- Also called lysosome associated membrane protein 2 (LAMP2)
- X linked
- Major constituent of lysosomal membranes (also LAMP1)
- Functions:
- Mutations cause Danon disease, a lysosomal glycogen storage disease with cardiomyopathy in adult women and men before age 20 years (N Engl J Med 2005;352:362, Circulation 2005;112:1612)
- Also, Wolff-Parkinson-White syndrome, myopathy, variable intellectual disability and retinopathy (Arch Ophthalmol 2007;125:231)
- Skeletal and cardiac muscle cells have intracytoplasmic vacuoles containing glycogen and autophagic material
- Levels decrease with age (J Cell Sci 2007;120:782)
- Binding of substrates to LAMP2 is limiting step in chaperone-mediated autophagy, a selective mechanism for the degradation of soluble cytosolic proteins in lysosomes (EMBO J 2006;25:3921)
- May be involved in infection induced involution of thymus via autophagy (Acta Biol Hung 2006;57:315)
- Facilitates MHC class II presentation of cytoplasmic antigens (Immunity 2005;22:571)
- Basophil activation antigen (Cytometry A 2004;61:62)
- Uses by pathologists: help differentiate cardiomyopathy due to Danon disease (LAMP2 negative) from other causes (LAMP2 positive) (Intern Med 2007;46:757)
- Positive staining - normal: lysosome membranes of various tissues, platelets (Thromb Haemost 1996;75:623)
- Negative staining: cardiac and skeletal muscle in Danon disease (Neuromuscul Disord 2003;13:708)
- Reference: OMIM: 309060 [Accessed 30 April 2021]
CD108
- Also called semaphorin 7A (SEMA7A) or John Milton Hagen (JMH) human blood group antigen
- A semaphorin (Wikipedia: Semaphorin [Accessed 30 April 2021])
- Receptors are plexin C1 and beta1 integrins
- Functions:
- Genetic variations may play a role in decreased bone mineral density and risk of vertebral fracture (J Hum Genet 2006;51:112)
- Extremely potent monocyte activator; stimulates chemotaxis and cytokine production (Scand J Immunol 2002;56:270)
- Stimulates axon growth and guidance during development (Nature 2003;424:398)
- Negative regulator of T cell responses (Immunity 2006;24:591)
- Expression is correlated with the establishment of dentin-pulp complex terminal innervation (Matrix Biol 2005;24:232)
- Positive staining - normal: erythrocytes, activated lymphocytes, odontoblasts, monocytes, keratinocytes, fibroblasts
- Reference: OMIM: 607961 [Accessed 30 April 2021]
CD109
- Also called platelet activation factor
- Glycosylphosphatidylinositol-anchored cell surface protein
- Carries the biallelic platelet-specific Gov antigen system
- Alloantibodies to HPA-15 residing on CD109 are implicated in refractoriness to platelet transfusion, fetal / neonatal alloimmune thrombocytopenia and posttransfusion purpura (Blood 2002;99:1692)
- Positive staining - normal:
- Activation antigen for platelets and T cells
- Subset of hematopoietic stem and progenitor cells (Exp Hematol 1999;27:1282)
- Myoepithelial cells (breast, prostate [basal cells] salivary and lacrimal glands) (Pathol Int 2007;57:245)
- Widely expressed in other tissues
- Negative staining: invasive ductal carcinoma (breast), prostate adenocarcinoma
- Reference: OMIM: 608859 [Accessed 30 April 2021]
Microscopic (histologic) images
CD103
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- CD103 is a heterodimeric transmembrane surface receptor that is expressed by several cell types of the immune system and is involved in cell to cell or cell to matrix interactions
- CD103 mediates cell adhesion, migration and lymphocyte homing through interaction with E-cadherin, which is expressed in epithelial cells
Essential features
- Diagnostic tool in the detection of hairy cell leukemia (HCL) and hairy cell leukemia variant (HCL-v)
- Aids in distinguishing hairy cell leukemia from other types of B cell lymphoproliferative disorders (in conjunction with additional markers) (Am J Clin Pathol 2009;131:586, Am J Clin Pathol 2011;136:625)
- High CD103+ tumor infiltrating lymphocyte (TIL) cell count is reported to be a favorable prognostic marker in a multitude of solid tumors (Cancers (Basel) 2021;13:6211, Clin Cancer Res 2014;20:434, J Immunol 2015;194:3475, Clin Cancer Res 2016;22:6290, Oncoimmunology 2014;3:e27668, J Urol 2015;194:556, Exp Ther Med 2018;15:4979, Sci Rep 2019;9:3808)
Terminology
- Integrin alpha Eβ7 (ITGAE)
- Integrin alpha E (αE)
- αE subunit first described as human mucosal lymphocyte 1 (HML1) antigen
Pathophysiology
- CD103 is a heterodimer complex; the integrin αE chain (CD103 in the strict sense) dimerizes exclusively with the β7 integrin subunit
- CD103 is the first integrin discovered that binds to a cadherin, namely E-cadherin
- Binding of CD103 is heterophilic
- αE subunit binds through its metal ion dependent coordination site (MIDAS) motif to the tip of the BC loop of E-cadherin (J Exp Med 2000;191:1555)
- β7 chain does not bind directly to E-cadherin but appears to have more of a regulatory function in this process
- CD103 mediates lymphocyte retention in epithelial tissues and allows immunocytes to maintain close contact with both peripheral lymphoid and nonlymphoid tissue (through binding to E-cadherin) (Nature 1994;372:190)
- Transforming growth factor β (TGFβ) has been found to consistently upregulate its expression
- This cytokine induces CD103 on human cytotoxic lymphocytes in conjunction with T cell receptor (TCR) activation
Clinical features
- Interaction of E-cadherin with integrin αE(CD103)β7 plays a significant role in effective tumor cell lysis (J Exp Med 2007;204:559)
- CD103 plays a key costimulatory role in cytotoxic T cell activation (Int J Cancer 2011;129:2417, Cancer Res 2011;71:328)
Interpretation
- Membranous (primarily) and cytoplasmic (variable intensity) with overlay of irregular cytoplasmic borders (consistent with projections) (Am J Clin Pathol 2013;139:220)
Uses by pathologists
- Diagnostic tool in the detection of hairy cell leukemia and hairy cell variant
- Aids in distinguishing hairy cell leukemia from other types of B cell lymphoproliferative disorders (in conjunction with additional markers) (Am J Clin Pathol 2009;131:586, Am J Clin Pathol 2011;136:625)
Prognostic factors
- High CD103+ tumor infiltrating lymphocyte cell count is reported to be a favorable prognostic marker in a multitude of solid tumors (Cancers (Basel) 2021;13:6211, Clin Cancer Res 2014;20:434, J Immunol 2015;194:3475, Clin Cancer Res 2016;22:6290, Oncoimmunology 2014;3:e27668, J Urol 2015;194:556, Exp Ther Med 2018;15:4979, Sci Rep 2019;9:3808)
- High CD8+, CD103+ tissue resident memory T cells (TRM) are associated with metastasis and poorer clinical outcome in cutaneous squamous cell carcinoma (cSCC) (J Immunother Cancer 2021;9:e001807)
Microscopic (histologic) description
- CD103 expression is uniform with high intensity in cases of bone marrow involvement by hairy cell leukemia (in a diffuse interstitial pattern, ≥ 50% involvement)
- CD103 expression follows the distribution of neoplastic cells in cases of a patchy intrasinusoidal / interstitial pattern of bone marrow involvement (low level, 15% involvement)
- Reference: Am J Clin Pathol 2013;139:220
Microscopic (histologic) images
Positive staining - normal
- Intestinal intraepithelial lymphocytes (IELs, T cells) (Eur J Immunol 1990;20:2201)
- Alloantigen induced regulatory CD8+ T cells (Tregs) (Hum Immunol 2008;69:737, J Immunol 2006;177:2775)
- Tissue resident memory T cells (TRM cells) (Nat Rev Immunol 2016;16:79, J Invest Dermatol 2018;138:23)
- FOXP3+ regulatory T cells (Tregs) (Int J Cancer 2011;129:2417)
- Classic dendritic cells (cDCs) in nonlymphoid tissue (J Am Soc Nephrol 2016;27:1344)
- CD11chighMHC class IIhigh dendritic cells (mucosal and epithelial sites) (Immunol Rev 2010;234:268)
- CD4+ natural regulatory T cells (nTreg) (J Allergy Clin Immunol 2006;118:1342)
Positive staining - disease
- Hairy cell leukemia (HCL) (Am J Clin Pathol 2009;131:586, Curr Oncol 2021;28:5148)
- Hairy cell leukemia variant (HCL-v) (Hematol Oncol Clin North Am 2006;20:1051, Curr Oncol 2021;28:5148)
- Enteropathy associated T cell lymphoma (EATL) (Am J Surg Pathol 2014;38:1557)
- Adult T cell leukemia / lymphoma (ATLL) (Am J Surg Pathol 2016;40:462, Am J Surg Pathol 2014;38:1557)
- Monomorphic epitheliotropic intestinal T cell lymphoma (MEITL) (Haematologica 2023;108:181)
Negative staining
- Angioimmunoblastic T cell lymphoma (AITL) (Am J Surg Pathol 2014;38:1557)
- T cell large granular lymphocytic leukemia (TLGL) (Am J Surg Pathol 2014;38:1557)
- Splenic marginal zone lymphoma (SMZL) (Blood 2016;127:2072, Am J Clin Pathol 2011;136:625, Mod Pathol 1998;11:601)
- < 10% cases positive by flow cytometry, < 25% cases by IHC
- Splenic diffuse red pulp small B cell lymphoma (SDRPL) (Histopathology 2002;40:22, Curr Oncol 2021;28:5148)
- Reports of cases that are positive
- 13/34 cases = 38% (Blood 2008;111:2253)
- 10/30 cases = 33% (Hematol Oncol 2011;29:47)
- Reports of cases that are positive
- Chronic lymphocytic leukemia (CLL) (Am J Clin Pathol 2011;136:625)
- Mantle cell lymphoma (MCL) (Am J Clin Pathol 2011;136:625)
- Follicular lymphoma (FL) (Am J Clin Pathol 2011;136:625)
- Mycosis fungoides (MF) (16 - 24%) (Am J Surg Pathol 2014;38:1557, Am J Surg Pathol 2016;40:462)
Sample pathology report
- Bone marrow, posterior iliac crest, aspirate and core biopsy:
- Hypercellular marrow with involvement by CD103+ mature B cell neoplasm (see comment)
- Comment: The trephine core biopsy shows intravascular and patchy interstitial infiltration by small to intermediate sized lymphoid cells with asymmetric cytoplasmic projections and occasional nucleoli. These cells are positive for CD20, bright CD11c, bright CD22, CD103 and show kappa light chain restriction. These cells are negative for CD5, CD10, CD25 and CD38.
- The overall morphologic and immunophenotypic features are consistent with involvement by a splenic origin lymphoma. Absence of CD25 coexpression argues against a diagnosis of classical hairy cell leukemia. The primary diagnostic considerations include hairy cell leukemia variant and splenic marginal zone lymphoma. An additional differential may include splenic diffuse red pulp lymphoma (SDRPL). The morphologic features reflect a low grade process. There is no overt large cell transformation observed.
- Correlation with clinical findings and additional pertinent laboratory and radiographic studies is recommended for comprehensive assessment. This case (core biopsy) was submitted for internal quality assurance review.
Additional references
Board review style question #1
A 59 year old man visits his primary care doctor to be evaluated for progressive weakness and decreased exercise tolerance. Physical examination shows splenomegaly and petechial bruises on the upper limbs bilaterally. Laboratory studies reveal pancytopenia. Peripheral smear reveals the findings in the image above and flow cytometry shows a mature monotypic B cell population coexpressing bright CD20, CD22, CD25, CD11c, CD103, FMC7, CD200 and lambda light chain restriction. Which of the following is the most likely diagnosis?
- Adult T cell leukemia / lymphoma (ATLL)
- Angioimmunoblastic T cell lymphoma (AITL)
- Hairy cell leukemia (HCL)
- Splenic diffuse red pulp small B cell lymphoma (SDRPL)
- T cell large granular lymphocytic leukemia (TLGL)
Board review style answer #1
C. Hairy cell leukemia (HCL). The immunoprofile (particularly coexpression of CD11c, CD25 and CD103) and cytologic features (intermediate sized lymphocytes with circumferential cytoplasmic projections) are most consistent with hairy cell leukemia. The alternate disease entities listed either do not (or seldomly) coexpress CD103 with the other markers listed above (i.e., AITL, TLGL, SDRPL) or have different cytologic features in the peripheral blood (i.e., ATLL shows multilobed nuclei flower cells in the peripheral blood).
Comment Here
Reference: CD103
Comment Here
Reference: CD103
Board review style question #2
A 40 year old man presents to his physician with fever and left upper quadrant pain. Subsequent clinical evaluation shows anemia and monocytopenia. A bone marrow biopsy evaluation reveals a B cell lymphoproliferative disorder with the following immunoprofile: CD20+, CD25+, CD103+, annexin A1+, DBA44+. A diagnosis of hairy cell leukemia is made. Which of the following is the characteristic staining pattern of CD103 in this disease entity?
- Cytoplasmic
- Membranous (primarily) and cytoplasmic
- Nuclear
- Perinuclear dot-like
- Perinuclear golgi
Board review style answer #2
B. Membranous (primarily) and cytoplasmic. The most characteristic immunohistochemical pattern of CD103 staining is described in the literature as membranous (primarily) and cytoplasmic (variable intensity) with overlay of irregular cytoplasmic borders (consistent with projections). Since CD103 is a transmembrane surface receptor, the CD103 antibody would bind primarily to the cell membrane; therefore, the alternate choices (nuclear, perinuclear golgi or dot-like and cytoplasmic) are incorrect.
Comment Here
Reference: CD103
Comment Here
Reference: CD103
CD105
Table of Contents
Definition / general | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Additional referencesDefinition / general
- Also called endoglin
- Regulatory component of TGF-beta receptor complex; mediates cellular response to TGF-beta 1
- Mutations cause Hereditary Hemorrhagic Telangiectasia type I (Am J Hum Genet 1997;61:68)
- Required for hemangioblast and early hematopoietic development (Development 2007;134:3041)
Uses by pathologists
- Specific and sensitive marker for tumor angiogenesis (better than CD31)
Prognostic factors
- Increased microvessel staining:
- Acute lymphoblastic leukemia in children (Leuk Res 2007;31:1741)
- Breast carcinoma (Am J Clin Pathol 2003;119:374, including node negative, Hum Pathol 2004;35:176)
- Chronic idiopathic myelofibrosis (Mod Pathol 2004;17:1513)
- Colorectal carcinoma (Mod Pathol 2004;17:197)
- Endometrial carcinoma (Gynecol Oncol 2006;103:1007)
- Esophageal adenocarcinoma (Hum Pathol 2006;37:861)
- Gastric carcinoma (Hum Pathol 2006;37:861)
- Hepatocellular carcinoma (BMC Cancer 2006;6:110)
- Meningioma (Acta Neuropathol 2007;114:147)
- Ovarian carcinoma (Int J Gynecol Cancer 2006;16:1789)
- Primary CNS lymphoma (J Neurooncol 2007;82:249)
- Prostate adenocarcinoma (Am J Clin Pathol 2007;127:572)
- Squamous cell carcinoma of head and neck (Virchows Arch 2006;448:768), including tongue (Laryngoscope 2006;116:1175)
- Other:
- Serum endoglin is associated with intrauterine growth restriction during pregnancy (J Clin Endocrinol Metab 2007;92:2831), preeclampsia (N Engl J Med 2006;355:992, Nat Med 2006;12:642), diabetic retinopathy (J Cell Mol Med 2005;9:692)
- Tissue endoglin is associated with progressive hepatic fibrosis in chronic HCV infection (J Viral Hepat 2006;13:625) and aortic atherosclerosis (J Atheroscler Thromb 2006;13:82)
Microscopic (histologic) images
Positive staining - normal
- Activated monocytes, erythroid precursors in marrow; syncytiotrophoblast, cytotrophoblast in first trimester (transient expression)
Positive staining - disease
- Endometriosis (Reprod Biol 2005;5:51), tumor microvessels (Rom J Morphol Embryol 2007;48:41)
Negative staining
- Normal endothelial cells (or weak)
Additional references
CD110-119
CD110
- Also called thrombopoietin receptor (TPO-R), myeloproliferative leukemia virus oncogene (MPL)
- Binding to thrombopoietin induces megakaryocyte proliferation and differentiation and prevents apoptosis
- Mutations present in some patients with congenital amegakaryocytic thrombocytopenia, characterized by severe congenital thrombocytopenia with no megakaryocytes in the bone marrow (Hum Mutat 2006;27:296)
- MPL mutations in myelofibrosis patients are associated with more severe anemia (Br J Haematol 2007;137:244)
- Thrombopoietin receptor agonists may be useful for treating thrombocytopenia (Blood 2007;109:4739)
- Uses by pathologists: differentiate essential thrombocythemia (variable but weak / negative staining) from reactive thrombocytosis (positive staining) (Blood 2002;99:4131)
- Positive staining - normal: hematopoietic stem cells and progenitor cells, megakaryocytes and progenitors, platelets (J Transl Med 2006;4:9)
- References: OMIM: 159530 [Accessed 29 April 2021], Gene: MPL proto-oncogene, thrombopoietin receptor [Accessed 29 April 2021]
Images hosted on other servers:
CD111
- Also known as poliovirus receptor related 1 (PRR1), nectin1
- Widely expressed adhesion molecule that is a component of the adherens junction; receptor for herpes simplex viruses 1 and 2
- Positive staining - normal: cells from myeloid, monocyte, megakaryocytes and erythroid lineage, epithelial cells, neurons, endothelium
CD112
CD114
- Also known as granulocyte colony stimulating factor receptor, G-CSFR
- Specific regulator of myeloid proliferation and differentiation
- Mutations present in some patients with severe congenital neutropenia
- Positive staining - normal: granulocytes (all), monocytes, platelets, endothelium, placenta, trophoblastic cells
- Positive staining - malignant: cultured tumor cells
- Negative staining: eosinophils, lymphocytes, erythrocytes
CD115
- Also known as c-fms, receptor for macrophage colony stimulating factor, CSF-1R
- Localized on cytoplasmic membrane; mediates biologic activity of CSF-1
- v-fms is a viral oncogene present in the feline McDonough sarcoma virus (has several substitute mutations)
- Related to platelet derived growth factor receptor, c-kit, vascular endothelial growth factor receptor, fibroblast growth factor receptor, high affinity nerve growth factor (TrkA)
- Deficiency causes reduced osteoclasts and macrophages, abnormal bone remodeling and osteopetrosis, abnormal breast development and decreased fertility
- Positive staining - normal: macrophages and precursors, osteoclasts, placental trophoblast, breast tissue, microglia, neurons, astrocytes
- Positive staining - malignant: 10% AML, some endometrial, ovarian and breast cancers, vascular smooth muscle cells in atheromas, choriocarcinoma cells
CD116
CD117
- See CD117
CD117
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Proto-oncogene activated in gastrointestinal stromal tumors (GISTs) (Cureus 2022;14:e20868, Appl Immunohistochem Mol Morphol 2005;13:205)
- Aka c-kit, KIT, stem cell factor receptor, mast cell growth factor
- Gene at 4q11-21
- Class III receptor tyrosine kinase (Appl Immunohistochem Mol Morphol 2005;13:205)
- Receptor for kit protein, a 145 kD tyrosine kinase growth factor receptor protein, important for development and survival of mast cells, hematopoietic stem cells, melanocytes, germ cells, interstitial cells of Cajal (Appl Immunohistochem Mol Morphol 2005;13:205)
Essential features
- Proto-oncogene activated in GISTs (Cureus 2022;14:e20868)
- Gene at 4q11-21
- Class III receptor tyrosine kinase
- Highlights mast cells (normal and abnormal) in the assessment of mast cell neoplasms
Terminology
- CD117 / KIT
- Also known as c-kit, stem cell factor receptor, mast cell growth factor (Appl Immunohistochem Mol Morphol 2005;13:205)
Pathophysiology
- Has activating or gain of function mutations in most GISTs, often at exon 11, less often at exons 9 and 13 (Hum Pathol 2002;33:484, Cancer Med 2020;9:6485, Cureus 2022;14:e20868)
- Tyrosine kinase activity of c-kit in GIST and BCR-ABL overexpression in chronic myeloid leukemia (CML) are inhibited by imatinib mesylate (Gleevec, STI571), a tyrosine kinase inhibitor used to treat these diseases (Clin Cancer Res 2022;28:1672)
- Mutated in mastocytosis, typically the D816V mutation
Interpretation
- Cytoplasmic staining
Uses by pathologists
- Confirming diagnosis of GIST (also see Positive staining - disease) (Cureus 2022;14:e20868)
- Staining of mast cells
- Staining of myeloid stem cells (myelodysplastic syndrome [MDS], acute myeloid leukemia [AML]: estimating quantity of blasts)
Microscopic (histologic) images
Positive staining - normal
- Interstitial cells of Cajal, hematopoietic progenitor cells, melanocytes, embryonic / fetal brain, endothelium, gonads, mast cells, breast epithelium, germ cells (Appl Immunohistochem Mol Morphol 2005;13:205)
Positive staining - disease
- Acute myeloid leukemia (Gastroenterology Res 2022;15:39, Appl Immunohistochem Mol Morphol 2005;13:205)
- Adenoid cystic carcinoma of salivary gland (strong staining)
- Angiomyolipoma (Am J Surg Pathol 2002;26:493)
- Angiosarcomas (50%) (Appl Immunohistochem Mol Morphol 2005;13:205)
- Epithelioid sarcoma (Appl Immunohistochem Mol Morphol 2005;13:205)
- Ewing sarcoma (Appl Immunohistochem Mol Morphol 2005;13:205)
- Gastrointestinal stromal tumor (Appl Immunohistochem Mol Morphol 2005;13:205)
- Hodgkin lymphoma (some Reed-Sternberg cells)
- Intra-abdominal fibromatosis (depends on antibody used) (Am J Surg Pathol 2001;25:549)
- Leiomyosarcoma (Appl Immunohistochem Mol Morphol 2005;13:205)
- Mast cell diseases (also positive for tryptase, CD43, CD68)
- Melanoma (Arch Pathol Lab Med 2006;130:343)
- Mesenteric fibromatosis (variable) (Am J Surg Pathol 2002;26:1296)
- Metanephric adenosarcoma (Am J Surg Pathol 2001;25:1451)
- Nasopharyngeal angiofibroma (Arch Pathol Lab Med 2003;127:1480)
- Osteosarcoma (Appl Immunohistochem Mol Morphol 2005;13:205)
- Rhabdomyosarcoma
- Seminomas / dysgerminomas (Hum Pathol 2002;33:1182, Appl Immunohistochem Mol Morphol 2005;13:205)
- Small cell carcinoma of the lung (Appl Immunohistochem Mol Morphol 2005;13:205)
- Synovial sarcoma (~10%, usually cytoplasmic staining)
- Thymic carcinoma (Appl Immunohistochem Mol Morphol 2005;13:205)
- 50% of solid pseudopapillary tumor (Mod Pathol 2006;19:1157)
Negative staining
- Alveolar soft part sarcoma, desmoplastic small round cell tumor, glomus tumor, leiomyoma (retroperitoneal, colorectal), leiomyosarcoma, myxoma (cardiac), schwannoma (colorectal), smooth muscle tumor of uncertain malignant potential, solitary fibrous tumor (Am J Surg Pathol 2002;26:486)
Sample pathology report
- Gastric biopsy:
- Gastrointestinal stromal tumor (see comment)
- Comment: Infiltrates of a well circumscribed spindle cell tumor with few mitoses (2 / 5 mm2). Immunohistochemically, the tumor is CD117+, DOG1+ and CD34+.
Board review style question #1
Board review style answer #1
CD120-129
Table of Contents
CD120 | CD121a | CDw121b | CD122 | CD123 | CD124 | CDw125 | CD126 | CD127 | CD128 | CD129CD120
- CD120a: aka TNFR1, receptor for tumor necrosis factor alpha and beta, type I; receptor binding to ligand causes apoptosis
- CD120b: aka receptor for tumor necrosis factor (TNF) alpha and beta, type II
CD121a
CDw121b
CD122
CD123
- See CD123
- Aka Interleukin 3 receptor alpha subunit
- Associates with the GM-CSF receptor (GMR beta)
- Uses by pathologists: important for diagnosis of blastic plasmacytic dendritic cell neoplasm (BPDCN)
- Positive staining - normal: plasmacytoid monocytes (bright with flow cytometry) (Am J Surg Pathol 2002;26:852)
CD124
CDw125
CD126
- Aka Interleukin 6 receptor
- Continuous expression of IL-6 and CD130, ligands for CD126, causes hypergammaglobulinemia, glomeruloproliferative nephritis and lymphoid infiltration in some organs
- Dysregulated stimulation may cause myeloma and plasmacytoma
- Positive staining - normal: T cells, monocytes, activated B cells, hepatocytes
CD127
CD128
- See CD181 / CD128
CD123
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Definition / general
- Interleukin 3 receptor alpha chain (IL3Rα)
- Upregulated and overexpressed in a variety of myeloid and lymphoid neoplasms
- CD123 is a biomarker for targeted therapy
Essential features
- CD123 serves as a diagnostic, prognostic and therapeutic marker in some hematologic malignancies, especially acute leukemia
- CD123 and TCF4 coexpression by immunohistochemistry is highly specific and sensitive for blastic plasmacytoid dendritic cell neoplasm (BPDCN)
- Tagraxofusp (SL-401) is a CD123 targeted therapy for BPDCN
Terminology
- IL3Rα
Pathophysiology
- Membrane receptor that heterodimerizes with the β common (βc) subunit to constitute the functional IL3 receptor (IL3R)
- IL3R is the IL3 specific member of the beta βc family of receptors, which also includes IL5R and granulocyte monocyte colony stimulating factor (GM CSF) receptor
- Functions in regulating growth, proliferation, survival and differentiation of hematopoietic cells, along with immunity and inflammatory response
- Downstream signaling is primarily through JAK / STAT, RAS / MAPK and phosphatidylinositol 3 kinase pathways (Cancers (Basel) 2020;12:3087)
Clinical features
- CD123 is a biomarker for targeted therapy in certain diseases, including blastic plasmacytoid dendritic cell neoplasm (BPDCN), acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL) (N Engl J Med 2019;380:1628, Clin Cancer Res 2017;23:3385, Haematologica 2019;104:749)
Interpretation
- Strongest level of CD123 staining is on plasmacytoid dendritic cells
- CD123 is expressed by endothelial cells
- CD123 is a membrane bound protein, resulting in a membranous pattern of staining by immunohistochemistry and surface expression by flow cytometry
- CD123 expression in normal karyotype AML is associated with FLT3-ITD and NPM1 mutations (Br J Haematol 2020;188:181)
- Reference: Am J Surg Pathol 2019;43:1429
Uses by pathologists
- Blastic plasmacytoid dendritic cell neoplasm (BPDCN) (Am J Surg Pathol 2019;43:1429)
- Mature plasmacytoid dendritic cell proliferations (Curr Hematol Malig Rep 2018;13:477)
- Systemic mastocytosis (Leukemia 2016;30:914)
- Hairy cell leukemia (Am J Clin Pathol 2011;136:625)
- Increased plasmacytoid dendritic cells in Kikuchi lymphadenitis and discoid (cutaneous) lupus erythematosus
Prognostic factors
- Prognostic impact of CD123 expression has not been established
Microscopic (histologic) images
Positive staining - normal
- Hematopoietic stem cells
- Endothelial cells
- Plasmacytoid dendritic cells
Positive staining - disease
- Blastic plasmacytoid dendritic cell neoplasm (BPDCN), with marked enhancement in specificity when used alongside TCF4, CD4, CD56, TCL1 and CD303, though CD303 can be negative in up to 56% (Am J Surg Pathol 2019;43:1429, Am J Surg Pathol 2014;38:673, Haematologica 2021;106:1047, Blood Adv 2019;3:4238)
- Mature plasmacytoid dendritic cell proliferations
- Systemic mastocytosis (Leukemia 2016;30:914)
- Hairy cell leukemia
- Acute myeloid leukemia (AML) subset, typically negative for TCF4 and positive for lineage markers
- Rare B cell acute lymphoblastic leukemia (B ALL) cases
Negative staining
- Lymphoma, including most cases of chronic lymphocytic leukemia (CLL), mantle cell lymphoma, follicular lymphoma and mycosis fungoides (Biomark Res 2014;2:4, Postepy Dermatol Alergol 2021;38:994)
- Hairy cell leukemia variant and splenic marginal zone lymphoma with villous lymphocytes (Biomark Res 2014;2:4)
- Carcinoma
- Various soft tissue neoplasms
- Merkel cell carcinoma
Board review style question #1
Patient presents with a skin tumor comprised of blastoid neoplastic cells involving the dermis and subcutaneous tissue without epidermotropism. Which immunohistochemical profile suits the diagnosis of blastic plasmacytoid dendritic cell neoplasm?
- AE1 / AE3 positive, chromogranin positive
- CD21 positive, CD23 positive
- CD34 positive, MPO positive
- TCF4 / CD123 positive, CD4 positive, CD56 positive, CD303 positive
Board review style answer #1
D. TCF4 / CD123 dual expression is highly sensitive and specific for blastic plasmacytoid dendritic cell neoplasm. Such staining is rarely encountered in other malignancies.
Comment Here
Reference: CD123
Comment Here
Reference: CD123
CD13
Table of Contents
Definition / general | Clinical features | Pathophysiology | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Myeloid antigen, although CD33 is more specific (OMIM #151530)
- Also called aminopeptidase N (APN)
Clinical features
- CD13+ may be poor prognostic indicator in Ph' negative B cell ALL (Leuk Res 2013;37:759)
- Mediates tumor angiogenesis (J Histochem Cytochem 2011;59:47, Blood 2007;110:142)
- Viruses: acts as receptor for human coronavirus 229E (J Virol 1998;72:6511), mediates CMV infection (J Immunol 2004;173:4897)
- CD13 autoantibodies are associated with chronic graft versus host disease after bone marrow transplantation (Bone Marrow Transplant 2010;45:1653)
- Caution: may be easy to induce CD13 expression with in vitro culture (Southeast Asian J Trop Med Public Health 2002;33 Suppl 2:155)
Pathophysiology
- Cleaves peptides at brush border of small intestine, renal proximal tubules and placenta
- Cleaves antigen peptides bound to MHC class II molecules of presenting cells
- Degrades neurotransmitters at CNS synaptic junctions
- Regulates sperm motility (Asian J Androl 2010;12:899)
Uses by pathologists
- Differentiate acute myelogenous leukemia / AML in Down's syndrome patients (usually CD13+, CD11b+) from transient myeloproliferative disorder (usually CD13-, CD11b-, Am J Clin Pathol 2001;116:204)
- Differentiate AML M0 (CD13+) from ALL (CD13-, Am J Clin Pathol 2002;117:380)
Microscopic (histologic) images
Positive staining - normal
- Granulocytes (most, but low levels in newbornss, Mod Pathol 1993;6:414), interdigitating dendritic cells, large granular lymphocytes (some), macrophages, mast cells, monocytes, myelomonocytes and osteoclasts
- Also bile duct canaliculi, central nervous system synapses, endothelial cells, endometrial stromal cells, fibroblasts, liver, perineurium of peripheral nerves, placenta, prostate secretory cells, renal proximal tubules (PLoS One 2013;8:e66750), respitatory epithelium, small intestine and sperm
Positive staining - disease
- Tumor vasculature (J Histochem Cytochem 2011;59:47)
- Acute basophilic leukemia
- Acute panmyelosis with myelofibrosis
- AML M1-M5 (75-95%), AML-M6 (usually) and myeloid sarcoma
- Anaplastic large cell lymphoma (47%, Am J Clin Pathol 2003;119:205, Arch Pathol Lab Med 2000;124:1804, leukemic-Am J Clin Pathol 2003;120:617)
- CLL (Hematology 2012;17:1332)
- CML (90%), CML in blast transformation (Mod Pathol 1998;11:1211), chronic myelomonocytic leukemia
- Chronic B cell lymphoproliferative disorders (Arch Pathol Lab Med 1995;119:53)
- Hepatocellular carcinoma (canalicular pattern, J Clin Pathol 2005;58:1069)
- Mast cell sarcoma (Am J Surg Pathol 2003;27:1013)
- MFH (Int J Oncol 2013;43:57)
- Pre B ALL, pre T ALL (occasionally, Exp Mol Pathol 2007;83:471)
Negative staining
- CLL/SLL (rarely positive, Am J Clin Pathol 2003;119:824)
- Prostatic adenocarcinoma (usually, Am J Pathol 2004;165:1543)
- Transient myeloproliferative disorder of Down's syndrome (usually)
CD130-139
Table of Contents
CD130 | CDw131 | CD132 | CD133 | CD134 | FLT3 / CD135 | CDw136 | CDw137 | CD138 | CD139CD130
- Aka gp 130
- Required for transducing biological activities of IL6, IL11, leukemia inhibitory factor, ciliary neurotrophic factor, oncostatin M and cardiotrophin-1
- IL6 and oncostatin M dependent activation of gp130 are involved in multiple myeloma
- Positive staining - normal: almost all cell types (low levels)
CDw131
CD132
- Aka common cytokine receptor gamma chain - receptor for IL-2, IL-4, IL-7, IL-9 and IL-15
- Mutation in humans causes X-linked severe combined immunodeficiency (no T cells, no NK cells)
- CD132 is a target molecule for gene therapy for X-SCID
- Positive staining - normal: T cells, B cells, NK cells, monocytes / macrophages, neutrophils
CD133
- Also known as Prominin 1, AC133
- Transmembrane glycoprotein expressed on the hematopoietic stem cells, endothelial progenitors and dermal derived stem cells capable of differentiating into neural cells
- Uses by pathologists: alternative to CD34 in selecting hematopoietic stem and progenitor cells for transplantation studies; marker of cancer stem cells (cells with tumor initiating potential) (Genes Chromosomes Cancer 2012;51:792)
- Clinical features:
- High expression is a poor prognostic factor in:
- Colorectal carcinoma (Mod Pathol 2010;23:450)
- Endometrial carcinoma (Hum Pathol 2010;41:1516)
- Hepatocellular carcinoma (Br J Cancer 2012;106:1997)
- Melanoma (childhood) (Mod Pathol 2010;23:376)
- Neuroblastoma (Histopathology 2012;60:1144)
- Ovarian carcinoma (Mod Pathol 2012;25:456)
- Note: for colorectal carcinoma, CD133 expression may be related to mutation or activity status of Ras-Raf pathway (Clin Cancer Res 2012;18:3132)
- High expression is a poor prognostic factor in:
- Positive staining - normal:
- Localized to microvilli and other plasma membrane protrusions
- CD34 bright hematopoietic stem and progenitor cells (umbilical cord blood-derived CD133+ cells can differentiate into endothelial cells and induce new blood vessel growth) (Front Biosci 2012;17:2247)
- Progenitor cells within nephron (Expert Opin Ther Targets 2012;16:157)
- Neural stem cells and other primitive cells such as retina
- Villous and extravillous cytotrophoblast, syncytiotrophoblast
- Positive staining - disease:
- Numerous malignancies
- Brain tumors (CD133+ cells have characteristics of endothelial progenitor cells) (Cancer Lett 2012;324:221)
- Negative staining: adult epithelial tissue, villous stroma
Microscopic (histologic) images
Images hosted on other servers:
CD134
FLT3 / CD135
- Also known as FMS-like tyrosine kinase 3, CD135
- Class III receptor tyrosine kinase that regulates hematopoiesis (US National Library of Medicine)
- Constitutive activation occurs by internal tandem duplication (ITD) (Arch Pathol Lab Med 2012;136:84); detection fast and inexpensive
- Most frequent molecular abnormality in AML
- Mutated in 10% with chronic myeloproliferative diseases (CMPD) or CMPD/myelodysplastic syndrome but not CML (Am J Clin Pathol 2006;126:530)
- Mutated in 2% with myelodysplastic syndrome (Am J Clin Pathol 2011;135:62)
- Immunophenotypic profile of TdT+ CD7+ CD13+ CD34+ CD117 (bright) predicts FLT3 mutations (100% sensitive, 94% specific) (Am J Clin Pathol 2012;137:213)
- Activated FLT3 inhibited by Sunitinib malate
- Uses by pathologists: subtype of AML (see AML with FLT3 mutations); associated with poor clinical outcome; FLT3 mutations in AML may be unstable (Mod Pathol 2012;25:1405)
Diagrams / tables
Images hosted on other servers:
CDw136
CDw137
CD138
- See CD138
CD139
CD138
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Transmembrane proteoglycan expressed in various normal and malignant tissues
- 1 of 4 members of the syndecan family, a cell surface protein involved in the regulation of cell proliferation, migration and organization of the cytoskeleton
- Syndecan derives from the Greek word syndein, which means to bind together (Oncotarget 2015;6:28693)
Essential features
- Used to distinguish and quantitate plasma cells in hematolymphoid tissues and as a biomarker for multiple myeloma cells
- CD138 expression is highly variable among different cancer types
- Both high and low expression levels can be associated with poor prognosis depending on the tumor type
Terminology
- Syndecan 1 (SDC1)
Pathophysiology
- Involved in cell proliferation, migration, adhesion and angiogenesis with loss of CD138 expression leading to enhanced motility and invasion of neoplastic cells (Oncotarget 2015;6:28693)
- Acts as coreceptor to bind growth factors and promote cell survival and proliferation; can also be shed into the surrounding cellular environment
- Has been implicated in the regulation of the Wnt signaling, focal adhesion kinase (FAK), nuclear factor kappa B (NFkB) and mitogen activated protein kinase (MAPK) pathways (J Histochem Cytochem 2015;63:465, Int J Mol Sci 2022;23:9037)
- Involved in leukocyte recruitment and extracellular matrix remodeling during injury repair (Front Immunol 2020;11:227)
Clinical features
- Expressed on cell surface of immature B cells and mature plasma cells
- Overexpressed on malignant plasma cells
Interpretation
- Predominantly membranous but sometimes expressed in the cytoplasm or nucleus
Uses by pathologists
- Used in routine diagnostic pathology to distinguish and quantitate plasma cells in hematolymphoid tissues (Dis Markers 2019;2019:4928315)
- Biomarker for multiple myeloma (Int J Mol Sci 2022;23:9037)
Prognostic factors
- CD138 expression levels generally decrease as tumor grade, stage and invasiveness increase; however, variable expression levels may depend on tumor type
- Expression levels are reduced in squamous cell lung cancer, advanced ovarian cancer, poorly differentiated head and neck squamous cell carcinomas and prostate cancer (Oncotarget 2015;6:28693)
- CD138 expression levels are increased in
- Neoplastic cells of urothelial carcinoma and correlates with high tumor grade, advanced stage and tumor recurrence
- Increased CD138 expression in gallbladder cancer is associated with lymph node metastasis and poor survival (Dis Markers 2019;2019:4928315)
- Most studies show increase of CD138 in breast carcinomas, which correlates with triple negative ductal tumors (negative for ER, PR and HER2) with poor survival (Oncotarget 2015;6:28693)
- Pancreatic cancer, with better prognosis for epithelial expression of CD138 versus stromal expression (Oncotarget 2015;6:28693)
- Some tumors lose CD138 membrane expression but show abnormal cytoplasmic or nuclear expression (Int J Mol Sci 2021;22:4227)
- Appearance of CD138 in tumor stroma is almost always a sign of poor prognosis (Int J Mol Sci 2021;22:4227)
Microscopic (histologic) description
- Expressed on mature plasma cells and immature B cells (Oncotarget 2015;6:28693)
- Expressed widely on the bone marrow hematopoietic cells, endothelial cells and on some breast cancer cells (Leukemia 2020;34:245)
- Negative for other hematolymphoid cells
Microscopic (histologic) images
Positive staining - normal
- Normal plasma cells and immature B cells of hematolymphoid organs, plasma cell malignancies
- Strong expression in normal squamous epithelium of various organs
- Goblet and columnar cells of the gastrointestinal tract (Dis Markers 2019;2019:4928315)
Positive staining - disease
- Multiple myeloma tumor cells (95%)
- Carcinomas with strong CD138 expression (tissue samples from microarray)
- Anal carcinoma (63.6%)
- Esophageal squamous cell carcinoma (78.8%)
- Colon adenoma (92%)
- Urothelial carcinoma pTa (90.5%)
- Squamous cell carcinoma of skin (61.9%)
- Basal cell carcinoma of skin (82.9%)
- Hepatocellular carcinoma (72.7%)
- Granular cell tumor (62.5%)
- Squamous cell lung carcinoma (61.9%) (Dis Markers 2019;2019:4928315)
- Invasive ductal breast carcinoma (90%) (Cancer Treat Res Commun 2021;27:100312, Anal Cell Pathol 2018;2018:9432375)
- Loss of membranous staining and the cytoplasmic accumulation of CD138 reflects a poorer outcome (Mol Carcinog 2019;58:2306)
Negative staining
- Low or absent expression in testicular germ cell tumors, sarcomas, melanoma and small cell urinary bladder carcinoma (Dis Markers 2019;2019:4928315)
Molecular / cytogenetics description
- Encoded on chromosome 2p24.1 (Cancer Treat Res Commun 2021;27:100312)
- Mutant KRAS has been shown to induce CD138 expression in pancreatic ductal adenocarcinoma cells (Am J Physiol Cell Physiol 2022;323:C29)
Sample pathology report
- Core biopsy, bone marrow:
- Multiple myeloma (see comment)
- Comment: The patient is a 57 year old man with symptoms of exertional fatigue, anemia and back pain. Immunohistochemistry was performed to quantify plasma cells (CD138) in addition to Ig kappa and lambda to establish clonality. CD138 positive cells represent 20 - 25% of total cellularity. Results will be correlated with flow cytometry and FISH.
Board review style question #1
Board review style answer #1
E. Plasma cells. CD138 is a useful marker of plasma cells and can help support a diagnosis of multiple myeloma. Answers B, C and D are incorrect because CD138 is not a useful marker in identifying T or B cells. While B cells may express CD138 during earlier stages of development, they lose expression of this marker at maturity. Answer A is incorrect because CD138 is rarely expressed on other hematopoietic cells; CD38 and not CD138 would be a better marker for activated T cells.
Comment Here
Reference: CD138
Comment Here
Reference: CD138
Board review style question #2
Increased expression of CD138 has been found in which of the following cancer types?
- Liposarcomas
- Melanomas
- Sarcomas
- Triple negative breast cancer
Board review style answer #2
D. Triple negative breast cancer. CD138 is expressed in most triple negative breast cancers (TNBC). The increased expression of CD138 may contribute to the formation of a tumor supportive microenvironment, promoting the aggressive growth and invasion of cancer cells that are commonly noted in TNBC. Answers A and C are incorrect because CD138 is rarely expressed in soft tissue tumors. Answer B is incorrect because expression of CD138 in melanomas is low to absent; however, low levels of staining have been observed in metastatic forms of melanoma.
Comment Here
Reference: CD138
Comment Here
Reference: CD138
CD140-149
Table of Contents
CD140 | CD141 (Thrombomodulin) | CD142 | CD143 | CD144 | CDw145 | CD146 | CD147 | CD148 | CD149CD140
- CD140a: also known as alpha platelet derived growth factor receptor
- CD140b: also known as beta platelet derived growth factor receptor
CD141 (Thrombomodulin)
- See Thrombomodulin
CD142
- Aka coagulation Factor III, thromboplastin, tissue factor
- Major initiator of clotting in normal hemostasis and many thrombotic diseases, via complex with factor VIIa
- Also binds zymogen factor VII, the inactive precursor form; once bound, a variety of serine proteases rapidly activate factor VII to VIIa via limited proteolysis
- Normally absent from all cells in direct contact with plasma
- Positive staining - normal: epidermal keratinocytes, glomerular epithelial cells and various other epithelia, adventitial cells of blood vessels, astrocytes, myocardium, Schwann cells, stromal cells of liver, pancreas, spleen and thyroid
CD143
- Aka angiotensin-converting enzyme, ACE, peptidyl dipeptidase A
- Involved in metabolism of angiotensin II and bradykinin; also cleaves substance P and LH-RH
- Patients with high activity have DD genotype, associated with MI, strokes, diabetic nephropathy
- Necessary for spermatozoa to bind to egg and associated with better penetration of egg
- Positive staining - normal: endothelial cells of small/medium arteries, lung capillary endothelium, proximal renal tubule brush borders, basal ganglia neuropil, granulosa cells, Leydig cells, variable on other cells
CD144
- Endothelial-specific cadherin localized at intercellular junctions
- Aka vascular endothelial-cadherin precursor, VE-cadherin, cadherin 5
- Cadherins are cell adhesion proteins that preferentially interact with themselves in a homophilic manner in connecting cells, thus contributing to the sorting of heterogeneous cell types
- Positive staining - normal: endothelial cells, brain
CDw145
- Endothelium cell marker
- Minimal information present as of 1Dec11
- Note: one paper indicates CD145 is equivalent to CD40L (Rev Clin Esp 2007;207:418), but this appears to be a typo; CD154 is equivalent to CD40L
- Positive staining - normal: endothelium; basement membrane of Bowman's membrane and tonsillar epithelium (CDw145 Worksheet Panel report-broken link)
CD146
- Aka melanoma cell adhesion molecule (MEL-CAM), cell surface glycoprotein MUC18
- May be a neural crest cell adhesion molecule during embryogenesis
- Associated with tumor progression and the development of metastasis in human malignant melanoma
- Sensitive but nonspecific marker of desmoplastic/spindle cell melanoma; use if suggestive histology, S100 positive, melanoma markers otherwise negative (Am J Surg Pathol 2001;25:58)
- Interpretation: membranous staining
- Positive staining - normal: vascular smooth muscle, endothelium, intermediate trophoblast in exaggerated placental sites and placental site trophoblastic tumors (Hum Pathol 1999;30:687), subpopulation of T cells, endothelium, smooth muscle, Schwann cells
- Positive staining - malignant
- Clear cell sarcoma (90%)
- Leiomyosarcomas (almost all)
- Melanoma (desmoplastic-84%, epithelioid melanomas-100%, advanced primary tumors and metastatic tumors)
- Melanotic schwannoma (100%)
- MPNST (27%), neurofibroma (40%)
- Prostatic adenocarcinoma and high grade PIN
- Squamous cell carcinomas (some)
- Vascular sarcomas (almost all)
- Negative staining: normal melanocytes, melanocytic nevi, cellular blue nevus, thin primary melanomas, placental site nodules (or focal), epithelioid trophoblastic tumors (or focal), cytotrophoblast, atypical fibroxanthoma
CD147
CD148
CD149
- CDw149 antibodies actually recognize a subset of CD47, also known as integrin-associated protein (IAP), present on leukocytes but not erythrocytes (Tissue Antigens 2000 ;56:258)
CD15
Table of Contents
Definition / general | Clinical features | Uses by pathologists | Case reports | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- A carbohydrate (not a protein) widely used for diagnosis of Hodgkin lymphoma
- Also known as LeuM1, Lewis X, 3-fucosyl-N-acetyl-lactosamine
- Mediates phagocytosis and chemotaxis
- Synthesis is directed by FUT4 (OMIM #104230) in lymphoid cells and mature granulocytes, and by FUT9 (OMIM #606865) in promyelocytes and monocytes
- References: Quality control for CD15
Clinical features
- Poor prognostic marker in acute promyelocytic leukemia (Leuk Res 2014;38:194)
- May be useful to differentiate recent antemortem from postmortem injuries (Int J Legal Med 2013;127:957)
- Helps differentiate pulmonary adenocarcinoma (CD15+) from mesothelioma (CD15-), although other markers are more specific
- May help define neural stem cells (Stem Cells 2009;27:2928)
Uses by pathologists
- Hodgkin lymphoma: membranous, diffuse cytoplasmic or Golgi staining of Reed-Sternberg cells; CD15 staining is used to confirm diagnosis, or to differentiate Hodgkin lymphoma (CD15+) from anaplastic large cell lymphoma (usually CD15-)
- Granulocyte marker
Case reports
- 64 year old woman with CD15+ pre-B ALL (Arch Pathol Lab Med 2001;125:1227)
Microscopic (histologic) images
Positive staining - normal
- Myeloid cells and eosinophils; activated B and T cells (including infectious mononucleosis); variable monocytes and basophils
- Kidney proximal convoluted tubules; small intestine Paneth cells (J Clin Pathol 1996;49:474)
Positive staining - disease
- Hodgkin lymphoma: Reed-Sternberg cells in classic and follicular Hodgkin lymphoma (Am J Clin Pathol 2002;117:29)
- 50% of carcinomas, including some colorectal carcinomas (Korean J Pathol 2013;47:340), ovarian / peritoneal serous tumors (Am J Surg Pathol 1998;22:1203), renal cell carcinomas
- 15% of peripheral T cell lymphoma (Am J Surg Pathol 2003;27:1513, Int J Oncol 2003;22:319)
- 5% of B cell lymphomas, including some B-CLL and pre-pre B ALL (Am J Clin Pathol 2002;117:380, Arch Pathol Lab Med 2001;125:1227)
- Some AML, particularly AML-M4 / M5 (flow cytometry is more sensitive than immunohistochemistry), some granulocytic sarcomas (Histopathology 1999;34:391), some histiocytic sarcomas
- Occasionally anaplastic large cell lymphoma (Am J Clin Pathol 2003;119:205, but usually negative, Am J Surg Pathol 2006;30:223)
- Note: EBV infections can have Reed-Sternberg-like cells that are focally CD15+ (Am J Surg Pathol 2010;34:1715, Am J Surg Pathol 2010;34:405)
Negative staining
- Non-activated lymphocytes; erythroid cells, histiocytes (usually), osteoblasts and platelets
- LP/L&H cells in nodular lymphocyte predominant Hodgkin lymphoma
- Diffuse large B cell lymphoma, hairy cell leukemia, post-transplant lymphoproliferative disorders and systemic mastocytosis (Hum Pathol 2001;32:545)
- Langerhans cell histiocytosis, mesothelioma at various sites (usually, Hum Pathol 2001;32:529)
CD150-159
Table of Contents
CD150 | CD151 | CD152 | CD153 | CD154 | CD155 | CD156a | CD156b | CD156c | CD157 | CD158 | CD158a | CD158b | CD159a | CD159cCD150
- Also known as signal lymphocyte activation molecule (SLAM)
- Costimulatory molecule on B lymphocytes and dendritic cells
- Positive staining - normal: thymocytes, CD45RO positive subpopulation of T cells, B cells, dendritic cells, endothelium
CD151
CD152
- Also known as cytotoxic T lymphocyte associated protein 4, CTLA4
- Negative regulator of T cell activation
- CTLA4 restriction fragment length polymorphisms are linked to various autoimmune disorders
- Shares sequence homology with CD28; also shares ligands CD80 and CD86 with CD28
- Positive staining - normal: activated but not resting T cells, activated B cells
- Reference: OMIM CD152
CD154
- Also known as CD40 ligand, CD40L, TNF related activation protein (TRAP)
- Regulates B cell function by engaging CD40
- Defective gene prevents immunoglobulin class switch and is associated with hyper IgM syndrome, autoimmune hematologic disorders, disorganized nodal follicular architecture and PAS positive plasmacytoid cells containing IgM, lymph nodes without germinal centers, shortened lifespan, often with gastrointestinal cancers (cholangiocarcinoma, hepatocellular carcinoma and adenocarcinoma) and Cryptosporidium parvum infection
- Positive staining - normal: T cells
CD155
CD156a
CD156b
CD156c
- Also known as ADAM10
- Protein belonging to a superfamily of metalloproteases (Anal Cell Pathol (Amst) 2015;2015:975436)
CD157
CD158
- Member of KIR (killer cell immunoglobulin like receptor) family, also called killer cell inhibitory receptors
- Binding by HLA class I molecules causes inhibition of NK or T cell cytotoxic activity
- Melanoma specific cytotoxic T lymphocytes may express KIR and regulate their ability to kill these tumors
- Terminology:
- CD158c: KIR2DS6 / KIRX
- CD158d: KIR2DL4
- CD158e1: KIR3DL1 / p70
- CD158e2: KIR3DS1 / p70
- CD158f: KIR2DL5 (Front Immunol 2017;7:698)
- CD158g: KIR2DS5
- CD158h: KIR2DS1 / p50.1
- CD158i: KIR2DS4 / p50.3
- CD158j: KIR2DS2 / p50.2
- CD158k: KIR3DL2 / p140
- CD158z: KIR3DL7 / KIRC1
- Positive staining - normal: natural killer cells (NK cells), some T cells
CD158a
CD158b
CD159a
CD159c
- Plays a role as a receptor for the recognition of MHC class I HLA-E molecules by natural killer cells and some cytotoxic T cells (Front Immunol 2018;9:686)
- Also known as NKG2C, KLRC2
- Positive staining - normal: natural killer cells and CD8+ T cells
CD160-169
Table of Contents
CD160 | CD161 | CD162 | CD163 | CD164 | CD165 | CD166 | CD167 | CD168 | CD169 | Microscopic (histologic) imagesCD160
- Aka BY55
- Expression tightly associated with peripheral blood NK cells and CD8+ T lymphocytes with cytolytic effector activity
- Positive staining - normal: circulating NK (CD56 dim, CD116+) and T cells, spleen, small intestinal intraepithelial lymphocytes
CD161
CD162
- Aka P-Selectin Glycoprotein Ligand 1 (PSGL-1)
- Important in adhesive interactions between circulating leukocytes and platelets and endothelial cells
- Mediates rolling on activated endothelium or activated platelets (which express P selectin / CD62P) and other leukocytes at inflammatory sites
- Site of binding of human granulocyte ehrlichiosis bacteria
- Positive staining - normal: myeloid cells, stimulated T cells
- CD162R:
- Aka PEN5
- Positive staining - normal: NK cells
CD163
- Hemoglobin / haptoglobin scavenger receptor
- Soluble form attenuates immune response
- Positive staining - normal: monocytes / macrophages
- Positive staining - disease: histiocytic sarcoma (Diagn Pathol 2007;2:7)
CD164
- Aka MUC-24, sialomucin
- Mucin-like cell surface glycoprotein that facilitates adhesion of CD34+ cells
- Regulates hematopoietic cell proliferation
- Positive staining - normal: small and large bowel epithelia; lung, thyroid epithelia
- Positive staining - disease: colorectal carcinoma, pancreatic adenocarcinoma
CD165
CD166
CD167
- Aka Discoidin Domain Receptor 1 (DDR1)
- Has homologous region to the Dicytostelium discoideum protein discoidin I in extracellular domain
- Tyrosine kinase receptor, may be important in cytoskeletal organization and the ability to align with other cells during aggregation
- Receptor tyrosine kinases help cells communicate with their microenvironment and regulate cell growth, differentiation and metabolism
- Activated by collagen types I - V, VIII
- May have a role in tumor invasion and metastasis
- Positive staining - normal: epithelial cells (breast, kidney, lung, GI, brain)
- Positive staining - disease: carcinomas (various)
CD168
CD169
- Aka sialoadhesin
- Macrophage restricted cellular interaction molecule that binds sialylated ligands
- Highly expressed on macrophages in chronically inflamed tissues, such as rheumatoid synovium and atherosclerotic plaques
- Positive staining - normal: macrophages (all sites but microglia)
- Negative staining: microglia
Microscopic (histologic) images
CD170-179
CD170
- Aka Sialic acid binding IG-like Lectin 5 (SIGLEC5)
- May function in cell-cell interaction
- Positive staining - normal: neutrophils
CD171
- Aka L1
- Adhesion molecule required for normal neurohistogenesis
- Mutations cause CRASH (Corpus callosum hypoplasia / agenesis, Retardation, Aphasia, Spastic paraplegia / shuffling gait and Hydrocephalus due to stenosis of aqueduct of Sylvius), an X linked neurologic disorder
- May mediate kidney branching morphogenesis, maintenance of lymph node architecture during immune response, costimulation of T cell activation in vitro
- Positive staining - normal: postmitotic neurons, glia, epithelial cells (some), lymphoid cells (some), myeloid (some), monocytes
CD173
CD174
CD175
- CD175:
- Aka Tn
- Simple mucin type carbohydrate antigen produced in the initial steps of mucin biosynthetic pathway, due to aberrant or incomplete glycosylation of mucins
- CD175s:
- Aka Sialyl Tn (STN)
- Carbohydrate associated with apomucins MUC1, MUC2; produced in the initial steps of mucin biosynthetic pathway
- Presence associated with aggressive tumors
- High pre-operative serum levels predict liver metastasis and poor prognosis after resection for gastric cancer
- Definitive Phase III trial of STN vaccine in metastatic breast cancer patients began 2001
- Positive staining - disease: carcinoma
CD176
CD177
CD178
- Aka CD95 ligand, Fas ligand (FasL)
- Important role in T cell mediated cytotoxicity; induces apoptosis in Fas expressing target cells
- Cells in immune privileged sites (testis, anterior chamber of eye, placenta) constitutively express FasL, which induces apoptosis in Fas expressing infiltrating T cells, minimizing inflammatory responses that might damage important physiologic functions at these sites
- May influence interaction of tumor cells with host immune system; theory is that FasL+ tumor cells induce apoptosis in infiltrating Fas+ mononuclear cells
- Fas-FasL binding triggers apoptosis in lymphocytes
- Mutations may be related to some cases of Systemic Lupus Erythematosis (SLE)
- Processed by metalloproteases which cause shedding of extracellular portion into blood (sFas L)
- Positive staining - normal: activated and cytotoxic T cells, testis, anterior chamber of eye, placenta; also Sertoli cells, neurons, thyroid epithelial cells
- Positive staining - tumors: Reed-Sternberg cells of Hodgkin’s lymphoma (nodular sclerosis and mixed cellularity) (Am J Surg Pathol 2001;25:388)
CD179
- CD179a:
- Aka VpreB1
- Associates noncovalently with CD179b to form surrogate light chain as component of preB cell receptor, which plays a critical role in early B cell differentiation
- CD179b:
- Aka lambda-5
- Associates noncovalently with CD179a to form surrogate light chain as component of preB cell receptor, which plays a critical role in early B cell differentiation
- Mutations impair B cell development and cause agammaglobulinemia
- Positive staining - normal: preB cells
CD180-189
Table of Contents
CD180 | CD181 | CD182 | CD183 | CD184 | CD185 | CD186 | CD187 | CD188 | CD189 | Diagrams / tables | Microscopic (histologic) imagesCD180
- Also called RP105
- Regulates B cell recognition of lipopolysaccharide, a membrane constituent of gram-negative bacteria
- Positive staining - normal: mantle zone and marginal zone B cells (strong), other B cells (weak/negative); peripheral blood monocytes, dendritic cells
CD181
- Also called CXCR1, IL8Ralpha; previously called CDw128A
- Chemokine receptor, powerful neutrophil chemotactic factor
- Positive staining - normal: neutrophils, basophils, T cell subset, monocytes, keratinocytes
- Positive staining - disease: T cells in allergic rhinitis (J Immunol 2004;172:268)
CD182
- Also called CXCR2; formerly called CD128b
- Interleukin 8 receptor beta subunit (IL8RB); binds multiple CXC chemokines including IL-8 (CXCL8)
- Chemokine receptor, powerful neutrophil chemotactic factor, particularly to sites of inflammation
- Interpretation: cytoplasmic staining
- Uses by pathologists: no significant uses by pathologists
- Positive staining - normal: mature granulocytes, keratinocytes, neuroendocrine cells, projection neurons (Arch Pathol Lab Med 2000;124:520)
- Positive staining - disease: carcinoid tumor (classic, atypical, metastatic), pituitary adenoma, pheochromocytoma, medullary carcinoma
- Negative staining: parathyroid cells; small cell carcinoma of lung / cervix, large cell lung neuroendocrine carcinoma, Merkel cell carcinoma, neuroblastoma, melanoma
CD183
- Also called CXCR3
- Receptor for some chemokines; binding of chemokines to CD183 induces integrin activation, cytoskeletal changes and chemotactic migration in inflammation-associated effector T cells
- CD183+ T cells detected in inflamed tissues of patients with juvenile rheumatoid arthritis, multiple sclerosis, sarcoidosis, hepatitis C
- Positive staining - normal: T cells in inflamed tissue, eosinophils, plasmacytoid dendritic cells, hematopoietic progenitors
- Negative staining: naïve T cells in peripheral blood
CD184
- Also called CXCR4, Stromal cell Derived Factor 1 (SDF1)
- Receptor for the CXC chemokine SDF-1
- Also major HIV/SIV co-receptor (with CCR5/CD195)
- Involved in B cell development, myelopoiesis, cardiac ventricular septum formation, blood vessel formation in GI tract, cerebellar granular cell development
- Positive staining - normal: all mature blood cells, blood progenitor cells, endothelial and epithelial cells, astrocytes, neurons
CD185
- Multipass membrane protein of CXC chemokine receptor family
- Also called CXCR5, BLR1 (Burkitt lymphoma receptor 1)
- Pathophysiology:
- Binds to B Lymphocyte Chemoattractant (BLC / CXCL13) (J Exp Med 1998;187:655)
- Involved in B cell migration into B cell follicles of spleen and Peyer patches (J Immunol 2009;182:2610)
- Critical for function of follicular helper T (TFH) cells
- May have role in survival and maintainance of cardiac structure upon pressure overload by regulating proteoglycans essential for correct collagen assembly (PLoS One 2011;6:e18668)
- May be important for ectopic mucosa associated lymphoid tissue neogenesis in chronic Helicobacter pylori induced inflammation (J Mol Med (Berl) 2010;88:1169)
- During HIV1 infection, altered expression of CXCR5 / CXCL13 may cause B cell dysfunction (Blood 2008;112:4401)
- Upregulated in rheumatoid arthritis synovial tissue and expressed in various cell types (Arthritis Res Ther 2005;7:R217)
- Interpretation: cytoplasmic staining
- Uses by pathologists: no significant uses by pathologists
- Positive staining - normal: mature B cells
- Positive staining - disease: Burkitt's lymphoma, mantle cell lymphoma; AIDS-related non-Hodgkin lymphoma (Blood 2009;113:4604, AIDS Res Treat 2010;2010:164586)
Microscopic (histologic) images
CD19
Table of Contents
Definition / general | Pathophysiology | Diagrams / tables | Clinical features | Uses by pathologists | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Common B cell marker (also CD20, CD79a, PAX5)
- Expressed by B cells and follicular dendritic cells
- Early B lineage-restricted antigen present on most pre-B cells, B-ALL and B-CLL cells (OMIM #107265)
Pathophysiology
- Forms a complex with CD21, CD81 and CD225 in the membrane of mature B cells
- Regulates B cell development, activation and differentiation (J Immunol 2003;171:5921)
- May define intrinsic and antigen receptor-induced signaling thresholds critical for clonal expansion of the B cell pool and humoral immunity (Curr Dir Autoimmun 2005;8:55, Science 1992;256:105, Exp Hematol Oncol 2012;1:36)
Clinical features
- Defects in CD19 cause immunodeficiency common variable type 3 (OMIM #613493), characterized by antibody deficiency, hypogammaglobulinemia, recurrent bacterial infections and an inability to mount an antibody response to antigen
- CD19 count may be useful to screen for B cell lymphoproliferative disorders (Clin Chem Lab Med 2011;49:115)
- Adoptive transfer of anti-CD19-chimeric antigen receptor-expressing T cells may be effective for B cell malignancies (Blood 2010;116:4099, Sci Transl Med 2013;5:177, Blood 2013;122:4129)
Uses by pathologists
- Detection of B cells
- Diagnosis of B disorders
- May be more sensitive than CD20 in detecting B cell acute leukemias (Zhongguo Shi Yan Xue Ye Xue Za Zhi 2005;13:943)
Positive staining - normal
- Pre-B cells, B cells; follicular dendritic cells
- Hematogones in bone marrow by flow cytometry
Positive staining - disease
- B cell lymphomas and leukemias, but often weak / negative in follicular lymphoma or diffuse large B cell lymphoma (Histopathology 2006;48:239, Cytometry B Clin Cytom 2005;63:28)
- Occasionally myeloid leukemias (AML - Am J Clin Pathol 1998;109:211, AML with t(8;21) - Oncogene 2010;29:2927, AML-M0 - Am J Clin Pathol 2001;115:876, CML blast phase - Am J Clin Pathol 2004;121:836)
- Occasionally anaplastic large cell lymphoma by flow cytometry (Am J Clin Pathol 2003;119:205)
- Rarely T cell lymphoma (Cytometry B Clin Cytom 2009;76:142, Case Rep Hematol. 2013;2013:183134)
Negative staining
- Plasma cells, basophils, mast cells
- Myeloma (Am J Clin Pathol 2004;121:482, Am J Clin Pathol 2012;137:377), most T cell lymphomas
- Often L&H cells in lymphocyte predominant Hodgkin lymphoma, often post-transplant B cell lymphoproliferative disorder
CD1a
Table of Contents
Definition / general | Clinical features | Uses by pathologists | Microscopic (histologic) images | Cytology images | Positive staining - normal | Positive staining - not malignant | Positive staining - tumors | Negative staining | Electron microscopy imagesDefinition / general
- T cell surface antigen (gene on #1q22-23, not MHC linked)
- CD1a+ T cells are normal component of T cell repertoire (Nat Immunol 2010;11:1102), important in dendritic cell presentation of glycolipids and lipopeptide antigens, particularly those that traffic through early endocytic and recycling pathways (J Immunol 2010;184:1235)
- Also called Leu6
- Activin A, a TGFβ family member induced by pro-inflammatory cytokines and involved in skin morphogenesis and wound healing, induces the differentiation of human monocytes into Langerhans cells in absence of TGFβ (PLoS One 2008;3:e3271)
Clinical features
- May identify myeloid dendritic cells that produce IL12 and Th1 CD4+ T cell polarization (Clin Exp Immunol 2009;155:523)
- May activate intrathyroidal T cells in Hashimoto thyroiditis and Grave disease (J Immunol 2005;174:3773)
- CD1A and CD1E polymorphisms contribute to polygenic susceptibility to multiple sclerosis (Int J Immunopathol Pharmacol 2011;24:175)
Uses by pathologists
- Interpretation: membranous staining
- Used to diagnose Langerhans cell histiocytosis and to exclude other entities that are CD1a negative
- Used to identify Langerhans cells in inflammatory or neoplastic disorders (Am J Dermatopathol 2009;31:527, Appl Immunohistochem Mol Morphol 2011;19:239, Colorectal Dis 2011;13:768)
Microscopic (histologic) images
Positive staining - normal
- Cortical thymocytes
- Immature dendritic cells (Langerin-, CD86-, HLA-DR low, CD40 low)
- Indeterminate cells (resemble Langerhans cells but no Birbeck granules on EM)
- Langerhans cells (Langerin+, CD86+)
Positive staining - not malignant
- Actinic cheilitis exhibiting epithelial dysplasia (J Mol Histol 2010;41:357)
- Barretts metaplasia of esophagus (Br J Cancer 2005;92:888)
- Dendritic cells in dermis / epidermis of benign inflammatory skin disorders including pseudolymphomatous folliculitis (Am J Surg Pathol 1999;23:1313)
- Periodontitis (gingiva, Oral Dis 2012;18:778, but see Indian J Dent Res 2010;21:396
- Primary biliary cirrhosis (up to 79%, Am J Surg Pathol 2012;36:732)
- Psoriasis (J Cutan Pathol 1995;22:223)
- Sickle cell anemia-monocytes (Hum Immunol 2004;65:1370)
- Spongiotic dermatitis and lichen planus (Arch Dermatol Res 2002;294:297)
Positive staining - tumors
- Langerhans cell histiocytosis (fairly specific)
- Cutaneous T cell lymphoma
- Myeloid leukemia
- Mycosis fungoides (variable)
- Papillary thyroid carcinoma (FNA, Cancer Cytopathol 2013;121:206)
- T-ALL (Am J Clin Pathol 2002;117:252)
- Thymoma (Histopathology 2002;40:152)
Negative staining
- B cells, follicular dendritic cells
- Dendritic cells in most cutaneous B cell lymphomas (or weak staining, Am J Clin Pathol 2001;116:72), dendritic cell neurofibroma, Erdheim-Chester disease, follicular dendritic cell tumor, histiocytic lymphoma / sarcoma, histiocytoma, interdigitating dendritic cell sarcoma, juvenile xanthogranuloma, sinus histiocytosis with massive lymphadenopathy
- PECOmas: CD1a negative, but may show aberrant cytoplasmic staining due to endogenous biotin (Hum Pathol 2011;42:369); prior report of CD1a+ PEComas at Pathol Int 2008;58:169
Electron microscopy images
CD20
Table of Contents
Definition / general | Essential features | Pathophysiology | Clinical features | Uses by pathologists | Case reports | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Flow cytometry description | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
Essential features
- Widely used B cell marker (also CD19, CD79a, PAX5)
- Retained on mature B cells until plasma cell differentiation
- Anti-CD20 therapy (e.g., rituximab) is available for treatment of non-Hodgkin B cell lymphoma and autoimmune diseases
Pathophysiology
- 33kd phosphoprotein with 3 hydrophobic regions that traverse the cell membrane, creating a structure similar to an ion channel that allows for the influx of calcium required for cell activation
- Initially expressed on B cells after CD19 / CD10 expression and before CD21 / CD22 and surface immunoglobulin expression; retained on mature B cells until plasma cell differentiation
- Delivers early signal in B cell activation
- FMC7 detects a conformational epitope on the CD20 molecule with probable cholesterol dependency (Cytometry 2001;46:98, Leukemia 2003;17:1384)
Clinical features
- Rituximab is a chimeric murine / human anti-CD20 antibody used to treat B cell lymphomas; treatment may cause selection of CD20 negative (but CD79a positive) tumor subclones (Am J Surg Pathol 2005;29:1399, Ann Hematol 2020;99:2141)
- Changes in morphology and CD20 expression after rituximab therapy vary widely (Am J Surg Pathol 2013;37:563, Ann Hematol 2020;99:2141)
- Rituximab is also used to treat autoimmune disorders, thrombotic thrombocytopenic purpura / hemolytic uremia syndrome (TTP / HUS), ABO incompatible transplantation and transplant rejection (Clin Immunol 2005;117:207, J Clin Aesthet Dermatol 2013;6:45, Ther Adv Neurol Disord 2018;11:1756286418773025, Neurology 2018;90:e1805, Clin Transplant 2005;19:423, Blood Transfus 2010;8:203, Animal Model Exp Med 2019;2:76, Transplant Proc 2005;37:1205, Int Rev Immunol 2019;38:118, Clin Transplant 2005;19:137, Clin J Am Soc Nephrol 2020;15:430, Am J Transplant 2018;18:927)
- Radioimmunotherapy with rituximab may be effective for follicular lymphoma and as myeloablative therapy followed by autologous stem cell support for relapsed / refractory B cell lymphoma (Clin Dev Immunol 2013;2013:875343, Oncotarget 2013;4:899)
- Dim CD20 expression on IgG4 plasma cells in IgG4 related lymphadenopathy may explain efficacy of rituximab in IgG4 related disease (Arch Pathol Lab Med 2013;137:1282, Eur J Intern Med 2020;74:92)
- Further anti-CD20 antibodies are ocrelizumab (mainly used in therapy of multiple sclerosis), ofatumumab (in use for relapsed CLL and multiple sclerosis) and obinutuzumab (in use for relapsed or refractory follicular lymphoma and advanced CLL) (Ther Adv Neurol Disord 2018;11:1756286418773025, N Engl J Med 2014;371:213, Neurology 2018;90:e1805, N Engl J Med 2017;377:1331, N Engl J Med 2019;380:2225)
- CD20 antigen may be expressed by reactive or lymphomatous cells of transformed mycosis fungoides as well as in other T cell lymphomas (see Positive staining - disease) (Am J Surg Pathol 2013;37:1845, Am J Dermatopathol 2013;35:833)
- CD20 mutation rarely causes common variable immunodeficiency 5 (OMIM: Membrane-Spanning 4 Domains, Subfamily A, Member 1; MS4A1 [Accessed 20 September 2021])
- Double hit lymphomas show reduced CD20 expression by flow cytometry (Am J Clin Pathol 2010;134:258)
Uses by pathologists
- Commonly used B cell marker used in the workup of benign and malignant processes
Case reports
- 21 year old man with nodular lymphocyte predominant Hodgkin lymphoma with large atypical cells (Case #284)
Microscopic (histologic) images
Contributed by Leonie Frauenfeld, M.D., Andrey Bychkov, M.D., Ph.D. and Kaveh Naemi, D.O.
Cases #101, 118, 127, 130, 284 and AFIP images
Positive staining - normal
- Most B cells (considered a pan-B cell antigen), also follicular dendritic cells
- Hematogones can be CD20+ (acquire CD20 during maturation) and a panel is useful in distinguishing them from leukemia cells (Am J Clin Pathol 2000;114:66, Blood 2001;98:2498)
Positive staining - disease
- 90% of B cell lymphomas, although B cell lymphomas are CD20 negative after rituximab and other B cell markers (CD19, CD79a, PAX5) should be used (Am J Clin Pathol 2006;126:534, Biomark Res 2017;5:5, Ann Hematol 2020;99:2141)
- 40% of pre-B acute lymphoblastic leukemia / lymphoblastic lymphoma (ALL / LBL) (Hematology Am Soc Hematol Educ Program 2018;2018:9)
- Also spindle cell thymomas (Am J Surg Pathol 1992;16:988, Diagn Pathol 2007;2:13)
- 80% of nodular lymphocyte predominant Hodgkin lymphoma, 20% of classic Hodgkin lymphoma (may be an adverse prognostic factor) (Br J Haematol 2004;125:701, PLoS One 2009;4:e6341, Br J Haematol 2019;184:45)
- Dimly expressed in T cells (benign and neoplastic, particularly in bone marrow), some myelomas (especially multiple myeloma with lymphoplasmacytoid morphology) and occasionally acute myelogenous leukemia (Am J Surg Pathol 2008;32:1593, Am J Clin Pathol 1996;106:78, Am J Clin Pathol 1994;102:483, Mod Pathol 2004;17:1217, Blood 2003;102:1070, Leuk Lymphoma 2016;57:335, Am J Clin Pathol 2013;140:519, Virchows Arch 2020;476:337)
- Certain T cell lymphomas such as MEITL have a 20% positivity rate for CD20 (Pathology 2020;52:128)
Negative staining
- Nonhematopoietic cells, most T cells, basophils, plasma cells and mast cells
- Note: staining does not work well with Bouin fixative
Flow cytometry description
- CD20 can be evaluated by flow cytometric immunophenotyping as well as immunohistochemical stains
- Dim or bright CD20 expression can provide clues to diagnoses
- Brighter expression in follicular lymphomas than normal B cells (Am J Clin Pathol 2005;124:576)
- In chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL), CD20 expression may be dim to negative
Sample pathology report
- Lymph node, excision:
- Diffuse large B cell lymphoma (DLBCL)
- Comment: Lymph node presents with effaced architecture and demonstrates a dense, sheet-like proliferation of immunoblastic cells with strong, homogeneous CD20 positivity. Additionally, the cells mark positive for CD10 and BCL6 but are negative for MUM1, according to a germinal center type DLBCL (Hans algorithm). The cells are positive for BCL2 and weakly positive for MYC (20%).
Board review style question #1
Board review style answer #1
Board review style question #2
CD20 is the target of monoclonal antibodies used in the therapy against
- Anaplastic large cell lymphoma
- Mycosis fungoides
- Rheumatoid arthritis
- T cell large granular lymphocytic leukemia (T-LGL)
Board review style answer #2
CD20-29
Table of Contents
CD20 | CD21 | CD22 | CD23 | CD24 | CD25 | CD26 | CD27 | CD28 | CD29 | Diagrams / tables | Microscopic (histologic) imagesCD20
- See CD20
CD21
- See CD21
CD22
- Pan B cell marker helpful for diagnosis of hairy cell leukemia
- Also called B lymphocyte cell adhesion molecule (BL-CAM), Sialic acid binding immunoglobulin-like lectin / Siglec-2
- Pathophysiology:
- Inhibits B cell receptor signaling via alpha 2,6 sialic acid ligand binding activity (Front Immunol 2012;2:96); also binds CD45 and has adhesion properties of a lectin (J Exp Med 2002;195:1207)
- May localize B cells in lymphoid tissues
- Ligand is CD75
- CD22 internalizes within the cell and recycles (Traffic 2014;15:255)
- Clinical features:
- Shows variability in flow cytometry expression between specimens from same patient, may be due to delayed processing (Am J Clin Pathol 2002;117:615, Cytometry B Clin Cytom 2011;80:83)
- Leukemic cells from infants with newly diagnosed preB leukemia may express CD22 with exon 12 deletion (Proc Natl Acad Sci U S A 2010;107:16852)
- Epratuzumab and other anti-CD22 antibodies may have therapeutic value as part of radioimmunotherapy
- Non-Hodgkin lymphoma (J Clin Oncol 2010;28:3709, Blood 2011;118:4053), including relapsed / resistant hairy cell leukemia (J Clin Oncol 2012;30:1822)
- ALL (Cancer 2013;119:2728, Lancet Oncol 2012;13:403)
- SLE and other autoimmune diseases (Blood 2013;122:3020)
- CD22 may be a component of immunotoxins (Eur J Immunol 2012;42:2792)
- Uses by pathologists:
- Pan B cell marker; helpful for diagnosis of hairy cell leukemia
- Aberrant CD22 expression is useful to detect monoclonal B cells of CLL admixed with benign polyclonal B cells (Am J Clin Pathol 2005;123:826)
- Positive staining - normal: B cells (considered a pan B cell antigen), dendritic cells and basophils
- Positive staining - disease:
- Hairy cell leukemia; also pre B ALL
- Blastic plasmacytoid dendritic cell neoplasm (Cytometry B Clin Cytom 2009;76:237)
- Staining of other B cell leukemias / lymphomas is variable (Am J Clin Pathol 2002;117:615)
- Negative staining:
- Myeloblasts, plasma cells
- Lung carcinoma (Cancer Res 2014;74:263, Cancer Res 2012;72:5556)
- Reference: OMIM: 107266 [Accessed 7 May 2021]
CD23
- See CD23
CD24
- Glycosylphosphatidylinositol anchor protein involved in cell adhesion and tumor metastasis
- Putative cancer stem cell marker
- Also called heat stable antigen homologue (HAS)
- Pathophysiology: small glycosylphosphatidylinositol anchor protein with mucin-like adhesion properties; promotes antigen dependent proliferation of B cells and prevents differentiation into plasma cells
- Clinical features:
- Ligand of P selectin on tumor cells that is associated with in vitro invasiveness and metastasis (Tumour Biol 2002;23:139, Cancer Res 2005;65:10783)
- Expressed in many solid tumors, promotes tumor growth,invasion and metastasis and confers resistance to some chemotherapeutic drugs (Eur Rev Med Pharmacol Sci 2013;17:1709)
- Marker of disseminated tumor cells in malignant pleural effusions (Int J Cancer 2013;133:2925)
- Breast cancer cells with CD44+ / CD24- phenotype are associated with:
- Stem cell properties (Mod Pathol 2012;25:185)
- Poor prognosis in triple negative (Hum Pathol 2012;43:364)
- Other breast tumors (Oncol Rep 2014;31:1127)
- Cancer stem cells: cells within tumor that possesses the capacity to self-renew and to cause the heterogeneous lineages of cancer cells that comprise the tumor
- Cancer stem cell hypothesis: a small subpopulation of cancer cells drives tumor initiation, growth and metastasis (Oncol Rep 2014;31:1127)
- Alleles / polymorphisms associated with autoimmune disease risk / progression, including:
- Inflammatory bowel disease (Int J Biol Markers 2014;29:e62)
- Multiple sclerosis (Proc Natl Acad Sci USA 2003;100:15041, Am J Transl Res 2012;4:347)
- CD24 polymorphism may serve as poor prognostic marker in esophageal cancer (Int J Biol Markers 2014;29:49)
- Uses by pathologists:
- Strong expression is a poor prognostic factor in carcinomas of:
- Bile duct (Cancer Lett 2006;235:34)
- Bladder (Oncol Lett 2013;6:96)
- Breast (with CD44) (Breast Cancer Res Treat 2012;133:979, PLoS One 2012;7:e43110)
- Colorectum (Clin Cancer Res 2005;11:6574)
- Gallbladder (Med Oncol 2012;29:1879)
- Liver (Clin Cancer Res 2009;15:5518)
- Lung: nonsmall (Br J Cancer 2003;88:231)
- Ovary (Am J Pathol 2002;161:1215)
- Pancreas (Pancreas 2014;43:380)
- Poor prognostic marker in glioma, osteosarcoma (J Biomed Biotechnol 2012;2012:517172, Clin Transl Oncol 2013;15:541)
- Strong expression is a poor prognostic factor in carcinomas of:
- Positive staining - normal:
- All B cells, granulocytes
- Also apocrine sweat glands, epithelial cells, fallopian tube, kidney cells, muscle, nucleus pulposus of intervertebral discs and some neurons (Proc Natl Acad Sci U S A 2006;103:6374)
- Positive staining - disease:
- Apocrine metaplasia of breast, exosomes (membrane vesicles 40 - 100 nm released by different cell types from a late endosomal cellular compartment) (Mol Oncol 2009;3:220, J Transl Med 2011;9:86)
- Most pre-B-ALL / lymphoblastic lymphoma, virtually all B cell lymphomas
- Breast cancer: ductal type has cytoplasmic expression, invasive micropapillary has strong expression with typical inverted apical membrane pattern (Breast 2012;21:165)
- Chordoma (Biochem Biophys Res Commun 2005;338:1890)
- Various solid carcinomas (Pathol Res Pract 2005;201:479)
- Biliary tract dysplasia / carcinoma (Hum Pathol 2010;41:1558)
- Lung cancer (J Clin Pathol 2013;66:256)
- Pancreatic ductal carcinoma and IPMN (Hum Pathol 2010;41:1466)
- Pleomorphic adenoma (salivary gland) (Histopathology 2013;62:1075)
- Wilm tumor (Hum Pathol 1990;21:536)
- Negative staining: plasma cells, T cells, monocytes, mast cells, red blood cells, platelets; also ovarian epithelium, multiple myeloma and chondrosarcoma
- Reference: OMIM: 600074 [Accessed 7 May 2021]
CD25
- Marker for hairy cell leukemia and systemic mastocytosis
- Also called IL-2 receptor alpha chain, IL2RA and TAC antigen (OMIM: 147730 [Accessed 7 May 2021])
- Pathophysiology:
- Exists in at least 3 forms: a high affinity dimer, an intermediate affinity monomer (beta subunit) and a low affinity monomer (alpha subunit)
- Considered an activation antigen (also CD30)
- CD4+ CD25+ cells are regulatory T cells (Treg) that (Cancer Res 2012;72:2162):
- Suppress the activation of self reactive T cells and prevent autoimmunity
- May prevent cytotoxic T cells from killing tumor cells (J Hepatol 2006;45:254, Zhongguo Shi Yan Xue Ye Xue Za Zhi 2006;14:119)
- CD4+ CD25+ cells also suppress NK cells (Proc Natl Acad Sci USA 2006;103;5460, J Immunol 2006;176:1582)
- May act directly on B cells (Blood 2006;107:3925)
- Clinical features:
- High levels of Treg by flow cytometry are associated with advanced stage in esophageal and gastric cancer (Cancer Immunol Immunother 2006;55:1064, Oncol Lett 2012;4:755)
- CD25 expression in advanced cutaneous T cell lymphoma associated with response to denileukin diftitox therapy, a recombinant fusion protein of diphtheria toxin and IL-2, which binds to CD25 (J Invest Dermatol 2006;126:575, Leuk Lymphoma 2013;54:69)
- Uses by pathologists:
- Marker for hairy cell leukemia but CD103 and CD123 may be more useful (Am J Clin Pathol 2011;136:625)
- Loss of CD25 distinguishes hairy cell leukemia from variant hairy cell leukemia or other disorders (Am J Clin Pathol 2009;131:586)
- Diagnose systemic mastocytosis (Mod Pathol 2012;25:516)
- Also specific in GI mucosal mast cells (Am J Surg Pathol 2007;31:1669)
- CD25+ cutaneous mast cells in urticaria pigmentosa may predict subsequent systemic mastocytosis (Am J Surg Pathol 2008;32:139)
- Part of diagnostic criteria for hemophagocytic lymphohistiocytosis is soluble CD25 / IL2 receptor ≥ 2,400 U/ml (Pediatr Blood Cancer 2007;48:124)
- Marker for hairy cell leukemia but CD103 and CD123 may be more useful (Am J Clin Pathol 2011;136:625)
- Positive staining - normal: activated B and T cells, macrophages, osteoblasts; some thymocytes, some myeloid precursors and some oligodendocytes; basophils have dim staining by flow cytometry (Arch Pathol Lab Med 2008;132:813)
- Positive staining - disease:
- Hairy cell leukemia (most, Am J Clin Path 2006;125:251)
- Anaplastic large cell lymphoma (Am J Clin Path 2003;119:205)
- Most B cell neoplasms, adult T cell leukemia / lymphoma (Am J Clin Pathol 2010;133:592)
- Reed-Sternberg-like cells in peripheral T cell lymphoma (Am J Surg Pathol 2003;27:1513)
- Hodgkin lymphoma (most), some AML
- Systemic mastocytosis (Arch Pathol Lab Med 2012;136:832)
- Acquired ocular toxoplasmosis (Arq Bras Oftalmol 2010;73:443)
- Idiopathic retroperitoneal fibrosis (Am J Surg Pathol 1993;17:482)
- Neuroblastoma
- Negative staining:
- Nonneoplastic mast cells (Am J Clin Path 2004;122:560)
- Marginal zone B cell lymphoma (Am J Clin Path 1996;105:277)
- T cell large granular leukemia / lymphoma (Am J Surg Pathol 2005;29:935)
- Often / usually variant hairy cell leukemia (Am J Clin Path 2005;123:132)
CD26
- Widely expressive dipeptidase with various clinical features (see below)
- Also called dipeptidyl-peptidase IV, DPP4, DDPIV, adenosine deaminase complexing protein 2 (OMIM: 102720 [Accessed 7 May 2021])
- Pathophysiology:
- Costimulatory molecule in T cell activation and proliferation
- Also regulates various chemokines and cytokines
- Cleaves amino-terminal dipeptides
- Key role in cell adhesion and invasion, plays a role in cell spreading and migration (BMC Cancer 2013;13:517)
- Either soluble in plasma or present on cell surface
- Clinical features:
- Acute kidney transplant rejection: associated with increased serum CD26 and CD26 inhibition reduces acute and accelerated rejection (Adv Exp Med Biol 2003;524:133)
- Colorectal carcinoma: marker of poor prognosis (PLoS One 2014;9:e98582, PLoS One 2014;9:e107470)
- Endometrial carcinoma: reduced expression (Am J Obstet Gynecol 2003;188:670)
- HIV infection: may have protective role (Virol J 2010;7:343)
- Lung: soluble CD26 in serum/pleural fluid may distinguish pleural mesothelioma (lower values) from pulmonary adenocarcinoma (PLoS One 2014;9:e115647)
- Lung: may function as tumor suppressor in non small cell lung carcinoma (Int J Cancer 2004;109:855)
- Lymphoma, T cell: absence of CD26 staining on peripheral blood CD4+ T cells by flow cytometry may be useful for diagnosis (Am J Clin Pathol 2001;115:885, Am J Clin Pathol 2008;129:146)
- Pregnancy: blastocyst implantation may occur by binding of endometrial CD26 to embryonal fibronectin (Mol Hum Reprod 2006;12:491)
- Prostate cancer: possible poor prognostic marker (J Res Med Sci 2013;18:647)
- Thyroid carcinoma: increased expression (Diagn Cytopathol 2002;26:366, Am J Clin Pathol 1991;96:306)
- In initial study, CD26high T cells elicit tumor immunity against multiple malignancies via enhanced migration and persistence (Nat Commun 2017;8:1961)
- No significant uses by pathologists
- Positive staining - normal:
- Activated T and B cells, basophils, macrophages, NK cells, thymocytes (mature)
- Epithelium: endometrium, hepatocytes, lung, prostate, renal proximal tubular cells, small intestine
- Also cytotrophoblast and extravillous trophoblast (J Clin Endocrinol Metab 2002;87:4287)
- Biliary canaliculae, endothelial cells, fibroblasts, mesothelial cells (Oncology 2002;63:158)
- Splenic sinus lining cells
- Positive staining - disease:
- Esophageal adenocarcinoma and Barrett's metaplasia (Hum Pathol 1999;30:1291)
- Prostate carcinoma, thyroid anaplastic carcinoma (reduced expression in undifferentiated versus differentiated areas (Am J Clin Pathol 2006;125:399)
- Wilm's tumor (Hum Pathol 1990;21:536)
- Negative staining: normal thyroid gland, T cells in peripheral blood of mycosis fungoides / cutaneous T cell lymphoma (40%) (BMC Clin Pathol 2002;2:5)
CD27
- See CD27
CD28
- Receptor important in CD4+ T cell activation, IL2 production and T helper 2 development (OMIM #186760)
- Plays a critical role in controlling the adaptive arm of the immune response (Blood 2005;105:13)
- Pathophysiology:
- T cells require 2 signals for full activation: (1) binding of the antigen / MHC complex on the antigen presenting cell to the T cell receptor; (2) interaction of CD28 with its ligands CD80 (B7-1) or CD86 (B7-2), found on activated B cells and called a costimulation signal
- Costimulatory signal induces T cell activation and survival, interleukin 2 production, T helper type 2 development and clonal expansion
- CD28 is a constitutive, high abundance, low affinity receptor; its binding also increases expression of CTLA4 (CD152), a structurally related cell surface receptor on T cells which competes with CD28 for the same ligands but has opposite effects (J Clin Immunol 2002;22:1, Curr Pharm Des 2006;12:149)
- CD8+, CD28+ T cells are antigen specific cytotoxic T cells (class I restricted) and constitute 90% of CD8+ T cells
- CD8+, CD28- T cells are suppressor T cells; loss of CD28 expression in T cells is associated with various infectious and autoimmune diseases and aging:
- Primary sclerosing cholangitis (Gastroenterology 2014;147:221)
- Hashimoto thyroiditis (BMC Endocr Disord 2013;13:34)
- Chronic hepatitis B virus infection (Biomed Rep 2014;2:270)
- Chronic bone infection (Clin Exp Immunol 2014;176:49)
- Unexplained spontaneous abortion and unexplained recurrent spontaneous abortion (Int J Gynaecol Obstet 2006;93:123)
- Aging; the frequency of CD28(null) T cells predicts immune incompetence in elderly; these T cells are functionally active and long lived but have no / limited proliferative capacity (Trends Immunol 2009;30:306)
- Clinical features:
- Contributes to genetic susceptibility to type 1 diabetes (Gene 2014;533:420)
- CD4+ CD28(null) cells are an independent predictor of mortality in heart failure (Atherosclerosis 2013;230:414)
- No significant clinical use by pathologists
- Positive staining - normal: CD4+ T cells (95%), CD8+ T cells (50%); activated B cells, thymocytes and plasma cells (some)
- Positive staining - disease: myeloma (95%) (Blood 2014;123:3770)
CD29
- Integrin component that mediates adhesion and is involved in homing to sites of inflammation
- Also called glycoprotein IIa (GP IIa), integrin beta-1 (ITGB1), fibronectin receptor beta subunit, VLA (CD49) beta chain
- Pathophysiology:
- Common beta subunit of integrins VLA1 to VLA6, which are also composed of alpha subunits alpha 1 to alpha 6 (CD49a - f)
- Combines with CD49a to form a receptor for collagen and laminin; this receptor may also be involved in cell to cell adhesion and play a role in inflammation and fibrosis
- Involved in lymphocyte and endothelial adhesion; important for lymphocyte trafficking and transvascular migration
- Promotes or inhibits apoptosis, depending on the ligands and apoptotic insults (Cancer Res 2003;63:8302)
- May help define neural lineage differentiation of stem cells (Stem Cells 2009;27:2928)
- Uses by pathologists: myoepithelial marker, although established markers (SMA, CD10, p63, S100, maspin, calponin, GFAP, smooth muscle myosin) are more commonly used
- Positive staining - normal: fibroblasts, platelets, T cells, monocytes, granulocytes (low), mast cells, endothelial cells and myoepithelium; also other diverse cell types
- Positive staining - disease:
- Bile duct epithelium in alcoholic liver disease (16%) (Arch Pathol Lab Med 1999;123:411)
- Breast metaplastic carcinoma (90%) (Am J Surg Pathol 2005;29:347)
- Breast sarcoma NOS if CD10+ (43%) (Am J Surg Pathol 2006;30:450)
- Liver cirrhosis and hepatocellular carcinoma (Zhonghua Gan Zang Bing Za Zhi 2010;18:353)
- Lung cancer (PLoS One 2013;8:e55714)
- Myeloma in bone marrow (Br J Haematol 2002;119:70)
- T cells in asthma (Pol Arch Med Wewn 2012;122:585)
- Trophoblasts in malignant gestational trophoblastic disease (Int J Gynecol Cancer 2013;23:749)
- Negative staining:
- Red blood cells, spermatogonia (Syst Biol Reprod Med 2013;59:233)
- Intravascular lymphomatosis (Hum Pathol 2000;31:220)
- References: OMIM: 135630 [Accessed 7 May 2021], Wikipedia: CD29, Cell Biochem Biophys 2014;70:601
Diagrams / tables
Microscopic (histologic) images
Images hosted on other servers:
CD200-209
CD200
- Aka OX2
- An immunoadhesin that may deliver immunosuppressive signals and regulate autoimmune disorders
- Inhibitory for macrophage lineage cells
- Positive staining - normal: follicular dendritic cells, thymocytes, B cells, T cells, neurons, kidney glomeruli, syncytiotrophoblast, endothelial cells
CD201
- Binds protein C in a calcium-dependent manner
- Aka Endothelial Protein C Receptor (EPC R), protein C receptor
- Protein C is a vitamin K dependent enzyme with major role in coagulation of blood; activated when thrombin binds to thrombomodulin on endothelium.
- Mutations in CD201 and thrombomodulin associated with late fetal loss; similar mutation associated with venous thromboembolism and myocardial infarction
- Positive staining - normal: endothelial cells (not in liver and kidney)
CD202b
- Aka Tie2 (Tyrosine kinase with Ig-like loops and Epidermal growth factor homology domains), aka Tek
- Receptor tyrosine kinase at #9p21, binds to angiopoietin-1
- May be earliest mammalian endothelial cell lineage marker
- Involved in vein morphogenesis and communication between endothelial and smooth muscle cells for remodeling and repair of blood vessels
- Defects associated with inherited venous malformations
- Positive staining - normal: endothelial cells, hematopoietic cells
CD203c
CD204
CD205
CD206
CD207
- Aka langerin (Langerhans cell specific c-type lectin)
- Functions as endocytic receptor
- Localized to Birbeck granules
- Mannose binding to this protein may cause antigen internalization into Birbeck granules and access to a nonclassical antigen-processing pathway
- Positive staining - normal: Langerhans cells (immature dendritic cells of epidermis and mucosa)
CD208
CD209
CD21
Table of Contents
Definition / general | Pathophysiology | Clinical features | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Receptor for Epstein Barr virus (EBV) and HHV8 (J Virol 2005;79:4651)
- Marker of dendritic cells (also CD23 and CD35)
- Also called CR2 (complement receptor type 2), C3d receptor and EBV receptor (OMIM #120650)
- Note: although CD21 is the receptor for EBV, it is not necessarily expressed in EBV+ tumors
Pathophysiology
- Forms a complex with CD19, CD81 and CD225 in the membrane of mature B cells; complex is often called the B cell coreceptor complex, because CD21 binds to antigens through attached C3d (or iC3b or C3dg) when the membrane IgM binds to the antigen, which results in a greatly enhanced response B cell response to the antigen (Wikipedia)
- Besides EBV and HHV8, also binds to breakdown products of complement component C3 (C3d), CD23 (plays a role in IgE synthesis) and possibly gamma interferon
- CD21/35 promotes protective immunity to Streptococcus pneumoniae through a complement-independent, but CD19-dependent pathway that regulates PD-1 expression (J Immunol 2009;183:3661)
- Follicular dendritic cells produce a different isoform of CD21 than B cells (J Exp Med 1997;185:165)
- Genetic CD21 deficiency is associated with hypogammaglobulinemia (J Allergy Clin Immunol 2012;129:801)
Clinical features
- Variable expression by flow cytometry in specimens from same patient (Am J Clin Pathol 2002;117:615)
- Hodgkin lymphoma: disruption of follicular dendritic cell-germinal cell clusters can be evaluated by CD21 and CD23
- Genetic variations are associated with susceptibility to:
- nasopharyngeal carcinoma (Oncol Rep 2013;30:11)
- systemic lupus erythematosus (Proc Natl Acad Sci USA 2007;104:3961, OMIM #610927)
Uses by pathologists
- CD21, CD23 and CD35 are dendritic cell markers
- Diagnosis of follicular dendritic cell sarcomas (Am J Surg Pathol 1996;20:944)
- Assess follicular dendritic cell meshwork infrastructure (Am J Clin Pathol 2005;124:182, Am J Surg Pathol 2001;25:388)
- Distinguish cutaneous or nodal marginal zone lymphoma from follicular lymphoma (Am J Surg Pathol 2001;25:732, Int J Surg Pathol 2005;13:73)
- Distinguish splenic littoral cell angioma (CD21+ lining cells) from splenic hamartomas (CD21-, Am J Surg Pathol 1997;21:827)
- Confirm that atypical cells have follicular dendritic origin in fine needle aspirates of hyaline-vascular Castleman disease (Diagn Cytopathol 2000;22:230)
- Differentiate invasive Quilty lesions (central aggregate of B cells with a rim of T cells admixed with capillary vessels) from cardiac acute cellular rejection (Am J Surg Pathol 2006;30:1008)
Microscopic (histologic) images
Positive staining - normal
- Mature B cells (particularly marginal and mantle cells), follicular dendritic cells, pharyngeal and cervical epithelial cells, some thymocytes and some T cells
Positive staining - disease
- Follicular dendritic cell tumor (Am J Surg Pathol 2004;28:988, Am J Surg Pathol 2001;25:721), hairy cell leukemia, B cell lymphomas (particularly mantle and marginal zone), hyaline vascular variant of Castleman disease (Am J Surg Pathol 2002;26:662), splenic littoral cell angiomas (lining cells are CD21+, Am J Surg Pathol 1997;21:827) and some T-ALL
Negative staining
- Basophils, fibroblastic reticulum cells and related tumors, interdigitating dendritic cells and related tumors (Am J Clin Pathol 2001;115:589), Langerhans cells and related tumors, plasma cells
- Dendritic cell neurofibroma with pseudorosettes (Am J Surg Pathol 2001;25:587)
- Histiocytic sarcoma (Am J Surg Pathol 2004;28:1133), indeterminate cell tumors in lymph nodes
- Inflammatory fibroid polyps of GI tract (Am J Surg Pathol 2004;28:107), inflammatory myofibroblastic tumor and splenic hamartomas
- Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease)
CD220-229
CD220
- Aka insulin receptor
CD221
CD222
CD223
- Aka Lymphocyte-Activation Gene 3 (LAG-3)
- Homologous to CD4
- Associates with MHC class II molecules on monocytes/dendritic cells, which are subsequently activated
- May help activated CD4+ and CD8+ T cells to fully activate monocytes and dendritic cells, leading to optimized MHC class I and class II T cell responses
- Positive staining - normal: activated T cells, activated NK cells
CD224
CD225
CD226
- Aka DNAM-1, Platelet and T cell Activation antigen 1 (PTA1)
- Mediates adhesion to an unknown ligand
- T cell expression increased in some patients with autoimmune disease and viral infection
- Positive staining - normal: NK cells, platelets, monocytes, subset of B and T cells
- Negative staining: granulocytes, erythrocytes
CD227
- See EMA / MUC1
CD228
CD23
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- CD23 is a low affinity immunoglobulin E (IgE) receptor
- Found on mature B cells, activated macrophages, eosinophils, follicular dendritic cells (FDCs), platelets and megakaryocytes (Sci Rep 2016;6:25629, Immunol Res 1992;11:252, World J Surg Oncol 2019;17:115, Eur J Immunol 1997;27:2212)
Essential features
- CD23 is a low affinity IgE receptor
- Differentiates small lymphocytic lymphoma (SLL) / chronic lymphocytic leukemia (CLL) (CD23+) from mantle cell lymphoma or MALT lymphoma (CD23-)
- B cell marker, particularly for SLL / CLL, mediastinal large B cell lymphoma, lymphoplasmacytic lymphoma and diffuse follicular lymphoma (Mod Pathol 2012;25:1637, Blood Adv 2020;4:5652)
- Distinguish nodal marginal zone lymphoma from follicular lymphoma by identifying a disrupted follicular dendritic cell pattern (Int J Surg Pathol 2005;13:73)
Terminology
- Low affinity IgE receptor, Fc fragment of IgE receptor, FCER
Pathophysiology
- Secretable type C lectin
- After physiologic germinal cell development, the follicular dendritic cell meshwork expands and follicular dendritic cells in the light zone of the germinal center become CD23 positive
- CD23 acts as a B cell growth and activation factor, promoting differentiation into plasma cells
- Shows variability in flow cytometry expression between specimens from same patient (Am J Clin Pathol 2002;117:615)
- CD21, CD23 and CD35 are dendritic cell markers
- Interactions with IgE:
- Membranous form regulates IgE synthesis through CD21 and IgE binding (J Exp Med 2005;202:751, Acta Crystallogr F Struct Biol Commun 2014;70:305)
- Soluble form also controls IgE synthesis and homeostasis in B cells (J Immunol 2012;188:3199)
- Membranous form mediates IgE related immune responses (Clin Rev Allergy Immunol 2005;29:61)
- IgE binding site of CD23 has extensive conformational plasticity (Mol Immunol 2013;56:693)
- Presentation of extremely low doses of antigen to T cells is enhanced by IgE dependent antigen focusing to CD23 (Immunology 2001;103:319)
- CD23 is noncovalently associated with HLA-DR and plays a role in endocytosis and recycling of the complex, which may contribute to the efficiency of antigen presentation (Immunology 2001;103:319)
Clinical features
- High expression on B cells in peripheral blood is associated with bullous pemphigoid (J Dermatol Sci 2004;35:53)
- CD23 antibodies may decrease adherence of Plasmodium falciparum infected erythrocytes (Cell Microbiol 2004;6:839)
- CD23 levels correlate with Plasmodium falciparum malaria severity (Acta Trop 2016;154:25)
- CD23 mediates antimycobacterial activity of human macrophages (Infect Immun 2009;77:5537)
- Polymorphisms are associated with atopy, increased risk of exacerbations in patients with asthma and high serum IgE levels (Am J Respir Cell Mol Biol 2014;50:263)
- Mantle cell lymphoma:
- Usually CD23-
- May have CD23 present with dim intensity by flow cytometry; however, these cases have high cyclin D1 levels (Am J Clin Pathol 2003;120:760, Am J Clin Pathol 2001;116:893, Am J Clin Pathol 2002;117:237)
- CD23+ cases may have better prognosis (Am J Clin Pathol 2008;130:166, Hum Pathol 2019;89:71, Curr Oncol Rep 2021;23:102)
- Rarely has CD23+ cells in peripheral blood (Am J Clin Pathol 2002;118:758)
- Chronic lymphocytic leukemia / CLL:
- High soluble CD23 is associated with aggressive disease and poorer prognosis (Leuk Lymphoma 2002;43:549, Clin Lab Haematol 2006;28:30, Cytometry B Clin Cytom 2014;86:91)
Interpretation
- Diffuse cell membrane staining, cytoplasmic staining
Uses by pathologists
- CD21, CD23 and CD35 are follicular dendritic cell markers
- Differentiate SLL / CLL (CD23+) versus mantle cell lymphoma or MALT lymphoma (CD23-)
- B cell marker, particularly for SLL / CLL, mediastinal large B cell lymphoma, lymphoplasmacytic lymphoma and diffuse follicular lymphoma (Mod Pathol 2012;25:1637, Blood Adv 2020;4:5652)
- Distinguish nodal marginal zone lymphoma from follicular lymphoma by identifying a disrupted follicular dendritic cell pattern in marginal zone lymphoma (Int J Surg Pathol 2005;13:73)
Microscopic (histologic) images
Virtual slides
Positive staining - normal
- Activated mature B cells expressing IgM or IgD (particularly mantle cells), activated monocytes / macrophages, T cell subsets, platelets, eosinophils, Langerhans cells, follicular dendritic cells and intestinal epithelium (encodes IgE receptor) (Gastroenterology 2005;129:928, Sci Rep 2016;6:25629, Immunol Res 1992;11:252, World J Surg Oncol 2019;17:115, Eur J Immunol 1997;27:2212)
Positive staining - disease
- B cell CLL / SLL (almost all cases; high levels) (Leuk Res 2002;26:809, Hum Pathol 1999;30:648)
- Atypical cases of CLL / SLL may have higher levels (Am J Clin Pathol 2001;116:655)
- Follicular dendritic cell sarcoma (Am J Surg Pathol 2001;25:721, Pathologica 2021;113:316, Cytopathology 2022;33:119, Medicine (Baltimore) 2021;100:e27209)
- Mediastinal large B cell lymphoma (70%) (Histopathology 2004;45:619, Blood 2021;138:136)
- Lymphoplasmacytic lymphoma (61%, usually dim intensity by flow cytometry) (Am J Clin Pathol 2005;124:414, Clin Lymphoma 2005;5:246)
- Hairy cell leukemia (17%) (Am J Clin Pathol 2006;125:251)
- Diffuse large B cell lymphoma (16%) (Histopathology 2010;56:217)
- Primary cutaneous follicle center lymphoma (38%) (Am J Surg Pathol 2002;26:733)
- Plasma cell myeloma (10%) with chromosome 11 abnormalities, with t(11;14)(q13;q32) (40%) (Br J Haematol 2010;149:292, Ann Diagn Pathol 2011;15:385)
- Plasma cell leukemia (Br J Haematol 2010;150:724)
- Postsplenectomy polyclonal B cell lymphocytosis (Int J Lab Hematol 2022;44:e32)
Negative staining
- Basophils, resting B cells
- Other B cell lymphomas, including Burkitt lymphoma, mantle cell lymphoma and marginal zone lymphoma; HHV8 associated germinotropic lymphoproliferative disorder and acute precursor B cell lymphoma / leukemia (Am J Surg Pathol 2005;29:1652, Am J Surg Pathol 1999;23:59, Mod Pathol 1998;11:967, Int J Clin Exp Pathol 2021;14:375, Am J Surg Pathol 2017;41:795, Am J Clin Pathol 2001;116:673, Curr Oncol 2021;28:5148)
- Most T cell lymphomas, inflammatory fibroid polyps of the gastrointestinal tract (although of dendritic cell origin), indeterminate dendritic cell tumor and interdigitating dendritic cell sarcoma (Am J Surg Pathol 2004;28:107, Hemasphere 2020;5:e511, J Int Med Res 2018;46:4791)
- Blastic plasmacytoid dendritic cell neoplasm (Clin Case Rep 2018;6:770)
- Epithelioid sarcoma (Am J Clin Pathol 2021;156:229)
- Classic Hodgkin lymphoma (Histopathology 2010;56:217)
- Plasmablastic lymphoma (Rev Esp Enferm Dig 2021 Dec 22 [Epub ahead of print])
- Abnormally developed CD23 negative B cells in AIOLOS defect patients (J Exp Med 2021;218:e20211118)
Sample pathology report
- Left axillary lymph node, excision:
- Left axillary lymph node excision infiltrated by chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL) with large proliferation centers; no signs of Richter transformation (see comment)
- Comment: A large lymph node with disrupted architecture due to a lymphocytic infiltrate with a vaguely nodular growth pattern. The infiltrate consists of small cells with round nuclei, mature chromatin and a barely visible cytoplasmic border. The nodular parts (so called proliferation centers) consist of small and large cells and some large prominent paraimmunoblasts.
- Immunohistochemically, the infiltrate is positive for CD20, CD5, CD23 and BCL2. The staining for CD3 shows numerous accompanying reactive T lymphocytes. The stains for cyclin D1, BCL6 and CD10 remain negative in the lymphocytic infiltrate but BCL6 and CD10 are positive in a few residual reactive germinal centers. The proliferation is high and polarized in the residual germinal centers and somewhat increased in the proliferation centers with a proliferation rate of about 20%.
Board review style question #1
Which tumor typically exhibits CD23 positivity?
- Blastic plasmacytoid dendritic cell neoplasm
- Follicular dendritic cell sarcoma
- HHV8 associated germinotropic lymphoproliferative disorder
- Indeterminate dendritic cell tumor
- Interdigitating dendritic cell sarcoma
Board review style answer #1
CD230-239
CD230
- Aka prion protein (“PRotein INfectious agent”)
- Mutations associated with Gerstmann-Straussler disease, Creutzfeldt-Jakob disease (CJD), familial fatal insomnia, which are neurodegenerative conditions transmissible by inoculation or inherited as autosomal dominant disorders
- Aberrant isoforms can act as an infectious agent in these disorders as well as in kuru and in scrapie in sheep
- Replication (infectivity) occurs as abnormal protein with conformational change recruits cellular prion and converts it into infective form with same conformational change
- Positive staining - normal: neurons (nonpathogenic isoform)
- Reference: OMIM 176640
CD231
- Aka T cell Acute Lymphoblastic Leukemia Antigen-1 (TALLA-1), TM4SF2, A15
- Involved in X-linked intellectual disability (Nat Genet 2000;24:167)
- Positive staining - normal: T cell acute lymphoblastic leukemia, neuroblastoma cells
- Positive staining - malignant: T cell acute lymphoblastic leukemia, neuroblastoma cells
- Negative staining: B cells, monocytes
CD232
CD233
- Aka band 3
- Erythrocyte membrane protein that functions as an anion (chloride/bicarbonate) exchanger and attachment site for cytoskeleton (where spectrin/actin bind to membrane lipid bilayer)
- Truncated form of CD233 is expressed in kidney and involved in acid secretion
- Mutations cause hereditary spherocytosis or distal renal tubular acidosis (due to defective acid secretion)
- Other mutations cause novel blood group antigens which form the Diego blood group system
- Southeast Asian ovalocytosis is due to heterozygous deletions, common where Plasmodium falciparum malaria is endemic, associated with abnormally rigid, stomatocytic erythrocytes, asymptomatic; children are protected against cerebral malaria
- Positive staining - normal: erythrocyte plasma membrane (strong), basolateral membrane of a-intercalated cells of the distal tubules and collecting ducts of the kidney
- Negative staining: all other cells
CD234
- Aka Duffy blood group antigen (Fy glycoprotein); erythrocyte chemokine receptor, Duffy Antigen Receptor for Chemokines (DARC)
- RBC receptor for Plasmodium vivax, a malarial parasite
- Negativity associated with sickle cell trait, due to common protection against malaria provided by both traits African-Americans often Duffy negative and resistant to P. vivax malaria
- Positive staining - normal: endothelial cells of postcapillary venules, Purkinje cells of cerebellum
- See also Duffy system
CD235
- Glycophorins A and B are major sialoglycoproteins of the human erythrocyte membrane; contain antigenic determinants for the MN blood group
- CD235a: also called glycophorin A
- CD235b: also called glycophorin B
- CD235ab: also called glycophorin A/B crossreactive antibodies
- Positive staining - normal: erythroid cells
- Positive staining - disease: AML-M6
- Negative staining: AML M0-M5, M7
CD236
CD238
- Aka Kell blood group antigen
- Positive staining - normal: erythroid cells
- See also Kell group
CD239
CD240-249
Table of Contents
CD240CE | CD240D | CD240DCE | CD241 | CD242 | CD243 | CD244 | CD245 | CD246 | CD247 | CD248 | CD249 | Diagrams / tables | Microscopic (histologic) imagesCD240CE
- Also called RH 30 CE, Rh blood group Cc and Ee blood group antigens; encodes RhC and RhE antigens on a single polypeptide
- On #1p36.11 adjacent to RH D gene
- Rh (rhesus) blood group system is second most clinically significant blood group after ABO; is most polymorphic blood group, with variations due to deletions, gene conversions and missense mutations
- Rh antigens are carried by an oligomer of two major erythroid specific polypeptides, the Rh (D and CcEe) proteins and the RhAG glycoprotein
- Rh proteins form a core complex critical to structure of erythrocyte membrane (Blood Rev 2006;20:93)
- May play a role in ammonia transport (J Biol Chem 2002;277:12499, Transfus Clin Biol 2006;13:132)
- Discrepant or doubtful serologic results can be resolved by sequence specific primer (PCR SSP) technique (Transfusion 2007;47:54S)
- Rarely causes hemolytic disease of newborn (Transfus Med 2000;10:305)
- Uses by pathologists: blood typing
- Positive staining - normal: erythroid cells
- References: Blood 2000;95:375, OMIM 111700
CD240D
- Also called RH30 D, Rh blood group D blood group antigen; is major antigen of the Rh system
- On #1p36.11 adjacent to RHCE gene
- Rh (rhesus) blood group system is second most clinically significant blood group after ABO; is most polymorphic blood group, with variations due to deletions, gene conversions and missense mutations
- Weak D, formerly called D(u), occurs in 0.2 to 1% of whites
- Exhibits reduced expression of D antigen (Blood 1999;93:385)
- Should not be labeled as Rh negative (Curr Opin Hematol 2006;13:476)
- Individuals are classified as Rh positive or negative based on presence or absence of highly immunogenic D antigen on red cell surface
- May have arisen historically by duplication of RHCE gene (Blood 2002;99:2272)
- Discrepant or doubtful serologic results can be resolved by sequence specific primer (PCR SSP) technique (Transfusion 2007;47:54S)
- Hemolytic disease of fetus and newborn: usually due to Rh negative woman whose partner is Rh+ or heterozygous and fetus is Rh+; woman has preexisting anti-RhD antibodies that cross placenta and harm fetus (Immunohematol 2006;22:188)
- Can use maternal plasma in alloimmunized pregnancies to determine fetal RhD status or for RHD and RHCE genotyping (Fetal Diagn Ther 2006;21:404, Prenat Diagn 2005;25:1079)
- Genotyping from amniotic fluid or chorionic villi sampling was performed in past but is more invasive (N Engl J Med 1998;339:1734, Clin Exp Med 2002;2:77)
- Rh positive mothers may rarely (0.15%) develop new antibodies (other than anti-RHD) in third trimester but no clinical significance (J Matern Fetal Neonatal Med 2007;20:59)
- Having Rh negative mother may be risk factor for autistic children, due to use of mercury containing Rho-immune globulin (J Matern Fetal Neonatal Med 2007;20:385)
- Uses by pathologists: blood typing
- Positive staining - normal: erythroid cells
- References: OMIM 111680, Wikipedia, eMedicine (Rh incompatibility)
CD240DCE
CD241
- Also called RH50 glycoprotein, RHAG, Rhesus blood group associated glycoprotein
- Located at #6p21.1 - p11
- Is a strictly required posttranscriptional factor regulating Rh membrane expression (Blood 2002;100:1038)
- Also appears to be an ammonium transporter and a CO2 channel (Proc Natl Acad Sci USA 2004;101:17222, FASEB J 2008;22:64)
- Defects cause Rh-null phenotype, associated with a chronic hemolytic anemia and spherostomatocytosis (OMIM 268150, J Biol Chem 1998;273:2207)
- Uses by pathologists: blood typing
- Positive staining - normal: erythroid cells
- Reference: OMIM 180297
CD242
- Also called intercellular adhesion molecule 4 (ICAM-4), Landsteiner-Wiener (LW) blood group protein
- Discovered with antibody raised in guinea pigs injected with the cells of rhesus monkeys but Rh designation had already been taken
- Binds to CD11a / CD18, CD11b / CD18 and CD11c / CD18 (Blood 2007;109:802)
- May be critical in erythroblastic island formation, where erythroid progenitors differentiate (Blood 2006;108:2064)
- May be ligand for platelet activated alpha IIb beta 3 integrin (J Biol Chem 2003;278:4892)
- In sickle cell disease, contributes to red cell endothelial cell adhesion and vasoocclusion (Transfus Clin Biol 2006;13:44)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: erythroid cells
- References: OMIM 111250
CD243
- See Stains-MDR
CD244
- Also called Natural Killer cell receptor 2B4
- Regulates NK and T cell function in multiple ways (J Immunol 2005;175:2045)
- Coexpression of 2B4 and CD160 defines a CD8+ T lymphocyte subpopulation with high cytolytic effector activity (Eur J Immunol 2006;36:2359)
- Binds to CD48 (J Immunol 2006;176:4646)
- CD244 - CD48 interactions prevent NK cells from killing each other (Blood 2007;110:2020)
- Functional changes are associated with X linked lymphoproliferative disease (J Exp Med 2000;192:337, J Immunol 2000;165:2932)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal:
- NK cells
- CD8+ T cells
- Monocytes and basophils (Eur J Immunol 1999;29:1676)
- Eosinophils (J Immunol 2005;174:110)
- Spleen (Tissue Antigens 1999;54:27)
- Reference: OMIM 605554
CD245
- Also called p220 / 240
- Very little information is available for CD245 directly; appears to be identical to NPAT (nuclear protein, ataxia-telangiectasia locus)
- NPAT links S phase cyclin E / Cdk2 kinase activity to replication dependent histone gene transcription (Biochemistry 2006;45:15915, Mol Cell Biol 2005;25:6140)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: T cells (some), other white blood cells with varying intensity
CD246
- See Stains-ALK
CD247
- Also called T cell receptor zeta chain
- Forms T cell-CD3 receptor complex with TCR alpha / beta and gamma / delta heterodimers and CD3 (gamma, delta and epsilon) (Proc Natl Acad Sci USA 1988;85:9709)
- Couples antigen recognition to several intracellular signal transduction pathways; low expression causes impaired immune response
- Low expression in tumor infiltrating T cells in various disorders:
- Cancer of kidney (Cancer Invest 2004;22:871)
- Cancer of stomach (Cancer 2002;94:1437)
- Hodgkin’s lymphoma (Blood 1996;88:236)
- Active tuberculosis (J Infect Dis 2006;194:1385)
- Systemic lupus erythematosus (J Immunol 2002;169:6048, Adv Med Sci 2006;51:181)
- Normal pregnancy but not preeclampsia (Am J Obstet Gynecol 2003;189:843)
- Defects cause primary T cell immunodeficiency (OMIM 610163)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: T cells
- Reference: OMIM 186780
CD248
- Also called endosialin, tumor endothelial marker 1 (TEM1)
- Cell surface glycoprotein associated with tumors: traditionally thought present in vascular endothelial cells (Proc Natl Acad Sci USA 1992;89:10832, J Biol Chem 2001;276:7408)
- May actually be marker of stromal fibroblasts (FEBS Lett 2005;579:2569)
- Not present (or weak) in nontumor associated endothelium
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal:
- Endometrium
- Embryos (Cancer Res 2001;61:6649)
- Fibroblasts and pericytes during lymphoid tissue development (FEBS Lett 2007;581:3550)
- RNA at low / moderate levels in many organs
- Positive staining - disease:
- MFH and other sarcomas, some capillaries and fibroblasts in carcinomas
- Endothelium of high grade brain tumors (J Neuropathol Exp Neurol 2004;63:1274)
- RNA at low / moderate levels in carcinomas (Cancer Immun 2005;5:10)
- Reference: OMIM 606064
CD249
- Also called ENPEP, glutamyl aminopeptidase, differentiation antigen gp160, aminopeptidase A
- Regulates blood pressure via renin-angiotensin system (J Biol Chem 2006;281:23503)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: kidney; also brain, heart, liver, lung, placenta, skeletal muscle, pancreas (Genomics 1993;17:657)
- Positive staining - disease:
- Cervical neoplasia (Lab Invest 2004;84:639)
- Renal cell carcinoma-some (Proc Natl Acad Sci USA 1993;90:7069)
- Reference: OMIM 138297
Microscopic (histologic) images
CD27
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Flow cytometry images | Molecular / cytogenetics description | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Tumor necrosis factor receptor (TNF) family member expressed on T and B cells
Essential features
- CD27 is a costimulatory receptor of the TNF receptor superfamily expressed on lymphocytes
- CD27 is triggered by its unique ligand CD70, which is expressed on immune cells and often in cancers
- Soluble CD27 can be measured in serum and is an indicator of the CD70 - CD27 interaction in vivo
- CD27 deficiency should be considered in patients with immunodeficiencies
- CD27 staining in flow cytometry can help detect immunodeficiencies
Terminology
- Also known as tumor necrosis factor receptor superfamily member 7 (TNFRSF7)
Pathophysiology
- CD27 is the receptor for its ligand CD70 (Int Immunol 1994;6:477)
- CD70 expression is tightly controlled in human tissues but often overexpressed in cancers (Pharmacol Ther 2015;155:1)
- CD27 is variably expressed on B, T and NK cells (J Immunol 1987;139:1589)
- CD27 is a costimulatory receptor (Int Immunol 1995;7:551)
- On T cells, CD27 activates NFκB and promotes cell survival, antigen receptor mediated proliferation and immune function (Curr Opin Immunol 2005;17:275)
- On B cells, CD27 augments Ig class switching and promotes plasma cell differentiation (Blood 2010;115:3051, Blood 1998;91:173)
- On NK cells, CD27 stimulates interferon gamma secretion (J Immunol 2000;164:1741)
- CD27 high and low NK cells represent functionally distinct subsets (J Immunol 2006;176:1517)
- On hematologic progenitor cells and leukemic stem cells, CD27 leads to Wnt pathway activation and promotes cell growth (J Clin Invest 2012;122:624)
- CD27 stimulation can lead to immune cell suppression depending on the duration and timing of signaling (Immunol Rev 2009;229:216)
- CD27 signaling increases the numbers of regulatory T cells and may promote tumor growth (Cancer Res 2012;72:3664)
- CD27 is a marker for IgG class switched memory (CD27+ IgD- IgM-) versus naïve B cells (CD27- IgD+ IgM+) (J Exp Med 1998;188:1679)
- Triggering of CD27 by CD70 leads to shedding of soluble CD27 from cells by a protease (J Immunol 1991;147:29)
- Soluble CD27 can be measured in serum and reflects the extent of CD27 / CD70 interactions in vivo (J Exp Med 2017;214:359)
Diagrams / tables
Clinical features
- Soluble CD27 has been explored as a promising marker of immune function and disease status in a range of infectious, immunologic and oncologic settings (J Immunol 2013;190:6250)
- Immunology
- CD27 deficiency can be seen in many cases of common variable immune deficiency (Blood 2002;99:1544)
- CD27 deficiency should be considered in all patients with hypogammaglobulinemia or unusually severe causes of EBV infection to allow for individualized treatment (J Allergy Clin Immunol 2012;129:787, Haematologica 2013;98:473)
- CD27 expression on lymphocytes is increased in patients with diffuse and limited cutaneous systemic sclerosis (Intractable Rare Dis Res 2020;9:99)
- High serum levels of soluble CD27 and increased CD27 negative memory B cells are associated with disease severity in systemic lupus erythematosus (Clin Rheumatol 1995;14:293, J Immunol 2007;178:6624)
- Oncology
- CD27 signaling can enhance T cell proliferation and differentiation to effector and memory T cells (ESMO Open 2020;4:e000629)
- CD27 is being investigated as a therapeutic target for hematolymphoid malignancies and solid tumors (Blood Adv 2020;4:1917, J Clin Oncol 2017;35:2028)
- Its agonistic antibody, varlilumab, is being studied as a potential immune modulator for cancer patients (ESMO Open 2020;4:e000629)
- CAR T cells costimulated with CD27 signaling have improved survival and enhanced function in vitro and in vivo (Blood 2012;119:696)
Interpretation
- Membranous staining
Uses by pathologists
- CD27 dim expression detected by flow cytometry is a marker of atypical plasma cells (see Diagrams / tables) (Br J Haematol 2022;196:1175)
- B cell phenotyping for evaluation of immunodeficiency syndromes and immune competence analysis by flow cytometry
- T cell phenotyping for evaluation of immunodeficiency syndromes and immune competence analysis by flow cytometry
Prognostic factors
- Solid tumors
- CD27 positive tumor infiltrating lymphocytes predict inferior survival in renal cell carcinoma (Clin Cancer Res 2015;21:889)
- CD27 negative tumor infiltrating lymphocytes are associated with an improved survival in high grade serous ovarian carcinoma (Clin Cancer Res 2012;18:3281)
- CD27 negative tumor infiltrating lymphocytes are associated with an improved survival in hepatocellular carcinoma (Clin Cancer Res 2013;19:5994)
- Hematolymphoid neoplasms
- Soluble CD27 is an independent unfavorable prognostic marker in acute myeloid leukemia (J Exp Med 2017;214:359)
- CD27 is highly expressed in high risk B cell progenitor acute lymphoblastic leukemia and associated with decreased survival (Blood Cancer J 2017;7:e575)
- Loss of CD27 expression indicates poor prognosis in multiple myeloma (Clin Immunol 2020;213:108363)
Microscopic (histologic) images
Positive staining - normal
- Immune cells (see Pathophysiology)
Positive staining - disease
- Myeloma (heterogeneous expression) (Br J Haematol 2006;132:168, Br J Haematol 2003;121:36)
- Adult T cell leukemia / lymphoma (100%, 17/17) (Am J Clin Pathol 2010;133:592)
- Chronic lymphocytic leukemia (100%, 18/18) (Blood 1995;85:3556)
- Mantle cell lymphoma (100%, 15/15) (Leuk Lymphoma 2002;43:1855)
- Burkitt lymphoma (100%, 6/6) (Leuk Lymphoma 2002;43:1855)
- Pro-B acute lymphoblastic leukemia (Leuk Lymphoma 2002;43:1855, Exp Hematol 2005;33:1500)
- CD27 positive hairy cell leukemia, Japanese variant (Virchows Arch 2016;468:375)
- Chronic myeloid leukemia, CD34 positive blasts (J Clin Invest 2012;122:624)
Negative staining
- Oncology
- Hairy cell leukemia (Haematologica 2005;90:266)
- Splenic diffuse red pulp lymphoma (Clin Lymphoma Myeloma Leuk 2016;16:S166)
- Immunology
- Chronic active EBV infection associated with CD27 deficiency (J Allergy Clin Immunol 2015;136:703)
Flow cytometry images
Molecular / cytogenetics description
- CD27 expression (based on mRNA detection by PCR) is higher in mycosis fungoides skin lesions than in healthy controls (Ital J Dermatol Venerol 2022;157:275)
Sample pathology report
- Peripheral blood, flow cytometry, quantitative B cell phenotyping analysis:
- Abnormal (see comment)
- Comment: A decrease of class switched memory B cells (CD19 positive, CD27 positive, IgM negative, IgD negative) is consistent with common variable immunodeficiency (CVID). Switched memory B cells are quantitatively decreased in relation to marginal zone B cells (CD19 positive, CD27 positive, IgM positive, IgD negative). This result is consistent with but not diagnostic of CVID. Quantitative B cell phenotyping is helpful for the classification and prognosis of CVID and should be considered in the context of clinical and other immunological and laboratory findings. Decreased class switched memory B cells may also be seen in some autoimmune diseases, secondary to certain medications and in patients with other hereditary syndromes.
Additional references
Board review style question #1
Board review style answer #1
D. CD70, the ligand of CD27, is often overexpressed in cancer. CD70 is overexpressed in many cancers and the CD27 / CD70 immune axis is utilized by cancers to escape immune surveillance (Oncoimmunology 2012;1:1604). The expression of CD27 in lymphoid and myeloid progenitor cells is tightly controlled. The expression pattern of CD27 is predominantly membranous. Clinical uses include immunophenotypic evaluation of plasma cell neoplasms and analysis of lymphocytes in patients with immunodeficiency syndromes.
Comment Here
Reference: CD27
Comment Here
Reference: CD27
CD270-279
CD270
- Also known as tumor necrosis factor receptor superfamily member 14 (TNFRSF14), Herpesvirus entry mediator (HVEM) (GeneCards)
- Ligand to B and T lymphocyte attenuator (BTLA, Diagn Pathol 2012;7:142)
- Acts as receptor for Herpes simplex virus (Virology 2014;448:185)
- Recurrent mutations associated with pediatric follicular lymphoma (Haematologica 2013;98:1237)
- Acquired mutations associated with worse prognosis in follicular lymphoma (Cancer Res 2010;70:9166)
- No uses for pathologists at this time
- Positive staining: T cells (constitutive or induced)
CD272 / BTLA
- B and T lymphocyte attenuator (BTLA) is a recently discovered inhibitory receptor belonging to the CD28 family
- Expressed by most lymphocytes; shares structural and functional similarities with CTLA4 / cytotoxic T-lymphocyte antigen-4 / CD152 and PD1 / programmed death 1 (PD1), although only 9-13% amino acid identify (Arch Immunol Ther Exp (Warsz) 2015;63:73)
- Interacts with CD270 / herpesvirus entry mediator (HVEM), a TNFR superfamily member found on T, B, NK, DC and other cells
- Has a negative regulatory role in diverse immune responses
- Expression on αβ T cells is likely associated with protective immune memory against Mycobacteria tuberculosis infection in patients with active pulmonary tuberculosis (Am J Transl Res 2014;6:494)
- May contribute to immune escape (Blood 2013;122:922, Cancer Res 2012;72:887)
- In mice, BTLA antibodies prevented graft versus host disease without global immunosuppression (J Exp Med 2010;207:2551)
- No uses for pathologists at this time
CD273
CD274
- See PDL1 22C3
CD278
- Also called ICOS
- Enhances basic T-cell responses to a foreign antigen, namely proliferation, secretion of lymphokines, upregulation of molecules that mediate cell-cell interaction and effective help for antibody secretion by B-cells
- Essential both for efficient interaction between T and B-cells and for normal antibody responses to T-cell dependent antigens
- Plays a critical role in CD40-mediated class switching of immunoglobin isotypes
- A type I membrane protein
- Defects cause ICOS deficiency (OMIM 607594), a form of common variable immunodeficiency characterized by recurrent bacterial infections of the respiratory and digestive tracts, but without splenomegaly, autoimmune disease, sarcoid-like granulomas, overt T cell immunodeficiency
- Present in: activated T cells, tonsillar T cells, fetal and newborn thymic medulla
- Reference: Swiss-Prot entry
CD279
- See PD1
CD278 / ICOS (pending)
[Pending]
CD280-289
CD281
- TLR1_HUMAN, Q15399, OMIM 601194, TLR1, Toll-like receptor 1 (Toll/interleukin-1 receptor-like) (TIL)
CD282
- TLR2_HUMAN, O60603, OMIM 603028, TLR2, TIL4, Toll-like receptor 2 (Toll/interleukin-1 receptor-like protein 4)
CD283
- TLR3_HUMAN, O15455, OMIM 603029 TLR3, Toll-like receptor 3
CD284
- TLR4_HUMAN, O00206, OMIM 603030, TLR4, toll-like receptor 4
CD289
- TLR9_HUMAN, Q9NR96, OMIM 605474, TLR9, Toll-like receptor 9
CD3
Table of Contents
Definition / general | Essential features | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Flow cytometry description | Flow cytometry images | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Common antibody for identifying T cells
- Member of immunoglobulin superfamily on 11q23
- Also called OKT3
Essential features
- Common antibody for identifying T cells
Pathophysiology
- CD3 is a cell surface complex composed of 4 distinct subunits; these subunits are chains of integral membrane glycoproteins that associate with T cell antigen receptor (TCR) and are required for TCR cell surface expression and signal transduction (Immunity 2006;24:133, Nature 2019;573:546)
- Delta (CD3ƍ) (OMIM: 186790 - CD3 Antigen, Delta Subunit [Accessed 18 March 2022])
- Epsilon (CD3ε) (OMIM: 186830 - CD3 Antigen, Epsilon Subunit [Accessed 18 March 2022])
- Gamma (CD3γ) (OMIM: 186740 - CD3 Antigen, Gamma Subunit [Accessed 18 March 2022])
- Zeta (CD3ζ, also called CD247) (OMIM: 186780 - CD247 Antigen [Accessed 18 March 2022])
- CD3 is expressed as either TCR alpha / beta or TCR gamma / delta heterodimers, coexpressed at cell surface with the TCR complex (Immunity 2006;24:133)
- CD3 is first expressed in the cytoplasm of developing T cells, then as they mature it moves to the membrane (Immunity 2006;24:133)
- Activation of the TCR by antigen peptides, presented via major histocompatibility complexes, induces phosphorylation of intracellular immunoreceptor tyrosine based activation motifs (ITAMs) in the CD3ζ subunits (Nature 2019;573:546)
Clinical features
- CD3 gamma, delta and epsilon defects cause autosomal recessive severe combined immunodeficiency (no T cells, although B cells and NK cells are normal) (Pediatr Allergy Immunol 2013;24:257, OMIM: 608971 - Severe Combined Immunodeficiency [Accessed 21 March 2022], Curr Opin Allergy Clin Immunol 2004;4:479)
- Anti-CD3 monoclonal antibodies as treatment:
- FDA approved to treat acute renal, cardiac or hepatic allograft rejection (antithymocyte antibody, ATG) (MAbs 2010;2:148)
- ATG is a polyclonal antibody, directed against multiple T cell epitopes
- In contrast to ATG, muromonab CD3, otelixizumab, teplizumab and visilizumab are monoclonal antibodies; in use for rejection, type 1 diabetes mellitus and inflammatory bowel disease (Lancet 2007;369:1641, Indian J Endocrinol Metab 2015;19:S58)
- Reverse steroid resistant acute graft rejection (J Immunol 2011;187:2015)
- Although initially thought to improve clinical parameters in new onset type 1 diabetes, phase III trials have been disappointing (N Engl J Med 2002;346:1692, Diabetes 2005;54:1763, Clin Dev Immunol 2011;2011:432016)
Interpretation
- Cytoplasmic positivity in immature T cells (cCD3), while negative surface CD3 (sCD3)
- Complete and membranous positivity in mature T cells (CD3)
- Reference: Histopathology 2000;36:544
Uses by pathologists
- Most specific T cell antibody; usually used to identify T cells in benign and malignant disorders; most antibodies are directed against epsilon chain
- CD3 in IHC stains both membrane and cytoplasm and stains both T cells and NK cells, thus NK cell processes / lymphomas are CD3 by IHC
- Flow cytometry can distinguish surface from cytoplasmic CD3 and therefore T cells (surface CD3+ from NK cells (surface CD3-)
- Flow cytometry can also distinguish T cells with surface CD3 (mature T cells) from T cells with cytoplasmic CD3 but without surface CD3 (T lymphoblasts)
- CD3 / CD20 combined immunostains are often performed in initial cytological evaluation of lymphoid rich pleural effusions but their cost effectiveness has been questioned (Diagn Cytopathol 2012;40:565)
- Does not improve detection of gluten sensitive enteropathy when H&E sections are normal (Mod Pathol 2013;26:1241)
Microscopic (histologic) images
Positive staining - normal
- Thymocytes, peripheral T cells (cytoplasmic expression at early T cell differentiation, then membranous expression) (Adv Biol Regul 2019;74:100638, Nat Methods 2017;14:531)
- NK cells (CD3 epsilon, cytoplasmic in 56%, not membranous); also Purkinje cells of cerebellum
- Note: nonspecific cytoplasmic staining may be present in plasma cells and macrophages (faint reactivity)
Positive staining - disease
- 80% of T cell lymphomas, NK cell lymphoma (cytoplasmic, not membranous), reactive T cells in lymphomatoid granulomatosis, lymphomatoid papulosis and precursor T cell acute lymphoblastic leukemia (pre-T ALL) (cytoplasmic staining, cCD3) (Rev Med Interne 2013;34:349, Adv Biol Regul 2019;74:100638)
- Small T lymphocytes surrounding LP cells in nodular lymphocyte predominant Hodgkin lymphoma (T cell rosettes, usually CD57+)
- Variable in B cell neoplasms (particularly in those with expression of EBV); e.g., in B cell non-Hodgkin lymphoma (B NHL) with plasmablastic differentiation, primary effusion lymphoma and pyothorax associated lymphoma (Mod Pathol 2018;31:718, Am J Surg Pathol 2022;46:353, Am J Surg Pathol 2002;26:724)
- Polykaryocytes (Warthin-Finkeldey) in various benign and malignant disorders (e.g., Kimura lymphadenitis, measles infections, HIV lymphadenitis) (Am J Clin Pathol 1992;97:179)
Negative staining
- B cells, histiocytes and histiocytic lesions, osteoblasts
- Most B cell lymphomas, but aberrant staining occurs
- Aberrant loss / dim positivity of CD3 in some cases of:
- Mycosis fungoides (Am J Clin Pathol 2000;114:467, Cytometry B Clin Cytom 2021;100:132, Blood 2005;105:3768)
- Anaplastic large cell lymphoma (Blood 2005;105:3768)
- Angioimmunoblastic T cell lymphoma (Am J Clin Pathol 2006;126:29, Blood 2005;105:3768)
- NK large granular lymphocyte leukemia
- Reed-Sternberg cells are negative in classic Hodgkin lymphoma (Cytometry B Clin Cytom 2019;96:116)
- LP cells in nodular lymphocyte predominant Hodgkin lymphoma are CD3- but may be surrounded by CD3+ T cell rosettes (Semin Hematol 1999;36:242)
- Small cell carcinoma, melanoma, myeloid sarcoma, Ewing sarcoma and posttransplant lymphoproliferative disorders
Flow cytometry description
- Adult T cell leukemia / lymphoma often has abnormally low CD3 T cell population (Am J Clin Pathol 2005;124:199, Virol J 2007;4:85)
- Angioimmunoblastic T cell lymphoma has decreased or absent CD3 expression (~60% of cases) (Leuk Lymphoma 2016;57:2804)
Sample pathology report
- Lymph node, excision:
- Peripheral T cell lymphoma, TBX21 (see comment)
- Comment: Lymph node with polymorphous infiltrate with atypical lymphocytic cells. The tumor cells are positive for CD3 with coexpression of CD4, CD2, CD5 and loss of CD7. CD8 marks reactive cytotoxic T cells. TFH markers (PD-1, ICOS, BCL6, CD10, CXCR13) remain negative. The tumor cells coexpress TBX21 / T bet and CXCR3 but remain negative in GATA3 and CCR4 (Blood 2019;134:2159).
Board review style question #1
Board review style answer #1
CD30
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- CD30 is a transmembrane, type I, glycoprotein receptor from the tumor necrosis factor receptor (TNFR) superfamily (Blood Cancer J 2017;7:e603, Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print], J Mol Recognit 2003;16:28, Oncologist 2022 Aug 10 [Epub ahead of print], Blood 1995;85:1, Histopathology 2022;81:55, Clin Adv Hematol Oncol 2014;12:1)
Essential features
- CD30 is a transmembrane, type I, glycoprotein receptor from the tumor necrosis factor receptor (TNFR) superfamily (Blood Cancer J 2017;7:e603, Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print], J Mol Recognit 2003;16:28, Oncologist 2022 Aug 10 [Epub ahead of print], Blood 1995;85:1, Histopathology 2022;81:55, Clin Adv Hematol Oncol 2014;12:1)
- BerH2 (J Mol Recognit 2003;16:28, Blood Cancer J 2017;7:e603, Am J Surg Pathol 2016;40:378, Blood 2014;124:2983)
- Most commonly used clone to fabricate the antibody and has good correlation with mRNA levels of CD30
- Composed of 2 linear epitopes with identical sequence
- Targetable biomarker (Oncologist 2022 Aug 10 [Epub ahead of print])
- High expression by neoplastic cells
- Low expression by normal cells
- Extracellular localization
Terminology
- Ki1 (J Mol Recognit 2003;16:28, Blood 1995;85:1)
- Discontinuous epitope of 2 regions
- Close to N terminus region
- Close to membrane spanning region
- Discontinuous epitope of 2 regions
- Ki2 (J Mol Recognit 2003;16:28)
- Single chain Fv linear fragment
- BerH2 (J Mol Recognit 2003;16:28, Blood Cancer J 2017;7:e603, Am J Surg Pathol 2016;40:378, Blood 2014;124:2983)
- Most commonly used clone and has good correlation with mRNA levels
- Composed by 2 linear epitopes with identical sequence
- TNFRSF8
Pathophysiology
- CD30 gene is located at 1p36
- Close to TNFR2 and OX40
- Molecular weight of the protein: 120 kD
- Mature form of CD30 protein is processed from a precursor weighing 84 kD and during transit in the Golgi complex gains weight through glycosylation
- 3 domains:
- Extracellular (361 amino acids)
- Flower-like configuration
- 2 subdomains: D1 and D2
- Similar sequence when compared to TNFR molecules: 6 cysteine rich stretches of amino acids
- Implications in antibody binding
- Soluble form of CD30 (sCD30) is an 85 - 88 kD protein detected in inflammatory scenario and it is a product of the extracellular domain
- Transmembrane (28 amino acids)
- Intracellular (188 amino acids)
- Contains several serine / threonine residues, which can be phosphorylated
- Docking sites for protein binding and signaling transduction
- Contains several serine / threonine residues, which can be phosphorylated
- Extracellular (361 amino acids)
- Expression and function are related to the composition and functionality of the immune microenvironment (Blood Cancer J 2017;7:e603, Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print], J Mol Recognit 2003;16:28, Oncologist 2022 Aug 10 [Epub ahead of print], Blood 1995;85:1, Histopathology 2022;81:55, Clin Adv Hematol Oncol 2014;12:1)
- First monoclonal antibody was derived from Hodgkin lymphoma cell lines and identified in 1982 (Blood Cancer J 2017;7:e603)
- Ligand is CD30L (or TNFSF8 or CD153) (Blood Cancer J 2017;7:e603, J Mol Recognit 2003;16:28)
- Type II glycoprotein
- Extracellular C terminal domain is similar to TNFα, TNFβ, FasL, CD40L and CD70
- Can be detected in activated lymphocytes, histiocytes and granulocytes
- Stimulation of CD30 transmembrane protein leads to receptor trimerization and transduction of the signal to TNFR associated factor (TRAF) proteins (TRAF1, TRAF2 and TRAF5) (Blood Cancer J 2017;7:e603, Histopathology 2022;81:55)
- Signaling complex may activate both MAPK / ERK1 / ERK2 and NFκB pathways
- Direct or indirect (via JunB) activation of antiapoptosis, prosurvival or activation effects
- Signaling complex may activate both MAPK / ERK1 / ERK2 and NFκB pathways
- Viral infection may induce activation of CD30 in both B and T cells (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print], Clin Adv Hematol Oncol 2014;12:1)
- Cells that carry Epstein-Barr virus (EBV), human immunodeficiency virus (HIV) and human T cell leukemia / lymphoma virus type I (HTLV1)
- Elevated expression in autoimmune diseases (Clin Adv Hematol Oncol 2014;12:1)
- Rheumatoid arthritis, primary progressive multiple sclerosis, localized scleroderma, systemic lupus erythematous, atopic dermatitis, asthma and allergic rhinitis
- Role in the development of graft versus host disease (GVHD) (Clin Adv Hematol Oncol 2014;12:1)
- Inhibition is linked to decreased incidence of GVHD
Diagrams / tables
Clinical features
- Targetable biomarker (Oncologist 2022 Aug 10 [Epub ahead of print])
- High expression by neoplastic cells
- Low expression by normal cells
- Extracellular localization
- CD30 antibody drug conjugate (ADC): brentuximab vedotin (BV) (Blood Cancer J 2017;7:e603, Oncologist 2022 Aug 10 [Epub ahead of print])
- Composed of an IgG1 monoclonal antibody SGN 30 in combination with mono methyl auristatin E (MMAE) and a cathepsin linker
- ADC binds to the CD30 positive cell
- Receptor endocytosis and MMAE release
- Leads to inhibition of tubulin formation and cell apoptosis
- Receptor endocytosis and MMAE release
- Indications of BV
- Classic Hodgkin lymphoma (CHL) after autologous stem cell transplant or failure of at least 2 major multiagent chemotherapies
- Systemic or primary cutaneous anaplastic large cell lymphoma or CD30 positive mycosis fungoides after failure of at least 1 multiagent chemotherapy
- Frontline treatment of peripheral T cell lymphomas that express CD30, in combination with cyclophosphamide, doxorubicin and prednisone
- There is no correlation between CD30 expression levels by immunohistochemistry and response to therapy
- CD30 specific chimeric antigen receptor T (CAR T) cells (Blood Cancer J 2017;7:e603, J Clin Oncol 2020;38:3794, Sci Rep 2022;12:10488, Front Immunol 2022;13:858021)
- 3 generations of anti-CD30 CAR T cells
- Phase I / II studies in relapsed / refractory CHL
- Association with anti-PD1 regimen can improve the efficacy of CD30 CAR T therapy
Interpretation
- Typically expressed in cytoplasmic / membrane compartments (Histopathology 2022;81:55)
- May have weak, moderate or strong intensity
- Golgi pattern can also be found isolated or in association with cytoplasmic / membrane staining
- Rare
- Nuclear staining is not acceptable
- May have a membrane enhancement in reactive mesothelial cells
Uses by pathologists
- Differential diagnosis and assessment of lymphomas in which the neoplastic cells universally express CD30 (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print], Oncologist 2022 Aug 10 [Epub ahead of print], Am J Clin Pathol 2022;158:173)
- Classic Hodgkin lymphoma (CHL)
- Anaplastic large cell lymphoma and subtypes
- Usually negative for IRF8, helping in the differential diagnosis with CHL
- Lymphomatoid papulosis
- Any degree of CD30 expression should be reported (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print])
- BerH2 is the most used (J Mol Recognit 2003;16:28)
- Recommendations for testing (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print])
- All cases of T cell lymphomas
- Relapsed / refractory setting of diffuse large B cell lymphoma or primary mediastinal B cell lymphoma
- Clinical trial requests
- IHC testing is the preferred methodology (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print])
- Recommendations for assay best performance
- Preanalytical phase
- Tissue should be fixed in 10% neutral pH, phosphate buffered formalin for 8 - 72 hours
- Analytical phase
- Follow protocols and control tissues from NordiQC
- Postanalytical phase
- Estimation of positive neoplastic cells: 0%, 1 - 10% and after in 10% increments (or ranges)
- Record descriptively the nonneoplastic cells in the background and if possible, estimate the percentage
- Excisional biopsy is the preferred tissue for testing; better than needle biopsies or fine needle aspirates
- Preanalytical phase
- Sensitivity of flow cytometry varies with the type of tumor and demands technical skill
- Recommendations for assay best performance
Prognostic factors
- Expression of CD30 is associated with outcomes in lymphomas in which there is a heterogeneous expression
- Decreased hazard of death in transformed mycosis fungoides (Am J Clin Pathol 2021;156:350)
- Poor overall and progression free survival in extranodal NK / T cell lymphoma cases with expression of CD30 in 50% or more of the neoplastic cells (Oncol Lett 2017;13:1211, BMC Cancer 2014;14:890)
- Expression of CD30 is correlated with presence of B symptoms and elevated serum lactate dehydrogenase
- Better outcomes in cases of diffuse large B cell lymphoma treated with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) (Hum Pathol 2017;60:160)
Microscopic (histologic) images
Contributed by Roberto N. Miranda, M.D.
Positive staining - normal
- Transient activated B, T and NK lymphocytes (Blood Cancer J 2017;7:e603, Oncologist 2022 Aug 10 [Epub ahead of print], J Pathol 2000;190:613)
- < 1% of circulating cells
- Range of expression intensities from weak to strong
- Stimulated B immunoblasts at the edge of the germinal center
- Subpopulations of CD4+ / CD45RO+ and CD8+ cells in lymph node and thymic medulla
- Faint reactivity in scattered lipoblasts, myoepithelial cells and decidual cells (J Pathol 2000;190:613)
- Heterogeneous positivity in activated mesothelium (J Pathol 2000;190:613)
- Early human fetal development tissues (Clin Adv Hematol Oncol 2014;12:1)
- 8 - 10 weeks: expression by all 3 germ layers
- 10 - 12 weeks: skin and hematolymphoid tissues
- After 12 weeks: hematolymphoid tissues
Positive staining - disease
- Classic Hodgkin lymphoma (CHL) (Blood Cancer J 2017;7:e603, Am J Clin Pathol 2022;158:173)
- Anaplastic large cell lymphoma (ALCL) and subtypes: defined as > 75% of the cells (Blood Cancer J 2017;7:e603, Am J Clin Pathol 2022;158:173)
- ALK+ ALCL
- ALK- ALCL
- Primary cutaneous ALCL
- Breast implant associated ALCL
- Lymphomatoid papulosis (J Eur Acad Dermatol Venereol 2020;34:59)
- Primary effusion lymphoma and variants (Onco Targets Ther 2018;11:3747)
- Primary mediastinal large B cell lymphoma (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print])
- EBV+ diffuse large B cell lymphoma (Blood Adv 2021;5:3227)
- Mediastinal gray zone lymphoma (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print])
- EBV+ large B cell lymphoma associated with breast implants (Mod Pathol 2021;34:2154)
- EBV+ mucocutaneous ulcer (Am J Clin Pathol 2017;147:129)
- EBV+ T and NK cell lymphoid proliferations and lymphomas of the childhood (Blood 2013;122:3101)
- Variable positivity in hydroa vacciniforme lymphoproliferative disorder and severe mosquito bite allergy
- Extranodal NK / T cell lymphoma but it can be detected in up to 47% of cases (Oncol Lett 2017;13:1211, BMC Cancer 2014;14:890, Chin J Cancer 2017;36:43)
- Mycosis fungoides (Blood Cancer J 2017;7:e603, Oncologist 2022 Aug 10 [Epub ahead of print], Histopathology 2022;81:55)
- Can be detected in up to 90% of the patients but usually has scattered positivity in the neoplastic cells; more consistent CD30 reactivity in cases of large cell transformation
- Usually located in the dermal neoplastic cells
- Variability within individual patients and individual lesions
- Primary cutaneous gamma delta T cell lymphoma; can be positive in up to 60% of cases (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print], Am J Surg Pathol 2017;41:431)
- Enteropathy associated T cell lymphoma (Blood 2014;124:2983, Gastroenterology 2007;132:1902)
- Frequent positivity but scattered: < 50% of the neoplastic cells
- Usually associated with anaplastic morphology
- Advanced systemic mastocytosis (Blood Cancer J 2017;7:e603)
- Hodgkin-like histiocytosis (Histopathology 2022;81:371)
- Embryonal carcinoma (Blood Cancer J 2017;7:e603, J Pathol 2000;190:613)
- Infectious mononucleosis (Blood 1995;85:1)
Negative staining
- Acute myeloid leukemia / myeloid sarcoma; reactivity weak in 30% of AML cases and negative in acute monocytic leukemias (Clin Lymphoma Myeloma Leuk 2013;13:307)
- Multiple myeloma (Leuk Lymphoma 2021;62:2845)
- Diffuse large B cell lymphoma; CD30 expressed in 10 - 15% of cases (Hum Pathol 2017;60:160, Mod Pathol 2015;28:1202)
- Follicular lymphoma (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print])
- Lymphomatoid granulomatosis (Am J Surg Pathol 2015;39:141)
- Plasmablastic lymphoma; expressed in 20 - 30% of cases (Blood 2015;125:2323)
- ALK+ large B cell lymphoma; 14% of cases were positive (Leuk Lymphoma 2021;62:2845)
- Nodular lymphocyte predominant Hodgkin lymphoma; when positive, reactivity is faint (Hematology Am Soc Hematol Educ Program 2017;2017:324)
- Sézary syndrome (Arch Pathol Lab Med 2022 Apr 26 [Epub ahead of print])
- Hepatosplenic T cell lymphoma (Blood 2014;124:2983)
- Adult T cell leukemia / lymphoma (Blood 2014;124:2983)
- Indolent T cell lymphoma of the gastrointestinal tract (Haematologica 2020;105:1895)
- Angioimmunoblastic T cell lymphoma (Am J Surg Pathol 2016;40:378)
- Majority of cases show scattered positive cells
- Can be positive in both B and T cell compartments
- Peripheral T cell lymphoma, not otherwise specified (Am J Surg Pathol 2016;40:378)
- Heterogeneous and scattered positivity
- Dermatopathic lymphadenopathy (Mod Pathol 2020;33:1104)
- Scattered immunoblasts in the background may be positive
- Kikuchi-Fujimoto disease (Appl Immunohistochem Mol Morphol 2018;26:274)
- Positivity in scattered immunoblasts
- Progressive transformation of germinal centers (Int J Pediatr Otorhinolaryngol 2002;65:195)
- Syphilis (Am J Dermatopathol 2022 Jul 19 [Epub ahead of print])
- Rare cases reporting strong and diffuse positivity in the lymphocytic infiltrate
- Inflammatory myofibroblastic tumor (Leuk Lymphoma 2021;62:2845)
- Malignant melanoma (Blood 1995;85:1)
- Seminoma (J Pathol 2000;190:613)
- Malignant mesothelioma (J Pathol 2000;190:613)
- Yolk sac tumor (J Pathol 2000;190:613)
- Choriocarcinoma (J Pathol 2000;190:613)
- Spermatocytic tumor (J Pathol 2000;190:613)
Molecular / cytogenetics description
- Chromosomal aberrations of the short arm of chromosome 1 are described in CHL, which could be related to the CD30 expression in this entity (Blood 1995;85:1)
Sample pathology report
- Right breast capsule, complete capsulectomy:
- Fibrous breast capsule with mild chronic inflammation
- No morphologic or immunophenotypic support for lymphoma
- Histologic sections of the right breast capsule show a fibrinous breast capsule with scattered small and mature lymphocytes. Synovium-like lining formation and silicone particles are occasionally seen. There are rare foci of breast glandular epithelium on the outer surface of the specimen.
- Immunohistochemical stains are performed and the cells are negative for CD30, while CD3 and CD20 highlight small and mature T and B lymphocytes, respectively.
- Left breast capsule, complete capsulectomy:
- Breast implant associated anaplastic large cell lymphoma (see comment)
- Tumor is confined to the inner surface of the peri-implant capsule (pathologic stage T1) and margins are negative
- Comment: According to clinical notes, the patient is a 52 year old woman with a history of bilateral breast implant placement 9 years ago due to aesthetic reasons. She noticed swelling of the left breast 10 months ago and it was initially attributed to capsular contracture and spontaneously resolved; however, 1 month ago, the swelling recurred with an ipsilateral accompanying effusion, which was aspirated. The cytologic and immunophenotypic examination showed neoplastic cells consistent with anaplastic large cell lymphoma and a bilateral complete capsulectomy was recommended.
- Histologic sections of the left breast capsule show a thick and fibrinous breast capsule with rare, large and atypical lymphocytes with hyperchromatic and irregular surface in the luminal side of the capsule. Associated with the atypical lymphocytes, there is a dense lymphocytic infiltrate composed predominantly of small and mature lymphocytes.
- Scrapings from the left breast implant surface show a high number of atypical cells with same cytological features of the capsule. Karyorrhectic debris is also present within the implant scrapings.
- Touch preparation slides performed on the left breast capsule show rare large cells with irregular, multilobated nuclei and moderate cytoplasm.
- Immunohistochemical stains are performed. The neoplastic cells are positive for CD2, CD5, CD8 and CD30 and are negative for CD3, CD4, CD7, CD10, CD56, TCR alpha beta and TCR gamma delta. Epstein-Barr virus encoding region (EBER) in situ hybridization is negative.
- In summary, the clinicopathological features are diagnostic of breast implant associated anaplastic large cell lymphoma.
Additional references
Board review style question #1
Which of the following is true about CD30 expression?
- CD30 belongs to tumor necrosis factor receptor superfamily
- High CD30 expression is required in lymphoma cells to predict better response to anti-CD30 therapy (brentuximab vedotin)
- It is a protein with exclusive extracellular domain
- Naïve normal B and T cells can express CD30
- There is an inconsistent correlation between the immunohistochemical expression of CD30 and mRNA levels
Board review style answer #1
A. CD30 belongs to tumor necrosis factor receptor superfamily. CD30 is a transmembrane glycoprotein, which belongs to tumor necrosis factor receptor superfamily. CD30, also known as BerH2, Ki1 or TNFRSF8, is a transmembrane glycoprotein receptor that belongs to the tumor necrosis factor receptor (TNFR) and was first identified in Hodgkin lymphoma cell lines but also expressed in normal activated B and T cells. This protein has an extracellular transmembrane and intracellular domains and the similarity of CD30 and other proteins of TNFR family is restricted only to the extracellular domain. Immunohistochemical expression of CD30 has a high concordance with mRNA levels. Interestingly, patients with any number of positive CD30+ cells in lymphoma cases can benefit from therapy with brentuximab vedotin, not only those cases that show all tumor cells positive for CD30.
Comment Here
Reference: CD30
Comment Here
Reference: CD30
Board review style question #2
Board review style answer #2
A. Classic Hodgkin lymphoma and anaplastic large cell lymphoma are typically positive for CD30, while nodular lymphocyte predominant Hodgkin lymphoma, follicular lymphoma and hepatosplenic T cell lymphoma are negative for CD30. Testicular embryonal but not choriocarcinoma is usually positive for CD30.
Comment Here
Reference: CD30
Comment Here
Reference: CD30
CD30-39
Table of Contents
CD30 | CD31 | CD32 | CD33 | CD34 | CD35 | CD36 | CD37 | CD38 | CD39 | Diagrams / tables | Microscopic (histologic) imagesCD30
- See CD30
CD31
- See CD31
CD32
- Low affinity receptor to the Fc region of IgG
- Also called Fc gamma RII
- Subtyped as:
- Fc gamma RIIa (OMIM: 146790 [Accessed 6 May 2021])
- RIIb (OMIM: 604590 [Accessed 6 May 2021])
- RIIc (OMIM: 612169 [Accessed 6 May 2021])
- Pathophysiology: low affinity receptor on white blood cells (see below) that binds to the Fc region of IgG immune complexes to remove foreign antigens
- Clinical features:
- Polymorphisms affects incidence or severity of some diseases, including:
- Antiphospholipid syndrome (Arthritis Rheum 2003;48:1930)
- IgA nephropathy (Nephrol Dial Transplant 2005;20:2439)
- Malaria (Am J Trop Med Hyg 2003;69:565)
- Myasthenia gravis (J Neuroimmunol 2003;144:143)
- Onchocerciasis (Am J Trop Med Hyg 2007;77:1074)
- Peripheral atherosclerosis (Thromb Haemost 2004;92:1273)
- Rheumatic fever (Clin Biochem 2004;37:925)
- Systemic lupus erythematosus (Arthritis Rheum 2002;46:1563)
- In dendritic cells, CD32a is considered an activating isoform and CD32b an inhibitory isoform; the balance between these receptors establishes a threshold of activation and enables immune complexes to mediate opposing effects on dendritic cell maturation and function (J Clin Invest 2005;115:2914)
- Polymorphisms affects incidence or severity of some diseases, including:
- Uses by pathologists: preincubation with CD16 / CD32 antibodies is commonly used to prevent nonspecific binding; no significant clinical use by pathologists
- Positive staining - normal:
- CD32a: monocytes, macrophages; B cells, basophils, eosinophils, granulocytes, NK cells, plasma cells (some), platelets
- CD32b: most broadly distributed Fc receptor; monocytes / macrophages; also basophils, B cells eosinophils, Langerhans cells, neutrophils, placenta endothelial cells, platelets; not NK cells
- CD32c: monocytes, macrophages, neutrophils, NK cells
- Positive staining - disease: follicular lymphoma, histiocytic sarcoma
- Negative staining: T cells (usually) (Immunology 1997;90:109)
CD33
- See CD33
CD34
- See CD34
CD35
- Dendritic cell marker
- Mediates cellular binding of particles and immune complexes that have activated complement
- Also called erythrocyte complement receptor 1 (CR1), C3b and C4b receptor
- Pathophysiology:
- Binds immune complexes coated with C3b or C4b and mediates their transport to and removal by the fixed phagocyte systems of the spleen and liver
- Cofactor for specific proteolytic cleavage of C3b and C4b by plasma serine protease factor I, which limits complement activation and produces ligands for other complement receptors
- The Knops, McCoy, Swain-Langley and York blood group antigens are located on CD35 (Blood Group Antigen Gene Mutation Database)
- Follicular dendritic cells form a reticular network in the lymphoid follicle necessary to retain and present native antigens (in the form of antigen antibody immune complexes) to B cells during the secondary immune response
- CD21, CD23 and CD35 are dendritic cell markers
- Clinical features:
- Reduced expression in erythrocytes in:
- Gallbladder carcinoma (World J Gastroenterol 2004;10:3480)
- Preeclampsia (Am J Reprod Immunol 2005;54:352)
- Severe acute respiratory syndrome (Clin Exp Immunol 2005;139:112)
- Mesangiocapillary glomerulonephritis, systemic lupus erythematosis (Arthritis Rheum 2004;50:3596)
- Acts as a malaria resistance gene and deficiencies of CR1 are protective against Plasmodium falciparum (Proc Natl Acad Sci USA 2004;101:272)
- Specific genotype is associated with sarcoidosis in females (Am J Respir Cell Mol Biol 2002;27:17)
- Reduced expression in erythrocytes in:
- Uses by pathologists:
- Diagnose follicular dendritic cell sarcoma (Am J Surg Pathol 1996;20:944)
- Highlight or confirm lack of dendritic cell germinal center meshwork
- For example: splenic B cell lymphoma (Am J Surg Pathol 2003;27:903)
- Positive staining - normal: follicular dendritic cells, erythrocytes; basophils, eosinophils, granulocytes, monocytes, macrophages (some), B cells, T cells (10%), NK cell subset, some astrocytes
- Positive staining - disease:
- Follicular dendritic cell sarcoma (Am J Surg Pathol 1998;22:1048, Mod Pathol 2002;15:50)
- Hodgkin lymphoma (Reed-Sternberg cells in 5%) (Am J Surg Pathol 1999;23:363)
- Inflammatory GI fibroid polyps (focal in stromal cells) (Am J Surg Pathol 2004;28:107)
- Splenic marginal zone lymphoma (some cases) (Am J Surg Pathol 2007;31:438)
- Occasionally other B cell lymphomas (J Appl Oral Sci 2009;17:248)
- Negative staining:
- Langerhans cells (normal and tumors)
- Fibroblastic reticulum cell tumor, gastrointestinal stromal tumor, histiocytic sarcoma (Am J Surg Pathol 1994;28:1133)
- Inflammatory myofibroblastic tumor (Am J Surg Pathol 1998;22:412)
- Interdigitating dendritic cell tumor (Am J Surg Pathol 1999;23:1141)
- Reference: OMIM: 120620 [Accessed 6 May 2021]
CD36
- Scavenger receptor with numerous physiologic functions
- Also known as platelet GPIV or GPIIIb, fatty acid translocase (FAT)
- Pathophysiology:
- Numerous potential physiologic functions (see Clinical Features below)
- Serves as a scavenger receptor for oxidized phospholipids, apoptotic cells and certain microbial pathogens (Trans Am Clin Climatol Assoc 2010;121:206)
- Receptor for thrombospondin, collagen, oxidized LDL
- Gives rise to Naka antigen
- Clinical features:
- Associated with platelet disorders:
- Acts as cell adhesion molecule in platelet adhesion and aggregation, platelet monocyte and platelet tumor cell interactions
- CD36 isoantibody may cause:
- Posttransfusion purpura and platelet transfusion refractoriness (Transfusion 1995;35:777)
- Life threatening hypotension and thrombocytopenia (Transfusion 2005;45:803)
- Hydrops fetalis (Thromb Haemost 2006;95:267)
- CD36 deficiency causes platelet glycoprotein IV deficiency (OMIM: 608404 [Accessed 6 May 2021])
- More common in Asians and Africans
- Divided into 2 subgroups
- Type I is characterized by platelets and monocytes / macrophages exhibiting complete CD36 deficiency
- Type II lacks the surface expression of CD36 in platelets but expression in monocytes / macrophages is near normal
- CD36 deficiency is associated with hyperlipidemia, insulin resistance and mild hypertension (Mol Cell Biochem 2007;299:19)
- Associated with atherosclerosis:
- Scavenger receptor for oxidized LDL and shed photoreceptor outer segments (Atherosclerosis 2006;184:15)
- Also transports long chain fatty acids
- Upregulated in familial combined hyperlipidemia (FASEB J 2005;19:2063)
- Genetic variations in CD36 are associated with susceptibility to coronary heart disease type 7
- CD36 may be taste receptor for fatty acids (J Clin Invest 2005;115:2965)
- Associated with malaria:
- Site of cytoadherence of Plasmodium falciparum infected erythrocytes to microvascular endothelial cells
- CD36 deficiency is frequent in sub Saharan Africa and Asia and is associated surprisingly with susceptibility to severe cerebral malaria
- Associated with Alzheimer’s disease:
- May mediate binding to fibrillar beta amyloid
- Present in microglia and endothelium in Alzheimer's disease
- Low levels on peripheral blood leukocytes in Alzheimer patients (Neurobiol Aging 2007;28:515)
- Associated with platelet disorders:
- Positive staining - normal:
- Platelets, monocytes, macrophages, basophils, endothelial cells, early erythroid cells, megakaryocytes
- Also adipose tissue, breast epithelial cells, cardiac muscle, Sertoli cells of testis (elderly men and those with hypospermatogenesis), skeletal muscle, splenic cells (Hum Pathol 2004;35:34)
- Positive staining - disease:
- Alzheimer’s disease (microglia, endothelial cells) (Am J Pathol 2002;160:101)
- AML M4 - M7, cervical LSIL (Hum Pathol 1994;25:73)
- CML (60%) (Mod Pathol 1998;11:1211)
- Gaucher cells (Am J Clin Path 2004;122:359)
- Myxoid liposarcoma (Am J Clin Path 1995;103:20)
- Plasmacytoid T cell lymphoma (Am J Clin Path 1990;93:822)
- Transient myeloproliferative disorder in Down’s syndrome (Am J Clin Path 2001;116:204)
- Negative staining: AML M0 - M2 (usually), AML M3 (Am J Clin Path 1998;109:211)
- References: OMIM: 173510 [Accessed 6 May 2021], Wikipedia: CD36 [Accessed 6 May 2021]
CD37
- Member of tetraspanin family (members have 4 hydrophobic domains, others are CD9, CD53, CD63, CD81, CD82 and CD151)
- Regulates T cell proliferation (J Immunol 2004;172:2953)
- Clinical features: inhibits IgA responses and regulates the anti-fungal immune response (PLoS Pathog 2009;5:e1000338)
- No significant clinical use by pathologists
- Positive staining - normal: B cells, T cells (low), neutrophils (low), monocytes (low), macrophages, dendritic cells
- Positive staining - disease: most B cell lymphomas, some T cell lymphomas (Leukemia 1994;8:1864)
- Negative staining: NK cells, platelets, erythrocytes, plasma cells; plasma cell neoplasms, pre-B-ALL (or low)
- Reference: OMIM: 151523 [Accessed 6 May 2021]
CD38
- See CD38
CD39
- Endothelial ATPase that blocks platelet activation
- Also called ectonucleoside triphosphate diphosphohydrolase (NTPDase1)
- Pathophysiology:
- Plasma membrane bound enzyme that hydrolyzes extracellular ATP and ADP to AMP (Platelets 2005;16:159)
- Acts as important inhibitor of platelet activation by blocking platelet aggregation responses to ADP
- Highly expressed on regulatory Foxp3(+) CD4 T cells
- May have a therapeutic anti-thrombotic effect (Semin Thromb Hemost 2005;31:234)
- Biochemical activity is lost at sites of acute vascular injury, such as in ischemia reperfusion and immune graft rejection (Blood Cells Mol Dis 2006;36:217)
- Also regulates vascular and immune cell adhesion and signaling events pivotal in inflammation (Biochem J 2006;396:23)
- Plasma membrane bound enzyme that hydrolyzes extracellular ATP and ADP to AMP (Platelets 2005;16:159)
- Clinical features:
- Increased expression in lymphocytes of HIV+ patients (Biochim Biophys Acta 2005;1746:129)
- Presence in coronary atheromatous plaque may prevent acute coronary syndromes (Am J Cardiol 2005;95:632)
- Expression in HIV correlates with progressive disease and viral load (J Virol 2011;85:1287)
- Can be used to isolate functionally active Treg from peripheral blood (J Immunol Methods 2009;346:55)
- No significant clinical use by pathologists
- Positive staining - normal:
- Activated B cells, cytotoxic T cells (Eur J Immunol 1992;22:2681)
- Monocytes, macrophages, NK cells
- Endothelial cells, Langerhans cells (J Invest Dermatol 2005;125:482)
- Pancreas (J Histochem Cytochem 2002;50:549)
- Placenta (Eur J Histochem 2004;48:253)
- Vascular smooth muscle
- Reference: OMIM: 601752 [Accessed 6 May 2021]
Microscopic (histologic) images
CD31
Table of Contents
Definition / general | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Cell adhesion molecule required for leukocyte transendothelial migration under most inflammatory conditions
- Most sensitive and specific endothelial marker in paraffin sections
Terminology
- Also known as platelet endothelial cell adhesion molecule (PECAM1, OMIM 173445), PECA1, GPIIA, endoCAM, CD31 / EndoCAM (Entrez Gene: platelet / endothelial cell adhesion molecule)
Pathophysiology
- Member of immunoglobulin superfamily
- Ligands are CD38 and vitronectin receptor (αvβ3 integrin, CD51 / CD61) (Cancer 2003;97:1914, J Cell Biol 1995;130:451)
- Cell adhesion molecule that is found on the surface of platelets, monocytes, neutrophils and some types of T cells
- Major constituent of endothelial intercellular junction
- Plays a key role in leukocyte trafficking across endothelium / transendothelial migration (Blood 2003;101:2816) and integrin activation
- Also important for angiogenesis and removal of aged neutrophils from body
- May mediate signal-transduction pathway regulating capacitation in spermatozoa (J Cell Sci 2005;118:4865)
- May act as a minor histocompatibility antigen in HLA identical stem cell transplantation (Bone Marrow Transplant 2005;36:151)
Clinical features
- CD31+ T cells (angiogenic T cells) have vasculoprotective and neovasculogenic qualities; undergo numerical and functional impairments with advancing age (J Appl Physiol 2010;109:1756)
- CD31+ Annexin V+ circulating microparticles are risk factor for cardiovascular disease (Eur Heart J 2011;32:2034)
Interpretation
- Membranous (not cytoplasmic) immunostain; endothelium is a positive internal control
- Potential pitfall: don't confuse CD31+ macrophages (granular, membranous expression) with a vascular tumor (Am J Surg Pathol 2001;25:1167)
Uses by pathologists
- Most sensitive and specific endothelial marker in paraffin sections; stains small and large vessels
- Confirms vascular origin of tumors, but may also stain nodal sinuses (J Clin Pathol 2003;56:638)
- Identifies/confirms vascular invasion (J Clin Pathol 2003;56:786, Arch Pathol Lab Med 2005;129:354), although D240 may be more sensitive (Am J Clin Pathol 2009;131:92, Am J Surg Pathol 2007;31:1825)
- Assesses tumor microvessel density, a possible prognostic factor, although D240 and endoglin / CD105 (Am J Clin Pathol 2008;129:578) may be more sensitive
Microscopic (histologic) images
Cases #107, 187, 77
Images hosted on other servers:
Normal structure:
Benign vascular tumors / processes:
Positive staining - normal
- Endothelial cells at cell junctions, including alveolar wall capillaries, glomeruli, sinuses in liver, lymphatics, spleen (J Histochem Cytochem 2006;54:385), megakaryocytes (Arch Pathol Lab Med 2002;126:618), pericytes, platelets
- Also basophils, granulocytes, Kupffer cells, macrophages, monocytes, NK cells, osteoclasts, plasma cells (extramedullary strong; bone marrow focal, J Clin Pathol 1997;50:490), T cells (some)
- Also brown fat (Arch Pathol Lab Med 2006;130:480), fibroblasts, spermatozoa, trophoblast (Mol Hum Reprod 1998;4:357)
Positive staining - disease
- Vascular lesions: angiosarcoma, benign vascular proliferations (Am J Surg Pathol 2002;26:328), blood vessels in tumors (usually), hemangioendothelioma (Am J Surg Pathol 2003;27:48, Am J Surg Pathol 2004;28:559), hemangioendothelioma-pseudomyogenic (variable, Am J Surg Pathol 2011;35:190), hemangioma, intravascular papillary endothelial hyperplasia (Hum Pathol 1996;27:986), Kaposi sarcoma (75% of AIDS-related cases, 58% of non AIDS related cases; Arch Pathol Lab Med 2012;136:301), littoral cell angioma of spleen, lymphangioendothelioma (Am J Surg Pathol 2000;24:1047), lymphangioma (Hum Pathol 2005;36:426), papillary endovascular angioendothelioma (Am J Surg Pathol 1999;23:1004), primary cutaneous epithelioid angiosarcoma (Am J Surg Pathol 2011;35:60), sclerosing angiomatoid nodular transformation of spleen (Am J Surg Pathol 2004;28:1268), splenic hamartoma
- Other lesions: breast DCIS-high grade (J Pathol 2001;194:254), cardiac myxoma, epithelioid sarcoma (focal in 7%, Hum Pathol 1999;30:934, Virchows Arch 2003;443:93), Ewing sarcoma / PNET (focal in 5%, Appl Immunohistochem Mol Morphol 2000;8:19), giant cell tumor of tendon sheath, granulocytic sarcoma (25%, Am J Clin Pathol 1994;102:55), hibernoma, histiocytes in granulomas, histiocytic sarcoma (Am J Surg Pathol 2004;28:1133), intimal sarcoma of large systemic vessels (Am J Surg Pathol 2005;29:1184), juvenile xanthogranuloma, Langerhans cell histiocytosis, lymphoblastic lymphoma (Appl Immunohistochem Mol Morphol 2000;8:19), plasmacytomas (50%), sinus histiocytosis with massive lymphadenopathy (Arch Pathol Lab Med 2003;127:341); rare in carcinoma and mesothelioma (Am J Clin Pathol 1998;110:374)
Negative staining
- B cells, epidermal Langerhans cells, vascular adventitial fibroblastic cells, vas deferens (Am J Clin Pathol 2009;132:893)
- Adenomatoid tumor (Appl Immunohistochem Mol Morphol 2012;20:173), aneurysmal fibrous histiocytoma, cellular angiofibroma (Mod Pathol 2011;24:82), gastrointestinal stromal tumor, giant cell fibroblastoma, lipomatous hemangiopericytoma (Hum Pathol 2000;31:1108), mesothelial cyst (Am J Surg Pathol 1997;21:334), mycobacterial pseudotumor (Am J Surg Pathol 1999;23:656), myeloma, nonvascular soft tissue tumors, peripheral T cell lymphoma, ovarian microcystic stromal tumors (Am J Surg Pathol 2011;35:1429), pseudoangiomatous stromal hyperplasia of breast, sclerosing hemangioma of lung (Arch Pathol Lab Med 2001;125:1335), sinonasal hemangiopericytoma, solitary fibrous tumor (Hum Pathol 1995;26:440)
CD33
Table of Contents
Definition / general | Pathophysiology | Clinical features | Uses by pathologists | Positive staining - normal | Positive staining - disease | Negative staining | Additional referencesDefinition / general
- Classic myeloid antigen (also CD13)
Pathophysiology
- Glycosylated transmembrane protein of sialic acid binding immunoglobulin-like lactic (siglec) family
- May mediate cell to cell adhesion; acts as receptor that inhibits the proliferation of normal and leukemic myeloid cells
Clinical features
- Gemtuzumab ozogamicin (anti-CD33 antibody), was previously used to treat AML (Wikipedia - Gemtuzumab ozogamicin, BioDrugs 2006;20:137, Cancer 2005;104:1442)
- Used for negative selection for stem cells
Uses by pathologists
- Distinguish myeloid (CD33+) and lymphoid leukemias (CD33-)
- Identify monocytes by flow cytometry
Positive staining - normal
- Progenitor and other myeloid cells (decreasing expression with maturation, Am J Pathol 2001;158:1473)
- Basophils, granulocytes (low level expression), mast cells (Am J Pathol 1996;149:1493), monocytes (most), NK cells, plasmacytoid dendritic cells, T cells (some, J Leukoc Biol 2006;79:46)
- Epidermal Langerhans cells (variable)
Positive staining - disease
- AML M0 (almost all, Am J Clin Pathol 2001;115:876), M1-M5 (75-85%), M7 (variable)
- ALK+ anaplastic large cell lymphoma (Am J Clin Pathol 2008;130:628), CML (90%), chronic myelomonocytic leukemia, myeloid / granulocytic sarcoma (J Clin Pathol 2005;58:325), transient myeloproliferative disorder (Am J Clin Pathol 2001;116:204)
- CD4+ CD56+ acute leukemias (Blood 2005;105:1256) and lineage negative malignancies (weak in 44%, Am J Surg Pathol 2005;29:1274)
- Myeloma and plasmacytoma (occasional reports)
- Burkitt’s lymphoma (J Clin Pathol 1993;46:778), SLL/CLL (Am J Clin Pathol 2003;119:824) or T-ALL (Am J Clin Pathol 2000;113:823)
- More intense in bone marrow than peripheral blood
Negative staining
- Pluripotent stem cells, B cells
- Most B and T cell lymphomas, blastic NK lymphoma (usually)
- Not expressed outside hematopoietic system
Additional references
CD34
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- 110kDa glycosylated transmembrane protein
- Marker of vascular endothelial cells
- Sensitive but not specific marker for neoangiogenesis
- May mediate attachment of hematopoietic stem cells to bone marrow extracellular matrix or directly to stromal cells, although specific function is unknown
Essential features
- Good marker for neoangiogenesis
- Helpful to distinguish liver lesions (focal nodular hyperplasia [CD34-] versus hepatocellular carcinoma [CD34+ in sinusoidal spaces])
- Screening marker to differentiate between soft tissue neoplasms
- Marker for hematopoietic progenitor cells - blasts
Terminology
- Hematopoietic progenitor cell antigen CD34
- CD34+ stromal cells are called dendritic interstitial cells
Pathophysiology
- Intercellular adhesion protein and cell surface glycoprotein; ligand is CD62L (L selectin)
- May mediate attachment of hematopoietic stem cells to bone marrow extracellular matrix or directly to stromal cells, although specific function is unknown
- CD34 staining defines adult hematopoietic stem cells but CD34+ cells can also differentiate into neural cells (Exp Neurol 2006;197:399)
Interpretation
- Membranous stain
- Endothelium acts as a positive internal control
- Staining represents presence of protein, not cross reactivity, despite wide range of tissues that are CD34+ (Am J Pathol 2000;156:21)
Uses by pathologists
- Dermatopathology and soft tissue
- Distinguish CD34+ dermal neoplasms, such as Kaposi sarcoma (CD34+), dermatofibrosarcoma protuberans (DSFP) (CD34+) and epithelioid sarcoma (often CD34+) from dermatofibroma (CD34-)
- Distinguish solitary fibrous tumor (CD34+) from desmoplastic mesothelioma (CD34-) (Hum Pathol 1995;26:428)
- Distinguish hemangiopericytoma (CD34+) from endometrial stromal sarcoma (CD34-) (Mod Pathol 2005;18:40)
- Classify other soft tissue tumors
- Hematopathology
- Distinguish lymphocyte rich thymoma (CD34+ cells) from T cell acute lymphoblastic leukemia (T ALL, CD34-) (Am J Clin Pathol 2004;121:268)
- Quantify and purify lymphohematopoietic stem cell / progenitor cells for research and for clinical bone marrow transplantation (Folia Histochem Cytobiol 2006;44:53, Breast Cancer 2005;12:178)
- Identify blasts in general and in hypoplastic marrows (Am J Clin Pathol 2010;134:749)
- Distinguish acute leukemia and myelodysplastic syndrome (CD34+ blasts present) from aplastic anemia (no blasts / low marrow CD34+ cells) (Leukemia 2006;20:458)
- Identify hematogones and megakaryocytes (CD34+), although not all myeloblasts are CD34+ (Arch Pathol Lab Med 2002;126:823)
- May support the diagnosis of essential thrombocythemia
- Poor prognostic factor in newly diagnosed acute myeloid leukemia (AML) (Neoplasma 2005;52:402)
- Other
- Determine vascularization of tumors or disease processes (Saudi Med J 2006;27:154)
- Distinguish vascular invasion (CD34+) from displaced epithelium (CD34-) (J Clin Pathol 2002;55:780)
- Confirm diagnosis of gastrointestinal stromal tumor (GIST) (Arch Pathol Lab Med 2002;126:1189)
- May confirm diagnosis of chronic intestinal pseudo-obstruction (Am J Surg Pathol 2003;27:228)
- Use with other stains to distinguish meningeal solitary fibrous tumor hemangiopericytoma from meningioma (Am J Surg Pathol 2015;39:1377)
- Determine microvessel density; high microvessel density (using CD34) is associated with
- Poorer prognosis in esophageal squamous cell carcinoma (J Clin Pathol 2001;54:940)
- Poor survival in nonsmall cell lung cancer (J Clin Pathol 2004;57:591)
- Prostate specific antigen (PSA) recurrence of prostate cancer (Am J Clin Pathol 2000;113:555)
Prognostic factors
- Poor prognostic factor in newly diagnosed acute myeloid leukemia (Neoplasma 2005;52:402)
- Determine microvessel density; high microvessel density (using CD34) is associated with
- Poorer prognosis in esophageal squamous cell carcinoma (J Clin Pathol 2001;54:940)
- Poor survival in nonsmall cell lung cancer (J Clin Pathol 2004;57:591)
- PSA recurrence of prostate cancer (Am J Clin Pathol 2000;113:555)
Microscopic (histologic) description
- Membranous
Microscopic (histologic) images
Positive staining - normal
- Endothelium of blood vessels (including alveolar wall capillaries and glomeruli but not hepatic sinusoids or splenic sinusoids), endothelium of some lymphatics (J Histochem Cytochem 2006;54:385)
- Hematopoietic progenitor cells / hematogones (less mature) (Am J Clin Pathol 2009;132:573)
- Also dendritic interstitial cells, dermal dendrocytes, endometrial stroma, endoneurium, fibroblasts, fibrocytes, follicle cells, interstitial cells of Cajal (20%), mast cells, megakaryocytes, neural stem cells in CNS, osteoblasts, perivascular stroma, umbilical cord blood, vascular adventitial fibroblastic cells in stomach (Mod Pathol 2003;16:293, Am J Pathol 2000;156:1157, Exp Neurol 2006;197:399, J Clin Pathol 2001;54:428)
Positive staining - disease
- Acral pseudolymphomatous angiokeratoma of children (APACHE) (J Cutan Pathol 2015;42:50)
- Acute lymphoblastic leukemia, pre-B (Am J Clin Pathol 2009;132:940, Am J Clin Pathol 2004;121:512)
- Alveolar soft part sarcoma (Indian J Ophthalmol 2017;65:889)
- Acute myeloid leukemia (40 - 60%) (Arch Pathol Lab Med 2003;127:42)
- Angioblastoma / tufted angioma (J Clin Pathol 2005;58:214)
- Angiofibroma, cellular (50%) (Mod Pathol 2011;24:82)
- Angiomyofibroblastoma (variable) (Arch Pathol Lab Med 2000;124:1679)
- Angiosarcoma (70%) (Am J Surg Pathol 1998;22:683)
- Benign epithelioid peripheral nerve sheath tumor (fibroblasts are CD34+) (Am J Surg Pathol 2005;29:39)
- Benign stromal spindle cell tumors (Cureus 2023;15:e41961)
- Blood vessels in tumors (Blood 1990;75:2417)
- Calcifying fibrous pseudotumor (Int J Surg Pathol 2002;10:189)
- Cellular blue nevus (J Cutan Pathol 2001;28:145)
- Cellular digital fibroma (J Cutan Pathol 2005;32:413)
- Chordoid glioma (focal) (Am J Surg Pathol 2002;26:1330)
- Chronic myelomonocytic leukemia (Blood Cancer Discov 2022;3:536)
- Congenital / infantile fibrosarcoma (Semin Diagn Pathol 2023;40:295)
- Cystic panfolliculoma surrounding fibrotic stroma is CD34+ (Arch Pathol Lab Med 2006;130:389)
- Dendritic fibromyxolipoma (Mol Clin Oncol 2021;14:7)
- Dendritic interstitial cells at margin of salivary gland tumors (Arch Pathol Lab Med 2001;125:232)
- Dermal dendrocytoma (Am J Dermatopathol 2002;24:50)
- Dermatofibrosarcoma protuberans (Br J Dermatol 1992;127:79, Am J Surg Pathol 2003;27:27)
- Elastofibroma (spindle cells) (Anticancer Res 2021;41:2211)
- Epithelioid hemangioendothelioma (Am J Clin Pathol 1991;96:25)
- Epithelioid sarcoma (50%) (Hum Pathol 1999;30:934, Am J Surg Pathol 1997;21:130)
- Fibroadenoma (breast) (Hum Pathol 2023;139:17)
- Fibroblastic connective tissue nevus (Am J Surg Pathol 2012;36:1509)
- Fibromas with solitary fibrous tumor-like features (Semin Diagn Pathol 2023;40:295)
- Fibrous hamartoma of infancy (Am J Surg Pathol 2014;38:394)
- Ganglioglioma (Acta Neuropathol Commun 2023;11:50)
- Gardner type fibroma of soft tissue (Semin Diagn Pathol 2023;40:295)
- Glioneural hamartoma (J Neuropathol Exp Neurol 2002;61:575)
- Gastric carcinoma, diffuse type (vascular adventitial fibroblastic cells) (J Clin Pathol 2004;57:970)
- Gastrointestinal stromal tumor (50 - 80%) (Am J Surg Pathol 2005;29:52)
- Giant cell angiofibroma (Am J Surg Pathol 2000;24:971)
- Giant cell fibroblastoma (Am J Surg Pathol 2003;27:27)
- Glomus tumor / glomangioma (variable) (J Cutan Pathol 1993;20:15, Tohoku J Exp Med 1997;182:241)
- Hamartomatous tumors of chronic drug resistant epilepsy
- Hemangioblastoma (J Int Med Res 2021;49:3000605211027774)
- Hemangioendothelioma (Medicine (Baltimore) 2023;102:e32914)
- Hemangioma (variable) (Am J Surg Pathol 1999;23:97)
- Hemosiderotic fibrohistiocytic lipomatous lesion (Mod Pathol 2000;13:1192)
- Hepatic sinusoids in conditions associated with altered vascular flow and neoplasms (Res Pract 2023;249:154741)
- Hepatocellular carcinoma (staining of almost all sinusoidal spaces) (Am J Surg Pathol 2008;32:433)
- Inflammatory fibrous polyps of stomach / GI tract (Hum Pathol 2002;33:307, Am J Surg Pathol 2004;28:107)
- Juxtaglomerular cell tumor (may be focal) (Am J Clin Pathol 2001;116:854, Am J Surg Pathol 2004;28:1098)
- Kaposiform hemangioendothelioma (Am J Surg Pathol 2004;28:559)
- Kaposi sarcoma (90%) (strong and diffuse in spindle cells) (J Clin Pathol 2002;55:619)
- Kaposi sarcoma-like pyogenic granuloma (J Clin Pathol 2002;55:619)
- Lipomatous hemangiopericytoma (Am J Surg Pathol 1997;21:195)
- Lipomatous tumors (benign and malignant) (Am J Surg Pathol 1997;21:195)
- Liposarcoma (myxoid, pleomorphic, well differentiated) (Am J Surg Pathol 2002;26:601)
- Lymphangioma (50%) (Hum Pathol 2005;36:426)
- Lymphangioendothelioma (Autops Case Rep 2023;13:e2023435)
- Lymphatic endothelial cells in tumors (Am J Pathol 2006;168:1045)
- Malignant fibrous histiocytoma (Pathol Res Pract 1997;193:51)
- Malignant peripheral nerve sheath tumors (low grade stronger / more frequent than high grade) (Am J Surg Pathol 2003;27:1337)
- Meningioma (some) (Am J Surg Pathol 2002;26:125)
- Metanephric adenofibroma (often) (Int J Clin Exp Pathol 2015;8:3250)
- Metanephric adenosarcoma of kidney (stroma only) (Am J Surg Pathol 2001;25:1451)
- Metanephric stromal tumor of kidney (patchy) (Am J Surg Pathol 2000;24:917)
- Microcystic adnexal carcinoma (Am J Surg Pathol 2001;25:464)
- Mucosal epithelioid nerve sheath tumors (Am J Surg Pathol 2005;29:1310)
- Myelodysplastic syndrome (myeloid blasts)
- Myofibroblastoma (breast, cervicovaginal, soft tissue) (Am J Surg Pathol 2001;25:1022)
- Myxoma of heart (Cardiovasc Pathol 2023;63:107511)
- Myxoma of soft tissue (50%) (In Vivo 2023;37:503)
- Neurofibroma (may be focal) (Am J Clin Pathol 2000;114:123)
- Nuchal fibrocartilaginous pseudotumor of soft tissue (Histol Histopathol 2014;29:831)
- Nuchal type fibroma (Histol Histopathol 2014;29:831)
- Onychomatricoma (Am J Dermatopathol 2010;32:1)
- Papillary thyroid carcinoma (BMC Med Imaging 2021;21:159)
- Paratesticular fibrous pseudotumor (Am J Surg Pathol 2010;34:569)
- Periductal stromal sarcoma of breast (Am J Surg Pathol 2003;27:343)
- Perineurioma (variable) (Am J Surg Pathol 2005;29:859)
- Phyllodes tumor of breast (more common if benign) (J Surg Res 2000;94:84)
- Pleomorphic fibroma of skin (Semin Diagn Pathol 2023;40:295)
- Pleomorphic hyalinizing angiectatic tumor (Arch Pathol Lab Med 2000;124:423)
- Primary renal myxofibrosarcoma (Pathol Res Pract 2015;211:619)
- Pseudoangiomatous stromal hyperplasia of breast (J Clin Pathol 1998;51:204, Am J Surg Pathol 1995;19:270)
- Pseudocyst of adrenal gland (Ann Diagn Pathol 2022;57:151888)
- Reactive angioendotheliomatosis of skin (Am J Dermatopathol 2015;37:581)
- Schwannoma (Antoni B areas) (Am J Clin Pathol 2000;114:123)
- Sclerosing angiomatoid nodular transformation of spleen (capillaries) (Am J Surg Pathol 2004;28:1268)
- Sclerosing hemangioma of lung (Sci Rep 2014;4:6102)
- Sclerosing liposarcoma (spindle and atypical cells) (Int J Surg Case Rep 2023;109:108513)
- Solitary fibrous tumor; expression may be lost in high grade areas (Am J Surg Pathol 1994;18:992, Hum Pathol 1995;26:440, Am J Surg Pathol 2009;33:1314)
- Solitary sclerotic fibroma of skin (J Cutan Pathol 2003;30:631)
- Spindle cell epithelioma of vagina (Am J Dermatopathol 2022;44:764)
- Spindle cell lipoma / pleomorphic lipoma (Am J Dermatopathol 2022;44:764)
- Storiform collagenoma (J Cutan Pathol 2020;47:291)
- Stromal sarcoma of prostate (Diagn Pathol 2012;7:173)
- Subconjunctival herniated orbital fat (Am J Surg Pathol 2007;31:193)
- Superficial acral fibromyxoma (Hum Pathol 2001;32:704)
- Superficial cervicovaginal myofibroblastoma (Pathology 2005;37:144)
- Superficial CD34 positive fibroblastic tumor (Pathology 2015;47:479)
- Thymoma (ectopic hamartomatous variant; otherwise weak) (Am J Surg Pathol 2005;29:1208)
- Transient myeloproliferative disorder (staining of blasts) (Am J Clin Pathol 2001;116:204)
- Vaginal mixed tumor / spindle cell epithelioma (Mod Pathol 2004;17:1243)
- Vulvar fibroma, prepubertal (Am J Surg Pathol 2004;28:1601)
Negative staining
- Normal hepatic sinusoids, bone marrow mast cells
- Adenomatoid tumor (Am J Surg Pathol 2003;27:969)
- Angiomyxofibromatous tumor (Am J Surg Pathol 2006;30:545)
- Anaplastic sarcoma of kidney (Mod Pathol 2018;31:169)
- Angiomyolipoma (Histopathology 2004;44:462)
- Atypical fibrous histiocytoma of skin (focal in 10%) (Am J Surg Pathol 2002;26:35)
- Benign fibrous histiocytoma (but deep tumors are often CD34+)
- Benign vascular proliferations in irradiated skin (Am J Surg Pathol 2002;26:328)
- Calcifying aponeurotic fibroma of soft tissue (Histopathology 2004;44:462)
- Carcinoma (Adv Anat Pathol 2020;27:114)
- Chondromyxoid fibroma (Ann Diagn Pathol 2023;66:152174)
- Clear cell sarcoma of kidney (Histopathology 2004;44:462)
- Desmoplastic fibroblastoma (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:e92)
- Epithelioid sarcoma-like hemangioendothelioma (Am J Surg Pathol 2003;27:48)
- Ewing sarcoma / primitive neuroectodermal tumor (PNET) (Ann Diagn Pathol 2023;65:152152)
- Fibroblastic polyp of colon (may be weak / focal) (Am J Surg Pathol 2004;28:374)
- Fibroepithelial polyp of renal pelvis (Urology 2009;73:929.e9)
- Fibromatosis (J Clin Pathol 2004;57:1119, Am J Surg Pathol 2002;26:1296)
- Follicular dendritic cell sarcoma
- Giant cell tumor of tendon sheath
- Gliosarcoma (Arch Pathol Lab Med 1997;121:129)
- Granulocytic sarcoma (47%) (Arch Pathol Lab Med 2001;125:1448)
- Hibernoma (but spindle cell subtype is CD34+) (Cancer Diagn Progn 2023;3:282)
- Histiocytic sarcoma (Am J Surg Pathol 2004;28:1133)
- Inflammatory myofibroblastic tumor (Pathol Res Pract 2023;242:154335)
- Interdigitating dendritic cell sarcoma (Am J Surg Pathol 2002;26:530)
- Leiomyoma (usually) and vascular leiomyoma (Am J Surg Pathol 2001;25:1355, J Clin Pathol 2002;55:395)
- Leiomyosarcoma (usually) (Arch Pathol Lab Med 2017;141:1072)
- Leukemia cutis (Am J Clin Pathol 2009;132:101)
- Littoral cell angioma of spleen (Am J Surg Pathol 1997;21:827)
- Low grade fibromyxoid sarcoma (Arch Pathol Lab Med 2017;141:1072)
- Mammary NOS type sarcoma (Am J Surg Pathol 2006;30:450)
- Melanoma (rarely CD34+) (J Cutan Pathol 2005;32:685)
- Mesothelial cyst (Am J Surg Pathol 1997;21:334)
- Mesoplastic nephroma (Histopathology 2004;44:462)
- Metaplastic carcinoma of breast, spindle cell type (J Clin Pathol 2023 Aug 16 [Epub ahead of print])
- Multicentric reticulohistiocytosis (J Rheumatol 2014;41:780)
- Myelolipoma (Am J Surg Pathol 2006;30:838)
- Myoepithelioma of breast (Cancers (Basel) 2022;14:476)
- Myofibrosarcoma of breast (Cancers (Basel) 2022;14:476)
- Myoid gonadal stromal tumor (Am J Clin Pathol 2014;142:675)
- Myointimoma (Int J Impot Res 2021;33:583)
- Myxofibrosarcoma (38%) (J Clin Pathol 2003;56:666)
- Nodular fasciitis (Radiol Case Rep 2023;18:1564)
- Ossifying fibromyxoid tumor (Diagn Cytopathol 2015;43:646)
- Paratesticular leiomyosarcoma (30%) (Integr Cancer Ther 2020;19:1534735419900554)
- PEComa (Am J Surg Pathol 2005;29:1558)
- Pigmented villonodular synovitis (Clin Podiatr Med Surg 2023;40:381)
- Plexiform fibrohistiocytic tumor (Clin Podiatr Med Surg 2023;40:381)
- Plexiform fibromyxoma (Am J Surg Pathol 2009;33:1624)
- Plexiform xanthomatous tumor (Am J Surg Pathol 2002;26:1302)
- Pseudomycogenic hemangioendothelioma (Am J Surg Pathol 2011;35:190)
- Reactive fibroblastic and myofibroblastic proliferation of vulva (Am J Surg Pathol 2011;35:110)
- Schwannoma (Int J Clin Oncol 2021;26:284)
- Sclerosing epithelioid fibrosarcoma of the kidney (Diagn Pathol 2015;10:186)
- Sclerosing epithelioid fibrosarcoma of soft tissue (Skeletal Radiol 2023 Jul 31 [Epub ahead of print])
- Sclerosing hemangioma of lung (Hum Pathol 2004;35:503)
- Sclerosing paraganglioma (Head Neck Pathol 2015;9:300)
- Sclerosing perineurioma (J Gen Intern Med 2022;37:3188)
- Sinonasal hemangiopericytoma (Arch Pathol Lab Med 2001;125:686)
- Synovial sarcoma (focal in 6% of monophasic tumors) (Am J Surg Pathol 2002;26:1434)
- Thymoma (BMC Cancer 2023;23:161)
Sample pathology report
- Left thoracic tumor, resection:
- Spindle cell lipoma (maximum 11.5 cm) (see comment)
- MDM2 FISH: negative (no gene amplification)
- Comment: In combination with the additional molecular examinations, the findings fit primarily with a spindle cell lipoma (MDM2 negative and CD34 positive). There is no evidence for liposarcoma / atypical lipomatous tumor and the criteria for the diagnosis of an atypical spindle cell lipomatous tumor are not fulfilled.
Board review style question #1
Board review style answer #1
A. CD34. Under the given answers CD34 is the distinguishing marker for soft tissue neoplasms and in the majority of GIST positive. Other markers supporting the diagnosis of GIST are DOG1 and c-KIT (CD117). Answers B and E are incorrect because desmin and SMA are usually negative in GIST but positive in leiomyoma. Answer D is incorrect because S100 is a strong marker for neuronal differentiation and should be negative in GIST (Curr Opin Gastroenterol 2019;35:555). Answer C is incorrect because EMA is highly expressed in carcinomas and not in GIST.
Comment Here
Reference: CD34
Comment Here
Reference: CD34
CD38
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Flow cytometry images | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Marker of cellular activation expressed by plasma cells, T cells, NK cells and other hematopoietic cell types during various stages of maturation
Essential features
- Marker of activation that is present on many hematopoietic cells, especially plasma cells
- Used clinically as a prognostic marker in chronic lymphocytic leukemia (CLL) as evaluated by flow cytometry
- CD38 expression in lymphoid neoplasms is not specific for any discrete disease entity
- Can be aberrantly expressed in carcinoma and melanoma
- Absence of CD38 (in conjunction with CD34 positivity) is used as a marker for bone marrow hematopoietic stem cells
Terminology
- Also known as ADP ribosyl cyclase 1 (Cytometry B Clin Cytom 2013;84:207)
- First described in 1980 as T cell differentiation antigen (T10) (Proc Natl Acad Sci U S A 1980;77:1588)
Pathophysiology
- CD38 is a single chain, 45 kDa transmembrane molecule with its coding gene sequence located on chromosome 4 (Cytogenet Cell Genet 1995;69:38)
- CD38 has multifunctional activity; it has enzymatic and adhesion molecule features, for example, participating in the NAD+ cell cycle, regulating intracellular calcium levels and playing a role as receptor for the platelet and endothelial cell adhesion molecule CD31 (Physiol Rev 2008;88:841, J Immunol 1998;160:395, Curr Pharm Des 2009;15:57)
- Binding of CD38 by agonistic antibodies has been shown to prevent apoptosis (Eur J Immunol 1994;24:1218)
- CD38 has been shown to be highly expressed on myeloid derived suppressor cells (JCI Insight 2018;3:97022)
Clinical features
- CD38 is highly expressed on most multiple myeloma cells; the anti-CD38 monoclonal antibody daratumumab is used therapeutically in multiple myeloma patients and the response to therapy was shown to be correlated with CD38 expression as measured by flow cytometry (Br J Haematol 1999;105:441, Leukemia 2002;16:30)
- Several other anti-CD38 antibodies, including bispecific anti-CD3 / CD38 antibodies, are in development or have recently been approved for treatment in multiple myeloma (e.g., isatuximab, approved March 2020) (Front Immunol 2018;9:2722, Front Immunol 2020;11:501)
- CD38 expression on CD8+ T cells is associated with risk of progression of HIV infection to AIDS, is associated with poor prognosis and may be used as surrogate marker for HIV RNA viral load (J Acquir Immune Defic Syndr Hum Retrovirol 1997;16:83, Cytometry B Clin Cytom 2009;76:375, J Acquir Immune Defic Syndr 2006;41:416)
- Autoantibodies to CD38 have been implicated in autoimmune related diabetes mellitus type 1 in children (J Pediatr Endocrinol Metab 2005;18:1417)
Interpretation
- CD38 expression is considered positive when the cell membrane shows strong and diffuse staining; the cytoplasm and nucleus should not stain with CD38 (Blood 2008;111:5173)
- Few studies have reported on the use and interpretation of anti-CD38 antibodies in tissue sections for diagnostic purposes; interpretation is difficult due to the prevalence of CD38 in many cell types and the necessity for quantitative assessment more amenable to flow cytometric studies (Am J Surg Pathol 2006;30:585)
Uses by pathologists
- Flow cytometry is the primary use of anti-CD38 antibodies in the pathology laboratory
- CD38 is used in conjunction with CD138 to identify plasma cells (see Flow cytometry images below) and with CD20 to differentiate germinal center B cells from mantle zone B cells (Am J Clin Pathol 2003;119:130)
- CD38 expression by plasma cells is used in minimal residual disease monitoring (Cytometry B Clin Cytom 2016;90:61)
- Bright expression of CD38 aids in the identification of hematogones (Leuk Lymphoma 2004;45:277)
- There is considerable confusion in the literature regarding CD38 and the unrelated antibody VS38 which targets the p63 antigen and is also used for detection of plasma cells in tissue sections and flow cytometry (Blood Cancer J 2018;8:117)
Prognostic factors
- Chronic lymphocytic leukemia with CD38 expression is associated with a more aggressive clinical course and shorter overall survival (J Clin Pathol 2002;55:180, Br J Haematol 2003;120:1017)
- Hairy cell leukemia with CD38 expression is associated with a more aggressive clinical course (Cancer Res 2015;75:3902)
- Acute myeloid leukemia with CD38 expression was shown to be associated with a favorable prognosis and high numbers of immature CD34+ / CD38- blasts in myeloid leukemia are associated with unfavorable prognosis (Leuk Res 2000;24:153, Leukemia 2019;33:1102)
- CD38 expression on multiple myeloma cells has been correlated to anti-CD38 treatment response (Blood 2016;128:959)
- In the future, CD38 expression in tissue sections could be used to monitor anti-CD38 therapy with (bispecific) antibodies for early detection of treatment resistance (loss of CD38 expression)
Microscopic (histologic) description
- Plasmacytoma: see Microscopic (histologic) images
Positive staining - normal
- Plasma cells, hematopoietic progenitor cells, NK cells, B and T cells, monocytes and basophils (Chem Immunol 2000;75:169)
- Neurons, small lymph vessels in intestinal tract and pancreatic islets, perivascular autonomic nerve terminals, double positive thymocytes, erythrocytes (Brain Res 1995;697:235, Virchows Arch 2002;441:605, J Biol Regul Homeost Agents 1998;12:81, Int Immunol 2003;15:1105, Hematology 2007;12:409)
Positive staining - disease
- B cell lymphoid neoplasms
- Multiple myeloma and other plasma cell neoplasms (Br J Haematol 1999;105:441, Best Pract Res Clin Haematol 2010;23:433)
- Plasmablastic lymphoma and plasmablastic plasma cell myeloma (Mod Pathol 2005;18:806, Mod Pathol 2010;23:991, Am J Surg Pathol 2004;28:736)
- High grade B cell lymphoma with MYC and BCL2 or BCL6 rearrangement (Am J Clin Pathol 2022;158:338, Mod Pathol 2022;35:419)
- Burkitt lymphoma (Diagn Pathol 2019;14:100)
- Primary effusion diffuse large B cell lymphoma (Am J Clin Path 1996;105:221, Mod Pathol 2010;23:773)
- Chronic lymphocytic leukemia / small lymphocytic lymphoma and Richter transformed large cell lymphoma (Am J Surg Pathol 2002;26:624, Am J Clin Path 2001;115:385)
- Atypical chronic lymphocytic leukemia only rarely expresses CD38 (Am J Clin Path 2001;116:655)
- Nodal marginal zone lymphoma (10/24) (Am J Surg Pathol 2003;27:762)
- Lymphoplasmacytic lymphoma (Am J Clin Path 2005;124:414)
- Potential use in distinguishing follicular lymphoma and follicular hyperplasia (Int J Clin Exp Pathol 2018;11:1046)
- T cell lymphoid neoplasms
- T lymphoblastic leukemia (Am J Surg Pathol 1992;16:1075)
- T cell lymphomas (peripheral T cell lymphoma, NOS [57% positive], angioimmunoblastic T cell lymphoma [80%], ALK negative [17%] and ALK positive [0%] anaplastic large cell lymphoma) (Am J Hematol 2017;92:E1, Cytometry B Clin Cytom 2006;70:142)
- NK / T cell leukemia (N Engl J Med 2016;375:1501)
- Myeloid neoplasms
- CD38 is heterogeneously expressed in acute myeloid leukemia (Haematologica 2019;104:e100)
- CD38 positivity is used as an inclusion criterion in clinical trials evaluating anti-CD38 therapies
- Other
- Various types of carcinoma and melanoma (Cancer Discov 2018;8:1156)
- Prostate carcinoma (Cancer Metab 2018;6:13)
- Glioma (J Immunol 2008;181:92)
- Transient myeloproliferative disorder (Am J Clin Path 2001;116:204)
- Various inflammatory lymphadenopathies: infectious mononucleosis, Kikuchi lymphadenitis (Am J Clin Path 2003;120:49, Am J Clin Path 1989;92:42)
Negative staining
- Absence of CD38 expression does not reliably exclude a given pathologic diagnosis based on currently available data
- CD38 surface expression may be reduced on multiple myeloma / plasma cells due to CD38 internalization induced by treatment with anti-CD38 antibodies (e.g., daratumumab) (Oncoimmunology 2018;7:e1486948)
- CD38 has been used in conjunction with CD117 in fluorescence activated cell sorting of mast cells from bone marrow samples (CD117 positive and CD38 negative cells) (Am J Pathol 1996;149:1493)
- CD4+ CD26- T cells in patients with a diagnosis of Sézary syndrome are typically negative for CD38 (Dis Markers 2022;2022:3424413)
Flow cytometry images
Sample pathology report
- Bone lesion, needle core biopsy:
- Monotypic kappa expressing plasma cell neoplasm, consistent with plasmacytoma (see comment)
- Comment: The needle core biopsy demonstrates a dense infiltration by a clonal plasma cell population with kappa light chain restriction. The neoplastic plasma cells are positive for CD38, CD138 and CD79a. Lambda light chains, CD20 and CD43 are not expressed. There are only scattered CD3 positive T cells. There is no amyloid deposition. In summary, the bone lesion represents a plasmacytoma; clinical, serological and imaging correlation is required.
Additional references
Board review style question #1
Which statement about CD38 is correct?
- CD38 is typically downregulated in neoplastic plasma cells
- CD38 is brightly expressed on hematogones
- CD38 expression is a specific marker for hairy cell leukemia
- In chronic lymphocytic leukemia / small lymphocytic lymphoma, CD38 expression is considered a favorable prognosis
Board review style answer #1
B. CD38 is brightly expressed on hematogones. Answer A is incorrect because plasma cells typically downregulate CD38 only after daratumumab therapy. Answer C is incorrect because CD38 expression in hematolymphoid cells is nonspecific but is typically brightly expressed by hematogones. Answer D is incorrect because in chronic lymphocytic leukemia, CD38 expression is a poor prognostic indicator.
Comment Here
Reference: CD38
Comment Here
Reference: CD38
CD4
Table of Contents
Definition / general | Pathophysiology | Diagrams / tables | Uses by pathologists | Microscopic (histologic) images | Flow cytometry images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Marker of T helper cells, important in T cell activation and receptor for HIV (Wikipedia, OMIM #186940)
- Also called OKT4
- At #12p13.31
Pathophysiology
- Nonpolymorphous glycoprotein belonging to immunoglobulin superfamily (Cell 1985;42:93)
- Expressed on surface of T helper cells; serves as coreceptor in MHC class II-restricted antigen induced T cell activation
- CD4+ CD25+ FOXP3+ regulatory T cells maintain peripheral tolerance and prevent autoimmunity (Curr Top Microbiol Immunol 2005;293:115), and may be prognostic factor in malignancies (Mod Pathol 2013;26:448, J Clin Invest 2013;123:2873)
- Serves as HIV receptor on T cells, macrophages and brain
- Downregulated by HIV proteins during AIDS progression (J Virol 2003;77:11536, J Biol Chem 2003;278:33912)
- Normally CD4 > CD8; in HIV patients, CD4 / CD8 ratio is inverted (i.e. CD4 < CD8) and patients are at risk for opportunistic infections, particularly if CD4 < 200
- Homologous to CD223
- Interpretation: staining is usually cytoplasmic and has membrane accentuation
Diagrams / tables
Uses by pathologists
- Common marker for T cells; used to classify lymphomas and inflammatory conditions
- Serum levels are marker of HIV disease progression and response to HAART therapy (CD4+ cells are killed by HIV, Am J Clin Pathol 2010;134:556), although serum levels also increased by transient stress (Am J Clin Pathol 2002;117:819)
- Serum levels used to diagnose idiopathic CD4 lymphocytopenia (Obstet Gynecol 2013;122:455)
Microscopic (histologic) images
Images hosted on other servers:
Positive staining - normal
- T helper cells, thymocytes (80 - 90%), granulocytes, macrophages, Langerhans cells and dendritic cells
- Expressed in specific regions of brain
Positive staining - disease
- Many post-thymic T cell leukemia / lymphomas and T cell lymphoproliferative disorders
- Cutaneous lymphomatoid granulomatosis (Am J Surg Pathol 2001;25:1111)
- Eccrinotropic lymphomatoid papulosis (Am J Clin Pathol 2003;119:731)
- Indolent small intestinal CD4+ T-cell lymphoma (PLoS One 2013;8:e68343)
- Indolent T cell lymphoblastic proliferations
- Dendritic / histiocytic neoplasms
- Blastic plasmacytoid dendritic cell neoplasm
- Granulomatous histiocytic lymphoma / sarcoma
- Other hematologic / inflammatory lesions
- Acute myeloid leukemia (M4, M5, Am J Clin Pathol 1995;104:204)
- Florid antiviral inflammatory response (Mod Pathol 2003;16:166)
- Kikuchi-Fujimoto disease (decreased CD4:CD8 ratio in affected areas of lymph node, in contrast to lymphoma, Am J Clin Pathol 2004;122:141)
- Pityriasis lichenoides
- Pyothorax associated lymphoma (some)
Negative staining
- NK cells / NK leukemia / lymphoma
- B cell lymphoma (usually)
- Hodgkins lymphoma (usually)
- Non-hematopoietic neoplasms
- Some T cell lymphomas
- CD7+ stem cell lymphoma
- Enteropathy associated T cell lymphoma (Am J Surg Pathol 2011;35:1557)
- Epidermotropic aggressive CD8+ cutaneous T cell lymphoma (J Am Acad Dermatol 2010;62:300)
- Hepatosplenic alpha / beta and gamma / delta lymphoma (Leuk Lymphoma 2012;53:609)
CD40-49
Table of Contents
CD40 | CD41 | CD42a | CD42b | CD42c | CD42d | CD43 | CD44 and CD44R | CD45 (LCA) | CD45RA | CD45RB | CD45RC | CD45RO | CD46 | CD47 | CD47R | CD48 | CD49 | Diagrams / tables | Microscopic (histologic) imagesCD40
- Costimulatory protein found on antigen presenting cells, required for their activation
- Also called TNF receptor superfamily member 5; ligand is CD40L (CD154)
- Pathophysiology:
- Plays a central role in regulating cell mediated immunity and antibody mediated immunity
- Also mediates T cell dependent immunoglobulin class switching, memory cell development and germinal center formation
- Clinical features:
- Cardiovascular disease:
- May mediate inflammatory component of atherogenesis
- Variation of CD40 gene is associated with coronary artery calcification in diabetes (Am Heart J 2006;151:706)
- CD40 / CD40L signaling contributes to:
- Inflammatory and prothrombogenic responses and brain infarction induced by middle cerebral artery occlusion and reperfusion (Circulation 2005;111:1690)
- Acute cerebral ischemia (Stroke 2003;34:1412)
- CD40 mediated platelet activation may play a role in thrombosis, inflammation and atherosclerosis (Circ Res 2003;92:1041)
- Effects may be mediated by soluble form of CD40L (Ann Med 2011;43:331)
- Has role in pathogenesis of various autoimmune disorders (Semin Immunol 2009;21:293)
- Mutations may cause hyper IgM disease type 3 with opportunistic infections due to inability of B cells to undergo type switching and to defective T cell mediated immunity (OMIM: 606843 [Accessed 6 May 2021], Blood 2003;102:4099)
- CD40 - CD40L binding may cause microglial activation and contribute to Alzheimer's disease (CNS Neurol Disord Drug Targets 2010;9:149)
- Epithelial CD40 may cause inflammatory disorders, generation of self tolerance and chronic rejection of allografts (Semin Immunol 2009;21:289)
- EBV LMP1 is a constitutively active functional mimic of CD40, utilizing TNFR associated factor adaptor proteins to induce signaling (J Biol Chem 2011;286:9948)
- Cardiovascular disease:
- No significant clinical use by pathologists
- Prognostic factors:
- Expression in > 50% of cells may have poor prognostic value in adult soft tissue sarcomas (Clin Cancer Res 2004;10:2824)
- CD40+ diffuse large B cell lymphomas are associated with favorable survival (Clin Cancer Res 2004;10:2824)
- Positive staining - normal:
- B cells, dendritic cells, macrophages, mast cells, monocytes, platelets
- Also astrocytes, endothelial cells, fibroblasts, keratinocytes, Langerhans cells (in oral mucosa), microglia, nevus cells, pancreatic islet cells, prostatic acini, other epithelial cells (Diabetologia 2005;48:268)
- Positive staining - disease:
- Kaposi sarcoma (Am J Pathol 1996;148:1387)
- Melanoma (Am J Pathol 1996;149:1953)
- Reed-Sternberg cells in Hodgkin lymphoma (70%) (Am J Pathol 1994;144:21)
- Most B cell lymphomas (70% of diffuse large B cell lymphoma), B-ALL (some)
- Carcinomas:
- Renal cell (Cell Immunol 2005;235:145)
- Squamous cell carcinoma of oral mucosa (J Oral Pathol Med 2006;35:268)
- Thyroid (Thyroid 2005;15:105)
- Negative staining: plasma cells, Gaucher cells, prostatic adenocarcinoma (Oncol Rep 2004;12:679)
- Reference: OMIM: 109535 [Accessed 6 May 2021]
CD41
- Platelet glycoprotein IIb, important for platelet aggregation
- Also called platelet glycoprotein IIb, GPIIb, platelet fibrinogen receptor alpha subunit
- Pathophysiology:
- Gene encodes integrin alpha chain 2b, which undergoes post-translational cleavage to yield disulfide linked light and heavy chains which join with integrin beta3 (CD61) to form a fibronectin receptor expressed in platelets, which is crucial for platelet aggregation through binding of soluble fibrinogen
- GP IIb / IIIa is also a receptor for fibrinogen, plasminogen, prothrombin, thrombosponin, vitronectin and von Willebrand factor
- Recognizes the sequence R-G-D in a wide array of ligands
- Downregulated by factor XIII and calpain (J Biol Chem 2004;279:30697)
- Clinical features: mutations cause Glanzmann thrombasthenia, with a tendency to bleed for prolonged periods following injury (OMIM: 273800 [Accessed 6 May 2021])
- Uses by pathologists:
- Identify platelets or megakaryocytes (marker is specific)
- Isolate platelets (Cytometry A 2005;65:84)
- Confirm diagnosis of AML M7
- Diagnose Glanzmann thrombasthenia
- Positive staining - normal:
- Platelets, megakaryocytes, hematopoietic progenitor cells (erythroid, myeloid, megakaryocytes) (Br J Haematol 1999;105:1044, Development 2002;129:2003)
- Mast cells (Exp Hematol 2005;33:403)
- Positive staining - disease: AML M7, blasts in transient myeloproliferative disorder (Am J Clin Pathol 2001;116:204)
- Negative staining: AML M0 to M6
- References: OMIM: 607759 [Accessed 6 May 2021], J Clin Invest 2005;115:3363, Arterioscler Thromb Vasc Biol 2003;23:945
CD42a
- CD42a - d complex is receptor for von Willebrand factor and thrombin
- Also called platelet glycoprotein GPIX, GP9
- Absence of CD42 complex (mutations in CD42a - c) causes Bernard-Soulier syndrome (giant platelet syndrome), a bleeding disorder with thrombocytopenia, prolonged bleeding time and giant platelets (OMIM: 231200 [Accessed 6 May 2021])
- Pathophysiology:
- CD42a - d complex is receptor for von Willebrand factor and thrombin
- This complex mediates adhesion of platelets to subendothelial matrices that are exposed in damaged endothelium and amplifies platelet response to thrombin
- GP-IX (CD42a) is a small membrane protein glycoprotein that forms a noncovalent complex with GP-Ib (CD42b)
- Actual binding site of vWF and thrombin is on CD42b
- No significant clinical use by pathologists
- Positive staining - normal: platelets and megakaryocytes
- Negative staining: red blood cells, T cells
- Reference: OMIM: 173515 [Accessed 6 May 2021]
CD42b
- CD42a - d complex is receptor for von Willebrand factor and thrombin
- Also called platelet GPIb alpha, glycoprotein Ib alpha
- Mutations are associated with Bernard-Soulier syndrome (giant platelet syndrome), a bleeding disorder with thrombocytopenia, prolonged bleeding time and giant platelets (OMIM: 231200 [Accessed 6 May 2021], Int J Hematol 2002;76:319)
- CD42b mutations also cause platelet type von Willebrand disease, which is known as pseudo von Willebrand disease (OMIM: 177820 [Accessed 6 May 2021])
- Reduced levels are associated with bleeding disorders in AML patients (Saudi Med J 2005;26:1095)
- Aspirin induces shedding of CD42d and CD42b from platelets (J Biol Chem 2005;280:39716)
- Various snake venoms induce platelet aggregation via CD42b, including:
- TVMA (but inhibits platelet aggregation) (Toxicon 2004;44:649, Xenotransplantation 2004;11:203)
- Alboluxin (Thromb Haemost 2002;87:692)
- Bilinexin (Thromb Haemost 2001;86:1277)
- CD42b physiology is part of bacterial virulence factors:
- Streptococcus sanguis, an oral bacteria causing infective endocarditis, adheres to platelets and platelet fibrin vegetations via CD42b (Br J Haematol 2005;129:101)
- Some strains of H. pylori induce platelet activation mediated by H. pylori bound vWF interacting with CD42b, which may promote peptic ulcer disease and H. pylori associated cardiovascular disease (Gastroenterology 2003;124:1846)
- Pathophysiology:
- CD42a - d complex (also called glycoprotein Ib-IX-V receptor) is the surface platelet receptor for von Willebrand factor on endothelium (particularly CD42b)
- Endothelial damage exposes vWF, which binds to platelets very quickly despite high shear pressures; this leads to platelet activation, then a change in the platelet GpIIb-IIIa receptor, which allows binding to surface bound fibrinogen and free fibrinogen; this leads to platelet crosslinking and aggregation
- Platelet activation apparently involves disruption of the macromolecular complex of GP-Ib with the platelet glycoprotein IX (GP-IX) and dissociation of GP-Ib from the actin binding protein
- GPIb alpha (CD42b) and GPIb beta (CD42c) form main part of VWF receptor
- CD42b also binds to thrombospondin-1, a glycoprotein in arteriosclerotic plaques, causing thrombus formation independent of von Willebrand factor (FASEB J 2003;17:1490)
- Platelet receptors are important in understanding thrombus formation (Haematologica 2009;94:700)
- Case reports: Bernard-Soulier disease variant (Arch Pathol Lab Med 2005;129:e214)
- Uses by pathologists: marker of megakaryocytes and platelets; diagnosis of AML M7; distinguish AML M7 (CD42b positive) from acute myelosis with myelofibrosis (usually CD42b negative) (Mod Pathol 2005;18:603)
- Positive staining - normal: platelets, megakaryocytes and megakaryoblasts
- Positive staining - disease: blasts in transient myeloproliferative disorder
- Reference: OMIM: 606672 [Accessed 6 May 2021]
CD42c
- CD42a - d complex is receptor for von Willebrand factor and thrombin
- Also called platelet GPIb beta, glycoprotein Ib beta
- Mutations are associated with Bernard-Soulier syndrome (giant platelet syndrome), a bleeding disorder with thrombocytopenia, prolonged bleeding time and giant platelets (OMIM: 231200 [Accessed 6 May 2021], Int J Hematol 2002;76:319)
- Reduced levels are associated with bleeding disorders in AML patients (Saudi Med J 2005;26:1095)
- Pathophysiology:
- CD42a - d complex is receptor for von Willebrand factor and thrombin
- GPIb alpha (CD42b) and GPIb beta (CD42c) form main part of VWF receptor
- CD42c also amplifies the platelet response to thrombin during platelet activation where thrombin is involved
- Platelet activation apparently involves disruption of the macromolecular complex of GP-Ib with the platelet glycoprotein IX (GP-IX) and dissociation of GP-Ib from the actin binding protein
- Case reports: mutation in Bernard-Soulier syndrome patient (J Thromb Haemost 2006;4:217)
- No significant clinical use by pathologists
- Positive staining - normal: platelets and megakaryocytes; also endothelium, heart and brain (J Clin Invest 1994;93:2417)
- References: OMIM: 138720 [Accessed 6 May 2021], Thromb Haemost 2001;86:1238
CD42d
- CD42a - d complex is receptor for von Willebrand factor and thrombin
- Also called platelet GP V, GP5
- Aspirin induces shedding of CD42d and CD42b from platelets (J Biol Chem 2005;280:39716)
- CD42d is the predominant target antigen in gold-induced autoimmune thrombocytopenia (Blood 2002;100:344)
- Deficiency does not appear to cause Bernard-Soulier syndrome (Blood 1999;94:4112)
- Pathophysiology:
- Part of CD42a - d complex
- May activate residual platelets in thrombocytopenia regardless of its origin as immune thrombocytopenic purpura or thrombocytopenia of aplastic pancytopenia (J Natl Med Assoc 2008;100:86)
- Also involved in binding of thrombin (Blood 1997;89:4355)
- No significant clinical use by pathologists
- Positive staining - normal: platelets and megakaryocytes
- Reference: OMIM: 173511 [Accessed 6 May 2021]
CD43
- See CD43
CD44 and CD44R
- See CD44
CD45 (LCA)
- See CD45 (LCA)
CD45RA
- See CD45RA
CD45RB
- CD45 isoform generated by alternative mRNA splicing of exon 5, leading to change in the extracellular domain of the molecule (J Exp Med 1987;166:1548)
- Influx of CD4+, CD45RB high T cells is present in inflammatory bowel disease; may be important in pathogenesis as they produce more proinflammatory cytokines than CD4+ CD45RB low T cells (J Leukoc Biol 2004;75:1010)
- Pathophysiology:
- CD45 is a high molecular weight transmembrane protein with intrinsic tyrosine phosphatase activity
- CD45 is heavily glycosylated and expressed at high levels on nucleated hematopoietic cells
- CD45 isoforms, including CD45RB, are generated by alternative mRNA splicing of exons 4 (CD45RA), 5 (CD45RB) and 6 (CD45RC), leading to changes in the extracellular domain of the molecule
- Down regulated in memory cells
- No significant clinical use by pathologists
- Positive staining - normal: similar staining as CD45, except not expressed in Langerhans cells and some T cells; B cells, most T cells, monocytes, macrophages and granulocytes (weak)
- Positive staining - disease: most leukemias and lymphomas
- Negative staining: some T cells; Langerhans cells, platelets; plasma cell neoplasms, Reed-Sternberg cells, some lymphoblastic lymphomas and some anaplastic large cell lymphomas
CD45RC
- CD45 isoform generated by alternative mRNA splicing of exon 6, leading to change in the extracellular domain of the molecule (J Exp Med 1987;166:1548)
- Protein tyrosine phosphatase, receptor type C; PTPRC gene
- CD45RC+ CD4+ cells and CD45RC- CD4+ T cells have different cytokine profiles (Th1-like and Th2-like respectively)
- CD45RC expression divides human T cells into functionally distinct subsets that are imbalanced in antineutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV); this may be a preexisting immune abnormality involved in the etiology of AAV (PLoS One 2009;4:e5287)
- Pathophysiology:
- CD45 is a high molecular weight transmembrane protein with intrinsic tyrosine phosphatase activity
- CD45 is heavily glycosylated and expressed at high levels on nucleated hematopoietic cells
- CD45 isoforms, including CD45RC, are generated by alternative mRNA splicing of exons 4 (CD45RA), 5 (CD45RB) and 6 (CD45RC), leading to changes in the extracellular domain of the molecule
- No significant clinical use by pathologists
- Positive staining - normal:
- Thymocytes, monocytes and dendritic cells
- High levels: B cells, NK and CD4+ T cells
- Intermediate levels: CD8+ T cells
- Negative staining: myeloid cells
- Reference: OMIM: 151460 [Accessed 7 May 2021]
CD45RO
- Marker of activated T cells
- Also called UCHL1, although this is also an abbreviation for ubiquitin carboxyl-terminal esterase L1, a gene expressed in neurons and whose mutations are associated with Parkinson's disease
- Low density of intratumoral CD45RO+ cells was poor prognostic factor for non-metastasized esophageal adenocarcinoma (BMC Cancer 2010;10:608)
- Increased CD45RO+ T cell infiltrate is present in:
- Atherosclerosis (Am J Pathol 1992;140:907)
- Diffuse large B cell lymphoma, MALT lymphoma (Am J Pathol 1997;151:1353)
- Hashimoto’s thyroiditis: interfollicular infiltrate (J Clin Pathol 2004;57:1258)
- Kikuchi’s disease, molar pregnancy (J Clin Pathol 1999;52:888)
- Ovarian carcinoma (Am J Pathol 1997;150:1723)
- Primary cutaneous neoplasms (Am J Pathol 1993;142:1556)
- Well nourished versus malnourished infected children (Clin Exp Immunol 2001;126:461)
- CD4+ CD45RO+ T cells are a major latent viral reservoir in HIV+ individuals (Am J Pathol 1992;140:15)
- Increased percentage of CD45RO+ peripheral blood T cells in patients with preeclampsia and psoriasis (Am J Obstet Gynecol 2002;187:889, Ann Univ Mariae Curie Sklodowska Med 2001;56:465)
- Pathophysiology:
- Most regulatory T cells in adults are CD45RO+; percentage increases with age (J Immunol 2010;184:4317)
- Ligand is CD22
- CD45RO+ T cells are more common than naïve T cells (CD45RA+) in inflammatory myopathies (Am J Pathol 1995;146:1178)
- Uses by pathologists: T cell marker for diagnosis and classification of lymphoma; identify T cell subsets (i.e. memory T cells)
- Positive staining - normal: memory and activated T cells, granulocytes, monocytes, macrophages and cortical thymocytes; some B cells
- Positive staining - disease:
- T cell lymphomas (75%), including:
- Angiocentric and angioimmunoblastic (Hum Pathol 2005;36:784)
- Cutaneous T cell, hepatosplenic alpha beta and gamma delta and peripheral NOS (Am J Clin Pathol 2010;133:281)
- AML (25%), histiocytic sarcoma (Am J Surg Pathol 2004;28:1133)
- Myeloma (some, both on tumor cells and in infiltrate) (J Clin Pathol 1998;51:432)
- Some plasma cell neoplasms
- Also Candida albicans (Am J Clin Pathol 2000;113:59)
- T cell lymphomas (75%), including:
- Negative staining: B cells (most), NK cells; B cell lymphoma (most), carcinoma and autoimmune lymphoproliferative syndrome (Am J Pathol 1998;153:1541)
CD46
- Antigen which helps downregulate the immune system
- Also called membrane cofactor protein (MCP), trophoblast leukocyte common antigen
- Pathophysiology:
- Has multiple isoforms but unlike CD45, they don’t appear to have clinical significance
- Cofactor for proteolytic cleavage of C3b and C4b by factor I (J Immunol 2002;168:6298)
- Prevents inappropriate complement activation, especially via alternative pathway, by limiting formation and function of C3 convertases
- Induces regulatory T cells (Nature 2003;421:388)
- Suppresses immune function by secreting IL-10 and may prevent autoimmunity; various pathogens (see below) appear to exploit this property by binding to CD46 to induce an immunosuppressive phenotype
- Clinical features:
- Receptor for:
- Adenovirus (various serotypes) (J Virol 2005;79:7503)
- HHV-6 (Cell 1999;99:817, J Biol Chem 2003;278:25964)
- Measles virus (Cell 1993;75:295)
- Neisseria gonorrhoeae (J Cell Biol 2002;156:951)
- Streptococcus pyogenes (Infect Immun 2008;76:3951)
- Expression is often increased on tumor cells
- Homozygosity for specific alleles is a high risk factor for some types of recurrent pregnancy loss (Hum Reprod 2006;21:818)
- Mutations predispose to familial hemolytic uremic syndrome atypical type 2 (Proc Natl Acad Sci USA 2003;100:12966)
- Receptor for:
- No significant clinical use by pathologists
- Positive staining - normal: all cells except erythrocytes and some bone marrow cells
- Negative staining: red blood cells
- References: OMIM: 120920 [Accessed 6 May 2021], Springer Semin Immunopathol 2005;27:345
CD47
- See CD47
CD47R
- May not be a current CD marker; information is based on older sources
- Designation for CDw149 which was deleted at the 7th HLDA Workshop (Tissue Antigens 2000;56:258)
- Poorly characterized, with little information available
- Also called Rh related antigen, MEM133
- Similar distribution as CD47 but dimmer
- Recognizes a clustered subset of CD47 (Tissue Antigens 2000;56:258)
- Positive staining: lymphocytes, monocytes, neutrophils (weak), eosinophils (weak) and platelets (weak)
- Negative staining: erythrocytes
CD48
- Activation associated cell surface glycoprotein active in lymphocytes
- Also called B lymphocyte activation marker blast 1
- Pathophysiology:
- Glycosyl phosphatidylinositol (GPI) anchored surface molecule that mediates T cell activation by binding to CD2 (J Immunol 2009;182:7672)
- Induces numerous effects in B and T lymphocytes, natural killer cells, mast cells and eosinophils, partly based on its interaction with 2B4 / CD244 (Int J Biochem Cell Biol 2011;43:25)
- Regulates NK cell effector function (Blood 2006;107:3181)
- Clinical features: mast cell response to M. tuberculosis is mediated by CD48 (J Immunol 2003;170:5590)
- No significant clinical uses for pathologists
- Positive staining - normal: lymphocytes, monocytes, granulocytes (weak)
- Negative staining: platelets, fibroblasts, epithelium, endothelium; usually dendritic cells (J Immunol 2005;175:3690)
- Reference: OMIM: 109530 [Accessed 6 May 2021]
CD49
- See CD49
Diagrams / tables
Microscopic (histologic) images
CD43
Table of Contents
Definition / general | Terminology | Pathophysiology | Clinical features | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Additional referencesDefinition / general
- Pan T cell marker important in T cell and neutrophil adhesion to endothelium
Terminology
- Also called leukosialin, sialophorin
Pathophysiology
- Serves as a ligand for E-selectin on T cells and may regulate T cell trafficking (Blood 2006;107:1421, J Immunol 2005;175:8042)
- Has both antiadhesive and proadhesive roles in neutrophil rolling (J Immunol 2008;181:3628)
Clinical features
- Has defective expression in T cells of males with Wiskott-Aldrich syndrome (MIM 301000)
Uses by pathologists
- Pan T cell marker
- Diagnosis of myeloid (granulocytic) sarcoma (J Clin Pathol 2005;58:211)
- Classify subtypes of T cell lymphomas and low grade B cell lymphomas
- Differentiate pulmonary MALT lymphoma (CD20+ CD43+) from lymphoid hyperplasia (CD43 negative, Am J Surg Pathol 2002;26:76)
Microscopic (histologic) images
Positive staining - normal
- Most T cells, activated B cells, B cells in terminal ileum (Appl Immunohistochem Mol Morphol 2005;13:138), plasma cells (Scand J Immunol 1991;33:211)
- Basophils, erythrocytes, granulocytes, hematogones (Br J Haematol 2005;128:820), macrophages (some), megakaryocytes, monocytes, NK cells, platelets (weak)
- Brain, Langerhans cells, thymocytes
Positive staining - disease
- T/NK cell lymphomas - anaplastic large cell (variable), CD4+/CD56+ hematodermic neoplasm / blastic NK (Am J Surg Pathol 2005;29:1274), hepatosplenic gamma-delta T cell, NK/T cell-nasal type (96%, Hum Pathol 2004;35:86), peripheral T cell, subcutaneous panniculitis-like
- B cell lymphomas - ALL (most), Burkitt’s (almost all), Burkitt’s-like (almost all, Am J Surg Pathol 2005;29:1652), lymphoblastic (variable), mantle cell (100%, Am J Clin Path 2003;119:218), marginal zone (variable, most common in salivary gland, stomach, and upper aerodigestive tract, Arch Pathol Lab Med 2007;131:1673), nodal marginal zone (variable, Am J Surg Pathol 2003;27:762), plasmablastic, SLL/CLL (Am J Clin Path 1999;112:319)
- Other: AML (including leukemia cutis, Am J Clin Pathol 2009;132:101), granulocytic sarcoma, hemangioma, Langerhans cell histiocytosis, mast cell disease (Am J Surg Pathol 2000;24:703), plasmacytoma; early colonic adenoma (Oncol Rep 2004;11:327)
Negative staining
- Colonic epithelium, follicular lymphoma, Hodgkin’s lymphoma, lymphoepithelioma-like thymic carcinoma, primary effusion lymphoma, splenic marginal zone lymphoma
Additional references
CD44
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | CD44R | Board review style question #1 | Board review style answer #1Definition / general
- Complex, transmembrane, multistructural adhesion glycoprotein
- Surface marker of cancer stem cells (Exp Hematol Oncol 2020;9:36, Methods Mol Biol 2018;1692:31)
Essential features
- Complex transmembrane adhesion glycoprotein
- Surface marker of cancer stem cells
- Plays a crucial role in cell adhesion, differentiation, migration and signaling (Exp Hematol Oncol 2020;9:36)
- CD44 might represent a therapeutic target in various tumor types
Terminology
- Cluster of differentiation CD44
- Nonkinase, transmembrane glycoprotein (J Hematol Oncol 2018;11:64)
- Also called Hermes antigen, HCAM or lymphocyte homing receptor (J Oral Maxillofac Pathol 2019;23:267)
- Also known as phagocytic glycoprotein 1 (Blood 2006;107:4149)
Pathophysiology
- Contributes to cellular adhesion through binding to hyaluronic acid (HA) and through inter CD44 binding by attached glycosylation moieties (J Cell Biol 1995;131:1623, J Oral Maxillofac Pathol 2019;23:267)
- Binding to HA induces the expression of inflammatory genes in macrophages, including Osteopontin, leading to aggregation of macrophages, lymphocytes and fibroblasts (Science 1996;271:509)
- Member of the cartilage link protein family
- Also binds to chondroitin, collagen, laminin and fibronectin (J Cell Biol 1992;116:817)
- Cytoplasmic tail initiates cell signaling pathways through binding to adaptor protein (Nat Rev Mol Cell Biol 2003;4:33)
- Splice variants provide proliferation initiating signals for lymphopoiesis, myelopoiesis and angiogenesis (J Clin Invest 1996;97:596, J Immunol 1997;159:2549)
- Also, expression is induced through the binding between CD44 promoter region and transcriptional factors Sp1, Egr1, P53, NFκB and ETS1 (J Oral Maxillofac Pathol 2019;23:267)
- Contributes to cancer cell division, proliferation and invasion through mediating protein kinases, intracellular pathways and proteinases (J Hematol Oncol 2018;11:64)
- Contributes to the adaptive plasticity of cancer cells (J Hematol Oncol 2018;11:64)
Clinical features
- Might represent a therapeutic target in various tumor types, including ovarian cancer (Front Oncol 2020;10:589601)
- High expression of CD44 is associated with recurrence and metastases in several cancer types, including gastric, colorectal and bladder cancer (Oncol Rep 2016;36:2852)
- Treatment is based on suppression of CD44 expression by peptide mimetics, aptamers and natural compounds (J Hematol Oncol 2018;11:64)
- CD44 deletion enhances the fibrogenic response, increases leukocyte infiltration and delays the accumulation of fibrillar collagen (Matrix Biol 2019;75-76:314)
Interpretation
- Membranous
Uses by pathologists
- Biomarker for cancer stem cells (Methods Mol Biol 2018;1692:31, Stem Cells Int 2016;2016:2087204)
- Prognostic marker in various cancer subtypes and a marker for rapid progression and metastasizing (Stem Cells Int 2016;2016:2087204, Front Oncol 2019;9:39)
- Differentiate reactive urothelium from urothelial carcinoma in situ (Med J Islam Repub Iran 2016;30:400, Am J Surg Pathol 2001;25:1074, Appl Immunohistochem Mol Morphol 2018;26:180)
Prognostic factors
- Increased expression is associated with invasiveness and increased chemotherapy resistance
- Might represent a therapeutic target in various tumor types
- CD44v high expression correlates to progression and poor outcome in various cancers, including non-Hodgkin lymphoma, hepatocellular carcinoma, breast, bone, ovarian, pancreatic, colorectal, bladder, gastric, head and neck squamous cell carcinomas, leukemias and lymphomas (Front Oncol 2020;10:589601)
Microscopic (histologic) description
- Positive cells should demonstrate a strong plasma membrane staining pattern
- Cells that lack membranous staining or demonstrate only cytoplasmic staining are considered negative
- Reference: PLoS One 2016;11:e0165253
Microscopic (histologic) images
Contributed by John Yahya I. Elshimali, M.D. and Maria Tretiakova, M.D., Ph.D.
Positive staining - normal
- Fallopian tube epithelium (Stem Cells 2012;30:2487)
- Myeloid cells in bone marrow biopsies, memory T cells, activated lymphocytes and other hematopoietic cells (Commun Integr Biol 2010;3:508)
- Also, high expression in white matter cells of the brain, epithelial cells in the stomach, colon, bladder, liver and cervix (Brain 2013;136:209, J Biol Chem 2013;288:16085, Stem Cells 2013;31:2024, Verh Dtsch Ges Pathol 1995;79:144, Clin Cancer Res 1995;1:1125)
- Proliferating cells and smooth muscle cells express high amounts of CD44 (J Oral Maxillofac Pathol 2019;23:267)
- CD44 is expressed in most cells, CD44v is expressed only in subpopulations of epithelial and hematopoietic cells, particularly during embryogenesis and hematopoiesis, on leukocytes during activation and frequently on cancer initiating cells (CIC) (Front Cell Dev Biol 2018;6:97)
- CD44v6: pancreatic ductal cells (Front Cell Dev Biol 2018;6:97)
Positive staining - disease
- Tubal intraepithelial carcinomas, serous tumors of the ovary, lung squamous cell carcinoma, breast cancer, soft tissue sarcomas (Biomolecules 2015;5:3051, PLoS One 2010;5:e14062, Breast Dis 2020;39:1, Virchows Arch 2000;436:574)
- Reactive urothelium (Med J Islam Repub Iran 2016;30:400, Am J Surg Pathol 2001;25:1074)
- Colorectal adenocarcinoma (CD44v) (Zhonghua Zhong Liu Za Zhi 1996;18:347)
- Head and neck squamous cell carcinoma (CD44v3-CD44v6-CD44v10) (Laryngoscope 2009;119:1518)
- B cell chronic lymphocytic leukemia CD44s (Front Immunol 2015;6:177)
- Pancreatic cancer (CD44v6) (J Oncol 2019;2019:3516973)
- Thyroid cancer (CD44v6) (Diagn Mol Pathol 2011;20:233)
- Prostate adenocarcinoma (CD44v6-CD44v9-CD44v10) (Lab Invest 2004;84:894)
- Leukemia and hematopoietic malignancies (CD44v8-10) (J Hematol Oncol 2018;11:64)
- Liposarcoma and clear cell sarcoma have lower expression of CD44 (J Oral Maxillofac Pathol 2019;23:267)
- Triple negative breast cancer: high expression (PLoS One 2013;8:e78259)
Negative staining
- Neuroblastoma (Mol Cell Biol 1991;11:5446)
- Basal and squamous cell carcinoma of the skin (Br J Dermatol 1996;134:465, Br J Dermatol 2009;160:1251)
- Bladder carcinoma in situ and normal urothelium (Med J Islam Repub Iran 2016;30:400, Am J Surg Pathol 2001;25:1074, Anal Quant Cytopathol Histpathol 2015;37:29)
Molecular / cytogenetics description
- Molecular mass of 85 - 200 kDa (Front Cell Dev Biol 2017;5:18)
- Single chain glycoprotein encoded by CD44 gene located on chromosome 11, (11p13) (Front Cell Dev Biol 2017;5:18)
- Known as the major hyaluronan (HA) receptor (Front Cell Dev Biol 2018;6:97)
- Has 2 isoforms: the standard isoform (CD44s) and the variant isoform (CD44v) (Exp Hematol Oncol 2020;9:36)
- Composed of an extracellular domain, a membrane proximal region, a transmembrane domain and a cytoplasmic tail
- Lacks TATA and CCAAT in upstream regulatory region (J Hematol Oncol 2018;11:64)
- CD44s is composed of 363 amino acids (aa) with a molecular mass of 37 kDa (J Oral Maxillofac Pathol 2019;23:267)
- CD44 is encoded by 19 exons, CD44s is encoded by 10 constant exons and CD44v is encoded by splicing and combination of the 10 exons and the other 9 variable exons (J Hematol Oncol 2018;11:64)
- Main specific ligand is hyaluronic acid (HA)
- Activation of CD44 in breast cancer by HA promotes cell proliferation through the expression of BCL2 and P glycoprotein (J Hematol Oncol 2018;11:64)
Sample pathology report
- Breast, right mastectomy:
- Invasive triple negative breast carcinoma (see comment)
- CD44 IHC (clone 156-3C11, Thermo Fisher Scientific)
- Comment: CD44 is a marker for cancer stem cell and a biomarker for embryonic stem cells. Surgically resected specimen was fixed in 10% buffered formalin and embedded in paraffin. Positive cells were defined as those demonstrating a strong plasma membrane staining pattern. Cells that lacked membranous staining were considered negative. Positive rates were semiquantitatively assessed. The tumor was considered positive since more than 5% of cancer cells revealed a CD44 positive staining pattern on the cell membrane.
CD44R
- Definition / general
- Variant isoform of CD44
- Also known as CD44v9 (Front Cell Dev Biol 2020;8:417)
- Potential marker for tumor initiating cells (Cancer Sci 2016;107:609)
- Pathophysiology
- Variant isoform of CD44 that is generated by alternative splicing of CD44 gene
- CD44v9 is associated with recurrence and poor response to chemotherapy due to reactive oxygen species suppression through stabilizing the glutamate-cystine transporter on the cytoplasmic membrane (Cancer Sci 2018;109:2801)
- Uses by pathologists
- Predicts prognosis and resistance to chemotherapy in hepatocellular carcinoma and invasive bladder cancer (Cancer Sci 2018;109:2801, Cancer Sci 2019;110:1431)
- High expression of CD44v9 is associated with rapid progression and cancer specific death in metastatic invasive bladder cancer (Front Cell Dev Biol 2020;8:417)
- Positive staining – disease
- Colonic adenocarcinoma, cholangiocarcinoma (Mediators Inflamm 2018;2018:4867234)
- High expression is associated with poor outcomes in esophageal squamous cell carcinoma, head and neck squamous cell carcinoma, gastric cancer, triple negative breast cancer, hepatocellular carcinoma, bladder cancer (Cancer Med 2018;7:6258, PLoS One 2015;10:e0116596, Br J Cancer 2013;109:379, Breast Cancer 2019;26:47, Cancer Sci 2018;109:2801, Urol Oncol 2016;34:337.e19)
Board review style question #1
A CD44 immunostain is shown above. Which of the following statements regarding CD44 is correct?
- CD44 deletion enhances the fibrogenic response, increases the kinetics of leukocyte infiltration and delays the accumulation of FAP+ fibroblasts
- CD44 is encoded by 20 exons, CD44v is encoded by 10 constant exons
- CD44v9 is associated with increased free survival in metastatic invasive bladder cancer
- The main ligand for CD44 is collagen
Board review style answer #1
A. CD44 deletion enhances the fibrogenic response, increases the kinetics of leukocyte infiltration and delays the accumulation of FAP+ fibroblasts. The main ligand for CD44 is hyaluronic acid (HA). CD44 is encoded by 19 exons; CD44s is encoded by 10 constant exons. CD44v9 is associated with poor prognosis in metastatic invasive bladder cancer.
Comment Here
Reference: CD44
Comment Here
Reference: CD44
CD45 (LCA)
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Ubiquitous cell surface marker of nucleated hematopoietic cells involved in the regulation and activation of the immune system
- Detectable by immunohistochemistry or flow cytometry
Essential features
- Receptor tyrosine phosphatase protein expressed on the cell surface of white blood cells and involved in B and T cell activation and signaling (Immunol Lett 2018;196:22)
- Used by pathologists to highlight inflammatory cells or determine the hematopoietic nature of tumors of unknown origin with high specificity
Terminology
- Leukocyte common antigen (LCA) or Ly-5
Pathophysiology
- High molecular weight (180 - 220 kDa) transmembrane protein with intrinsic tyrosine phosphatase activity
- Involved in regulating thymic selection and B and T cell antigen receptor mediated activation (Hum Pathol 2017;62:83)
Clinical features
- Different subsets of immune cells express different isoforms of CD45 due to variable exon splicing (Immunol Lett 2018;196:22):
- Mutations in CD45 have been implicated in cases of autosomal recessive T cell negative, B cell positive, NK cell positive severe combined immunodeficiency (Immunol Lett 2018;196:22, OMIM: Severe Combined Immunodeficiency, Autosomal Recessive, T Cell Negative, B Cell Positive, Nk Cell Positive [Accessed 13 January 2022])
Interpretation
- Membranous / cytoplasmic staining
Uses by pathologists
- Confirm the hematopoietic nature of tumors
- Highlight inflammatory cells, for example in lymphocytic myocarditis or Sjögren syndrome (Hum Pathol 2017;62:83, J Oral Pathol Med 2021;50:98)
Prognostic factors
- Strong expression of CD45 may predict a worse prognosis in certain hematologic malignancies, including pediatric B cell progenitor acute lymphoblastic leukemia and multiple myeloma (Blood Cells Mol Dis 2021;89:102562, Leuk Res 2016;44:32)
- Tumor infiltrating lymphocytes, which can be highlighted by CD45, may predict a more favorable prognosis in solid tumors, like colorectal cancer or small cell carcinoma (Science 2006;313:1960, Chest 2013;143:146)
Microscopic (histologic) images
Positive staining - normal
- White blood cells, including granulocytes, lymphocytes, eosinophils, basophils (dim), monocytes, macrophages / histiocytes, mast cells and plasma cells; not including red blood cells and their precursors, megakaryocytes or platelets (Immunol Lett 2018;196:22)
Positive staining - disease
- Acute leukemias, including acute myeloid leukemia, acute lymphoblastic leukemias and leukemia cutis (Methods Mol Biol 2017;1633:33, J Hematol 2018;7:124)
- Acute myeloid leukemia blasts have a lower CD45 mean fluorescence intensity in flow cytometry than other circulating white blood cells, allowing them to be identifed as a distinct population (blast gate) (Leukemia 1997;11:1878, Am J Clin Pathol 2012;137:800)
- B lymphoblastic leukemia / lymphoma can be negative; if positive, it is usually dimly expressed and the strong expression has been described as associated with a worse prognosis in B cell progenitor acute lymphoblastic leukemia (Blood Cells Mol Dis 2021;89:102562)
- B and T cell lymphomas (most), including the lymphocyte predominant (LP) cells of nodular lymphocyte predominant Hodgkin lymphoma (Leuk Res 2008;32:263)
- Plasma cell neoplasms (variable) (Blood Cells Mol Dis 2004;32:293)
- Histiocytic tumors such as histiocytic sarcoma (Diagn Cytopathol 2018;46:790)
- Mast cell disorders, such as systemic / cutaneous mastocytosis, mastocytoma (Am J Clin Pathol 2015;143:527)
- Blastic plasmacytoid dendritic cell neoplasm (J Hematol 2018;7:124)
- Candida albicans yeast forms (Am J Clin Pathol 2000;113:59)
- Rarely carcinomas, particularly undifferentiated / neuroendocrine neoplasms or necrotic tumors (Mod Pathol 1998;11:1204, Am J Clin Pathol 1998;110:641)
Negative staining
- Red blood cells, megakaryocytes, osteoblasts and platelets (Methods Cell Biol 2011;103:221)
- Reed-Sternberg cells of classic Hodgkin lymphoma (Appl Immunohistochem Mol Morphol 2016;24:535)
- Anaplastic T cell lymphomas, plasma cell neoplasms and acute lymphoblastic leukemia / lymphoma neoplasms can occasionally have negative expression of CD45 (Appl Immunohistochem Mol Morphol 2016;24:535)
- ALK positive anaplastic large cell lymphoma may sometimes be negative for CD45 by immunohistochemistry but CD45 positive by flow cytometry (Am J Clin Pathol 2007;127:707)
- Epithelial tumors, germ cell tumors, melanoma, mesothelioma, sarcoma (note that infiltrating lymphocytes are CD45 positive and must be distinguished from tumor cells) (Appl Immunohistochem Mol Morphol 2016;24:535)
Sample pathology report
- Lymph node, right cervical excision:
- Nodular lymphocyte predominant Hodgkin lymphoma (see comment)
- Comment: There is total replacement of the nodal architecture by expansive vague nodules of small lymphocytes with sparse, relatively large tumor cells with multilobulated or round nucleus, thin nuclear membrane, finely granular chromatin and variable, small nucleoli (popcorn cells). The tumor cells are immunoreactive for CD45, CD20 and CD19 and negative for CD15 and CD30, which confirms the diagnosis.
Board review style question #1
CD45 expression is consistently seen in most hematopoietic neoplasms and it is considered a specific marker when investigating neoplasms of unknown primary origin; however, CD45 can be negative in a subset of hematopoietic neoplasms. Which of the following hematopoietic neoplasms is positive for CD45 in nearly all cases?
- Acute megakaryoblastic leukemia
- B lymphoblastic leukemia / lymphoma (B-ALL)
- Classic Hodgkin lymphoma (CHL)
- Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL)
- Plasma cell neoplasm
Board review style answer #1
D. Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL). CD45 is positive in nearly all cases and it is an important marker together with other B cell markers (CD20, PAX5, CD19, CD79a, CD75, OCT2 and BOB1) in differentiating classic Hodgkin lymphoma (CHL) and NLPHL. Sometimes the background staining of the hematopoietic cells can make the interpretation of CD45 difficult; however, the absence of staining in back to back Reed-Sternberg / Hodgkin cells or consistent positive staining in lymphocyte predominant (LP) cells are helpful in the differentiation of these lesions. All the other hematopoietic neoplasms listed on the question can have negative expression of CD45.
Comment Here
Reference: CD45
Comment Here
Reference: CD45
CD45RA
Table of Contents
Definition / general | Pathophysiology | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Marker of naive T cells
- Also called protein tyrosine phosphatase receptor type C
- Cord blood has higher percentage of CD45RA helper T cells than adult blood (Am J Clin Pathol 1996;105:38)
- In adults, CD45RA+ cells may prevent autoimmune disease (Blood 2006;107:2830)
- Reduced numbers of CD45RA+ CD4+ T cells are associated with children with biliary atresia (Transplant Proc 2003;35:3026); primary biliary cirrhosis (Scand J Gastroenterol 2003;38:421), fetal distress (Biol Neonate 2004;85:61) and preeclampsia (Am J Obstet Gynecol 2002;187:889)
Pathophysiology
- CD45 isoforms [functionally similar proteins with similar but not identical amino acid sequence], including CD45A, are generated by alternative mRNA splicing of exons 4 (CD45RA), 5 (CD45RB) and 6 (CD45RC), leading to changes in the extracellular domain of the molecule (J Exp Med 1987;166:1548)
- CD45RA+ T regulatory cells are converted to CD45RO+ T regulatory cells after activation (J Immunol 2010;184:4317)
- High molecular weight transmembrane protein with intrinsic tyrosine phosphatase activity
- Heavily glycosylated, and expressed at high levels on nucleated hematopoietic cells
Uses by pathologists
- Differentiate naive T cells (CD45RA+) from memory T cells (CD45RO+), but not in adult allogeneic hematopoietic cell transplant recipients (Bone Marrow Transplant 2003;32:609)
Microscopic (histologic) images
Positive staining - normal
- B cells, NK cells, naive / resting T cells (those not exposed to antigens), medullary thymocytes and plasmacytoid dendritic cells (Am J Pathol 2001;159:237)
Positive staining - disease
-
Hematologic malignancies:
- B cell lymphomas (most), hairy cell leukemia (Hum Pathol 1992;23:172)
- CD8+ primary cutaneous T cell lymphoma (Am J Pathol 1999;155:483)
- CD4(+) CD56(+) lineage-negative malignancies (Am J Surg Pathol 2005;29:1274)
- Progressive transformation of germinal centers
- Reed-Sternberg cells in lymphocyte predominant Hodgkin’s lymphoma (Am J Surg Pathol 1999;23:27)
- Autoimmune lymphoproliferative syndrome (Am J Pathol 1998;153:1541)
- Effector memory T cells in lesional epidermis (Am J Pathol 2002;161:1337)
- CD4+ memory T cells after bone marrow grafts (Eur J Immunol 1999;29:3987)
- Terminally differentiated CD8+ memory T cells (Arthritis Res Ther 2003;5:R91)
Other:
Negative staining
- Basophils, endothelial cells, Langerhans cells, memory T cells (usually), most T cell lymphomas and most plasma cell neoplasms
CD47
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- CD47 is a ubiquitously expressed marker of self ("don't eat me" signal) and functions as an antiphagocytic molecule on the cell surface by binding the inhibitory molecule SIRPα on immune cells (e.g. macrophages) (Science 2000;288:2051)
Essential features
- Expressed in most tissues and primarily acts as a marker of self
- Overexpressed on solid tumors and hematolymphoid malignancies to evade immune control
- Limited diagnostic utility but may be used as a prognostic or predictive marker in the future
Terminology
- Integrin associated protein (IAP) (J Cell Biol 1990;111:2785)
- Antigenic surface determinant protein OA3 (Biochem J 1994;304:525)
- "Don't eat me" signal (Mol Immunol 2003;40:85)
- Myeloid immune checkpoint (Nat Rev Clin Oncol 2019;16:275)
Pathophysiology
- Transmembrane protein that forms complexes with integrin αvβ3 and other integrins (J Cell Biol 1990;111:2785)
- Receptor for thrombospondin-1 and signal regulatory protein alpha (SIRPα) (J Biol Chem 1999;274:559, Blood 1999;94:3633)
- Interaction of CD47 with SIRPα on macrophages and dendritic cells can downregulate immune cell activity by activating protein phosphatases such as SHP-1 and inhibiting cytokine synthesis (J Exp Med 1999;190:1175, J Immunol 2000;164:2193, J Immunol 2001;167:2547)
- Red blood cells lacking CD47 are quickly eliminated from circulation by splenic macrophages (Leuk Lymphoma 2004;45:1319)
- A complex mechanism involving conformational changes of the CD47-SIRPα complex has been suggested to impart a prophagocytic effect on red blood cells (Blood 2012;119:5512)
- Calreticulin, a molecular chaperone and endoplasmatic reticulum protein, is expressed on the surface of stressed / senescent cells and cancer cells
- Calreticulin is the dominant prophagocytic ("eat me") signal on cancer cells and is counteracted by overexpression of CD47 (Sci Transl Med 2010;2:63ra94)
- Involved in platelet aggregation, epithelial and endothelial leukocyte adhesion, migration of immune cells and activation of T cells (Trends Cell Biol 2001;11:130)
- Monoclonal anti-CD47 antibodies can reduce tumor cell growth in vitro, in xenograft tumor models and in vivo (Nat Med 1999;5:1277, Proc Natl Acad Sci U S A 2012;109:6662, PLoS One 2015;10:e0137345, Cell Death Dis 2018;9:544, N Engl J Med 2018;379:1711)
Clinical features
- Oncology
- CD47 is a promising therapeutic target and anti-CD47 therapies for advanced solid tumors and hematolymphoid malignancies have preliminary results (N Engl J Med 2018;379:1711, J Clin Oncol 2019;37:946, Front Oncol 2020;9:1380)
- Increased expression in response to chemotherapy (Proc Natl Acad Sci U S A 2018;115:E1239)
- Decreased expression in response to radiotherapy (Int J Cancer 2013;133:120)
- Associated with response to trastuzumab therapy and poor prognosis in breast cancer (Proc Natl Acad Sci U S A 2011;108:18342, Oncol Lett 2019;18:3249)
- Transfusion medicine
- Highly expressed on red blood cells and anti-CD47 therapy causes interferences with pretransfusion testing (Transfusion 2019;59:730)
- Expressed on stored red blood cells decreases over time (Transfus Apher Sci 2002;27:233)
- Increased in red blood cells in sickle cells patients in response to treatment with hydroxyurea (Haematologica 2008;93:502)
Interpretation
- Cell membrane staining
- Cytoplasmic staining may also be observed but the significance of this finding is unclear
Uses by pathologists
- Cytological diagnosis of body cavity effusions: a 2 marker panel of CD47 (high expression) and BRCA1 associated protein 1 (BAP1; loss) can discriminate diffuse malignant mesothelioma from reactive pleural effusions with a sensitivity of 78% and a specificity of 100% (Oncoimmunology 2017;7:e1373235)
Prognostic factors
- Overexpressed on circulating leukemia cells in acute myeloid leukemia and associated with a poor prognosis (Leuk Res 2015;39:749, Cell 2009;138:271, Cell 2009;138:286)
- Overexpressed on acute lymphoblastic leukemia and associated with a poor prognosis (Cancer Res 2011;71:1374)
- Overexpressed on non-Hodgkin B cell lymphomas and confers a worse prognosis (Cell 2010;142:699)
- Predictor of poor overall survival in ovarian carcinoma, glioma and glioblastoma (Proc Natl Acad Sci U S A 2012;109:6662)
Microscopic (histologic) images
Positive staining - normal
- First described in red blood cells and other hematopoietic cells (J Cell Biol 1990;111:2785)
- Expressed in all tissue types based on mRNA studies and 4 splice variants with different tissue distribution are known (J Cell Sci 1995;108:3419)
Positive staining - disease
- Cholangiocarcinoma (Transl Oncol 2019;12:217)
- Colorectal carcinoma (Pathobiology 2019;86:182)
- Gastric adenocarcinoma (Oncol Lett 2017;14:801)
- Ovarian carcinoma (79.2%) (Gynecol Oncol 2016;143:393)
- Endometrial carcinoma (J Immunol Res 2018;2018:6156757)
- Small cell lung cancer (J Clin Invest 2016;126:2610)
- Non small cell lung cancer (Cancer Med 2020;9:2390)
- Mesothelioma (63%) (Oncoimmunology 2017;7:e1373235)
- Anaplastic thyroid cancer (Thyroid 2019;29:979)
- Squamous cell carcinoma of the head and neck (Int J Cancer 2013;133:120, Cells 2019;8:1658, Oncoimmunology 2018;7:e1397248)
- Bladder cancer (Cent European J Urol 2017;70:349)
- Breast cancer (Nat Commun 2017;8:14802)
- Leiomyosarcoma (Proc Natl Acad Sci U S A 2012;109:6656)
- Lymphoid malignancies (Cell 2010;142:699)
- Acute lymphoblastic leukemia (Cancer Res 2011;71:1374)
- Chronic lymphocytic leukemia (Nat Med 1999;5:1277)
- Hodgkin lymphoma (Clin Transl Oncol 2020;22:782)
- T cell lymphoma (Blood 2019;134:1430)
- Myeloid malignancies
- Acute myeloid leukemia (Cell 2009;138:271, Cell 2009;138:286)
- Myelodysplastic syndrome (Leuk Res 2013;37:907)
- Chronic myelogenous leukemia (Cell 2009;138:271)
- Myeloma (Leukemia 2012;26:2538)
- Glioma and glioblastoma (Proc Natl Acad Sci U S A 2012;109:6662)
- Atherogenesis is associated with increased CD47 expression (Arterioscler Thromb Vasc Biol 2008;28:615, Nature 2016;536:86)
Negative staining
- Rh null red blood cells show a lack of CD47 on erythrocytes (Br J Haematol 2004;125:412)
- No increase in CD47 expression in myeloproliferative neoplasm hematopoietic progenitor cells, such as in myelofibrosis, polycythemia vera and essential thrombocytosis (Braz J Med Biol Res 2018;52:e7784, Cell 2009;138:271)
- Reduction in CD47 expression in monocytes is associated with disease severity in patients with burns (Burns 2011;37:94)
Sample pathology report
- Pleural fluid, thoracentesis:
- Positive for malignant cells, favor mesothelioma (see comment)
- Comment: The cytology slide shows numerous three dimensional cell clusters and atypical single cells. Immunostains for calretinin, CK5/6, D2-40 and CD47 are positive. Immunostains for Ber-EP4, TTF1 and BAP1 are negative. The combined morphological and immunohistochemical features are consistent with an atypical mesothelial proliferation, favor malignant mesothelioma. Correlations with the clinical and imaging findings, as well as the patient history are necessary. A pleural biopsy may be valuable to further classify the disease process.
Additional references
Board review style question #1
Board review style answer #1
B. CD47 is antiphagocytic by binding SIRPα on effector immune cells. CD47 can be thought of as an innate immune checkpoint and marker of self. In contrast, calreticulin is prophagocytic and its effect is controlled by the expression of CD47. Both molecules are highly expressed in mesothelioma and other cancer types. CD47 was first discovered in erythrocytes.
Comment Here
Reference: CD47
Comment Here
Reference: CD47
CD49
CD49a
Definition / general
- Integrin alpha 1 chain, which combines with beta1 subunit (CD29) to form a receptor for collagen and laminin
- Also called very late antigen (VLA) alpha 1 chain, integrin alpha 1 chain and ITGA1
- Mesenchymal stem cells are selected from bone marrow by CD49+ with flow cytometry (Br J Haematol 2003;122:506, J Mol Histol 2007;38:449)
- Reference: OMIM #192968
Pathophysiology
- Integrins are integral cell-surface proteins composed of an alpha chain and a beta chain; a given chain may combine with multiple partners resulting in different integrins
- Very late activation proteins (VLA) are a family of integrins originally identified on activated human T cells, later on fibroblasts and platelets
- CD49a combines with beta1 subunit (CD29) to form a receptor for collagen and laminin; this receptor may also be involved in cell-cell adhesion and play a role in inflammation and fibrosis
- CD49a contributes to beta cell functions important for pancreatic islet morphogenesis and glucose homeostasis (J Biol Chem 2004;279:53762)
Uses by pathologists
- No significant clinical use by pathologists
Positive staining - normal
- Activated B and T cells, monocytes, fibroblasts, platelets, endothelial cells and smooth muscle cells
CD49b
Definition / general
- Platelet receptor that mediates adhesion to subendothelial tissue after endothelial damage
- Also called very late antigen (VLA) alpha 2 chain
- Called GP Ia / IIa receptor (integrin alpha2beta1) on platelets
- Associated with neonatal alloimmune thrombocytopenia (CD49b is BRa) (Vox Sang 1988;54:101)
- Elevated numbers of peripheral blood CD18(high) CD49b+ T cells are associated with severe uncontrolled asthma (Int Arch Allergy Immunol 2006;140:139)
- CD49b C807T polymorphism is associated with:
- High density of alpha2beta1 receptor on platelets (Arterioscler Thromb Vasc Biol 2005;25:1756)
- Severe retinopathy in patients with diabetes > 25 years (Thromb Haemost 2003;89:142)
- Ischemic strokes in young monozygotic twins (Blood Coagul Fibrinolysis 2003;14:83)
- Reference: OMIM #192974
Pathophysiology
- Receptor for laminin, collagen, fibronectin and E-cadherin
- Responsible for platelet adhesion to subendothelial tissue; after endothelial damage, circulating platelets via platelet surface GP Ib-IX-V complex contact subendothelial vWF bound to collagen; this initial contact slows down the platelets, allowing platelet CD49b to bind to endothelial collagen; this stops the platelets and contributes to their activation and aggregation (Blood 2005;105:1986)
- CD49b mediates disassembly of actin cytoskeleton stress fibers and focal adhesions, leading to block of endothelial cell migration and angiogenesis (J Cell Biol 2004;166:97)
- May be a immunodominant minor histocompatibility antigen (Blood 1998;92:2169)
Uses by pathologists
- No significant clinical use by pathologists
Positive staining - normal
- Platelets, activated B & T cells, monocytes, megakaryocytes and NK cells (most)
Videos
Platelet adhesion and aggregation
CD49c
Definition / general
- Major receptor for laminin; also a receptor for collagen, fibronectin and thrombospondin
- Also called very late antigen (VLA) alpha 3 chain (VLA-3), ITGA3
- Common integrin is alpha3beta1, which is CD49c and CD29
- Has 2 isoforms produced by alternate splicing: alpha-3A and alpha-3B
- Tumor cell alpha3beta1 binds to exposed basement membrane on pulmonary vessels to cause tumor cell arrest and early colony formation (J Cell Biol 2004;164:935)
- May play a role in peritoneal dissemination of gastric carcinoma (Cancer Res 2004;64:6065)
- May mediate invasion of melanoma cells (Clin Exp Metastasis 2002;19:127)
- Reference: OMIM #605025
Pathophysiology
- Binds to laminin 10/11, the major basement membrane component on many adult tissues, suggesting that it has a central role in adhesion of epithelial cells with basement membrane (J Biochem 2003;134:497)
- Mediates angiogenesis through both repression and promotion (Am J Pathol 2010;177:1534, J Cell Sci 2009;122:1778)
Uses by pathologists
- No significant clinical use by pathologists
Positive staining - normal
- B & T cells, most nonhematopoietic cells; lens capsule (Eye (Lond) 2003;17:473)
Negative staining
- Platelets
CD49d
Definition / general
- Receptor for fibronectin, thrombospondin and VCAM1 / CD106
- Also called very late antigen (VLA) alpha 4 chain (VLA4), ITGA4
- Relevant to tumor progression and metastasis
- Increased expression during relapse in multiple sclerosis (J Neuroimmunol 2005;166:189)
- Treatment with alpha4 integrin antagonist natalizumab led to fewer inflammatory brain lesions and fewer relapses in patients with relapsing multiple sclerosis (N Engl J Med 2003;348:15)
- Although it is also associated with progressive multifocal leukoencephalopathy (Neurol Res 2006;28:299)
- Reference: OMIM #192975
Pathophysiology
- Combines with CD29 to form alpha4 beta1 integrin
- Has role in cell-cell interactions, cell adhesion to the extracellular matrix
- Integrins alpha4beta1 and alpha4beta7 are receptors for fibronectin
- Integrin alpha4beta1 is also a receptor for VCAM1 / CD106, MAdCAM1 and thrombospondin
- Avidity (binding strength) of cells expressing alpha4beta1 integrin can be rapidly changed by chemokines and chemoattractants
- Integrin anchorage to cytoskeleton enhances the mechanical stability of its adhesive bonds under strain and promotes its ability to mediate leukocyte adhesion under physiological shear stress conditions (J Cell Biol 2005;171:1073)
- Promotes (a) lymphocyte migration into tissue by strengthening lymphocyte adhesion to endothelial cells, (b) rolling of T cells in vascular lumen on VCAM-1 of endothelium, (c) homing of T cell subsets to Peyer's patches, (d) differentiation of hematopoietic precursor cells by adhesion to bone marrow stromal cells
Uses by pathologists
- Surface expression has prognostic significance in chronic lymphocytic leukemia (Leuk Res 2011;35:750, Br J Haematol 2008;140:537)
Positive staining - normal
- Macrophages, T and B cells, eosinophils, basophils, NK cells, dendritic cells, Langerhans cells, myeloid cells, erythrocyte precursors and thymocytes
- Also basal epidermal layer
Positive staining - disease
- Found in suprabasal skin during wound healing and psoriasis
- Melanoma, ALL and AML
Negative staining
- Erythrocytes, platelets and neutrophils
CD49e
Definition / general
- Fibronectin and fibrinogen receptor
Terminology
- Also called very late antigen (VLA) alpha 5 chain (VLA5), ITGA5, fibronectin receptor (FNRA)
Physiology
- Recognizes the sequence R-G-D in fibronectin and fibrinogen, mediating its adhesion function
Clinical features
- Important in wound reepithelialization (Larjava: Keratinocyte Interactions with Fibronectin During Wound Healing)
- Weakening of tumor cell adhesion strength, controlled by alpha5beta1, may mediate tumor cell motility (Mol Biol Cell 2005;16:51)
- Arginine-glycine-aspartic acid (RGD) sequence present on HIV Tat protein mediates vascular cell migration and invasion by binding to the alpha5beta1 and alphavbeta3 integrins, promotes angiogenesis and Kaposi sarcoma (Blood 1999;94:663)
- Persistently reduced expression of blood monocyte CD49e is an adverse prognostic marker in HIV (AIDS 2009;23:2247)
Uses by pathologists
- No significant clinical use by pathologists
Immunofluorescence images
Contributed by Vincent Achard, M.D., Ph.D.
Positive staining - normal
- T cells, early and activated B cells, platelets, monocytes, neutrophils
Additional references
CD49f
Definition / general
- Forms laminin and thrombospondin receptors
Terminology
- Also called very late antigen (VLA) alpha 6 chain (VLA6), ITGA6
Physiology
- Forms laminin receptor on platelets (with CD29 / alpha6beta1) and on epithelial cells (with CD104 / alpha6beta4); alpha6beta1 is also part of the thrombospondin receptor (J Biol Chem 2003;278:40679)
- Important for formation of hemidesmosomes on stratified squamous and transitional epithelia
Clinical features
- Commonly overexpressed in pre B-ALL; may be useful marker to detect minimal residual disease (Cytometry B Clin Cytom 2009;76:150)
- Alpha6beta1 is expressed on pancreatic cancer cells during invasion and metastasis formation (BMC Cell Biol 2006;7:8)
- In junctional epidermolysis bullosa with pyloric atresia, patients have antibodies to alpha6beta4 (J Clin Invest 1997;99:2826)
- Epitope within alpha6 protein may be site of binding of antibodies in oral pemphigoid (J Immunol 2006;176:1968)
Uses by pathologists
- No significant clinical use by pathologists
Positive staining - normal
- Epithelial cells, memory T cells, monocytes, platelets, megakaryocytes, thymocytes
Additional references
CD5
Table of Contents
Definition / general | Pathophysiology | Clinical features | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Important in identification of T cells and most T cell lymphomas, some low grade B cell lymphomas, thymic carcinoma
Pathophysiology
- Belongs to ancient scavenger receptor superfamily; at 11q13; binds to CD72
- CD5+ B cells, which may arise from B-1 cells (subset of B cells) produce "generalist antibodies" using germline (nonmutation) configuration of gene segments - polyreactive low affinity "natural" antibodies (usually IgM) to exogenous antigens (tetanus toxoid, lipopolysaccharide) as well as autoreactive antibodies (Immunol Lett 1993;38:159)
- First line of defense against antigens; have a low activation threshold; are the only line of defense for those who cannot produce specific antibody
- May mediate hepatitis C infection of T cells (J Virol 2012;86:3723)
Clinical features
- CD5 production elevated in rheumatoid arthritis (represents 27 - 52% of circulating B cells vs 20% normally)
- Key regulator of immune response including antitumor response (Curr Opin Immunol 2011;23:310, Oncoimmunology 2013;2:e22841)
- Abnormalities may produce autoimmunity (Immunol Res 2002;26:255, Autoimmun Rev 2009;8:349)
- Serum % CD5+ B cells may predict relapse in ANCA+ vasculitis after rituximab treatment (Clin J Am Soc Nephrol 2013;8:382)
Uses by pathologists
- Marker for CLL, mantle cell lymphoma (only rarely is CD5-), T cells (normal and malignant), thymic carcinoma (Arch Pathol Lab Med 2008;132:1346, Int J Clin Exp Pathol 2010;3:430)
Microscopic (histologic) images
Positive staining - normal
- Thymocytes, almost all T cells
- B cells in fetal spleen and cord blood; B cells in bone marrow (particularly stage 3 hematogones and mature B cells), B cells in peritoneal and pleural cavities, some B cells in mantle zone of spleen and lymph nodes (12% of B cells in peripheral blood) (Am J Clin Pathol 2009;132:733, Am J Clin Pathol 2004;121:368)
Positive staining - disease
- B cell CLL / SLL, mantle cell lymphoma, most T cell malignancies, thymic carcinoma (almost all), CASTLE (thyroid tumor)
- Occasionally / rarely
- Atypical thymoma (some)
- Burkitt lymphoma (rare)
- Diffuse large B cell lymphoma (10%, usually aggressive) (Am J Clin Pathol 2009;131:339, Int J Clin Exp Pathol 2013;6:985)
- Follicular lymphoma-aggressive variant (rare) (Am J Clin Pathol 2005;12:182, Am J Clin Pathol 2000;114:912)
- Lymphoplasmacytic lymphoma (rare) (J Korean Med Sci 2011;26:824)
- MALT lymphoma (Hum Pathol 2012;43:1436)
- NK/T cell lymphoma (variable)
- Splenic lymphoma with villous lymphocytes (19%)
- Breast ductal carcinoma NOS stains with CD5 clone 4C7 (Arch Pathol Lab Med 2001;125:781)
Negative staining
- Various T cell lymphomas: enteropathy associated, hepatosplenic alpha-beta and gamma-delta, large granular lymphocytic lymphoma
- Most B cell lymphomas other than mantle cell or CLL (although there rarely are CD5+ variant forms), Reed-Sternberg cells in Hodgkin lymphoma
CD50-59
Table of Contents
CD50 | CD51 | CD52 | CD53 | CD54 | CD55 | CD56 | CD57 | CD58 | CD59 | Microscopic (histologic) imagesCD50
- Also known as ICAM-3, the third counter receptor for LFA-1 (CD54)
- Provides adhesion signals important in B-T cell interactions and regulates leukocyte morphology
- May predict resistance to radiation therapy in cervical cancer (Int J Cancer 2005;117:194)
- Costimulator for HIV1 replication (J Virol 2004;78:6692, J Virol 2002;76:32)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal:
- Leukocytes including:
- Eosinophils and mast cells (J Allergy Clin Immunol 2003;111:1024, Cell Adhes Commun 1999;7:195)
- Epidermal Langerhans cells and endothelial cells (J Invest Dermatol 1995;104:995, J Vasc Res 2004;41:28)
- Leukocytes including:
- Positive staining - disease: synovium in rheumatoid arthritis (Arthritis Rheum 2003;48:360)
- Negative staining: nonhematopoietic cells, platelets (J Clin Invest 1994;94:1243)
- References: OMIM #146631
CD51
- Also called integrin alpha chain V or vitronectin receptor alpha chain
- Integrins are membrane receptors for extracellular matrix mediated cell adhesion and migration, cytoskeletal organization, cell proliferation, cell survival and differentiation
- Integrins are composed of an alpha chain and a beta chain
- Alpha V integrins are a subset of integrins with a common alpha V subunit combined with beta subunits 1, 3, 5, 6 or 8
- The beta chain of the vitronectin receptor is CD61
- Most alpha V integrins recognize the RGD (Arg-Gly-Asp) sequence in various ligands such as vitronectin, fibronectin, osteopontin, bone sialoprotein, thrombospondin, fibrinogen, von Willebrand factor, tenascin or agrin
- Alpha V beta 3 integrin may mediate melanoma progression (Oncogene 2005;24:4710)
- CD51 on some dendritic cells serves as adenovirus receptor (J Leukoc Biol 2006;79:1271)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: endothelial cells, megakaryocytes, osteoclasts, monocytes and macrophages, placenta cytotrophoblast and Hofbauer cells and fibroblasts (Histochemistry 1991;96:169, Acta Histochem 2003;105:253)
- Positive staining - disease: osteoclast disorders including osteoclast-like giant cell neoplasms and inflamed synovium (Mod Pathol 2006;19:161, Ann Rheum Dis 1993;52:182)
- Negative staining: cartilage (Ann Rheum Dis 2000;59:448)
- Reference: OMIM #193210
CD52
- Also called Campath-1 and epididymal secretory protein E5
- CD52 antibodies are lytic for target cells, both with human complement and via antibody dependent cellular cytotoxicity
- Uses by pathologists:
- Antibodies (Alemtuzumab) are used for long term depletion of T lymphocytes from donor marrow to prevent graft versus host disease (Bone Marrow Transplant 2000;26:69, Transplantation 1999;67:620)
- Also to treat refractory CLL; high serum levels are poor prognostic marker in CLL (Cancer 2004;101:999)
- May treat other malignancies (see CD52+ disorders below), including pure red blood cell aplasia (Br J Haematol 2003;123:278)
- Differentiates eosinophils (CD52++) from neutrophils (CD52 weak / negative)
- Positive staining - normal: thymocytes, lymphocytes, monocytes / macrophages, eosinophils, mast cells and epithelial cells lining the male reproductive tract (Clin Lymphoma Myeloma 2006;6:478)
- Positive staining - disease:
- Most lymphoid malignancies (variable levels), including (J Clin Pathol 1994;47:313):
- Lymphoplasmacytic lymphoma (100%) (Am J Clin Pathol 2005;124:414)
- Myeloma (5 - 10%) (Am J Clin Pathol 2004;121:482)
- Hairy cell leukemia (Am J Hematol 2003;74:227)
- T cell large granular lymphocytic leukemia, Langerhans cell histiocytosis (Leuk Lymphoma 2005;46:723, Pediatr Blood Cancer 2005;44:251)
- Most lymphoid malignancies (variable levels), including (J Clin Pathol 1994;47:313):
- Negative staining: neutrophils, Langerhans cells (normal), lymphocytes in paroxysmal nocturnal hemaglobinuria and Reed-Sternberg cells in Hodgkin’s lymphoma
- Reference: OMIM #114280
CD53
- Most specific and reliable panleukocyte marker
- Encodes member of tetraspanin family, a cell surface protein with 4 hydrophobic domains that mediate signal transduction
- Also has adhesion / activation functions
- Upregulated in macrophages exposed to lipopolysaccharide (Mol Cells 2004;17:125)
- May transduce CD2 generated signals in T cells and natural killer cells
- May be a thymocyte selection marker, with CD69 (Int Immunol 2002;14:249)
- Familial deficiency is associated with recurrent infectious diseases (Clin Diagn Lab Immunol 1997;4:229)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: leukocytes; also dendritic cells, osteoclasts and osteoblasts and mesangial cells (Kidney Int 2003;63:534)
- Positive staining - disease: radioresistant tumor cells
- Negative staining: platelets, red blood cells and nonhematopoietic cells
- Reference: OMIM #151525
CD54
- Also called ICAM-1 (intercellular adhesion molecule 1)
- Ligand for LFA-1 (CD50)
- Receptor for:
- Rhinovirus (Proc Natl Acad Sci U S A 1991;88:7993)
- Malaria infected erythrocytes (Infect Immun 2006;74:3262, Proc Natl Acad Sci U S A 2000;97:1766)
- Involved in adhesion of neutrophils to endothelium at site of inflammation
- Reacts with CD11a / CD18 or CD11b / CD18, resulting in immune reaction or inflammation
- Reduced expression in endometrial cells may contribute to endometriosis (Immunol Lett 2002;80:49)
- Positive staining - normal: broad, B and T cells and B cell precursors, monocytes, osteoclasts, endothelial cells and epithelial cells (various)
- Positive staining - tumors: keratoacanthoma (more in fully developed lesions with inflammatory infiltrate), cutaneous squamous cell carcinoma (focal if well differentiated, intense if poorly differentiated) (Mod Pathol 2003;16:8)
- Negative staining: intravascular B cell lymphoma
- Reference: OMIM #147840
CD55
- Also called complement decay accelerating factor (DAF)
- Gene encodes Cromer blood group
- Binds C3bBb (alternative pathway convertase) and C4b2a (classical pathway convertase) to accelerate decay of the C3 convertases; protects against inappropriate complement activation (J Biol Chem 2005;280:2569)
- Receptor for CD97, echovirus and Coxsackie B virus (Proc Natl Acad Sci U S A 2002;99:10325, J Virol 1998;72:9407)
- Also is part of lipopolysaccharide-induced receptor complex (Eur J Immunol 2003;33:1399)
- Genetic defects that cause a reduction or loss of both CD59 and CD55 on erythrocytes produce paroxysmal nocturnal hemoglobinuria (PNH); also cause defective platelets, granulocytes, erythrocytes and possibly lymphocytes
- CD55 deficiency is common in patients treated with Campath (anti-CD52), which may predispose to PNH (Transplant Proc 2006;38:1750)
- A minor population of CD55 - CD59 negative granulocytes and red blood cells predicts a good response to immunosuppressive therapy in patients with acquired aplastic anemia (Blood 2006;107:1308)
- Loss of CD55 is associated with poor prognosis in breast cancer (Clin Cancer Res 2004;10:2797)
- However high expression is associated with poor prognosis in colorectal carcinoma (Cancer Immunol Immunother 2003;52:638)
- Case reports: pregnant woman in her early 40's with thrombocytopenia due to PNH (Univ Pittsburgh Case #419)
- Uses by pathologists: diagnosis of PNH (Am J Clin Pathol 2006;126:781)
- Positive staining - normal: all hematopoietic cells and all cell types in intimate contact with complement proteins; also epithelial cells lining extracellular compartments, body fluids and extracellular matrix
- Reference: OMIM #125240
CD56
- See CD56
CD57
- See CD57
CD58
- Also called LFA-3 (lymphocyte function associated antigen)
- Ligand for CD2 (J Mol Biol 2001;312:711)
- Mediates adhesion between:
- NK cells and target cells (J Immunol 2003;170:294)
- Antigen presenting cells and T cells (Cell 1999;97:791)
- Thymocytes and thymic epithelial cells
- High serum levels in Hepatitis B, associated with liver cell damage (World J Gastroenterol 2006;12:4237)
- Uses by pathologists: detect minimal residual disease in pre-B-ALL (Haematologica 2003;88:1245)
- Positive staining - normal: leukocytes (but not mature B cells), pre B cells, erythrocytes, endothelial cells, epithelial cells, fibroblasts and cardiac muscle (J Clin Pathol 1990;43:893)
- Positive staining - diseases: pre-B-ALL (Am J Clin Pathol 2005;123:119)
- Negative staining: mature B cells
- Reference: OMIM #153420
CD59
- Also called protectin, complement regulatory molecule
- Regulates complement mediated cell lysis by inhibiting formation of membrane attack complex (MAC); binds to C8 or C9 components, preventing incorporation of multiple copies of C9 required for complete formation of osmolytic core
- Also makes cells susceptible to NK cell mediated cytotoxicity (J Immunol 2006;176:2915)
- Genetic defects that reduce both CD59 and CD55 on erythrocytes produce paroxysmal nocturnal hemoglobinuria (PNH); also cause defective platelets, granulocytes, erythrocytes and possibly lymphocytes
- Low CD59 levels may also cause PNH-like symptoms after Campath therapy (Transplant Proc 2006;38:1750)
- Not a particularly good marker for detecting PNH+ monocytes (Am J Clin Pathol 2006;126:781)
- In diabetes, glycation may inhibit CD59, causing MAC deposition in vessels, leading to vascular complications (Diabetes 2004;53:2653)
- May resist complement mediated lysis via a surface CD59 like protein:
- Naegleria (Infect Immun 2006;74:1189)
- Borrelia (J Immunol 2003;170:3214)
- HIV (J Gen Virol 1997;78:1907)
- Uses by pathologists: no significant clinical use by pathologists
- Positive staining - normal: most cells
- Positive staining - disease: squamous cell carcinoma of head and neck (J Oral Pathol Med 2006;35:560)
- Reference: OMIM #107271
Microscopic (histologic) images
Images hosted on other servers:
CD56
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Interpretation | Case reports | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Homophilic binding glycoprotein with a role in cell - cell adhesion (Wikipedia: Neural Cell Adhesion Molecule [Accessed 8 February 2023])
Essential features
- Marker of natural killer (NK) cells and NK lymphomas
- Subsets of T cell lymphomas can show expression of CD56
- Sensitive marker for neuroendocrine tumors in the majority of small cell carcinoma / carcinoid tumors
- Not specific for neuroendocrine differentiation; should always be used in conjunction with other markers of neuroendocrine lineage (synaptophysin, chromogranin)
Terminology
- CD56 antigen is a 140 kDa isoform of the neural cell adhesion molecule (NCAM)
- Posttranslational modifications to the polypeptide include N and O glycosylations, acylation, sulphation and phosphorylation
- Different NCAM isoforms have molecular weights ranging from 135 to 220 kDa
- CD56 antigen is moderately expressed on a subpopulation of peripheral blood large granular lymphocytes and on all cells with NK activity; it is also expressed by subsets of T lymphocytes
- CD56 antibodies do not react with granulocytes, monocytes or B cells
- Reference: Beckman Coulter: CD34 Antibodies [Accessed 19 July 2023]
Pathophysiology
- Nerves
- Regulates homophilic (like - like) interactions between neurons and between neurons and muscle
- Associates with fibroblast growth factor receptor and stimulates tyrosine kinase activity of receptor to induce neurite outgrowth
- When neural crest cells stop making NCAM and N-cadherin and start displaying integrin receptors, cells separate and migrate (J Cell Sci 2002;115:283)
- Hematopoiesis
- Prototypic marker of NK cells
- Also presents on a subset of CD4+ and CD8+ T cells
- NK cells include a less mature (CD56 [bright] / CD16-) subset that is more common in lymph nodes and a more mature (CD56 [dim] / CD16+) subset that is more numerous in peripheral blood (Hum Pathol 2011;42:679)
- Adhesion
- Contributes to cell - cell or cell - matrix adhesion during development
Interpretation
- Membranous expression is interpreted as positive staining
Case reports
- 6 year old girl with B cell acute lymphoblastic leukemia (B ALL) and CD56 and CD57 coexpression (Pediatr Hematol Oncol 2004;21:677)
- 56 year old woman with CD56+ plasma cell leukemia (University of Pittsburgh: Case 470 [Accessed 8 February 2023])
Uses by pathologists
- Marker of NK cells and NK lymphomas
- Detects residual myeloma and residual acute myeloid leukemia in bone marrow (Am J Clin Pathol 2009;132:60, Am J Clin Pathol 2008;129:934)
- Differentiates plasma cells in myeloma (CD56+) from reactive plasmacytosis or monoclonal gammopathy of undetermined significance (MGUS) (CD56-) (Am J Pathol 2002;160:1293, Am J Clin Pathol 2009;132:728)
- Detects neuroendocrine disorders (J Clin Pathol 2002;55:535)
- Particularly if extensive crush artifact (J Clin Pathol 2005;58:978)
- Other neuroendocrine markers are synaptophysin and chromogranin
- Predicts poor prognosis for cutaneous lymphoproliferative disorders other than cutaneous T cell lymphoma (J Clin Pathol 2007;60:981)
- Most uterine smooth muscle neoplasms express CD56 (Int J Gynecol Pathol 2021;40:315)
Prognostic factors
- Myelomas that are negative for CD56 may have a poorer prognosis (Leuk Lymphoma 2004;45:61)
- Preliminary study suggests CD56+ lymphocytes may be associated with regression of melanoma (Hum Pathol 2011;42:1960)
Microscopic (histologic) images
Positive staining - normal
- NK cells (80 - 90%), large granular lymphocytes, activated T cells, osteoblasts
- Cerebellum and cortex at neuromuscular junctions, neuroendocrine tissue, neurons (membranous pattern), glia
- Ovarian stromal cells
- Rete testis cells (clusters of sloughed cells in hydrocele and spermatocele specimens may mimic small cell carcinoma) (Hum Pathol 2010;41:88)
- Skeletal muscle
Positive staining - disease
- Hematopoietic disorders
- Acute myeloid leukemia (variable) (Am J Clin Pathol 2007;128:550, Am J Clin Pathol 2009;132:101)
- Blastic plasmacytoid dendritic cell neoplasm (Arch Pathol Lab Med 2007;131:149)
- Enteropathy associated T cell lymphoma (Am J Clin Pathol 2007;127:701, Am J Surg Pathol 2011;35:1557)
- Myeloid sarcoma (variable) (Am J Clin Pathol 2000;114:807)
- Myelofibrosis (Am J Clin Pathol 2010;133:314)
- Myeloma, NK / T cell lymphoma (Am J Clin Pathol 2008;130:343, Am J Surg Pathol 2011;35:1195)
- Pediatric anaplastic large cell lymphoma (some) (Arch Pathol Lab Med 2006;130:1859)
- Primary cutaneous gamma delta T cell lymphoma (Cureus 2023;15:e35442)
- Other
- Alveolar rhabdomyosarcoma (Hum Pathol 2009;40:341, Mod Pathol 2008;21:795)
- Cardiac ischemic damage (Verh Dtsch Ges Pathol 2004;88:246)
- Extrahepatic biliary atresia (Am J Surg Pathol 2003;27:1454)
- Meningiomas and pulmonary meningothelial-like nodules (Am J Surg Pathol 2009;33:487)
- Intrahepatic clear cell cholangiocarcinoma (Am J Surg Pathol 2007;31:902)
- Merkel cell carcinoma (J Dermatol Sci 2003;31:219)
- Mesotheliomas (some)
- Neuroblastoma (adult) (World Neurosurg 2022;159:e23)
- Merkel cell carcinoma (Mod Pathol 2007;20:1113)
- Neuroendocrine carcinomas (Am J Surg Pathol 2006;30:684, Am J Clin Pathol 2010;133:618)
- Ovarian fibroma, fibrothecoma, leiomyoma (Am J Surg Pathol 2008;32:884)
- Ovarian sex cord stromal tumors (Int J Gynecol Pathol 2021;40:315)
- Pancreatic neuroendocrine tumor and solid pseudopapillary tumor (usually) (Mod Pathol 2006;19:1409)
- Pheochromocytoma (World J Surg Oncol 2022;20:185)
- Small cell carcinomas of cervix, lung and prostate (Int J Gynecol Pathol 2005;24:113, Am J Surg Pathol 2006;30:705)
- Sustentacular cell tumor (Am J Surg Pathol 2006;30:268)
- Synovial sarcoma (usually) (Mod Pathol 2006;19:659)
- Thyroid tumors (various) (Am J Clin Pathol 2003;120:64, Am J Surg Pathol 2010;34:1582)
- Uterine plexiform tumor / tumorlet
- Wilms tumor (Am J Surg Pathol 2009;33:454)
Negative staining
- Normal: B cells, granulocytes, monocytes, plasma cells
- Acute lymphocytic leukemia (ALL), large granular NK cell lymphocytosis (some cases), peripheral T cell lymphoma, plasma cell leukemia, primitive neuroectodermal tumors (PNET) / Ewing sarcoma, subcutaneous panniculitis-like T cell lymphoma (Am J Pathol 2004;165:1117, Arch Pathol Lab Med 2009;133:303)
- Chronic myelomonocytic leukemia (occasionally positive) (Leukemia 1993;7:1570)
- Ossifying fibromyxoid tumor of soft parts (43% positive) (Am J Surg Pathol 2011;35:1615)
Sample pathology report
- Lower right lung lobe, mucosal biopsies:
- Atypical carcinoid / neuroendocrine tumor of the lung with associated areas of necrosis and portions of respiratory mucosa (see comment)
- Comment: In this case, a neuroendocrine tumor of the lung is present, which shows areas of necrosis. Although the mitotic count in this section is low, the presence of necrosis advocates the diagnosis of an atypicial carcinoid.
- The neoplastic cells are positive for CD56, synaptophysin, chromogranin A and express SSTR2.
Additional references
Board review style question #1
Board review style answer #1
C. It is a marker of natural killer (NK) cells and NK lymphomas. Answers B and D are incorrect because these cells are typically negative for CD56. Answer A is incorrect because although it can differentiate MGUS from myeloma, MGUS plasma cells are CD56- and myeloma plasma cells are CD56+.
Comment Here
Reference: CD56
Comment Here
Reference: CD56
CD57
Table of Contents
Definition / general | Case reports | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Positive staining - tumors | Negative stainingDefinition / general
- Also called Leu7, beta-1,3-glucuronyltransferase 1 and glucuronosyltransferase P
- Glycoprotein with cell adhesion functions
- May define a phenotype associated with replicative senescence in HIV specific CD8+ T cells (Blood 2003;101:2711)
- References: OMIM #151290
Case reports
- 6 year old girl with B-ALL, CD56 and CD57 coexpression (Pediatr Hematol Oncol 2004;21:677)
Uses by pathologists
- Marker of NK cells and neuroendocrine tumors, helps distinguish high grade prostatic adenocarcinoma (CD57+) from high grade urothelial carcinoma (CD57-)
Microscopic (histologic) images
Positive staining - normal
- NK subset, T cell subset, neuroectodermal tissue, retina, brain, prostate and renal proximal tubules
Positive staining - disease
- Leukemia / lymphomas: autoimmune lymphoproliferative syndrome, hepatosplenic T cell lymphoma (some), nodular lymphocyte predominant Hodgkin lymphoma (CD57+ rosettes in 50%, Am J Clin Pathol 2003;119:192), pre T-ALL (occasional) and T-cell large granular lymphocytic leukemia (some)
- Nerve sheath origin lesions: benign epithelioid nerve sheath tumor (Am J Surg Pathol 2005;29:39), chordoma, dendritic cell neurofibroma with pseudorosettes (Am J Surg Pathol 2001;25:587), melanotic neuroectodermal tumor of infancy, MPNST (expression decreases with tumor grade, Am J Surg Pathol 2003;27:1337) and nerve sheath myxoma (Am J Surg Pathol 2005;29:1615)
Positive staining - tumors
- Other: carcinoid tumors, desmoplastic nested spindle cell tumor of liver (Am J Surg Pathol 2005;29:1), desmoplastic small round cell tumor (Am J Surg Pathol 1998;22:1314), germ cell tumor (embryonal carcinoma, seminoma), mesenchymal chondrosarcoma, metanephric adenoma (Am J Surg Pathol 2001;25:1290), neuroendocrine carcinoma of prostate (Am J Surg Pathol 2006;30:684) and other sites, PNET, prostatic adenocarcinoma, renal carcinoid, renal clear cell carcinoma (some), small cell carcinoma of lung and other sites, spindle cell thymoma (Am J Surg Pathol 2001;25:111), synovial sarcoma and thyroid papillary carcinoma (Cancer 2006;108:331)
Negative staining
- B cells, monocytes, red blood cells and platelets; NK/T cell lymphoma-nasal type, Wilm’s tumor
CD60-69
Table of Contents
CD60 (CDw60) | CD60a | CD60b | CD60c | CD61 | CD62 | CD63 | CD64 | CD65 | CD65s | CD66 | CD66b (formerly CD67) | CD66c | CD66d | CD66e / CEA | CD66f | CD68 | CD69 | Microscopic (histologic) imagesCD60 (CDw60)
- Use of CD60, CDw60 and CD60a, CD60b and CD60c is inconsistent
- Not proteins but oligosaccharides present on gangliosides
- Antibodies provide costimulatory signals for T cells
- Expressed on most T cells in autoimmune lesions (Immunol Invest 2001;30:67)
- CD8+ CD60+ T cells may regulate IgE memory responses and isotype switching (Hum Immunol 2005;66:1029)
- Associated with Th1 immune response in skin (Br J Dermatol 2003;149:739)
- No significant clinical use by pathologists
- Positive staining - normal:
- Platelets, T cells (30%), thymic epithelium, activated keratinocytes, melanocytes, synovial fibroblasts, glomeruli, smooth muscle cells and astrocytes (Carbohydr Res 2000;329:791)
- Also epithelium of reproductive system, exocrine and endocrine glands (Histochem J 2000;32:447)
- Positive staining - disease: T cells in rheumatoid arthritis and psoriasis, monocytes in cutaneous T cell lymphoma (Acta Derm Venereol 2001;81:263)
- Negative staining: B cells, granulocytes and monocytes
- Reference: Glycoforum: Glycolipid [Accessed 5 May 2021]
CD60a
CD60b
- 9-O-acetyl-GD3 - carbohydrate structure
- Intracellular regulators of apoptosis in T lymphocytes (Glycobiology 2011;21:1161)
- Expressed during rat central nervous system development and mainly associated with neuronal migration (Stem Cells Int 2017;2017:5759490)
- Other names: UM4D4
- Positive stains: subsets of CD4+ and CD8+ peripheral T cells, platelets and monocytes
CD60c
CD61
- See CD61
CD62
- See Selectins
CD63
- See CD63
CD64
- Also called Fc gamma RI, CD64A
- High affinity receptor binds to Fc region of IgG
- Important in phagocytosis via receptor mediated endocytosis of IgG antigen complexes
- Mediates antigen capture for presentation to T cells, antibody dependent cellular cytotoxicity, release of cytokines and reactive oxygen intermediates
- Also binds to C reaction protein and mediates its effects (J Biol Chem 2005;280:25095)
- Denge fever immune complexes enter macrophages via CD64 (J Virol 2006;80:10128)
- Uses by pathologists:
- High neutrophil CD64 levels predict sepsis (Arch Pathol Lab Med 2006;130:654, Lab Hematol 2005;11:137)
- Early onset of infection in neonates (Pediatr Res 2004;56:796)
- Infection in rheumatoid arthritis patients (J Rheumatol 2006;33:2416)
- Positive staining - normal: antigen presenting cells including macrophages / monocytes, activated granulocytes and dendritic cells; also early myeloid cells
- Positive staining - disease: AML M3 (usually); M4, M5, M0 - M2 (variable) (Am J Clin Pathol 1998;110:797)
- Negative staining: AML M7
- Reference: OMIM: 146760 [Accessed 5 May 2021]
CD65
- Also called VIM2, ceramide dodecasaccharide, dimeric sialyl CD15
- Adhesive carbohydrate (not a protein) that appears to be significant risk factor for extravascular AML infiltration (Leuk Res 2001;25:847)
- Uses by pathologists: myeloid antigen used in flow cytometry
- Positive staining - normal: myeloid cells, monocytes
- Positive staining - disease: AML
- Negative staining: lymphocytes
CD65s
- Also called sialylated CD65
- Carbohydrate antigen, not a protein
- Appears when CD34 antigen disappears
- Antibodies may either recognize CD65s (sialylated) or CD65 (nonsialylated)
- Uses by pathologists: for acute leukemia cell typing and to identify a subset of pre-B ALL (Am J Clin Pathol 2002;117:380)
- Positive staining - normal: granulocytes, monocytes
- Positive staining - disease: myeloid leukemia, low levels in AML M0 - M1 (Leukemia 2003;17:1544)
CD66
- Also called CEACAM1, biliary glycoprotein, BGP, C-CAM, CD66A
- Primordial protein of carcinoembryonic antigen (CEA) family
- Cell adhesion molecule capable of activating neutrophils
- Receptor for Neisseria gonorrhoeae and N. meningitides; binding prevents epithelial detachment, a defense mechanism that hinders colonization (J Cell Biol 2005;170:825)
- CD66a+ B cells are also killed by N. gonorrhoeae (Infect Immun 2005;73:4171)
- With osteopontin, may mediate invasion of extravillous trophoblast at maternal fetal interface (J Clin Endocrinol Metab 2005;90:5407)
- Interactions with CEA inhibit NK cell cytotoxicity (J Immunol 2005;174:6692)
- Downregulated in:
- Breast (J Histochem Cytochem 1997;45:957)
- Colorectal, endometrial, hepatocellular, prostate (particularly Gleason grade 4/5) (Hum Pathol 2002;33:290)
- Renal cell carcinoma (J Pathol 2004;204:258)
- Uses by pathologists: expression predicts metastases in cutaneous melanoma (J Clin Oncol 2002;20:2530)
- Positive staining - normal: granulocytes, lymphocytes, epithelial cells, endothelial cells, prostate glands and ducts (dense), bile canaliculi between liver cells, extravillous trophoblast (Am J Pathol 2000;156:1165)
- Positive staining - disease: low grade prostate carcinoma
- Negative staining: high grade (Gleason 4/5) prostate carcinoma
- Reference: OMIM: 109770 [Accessed 5 May 2021]
CD66b (formerly CD67)
- Also called CEACAM8. NCA-95 and CGM6; formerly CD67
- Cell adhesion molecule capable of activating neutrophils
- Increased expression on peripheral blood neutrophils and eosinophils of rheumatoid arthritis patients (Scand J Immunol 1999;50:433)
- Uses by pathologists: marker for granulocytes
- Positive staining - normal: granulocytes
- Positive staining - disease: chronic myelogenous leukemia, cardiomyocytes in areas of infarction (Cancer Res 1990;50:6534, Cardiovasc Res 1999;41:603)
CD66c
- Also called nonspecific cross reactive antigen, CEACAM6, NCA 50/90
- Cell adhesion molecule capable of activating neutrophils
- No significant clinical use by pathologists
- Positive staining - normal: granulocytes
- Positive staining - disease: ALL (43%) (BMC Cancer 2005;5:38)
- Reference: OMIM: 163980 [Accessed 5 May 2021]
CD66d
- Also called CEACAM3, CGM1
- Cell adhesion molecule capable of activating neutrophils
- Has important role in control of pathogens by the innate (opsonin independent) immune system (Wikipedia: Innate Immune System [Accessed 5 May 2021], J Exp Med 2004;199:35)
- Used by Neisseria. gonorrhoeae, Moraxella catarrhalis and Hemophilus influenzae to anchor themselves to and invade host cells
- N. gonorrheae has an opacity associated (Opa) protein that binds to CEACAM3 (J Biol Chem 2001;276:17413)
- No significant clinical use by pathologists
- Positive staining - normal: granulocytes
- Reference: OMIM: 609142 [Accessed 5 May 2021]
CD66e / CEA
- See CD66e / CEA
CD66f
- Also called pregnancy specific beta 1 glycoprotein, PSG1
- May be involved in immune regulation, protection of fetus from maternal immune system
- Released into maternal circulation during pregnancy
- Low levels in maternal blood predict spontaneous abortion
- No significant clinical use by pathologists
- Positive staining - normal: syncytiotrophoblasts, fetal liver and myeloid cells
- Positive staining - disease: hydatidiform and invasive moles, choriocarcinoma (J Clin Pathol 1977;30:19)
- Reference: OMIM: 176390 [Accessed 5 May 2021]
CD68
- See CD68
CD69
- Also called activation inducer molecule (AIM), early activation antigen (EA1)
- Earliest inducible cell surface glycoprotein acquired during lymphoid activation
- Involved in early events of T cell, NK cell, monocyte and platelet activation
- Associated with Th1 T cell differentiation and associated cytokines (IL2, TNF alpha, interferon gamma) (Hum Pathol 2002;33:330)
- Highly expressed on T cells from inflammatory infiltrates of rheumatoid arthritis, viral hepatitis and autoimmune thyroid disorders (Clin Exp Rheumatol 2004;22:331)
- Expression on CD3+ and CD8+ peripheral blood T cells correlates with acute graft rejection in renal allograft recipients (Transplantation 2003;76:190)
- May promote lymphocyte retention in lymphoid organs (Nature 2006;440:540)
- No significant clinical use by pathologists
- Positive staining - normal: activated T cells, B cells, NK cells, neutrophils, eosinophils, epidermal Langerhans cells, platelets and thymocytes
- Positive staining - disease: peripheral T cell lymphoma (Am J Clin Pathol 2003;120:866)
- Reference: OMIM: 107273 [Accessed 5 May 2021]
Microscopic (histologic) images
Images hosted on other servers:
CD61
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Membrane glycoprotein that associates with CD41 to form a heterodimeric complex (CD61 / CD41); dominant integrin on platelets that is essential for normal platelet function (J Hematol Oncol 2019;12:26)
- CD61 binds to several matrix proteins, including fibrinogen, which is important to blood clotting (Alberts: Molecular Biology of the Cell, 4th Edition, 2002)
Essential features
- CD61, also known as GP3A and β3 integrin, is an adhesion receptor on the membrane of cells with a megakaryocytic lineage (Histol Histopathol 2002;17:347, F1000Res 2016;5:F1000)
- CD61 forms heterodimer with CD41 known as glycoprotein IIb - IIIa complex
- CD61 is encoded by ITGB3 gene
- Dominant integrin on platelets and is highly expressed
- Important mediator of platelet aggregation
- Activated glycoprotein IIb - IIIa complex binds fibrinogen or von Willebrand factor to bridge platelets together
- CD61 is encoded by ITGB3 gene
- CD61 can promote invasion and migration in tumors (Am J Transl Res 2019;11:7195)
Terminology
- β3 integrin (ITGB3)
- Integrin subunit beta 3
- GP3A
Pathophysiology
- Platelet aggregation is mediated by binding of fibrinogen to sites on the glycoprotein IIb - IIIa receptor complex (Biochem J 1995;309:613)
- Hereditary defect of glycoprotein IIb - IIIa receptor complex causes Glanzmann thrombasthenia, an autosomal recessive bleeding disorder (Transfus Med Rev 2016;30:92)
- TGFβ is the main upstream factor of integrins and when elevated, leads to increased levels of mesenchymal-like cancer cells (Am J Transl Res 2019;11:7195)
Clinical features
- Expressed on macrophages, endothelial cells, fibroblasts, megakaryocytes, osteoclasts, mast cells and platelets
- Present in normal tissue and tumors (Histol Histopathol 2002;17:347)
Interpretation
- Membrane, intracellular
- Cytoplasmic expression in megakaryocytes and platelets
Uses by pathologists
- Identify platelets, megakaryocytes and platelet thrombi
- Count platelets in thrombocytopenic patients (Br J Haematol 2001;112:584)
Prognostic factors
- CD61 upregulation is related to poor survival on non-small cell lung cancer, breast cancer, cervical cancers, pancreatic ductal adenocarcinomas, T cell acute lymphoblastic leukemia and gliomas (Transl Lung Cancer Res 2019;8:323, Am J Transl Res 2019;11:7195, Commun Biol 2021;4:490)
Microscopic (histologic) description
- CD61 is expressed on platelets, megakaryocytes, monocytes, macrophages and endothelial cells (Barclay: The Leucocyte Antigen Factsbook, 2nd Edition, 1997)
- CD41 interacts with CD61 to form the glycoprotein IIb - IIIa receptor complex
- Expressed on platelets and megakaryocytes
- CD41 interacts with CD51 to form the vitronectin receptor
- Expressed on endothelial cells, monocytes, platelets and osteoclasts
- CD41 interacts with CD61 to form the glycoprotein IIb - IIIa receptor complex
Microscopic (histologic) images
Positive staining - normal
- Cytoplasmic staining of normal and abnormal megakaryocytes, platelets, occasional endothelial cells, some myeloid precursor cells
Positive staining - disease
- Useful in identifying micromegakaryocytes, abnormal megakaryocytes and megakaryoblasts in cases of acute megakaryoblastic leukemia, myeloproliferative disorders and myelodysplastic syndromes (Am J Clin Pathol 2018;150:461, Virchows Arch B Cell Pathol Incl Mol Pathol 1992;62:275)
- CD61 may assist in marking tumor associated thrombi in follicular thyroid carcinoma in order to distinguish true vascular invasion from mimics (Head Neck Pathol 2020;14:399)
- Identification of microthrombi in renal biopsies from patients with lupus nephritis and those receiving calcineurin inhibitor therapy (Head Neck Pathol 2020;14:399)
Negative staining
- Acute myeloid leukemia without maturation (AML M0 - M6) (Arch Pathol Lab Med 2011;135:44)
Molecular / cytogenetics description
- Glanzmann thrombasthenia is caused by a defect in the platelet integrin receptor essential to platelet aggregation and hemostasis
- Mutations involve missense, nonsense, frameshift or point mutations in ITGA2B or ITGB3 genes located on chromosome 17q21 (Orphanet J Rare Dis 2006;1:10)
Sample pathology report
- Bone marrow aspirate:
- Acute leukemia of ambiguous lineage, NOS (see comment)
- Comment: A 68 year old man presented with suspected leukemia. Bone marrow aspiration revealed 85% blasts with positive expression for CD34, CD7, TdT, CD33, CD117 and CD61, while being negative for MPO, CD19, CD22, CD79a and CD3.
Board review style question #1
An infant is evaluated for bleeding of the gums and ongoing nose bleeds. A complete blood count comes back with normal platelet count but prolonged bleeding time. Evaluation by flow cytometry and IHC indicates markedly decreased CD41 and CD61. Genetic sequencing indicated mutated ITGA2B. What is the most likely diagnosis?
- Factor V Leiden
- Glanzmann thrombasthenia
- Hemophilia B (characterized by deficiency in factor VIII or IX, caused by X linked recessive trait)
- Von Willebrand disease
Board review style answer #1
B. Glanzmann thrombasthenia. Significantly decreased levels of CD41 and CD61 is diagnostic for Glanzmann thrombasthenia. Answer A is incorrect because factor V Leiden involves a mutated F5 gene resulting in thrombophilia. Answer C is incorrect because hemophilia B is caused by an X linked recessive trait, not a mutated ITGA or ITGB gene. Answer D is incorrect because von Willebrand disease is caused by variants in the VWF gene.
Comment Here
Reference: CD61
Comment Here
Reference: CD61
Board review style question #2
Board review style answer #2
B. Megakaryocytes. CD61 is a glycoprotein found on megakaryocytes, platelets and their precursors. Answer A is incorrect because granulocytes are identified by CD66b. Answer C is incorrect because plasma cells are distinguished by their expression of CD38 and CD138. Answer D is incorrect because other CD markers such as CD3, CD4 and CD8 are used to identify this cell type.
Comment Here
Reference: CD61
Comment Here
Reference: CD61
CD63
Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Additional referencesDefinition / general
- Also called NKI-C3 (J Natl Cancer Inst 1992;84:422), lysosomal membrane-associated glycoprotein 3, LAMP-3, melanoma associated antigen and ME491
- Member of tetraspanin superfamily of integral membrane proteins - tetraspanins form lateral associations with integrins and may act as organizers of multimolecular networks that modulate integrin mediated signaling, cell morphology, motility and migration
- Intracellular lysosomal / endosomal / granule protein, in Weibel-Palade bodies of endothelium and in azurophil granules of neutrophils (Am J Pathol 1994;144:1369)
- Serves as adaptor protein that links its interaction partners to the cell’s endocytic machinery (Proc Natl Acad Sci U S A 2003;100:15560)
- Marker of platelet activation that is transported to surface after activation; also modulates platelet spreading on immobilized fibrinogen (Thromb Haemost 2005;93:311)
- Associated with early stages of melanoma progression (Cancer Res 1988;48:2955)
- Deficiency associated with Hermansky-Pudlak syndrome (OMIM #203300)
- High pre-kidney transplant levels are associated with acute rejection (Transplant Proc 2003;35:1360)
- Used for basophil activation tests (Allergy 2006;61:1084)
- CD63 pathway from host multivesicular bodies provides essential lipids to Chlamydia to maintain productive intracellular infection (J Cell Sci 2006;119:350)
Uses by pathologists
- Marker of melanoma (although non-specific) and melanocytic tumors
- May be useful for other tumors (see below)
Positive staining - normal
- Activated platelets, endothelium, fibroblasts, macrophages, mast cells and osteoclasts
- Weakly expressed on B and T cells and granulocytes
- Also bronchial glands, neural tissue (brain white matter and peripheral nerves), nevi, salivary glands, smooth muscle and synovial lining cells
Positive staining - disease
- Angiomyolipoma (100%) (Arch Pathol Lab Med 2001;125:751)
- Atypical fibroxanthoma (33%)
- Breast carcinoma (100%) (Am J Pathol 1998;153:973)
- Carcinoids (some)
- Cellular fibrous histiocytoma (50%)
- Cellular neurothekeoma (81%) (Mod Pathol 2004;17:230)
- Clear cell fibrous papule of nose (83%) (Am J Dermatopathol 2005;27:296)
- Deciduoid mesothelioma (67%) (Am J Surg Pathol 2000;24:285)
- Dermatofibrosarcoma protuberans (90%) (Am J Clin Pathol 1992;97:478)
- Histiocytic sarcoma
- Juvenile xanthogranuloma (60%)
- Melanoma (90%)
- Primitive nonneural granular cell tumors of skin (90%) (Am J Surg Pathol 2005;29:927)
- Renal oncocytoma (apical and polar staining)
- Renal chromophobe carcinoma-eosinophilic variant (diffuse staining) (Virchows Arch 2005;447:938)
- Reticulohistiocytoma (50%)
- Thyroid medullary carcinoma (some)
- Xanthoma (80%)
Negative staining
- Epithelioid cell histiocytoma, Langerhans cell histiocytosis
Additional references
CD68
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Lysosomal associated transmembrane glycoprotein that is present in a variety of normal and neoplastic cell types and is primarily used as a marker to identify histiocytes and histiocytic tumors
Essential features
- Lysosomal marker used to identify histiocytic and monocytic cells with limited specificity
- KP1 and PGM1 are the 2 most commonly used antibody clones, with PGM1 being the slightly more specific marker
Terminology
- Lysosomal associated membrane protein 4 (LAMP4)
- Gp110
- Scavenger receptor class D member 1 (SCARD1)
- Macrosilian (murine analog)
- KP1 (common antibody clone)
- PGM1 (common antibody clone)
- EBM11 (less commonly used antibody clone)
- KiM6 and KiM7 (less commonly used antibody clones)
Pathophysiology
- Mucin rich transmembrane glycoprotein (110 kDa), encoded by a gene on chromosome 17p13 (Blood 1993;81:1607, Lab Invest 2017;97:4)
- CD68 primarily localizes to lysosomes and endosomes; a smaller fraction circulates to the cell surface (Lab Invest 2017;97:4)
- Macrophage CD68 is upregulated in response to inflammatory stimuli (Proc Natl Acad Sci U S A 1996;93:14833, Atheroscler Thromb 2002;9:57)
- CD68 can bind apoptotic cells, phosphatidylserine and oxidized low density lipoprotein (Proc Natl Acad Sci U S A 1996;93:14833, Proc Natl Acad Sci U S A 28;92:1396, Proc Natl Acad Sci U S A 1995;92:1391)
Interpretation
- Dot-like granular or diffuse cytoplasmic stain (Mod Pathol 2011;24:390, Scand J Immunol 2020;92:e12889, Melanoma Res 2019;29:237)
Uses by pathologists
- Histiocytic malignancies are usually CD68 positive (Am J Clin Pathol 2004;122:794)
- CD68 is used to diagnose histiocytic sarcoma, which usually expresses at least 2 of the following markers: CD68, CD163, CD4, lysozyme (Blood 2016;127:2672)
- Myeloid / monocytic sarcoma is usually CD68 positive (Leukemia 2007;21:340)
- PGM1 is more specific to monocyte / macrophages than KP1, which is widely reactive (Ann Rheum Dis 2004;63:774)
- Renal cell carcinoma with t(6;11) is consistently KP1 positive and PGM1 negative, whereas epithelioid angiomyolipoma is KP1 and PGM1 positive (Mod Pathol 2018;31:474)
- Double staining of CD68 and CD31 can aid in the diagnosis of antibody mediated rejection by labeling intracapillary macrophages (Am J Transplant 2019;19:3149)
- CD68 can aid in identification of chronic granulomatous disease (CGD) in patients with colonic inflammation; CGD patients have a significantly smaller average of CD68 positive cells per mm2 of lamina propria (242.3 cells/mm2) than patients with Crohn’s disease (1,104.2 cells/mm2) and the control group (565.4 cells/mm2) (Inflamm Bowel Dis 2009;15:1213)
- CD68 can aid in the differential diagnosis between cellular fibrous histiocytoma (83% KP1 positive) and dermatofibrosarcoma protuberans (6% KP1 positive) (J Cutan Pathol 2006;33:353)
- Primary cutaneous acral CD8 positive T cell lymphoproliferative disorder shows dot-like CD68 positivity, allowing it to be distinguished from other primary or secondary cutaneous CD8 positive T cell lymphomas (Br J Dermatol 2015;172:1573)
Prognostic factors
- Elevated numbers of CD68 positive tumor associated macrophages (TAMs) correlate with negative survival outcomes in many cancer types; TAMs are predominantly M2 macrophages, which can promote tumor growth / spread through the secretion of MMP9, VEGF, EGF and TGF1 (Clin Transl Oncol 2016;18:251)
- Anaplastic large cell lymphoma (ALCL): increased intratumoral TAMs correlate with an adverse outcome in anaplastic lymphoma kinase negative ALCL (Histopathology 2014;65:490)
- Breast cancer: increased TAMs predict worse cancer specific survival and a shorter disease free interval; patients with lower TAM levels showed improved metastasis free survival (J Clin Pathol 2012;65:159, Int J Cancer 2012;131:426)
- Diffuse large B cell lymphoma: TAMs are associated with a favorable prognosis when patients are treated with rituximab in addition to multiagent chemotherapy and with a poor outcome when rituximab is not given (Haematologica 2015;100:143)
- Classical Hodgkin lymphoma: studies have suggested elevated TAM expression as a negative indicator of survival in classical Hodgkin lymphoma; however, this association has been disputed (Leuk Lymphoma 2011;52:1913, N Engl J Med 2010;362:875, Diagn Pathol 2020;15:10, BMC Med 2016;14:159, Ann Oncol 2012;23:736)
- Follicular lymphoma: TAMs are associated with adverse outcomes in chemotherapy treated patients; in contrast, after a rituximab and chemotherapy combination regimen, high TAM content is correlated with longer overall survival (Clin Cancer Res 2007;13:5784)
- Hepatocellular carcinoma: density of peritumoral TAMs is associated with poor recurrence free survival and poor overall survival (PLoS One 2013;8:e59771)
- Squamous cell carcinoma of the head and neck: increased TAMs are associated with worse relapse free survival, worse disease specific survival and worse overall survival (Head Neck 2016;38:1074, Oral Oncol 2015;51:90)
- Myxoid liposarcoma: increased TAMs are associated with poorer overall survival rate (Br J Cancer 2015;112:547)
- Urothelial carcinoma: a high CD68/CD3 positive ratio identifies a bad prognosis group among muscle invasive cases (Urol Oncol 2014;32:791)
- Brain tumors: CD68 TAMs are associated with higher tumor grade in astrocytoma (Clin Cancer Res 2013;19:3776)
Microscopic (histologic) images
Virtual slides
Positive staining - normal
- Highly expressed in cells of mononuclear phagocyte lineage, including macrophages, microglia, osteoclasts, tissue histiocytes, Kupffer cells (IHC KP1), multinucleated giant cells (IHC KP1), Langerhans cells (IHC KP1), Hofbauer cells (IHC PGM1) (J Clin Pathol 1989;42:414, J Leukoc Biol 2012;92:723, Head Neck Pathol 2009;3:95, Am J Clin Pathol 1989;92:273, Pediatr Dev Pathol 2010;13:300)
- Comparably high expression reported in fibroblasts (IHC KP1, EBM11) and endothelial cells (IHC KP1, FCM KP1) (Ann Rheum Dis 2004;63:774, Scand J Immunol 2008;67:453, Verh Dtsch Ges Pathol 2003;87:215)
- Lower expression in neutrophils (ICC KP1), CD34 positive progenitor cell subsets (IHC KiM7), adipocytes (IF and FCM), activated T and B cells, gamma delta T cells and NK cells (IHC KP1, EMB11; FCM KP1, EMB11) (Int Immunol 1990;2:973, Blood 1995;86:4115, FEBS Lett 2005;579:5631, Hum Pathol 1994;25:872, Scand J Immunol 2008;67:453)
- Other myeloid cells such as basophils (ICC KP1) and mast cells (IHC KP1) (Int Immunol 1990;2:973, J Clin Pathol 1990;43:719)
- Intimal smooth muscle cells of human arteries (ICC KP1), fetal small intestinal inclusions (Atherosclerosis 1997;135:19, Cesk Patol 2001;37:7)
Positive staining - disease
- Benign tumors:
- Calcifying aponeurotic fibroma (KP1: 100%) (Hum Pathol 1998;29:1504)
- Cellular fibrous histiocytoma (KP1: 83%) (J Cutan Pathol 2006;33:353)
- Chondroid lipoma (KP1: 82%) (Am J Surg Pathol 1993;17:1103)
- Angiomyolipoma (PGM1 and KP1) (Mod Pathol 2012;25:100)
- Epithelioid angiomyolipoma (PGM1 in 40 - 80% of cells, 100% of cases; KP1 in 50 - 90% of cells, 100% of cases in one study; PGM1 and KP1 in 100% of cases in another study) (Mod Pathol 2012;25:100, Mod Pathol 2018;31:474)
- Giant cell tumor of the bone (strong positivity in osteoclast-like giant cells in 100% of cases, weaker and less frequent positivity in stromal cells in one study; positivity in osteoclast-like giant cells in another study) (Hum Pathol 1996;27:754, J Clin Orthop Trauma 2016;7:109)
- Giant cell tumor of soft tissue (strong positivity in osteoclast-like giant cells in 87% of cases, positivity in mononuclear cells in 73% of cases) (Am J Surg Pathol 2000;24:386)
- Granular cell tumor (KP1 strong positivity: 100%) (Arch Pathol Lab Med 2004;128:771)
- Malignant granular cell tumor of soft tissue (KP1: 65%) (Am J Surg Pathol 1998;22:779)
- Granuloma annulare (KP1: 86%; PGM1: 100%) (J Cutan Pathol 2002;29:590)
- Juvenile xanthogranuloma (100% in one study; KP1: 100% in another study) (Am J Surg Pathol 2003;27:579, Am J Dermatopathol 2001;23:104)
- Kikuchi disease (Kikuchi-Fujimoto disease of the lymph node) (KP1: 100%; PGM1: 100%) (Am J Surg Pathol 1999;23:1040, Am J Surg Pathol 1995;19:798, Am J Pathol 2001;159:915)
- Mycobacterial pseudotumor (Am J Surg Pathol 1999;23:656, Iran J Med Sci 2018;43:94)
- Multicentric reticulohistiocytosis (KP1) (Am J Dermatopathol 1994;16:577)
- Cellular neurothekeoma (KP1: 46 - 59%) (Am J Surg Pathol 2007;31:1103, Mod Pathol 2014;27:701)
- Nodular fasciitis (KP1: 92%) (Am J Surg Pathol 1991;15:942)
- Pleomorphic xanthoastrocytoma (Folia Neuropathol 2003;41:89)
- Schwannoma (KP1: 80%) (Int Pharmacopsychiatry 1977;12:72, Mod Pathol 1993;6:463)
- Splenic littoral cell angioma (KP1: 100%) (Am J Surg Pathol 1997;21:827, Am J Surg Pathol 2006;30:1036)
- Solitary reticulohistiocytoma of the skin (KP1) (Am J Surg Pathol 2006;30:521)
- Tenosynovial giant cell tumor (Hum Pathol 2003;34:670)
- Localized type (previously giant cell tumor of the tendon sheath) (Hum Pathol 1995;26:771, Tumorit 1997;83:841)
- Diffuse type (previously pigmented villonodular synovitis) (Hum Pathol 2003;34:65, Hum Pathol 1995;26:771)
- Carcinoma:
- Fibrolamellar carcinoma of the liver (KP1 strong positivity: 97%) (Mod Pathol 2011;24:390)
- Osteoclast-like giant cells in tumors of pancreas and urinary tract (KP1: 100%) (Arch Pathol Lab Med 1998;122:266, Mod Pathol 2006;19:161)
- Renal cell carcinoma with t(6,11) (KP1: 100%) (Mod Pathol 2018;31:474)
- Hematologic malignancies:
- Acute myeloid leukemia (AML): KP1 in most AML subtypes (Am J Clin Pathol 2000;113:814, Am J Clin Pathol 2004;122:794)
- Chronic myeloid leukemia (chronic myelogenous leukemia) (KP1 and PGM1: 100%) (Am J Clin Pathol 2004;122:794, Mod Pathol 2006;19:1536)
- Chronic myelomonocytic leukemia (KP1 and PGM1: 100%) (Am J Clin Pathol 2004;122:794, Mod Pathol 2006;19:1536)
- Hairy cell leukemia (KP1: 78 - 100%) (Am J Pathol 1989;135:1089, Pathol Oncol Res 2015;21:203, Mod Pathol 1996;9:982)
- Myelodysplasia bone marrow nodules (KP1 and PGM1 in one study; PGM1: 100% in another study) (Am J Clin Pathol 2003;120:874, Am J Hematol 2005;79:329)
- Small lymphocytic lymphoma (KP1: 83 - 87%) (Hum Pathol 1993;24:886, Am J Clin Pathol 1995;103:425)
- Erdheim-Chester disease (KP1: 100%) (Am J Surg Pathol 1999;23:17)
- Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy) (KP1 in one study; KP1 and PGM1: 100% in another study) (Mod Pathol 2001;14:172, Am J Clin Pathol 2004;122:794)
- Langerhans cell histiocytosis (100% in one study; KP1 and PGM1: 96% in another study) (Blood 2001;97:1241, Histopathology 2002;41:1)
- Primary cutaneous acral CD8+ T cell lymphoma (dot-like positivity) (J Am Acad Dermatol 2021;85:1073)
- Histiocytic sarcoma (KP1: 86 - 100%; PGM1: 100%) (Am J Surg Pathol 2004;28:1133, Mod Pathol 2005;18:693, Cancer Cytopathol 2017;125:604)
- Myeloid / monocytic sarcoma (KP1: 100%; PGM1: 51%) (Leukemia 2007;21:340)
- Mastocytosis and mast cell disease (KP1: 100%) (Am J Surg Pathol 2000;24:703)
- Sarcoma:
- Angiosarcoma (KP1: 60%) (Virchows Arch 1994;424:635)
- Angiomatoid fibrous histiocytoma (65 - 95%) (Pathology 2014;46:199, Pediatr Dev Pathol 2012;15:181)
- Phyllodes tumor (benign and malignant, stromal component, KP1: 75%) (Virchows Arch 1994;424:635)
- Follicular dendritic cell sarcoma (92%; KP1: 100% in one study; KP1 and PGM1: 62% in another study) (Diagn Pathol 2010;5:67, Am J Surg Pathol 1998;22:1048, Histopathology 2002;41:1)
- Inflammatory myofibroblastic tumor (previously inflammatory pseudotumor) - hepatic (KP1: 100%); splenic (KP1: 60%) (Mod Pathol 2007;20:884, Arch Pathol Lab Med 2001;125:379)
- Interdigitating dendritic cell sarcoma (92%) (Diagn Pathol 2010;5:67)
- Leiomyosarcoma (KP1: 89%; some PGM1) (Virchows Arch 1994;424:635)
- Malignant peripheral nerve sheath tumor (neurofibrosarcoma) (KP1: 67%) (Virchows Arch 1994;424:635)
- Myxoinflammatory fibroblastic sarcoma (KP1 and PGM1: 68 - 80%) (Ann Diagn Pathol 2002;6:272, Am J Surg Pathol 1998;22:911, J Cutan Pathol 2008;35:186)
- Undifferentiated embryonal sarcoma of the liver (KP1: 67%) (Am J Surg Pathol 1991;15:615)
- Undifferentiated pleomorphic sarcoma (malignant fibrous histiocytoma) (KP1: 72 - 79%; of the breast, KP1: 71%) (Am J Clin Pathol 1992;97:759, Am J Clin Pathol 1995;103:425, Ann Diagn Pathol 2011;15:407)
- Other:
- Chronic intervillositis (positivity in 90% of mononuclear cells in intervillous spaces, in 100% of cases) (Hum Pathol 2000;31:1389)
- Crystal storing histiocytosis (KP1: 100%) (Histopathology 2016;68:482)
- Desquamative interstitial pneumonia (diffuse and extensive intra-alveolar deposition of alveolar CD68 positive macrophages) (KP1) (Am J Respir Crit Care Med 1997;156:2003)
- Diffuse alveolar damage (DAD) (positive association of PGM1 macrophage infiltrates with DAD) (Nat Commun 2020;11:5086)
- Gaucher disease (100%) (Am J Clin Pathol 2004;122:359, Acta Med Croatica 2001;55:131)
- Malakoplakia (Diagn Pathol 2020;15:97)
- Plexiform fibrohistiocytic tumor (KP1: 55 - 100%) (Am J Surg Pathol 1999;23:662, Histopathology 1991;19:503, Am J Surg Pathol 2009;33:905)
- Rheumatoid nodules (KP1: 93%; PGM1: 100%) (J Cutan Pathol 2002;29:590)
- Steatohepatitis (Mod Pathol 2002;15:699)
- Whipple disease (Hum Pathol 2003;34:589)
- Xanthogranulomatous pyelonephritis (Arch Pathol Lab Med 2005;129:e209)
- Xanthoma (Hum Pathol 2003;34:814)
Negative staining
- Anaplastic large cell lymphoma (KP1: 10%) (Hum Pathol 1993;24:886)
- Atypical fibrous histiocytoma (Am J Surg Pathol 2002;26:35)
- Hemangiopericytoma (KP1: 50%) (Virchows Arch 1994;424:635)
- Liposarcoma (KP1: 33%) (Virchows Arch 1994;424:635, Am J Clin Pathol 1995;103:425)
- Osteosarcoma (KP1: 33%) (Am J Clin Pathol 1995;103:425)
- Rhabdomyoma (adult and fetal) (ORL J Otorhinolaryngol Relat Spec 1998;60:178, Hum Pathol 1993;24:754)
- Synovial sarcoma (KP1: 14%, weak staining) (Virchows Arch 1994;424:635)
- Dermatofibrosarcoma protuberans (KP1: 6%) (J Cutan Pathol 2006;33:353)
Sample pathology report
- Skin, biopsy:
- Diagnosis: myeloid / monocytic sarcoma (see comment)
- Comment: The skin biopsy shows a dense infiltrate of intermediate sized cells with open and dispersed chromatin, irregular nuclear contours, variable amounts of cytoplasm and frequent mitotic figures. Areas of tumoral necrosis are present. Immunohistochemical stains show that the atypical infiltrate are positive for CD4, CD33, CD43, CD68 (KP1) and CD68 (PGM1). The atypical cells are negative for CD3, CD20, PAX 5, CD34, CD56, CD123 and muramidase. A Ki67 stain is positive in 90% of tumor cell nuclei. In summary, these findings represent involvement by myeloid / monocytic sarcoma.
Board review style question #1
Which of the following marker combinations fits the immunoprofile of Langerhans cell histiocytosis (LCH)?
- CD68 negative, CD1a negative, CD207 (langerin) negative
- CD68 negative, CD1a positive, CD207 (langerin) positive
- CD68 positive, CD1a negative, CD207 (langerin) negative
- CD68 positive, CD1a positive, CD207 (langerin) positive
Board review style answer #1
D. CD68 positive, CD1a positive, CD207 (langerin) positive. LCH cells are positive for CD68, a traditional histiocyte marker, as well as CD1a and CD207 (langerin), typical Langerhans cell markers. CD1a and CD207 positivity (as opposed to answer choice C) can distinguish surrounding CD68 positive macrophages from LCH cells.
Comment Here
Reference: CD68
Comment Here
Reference: CD68
Board review style question #2
CD68 IHC can be helpful in which of the following differential diagnostic scenarios?
- Chronic granulomatous disease versus Whipple disease
- Clear cell renal cell carcinoma versus chromophobe renal cell carcinoma
- Reticulohistiocytoma versus neurothekeoma
- Rhabdomyoma versus granular cell tumor
- Rheumatoid nodules versus granuloma annulare
Board review style answer #2
D. Rhabdomyoma versus granular cell tumor. Granular cell tumors are diffusely CD68 positive whereas rhabdomyomas are CD68 negative. Chronic granulomatous disease and Whipple disease are both marked by an abundance of CD68 positive macrophages in the lamina propria (A). Clear cell renal cell carcinoma and chromophobe renal cell carcinoma are CD68 negative (B). Reticulohistiocytoma is uniformly CD68 positive, while (cellular) neurothekeoma may be positive in over half of cases (C). Rheumatoid nodules and granuloma annulare both contain many CD68 positive macrophages (E).
Comment Here
Reference: CD68
Comment Here
Reference: CD68
CD70
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Definition / general
- Ligand to CD27 that is transiently upregulated upon stimulation of immune cells and delivers a costimulatory signal to T cells
Essential features
- Transmembrane protein and unique ligand to CD27
- Expressed on lymphocytes and dendritic cells (Curr Opin Immunol 2005;17:275)
- Provides stimulatory signal for T cell development and activation (Curr Opin Immunol 2005;17:275)
- Provides complex (and incompletely understood) signaling for B cell development (Semin Arthritis Rheum 2016;45:496)
- Expressed on various solid tumors and hematolymphoid malignancies and may impart a poor prognosis
Terminology
- Tumor necrosis factor ligand superfamily member 7 (TNFSF7)
- CD27 ligand (CD27L)
- Ki24 antigen (Blood 1985;66:848)
Pathophysiology
- Transiently upregulated during lymphocyte activation (J Immunol 1994;152:1756)
- Regulated by activation signals received via toll-like receptors (TLRs), CD40 and the antigen receptor MHC II (Semin Arthritis Rheum 2016;45:496)
- Only characterized ligand to CD27 with bidirectional signaling activity
- Can be upregulated on leukemia cells after tyrosine kinase inhibitor therapy (Sci Transl Med 2015;7:298ra119)
- Reverse signaling through CD70 enhances NK cell function and immunosurveillance of CD27 expressing B cell malignancies (Blood 2017;130:297)
- Regulatory T cells can gain CD70 expression after prolonged stimulation, curbing their suppressive activity on other T cells (Commun Biol 2020;3:375)
Clinical features
- Targeting CD70 has shown promise in xenograft models and a phase 1 study using the monoclonal antibody cusatuzumab (Blood 2011;117:4304, Nat Med 2020;26:1459)
- Genetic polymorphisms in CD70 may cause susceptibility to EBV driven malignancies (J Exp Med 2017;214:91)
- CD70 specific CAR T cells show anti-AML activity in murine AML xenograft models (Blood 2021;138:318, J Immunother Cancer 2022;10:e003289)
Interpretation
- Membranous and cytoplasmic staining (Clin Cancer Res 2008;14:7763)
Uses by pathologists
- No current clinical use by pathologists
Prognostic factors
- High CD70 expression is associated with poor overall survival in
- Glioblastoma (Int J Cancer 2017;141:1434)
- Ovarian serous carcinoma (Onco Targets Ther 2013;6:615)
- Pleural mesothelioma (J Pathol 2020;250:205)
Positive staining - normal
- Temporarily expressed on activated T and B cells (Eur J Immunol 1996;26:2964)
- Stromal cells of thymic medulla (Int Immunol 1994;6:477)
- NK cells (J Immunol 1999;163:5358)
Positive staining - disease
- B cell lymphomas
- Expressed on chronic lymphocytic leukemia cells (89%, 17/19) (Blood 1995;85:3556)
- Diffuse large B cell lymphoma (Genes Chromosomes Cancer 2013;52:764)
- Follicular lymphoma (77%, 20/26) (Invest New Drugs 2019;37:297)
- Waldenström macroglobulinemia (100%, 6/6) (Blood 2008;112:4683)
- Hodgkin lymphoma (Reed-Sternberg cells) (100%, 33/33) (Clin Cancer Res 2008;14:7763, Blood 1985;66:848)
- T cell lymphomas
- Peripheral T cell lymphoma (85%) (Histopathology 2022;81:272)
- Mycosis fungoides (95%) (Blood Adv 2022;6:2290)
- Primary cutaneous anaplastic large cell lymphoma (100%) (Blood Adv 2022;6:2290)
- ALK positive / negative anaplastic large cell lymphoma (78% / 50%) (Blood Adv 2022;6:2290)
- Adult T cell leukemia / lymphoma (J Virol 2008;82:3843)
- Acute myeloid leukemia (86 - 100%) (Cancer Cell 2017;32:506, J Exp Med 2017;214:359)
- EBV associated malignancies
- Nasopharyngeal carcinoma (88%, 16/18) (Am J Pathol 1995;14:1152)
- Carcinoma
- Clear cell renal cell carcinoma (64%, 46/72) (Cancer Res 2006;66:2328)
- Thymic carcinoma (88%, 7/8) (Am J Surg Pathol 2000;24:742)
- Pulmonary sarcomatoid carcinoma (Eur J Cancer 2022;169:106)
Negative staining
- Carcinoma (Br J Cancer 2010;103:676)
- Lung (10%, 17/172)
- Breast (2%, 5/204)
- Pancreatic (25%, 35/140)
- Ovarian (15%, 37/241)
- Colon (9%, 17/194)
- Thymoma (0%) (Front Oncol 2022;11:808396)
- Thymic neuroendocrine tumor (0%) (Front Oncol 2022;11:808396)
- Osteosarcoma (19%, 16/83) (Cancer Cell Int 2015;15:31)
- Papillary renal cell carcinoma (40%) (Cancer Res 2006;66:2328)
- Mesothelioma (20%, 34/138) (J Pathol 2020;250:205)
- Melanoma (16%, 15/96) (Br J Cancer 2010;103:676)
- Glioblastoma (10 - 42%) (Cancer Res 2002;62:2592, Br J Cancer 2010;103:676)
- Multiple myeloma (42%, 13/31) (Clin Cancer Res 2008;14:7763)
Board review style question #1
Board review style answer #1
D. CD70 is transiently expressed by activated immune cells. CD70 is the ligand to CD27. It is expressed in a majority of B and T cell lymphomas and is usually negative in plasma cell neoplasms.
Comment Here
Reference: CD70
Comment Here
Reference: CD70
CD70-79
Table of Contents
CD70 | CD71 | CD72 | CD73 | CD74 | CD75 | CD75s / CDw76 | CD77 | CDw78 | CD79a | CD79b | Microscopic (histologic) imagesCD70
- See CD70
CD71
- See CD71
CD72
- Cell surface protein expressed exclusively on B cells
- Regulates mature B cell differentiation, prevents differentiation of naive B cells into plasma cells (Eur J Immunol 2005;35:2325)
- Ligand of CD5 and CD100 (J Immunol 1992;148:1630, Int Immunol 2005;17:1277)
- Not the same as DBA.44 (abstract in the following article is apparently wrong) (Am J Surg Pathol 1996;20:613)
- Increased nucleotide mutation of CD72 mRNA accounts for decreased CD72 expression in B cells of teenage SLE patients (Pediatr Allergy Immunol 2006;17:565)
- Uses by pathologists: marker of B cells (not commonly used)
- Positive staining - normal: B cells only
- Positive staining - disease: B cell lymphoma
- Negative staining: plasma cells (Am J Hematol 1992;41:151)
- Reference: OMIM: 107272 [Accessed 4 May 2021]
CD73
- Also called ecto-5'-nucleotidase
- Catalyzes dephosphorylation of ribo and deoxyribonucleotides to their corresponding nucleosides, such as 5’ AMP to adenosine
- Mediates costimulatory signals in T cell activation
- Mediates lymphocyte adhesion to dendritic cells and endothelium (Blood 1996;88:1755, J Immunol 2000;165:5411)
- May protect against vascular inflammation and neointima formation (Circulation 2006;113:2120)
- May be a lymphocyte maturation marker
- No significant clinical use by pathologists
- Positive staining - normal: B and T cell subset, endothelial cells, follicular dendritic cells and epithelial cells
- Reference: OMIM: 129190 [Accessed 4 May 2021]
CD74
- Also called LN2, HLA-DR associated invariant chain
- Gamma chain antigen associated with MHC class II antigen and antigen presentation
- MHC class II chaperone stabilizes alpha / beta heterodimers in a complex soon after synthesis and directs transport of the complex from the endoplasmic reticulum to compartments, where peptide loading of class II takes place
- H. pylori urease binds to CD74 on gastric epithelial cells and upregulates CD74 expression (Infect Immun 2006;74:1148, J Immunol 2005;175:171)
- Has important role in mucosal immunity
- Receptor for macrophage migration inhibitory factor, a proinflammatory cytokine (J Immunol 2006;177:8730)
- Associated with perineural invasion in pancreatic carcinoma (Clin Cancer Res 2006;12:2419)
- Uses by pathologists: B cell marker (not commonly used)
- Positive staining - normal: B cells, activated T cells, macrophages, interdigitating dendritic cells, activated endothelial and epithelial cells
- Positive staining - disease:
- Many B cell lymphomas, myeloma (Clin Cancer Res 2004;10:6606)
- Some T cell lymphomas, Reed-Sternberg cells, many myeloid leukemias and Langerhans cell histiocytosis
- Renal clear cell and chromophobe carcinoma (most) (Am J Pathol 2001;158:1639)
- Negatie staining: renal oncocytoma
- Reference: OMIM: 142790 [Accessed 5 May 2021]
CD75
- Also called lactosamines, LN1; formerly CDw75
- Carbohydrate, not a protein (Cell 1992;68:1003)
- Ligand for CD22 (Cell 1991;66:1133)
- A neuraminidase sensitive lymphocyte cell surface differentiation antigen
- Strong expression associated with better prognosis in follicular center cell lymphoma (J Pathol 2006;209:352)
- Uses by pathologists: marker of follicular center cell lymphoma; identify Reed-Sternberg cells (not commonly used)
- Positive staining - normal: mature B cells (germinal center derivation), erythrocytes, some T cells and some epithelial cells
- Positive staining - disease: popcorn cells of lymphocyte predominance Hodgkin’s lymphoma, many B cell lymphomas (Histopathology 1999;35:209)
- Reference: Arch Pathol Lab Med 2002;126:862
CD75s / CDw76
- CDw76 renamed CD75s at 7th HLDA Workshop
- Alpha 2, 6 sialylated lactosamines
- A carbohydrate, not a protein
- Marker of murine CD8+ suppressor T cells (Int Immunol 2003;15:1389)
- No significant clinical use by pathologists
- Positive staining - normal: B cells, some T cells
CD77
- Also called globotriaosylceramide, CD77 synthase (OMIM: 607922 [Accessed 5 May 2021])
- pK blood group antigen on erythrocytes
- Carbohydrate, not a protein
- Endothelial receptor for verotoxins from Shigella dysenteriae and E. coli (J Biol Chem 2006;281:10230)
- Also expressed by liver flukes (Biol Chem 2001;382:195)
- Interacts with CD19 (J Cell Physiol 1998;176:281)
- Mediates apoptosis of renal vascular endothelial cells and intestinal epithelial cells, resulting in hemolytic uremic syndrome
- Does not discriminate centroblasts from centrocytes
- Uses by pathologists: identify germinal center cells
- Positive staining - normal:
- B cells (centrocytes, centroblasts, plasmablasts) (J Immunol 2006;177:4341)
- Megakaryoblasts and platelets (J Biol Chem 2002;277:11247)
- Positive staining - disease: Burkitt's lymphoma
CDw78
- Deleted at 7th HLDA Workshop (reasons unknown)
- Defines a conformation of MHC class II molecules bound to peptides acquired through trafficking to lysosomal antigen processing compartments and not MHC class II molecules associated with tetraspanins (J Immunol 2006;177:5451)
- Appears on B cells following HLA-DR and preceding CD10, CD19, CD22 and CD37
- No significant clinical use by pathologists
- Positive staining - normal: B cells
CD79a
- See CD79a
CD79b
- See CD79b
Microscopic (histologic) images
CD71
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Interpretation | Uses by pathologists | Less common usage | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- CD71 is an integral membrane protein that mediates the uptake of transferrin iron complexes
- In human tissues, CD71 is more highly expressed in placental syncytiotrophoblast, myocytes, hepatocytes, basal keratinocytes, endocrine cells of the pancreas, spermatocytes and erythroid precursors
- CD71 is present on actively proliferating cells, essential for iron transport into proliferating cells (benign and malignant)
- Can be expressed by tumor cells; for example, in breast cancers and squamous cell carcinomas of the esophagus
- Level of transferrin receptor is higher in early erythroid precursors during the intermediate normoblast phase, after which expression decreases through the reticulocyte phase
Essential features
- CD71 is a robust immunohistochemical marker in gestational pathology, used for identifying nucleated red blood cells that can help in excluding a complete mole, and for identifying chorionic villi to demonstrate gestation even in the case of massive necrotic hemorrhagic modifications
- In hematopathology, CD71 is very useful because it is expressed only by erythroid precursors within the normal hematopoietic marrow and spleen and can aid in the correct identification of all erythroid precursors
- CD71 expression is important for the diagnosis of the acute myeloid leukemia M6 (acute erythroleukemia)
Terminology
- Also known as transferrin receptor
Pathophysiology
- It is a homodimeric glycoprotein of 760 amino acids that binds to diferric transferrin at the cell surface
- Binding is followed by the internalization, a mechanism partially regulated by hereditary hemochromatosis protein; diferric iron is subsequently released from transferrin owing to endosomal acidification
Interpretation
- To be considered positive, immunohistochemistry for CD71 must stain cell membrane
- Other locations of staining (e.g. nucleus) are considered not reliable
Uses by pathologists
- CD71 is a robust immunohistochemical marker for the detection of nucleated red blood cells and chorionic villi, especially in presence of necrosis (Appl Immunohistochem Mol Morphol 2016;24:215)
- Demonstration of nucleated red blood cells can be important in molar pathology, helping to exclude a complete mole (Appl Immunohistochem Mol Morphol 2016;24:215)
- Used to detect micronucleated reticulocytes / Howell-Jolly bodies by flow cytometry, also used to test for erythropoietin doping by athletes (Mutat Res 2003;542:77)
- In hematopathology, CD71 is very useful because it is expressed only by erythroid precursors within the normal hematopoietic marrow and spleen
- CD71 has particular utility for identification of erythroid precursors, differently from glycophorin that marks all types of red blood cells
- In hematopathology, it is useful in identifying erythroid precursors in red blood cell hypoplasia and hyperplasia, with or without dyspoietic features (Am J Surg Pathol 2011;35:723)
Less common usage
- CD71 is also useful in the cytometry evaluation of childhood acute lymphoid leukemia, giving potential information regarding patient survival (Folia Histochem Cytobiol 2012;50:304)
- In lymph node neoplastic pathology, using flow cytometry, CD71 may be a useful tool in the differential diagnosis between primary mediastinal large B cell lymphoma and diffuse large B cell lymphoma, NOS and in the differential diagnosis between Burkitt lymphoma and CD10+ diffuse large B cell lymphoma, NOS (Cytometry B Clin Cytom 2018;94:459, Am J Clin Pathol 2012;137:665)
Microscopic (histologic) images
Positive staining - normal
- Erythroid precursors, placental syncytiotrophoblast, myocytes, hepatocytes, basal keratinocytes, endocrine cells of the pancreas, spermatocytes and capillary endothelium in the brain
- Tumor cells may express this marker
Positive staining - disease
- CD71 is an essential marker in the diagnosis of myeloproliferative neoplasms and myelodysplastic syndromes, using both flow cytometry and immunohistochemistry (Cytometry B Clin Cytom 2015;88:125, Haematologica 2017;102:308, Appl Immunohistochem Mol Morphol 2016;24:51)
- CD71 could be useful in flow cytometry to discriminate between follicular lymphoma (FL) and CD10+ large B cell lymphomas (LBCL), because its fluorescence intensity is higher in LBCL (Am J Clin Pathol 2006;126:39, Am J Clin Pathol 2012;137:665)
- Another useful application of CD71 in flow cytometry regards its determination for the diagnosis of acute lymphoid leukemia (Folia Histochem Cytobiol 2012;50:304, Endocr Metab Immune Disord Drug Targets 2018;18:610)
- Its expression is important for the diagnosis of the acute myeloid leukemia M6 (acute erythroleukemya) (Leuk Lymphoma 2014;55:892)
- CD71 can be also detected by flow cytometry in neoplastic cells of primary effusion lymphoma (APMIS 2009;117:222)
- CD71 could be useful in the diagnosis of breast implant associated ALK anaplastic large cell lymphoma, which shows positivity in the neoplastic cells (Clin Cancer Res 2012;18:4549)
Board review style question #1
- In gestational pathology, what can CD71 be used for?
- CD71 is a useful marker in gestational pathology only in addition with beta HCG immunohistochemistry
- CD71 is not a useful marker in gestational pathology
- For staining chorionic villi, also in case of necrotic hemorrhagic modifications and for staining nucleated red blood cells
- Only for highlighting nucleated red blood cells
- Only for highlighting the presence chorionic villi
Board review style answer #1
C. For staining chorionic villi, also in case of necrotic hemorrhagic modifications and for staining nucleated red blood cells. CD71 is a very useful marker in gestational pathology. It stains chorionic villi, even in case of massive necrotic hemorrhagic modifications. In these cases, CD71 is of great help since hematoxylin eosin staining cannot always permit their identification. It is also useful since it stains nucleated red blood cells that can help in excluding the presence of a complete mole in gestational pathology.
Comment Here
Reference: CD71
Comment Here
Reference: CD71
Board review style question #2
Board review style answer #2
B. Erythroid precursors. CD71 is a very helpful marker for staining erythroid precursors.
Comment Here
Reference: CD71
Comment Here
Reference: CD71
CD79a
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- CD79a, identified as the alpha chain of the B cell antigen receptor complex, is a transmembrane protein synthesized by the CD79A gene located on chromosome 19
- Expressed over full range of B cell development from early B cell precursors, preceding immunoglobulin heavy chain gene rearrangement and persisting through B cell maturation (Blood 1995;86:1453, Appl Immunohistochem Mol Morphol 2001;9:97)
Essential features
- CD79a / CD79b are membrane bound immunoglobulins that form the B cell receptor (BCR) complex
- Expressed from early B cell precursors until advanced plasma cell stages (Blood 1995;86:1453)
- Membranous and cytoplasmic expression useful for confirming B cell lineage or following therapy with monoclonal antibodies against other B cell antigens
Terminology
- Also called MB1 membrane glycoprotein, IgMα and Igα
Pathophysiology
- CD79a, a 226 amino acid membrane protein, is the product of the human mb1 gene situated on chromosome 19, specifically at band q13.2 (OMIM: CD79A Antigen; CD79A [Accessed 23 January 2024])
- Has single extracellular immunoglobulin domain, a transmembrane domain and an intracytoplasmic signaling domain with an immunoreceptor tyrosine based activation motif (ITAM)
- Heterodimerizes with CD79b (B29) and constitutes an integral component of the B cell receptor (BCR) complex
- CD79a's cytoplasmic domain enables signal transduction via antigen binding to the BCR, causing rapid protein tyrosine phosphorylation and activation of pathways through the immunoreceptor tyrosine based activation motif (ITAM) (Front Immunol 2018;9:665)
- CD79a and CD79b are required for surface IgM expression in human B cells (J Immunol 2022;209:2042)
Clinical features
- Deletions or mutations in the genes encoding CD79a lead to developmental arrest at the pre-B cell stage and can be a cause of agammaglobulinemia (J Clin Invest 1999;104:1115)
- Plays an important functional role in maintaining the immature, immune suppressive phenotype of myeloid derived suppressor cells (MDSC) and in inducing the secretion of protumorigenic cytokines, thus, may be a novel target for cancer therapy (PLoS One 2013;8:e76115)
- Impairment of the glycosylation of μ and CD79a chains is associated with lower levels of expression of IgM in chronic lymphocytic leukemia (Blood 2005;105:2933)
- Synovial infiltration of CD79a positive B cells correlates with joint destruction in rheumatoid arthritis (J Rheumatol 2011;38:2301)
- Aberrant staining in megakaryocytes in postinduction acute lymphoblastic leukemia (ALL) cases (cytoplasmic and granular) (Hum Pathol Case Rep 2021;23:200467)
- Aberrant CD79a positivity in erythroid precursors postchemotherapy in lymphoma patients can complicate minimal residual disease detection after rituximab treatment (Haematologica 2007;92:855)
Interpretation
- Membranous and cytoplasmic expression is considered positive; pro-B cells may only show cytoplasmic expression (J Immunol 1991;147:2474)
Uses by pathologists
- Used as a pan-B cell marker in immunohistochemistry
- Used to differentiate ALL from other pediatric small blue round cell tumors (Appl Immunohistochem Mol Morphol 2001;9:97)
- Used to confirm B cell lineage in rituximab treated B cell neoplasms (Blood Res 2022;57:55)
- Used as part of a panel to differentiate classic Hodgkin lymphoma from nodular lymphocyte predominant Hodgkin lymphoma and aggressive B cell lymphomas that may show Hodgkin-like features (Appl Immunohistochem Mol Morphol 2016;24:535)
Prognostic factors
- Some studies report that cytoplasmic CD79a expression is associated with lower survival odds than classical acute myeloid leukemia (AML) with t(8;21)(q22;q22) (Korean J Lab Med 2007;27:388)
- Cytoplasmic CD79a can be used in monitoring of relapse in B ALL post-CD19 chimeric antigen receptor (CAR) T cell therapy (Leuk Lymphoma 2022;63:426)
- CD79a may have independent prognostic relevance for CNS involvement and CNS relapse in pediatric B cell precursor ALL (Commun Biol 2021;4:73)
- CD79a positivity may be associated with worse prognosis in classic Hodgkin lymphoma compared to CD79a negative classic Hodgkin lymphoma (J Clin Exp Hematop 2020;60:78)
Microscopic (histologic) description
Microscopic (histologic) images
Positive staining - normal
- B lymphocytes (mature and immature) and plasma cells (J Immunol 1991;147:2474)
- Follicular mantle zone more strongly labeled than germinal center B cells; in spleen, marginal zones are strongly labeled (Appl Immunohistochem Mol Morphol 2001;9:97)
- Expressed weakly and transiently in early T cell differentiation (J Pathol 2002;197:341)
Positive staining - disease
- B cell lymphoid neoplasms
- Most low grade B cell lymphomas (membranous and cytoplasmic often with perinuclear accentuation) (Blood 1995;86:1453)
- Weak expression may be seen in follicular lymphoma (Am J Surg Pathol 2002;26:1458)
- B ALL (90% of cases, cytoplasmic, may be weak and focal) (Blood 1993;82:853)
- Diffuse large B cell lymphomas (Appl Immunohistochem Mol Morphol 2001;9:97)
- Primary mediastinal large B cell lymphomas (heterogenous pattern); discordant mb1+ / Ig- expression occurs commonly in mediastinal large B cell lymphomas (Appl Immunohistochem Mol Morphol 2001;9:97, Am J Clin Pathol 2021;156:497)
- Nodular lymphocyte predominant Hodgkin lymphoma (faint) (Am J Clin Pathol 2003;119:192)
- T cell histiocyte rich large B cell lymphomas (60% of cases, weak expression) (Am J Surg Pathol 2002;26:1458)
- Myeloma / plasmacytoma (50% of cases positive) (Appl Immunohistochem Mol Morphol 2001;9:97)
- Can be used together with other markers to identify mixed phenotype acute leukemia (Arch Pathol Lab Med 2017;141:1462)
Negative staining
- Anaplastic large cell lymphoma (Hum Pathol 2004;35:455)
- T cell neoplasms
- Few T ALL may be positive (10 - 40% of cases, weak to moderate cytoplasmic positivity, 30 - 100% of leukemic cells) (J Pathol 1998;186:140, Am J Clin Pathol 2000;113:823, Cancer Res 2004;64:7399)
- Some extranodal NK / T cell lymphomas are positive (Mod Pathol 2000;13:766)
- Classic Hodgkin lymphoma (18% of cases are positive) (Mod Pathol 2004;17:1531)
- Acute myeloid leukemias; however, aberrant CD79a expression can be seen in AML cases with RUNX1 mutations and t(8; 21) (Am J Clin Pathol 2000;113:823, Pathobiology 2019;86:162)
- Myeloid sarcoma (Int J Lab Hematol 2011;33:555)
Sample pathology report
- Cervical lymph node, excisional biopsy:
- Nodular lymphocyte predominant Hodgkin (B cell) lymphoma (see comment)
- Comment: Histologic sections show lymphoid infiltrate in diffuse and vaguely nodular patterns. The lymphoma cells are large with scant to moderate cytoplasm and large nuclei with fine chromatin (LP cells). These cells are in a background of numerous small, mature lymphocytes and epithelioid histiocytes. Immunohistochemical stains show the large, abnormal cells are positive for CD20, CD45, CD79a, BCL6 and PAX5. They are negative for CD3, CD4, CD5, CD8, CD10, CD15, CD30, ALK1, BCL2 and fascin. The large, abnormal cells overlap networks of CD21 positive follicular dendritic cells. Chromogenic in situ hybridization studies with probes for Epstein-Barr virus (EBV) encoded small RNA (EBER) are negative. PD-1 is positive on small, mature T cells surrounding the LP cells.
Additional references
Board review style question #1
Board review style answer #1
A. Complete absence of expression. Despite originating from B cells, Hodgkin and Reed-Sternberg (HRS) cells in classic Hodgkin lymphoma exhibit a disrupted B cell program, resulting in the loss or downregulation of numerous B cell markers. These include pan-B cell antigens, such as CD19, CD20, CD22 and CD79a, as well as B cell transcription factors, such as OCT2, BOB.1 and BCL6. Answers B and D are incorrect because they do not represent the usual pattern of expression in Hodgkin lymphoma. Answer C is incorrect because some cases may show weak expression of CD79a but it is not the typical pattern.
Comment Here
Reference: CD79a
Comment Here
Reference: CD79a
CD79b
Table of Contents
Definition / general | Uses by pathologists | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Also called B29, B cell antigen receptor complex associated protein beta-chain
- Encodes the Ig-beta protein of the B cell antigen receptor; the receptor also includes Ig-alpha protein (CD79a) and surface immunoglobulin
- First expressed in cells with Ig µ chains and remains expressed throughout B cell differentiation to plasma cells
- References: OMIM #147245
Uses by pathologists
- Distinguish CLL from other B cell disorders if intensity of staining is considered (J Clin Pathol 2002;55:180)
Positive staining - normal
- B cells, plasma cells
Positive staining - disease
- B cell lymphoma and lymphoproliferative disorders: CLL (18%, Arch Pathol Lab Med 2003;127:561), CLL with IgM paraproteins (58%, Am J Clin Pathol 2005;123:594) and lymphoplasmacytic lymphoma (85%, Am J Clin Pathol 2005;124:414)
Negative staining
- Hairy cell leukemia (usually)
CD8
Table of Contents
Definition / general | Pathophysiology | Diagrams / tables | Clinical features | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Flow cytometry imagesDefinition / general
- Cytotoxic T cell marker (Wikipedia); CD8+ cells are called T cell suppressor cells, cytotoxic T cells
- Also called OKT8
Pathophysiology
- Cell surface glycoprotein, member of immunoglobulin superfamily; at 2p12
- Heterodimer of an alpha (CD8A, OMIM #186910 ) and a beta chain (CD8B, OMIM #186730 ) linked by two disulfide bonds; each chain has significant homology to immunoglobulin variable light chains; is present as a heterodimer on thymocytes and as homodimer on peripheral blood T cells
- Both the CD8 antigen (acting as a coreceptor) and the T cell receptor recognize antigens displayed by an antigen presenting cell (APC) in the context of class I MHC molecules; CD8 binds to non-polymorphic region of class I molecules; may increase avidity of interactions between cytotoxic T cell and target cell during antigen-specific activation
- Can kill target cells by recognizing peptide-MHC complexes on them or by secreting cytokines capable of signaling through death receptors on target cell surface
- CD8 alpha cells promote survival and differentiation of activated T cells into memory CD8+ T cells
- CD8 T cell clonal expansions occurr in normal young (PLoS One 2011;6:e21240) and elderly adults (Immunol Rev 2005;205:170)
- May contribute to initiation, progression and regulation of autoimmune responses (Curr Opin Immunol 2005;17:624)
Clinical features
- Lymphocytic infiltrate in lymphoepithelioma-like carcinomas is often CD8+ in cervix (Arch Gynecol Obstet 2009;280:725), esophagus (Hum Pathol 2003;34:407), liver (World J Gastroenterol 2008;14:4694) and lung (Am J Surg Pathol 2002;26:715)
- Mutations in alpha chain cause CD8 deficiency, with recurrent bacterial infections (J Clin Invest 2001;108:117)
- Accumulate in advanced atherosclerotic plaques (Hum Pathol 2008;39:1756)
Uses by pathologists
- Marker of T cells (normal and malignant)
- Marker of cytotoxic / suppressor T cells
- Classify lymphomas
- Differentiate splenic hamartoma (CD8+) from hemangioma or littoral cell angioma (CD8-)
- Note: use of CD3, CD8 does NOT improve detection of gluten-sensitive enteropathy in duodenal biopsies (Mod Pathol 2013 Apr 5 [Epub ahead of print])
Microscopic (histologic) images
Positive staining - normal
- Cortical thymocytes (70-80%), T cells (25-35% of mature peripheral T cells, mostly cytotoxic T cells), NK cells (30%) and dendritic cells
- Splenid littoral cells but not littoral cell angioma (Arch Pathol Lab Med 2019;143:1093)
Positive staining - disease
- T cell lymphoma, post-thymic (some)
- Heterotopic ovarian splenoma, Hodgkin lymphoma-nodular lymphocyte predominant (reactive T cells are CD4+ CD8+ in 58%, Am J Clin Pathol 2006;126:805)
- Melanoma (CD4+ CD8+ in 60%, PLoS One 2010;5:e8437)
- Mycosis fungoides - epidermotrophic lymphocytes, NK/T cell lymphoma (variable)
- Splenic hemartoma-sinus lining cells, subcutaneous panniculitis-like T cell lymphoma
- Rare: B-CLL (Am J Clin Pathol 2009;132:186), lymphomatoid papulosis, type "D" (Am J Clin Pathol 2006;125:490, Am J Surg Pathol 2010;34:1168), mantle cell lymphoma (Am J Clin Pathol 1998;109:689)
Negative staining
- Adult T cell leukemia / lymphoma, littoral cell hemangioma of spleen
CD9
Table of Contents
Definition / general | Pathophysiology | Clinical features | Diagrams / tables | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative stainingDefinition / general
- Cell surface protein that mediates adhesion, migration, signal transduction
- Also called tetraspanin CD9, motility related protein 1 (MRP1) [note: MRP is multidrug resistance associated protein]
- Antibodies are used to purge bone marrow in acute lymphoblastic leukemia prior to peripheral stem cell bone marrow transplant (Am J Pediatr Hematol Oncol 1993;15:162)
Pathophysiology
- Member of transmembrane 4 superfamily (tetraspanin family); tetraspanins have 4 hydrophobic domains, organize multimolecular complexes in plasma membrane; each tetraspanin associates specifically with integrins and other tetraspanins, forming primary complexes and leading to molecular network of interactions, the "tetraspanin web"
- Regulates cell motility, development, activation, growth and adhesion (Blood 2011;117:1840), differentiation (OMIM #143030), fertilization (oocyte CD9 is required for sperm-egg fusion)
- Regulates paranodal junction formation (between neurons and glia)
- Required for microparticle release from coated-platelets (Platelets 2009;20:361); triggers platelet activation and aggregation
- Supports myotube maintenance and promotes muscle cell fusion
- Downregulation in ovarian carcinoma may promote tumor dissemination (Cancer Res 2005;65:2617)
- May suppress metastasis in small cell lung cancer by promoting apoptosis via calretinin expression (Cancer Res 2010;70:8025, FEBS Open Bio 2013;3:225)
- May mediate invasion by upregulating MMP9 (PLoS One 2013;8:e67766)
Clinical features
- Favorable prognostic marker for gallbladder carcinoma (World J Surg Oncol 2012;10:92), gastric GIST (Cancer Sci 2011;102:883), malignant mesothelioma (Oncol Rep 2013;29:21), oral squamous cell carcinoma (Oral Oncol 2010;46:166)
- Poor prognosis factor in gastric carcinoma (Pathol Res Pract 2010;206:607)
Uses by pathologists
- No significant clinical use by pathologists
Microscopic (histologic) images
Images hosted on other servers:
Normal tissue:
Various tumors:
Positive staining - normal
- Pre B cells, B cell subset, activated T cells, basophils, eosinophils (Am J Respir Cell Mol Biol 2012;46:188), macrophages, megakaryocytes, plasma cells, plasma cell precursors in germinal centers (Biochem Biophys Res Commun 2013;431:41), platelets
- Brain, cardiac muscle, GI system, kidney (glomeruli, tubules and collective ducts), liver, lymphatic epithelium, ovarian surface epithelium, peripheral nerve, skin, spleen, thyroid, tonsil
Positive staining - disease
- Pre-B ALL, acute promyelocytic leukemia, astrocytoma (J Histochem Cytochem 2002;50:1195), mast cell disease
- Vascular tumors: angiosarcoma, juvenile nasopharyngeal angiofibroma, Kaposi sarcoma (Mod Pathol 2003;16:1028)
Negative staining
- Red blood cells, renal collecting duct carcinomas (almost all)
CD90-99
Table of Contents
CD90 | CD91 | CDw92 | CD93 | CD94 | CD95 | CD96 | CD97 | CD98 | CD99 | Microscopic (histologic) imagesCD90
- Also called Thy-1
- May mediate differentiation of hematopoietic stem cells and synaptogenesis in the CNS
- CD34+ CD90+ cells include hematopoietic stem cells that serve as autologous grafts to replace the bone marrow in patients with malignancies (Biol Blood Marrow Transplant 2000;6:262)
- Mediates adhesion of various white blood cells to activated endothelial cells (J Immunol 2004;172:3850)
- Uses by pathologists: hematopoietic stem cell marker
- Positive staining - normal:
- Immature hematopoietic stem cells, neurons, connective tissue, activated endothelial cells, fibroblasts (variable) (Am J Pathol 2003;163:1291)
- Keratinocyte stem cells (Br J Dermatol 2006;154:1062)
- Negative staining - disease: Ewing sarcoma and some rhabdomyosarcomas (Am J Clin Pathol 2003;119:643)
CD91
- Low density lipoprotein receptor related protein 1 (LRP1); also called alpha 2 macroglobulin receptor
- Large scavenger receptor that mediates the uptake and degradation of various ligands
- Binds to apoE containing lipoproteins and mediates chylomicron remnant clearance from the plasma
- May suppress thyroid carcinoma invasion by clearing urokinase plasminogen activator (Int J Biochem Cell Biol 2006;38:1729)
- Increased CD91 surface expression on CD14(+) monocytes is associated with the apparent HIV1 resistance observed in HIV exposed but seronegative subjects (J Leukoc Biol 2005;78:37)
- Increased expression on monocytes in melanoma patients is associated with slow progression (Clin Exp Immunol 2004;138:312)
- Part of pathway of C1q mediated apoptotic clearance (Arthritis Rheum 2006;54:1543)
- Also a cell surface receptor for heat shock protein gp96 and others (Arch Pathol Lab Med 2003;127:178)
- No significant clinical use by pathologists
- Positive staining - normal:
- Fibroblasts, dendritic cells (Immunobiology 2006;211:407)
- Macrophages; liver, brain, lung
- References: J Thromb Haemost 2005;3:1884, OMIM: 107770 [Accessed 4 May 2021]
CDw92
- Also called choline transporter-like protein 1 (CTL1), Solute carrier family 44 member 1 (SLC44A1)
- Produces membrane lipid phosphatidylcholine (Exp Biol Med (Maywood) 2006;231:490)
- No significant clinical use by pathologists
- Positive staining - normal: B cells, T cells (most), monocytes, NK cells (some), neutrophils, fibroblasts (weak), endothelial cells
- References: OMIM: 606105 [Accessed 4 May 2021], J Immunol 2001;167:5795
CD93
- Also called complement component C1q receptor, C1qR
- No longer believed to be part of receptor complex for C1q (J Immunol 2002;168:5222)
- Enhances phagocytosis in monocytes and macrophages upon interaction with soluble defense collagens
- Also enhances phagocytosis via mannan binding lectin, an important part of the innate immune defense (J Biol Chem 2001;276:43087)
- Receptor for pulmonary surfactant protein A
- Has role in intercellular adhesion
- Soluble form present in plasma (J Immunol 2005;175:1239)
- No significant clinical use by pathologists
- Positive staining - normal:
- Granulocytes, monocytes, platelets, endothelial cells (J Leukoc Biol 2001;70:793)
- Microglia (J Immunol 2001;166:7496)
- Stem cells (rare, Proc Natl Acad Sci USA 2002;99:10441)
- Negative staining: lymphocytes
- Reference: OMIM: 120577 [Accessed 4 May 2021]
CD94
- Also called natural killer cell antigen, kP43, killer cell lectin-like receptor subfamily D member 1, KLRD1
- Receptor for MHC class I HLA-E molecules present on NK cells and some cytotoxic T cells
- Inhibits NK cell activation by disrupting the actin network where the NK cell contacts its ligand (J Immunol 2006;177:3590)
- Increased numbers of CD94+ NK cells in active and inactive ulcerative colitis (Hepatogastroenterology 2001;48:1316)
- Increased number of CD94+ T cells in chronic plaque psoriasis (Br J Dermatol 2006;155:318)
- Uses by pathologists:
- NK cell marker; favorable prognostic marker for lymphoblastic lymphoma (Blood 2005;106:3567)
- Nasal type, extranodal NK / T cell lymphoma (Blood 2003;102:2623)
- Positive staining - normal: NK cells, CD8+ T cells
- Positive staining - disease: T cell large granular lymphocyte leukemias (Am J Clin Pathol 2005;124:937)
- Reference: OMIM: 602894 [Accessed 4 May 2021]
CD95
- See CD95
CD96
- Also called T cell activated increased late expression (TACTILE)
- May be involved in adhesion of activated T and NK cells late in immune response
- Binds CD155
- No significant clinical use by pathologists
- Positive staining - normal: activated T cells and NK cells, B cells (low levels)
- Positive staining - disease: T-ALL (Exp Hematol 1998;26:1209)
- References: J Immunol 2004;172:3994, OMIM: 606037 [Accessed 4 May 2021]
CD97
- Binds to CD55 and G protein coupled receptors
- May be involved in cell adhesion and signaling processes early after leukocyte activation
- May be involved in migration of neutrophils (J Immunol 2004;172:1125)
- Highly expressed at sites of inflammation in skin, lung and rheumatoid arthritis
- May contribute to angiogenesis associated with tumors (Blood 2005;105:2836)
- Glycosylation causes CD97 to show two different epitopes, EGF and Stalk (Int J Cancer 2004;112:815)
- No significant clinical use by pathologists
- Positive staining - normal: activated T > B cells, monocytes / macrophages, dendritic cells, granulocytes, smooth muscle cells
- Positive staining - disease:
- GI carcinomas (Oncol Rep 2005;14:1413, Am J Clin Pathol 2002;118:699)
- Thyroid carcinoma (stronger if undifferentiated) (J Clin Endocrinol Metab 1999;84:1104)
- Negative staining: microglia
- References: Tissue Antigens 2001;57:325, OMIM: 601211 [Accessed 4 May 2021]
CD98
- Also called SLC3A2
- Heavy chain of amino acid transporters (J Cell Sci 2005;118:889)
- Involved in cell fusion necessary for syncytiotrophoblast formation (J Physiol 2003;550:3)
- Strongly expressed by neoplastic cells; expression contributes to transformation by promoting anchorage and serum independent growth (J Biol Chem 2004;279:54731)
- No significant clinical use by pathologists
- Positive staining - normal: broad
- Positive staining - malignant: all tumor cells
- Reference: OMIM: 158070 [Accessed 4 May 2021]
CD99
- See CD99
Microscopic (histologic) images
CD95
Table of Contents
Definition / general | Prognostic factors | Diagrams / tables | Uses by pathologists | Positive staining - normal | Positive staining - disease | Negative staining | Additional referencesDefinition / general
- Also called Fas, Apo-1, TNF receptor superfamily member 6, TNFRSF6
- Cell surface membrane receptor that activates apoptotic pathways when bound by Fas ligand (FasL, CD178)
- Extrinsic pathway: activation leads to assembly of a death inducing signaling complex (DISC) consisting of CD95, the Fas-associated death domain (FADD) adapter protein, the initiator caspase-8 (previously called FLICE or MACH) and cellular FLICE inhibitory protein (cFLIP), a regulatory protein that can block or promote autoproteolytic conversion of pro-caspase-8 to caspase-8 within the DISC; caspase 8 activates a cascade of caspases that ultimately activates caspase 3, which mediates apoptosis
- Intrinsic pathway: involves release of cytochrome c from mitochondria, which complexes with apoptosis inducing factor 1, procaspase 9 and ATP, leading to caspase 9 activation, which activates caspase 3
- Fas-FasL system mediates extra-thymic self-tolerance (FasL+ cells induce apoptosis in infiltrating Fas+ lymphocytes in testis, cornea), T cell mediated cytotoxicity, apoptosis during development, halting of immune response
- Defects in Fas-Fas ligand pathway (usually Fas but occasionally FasL germline mutations) cause autoimmune lymphoproliferative syndrome, a rare childhood disorder associated with B cell lymphomas, classic Hodgkin’s lymphoma and nodular lymphocyte predominant Hodgkin’s lymphoma (Leuk Lymphoma 2004;45:423)
- CD95 downregulation may reduce CD4+ T cells in HIV (Arch Pathol Lab Med 2002;126:28)
- May be involved in clearance of benign ovarian epithelial inclusion cysts; derangement in pathway may cause ovarian surface epithelial carcinomas (Hum Pathol 2005;36:971)
- Polymorphisms in Fas or FasL: associated with increased risk of autoimmune hepatitis (Am J Gastroenterol 2005;100:1322), increased risk of type II diabetes (Genes Immun 2006;7:316); Fas -670 AG genotype is associated with increased risk of preterm premature rupture of membranes (Am J Obstet Gynecol 2005;193:1132); Fas -670 AA genotype is associated with reduced liver graft survival (Tissue Antigens 2006;67:117); FAS -1377AA genotype is associated with increased risk of lung cancer (J Med Genet 2005;42:479)
Prognostic factors
- Reduced Fas expression is a poor prognostic factor for breast carcinoma (Clin Cancer Res 2004;10:1360), colorectal carcinoma (Carcinogenesis 2006;27:1113), retinoblastoma (Ocul Immunol Inflamm 2003;11:107) and urothelial carcinoma (Br J Cancer 2005;93:544), but reduced Fas expression is a favorable prognostic factor in primary nodal diffuse large B cell lymphoma (Am J Hematol 2006;81:307) and subcutaneous panniculitis-like lymphoma (Am J Clin Pathol 2004;121:408)
Uses by pathologists
- Prognostic factors (above)
Positive staining - normal
- Activated B cells, activated T cells (initially extra but nonfunctional Fas), resting T cells (low levels), numerous epithelium and connective tissue
Positive staining - disease
- Barrett’s esophagus (Hum Pathol 2002;33:686)
- Hashimoto’s thyroiditis (thyroid epithelial cells)
- Ovarian cystadenoma and serous borderline tumors
- Reed-Sternberg cells in classic Hodgkin’s lymphoma (Am J Surg Pathol 2001;25:388)
Negative staining
- Invasive ovarian carcinoma
Additional references
CD99
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Transmembrane protein with various functions and limited diagnostic utility
- In the differential diagnosis of small round blue cell tumors
Essential features
- Exists in 2 isoforms and has variable oncogenic and tumor suppressor functions
- Positivity for CD99 is not specific but its absence rules out Ewing sarcoma in the workup of a small blue round cell tumor
- Dot-like staining pattern has been reported in several disease entities but has so far not been proven to be diagnostically useful
Terminology
- Also called MIC2, T cell surface glycoprotein E2, p30 / 32 protein (