- Acquired benign lesion of acral (limb or other extremity) skin
- Also known as acral fibrokeratoma and acquired periungual fibrokeratoma
- Middle aged adults
- Men > women
- Classically located on fingers and toes but can occur elsewhere on acral skin
- Etiology unknown
- Trauma has been implicated but no studies have substantiated that hypothesis
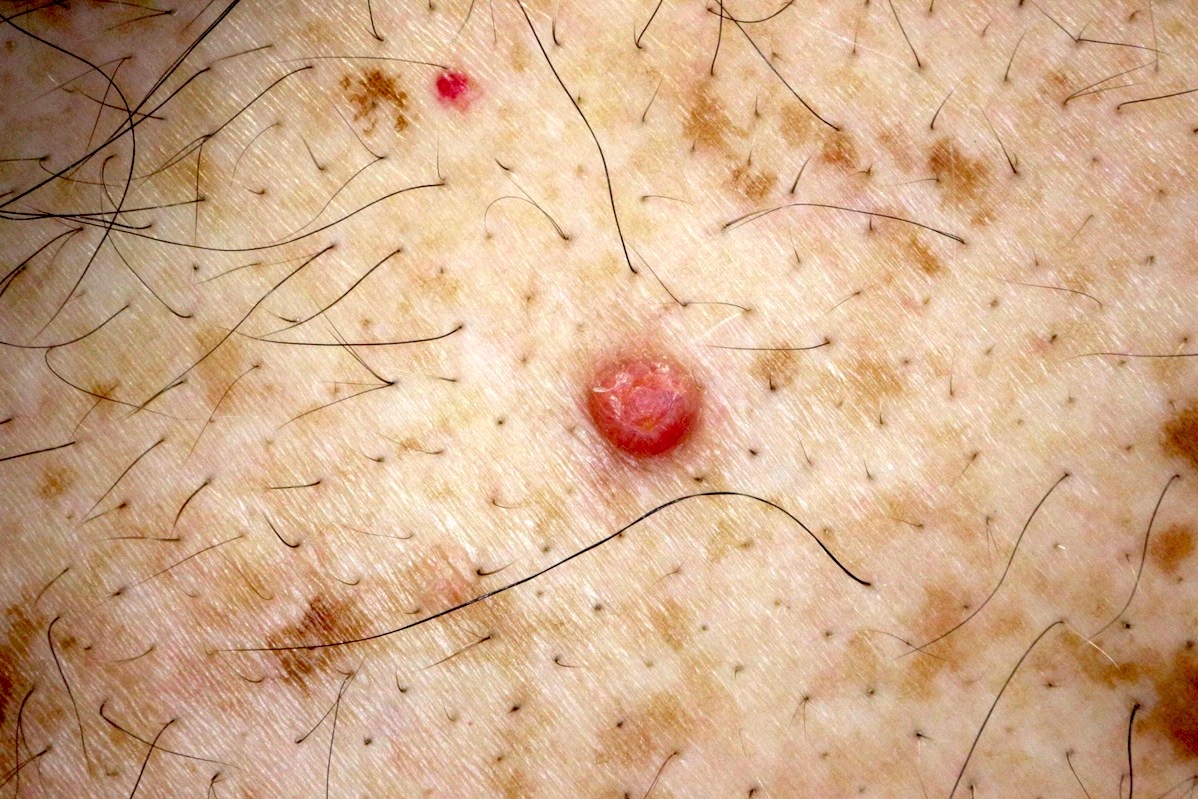
- Skin colored, slow growing firm nodule, from a few millimeters to over 1 cm in size
- Rare giant variants have been described (Ann Dermatol 2011;23:64)
- Hyperkeratotic collarete at base is characteristic
- May have prominent verruciform surface resembling a verruca or cutaneous horn
- 15 year old boy with acquired fibrokeratoma presenting as multiple plantar nodules (Dermatol Online J 2010;16:5)
- 18 year old woman with giant acquired digital fibrokeratoma occurring on left great toe (Ann Dermatol 2011;23:64)
- 35 year old man with acquired digital fibrokeratoma accompanied by pyogenic granuloma (Dermatol Online J 2009;15:8)
- 50 year old man with acquired fibrokeratoma presenting as a giant pedunculated lesion (Dermatol Online J 2008;14:10)
- Benign, although appearance or discomfort may prompt treatment
- Excision is curative
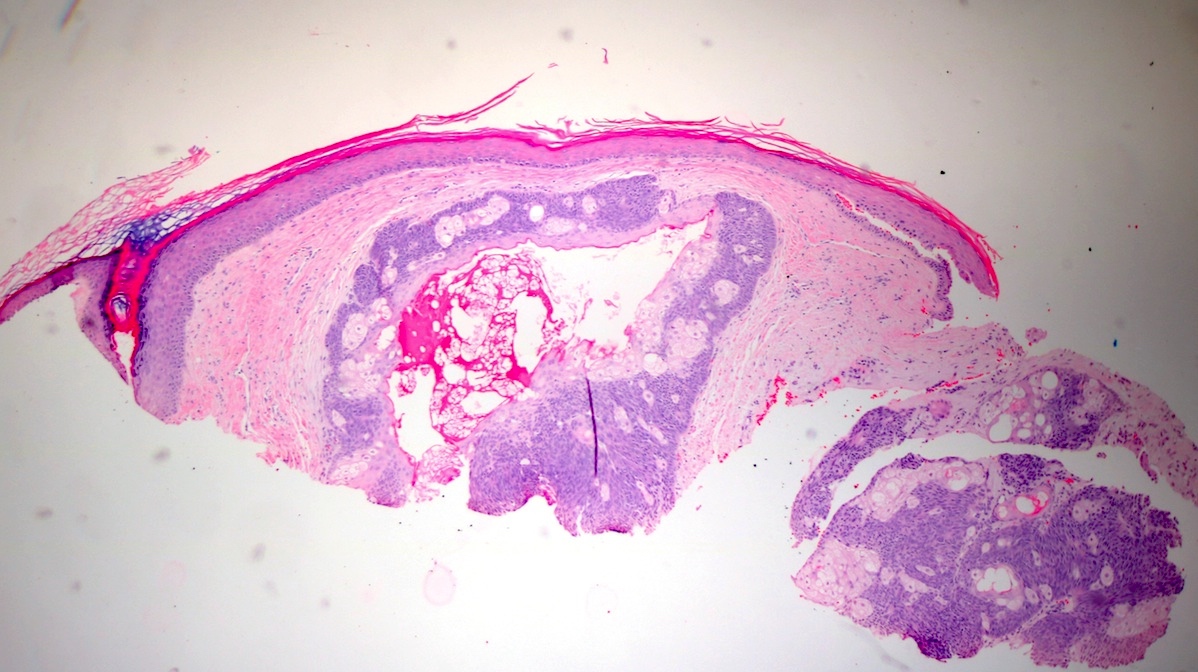
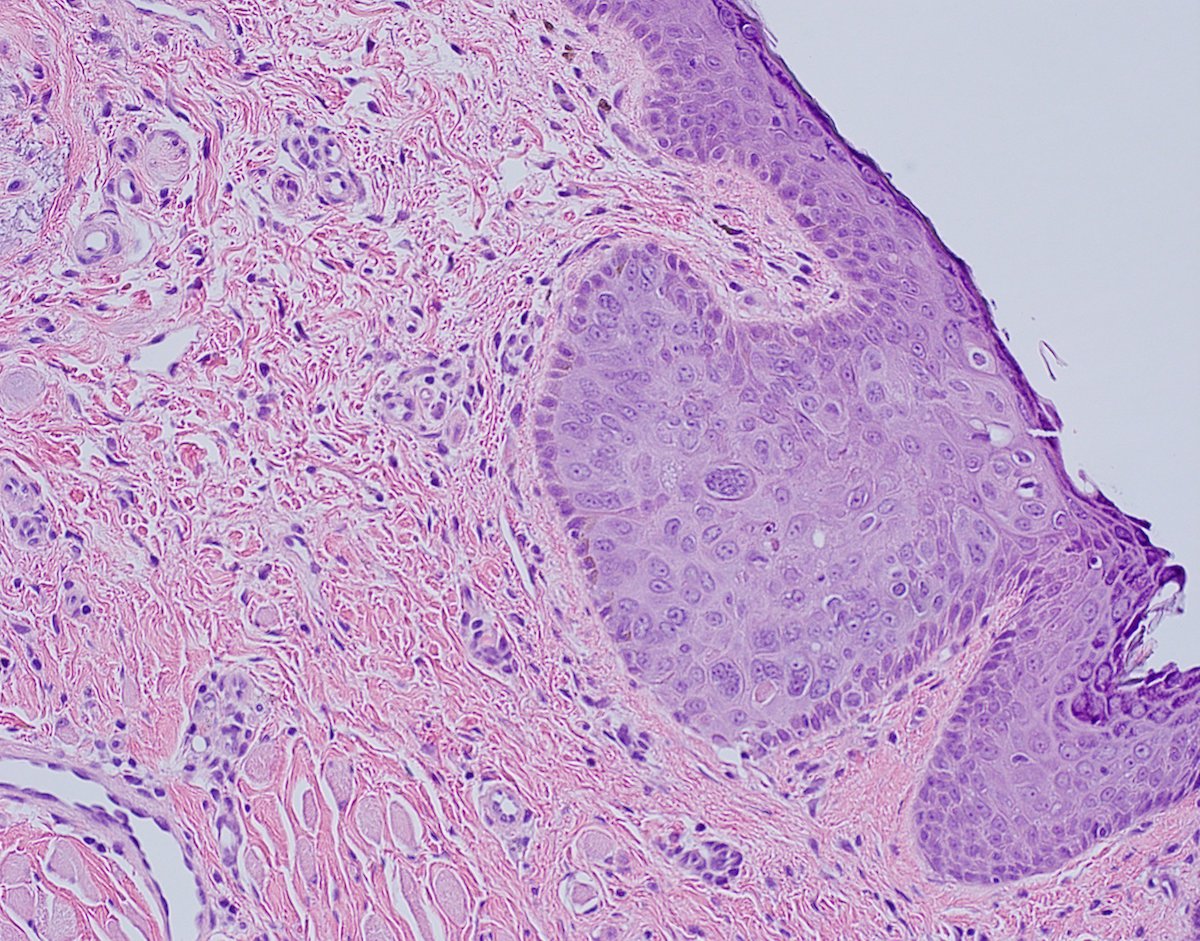
- Pedunculated to dome shaped nodule on acral skin
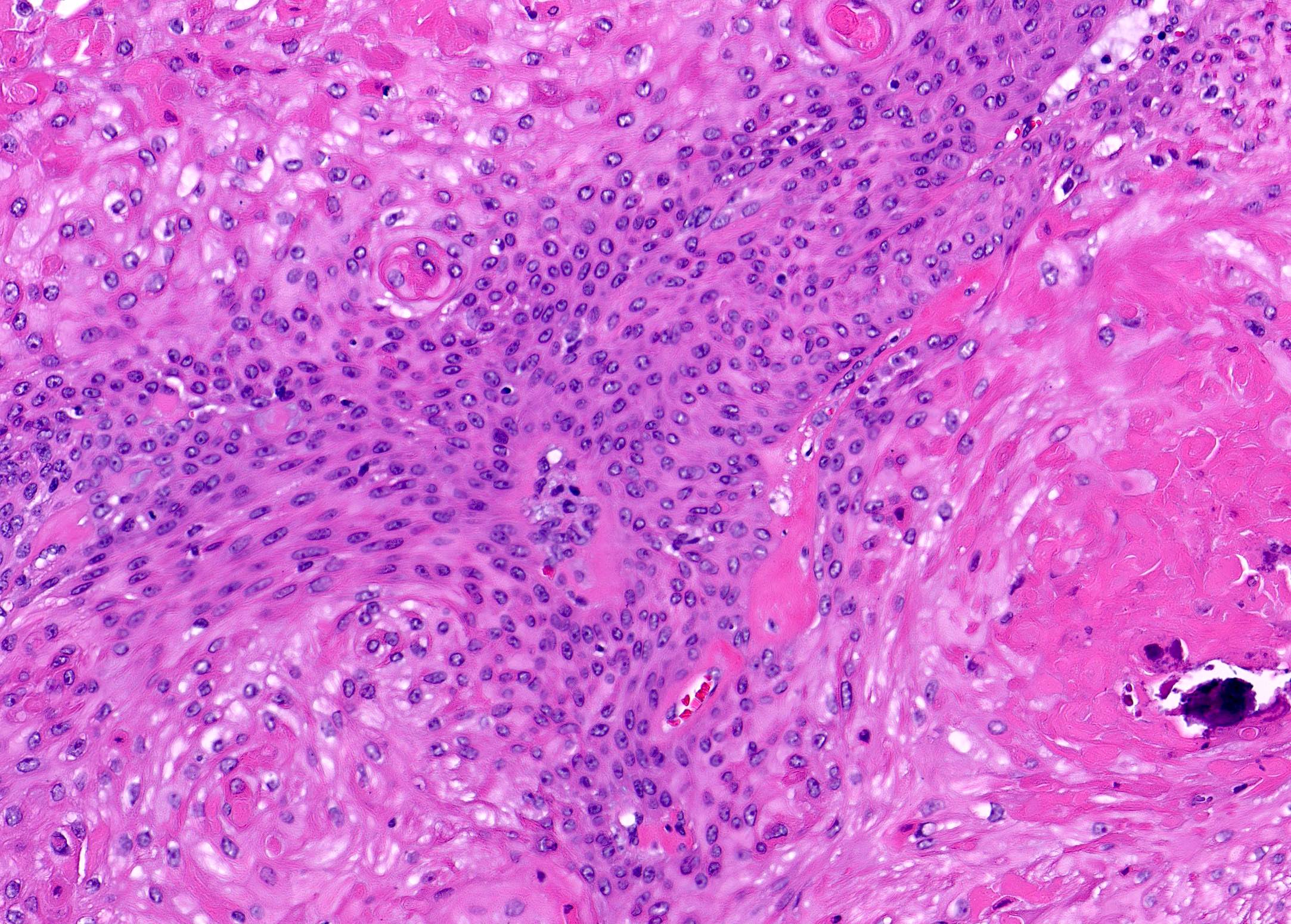
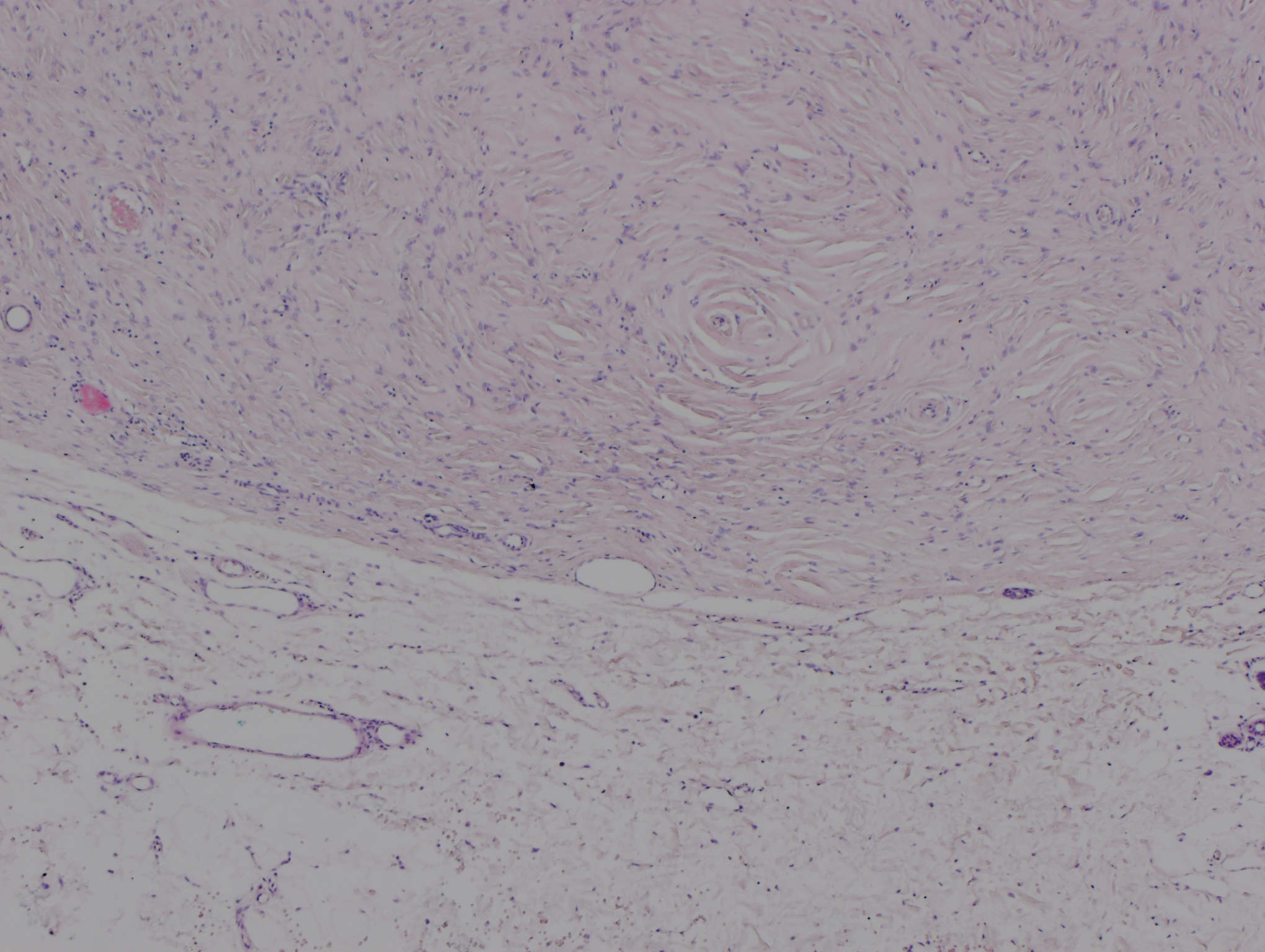
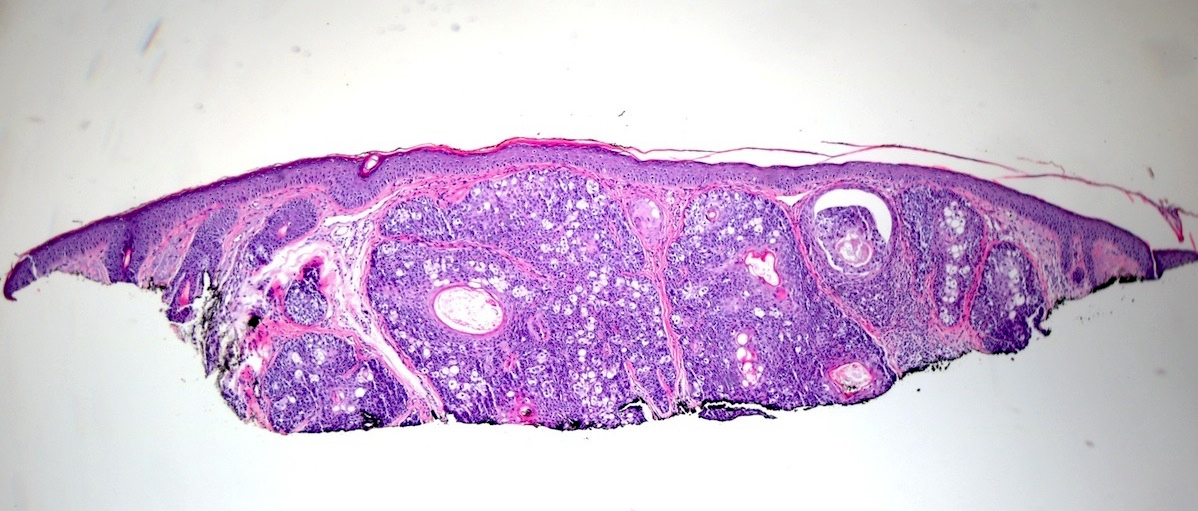
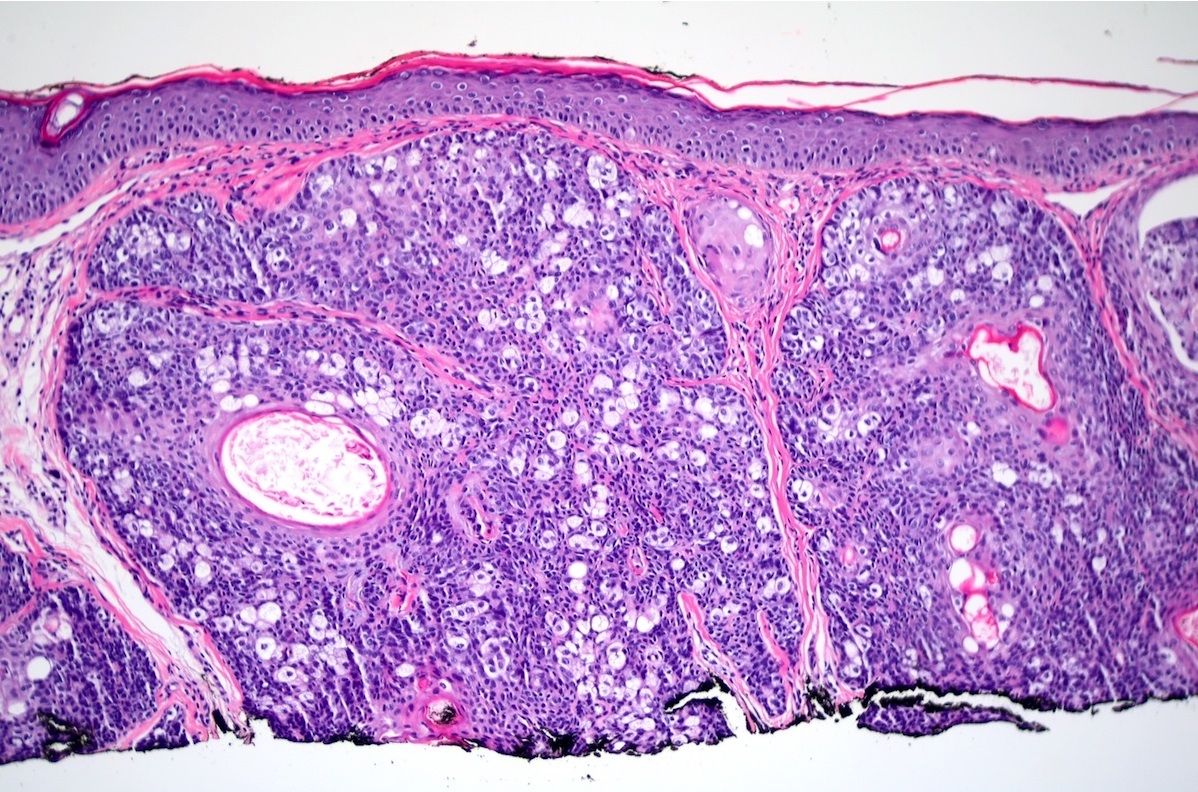
- Polypoid lesion with variably hyperplastic epidermis covering a dermal proliferation composed of dense collagen fibers and variable amounts of mature fibroblasts, small blood vessels and elastic tissue (J Am Acad Dermatol 1985;12:816)
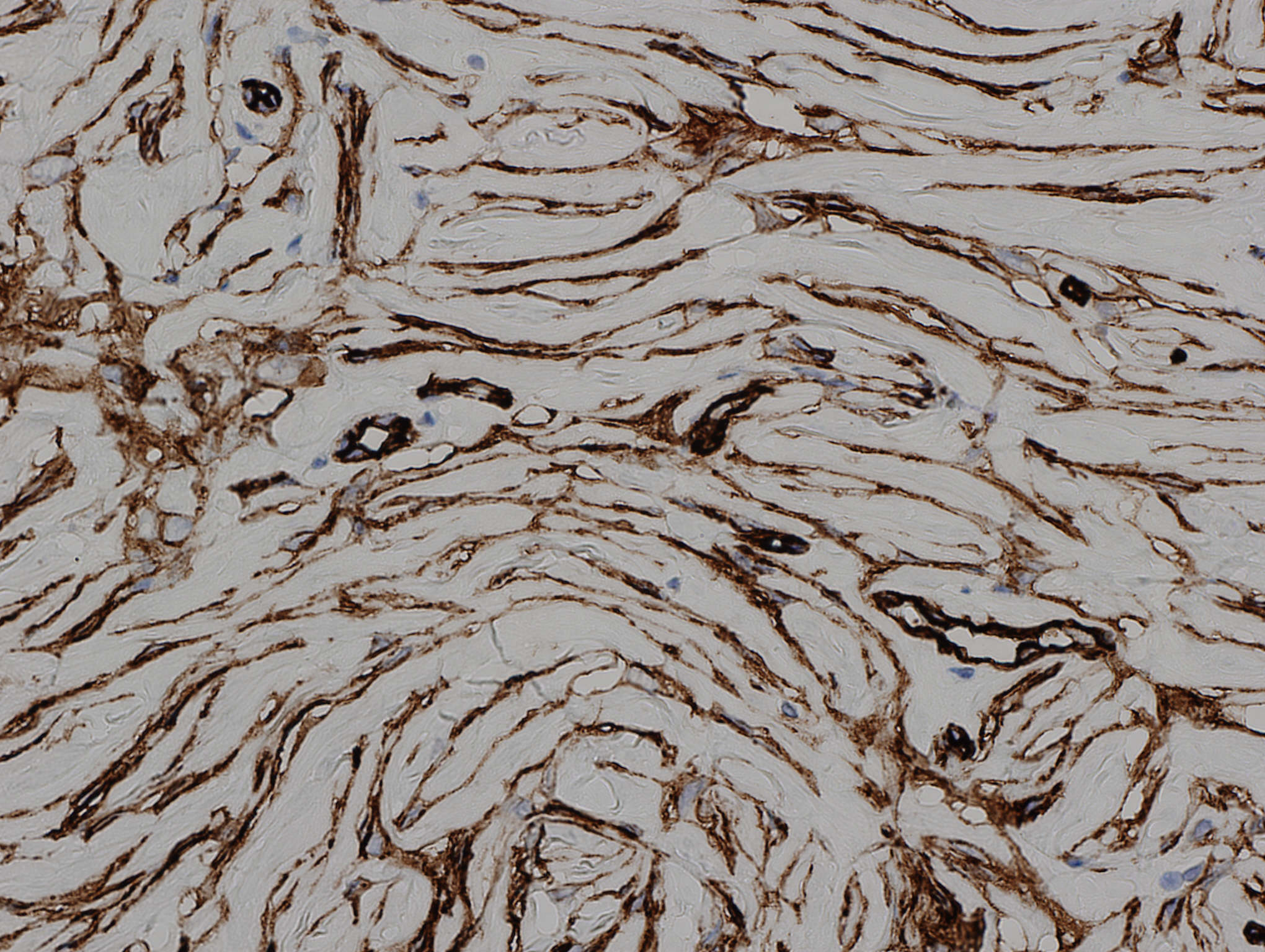
- Thickened collagen in dermis is oriented predominantly in the vertical direction
- Stellate stromal cells may be present
- Covered by variably acanthotic epidermis with hyperkeratotic orthokeratosis
- Lesion merges with adjacent normal dermis
- Neural structures are absent or inconspicious
- Lacks adnexal structures
Contributed by Hillary Rose Elwood, M.D.
Images hosted on other servers:
- Noncontributory
- Acrochordon: non acral location, pedunculated, less hyperkeratotic, less dense connective tissue
- Hypertrophic scar: normal or atrophic epidermis, dermal band of fibroblasts and dense collagen, blood vessels oriented perpendicular to epidermis
- Periungual fibroma (Koenen tumor): similar/identical histology, distinction is predominantly based on clinical findings (i.e. location, multiple lesions, patient with tuberous sclerosis); some have noted that periungual fibromas can have prominent stellate atypical myofibroblasts, may have a more prominent vascular component, and may lack the epidermal changes of digital fibrokeratoma (Arch Dermatol 1995;131:1465)
- Supernumerary digit: has prominent neural structures (i.e. peripheral nerves or tactile corpuscles), sometimes cartilage/bone is present; most are related to the fifth digit
- Intraepidermal keratinocytic lesion secondary to solar damage
- Most common precursor of cutaneous squamous cell carcinoma (SCC)
- Most common precursor of cutaneous squamous cell carcinoma
- Secondary to solar damage
- Epidermal dysplasia that is not full thickness
- Parakeratosis, dermal solar elastosis and mild dermal lymphocytic infiltrate
- Solar keratosis, senile keratosis, keratinocytic intraepithelial neoplasia
- Advancing age, usually > 40 years old
- Pale skin (Curr Probl Dermatol 2015;46:1)
- Sun exposure (Curr Probl Dermatol 2015;46:1)
- Prolonged immunosuppression (Curr Probl Dermatol 2015;46:1)
- M > F (Curr Probl Dermatol 2015;46:1)
- Sun exposed sites: face, scalp, upper chest and distal arm (Curr Probl Dermatol 2015;46:1)
- Cumulative solar damage causes a high mutation burden in the germinative (basal) layer of keratinocytes
- Chronic sun damage (ultraviolet UVB radiation and UVA to a lesser extent)
- Chronic immunosuppression
- Arsenic exposure
- PUVA therapy
- Chronic cutaneous inflammation
- βHPV (Viruses 2017;9:187)
- High prevalence rates and viral loads in actinic keratoses
- Virus, when combined with UV exposure, may play a role in progression to SCC
- Single or multiple erythematous and hyperkeratotic macules or papules
- Usually < 1 cm in diameter
- Sometimes pigmented or ulcerated
- Chronic sun damage of background skin
- Reference: J Drugs Dermatol 2010;9:1125
- Usually by clinical examination
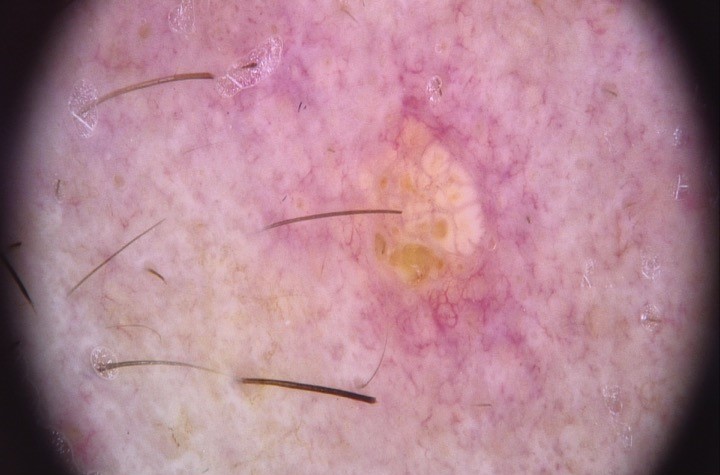
- Dermoscopy shows erythematous to brown networks, irregular hyperpigmented follicular openings, grey dots and lineal or circular structures; surface scales are common (Curr Probl Dermatol 2015;46:70)
- In vivo reflectance confocal microscopy shows a disarranged or mildly atypical honeycomb pattern (Eur J Dermatol 2016;26:549)
- Can remain stable for long periods or regress
- Rate of transformation to SCC: closer to 1/100 (from 1/10 to 1/1000 in different studies)
- Proliferative variant has higher risk of invasion
- 2 main pathways for progression to SCC (J Eur Acad Dermatol Venereol 2018;32:581):
- Classical: atypical basal keratinocytes in an actinic keratosis invade the mid to upper epidermis and transform to invasive SCC
- Differentiated: invasive SCC develops directly from actinic keratosis with dysplasia limited to the basal layer
- 54 year old man with a dark lesion on his nasal tip; biopsy revealed pigmented actinic keratosis (Cureus 2019;11:e4721)
- 68 year old woman with non small cell lung adenocarcinoma with eruptive inflamed actinic keratosis consequent to systemic chemotherapy (Dermatol Online J 2017;23:13030/qt77s2r0p9)
- 72 year old woman developed an acute inflammation of her actinic keratosis while on oral capecitabine chemotherapy for rectal adenocarcinoma (J Cutan Med Surg 2012;16:298)
- 77 year old woman with seborrheic keratosis that transformed into bowenoid actinic keratosis (Case Rep Dermatol 2020;12:19)
- Excision
- Cryosurgery
- Topical drugs: 5-fluorouracil, ingenol mebutate, diclofenac or imiquimod
- 5-fluorouracil is the most effective and most cost effective treatment
- Photodynamic therapy
- Above methods often combined
- References: J Eur Acad Dermatol Venereol 2017;31:13, Australas J Dermatol 2020 Aug 25 [Epub ahead of print]
- See Clinical images
- Frozen section not performed as lesion is precancerous
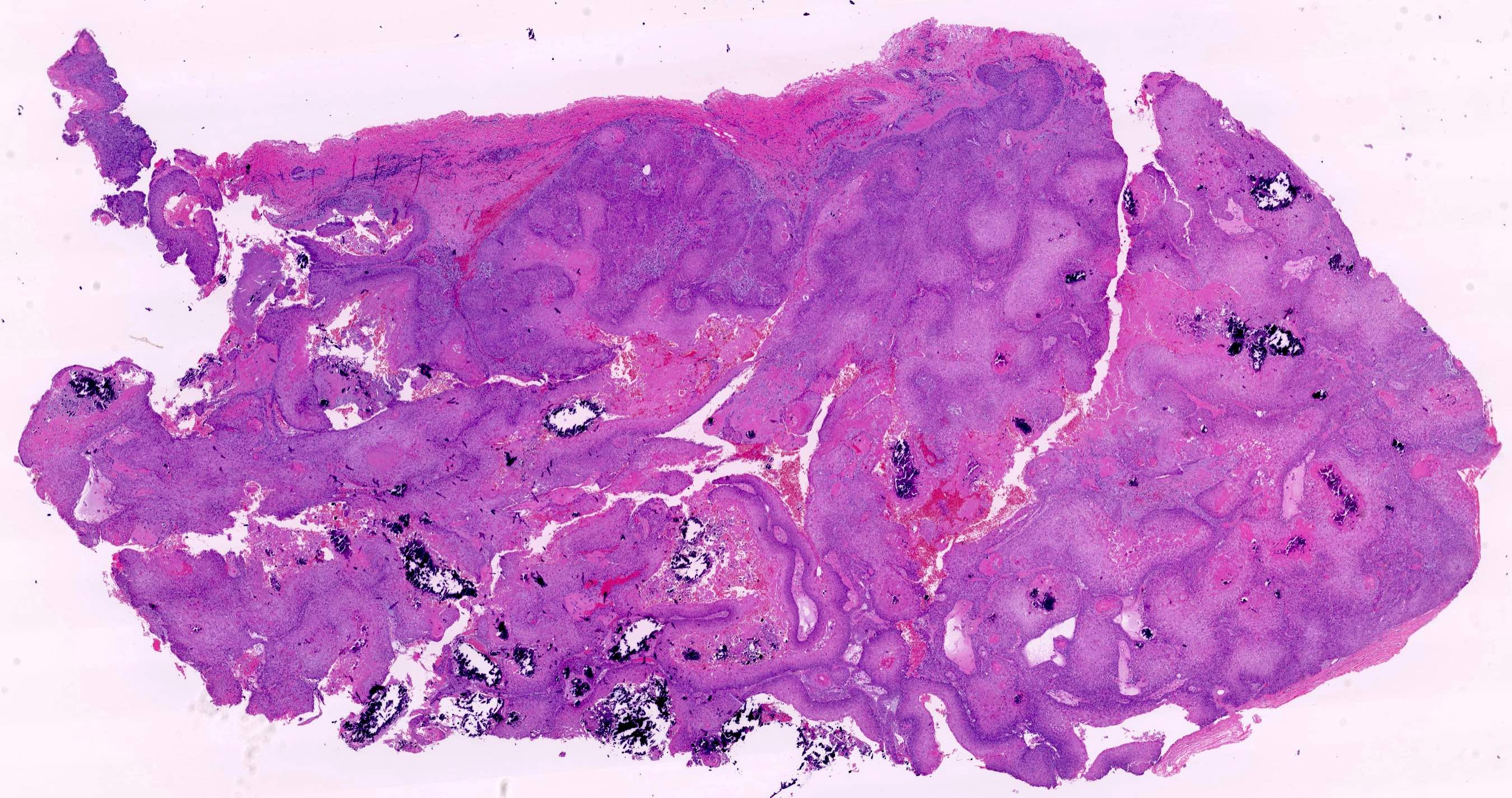
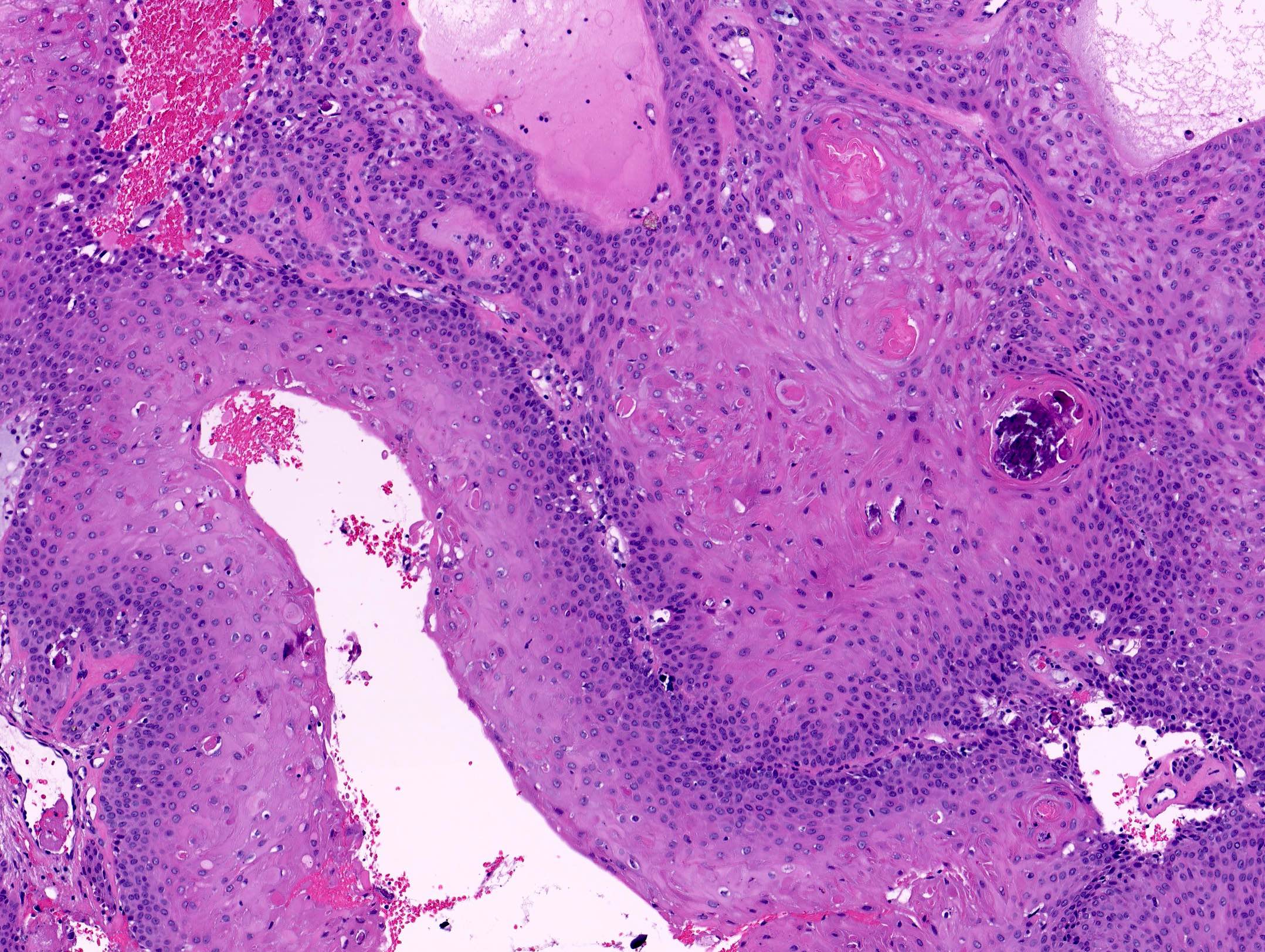
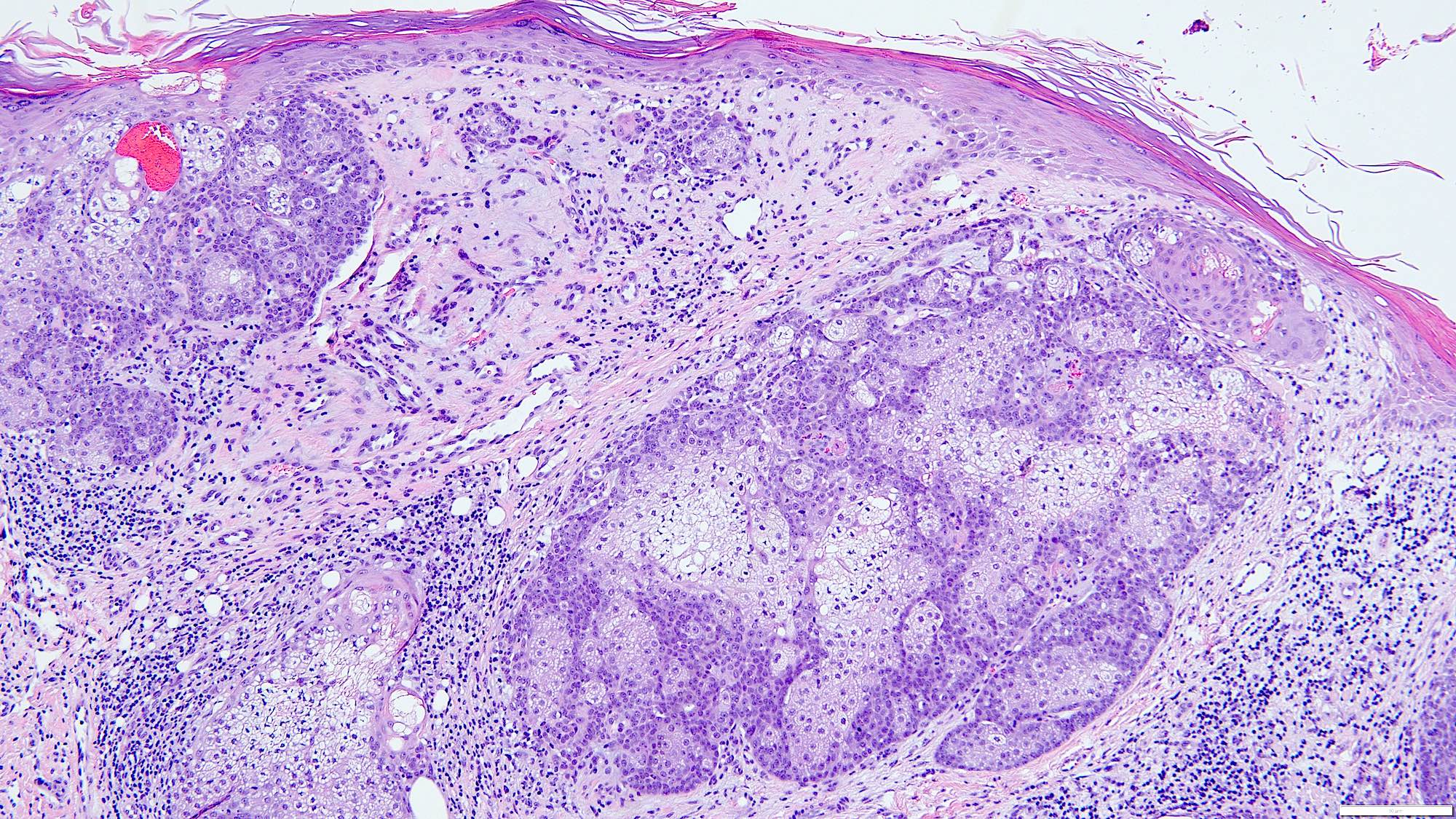
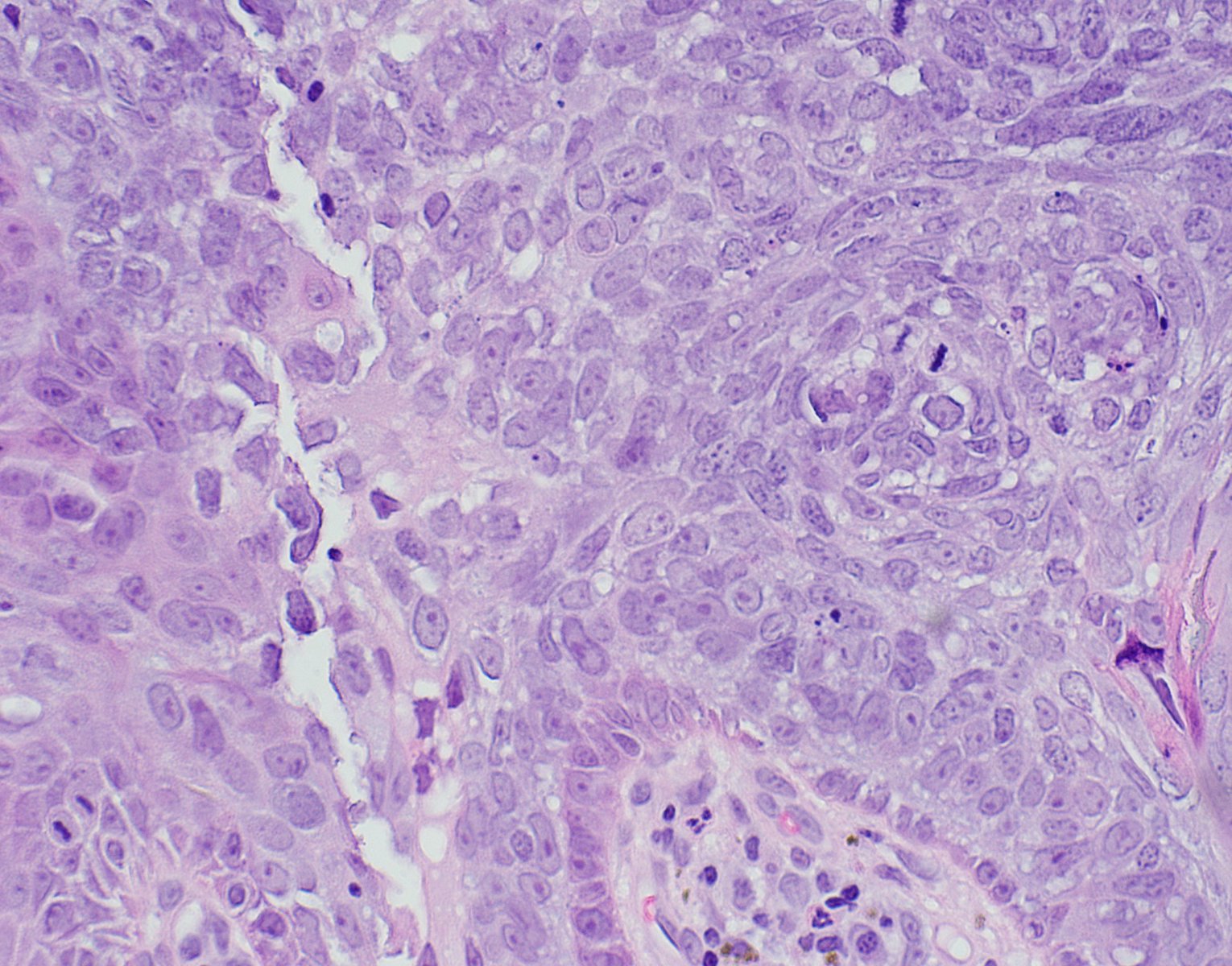
- Atypia of basal keratinocytes with loss of polarization, crowding and overlapping
- Can progress to involve the mid to upper epidermal layers
- Can extend along adnexal structures; typically limited to infundibular extension
- Never full thickness
- Typically, mild acanthosis with occasional downward buds; tangential sectioning of these buds can prompt overdiagnosis of superficially invasive SCC but these do not represent actual squamous pearls
- Focal parakeratosis
- Flag sign: occasional columns of grey loose keratin above preserved acrosyringiums (known as Freudenthal funnels) alternate vertically with eosinophilic compact hyperkeratosis
- Lost / attenuated granular layer
- Dermal changes: solar elastosis, mild inflammatory infiltrate (usually lymphocytes; plasma cells present in longstanding lesions)
- Variants:
- Hypertrophic / hyperplastic: prominent irregular acanthosis, parakeratosis and orthokeratosis
- Atrophic: thin epidermis
- Lichenoid: band-like lymphocytic infiltrate of papillary dermis, basal keratinocytes with scattered apoptosis and vacuolar change
- Acantholytic: suprabasal clefting between atypical keratinocytes
- Pigmented: increased melanin in the basal keratinocytes and melanocytes; melanophages in the papillary dermis
- Proliferative: dermal projections of nested atypical keratinocytes; dense dermal inflammation
- Bowenoid: near full thickness atypia, usually focal
- Pagetoid: pale cells
Contributed by María-Teresa Fernández-Figueras, Ph.D.
- p53 (50%)
- Cyclin D1 (50%)
- Increased Ki67 expression
- MelanA can be positive in pigmented lesions (Am J Dermatopathol 2009;31:305)
- Main driver mutations present in cutaneous invasive squamous cell carcinoma such as TP53, NOTCH1 and NOTCH2 are already present in actinic keratosis
- MAPK pathway seems to play a leading role in invasion
- References: Nat Commun 2018;9:3667, Clin Cancer Res 2019;25:2379, Br J Cancer 2014;110:520
Tutorial on actinic keratosis histopathology
- Skin, forehead, curettage:
- Fragments of hypertrophic actinic keratosis (see comment)
- Comment: Due to fragmentation, small areas of in situ or invasive squamous cell carcinoma cannot be ruled out.
- Actinic cheilitis:
- Similar histologically but in case of invasion the risk of metastasis is 11% (StatPearls: Actinic Cheilitis [Accessed 22 March 2021])
- Squamous cell carcinoma:
- In situ: full thickness epidermal dysplasia
- Invasive:
- Isolated dermal squamous cells or pearls
- Dermal desmoplasia
- Pseudomaturation with large keratinized cells close to the dermal collagen
- Finger-like projections of proliferative actinic keratosis are challenging to differentiate from invasion, especially when tangentially sectioned
- Bowen disease (classical):
- Involves non sun exposed areas
- Full thickness atypia of keratinocytes
- Sharply delineated
- Gives rise to nonactinic related invasive tumors with higher metastatic risk (J Eur Acad Dermatol Venereol 2019;33:11, J Cutan Pathol 2006;33:261)
- Benign lichenoid keratosis:
- Also known as lichen planus-like keratosis: resembles a lichen planus and often shows hypergranulosis (Dermatol Reports 2011;3:e25)
- Sharply demarcated
- Mild reactive keratinocyte atypia
- Dysmaturatative drug eruptions:
- In patients receiving chemotherapeutic drugs (J Eur Acad Dermatol Venereol 2016;30:638)
- Atypical starburst-like or ring-like mitoses are common
- Dyskeratosis of basal and suprabasal layers of the epidermis
- Occasional squamous syringometaplasia
- Grover disease (transient acantholytic dermatosis):
- Lesions show dismaturation and lentiginous silhouette (Am J Dermatopathol 2010;32:541)
- Areas of acantholysis or dyskeratosis can be present in actinic keratosis but the phenomenon of acantholytic dyskeratosis favors the diagnosis of Grover disease
Which of the following is true about the entity shown in the photo above?
- Clinically ranges from small papules to pustulous plaques or erythroderma
- It is frequently located in the genital area
- It is the most common precursor of cutaneous invasive squamous cell carcinoma
- Nodular growth pattern is considered a low risk variant
- p16 is positive in high risk cases
Comment Here
Reference: Actinic keratosis
- BerEP4
- EMA
- MelanA
- p16
- p53
Comment Here
Reference: Actinic keratosis
- CD20
- HMB45
- MelanA
- Sox10
- Vimentin
Comment Here
Reference: Actinic keratosis
- Rare, slow growing cutaneous adnexal tumor with 3 major histologic patterns: tubular, cribriform and solid
- Morphologically indistinguishable from adenoid cystic carcinoma at other sites; must rule out cutaneous extension from salivary gland malignancy or metastasis from other locations
- More indolent than salivary gland counterpart (Am J Surg Pathol 2013;37:1603)
- Primary cutaneous adenoid cystic carcinoma (PCACC) is a rare adnexal tumor with different histopathologic growth patterns, including cribriform, tubular and solid variants
- Perineural invasion is a common feature and may explain the high recurrence level
- Diagnosis is confirmed only after ruling out metastatic disease through thorough clinical history and imaging studies
- 60% of PCACC cases exhibit MYB overexpression, which is mediated by MYB::NFIB fusion or other MYB chromosomal abnormalities
- ICD-O: 8200/3 - adenoid cystic carcinoma
- ICD-11: 2C33 & XH4302 - adnexal carcinoma of skin & adenoid cystic carcinoma
- Occurs predominantly in middle aged and elderly individuals; median age is 62 years (JAAD 2021;85:245)
- M:F ratio ranges from 0.79:1 to 1.6:1 (JAAD 2021;85:245, Histopathology 2022;80:407, Am J Surg Pathol 2013;37:1603)
- Head and neck (particularly the scalp) is the most frequently involved site, followed by the trunk, upper limbs / limb girdle and lower limb / limb gridle (Histopathology 2022;80:407)
- Unclear; previously thought to arise from eccrine glands
- Recent hypotheses support apocrine or modified apocrine glands as an origin (Dermatol Online J 2013;19:5)
- ~60% of PCACC cases harbor MYB gene activation (J Cutan Pathol 2017;44:201)
- Unknown
- Solitary, slow growing mass; often present for several years prior to diagnosis (Histopathology 2022;80:407)
- Usually skin colored
- Some may be indurated, tender or ulcerate; in the scalp, symptoms may involve localized alopecia (Rare Tumors 2011;3:e3)
- Size range: 1.0 - 5.0 cm, with a median of 2.0 cm (Am J Surg Pathol 2013;37:1603)
- Essential
- Histology with 2 types of lumina, including true small bilayered ducts (with or without secretion) and pseudocysts containing basophilic mucinous material in multinodular neoplasm
- 2 main cell types: ductal and myoepithelial cells
- Desirable
- Cylindroma-like appearance
- Perineural invasion
- Coexpression of MYB and CD117
- Demonstration of MYB or MYBL1 rearrangements in selected cases
- Metastasis is rare (typically to lymph nodes or lungs) and associated with high grade transformation (Histopathology 2022;80:407)
- Recurrence is very common, primarily attributed to perineural invasion (Am J Surg Pathol 2013;37:1603)
- Vulva and perigenital sites may correlate with more aggressive disease / metastases, possibly due to the abundance of nerve tissue in this area; however, larger studies are needed to validate this supposition (Am J Surg Pathol 2013;37:1603)
- Factors that may reflect a more biologically aggressive tumor (Histopathology 2022;80:407)
- Longest diameter of the lesion (≥ 1 cm)
- Involvement of subcutaneous fat tissue and widely infiltrative border
- Grade III / high grade transformation
- In multivariate analysis of 451 cases, more recent year of diagnosis, advanced patient age and advanced stage were associated with poorer outcomes (JAAD 2021;85:245)
- 62 year old man with painful and erythematous nodule on his left chest (Exp Oncol 2022;44:174)
- 67 year old woman with firm mobile nodule on her lower back (Cureus 2023;15:e49099)
- 70 year old woman with slow growing, painless, solid to cystic, skin colored lesion on her scalp (Skin Health Dis 2022;2:e118)
- 79 year old man with an asymptomatic, slow growing lesion on the abdomen (Dermatol Online J 2020;26:13030)
- 83 year old man with a 10 year history of nodule on lower leg (J Surg Case Rep 2019;2019:rjz201)
- Wide surgical excision to prevent recurrence
- Mohs surgery has been performed for better control of surgical margins (JAMA Dermatol 2013;149:1343)
- Smooth surface with a firm consistency and a tan-gray color
- Frozen sections are only utilized to confirm diagnosis or verify that the surgical margins were negative
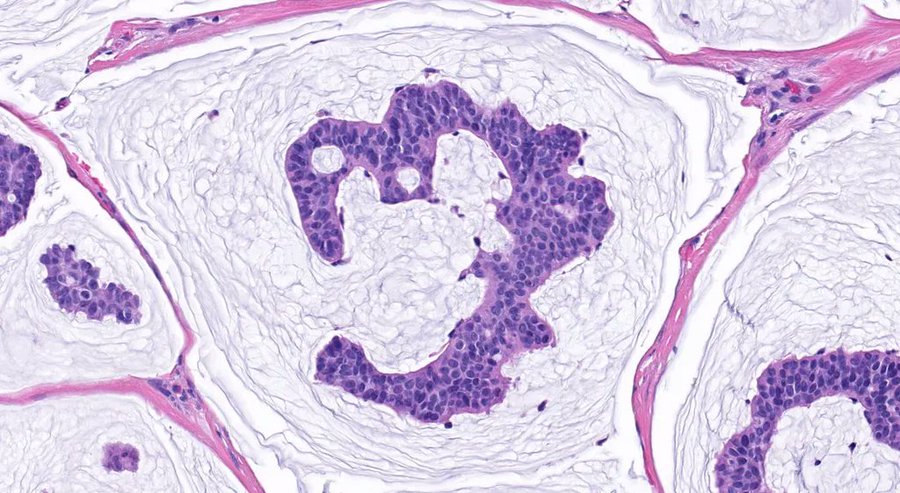
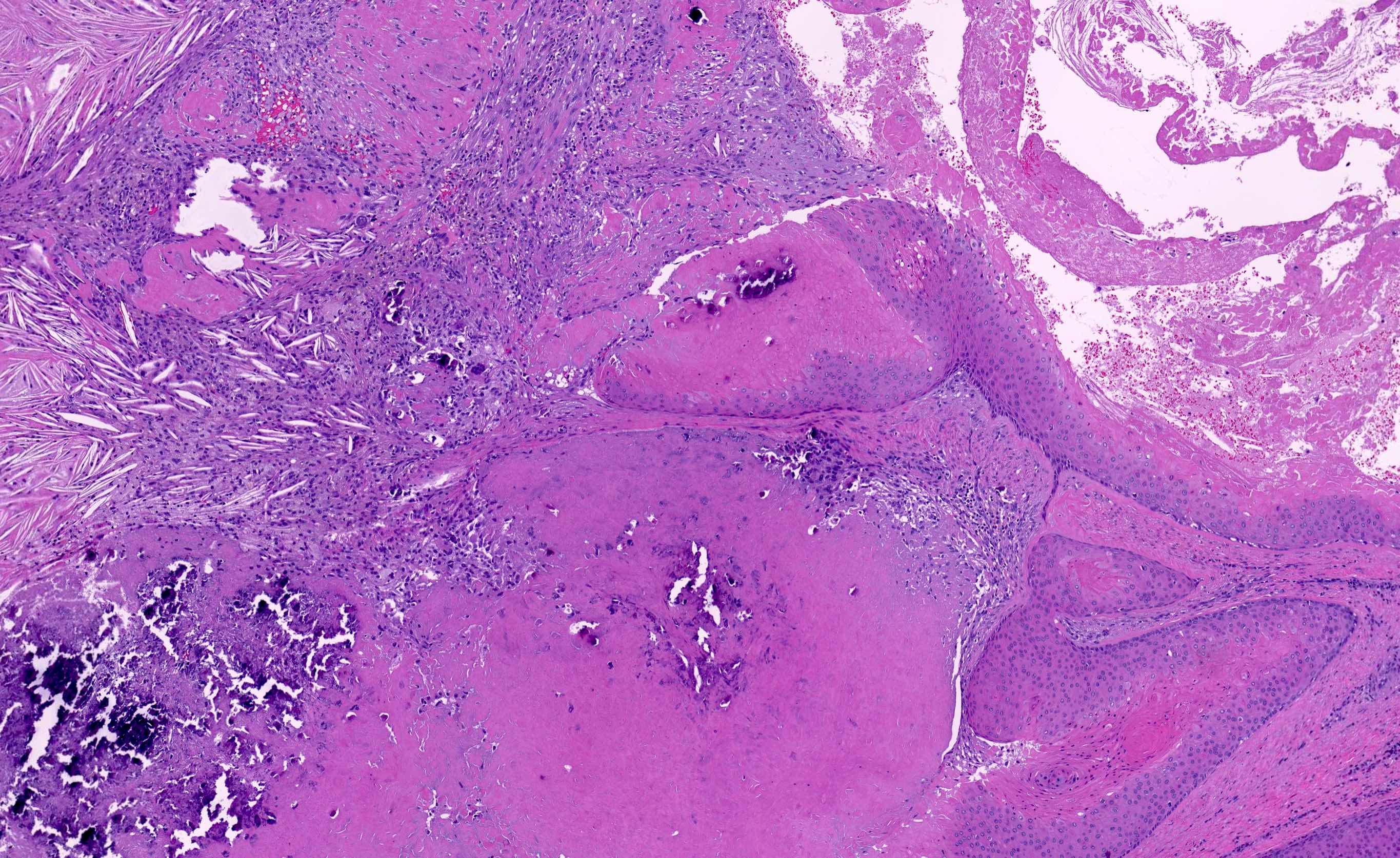
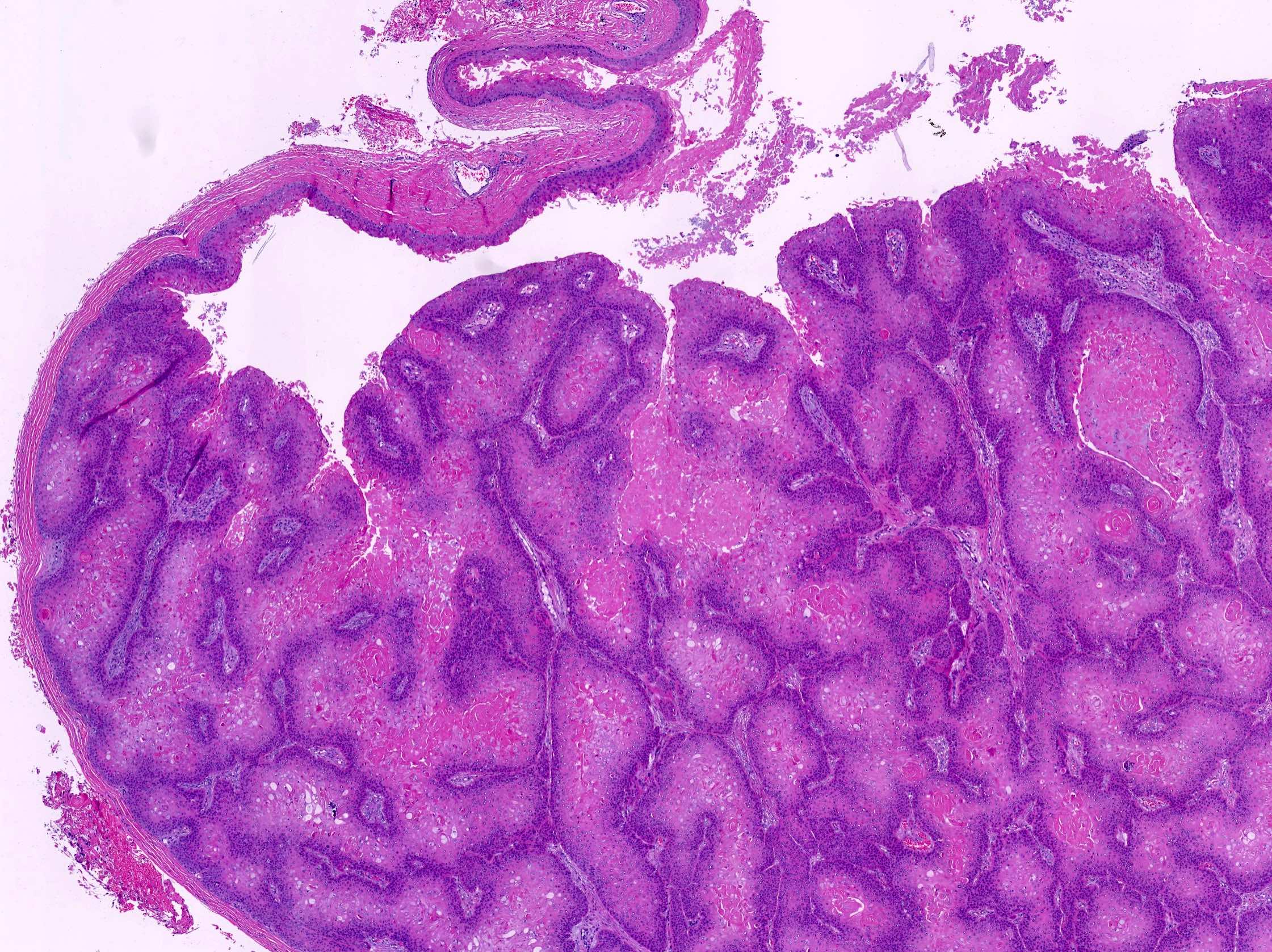
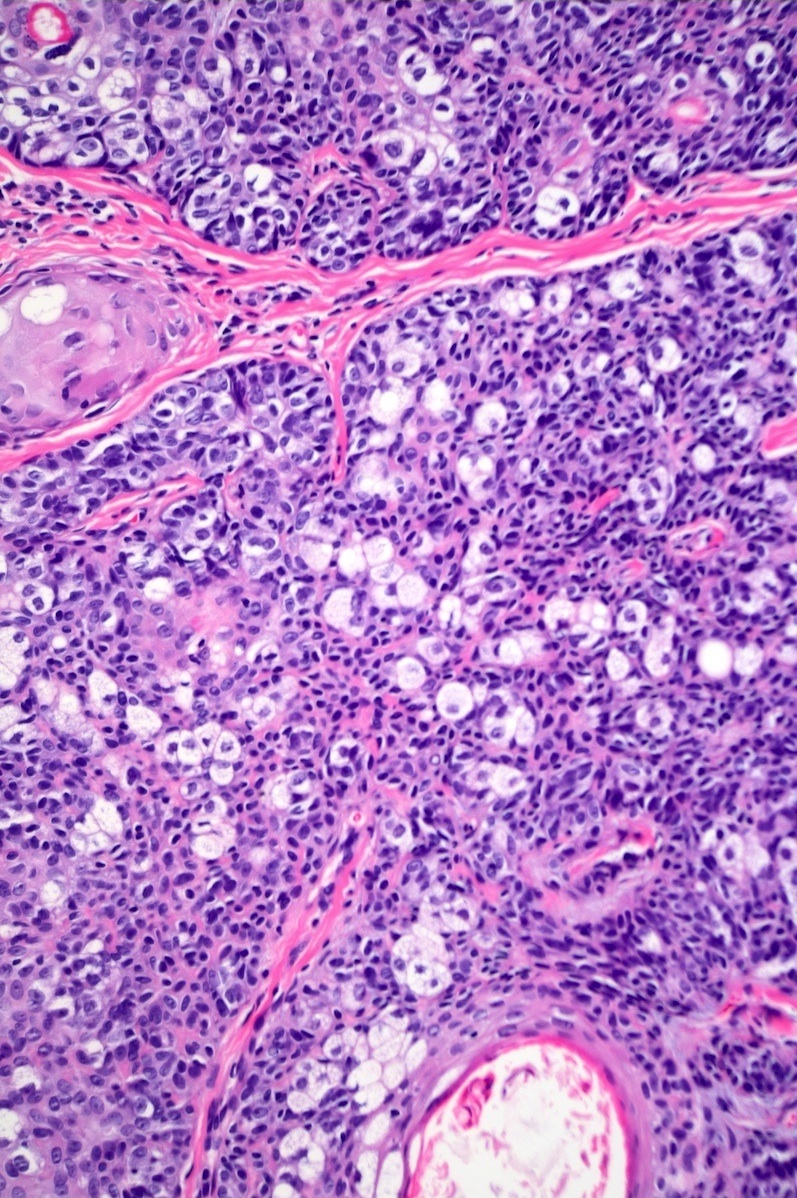
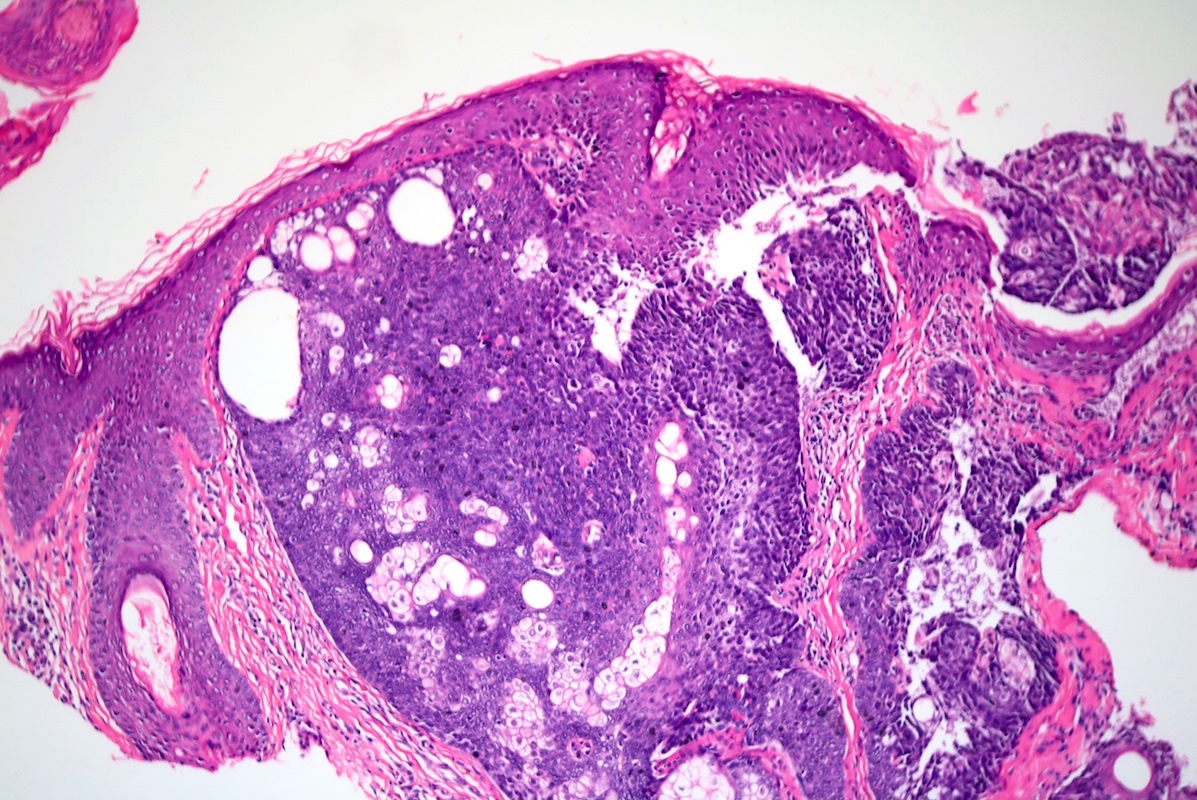
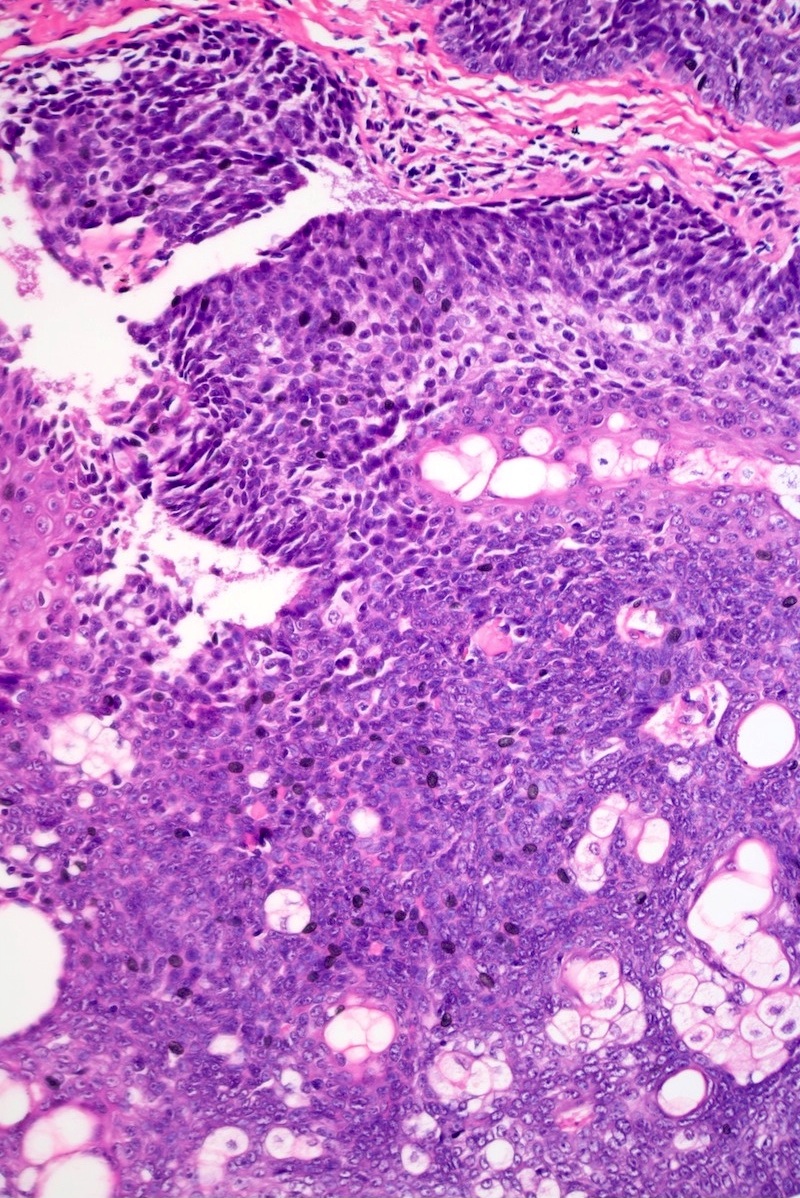
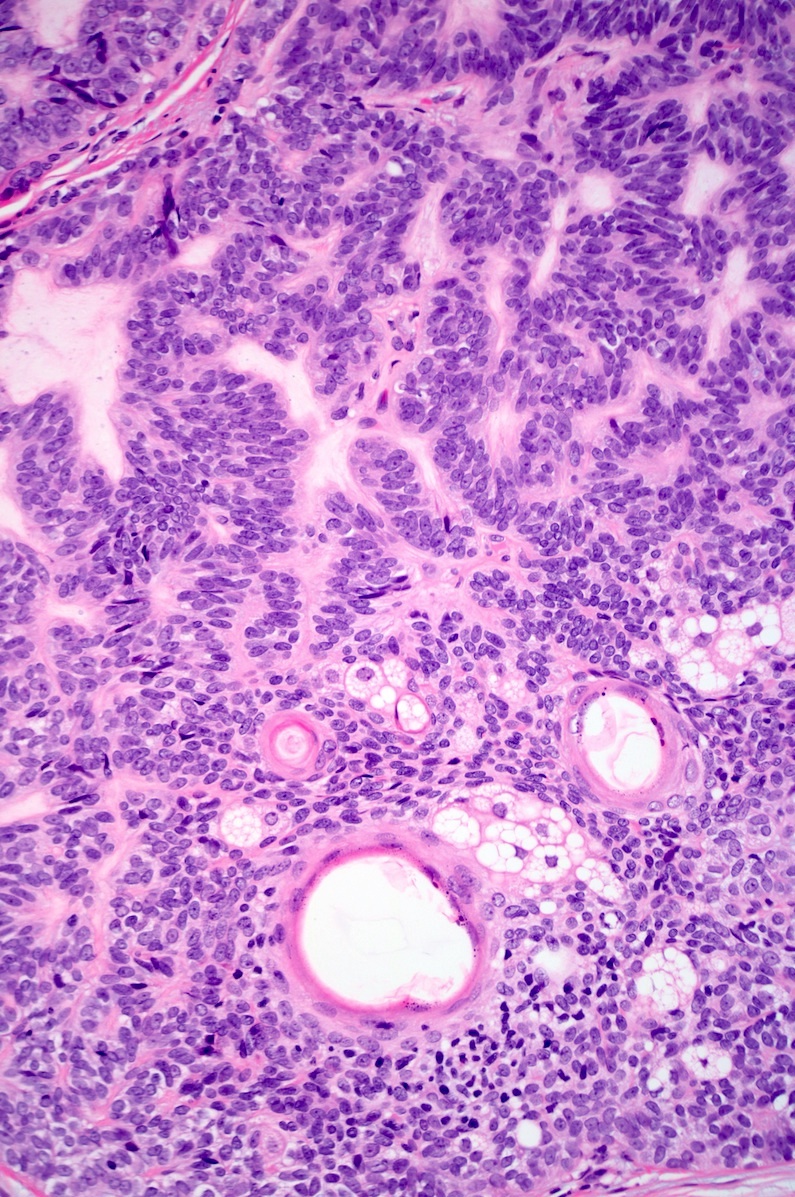
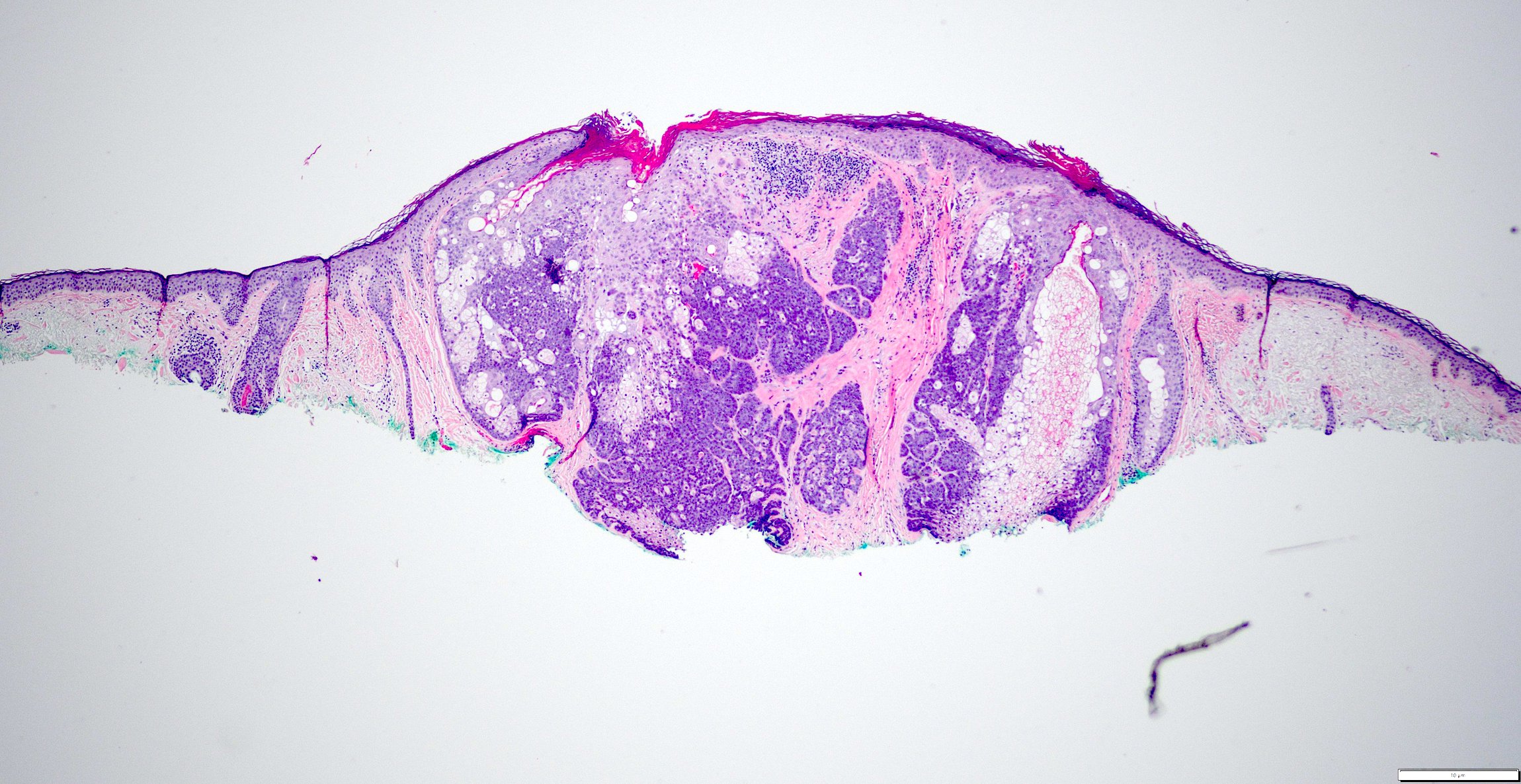
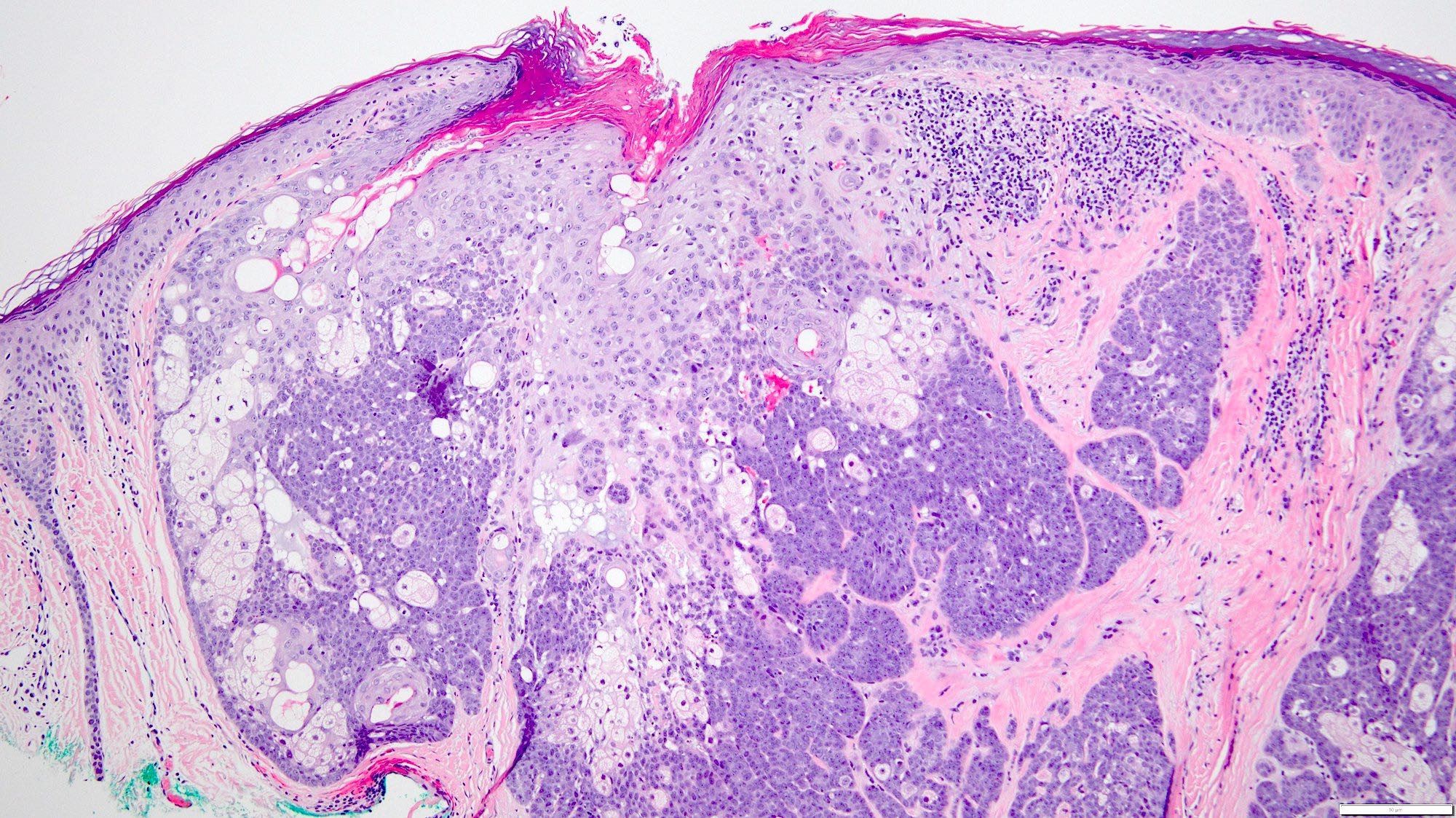
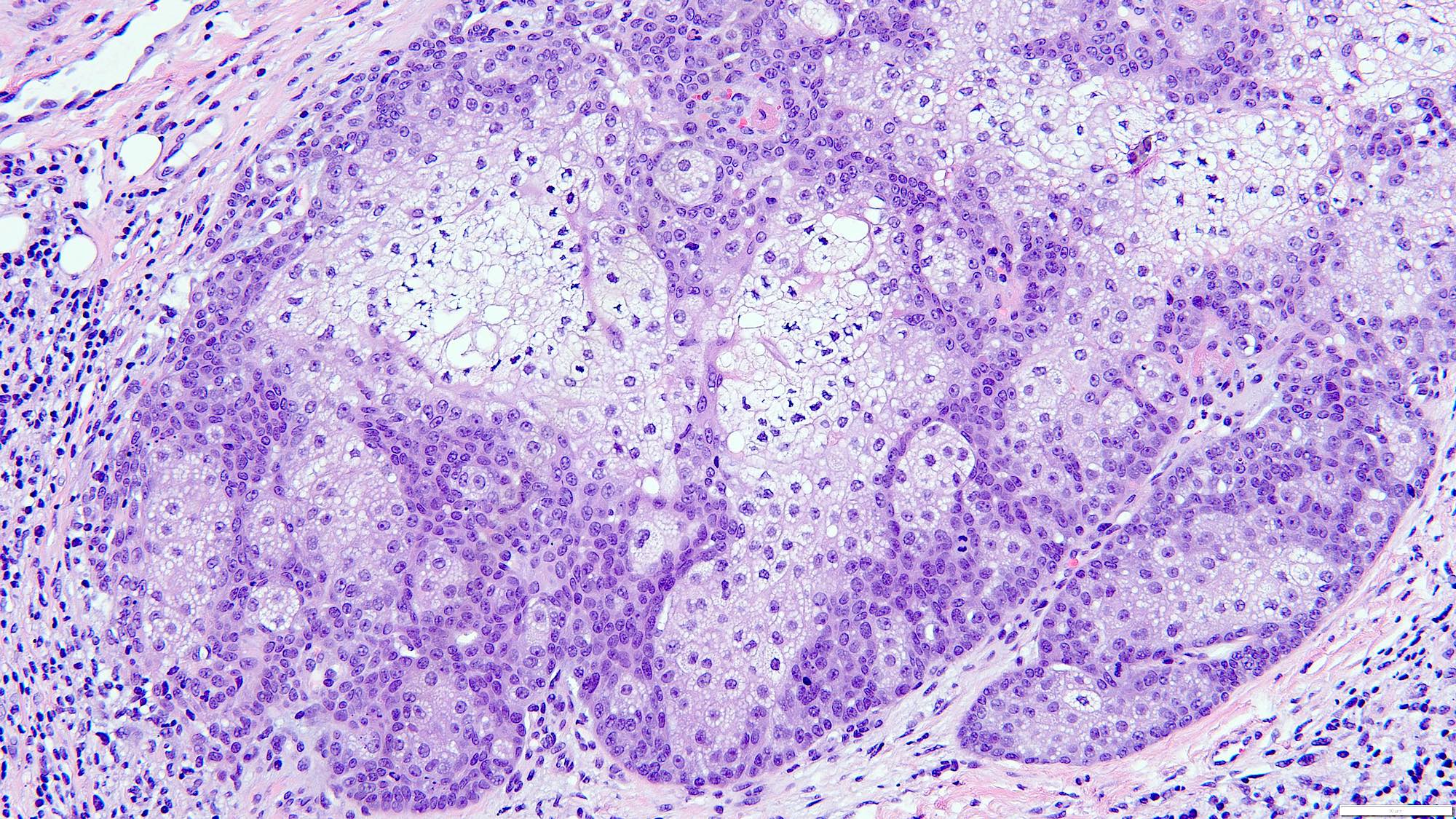
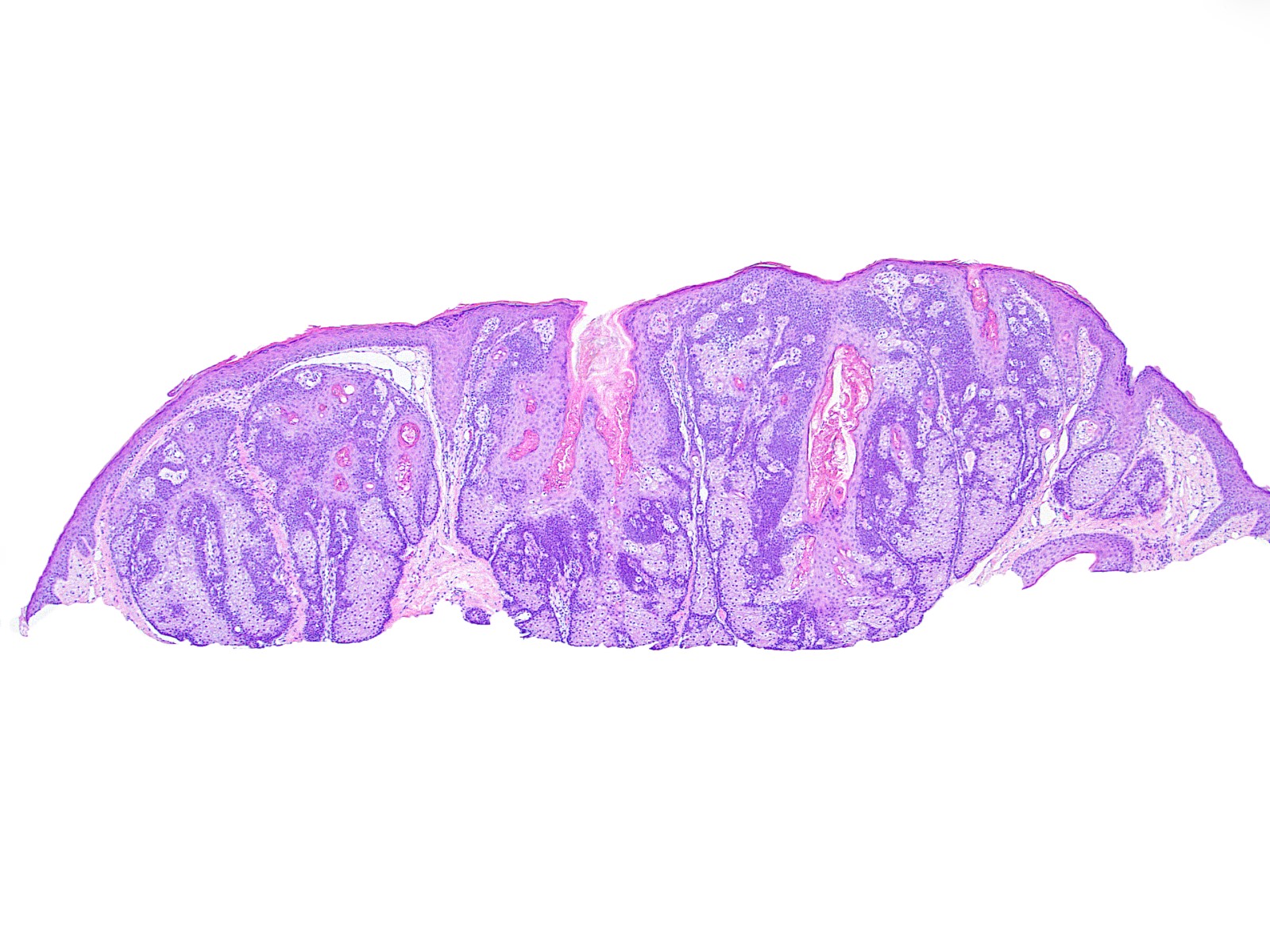
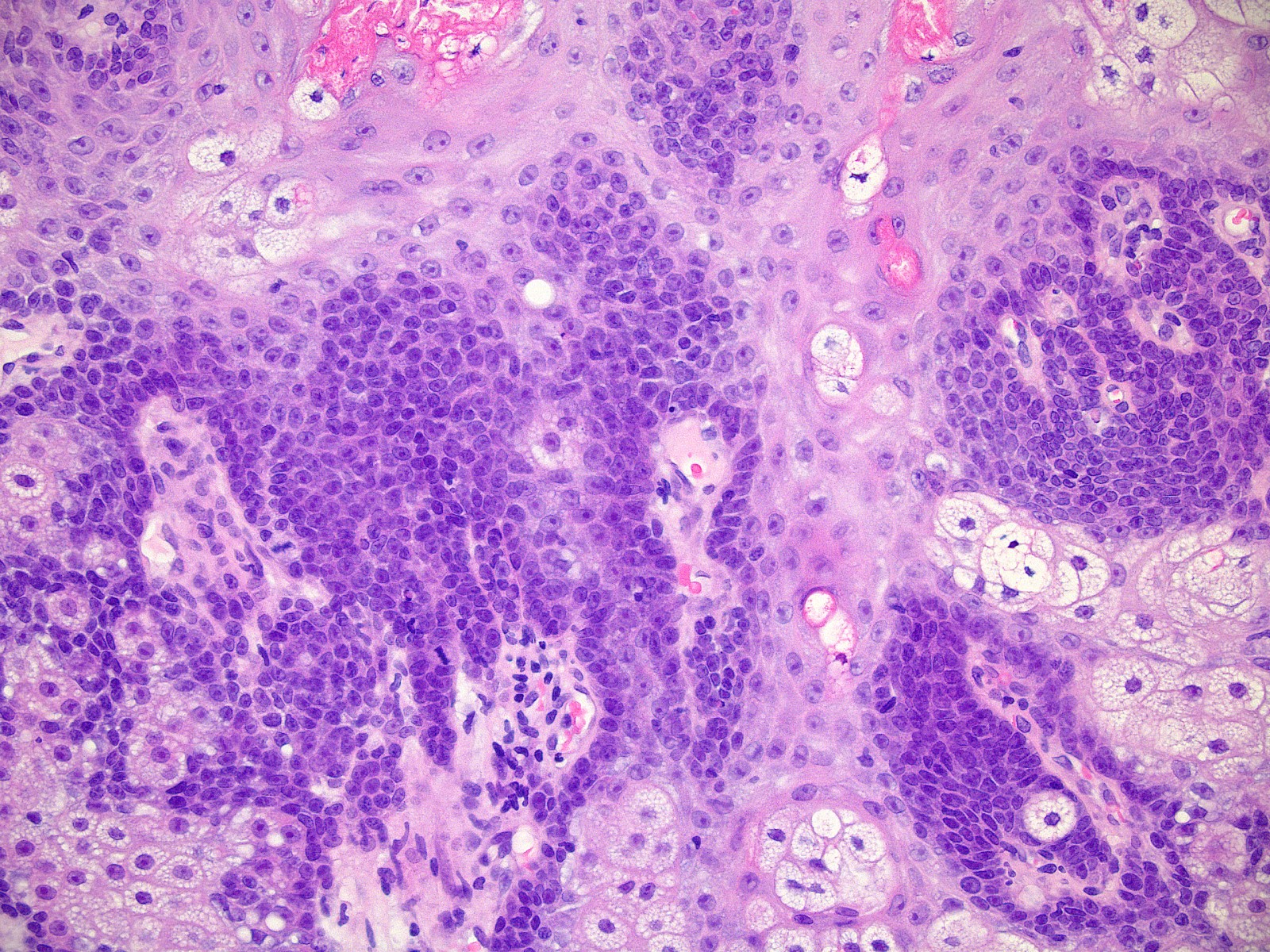
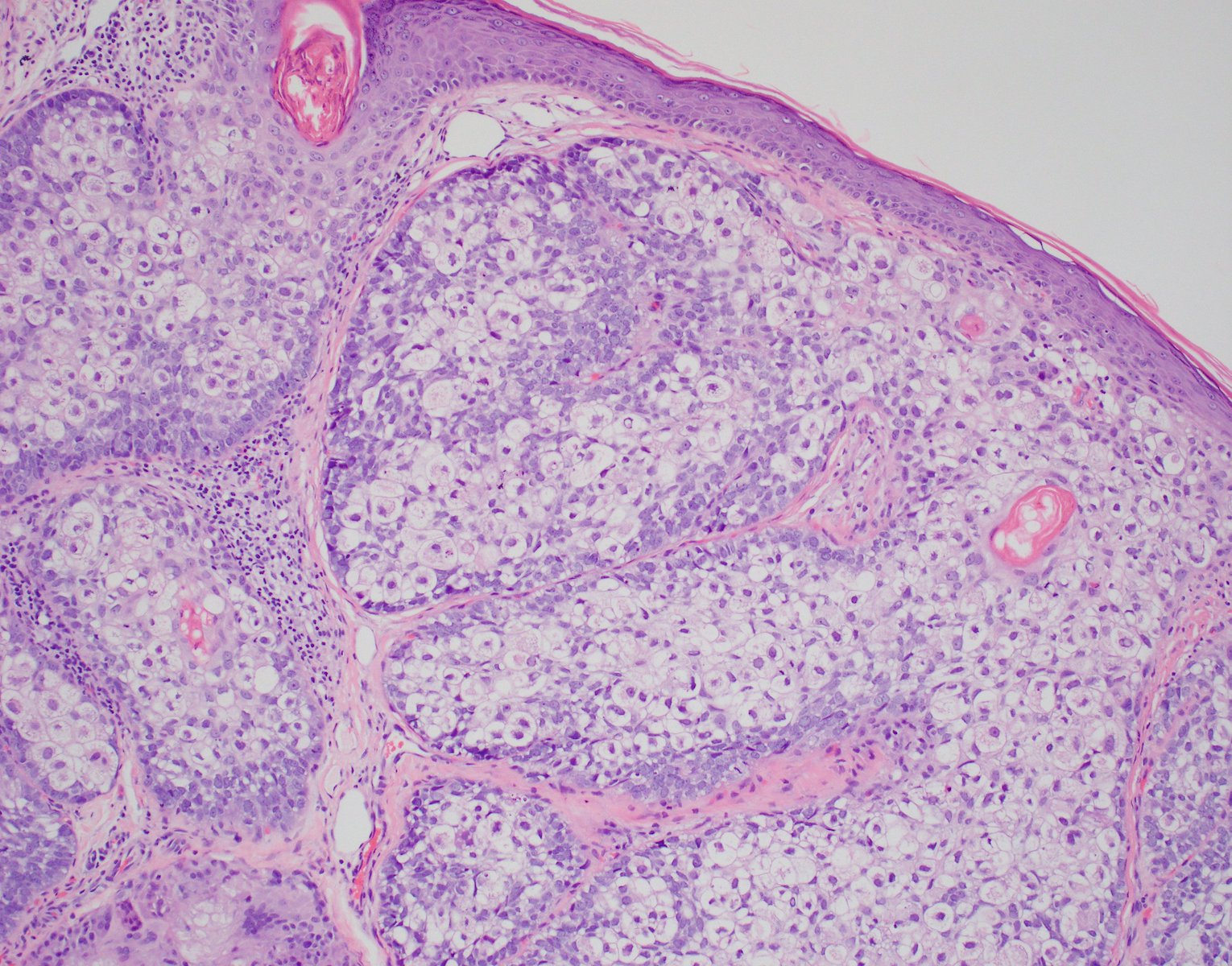
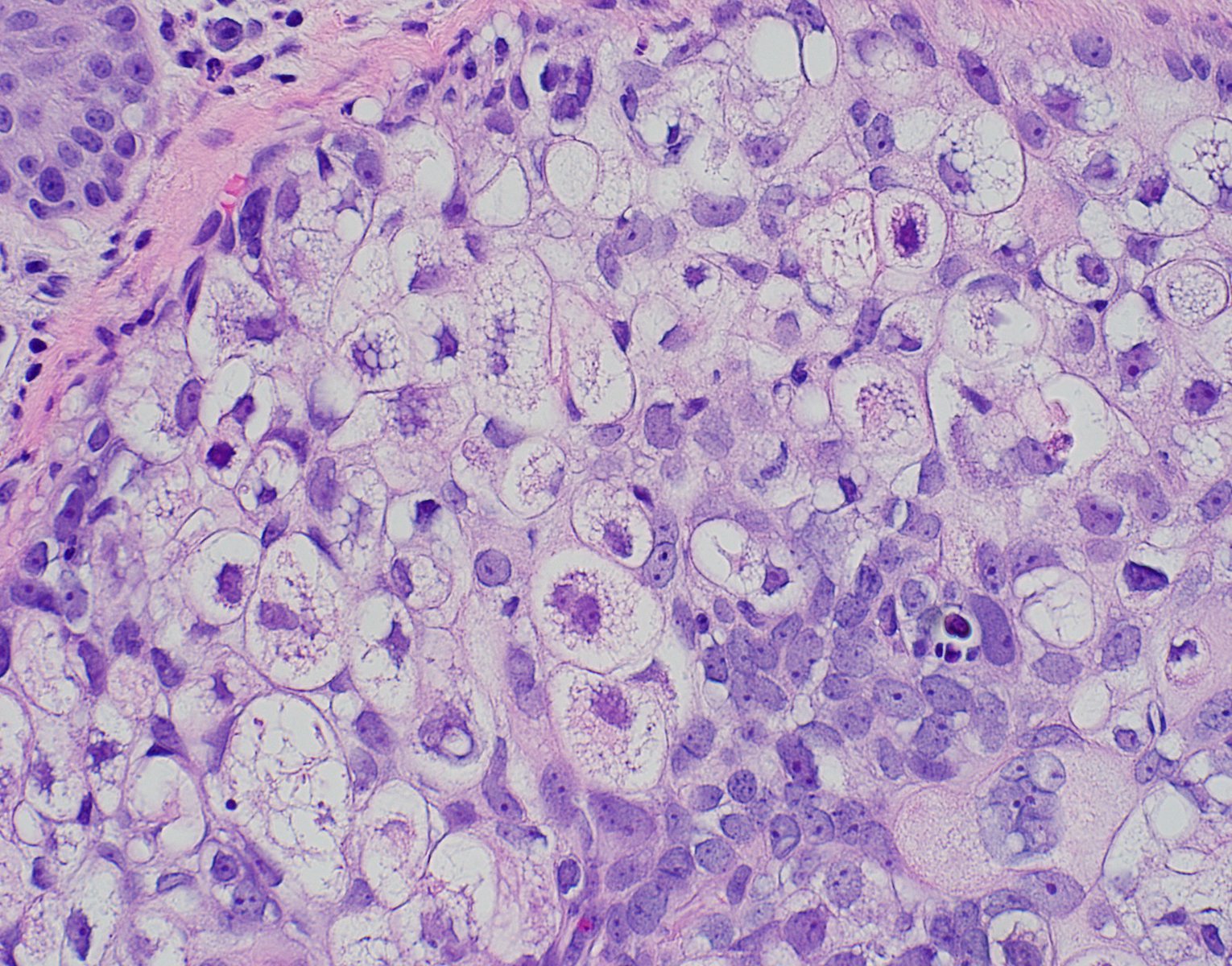
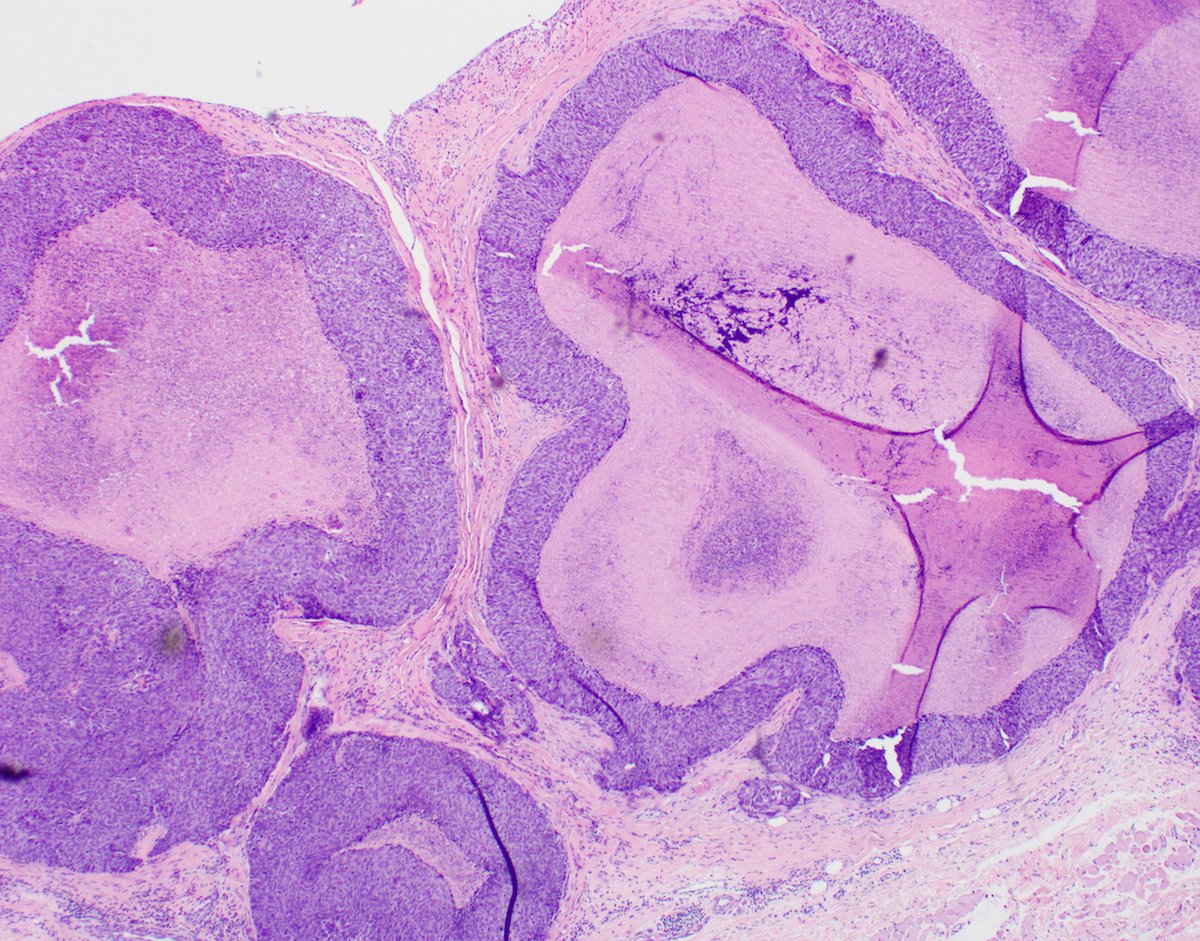
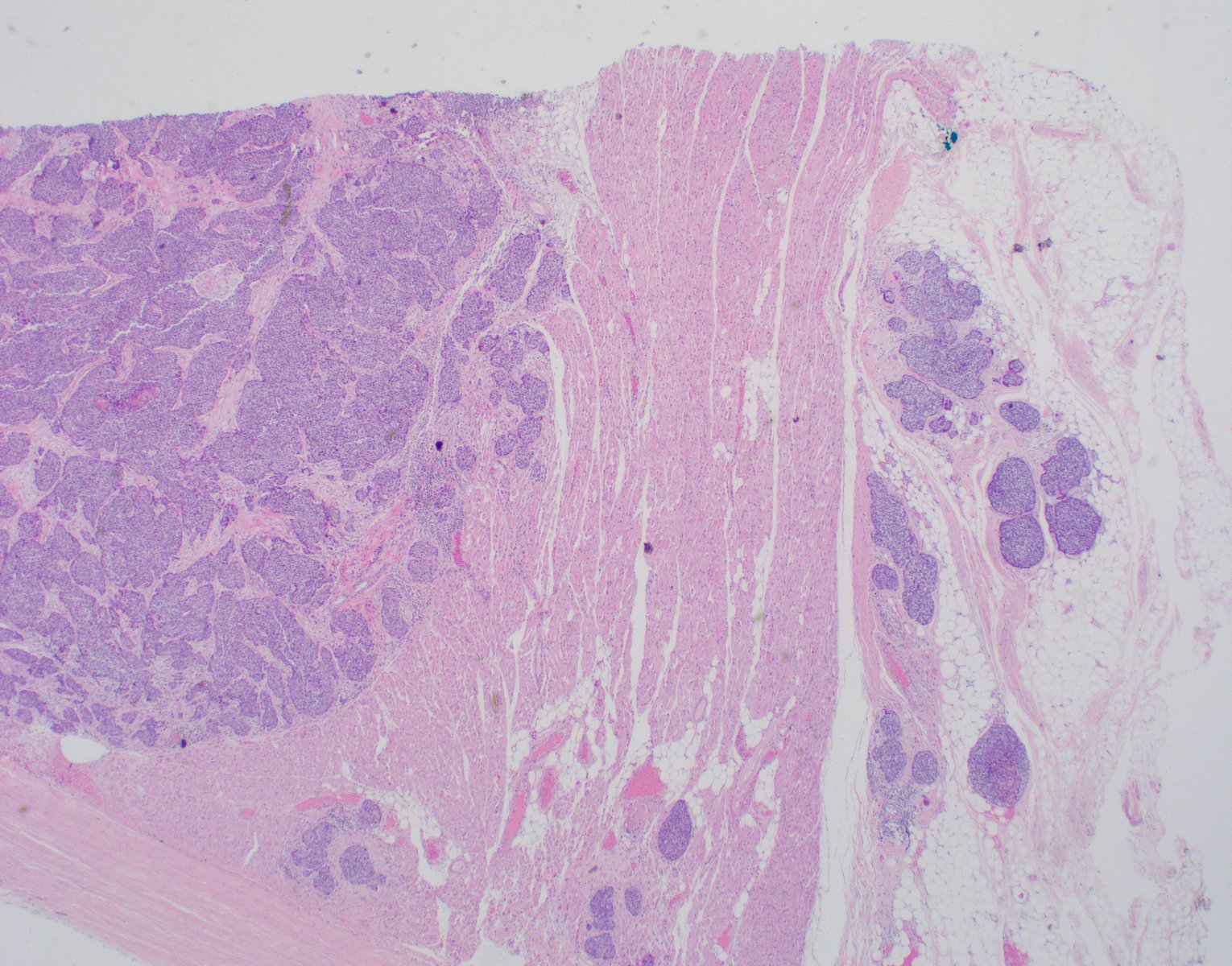
- Shows the characteristic histologic findings of PCACC: basaloid cells within dermis, arranged in cords and islands forming tubular structures and cribriform patterns
- Poorly circumscribed, dermal based basaloid neoplasm with numerous ductular and cystic spaces
- Often with subcutaneous extension; epidermal involvement unusual but has been reported (Am J Dermatopathol 2019;41:619)
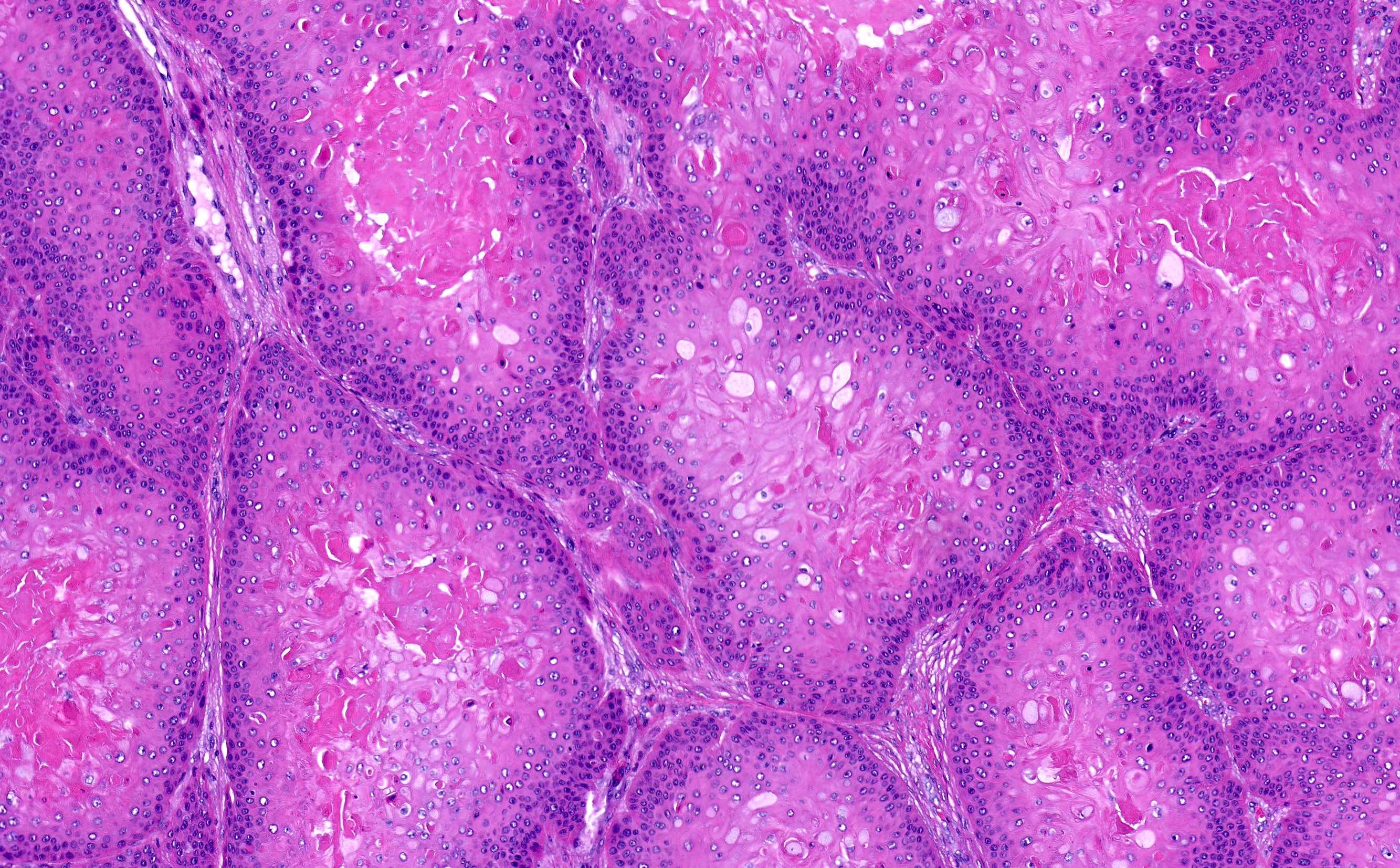
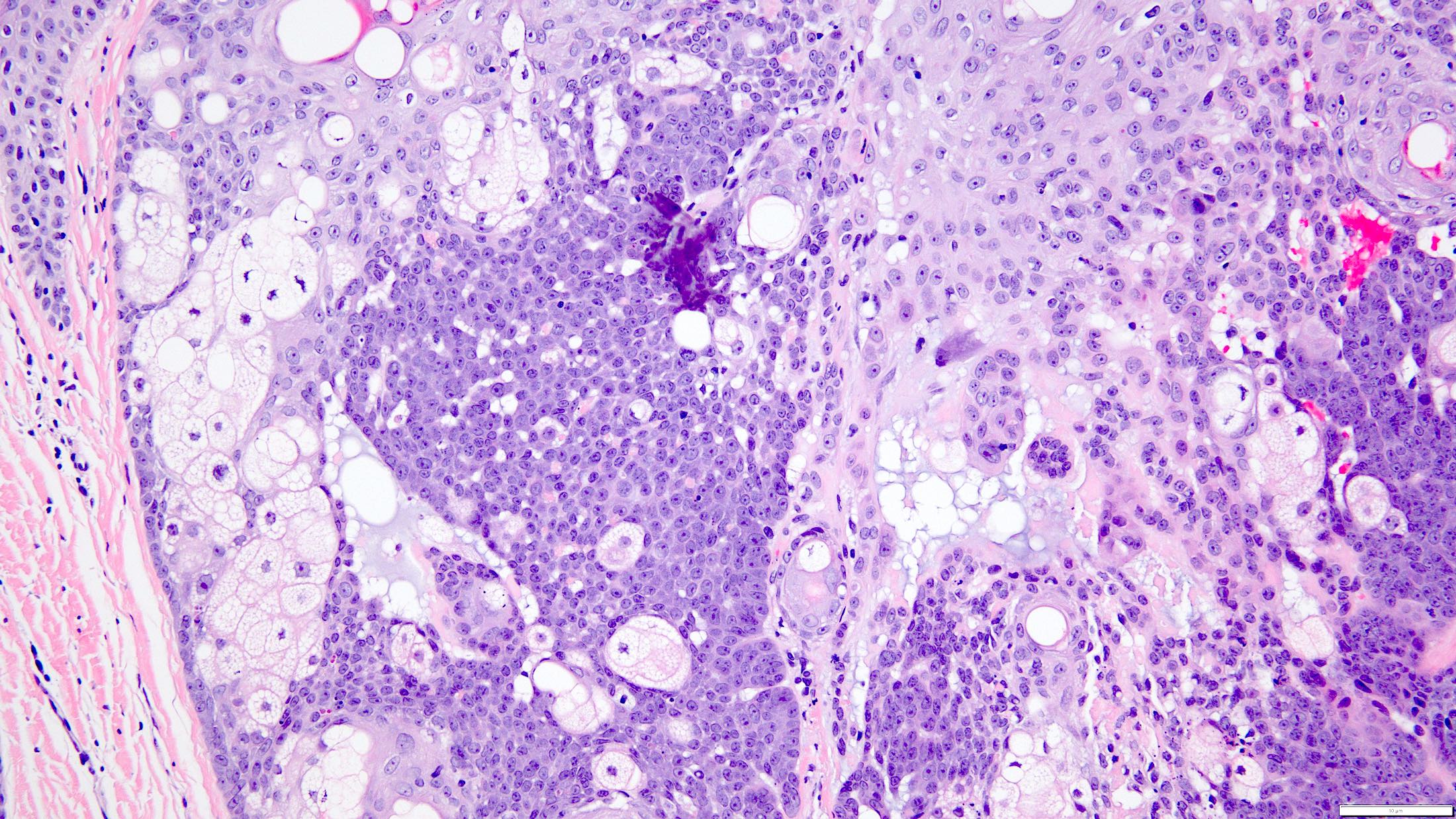
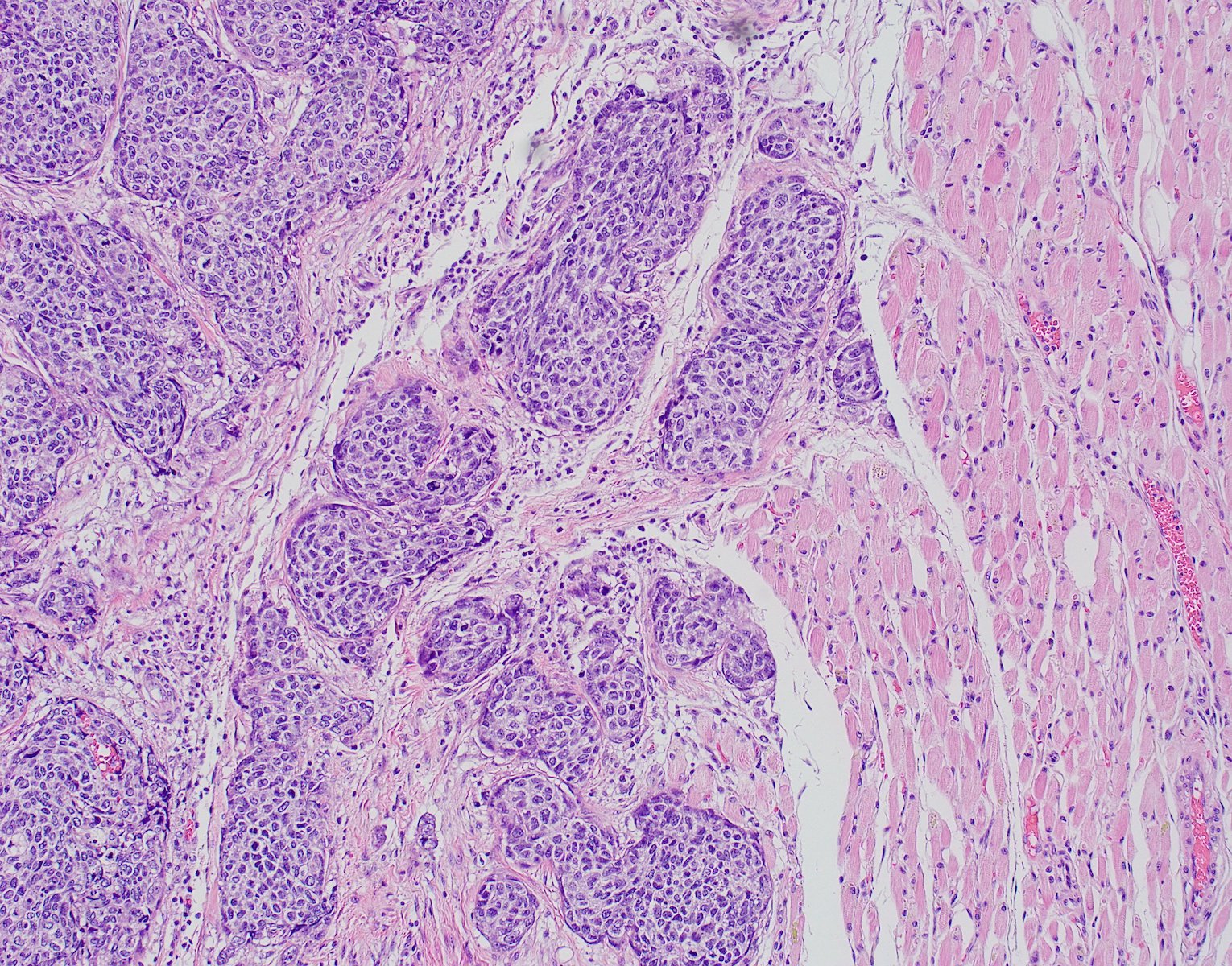
- An essential diagnostic feature is the coexistence of true small bilayered ducts and pseudocysts (Histopathology 2022;80:407)
- Sparse ductal structures composed of inner epithelial cells surrounded by an outer layer of basal / myoepithelial cells; intraluminal secretion may be present
- Cystic spaces (larger than ducts) contain abundant basophilic mucinous material or hyalinized eosinophilic material
- Deposition of hyaline basement membrane material on the intraluminal aspect of cystic spaces
- Mixture of cribriform, tubular and solid patterns (Am J Surg Pathol 2013;37:1603)
- Cells are typically small and monomorphic appearing with hyperchromatic nuclei and scant cytoplasm
- Mitotic activity is typically low
- Perineural invasion is a common finding
Grading criteria (Histopathology 2022;80:407)
| Grade I | Grade II | Grade III | |
| Histologic features |
|
|
|
| Solid area | None | < 30% | > 30% |
| Cytologic features | No cellular atypia | Atypia > grade I but < grade III | Significant cellular atypia |
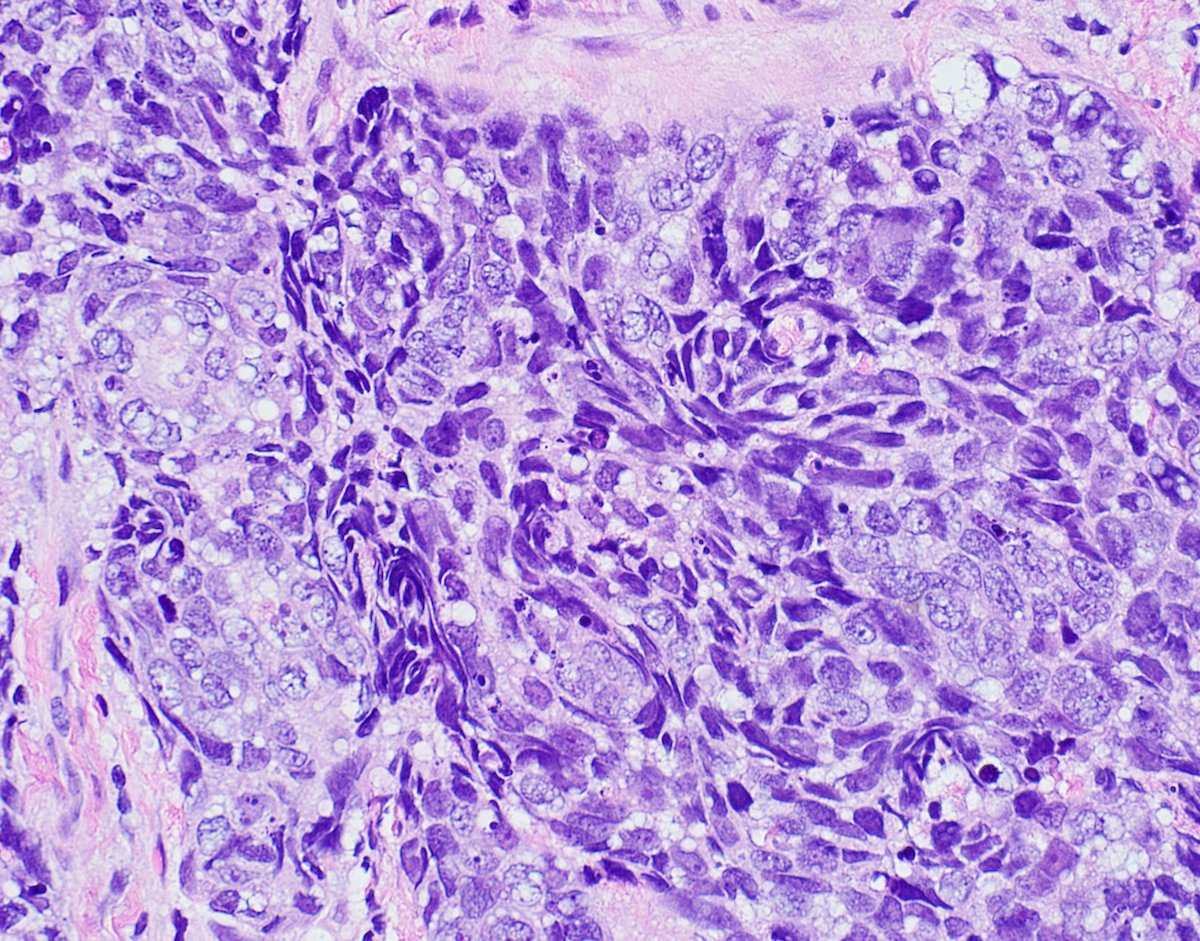
- High grade transformation (HGT), previously known as dedifferentiation
- Distinct population of anaplastic cells with loss of the biphasic ductal - myoepithelial differentiation
- Loss of myoepithelial cell differentiation is more usual; however, 1 PCACC case with HGT showed loss of epithelial cell differentiation and was diagnosed as myoepithelial carcinoma
- Nuclear enlargement, higher mitotic counts and necrosis are commonly seen
- Distinct population of anaplastic cells with loss of the biphasic ductal - myoepithelial differentiation
- HGT should be differentiated from solid type adenoid cystic carcinoma (ACC)
- With HGT, solid transformed areas are
- Separated from the tubular / cribriform component
- Have higher p53 and Ki67 expression
- Solid type ACC
- Solid cell nests are intermixed with cribriform and tubular structures throughout the tumor
- With HGT, solid transformed areas are
Contributed by Haya Homsi, M.D., M.P.H. and Shira Ronen, M.D.
- EMA, CEA monoclonal (mCEA), CK15 highlight the luminal cells in recognizable ductal structures (Am J Surg Path 2015;39:1347)
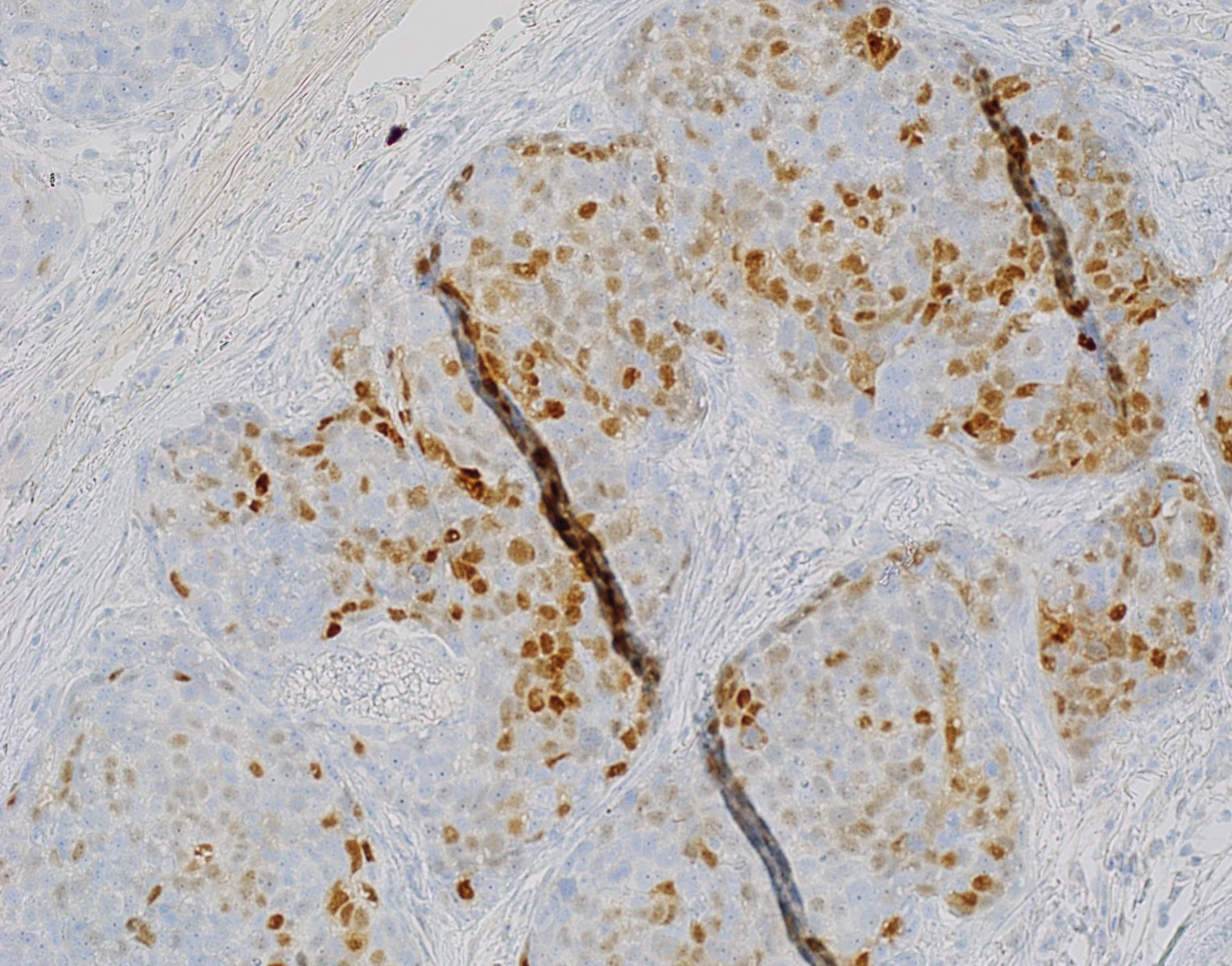
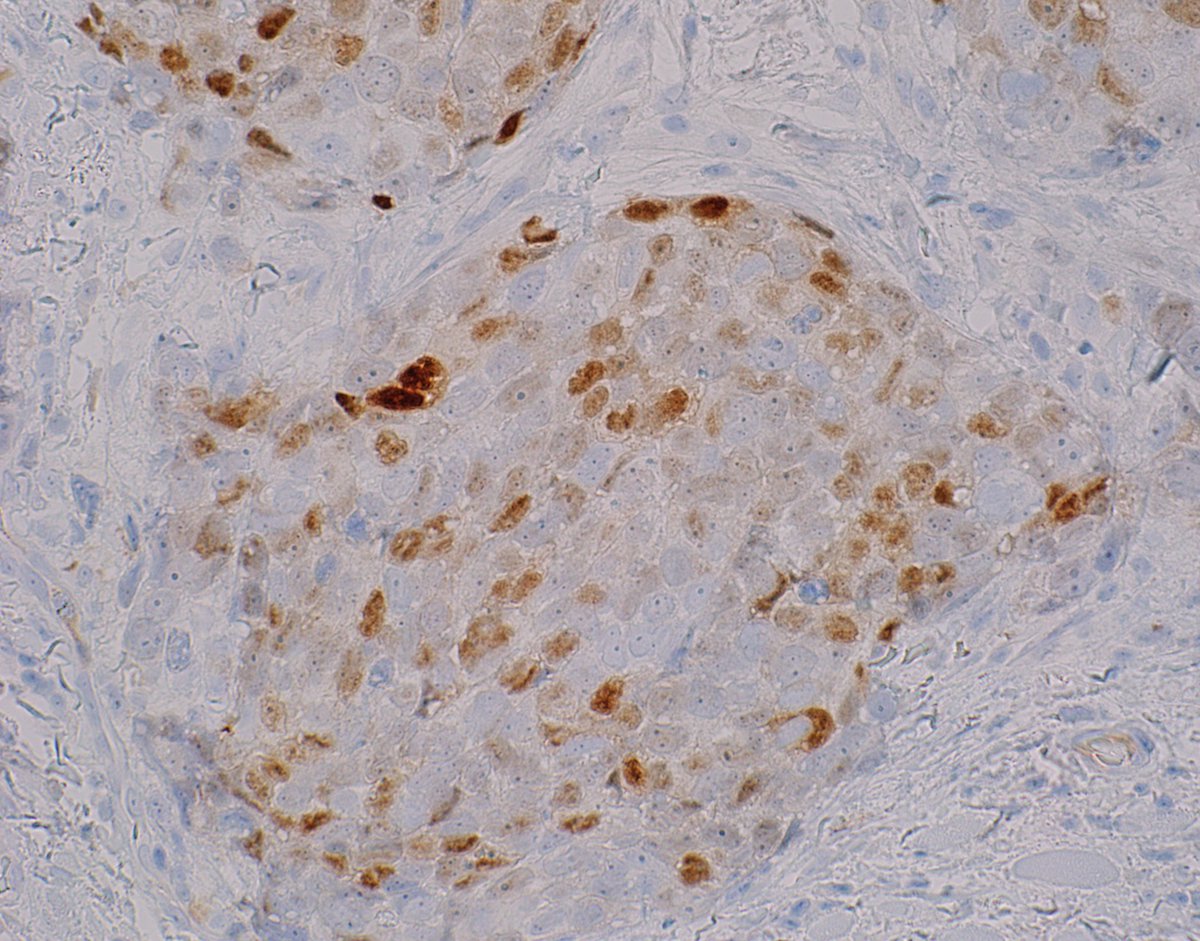
- CK7, CD117 (KIT), CD43 and BerEP4 (focally to diffusely positive) (Histopathology 2022;80:407, Case Rep Pathol 2017;2017:7949361, Pathology 2015;47:130)
- Myoepithelial cells surrounding ducts and pseudocysts stain positive for S100, p63, SMA, SMMS1, SOX10, MSA, calponin, GFAP, CK5/6 and 34 beta E12 (Am J Surg Pathol 2013;37:1603)
- Basophilic mucinous material within cystic spaces stains with mucicarmine, Alcian blue and colloidal iron (JAAD 1987;17:113)
- Hyalinized eosinophilic material surrounding true lamina gives a positive periodic acid-Schiff (PAS), diastase resistant reaction (J Oncol 2010;2010:469049)
- Basement membrane expresses collagen type IV; laminin is less marked (Am J Surg Pathol 2013;37:1603)
- MYB: it is crucial to highlight that the sole expression of MYB through immunostaining does not suffice for diagnosing PCACC as it is not specific and can be seen in other adnexal tumors, such as cylindromas (Histopathology 2022;80:407, J Cutan Pathol 2017;44:444, Am J Dermatopathol 2017;39:279)
- ~60% of PCACC cases have been found to harbor MYB gene activations, either through MYB chromosomal abnormalities or MYB::NFIB fusion (J Cutan Pathol 2017;44:201)
- Less commonly, MYBL1 gene alterations have also been reported (Am J Dermatopathol 2018;40:721)
- According to one study, detection of MYB gene alterations does not necessarily correlate with MYB protein expression (i.e., MYB immunohistochemistry staining) (Histopathology 2022;80:407)
Primary cutaneous adenoid cystic carcinoma
- Skin, forehead, excision
- Adenoid cystic carcinoma (see comment)
- Comment: Sections demonstrate an excision specimen containing multiple foci of basaloid nodules with a cribriform architecture and duct formation. Lumen spaces are filled with blue mucin and eosinophilic basement membrane-like material. Cytologically, the tumor cells show scant to moderate pale eosinophilic cytoplasm and oval nuclei with vesicular chromatin. Significant pleomorphism and mitotic activity is not appreciated. Solid growth is not identified. Perineural invasion is present. The margins are negative for tumor.
- To further characterize this case, immunohistochemical stains with SMMS1, CD117 and SOX10 were performed and compared with appropriate controls. The tumor is positive for SOX10, CD117 and SMMS1.
- Molecular studies detected MYB gene rearrangement.
- The histologic and immunohistochemical findings support the diagnosis of adenoid cystic carcinoma. This could be a primary cutaneous lesion but a metastasis from a salivary gland tumor cannot be excluded. An appropriate clinical evaluation to rule out that possibility is recommended.
- Metastatic adenoid cystic carcinoma:
- Can only exclude based on clinical history and imaging studies
- CK15 and vimentin may have some discriminatory value in differentiating between primary cutaneous and salivary gland ACCs; one study found that CK15 and vimentin showed diffuse positivity in 36% and 57% of PCACCs, respectively, whereas all salivary ACCs were negative or only focally positive for either CK15 or vimentin (Am J Surg Path 2015;39:1347)
- Basal cell carcinoma (adenoid type):
- Peripheral palisading
- Retraction artifact
- Mucinous stroma
- Attachment to epidermis often present
- Lack of true ductal structures with myoepithelial cells
- Focal areas of conventional basal cell carcinoma
- Cutaneous secretory carcinoma (Am J Surg Pathol 2017;41:62):
- Back to back tubules and microcysts with intraluminal secretions
- Positive for S100, mammaglobin, STAT5A and NTRK
- Primary cutaneous mucinous carcinoma:
- Primary cutaneous cribriform tumor (J Cutan Pathol 2005;32:577):
- Interconnected cribriform lesion that varies in size and shape
- Focal solid areas
- More eosinophilic cells
- Lacks myoeithelial cells
- Perineural invasion not a common feature
- Cylindroma / spiradenoma:
- Cylindroma: absence of prominent cystic / ductal spaces with mucin
- Spiradenoma: presence of dilated vascular spaces and numerous lymphocytes
- Lack perineural invasion
- Recognition of the typical areas
- Cylindroma: well circumscribed, symmetrical lesion composed of multiple aggregates of basaloid cells surrounded by a prominent basement membrane that appear to fit together in jigsaw puzzle arrangement
- Spiradenoma: regular nodules of small basaloid cells admixed with lymphocytes and basement membrane material
Comment Here
Reference: Adenoid cystic carcinoma (primary cutaneous)
- CYLD
- BHD
- EGFR
- MYB
Comment Here
Reference: Adenoid cystic carcinoma (primary cutaneous)
- Benign fibrohistiocytic tumor consisting of dermal dendritic cells
- Common benign lesion composed of stellate, factor XIIIa positive stromal cells
- Most common variant referred to as fibrous papule when present on the central face
- Solitary angiofibroma on the central face referred to as fibrous papule
- Multiple angiofibromatous lesions in tuberous sclerosis referred to as adenoma sebaceum
- On the penis, referred to as pearly penile papules
- Middle aged adults (J Invest Dermatol 1965;45:194)
- Multiple facial lesions can be seen in tuberous sclerosis, multiple endocrine neoplasia type I (MEN 1), neurofibromatosis II and Birt-Hogg-Dubé
- Central face, particularly on the nose
- Unknown at this time
- Unclear
- Thought to represent a proliferative reactive process of dermal dendritic cells (J Cutan Pathol 1989;16:194)
- Dome shaped, skin colored papules measuring a few millimeters
- Asymptomatic
- Diagnosis can be made on biopsy
- Dermoscopy may show milky white or pink background with telangiectasia (StatPearls: Cutaneous Angiofibroma [Accessed 3 December 2021])
- 39 year old woman with a dome shaped papule on the nose (J Cutan Pathol 2009;36:381)
- 45 year old woman with multiple facial papules since her 20s (JAAD Case Rep 2019;5:368)
- 63 year old man with a flesh colored papule on the left nasal ala present for many years (J Cutan Pathol 1991;18:284)
- For cosmetic purposes, can be removed by excisional / shave biopsy or electrosurgery
- Slightly raised dermal lesion composed of collagenous stroma with increased vasculature
- Increased stromal cells with varying morphology
- Cells can be plump, spindle shaped, stellate or multinucleate
- Mitotic figures are rare
- Epidermis uninvolved but can appear flattened or atrophic
- Can have overlying junctional melanocytic hyperplasia
- Useful clue in partially / limited biopsies
- However, overdiagnosis (atypical junction melanocytic hyperplasia or melanoma in situ) is a pitfall that should be avoided
- Histologic variants exist:
- Granular cell change: stromal cells with coarse cytoplasmic granules (J Cutan Pathol 1991;18:284)
- Clear cell change: stromal cells with clear vacuolated cytoplasm (J Eur Acad Dermatol Venereol 2007;21:1267)
- Other rare variants include hypercellular, pigmented, pleomorphic, inflammatory and epithelioid fibrous papules (J Cutan Pathol 2005;32:424)
Contributed by Gregory A. Hosler, M.D., Ph.D.
Contributed by Hillary Rose Elwood, M.D.
- Factor XIIIa: positive in stellate stromal cells (J Am Acad Dermatol 1988;19:1102)
- CD34: may also be positive (J Am Acad Dermatol 1996;35:342)
- NKI-C3: positive in clear cell variant (Am J Dermatopathol 2005;27:296)
- S100 and cytokeratins
- Stellate stromal cells with ultrastructural features of fibroblasts, rather than melanocytic or Schwann cell differentiation (Am J Dermatopathol 1979;1:349)
- Fibrous papule was previously suggested to represent fibrosed dermal nevi (Am J Dermatopathol 1979;1:345)
Fibrous papule (angiofibroma)
by Dr. Gardner
- Skin, nasal tip, shave biopsy:
- Fibrous papule
- Adenoma sebaceum (angiofibroma of tuberous sclerosis):
- Fewer bizarre dermal stromal cells than in fibrous papule
- Vessels are smaller and likely to show more concentric fibrosis
- Pearly penile papules:
- Absence of pilosebaceous follicles
- Multiple in number and located on the penis
- Angioma:
- Proliferation of ectatic vessels
- Lacks stellate stromal cells
- Fibrosing / sclerotic nevus:
- Lacks stellate cells and cellular stroma
- S100 positive
- Pleomorphic fibroma:
- Pleomorphic cells can resemble those occasionally present in fibrous papule
- More commonly located on the truck and extremities
- Lacks vascularity
- Scar:
- Horizontal orientation of fibroblasts with vertically oriented blood vessels
Comment Here
Reference: Angiofibroma / fibrous papule
- Brooke-Spiegler syndrome
- Cowden syndrome
- Gardner syndrome
- Reed syndrome
- Tuberous sclerosis
Comment Here
Reference: Angiofibroma / fibrous papule
- Benign vascular lesion characterized by superficial vascular ectasia and overlying epidermal hyperplasia (acanthosis or hyperkeratosis)
- Lesions may be solitary or multiple / diffuse
- Five types with similar histology:
- Angiokeratoma of Mibelli: seen in children and adolescents on dorsum of toes and fingers
- Angiokeratoma of Fordyce: scrotal skin of elderly
- Angiokeratoma corporis diffusum: clustered papules in a bathing suit distribution; associated with Anderson-Fabry disease (X-linked recessive lysosomal storage disease)
- Angiokeratoma circumscriptum: least common type, usually congenital, associated with nevus flammeus, cavernous hemangioma
- Idiopathic solitary or multiple angiokeratomas
- Benign vascular lesion
- Characterized by superficial vascular ectasia and overlying epidermal hyperplasia
- May occur in a variety of clinical settings
- Associated with Anderson-Fabry disease (X-linked recessive lysosomal storage disease)
- 17 year old boy and 21 year old woman with solitary tumors (J Clin Diagn Res 2015;9:WD01)
- 39 year old man with a family history of Fabry disease (Dermatol Online J 2011;17:5)
- 72 year old man with multiple penile shaft eruptions (An Bras Dermatol 2015;90:150)
- Small red to brown / black papule or nodule with verrucous surface, can be clustered
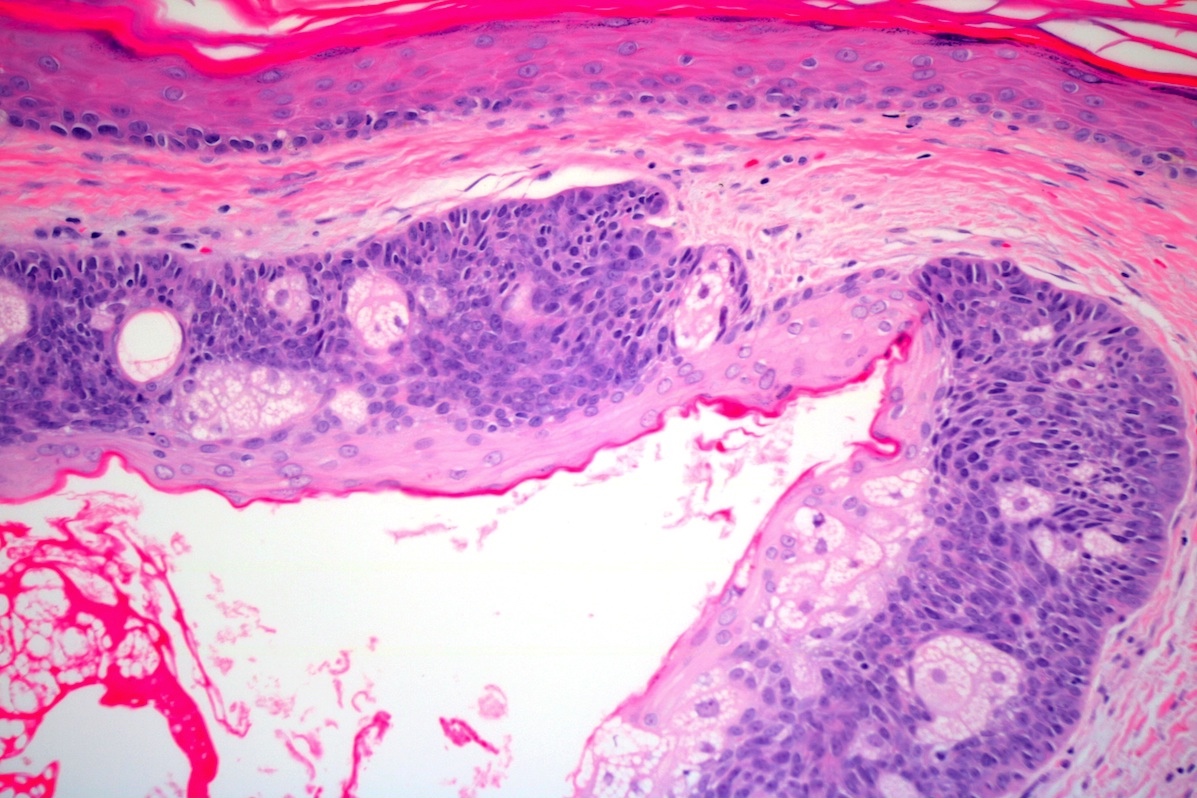
- Vascular ectasia of the papillary dermis which may appear to extend into the epidermis
- Overlying epidermal hyperplasia characterized by acanthosis, elongation of the rete and hyperkeratosis, with the epidermis encircling the dilated vascular spaces
- Often thrombosis within the vascular ectasia
Contributed by Sabrina C. Sopha, M.D, Joel Tjarks, M.D., Angel Fernandez-Flores, M.D., Ph.D. and @RaulSGonzalezMD on Twitter
- In patients with Anderson-Fabry disease, see lipid bodies and lamellar inclusions in endothelial cells, pericytes and smooth muscle cells in angiokeratomas
- Hemangioma (verrucous, lobular capillary, etc.)
- Lymphangioma
- Venous lake
- Clinical differential diagnosis may include pigmented / melanocytic lesions due to thrombosis
- Angiolymphoid hyperplasia with eosinophilia (ALHE) is a rare, benign vascular neoplasm characterized by proliferation of blood vessels along with inflammatory infiltrate rich in eosinophils
- Nonmalignant vasoproliferative lesion
- Predominant epithelioid or histiocytoid endothelial cells
- Papules or nodules
- Mixed inflammatory infiltrate composed of lymphocytes, plasma cells and eosinophils
- Angiolymphoid hyperplasia with eosinophilia
- Epithelioid hemangioma
- Obsolete terms
- Histiocytoid hemangioma
- Angiomatous nodule
- Pseudopyogenic granuloma
- Inflammatory angiomatous nodule
- ICD-10: L98.8 - other specified disorders of the skin and subcutaneous tissue
- Most common in middle aged adults
- Slight female preponderance
- More frequent in Asian populations, particularly in individuals of Japanese and Chinese descent (J Am Acad Dermatol 2016;74:506)
- Most common sites are skin and subcutaneous tissue of head and neck, particularly the face, scalp and ear lobes (Int J Surg Pathol 2016;24:59)
- Less common sites are limbs, oral mucosa and genitalia
- Pathophysiology of ALHE is likely multifactorial, involving a complex interplay of angiogenesis, immune dysregulation and possibly genetic and environmental factors (Dermatol Pract Concept 2018;8:28)
- Initial inflammatory event or injury to the blood vessels triggers a cascade of events leading to the proliferation of blood vessels known as angiogenesis
- Eosinophils are known to have a role in allergic and inflammatory response
- Presence of eosinophils is very much suggestive of a dysregulated immune response
- Inflammatory mediators released by eosinophils may be a contributing factor to the vascular changes seen in ALHE
- Other possible contributing factors are
- Arteriovenous shunting
- Local trauma
- Elevated serum estrogen levels
- Idiopathic condition
- Theories include vascular abnormalities, immunologic factors, inflammatory response, infectious agents, genetic factors, hormonal factors (Open Access Maced J Med Sci 2017;5:423)
- Slow growing cutaneous lesions
- Can be single or multiple
- Firm, red to violaceous (purple) nodules or papules (J Am Acad Dermatol 2016;75:e19)
- Size ranges from a few millimeters to centimeters
- Sometimes can be pruritic and occasionally ulcerate (Dermatol Pract Concept 2021;11:e2021003)
- Rarely associated with tenderness / pain
- Some patients may experience regional lymphadenopathy near the affected area
- Systemic involvement is rare
- Can be clinically mistaken for hemangioma or other vascular lesions
- Peripheral eosinophilia has been reported in few cases (Indian J Dermatol 2020;65:556)
- Definite diagnosis requires a biopsy and histopathological examination
- Imaging modalities can help distinguish ALHE from other vascular or soft tissue lesions (J Am Acad Dermatol 2016;74:506)
- Additional diagnostic tests can be performed to rule out the other causes of eosinophilia, if clinically indicated (J Am Acad Dermatol 2016;74:506)
- Eosinophilia and elevated IgE levels may be present in patients with ALHE (Indian J Dermatol 2020;65:556)
- Radiology is typically not required
- Ultrasound shows isoechoic or hypoechoic masses with increased blood flow (Open Access Maced J Med Sci 2017;5:423)
- Benign localized disease with indolent course
- Does not regress without intervention
- Recurrence is a common feature; can appear at the same site or in different locations (Indian Dermatol Online J 2017;8:267)
- 13 year old Caucasian girl with bilateral, huge, protruding and yellowish nostril masses (J Med Case Rep 2018;12:89)
- 21 year old woman presented with multiple erythematous to skin colored, dome shaped, firm papules and plaques (BMJ Case Rep 2018;2018:bcr2017223447)
- 28 year old woman presented with multiple, well delimited, infracentimetric erythematous papules with a smooth surface on the left frontal, temporal and preauricular regions (Acta Dermatovenerol Croat 2019;27:40)
- 37 year old Filipino man with lesions located on the central face (J Clin Aesthet Dermatol 2021;14:49)
- 48 year old woman presented with a painful subungual nodule of the left first fingernail (Dermatol Online J 2017;23:13030)
- Total surgical excision is the current treatment of choice
- Other treatment options include laser therapy and corticosteroid injections (J Am Acad Dermatol 2013;68:e48)
- Single or multiple, dome shaped, light pink to red brown papules or subcutaneous masses with no specific distinguishing surface features (J Am Acad Dermatol 2016;74:506)
- Size may range from few millimeters to a centimeter
- There might be erosion or crust formation of the surface (J Am Acad Dermatol 2016;74:506)
- Dermal based lesion with extension into the subcutaneous tissue
- Proliferation of vascular channels as nests and cords of endothelial cell proliferations with admixed lymphocytes, plasma cells and eosinophils, accompanied by hemorrhage and proliferation of thick and thin walled blood vessels (Dermatol Pract Concept 2018;8:28)
- Endothelial cells show large vesicular nuclei with acidophilic and sometimes vacuolated cytoplasm, imparting a hobnail appearance (Clin Colorectal Cancer 2010;9:179)
- Mitoses can be seen but lack atypical features and anaplasia
- Eosinophilia is usually a striking feature
- Stroma may show varying degrees of fibrosis, which can be a contributing factor to the firmness observed clinically (StatPearls: Angiolymphoid Hyperplasia With Eosinophilia [Accessed 19 January 2024])
- Plump polygonal endothelial cells with vesicular nuclei and deeply eosinophilic cytoplasm (Diagn Cytopathol 2021;49:E7)
- Background shows eosinophils and lymphocytes
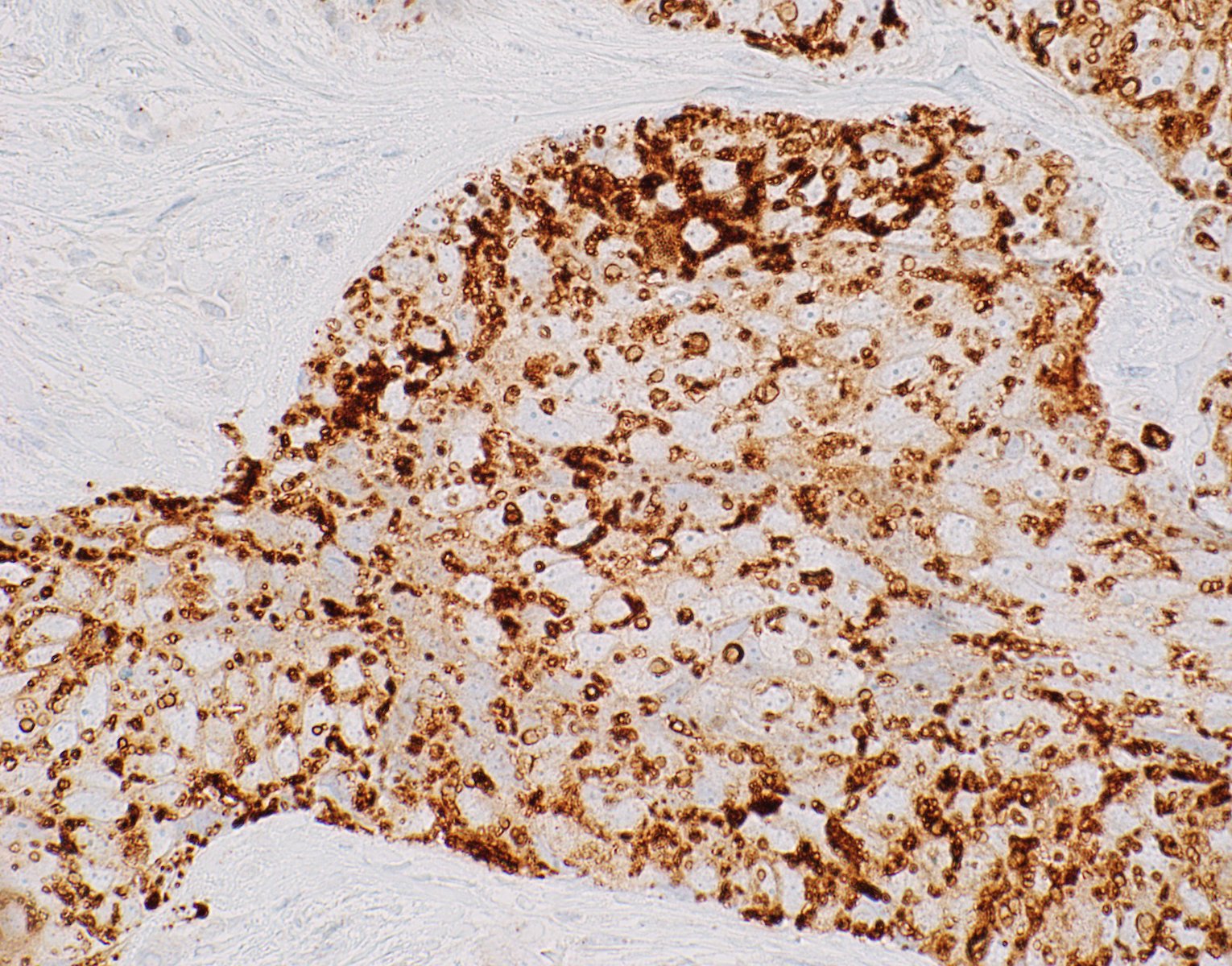
- CD31: strong staining in endothelial cells
- CD34: lesser reactivity as compared to CD31 (Am J Surg Pathol 2004;28:523)
- Factor VIII related antigen: weak positive but not as specific as CD31 (Am J Surg Pathol 2004;28:523)
- FOSB: strong nuclear expression in endothelial cell (J Cutan Pathol 2018;45:395)
- Electron microscopy of ALHE reveals features that support the endothelial origin (Ann Pathol 1985;5:271)
- Molecular basis of ALHE is limited and further studies are needed to be done to understand the underlying genetic and molecular alterations driving this condition
Angiolymphoid hyperplasia with eosinophilia
- Right cheek, excision:
- Angiolymphoid hyperplasia with eosinophilia (see comment)
- Comment: Histologic sections consist of skin with a dermal based lesion composed of proliferation of vascular channels accompanied by inflammatory infiltrate. Endothelial cells are showing epithelioid morphology with hobnail nuclei. The inflammatory infiltrate is composed of lymphocytes, plasma cells and eosinophils. The lesion appears to be completely excised and excision is curative.
- Kimura disease (An Bras Dermatol 2017;92:392):
- More common in young Asians
- Age range: second to sixth decades
- Most have lymph node involvement
- Peripheral eosinophilia is usually present
- Vascular proliferation is less notable than in ALHE, lacks plump endothelial cells
- Angiosarcoma (Arch Pathol Lab Med 2015;139:683):
- Occurs in older age group
- Cutaneous involvement is rare
- Irregular vascular channels and fascicular arrangement
- Mitotic activity, pleomorphism and nuclear hyperchromasia
- Epithelioid hemangioendothelioma (Diagn Pathol 2014;9:131):
- Wide age range
- Any location
- Strands, cords and nests of vacuolated endothelial cells separated by myxohyaline stroma
- WWTR1::CAMTA1
- Kaposi sarcoma (Cutis 2013;92:110):
- Skin is the most common location
- Spindle cell proliferation with slit-like vascular spaces
- Stain positively with HHV8
- Pyogenic granuloma (Cutis 2013;92:110):
- Very common
- Rapidly growing polypoid red mass
- Capillary sized vessels separated by fibromyxoid stroma, not seen in ALHE
- Common in head and neck area
- HHV8 is usually positive
- Inflammatory infiltrate in the lesion is composed of eosinophils only
- Presence of mitosis is suggestive of malignancy
- Shows strong positivity with all vascular markers
Comment Here
Reference: Angiolymphoid hyperplasia with eosinophilia
Comment Here
Reference: Angiolymphoid hyperplasia with eosinophilia
- Malignant neoplasm with vascular differentiation
- Infiltrative vascular neoplasm with broad histologic profile ranging from a well differentiated neoplasm with frank vascular differentiation to a poorly differentiated tumor with epithelioid or spindled cells
- May mimic poorly differentiated carcinoma, inflammatory process, lymphoma or melanoma
- Also known as hemangiosarcoma
- Classically arises in one of three scenarios:
- Head and neck of the elderly
- Chronic lymphedema
- Postradiation (usually in the setting of breast cancer)
- Sun exposed skin of the elderly (head and neck); breast with history of lymphedema or radiation therapy
- Wide age range (most common in adults)
- Presents as purple nodules or plaques
- Highly aggressive
- Frequent recurrence and metastasis
- Poor prognosis - high mortality
- Epithelioid tumors are often more aggressive
- 80 year old woman with secondary angiosarcoma postradiation and breast conserving therapy (J Clin Imaging Sci 2015;5:45)
- Surgical resection with negative margins
- Chemotherapy is occasionally used
- Violet elevated nodules with ill defined margins
- Infiltrating, freely anastomosing channels lined by spindled to epithelioid endothelial cells with variable atypia, surrounding adnexae and dissecting dermal collagen
- Endothelial cells may have multilayered appearance
- May have free floating intraluminal endothelial cells (“fish in the creek”)
- MYC (8q24) amplification seen in great majority radiation / lymphedema associated tumors
- Atypical fibroxanthoma
- Atypical vascular lesion
- Hemangioma
- Kaposi sarcoma
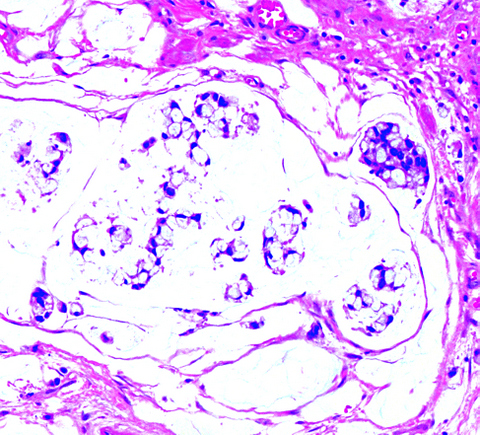
- Benign dermal adnexal neoplasm of apocrine derivation
- Most common location is scalp, typically in women (M:F ratio is 1:2)
- Also called apocrine adenoma, tubular adenoma, tubulopapillary hidradenoma, papillary tubular adenoma
- Associated with organoid nevus, nevus sebaceus of Jadassohn and syringocystadenoma papilliferum (SCAP)
- Rarely occurs in nose, eyelid, leg, trunk, axilla, chest, external auditory meatus, cheek, vulva
- Clinically asymptomatic, sometimes smooth, sometimes irregular, well-defined nodule
- Usually < 2 cm but reported up to 7 cm
- 12 year old girl with tubular apocrine adenoma and syringocystadenoma papilliferum of back (Ann Dermatol 2011;23:S151)
- 25 year old man with lipomatous apocrine adenoma with syringocystadenoma papilliferum (Head Neck Oncol 2011;3:36)
- 48 and 60 year old women with tubular adenoma of skin with follicular and sebaceous differentiation (Am J Dermatopathol 2006;28:142)
- 61 year old woman with tubular apocrine adenoma of nose (Eur J Dermatol 2011;21:132)
- 63 year old man with tubular apocrine adenoma mimicking basal cell carcinoma (J Am Acad Dermatol 2014;71:e45)
- Tubular apocrine adenoma on trunk with follicular differentiation (J Dermatol 2012;39:653)
- Complete excision is curative
- Malignant transformation is rare
- Firm, slow growing, dermal or cutaneous skin colored nodule
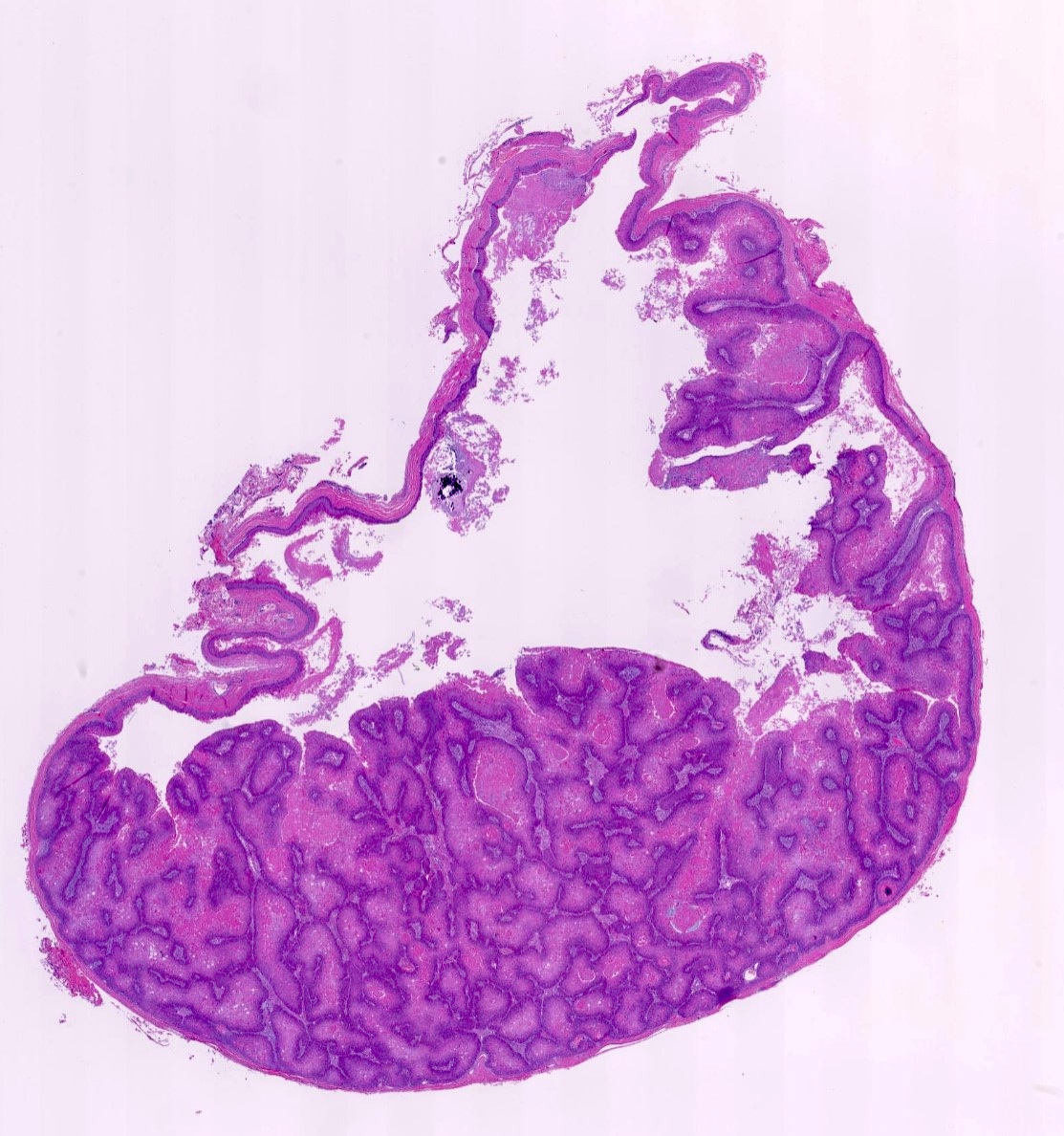
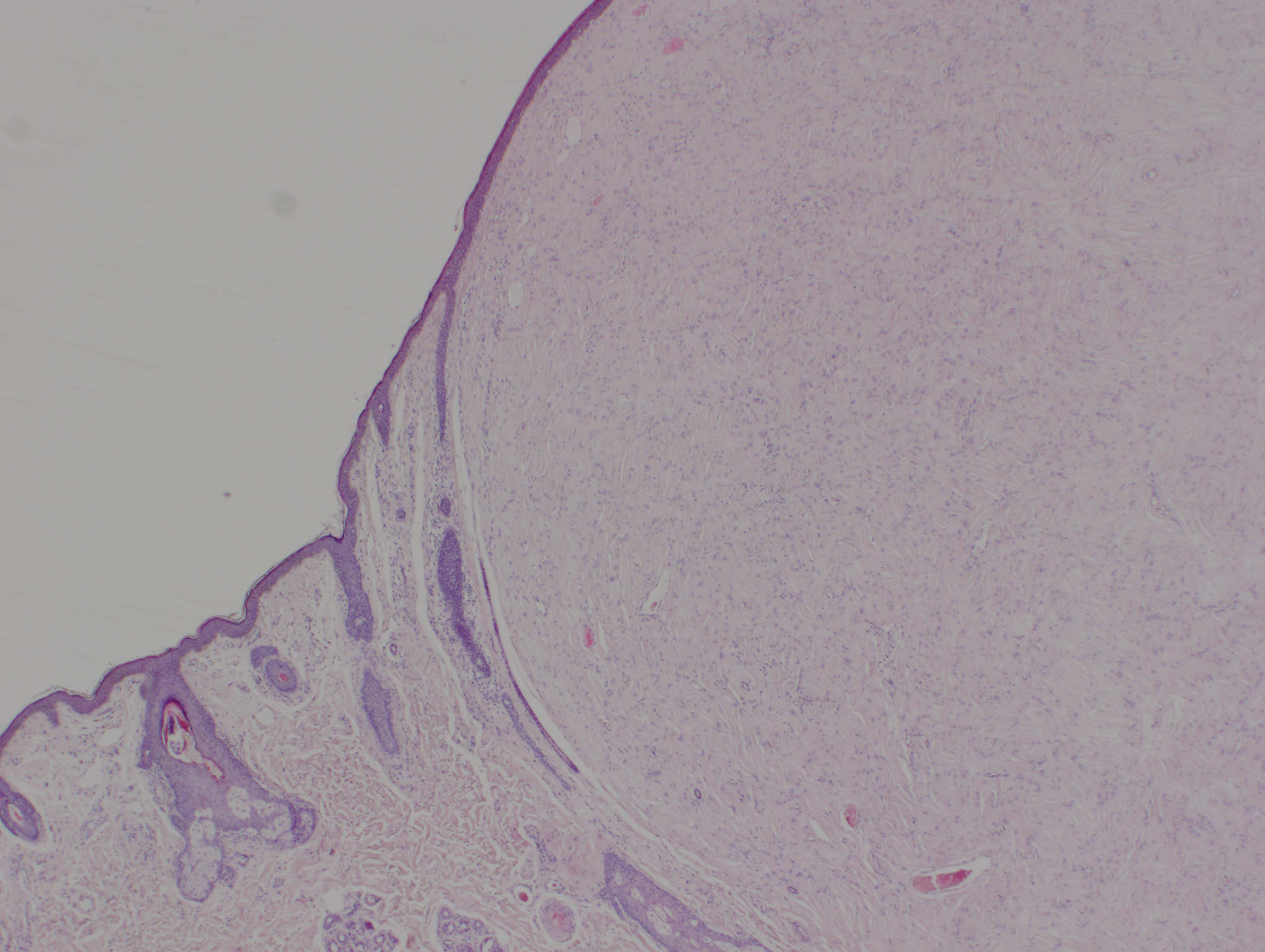
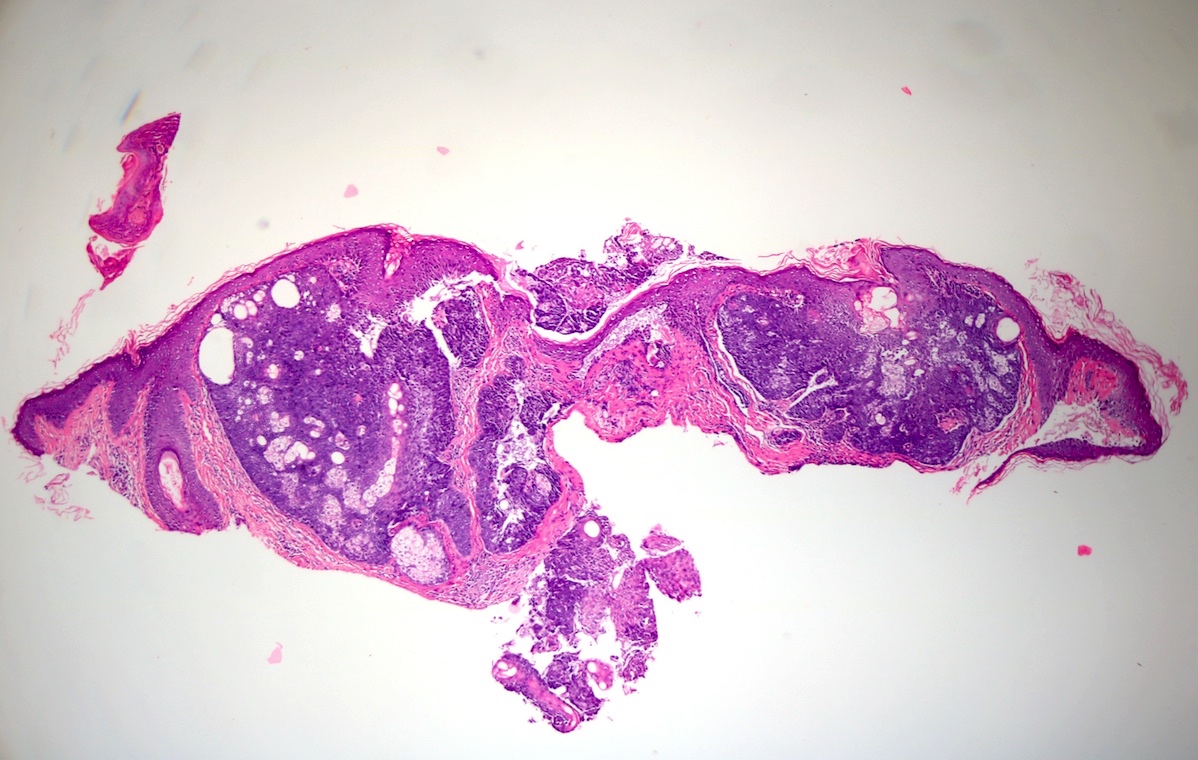
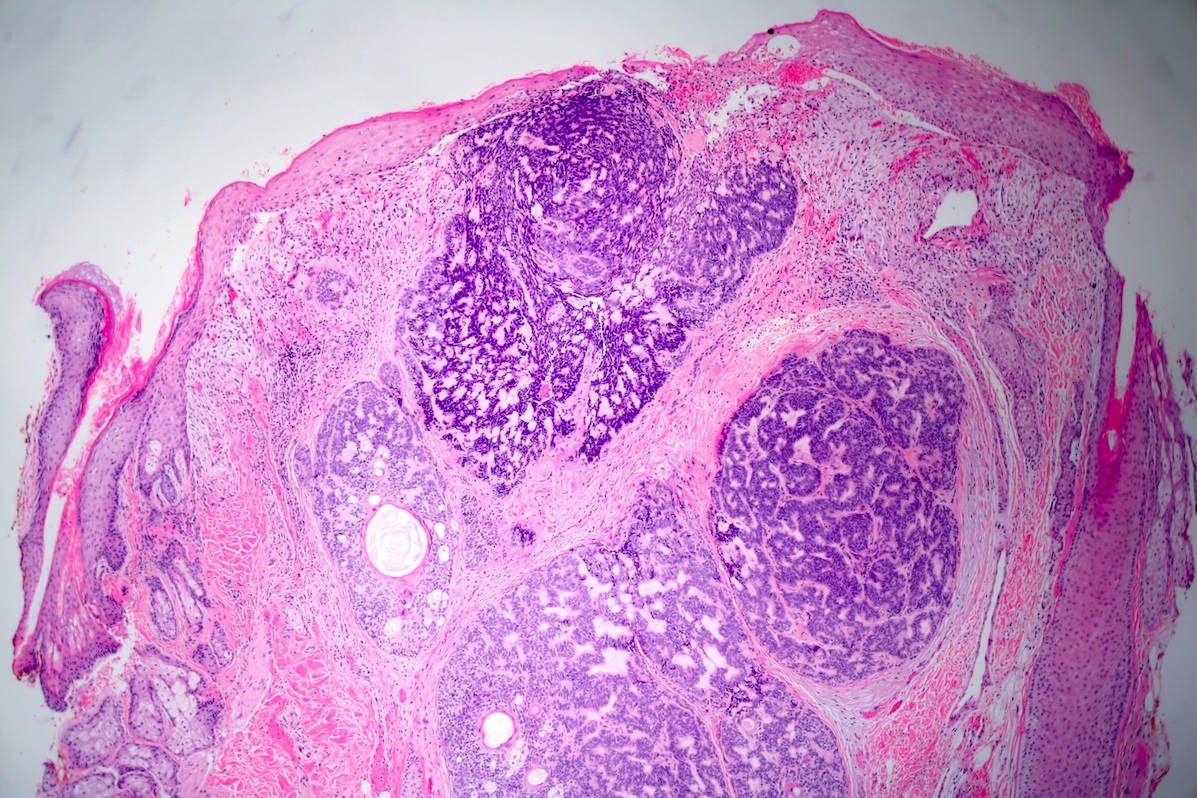
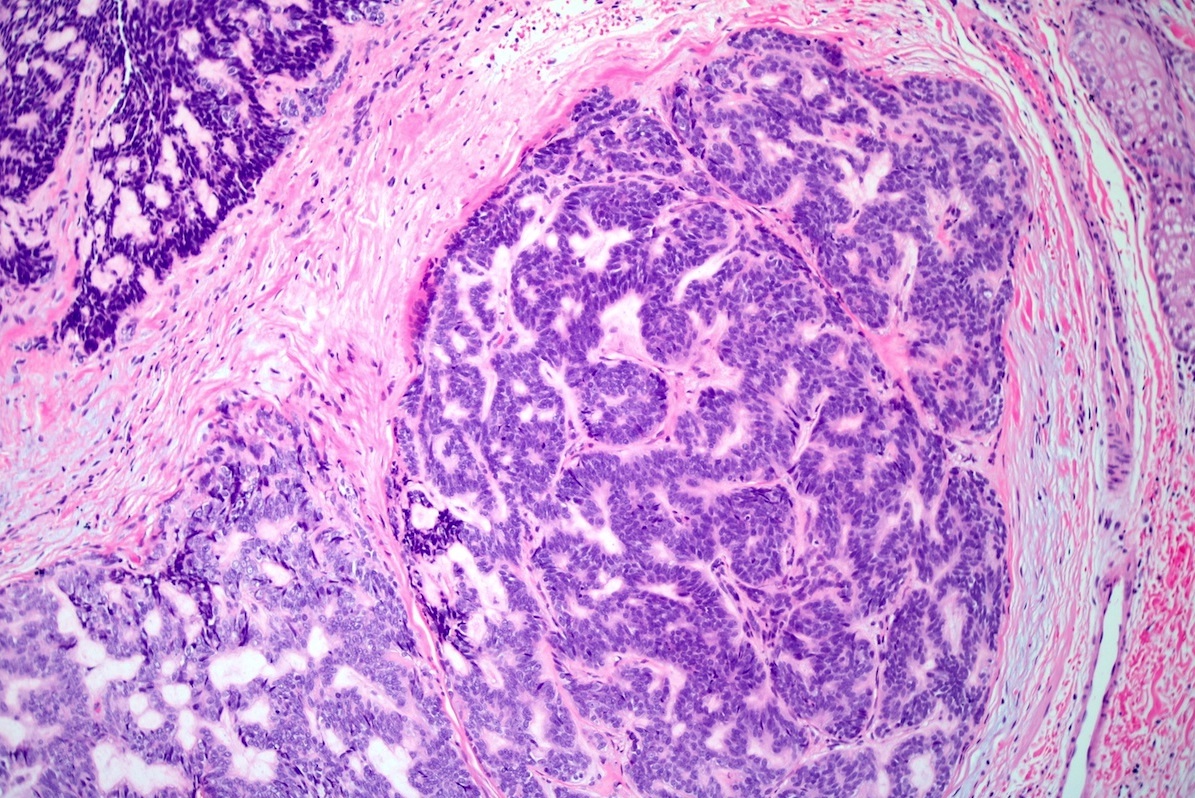
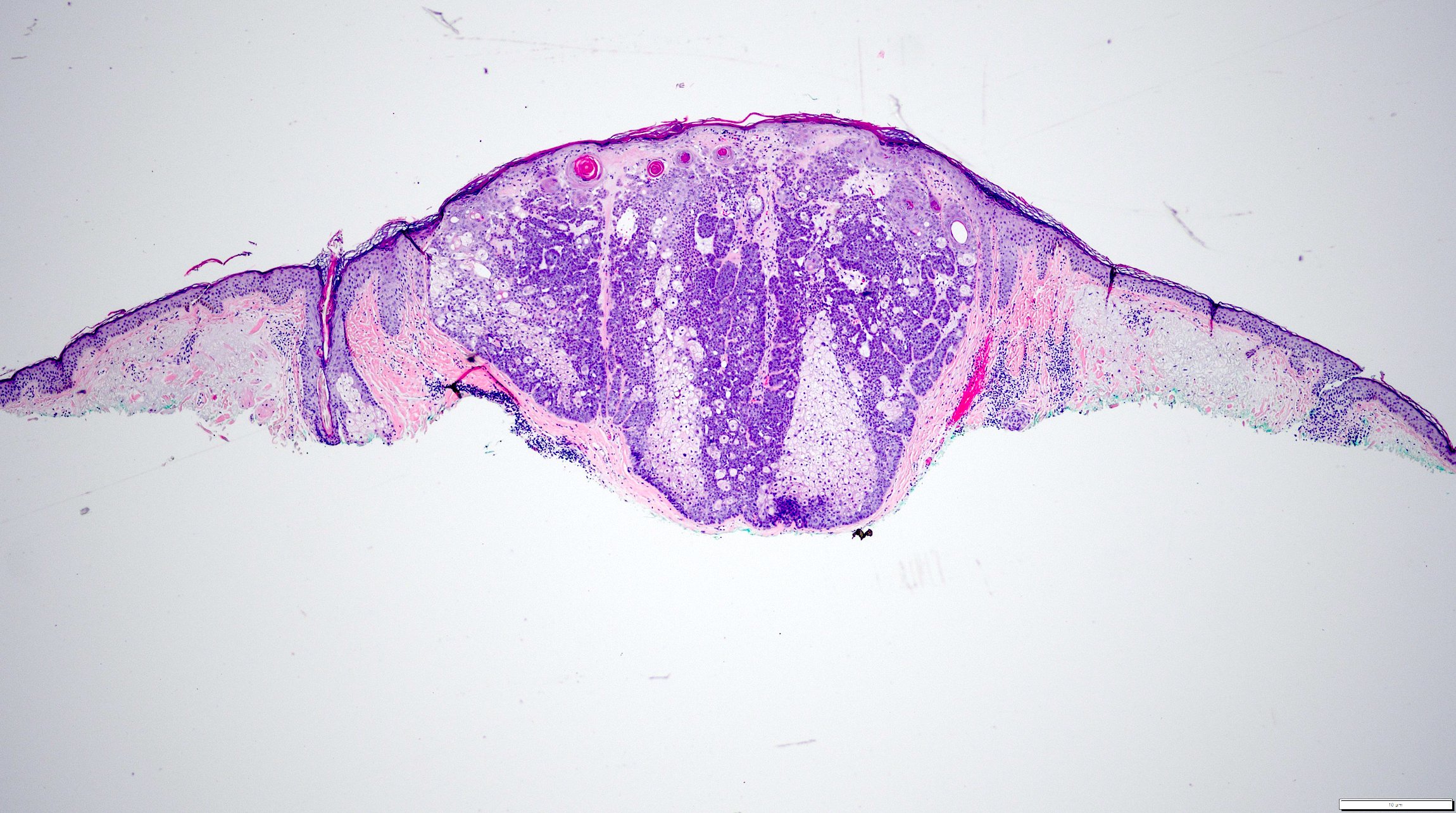
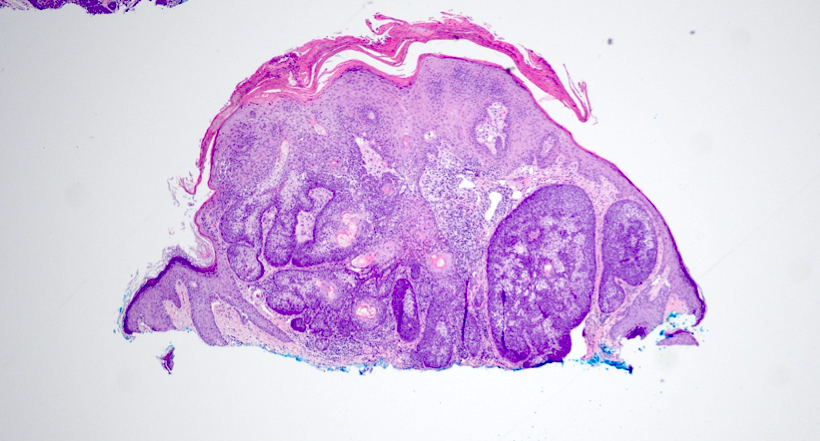
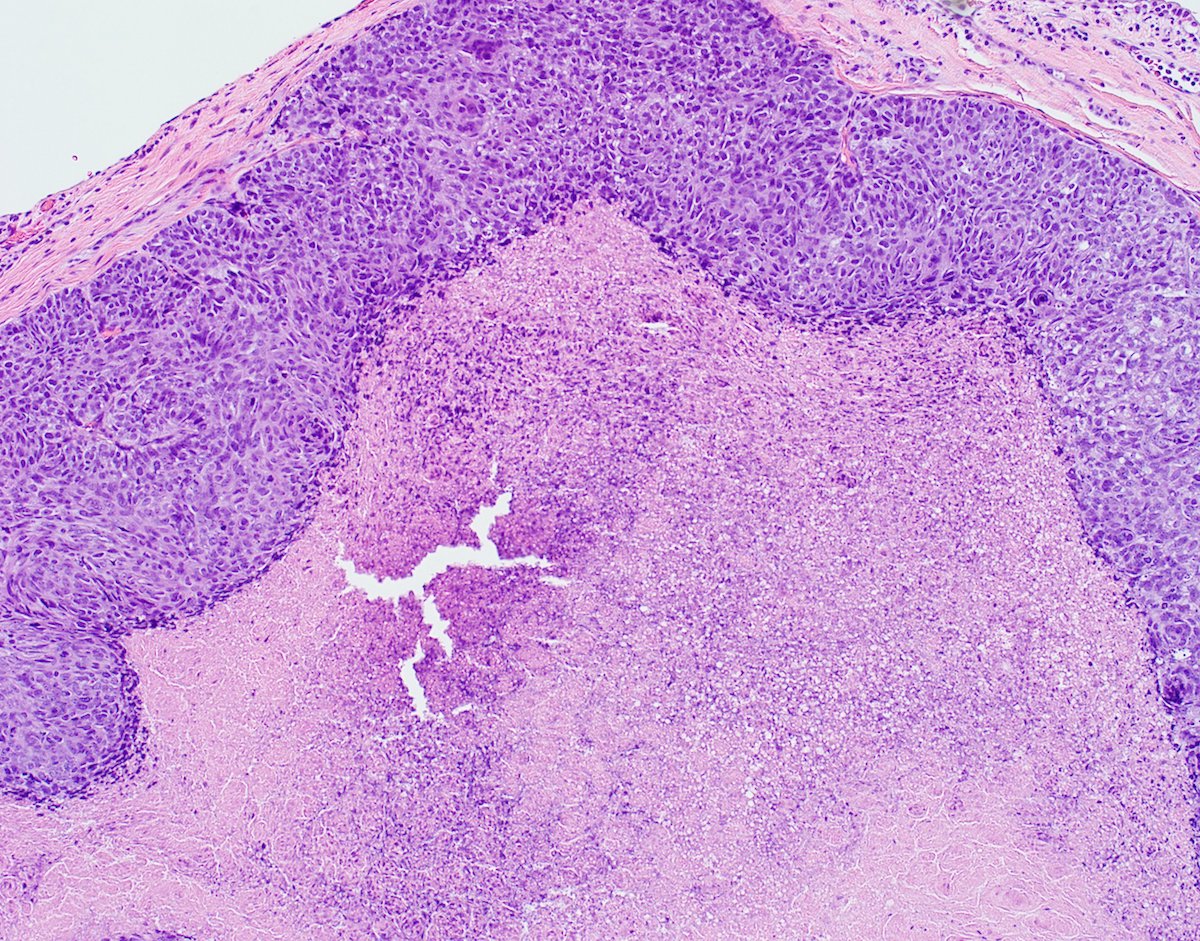
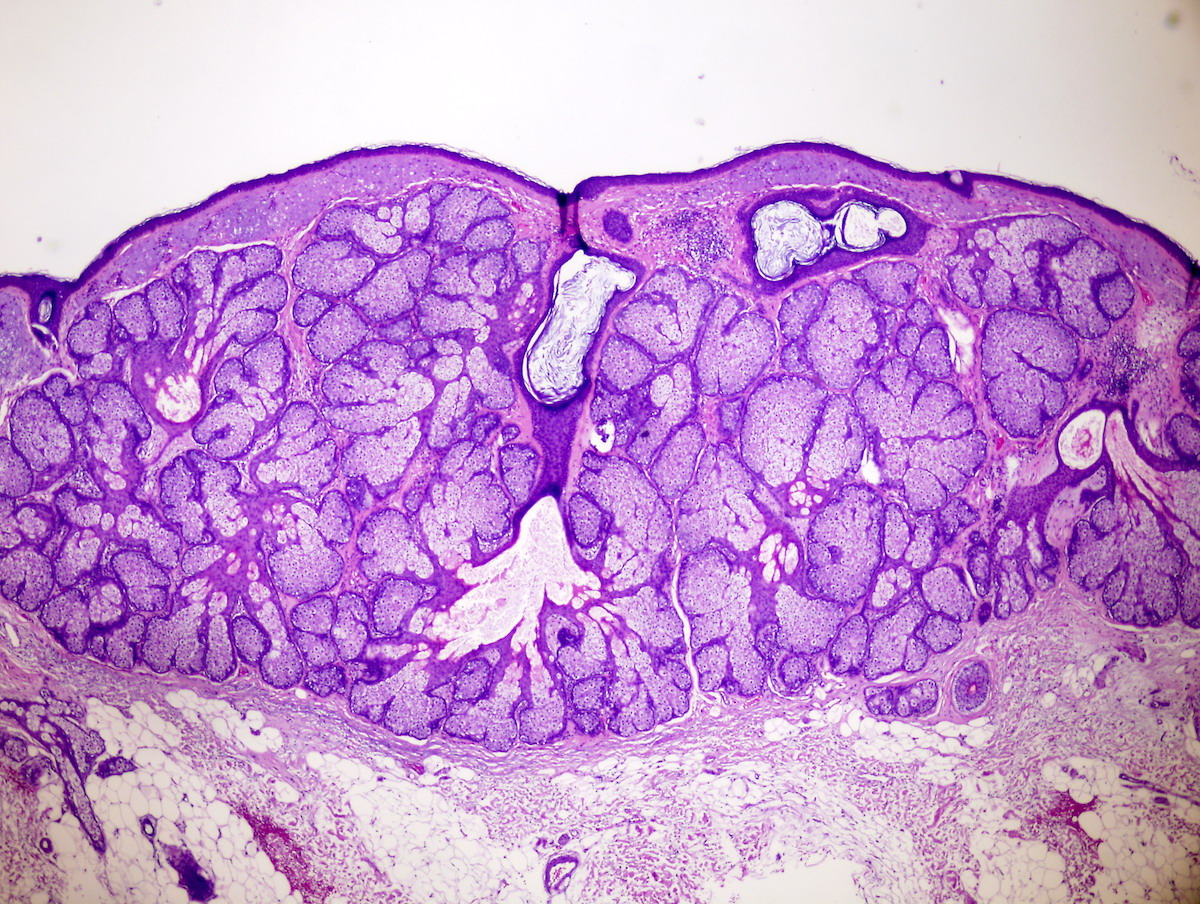
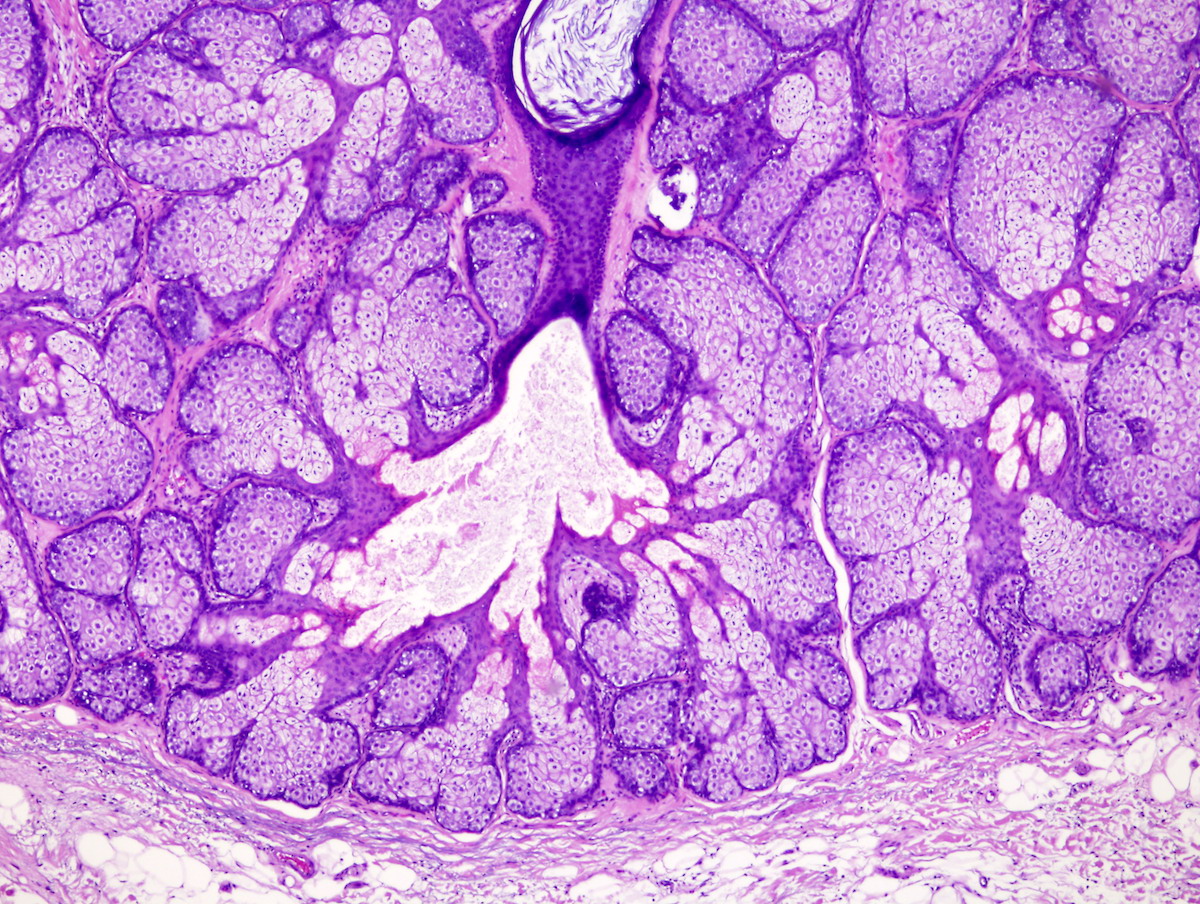
- Well circumscribed dermal neoplasm that may extend into subcutis
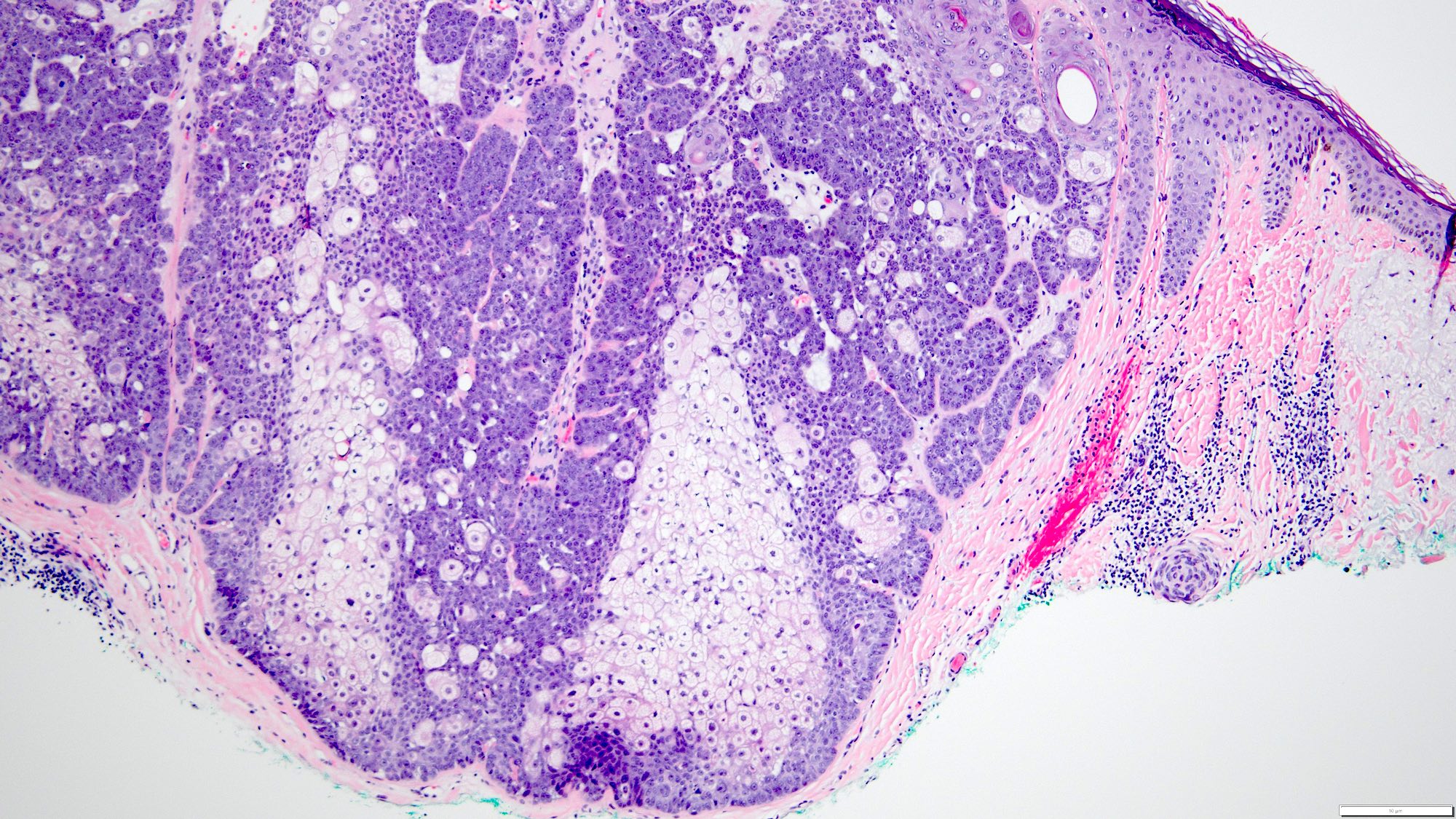
- Lobular pattern of dermal and subcutaneous tubular apocrine structures often encased by a fibrous, sometimes hyalinized stroma
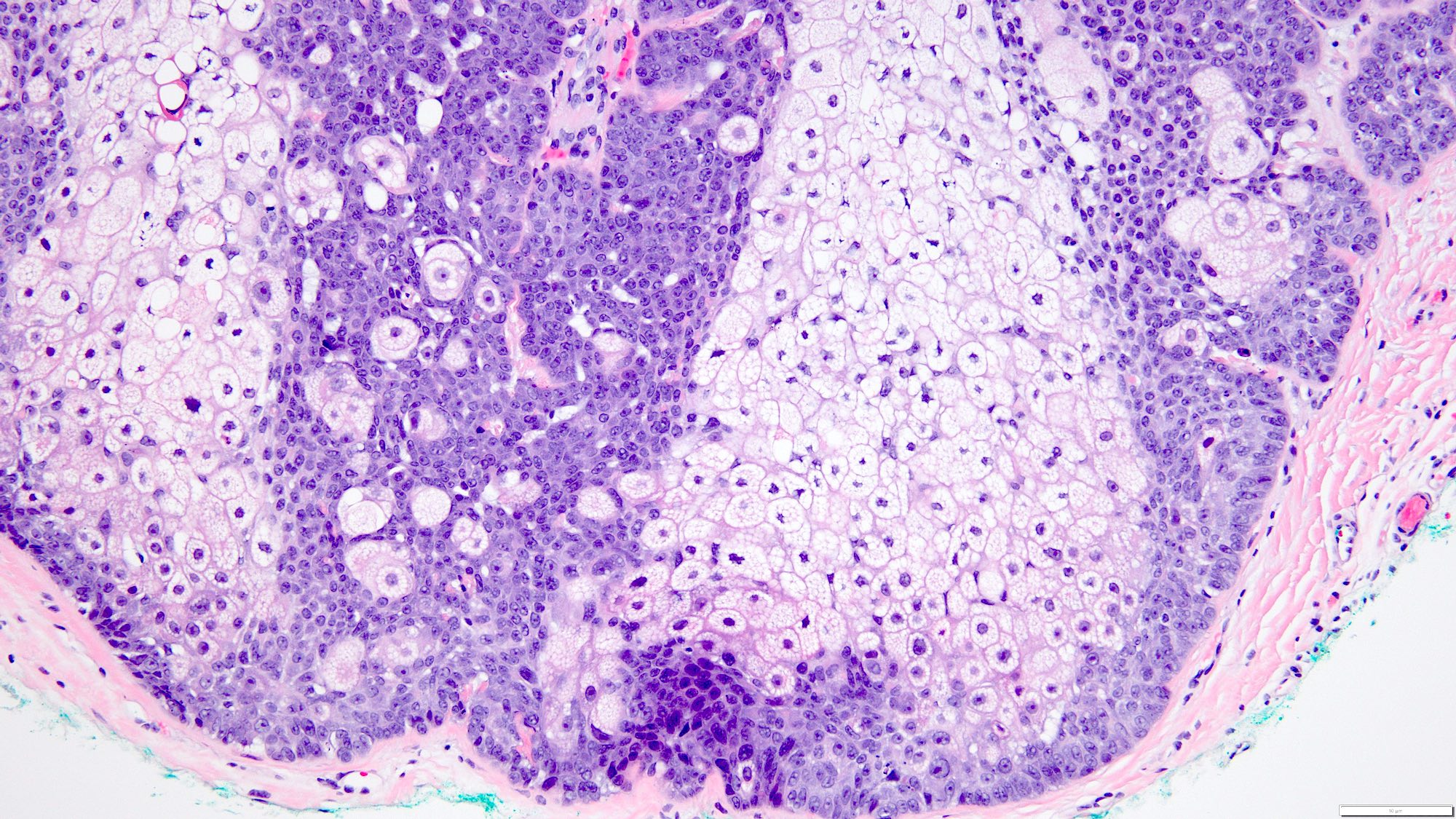
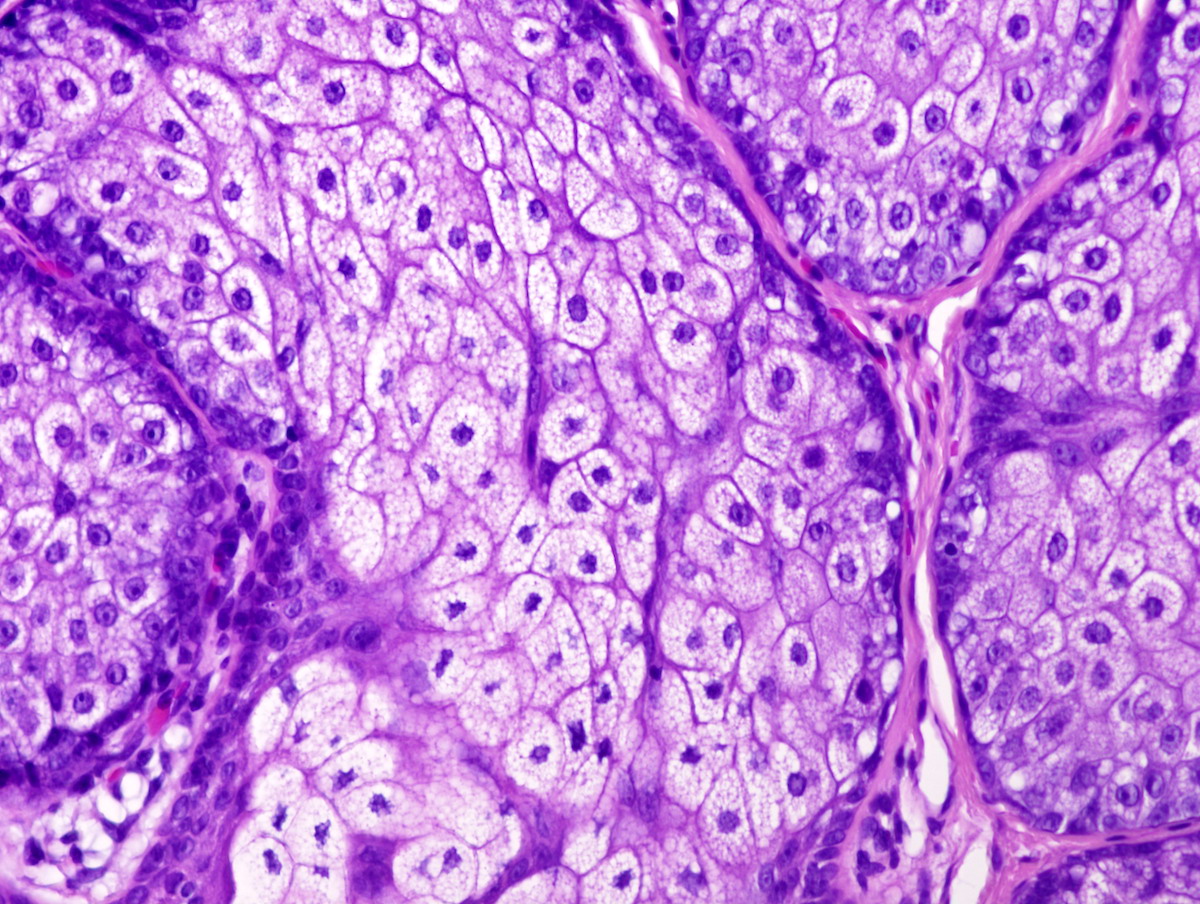
- Lobules have dilated, variably sized tubules lined by two layers of epithelial cells
- Pseudopapillae are common, but true papillae are more often associated with SCAP
- Decapitation secretion by apical layer
- Cuboidal to columnar cells with eosinophilic cytoplasm and round bland nuclei
- Often hyaline and clear cell change
- May show cyst formation with papillae or pseudopapillae protruding into the lumen
- Variable overlyng epidermal hyperplasia
- Rare connection with overlying epidermis
- Tall columnar cells on basal lamina forming acini
- Cells lining tubules have luminal villi and apical pinching
- Conspicuous mitochondria, prominent golgi
- Lipid rich cytoplasmic secretory vacuoles
- Decapitation secretion (J Am Acad Dermatol 1984;11:639)
- Apocrine cystadenoma: more dilated, cystic spaces rather than tubules
- Hidradenoma papilliferum: often has complex arborizing papillae, with more closely arranged tumor cells and glands
- Limited to female genital region
- Papillary apocrine carcinoma: more cytologic atypia, irregular nuclear contours and a higher mitotic rate
- Papillary eccrine adenoma: classically has features of eccrine rather than apocrine derivation; lacks decapitation secretion; different clinical presentation and distribution
- Syringocystadenoma papilliferum:
- Usually connects to epidermis
- Fibrovascular cores within papillary structures
- Plasma cells within stroma
- Tubular apocrine adenoma may be a variant
- Benign dermal adnexal neoplasm of apocrine derivation
- Associated with organoid nevus, nevus sebaceus of Jadassohn and syringocystadenoma papilliferum (SCAP)
- In most cases shows an apocrine differentiation but eccrine differentiation may be present as well
- Reference: Int J Mol Sci 2021;22:5077
- Rare, benign adnexal neoplasm
- Most common location is the scalp but can occur on other sites (Hum Pathol 2018;73:59)
- Microscopically, it is a well circumscribed intradermal tumor composed of tubules lined by 2 cell layers or more in a fibrous, sometimes hyalinized stroma
- Also called apocrine adenoma, tubular adenoma, tubulopapillary hidradenoma, papillary tubular adenoma
- Considerable overlap with papillary eccrine adenoma; may be part of the same spectrum (Am J Dermatopathol 1992;14:149, Am J Dermatopathol 1993;15:482, Int J Mol Sci 2021;22:5077)
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
- Age distribution of apocrine tubular adenoma is very wide, ranging from 28 to 85 years according to one study (Hum Pathol 2018;73:59)
- Most common location is scalp
- Rarely occurs in the nose, eyelid, leg, trunk, axilla, chest, external auditory meatus, cheek, vulva
- Associated with organoid nevus, nevus sebaceus of Jadassohn and syringocystadenoma papilliferum (SCAP) (J Cutan Pathol 1989;16:230)
- BRAF p.V600E mutations are detected in 50 - 64% of syringocystadenomas papilliferum and 66% of tubular adenomas, respectively (Cancers (Basel) 2022;14:476)
- BRAF and KRAS mutations may be present (Hum Pathol 2018;73:59)
- Clinically asymptomatic, well defined nodule
- Usually < 2 cm but reported up to 7 cm
- Skin biopsy
- Lesion is benign and recurrence following excision is uncommon
- 34 year old woman with 10 year history of foot nodule consistent with tubular apocrine adenoma (J Dermatol 2019;46:e45)
- 36 year old woman with an asymptomatic tubular apocrine adenoma of the vulva (Indian Dermatol Online J 2018;9:346)
- 63 year old man with recurrence of a tubular apocrine adenoma of the left upper eyelid after incomplete excision (Saudi J Ophthalmol 2019;33:304)
- Complete excision is curative
- Malignant transformation is rare
- Firm, slow growing, dermal or cutaneous, skin colored nodule
- May arise in the dermis without any epidermal connection
- Well circumscribed dermal neoplasm that may extend into subcutis
- Lobular pattern of dermal and subcutaneous tubular apocrine structures often encased by a fibrous, sometimes hyalinized stroma
- Lobules have dilated, variably sized, well formed tubules lined by 2 layers of epithelial cells
- Pseudopapillae are common but true papillae are more often associated with SCAP
- Decapitation secretion by apical layer and flattened outer myoepithelial layer
- Cuboidal to columnar cells with eosinophilic cytoplasm and round bland nuclei
- Often hyaline and clear cell change
- May show cyst formation with papillae or pseudopapillae protruding into the lumen
- Variable overlying epidermal hyperplasia
- Rare connection with overlying epidermis
- References: J Cutan Pathol 1987;14:114, Saudi J Ophthalmol 2019;33:304, Int J Mol Sci 2021;22:5077
- Tall columnar cells on basal lamina forming acini
- Cells lining tubules have luminal microvilli and apical pinching
- Conspicuous mitochondria, prominent Golgi
- Lipid rich cytoplasmic secretory vacuoles
- Decapitation secretion (J Am Acad Dermatol 1984;11:639)
- BRAF p.V600E mutations are detected in 50 - 64% of syringocystadenomas papilliferum and 66% of tubular adenomas, respectively (Cancers (Basel) 2022;14:476)
- BRAF and KRAS mutations may be present (Hum Pathol 2018;73:59)
- Skin, scalp, shave biopsy:
- Apocrine tubular adenoma
- Apocrine cystadenoma:
- More dilated, cystic spaces rather than tubules
- Hidradenoma papilliferum:
- Often has complex arborizing papillae, with more closely arranged tumor cells and glands
- Limited to female genital region
- Papillary apocrine carcinoma:
- More cytologic atypia, irregular nuclear contours and a higher mitotic rate along with infiltrative growth
- Papillary eccrine adenoma:
- Classically has features of eccrine rather than apocrine derivation
- Lacks decapitation secretion
- Different clinical presentation and distribution
- Syringocystadenoma papilliferum:
- Usually connects to epidermis
- Fibrovascular cores within papillary structures
- Plasma cells within stroma
- Tubular apocrine adenoma may be a variant
- Associated with Cowden syndrome
- Associated with mucinous carcinoma
- Most common in the extremities
- Sometimes associated with syringocystadenoma papilliferum
Comment Here
Reference: Apocrine tubular adenoma
Comment Here
Reference: Apocrine tubular adenoma
- Arsenic is a well water contaminant, used in industrial, mining, agricultural (pesticide) and medicinal (chemotherapy) substances (Toxicol Sci 2011;123:305)
- Often causes hyperkeratotic lesions of skin called arsenical keratoses
- Risk factor for Bowen disease, squamous cell carcinoma, basal cell carcinoma and carcinomas of lung, bladder and kidney
- Skin related problems are rare in U.S.
- Acute arsenical dermatitis or long term sequelae as a diffuse erythematous papular or pustular bullous dermatosis that can progress to exfoliative dermatitis
- "Rain drops on a dusty road": hyperpigmented macules with small foci of hypopigmentation and darker hyperpigmentation in trunk, areola and flexural
- Transverse white nail striations
- Palmar and plantar keratoses 2+ years after exposure; may transform to Bowen’s disease, squamous cell carcinoma and superficial basal cell carcinoma
- Thick, compact hyperkeratosis and parakeratosis, resembling hypertrophic actinic keratoses (eMedicine: Arsenical Keratosis [Accessed 24 August 2018])
- Numerous vacuolated keratinocytes without solar elastosis are suggestive
- May have atypia of keratinocytes
- Rare low grade malignant cutaneous tumor of uncertain differentiation
- First described in the 1960s by EB Helwig (Arch Pathol Lab Med 2016;140:376)
- Low grade malignant cutaneous neoplasm
- Usually presents on the sun exposed skin (e.g. head and neck) of elderly patients with a slight male predominance
- Histologically, a dermal based, well circumscribed tumor composed of pleomorphic, irregularly arranged, spindled to epithelioid cells with numerous mitotic figures
- Diagnosis of exclusion that requires the evaluation of multiple immunohistochemical studies to rule out other differential diagnoses
- Size, substantial involvement of the subcutis or beyond, perineural invasion, lymphovascular invasion or necrosis may suggest a diagnosis of pleomorphic dermal sarcoma instead
- Dermal variant of superficial undifferentiated pleomorphic sarcoma / malignant fibrous histiocytoma
- ICD-O: 8830/1 - atypical fibroxanthoma
- Elderly patients with a slight male predominance (Am J Dermatopathol 2010;32:533)
- Rarely, young patients with Li-Fraumeni syndrome or xeroderma pigmentosum
- Sun exposed skin (usually head and neck)
- Unclear but likely associated with ultraviolet induced damage
- Associations with ultraviolet radiation exposure and ultraviolet radiation signature mutations in TP53, Li-Fraumeni syndrome, xeroderma pigmentosum, radiotherapy, immunosuppression, organ transplantation
- Rapidly growing, single red to pink nodule or polypoid tumor
- Usually less than 2 cm in diameter (Am J Dermatopathol 2010;32:533)
- May be ulcerated (J Cutan Pathol 2010;37:301)
- Clinical differential may include squamous cell carcinoma or basal cell carcinoma
- Diagnosis of exclusion
- Requires use of ancillary techniques (i.e. immunohistochemistry panels) to rule out other differential diagnoses
- Rendering a definitive diagnosis on superficial biopsies alone may be difficult, given the differential diagnosis of pleomorphic dermal sarcoma
- Low grade tumor with an almost always benign clinical course
- Recurrence may occur due to incomplete surgical removal
- Metastasis is rare (Am J Dermatopathol 2015;37:455)
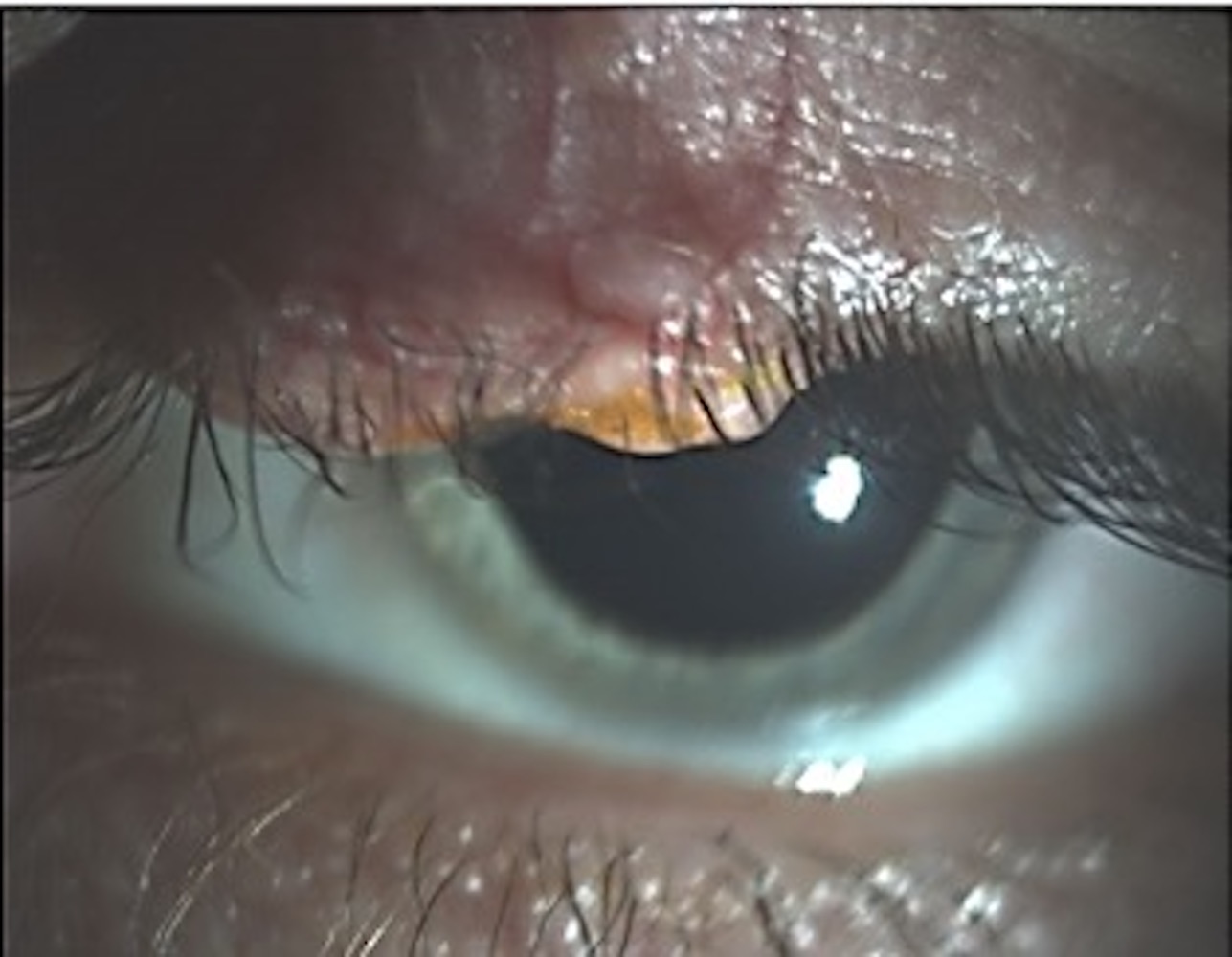
- 24 year old man with xeroderma pigmentosum and a rapidly growing conjunctival mass (Ocul Oncol Pathol 2015;1:254)
- 72 year old man with an ulcerated nodule on the lower leg (J Cutan Pathol 2017;44:951)
- 74 year old man with a mass on the ear (An Bras Dermatol 2019;94:239)
- 75 year old man with an intermittently bleeding nodule on the left temple and 90 year old man with a violaceous nodule on the vertex of the scalp (JAAD Case Rep 2018;4:292)
- Complete surgical removal with wide local excision or Mohs micrographic surgery (Dermatol Clin 2019;37:253)
- Single red to pink nodule or polypoid tumor, usually less than 2 cm in diameter and may be ulcerated and covered with serum crust
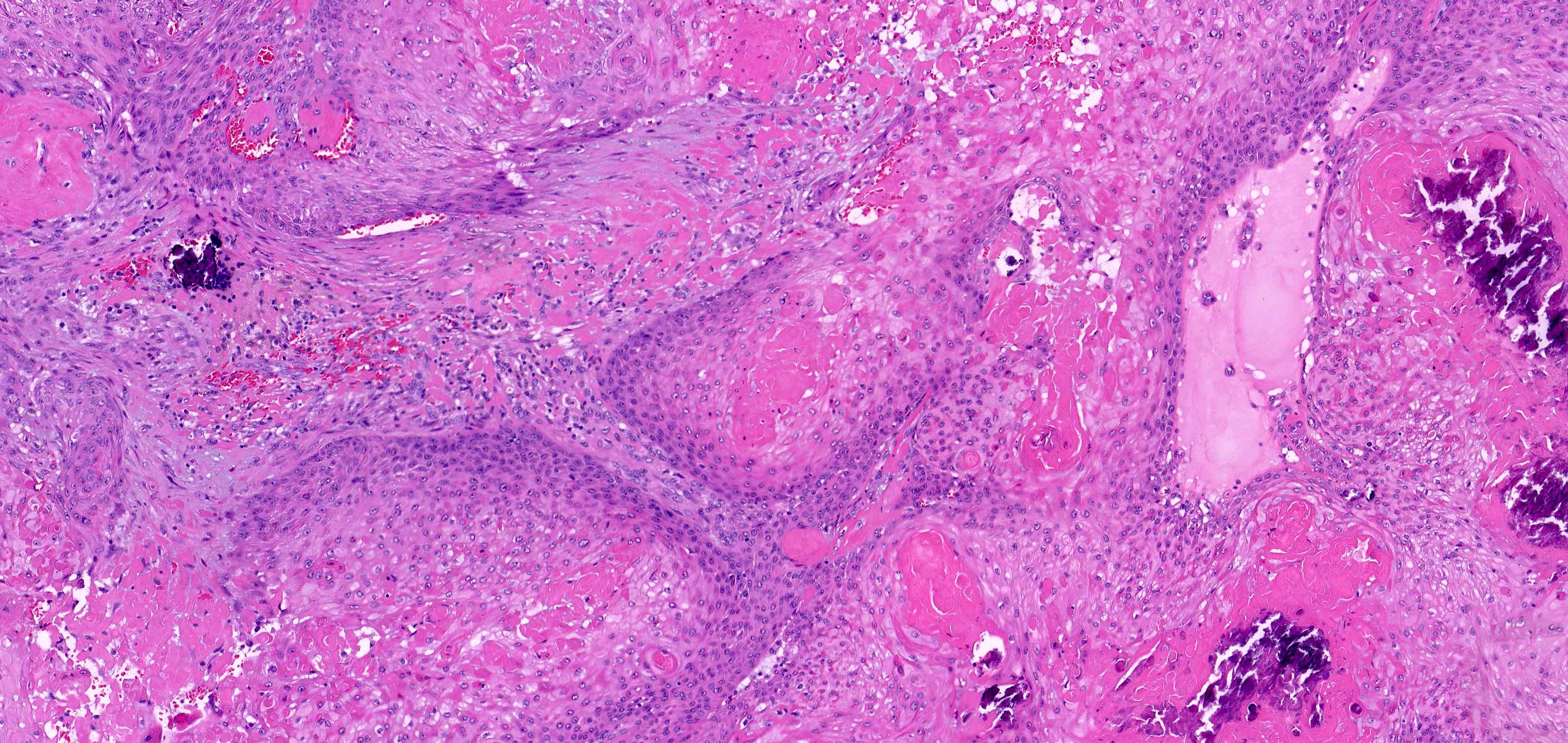
- Dermal based, well circumscribed tumor
- Composed of irregularly arranged spindled to epithelioid cells with no involvement of the subcutis
- Necrosis, lymphovascular invasion and perineural invasion should not be present
- Cytomorphologically, lesional cells are highly bizarre and atypical, with marked pleomorphism in size and shape, abundant eosinophilic cytoplasm, occasional multinucleation and numerous mitotic figures, including atypical forms
- Epidermal collarette, ulceration and actinic changes, including prominent solar elastosis, may be present
- No connection to the overlying epidermis and no in situ component
- Histologic variants (Am J Dermatopathol 2010;32:533):
- Spindle cell (Am J Dermatopathol 2015;37:509)
- Clear cell
- Granular cell (Cesk Patol 2014;50:34)
- Keloidal (Am J Dermatopathol 2010;32:713)
- Myxoid
- Pseudoangiomatous (Ann Diagn Pathol 2013;17:502)
- Pigmented (Histopathology 1998;33:537)
- Plaque-like
- May have forms with osteoclast giant cells, osteoid and chondroid formation (Am J Dermatopathol 2010;32:533)
- Nonspecific: CD10, CD99, procollagen 1, vimentin (Australas J Dermatol 2005;46:235, Stomatologiia (Mosk) 2005;84:36, J Cutan Pathol 2007;34:415, Am J Clin Pathol 2002;117:126)
- May be positive for CD68, CD163, CD117, MITF, factor XIIIa, CD31, MelanA and HMB45 in multinucleated giant cells, SMA, EMA, p63 (Am J Dermatopathol 2008;30:34, Am J Dermatopathol 2014;36:888, J Cutan Pathol 2010;37:301, Am J Dermatopathol 2010;32:533)
- Genetics are currently poorly understood
- FAT1, NOTCH1/2, CDKN2A, TP53, TERT mutations (Mod Pathol 2018;31:418)
- Loss of 9p and 13q, gain of 8q, gain of CDKN2A (Clin Sarcoma Res 2019;9:2)
- TERT promoter mutations (Mod Pathol 2014;27:502)
Atypical fibroxanthoma and mimics
Atypical fibroxanthoma pearls
- Vertex scalp, skin shave:
- Malignant spindle cell neoplasm predominantly in dermis, consistent with atypical fibroxanthoma, present at tissue edges (see comment)
- Comment: Sections show a dermal, poorly differentiated pleomorphic neoplasm, characterized by large and bizarre spindled to epithelioid cells with abundant eosinophilic cytoplasm, occasional multinucleation and numerous mitotic figures. Adjacent dermis contains solar elastosis. The overlying epidermis does not have a connection to the tumor. Immunohistochemical studies show that lesional cells are positive for CD68 and negative for CAM5.2, AE1 / AE3, CD31 and S100. Overall, these features support the above interpretation.
- Pleomorphic dermal sarcoma:
- Histologically similar to atypical fibroxanthoma but larger and shows substantial involvement of the subcutis or beyond, perineural invasion, lymphovascular invasion or necrosis
- Behaves in a more aggressive manner than atypical fibroxanthoma
- Melanoma:
- Usually associated with an in situ component in the overlying epidermis
- Melanin pigment, lymphovascular invasion, perineural invasion, involvement of the subcutis and microsatellites may also be present
- Lesional cells are positive for melanocytic immunohistochemical markers (e.g. SOX10, S100, MelanA, HMB45, tyrosinase and MITF), although reactivity to melanocytic markers other than S100 and SOX10 may be lost in spindle cell / desmoplastic variants
- Squamous cell carcinoma:
- Usually associated with a connection to the overlying epidermis and an in situ component
- Keratin, intercellular bridging, invasion of the subcutis, perineural invasion and lymphovascular invasion may be present
- Lesional cells are positive for p40 (Am J Surg Pathol 2014;38:1102)
- Angiosarcoma:
- Atypical fibrous histiocytoma:
- Usually presents in younger patients, lacks prominent actinic changes and may have areas of classic dermatofibroma in the periphery of the tumor
- Leiomyosarcoma:
- Usually positive for smooth muscle markers, such as smooth muscle myosin and desmin
- Metastatic carcinoma:
- Should be considered in the differential diagnosis for patients with a known history of carcinoma
- Lesional cells are usually positive for pancytokeratin and other immunohistochemical markers similar to the primary tumor
- Superficial CD34+ fibroblastic tumor:
The finding of which of the following additional histologic features in the lesion shown above would most likely favor a diagnosis of melanoma over atypical fibroxanthoma?
- Presence of an in situ component
- Presence of numerous mitotic figures, including atypical forms
- Presence of pigment
- Reactivity for MITF
Comment Here
Reference: Atypical fibroxanthoma
- CD10
- p40
- S100
- Smooth muscle myosin
Comment Here
Reference: Atypical fibroxanthoma
- Superficial dermal based smooth muscle tumor which is biologically different from deep leiomyosarcoma
- Typically larger than leiomyomas with vascular invasion
- Recurs, but only rarely metastasizes
- May be associated with HIV infection
- 59 year old woman with painless skin nodule (J Med Case Reports 2007;1:180)
- 67 year old woman with neck lesion (Cases J 2010;3:52)
- Cellular lesions of smooth muscle type cells with atypia, necrosis and mitotic activity
- May have prominent vascular pattern, clear cell features, desmoplasia
- HHF35 (90%), alpha smooth muscle actin (90%), vimentin, desmin (75%) (Cancer 2009;115:4186)
- Basal cell carcinoma (BCC) arises from the interfollicular or follicular epithelium
- Most common malignant tumor type in humans
- Local aggressive course
- Low disease associated death rate; metastases to lung and bone exceptionally rare
- When multiple, associated with a number of genetic conditions, including basal cell nevus (Gorlin), Bazex-Dupré-Christol, Rombo syndromes and xeroderma pigmentosum
- Nests of basaloid cells with peripheral palisading associated with a fibromyxoid stroma
- Basal cell epithelioma
- Rodent ulcer
- Basalioma
- Fibroepithelioma of Pinkus
- ICD-O:
- 8090/3 - Basal cell carcinoma, NOS
- 8097/3 - Nodular basal cell carcinoma
- 8091/3 - Superficial basal cell carcinoma
- 8097/3 - Micronodular basal cell carcinoma
- 8092/3 - Infiltrating basal cell carcinoma
- 8092/3 - Morpheaform basal cell carcinoma
- 8094/3 - Basosquamous carcinoma
- 8090/3 - Pigmented basal cell carcinoma
- 8092/3 - Basal cell carcinoma with sarcomatoid differentiation (metaplastic BCC)
- 8090/3 - Basal cell carcinoma with adnexal differentiation
- 8093/3 - Fibroepithelial basal cell carcinoma
- N/A - Basomelanocytic tumor
- Most common cancer type in fair skinned people (Br J Dermatol 2017;177:359)
- Highest rate is observed in Australia (1,000/100,000 person years) (Br J Dermatol 2012;166:1069)
- More frequent:
- Middle aged adults with increasing incidence with age
- People with I - II Fitzpatrick skin phototype (Cancer Epidemiol 2013;37:534)
- Male (M:F = 1.5:1)
- Number of cases is increasing every year worldwide, especially among young age group, with a predilection for women (Br J Dermatol 2012;166:1069, Pediatrics 2014;134:e4)
- Tumors that occur in younger age group tend to behave in an aggressive fashion (Br J Plast Surg 2000;53:393)
- Sun exposed skin (G Ital Dermatol Venereol 2014;149:423)
- 64% on the head region (most often nodular variant)
- 24% on the trunk (most often superficial variant)
- Rare areas such as anogenital region, nail unit, palm and sole (J Cutan Pathol 2018 Jun 19 [Epub ahead of print])
- UV radiation induced carcinogenesis
- Mutations in TP53 gene
- PTCH1 gene mutations
- Activating mutations in SMO gene
- Other genes including mutations in the CDKN2A gene and RAS genes
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- UV radiation (sun damage and indoor tanning) (Cancer 1990;65:2811, Am J Epidemiol 1999;150:459, Pediatrics 2014;134:e4)
- Ionizing radiation (J Natl Cancer Inst 1996;88:1848)
- Arsenic exposure (J Dermatol 2017;44:1374)
- Genetic conditions
- Nevoid basal cell carcinoma syndrome (Gorlin syndrome) (Lancet 1992;339:581)
- Xeroderma pigmentosum (J Invest Dermatol 2012;132:785)
- Bazex-Dupré-Christol syndrome (NIH: Bazex-Dupre-Christol syndrome [Accessed 15 December 2020])
- Oculocutaneous albinism (BMC Cancer 2014;14:157)
- Muir-Torre syndrome
- Smoking (J Am Acad Dermatol 2002;46:706)
- Nevus sebaceus (J Am Acad Dermatol 2000;42:263)
- Immunosuppression (Lancet 1998;351:623, J Am Acad Dermatol 2003;49:397, Arch Dermatol 2001;137:459)
- Nodular variant usually presents as a pearly pink or flesh colored papule or nodule with arborizing and branching vessels (Br J Dermatol 2002;147:41)
- In the past, ulceration of a nodular BCC gave rise to the term rodent ulcer
- Tumor with ulceration has characteristic rolled borders
- Superficial variant presents with scaly macules, patches or plaques with an erythematous surface
- Pigmented variant resembles a nodular or superficial BCC but has a pigmented surface and can be clinically mistaken for a melanoma
- Neglected tumors may result in massive skin, soft tissue and bone destruction with severe disfiguration
- Clinical features
- Dermatoscopy
- Histological features
- Histological type associated with risk of local recurrence
- Lower risk: nodular, superficial, pigmented, infundibulocystic, fibroepithelial
- Higher risk: basosquamous, sclerosing / morpheaform, keloidal, infiltrating, BCC with sarcomatoid differentiation and micronodular variants
- Circumscription of tumor margins
- Presence of perineural and lymphovascular invasion
- Status of surgical margins
- Tumor size
- Localization (part of skin affected, e.g. head and neck, trunk, etc.)
- History of nonmelanoma skin cancer
- Radiation therapy
- PUVA therapy
- Immunosuppression
- Reference: NCCN: Basal Cell Skin Cancer Evidence Blocks [Accessed 15 December 2020]
- 55 year old Caucasian man with BCC on the left forearm presenting with ulcerative axillary lymph node and pulmonary metastases (Case Rep Oncol Med 2018;2018:3485326)
- 65 year old man with clear cell BCC on upper chest (Patholog Res Int 2011;2011:386921)
- 65 year old man with neglected BCC on posterior neck presenting with diffuse skeletal metastases (JAAD Case Rep 2018;4:678)
- 76 year old Caucasian man with basosquamous carcinoma with lymphovascular invasion on left lateral shoulder (Cureus 2018;10:e3401)
- 79 year old woman with massive basosquamous carcinoma of back (Oxf Med Case Reports 2017;2017:omw095)
- 90 year old woman with infiltrative BCC on left shin that was clinically diagnosed as tinea corporis (Dermatol Online J 2018;24:13030)
- Surgery
- Mohs micrographic surgery
- Curettage and electrodesiccation for tumors with lower risk of local recurrence
- Radiation therapy
- Topical treatment (5-fluorouracil, imiquimod)
- Photodynamic therapy with aminolevulinic acid or porfimer sodium
- Nicotinamide (can be used for prophylactic treatment)
- Systemic therapy (sonidegib and vismodegib are hedgehog pathway inhibitors [HhIs])
- Reference: NCCN: Basal Cell Skin Cancer Evidence Blocks [Accessed 15 December 2020]
- Variable, mirroring the clinical variants described above
- Mohs micrographic surgery technique is one of the most often used options for assessment of margins of surgery specimens (Dermatol Surg 2019;45:S57)
- Mohs surgery shows excellent 5 year cure rates: primary 99%, recurrent 94.4% (J Dermatol Surg Oncol 1989;15:315)
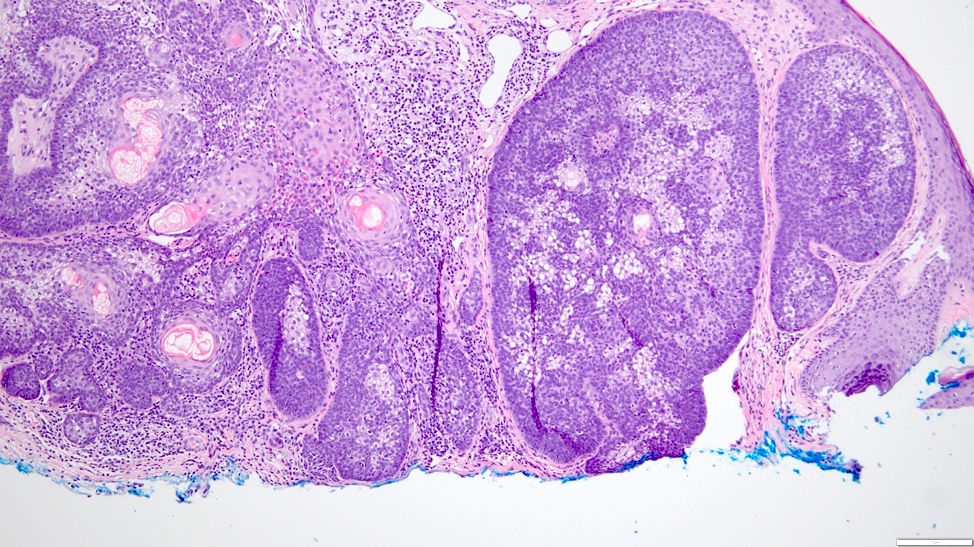
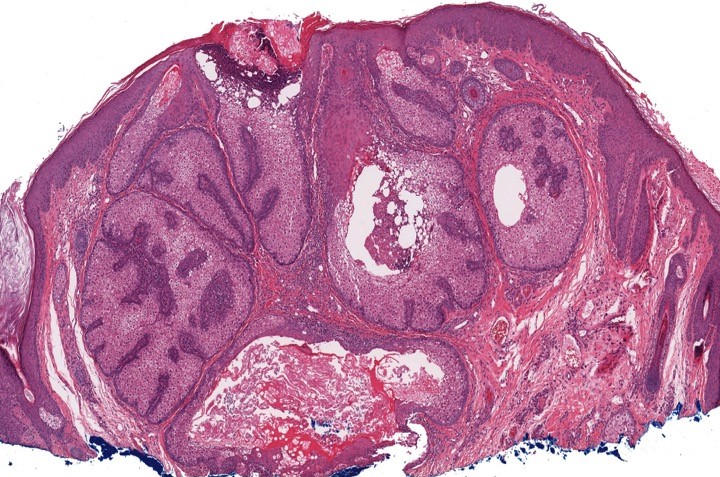
- Nodular and nodulocystic BCC
- Relatively circumscribed mass
- Epidermal or follicular attachment variably present
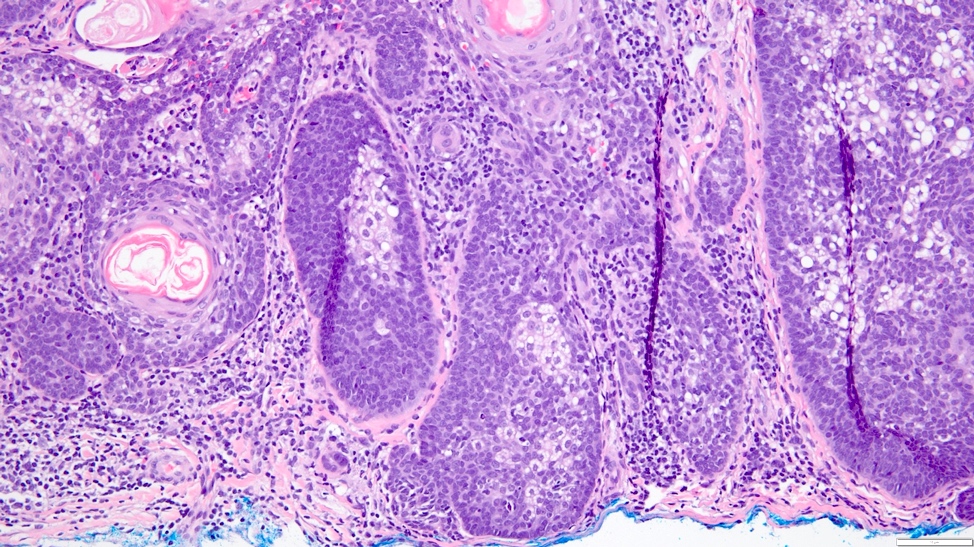
- Large basaloid lobules with peripheral nuclear palisade
- Lobules may be solid or show central cyst formation due to excessive mucin production
- Fibromyxoid stroma
- Cleft formation between tumor lobules and stroma
- Pleomorphism is generally mild
- Variable mitotic activity and apoptosis
- Sometimes necrosis en masse
- Adenoid BCC
- Reticulate pseudoglandular pattern of basaloid cells
- Mucinous stroma
- Can mimic true gland formation, resulting in diagnostic confusion with a sweat gland adenocarcinoma, e.g. adenoid cystic carcinoma
- Micronodular BCC
- Small basaloid nests
- Peripheral palisading less prominent
- Retraction artifact usually absent
- Can diffusely infiltrate the dermis and extend into the subcutis
- Infiltrative BCC
- Small irregular clumps of basaloid cells
- Limited peripheral palisading
- Stroma loose and mucin may be prominent
- Extensive spread
- Perineural invasion can be seen
- Morpheaform (sclerosing, morphoeic) BCC
- Thin strands and nests of basaloid cells
- Limited peripheral palisading
- Stroma is dense and sclerotic
- Extensive spread
- Perineural invasion can be seen
- Keratotic BCC
- Horn cyst formation
- Basosquamous (metatypical) BCC
- Biphasic tumor
- Foci of neoplastic squamous differentiation
- Pigmented BCC
- Nodular and superficial variants can be pigmented
- Colonization of tumor's complexes with melanocytes
- Stromal melanophages
- Superficial BCC
- Isolated basaloid lobules projecting from the lower margin of the epidermis
- Ulcerative BCC
- Ulceration
- Highly infiltrative growth pattern
- Less commonly nodulocystic variant with ulceration
- BCC, fibroepitheliomatous type (fibroepithelioma of Pinkus)
- Anastomosing strands and cords of basaloid cells connected to the epidermis
- Peripheral nuclear palisading with a formation of follicular germ-like structures
- Rarely, isthmic differentiation is present
- Fibrotic stroma that can differentiate towards follicular papillae in the areas of germ-like structure formation
Rare variants
- Pleomorphic (giant cell, BCC with monster cells) BCC
- Mitotic activity
- Apoptosis
- Сellular pleomorphism and giant cell formation
- Atypia has no prognostic significance
- Clear cell BCC
- Focal or total clear cell change with clear to finely granular eosinophilic cytoplasm due to lysosomal degeneration
- Peripheral palisading is usually preserved
- Signet ring cell BCC
- Tumor cells with laterally displaced nuclei
- May show positivity for S100 protein, glial fibrillary acidic protein and smooth muscle actin, suggesting myoepithelial differentiation
- Referred to as BCC with myoepithelial differentiation
- Granular BCC
- Tumor cells with abundant granular eosinophilic cytoplasm
- BCC with differentiation towards adnexal structures
- Tumor complexes can show differentiation towards sebaceous, follicular, eccrine or apocrine structures
- Infundibulocystic BCC
- Synonym: BCC with follicular differentiation
- Superficial dermal proliferation of basaloid cells arranged in anastomosing cords and strands
- Peripheral palisading is present
- Stroma is typically scanty
- Infundibular cysts are present
- Metaplastic BCC
- Stromal malignant metaplastic features (carcinosarcoma)
- Chondroid, osteoid and smooth muscle differentiation may be seen
- BCC with matricial differentiation (shadow cell BCC)
- Tumor cells show differentiation towards matricial cells of the hair follicle displaying shadow cells and trichohyaline granules
- Keloidal BCC
- Stroma shows thick, sclerotic collagen bundles
- BCC with thickened basement membrane
- Tumor complexes surround by thickened basement membrane
- Basomelanocytic tumor
- Combined and intermixed basal cell and melanomatous elements
- BCC with neuroid type nuclear palisading
- Central nuclear palisading reminiscent of that seen in schwannoma
Contributed by Antonina Kalmykova, M.D., Phillip H. McKee, M.D., Sate Hamza, M.D., Eduardo Calonje, M.D.,
Wayne Grayson, M.B.Ch.B., Ph.D., James Sampson, M.B.B.S., M.Sc. and Assia Bassarova, M.D., Ph.D.
- Sensitivity and specificity of exfoliative cytology estimate 97.5% (95% CI 94.5% to 98.9%) and 90.1% (95% CI 81.1% to 95.1%) respectively and can result in wrong or false positive result (Cochrane Database Syst Rev 2018;12:CD013187)
- Complexes of tightly packed basaloid cells with palisading in the periphery
- High nuclear/cytoplasmic ratio, minimal atypia and mitotic activity
- CK AE1 / AE3 (100%), BerEP4 (80 - 100%), p63 (100%), CAM 5.2 (20 - 95%), androgen receptor (33 - 66%), p53 (74.5 - 83%), 34 beta E12 (high molecular weight CK), BCL2 (diffuse pattern), CD10 (positive in tumor cells, negative in stroma) (Dermatopathology (Basel) 2015;2:15, Arch Pathol Lab Med 2017;141:1490, Rom J Morphol Embryol 2018;59:1115, Am J Pathol 1992;141:25)
- CK20, adipophilin, SOX10, S100, MelanA / MART1, HMB45, CD34, CD44 (Dermatopathology (Basel) 2015;2:15)
- Usually negative: CK7 (0 - 70%), CEA (0 - 20%), EMA (0 - 6%) (Dermatopathology (Basel) 2015;2:15, Arch Pathol Lab Med 2017;141:1490, Rom J Morphol Embryol 2018;59:1115, Am J Pathol 1992;141:25)
- Chromosomal gains at 6p (47%), 6q (20%), 9p (20%), 7 (13%) and X (13%)
- Regional loss on 9q in 33% of tested tumors encompassing 9q22.3 to which the Patched gene has been mapped (J Invest Dermatol 2001;117:683)
BCC discussed by Dr. Jerad Gardner
Malignant keratinocytic neoplasms discussed by Dr. Clay J. Cockerell
- Face, excision:
- Nodular basal cell carcinoma (LVI0 Pn0 R0) (ICD-O code 8097/3) (see synoptic report)
- Synoptic report:
- Tumor site: face
- Procedure: excision
- Histological type: nodular basal cell carcinoma
- Depth of invasion: 2.5 mm
- Tumor size (greatest dimension): 7 mm
- Anatomic level (Clark level): IV
- Lymphovascular invasion (LVI): 0
- Perineural invasion (Pn): 0
- Peripheral margins: uninvolved
- Deep margin: uninvolved
- Reference: NCCN: Basal Cell Skin Cancer Evidence Blocks [Accessed 15 December 2020]
- Follicular induction (also known as follicular basal cell hyperplasia, epidermal basaloid cell hyperplasia and basaloid epidermal proliferation) versus superficial BCC:
- Usually seen above dermatofibroma, less common above nevi
- Follicular differentiation (germinative buds and papillary mesenchymal bodies) shows clear cell hyperplasia, epidermal hyperplasia between sites of follicular induction
- No atypical nuclei, increased mitotic figures or apoptotic bodies
- CK20+ colonizing Merkel cells
- Trichoepithelioma / trichoblastoma versus nodular BCC:
- Delicate perifollicular-like stroma with small spindled cells
- Papillary mesenchymal bodies
- No prominent cleft retraction, myxoinflammatory stroma, significant mitotic activity (is sometimes marked in trichoblastoma and should not be misconstrued as implying malignant trichoblastoma), cytologic atypia or tumor necrosis
- Desmoplastic trichoepithelioma versus morpheaform BCC:
- Does not extend into the deep dermis
- Architectural symmetry, horn cysts with calcification, granulomatous inflammation and follicular / sebaceous / infundibular differentiation
- No mitotic figures, ductal differentiation, cytologic atypia, tumor to stroma clefting or perineural infiltration
- CK20+ colonizing Merkel cells, androgen receptor-
- PHLDA1+ (highly specific for trichoepithelioma / trichoblastoma, although expression in micronodular BCC has been reported)
- Note: no single IHC marker can differentiate trichoepithelioma and BCC
- Basaloid follicular hamartoma versus infundibulocystic BCC:
- Tumor of follicular infundibulum versus superficial BCC:
- Syringoma versus morpheaform BCC:
- Squamous cell carcinoma (basaloid, clear cell, sarcomatoid):
- Shows an intraepidermal component, pagetoid spread
- No peripheral palisading, clefting or myxoinflammatory stroma
- Areas with conventional features like keratinization, keratin pearls
- BerEP4- (also absent in squamous areas of basosquamous carcinoma)
- EMA+ (may be expressed in squamous areas of BCC), CD44+
- Microcystic adnexal carcinoma versus morpheaform BCC:
- Superficial keratocysts (infundibular or isthmic), ductal differentiation with eosinophilic luminal secretions
- Frequently invades nerves (can't discriminate)
- No peripheral palisading, mitotic activity, tumor to stroma retraction or myxoinflammatory stroma
- CEA+, EMA+ in ductal structures
- CK15+, BerEP4 variable (mixed reports)
- p63 highlights ductal myoepithelial cells
- Sebaceous carcinoma versus BCC (nodular, clear cell):
- Intraepidermal pagetoid spread
- No peripheral clefting
- May have evidence of sebaceous, lobular architecture
- Often relatively greater cytologic atypia and less basaloid morphology
- Diffuse androgen receptor+ (versus focally positive in BCC)
- Low molecular weight CK+, EMA+
- BerEP4-, adipophilin+, perilipin+
- Merkel cell carcinoma:
- Rarely may show intraepidermal with pagetoid spread
- No / focal peripheral palisading
- Homogenous salt and pepper chromatin
- Nuclear molding
- Abundant mitotic activity and necrosis
- MCPyV 70 - 80% (highly specific marker)
- CK20+ (paranuclear, dot-like pattern)
- Neuroendocrine markers expressed but rarely also positive in BCC
- Adenoid cystic carcinoma versus adenoid BCC:
- Well defined cribriform patterns
- No peripheral palisading, continuity with the epidermis or adjacent hair follicle or retraction artifacts between the tumor islands and stroma
- Typically shows hyaline material lining the lumina of the ducts and sometimes also present in the stroma
- CD117+ (20% of BCC CD117+), CD43+ (40%), CK7+, CEA+, EMA+ (in ductal structures)
- p63+, SMA+, calponin+ (myoepithelial cell population at periphery of tumor islands)
- Clear cell melanoma (balloon cell melanoma) versus clear cell BCC:
- Clear cell eccrine porocarcinoma versus clear cell BCC:
- Clear cell hidradenocarcinoma versus clear cell BCC:
- Trichilemmal carcinoma versus clear cell BCC:
- Pilomatrix carcinoma versus BCC with matricial differentiation:
- No conventional areas of BCC
- Pigmented reticulated seborrheic keratosis versus BCC with follicular differentiation:
- No peripheral palisading, myxoinflammatory stroma, peripheral clefting, atypical nuclei, increased mitotic figures or apoptotic bodies
- CK20+ colonizing Merkel cells may be present
- Cylindroma versus BCC with thick basement membrane:
- Rare, benign cutaneous lesion associated with inherited syndromes
- Confused histologically with infundibulocystic basal cell carcinoma
- Benign cutaneous hair follicle hamartoma
- Can occur as papule(s) or plaque
- May be solitary, linear or diffuse in distribution (Indian J Dermatol Venereol Leprol 2019;85:60)
- Confused histologically with basal cell carcinoma or other benign basaloid dermal growths
- May occur spontaneously or as the result of inherited disorders
- Basaloid follicular hamartoma
- Generalized basaloid follicular hamartoma syndrome: autosomal dominant variant
- Linear unilateral basal cell nevus with comedones: childhood form occurring in a linear distribution, often along the lines of Blaschko and may have associated comedones
- Generalized hair follicle hamartoma: multiple basaloid follicular hamartomas and coexisting alopecia and myasthenia gravis (Patterson: Weedon's Skin Pathology, 4th Edition, 2015, Chapter 33)
- ICD-10: Q82.5 - congenital nonneoplastic nevus
- Associated with certain autoimmune diseases: myasthenia gravis, alopecia, systemic lupus erythematosus
- Happle-Tinschert syndrome (Dermatology 2009;218:221)
- Bazex syndrome, aka Bazex-Dupre-Christol syndrome (X-linked dominant)
- Nevoid basal cell carcinoma syndrome, aka Gorlin syndrome, aka basal cell nevus syndrome
- Generalized basaloid follicular hamartoma (autosomal dominant mutation) (J Cutan Pathol 2008;35:477)
- Brown-Crounse syndrome
- Skin of the face, trunk, limbs, scalp, axilla and pubic area
- Distribution may be localized or generalized depending on the variant (Arch Pathol Lab Med 2010;134:1215)
- Can occur sporadically or in association with genetic mutations
- Mutated PTCH (protein patched homolog) gene leads to disrupted tumor suppressor function
- PTCH abnormally binds sonic hedgehog (Shh), a protein signal involved in embryogenesis
- Constitutive activation of downstream signaling in transcription factors like Gli-1 and abnormal growth ensues (Arch Pathol Lab Med 2010;134:1215)
- Associated with autoimmune disease
- May occur as solitary or multiple hypopigmented to hyperpigmented papules, commonly over the central face
- May occur as a plaque or coalescing papules
- Lesions may be associated with alopecia, hypertrichosis or open comedones (J Cutan Pathol 2008;35:477)
- Unilateral variants may follow lines of Blaschko and can be associated with underlying neurological findings (Korean J Radiol 2014;15:534)
- Diagnosis relies on recognizing the specific pathologic features
- Correlation with clinical findings is required
- Some authors have discussed the utility of immunohistochemical studies in distinguishing basaloid follicular hamartoma from basal cell carcinoma (Arch Pathol Lab Med 2017;141:1490)
- Significant morphologic overlap between other benign tumors of the follicular infundibulum as well as infundibulocystic basal cell carcinoma exists; some have argued that infundibulocystic basal cell carcinoma and basaloid follicular hamartoma are the same entity (J Cutan Pathol 2014;41:916)
- 3 month old and 8 year old boys with Blaschkoid hypopigmented papules (Pediatr Dermatol 2017;34:e196)
- 5 year old and 9 year old sisters with malar papules and comedones (J Cutan Pathol 2008;35:477)
- 7 year old boy with truncal hypopigmented papules and ipsilateral medulloblastoma, diagnosed with Happle-Tinschert syndrome (Dermatology 2009;218:221)
- 9 year old boy with unilateral papules over the chest with associated limb shortening and ipsilateral hemimegalencephaly diagnosed with Happle-Tinschert syndrome (Korean J Radiol 2014;15:534)
- 27 year old woman with Gorlin syndrome and many basaloid follicular hamartomas over the upper body (Pediatr Dermatol 2018;35:e396)
- 47 year old woman with generalized basaloid follicular hamartoma syndrome who developed basal cell carcinoma in a pre-existing basaloid follicular hamartoma (Am J Dermatopathol 2015;37:e37)
- 64 year old man with an isolated hyperpigmented macule over the cheek (Dermatol Online J 2017;23:15)
- 70 year old man with flesh colored firm papule and central depression over the forehead (Ann Dermatol 2010;22:229)
- Three siblings with consanguineous parents and generalized basaloid follicular hamartoma (Arch Dermatol 1995;131:454)
- Not officially considered a premalignant lesion
- Close follow up to monitor for progression to basal cell carcinoma should be considered
- Some patients may be at greater risk for development of malignancy such as those with basal cell nevus syndrome
- Those that arise in the setting of autoimmune disease may resolve with treatment of the corresponding autoimmune disorder
- Surgical excision with carbon oxide laser therapy and dermabrasion have been successfully used in a 14 year old boy with unilateral facial basaloid follicular hamartoma with no recurrence at 11 years (J Dermatol 2017;44:e278)
- Pulsed dye laser therapy was used with some success in the treatment of acquired basaloid follicular hamartomas on the face of a 68 year old man (J Clin Aesthet Dermatol 2018;11:39)
- Three children with basal cell nevus syndrome who had extensive basal cell carcinomas and basaloid follicular hamartomas were treated with 5-aminolevulenic acid photodynamic therapy with satisfactory cosmetic results lasting at least 6 years (Arch Dermatol 2005;141:60)
- Oral and topical retinoids have been used with some efficacy in an isolated case (J Am Acad Dermatol 2003;49:1067)
- Basaloid follicular hamartomas may be seen on frozen section, especially during Mohs surgery
- The same diagnostic criteria apply for frozen section diagnosis as for the evaluation of paraffin embedded tissue
- Distinguishing between basaloid follicular hamartoma and basal cell carcinoma on frozen section is challenging
- Anastomosing strands of basaloid and squamoid cells with connection to the overlying epithelium
- Should only arise where normal hair follicles are present
- Bland cells without atypia, mitoses or apoptotic bodies
- Loose, cellular or myxoid stroma
- Horns, cysts and pigmentation may be present
- If peripheral palisading and retraction are present, they should be focal and less than the amount typically seen within basal cell carcinoma (Arch Pathol Lab Med 2010;134:1215)
- BCL2: stains peripheral basaloid cells; a diffuse staining pattern is observed in all basaloid cells in basal cell carcinoma
- CD34: stains the stroma around basaloid cells; the stroma in basal cell carcinoma may only rarely stain with CD34 (J Cutan Pathol 2001;28:538)
- CD10: stains the stroma around basaloid cells; both the stroma and basaloid cells in basal cell carcinoma may stain with CD10
- P40: strongly positive in basaloid cells
- CK20: focal positivity has been reported (J Cutan Pathol 2014;41:916)
- There is no specific immunohistochemical study for basaloid follicular hamartoma and studies analyzing sensitivity and specificity of markers are limited by the availability of this rare tumor
- Immunohistochemistry has not been widely studied in basaloid follicular hamartoma
- Targeted next generation sequencing may be helpful in the diagnosis of patients with syndromic phenotypes
- The first family described with generalized basaloid follicular hamartoma was in North Carolina; there were 6 generations of affected members who had multiple flesh colored and hyperpigmented papules over the face, neck, trunk and arms, palmar / solar pits, scalp alopecia, milia and comedones (J Am Acad Dermatol 2000;43:189)
- The PTCH1 gene on chromosome 9q23 is implicated in both generalized basaloid follicular hamartoma syndrome (GBFH) and Gorlin syndrome; basaloid follicular hamartomas occur in both syndromes and some have suggested that these two diseases are on a spectrum (Anticancer Res 2018;38:471)
- Basal cell nevus syndrome may also arise as a result of PTCH2 mutation or SUFU mutation, a signaling molecule in the same pathway; as opposed to generalized basaloid follicular hamartoma syndrome, basal cell nevus syndrome is defined by the presence of jaw keratocysts, calcification of the falx cerebri, bifid ribs and macrocephaly
Clinical phenotype and molecular genetics of Basal cell nevus syndrome
- Skin, cheek, biopsy:
- Cutaneous adnexal neoplasm, morphologically consistent with basaloid follicular hamartoma (see comment)
- Comment: Basaloid follicular hamartoma demonstrates significant overlap between basal cell carcinoma and has been shown to progress to malignancy in some cases. Increased surveillance or complete surgical excision may be required depending upon the clinical circumstances.
- Microscopic description: Anastomosing cords of bland basaloid cells with peripheral palisading and surrounding cellular stroma. Rare papillary mesenchymal bodies are noted. Absent are mitoses, apoptotic bodies and atypical nuclear features.
- Infundibulocystic basal cell carcinoma:
- Strikingly similar appearance to basaloid follicular hamartoma but is more likely to have atypia and mitoses
- Stromal retraction should be more prominent in basal cell carcinoma
- Some have discussed the presence of a myxoinflammatory stroma as a helpful distinguishing feature
- Clinical correlation and immunohistochemistry may aid in the diagnosis (Arch Pathol Lab Med 2017;141:1490)
- Trichoepithelioma / trichoblastoma:
- Benign tumor composed of separate islands of basaloid cells which may have peripheral palisading
- Islands may branch and are surrounded by a loose to fibrotic stroma
- Papillary mesenchymal bodies may be seen
- The presence of distinct rounded islands as opposed to multiple branching anastomoses signals the diagnosis
- Tumor of the follicular infundibulum:
- Helpful distinguishing features are a growth pattern along the dermal epidermal junction resembling superficial basal cell carcinoma with fenestrated areas
- Another helpful feature is the presence of pale staining glycogen containing cells that are reminiscent of trichilemmoma
- Pilar sheath acanthoma:
- Cystically dilated follicle with radiating acanthotic epithelial projections
- Trichofolliculoma:
- Central large dilated follicle surround by smaller secondary follicles
Explanation: A) Basal cell carcinoma should have atypia; C) While, syringoma will have basaloid cells in the dermis, they are separate, small “comma-shaped” islands; D) Trichoblastoma will have rounded basaloid islands in the dermis that may focally connect as opposed to the more predominantly branching stranded pattern of basaloid follicular hamartoma; E) The classic intensely eosinophilic basement membrane material normally found in spiradenoma is lacking in this biopsy as is the “blue balls in the dermis” architecture
Reference: Basaloid follicular hamartoma
Comment Here
- Basaloid follicular hamartoma has been reported to occur in both sporadic and syndromic forms. With which of the following syndromes is basaloid follicular hamartoma associated?
- Birt-Hogg Dubé syndrome
- Gorlin Syndrome
- Lynch Syndrome
- Rothmund Thomson
- Tuberous sclerosus
Explanation: A) Birt-Hogg Dubé is associated with fibrofolliculoma, trichodiscomas and acrochordons; C) the Muir-Torre variant of Lynch is associated with sebaceous adenoma, sebaceous adenocarcinoma and squamous cell carcinoma; D) Rothmund Thomson is characterized by poikiloderma and increased risk of basal cell carcinoma and squamous cell carcinoma among other findings; E) Tuberous sclerosis is associated with angiofibromas, subungual fibromas, connective tissue hamartomas (Shagreen patch) and hypomelanotic macules
Reference: Basaloid follicular hamartoma
Comment Here
- Sharply demarcated pigmented macule, often with localized hypertrichosis (eMedicine)
- Dermoscopy: network, focal hypopigmentation, skin furrow hypopigmentation, hair follicles, perifollicular hypopigmentation and vessels (Dermatology 2006;212:354)
- Also called pigmented hairy epidermal nevus, Becker's melanosis
- Becker's nevus syndrome: Becker's nevus with congenital abnormalities (J Am Acad Dermatol 2004;51:965)
- First described by Becker in 1948 (Arch Dermatol 1948;60:155)
- Present in 0.5% of young men (Ann Dermatol Venereol 1981;108:41)
- Sex ratio close to 1:1 despite apparent increase in women due to association with breast hypoplasia (An Bras Dermatol 2010;85:379)
- Associated with high localized androgen receptor expression (J Am Acad Dermatol 1984;10:235, J Am Acad Dermatol 2008;59:834)
- May be associated with hypoplasia of ipsilateral breast (Arch Iran Med 2006;9:68), aplasia of ipsilateral pectoralis major muscle, limb shortening, lipoatrophy (Clin Exp Dermatol 2002;27:27), spina bifida and scoliosis
- Occasionally associated with melanoma, but overall no known increased risk (Dermatologica 1991;182:77)
- Possible association with Kabuki Syndrome (Dermatol Online J 2011;17:1)
- Usually back, shoulder or chest
- Sharply demarcated, unilateral, hyperpigmented tan macule on back, shoulder or chest
- Hypertrichosis in 50%
- 12 year old girl with coexisting segmental nevus depigmentosus (Australas J Dermatol 2007;48:224)
- 18 year old man with bilateral nevus (Indian J Dermatol Venereol Leprol 2008;74:73)
- 24 year old man with hypopigmented pityriasis versicolor developing on pre-existing Becker's nevus (Indian J Dermatol Venereol Leprol 2002;68:43)
- Laser (Br J Dermatol 2005;152:308)
- Spironoactone may improve associated breast hypoplasia (J Dermatol 2003;30:154)
- Increased basal layer pigmentation, mild acanthosis, hyperkeratosis and regular elongation of rete ridges
- Variable hypertrichosis
- Areas associated with smooth muscle hamartoma have more pronounced smooth muscle bundles irregularly dispersed within the dermis and unrelated to either hair follicles or vascular channels
- Does not actually contain nevus cells
- Congenital smooth muscle hamartoma
- Congenital tumor (extremely rare in skin) containing tissue components from all 3 germinal layers
- Very rare with only scattered case reports
- Lesions present at birth
- Locations vary including face, back, neck, knee
- A cystic teratoma in skin (Am J Dermatopathol 1985;7:383, Histopathology 1996;29:384)
- Benign cutaneous cystic teratoma (J Cutan Pathol 1982;9:345)
- Cystic structure with elements from all 3 germinal layers (ectoderm, endoderm and mesoderm)
- Variable tissue types may be present from the germinal layers:
- Superficial ectoderm such as epidermis and appendages
- Neuroectoderm (nervous tissue)
- Mesoderm such as connective tissue, striated and smooth muscle
- Endoderm such as respiratory epithelium, thyroid tissue, GI mucosa
- Rare benign lymphovascular proliferation of unknown etiology, initially described in 1990 (J Am Acad Dermatol 1990;23:229)
- Delicate, thin walled, endothelium lined dilated vascular spaces involving the superficial dermis
- Intravascular papillary stromal projections resemble papillary endothelial hyperplasia
- Deeper in dermis, vascular spaces collapse and dissect dermal collagen in angiosarcoma-like pattern
- Also called acquired progressive lymphangioma
- ICD-10: D18.1 - lymphangioma, any site
- Uncommon; around 50 reported cases in English literature
- Wide age distribution
- No sex predilection
- Trunk / limbs usually; other sites have been described
- Favored to be a benign vascular malformation rather than a true neoplasm
- Some cases possibly related to trauma
- Bruise-like red-brown patch or plaque with indolent growth
- May be nodular, fluctuant and rubbery
- Drainage of serous fluid has been reported (Clin Exp Dermatol 2009;34:e341, Ann Acad Med Singapore 2011;40:106, J Cutan Pathol 2015;42:217)
- 1 year old boy with extensive acquired progressive lymphangioma (Pediatr Dermatol 2018;35:486)
- 2 year old patient with alopecia lesions in scalp (Cir Pediatr 2000;13:170)
- 32 year old man with tumor in hypogastric region (Actas Dermosifiliogr 2010;101:792)
- 75 year old man with giant benign lymphangioendothelioma (J Cutan Pathol 2012;39:950)
- HIV+ man with acquired progressive lymphangioma (J Cutan Pathol 2007;34:882)
- 4 cases of benign lymphangioendothelioma (J Cutan Pathol 2013;40:945)
- Complete excision is usually curative but not necessary
- May recur
- Reports of regression with sirolimus (J Am Acad Dermatol 2014;71:e221), pulsed dye laser (Dermatol Surg 2014;40:218), 5% imiquimod (Pediatr Dermatol 2017;34:e302)
- Delicate, thin walled, endothelium lined dilated vascular spaces involving the superficial dermis
- Intravascular papillary stromal projections resemble papillary endothelial hyperplasia
- Deeper portion of lesions have vascular space collapse and dissect collagen bundles, mimicking patch stage Kaposi sarcoma
- Preexisting vessels and adnexal structures of the dermis also appear dissected by newly formed vascular channels
- Smooth muscle often focally present around vascular spaces
- Endothelial cells may hobnail, may form morula resembling giant cells
- Crowding of endothelial cells present but no endothelial atypia
- Vascular spaces lack erythrocytes and hemosiderin deposits
- No mitotic figures
- Kaposi sarcoma: HHV8+; usually demonstrates slit-like vasculature without marked dilation of vessels and plasma cell infiltrate
- Atypical vascular lesion: demonstrates more endothelial prominence and atypia; associated with radiation
- Angiosarcoma: dissects through dermal collagen with significant atypia, atypical intraluminal cells, endothelial stacking (multilayering) and mitoses
- Superficial lymphangioma (lymphangioma circumscriptum): congenital hamartoma often associated with cytogenetic abnormalities; typically does not dissect dermal collagen but may show dilated superficial dermal vessels
- Targetoid hemosiderotic hemangioma (hobnail hemangioma): may have similar infiltration pattern to benign lymphangioendothelioma; endothelial cells protruding into vascular lumen (hobnail cells); deep stromal hemosiderin deposition
- CD31
- CD34
- D2-40
- ERG
- HHV8
- Delicate thin walled vessels
- Frequent mitotic figures
- Hobnail endothelial cells
- Infiltration into the deep dermis
- Intravascular papillary stromal projections
Comment Here
Reference: Benign lymphangioendothelioma / acquired progressive lymphangioma
- Previously called intraepidermal epithelioma
- Not clearly defined
- Likely heterogeneous group of disorders (Am J Dermatopathol 2011;33:492) including irritated seborrheic keratosis, eccrine poroma and other intraepidermal sweat gland tumors
- Malignant dermal tumor with epithelioid and spindled cells of uncertain origin with partial melanocytic differentiation and CRTC1::TRIM11 translocation
- Histological features include a dermal / subcutaneous circumscribed tumor composed of fascicles and nests of monomorphic epithelioid and spindle cells with prominent nucleoli divided by delicate collagen septa, no / very rare pigment
- Immunohistochemical features include consistent diffuse SOX10 and MITF staining; S100, MelanA and HMB45 stains are variable
- Defined by identifying CRTC1::TRIM11 translocation
- No evidence of EWSR1 rearrangement
- Appears to have at least some malignant potential, although cases and follow up are limited
- Cutaneous melanocytic tumor with CRTC1::TRIM11 fusion
- Not recommended: cutaneous melanocytoma with CRTC1::TRIM11 fusion
- Age: broad range (5 - 87); median age of 42 (Histopathology 2023;82:368)
- No clear gender bias (Am J Surg Pathol 2022;46:1457)
- Broad anatomic distribution
- Limbs (64%) appear to be involved more often than trunk (20%) and head (2%) based on current case reports (Am J Surg Pathol 2022;46:1457)
- 2 cases of oral and nasal mucosal involvement (Am J Surg Pathol 2022;46:1457)
- Exact mechanism of how the CRTC1::TRIM11 fusion transcript causes neoplasia is not known; hypotheses include
- CRTC1::TRIM11 fusion deletes a protein - protein interaction site on TRIM11 that is involved in directing misfolded proteins towards proteasomes for degradation (Cureus 2022;14:e33179)
- CRTC1::TRIM11 fusion retains an interaction site with CREB1, which in turn may drive expression of MITF; MITF acts like an oncogene and can drive MITF synthesis (Am J Surg Pathol 2022;46:1457)
- Unknown
- Discrete, slowly growing, skin colored nodule without pigmentation (Am J Surg Pathol 2022;46:1457)
- Biopsy
- Defined by molecular findings
- Lobulated lesion on imaging
- May be positron emission tomography (PET) avid
- Limited case reports and follow up available but appears more indolent than melanoma and clear cell sarcoma at the time of writing
- 4 of 48 published cases reported have shown regional or distant metastasis (Am J Surg Pathol 2022;46:1457, Histopathology 2023;82:368, Am J Surg Pathol 2019;43:861, J Cutan Pathol 2024;51:181)
- A recent additional case of CRTC1:TRIM11 cutaneous tumor (CTCT) with regional lymph node metastasis was presented at the American Society of Dermatopathology in 2023 (Tseng, et al.: CRTC1::TRIM11 Cutaneous Tumor With Ulceration and Sentinel Lymph Node Metastasis, oral presentation at American Society of Dermatopathology, Oct 2 - 8, 2023)
- 5 year old girl with right upper arm lesion (J Cutan Pathol 2022;49:1025)
- 27 year old man with fourth finger mass (Cureus 2022;14:e33179)
- 77 year old man with right thigh lesion (Pathol Int 2019;69:496)
- Other than complete surgical excision, optimal treatment is unknown
- Circumscribed tumors with pale, firm cut surface without pigmentation
- Mean size: 1.4 cm (0.4 - 5.1 cm) (Histopathology 2023;82:368)
- Morphology is uniform and resembles clear cell sarcoma
- Circumscribed, unencapsulated dermal nodule, no / very rare pigment, with only rare cases showing epidermal involvement (J Cutan Pathol 2022;49:1025)
- Some cases show extension into subcutis (Am J Surg Pathol 2019;43:861)
- Characteristic pattern of nests and intersecting (occasionally herringbone to vaguely palisaded) fascicles of uniform epithelioid to spindled cells with intervening delicate collagen bands (Am J Surg Pathol 2022;46:1457)
- Abundant pale eosinophilic cytoplasm, monomorphic nuclei with vesicular chromatin and prominent nucleoli
- Mitotic figures present (Am J Surg Pathol 2022;46:1457)
- Necrosis reported but uncommon (Am J Surg Pathol 2022;46:1457)
- Lymphovascular and perineural invasion uncommon (Am J Surg Pathol 2022;46:1457)
- Pigment and multinucleate giant cells may very rarely be seen
- A recent case of CTCT with ulceration was reported (Tseng, et al.: CRTC1::TRIM11 Cutaneous Tumor With Ulceration and Sentinel Lymph Node Metastasis, oral presentation at American Society of Dermatopathology, Oct 2 - 8, 2023)
Contributed by Zaid Saeed Kamil, M.B.Ch.B., Stephen M. Smith, M.D. and Calvin Tseng, M.D.
- SOX10 diffuse positive in all cases (Am J Surg Pathol 2022;46:1457)
- MITF diffuse positive in majority of cases (J Cutan Pathol 2022;49:1025)
- S100 diffuse positive in 44%, partial positive in 36% (Am J Surg Pathol 2022;46:1457)
- MelanA diffuse positive in 9%, partial positive in 52% (Am J Surg Pathol 2022;46:1457)
- HMB45 diffuse positive in 4%, partial positive in 52% (Am J Surg Pathol 2022;46:1457)
- Ki67 5 - 20% (Am J Surg Pathol 2018;42:382)
- Pan-TRK diffuse cytoplasmic positive in 57%, partial cytoplasmic positive in 36% despite lack of TRK mutations (Am J Surg Pathol 2022;46:1457)
- TRIM11 diffuse nuclear positive in 94% (Am J Surg Pathol 2022;46:1457)
- CRTC1::TRIM11 fusion (Am J Surg Pathol 2022;46:1457)
- No EWRS1 rearrangement (Am J Surg Pathol 2022;46:1457)
- No melanoma driver mutations (Am J Surg Pathol 2022;46:1457)
- No NTRK fusions despite positivity for pan-TRK immunohistochemistry (Am J Surg Pathol 2018;42:382)
CRTC::TRIM11 cutaneous tumor
- Skin, amputation, right fifth toe:
- CRTC1::TRIM11 cutaneous tumor (see comment)
- Comment: The neoplasm is composed of intersecting fascicles and nests of relatively uniform epithelioid and spindled cells with intervening bands of fibrocollagenous stroma. The neoplastic cells have abundant amounts of amphophilic to eosinophilic cytoplasm and moderately pleomorphic nuclei with prominent nucleoli. Mitotic figures including deep mitoses are identified. There is no evidence of necrosis, lymphovascular invasion or perineural invasion. The neoplastic cells are diffusely positive for SOX10, patchy positive for S100 and negative for MelanA and HMB45. Molecular analysis demonstrated the presence of CRTC1::TRIM11 fusion. Overall, the features are compatible with the recently described CRTC1::TRIM11 cutaneous tumor. Based on the limited reported cases and limited follow up data, the clinical course was indolent in most of the reported cases. However, 4 of the reported cases presented with regional nodal metastasis or distant metastasis as of January 2024. The available data at the time of this report suggest that these tumors have at least some malignant potential.
- Clear cell sarcoma:
- Predominantly affects adults ages 30 - 40s
- Often deeper location (associated with tendons or aponeuroses)
- Infiltrative growth
- May have clear cells and melanin pigment
- Wreath-like multinucleated tumor giant cells
- More consistently expresses S100, MelanA and HMB45
- Has ESWR1 translocations, most commonly EWSR1::ATF1 or EWSR1::CREB1
- Lacks CRTC1::TRIM11 fusion
- More aggressive behavior
- Melanoma:
- In situ component (may not be present for previously excised melanoma, metastatic melanoma or primary dermal melanoma)
- Infiltrative growth
- Pleomorphic cytology
- Pigment production
- More consistently expresses S100, MelanA and HMB45 (other than in desmoplastic melanoma)
- PRAME positive
- Has melanoma driver mutations
- Lacks CRTC1::TRIM11 fusion
- More aggressive behavior
- Spitz tumor:
- Cellular blue nevus:
- Myoepithelial tumors:
- Epithelioid schwannoma:
- MITF negative
- 40% show loss of INI1 (Am J Surg Pathol 2017;41:1013)
- Lacks CRTC1::TRIM11 fusion
- Epithelioid MPNST:
- PEComa:
- MITF pathway activated melanocytic tumors:
A superficial dermal tumor with the above histology is identified. IHC shows diffuse SOX10 positivity, diffuse MITF positivity, partial S100 positivity, partial MelanA positivity and partial HMB45 positivity. PRAME IHC is negative. Molecular investigations identify a CRTC1::TRIM11 fusion. Is it important to differentiate this entity from melanoma and clear cell sarcoma and why?
- No, as this entity currently appears to behave similarly to melanoma and clear cell sarcoma
- No, as this entity is currently thought to be a subtype of melanoma
- Yes, as this entity currently appears to behave less aggressively than melanoma and clear cell sarcoma
- Yes, as this entity currently has specific targeted treatments available
Comment Here
Reference: CRTC1:TRIM11 cutaneous tumor
- Absence of mitotic activity
- Presence of an epidermal component
- Presence of CRTC1::TRIM11 fusion
- Presence of infiltrative growth
Comment Here
Reference: CRTC1:TRIM11 cutaneous tumor
- Benign epidermal tumor, typically of the leg, with acanthosis and accumulation of glycogen in keratinocytes leading to pale staining cytoplasm
- Benign intraepithelial tumor composed of pale staining, glycogen rich keratinocytes
- Pink to tan papule or plaque on the distal lower extremity of older adults
- Histologic features include bland, pale keratinocytes with abrupt transition to normal epidermis, often associated with psoriasiform hyperplasia with scattered neutrophils
- Pale cell acanthoma (of Degos)
- Degos acanthoma
- Acanthome cellules claires of Degos and Civatte (StatPearls: Clear Cell Acanthoma [Accessed 21 July 2023])
- 80% of cases on legs
- No gender proclivity
- Occurs most commonly between ages 50 and 70 (Dermatopathol 2020;7:26)
- Distal lower extremities of middle aged and older individuals
- Other sites reported, in order of frequency: trunk, especially back, abdomen, head, upper extremities (StatPearls: Clear Cell Acanthoma [Accessed 21 July 2023])
- Possible upregulation of KGF (keratinocyte growth factor)
- Defect in phosphorylase enzyme leads to intracellular glycogen accumulation
- Reference: Exp Dermatol 2006;15:762
- Unknown
- Hypotheses
- Inflammatory epithelial hyperplasia (reactive)
- Produces similar cytokeratin as in psoriasis (Dermatopathol 2020;7:26)
- Associated with other inflammatory dermatoses, such as stasis dermatitis, bacterial and viral dermatoses, atopic dermatitis and insect bite reactions (Dermatopathol 2020;7:26)
- Variation of seborrheic keratosis
- Inflammatory epithelial hyperplasia (reactive)
- Well demarcated, pink to brown papule or plaque
- Usually 0.5 - 2.0 cm in diameter
- Peripheral rim of scale and central erythema with puncta that bleed easily upon trauma
- Associated with crust from weeping
- Polypoid, pigmented and giant variants (up to 6 cm) have been described
- Dermoscopic findings
- Dotted blood vessels lined up in strings with white surrounding halo
- Vascular lines may be coiled (glomerular) or more rarely in a hairpin-like structure
- References: J Am Acad Dermatol 2015;72:S47, Dermatopathol 2020;7:26
- Skin biopsy or excision
- 22 year old woman with clear cell acanthoma with melanophages simulating a spitz nevus (Dermatol Pract Concept 2021;11:e2021089)
- 33 year old woman with clear cell acanthoma developing in epidermal nevus (J Dermatol 1997;24:601)
- 58 year old woman with erythematous lesion on the hard palate (Head Neck Pathol 2020;14:535)
- 60 year old woman with clear cell acanthoma developing on a psoriatic plaque (Br J Dermatol 2000;142:842)
- 64 year old man with lower leg lesion and ichthyosis (Arch Dermatol 1972;105:371)
- 78 year old man with clear cell acanthoma with malignant cytologic features (Dermatopathol 2022;9:355)
- Preferred management is with complete removal
- Location, size and number of lesions should be considered
- Methods
- Shave removal or curettage followed by electrofulguration
- Electrofulguration alone
- Surgical excision
- Cryotherapy or carbon dioxide laser (when there are multiple lesions)
- Reference: StatPearls: Clear Cell Acanthoma [Accessed 21 July 2023]
- Well demarcated, pink to brown papule or small plaque
- Bland, intraepithelial tumor of clear, glycogen rich keratinocytes
- Abrupt transition to normal epidermis (Dermatopathology (Basel) 2020;7:26)
- Often in a pattern of psoriasiform hyperplasia
- Parakeratosis
- Typically lacks the thinning of the suprapapillary plate seen in psoriasis
- With or without colonization with melanocytes
- Often the vessels within the dermal papillae are dilated, tortuous and run vertically up the papillae
- Often spares hair follicles / adnexal structures
- Some cases have hyperplasia of underlying sweat ducts
- Reference: Dermatopathology (Basel) 2020;7:26
- PAS (diastase sensitive due to glycogen accumulation)
- Keratin, filaggrin and involucrin
- Strong diffuse EMA (epithelial membrane antigen) positivity
- References: J Cutan Pathol 1988;15:27, Br J Dermatol 1967;79:249
- Carcinoembryonic antigen (CEA)
- Phosphorylase negative (cytochemical stain), except in the basal layer
- References: J Cutan Pathol 1988;15:27, Br J Dermatol 1967;79:249
Clear cell acanthoma
- Skin, right lower leg, biopsy:
- Clear cell acanthoma
- Squamous cell carcinoma in situ:
- Squamous cell carcinoma in situ may have clear cell variant
- Cells are pleomorphic with increased N:C ratio
- Has full thickness atypia
- Psoriasis vulgaris:
- Elongation of rete ridges, thinning of suprapapillary plates
- Lymphocytic infiltrate in upper and middle portions of dermis
- Lacks the sharply demarcated lateral boundaries and glycogenation
- Lacks string-like arrangement of vessels on dermoscopy
- Seborrheic keratosis:
- Hyperkeratotic with horn pseudocysts
Comment Here
Reference: Clear cell acanthoma
- Rare condition of unknown histogenesis and pathogenesis, predominantly described in Asian children
- Originally proposed to be related to Toker's clear cells of the nipple (Am J Surg Pathol 1987;11:827)
- May be a genetic predisposition based on positive family history in some cases
- Manifests in early childhood, majority before age 2
- Rare in adults
- No gender predilection
- Predominantly described in Asian and Hispanic populations
- Presents as multiple white hypopigmented macules or papules most commonly on the pubic area and lower abdomen
- Less commonly on face, chest, anterior trunk, axilla
- Can be linear, and may develop along the 'milk line'
- Range from 2 - 10 mm in size
- Usually 10 - 20 lesions, with range from 5 to more than 100
- Hypopigmented to depigmented macules or barely palpable papules
- 16 month old girl and 2 year old boy (Arch Pathol Lab Med 2004;128:e149, Dermatol Online J 2008;14:19)
- 18 month old boy and 6 year old sister (Arch Dermatol 2007;143:358)
- Clear cell papulosis (pagetoid papulosis) in a non-Asian patient (Dermatology 2001;203:260)
- Benign asymptomatic lesions, no known treatments
- Lesions may decrease in number or disappear over time (J Am Acad Dermatol 2010;63:266)
- Small hypopigmented macules or papules
- Intraepidermal oval to round cells with ample pale clear cytoplasm, single or in clusters
- Clear cells predominantly among basal cells but some may be in the suprabasal epidermal layers
- Larger than adjacent keratinocytes
- Nucleoli tiny or indistinct
- Mitotic figures rare and no pleomorphism
- Epidermis mildy acanthotic with mild hyperkeratosis
- Decreased to absent pigmentation of basal epidermis (can be highlighted by Fontana-masson stain)
- GCDFP-15, pancytokeratin, CK7, CAM5.2, low molecular weight keratin, CEA, EMA
- Variably stained by mucin stains including PAS, mucicarmine, Alcian blue, colloidal iron
- Paget disease: histologic mimic - distinction is predominantly based on clinical findings (i.e. age of patient, location, number of lesions and clinical appearance)
- Pagetoid dyskeratosis: an incidental histologic finding - cells with a pyknotic nucleus, a clear halo, and a rim of pale cytoplasm; clear cells at higher levels in epidermis, negative for PAS / mucicarmine,
- Also called desmoplastic fibroblastoma
- Rare paucicellular tumor consisting of dense collagen fibers with scattered stellate and spindled fibroblasts involving the subcutis or skeletal muscles
- Benign clinical behavior with no reported tumor recurrence
- Most frequently found in the subcutis, with up to 25% found in the skeletal muscles (Hum Pathol 1998;29:676)
- Essential to distinguish from other more aggressive fibroblastic and myofibroblastic neoplasms
- Treatment is simple excision
- Desmoplastic fibroblastoma
- ICD-O: 8810/0 - desmoplastic fibroblastoma
- ICD-11: EE6Y & XH2ZF3 - other specified fibromatous disorders of skin and soft tissue & desmoplastic fibroblastoma
- Rare (largest series is 63 cases) (Hum Pathol 1998;29:676)
- M:F = 4:1
- Median age of 50 - 60 years
- Most common in upper extremities (Am J Surg Pathol 1995;19:1077)
- Followed by lower extremities (Hum Pathol 1998;29:676)
- Rarely head and neck (Clin Case Rep 2022;10:e6029)
- Translocation involving the long arm of chromosome 11, particularly 11q12
- Reported translocations include t(2;11)(q31;q12) and t(11;17)(q12;p11.2) (Cancer Genet Cytogenet 2004;149:161, Cancer Genet Cytogenet 2009;192:73, Cancer Genet 2011;204:569)
- 11q12 rearrangement results in the overexpression of FOSL1 (Histopathology 2016;69:1012, Lab Invest 2012;92:735, J Pathol 2023;259:119)
- Unknown at this time
- Solitary, painless, slow growing nodule (Hum Pathol 1998;29:676, In Vivo 2021;35:69)
- Size ranges from 1 to 20 cm (median size: 3 cm) (Hum Pathol 1998;29:676, In Vivo 2021;35:69)
- Histopathology is the gold standard for definitive diagnosis
- Relatively well defined, lobulated, increased soft tissue density (Skeletal Radiol 2019;48:637)
- Simple excision is curative
- No recurrence or metastasis reported (Am J Surg Pathol 1995;19:1077, Hum Pathol 1998;29:676)
- 45 year old man with mass in supraclavicular region (Ear Nose Throat J 2022 Aug 27 [Epub ahead of print])
- 56 year old woman with mass in the pleural cavity (Thorac Cancer 2021;12:2961)
- 61 year old man with painless mass on the left ring finger (Case Rep Oncol 2023;16:478)
- 66 year old woman with axillary mass (Case Rep Orthop 2020;2020:9780263)
- 79 year old man with chest wall mass (Surg Case Rep 2021;7:86)
- Surgical excision
- Firm, well circumscribed, lobulated mass (Hum Pathol 1998;29:676)
- Uniform white-gray cut surface
- No necrosis or hemorrhage
- Intraoperative frozen section analysis is usually not performed
- Well circumscribed but may infiltrate fat or less commonly skeletal muscles (Hum Pathol 1998;29:676)
- Hypocellular with fibromyxoid or collagenous stroma
- Bland spindled to stellate shaped fibroblasts
- Minimal vasculature
- Minimal to absent mitotic activity
- Cytology is usually not performed
- Immunohistochemical (IHC) stains are usually not needed for diagnosis
- Most IHC stains are nonspecific
- Diffuse and strong nuclear reactivity with FOSL1 (In Vivo 2021;35:69)
- Variable SMA positive
- Rare focal keratin expression
- CD34
- Desmin
- S100
- EMA
- Beta catenin
- MUC4
- References: In Vivo 2021;35:69, J Cutan Pathol 2024;51:70
- Electron microscopy is not usually performed
- Tumor cells show features of fibroblasts and myofibroblasts
- Translocations involving 11q12, including t(2;11)(q31;q12) and t(11;17)(q12;p11.2) (Cancer Genet Cytogenet 2004;149:161, Cancer Genet Cytogenet 2009;192:73, Cancer Genet 2011;204:569)
Desmoplastic fibroblastoma (collagenous fibroma) versus sclerotic / plywood fibroma
Desmoplastic fibroblastoma (collagenous fibroma)
- Skin, chest, biopsy:
- Collagenous fibroma (desmoplastic fibroblastoma) (see comment)
- Comment: Sections demonstrate a well circumscribed hypocellular proliferation of stellate fibroblasts in a collagenous stroma, consistent with a collagenous fibroma (desmoplastic fibroblastoma).
- Desmoid type fibromatosis:
- Predominantly affects young adults (mean age: 41)
- Deep seated soft tissue tumors, subdivided into extra-abdominal, abdominal and intra-abdominal
- May be associated with Gardner syndrome
- Locally aggressive, nonmetastasizing
- Long fascicles of bland fibroblasts and myofibroblasts
- Usually more cellular than collagenous fibroma, except for the hypocellular variant
- Conspicuous thin walled blood vessels with perivascular edema and lymphoid aggregates
- Beta catenin nuclear staining
- Mutations CTNNB1 (sporadic) and APC (familial)
- Low grade fibromyxoid sarcoma:
- Predominantly affects young adults (mean age: 35 - 45)
- Deep seated soft tissue tumors of proximal extremities and trunk
- Protracted clinical course with high risk of local recurrence and late metastasis
- Short fascicles of bland spindle fibroblasts in alternating myxoid and collagenous stroma
- Curvilinear blood vessels (Int J Clin Exp Pathol 2018;11:5860)
- MUC4 positive
- FUS::CREB3L2, FUS::CREB3L1 and rarely EWSR1::CREB3L1 fusions
- Fibroma of tendon sheath:
- Predominantly affects young to middle aged adults (median age: 31)
- Arises from synovium of tendon sheath in small distal joints
- 5 - 10% risk of recurrence
- Well circumscribed paucicellular tumor with bland fibroblasts, collagenous stroma and slit-like vessels
- SMA positive; may be focal
- Desmin and nuclear beta catenin negative
- USP6 gene rearrangement by FISH
- t(2;11)(q31;q12)
- t(7;16)(q32-34;p11) FUS::CREB3L2 fusion
- t(17;22)
- USP6 gene rearrangement
Comment Here
Reference: Collagenous fibroma
Comment Here
Reference: Collagenous fibroma
- Rare connective tissue hamartoma derived from cells of mesodermal origin
- May be syndromic (Proteus syndrome, tuberous sclerosis, others) or isolated (collagenoma)
- 8 year old girl with connective tissue nevus with zosteriform distribution (Pediatr Dermatol 2007;24:557)
- 8 year old boy with linear connective tissue nevus (Pediatr Dermatol 2007;24:439)
- 25 year old man with 40 nodules / papules distributed in zosteriform pattern (Am J Dermatopathol 2007;29:303)
- Benign vascular tumor comprised of solid sheets of epithelioid endothelial cells in the superficial dermis
- May be mitotically active
- Strongly positive for vascular markers
- Benign clinical behavior with no reported adverse outcomes
- Located in superficial dermis, well circumscribed, sheets of epithelioid cells with intracytoplasmic vacuoles
- Significant histomorphologic overlap with epithelioid hemangioma (EH) / angiolymphoid hyperplasia with eosinophilia (ALHE)
- Essential to distinguish from other more aggressive epithelioid neoplasms
- Treatment is simple excision
- CEAN
- Very rare (< 70 cases reported in the English literature) (J Cutan Pathol 2022;49:765)
- Wide age range (14 - 84 years old)
- Slight male predominance (M:F = 1.4:1)
- Most commonly trunk and extremities (J Cutan Pathol 2022;49:765)
- Can also occur on head and neck
- Nasal cavity
- Largely unknown at this time
- Some experts suggest it may be reactive (Am J Dermatopathol 2004;26:14)
- Some experts consider it to be a variant of EH / ALHE (Am J Dermatopathol 2008;30:16)
- Unknown at this time
- Most commonly a solitary lesion but may be multiple
- Red to violaceous vascular nodule; may be painful
- Histopathology is the gold standard for definitive diagnosis
- Dermal based, palpable; imaging studies are usually not necessary
- In cases involving nasal cavity, a homogenous mass is seen on noncontrast CT
- Generally does not recur (Am J Dermatopathol 2004;26:14, J Cutan Pathol 2022;49:765)
- No reports of distant metastasis
- 19 year old man with left foot mass (World J Clin Cases 2020;8:600)
- 28 year old woman with right breast nodule (Indian Dermatol Online J 2019;10:463)
- 30 year old man with nodule in pre-existing port wine stain on the chest (Acta Derm Venereol 2017;97:135)
- 84 year old man with multiple papules on scalp and neck (Am J Dermatopathol 2011;33:831)
- Surgical excision
- Well circumscribed, solid, hemorrhagic nodule in the dermis (Indian Dermatol Online J 2019;10:463)
- Frozen sections usually not performed
- Dermal based (Acta Derm Venereol 2017;97:135, Am J Dermatopathol 2008;30:16)
- Well circumscribed
- Nodular proliferation of epithelioid cells with vesicular chromatin, prominent nucleoli and abundant eosinophilic to clear cytoplasm
- Mitotic figures can be present but not numerous (up to 5/10 high power fields) and without atypical forms
- In exceptional cases, moderate cytologic has been reported (Diagn Pathol 2018;13:50)
- Vascular channel formation is focal but intracytoplasmic lumina are common
- Vascular channels are lined by a single layer of constituent cells
- Mild background chronic lymphoplasmacytic inflammation with scattered eosinophils
- Hemosiderin deposition may be seen
- Skin, chest, biopsy:
- Cutaneous epithelioid angiomatous nodule (see comment)
- Comment: The biopsy demonstrates a well circumscribed nodule, comprised of sheets of epithelioid cells in the superficial dermis. The epithelioid cells are relatively monomorphous and have intracytoplasmic vacuoles. Rare vascular channel formation is noted. A mild stromal lymphocytic and eosinophilic inflammatory infiltrate is present at the periphery. Immunohistochemistry shows that the epithelioid cells are positive for CD34 and ERG. The overall histopathologic and immunohistochemical findings are consistent with cutaneous epithelioid angiomatous nodule, a benign vascular neoplasm with a very low risk of local recurrence and no metastatic potential.
- Epithelioid hemangioma (EH) / angiolymphoid hyperplasia with eosinophilia (ALHE):
- More commonly affects head and neck (Adv Anat Pathol 2019;26:186)
- Considerable histopathologic overlap with CEAN
- More prominent, well formed vasculature
- May involve deep dermis and subcutis
- Hobnail-like endothelial cells
- FOS gene rearrangement may be found in a subset of intraosseous and soft tissue lesions (Am J Surg Pathol 2015;39:1313)
- FOSB fusion with ZNF36 or WWTR1 reported in rare EHs with atypical features (Genes Chromosomes Cancer 2014;53:951)
- Some experts think that CEAN is a variant of EH / ALHE
- Epithelioid angiosarcoma:
- Infiltrative, architecturally complex (Adv Anat Pathol 2019;26:186)
- Significant cytologic atypia
- Mitotic figures, including atypical forms
- May have necrosis
- Destruction of native structures
- Epithelioid hemangioendothelioma:
- Cords and nests of epithelioid, lightly eosinophilic cells (Adv Anat Pathol 2019;26:186)
- Nonvasoformative
- Fibromyxoid stroma
- Cytologic atypia and mitotic figures common
- WWTR1::CAMTA1 fusion (Genes Chromosomes Cancer 2011;50:644)
- YAP1::TFE3 fusion (Genes Chromosomes Cancer 2013;52:775)
- Nonvascular neoplasms:
Comment Here
Reference: Cutaneous epithelioid angiomatous nodule
- Indolent
- Locally aggressive
- Potentially metastatic
- Recurs frequently
Comment Here
Reference: Cutaneous epithelioid angiomatous nodule
- Benign nonepithelial tumors arising from mesodermal tissue
- Common benign cutaneous tumor
- On eyelids, flexural areas
- F = M
- Associated with trauma, obesity, diabetes mellitus, pregnancy
- Acrochordon, soft fibroma, fibroma molle, skin tag
- 50+ years of age (Dermatologica 1987;174:180)
- Incidence: 46 - 64% in people > 50 years (Dermatologica 1987;174:180)
- F = M (Dermatologica 1987;174:180)
- Causal connections: obesity (Eur J Dermatol 2012;22:106)
- Eyelids
- Flexural areas: axillae, groin
- Lateral neck
- Inframammary
- Trauma → mast cell recruitment → upregulation of TNF-α → fibroblast proliferation and mitogenicity (Indian J Dermatol 2011;56:641)
- Growth factors → keratinocyte and fibroblast proliferation (Clin Cosmet Investig Dermatol 2019;12:255)
- Loss / downregulation of hamartin and tuberin (inactivating tumor suppressor proteins) (J Cutan Pathol 2004;31:383)
- Human papillomavirus (HPV) (Iran J Basic Med Sci 2012;15:840)
- The etiology is not clear nor the same for every FEP; reported associations include:
- Trauma (Indian J Dermatol 2011;56:641)
- Diabetes mellitus, metabolic syndrome (Eur J Dermatol 2012;22:106)
- Polycystic ovary syndrome (Australas J Dermatol 2019;60:70)
- Hormonal replacement therapy (Australas J Dermatol 2019;60:70)
- Acromegaly (Acta Dermatovenerol Croat 2013;21:224)
- HPV 6 and 11 (Indian J Dermatol Venereol Leprol 2008;74:222)
- Lymphedema (APMIS 2008;116:215)
- Clinical appearance:
- Small soft papules, pedunculated or filiform, 2 - 5 mm, rough surface
- Pendulous fibromas can be large (several centimeters) (Australas J Dermatol 2019;60:70)
- May be multiple (Dermatologica 1987;174:180)
- Look for associated disease / physiologic states including:
- Diabetes mellitus / insulin resistance (Eur J Dermatol 2012;22:106)
- Hyperlipidemia
- Familial predisposition
- Pregnancy (J Am Acad Dermatol 1984;10:929)
- Lymphedema (APMIS 2008;116:215)
- Characteristic clinical features and histopathology
- Benign
- 19 year old woman presents with an 18 month history of a slowly enlarging and painless 20 cm vulval mass (BMJ Case Rep 2019;12:e230449)
- 23 year old woman presents with a 9 year history of a progressively enlarging vulval mass (Australas J Dermatol 2019;60:70)
- 55 year old man presents with a painless swelling on his right back (Dermatol Surg 2009;35:1804)
- 57 year old man presents with swelling of the nasal conjunctiva and a 2 year old boy presents with numerous swellings around the right lower eyelid and ocular surface (Arq Bras Oftalmol 2019;82:239)
- 63 year old man presents with a 4 month history of lower urinary tract symptoms (APMIS 2008;116:215)
- Topical anesthetic may be used prior to procedure (Aesthetic Plast Surg 2015;39:644)
- Surgical removal / snip excision (Aesthetic Plast Surg 2015;39:644)
- Cryotherapy (Aesthetic Plast Surg 2015;39:644)
- Shave excision (Aesthetic Plast Surg 2015;39:644)
- Electrodissection (Am Fam Physician 2002;66:1259)
- Ligation (J Dermatol Surg Oncol 1994;20:151)
- Sessile or pedunculated polyp
- 2 - 5 mm to several centimeters (Australas J Dermatol 2019;60:70)
- Surface smooth or filiform
- Smaller ones may be pigmented
- Larger ones are skin colored
- Epidermis may be hyperplastic and papillomatous and may have keratotic cysts and pigment in basal epidermal keratinocytes
- Loose fibrocollagenous stroma, abundant vessels
- Usually no adnexa
- Variable adipose tissue in larger ones - lipofibroma
- Traumatic changes: lichen simplex chronicus, epidermal necrosis, ulceration, pagetoid dyskeratosis, lichen sclerosus-like change (Am J Dermatopathol 2006;28:478, Am J Dermatopathol 2019;41:e64)
- Pseudosarcomatous change: pleomorphic stellate stromal cells, multinucleated stromal cells, myxoid to collagenous stroma (Ann Diagn Pathol 2008;12:440)
- On IHC, the pleomorphic cells stain diffusely for vimentin; there is variable staining for CD34 and factor 13a and the cells do not stain for SMA or desmin (Ann Diagn Pathol 2008;12:440)
- Some of the lesions with pseudosarcomatous change overlap with pleomorphic fibroma
- A subset of cellular pseudosarcomatous fibroepithelial polyps occurs in the female genital tract including the vulva (Am J Surg Pathol 2000;24:231)
- Left neck, shave biopsy:
- Fibroepithelial polyp / acrochordon (see comment)
- Comment: A polyp covered by mildly acanthotic epidermis with mild hyperkeratosis. There is a mildly cellular fibrovascular core with scattered dilated small thin walled vessels and a sparse lymphocytic infiltrate. Dysplasia or malignancy is not seen.
- Polypoid / papillary variants of:
- Seborrheic keratosis (Arch Dermatol 1996;132:1459):
- Generally lacks the fibrovascular core of a fibroepithelial polyp
- Dermatosis papulosa nigra:
- Considered to be a seborrheic keratosis; however, it has a well developed fibrous stroma
- It is a clinically distinct entity (Clin Dermatol 2017;35:491)
- Verruca vulgaris / squamous cell papilloma (Australas J Dermatol 2019;60:70):
- Epidermal papillomatosis with coarse hypergranulosis
- May have koilocytosis
- Hyperkeratosis with columns of parakeratosis
- Melanocytic nevus (Arch Dermatol 1996;132:1459):
- Melanocytic proliferation within the polyp
- Commonly intradermal or compound
- Neurofibroma (Australas J Dermatol 2019;60:70):
- Cellular stromal proliferation of spindle cells with wavy nuclei
- Mast cells within the lesion
- Hemangioma and pyogenic granuloma (Arch Dermatol 1996;132:1459):
- Large number of vessels in the stroma
- Fibroepithelial tumor of Pinkus:
- Thin anastomosing strands of basaloid or squamous keratinocytes projecting downward from the epidermis in a fenestrated pattern
- Abundant fibrous stroma (Am J Dermatopathol 2005;27:149)
- Polypoid trichodiscomas and fibrofolliculomas in Birt-Hogg-Dubé syndrome:
- Infundibular structures in the stroma (Am J Dermatopathol 1999;21:369)
- Accessory tragus:
- Most commonly preauricular
- Vellus hairs, eccrine glands, adipose tissue and cartilage in the stroma (J Am Acad Dermatol 2007;56:AB54)
- Supernumerary digit:
- Congenital
- Increased peripheral nerves in the stroma (Arch Dermatol 1973;108:223)
- Acquired digital fibrokeratoma:
- Acral skin
- Marked epidermal acanthosis and hyperkeratosis
- Thickened stromal collagen parallel to the long axis of the lesion (J Am Acad Dermatol 1985;12:816)
- Seborrheic keratosis (Arch Dermatol 1996;132:1459):
Comment Here
Reference: Cutaneous fibroepithelial polyps
Comment Here
Reference: Cutaneous fibroepithelial polyps
- Rare neoplasm characterized by marked mononuclear infiltrate that appears to be integral component of tumor
- May be related to eccrine spiradenoma
- 70 year old Japanese man with lesion on face (Case Rep Dermatol 2012;4:50)
- Firm, well-demarcated nodule
- Multiple rounded lobules of basaloid cells with some peripheral palisading, focal keratinization, occasional duct formation and mixed with small lymphocytes
- Stroma: Alcian blue
- Ducts: AE1/AE3
- Basal cell carcinoma
- Trichoblastoma
- Heterogeneous group of disorders with benign T or B cell lymphocytic infiltrates in the skin that mimic cutaneous lymphomas both clinically and histologically (J Am Acad Dermatol 1998;38:877)
- Typically presents as a solitary nodule in the head and neck region
- Spontaneous regression is common; excellent prognosis
- Idiopathic; however, some cases are associated with specific antigenic stimuli or triggering factors (e.g., drugs, tattoos, vaccinations, arthropod bites and infections)
- Classically characterized by a dermal lymphoid infiltrate composed predominantly of reactive polyclonal lymphocytes with a variable admixture of other inflammatory cells
- Although typically absent, clonal T or B cell populations can occasionally be seen in cutaneous lymphoid hyperplasia
- Pseudolymphoma, lymphocytoma cutis, lymphadenosis benigna cutis
- Can affect all age groups
- Slight female predilection; M:F = 1:2 - 3 (Hum Pathol 2003;34:617)
- Can involve any area of the skin
- Most commonly arises in the head and neck regions (particularly the face), followed by the extremities and trunk
- Largely unknown but thought to be a reactive process to certain antigenic stimuli
- Often idiopathic
- Various antigenic stimuli or triggering factors (e.g., medications, tattoos, vaccinations, arthropod bites, infections with various pathogens, especially with Borrelia burgdorferi) have been reported (Hum Pathol 2003;34:617, Acta Derm Venereol 2018;98:310, J Cutan Pathol 2020;47:76)
- Solitary nodule or localized cluster of red to violaceous papulonodules
- Requires thorough clinical and histopathologic evaluation and acquisition of appropriate clinical history to identify possible triggering factors
- In the absence of an identifiable triggering factor, it may pose a diagnostic challenge to pathologists and may potentially be misdiagnosed as a neoplastic process, especially if clonality is found in the cutaneous infiltrate
- Historically divided into 3 categories based on the predominant cell type in the infiltrate (J Am Acad Dermatol 1998;38:877, Hum Pathol 2003;34:617):
- B cell predominant type
- T cell predominant type
- Mixed B cell / T cell type
- Newly proposed classification divides cutaneous lymphoid hyperplasia into 4 major groups, based on both histologic and clinical features (J Cutan Pathol 2020;47:76):
- Nodular cutaneous lymphoid hyperplasia
- Cutaneous lymphoid hyperplasia mimicking mycosis fungoides or other cutaneous T cell lymphomas
- Other cutaneous lymphoid hyperplasia with distinct clinical features (e.g., acral pseudolymphomatous angiokeratoma, T cell rich angiomatoid polypoid pseudolymphoma, primary cutaneous angioplasmocellular hyperplasia, lymphoplasmacytic plaque, cutaneous plasmacytosis)
- Intravascular cutaneous lymphoid hyperplasia
- Nodular type is the most common form and encompasses nodular B cell cutaneous lymphoid hyperplasia, Borrelia associated nodular B cell cutaneous lymphoid hyperplasia (also known as lymphocytoma cutis or lymphadenosis benigna cutis), nodular T cell and mixed cutaneous lymphoid hyperplasia and nodular CD30+ cutaneous lymphoid hyperplasia (J Cutan Pathol 2020;47:76)
- Benign clinical course
- Spontaneous regression is common following excision or topical / intralesional corticosteroids
- May rarely recur
- Almost never progresses to an overt lymphoma (although rare anecdotal examples of such progression have been described) (Am J Pathol 1989;135:13, Hum Pathol 2003;34:617)
- 25 year old woman with pruritic papulovesicular lesions on the right shoulder (J Investig Allergol Clin Immunol 2018;28:199)
- 36 year old woman with a pruritic erythematous nodule on the left forearm (Indian J Dermatol Venereol Leprol 2021;87:748)
- 48 year old woman with a red erythematous nodule on the right medial cheek (CMAJ 2018;190:E398)
- 78 year old woman with a pink papule on the right arm (JAAD Case Rep 2022;20:26)
- 81 year old woman with a rapidly enlarging, solitary lesion on the left lateral trapezial neck (Am J Dermatopathol 2022;44:226)
- Observation
- Antibiotics, topical or intralesional corticosteroids, surgical excision or localized radiotherapy
- Less commonly, intralesional rituximab or methotrexate (Clin Lymphoma Myeloma Leuk 2011;11:286, Dermatol Online J 2021;27)
- Dermal lymphoid infiltrate, forming nodules or diffuse sheets (particularly in nodular cutaneous lymphoid hyperplasia), without significant epidermal involvement
- Grenz zone, between the dermal infiltrate and the overlying epidermis, is frequently found
- Perivascular and periadnexal distribution patterns may also be seen
- Although typically intradermal, the infiltrate may also occasionally extend into the superficial subcutis
- Prominent lymphocytic exocytosis may occasionally be seen mimicking other cutaneous T cell lymphomas, such as mycosis fungoides
- Infiltrate predominantly composed of small to medium sized lymphocytes, often indistinguishable from those seen in primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder, with variable admixture of other inflammatory cells (e.g., histiocytes, eosinophils, plasma cells)
- Well formed reactive germinal centers may or may not be seen
- If present, reactive germinal centers often show tingible body macrophages and preservation of polarity and mantle zone
- Immunophenotype is variable depending on the predominant component of the infiltrate (Hum Pathol 2003;34:617)
- In general, the infiltrate is composed of mixed T cells (CD3+) and B cells (CD20+)
- Although variable depending on the subtypes of cutaneous lymphoid hyperplasia, T cell component may show an increased CD4:CD8 ratio
- B cell component expresses CD20, CD79a and BCL6
- Subset of T cells may express follicular helper T cell markers (PD-1, BCL6, CXCL13)
- Plasma cells are usually polytypic (mixed kappa and lambda positive plasma cells)
- T cell component may show partial loss of CD7 and less commonly, CD5 (loss of pan T cell markers, particularly isolated loss of CD7, however, is not pathognomonic for neoplastic processes)
- B cell component lacks BCL2, CD5 or cyclin D1 expression; the mantle zone cells will express BCL2 in cases with well formed germinal centers
- B cell component lacks CD43 coexpression
- CD30, EBER
- CD30 can be positive in T cell variants, particularly with persistent arthropod bite reactions, molluscum contagiosum, HSV infection, etc.
- Scattered cells versus sheets or clusters and weak staining may favor CLH over neoplasia
- Typically, clonal T or B cell population is absent
- Clonal T cell gene rearrangements or immunoglobulin heavy chain gene rearrangements may occasionally be seen (so called, clonal cutaneous lymphoid hyperplasia; reported frequency varies from 4 - 62% depending on the published series) (Hum Pathol 2003;34:617, Arch Dermatol 1999;135:168, Am J Dermatopathol 2005;27:375, Arch Dermatol 2006;142:1561, Am J Surg Pathol 1995;19:12, Am J Pathol 1989;135:13)
- Skin, right arm, punch:
- Nodular dermal lymphohistiocytic infiltrate admixed with scattered eosinophils, consistent with cutaneous nodular hyperplasia (see comment)
- Comment: Sections show a nodular dermal lymphoid infiltrate without significant epidermal involvement. There is a grenz zone between the dermal infiltrate and the overlying epidermis. The infiltrate is forming nodules in the superficial and deep dermis, with focal perivascular and periadnexal distribution patterns and is predominantly composed of lymphocytes and histiocytes. Scattered eosinophils are also noted. Definitive germinal center formation is not identified. Immunohistochemical studies highlight the infiltrate to be composed of mixed CD3+ T cells and CD20+ B cells. The CD3+ T cells show a CD4:CD8 ratio of approximately 4:1. Anti-CD4 also highlights numerous background histiocytes. Anti-CD30 highlights scattered cells admixed within the infiltrate. Anti-PD-1 highlights areas with slightly increased PD-1+ T cells. Kappa and lambda by in situ hybridization fail to reveal increased monotypic plasma cells. Special stains (Fite, Gram and PAS) are negative for definitive fungal and bacterial (including mycobacterial) organisms. If available, correlation with the results of microbiology cultures is necessary. The histologic differential diagnoses include primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder and cutaneous lymphoid hyperplasia. Additional molecular studies by polymerase chain reaction for T cell receptor gene rearrangements fail to reveal monoclonal pattern of amplification of both TCRB and TCRG. Taken together, these morphologic, immunophenotypic and molecular features are consistent with cutaneous lymphoid hyperplasia in the appropriate clinical context. Clinical pathologic correlation and a close follow up are necessary.
- Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder:
- Distinction from cutaneous lymphoid hyperplasia (particularly nodular T cell and mixed type) is challenging due to frequently overlapping histologic (i.e., dense lymphoid infiltrate composed of small to medium sized lymphocytes involving the dermis or subcutis), immunophenotypic (i.e., CD3+, CD4+, CD8-, CD30- phenotype) and clinical (i.e., solitary plaque or nodule on the head and neck region) features
- Loss of 1 or more pan T cell markers (CD2, CD5 and CD7) more frequently seen in primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder than in cutaneous lymphoid hyperplasia
- Clonal T cell receptor gene rearrangements more commonly seen in primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder than in cutaneous lymphoid hyperplasia
- Presence of monoclonality, in the absence of identifiable triggering factors, favors primary cutaneous + small / medium T cell lymphoproliferative disorder over cutaneous lymphoid hyperplasia
- Primary cutaneous marginal zone B cell lymphoma:
- Simulates Borrelia associated nodular B cell cutaneous lymphoid hyperplasia
- Sheets of plasma cells and Dutcher bodies more frequently seen in primary cutaneous marginal zone B cell lymphoma than in cutaneous lymphoid hyperplasia
- Neoplastic B cells express BCL2 while lacking immunoreactivity for CD5, CD10, BCL6 and cyclin D1
- Neoplastic B cells may coexpress CD43
- Monotypic plasma cells with light chain restriction (either kappa or lambda) more frequently seen in primary cutaneous marginal zone B cell lymphoma than in cutaneous lymphoid hyperplasia
- Clonal immunoglobulin heavy chain gene rearrangements are more commonly seen in primary cutaneous marginal zone B cell lymphoma than in cutaneous lymphoid hyperplasia
- Mycosis fungoides:
- Cutaneous lymphoid hyperplasia may histologically mimic mycosis fungoides, particularly if the infiltrate is T cell predominant and shows prominent lymphocytic exocytosis
- Neoplastic cells of mycosis fungoides, however, typically exhibit cytologic atypia with hyperchromatic nuclei with irregular convoluted nuclear contours
- Both mycosis fungoides and cutaneous lymphoid hyperplasia can show an increased CD4:CD8 ratio in the infiltrate
- Presence of patches / plaques favors mycosis fungoides over cutaneous lymphoid hyperplasia
- Primary cutaneous follicular center lymphoma:
- May simulate nodular B cell cutaneous lymphoid hyperplasia
- Neoplastic follicles lack tingible body macrophages and have attenuated or absent mantle zones
- Neoplastic B cells express BCL6, CD10 (variable; positive in follicular pattern but generally negative in diffuse pattern) while typically lacking immunoreactivity for BCL2
Which of the following features would most likely favor a diagnosis of cutaneous lymphoid hyperplasia over primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder?
- Dermal lymphoid infiltrate predominantly composed of small to medium sized pleomorphic T cells
- Presence of B cells coexpressing CD43
- Presence of T cell receptor beta (TCRB) and gamma (TCRG) gene rearrangements
- Recent history of vaccination to the same site with an erythematous nodule
- Presence of PD-1+ and CXCL13+ cells in the infiltrate
Comment Here
Reference: Cutaneous lymphoid hyperplasia
- Clonal T cell receptor beta (TCRB) and gamma (TCRG) gene rearrangements are never found in cutaneous lymphoid hyperplasia
- Cutaneous lymphoid hyperplasia frequently progresses to a lymphoma
- Diagnosis of cutaneous lymphoid hyperplasia requires clinical and pathologic correlation
- Presence of monotypic plasma cells with kappa light chain restriction always favors a diagnosis of primary cutaneous marginal zone B cell lymphoma over cutaneous lymphoid hyperplasia
- Triggering factors or etiologic agents are always identified in cutaneous lymphoid hyperplasia
Comment Here
Reference: Cutaneous lymphoid hyperplasia
- Most cutaneous mast cell disorders have a good prognosis
- Mastocytosis: monomorphic population of mast cells with rare eosinophils
- Telangiectasia macularis eruptive perstans (TMEP): telangiectatic light or dark brown macules
- Urticaria pigmentosa: common form of mastocytosis, numerous small yellow brown papules, become hives when rubbed
- At birth or during the first 3 months of life
- May present with flushing attacks due to high histamine content
- Spontaneous involution frequently occurs
- CD117 mutations in patients with mastocytosis
- Urticaria pigmentosa: most common form of mastocytosis of skin; usually childhood onset of multiple brown macules; systemic variant is malignant and involves liver, spleen, bone marrow, lymph nodes and occasionally peripheral blood (mast cell leukemia)
- Darier's sign: stroking skin releases histamine, causing hives
- Dermatographism: dermal edema resembling hives due to stroking with pointed instrument
- Description:
- Solitary lesion, or small group as part of urticaria pigmentosa
- Affect extremities and trunk, not palms and soles
- May blister
- Red, brown pink or yellow nodules, or plaques measuring up to 1.0 cm
- 2 year old boy with itchy brown skin macules (Case of the Week #344)
- 53 year old man with erythematous macules and telangiectasia on arm (J Clin Aesthet Dermatol 2011;4:52)
- Within the macules and plaque, mast cells are predominantly in papillary dermis
- Mast cells are round or spindle shaped with abundant eosinophilic cytoplasm, distinct cytoplasmic boundaries, large pale nuclei
- Eosinophils are often present
- Also edema of papillary dermis, subepidermal vesiculation
- Bullous mastocytosis may be diagnosed by Tzank smear; infiltrate may be slight and perivascular
- In telangiectasia macularis eruptive perstans, features may be subtle, with increased mast cells around dilated superficial capillaries, basal cell hyperpigmentation of overlying epidermis, superficial lymphohistiocytic infiltrate
- Toluidine blue and Giemsa demonstrate metachromasia (granules are purple red)
- Leder (chloroacetate esterase), CD117 / c-kit
- Normal skin or dermatoses:
- Must search to find mast cells even with special stains
- Chronic dermatitis, nodular prurigo, and venous stasis:
- Typically associated with granulation tissue and foci of neovascularization
- Benign adnexal tumor of the skin composed of mesenchymal and sweat gland components
- Morphologically identical to pleomorphic adenoma / benign mixed tumor of salivary gland
- Most mixed tumors have both eccrine and apocrine components
- Most are currently classified as apocrine type
- Slow growing, painless nodule on head and neck
- Benign tumor of sweat glands with a myxoid stroma and cartilaginous metaplasia (Stedman: Medical Dictionary, 28th Edition, 2006)
- Other names include:
- Apocrine mixed tumor
- Eccrine mixed tumor
- Benign mixed tumor of skin
- Chondroid syringoma
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
- Less than 0.1% of cutaneous tumors (Dermatol Surg 2003;29:179)
- Middle aged men most commonly affected (J Am Acad Dermatol 2007;57:467)
- Head and neck region involvement is common (nose most common site)
- Extremities are less common (axilla most common site)
- Rare cases of scrotum reported (J Int Med Res 1996;24:482, Int J Urol 2008;15:944)
- Benign adnexal proliferation with a wide range of differentiation and metaplastic changes in its epithelial, myoepithelial and stromal components
- Unclear
- Benign; rarely recurs
- No distinctive clinical characteristics but may mimic pilomatricoma
- Most often seen in middle aged men; mean age at presentation is 48 years
- Most commonly in nose, followed by cheek and upper lip
- Face / head and neck > extremities, trunk or back
- Calcification / ossification may occur
- Typically small (0.5 - 3 cm) and painless
- No specific findings on dermoscopy
- Rapid, ulcerative growth can be seen in malignant mixed tumor
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- Biopsy required for diagnosis
- Findings are not highly specific for chondroid syringoma over other dermal and soft tissue neoplasms (Australas Radiol 2001;45:240)
- MRI can be helpful to determine the extent and depth of the lesion and relation to anatomic structures in large tumors
- In the few cases studied, radiography of malignant chondroid syringoma tends to show higher signal intensity and enhancement (Australas Radiol 2001;45:240)
- Benign, with rare recurrence
- Malignant counterpart (malignant chondroid syringoma) rare with high rate of metastasis (60%) and death (25%) and should be ruled out on microscopic morphology (Pathology 1994;26:237)
- 14 year old boy with eccrine spiradenoma with chondroid syringoma in Blaschkoid distribution (Indian J Dermatol Venereol Leprol 2009;75:600)
- 20 year old man with chondroid syringoma with extensive bone formation (J Clin Diagn Res 2014;8:FD15)
- 34 year old man with rapidly growing chondroid syringoma of external auditory canal (Case Rep Med 2011;2011:589680)
- 43 year old woman with chondroid syringoma of arm (Dermatol Online J 2006;12:14)
- 47 and 59 year old men whose tumors had prominent pilomatricomal component (J Cutan Pathol 2009;36:882, J Cutan Pathol 2012;39:718)
- 53 year old man with chondroid syringoma in the middle finger (Hand Surg Rehabil 2021;40:353)
- 55 year old man with 10 x 10 cm chondroid syringoma (Dermatol Surg 2003;29:977)
- 67 year old man with lipomatous mixed tumor with follicular differentiation (J Cutan Pathol 2006;33:389)
- 72 year old man with chondroid syringoma of the toe (Medicine (Baltimore) 2018;97:e9825)
- Apocrine mixed tumors of the skin with architectural or cytologic atypia (Am J Surg Pathol 2007;31:1094)
- Cutaneous apocrine mixed tumor with intravascular tumor deposits (Am J Dermatopathol 2011;33:775)
- Surgical excision is curative
- Recurrence is rare
- Electrodissection and CO2 laser have been used with slightly higher recurrence rate
- Reference: Dermatology Advisor: Chondroid Syringoma (Mixed Tumor of the Skin) [Accessed 17 June 2021]
- Nodular, circumscribed, nonulcerated, with marked variation in size
- Cut surfaces are tan-white, often with grossly apparent chondroid component
- Slow growing, painless, firm, deep dermal to subcutaneous nodule
- Well circumscribed but unencapsulated, multilobulated mass (separated by fibrous septae) centered in deep dermis or subcutaneous fat, with a prominent chondroid or myxoid stroma enveloping benign bland appearing epithelial and myoepithelial cells that form secondary structures (glands, ducts, cysts, reticular lace-like networks, nests)
- Biphasic, with both epithelial and stromal components
- Epithelial: elongated branching tubular structures with 2 cell layers
- Outer layer is cuboidal or columnar; inner layer is columnar with eosinophilic cytoplasm
- Decapitation type secretion, often squamous metaplasia and basal nuclei
- Often has areas of apocrine, follicular and sebaceous differentiation
- Presence of any follicular or sebaceous features rules out pure eccrine mixed tumor
- Wide array of morphologies can be seen with all types of differentiation along the folliculosebaceous unit
- Occasional cases have neoplastic tubules connecting directly to normal follicular infundibulum
- Follicular differentiation is the most common type of change in the epithelium and may include:
- Keratinous cysts with infundibular keratinization
- Isthmic epithelium
- Hair bulbs with papillary mesenchyme
- Matrical differentiation with basaloid, transitional and ghost cells
- Trichohyaline granules
- Vellous hair shafts
- Anagen differentiation
- Sebaceous differentiation may include single cells or islands of mature sebocytes
- Metaplastic epithelial changes include clear cell change, columnar change, cytoplasmic vacuolization (may be abortive luminal differentiation), hobnailing, mucinous, oxyphilic, squamous
- Metaplastic myoepithelial changes include clear cell change, collagenous spherulosis, hyaline cells, plasmacytoid cells, spindled cells
- Stroma: chondroid, mucoid or focally fibrous / hyaline
- Metaplastic stromal changes include adipocytic, chondroid and osseous metaplasia
- Adipocytic metaplasia may be extensive; some adipocytes may have Lochkern nuclei with a single small vacuole indenting the nucleus that resemble lipoblasts
- Epithelial: elongated branching tubular structures with 2 cell layers
- In contrast to eccrine mixed tumors, apocrine mixed tumors do not have clear cell change, cribriform areas, osseous metaplasia (prominent), physaliferous-like cells, pseudorosettes
- No pleomorphism or necrosis, sparse mitoses
- Benign tumors may have:
- Asymmetry
- Mild nuclear pleomorphism within the ductal component
- Multinucleated, bizarre, hyperchromatic cells
- Infiltrative or pushing borders
- Features suggestive of malignant transformation include:
- Severe atypia
- Markedly increased cellularity
- Increased mitotic rate
- Destruction of surrounding tissue
- Tumor necrosis
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- Many epithelial cells with bland nuclei in a chondromyxoid background
- Marked nuclear pleomorphism and prominent nucleoli may be used to identify malignant features on fine needle aspiration (Acta Cytol 1998;42:1155)
- Findings for diagnosis of chondroid syringoma on fine needle aspiration (Acta Cytol 2010;54:183)
- Fibrillary chondromyxoid background
- Prominent cellular component of epithelial and myoepithelial cells
- Absence of atypia and tumor diathesis (however, histology still required for definitive exclusion of malignant features)
- Immunohistochemistry generally not required for diagnosis
- Inner epithelial layer: keratin, EMA, CEA, GCDFP-15, actin, cytokeratin 15
- Outer myoepithelial layer / stromal component: S100, SOX10, NSE, GFAP, SMA, calponin, p63
- Variable SMA, GFAP
- p53 positivity of varying intensity
- PLAG1 nuclear expression in apocrine mixed tumors (Am J Dermatopathol 2020;42:251)
- Desmin (usually) (J Clin Pathol 2007;60:145)
- p16 negative, in contrast to strong nuclear positivity in malignant chondroid syringoma (CRCP 2015;2:28)
- Positive for gene rearrangement of PLAG1 in largest study to date but lacks the characteristic translocations of PLAG1 seen in pleomorphic adenoma of salivary gland (Genes Chromosomes Cancer 2012;51:140, Virchows Arch 2011;459:539)
- Small subset with ESWR1 rearrangement (Mod Pathol 2011;24:1444)
- Skin, nose, biopsy:
- Chondroid syringoma (benign cutaneous mixed tumor)
- Microscopic description: Histologic sections demonstrate a well circumscribed nodular dermal (subcutaneous) neoplasm. The tumor consists of cords and islands of banal epithelial cells set in a variably fibrous and chondromyxoid stroma, creating a biphasic appearance. Ductal structures are present, with inner epithelial and outer myoepithelial layers evident. Cystic (or other metaplastic) change is seen. There is minimal nuclear atypia and mitoses are not abundant.
- Cutaneous chondroma:
- Lacks the epithelial and myoepithelial elements
- Malignant mixed tumor / malignant chondroid syringoma:
- Necrosis, infiltrative growth, marked pleomorphism and greater cellularity
- Metastatic carcinoma:
- Can often be distinguished based on immunohistochemistry and cytologic features of malignancy
- Parachordoma:
- Rare, no true ducts, actin negative, presence of physaliferous cells, arises adjacent to tendon and synovium in extremities
- Now often considered a variant of myoepithelioma
- Collagenous spherulosis:
- More common in breast, lumina contain dense eosinophilic secretion, no biphasic appearance
- Hidradenoma papilliferum:
- No chondroid matrix, not biphasic
- Myopeithelioma / adenomyoepithelioma of the skin:
- More common on extremities, myoepithelial areas should predominate, lacks luminal epithelial cells
- Negative for cytokeratin and CEA
- Other adnexal tumors with apocrine differentiation
Features that are most suggestive of malignant behavior in mixed tumor are
- Asymmetry, osseous metaplasia and scattered pleomorphic cells
- Cytoplasmic vacuolization and plasmacytoid cells
- Increased cellularity and necrosis
- Infiltrative borders and asymmetry
- Infiltrative borders and bizzare, multinucleated cells
Comment Here
Reference: Chondroid syringoma
- EWSR1 amplification
- EWSR1 rearrangement
- HMGA2 fusion
- PLAG1 deletion
- PLAG1 rearrangement
Comment Here
Reference: Chondroid syringoma
- Benign tumor with debated origin from eccrine sweat glands or hair follicles
- Also called turban tumor, particularly when a large, multicentric scalp tumor
- Autosomal dominant, multiple tumors of children / teenagers that may also involve trunk and extremities
- In association with spiradenoma, trichoepithelioma, milia or membranous variant of basal cell adenoma of salivary glands
- Due to mutations in CYLD gene at chromosome 16q12-13
- Rarely undergoes malignant transformation
- Features of cylindroma and eccrine spiradenoma
- Benign
- Solitary or multiple
- Familial inheritance possible
- Typically, solitary exophytic painless tumors (Lancet Oncol 2015;16:e460)
- Can develop multiple scalp lesions (turban tumor) (Int J Dermatol 2015;54:275)
- Multiple cylindromas associated with cylindromatosis gene (CYLD) mutations and Brooke-Spiegler syndrome; associated with earlier development (Lancet Oncol 2015;16:e460)
- Single lesions associated with MYB gene mutations (J Pathol 2016;239:197)
- Cutaneous or dermal cylindromas
- Turban tumor
- Salivary cylindroma or cystic adenoid carcinoma
- F > M (Dermatol Clin 2017;35:61)
- Middle aged and elderly women (Int J Dermatol 2015;54:275)
- Head, neck and scalp (Int J Dermatol 2015;54:275)
- Unclear pathophysiology, currently debated to be from eccrine, apocrine or follicular origin (Int J Dermatol 2015;54:275)
- MYB gene fuses with NFIB gene forming single sporadic tumors (J Pathol 2016;239:391)
- Germ line mutation on CYLD tumor suppressor gene on chromosome 16 leads to Brooke-Spiegler syndrome; autosomal dominant inheritance pattern (Head Neck Pathol 2016;10:125)
- Currently unknown
- Solitary or multiple
- Primarily on head, neck and scalp
- Usually ages 40+ years
- F > M
- Rarely associated with similar tumors in major salivary glands
- Rare malignant transformation, local infiltration common (Lancet Oncol 2015;16:e460)
- Brooke-Spiegler syndrome associated with spiradenoma and trichoepithelioma formation (Dermatol Clin 2017;35:61)
- Diagnosis based on biopsy histology (Dermatol Clin 2017;35:61)
- Consider genetic testing in patients with multiple cylindromas, spiradenomas or trichoepitheliomas and in patients with one of these solitary tumors and a first degree relative with any of these tumors (Dermatol Clin 2017;35:61)
- MRI imaging utilized with suspected malignant transformation of scalp tumors to detect intracranial invasion (Lancet Oncol 2015;16:e460)
- Rarely undergo malignant transformation (poorly established rate) with slightly higher risk in Brooke-Spiegler patients (Dermatol Pract Concept 2015;5:61)
- Salivary cylindromas are malignant with a poor 15 - 20 year survival (10 - 30%) (Curr Opin Otolaryngol Head Neck Surg 2017;25:147)
- 38 year old man with numerous scalp cylindromas (Natl J Maxillofac Surg 2012;3:59)
- 58 year old man with facial cylindroma clinically mimicking basal cell carcinoma (Indian Dermatol Online J 2016;7:203)
- 73 year old woman with large pedunculated facial cylindroma (Open Access Maced J Med Sci 2018;6:1868)
- 75 year old man with cylindroma of the external ear (BMJ Case Rep 2016;2016:212035)
- 83 year old woman with Brooke-Spiegler syndrome presenting with malignant cylindromas (Dermatol Pract Concept 2015;5:61)
- Treatment for cylindromas with CYLD mutations or tumors that are disfiguring or uncomfortable is with surgical excision (Dermatol Clin 2017;35:61)
- Mohs micrographic surgery may be necessary with recurrent tumors to confirm histologic clearance (Lancet Oncol 2015;16:e460)
- Radiotherapy is contraindicated as it can further induce DNA damage (Dermatol Clin 2017;35:61)
- Pink-red dome shaped nodule with smooth surface
- Compact nests of basaloid cells that fit together like a jigsaw puzzle, surrounded by thick basement membrane (Dermatol Clin 2017;35:61)
- Cylindrical shape appreciated in cross section (Dermatol Clin 2017;35:61)
- 2 groups of cells:
- Undifferentiated peripheral palisading epithelial cells with small dark nuclei
- Centrally located increasingly differentiated ductal cells with large pale nuclei (Dermatol Clin 2017;35:61)
- CK7 (in central basaloid cells), CK8 (J Cutan Pathol 2009;36:190)
- EMA and CEA in ducts (Indian J Dermatol 2012;57:141)
- PAS highlights hyaline in basement membrane (Indian Dermatol Online J 2016;7:203)
- Differentiation towards intradermal coiled duct region of eccrine sweat glands
- Compact small cells with dark nuclei on the periphery with larger cells containing light colored nuclei more centrally
- Ductal structures and thick hyaline bands present
- Mutation in CYLD on chromosome 16 associated with multiple familial cylindromas
- MYB gene mutations associated with sporadic cylindromas
- Chromosome 16 CYLD mutation common
- CYLD codes for recessive cylindromatosis familial tumor suppressor gene a ubiquitin specific protease (Lancet Oncol 2015;16:e460)
- Majority of mutations are frameshift and result in truncated proteins (Hum Mutat 2009;30:1025)
- Mutations detected in 84% of reported Brooke-Spiegler patients and 88% in familial cylindromatosis (Hum Mutat 2009;30:1025)
- MYB activation (~12%) and MYB-NFIB fusion oncoproteins (~55%) present in sporadic tumors (J Pathol 2016;239:197)
Spiradenoma and cylindroma sweat gland tumor
- Forehead, excision:
- Benign adnexal tumor (see comment)
- Comment: There are cylindrically shaped nests of epithelial cells arranged in a jigsaw pattern surrounded by thick hyaline basement membrane. Immunohistochemically the tumor nests are express CK7 and 8 positivity, with EMA and CEA positivity in the accompanying duct structures. Tumor is CK20, GCDFP-15, ER and PR negative. These features support the diagnosis of cylindroma.
- Malignant transformation is unlikely. If multiple tumors are present, consider genetic testing for CYLD mutations as this is associated with Brooke-Spiegler.
- Trichoepithelioma:
- Hair follicle tumor with basaloid cells in nests surrounded by dense fibrous stroma and spindle cells
- Mucin pools may be present within basaloid nests
- Lack of clefting distinguishes from basal cell carcinoma
- Spiradenoma:
- Can occur both separately and in combination with cylindromas
- Similar formation with peripheral small basaloid cells and larger paler cells centrally
- Lobulated tumor islands separated by thin fibrous tissue containing blood vessels
- Basal cell carcinoma:
- Lacks tight hyaline membrane separating epithelial islands
- Mucinous stroma with clefting artifact present
- A 31 year old woman who was previously diagnosed with Brooke-Spiegler syndrome has developed three painless cutaneous tumors on her scalp. Tumor biopsy shows a jigsaw pattern of basaloid ovoid nests of tumor lobules located within the dermis, ductal structures and thick hyaline bands. Which of the following is true concerning this adnexal tumor?
- It can appear both separately and in conjunction with spiradenomas
- It most commonly appears on elderly males
- Malignant transformation occurs frequently
- Tumors are normally found on the lower extremities
Comment Here
Reference: Cylindroma
- A 26 year old woman presents with multiple tumors on her scalp, neck and face. She otherwise feels well. Her mother has similar appearing tumors that have previously been diagnosed as cylindromas and spiradenomas. This is her first time seeking diagnosis as her tumors are disfiguring but generally painless. Testing for mutation in which gene should be recommended for this patient?
- CYLD
- MYB
- MYB-NFIB
- No genetic testing is recommended
- Dermatofibromas (also known as fibrous histiocytomas) are a spectrum of benign dermal based lesions with fibroblastic and histiocytic differentiation
- There is debate as to whether dermatofibroma is a reactive or neoplastic process
- Benign dermal based, nodular proliferation of fibroblasts and histiocytes
- Collagen trapping at periphery and follicular induction commonly seen
- IHC is nonspecific for dermatofibroma
- Benign fibrous histiocytoma and fibrous histiocytoma
- Common
- All races
- All ages; most common in third and fourth decades
- F > M
- Reference: Am J Surg Pathol 1990;14:801
- Typically occurs on distal extremities (legs > arms > trunk)
- May present on any part of the skin surface
- Cause unknown
- No evidence associates it with insect bites or trauma
- Unclear whether a reactive or neoplastic process
- Cytogenetic data has shown clonality, arguing in favor of a neoplastic process (J Cutan Pathol 2000;27:36, Histopathology 2000;37:212)
- Multiple dermatofibromas may occur in immunosuppressed populations (Eur J Dermatol 1999;9:45)
- Painless
- 5 mm - 2 cm
- Variable color: skin colored to brown to purple
- Variable shape: plaques, nodules or polyps
- Covered by intact skin
- Suspected by pinching the nodule between the fingers and observing that the tumor is fixed within the dermis
- Pinch sign: overlying skin dimples on pinching the lesion (An Bras Dermatol 2014;89:472)
- Combination of clinical and histologic findings
- Excellent prognosis (Am J Surg Pathol 1990;14:801)
- Cellular, atypical, aneurysmal and deep subtypes associated with higher risks of local recurrence (Am J Surg Pathol 1994;18:668, Eur J Dermatol 1998;8:122)
- Very rarely metastasize (Am J Surg Pathol 2008;32:354, Am J Surg Pathol 2002;26:35, Mod Pathol 2013;26:256)
- 2 young children with tumors of skin and conjunctiva and coexisting xeroderma pigmentosum (Arch Pathol Lab Med 1991;115;910)
- 19 year old man with corneoscleral tumor (Br J Ophthalmol 2002;86:477)
- 25 year old man with cystic lesion on calf (Cureus 2020;12:e6736)
- 25 year old man with external auditory canal tumor (Ear Nose Throat J 2019;98:396)
- 36 year old woman with blue-gray pigmented lesion (An Bras Dermatol 2017;92:92)
- 40 year old woman with multiple dermatofibromas associated with pregnancy (Dermatol Online J 2019;25:13030)
- 42 year old man with swelling over the occipital region (J Clin Diagn Res 2017;11:ED08)
- 43 and 48 year old women and 60 year old man with conditions associated with multiple dermatofibromas (Dermatol Online J 2017;23:13030)
- 51 year old woman with swelling of lower jaw (J Clin Diagn Res 2016;10:ZD24)
- 62 year old woman with unusual presentation of dermatofibroma on the face (Clin Case Rep 2019;7:672)
- 85 year old man with lump on his back (Int J Surg Case Rep 2019;60:299)
- Complete excision is curative
- Wide local excision is adequate to prevent recurrence
- Spontaneous regression has been reported
Images hosted on other servers:
- Most classic pattern: pigment network and central white patch
- Wide range of presentations
- Symmetric and predominantly dermal based
- Relatively circumscribed but have irregular and unencapsulated borders
- Patterns range from diffuse to reticular to hemangioma-like to keloid-like
- Classic pattern: storiform, pinwheel or curlicue pattern
- Made up of spindled fibroblasts or histiocytes
- Some areas densely cellular, while others are sclerotic and hypocellular
- Early lesions: more cellular
- Later lesions: more sclerotic
- Spindled cells: thin, elongated nuclei with pointed ends and eosinophilic cytoplasm
- Histiocytic cells: epithelioid shaped cells with abundant pale cytoplasm
- May see varying amounts of inflammatory cells
- Cytologic atypia and pleomorphism are variable
- Mitotic activity is variable
- Touton giant cells and ringed lipidized siderophages may be present
- Collagen trapping at periphery
- Spheres of eosinophilic collagen (collagen balls) surrounded by the fibroblast proliferation
- Grenz zone (sparing of the superficial papillary dermis) commonly seen
- Follicular or sebaceous induction and basilar hyperpigmentation
- Tumor may extend into superficial fat
- Numerous histological subtypes (An Bras Dermatol 2014;89:472):
- Aneurysmal and hemosiderotic variants are both characterized by numerous multinucleate cells and prominent hemosiderin deposition due to red blood cell extravasation; distinction between these two is the pseudovascular spaces with blood in aneurysmal type (Histopathology 1995;26:323)
- Hemosiderotic frequently has extracellular hemosiderin pigmentation present
- Deep fibrous histiocytoma: may extend into hypodermis (Am J Surg Pathol 2008;32:354)
- Cellular: highly cellular and look blue at low power with thick collagen bundles (Am J Surg Pathol 1994;18:668)
- Lipidized: also known as 'ankle type' Am J Dermatopathol 2000;22:126
- Atypical: also has prominent pleomorphism, mitotic activity including atypical forms (Am J Dermatopathol. 1987 Oct;9(5):380)
- Epithelioid fibrous histiocytoma: epidermal collarette, binucleate cells (Mod Pathol 2015;28:904)
Contributed by Brandon Zelman, D.O. and Jodi Speiser, M.D.
AFIP images
Aneurysmal
Cellular
- Most useful stain based on evidence is CD163; factor XIIIa is variable in dermatofibroma; CD68 and CD10 are less specific for fibrohistiocytic lineage
- Ki67 and PHH3 can also be used to show increased proliferation index in dermatofibroma (compared to low index in dermatofibrosarcoma protuberans) (Am J Dermatopathol 2017;39:504)
- ALK nuclear and cytoplasmic reactivity in epithelioid fibrous histiocytoma due to ALK rearrangement and overexpression
- Staining pattern is highly variable and nonspecific but the following stains may be positive:
- Factor XIIIa, CD163, CD10
- Factor XIIIa is usually negative in dermatofibrosarcoma protuberans
- CD68 may highlight histiocytic cells (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- Factor XIIIa, CD163, CD10
- CD34 shows a characteristic staining pattern:
- CD34 is usually positive in the periphery of dermatofibroma, and negative in the middle
- CD34 is positive in dermatofibrosarcoma protuberans
- CD34 peripheral staining in dermatofibroma is observed in cellular dermatofibroma and deep FH and is weak and patchy
- CD34 is strong and diffuse throughout dermatofibrosarcoma protuberans
- S100, HMB45, MelanA / MART1, nestin (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
Dermatofibroma
Anerysmal fibrous histiocytoma
Cellular dermatofibroma
Lipidized dermatofibroma
- Skin, right arm, excision:
- Dermatofibroma
- Skin, left shin, excision:
- Dermatofibroma (see comment)
- Comment: Immunohistochemical stains were performed on the above specimen. The cells are positive for factor XIIIa and negative for CD34. This supports the above diagnosis.
- Dermatofibrosarcoma protuberans (DFSP):
- Lower mitotic activity
- Greater cellularity
- Absence of inflammation
- Involvement of subcutis is infiltrative and extensive rather than pushing and focal in deep and cellular variants of fibrous histiocytoma
- CD163 is negative
- Monotonous cells
- Usually deeper, with adnexal structures and fat within
- CD34+ and factor XIIIa-
- COL1A1::PDGFB fusion
- Melanoma, especially desmoplastic type:
- S100+
- Prominent lymphoid aggregates
- Dermatomyofibroma:
- Corkscrew nuclei running parallel to epidermis
- Respects adnexal structures
- Thick elastic fibers present
- Dermal scar:
- Loss of dermal papilla and adnexal structures
- Dense collagen fibers run parallel to dermal epidermal junction
- Factor XIIIa-
- Neurofibroma:
- Mucinous stroma
- Slightly wavy spindle cells with loose appearance
- Mast cells
- Poor circumscription
- S100+
- CD34+ plaque-like dermal fibroma
- Nodular fasciitis
- Atypical fibroxanthoma
- Cellular proliferation involves both the epidermis and dermis
- CD34 is positive at the center of the lesion
- Collagen trapping is seen at the periphery of the lesion
- Deep margins of the lesion typically show extensive infiltration
Comment Here
Reference: Dermatofibroma (cutaneous fibrous histiocytoma)
- S100- / CD34- / CD163+ / MART1-
- S100- / CD34+ / CD163+ / MART1-
- S100+ / CD34- / CD163- / MART1+
- S100+ / CD34- / CD163+ / MART1-
- S100+ / CD34+ / CD163+ / MART1-
Comment Here
Reference: Dermatofibroma (cutaneous fibrous histiocytoma)
- Locally aggressive, superficial mesenchymal neoplasm with fibroblastic differentiation
- Locally aggressive, superficial mesenchymal neoplasm with fibroblastic differentiation
- Virtually all cases contain fusion genes; COL1A1::PDGFB is the most common fusion product, although others have recently been reported
- Fibrosarcomatous transformation imparts an increased risk of recurrence and metastasis
- Rare, though one of the most common sarcomas of the skin / subcutis
- Occurs over a wide age range but most commonly in early to mid adulthood (Cancer 1962;15:717, Am J Surg 1966;111:638)
- Both men and women affected, with some debate as to whether there is a slight male or female predilection (J Am Acad Dermatol 2007;56:968)
- Can ostensibly involve any area of skin but the trunk and extremities are the most common locations
- Tumors are generally presumed to occur sporadically
- Virtually all cases contain fusion genes; COL1A1::PDGFB is the most common fusion product, although others have been reported
- Possible association with adenosine deaminase deficient severe combined immunodeficiency (J Allergy Clin Immunol 2012;129:762)
- Classically an exophytic, nodular cutaneous mass; however, often initially presents as a flat plaque (JAMA Netw Open 2019;2:e1910413)
- Initially may show persistent slow growth, often for many years, then sudden progression (Cancer 1962;15:717)
- Fibrosarcomatous transformation is associated with metastatic potential (Cancer 2000;88:2711)
- Tumors are morphologically distinctive and frequently amenable to classification based on H&E
- Immunohistochemistry for CD34 is a useful adjunct since most cases are diffusely positive
- Molecular testing is helpful, particularly in the context of limited sampling or unusual morphology
- Imaging findings are nonspecific but in general show a well defined, subcutaneous soft tissue mass with intermediate to marked enhancement on contrast enhanced CT and MRI (Medicine (Baltimore) 2015;94:e1001)
- So called claw sign may be seen in some cases (J Med Imaging Radiat Oncol 2017;61:9)
- Incomplete resection is a risk factor for recurrence
- Fibrosarcomatous transformation (fibrosarcoma ex DFSP) imparts an increased risk of recurrence and metastasis (Am J Surg Pathol 2006;30:436)
- Metastases typically occur following multiple local recurrences
- Increased age, male sex and tumor size are associated with worse overall survival (JAMA Dermatol 2016;152:1365)
- 21 year old man with history of Cowden syndrome and scalp tumor (Am J Dermatopathol 2016;38:e40)
- 23 year old man and 28 year old woman with fibrosarcomatous transformation occurring on the scalp (BMJ Case Rep 2016;2016:bcr2016215427)
- 30 year old woman with longstanding history of a small abdominal wall mass (Case #485)
- 37 year old man with recurrent dermatofibrosarcoma protuberans, refractory to therapy (Onco Targets Ther 2018;11:2439)
- 44 year old woman with vulvar myxoid dermatofibrosarcoma protuberans (Am J Dermatopathol 2016;38:226)
- 47 year old man with dermatofibrosarcoma protuberans in the inguinal region (Ann Dermatol 2016;28:629)
- 60 year old man with metastatic fibrosarcomatous dermatofibrosarcoma protuberans treated with imatinib mesylate (Dermatol Ther 2022;35:e15736)
- Wide local excision is considered the mainstay of treatment for localized disease (Cancer 2019;125:735)
- Advanced disease may also require consideration of imatinib or radiotherapy (Eur J Cancer 2015;51:2604, JAMA Dermatol 2019;155:361, J Eur Acad Dermatol Venereol 2016;30:1107)
- Initially, plaque-like dermal / subcutaneous thickening; progresses to raised firm multinodular mass (Cancer 1962;15:717)
- Tumor is usually centered in dermis with extension into subcutaneous tissue; occasionally, subcutaneous involvement only (Am J Dermatopathol 2008;30:327)
- Variable size (0.5 cm to > 10 cm) (Cancer 1962;15:717)
- Gray-white, firm; may be myxoid or gelatinous (Cancer 1962;15:717)
- Tumors are generally centered within the dermis or subcutis and characterized by spindle cells with a storiform to whorled pattern
- Cytoplasm is generally abundant and eosinophilic; nuclei are monomorphic and ovoid to elongated with variable mitotic activity
- Tumors infiltrate and expand fibrous septa; interdigitation among lobules of fat yields a honeycomb pattern
- Adnexal structures are typically spared
- Stroma may be collagenous, myxoid or microcystic
- Multiple variants exist, including those with
- Giant cells (Histopathology 1990;17:165)
- Melanin pigmentation (Bednar tumor) (Am J Surg Pathol 1985;9:630, Histopathology 1988;13:631)
- Myoid differentiation (J Cutan Pathol 1996;23:30)
- Myxoid stroma (Am J Surg Pathol 1983;7:445, Am J Dermatopathol 2007;29:443, Am J Surg Pathol 2007;31:1371)
- Pseudocystic change (J Cutan Pathol 2012;39:356)
- So called sarcomatous transformation (mimics undifferentiated pleomorphic sarcoma) (Am J Dermatopathol 2011;33:354)
- Fibrosarcomatous transformation denotes those with cellular spindle cell fascicles or a herringbone pattern
- Generally with greater atypia and mitotic activity
- CD34 expression may be diminished / absent
Contributed by Brendan C. Dickson, M.D., M.Sc.
- CD34: may be diminished / absent with fibrosarcomatous transformation
- Vimentin
- p53: with fibrosarcomatous transformation (Am J Surg Pathol 2006;30:436)
- Fontana-Masson (Bednar tumor)
- Factor XIIIa
- S100, HMB45, MelanA, Fontana-Masson: usually negative but positive in dendritic melanocytic cells in pigmented DFSP (Bednar tumor)
- Desmin
- Smooth muscle actin: positive in the context of myoid differentiation
- CD31
- ERG
- AE1 / AE3
- Prussian blue
- Reference: J Cutan Pathol 1996;23:30
- Ultrastructural features are compatible with fibroblasts (J Cutan Pathol 1979;6:265, Virchows Arch A Pathol Anat Histol 1981;391:165)
- Long ramified processes with primitive junctions (Ultrastruct Pathol 2006;30:283)
- Multivesicular buds (structures containing microvesicles abutting from the cell membrane) frequently present (Ultrastruct Pathol 2006;30:283)
- Early cytogenetic studies identified a supernumerary ring chromosome in most cases; this led to the identification of t(17;22)(q22;q13) (Cancer Genet Cytogenet 1990;49:273, Am J Pathol 1995;147:1553, Cancer Genet Cytogenet 1996;89:88)
- Most common fusion is COL1A1::PDGFB (Genes Chromosomes Cancer 1995;13:62, Nat Genet 1997;15:95)
- Less common fusions include
- COL1A2::PDGFB (JAMA Dermatol 2015;151:1330)
- COL6A3::PDGFD (Mod Pathol 2018;31:1683, Genes Chromosomes Cancer 2018;57:437)
- EMILIN2::PDGFD (Mod Pathol 2018;31:1683)
- TNC::PDGFD (Diagn Pathol 2021;16:63)
- Of note: there is molecular pleiotropy with the COL1A1::PDGFB gene fusion, which has also been reported in a subset of uterine mesenchymal neoplasms (Mod Pathol 2019;32:1008, Gynecol Oncol Rep 2019;31:100523)
- Skin, back, biopsy:
- Dermatofibrosarcoma protuberans (see comment)
- Comment: Within the dermis and subcutis there is a spindle cell neoplasm with a storiform pattern. The cytoplasm is eosinophilic. The nuclei are ovoid and monomorphic with rare mitotic activity. There is sparing of adnexal structures and infiltration of the subcutaneous fat with a honeycomb pattern. The cells are diffusely positive for CD34; they are negative for desmin, smooth muscle actin, S100 and keratin (AE1 / AE3).
- Cellular fibrous histiocytoma:
- Plump spindle cells with peripheral collagen entrapment
- Inflammation is often present, including foamy macrophages, lymphocytes and plasma cells; occasionally multinucleated giant cells (J Cutan Pathol 2012;39:747)
- Immunohistochemistry for CD34 may highlight peripheral dermal fibroblasts; rarely, tumors may be positive (J Cutan Pathol 2012;39:747)
- Cutaneous leiomyosarcoma:
- Plump spindle cells with a fascicular architecture
- Ovoid / cigar shaped nuclei, atypical mitoses may be identified
- Immunohistochemistry typically positive for desmin and h-caldesmon and negative for CD34
- Solitary fibrous tumor:
- Spindle cells with a patternless distribution; prominent branching vasculature
- Keloid-like collagen bundles
- Immunohistochemistry will also be positive for STAT6
Comment Here
Reference:Dermatofibrosarcoma protuberans (DFSP)
- COL1A1::PDGFB
- EWSR1::FLI1
- FUS::DDIT3
- JAZF1::SUZ12
- MYB::NFIB
- EWSR1::FLI1: Ewing sarcoma
- FUS::DDIT3: myxoid liposarcoma
- JAZF1::SUZ12: low grade endometrial stromal sarcoma
- MYB::NFIB: adenoid cystic carcinoma
Comment Here
Reference: Dermatofibrosarcoma protuberans (DFSP)
Comment Here
Reference: Dermatofibrosarcoma protuberans (DFSP)
- COL6A3::CSF1
- COL1A1::PDGFB
- COL6A3::PDGFD
- COL1A1::USP6
Comment Here
Reference: Dermatofibrosarcoma protuberans (DFSP)
- Distinct cutaneous plaque-like proliferation of fibroblasts and myofibroblasts (J Cutan Pathol 1992;19:85, Br J Dermatol 1993;129:69)
- Also called cutaneous myofibroma
- Women > men, usually age 20 - 39, but occasionally in children (J Cutan Pathol 2011;38;967)
- Upper arms, neck or trunk
- Pediatric cases more often in neck
- 4 month old boy with development of dermatomyofibroma (Ann Dermatol 2011;23:S72)
- Two young women with dermatomyofibroma (J Cutan Pathol 1994;21:371)
- Reddish brown plaque or nodule
- Fascicles of monomorphic spindle cells parallel to epidermis
- Dermatofibroma
- Diffuse neurofibroma
- Keloid (gross)
- Plaque stage DFSP
- Other tumors with myofibroblastic differentiation
- Benign epidermal growth presented as hyperpigmented or skin colored papules on face and neck, most commonly found on patients with darker phototypes (Fitzpatrick type IV, V or VI)
- Likely a variant of seborrheic keratosis
- Small (several millimeters) hyperpigmented or flesh colored papules seen most commonly in patients with skin of color, particularly darker phototypes (Fitzpatrick type IV, V or VI)
- Increase in size and number of papules with aging
- Familial
- Clinical: filiform, verrucous or pedunculated pigmented papule
- Histology: acanthosis, papillomatosis, hyperkeratosis and hyperpigmentation
- First described in 1925 by Dr. Aldo Castellani
- Seborrheic keratosis
- ICD-10: L82.1 - other seborrheic keratosis
- Common in patients with skin of color, particularly darker phototypes (Fitzpatrick type IV, V or VI), affecting 10 - 75% of the population (Clin Dermatol 2017;35:491)
- Onset often late in adolescence, increasing numbers with age, common in adulthood and age > 60 years
- Familial in majority of cases (Int J Dermatol 2017;56:957)
- F:M = 2:1
- Mainly in photoexposed areas: head, neck and upper trunk
- Not entirely known
- Frequent positive family history and possible genetic predisposition
- Somatic activation mutation in FGFR3 has been rarely reported (Br J Dermatol 2010;162:508)
- Cumulative ultraviolet (UV) exposure may play a role
- Not entirely known
- Aging
- UV exposure
- Round, 1 - 5 mm, skin colored to hyperpigmented fleshy papules mimicking skin tags, warts or seborrheic keratoses
- Filiform to sessile, smooth surface to wrinkled papules in a symmetric distribution
- Distribution is typically head and neck, upper chest
- Generally asymptomatic papules without crusting, scaling or ulceration
- No spontaneous resolution (Int J Dermatol 2017;56:957)
- Diagnosis is usually clinical
- Dermatoscopy: fissures and ridges in a cerebriform pattern in 59% of cases, comedo-like openings in 27% and milia-like cysts (Int J Dermatol 2017;56:957)
- Biopsy often performed if concerned for malignancy
- Histologic findings are confirmatory
- No risk for transforming to malignancy
- Never regresses spontaneously
- 3 year old boy with dermatosis papulosa (Pediatr Dermatol 1993;10:356)
- 9 year old girl with early onset dermatosis papulosa nigra (Br J Dermatol 2016;174:1148)
- 32 year old woman with superimposed segmental dermatosis papulosa nigra (Clin Exp Dermatol 2020;45:521)
- 42 year old black woman with eruptive dermatosis papulosa nigra as a possible sign of internal malignancy (Int J Dermatol 2007;46:186)
- Not necessary; for cosmetic purposes
- Caution in choosing treatment option due to tendency of darker skin to dyspigmentation
- Snip excision with scissors
- Light curettage with or without anesthesia
- Electrodesiccation (Dermatol Surg 2009;35:1079)
- Cryotherapy
- Potassium titanyl phosphate (KTP), pulse dye laser (PDL), Nd:YAG and carbon dioxide lasers (Indian J Dermatol 2015;60:321, Dermatol Surg 2010;36:1968)
- Round to filiform, skin colored or hyperpigmented polyp / papule ranging from 1 - 5 mm
- Irregular acanthosis of epidermis, hyperkeratosis and papillomatosis
- Elongated and interconnected rete ridges with hyperpigmentation of basal layer
- No increase in melanocyte number
- Keratin filled invagination of epidermis
- Prominent and well developed fibrous stroma within papillomatous acanthotic structures
- Similar features to reticulate and acanthotic types of seborrheic keratosis (Int J Dermatol 2017;56:957)
- No stains are required to make the diagnosis
- Pancytokeratin and high molecular weight cytokeratin positive
- Skin, right shoulder, shave biopsy:
- Dermatosis papulosa nigra
- Seborrheic keratosis:
- Essentially identical histopathologic features
- Distinguishing features are predominantly clinical
- Not all clinicians agree with dermatosis papulosa nigra being a variant of seborrheic keratosis
- Affects all skin types, including lighter skin phototypes (Fitzpatrick skin type I to II) (Int J Dermatol 2007:46:45)
- Not limited to sun exposed areas
- Can be larger in size (up to several cm)
- Verruca vulgaris:
- Papillomatosis, tiers of parakeratosis, valleys of hypergranulosis and dilated papillary dermal blood vessels
- Acrochordon / fibroepithelial polyp / skin tag:
- Polypoid fragment of skin lined by unremarkable (not significantly acanthotic) epidermis with abundant loose fibrocollagenous stroma, abundant vessels and no adnexal structures
- Melanocytic nevi:
- Nest of melanocytes in dermoepidermal junction or within dermis
- Actinic keratosis:
- Proliferation of atypical keratinocytes at basal layer, loss of granular layer, parakeratosis, solar elastosis in dermis
(Disclaimer: this question has not been reviewed or approved by Dr. Shalin)
65 year old woman with darkly pigmented skin (Fitzpatrick type V) presented with multiple pigmented lesions on her cheek with the microscopic features shown above. What is the best diagnosis?
- Actinic keratosis
- Cutaneous fibroepithelial polyp
- Dermatosis papulosa nigra
- Verruca vulgaris
Comment Here
Reference: Dermatosis papulosa nigra
What are the most important histology findings of dermatosis papulosa nigra?
- Increased melanocyte proliferation in epidermis
- Papillomatosis, acanthosis and hyperkeratosis
- Papillomatosis, parakeratosis, valleys of hypergranulosis and dilated papillary dermal blood vessels
- Parakeratosis, proliferation of atypical keratinocytes at basal layer and loss of granular layer
Comment Here
Reference: Dermatosis papulosa nigra
- Benign cutaneous developmental anomaly
- Arises from the entrapment of ectodermal elements along the lines of embryonic closure
- Derived from both ectoderm (stratified squamous epithelium) and mesoderm (cutaneous adnexal structures)
- Most commonly on the lateral aspect of the upper eyelid
- Can be complicated by intracranial involvement
- Total resection of the cyst, along with the adhesions and sinuses, is crucial
- Cystic teratoma (not true teratoma), nasal dermoid sinus cyst (when located in sinus)
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
- One of the most common pediatric skull tumors
- Accounts for about 15.4 - 58.5% of all scalp and skull masses in pediatric patients (World Neurosurg 2018;120:119)
- Incidence roughly 3 per 10,000 pediatric patients
- Mostly are congenital (40%) but not all of them are diagnosed at birth
- About 60% of cases discovered in children 5 years old or younger (World Neurosurg 2018;120:119, Pediatr Dermatol 2013;30:706)
- Cases in adulthood have also been reported (World Neurosurg 2018;120:119)
- No significant predominance for sex and race
- Most common: lateral aspect of the upper eyelid (Pediatr Dermatol 2019;36:999)
- Other: midline of neck, nasal root, nose, forehead, the mastoid area, anterior chest and scalp (J Pediatr Surg 1990;25:294)
- Rare: mid chest, sacrum, perineum, scrotum, penis and ear (Pediatr Dermatol 2013;30:706)
- Results from incomplete closure of the neural tube during the third to fifth week of fetal development (Case Rep Neurol Med 2021;2021:9917673)
- Arises from traumatic sequestration of cutaneous tissues along the embryonal lines of closure (Pediatr Dermatol 2019;36:999)
- Derived from both ectoderm (stratified squamous epithelium) and mesoderm (cutaneous adnexal structures)
- Trichilemmal differentiation rarely seen in the lining of the cyst (Ophthalmic Plast Reconstr Surg 2017;33:e116)
- Some authors propose an embryological origin for these cysts, particularly in the nasal form (Cleft Palate Craniofac J 2005;42:51)
- Mostly unknown
- Usually a solitary, pale to flesh colored, nontender, noncompressible, firm, nonpulsatile, deep seated, predominantly subcutaneous nodule (Pediatr Dermatol 2019;36:999)
- Hair protruding from a cyst is pathognomonic (Cleft Palate Craniofac J 1991;28:87)
- May lie dormant for a period of time and then grow and become clinically manifest because of enlargement, rupture or sometimes extension to surrounding structures (World Neurosurg 2018;120:119)
- Based on clinical features, imaging modalities and histopathological findings
- CT imaging is better at delineating the changes in bony erosions
- Magnetic resonance imaging (MRI) is the preferred means of revealing evidence of intracranial extension
- Ultrasound (USG) demonstrates a well defined homogenous and hypoechoic cystic lesion
- Radiological features include characteristic signal intensities, absence of perilesional edema and the presence of well defined margins to the cyst (Case Rep Neurol Med 2021;2021:9917673)
- Overall prognosis good, especially when there is no intracranial or intraspinal extension (Pediatr Dermatol 2013;30:706)
- Aspiration or biopsies have the potential to cause infection, further leading to osteomyelitis, meningitis or cerebral abscess (Case Rep Neurol Med 2021;2021:9917673, J Pediatr Surg 1990;25:294)
- Squamous cell carcinoma very rarely develops in the wall of the cyst (Int Orthop 1995;19:185)
- Rarely, the development of carcinosarcoma has been described (J Med Case Rep 2017;11:11)
- 14 year old boy with a painless swelling in left upper part of chest wall of 2 years' duration (BMJ Case Rep 2019;12:e228831)
- 22 year old woman with a gradually enlarging mass in the right retroauricular region (Acta Biomed 2021;92:e2021075)
- 40 year old woman with a painless swelling of the lower eyelid of 20 years' duration (BMJ Case Rep 2013;2013:bcr2013200686)
- 42 year old Sri Lankan Tamil man presented with a large cystic swelling in his submental region (J Med Case Rep 2017;11:11)
- 75 year old man presented with a soft, painless mass on his left upper back (Radiol Case Rep 2021;16:1127)
- 15 cases of orbital dermoids representing 6% of orbital tumors (Br J Ophthalmol 1984;68:642)
- Complete surgical resection is the treatment of choice
- Imaging done prior to determine the extent of underlying tissue involvement
- Resected carefully to avoid spilling of contents intracranially
- Recurrences have been reported in case of incomplete excision (Pediatr Dermatol 2013;30:706)
- Well defined wall lined by stratified squamous epithelium with mature skin appendages (hair follicles and sebaceous glands) and a lumen filled with keratin and hair shafts (Yale J Biol Med 2014;87:349, Pediatr Dermatol 2013;30:706)
- Occasionally, smooth muscle may be present but in contrast to benign cystic teratoma, cartilage and bone has not been described (Yale J Biol Med 2014;87:349)
- Eccrine sweat glands present in 35% of cases and apocrine glands in 15%
- Ruptured cyst with evidence of granulomatous inflammation with giant cells, most concentrated around exposed hair follicles
- Implantation dermoid cysts have no adnexal structures and therefore, they are easily distinguished from congenital forms on histology (BMJ Case Rep 2019;12:e228831)
- CK6 (positive in epidermoid cyst, indicating cell hyperproliferation)
Cutaneous dermoid cyst
- Skin, right lower eyelid, excision:
- Dermoid cyst
- Skin, left shin, excision:
- Dermoid cyst (see comment)
- Comment: The sections show a dermal cyst lined by stratified squamous epithelium with attached sebaceous gland and hair follicle. The lumen contains loose keratin flakes and scattered hair shafts.
- Epidermal inclusion cyst / epidermoid cyst:
- Smooth, dome shaped firm, skin colored nodule that is freely movable on palpation and sometimes has a small, dilated punctum
- Lined only by stratified squamous epithelium; no adnexal structures identified
- Lumen contains abundant keratin flakes
- Vellus hair cyst:
- Multiple, small, smooth, skin colored, reddish, bluish, yellowish, brown, violaceous or grayish papules
- Mid dermal cyst containing laminated keratin and many vellus hairs
- Epithelial lining consists of several layers of squamous epithelium, often with a granular cell layer
- Steatocystoma:
- Skin colored to yellowish dermal cystic papules or nodules
- Cyst lined by stratified squamous epithelium without a granular layer with attached sebaceous gland
- Diagnostic, corrugated eosinophilic layer lining luminal surface
- Congenital dermoid fistula:
- Presents at birth as a superficial fistula tract
- Pilomatrixoma:
- Benign tumor arising from hair matrix
- Solid nests of basaloid cells undergoing abrupt trichilemmal type keratinization
- Ghost cells, calcification or ossification with extramedullary hematopoiesis and frequent rupture leading to giant cell reaction
- Encephalocele:
- Can also be found in glabella area
- Compressible / soft and bluish in color
- Typically transilluminate
- Nasal glioma:
- Pilar / trichilemmal cyst:
- Firm and well circumscribed nodule on palpation
- Lined by stratified squamous epithelium, which lacks granular layer
- Contains dense eosinophilic keratin
- Teratoma:
- Represents true neoplasm comprised of tissues from all 3 germ layers: ectoderm, mesoderm and endoderm
- Biopsy
- Excision
- MRI
- Radiograph (Xray)
Comment Here
Reference: Dermoid cyst
What findings in the above picture are specific to dermoid cyst?
- Cyst lined by stratified squamous epithelium and abundant keratin flakes
- Cyst lined by stratified squamous epithelium and sebaceous glands
- Cyst lined by stratified squamous epithelium with multiple hair shafts
- Cyst lined by stratified squamous epithelium with retained the granular layer
- Cyst lined by stratified squamous epithelium, sebaceous glands and hair follicle
Comment Here
Reference: Dermoid cyst
- Malignant adnexal tumor with a marked predilection of acral sites
- Helwig first described as eccrine acrospiroma in 1979 (J Cutan Pathol 1987;14:129)
- Malignant adnexal tumor with a marked predilection of acral sites
- Usually fingers and toes, rarely palm and sole
- Clinically confused with a cystic lesion
- Tumor cells are basaloid / cuboidal to low columnar epithelial cells and myoepithelial cells with mild to moderate cytologic atypia
- Rarely, metastasis to lung and lymph node
- Also called digital papillary eccrine adenoma, aggressive digital papillary adenoma, digital adenocarcinoma
- ICD-O: 8408/3 - Digital papillary adenocarcinoma
- About 200 cases reported (Am J Surg Pathol 2012;36:1883, Dermatol Surg 2018;44:911, Ann Diagn Pathol 2015;19:381, J Am Acad Dermatol 2017;77:549, Br J Dermatol 2019;180:1150)
- 0.08 cases/1,000,000 (Dermatol Surg 2018;44:911)
- M:F = 74:20 (~4:1) (Dermatol Surg 2018;44:911)
- 14 - 83 years (average 52 years)
- Most common in Caucasians (Dermatol Surg 2018;44:911)
- Mortality in 2.1% (Dermatol Surg 2018;44:911)
- Usually digits (fingers and toes), rarely palm and sole, hands are more common (> 80%) than feet
- Rarely, face (2 cases), thigh (1 case) (Dermatol Surg 2018;44:911, Medicine (Baltimore) 2016;95:e4110)
- Ultrastructural finding (see below) and eccrine glands are abundant in acral sites
- This is because digital papillary adenocarcinoma is an eccrine tumor
- Some patients have trauma
- Slow growing, asymptomatic nodule (average 1.7 cm, range: 0.4 - 4.3 cm)
- Clinically confused with a cystic lesion, ulceration is rare
- Pain may occur if the tumor involves the underlying bone, joint, nerves
- Rarely, metastatic disease (lung, lymph node) (Am J Surg Pathol 2012;36:1883, J Am Acad Dermatol 2017;77:549)
- Clinically, may be suspected from the site of origin and clinical course
- Histologic examination of tissue provides a definitive diagnosis
- Local recurrence and metastasis are 5 - 21% and 26 - 50%
- Histopathological features appear not to be predictive
- Delayed occurrence of metastases and a protracted course, long term follow up is necessary (Am J Surg Pathol 2012;36:1883)
- A man in his 20s (Dermatol Online J 2018;24)
- 53 and 65 year old men (Int J Dermatol 2017;56:1061)
- 54 year old Indian man with heel tumor (Clin Med Insights Case Rep 2019;12:1179547619828723)
- 67 year old right hand dominant man (Case Reports Plast Surg Hand Surg 2019;6:29)
- 89 year old Caucasian man (Dermatol Surg 2019 Sep 26 [Epub ahead of print])
- Complete excision or amputation of the affected digit
- Sentinel lymph node biopsy may translate into decreased local recurrence and metastasis (S Afr Med J 1989;76:593)
- The role of chemotherapy remains unclear (J Clin Oncol 2013;31:e386)
- Radiation can be used effectively at conventional palliative doses (J Clin Oncol 2013;31:e386)
- FGFR or BRAF targeted therapy may be useful (Br J Dermatol 2019;180:1150, Ann Diagn Pathol 2015;19:381)
- Well circumscribed multinodular tumors within dermis and superficial subcutis
- Solid and cystic portions, papillary projections, tubular or ductal structures (Am J Surg Pathol 2012;36:1883)
- Occasionally show infiltrative margin
- Uncommonly epidermal hyperplasia (3/31), ulceration (2/31), focal epidermal connection (1/31) (Am J Surg Pathol 2012;36:1883)
- Tumor cells are basaloid, cuboidal to low columnar epithelial cells and myoepithelial cells with mild to moderate cytologic atypia
- Severe cytologic atypia (3/31) and tumor necrosis (6/31) is noted in a small subset of tumors (Am J Surg Pathol 2012;36:1883)
- Mitoses may be inconspicuous or frequent (1 - 15 mm2) (Am J Surg Pathol 2012;36:1883)
- Spindle cell, squamoid differentiation, clear cell changes may be encountered (Am J Surg Pathol 2012;36:1883)
- Pancytokeratin, CK7 diffusely positive
- S100 protein, ER, PR, AR in 50% of cases (J Am Acad Dermatol 2017;77:549)
- Inner cell layer: EMA, CEA (highlights luminal border of tubules) (Am J Surg Pathol 2012;36:1883)
- Myoepithelial cell (outer cell) layer: SMA, calponin, p63, focally D2-40, CK14
- Ultrastructural studies demonstrated three types of neoplastic cells: clear cells, dark cells and myoepithelial cells
- Some dark cells have dense granules (J Cutan Pathol 1987;14:129)
- BRAFV600E (1/9) (Ann Diagn Pathol 2015;19:381)
- Tumor overexpression of FGFR2 (6/6) (Br J Dermatol 2019;180:1150)
- Skin, left ring finger, punch biopsy:
- Digital papillary adenocarcinoma (see comment)
- Comment: The histopathological examination shows a well circumscribed multinodular tumor within the dermis to superficial subcutis. It shows solid and cystic portions with focal papillary projections and tubular structures. Two cell layers are present; inner cells are cuboidal epithelial cells with mild to moderate cytologic atypia and outer cells are myoepithelial cells. Some mitoses are seen (1 - 3 mm2). The inner layer is immunoreactive for EMA and CEA which highlighted the luminal border of tubules. The myoepithelial cell (outer cell) layer is positive for SMA, calponin and p63. These histologic features are consistent with digital papillary adenocarcinoma.
- Hidradenoma:
- Lack of papillary structures and cytologic atypia
- Diffuse immunohistochemical positivity for p40 and p63; absence of S100 and SMA
- Fusion gene CRTC1/MAML2 detected in 50% (particularly in those with clear cell features) or CRTC3/MAML2 (Am J Surg Pathol 2019 Dec 23 [Epub ahead of print], Genes Chromosomes Cancer 2007;46:559, Hum Pathol 2017;70:55)
- Papillary eccrine adenoma:
- Rare or absent solid areas
- Absence of infiltrative growth pattern, significant cytologic atypia and pleomorphism
- Mitoses are usually absent but can be scant (Am J Surg Pathol 2019 Dec 23 [Epub ahead of print])
- Apocrine hidrocystoma / apocrine cystadenoma:
- Exceptionally rare on the distal extremities
- Cytologic atypia in cystic and papillary tumors on the distal extremities exclude this diagnosis (Surg Pathol Clin 2017;10:383)
- Microcystic adnexal carcinoma:
- infiltrative growth in a desmoplastic stroma
- Predominantly duct differentiation (Surg Pathol Clin 2017;10:383)
- Hidradenocarcinoma:
- Lack of two cell layers (Surg Pathol Clin 2017;10:383)
- Epithelial myoepithelial carcinoma / adenomyoepithelial carcinoma (tumor):
- Controversial; past reported cases might include epithelial myoepithelial carcinoma or adenomyoepithelial carcinoma
- These tumors are very rare; there are not enough cases to distinguish them
- Further examination is needed by correcting many cases (Dermatol Pract Concept 2014;4:33, J Dermatol 2018;45:357)
- Controversial; past reported cases might include epithelial myoepithelial carcinoma or adenomyoepithelial carcinoma
- Metastatic adenocarcinoma:
- Lack of two cell layers (especially myoepithelial cell) (Pathology 2013;45:55)
- A 56 year old man presented with a tumor on his middle finger. The tumor shows solid and cystic areas with focal papillary projections and tubular structures. Which of the following is most likely the correct diagnosis?
- Apocrine hidrocystoma
- Bowen disease
- Digital papillary adenocarcinoma
- Hidradenoma
- Papillary eccrine adenoma
- Which of the following is true about digital papillary adenocarcinoma?
- Dual layered cystic structures are characteristic
- It arises only in digits
- It does not occur in young people
- Tumor does not show metastasis
Reference: Digital papillary adenocarcinoma
Comment Here
- Rare benign hamartoma of eccrine glands and blood vessels that often occurs in the extremities (Ann Dermatol 2013;25:208)
- May be present at birth or develop during childhood (Dermatology Online Journal 2009;15:10)
- May be painful and be associated with hyperhidrosis, which can be helpful in diagnosis
- Typically slow growing with benign behavior
- 3 month old child with painful nodule on finger (Case of the Week #324)
- Simple excision is usually curative, but is reserved for painful and cosmetically disfiguring lesions (Ann Dermatol Venereol 1997;124:623, Pediatr Dermatol 2009;26:316)
- 2.0 x 1.5 cm skin covered nodule; cut section showed a homogenous dark brown appearance (Case of the Week #324)
- Increased number of eccrine glands in the superficial dermis, with blood vessels between and around the glands and ducts
- Vessels varied in size, but were predominantly small and lined by endothelial cells
- Other areas of dermis showed smooth muscle bundles, fat cells and focal areas of myxoid change (Case of the Week #324)
- Angiokeratoma
- Eccrine nevus
- Glomus tumor
- Hemorrhage (Ann Dermatol 2011;23 Suppl 1:S84)
- Macular telangiectatic mastocytosis
- Nevus flammeus
- Smooth muscle hamartoma
- Benign (multi) nodular solid tumor showing eccrine differentiation
- Benign neoplasm, excision is curative
- Predilection for head and neck
- Usually asymptomatic but can be painful, belonging to the painful skin tumors in the acronym BLEND TAN EGG (blue rubber bleb nevus, leiomyoma, eccrine spiradenoma, neuroma, dermatofibroma, tufted angioma, angiolipoma, neurilemmoma, endometrioma, granular cell tumor, glomus tumor) (Indian J Dermatol Venereol Leprol 2019;85:231)
- Association with the Brooke-Spiegler syndrome
- Multiple dark nests of cells confined to dermis (blue balls in the dermis) composed of 2 epithelial cell types: small dark peripheral cells and larger pale central cells, with intratumoral lymphocytes
- Spiradenoma
- Eccrine spiradenoma
- Usually in adults
- Rarely congenital or infants (Arch Craniofac Surg 2017;18:211)
- Head / face and neck
- Other sites (extremities and trunk) less common
- Commonly presenting as solitary nodule
- Rarely as multiple lesions in combination with other types of adnexal tumors as part of the Brooke-Spiegler syndrome
- Predilection site: head and neck area, less commonly trunk and extremities
- Usually asymptomatic, although often cited as a painful skin tumors in the acronym BLEND TAN EGG (blue rubber bleb nevus, leiomyoma, eccrine spiradenoma, neuroma, dermatofibroma, tufted angioma, angiolipoma, neurilemmoma [schwannoma], endometrioma, granular cell tumor, glomus tumor) (Indian J Dermatol Venereol Leprol 2019;85:231)
- Firm, round and smooth surface nodule
- Skin colored, gray-pink, reddish or blue
- Small, usually 1 - 3 cm in size, may be larger, rare giant variants
- Clinical examination and dermoscopy
- Excisional biopsy for a definitive diagnosis (Arch Craniofac Surg 2017;18:211)
- Benign neoplasm
- Malignant transformation is a very rare phenomenon with the malignant component classified into basal cell adenocarcinoma-like, low grade pattern, basal cell adenocarcinoma-like, high grade pattern, invasive adenocarcinoma, NOS, sarcomatoid carcinoma / carcinosarcoma and malignant epithelial myoepithelial carcinoma (Am J Surg Pathol 2009;33:705, Int J Surg Pathol 2020;28:427)
- 23 year old woman with zosteriform spiradenoma and spiradenocarcinoma (Indian Dermatol Online J 2015;6:S30)
- 28 year old woman with multiple supraclavicular subcutaneous nodules and intermittent pain (J Cytol 2017;34:39)
- 47 year old woman with shin lump (J Vasc Surg Cases Innov Tech 2019;5:583)
- 75 year old woman with auricular nodule (Ear Nose Throat J 2019;98:545)
- 84 year old woman with nipple mass (Histol Histopathol 2019;34:909)
- Complete excision is curative
- Usually less than 1 cm, rarely can be larger
- Gray-pink or blue nodule
- Either uninodular or multinodular tumor centered within the dermis
- Extension into the subcutaneous tissue is common
- Usually not connected to epidermis (Arch Craniofac Surg 2017;18:211)
- Not typically submitted for frozen section
- Histologic features described below
- Might be mistaken for basal cell carcinoma at the time of Mohs surgery (Wien Med Wochenschr 2018;168:218)
- Circumscribed uninodular or multinodular basophilic tumor (see Figure 1)
- Mostly centered in the dermis (blue balls)
- Some tumors are encapsulated (see Figure 2)
- Extension into the subcutis is common
- 2 cell populations in the neoplastic nodules: centrally located large pale cells and small dark basaloid cells at the periphery (see Figure 3)
- Neoplastic cells are arranged in trabecular, reticular or solid fashion
- Intratumoral lymphocytes as an integral component of the tumor (see Figure 3)
- Tubular / ductal structures (see Figure 4) and PAS positive basement membrane material (see Figure 5)
- Stroma between the nests of epithelial cells is often edematous with prominent vascularity (see Figure 6); may be hyalinized (see Figure 7)
- Vessels may be widely dilated (see Figure 7) / hemangiopericytoma-like
- Many T lymphocytes and Langerhans cells often scattered throughout lobules
- Mitoses extremely rare
- Morphologic variations:
- Architectural variations:
- Cystic changes (see Figure 8)
- Adenomatous (see Figure 9) (Am J Dermatopathol 2008;30:436)
- Adenomyoepitheliomatous component (see Figure 10) (Int J Surg Pathol 2020;28:427)
- Adenoid cystic-like pattern cylindromatous features (see Figure 11)
- Trichoepitheliomatous / trichoblastomatous differentiation
- Cytologic variations:
- Stromal variation: edematous, myxoid, lipomatous metaplasia, osseous metaplasia, myoid metaplasia
- Architectural variations:
- Rare case reports describing the fine needle aspiration (FNA) cytologic findings of spiradenoma
- Tight multilayered clusters of uniform benign cuboidal epithelial cells along with spindle shaped myoepithelial cells and occasional lymphocytes (J Lab Physicians 2014;6:130)
- Prominent basement membrane deposition with an irregular tubular and nesting growth pattern and bland basaloid cells (Acta Cytol 1990;34:275)
- Intraluminal material is PAS positive, diastase resistant
- Both cell populations (dark and pale) are positive for CK7, CK8 and CK18
- CEA and EMA highlight the ductal components
- S100 (see Figure 14) and SMA (see Figure 15) highlight myoepithelial cells
- Beta catenin positive (nuclear) (J Cutan Pathol 2011;38:657)
- Immunopositivity for IKH4 is supportive of eccrine differentiation over apocrine (J Cutan Pathol 1998;25:100)
- Lobules separated by amorphous / fibrillar material
- Large pale cell has mitochondria, vesicles, glycogen in cytoplasm (J Invest Dermatol 1962;38:289)
- Axin and GSK-3β (both induce degradation of beta catenin) downregulated (J Cutan Pathol 2011;38:657)
- Mutations in the tumor suppressor gene, CYLD (Nat Commun 2019;10:2213)
- Missense mutations in the alpha kinase domain of the ALPK1 gene (Nat Commun 2019;10:2213)
- p53 loss of function mutations described in rare cases of malignant transformation / spiradenocarcinoma (Nat Commun 2019;10:2213)
Spiradenoma: 5 minute pathology pearls
Spiradenoma and cylindroma: sweat gland tumor pathology
Spiradenoma for beginners
- Skin, left cheek, excision:
- Spiradenoma, completely excised with negative surgical margins
- Negative for malignancy
- Cylindroma:
- Closely related tumor with morphologic overlap but generally more abundant eosinophilic material around clusters of dark cells with jigsaw pattern and usually lack of lymphocytes
- Poroma:
- Only basaloid cells, absence of the second pale cell population and intratumoral lymphocytes
- Spiradenocarcinoma / malignant spiradenoma / carcinoma ex spiradenoma:
- Infiltrative growth and nuclear atypia, arising from spiradenoma (both components identified)
- Composed of nests of a single cell type, forming dark nests in the dermis
- Even with complete excision, local recurrence is typical
- Intratumoral lymphocytes are a common component
- Usually centered in the epidermis
- Birt-Hogg-Dube syndrome
- Brooke-Spiegler syndrome
- Cowden syndrome
- Tuberous sclerosis
- Rare, benign eccrine proliferation of anastomosing cords with ductal structures set in a fibrovascular stroma, often located on the extremities
- Erythematous, solitary or multiple papules and nodules often on acral sites
- Association with Schöpf-Schulz-Passarge syndrome and Clouston syndrome
- Thin anastomosing cords and strands of basaloid monomorphous cuboidal cells extending from the basal layer of epidermis into dermis with ductal structures and set in a fibrovascular stroma
- Eccrine syringofibroadenoma (of Mascaro)
- Other names include
- Eccrine syringofibroadenomatous hyperplasia
- Acrosyringeal adenomatosis
- Eccrine poromatosis
- Linear eccrine poroma
- Acrosyringeal nevus or acrosyringeal nevus of Weedon and Lewis
- Nevus syringoadenomatosus papilliferum
- Rare
- Wide age range, most cases presenting in the seventh to eighth decade (Am J Dermatopathol 1992;14:328)
- Schöpf-Schulz-Passarge syndrome associated cases usually present in adolescence; slightly later presentation in Clouston syndrome
- No clear racial or gender predilection
- Predilection for extremities, especially acral sites
- Several nonacral sites, such as eyelid, perianal region and scalp, reported (Sultan Qaboos Univ Med J 2013;13:328, Indian J Dermatol 2017;62:548, J Cutan Aesthet Surg 2022;15:335)
- Morphologic, immunohistochemical and electron microscopic evidence supports origin from eccrine duct cells
- Reactive subtype postulated to be induced by repair / remodeling process (An Bras Dermatol 2021;96:255)
- Unclear; neoplastic / tumoral, hamartomatous and reactive origins postulated
- Presence in ectodermal dysplasia supports a tumoral or hamartomatous process (J Dermatol 2022;49:e451)
- Rare cases with malignant transformation support a neoplastic process (Am J Dermatopathol 2020;42:780)
- Cases with associated inflammatory dermatoses and benign or malignant epithelial neoplasms support a reactive process (An Bras Dermatol 2021;96:255)
- Presents as slow growing, solitary or multiple, flesh colored nodule(s)
- 5 major clinical types (J Am Acad Dermatol 1997;36:569)
- Solitary: most common form, often on lower extremities
- Multiple with hidrotic ectodermal dysplasia (Schöpf-Schulz-Passarge syndrome and Clouston syndrome): palms and soles, younger patients (15 - 25 years old)
- Multiple without associated cutaneous findings: palms and soles
- Nevoid (i.e., nonfamilial unilateral linear eccrine syringofibroadenoma [ESFA]): rare, unilateral linear papules and plaques
- Reactive, as can be seen in association with the following
- Inflammatory dermatoses / processes (i.e., erosive lichen planus, uncontrolled psoriasis, bullous pemphigoid, epidermolysis bullosa, primary cutaneous amyloidosis, thermal scar, venous stasis, chronic diabetic foot ulcer, neuropathy, peristomal skin)
- Infectious etiologies (i.e., leprosy, HPV)
- Neoplasms / tumors (i.e., nevus sebaceus, clear cell acanthoma, acantholytic dyskeratotic acanthoma, squamous cell carcinoma, basal cell carcinoma and Merkel cell carcinoma)
- Associated syndromes
- Schöpf-Schulz-Passarge syndrome (OMIM: Schopf-Schulz-Passarge Syndrome; SSPS [Accessed 11 October 2023])
- Autosomal recessive disorder due to a homozygous mutation of the WNT10A gene (chromosome 2q35)
- Clinical features include palmoplantar keratoderma, hypodontia, hypotrichosis, hyperhidrosis, eyelid hidrocystomas, nail dystrophy and eccrine syringofibroadenoma (Br J Dermatol 2014;171:1211, J Cutan Pathol 2020;47:987)
- Clouston syndrome (OMIM: Clouston Syndrome [Accessed 11 October 2023])
- Autosomal dominant disorder due to heterozygous mutations in the gap junction beta 6 (GJB6) gene (chromosome 13q12.11) that encodes gap junction protein beta 6 (i.e., connexin 30) (Front Med 2023;17:330)
- Clinical features include palmoplantar keratoderma, alopecia, nail dystrophy and eccrine syringofibroadenoma (Int J Dermatol 2019;58:e143)
- Schöpf-Schulz-Passarge syndrome (OMIM: Schopf-Schulz-Passarge Syndrome; SSPS [Accessed 11 October 2023])
- Biopsy / histologic examination and clinicopathologic correlation necessary for diagnosis
- Benign lesion(s)
- 1 case of reactive ESFA with spontaneous involution (Clin Exp Dermatol 2009;34:e66)
- Rare malignant transformation in longstanding lesions (Am J Dermatopathol 2020;42:780)
- 31 year old man with perianal ESFA following deep bacterial infection (Indian J Dermatol 2017;62:548)
- 36 year old woman with palmar syringofibroadenoma-like lesions in the setting of Clouston syndrome treated with CO2 ablative laser (JAAD Case Rep 2023:39:61)
- 72 year old woman with reactive ESFA in association with a Merkel cell carcinoma excision scar (Am J Dermatopathol 2023;45:137)
- 77 year old man with ESFA associated with basal cell carcinoma (Dermatol Surg 2018;44:738)
- 97 year old woman with acantholytic dyskeratotic acanthoma accompanying syringofibroadenomatous hyperplasia (J Cutan Pathol 2021;48:451)
- Single lesions treated by surgical excision or cryotherapy (J Am Podiatr Med Assoc 2016;106:237)
- Therapy for cases with multiple lesions depends on size and location
- Laser therapy with dual pulse width flashlamp (Dermatol Surg 1999;25:418)
- Etretinate oral therapy in diffuse lesions (J Dermatol 1999;26:36)
- CO2 laser (JAAD Case Rep 2023:39:61)
- Radiotherapy (Dermatol Ther 2010:23:S20)
- Topical corticosteroids (An Bras Dermatol 2021;96:255)
- Verrucous erythematous papules, nodules and ulcerative plaques
- Multiple nodules may be arranged in a symmetrical or unilateral nevoid fashion
- Proliferation of thin anastomosing reticulated epithelial cords and strands often forming a lattice and extending from the epidermis into the dermis (J Cutan Aesthet Surg 2022;15:335)
- Lesional cells are monomorphous, basaloid, cuboidal and slightly smaller than adjacent keratinocytes
- Epithelial cords contain structures resembling eccrine ducts (Ann Dermatol 2020;32:57)
- Background fibrovascular stroma
- Periductal / ductal structures: CEA, EMA, involucrin, filaggrin, CK6, CK8, CK10, CK18, CK19 (Am J Dermatopathol 1996;18:207, Am J Dermatopathol 2000;22:171)
- Strands and sheets of cells: CK6, AE1, MNF116, AE3, CK 34 beta E12 (Am J Dermatopathol 2000;22:171, J Cutan Pathol 2000;27:164)
- Strands and sheets of cells: cytokeratin KL1, CK10 (J Cutan Pathol 2000;27:164)
- Tumor cells with tonofilaments / desmosomes, numerous glycogen granules
- Basal lamina
- Globular keratohyalin granules around ducts / cysts
- No lamellar granules
- Poorly developed cornified cell envelopes (Am J Dermatopathol 1996;18:207)
Eccrine syringofibroadenoma: rare skin adnexal tumor / pattern
- Leg, shave biopsy:
- Benign appendageal neoplasm with eccrine differentiation consistent with an eccrine syringofibroadenoma (see comment)
- Comment: The lesion extends to the deep margin. The specimen exhibits an epidermal based proliferation of monomorphous basaloid cells arranged as anastomosing cords forming a lattice with intermixed ductal structures and set in a fibrovascular stroma. These findings support the histologic diagnosis.
- Fibroepithelioma of Pinkus:
- Buds of basaloid epithelium characteristic for basal cell carcinoma
- No duct formation noted within the anastomosing epithelial cords
- Poroma and hidroacanthoma simplex:
- Shares eccrine histogenesis
- Lacks the reticular and corded architecture of ESFA
- Porocarcinoma:
- Lacks corded architecture
- Has malignant cytologic changes
- Tumor of the follicular infundibulum:
- Shares anastomosing strands but forms a plate-like structure in the dermis and lacks ductal structures
- Squamous cell carcinoma with ductal differentiation:
- Infiltrative pattern with cytologic atypia
A 74 year old woman presents with a 1 year history of asymptomatic, erythematous papules on the left heel. A subsequent shave biopsy is performed (see image above). Few intermixed ducts in the epithelial cords are also noted on examination of multiple tissue levels. What is the best histologic diagnosis for this lesion?
- Basal cell carcinoma, infiltrative type
- Eccrine syringofibroadenoma
- Porocarcinoma
- Poroma
- Squamous cell carcinoma
Comment Here
Reference: Eccrine syringofibroadenoma
- Birt-Hogg-Dubé
- Brooke-Spiegler
- Rubinstein-Taybi
- Schöpf-Schulz-Passarge
Comment Here
Reference: Eccrine syringofibroadenoma
- Low grade adenocarcinoma of cutaneous sweat gland origin
- Predilection for the eyelids of older women
- Rare, low grade adenocarcinoma of sweat gland origin that often arises on or near the eyelids of older women
- Can recur if incompletely excised and may be a precursor to mucinous carcinoma; however, there are no reported cases of metastases
- Must be distinguished from metastatic adenocarcinoma; resembles mammary solid papillary carcinoma / endocrine ductal carcinoma with cystic and solid architecture (solid components show cribriform, papillary and pseudopapillary patterns punctuated by mucin filled spaces)
- Key feature is neuroendocrine expression; elaboration of a myoepithelial layer by immunohistochemistry is helpful to confirm primary cutaneous origin and exclude metastatic adenocarcinoma
- C44.191 (eyelid): other specified malignant neoplasm of skin of unspecified eyelid, including canthus
- Higher incidence among women than men (Am J Surg Pathol 2005;29:1330)
- Often elderly adults, not described in children
- Head and neck, eyelid most common
- Given the low incidence of this disease, its etiology is incompletely understood
- Tumor is thought to be analogous to mammary solid papillary carcinoma / endocrine ductal carcinoma in situ of and exhibits a similar immunophenotype, including evidence of a surrounding myoepithelial cell layer
- Lesions can be solitary or less often multiple (regional)
- Translucent cyst (sometimes multiloculated) may resemble hidradenoma
- Cases with lesser developed cystic components appear as skin colored nodules
- Diagnosis requires correlations with immunohistochemistry, clinical history and clinical examination findings to exclude metastatic adenocarcinomas from breast, salivary gland or viscera
- No reported cases of metastasis
- Some cases have contiguous primary cutaneous mucinous carcinoma
- Recurrence is common when the tumor is incompletely excised
- 71 year old woman with a papule on her left upper eyelid (Am J Dermatopathol 2016;38:636)
- 75 year old woman with a skin colored eyelid nodule and a left breast mass (Am J Dermatopathol 2015;37:425)
- 83 year old woman with nodules on her bilateral lower eyelids (Am J Dermatopathol 2016;38:789)
- Excision or Moh's micrographic surgery
- Nodular, often multilobulated dermal tumor with solid areas and cystic spaces
- Solid areas may show cribriform architecture or pseudorosettes, papillae with fibrovascular cores or smaller pseudopapillae
- Solid areas are often punctuated by mucin filled cystic spaces that range in appearance from small holes and clefts to large, hidrocystoma-like components
- Some lesions closely resemble hidrocystoma on low power but show multilayering of neoplastic cells and Roman bridges analogous to breast ductal carcinoma in situ
- Lesions frequently appear contiguous with benign ducts
- Most lesions have an inconspicuous and discontinuous myoepithelial cell layer surrounding them; however, there is disagreement as to whether to classify endocrine mucin producing sweat gland carcinoma as purely in situ carcinoma or invasive adenocarcinoma (Am J Surg Pathol 2005;29:1330, Am J Dermatopathol. 2013;35:117, Requena: Cutaneous Adnexal Neoplasms, 1st Edition, 2018)
- Has 1 to 3 layers of bland columnar secretory cells with occasional apical snouts, intracellular and extracellular mucin, moderate amounts of cytoplasm with a basophilic hue, ovoid nuclei (slightly larger than those of surrounding eccrine ductal epithelia), bland or sometimes stippled nuclear chromatin and minimal to no nuclear pleomorphism or mitotic activity (Am J Surg Pathol 2005;29:1330)
- Lesions are sometimes contiguous with primary cutaneous mucinous carcinoma (or adjacent acellular pools of mucin suspicious for mucinous carcinoma) or have a component of infiltrative nests of cells with mild nucleomegaly and hyperchromasia
- Neuroendocrine expression: NSE, synaptophysin, chromogranin, CD56, INSM1
- Mucicarmine highlights intracellular and extracellular mucin
- CK7, ER / PR, GCDFP-15 and GATA3 (Am J Dermatopathol 2016;38:789) are also positive in adenocarcinoma of breast and salivary gland and cannot distinguish it from endocrine mucin producing sweat gland carcinoma
- Calponin, SMA and p63 highlight myoepithelial layer around the dermal nodules and intraductal components, providing evidence of a primary cutaneous origin but care should be taken not to overinterpret staining of adjacent benign eccrine structures
- AE1 / AE3, CAM 5.2, EMA, E-cadherin, CD57, CEA (patchy in areas with ductal differentiation)
- Cytogenetics reveal diploidy (J Dermatol 1994;21:117, Am J Dermatopathol 2000;22:166)
- No mutations in TP53, PIK3CA, AKT1, KRAS, GNAS and EGFR or HER2/neu amplifications have been identified to date in EMPSGC or cutaneous mucinous carcinoma (Am J Dermatopathol 2000;22:166, Am J Surg Pathol 2005;29:764, Am J Dermatopathol 2016;38:636, Am J Surg Pathol 2005;29:764, J Cutan Pathol 2020 [Online ahead of print])
- Skin, left upper eyelid, shave:
- Endocrine mucin producing sweat gland carcinoma, present at the peripheral edge and base of specimen (see comment)
- Comment: The bland cytomorphology, evidence of neuroendocrine expression (INSM1 stains tumoral nuclei and synaptophysin stains tumoral cytoplasm) and variable presence of a p63 positive myoepithelial layer surrounding the lesion together support this diagnosis.
- Apocrine adenoma:
- Extensive decapitation secretion, absence of neuroendocrine differentiation, absence of mucin and enlarged epithelioid nuclei with conspicuous nucleoli
- Apocrine carcinoma:
- High grade cytologic atypia exceeding that of endocrine mucin producing sweat gland carcinoma (EMPSGC), usually no mucin production
- Basal cell carcinoma:
- Rare cases exhibit neuroendocrine differentiation; however, palisading of peripheral cells with retraction of the adjacent stroma and increased apoptoses and mitoses favor the latter
- Dermal duct tumor:
- Absence of neuroendocrine differentiation, no cribriform architecture or mucin filled clefts, more prominent ductular differentiation with secretory spaces lined by cuticle, foci of necrosis
- Hidrocystoma:
- Bland lining lacks architectural complexity, cytologic atypia or neuroendocrine marker expression
- Nodular hidradenoma:
- Also has variable cystic and solid conformation but an absence of neuroendocrine differentiation, attachment to the epidermis and vascular spaces favor hidradenoma and a greater diversity of cell types including eosinophilic polygonal cells, squamous cells, clear cells and goblet cells
- Primary cutaneous mucinous adenocarcinoma:
- May be contiguous with EMPSGC suggesting that EMPSGC could be a precursor lesion; small cribriform or tubular islands of epithelioid cells in pools of mucin partitioned by strands of dermal collagen
- CK7
- CK20
- GATA3
- p63
Comment Here
Reference: Endocrine mucin producing sweat gland carcinoma
- Eyelid
- Inferior helix
- Nasal ala
- Scalp
Comment Here
Reference: Endocrine mucin producing sweat gland carcinoma
- This topic discusses features of cutaneous endometriosis only - a general discussion of endometriosis is found in the Ovary topic
- Ectopic endometrial tissue, usually described in pelvic organs, but 0.5% - 1.0% of cases are cutaneous
- Women of reproductive age, often due to iatrogenic seeding of umbilicus during C-section (Villar’s nodule) but may occur in almost any site
- Carcinoma rarely arises in preexisting endometriosis
- Women with endometriosis may have mildly increased risk of melanoma (Int J Epidemiol 2009;38:1143)
- 35 year old woman with menstruating cutaneous lesion of umbilicus (J Med Case Reports 2009;3:9326)
- 37 year old woman with umbilical nodule (Dermatol Online J 2011;17:5)
- Gonadotropin releasing hormone analogues
- Excision
- Dark red to bluish nodule, may form cystic structure
- Endometrial glands, endometrial stroma and hemorrhage
- May have marked decidual changes
- Sweat gland tumor
- Urachal duct cyst
- Pyogenic granuloma
- Hernia
- Residual embryonic tissue
- Primary or metastatic adenocarcinoma (Sister Joseph's nodule)
- Cutaneous endosalpingiosis
- Benign skin tumor
- Cystic mass containing keratin
- Cystic mass with soft white keratin contents
- Histologically cystic mass with squamous epithelium and keratin flakes
- Epidermoid cyst, epidermal cyst, epidermal inclusion cyst, infundibular cyst
- ICD-10: L72.0 - epidermal cyst
- Young and middle aged adults are most often affected (Int J Trichology 2017;9:108)
- M = F
- Face, neck, trunk, perineal area, cerebellopontine angle
- Less commonly spine, intrapancreatic accessory spleen
- Follicular orifice becomes plugged with bacteria and keratin, leading to cystic dilation and entrapment of keratin debris
- Presence of multiple epidermal inclusion cysts has been documented in Gardner syndrome, a variant of familial adenomatous polyposis with benign osteomas and intestinal fibromatoses
- Less frequently, patients may have lipomas, pilomatrixomas (including epidermoid cysts with pilomatrical lining) or leiomyomas
- Multiple and large epidermoid cysts may occur with the use immunosuppressants in the posttransplantation setting, for example, with cyclosporine or tacrolimus (Cutis 1992;50:36, Ann Dermatol 2011;23:S182)
- May complicate penetrating trauma to skin, such as a sewing needle, with resultant implantation of squamous epithelium into the dermis (Turk J Pediatr 2011;53:108)
- Present as smooth dome shaped swellings varying in size from a few millimeters to a few centimeters (Ann Dermatol 2017;29:33)
- Usually occur on the face, neck or trunk but can occur anywhere
- Overlying skin may be taut with the pressure of the cyst and have a central punctum
- Generally occurs in postpubertal individuals
- Freely mobile unless ruptured, in which case a foreign body giant cell reaction may make them more adherent to surrounding connective tissue
- May become painful and inflamed with external manipulation
- Cyst contents white, cheesy macerated keratin that may have an odor
- Often based on clinical examination
- Pathological diagnosis relies on recognizing the cyst wall and contents
- In cases of extensive foreign body giant cell reaction or fibrosis, the classic features may not be visualized as readily and a diligent search for keratin flakes may lead to diagnosis
- No specific laboratory findings
- Ultrasound:
- Subcutaneous rounded structure that is mostly anechoic or hypoechoic with focal present inner echoes (pseudotestis appearance) representing cystic debris
- MRI:
- Fluid-like enhancement
- High intensity of cyst contents on T2 weighted images and peripheral cyst wall enhancement with T1 gadolinium enhancement
- Cyst rupture results in irregular enhancement (AJR Am J Roentgenol 2006;186:961)
- 7 year old boy with epidermal inclusion cyst infected by molluscum contagiosum virus (J Dtsch Dermatol Ges 2018;16:1143)
- 40 year old woman with recurrent spinal epidermoid cysts with atypical hyperplasia (Medicine 2017;96:e8950)
- 51 year old man with squamous cell carcinoma arising in a 30 year old perineal epidermal inclusion cyst (World J Surg Oncol 2018;16:155)
- 63 year old man with epidermal inclusion cyst containing a splinter with nonpigmented fungi (J Cutan Pathol 2018;45:954)
- 73 year old man with squamous cell carcinoma arising in an epidermoid cyst with human papillomavirus changes (Clin Exp Dermatol 2018;43:201)
- Complete excision of the cyst is curative
- Pearly glistening cyst with creamy contents
- Subepidermal cyst that may or may not open into the overlying epidermis
- Cyst lining composed of stratified squamous epithelium with a granular layer
- Cyst wall does not contain eccrine glands, sebaceous glands or hair follicles
- Cyst contents composed of abundant keratin flakes
- Foreign body giant cell reaction is frequently present in ruptured cysts
- Melanoma, basal cell carcinoma and squamous cell carcinoma have been reported in association with epidermal inclusion cysts (J Am Acad Dermatol 2013;68:e6, J Cutan Med Surg 2015;19:105)
Contributed by the University of Colorado Department of Pathology, Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
- Anucleate keratinizing squamous cells with some nucleated squamous cells
- Frequent erythrocytes, leukocytes, multinucleated giant cells and cholesterol crystals (J Nat Sci Biol Med 2014;5:460)
- Skin, neck, excision:
- Epidermal inclusion cyst
- Microscopic description: Cyst lined by squamous epithelium with granular layer containing lamellated keratin.
- Proliferating epidermoid cyst:
- May show carcinomatous changes, invasion and be locally aggressive
- Trichilemmal (pilar) cyst:
- Lack a granular layer in the cyst lining
- Dense lamellated keratin cyst contents
- More likely to occur on the scalp
- Pilomatricoma:
- Eosinophilic cellular outlines of squamous cells ("ghost cells") in addition to the more basophilic matrical cells
- More likely to occur in a pediatric population
- Hybrid cyst:
- Demonstrates features of both an epidermal and trichilemmal cyst
- Dermoid cyst:
- Similar in appearance
- Has adnexal structures (ie. sebaceous glands) in cyst wall
- Arises at sites of embryonic closure such as the lateral eyebrow
- Pilonidal sinus:
- Sinus tract surrounded by epithelium and mixed inflammation
- Characteristically contains broken hair shafts
- Steatocystoma:
- Compressed sebaceous gland within the cyst wall
- Characteristic wavy eosinophilic crenulated cuticle of the lining
- Odontogenic keratocyst:
- Attenuated squamous epithelium with parakeratosis
- Retraction of epithelium with basal palisade can be a helpful finding
- Often filled with keratin debris like epidermoid cyst
- Angiosarcoma
- Epidermoid cyst
- Lymphadenitis
- Pilar cyst
- Spindle cell lipoma
- Epidermal nevus is a developmental malformation that involves the epidermis and clinically manifests as a discrete congenital linear patch or plaque along the Blaschko lines
- Histologically characterized by a hamartomatous keratinocyte proliferation that results in epidermal papillomatosis and acanthosis with no associated adnexal structures
- Here, the term epidermal nevus is discussed within a narrow definition and does not include organoid, sebaceous, eccrine and pilar nevi
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- Hamartomatous proliferation of the epidermis with no associated adnexal structures, commonly presenting at birth
- Clinically presents as single to multiple coalescing small pale to dark brown plaques, occasionally markedly papillomatous or hyperkeratotic in a Blaschko linear distribution
- It is estimated that 33% of patients with epidermal nevi have other organ involvement and occurrence is associated with multiple syndromes
- Commonly caused by mosaic postzygotic activating mutations in FGFR2 / FGFR3, PIK3CA or RAS genes in the epidermis, occurring in early embryonic development
- Development of malignant neoplasms in epidermal nevi is a rare phenomenon and almost always occurs during adulthood
- Epithelial nevus
- Essentially a synonym for epidermal nevus; though both terms are used frequently to cover hamartomas of the epidermis along with those with adnexal malformations, this page uses the term epidermal nevus to discuss nevi arising from the epidermal keratinocytes only
- Common keratinocyte nevus
- Linear epidermal nevus (Am J Dermatopathol 2014;36:430)
- Linear verrucous epidermal nevus
- Nonorganoid epidermal nevus (Dermatol Online J 2010;16:12)
- Typically present at birth or develops in early childhood, with a prevalence of ~1 in 1,000 live newborns (Pediatr Dermatol 2004;21:432)
- F = M
- Secondary tumors are infrequent compared to organoid epidermal nevi (Dermatol Pract Concept 2022;12:e2022087)
- Extremely low rate of malignant transformation (Clin Exp Dermatol 2019;44:238)
- Can be associated with the following syndromes
- Schimmelpenning-Feuerstein-Mims syndrome (organoid nevi, abnormalities of the central nervous system and eyes, oral lesions and skeletal defects)
- Phakomatosis pigmentokeratotica type I (capillary malformations and epidermal nevus)
- Nevus comedonicus syndrome (ocular, skeletal and neural abnormalities, ipsilateral congenital cataract and malformations of fingers and toes) (Pediatr Dermatol 2021;38:359)
- Angora hair nevus syndrome (Angora hair nevus ocular, skeletal and neural abnormalities)
- Becker nevus syndrome (Becker nevus, poor unilateral breast or nipple development, supernumerary nipples, loss of subcutaneous fat, loss of axillary hair, musculoskeletal abnormalities)
- Proteus syndrome (overgrowth of skin and connective tissue)
- Type II segmental Cowden disease (neural defects, overgrowth of limbs and toes, polyps and nevi)
- Fibroblast growth factor receptor 3 epidermal nevus syndrome (keratinocytic epidermal nevus, acanthosis nigricans and neurological abnormalities) (J Pediatr Neurosci 2014;9:66)
- CHILD syndrome (congenital hypoplasia with ichthyosiform nevus and limb defects)
- Associated with several other less well defined epidermal nevus syndromes
- Reference: DermNet: Epidermal Naevus [Accessed 28 July 2023]
- Nearly all lesions occur on the neck, trunk and extremities
- Rare sites of presentation include intraoral and the face
- Epidermal nevi typically result from a postzygotic somatic mutation in an embryotic cell
- This leads to genetic mosaicism and the phenotypic consequence of the somatic mutation depends on how early the mutation arises, with very early mutations leading to extensive epidermal nevi and organ involvement (Dermatol Online J 2010;16:12)
- Epidermal nevi exhibit diverse clinical patterns, which can be attributed to a variety of histological patterns
- Epidermal nevi typically present as multiple warty brown patches or plaques along the lines of Blaschko
- Epidermal nevi can form a linear or zosteriform lesion
- At puberty, lesions become thicker, more verrucous and hyperpigmented (Curr Derm Rep 2012;1:186)
- Terms for different clinical patterns
- Nevus verrucosus (verrucous epidermal nevus): localized wart-like lesions
- Nevus unius lateris: unilateral, long, linear lesions on the extremities
- Ichthyosis hystrix: large, bilateral nevi on the trunk
- En bloc movement on the wobble test (characteristic of an epidermal growth)
- Patches of discoloration with minimal scale as a presentation have been described
- Epidermal nevi measure a few millimeters to several centimeters in length
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- Usually clinically suspected and diagnosed
- Skin biopsy may be required for confirmation or assessment of neoplasms developing in the lesion
- Generally, an epidermal nevus will persist indefinitely and follow a benign course
- It is estimated that 33% of patients with epidermal nevi have other organ involvement (Indian Dermatol Online J 2015;6:37)
- Benign secondary tumors have been reported arising from epidermal nevi showing divergent differentiation (e.g., toward sweat ducts in poromas and syringocystadenoma papilliderums) (Dermatol Pract Concept 2022;12:e2022087, Am J Dermatopathol 2014;36:430)
- Incidence of development of malignant neoplasms (e.g., basal cell carcinoma, keratoacanthoma and squamous cell carcinoma) in epidermal nevi is very rare (Case Rep Dermatol 2013;5:272)
- 10 month old girl with epidermal nevus syndrome with a PTCH1 gene mutation and cerebral infarction (J Med Case Rep 2022;16:343)
- 22 year old woman with a keratinocytic epidermal nevus and ipsilateral breast hypoplasia (Int J Womens Dermatol 2019;5:181)
- 28 year old woman developed syringocystadenoma papilliferum and eccrine poroma in a verrucous epidermal nevus (Dermatol Pract Concept 2022;12:e2022087)
- 31 year old man with adult onset verrucous epidermal nevus overlying an implanted cardioverter defibrillator (JAAD Case Rep 2023;34:58)
- Topical treatments (i.e., retinoic acid or 5-fluorouracil) are used to improve the cosmetic appearance of epidermal nevi by removing the keratotic surface
- Smaller lesions can be surgically excised
- Larger lesions can be treated by laser or cryotherapy
- Pulsed erbium: yttrium aluminium garnet (YAG) laser is effective and has a low incidence of scarring (Dermatol Surg 2004;30:378)
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- Well defined, elevated, tan verrucous linear plaque
- Epidermal nevus can show a spectrum of histological patterns with occasionally more than 1 pattern existing in a single lesion; the patterns are described below
- Common keratinocyte pattern (> 60% of cases)
- Hyperkeratosis (occasionally columns of parakeratosis)
- Irregular acanthosis
- Broad papillomatosis with flat vertical peaks
- Sharply demarcated from the adjacent normal epidermis
- Occasional focal thickening of the granular layer
- Hyperpigmentation of the basal keratinocytes
- Uncommonly has associated mild inflammation or perivascular lymphocytes
- Seborrheic keratosis-like pattern
- Hyperkeratosis
- Acanthosis and papillomatosis (with flattening of the lower border, Mesa sign)
- Horn pseudocysts
- Verrucoid pattern
- Hyperkeratosis (orthokeratosis and parakeratosis)
- Vacuolated cells in the granular and upper spinous layer
- Increased keratohyaline granules
- No prominent vascularity in the papillary dermis (typical of verruca vulgaris)
- Acrokeratosis verruciformis pattern
- Marked hyperkeratosis
- Acanthosis and papillomatosis with peaks resembling church spires
- Thickened granular layer
- Porokeratotic pattern
- Orthokeratosis and acanthosis are less prominent that other variants of epidermal nevus
- Parakeratotic columns (with focal occasional vacuolated keratinocytes below)
- Cornoid lamellae (with a focal absent granular layer below)
- Focal acantholytic dyskeratotic Darier disease-like pattern
- Hyperkeratosis
- Acanthosis and papillomatosis
- Acantholytic dyskeratotic cells (corps ronds) and acantholytic basophilic keratinocytes (grains) in the granular layer and spinous layers
- Scattered acantholytic spinous cells above suprabasal clefts
- Acanthosis nigricans-like pattern (Australas J Dermatol 1983;24:130)
- Hyperkeratosis
- Papillomatosis
- Mild irregular acanthosis with poorly developed rete ridges
- Hailey-Hailey disease-like pattern (Br J Dermatol 1985;112:349)
- Mild hyperkeratosis
- Papillomatosis
- Suprabasal acantholysis, similar to a dilapidated brick wall
- Rare dyskeratotic cells
- Incontinentia pigmenti-like (verrucous phase) pattern (Pediatr Dermatol 1985;3:69)
- Hyperkeratosis (vertical parakeratosis)
- Acanthosis and papillomatosis
- Thickened granular layer
- Many individual dyskeratotic cells within the epidermis
- Epidermolytic hyperkeratosis pattern (Australas J Dermatol 1983;24:130)
- Hyperkeratosis
- Acanthosis and papillomatosis
- Perinuclear vacuolization
- Increased irregularly shaped keratohyaline granules
- Indistinct cell borders
- Inflammatory linear verrucous epidermal nevus (ILVEN), epidermal nevus with skyline basal cell layer (PENS) and nevus comedonicus are regarded as distinct entities, although they are sometimes included as histological patterns of epidermal nevus
- Reference: Am J Dermatopathol 1982;4:161
- Typically not required for diagnosis
- 40% of epidermal nevi harbor a postzygotic activating mutation in FGFR3 and PIK3CA
- Another 40% harbor a RAS (i.e., KRAS, NRAS, HRAS) postzygotic activating mutation (typically HRAS G13R)
- Another 5 - 10% harbor an embryonic postzygotic FGFR2 activating mutation (J Invest Dermatol 2016;136:1718)
- Missense mutation c.109G>T in PTCH1 gene was detected in a patient with epidermal nevi and cerebral infarction (J Med Case Rep 2022;16:343)
- Skin, neck, excision:
- Epidermal nevus (see comment)
- Comment: Histological examination demonstrates skin to the subcutis with a lesion comprising an acanthotic and papillomatous epidermis with overlying hyperkeratosis. The underlying dermis appears unremarkable with no abnormal pilosebaceous units identified. There is no evidence of an associated neoplastic growth or malignancy in the material examined.
- Nevus sebaceus (of Jadassohn):
- Clinically often presents as a single yellow patch of alopecia on the scalp
- Histologically similar epidermal changes, though with additional sebaceous gland alterations and ectopic dilated apocrine glands
- Seborrheic keratosis:
- Unusual diagnosis in children / young adults
- Histologically similar, though more likely to have pseudohorn cysts, squamous eddies and compact basaloid cells
- Verruca vulgaris:
- Papillomatosis, hypergranulosis and hyperparakeratosis
- Elongated rete ridges with inward bending at the edge of the lesion
- Intracorneal hemorrhage and ectatic capillaries
- Koilocytes may be seen
- Acanthosis nigricans:
- Usually found in flexural areas of the body, particularly the axilla
- Associated with an underlying metabolic disorder or malignancy
- Usually, lesser degrees of hyperkeratosis and papillomatosis
- Inflammatory linear verrucous epidermal nevus:
- Alternating orthokeratosis and parakeratosis
- Psoriasiform epidermal hyperplasia
- Prominent granular layer underlies the orthokeratosis while the epidermis under the parakeratosis lacks a granular layer
- Mild perivascular lymphocytic infiltrate in the upper dermis
- Nevus with skyline basal cell layer (PENS):
- Mild orthohyperkeratosis, slight papillomatosis and broad acanthosis
- Distinctly palisaded basilar layer with a widened space separating this layer from the overlying spinous layer keratinocytes
- Confluent and reticulated papillomatosis (CARP) (of Gougerot and Carteaud):
- Clinically confluent patches or plaques centrally with a reticular pattern peripherally around the upper trunk, neck and axillae
- Usually, lesser degrees of hyperkeratosis and papillomatosis
- Acanthosis is present in the base of the papillae
Comment Here
Reference: Epidermal nevus
- Germline activating mutation in FGFR3
- Germline inactivating mutation in FGFR3
- Postzygotic activating mutation in FGFR3
- Postzygotic inactivating mutation in FGFR3
- Somatic activating mutation in FGFR3 after birth
Comment Here
Reference: Epidermal nevus
- Cutaneous acanthotic benign lesion with epidermolytic hyperkeratosis spanning more than 50% of its surface
- Solitary or multiple lesions with acanthosis and epidermolytic hyperkeratosis
- Epidermolytic hyperkeratosis spanning > 50% of the lesion surface
- M = F (J Cutan Pathol 2019;46:305)
- Mean age: 58 years old (J Cutan Pathol 2019;46:305)
- Extragenital (67% of cases): head and neck, upper limbs, trunk or back, lower limbs (uncommon), oral (uncommon)
- Genital (33% of cases): vulvar, penile, perianal, perineal, scrotal
- Somatic hotspot mutations in the Arg156 position of KRT10, also known to cause epidermolytic ichthyosis (germline) (J Cutan Pathol 2020;47:524)
- Not HPV related (J Cutan Pathol 2020;47:524)
- Most frequently a single lesion but may be multiple (5% of instances) (J Cutan Pathol 2019;46:305)
- Erythematous, skin colored or brown papules or nodules with scale
- Multiple epidermolytic acanthomas are more likely to be found on genital sites
- Can be confused with condyloma (J Cutan Pathol 2019;46:305)
- May be pruritic
- Dermoscopy may show pearly white areas, irregular pigmented grooves and peripheral pigmented radial streak-like areas (J Am Acad Dermatol 2017;77:e37)
- H&E stain with light microscopy
- Benign
- 40 year old man with multiple epidermolytic acathomas on the fingers, mimicking flat warts (Case Rep Dermatol 2017;9:98)
- 49 year old man with multiple pruritic epidermolytic acanthomas on the scrotum (Actas Dermosifiliogr 2018;109:81)
- 56 year old man with epidermolytic acanthoma on the lower back and related dermoscopy findings (J Am Acad Dermatol 2017;77:e37)
- 57 year old man with solitary penile pidermolytic acanthoma mimicking condyloma (Dermatopathology (Basel) 2019;6:23)
- 58 year old woman with a solitary vulvar epidermolytic acanthoma mimicking condyloma (Int Angiol 1988;7:19)
- 71 year old Caucasian man with an oral solitary epidermolytic acanthoma (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:e208)
- Surgical excision
- Liquid nitrogen (Case Rep Dermatol 2017;9:98)
- Topical imiquimod (J Dermatol 2007;34:267)
- Topical calcipotriol (J Dermatol 2013;40:144)
- Acanthosis and epidermolytic hyperkeratosis (covering > 50% of the lesion surface) (J Cutan Pathol 2019;46:305)
- Low power architecture generally resembles seborrheic keratosis (J Cutan Pathol 2019;46:305)
- Epidermolytic hyperkeratosis consists of lace-like degeneration of the midspinous epithelial layer, perinuclear vacuolization, epithelial eosinophilia and finely speckled keratohyaline granules (J Cutan Pathol 2019;46:305)
- 3 architectural patterns of solitary epidermolytic acanthoma have been described: papillomatous, cup shaped and acanthotic (J Eur Acad Dermatol Venereol 2011;25:175)
- Solitary and multiple epidermolytic acanthomas display similar histopathological findings (J Cutan Pathol 2019;46:305)
- Not usually performed
Epidermolytic hyperkeratosis
- Skin, left forearm, punch biopsy:
- Epidermolytic acanthoma
- Seborrheic keratosis:
- Acanthosis and papillomatosis but no epidermolytic hyperkeratosis
- Focal incidental epidermolytic hyperkeratosis may be present
- Still classified as seborrheic keratosis if covering < 50% of the surface
- Verruca or condyloma:
- Hypergranulosis and finely speckled keratohyaline granules
- No lace-like reticular degeneration
- No dense cytoplasmic eosinophilia
- HPV induced
- Incidental epidermolytic hyperkeratosis in another acanthotic lesion:
- Epidermolytic hyperkeratosis is found spanning < 50% of the lesion surface
- Epidermolytic ichthyosis (formerly bullous congenital icthyosiform erythroderma):
- Generalized desquamating plaques rather than a solitary lesion
- Hereditary ichthyosiform condition due to alterations in keratin genes
- Overlapping histology with solitary epidermolytic acanthoma, clinicopathologic correlation is crucial
- Clear cell acanthoma:
- Pale epithelial cells with acanthosis but no epidermolytic hyperkeratosis
- Solitary keratosis with hypergranulotic dyscornification:
- Dense keratohyaline granules rather than finely speckled
- Both may display eosinophilic cytoplasm but perinuclear vacuolization is more characteristic of epidermolytic acanthoma
- Hypergranulotic dyscornification may be a focal incidental finding in other lesions
Comment Here
Reference: Epidermolytic acanthoma
Comment Here
Reference: Epidermolytic acanthoma
- May originate from intraepidermal portion of sweat glands or primitive basal cells with ability to differentiation towards glandular elements
- Labia majora, scrotum and perineum are most common sites
- Due to underlying carcinoma in 10 - 20% of cases of vulvar disease
- 66 year old woman with vulvar Paget disease (BMC Cancer 2010;10:405)
- Complete surgical excision
- Erythematous, eczematous or ring shaped
- Often multicentric, extensive, pigmented
- Malignant cells in epidermis with differentiation towards local glandular structures
- Almost always simultaneous involvement of eccrine glands or hair follicles
- Dermal invasion is rare in vulva, more common in perianal region)
- Single, clusters or glandular formations of large cells with pale, vacuolated cytoplasm, usually just above basal layer of epidermis
- May have cleft-like spaces between Paget cells and neighboring keratinocytes
- No intercellular bridges, no dyskeratosis
- Cells with glandular differentiation, not melanocytes or keratinocytes
- Clear cell papulosis
- Metastatic epidermotropic carcinomas
- Melanocytic lesions
- Pagetoid actinic keratosis
- Pagetoid Bowen disease
- Considered a hamartoma of hair follicle
Birt-Hogg-Dubé syndrome
- Folliculofibroma associated with Birt-Hogg-Dubé (BHD) syndrome
- Autosomal dominant, multiple folliculomas on head and neck, acrocordons and trichodiscomas; also renal cell carcinoma [various types], renal oncocytoma and oncocytic hybrid tumors, lung cysts and spontaneous pneumothorax)
- Human gene at 17p11.2 encodes folliculin, normally expressed in skin and adnexae (Mod Pathol 2004;17:998)
- Frameshift mutations occur in BHD causing premature protein termination
- 54 year old man with papules on cheeks (Ann Dermatol 2011;23:S193)
- Multiple skin-colored papules
- Thin epidermal strands originating from a central hair follicle with prominent connective tissue
- Mantleoma
- Perifollicular fibroma
- Trichodiscoma
- Trichofolliculoma
- Dermal or subcutaneous tumor with abundant granular cytoplasm and Schwannian differentiation
- Nonneural variant (primitive polypoid granular cell tumor) shows similar granular cytomorphology but does not have immunohistochemical evidence of Schwannian differentiation
- A predominantly dermal based tumor composed of cells with abundant eosinophilic to basophilic granular cytoplasm
- Often have an infiltrative configuration
- Tumors demonstrate Schwannian differentiation (S100+, SOX10+)
- Epidermis can exhibit pseudocarcinomatous hyperplasia in a subset of cases
- Also known as Abrikossoff tumor and granular cell schwannoma (Arch Otolaryngol 1968;88:174)
- Originally described as granular cell myoblastoma, given the resemblance to skeletal muscle myocytes (Am J Pathol 1947;23:721)
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
- Slightly higher incidence in women (Cancer 1987;60:220)
- Mainly adults but has wide age range of presentation (J Surg Oncol 1980;13:301)
- Common sites are trunk, upper limbs and head / neck
- May also arise on feet, hands, anogenital region and breast
- Dysregulation of endosomal pH due to inactivation of accessory proteins of the vacuolar H+ ATPase can give rise to conventional granular cell tumors (Nat Commun 2018;9:3533)
- A subset of nonneural granular cell tumors (S100-) harbor ALK gene fusions (Am J Surg Pathol 2018;42:1133)
- Harboring multiple tumors has been associated with Noonan syndrome and LEOPARD syndrome (Eur J Pediatr Surg 2013;23:257, Clin Genet 2009;75:185)
- Slowly growing papule or nodule; rarely ulcerates (Adv Anat Pathol 1999;6:186)
- Rare cases can exhibit multiple lesions (Cutis 2002;69:343)
- Fanberg-Smith et al. proposed diagnostic criteria for atypical and malignant tumors (Am J Surg Pathol 1998;22:779):
- Increased N:C ratio
- Nuclear pleomorphism
- Necrosis, tumor type
- Spindling of tumor cells
- Vesicular nuclei with prominent nucleoli
- > 2 mitoses per 10 high power fields
- Atypical: 1 - 2 features
- Malignant: > 2 features
- Nasser et al. proposed diagnostic criteria for granular cell tumor of uncertain malignant potential and malignancy (Pathol Res Pract 2011;207:164):
- Necrosis, single cell or en masse
- > 2 mitoses per 10 high power fields
- Uncertain malignant potential: 1 - 2 features
- Malignant: evidence of metastatic disease
- 48 year old woman with upper back nodule (Indian J Dermatol 2015;60:322)
- 51 year old woman with left posterior chest wall mass and lymph node metastases (Am J Dermatopathol 2015;37:334)
- 53 year old woman with an enlarging left lower abdominal nodule (Am J Dermatopathol 2010;32:370)
- 54 year old patient with toe lesion (Dermatol Res Pract 2010;2010:184125)
- 69 year old woman with a rapidly enlarging firm neck mass (Am J Dermatopathol 2017;39:e50)
- Benign and malignant tumors are typically treated with wide local excision (J Surg Oncol 1980;13:301)
- Mohs micrographic surgery is an option for anatomic sites in which conservative re-excision is desired (Case Rep Oncol Med 2012;2012:453569)
- Grayish white to pale yellow
- Oftentimes, not well circumscribed
- Infiltrative or circumscribed architecture
- Can involve the subcutis
- Large polygonal cells with abundant eosinophilic granular cytoplasm and small, central nuclei
- Epidermis can show pseudocarcinomatous hyperplasia
- Lysosomal macroinclusions (pustulo-ovoid bodies of Milian) are usually present (J Cutan Pathol 2007;34:405)
- Can exhibit accentuation around arrector pili muscles or peripheral nerves (J Clin Pathol 2014;67:19)
- Nonneural granular cell tumors (S100-) can exhibit nucleomegaly, pleomorphism and variable mitotic activity (Am J Surg Pathol 1991;15:48, Histopathology 2005;47:179)
Contributed by Jarish Cohen, M.D., Ph.D.
- PASD, Sudan Black B, S100 (except for nonneural granular cell tumors), SOX10, NSE
- Variable staining for vimentin, CD68, NKI-C3 (CD63), MITF, CD56
- A subset of nonneural granular cell tumors express ALK
- References: Cancer 1982;49:1624, Histopathology 2012;61:997, Diagn Histopathol 1982;5:205, Cancer 1989;64:1455, Dermatology 1993;186:106, Am J Dermatopathol 2007;29:22, Hum Pathol 2015;46:813, Am J Surg Pathol 2018;42:1133
- HMB45, MelanA, AE1 / AE3, EMA, desmin
- Nonneural granular cell tumor is negative for S100
- References: Am J Dermatopathol 2007;29:22, Am J Surg Pathol 1991;15:48
- Membrane bound cytoplasmic granules containing lysosomes of varying sizes (J Cutan Pathol 1981;8:277, Oral Surg Oral Med Oral Pathol 1977;44:227, Ultrastruct Pathol 2018;42:304)
- Larger secondary lysosomes can be seen
- Some membrane bound granules contain aggregates of virus-like particles
- Some lesional cells contain long spacing collagens (Luse bodies)
- Variably abundant basal lamina material may be seen
- Inactivating ATP6AP1 and ATP6AP2 somatic mutations are highly prevalent in conventional granular cell tumors (Nat Commun 2018;9:3533, Genes Chromosomes Cancer 2019;58:37)
- A subset of nonneural granular cell tumors harbor ALK gene fusions (Am J Surg Pathol 2018;42:1133, J Cutan Pathol 2020;47:1026)
Granular cell tumor
- Skin, left antecubital fossa, shave biopsy:
- Granular cell tumor (granular cell schwannoma) (see comment)
- Comment: The lesional cells are positive with an immunostain for SOX10 protein, a finding that is typical of this entity.
- Skin, left thigh, shave biopsy:
- Nonneural granular cell tumor (see comment)
- Comment: The biopsy shows a polypoid mass of large, oval cells with ample pallid and both finely and coarsely granular cytoplasm, with some pustulo-ovoid bodies. The lesional cells are S100 negative, MITF negative and NKI-C3 strongly positive. An ALK immunostain shows moderate patchy positivity. A phosphohistone H3 shows that cells in mitosis are exceedingly rare, under 1/mm2. The histopathologic and immunohistochemical findings are consistent with nonneural granular cell tumor (also known as primitive polypoid granular cell tumor).
- Melanocytic neoplasms (J Am Acad Dermatol 2004;50:765):
- Leiomyosarcoma (Am J Dermatopathol 1988;10:234, Am J Dermatopathol 1999;21:307):
- Positive for desmin and alpha smooth muscle type
- Negative for S100 and SOX10
- Atypical fibroxanthoma (AFX) (J Cutan Pathol 2005;32:314, J Cutan Pathol 2010;37:380, Am J Dermpathol 2021;43:831):
- A subset of AFX can demonstrate an infiltrative silhouette and cells with abundant granular cytoplasm
- Most AFX will display elevated mitotic activity with atypical forms, prominent nuclear pleomorphism and arise in the setting of marked solar elastosis
- Negative for S100 and SOX10
- Granular AFX may show positive ALK staining that is not reflective of an underlying gene fusion
- Dermatofibroma (benign fibrous histiocytoma) (Dermatology 1999;199:54):
- Xanthoma:
- Reticulohistiocytoma:
- Adult type rhabdomyoma:
- Can be composed of sheets of polygonal cells with abundant eosinophilic, variably granular cytoplasm
- Usually demonstrates cross striations
- Positive for desmin, actin - muscle specific and myogenin
- Negative for S100
- Alveolar soft part sarcoma:
- A 40 year old woman presents with a nodule on her trunk. The lesion is biopsied and shows a dermal based proliferation of cells with abundant eosinophilic granular cytoplasm. Which of the following statements is true?
- The abundant granular cytoplasm is indicative of numerous membrane bound cytoplasmic granules containing aggregates of mitochondria
- An S100 or SOX10 stain is negative in most tumors
- Perineural accentuation of cellularity is a feature of malignancy
- These tumors can display infiltrative architecture and can sometimes involve the subcutaneous fat
Comment Here
Reference: Granular cell tumor
- Which of the following statements about granular cell tumors is true?
- A subset are negative for S100 and other neural markers and can have a polypoid appearance
- Atypical features include association with pseudocarcinomatous hyperplasia and accentuation around peripheral nerves
- NF1 is commonly mutated in conventional granular cell tumors
- Tumors never demonstrate metastatic potential
Comment Here
Reference: Granular cell tumor
- Rare, congenital, hamartomatous proliferation of mature vellus hairs
- Also known as congenital vellus hamartoma
- Usually present at birth or early childhood
- Solitary skin colored papule, less than 1 cm in greatest dimension
- Sometimes with hypertrichosis
- Most commonly on head and neck
- Rarely multiple or arranged in a linear distribution, following the lines of Blaschko (J Am Acad Dermatol 2002;46:S125)
- 2 year old boy with nose nodule (Pediatr Dermatol 2008;25:60)
- 26 year old man with small soft nodules on his nose since childhood (Eur J Dermatol 2008;18:185)
- Hair follicle nevus with features of comedo nevus (Am J Dermatopathol 2016;38:e81)
- Increased numbers of closely situated mature vellus hair follicles
- Some are associated with small sebaceous glands or have thickened perifollicular fibrous sheaths
- Follicles may be located abnormally high within the dermis
- No cartilage (seen in accessory tragus), central cysts or a central canal (seen in trichofolliculoma)
- Accessory tragus: also has increased vellus hairs, but usually has other types of tissue (i.e. mature adipose tissue or cartilage); location around the ear is also helpful
- Trichofolliculoma: has central cyst or canal; deeper levels may be necessary to find trichofolliculoma in a lesion that resembles hair follicle nevus
- Benign tumor composed of circumscribed proliferation of predominantly small capillary sized blood vessels
- See also these related soft tissue topics: anastomosing hemangioma, cystic / cavernous lymphangioma, epithelioid hemangioma, intramuscular angioma, lymphangioendothelioma, lymphangioma, lymphangiomatosis, venous hemangioma
- Most cases arise in children, with equal gender distribution
- Composed of small capillary sized blood vessels with a larger feeding vessel commonly present
- Most cases are treated with topical or systemic beta blockers in isolation or in combination with other modalities like laser therapy, excision, etc.
- Recurrence is uncommon and only exceptional examples show malignant transformation
- Hemangioma is commonly used with a qualifier (e.g. congenital hemangioma)
- Most common tumor of childhood and infancy (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2019)
- M = F; gender predilection is variable for site specific examples, like synovial hemangioma (Eur J Orthop Surg Traumatol 2019;29:1291)
- Common in Klippel-Trenaunay syndrome, PHACE syndrome and LUMBAR syndrome (Surg Neurol Int 2018;9:205, StatPearls: PHACE Syndrome [Acessed 13 October 2021], Med Arch 2021;75:158, Actas Dermosifiliogr 2017;108:475)
- Most are superficial, commonly in head and neck region
- Hepatic hemangiomas are common in infants
- Deep visceral or skeletal location is rare but well documented (J Cancer Res Ther 2020;16:938, World J Gastroenterol 2020;26:11, BMC Musculoskelet Disord 2021;22:27, J Optom 2017;10:79)
- Specific pathogenesis has not been fully understood
- Currently regarded as a multifactorial condition, resulting in endothelial proliferation, with uncontrolled angiogenesis and abnormal function of downstream pathways (notably HIF1α, VEGF and PI3K / Akt) (Biomed Res Int 2021;2021:5695378)
- Not known
- Superficial: red to purple papules, nodules or ill defined elevations (Semin Cutan Med Surg 2016;35:108)
- Cavernous hemangiomas present as port wine nevi
- May be associated with von Hippel-Lindau disease (Can Med Assoc J 1969;101:135)
- Visceral: hemoptysis, visual field defects, localized pressure effects, mass effect (Medicine (Baltimore) 2018;97:e11203, J Optom 2017;10:79, Ital J Pediatr 2020;46:157, J Cancer Res Ther 2020;16:938, Ann Thorac Cardiovasc Surg 2019;25:71, J Pak Med Assoc 2018;68:1846, J Int Med Res 2020;48:300060520954718)
- Presence of more than 5 cutaneous lesions has increased chance of visceral involvement (Pediatrics 2008;122:360)
- Hepatic hemangioma: abdominal distension and discomfort when more than 5 cm in size; most are asymptomatic (J Hepatobiliary Pancreat Sci 2017;24:417)
- Skeletal: mostly asymptomatic; rarely present with localized symptoms, such as bone pain and pathological fracture (BMC Musculoskelet Disord 2021;22:27)
- Infantile hemangioma: small at birth; grows up to 6 months of age and involutes after first year of life (Hum Pathol 2000;31:11)
- Congenital hemangioma: maximum size at birth, lacks growth phase, either involutes partially (partially involuting congenital hemangioma [PICH]) or completely (rapidly involuting congenital hemangioma [RICH]) or requires treatment / intervention (noninvoluting congenital hemangioma [NICH]) (Semin Pediatr Surg 2014;23:162, BMJ Paediatr Open 2020;4:e000816)
- Requires correlation of detailed history and physical examination with microscopic features, as the latter overlaps for various clinical presentations
- Transient mild to moderate thrombocytopenia due to consumption may be seen in rapid growth phase (F1000Res 2019;8:F1000)
- Mostly required for extracutaneous cases
- Skeletal (bone) hemangiomas: radiology is highly nonspecific (BMC Musculoskelet Disord 2021;22:27)
- Ultrasound: highly effective; shows well defined mass with high vascularity
- Contrast enhanced ultrasonography (CEUS): gold standard for hepatic hemangiomas (Korean J Radiol 2000;1:191)
- High flow in proliferative phase of infantile hemangioma; slow flow in involuted phase
- Central high flow for NICH; slow flow for RICH
- Fluttering sign: recently described feature for grayscale ultrasound in hepatic hemangiomas (Ultrasound Med Biol 2021;47:941)
- MRI: useful in deep locations to estimate extent of tissue involvement
- Infantile hemangioma: hyperintense on T2; isointense on T1 with postcontrast enhancement
- Congenital hemangioma: heterogeneous appearance on MRI
- CT scan: hypodense, with postcontrast enhancement of periphery (World J Gastroenterol 2020;26:11)
- Most common complications in superficial lesions include ulceration and permanent skin changes, like scarring (Semin Cutan Med Surg 2016;35:108, Semin Pediatr Surg 2014;23:162)
- Recurrence if larger or deep lesions are incompletely excised or inadequately treated (Acta Ophthalmol 2020;98:679, Int J Surg Case Rep 2019;60:319)
- Large lesions may contribute to high output cardiac failure (Interv Neuroradiol 2017;23:102)
- Only exceptional examples show malignant transformation (Am J Surg Pathol 2002;26:1319)
- 3 month old girl with facial lesion and intussusception (Oman Med J 2020;35:e204)
- 14 year old boy with right sided hearing loss (Einstein (Sao Paulo) 2018;16:eRC4509)
- 32 year old woman with progressive loss of vision (J Ophthalmic Vis Res 2012;7:244)
- 49 year old woman with lumbar pain (Medicine (Baltimore) 2019;98:e14001)
- 84 year old man with BI RADS III mass in right breast (Am J Case Rep 2018;19:1425)
- Aims at stopping the growth of lesion
- Systemic and topical beta blockers, alone or in combination with steroids or surgery, may be useful depending on age, site and size of lesion (Turk J Pediatr 2017;59:254)
- Laser treatments, embolization and sclerotherapy or a combination of different modalities have all been described to be useful depending on individual cases (J Optom 2017;10:79, J Int Med Res 2020;48:300060520977589, Intern Med 2020;59:1727, Am J Case Rep 2021;22:e931042)
- Proanthocyanidins are under research as potential therapeutic options for infantile hemangioma (Biomed Res Int 2021;2021:5695378)
Contributed by Nasir Ud Din, M.B.B.S.
Images hosted on other servers:
- Deep lesions are well circumscribed and solid to cystic, with dilated vessels and with or without thrombus formation (Pediatr Radiol 2010;40:S63)
- May be polypoid with a stalk (Ann Thorac Cardiovasc Surg 2019;25:71)
- Lobules of capillary sized vascular channels, lined by single layer of flattened endothelial cells
- Large feeding vessel is usually seen at the deeper aspect
- Associated lymphocyte infiltrate may be seen (Cardiovasc Pathol 2017;28:59)
- Anastomosing hemangioma: anastomosing vascular channels lined by flattened endothelium; deep occurrence
- Angiomatosis: involvement of multiple tissue planes with irregular and poorly circumscribed edges
- Cavernous hemangioma: shows predominantly ectatic channels
- Congenital hemangioma:
- Solid appearance in rapid growth phase with poorly canalized vessels and mitotically active endothelium
- Surrounding pericyte layer is present
- With maturation, the lumina become prominent and blood flow ensues
- Combination of solid and vascular areas in varying proportions may be seen
- Noninvoluting congenital hemangioma (NICH) shows well formed capillaries and vascular channels
- Involuting examples show thickening of basement membranes and fibrosis in the background
- Epithelioid hemangioma:
- Well formed small vessels are lined by plump endothelial cells with abundant eosinophilic cytoplasm and round enlarged nuclei, accompanied by abundant eosinophils in the background
- Lobulated, well demarcated with maturation of vascular lumina at the periphery
- Glomeruloid hemangioma: resembles glomerular capillaries
- Hobnail hemangioma: hobnail nuclei protruding into vascular lumina; circumscribed
- Infantile hemangioma:
- Proliferation of capillary lobules; has a distinct natural history involving three stages (i.e., proliferation, partial regression and complete regression):
- Early proliferative stage: lobules of immature dendritic type cells with intervening stroma, large feeding vessels and occasional presence of perineural involvement
- Early regression: capillaries dilate and eventually start disappearing; apoptotic debris in basement membrane with increased numbers of pericapillary mast cells.
- Late regression / end stage: ghosts of capillaries, rings of basement membrane with rare endothelial cells having immunophenotype of placental capillaries (GLUT1, LeY, CD15, CCR6, IDO and IGF2 positive)
- Proliferation of capillary lobules; has a distinct natural history involving three stages (i.e., proliferation, partial regression and complete regression):
- Intramuscular angioma:
- Arises within skeletal muscle in association with variable amount of mature adipose tissue, phleboliths and metaplastic bone formation
- Shows a combination of lymphatics, variable sized veins and arteriovenous component
- Lobular capillary hemangioma / pyogenic granuloma: ulceration with dense mixed inflammation
- Microvenular hemangioma:
- Poorly defined, in superficial and deep dermis
- Small venule-like channels lined by single layer of endothelial cells which lack mitotic activity, surrounded by single layer of pericytes; these venules appear to dissect hyalinized collagen bundles of the dermis but lack multilayering and HHV8 positivity
- Sinusoidal hemangioma:
- Well demarcated proliferation of dilated, congested and thin vascular channels anastomosing in a sinusoidal manner
- Intervening stroma is scant and scant smooth muscle may be present in the wall
- Mitotic activity is not seen
- Spindle cell hemangioma: proliferating spindle cells with intraluminal phleboliths
- Verrucous hemangioma: hyperkeratosis and involvement of several tissue planes
Contributed by Nasir Ud Din, M.B.B.S.
- Aspiration is not advised, as there is high risk of uncontrolled bleeding
- CD31 (PECAM1): cytoplasmic and membranous positivity; highly sensitive and very specific for vascular differentiation
- CD34: cytoplasmic and membranous positivity; less specific
- ERG: nuclear positivity, stains all vascular tumors, more specific than FLI1
- GLUT1: positive in infantile hemangioma and negative in congenital hemangioma
- FLI1: nuclear positivity; stains all vascular tumors
- von Willebrand factor (vWF): granular cytoplasmic positivity
- Thrombomodulin (CD141): cytoplasmic positivity
- Ulex europaeus agglutinin I (UEAI): membranous staining, sensitive but nonspecific, also stains epithelial cells (Arch Histol Cytol 2004;67:187)
- Claudin5: component of endothelial tight junctions; highly sensitive but less specific
- Podoplanin (D2-40): more specific for lymphatic differentiation (Blood 2019;134:1912)
- Vascular endothelial growth factor receptor 3 (VEGFR3): membrane staining
- PROX1: suggested marker of neoplastic endothelial cells (Am J Surg Pathol 2012;36:351)
- CIZ1: nuclear protein; upregulated in mucosal hemangiomas (Pathol Oncol Res 2019;25:1653)
- WT1: variable cytoplasmic positivity in vascular neoplasms (Am J Dermatopathol 2011;33:569)
- HHV8: kaposi sarcoma (Arq Bras Oftalmol 2021 Sep 10 [Epub ahead of print])
- TFE3: high grade epithelioid hemangioendothelioma (Mod Pathol 2020;33:591)
- SMA: pericytes and vascular smooth muscle stain positive
- Desmin: vascular smooth muscle stains positive
- Cytokeratin: variable positivity may be seen in some examples of angiosarcoma; however, mostly negative (Case Rep Med 2016;2016:8919012)
- Not required for diagnosis in routine cases
- Endothelial cells show cytoplasmic folds on luminal surface, junctional complexes and cytoplasmic pinocytic vesicles (Cancer Res 1990;50:4787)
- Not required for routine diagnosis of hemangioma
- May be helpful in difficult cases
- RASA1 mutations: arteriovenous malformations, Klippel-Trenaunay syndrome, Sturge-Weber syndrome, Parker-Weber syndrome (Am J Hum Genet 2003;73:1240, Br J Dermatol 2008;158:1035, Hereditas 2018;155:24)
- GNAQ mutation: Sturge-Weber syndrome (N Engl J Med 2013;368:1971)
- PDGFRβ and its downstream signaling pathways (PI3K / Akt / mTOR) are activated in infantile hemangioma (J Invest Dermatol 2019;139:1574)
- More relevant in intermediate and malignant vascular lesions
Spindle cell hemangioma
Cutaneous vascular tumors
- Liver, lobectomy:
- Benign vascular lesion, consistent with hemangioma (see comment)
- Comment: The tumor is completely excised with free margins. Evidence of embolization is seen, with presence of acellular material within the lumina of large caliber vessels, accompanied by areas of infarction within the lesion.
- Granulation tissue:
- Sites of trauma, commonly cutaneous or mucosal
- Shows associated inflammatory infiltrate and edema
- Feeding vessels are not seen commonly
- Lobular capillary hemangioma is common mimicker
- Correlation with clinical history is important
- Hemangioendothelioma:
- Mimics proliferating phase of congenital hemangioma
- Retiform type mimics hobnailing seen in proliferating phase of congenital hemangioma
- Not well circumscribed
- Clinical presentation with consumptive coagulopathy is common in both
- May be associated with other anomalies
- Requires more aggressive treatment
- Kaposi sarcoma:
- Mimics proliferating phase of congenital hemangioma due to compact cellularity and slit-like spaces
- Eosinophilic hyaline globules are not seen in hemangioma
- HHV8 association is not seen in hemangioma
- Requires aggressive treatment
- Angiosarcoma:
- Malignant vascular tumor with infiltrative growth
- Marked nuclear pleomorphism and brisk mitotic activity
- Visceral location is more common compared to hemangioma
A newborn shows a nodular growth on his scalp. Over the next couple of weeks, the lesion starts shrinking. Despite reassurances from the pediatrician, the parents insist on excision. Upon pathological examination, it shows a network of capillary sized vessels with large feeding vessels near the base, shown in the above photomicrograph. The diagnosis in this case is
- Infantile hemangioma
- Noninvoluting hemangioma
- Partially involuting hemangioma
- Rapidly involuting hemangioma
Comment Here
Reference: Hemangioma
A 9 year old boy presents with a purple nodular / bosselated lesion on the left leg, with involvement of the plantar and dorsal aspects of foot (as shown in the clinical photograph). He has had this lesion since birth and it has grown with him since then. The microscopic examination shows well formed vascular channels of variable size lined by a single layer of endothelial cells. The most likely diagnosis in this case is
- Birth mark
- Infantile hemangioma
- Kaposiform hemangioendothelioma
- Lobular capillary hemangioma
- Noninvoluting congenital hemangioma
Comment Here
Reference: Hemangioma
- Benign dermal nodule of eccrine / apocrine gland derivation (Middle East Afr J Ophthalmol 2010;17:374)
- Presents as a slow growing, nodular, solid or cystic cutaneous mass usually measuring up to 3 cm in diameter (Dermatology 2016;232:78)
- Characterized by variably sized nests and nodules of epithelial cells within the upper or mid dermis, typically with no overlying connection to the epidermis (J Clin Pathol 2007;60:145)
- Also known as nodular hidradenoma, eccrine acrospiroma, clear cell hidradenoma, eccrine sweat gland adenoma and solid cystic hidradenoma
- Frequently occurs in the third to fifth decade of life with a slight predominance in females (Case Rep Oncol 2018;11:298)
- Typically located on the head, neck and limbs (although any site may be affected) (Case Rep Oncol 2018;11:298)
- Presents as a slow growing, nodular, solid or cystic cutaneous mass usually measuring up to 3 cm in diameter (Dermatology 2016;232:78)
- Overlying skin can be skin colored, erythematous or blue and may exhibit superficial ulceration or serous discharge (Indian Dermatol Online J 2016;7:410)
- 13 year old boy with nodular hidradenoma on the upper arm (Australas J Dermatol 2017;58:e135)
- 20 year old woman with nodular hidradenoma on the breast (Lab Med 2019;50:320)
- 61 year old woman with clear cell hidradenoma on the chin (J Craniofac Surg 2017;28:e454)
- Recurrence rate of 12% if not completely excised (J Clin Pathol 2007;60:145)
- Solitary well circumscribed dermal nodule (Int J Gynecol Pathol 2008;27:457)
- Well circumscribed but unencapsulated, lobulated / cystic mass with variably sized nests and nodules of epithelial cells within the upper or mid dermis, typically with no overlying connection to the epidermis (J Clin Pathol 2007;60:145)
- Shows both solid and cystic components (Arch Pathol Lab Med 2005;129:e113)
- Solid portion composed of 2 types of cells: polyhedral cells with basophilic cytoplasm and glycogen containing clear cells with eccentric round nucleus
- Cystic areas secondary to degeneration of tumor cells
- Tubular lumina are lined by cuboidal or columnar secretory cells (J Oral Maxillofac Pathol 2013;17:136)
- Fibrovascular, collagenous or hyalinized stroma (J Cutan Pathol 2007;34:497, Arch Pathol Lab Med 2005;129:e113)
- Focal apocrine decapitation secretion, squamous differentiation, squamous eddy formation, keratinization, mucinous change or sebaceous differentiation can be seen (Am J Dermatopathol 2012;34:461, J Cutan Pathol 2007;34:801, J Cutan Pathol 2007;34:497)
- Malignant hidradenocarcinoma presents with infiltrative growth pattern, nuclear atypia and pleomorphism, predominantly solid cell islands, angiolymphatic invasion, necrosis and ≥ 4 mitoses per 10 high power fields (Middle East Afr J Ophthalmol 2010;17:374, Mod Pathol 2009;22:600)
- Variants:
- Clear cell hidradenoma (Cutis 2014;94:268)
- Has a biphasic cellular population: (1) round, fusiform, or polygonal cells with vesicular nuclei and eosinophilic cytoplasm and (2) cells with clear cytoplasm and often eccentrically located nuclei
- Solid cystic hidradenoma (Arch Pathol Lab Med 2005;129:e113)
- Shows both solid and cystic components
- Cysts probably represent cystic degeneration
- Mucinous hidradenoma (J Cutan Pathol 2007;34:497)
- Demonstrates diffuse and prominent mucinous cell proliferation
- Poroid hidradenoma (Ann Dermatol 2021;33:289)
- Has architectural features of the apocrine hidradenoma and cytological features of poroid and cuticular cells
- Poroid cells are uniform, small cuboidal cells with an oval to round nuclei
- Cuticular cells have an abundant eosinophilic cytoplasm with a larger nucleus that shows occasional multinucleation
- Pigmented nodular hidradenoma (Arch Dermatol 1971;104:117)
- Shows melanin pigmentation
- Clear cell hidradenoma (Cutis 2014;94:268)
- AE1 / AE3 and other low molecular weight cytokeratins, EMA, CEA (J Cytol 2011;28:235, J Clin Pathol 2007;60:145)
- Some cases show partial staining with SMA, p63, actin-muscle specific (J Cytol 2011;28:235)
- Stains are not particularly helpful in the diagnosis of this entity and can be misleading
- Some cases show partial staining with SMA, p63, actin - muscle specific (J Cytol 2011;28:235)
- CD10 is typically negative
- t(11;19) translocation has been reported (Am J Dermatopathol 2007;29:457)
- Skin, neck, excision:
- Hidradenoma, extending to the deep margin
- Metastatic renal cell carcinoma
- Absence of ductal differentiation/sweat production
- Positive for PAX8 and CD10
- Negative for p63
- Basal cell carcinoma with eccrine differentiation:
- Peripheral palisading and no cystic areas
- Stromal epithelial retraction
- Epidermal connection
- Hidradenocarcinoma:
- Greater cytologic atypia, mitoses and infiltrative
- Squamous cell carcinoma:
- Epidermal connection, keratin pearls and infiltrative
- Absence of secretory differentiation
- Trichilemmoma:
- Broad connection with the epidermis
- CD34, thickened hyalinized basement membrane and peripheral cell palisading
- Poroma:
- Epidermal connection and broad, anastomosing cords
- Cells are more basaloid while cells of hidradenoma are more eosinophilic
- Recurrent YAP1-MAML2 and YAP1-NUTM1 fusions identified in a subset
- Cylindroma:
- Jigsaw puzzle pattern
- Hyaline globules and thickened basement membranes
- Hidradenoma papilliferum is a benign dermal papulonodular tumor almost always found in the vulva / perianal region of women
- Benign neoplasm of modified anogenital mammary-like glands, predominantly found in the vulva / perianal region of women
- Histopathology features include characteristic dermal maze-like growth with papillary / glandular / cyst-like architecture, often with apocrine differentiation
- Also referred to as papillary hidradenoma
- Predominantly women; ages 30 - 80 (Arch Gynecol Obstet 2011;284:1015, Clin Exp Dermatol 2020;45:1035)
- Ectopic hidradenoma papilliferum is only slightly more common in women (Am J Dermatopathol 2003;25:176)
- Vulva or perianal region
- Rarely involves ectopic sites (head, neck, chest, abdomen) (Indian J Pathol Microbiol 2018;61:287)
- 60% of ectopic HP is present in head and neck region, including eyelid, forehead, face, external auditory canal, post auricular region
- Thought to arise from modified apocrine glands in eyelids / external auditory canal or heterotopic apocrine glands
- Rare case reports of sebaceous differentiation in ectopic HP (Pathology 2019;51:362)
- Favored to arise from anogenital mammary-like glands (Am J Dermatopathol 2012;34:104)
- Unknown
- Solitary dermal or subcutaneous nodule, < 1 - 2 cm
- Usually asymptomatic but can present with pain, pruritis, discharge or ulceration / bleeding (Calonje: McKee's Pathology of the Skin, 4th Edition, 2011)
- Clinical diagnosis confirmed with biopsy
- May cause Bartholin cyst or abscess; can be misdiagnosed as such (Arch Gynecol Obstet 2011;284:1015)
- Generally excellent prognosis and curative with complete excision
- Can very rarely transform into malignant hidradenocarcinoma papilliferum or aggressive adenosquamous carcinoma (Gynecol Oncol 1989;35:395)
- 16 year old boy with upper and lower eyelid lesions (Indian J Pathol Microbiol 2018;61:287)
- 35 and 39 year old women with perianal mass and hemorrhoids (Ann Coloproctol 2019;35:361)
- 36 year old man with left areolar papule (An Bras Dermatol 2018;93:474)
- 38 year old woman with painful vaginal mass (J Med Case Rep 2021;15:162)
- 56 year old man with unilateral hearing loss and an external auditory canal mass (Ann Med Surg (Lond) 2019;49:41)
- Conservative surgical excision or excision with wide margins (Arch Gynecol Obstet 2011;284:1015)
- Solid, skin colored papule, usually < 1 - 2 cm
- Well circumscribed dermal maze-like or arborizing proliferation (rarely connected to epidermis), with a combination of papillary, cystic or glandular architecture
- 2 types of epithelia:
- Luminal layer of tall, columnar cells; cuboidal cells with eosinophilic cytoplasm, decapitation secretion and small, round nuclei (apocrine differentiation)
- Can occasionally exhibit clear cell change (lamprocyte-like changes) (Pathology 2019;51:362)
- Underlying layer of thin or cuboidal myoepithelial cells (Am J Dermatopathol 2006;28:322, Ann Coloproctol 2019;35:361)
- Luminal layer of tall, columnar cells; cuboidal cells with eosinophilic cytoplasm, decapitation secretion and small, round nuclei (apocrine differentiation)
- Entrapment of epithelial cells in connective tissue may mimic infiltrative pattern (Arch Gynecol Obstet 2011;284:1015)
- May have connection to the epidermis with associated dermal plasma cell infiltrate (mimics syringocystadenoma papilliferum) (Am J Dermatopathol 2016;38:598)
- Stromal changes: dense stromal plasma cell infiltrate, sclerosis, hyperplasia of myofibroblast-like cells, foamy macrophages
- Metaplasia occasionally present
- Most commonly oxyphilic (eosinophilic, granular cytoplasm, conspicuous nucleoli, occasional pleomorphism), oftentimes leading to misdiagnosis of malignancy (Am J Dermatopathol 2005;27:102)
- Rarely squamous or mucinous metaplasia
- Remnants of anogenital mammary-like glands (AGMLG) often present
- Epithelium of these glands can be normal or exhibit columnar cell change or columnar cell hyperplasia (Am J Dermatopathol 2016;38:598)
- Mitotic rate can be variable and sometimes high but high mitotic rate does not correlate with an aggressive outcome (Am J Dermatopathol 2006;28:322)
- Rare case reports with sebaceous differentiation (in association with ectopic HP) and extramammary Paget disease (J Dermatol 2006;33:256, Am J Dermatopathol 2016;38:598)
- Described to harbor mutations in genes involved in PI3K/ATK/MAPK signaling pathways (Pathology 2019;51:362)
- Non-PI3K/AKT mutated cases display mutations in various other genes (PIK3CA PIK3R1, SYNE1, AR, IL6ST, PDGFRB, KMT2C, AR, BTK, DST, KAT6A, BRD3, RNF213, USP9X, ADGRB3, MAGI1, and IL7R) involved in PI3K/AKT signaling
- Rare cases described mutations in BRAF, APC, ERBB4 (Genes Chromosomes Cancer 2016;55:113)
Diagnostic pearls of hidradenoma papilliferum
- Skin, vulva, biopsy:
- Diagnosis: hidradenoma papilliferum (see comment)
- Comment: The biopsy contains a sharply circumscribed, maze-like glandular and papillary architecture without connection to overlying epithelium. The glands are lined by an inner layer of cuboidal cells and an outer layer of myoepithelial cells. Mitotic figures are rare. The morphologic features are most consistent with hidradenoma papilliferum.
- Syringocystadenoma papilliferum:
- Frequently connects to epidermis
- Associated with characteristic plasma cell infiltrate
- More common on head and neck
- Hidradenocarcinoma papilliferum:
- Asymmetric, infiltrative growth pattern, cytologic atypia, cribriform structures (Am J Dermatopathol 2006;28:322)
- Tubular apocrine adenoma:
- Predominantly tubular structures
- Less complex architecture
- Papillary eccrine adenoma:
- Eccrine differentiation
A 57 year old woman develops a lesion on her vulva. Excision of the lesion shows a glandular and papillary proliferation (shown above). Which of the following is true concerning this lesion?
- Higher mitotic activity indicates worse prognosis
- It is often associated with a plasma cell infiltrate
- It is positive for EMA and GCDFP-15
- Malignant transformation occurs frequently
- Uncommon benign adenomatous cystic proliferation derived from apocrine glands
- Also called apocrine hidrocystoma, although apocrine cystadenoma may be preferable for lesions with true papillary projections and active epithelial secretions; these lesions are usually small (< 2 cm), on face of older adults (see also J Cutan Pathol 1997;24:249)
- Despite its apocrine derivation, rare at sites rich in normal apocrine glands (groin, axilla, anogenital region, eyelids [Moll's glands], ears [ceruminous glands])
- Usually solitary, but multiple lesions have been documented
- Often occurs as cystic lesion of head and neck (commonly check), rarely in axilla
- Similar lesion on eyelid known as Moll's gland cyst
- Presents as intradermal, moderately firm, dome-shaped, translucent, blue, bluish-black or purple cystic nodule up to 1 cm
- No gender preference
- Lesions on face, also called Robinson variant, usually in middle aged women
- Solitary lesions are not familial, but multiple apocrine hidrocystomas are a feature of ectodermal dysplasia (Acta Derm Venereol 2008;88:607) and focal dermal hypoplasia (Goltz syndrome)
- Although solitary apocrine hidrocystomas lack seasonal variation, multiple lesions in some patients worsen in summer or with excessive heat and improve during winter
- May be precursor to apocrine carcinoma
- 29 year old woman with apocrine cystadenoma of axillary tail (Breast J 2013;19:109)
- 41 year old man with giant multicystic cystadenoma of Cowper's gland (Int Braz J Urol 2013;39:741)
- 58 year old man with giant multi-loculated apocrine hidrocystomas (Dermatol Online J 2010;16:16)
- 58 year old woman with apocrine hidrocystoma of cheek (Arch Plast Surg 2012;39:86)
- 64 year old man with apocrine hidrocystoma of lower lip (Head Neck Pathol 2014;8:117)
- 75 year old man with multiple apocrine hidrocystomas (J Clin Diagn Res 2013;7:171)
- Complete excision recommended
- Unilocular cystic lesion with clear to brown fluid
- Large unilocular or multilocular cystic space within dermis
- Fibrous pseudocapsule is often present
- Typically, cystic spaces are lined by double layer of epithelial cells: an outer layer of flattened vacuolated myoepithelial cells and an inner layer of tall columnar cells with eosinophilic cytoplasm and basally located, round or oval vesicular nuclei
- Decapitation secretion is usually present
- Often adjacent to hyperplastic apocrine glands
- AE1 / AE3
- PAS-positive, diastase resistant granules may be evident in the cytoplasm of the inner lining cells and occasionally iron or melanin is also demonstrable
- Myoepithelial layer: smooth muscle actin (SMA), p63
- HER2: see Mod Pathol 2004;1:28
- Two types of cells: secretory cells with granules resembling lipid droplets, and basal (myoepithelial) cells
- Lumen filled with cytoplasmic fragments detached from apical portions of secretory cells (Arch Dermatol 1979;115:194)
- Eccrine cystadenoma
- Eccrine hidrocystoma
- Also called Masson hemangioma (Am J Dermatopathol 2003;25:71)
- Often on fingers and in hemorrhoids
- In skin, associated with preexisting pyogenic granuloma or hemangioma, vascular malformations or hemangiomas of blue rubber bleb nevus syndrome
- Due to exuberant recanalization of a thrombus
- May be secondary to trauma or superimposed on pyogenic granuloma or cavernous hemangioma
- Slow growing, tender, blue red, deep dermal to subcutaneous mass
- Rarely recurs after excision
- 70 year old woman with 1 cm lesion on buccal mucosa (Case Rep Dermatol 2010 2;1:22)
- Dilated vessel contains papillary proliferation of plump endothelial cells without atypia overlying fibrous tissue
- Fibrin deposition and thrombi present
- Variable pleomorphism and stratification, no/rare mitotic figures, no necrosis, no solid cellular areas
- Angiosarcoma: infiltrating, freely anastomosing channels lined by spindled to epithelioid endothelial cells with marked atypia, surrounding adnexae and dissecting dermal collagen
- Benign tumor of the follicular infundibulum
- Benign, endophytic follicular tumor with characteristic presence of squamous eddies
- Inverted follicular keratosis (IFK)
- More common in males and older individuals
- Multiple lesions may be associated with Cowden syndrome (Acta Derm Venereol 1976;56:337)
- Although this association may be as a result of its resemblance to trichilemmoma
- Most commonly on the head and neck (~90% of cases) but can also be found on extremities or trunk
- Predilection for cheeks and upper lip (Am J Dermatopathol 1983;5:467)
- Can involve eyelids (Am J Ophthalmol 1979;87:810)
- Unknown at this time
- Regarded by some as a variant of seborrheic keratosis
- Solitary flesh colored nodular or filiform lesion
- Typically 0.3 - 1 cm in diameter (J Cutan Pathol 1984;11:387)
- Can be made on biopsy
- 24 year old woman with a vulvar lesion (Int J Gynecol Pathol 2000;19:369)
- 55 year old woman with a keratotic lesion of the lip (Pan Afr Med J 2014;18:304)
- 63 year old man with a skin colored plaque on the eyelid (Indian J Dermatol Venereol Leprol 2021;87:455)
- Biopsy is usually curative
- Larger lesions treated by complete excision
- Well circumscribed, endophytic tumor with large lobules or finger-like extensions that resemble expanded follicles
- Variable number of squamous eddies
- Occasional mitoses within peripheral basaloid cells
- Histologic variants have been described (J Cutan Pathol 1984;11:387):
- Papillomatous wart-like: exophytic with overlying hyperkeratosis and parakeratosis
- Keratoacanthoma-like: central exoendophytic mass
- Cystic type: irregular clefts within tumor and formation of small cysts
- BCL2: positive dendritic cells are present in increased numbers in the suprabasal areas, compared to seborrheic keratosis (J Cutan Pathol 2006;33:498)
Inverted follicular keratosis:
5 minute pathology pearls
Inverted follicular keratosis with great squamous eddies
- Skin, upper cutaneous lip, shave biopsy:
- Inverted follicular keratosis
- Irritated seborrheic keratosis:
- Presence of squamous eddies; however, lacks endophytic growth
- Tricholemmoma:
- Similar lobulated, endophytic architecture
- Clear glycogenated cells, palisaded basilar layer and thickened basement membrane
- Verruca vulgaris:
- More exophytic than endophytic with inward curving papillomatosis, coarse hypergranulosis and koilocytes
- Associated with human papillomavirus
Comment Here
Reference: Inverted follicular keratosis
- Rare, sporadic, benign disorder which results from the proliferation of factor XIIIa positive dendritic cells
- Most common form of non-Langerhans cell histiocytosis
- Typically a disorder of early childhood
- Juvenile xanthogranuloma (JXG) is a rare, benign proliferative non-Langerhans cell histiocytic proliferation
- Occurs predominantly in young children
- Clinically, it presents as a solitary red-brown, yellowish papule or nodule, most often on the head and neck area
- Systemic JXG is rare and may involve any organ system
- Histologically characterized by the presence of histiocytes, foam cells and Touton giant cells
- Generally follows a benign course with spontaneous resolution over a period of a few years
- Cutaneous JXG is usually self limited
- Cases of ocular JXG should be referred to an ophthalmologist
- Symptomatic systemic JXG may require treatment
- Nevoxanthoendothelioma, xanthoma multiplex, juvenile xanthoma, multiple eruptive xanthoma in infancy, congenital xanthoma tuberosum, xanthoma neviforme and juvenile giant cell granuloma
- ICD-10: D76.3 - Other histiocytosis syndromes
- Incidence is unknown
- Between 40 - 70% of cases arise in the first year of life
- More than 15 - 20% of patients have lesions at birth
- Adult onset accounts for 10% of cases
- M:F = ~1.4:1 (Actas Dermosifiliogr 2020;111:725)
- Has been associated with juvenile chronic myelogenous leukemia and neurofibromatosis type I (Br J Dermatol 2017;176:481)
- Presents as a solitary cutaneous nodule on the head, neck or trunk
- Occasionally extracutaneous presentation of nodules occurs within the eye (most common), soft tissues or visceral organs
- Ocular JXG is usually unilateral and most often develops before the age of 2
- Hyphema and glaucoma are serious complications of ocular JXG
- Systemic involvement is rare, occurring in less than 5% of cases
- Reference: Actas Dermosifiliogr 2020;111:725
- Unknown at this time
- Cause is unknown
- Suggested that histiocytes possibly react to a traumatic or infectious stimuli by progressive lipidation
- 2 clinical variants have been described: a small and a large nodular form; both present as red-brown, dome shaped papules
- Small nodular form usually consists of multiple 2 - 5 mm sized papules, whereas the large nodular form is characterized by 1 or a few nodules 1 - 2 cm in diameter; these 2 forms can coexist
- Has been associated with insulin dependent diabetes mellitus, aquagenic pruritus, urticaria pigmentosa and cytomegalovirus infection
- Most adult patients have solitary lesions
- Reference: Actas Dermosifiliogr 2020;111:725
- Diagnosis is made clinically based on the typical appearance of lesions on physical examination in most cases
- On dermoscopy, the setting sun sign is described, which corresponds to a yellow-orange, central area surrounded by a peripheral border with branched, linear telangiectasias (An Bras Dermatol 2018;93:138)
- In older lesions, white and yellow globules are most commonly seen on dermoscopy because of the more lipidized cells (An Bras Dermatol 2018;93:138)
- Has a good prognosis; lesions usually regress spontaneously
- Cases of liver or central nervous system involvement may rarely be fatal
- 31 week preterm newborn with multiple skin lesions whose clinical, histological and immunohistochemical findings were consistent with juvenile xanthogranuloma (Rev Paul Pediatr 2019;37:257)
- 14 month old and 14 year old girls with oral JXG affecting the lower lip and the soft palate, respectively (Pediatr Dent 2017;39:238)
- 12 year old girl with a slowly growing yellowish polypoid lesion on the posterior scalp (Am J Dermatopathol 2017;39:773)
- Self limited
- No treatment is usually required
- Excision can be done for cosmetic concerns
- Reference: Actas Dermosifiliogr 2020;111:725
- Demarcated dense dermal infiltrate of foamy histiocytes that can extend to the subcutis in large lesions
- Scattered Touton giant cells are characteristic
- Can have loss of the rete ridges and ulceration
- Lymphocytes, plasma cells, eosinophils and some neutrophils can be observed
- Early lesions usually have monomorphous histiocytes with abundant eosinophilic cytoplasm
- In older lesions, the histiocytes become more xanthomatous by developing lipid in their cytoplasm, creating a foamy appearance
- Reference: Actas Dermosifiliogr 2020;111:725
Contributed by Lamiaa Hamie, M.D., M.Sc. and Ossama Abbas, M.D.
Contributed by Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
- HAM56
- CD68
- Factor XIIIa
- CD163
- Reference: Actas Dermosifiliogr 2020;111:725
- Langerin (CD207)
- CD1a
- S100 (not always)
- Reference: Actas Dermosifiliogr 2020;111:725
Brief review of JXG
- Right arm, excision:
- Xanthogranuloma (see comment)
- Comment: Dense sheets of histiocytes infiltrating the dermis and the upper portion of the subcutaneous fat. Numerous multinucleated giant cells of the Touton cell type. In addition, clinicopathologic correlation may be helpful.
- Langerhans cell histiocytosis:
- LCH cells are positive for S100 protein, CD1a and langerin (CD207)
- Intracytoplasmic Birbeck granules are seen on electron microscopy
- Systemic manifestations include osteolytic bone lesions, diabetes insipidus, hepatosplenomegaly and lymphadenopathy
- Papular xanthoma:
- Multiple yellow-red papules
- Mainly on the trunk
- Fewer Touton cells than JXG
- Factor XIIIa is more likely to be negative
- Tuberous xanthoma:
- Occurs in areas of pressure
- Associated with hypercholesterolemia and high LDL
- Consists of dermal aggregates of foam cells, no Touton cells or inflammatory cells
- Spitz nevus:
- Nests of spindle and epithelioid cells within a uniformly hyperplastic epidermis
- Melanocytic immunostaining with S100, MelanA (MART1) and tyrosinase
- Mastocytoma:
- Reddish golden-brown papules
- Can display Darier sign
- Can be pruritic
- Mast cells in the papillary dermis
- Dermatofibroma:
- Brownish papules
- Mainly on the extremities
- May arise after trauma
- Older age group
- Dermal spindle shaped proliferation with collagen trapping
- Reticulohistiocytoma:
- More prominent nucleoli
- Few to no Touton giant cells
- More likely to be punctuated by inflammatory foci
- Ground glass cytoplasm (can be seen in some JXGs)
- Erdheim-Chester disease:
Comment Here
Reference: Juvenile xanthogranuloma
- HAM56
- CD207
- Factor XIIIa
- CD163
- CD68
Comment Here
Reference: Juvenile xanthogranuloma
- Abnormal fibroblast reaction to injury
- Usually in people of African descent, often in earlobe
- High rate of recurrence after excision
- Corticosteroid injection
- Wide bands of collagen with large, brightly eosinophilic, glassy fibers
- Also parallel fibroblasts and myofibroblasts
- Mucinous pools after steroid injection
- Epigenetic alteration in fibroblast DNA and acetylation of histone proteins (J Invest Dermatol 2010;130:2489)
- Complication of acne
- Hyperplastic scar
- Keloidal dermatofibroma
- Result of abnormal fibroblast activity in response to skin trauma or inflammation resulting in increased production of collagen and growth factors
- Nodule or mass forming scar that extends beyond the site of initial injury
- Benign and potentially disfiguring fibrous tumor caused by increased fibroblast activity in response to skin trauma, causing increased collagen and growth factor production
- Common in individuals with darker skin and most common in African Americans (Cureus 2022;14:e23503)
- In comparison to hypertrophic scars, keloids extend beyond the site of initial injury
- Persist until treated, commonly by a combination of intralesional corticosteroids and surgical excision
- Recurrence is common despite treatment (Am Fam Physician 2009;80:253)
- Keloid scar
- Common in < 30 years of age (Am Fam Physician 2009;80:253)
- Commonly seen after ear piercings
- Most common in Black and darker pigmented individuals
- Positive family history increases risk of development
- Any site of trauma or injury to the skin can be affected
- Typically occurs in the head and neck region, including upper part of the back, deltoids and presternal areas
- Characteristically occurs on the earlobes from ear piercings
- Exact pathophysiology is unknown
- Commonly accepted to be due to a dysregulated fibroblastic phase of wound healing, in which fibroblasts have increased proliferative activity and decreased apoptosis resulting in increased collagen, extracellular matrix and cytokine production (J Clin Aesthet Dermatol 2020;13:33, StatPearls: Keloid [Accessed 28 July 2023])
- Primary drivers of keloid formation are considered to be transforming growth factor beta (TGFβ) and platelet derived growth factor (PDGF) (StatPearls: Keloid [Accessed 28 July 2023])
- TGFβ promotes chemotaxis of fibroblasts to the site of inflammation and produces collagen
- Abnormalities in this pathway lead to fibrosis and an abnormal scar response
- Caused by genetic and environmental factors
- Can occur as a result of increased tension in a wound
- Occurs in susceptible individuals after any type of skin trauma including surgery, piercings, acne, tattooing, insect bites, burns, lacerations, abrasions, vaccinations and any other process resulting in cutaneous inflammation (StatPearls: Keloid [Accessed 28 July 2023])
- Occurs after trauma to the skin
- Keloids can take on various shapes depending on site of injury (Scars Burn Heal 2021;7:2059513120980320)
- Ranges in color from flesh colored to red or brown
- Initial presentation commonly includes erythema, pruritis or pain (Scars Burn Heal 2021;7:2059513120980320)
- Rubinstein-Taybi and Goeminne syndromes are rare genetic conditions that are associated with an increased risk of developing keloids (StatPearls: Keloid [Accessed 28 July 2023])
- Diagnosis is made clinically but lesions may be biopsied for confirmation or excised for cosmetic purposes
- Benign but may cause symptoms including pain and pruritus
- Persists unless treated; most commonly removed for cosmetic reasons and if symptomatic
- Despite treatment, recurrence is common (Scars Burn Heal 2021;7:2059513120980320)
- 20 year old woman with development of nodules on earlobes after ear piercing (Malays Fam Physician 2020;15:83)
- 23 year old man with posterior ear lobe mass (Am Fam Physician 2018;98:603)
- 24 year old woman with recurrence 8 years after keloid resection (Medicine (Baltimore) 2023;102:e33444)
- 57 year old man with scar formation several months after trauma (J Pharm Bioallied Sci 2021;13:S871)
- Complete surgical excision
- In conjunction with complete surgical excision, intralesional corticosteroid injections imiquimod, bleomycin or radiotherapy can be used to decrease the risk of recurrence (Dermatol Ther 2022;35:e15425)
- Compression bandages, silicone dressings, cryotherapy, laser therapy and intralesional 5-fluorouracil are also treatment options
- Nodular or raised and irregularly shaped dermal skin lesion (Scars Burn Heal 2021;7:2059513120980320)
- Varies in color, can be flesh colored to red or brown
- Smooth, firm and rubbery
- Characteristic keloidal collagen is composed of broad, homogeneous, brightly eosinophilic bands of hyalinized collagen bundles
- Keloidal collagen in often described as bubble gum-like collagen
- Collagen bands are haphazardly arranged or form a nodular lesion in the reticular dermis sparing the papillary dermis (Am J Dermatopathol 2004;26:379)
- Focal aggregates of fibroblasts can be seen in between or around the collagen bands (Scars Burn Heal 2021;7:2059513120980320)
Dr. Gardner explains histological findings of keloids
- Skin, ear lobe, excision:
- Keloid
- Hypertrophic scar:
- Does not grow outside of wound margins
- Can regress on its own
- Does not contain keloid type collagen bundles on histological exam
- Dermatofibroma:
- Positive dimple sign on physical exam; lesion develops a central depression when lateral pressure is applied
- More common on the lower legs
- No history of preceding trauma
- Dermatofibrosarcoma protuberans:
- No history of trauma
- Harbors translocation t(17;22)(q22;q13) that results in a COL1A1::PDGFB fusion gene
- Most commonly found on the chest, shoulders and limbs
- Lobomycosis:
Comment Here
Reference: Keloid
- Complete resolution
- Increase in propensity for development of squamous cell carcinoma
- Melanoma in situ
- Recurrence
Comment Here
Reference: Keloid
- Keloids grow beyond the wound site
- Keloids have an increased propensity for malignant transformation
- Keloids never recur after treatment
- Keloids occur exclusively in pigmented skin
Comment Here
Reference: Keloid
- Keratoacanthoma (KA) is a well differentiated, cutaneous squamous cell carcinoma, which often spontaneously regresses
- Regression is thought to be due to immune mediated destruction of squamous cells
- For lesions that are entirely resected, can diagnose as "well differentiated squamous cell carcinoma, keratoacanthoma type”
- For lesions that are not entirely histologically examined, can diagnose as "well differentiated squamous cell carcinoma with features of keratoacanthoma”
- Common, represents approximately up to 30% of cases of cutaneous squamous cell carcinoma (SCC)
- Dome shaped tumor with central keratinous plug in sun exposed areas
- May become large, up to 10 cm (called giant KA)
- Good prognosis; vast majority of cases spontaneously regress
- Agglomerate KA (variant)
- KA centrifugum (variant)
- Giant KA (variant)
- Subungual KA (variant)
- Intraoral KA (variant)
- Older adults, mean age mid 60s (Indian J Dermatol 2011;56:435)
- M:F = 3:1 (Indian J Dermatol 2011;56:435)
- Head and neck most common sites, followed by extremities (Open Access Maced J Med Sci 2018;6:531)
- Tumor stems from follicular infundibulum related to chronic solar (UV) damage (Indian J Dermatol 2011;56:435)
- Undergoes 3 clinical stages: proliferative, mature, involutional / resolving (Arch Craniofac Surg 2015;16:92)
- Typically solitary but may present with multiple tumors (Acta Biomed 2019;90:580)
- Excisional biopsy preferred to show suggestive histopathology
- Nonfatal tumor
- Can regress; however, final size prior to regression is difficult to predict (J Am Acad Dermatol 2016;74:1220)
- Recurrence is uncommon with surgical removal
- Self limited proliferation with low probability of malignant transformation (more often associated with perineural invasion) (Acta Biomed 2019;90:580)
- 34 year old woman with rapidly growing conjunctival mass (Rev Hosp Clin Fac Med Sao Paulo 2004;59:135)
- 56 year old man with giant variant keratoacanthoma of the cheek (Arch Craniofac Surg 2015;16:92)
- 61 year old man with rapidly occurring forearm keratoacanthoma over 11 days (Cutis 2015;95:E7)
- 74 year old man with keratoacanthoma of the palm (Cureus 2018;10:e2331)
- 79 year old man with keratoacanthoma of the forehead with venous invasion (Dermatol Pract Concept 2012;2:204a03)
- 92 year old man with keratoacanthoma of the left cheek with perineural invasion (Acta Biomed 2019;90:580)
- Monitoring for spontaneous regression; often leaves atrophic hypopigmented scar (Indian J Dermatol 2011;56:435)
- Typically treated with complete surgical excision; Mohs surgery performed dependent on location (Ann Dermatol 2011;23:357)
- Electrosurgery, cryosurgery, laser surgery, systemic or topical chemotherapy occasionally utilized (J Dent (Shiraz) 2014;15:91)
- Radiotherapy can be utilized with reoccurrence or potential large cosmetic disfigurement with surgery; typically not utilized in young adult patients (J Am Acad Dermatol 1990;23:489)
- Typically large, scaly, dome shaped tumor with central keratinous plug
- Low power magnification shows large, well differentiated squamous tumor with central keratin filled crater
- Surrounding epidermis forms a lip around the invaginating crateriform tumor
- Tumor is composed of bland squamous cells with abundant eosinophilic or glassy cytoplasm and enlarged hyperchromatic to vesicular appearing nuclei
- Mitotic activity and cellular atypia are usually seen at the periphery of tumor
- Intraepidermal neutrophilic microabscesses and keratin horn pearls are seen within the tumor
- Regressing tumors show epidermal atrophy, bland cytologic features, dermal inflammation and fibrosis at the periphery of tumor
- Ki67 in tumor lobule basal cells (Oncol Lett 2017;13:2539)
- CK17 in the suprabasal cells with central staining pattern (Oncol Lett 2017;13:2539)
- PAS in outer root sheath of hair follicle and epithelial tumor cells (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:310)
- CK6 and CK10 in tumor islands (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:310)
- CK14 epithelial basal layer (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:310)
- CK10 spinous and granular layers (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:310)
- Ki67 in suprabasal cells (Oncol Lett 2017;13:2539)
- CK17 weak / negative in tumor lobules (Oncol Lett 2017;13:2539)
- Transforming growth factor beta receptor 1 can cause multiple self healing squamous epithelioma (MMSE); most common cause of multiple KA
- Germline mutations of hMSH2 and hMLH1 mismatch repair genes causing Muir-Torre syndrome have been implicated in solitary and multiple KA formation
- BRAF kinase inhibitors utilized to treat KA has been reported to induce reactive KA by paradoxical activation of the ERK MAPkinase pathway
- Reference: Exp Dermatol 2016;25:85
Keratoacanthoma
- Skin, left cheek (clinical keratoacanthoma), excision:
- Well differentiated squamous cell carcinoma, keratoacanthoma type (see comment)
- Comment: Well differentiated hyperplastic squamous epithelium with crater-like depression with keratin horn pearls present centrally. Enlarged hyperchromatic vesicular nuclei present along with glassy appearing cytoplasm.
- Conventional, well differentiated squamous cell carcinoma:
- Shows greater cellular atypia and mitotic activity
- Intraepidermal neutrophilic microabscesses and tissue eosinophilia less common
- May be difficult to distinguish in superficial biopsies
- Verrucous carcinoma:
- Shows prominent endophytic and exophytic growth
- Lacks central crateriform architecture
- Also has bland cytologic features
- May be difficult to distinguish in superficial biopsies
A 62 year old man presents with a single, solitary, skin colored tumor that has a crater-like appearance with central keratin buildup on his left forearm. It appeared spontaneously and has grown rapidly over the past 3 weeks. It is painless to the touch but is cosmetically displeasing. He has no other skin conditions. The tumor is excised and a microscopic image is shown above. Which of the following is true concerning this skin lesion?
- It is a variant of basal cell carcinoma
- The underlying cause for this tumor is typically due to a genetic mutation
- The malignant potential of this tumor is high and it must be removed immediately
- This tumor has the potential to completely spontaneously regress
Comment Here
Reference: Keratoacanthoma
- Peripheral palisading and clefting are also likely to be seen under the microscope
- It has overlapping features of squamous cell carcinoma
- Due to its rapid growth, this tumor is likely to metastasize
- Excessive UV damage plays no role in pathogenesis
Comment Here
Reference: Keratoacanthoma
- Benign intraepidermal lesion composed of large keratinocytes
- Debate as to whether this represents a distinct entity or a reaction pattern within a solar lentigo (Int J Dermatol 2003;42:36)
- Recent study suggests large cell acanthoma is a solar lentigo with cellular hypertrophy (J Cutan Pathol 2014;41:733)
- 62 year old man with multiple disseminated large cell acanthomas of the skin associated with HPV6 (J Am Acad Dermatol 2005;53:335)
- Conjunctival lesion with histological features similar to large cell acanthoma (J Cutan Pathol 2010;37:1103)
- Light-tan to dark brown, well circumscribed macule or patch
- Few millimeters to centimeters in diameter
- Typically on sun exposed skin
- Clinically resembles a seborrheic or actinic keratosis
- Atrophic or acanthotic epidermis containing larger than usual keratinocytes (~2x normal epidermal keratinocytes)
- Usually well demarcated from adjacent epidermis
- Basal layer may appear hyperpigmented; sometimes conspicuous rete ridges
- Orthokeratosis; may have hypergranulosis
- Minimal nuclear pleomorphism
- Basal mitoses only
- Bowen's disease / squamous cell carcinoma in situ: full thickness keratinocytic atypia with mitoses throughout, often parakeratosis
- Pigmented actinic keratosis: keratinocytic atypia limited to basal layer and lower spinous layer, solar elastosis, occasional parakeratosis
- Solar lentigo: no enlarged keratinocytes
- Divided into lesions of nipple or scrotum, pilar leiomyoma or solitary angioleiomyoma (vascular leiomyoma) usually in subcutis
- May be very painful
- Familial cutaneous leiomyomatosis (Reed syndrome):
- Due to mutation in fumarate hydratase, may be associated with renal cell carcinoma (Dermatol Online J 2005;11:21)
- Arises from arrector pili muscles
- Superficial, small, multiple, painful
- May be due to hereditary leiomyomatosis and renal cell cancer syndrome (J Urol 2007;177:2074)
- May be associated with germline mutations in the fumarate hydratase gene (Nat Genet 2002;30:406, Cancer Genet Cytogenet 2008;183:83)
- 51 year old woman with multiple cutaneous and uterine leiomyomatosis (Dermatol Online J 2005;11:21)
- 79 year old man with hereditary leiomyomatosis and renal cell carcinoma syndrome (Dermatol Online J 2008;14:16)
- Avoidance of cold
- Possibly nifedipine, nitroglycerine, phenoxybenzamine (block smooth muscle contraction) (Dermatol Online J 2005;11:21)
- Possibly botulinum toxin type A (Dermatology 2009;218:44)
- Possibly excision with dermal skin template for multiple tumors, carbon dioxide laser ablation (J Cutan Med Surg 2009;13:102)
- Intersecting smooth muscle fascicles
- May have scattered bizarre hyperchromatic nuclei (symplastic leiomyoma)
- No atypia, no mitotic activity, no necrosis
- Pilar leiomyoma:
- Dermal intersecting fascicles of eosinophilic spindle cells with plump, cigar shaped nuclei with dermal collagen bundles
- Almost all patients with multiple skin leiomyomas have germline fumarate hydratase mutation (Arch Dermatol 2005;141:199)
- Cutaneous leiomyomas are benign tumors originating from arrector pili (piloleiomyoma), vascular (angioleiomyoma), periareolar and genital smooth muscle cells (genital leiomyoma)
- Cutaneous piloleiomyomas may be sporadic or associated with the autosomal dominant syndrome multiple cutaneous and uterine leiomyomatosis (also known as Reed syndrome or hereditary leiomyomatosis and renal cell cancer)
- Cutaneous leiomyomas are benign dermal tumors of smooth muscle cells arranged in interlacing fascicles
- Leiomyomas may be differentiated from other spindle cell tumors due to their positivity for both SMA and desmin
- Cutaneous piloleiomyomas can be sporadic or inherited in association with multiple cutaneous and uterine leiomyomatosis (also known as Reed syndrome or hereditary leiomyomatosis and renal cell cancer)
- ICD-10: D21.9 - benign neoplasm of connective and other soft tissue, unspecified
- Leiomyomas are typically diagnosed in young and middle aged adults; however, they can occur in children
- Frequency of piloleiomyomas is about equal in males and females and it is unknown whether a sex predominance exists for genital leiomyomas; there is no known racial predilection for cutaneous leiomyomas (StatPearls: Cutaneous Leiomyomas [Accessed 10 April 2024])
- Angioleiomyomas have been further split by some authors into solid (more common in females), cavernous and venous subtypes (cavernous and venous being more common in males) (Laryngoscope 2004;114:661)
- Cutaneous leiomyomas can occur anywhere on the body
- Germline heterozygous mutations of the fumarate hydratase gene are found in cutaneous piloleiomyomas associated with the autosomal dominant syndrome multiple cutaneous and uterine leiomyomatosis (also known as Reed syndrome or hereditary leiomyomatosis and renal cell cancer)
- Fumarate hydratase missense mutations are associated with decreased enzyme activity suggesting a tumor suppressor role (J Mol Diagn 2005;7:437)
- Little is known about the etiology of sporadic cutaneous leiomyomas (Int J Mol Med 2004;13:13, Cancer Genet Cytogenet 2006;170:58, Cancer Genet Cytogenet 2010;199:21)
- Recurrent losses in chromosome 22 and recurrent gains in Xq have been reported in few cases of sporadic angioleiomyomas
- Few studies have examined cytogenetics of genital leiomyomas
- No consistent mutations have been identified in sporadic piloleiomyomas to date
- Cutaneous leiomyomas can be solitary or multiple; when multiple, they may be clustered or linear in distribution
- They present as skin colored or red-brown, firm papules and nodules
- Pain and cold sensitivity are common complaints
- Genital leiomyomas may be pedunculated and are less likely to be painful compared to other subtypes
- Diagnosis is often made by histopathology
- Imaging including computed tomography (CT), magnetic resonance imaging (MRI) and ultrasound can be performed
- Germline mutations of the fumarate hydratase gene are diagnostic of multiple cutaneous and uterine leiomyomatosis (also known as Reed syndrome or hereditary leiomyomatosis and renal cell cancer)
- Imaging is not routinely performed for cutaneous leiomyomas
- Characteristic imaging findings of angioleiomyomas have been described
- On ultrasound, angioleiomyomas are often described as well defined, solid, round and homogenous; echogenicity and vascularity are variable; Doppler ultrasound can be used to evaluate vasculature and presence of feeding vessels (Korean J Radiol 2018;19:752)
- Signal intensity of angioleiomyomas on MRI can be similar or hyperintense compared to skeletal muscle on T1 weighted images; a dark reticular signal on T2 weighted images has been proposed as a characteristic feature of angioleiomyomas (Skeletal Radiol 2022;51:837)
- Calcifications due to degenerative change can be seen on CT
- Cutaneous leiomyomas are slow growing and can increase in number over time
- Excised solitary, sporadic cutaneous leiomyomas have an excellent prognosis with low recurrence rates (J Oral Maxillofac Pathol 2013;17:281)
- Malignant transformation is rare in cutaneous leiomyomas
- Leiomyosarcomas have been described in patients with multiple cutaneous and uterine leiomyomatosis (also known as Reed syndrome or hereditary leiomyomatosis and renal cell cancer); subcutaneous extension is a poor prognostic factor in leiomyosarcoma (JAAD Case Rep 2015;1:150, J Am Acad Dermatol 2014;71:919)
- Presence of multiple cutaneous piloleiomyomas is cause for further work up due to the association of the following malignancies with multiple cutaneous and uterine leiomyomatosis (also known as Reed syndrome or hereditary leiomyomatosis and renal cell cancer)
- Renal cell cancers, most commonly type II papillary renal cell carcinoma
- Cutaneous and uterine leiomyosarcomas
- Cases have been reported of breast cancer, bladder cancer, gastrointestinal stromal tumors, adrenal tumor, testicular and ovarian tumors; however, it is unknown whether these are coincidental or related (GeneReviews: FH Tumor Predisposition Syndrome [Accessed 10 April 2024])
- 24 year old woman with painful lesions of the back and left shoulder (J Clin Aesthet Dermatol 2011;4:37)
- Woman in her 30s with painful nodules of the head, neck and lower extremities (JAMA Dermatol 2016;152:1041)
- 36 year old woman with multiple papules of the right upper extremity and chest (Clin Case Rep 2023;11:e6904)
- 41 year old woman with a tender nodule on the right heel (Cureus 2018;10:e3419)
- Surgical excision can be performed when practical for symptomatic lesions or for elective removal
- Conservative but complete excision should be advised if atypical features are present on histopathology
- Alternative destructive interventions include CO2 laser, electrodessication and cryosurgery
- Topical, intralesional and systemic treatments for symptomatic relief may be indicated (J Am Acad Dermatol 2017;77:149)
- Topical options include nitroglycerin, lidocaine and capsaicin
- Use of intralesional botox has been reported
- Systemic treatment options include gabapentin, pregabalin, NSAIDs, calcium channel blockers, doxazosin, nitroglycerin, phenoxybenzamine and duloxetine
- Smooth muscle cells have elongated, thin nuclei with blunt ends; they are often described as cigar shaped with pink, eosinophilic cytoplasm
- Perinuclear vacuoles made of glycogen may be seen (Am J Dermatopathol 1997;19:2)
- Well circumscribed tumor consisting of fascicles and interlacing smooth muscle bundles
- Piloleiomyomas are nonencapsulated while angioleiomyomas can be encapsulated
- Angioleiomyomas have prominent vessels described as slit-like or round; smooth muscle layers surrounding the vessels interlace with surrounding smooth muscle fascicles
- Overlying epidermal changes such as acanthosis and hyperkeratosis can be seen
- Cytologic atypia is usually absent and mitotic activity is negligible
- Presence of nuclear atypia and degenerative features have been described in symplastic leiomyomas (Dermatol Surg 2004;30:1249)
- Smooth muscle actin (SMA)
- Desmin
- Muscle specific actin (MSA)
- h-caldesmon
- Variable cytokeratin
- Variable EMA
- S100
- SOX10
- HMB45
- CD34
- Fumarate hydratase: loss of fumarate hydratase expression can be seen in piloleiomyomas associated with multiple cutaneous and uterine leiomyomatosis (also known as Reed syndrome or hereditary leiomyomatosis and renal cell cancer); sensitivity 70%, specificity 97.6% (Am J Surg Pathol 2017;41:801)
- For piloleiomyomas, fumarate hydratase gene mutations can be identified using a variety of methods including sequencing and copy number analyses; a variant specific test can be used if there is a known germline pathogenic variant
- Fumarate hydratase activity can be measured in fibroblasts or leukocytes (GeneReviews: Fumarate Hydratase Deficiency [Accessed 10 April 2024])
Pilar leiomyoma video
by Dr. Jerad Gardner
Angioleiomyoma video
by Dr. Jerad Gardner
- Skin, right shoulder, shave biopsy:
- Piloleiomyoma (see comment)
- Comment: This is a dermal tumor consisting of interlacing fascicles of smooth muscle cells. Cellular atypia and mitoses are not identified. The tumor is positive for SMA.
- Leiomyosarcoma:
- Marked cytologic atypia
- Frequent mitoses
- Necrosis
- Subcutaneous extension
- Congenital smooth muscle hamartoma:
- Presentation in infancy, can see overlying epidermal changes
- May see hypertrichosis
- Becker nevus:
- May see hyperpigmentation
- Variable hypertrichosis
- Spindled squamous cell carcinoma:
- Pleomorphism
- Cytokeratin+
- Variable SMA
- Atypical fibroxanthoma (AFX):
- Spindle cell melanoma:
- Dermatomyofibroma:
- Horizontal arrangement of spindled cells
- Desmin negative
- Neurofibroma:
- S100+
- Cells have scant cytoplasm and are loosely arranged
- Dermatofibroma:
- Myoepithelioma:
- S100+
- EBV associated smooth muscle tumor:
- EBER ISH +
A 25 year old man presents with multiple red-brown, painful papules on the right upper back. On histopathology, there is a dermal nodule with fascicles of spindle cells with eosinophilic cytoplasm. Tumor cells are positive for SMA and desmin and are negative for S100. What is the diagnosis?
- Atypical fibroxanthoma
- Dermatomyofibroma
- Leiomyoma
- Neurofibroma
Comment Here
Reference: Leiomyoma
A 36 year old woman presents for excision of a painful, slowly enlarging nodule on the thigh present for many years. Her father has history of papillary type 2 renal cell carcinoma. Mutation in which of the following enzymes is implicated in this genetic syndrome?
- Alpha galactosidase A
- Ferrochelatase
- Fumarate hydratase
- Uroporphyrinogen decarboxylase
Comment Here
Reference: Leiomyoma
- Skin involvement ("leukemia cutis") occurs in 5% with CML, 8% with CLL, 10% with monocytic leukemia
- Myeloid leukemia with monocytic differentiation more commonly involves the skin than other types of myeloid leukemia
- Usually is abnormal peripheral blood count at diagnosis
- Skin involvement is rarely initial manifestation of recurrence (Am J Clin Pathol 2008;129:130)
- May also have accompanying vasculitis (Am J Clin Pathol 1997;107:637)
- Aggressive behavior and short survival (J Am Acad Dermatol 1999;40:966)
- 68 year old woman with history of AML (Case of Week #140)
- Systemic chemotherapy directed at eradicating the leukemic clone
- Multiple nodules / papules
- In CLL, may be perivascular, periadnexal, nodular or band-like dermal infiltrate
- Infiltrate in leukemic patients is often NOT neoplastic, but reactive
- AML: dermis and superficial subcutaneous fat are diffusely infiltrated by a monotonous population of large cells with a high nuclear to cytoplasmic ratio, round to slightly irregular nuclear contours, finely dispersed chromatin and prominent nucleoli
- Myeloblasts: chloroacetate esterase (Leder stain), myeloperoxidase
- Very common; rapidly growing polypoid red mass surrounded by thickened epidermis, often in finger or lips
- Also called granuloma pyogenicum, lobular capillary hemangioma
- May be associated with keratinous cyst
- Benign, often regresses spontaneously
- May be disseminated, occur within port wine stains, be in deep dermis / subcutis or be intravenous
Variants:
- Classic polypoid, dermal, subcutaneous, intravenous, eruptive, with multiple satellites
- None or excision (may recur as multiple satellites)
- Fleshy cutaneous tumor
- Lobular pattern of vascular proliferation with inflammation and edema resembling granulation tissue
- Thin epidermis at top with variable ulceration
- Acanthosis and hyperkeratosis at sides
- Central branching vessel is called capillary or vascular lobule, with no / rare red blood cells, surrounded by endothelial cells
- Variable mitotic activity
- Deep lesions often lack edema and inflammation
- Acrodermatitis
- Bacillary angiomatosis
- Benign (infantile) hemangioendothelioma
- Reactive angioendotheliomatosis
- Venous stasis
- Verruga peruana
- Exceptionally rare and poorly differentiated cutaneous carcinoma with prominent reactive inflammatory infiltrate
- Mimics undifferentiated nasopharyngeal carcinoma (Rare Tumors 2013;5:e47)
- WHO defines these tumors (in nasopharynx/sinonasal cavity) as lymphoepithelial carcinoma
- Importantly, cutaneous LELC is NOT associated with Epstein Barr virus (EBV) infection
- Older to elderly adult patients (Dermatol Online J 2008;14:12)
- Approximately equal incidence of females and males
- Head and neck most common site
- In skin, no apparent relationship with EBV (Dermatol Online J 2008;14:12, Am J Dermatopathol 1996;18:478)
- This is in contrast to consistent EBV association with similar tumors from lung, salivary glands, stomach, thymus, nasopharynx and sinonasal cavity
- Uncertain origin (Dermatol Online J 2008;14:12)
- Unclear whether a poorly / undifferentiated squamous cell carcinoma versus poorly differentiated adnexal neoplasm
- Usually firm, variably colored, face or neck plaque, papule or nodule (Dermatol Online J 2008;14:12)
- 73 year old woman with vulvar tumor (Diagn Pathol 2011 Jan 10;6:4)
- 85 and 87 year old men (Dermatol Online J 2012;18:7, Rare Tumors 2013;5:e47)
- 89 year old woman (Dermatol Online J 2008;14:12)
- Wide local excision or Moh's microsurgery to ensure complete removal
- Radiation reserved for recurrence or lymph node involvement (Case Rep Oncol Med 2012;2012:241816)
- Generally low recurrence and metastatic potential with complete excision (in contrast to nasopharyngeal counterpart)
- Rare lymph node metastasis (Am J Dermatopathol 2006;28:211) or death from disease
- With Diagnostic criteria:
- Well circumscribed lobules, nests or small aggregates of large, cohesive, epithelioid cells closely associated with a dense, mixed T and B lymphocytic and plasmacytic infiltrate (Rare Tumors 2013;5:e47)
- Biphasic nature may be more apparent at high magnification
- The epithelioid component generally lacks connection with the epidermis
- Cells are often polygonal and display poorly defined eosinophilic cytoplasm, vesicular nuclei with prominent nucleoli and increased mitotic activity, including atypical mitotic figures (Dermatol Online J 2008;14:12)
- Focal ductular differentiation or trichilemmal keratinization rarely reported (J Cutan Pathol 1991;18:93)
- Mandatory dense inflammatory infiltrate (polymorphous and polytypic) surrounding and intermingling with epithelial tumor cells
- Lymphoid infiltrate may obscure the epithelial component
- When inflammation predominates, may mimic lymphoproliferative disorder
- Well circumscribed lobules, nests or small aggregates of large, cohesive, epithelioid cells closely associated with a dense, mixed T and B lymphocytic and plasmacytic infiltrate (Rare Tumors 2013;5:e47)
Contributed by Sara Shalin, M.D., Ph.D.
Images hosted on other servers:
- Melanoma markers: S100 and HMB45
- Neuroendocrine markers: chromogranin, synaptophysin and CD56
- EBER (EBV encoded RNA in situ hybridization)
- Cutaneous lymphadenoma
- Lymphoma
- Melanoma
- Merkel cell carcinoma
- Metastatic disease from nasopharyngeal carcinoma
- Poorly differentiated inflamed carcinoma
- Lymphomatoid papulosis (LyP) is a chronic and self healing CD30+ lymphoproliferative disorder characterized by recurrent erythematous papules / nodules on skin (J Am Acad Dermatol 2016;74:59, Blood 2019;133:1703, Am J Clin Dermatol 2016;17:319, J Clin Oncol 2015;33:3759, Semin Diagn Pathol 2017;34:22, Am J Surg Pathol 2013;37:1173, Blood 2000;95:3653)
- Lymphomatoid papulosis (LyP) is a chronic and self healing CD30+ lymphoproliferative disorder characterized by recurrent erythematous papules / nodules on skin; as such it conveys a benign clinical course (J Am Acad Dermatol 2016;74:59, Blood 2019;133:1703, Am J Clin Dermatol 2016;17:319, J Clin Oncol 2015;33:3759, Semin Diagn Pathol 2017;34:22, Am J Surg Pathol 2013;37:1173, Blood 2000;95:3653)
- More common in trunk and extremities but can affect any body part (J Am Acad Dermatol 2016;74:59, Am J Clin Dermatol 2016;17:319)
- Single or clustered red or purple papules and small nodules (< 2.0 cm) with different stages of development; spontaneous regression in few weeks and indolent clinical course (Hematol Oncol 2019;37 Suppl 1:43, J Am Acad Dermatol 2016;74:59, Arch Dermatol 2009;145:966, Semin Diagn Pathol 2017;34:22, Clin Exp Dermatol 2018;43:137)
- Most patients don’t require specific treatment (J Am Acad Dermatol 2016;74:59, Am J Surg Pathol 2013;37:1173, Clin Exp Dermatol 2018;43:137, Blood 2000;95:3653)
- ICD-O: 9718/1 - lymphomatoid papulosis
- Primary cutaneous CD30+ lymphoproliferative disorders include primary cutaneous anaplastic large cell lymphoma and lymphomatoid papulosis and account for 25% of all cutaneous T cell lymphomas (Hematol Oncol 2019;37 Suppl 1:43, Semin Diagn Pathol 2017;34:22)
- Rare condition in general population and has an incidence of 1.2 to 1.9 cases per 1 million people (Cancer 1992;70:2951)
- Incidence peaks in the fifth decade but can affect all age groups (J Am Acad Dermatol 2012;66:928, J Am Acad Dermatol 2016;74:59, Am J Clin Dermatol 2016;17:319)
- M > F (J Am Acad Dermatol 2012;66:928, J Am Acad Dermatol 2016;74:59)
- In general is more common in Caucasians (Semin Diagn Pathol 2017;34:22)
- Lymphomatoid papulosis type B is more common in Hispanics (J Am Acad Dermatol 2016;74:59)
- More common in trunk and extremities but can affect any body part (J Am Acad Dermatol 2016;74:59, Am J Clin Dermatol 2016;17:319)
- Oral and mucosal involvement is rare (Semin Diagn Pathol 2017;34:22)
- No etiologic factors identified (e.g., not associated with EBV)
- One case report associated with HTLV-1 (Eur J Dermatol 2016;26:194)
- Some cases that show progression to anaplastic large cell lymphoma show resistance to CD30 ligand and mutations of TGF-β (Semin Diagn Pathol 2017;34:22)
- Most patients are previously asymptomatic and lack underlying disease; a subset of cases arises in patients with history of mycosis fungoides
- Clusters of red or purple papules and small nodules (< 2.0 cm each) with different stages of development, spontaneous regression in few weeks and indolent clinical course (Hematol Oncol 2019;37 Suppl 1:43, J Am Acad Dermatol 2016;74:59, Arch Dermatol 2009;145:966, Semin Diagn Pathol 2017;34:22, Clin Exp Dermatol 2018;43:137)
- Less commonly, single or multiple crops; the disease can persist from several weeks to years (J Am Acad Dermatol 2016;74:59, Semin Diagn Pathol 2017;34:22, Clin Exp Dermatol 2018;43:137)
- The severity of lesions is defined as: mild (< 12 lesions), moderate (12 - 50 lesions) and severe (> 50 lesions) (J Am Acad Dermatol 2016;74:59)
- Dermoscopic appearance may coexist in different stages of progression and involution (J Eur Acad Dermatol Venereol 2018;32:e198, Arch Dermatol 2009;145:966):
- Pinkish or light brown papules with homogeneous areas and delicate dotted vascular pattern in the periphery
- Papules with centripetal and tortuous irregular vessels
- Crusts and papules with central scale and vascular pattern sparing the center in mature lesions
- Papule with central necrotic ulceration denotes old lesion
- Post inflammatory pigmentation macule
- Pruritus is the primary symptom in about half of patients (J Am Acad Dermatol 2016;74:59)
- The correct diagnosis requires (J Am Acad Dermatol 2016;74:59, Am J Clin Dermatol 2016;17:319, Semin Diagn Pathol 2017;34:22, Blood 2000;95:3653):
- A clinical history of crops of lesions with spontaneous regression
- Typical histological findings
- Typical immunohistochemical findings
- Excellent prognosis (Hematol Oncol 2019;37 Suppl 1:43, Semin Diagn Pathol 2017;34:22, J Am Acad Dermatol 2012;66:928, Blood 2000;95:3653)
- Around 5% of patients die of disease over a median period of 4 years, particularly those patients with underlying cutaneous lymphoma (J Am Acad Dermatol 2016;74:59)
- Histologic types do not have prognostic significance (Blood 2019;133:1703)
- Clinical follow up is recommended, since there is a risk of developing a second lymphoid malignancy (e.g. mycosis fungoides and Hodgkin lymphoma) (Hematol Oncol 2019;37 Suppl 1:43, J Clin Oncol 2015;33:3759, Semin Diagn Pathol 2017;34:22, Clin Exp Dermatol 2018;43:137, J Am Acad Dermatol 2012;66:928, Blood 2000;95:3653)
- Patients with T cell receptor gene rearrangement or a mixed type of lymphomatoid papulosis have a higher risk of progressing to lymphoma (J Am Acad Dermatol 2012;66:928)
- Men, lymphomatoid papulosis type B and lymphomatoid papulosis type C are associated with increased risk of lymphoma development (J Am Acad Dermatol 2016;74:59)
- Lymphomatoid papulosis type A and lymphomatoid papulosis type D are less frequently associated with lymphoma development (J Am Acad Dermatol 2016;74:59)
- Lymphomatoid papulosis type A is the more prevalent subtype associated with early relapse (Clin Exp Dermatol 2018;43:137)
- 7 year old girl with lymphomatoid papulosis type A and pseudocarcinomatous hyperplasia (J Cutan Pathol 2016;43:430)
- 14 year old girl with lymphomatoid papulosis type C of the eyelid (Orbit 2014;33:395)
- 27 year old man with extensive lymphomatoid papulosis type A (Case Rep Dermatol Med 2019;2019:1765210)
- 46 year old woman with Waldenström macroglobulinemia and lymphomatoid papulosis (J Dermatol 2005;32:132)
- 46 year old woman with γδ lymphomatoid papulosis type D mimicking primary cutaneous γδ T cell lymphoma (JAAD Case Rep 2019;5:264)
- 70 year old man with rheumatoid arthritis and lymphomatoid papulosis type E preceding and coexisting with mycosis fungoides (J Cutan Pathol 2015;42:1018)
- 84 year old man with chronic lymphocytic leukemia / small lymphocytic lymphoma and lymphomatoid papulosis type A (Dermatol Online J 2018;24:6)
- Most patients don’t require specific treatment (J Am Acad Dermatol 2016;74:59, Am J Surg Pathol 2013;37:1173, Clin Exp Dermatol 2018;43:137, Blood 2000;95:3653)
- Treatments aimed towards symptom relief and faster regression:
- Psoralen ultraviolet A (PUVA) (Hematol Oncol 2019;37 Suppl 1:43, J Am Acad Dermatol 2016;74:59, Clin Exp Dermatol 2018;43:137, Blood 2000;95:3653)
- Related to longer disease free survival (DFS): 10 to 36 months (Clin Exp Dermatol 2018;43:137)
- Topical corticosteroids (J Am Acad Dermatol 2016;74:59, Clin Exp Dermatol 2018;43:137, Blood 2000;95:3653)
- Brentuximab vedotin is an active and well tolerated option and has 100% response rate (J Am Acad Dermatol 2016;74:59, J Clin Oncol 2015;33:3759)
- Bexarotene (J Am Acad Dermatol 2016;74:59)
- Low dose methotrexate (Hematol Oncol 2019;37 Suppl 1:43, Clin Exp Dermatol 2018;43:137)
- Psoralen ultraviolet A (PUVA) (Hematol Oncol 2019;37 Suppl 1:43, J Am Acad Dermatol 2016;74:59, Clin Exp Dermatol 2018;43:137, Blood 2000;95:3653)
- Lymphomatoid papulosis is characterized by a wedge shaped pattern, with a wide superficial base and the tip at the bottom, usually deep dermis and less frequently into the subcutaneous tissue
- The most characteristic appearance is the presence of few to numerous large cells with a Hodgkin or Hodgkin-Reed Sternberg admixed with a reactive background of small lymphocytes and less frequently eosinophils, plasma cells and histiocytes
- The microscopic appearance and immunophenotype of large cells is variable and led to subclassification of lymphomatoid papulosis into different categories (J Am Acad Dermatol 2016;74:59, Blood 2019;133:1703, Semin Diagn Pathol 2017;34:22, J Am Acad Dermatol 2013;68:809, J Am Acad Dermatol 2012;66:928, Am J Clin Pathol 2003;119:731, Am J Surg Pathol 2010;34:1168, Am J Surg Pathol 2013;37:1)
- Type A: wedge shaped and extensive lymphoid infiltrate with neutrophils, eosinophils and histiocytes; CD30+ cells are scattered and the overall histologic appearance mimics classic Hodgkin lymphoma
- Type B: epidermotropism and band-like distribution of small to medium atypical lymphocytes with cerebriform nuclei, without CD30+ expression and mimics mycosis fungoides, patch stage
- Type C: sheets of large cells, uniformly positive for CD30, with or without epidermotropism and few admixed inflammatory cells; the lesion mimics primary cutaneous anaplastic large cell lymphoma
- Type D: atypical small to medium lymphoid infiltrate with epidermotropism; the neoplastic cells express CD30 and CD8 and mimic pagetoid reticulosis
- Type E: angiocentric and angiodestructive pleomorphic lymphoid infiltrate of small to medium size lymphocytes; there are scattered large cells, positive for CD30 and the overall appearance is that of an aggressive lymphoma such as extranodal T/NK cell lymphoma, nasal type; EBER is negative
- Lymphomatoid papulosis with DUSP22-IRF4 rearrangement: biphasic growth pattern with pagetoid reticulosis-like epidermotropism of small to medium size cerebriform lymphocytes that lack CD30; the second component is dermal or periadnexal and the atypical lymphocytes express CD30+
- Rare forms
- Folliculotropic: perifollicular infiltrate of atypical lymphocytes, cystic dilatation of hair follicle, rupture of hair follicle, hyperplasia of the follicular epithelium, intrafollicular pustules (neutrophil collections) and follicular mucinosis
- Syringotropic: eccrine units with periglandular infiltrate
- Granulomatous: mononuclear infiltrate with perivascular, eccrinotropic and neurotropic distribution associated with noncaseating granulomas
Contributed by Roberto N. Miranda, M.D.
- Activate T helper phenotype (Semin Diagn Pathol 2017;34:22)
- Usually CD8 negative (Semin Diagn Pathol 2017;34:22)
- Variable loss of pan T cell antigens (Semin Diagn Pathol 2017;34:22)
| Type of LyP | Reference | CD2 | CD3 | CD4 | CD5 | CD7 | CD8 | CD30 | Other markers |
| Type A | Blood 2019;133:1703 | +/- | + | + | +/- | +/- | - | + | TIA1+ |
| Type B | Blood 2019;133:1703 | +/- | + | + | +/- | +/- | - | - | TIA1+ |
| Type C | Blood 2019;133:1703 | +/- | + | + | +/- | +/- | - | + | TIA1+ |
| Type D | Am J Surg Pathol 2010;34:1168 | + | + | - | - | - | + | + | TIA1+, βF1+, CD56-, EBER- |
| Type E | Am J Surg Pathol 2013;37:1 | + | + | -/+ | + | +/- | + | + | CD45RA-, CD45RO+/-, TIA1+, βF1+, EBER- |
| LyP with DUSP22-IRF4 rearrangement | Am J Surg Pathol 2013;37:1173 | +/- | + | - | +/- | +/- | +/- | + | CD15+, TIA1-, Ki67 (> 80%), TCR-β+ |
| Folliculotropic LyP | J Am Acad Dermatol 2013;68:809 | + | + | + | +/- | - | - | + | |
| Granulomatous LyP | Am J Clin Pathol 2003;119:731 | + | + | + | + | - | - | + |
- Monoclonal rearrangement of the T cell receptor (TCR) is usually detected (Semin Diagn Pathol 2017;34:22)
- Recurrent NPM-TYK2 gene fusion induces activation of STAT signaling pathway (Blood 2014;124:3768)
- DUSP22-IRF4 rearrangement cases have characteristic features (Am J Surg Pathol 2013;37:1173)
- 6p25.3 translocation
- More common in older patients
- Localized lesions and clinical presentation suggesting benign inflammatory dermatoses or epithelial tumors
- Histologically has a bimodal pattern, with epidermotropic cells appearing small and uniform while dermal cells are large and CD30+
- Skin of left ear, excisional biopsy:
- CD30 positive T cell lymphoproliferative disorder, with extensive ulceration and necrosis, most consistent with lymphomatoid papulosis (see comment)
- Comment: According to outside pathology report, the patient has a history of left ear abscess. No other clinical history is available at this time.
One routinely stained slide shows four sections of squamous lined tissue with underlying lymphoid neoplasm and minimal remnants of skin that includes sebaceous glands and hair follicle. There is extensive ulceration and a dense diffuse infiltrate of large cells with vesicular nuclei, irregular nuclear outlines and occasional prominent nucleolus. Few mitotic figures are noted. Extensive coagulative necrosis, as well as suppurative necrosis is noted. Rare areas show perivascular viable cells surrounding by extensive necrosis.
The immunohistochemical studies reveal the large neoplastic cells are positive for CD2, CD3, CD4, CD5, CD30 and a subset were positive for CD117 and TIA1. The aberrant cells are negative for CD10, CD20, ALK-1, PAX-5, cytokeratin, CD7, CD8, CD56, ALK and EBER.
The features of this lesion are consistent with primary cutaneous CD30 positive T cell lymphoproliferative disorder, that encompasses lymphomatoid papulosis and cutaneous anaplastic large cell lymphoma. The final diagnosis of this relies on the clinical history. The differential diagnosis includes peripheral T cell lymphoma or ALK negative anaplastic large cell lymphoma with cutaneous involvement or transformation of mycosis fungoides. To exclude these possibilities, clinical correlation and staging studies are recommended.
| LyP Type A | Primary cutaneous anaplastic large cell lymphoma | |
| Reference | Blood 2019;133:1703 | Am J Dermatopathol 2017;39:877 |
| Age | Fifth decade | Seventh decade |
| Gender (M:F) | 2 - 3:1 | 2 - 3:1 |
| Clinical Features | Papular, papulonodular or nodular, < 2 cm | Localized nodule or papule, usually > 2 cm |
| Microscopy | Wedge shaped and large lymphoid infiltrate with neutrophils, eosinophils and histiocytes | Diffuse and uniform dermal infiltrate of anaplastic large cells |
| Immunophenotype | CD3+, CD4+, CD8-, CD30+ | CD3+/-, CD4+, CD8-, CD30+ |
| Treatment | None for spontaneous regression; symptomatic treatment for relief | Excision, radiation or chemotherapy, alone or combined |
| Outcomes | Excellent | Excellent |
| LyP Type B | Early stage mycosis fungoides | |
| Reference | Blood 2019;133:1703 | An Bras Dermatol 2018\;93:546 |
| Age | Fifth decade | Sixth decade |
| Gender (M:F) | 2 - 3:1 | 5:4 |
| Clinical Features | Papular, papulonodular or nodular | Patches and plaques |
| Microscopy | Epidermotropism and band-like distribution of small / medium atypical lymphocytes with cerebriform nuclei (MF-like) | Cerebriform cells with epidermotropism, predominate along basal layer of epidermis |
| Immunophenotype | CD4+, CD8-, CD30- | CD4+, CD7-, CD8-, CD30- |
| Treatment | Spontaneous regression or symptomatic treatment | Ultraviolet light |
| Outcomes | Excellent | Good |
| LyP Type C | Primary cutaneous anaplastic large cell lymphoma | |
| Reference | Blood 2019;133:1703 | Am J Dermatopathol 2017;39:877 |
| Age | Fifth decade | Seventh decade |
| Gender (M:F) | 2 - 3:1 | 2 - 3:1 |
| Clinical Features | Papular, papulonodular or nodular; < 2 cm | Localized nodule or papule, > 2 cm |
| Microscopy | Sheets of large lymphocytes with or without epidermotropism and few admixed inflammatory cells | Diffuse dermal infiltrate of anaplastic morphology |
| Immunophenotype | CD4+, CD8-, CD30+ (uneven) | CD3+/-, CD4+, CD8-, CD30+ (uniform) |
| Treatment | Spontaneous regression or symptomatic treatment | Radiation or chemotherapy, alone or combined |
| Outcomes | Excellent | Good |
| LyP Type D | Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma | |
| Reference | Am J Surg Pathol 2010;34:1168 | Mod Pathol 2017;30:761 |
| Age | Third decade | Fourth decade |
| Gender (M:F) | 6:3 | 5:2 |
| Clinical Features | Papules and small nodules | Ulcerative patches or plaques |
| Microscopy | Epidermotropism with pagetoid reticulosis-like | Small to intermediate size lymphocytes with epidermotropism |
| Immunophenotype | CD2+, CD3+, CD4-, CD8+, CD30+, TIA1+ | CD2-, CD3+, CD7+, CD8+, CD30-, CD56- |
| Treatment | Spontaneous regression or symptomatic treatment | Chemotherapy, stem cell transplant |
| Outcomes | Excellent | Poor |
| LyP Type E | Extranodal NK/T cell lymphoma, nasal type | |
| Reference | Am J Surg Pathol 2013;37:1 | Blood 2019;133:1703, Curr Hematol Malig Rep 2016;11:514 |
| Age | Sixth decade | Fifth and sixth decade |
| Gender (M:F) | 3:1 | 2:1 |
| Clinical Features | Recurrent papular lesions with rapid progression to hemorrhagic necrotic ulcers | Necrotic lesions |
| Microscopy | Angiocentric and angiodestructive pleomorphic lymphoid infiltrate of small / medium size | Atypical lymphocytes; angiocentric and angiodestructive in most cases |
| Immunophenotype | CD2+, CD3+, CD4-/+, CD8+, CD30+, TIA1+ | CD3-, CD4-, CD5-, CD8-, CD30+, CD56+, TIA1+, EBER+ |
| Treatment | Spontaneous regression or symptomatic treatment | Progressive disease |
| Outcomes | Excellent | Poor |
| LyP with DUSP22-IRF4 rearrangement | Transformed mycosis fungoides | |
| Reference | Am J Surg Pathol 2013;37:1173 | Pathology 2014;46:610 |
| Age | Eighth decade | Seventh decade |
| Gender (M:F) | 9:2 | 1.1:1 |
| Clinical Features | One or multiple eruptive and papulonodular lesions in a single body area | Patches, plaques and tumor |
| Microscopy | Biphasic growth pattern and epidermotropism and periadnexal small to medium size cerebriform cells | Cerebriform with increased large cells in dermis |
| Immunophenotype | CD3+, CD4-, CD8+/- | CD3+, CD4-, CD7-, CD8-, CD30+/- |
| Treatment | Spontaneous regression or symptomatic treatment | Radiation, chemotherapy |
| Outcomes | Excellent | Poor |
| Folliculotropic LyP | Folliculitis | |
| Reference | J Am Acad Dermatol 2013;68:809 | Folliculitis |
| Age | Sixth decade | Variable |
| Gender (M:F) | 9:2 | Variable |
| Clinical Features | Follicular pustules | Superficial folliculitis |
| Microscopy | Perifollicular infiltrate of atypical lymphocytes and follicular mucinosis | Moderate mixed inflammatory cells in the follicular ostium |
| Immunophenotype | CD3+, CD4+, CD30+ | Nonclonal |
| Treatment | Spontaneous regression | Topical treatment |
| Outcomes | Excellent | Excellent |
| Granulomatous LyP | Discoid lupus erythematous | |
| Reference | Am J Clin Pathol 2003;119:731 | Arch Dermatol 2009;145:249 |
| Age | Fifth decade | Fifth decade |
| Gender (M:F) | 5:4 | 1:2 |
| Clinical Features | Nodules | Discoid lesions |
| Microscopy | Noncaseating granulomas associated with mononuclear infiltrate with perivascular, eccrinotropic and neurotropic distribution | Edema and a mild infiltrate of inflammatory cells (lymphocytes) in upper dermis |
| Immunophenotype | CD3+, CD4+, CD5-, CD7-, CD8-, CD30+ | CD3+, CD4+; no loss of T cell antigens |
| Treatment | Spontaneous regression | Systemic agents, Phototherapy |
| Outcomes | Excellent | Excellent |
- ETV6-ABL
- EML4-ALK
- DUSP22-IRF4
- NPM-TYK2
- Type A and B
- Type B and C
- Type C and D
- Type D and E
- Benign pigmented lesion composed of melanocytes and keratinocytes
- Best regarded as a variant of seborrheic keratosis
- Oral melanoacanthoma or melanoacanthosis is clinically distinct from cutaneous melanoacanthoma
- Oral melanoacanthoma is likely reactive, possibly a form of postinflammatory hypermelanosis, and not a tumor-like proliferation
- It is not discussed as part of this topic
- 58 year old woman with multifocal cutaneous melanoacanthoma with ulceration (Indian J Dermatol Venereol Leprol 2011;77:699)
- 65 year old man with giant melanoacanthoma mimicking melanoma (Indian J Dermatol 2011;56:79)
- Pigmented plaque, papule or nodule with dull surface
- Usually solitary and slow growing lesion on head and neck or trunk of older individuals
- Can clinically mimic a seborrheic keratosis or melanoma
- Large variants have been described, up to 3 cm or more
- Resembles a seborrheic keratosis with acanthotic or slightly verrucous epidermis containing small cuboidal keratinocytes and numerous dendritic melanocytes
- The dendritic melanocytes are heavily pigmented with abundant melanin granules
- Most melanin pigment is contained within the dendritic melanocytes with little transfer to adjacent keratinocytes
- Dendritic melanocytes express usual markers of melanocytic differentiation (i.e. S100, HMB45, MelanA)
- Often has overlying compact eosinophilic parakeratosis even when not irritated
- No significant cytologic atypia present
- Composed of benign keratinocytes and dendritic melanocytes
- Incomplete transfer of pigment from melanocytes to keratinocytes, normal population of Langerhan cells (J Cutan Pathol 1978;5:127)
- Melanoma:
- While the dendritic melanocytes in melanoacanthoma might be confused for intraepidermal spread of melanocytes, the melanocytes lack atypia and are part of a background keratinocytic proliferation
- Pigmented hidroacanthoma / poroma:
- Contains discrete smooth bordered intraepidermal cellular aggregates with ductal differentiation
- Melanin pigmentation not restricted to pigmented melanocytes
- Pigmented squamous cell carcinoma in situ:
- Full thickness intraepidermal keratinocytic atypia with mitoses and pigment in keratinocytes
- Seborrheic keratosis:
- Melanoacanthoma is a variant of seborrheic keratosis so the distinction is not critical
- Some might sign out melanoacanthoma as seborrheic keratosis, or might use melanoacanthoma with the additional descriptor of 'benign variant of seborrheic keratosis with prominent dendritic melanocytes'
- Scalp nodule that often arises during infancy containing meningothelial cells; may be diagnosed later in life
- Also called rudimentary meningocele or hamartoma of scalp with ectopic meningothelial elements
- Related to meningioma of skin
- 9 year old girl with scalp lesion (Pediatr Dermatol 2011;28:677)
- 78 year old man with scalp lesion (Eur J Dermatol 2011;21:255)
- Whorls or dissecting pattern of meningothelial cells in dermis and subcutis
- Often psammoma bodies and cartilage
- Center of lesion may have long cleft
- Adipose tissue, blood vessels, nerves admixed with lesion
- Merkel cell carcinoma (MCC) is an uncommon and highly aggressive primary cutaneous neuroendocrine carcinoma
- Merkel cell carcinoma is a highly aggressive primary cutaneous neuroendocrine carcinoma primarily affecting elderly and immunosuppressed individuals
- Diagnosis requires microscopic evaluation as the clinical appearance is nonspecific and can mimic a variety of benign and malignant skin lesions
- There is emerging evidence of distinct Merkel cell polyomavirus associated and UV mediated oncogenetic pathways
- Distinction between primary cutaneous Merkel cell carcinoma and metastatic neuroendocrine carcinoma in the skin requires immunohistochemical and clinical pathologic correlation
- Originally described as trabecular carcinoma by Toker in 1972
- Primarily affects elderly Caucasians, seventh decade and older (J Am Acad Dermatol 2018;78:457)
- Rising incidence due to aging population and improved recognition (J Am Acad Dermatol 2018;78:457, Nat Rev Dis Primers 2017;3:17077)
- M > F (J Am Acad Dermatol 2018;78:457)
- Sun exposed skin: head and neck > extremities > trunk (J Cutan Pathol 2010;37:20)
- Emerging evidence of distinct oncogenetic pathways: majority of cases (up to ~80%) are associated with Merkel cell polyomavirus while minority are UV mediated (Eur J Cancer 2017;71:53)
- Risk factors: advanced age, chronic sun exposure, fair skin, immune suppression (e.g. organ transplantation, HIV infection, chronic lymphocytic leukemia, autoimmunity) (Head Neck Pathol 2018;12:31)
- Painless and rapidly growing flesh colored or red-violaceous nodule
- AEIOU acronym for clinical characteristics (J Am Acad Dermatol 2008;58:375):
- Asymptomatic / lack of tenderness
- Expanding rapidly
- Immune suppression
- Older than age 50
- UV exposed site
- Biopsy or surgical excision
- Distinction between primary cutaneous Merkel cell carcinoma and metastatic neuroendocrine carcinoma in the skin is based on the immunohistochemical profile of the tumor and clinical pathologic correlation (i.e. clinically exclude prior malignancy and potential noncutaneous sources of metastases)
- CT: isoattenuating or hyperattenuating areas in soft tissue
- MRI: enhances with contrast
- Fluorodeoxyglucose PET / CT: avid hypermetabolic activity (AJR Am J Roentgenol 2013;200:1186)
- Factors relevant to staging for Merkel cell carcinoma include tumor size, depth of invasion, locoregional nodal involvement and disseminated metastasis
- Negative clinical prognostic indicators: advanced disease stage at diagnosis (most important), age > 60, male gender, head and neck site, immunosuppression, Merkel cell polyomavirus negative subtype (Curr Opin Oncol 2019;31:72)
- ~60% present with local disease, ~30% with nodal disease and ~10% with distant disease (Ann Surg Oncol 2016;23:3564)
- High mortality
- Rarely, complete spontaneous regression of the tumor can occur (J Cutan Pathol 2016;43:1150)
- 51 year old man with concurrent metastatic Merkel cell carcinoma and cutaneous squamous cell carcinoma in the same lymph node (Am J Dermatopathol 2019;41:e61)
- 54 year old man with primary retroperitoneal Merkel cell carcinoma (Int J Surg Case Rep 2016;19:21)
- 64 and 68 year old men, organ transplant recipients, with Merkel cell carcinoma (JAAD Case Rep 2015;1:S29)
- 65 year old man with primary Merkel cell carcinoma of the parotid gland diagnosed on cytopathology (Cytopathology 2017;28:552)
- 96 year old woman with spontaneous regression (Cutis 2018;101:301)
- Multidisciplinary approach with wide local excision and sentinel lymph node biopsy in clinically node negative patients with or without adjuvant radiotherapy
- Emergence of immune checkpoint blockade therapy, targeting PDL1 / PD1 pathway, for advanced disease (N Engl J Med 2016;374:2542, Lancet Oncol 2016;17:1374)
- Chemotherapy generally ineffective and reserved for palliation
- Single modality radiotherapy for inoperable tumors
- Fleshy to tan-brown lesion with nodular or ill defined silhouette
- Variable ulceration
- Expansile, nodular or diffusely infiltrative tumor within the dermis, variably in subcutis
- Variable mixture of nodules, sheets, nests and trabeculae of neoplastic cells
- Intraepidermal tumor (or component) is occasionally present
- Generally, small round blue cell tumor with high N:C ratio, round / oval nuclei, finely dispersed chromatin (salt and pepper), indistinct nucleoli and scant cytoplasm
- Conspicuous mitoses and apoptotic bodies
- Variable nuclear molding and crush artifact
- Majority of cases display pure neuroendocrine morphology (pure Merkel cell carcinoma)
- Minority of cases feature neuroendocrine and other elements (combined Merkel cell carcinoma) such as divergent differentiation (e.g. squamous, sarcomatoid) or intimate association with other cutaneous neoplasms (most commonly in situ or invasive squamous cell carcinoma)
- Hypercellular specimen featuring small to medium sized neoplastic cells, dispersed and arranged in cohesive, disorganized groups with nuclear molding
- Neoplastic cells display uniform, round / oval nuclei with fine stippled chromatin, inconspicuous nucleoli, scant cytoplasm and high N:C ratio
- Apoptotic bodies, necrotic debris and mitoses are frequent
- Broad spectrum keratins: CAM 5.2, AE1 / AE3 (paranuclear, cytoplasmic or mixed pattern)
- CK20 (classic dot-like paranuclear pattern)
- Chromogranin, synaptophysin, CD56, neuron specific enolase
- Neurofilament (dot-like pattern)
- Variable MCPyV (nuclear pattern)
- Can express PAX5, TdT, BCL2, CD99, FLI1
- Intracytoplasmic membrane bound, dense core neurosecretory granules
- Paranuclear aggregates of keratin filaments
- Divergent genetic profiles for MCPyV+ and MCPyV- tumors
- MCPyV- tumors harbor TP53 and RB1 gene mutations, UV signature mutations and overall higher mutational burden (Oncotarget 2016;7:3403, Cancer Res 2015;75:5228)
- Left temple skin, lesion, shave excision:
- Merkel cell carcinoma (see relevant parameters below)
- Tumor size: ___ cm (maximum clinical tumor diameter; if unavailable use maximum gross or microscopic measurement)
- Depth of involvement (dermis only, involvement of fascia, muscle, cartilage or bone or unclear, due to superficial sampling)
- Morphology (pure or combined)
- MCPyV status (positive or negative)
- Lymphovascular involvement (present or absent)
- Margin status (involved or uninvolved)
- Merkel cell carcinoma (see relevant parameters below)
- Left ear, tumor, wide excision:
- Merkel cell carcinoma (see synoptic report)
- Refer to the International Collaboration on Cancer Reporting (ICCR) Histopathology Reporting Guide (1st Edition, 2019) and CAP reporting guidelines for Merkel cell carcinoma and Merkel cell carcinoma staging
- Basal cell carcinoma:
- Displays budding from epidermal base, peripheral palisading of nuclei, myxoid stroma and peritumoral stromal retraction
- Negative: CK20, MCPyV, neurofilament
- Metastatic neuroendocrine carcinoma:
- May be morphologically indistinguishable
- Positive: variable TTF1, CK7, CDX2, MASH1, PAX8, calcitonin
- Negative: CK20, MCPyV, neurofilament
- Lymphoma / leukemia:
- Small cell melanoma:
- Ewing sarcoma:
- Rare, small round blue cell tumor
- Characteristic EWSR1 translocation
- Negative: CK20, MCPyV
- Caveat: both can express CD99, FLI1, neuron specific enolase
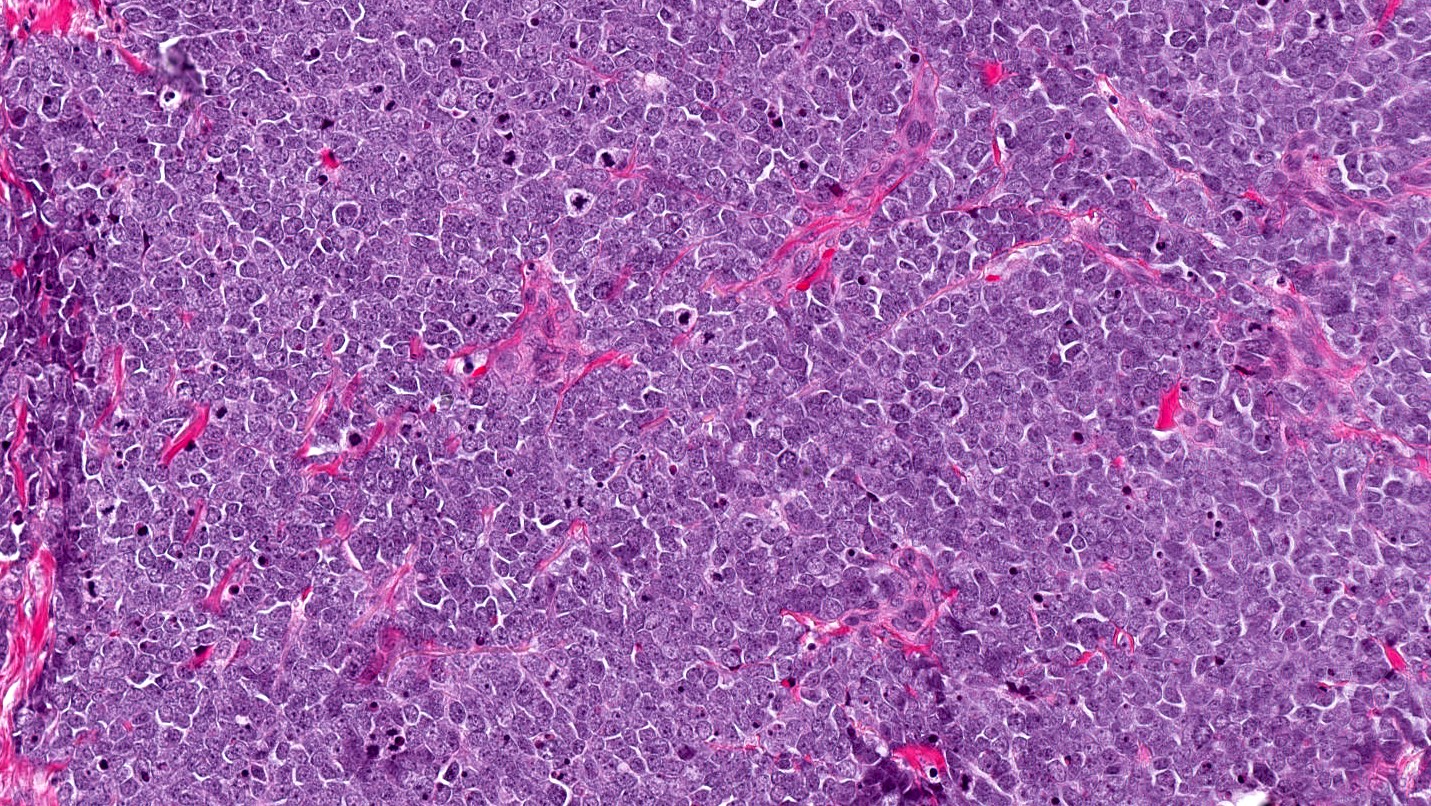
- Clinical course is indolent
- Middle aged females are primarily affected
- Morphological features alone cannot distinguish between primary cutaneous disease and metastasis from a noncutaneous source
- Nuclear pattern of CK20 expression is classic
- Site of predilection is the trunk
Comment Here
Reference: Merkel cell carcinoma
- CD45
- CK7
- CK20
- S100
- TTF1
Comment Here
Reference: Merkel cell carcinoma
- Cutaneous metastases from many internal organ sites or soft tissue sarcomas are uncommon (J Surg Case Rep 2014 Sep 9;2014)
- Men: usually from lung (25%), colon, melanoma, kidney, upper aerodigestive tract
- Women: usually from breast (69%), lung, melanoma, kidney, ovary
- Metastasis is often close to site of primary
- Local recurrence / regional metastasis most commonly occurs upon anterior chest wall
- Scalp is tmost commonly observed distant metastatic site
- 73 year old woman with cutaneous metastases as only sign of extranodal tumor spread (ISRN Surg 2011;2011:902971)
- 83 year old woman with herpetiform cutaneous metastases from transitional cell carcinoma of bladder (J Clin Pathol 2006;59:1331)
- 91 year old woman with seven month history of redness and swelling around her right eye (BMJ 2007;334:1228)
- Treat underlying malignancy, possible excision of metastasis
- Often multiple, firm, nonulcerated nodules, but may be solitary
- Poorly differentiated adenocarcinoma within dermis and often underlying subcutaneous tissue
- Tumor cells in sheets or clusters or as single detached cells
- Either abortive gland formation or "signet ring" cells (with central, cleared mucin-filled space which compresses and marginalizes the cell nucleus)
- Tumor cells may show a "single file" appearance (metastatic lobular breast carcinoma)
- Cytologic atypia in small to large epithelioid cells, often with striking nuclear pleomorphism
- Tumor cells may produce mucin, or mucinous debris may separate collagen bundles
- Variable desmoplasia or sclerosis of dermal collagen
- Immunohistochemical studies are often essential for diagnosis of cutaneous metastasis by breast carcinoma
- Tumor cells are usually positive for CK7, mammoglobin, or GCDFP-15
- May be positive for estrogen receptor (ER), progesterone receptor (PR), and HER2/neu
- Carcinoembryonic antigen (CEA) may highlight gland or signet ring cell lumina
- CK5/6 or p63 may distinguish primary apocrine or eccrine adnexal neoplasms (positive) from metastatic breast adenocarcinoma (generally negative)
- Dermatofibrosarcoma protuberans: may resemble metastatic signet ring cell carcinoma
- Merkel cell carcinoma: resembles neuroendocrine metastases
- Sweat gland tumor: may resemble metastatic renal cell carcinoma
- Microcystic adnexal carcinoma is a rare malignant adnexal tumor with sweat duct and follicular differentiation
- Malignant adnexal carcinoma with sweat duct and follicular differentiation
- Most commonly occurs on the face of elderly White patients
- Histopathology shows deep tumor extension with perineural invasion and may show the presence of lymphoid aggregates
- Tumors may be locally aggressive and Mohs micrographic surgery is the mainstay of treatment
- Sclerosing sweat duct carcinoma
- Malignant syringoma
- Sweat gland carcinoma with syringomatous features
- Locally aggressive adnexal carcinoma
- Reference: Mod Pathol 2008;21:178
- Most common in White patients
- Median age: 68 years old
- Possible associations
- Prior radiation
- Immunosuppressed states
- Ultraviolet (UV) exposure
- References: JAMA Dermatol 2019;155:1059, Am J Clin Oncol 2010;33:125, Dermatol Surg 2000;26:531, Mod Pathol 2020;33:1092, J Cutan Pathol 1999;26:48, Mil Med 2019;184:948
- Left side of the face in U.S. population
- Face, particularly on the lips, perioral, nasolabial, periorbital regions
- Uncommon: axilla, trunk, extremities, genitalia
- References: Arch Dermatol 2000;136:1355, JAMA Dermatol 2019;155:1059
- Mutations
- No signature mutation to date
- TP53 is the most common mutation (22%)
- JAK1 (17%)
- Other oncogenes (JAK2, MAF, MAFB, JUN, FGFR1)
- Individual cases may harbor ultraviolet pattern of mutations
- References: Mod Pathol 2020;33:1092, JAMA Dermatol 2019;155:1059
- Largely unknown at this time
- Some cases associated with prior radiation, both ultraviolet and therapeutic
- References: Mod Pathol 2020;33:1092, JAMA Dermatol 2019;155:1059
- Firm, yellow or flesh colored papule, plaque or nodule
- Mean size at diagnosis: 2.8 cm
- Rarely metastasizes
- Reference: JAMA Dermatol 2019;155:1059
- Skin biopsy that obtains adequate tissue depth (i.e., punch, incisional, excisional) (JAMA Dermatol 2019;155:1059)
- Proposed adverse prognostic factors (Dermatol Surg 2004;30:957, J Am Acad Dermatol 2018;79:756)
- Perineural invasion
- Regional lymph node metastasis
- Visceral metastasis
- Tumor recurrence
- 46 year old woman with microcystic adnexal carcinoma of the left upper eyelid (Medicine (Baltimore) 2023;102:e34709)
- 54 year old woman with a medical history of liver transplantation (JAAD Case Rep 2020;10:126)
- 55 year old man with microcystic adnexal carcinoma of the right heel (Ann Dermatol 2023;35:S215)
- 83 year old man with microcystic adnexal carcinoma colliding with squamous cell carcinoma (JAAD Case Rep 2020;6:479)
- 83 year old woman with microcystic adnexal carcinoma treated with radiation therapy (SAGE Open Med Case Rep 2020;8:2050313X20953114)
- 86 year old woman with microcystic adnexal carcinoma of the vulvar region (JAAD Case Rep 2023;38:72)
- Mohs micrographic surgery
- Radiation therapy can be considered when surgery is not feasible
- Imaging is not routinely recommended
- References: JAMA Dermatol 2019;155:1059, Arch Dermatol 2000;136:1355, Cancer Radiother 2023;27:349
- Features of both eccrine and follicular differentiation
- Poorly circumscribed and deeply infiltrating
- Extension into the subcutaneous adipose tissue and skeletal muscle
- Superficial pseudohorn cysts containing lamellar keratin
- Small aggregates of epithelioid cells with curved and angulated shapes, sometimes referred to as having a tadpole-like morphology
- Deeper components typically have smaller tumor aggregates and can be a single cell layer thick
- Some islands of tumor cells will show ductal differentiation with luminal centers lined by a pink cuticle
- Dense fibrous stroma consisting of thick collagen bundles that surround the tumor aggregates
- Mild cytologic atypia with often bland appearing cells characterized by monomorphic nuclei and scant cytoplasm
- Lymphoid aggregates adjacent to or in association with tumor
- Incidental calcifications can be present
- Mitotic figures are often absent
- Perineural invasion is a common feature
- References: Mod Pathol 2008;21:178, Mod Pathol 2006;19:S93
Microcystic adnexal carcinoma by Dr. Jerad Gardner
- Skin, left cheek, punch biopsy:
- Microcystic adnexal carcinoma (see comment)
- Comment: The sections reveal a deeply infiltrating carcinoma with ductal and follicular differentiation. There are surrounding lymphoid aggregates and focal perineural invasion.
- Desmoplastic trichoepithelioma:
- Not deeply invasive
- Central dell
- Rare reports of perineural invasion (J Cutan Pathol 2012;39:317)
- CK20 positive Merkel cells retained (J Cutan Pathol 2008;35:174)
- Median age: 52 years (J Am Acad Dermatol 2010;62:102)
- CK19 negative (22 - 57%)
- Morpheaform basal cell carcinoma (J Clin Pathol 2007;60:145):
- Syringoma (J Clin Pathol 2007;60:145):
- Lacks horn cysts
- Clear cell variant
- Not deeply invasive
- No perineural invasion
- Typically located on eyelids (unless eruptive)
Comment Here
Reference: Microcystic adnexal carcinoma
- Angiolymphatic invasion
- Distant organ metastasis
- Lymph node metastasis
- Perineural invasion
Comment Here
Reference: Microcystic adnexal carcinoma
- Depth of invasion
- Presence of ductal differentiation
- Presence of follicular differentiation
- Sclerotic stroma
Comment Here
Reference: Microcystic adnexal carcinoma
- Mucoepidermoid carcinoma
- Very rare in skin (~30 cases reported)
- Probable sweat gland origin
- Resembles similar tumor of salivary gland
- Usually low to intermediate grade, some higher grade tumors perhaps better classified as adenosquamous carcinoma
- Adenosquamous carcinoma
- Adenosquamous carcinoma (ASC) is rare malignancy of squamous and glandular differentiation
- Usually men with lesions on face, scalp or upper extremities (Arch Dermatol 2009;145:1152)
- Aggressive behavior (Oncol Lett 2014;7:1941)
- Tumor thickness, perineural invasion and patient immunosuppression are associated with more aggressive local disease (Arch Dermatol 2009;145:1152)
- Adenosquamous carcinoma
- Frequent confusion in the literature regarding this entity in the head and neck and high grade mucoepidermoid carcinoma (Int J Clin Exp Pathol 2014;7:1809)
- More common in organs where adenocarcinoma arises frequently, including stomach, intestines and uterus (Oncol Lett 2014;7:1941)
- Adenosquamous carcinoma
- Although its pathogenesis is largely unknown, 4 hypotheses have been proposed:
- Malignant transformation of both squamous and glandular-like cells originating from pleiotropic epithelial stem cells
- Tumorigenesis of squamous metaplasia in columnar epithelium
- Transdifferentiation of adenocarcinoma to squamous cell carcinoma
- Coexistence of both carcinomas (World J Surg Oncol 2013;11:124)
- Although its pathogenesis is largely unknown, 4 hypotheses have been proposed:
- Adenosquamous carcinoma
- Neoplasm composed of an admixture or separate areas of squamous cell carcinoma and adenocarcinoma
- Criteria for squamous cell carcinoma component are 2 or more of these features:
- Intercellular bridging
- Keratin pearl formation
- Parakeratotic differentiation
- Individual cell keratinization
- Cellular arrangement showing a pavementing or mosaic pattern
- Criterion for adenocarcinoma component is demonstration of intracytoplasmic mucin
- World Health Organization Classification does not require intracytoplasmic mucin for diagnosis of adenocarcinoma in the presence of true glandular formation (Int J Clin Exp Pathol 2014;7:1809)
- Mucoepidermoid carcinoma
- 66 year old man with ear tumor (J Cutan Pathol 1991;18:56)
- 72 year old man with tumor arising within nevus sebaceus of Jadassohn on forehead (J Cutan Pathol 2003;30:652)
- 76 and 79 year old men (Int J Surg Pathol 2015;23:161, Am J Surg Pathol 2005;29:131) with tumors of cheek and axilla
- 81 year old man with tumor infiltrating parotid gland (Eur Rev Med Pharmacol Sci 2012;16:26)
- Adenosquamous carcinoma
- 71 year old woman with adenosquamous carcinoma of tongue (Int J Clin Exp Pathol 2014;7:1809)
- 76 year old woman with adenosquamous carcinoma of conjunctiva (Oncol Lett 2014;7:1941)
- Adenosquamous carcinoma
- Surgical excision or Mohs microsurgery are common treatment options (Head Neck Pathol 2011;5:108)
- Locoregional recurrence is not uncommon
- Mucoepidermoid carcinoma
- Up to 0.6 cm, ulcerated and nonencapsulated
- Flesh colored nodules, painless
- Adenosquamous carcinoma
- White nodular infiltrate into subcutaneous tissue
- Mucoepidermoid carcinoma
- Circumscribed tumor, may not be attached to surface
- Multilobulated nodulocystic tumor extending throughout dermis, exhibiting glandular and squamoid differentiation
- Dermal lobules or cystic growth of low grade epidermoid, intermediate, mucinous cells and clear cells
- Cribiform nests of epidermoid cells contain glandular spaces with mucin
- Nuclei are mildly atypical and contain scattered mitotic figures
- Peritumoral fibrosis is common
- May have focal perineural invasion
- Adenosquamous carcinoma
- Infiltrative islands of squamous cell carcinoma with admixed mucin containing glandular structures, adenomatous changes and acinar formation
- Glandular structures lined by low columnar epithelium, sometimes lined by an eosinophilic cuticle (ductular differentiation)
- Perineural invasion relatively common (Arch Dermatol 2009;145:1152)
- Mucoepidermoid carcinoma
- Adenosquamous carcinoma
- CK7, CEA and CA19-9 in adenocarcinoma component
- Alcian blue (pH 2.5), mucicarmine or PAS will identify the epithelial mucin
- p63 and p40 in squamous component (Int J Clin Exp Pathol 2014;7:1809)
- Mucoepidermoid carcinoma
- CRTC1 rearrangements have been detected in cutaneous MEC (like salivary gland MEC) but translocation t(11,19) or MAML2 rearrangements not seen (unlike salivary gland MEC) (Br J Dermatol 2009;161:925)
- Adenosquamous carcinoma:
- High grade tumor, often involves epidermis, adenocarcinoma component is well differentiated
- Metastatic salivary gland tumor:
- Usually high grade
- Mucinous metaplasia
Adenosquamous carcinoma
- Adenocarcinoma (primary versus metastatic)
- Acantholytic squamous cell carcinoma
- Mucoepidermoid carcinoma
- Rare disorder of women ages 40 - 50, with widespread cutaneous papules and nodules (eMedicine)
- Often associated with a destructive arthritis and internal malignancy
- Tumor cells are histiocytes and multinucleated giant cells containing abundant eosinophilic cytoplasm with a "ground glass" appearance
- Formerly called lipoid dermatoarthritis
- Usually women 40 - 50 years
- Histiocytic origin (Am J Surg Pathol 1990;14:687)
- Skin lesions on the hands, especially at the base of the nails
- Lesions may also be on the face, ears, arms, scalp or mucosal surfaces
- "Coral beads" and vermicular erythematous lesions bordering nostrils are pathognomonic (J Eur Acad Dermatol Venereol 2001;15:524)
- Lesions vary from small papules to lesions several centimeters across, and are usually skin colored, yellow or reddish brown
- Recommended to screen patients for malignancy (Rheumatology 2008;47:1102), since accompanied by neoplasm in 28% of cases
- May be a paraneoplastic process (J Am Acad Dermatol 1998;39:864), or association with neoplasm may be due to reporting bias (eMedicine)
- Associated with destructive arthritis
- 6 year old girl (J Rheumatol 1998;25:794)
- 33 year old woman with generalized systemic involvement (Clin Exp Dermatol 2004;29:373)
- 34 year old woman with papular lesions on hands and face (Case of the Week #153)
- 61 year old man with associated liver carcinoma (Case Rep Dermatol 2012;4:163)
- Relapse of multicentric reticulohistiocytosis before relapse of associated neoplasm (Med Pediatr Oncol 1985;13:273)
- No consistently reliable treatment (Ryumachi 1993;33:68)
- TNF inhibitors (Arch Dermatol 2008;144:1360), aminobisphosphonates (Arthritis Rheum 2003;48:3538) and immunosuppressive drugs (Dermatol Online J 2009;15:2) have been effective only in individual cases
- Prominent oncocytic histiocytes and multinucleated giant cells with eosinophilic, “ground glass” cytoplasm
- Solitary reticulohistiocytoma: younger age, solitary lesions usually not on digits or face (Am J Surg Pathol 2006;30:521)
- Epithelioid fibrous histiocytoma: usually < 1 cm on extremities, usually no giant cells, primarily myofibroblastic, not histiocytic
- Epithelioid sarcoma: deep seated tumor with markedly atypical cells that form granuloma-like clusters with central necrosis; tumor cells are EMA+, keratin+, CD68-
- Granulomatous inflammation: well formed granulomas and prominent lymphocytes, no large epithelioid histiocytes with eosinophilic glassy cytoplasm
- Histiocytic sarcoma: typically forms a large mass of epithelioid histiocytes with significant nuclear atypia and mitotic activity
- Juvenile xanthogranuloma: usually children, has scattered Touton type histiocytic giant cells and numerous eosinophils, but large epithelioid histiocytes are not prominent
- Rosai-Dorfman disease: associated with adenopathy; histiocytes are pleomorphic and S100+
- Uncommon cutaneous lesion
- Vascular and fibrohistiocytic lineage are hypothesized
- Characterized by odd multinucleated fibroblasts, superficial fibrosis and thickening of superficial papillary dermal vessels
- Presence of odd multinucleated fibroblasts
- Presence of superficial parallel fibrosis
- Presence and thickening of superficial papillary dermal vessels
- Absence of perifollicular fibrosis
- M = F according to the largest series with histopathological review (J Cutan Pathol 2019;46:563)
- But F > M according to prior literature review (Am J Dermatopathol 2015;37:222)
- Mean age 56 years for both sexes (J Cutan Pathol 2019;46:563)
- 2 cases associated with chronic hepatitis B and C (J Cutan Pathol 2019;46:563, J Cutan Pathol 2019;46:678)
- Certain authors postulate that MCAH-like changes can exist, although not as a distinct solitary papule clinically and more as a focal histologic finding aside or within another dermatologic process (Am J Dermatopathol 2010;32:415)
- Generalized form may be associated with systemic disease or abnormal immune states (J Cutan Pathol 2017;44:125)
- Dorsal hands or fingers most frequent; when multiple lesions are found, they are most likely to affect the hands or fingers (J Cutan Pathol 2019;46:563)
- Lower extremities
- Trunk or back
- Head and neck (rare, most often these are fibrous papules with multinucleated stromal cells, not multinucleate cell angiohistiocytoma)
- Currently unknown
- Role for increased mast cells had been postulated but when mast cell counts were compared with counts of normal skin, no difference was found (J Cutan Pathol 2019;46:563)
- Role for fibroblasts, given the increased intralesional elastic fibers in generalized multinucleate cell angiohistiocytoma, has been postulated (J Dermatol 2021;48:114)
- Role for estrogen receptor alpha overexpression has been proposed (Am J Dermatopathol 2010;32:655)
- Unknown
- Dull red papules and nodules
- Lesions may be single, multiple or generalized (rare)
- Reference: J Cutan Pathol 2019;46:563
- Made on H&E stain with light microscopy in conjunction with clinical findings
- Benign
- May recur (Am J Dermatopathol 2010;32:655)
- 28 year old woman with congenital chronic hepatitis B with multinucleate cell angiohistiocytoma and with cutaneous plasmacytosis (J Cutan Pathol 2019;46:678)
- 42 year old woman with generalized multinucleate cell angiohistiocytoma (J Cutan Pathol 2017;44:125)
- 42 year old man with generalized multinucleate cell angiohistiocytoma with involvement of palms and soles (Indian J Dermatol Venereol Leprol 2018;84:468)
- 42 year old man with Kaposi sarcoma-like multinucleate cell angiohistiocytoma complicating an iatrogenic arteriovenous fistula (Eur J Dermatol 2010;20:642)
- No standard first line therapy; without treatment, course is indolent and progressive and spontaneous remission is rare
- Numerous treatment modalities have shown success:
- Intralesional corticosteroids (An Bras Dermatol 2020;95:480)
- Surgical excision (An Bras Dermatol 2020;95:480)
- Potassium-titanyl-phosphate laser in combination with intralesional corticosteroids (JAAD Case Rep 2019;5:880)
- Fractionated ablative carbon dioxide (CO2) laser (JAAD Case Rep 2019;5:297)
- Pulsed dye laser (Clin Exp Dermatol 2016;41:312)
- Intense pulsed light (Dermatol Surg 2009;35:1141)
- Argon laser (Br J Dermatol 1995;133:308)
- Presence of odd multinucleated, stellate fibroblasts with stretched out cytoplasmic extensions; multinucleated cells may be scant and may require additional tissue levels (Dermatol Online J 2009;15:4)
- Presence of superficial parallel fibrosis (J Cutan Pathol 2019;46:563)
- Presence and thickening of superficial papillary dermal vessels (J Cutan Pathol 2019;46:563)
- May show moderately increased number of blood vessels
- Absence of perifollicular fibrosis (found in the fibrous papule of the nose) (J Cutan Pathol 2019;46:563)
- May be acanthotic or flat architectural profile, with generally a normal basket woven stratum corneum (Dermatol Online J 2009;15:4)
- Eosinophils are very rarely encountered (Cutis 2017;100:429)
- Immunohistochemistry is seldom contributory for the diagnosis (J Cutan Pathol 2019;46:563)
- Multinucleated cells: variably CD68, vimentin and factor XIIIa positive (Dermatol Online J 2009;15:4)
- Mast cells, plasma cells and prominent vessels may be highlighted with their respective markers (J Cutan Pathol 2019;46:563)
- Multinucleated cells are generally CD163, CD34 and factor VIII negative (J Cutan Pathol 2019;46:563)
- Skin, left dorsal hand, punch biopsy:
- Multinucleate cell angiohistiocytoma (see comment)
- Comment: Sections show superficial parallel fibrosis, thickened and abundant papillary dermal vessels and stellate multinucleated cells consistent with multinucleate cell angiohistiocytoma.
- Fibrous papule of the nose:
- Can also show prominent superficial papillary dermal vessels and multinucleated cells but the fibrosis is not parallel to the epidermis
- Shows concentric perifollicular fibrosis in most instances, unlike multinucleate cell angiohistiocytoma
- Much more commonly seen on the face / nose (J Cutan Pathol 2019;46:563)
- Dermatofibroma:
- More common on lower extremities
- Atrophic vascular variant of dermatofibroma may mimic multinucleate cell angiohistiocytoma
- Fibrosis in dermatofibroma is more storiform, rather than parallel to the epidermis
- May also show multinucleated cells and factor XIIIa positivity
- Follicular induction and beta catenin positivity in underlying dermal fibroblasts is frequent in dermatofibroma but absent in multinucleate cell angiohistiocytoma (J Cutan Pathol 2019;46:563)
- Telangiectasia macularis eruptive perstans:
- Eosinophils are frequent in the inflammatory infiltrate of telangiectasia macularis eruptive perstans but very rare in multinucleate cell angiohistiocytoma
- Multinucleated cells in telangiectasia macularis eruptive perstans are slightly different, showing < 3 nuclei, contrarily to multinucleate cell angiohistiocytoma
- Mast cell counts are elevated in telangiectasia macularis eruptive perstans compared with multinucleate cell angiohistiocytoma or normal skin (J Cutan Pathol 2019;46:563)
There are multiple red papules on the dorsal hands with multinucleated stromal cells, thickened superficial papillary dermal vessels and superficial dermal fibrosis arrayed in parallel to the epidermis. What is the best diagnosis?
- Dermatofibroma
- Fibrous papule
- Multinucleate cell angiohistiocytoma (MCAH)
- Telangiectasia macularis eruptive perstans (TMEP)
Comment Here
Reference: Multinucleate cell angiohistiocytoma
Comment Here
Reference: Multinucleate cell angiohistiocytoma
- Peripheral T cell lymphoma derived from mature, post-thymic T lymphocytes
- Presents as cutaneous patches and can progress to plaques, tumors and erythroderma
- While most patients experience an indolent course, the lymph nodes, bone marrow and viscera can become involved in advanced stage disease
- Mycosis fungoides (MF) is a clinical diagnosis that requires strong correlation with histopathologic and sometimes molecular findings to exclude benign inflammatory diseases, more aggressive primary cutaneous lymphomas, and extracutaneous lymphomas that can involve the skin
- Conventional MF begins as eczematoid or psoriasiform patches and plaques that arise in a "bathing trunk" distribution
- MF often behaves as an indolent lymphoma with excellent overall survival; however, a minority of patients experience disease progression with fungating tumors, erythroderma and extracutaneous spread
- Biopsies from developed patches and plaques of MF show band-like papillary dermal lymphoid infiltrates with background fibroplasia, lymphocytes tagging the junction and migrating to the epidermis as single cells and Pautrier microabscesses, lymphoid cytologic atypia and an absence of findings that would otherwise suggest a spongiotic, psoriasiform or interface dermatitis; there are many histologic variants
- Immunohistochemistry is generally more useful to exclude other lymphomas than to confirm a diagnosis of MF
- Clonality testing can sometimes solidify a diagnosis when findings from pairs of temporally or anatomically separate samples are compared together
- Mycosis fungoides (MF)
- Cutaneous T cell lymphoma
- Higher incidence among men than women
- Median age at diagnosis in 50s
- Wide age range, predominantly older adults
- Children more likely to have the hypopigmented variant
- Photoprotected "bathing trunk" distribution involving the buttock, trunk and proximal limbs is found in most cases; however, mycosis fungoides can arise anywhere on the body
- Pathophysiology is incompletely understood due to the clinical and immunophenotypic heterogeneity of this entity
- Cells of origin are skin honing, effector memory T cells in contrast with the central memory T cell phenotype encountered in Sézary syndrome
- In skin limited disease, the cells most often show a tissue resident memory T cell phenotype and less frequently a migratory memory T cell phenotype (Sci Transl Med 2015;7:308ra158)
- Immunological milieu of mycosis fungoides (MF) is enhanced for Th2 gene expression and Th2 associated cytokine production (Am J Hematol 2016;91:151)
- NFkB has been associated with B cell lymphomagenesis and is constitutively activated in MF (Am J Hematol 2016;91:151)
- STAT activation, cyclin upregulation and loss of RB1 have been identified in some MF cohorts (Am J Hematol 2016;91:151)
- Cytogenetic and comparative genomic hybridization have demonstrated loss of 9p21 (including the CDKN2a - CDKN2B locus) in some cases of large cell MF and tumor stage MF (Am J Hematol 2016;91:151)
- Recurrent chromosomal translocations are rare in comparison with B cell lymphomas (Am J Hematol 2016;91:151)
- Must exclude HTLV1 infection because some cases of adult T cell leukemia / lymphoma closely mimic mycosis fungoides (MF) at presentation
- Human leukocyte antigen (HLA) type associations and rare familial cases suggest genetic predisposition in some patients
- Some medications are associated with the development of T cell dyscrasias that resemble MF and resolve when the offending drug is withdrawn
- Infrequently, drug associated T cell infiltrates persist and behave as MF following agent withdrawal, suggesting that some medications can actually induce MF
- Must avoid overdiagnosis if equivocal findings, but underdiagnosis may lead to treatments that suppress antitumor immunity and foster disease development
- Can mimic spongiotic or psoriasiform dermatitis, wax and wane and elude a definitive diagnosis for years to decades
- Begins as a skin limited disease
- Classic patches are erythematous and heterogeneous in size and shape with fine scale and variable atrophy
- Increased risk of other malignancies including synchronous lymphoma
- Usually indolent, but may progress to infiltrative plaques, tumors and erythroderma reminiscent of Sézary syndrome
- Lymph node involvement, visceral involvement and rarely bone marrow involvement can occur with disease progression
- Advanced stage disease is associated with loss of T cell repertoire causing infection and death
- Variants include poikilodermatous, hypopigmented, granulomatous, folliculotropic, syringotropic and palmoplantar mycosis fungoides
- Mycosis fungoides (MF) is a clinical diagnosis and a diagnosis of exclusion, using clinical, histologic and molecular data
- Must exclude inflammatory dermatitis (in particular spongiotic, psoriasiform and lichenoid diseases),drug induced reactions and dyscrasias, cutaneous dissemination of extracutaneous peripheral T cell lymphoma, indolent cutaneous lymphoproliferative disorder or aggressive primary cutaneous lymphoma
- Elevated lactate dehydrogenase (LDH) is an independent prognostic marker of worse survival
- Smear, flow cytometry and clonality testing can detect involvement in the peripheral blood
- HTLV1 serologic studies may be required to exclude adult T cell leukemia / lymphoma
- Independent prognostic markers of worse survival include clinical stage IV disease, age older than 60 years, large cell transformation and elevated lactate dehydrogenase (LDH) (J Clin Oncol 2015;33:3766)
- T category is based on the percentage of skin surface involvement and the lesional morphology (patchy, plaque, tumor or erythroderma)
- N category is based on the presence of dermatopathic lymphadenopathy, lymphoma cells and evidence of clonality in addition to the extent of nodal involvement by lymphoma
- M category is based on the presence or absence of visceral involvement
- Peripheral blood staging is based on the quantity of abnormal lymphocytes (blood tumor burden) and presence or absence of clonality
- Median survival for stage IA (< 10% skin surface involvement by patches or plaques) is ≥ 20 years
- Median survival beyond stage III (> 80% skin surface confluence / erythroderma) is approximately 5 years
- 33 year old woman with a 7 year history of alopecia (J Cutan Pathol 2016;43:1179)
- 52 year old man with psoriasiform plaques on his palms and soles (Case Rep Dermatol 2009;1:60)
- 52 year old man with a 4 year history of intermittent, symmetrically distributed annular red patches on his trunk and extremities (JAAD Case Rep 2017;3:288)
- An array of treatments and clinical trials exists
- Treatment is tailored to each patient depending on clinical findings, stage, prognosis and disease comorbidities
- Comprehensive information: NIH: Mycosis Fungoides (Including Sézary Syndrome) Treatment (PDQ®) [Accessed 12 February 2018]
- Photodynamic therapy: J Am Acad Dermatol 2016;74:27
- Retinoids: J Am Acad Dermatol 2003;49:801
- Targeted therapies: Lancet 2017;390:555
- Biologic therapies: Blood 2015;125:71
- Radiation therapy: Arch Dermatol 2011;147:561
- Chemotherapies: Blood 2015;125:71
- Transplant: J Clin Oncol 2014;32:3347
- Early lesions are sometimes histologically indistinguishable from more common inflammatory skin diseases
- Band-like papillary dermal lymphoid infiltrate
- Intraepidermal lymphocytes out of proportion with spongiosis (epidermotropism) ± Pautrier microabscesses
- Lymphocytes tagging the junction and within the epidermis may have haloes and can show variable nuclear pleomorphism, nuclear contour irregularity (cerebriform cytomorphology can be difficult to appreciate on biopsies) and hyperchromasia
- Dermal reticular fibroplasia with space between single lymphocytes
- Absences of features that would otherwise suggest a diagnosis of spongiotic dermatitis, drug hypersensitivity reaction, psoriasis or interface dermatitis
- Tumors can show an absence of epidermotropism and can involve the fibroadipose tissue
- Large cell transformation should always be reported when present and is defined as cells ≥ 4x size of a small lymphocyte comprising > 25% of total infiltrate
- In general, immunohistochemistry is more helpful to exclude other lymphomas than to confirm a diagnosis of mycosis fungoides
- Immunophenotype is variable and can change with large cell transformation and stage progression
- Mature T cell phenotype (CD45RO+, TCR β+, CD2+, CD3+, CD4+ [frequent], CD8+ [infrequent], CD5+, CD7+) is most commonly observed
- Loss of CD2 or CD5 favors mycosis fungoides over inflammatory diseases such as eczema and psoriasis
- Partial loss of CD7 is common; however, this equivocal finding is also present in benign dermatoses
- TCR γ staining should raise consideration for gamma delta T cell lymphoma; however, there are clinically annotated cases of mycosis fungoides that have exhibited this immunophenotype
- CD8 and cytotoxic marker (TIA1, granzyme) expression should raise consideration for primary cutaneous CD8+ aggressive epidermotropic T cell lymphoma
- EBER staining of lesional cells should raise consideration for extranodal NK / T cell lymphoma, nasal type
- Clonal rearrangement of the T cell receptor can be helpful if histology is nonspecific and clinical findings are strongly suggestive, but identification of clonality in a single biopsy is considerably less specific than identification of the same clone in multiple biopsies taken at different times or from different sites
- Clones can persist in pityriasis lichenoides spectrum disease and other T cell dyscrasias that do not behave as lymphoma
- Skin, left flank, punch biopsy:
- Epidermotropic T-cell infiltrate, suspicious for mycosis fungoides (see comment)
- Comment: This lesion has Pautrier-type microabscesses comprised of CD4+ T-cells that express TCR-beta and show a loss of CD2 expression. Background features of clinically considered psoriasis are not identified, and a PASd stain is negative for intracorneal fungal elements. No folliculotropism is identified. No evidence of large cell transformation is identified. Correlations with clinical and laboratory findings are essential to confirm the above impression.
- Erythroderma:
- Acute graft versus host disease: subtle interface dermatitis with satellite cell necrosis
- Adult T cell leukemia / lymphoma: distinction often requires correlations with clinical history and serologic studies
- Atopic dermatitis: lymphocyte exocytosis proportionate to the degree of spongiosis; however, intraepidermal edema with eosinophils also can be present in mycosis fungoides so paired clonality studies may be helpful
- Chronic actinic dermatitis: clinical history, paired clonality studies
- Erythrodermic drug reaction: clinical correlation is necessary
- Paraneoplastic erythroderma: clinical correlation is necessary
- Pemphigus: an unusual cause of erythroderma; however, an absence of acantholysis and direct / indirect immunofluorescence findings could exclude this unlikely possibility
- Pityriasis rubra pilaris: clinical correlations can be extremely helpful and additionally, PRP can show alternating ortho and parakeratosis, thickening of suprapapillary plates, follicular plugs and focal acantholysis
- Psoriasis: dilated and tortuous papillary dermal vessels, attenuation of the suprapapillary plates, confluent parakeratotic crust with neutrophils and attenuation of the granular layer are helpful features but close clinical correlations and paired clonality testing are sometimes necessary
- Sézary syndrome: clinical correlations are necessary
- T cell prolymphocytic leukemia: clinical correlations would exclude mycosis fungoides (MF)
- Patch / plaque:
- Adult T cell leukemia / lymphoma: clinical correlations, HTLV1 serology
- Chronic actinic dermatitis: photodistribution should raise doubts about MF; however, paired clonality studies may be necessary in some cases
- Extranodal NK / T cell lymphoma nasal type: EBER+, angiodestructive
- Interface dermatitis: vacuolar degenerative changes, keratinocyte necrosis
- Lichenoid interface dermatitis: colloid body formations
- Mycosis fungoides-like drug reaction: clinical correlations are required
- Pityriasis rubra pilaris: clinical correlations can be extremely helpful and additionally, PRP can show alternating ortho and parakeratosis, thickening of suprapapillary plates, follicular plugs and focal acantholysis
- Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma: ulcerated plaques and tumors; furthermore, histology will show dense epidermotropic infiltrates of enlarged CD8 positive cells filling the epidermis without Pautrier microabscesses
- Primary cutaneous gamma delta T cell lymphoma: violaceous and sometimes ulcerated plaques and tumors comprised of TCR gamma+ lymphocytes
- Some show a predominantly epidermotropic pattern reminiscent of MF
- Another, potentially more aggressive variant shows adipotropism mimicking tumor stage / large cell MF and subcutaneous panniculitis-like T cell lymphoma
- Psoriasis: dilated and tortuous papillary dermal vessels, attenuation of the suprapapillary plates, confluent parakeratotic crust with neutrophils and attenuation of the granular layer are helpful features but close clinical correlations and paired clonality testing are sometimes necessary
- Secondary cutaneous involvement by an extracutaneous peripheral T cell lymphoma: clinical correlations are required
- Secondary syphilis: vacuolar interface changes, conspicuous endothelial swelling and a preponderance of plasma cells; immunohistochemistry or silver stain may highlight treponemes
- Spongiotic dermatitis: lymphocyte exocytosis proportionate to the degree of spongiosis; however, intraepidermal edema with Langerhans cells also can be present in mycosis fungoides so paired clonality studies may be helpful
- T cell prolymphocytic leukemia: clinical correlations would exclude MF
- Dermatophyte: PASd+ hyphae and yeast present in the stratum corneum
- Tumor:
- Lymphomatoid papulosis: clinical correlations (waxing and waning course), diffuse CD30 expression (this can also be seen in large cell MF) and paired clonality testing
- Primary cutaneous anaplastic large cell lymphoma: clinical correlations, diffuse CD30 expression (this can also be seen in large cell MF) and paired clonality testing
- Primary cutaneous CD4+ small / medium sized pleomorphic T cell lymphoproliferative disorder: clinical correlations (solitary lesion with no history of mycosis fungoides), polymorphous T cell infiltrate with T follicular helper immunophenotype (this immunophenotype can also be seen in MF), PD1+ rosettes, low Ki67 expression with positive cells distributed evenly throughout the lesion
- Primary cutaneous gamma delta T cell lymphoma: violaceous and sometimes ulcerated plaques and tumors comprised of TCR gamma+ lymphocytes
- Some show a predominantly epidermotropic pattern reminiscent of MF
- Another, potentially more aggressive variant shows adipotropism mimicking tumor stage / large cell MF and subcutaneous panniculitis-like T cell lymphoma
- Secondary cutaneous involvement by an extracutaneous peripheral T cell lymphoma: clinical correlations are required
- Subcutaneous panniculitis-like T cell lymphoma: clinical correlation can exclude MF; SPTCL can demonstrate epidermotropism but not to the extent of MF, CD8+ phenotype, Ki67 hotspots in the fat comprised of cytotoxic T cells rimming adipocytes
- General mycosis fungoides: Clin Lab Med 2017;37:527, Am J Hematol 2016;91:151, Sci Transl Med 2015;7:308ra158, J Clin Oncol 2015;33:3766, J Cutan Pathol 2001;28:174
- Pediatric mycosis fungoides: Pediatr Dermatol 2017;34:547, Actas Dermosifiliogr 2017;108:564
- Folliculotropic mycosis fungoides: J Am Acad Dermatol 2016;75:347, Arch Dermatol 2008;144:738
- Hypopigmented mycosis fungoides: Int J Dermatol 2018;57:306, J Eur Acad Dermatol Venereol 2017;31:808
- Palmoplantar mycosis fungoides: Arch Dermatol 2007;143:109, Dermatology 2002;205:239
- Biopsy revealing Pautrier microabscesses
- History of cutaneous patches at disease onset
- HTLV1 serology
- Immunohistochemistry with CD25
Comment Here
Reference: Mycosis fungoides
- History of cutaneous patches at disease onset
- Involvement of the bone marrow
- Presence of atypical lymphocytes on peripheral smear
- Presence or absence of epidermotropism from the biopsy
Comment Here
Reference: Mycosis fungoides
- Indolent, T cell cutaneous proliferative disorder related to mycosis fungoides
- Also called Woringer-Kolopp disease; disseminated lesions called Ketron-Goodman disease
- 2:1 male to female incidence
- Usually solitary lesion on distal extremities
- Treatment may include electron beam, pharmacological intervention, psoralen plus ultraviolet A (PUVA) photochemotherapy, radiotherapy, or surgery (J Clin Aesthet Dermatol 2010;3:46)
- Solitary erythematosquamous patch with monomorphic intraepidermal infiltrate of mycosis fungoides-like cells, in Paget's disease type pattern
- Special variants to be added include the WHO-EORTC variants including folliculotropic/adnexotropic MF and granulomatous slack skin syndrome. Rarer variants like pigmented purpura-like etc can be mentioned
- 24 year old woman with slowly enlarging plaque (J Clin Aesthet Dermatol 2010;3:46)
- 84 year old man with 2 year history of erythematous patches (Case Rep Dermatol 2009;1:39)
- Tumors with myoepithelial cells but no epithelial cells (Hum Pathol 2004;35:14)
- Usually benign lesions of extremities, but should be completely excised
- May recur locally, rarely metastasize
- Usually male, mean age 22 years (range 10 - 63 years)
- Part of a continuum with mixed tumors (ductal structures but few myoepithelial cells)
- Mitotic activity may predict more aggressive tumor
- Mean 1 cm, range 0.5 to 2.5 cm
- Well circumscribed dermal lesions, not connected to epidermis, may extend into superficial subcutis
- Either composed of:
- Solid proliferation of ovoid, spindled, histiocytoid or epithelioid cells with abundant eosinophilic syncytial cytoplasm and little stroma; or
- Reticular architecture with epithelioid, plasmacytoid or spindle cells in myxoid or hyalinized stroma
- Cells have ovoid / spindled nuclei, mild pleomorphism, small necrotic areas, fatty metaplasia, minimal mitotic figures (0 - 6 / 10 HPF), no ductal differentiation
- Required for diagnosis by Fletcher: EMA+ or keratin+, S100, GFAP (50%)
- Muscle markers calponin, smooth muscle actin (57%) or muscle specific actin (HHF)
- Benign mixed tumor
- Cellular neurothekeoma: nested architecture, sclerotic dermal collagen, NKI-C3+, S100-, EMA-, keratin-
- Epithelioid benign fibrous histiocytoma: lower limbs, circumscribed, polypoid, plump and often binucleate epithelioid cells, may entrap dermal collagen, keratin-, myogenic markers-, S100-
- Epithelioid sarcoma: distal extremities of young adults, infiltrates along fibrous septa and fascial planes, discontinuous growth, S100-, GFAP-
- Leiomyoma
- Myoepithelial carcinoma
- Spitz nevus: large epithelioid melanocytes with prominent nucleoli, junctional component, downward maturation, HMB45+, S100+, EMA-, keratin-, myogenic markers-
- Superficial tumor, first described in 1980
- Originally, derivation thought to be from nerve sheath; now thought to derive from fibroblasts with ability to differentiate into myofibroblasts and to recruit histiocytes (Am J Surg Pathol 2007;31:1103)
- Usually head, upper extremities or shoulder girdle
- Solitary, superficial, slow growing mass up to 2 cm
- 60% women, mean age 17 years (range 2 - 85 years), 80% are < age 30 at initial diagnosis
- 5 month old boy with thumb swelling (Indian J Dermatol 2009;54:59)
- 19 year old woman with painful subcutaneous nodule on lower back (Dermatol Online J 2009;15:3)
- 66 year old man with painless swelling in eyelid (Indian J Ophthalmol 2008;56:334)
- Excision, may recur
- Cellular, myxoid or mixed subtypes
- Involves dermis or subcutis
- Multinodular mass with myxoid matrix and peripheral fibrosis
- Whorled or focally fascicular patterns of spindled and epithelioid mononuclear cells with abundant cytoplasm, indistinct cell borders
- Margins usually positive; usually occasional multinucleated giant cells
- Variable nuclear atypia
- Median 4 MF / 25 HPF, may have 10+ MF / 25 HPF, may be atypical
- Nodules of mature fat tissue within dermis
- Either solitary or multiple
- Also called nevus lipomatosus cutaneous superficialis and dermolipoma
- Not a WHO diagnosis
- First described in 1921 by Hoffman and Zurhelle
- Considered to be a developmental anomaly or hamartoma
- Uncommon
- At birth or by age 20 years
- Buttocks or upper thighs
- Either solitary (more common) or multiple type of Hoffmann-Zurhelle (Tunis Med 2006;84:800)
- 7 year old girl with congenital lesion of calf (J Postgrad Med 2005;51:47)
- 12 year old girl with neck lesion (Indian J Dermatol Venereol Leprol 2006;72:66)
- 33 year old man with slow growing cutaneous plaque of lumbar region (Patholog Res Int 2011;2011:105973)
- 45 year old man with lower back lesion (Indian J Dermatol Venereol Leprol 1994;60:39)
- 51 year old man with lesion on pinna for 15 years (Dermatol Online J 2010;16:12)
- Excision - does not recur
- Soft yellow papules
- Mature adipocytes in dermis
- No encapsulation or connection with subcutaneous fat
- No distinct epidermal changes
- Nevus sebaceus of Jadassohn (sebaceous nevus, organoid nevus) is a hamartoma that is histologically characterized by a complex and abnormal proliferation of epidermis and adnexal structures
- Clinically manifests as a congenital, yellow-orange mamillated patch / plaque with alopecia typically occurring on the scalp and face
- Hamartomatous proliferation of epidermis and adnexal structures that commonly presents at birth as a single yellow patch of alopecia on the scalp, becomes verrucous during childhood and puberty and shows variable enlargement during adulthood (due to development of a range of often benign and occasionally / rarely malignant tumors)
- Unusual anatomical presentation and appearance as well as rare association with systemic syndromes (often with neurologic and developmental abnormalities) can occur
- New genomic data suggest that nevus sebaceus may represent a mosaic RASopathy, often originating from a portion of skin with HRAS / KRAS mutations; this further explains the rare association with other developmental syndromes and intralesional growth of neoplasms
- The common types of secondary neoplasm include syringocystadenoma papilliferum, trichoblastoma-like tumor, trichilemmoma and sebaceous neoplasms
- Development of malignant neoplasms (mainly basal cell carcinoma) in nevus sebaceus is a rare phenomenon (< 1% of lesions in a large series) and almost always occurs during adulthood
- Organoid nevus; though sometimes used as a generic term for the group of cutaneous hamartomatous lesions (see epidermal nevus)
- Nevus sebaceous; a common misspelling combining the Latin term nevus sebaceus with the English equivalent term sebaceous nevus
- ICD-10: Q82.5 - congenital nonneoplastic nevus
- Present at birth or develops in early childhood, with a prevalence of 0.3% in newborns
- F = M
- Affects all races and ethnicities
- Very low rate of malignant transformation, estimated to be ~0 - 0.8% (CMAJ 2019;191:E765)
- Can be associated with the following syndromes:
- Phacomatosis pigmentokeratotica
- SCALP syndrome (sebaceus nevus syndrome, CNS symptoms, aplasia cutis, limbal dermoid and pigmented nevus with neurocutaneous melanosis)
- Linear sebaceus nevus syndrome, i.e Schimmelpenning–Feuerstein–Mims syndrome (organoid nevi, abnormalities of the central nervous system and eyes, oral lesions and skeletal defects)
- Up to 19% are associated with a secondary benign lesion (J Am Acad Dermatol 2014;70:332)
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- Nearly all lesions occur on the scalp, forehead or face
- Rare sites of presentation include trunk, breast, extremities and perineal region (Medicine (Baltimore) 2021;100:e25047)
- Nevus sebaceus is now considered as a mosaic RASopathy with postzygotic somatic mutations of the Ras protein family, mainly due to HRAS and rarely KRAS mutations, in a section of the skin
- RAS mutations are also present in secondary tumors in nevus sebaceus (e.g., trichoblastomas)
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- No relevant etiology
- While HPV infection had been speculated to be an etiological factor, further and more comprehensive research has failed to establish a link between HPV infection and development of nevus sebaceus (J Am Acad Dermatol 2008;59:279, Pediatr Dermatol 2014;31:326)
- Clinical appearance of the lesion can change over time
- In infancy, nevus sebaceus is usually a smooth hairless patch
- During puberty (under hormonal influence), it can undergo rapid growth becoming more verrucous with tightly arranged yellowish waxy papules
- In adulthood, further enlargement can occur due to the development of intralesional neoplasms
- Nevus sebaceus, often in the form of a giant lesion involving large areas of head and neck, can be associated with a range of ophthalmic and neurologic anomalies (nevus sebaceus syndrome); seizures and neurologic anomalies have also been reported as part of epidermal nevus syndrome (CMAJ 2019;191:E765, Pediatr Dermatol 1999;16:211)
- Linear and zosteriform presentations have been described
- Usually clinically suspected and diagnosed
- Skin biopsy may be required for confirmation or assessment of secondary benign or rarely malignant neoplasms developing in the lesion
- Generally, nevus sebaceus will follow a benign course
- Incidence of development of malignant neoplasms (e.g., basal cell carcinoma, squamous cell carcinoma, sebaceous carcinoma) in nevus sebaceus is extremely rare (< 1%); a significantly higher rate (up to 20%) reported in some older studies is likely due to misclassification and inclusion of trichoblastoma-like tumors (J Dermatol 2016;43:175, CMAJ 2019;191:E765)
- 13 year old girl with nevus sebaceus and secondary squamous cell carcinoma (Cutis 2019;103:E17)
- 48 and 82 year old women with malignant tumors arising from nevus sebaceus (Diagnostics (Basel) 2022;12:1448)
- 67 year old woman with nevus sebaceus and multiple secondary neoplasms (Dermatol Online J 2020;26:13030)
- Generally safe to observe
- Surgical excision as a cosmetic procedure or to remove a secondary neoplasm
- Superficial procedures such as shave removal, dermabrasion or laser resurfacing are typically unsuccessful due to incomplete removal of the lesion (Am J Clin Dermatol 2015;16:197)
- Well defined, hairless yellow patches or plaques, 1 - 6 cm in diameter
- Some with mamillated or waxy appearance
- Reference: Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
- Well circumscribed and complex proliferation and alteration of epidermis and adnexal structures that often changes with age
- Prepubertal lesions are broad with primitive hair follicles and markedly decreased terminal hairs (hair follicles are usually vellus)
- Sebaceous glands can be increased or decreased based on the age and associated hormonal effect and can show an abnormal distribution and configuration; they can also be located higher than normal in the dermis without connection to a hair follicle and with direct opening onto the epidermal surface
- Additional features are variably seen and include:
- Increased acanthosis, papillomatosis and basal epidermal melanin pigmentation
- Presence of an inflammatory infiltrate
- Ectopic apocrine glands (up to half of cases and occasionally dilated)
- Anomalous ductal sweat gland structures resembling eccrine hyperplasia
- Secondary neoplasms occur, namely trichoblastoma-like tumor, trichilemmoma, syringocystadenoma papilliferum and sebaceous gland neoplasms
- References: Int J Dermatol 2016;55:193, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
Contributed by Ronan Knittel, M.D. and Sara C. Shalin, M.D., Ph.D.
- Typically not required for diagnosis
- Associated with activating HRAS p.Gly13Arg and KRAS p.Gly12Asp mutations (J Invest Dermatol 2013;133:824)
- Deletion of PTCH gene has also been implicated in pathogenesis in limited studies; further confirmation is required (Cancer Res 1999;59:1834)
- Activating FGFR2 mutations appear fairly specific for cerebriform nevus sebaceus (J Eur Acad Dermatol Venereol 2021;35:2085)
- Postzygotic mosaic NRAS mutation was identified in a nevus sebaceus in a patient with Schimmelpenning syndrome (Am J Med Genet A 2015;167A:2223)
Nevus sebaceus in 5 minutes
Nevus sebaceus
Nevus sebaceus with associated benign hair follicle tumors
Nevus sebaceus (not SebaceOus!)
- Skin, scalp, excision:
- Nevus sebaceus (see comment)
- Comment: The sections of scalp skin demonstrate a well circumscribed broad area of epidermal and adnexal proliferation. The lesion is characterized by marked epidermal acanthosis, papillomatosis and hyperkeratosis overlying lobules of hyperplastic and abnormally configured sebaceous glands. There are dilated apocrine glands in the dermis with a superficial dermal lymphoplasmacytic inflammation. There is no evidence of an associated neoplastic growth or malignancy in the material examined.
- Epidermal nevus:
- Often clinically presents on the extremities, trunk and neck as linear lesions following Blaschko lines
- Histologically similar epidermal changes but without sebaceous gland alterations
- Mesa sign (i.e., the tips of the epidermal papillations are flattened)
- Normal dermis, usually with no associated adnexal structures
- Sebaceous hyperplasia:
- Increased sebaceous glands, usually with no primary epidermal changes
- Seborrheic keratosis:
- Unusual diagnosis in children / young adults
- Some overlapping epidermal changes without adnexal / sebaceous alterations
- Presence of keratin horn cysts and squamous eddies
- Acanthosis nigricans:
- Usually in flexural areas of the body, particularly the axilla
- Associated with an underlying metabolic disorder or malignancy
- Hyperkeratosis and papillomatosis but mild acanthosis and no dermal inflammation or adnexal / sebaceous alterations
An incisional biopsy from the scalp of a 2 year old boy was performed; the histology is shown above. Which of the following alterations is most likely to occur in the lesion during puberty if not completely excised?
- Development of secondary malignant neoplasms
- Enlargement due to sebaceous gland hyperplasia
- Epidermal atrophy
- Spontaneous regression
Comment Here
Reference: Nevus sebaceus of Jadassohn
- Bronchogenic cysts presenting in the skin are very rare, with fewer than 70 cases reported
Cutaneous ciliated cyst
- Also called cystadenoma, cutaneous Müllerian cyst
- Usually extremities of teenage girls
- May have Müllerian derivation in females, distinct fetal eccrine duct origin in males
- Solitary lesion which presents shortly after menarche on limb of young females (12 - 42 years)
- Also described in males and at atypical sites including back, shoulder, scalp, cheek
- Most are present at birth on the precordium or overlying the suprasternal notch
- Occasionally occur near shoulder, back, scapula, neck, abdomen or chin or present at a later age
Cutaneous ciliated cyst
- Thigh > buttock > calf > foot
- Believed to form from buds or diverticula that separate from foregut during development of the tracheobronchial tree
- May be intrapulmonary or peripheral
- Cutaneous bronchogenic cysts may result from subsequent sequestration outside the chest cavity following fusion of the mesenchymal bars of the sternum or from active migration prior to fusion
Cutaneous ciliated cyst
- Lesions on limbs of young females are generally thought to be of Müllerian (paramesonephric) derivation, representing a migration abnormality of fetal development (heterotopia)
- Cysts arising at other sites and in males may represent metaplasia of lining of a pre-existent simple cyst of sweat duct derivation or have an entirely different histogenesis
- 80% males
- Variable presentation as cutaneous cystic nodule, sinus or papillomatous growth
- Usually asymptomatic but may be tender or painful
- Rarely are multiple
- Treatment is surgical resection, if clinically indicated
Cutaneous ciliated cyst
- Located in deep dermis or subcutaneous tissue
- Usually asymptomatic
- 2 year old boy with scapular cyst (Dermatol Online J 2012;18:12)
- 21 year old woman with multiple cysts on neck and scalp (Acta Dermatovenerol Alp Pannonica Adriat 2008;17:69)
Cutaneous ciliated cyst
- 16 year old girl with cutaneous ciliated cyst on finger (Am J Dermatopathol 2012;34:335)
- 18 year old woman with cutaneous ciliated cyst over knee (J Cutan Aesthet Surg 2011;4:158)
- 48 year old woman with cystic lesion on right heel (Dermatol Online J 2011;17:6)
- Surgical excision
- Skin nodule
Cutaneous ciliated cyst
- Soft to cystic, solitary, movable, nontender, fluctuant swelling
- Cutaneous bronchogenic cyst occurs within dermis or subcutaneous tissue
- Lining is usually thrown into small folds
- Epithelium is invariably ciliated, pseudostratified cuboidal or columnar, with mucus secreting goblet cells in 50% of cases
- May have nonciliated cuboidal, columnar and stratified squamous epithelium
- Smooth muscle supports the mucosa in 8% of cases
- Lymphoid follicles are found in 25% of cases and appear to be part of a secondary inflammatory response
- Occasionally seromucinous glands or cartilage are present
- Cutaneous lung tissue heterotopia, in which fully developed bronchioles and alveoli are present, is considered a variant
Cutaneous ciliated cyst
- Unilocular or multilocular cyst with intraluminal papillary projections of lining resembling fallopian tube
- Cuboidal to columnar ciliated epithelium with frequent pseudostratified foci
- Deep to the epithelium lie well vascularized parallel bundles of collagen but smooth muscle is not present
- Occasional: squamous metaplasia, intercalated dark cells
- Rare: mucin secreting cells, apocrine-like features
Images hosted on other servers:
Bronchogenic cyst
Cutaneous ciliated cyst
- Ciliated columnar cells with abundant cytoplasm and eccentric nuclei in proteinaceous or clean background (J Cutan Aesthet Surg 2010;3:181)
Cutaneous ciliated cyst
- Ultrastructurally, cilia have characteristic morphology with a central pair of microtubules, 9 radially orientated pairs of microtubules, basal bodies, cross striated rootlets
- Heterotopic rests
- Mature cystic teratoma
- Thyroglossal duct cyst
Cutaneous ciliated cyst
- Branchial and thymic cysts
- Bronchogenic cyst
- Mature cystic teratoma
- Thyroglossal duct
- Also called solitary circumscribed neuroma
- Common, often on face; often due to trauma or surgery
- Also known as solitary circumscribed neuroma
- Small solitary papule
- Spindle lesion with palisading, occasionally epithelioid cells, lesion is not truly encapsulated
- A cutaneous glandular neoplasm
- Eccrine or apocrine in origin
- First described by Rulon and Helwig in 1977 (Arch Dermatol 1977;113:596)
- A benign neoplasm (by some) and papillary adenocarcinoma in situ (by others) (Dermatol Pract Concept 2014;4:23)
- May be an analogue of micropapillary ductal carcinoma in situ of the breast
- Solitary nodule, mostly in lower extremity of young black women
- Well circumscribed in the dermis, composed of tubules with intraluminal papillary, micropapillary or cribriform and peripheral flat myoepithelial cells
- Nuclear hyperchromasia, single cell necrosis and mitotic figures present
- Called tubulopapillary hidradenoma by Falck and Jordaan in 1986 (Am J Dermatopathol 1986;8:64)
- Considerable overlap with apocrine tubular adenoma; may be part of the same spectrum (Am J Dermatopathol 1992;14:149, Am J Dermatopathol 1993;15:482)
- Significant similarities with nipple adenoma (Hum Pathol 2018;73:59)
- Papillary adenocarcinoma in situ was proposed in 2014 (Dermatol Pract Concept 2014;4:23)
- Usually occurs in young people
- Blacks > whites
- Women > men
- Usually extremities, lower more than upper
- Poorly understood; may be associated with nevus sebaceus
- Similar to nipple adenoma, BRAF V600E and KRAS mutations were frequently reported (Hum Pathol 2018;73:59)
- Unknown
- Solitary (almost always)
- Flesh-colored papule or nodule
- Dermal based neoplasm
- May mimic a basal cell carcinoma (J Am Acad Dermatol 2014;71:e45)
- Incisional or excisional biopsy should be performed with histologic examination for a definite diagnosis
- Excellent prognosis; no recurrence following simple conservative complete excision
- Can have recurrence / persistence after incomplete removal
- 35 year old Caucasian man with heel tumor (J Foot Ankle Surg 2000;39:249)
- 45 year old African American man with papillary eccrine adenoma (J Dermatol Sci 1990;1:65)
- 52 year old woman with foot lesion (Am J Dermatopathol 1993;15:150)
- 63 year old woman with thigh tumor (Dermatologica 1991;182:47)
- 4 cases of papillary adenocarcinoma in situ of the skin (Dermatol Pract Concept 2014;4:23)
- Simple surgical excision
- Nodular, well circumscribed and often asymmetrical from scanning magnification
- Tubular or cystic structures with intraluminal papillary, micropapillary or cribriform growth (common)
- Ductal lining is bilayered with luminal cuboidal cells and peripheral flat myoepithelial cells
- Occasional findings
- Variable clear cell change and squamous differentiation
- Nuclear hyperchromasia (Dermatol Pract Concept 2014;4:23)
- Mitotic figures (Dermatol Pract Concept 2014;4:23)
- Necrosis of single cells or necrosis en masse (Dermatol Pract Concept 2014;4:23)
- Inner epithelial cells: EMA, CAM 5.2, CK7, CK8, CEA (Clin Exp Dermatol 1990;15:425, J Cutan Pathol 1998;25:59)
- Outer myoepithelial cells: S100, calponin, p63, CK14 and SMA (J Cutan Pathol 1998;25:59)
- Cells of the inner layer have features of eccrine secretory (clear) cells
- Cells of the outer layer have characteristics of both ductal basal cells and glandular myoepithelial cells (J Dermatol Sci 1990;1:65)
- Skin, right foot, excision:
- Papillary glandular neoplasm (see comment)
- Margins negative for tumor
- Comment: The findings are consistent with a papillary eccrine adenoma (also called papillary adenocarcinoma in situ).
- Aggressive digital papillary adenocarcinoma:
- Digit predilection, more cellularity, solid growth, proliferation of both epithelial and myoepithelial cells (epithelial myoepithelial carcinoma) (Clin Exp Dermatol 2014;39:223, J Cutan Pathol 2017;44:410, Am J Dermatopathol 2018;40:152)
- Microcystic adnexal carcinoma:
- Face predilection, infiltrative, deep involvement, multiple keratin cysts, perineural invasion
- Syringocystadenoma papilliferum:
- Face predilection, squamous and glandular epithelium, decapitation secretion, many plasma cells, usually associated with nevus sebaceus
- Hidradenoma papilliferum:
- Female genital predilection, packed elongated tubular structures, decapitation secretion
- Nipple adenoma:
- Nipple location, fundamentally the same
- Papillary adenocarcinoma:
- Infiltrative, loss of myoepithelial cells at least in some foci (Dermatol Pract Concept 2014;4:23)
A 41 year old African American woman with a solitary, 1 cm nodule localized on the right leg comes to the office. Incisional biopsy was performed and the findings are illustrated above. Which of the following statements regarding this neoplasm is correct?
- Identical features may be seen in nipple adenoma
- It is composed of solid proliferation of both myoepithelial cells and epithelial cells
- Many plasma cells are present
- Myoepithelial cell layer may be absent at the periphery of some tubular structures
- This is an aggressive neoplasm with a high rate of metastasis (15%)
Comment Here
Reference: Papillary eccrine adenoma
- BRAF V600E
- CYLD1
- FLCN
- MLH1
- PTCH
Comment Here
Reference: Papillary eccrine adenoma
- Pilomatricoma is a benign skin adnexal tumor originating from hair matrix and cortex
- Benign skin adnexal tumor originating from hair matrix and cortex
- Most commonly occurs in head and neck, extremities and trunk in children
- Grossly appears as circumscribed hard dermal tumor with cheesy material
- Most cases behave indolently without recurrences
- Pilomatrixoma
- Calcifying epithelioma of Malherbe (not recommended)
- ICD-O: 8110/0 - pilomatrixoma, NOS
- ICD-11: 2F22 & XH9E37 - benign neoplasms of epidermal appendages & pilomatricoma, NOS
- Pilomatricoma, being the most common adnexal neoplasm in children, favors young age (Actas Dermosifiliogr 2010;101:771)
- However, a wide age range has been described from 3 months to 93 years
- Females are affected slightly more than males
- Usually solitary but multiple lesions can occur (Int J Dermatol 2017;56:1032)
- Head and neck are the most common sites of involvement, followed by upper and lower extremities and then trunk
- Ear (J Pediatr 2011;158:511, Ear Nose Throat J 2013;92:34)
- Eyelid (Int J Trichology 2011;3:31)
- Digits
- Male breast (Breast J 2019;25:1012)
- Pilomatricoma development is associated with mutations in CTNNB1 gene located in the exon 3 region encoding beta catenin, a 92 kDa molecule involved in cell - cell adhesion
- As an integral component of Wnt signaling pathway, beta catenin monitors cell proliferation, differentiation and survival
- Beta catenin expression in hair matrix during human embryogenesis signifies its importance in hair follicle development and thus pilomatricoma origin
- BCL2 oncoprotein is also implicated in its development (Arch Pathol Lab Med 2014;138:759)
- Although pilomatricoma are usually not hereditary, familial cases have been recognized
- Familial forms have been seen in myotonic dystrophy Curschmann-Steinert (an uncommon autosomal dominant disorder characterized by hypotonia, muscle wasting, cataracts, hypogonadism, progressive mental retardation and frontal baldness), familial adenomatous polyposis related syndromes (including Gardner syndrome), Turner syndrome, Rubinstein-Taybi syndrome, trisomy 9, gliomatosis cerebri (Paller: Hurwitz Clinical Pediatric Dermatology - A Textbook of Skin Disorders of Childhood and Adolescence, 5th Edition, 2015, Pediatr Dermatol 2020;37:9, An Bras Dermatol 2020;95:619, Pediatr Dermatol 2009;26:75)
- Rare association with Kabuki syndrome has also been described as characterized by ectodermal abnormalities (Pediatr Dermatol 2013;30:253)
- Multiple giant pilomatricoma were reported with familial Soto syndrome, panhypopituitarism, MYH associated polyposis and DICER1 syndrome (Pediatr Dermatol 2008;25:122)
- Constitutional mismatch repair deficiency (CMMRD) syndrome, biallelic mutations in DNA mismatch repair genes (MLH1, MSH2, MSH6 or PMS2) (Pediatr Dermatol 2020;37:1139)
- Germline mutation in PLCD1 has been identified as the genetic cause of familial multiple pilomatricomas (FMPs); PLCD1 is essential for maintaining skin function (J Invest Dermatol 2021;141:533)
- Pilomatricoma presents as slow growing, dermal based, asymptomatic nodule measuring 0.5 - 3 cm (Arch Argent Pediatr 2019;117:340)
- Flesh colored to white, firm papules / nodules that may have an overlying pink to blue hue (Paller: Hurwitz Clinical Pediatric Dermatology - A Textbook of Skin Disorders of Childhood and Adolescence, 5th Edition, 2015)
- Pain, pruritus or discharge can occur at times (Arch Craniofac Surg 2020;21:288)
- Occasionally, skin ulceration may be seen simulating squamous cell carcinoma (Int J Trichology 2012;4:280)
- Rare appearances may include bullous / anetodermal / lymphagiectatic, giant, perforating, pigmented lesions, keloid-like (J Cutan Pathol 2009;36:67, Indian J Dermatol Venereol Leprol 2020;86:55, Pediatr Dermatol 2013;30:e68, Int J Clin Exp Pathol 2013;6:1890, Case Rep Dermatol 2022;14:230)
- Recently a pseudocystic presentation has been documented (Australas J Dermatol 2021;62:60)
- Generally very hard, owing to calcification; skin lesions that are calcified tend to display positive teeter totter and tent signs
- Teeter totter sign is observed when applying downward pressure to one end of the lesion causes the other end to spring upwards in the skin
- Tent sign appears when the skin overlying the lesion is stretched, revealing multiple facets and angles, resembling a tent
- Clinical examination alone may not be diagnostic (Am J Dermatopathol 2018;40:631)
- Imaging studies ultrasound, computed tomography and magnetic resonance imaging are helpful; ultrasonography has a high positive predictive value (95.56%) (Arch Craniofac Surg 2020;21:288)
- Ultrasound
- Pilomatricoma present as heterogeneous, well demarcated, hypoechoic mass between the deep dermis and the subcutis on ultra high frequency ultrasonography
- Most common features are internal echogenic foci (calcifying), hypoechoic rim and posterior shadowing (J Ultrasound 2008;11:76, Front Med (Lausanne) 2021;8:673861)
- CT scan
- Appear well demarcated, subcutaneous masses with various levels of calcification
- Inflammatory cell infiltration into fat may result in peritumoral fat stranding on fat suppressed, T2 weighted images (Radiol Med 2019;124:1049)
- Rare tumor recurrence of ~1 - 2% is reported with incomplete primary excision (Arch Craniofac Surg 2020;21:288, Am J Dermatopathol 2018;40:631)
- In rare cases, can undergo malignant transformation
- Most of the reported cases of malignant transformation have occurred in adults, typically in their 40s or 50s
- However, there have been rare cases reported in children as well
- Risk of malignant transformation appears to be higher in large or longstanding pilomatricoma and in those that have been previously treated with radiation therapy (J Dermatol 2010;37:735)
- 6 year old girl with a painful swelling over the left buttock (Ann Med Surg (Lond) 2022;84:104847)
- 9 year old girl with keloid-like tumor on posterior part of the auricle (Case Rep Dermatol 2022;14:230)
- 34 year old pregnant woman with rapidly growing giant parotid tumor (Arch Craniofac Surg 2020;21:176)
- 69 and 76 year old men with melanocytic matricoma (JAAD Case Rep 2023;33:51)
- 87 year old woman with a scalp tumor (Cureus 2022;14:e30661)
- Surgical excision is curative
- Hard calcified, may be nodulocystic
- Circumscribed edges, lobulated
- Keratinous material appears cheesy while calcified areas are gritty
- Rare ossified area will be difficult to cut
- Lobulated and circumscribed dermal based neoplasm
- Islands of basaloid cells exhibiting abrupt keratinization, without intervening granular layer (trichilemmal keratinization)
- Ghost / shadow cells, may predominate
- Basaloid cells show mitotic activity; however, abnormal mitoses are absent
- Intermediary cells progressively more eosinophilic cytoplasm, with pyknotic nucleus
- Tumor keratin may elicit inflammatory response with foreign body giant cells, granuloma, cholesterol clefts and calcification
- Uncommonly metaplastic bone formation is present along with extramedullary hematopoiesis (Cureus 2022;14:e30661)
- Hemosiderin, melanin and amyloid deposition has been reported
- Occasionally tumors exhibit some atypical features that suggest a potential for malignancy but does not fully meet the criteria for pilomatrix carcinoma; these features include a focal infiltrative pattern at the periphery, variable cytological atypia, increased mitotic rate (up to 5/high power field) and irregular foci of central necrosis (Case Rep Dermatol 2021;13:98)
- Histological patterns: pigmented, proliferating, nodulocystic, perforating, bullous, pilomatricoma with osseous metaplasia, melanocytic matricoma (JAAD Case Rep 2023;33:51)
Contributed by Nasir Ud Din, M.B.B.S. and Andrey Bychkov, M.D., Ph.D.
- Clusters of basaloid cells with round to ovoid nuclei, nucleated squamous cells and anucleated squames as well as clusters of shadow cells are consistent with the characteristics typically seen in pilomatricoma (Diagn Pathol 2018;13:65)
- Foreign body giant cells may be present; markedly calcified lesion may yield scanty material (Int J Trichology 2012;4:280)
- Shadow cells are specialized cells, the result of a process called shadow cell degeneration, in which the cells lose their nuclei and undergo a series of structural changes
- Cytoplasm of shadow cells often contains basophilic (blue) granules, which are thought to represent remnants of the cellular organelles
- Pancytokeratin, cytokeratin 5/6
- Hard keratins hHa1, hHa2 and hHa5 are positive in pilomatricoma but not in other tumors of follicular origin
- Beta catenin: nuclear and membrane positivity in basaloid cells, negative in transitional and shadow cells (J Dermatol 2010;37:735)
- BCL2
- CDX2 (Hum Pathol 2022;129:1)
- LEF1 (Childs Nerv Syst 2023;39:821)
- Cyclin D1
- ER, PR
- CD10 and CD138 (Rom J Morphol Embryol 2018;59:917)
- Connexin 43 (Cx43) gap junction protein: Cx43 expression is preserved in benign cutaneous tumors with follicular differentiation (Am J Dermatopathol 2019;41:810)
- PHLDA1 (Am J Dermatopathol 2022;44:129)
- BerEP4
- CK15
- Mart1 and SOX10: negative in basaloid cells (Indian J Dermatol 2021;66:525)
- Cell differentiation and keratinization in shadow cells is similar to the process in the cortex of hair
- Shadow cells are fully keratinized that form a mantle around nuclear remnants
Diagnostic pearls of pilomatricoma in superficial biopsy
Pilomatricoma: mini tutorial
- Left cheek, excision biopsy:
- Pilomatricoma (see comment)
- Comment: There is a well circumscribed, lobulated, dermal based adnexal neoplasm comprising of many islands of basaloid cells with scattered mitoses. These cells exhibit abrupt keratinization transforming to shadow cells. Surrounding stroma has histiocytes, foreign body giant cell reaction and foci of calcification. There is no evidence of atypical mitoses, nuclear anaplasia or destructive infiltration into the surrounding tissue. Immunohistochemical stain beta catenin shows nuclear positivity in basaloid cells. Features are consistent with pilomatricoma, a benign adnexal tumor with hair matrix differentiation. The tumor is completely excised. Local recurrence is uncommon following complete excision.
- Basal cell carcinoma:
- Sun exposed areas of skin
- Most often seen in older individuals
- May occur in children in association with basal cell nevus syndrome, xeroderma pigmentosum and organoid nevus
- Nests of basaloid cells palisade at periphery
- Stromal retraction and mucin
- High mitotic activity
- Most show connection to epidermis
- Lacks anucleate shadow cells
- BerEP4 positive
- Basal cell carcinoma with matrical differentiation:
- Typical features of basaloid cells predominate with foci of matrical differentiation
- Pilomatrix carcinoma:
- Older adults; case reports document occurrence in children and young adults, mostly de novo
- Rare cases arise from existing pilomatricoma
- Pleomorphic basaloid cells
- Prominent nucleoli
- High mitotic activity, necrosis, lymphovascular invasion (rare)
- Locally aggressive behavior, infiltrating borders
- Local recurrence common
- Metastases may rarely occur, involving regional lymph nodes and lungs
- Squamous cell carcinoma:
- Intercellular bridges
- Epidermoid keratinization
- Keratin pearl formation
- Lacks shadow cells
- Merkel cell carcinoma:
- Small cells hyper chromatic nuclei; stippled (salt and pepper) nuclear chromatin pattern
- Lacks anucleate shadow cells
- Immunoreactive for neuroendocrine markers, such as chromogranin, synaptophysin, CD56 and CD57
- Dot positivity for CK20
- Epidermal cysts of Gardner syndrome:
- Changes of pilomatricoma can occur
- Other follicular tumors showing matrical differentiation, including
- Trichoblastoma:
- Circumscribed, dermal basaloid tumor without surface connection
- Stromal induction and formation of primitive hair bulbs
- Trichoepithelioma:
- Dermal based, focal epidermal connection, branching nests of basaloid cells
- Aggregations of fibroblasts as abortive attempts to form papillary mesenchyme (papillary mesenchymal bodies)
- Small keratinous cysts
- Panfolliculoma:
- Rare, advanced follicular differentiation
- Overlap features between trichoblastoma and matricoma
- All elements of follicular differentiation
- Trichoblastoma:
- Ghost cells may also be found in noncutaneous tumors, such as calcifying cystic odontogenic tumor (CCOT), dentinogenic ghost cell tumor, odontogenic ghost cell carcinoma and craniopharyngioma; occasionally, these cells are also seen in odontomas, ameloblastoma, adenomatoid odontogenic tumor and ameloblastic fibroma (J Pharm Bioallied Sci 2015;7:S142)
- Beta catenin
- CK5/6
- Ki67
- p40
- p53
Comment Here
Reference: Pilomatrixoma
A 20 year old man had multiple gradually enlarging, itchy scalp tumors for the past 2 years. On examination it was hard nodule and overlying skin was stretched, revealing multiple facets and angles resembling a tent. The excision specimen revealed features as shown in the photomicrograph above. The patient's history is significant for total colectomy a year ago with more than 100 polyps. What is the patient suffering from?
- Gardner syndrome
- Gliomatosis cerebri
- Myotonic dystrophy
- Rubinstein-Taybi syndrome
- Turner syndrome
Answer C is incorrect because myotonic dystrophy is part of a group of autosomal dominant disorders with high penetrance that show skeletal and respiratory muscle weakness and myotonia. Other findings may be cardiac muscle abnormalities and conduction defects, cataracts, daytime somnolence and endocrine disorders.
Answer E is incorrect because in Turner syndrome, patients are female and lack part or all of the second sex chromosome. Characteristic features include short stature, premature ovarian failure and high risk for various phenotypic abnormalities (e.g., high palate, nail dysplasia, low posterior hairline, widely spaced nipples, webbed neck and low set or malrotated ears), as well as other medical problems such as cardiovascular defects, skeletal anomalies and autoimmune disorders. It is suggested that growth hormone (or its effector molecule insulin-like growth factor 1) and estrogen may promote hair follicle growth and inhibit apoptosis, as well as produce pilomatricomas.
Answer D is incorrect because Rubinstein-Taybi syndrome is a rare genetic disorder characterized by mental retardation and multiple congenital anomalies. It involves broad thumbs and toes, short stature, distinctive facial features and varying degrees of intellectual disability. Low set ears, cataracts, microcephaly and cryptorchidism may also be seen.
Answer B is incorrect because gliomatosis cerebri is a diffuse growth pattern of glioma that invade multiple lobes of the brain. By definition, more than 2 brain regions have to be affected and symptoms include epilepsy, headaches and behavioral changes.
Comment Here
Reference: Pilomatrixoma
- An undifferentiated pleomorphic tumor with overlapping features of atypical fibroxanthoma but a higher rate of local recurrence and metastasis
- Undifferentiated pleomorphic tumor involving the dermis that histologically looks like an atypical fibroxanthoma and has any of the following:
- Size > 2 cm
- Shows extensive involvement of deeper tissue (subcutis, skeletal muscle, fascia)
- Necrosis
- Perineural
- Lymphovascular invasion
- Pleomorphic dermal sarcoma (PDS)
- Undifferentiated pleomorphic sarcoma of the skin
- Superficial malignant fibrous histiocytoma (terminology no longer used)
- ICD-10: C49.9 - malignant neoplasm of connective and soft tissue, unspecified
- Predominantly affects elderly patients on sun damaged skin
- Median decade: ninth (Am J Surg Pathol 2012;36:1317)
- M > F (Cancer 1973;31:1541)
- Head and neck, predilection for scalp
- Ultraviolet radiation induced damage and immunosuppression
- Rapidly growing nodules or plaques, often > 2 cm (Am J Surg Pathol 2012;36:1317)
- Ulceration can be present
- Dependent on clinical and tissue pathologic correlation
- Local recurrence rate of 20 - 30% (Am J Surg Pathol 2012;36:1317, J Cutan Pathol 2016;43:101)
- Median time to recurrence: 10 months (Am J Surg Pathol 2012;36:1317)
- Metastatic rate of 10 - 20% (Am J Surg Pathol 2012;36:1317, J Cutan Pathol 2016;43:101)
- Presence of metastatic disease associated with increased mortality
- 58 year old woman with a multifocal tumor arising in areas of alpha-1-antitrypsin deficiency panniculitis and a history of lung transplantation (J Med Case Rep 2019;13:169)
- 69 year old man with an enlarging, asymptomatic nodule on his forehead (An Bras Dermatol 2018;93:307)
- 77 year old man with a large nodular scalp lesion (Cureus 2018;10:e2979)
- 91 year old woman with a mass on the lateral aspect of the right upper eyelid (Ann Dermatol 2016;28:632)
- Surgery is gold standard
- Adjuvant radiation employed in setting of metastatic or locally recurrent, unresectable disease (Curr Treat Options Oncol 2017;18:50)
- Dermal based lesion composed of pleomorphic cells with vesicular nuclei and prominent nucleoli (Cancer 1973;31:1541)
- Cells can be spindled or epithelioid, often with admixed multinucleated giant cells
- Cells can be arranged in sheets and fascicles
- Necrosis often present
- Perineural and lymphovascular invasion can be seen
- Infiltration into subcutis, skeletal muscle or fascia
- Additional findings include myxoid change, pseudoangiomatous growth and storiform growth (Am J Surg Pathol 2012;36:1317)
- CD10
- Actin - alpha smooth muscle (usually nonspecific staining)
- References: J Cutan Pathol 2018;45:880, Am J Surg Pathol 2012;36:1317
- Both high and low weight cytokeratins: AE1 / AE3, 34betaE12 / HMWCK / high molecular weight, CK5 / 6
- p40
- Desmin, S100 protein, SOX10, MelanA
- Reference: J Cutan Pathol 2018;45:880
- 50 - 70% NOTCH1 / 2 and FAT1 mutations (Mod Pathol 2018;31:418)
- TERT promoter mutations in > 70% (Mod Pathol 2014;27:502)
- TP53 mutations in > 80% (Mod Pathol 2018;31:418)
- Skin, scalp, excision:
- Pleomorphic dermal sarcoma
- Tumor measures 3.5 cm in greatest dimension and extensively involves the subcutaneous tissue
- Necrosis is present: 30%
- Lymphovascular invasion is not identified
- Perineural invasion is not identified
- Margins are negative
- Atypical fibroxanthoma:
- May be identical histologically, especially if only a superficial shave biopsy is performed
- Tends to have a well circumscribed and pushing border with less infiltration into deep soft tissue
- Should not have perineural invasion
- Should not have lymphovascular invasion
- More than a minute focus of necrosis should raise suspicion
- Cutaneous leiomyosarcoma:
- Will also be dermal based
- Composed of intersecting fascicles of spindled cells with eosinophilic cytoplasm
- Intersecting fascicles will often create halo effect around nuclei cut on cross section
- Should express multiple smooth muscle markers such as desmin, caldesmon, actin - alpha smooth muscle
- Actin - alpha smooth muscle expression by itself is not enough to call leiomyosarcoma
- Sarcomatoid squamous cell carcinoma:
- May have overlying dysplasia of epithelium
- Should express cytokeratins and p63 / p40
- Cellular neurothekeoma:
- Also occurs in the head and neck region
- Occurs in young females instead of elderly males
- Microscopically composed of sheets and nest of spindled and epithelioid cells with gray cytoplasm with cytologic atypia and mitoses
- Usually shows variable expression of CD10, microphthalmia transcription factor (MITF) and actin - alpha smooth muscle
- For board testing purposes, NKI-C3+ and S100A6+
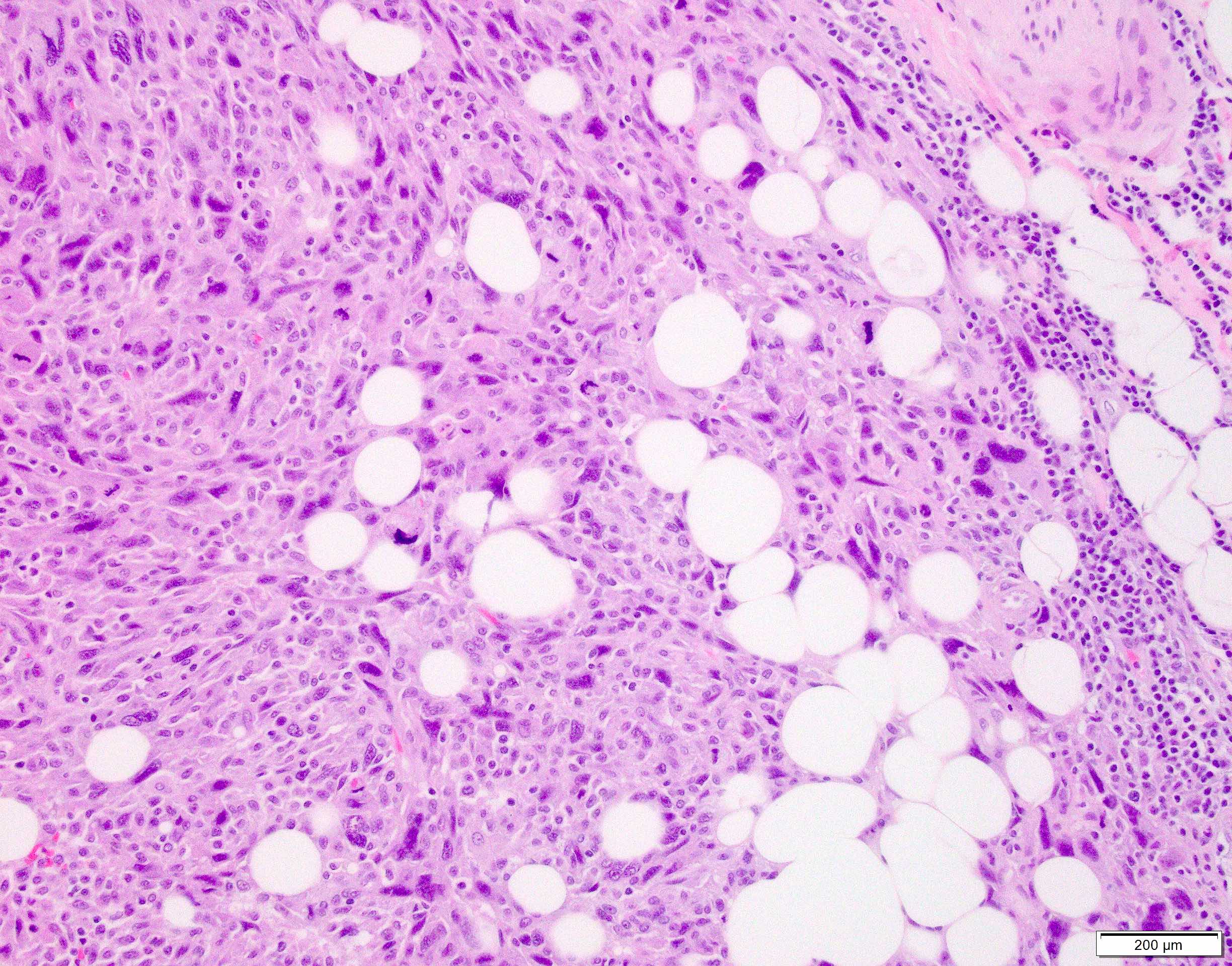
- Atypical fibroxanthoma
- Leiomyosarcoma
- Pleomorphic dermal sarcoma
- Sarcomatoid squamous cell carcinoma
- Atypical fibroxanthoma
- Leiomyosarcoma
- Pleomorphic dermal sarcoma
- Sarcomatoid squamous cell carcinoma
- Polypoid or dome-shaped cutaneous nodule with sparse cellularity and cytologic atypia of fibroblasts
- Not a WHO diagnosis
- First described in 1989 (Am J Surg Pathol 1989;13:107)
- Usually trunk, extremity or head (Clin Exp Dermatol 1998;23:22)
- Related entities: may be a variant of skin tag (acrochordon) with cytologic atypia
- Flesh-colored polyp resembling skin tag (acrochordon)
- 38 year old woman with a flesh-colored forehead nodule (Arch Pathol Lab Med 2005;129:e21)
- 38 year old man (J Cytol 2013;30:71)
- 66 year old woman with subungual tumor (J Cutan Pathol 2003;30:569)
- 75 year old man with myxoid pleomorphic fibroma that supposedly progressed to myxofibrosarcoma (Australas J Dermatol 2003;44:287)
- Resembles fibroepithelial polyp but with enlarged, bizarre, smudged, hyperchromatic nuclei, thick collagen bundles and rare mitotic figures; may be sclerotic (Am J Dermatopathol 2002;24:54) or have myxoid foci (Am J Dermatopathol 1998;20:502)
- Single lying and few clusters of pleomorphic cells with some monster cells and scant cytoplasm (J Cytol 2013;30:71)
- Angiofibroma: pleomorphic cells are similar, but have marked vascularity
- Atypical fibrous histiocytoma / dermatofibroma with monster cells: storiform pattern, more cellular, foam cells, hemosiderin laden macrophages, CD34- (Am J Dermatopathol 1999;21:414)
- Atypical fibroxanthoma: more cellular, more mitotic figures
- Atypical lipomatous tumor: may be in differential when pleomorphic fibroma has entrapped adipose cells, but atypical lipomatous tumor has 12q15/MDM2 amplification by FISH (J Cutan Pathol 2013;40:379)
- Dermal pleomorphic liposarcoma: high-grade sarcoma with pleomorphic lipoblasts (J Cutan Pathol 2013;40:734, Am J Surg Pathol 2012;36:1047)
- Giant cell fibroblastoma: young children
- First described by Suster and Wong in 1994 (Histopathology 1994;25:31)
- Uncommon, low grade, malignant adnexal tumor
- Histologically, the lesions are characterized by a cellular proliferation showing a combination of growth patterns, including trabecular, solid, tubular, cribriform or adenoid cystic and pseudopapillary (Am J Dermatopathol 2018;40:580)
- Marked predilection for the distal extremities
- Polymorphous sweat gland carcinoma
- Polymorphous low grade sweat gland carcinoma
- PSGC
- ICD-O-3 topography code: C44 - Skin
- Middle aged to older patients
- No sex preference (Am J Dermatopathol 2018;40:580)
- Favors the extremities (10 cases), followed by head and neck (4 cases) and the trunk (2 cases) (J Am Acad Dermatol 2002;46:914, Ann Pathol 1996;16:442)
- Slow growing, skin colored, firm dermal nodule measuring 1 - 8.5 cm (Am J Dermatopathol 2018;40:580)
- 51 year old man with a slow growing tan‐brown nodule on the left upper chest of 1 year's duration (J Cutan Pathol 2016;43:594)
- 54 year old woman with a 1 cm slow growing nodule on the elbow (J Cutan Pathol 2016;43:594)
- 56 year old man with multiple large skin nodules (J Am Acad Dermatol 2002;46:914)
- 60 year old man with a 20 - 30 mm, skin colored, mobile, firm tumor (Histopathology 2020;76:779)
- Patient with polymorphic sweat gland adenocarcinoma (Ann Pathol 1996;16:442)
- Complete excision with conservative margins has been recommended as the preferred modality of treatment
- Characterized by an admixture of multiple growth patterns within the same lesion, including trabecular, solid, tubular, cylindromatous and pseudopapillary, as well as prominent stromal changes, including hyalinization, hemorrhage, calcification and cystic changes
- Tumors grow within the dermis in a generally well demarcated, pushing border but rarely can show infiltration at the edges
- Parts of the tumor also show glandular differentiation and adnexal differentiation, such as abortive hair follicle formation and numerous squamous eddies
- Tumors are predominantly composed of large epithelioid cells with atypical nuclei and abundant eosinophilic cytoplasm
- Smaller cells with darker, angulated nuclei are scattered throughout the tumor
- Spindling of tumor cells can be seen focally
- Mitoses are present and can vary from case to case
Contributed by Shira Ronen, M.D.
- Strong positivity for cytokeratin AE1 / AE3, CK5/6, p40, p63 and p16 (Am J Dermatopathol 2018;40:580)
- MIB1 proliferation index is very high
- Focal expression of the neuroendocrine markers CD56 and chromogranin
- Negative for CD117, CEA, S100, vimentin, EMA, DOG1, estrogen receptor, progesterone receptor, synaptophysin, SMA, HBME-1 and mammaglobin (Am J Dermatopathol 2018;40:580)
- Negative for MYB-NFIB fusion
- Neck mass, excision:
- Polymorphous sweat gland carcinoma (see comment)
- Comment: Sections show a relatively well demarcated tumor involving the dermis without a connection to the epidermis. The tumor shows multiple growth patterns including solid, trabecular, tubular and focal cribriform. Prominent hemorrhage, cystic changes and calcifications are seen. The cells are mostly epithelioid with prominent nucleoli and eosinophilic cytoplasm. Scattered mitotic figures are also observed. There is no evidence of significant cytologic atypia or necrosis. Overall, in the absence of a known or occult primary malignancy, the tumor is most consistent with a polymorphous sweat gland carcinoma. A clinical workup to exclude the possibility of metastasis, as clinically indicated, is recommended.
- Adenoid cystic carcinoma (ACC) (Am J Dermatopathol 1986;8:2):
- ACC is characterized by monomorphic basaloid cells, which are arranged in tubules, elongated nests and cords
- There are typically numerous cystic and ductular spaces with a prominent cribriform pattern
- In comparison, polymorphous sweat gland carcinoma is characterized by striking variegation of histologic growth patterns, including glandular, trabecular, solid, cylindromatous and cribriform areas within the same tumor mass
- MYB overexpression
- Consistently expresses EMA
- Positive for CD117, CEA, S100 and vimentin
- Basal cell carcinoma (Am J Dermatopathol 1986;8:2):
- Retains striking peripheral nuclear palisading and stromal retraction
- Metastases from internal malignancies:
- Benign and malignant adnexal neoplasm, such as ductal eccrine carcinoma, microcystic carcinoma and papillary digital eccrine carcinoma:
- Key difference is the striking variegation of histologic growth patterns seen in polymorphous sweat gland carcinoma that would not be seen in other adnexal neoplasms
- It is characterized by an admixture of multiple growth patterns within the same lesion
- The most common location is the abdomen
- The tumor is common
- This tumor shows MYB-NFIB fusion
- It is a fast growing tumor
Comment Here
Reference: Polymorphous sweat gland carcinoma
- CD117 and CEA
- p63 and p16
- Vimentin and cytokeratin AE1 / AE3
- Chromogranin and S100
- DOG1 and p40
Comment Here
Reference: Polymorphous sweat gland carcinoma
- Skin disorder of abnormal clonal keratinization with various clinical expressions and subtypes
- Characterized by 1 or more variably sized lesions on the skin that are rimmed by a hyperkeratotic border
- Keratinization disorder resulting from abnormal clonal expansion of keratinocytes
- Histologic hallmark is cornoid lamella, a column of parakeratosis with underlying dyskeratosis with reduction of keratohyalin granules (Indian J Dermatol Venereol Leprol 2022;88:291)
- Some subtypes premalignant
- Subtypes include
- Porokeratosis of Mibelli
- Disseminated actinic porokeratosis (DSAP)
- Disseminated superficial porokeratosis (DSP)
- Linear porokeratosis
- Eruptive disseminated porokeratosis (EDP)
- Porokeratosis palmaris et plantaris disseminate
- Punctate porokeratosis
- Porokeratosis ptychotropica
- Penoscrotal porokeratosis
- Follicular porokeratosis
- Disseminated superficial actinic porokeratosis
- Disseminated superficial porokeratosis
- Porokeratosis of Mibelli
- Linear porokeratosis
- Eruptive disseminated porokeratosis
- Porokeratosis palmaris et plantaris disseminata
- Punctate porokeratosis
- Porokeratosis ptychotropica
- Penoscrotal porokeratosis
- Follicular porokeratosis
- Porokeratoma
- Most common subtype is DSAP
- Third or fourth decades of life (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- F > M, mostly on sun exposed skin (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Porokeratosis of Mibelli, DSP and linear porokeratosis are seen in children (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- DSP resembles DSAP but occurs in younger patients and involves both sun exposed and non-sun exposed skin (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Linear porokeratosis has a predilection for males (2 - 3:1) (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- EDP is associated with hepatic, digestive and hematologic malignancy in 33% of cases (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Varies per subtype
- DSAP: arms, legs, occasionally shoulders and back (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Porokeratosis of Mibelli: trunk or limbs, 1 or more lesions (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Linear porokeratosis: presents in a similar distribution to DSAP but with linear configuration (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Porokeratosis palmaris et plantaris disseminata: palms or soles; may spread to trunk, limbs or mucous membranes (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Punctate porokeratosis: palms and soles, with multiple seed-like keratotic papules (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Porokeratosis ptychotropica: buttocks and perianal region (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Penoscrotal porokeratosis: shaft of penis and anterior scrotum (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Follicular porokeratosis: face (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Porokeratoma: solitary lesions on limbs
- Abnormalities in the mevalonate pathway (Indian J Dermatol Venereol Leprol 2022;88:291)
- Affect sterol and cholesterol biosynthesis
- Results in abnormal differentiation of keratinocytes
- Immunosuppression may result in dysregulated proliferation of abnormal keratinocyte clones (Indian J Dermatol Venereol Leprol 2022;88:291)
- Malignant transformation if allelic loss associated with p53 overexpression (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Unclear etiology
- Genetic factors (Am J Clin Dermatol 2017;18:435, Indian J Dermatol Venereol Leprol 2022;88:291)
- 5 loci have been identified on chromosomes 1, 12, 15, 16 and 18 for DSAP (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Ultraviolet (UV) radiation or sun exposure (Am J Clin Dermatol 2017;18:435, Indian J Dermatol Venereol Leprol 2022;88:291)
- Immunosuppression
- Others: electron beam therapy, radiation therapy, transplant procedures, trauma, chronic renal failure, chronic liver disease, infections, hematological malignancies including lymphomas, HIV infection, hepatitis C infection, Crohn's disease and medications such as etanercept and adalimumab (Indian J Dermatol Venereol Leprol 2022;88:291)
- Genetic factors (Am J Clin Dermatol 2017;18:435, Indian J Dermatol Venereol Leprol 2022;88:291)
- Different subtypes may have different triggers
- DSAP and porokeratosis palmaris et plantaris disseminata: UV radiation (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- EDP: hepatotropic viruses and malignancies (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- DSP: immunosuppression (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Porokeratosis ptychotropica and penoscrotal porokeratosis: trauma and scratching (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Commonly characterized by atrophic center, bordered by a peripheral, hyperkeratotic ridge (cornoid lamella)
- Slight increase in malignant transformation (basal cell and squamous cell carcinoma)
- DSAP
- Multiple, small, annular, skin colored to hyperpigmented papules surrounded by a hyperkeratotic ridge (Actas Dermosifiliogr (Engl Ed) 2020;111:545, Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- Distributed symmetrically on the extremities > trunk in sun exposed areas (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- May worsen during summer months due to increased UV
- Porokeratosis of Mibelli
- Small papules with a keratotic ridge that evolve into larger plaques on the trunk and extremities (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Most common subtype of childhood
- Occurs in adults in the setting of immunosuppression (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Linear porokeratosis
- Distributed along Blaschko lines
- Strongest association with skin cancer (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- EDP
- Abrupt onset and progressive course (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Intensely pruritic (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Eruptive pruritic papular porokeratosis
- Inflammatory form of disseminated superficial porokeratosis
- Spontaneously resolves in most individuals (Dermatol Online J 2020;26:13030)
- Clinical diagnosis
- Dermoscopy or biopsy helpful if atypical presentation (Actas Dermosifiliogr (Engl Ed) 2020;111:545)
- Dermoscopy: blue-brown dots on homogenous central discoloration flanked by a 2 layered, raised, hyperkeratotic rim (double track sign) (Actas Dermosifiliogr (Engl Ed) 2020;111:545, Indian J Dermatol Venereol Leprol 2022;88:291)
- Take biopsy from the edge of the peripheral rim to visualize the cornoid lamella
- Reflectance confocal microscopy to identify the cornoid lamella (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- Iodine and self tanning lotions highlight lesions (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- Prognosis varies depending on subtype and severity
- Often a chronic condition refractory to treatment
- Rarely, lesions may spontaneously resolve
- Malignant transformation is rare
- Greatest risk: large lesions, longstanding duration, linear subtype (Dermatol Surg 1996;22:339)
- 8 year old Chinese boy with keratotic papules on the bottom of his foot (World J Clin Cases 2022;10:11585)
- 25 year old man with a single pruritic, ulcerated, indurated, nontender plaque on the buttocks (SAGE Open Med Case Rep 2022;10:2050313X221139559)
- 30 year old man with multiple pruritic, dark, raised skin lesions over the trunk, face and upper limbs (J Family Med Prim Care 2022;11:1195)
- 68 year old woman with diffuse, hyperkeratotic, scaly, lichenoid plaques on the buttocks (J Yeungnam Med Sci 2023;40:423)
- 89 year old Black woman with hyperkeratotic and filiform papules on the bilateral palms and soles (Proc (Bayl Univ Med Cent) 2020;33:415)
- No standard treatment
- Long term follow up
- Sun protection recommended for all patients
- Reported treatment options include excision, cryosurgery, electrocautery, carbon dioxide laser, topical 5-fluorouracil, keratolytics, imiquimod, vitamin D analogues and topical retinoids (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- Topical cholesterol / lovastatin has been shown to be effective, particularly in DSAP (J Am Acad Dermatol 2020;82:123)
- Screen for hepatobiliary or hematologic malignancy in EDP
Images hosted on other servers:
- Cornoid lamella (Actas Dermosifiliogr (Engl Ed) 2020;111:545, Indian J Dermatol Venereol Leprol 2022;88:291)
- Column of parakeratosis at 45 degree angle
- Underlying dyskeratosis with focal loss of granular layer
- Dilated capillaries in the papillary dermis are associated with a lymphocytic infiltrate (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- Most prominent inflammatory changes are seen in DSAP
- Central to coronoid lamella, epidermis may be atrophic, normal thickness or acanthotic
- Central interface dermatitis or psoriasiform dermatitis possible
- Solar elastosis possible in DSAP
- Multiple cornoid lamellae can be seen in porokeratosis ptychotropica or penoscrotal porokeratosis
- PAS special stain reportedly highlights granules within the corneocytes of the cornoid lamella, rarely required
Short video discussing porokeratosis (pathology pearls)
- Skin, right upper arm, skin shave:
- Porokeratosis (see comment)
- Comment: Sections show tiers of parakeratosis overlying dyskeratotic keratinocytes. If multiple lesions are present clinically, a diagnosis of DSAP should be considered.
- Skin, right scrotum, skin shave:
- Porokeratosis (see comment)
- Comment: Sections show acanthosis with multifocal columns of parakeratosis overlying dyskeratotic keratinocytes. At this anatomic site, the findings are consistent with a diagnosis of penoscrotal porokeratosis.
- Porokeratoma:
- Benign acanthoma (Am J Surg Pathol 2007;31:1897)
- Characterized by multiple cornoid lamellae embedded within a single verrucous lesion (Am J Dermatopathol 2022;44:748)
- Verrucae:
- Epidermal acanthosis, papillomatosis with tiers of parakeratosis and koilocytosis
- Actinic keratosis:
- Gritty papules in sun exposed sites
- Histology with lower keratinocyte atypia and disorder
- Cornoid lamella uncommonly seen
- Psoriasis:
- Regular acanthosis with parakeratosis and intracorneal neutrophils (Munro microabscesses)
- Porokeratotic eccrine ostial and dermal duct nervus:
- An eccrine hamartoma with punctate hyperkeratotic papules affecting the palms and soles
- Histologically and clinically could appear like punctate porokeratosis but cornoid lamellae are limited to eccrine ostia
- Tinea corporis (Am J Clin Dermatol 2022;23:37):
- Foci of parakeratosis with intracorneal hyphae
A 40 year old woman presented with an erythematous, annular macule with a thread-like, raised border on her arm. She had several similar lesions on her extensor arms. What is the most likely diagnosis?
- Disseminated superficial actinic porokeratosis
- Guttate psoriasis
- Macular seborrheic keratoses
- Nummular eczema
- Tinea corporis
Answer B is incorrect because guttate psoriasis is a variant of psoriasis that presents in children and adolescents following streptococcal infection (StatPearls: Guttate Psoriasis [Accessed 7 August 2023]). Although guttate psoriasis may also present as lesions over the extensor surfaces, biopsy would reveal a psoriasiform reaction pattern. There is less acanthosis than seen in psoriasis vulgaris. Other features of psoriasis include dilated superficial blood vessels, parakeratosis and neutrophils in the stratum corneum (microabscesses of Munro) (StatPearls: Guttate Psoriasis [Accessed 7 August 2023]).
Answer C is incorrect because seborrheic keratoses are benign lesions that classically present as waxy papules or plaques with a stuck on appearance. Histologic features include hyperkeratosis, acanthosis and papillomatosis (Dermatol Online J 2019;25:13030).
Answer D is incorrect because nummular eczema is a chronic skin condition characterized by oval or coin shaped, erythematous, eczematous plaques. These lesions are usually symmetrically distributed with a predilection for the lower and upper extremities (Recent Pat Inflamm Allergy Drug Discov 2020;14:146). Predominant features of eczema are spongiosis, acanthosis and exocytosis of inflammatory cells.
Answer E is incorrect because tinea corporis is a superficial dermatophyte infection that may clinically resemble porokeratosis due to its annular appearance. Histopathology shows hyphal forms in the stratum corneum.
Comment Here
Reference: Porokeratosis
- Bowen disease
- Condyloma acuminatum
- Penoscrotal porokeratosis
- Verruciform xanthoma
- Zoon balanitis
Answer A is incorrect because Bowen disease is a form of in situ squamous cell carcinoma. Although Bowen disease may present similarly to porokeratosis, it is rare in patients younger than 30 years of age (Indian Dermatol Online J 2022;13:177). Histopathology would demonstrate full thickness keratinocyte atypia (Indian Dermatol Online J 2022;13:177).
Answer B is incorrect because condyloma acuminata are anogenital warts caused by the human papillomavirus (HPV), most commonly HPV strains 6 and 11 (StatPearls: Condyloma Acuminata [Accessed 19 January 2024]). Similar to porokeratosis, condyloma acuminata display hyperkeratosis on histopathological evaluation. However, distinctive koilocytes are also expected. Additionally, condyloma acuminata lesions are usually found in groups that may coalesce into larger lesions and most often present as fleshy papules that range in size.
Answer D is incorrect because verruciform xanthoma is a rare mucocutaneous verrucopapillary lesion that is not associated with dyslipidemia. Histopathology demonstrates epithelial hyperplasia with prominent parakeratinization. The histological hallmark is the presence of foam cells or xanthoma cells confined to the connective tissue papillae (J Oral Maxillofac Pathol 2019;23:43).
Answer E is incorrect because Zoon balanitis is a nonvenereal condition that most commonly affects middle aged to older uncircumcised men. It most commonly presents as a single shiny erythematous plaque on the glans penis. Early cases will reveal thickening of the epidermis, parakeratosis and a patchy lichenoid infiltrate of lymphocytes and numerous plasma cells. Atrophy of the epidermis, superficial erosions, scattered neutrophils in the upper epidermis, scant spongiosis and a denser plasmacytic infiltrate may be seen in later stages (Indian J Sex Transm Dis AIDS 2016;37:129).
Comment Here
Reference: Porokeratosis
- Benign glandular adnexal tumor that usually originates from cells of the outer layer of the acrosyringium and terminal eccrine duct
- Has both eccrine and apocrine origin (AMA Arch Derm 1956;74:511)
- Malignant counterpart is referred to as porocarcinoma
- Single, slow growing, asymptomatic, well circumscribed, smooth, skin colored to red, slightly scaly papule or nodule
- Most commonly on palms and sole or sides of the foot
- Well circumscribed broad anastomosing bands of poroma cells with sharp demarcation from adjacent keratinocytes
- Excellent prognosis with simple excision
- Eccrine poroma / hidroacanthoma simplex / dermal duct tumor, apocrine poroma
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
- M = F (Arch Craniofac Surg 2017;18:44)
- Most commonly affects adults (Ann Dermatol 2011;23:250)
- Presentation in childhood and congenital onset are unusual (J Eur Acad Dermatol Venereol 2008;22:366)
- Eccrine porocarcinoma:
- Also known as malignant eccrine poroma
- Develops after several years from a pre-existing poroma
- Most commonly affects elderly, with F > M
- Tumors are often ulcerated and many bleed on trauma
- Most commonly on palms and sole or sides of the foot (AMA Arch Derm 1956;74:511)
- Occasionally on the head, neck, scalp, chest, abdomen, proximal extremities and the external auditory canal (J Am Acad Dermatol 2001;44:48, Otolaryngol Head Neck Surg 2003;128:439)
- Falls under the broad category of poroid neoplasms or acrospiromas
- Poroid neoplasms include the eccrine poroma, apocrine poroma, hidroacanthoma simplex and dermal duct tumor (Clin Exp Dermatol 2014;39:119)
- Eccrine poroma: derived from cells of the outer layer of the acrosyringium and the upper dermal eccrine duct, both epidermal and dermal (AMA Arch Derm 1956;74:511)
- Apocrine poroma: reflects the common embryological ancestry of the 3 units (the folliculosebaceous apocrine unit) (Pathologe 2014;35:456)
- Exact etiology is unknown (World J Surg Oncol 2011;9:94)
- No family predilection has been identified for the development of poromas
- Rare cases are associated with radiation therapy or chronic scarring (J Eur Acad Dermatol Venereol 2007;21:1128, Am J Dermatopathol 2013;35:615)
- Asymptomatic, slow growing, solitary, sessile, skin colored to red, slightly scaly nodule, papule or plaque (Int J Dermatol 2014;53:1053)
- Less commonly pigmented or pedunculated (J Dermatol 1990;17:555)
- Occasionally reported with Bowen disease, pregnancy and hypohidrotic ectodermal dysplasia (Ann Dermatol 2018;30:222, Arch Dermatol 1977;113:472)
- Rarely reported as arising within nevus sebaceous (Case Rep Dermatol 2016;8:80)
- Rarely, multiple poromas known as poromatosis can occur following chemotherapy or radiotherapy (Ann Dermatol 2020;32:422)
- Dermoscopic findings: white interlacing areas around vessels, yellow structureless areas, milky red globules, poorly visualized vessels and branched vessels with rounded endings (J Eur Acad Dermatol Venereol 2018;32:1263, Clin Case Rep 2021;9:1601)
- Clinical appearance confirmed by characteristic histologic findings
- Excellent; most cases do not show aggressive behavior
- Rarely progresses to porocarcinoma (World J Surg Oncol 2011;9:94)
- Poromatosis is of cosmetic concern for the patient (Skin Appendage Disord 2015;1:95)
- 40 year old woman with an asymptomatic red to brown colored hemorrhagic crusted nodule on the left forearm (Ann Dermatol 2011;23:250)
- 58 year old man had painless, progressive mass below the left temporal eyebrow for 8 years (Indian J Ophthalmol 2020;68:2522)
- 64 year old man with papules near his left nipple and left ankle (Dermatol Online J 2008;14:3)
- 67 year old man initially presented with a nonpainful, exophytic and pigmented lesion on scalp (Am J Case Rep 2019;20:179)
- 70 year old nondiabetic man presented with mass over the medial aspect of his right upper eyelid (Indian J Ophthalmol 2019;67:131)
- 74 year old man with a 4 year history of nodules on the chest and back (An Bras Dermatol 2017;92:550)
- No treatment is necessary
- Simple excision with shave or electrosurgical destruction is curative
- Reference: StatPearls: Poroma [Accessed 30 September 2021]
- Solitary, well circumscribed, smooth, pink to red papule, nodule or plaque (Int J Dermatol 2014;53:1053)
- Eccrine poroma:
- Well circumscribed
- Replaces the epidermis and extends into the dermis in broad anastomosing bands
- Poroma cells are monomorphic, small, cuboidal with basophilic round nuclei, inconspicuous nucleoli and compact eosinophilic cytoplasm
- Sharp demarcation present between the normal keratinocytes and poroma cells
- Devoid of peripheral palisading
- Ductal lumina with single row of luminal cells covered by eosinophilic lining or cystic spaces devoid of any formal lining
- Cells are united by conspicuous intercellular bridges and supported by a delicate fibrovascular stroma (J Dermatol 1980;7:263)
- Poroma cells usually contain glycogen (Int J Dermatol 2014;53:1053)
- Occasionally, pigmented variants with associated dendritic melanocytes and tumor cell melanin deposition (J Dermatol 2010;37:542, J Eur Acad Dermatol Venereol 2008;22:303)
- Dystrophic calcification and transepidermal elimination of tumor nests are exceptional findings (J Dermatol Case Rep 2009;3:38, J Dermatol 1997;24:539)
- Apocrine poroma:
- Shows sebaceous differentiation with the occasional presence of follicular differentiation and foci of apocrine-like features (J Cutan Pathol 2001;28:101)
- Anastomosing trabeculae, displaying multiple points of origin from the epidermis and located largely in the papillary and upper reticular dermis
- Cells are small and uniform with scanty cytoplasm and round to oval nuclei united by inconspicuous intercellular bridges
- Foci of ductal differentiation with a well developed eosinophilic cuticle
- Follicular differentiation in the form of epithelial lobules (Am J Dermatopathol 1999;21:31)
- Sebaceous cells, singly and in clusters with bubbly cytoplasm and crenated nuclei is an infrequent feature (Am J Dermatopathol 1996;18:1)
- Eccrine porocarcinoma:
- May remain completely intraepidermal (in situ porocarcinoma) but is more often associated with an invasive dermal component
- Poroma cells, with typical ductal lumina, associated with cytological features of malignancy, including nuclear and cytoplasmic pleomorphism, nuclear hyperchromatism and mitotic activity (Am J Surg Pathol 2001;25:710)
- Prone to have local recurrence (17%) and is occasionally associated with nodal metastases (19%); however, systemic spread is rare (11%) (Am J Surg Pathol 2001;25:710)
- CK5/6, CK7, EMA, CEA, CAM5.2, CD117, diastase PAS (J Cutan Pathol 1999;26:232)
- S100 protein in the diagnoses of recurrent and metastatic dedifferentiated eccrine porocarcinoma (Ann Dermatol 2013;25:348)
- BerEP4, S100 (benign poroma) (Recent Results Cancer Res 1995;139:303)
- Cells have numerous connecting desmosomes, cytoplasmic tonofilaments, glycogen granules and intracytoplasmic lumina (J Dermatol 1980;7:263)
- p53 expression is a feature of both poroma and porocarcinoma (Am J Dermatopathol 2001;23:402)
- p16 overexpression is only seen in porocarcinoma (J Cutan Pathol 2019;46:659)
- Skin, left palm, excision:
- Eccrine poroma, extending to the deep margin
- Hidroacanthoma simplex:
- Entirely intraepidermal
- Discrete circumscribed populations of poroma cells within an irregularly acanthotic epidermis
- Dermal duct tumor:
- Entirely intradermal, the epidermis is unaffected
- Large lobules of uniform poroma cells in the mid and lower dermis
- Basal cell carcinoma:
- Squamous cell carcinoma (SCC):
- Lacks evidence of ductal differentiation
- Squamous differentiation abundant, eosinophilic cytoplasm with keratin pearls, intercellular bridges and keratinization
- Greater cytologic atypia, dyskeratotic cells
- Irritated / clonal seborrheic keratosis (SK):
- Shows follicular differentiation with keratinizing pseudohorn cysts, no ductal differentiation
- Cells are typically larger than in poroma
- Hidradenoma:
- Nests and nodules of epithelial cells lacking epidermal connection
- Shows both solid and cystic components
- More commonly shows clear cell features
- Eccrine syringofibroadenoma:
- Benign eccrine proliferation
- Thin anastomosing reticulated cords and strands of basaloid monomorphous cuboidal cells extending from the basal layer of epidermis into dermis
- Loose fibrovascular stroma
- Glomerular
- Hairpin
- Mosaic
- Hairpin and glomerular
- Hairpin and mosaic
Comment Here
Reference: Poroma
Which of the following is true about eccrine poroma?
- Most commonly occurs on central part of the body: frontal scalp, anterior chest and around umbilicus
- No distinct demarcation between the poroma cells and adjacent keratinocytes
- Presence of monomorphic, basaloid cells with peripheral palisading
- Presence of sheets and trabeculae of monomorphic, round basophilic cells containing scattered duct-like structures
Comment Here
Reference: Poroma
- Primary cutaneous lymphoma composed of large cells with an anaplastic, pleomorphic or immunoblastic cytomorphology with > 75% malignant cells positive for CD30 (Am J Dermatopathol 2017;39:877, Elder: WHO Classification of Skin Tumours, 4th Edition, 2018)
- Primary cutaneous lymphoma composed of large cells with an anaplastic, pleomorphic or immunoblastic cytomorphology with > 75% malignant cells positive for CD30 (Am J Dermatopathol 2017;39:877, Elder: WHO Classification of Skin Tumours, 4th Edition, 2018)
- 80% of cases present as a cutaneous localized nodule or papule with or without ulceration (Pathology 2020;52:100)
- Diffuse dermal infiltrates with cohesive sheets of tumor cells with anaplastic morphology (round to irregularly shaped nuclei, prominent eosinophilic nucleoli and abundant cytoplasm); nonanaplastic appearance (pleomorphic or immunoblastic) is seen in 20% of cases (Pathology 2020;52:100, Am J Dermatopathol 2017;39:877)
- Primary cutaneous anaplastic large cell lymphoma is included under the umbrella term CD30+ T cell lymphoproliferative disorders (Am J Dermatopathol 2017;39:877)
- ICD-O: 9718/3 - primary cutaneous anaplastic large cell lymphoma
- 25 - 30% of primary cutaneous lymphomas; second most common type of cutaneous T cell lymphoma (J Cutan Pathol 2017;44:570)
- M:F = 2:1 - 3:1 (Am J Dermatopathol 2017;39:877, Elder: WHO Classification of Skin Tumours, 4th Edition, 2018)
- Median age: 60 years (J Cutan Pathol 2017;44:570)
- Pediatric and congenital cases are rare (Am J Dermatopathol 2015;37:398)
- Common sites: face, trunk and extremities (J Am Acad Dermatol 2016;74:1135, J Cutan Pathol 2017;44:570)
- Leg involvement is associated with extensive and multiple skin lesions
- 80% of cases present as a cutaneous localized nodule or papule with or without ulceration (Pathology 2020;52:100)
- Multifocal lesions in 20% of cases (Blood 2000;95:3653)
- Extra cutaneous dissemination (mainly to regional lymph nodes) in 10% of cases (Blood 2000;95:3653)
- Skin lesions can regress spontaneously or can progress or relapse (Blood 2000;95:3653)
- Prognosis is similar for patients with localized or multifocal skin lesions: 90% 10 year overall survival (Blood 2000;95:3653, J Am Acad Dermatol 2003;49:1049)
- 10 day old neonate with congenital primary cutaneous anaplastic large cell lymphoma (Am J Dermatopathol 2015;37:398)
- 18 year old man with primary cutaneous anaplastic large cell lymphoma (J Cancer Res Ther 2015;11:656)
- 8 men, age 46 and older, with primary cutaneous anaplastic large cell lymphoma small cell variant (Am J Dermatopathol 2017;39:877)
- 73 year old man with tumor in parotideomasseteric region initially diagnosed as discoid lupus (Medicine (Baltimore) 2018;97:e9645)
- 81 year old cardiac transplant recipient with primary cutaneous anaplastic large cell lymphoma (Am J Dermatopathol 2016;38:461)
- Radiation or chemotherapy, alone or combined (Arch Craniofac Surg 2019;20:207)
- Excision plus radiotherapy for solitary nodules
- Low dose methotrexate (5 - 20 mg/wk) for multifocal lesions (Arch Craniofac Surg 2019;20:207)
- Brentuximab vedotin (anti-CD30) for refractory cases (Arch Craniofac Surg 2019;20:207)
- Skin nodule with or without ulceration (J Am Acad Dermatol 2016;74:1135, J Cutan Pathol 2017;44:570)
- Diffuse dermal infiltrates with cohesive sheets of tumor cells with anaplastic morphology (round to irregularly shaped nuclei, prominent eosinophilic nucleoli and abundant cytoplasm); nonanaplastic appearance (pleomorphic or immunoblastic) is seen in 20% of cases (Pathology 2020;52:100, Am J Dermatopathol 2017;39:877)
- Epidermotropism is marked in cases with DUSP22-IRF4 rearrangement (Histopathology 2015;66:846)
- Cerebriform lymphocytes are not identified
- Variable degrees of inflammatory infiltrate, reactive lymphocytes are common in the periphery of the lesions (Br J Dermatol 2003;148:580)
- Ulcerated lesions may have lymphomatoid papulosis-like histology with abundant reactive T cells, histocytes, eosinophils, neutrophils and a low number of CD30+ cells (Am J Surg Pathol 2014;38:1203; J Cutan Pathol 2015;42:610)
- CD30 in more than 75% of neoplastic cells (Am J Dermatopathol 2017;39:877, Elder: WHO Classification of Skin Tumours, 4th Edition, 2018)
- Activated CD4 T cell immunophenotype (J Cutan Pathol 2017;44:570)
- CD45 (J Cutan Pathol 2017;44:570)
- Cytotoxic proteins: granzyme B, TIA1 and perforin (J Cutan Pathol 2017;44:570)
- CD15 (~40%) (Br J Dermatol 2009;161:121)
- Variable loss of CD2, CD5, CD7 and CD3 (J Invest Dermatol 1997;109:636)
- CD8 usually negative but can be CD4-/CD8+ or CD4+/CD8+ (Am J Dermatopathol 2014;36:153)
- EMA and ALK (J Clin Pathol 2000;53:445)
- CD56 (J Cutan Pathol 2000;27:392)
- Clonal TRB or TRG rearrangements in > 90% (J Cutan Pathol 2017;44:570)
- Rearrangements of:
- DUSP22-IRF4 locus in 6p25.3 in 20 - 57% (J Invest Dermatol 2010;130:816)
- NPM1-TYK2 in ~5% (Blood 2014;124:3768)
- Rare case with translocations involving ALK gene at 2p23 (Histopathology 2015;66:846)
- Chromosomal imbalances (J Invest Dermatol 2010;130:563):
- Gains in 7q, 17q, 21
- Losses in 3p, 6q, 8p, 13q
- Skin, punch biopsy:
- CD30 lymphoproliferative disorder, mostly consistent with cutaneous ALK- anaplastic large cell lymphoma, in the appropriate clinical context (see comment)
- Comment: The section shows an extensive dermal infiltrate composed predominantly of medium to large sized lymphocytes and admixed neutrophils and histiocytes. Scattered mitotic figures are noted. There is epidermal ulceration and extensive neutrophilic serum crust that prevents the evaluation of epidermotropism. Immunohistochemical studies show that the large lymphoid cells are diffusely positive for CD30. CD3 and CD20 label a mixed population of T and B small lymphocytes in the background; the large cells are only focally positive for CD3 and are negative for CD20. The large cells are also partially positive for CD4, while CD8 highlights very rare background lymphocytes. TCR beta labels background lymphocytes while TCR gamma is essentially negative. CD56, EBER and ALK1 are negative.
- Lymphomatoid papulosis (LyP) type C
- Multiple lesions arranged in crops < 10 mm with history of regression favor lymphomatoid papulosis
- Large cell transformation of mycosis fungoides
- Clinical history characteristic of mycosis fungoides: patches, plaques, tumors
- Look for typical features of mycosis fungoides at margins of lesion
- Often IHC positive for pan T cell antigens but negative for CD7
- Systemic ALK- anaplastic large cell lymphoma with cutaneous involvement
- Peripheral lymph nodes affected
- Systemic ALK+ anaplastic large cell lymphoma with cutaneous involvement
- Peripheral T cell lymphoma NOS with cutaneous involvement
- B symptoms and evidence of disseminated disease
- Usually spares epidermis
- IHC: CD30-, CLA-
- Subcutaneous panniculitis-like T cell lymphoma
- Primary cutaneous gamma-delta T cell lymphoma
- Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma
- Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder
- Primary cutaneous large B cell lymphoma (PCLBCL) composed exclusively of centroblasts and immunoblasts, typically arising in the leg
- Aggressive B cell neoplasm predominantly affecting older women
- Histologic evaluation shows large neoplastic B cell lymphoma composed exclusively of centroblasts and immunoblasts
- Neoplastic cells are positive for CD20, CD79a, strong staining for MUM1 and BCL2, while negative for CD10 and EBER
- Treatment involves R-CHOP (rituximab, cyclophosphamide, hydroxydaunomycin, oncovin, prednisone) or local radiotherapy (solitary lesions)
- 2.6% of all primary cutaneous lymphomas, 20% of all primary cutaneous B cell lymphomas (Arch Dermatol 2007;143:1144)
- M:F = 1:3 (Blood 2019;133:1703)
- Elderly patients, median age is seventh decade of life (Blood 2009;113:5064)
- To date, no reported cases in children (Semin Diagn Pathol 2017;34:85)
- Unilateral lower limb (80% of cases) (Blood 2019;133:1703)
- 2.0 - 5.0 cm, erythematous to violaceous nodules (Int J Radiat Oncol Biol Phys 2013;87:719)
- Up to 12% of cases arise at other sites, such as the CNS (Blood 2005;106:2491, J Eur Acad Dermatol Venereol 2016;30:186)
- Not clearly understood
- B cells undergo aberrant somatic hypermutation; process of affinity maturation of immunoglobulins by somatic hypermutation in regions of the genome that do not encode immunoglobulin genes
- May occur in oncogene containing gene loci
- Loss of high fidelity DNA repair mechanisms
- Not clearly understood
- Arises de novo
- Predisposing factors:
- Chronic antigenic stimulation by viral and bacterial infections
- Possible association:
- Hepatitis C virus (HCV) (An Bras Dermatol 2015;90:687)
- Clinically aggressive with a high rate of relapse or dissemination
- Recurrence in 55 - 70% of patients (Semin Diagn Pathol 2017;34:85)
- 5 year overall survival is 50 - 60% (Blood 2019;133:1703)
- Extensive clinical history (e.g. presence of B symptoms, fever, weight loss, etc.)
- Thorough physical examination
- Tissue biopsy of skin lesion with ancillary testing (flow cytometry, FISH, mutation next generation sequencing studies)
- Complete blood count with differential (CBC w/ diff):
- Lymphocytosis, atypical lymphocytes (if leukemic involvement)
- Comprehensive blood chemistry (CMP)
- Including liver and kidney analysis
- Lactate dehydrogenase (LDH):
- Elevated (indicator of tumor lysis)
- Serum Beta2 microglobulin:
- Variable (indicator of tumor mass) (An Bras Dermatol 2015;90:687)
- FDG avid and hypermetabolic subcutaneous nodules on FDG-PET imaging (Clin Nucl Med 2016;41:65)
- Unfavorable prognosis:
- Multiple skin lesions at diagnosis
- Loss of CDKN2A and CDKN2B gene loci on chromosome 9p21.3 due to promotor methylation or gene deletion (up to 67% of cases)
- MYD88 L265P mutation (Am J Surg Pathol 2018;42:1488)
- Favorable prognosis:
- Solitary skin lesion at diagnosis
- Addition of rituximab to CHOP regimen
- 41 year old woman with longstanding history of systemic lupus erythematosus presents with an enlarging, well demarcated 3 x 2 cm firm, multilobed, red violaceous, nontender nodule over the left shoulder (J Cutan Med Surg 2016;20:579)
- 72 year old woman with a solitary, 3 cm upper arm nodule for 1 month duration (J Dermatol 2017;44:608)
- 74 year old woman presenting with a painful, left lower leg lesion that was enlarging over 5 months (Cutis 2018;102:E31)
- 82 year old woman with asymptomatic, growing lesions over the past year (Actas Dermosifiliogr 2014;105:78)
- 83 year old man with history of pleomorphic sarcoma treated with radiotherapy, presents with a large, partially ulcerated cutaneous lesion in the region of prior radiation (J Gen Intern Med 2015;30:371)
- 85 year old woman with disseminated solid nodularities (1 - 2 cm) on the face and upper extremities (Am J Dermatopathol 2017;39:e44)
- Local radiation or surgery for solitary lesions (Dermatol Clin 2015;33:835)
- R-CHOP: rituximab, cyclophosphamide, hydroxydaunomycin, oncovin, prednisone
- Bortezomib (NFkB inhibitor)
- Ibrutinib (oral tyrosine kinase pathway inhibitor)
- Superficial and deep dermal involvement by intermediate to large, monotonous, diffuse sheets of centroblasts (round, noncleaved nuclei with vesicular chromatin and one to multiple small nucleoli) and immunoblasts (large, oval nuclei with vesicular chromatin and one prominent nucleolus) (Semin Diagn Pathol 2017;34:85)
- Epidermis spared (may be ulcerated)
- Brisk mitotic activity frequently seen (Histopathology 2019;74:1067)
- Apoptosis, karyorrhexis, cytoplasmic fragments (Am J Surg Pathol 2018;42:1488)
- Small B cells and follicular dendritic cell meshworks (CD21+ / CD35+) are often absent
- Rare reactive, perivascular T cells may be present
- Neoplastic B cells resemble normal B cells that give rise to them
- Centroblasts and immunoblasts cells
- Similar gene expression profile as DLBCL, activated B cell-like type (Blood 2005;105:3671)
- Interface FISH: translocation of IGH genes with MYC or BCL6
- DNA amplification of 18q21.31-21.33, including BCL2 and MALT1 genes, are identified in 67% of cases by array comparative genomic hybridization and FISH (J Clin Oncol 2006;24:296)
- Loss of CDKN2A and CDKN2B gene loci on chromosome 9p21.3 due to promoter methylation or gene deletion (up to 67% of cases)
- Other mutations: MYD88 L265P (60%), TNFAIP3 (40%), CD79B (20%), CARD11 (10%)
- Left thigh, biopsy:
- Primary cutaneous diffuse large B cell lymphoma, leg type; nongerminal center, double expressing (BCL2+ MYC+) involving superficial and deep dermis
- Microscopic description and additional studies:
- H&E sections reveal diffuse sheets of an atypical lymphocyte population infiltrating the dermis while sparing the epidermis. The atypical cells are medium to large in size with moderate amount of cytoplasm, enlarged round nuclei with vesicular chromatin. Some cells show a single prominent nucleolus (immunoblasts-like) while others display multiple smaller nucleoli (centroblasts-like). Brisk mitotic activity is noted (up to 4/hpf). No areas of geographic necrosis is present. No granulomas seen on sections examined.
- Immunochemistry show atypical large lymphoid cells are positive for CD45 (LCA), CD20, CD79a, MUM1, BCL6, BCL2 (> 95%), MYC (weak 40%), MIB1/Ki67 proliferative fraction of 80 - 90% while negative for CD3, CD10, P53 (< 3%), CD99, CD30 (< 1%), CHR, KER903, S100, TTF1, CK20, SYNAP.
- In situ hybridization for EBV encoded viral RNA (EBER) is NEGATIVE.
- PAS, GMS and AFB stains are negative for microorganisms.
- Karyotype: nuc ish(BCL6x2),(D8Z2x2)(MYC,IGH)x3(MYC con IGHx2),(IGHx3,BCL2x2),(MYCx2)(5'MYC sep 3'MYCx1).
- Report: Multiplex FISH x4 was performed on paraffin embedded tissue: nuc ish(BCL6x2) [191/200], (D8Z2x2)(MYC,IGH)x3(MYC con IGHx2) [130/200], (IGHx3,BCL2x2) [123/200], (MYCx2)(5'MYC sep 3'MYCx1) [124/200].
- Interpretation: Interphase FISH results are consistent with a 65% of cells showing MYC-IGH [t(8;14)] fusion POSITIVE signal pattern. Cells were IGH-BCL2 fusion negative and BCL6 (3q27) gene rearrangement was NOT detected. Although the hallmark of Burkitt lymphoma is the presence of MYC-IGH rearrangement, approximately 10% of DLBCL cases will contain a MYC rearrangement and an aggressive clinical course (Arch Pathol Lab Med 2015;139:602).
- Next generation mutation studies show:
- Biomarker findings
- Microsatellite status - MS-stable
- Tumor mutational burden - TMB-intermediate (7 Muts/Mb)
- CDKN2A/B loss
- ETV6 rearrangement exon 4
- MED12 R817H
- MLL2 H313fs*20
- MYD88 L265P
- PRDM1 splice site 291+1G > T
- Primary cutaneous follicle center lymphoma:
- Marginal zone lymphoma:
- Mantle cell lymphoma, blastoid variant:
- Primary cutaneous T cell lymphoma:
- EBV+ large B cell lymphomas of skin:
- Positive for EBV
- Lymphomatoid granulomatosis (LyG):
- Positive for EBV
- Plasmablastic lymphoma:
- Positive for EBV, may lack B cell markers
- Intravascular DLBCL:
- Intravascular neoplastic cells rather than diffuse infiltration
- Skin involvement of B cell acute lymphoblastic lymphoma (B-ALL):
- Venous leg ulcers:
- Lower extremity ulcerated lesions with mixed inflammatory infiltrate, no evidence of clonality
- Granuloma annulare:
- Dermal lymphophistiocytic infiltrate with mucin deposition, no overlying skin changes, associated with diabetes
- Necrobiosis lipoidica:
- Palisading, necrobiotic granuloma with histiocytes, eosinophils and giant cells in dermis and subcutaneous fat, plasma cells almost always present
- Sarcoidosis:
- Nonnecrotizing granulomatous reaction with lymphocytes, eosinophils and plasma cells
- Erythema nodosum:
- Perivascular and periadnexal inflammatory infiltrate (lymphocytes, histiocytes, neutrophils) with nonnecrotizing granulomatous inflammation (giant cells)
- Lupus erythematosus
- Leprosy (lepromatous):
- Macrophage localized in ill defined dermal aggregates, few lymphocytes, caused by Mycobacterium leprae
- Drug reaction
- A 78 year old woman with no known clinical history presents with a solitary, violaceous, 4.3 cm papule on her left shin. Patient denies any history of recent travel, allergies or sexually transmitted infections. Biopsy reveals sheets of large round cells with vesicular chromatin and 1 to multiple prominent nucleoli infiltrating the dermis. The tumor cells are positive for CD20, MUM1 and BCL6, while negative for EBV, CD4, CD5, CD30 and ALK. What additional immunohistochemical stain will help differentiating this diagnosis from primary cutaneous follicle center lymphoma?
- BCL1 (cyclin D1)
- BCL2
- CD19
- CD23
- CD79a
Comment Here
Reference: Diffuse large B cell lymphoma - leg
- Which of the following factors can be used as a predictor of an unfavorable prognosis for the above lymphoma entity?
- EBV positivity
- Gender
- Lack of MYD88 L265P mutation
- Presence of multifocal lesions
- Presence of t(14;18)(q32;q21) translocation
- Low grade B cell lymphoma arising in skin composed of follicular center B cells without evidence of systemic / nodal involvement at the time of diagnosis
- Mainly centrocytes; predominantly large centrocytes
- Follicular, diffuse or follicular and diffuse growth pattern
- Presence of monoclonal B cells in the right clinical and pathologic context can support a diagnosis of primary cutaneous follicle center lymphoma (PCFCL)
- Diffuse growth of centroblasts and immunoblasts excludes this diagnosis
- Clinically and genetically distinct from nodal follicular lymphoma
- Obsolete names include reticulohistiocytoma of the dorsum and Crosti lymphoma (J Am Acad Dermatol 1988;19:259)
- ~10% of all primary cutaneous lymphomas
- Most common (~50%) type of primary cutaneous B cell lymphomas
- Middle aged adults (i.e. 50 - 60 years)
- M:F = ~1.5:1
- Reference: Blood 2005;105:3768
- Mainly head or trunk (Int J Radiat Oncol Biol Phys 2013;87:719, J Clin Oncol 2007;25:1581)
- No definitive risk factors identified and no identified hereditary predisposition (StatPearls: Primary Cutaneous Follicle Center Lymphoma [Accessed 7 June 2021])
- Low grade lymphoma of follicle center B cells
- No systemic or nodal involvement at diagnosis
- Reference: Arch Pathol Lab Med 2018;142:1313
Table 1: differential diagnosis of primary cutaneous follicle center B cell lymphoma
| Criteria | Primary cutaneous follicle center lymphoma (PCFCL) | Secondary follicular lymphoma | Primary cutaneous marginal zone lymphoma | Primary cutaneous diffuse large B cell lymphoma, leg type |
| Age | 50 - 60 years | ~60 years | ~55 years | 70 years |
| Gender | M > F | M > F | M > F | F > M |
| Stage | Low (I - II) | High (III - IV) in majority of cases | Low, limited to skin | Low to high |
| Most common location | Head and neck | Variable | Trunk, arms or head | Lower leg(s) |
| Extracutaneous spread | Absent | Present, variable | Rare (< 10%) | Present, ~30% |
| Histology | Mixture of centrocytes and centroblasts (no grading required) in follicular, follicular and diffuse or diffuse growth patterns; background fibrosis and sclerosis with stromal reaction present | Mixture of centrocytes and centroblasts in follicles (grading based on number of centroblasts); background fibrosis and sclerosis with stromal reaction present | Polymorphous: small lymphocytes, small to medium sized marginal zone (centrocyte-like) cells with pale cytoplasm, lymphoplasmacytic cells, plasma cells and occasional large, transformed lymphoid cells | Centroblasts or immunoblasts (large noncleaved cells) in diffuse growth pattern; no background stromal reaction |
| BCL2 (IHC) | Negative to weak positive | Usually positive | Usually positive | Positive |
| CD10 | Positive in follicular pattern (< 25%); negative in diffuse pattern | Positive (usually) | Negative | Negative |
| BCL6 (IHC) | Positive (~100%) | Positive (usually) | Negative | Positive or negative |
| Ki67 | Variable, usually > 30% | Low (except for high grade) | ||
| BCL2 rearrangement / t(14;18) | Absent (10 - 40% can be positive) | Positive (~85%) | Absent | Present (~50%) |
| BCL6 or MYC rearrangements | Absent | Variably present | Rare cases with BCL6 rearrangement | BCL6 (30%), MYC (30%) |
| Cytogenetic findings | Deletion of 14q32.33; c-REL amplifications (~60%) | Complex |
| Inactivation / deletion of CDKN2a (9p21.3) & CDKN2B genes, deletion of 6q arm (BLIMP1; 60%) |
| Molecular findings | Mutations in any chromatin modifying genes (CREBBP, EZH2, KMT2D, EP300) are seen in < 10% of cases; gene expression profiling similar to germinal center B cell-like type DLBCL | Mutations in any chromatin modifying genes (CREBBP, EZH2, KMT2D, EP300) are common | MYD88 (6%), FAS (63%), SLAMF1 (24%), SPEN (18%) and NCOR2 (13%) | MYD88 (60%), CD79B (20%), CARD11 (10%), TNFAIP3 / A20 (40%); gene expression profiling similar to activated B cell-like type |
| Prognosis | Favorable, 95% at 5 years (disease free survival) | Variable, 20 - 75% at 5 years | 95 - 100% at 5 years | Variable, ~50% at 5 years |
- Single, raised nodule or plaque
- Satellite lesions in a localized area are common
- ~15% of patients have multifocal lesions
- Commonly scalp, forehead or trunk
- ~5% of patients present with lesions on the leg
- Intact epidermis
- Mildly erythematous
- References: J Clin Oncol 1999;17:2471, StatPearls: Primary Cutaneous Follicle Center Lymphoma [Accessed 7 June 2021], Blood 2000;95:3922
- Diagnosis made by:
- Histology and immunohistochemical evaluation of a skin biopsy
- Lymphoma involving the dermis, with follicular to diffuse growth pattern
- Mixture of centrocytes and centroblasts
- Histology and immunohistochemical evaluation of a skin biopsy
- Diagnosis is supported by:
- Flow cytometry immunophenotyping, if performed
- Immunoglobulin heavy / light chain gene rearrangement studies, if performed
- Reference: StatPearls: Primary Cutaneous Follicle Center Lymphoma [Accessed 7 June 2021]
- PET / CT: negative for lymphadenopathy
- Dissemination to extracutaneous sites is uncommon (< 10% of patients) (J Clin Oncol 2006;24:1376)
- Excellent prognosis
- 5 year survival rate of > 95%
- Cutaneous relapses after initial treatment: ~30% of patients
- If left untreated, the skin lesions gradually increase in size over years but dissemination to extracutaneous sites is uncommon (< 10%)
- Prognosis is good regardless of:
- Growth pattern (follicular or diffuse)
- Number of centroblasts / immunoblasts
- Presence or absence of t(14;18) and BCL2 expression
- Presence of either localized or multifocal skin disease
- Cutaneous relapse (J Clin Oncol 2007;25:1581, Blood 2008;11:1600, Int J Radiat Oncol Biol Phys 2015;92:32)
- Additional references: J Clin Oncol 2006;24:1376, J Clin Oncol 2007;25:1581
- 16 year old girl with primary cutaneous follicle center lymphoma (J Cutan Pathol 2021;48:663)
- 40 year old man who presented with a scalp mass (Am J Case Rep 2019;20:1273)
- 77 year old woman favored to represent primary cutaneous marginal zone lymphoma on an initial punch biopsy and PCFCL with extensive plasmacytic differentiation (J Cutan Pathol 2021 Mar 31 [Epub ahead of print])
- Single cutaneous lesion
- Local therapy with:
- Either surgical excision or local radiation
- In case of cutaneous relapse: radiotherapy
- Generalized skin lesions:
- Systemic intralesional administration of rituximab or systemic rituximab
- Local therapy with:
- Reference: Blood 2008;11:1600
- Infiltrate is based in the superficial dermis:
- Lymphoma may involve the entire dermis
- Often follicles of the tumor extending into the subcutis
- Perivascular, periadnexal, nodular and diffuse infiltrates
- Follicles are ill defined; lack tingible body macrophages and mantle zone
- Intact grenz zone
- Growth pattern varies:
- Follicular (mainly head and neck)
- Follicular and diffuse
- Purely diffuse (primarily trunk)
- Mixture of centrocytes and centroblasts
- Large cells are variable and can be polylobated
- Predominance of large centrocytes (large cleaved cells), may be spindle shaped
- Variable numbers of centroblasts
- T cells are abundant
- No WHO grading of lymphoma required as in nodal / systemic follicular lymphoma
- Reference: Arch Pathol Lab Med 2018;142:1313
- Cells resembling centrocytes and centroblasts (Jaffe: Hematopathology, 2nd Edition, 2016)
- Large centrocytes: dispersed chromatin and small nucleoli
- Large noncleaved cells: prominent and paracentral nucleoli
- CD10 is positive in < 25% of cases
- Positive in follicular pattern and usually negative in diffuse pattern (J Clin Oncol 2007;25:1581)
- BCL2 (usually negative but may show faint staining in a minority of neoplastic cells) (J Clin Oncol 2007;25:1581)
- Expression of BCL2 in > 50% of the neoplastic B cells: 11% of cases
- Combination of positive staining for both BCL2 and CD10 highly suggests secondary skin involvement by follicular lymphoma (Mod Pathol 2020;33:96)
- CD5 and T cell markers
- IRF4 / MUM1
- FOXP1
- CD43
- Restricted light chain expression in ~75% of cases (Am J Dermatopathol 2014;36:781)
- Similar gene expression profile as germinal center B cell subtype DLBCL
- Clonally rearranged immunoglobulin heavy and light chain genes
- BCL2 rearrangement or t(14;18): generally absent but can be positive in 10 - 40% of cases (Blood Adv 2021;5:649, Hum Pathol 2020;106:93)
- A subset of PCFCLs have 1p36 deletion
- Amplification of REL is often seen
- Deletion of chromosome 14q32.33 is rare
- References: Arch Pathol Lab Med 2018;142:1313, J Clin Oncol 2006;24:296
- Skin, left cheek, biopsy
- Low grade follicular lymphoma involving skin (see comment)
- Comment: Histologic sections demonstrate skin involved by lymphoma. The lymphoma has a vague nodular pattern and is composed of a mixture of large noncleaved and small cleaved lymphoid cells with predominance of small lymphoid cells. The epidermis is unremarkable. No epidermotropism noted. Plasma cells are not increased. Immunohistochemical studies performed demonstrate that the neoplastic cells are positive for CD10, CD20, PAX5, BCL6 and are negative for BCL2, cyclin D1 and MUM1. CD3 and CD5 highlight small reactive lymphocytes in the background. Ki67 demonstrates a proliferation index of ~20%.
- In the appropriate clinical setting, this neoplasm involving the skin is consistent with primary cutaneous follicle center cell lymphoma. Clinical correlation and staging studies may help to confirm this diagnosis. If the neoplasm is systemic, this follicular lymphoma can be classified as low grade.
- Reactive follicular hyperplasia:
- Follicles are well defined
- Polymorphous infiltrate
- Presence of tingible body macrophages
- Intact mantle zone
- Polyclonal with molecular studies and flow cytometry
- Spontaneous resolution
- Secondary involvement by systemic / nodal follicular lymphoma (Am J Surg Pathol 2016;40:127):
- Clinical features: lymphadenopathy or B symptoms present
- Strong CD10 and BCL2 expression
- t(14;18) identified in most follicular lymphoma (> 75% of cases)
- Rearrangements of BCL6: more common in the systemic type of follicular lymphoma than PCFCL
- Common mutations in ≥ 1 of chromatin modifying genes including CREBBP, KMT2D, EZH2, EP300 and TNFRSF14 (immune modulation) genes
- Recent study identified 3 criteria (i.e., presence of BCL2 rearrangement, mutations in ≥ 2 of the chromatin modifying genes [CREBBP, KMT2D, EZH2 and EP300] and proliferation index [Ki67 < 30%]) that predict a high likelihood of concurrent / systemic follicular lymphoma (Blood Adv 2021;5:649)
- Primary cutaneous marginal zone lymphoma (PCMZL):
- With or without monocytoid lymphocytes in histopathology
- With or without Dutcher bodies
- Inside out appearance of follicles
- Germinal center cells are at the periphery of a B cell aggregate
- BCL6 and CD10 negative, BCL2 positive
- CD43+
- Monotypic light chain expression (especially in plasma cells)
- Mutations: FAS (63%), SLAMF1 (24%), SPEN (18%) and NCOR2 genes (13%)
- Primary cutaneous diffuse large B cell lymphoma, leg type:
- Most frequently located on lower extremities
- Sheets of the large cell (centroblasts and immunoblasts)
- Positive for BCL2, MUM1, IgM and FOXP1
- MYD88 mutations (~70%)
- Amplification of BCL2
- Rearrangements in MYC (30%) and BCL6 (rare cases)
- Loss in 9p21.3 (CDKN2A gene) in a large subset of cases (66% of cases)
- References: J Clin Oncol 2007;25:1581, Am J Surg Pathol 2010;34:1043, J Invest Dermatol 2017;137:2450, J Clin Oncol 2006;24:296, Blood 2019;133:1703
A 50 year old man presented with a solitary and erythematous lesion on the scalp for ~3 weeks. He does not recall any similar lesion(s) in the past. On physical exam, no splenomegaly or lymphadenopathy is noted. A skin biopsy is performed and a diagnosis of primary cutaneous follicle center B cell lymphoma is rendered. Which of the following statements regarding this lesion is most accurate?
- Deletions of a small region on chromosome 9p21.3 containing CDKN2A and CDKN2B gene loci are frequently reported
- They are generally BCL2 negative, have a good prognosis and do not require grading for prognosis
- Majority of these lesions have t(14;18) translocation or BCL2 gene rearrangement
- MYD88 mutation is frequently reported in this lesion
Comment Here
Reference: Primary cutaneous follicle center lymphoma
- CD20+, CD10-, BCL2+, BCL6+ with IGH-BCL2 gene rearrangement
- CD20+, CD10-, BCL2-, BCL6+with IGH-BCL2 gene rearrangement
- CD20+, CD10-, BCL2-, BCL6+ in the absence of IGH-BCL2 gene rearrangement
- CD20+, CD10+, BCL2+, BCL6+ with IGH-BCL2 gene rearrangement
- CD20+, CD10-, BCL2-, BCL6- in the absence of IGH-BCL2 gene rearrangement
Comment Here
Reference: Primary cutaneous follicle center lymphoma
- B cell lymphoma derived from mature, predominantly postgerminal center B cells
- Subsumed under the 2016 revised World Health Organization classification of extranodal marginal zone B cell lymphoma of mucosa associated lymphoid tissue (MALT lymphoma) (Blood 2016;127:2375)
- Nodule or coalescing papules on the torso or upper extremities; lesions are often localized
- Excellent overall survival with rare reports of transformation to a more aggressive phenotype
- Primary cutaneous marginal zone B cell lymphoma (CMZL) is an indolent lymphoma with a nonspecific postgerminal center B cell phenotype that often presents as coalescing papules or a nodule on the torso or upper extremity of middle aged adults
- Excellent prognosis, rarely disseminates beyond skin and exceptionally rare cases show progression to an aggressive blastic or large cell appearance
- Comprised of 2 subtypes with distinct histomorphologic findings, a nonclass switched subtype that shares many similarities with extracutaneous marginal zone lymphomas and a class switched subtype that may be accompanied by a preponderance of reactive T and B lymphocytes
- Colonization of germinal center follicles by lymphoma is a helpful feature for making the diagnosis; however, CMZL should never exhibit a germinal center immunophenotype and should not be comprised of large and mitotically active cells
- Demonstration of a light chain restriction by in situ hybridization (or immunohistochemistry) or a clonally rearranged immunoglobulin heavy chain gene by PCR is more common in CMZL than in reactive cutaneous lymphoid hyperplasias; however, clonality is not pathognomonic of lymphoma
- Extranodal marginal zone B cell lymphoma of mucosa associated lymphoid tissue (MALT lymphoma)
- C88.4: extranodal marginal zone B cell lymphoma of mucosa associated lymphoid tissue (MALT lymphoma)
- Young to middle aged men and women, rare childhood cases
- Approximately 30% of cutaneous B cell lymphoma
- Variable but most frequently involves the trunk and upper extremities
- Many lesions are solitary or localized / regional; generalized spread in a minority of cases
- Extracutaneous dissemination is exceptional and should raise suspicion for cutaneous dissemination of an extracutaneous lymphoma (e.g. of splenic or nodal origin)
- Etiology is poorly understood, although thought to evolve in the setting of cutaneous lymphoid hyperplasia resulting from a variety of antigenic triggers
- Chronic antigenic stimulation may lead to immune dysregulation (analogous to the role of chronic Helicobacter pylori infection in the pathogenesis of gastric MALT lymphoma) (J Cutan Pathol 1997;24:457)
- Two distinct subcategories
- Nonclass switched
- More closely resembles extracutaneous MZL in that it arises in the setting of chronic Th1 type inflammation with increased production of Th1 associated cytokines including IFNƴ and IL2 (Blood 2008;112:3355)
- Borrelia burgdorferi antigen has been identified in a subset of cases from Europe but not in cases from the U.S. or Japan (J Cutan Pathol 1997;24:457, Am J Surg Pathol 2000;24:1279)
- Heavy chain class switched
- Majority of cutaneous MZL, is histologically distinct from extracutaneous MZL and arises in the setting of chronic Th2 type inflammation
- May arise in individuals with an allergic or atopic diathesis (Am J Surg Pathol 2010;34:1830)
- Nonclass switched
- Some cases associated with medications including methotrexate, cyclosporine, antidepressants and antihistamines (J Cutan Pathol 2006;33:1)
- Infectious disease associations have also included Helicobacter pylori, Hepatitis C and Epstein Barr virus
- Autoimmune disease associations include polyarteritis nodosa, Sjögren syndrome, rheumatoid arthritis, Hashimoto thyroiditis and ulcerative colitis (Appl Immunohistochem Mol Morphol 2004;12:216)
- Recurrent mutations involving FAS that affected the death domain of the apoptosis regulating FAS / CD95 protein were recently identified in 24 of 38 cases (J Invest Dermatol 2018 Feb 23 [Epub ahead of print])
- Erythematous to violaceous nodule or plaque comprised of coalescing papules
- Clinical correlation (complete history, review of systems, physical examination, complete blood count and imaging studies) are required to exclude skin involvement by lymphoma of extracutaneous origin
- Serologic testing for Borrelia burgdorferi may be helpful for excluding reactive lymphoid hyperplasia within Europe (no demonstrable association between the organism and CMZL in U.S. or Japan)
- Excellent 5 year overall survival of > 95%
- Small minority (4%) experience dissemination beyond the skin (J Am Acad Dermatol 2013;69:357)
- Relapse occurs in less than half of patients and is more common in patients with multifocal skin involvement (J Am Acad Dermatol 2013;69:357)
- Rare cases undergo transformation to an aggressive, blastic or large cell phenotype analogous to what is reported in splenic B cell lymphoma (APMIS 2007;115:1426)
- 15 year old boy with a 3 cm erythematous plaque on the left forearm (J Cutan Pathol 2006;33:1)
- 33 year old man with chronic active hepatitis B and multiple cutaneous nodules (J Cutan Pathol 2011;38:342)
- 60 year old woman with nodules on both of her elbows (Dermatol Online J 2015;21:qt9s15929m)
- Excision, radiotherapy and intralesional steroids for skin limited localized disease
- Withdrawal of any agent associated with this disease, often an antihistamine or antidepressant, could also be considered
- In general, CMZL exhibits a nodular and diffuse architecture described as having a grenz zone and a bottom heavy appearance (no tapering with descent to the deep dermis and superficial subcutis)
- Neoplastic B cells can have 3 appearances
- Monocytoid appearance
- Cleaved nuclei reminiscent of centrocytes
- Small round cells reminiscent of CLL / SLL
- Plasma cells and plasmacytoid cells may be conspicuous at the periphery of dermal nodules
- Nonclass switched CMZL often has dense sheets and nodules filling the dermis
- Class switched CMZL often has a preponderance of T cells and reactive germinal B cell follicles accompanying the neoplastic B cell population, which ranges in appearance from dense nodules to perivascular infiltrates or sometimes sparse, scattered cells
- Class switched CMZL can show variable plasmacytic differentiation and extreme examples were formerly called immunocytoma (dense perivascular plasma cell aggregates and binucleated forms, nuclear pleomorphism and Dutcher bodies are helpful hints to this diagnosis)
- Kappa or lambda light chain restriction in plasma cells or plasmacytoid forms has greater sensitivity for the detection of B cell monoclonality in CMZL than PCR detection of clonal IGH rearrangement
- B cells most often exhibit a mature, postgerminal center immunophenotype
- CD20 (may not be detected in patients who have received rituximab)
- CD79a
- BCL2
- CD43 (not always expressed)
- Colonization of germinal center follicles by neoplastic B cells (lymphoma cells are present within former germinal center follicles delineated by CD21 positive follicular dendritic cell networks and may surround diminished germinal centers that express BCL6 and CD10)
- T cells can may outnumber B cells and show a preponderance of CD4 positive forms with numerous cells expressing T follicular helper markers (PD-1 and BCL6)
- CXCR3, while not necessary for diagnosis, is more likely to be expressed in nonclass switched CMZL (Th1 dominant) along with IgM (the same as extracutaneous MZL)
- CXCR3 is less likely to be expressed in class switched CMZL (Th2 dominant) along with IgG (most cases) and or other isotypes in a minority of cases (Blood 2008;112:3355)
- Clonal rearrangement of the immunoglobulin heavy chain supports the diagnosis; however, this test suffers from low sensitivity owing to the fact that a large proportion of the infiltrate can be comprised of reactive T and B cells
- Trisomy 3 is present in at least 60% (Blood 1995;85:2000) with trisomy 7, 12 and 18 in a smaller subset of cases
- Rare cases show t(11;18)(q21;q21) resulting in API2-MALT1 fusion
- Rare cases show t(14;18) involving IGH / BCL2 or IGH / MLT1 (Am J Surg Pathol 2003;27:702)
- Report of t(3;14) IGH - FOXP1 (Leukemia 2005;19:652)
- 7q deletions, which can also be seen in some splenic lymphomas, have been described in a subset of cases including ones that underwent transformation to an aggressive blastic phenotype (Am J Dermatopathol 2013;35:319)
- Skin, left upper chest, excision:
- Clonal B cell infiltrate, suspicious for cutaneous marginal zone lymphoma (see comment)
- Comment: The dense dermal infiltrate comprised of small, mature B cells colonizes germinal center follicles. In the provided context of a solitary nodule on the chest of an adult, the immunophenotype and evident lambda light chain restriction provide support for a diagnosis of primary cutaneous marginal zone lymphoma. Correlation with clinical features is essential in order to confirm this impression.
- Chronic lymphocytic leukemia / small lymphocytic lymphoma: CD5+ / CD23+
- Cutaneous lymphoid hyperplasia: clinical correlation helpful
- Does not usually have a bottom heavy infiltrate
- No light chain restriction or clonal IGH rearrangement
- Preservation of germinal center follicles
- Diffuse large B cell lymphoma: preponderance of large B cells with increased mitotic activity and Ki67 proliferation rate; B cells predominate in the infiltrate
- Follicular lymphoma: clinical correlation, BCL2+ cells that co-express germinal center B cell markers (CD10, STMN1, HGAL, LMO2) extending beyond CD21+ dendritic cell networks in contrast to colonization of germinal center follicles present in CMZL
- Lymphoplasmacytic lymphoma: rare reports in the skin
- Clinical correlation is required
- LPL can be challenging to distinguish from CMZL with extensive plasmacytic differentiation as they share a similar immunophenotype and the latter can rarely produce Waldenström macroglobulinemia
- Mantle cell lymphoma: cyclin D1+
- Myeloma (plasmacytoma): clinical correlation
- Primary cutaneous CD4 positive small / medium sized pleomorphic T cell lymphoproliferative disorder: clinical correlation may be necessary to distinguish from T cell rich CMZL
- Usually a solitary lesion on the head and neck of a middle aged woman
- Clonally rearranged T cell receptor
- No B cell clone by immunohistochemistry or clonal IGH rearrangement
- High percentage of PD-1+ cells including enlarged forms (Am J Surg Pathol 2010;34:1830)
- Primary cutaneous follicle center lymphoma: BCL6+ cells or less frequently BCL2+ cells that co-express germinal center B cell markers (CD10, STMN1, HGAL, LMO2) extending beyond CD21+ dendritic cell networks in contrast to colonization of germinal center follicles present in CMZL
- Pseudolymphomatous folliculitis: clinical correlation helpful
- Folliculocentric mixed inflammatory infiltrate
- Often with perivascular granulomas and florid reactive follicular epithelial changes reminiscent of pseodueptheliomatous hyperplasia
- Splenic lymphoma: clinical correlation required, cases with cutaneous involvement can be indistinguishable from CMZL (Histopathology 2002;40:22)
- Tumid lupus erythematosus: clinical correlation, periadnexal and perivascular inflammation with interstitial mucin deposition and superficial dermal edema
- BCL2
- BCL6
- CD79a
- PD-1
Comment Here
Reference: Cutaneous marginal zone lymphoma / MALT
- B cells with a germinal center phenotype extending beyond CD21+ dendritic cell networks
- Confluent Ki67 expression by neoplastic B cells throughout the germinal center follicles
- Presence of circumscribed dermal aggregates
- Presence of kappa light chain-restricted plasma cells
Comment Here
Reference: Cutaneous marginal zone lymphoma / MALT
- Also called adenocystic carcinoma
- Scalp of elderly patients
- Caucasian > Black > Asian
- 50 year old woman with gluteal mass (Indian J Pathol Microbiol 2009;52:225)
- 51 year old woman with slowly growing scalp nodule (Case of the Week 413)
- 58 year old Jamaican man with mass on left cheek (Dermatol Surg 2011;37:1192)
- Slow growing, solitary, asymptomatic, flesh colored nodule with a slightly translucent surface
- Resembles mammary colloid carcinoma with lakes of mucin containing small tumor cell clusters
- May also have an infiltrating ductal pattern
Contributed by Mark R. Wick, M.D., Case #413 and @JMGardnerMD on Twitter
Images hosted on other servers:
- Metastatic breast mucinous carcinoma: CK7+, 60% are p63+, otherwise negative (J Cutan Pathol 2010;37:411)
- Metastatic colonic mucinous carcinoma: CK20+
- Proliferating pilar tumor (PPT) is an uncommon neoplasm within the dermis or subcutis that arises from the isthmus region of the outer root sheath of the hair follicle
- Generally develops from a pilar cyst (sometimes following trauma) but may also arise de novo
- Most commonly arises on the scalp of elderly women
- Histologically resembles a trichilemmal cyst but with central lobules of squamous proliferation and variable atypia and mitotic figures
- Complete excision and clinical follow up is recommended due to the small risk for recurrence and metastasis
- Proliferating pilar cyst
- Proliferating trichilemmal cyst
- Elderly women are most commonly affected (80% of cases arise in females) (Am J Clin Pathol 2004;122:566)
- Scalp (85%), less commonly on the trunk (Am J Clin Pathol 2004;122:566)
- Proliferating pilar tumors are believed to arise from pilar cysts; however, it remains unknown what triggers the proliferative activity (Dermatol Surg 2007;33:1102)
- Trauma and inflammation have been suggested as the triggers in some cases (J Dermatol Surg Oncol 1987;13:1339)
- Genetic basis of hereditary pilar cysts has been reported as mutations in PLCD1; it is not known whether proliferating pilar tumors share this genetic alteration (Sci Rep 2020;10:6035)
- Slowly growing nodule on the scalp
- Lesions are generally well circumscribed, although they may be multinodular
- Tend to shell out from surrounding tissue upon surgical excision, similar to pilar cysts
- Average size is several centimeters; however, tumors up to 25 cm have been reported (Cancer 1971;28:701)
- Based on histopathologic findings following skin biopsy or excision of the nodule
- Nonscalp location, recent rapid growth, size > 5 cm and histologic features of extensive necrosis, high mitotic activity, poor circumscription with areas of invasion and cytologic atypia are all concerning for more aggressive or malignant behavior (J Cutan Pathol 2003;30:492)
- Local recurrence rate is 6.6%; risk of lymph node involvement is 2.6% (Am J Clin Pathol 2004;122:566)
- 33 year old woman with multiple proliferating pilar tumors and a porokeratotic adnexal ostial nevus (JAAD Case Rep 2020;6:344)
- 46 and 54 year old women with proliferating pilar tumors treated with Mohs micrographic surgery (J Drugs Dermatol 2021;20:1346)
- 76 year old woman with a proliferating trichilemmal cyst with delayed treatment due to COVID outbreak (Front Surg 2021;8:680160)
- Complete surgical excision, either via wide local excision or Mohs micrographic surgery (Dermatol Surg 2007;33:1102)
- If the lesion was enucleated in its entirety, well circumscribed and without other concerning histologic features, additional surgical therapy is not required
- Ongoing surveillance to monitor for recurrence or metastasis is recommended
- Encapsulated, pearly white nodule; may be multinodular
- Features of a pilar cyst with abrupt trichilemmal keratinization with additional extensive epithelial proliferation within the center of the cystic space
- Mitotic activity and cytologic atypia may be variable
- Invasion into the surrounding soft tissue should not be present
- Grading criteria as suggested by Ye et al. stratifies proliferating pilar tumors into 3 groups based on histologic characteristics (Am J Clin Pathol 2004;122:566):
- Group 1:
- Circumscribed silhouettes with pushing margins, modest nuclear atypia and an absence of pathologic mitoses, necrosis and invasion of nerves or vessels
- Behaves in a benign manner
- Group 2:
- Similar to group 1 but manifest irregular, locally invasive silhouettes with involvement of the deep dermis and subcutis
- Small risk of local recurrence
- Group 3:
- Invasive growth patterns, marked nuclear atypia, pathologic mitotic forms and geographic necrosis, with or without the involvement of nerves or vascular structures
- Potential for regional recurrence and metastasis
- Group 1:
Contributed by Viktoryia Kazlouskaya, M.D., Ph.D. and Colleen J. Beatty, M.D.
Proliferating pilar tumor overview by Dr. Gardner
- Skin, scalp, biopsy:
- Proliferating pilar tumor (see comment)
- Comment: Examination reveals a well circumscribed nodule composed of lobules of proliferative squamous epithelium showing trichilemmal keratinization with an adjacent typical pilar cyst. No significant cytologic atypia or atypical mitoses are observed. The lesion appears to be excised in total; however, clinical correlation and follow up are recommended.
- Pilar (trichilemmal) cyst:
- Well circumscribed cyst lined by stratified squamous epithelium exhibiting trichilemmal keratinization
- Squamous cell carcinoma:
- Malignancy of epidermal keratinocytes exhibiting invasion and variable degrees of atypia
- Key differentiators are absence of areas of trichilemmal keratinization and a lack of staining with markers of outer root sheath differentiation
- Malignant proliferating pilar tumor:
- Features of a proliferating pilar tumor but with invasion into the surrounding tissue along with atypical mitoses, marked nuclear atypia and geographic necrosis
- Cyst with eosinophilic cuticle and associated sebaceous glands
- Cystic lining with granular layer and keratinization
- Lobules of squamous epithelium arising within a cyst with trichilemmal keratinization
- Proliferation of hair matrical cells and ghost cells
Comment Here
Reference: Proliferating pilar tumor
- Solitary lesions are known as circumscribed storiform collagenoma
- Some cases may represent folliculitis
- May be associated with Cowden disease
- 60 year old woman with clinical basal cell carcinoma (Case of Week #190)
- Bland, well circumscribed hypocellular lesion with focal heavy collagen deposition
- Benign sebaceous neoplasm composed of basaloid cells and mature sebocytes
- Associated with Muir-Torre syndrome (MTS) but can also be an isolated (sporadic) tumor
- Sebaceoma, as a term, is used for tumors with > 50% basaloid cells and sebaceous adenoma is used for tumors with < 50% basaloid cells
- Sebaceous epithelioma, as a term, is confusing and is best not used
- Sebaceous epithelioma could refer to a low grade form of sebaceous carcinoma, a basal cell carcinoma with sebaceous differentiation or sebaceous proliferations of uncertain potential and thus is not a useful term
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
- F:M = 4:1
- Wide age range but the majority of patients are in the sixth to ninth decades
- Primarily occurs on the face and scalp
- Occurrence on non head and neck regions should prompt consideration of Muir-Torre syndrome
- Yellow to orange or flesh colored papule, nodule or tumor
- Muir-Torre syndrome (MTS) is considered a phenotypic variant of hereditary nonpolyposis colorectal carcinoma syndrome (HNPCC, Lynch syndrome) and is caused by germline mutations in one allele of the DNA mismatch repair (MMR) genes, most commonly MLH1, MSH2, MSH6 and PMS2
- MTS is associated with sebaceous neoplasia (most commonly sebaceous adenoma), colorectal, GU and other visceral adenocarcinomas
- MSH2 is the gene most commonly mutated in MTS
- If there is concern for MTS (personal or family history of colorectal, GU or breast cancer; or an older patient with numerous sebaceous neoplasms, especially not on the head and neck), further testing for MMR IHC or microsatellite instability can be performed
- IHC cannot differentiate between loss of MLH1 expression caused by a germline mutation versus a somatic hypermethylation - some germline missense mutations may be erroneously interpreted as normal by IHC, because they may result in an antigenically intact but nonfunctional protein
- Microsatellite instability analysis (MSI): performed on formalin fixed tissue, is more sensitive at detecting patients with germline MMR defects than IHC
- Results are either MSI-H (high degree of MSI) or MSI-L (low degree of MSI)
- Germline mutation analysis: blood leukocyte genomic sequencing is preferred to identify germline mutations in the MLH1, MSH2, MSH6 and PMS2 genes - if there are no germline mutations, but the tumor shows MMR deficiency, there may be involvement of other MMR proteins, somatic mutations or hypermethylation of the promoter region
- Sebaceomas can be sporadic, not associated with MTS
- Loss of nuclear staining for MLH1, MSH2, MSH6 or PMS2 suggests microsatellite instability (MSI) and supports a diagnosis of Muir-Torre syndrome
- Mutations in MLH1 and MSH2 have the most severe effect, producing a high frequency MSI phenotype
- When MSH2 is deficient, MSH6 usually is as well, because protein products of MSH2 and MSH6 form a heterodimer MMR recognition factor
- MSH6 is unstable without MSH2 and is quickly degraded
- Once the diagnosis is established, no further treatment is needed
- However, complete excision should be considered if the tumor is only partially biopsied or there is concern for basal cell carcinoma with sebaceous differentiation or sebaceous carcinoma
- Dermal nodule with variable epidermal involvement consisting of basaloid cells and mature sebocytes
- Greater than 50% of the tumor is made up of basaloid cells
- Variants of sebaceoma have been described with carcinoid-like, reticulated, cribriform, rippled and Verocay body-like features
- EMA, D2-40, Factor XIIIa (clone AC-1A1) nuclear
Muir-Torre Syndrome
- Basal cell carcinoma with sebaceous differentiation:
- Predominantly shows peripheral palisading and cleft formation with incidental sebaceous differentiation
- BerEP4 staining is positive in basal cell carcinoma and negative in sebaceoma
- Sebaceous adenoma:
- Tumor with < 50% basaloid cells, as opposed to a sebaceoma which has > 50% basaloid cells
- Sebaceous carcinoma:
- Has more nuclear pleomorphism, nucleolar prominence and mitotic activity than sebaceoma, infiltrative growth pattern
- Trichoblastoma with sebaceous differentiation:
- Look for focal hair differentiation and papillary mesenchymal bodies
- What is the most common skin tumor associated with Muir-Torre syndrome?
- Basal cell carcinoma
- Sebaceoma
- Sebaceous adenoma
- Sebaceous carcinoma
- What is the most common mutation seen in Muir-Torre syndrome?
- MLH1
- MSH2
- MSH6
- PMS2
- Benign sebaceous neoplasm consisting of an admixture of mature sebocytes and predominantly immature basaloid cells (> 50% of the neoplasm)
- Associated with Muir-Torre syndrome (MTS) but can also be an isolated (sporadic) tumor (Am J Dermatopathol 2000;22:155)
- Benign adnexal neoplasm that clinically presents as a solitary, yellow-tan papule / nodule
- Histologic sections show well circumscribed cellular lobules composed of predominant immature basaloid cells (> 50% of the lesion) with admixed mature sebocytes
- Associated with Muir-Torre syndrome
- Sebaceous epithelioma, as a term, is confusing and is best not used
- Sebaceous epithelioma could refer to a low grade form of sebaceous carcinoma, a basal cell carcinoma with sebaceous differentiation or sebaceous proliferations of uncertain potential and thus is not a useful term
- ICD-O: 8410/0 - sebaceoma
- ICD-11: 2F22 & XH0QL4 - benign neoplasms of epidermal appendages & sebaceoma
- Female predominance (Am J Dermatopathol 2002;24:294, Am J Dermatopathol 1984;6:7)
- Majority in the sixth to ninth decades (Ann Dermatol Venereol 2016;143:814)
- Mean age at diagnosis is 70 years (Am J Dermatopathol 1984;6:7)
- Most common location is the face and scalp
- Less frequently on the trunk or extremities and should prompt consideration of Muir-Torre syndrome (Am J Dermatopathol 2001;23:58, J Am Acad Dermatol 1996;34:47, Am J Dermatopathol 1984;6:7)
- Sebaceomas commonly have mutation of RAS family genes (HRAS and KRAS), TP53, CDKN2A, EGFR and CTNNB1 when examined by next generation sequencing
- Abnormalities of TP53 were most frequently found (Pathology 2016;48:454)
- Sebaceomas are associated with defective mismatch repair proteins, manifesting as loss of expression of mismatch repair gene products, including MLH1, MSH2, MSH6 and PMS2; a subset of these are related to Muir-Torre syndrome (J Cutan Pathol 2009;36:613, Arch Pathol Lab Med 2014;138:1685, J Am Acad Dermatol 2016;74:558, Am J Dermatopathol 2017;39:239, Mod Pathol 2011;24:1004, Histopathology 2010;56:133, Am J Dermatopathol 2021;43:174)
- Yellow-orange or flesh colored papule, nodule or tumor (Am J Dermatopathol 1984;6:7, Am J Dermatopathol 2002;24:294)
- Usually a single lesion but can be multifocal in association with Muir-Torre syndrome (Am J Dermatopathol 2000;22:155)
- Muir-Torre syndrome is considered a phenotypic variant of hereditary nonpolyposis colorectal carcinoma syndrome (HNPCC, Lynch syndrome) and is caused by germline mutations in one allele of the DNA mismatch repair (MMR) genes, most commonly MLH1, MSH2, MSH6 and PMS2
- Muir-Torre syndrome is associated with sebaceous neoplasia (most commonly sebaceous adenoma), colorectal, genitourinary (GU) and other visceral adenocarcinomas
- Defective MMR gene products have been observed in association with sebaceoma, including MLH1, MSH2, MSH6 and PMS2; a subset of these are related to Muir-Torre syndrome (J Cutan Pathol 2009;36:613, Arch Pathol Lab Med 2014;138:1685, J Am Acad Dermatol 2016;74:558, Am J Dermatopathol 2017;39:239, Mod Pathol 2011;24:1004, Histopathology 2010;56:133, Am J Dermatopathol 2021;43:174)
- MSH2 is the gene most commonly mutated in Muir-Torre syndrome
- If there is concern for Muir-Torre syndrome (personal or family history of colorectal, GU or breast cancer; an older patient with numerous sebaceous neoplasms, especially not on the head and neck), further testing for MMR IHC or microsatellite instability can be performed
- IHC cannot differentiate between loss of MLH1 expression caused by a germline mutation versus a somatic hypermethylation; some germline missense mutations may be erroneously interpreted as normal by IHC because they may result in an antigenically intact but nonfunctional protein
- Microsatellite instability (MSI) analysis, performed on formalin fixed tissue, is more sensitive at detecting patients with germline MMR defects than IHC
- Results are either MSI-H (high degree of MSI) or MSI-L (low degree of MSI)
- Germline mutation analysis: blood leukocyte genomic sequencing is preferred to identify germline mutations in the MLH1, MSH2, MSH6 and PMS2 genes; if there are no germline mutations but the tumor shows MMR deficiency, there may be involvement of other MMR proteins, somatic mutations or hypermethylation of the promoter region
- Head and neck sebaceomas tend to be MMR stable as compared to sebaceomas outside the head and neck regions, which tend to be MMR deficient (Am J Surg Pathol 2008;32:936, Am J Dermatopathol 2021;43:174)
- Other mutations have been identified in sebaceoma with next generation sequencing studies, including TP53 (most common), RAS family genes (HRAS and KRAS), CDKN2A, EGFR and CTNNB1 (Pathology 2016;48:454)
- Sebaceoma can arise in a pre-existing sebaceous nevus (Pathology 2016;48:454)
- Solitary, yellow-tan papules / nodule (Am J Dermatopathol 1984;6:7)
- Well circumscribed cellular lobules comprised mostly of small monomorphic immature but cytologically benign basaloid cells admixed with fewer mature sebocytes (< 50%), haphazardly distributed throughout the tumor (Histopathology 2010;56:133)
- Sebaceomas have excellent prognosis and can be treated with conservative excision (Histopathology 2010;56:133)
- Loss of nuclear staining for MLH1, MSH2, MSH6 or PMS2 suggests MSI, supports a diagnosis of Muir-Torre syndrome and increases the risk of associated visceral malignancies (J Cutan Pathol 2009;36:613, J Am Acad Dermatol 2016;74:558, Arch Pathol Lab Med 2014;138:1685)
- Transformation to sebaceous carcinoma is rare (J Cutan Pathol 2016;43:64, J Cutan Pathol 2013;40:676)
- 48 year old man who presented with a pea sized growth in his left arm (Indian J Pathol Microbiol 2022;65:465)
- 71 year old woman had a dome shaped, slightly erythematous nodule on the anterior scalp (Am J Dermatopathol 2001;23:437)
- 76 year old woman with a 3 mm solitary pink papule on the nose (Skin Res Technol 2022;28:886)
- Once the diagnosis is established, no further treatment is needed if the biopsy margins are negative
- However, complete excision should be considered if the tumor is only partially biopsied or there is concern for basal cell carcinoma with sebaceous differentiation or sebaceous carcinoma
- Dermal based tumor with rare epidermal attachments
- Consists of variably sized, discrete nodules that lack lobular organization architecture (Am J Dermatopathol 1984;6:7, Am J Dermatopathol 2002;24:294, Am J Dermatopathol 2001;23:58, J Am Acad Dermatol 1990;22:533)
- Cytologically, the sebocytes have multiple cytoplasmic vacuoles and scalloped nuclei; the immature basaloid component features frequent mitotic activity but lacks atypical forms or necrosis
- Cystic spaces and duct-like structures are often present, displaying an eosinophilic cuticle and occasional holocrine secretions (Surg Pathol Clin 2017;10:367, Ann Dermatol Venereol 2016;143:814, Am J Dermatopathol 1984;6:7)
- Moreover, apocrine differentiation, infundibulocystic structures and squamous metaplasia can also be seen (Am J Dermatopathol 2016;38:678)
- Based on the growth patterns, sebaceoma variants can be described as follows: reticulated (rippled), cribriform, sinusoidal / labyrinthine, carcinoid-like and glandular configurations have been described in sebaceoma, sometimes even within the same neoplasm (Dermatol Online J 2016;22:13030/qt03s2g1c8, Am J Dermatopathol 2009;31:364, Ann Dermatol Venereol 2016;143:814, Am J Dermatopathol 2005;27:195, Am J Dermatopathol 2018;40:479)
- MMR deficient sebaceous neoplasms more often show cystic change, intratumoral mucin, squamous metaplasia, ulceration, a lymphocytic infiltrate and intertumoral heterogeneity compared to MMR stable sebaceous neoplasms (Am J Dermatopathol 2021;43:174)
Contributed by Jerad Gardner, M.D., Jennifer Kaley, M.D., Yazan Alhalaseh, M.D. and Dinesh Pradhan, M.D.
- BerEP4 is negative in sebaceoma (as compared to basal cell carcinoma [BCC], which has positive BerEP4) (Histopathology 2007;51:80)
- Low p53 and Ki67 profile as compared to sebaceous carcinoma which has diffuse p53 expression and high Ki67 proliferation rate (N Am J Med Sci 2015;7:275)
- MLH1, MSH2 and MSH6 may be lost in patients with Muir-Torre syndrome
Muir-Torre syndrome
- Skin, scalp nodule; biopsy:
- Sebaceoma
- Basal cell carcinoma with sebaceous differentiation:
- Predominantly shows peripheral palisading, mucinous stroma and retraction artifact with incidental sebaceous differentiation
- BerEP4 staining is positive in basal cell carcinoma and negative in sebaceoma (Histopathology 2007;51:80)
- EMA and D2-40 are negative in BCC
- Sebaceous adenoma:
- Preserved lobular architecture with distinct and regular maturation (similar to the normal sebaceous gland)
- Tumor with < 50% basaloid cells, as opposed to a sebaceoma, which has > 50% basaloid cells
- Sebaceous carcinoma:
- Has more nuclear pleomorphism, nucleolar prominence, mitotic activity and infiltrative growth pattern, as compared to sebaceoma
- Diffuse p53 expression and high Ki67 proliferation rate (N Am J Med Sci 2015;7:275)
- Trichoblastoma with sebaceous differentiation:
- Look for focal hair differentiation and papillary mesenchymal bodies
- EMA
- D2-40
- BerEP4
- Factor XIIIa
Comment Here
Reference: Sebaceoma
- p53
- Ki67
- Adipophilin
- EMA
- p53 and Ki67
Comment Here
Reference: Sebaceoma
Comment Here
Reference: Sebaceoma
- Benign neoplasm composed of mature sebaceous lobules with the expansion of germinative basaloid cell layers at the periphery
- Associated with Muir-Torre syndrome, especially when it arises outside the head and neck region (Histopathology 2010;56:133)
- Unrelated to adenoma sebaceum (facial angiofibromas of tuberous sclerosis)
- Well circumscribed, multilobulated tumor
- Increased number of basaloid germinative cells of more than 2 layers
- Shows distinct maturation, meaning that the basaloid germinative cells are usually at the periphery and the sebaceous cells are located centrally
- Associated with Muir-Torre syndrome, a variant of Lynch syndrome with mutations in the DNA mismatch repair (MMR) genes
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
- Mostly in older people with a mean age of 60 years (Ann Dermatol 2019;31:14)
- Mostly in the head and neck, particularly on the face and scalp
- Subset of these lesions has inactivating mutations in LEF1 affecting the Wnt / β catenin pathway, which is important in sebaceous differentiation (Nat Med 2006;12:395)
- Clinically presents as a yellow or pink-tan papule or nodule
- Clinically can be mistaken for basal cell carcinoma
- Muir-Torre syndrome (MTS) is a clinical variant of Lynch syndrome, which is defined as at least 1 sebaceous neoplasm (sebaceous adenoma, sebaceoma and sebaceous carcinoma) or keratoacanthoma and at least 1 Lynch syndrome related internal cancer
- MTS is caused by germline variants in the DNA mismatch repair (MMR) genes encoding for MSH2 and MLH1, accounting for most of the cases
- Isolated mutations in MSH6 and PMS2 account for a small minority of cases (J Cutan Pathol 2017;44:931)
- MUTYH associated polyposis (MAP) is an autosomal recessive disorder associated with colorectal polyps (adenomas) and adenocarcinomas that can also be associated with cutaneous sebaceous neoplasms, closely imitating MTS (Am J Dermatopathol 2016;38:915)
- Overall quality of evidence in support of MMR IHC reflex testing on MTS associated cutaneous neoplasms is weak to moderate
- Some pathologists do targeted testing specially if patient has multiple sebaceous neoplasms, outside the head and neck or history of colorectal, breast or urothelial cancer (J Cutan Pathol 2017;44:931)
- Diagnosis is made using clinical examination and biopsy
- Solitary tumors are treated by complete surgical removal with a 100% cure rate
- Incomplete removal has occasionally resulted in local recurrence (Pathology 2017;49:688)
- 57 year old man with a history of colon cancer diagnosed at age 32 and multiple sebaceous adenomas (Cureus 2021;13:e14582)
- 60 year old man, with a history of kidney transplantation 11 years prior, presented with new lesion on his left lower abdomen, which was sebaceous adenoma (JAAD Case Rep 2019;5:818)
- 68 year old man presented to the dermatology clinic with a solitary enlarging, bleeding lesion on his right central zygoma (Dermatol Arch 2019;3:77)
- Because sebaceous adenomas are benign, treatment for most individuals is conservative management, although bothersome lesions can be removed for patient comfort
- Consider complete excision also if the lesion is partially biopsied or of clinical concern for carcinoma with sebaceous differentiation (Pathology 2017;49:688)
- Well circumscribed superficial dermal nodule with sharp demarcation from the underlying tissue
- Well circumscribed, nodular growth of lobules consist of admixture of basaloid cells and mature sebocytes
- Some lobules may communicate directly with the surface epithelium
- Basaloid cells are usually located at the periphery of lobules and sebaceous cells with intracytoplasmic lipid vacuoles, which are usually located at the center of lobules
- Basaloid cells are composed of expanded germinative layer, with more than the normal 2 cell layers seen in mature sebaceous glands or sebaceous hyperplasia but still less than 50% of the tumor volume (> 50% is seen in sebaceoma / sebaceous epithelioma)
- Increased mitotic activity is sometimes seen in the basaloid cell component (Surg Pathol Clin 2017;10:367)
- Diagnosis is usually made by standard histology; the following immunostains can be used to confirm sebaceous origin:
- Adipophilin: membranous vesicular pattern of staining is suggestive of intracellular lipids (Mod Pathol 2010;23:567)
- Androgen receptor (AR)
- Preferentially expressed antigen in melanoma (PRAME) may show a cytoplasmic and perinuclear (but not nuclear) pattern (J Cutan Pathol 2021;48:1252)
- CK7
- D2-40 (Podoplanin)
- Epithelial membrane anttigen (EMA)
Sebaceous adenoma: 5 minute pathology pearls by Dr. Jerad Gardner
- Skin, right cheek, shave biopsy:
- Sebaceous adenoma
- Sebaceous hyperplasia:
- Hyperplastic sebaceous lobules
- Located slightly higher in the dermis than normal
- Individual lobules are increased in number but are not significantly different in size compared to normal
- Basaloid layer is not expanded
- Sebaceoma / sebaceous epithelioma:
- Tumor consists of a random admixture of basaloid cells and mature sebocytes with loss of regular maturation that is seen in sebaceous adenoma
- No nuclear pleomorphism and mitotic activity is generally sparse; however, it can sometimes be prominent
- No peripheral palisading or cleft formation
- Sebaceous carcinoma:
- Significant nuclear pleomorphism, nucleolar prominence and conspicuous mitotic activity
- Although in well differentiated variants, the tumor may have a smooth regular margin
- Less well differentiated examples typically show an infiltrating border
- Basal cell carcinoma with sebaceous differentiation:
- Features of basal cell carcinoma with proliferation of palisading basaloid cells, retraction artifact and loose mucinous stroma
- Within these nodules are foci of variable numbers of mature sebocytes
- EMA- and BerEP4+ (Can J Ophthalmol 2014;49:326)
- Trichoblastoma with sebaceous differentiation:
- Papillary mesenchymal bodies are often present
- Peripheral nuclear palisading and stromal induction are also generally present
- Balloon cell melanoma:
- Other lesions with clear cell differentiation (e.g., metastatic renal clear cell carcinoma)
Comment Here
Reference: Sebaceous adenoma
- CYLD
- Folliculin
- MLH1
- PTCH
- PTEN
Comment Here
Reference: Sebaceous adenoma
- Malignant neoplasm with sebaceous differentiation
- Generally classified into periocular and extraocular
- Mostly occurs sporadically in elderly patients with an equal gender distribution; periocular locations have a female predominance (Curr Treat Options Oncol 2017;18:47, Onco Targets Ther 2018;11:3713)
- Periocular versus extraocular
- Atypical sebocytes can be well, moderately or poorly differentiated
- May rarely occur in association with Muir-Torre syndrome, an autosomal dominant syndrome characterized by a sebaceous neoplasm (adenoma, sebaceoma or carcinoma) and occasionally keratoacanthoma associated with a visceral malignancy (Dermatol Surg 2015;41:1)
- Aggressive tumor with 5 year survival rate of 92.7%
- Treatment is primarily surgical excision
- Sebaceous gland carcinoma
- Sebaceous cell carcinoma
- Meibomian gland carcinoma (J Korean Med Sci 2017;32:1351)
- ICD-10: C44.1392 - sebaceous cell carcinoma of skin of eyelid, including canthus
- 0.2 - 4.6 % of all malignant cutaneous tumors and the third most common eyelid malignancy (Curr Treat Options Oncol 2017;18:47)
- More frequent:
- Patient age > 40
- Asian (periocular) (StatPearls: Sebaceous Gland Carcinoma [Accessed 30 March 2021])
- Most common in periocular area, head and neck but can arise from any sebaceous gland of the skin (StatPearls: Sebaceous Gland Carcinoma [Accessed 30 March 2021])
- Periocular (75%) > extraocular (25%) in most studies; however, more recent studies suggest the opposite (Dermatol Surg 2015;41:1, Cancer 2008;113:3372)
- Periocular:
- 1.0 - 3.2% of all malignant eyelid tumors
- Upper eyelid > lower eyelid
- Originates from meibomian glands, Zeiss glands, caruncle or skin of eyebrow (Curr Treat Options Oncol 2017;18:47)
- Extraocular:
- Occurs on the head and neck mostly, then rarely on the trunk, extremities, genitalia, external auditory meatus
- Very rarely can occur in extracutaneous sites, such as lungs, salivary glands and breast (Dermatol Pract Concept 2012;2:39, J Korean Med Sci 2017;32:1351)
- Can rarely occur in a nevus sebaceus of Jadassohn (J Dermatol 2016;43:175)
- Unknown
- Radiation
- Immunosuppression
- Muir-Torre syndrome: autosomal dominant syndrome with mutation in one or more of the mismatch repair genes (MLH1, MSH2, MSH6 PMS2) and associated microsatellite instability
- Production of nitrosamines (food or medication)
- Retinoblastoma (Onco Targets Ther 2018;11:3713)
- Periocular: presents as a yellow to pink, painless, rapidly enlarging, firm papule, nodule or cystic lesion (Curr Treat Options Oncol 2017;18:47)
- Extraocular: presents as yellowish nodule, often with ulceration (StatPearls: Sebaceous Gland Carcinoma [Accessed 30 March 2021])
- Biopsy is essential for the diagnosis (Curr Treat Options Oncol 2017;18:47)
- Radiologic studies may help to reveal bone destruction or soft tissue involvement by the tumor (Curr Treat Options Oncol 2017;18:47)
- 5 year relative survival rate: 92.7% (J Am Acad Dermatol 2016;75:1210)
- Overall prognosis for localized disease after complete excision is good
- Most significant predictor of reduced survival is the presence of metastatic disease at the time of diagnosis
- Other factors: multicentricity, pagetoid spread, perineural vascular and lymphatic invasion, poorly differentiated cytology, periocular location, primary site on the ear or lip, tumor size (> 10 mm), black race (Curr Treat Options Oncol 2017;18:47, Dermatol Surg 2015;41:1)
- Sebaceous carcinoma may metastasize in 2.4% of the cases; the majority of metastases occur within the first 2 years after initial treatment (Head Neck 2012;34:1765)
- 37 year old woman with Muir-Torre syndrome associated sebaceous carcinoma occurring in the setting of lipedematous scalp (Case Reports Plast Surg Hand Surg 2020;7:124)
- 55 year old woman presenting with asymptomatic nodular ulcerating lesions on the right side of the vulva (Indian J Dermatol Venereol Leprol 2017;83:221)
- 59 year old woman with disseminated subcutaneous nodules with history of previously treated sebaceous cell carcinoma (Am J Case Rep 2018;19:1192)
- 67 year old woman with longstanding history of an ovarian dermoid cyst (Gynecol Oncol Rep 2018;26:37)
- Wide local excision or Mohs micrographic surgery are the best initial treatment options
- Sentinel lymph node biopsy for periorbital sebaceous carcinoma > 10 mm in diameter
- Radiation therapy and systemic chemotherapy are only used for patients who are poor surgical candidates or those with recurrent or metastatic disease
- Immunohistochemistry to evaluate for microsatellite instability (MSH2, MSH6, MLH1, PMS2) should be offered on sebaceous carcinoma specimens, especially extraocular ones, to screen for Muir-Torre syndrome
- Evidence of orbital invasion on imaging necessitates exenteration (Dermatol Surg 2015;41:1)
- Papule, nodule or cystic lesion
- Lipid and fat staining with frozen sections have been used in the past
- Architecture: usually sheets or lobules separated by fibrovascular stroma
- Dermal based tumor with focal connection to the epidermis or follicular epithelium
- Can be rounded nodular aggregates or angulated infiltrative aggregates
- Can appear cystic with central comedo type necrosis
- Less commonly, can have a broad superficial intraepidermal pattern
- Cytology: classified as poorly, moderately or well differentiated
- Well differentiated: increased proportion of mature appearing sebocytes (multivacuolated cells) with nuclear indentation relative to basaloid undifferentiated cells
- Mild pleomorphism, minimal mitoses and necrosis
- Moderately to poorly differentiated: higher proportion of atypical basaloid (undifferentiated) cells with minimal differentiation toward multivacuolated cells
- Prominent pleomorphism and atypia, frequent mitoses and necrosis
- Well differentiated: increased proportion of mature appearing sebocytes (multivacuolated cells) with nuclear indentation relative to basaloid undifferentiated cells
- Pagetoid (or intraepidermal sebaceous carcinoma, sebaceous carcinoma in situ) tumor growth is much more commonly observed in periocular than in extraocular locations, where it is rare
- Can exhibit squamous metaplasia or focal apocrine differentiation
- References: Dermatol Surg 2015;41:1, Curr Treat Options Oncol 2017;18:47, Int J Surg Pathol 2019;27:432, J Korean Med Sci 2017;32:1351
Contributed by Bonnie Lee, M.D. and Maria Del Valle Estopinal, M.D.
- Androgen receptor
- Adipophilin - membranous vesicular pattern (a granular pattern is considered negative)
- Keratin
- EMA
- LeUM1
- Ki67 - increased relative to sebaceous adenoma and sebaceoma
- p53 - increased relative to sebaceous adenoma and sebaceoma
- BerEP4
- References: Onco Targets Ther 2018;11:3713, Curr Opin Ophthalmol 2018;29:445
- Skin, right elbow, shave biopsy:
- Well differentiated sebaceous neoplasm with severe nuclear atypia, consistent with sebaceous carcinoma (G1)
- Tumor measures at least 5.5 mm in greatest dimension
- Margins cannot be evaluated in the plane of sections examined
- No definite lymphovascular or perineural invasion identified
- American Joint Committee on Cancer pathologic staging (8th edition): pT1 pNx (Amin: AJJC Cancer Staging Manual, 8th edition, 2017)
- Left lower eyelid, wedge excision:
- Recurrent, sebaceous cell carcinoma in situ, moderately differentiated involving the skin of the left lower eyelid
- Tumor size: 0.7 mm
- Lymphovascular space invasion: not identified
- Perineural invasion: not identified
- Mitotic rate: 5 mitoses per square mm
- Surgical margins: nasal, temporal, inferior and deep margins are negative for sebaceous carcinoma
- Microsatellite instability markers for sebaceous carcinoma: positive (retained) nuclear staining for MLH1, PMS2, MSH2 and MSH6
- Pathologic staging: pTIs
- IHC stains: androgen receptor - positive in tumor cells; adipophilin - positive in tumor cells; BerEP4: negative in tumor cells
- Basal cell carcinoma with sebaceous differentiation:
- Clear cell squamous cell carcinoma:
- Balloon cell melanoma:
- Metastatic clear cell carcinoma (renal):
- Clear cell sarcoma:
A 75 year old woman had an excisional biopsy for a rapidly growing mass in her upper eyelid. Histologic details are shown in the image above. Which of the following is true regarding this entity?
- Pagetoid spread is more common in periocular location
- Radiation therapy is the first line treatment
- Surgical excision is not helpful
- This tumor is S100 positive
Comment Here
Reference: Sebaceous carcinoma
- Adipophilin
- Androgen receptor
- CEA
- EMA
Comment Here
Reference: Sebaceous carcinoma
- Most common sebaceous gland lesion
- Usually elderly patients on nose or cheeks
- Umbilicated yellowish papules
- Expansion of normal lobular sebaceous gland architecture without thickening of peripheral germinative layer of seboblasts
- Other disorders with sebaceous differentiation
- Sebaceous adenoma
- Common, benign keratinocyte proliferation of middle aged and elderly
- Benign
- Clinical: waxy, brown slow growing papule
- Histologic:
- Proliferation of basaloid keratinocytes without atypia
- Acanthosis and hyperkeratosis most often with horn pseudocysts
- Senile wart
- Seborrheic wart
- ICD-10: L82 - seborrheic keratosis
- Most common benign skin tumor
- Age > 50; incidence increases with age
- M = F
- Lighter skinned individuals (StatPearls: Seborrheic Keratosis [Accessed 28 September 2021])
- Head, neck, trunk (most common)
- Genitals (rare)
- Never on palms, soles or mucosal surfaces
- Reference: StatPearls: Seborrheic Keratosis [Accessed 28 September 2021]
- Immature benign keratinocyte proliferation
- Multiple somatic mutations (Oncotarget 2017;8:36639)
- Most common:













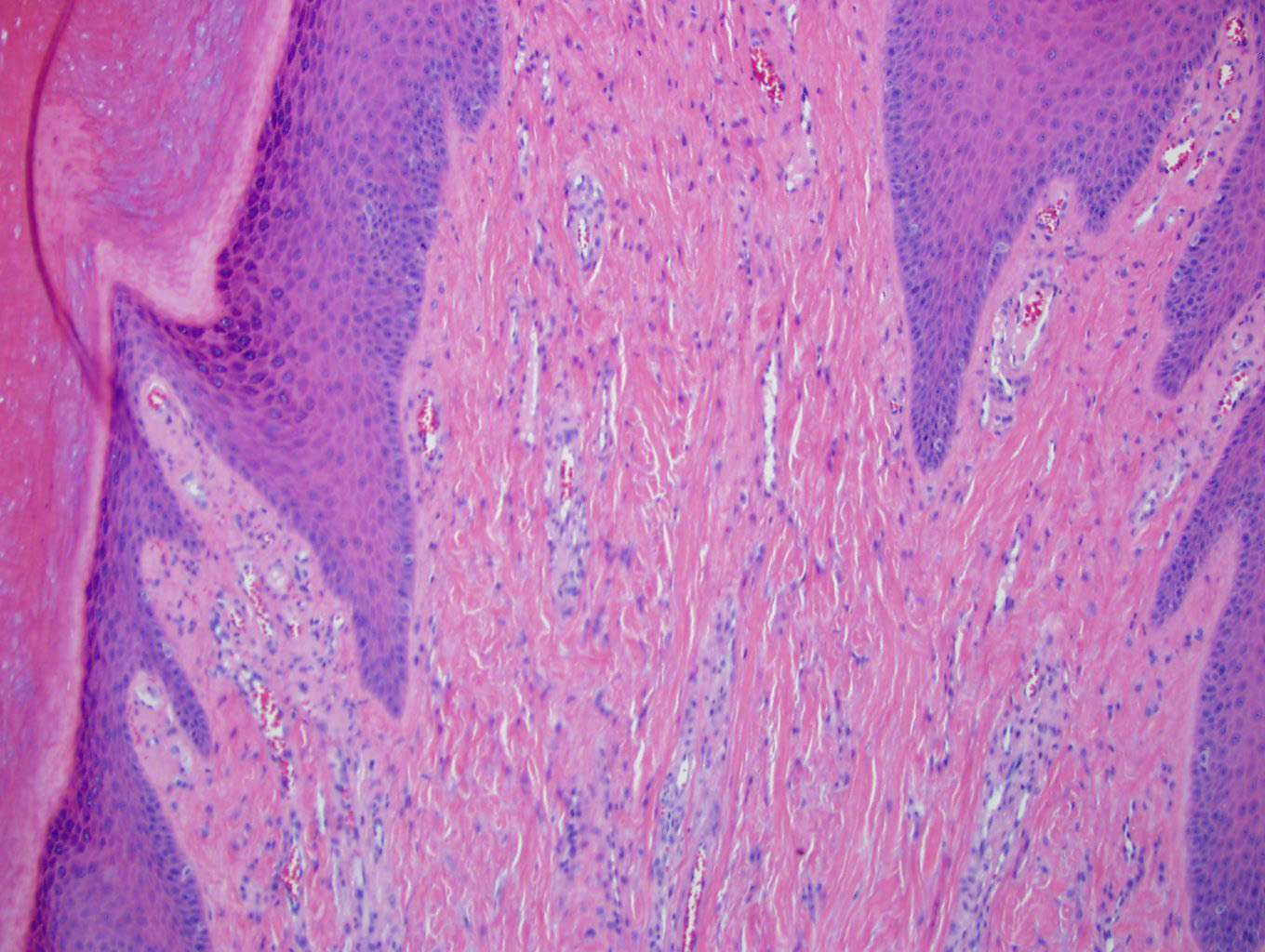
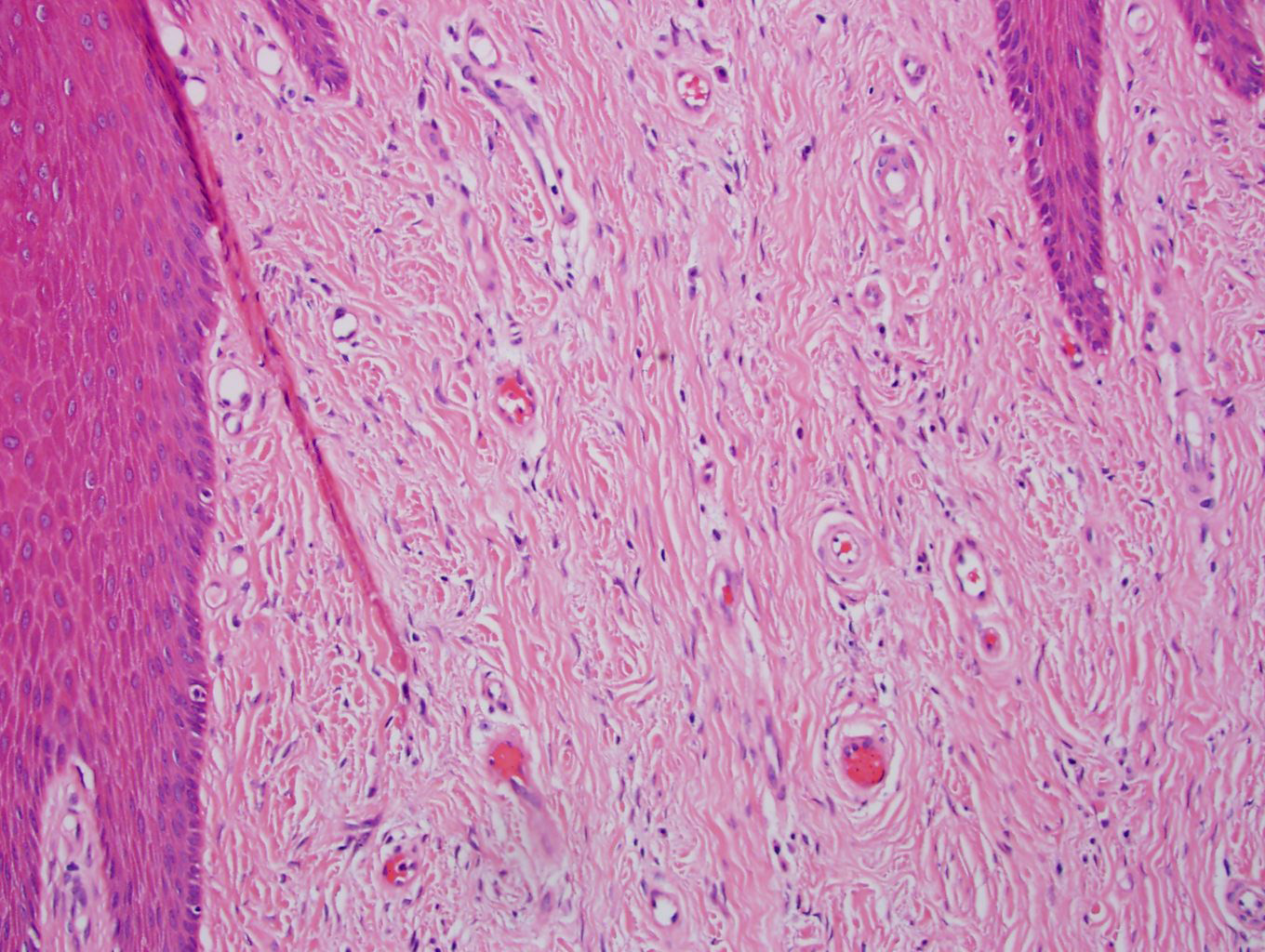











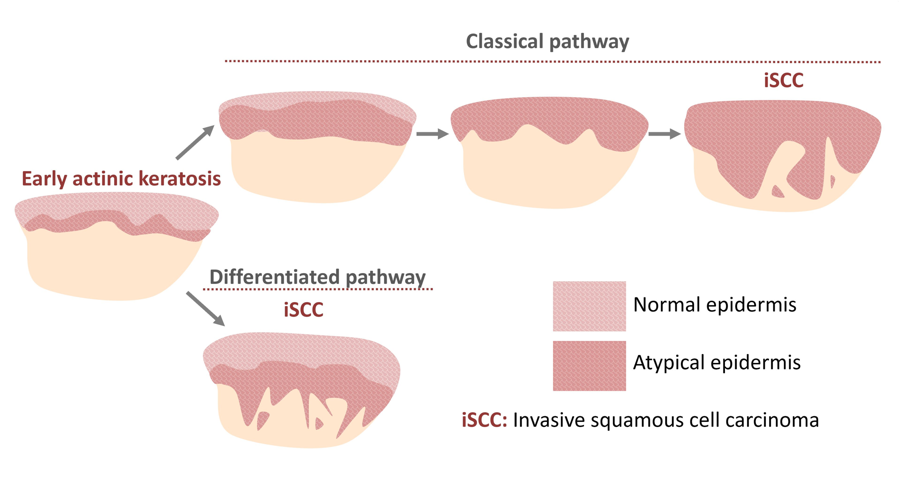


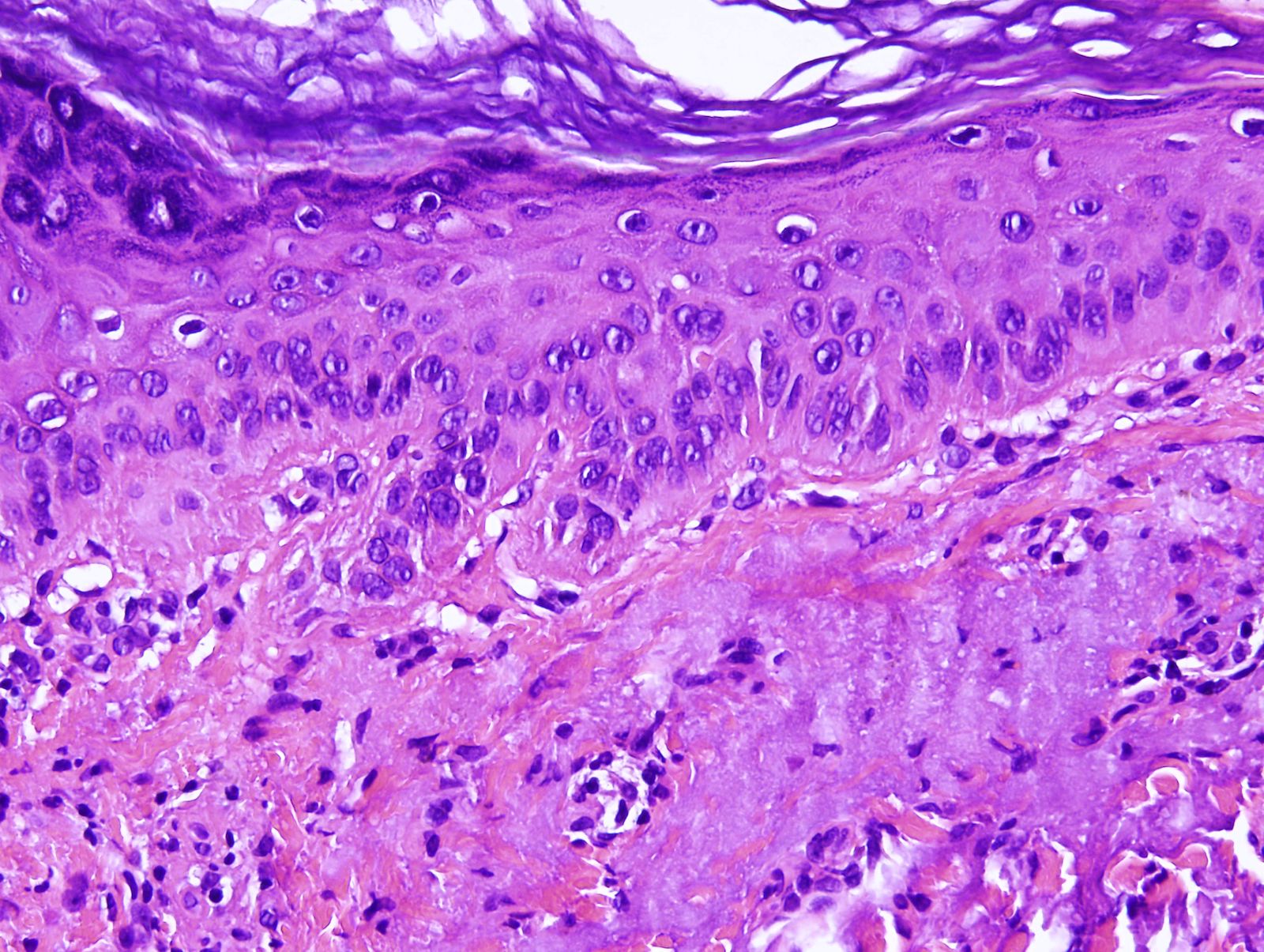

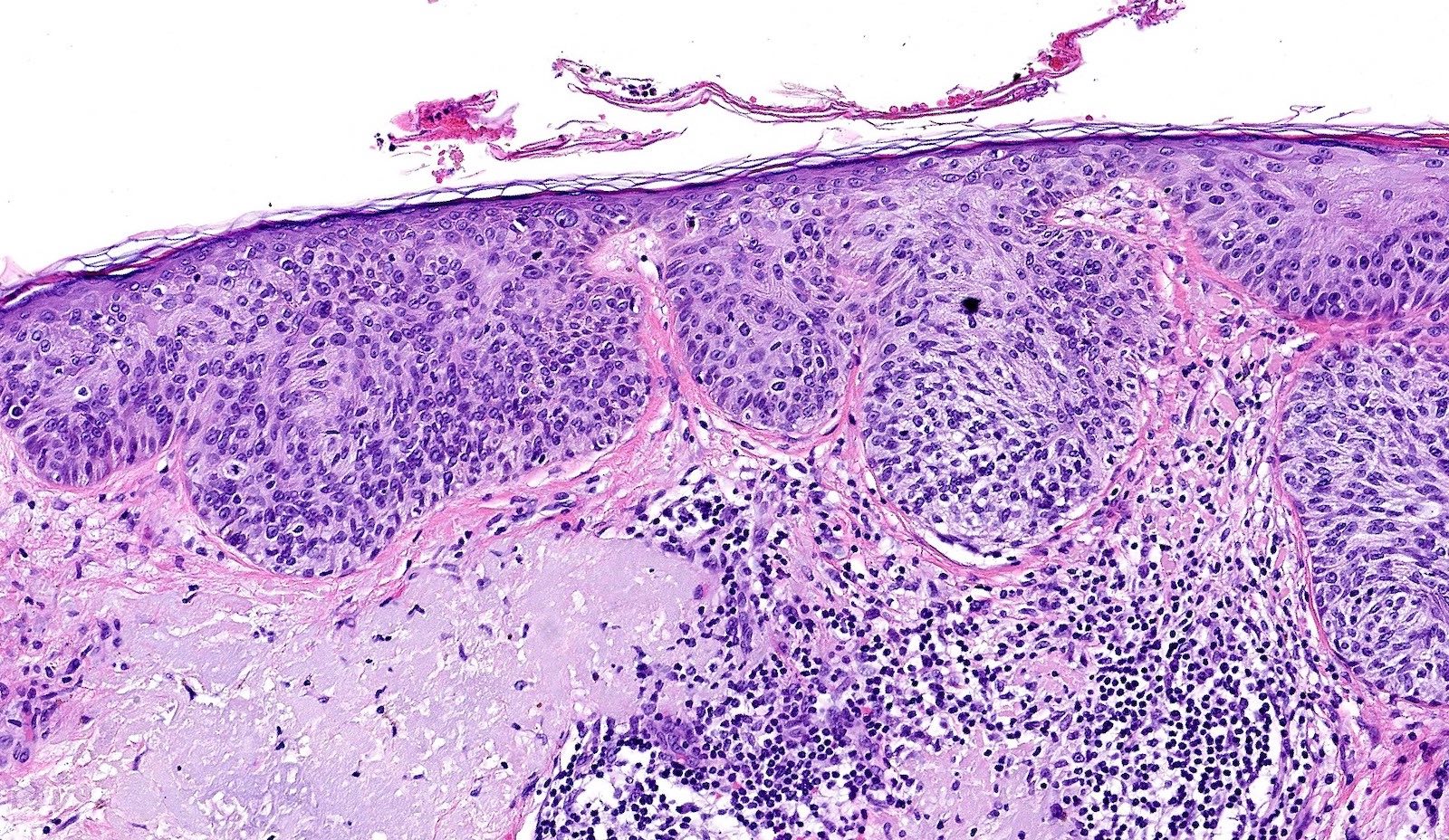



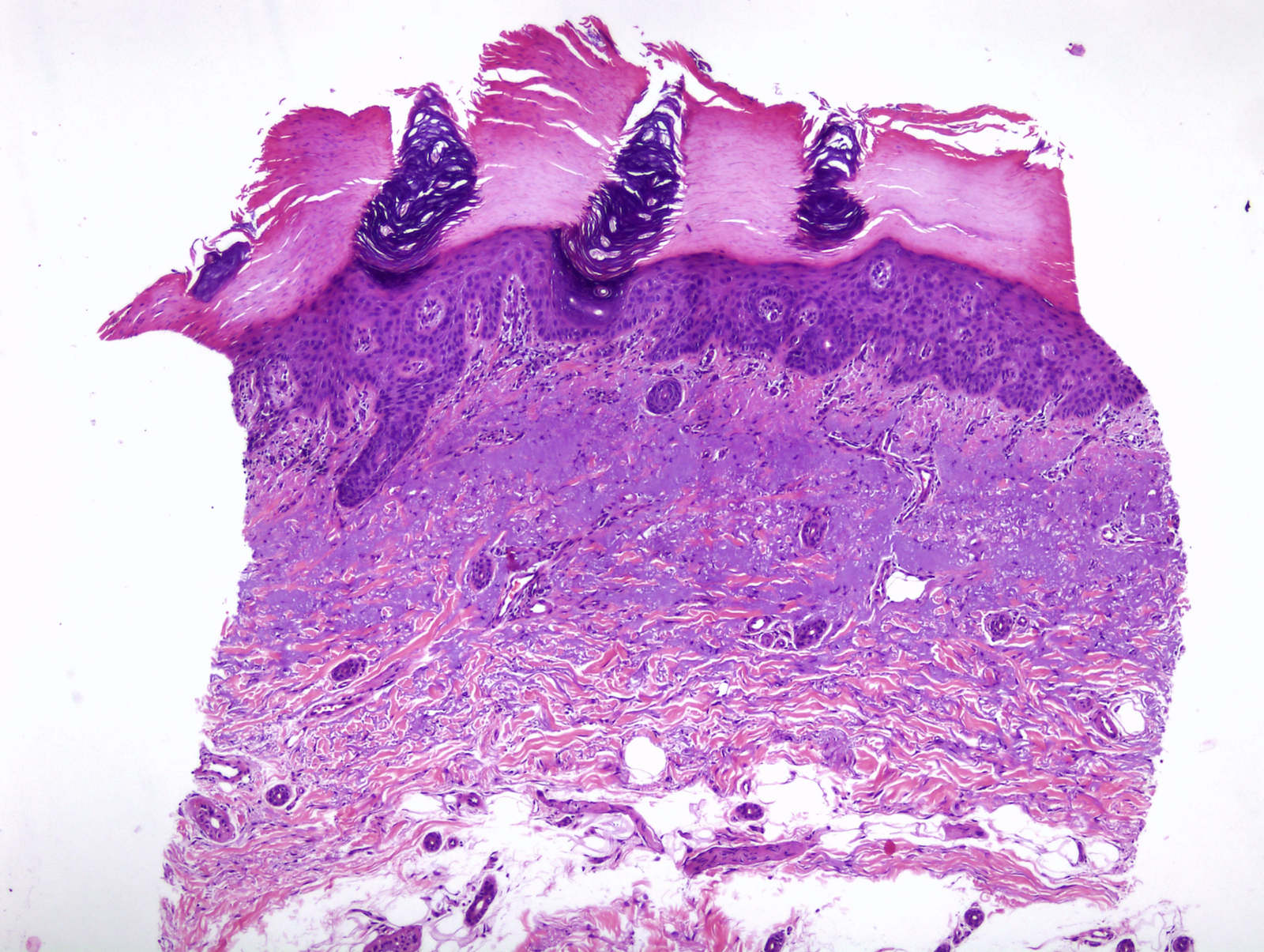
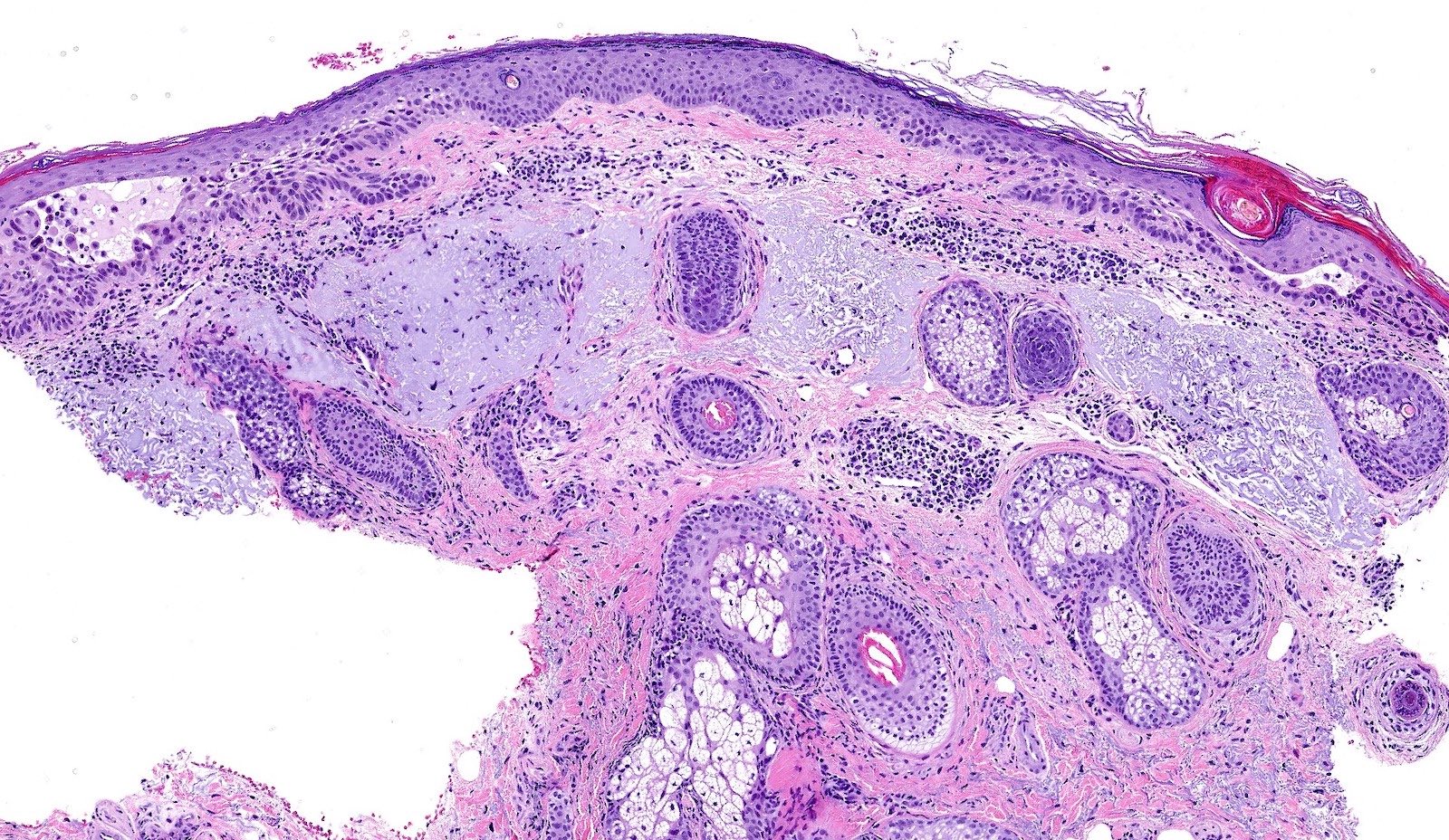

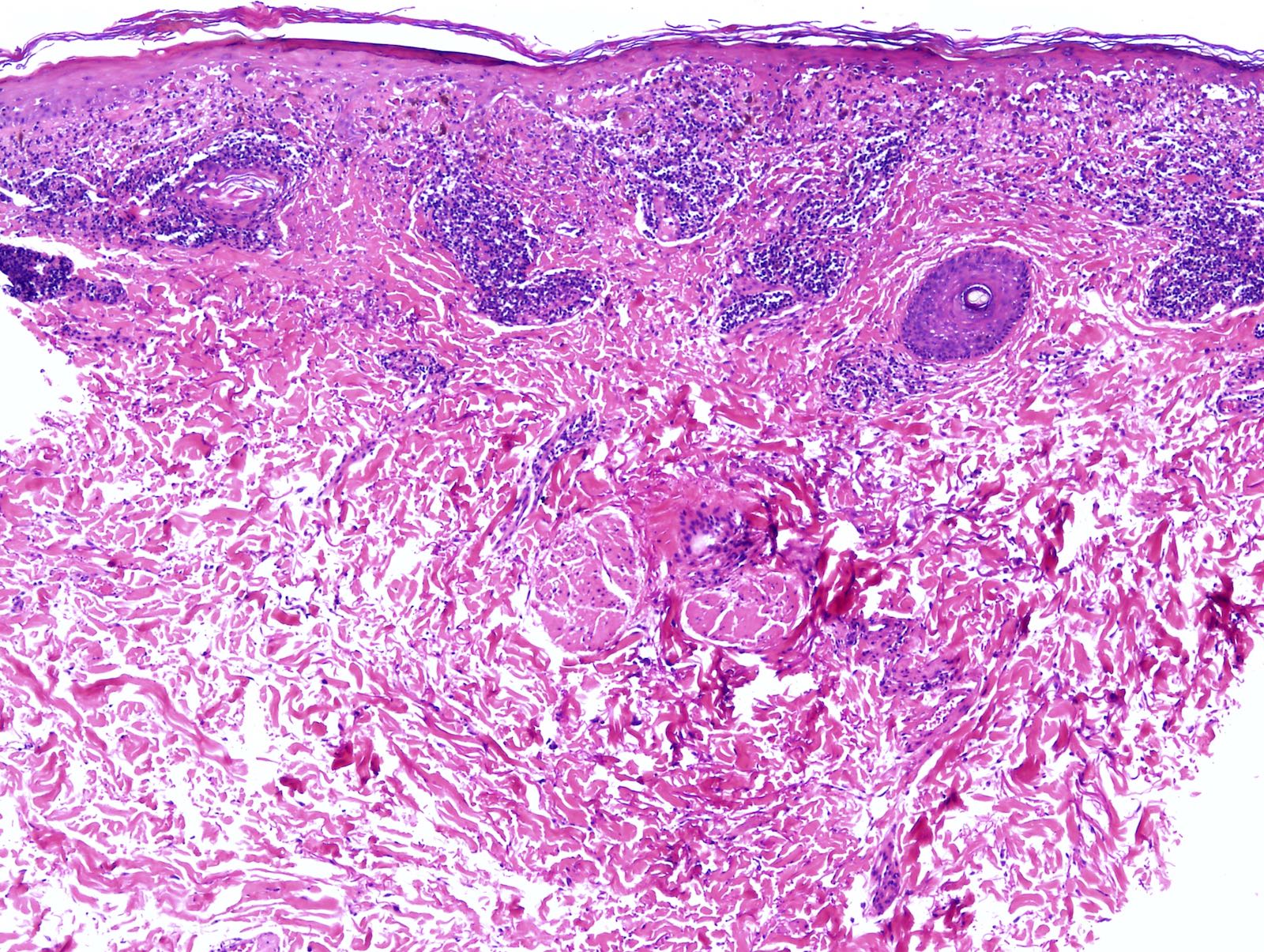
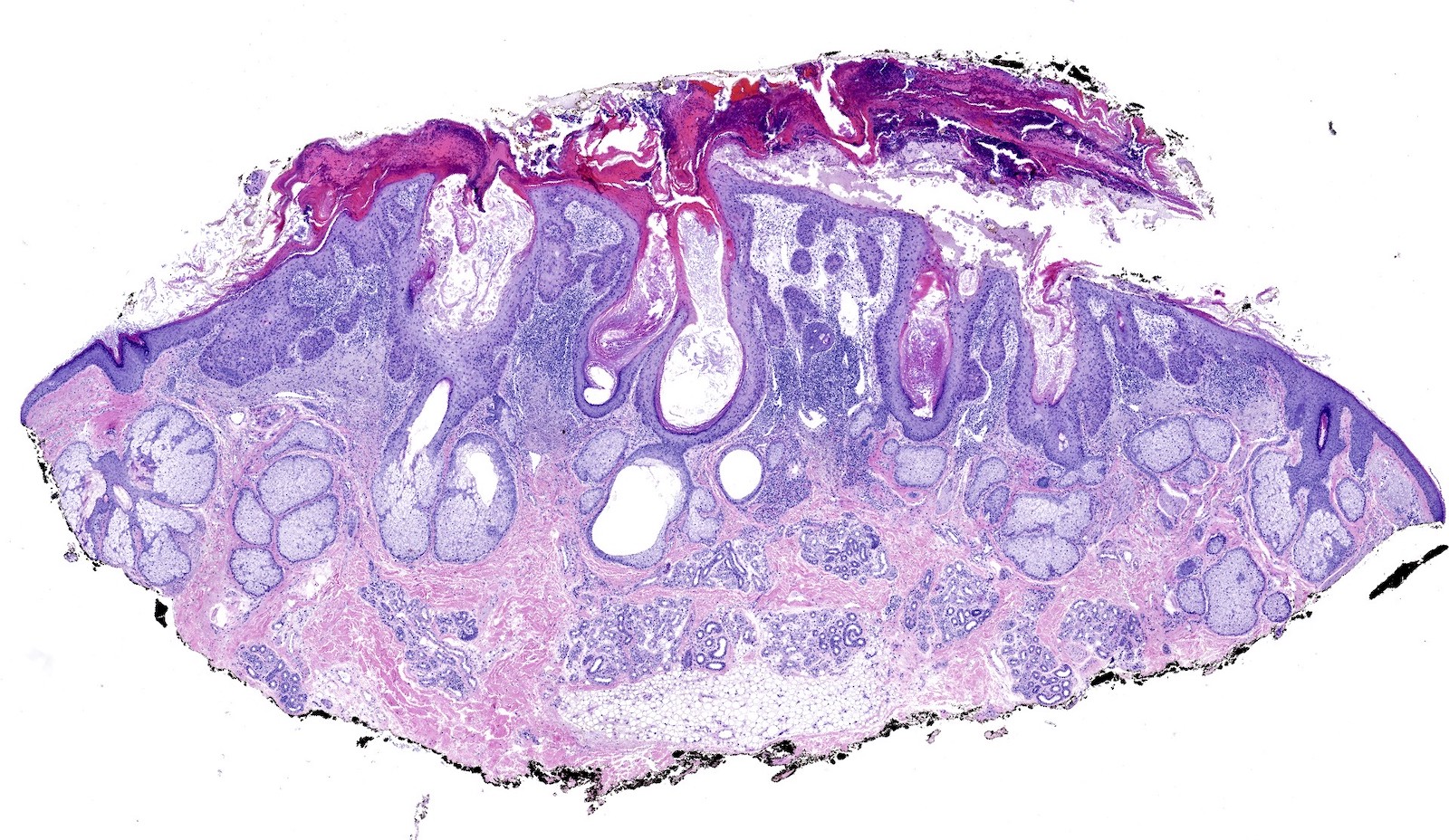


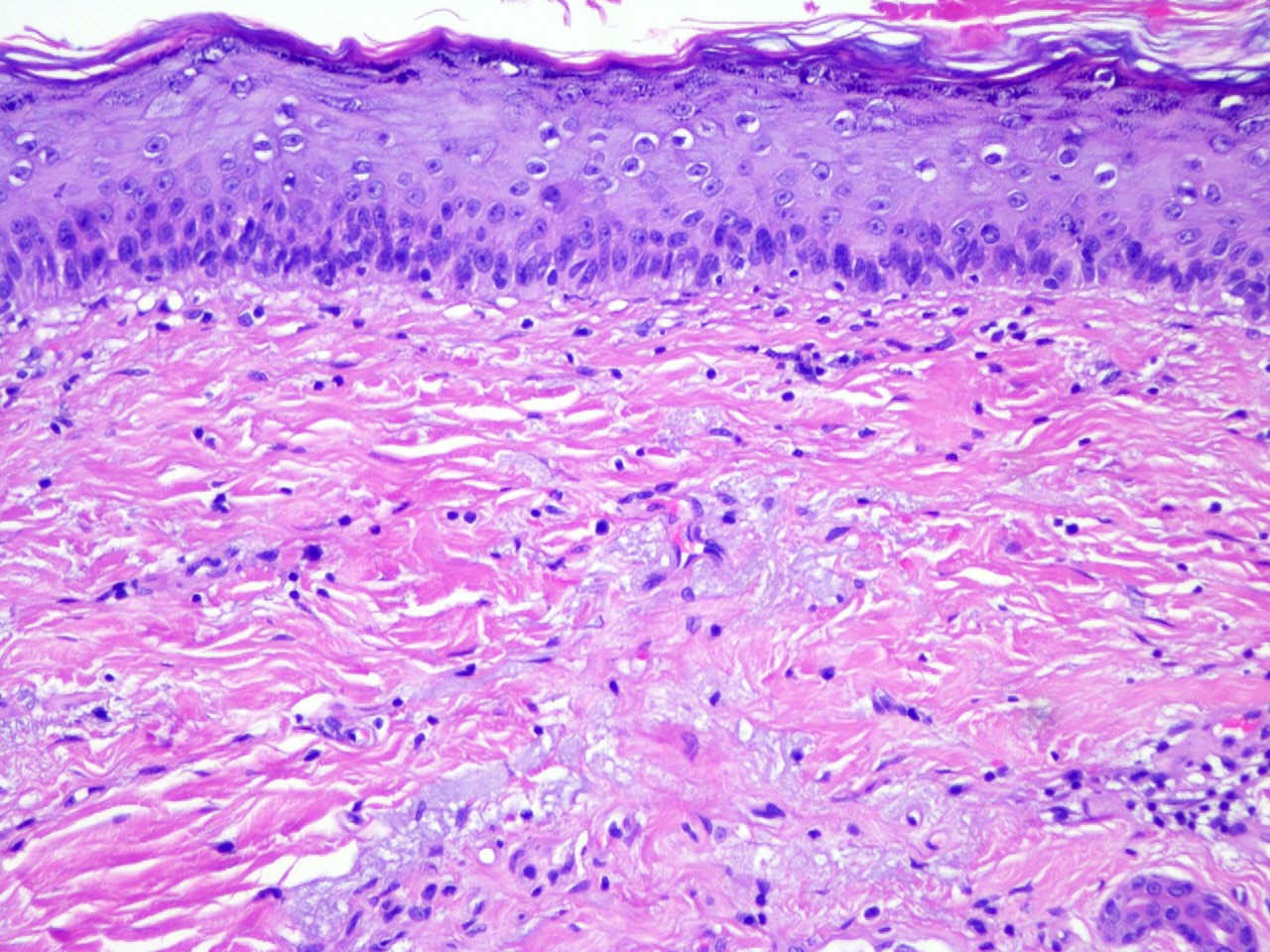
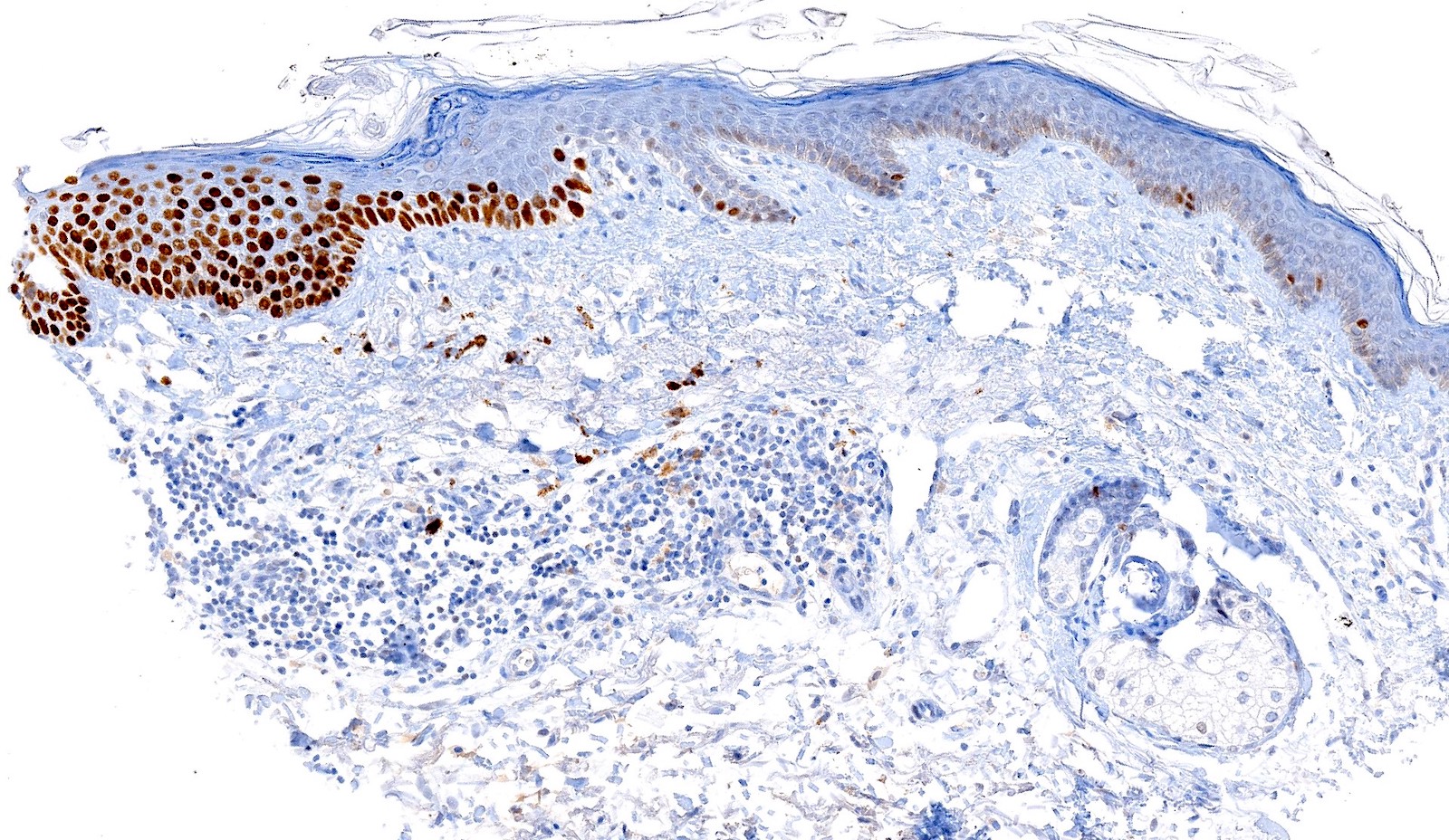


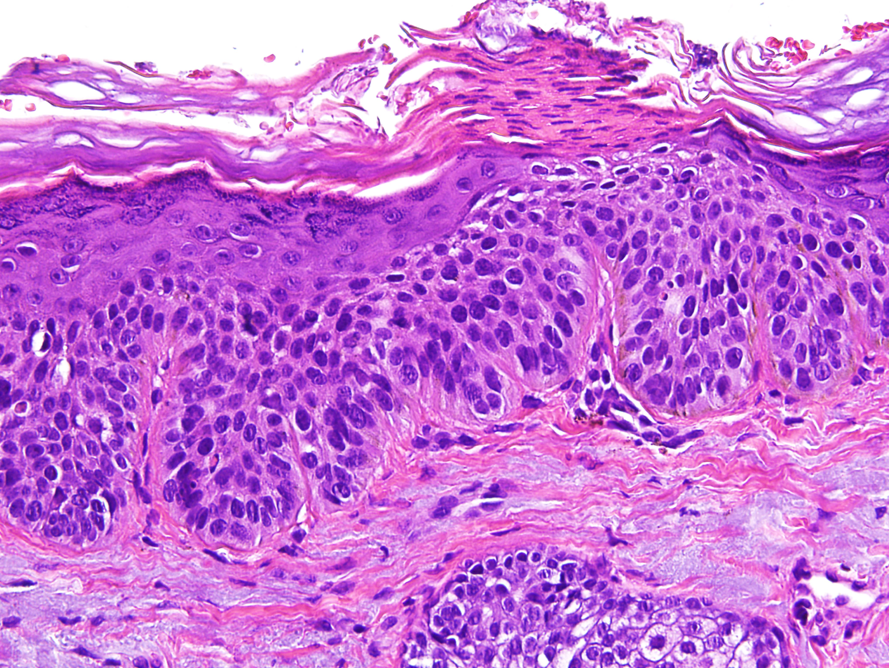







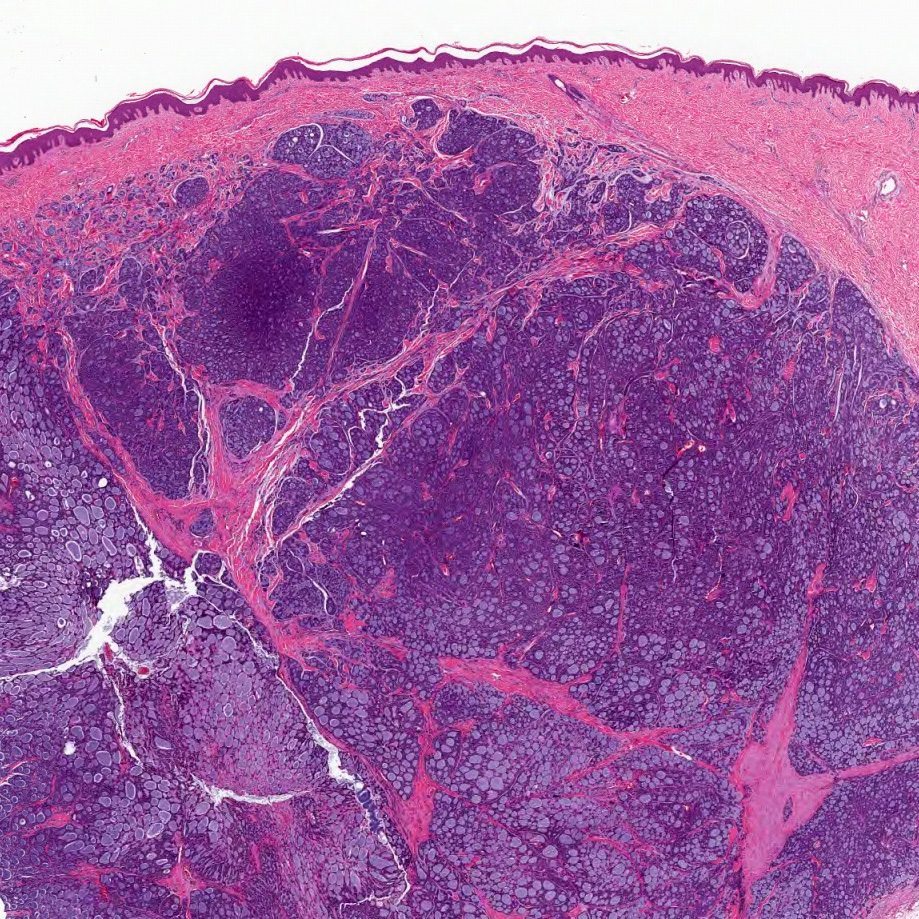
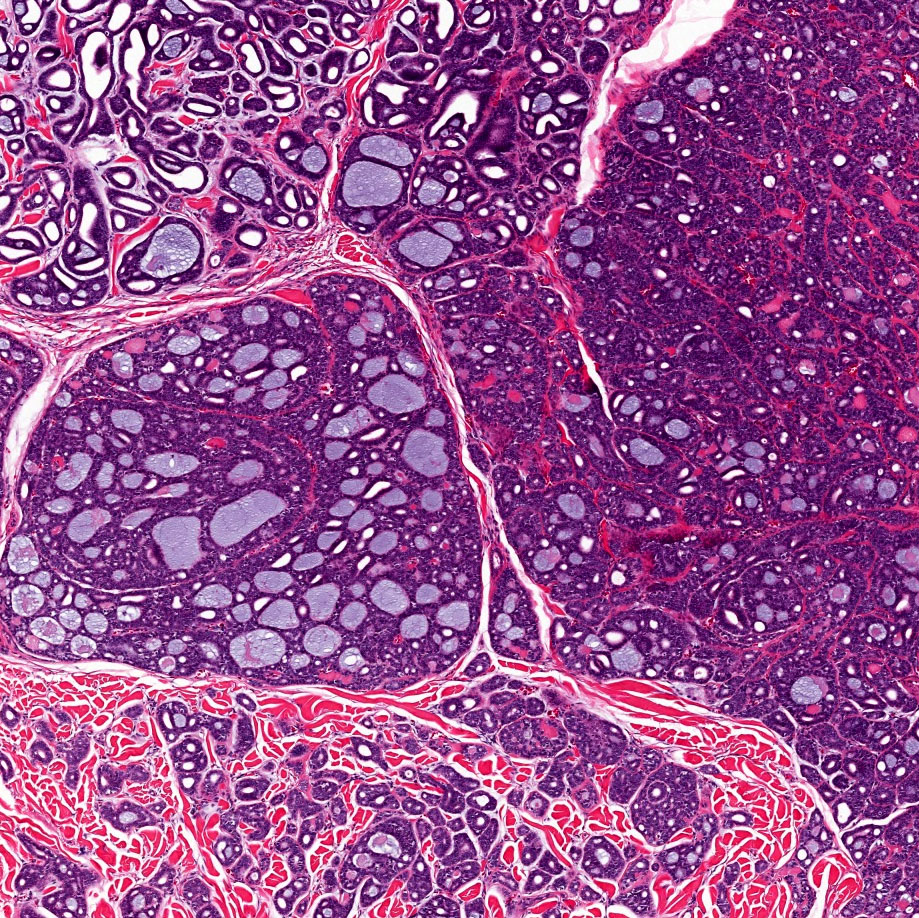
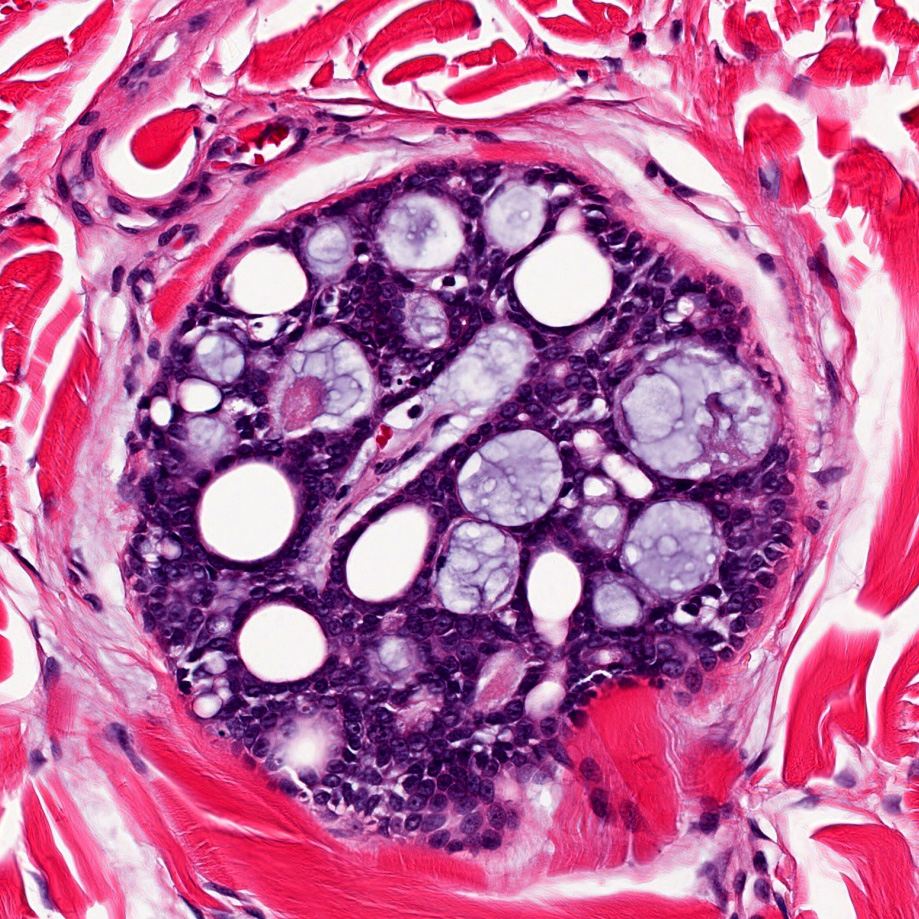
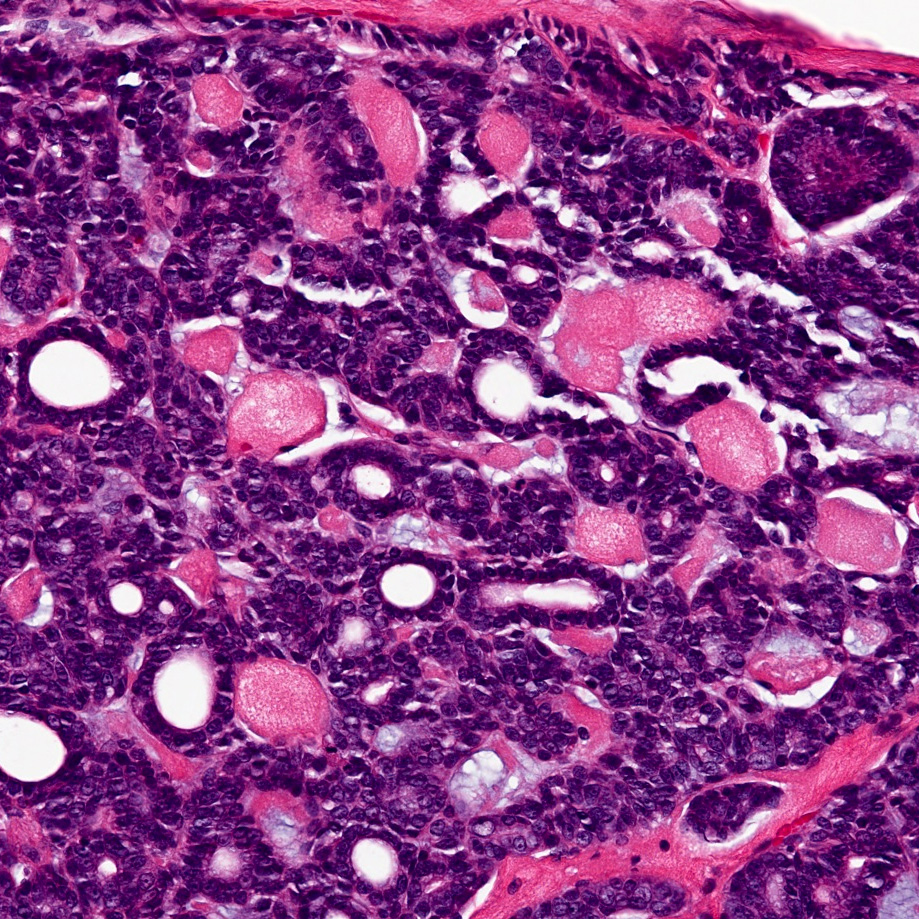
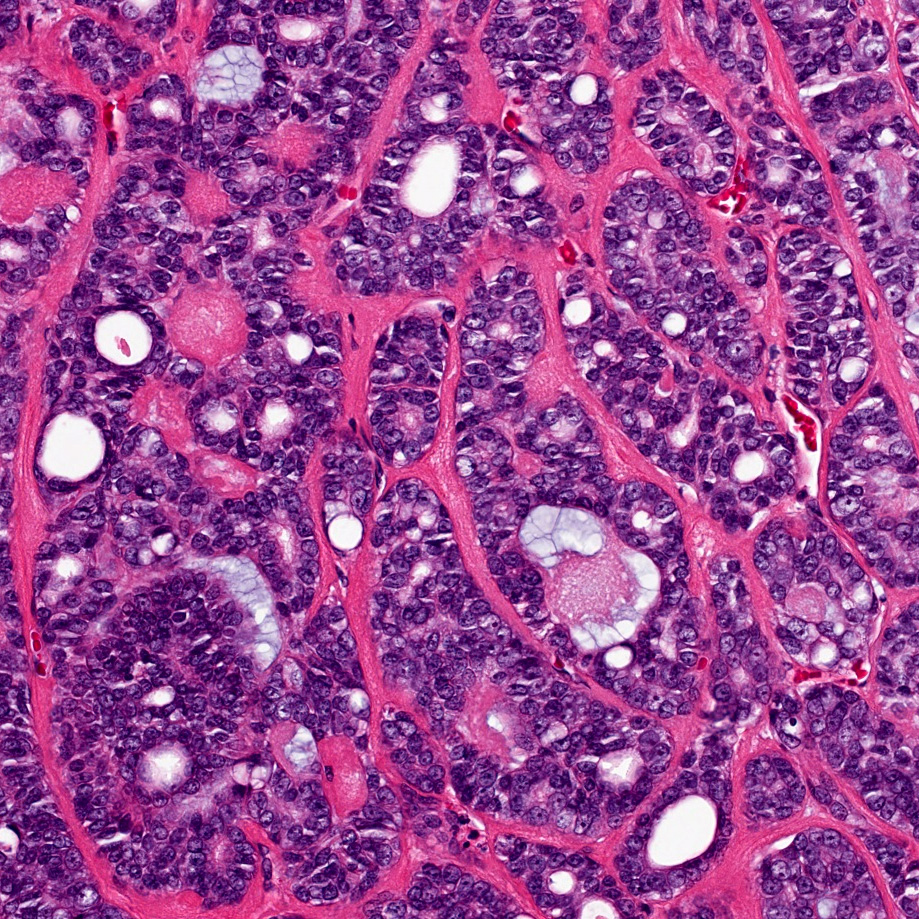
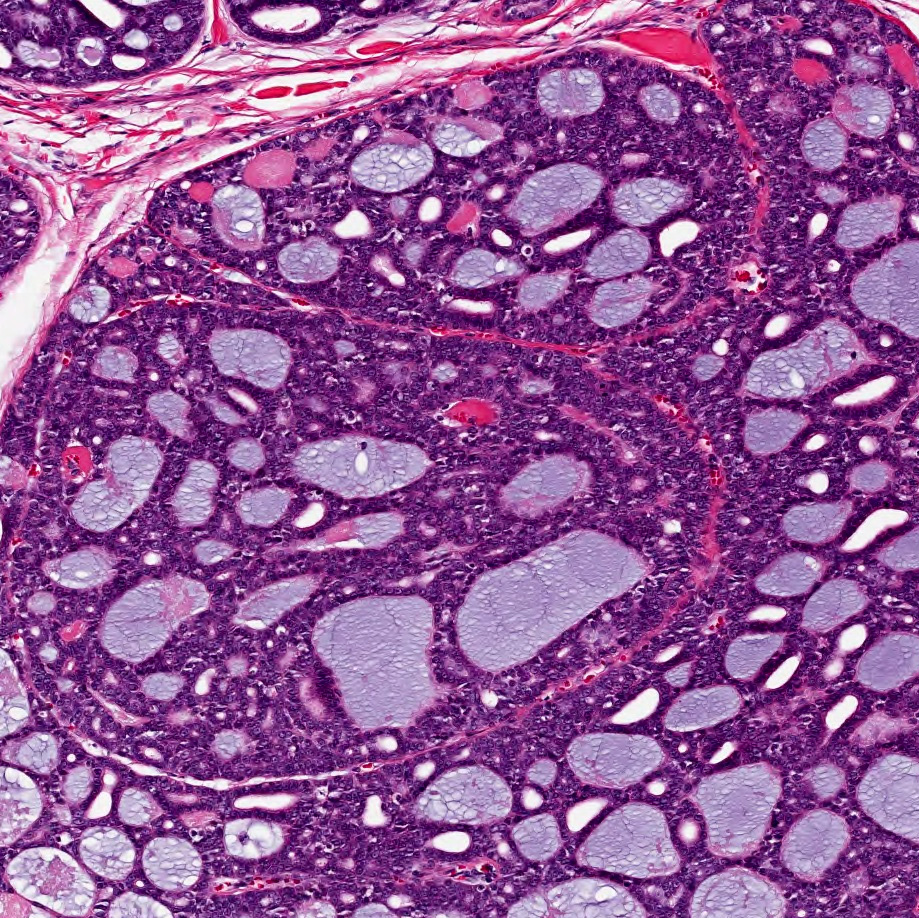
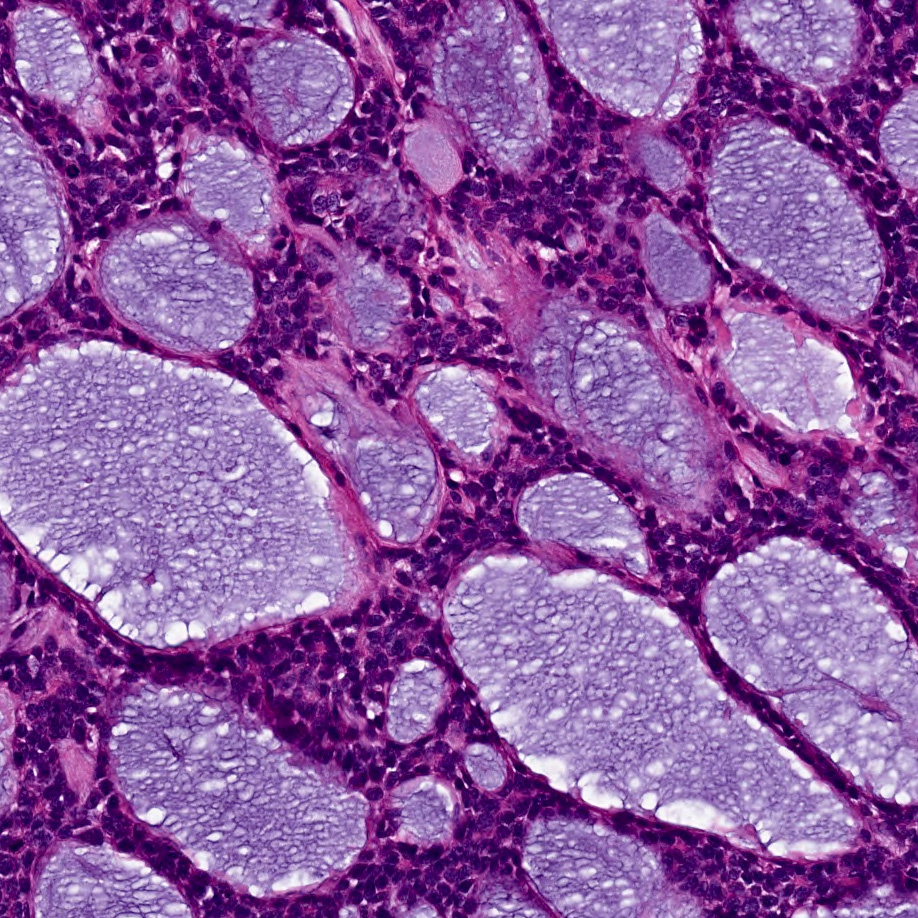
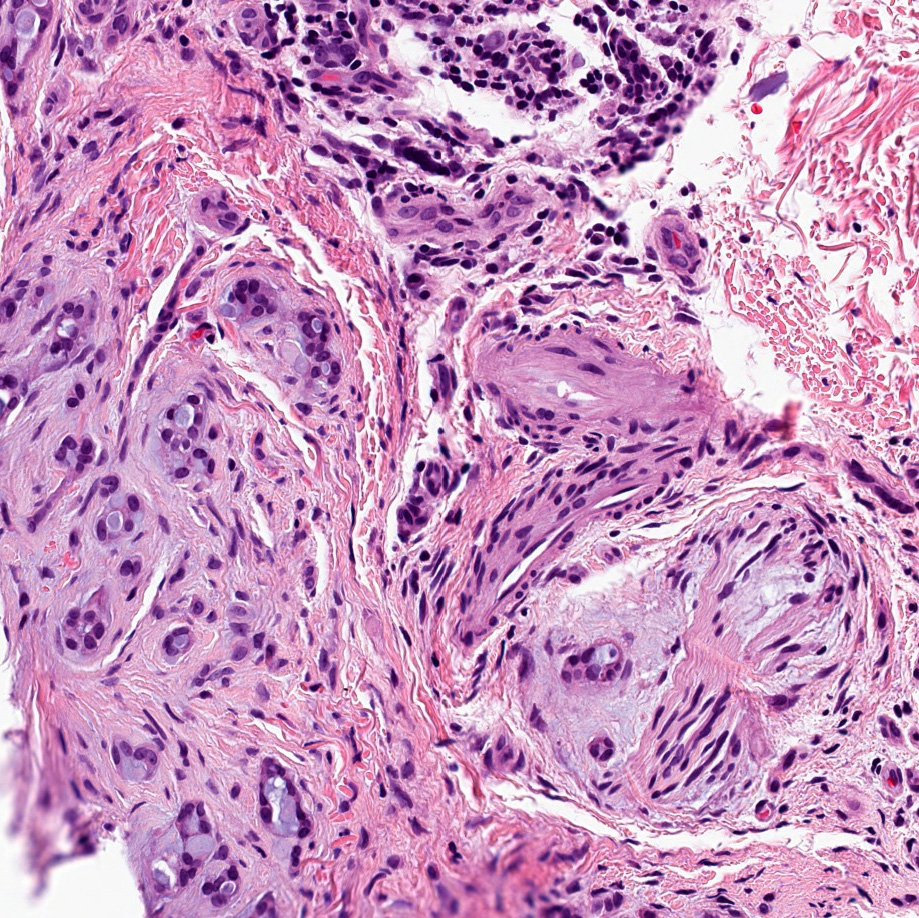
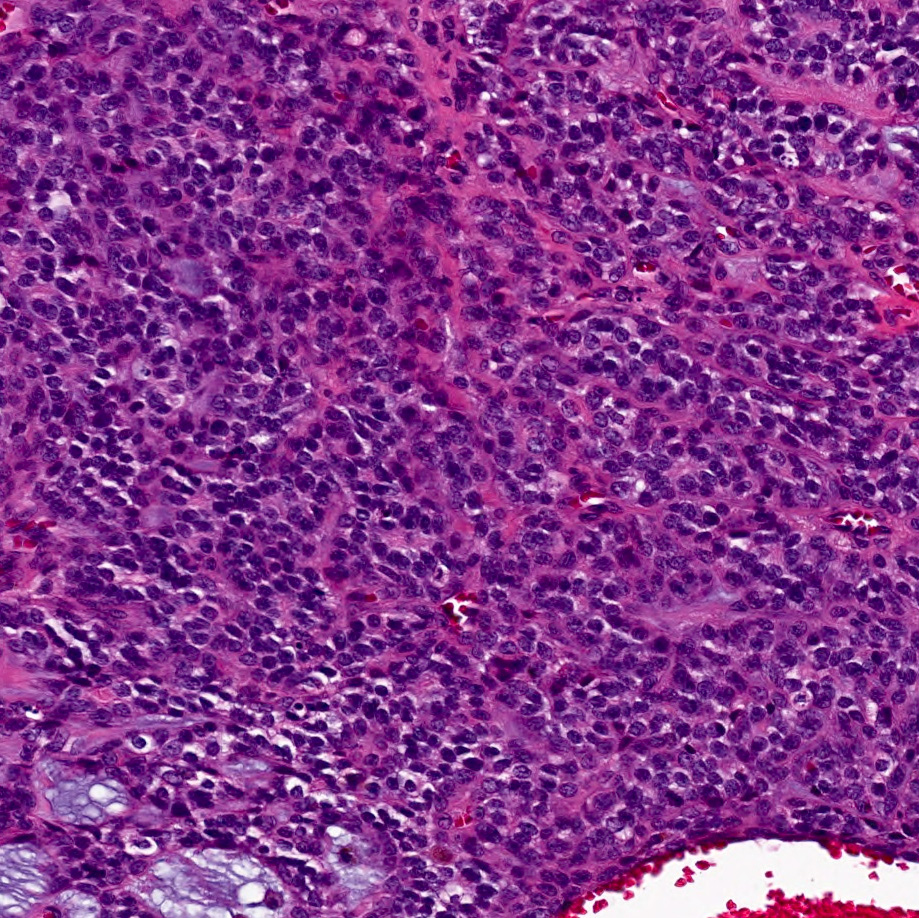
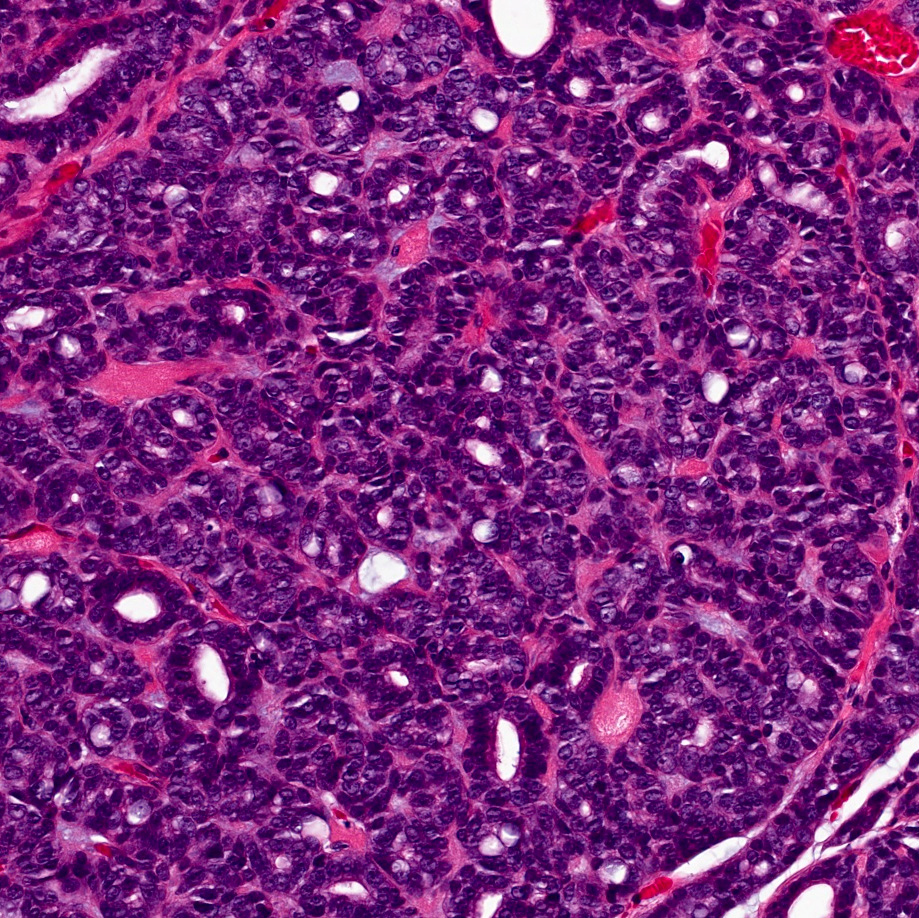
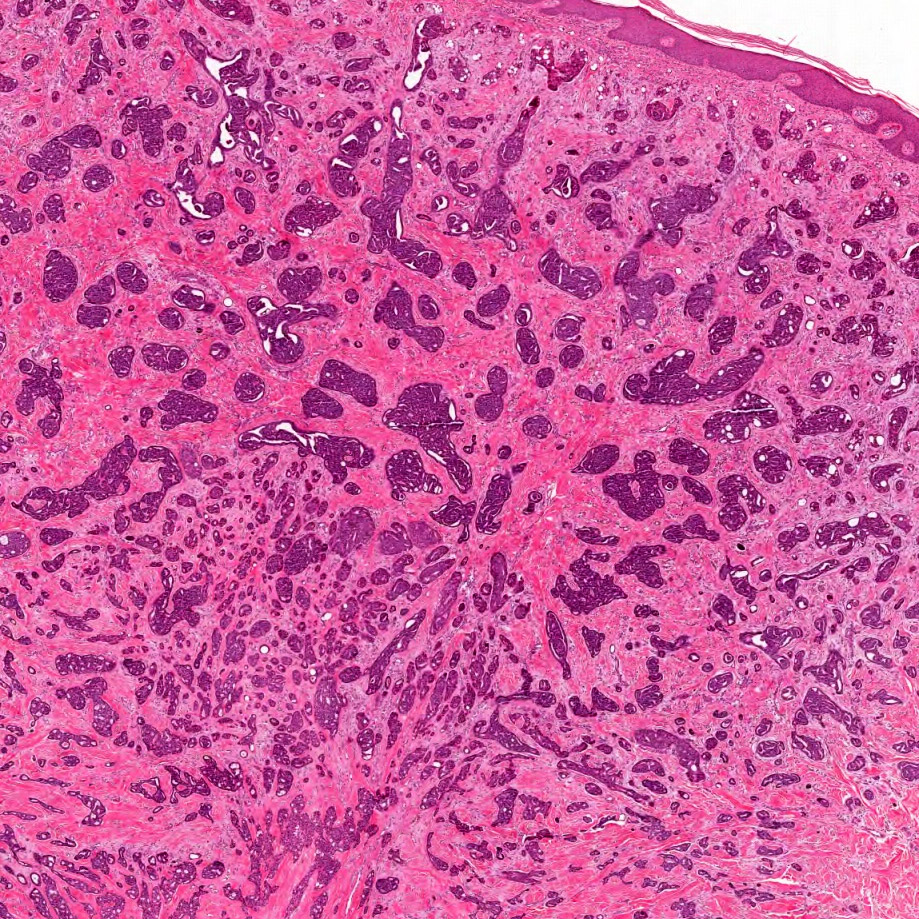
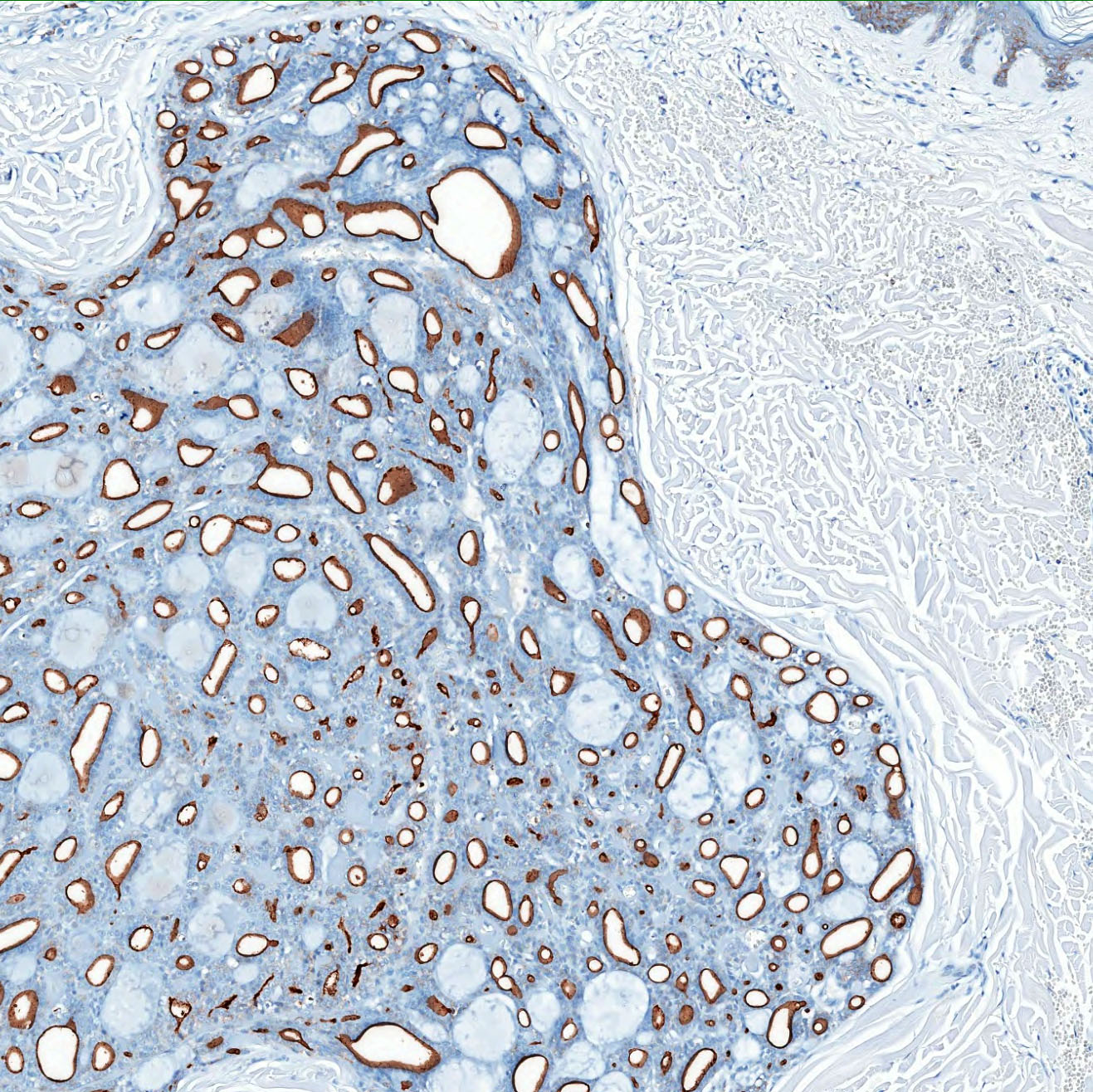
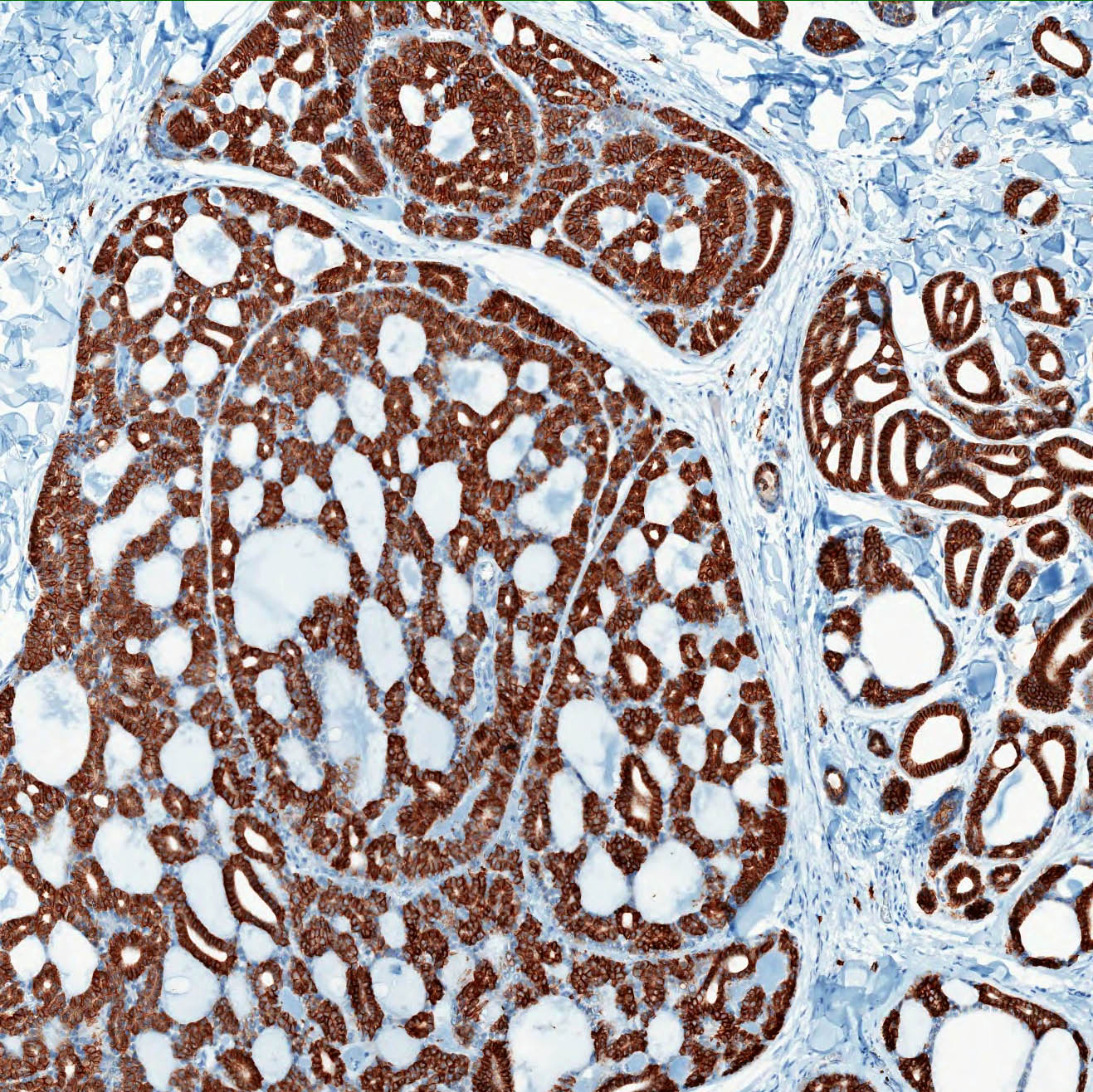
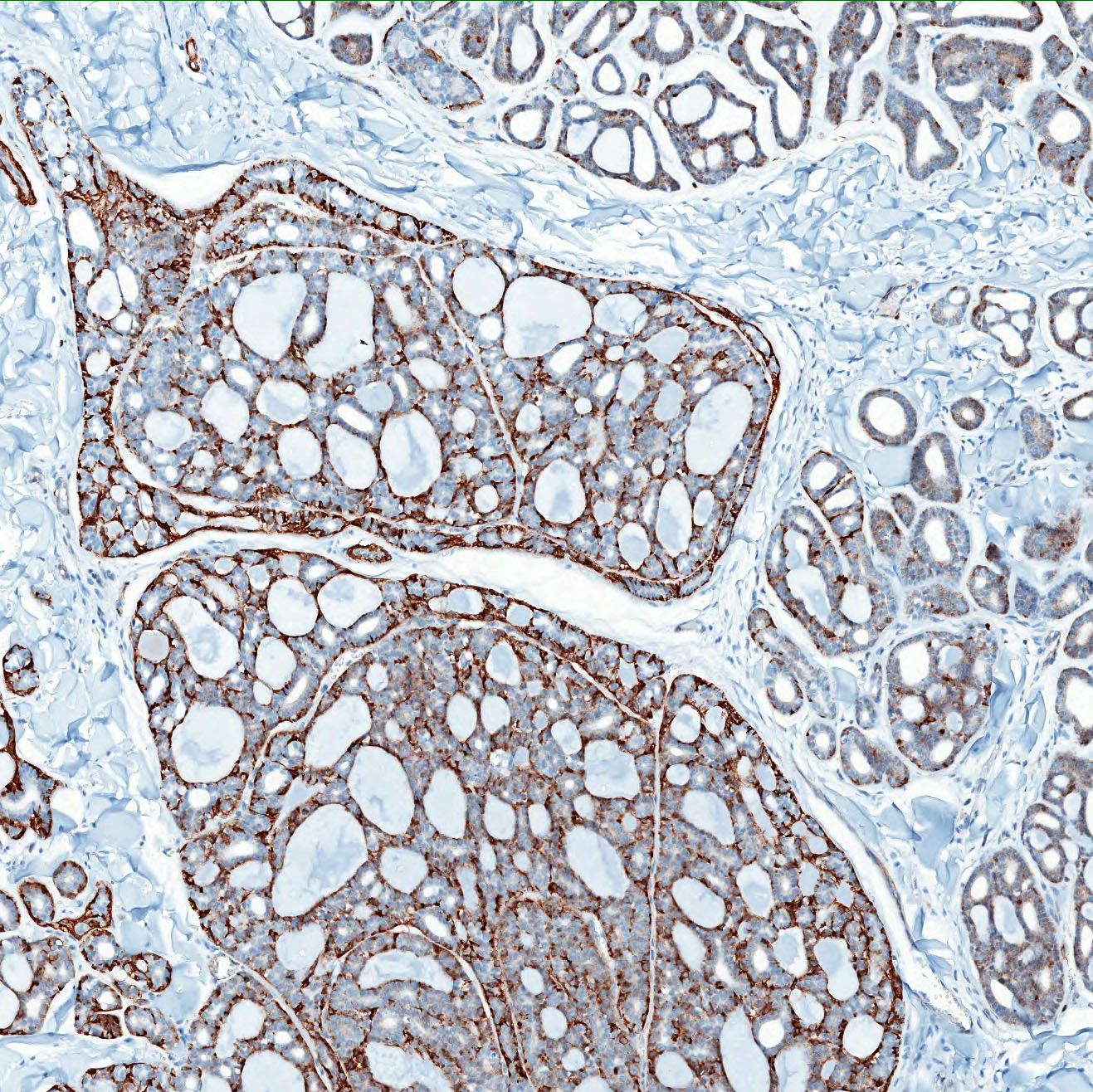
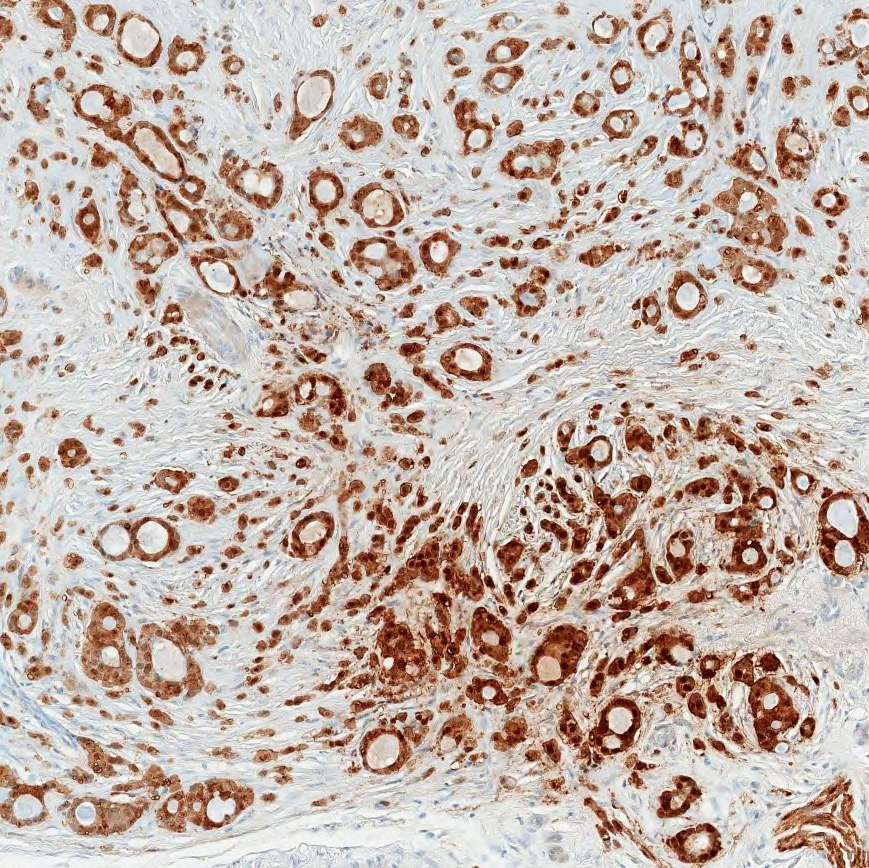

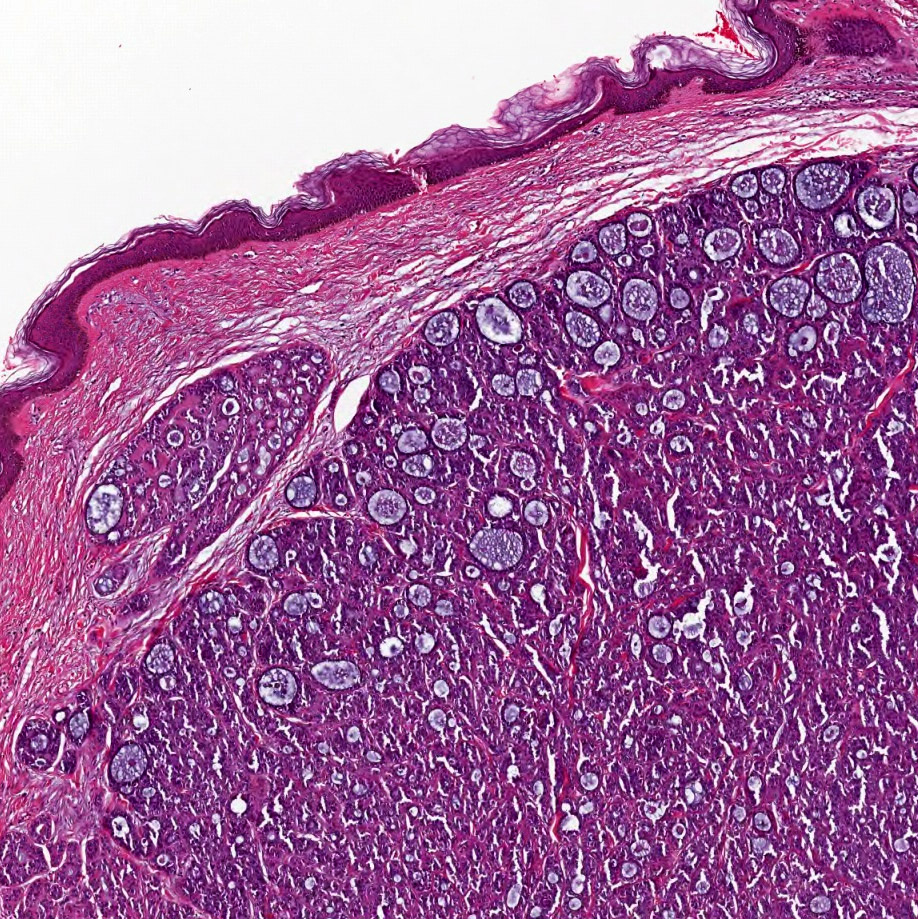



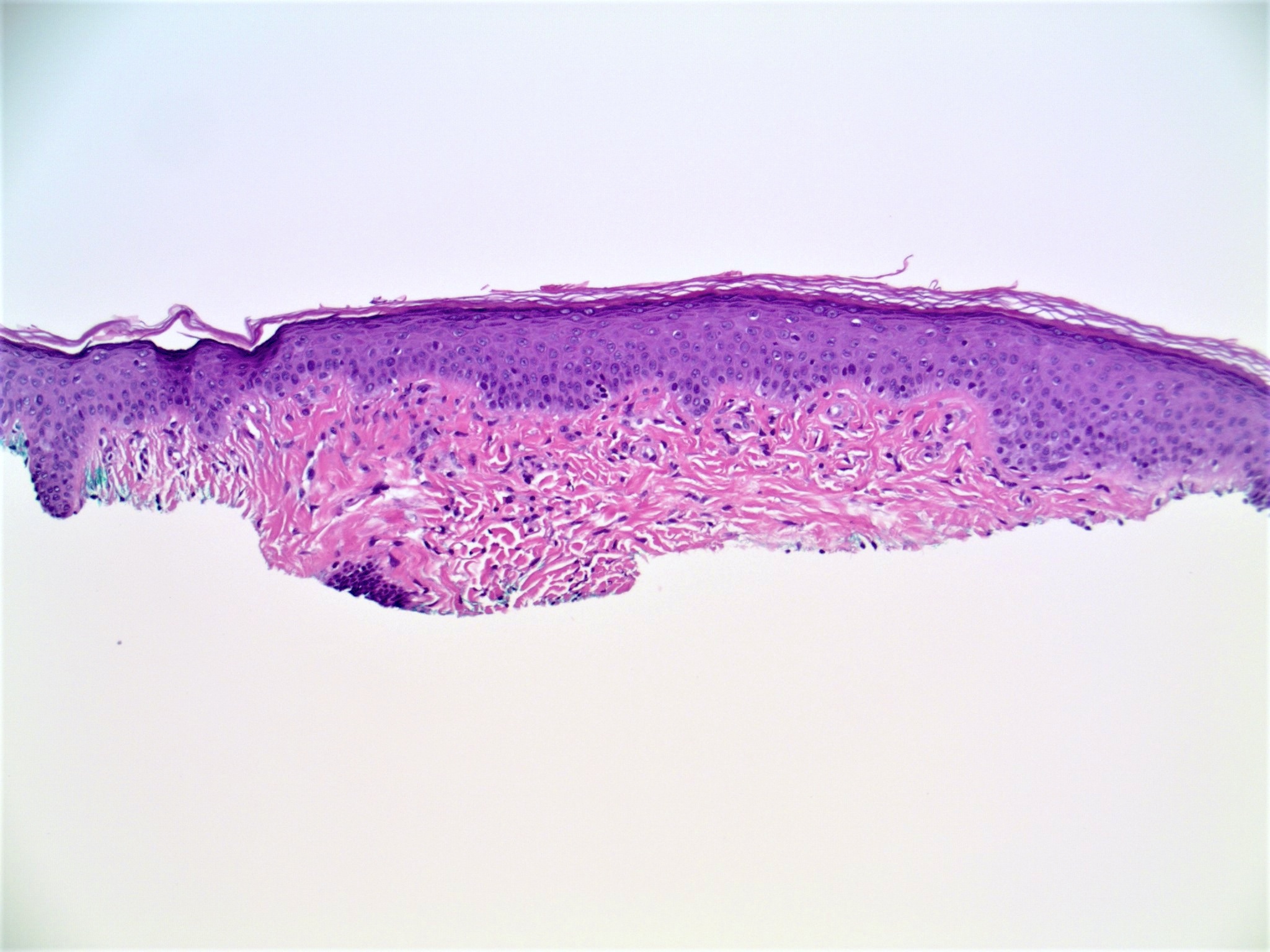
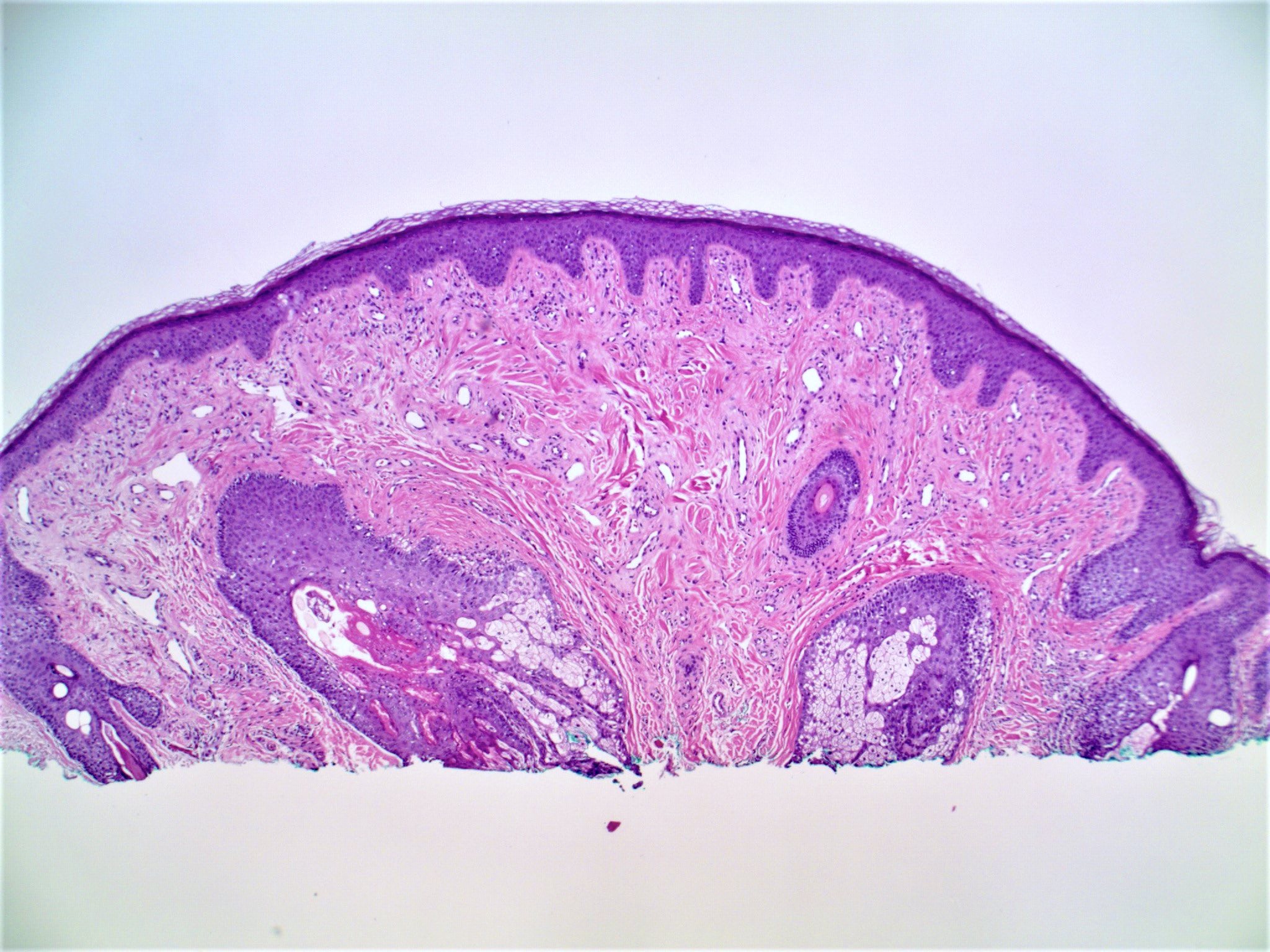
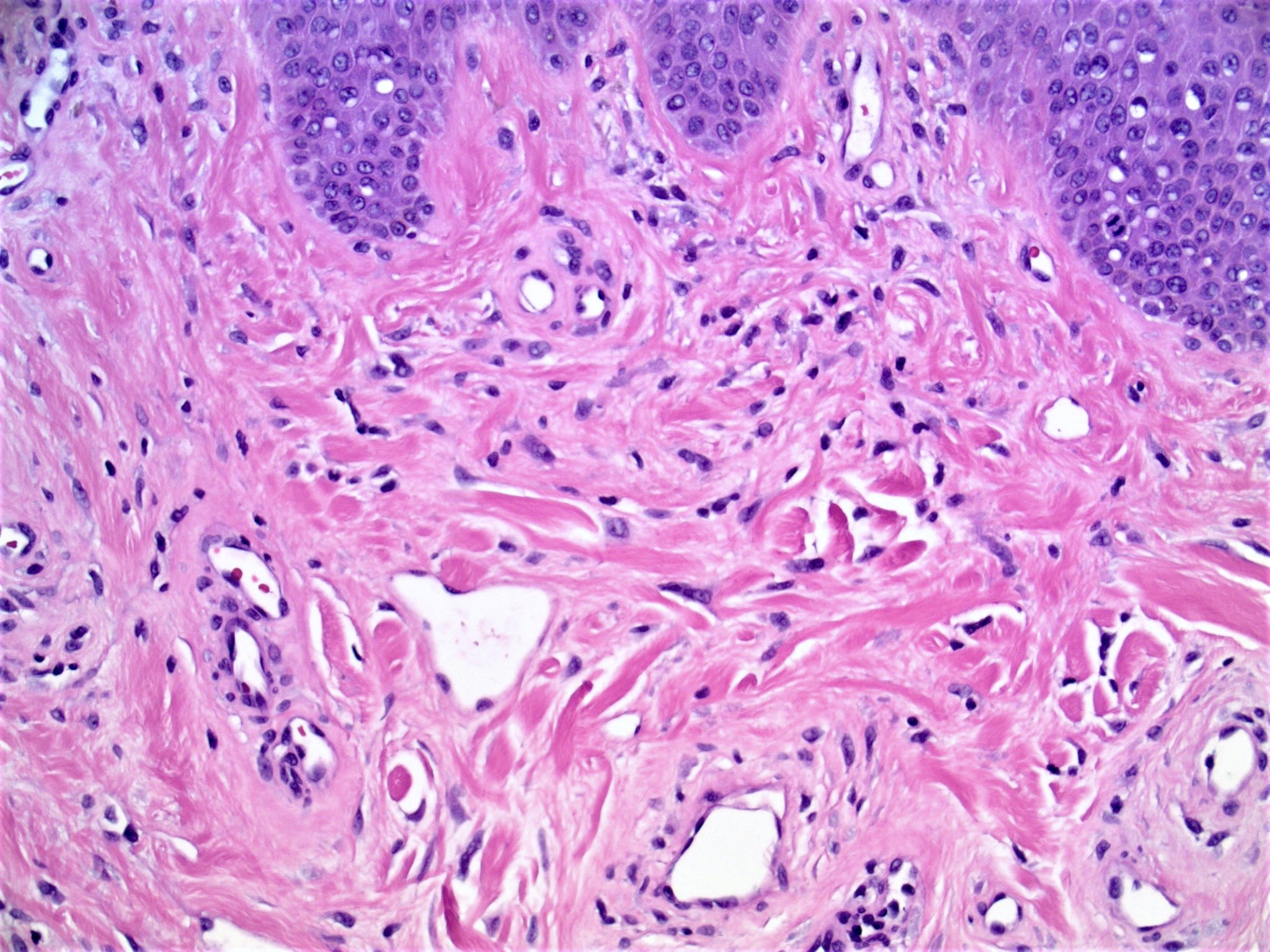
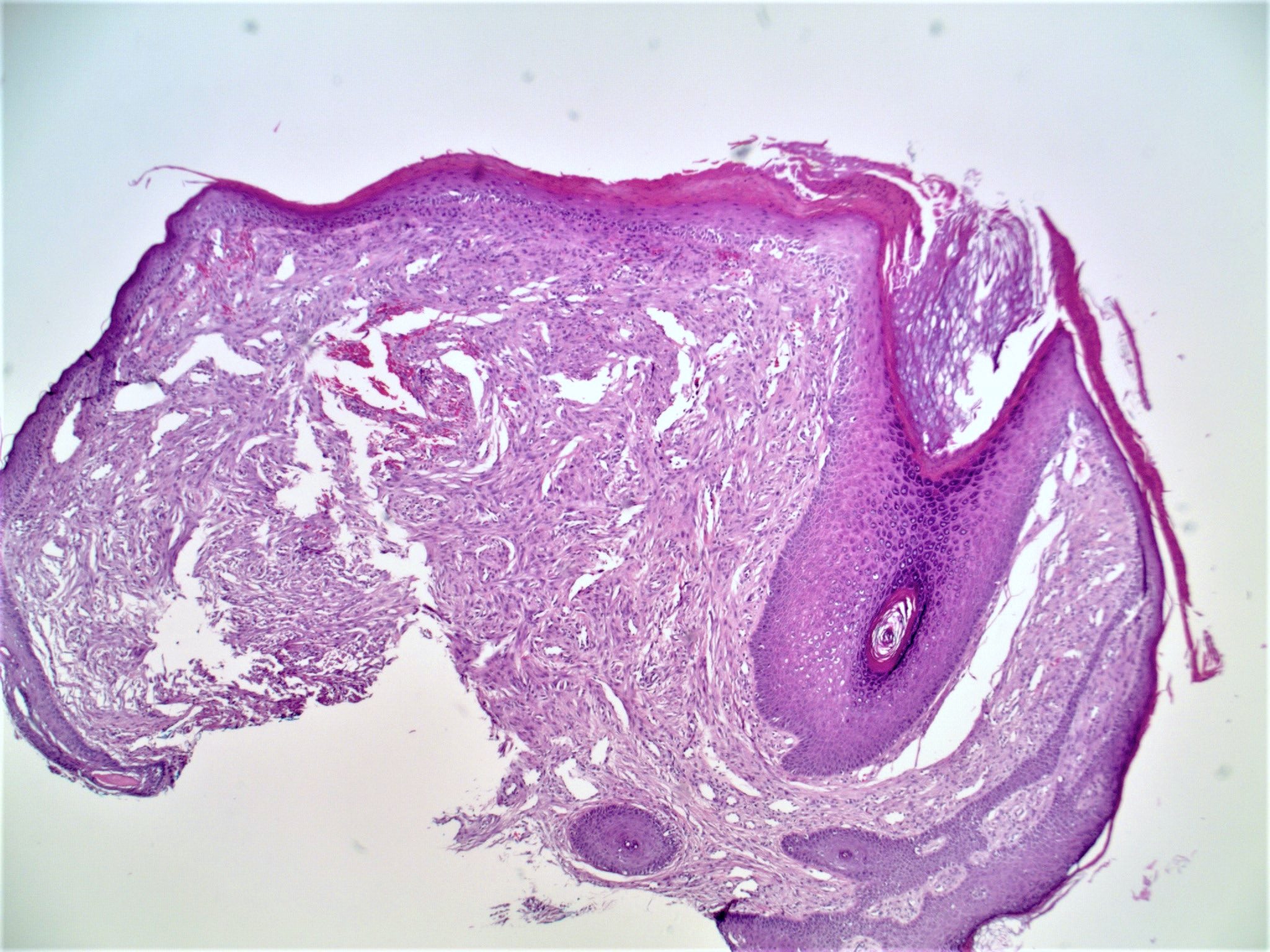
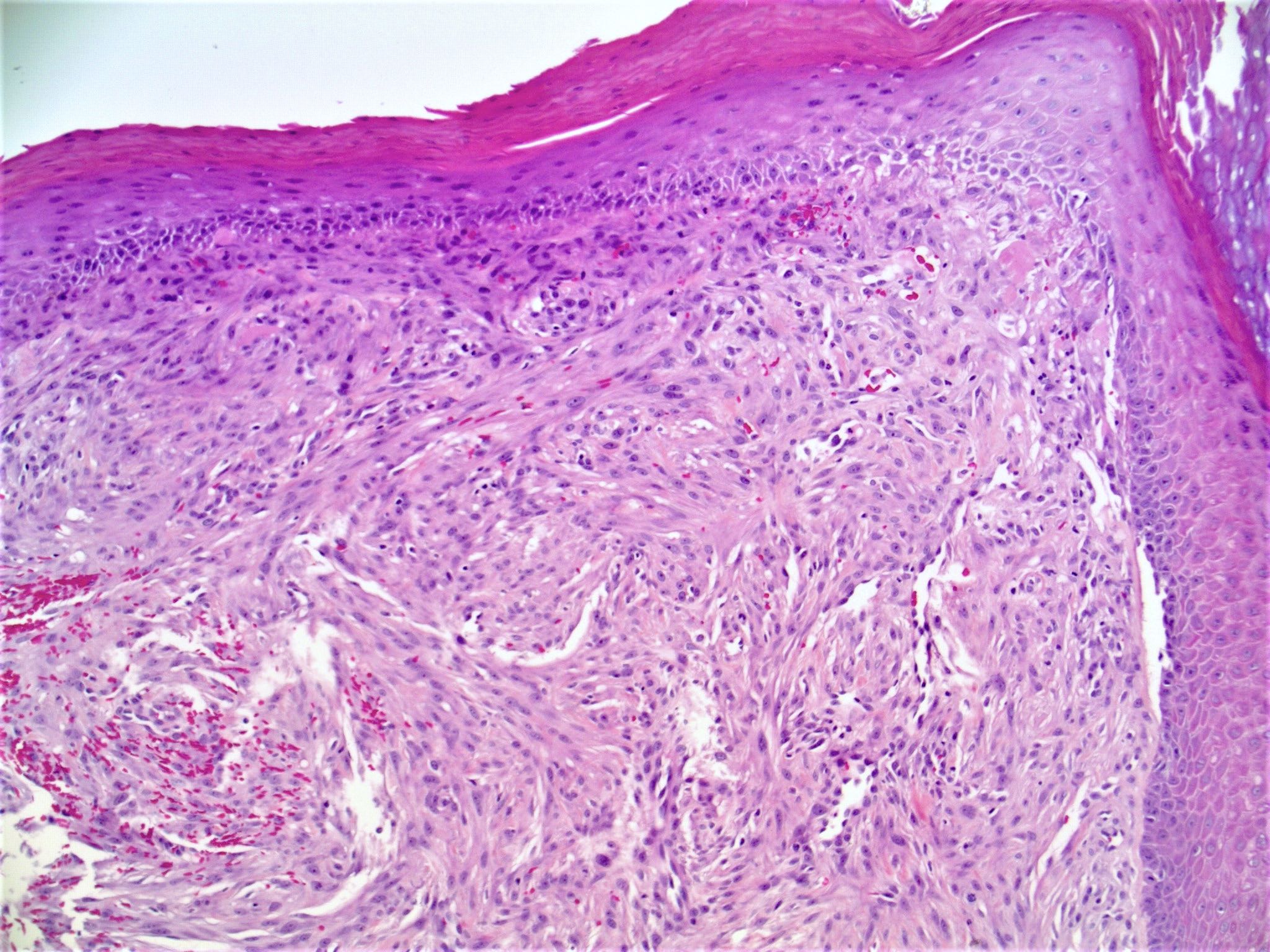
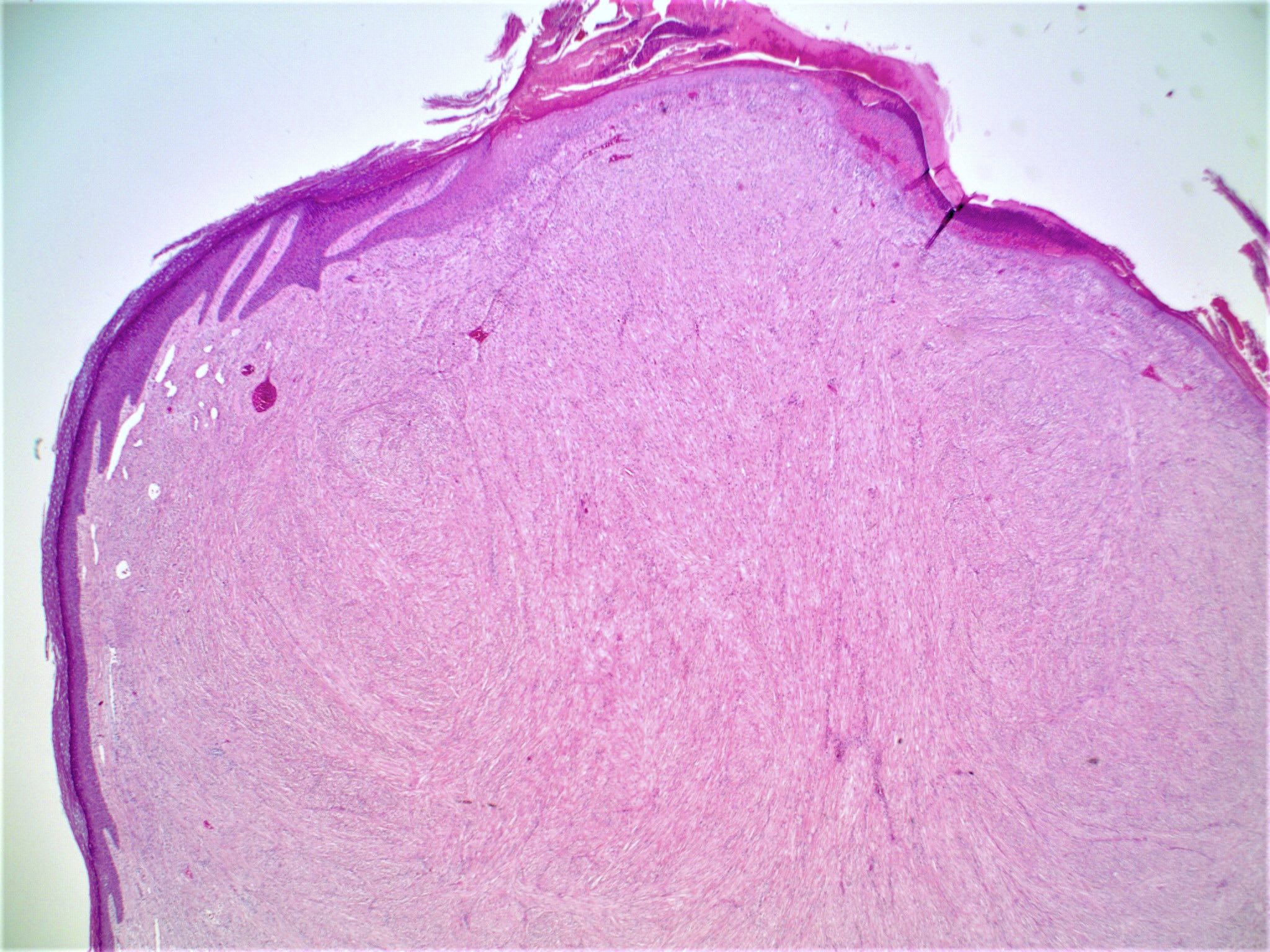
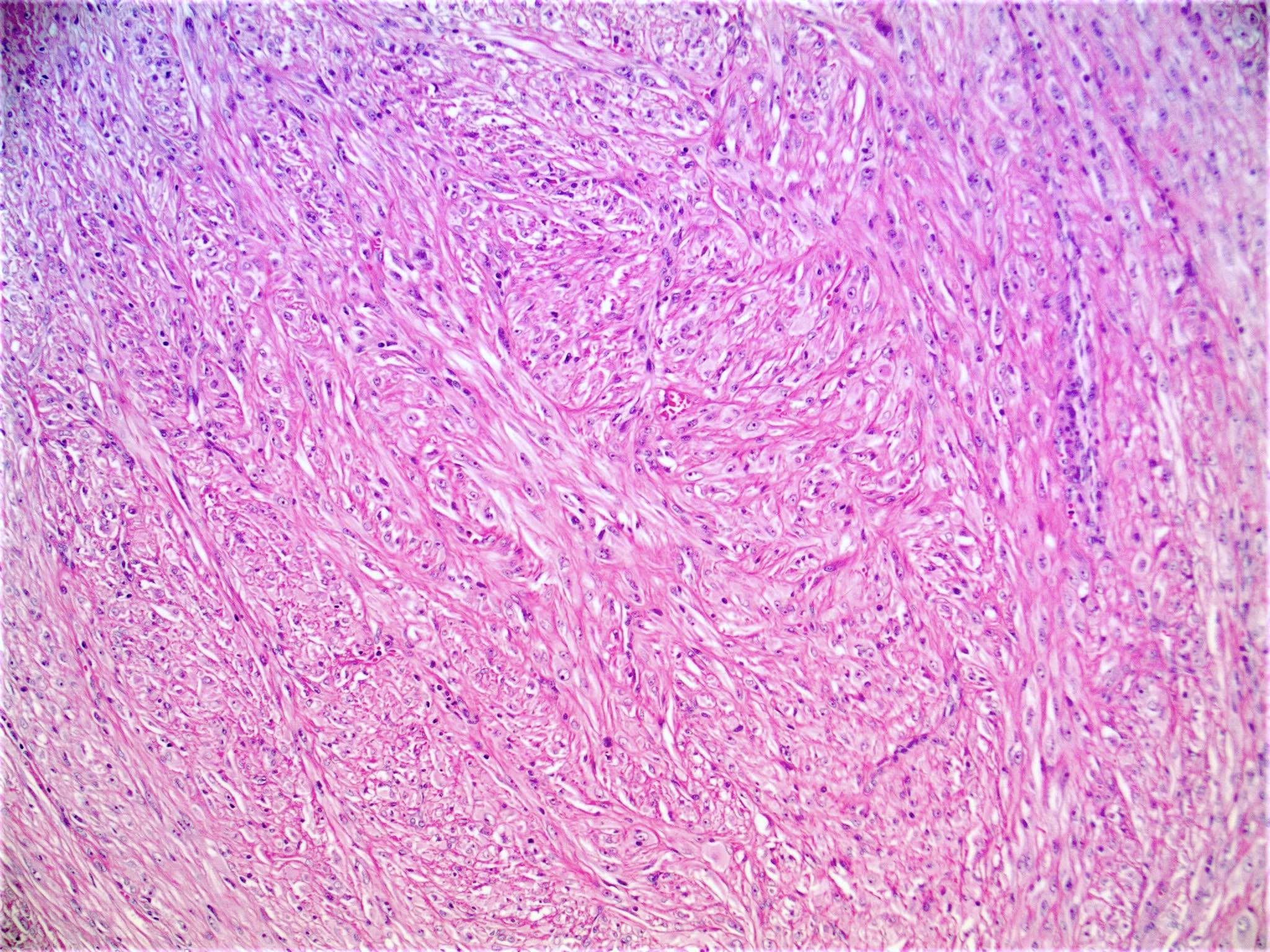
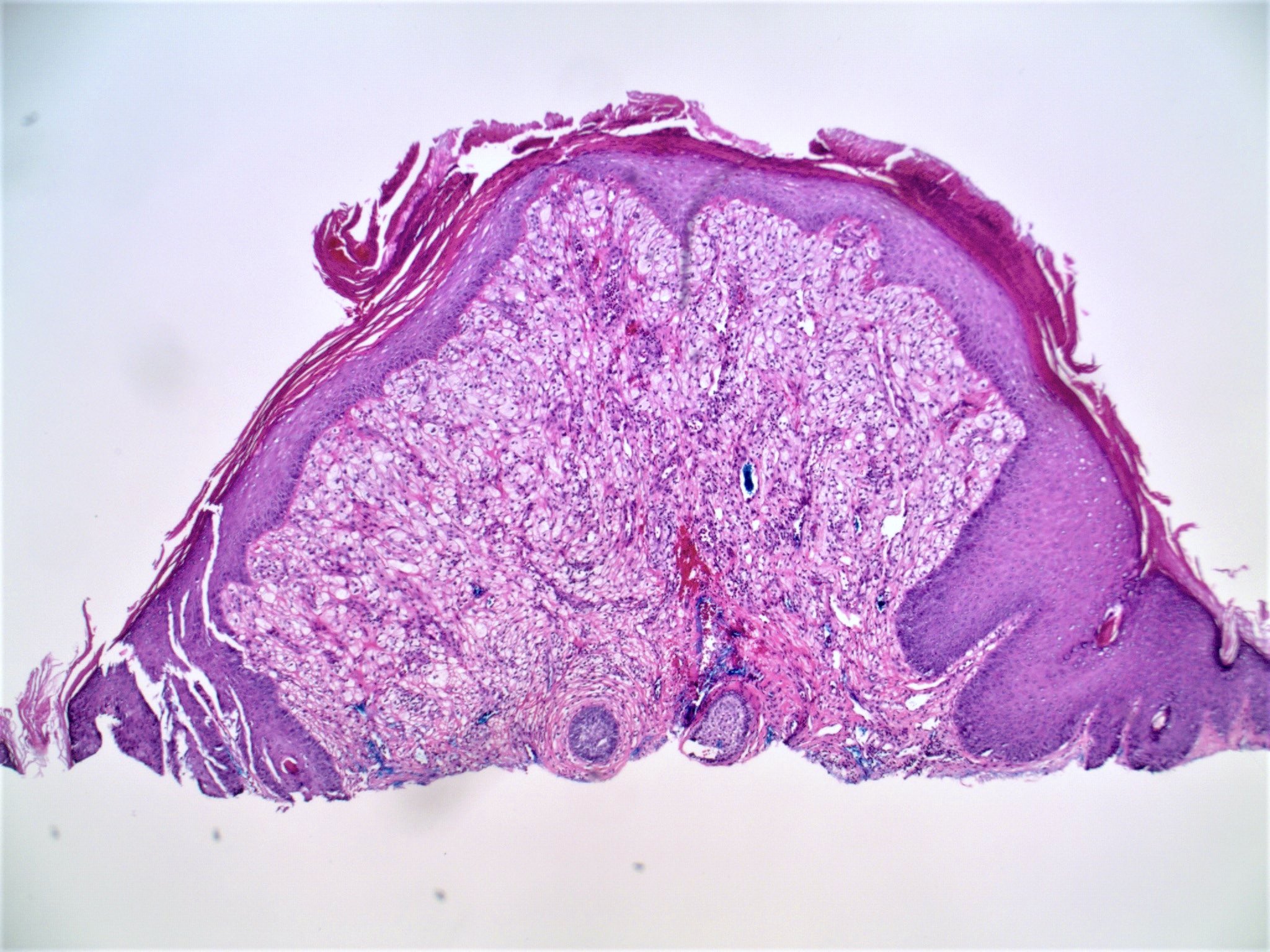
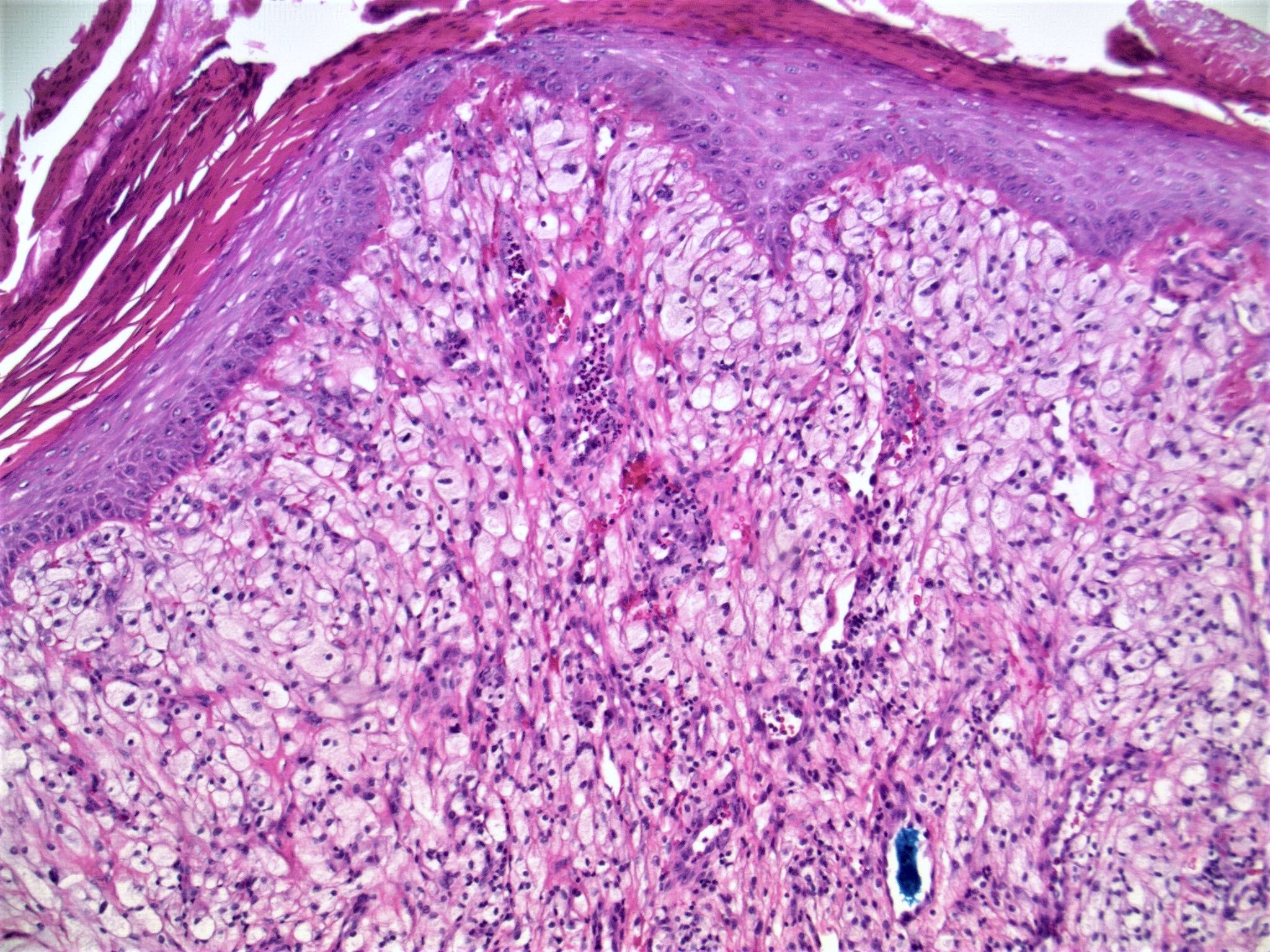
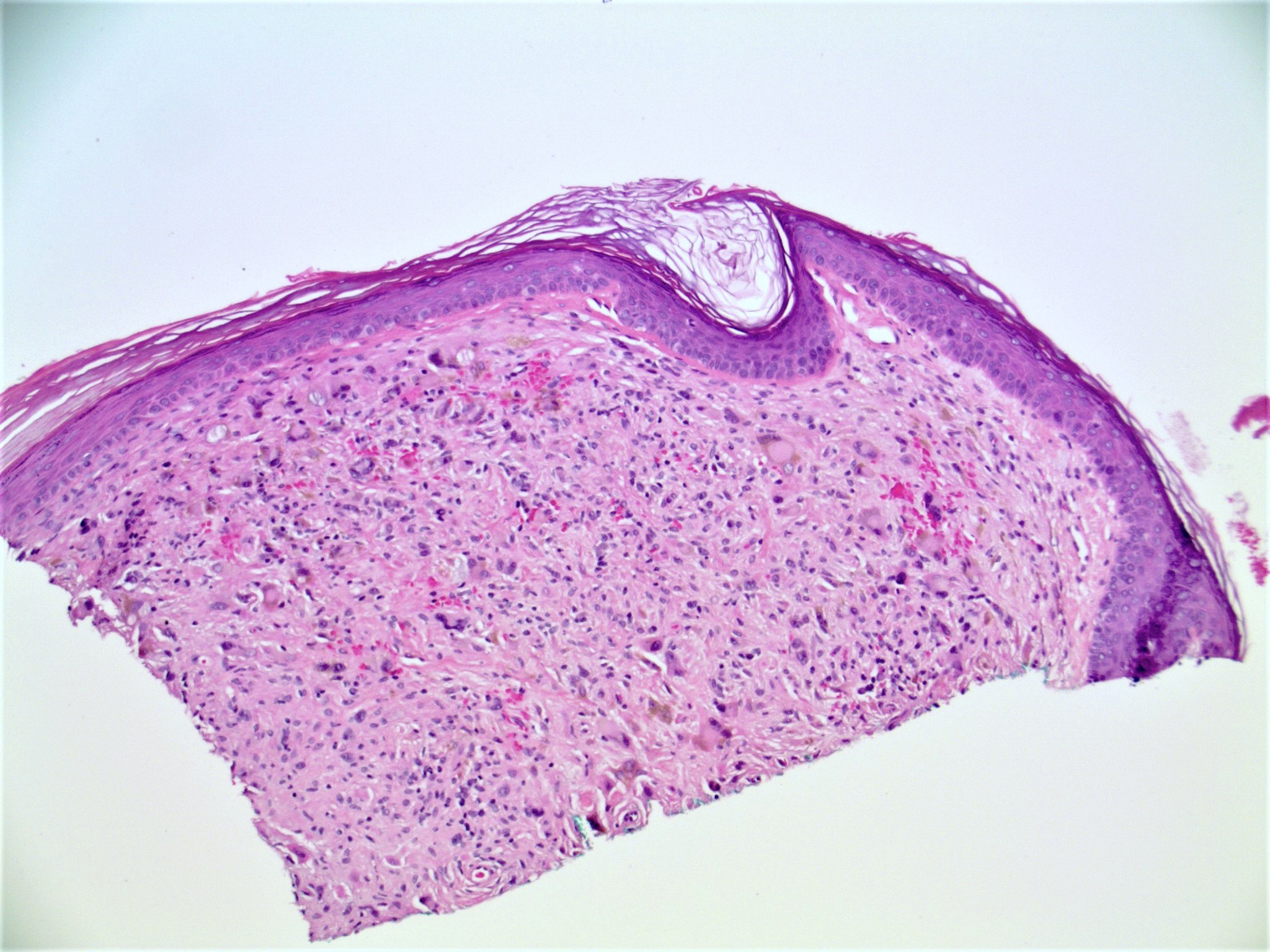
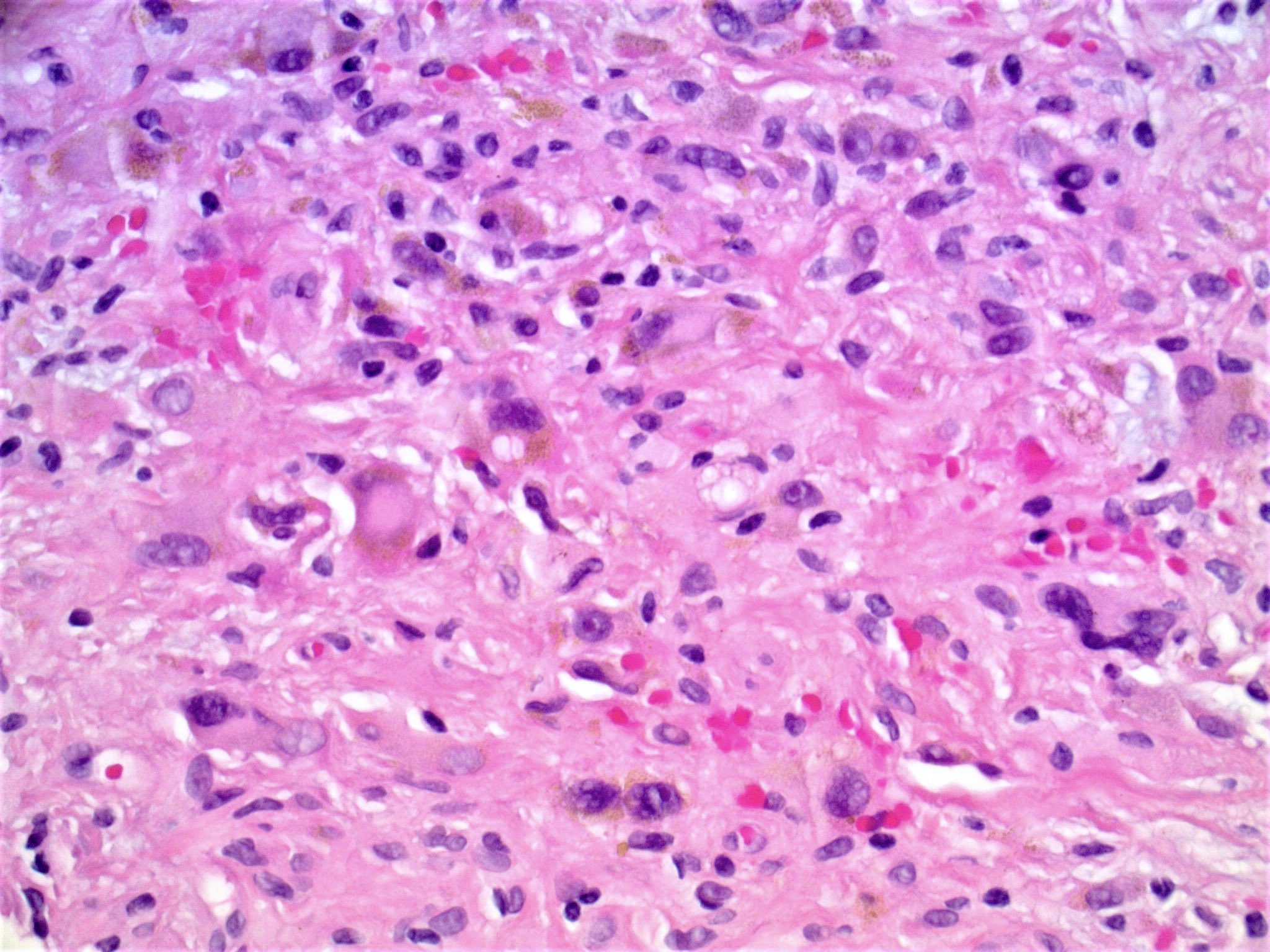
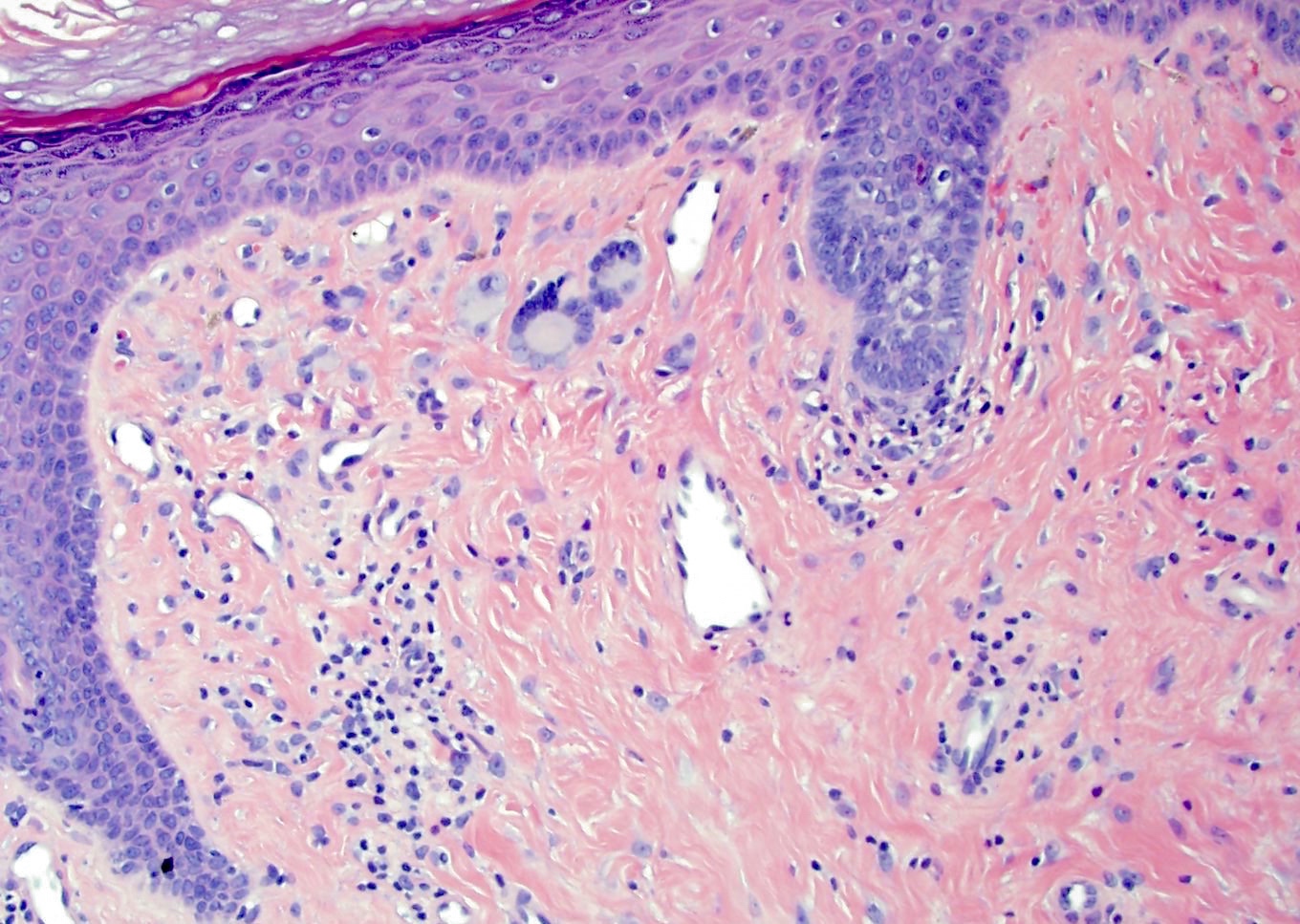
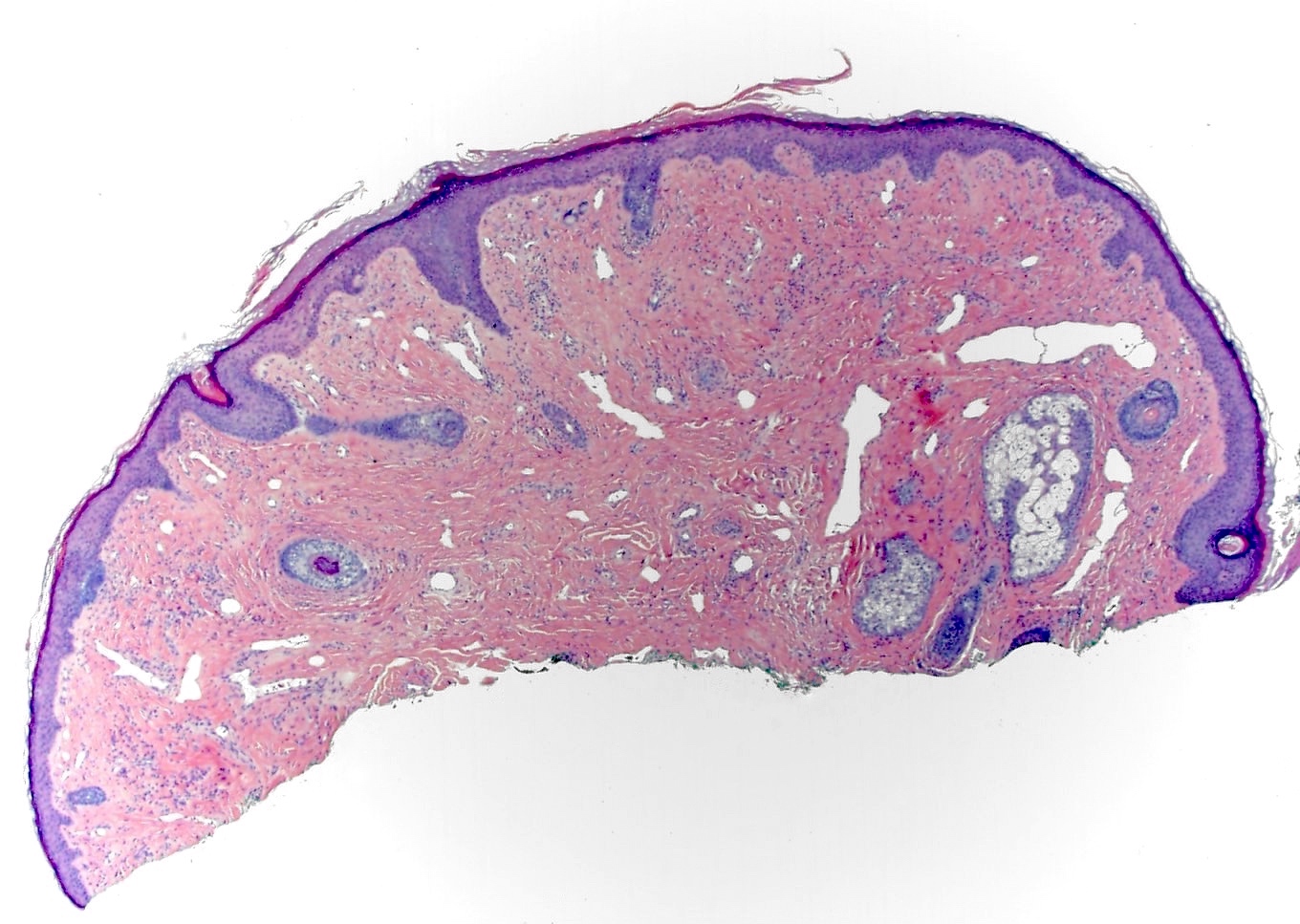
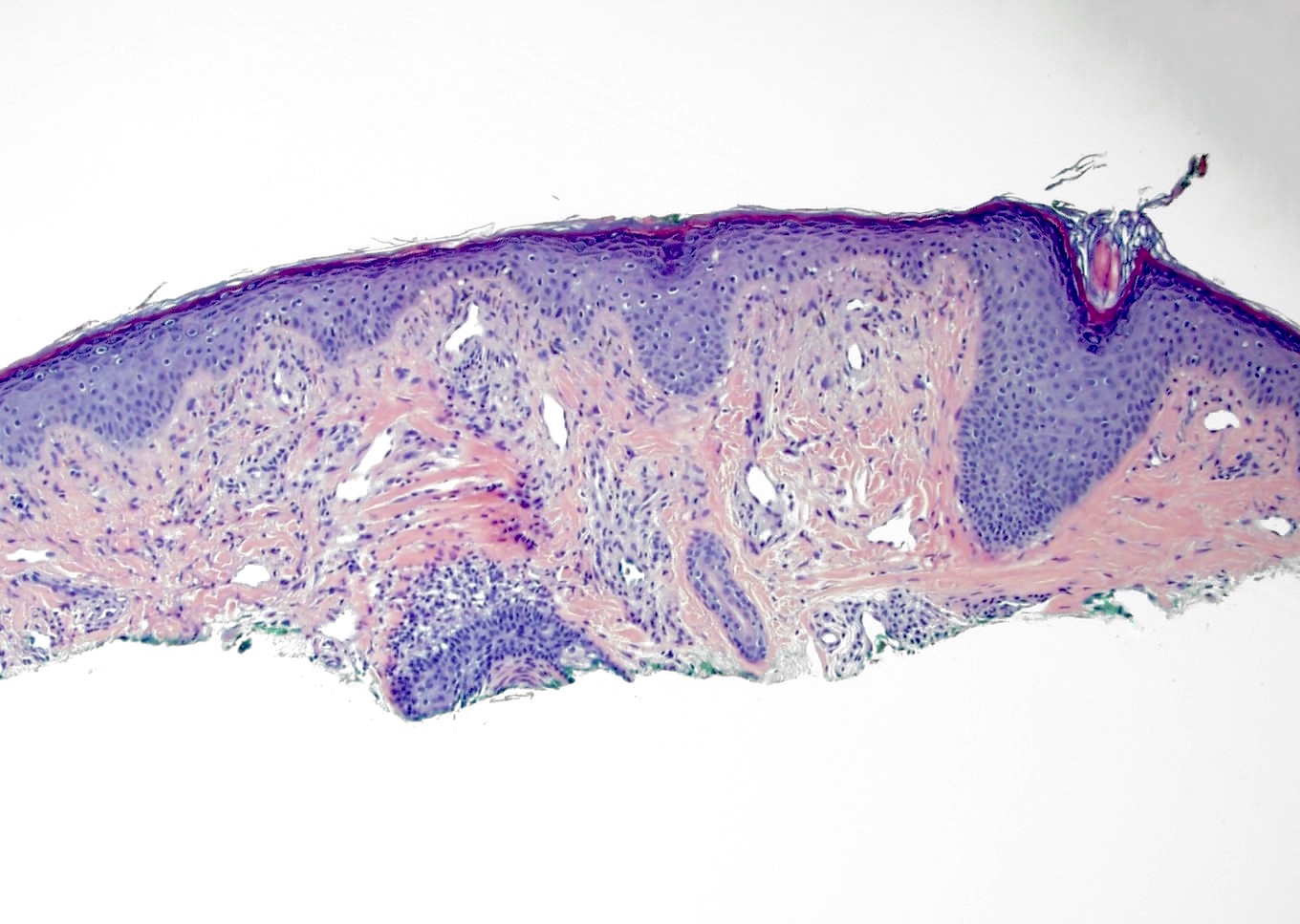
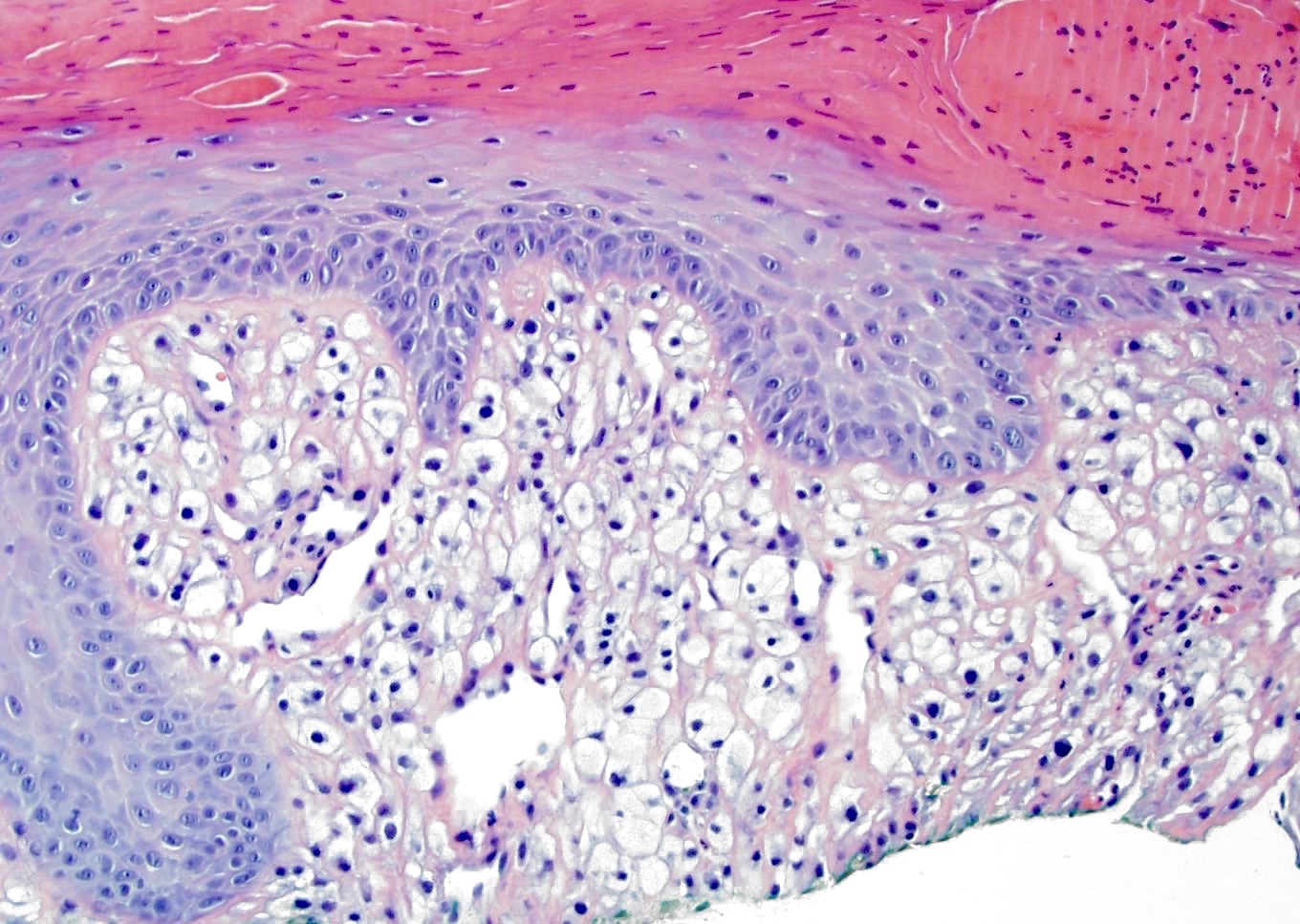



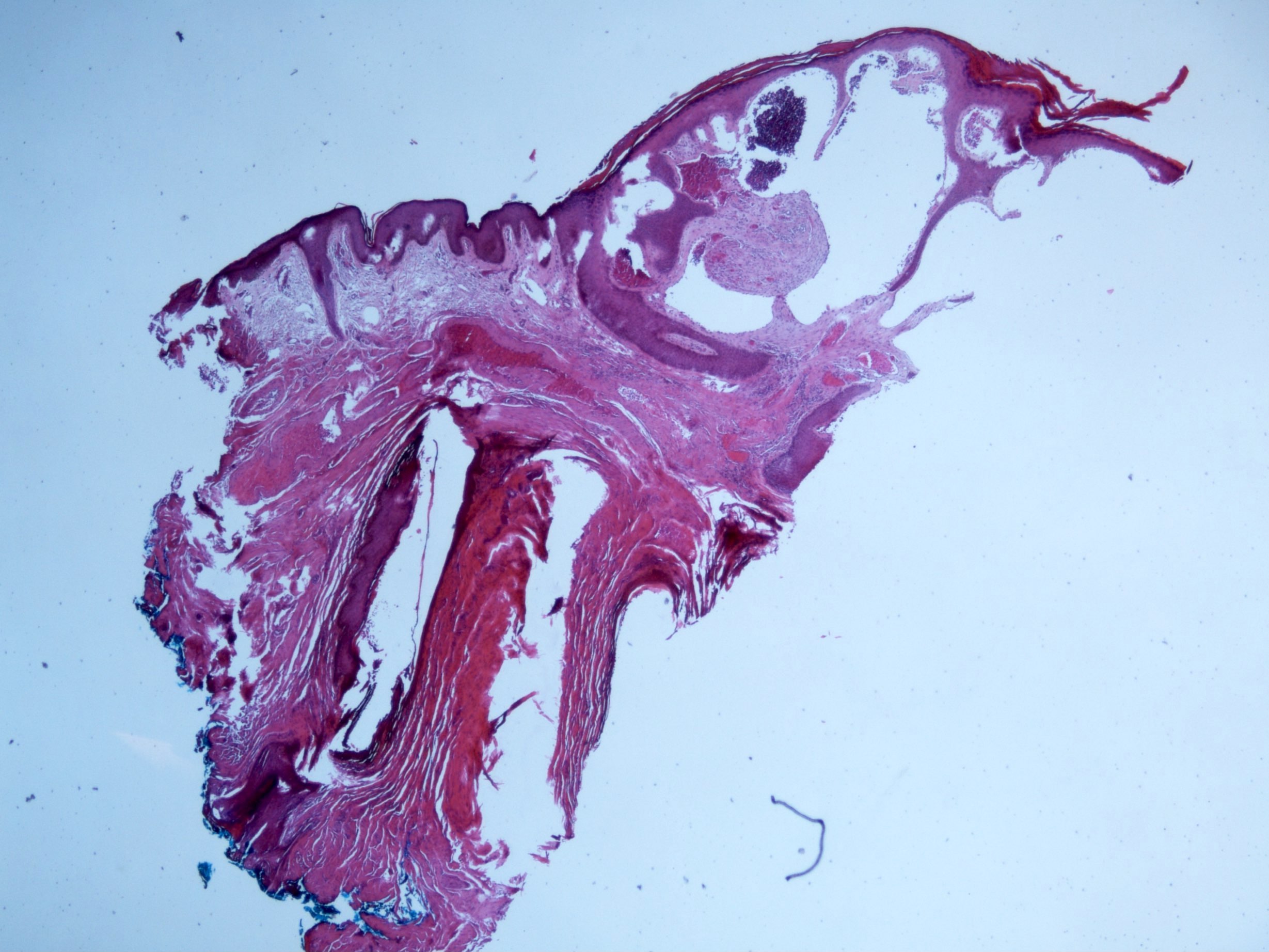
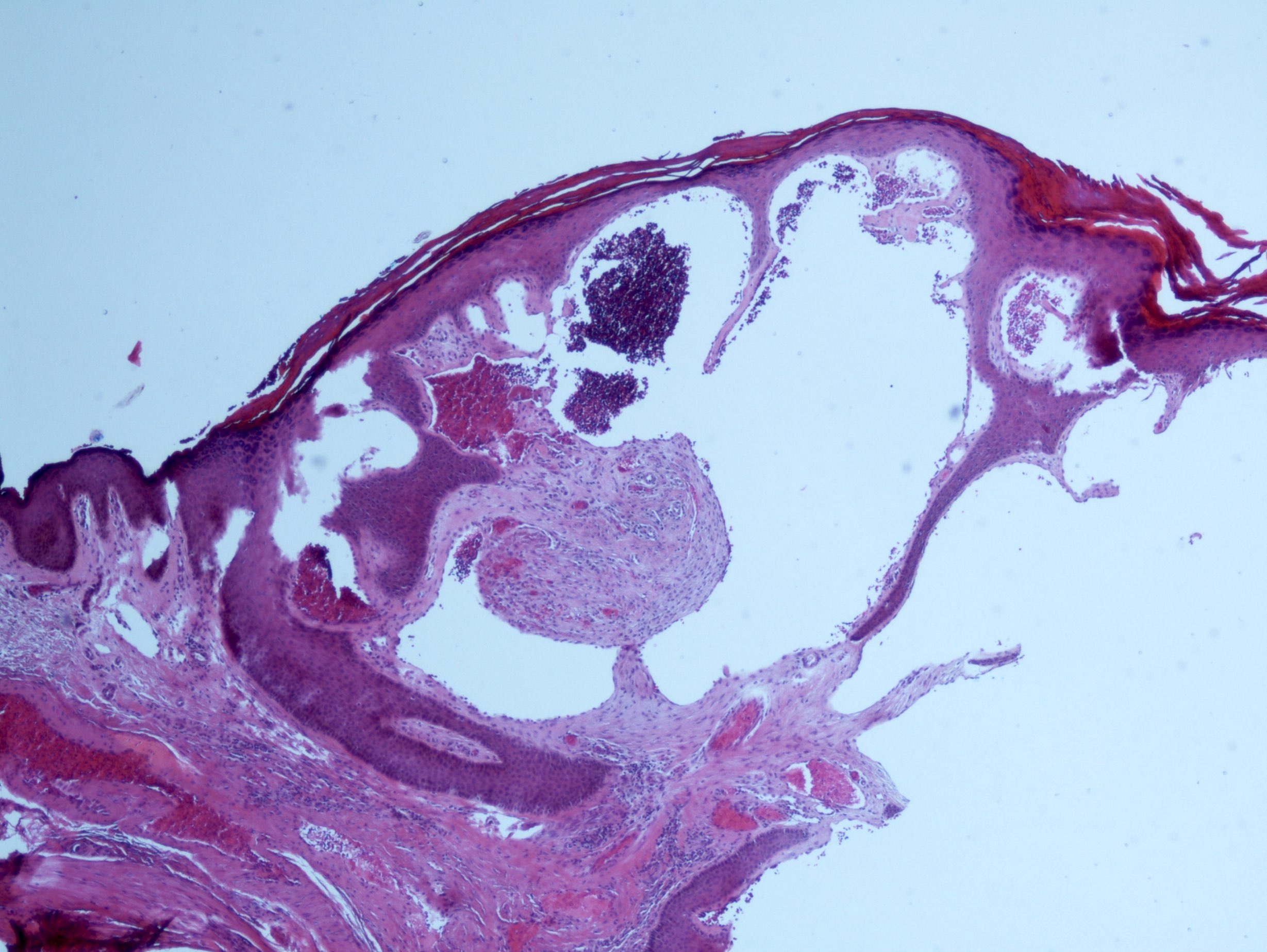

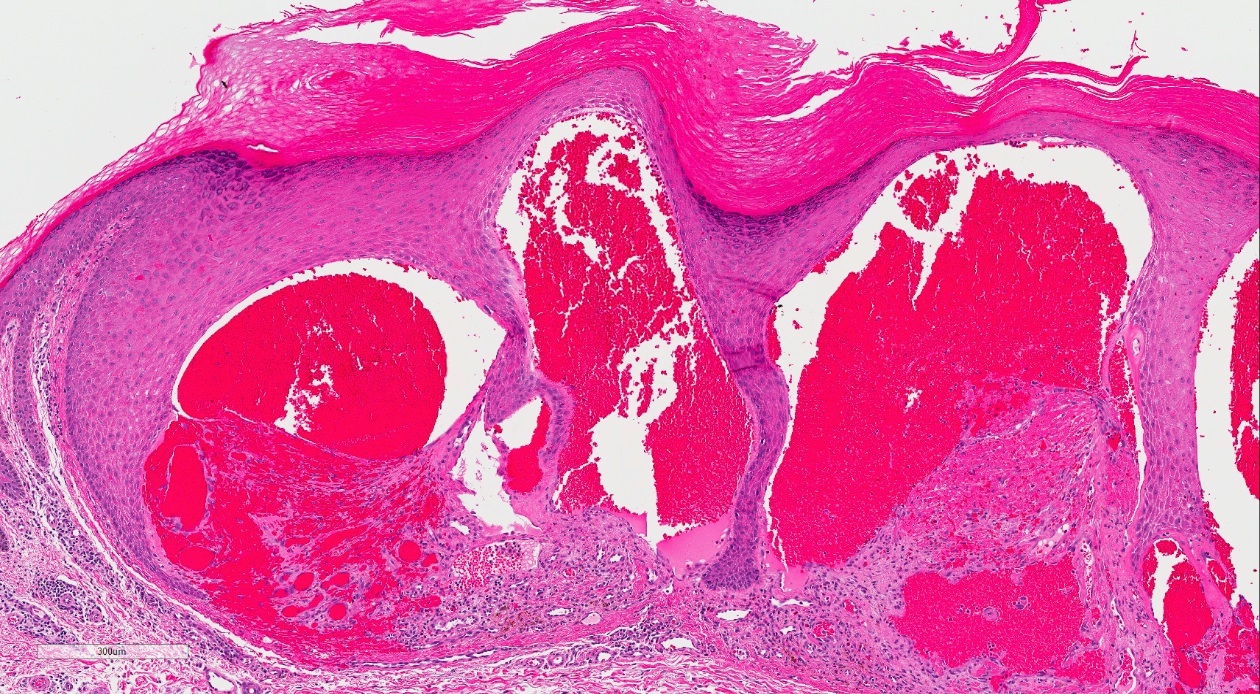
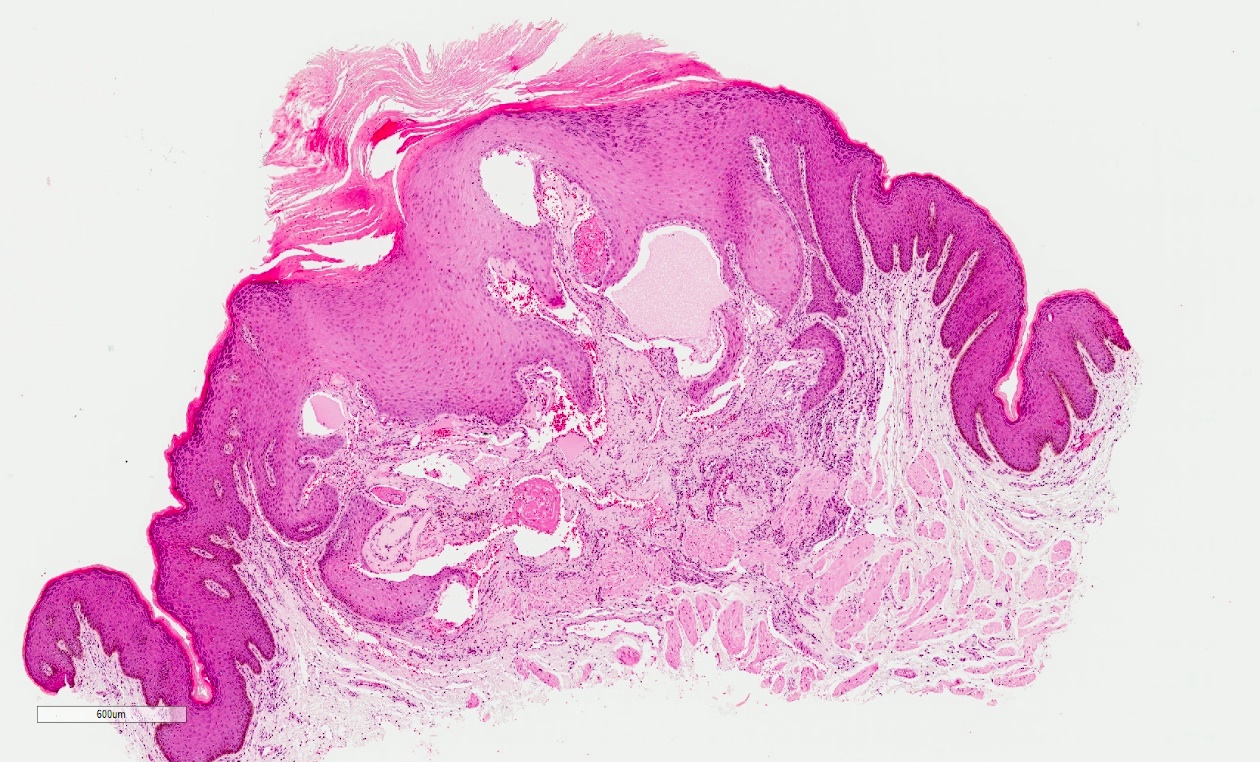
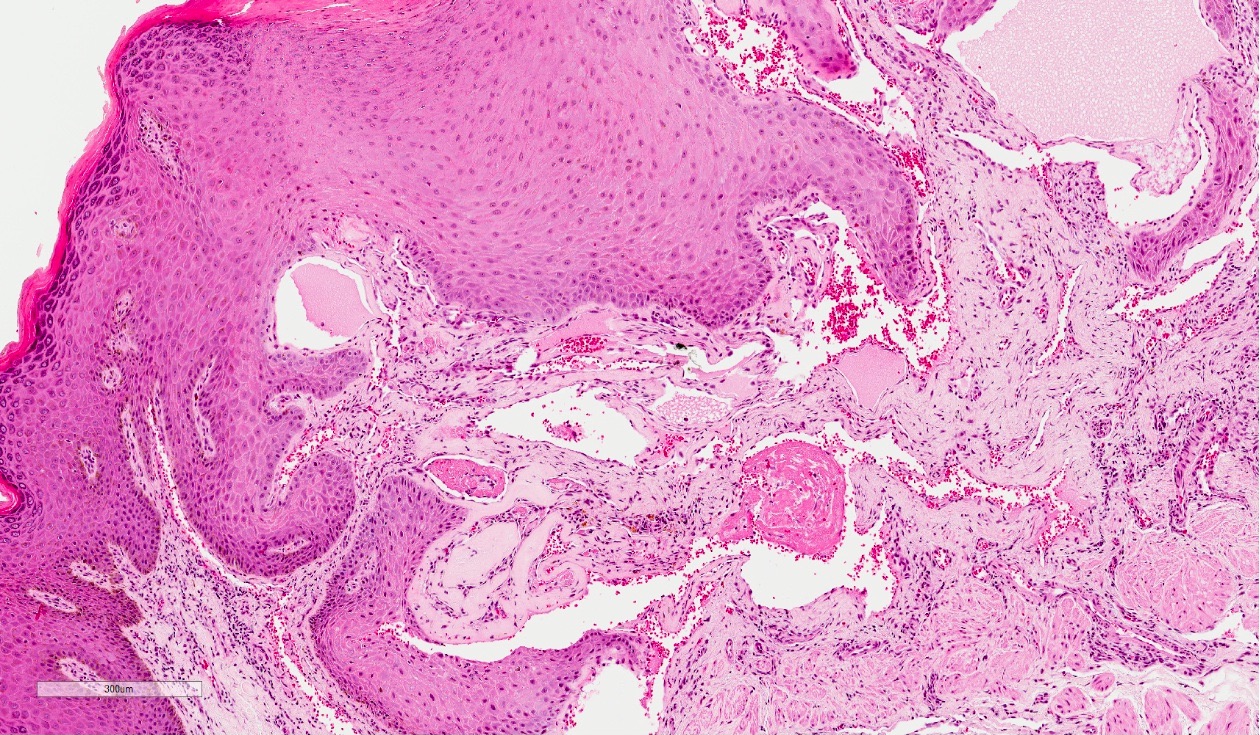
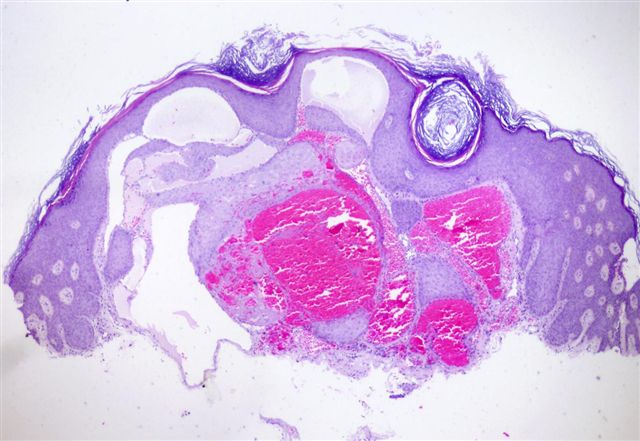

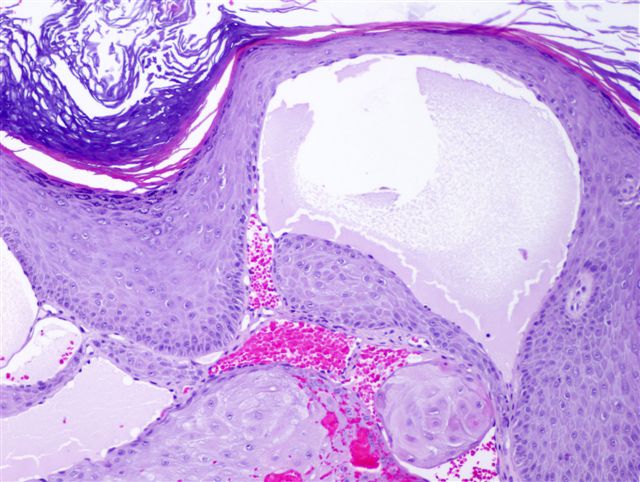
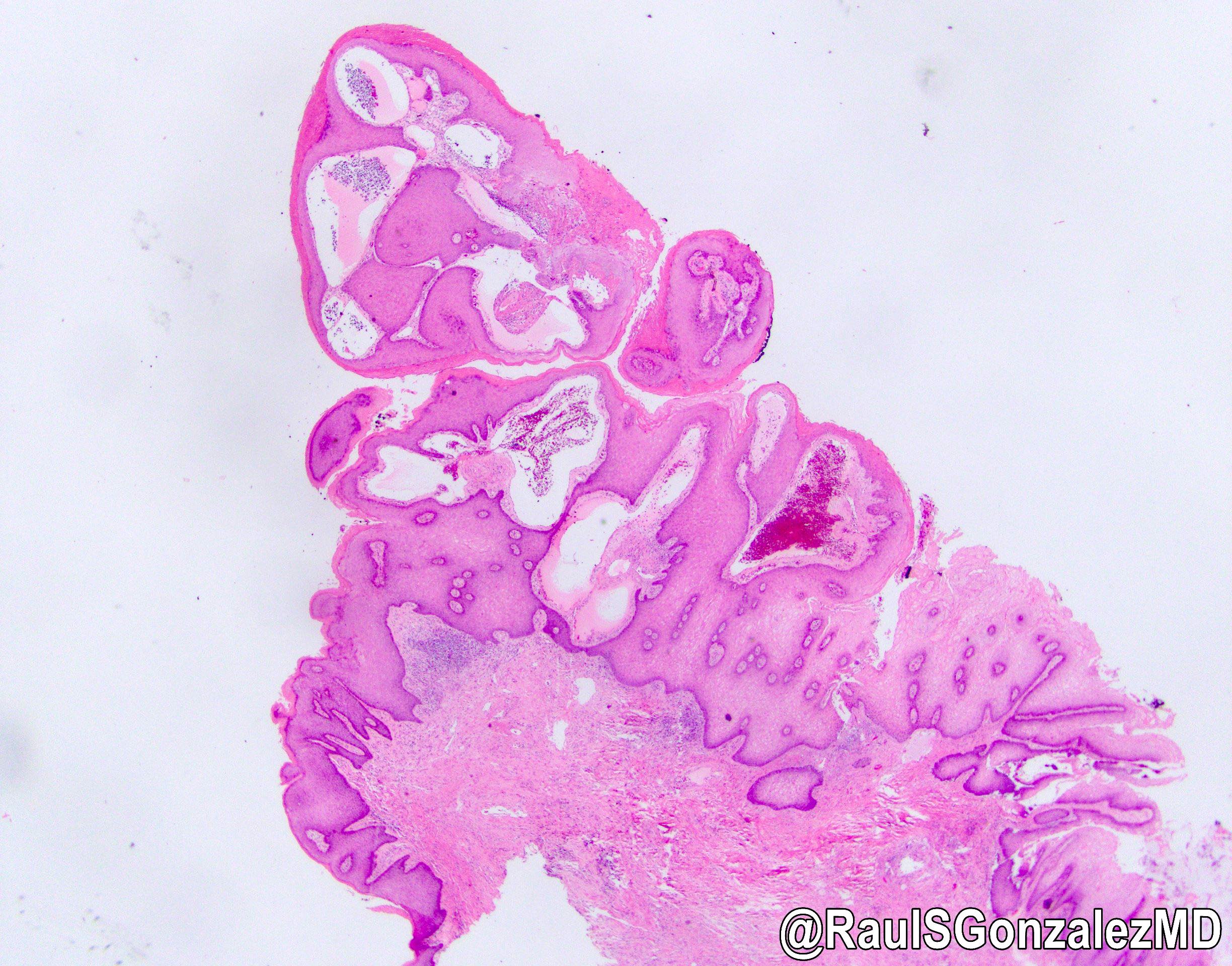







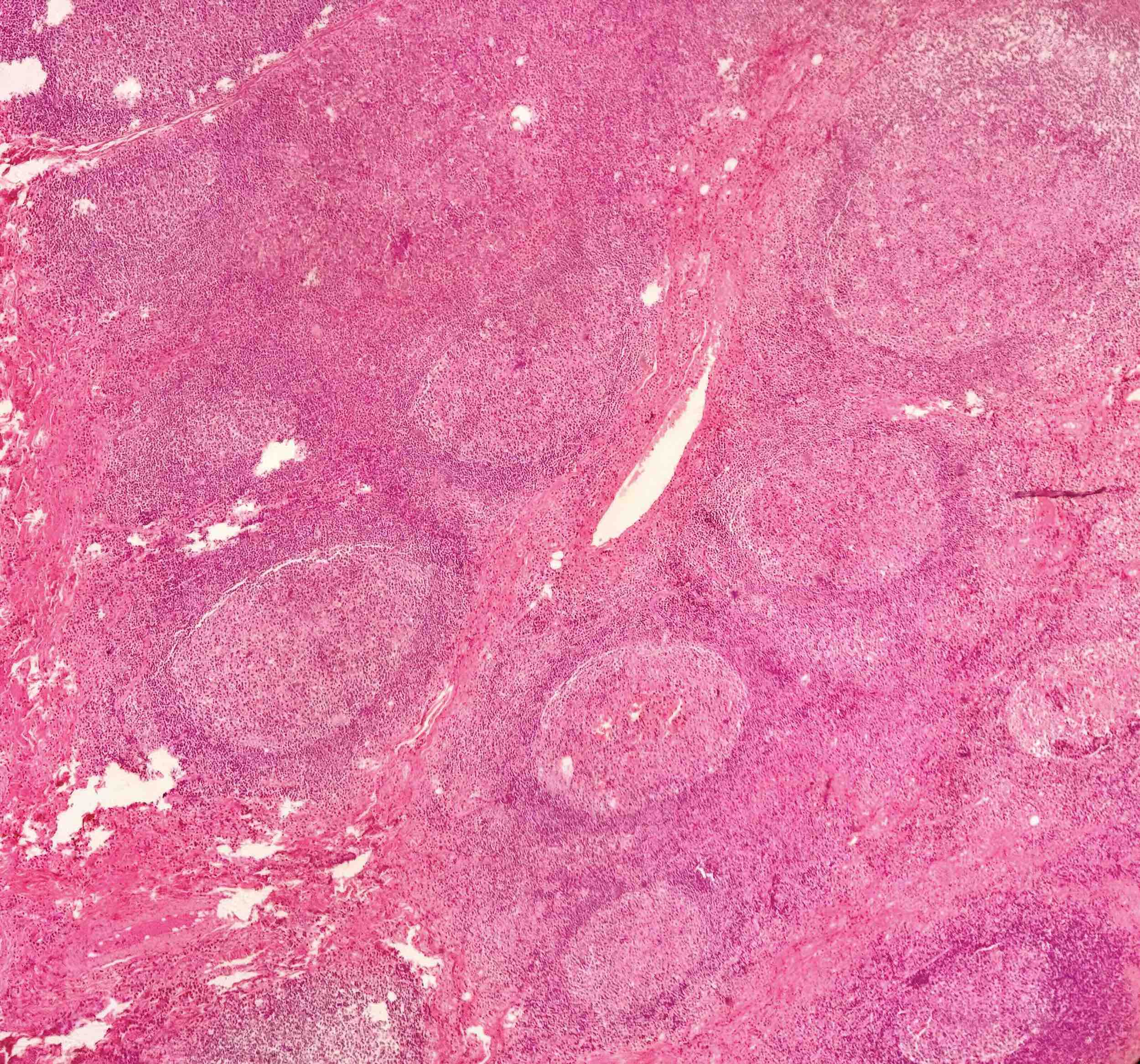
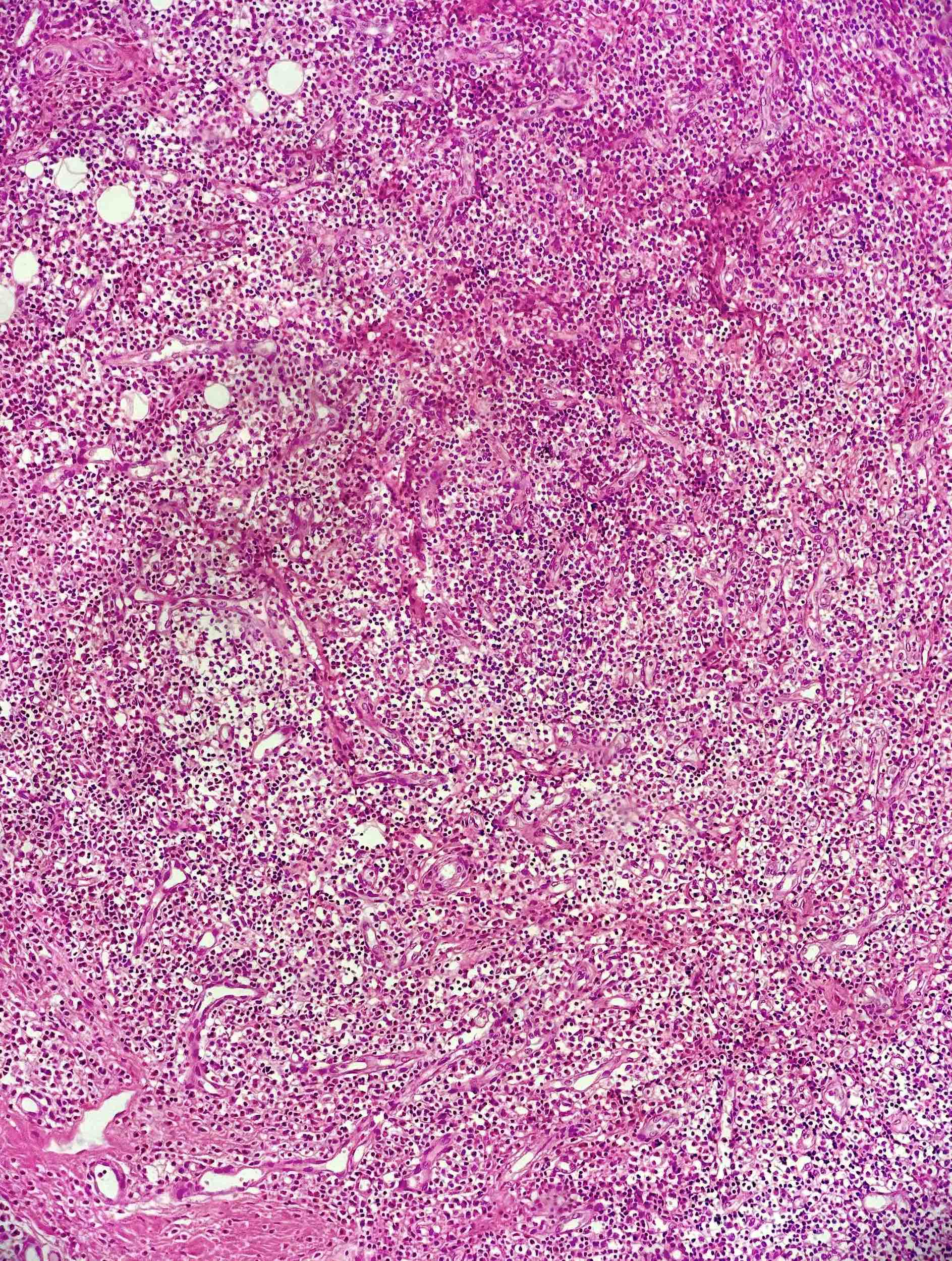
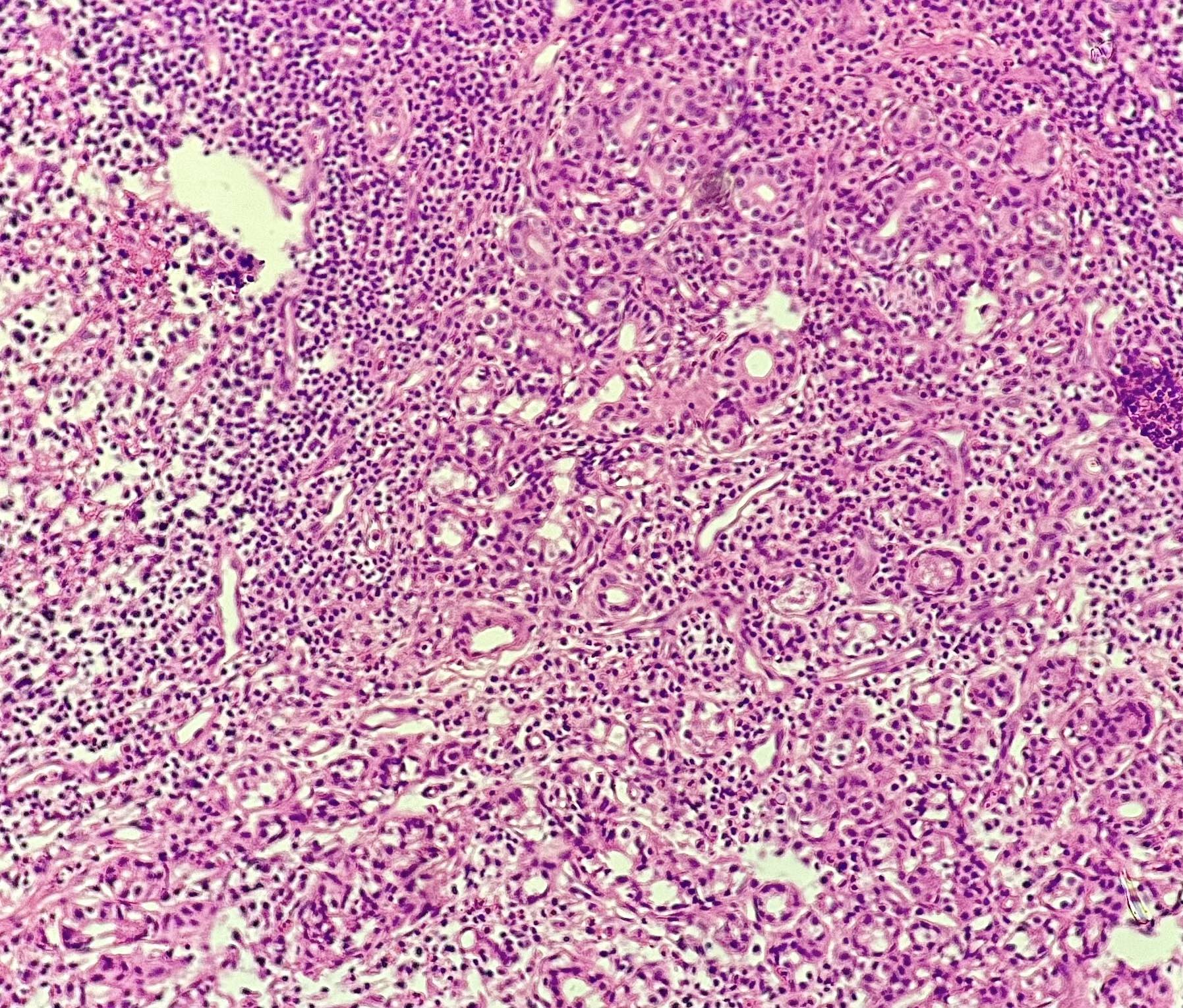
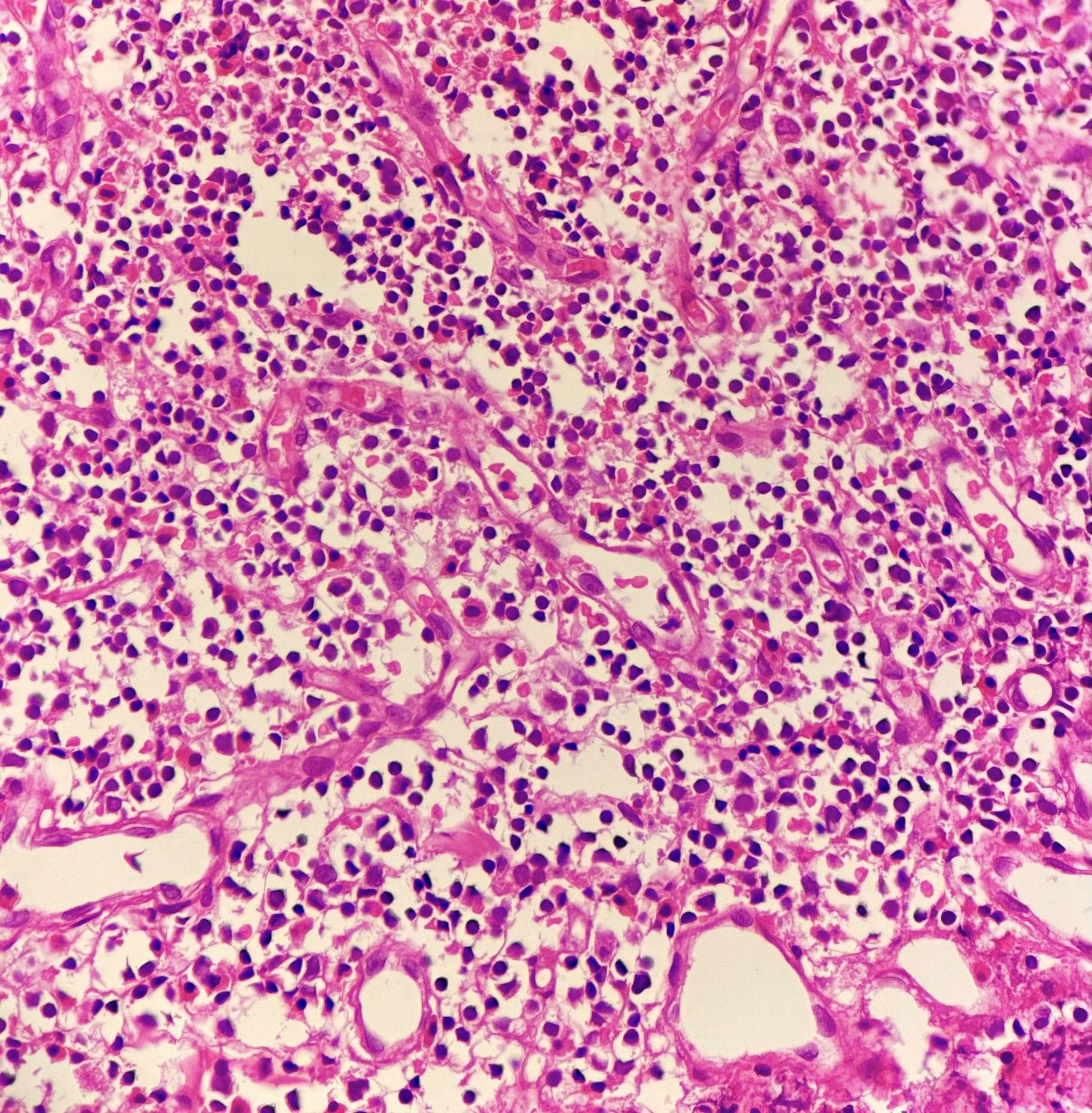
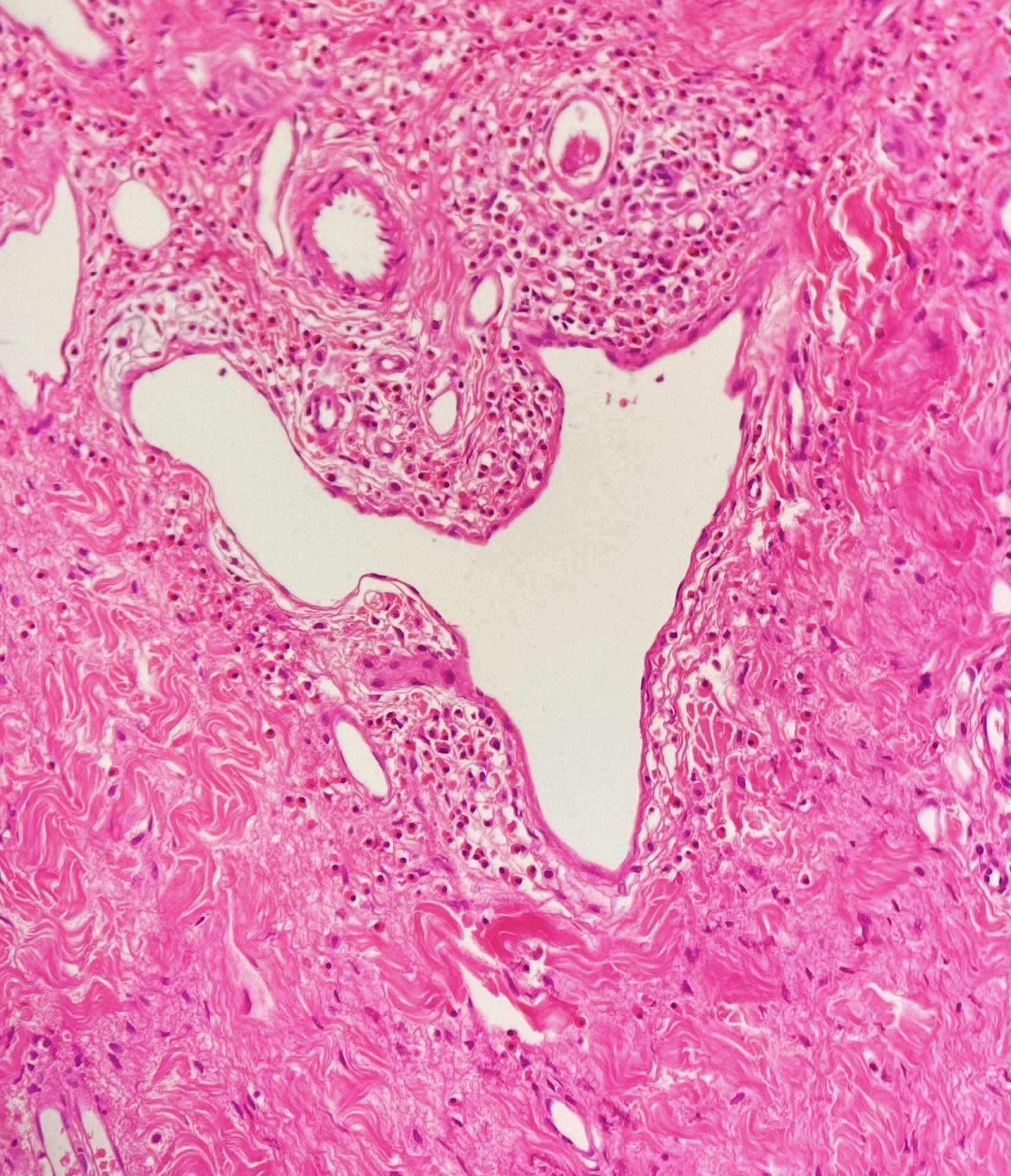
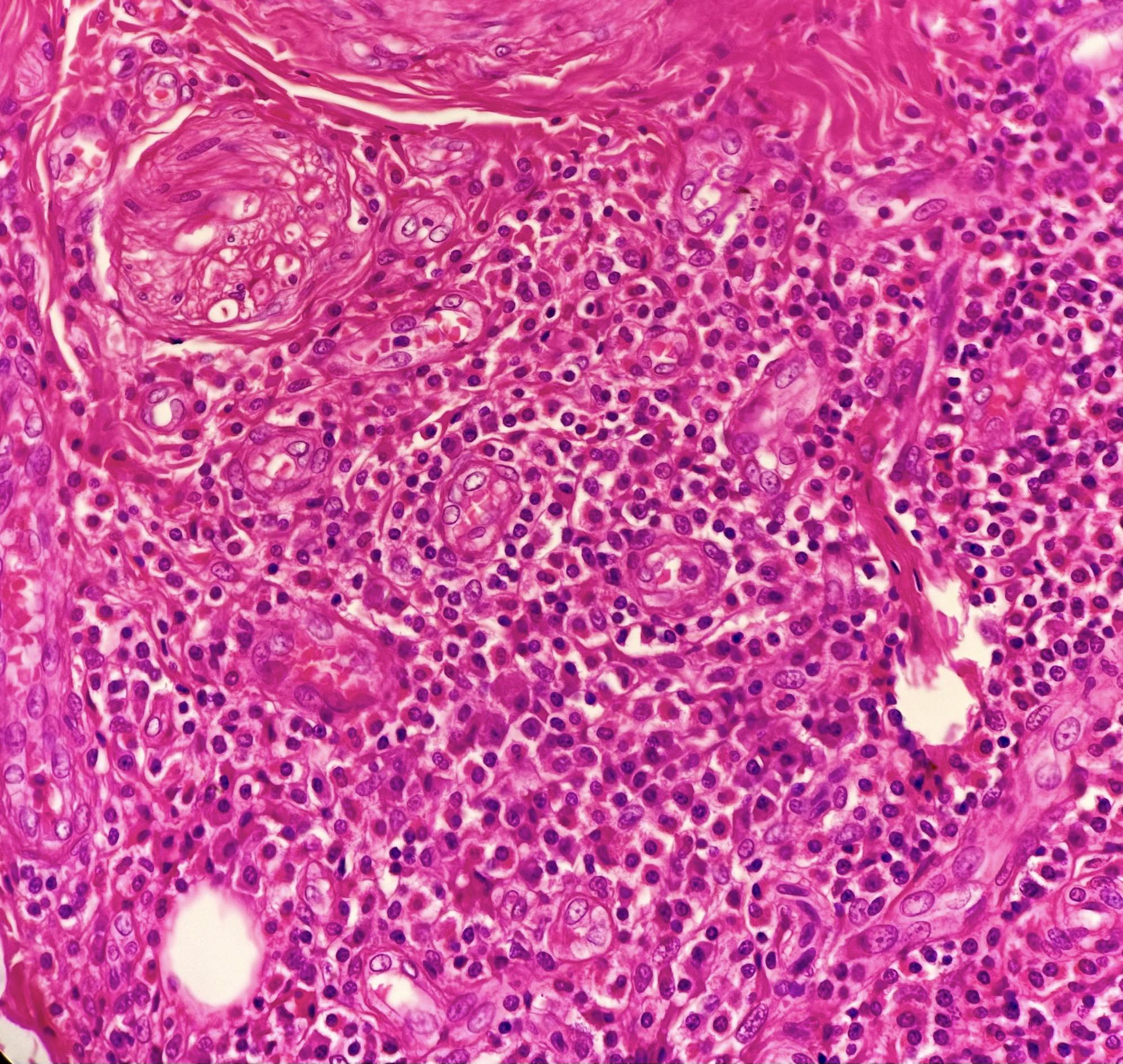





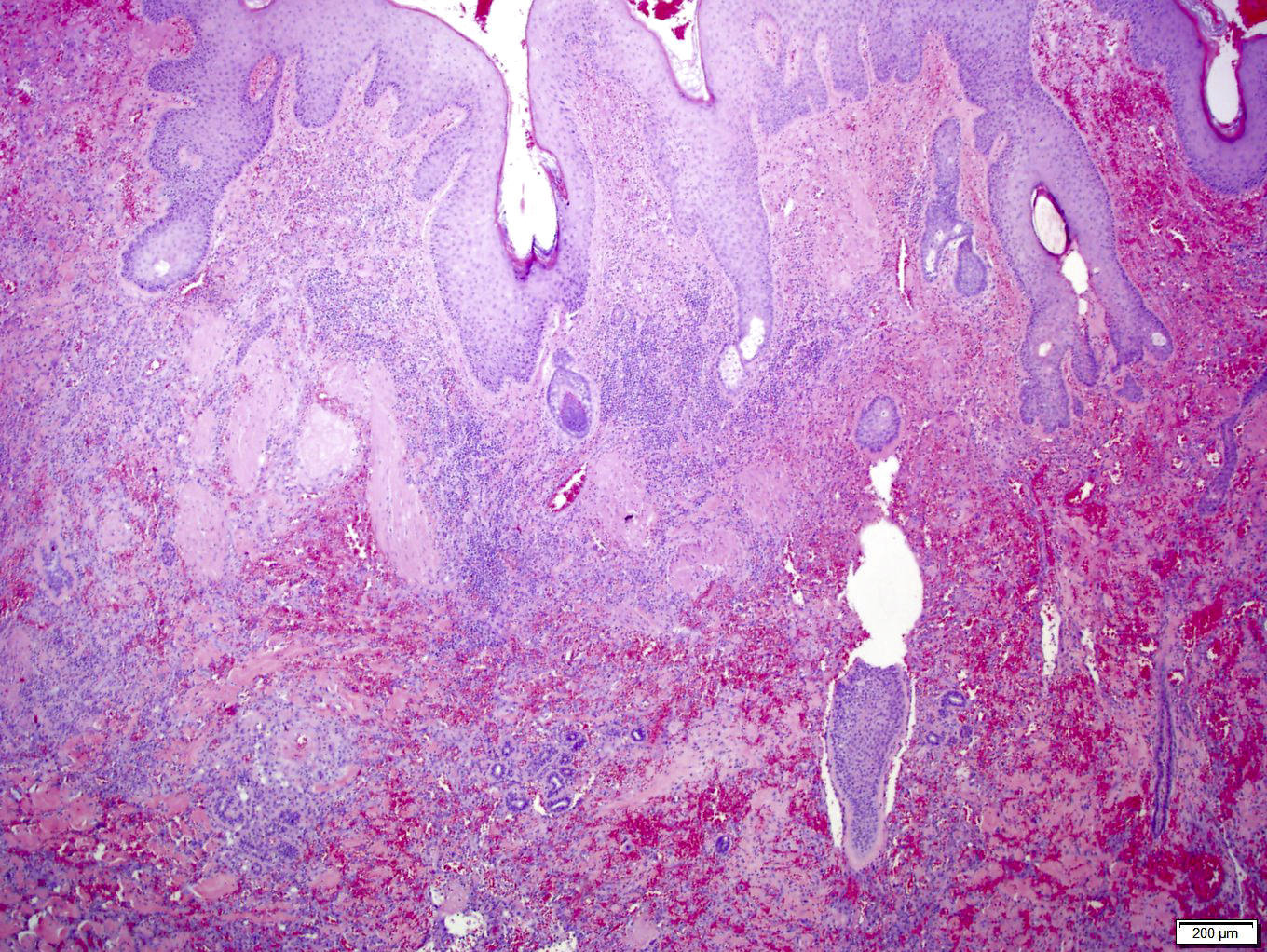
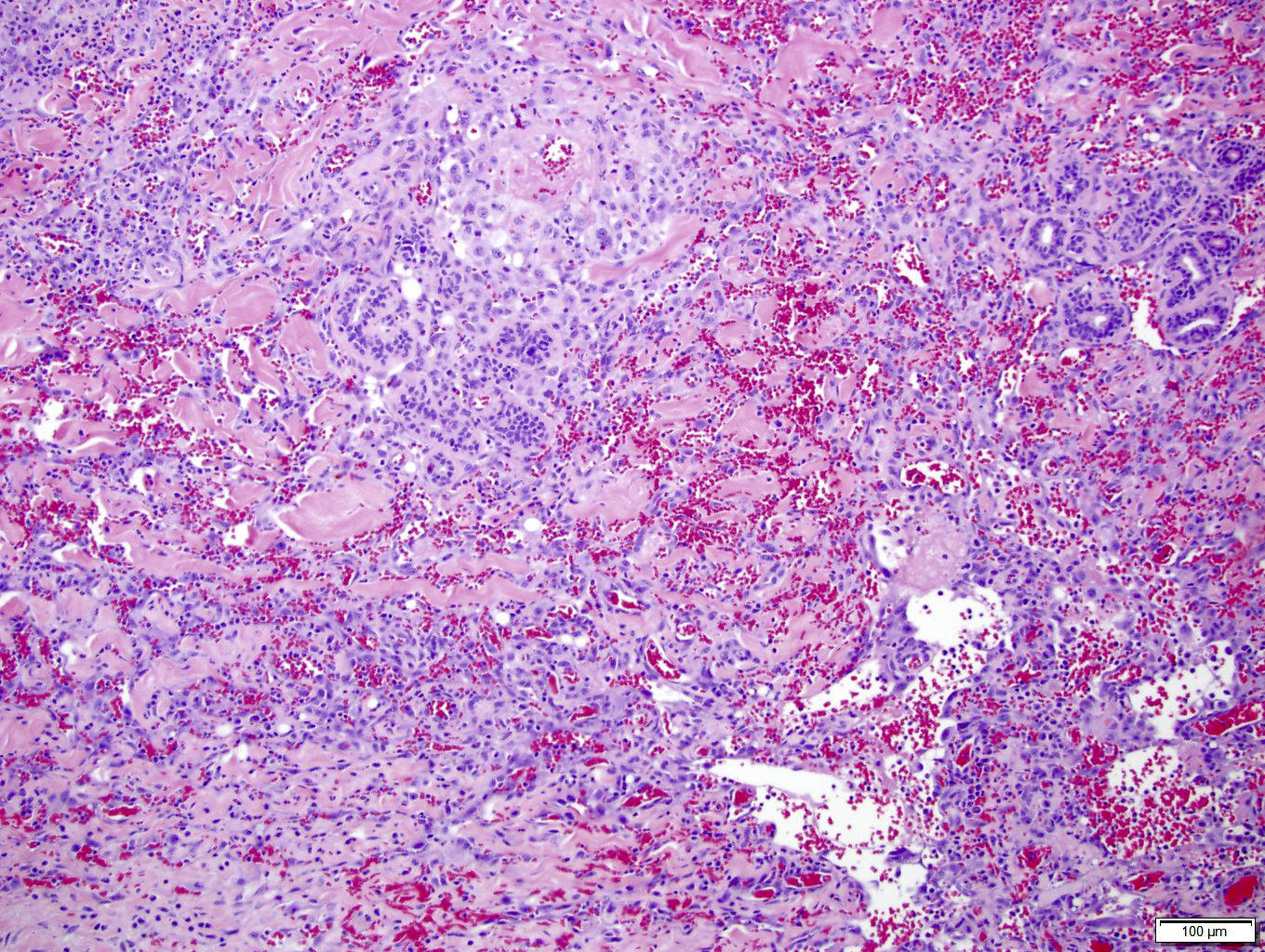
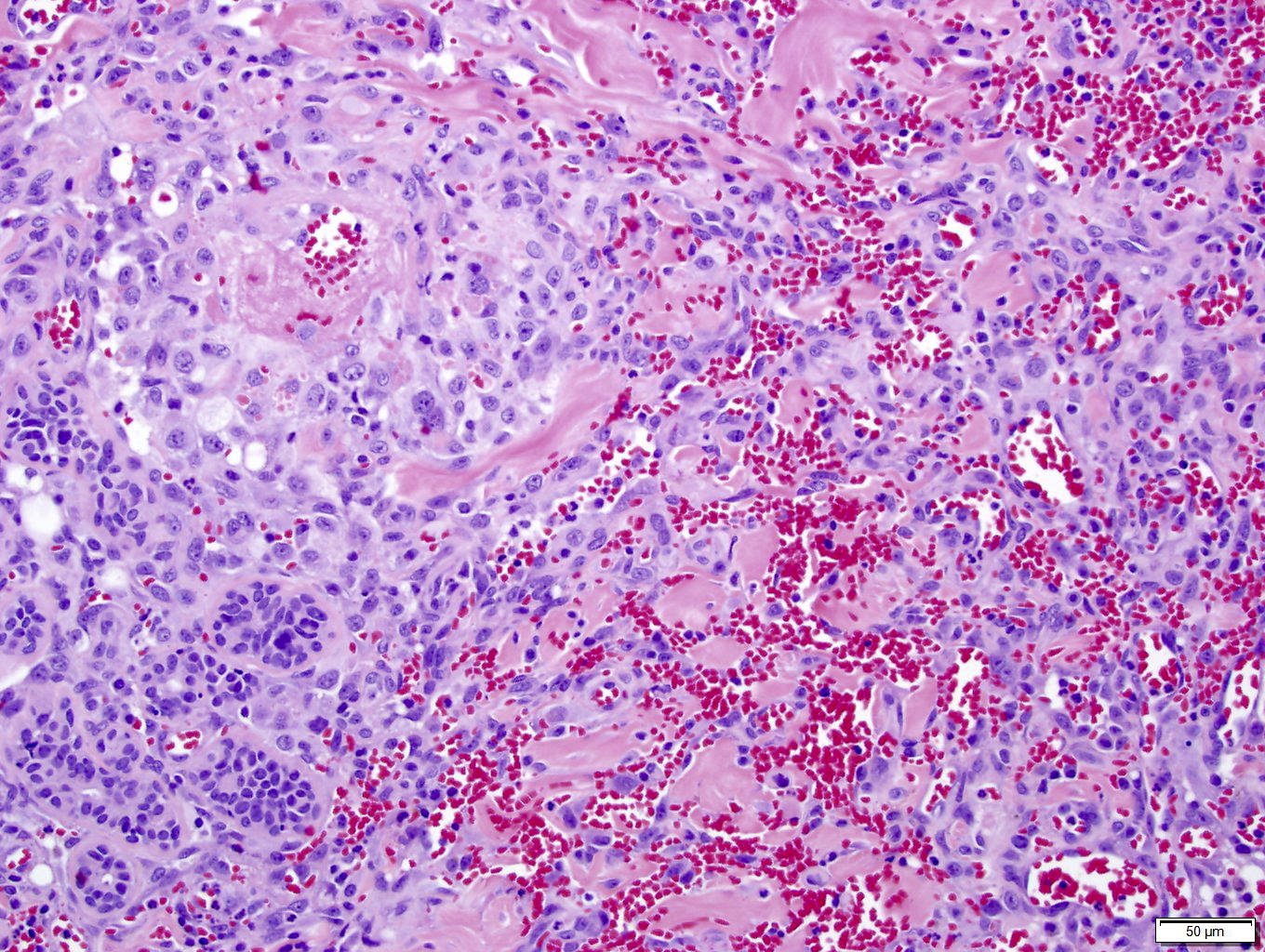
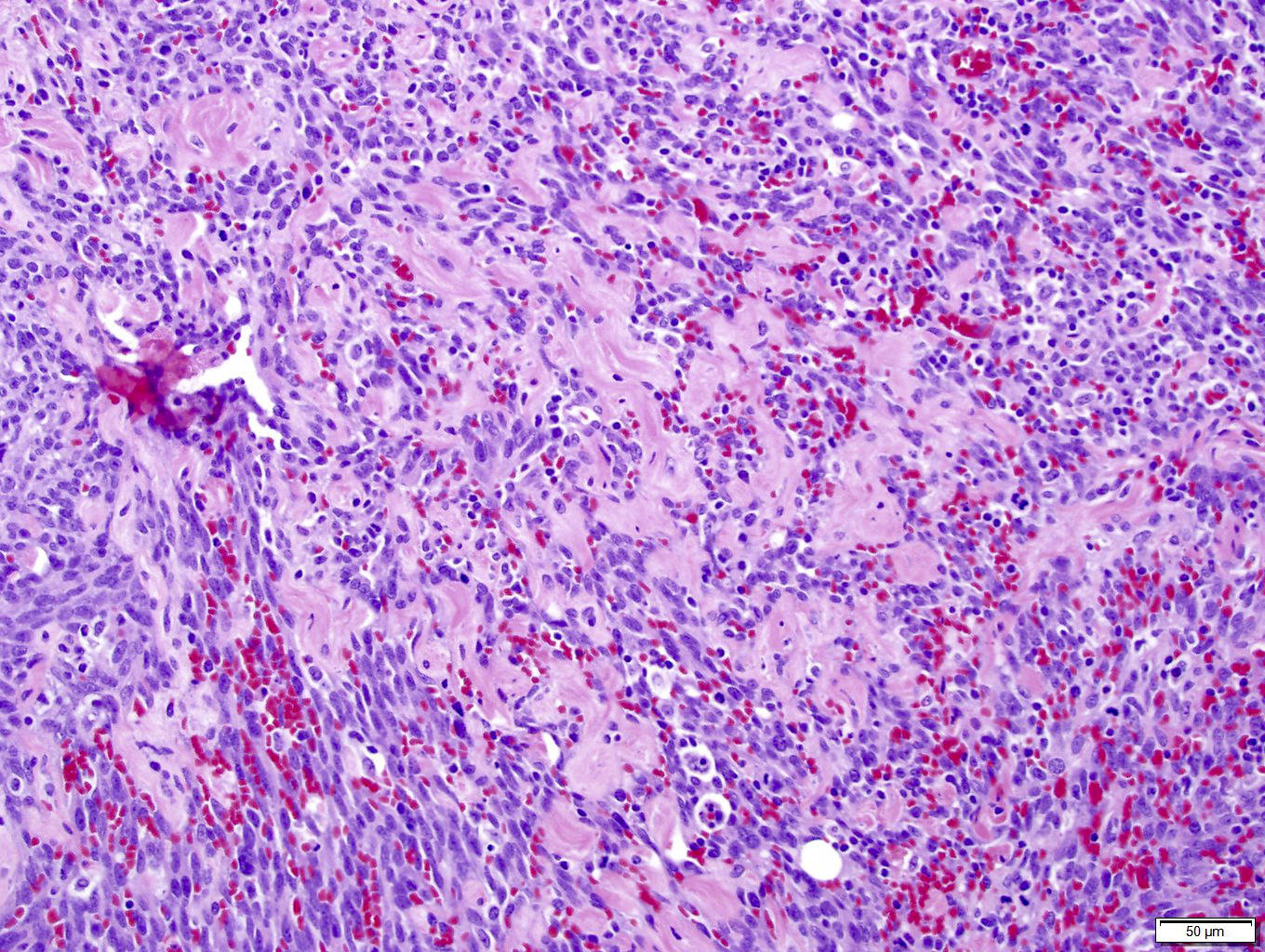
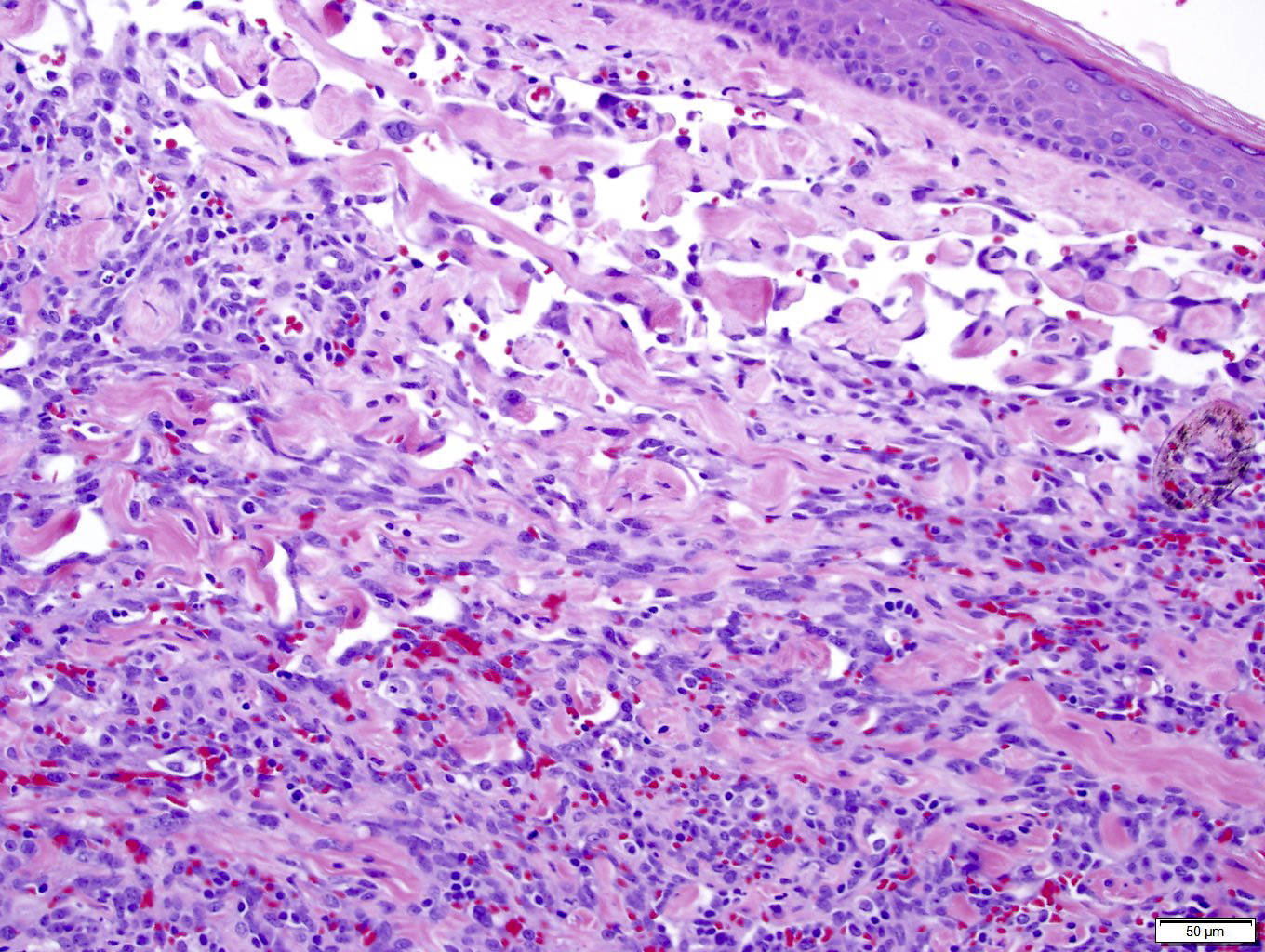
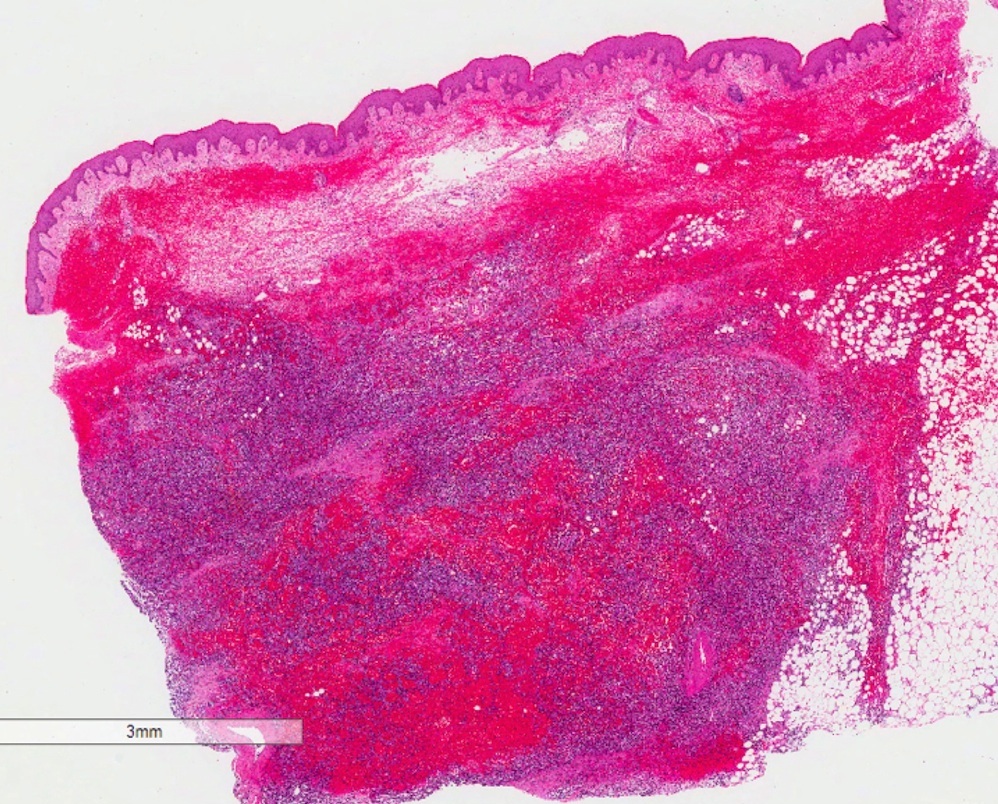
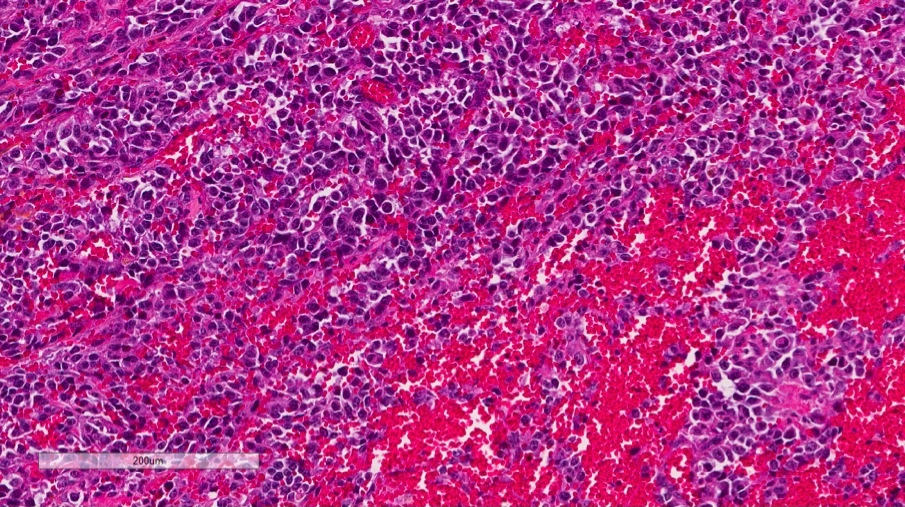
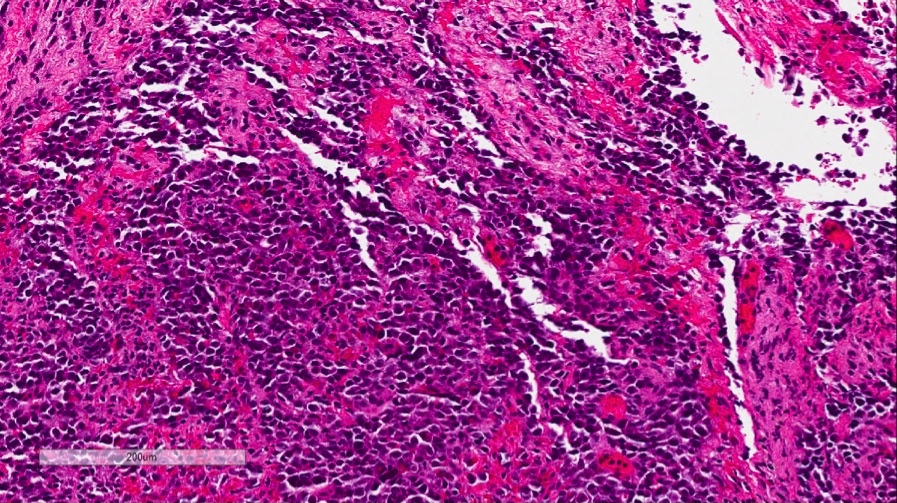


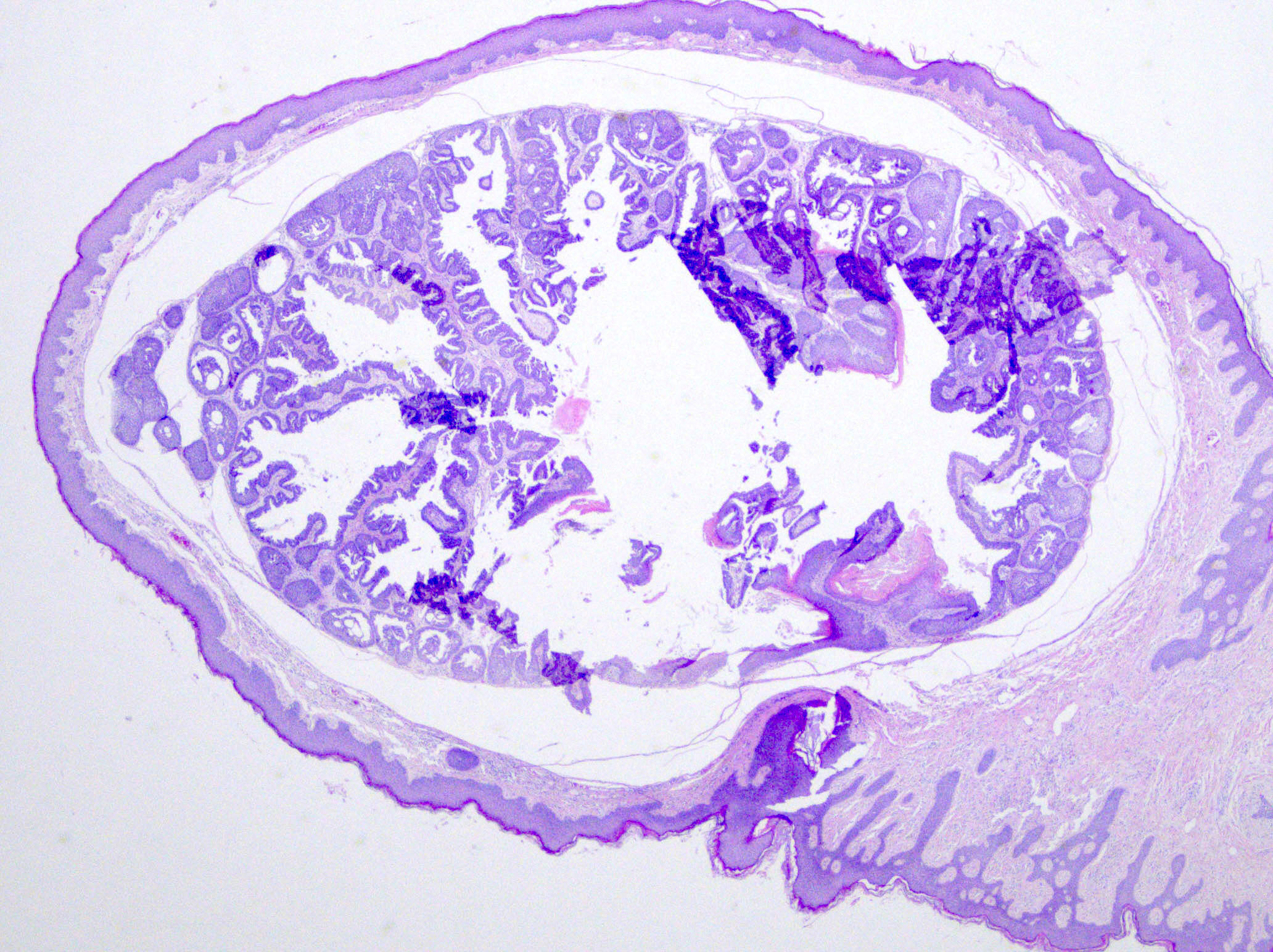
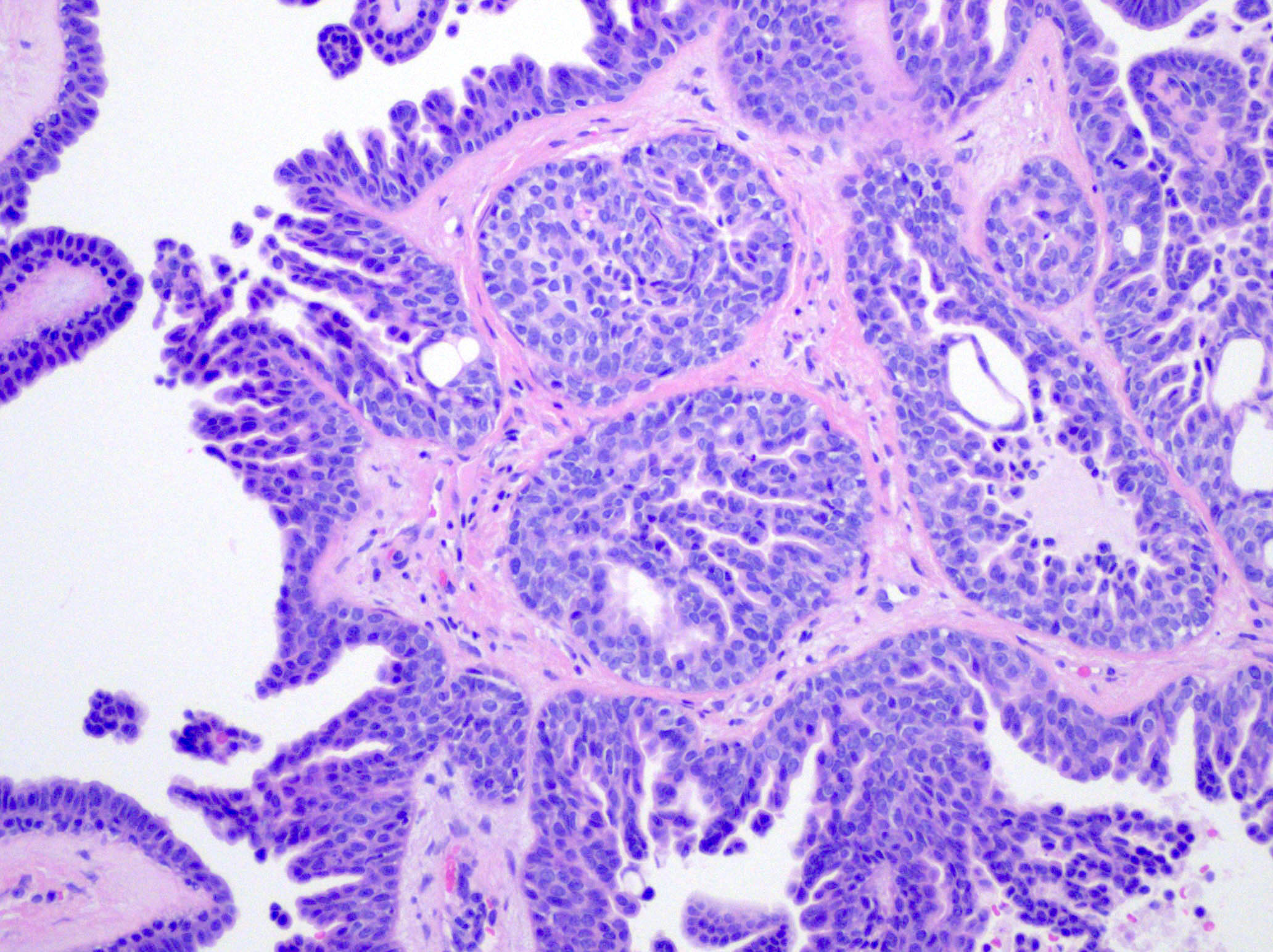
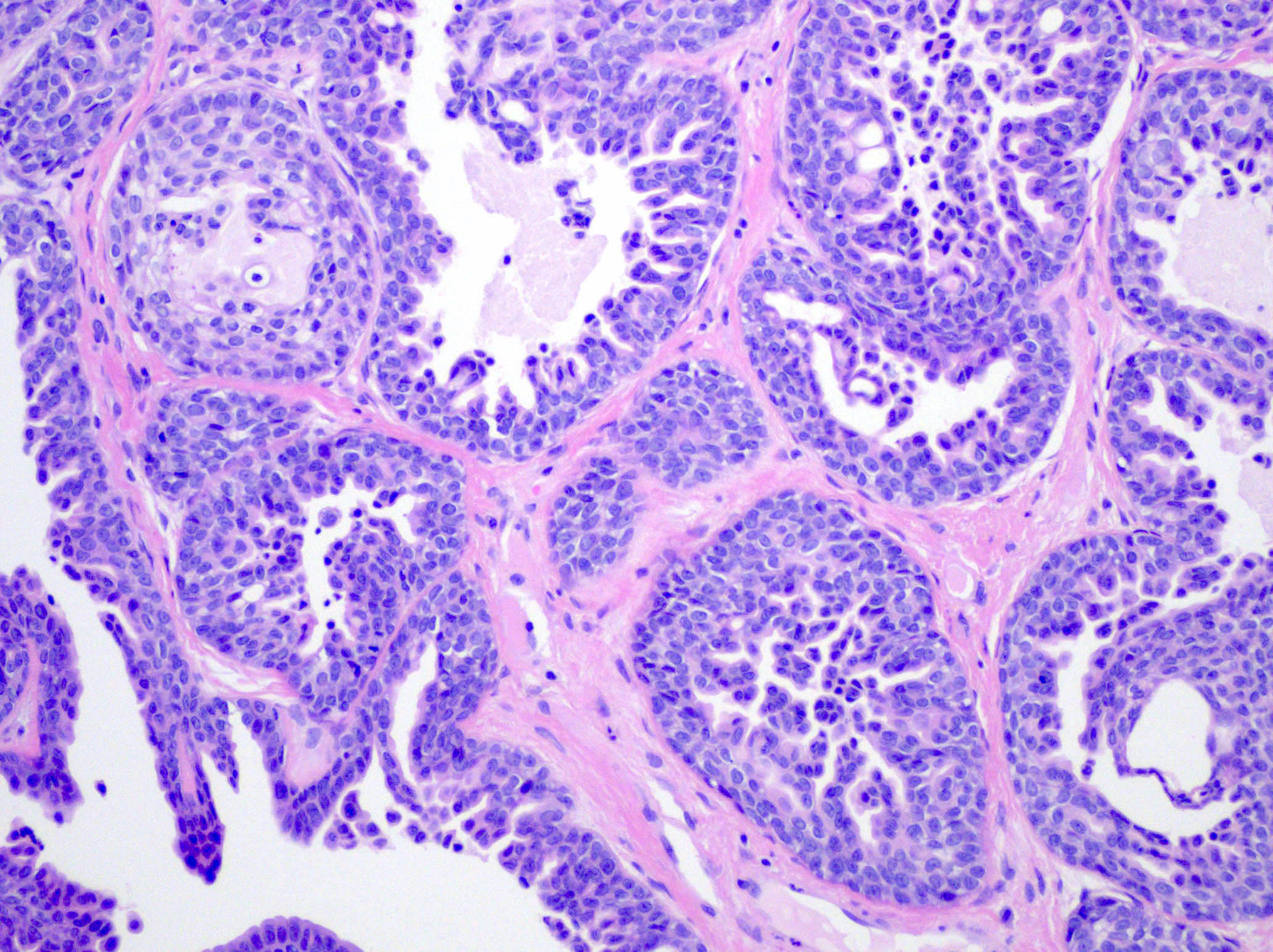
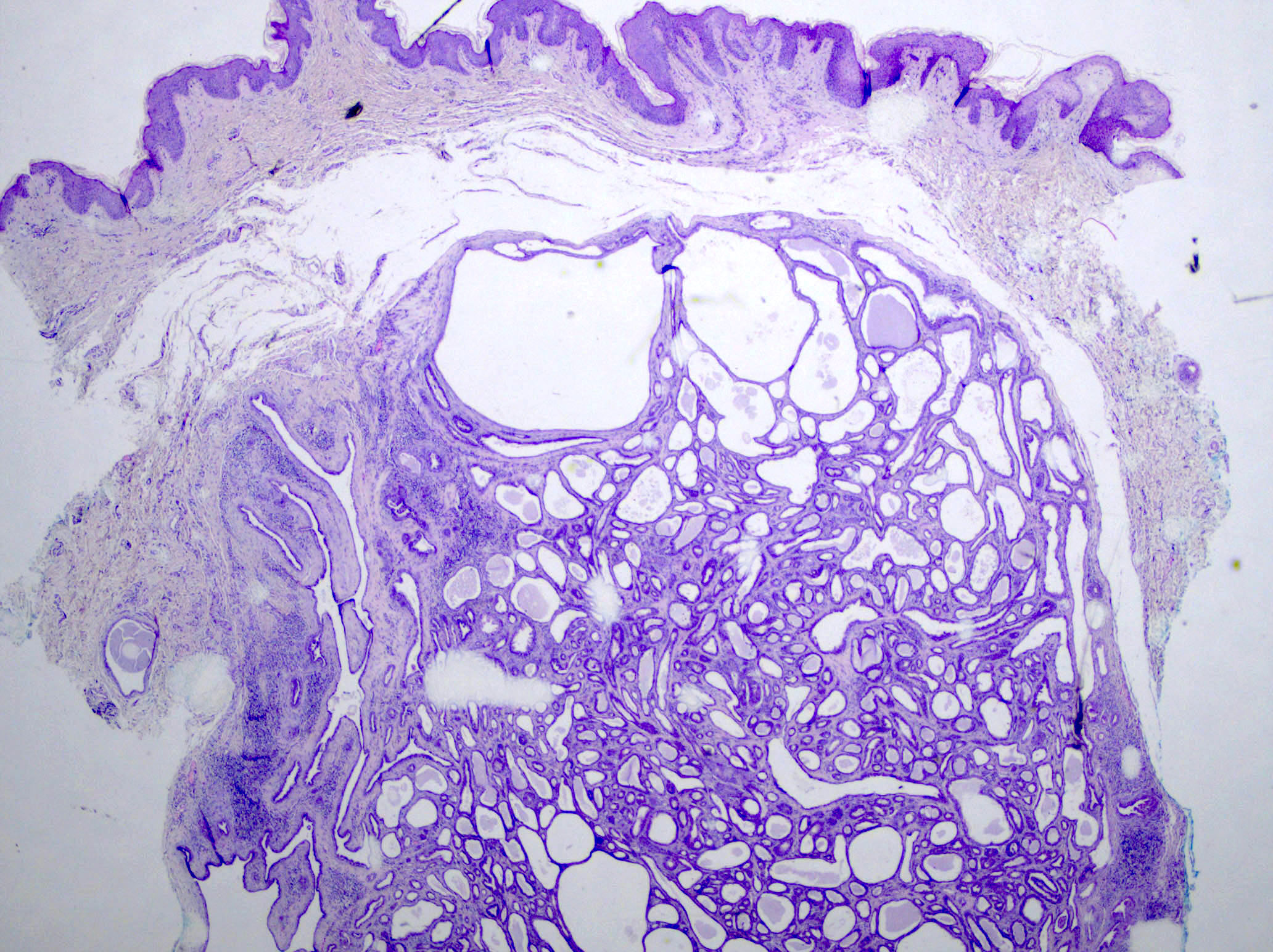
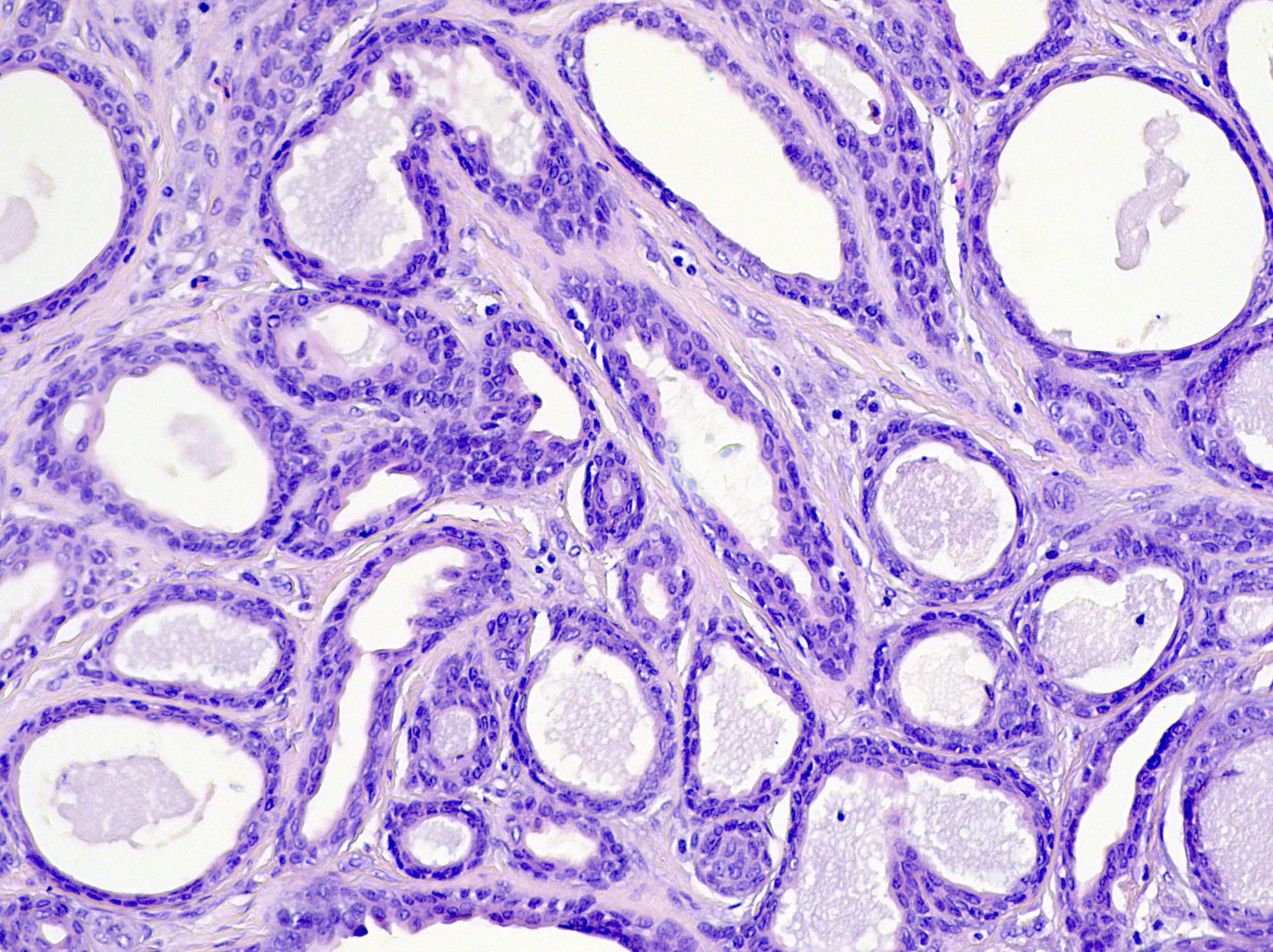
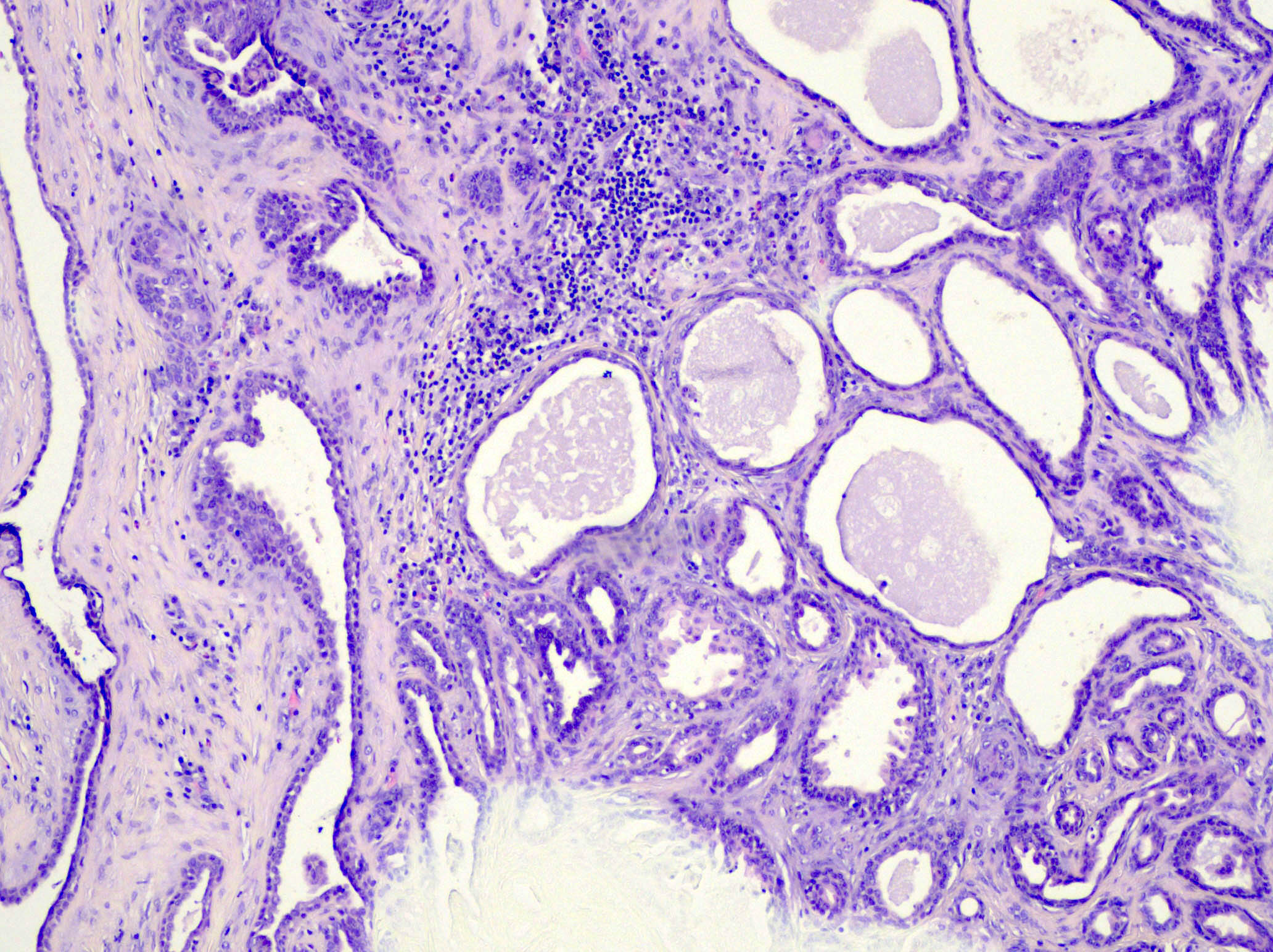
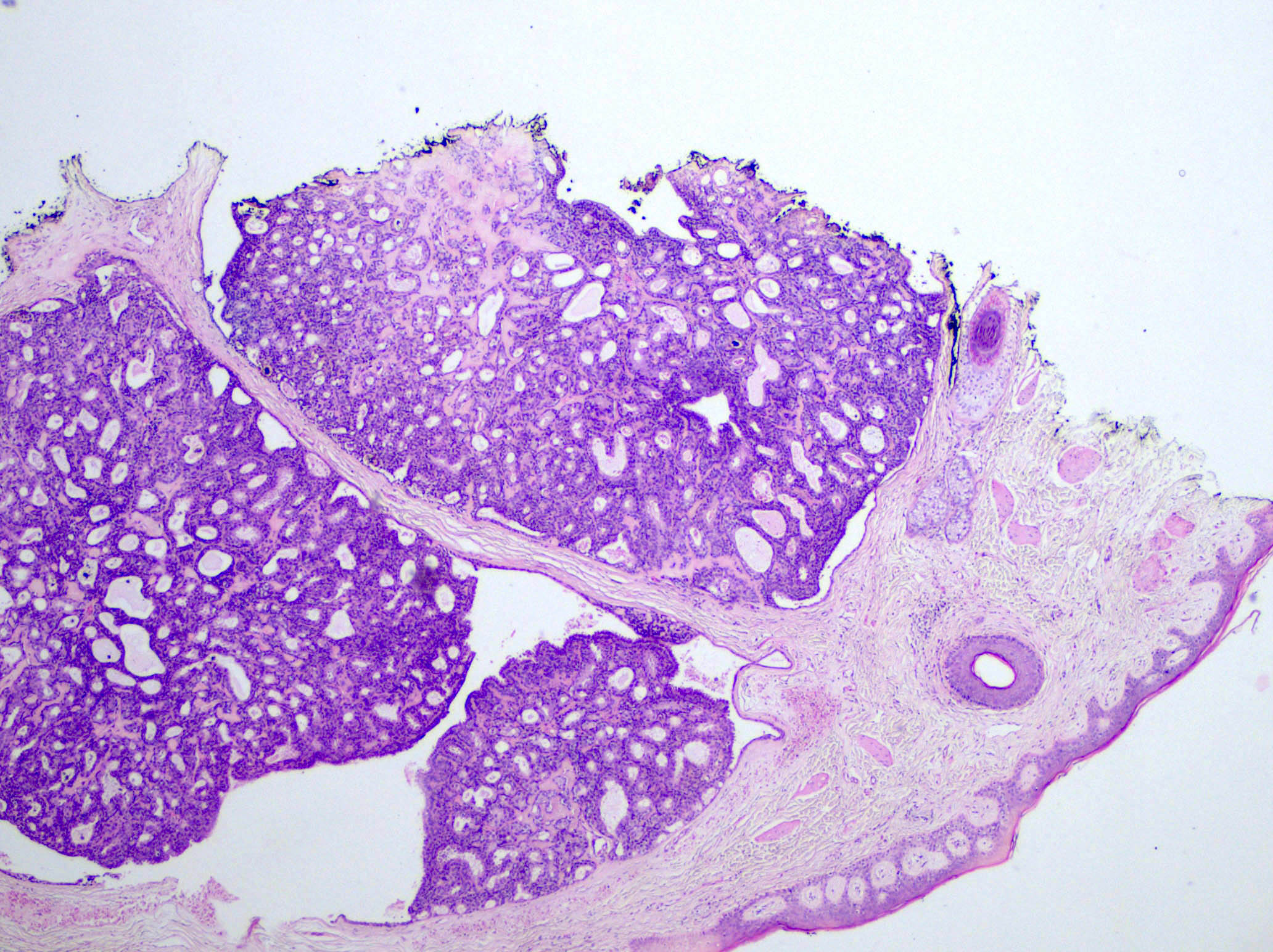
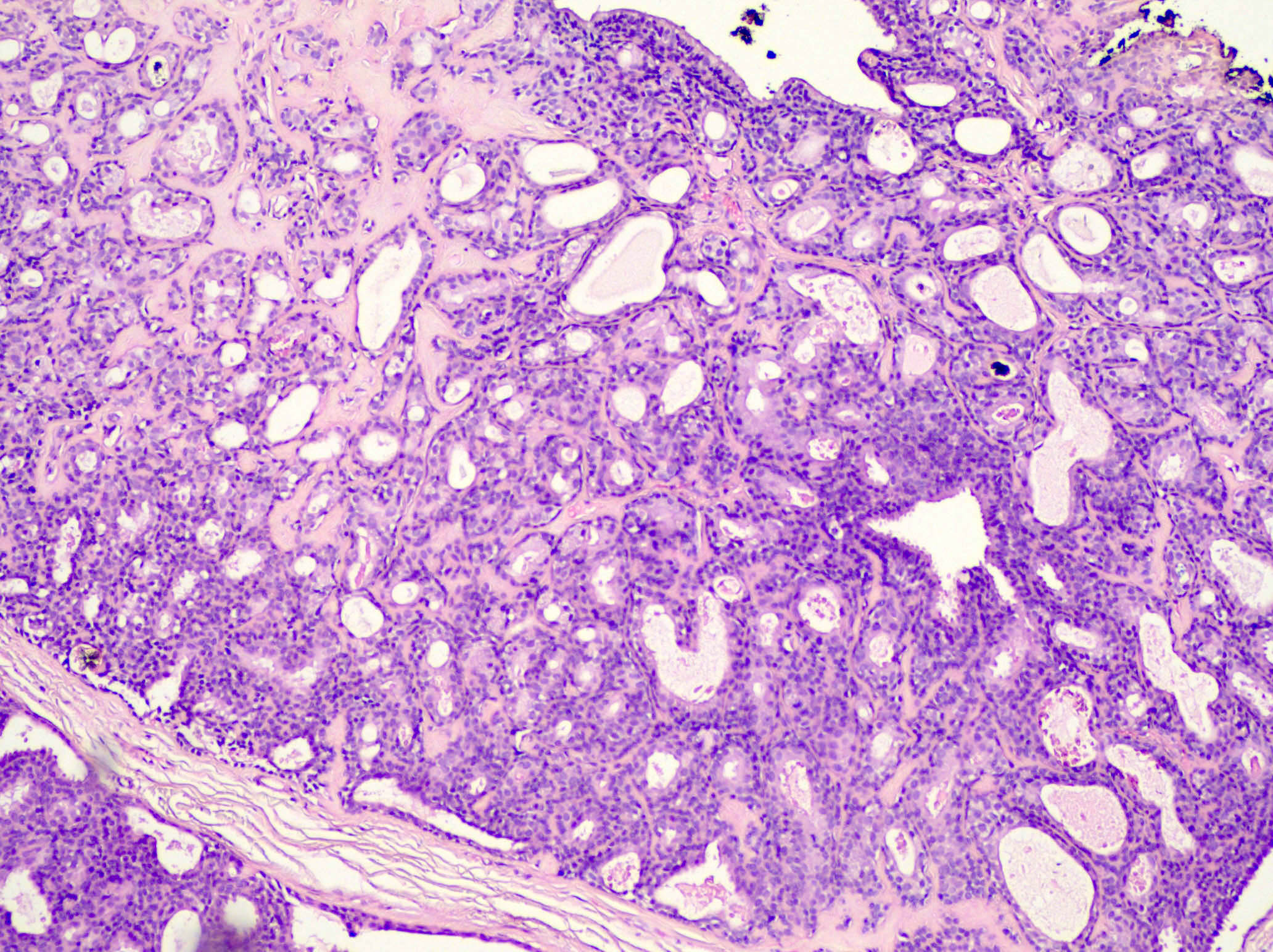
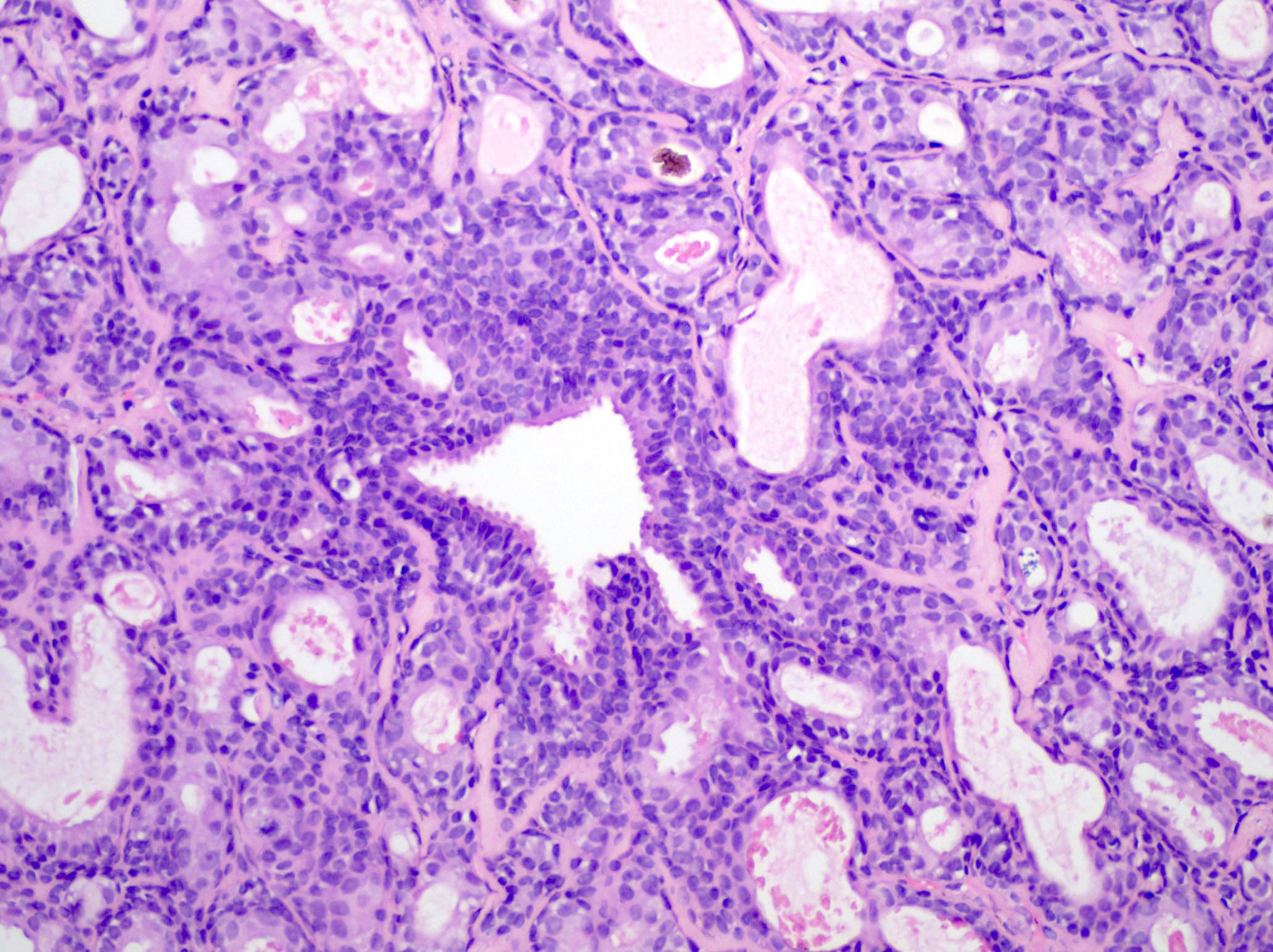


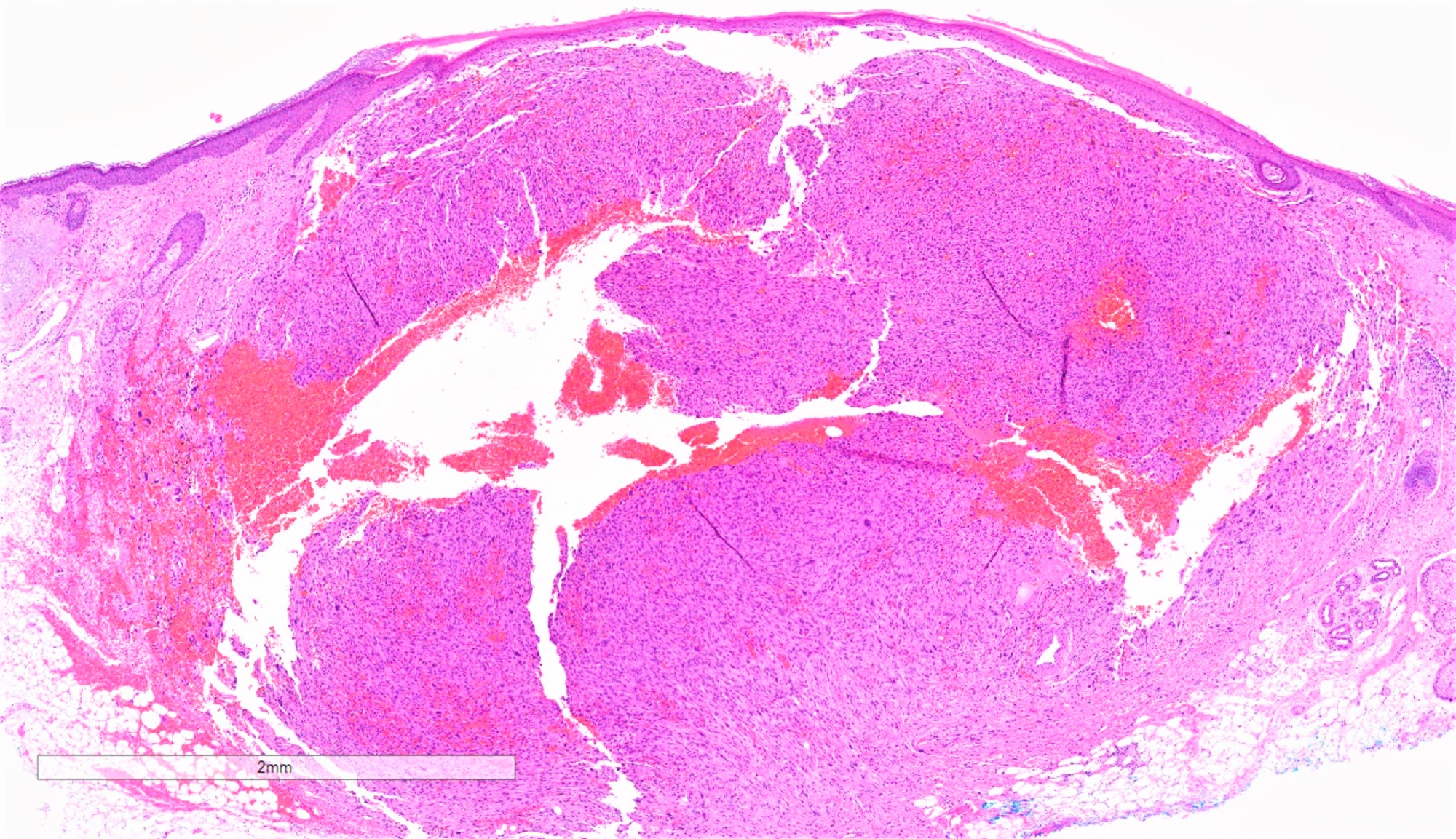
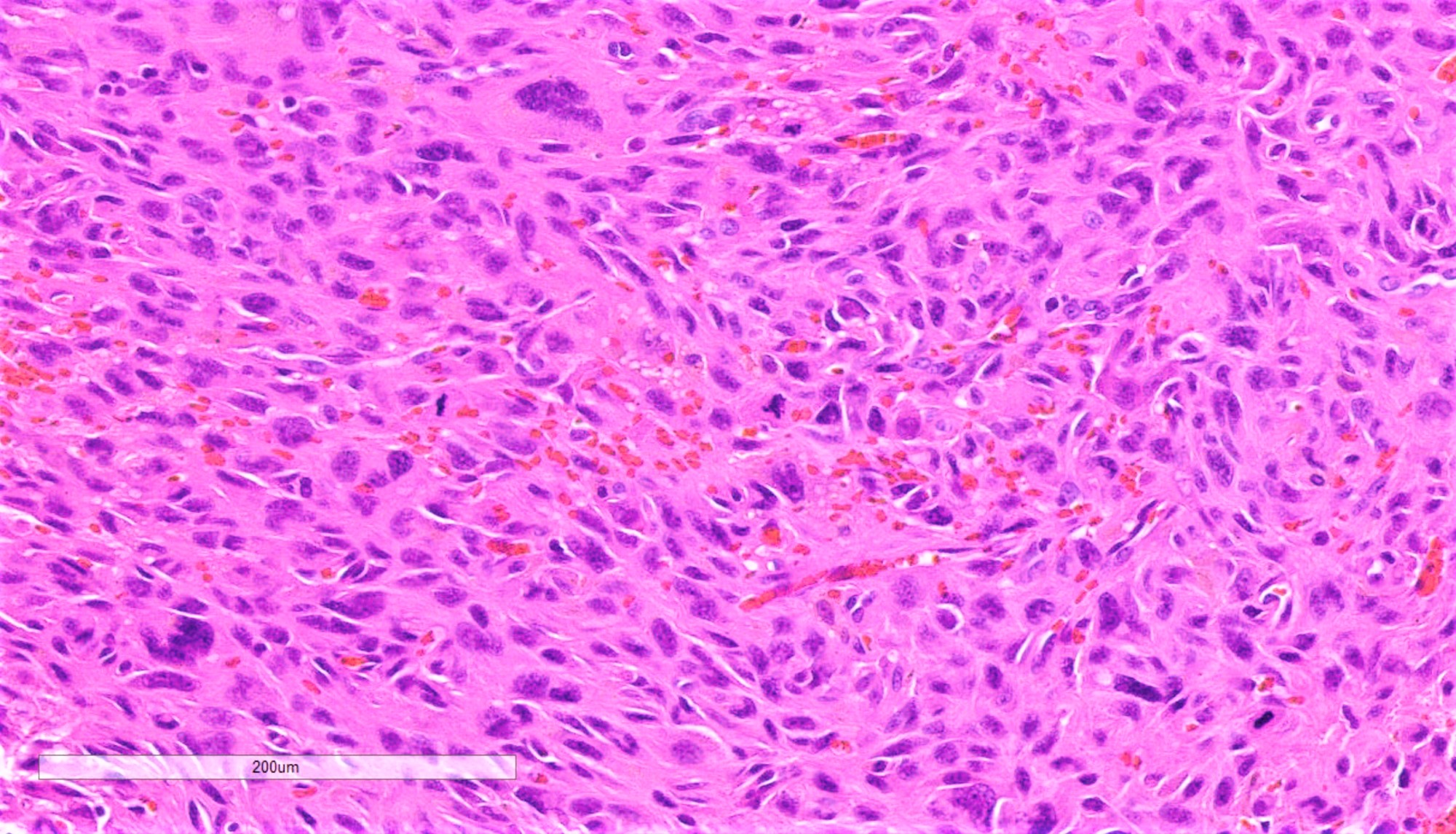
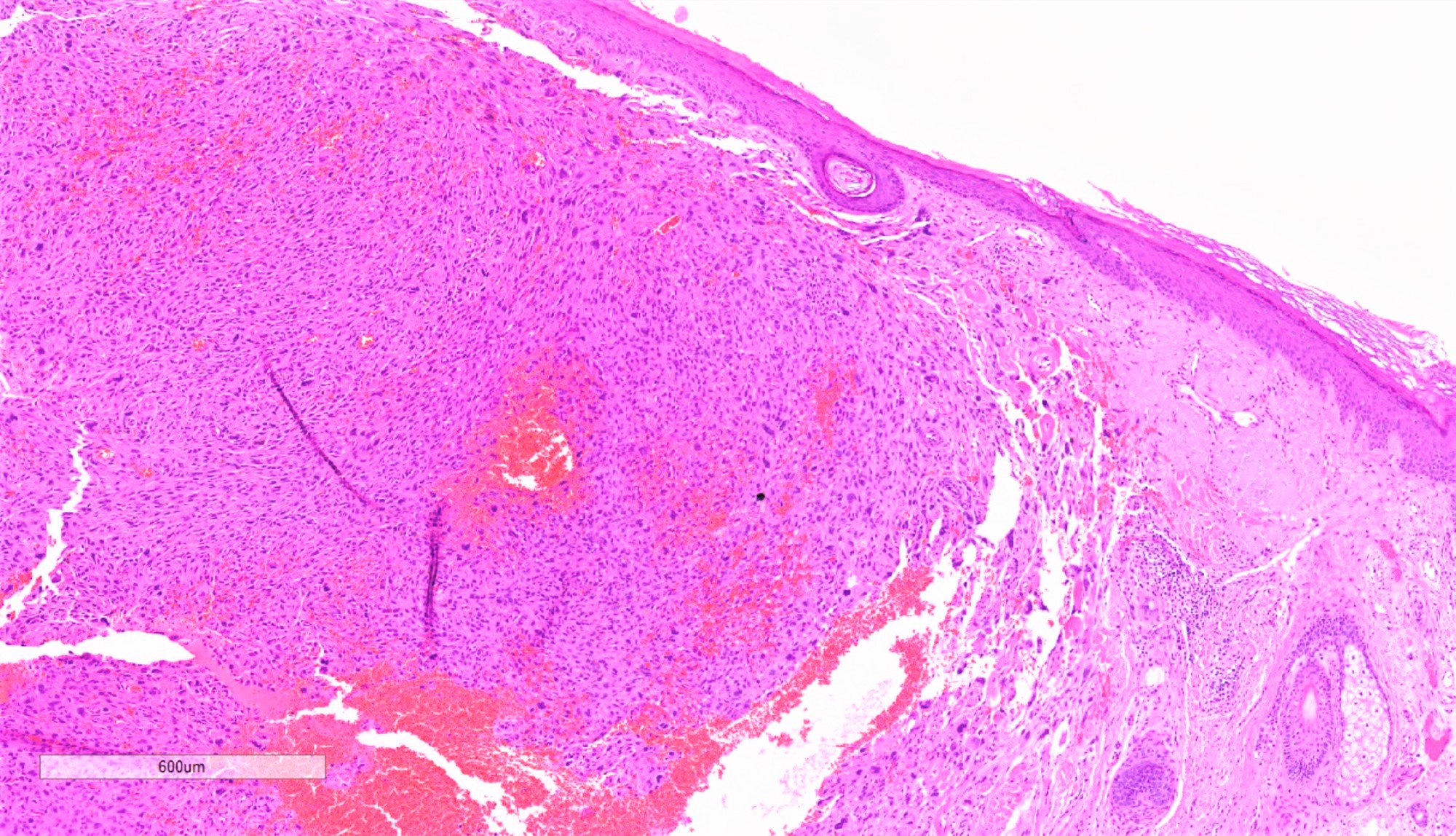
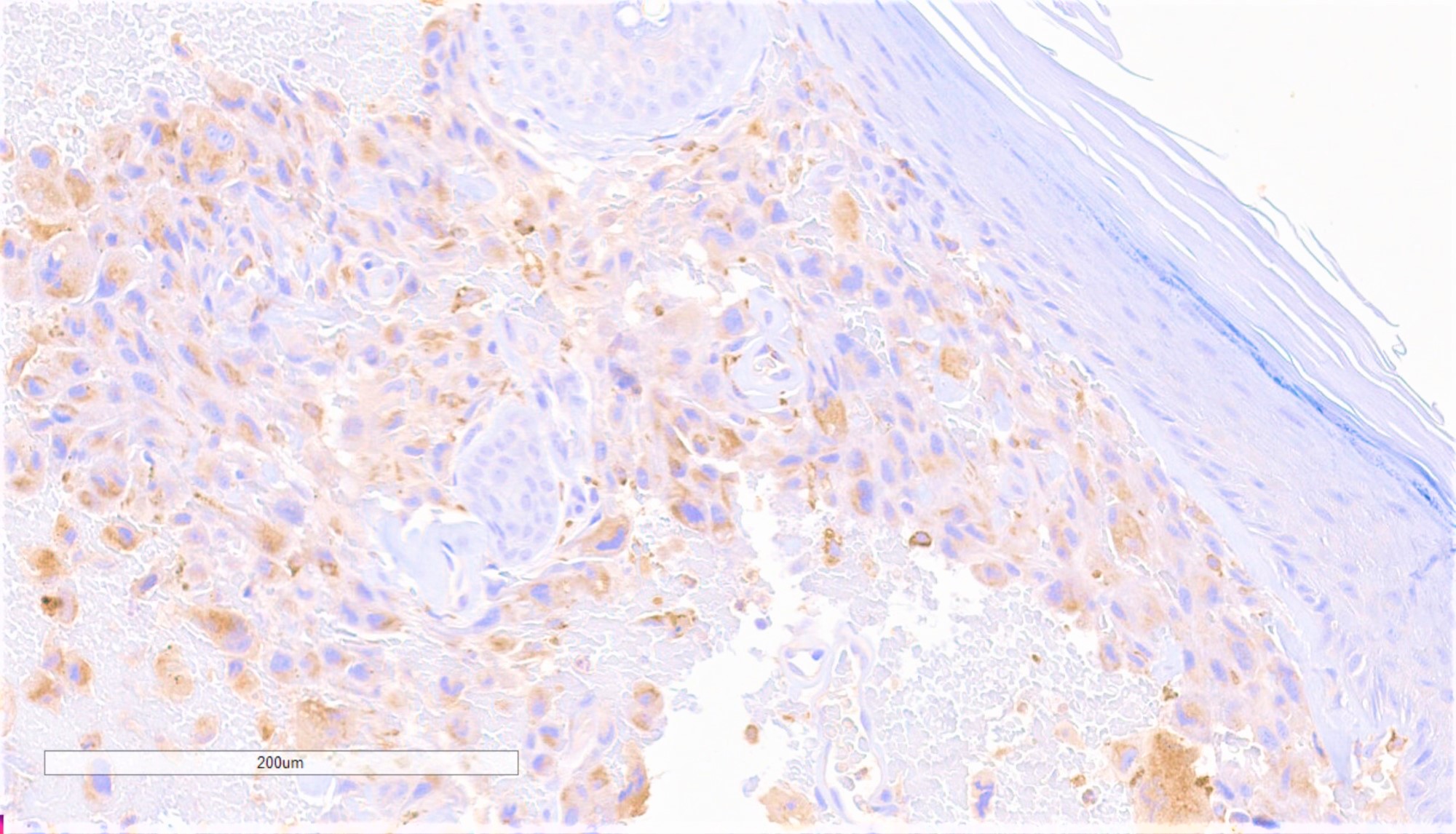
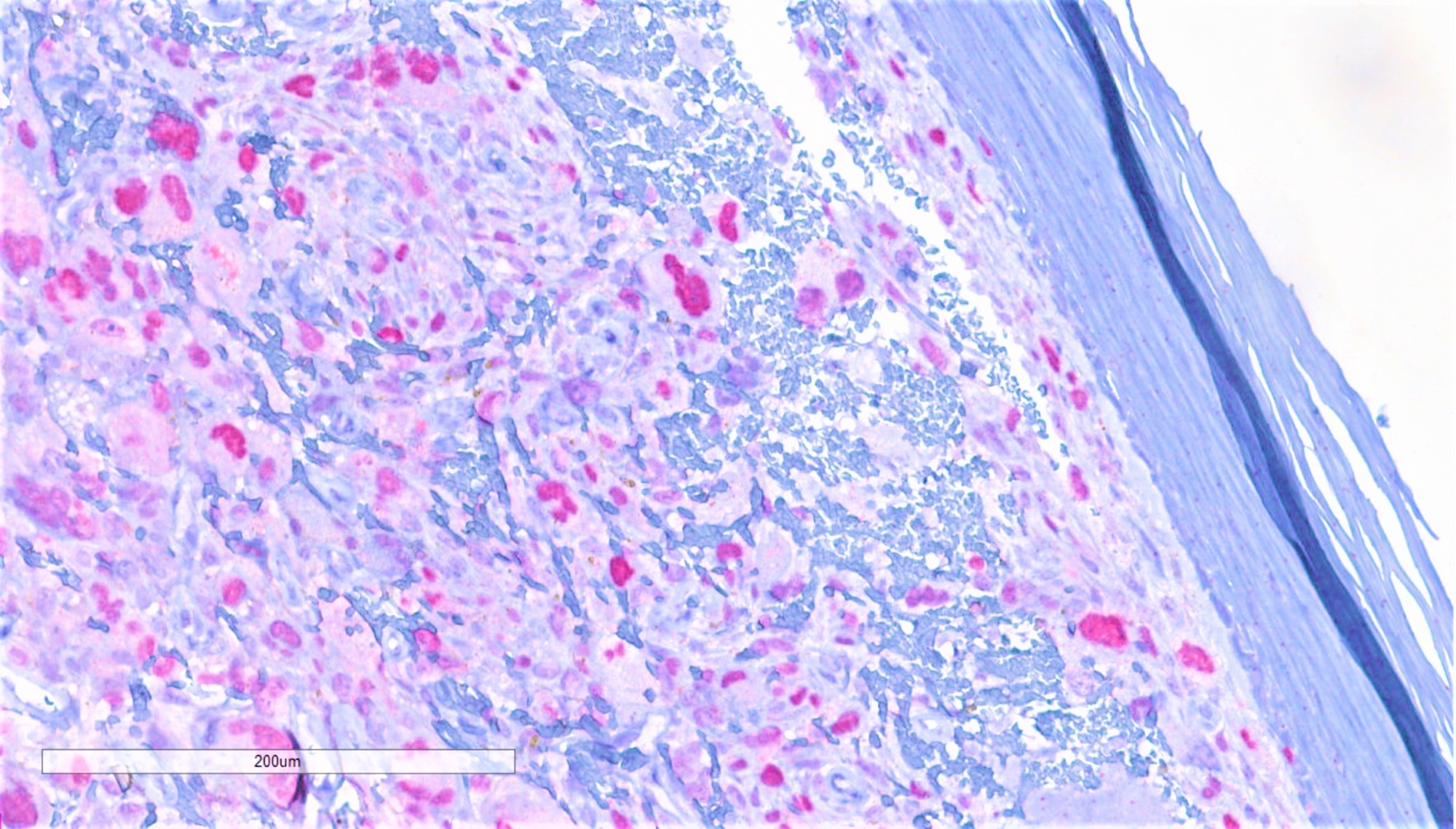




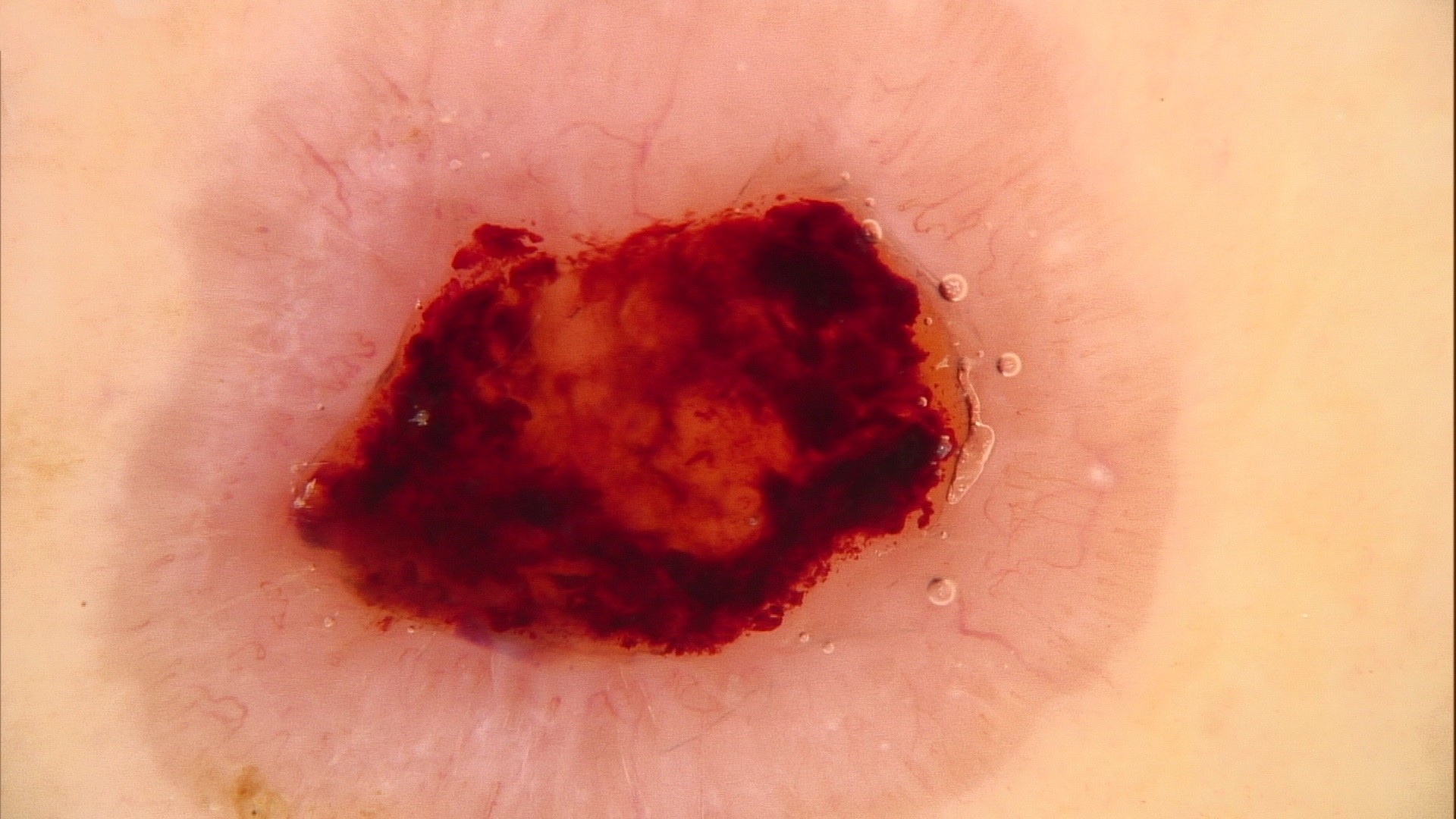







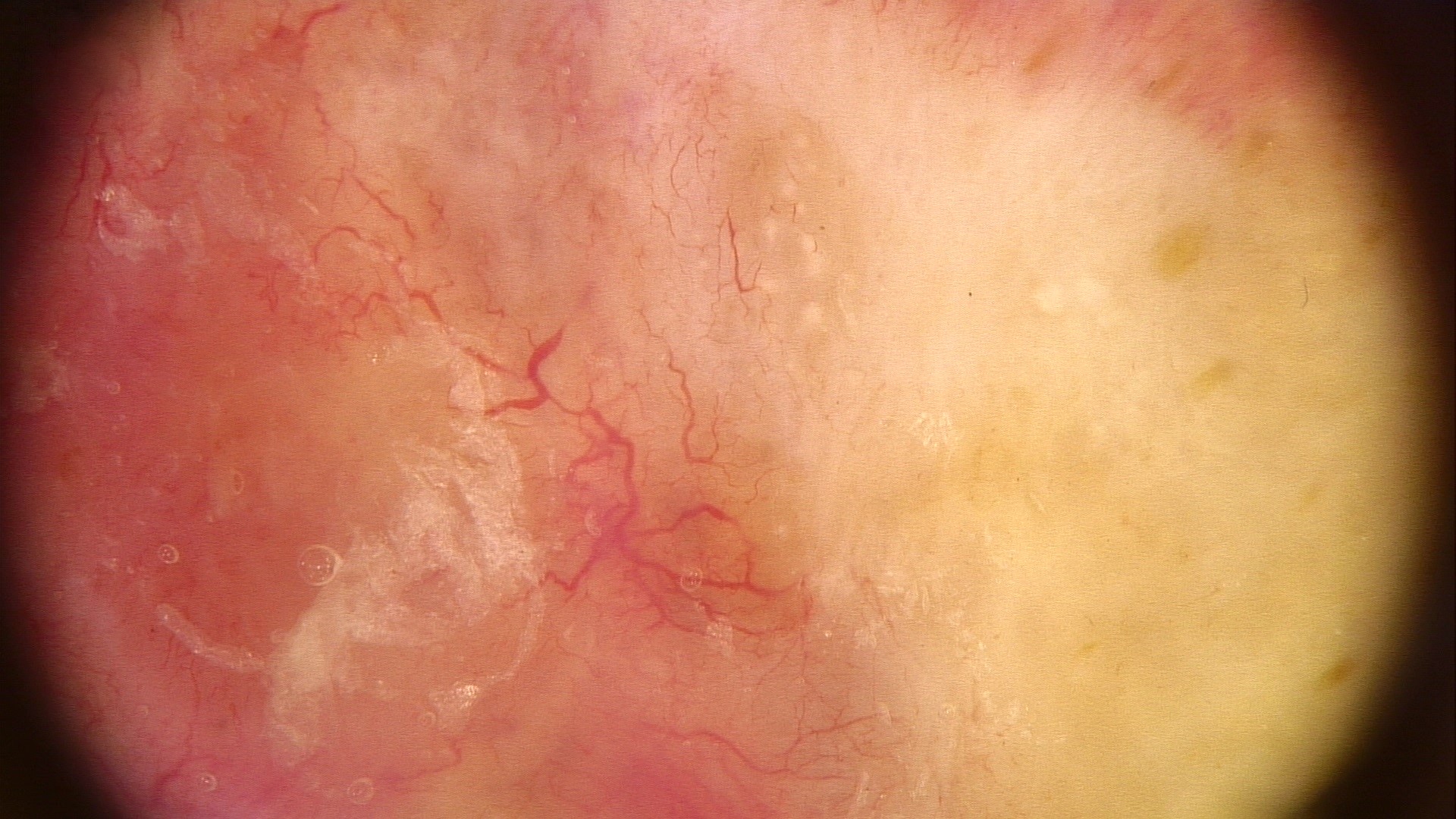
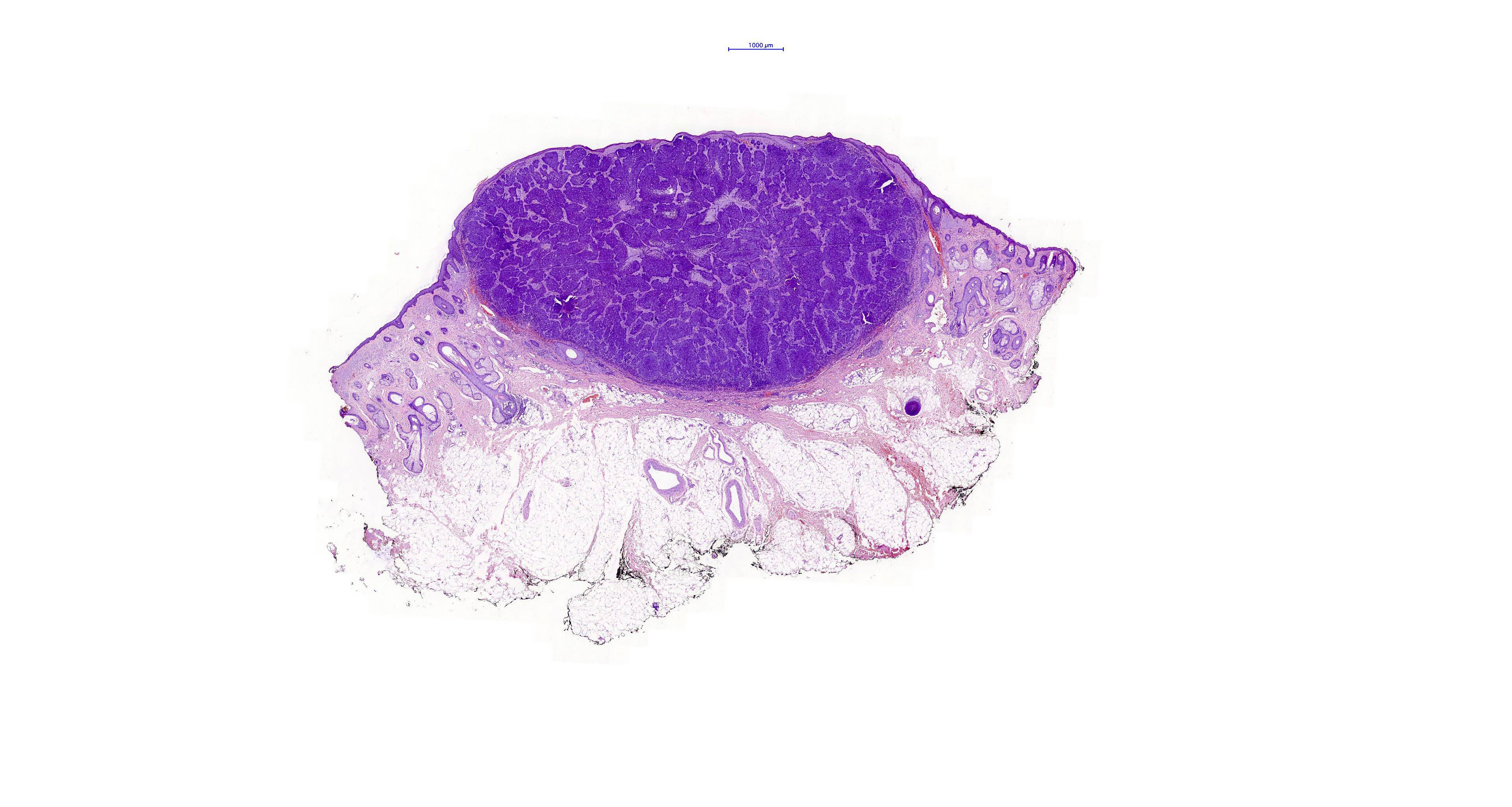
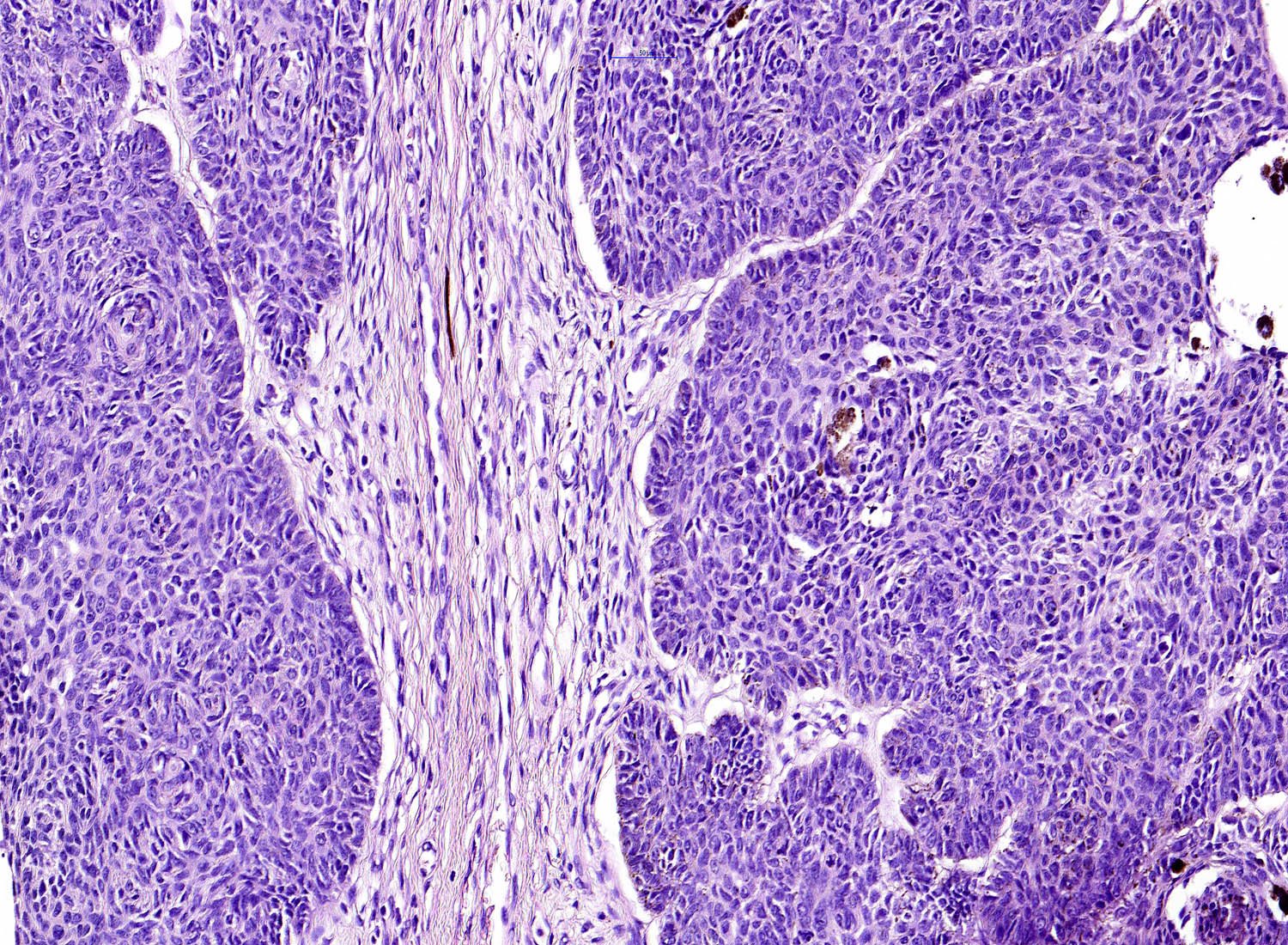
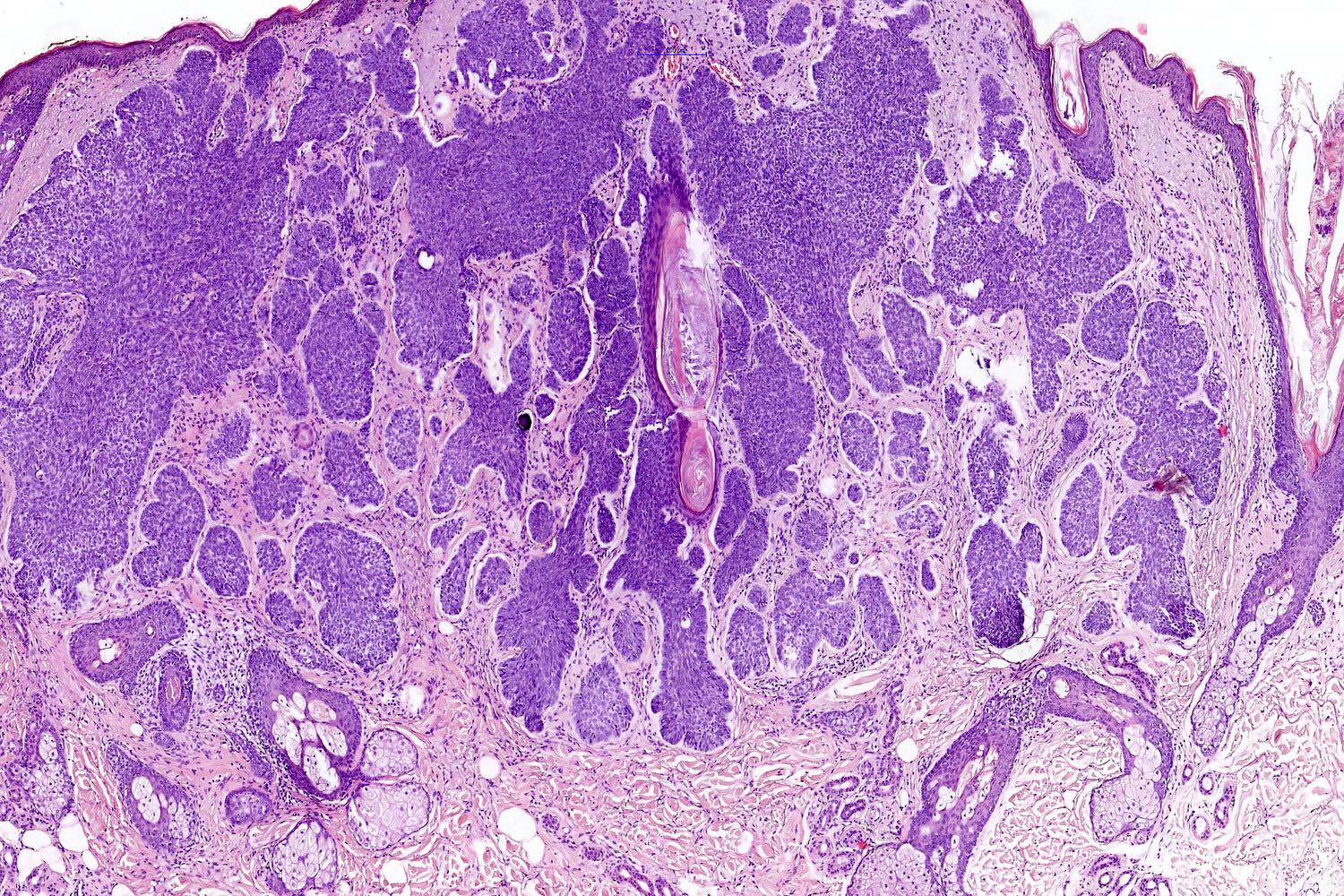
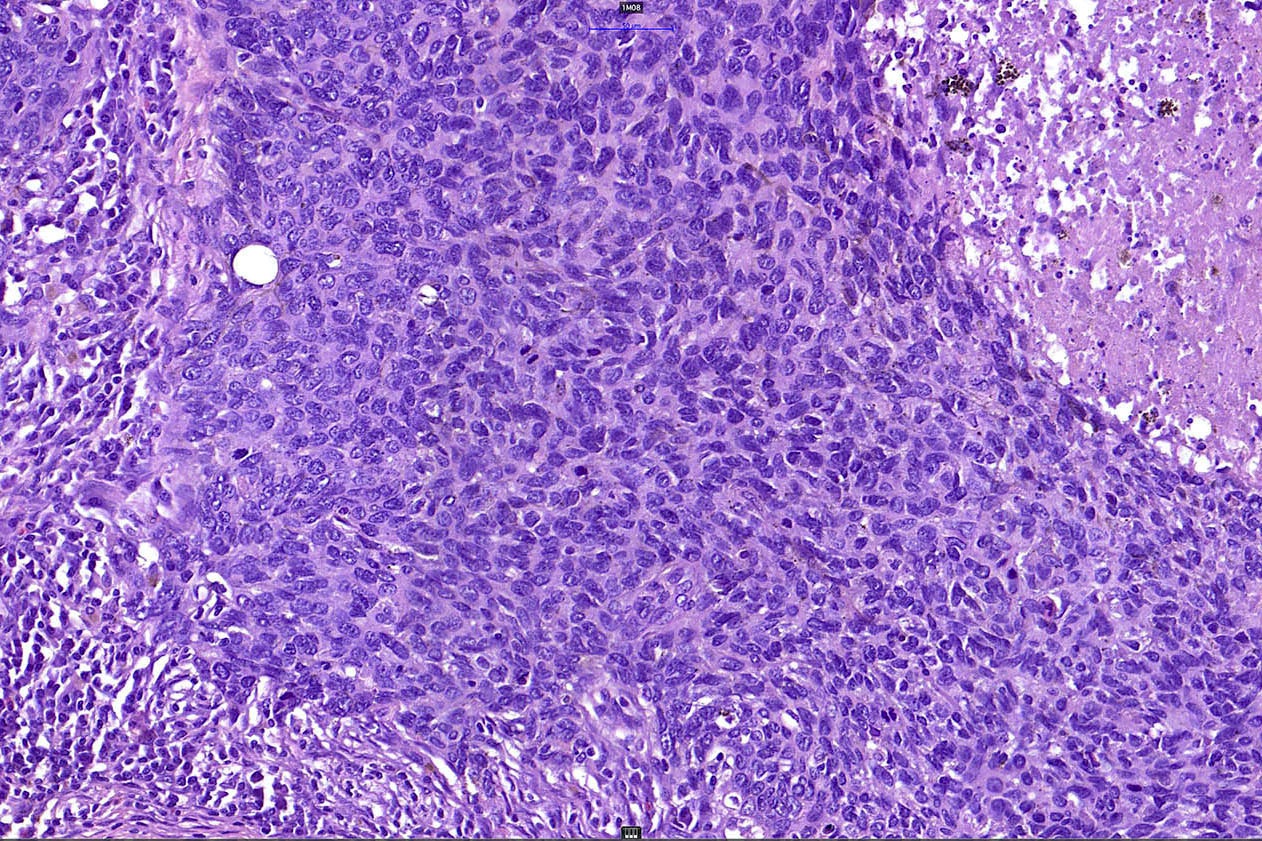

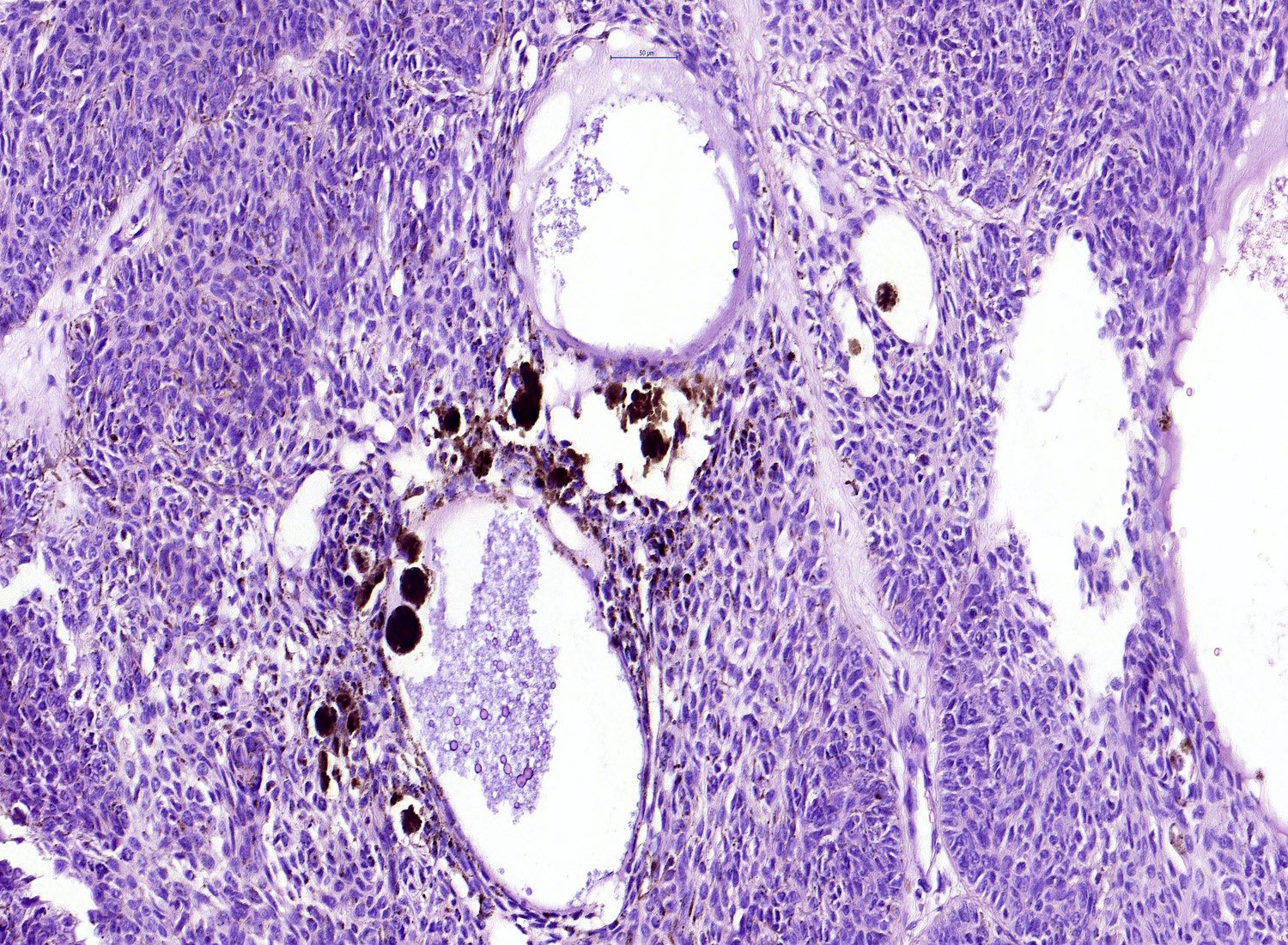
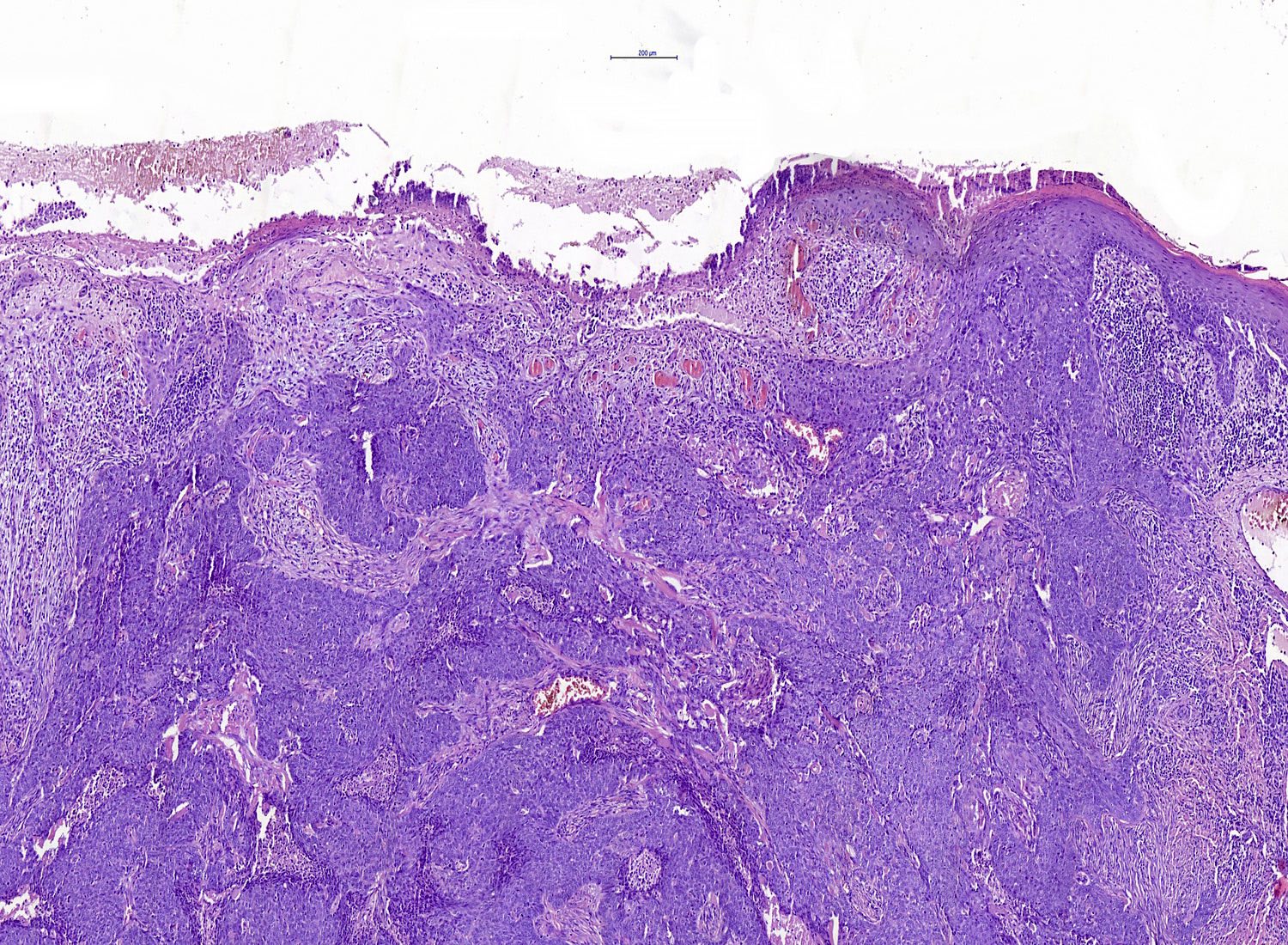
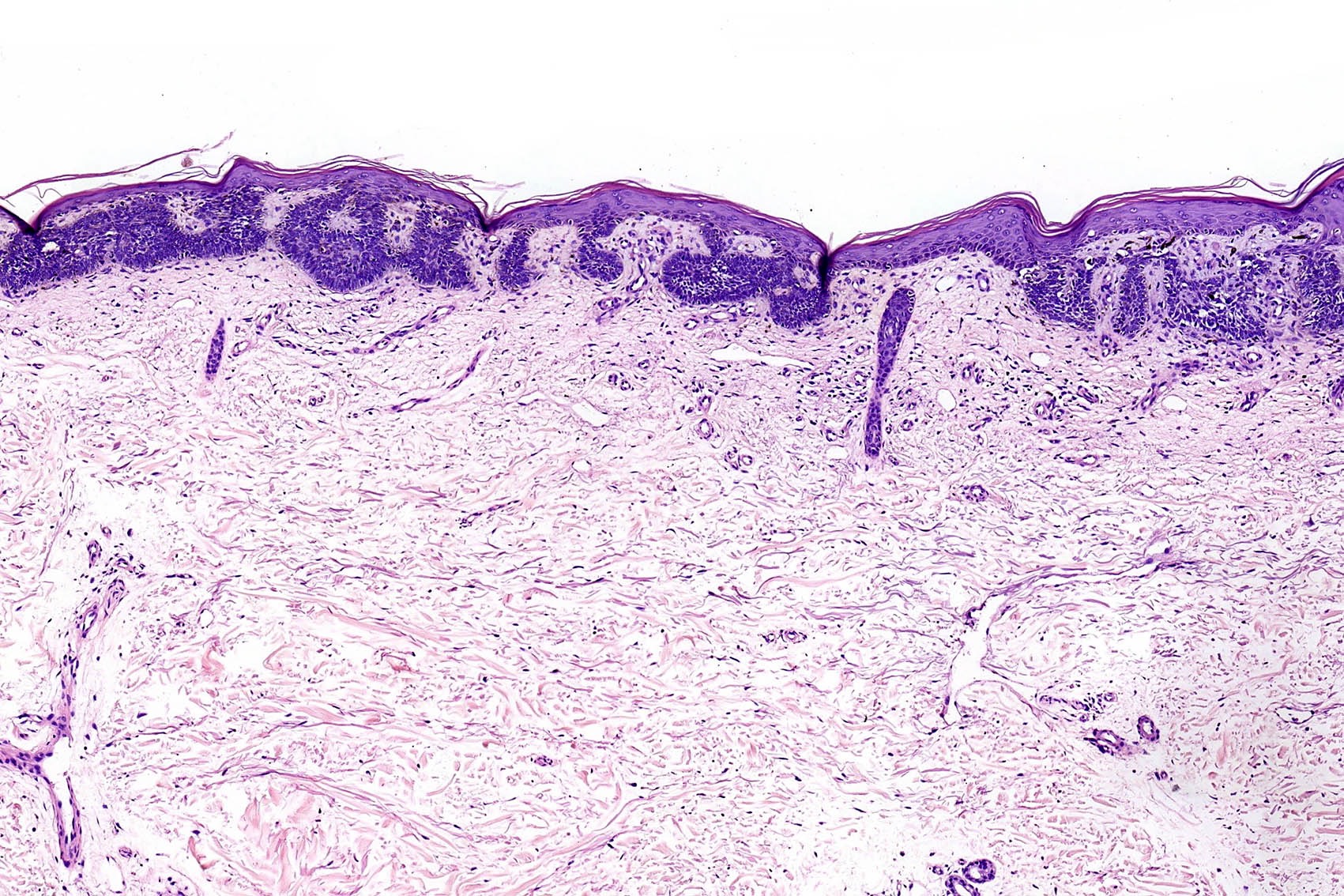
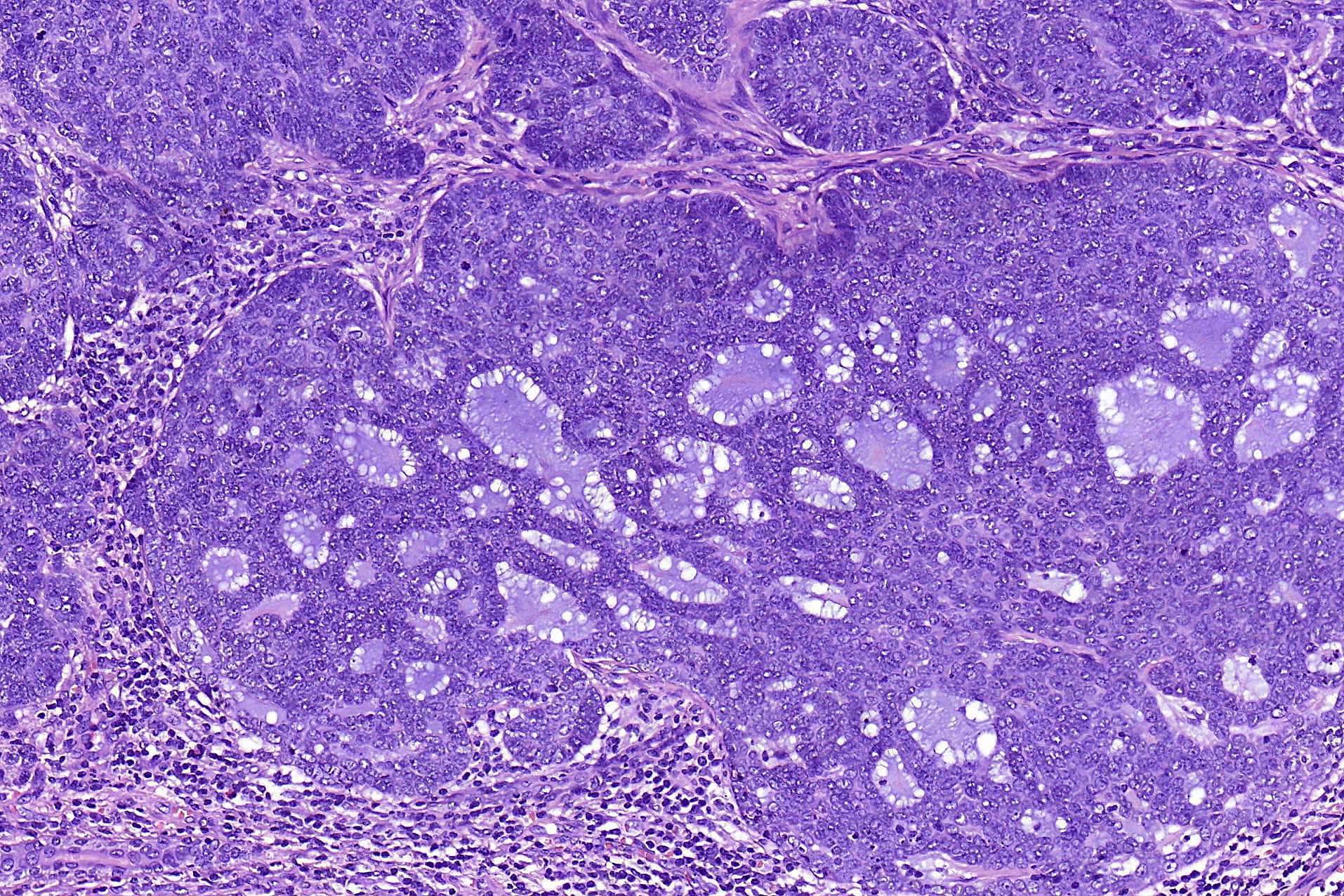
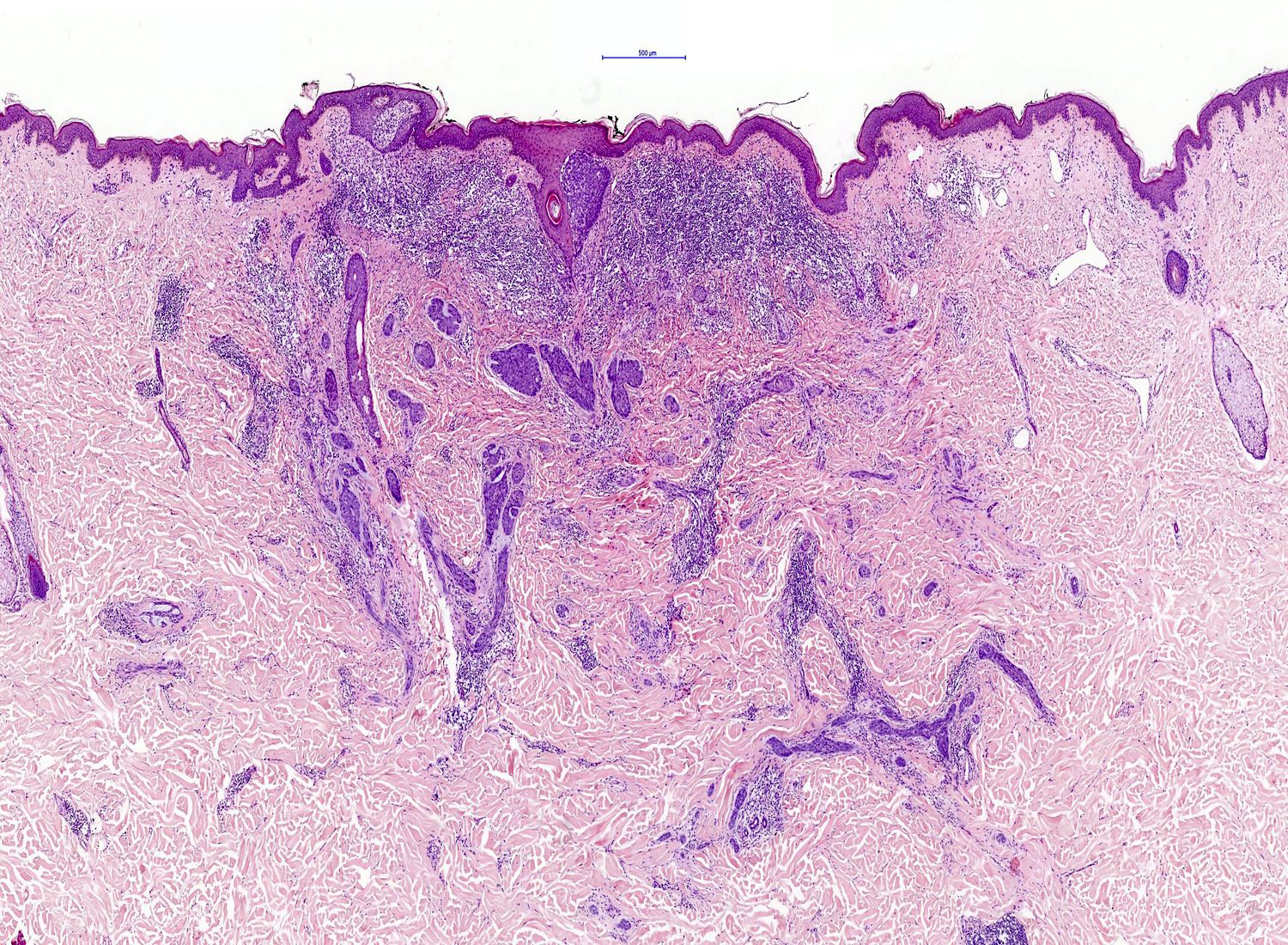
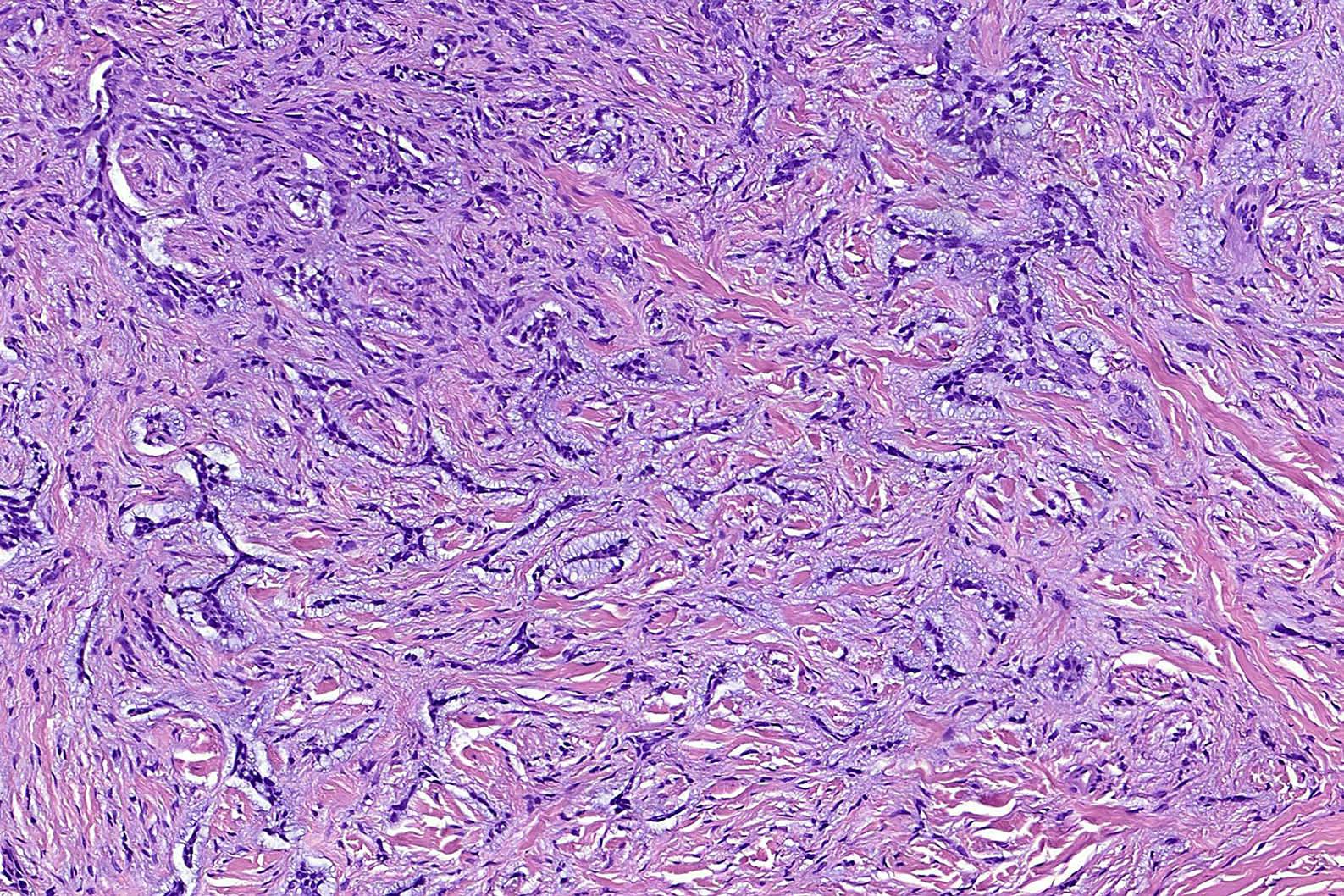
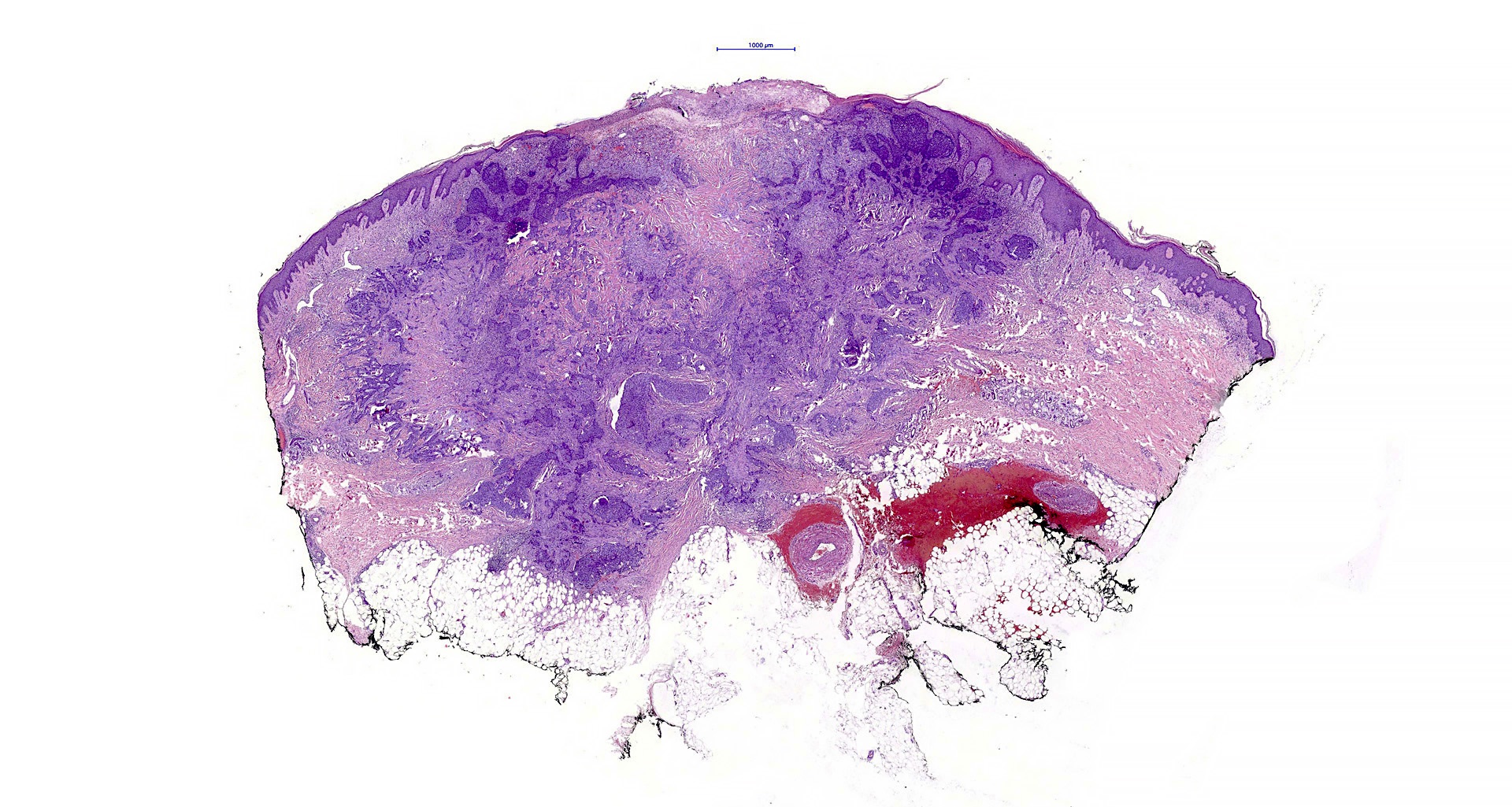
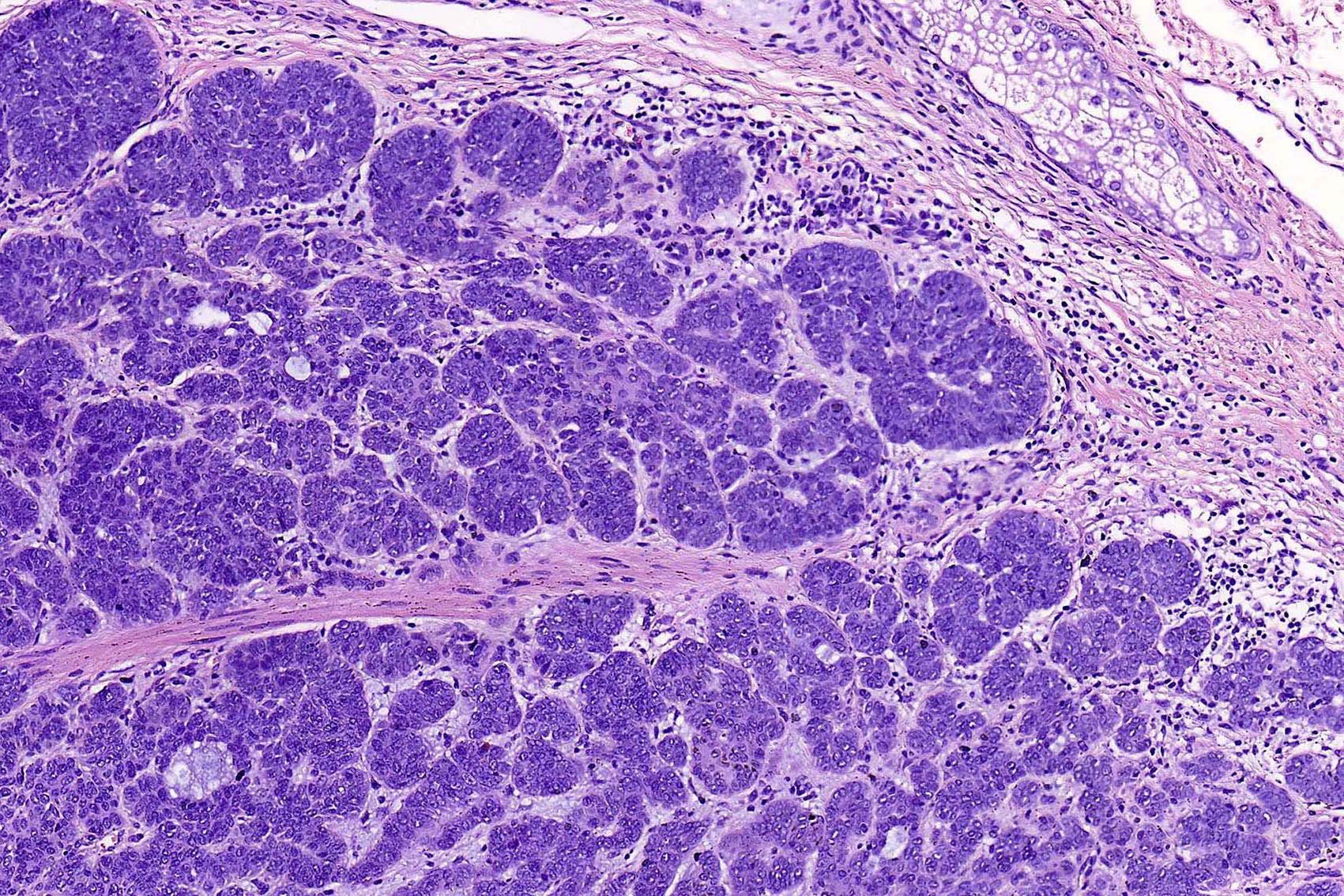
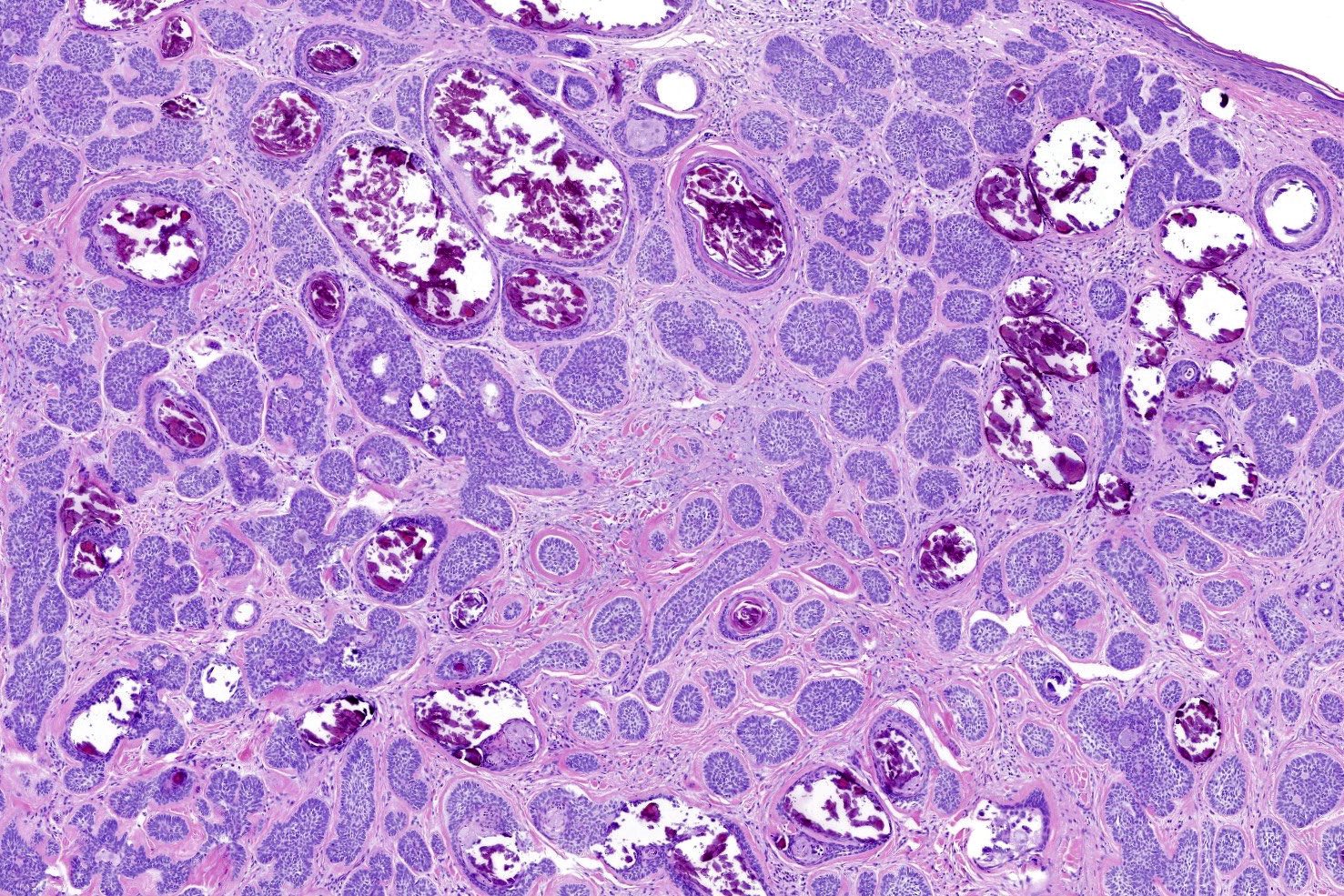
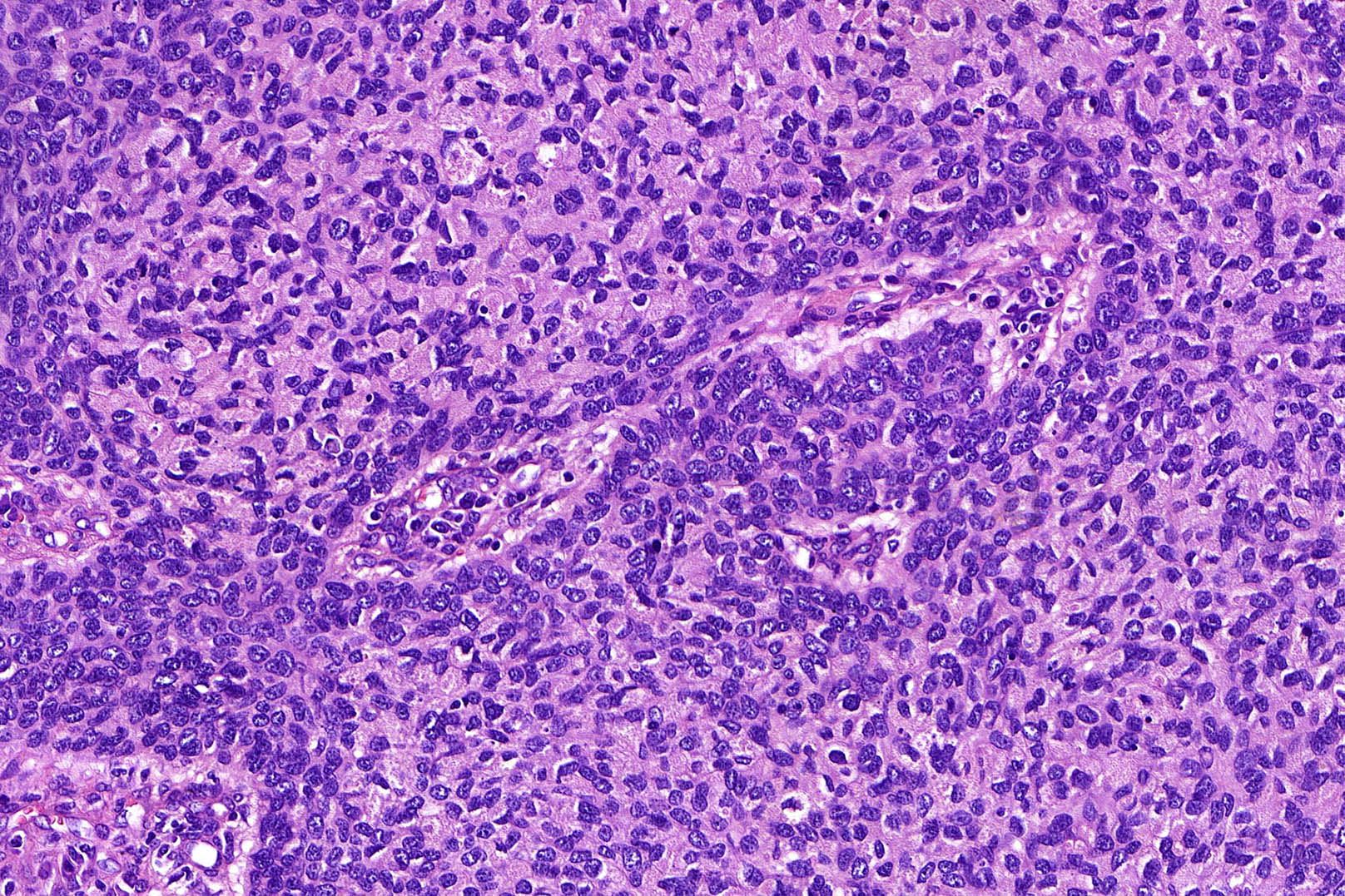
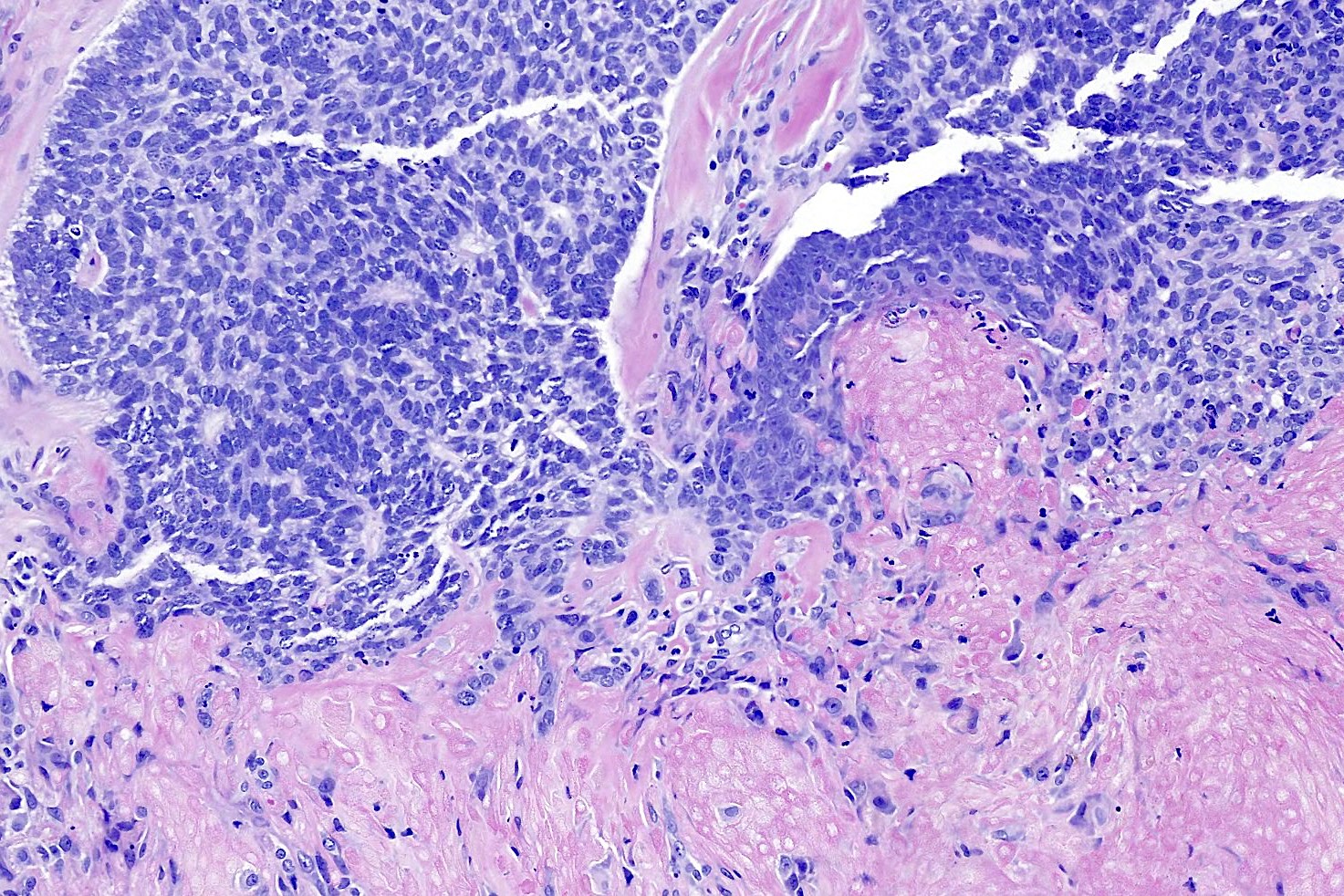
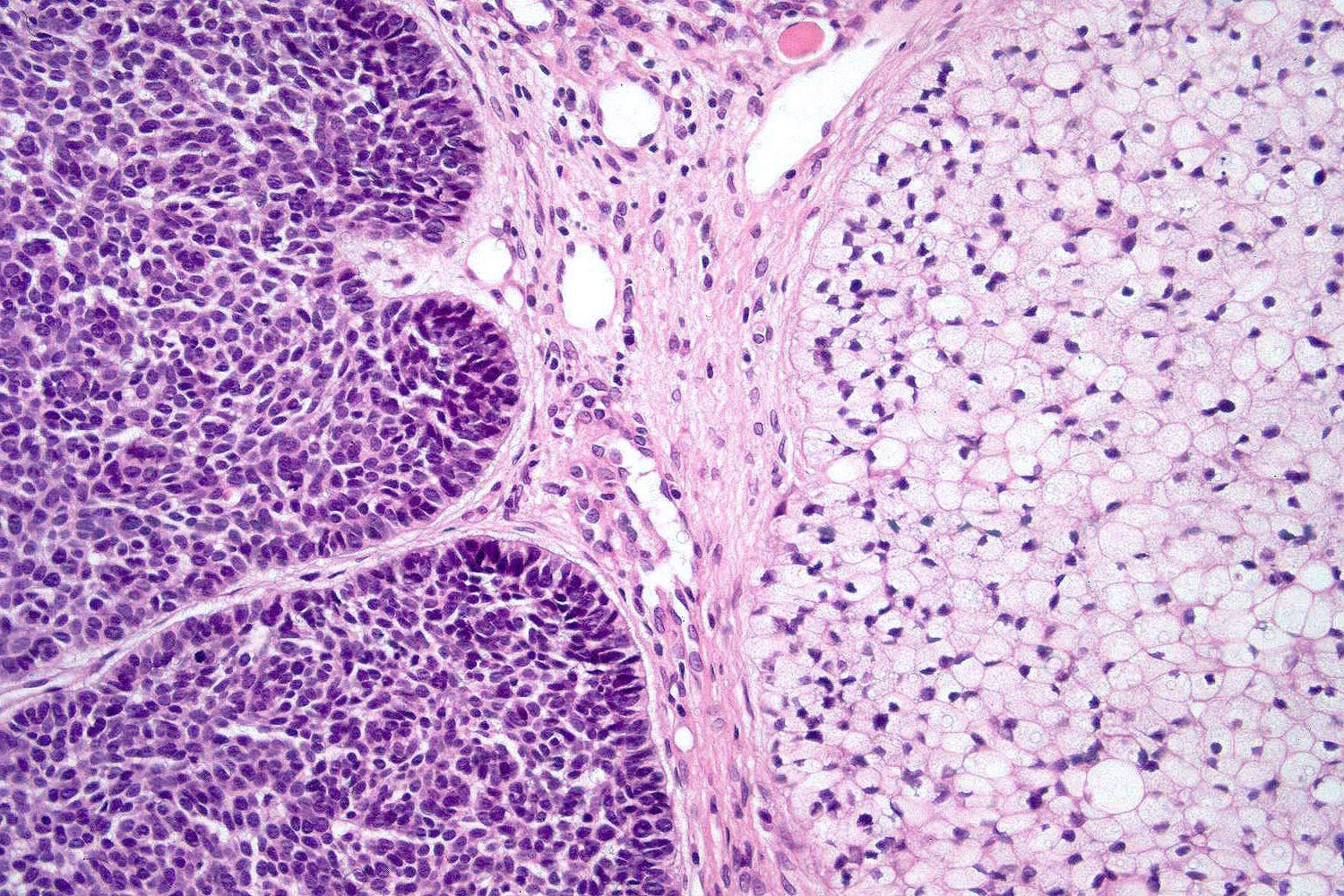
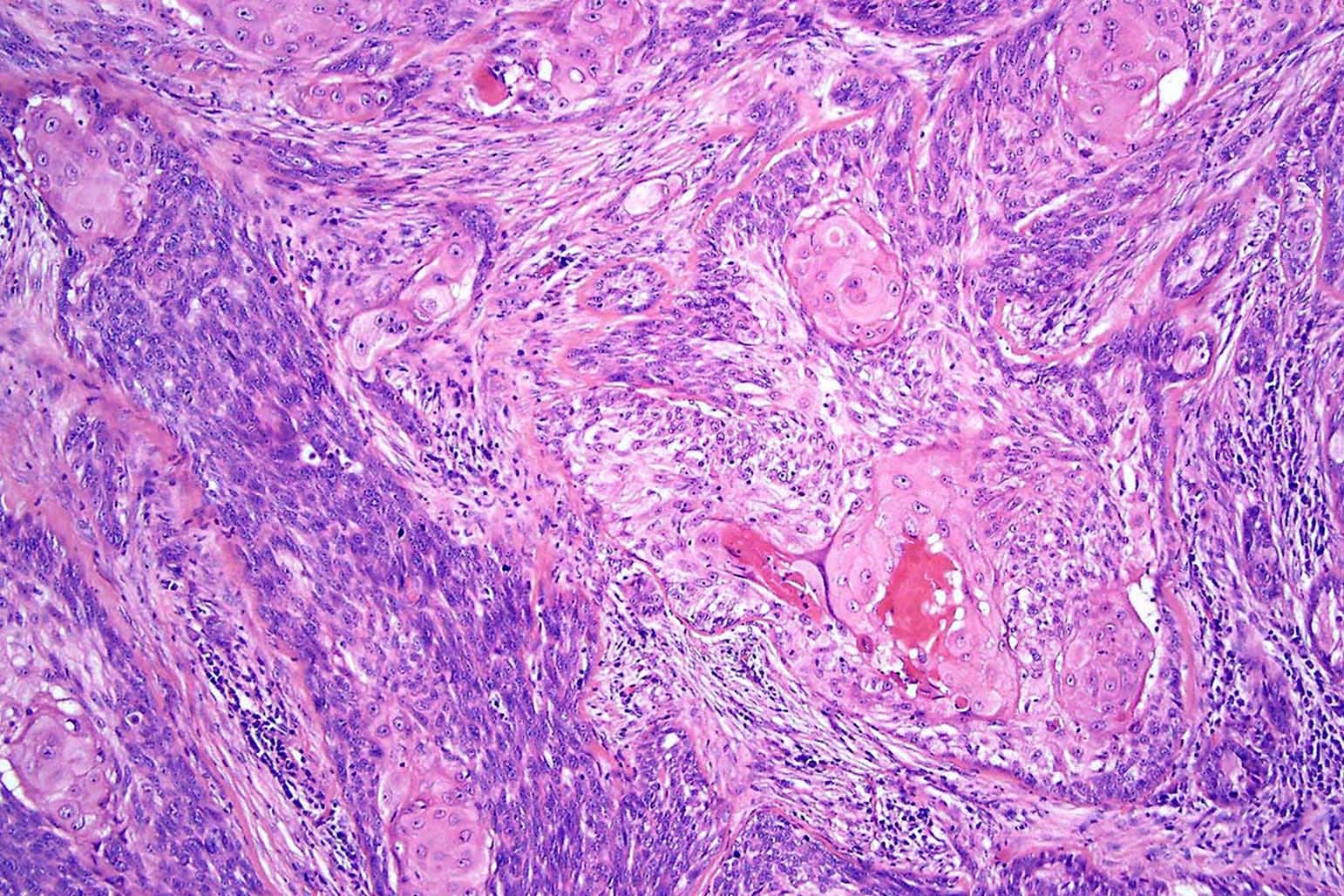
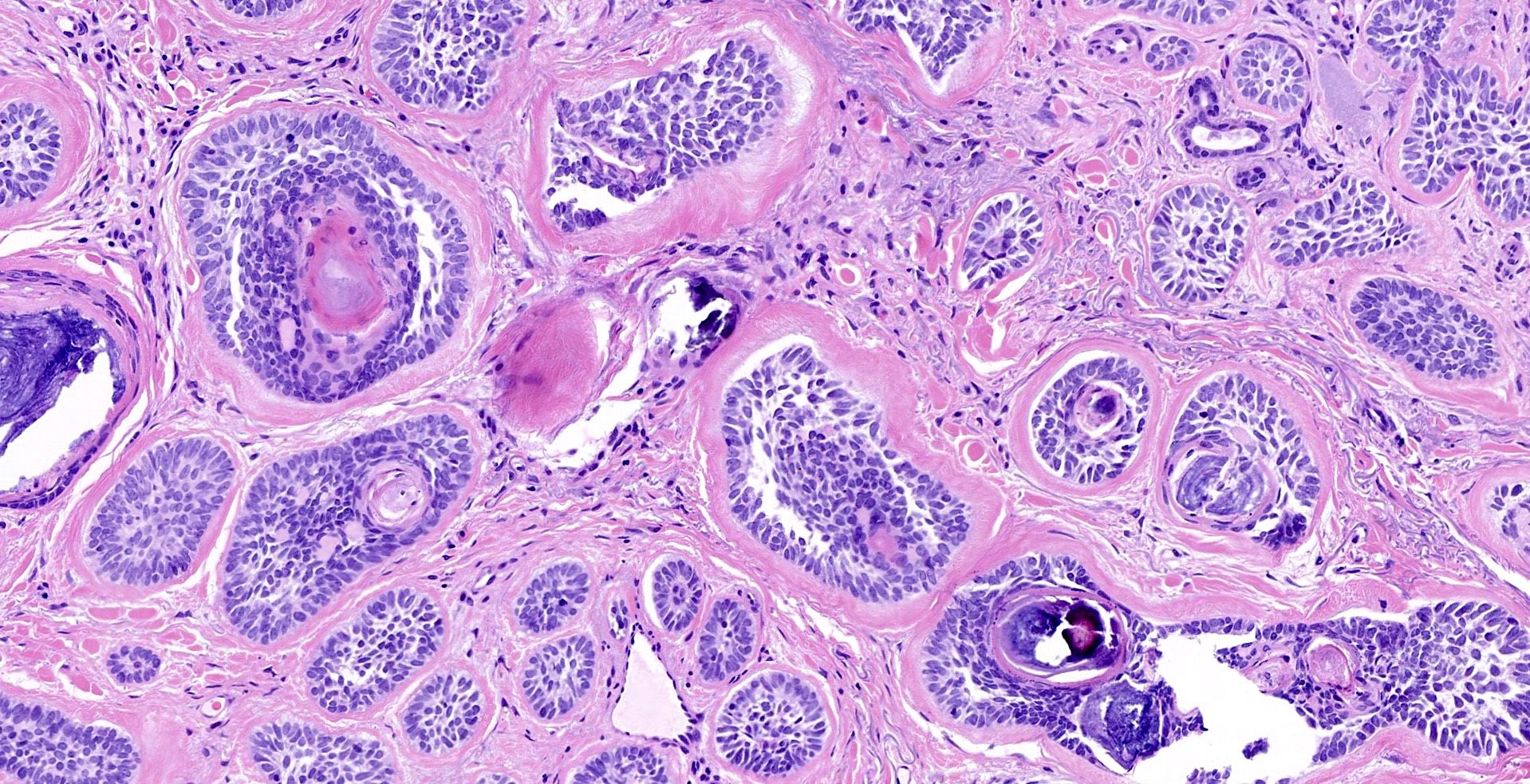
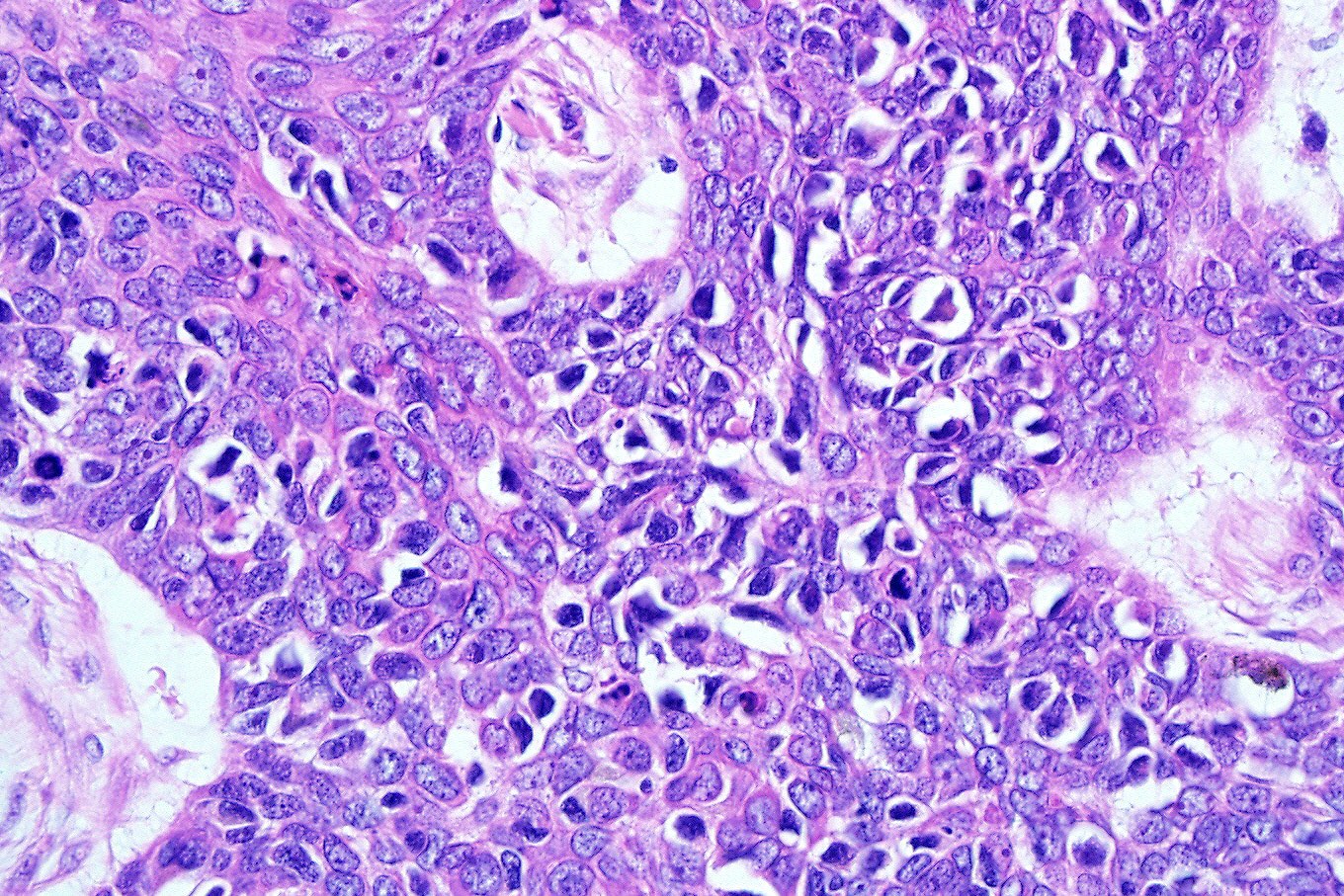
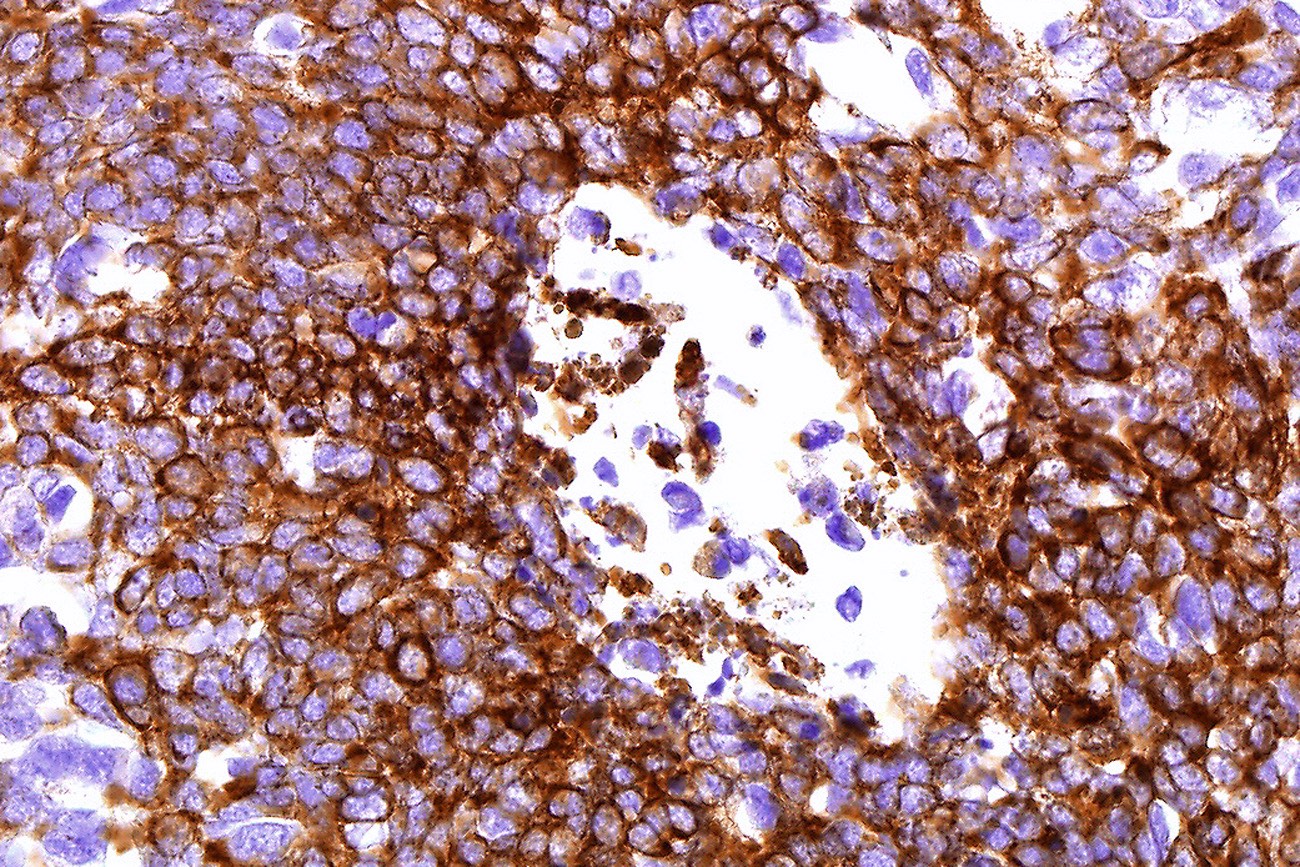
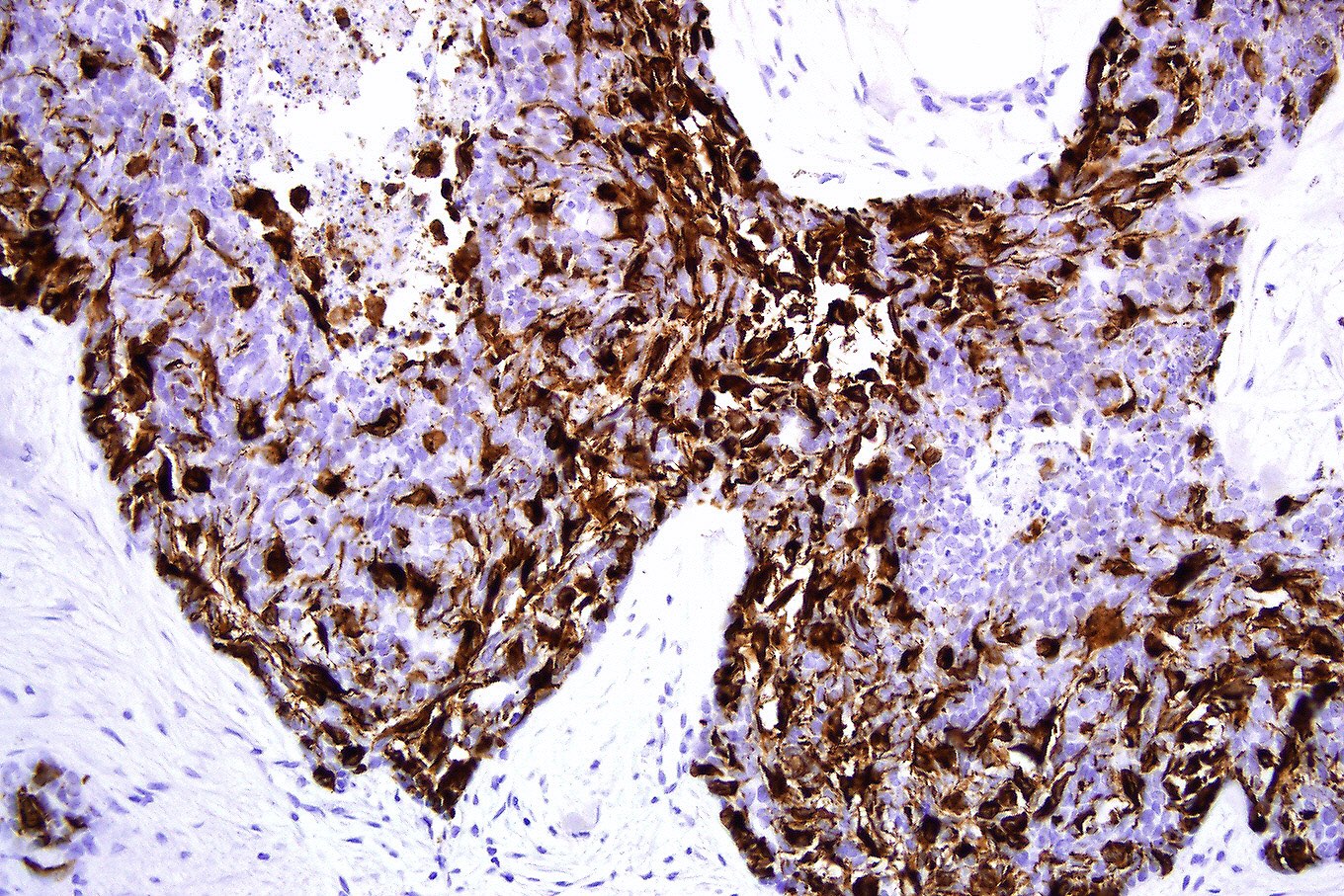
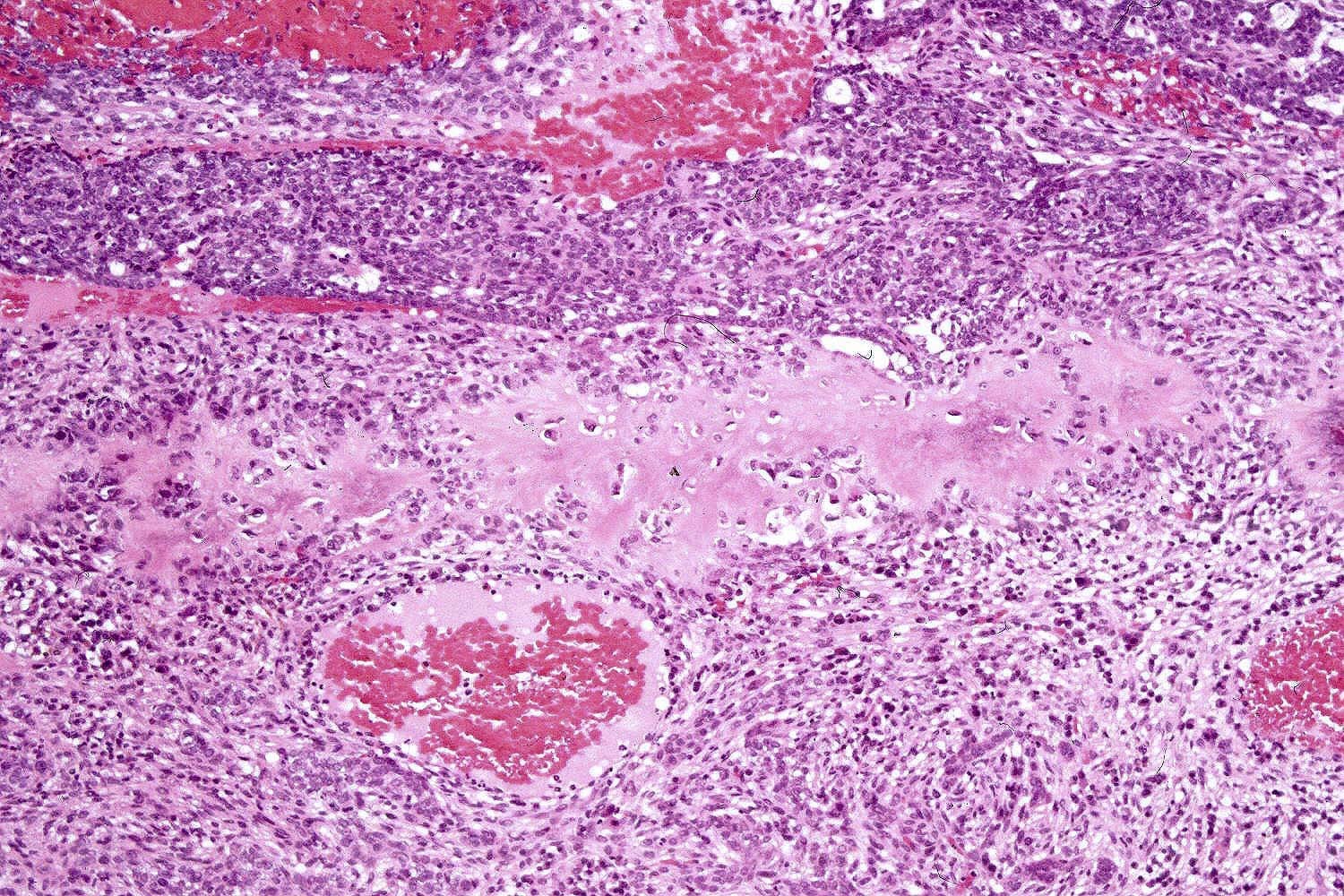
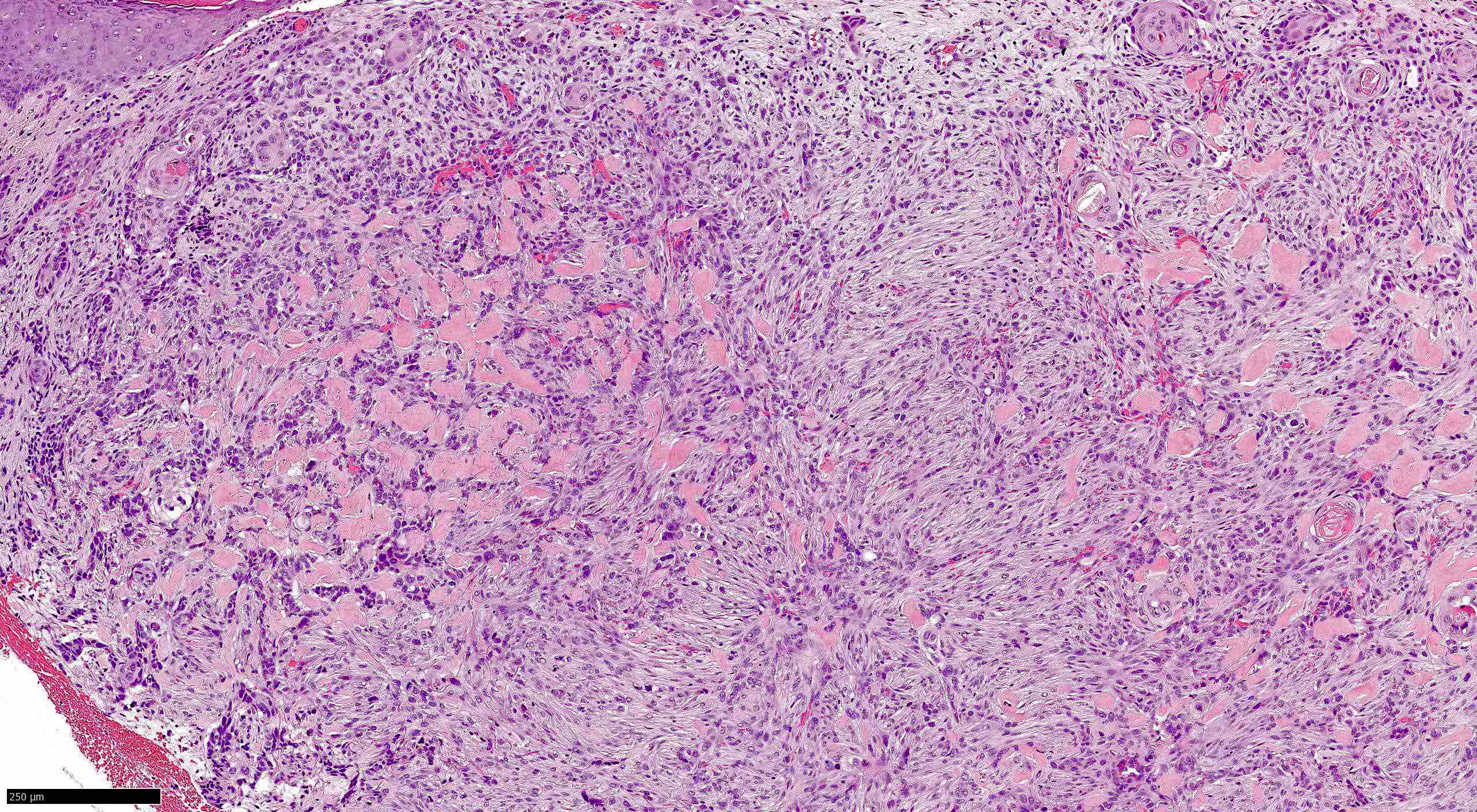
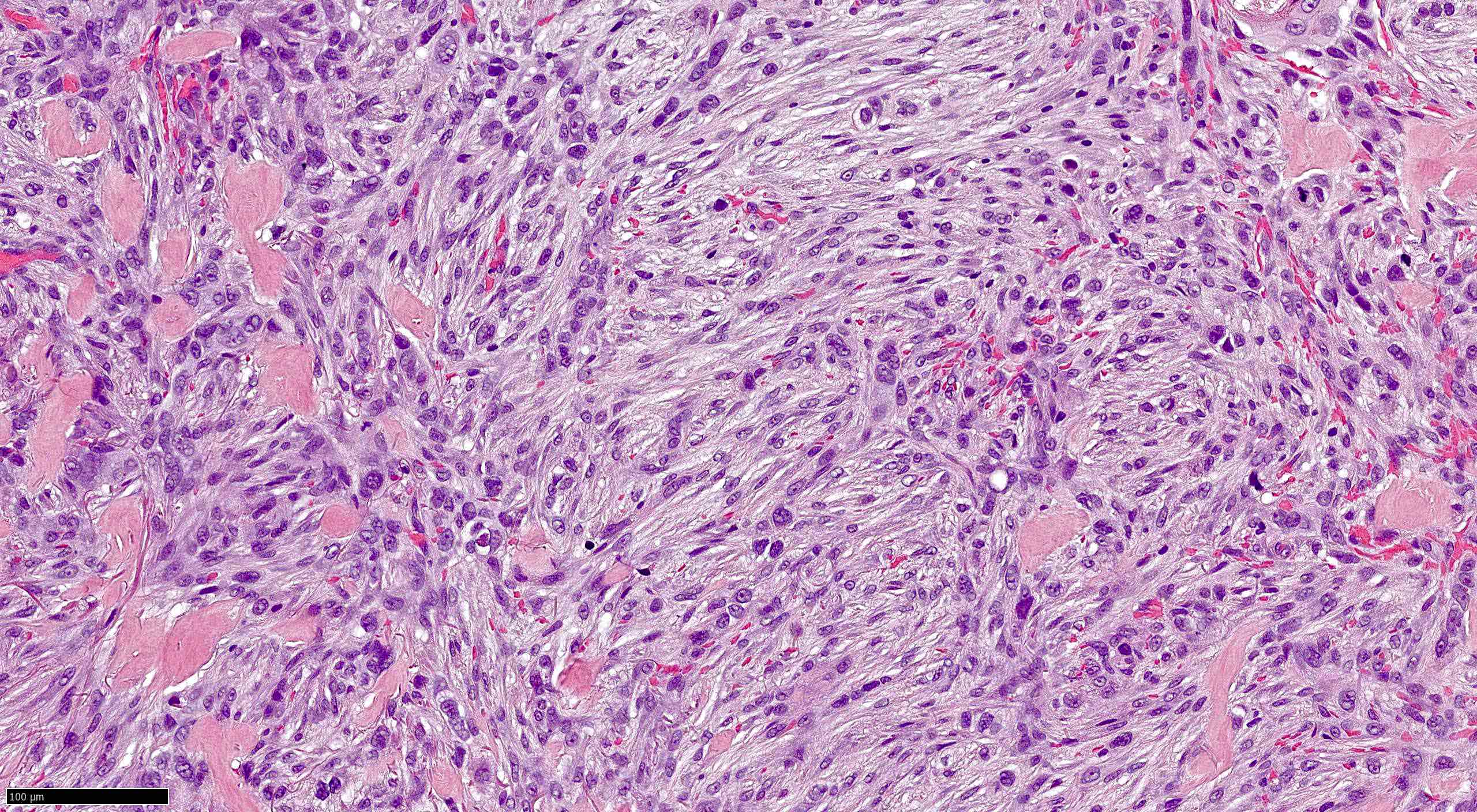
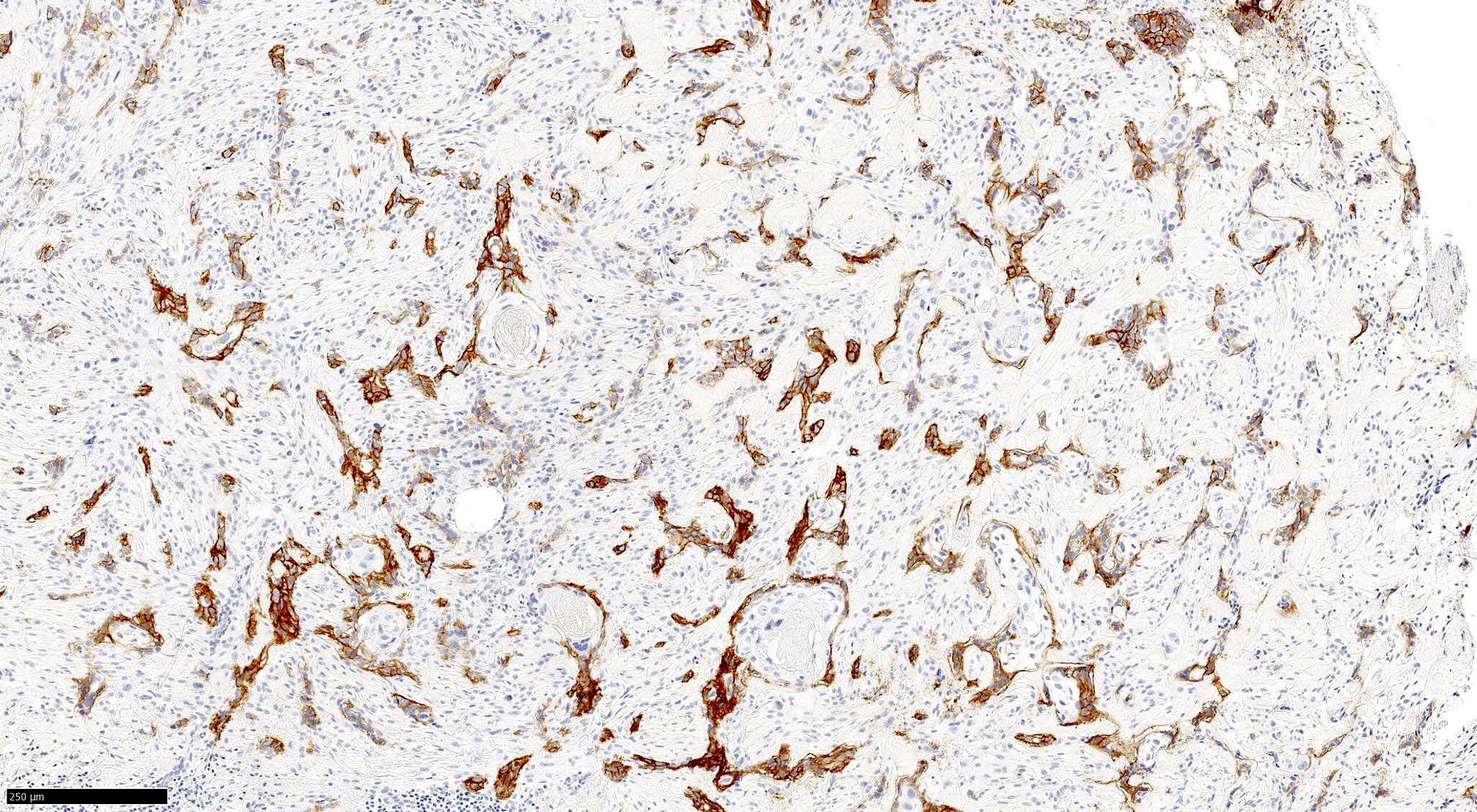
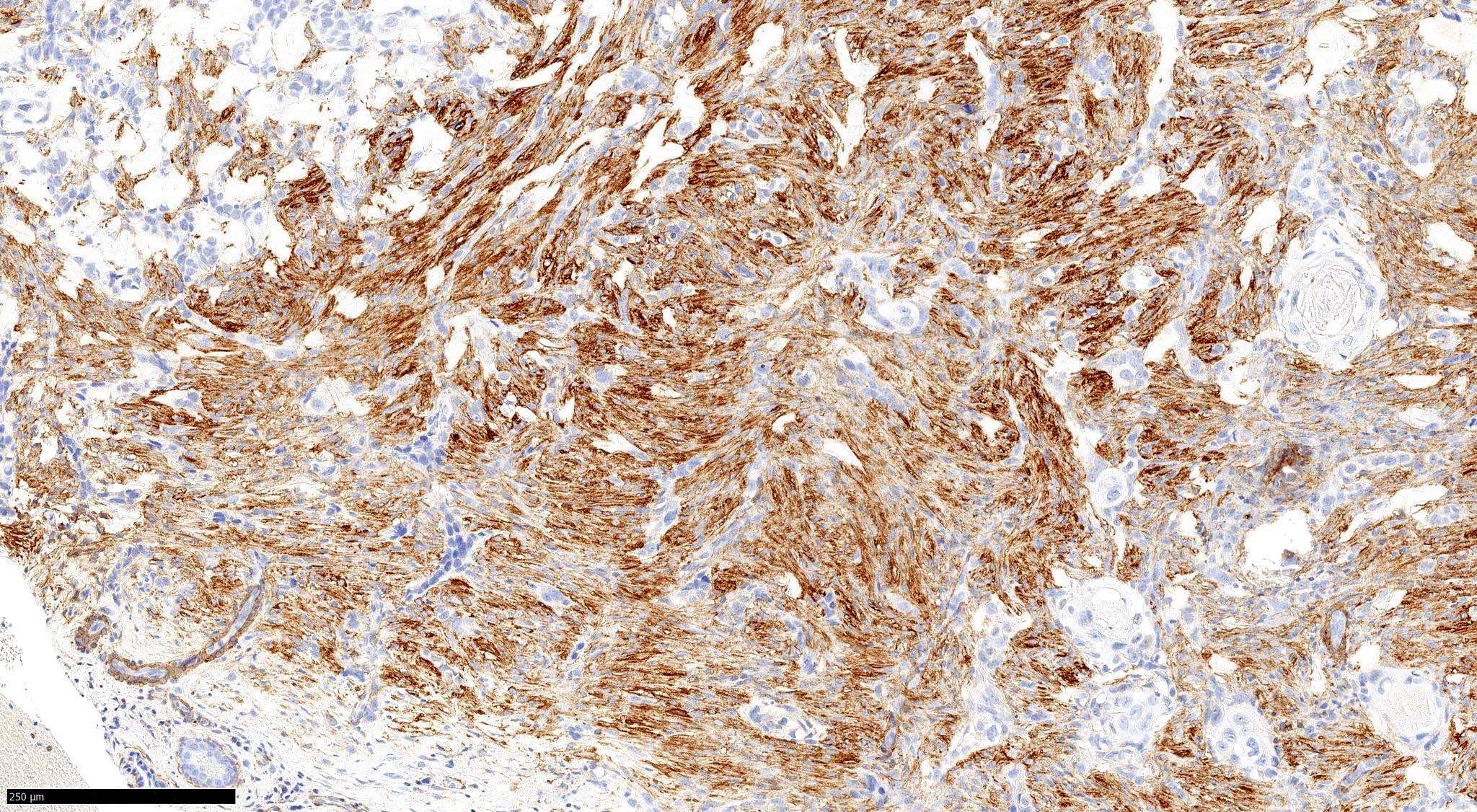


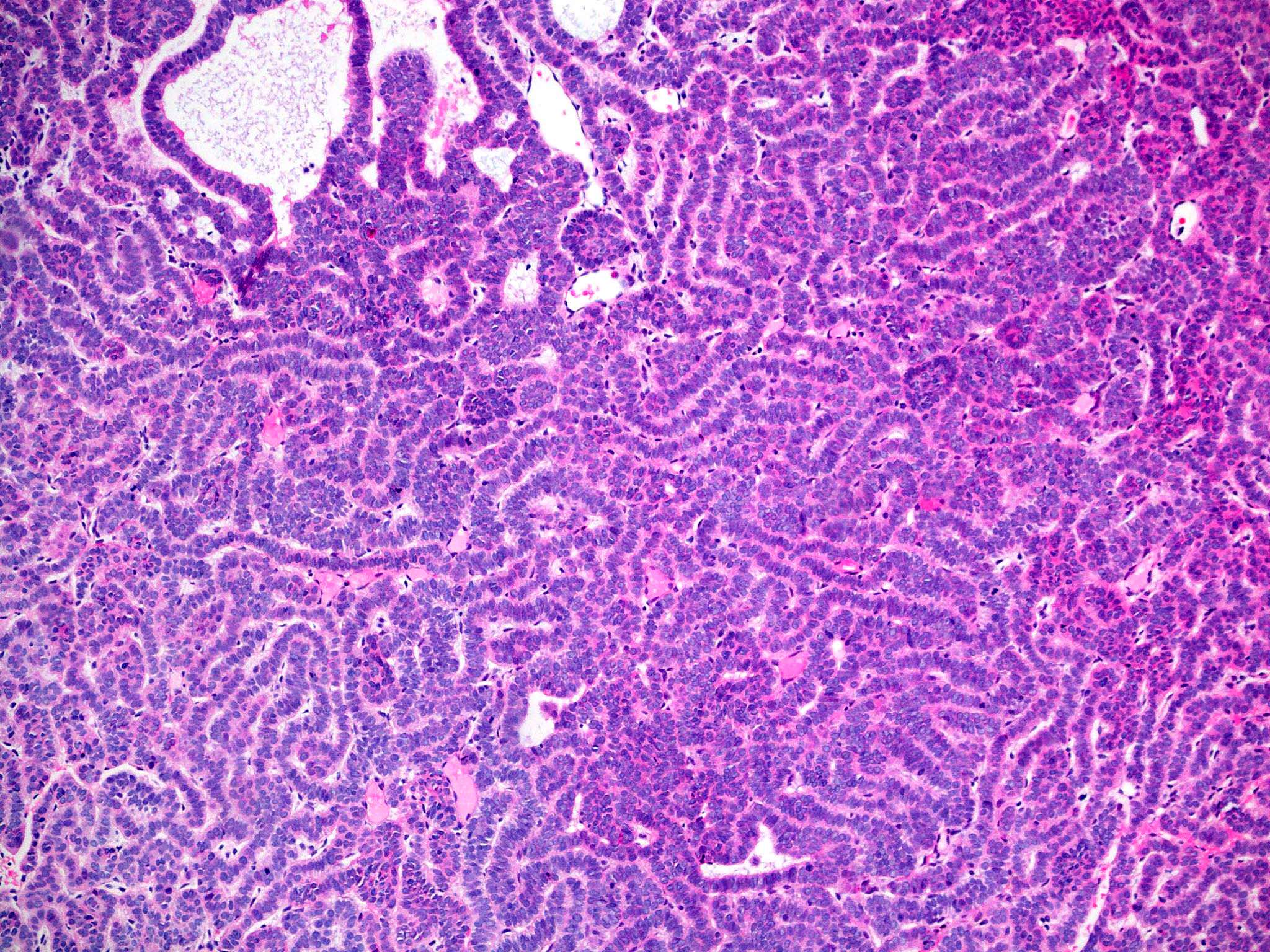
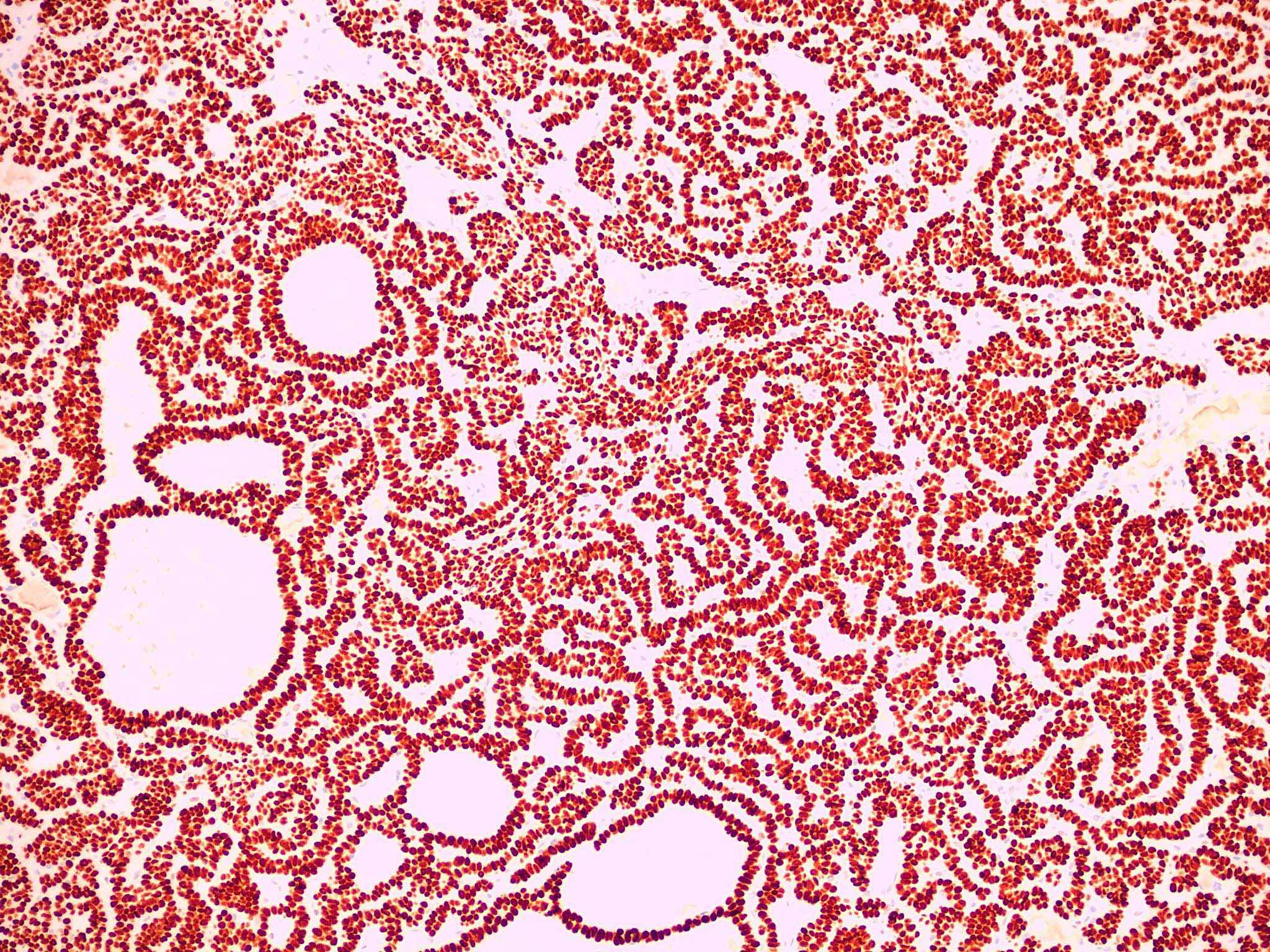
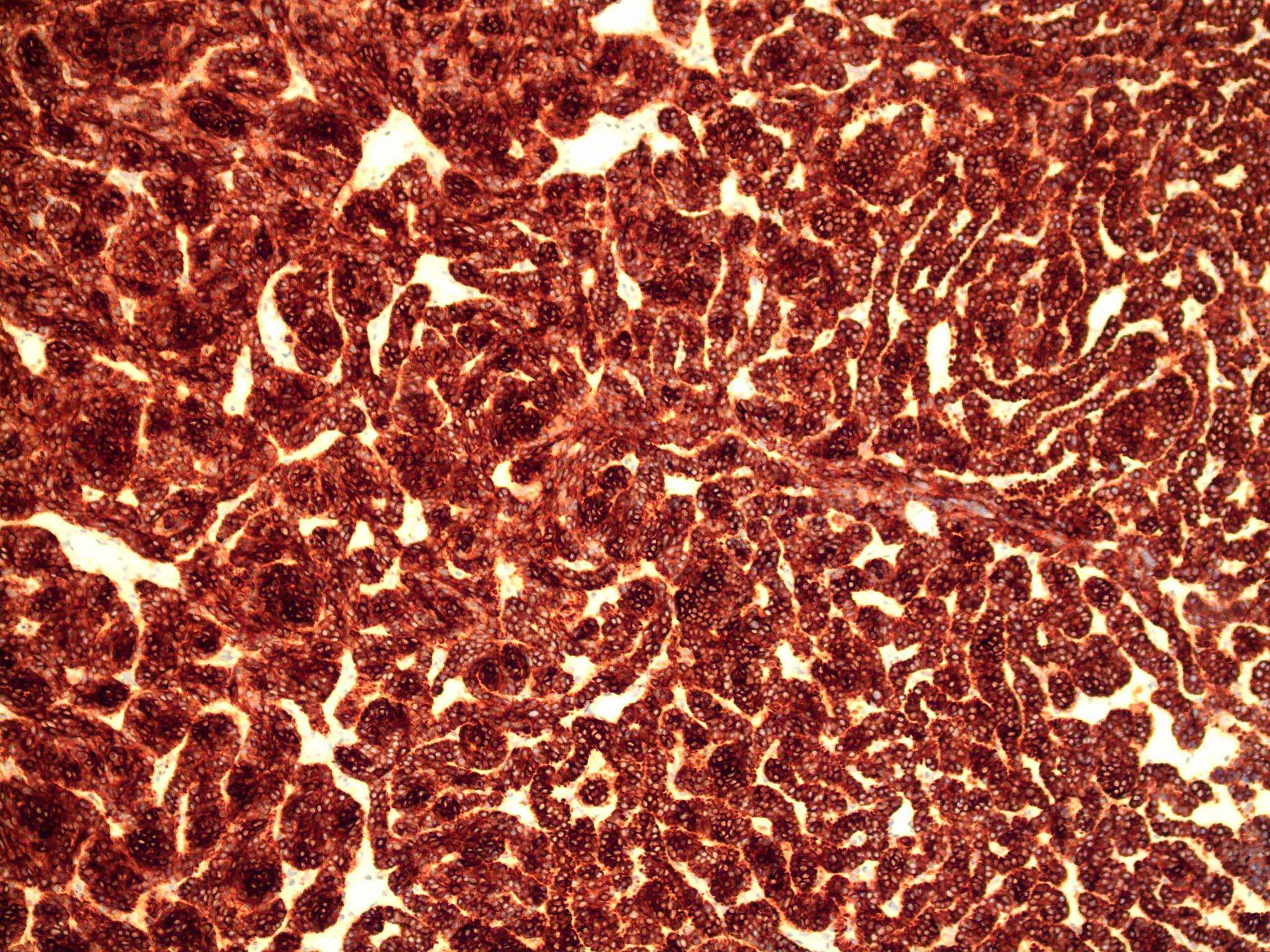
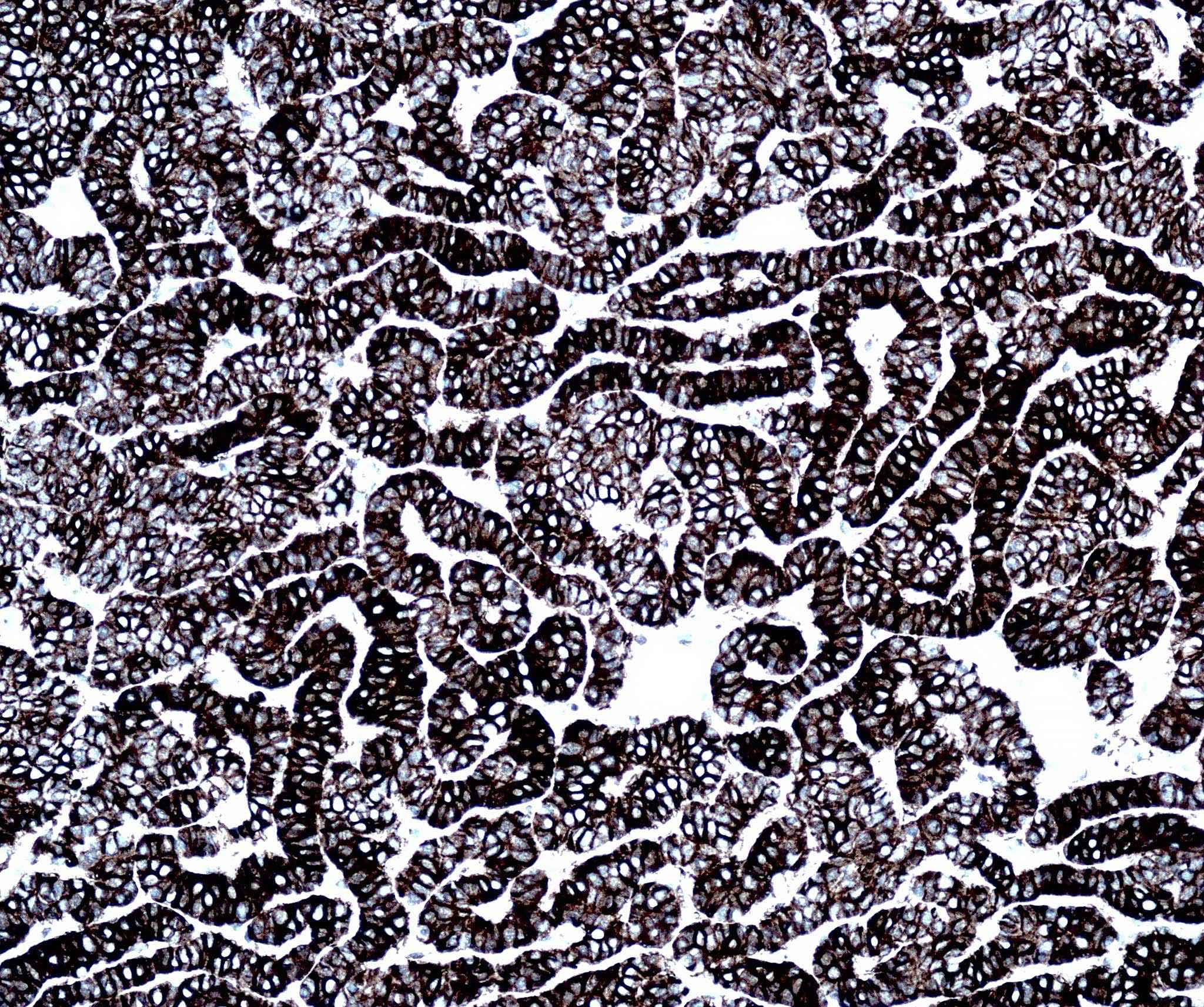

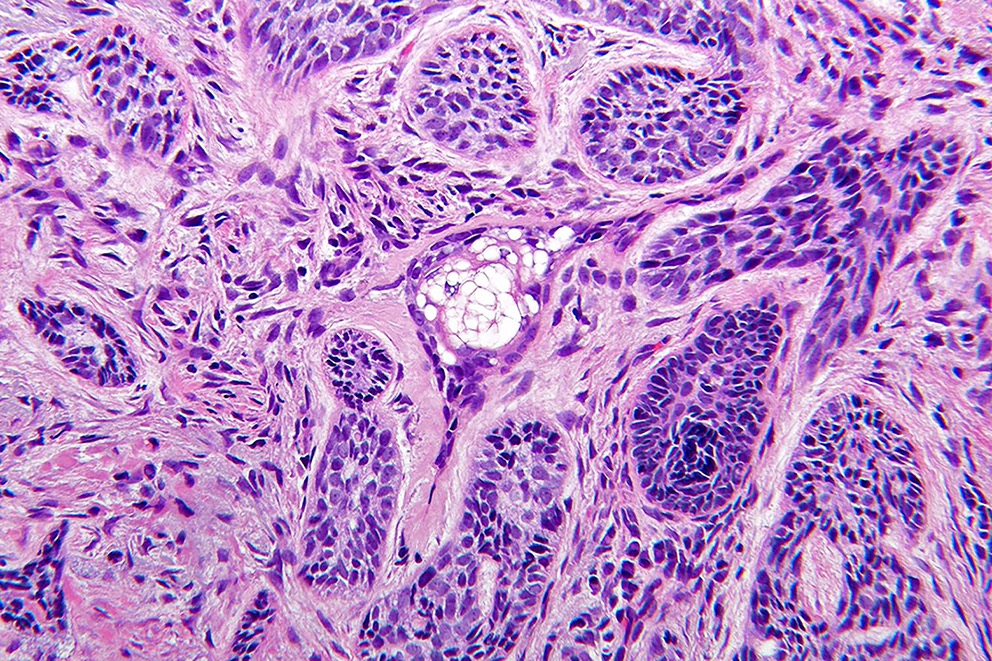



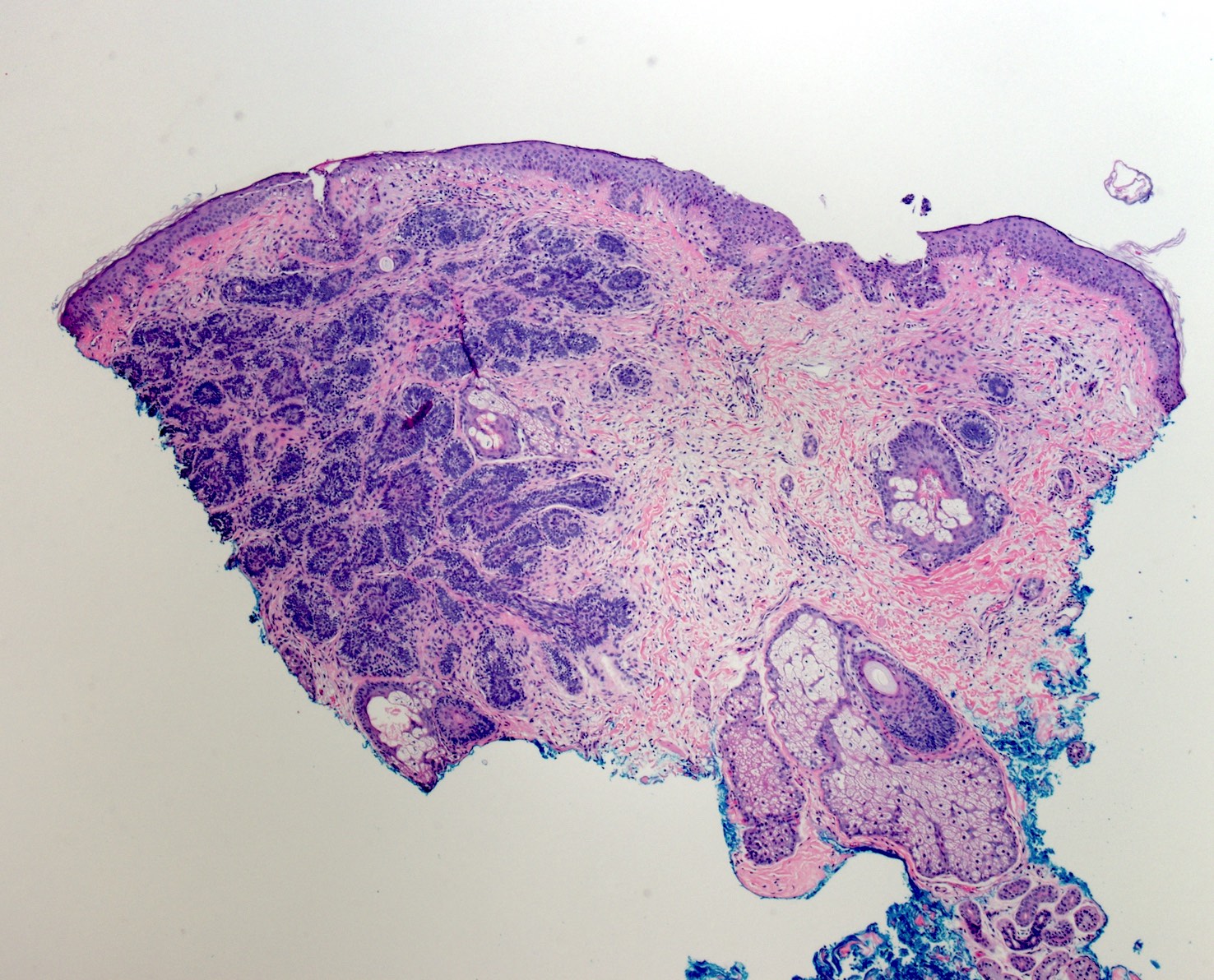
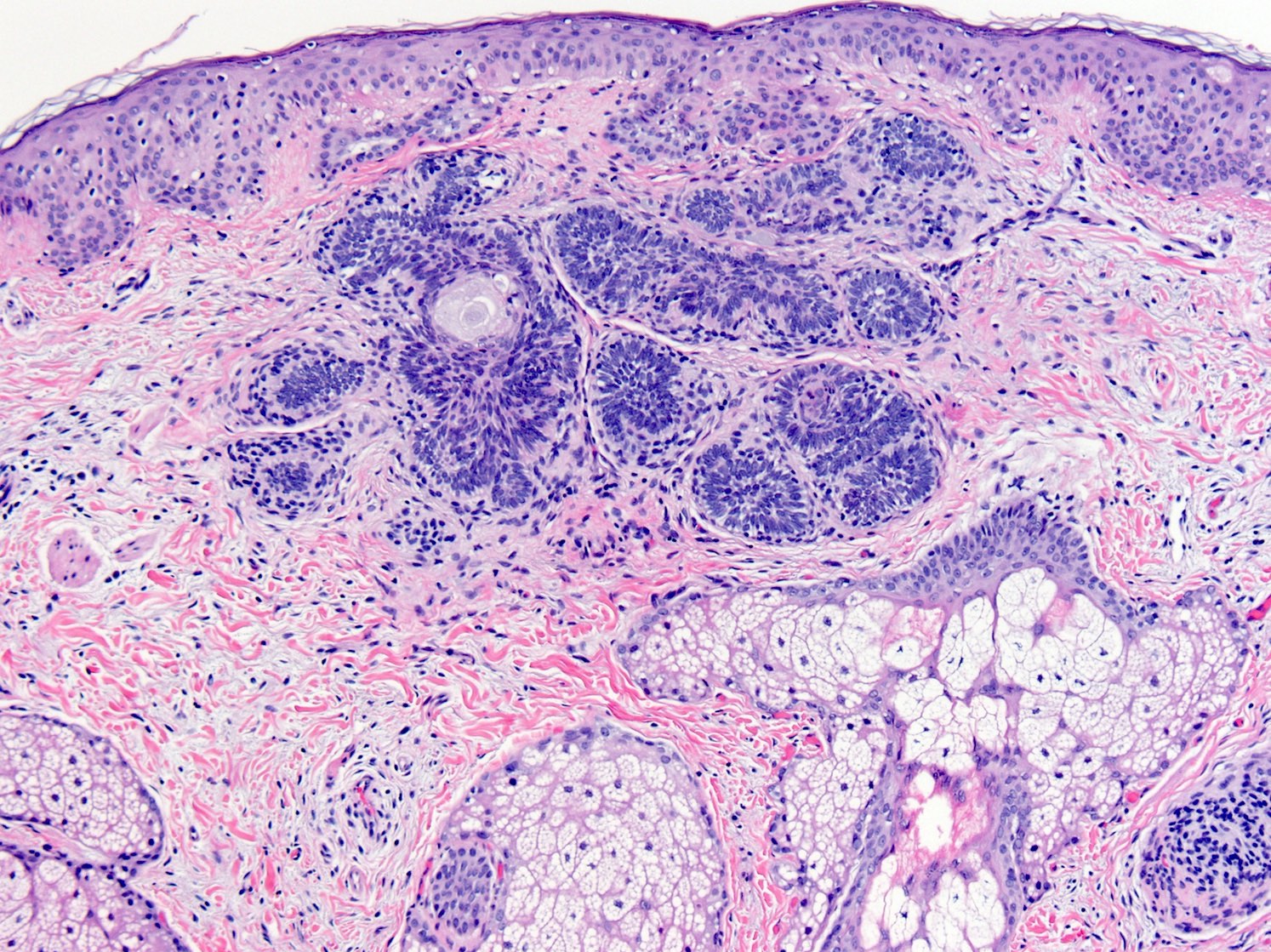
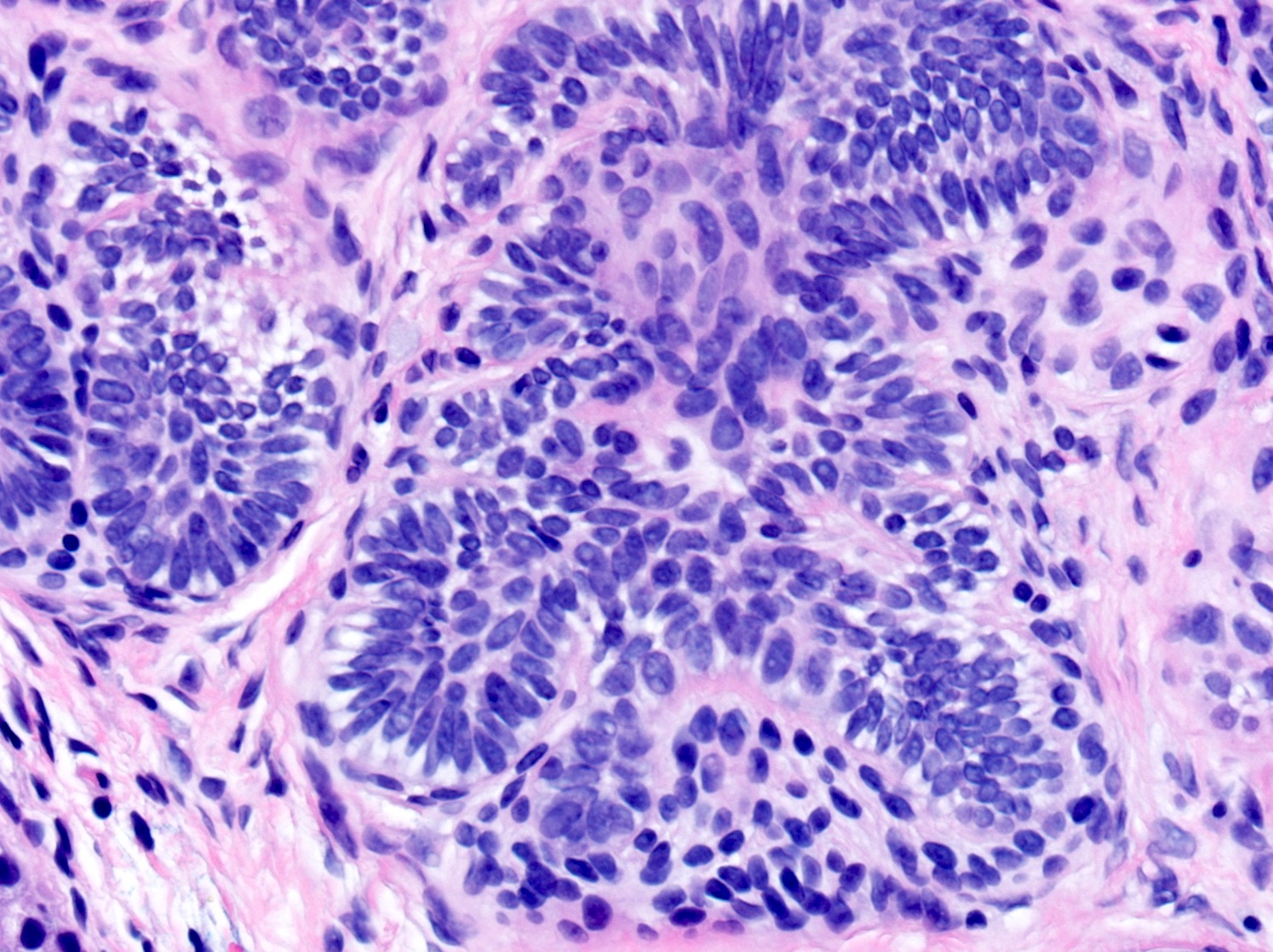
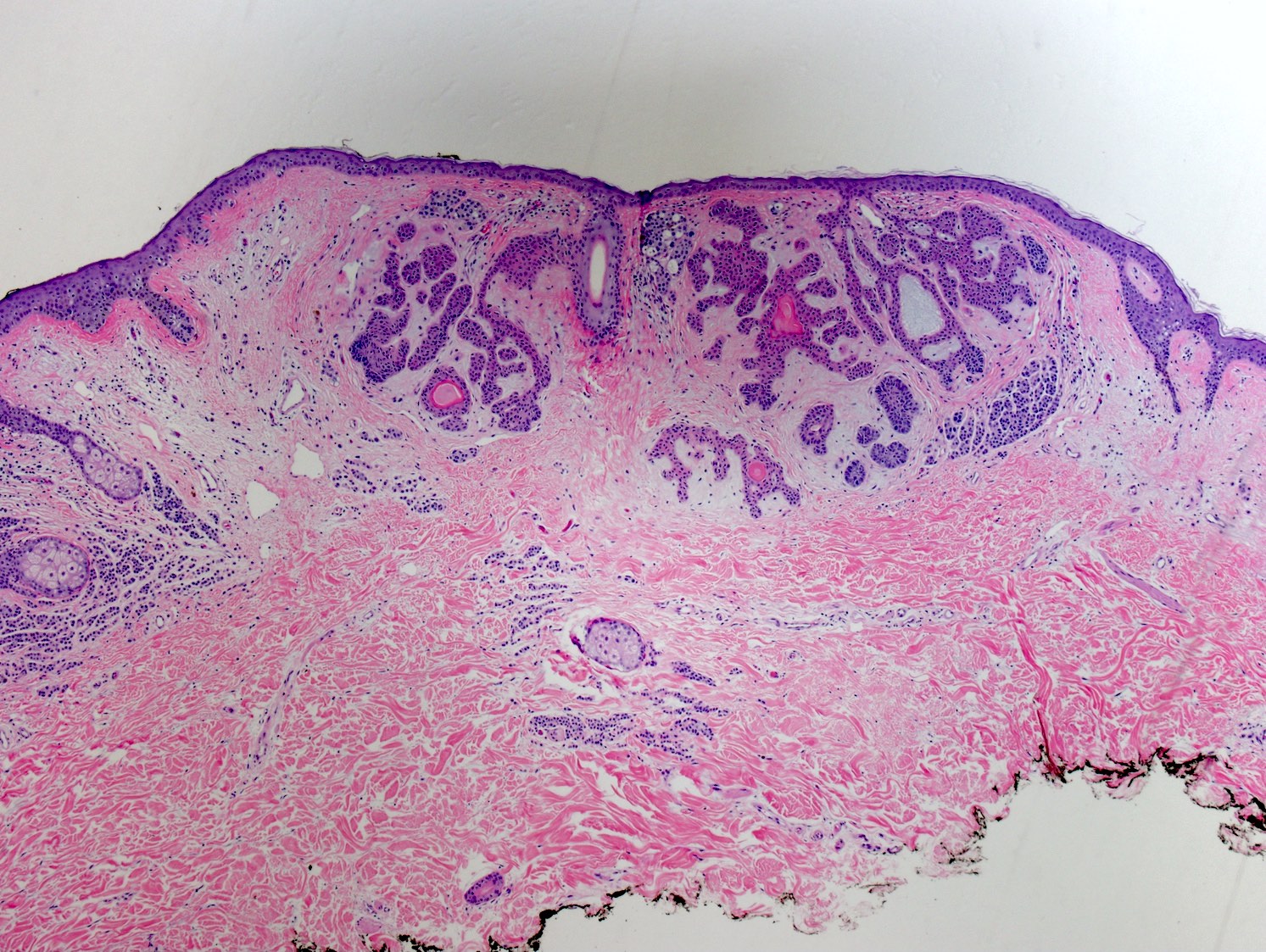
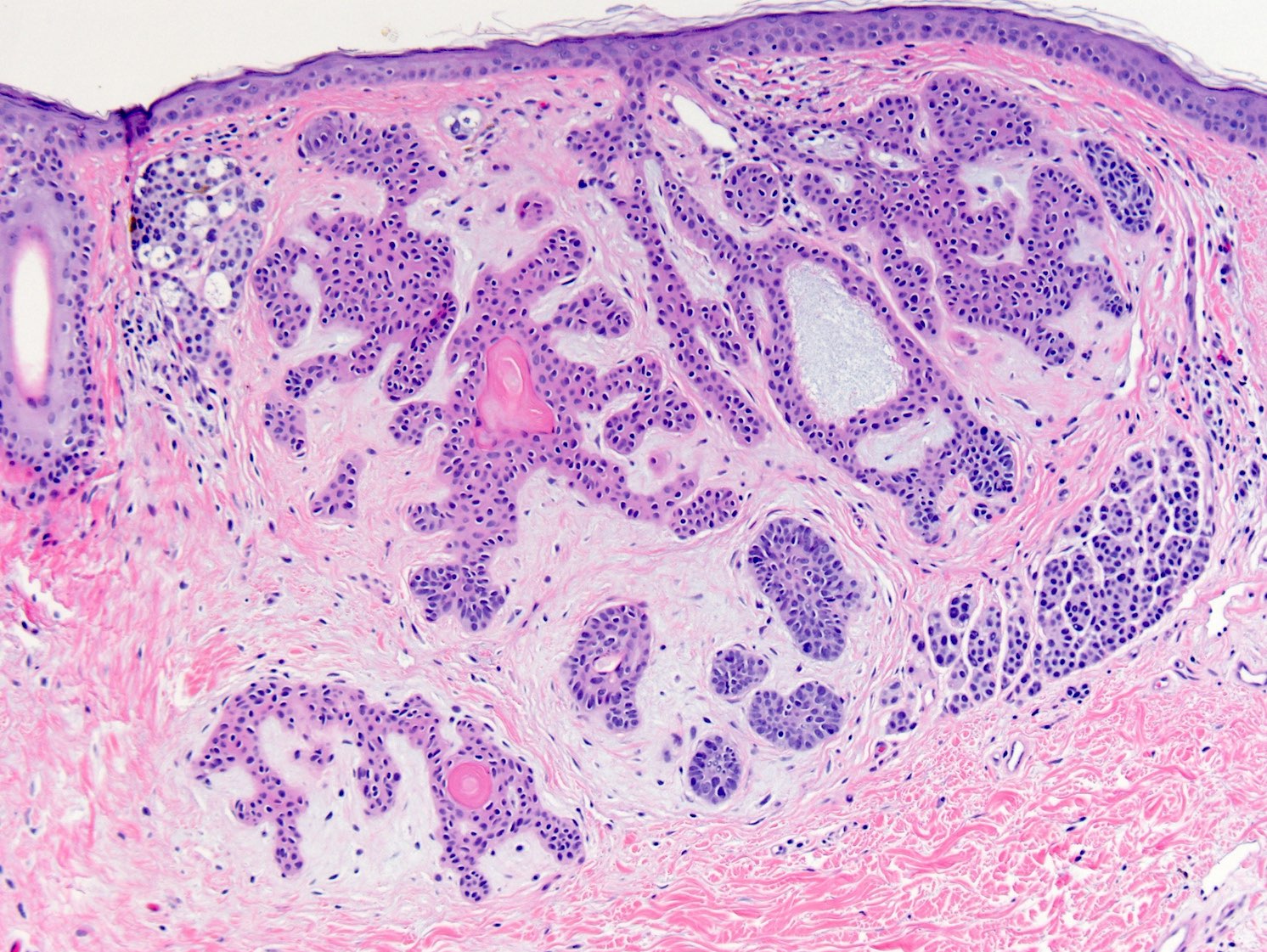
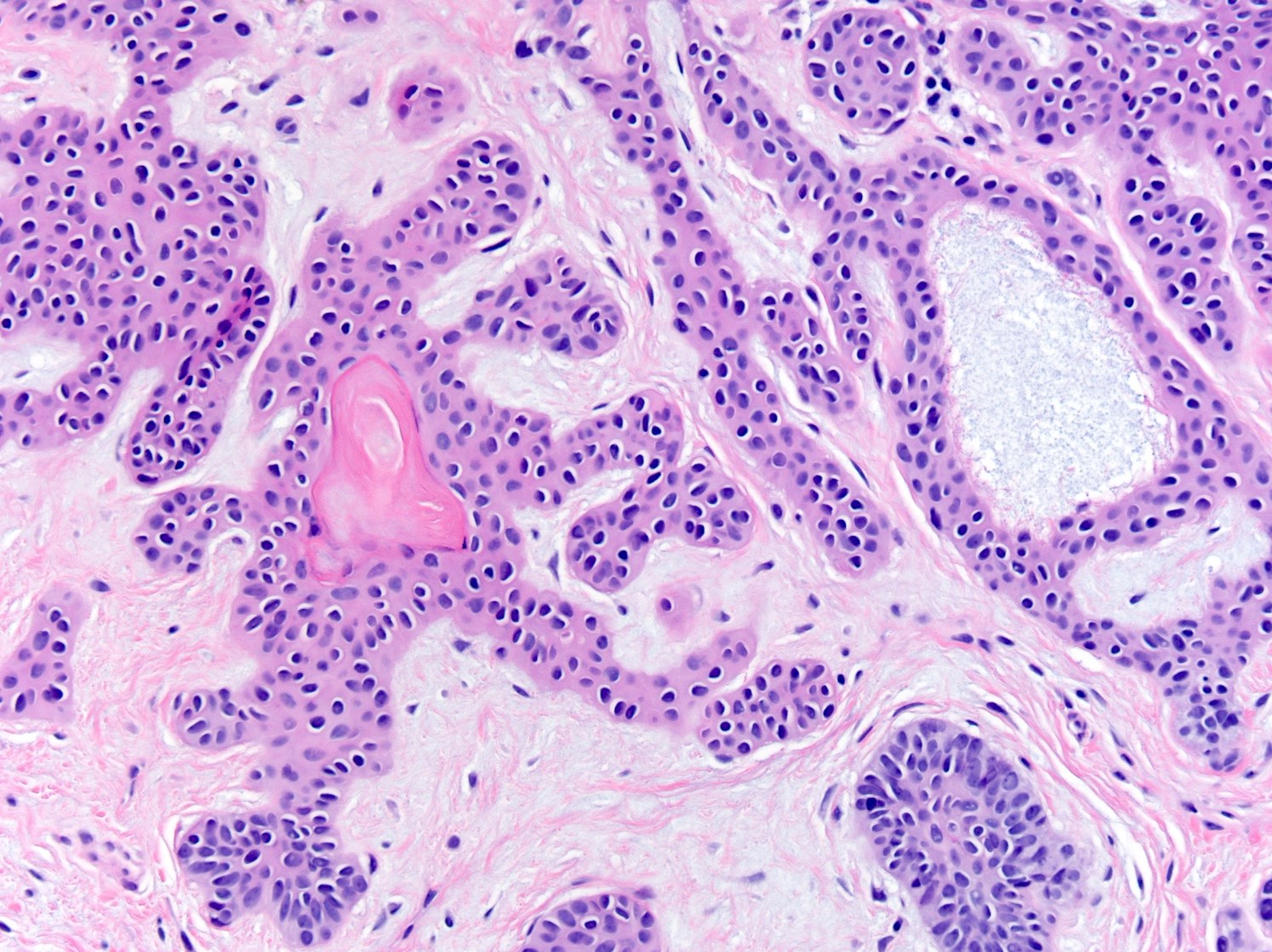
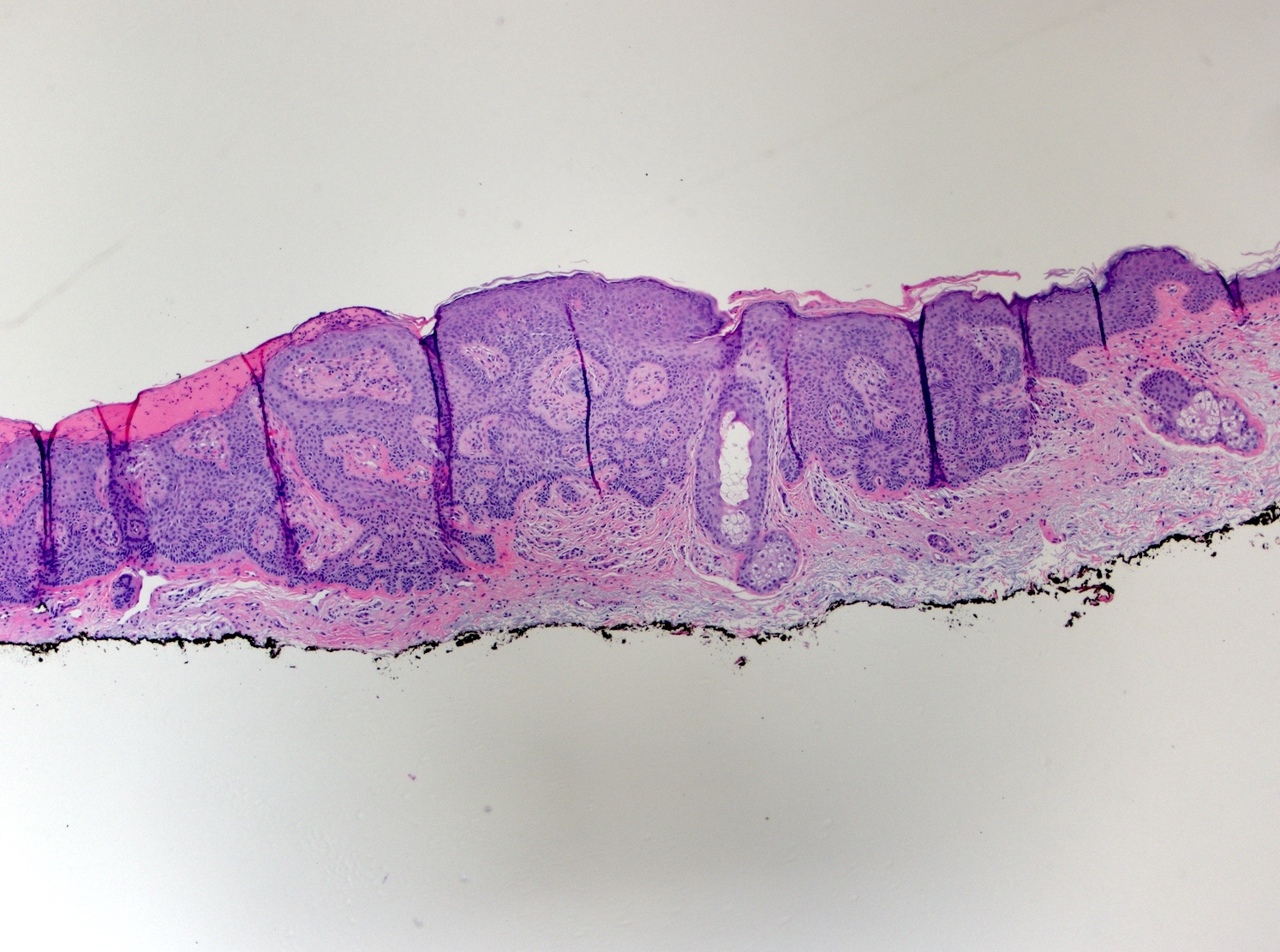
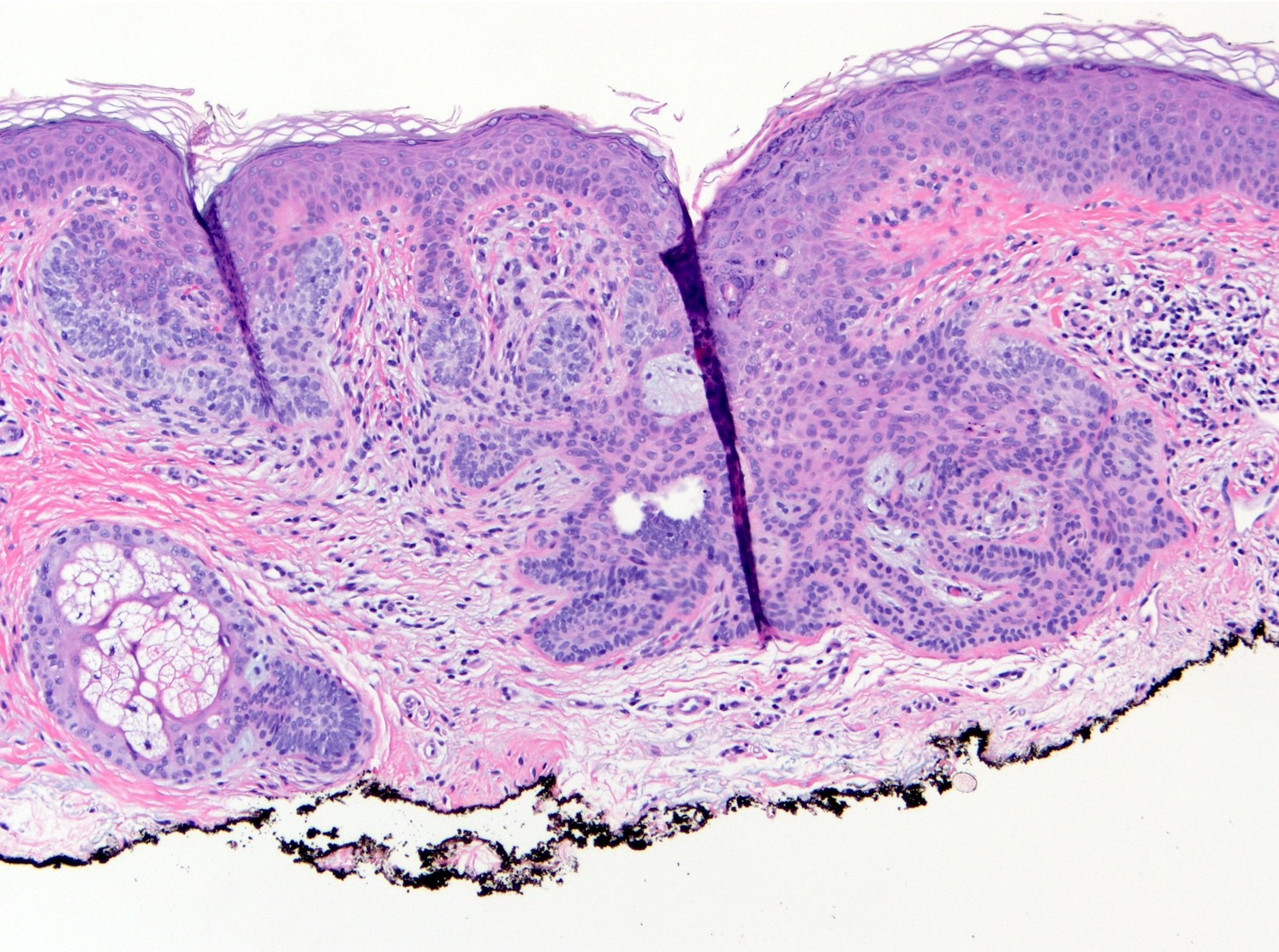
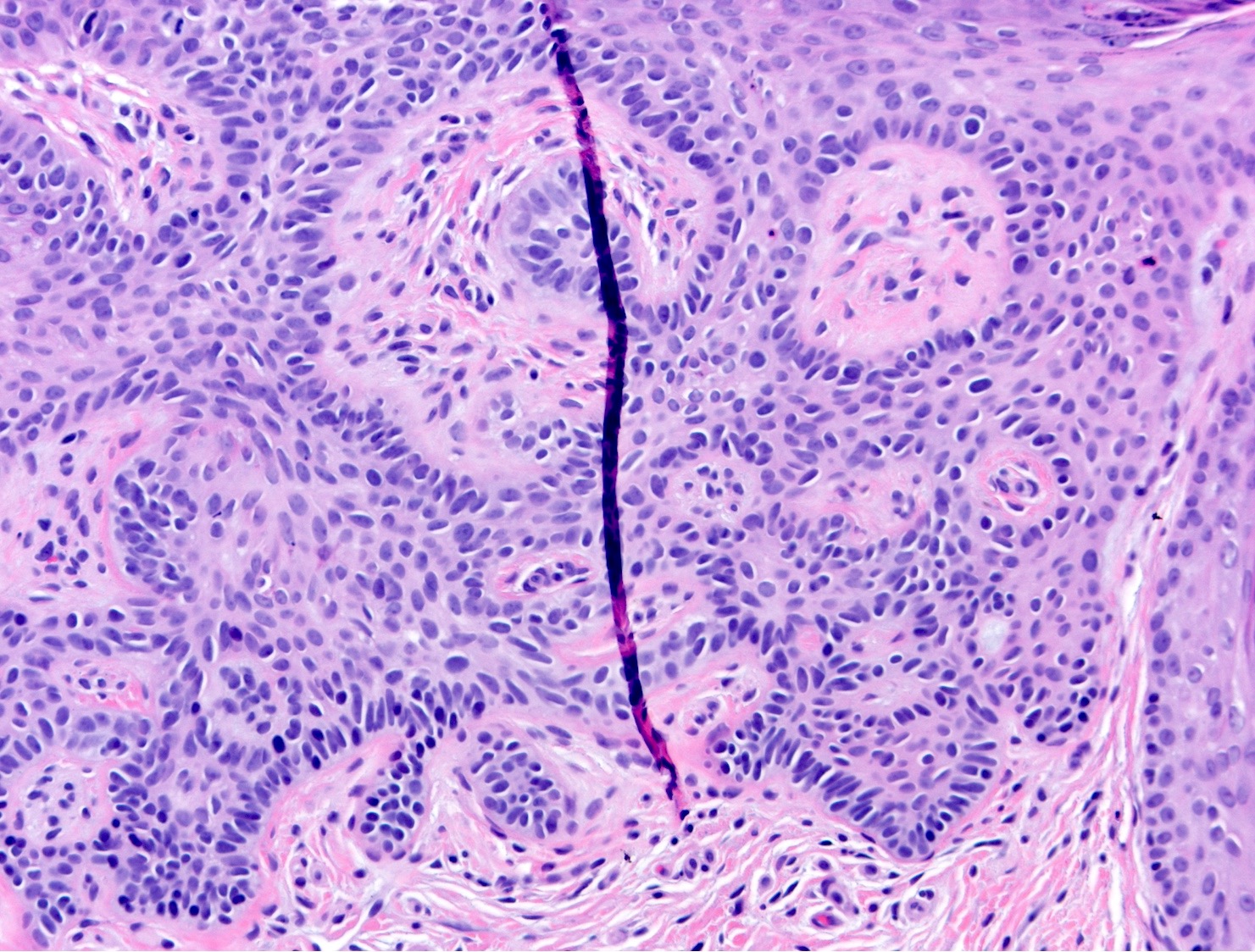
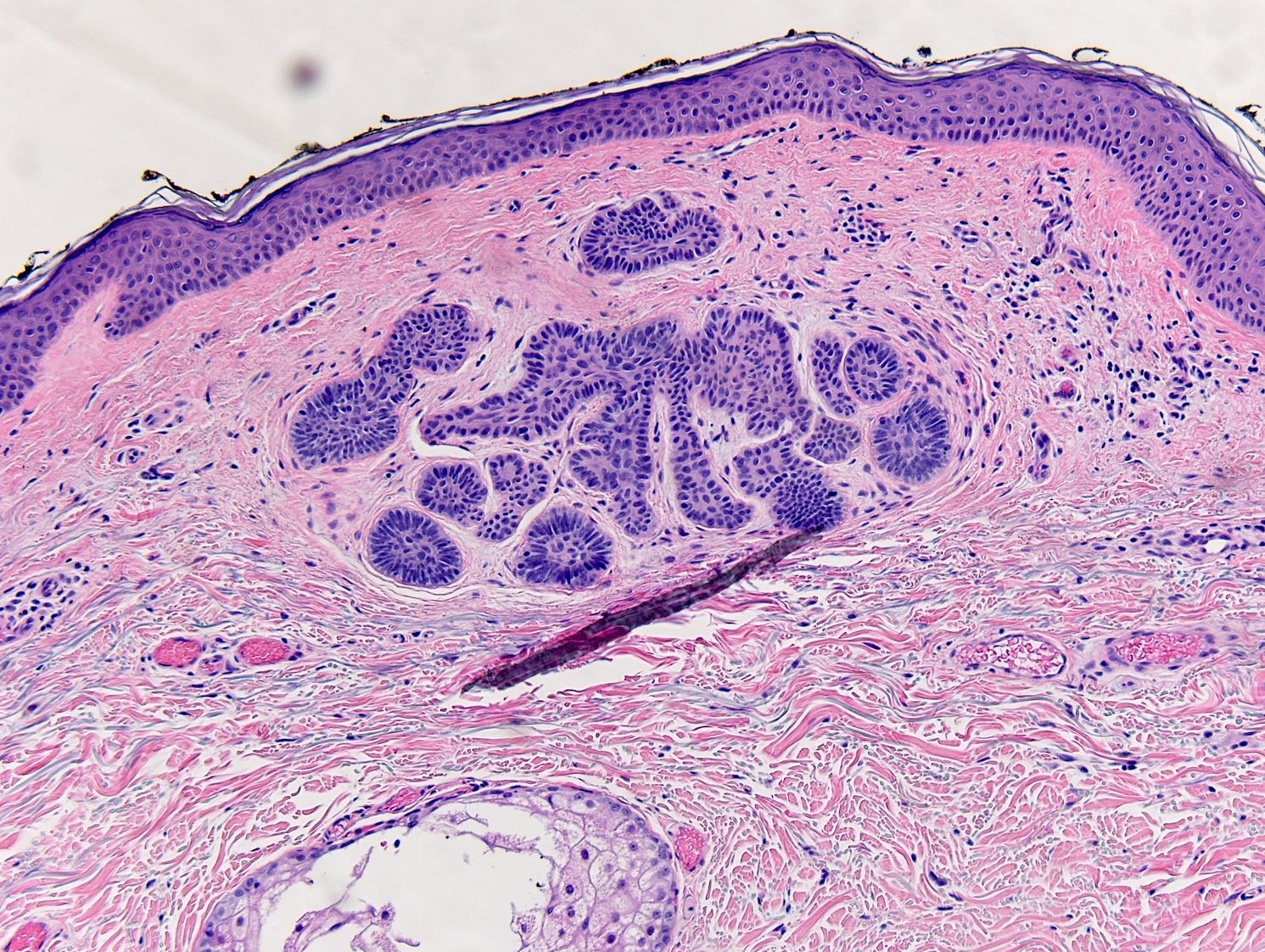
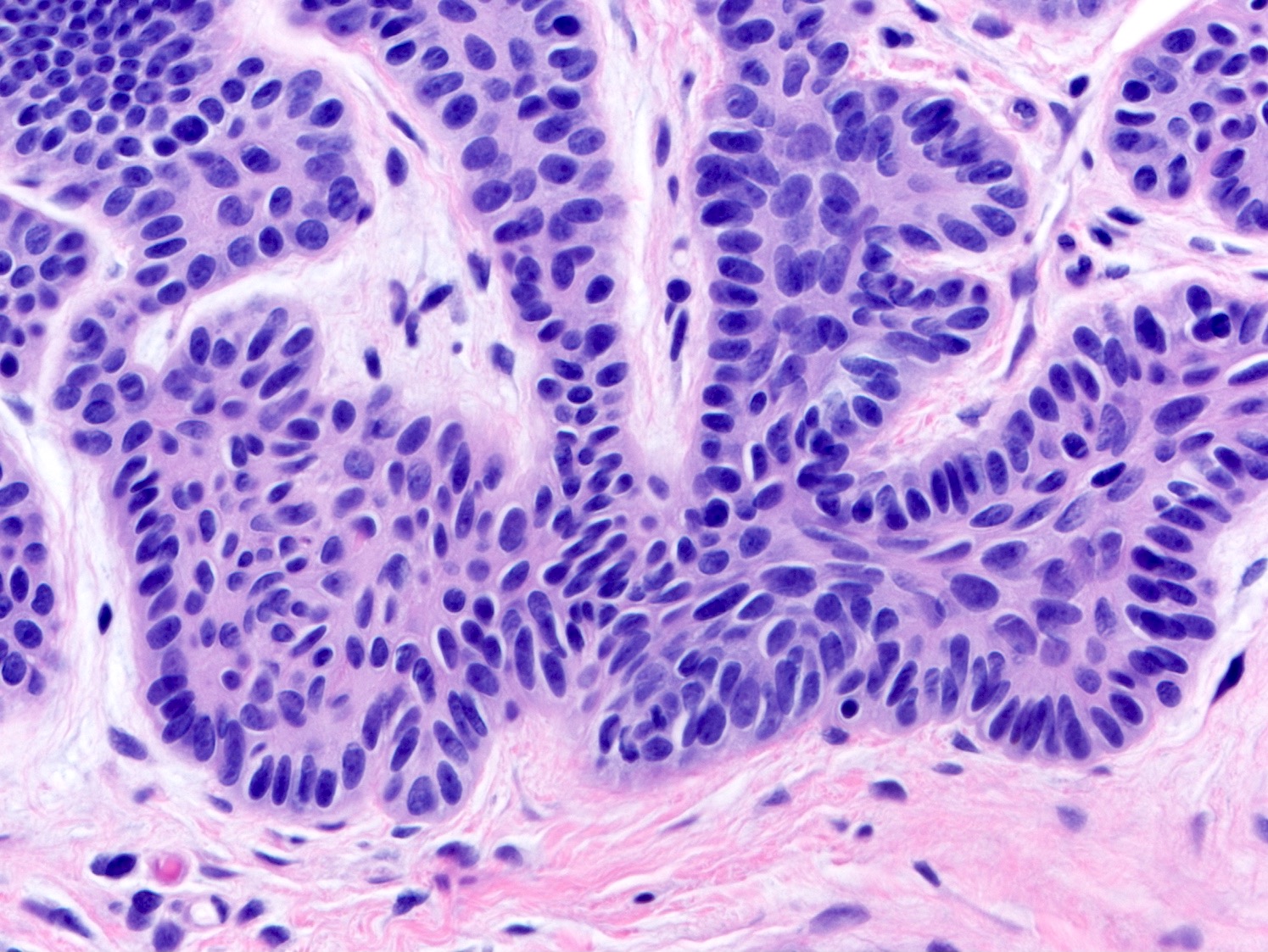
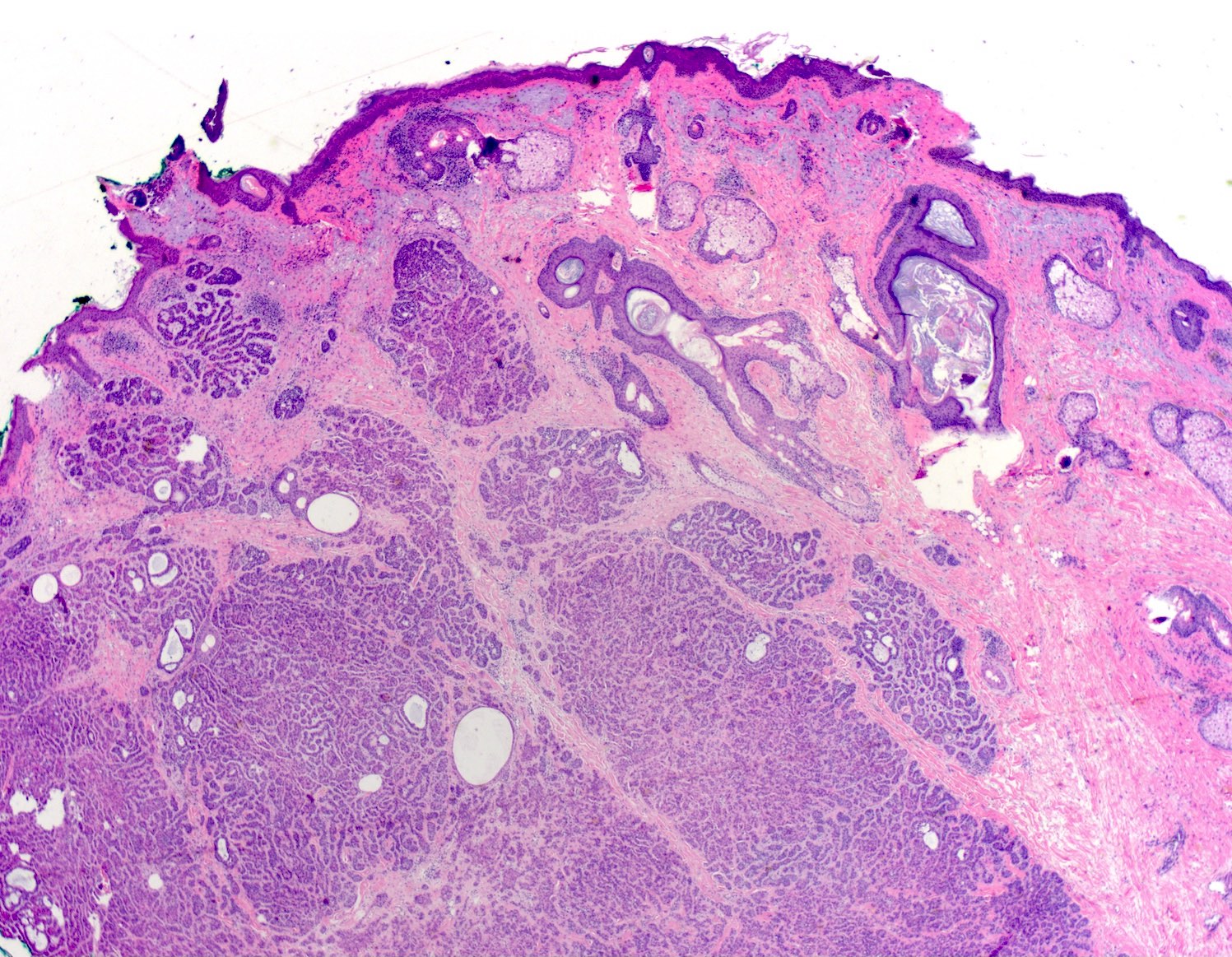
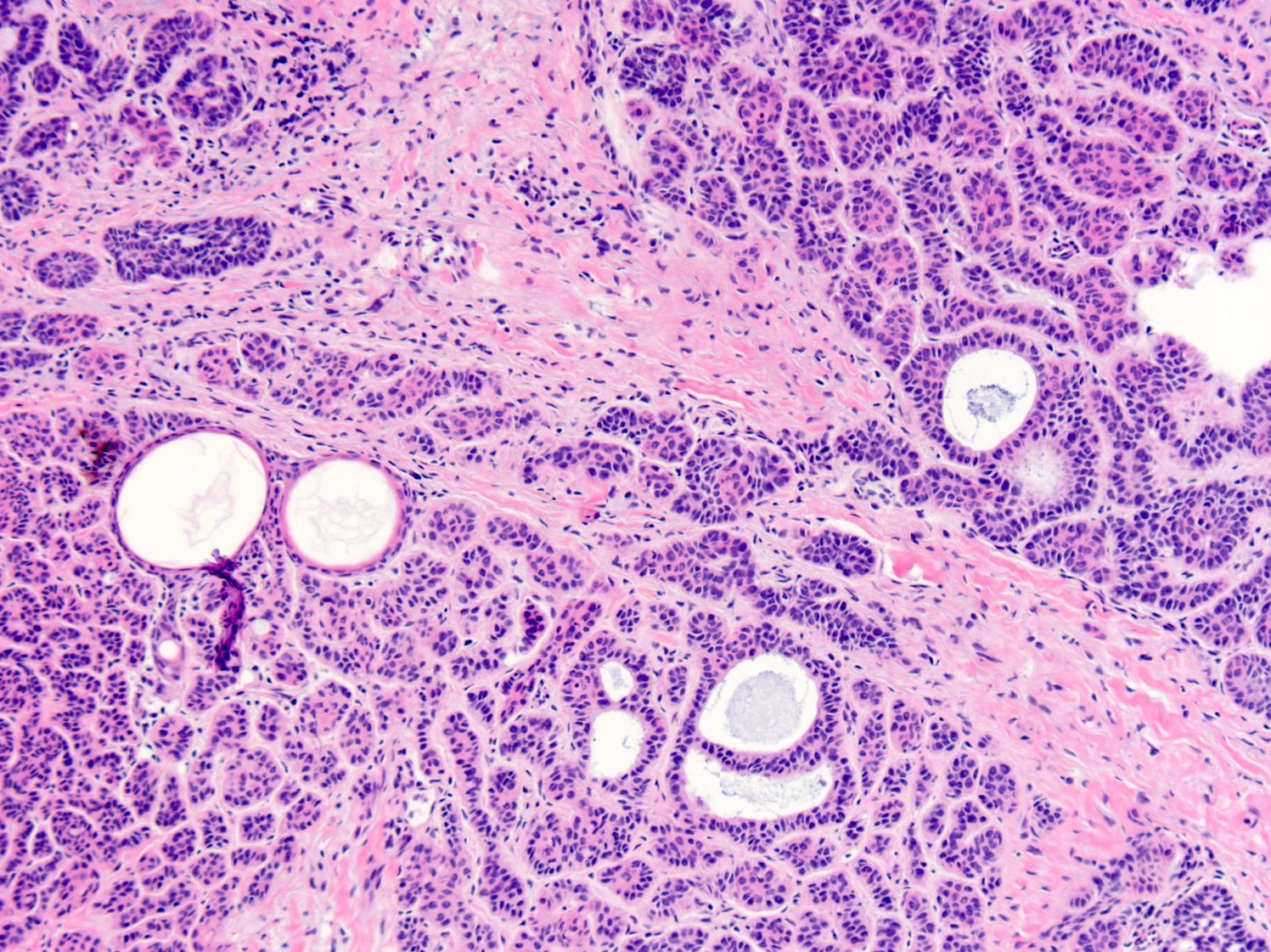

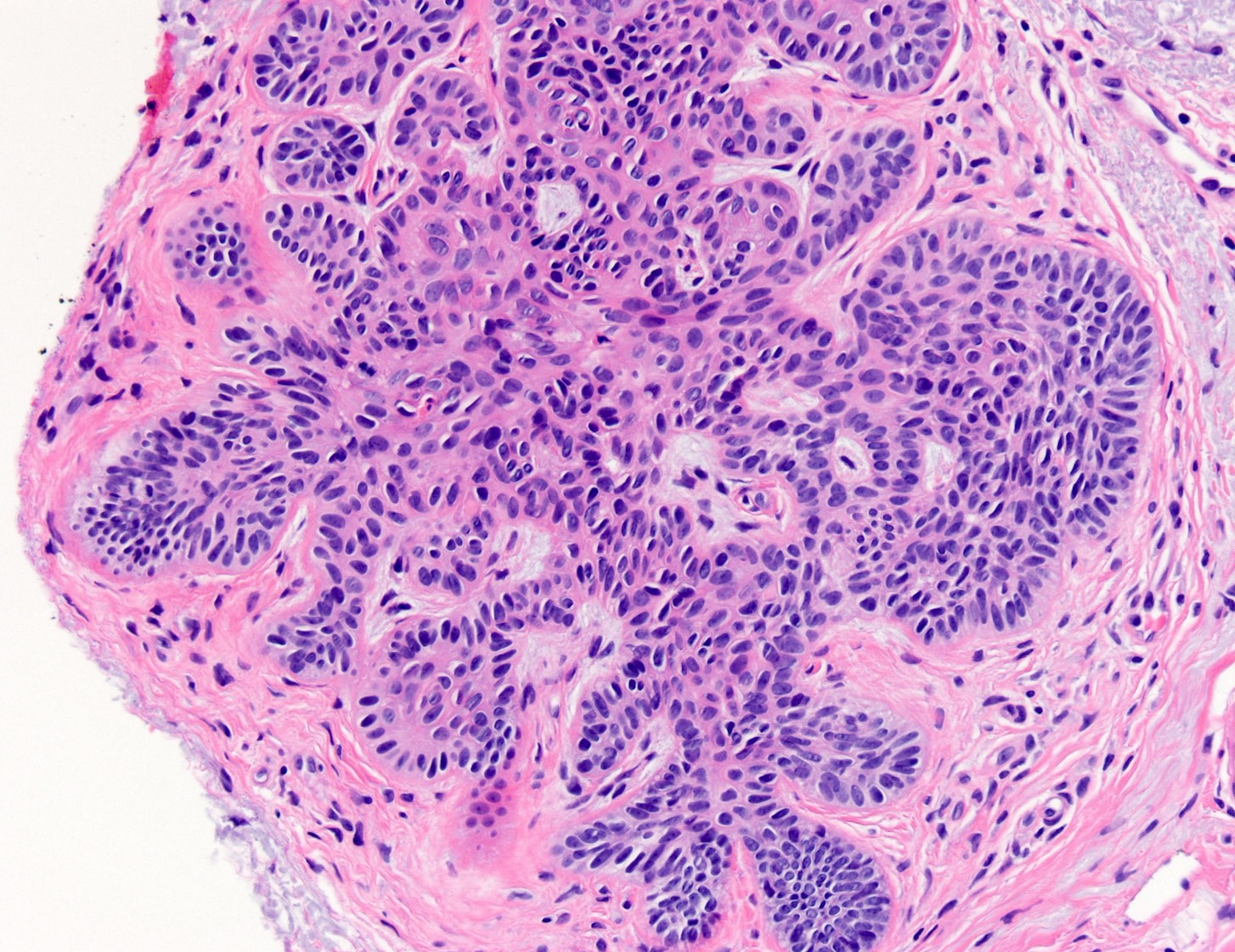
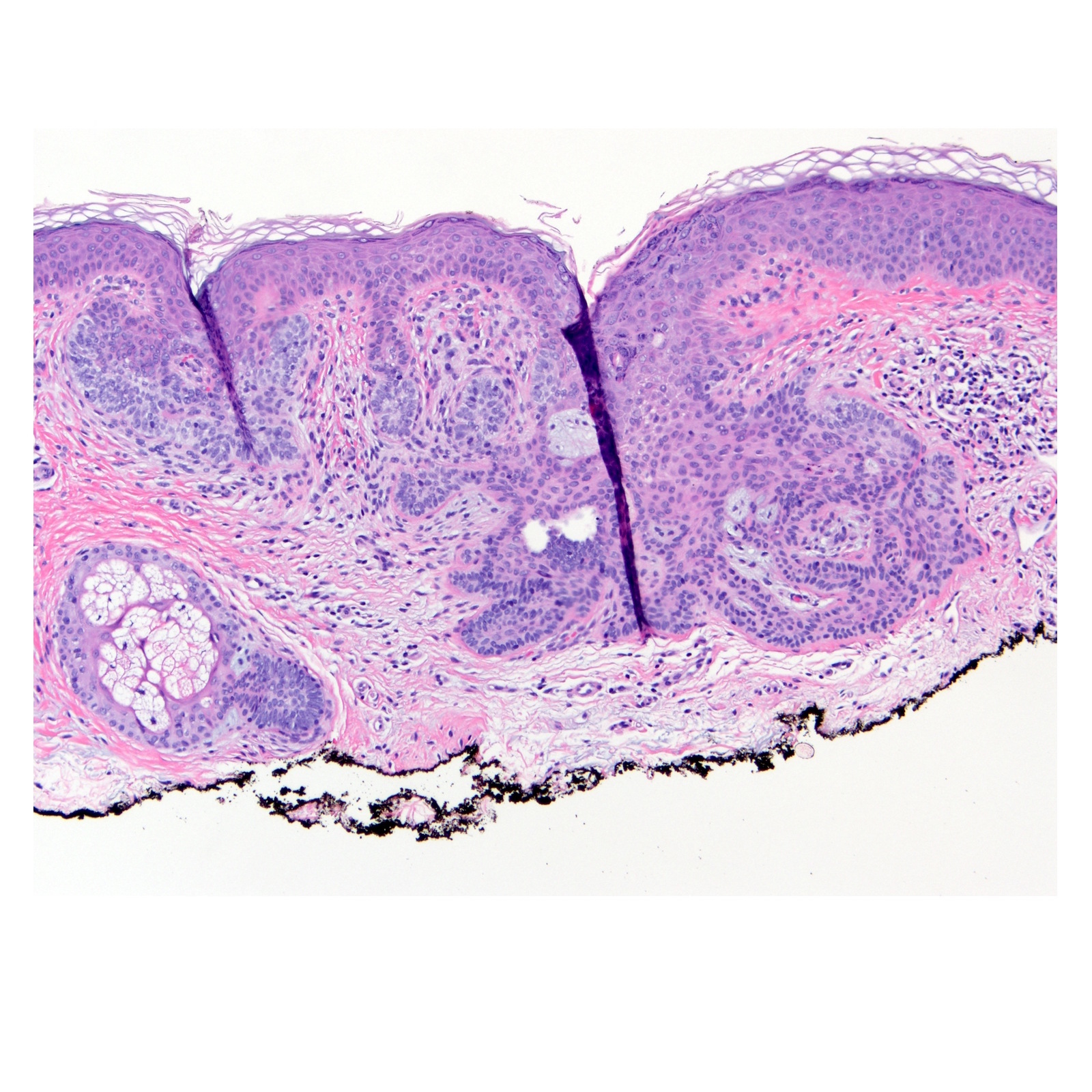

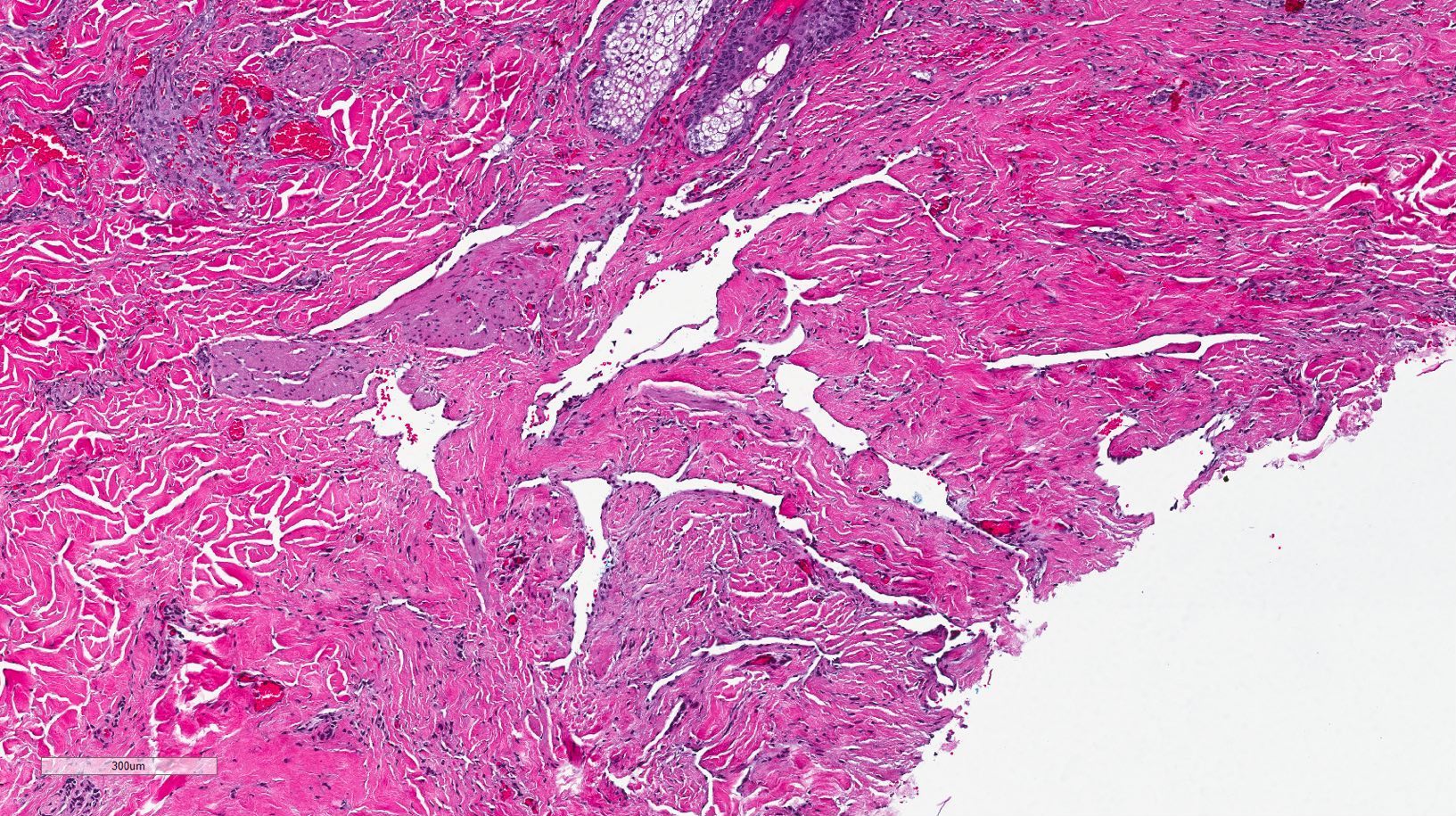
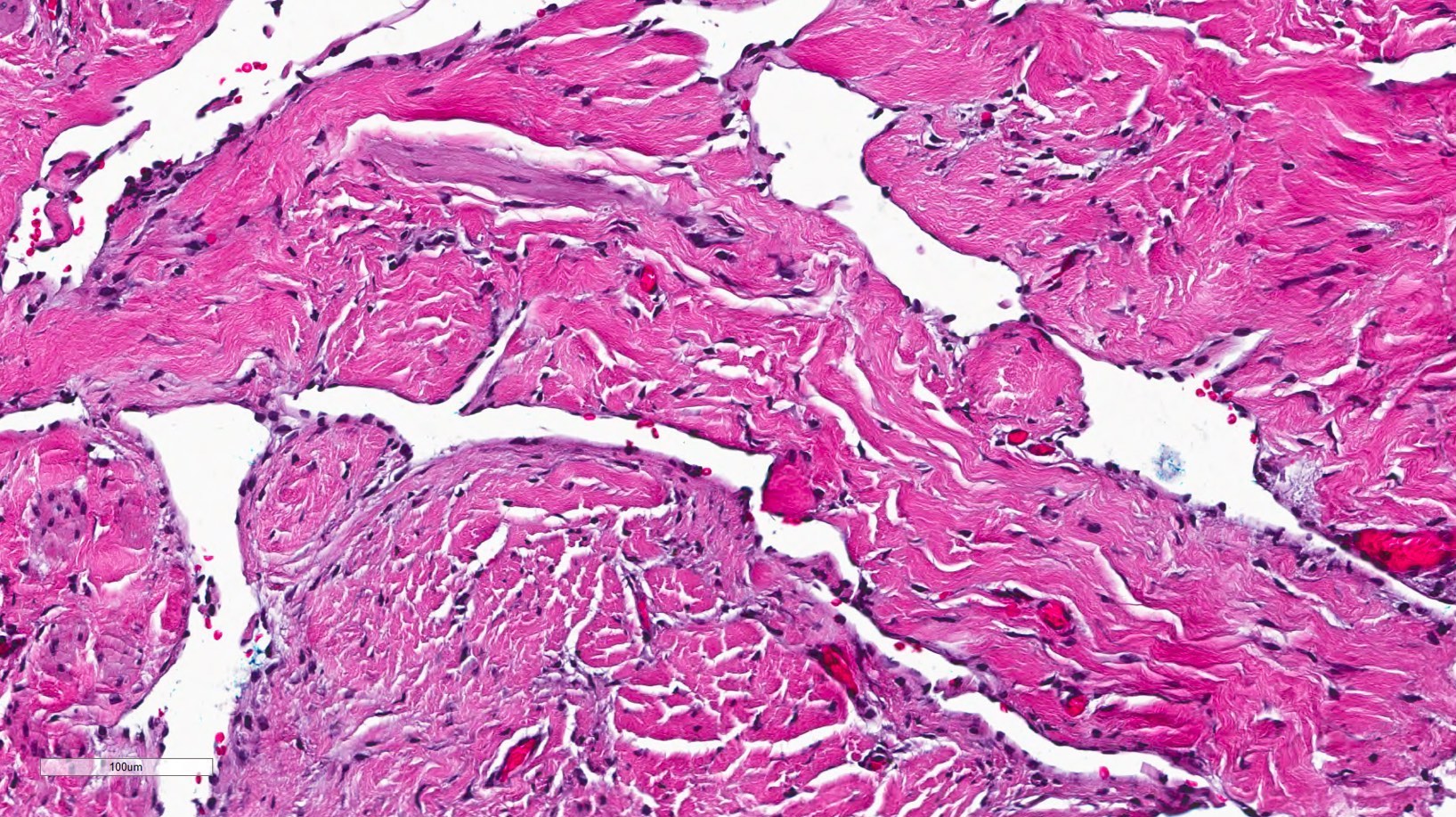
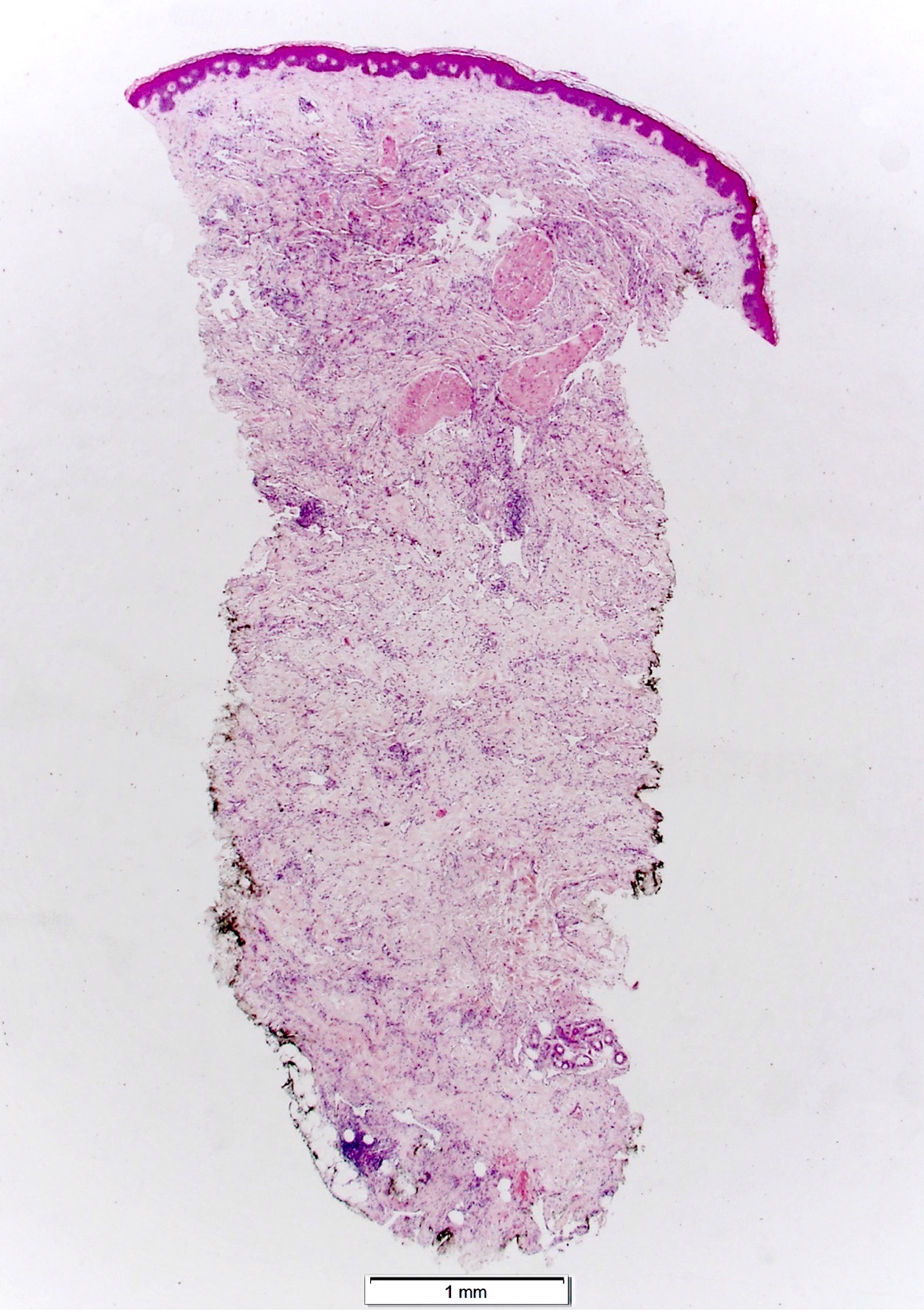

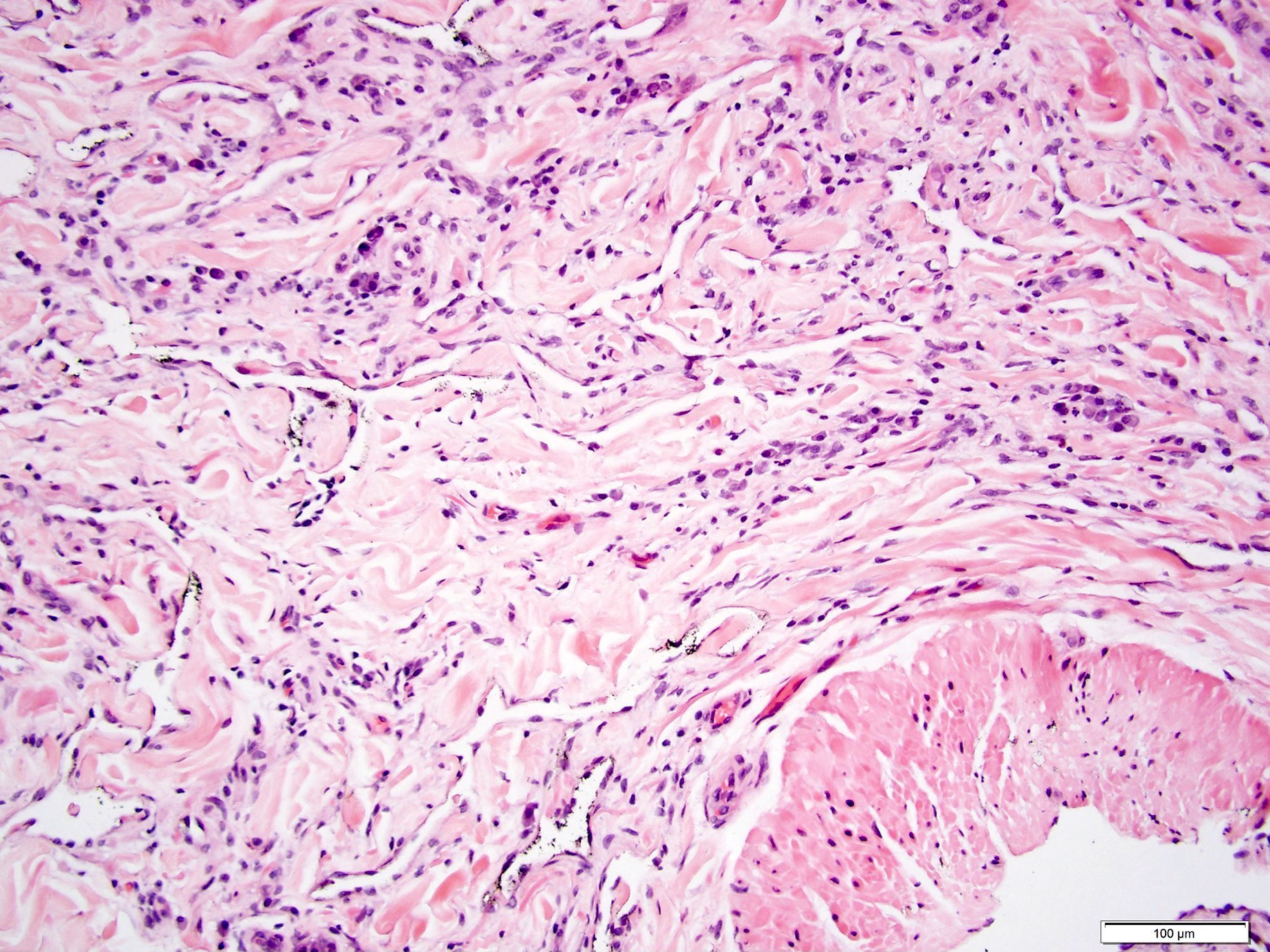

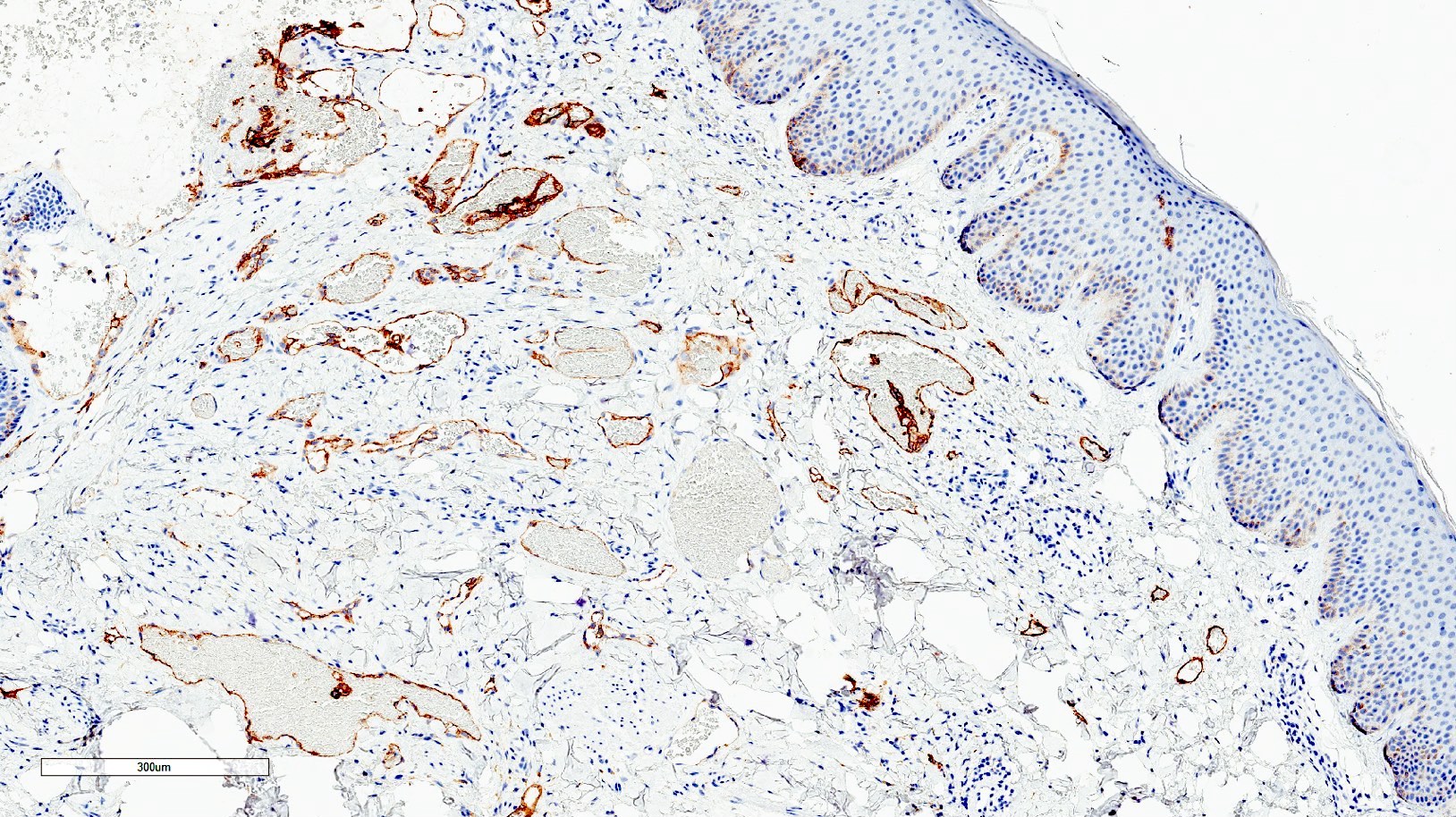
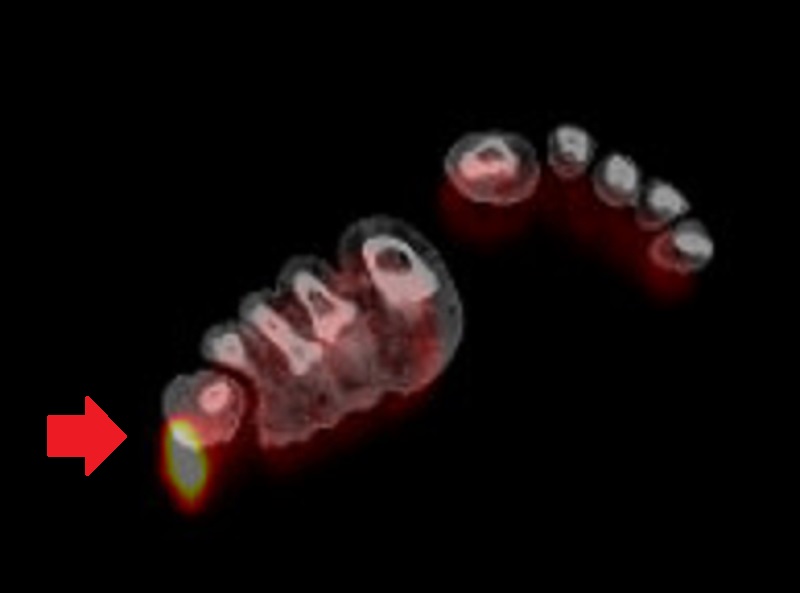




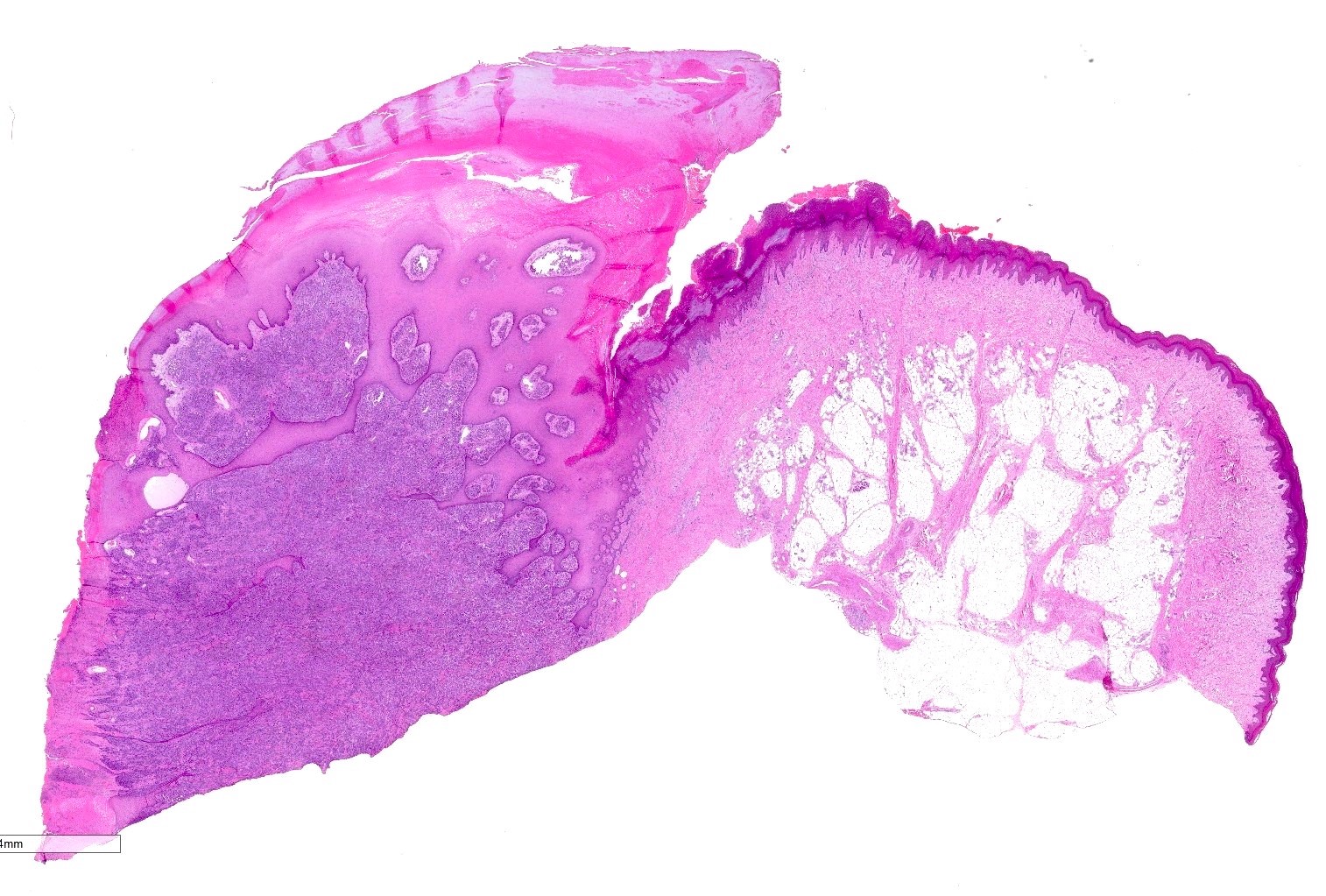
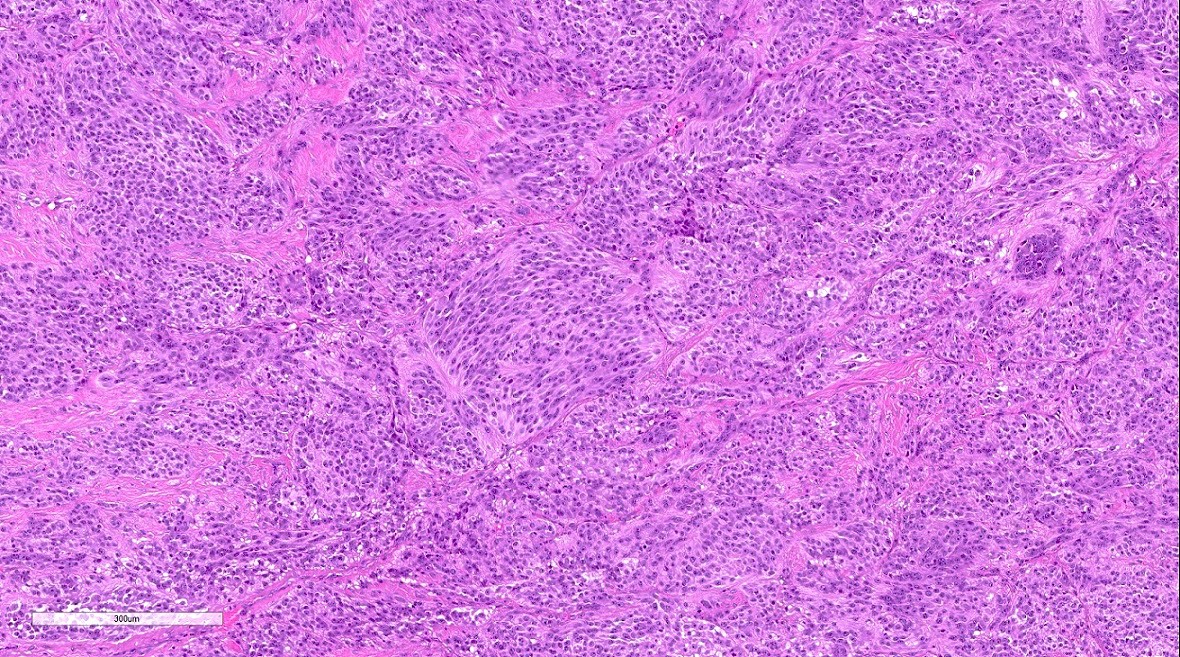
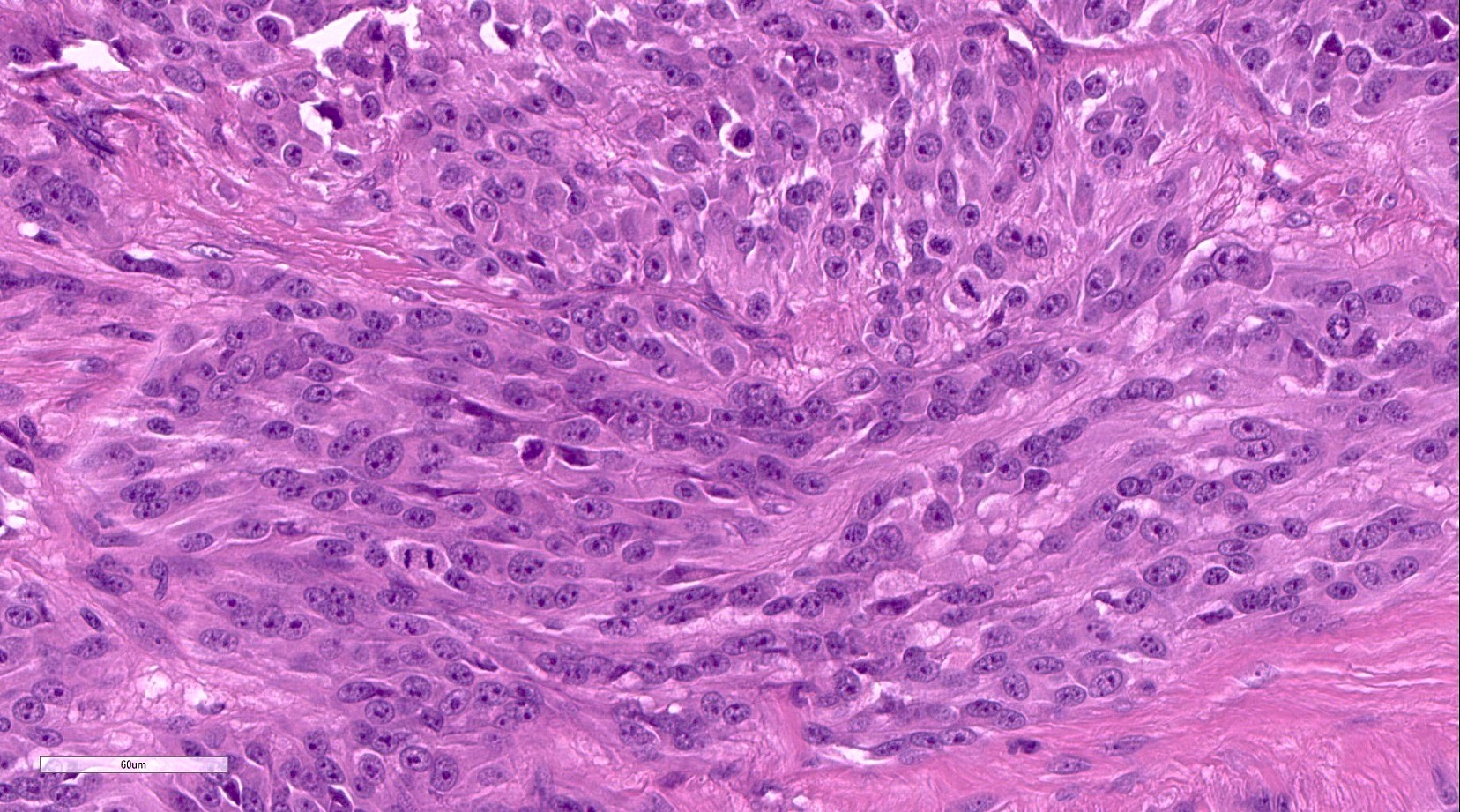
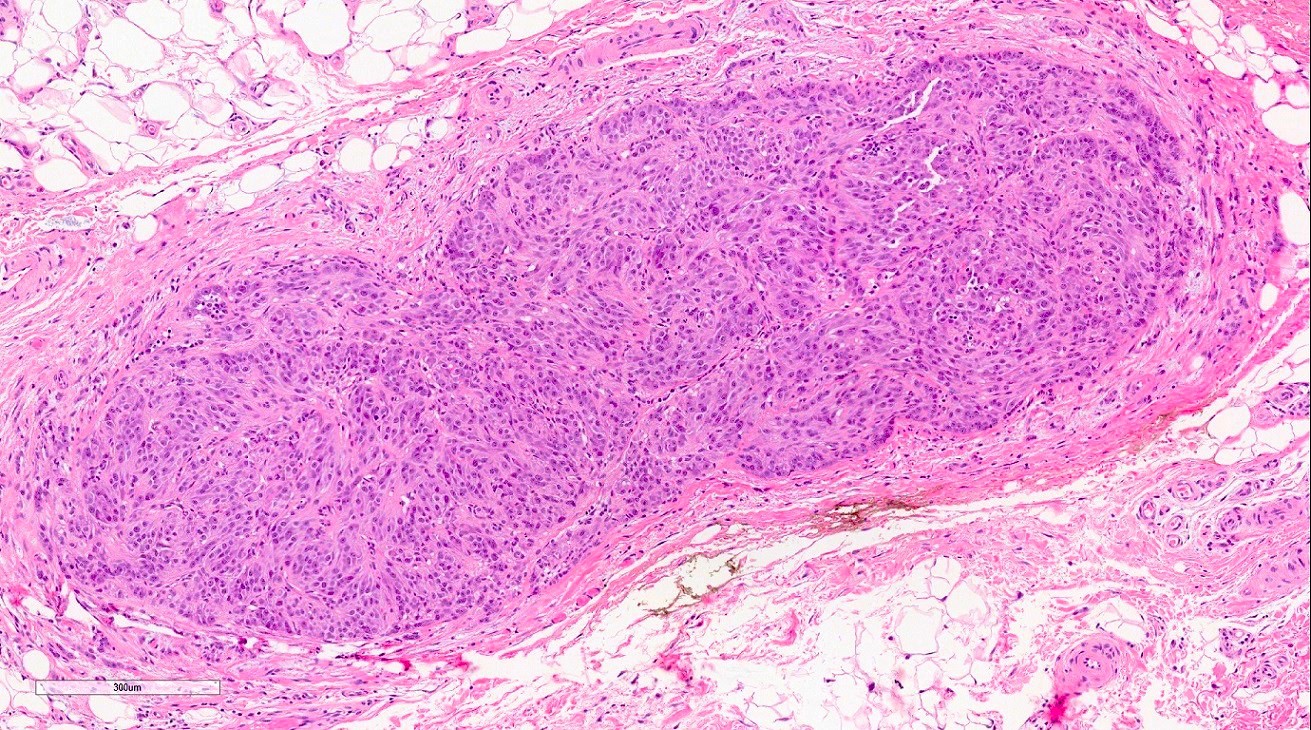

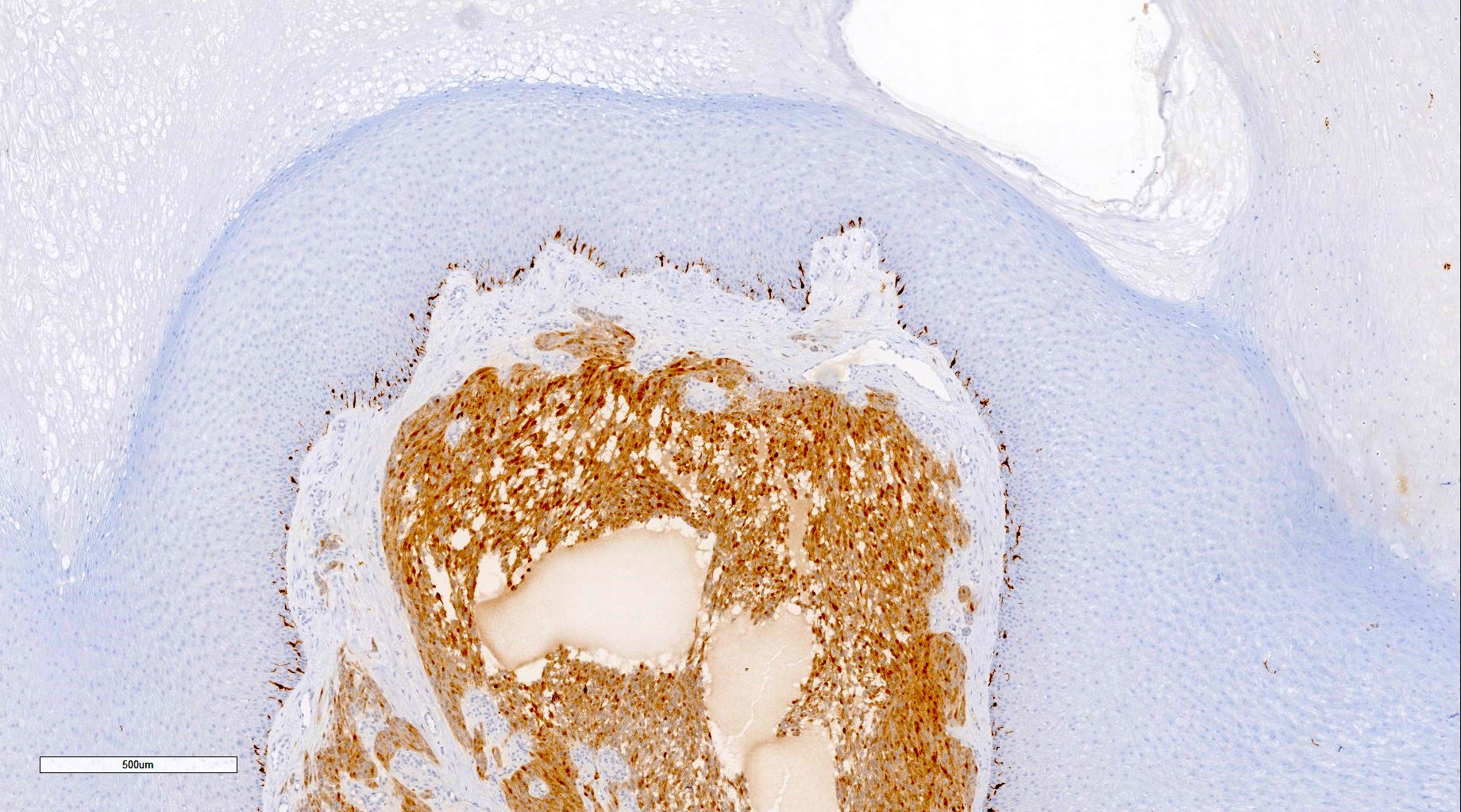

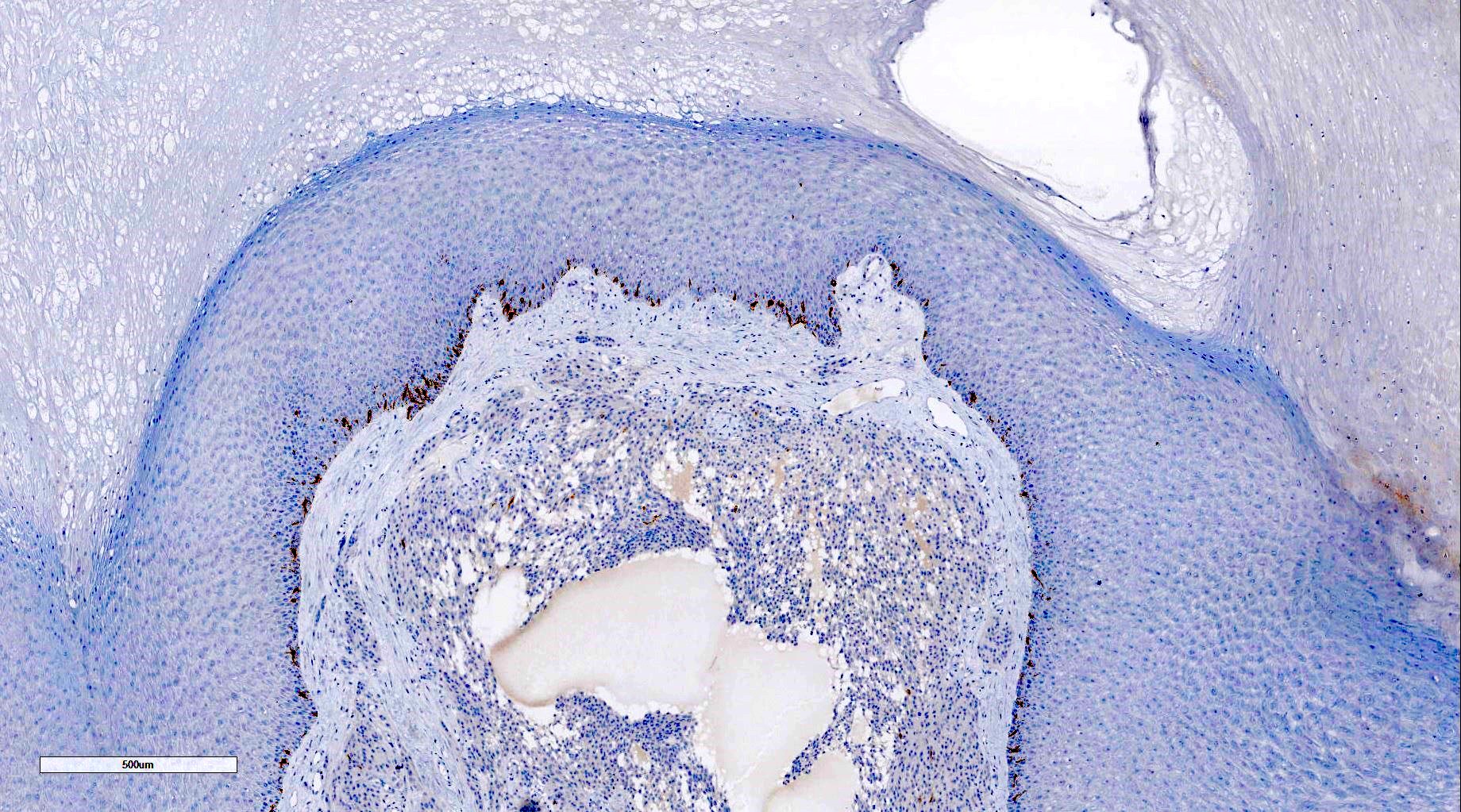
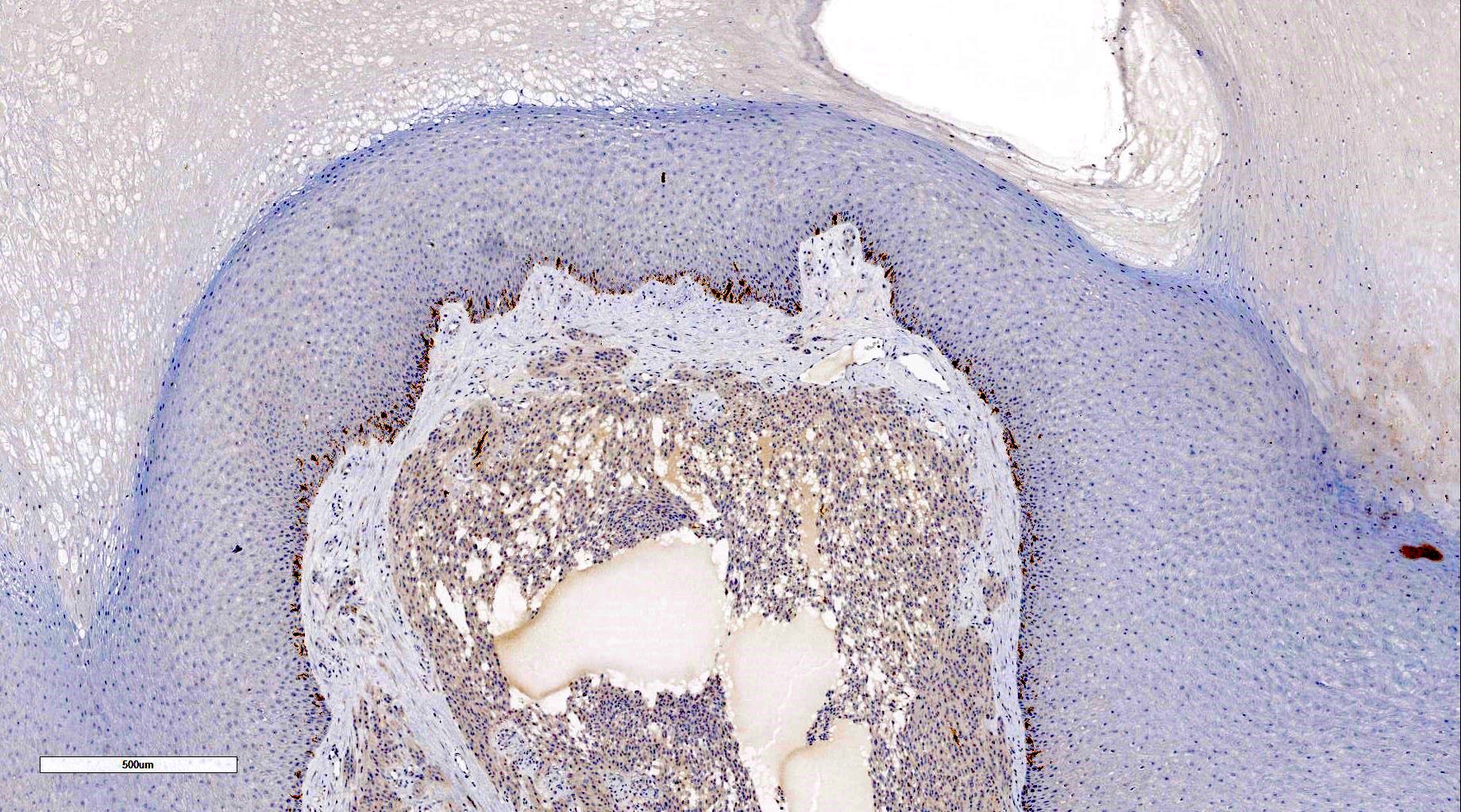
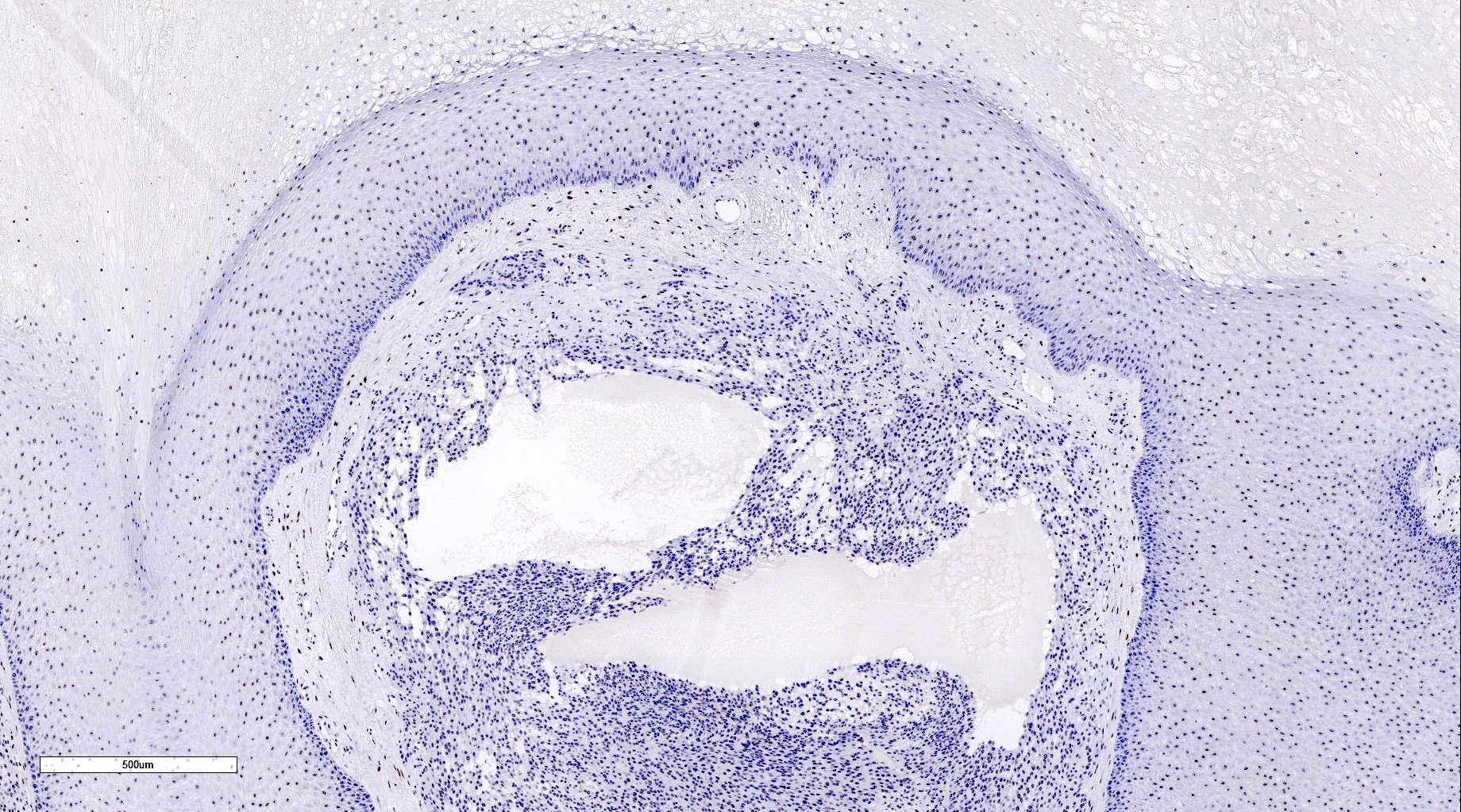

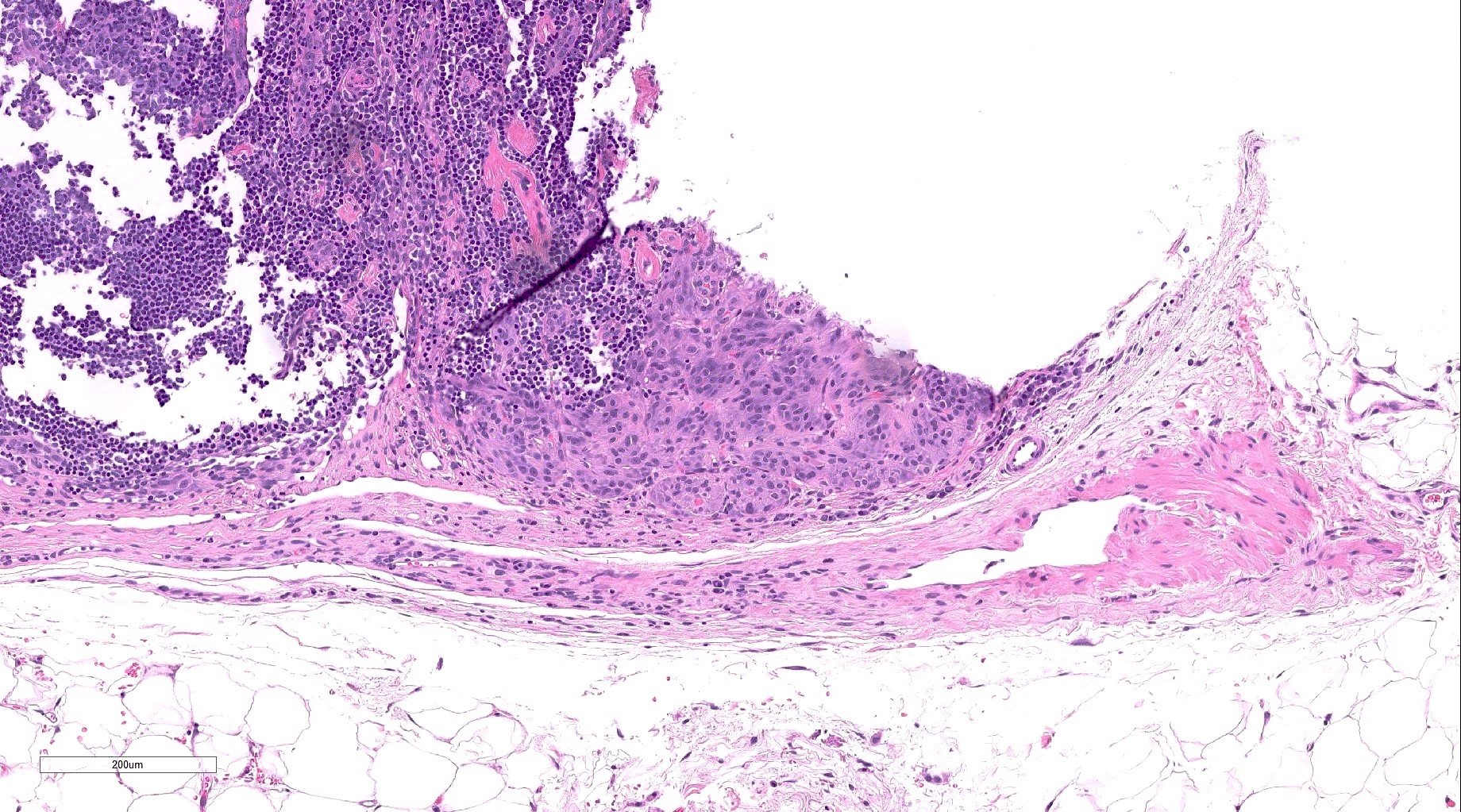
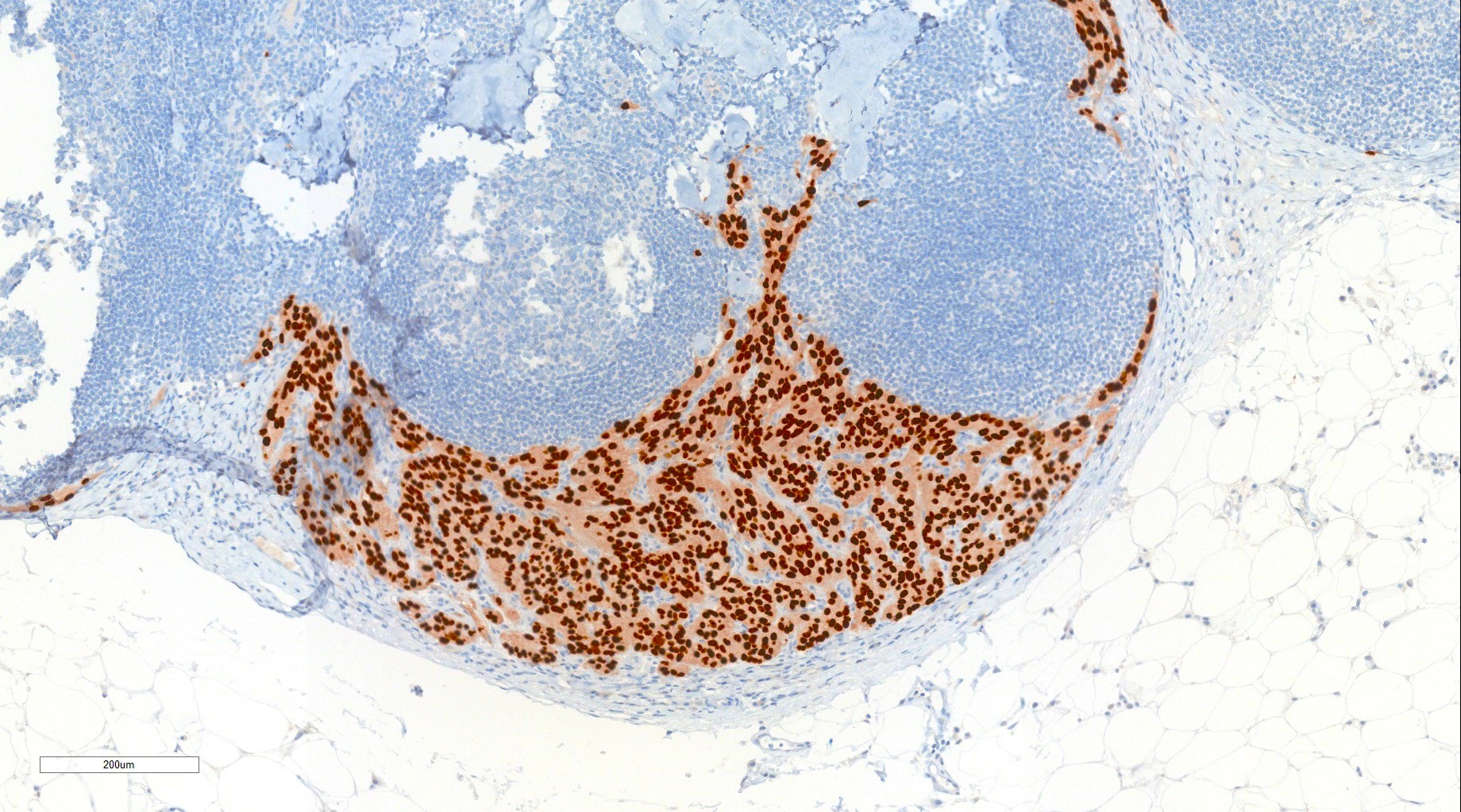
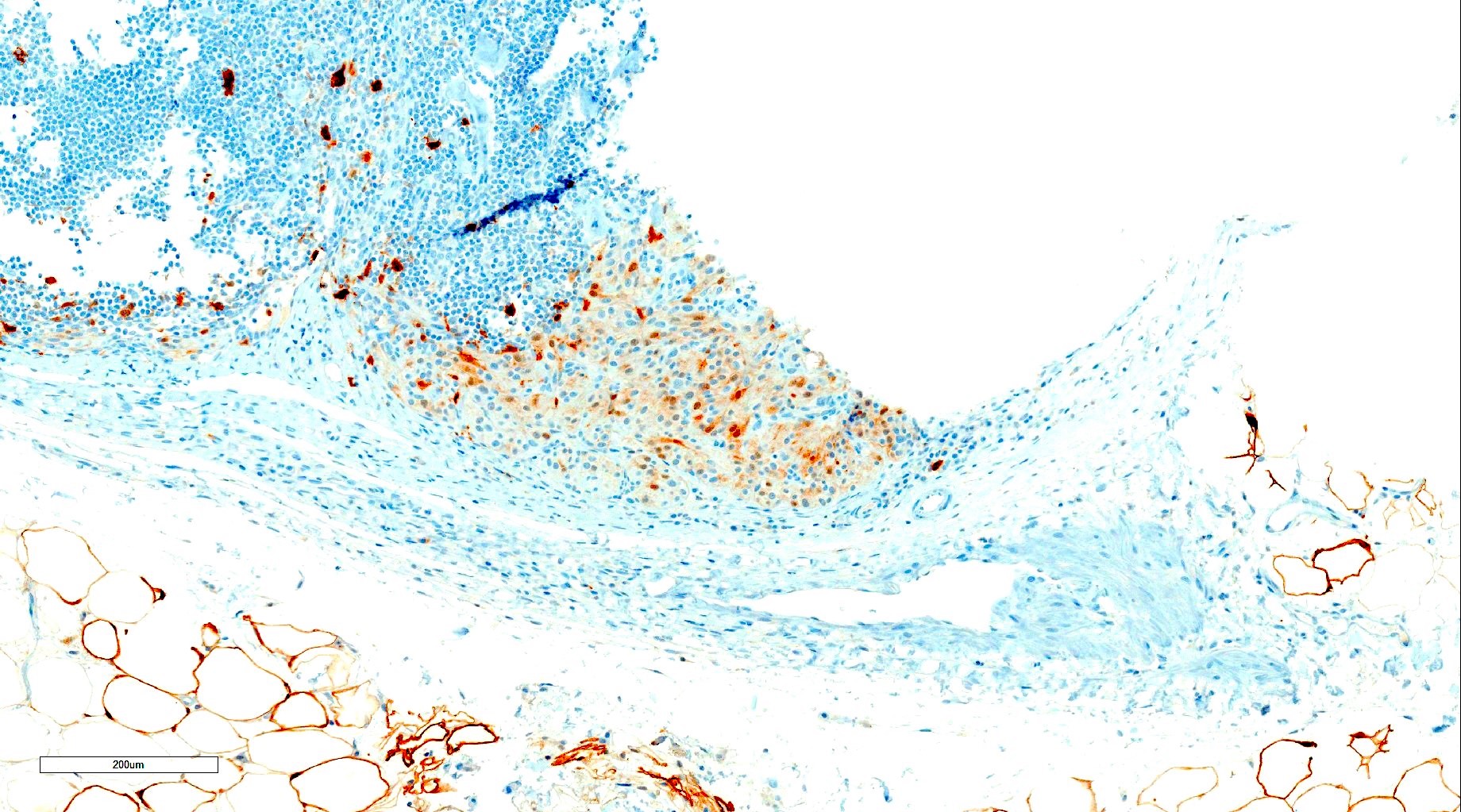
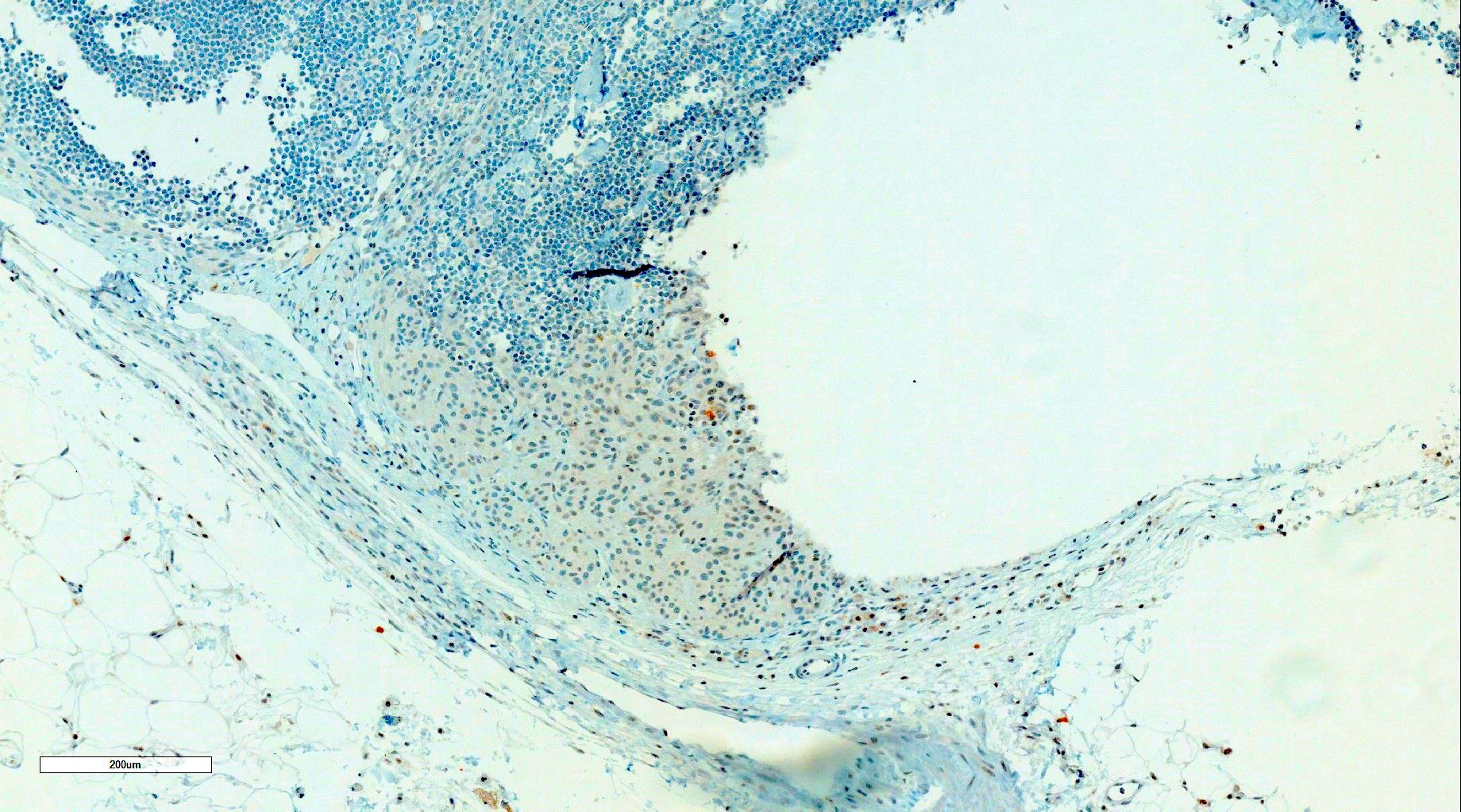


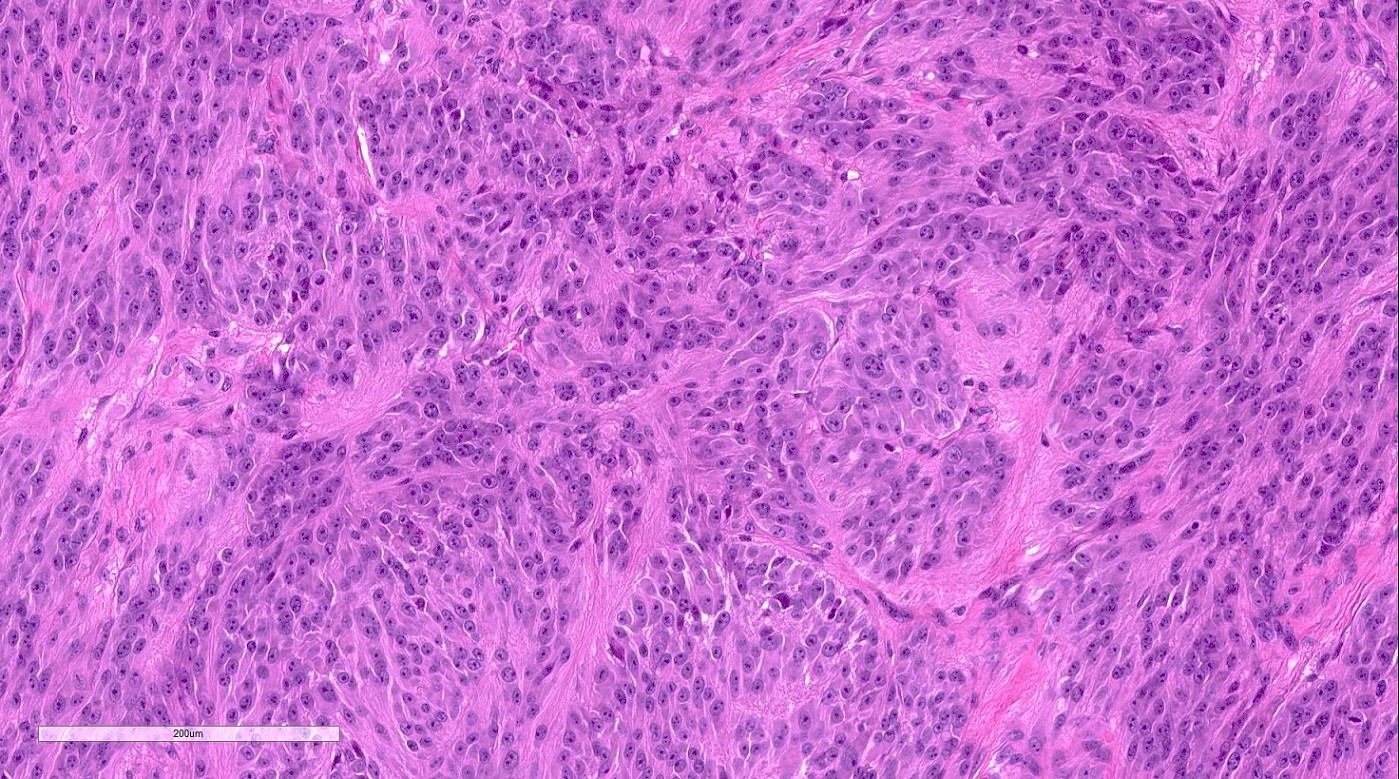



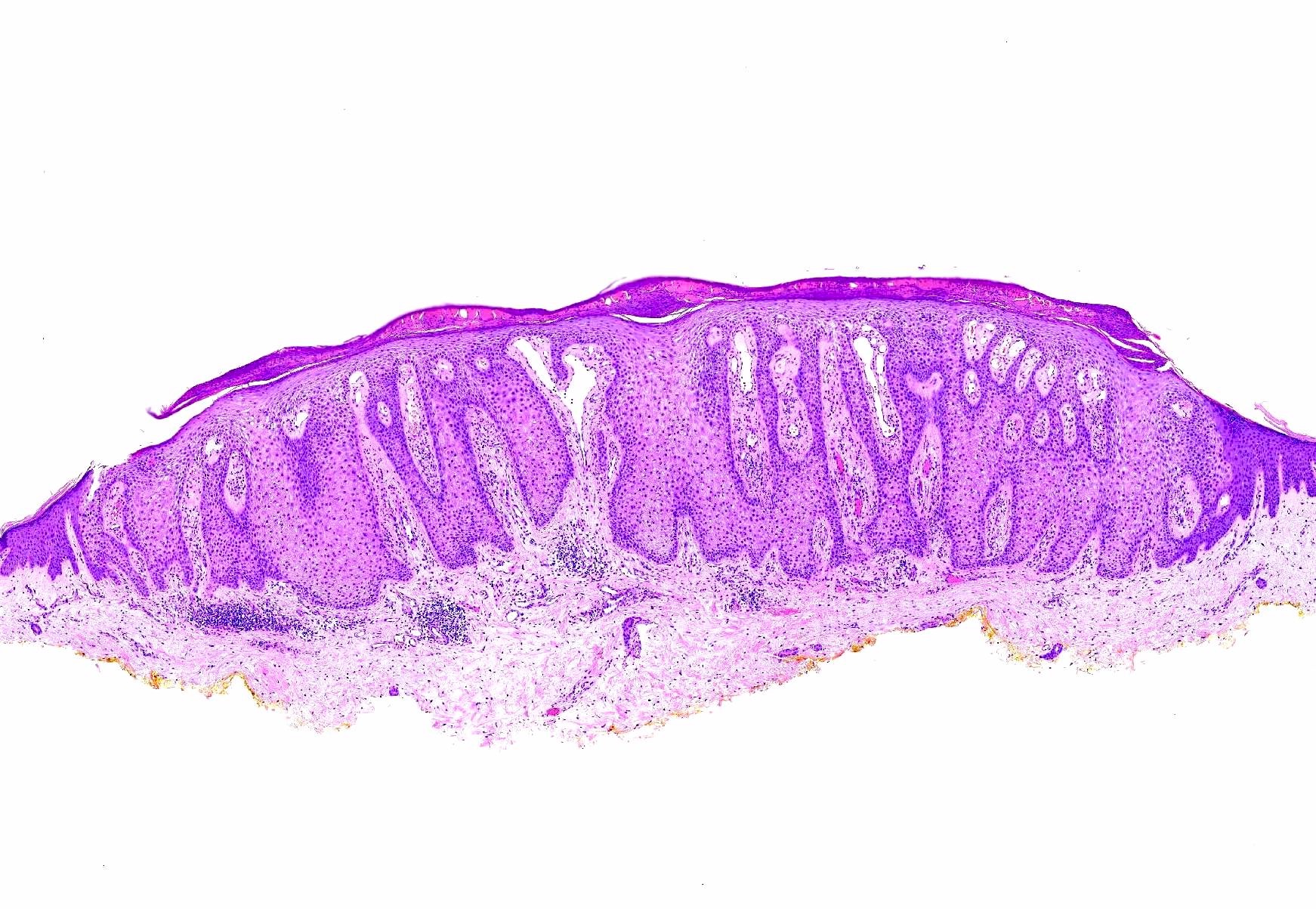
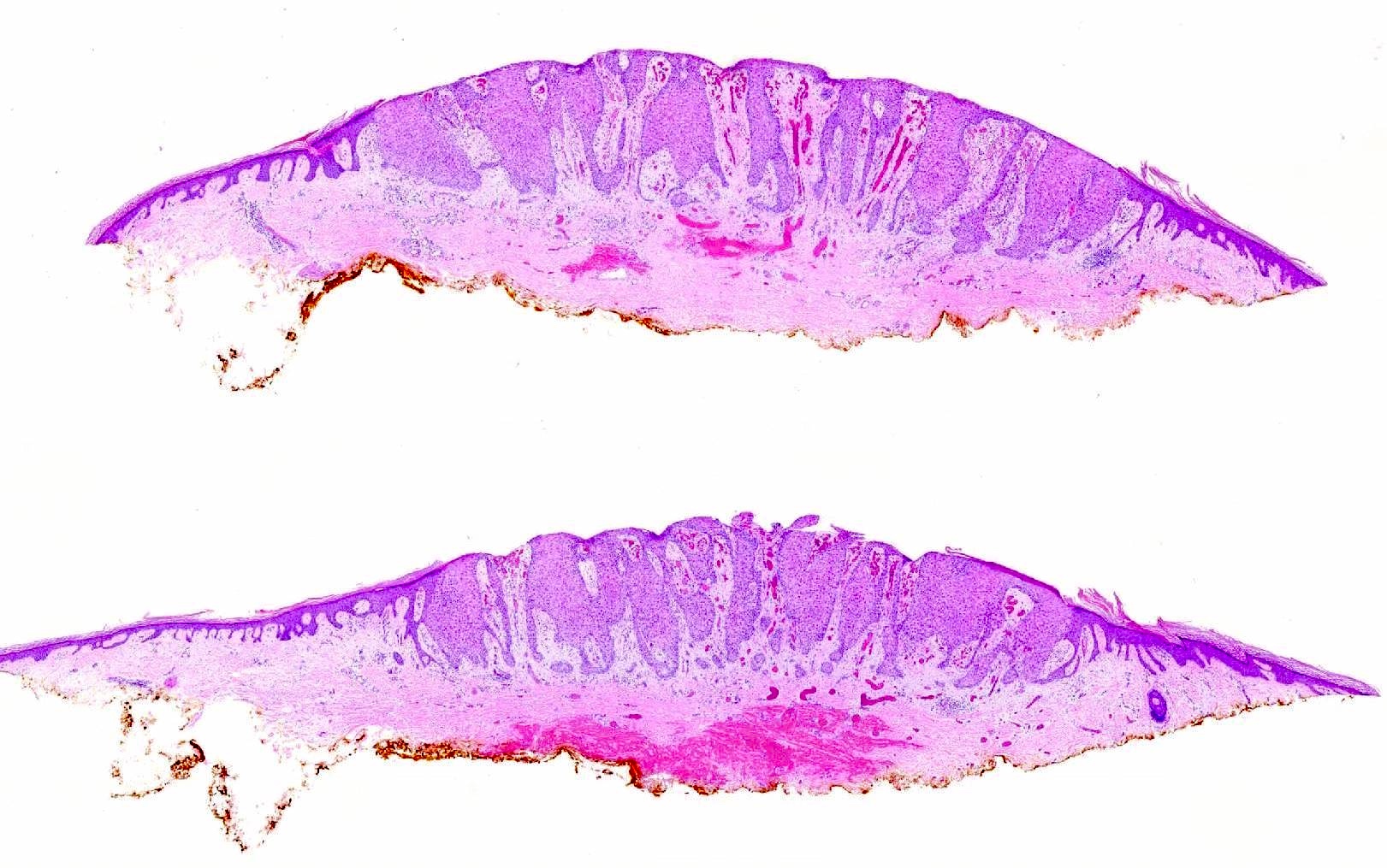

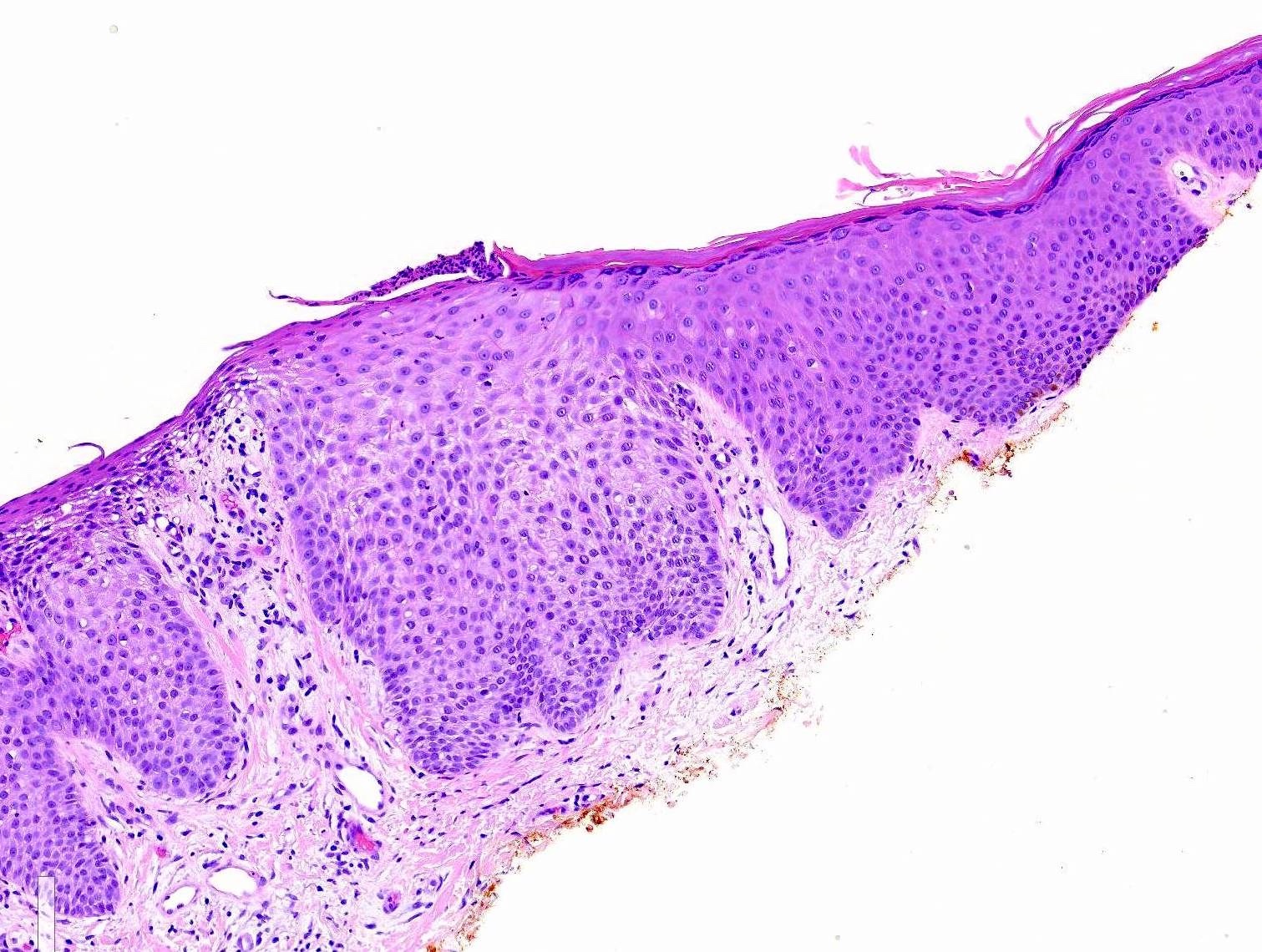
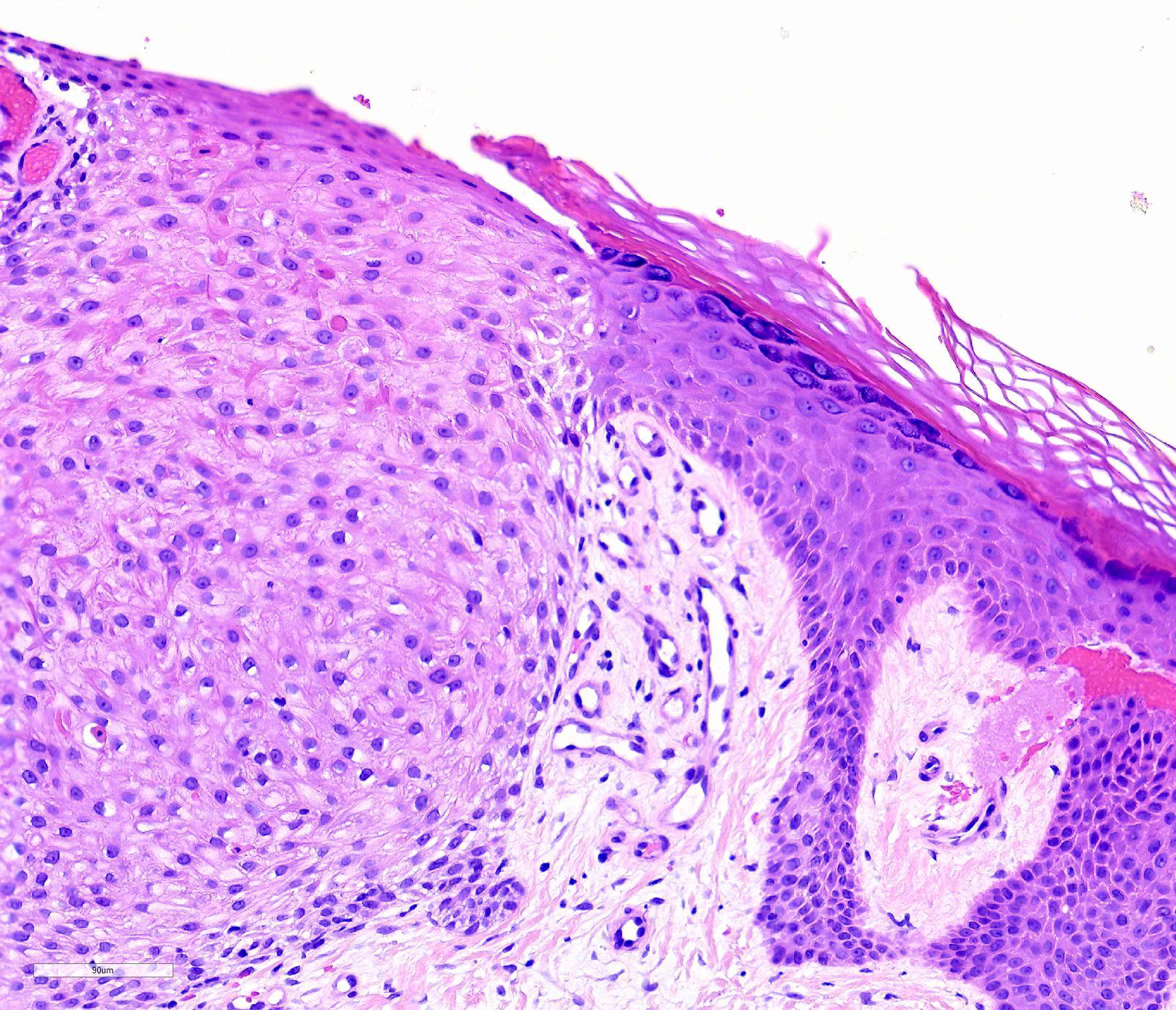
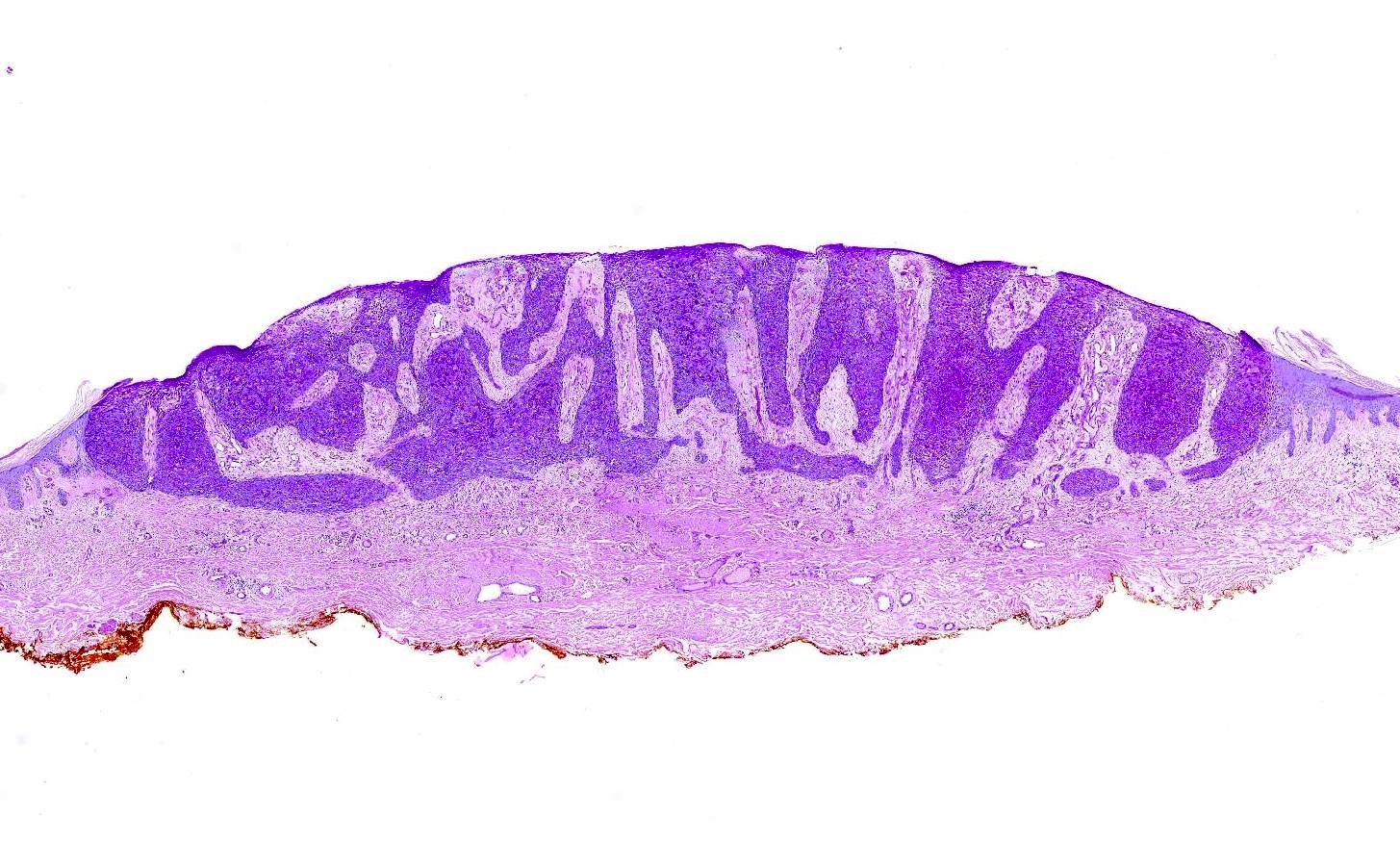











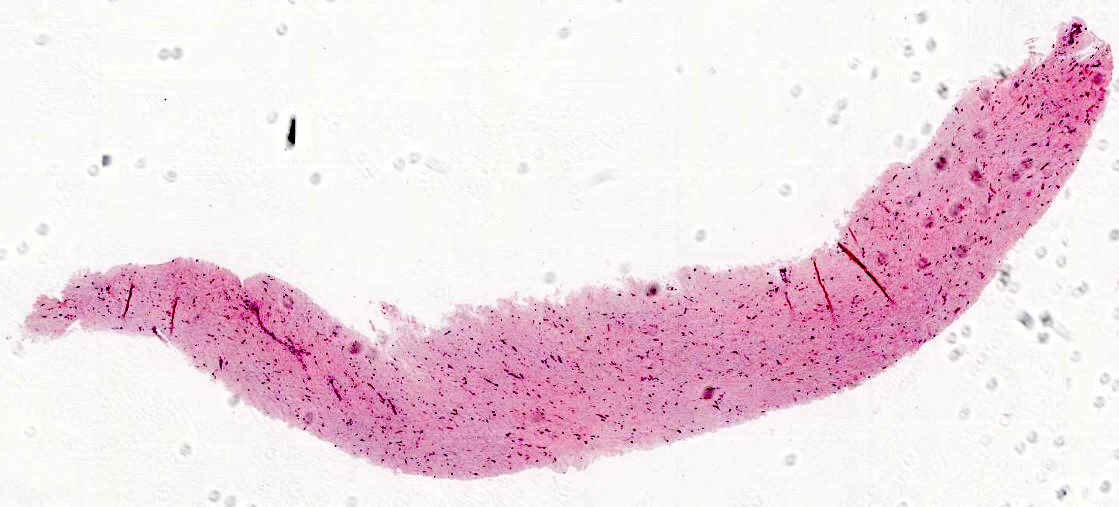
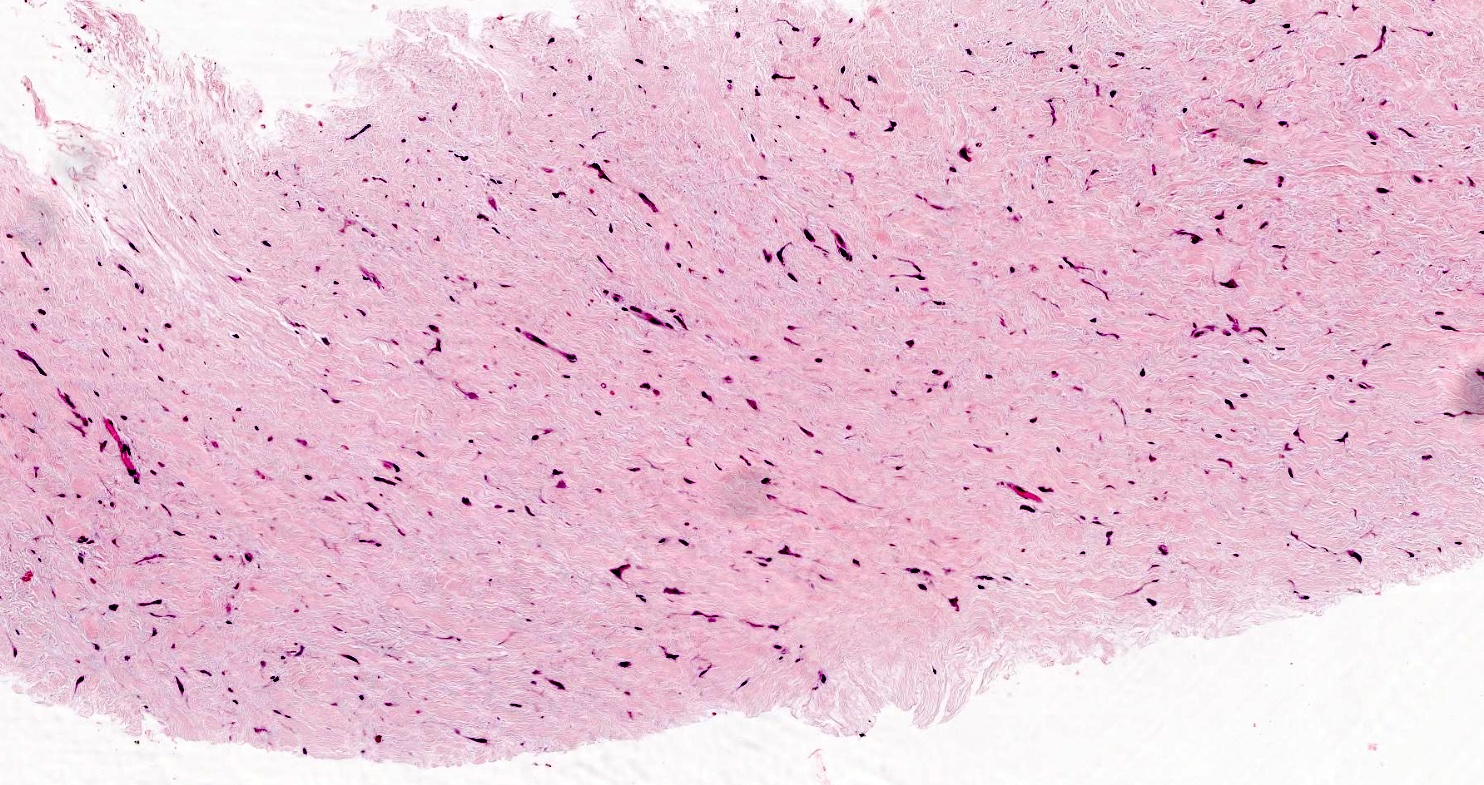
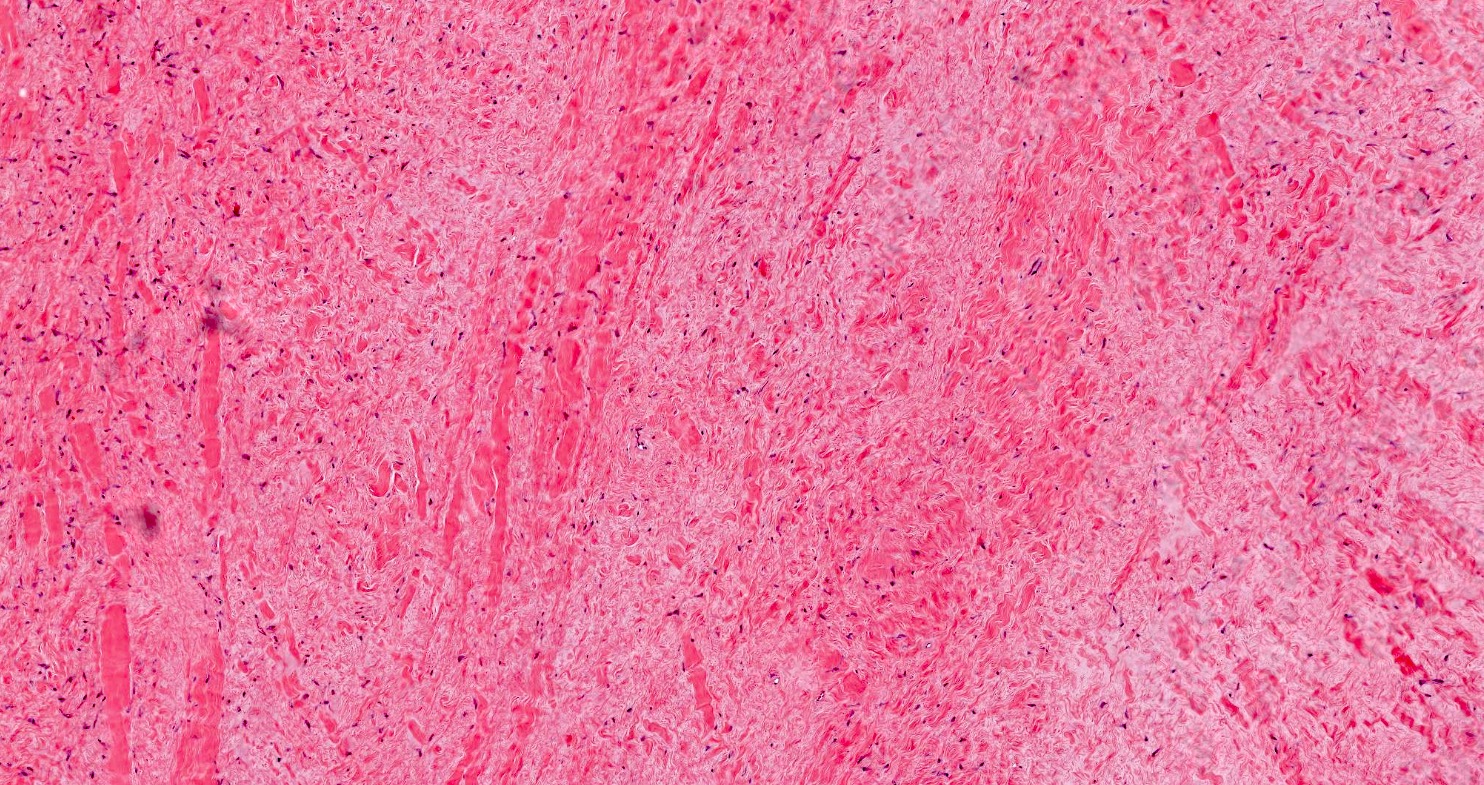
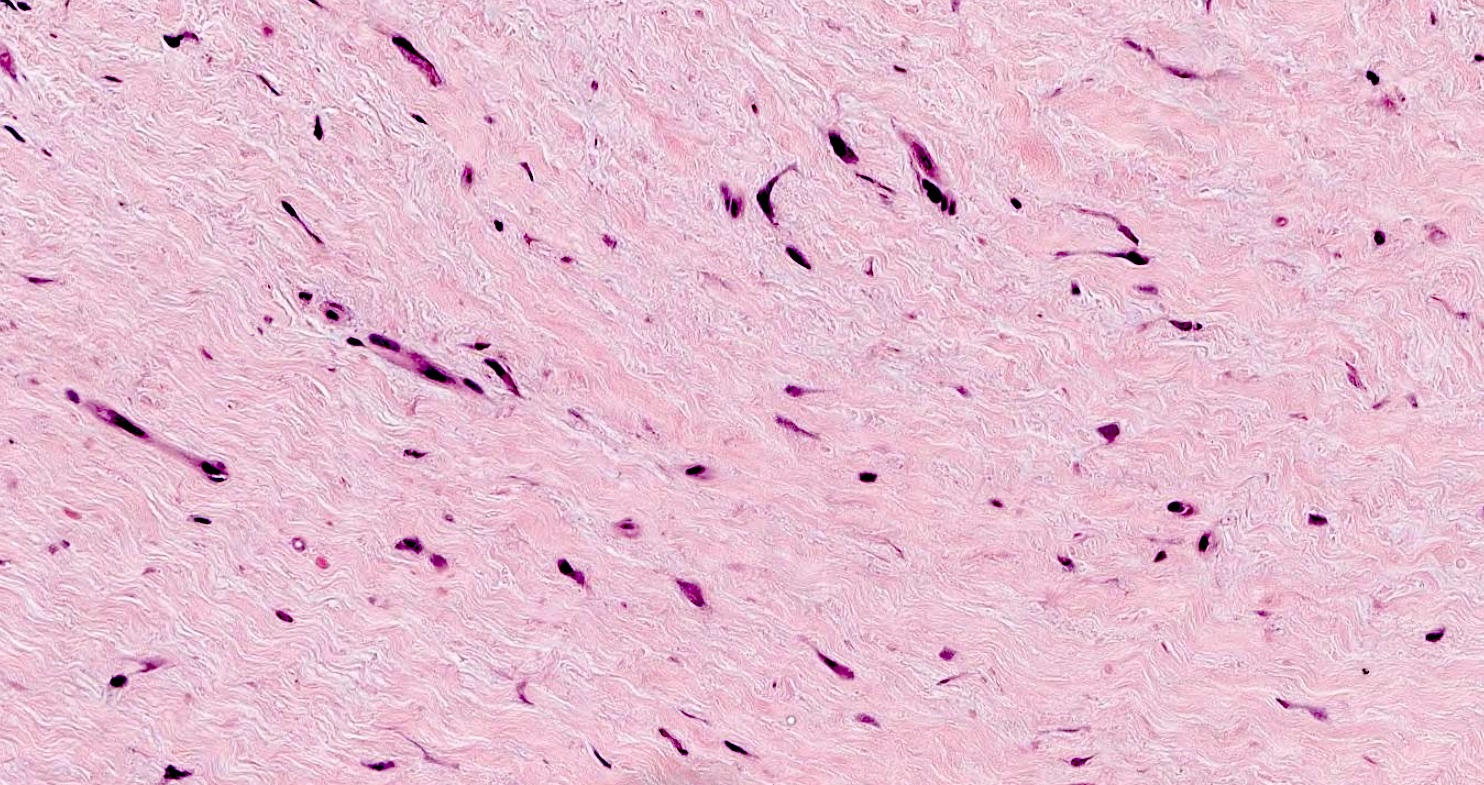
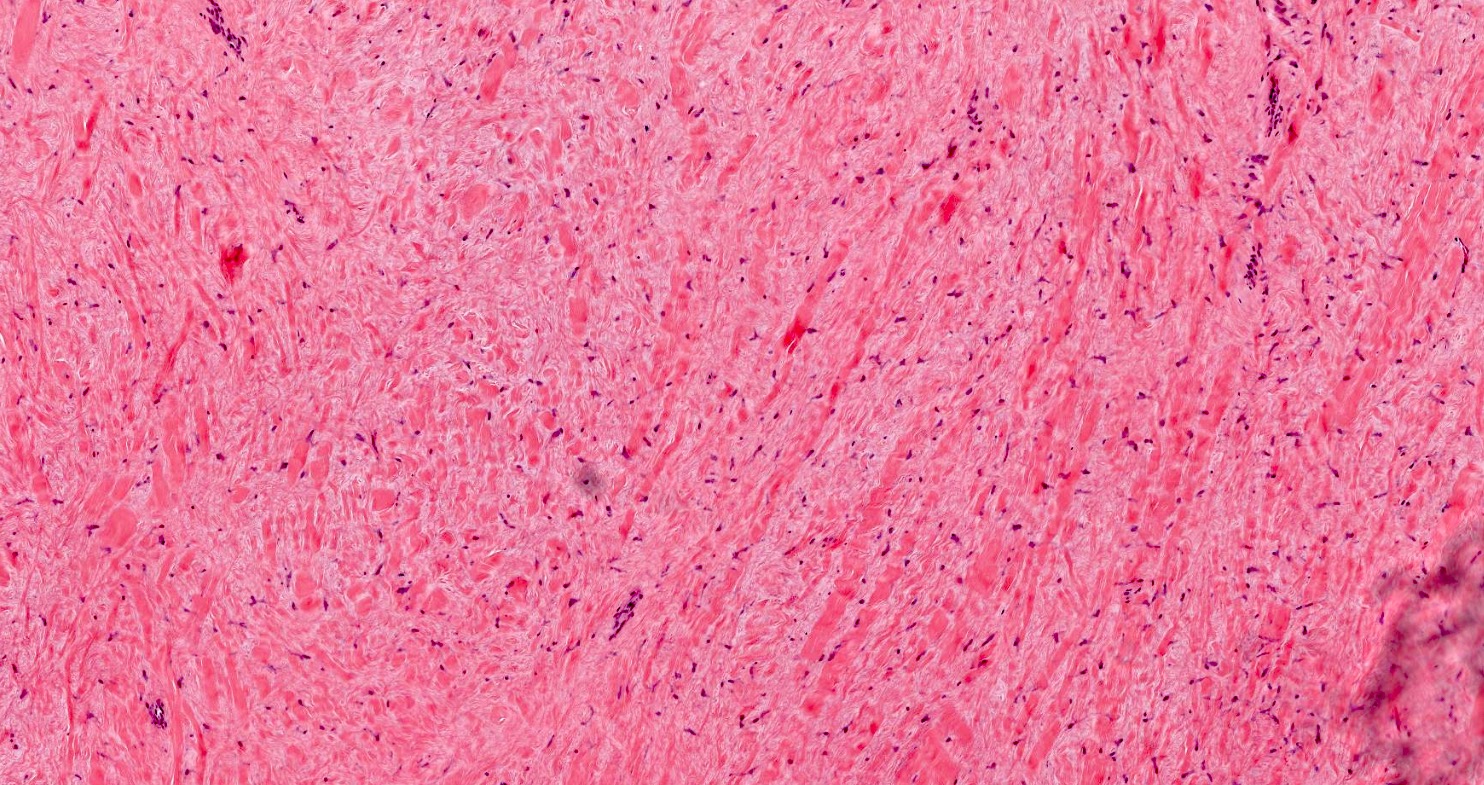
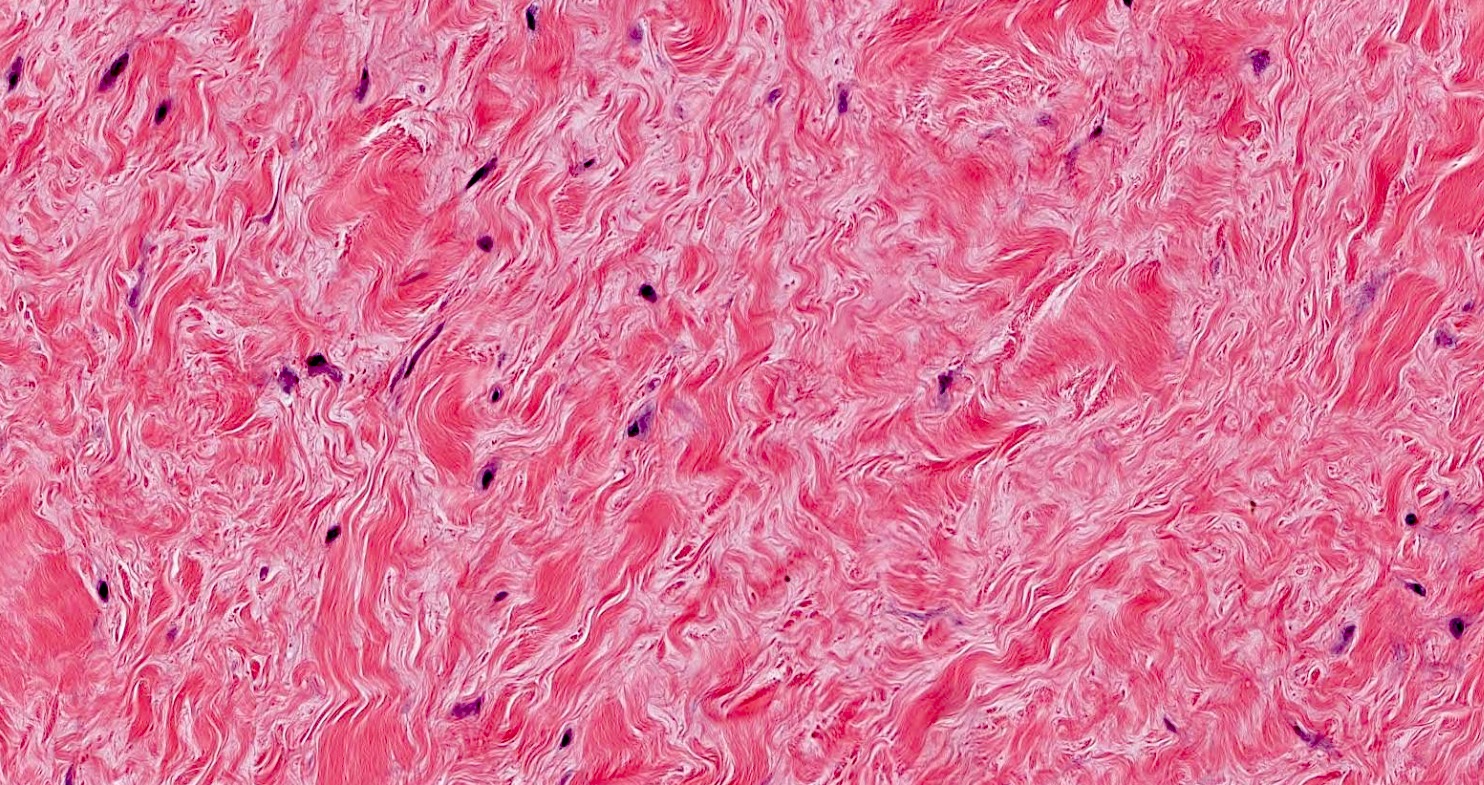



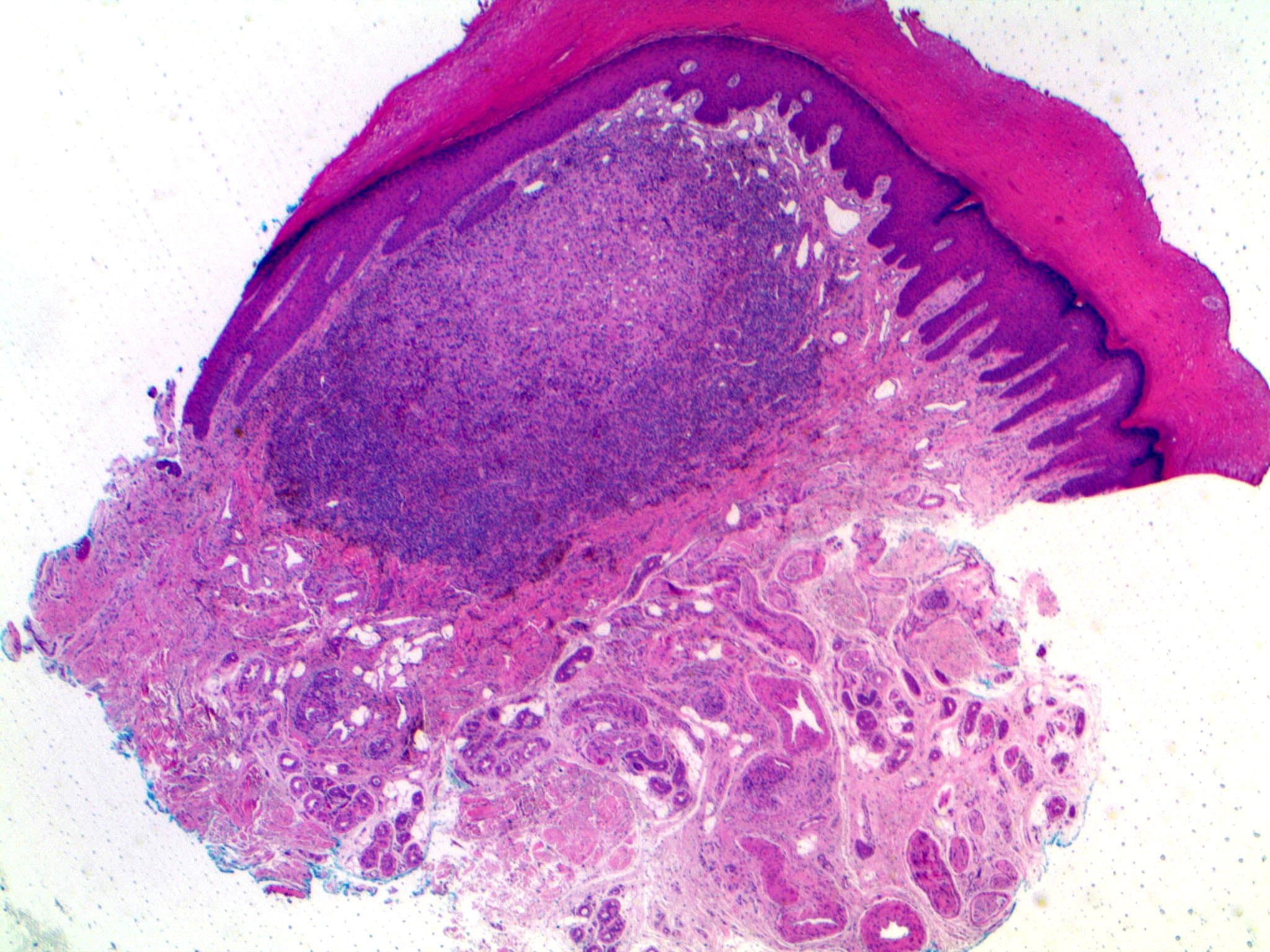
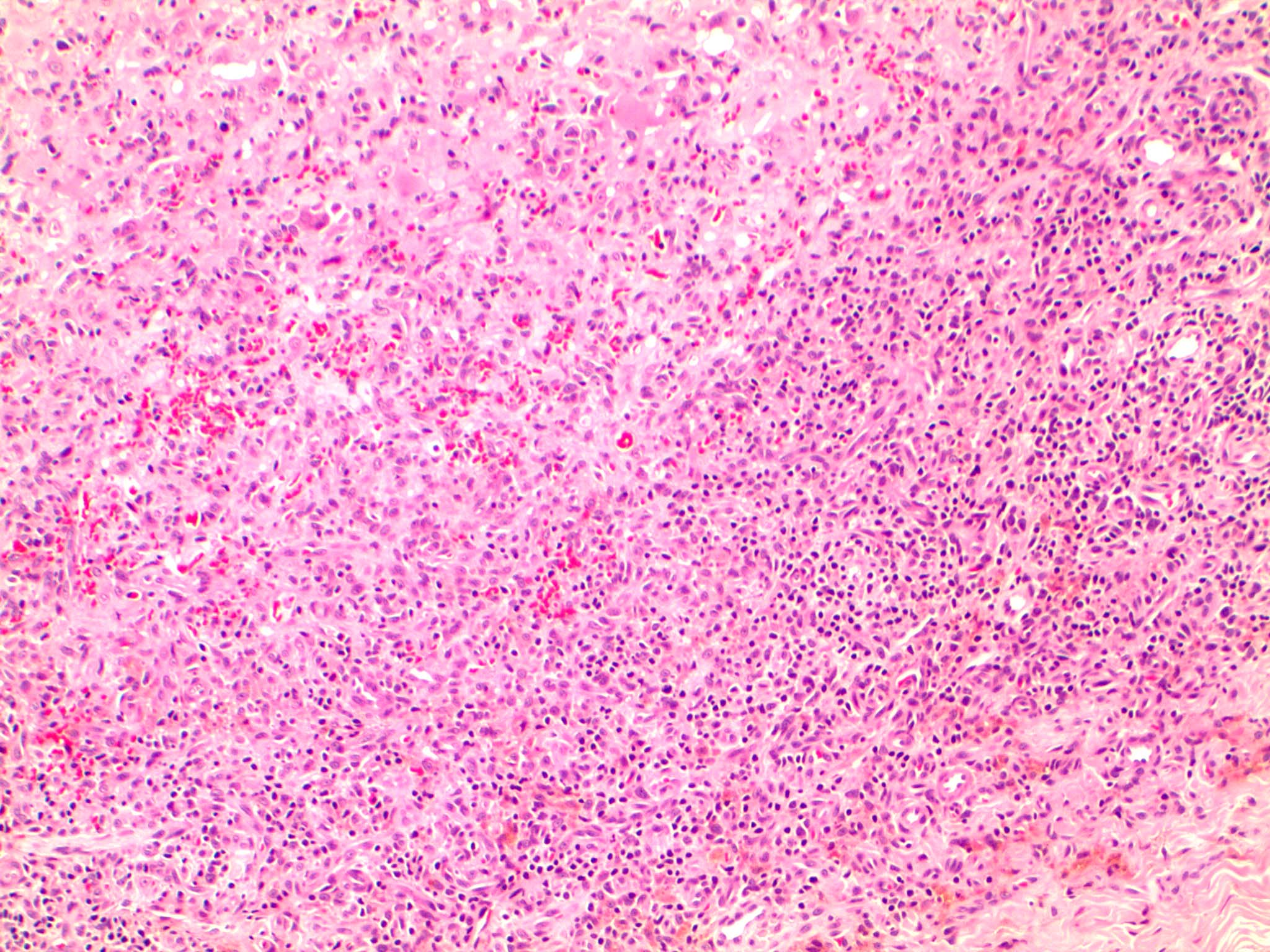
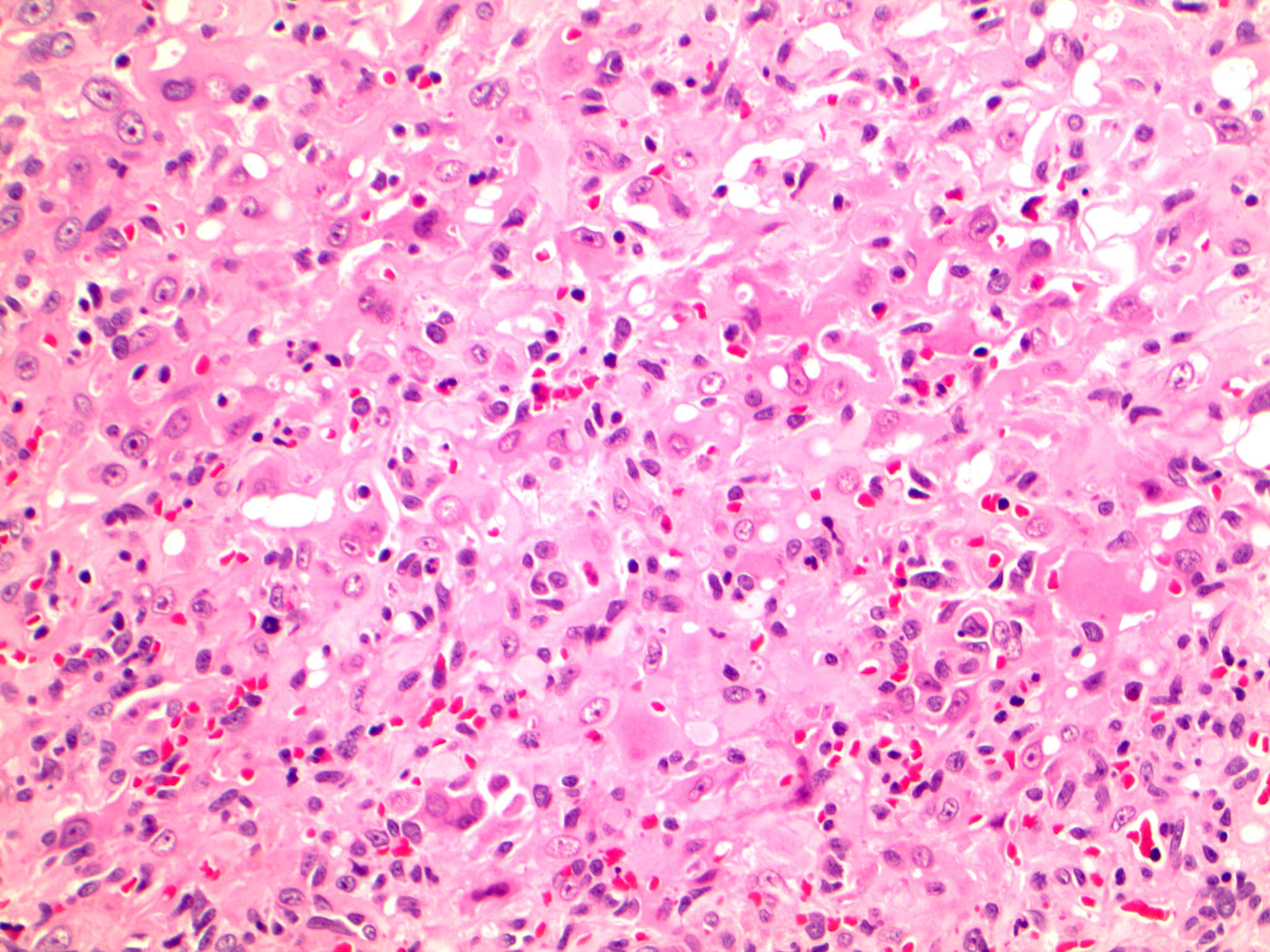
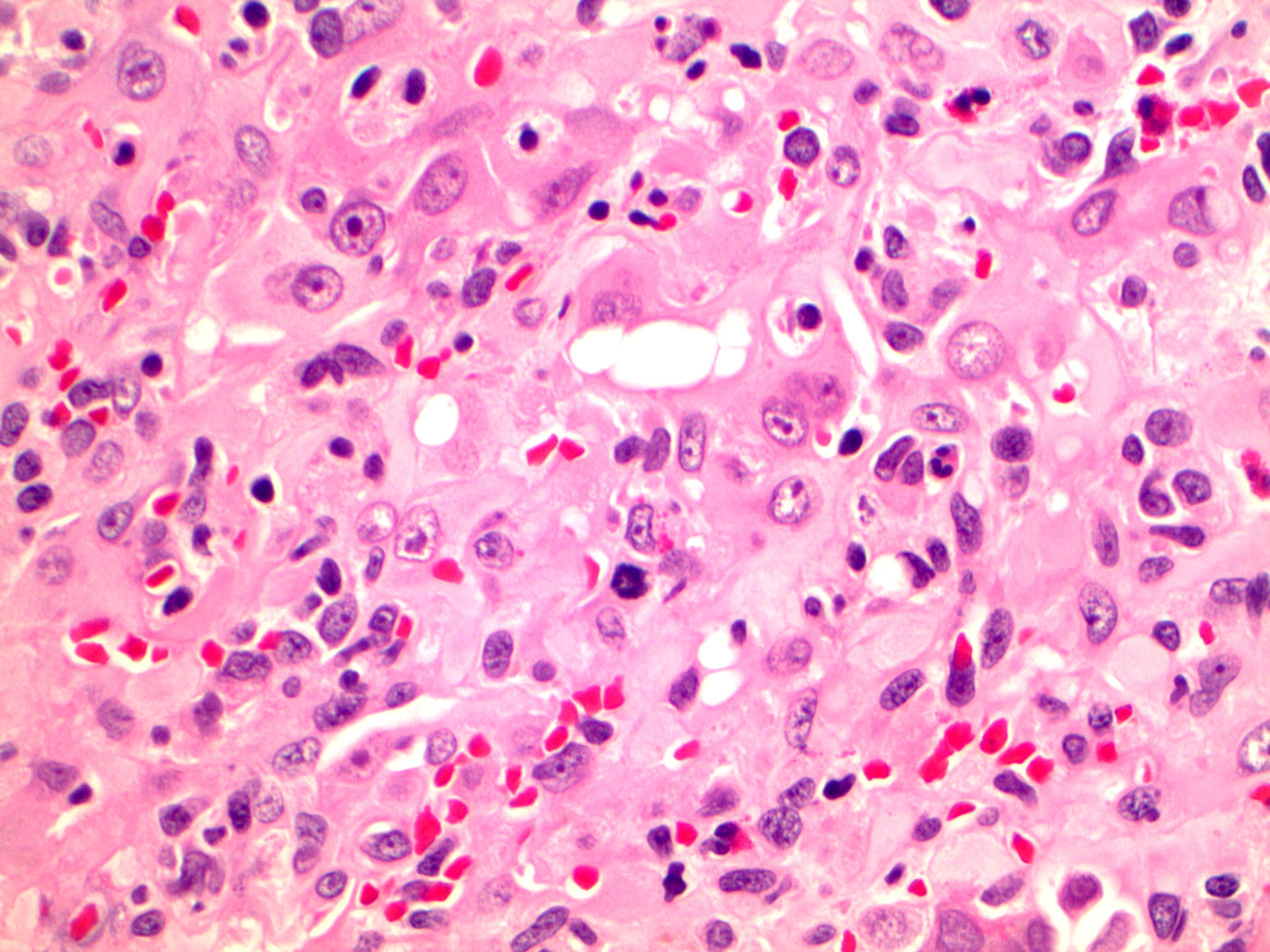
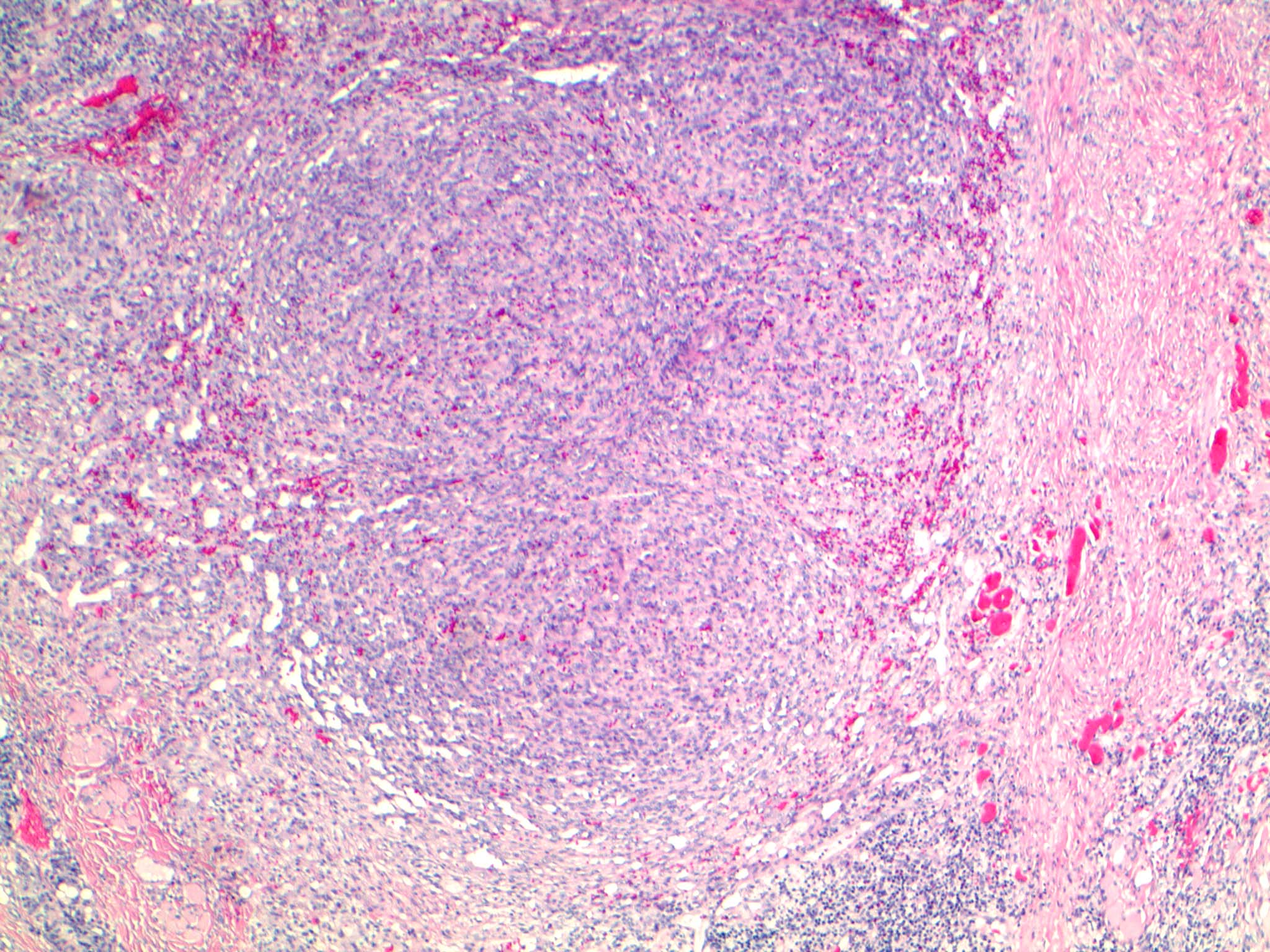
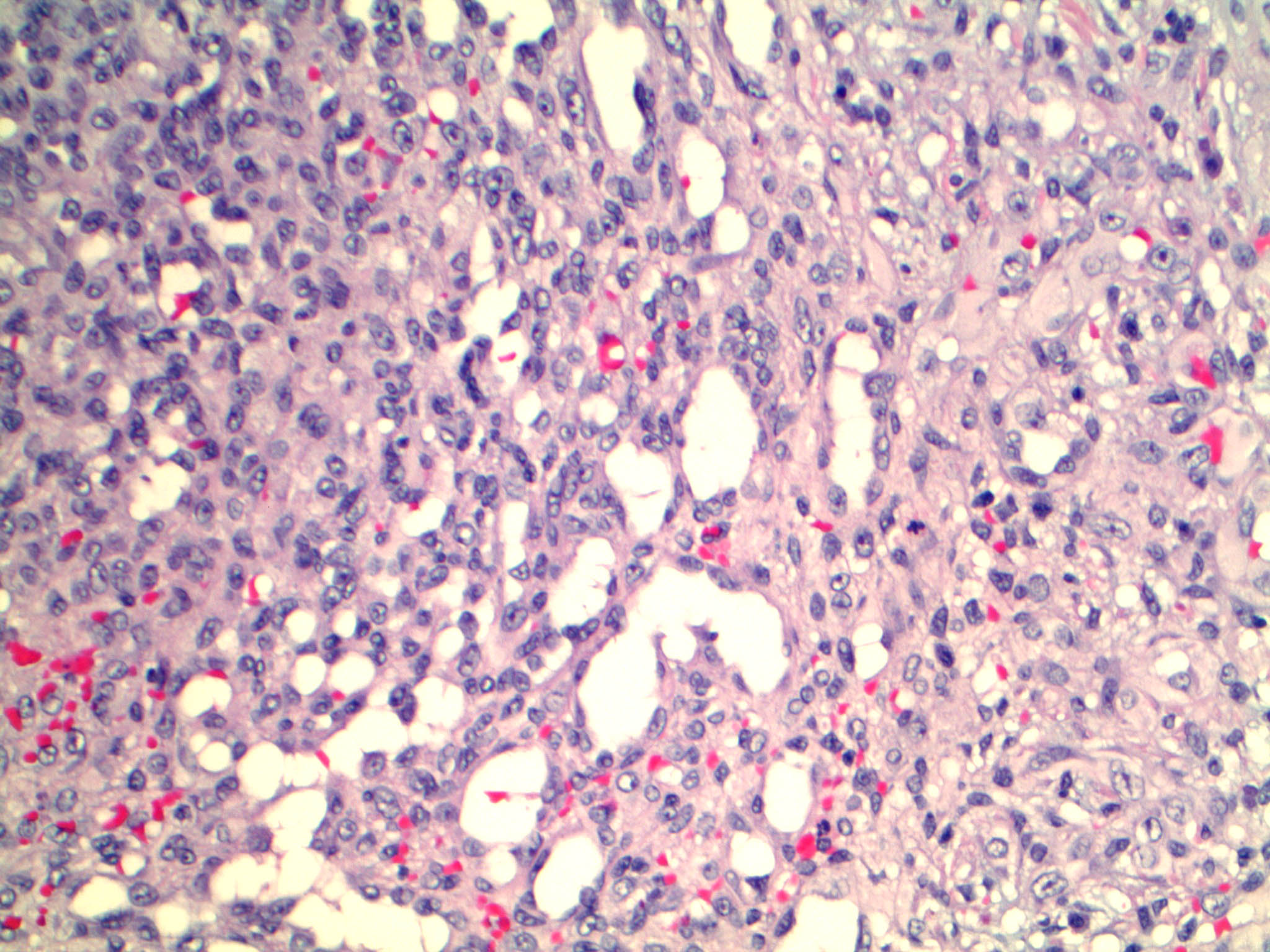
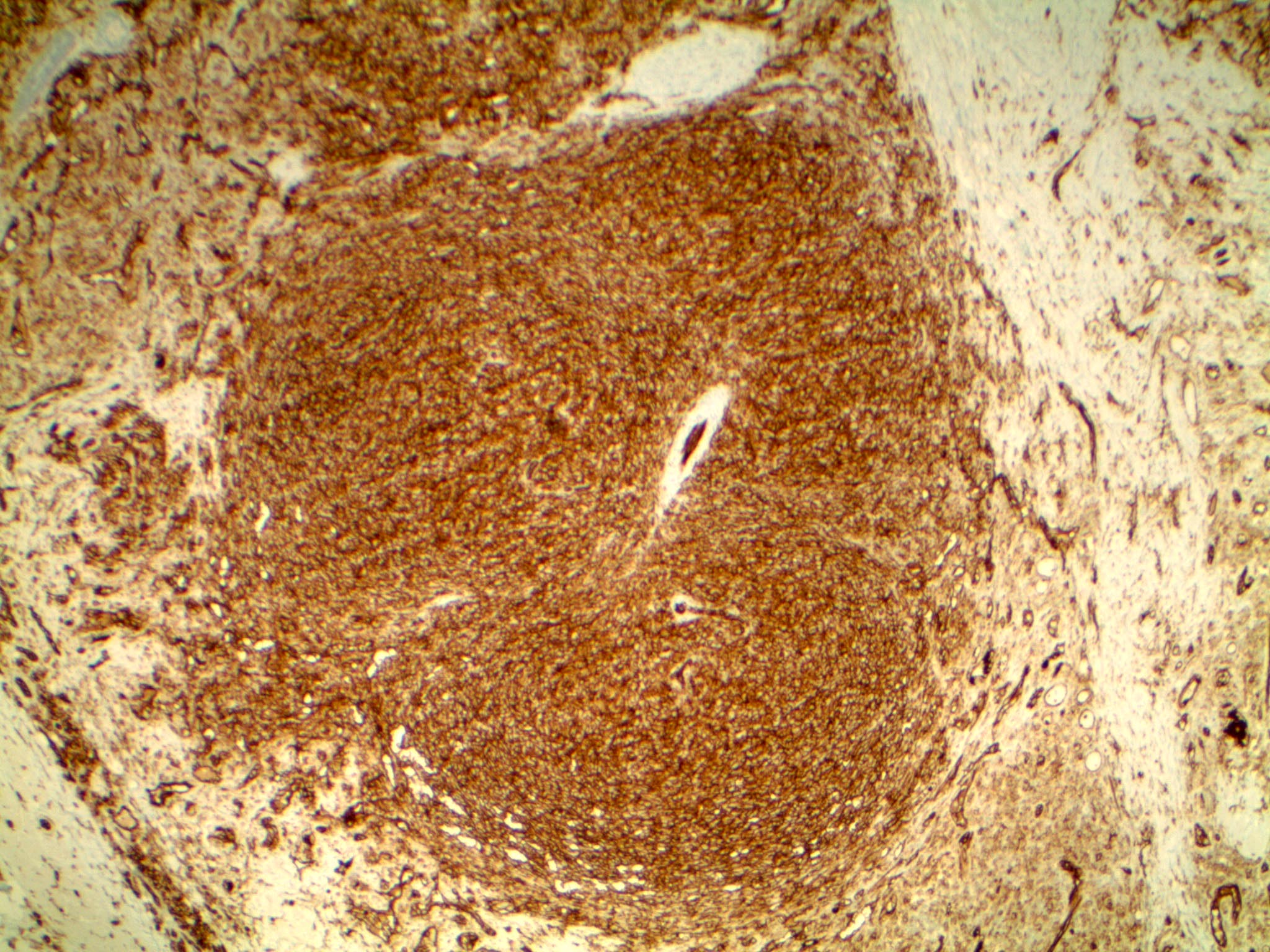
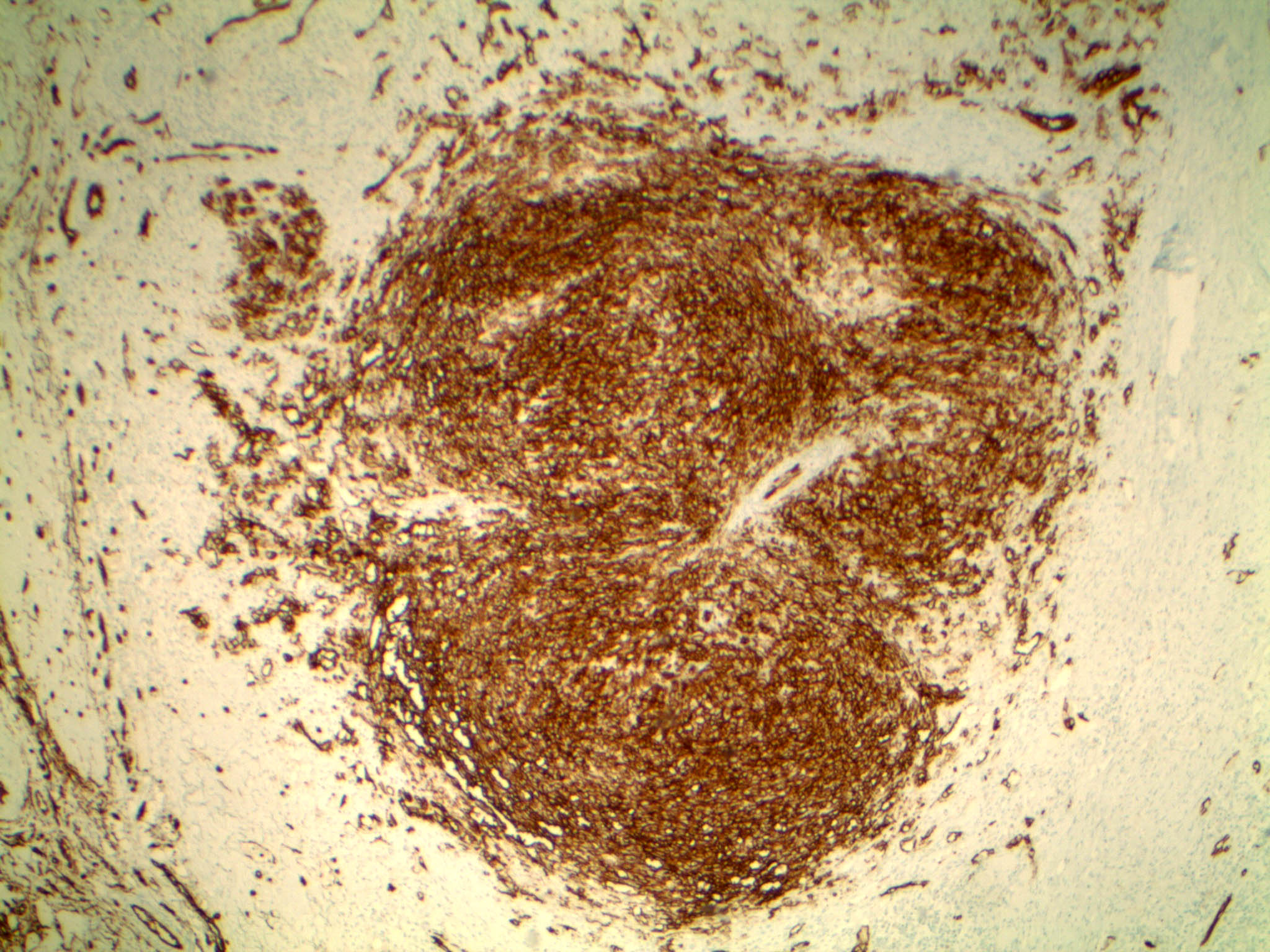






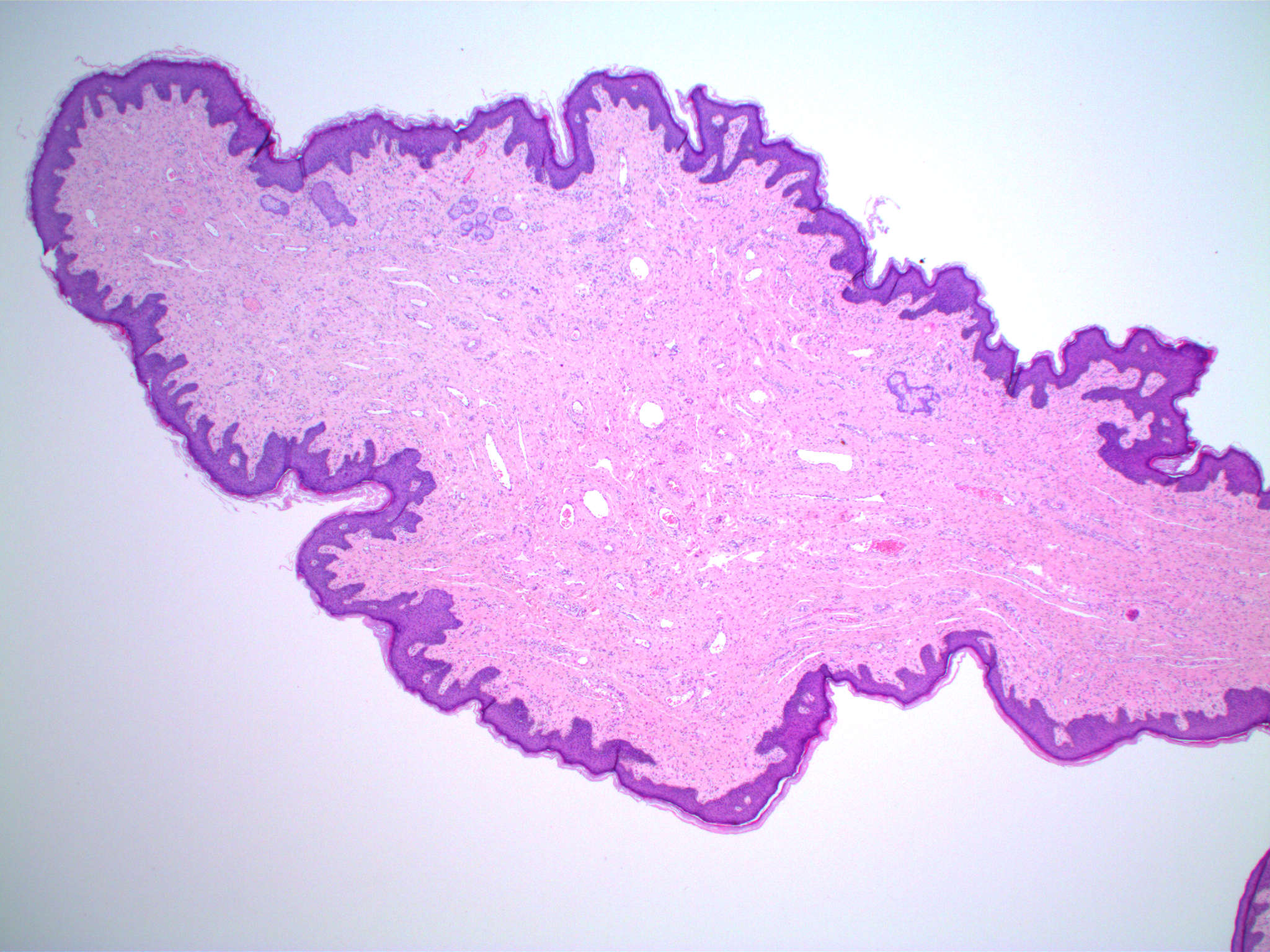
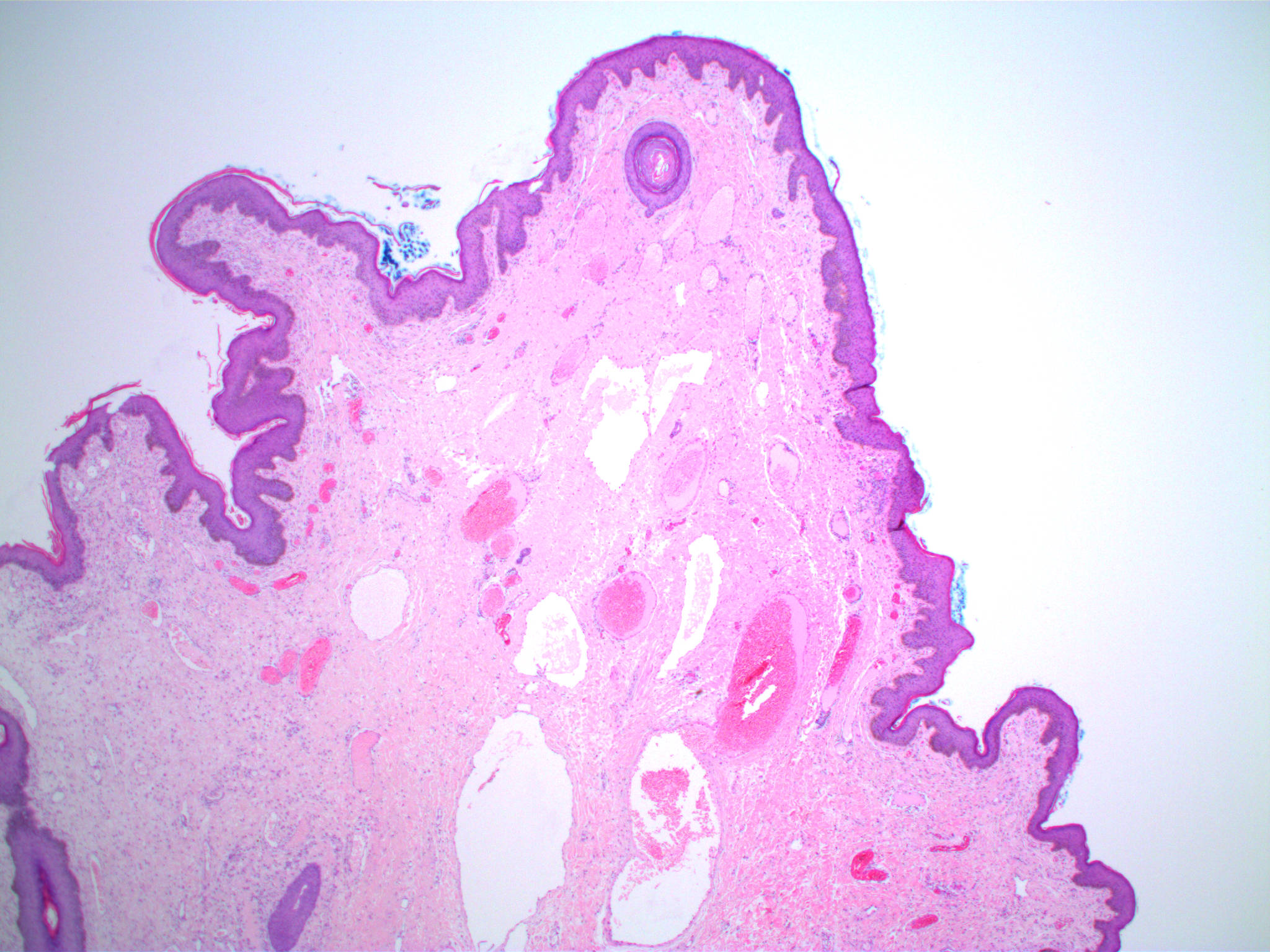
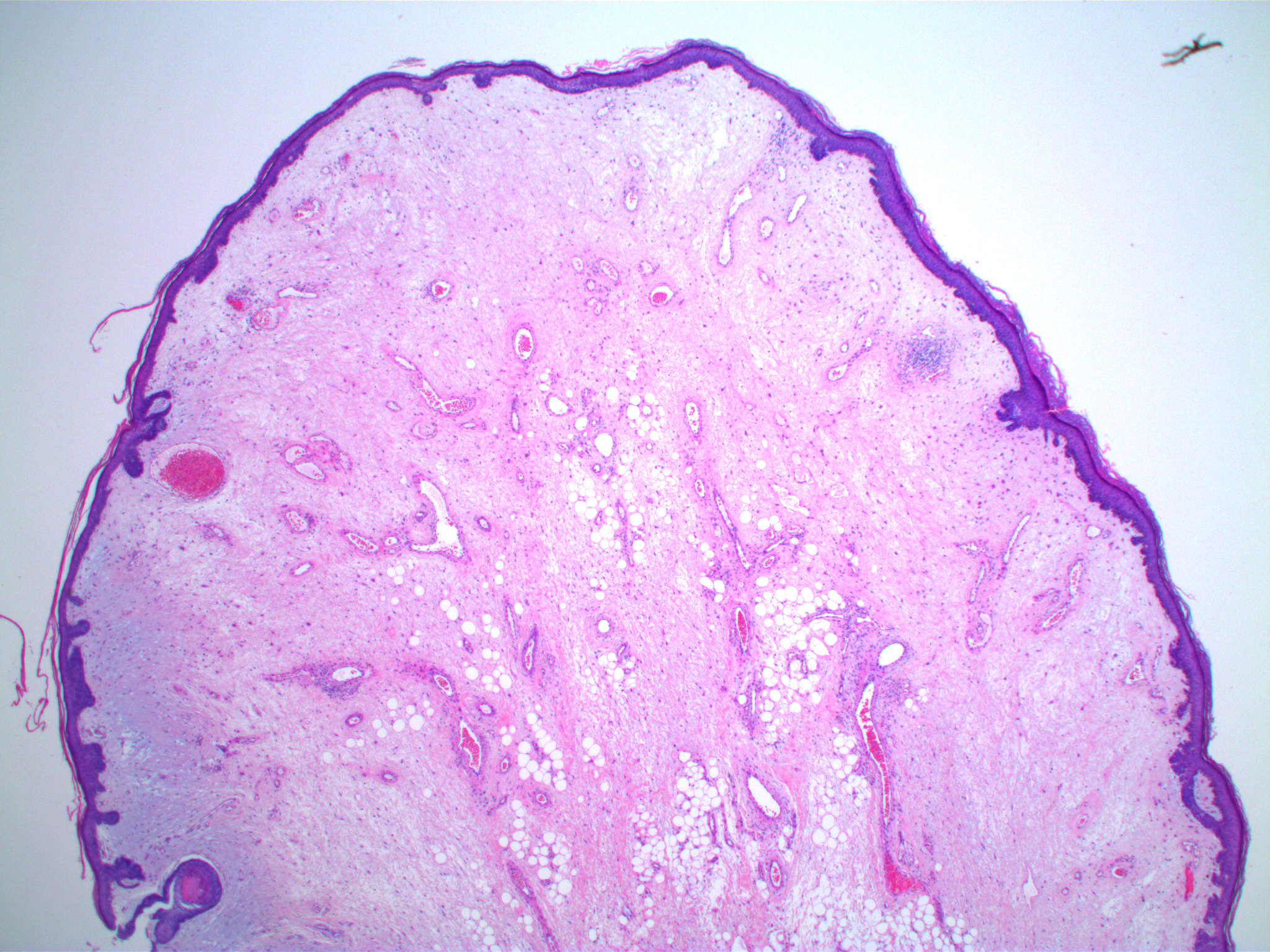
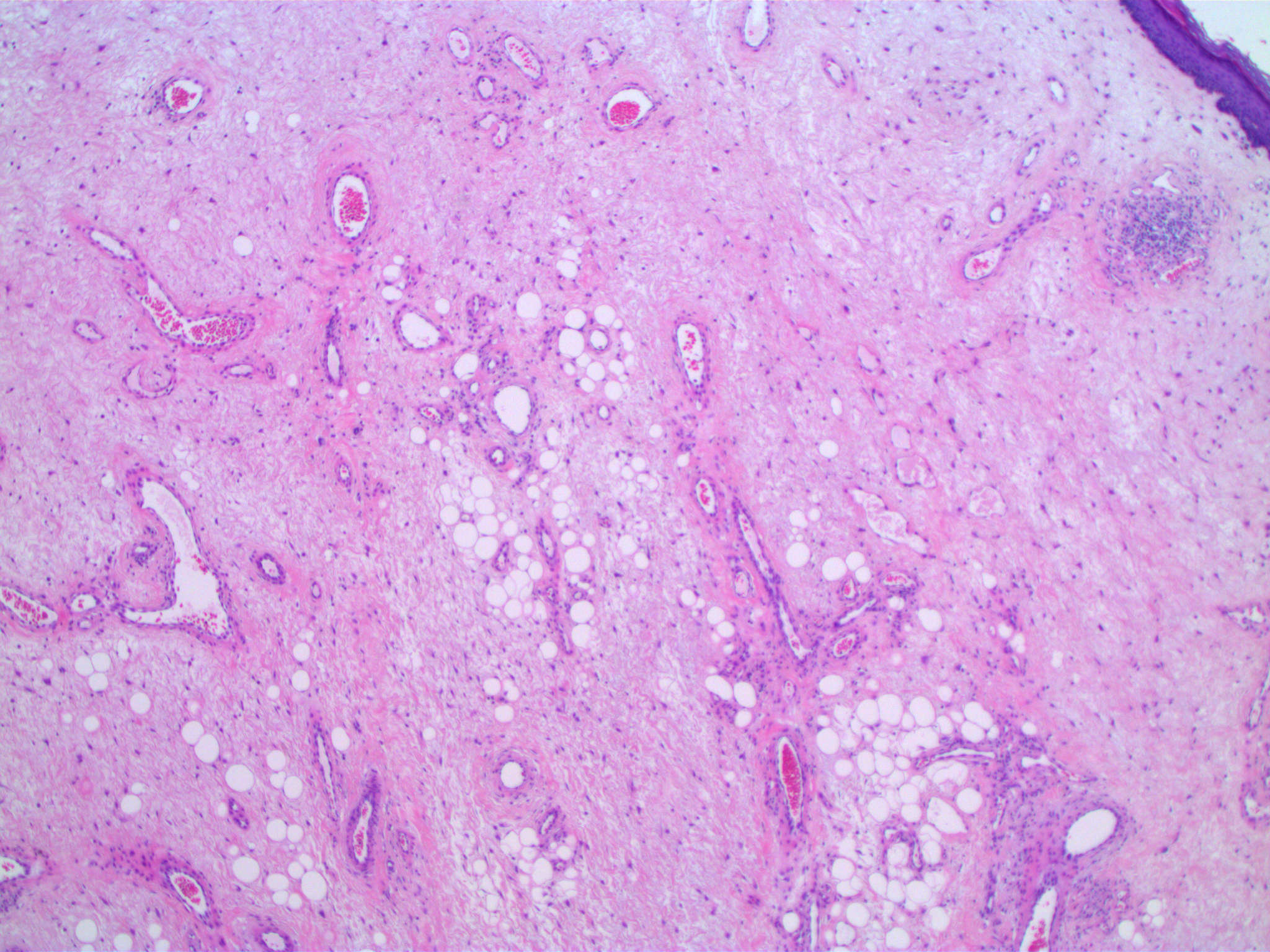

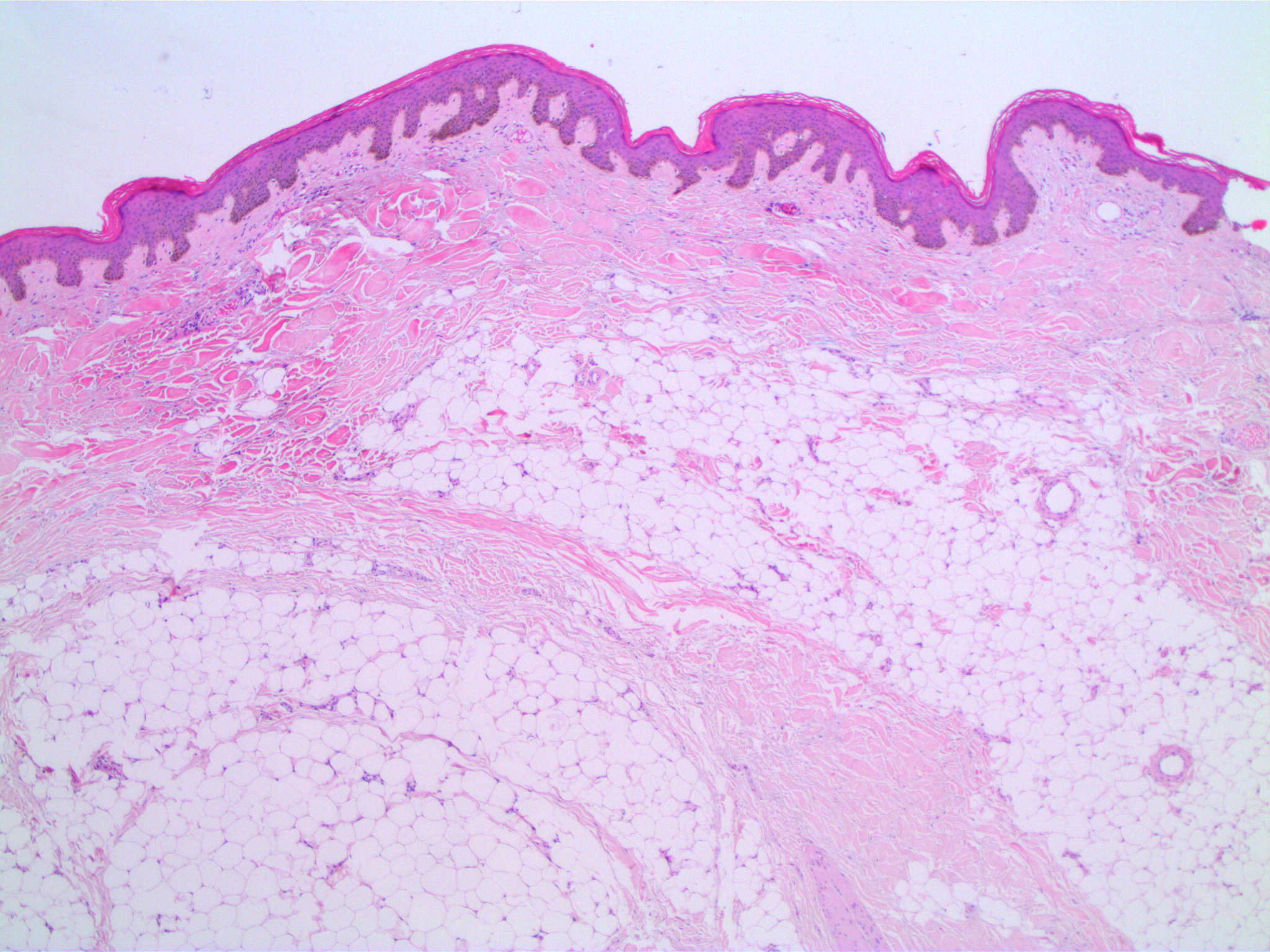
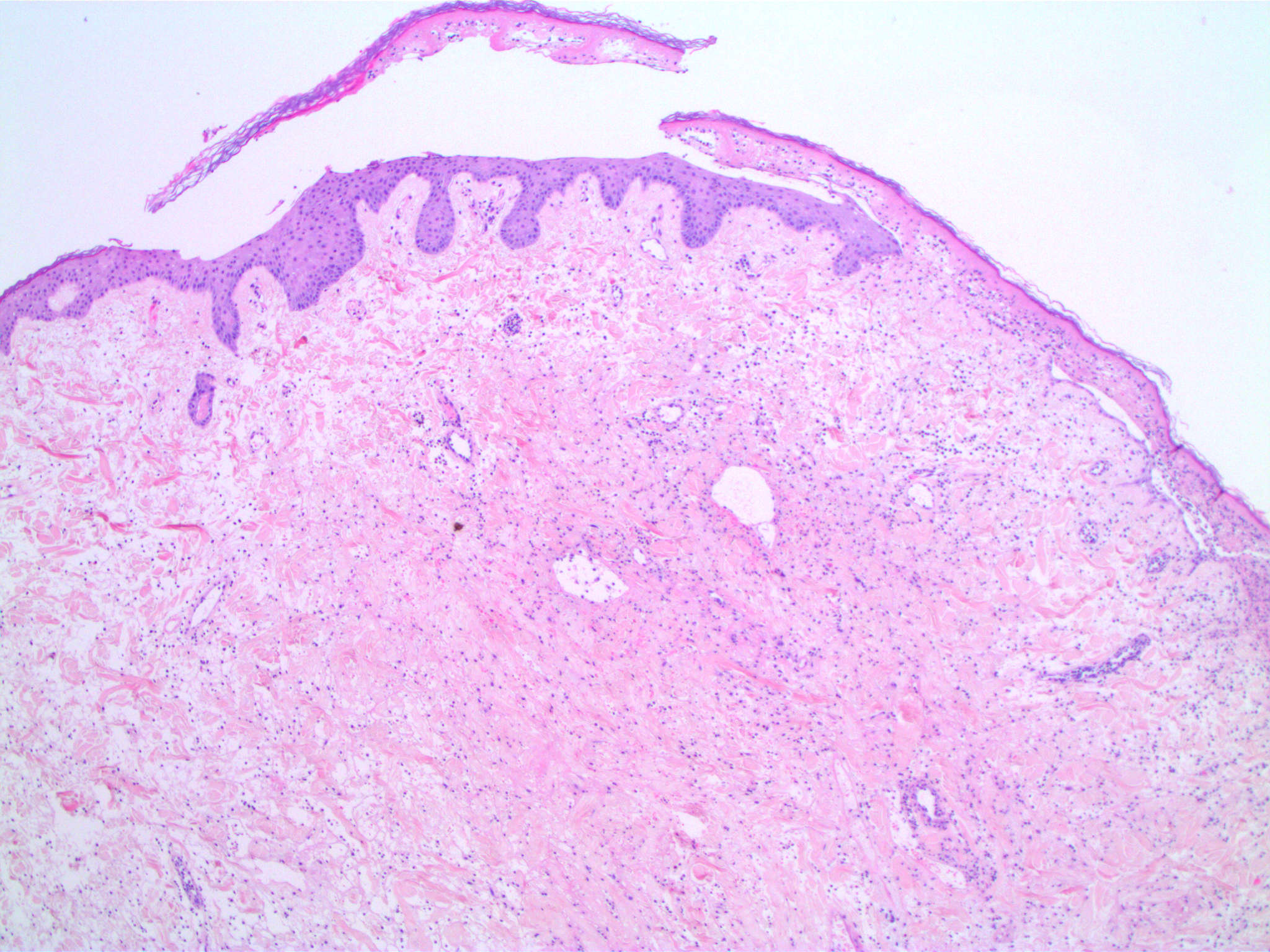
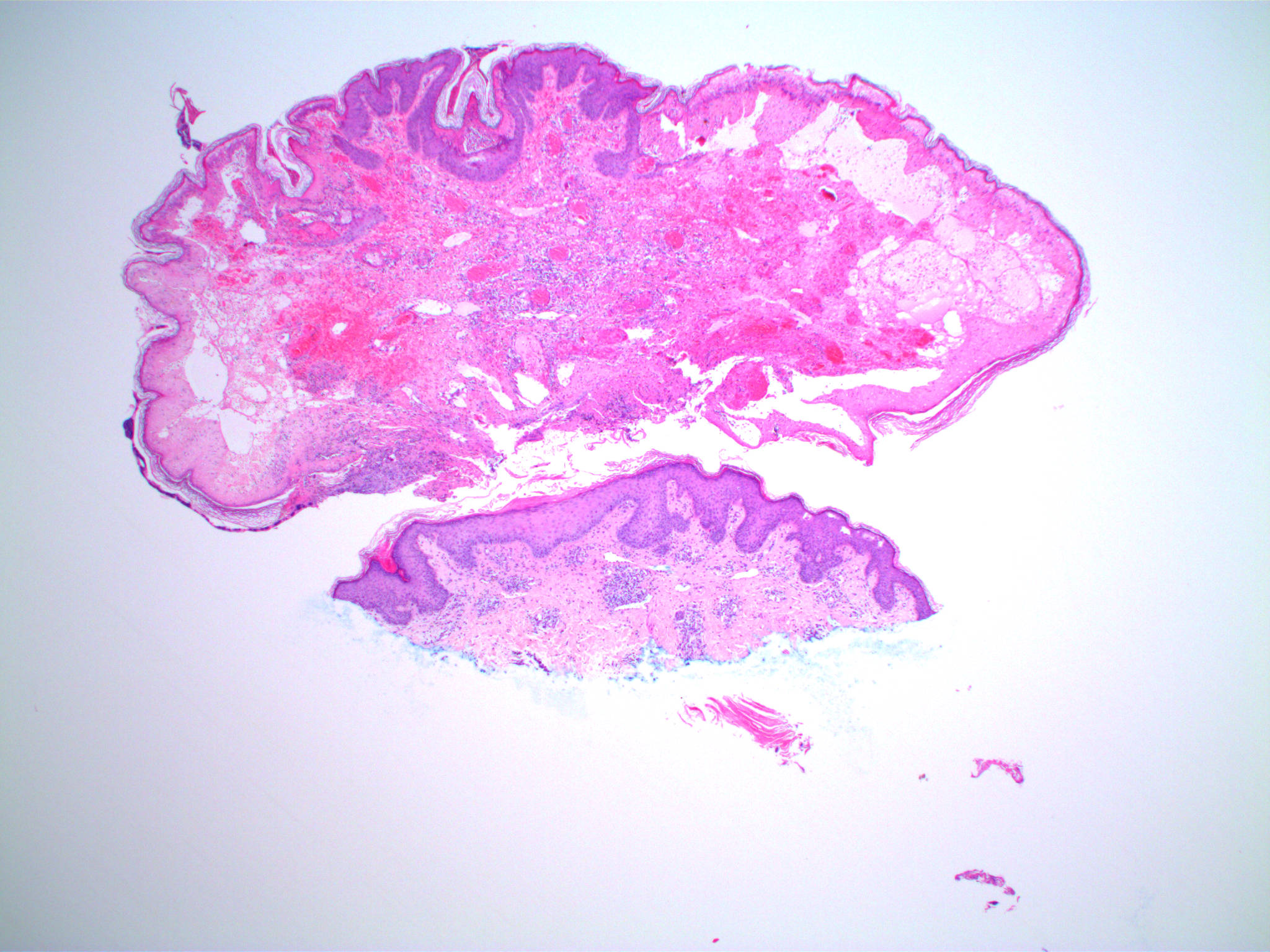


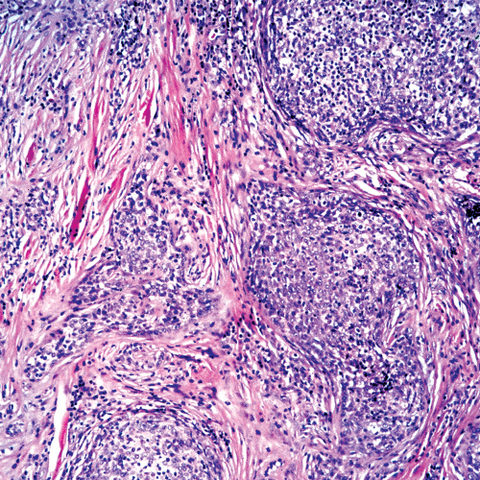
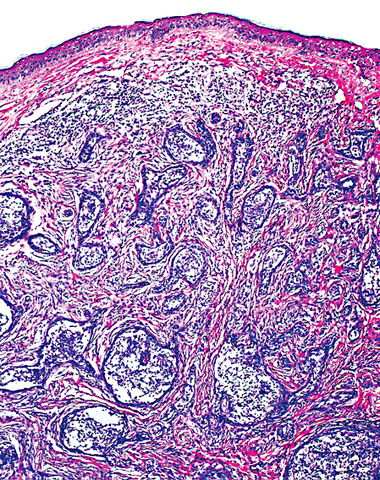
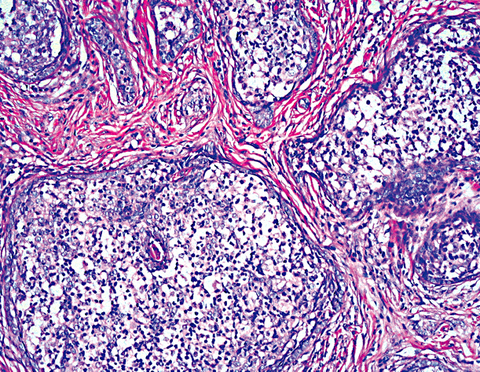
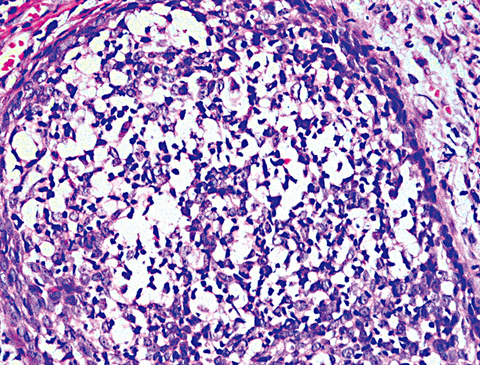
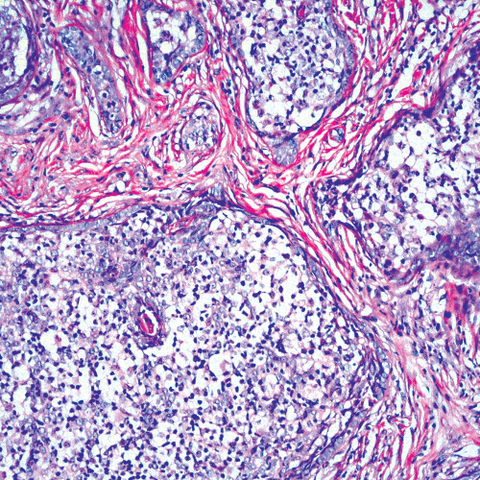





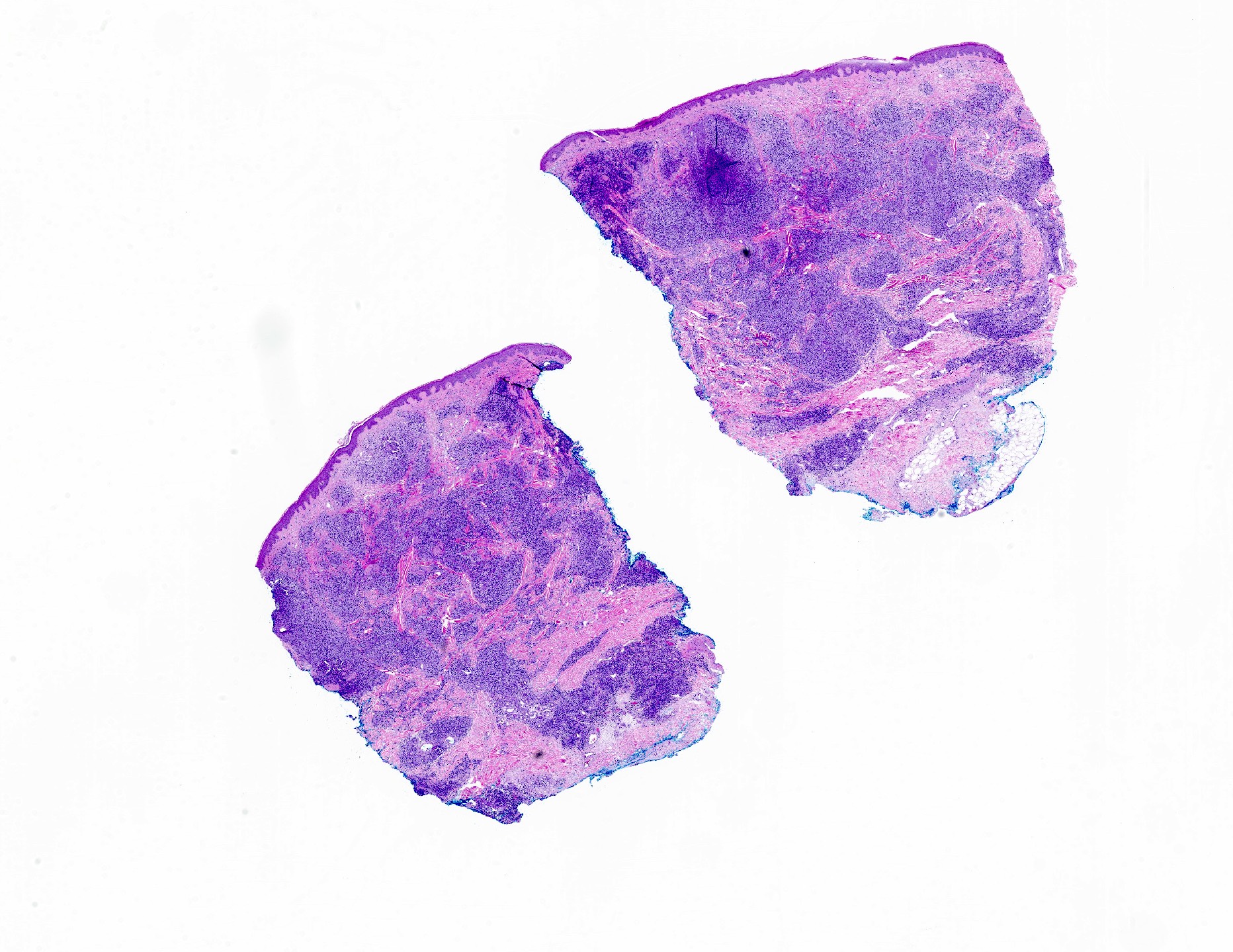
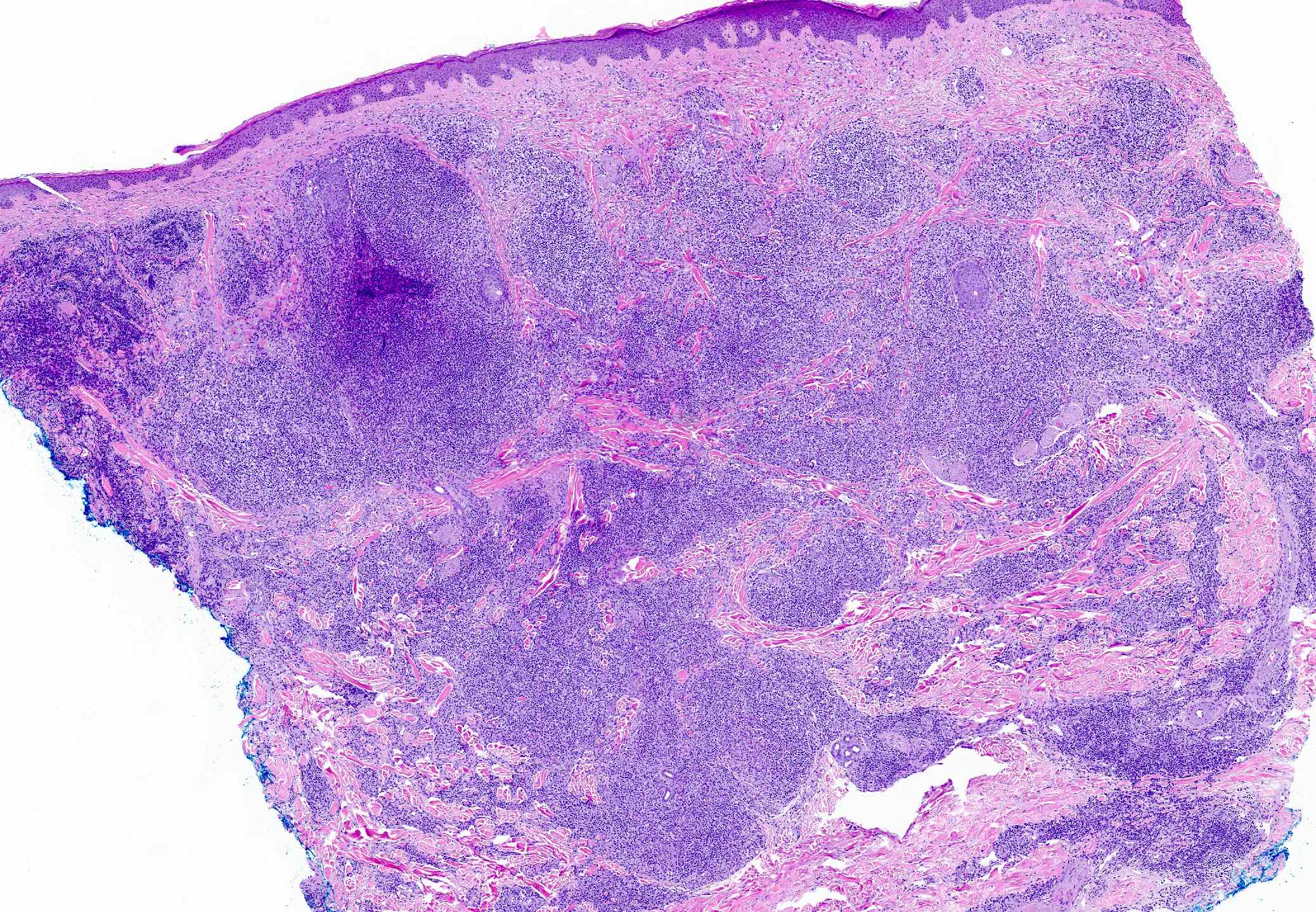
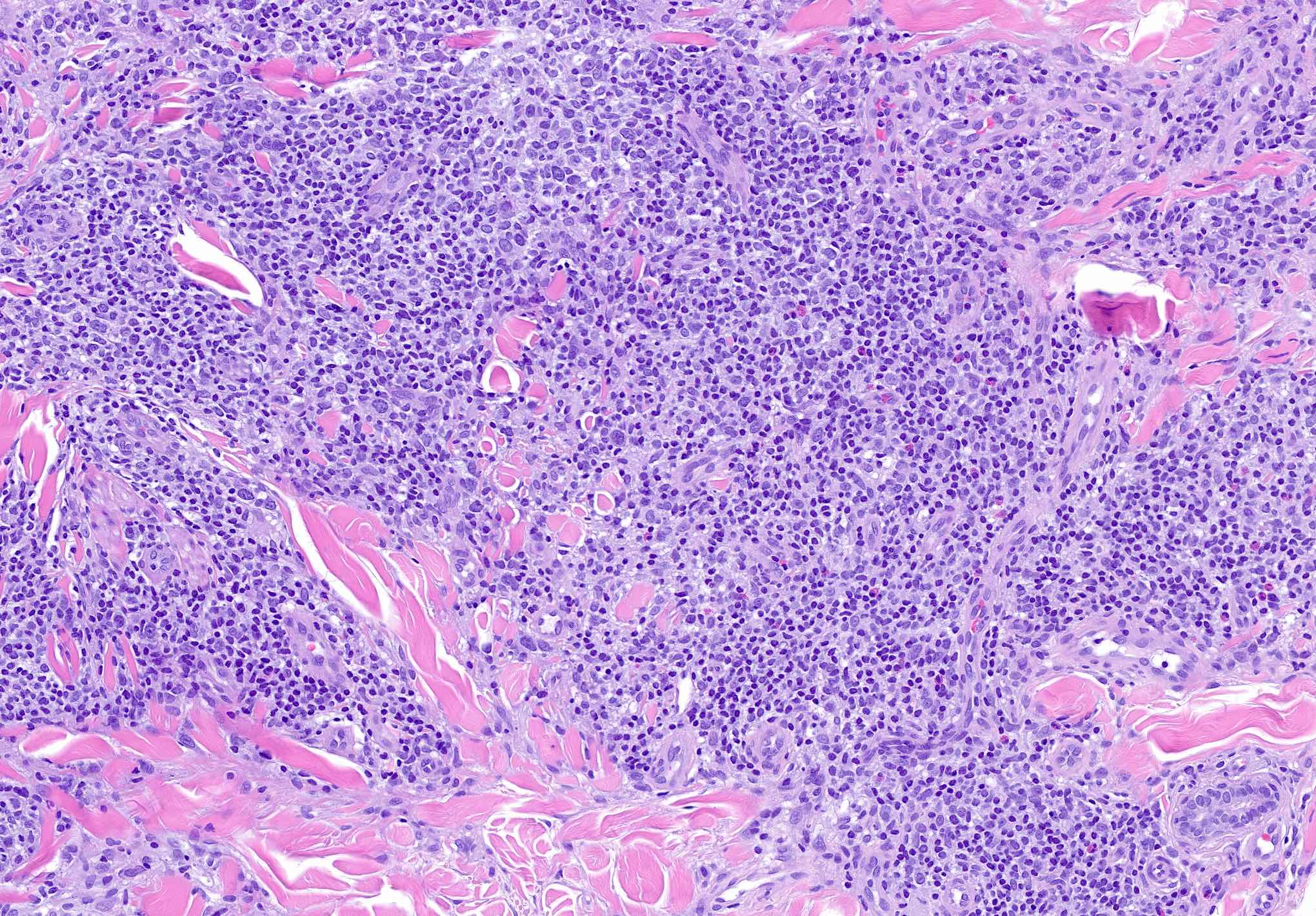
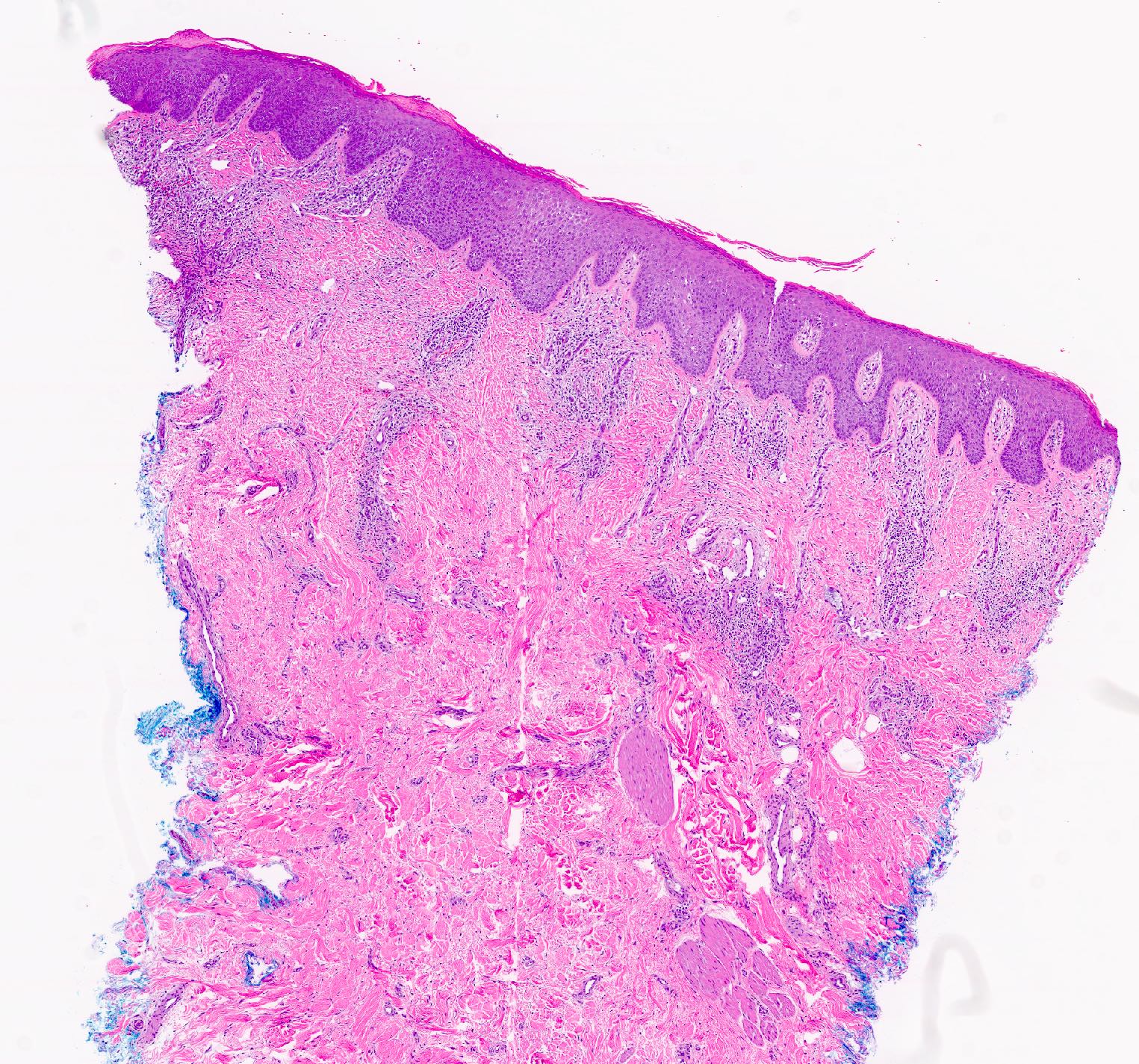
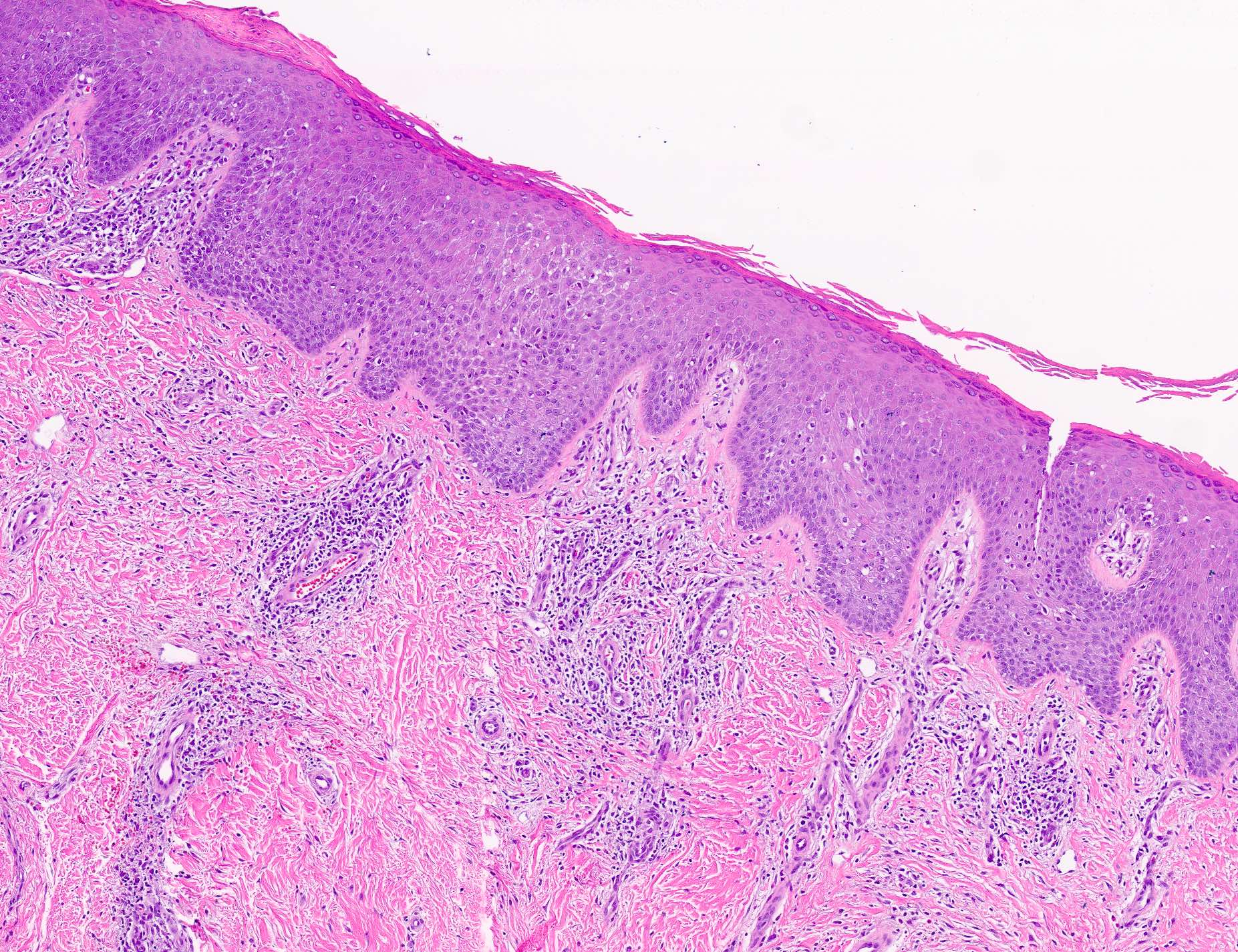
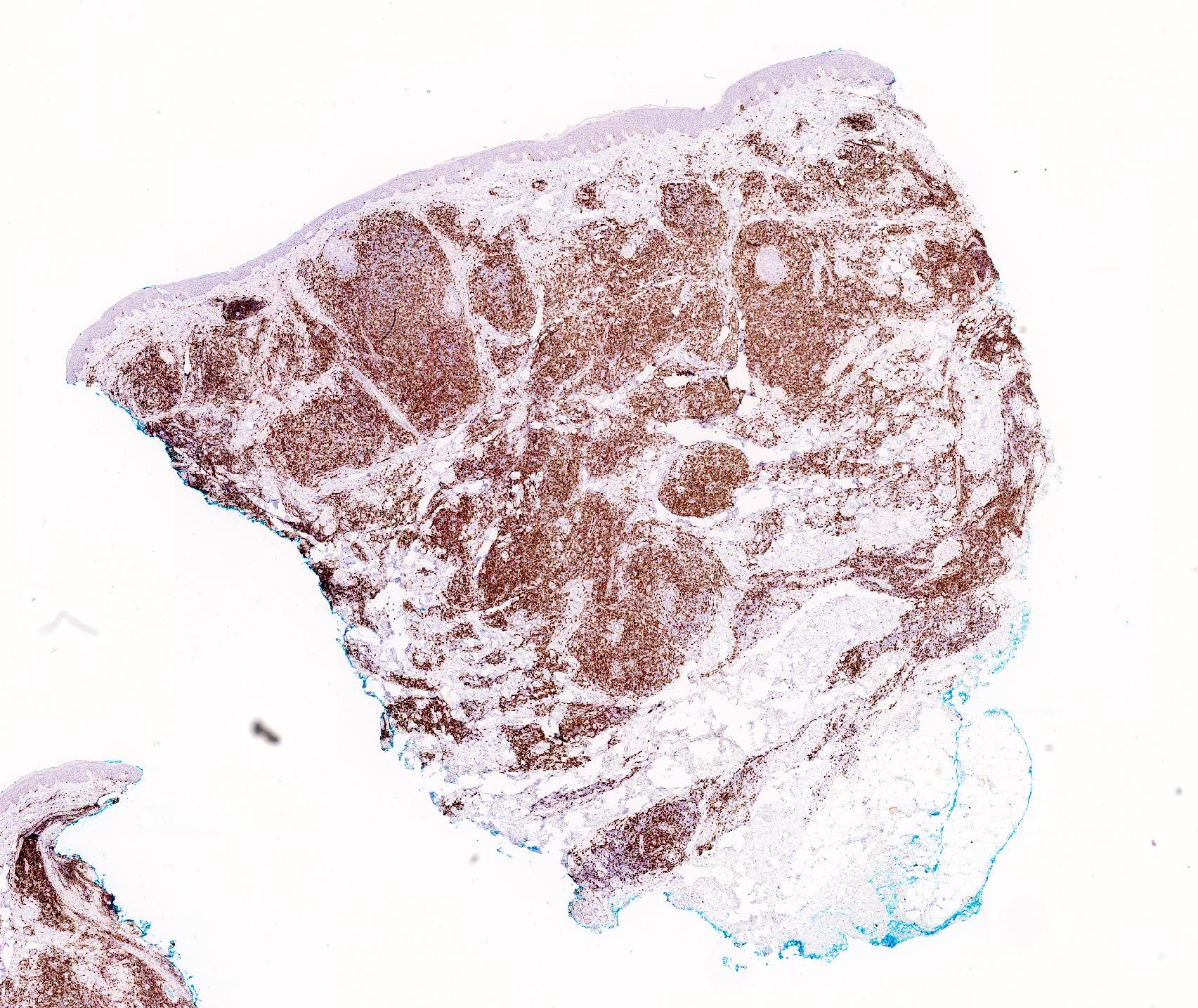
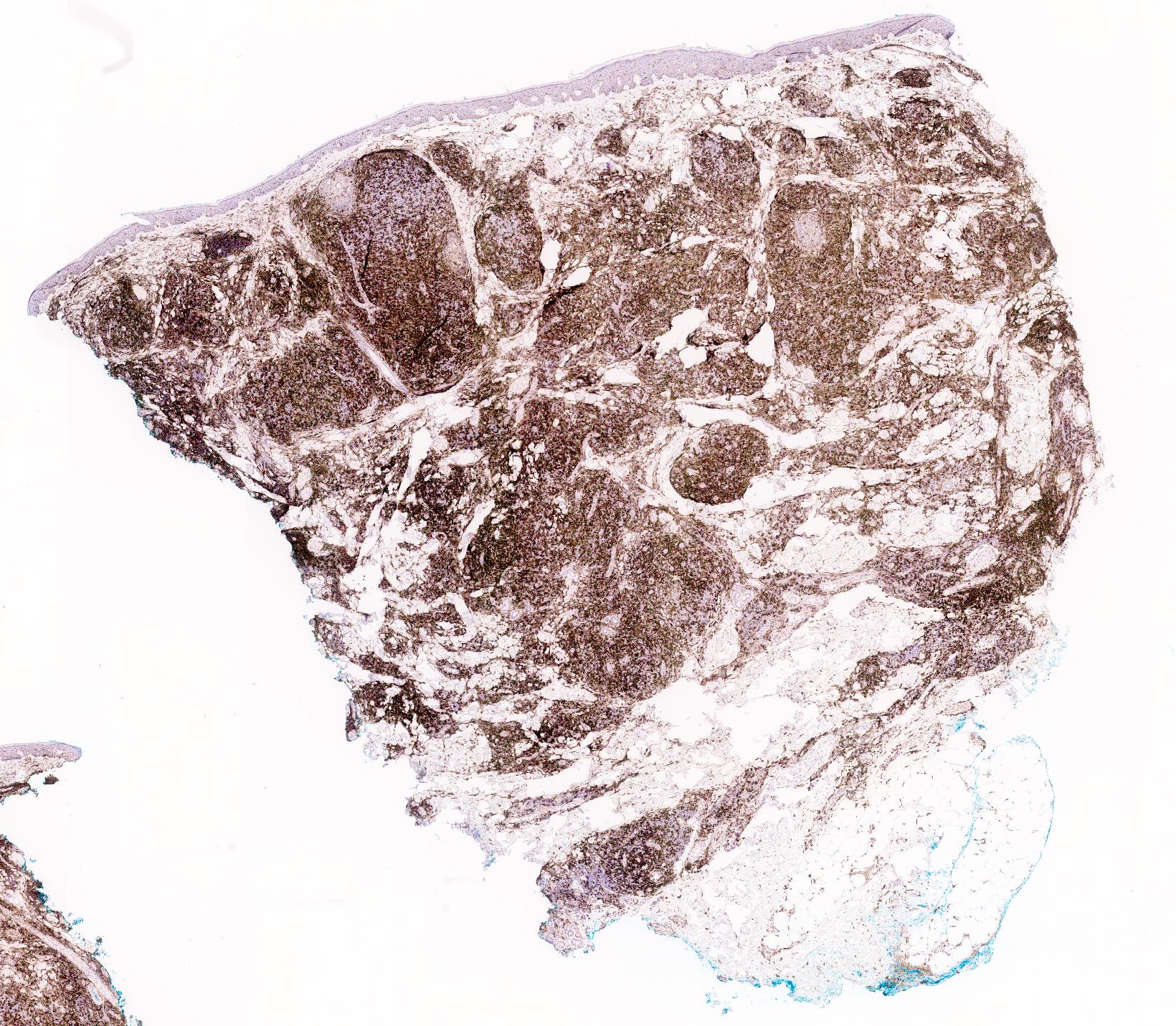
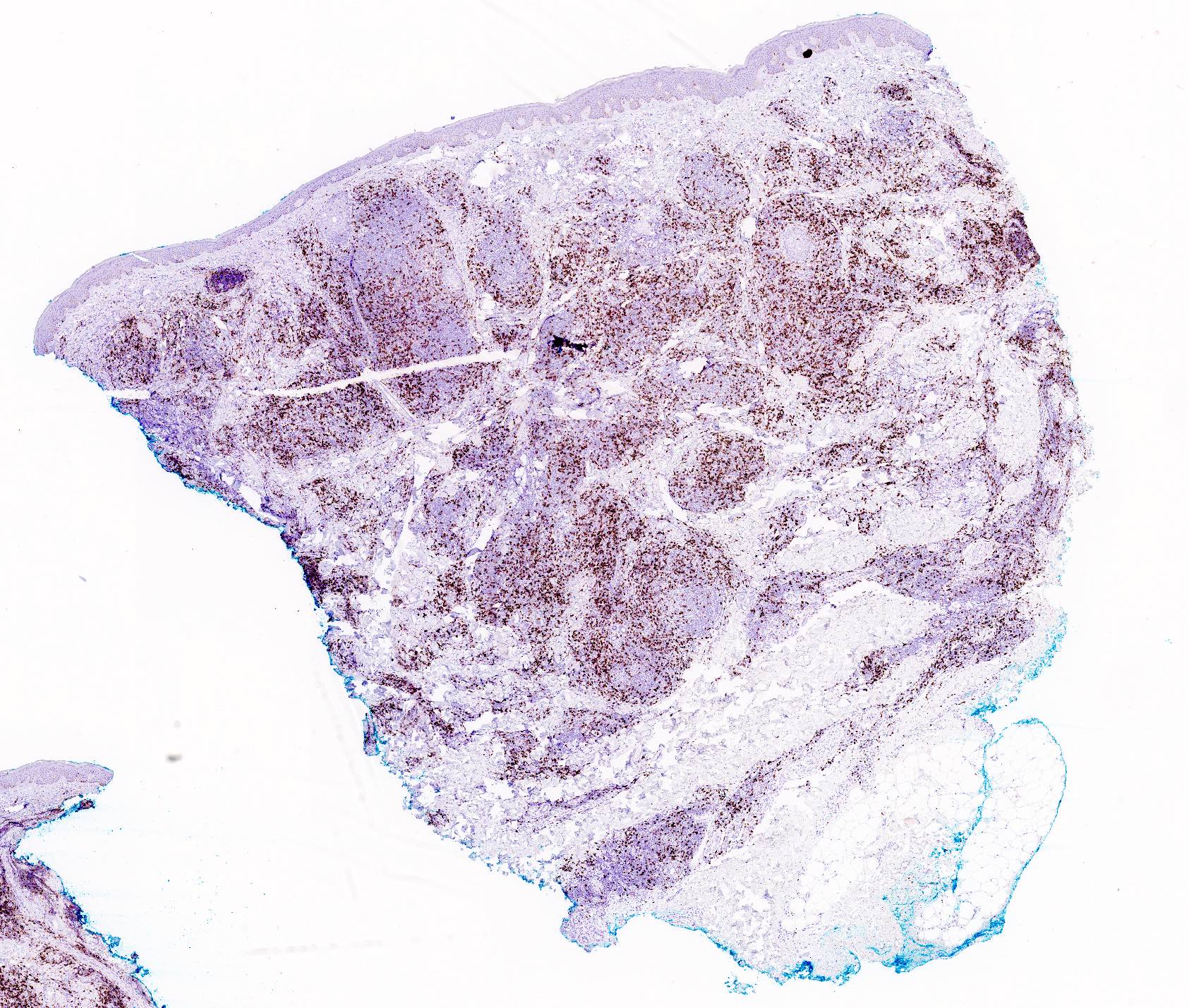
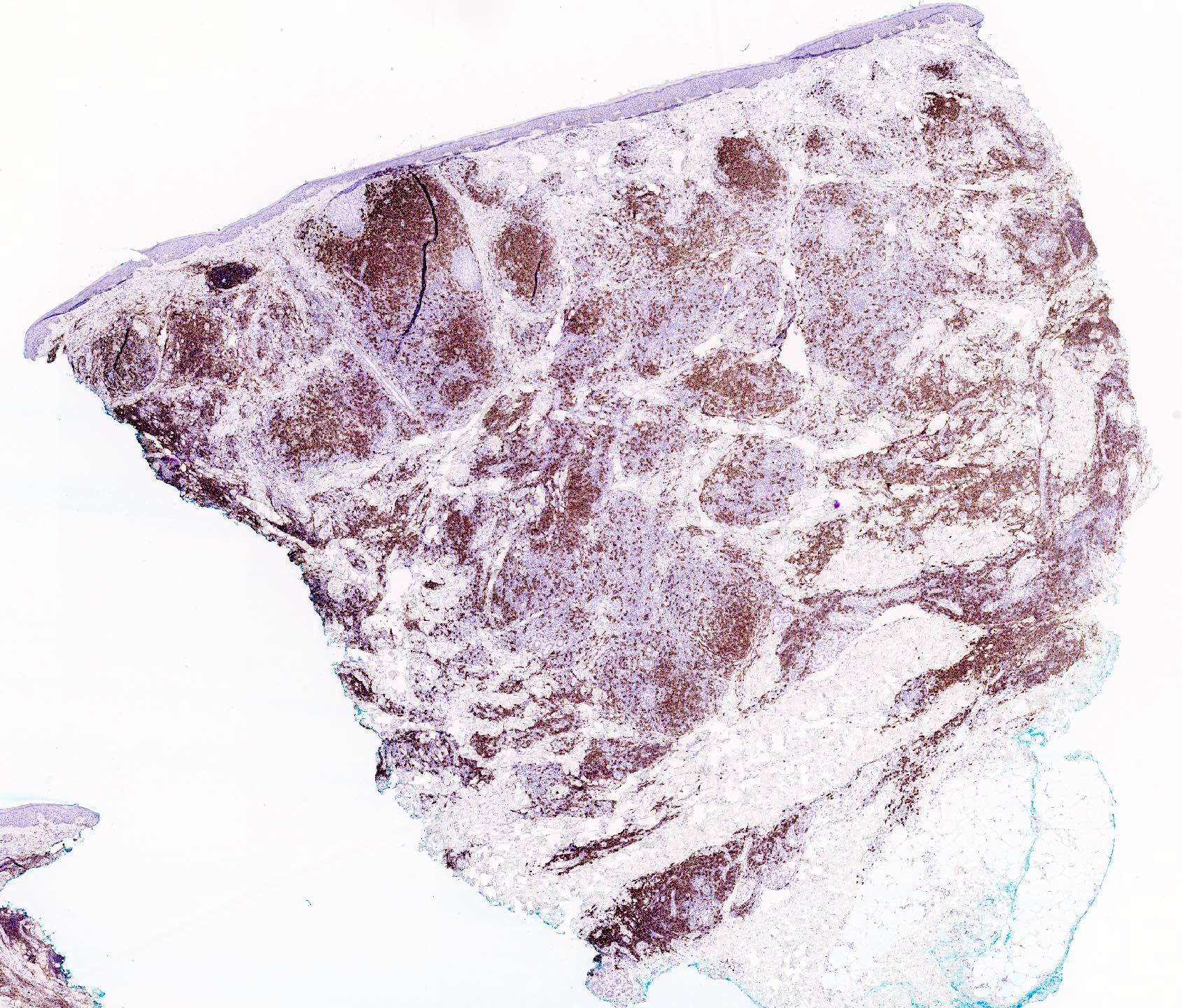
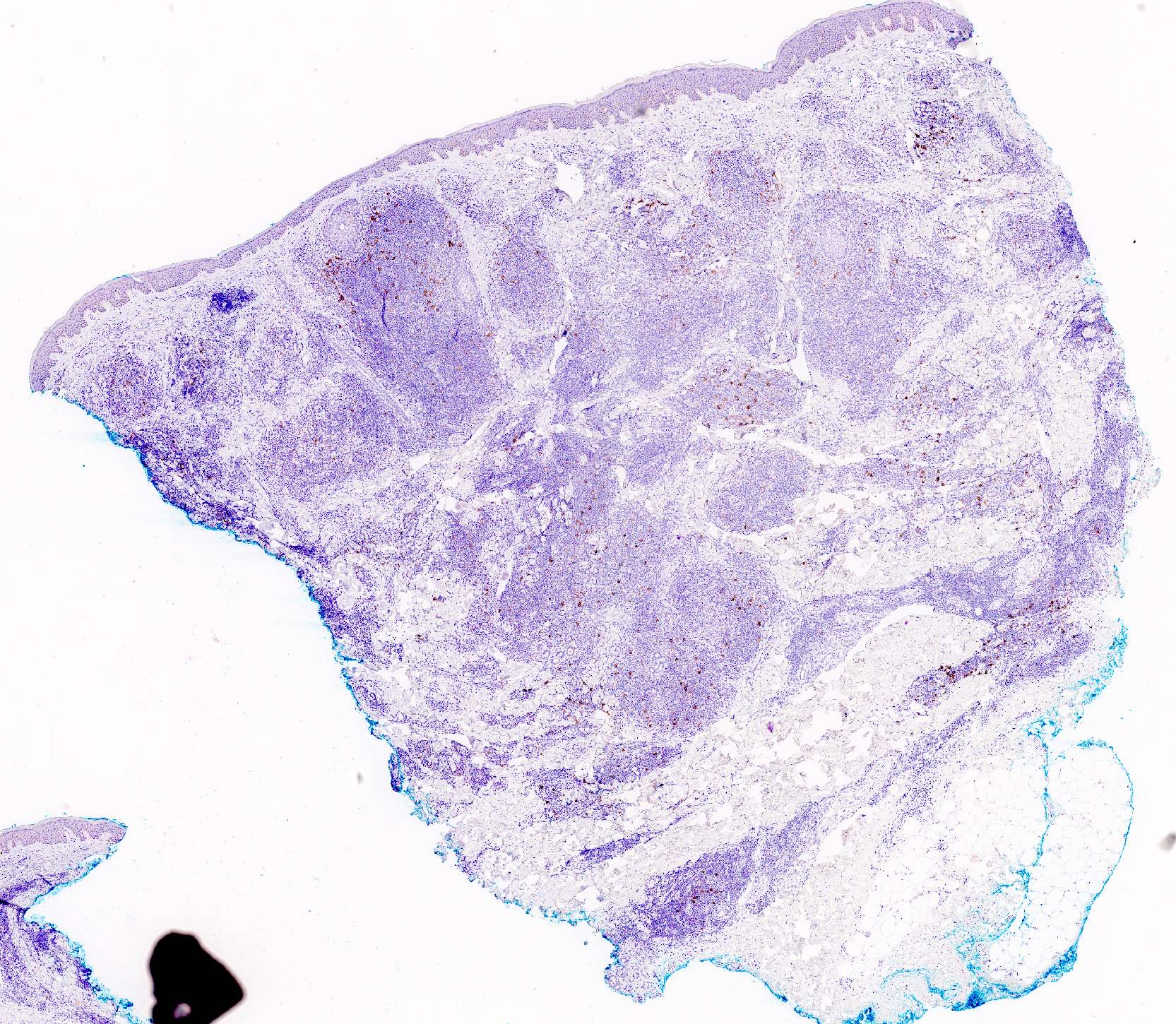
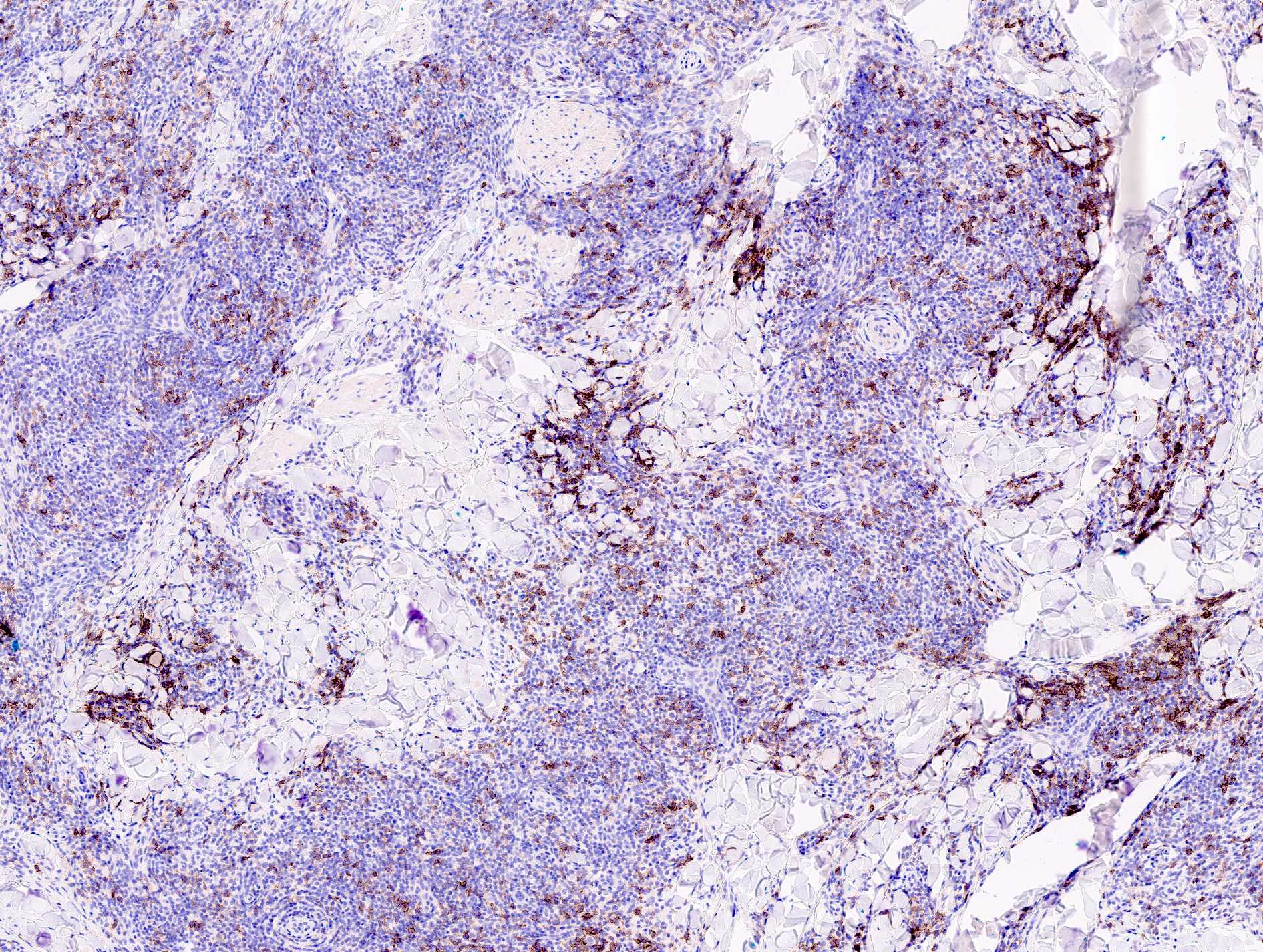
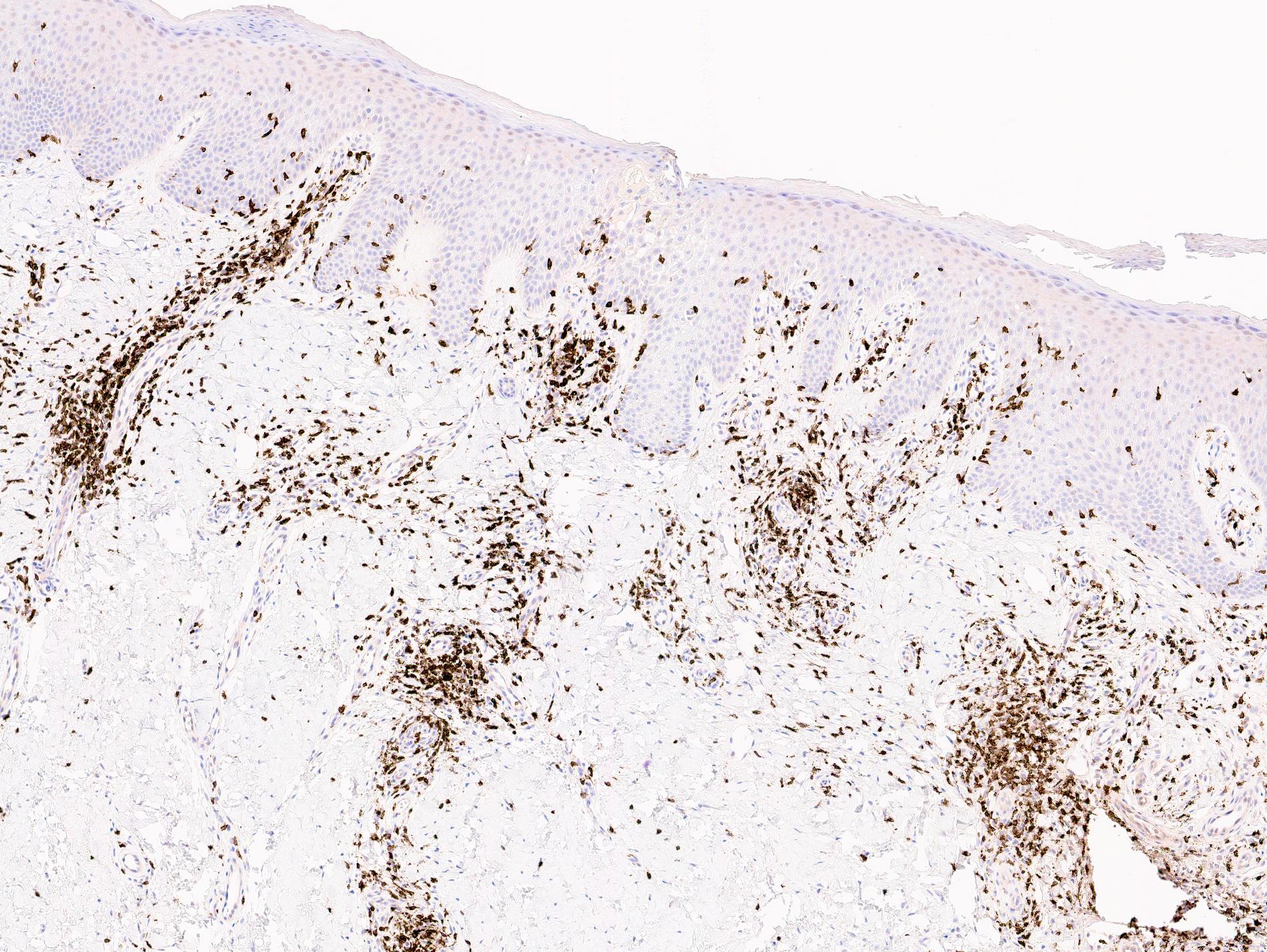
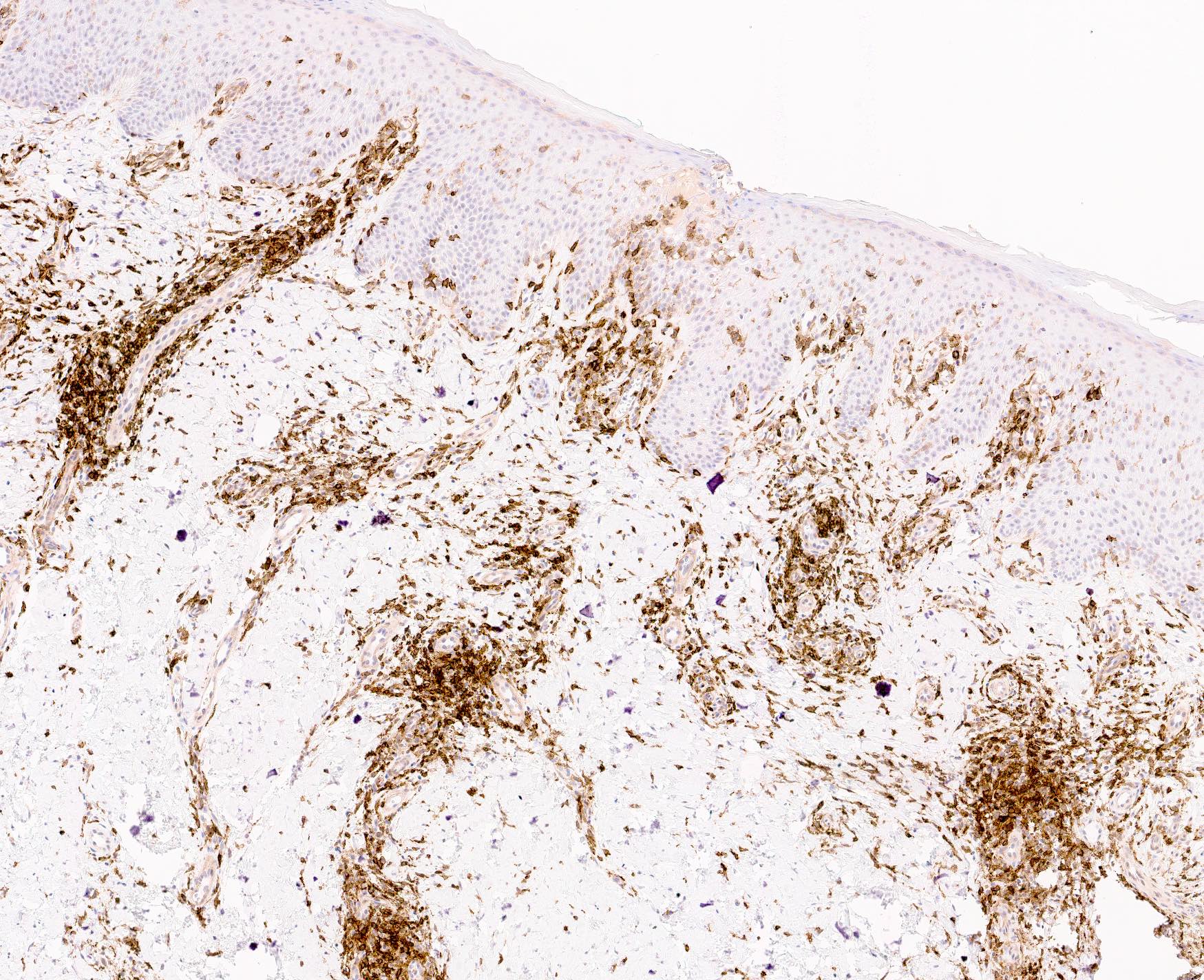
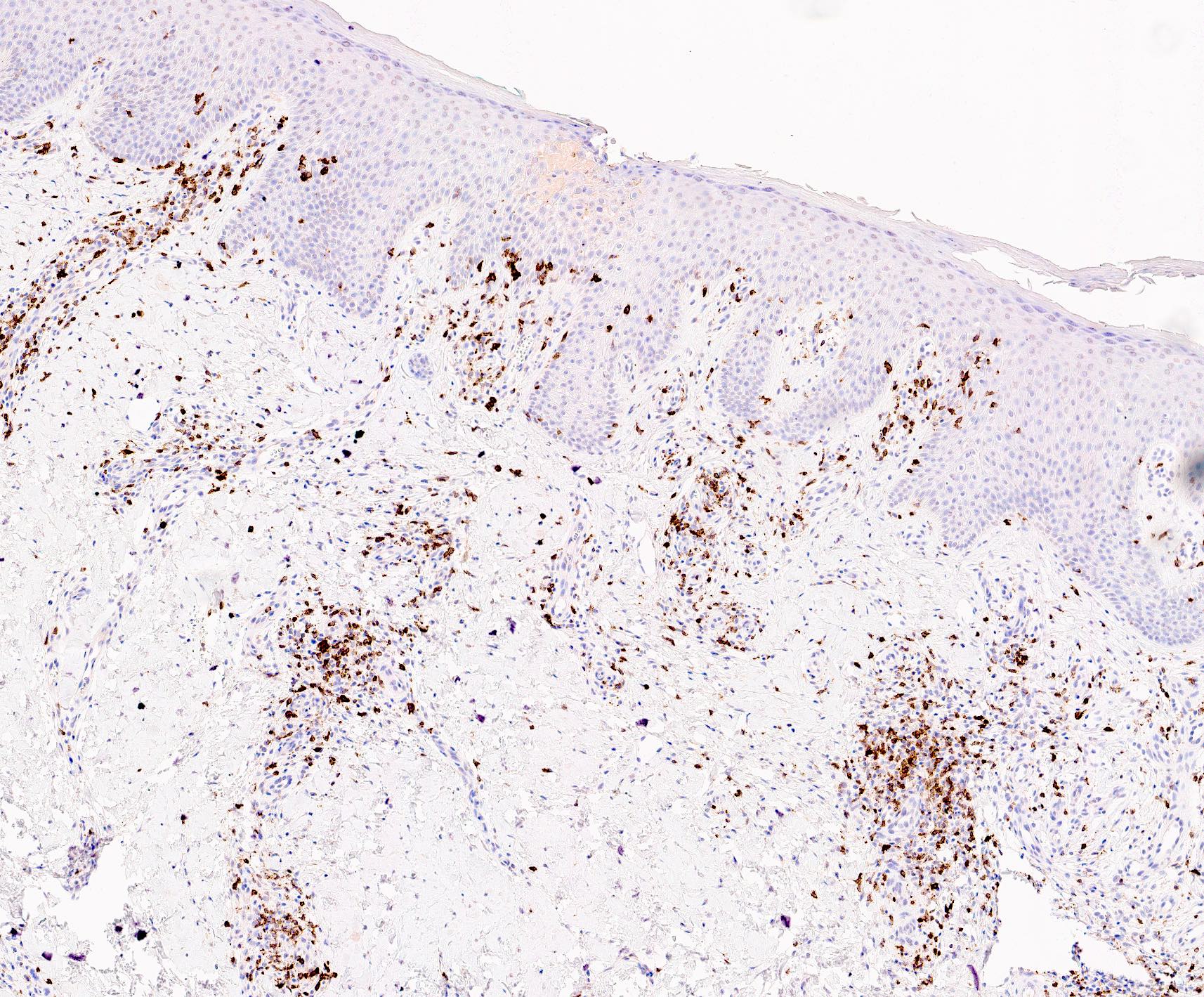
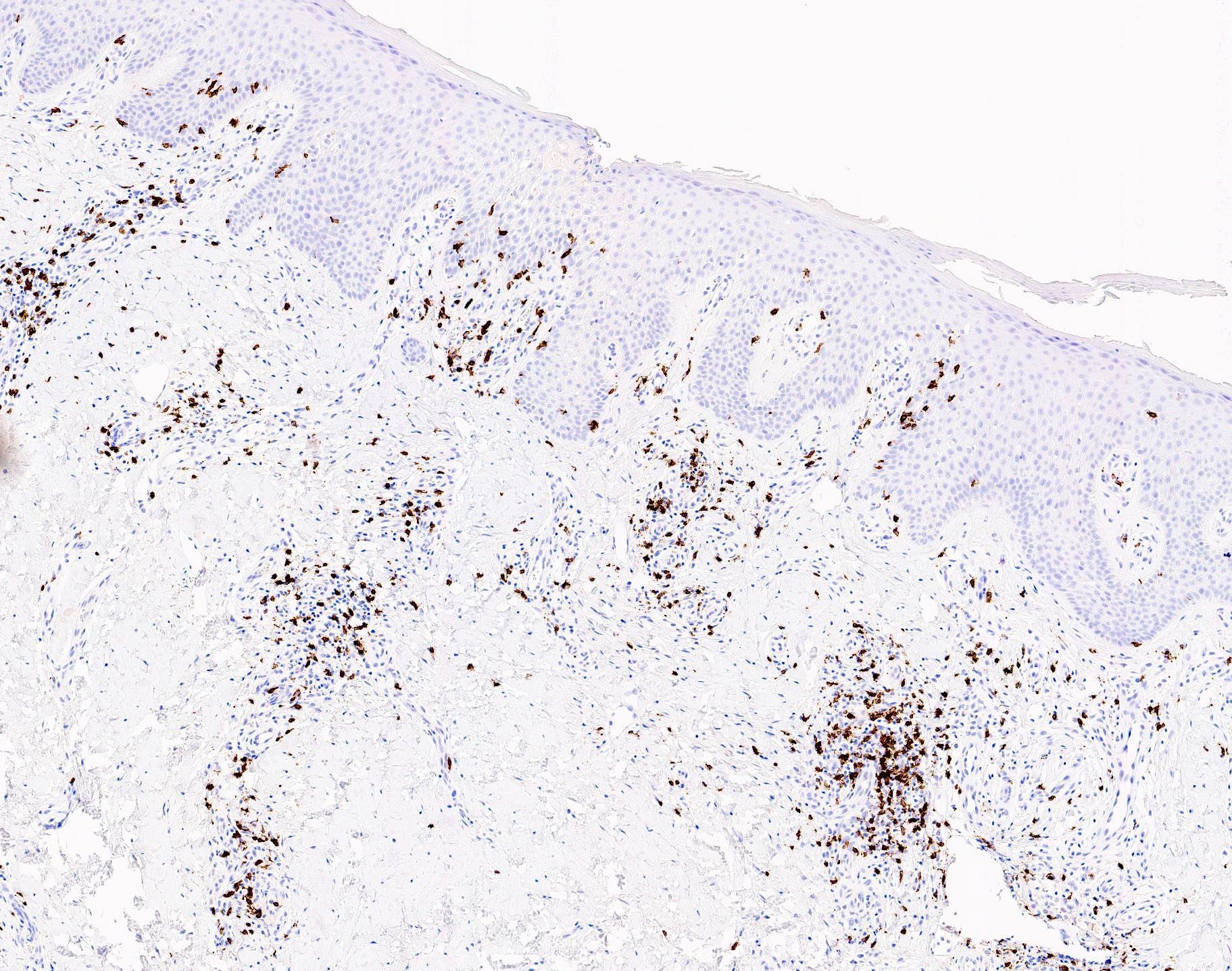
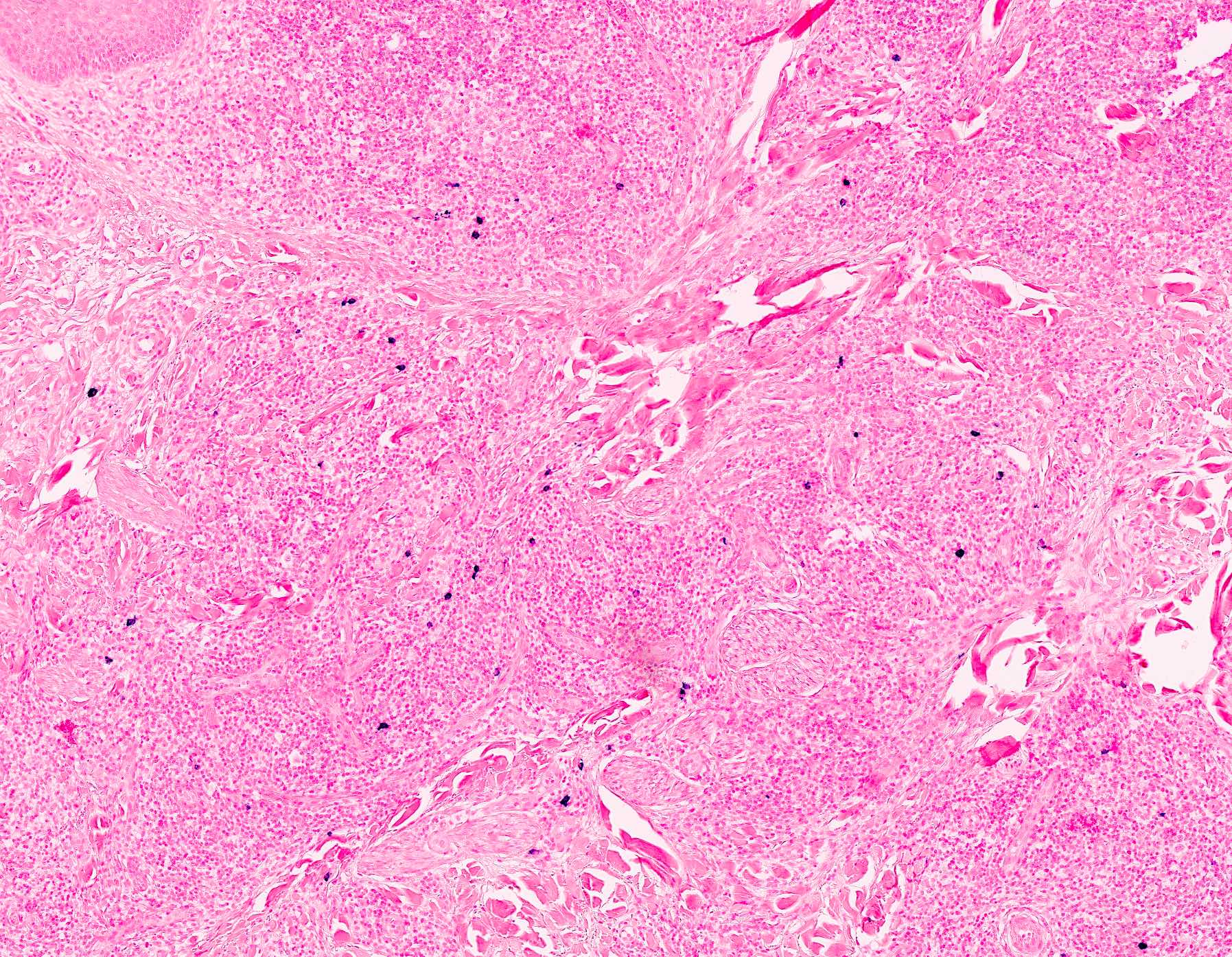
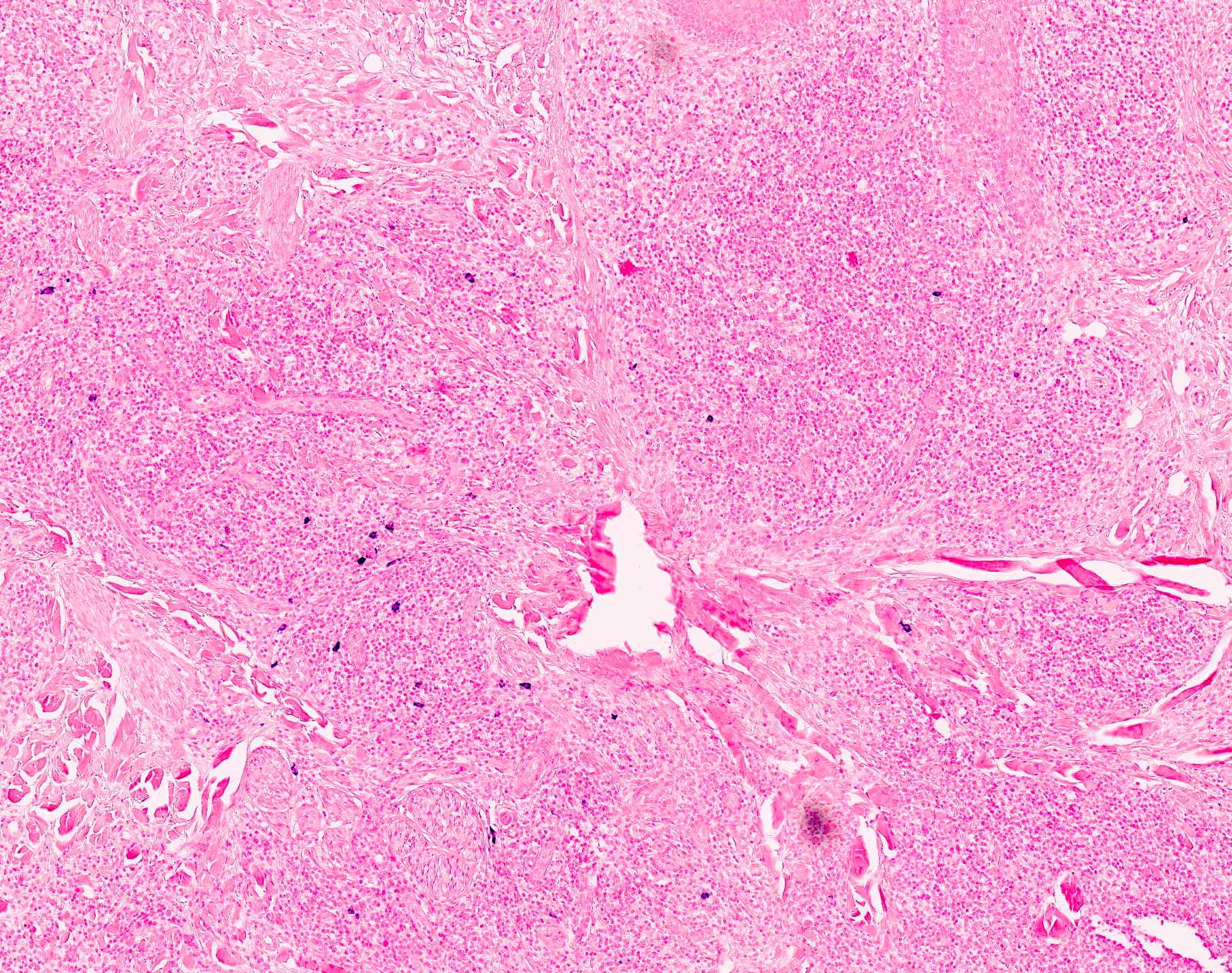



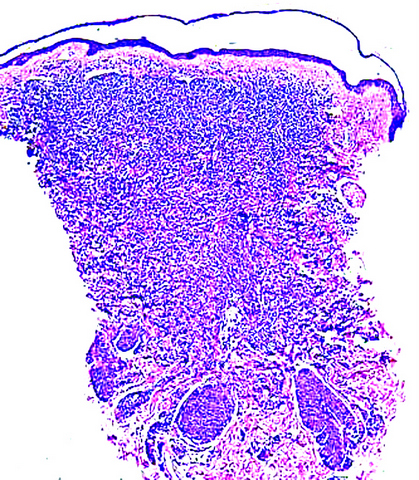
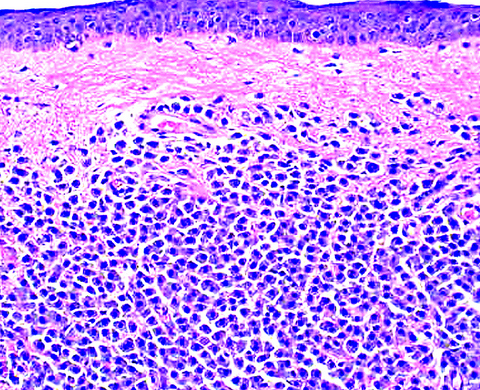
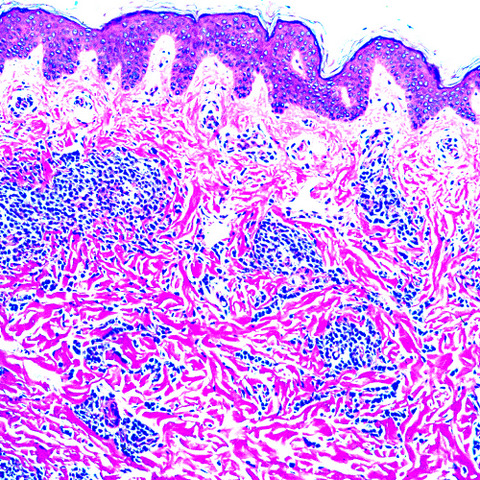
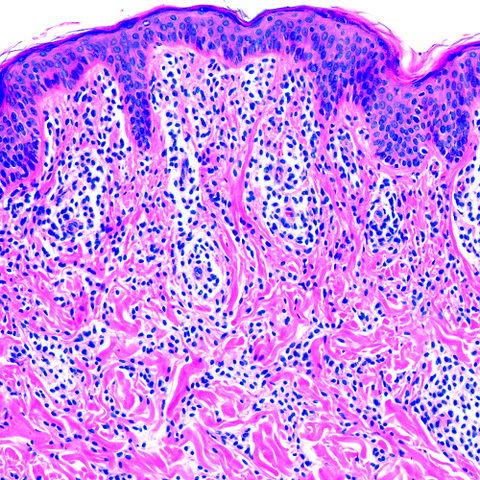

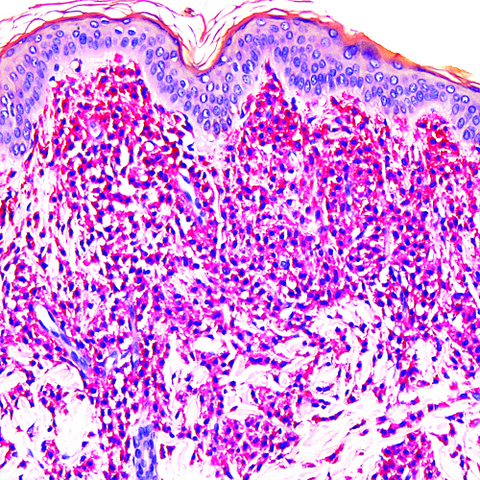
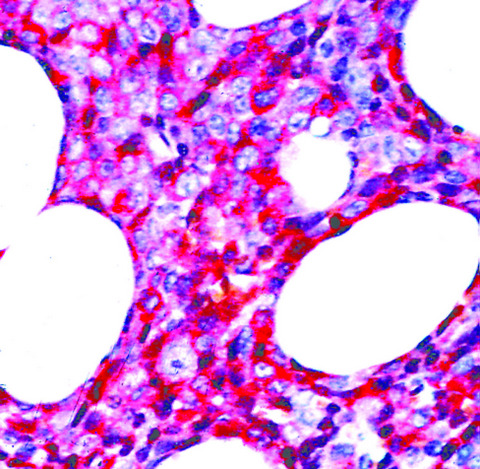
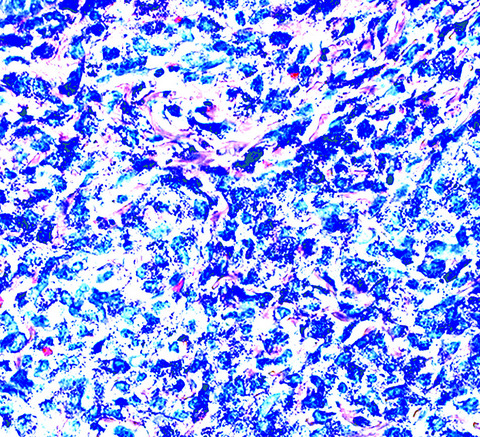
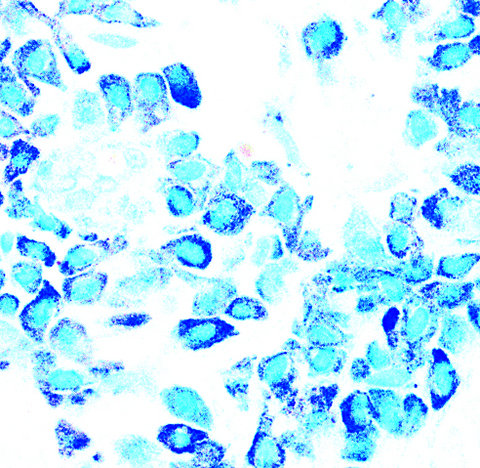

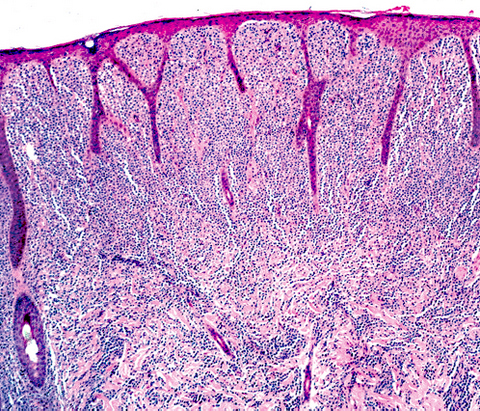
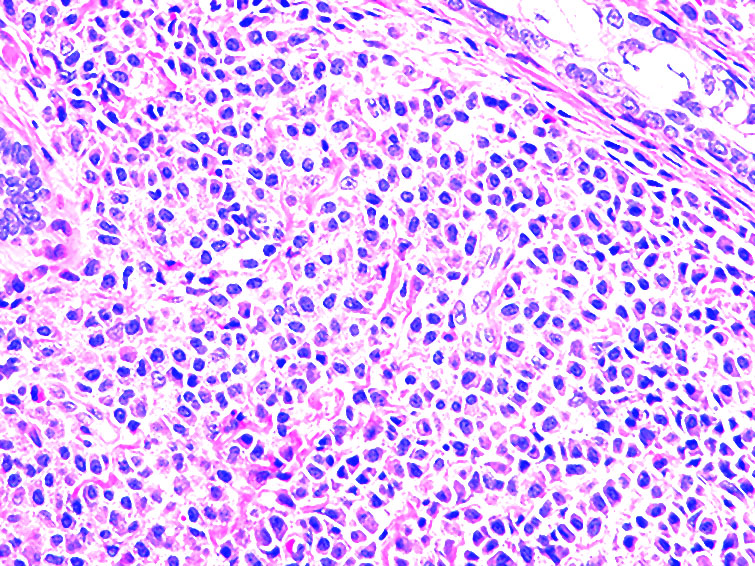
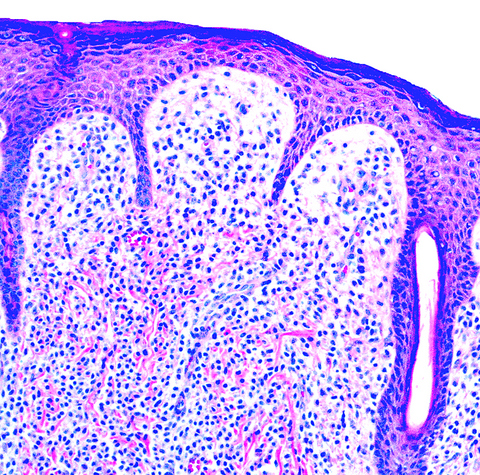

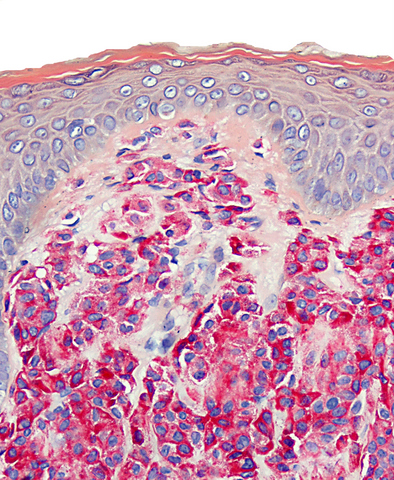
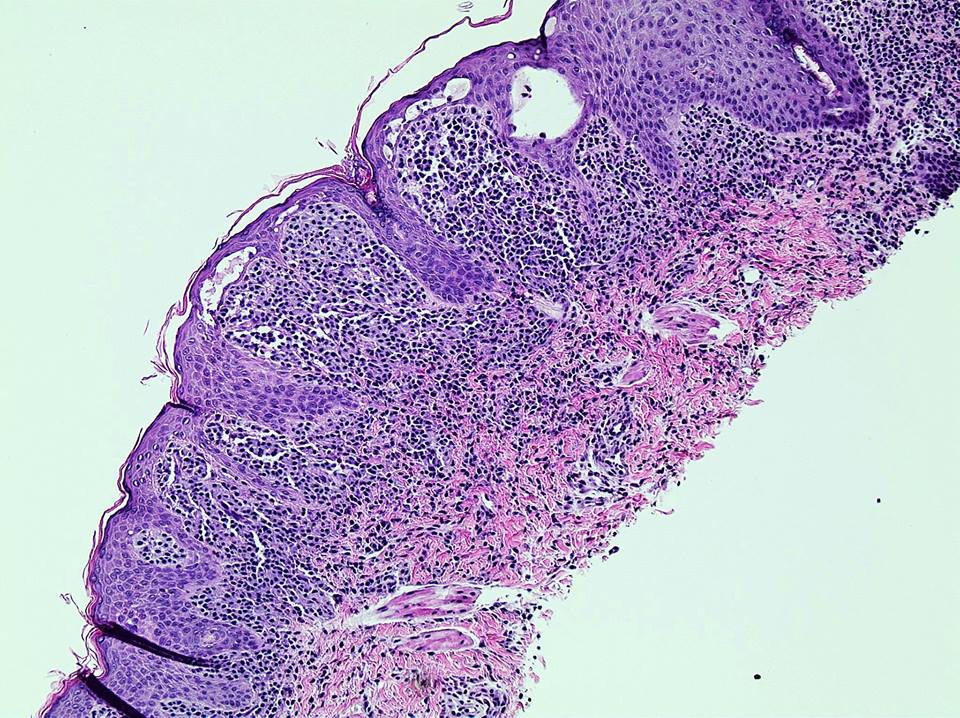
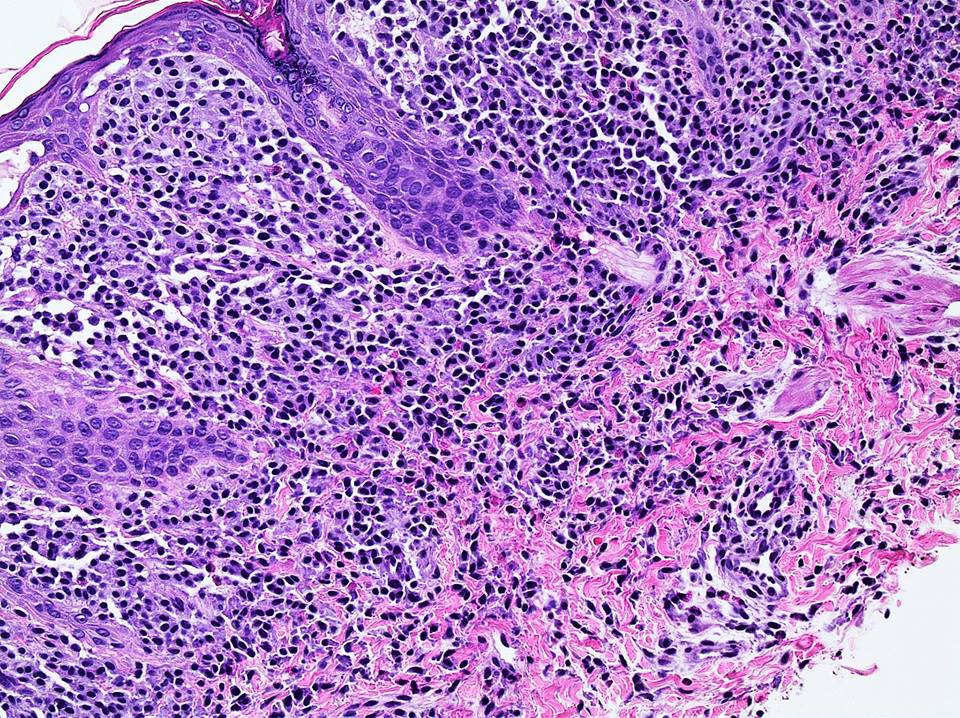
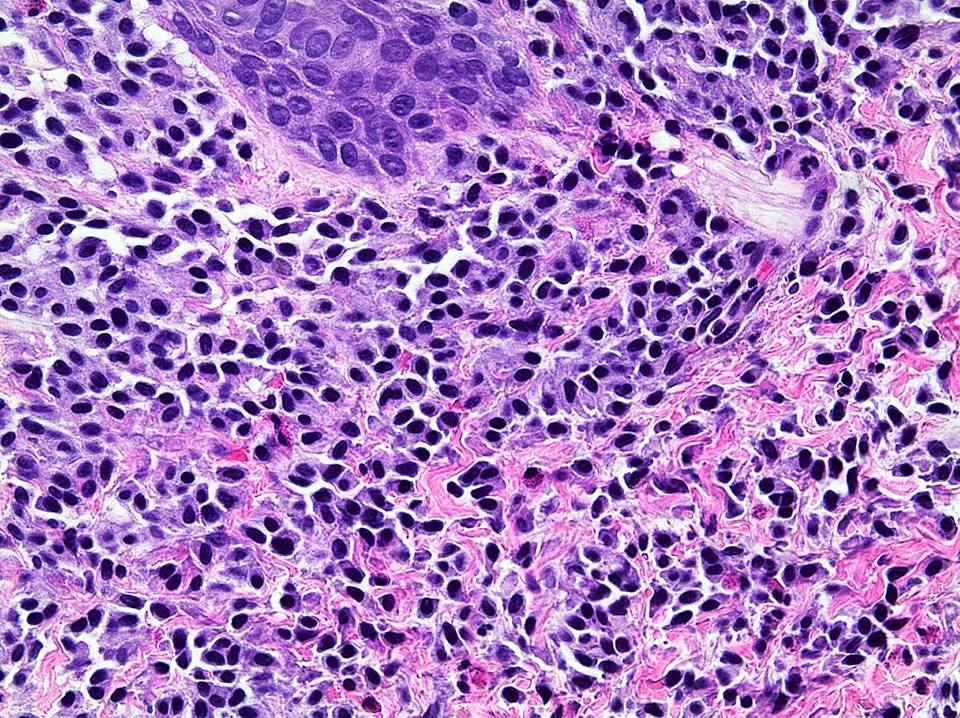
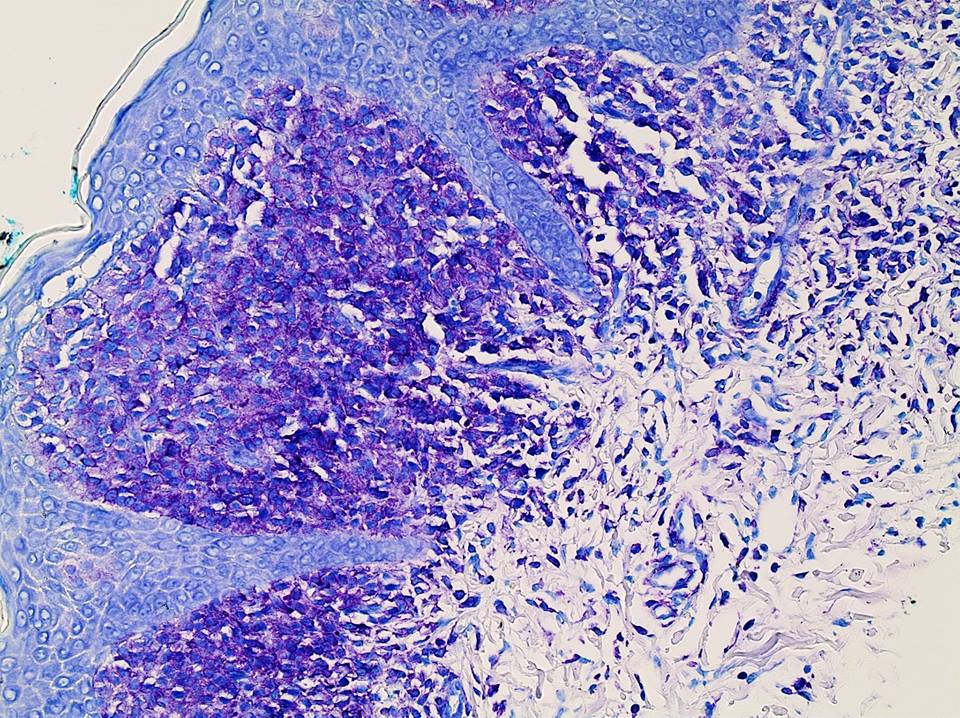
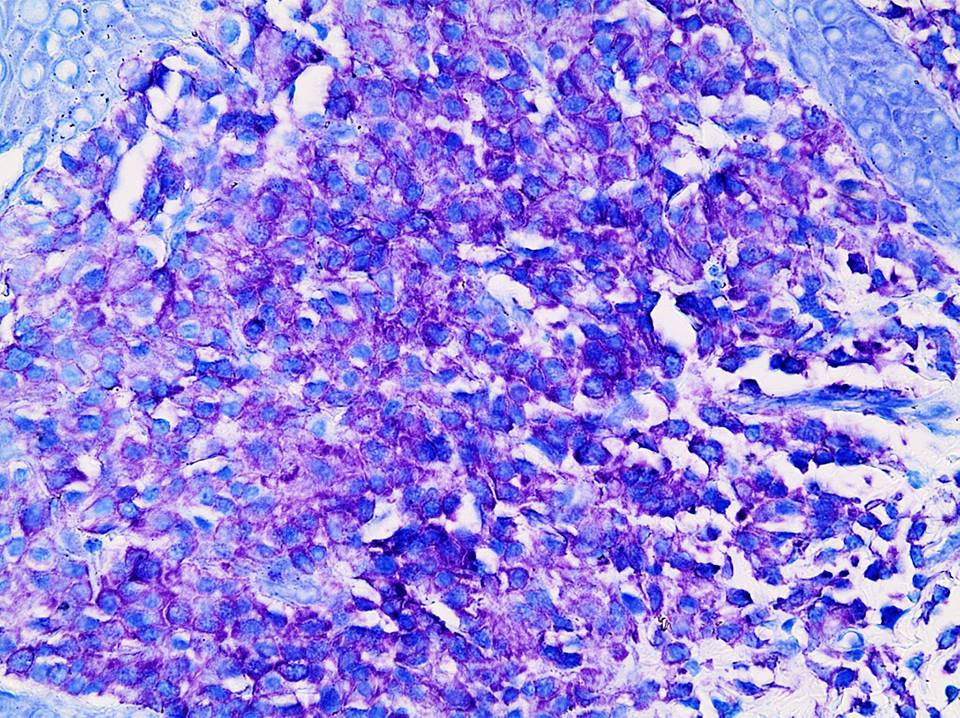




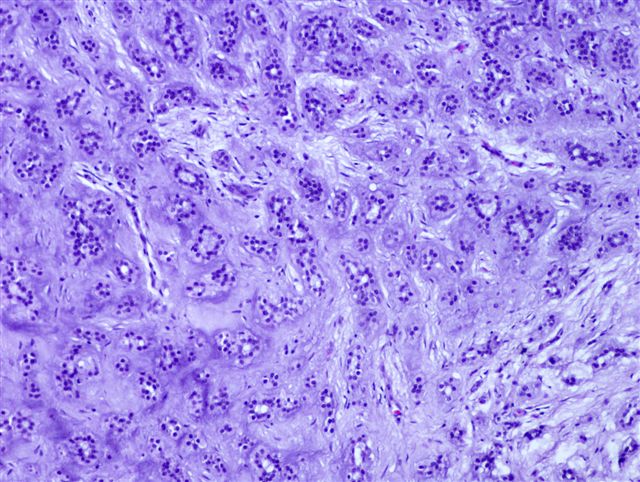
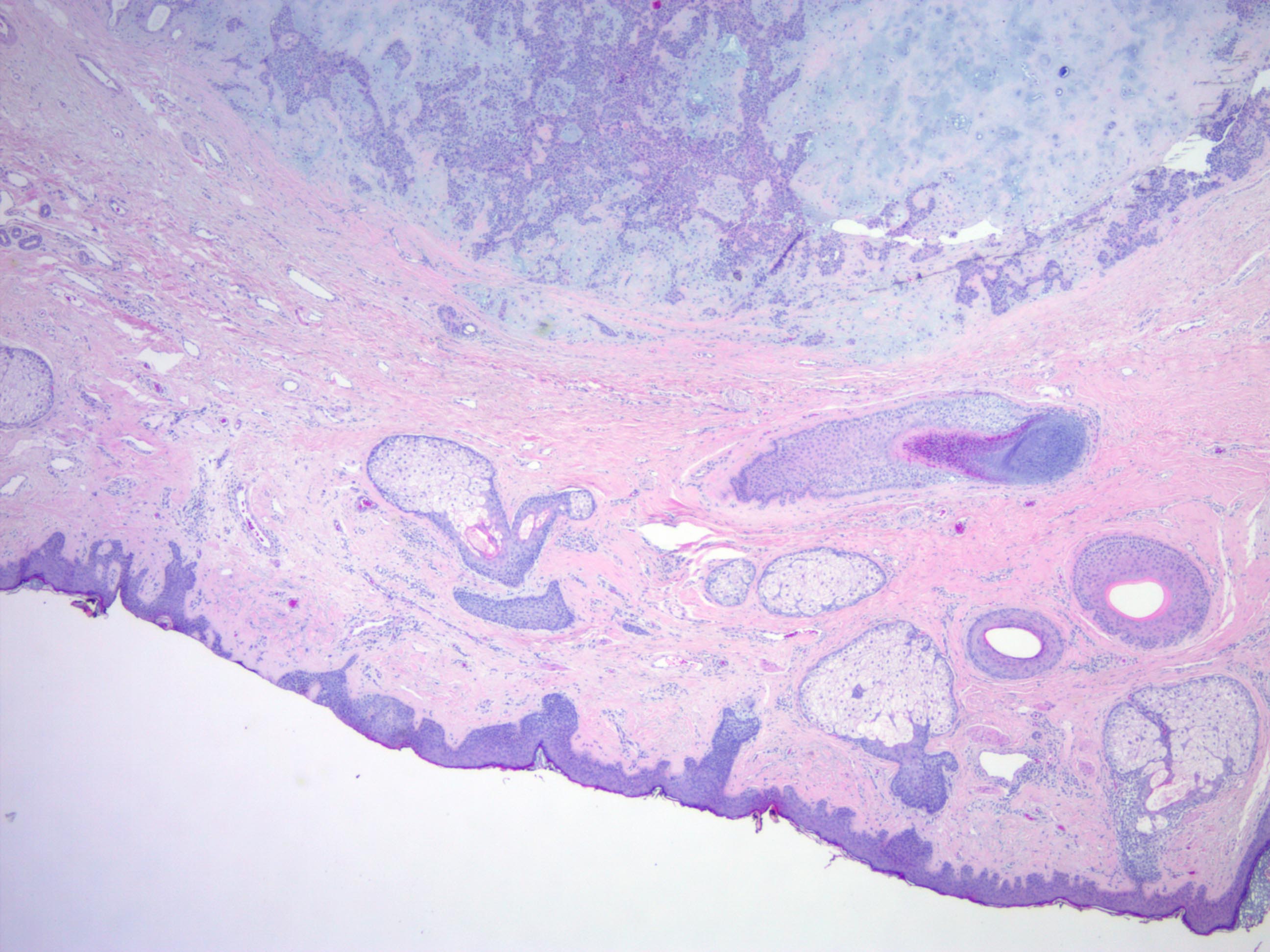
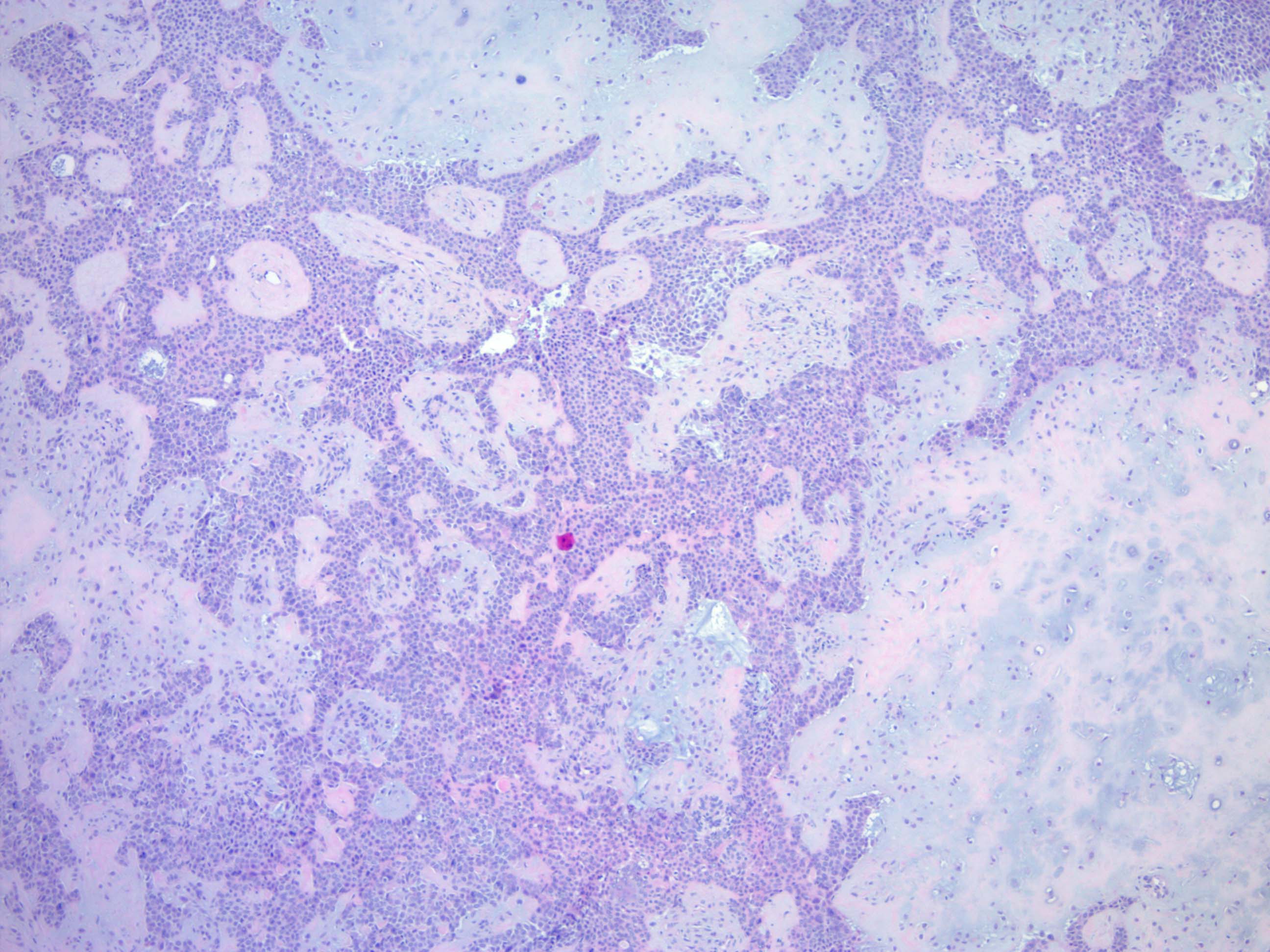
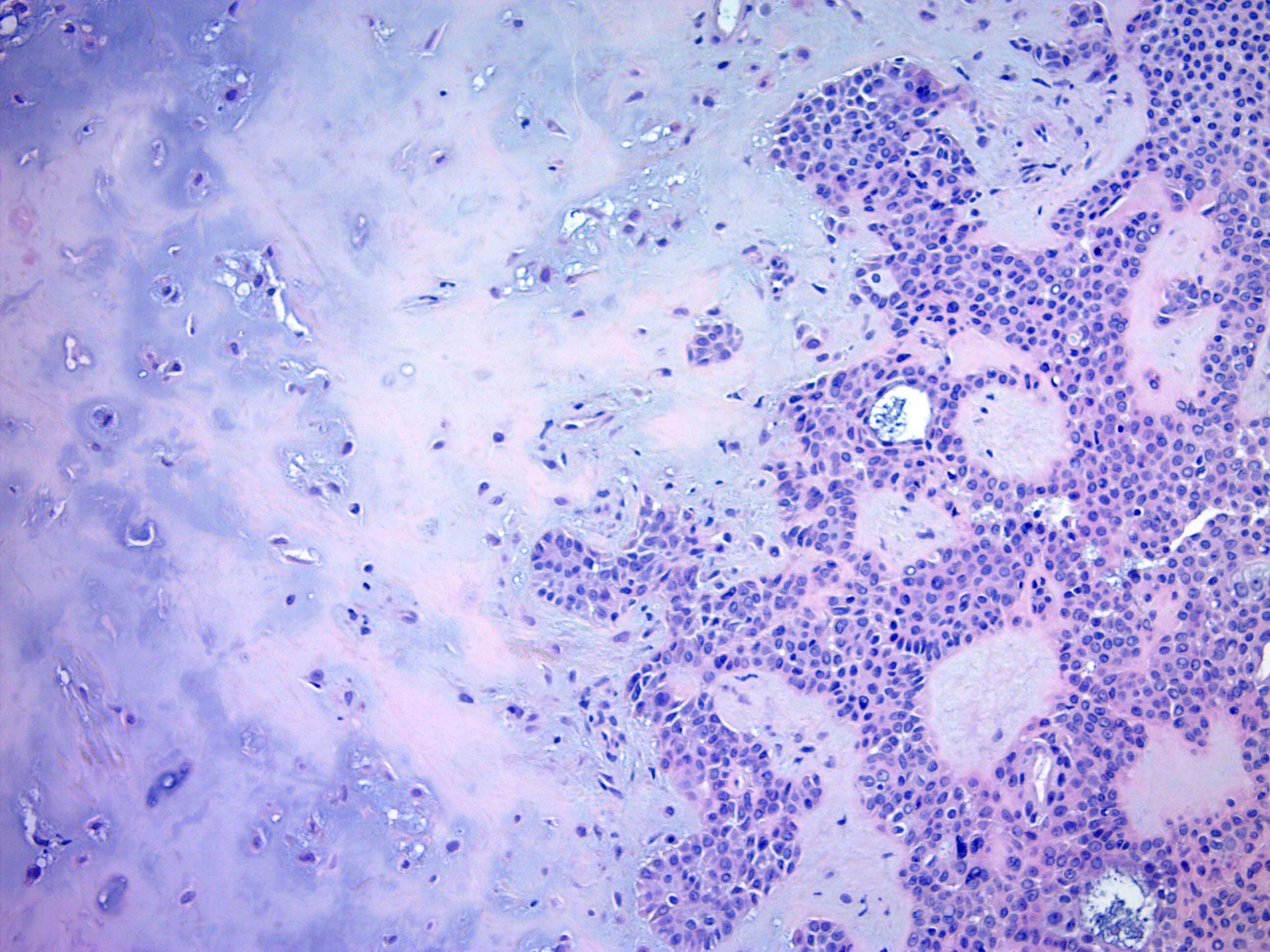
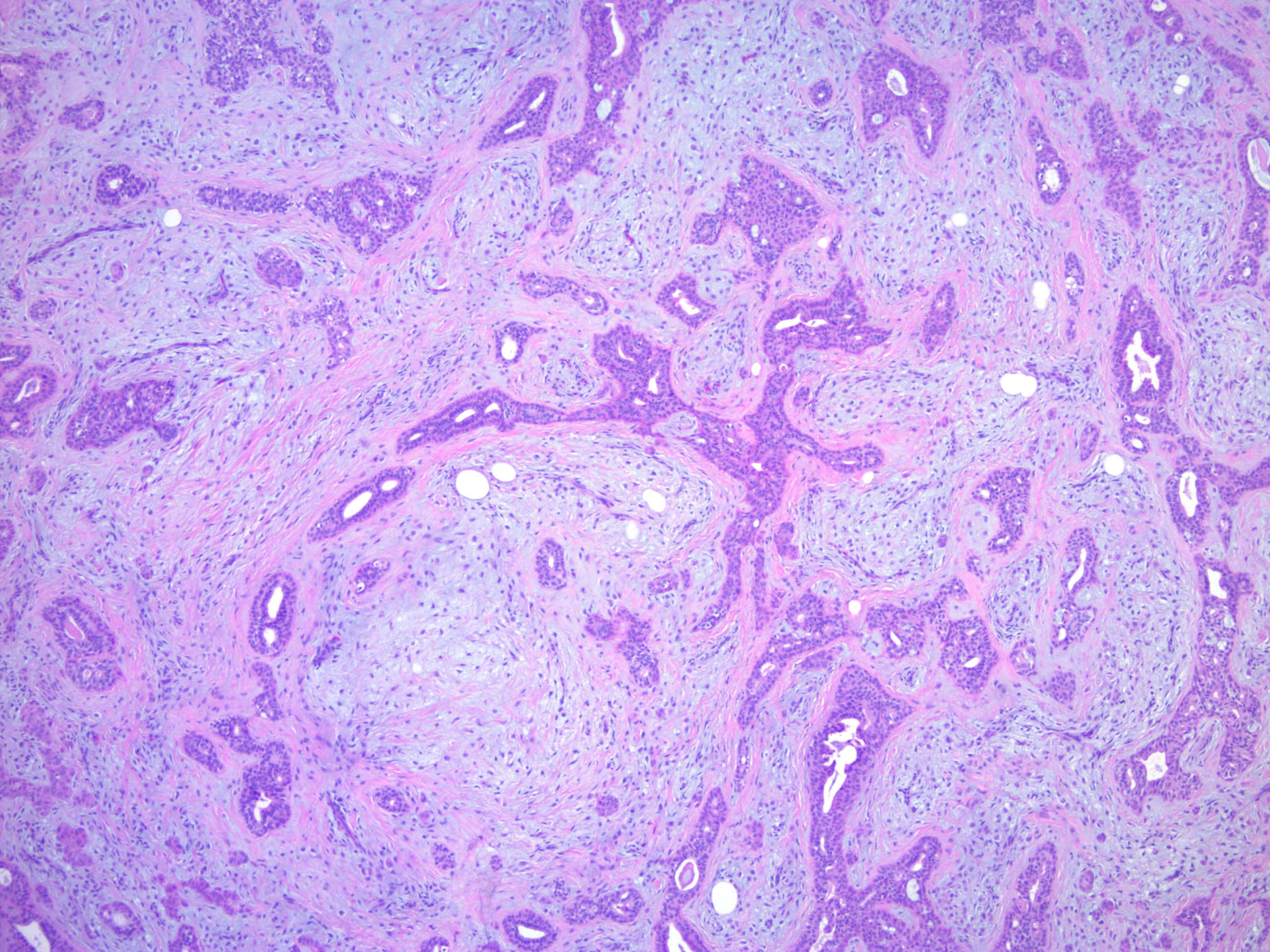
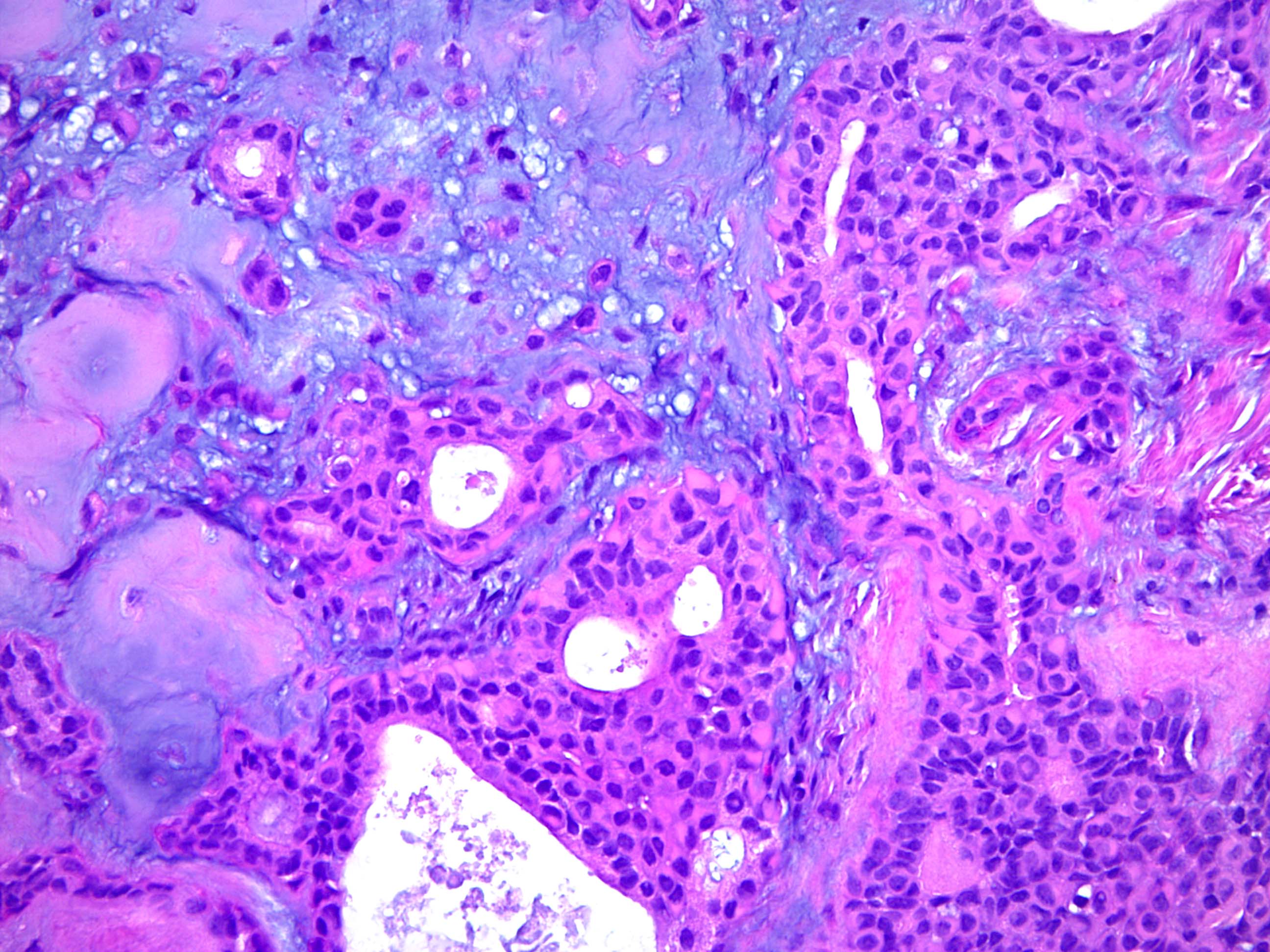
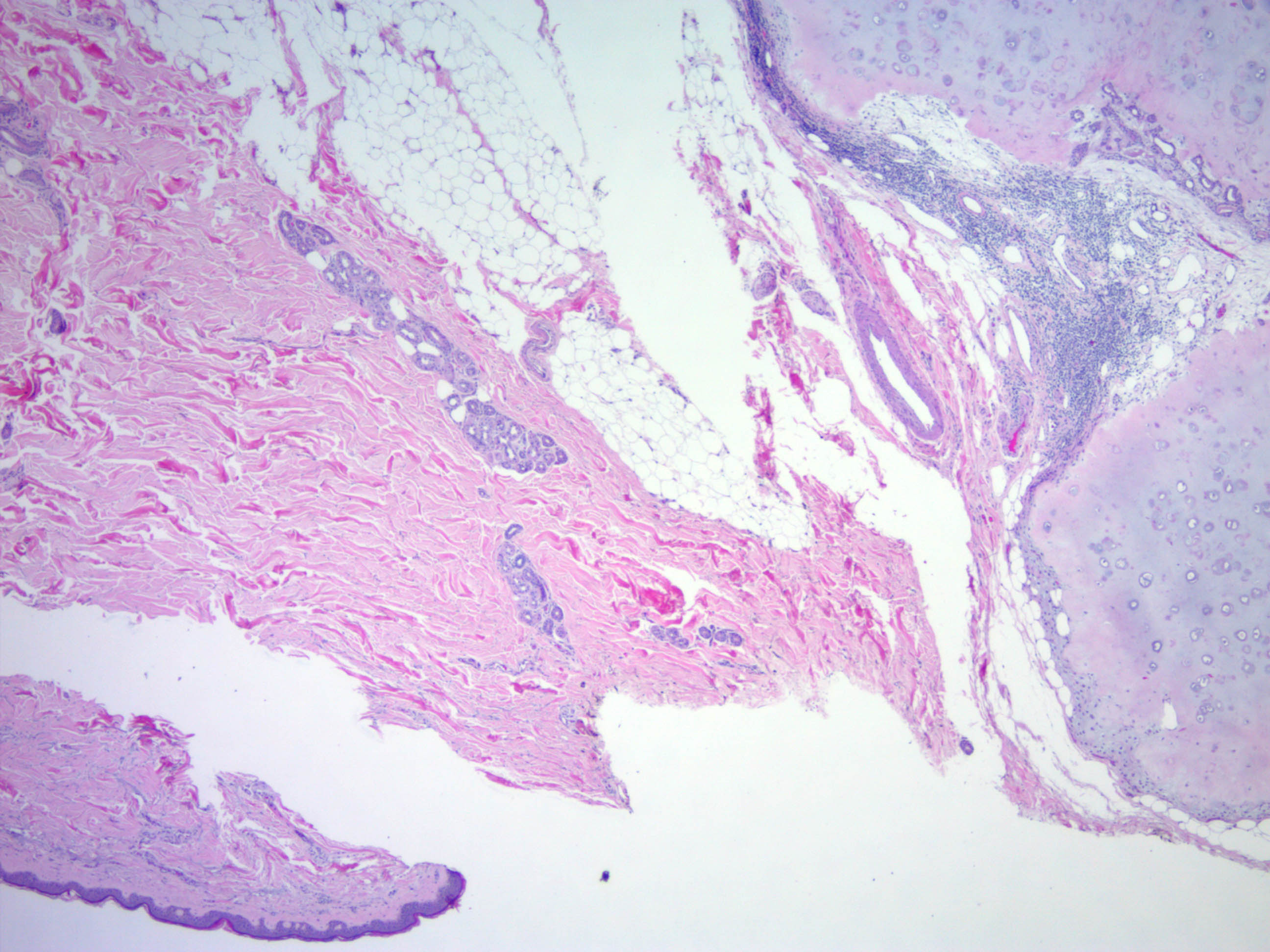
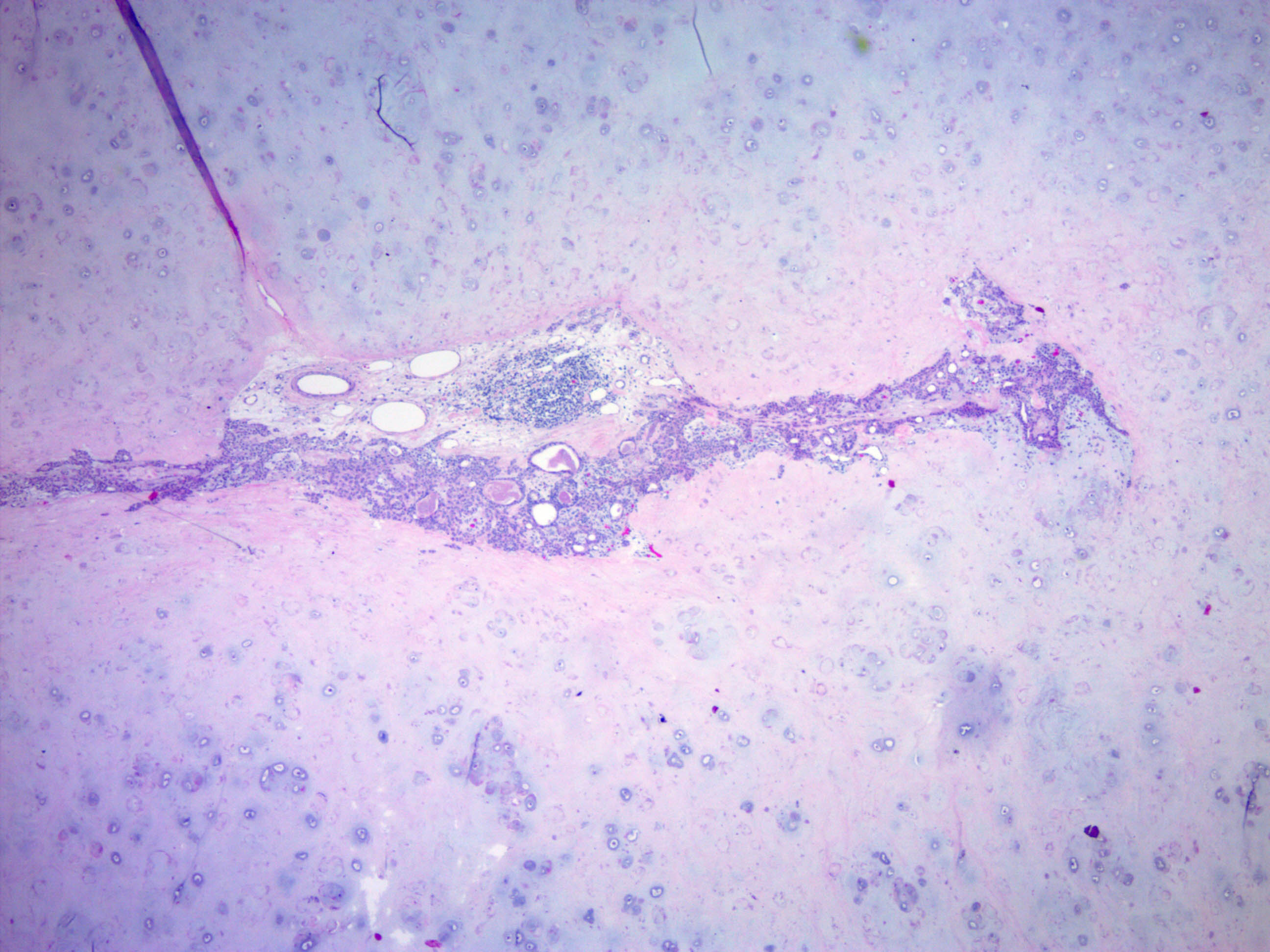
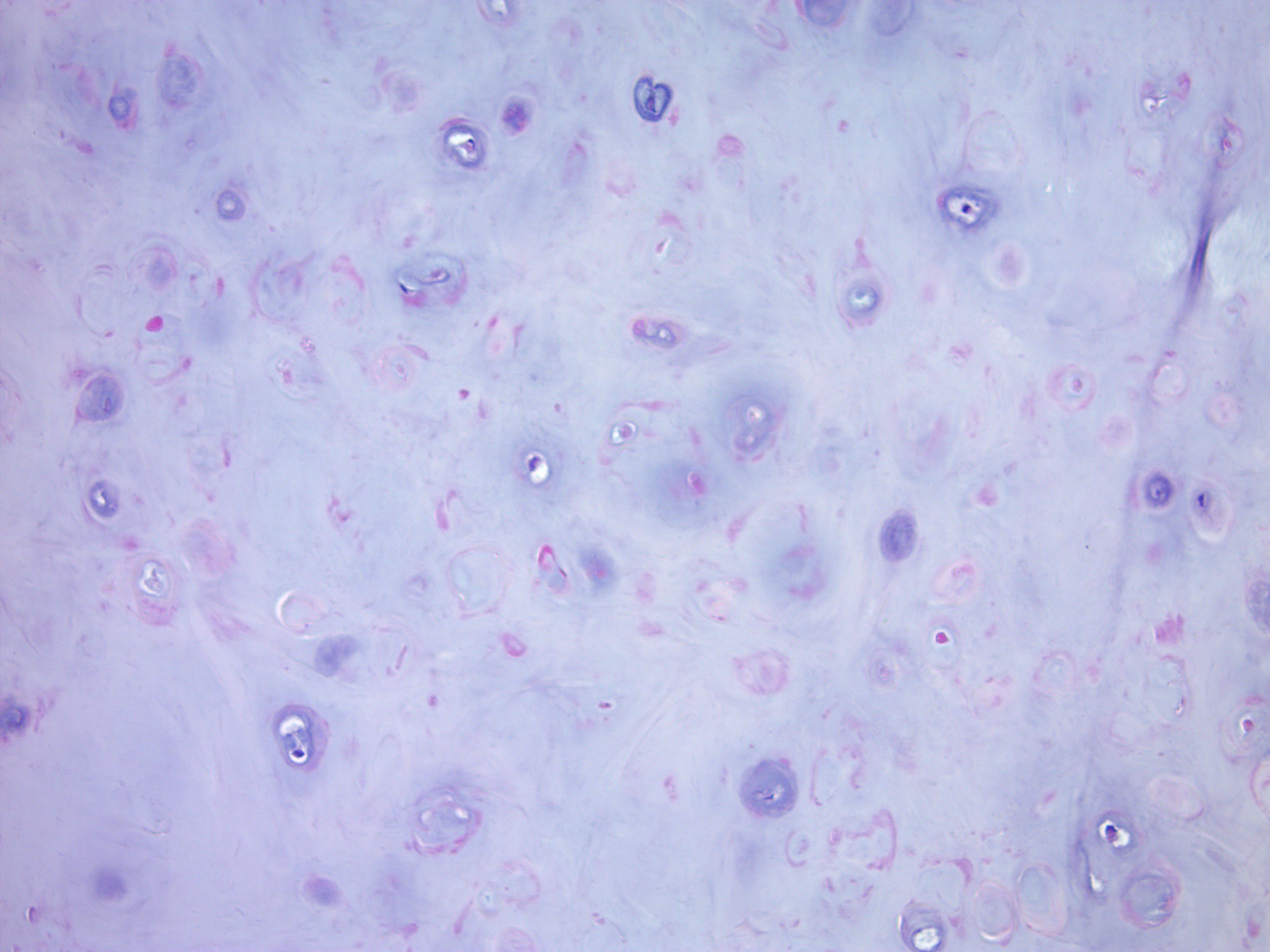
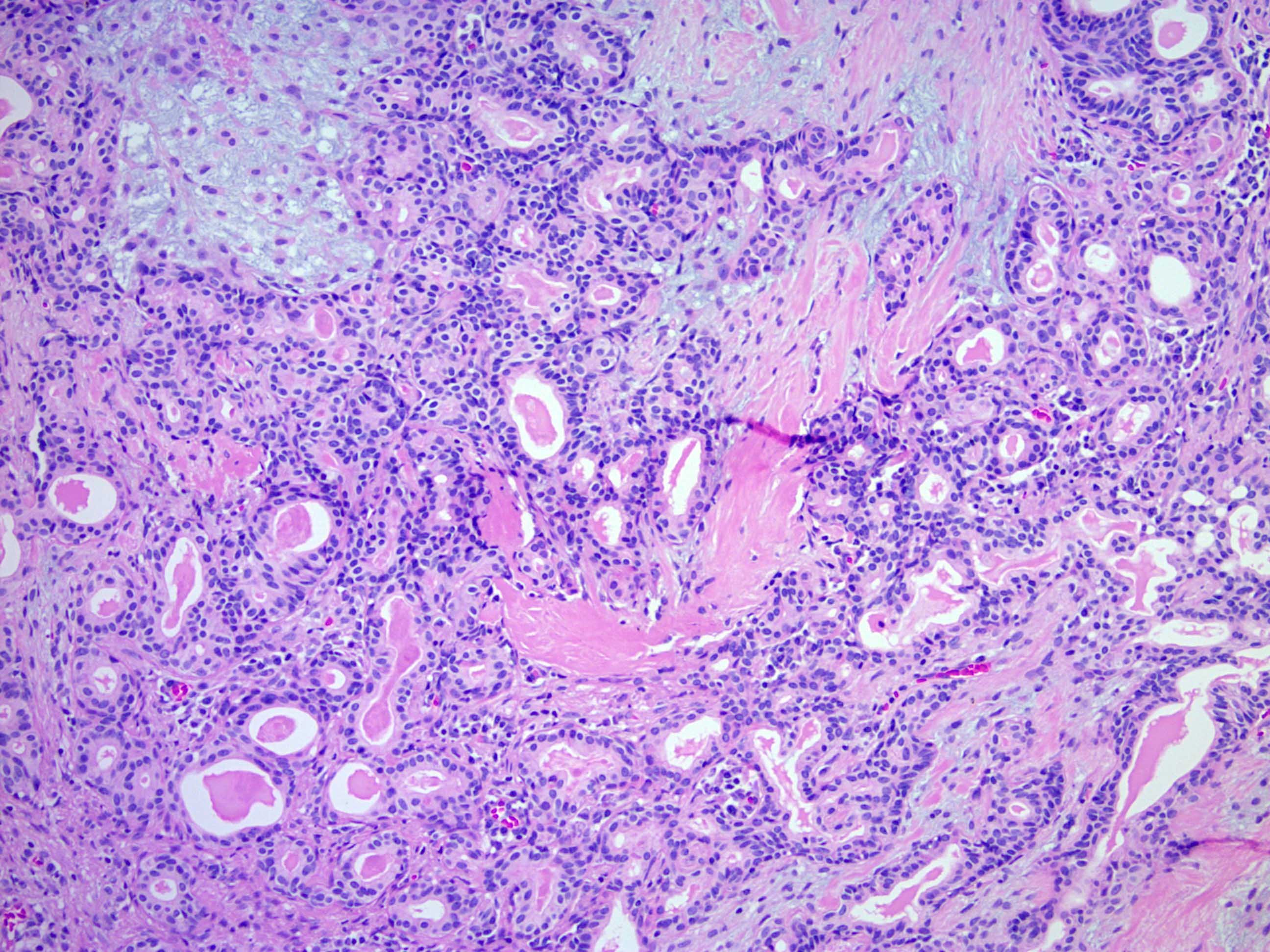
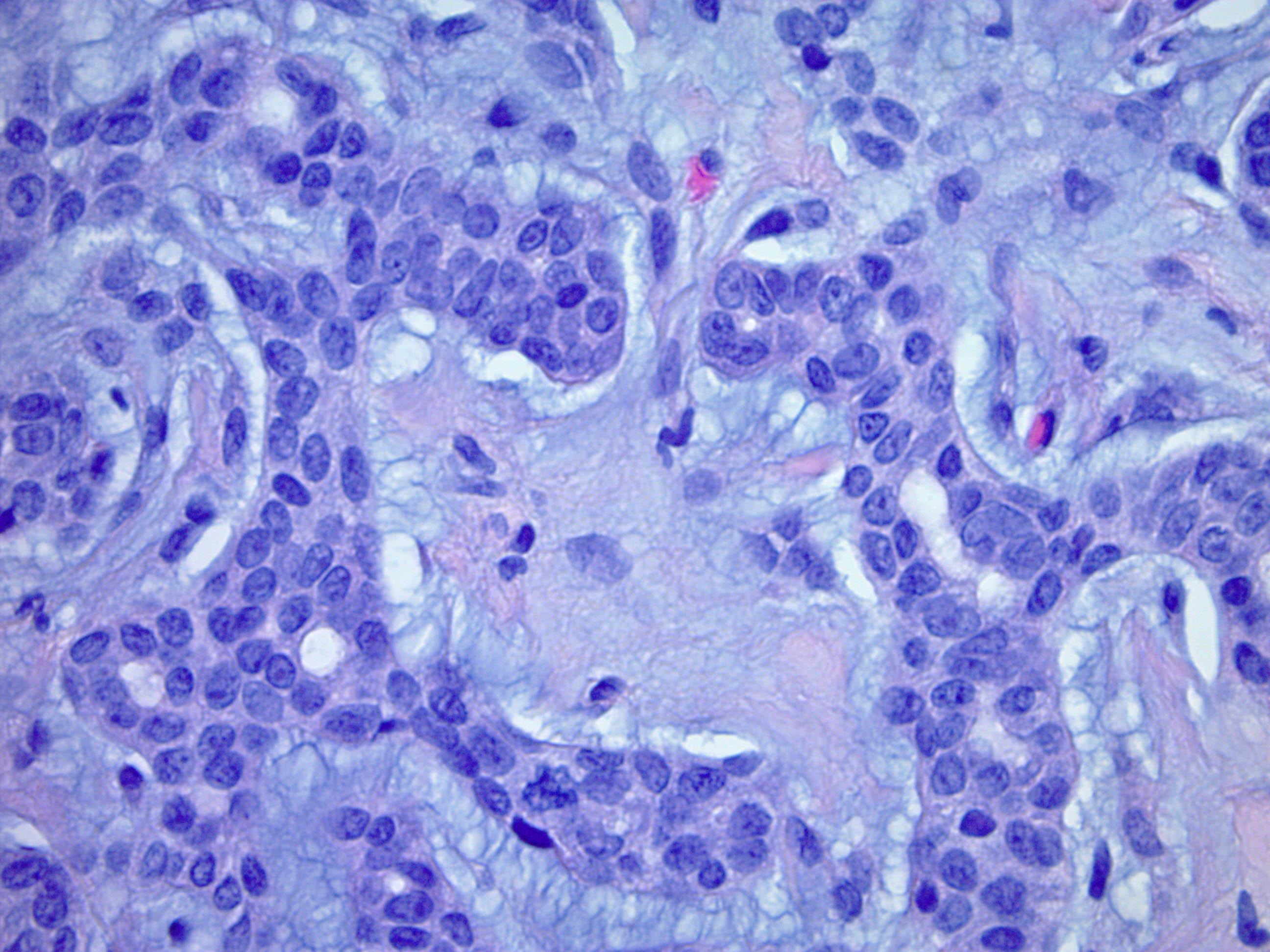
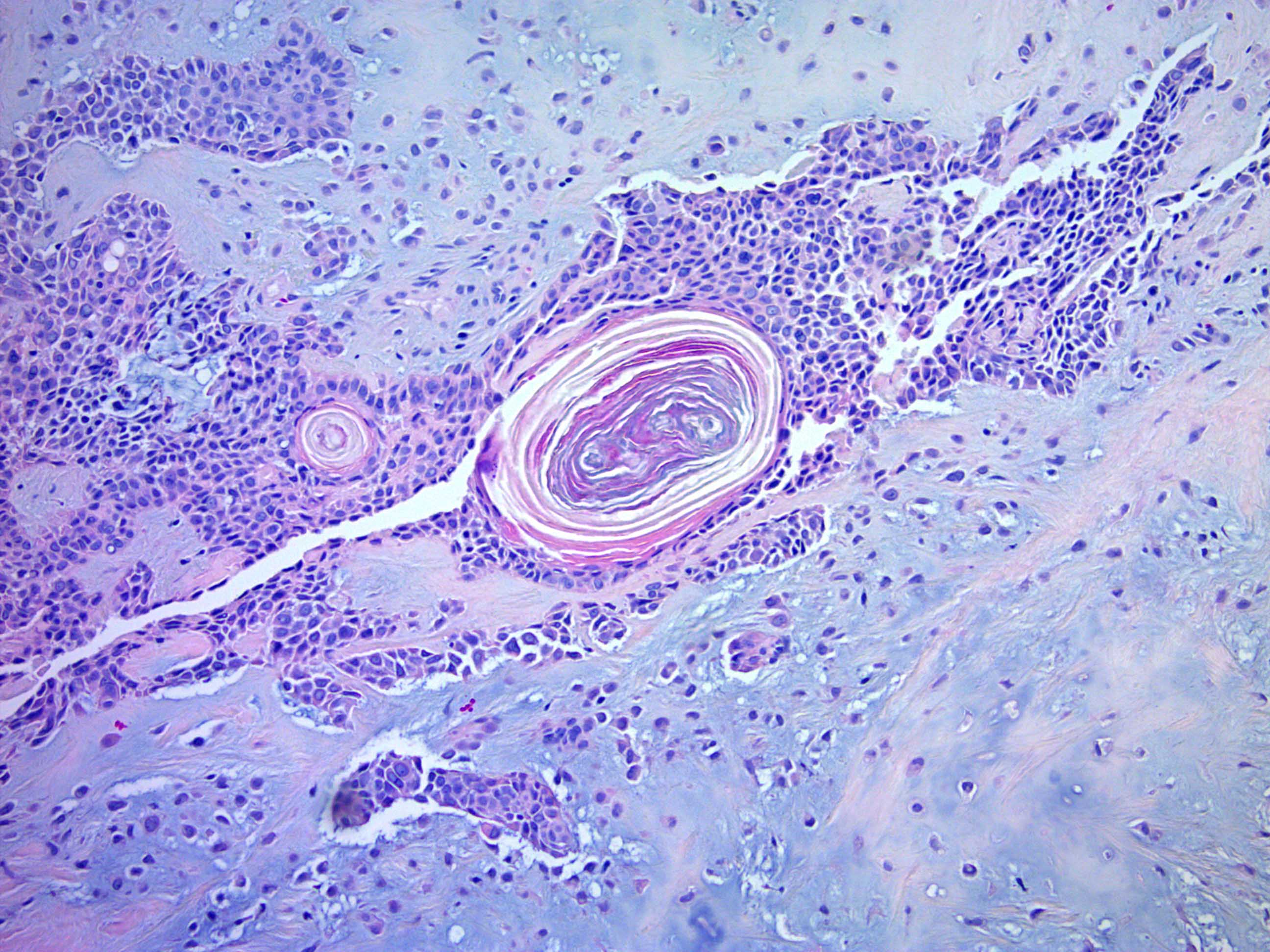
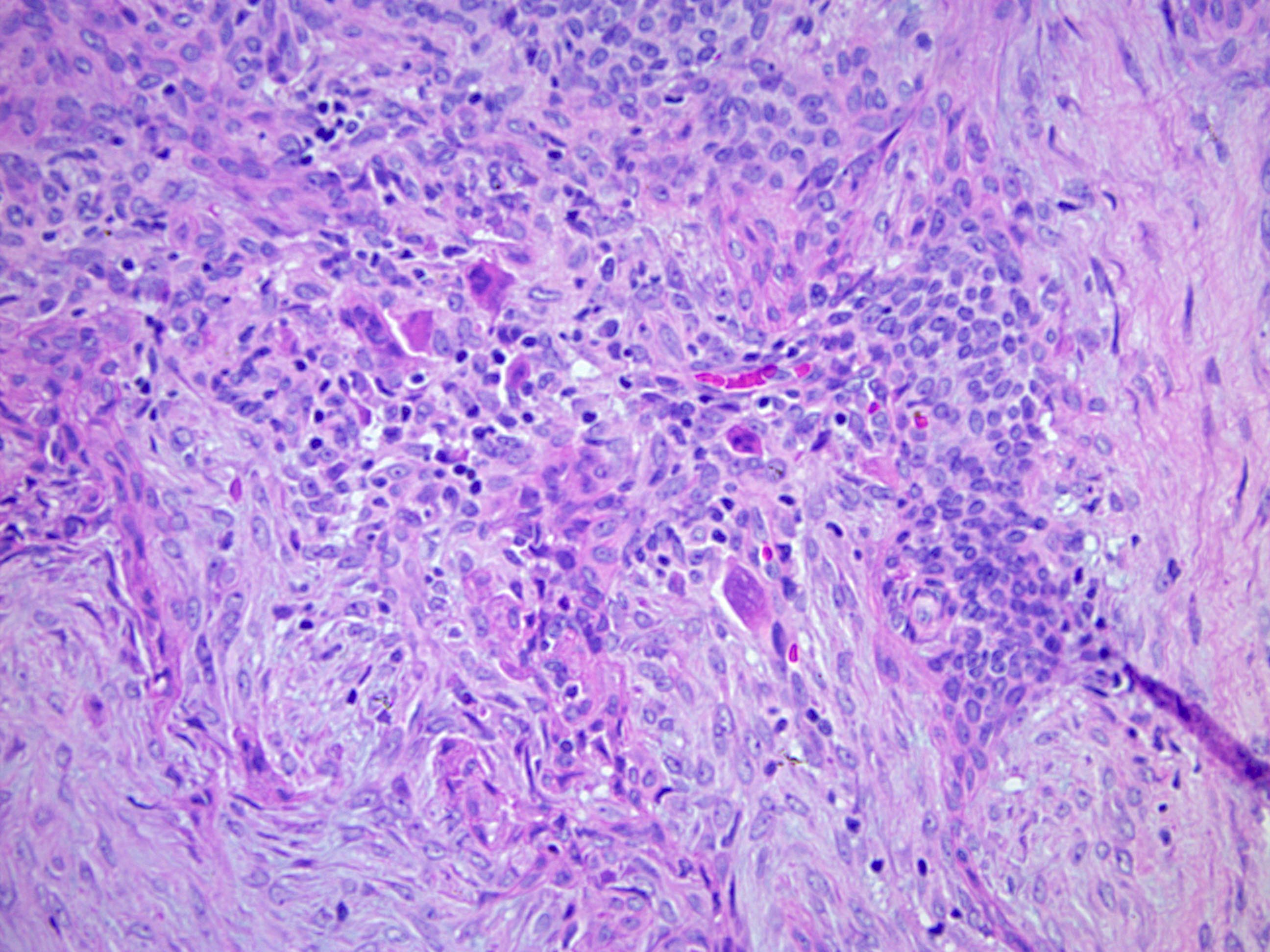








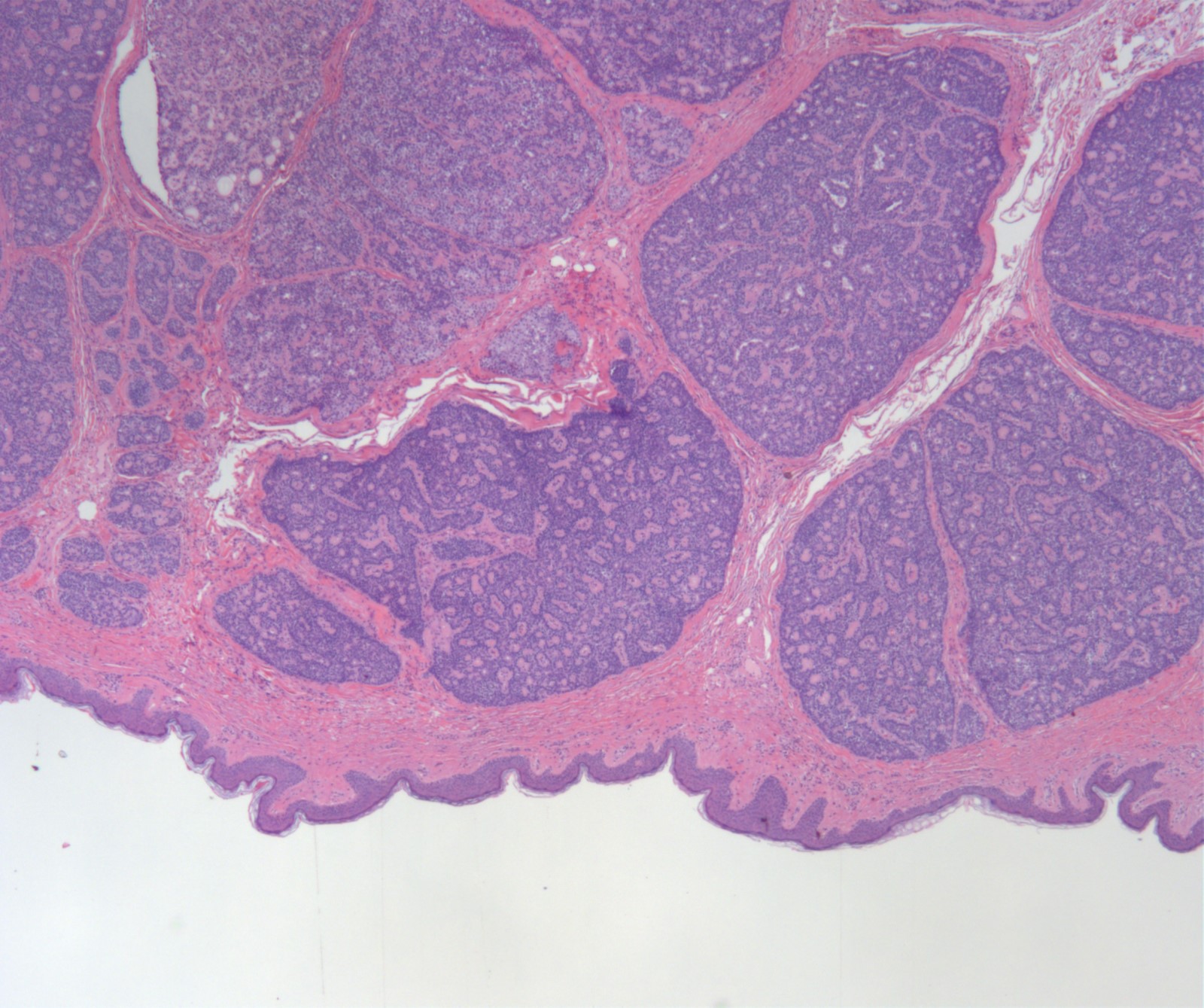
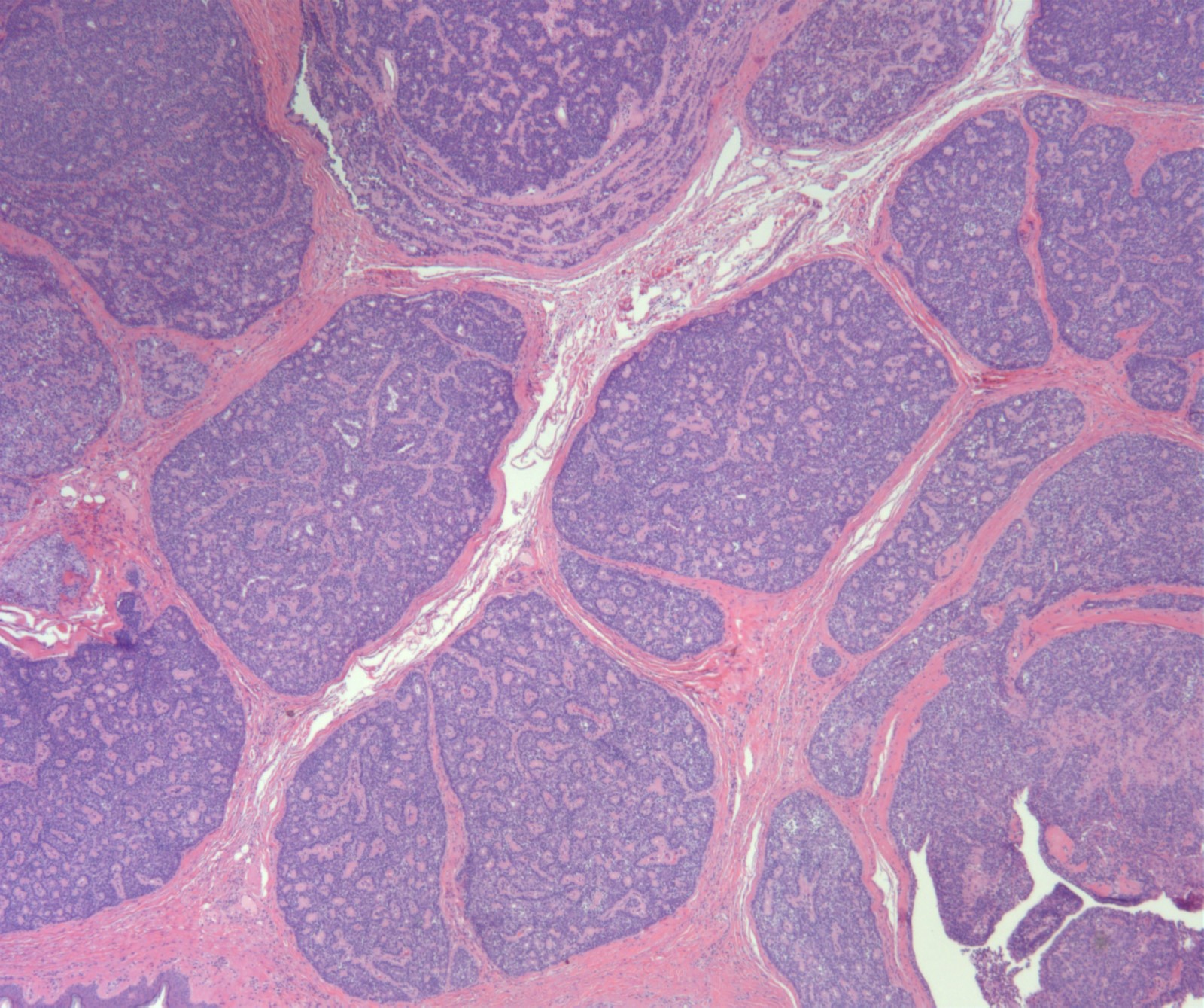
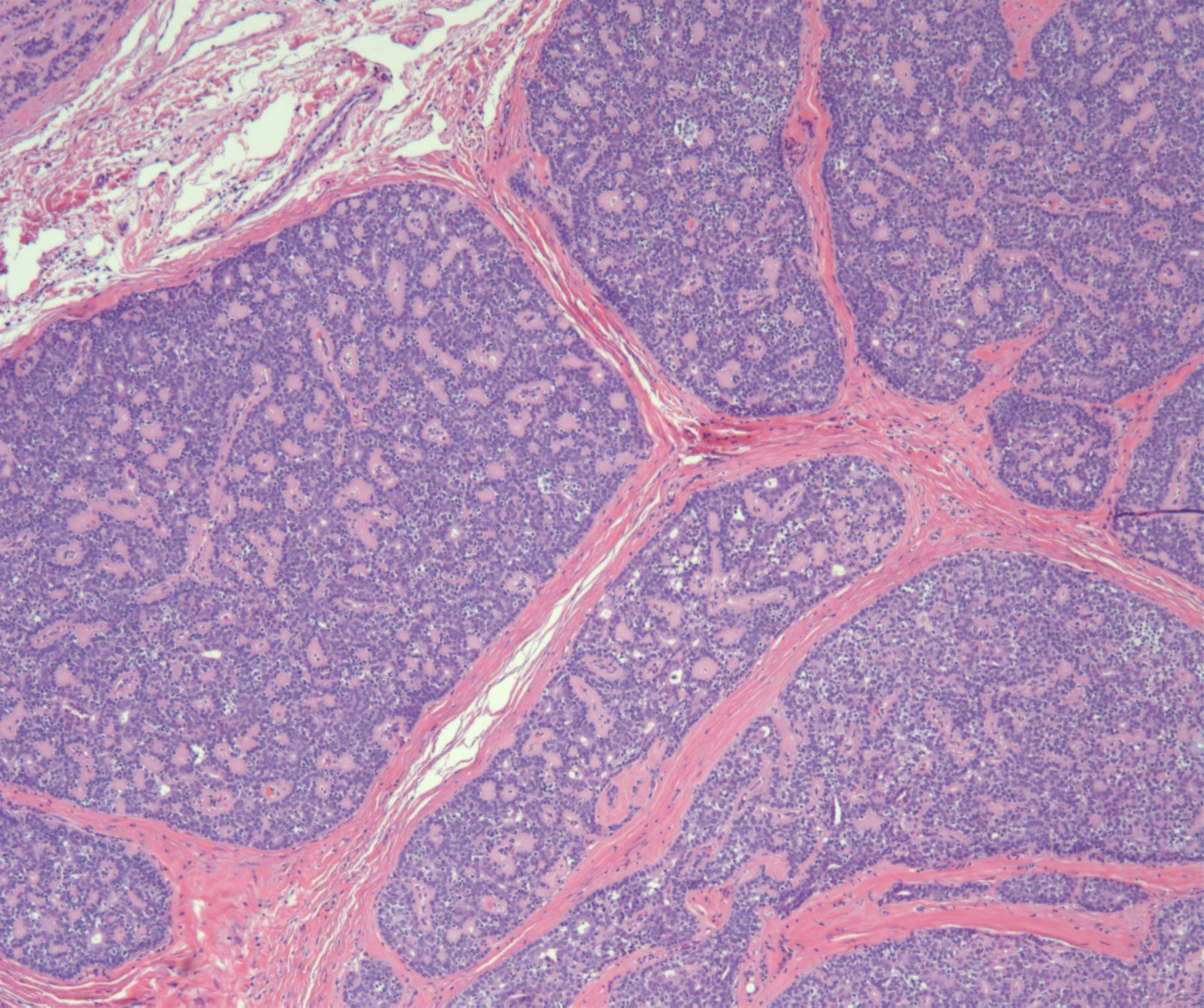

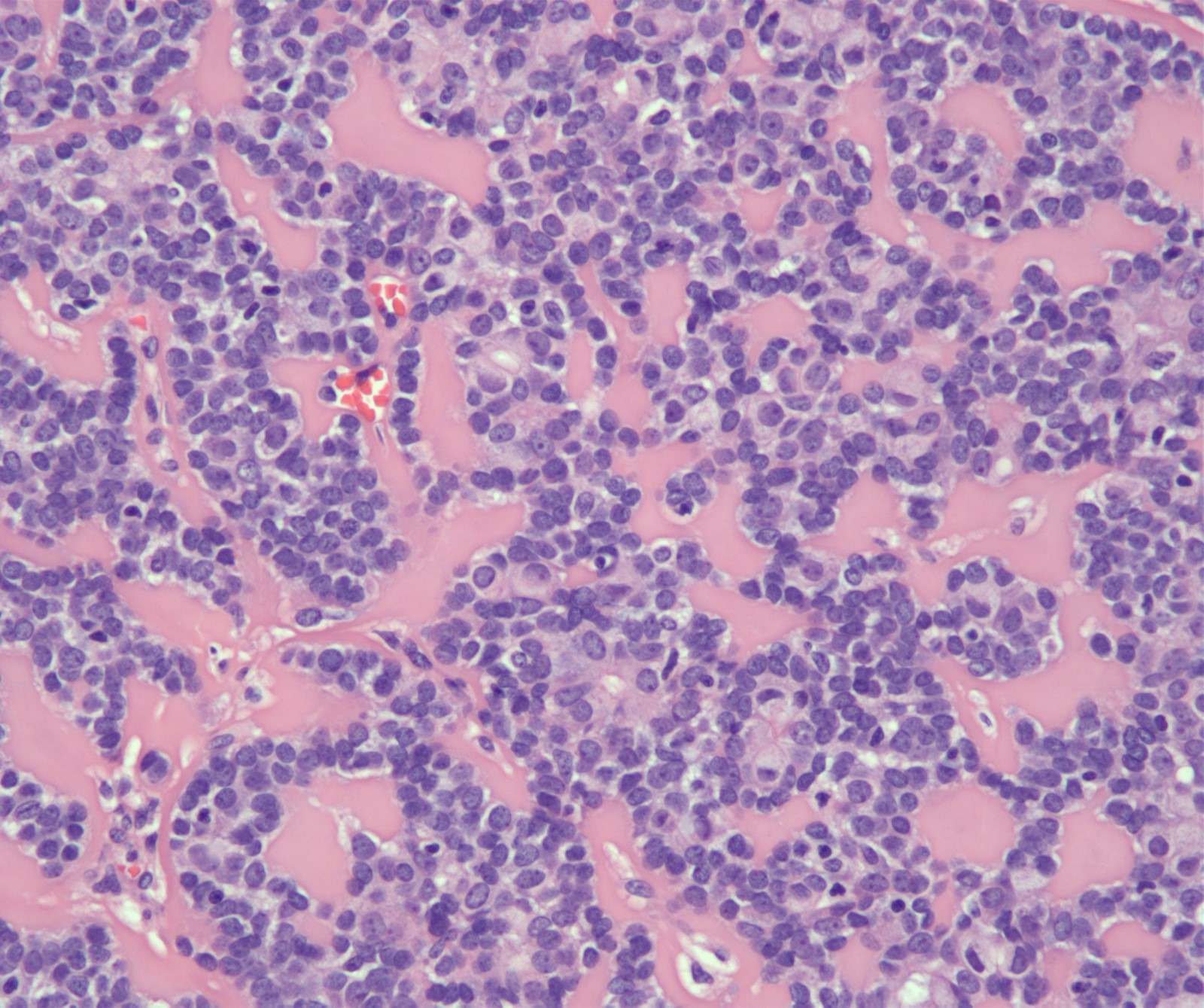

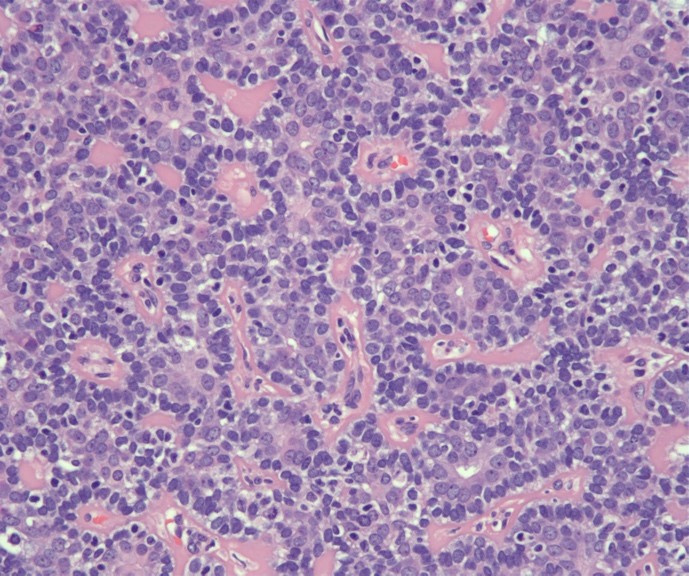

















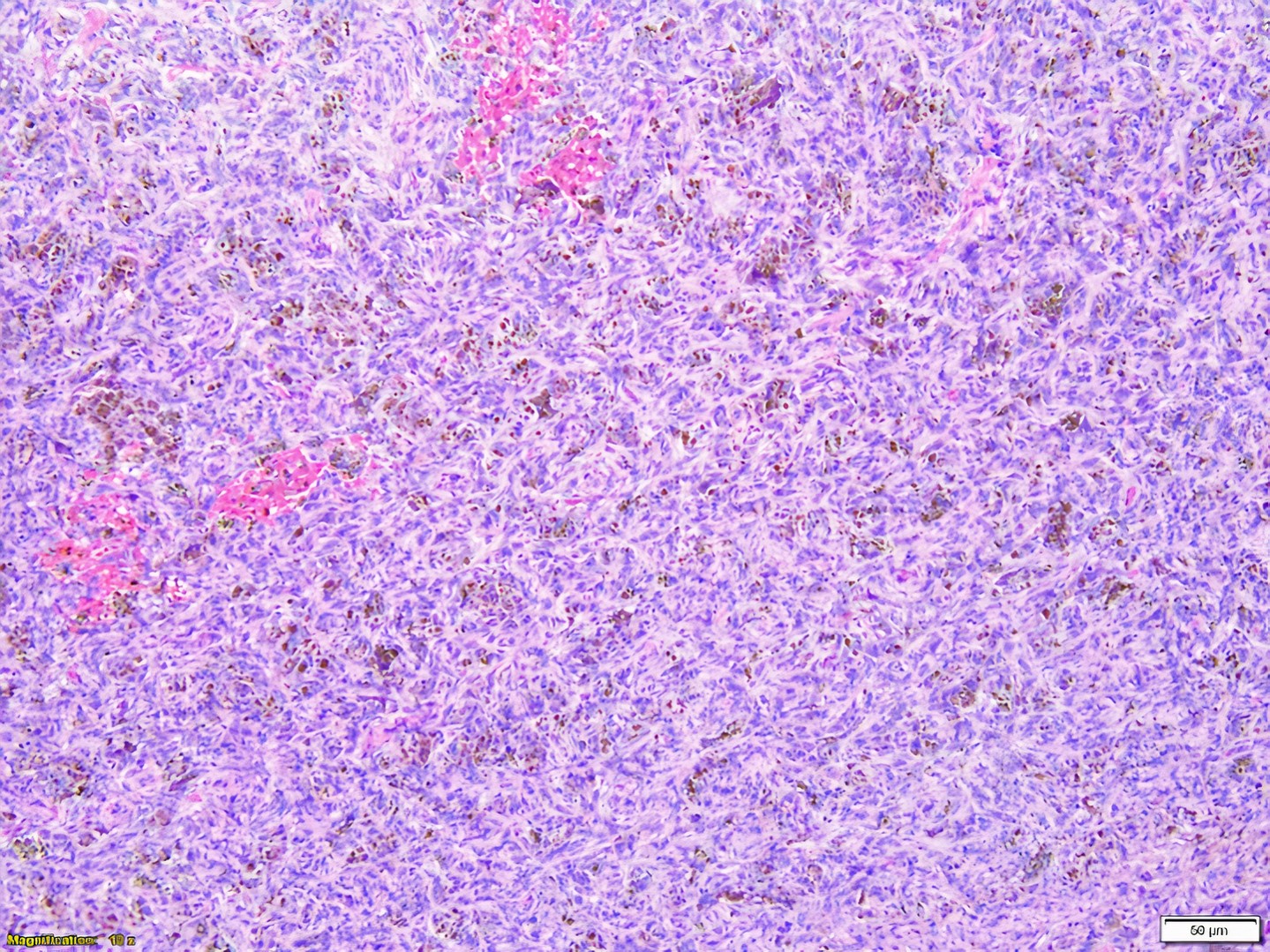
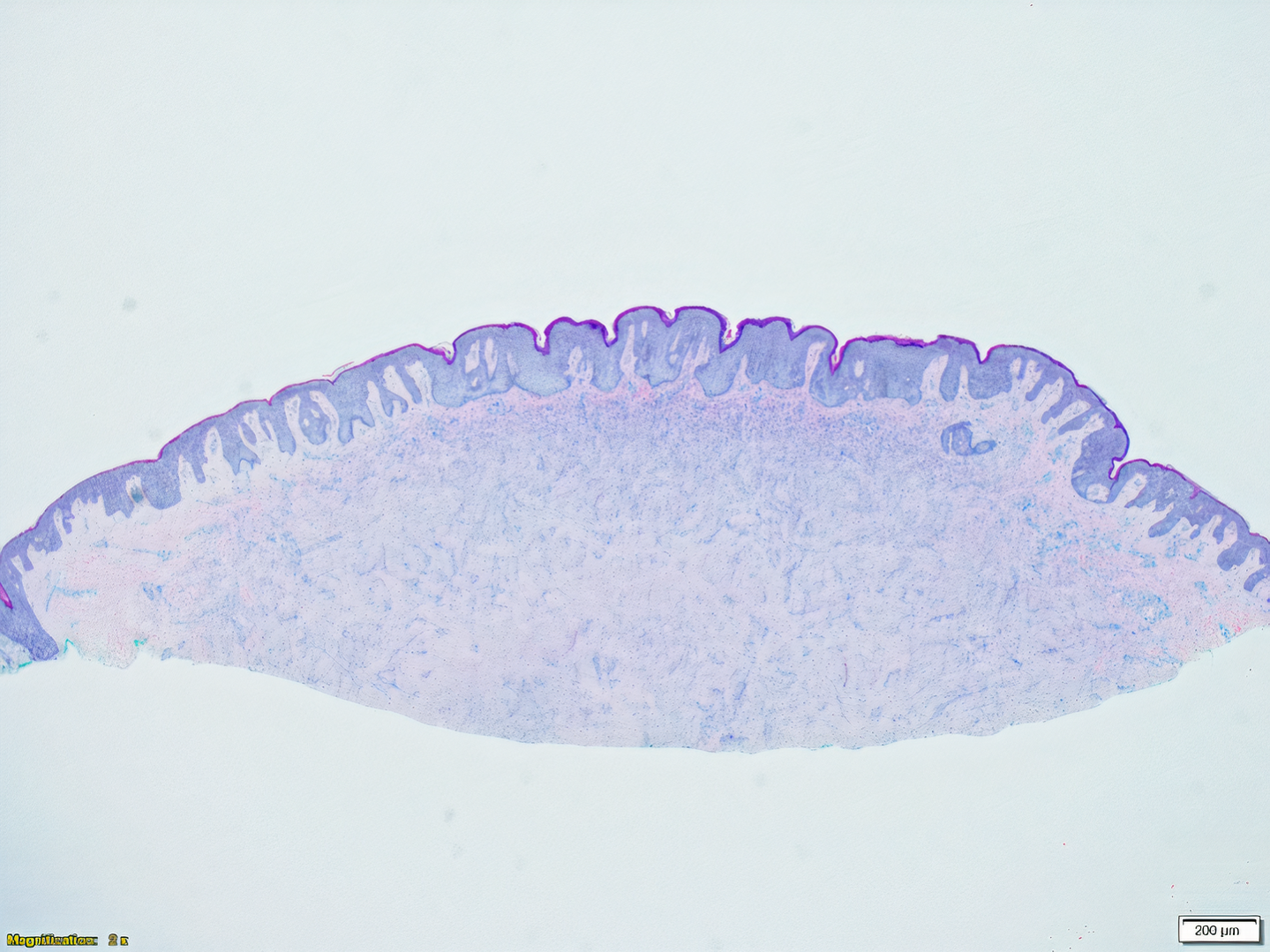
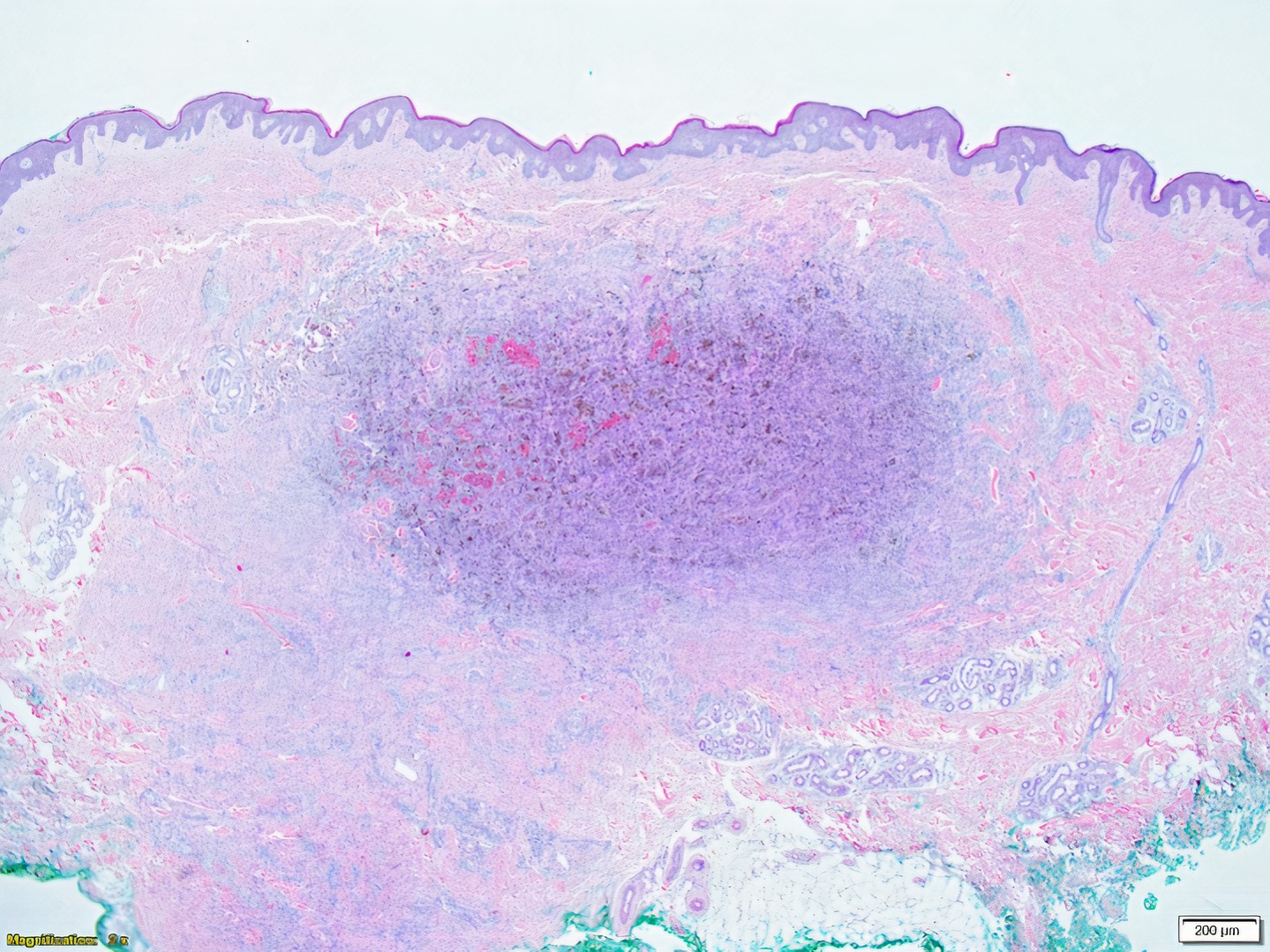
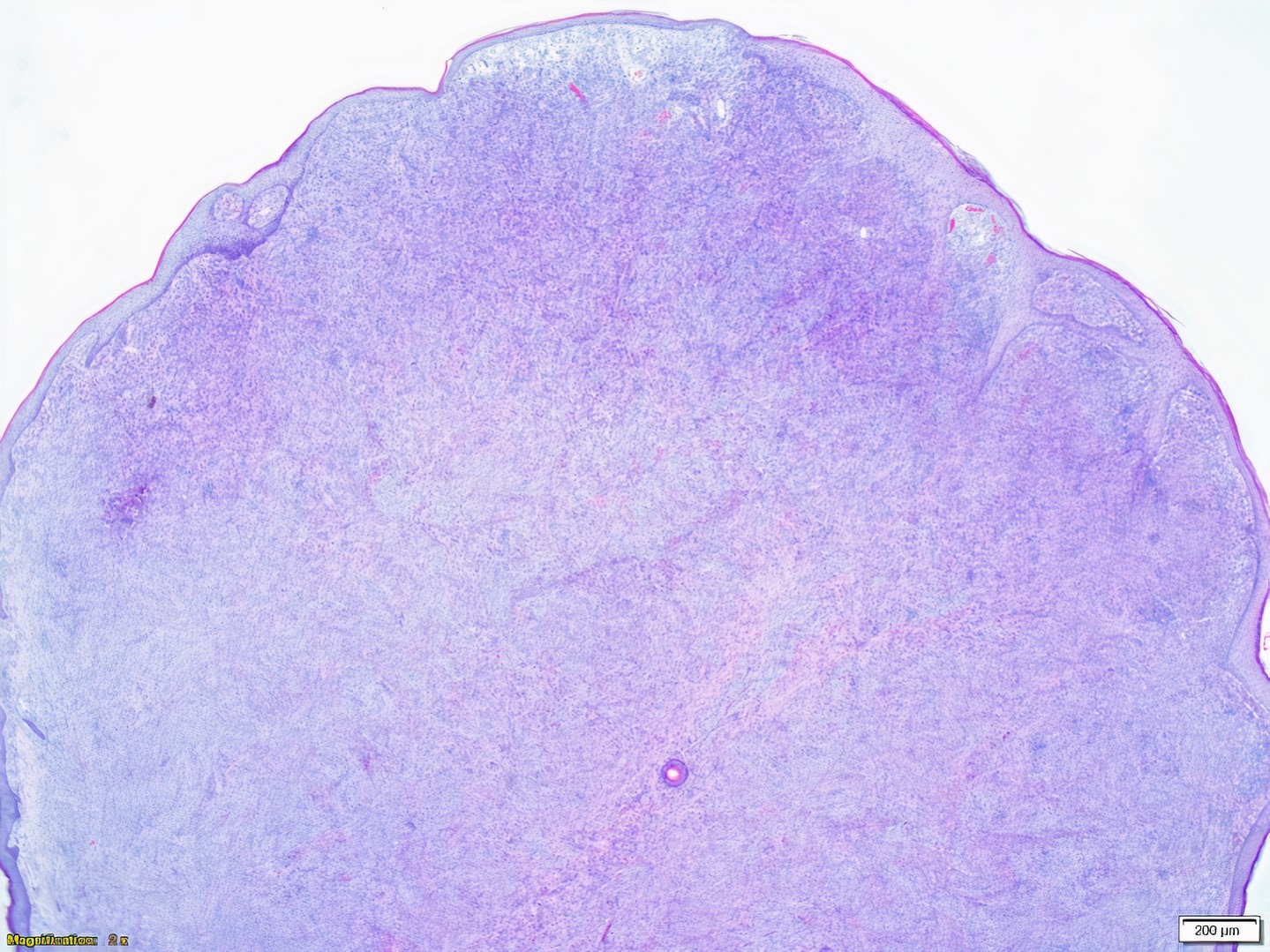

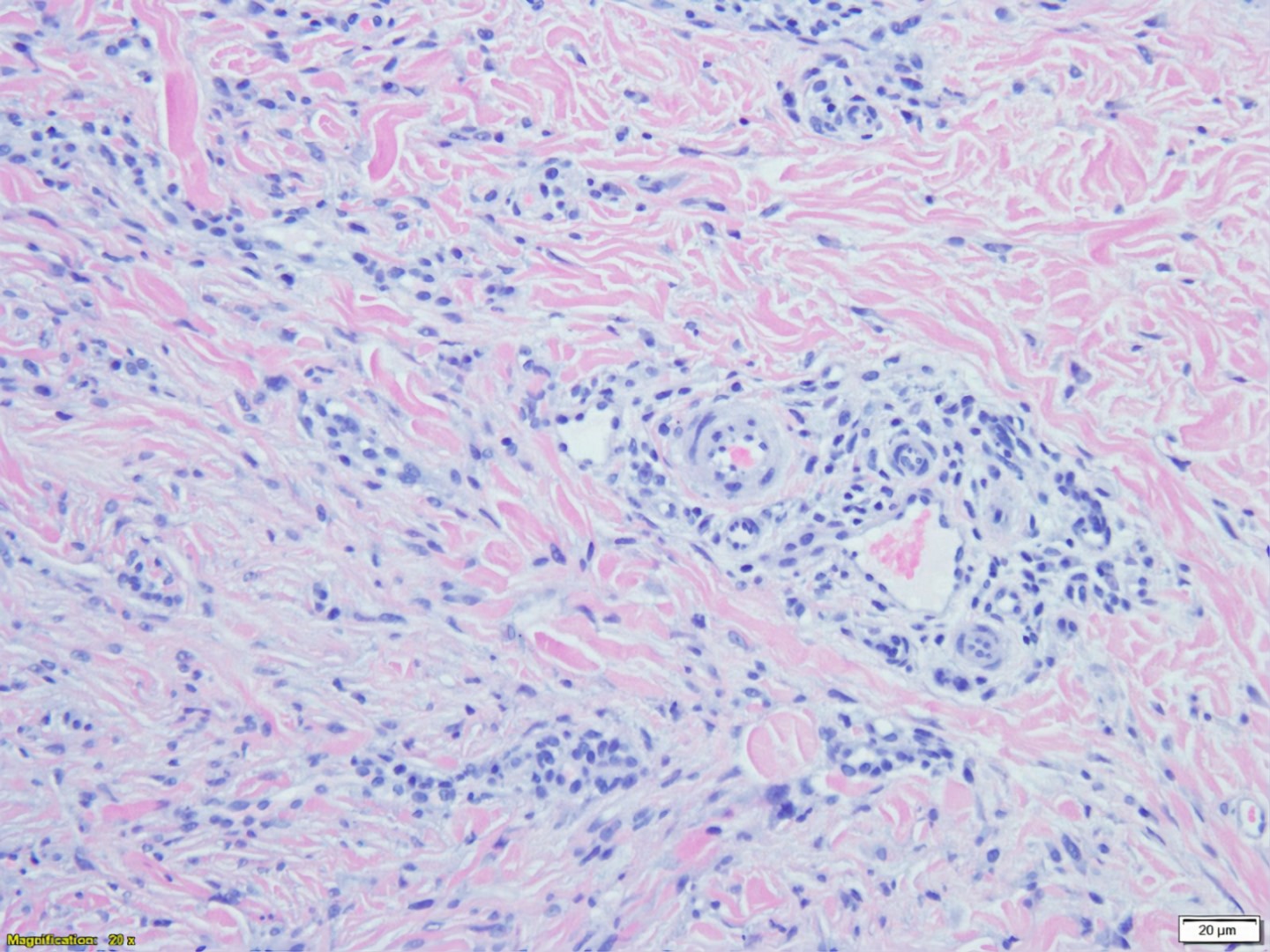
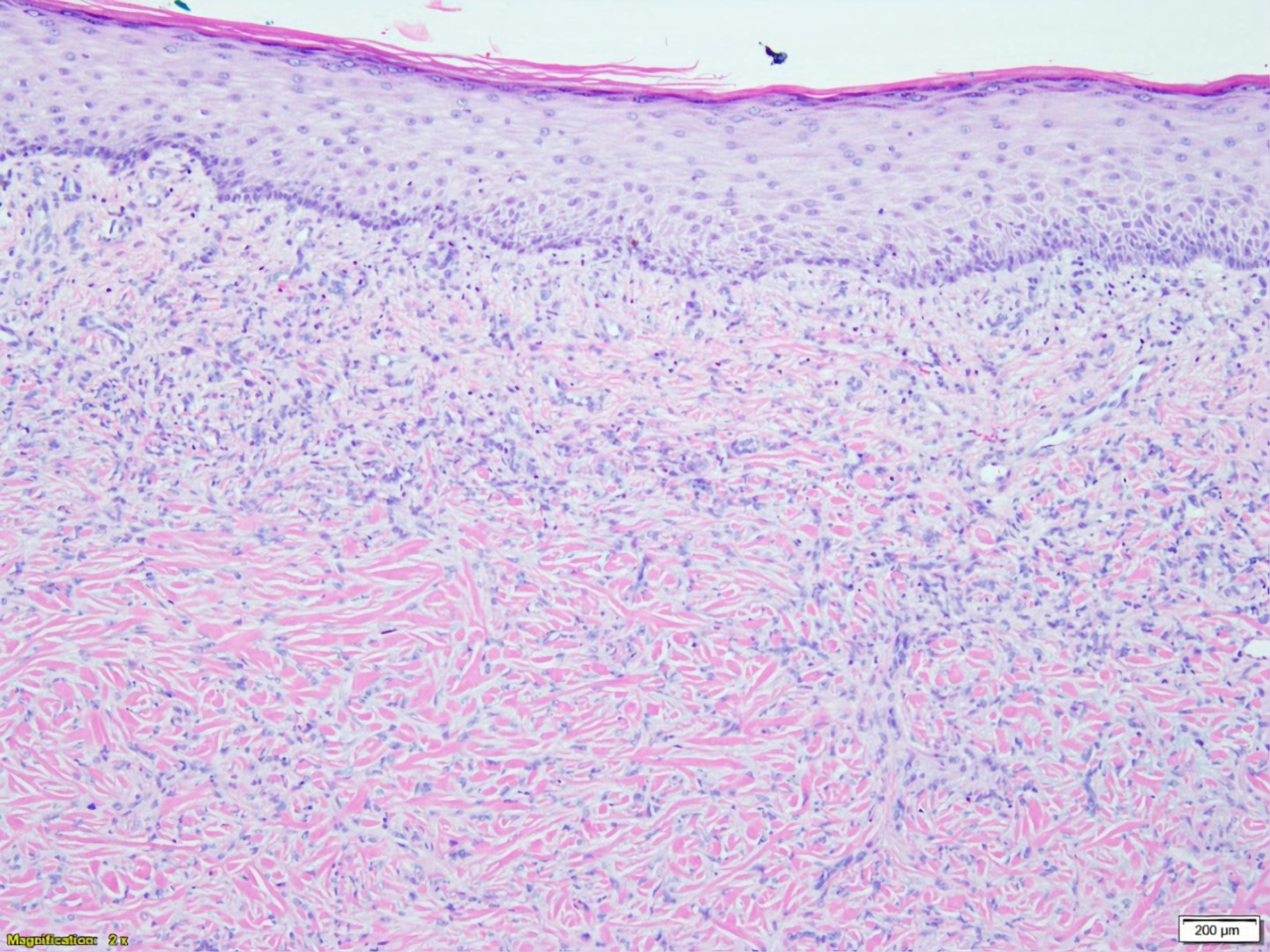
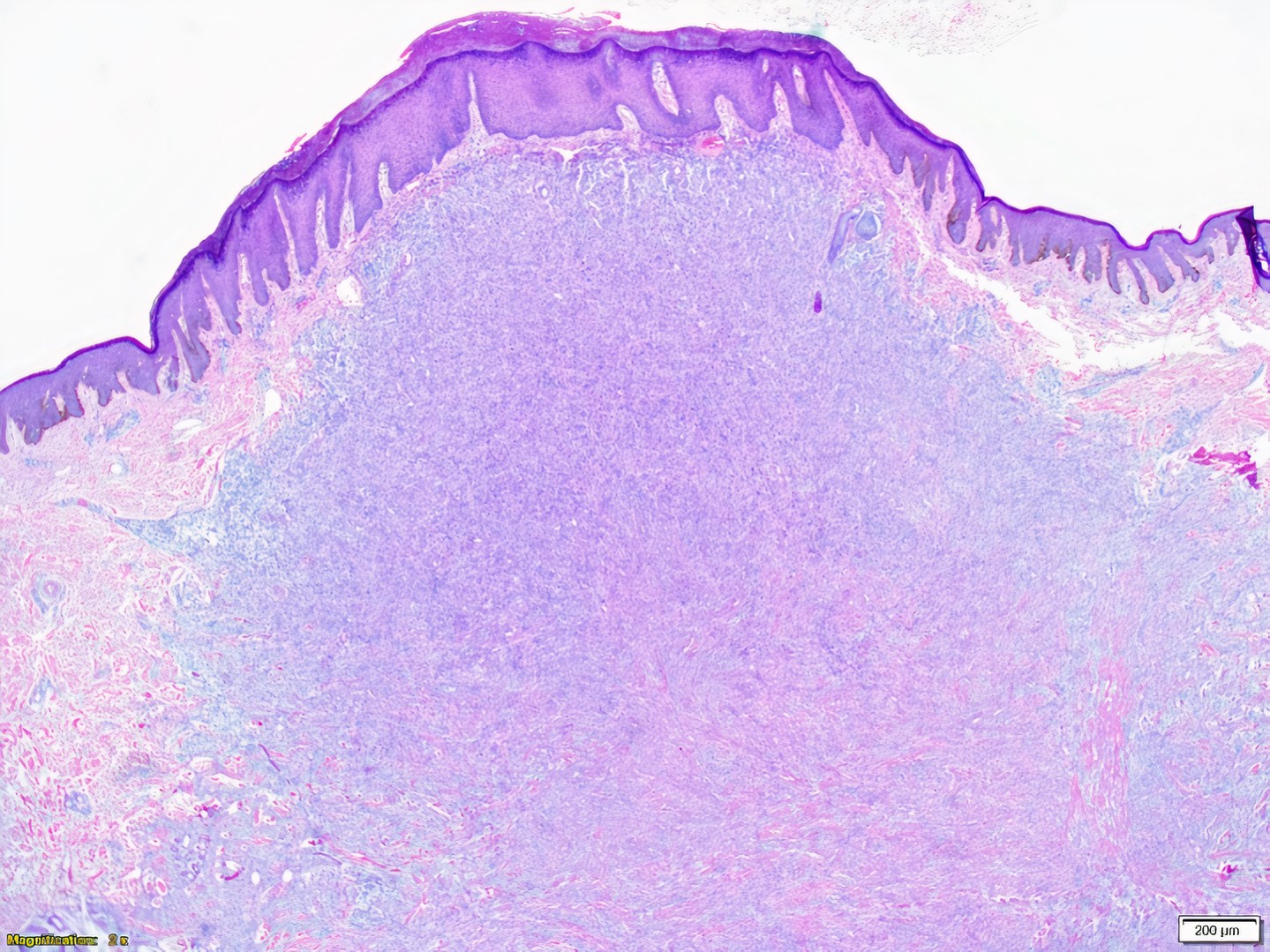
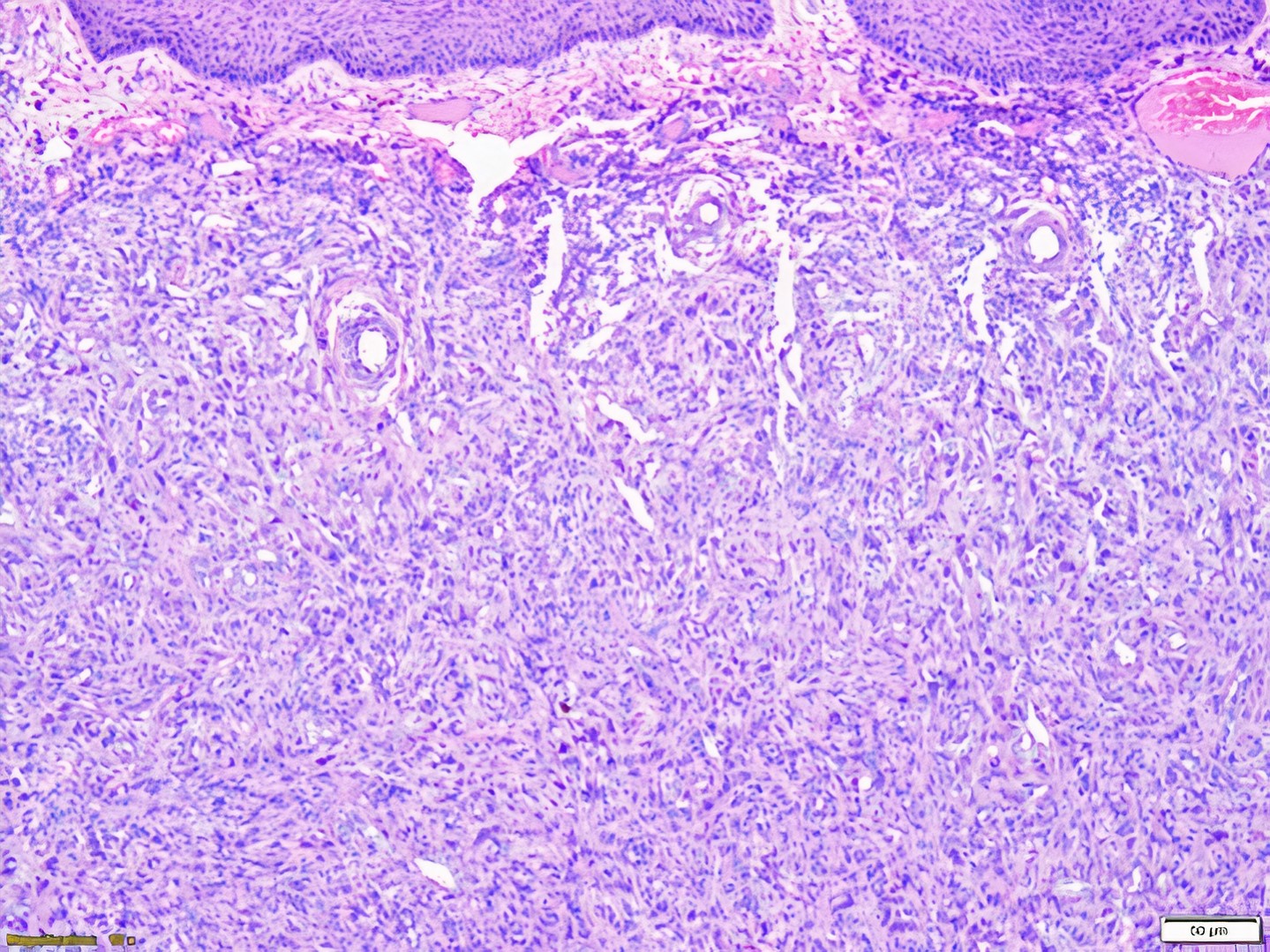
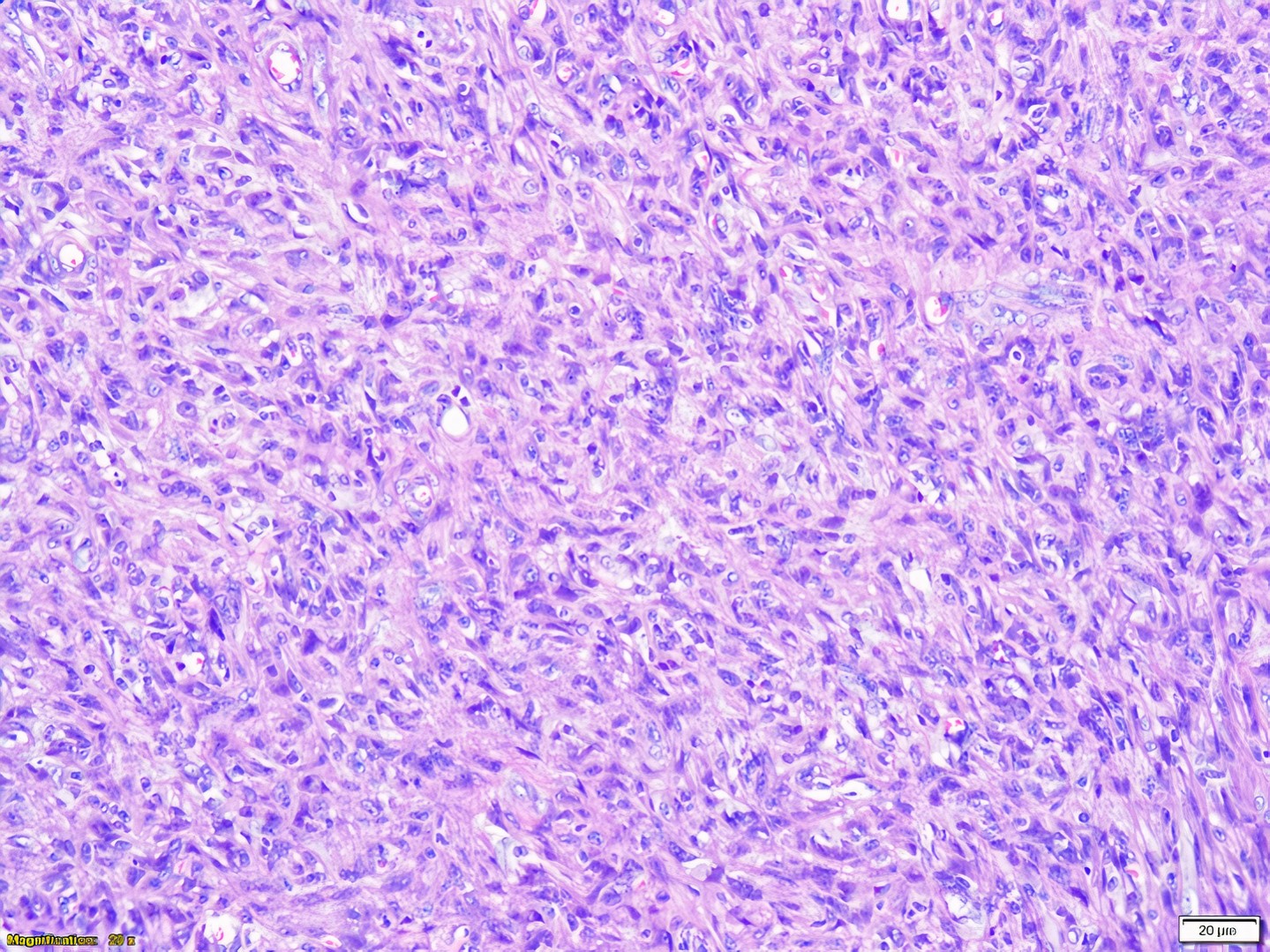
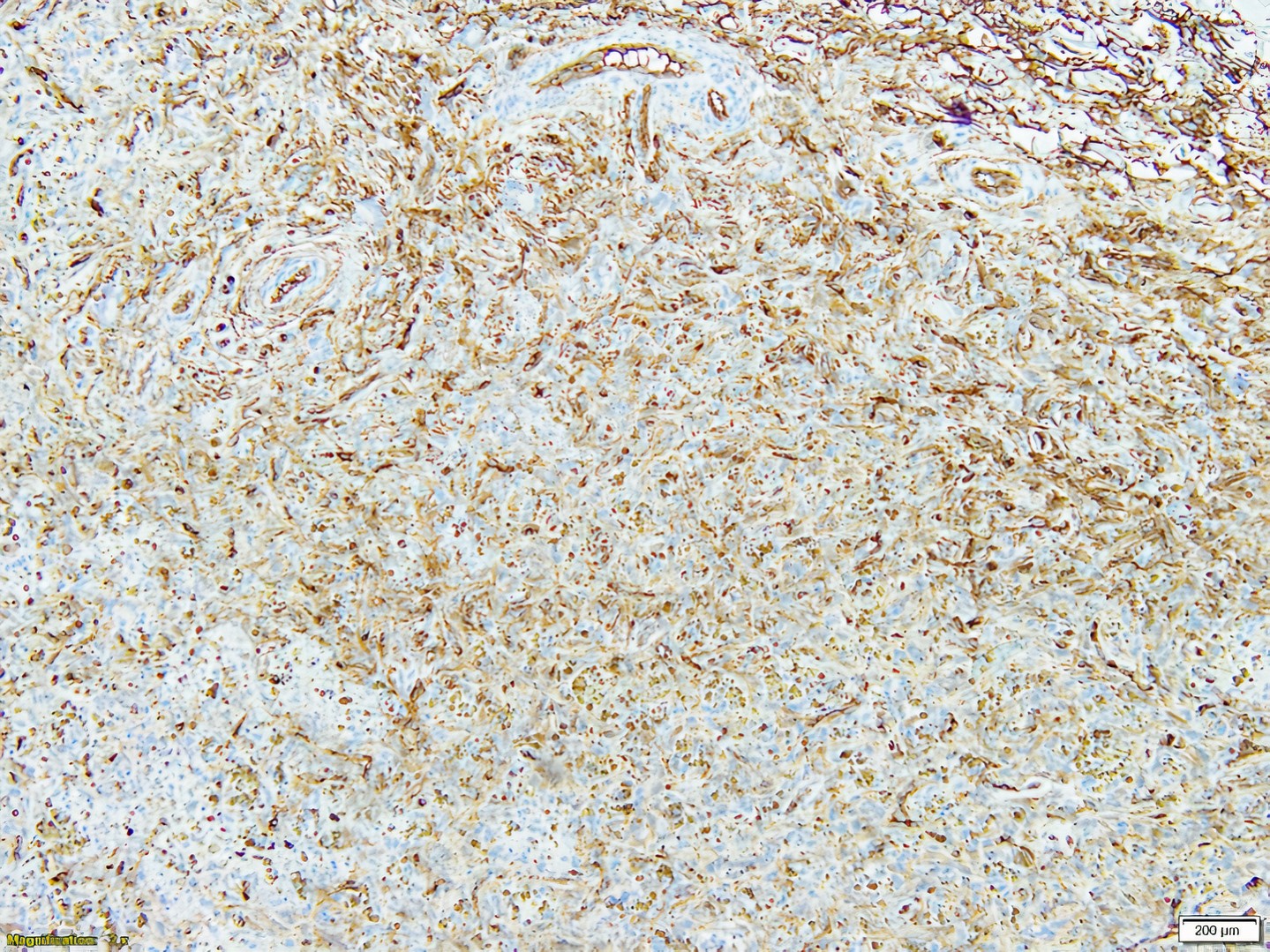
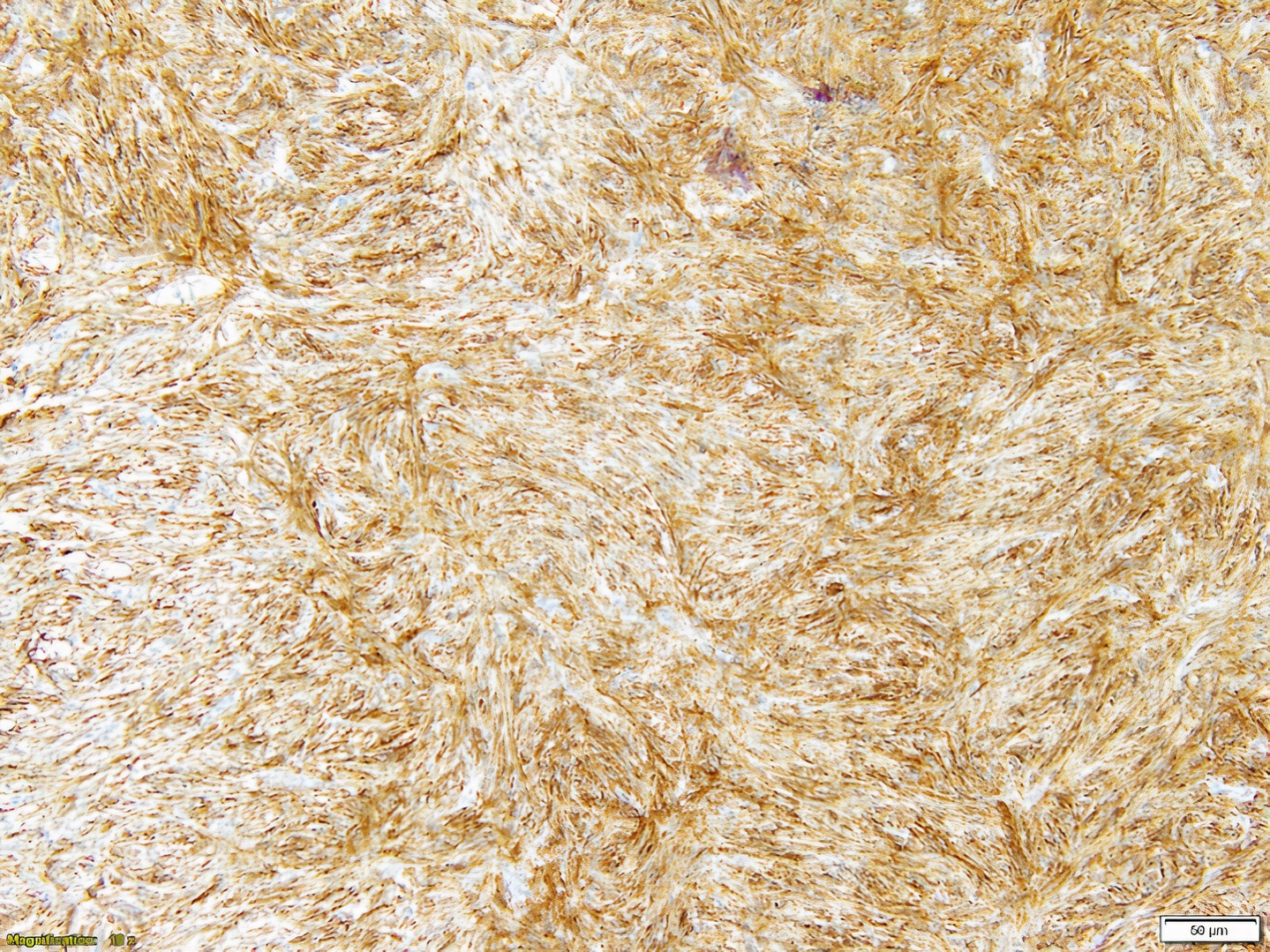
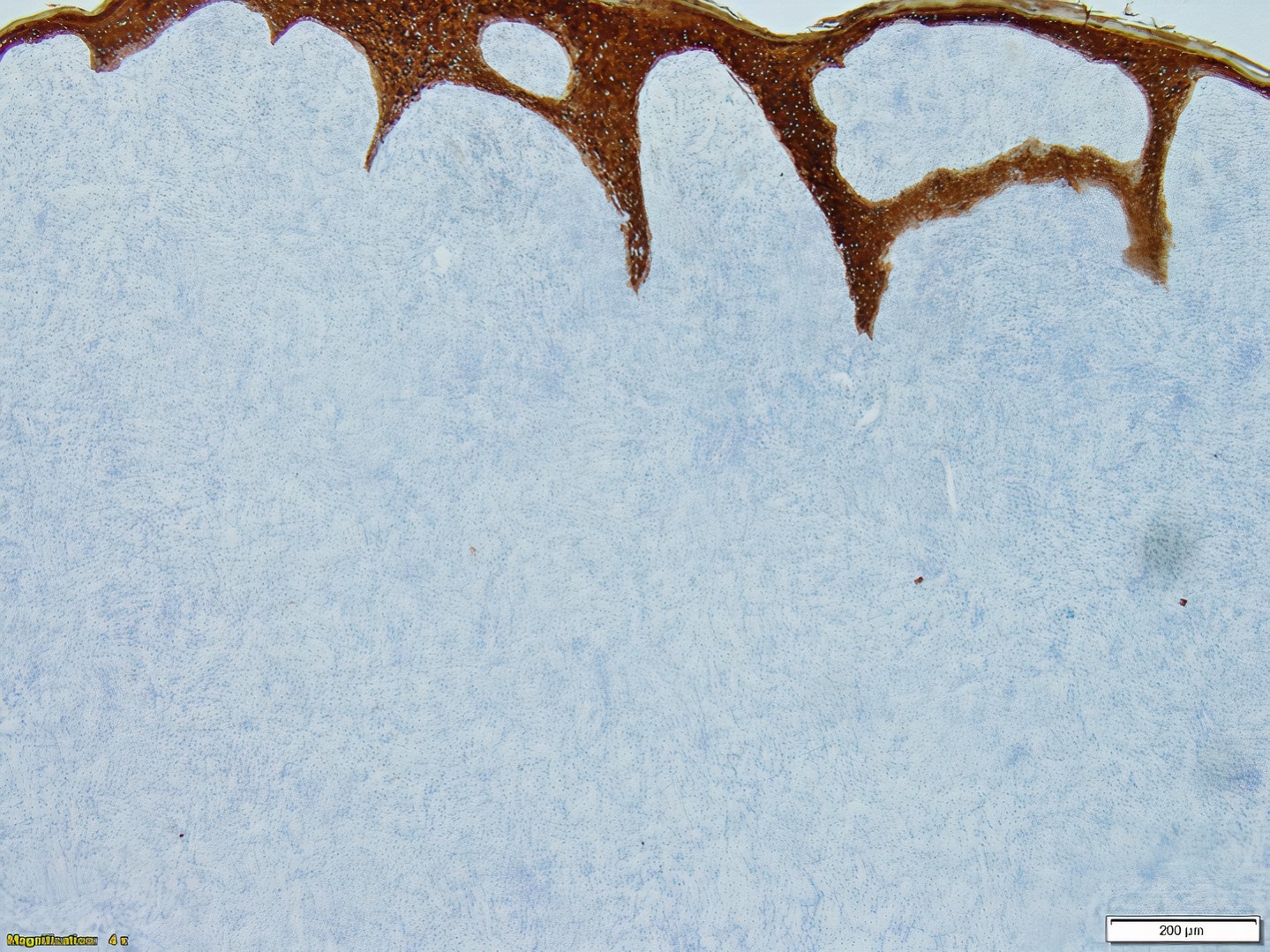

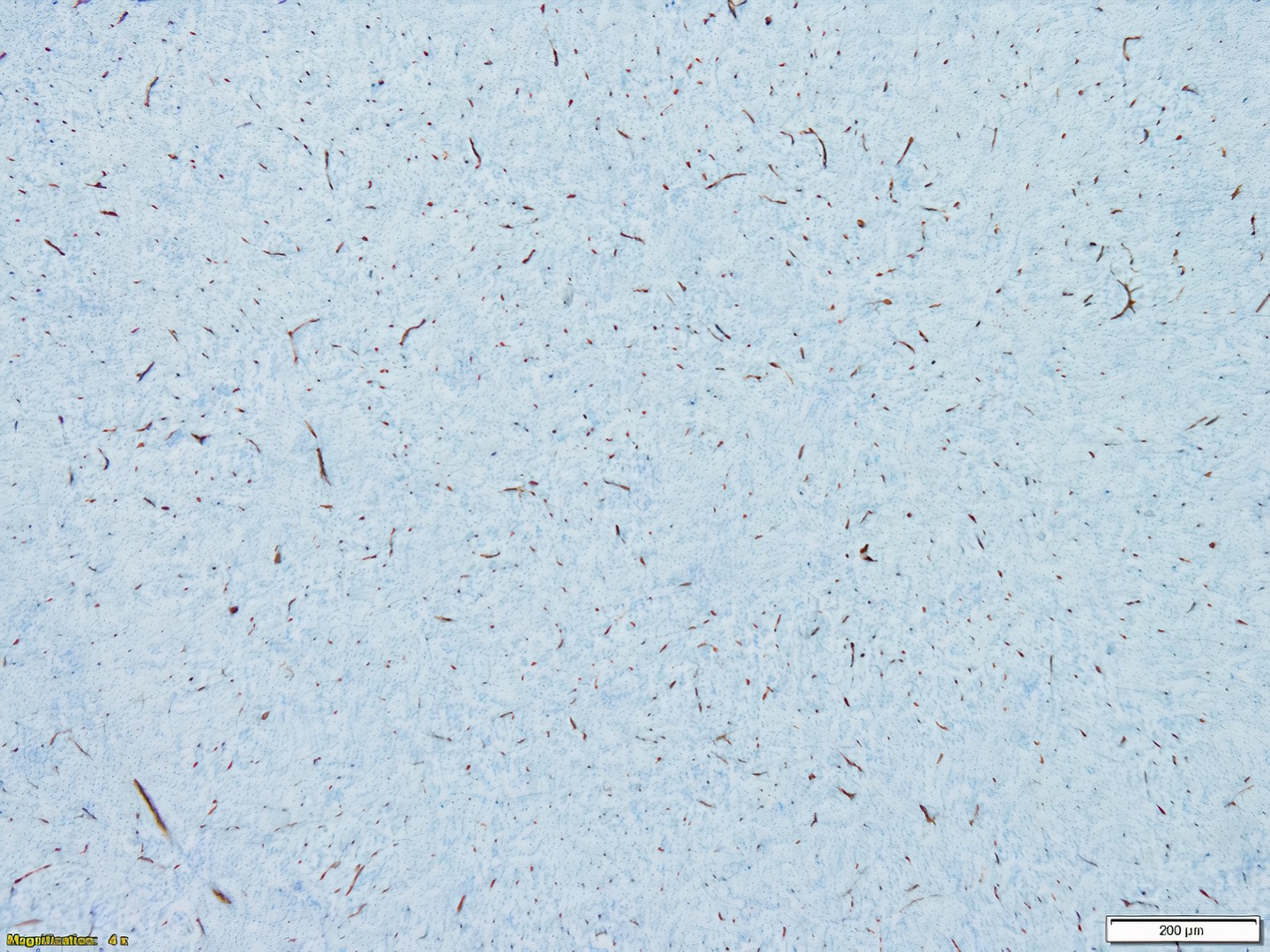
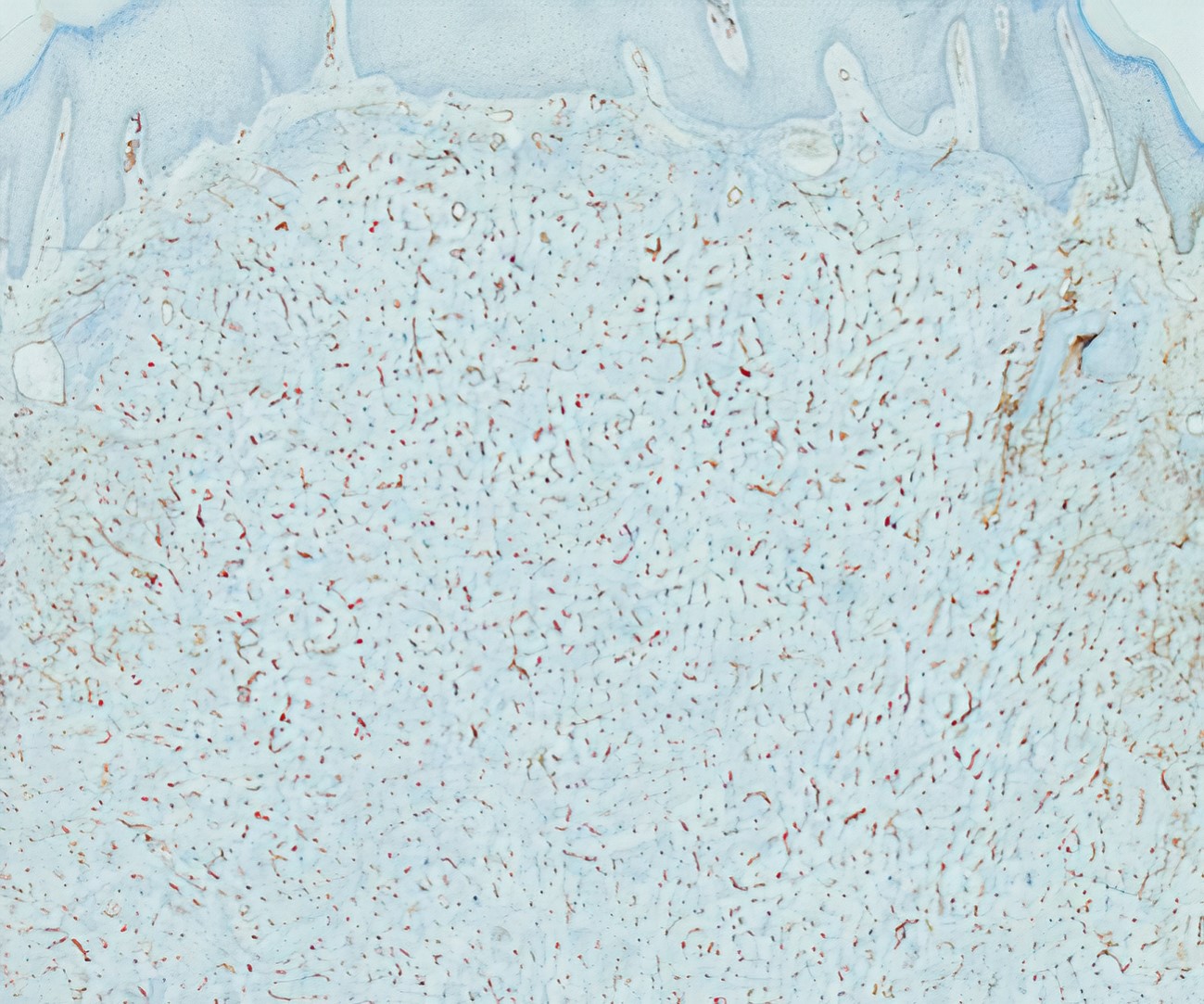
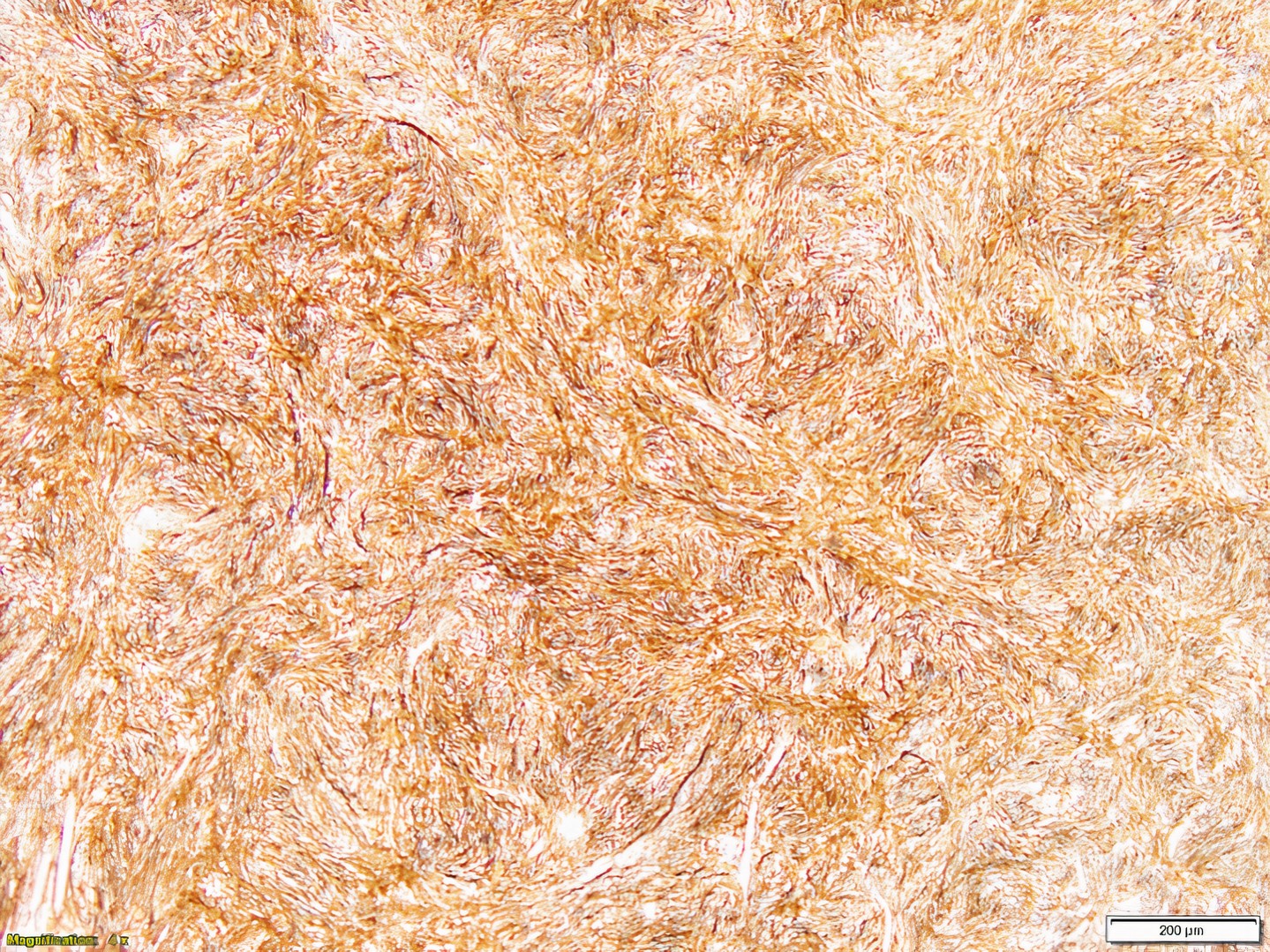
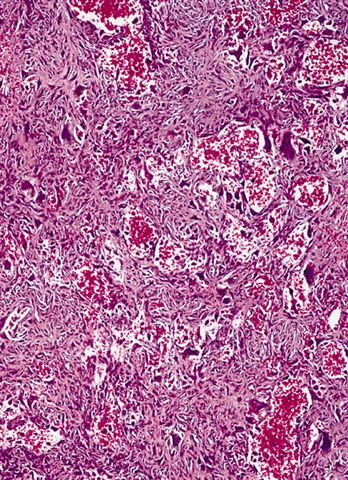
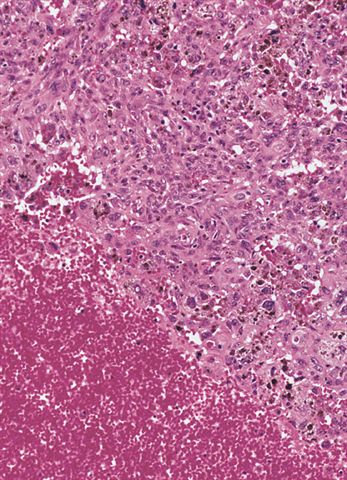
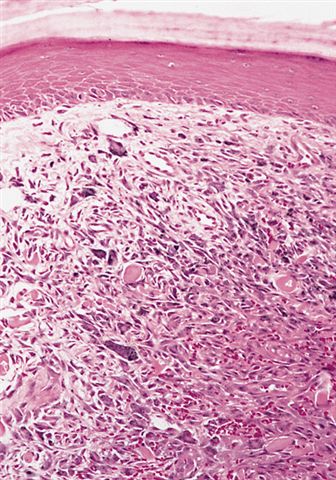
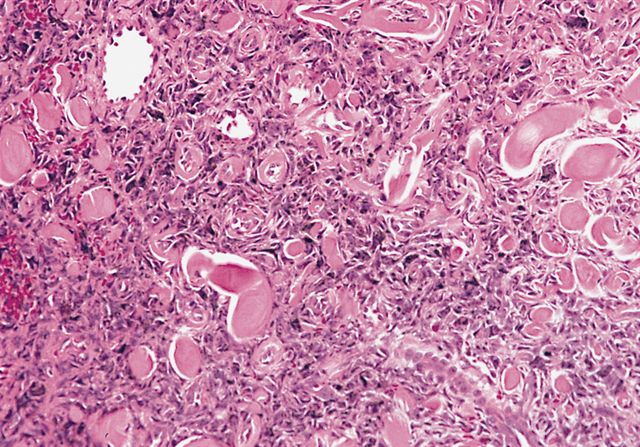

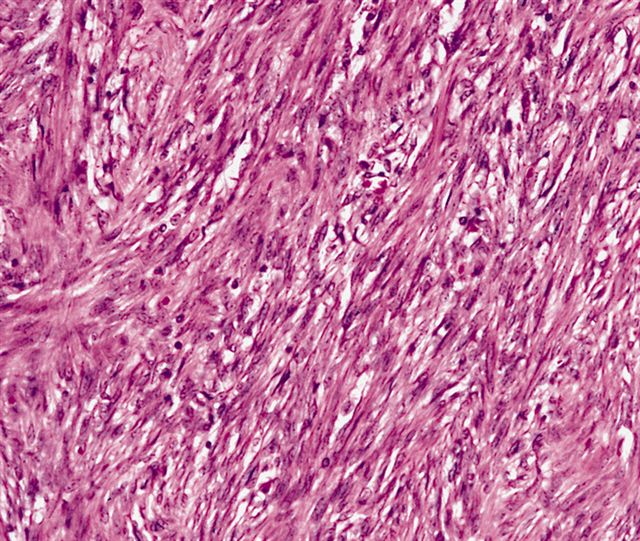
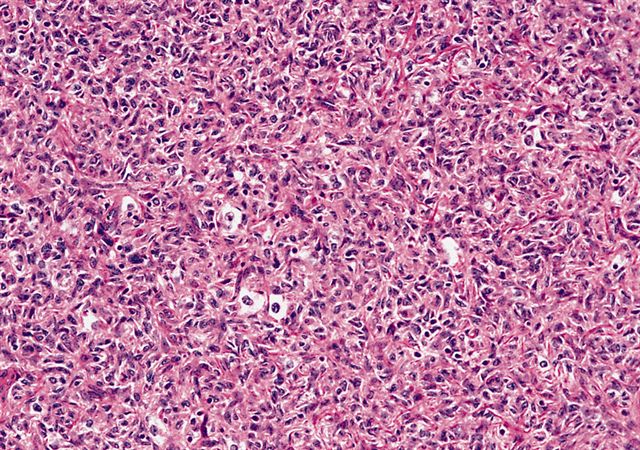
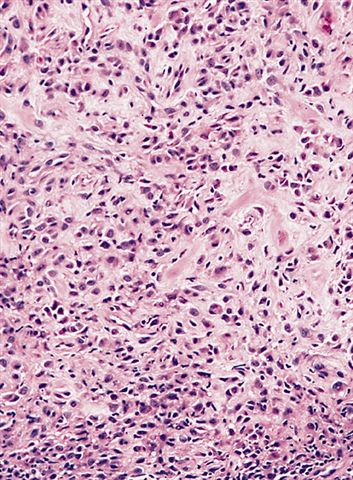
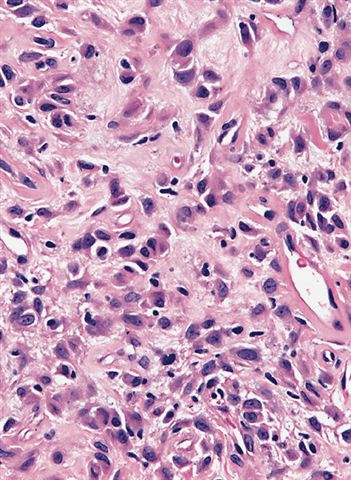
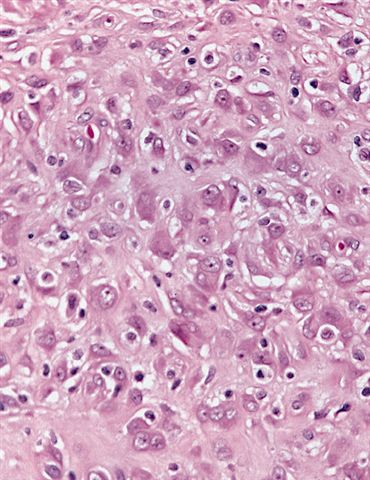





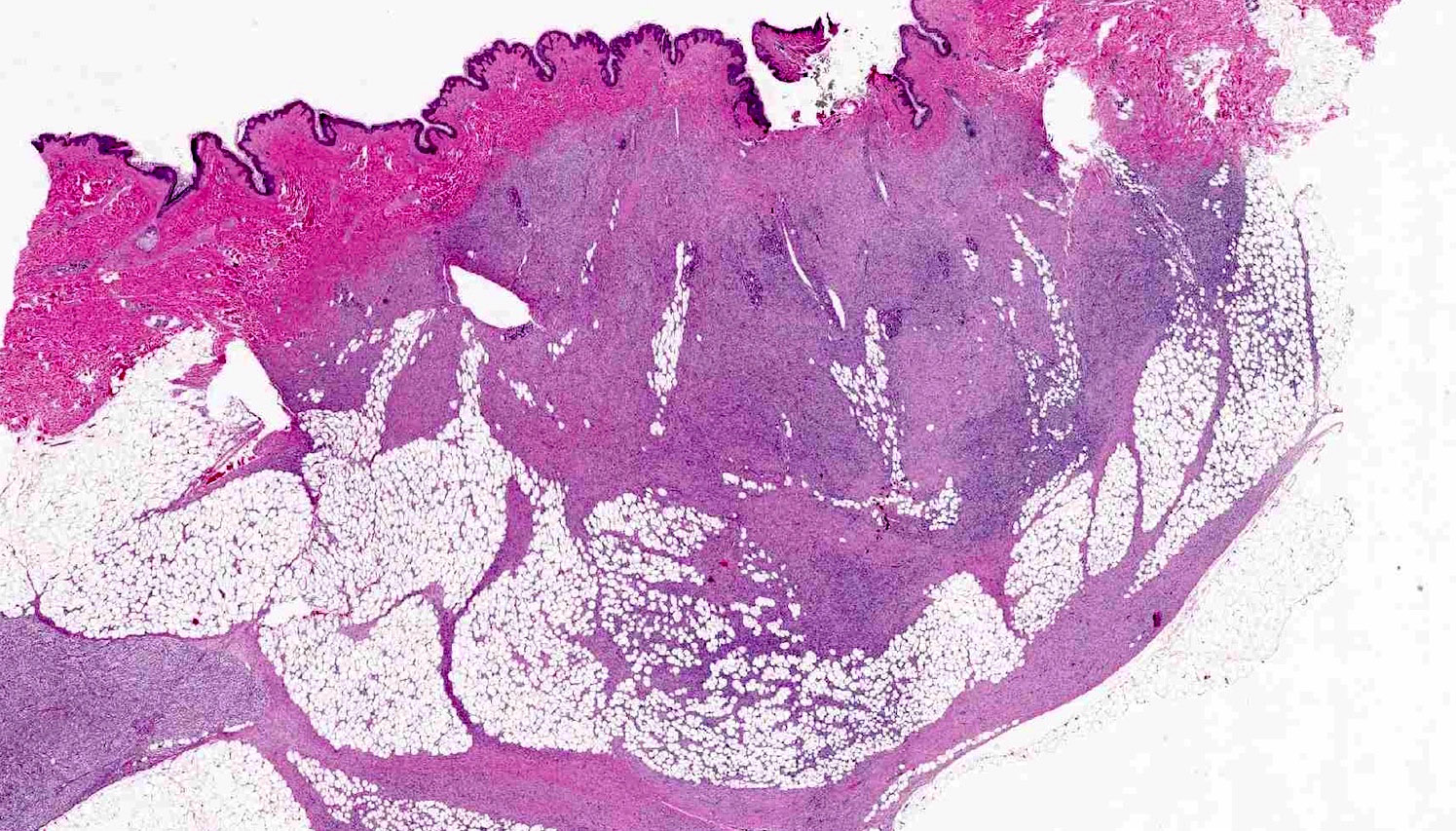
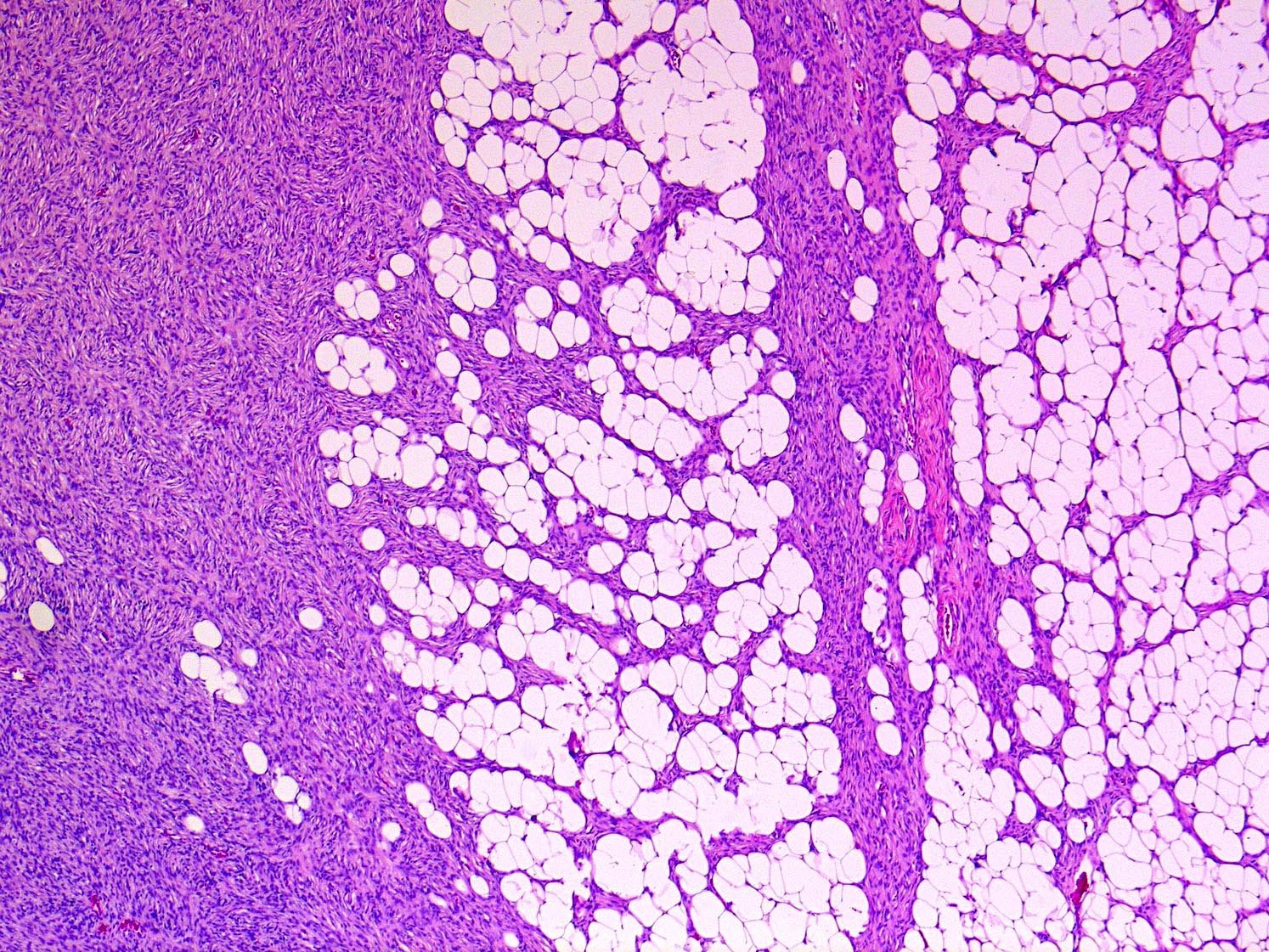
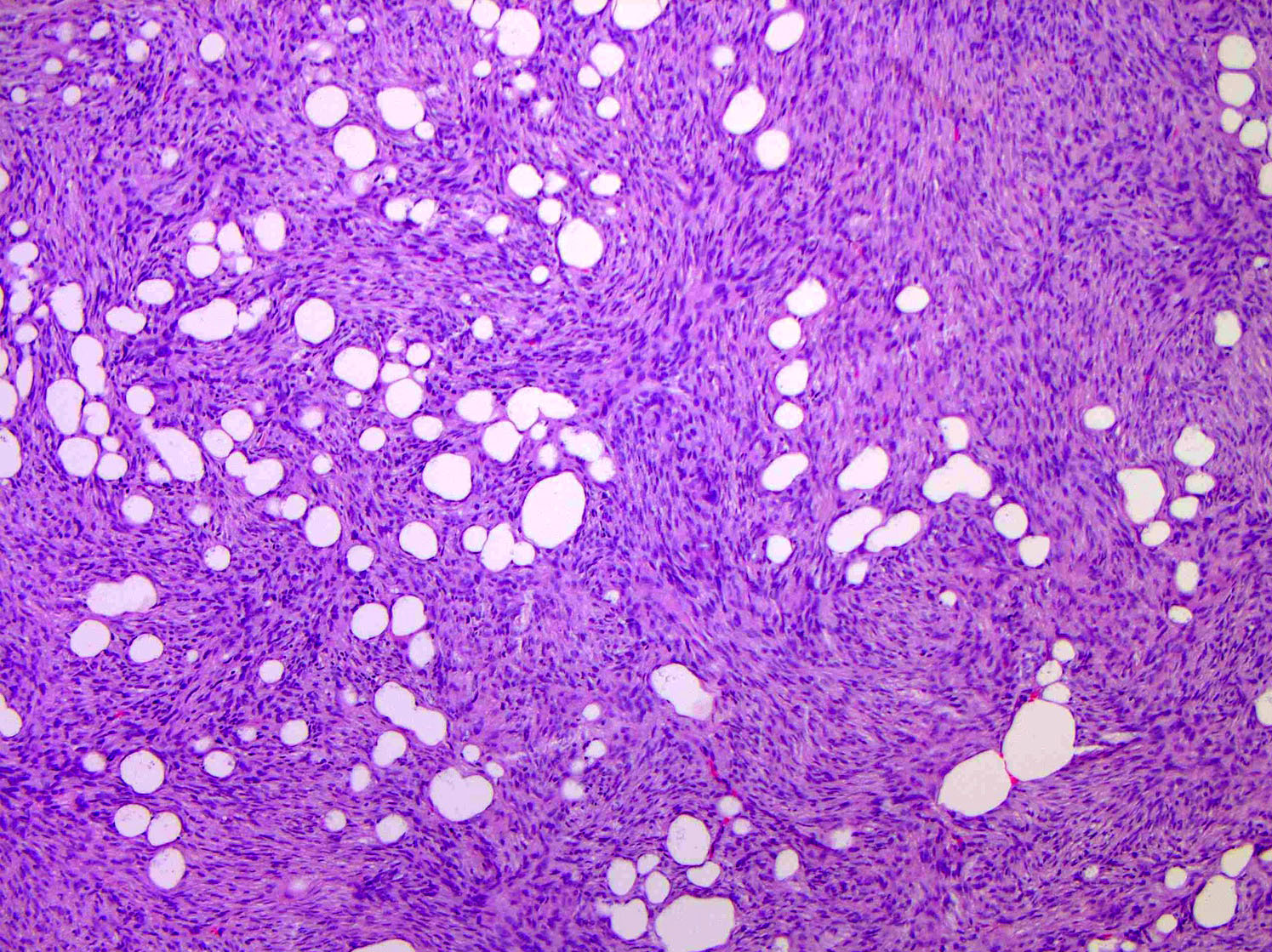
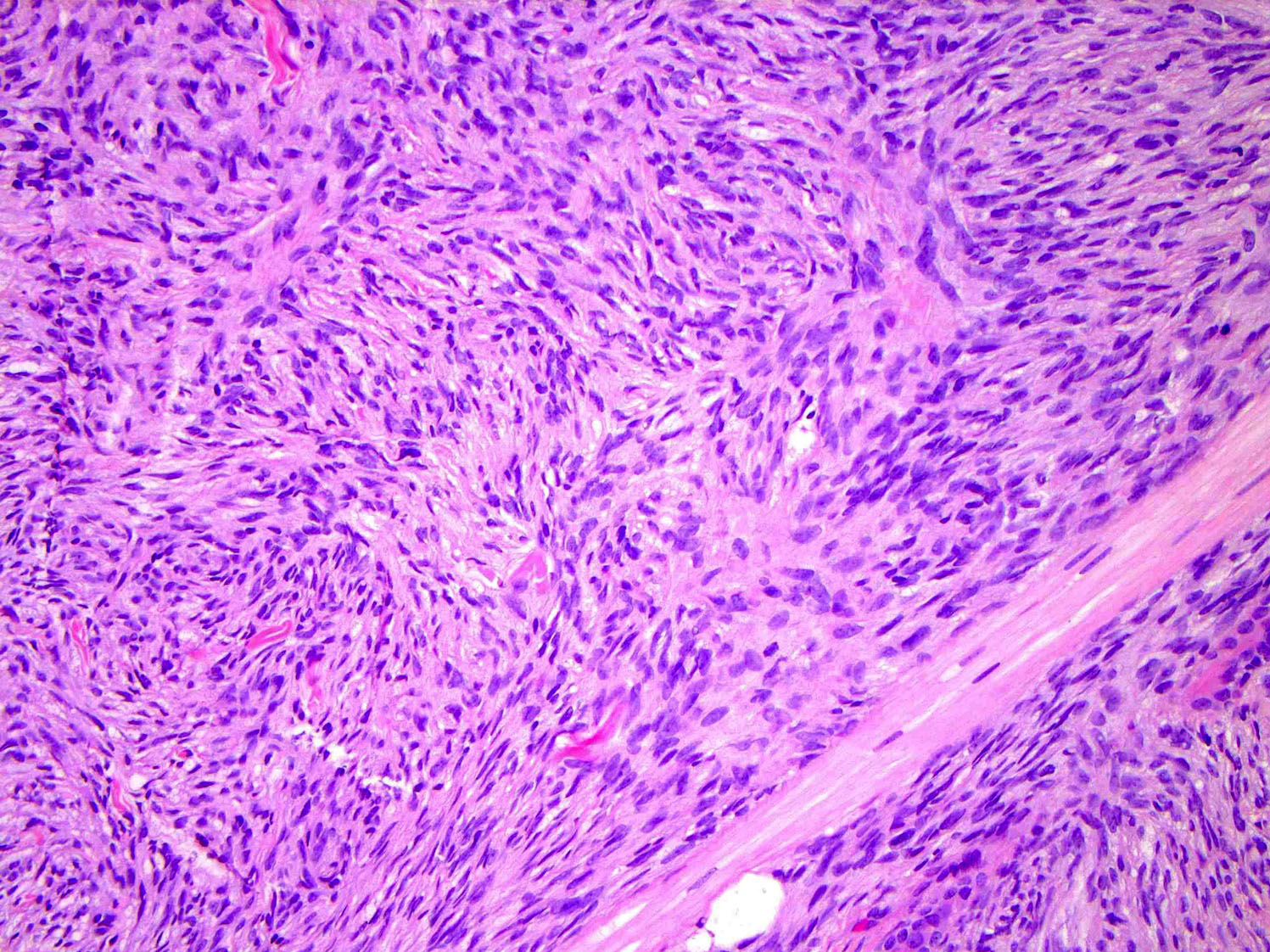
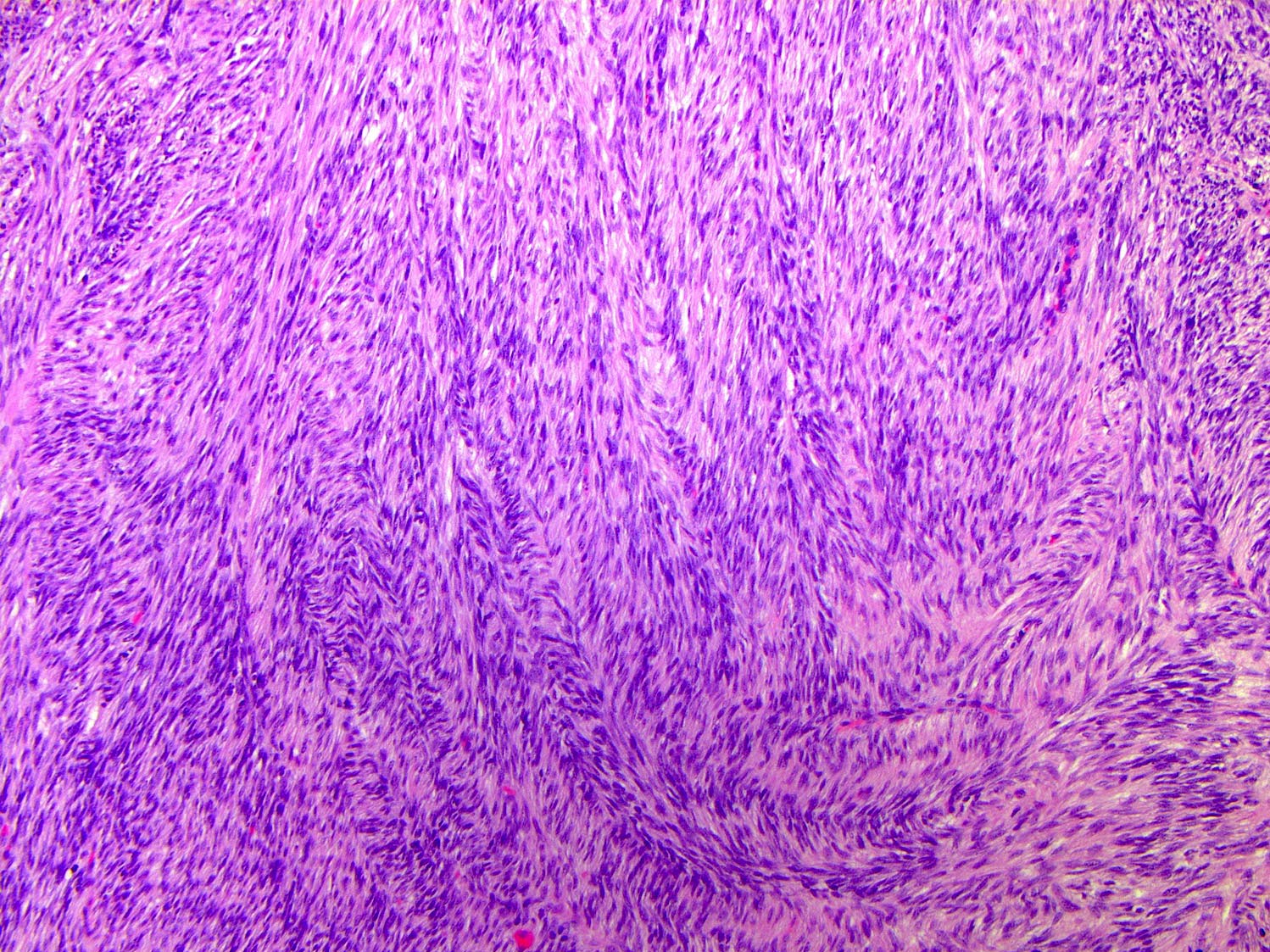
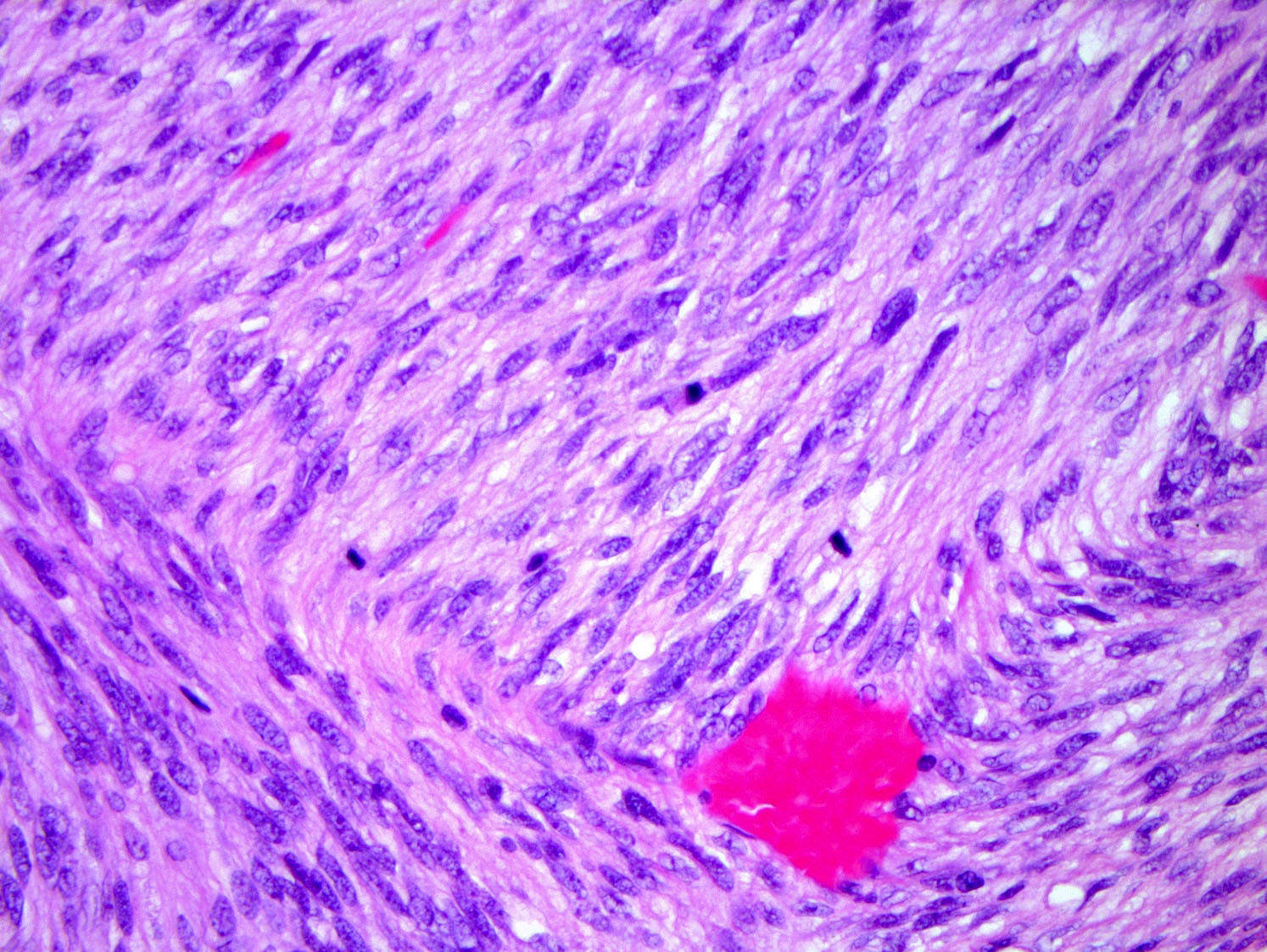
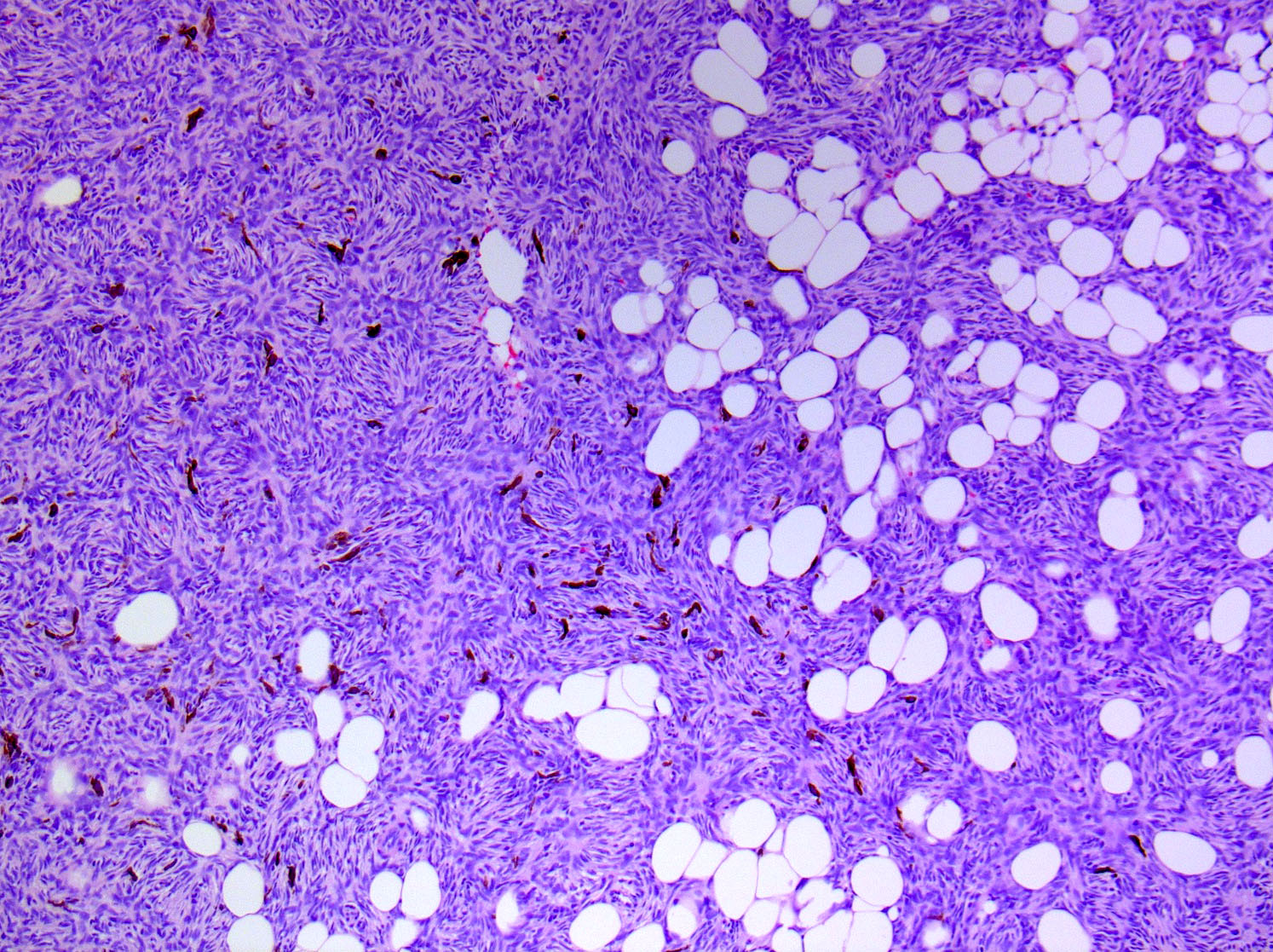
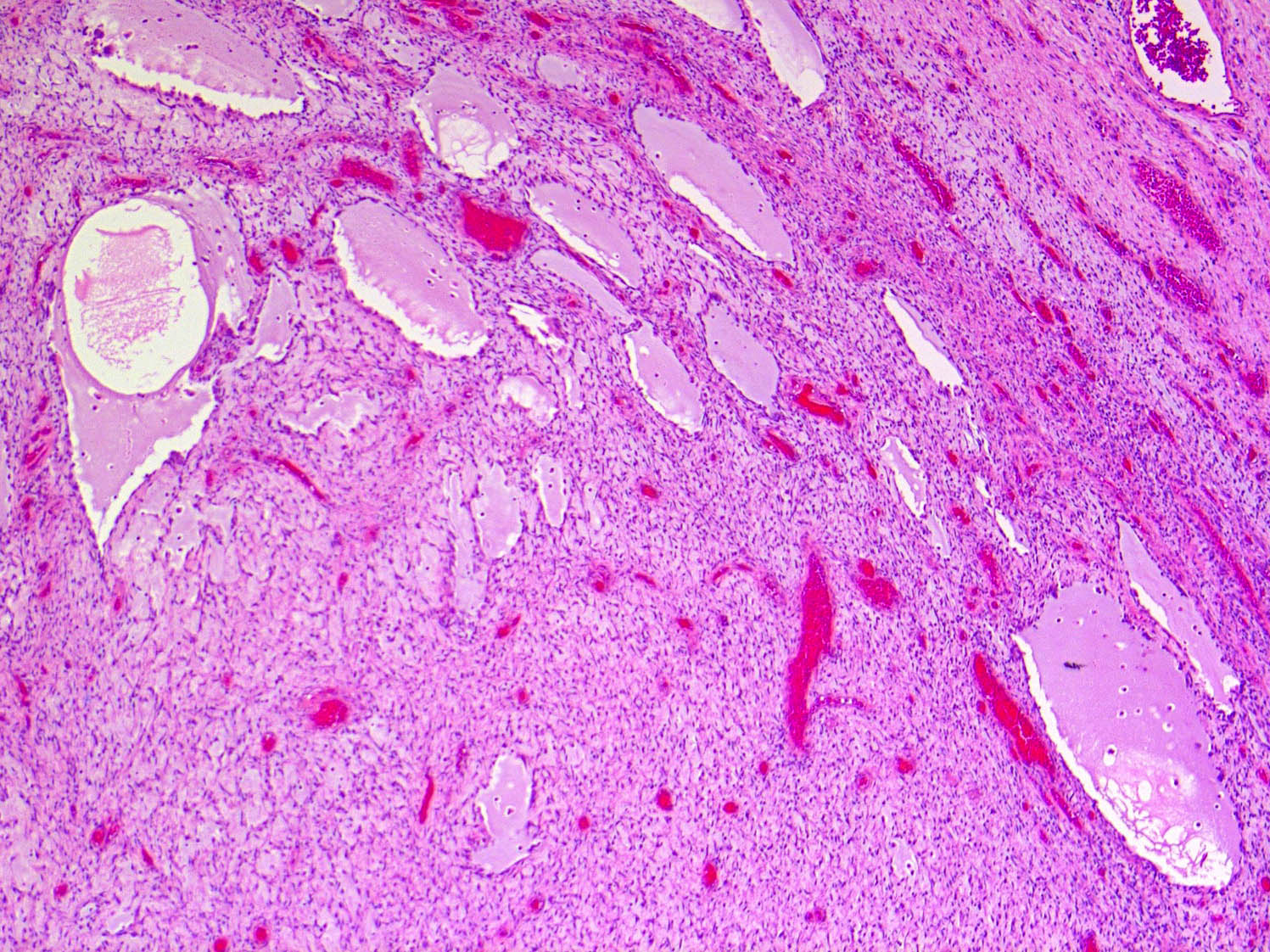
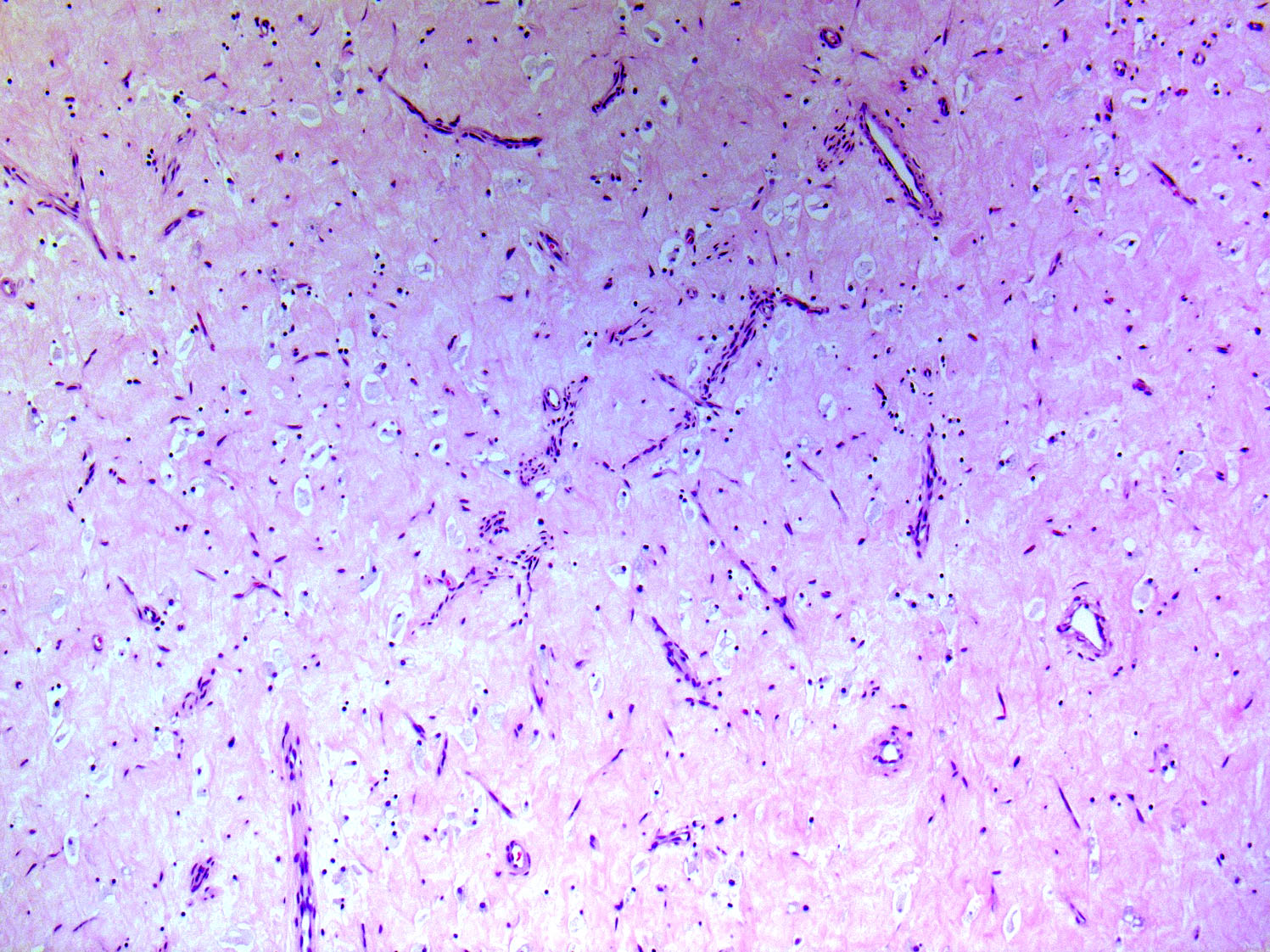

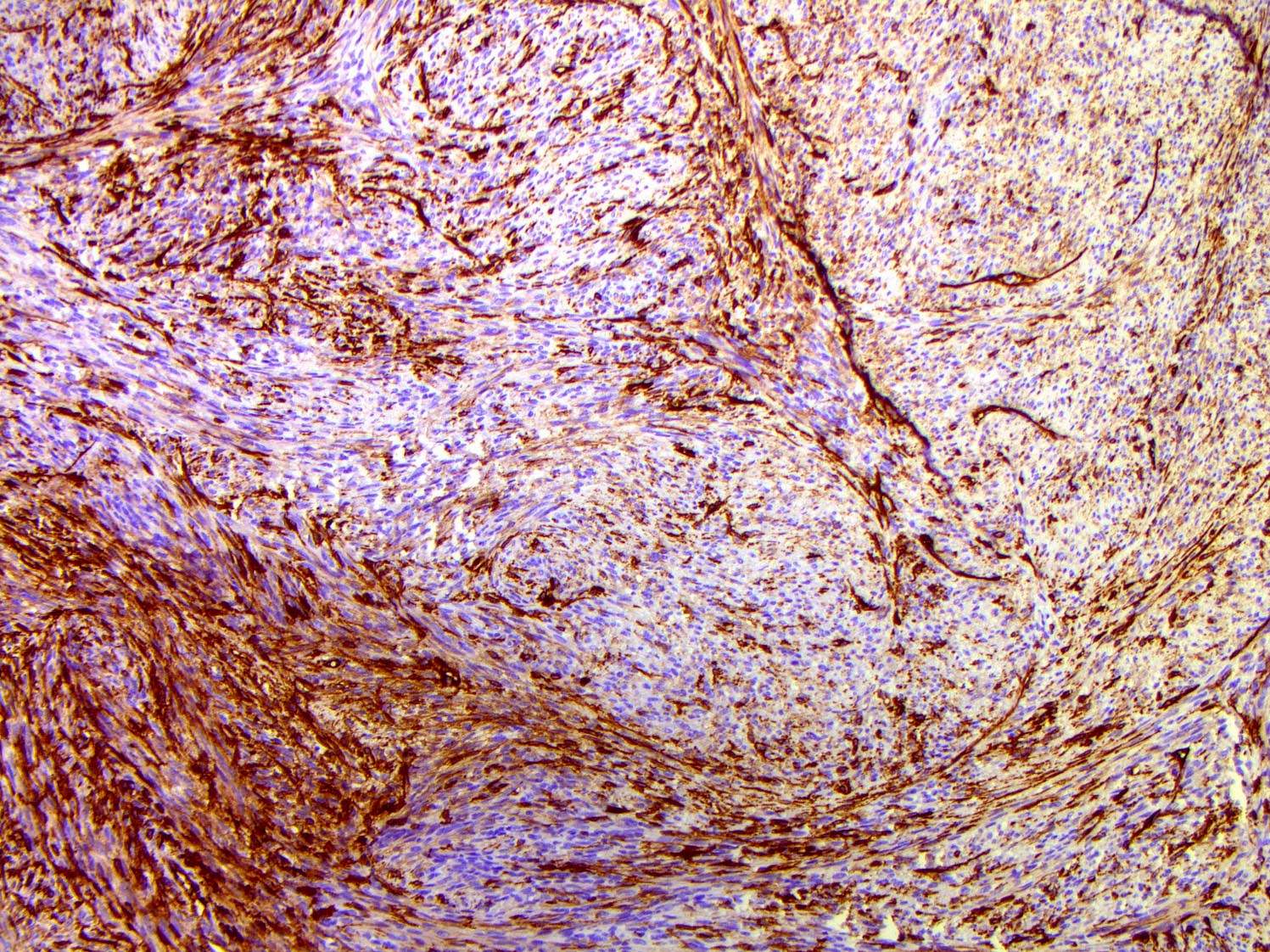







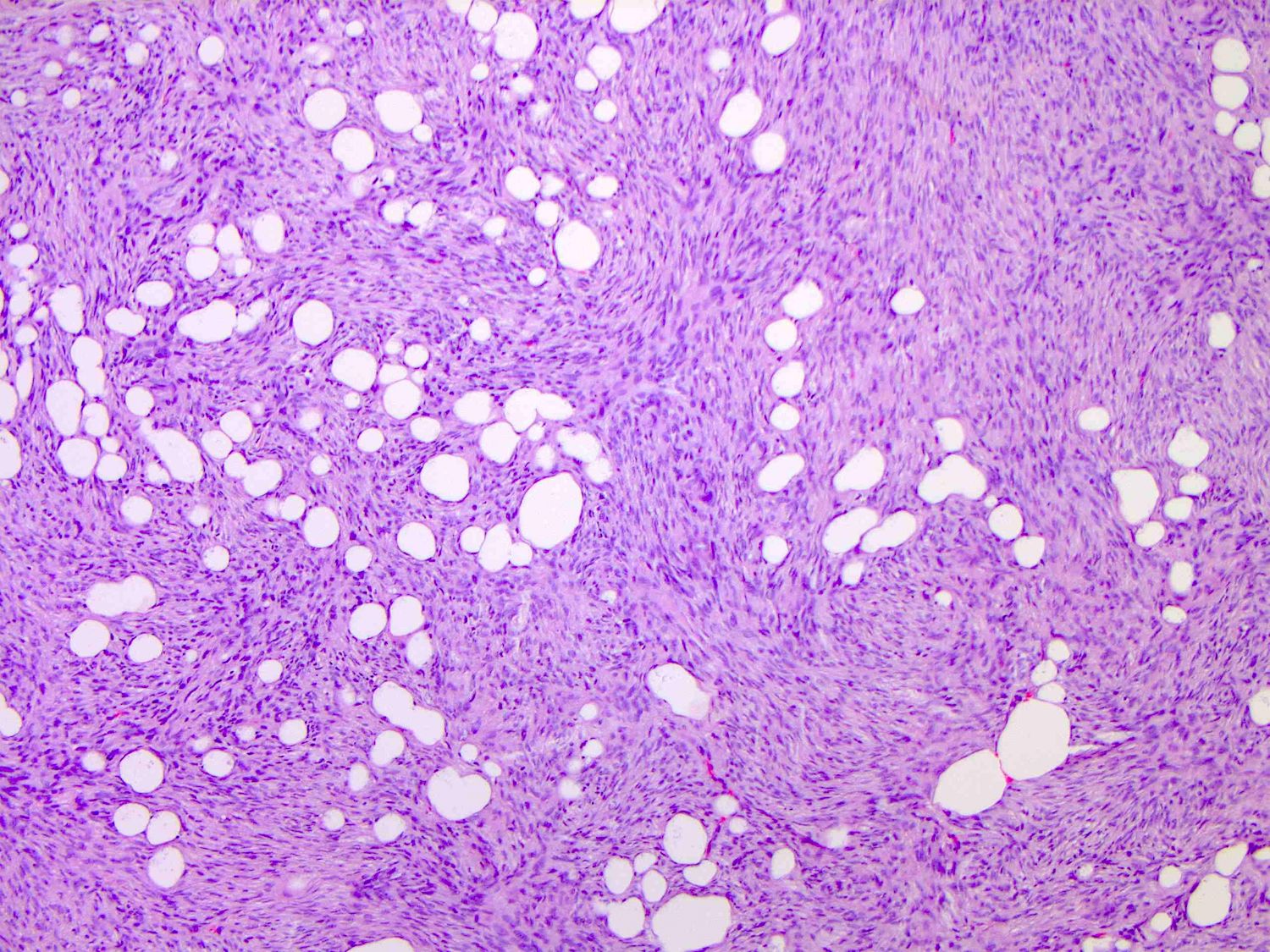
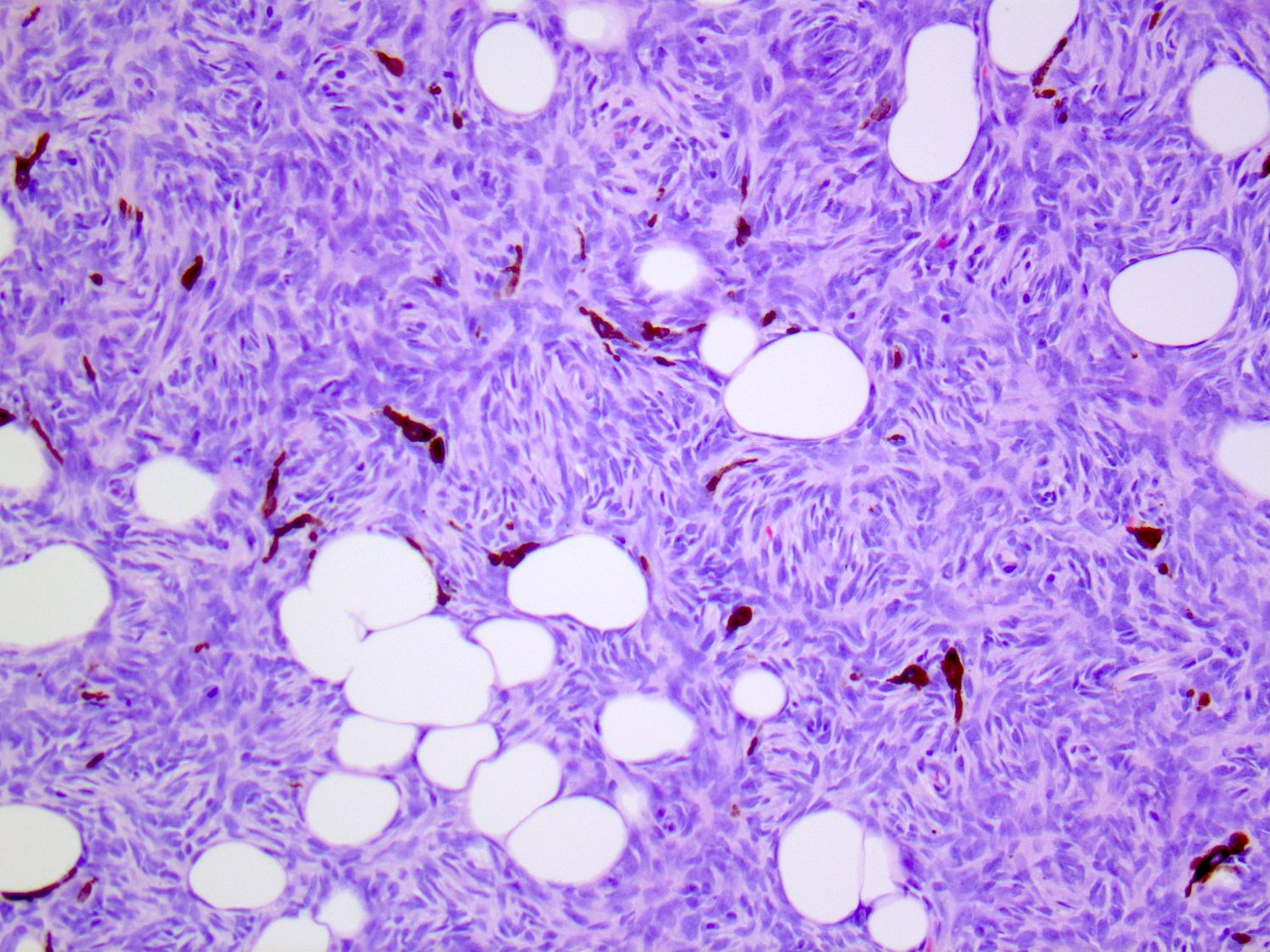


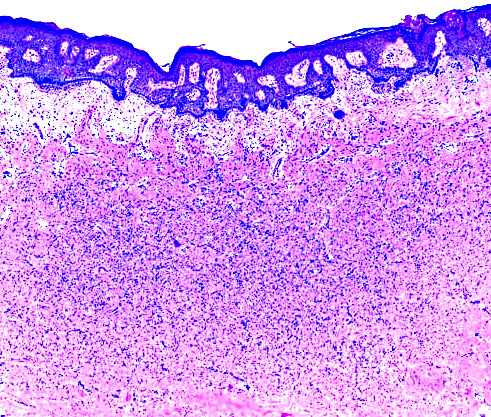
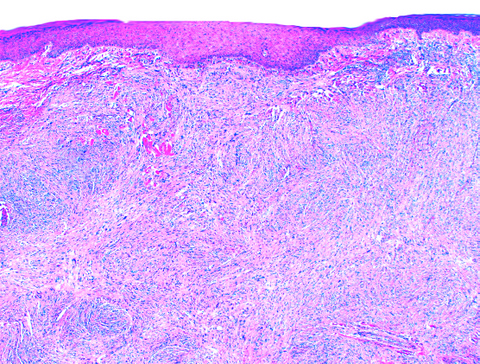
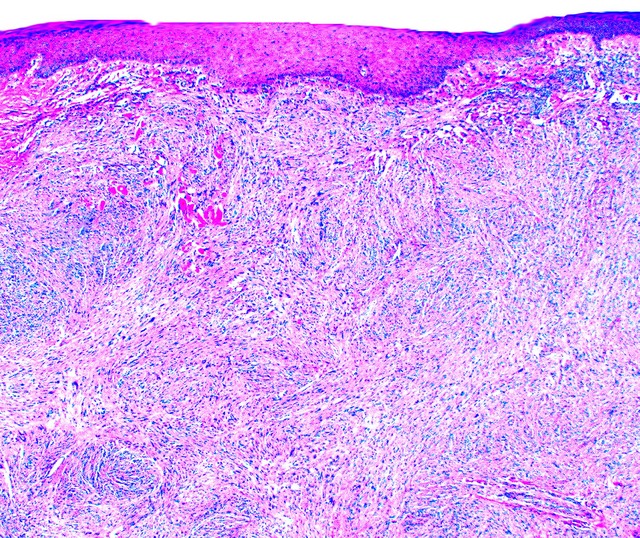
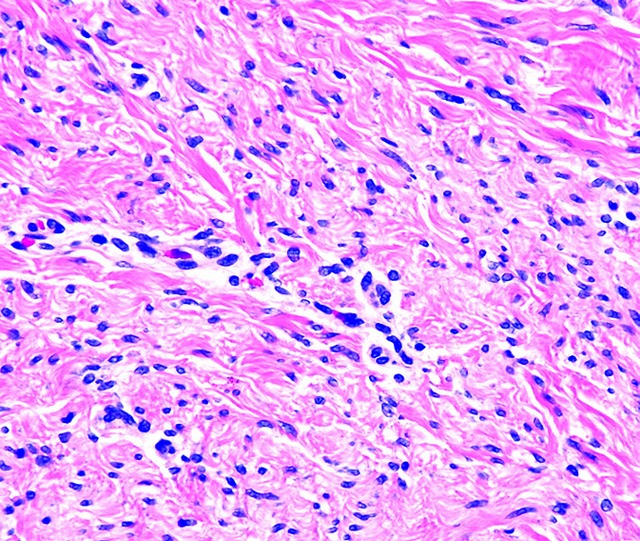
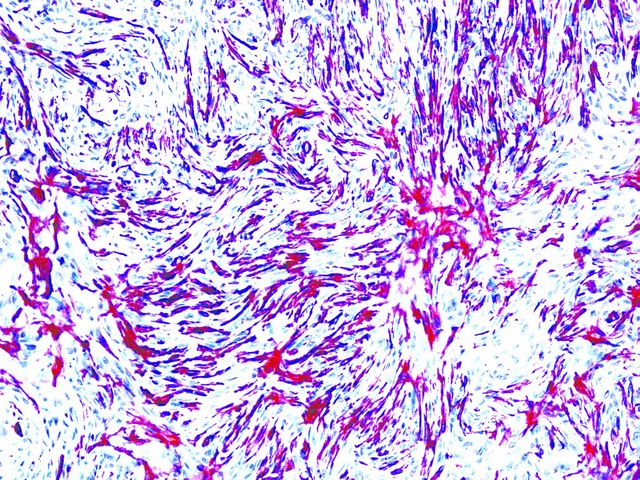





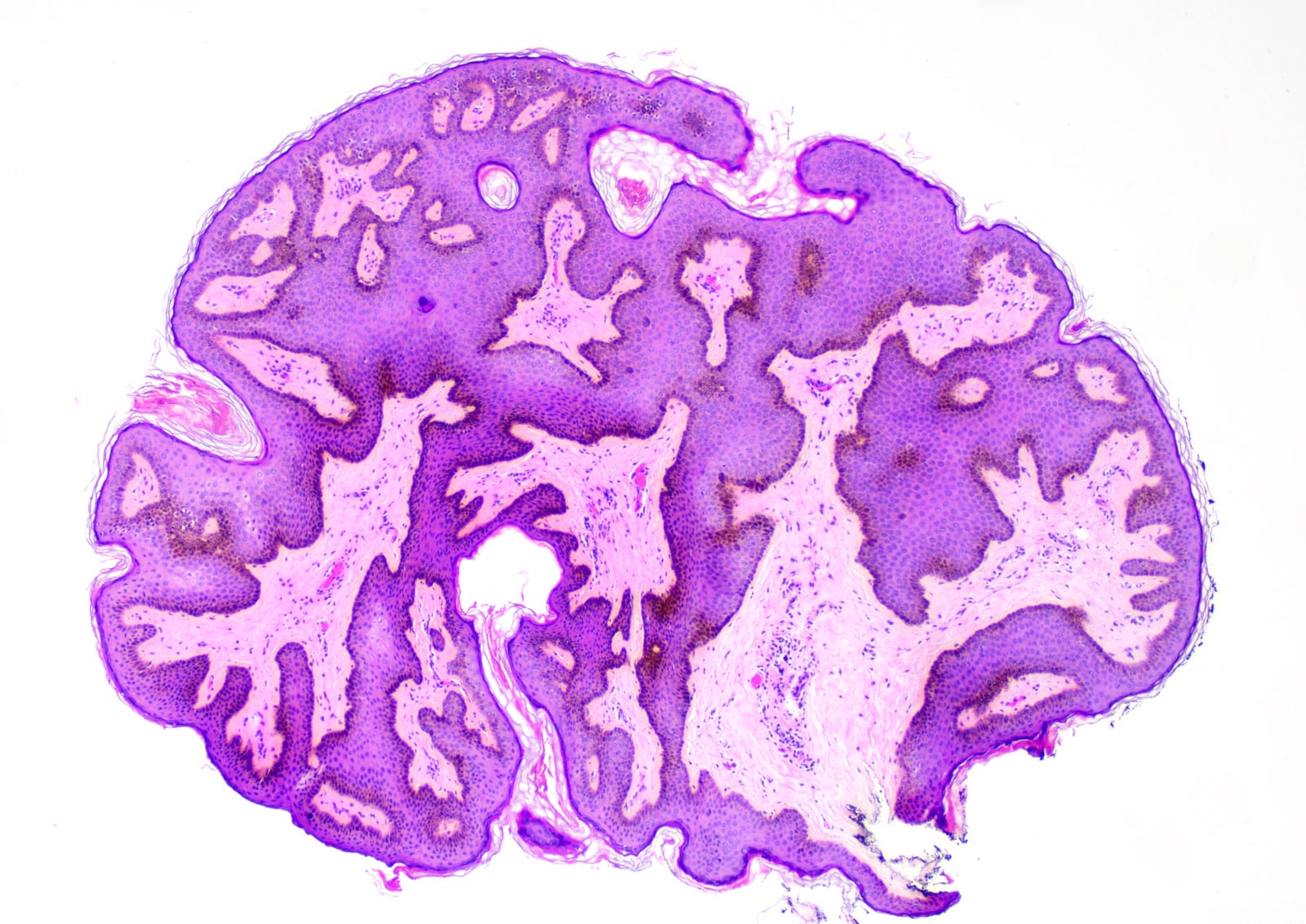
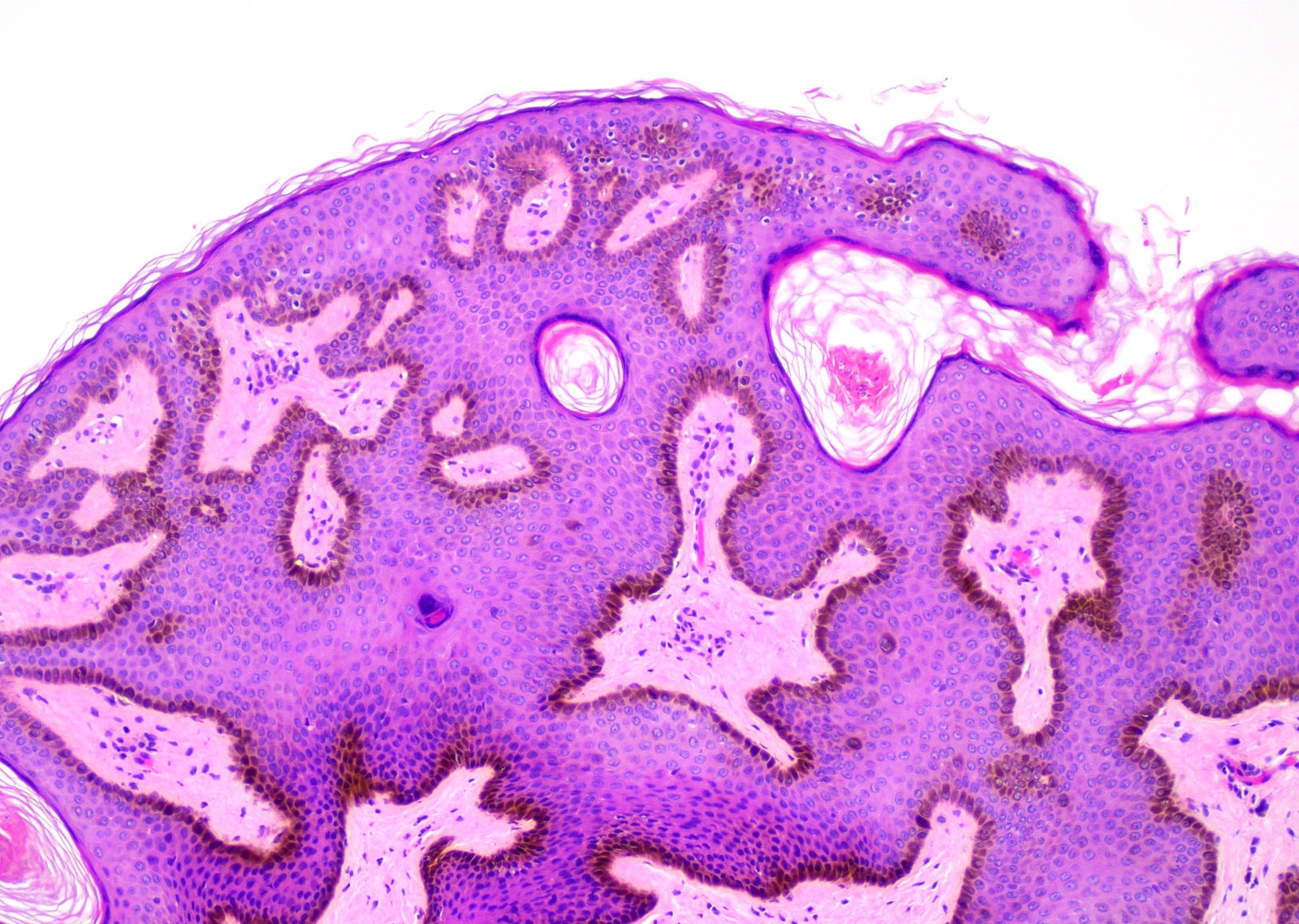
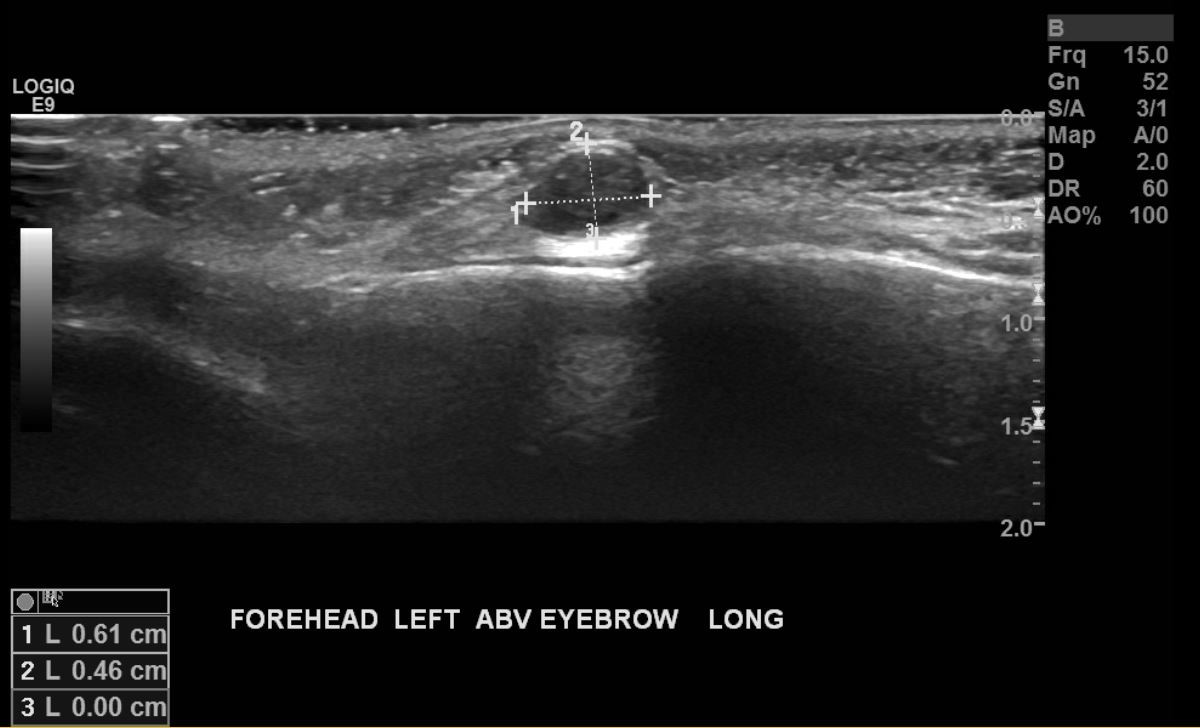
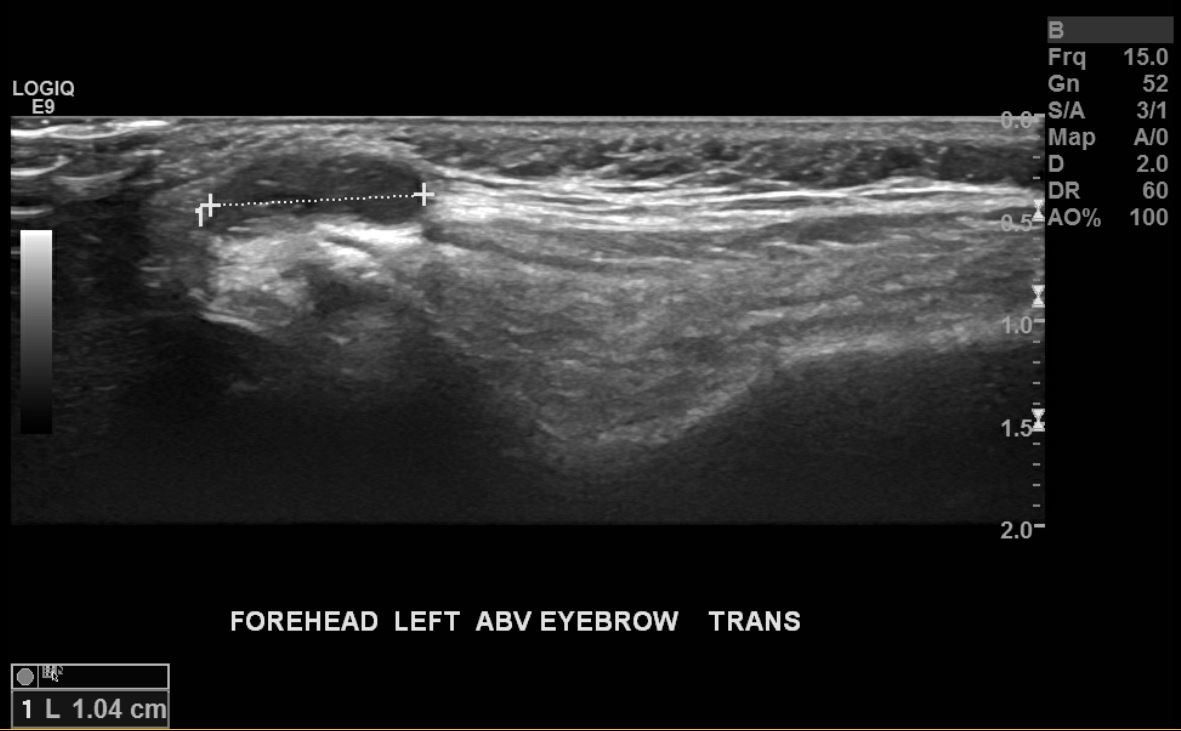





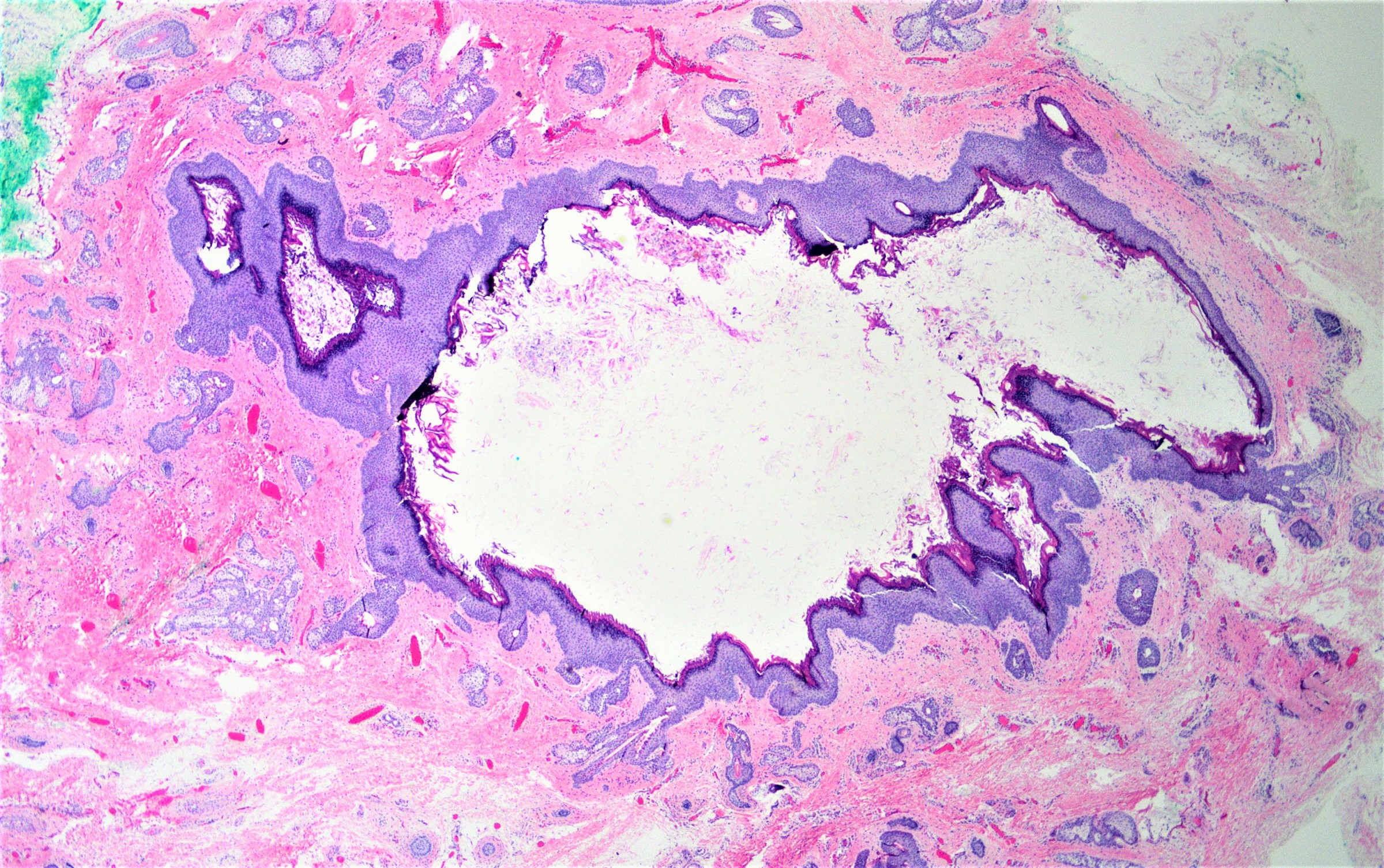
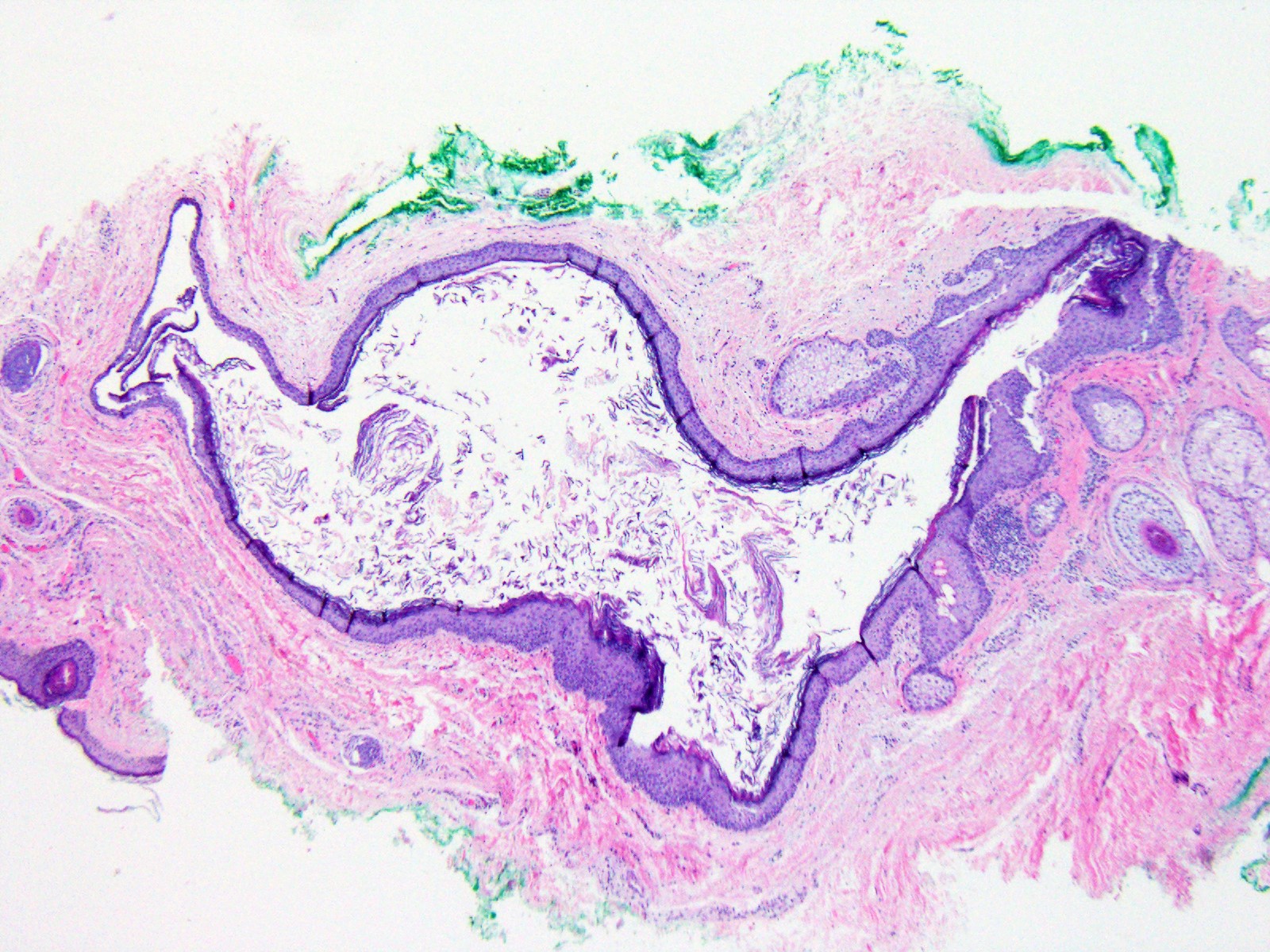
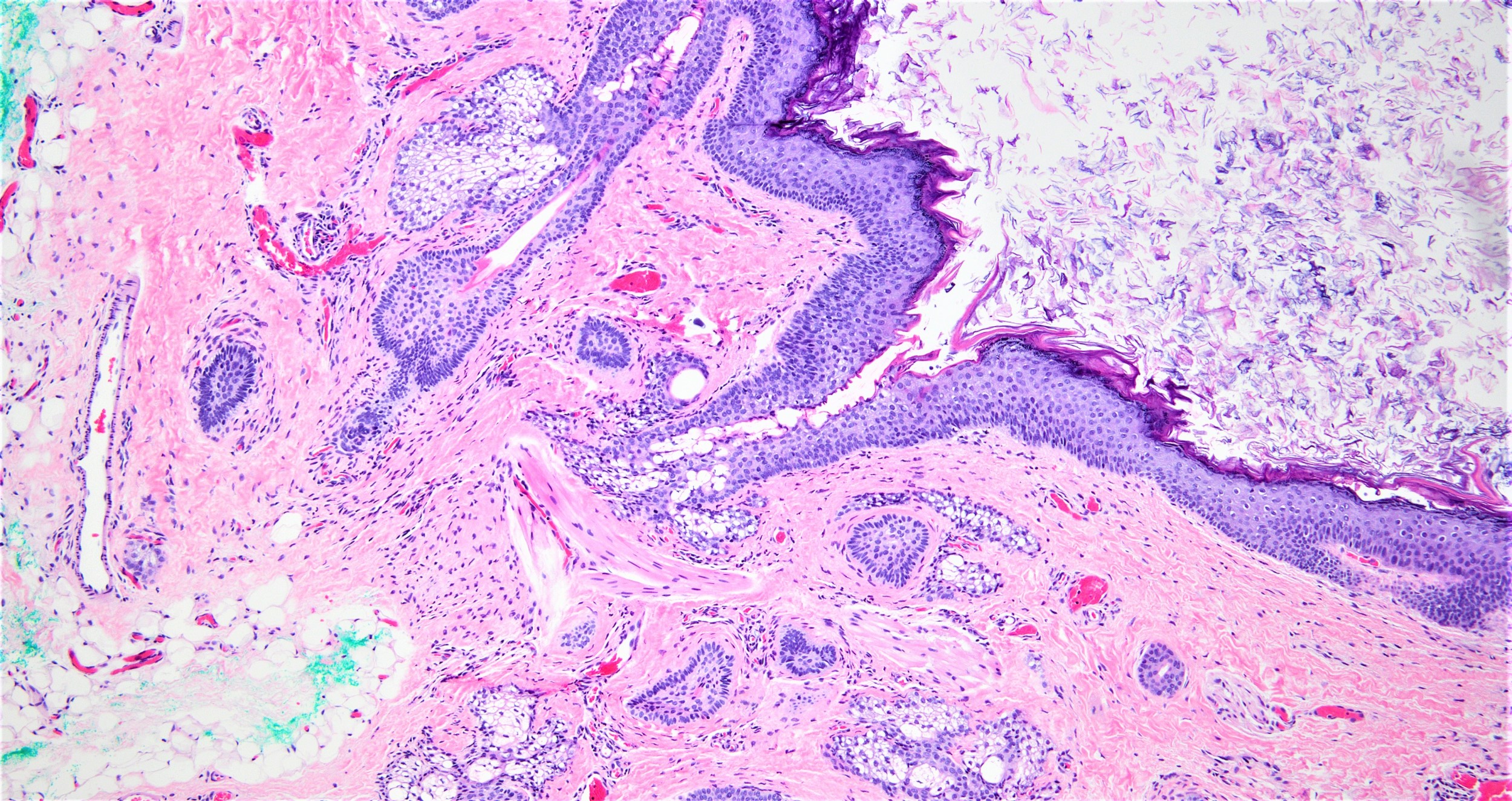
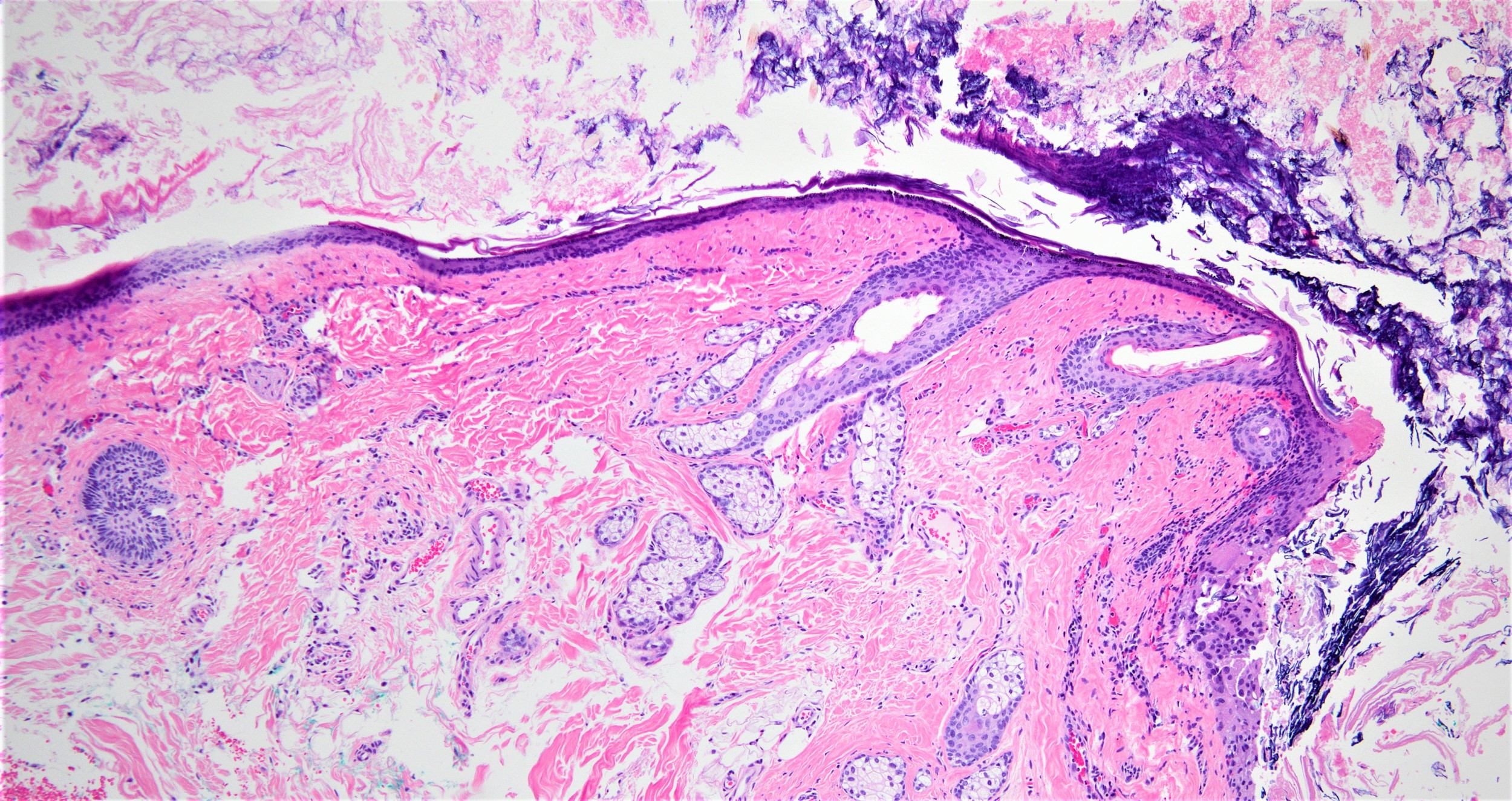
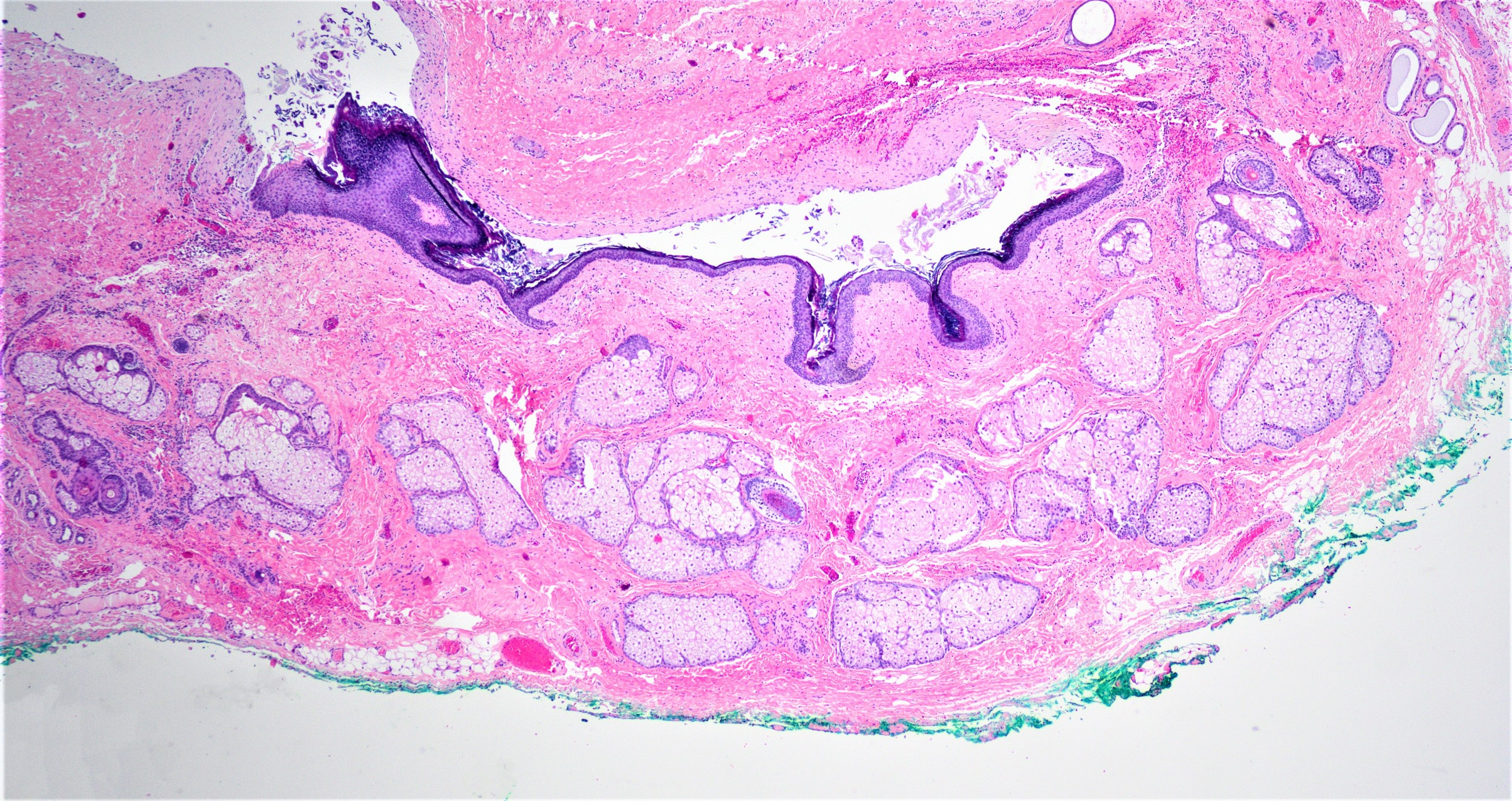
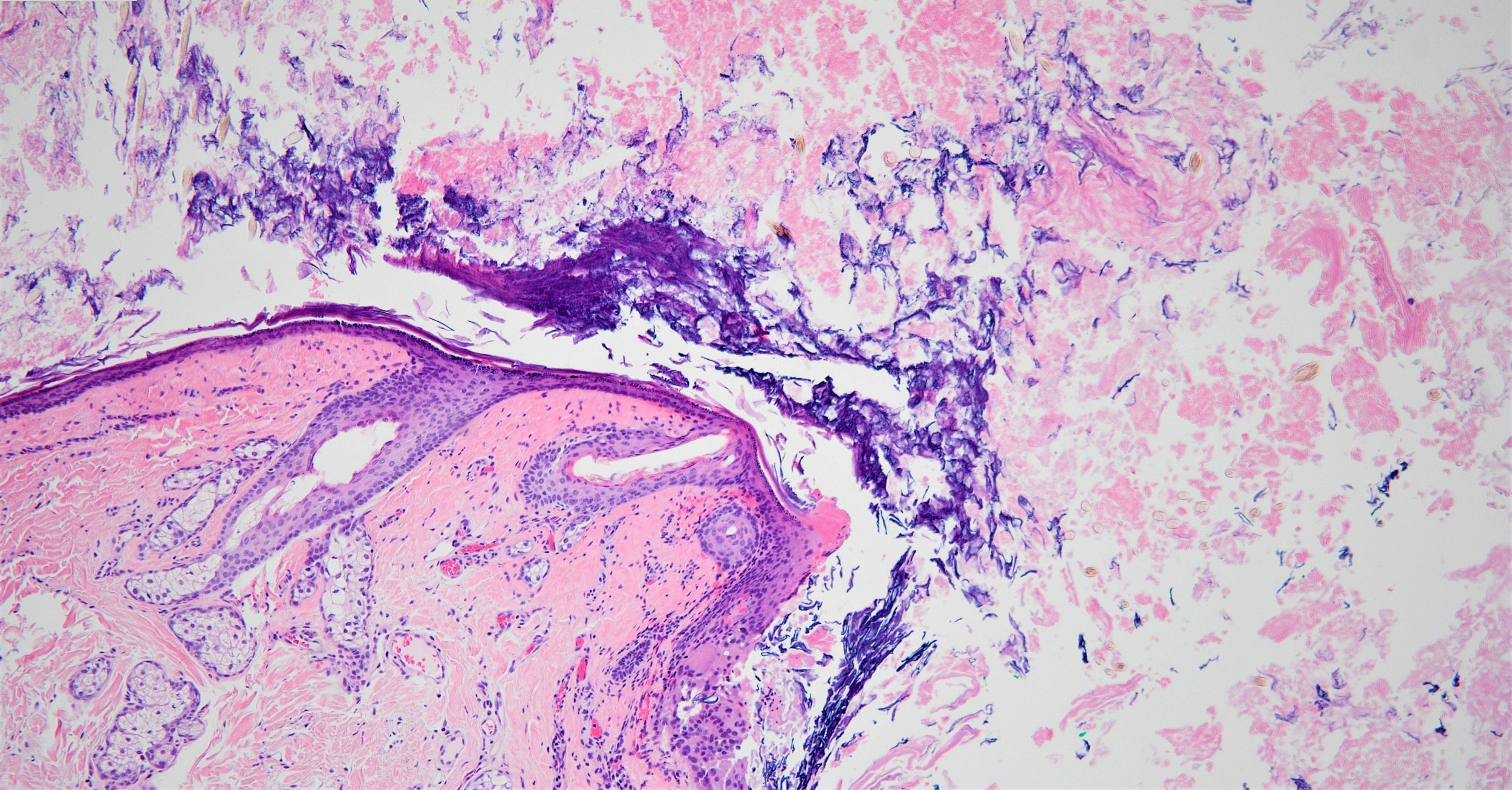
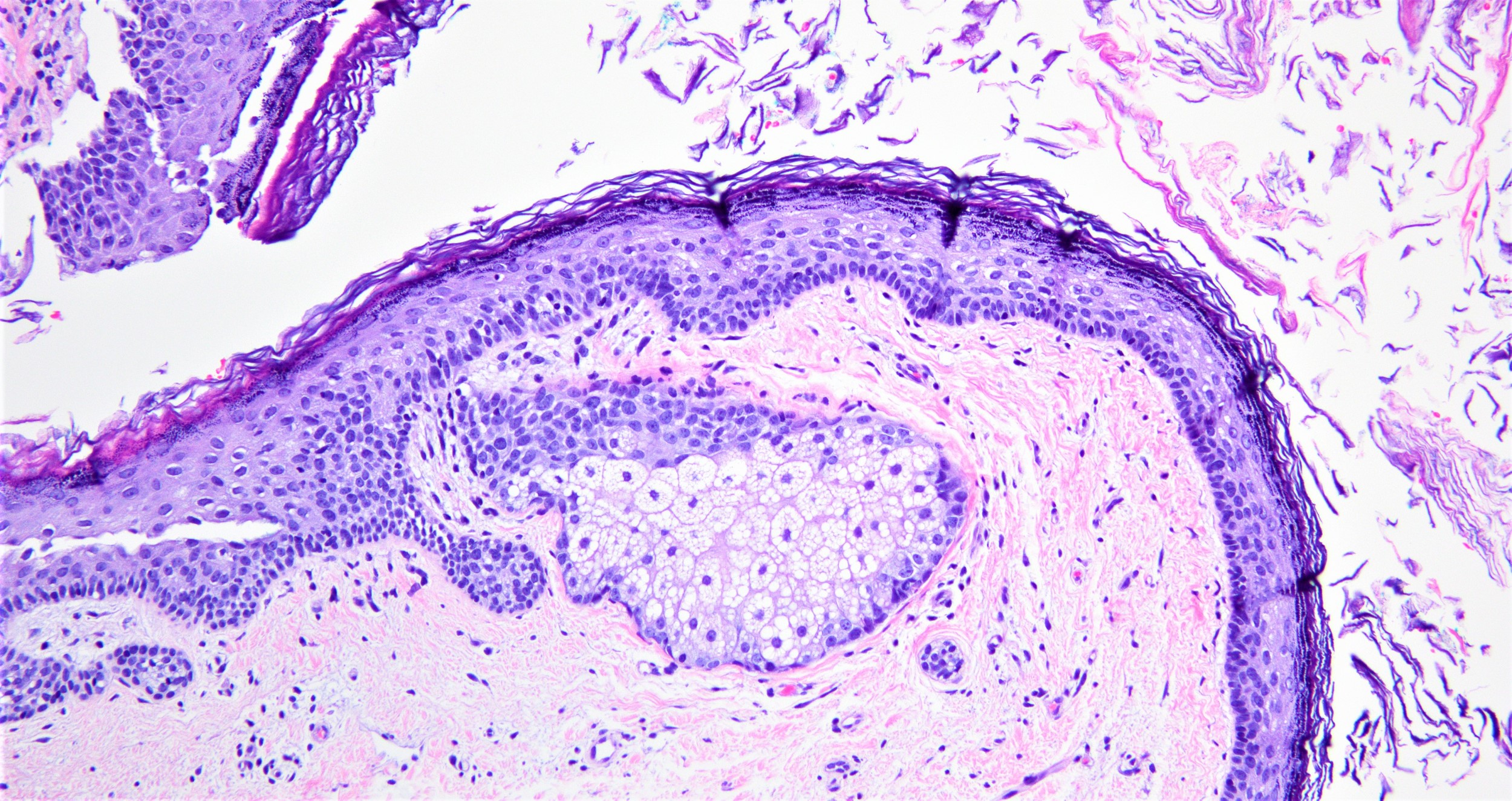
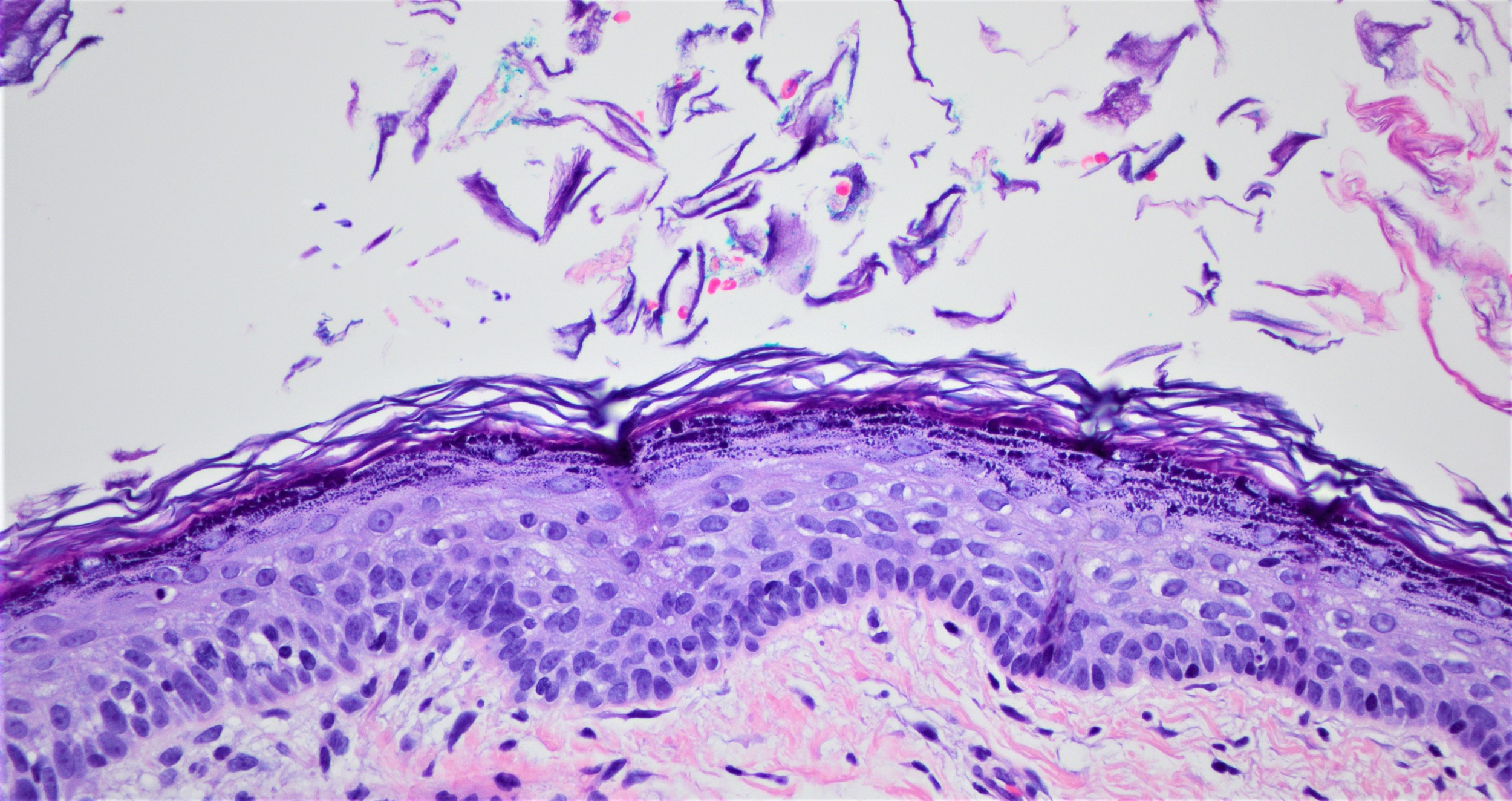
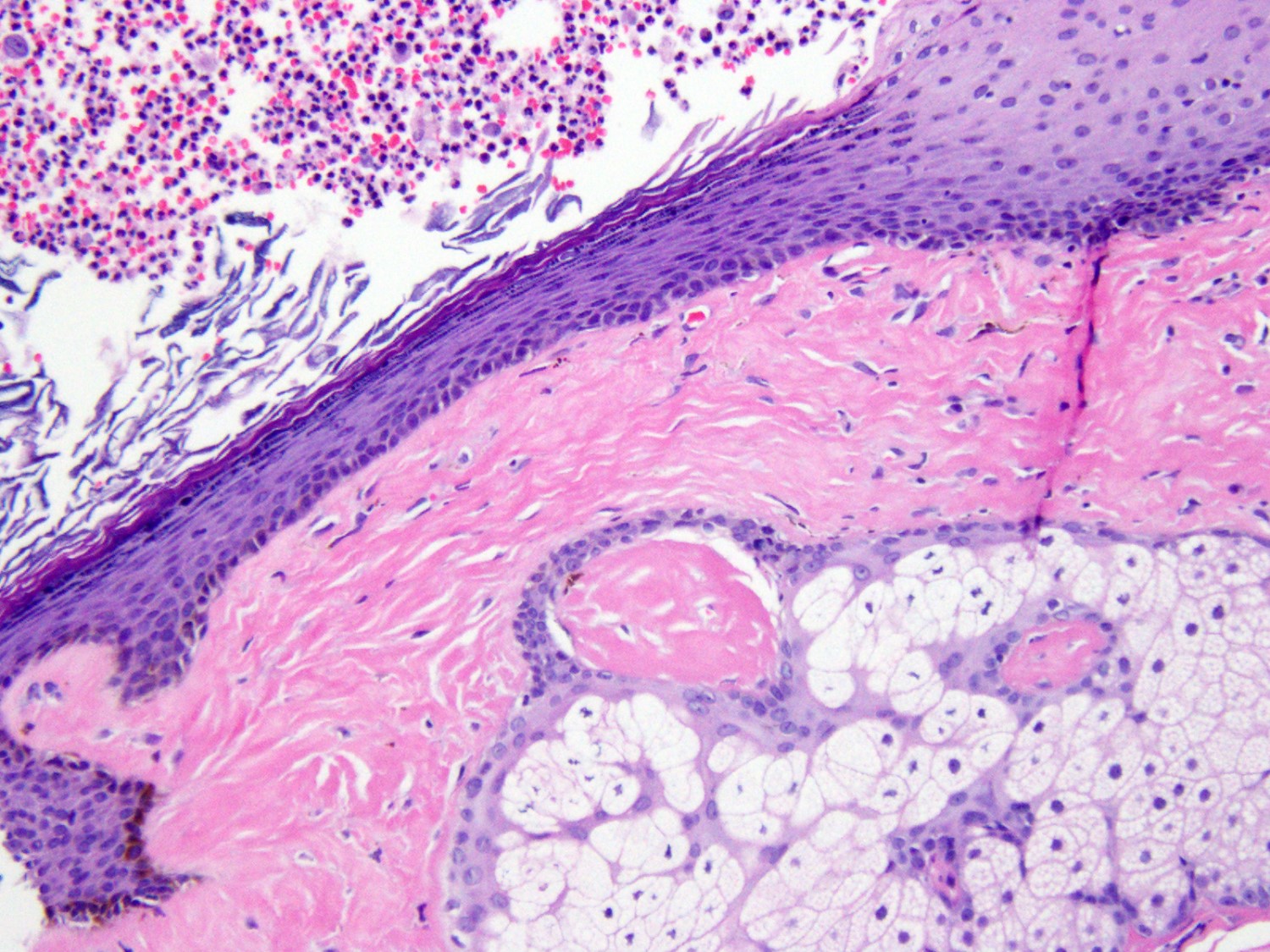
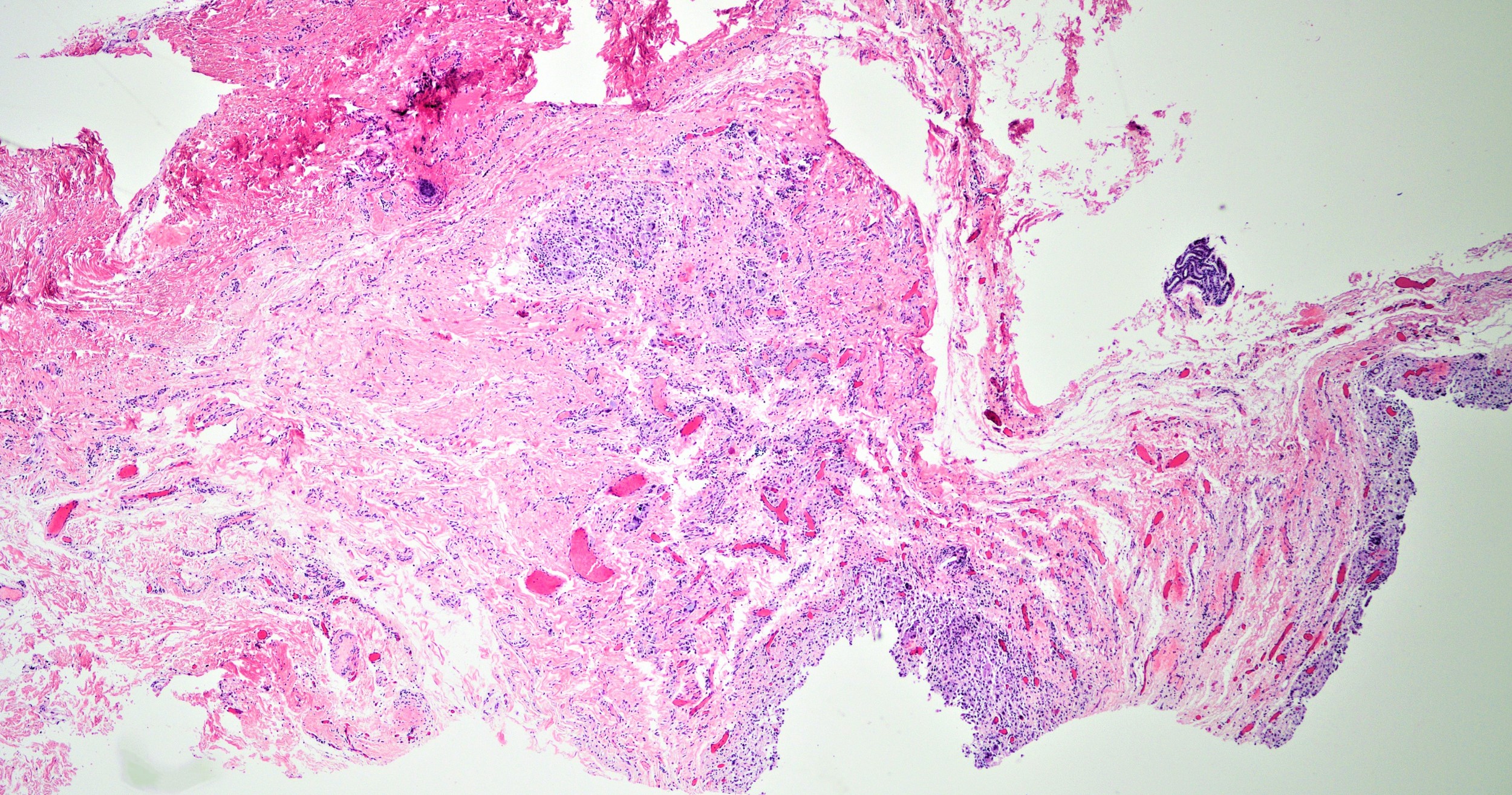
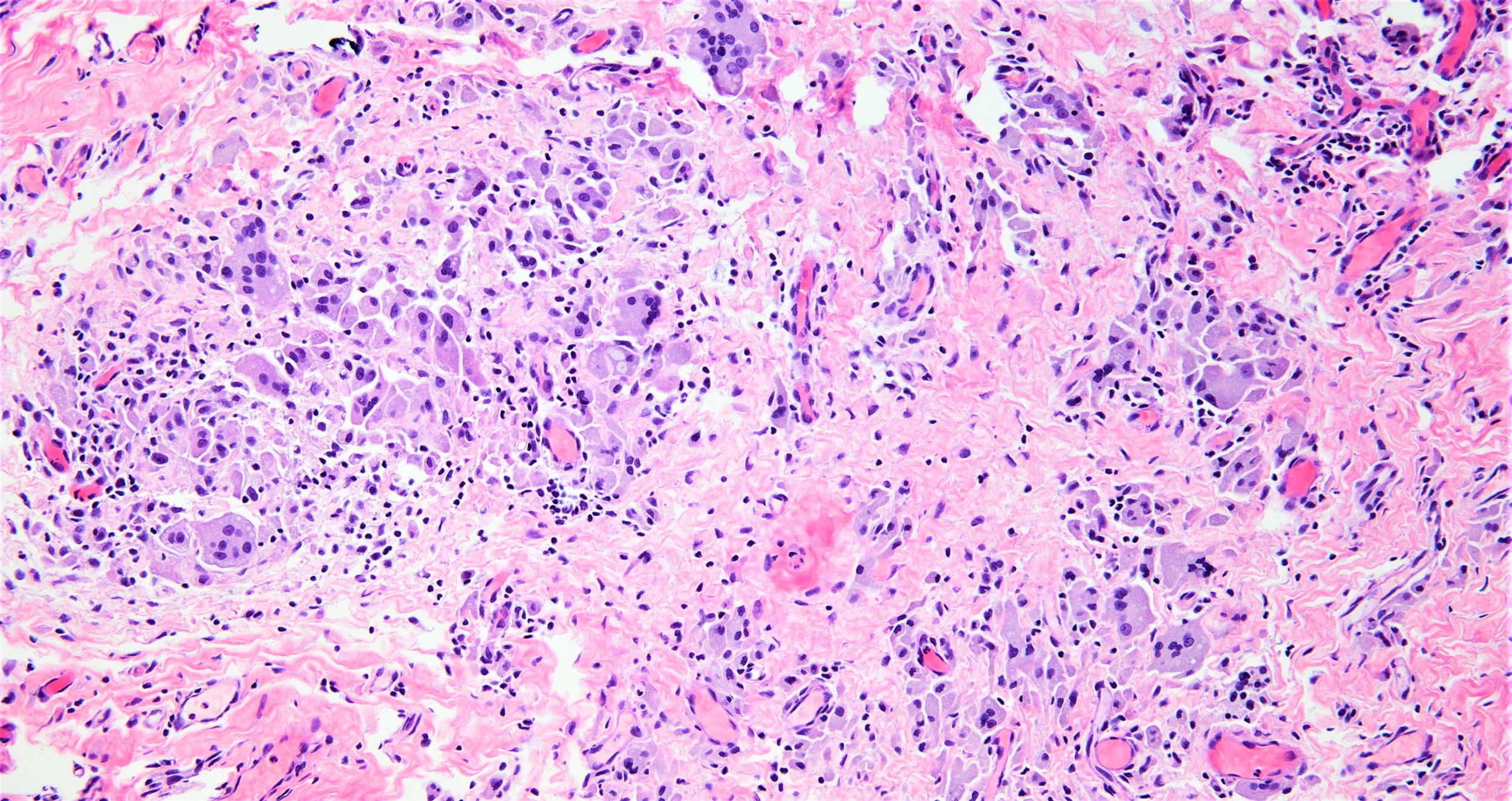

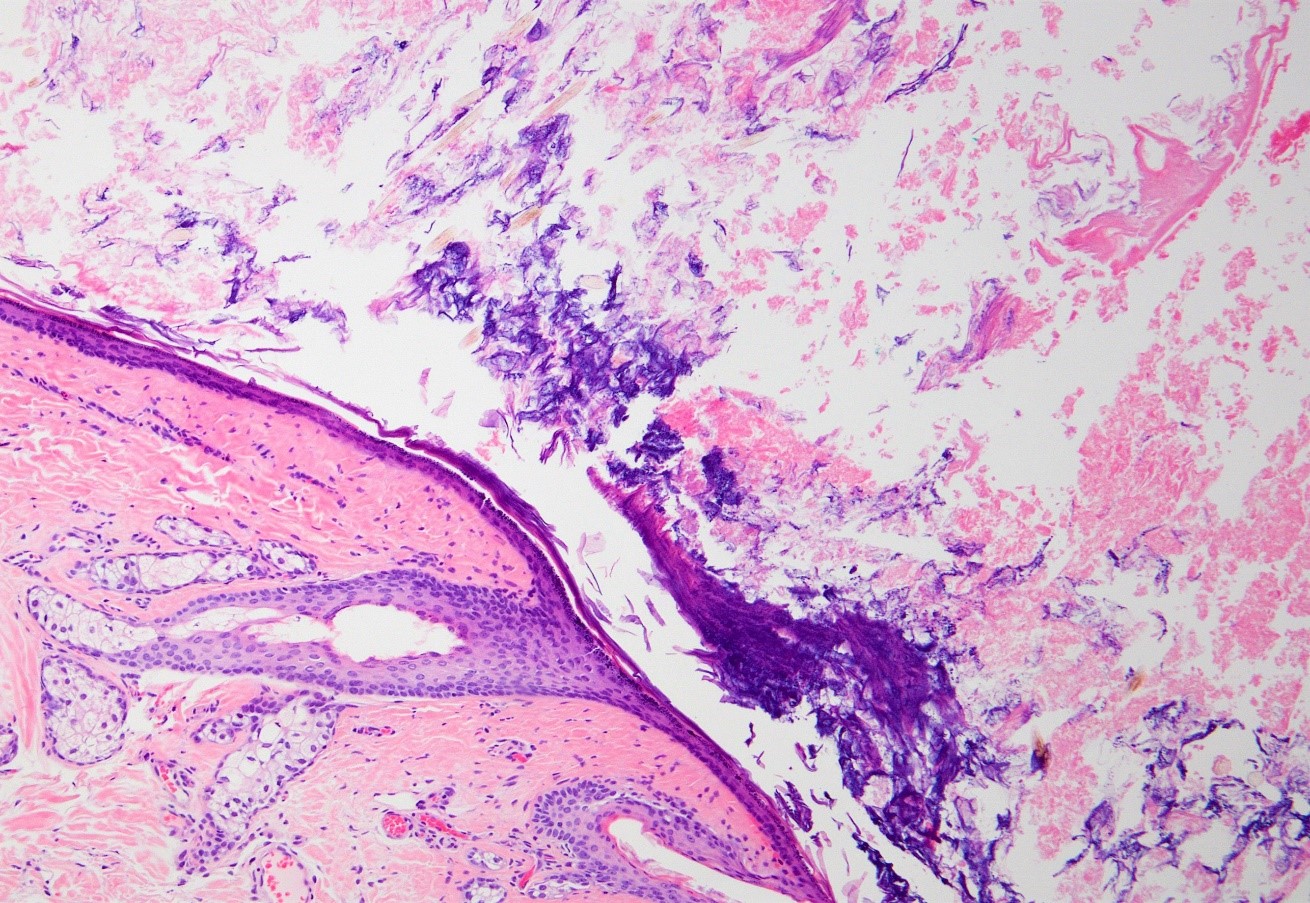



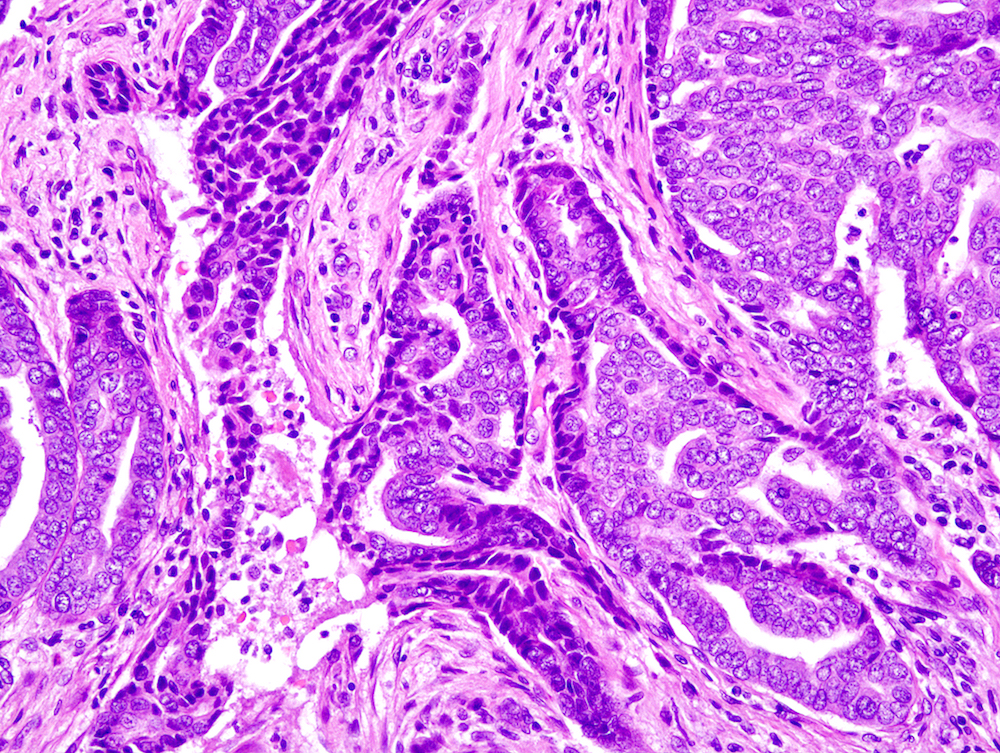
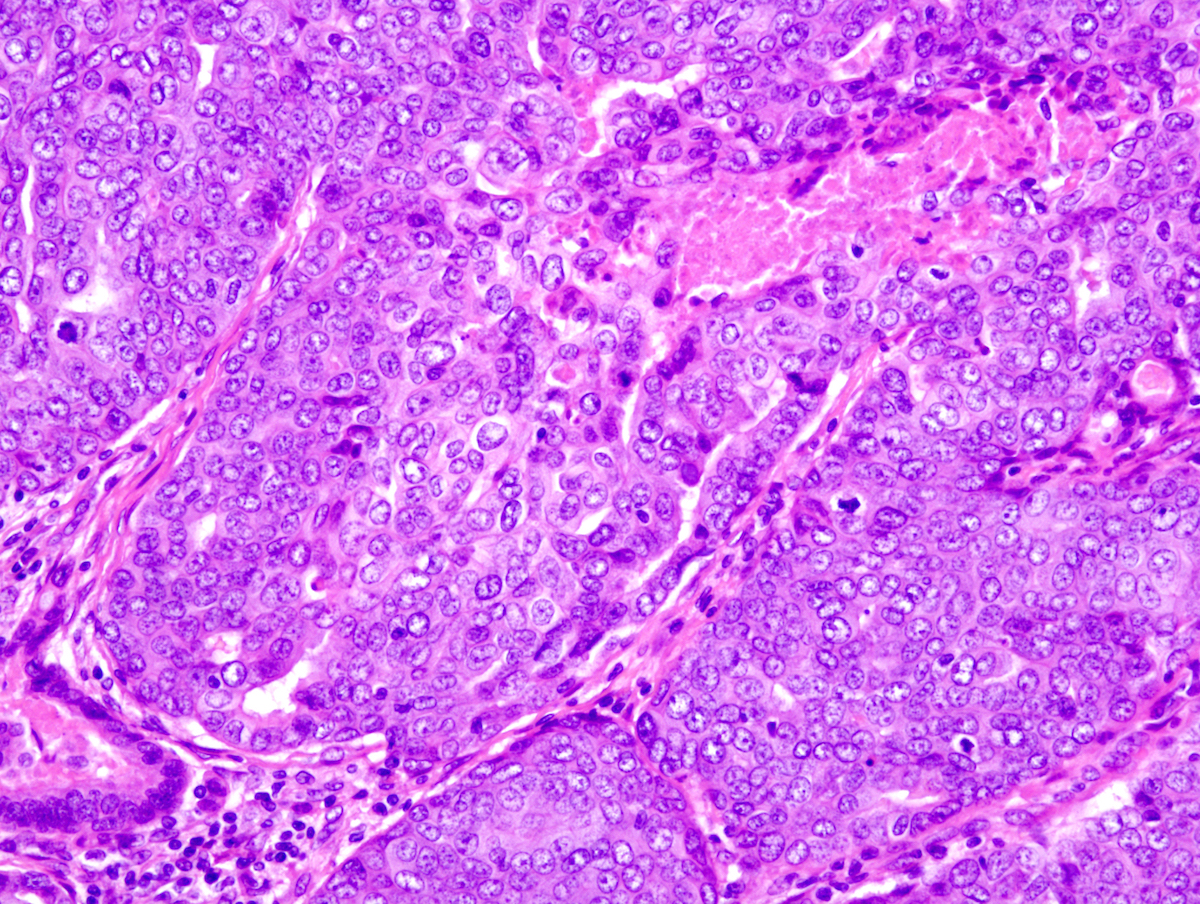







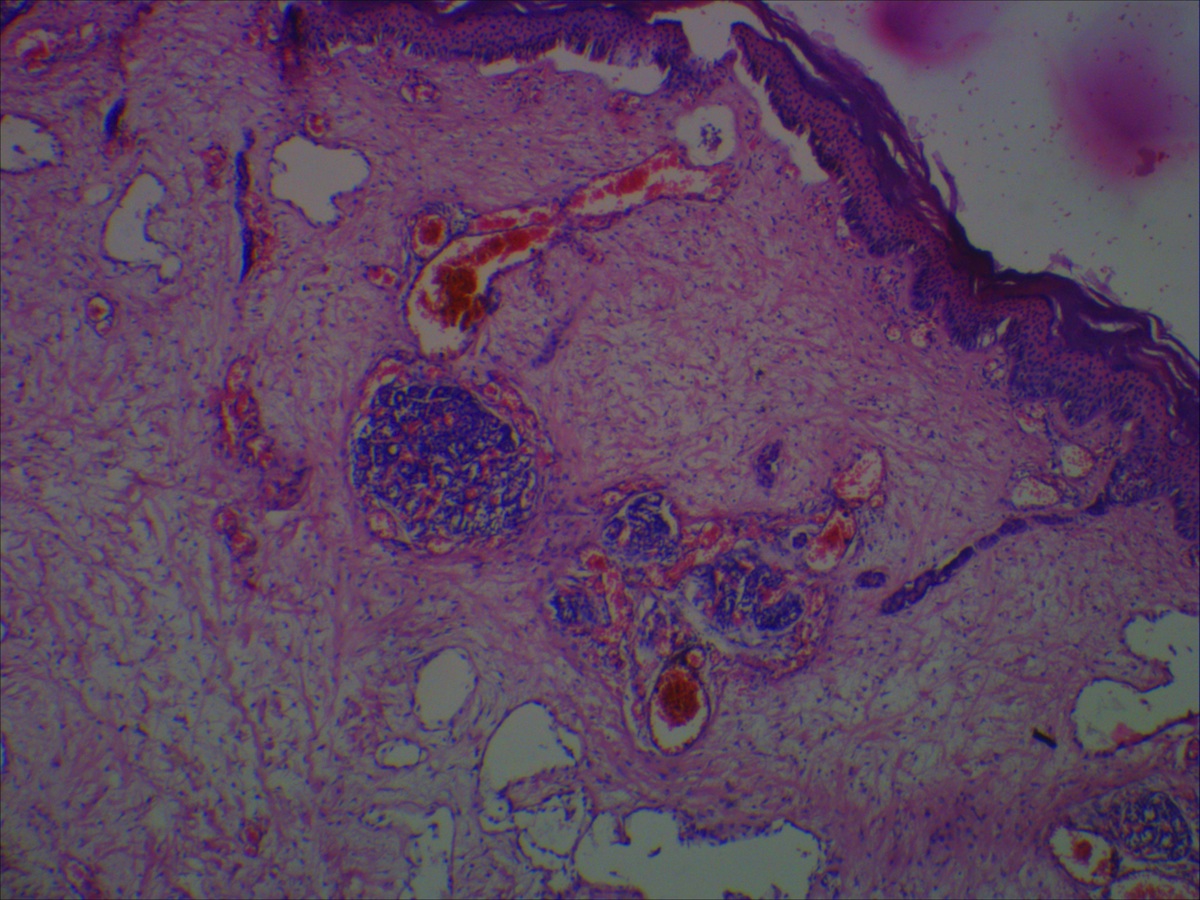
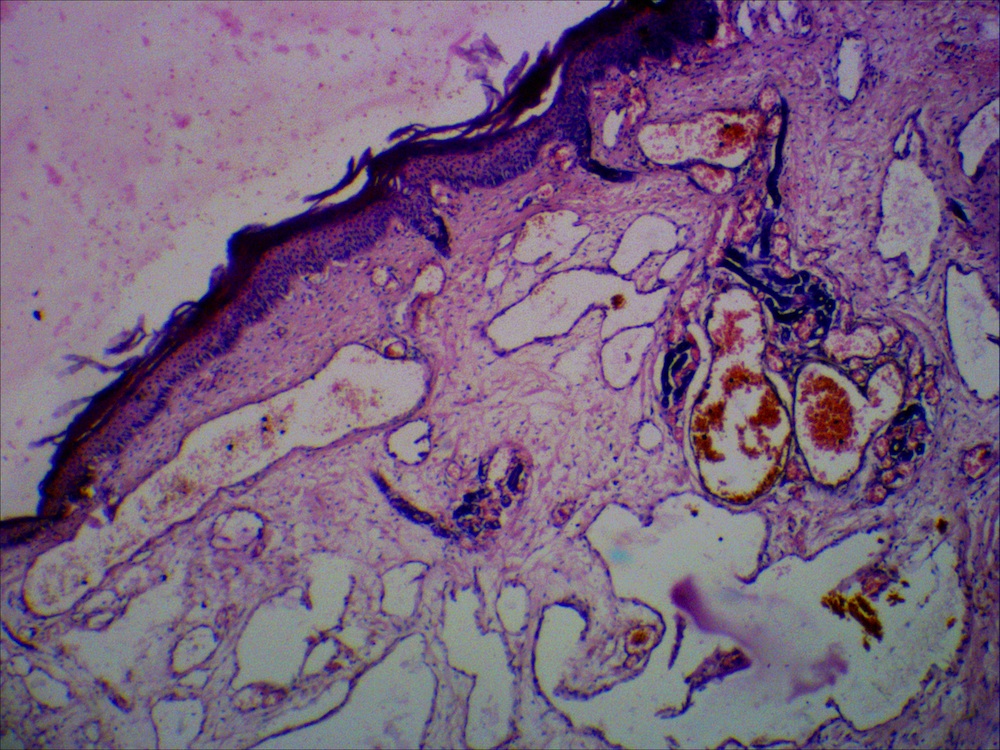
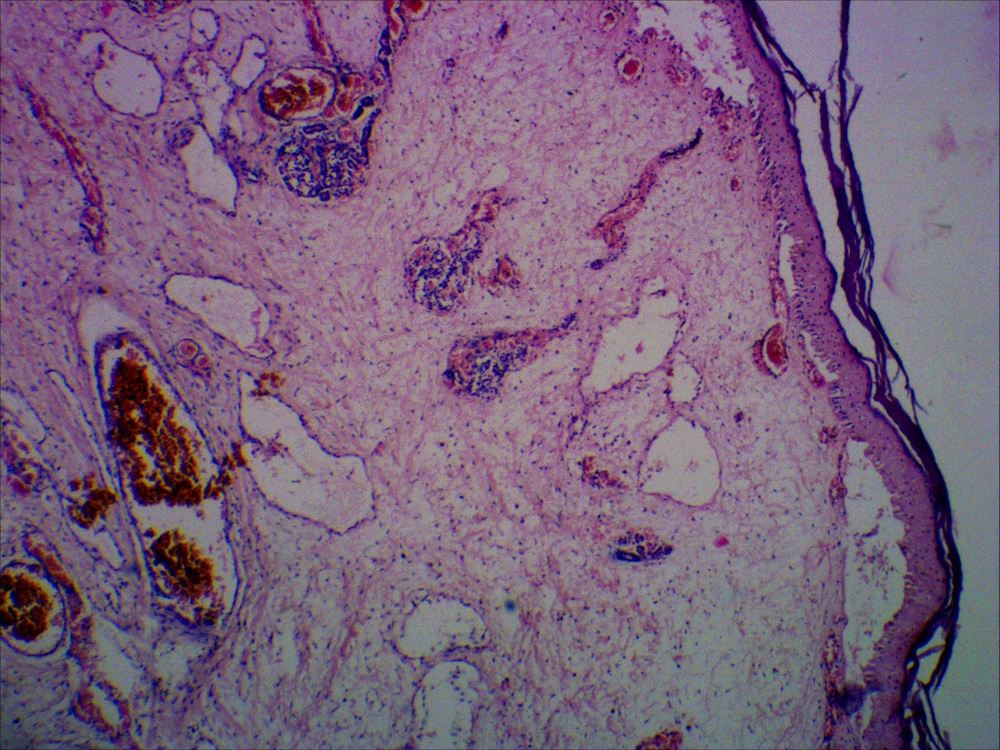
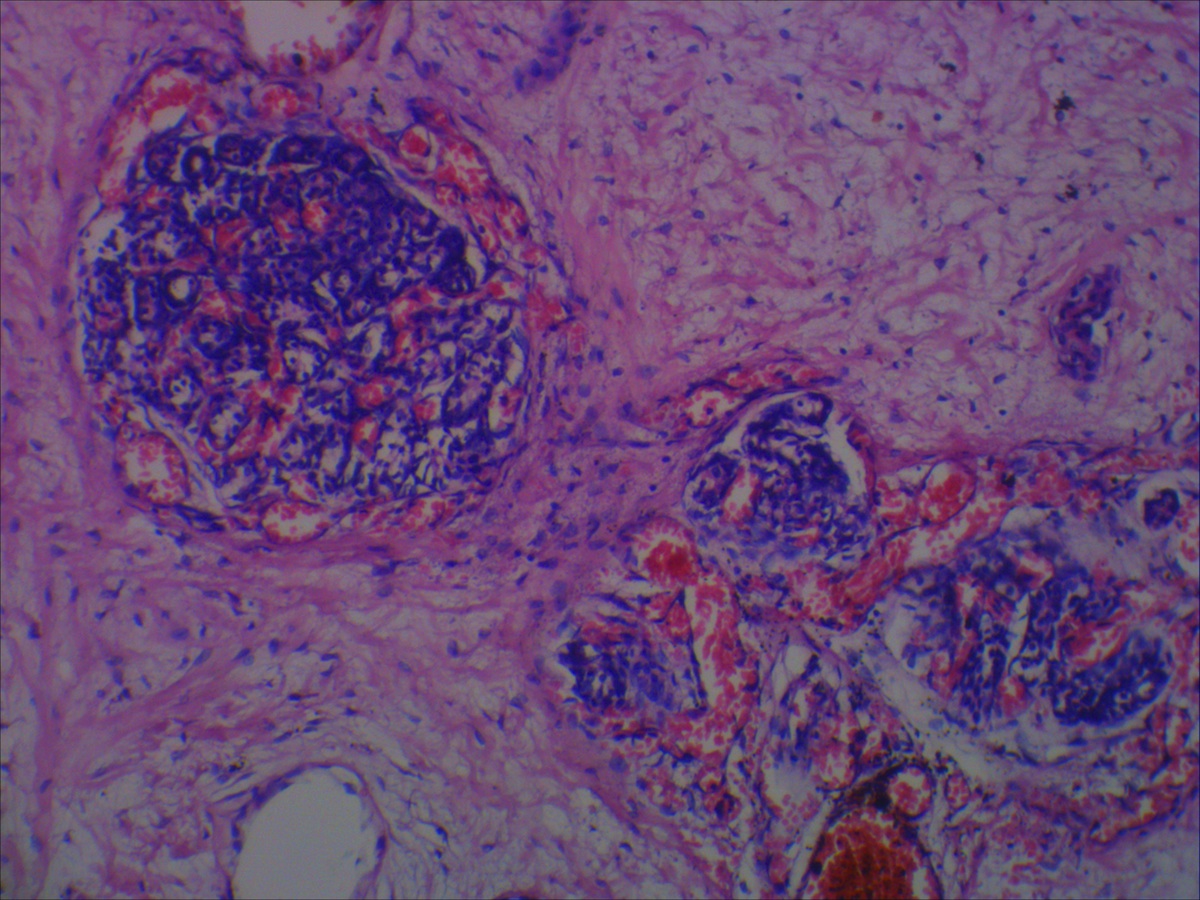
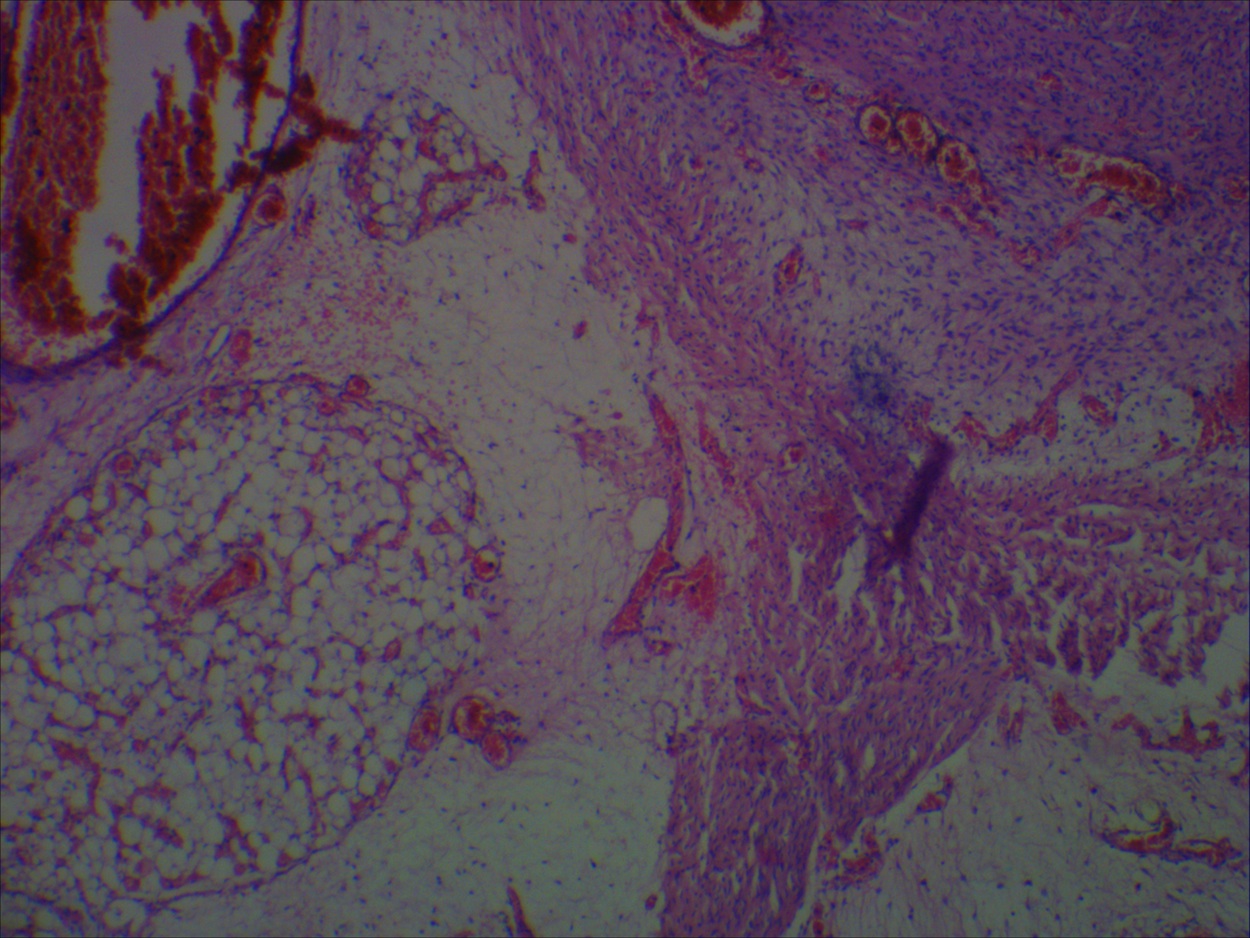
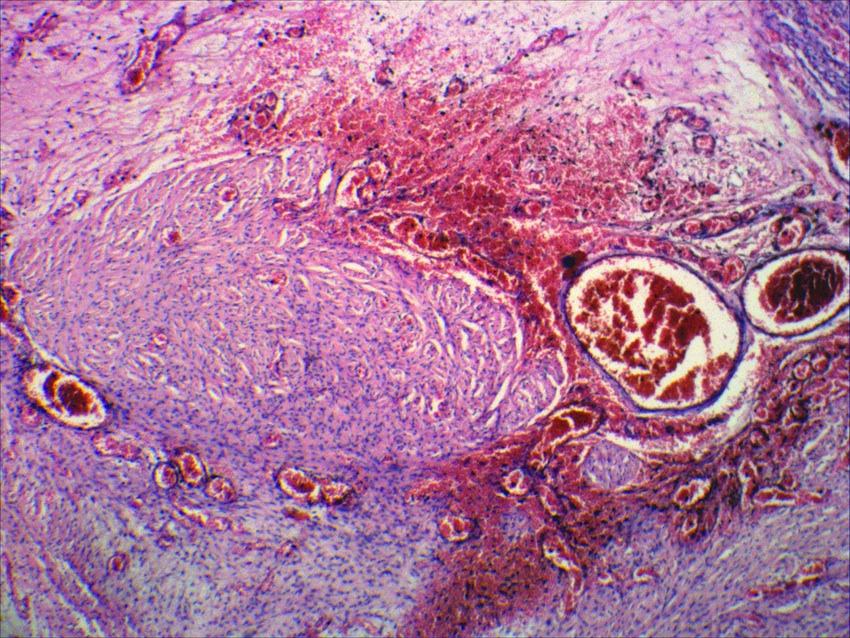
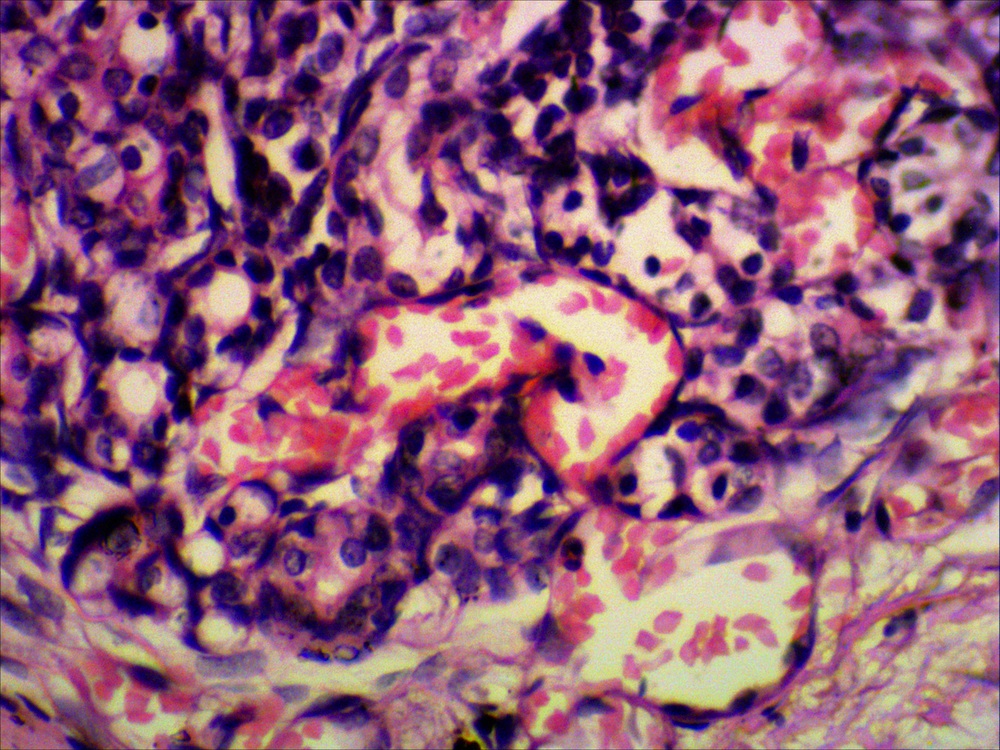
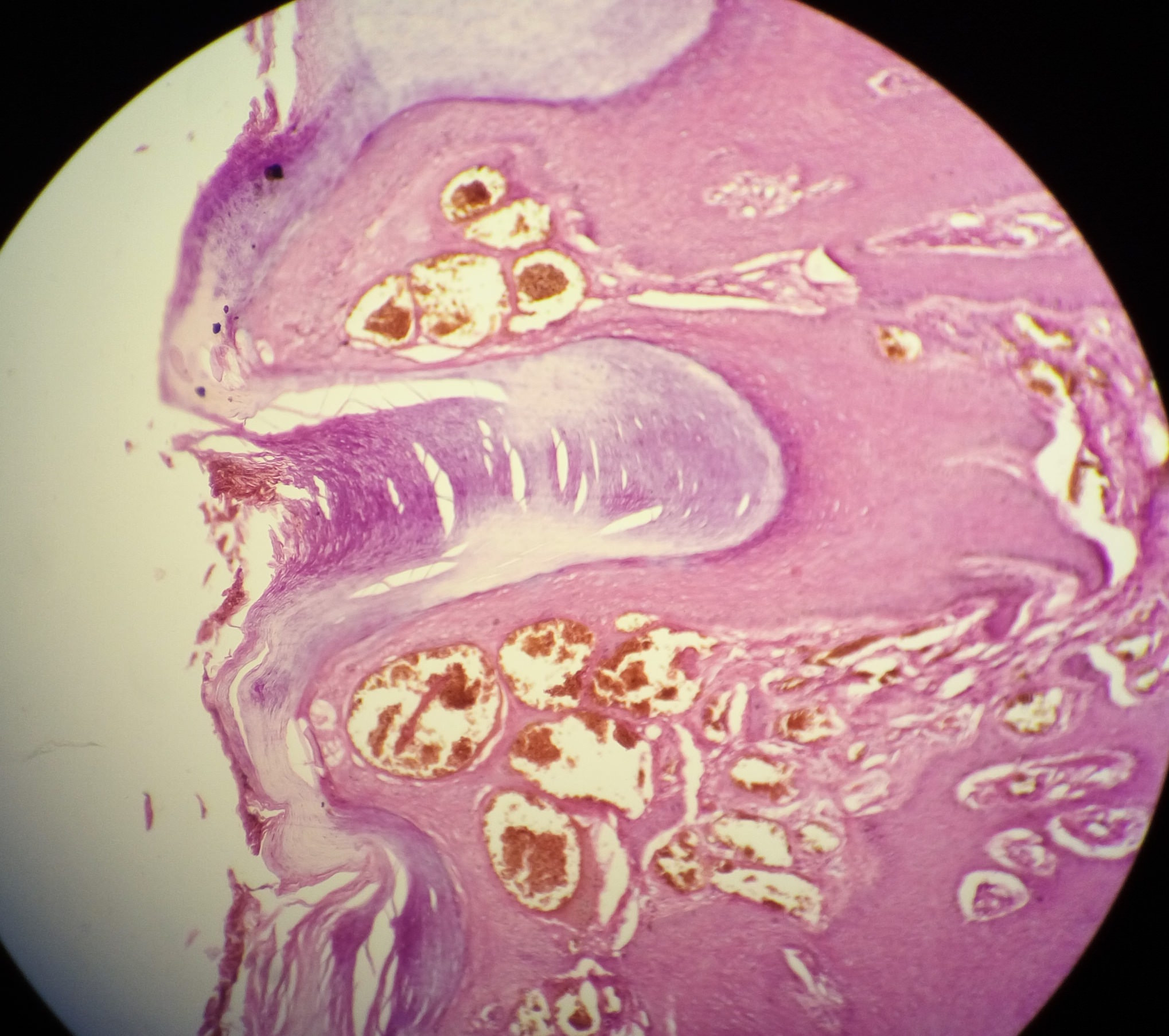

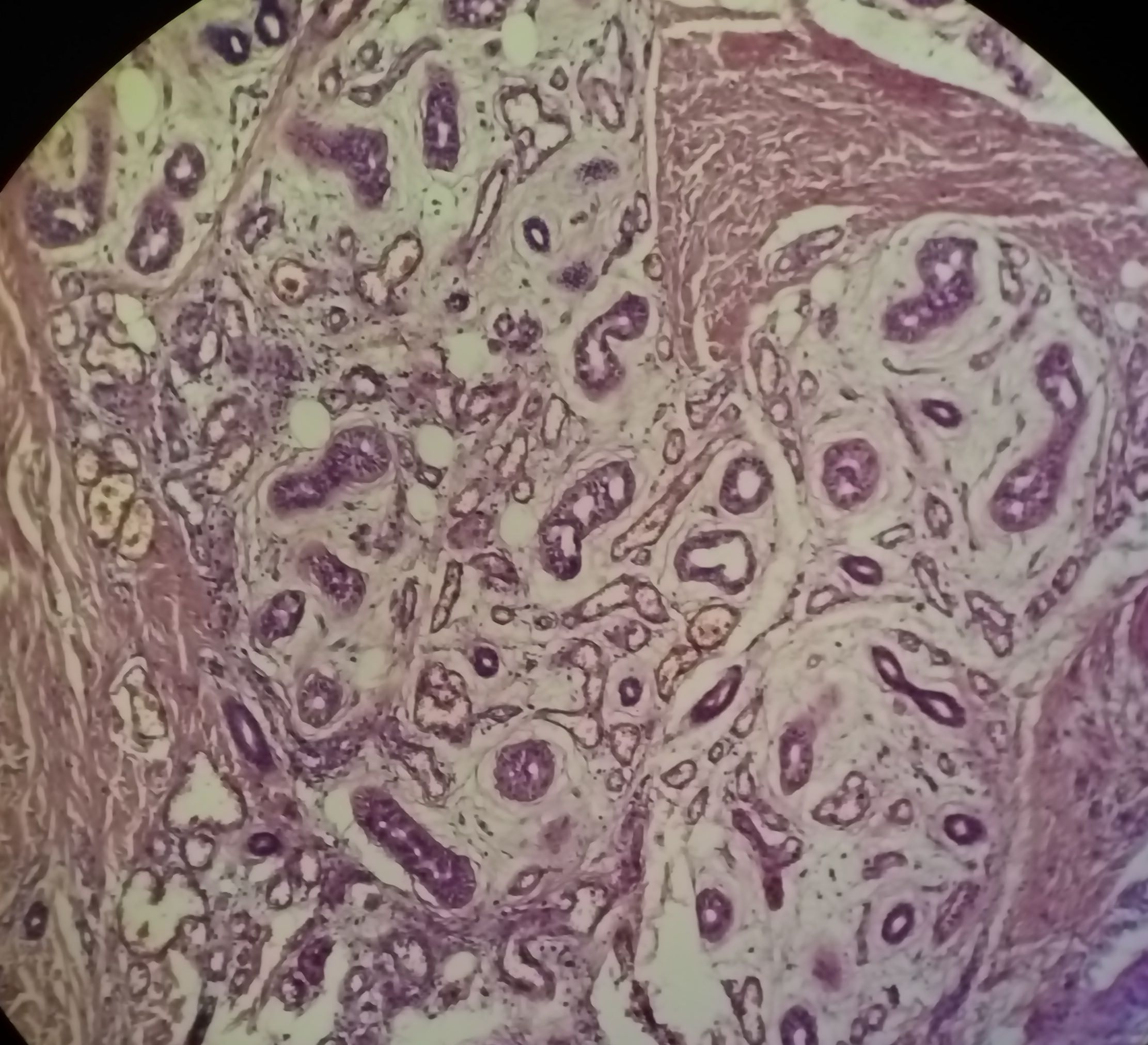

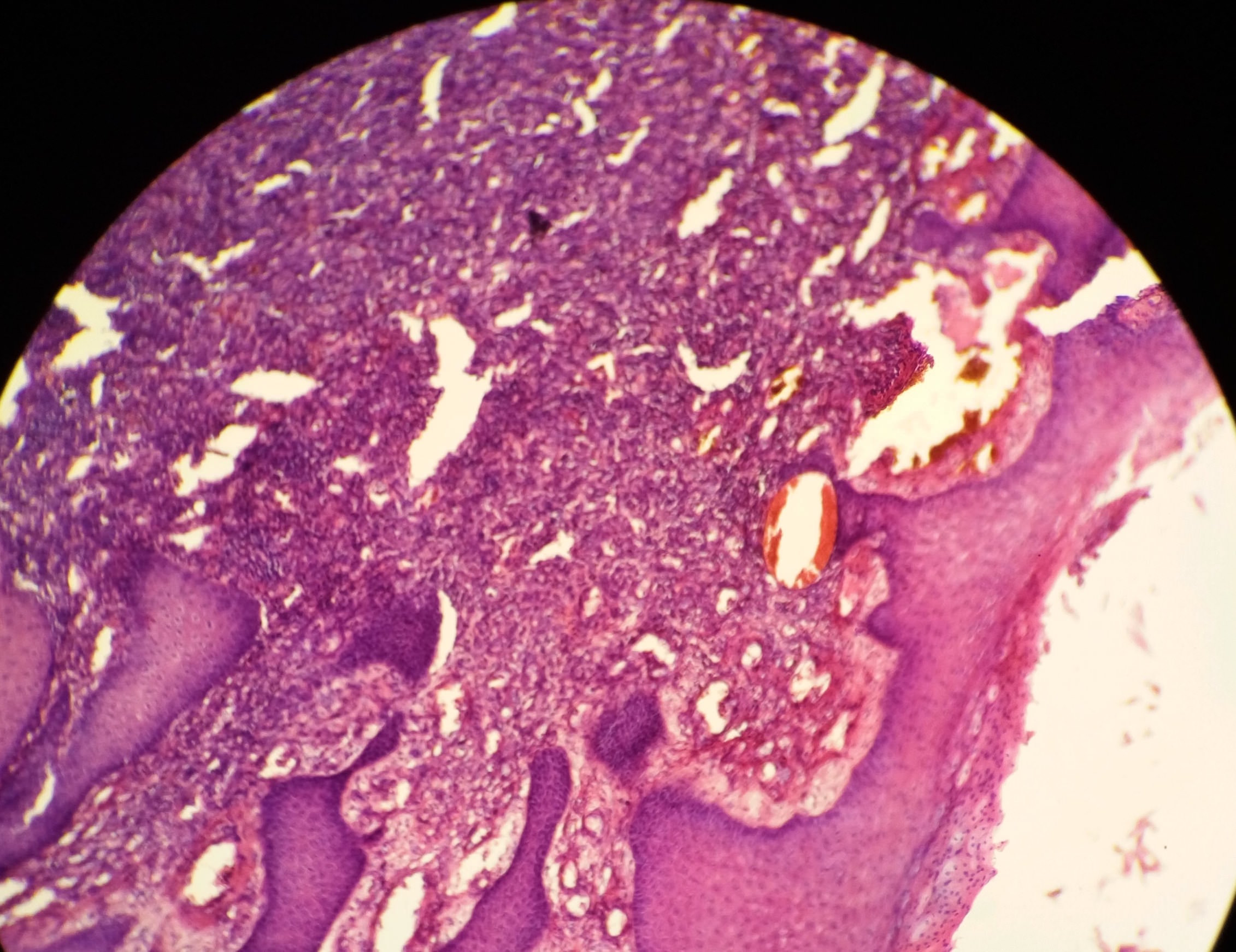







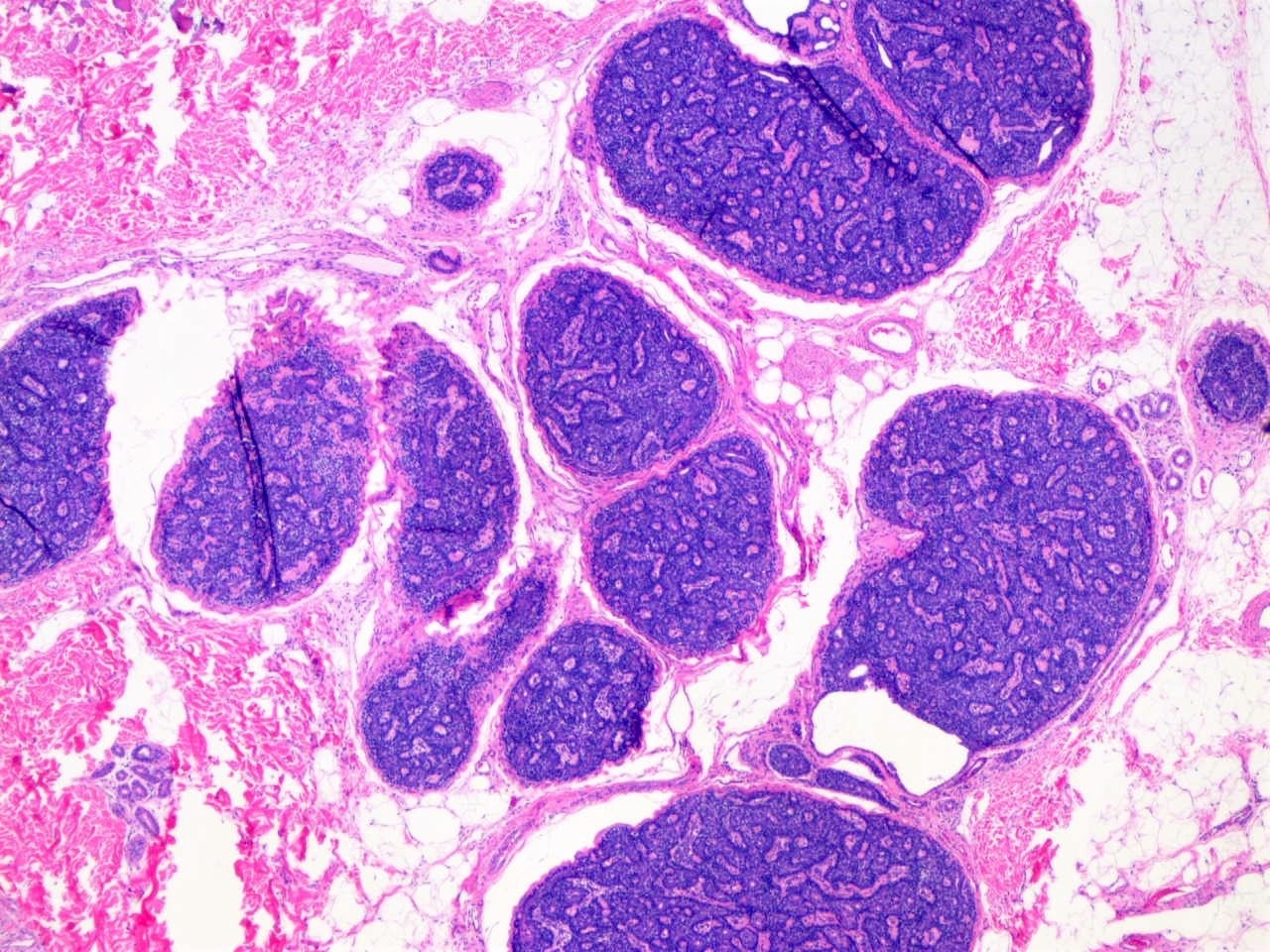
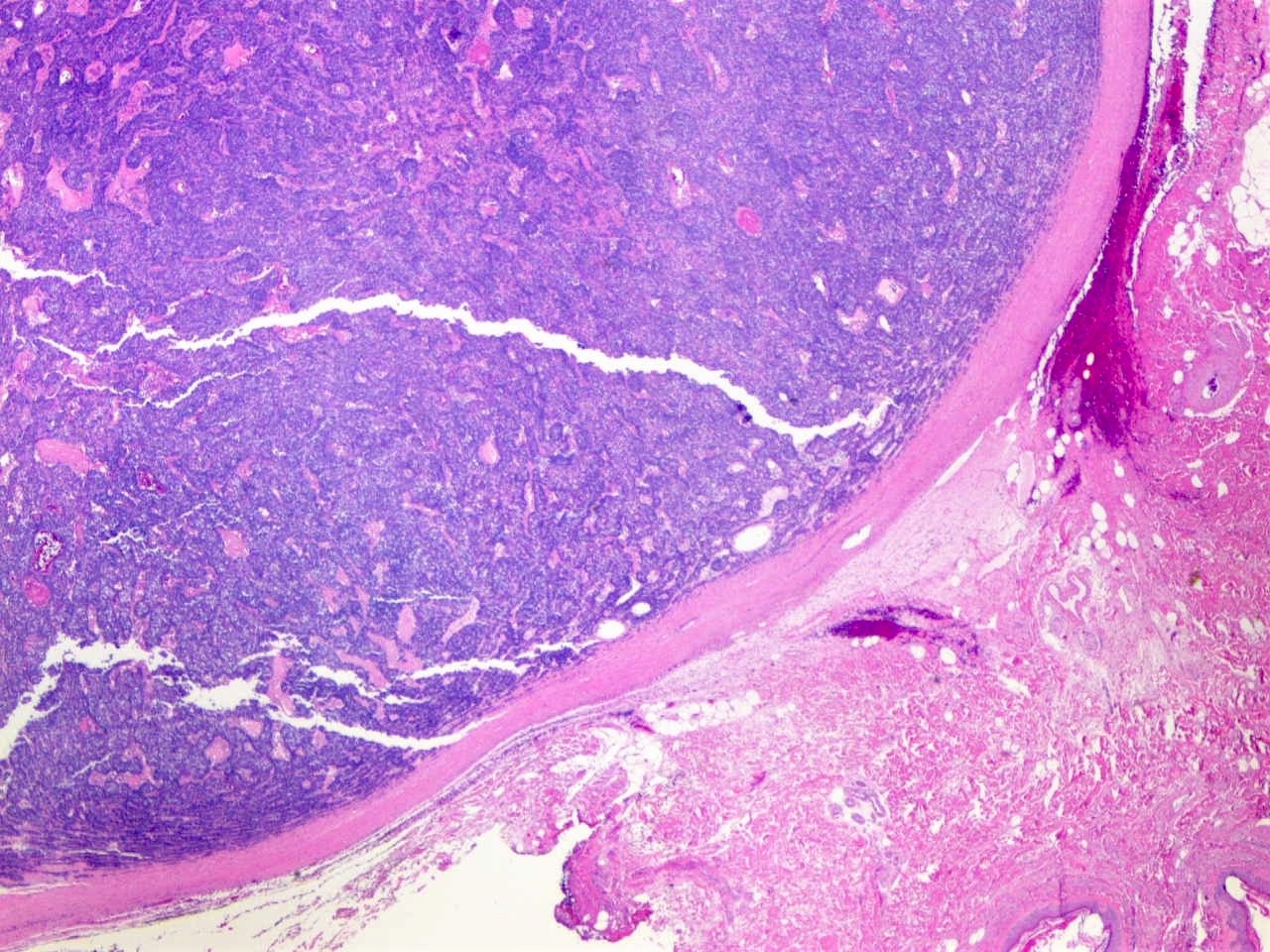
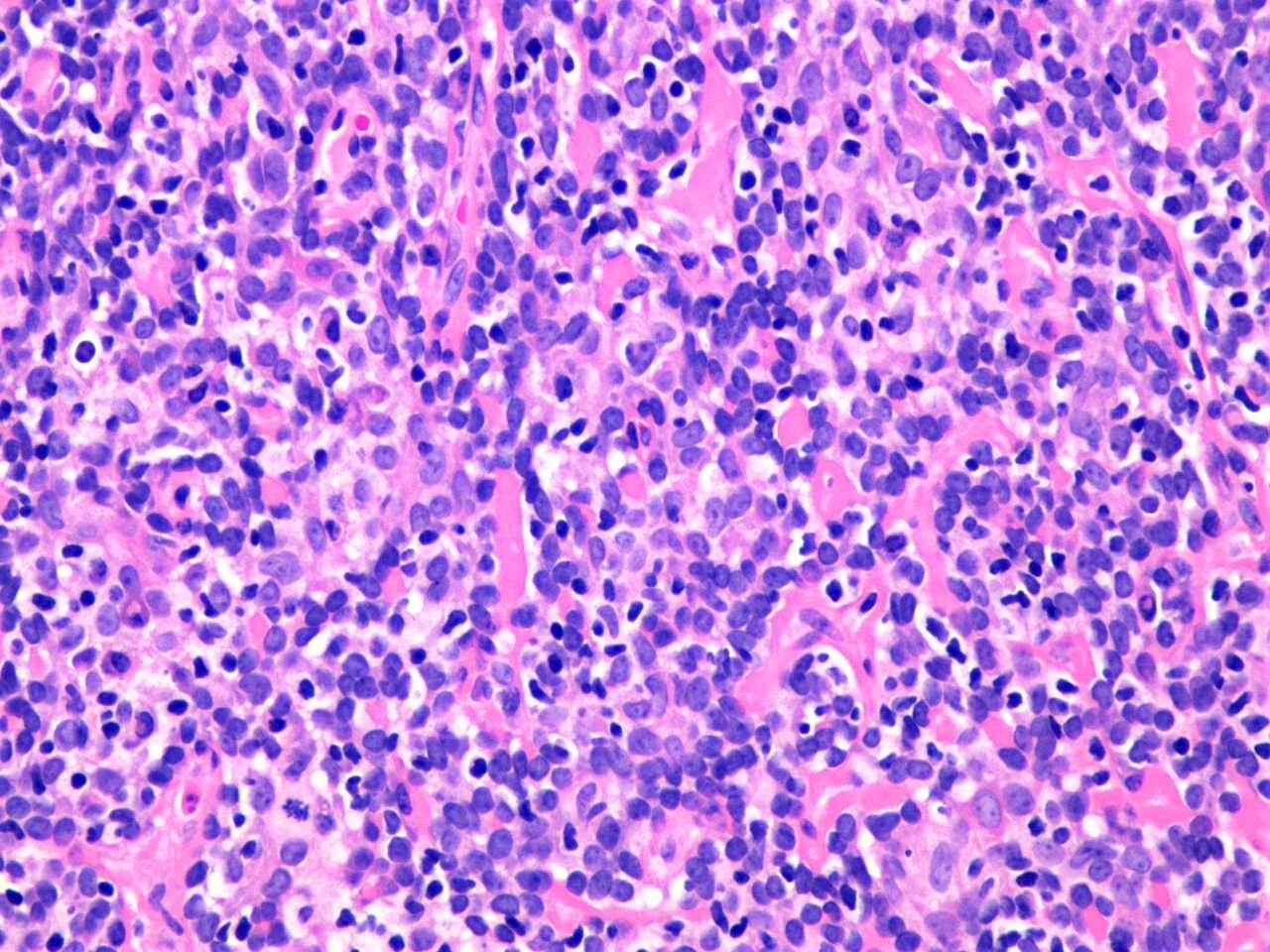
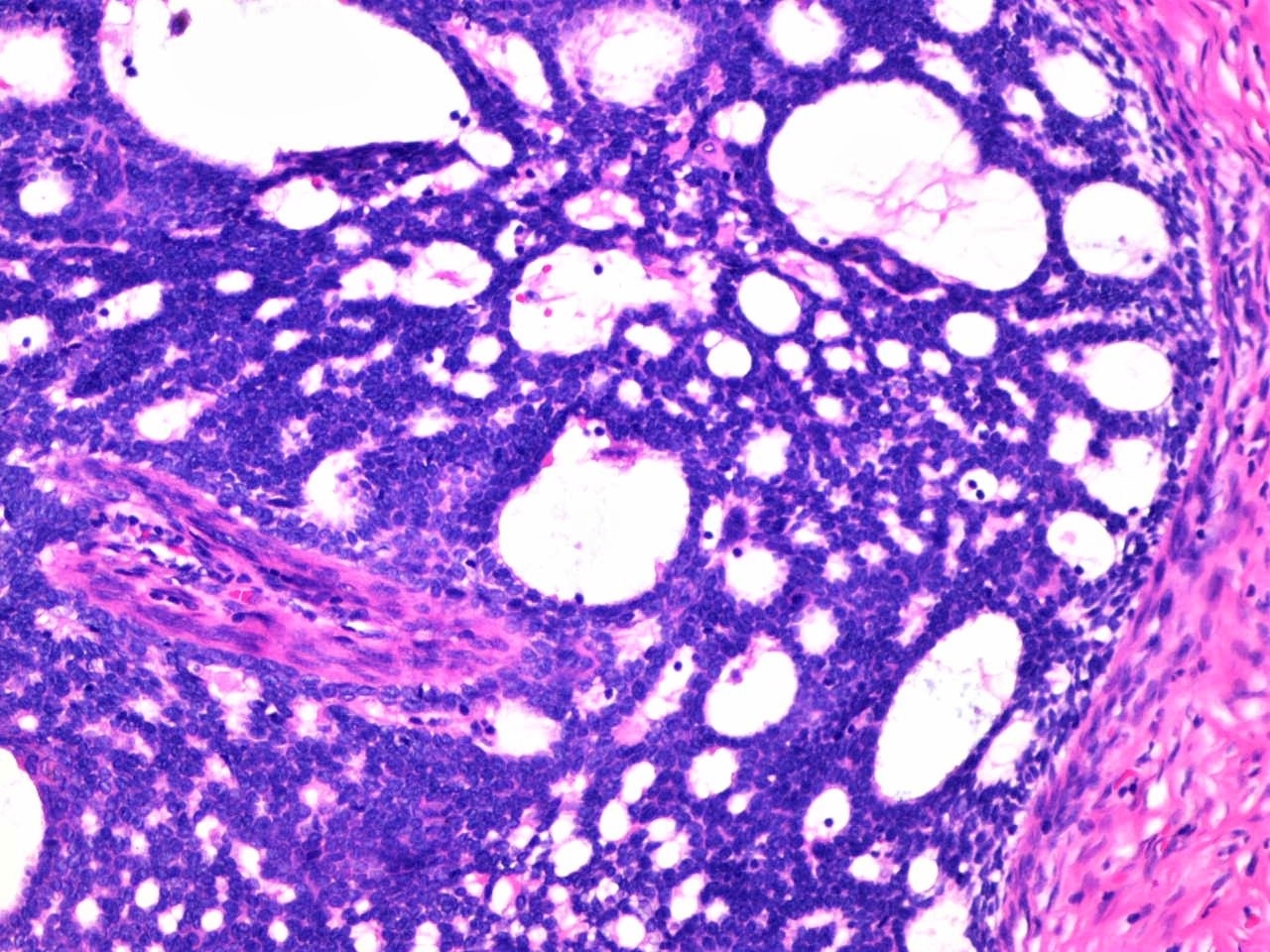
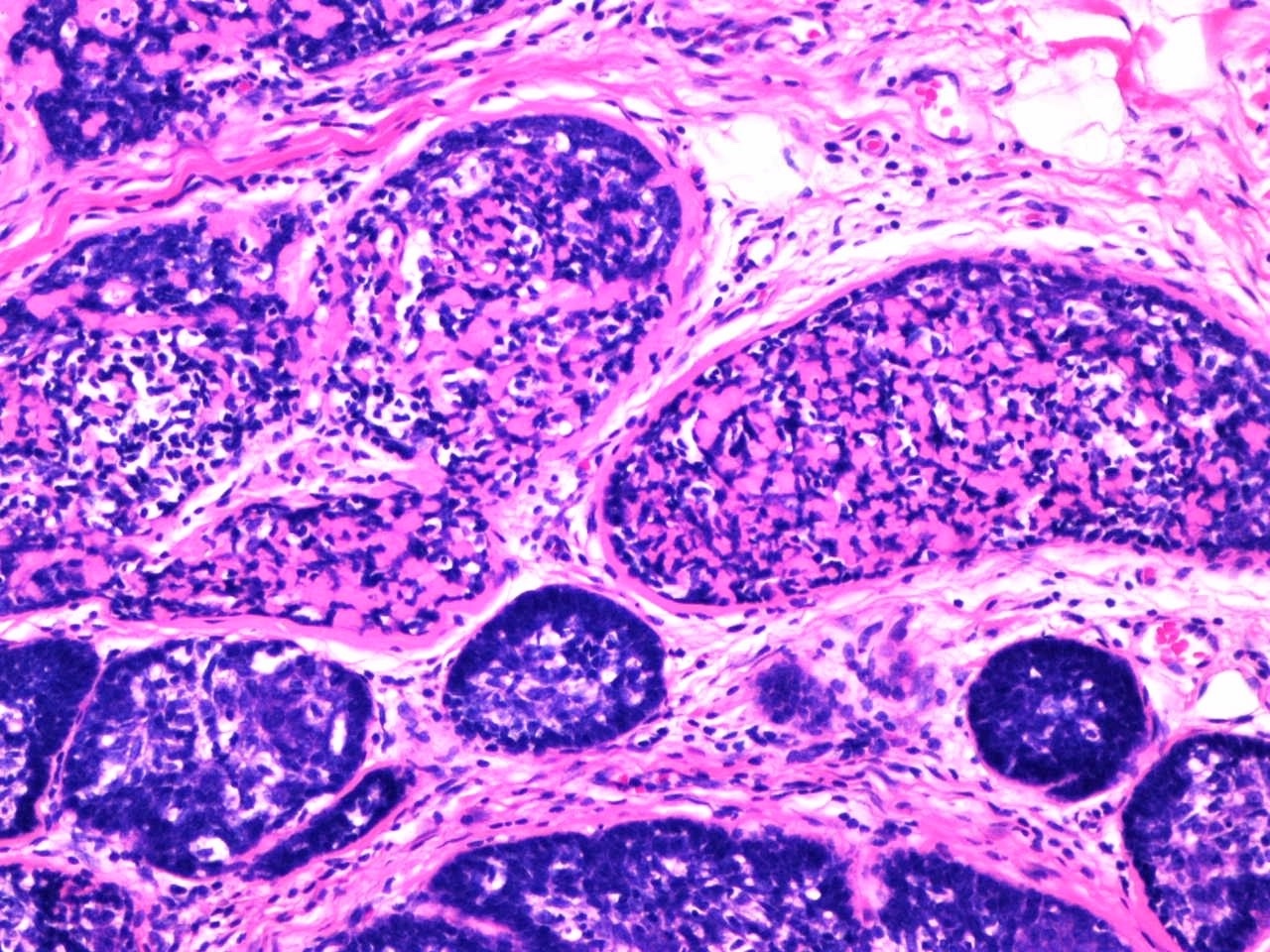

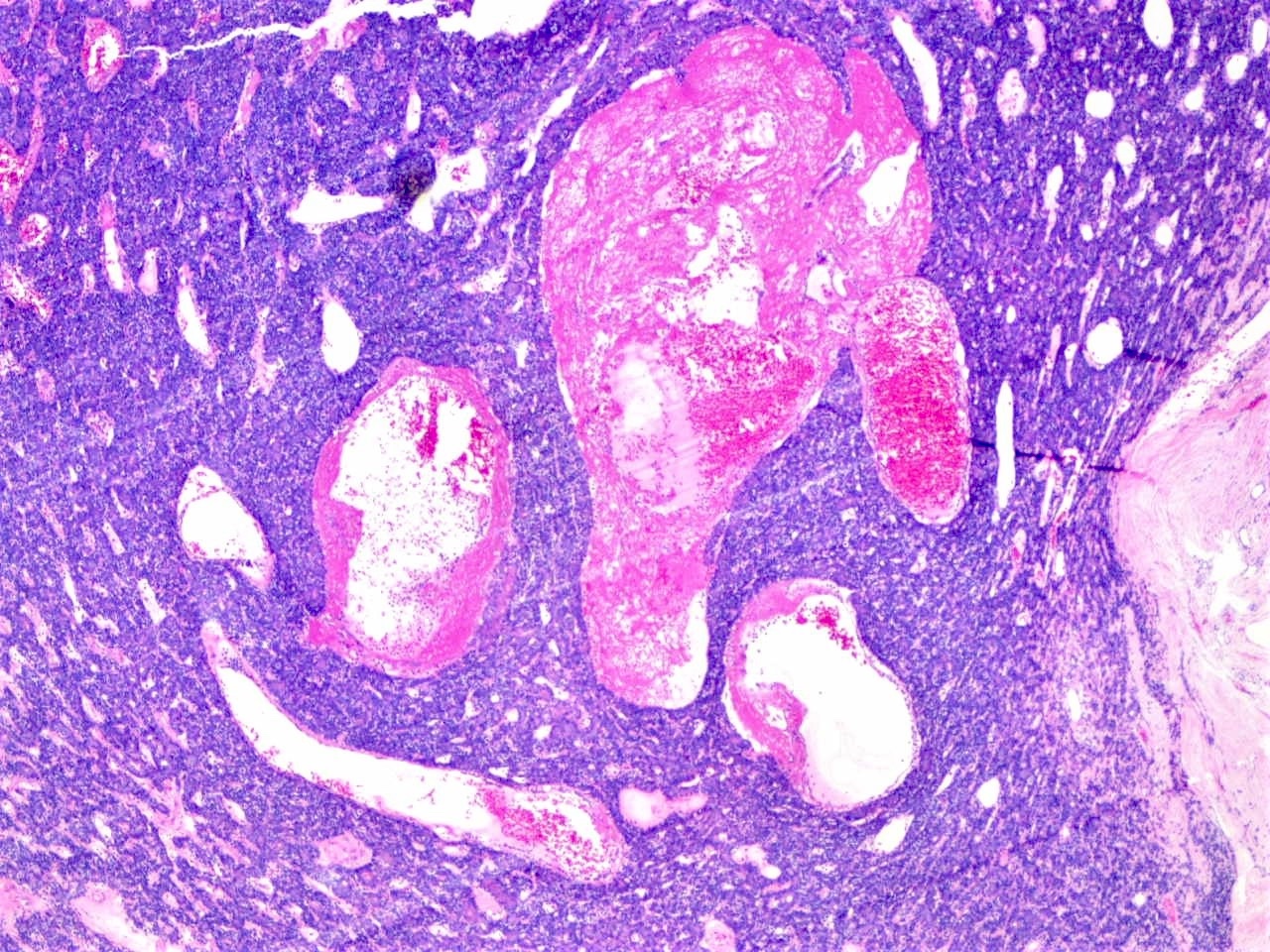
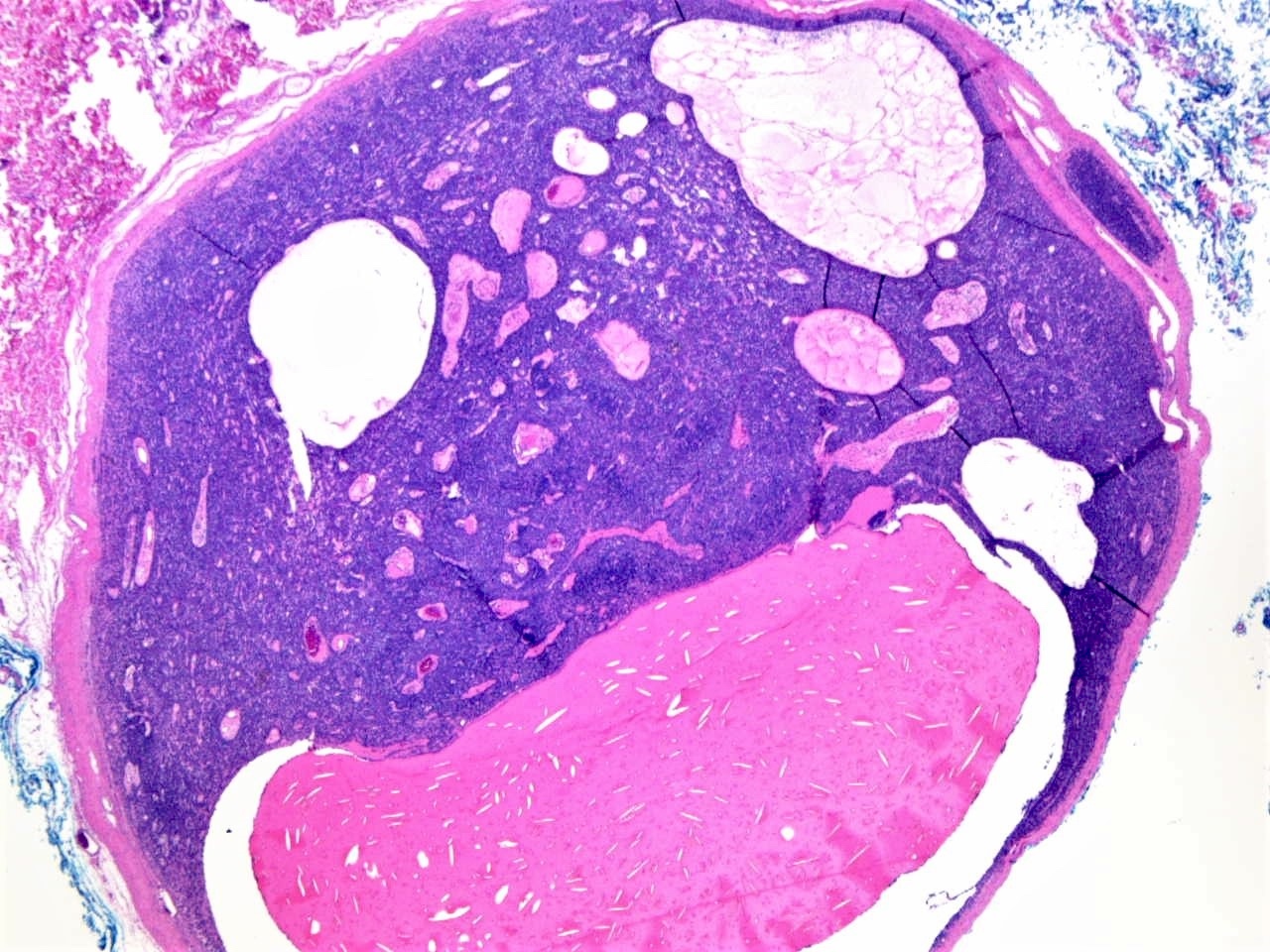
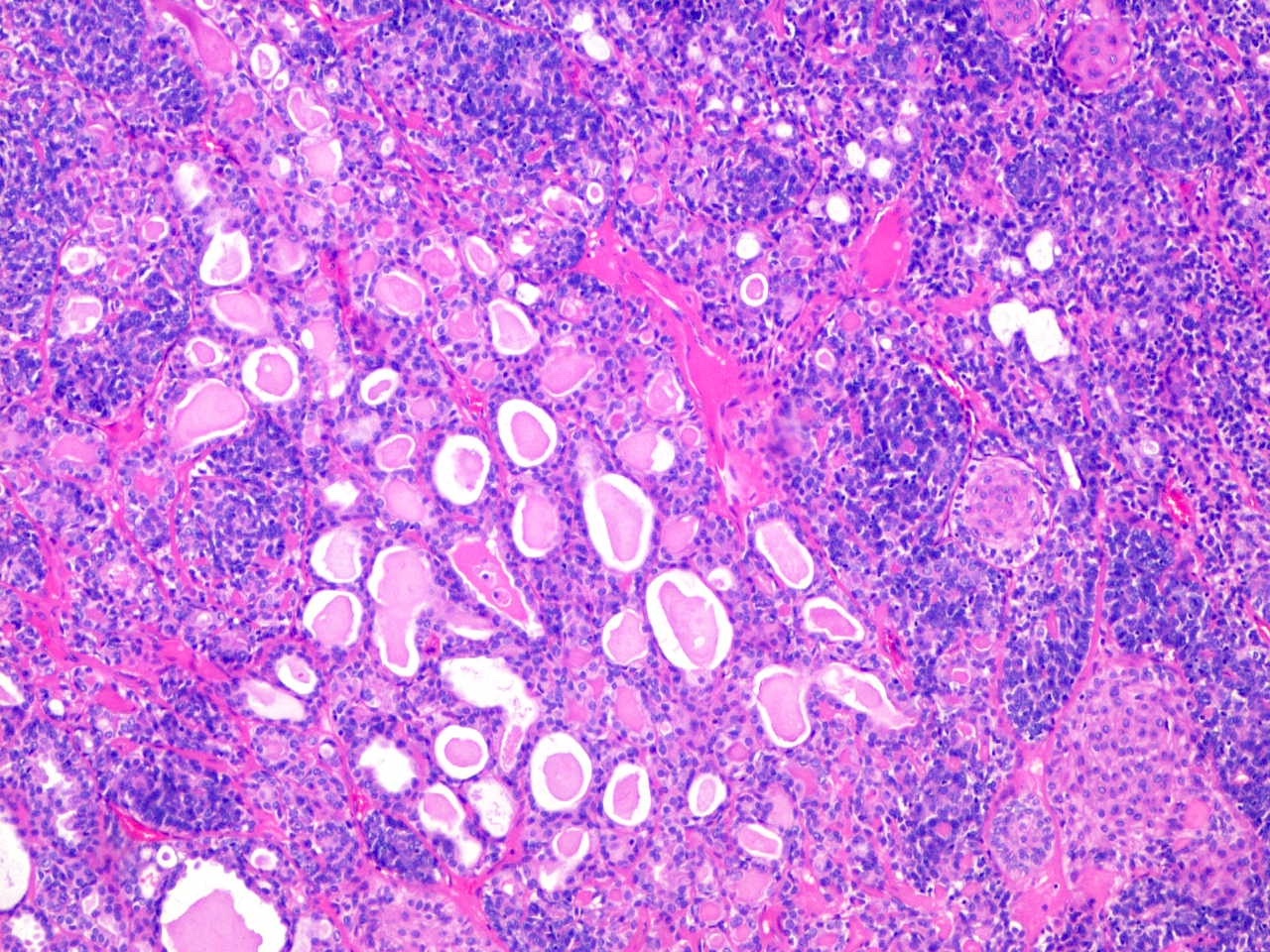
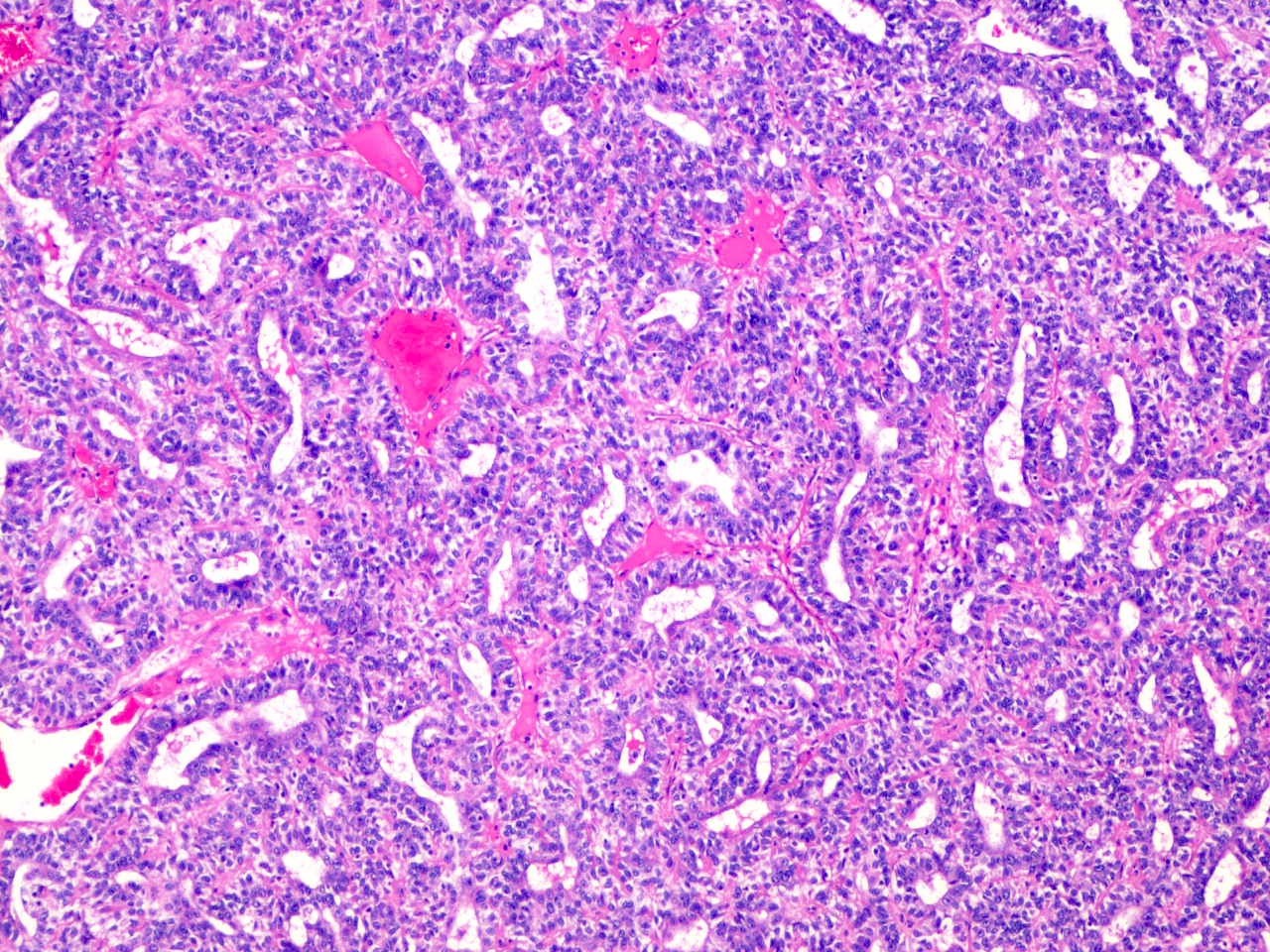
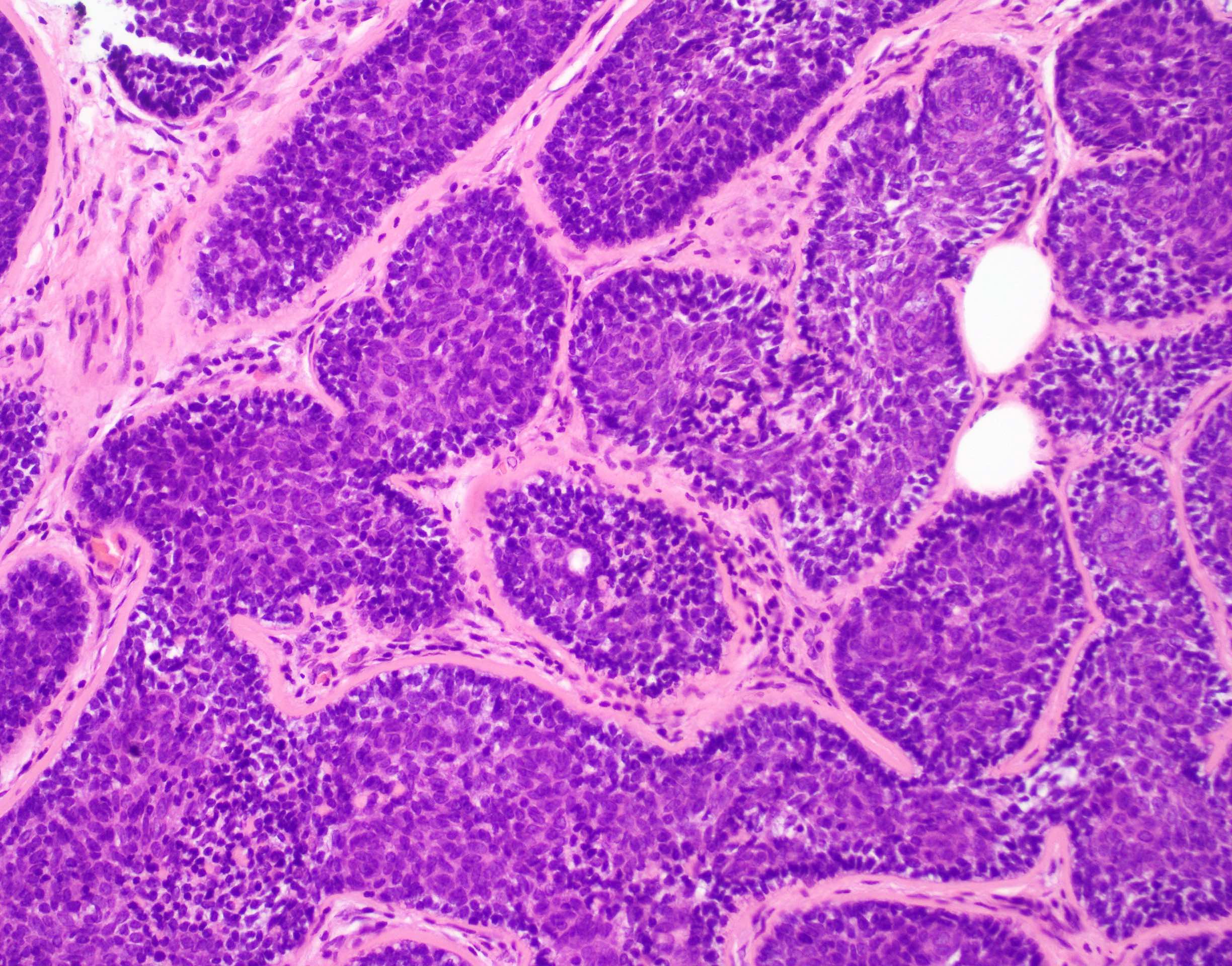
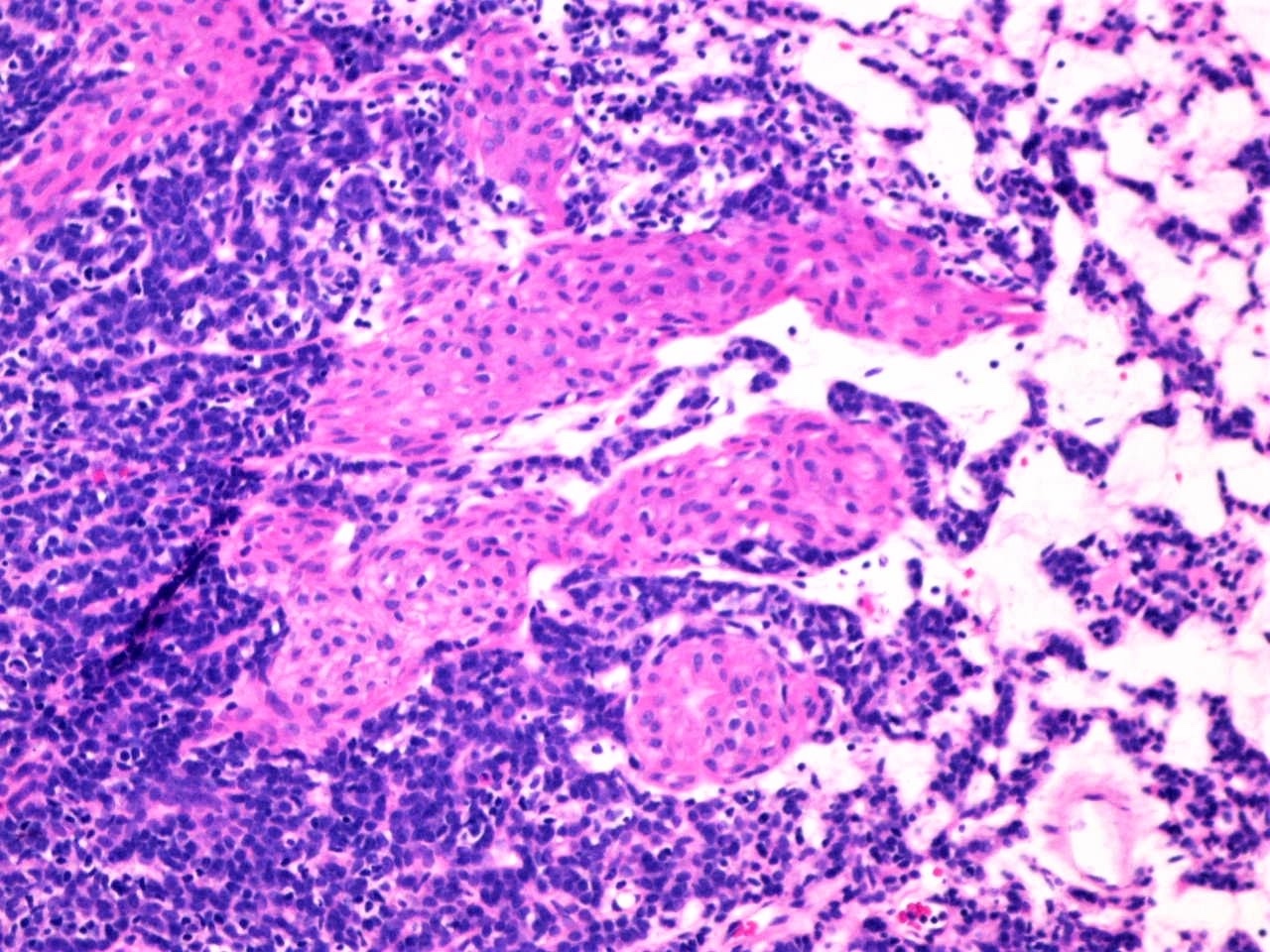
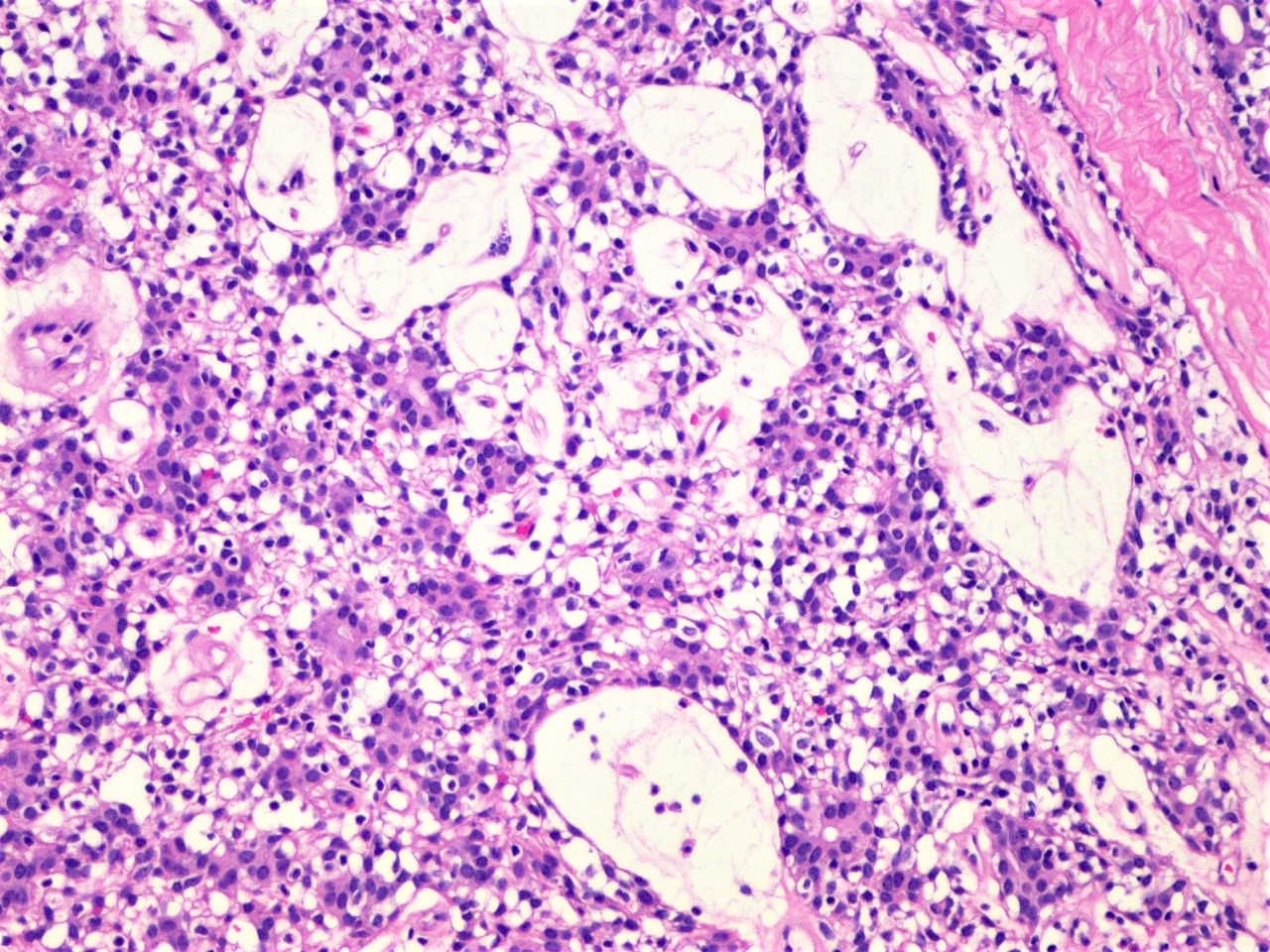
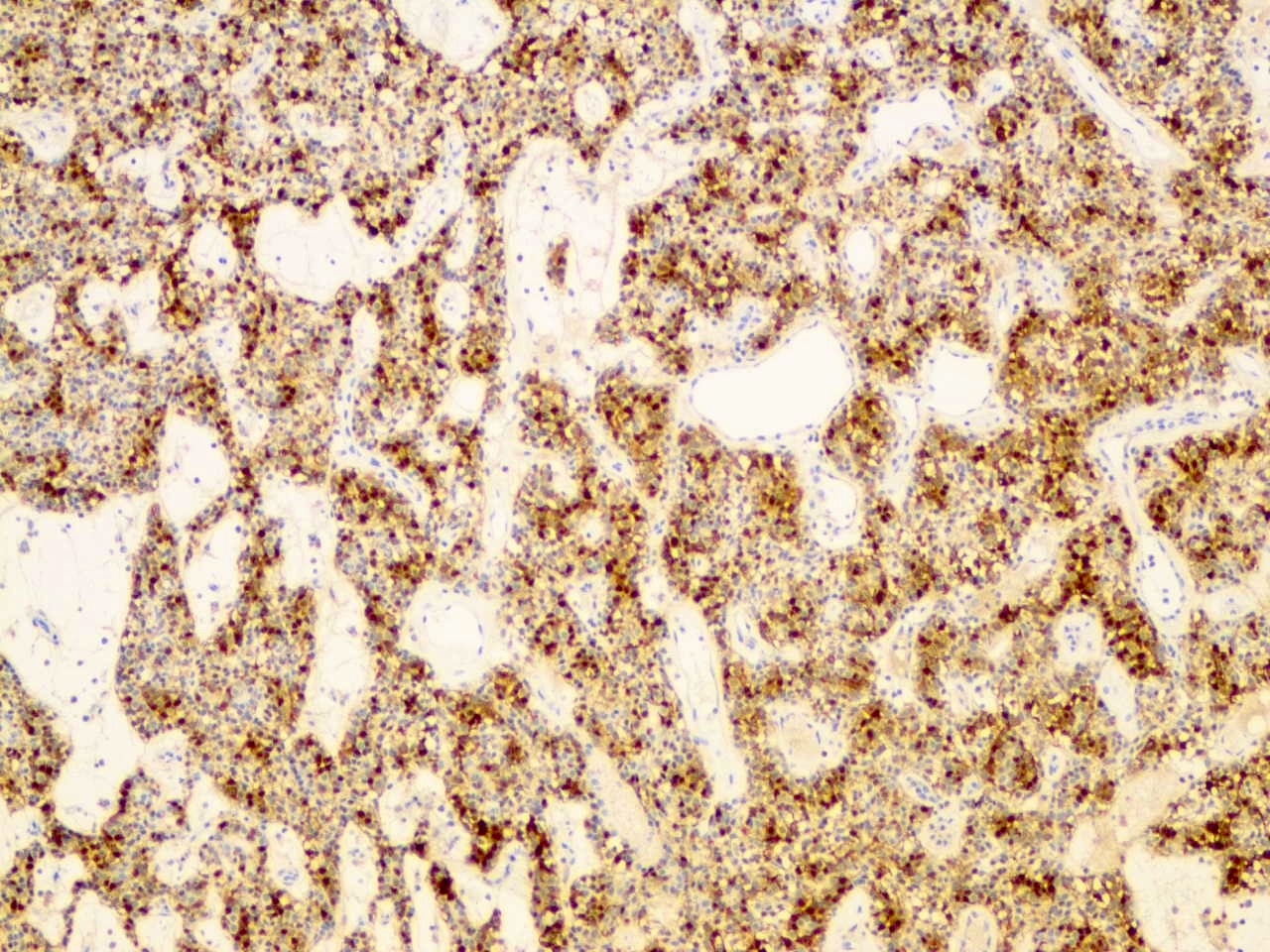
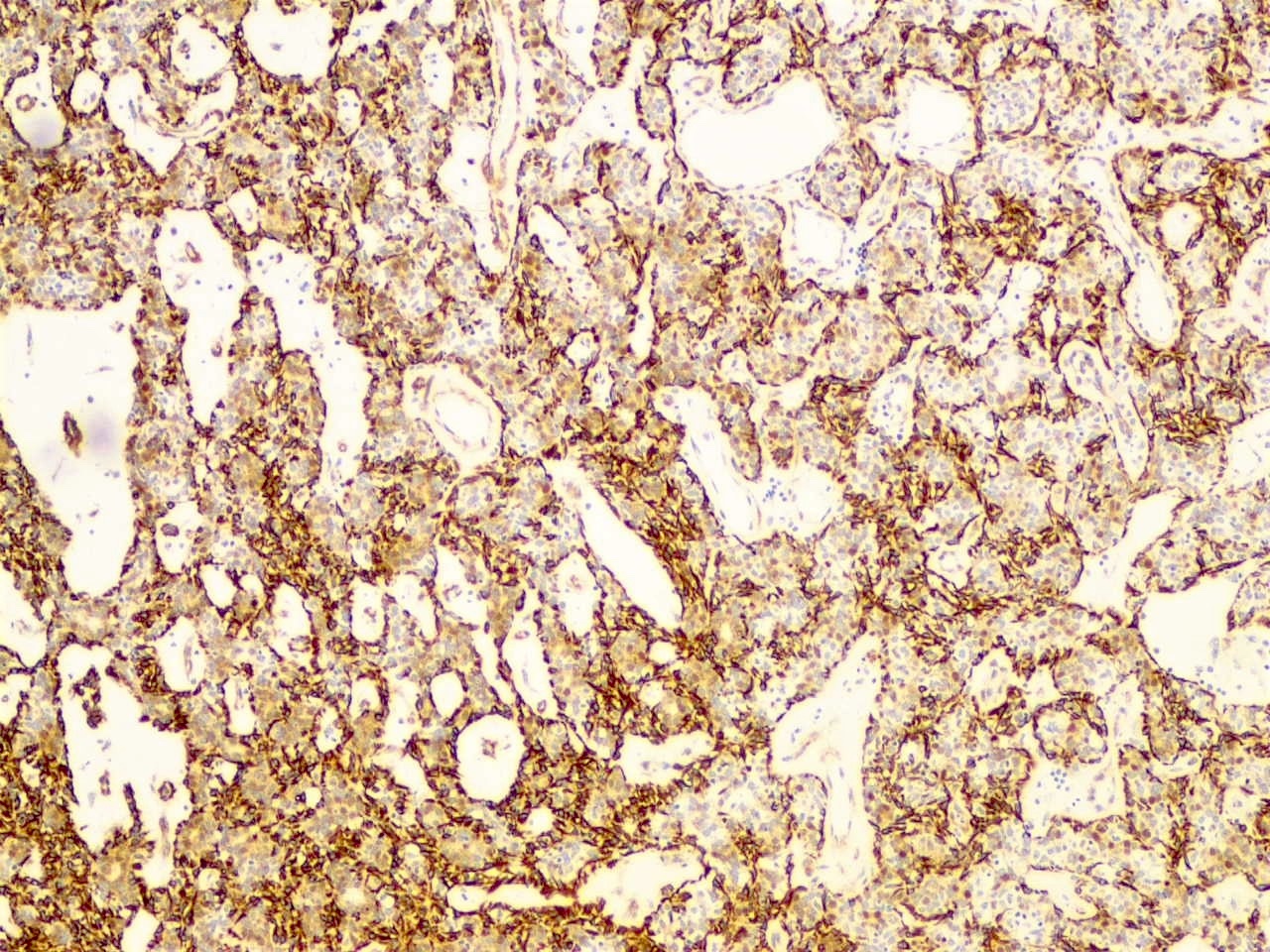









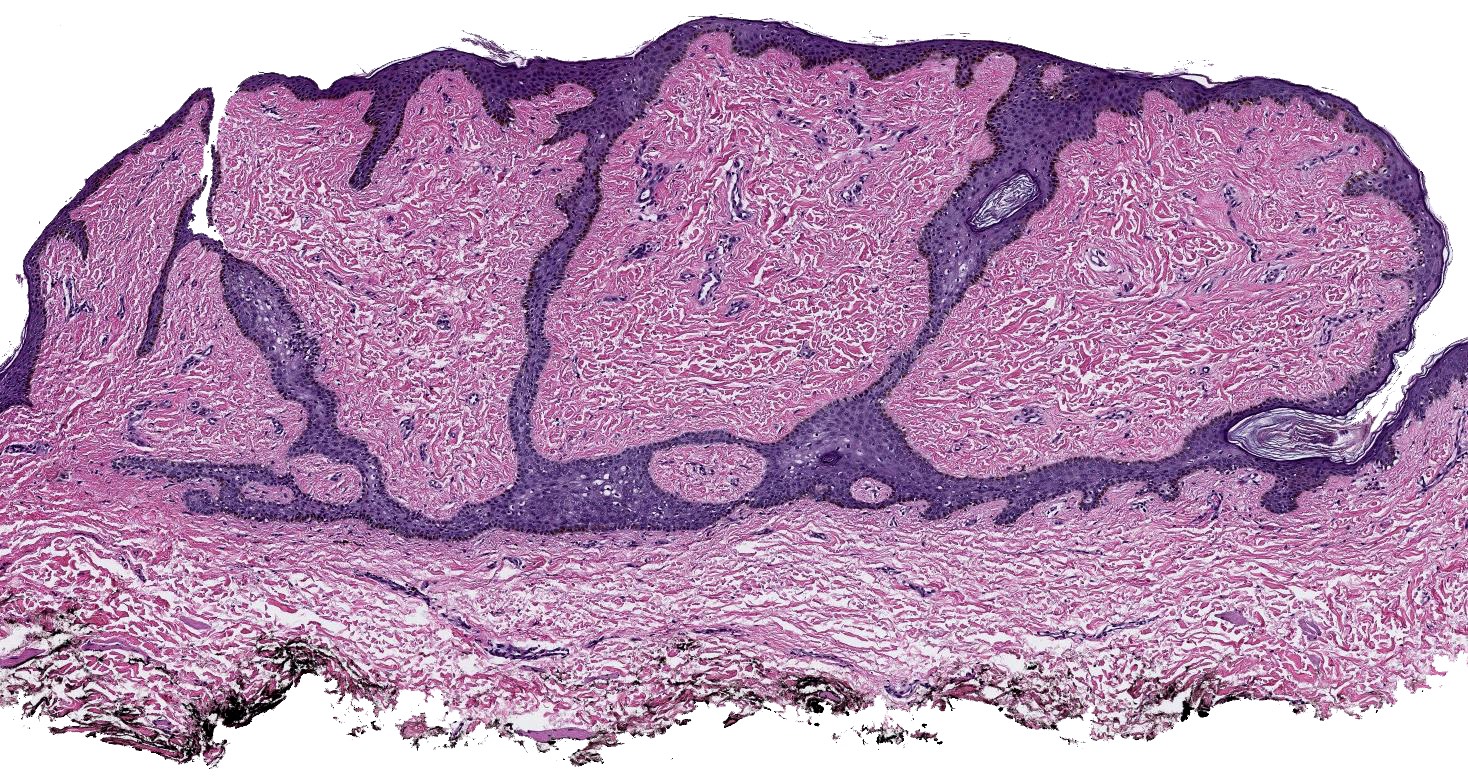
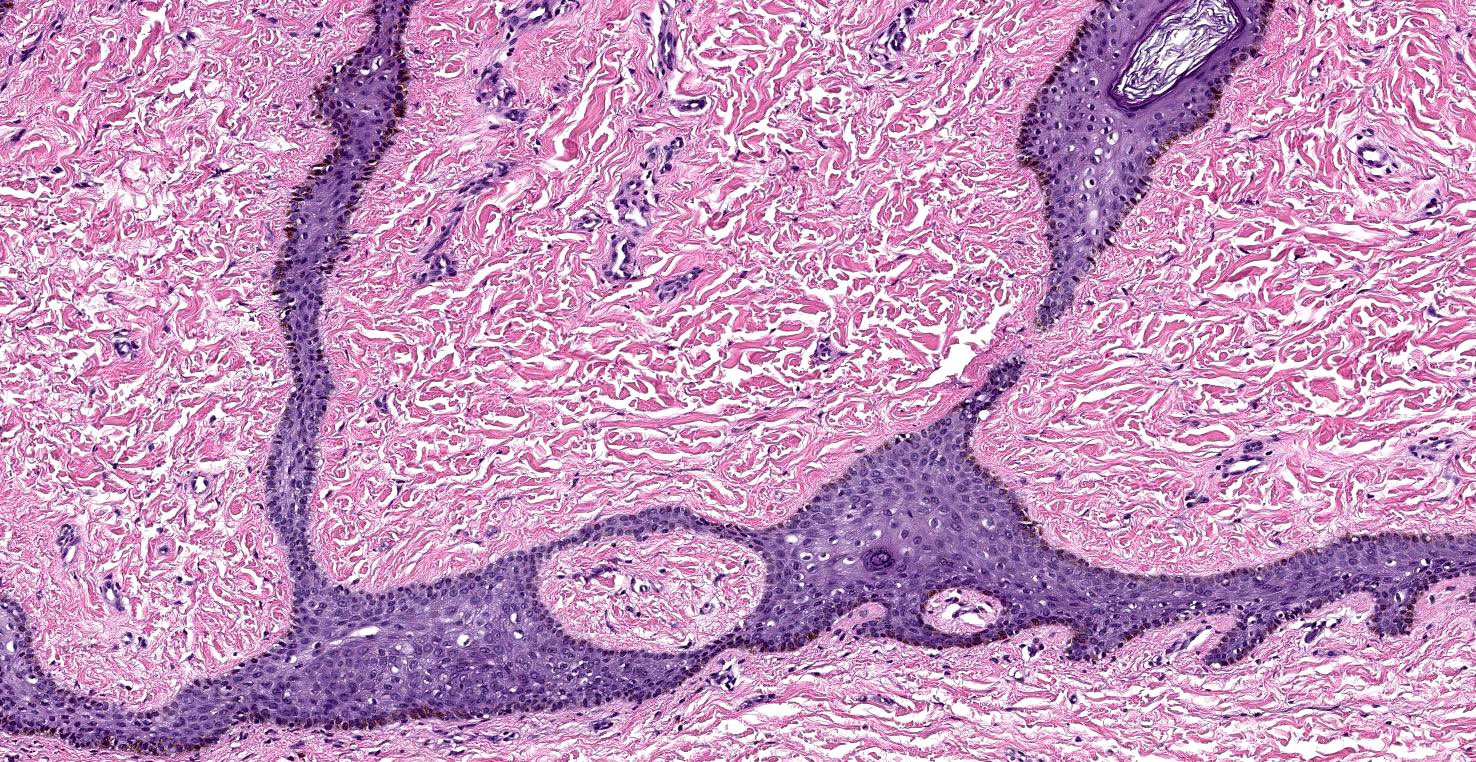
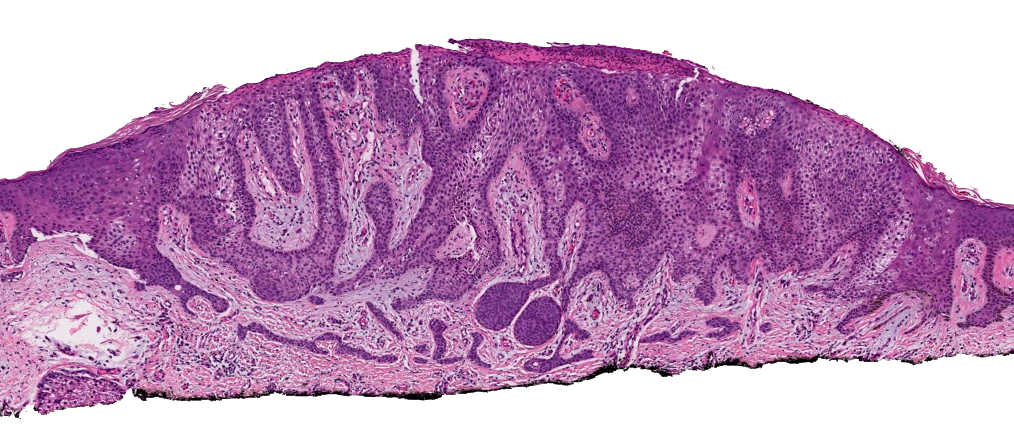
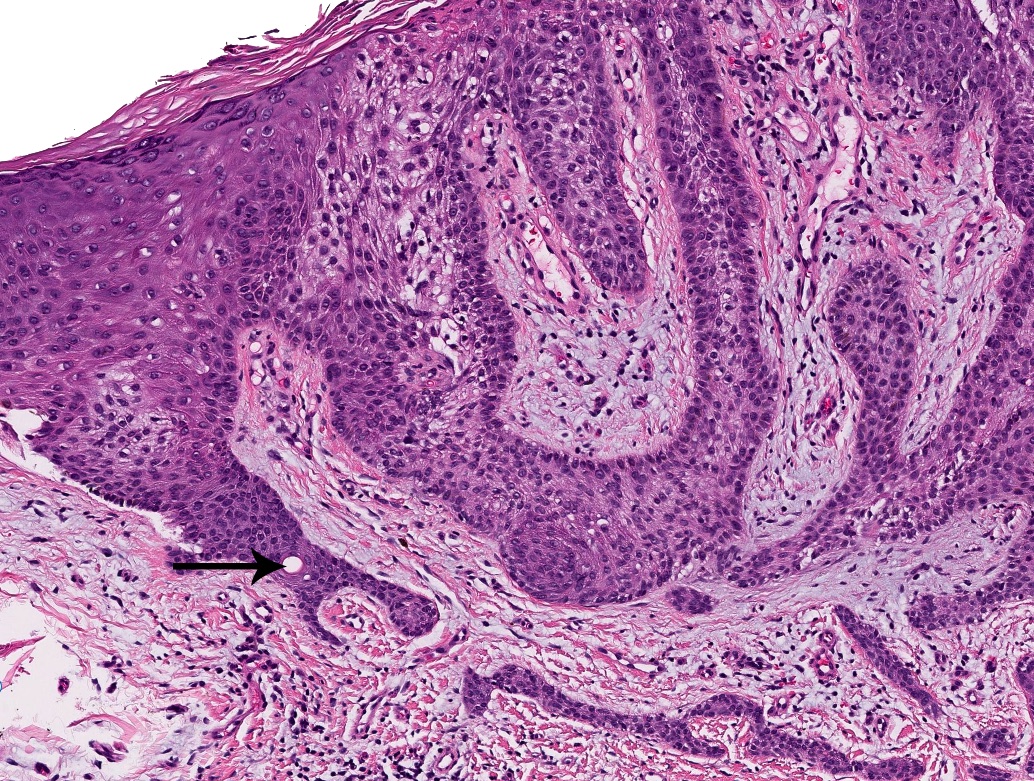
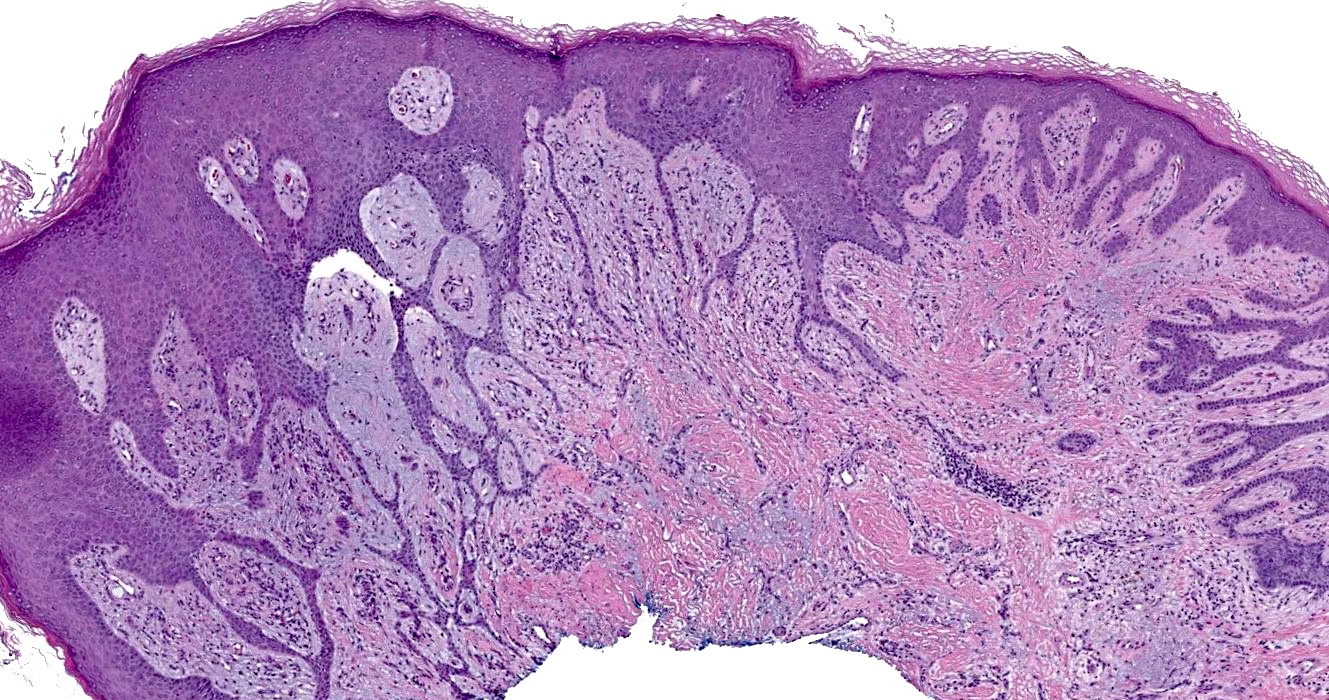
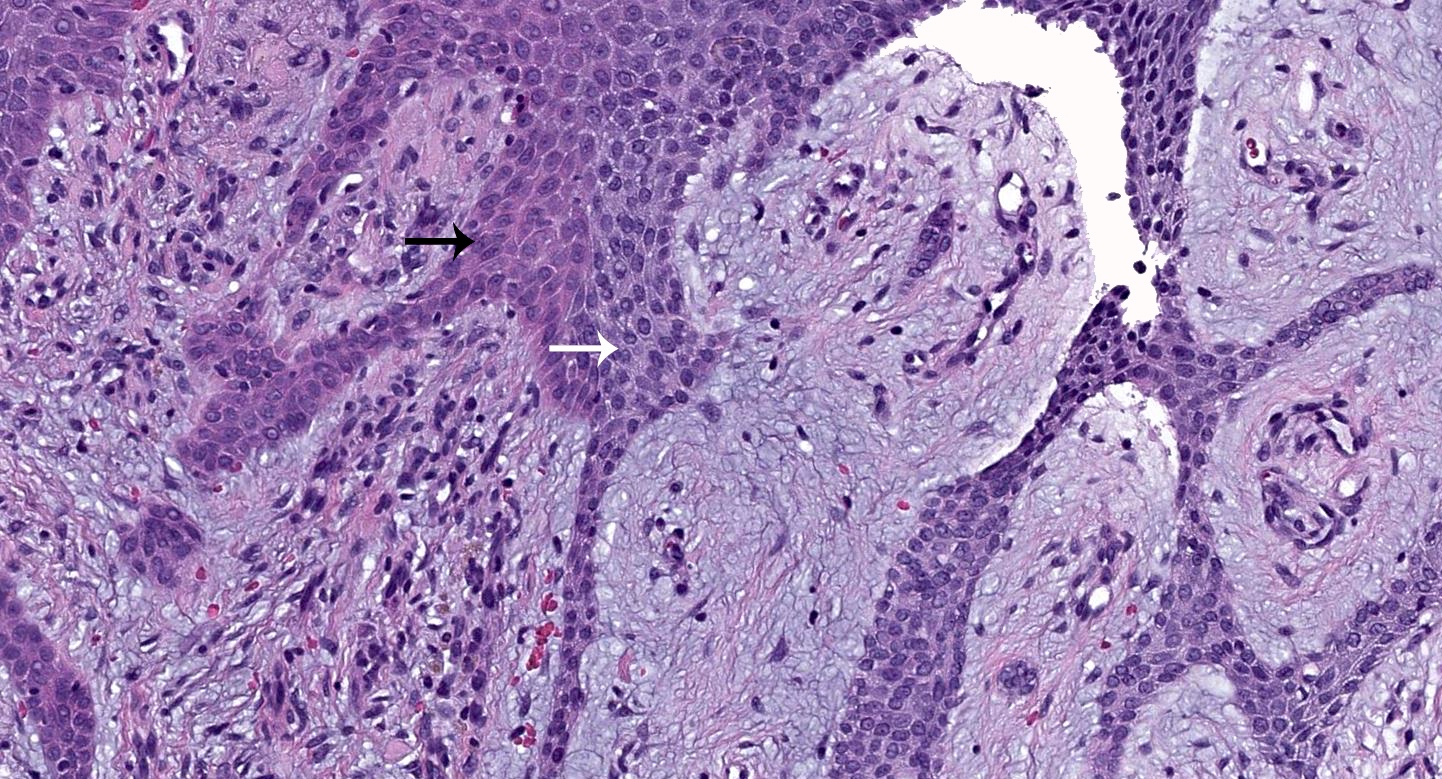

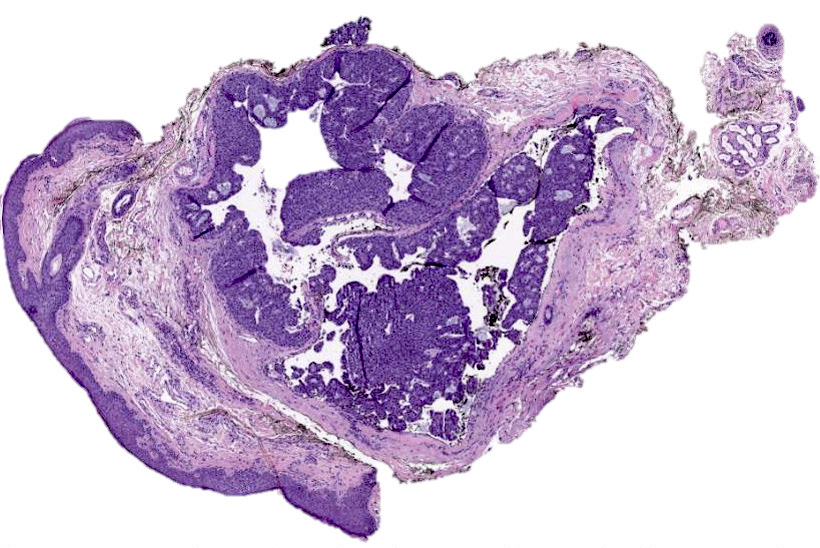

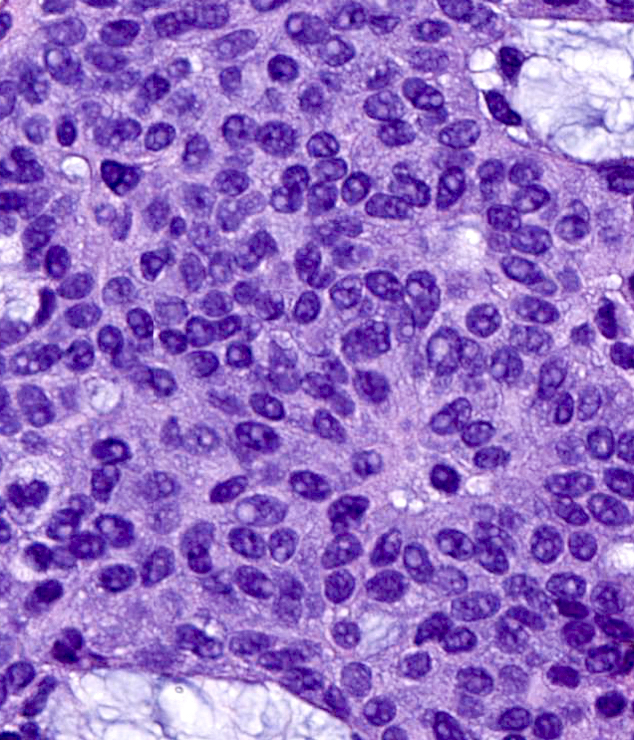
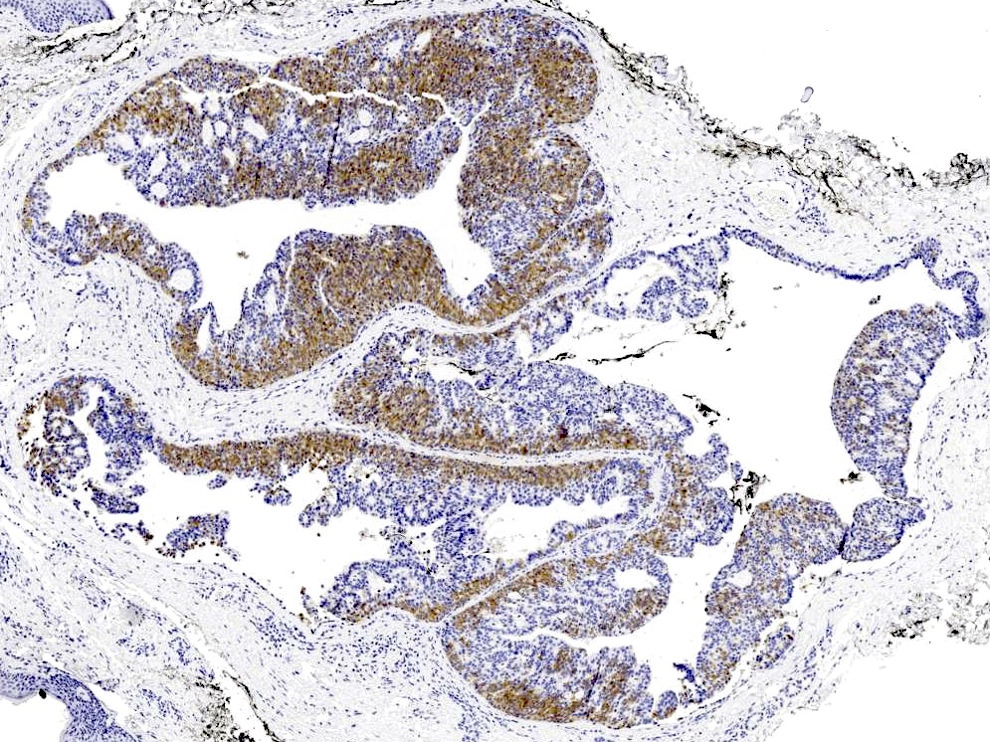
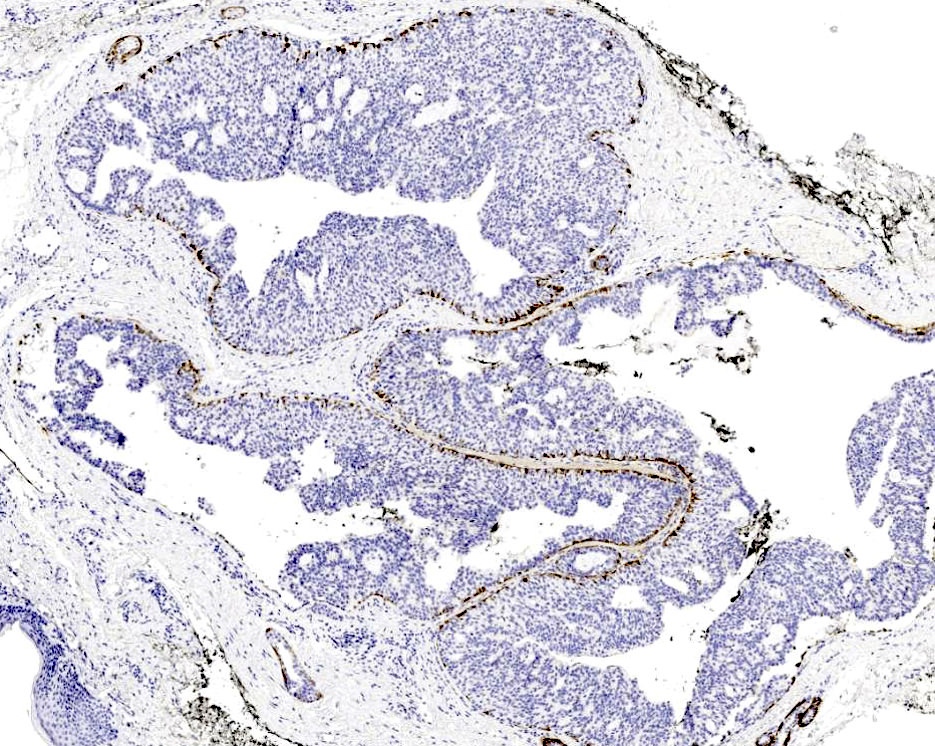
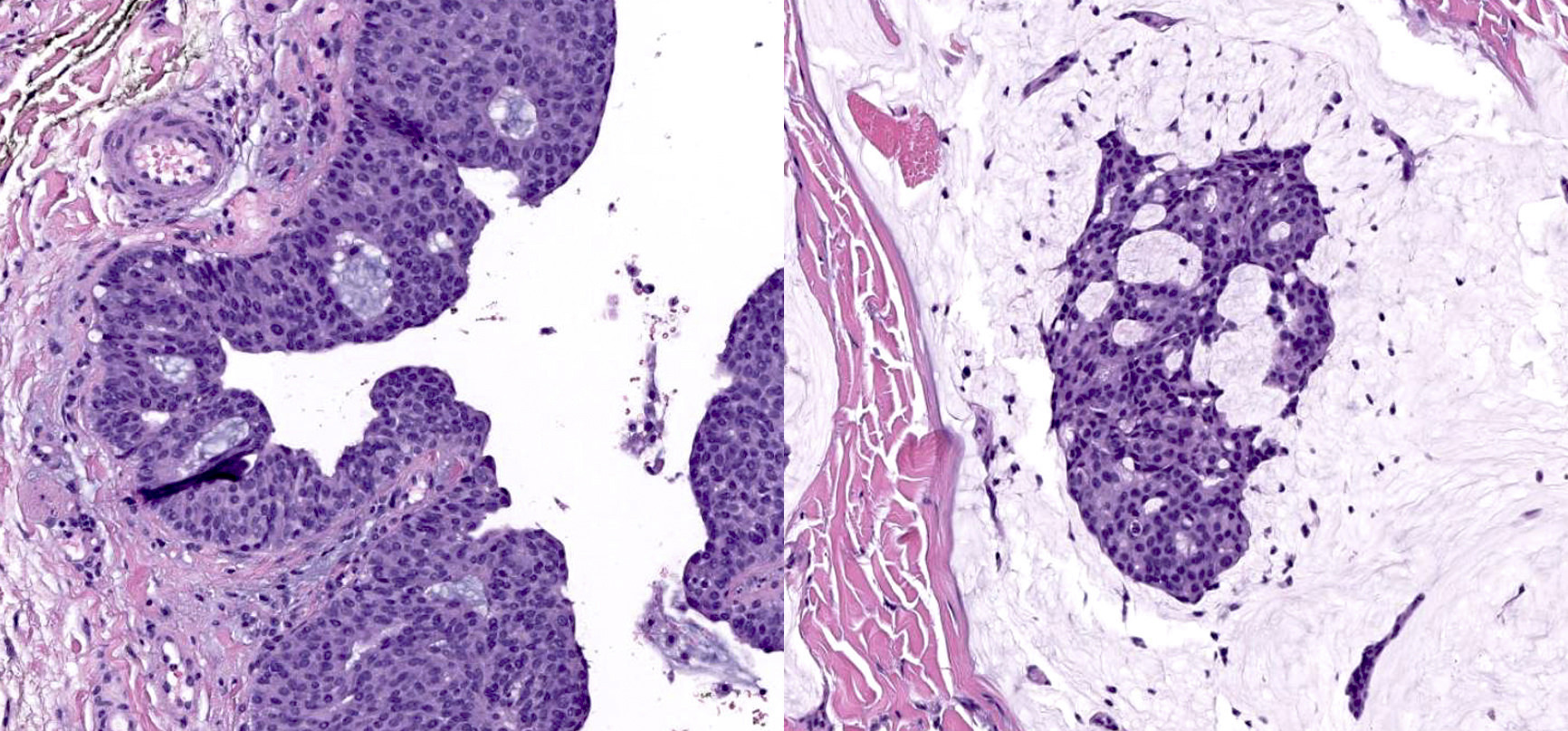












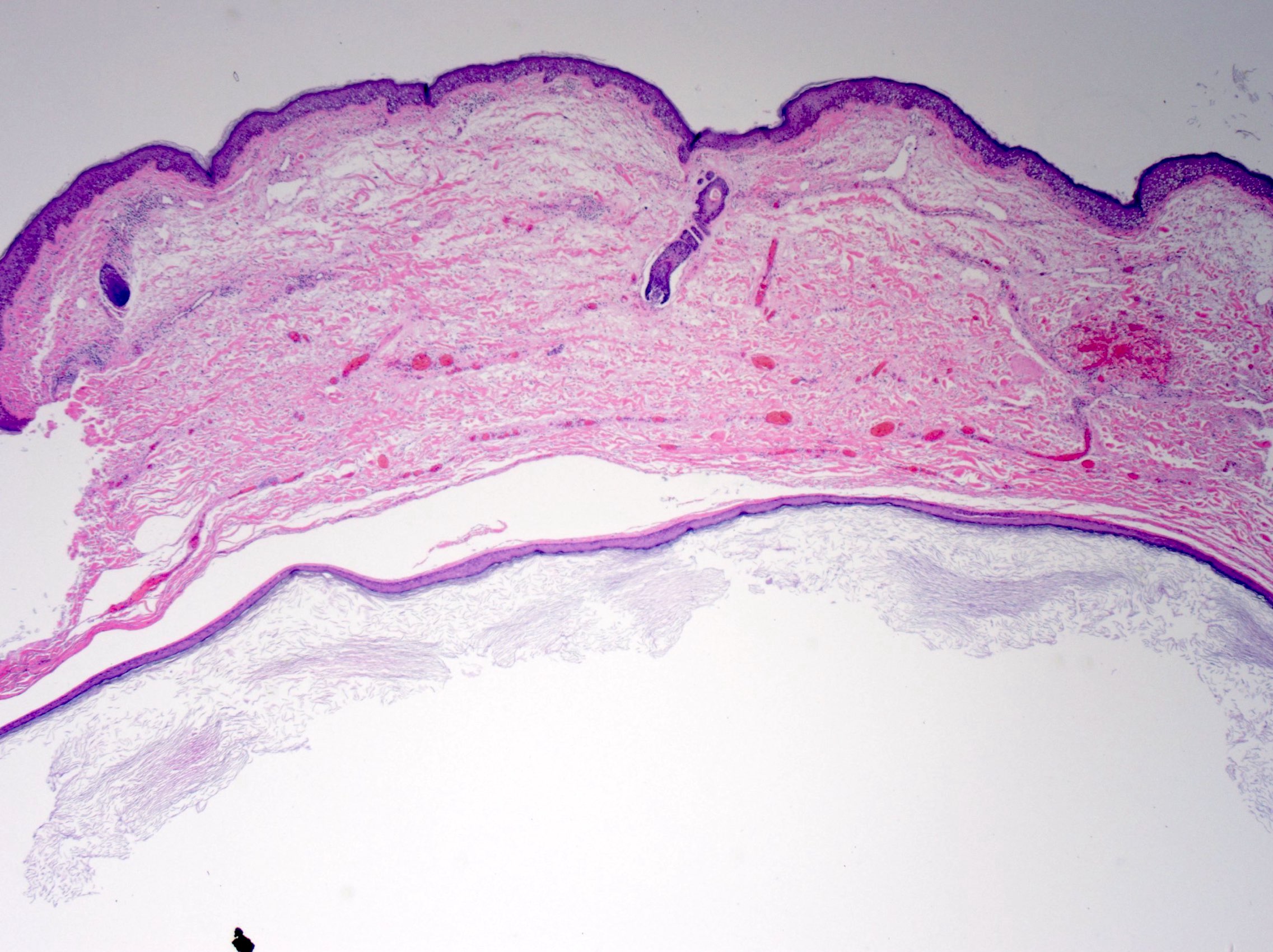
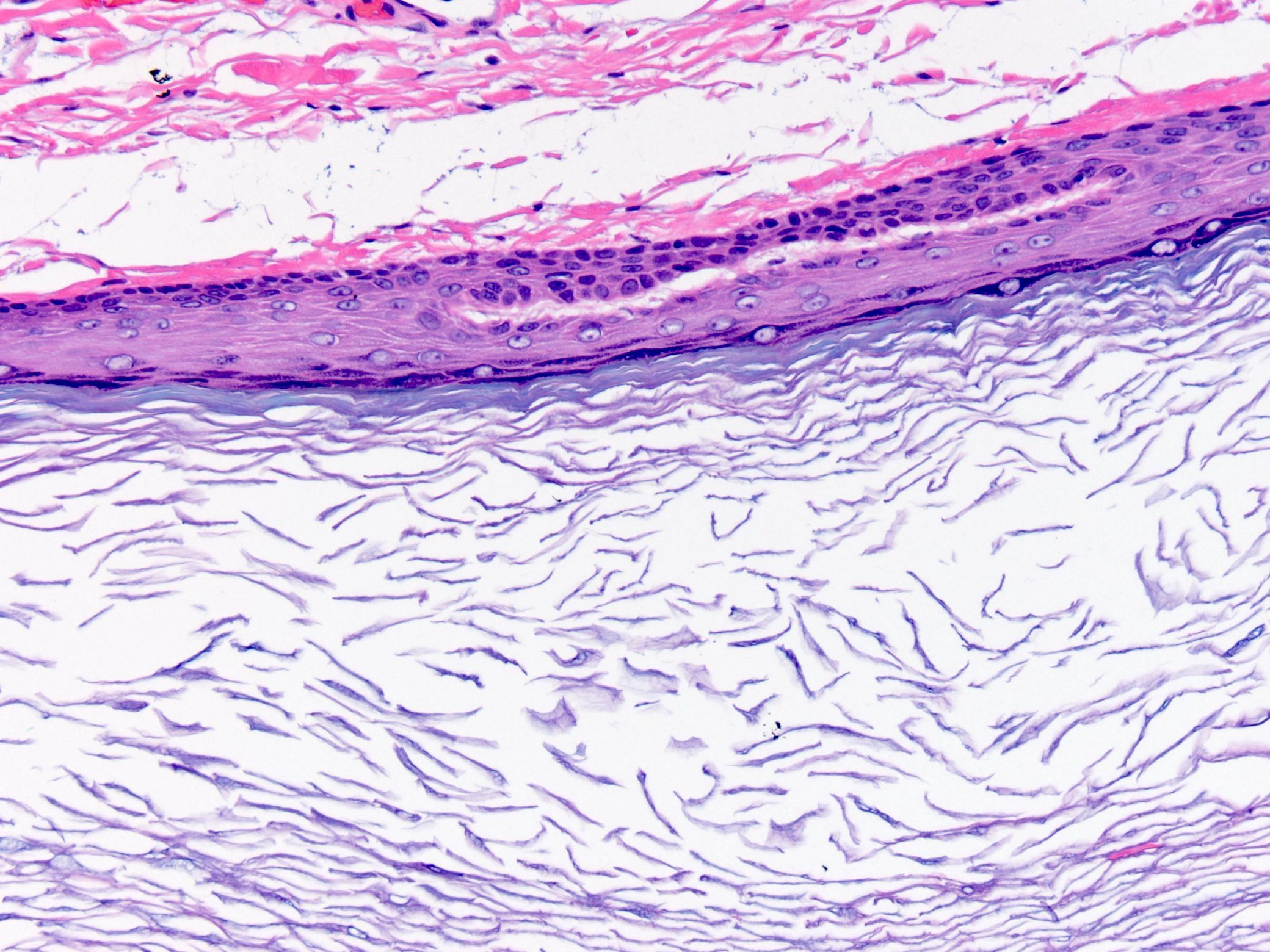
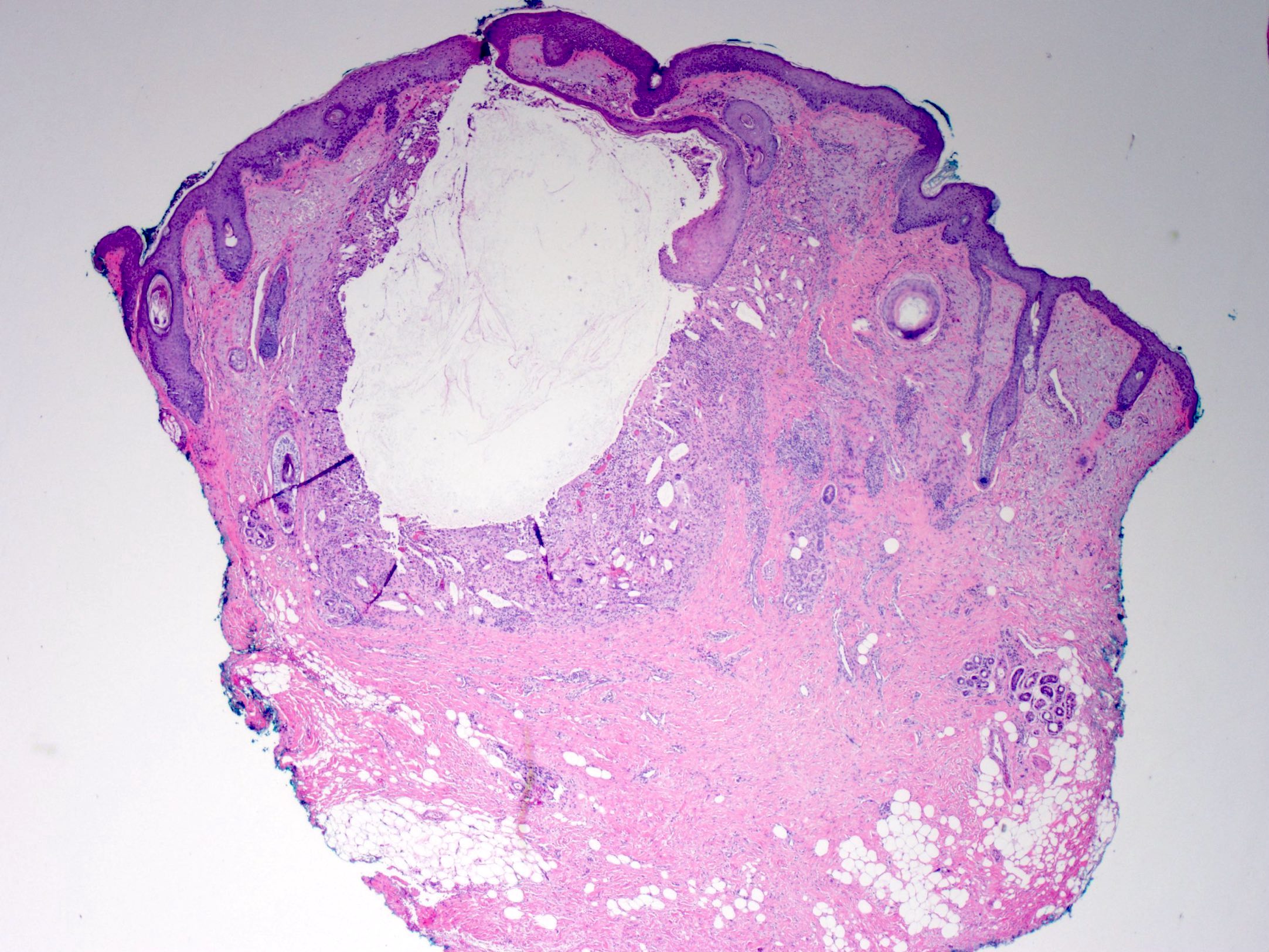
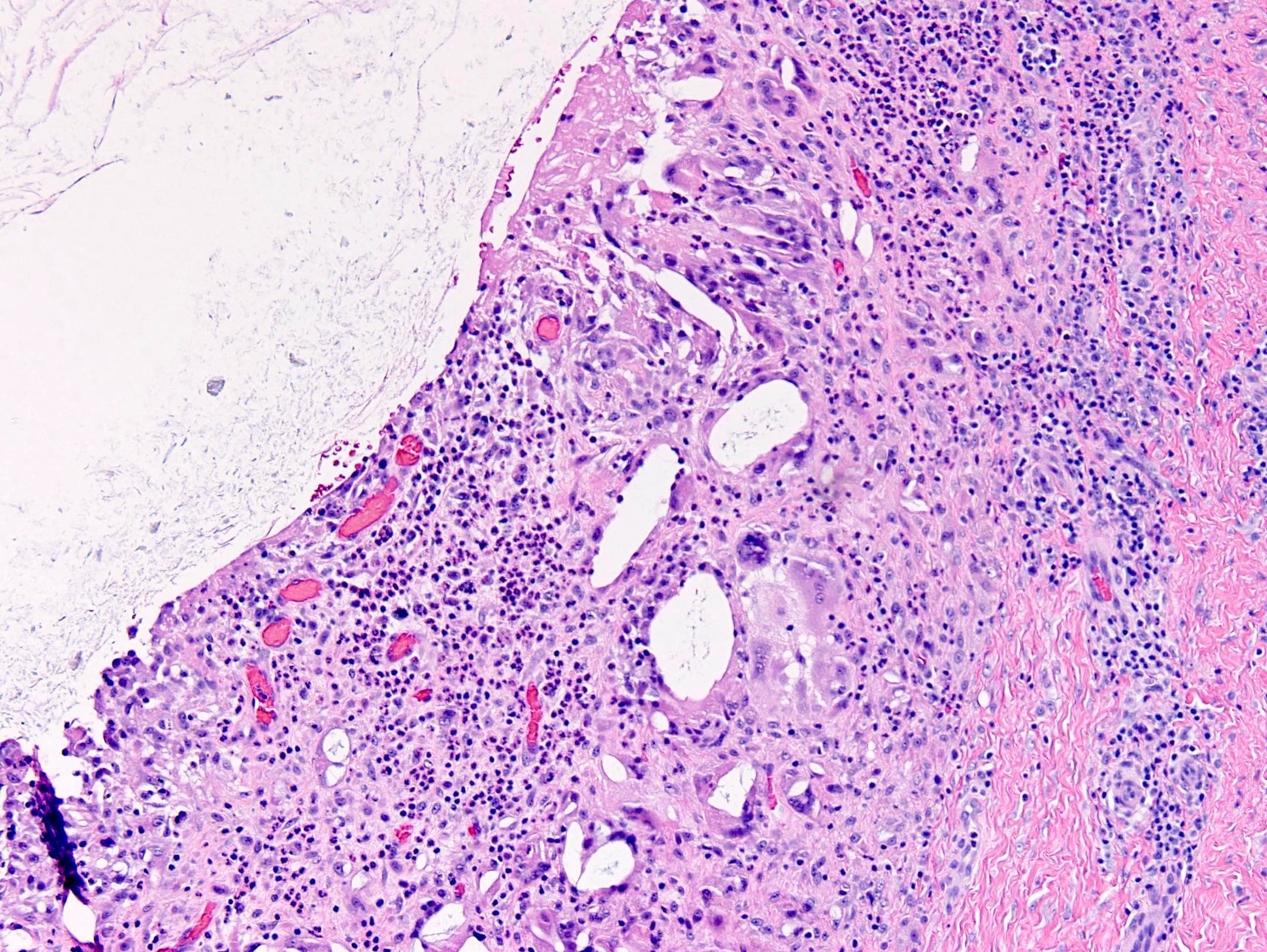
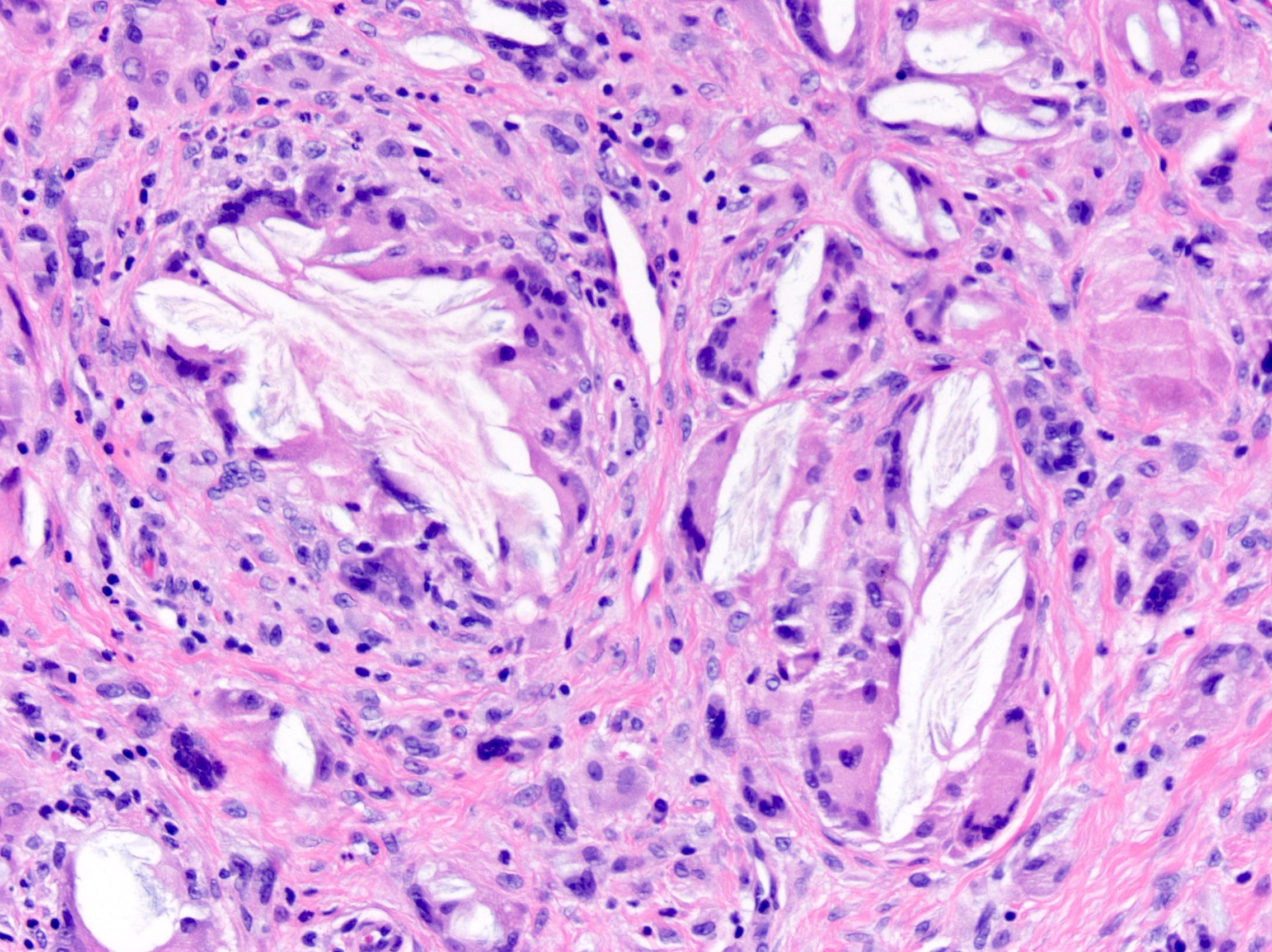
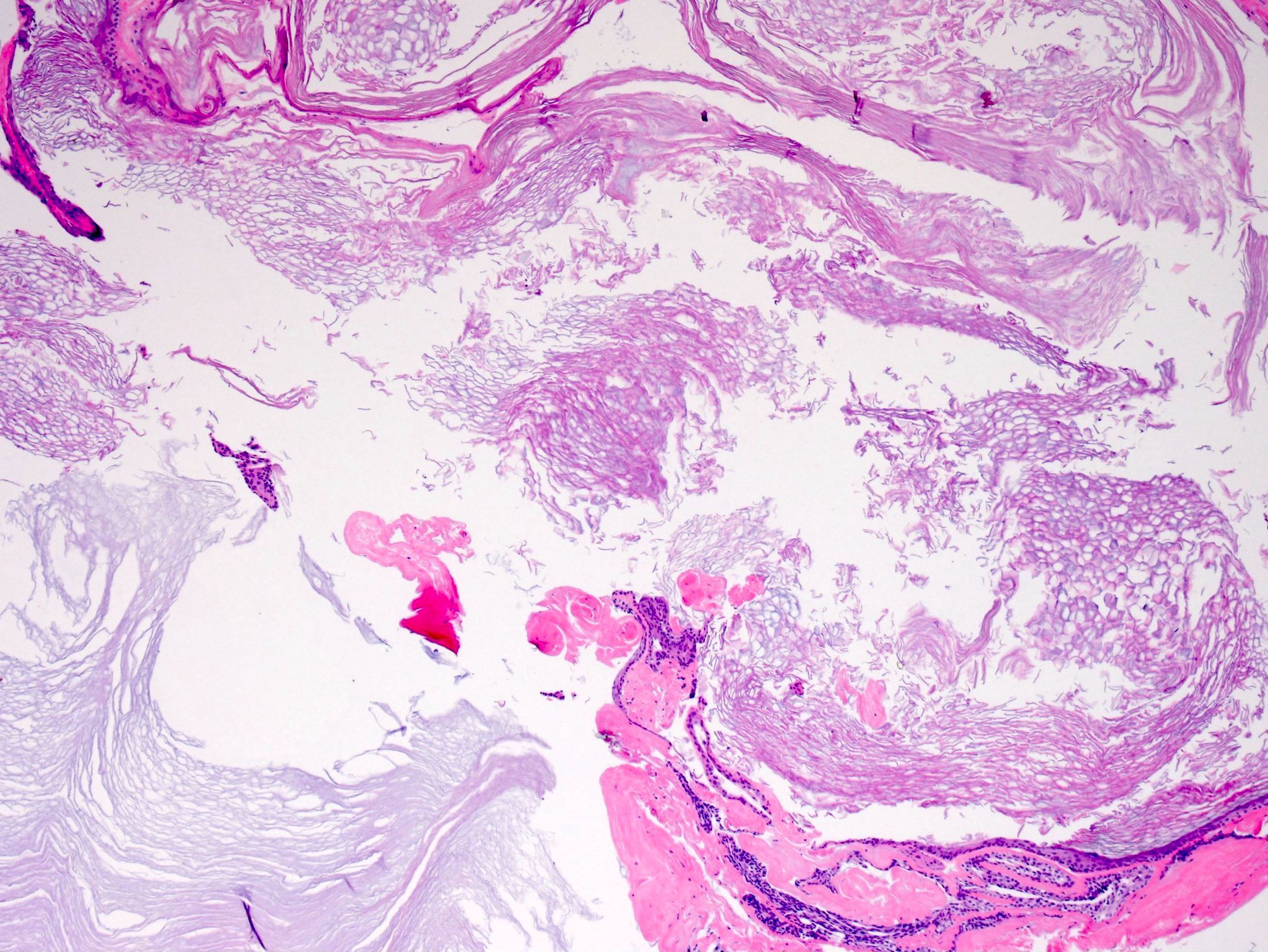

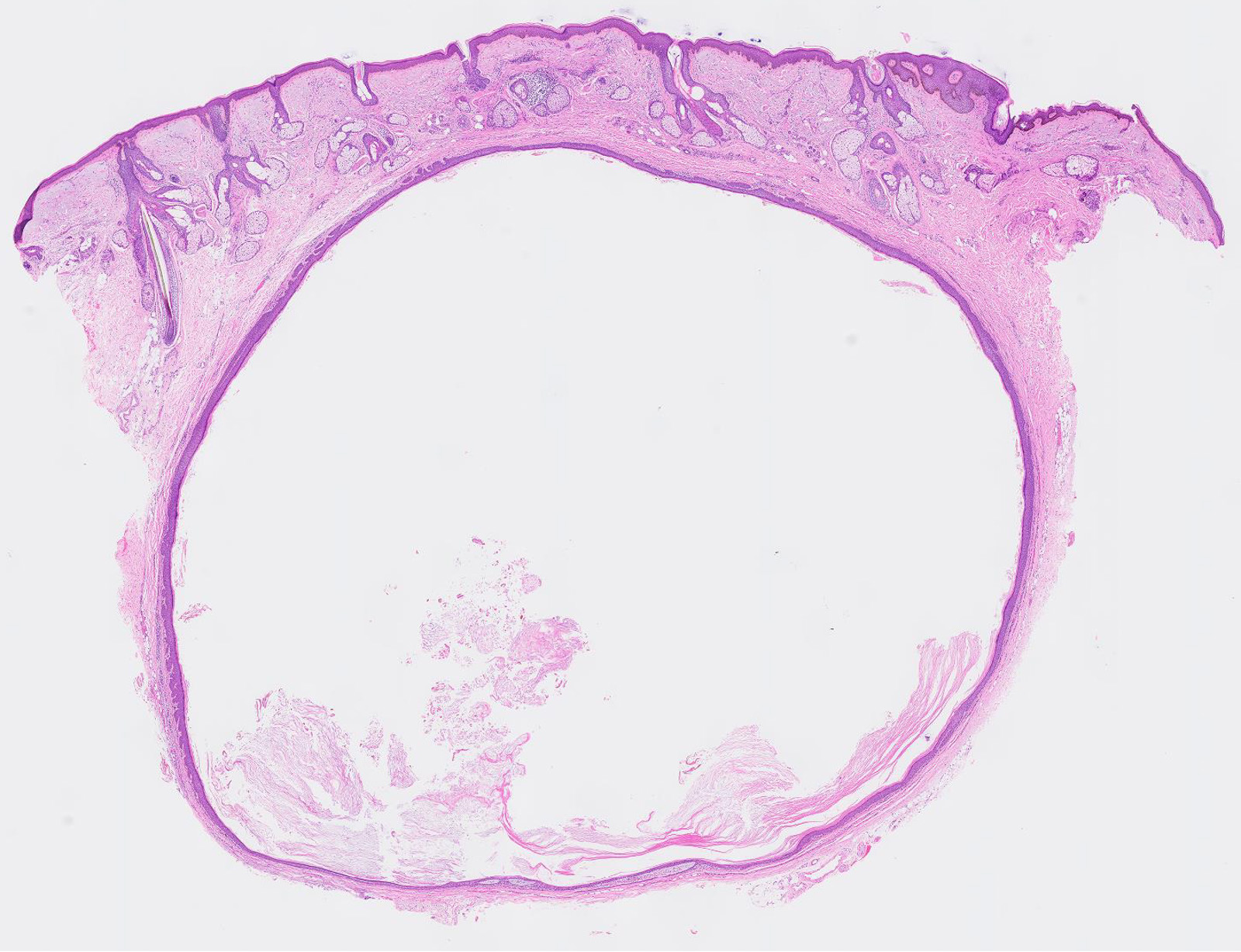
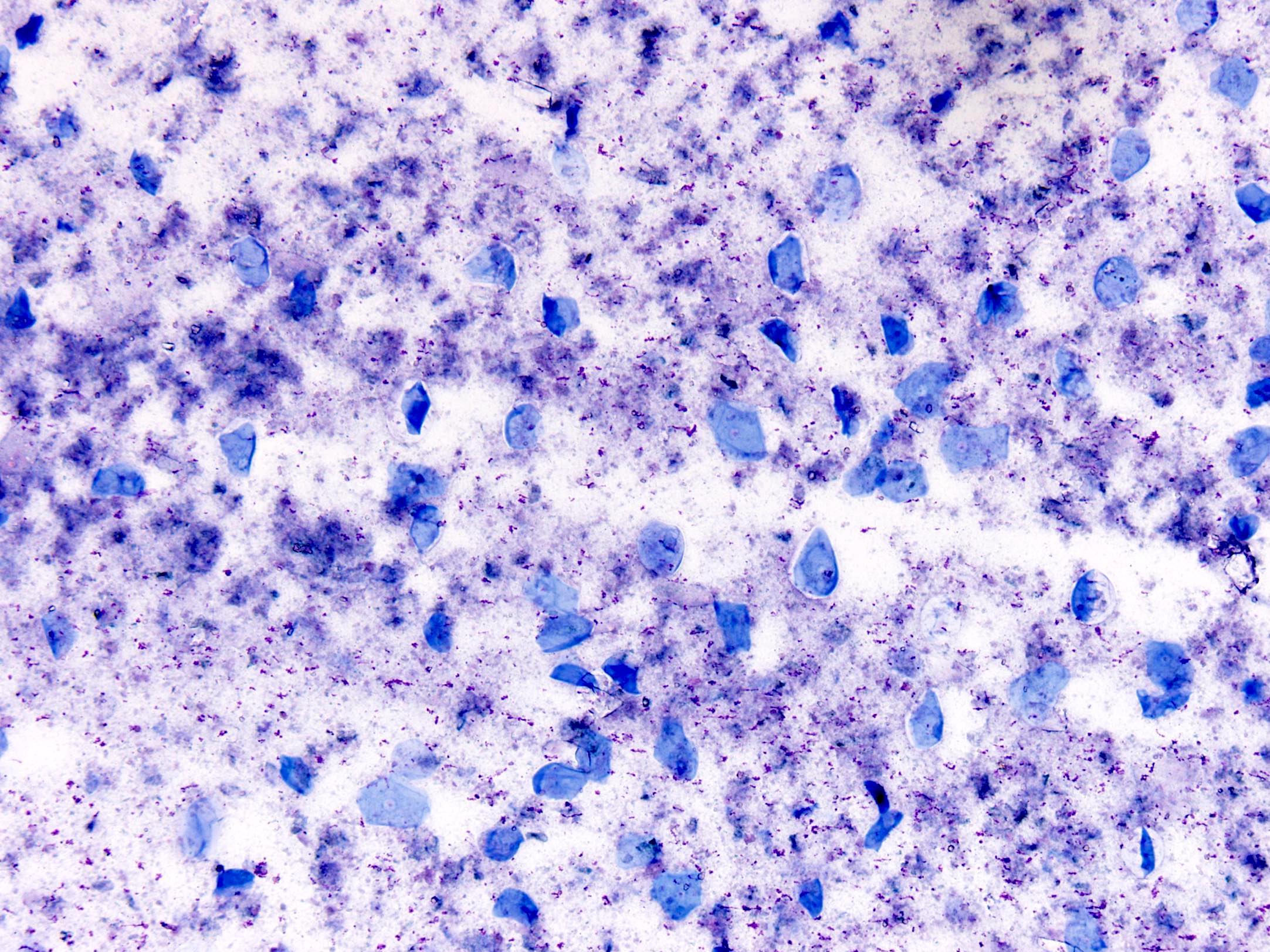
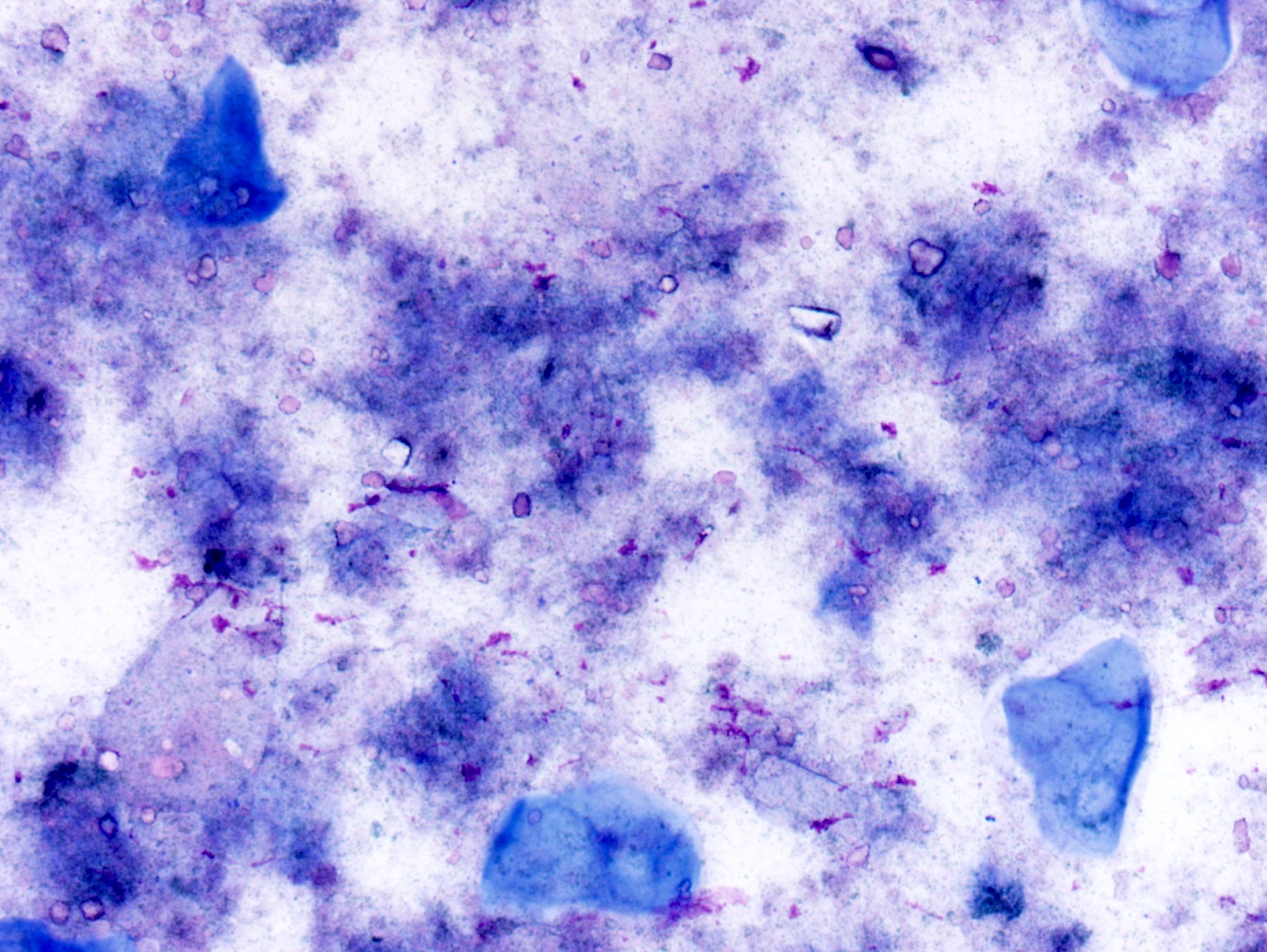
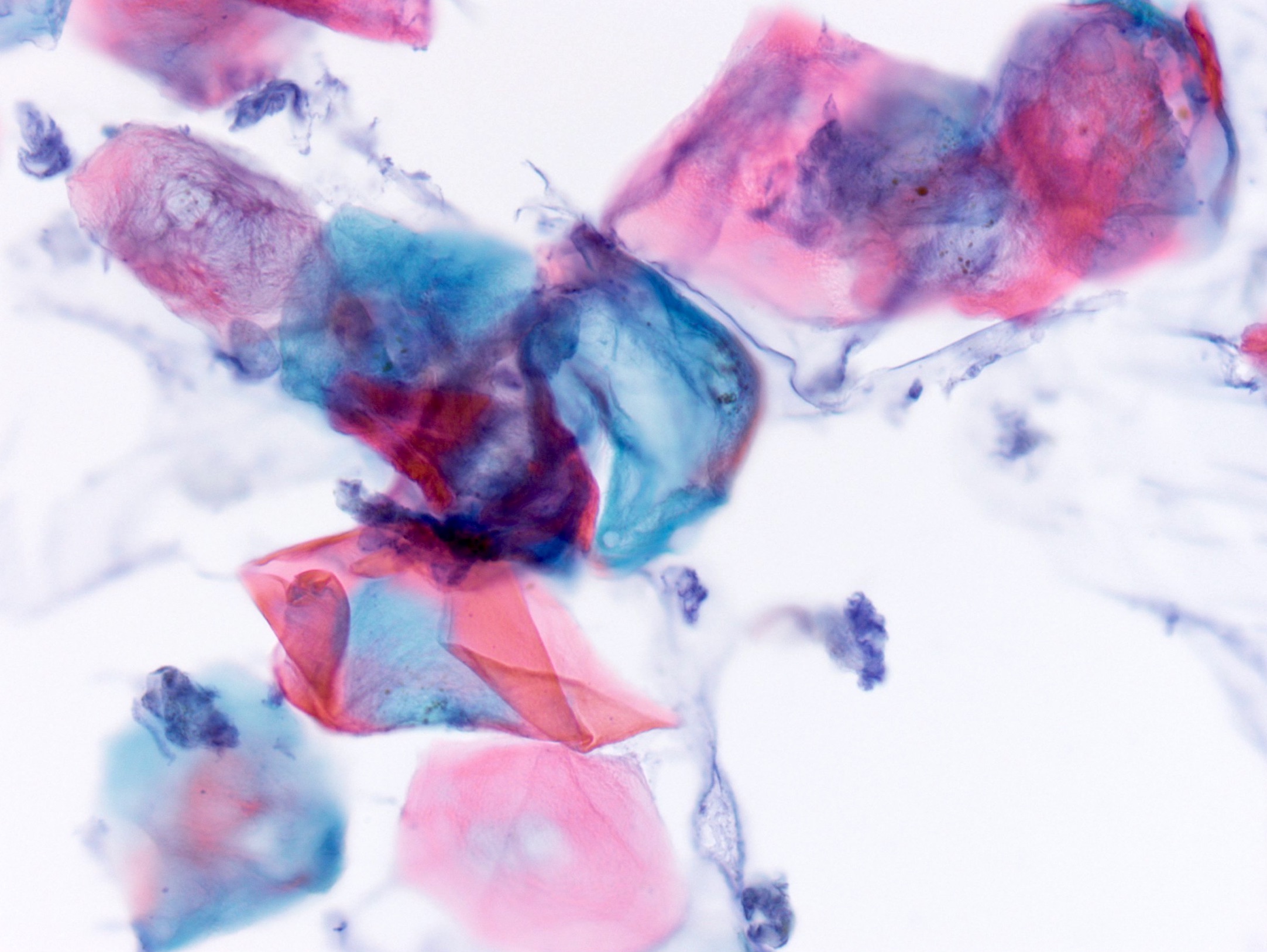







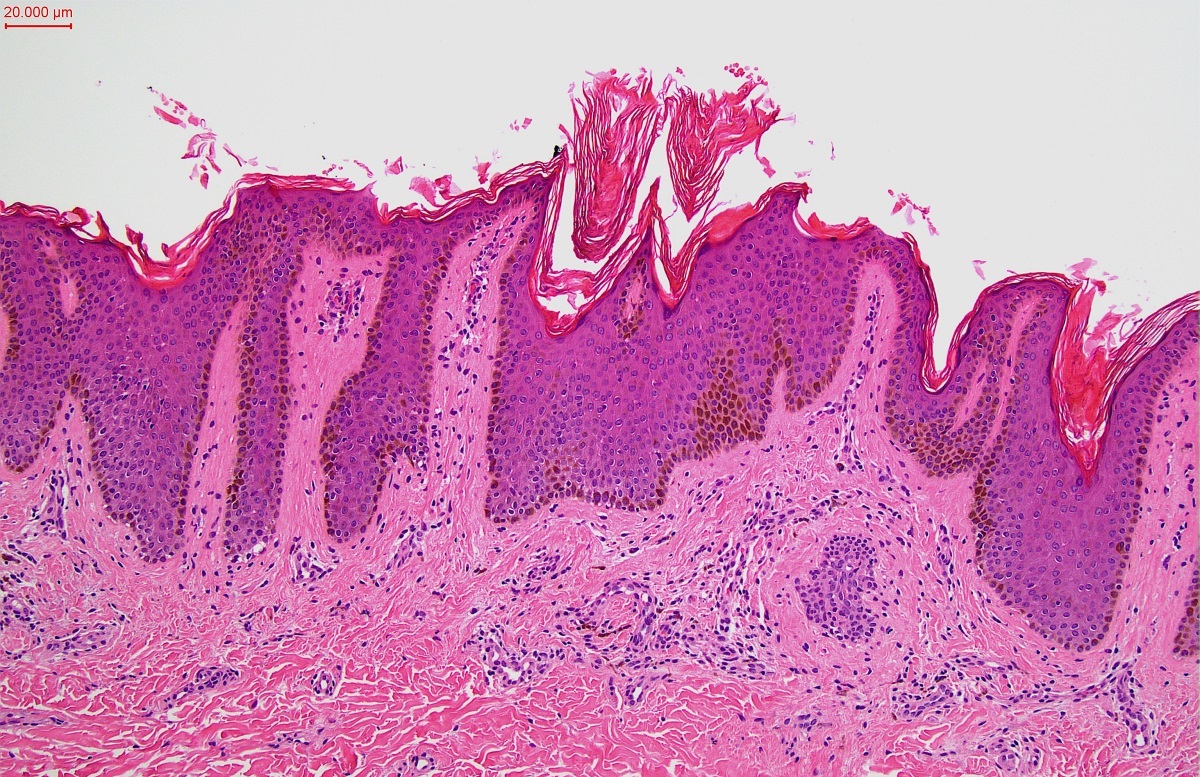
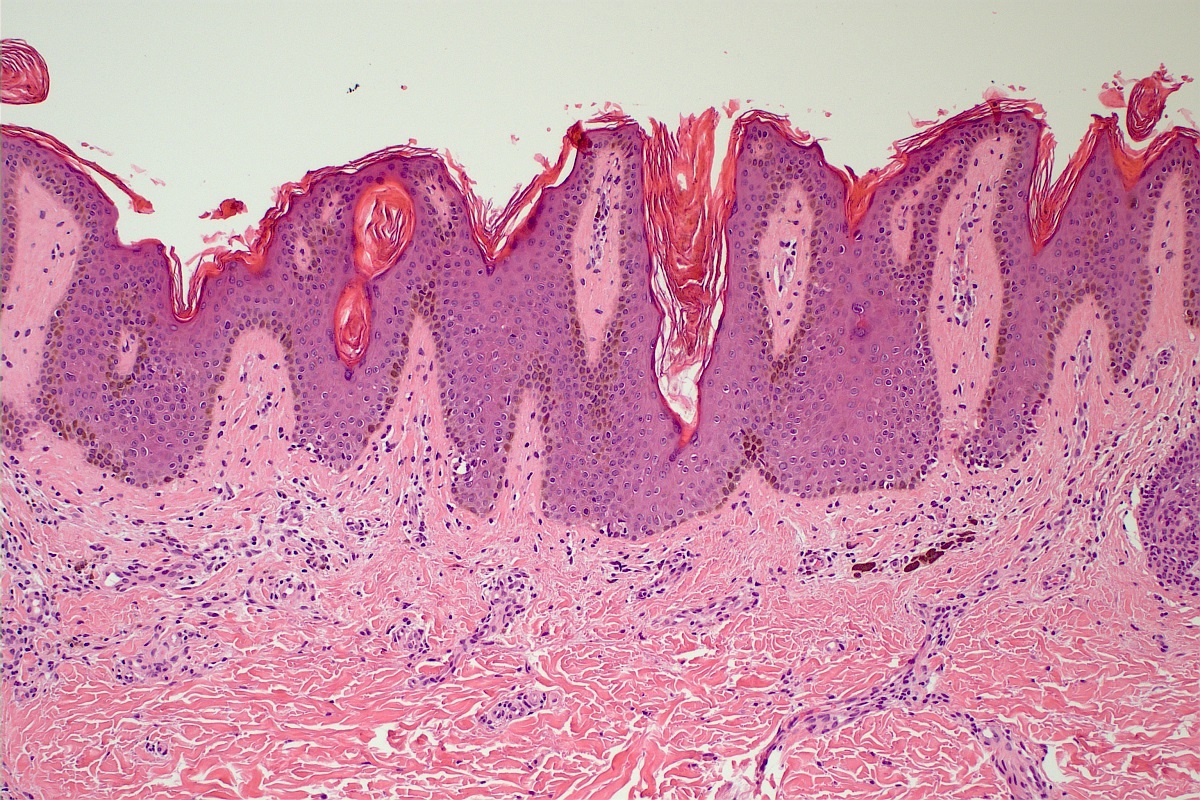
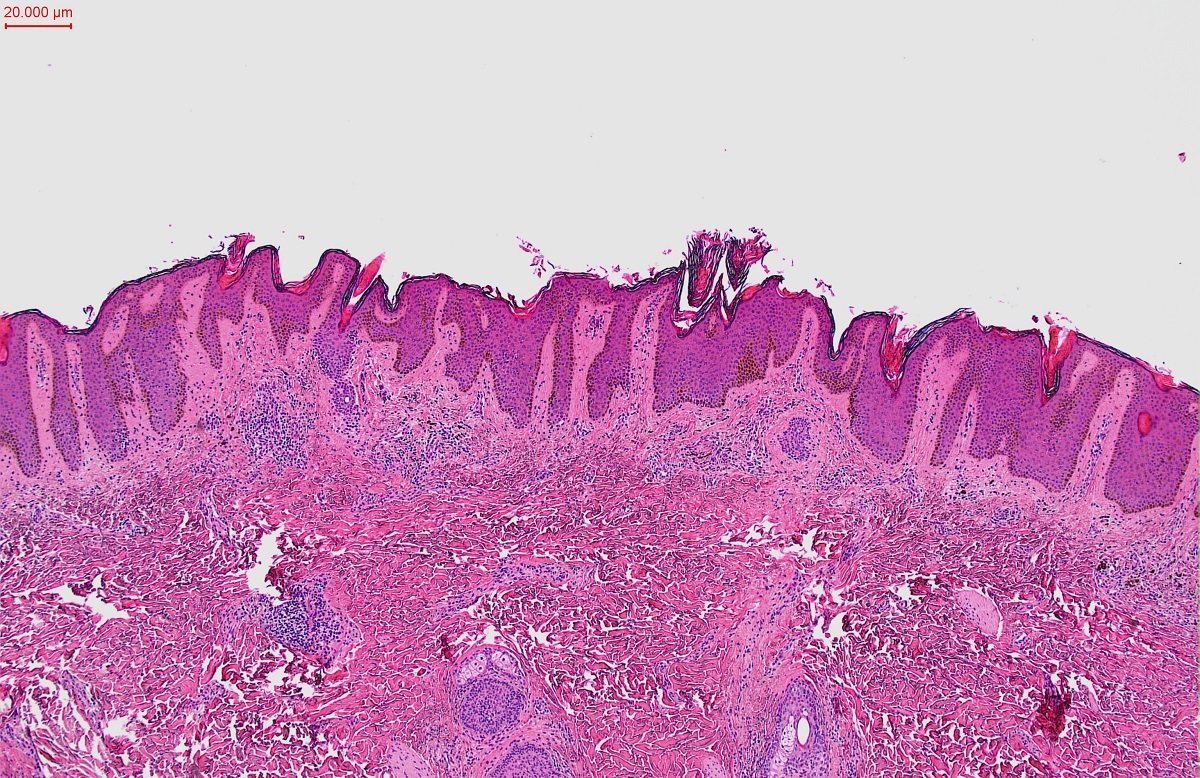
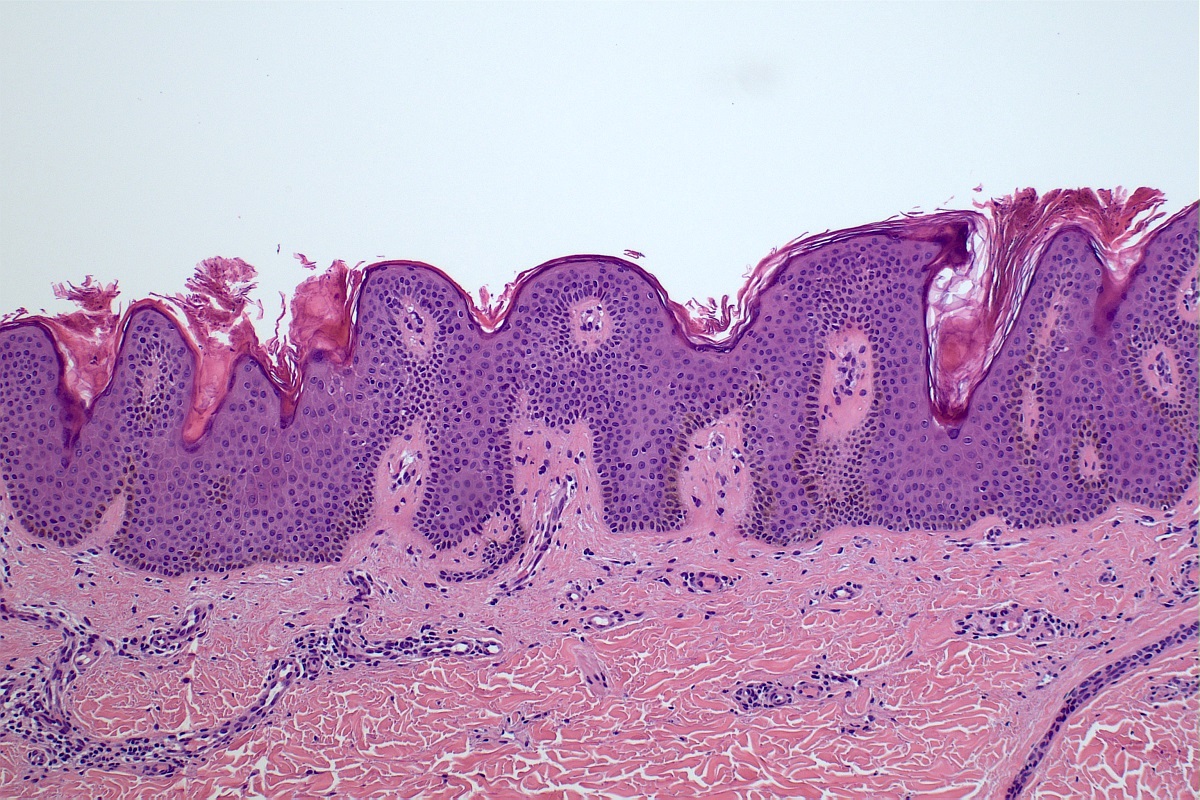
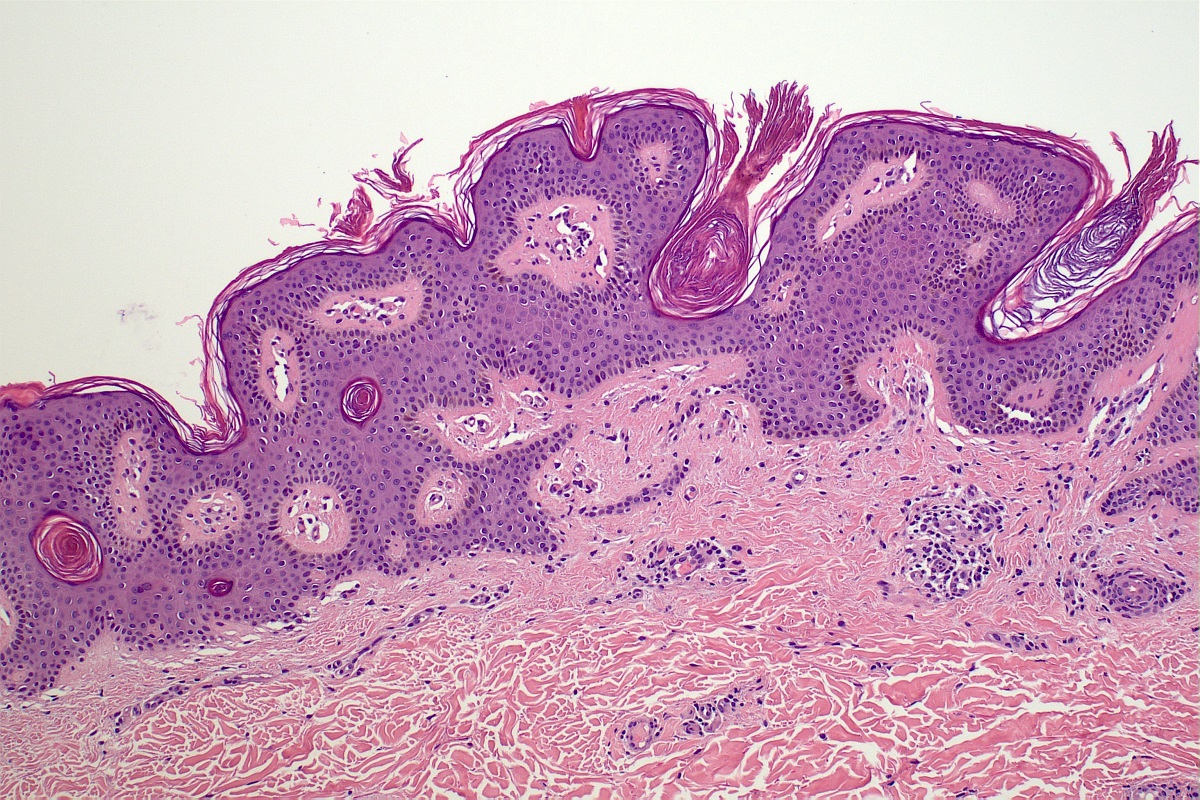

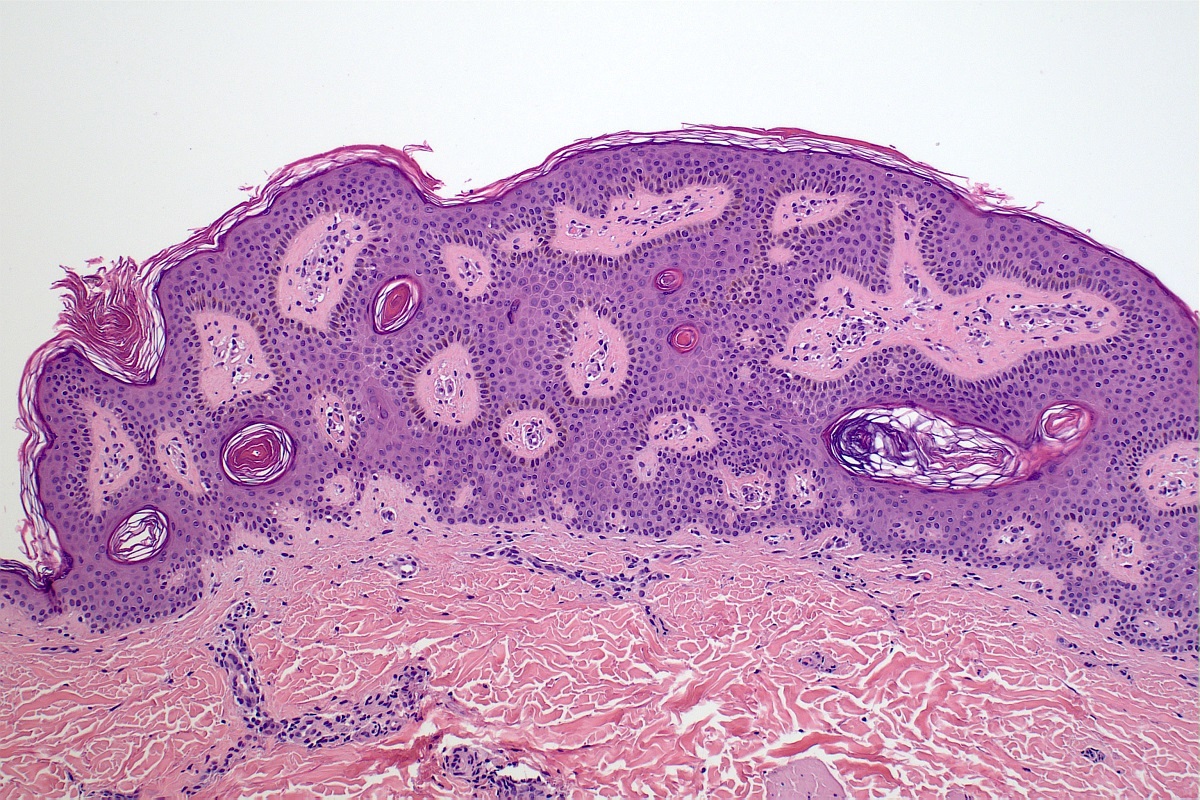
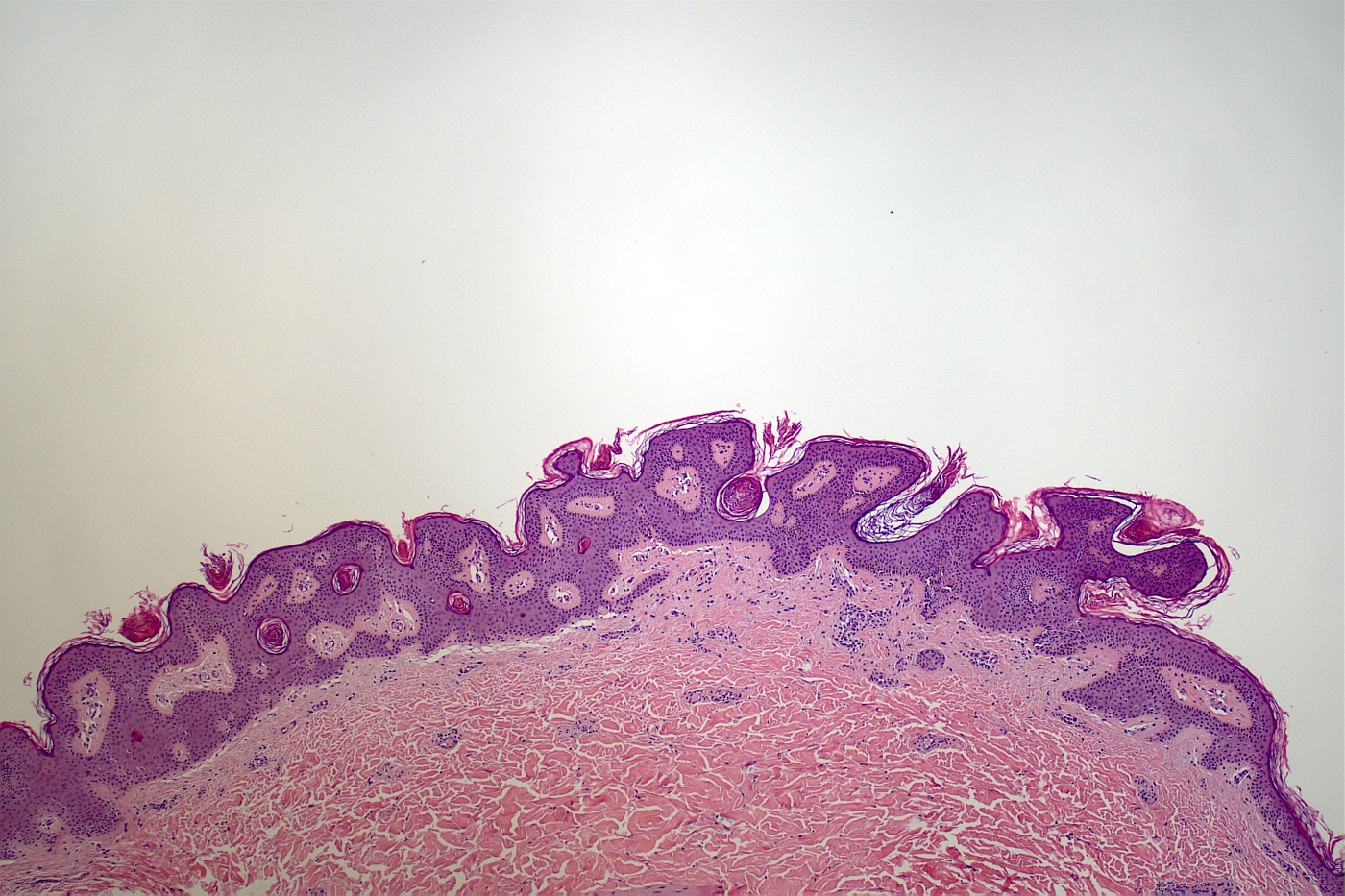
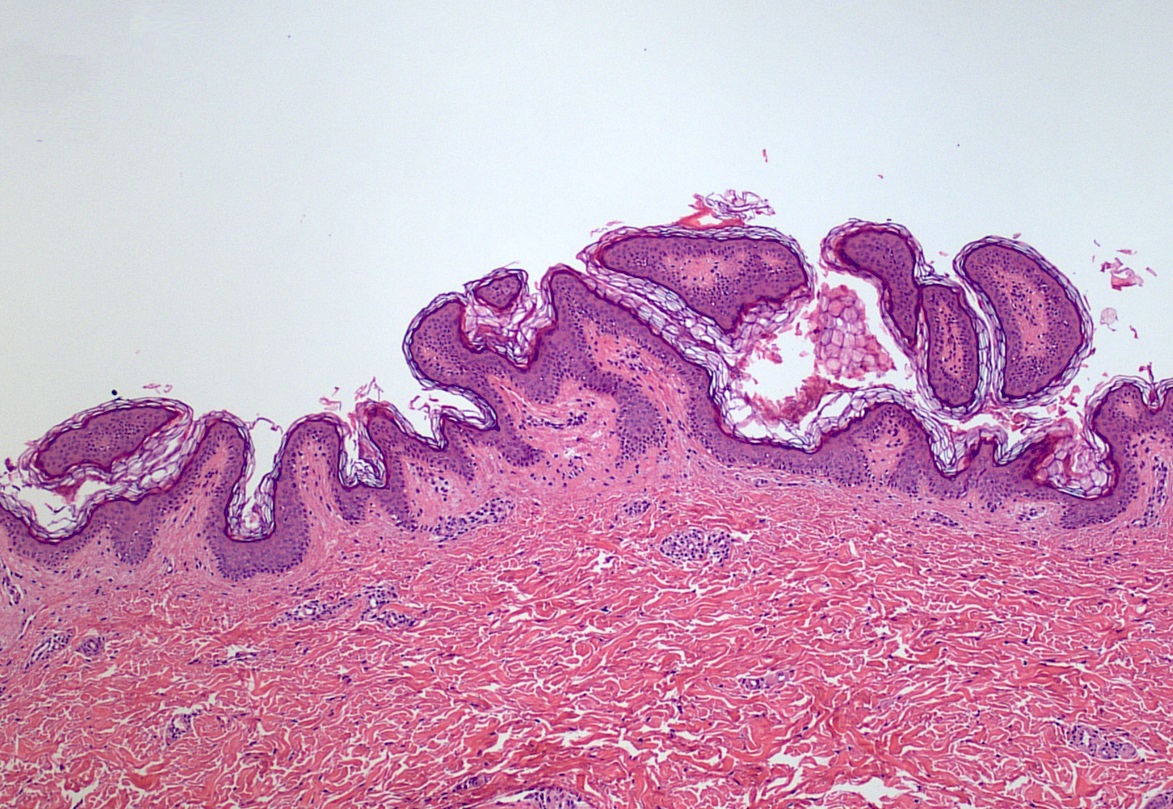
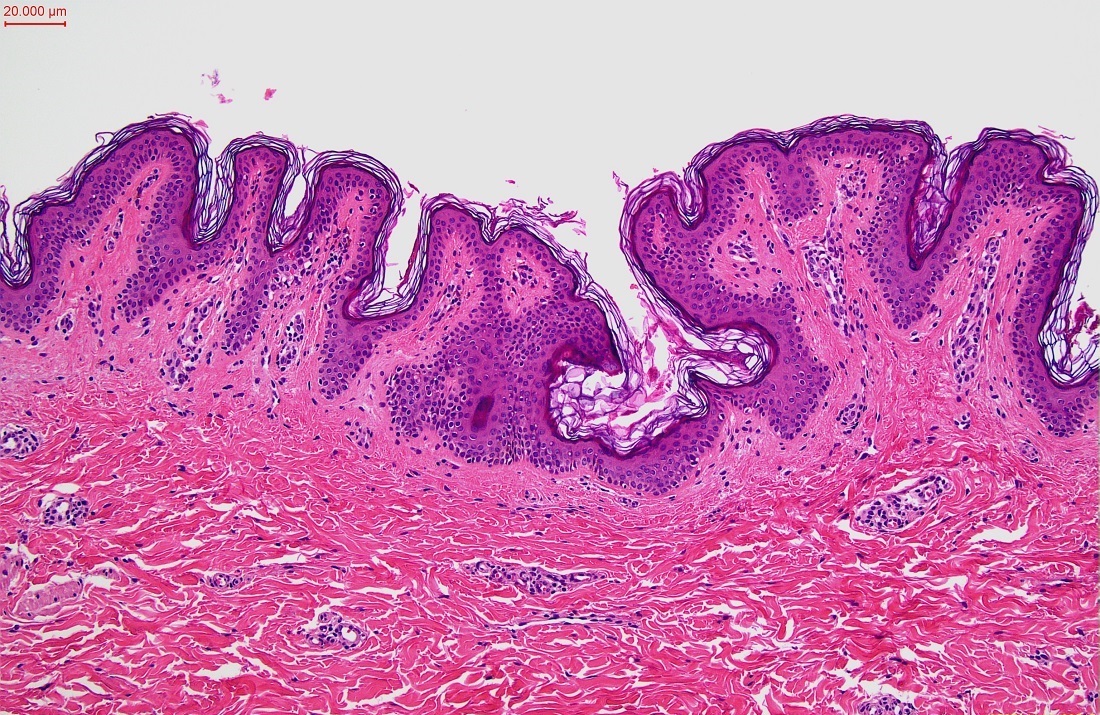
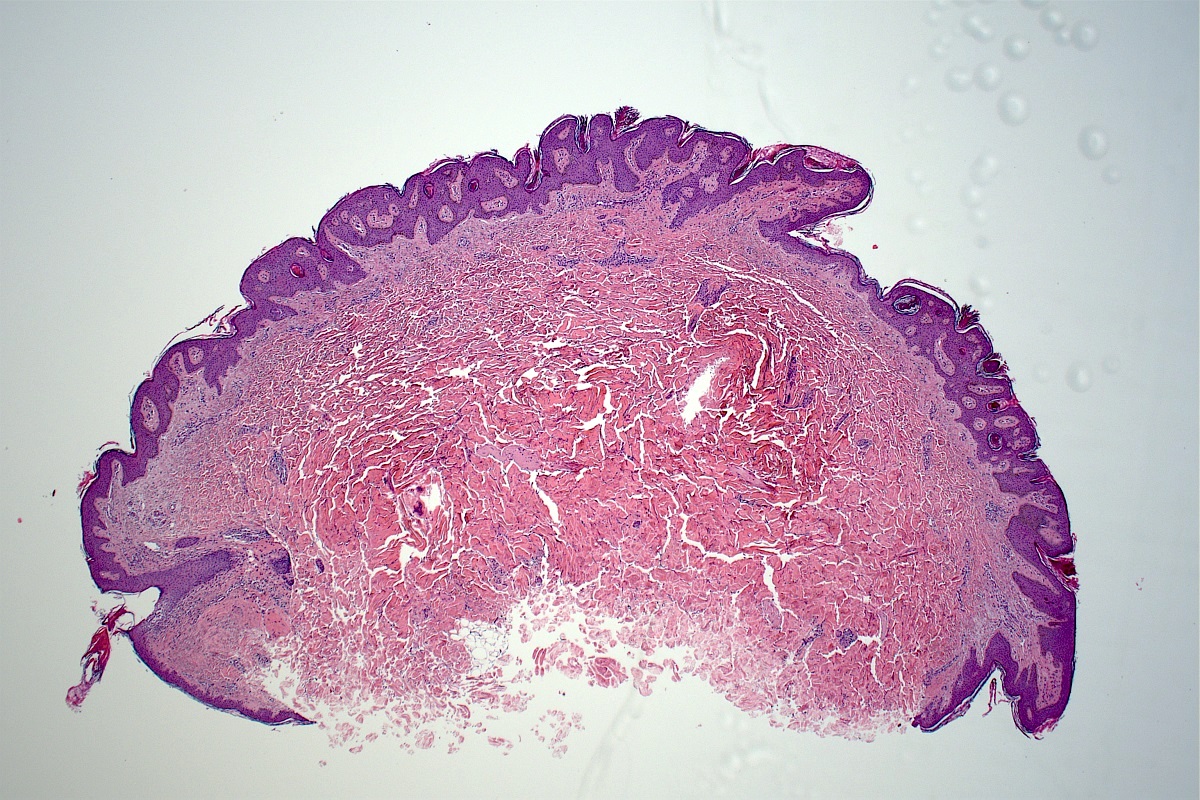
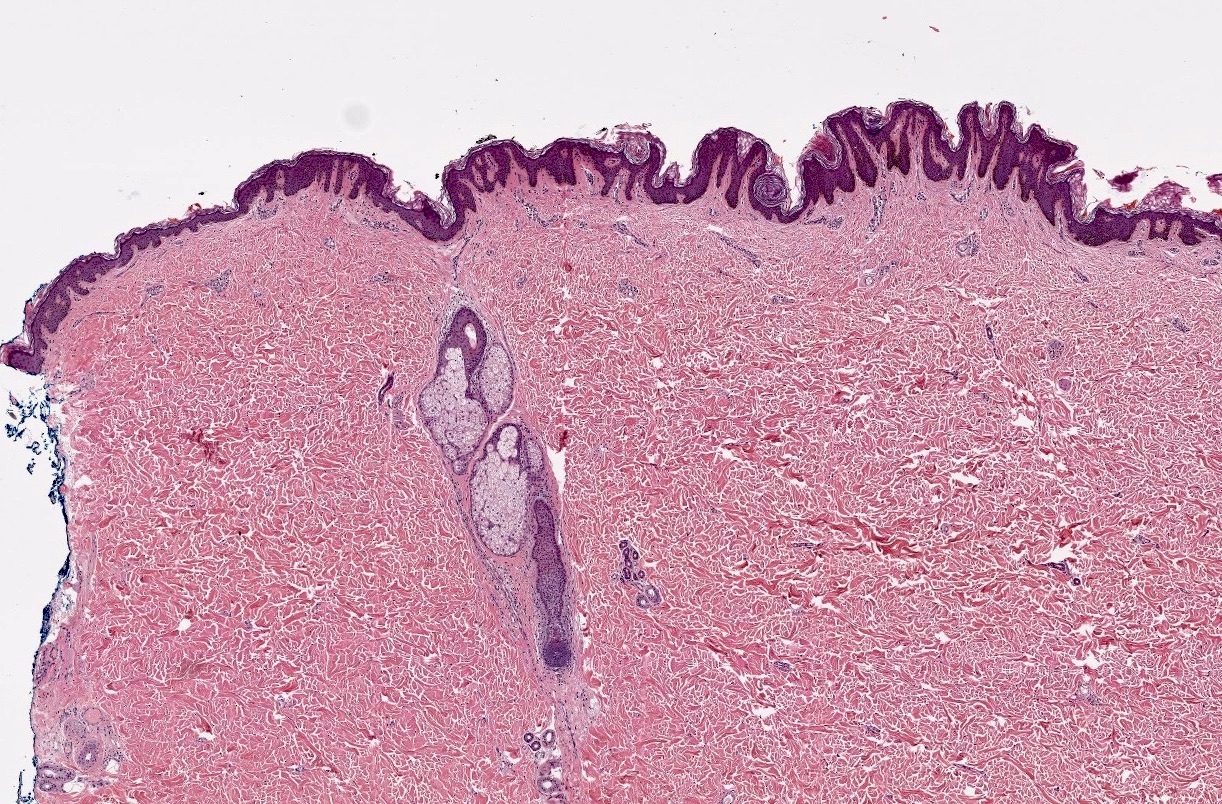
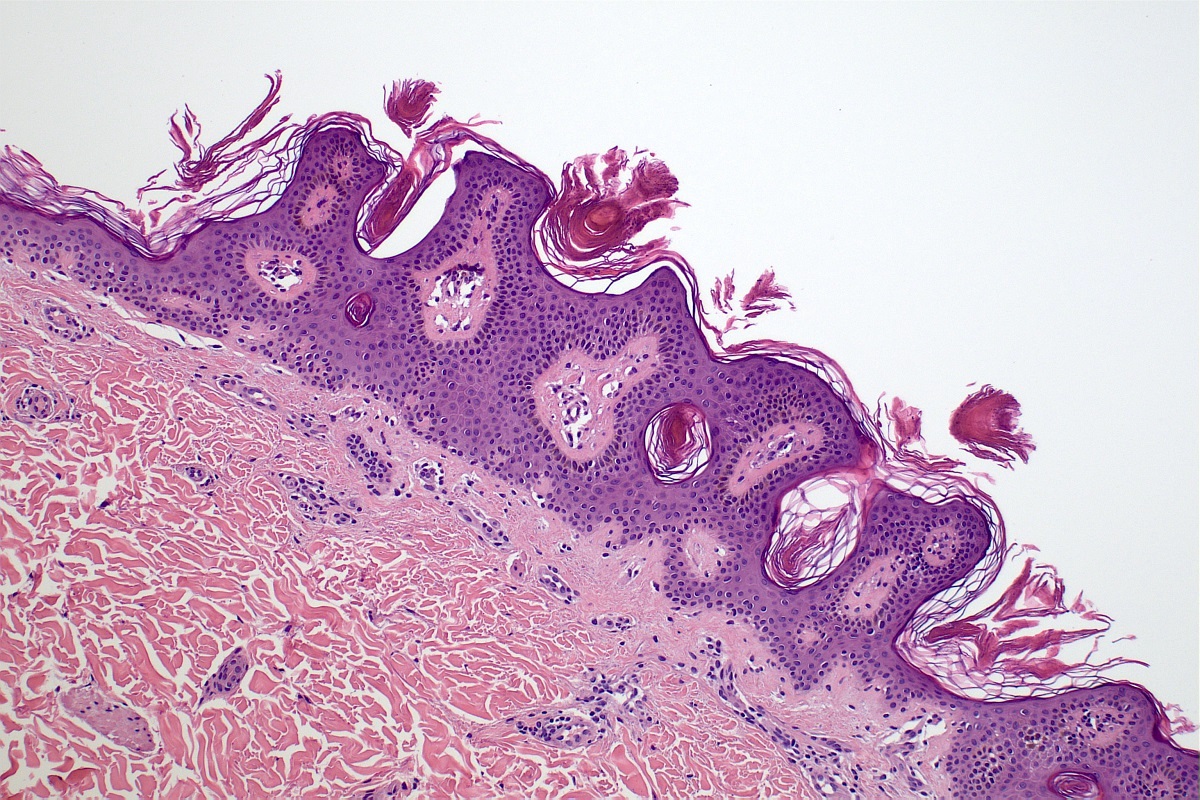

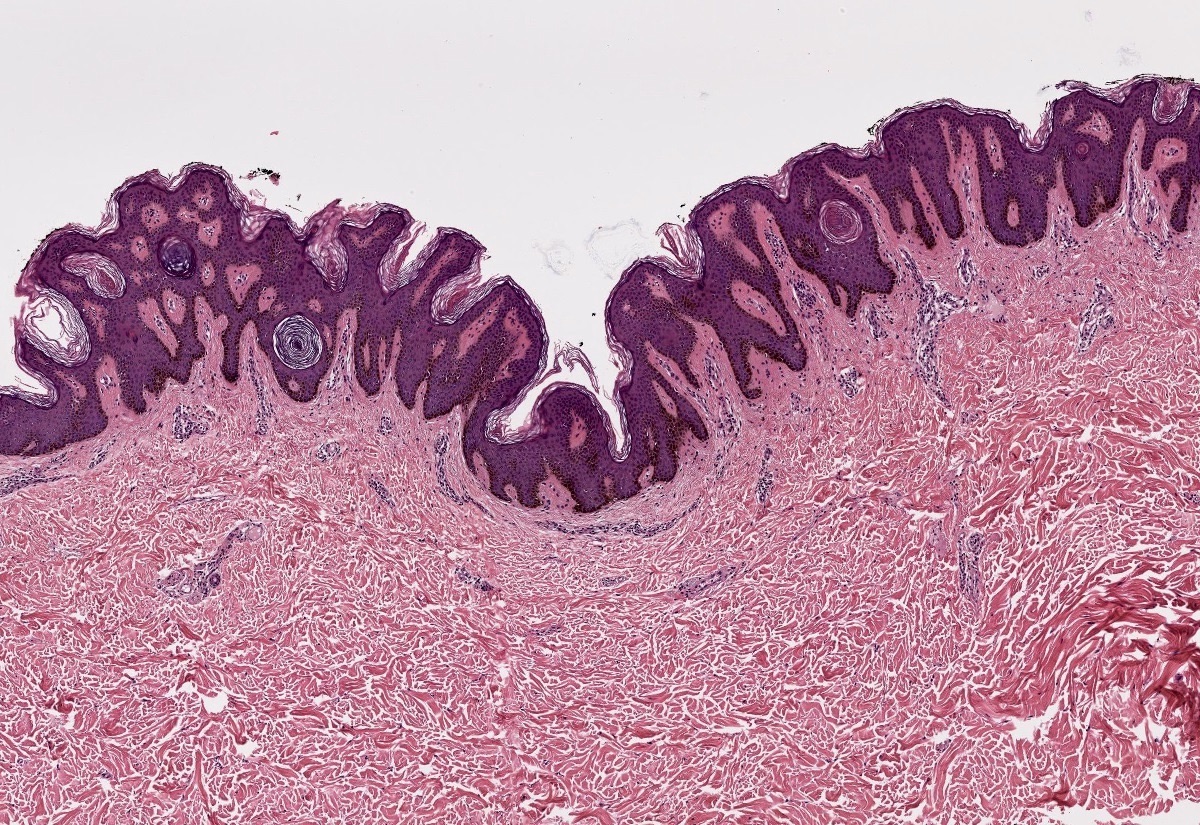


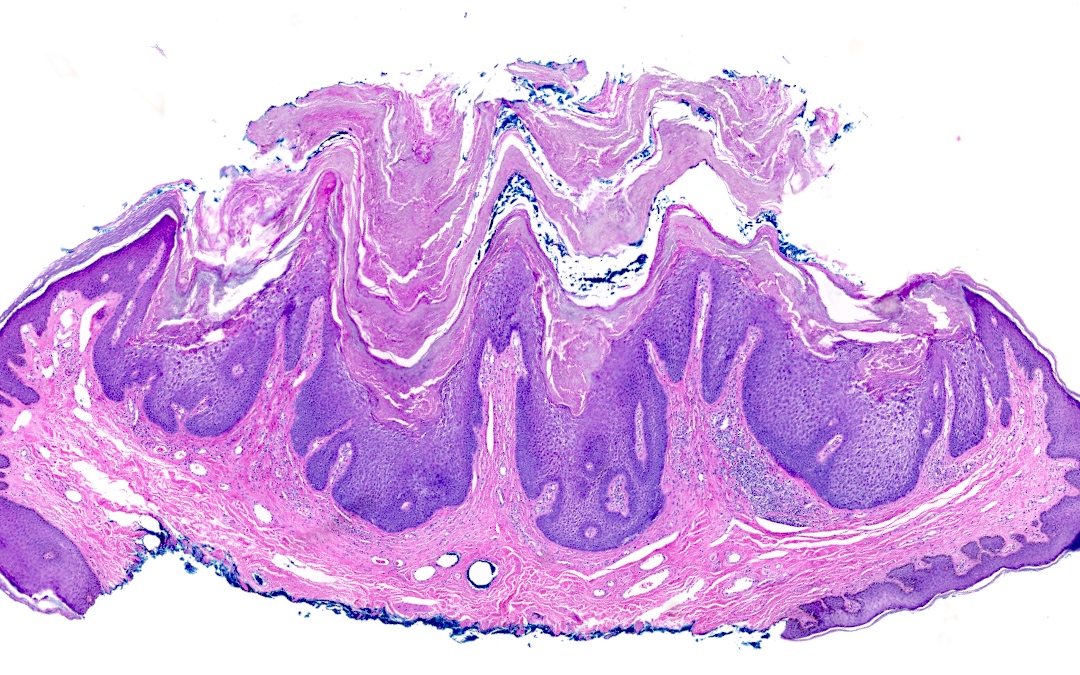
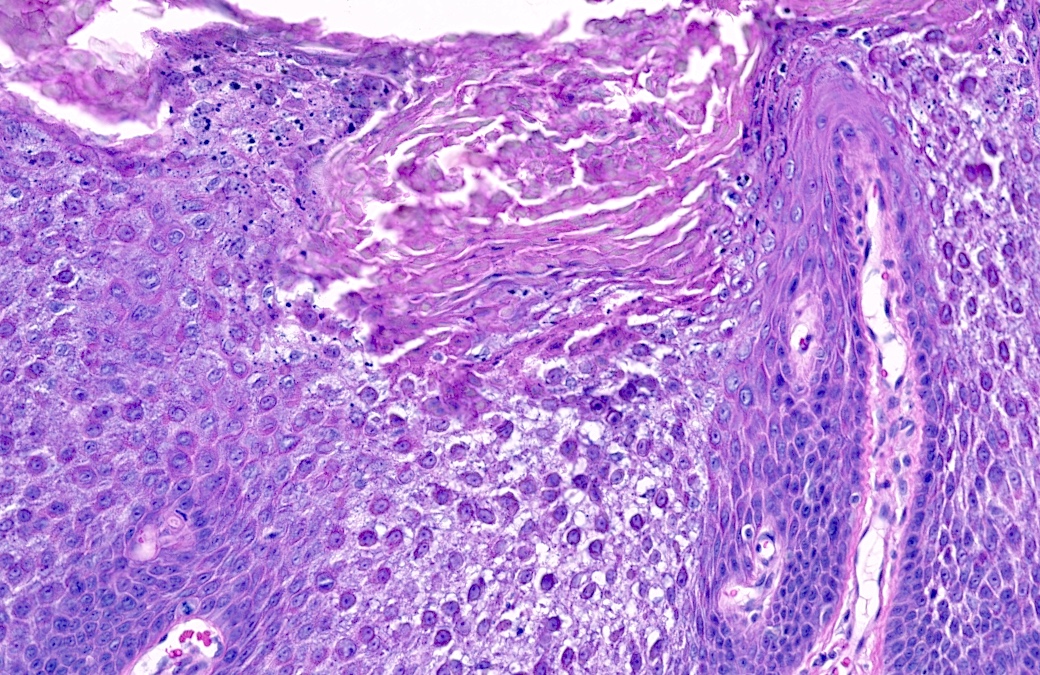
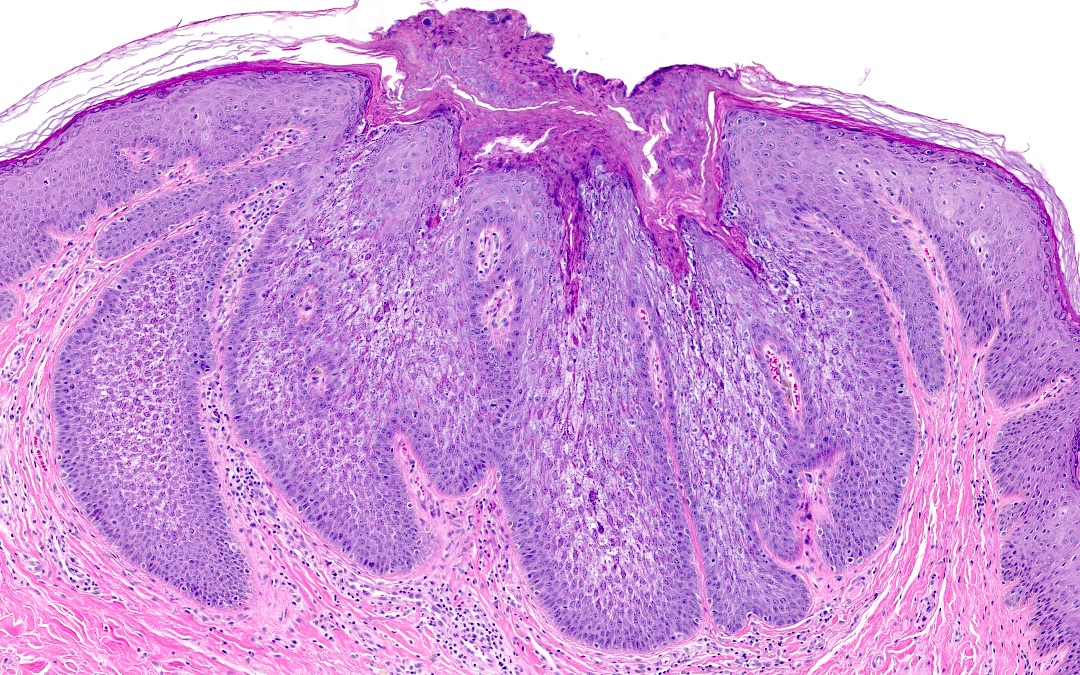
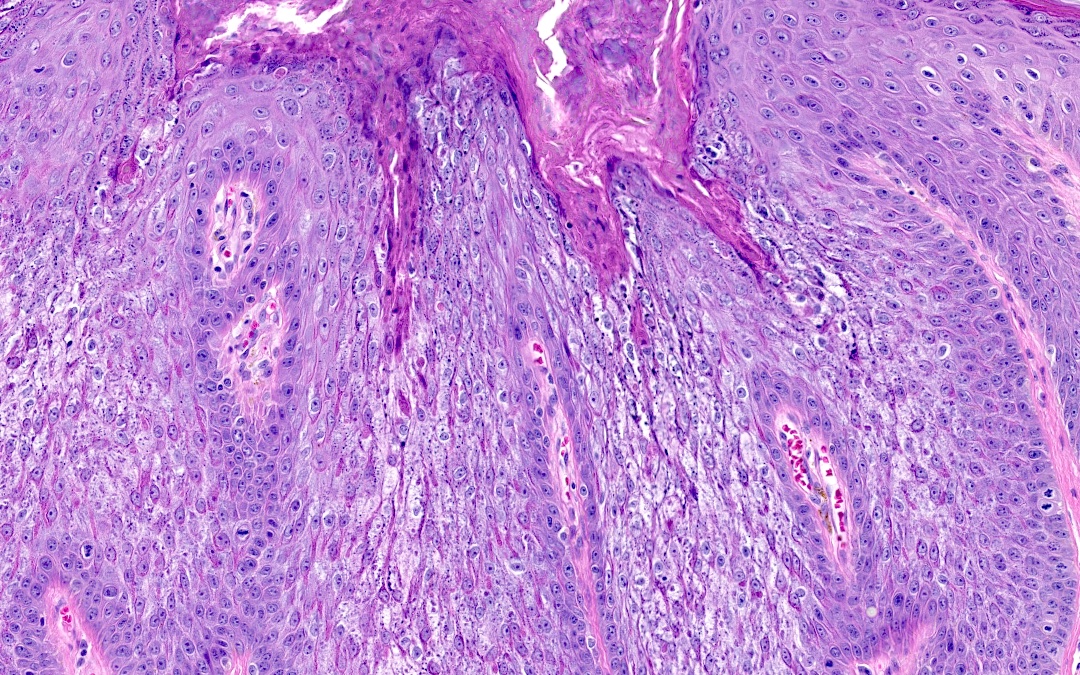


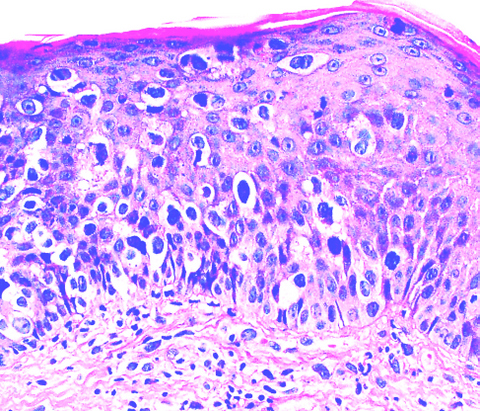
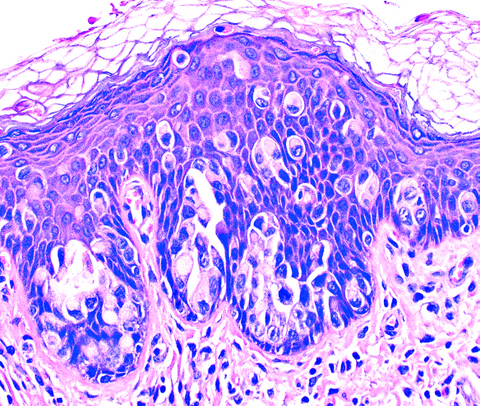
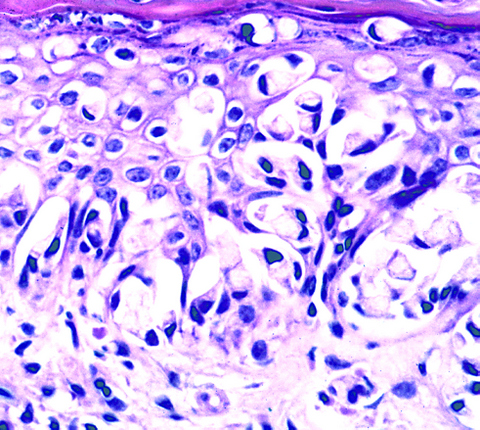
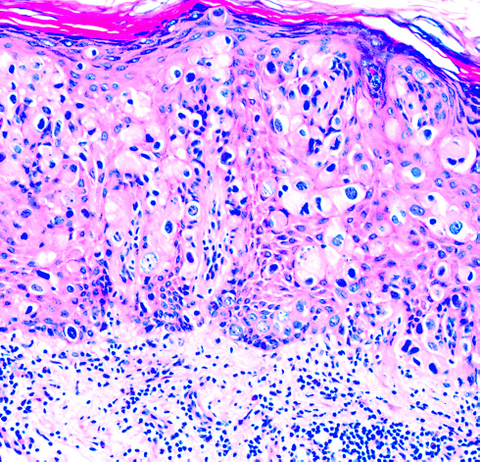
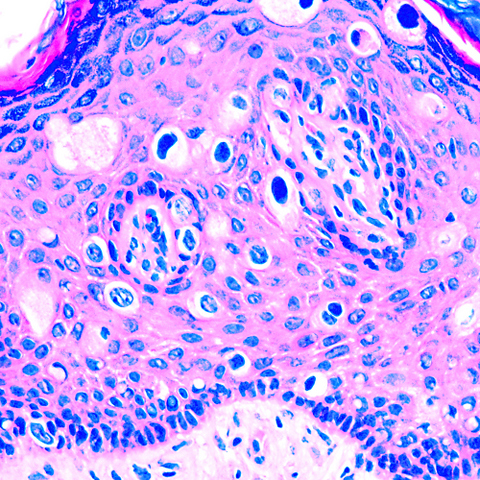
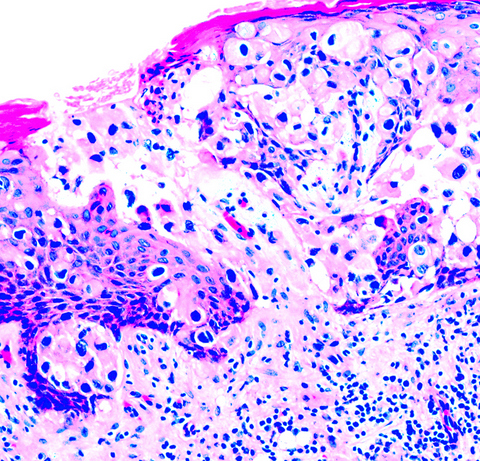
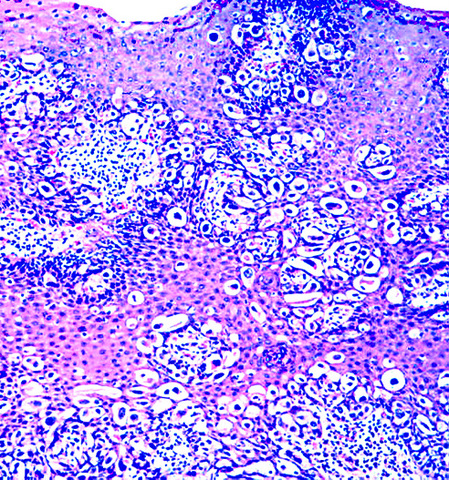
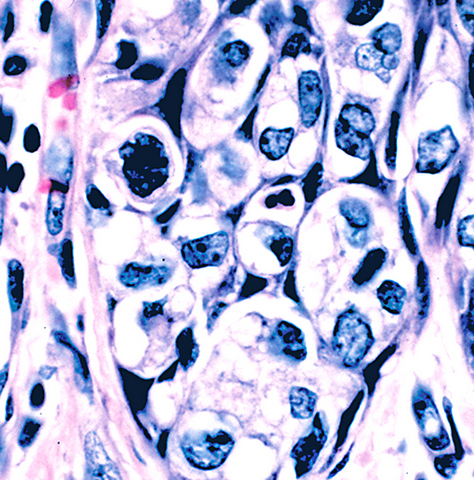
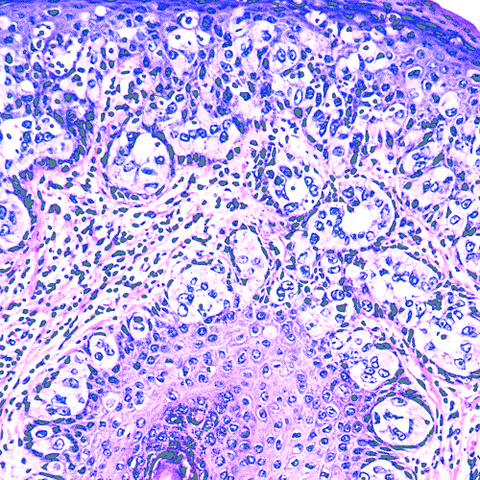
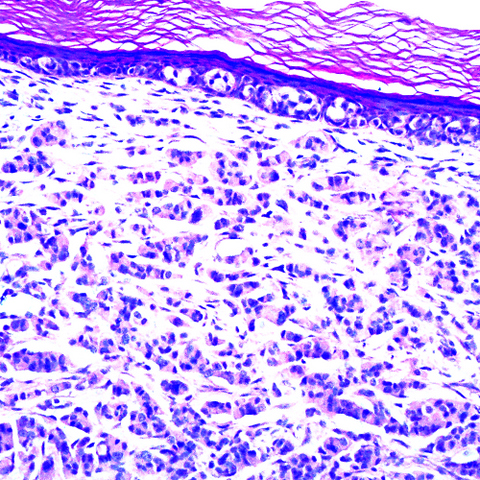
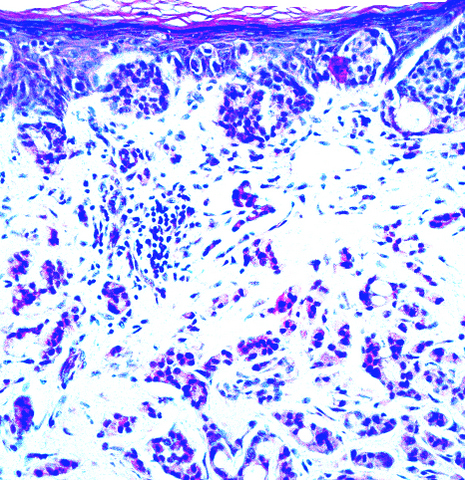
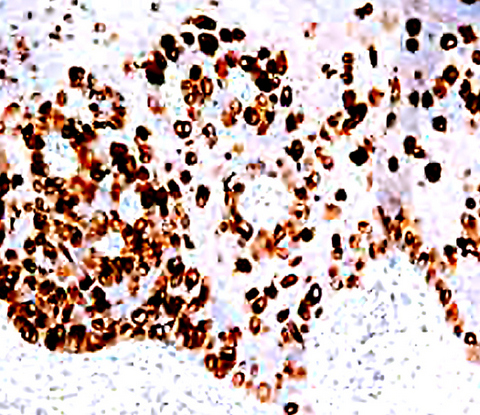
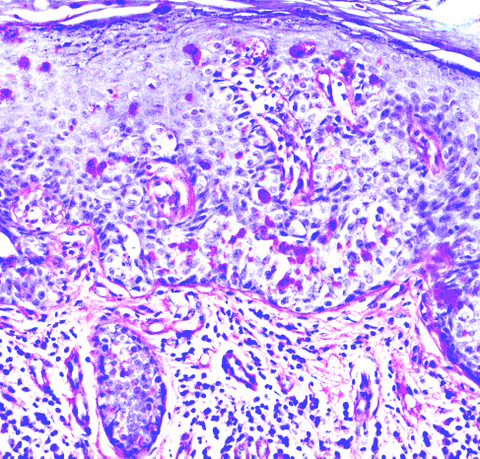
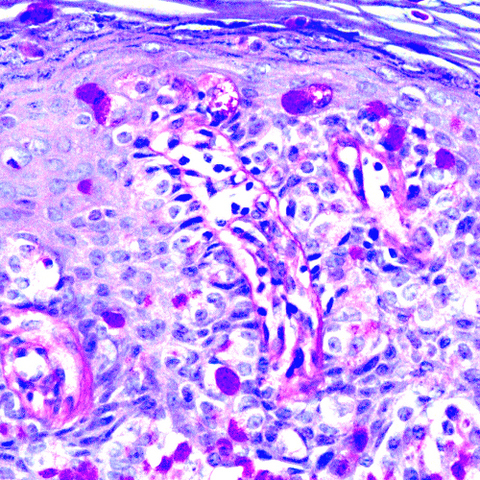















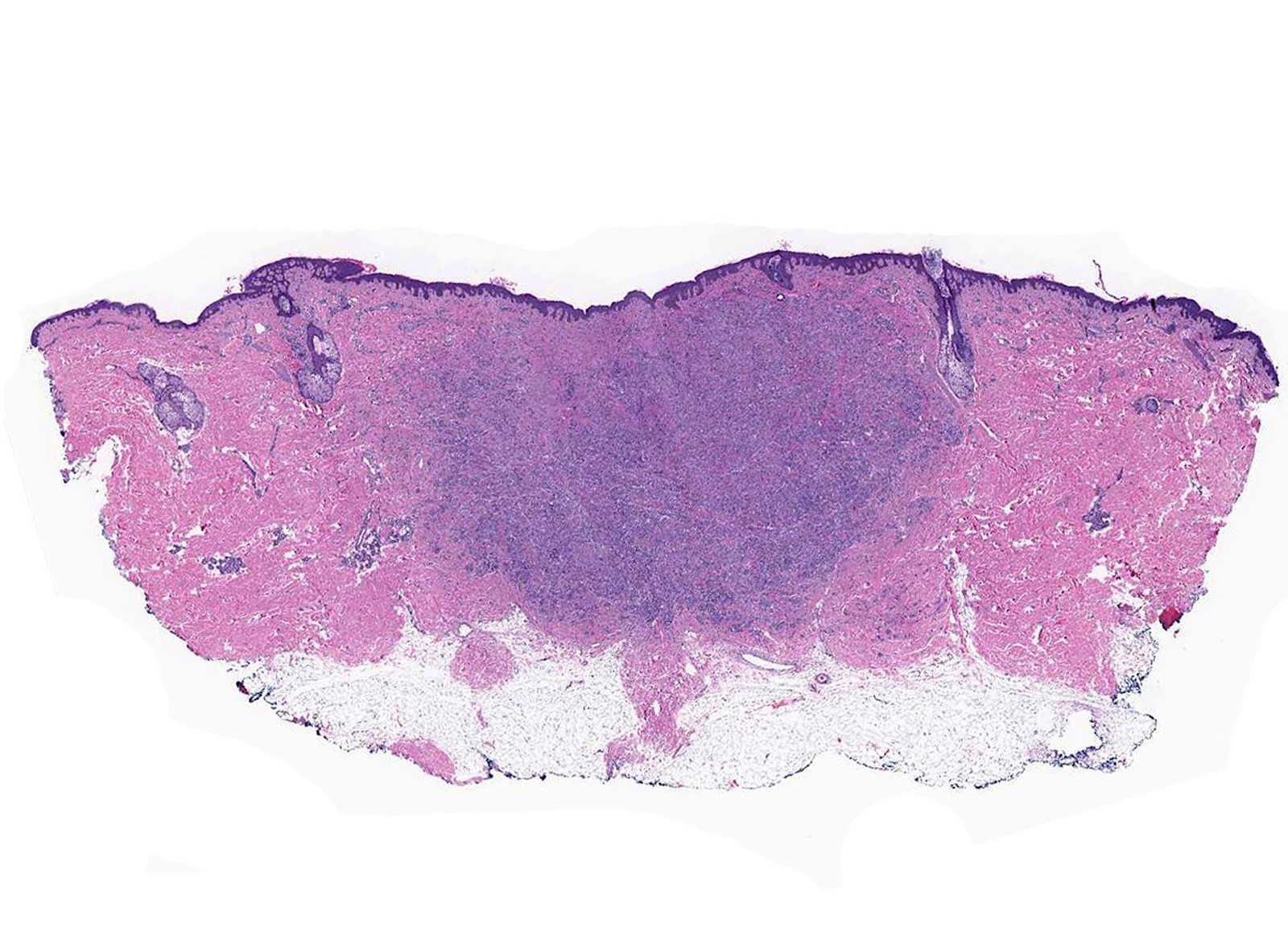
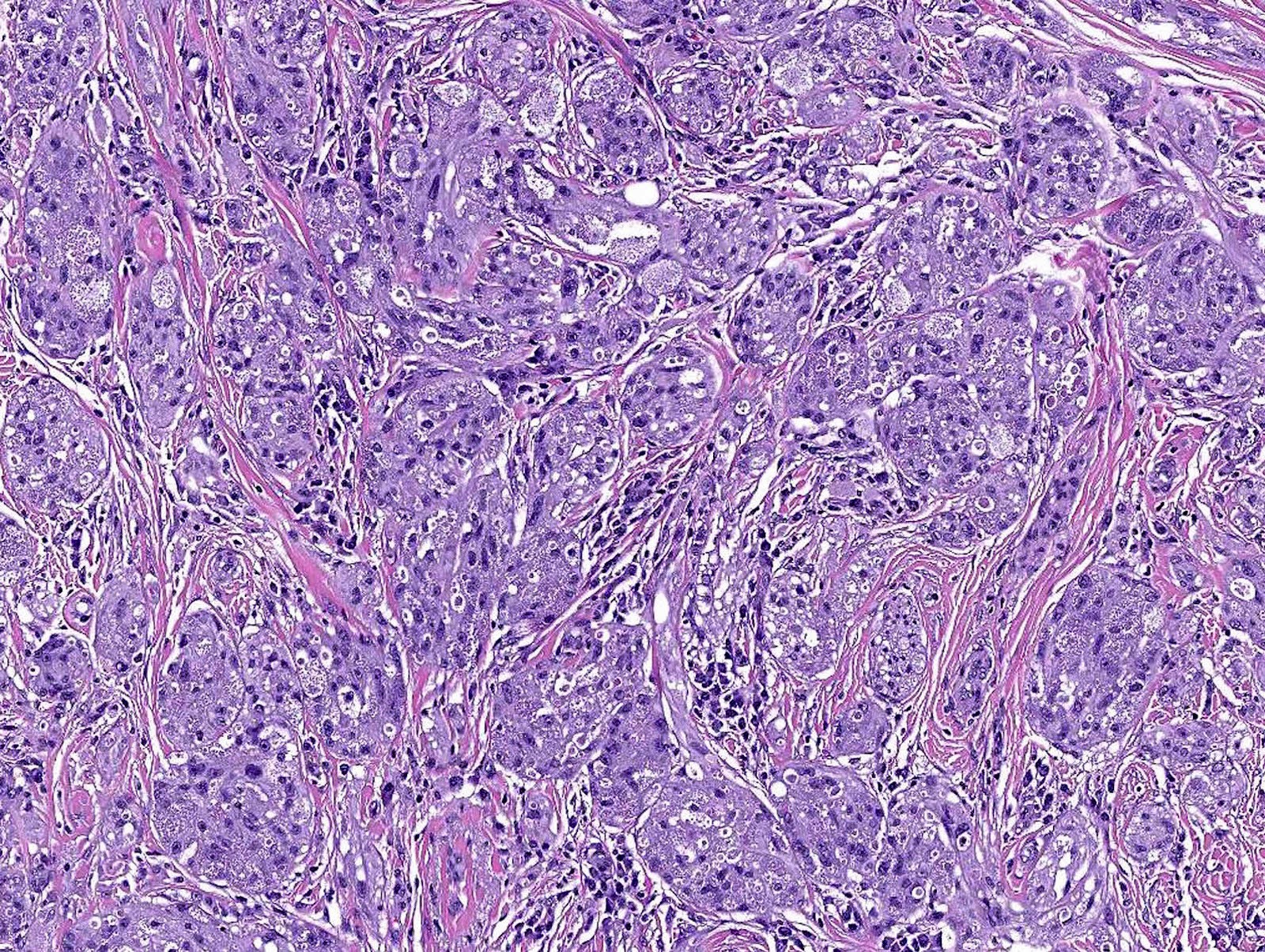
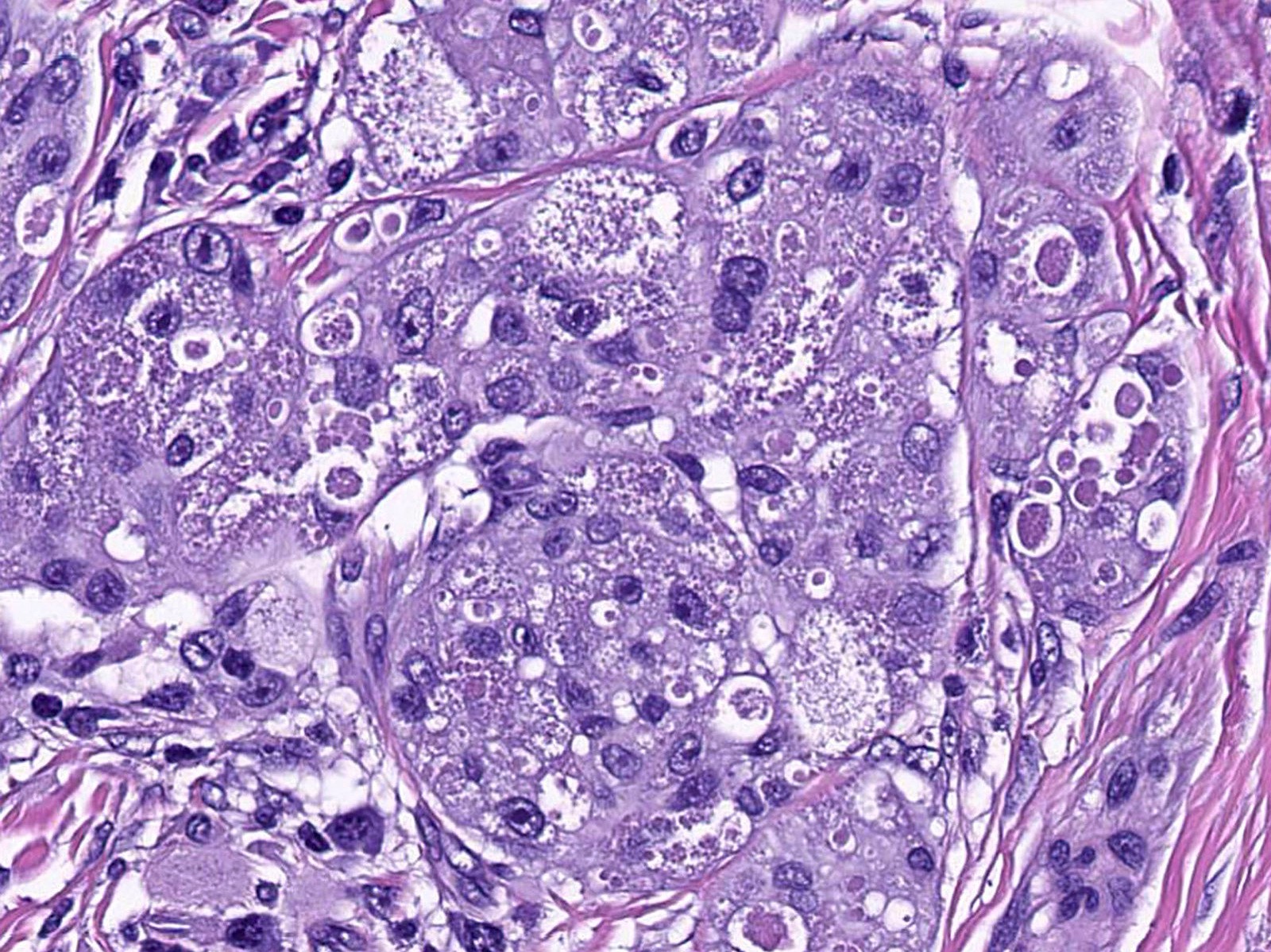
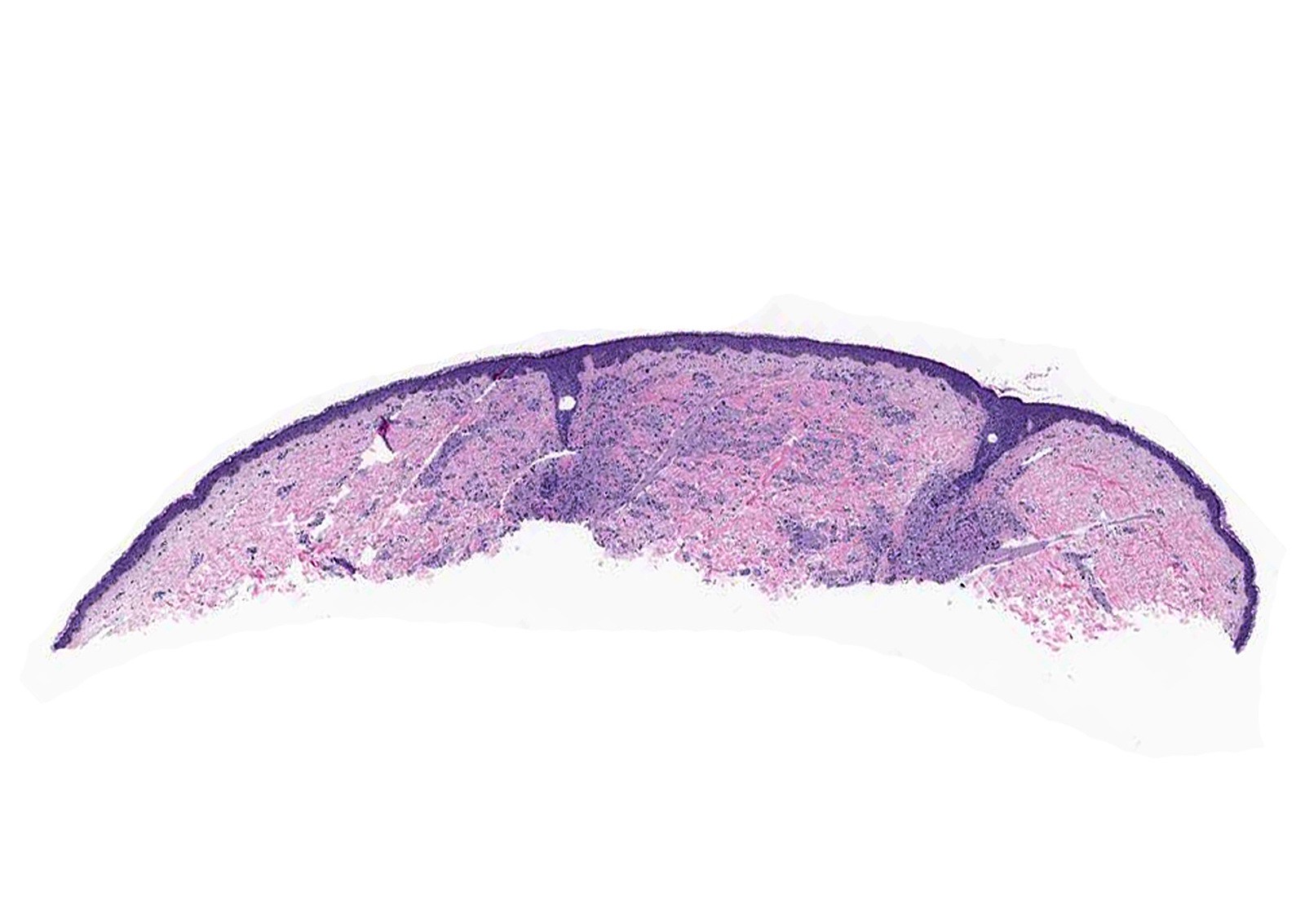
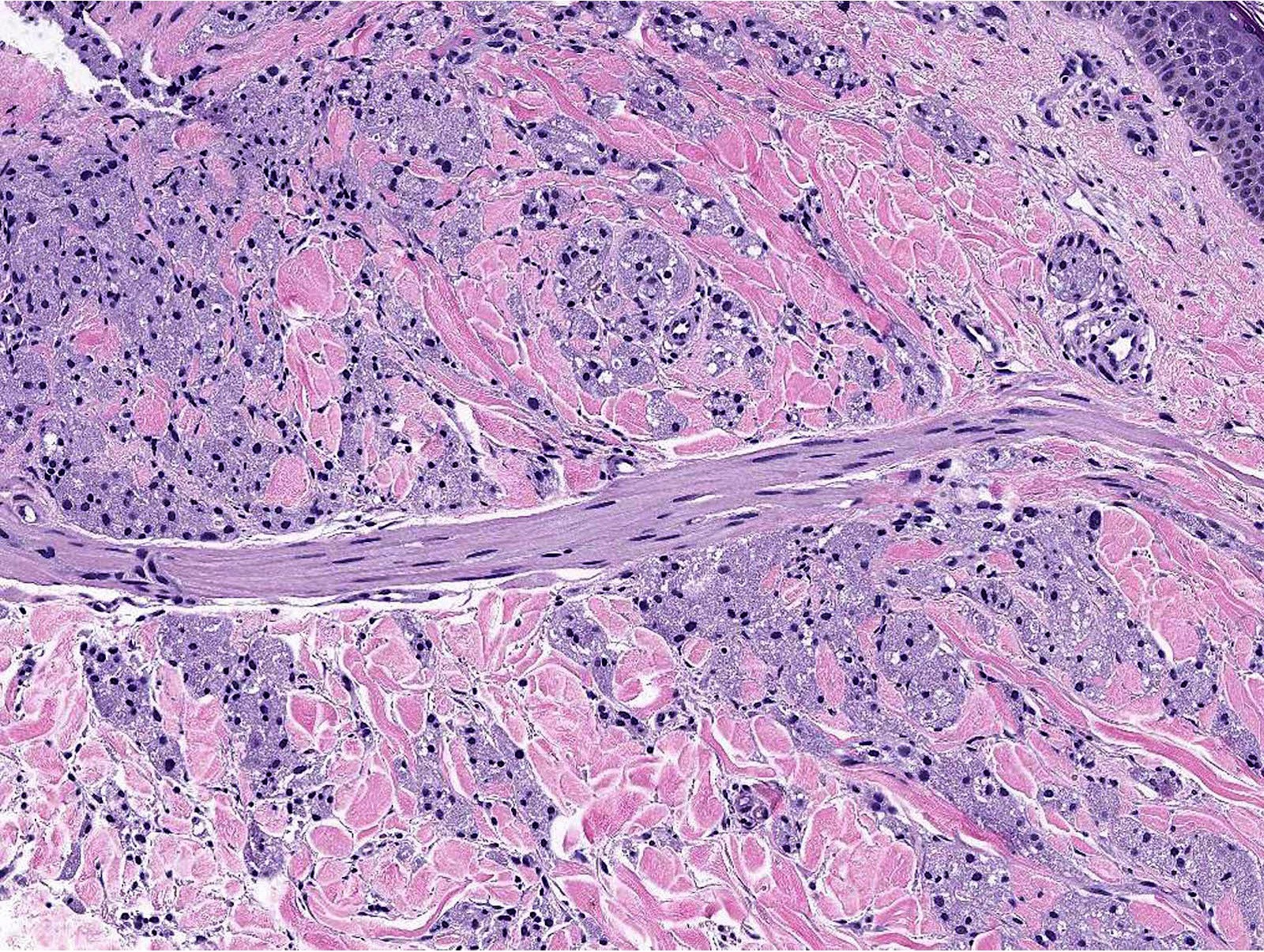

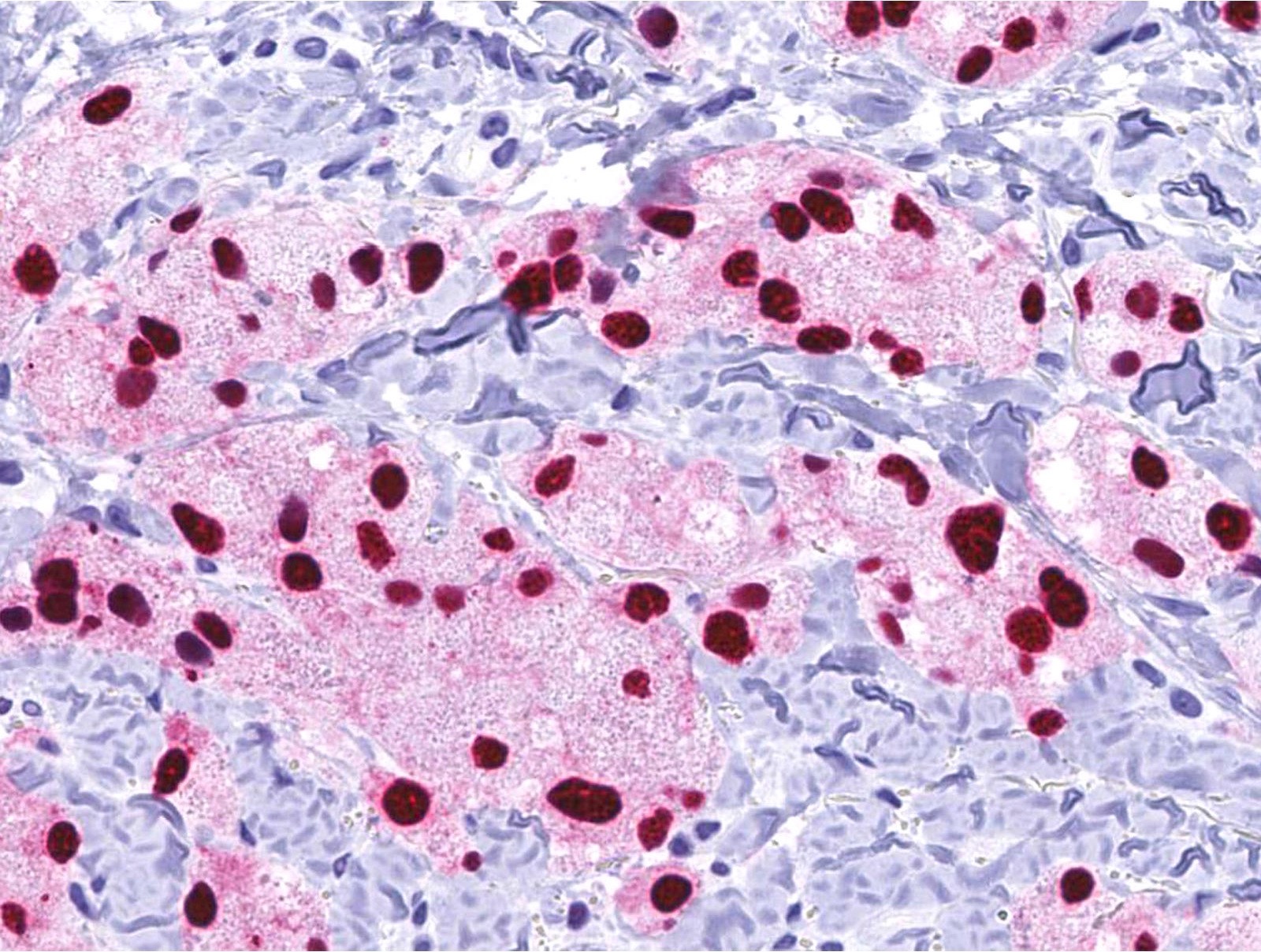
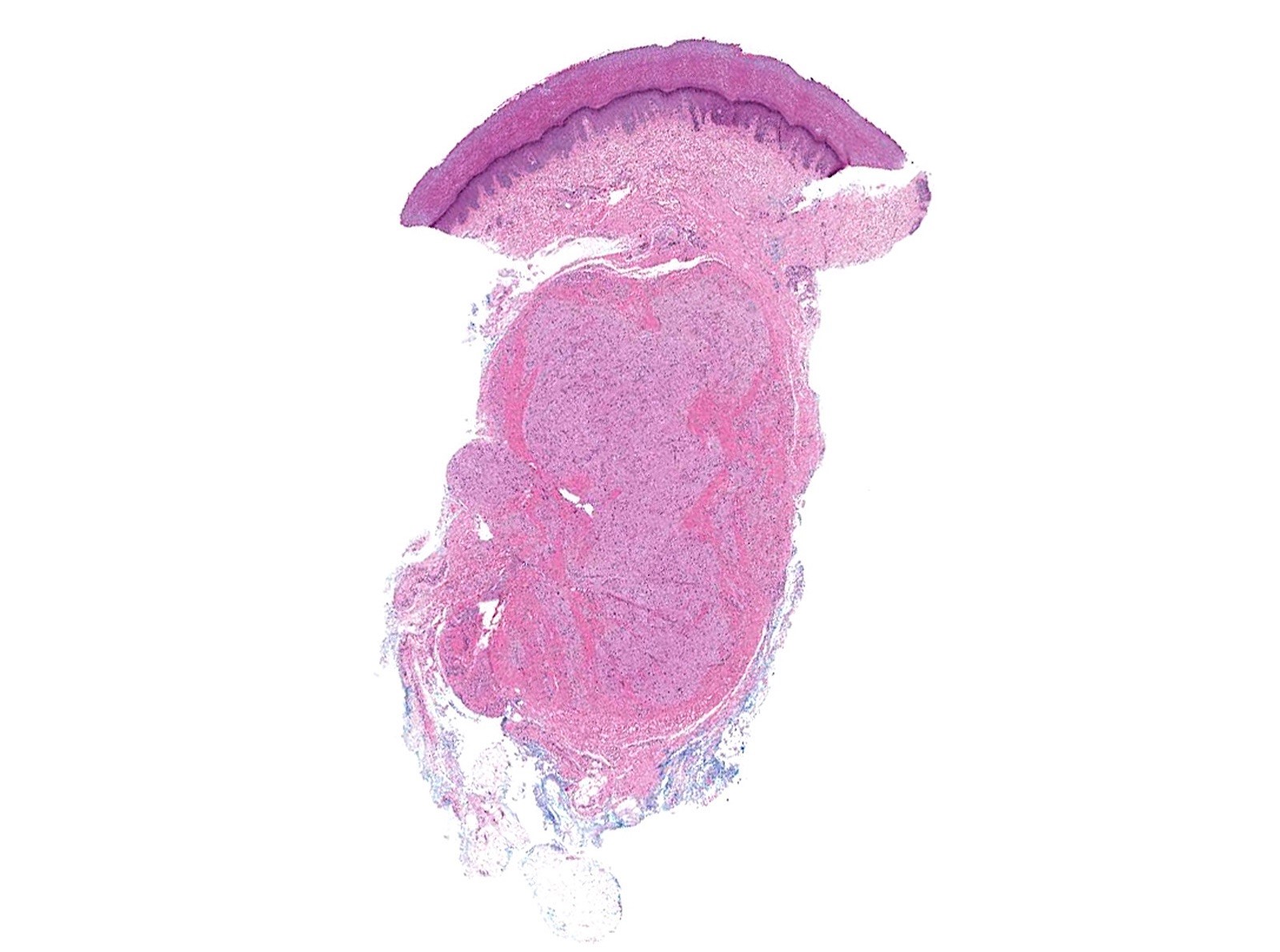

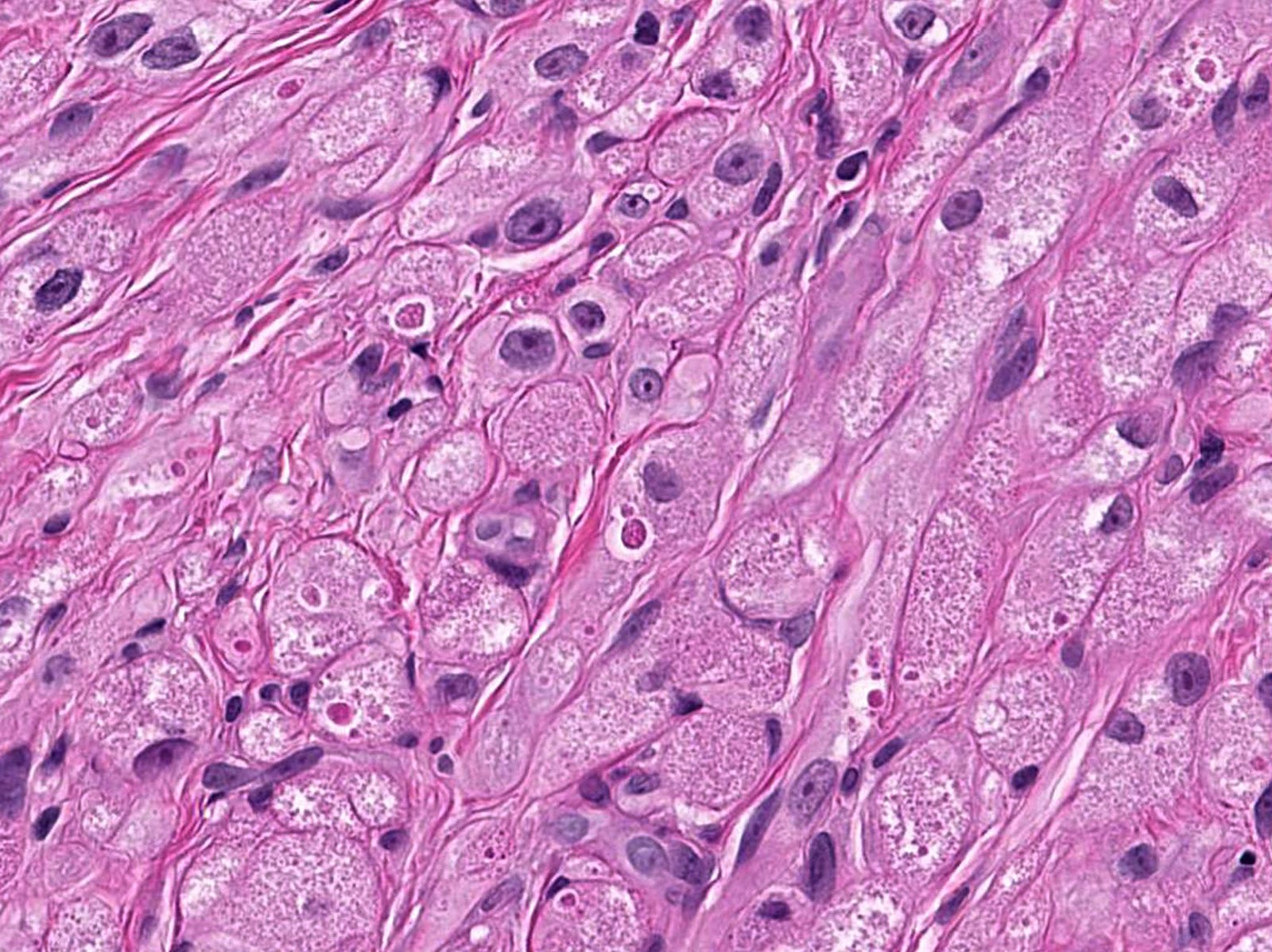



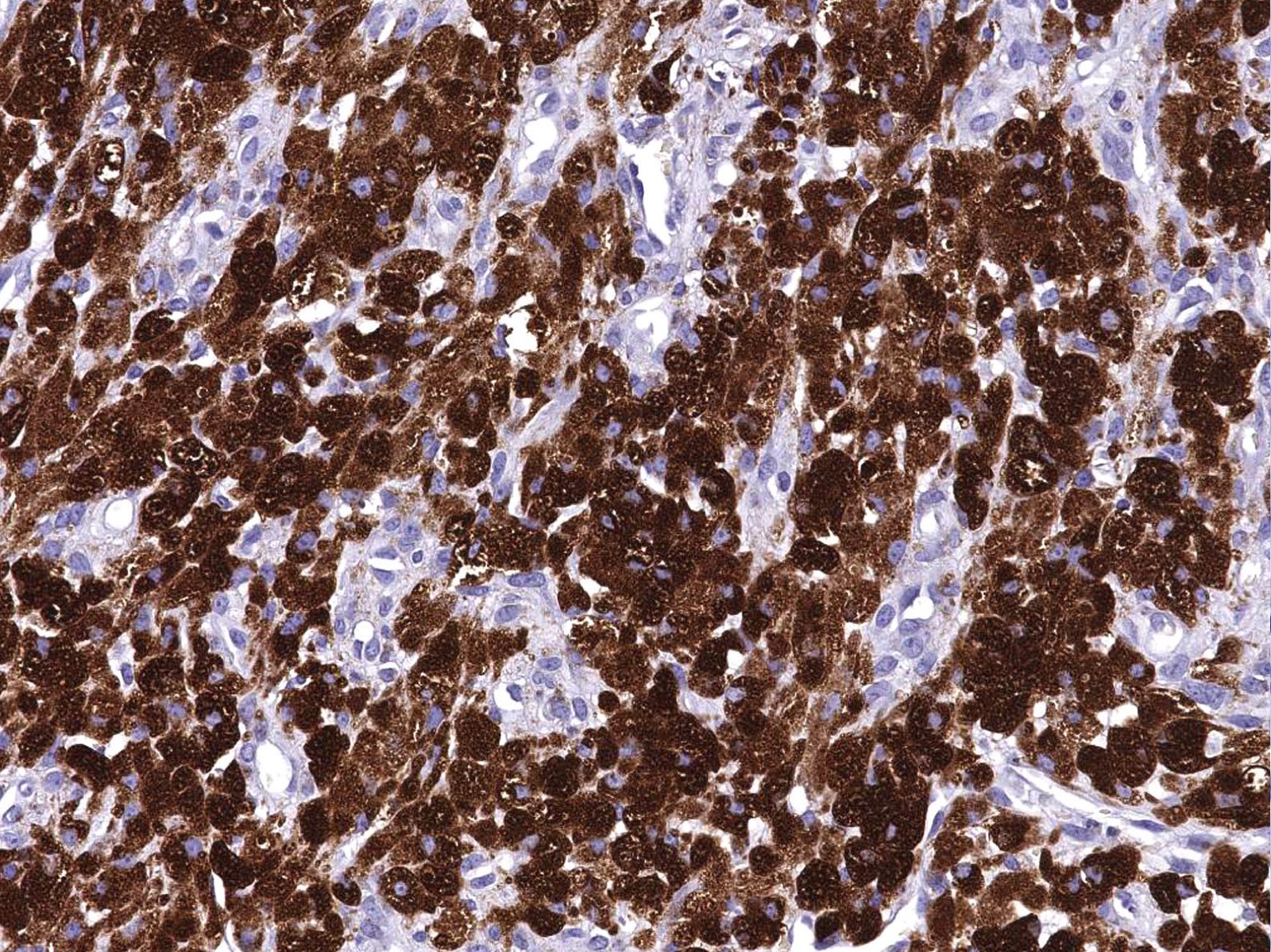
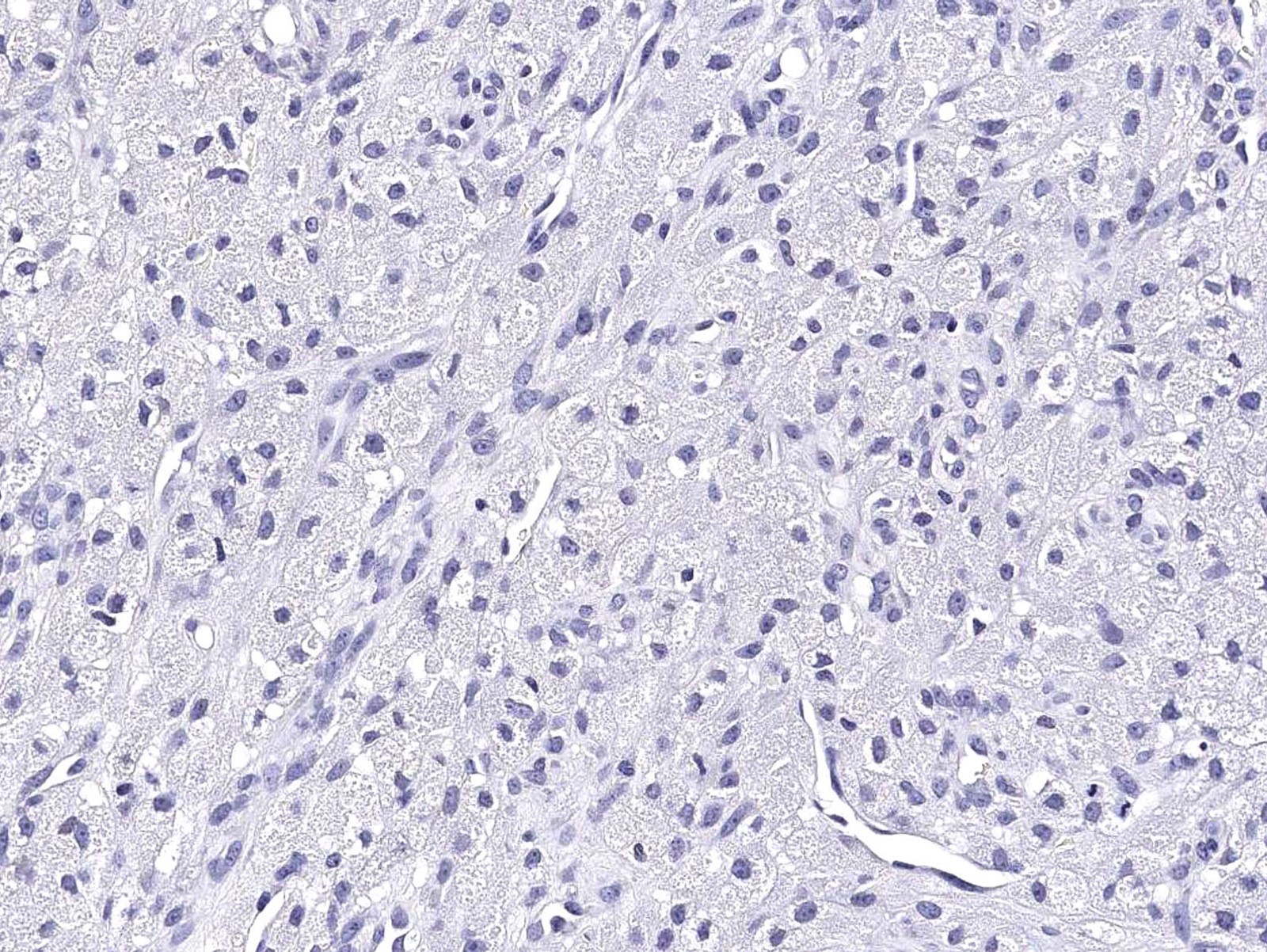
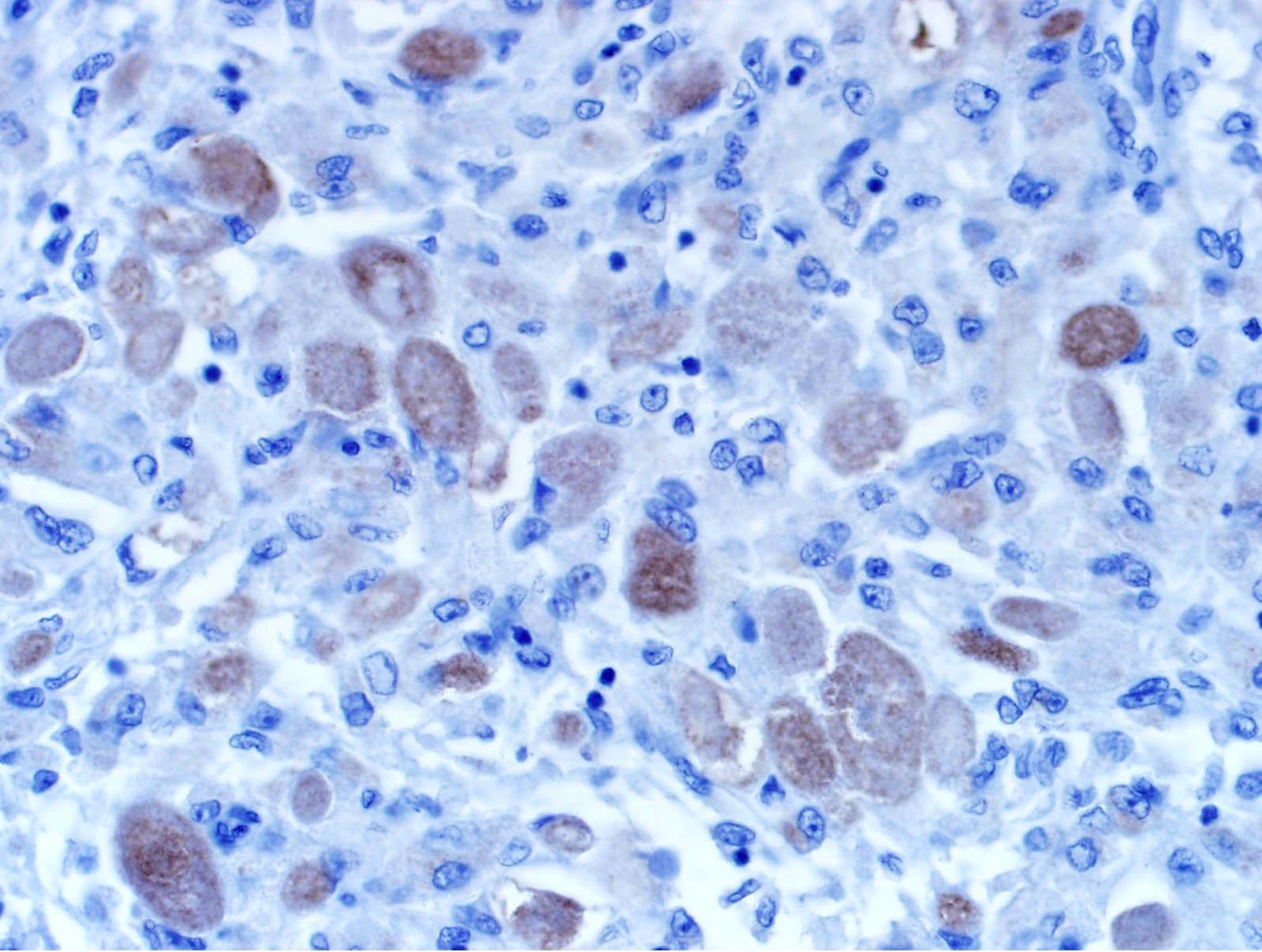
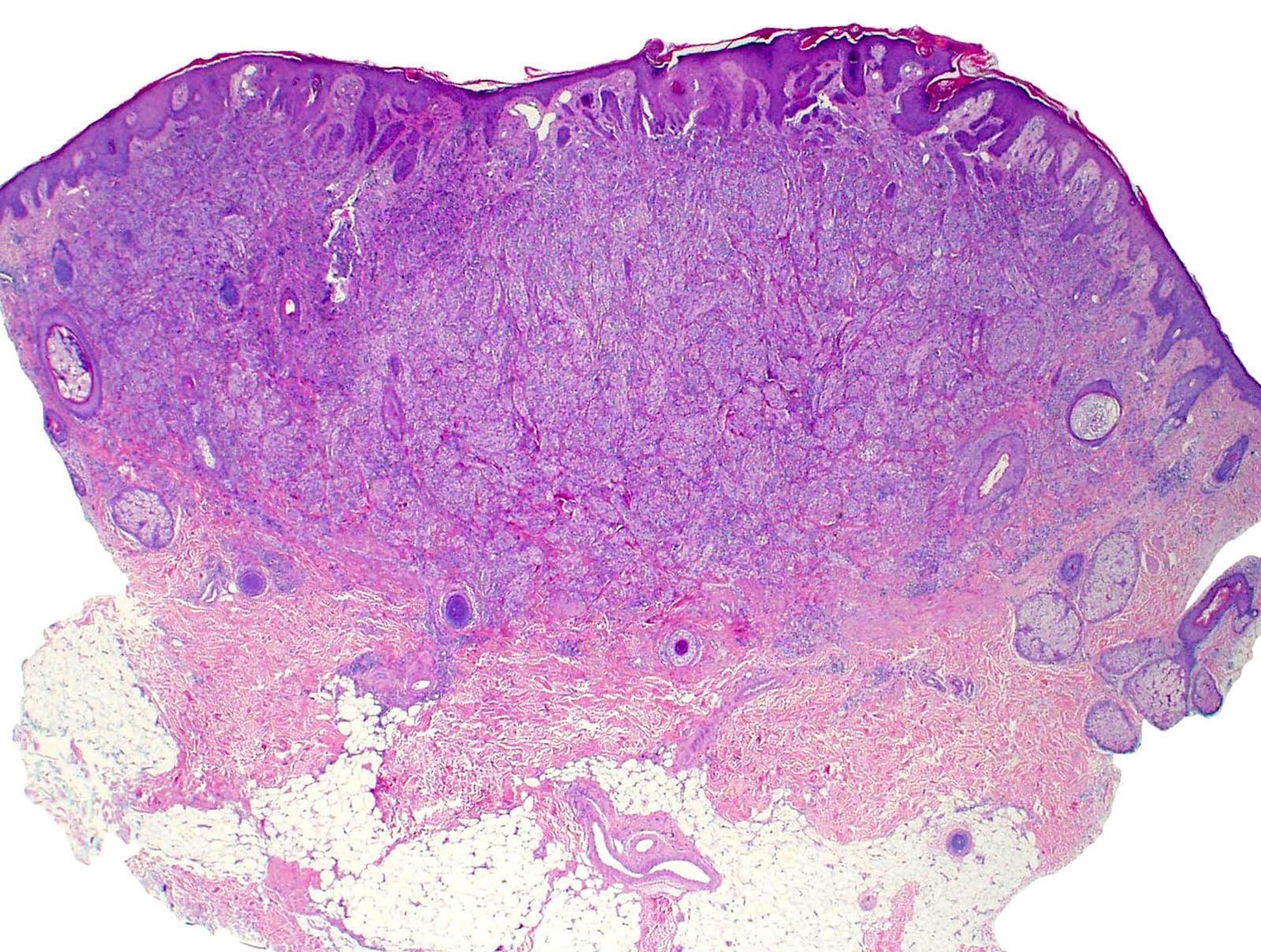
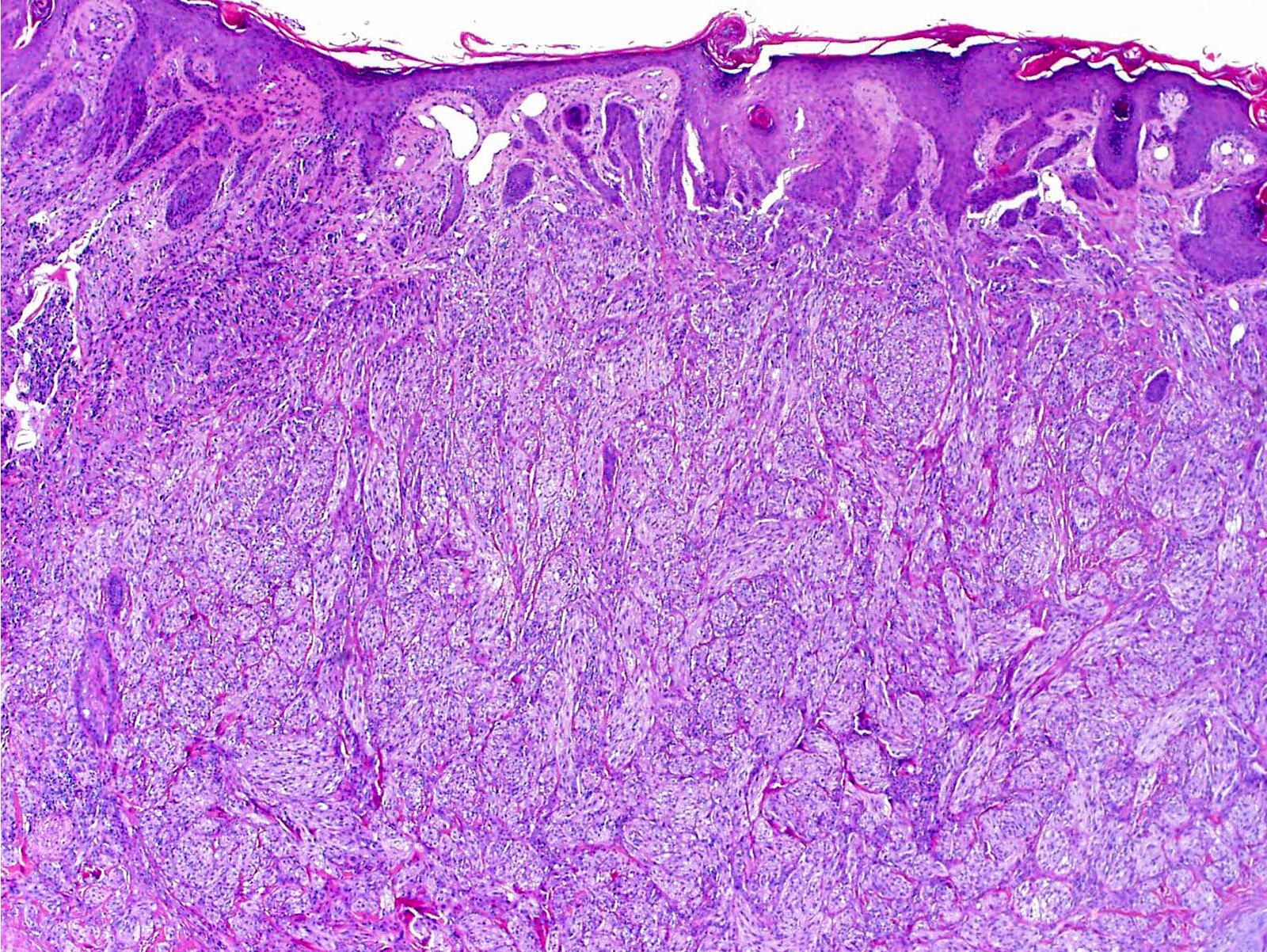
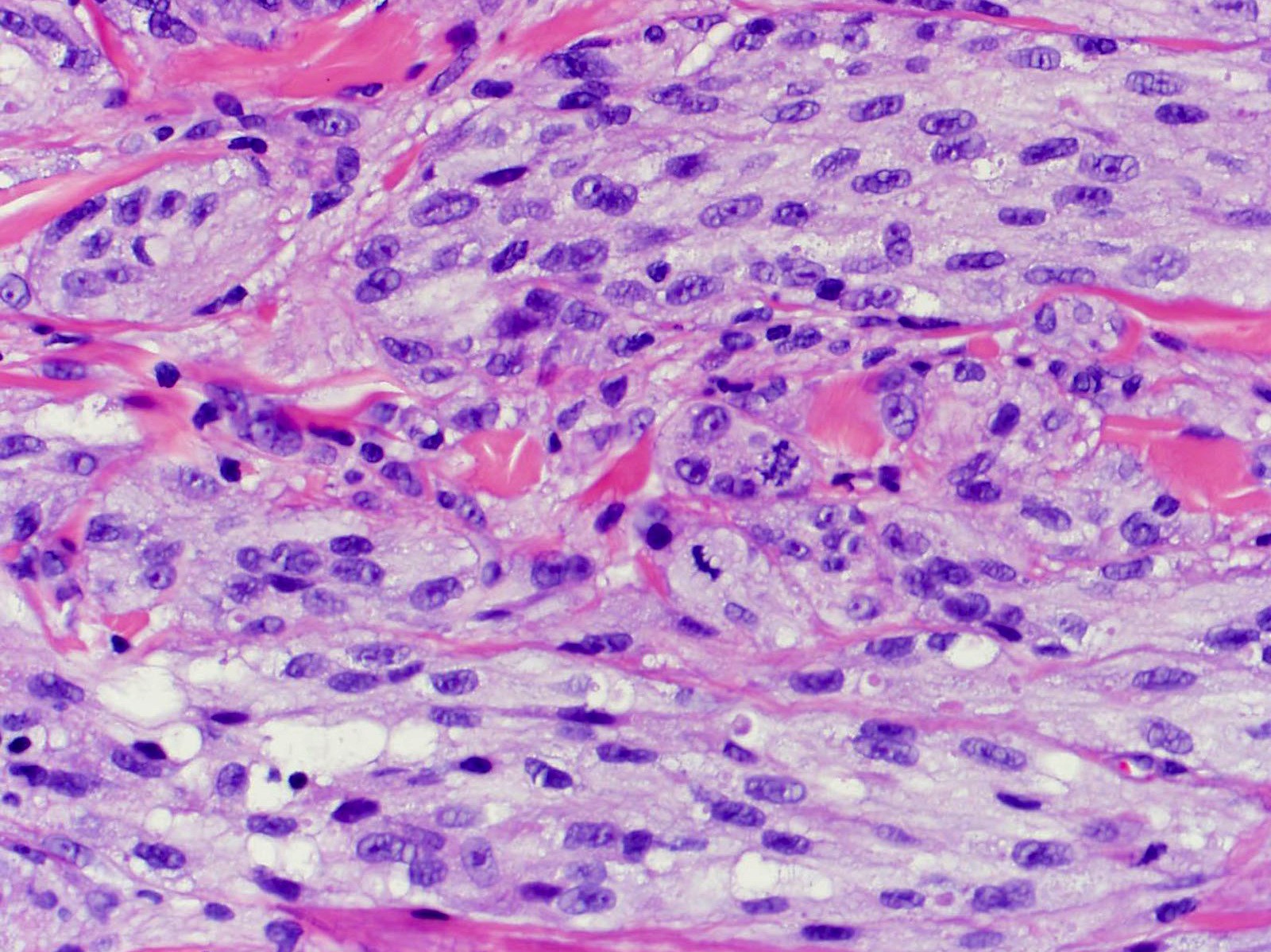























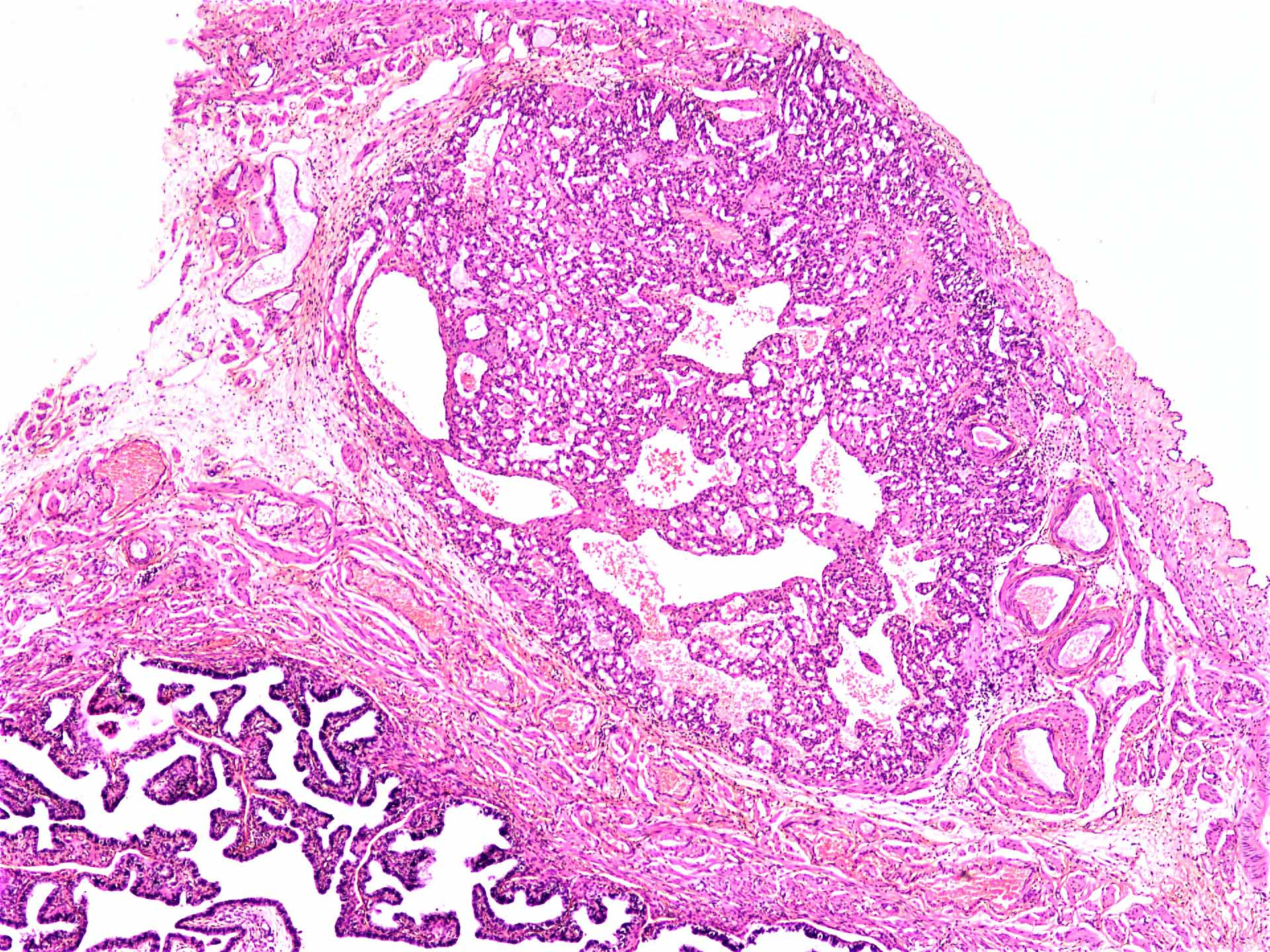
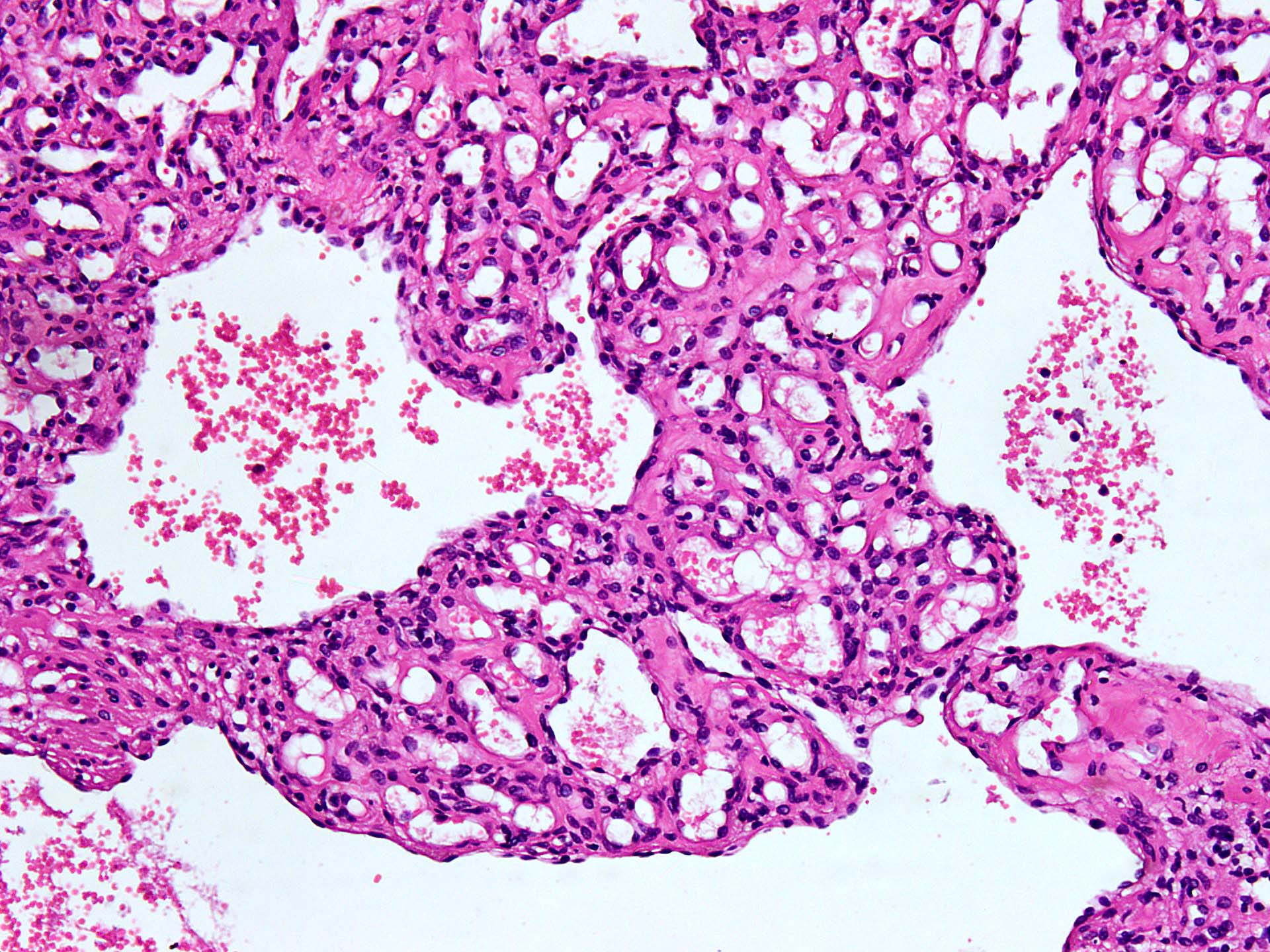
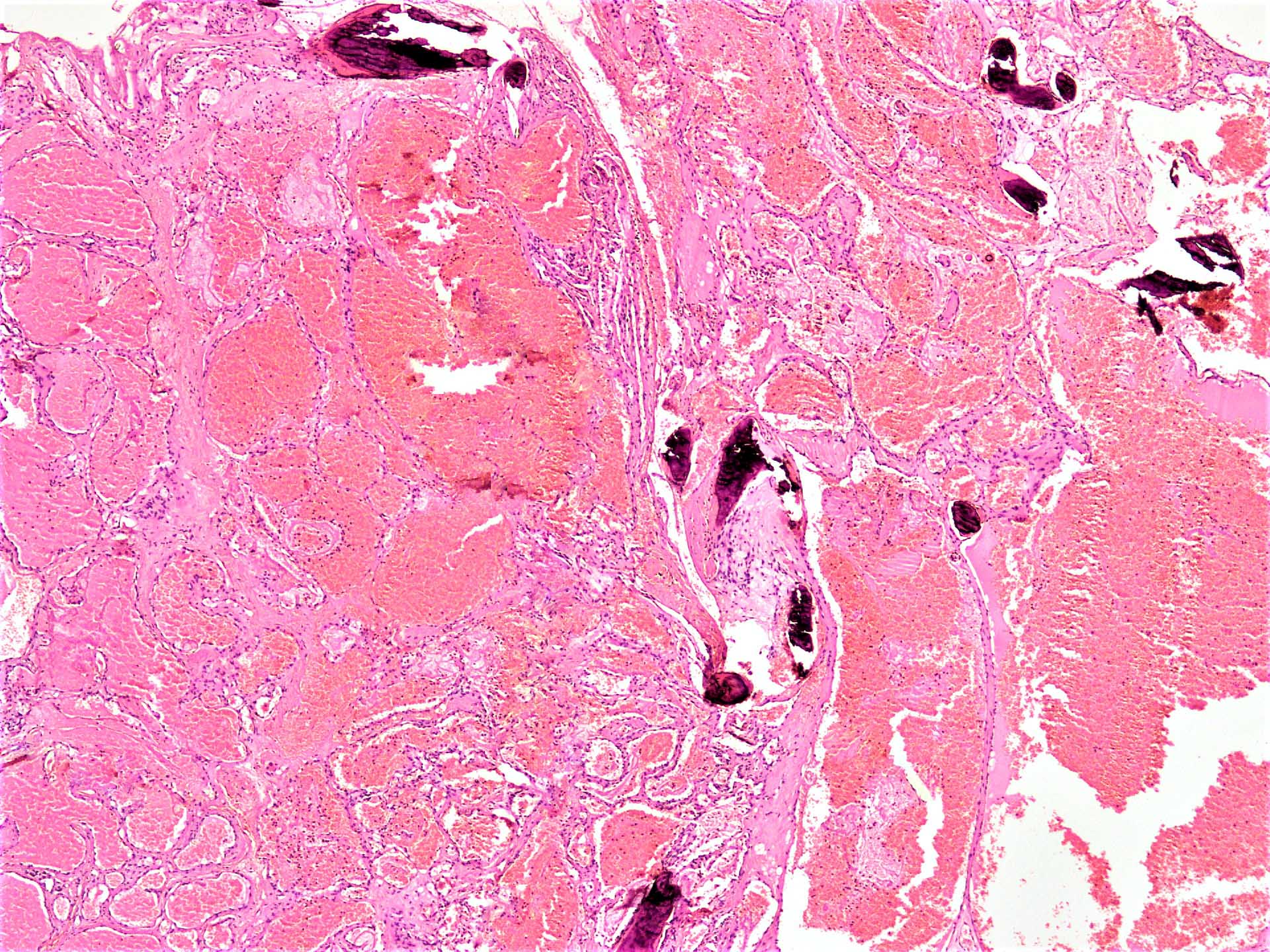
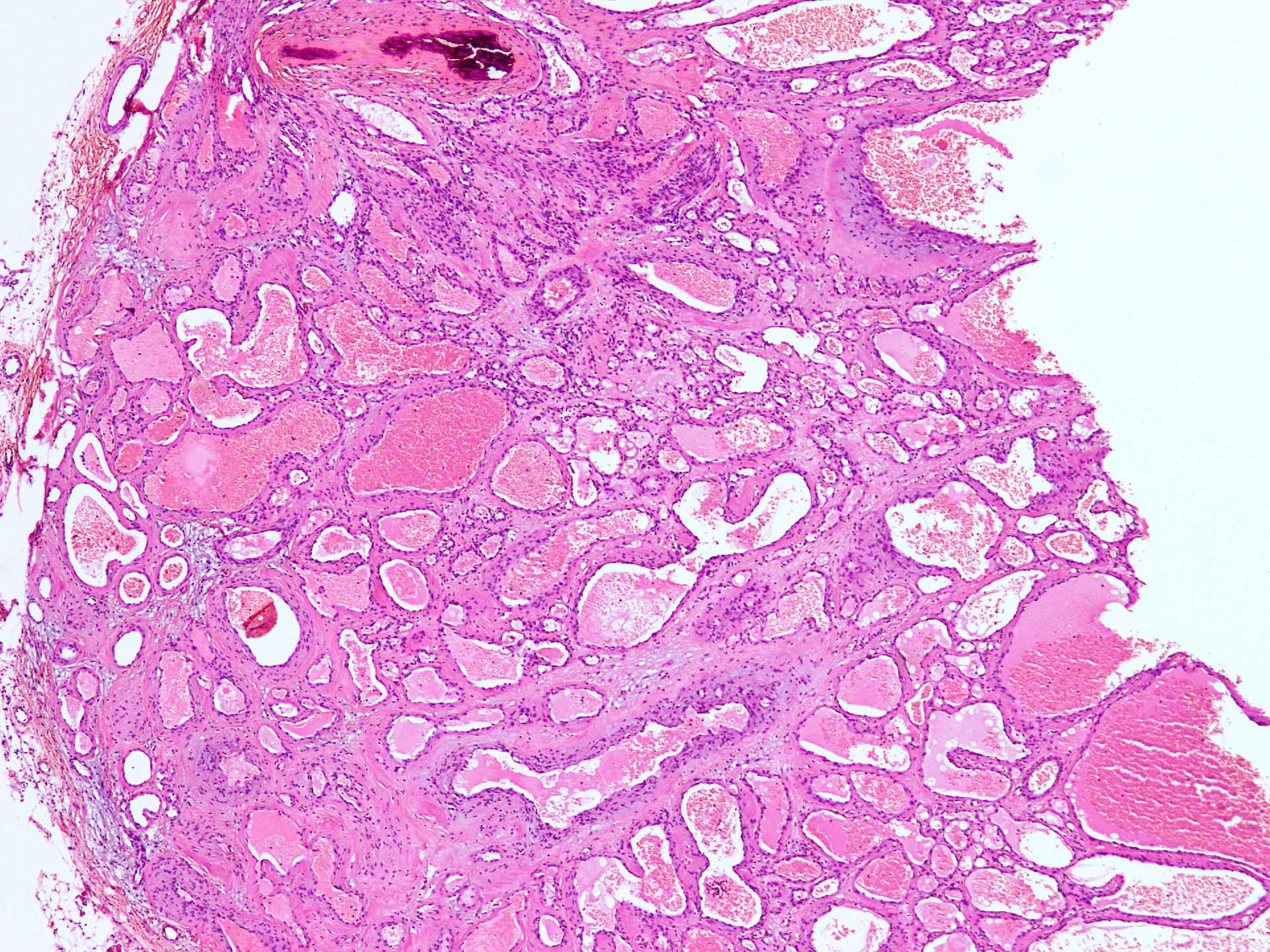
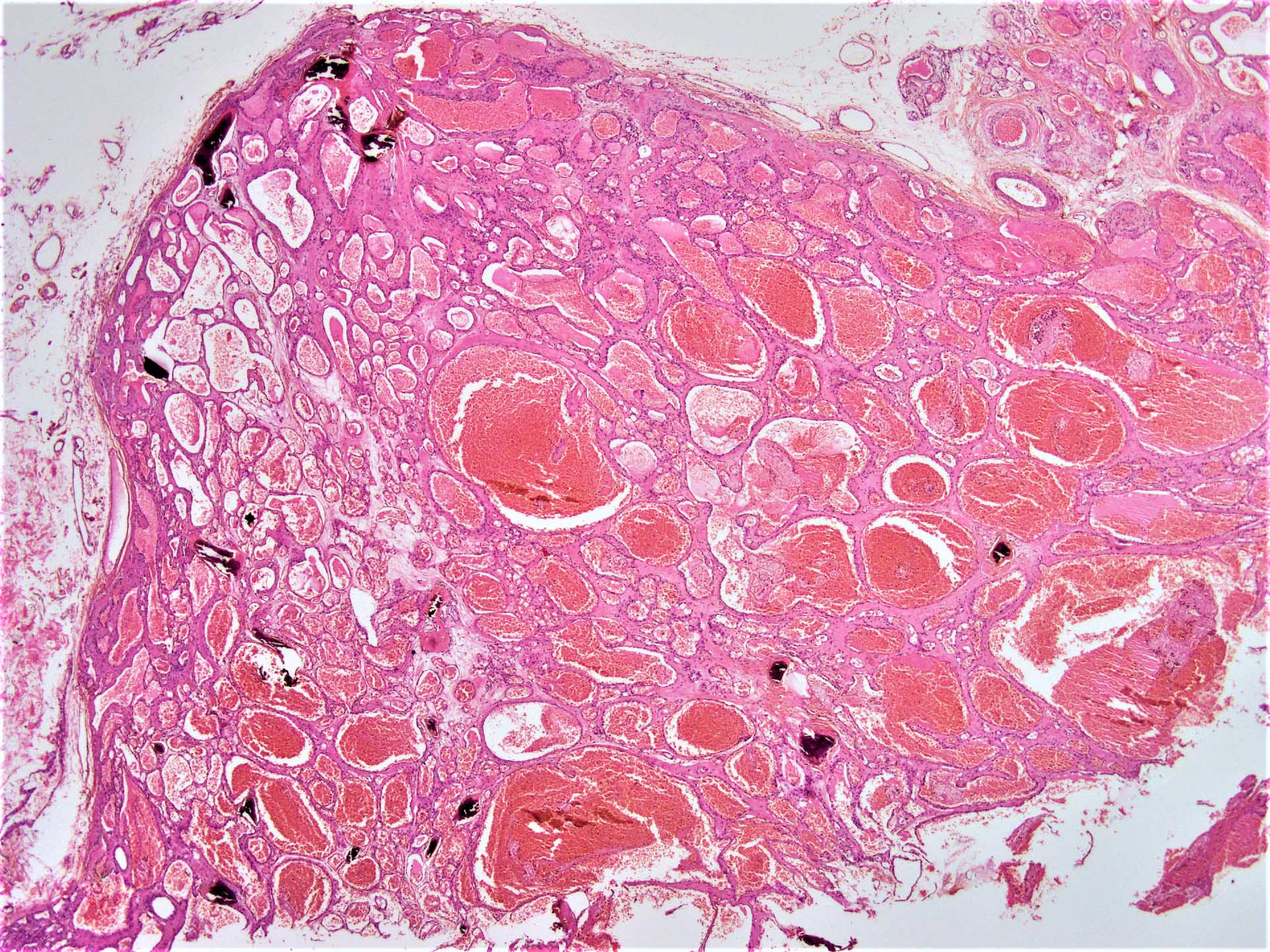
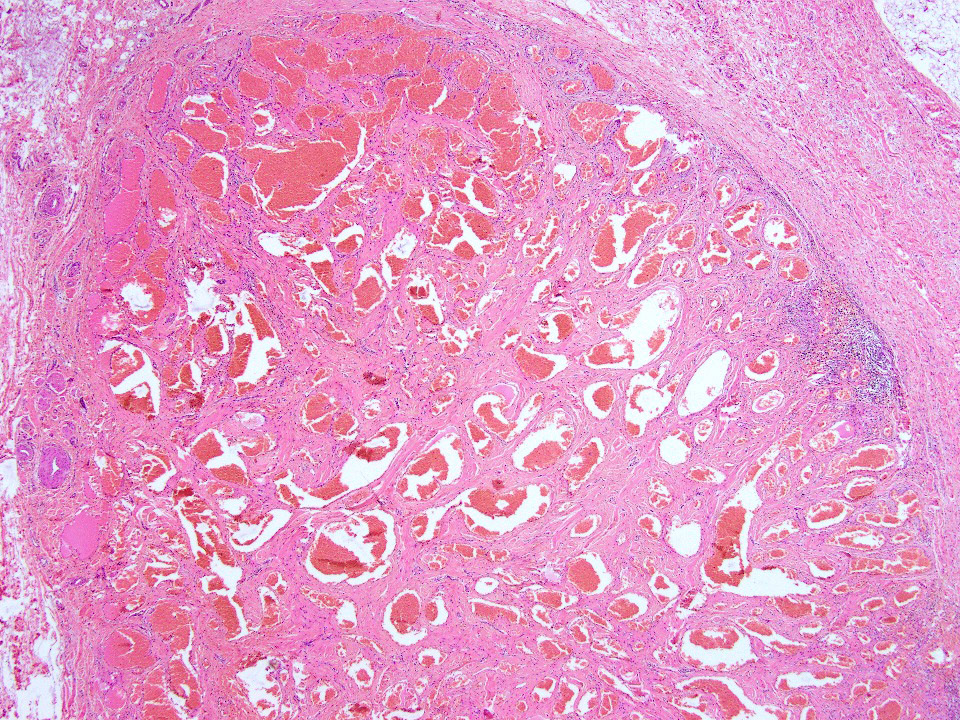
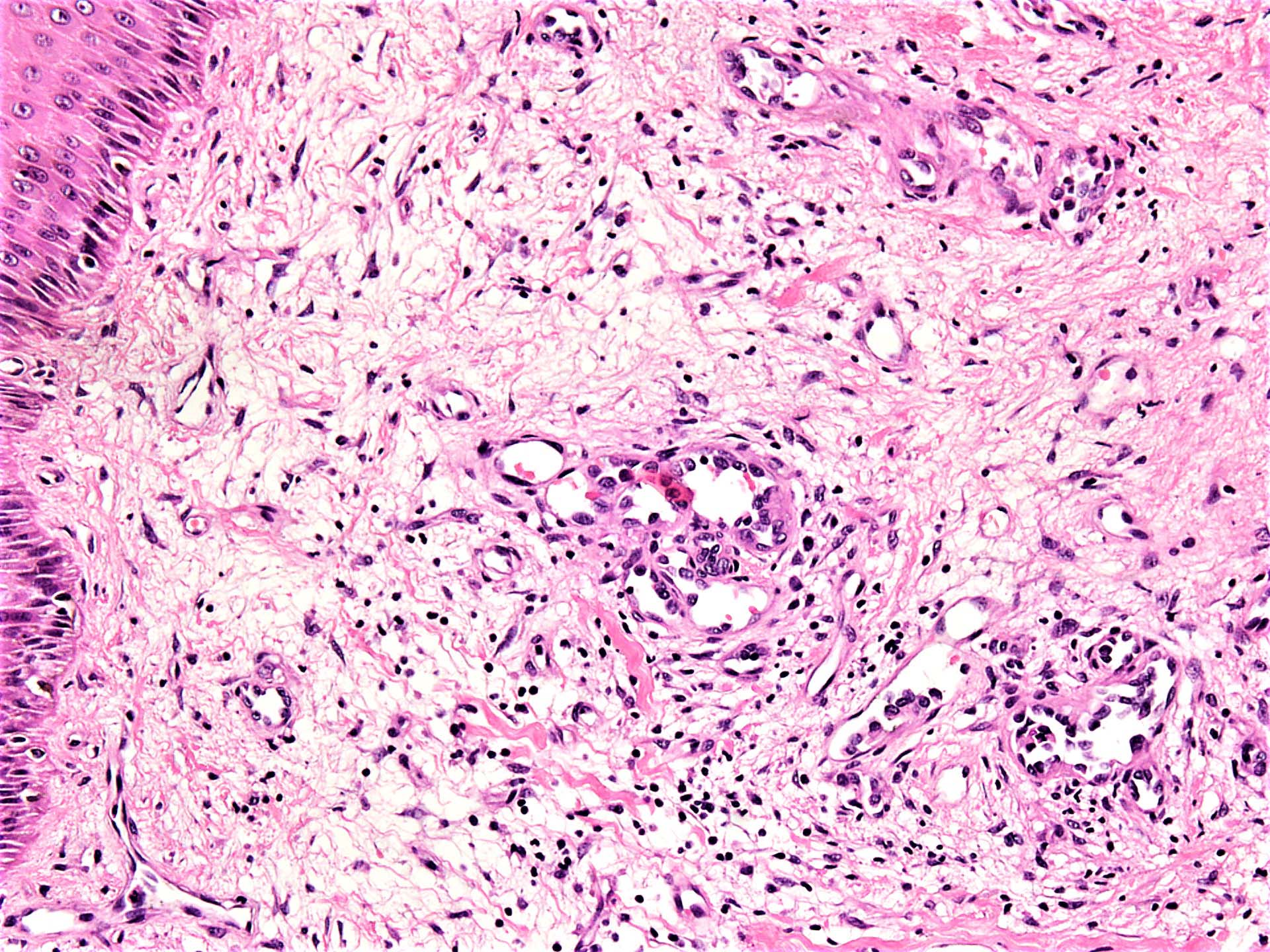
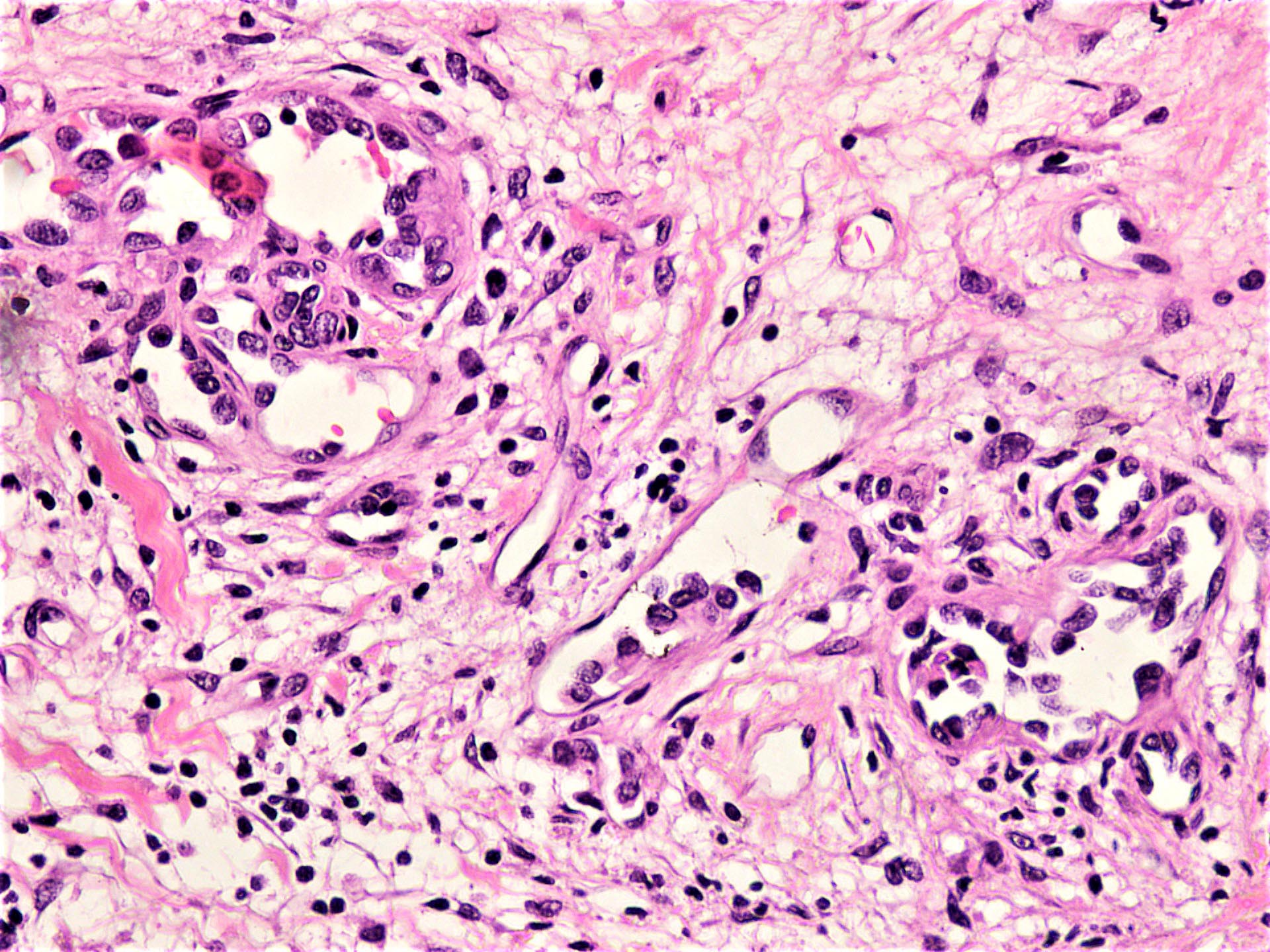
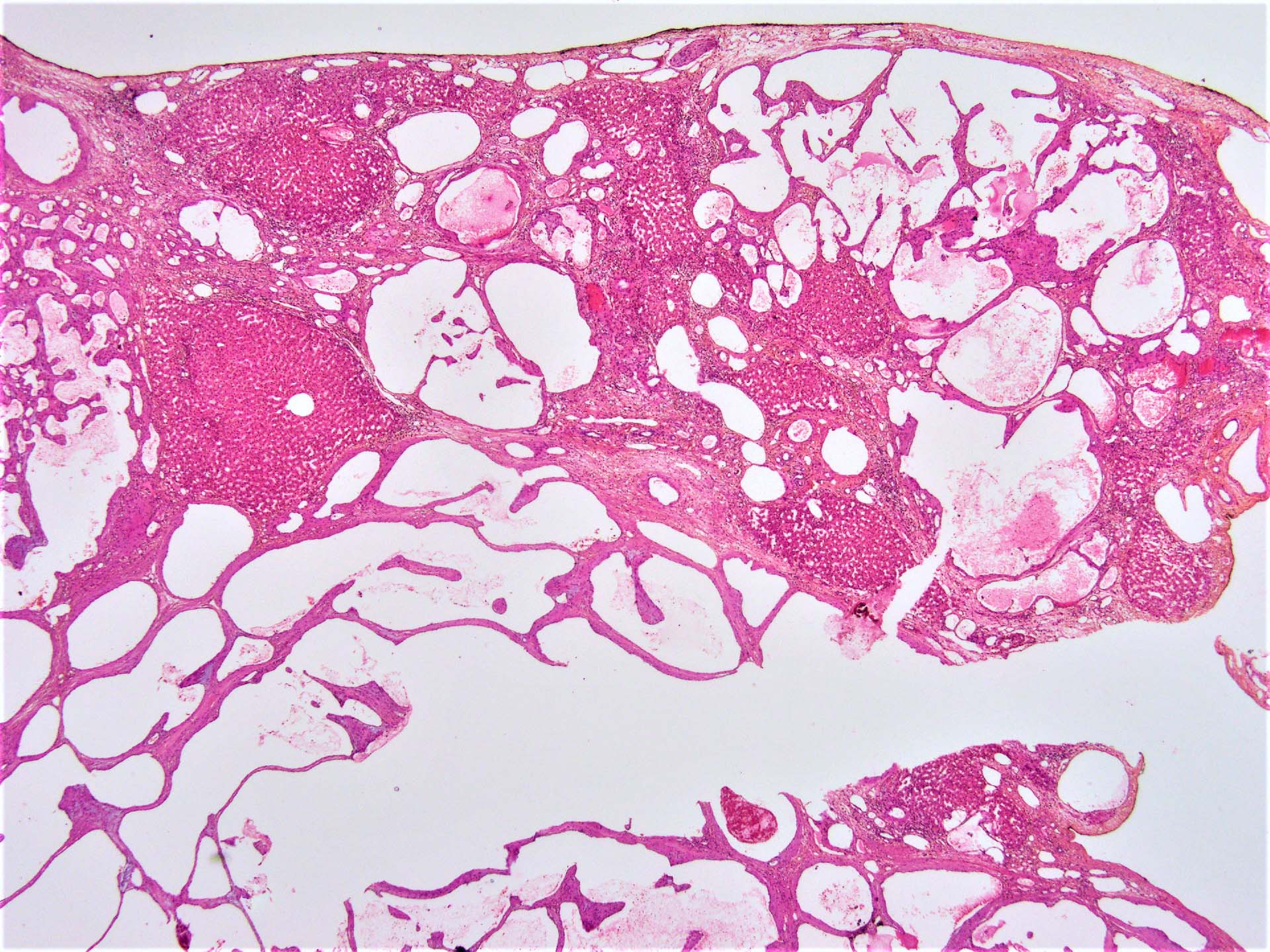
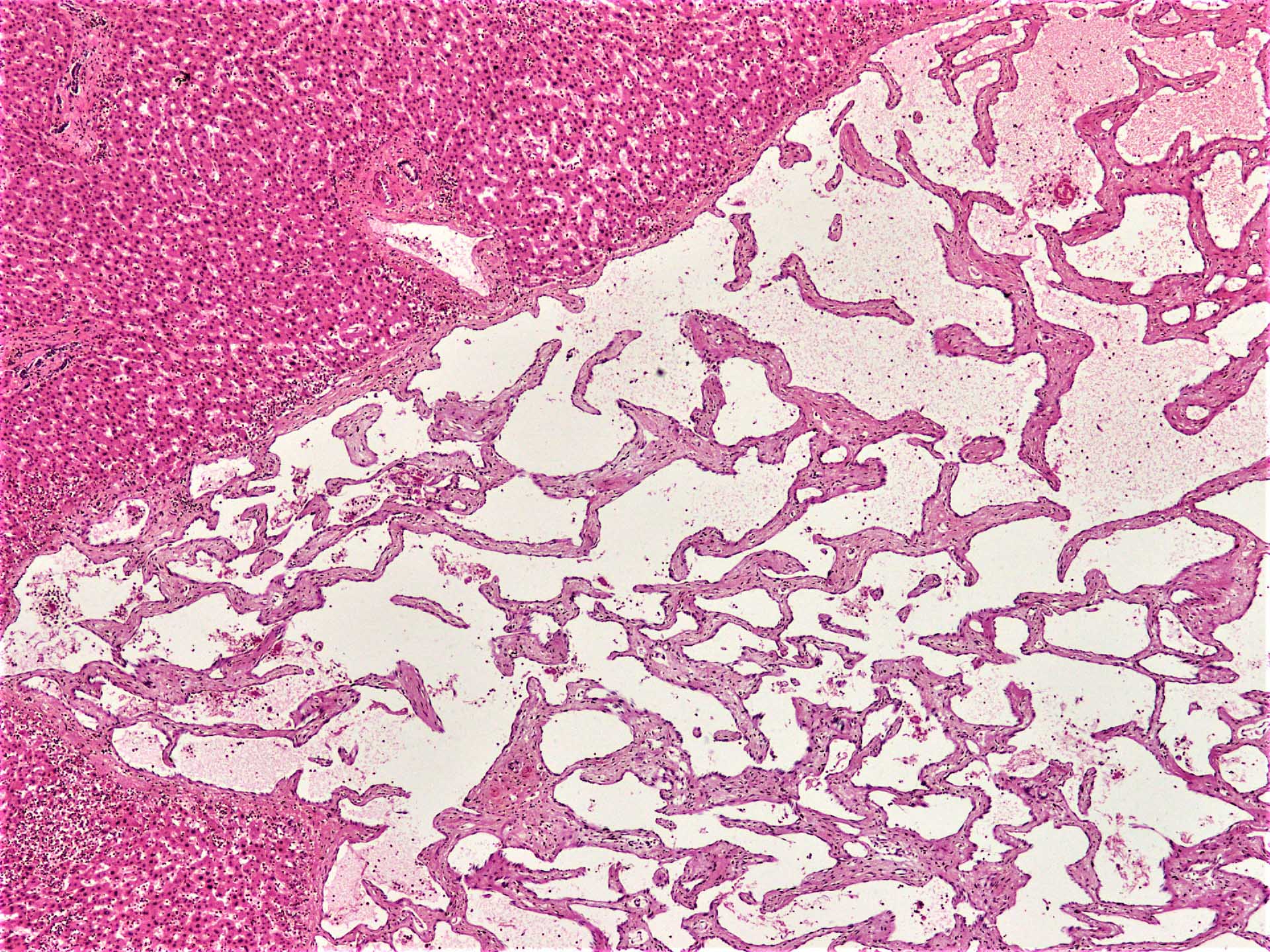
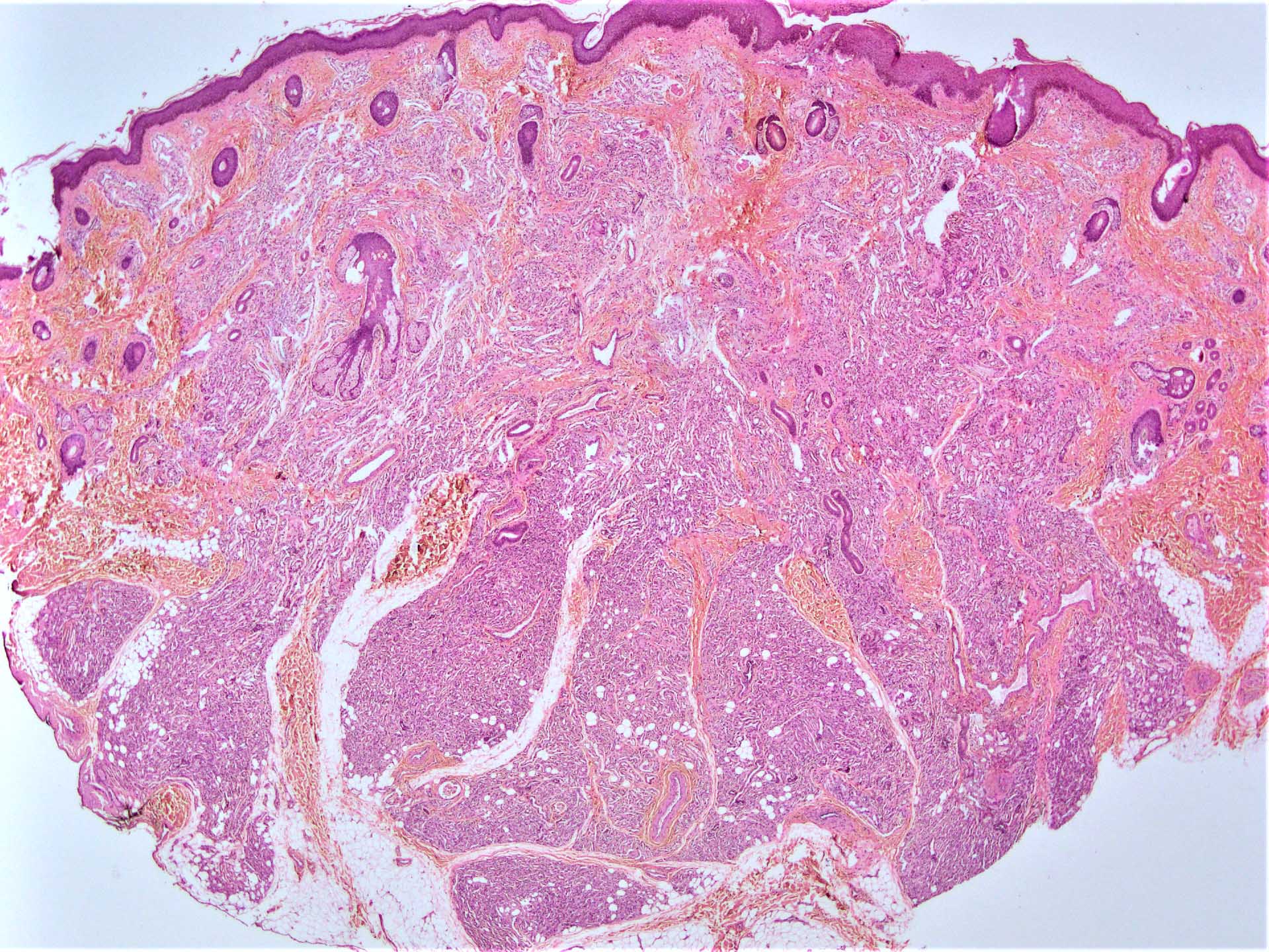
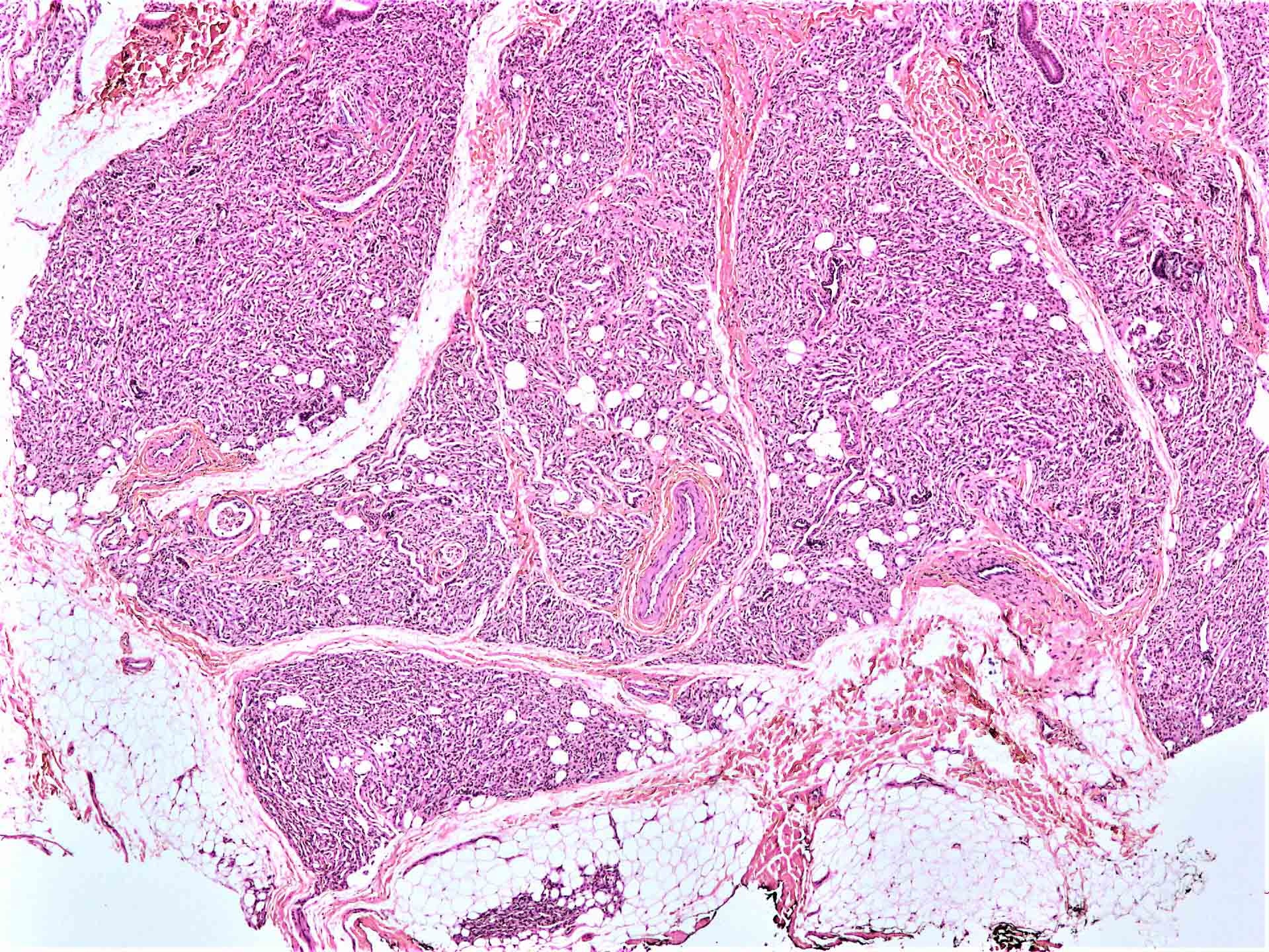
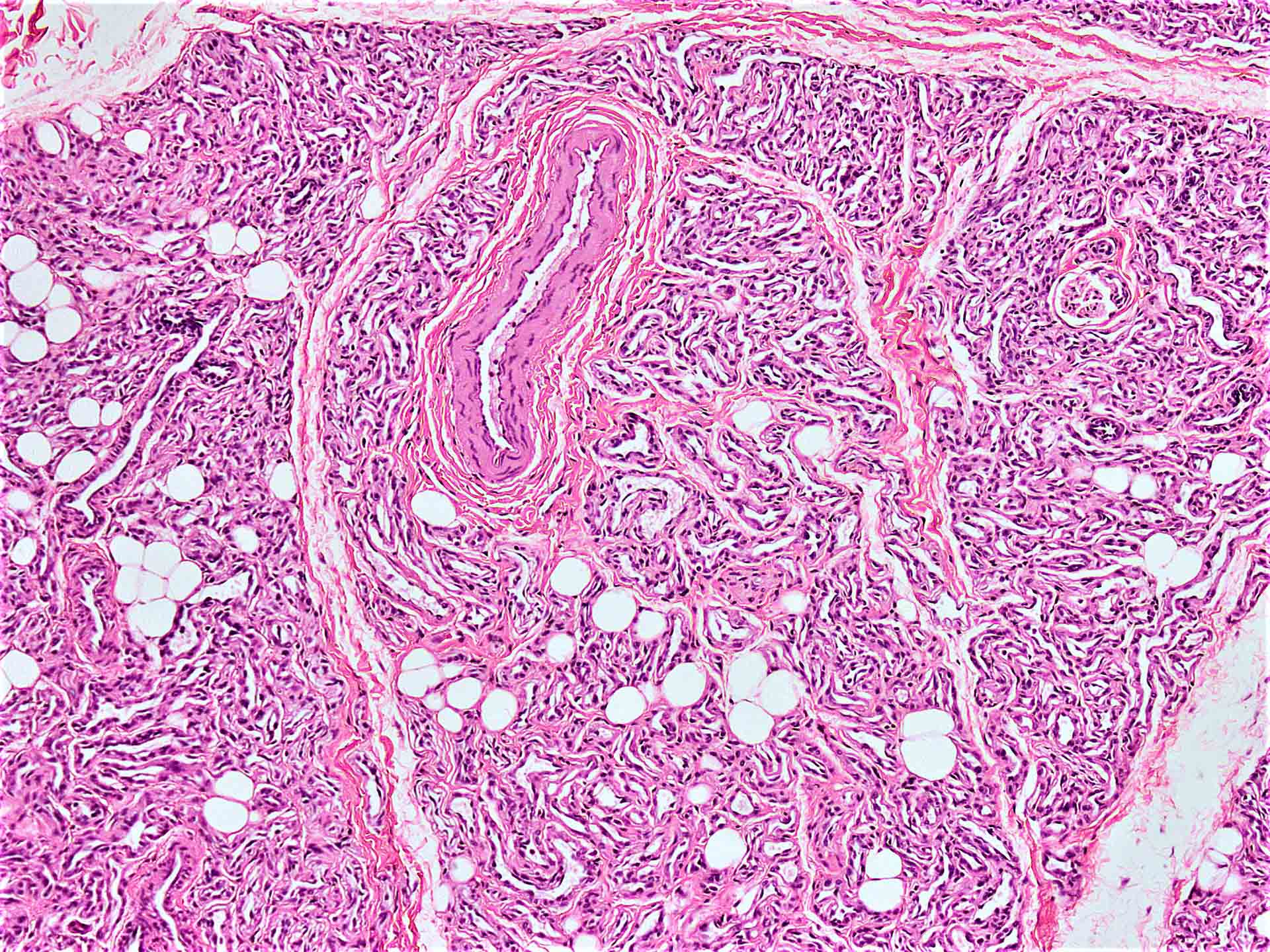
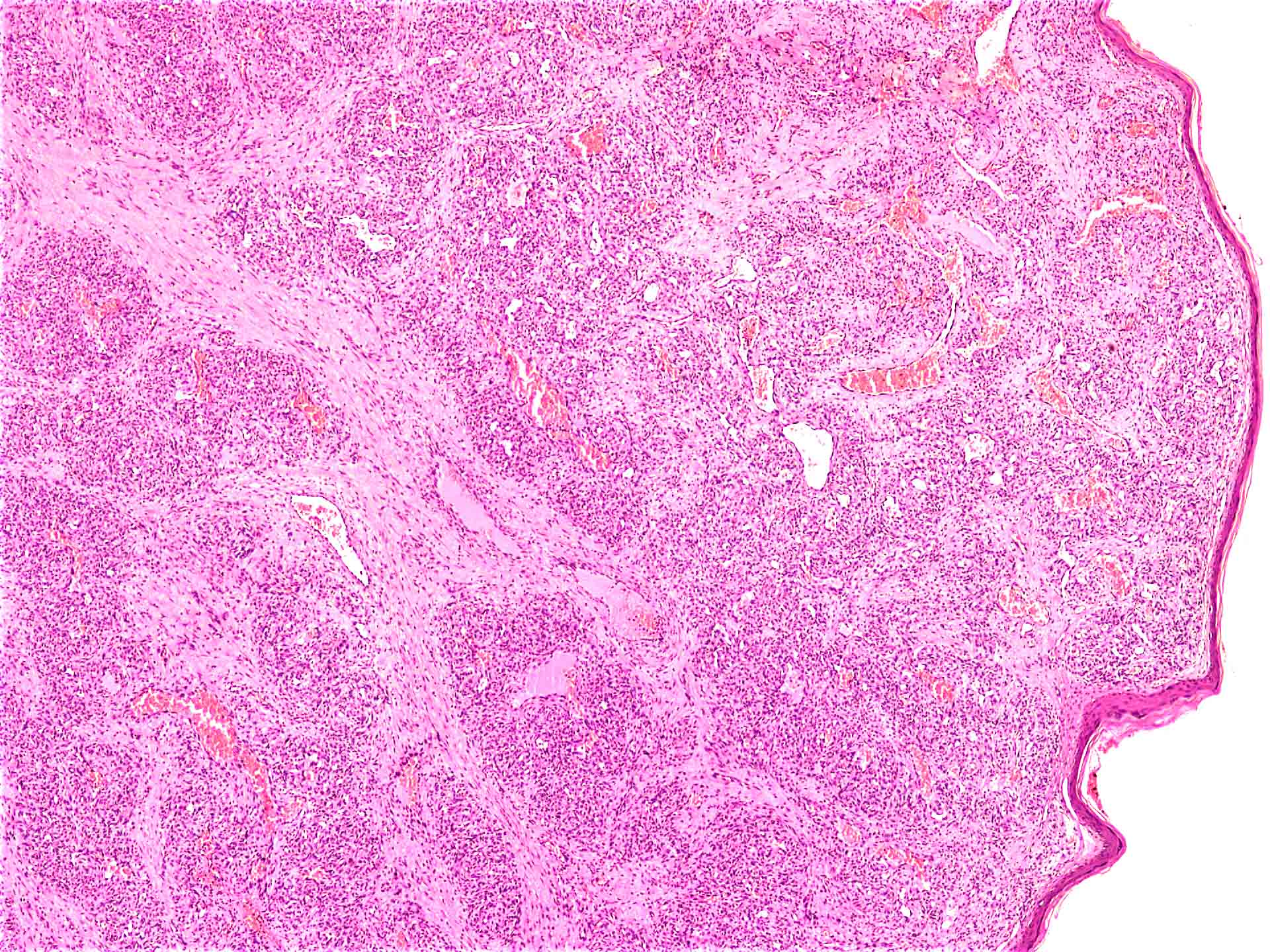
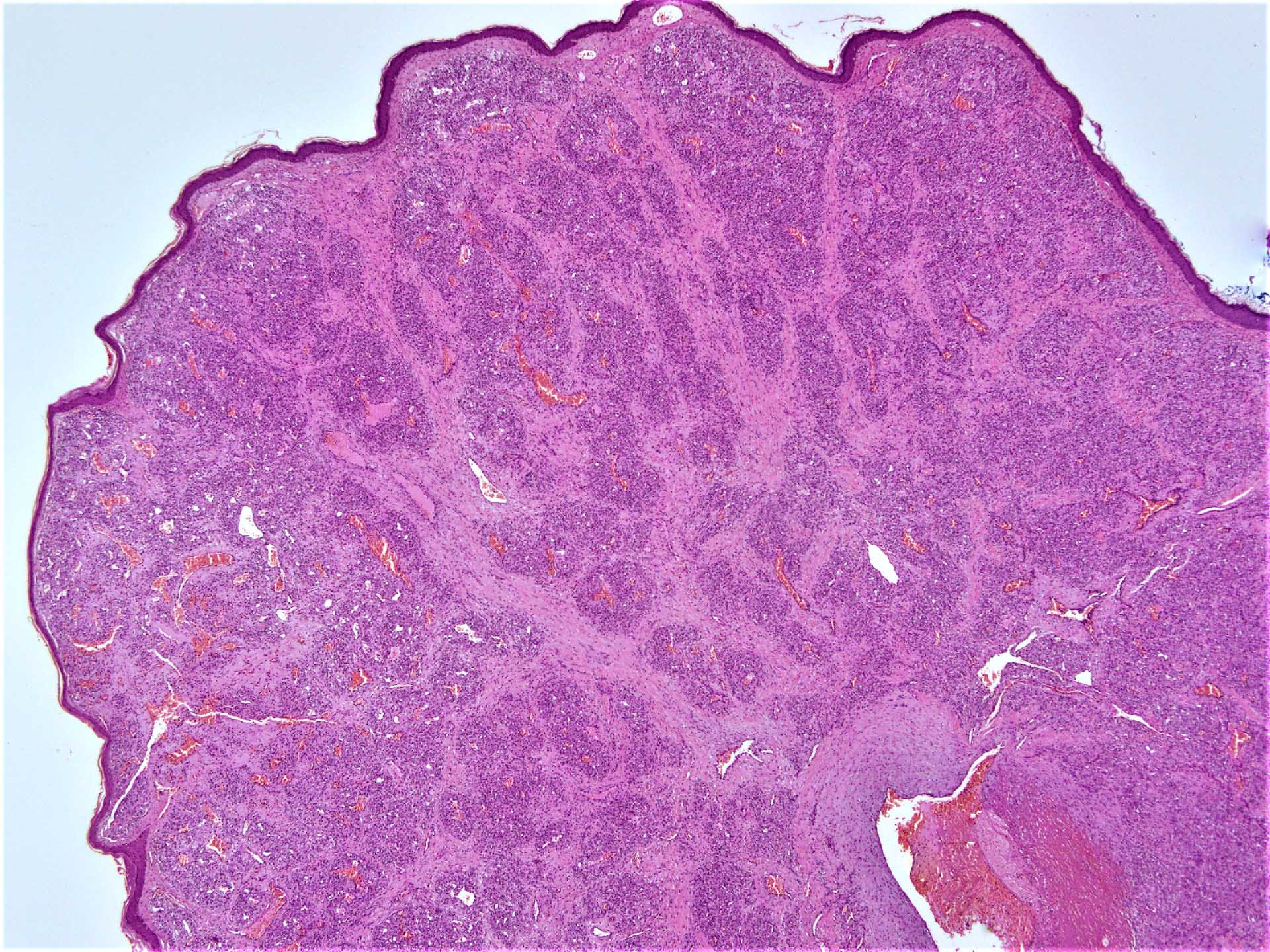
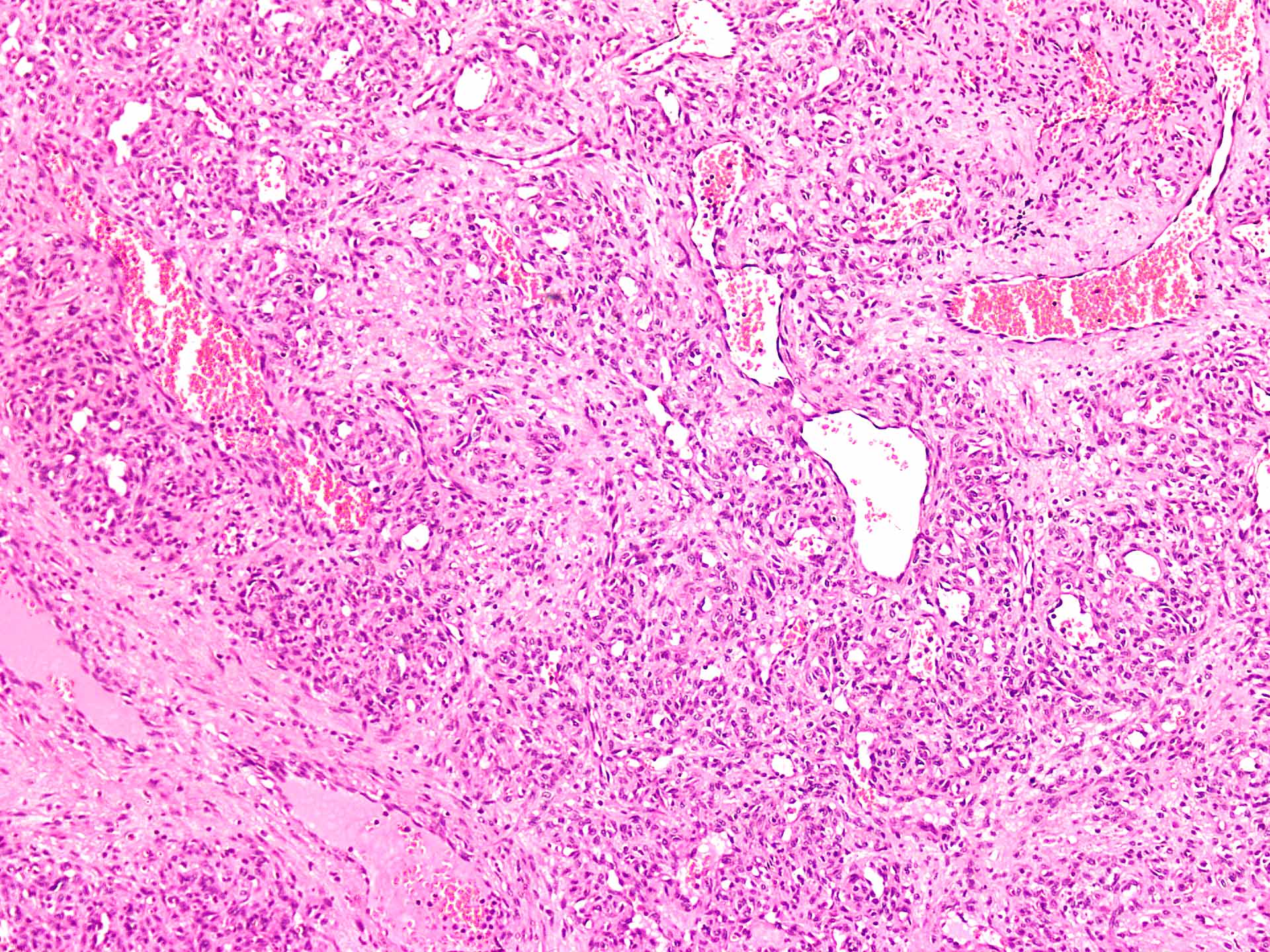
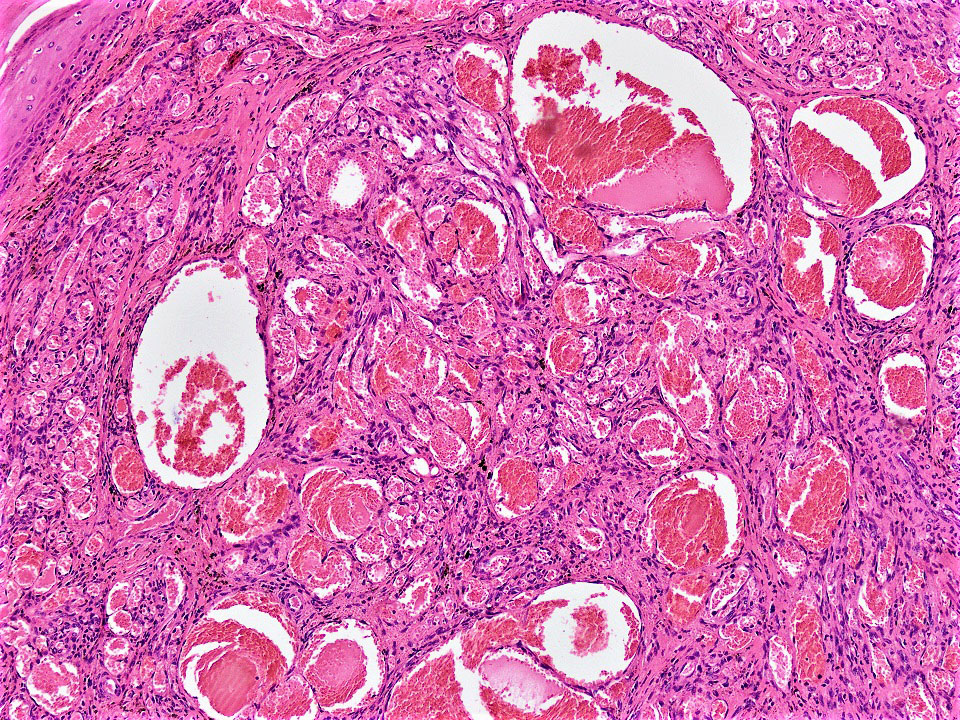
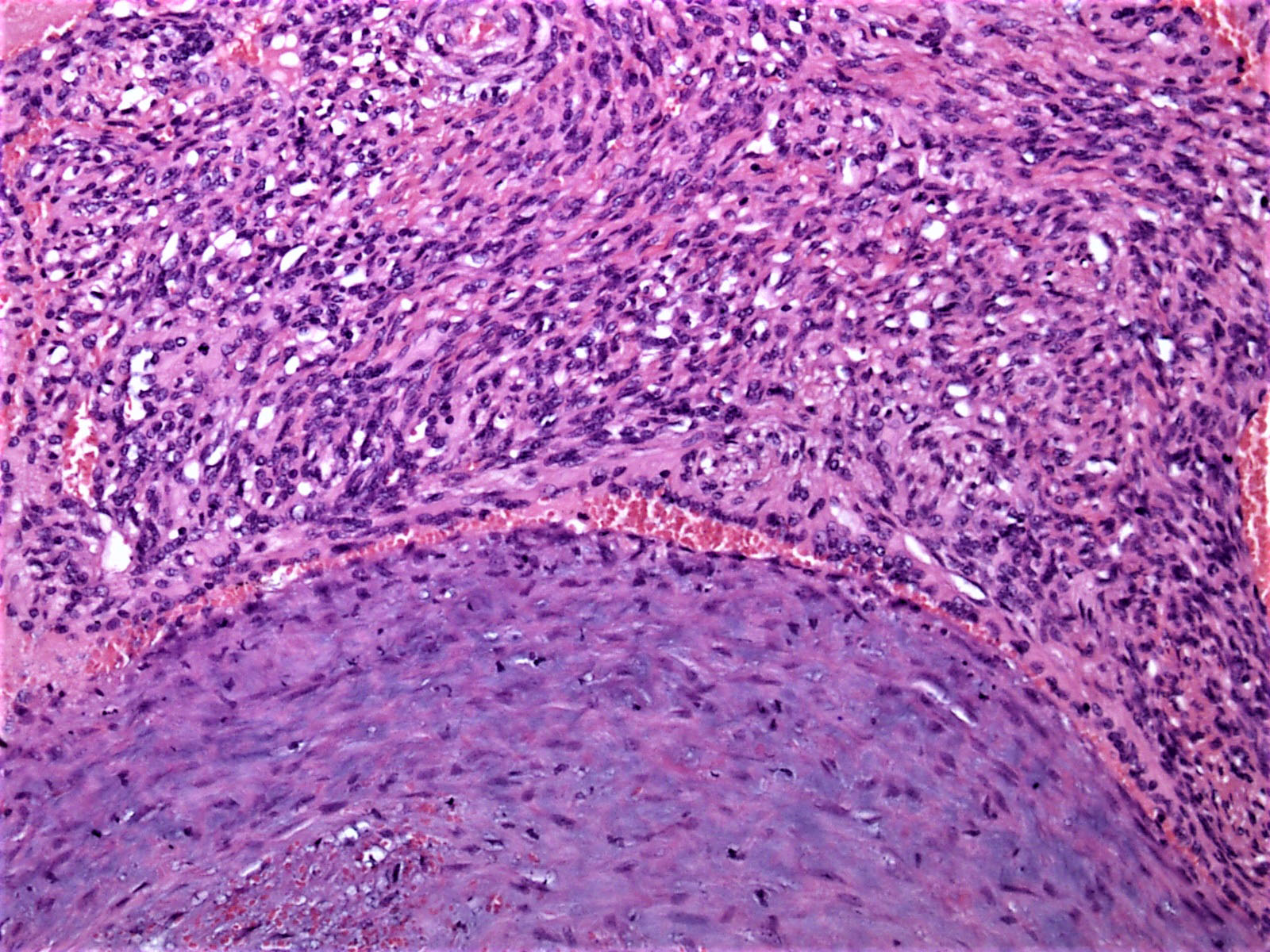
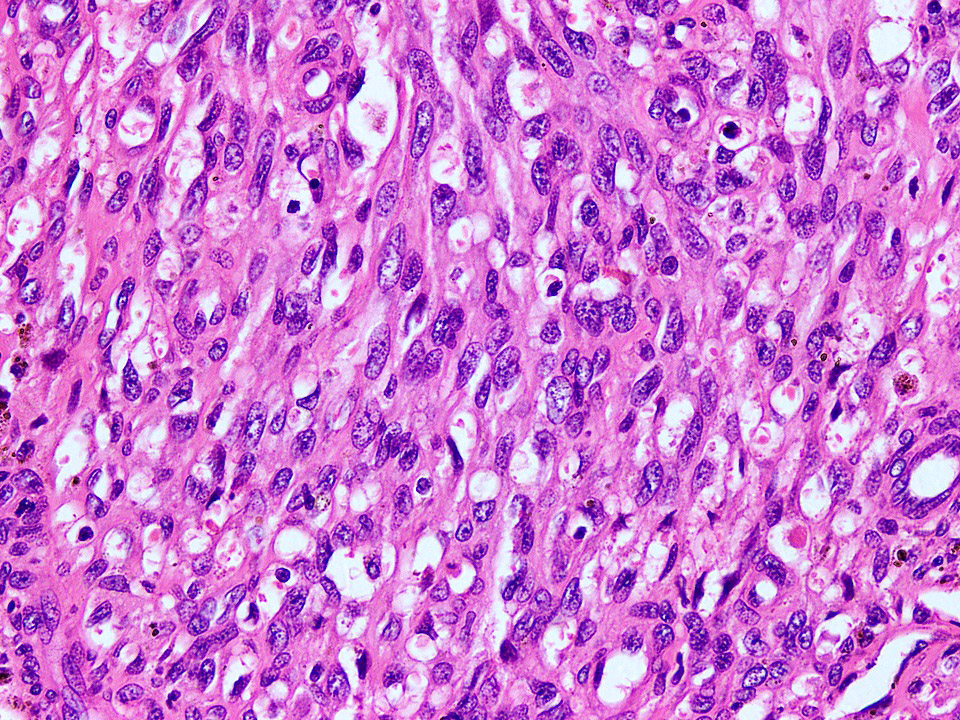
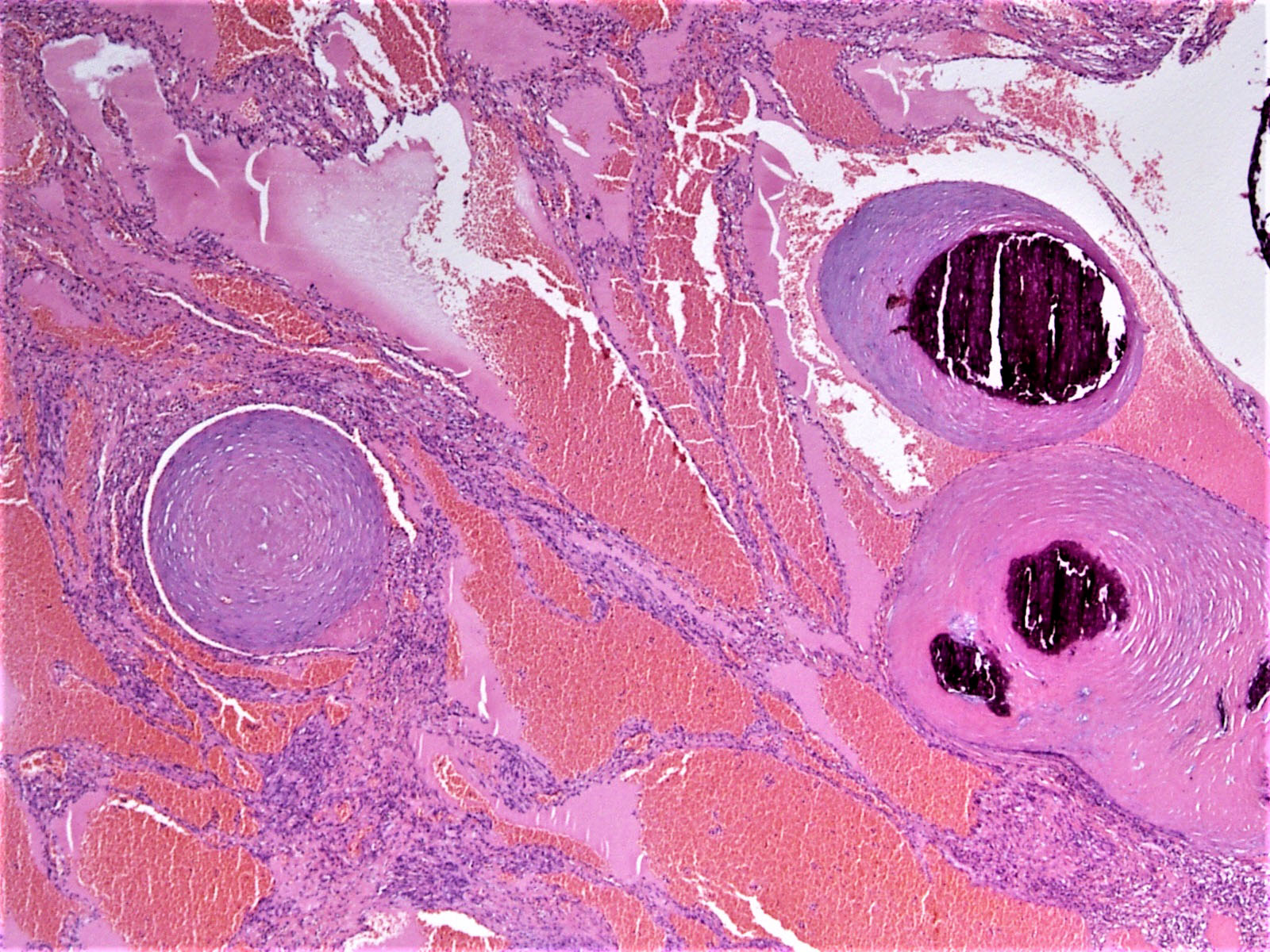
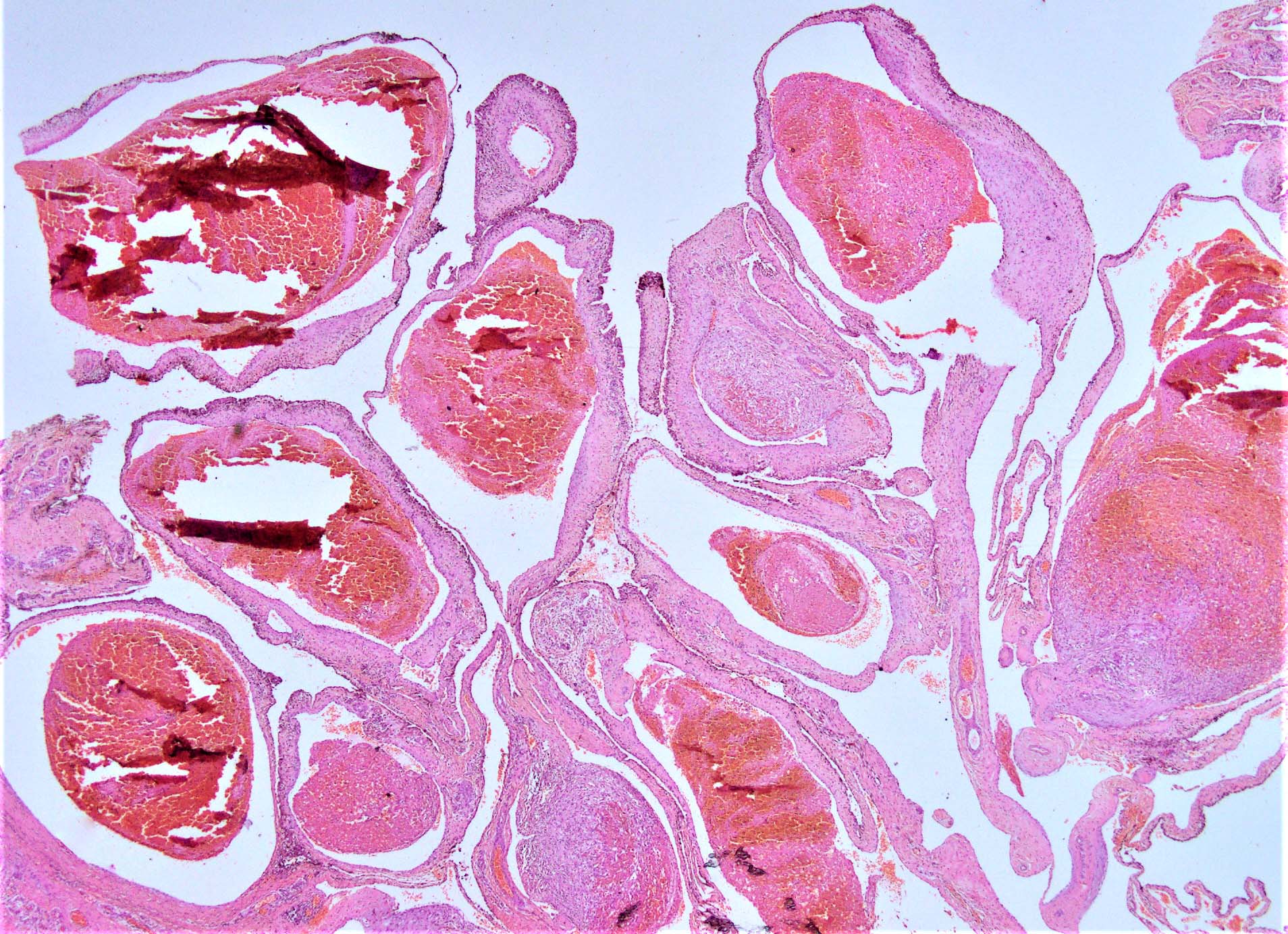
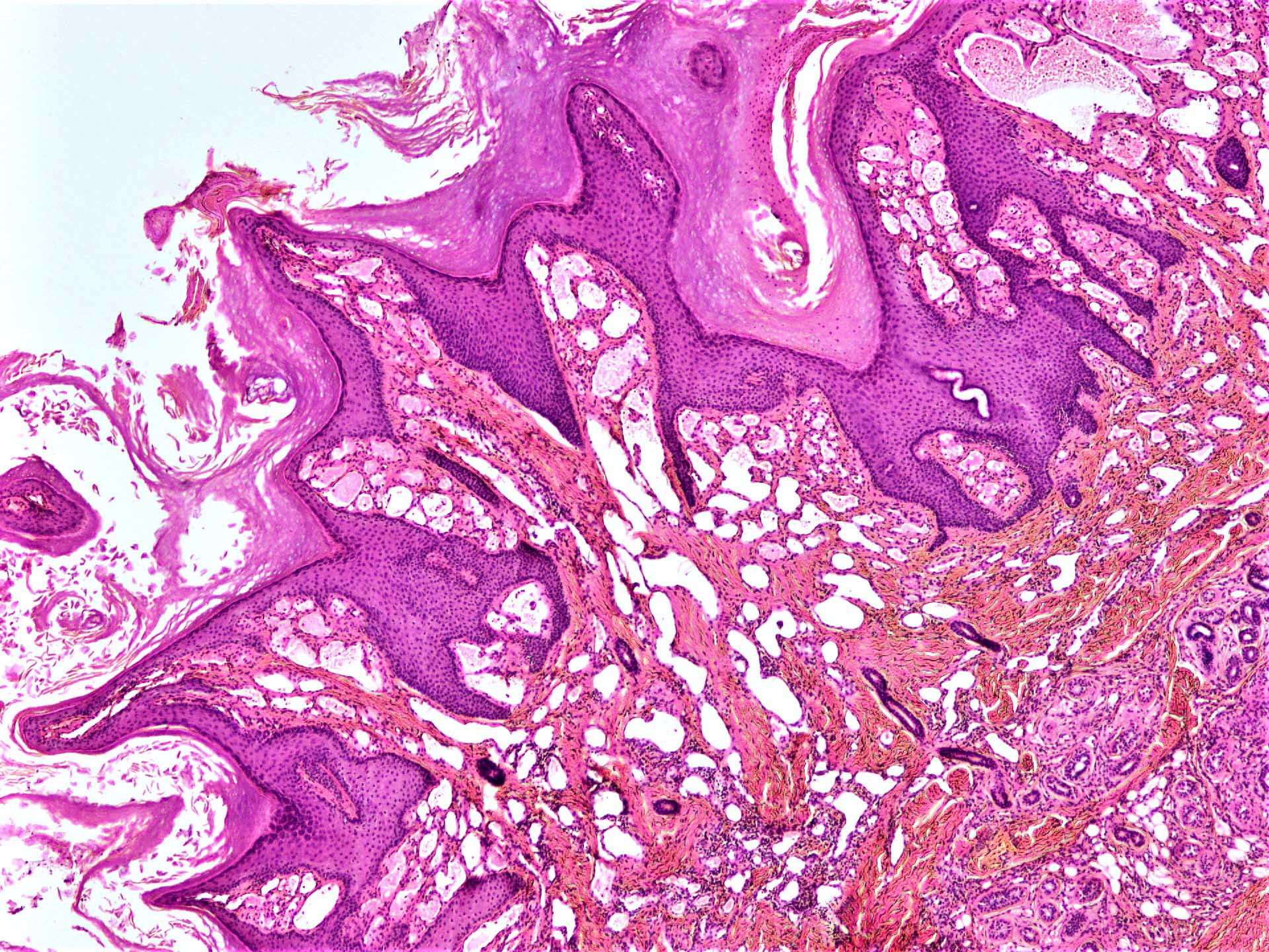








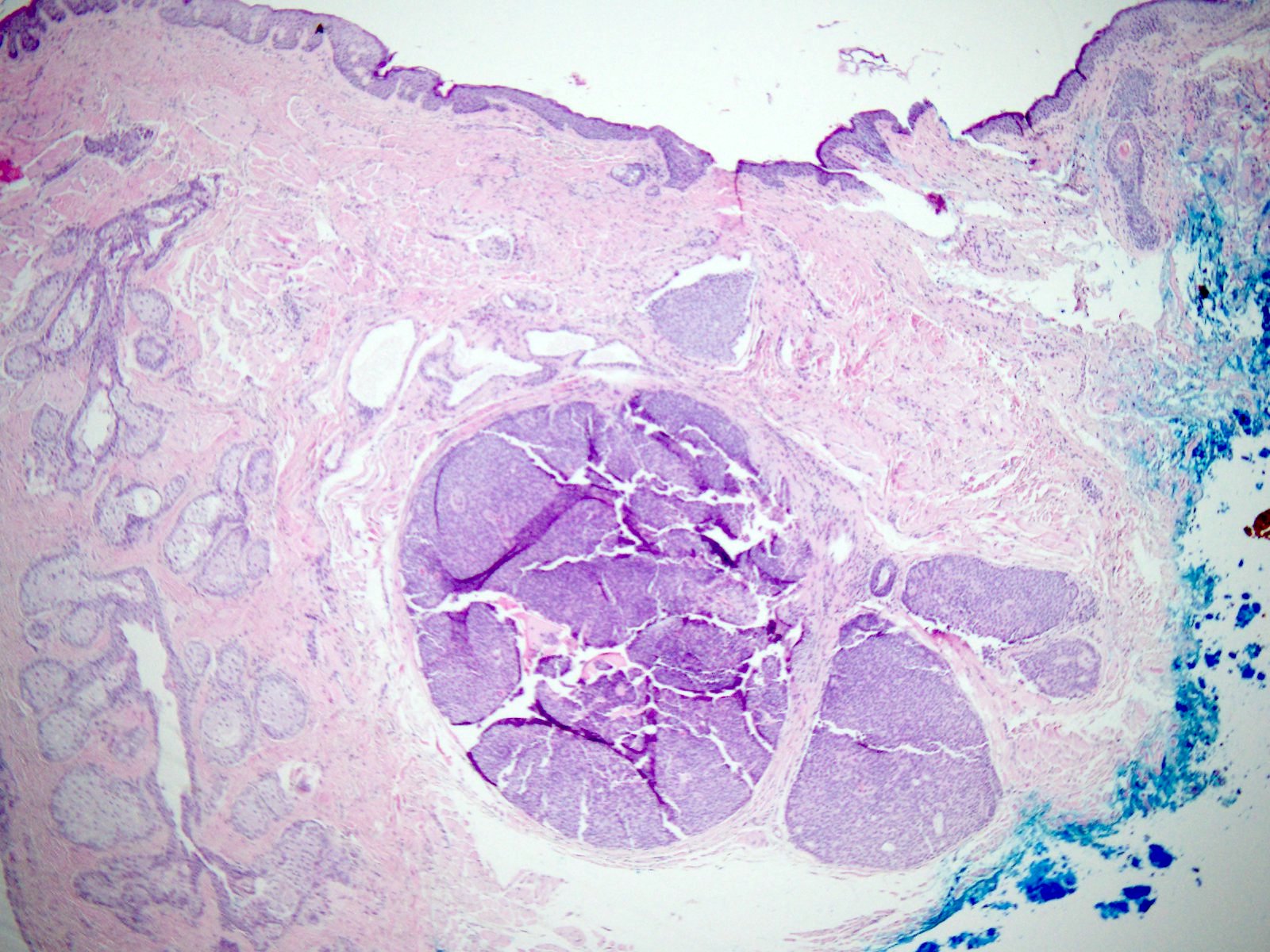
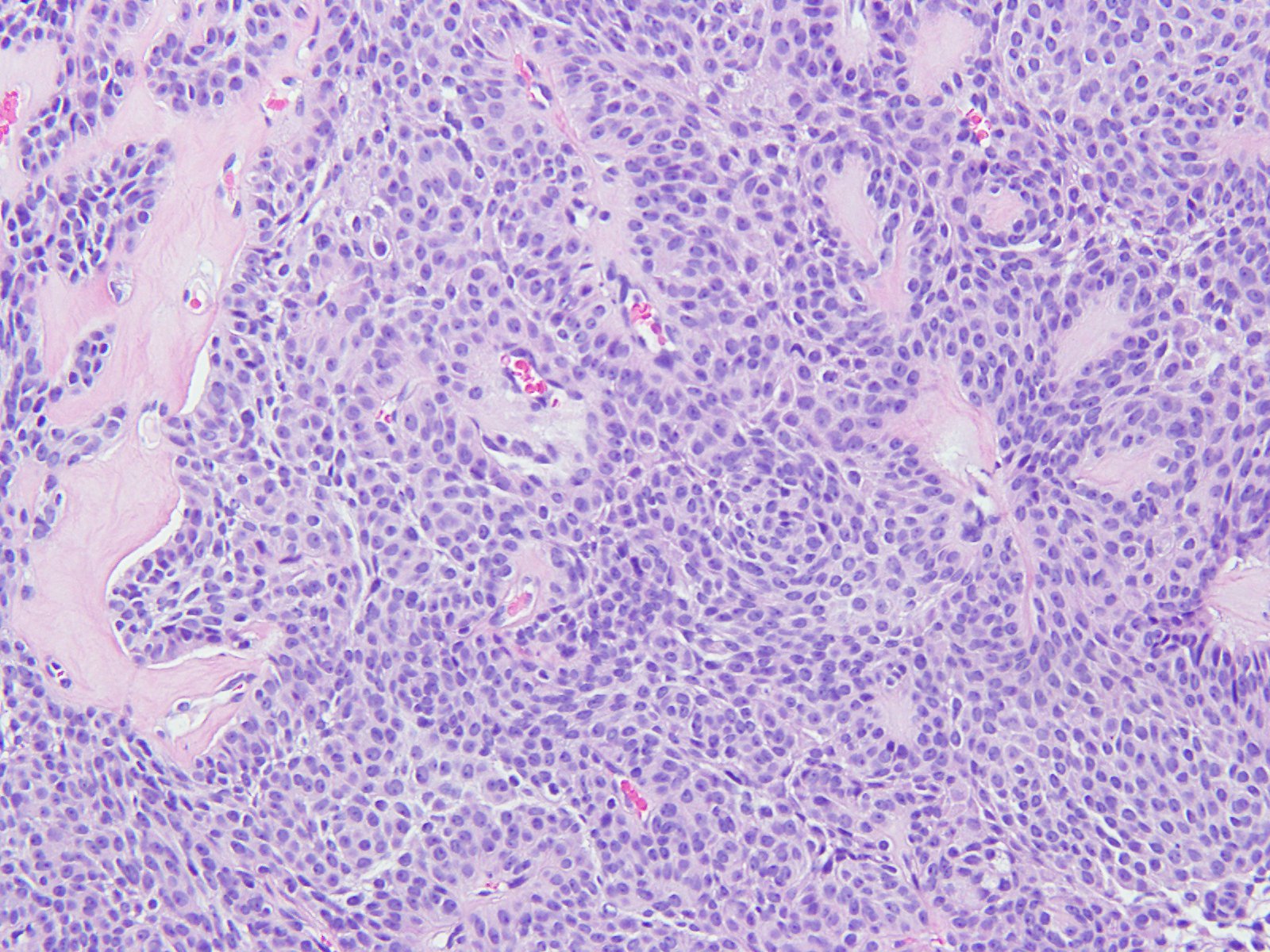
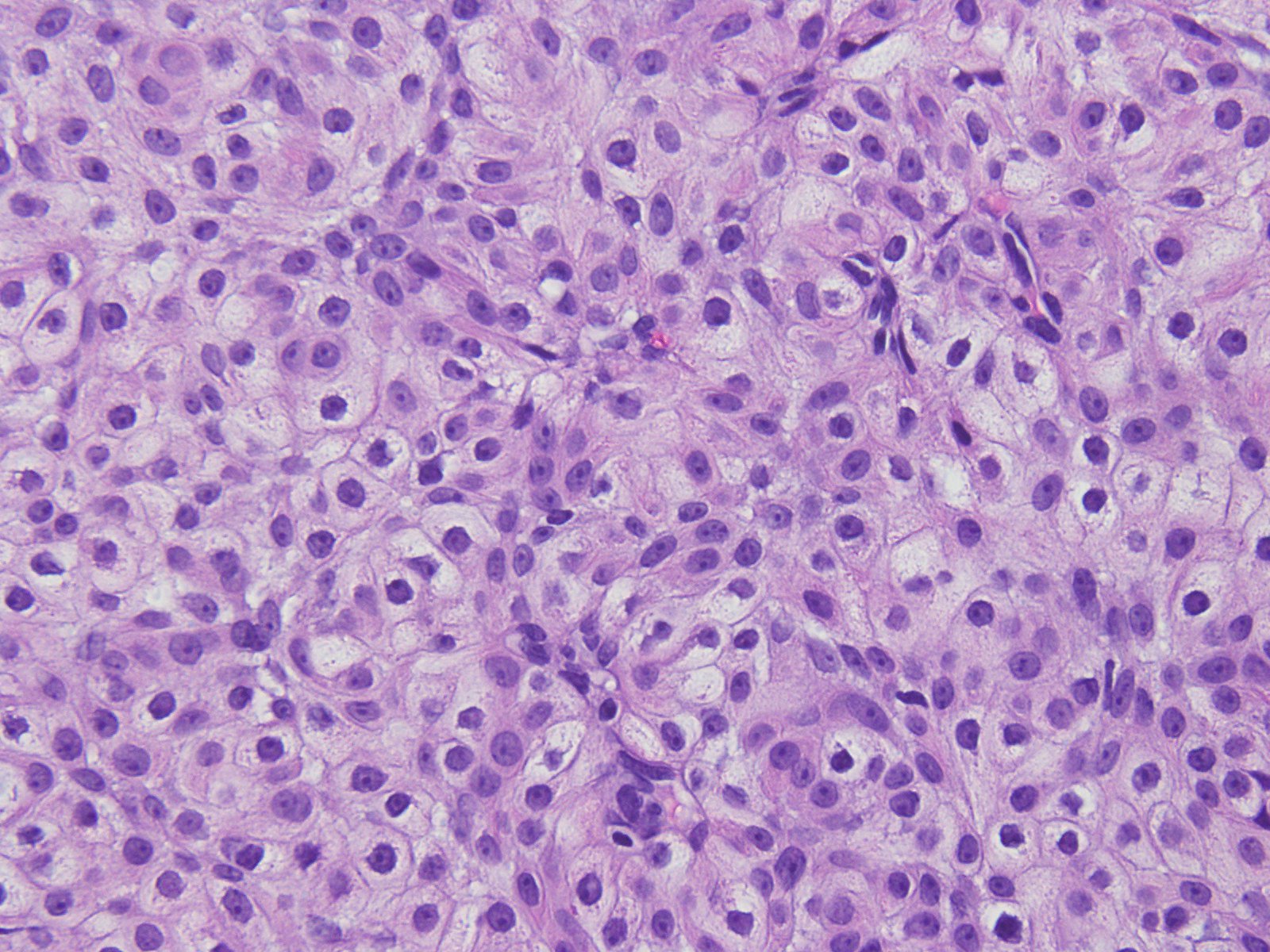
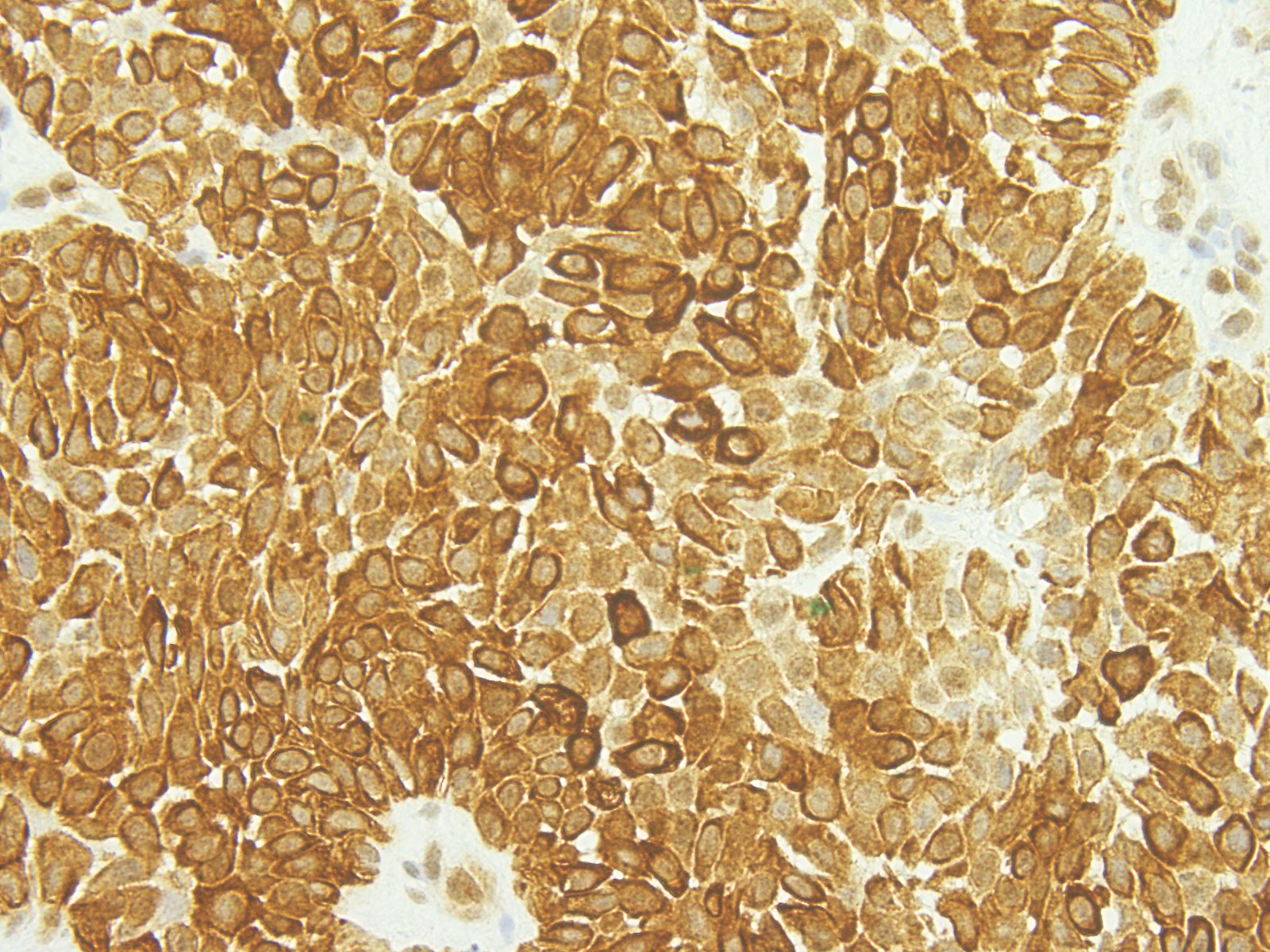
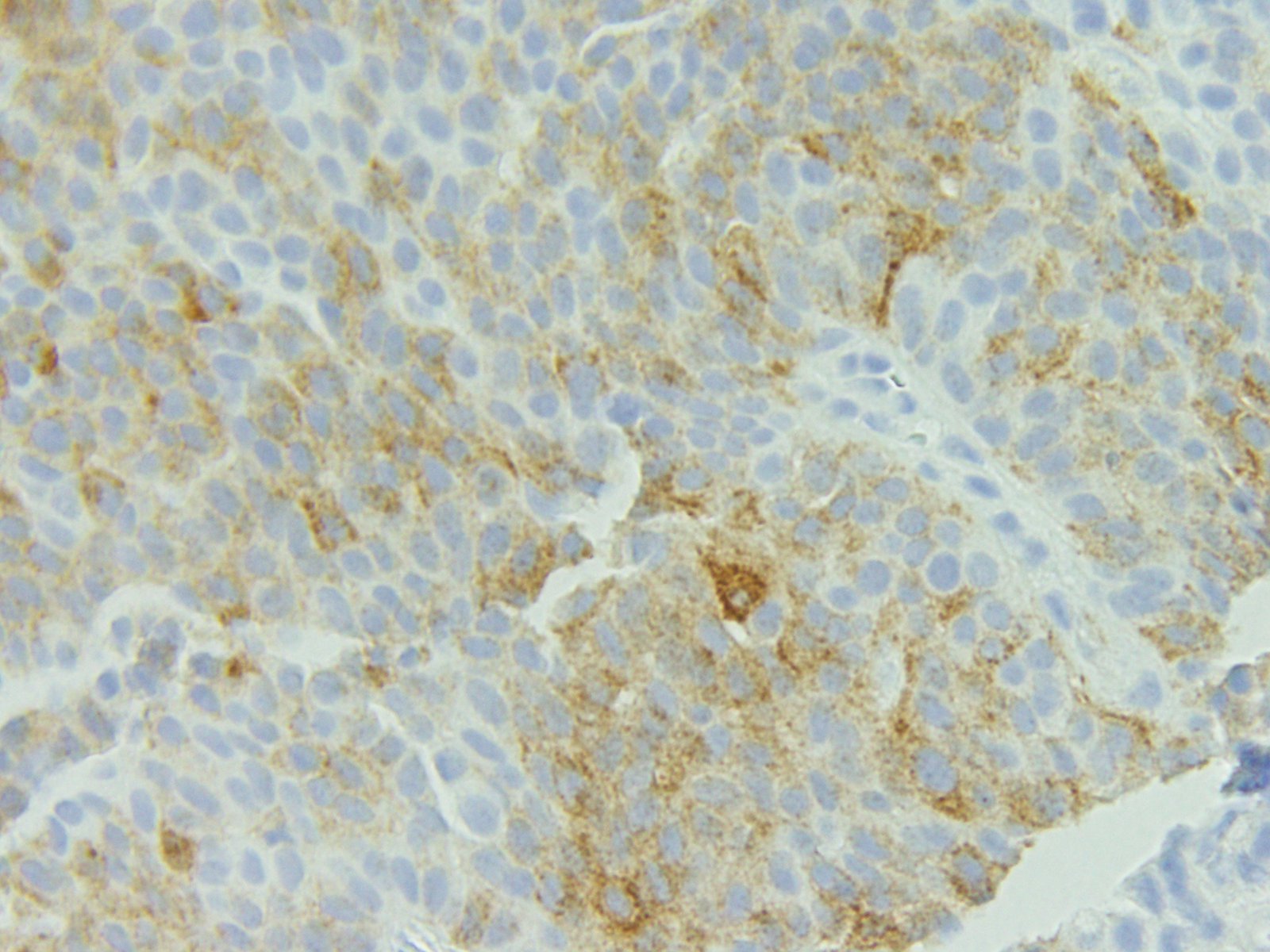




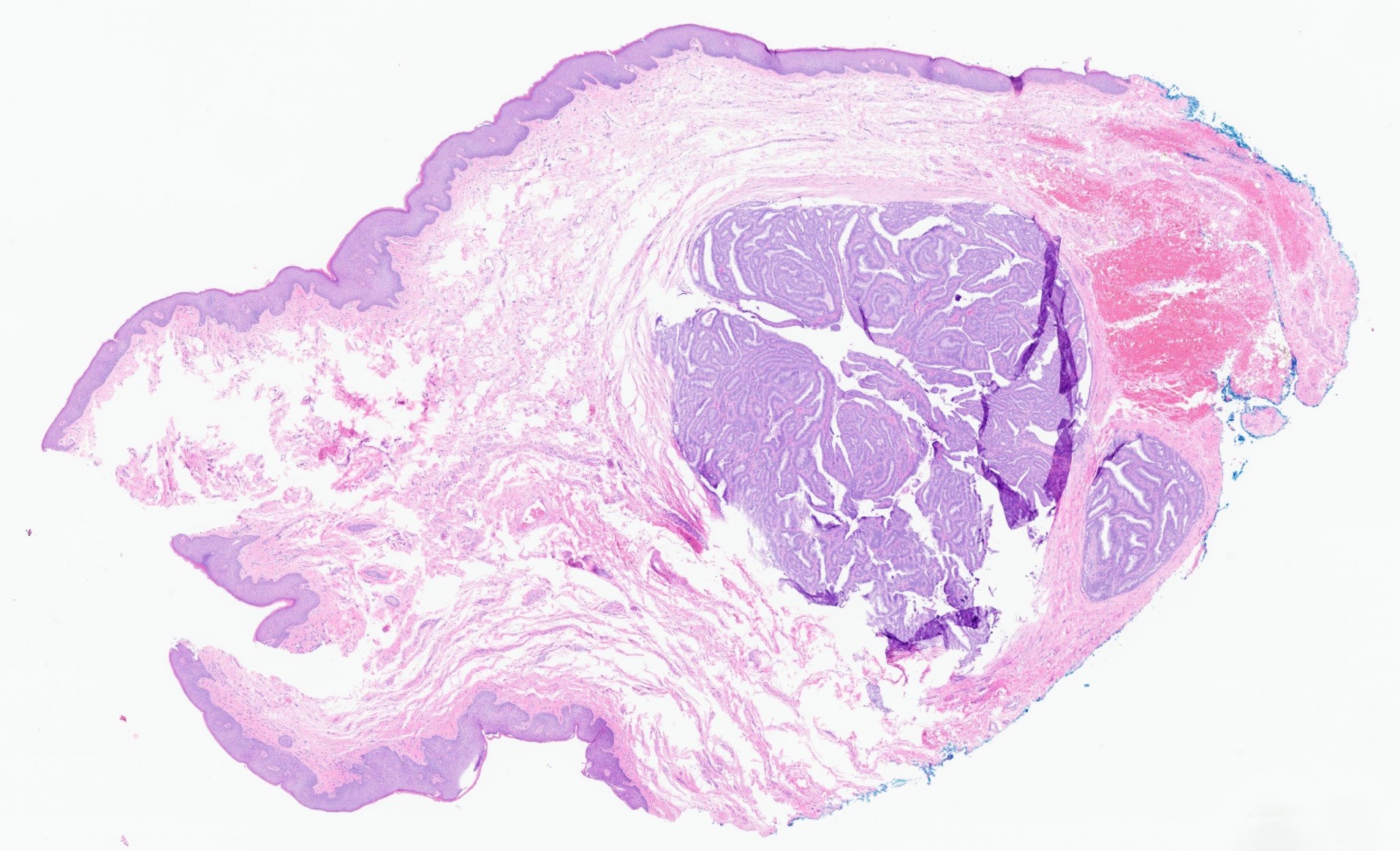
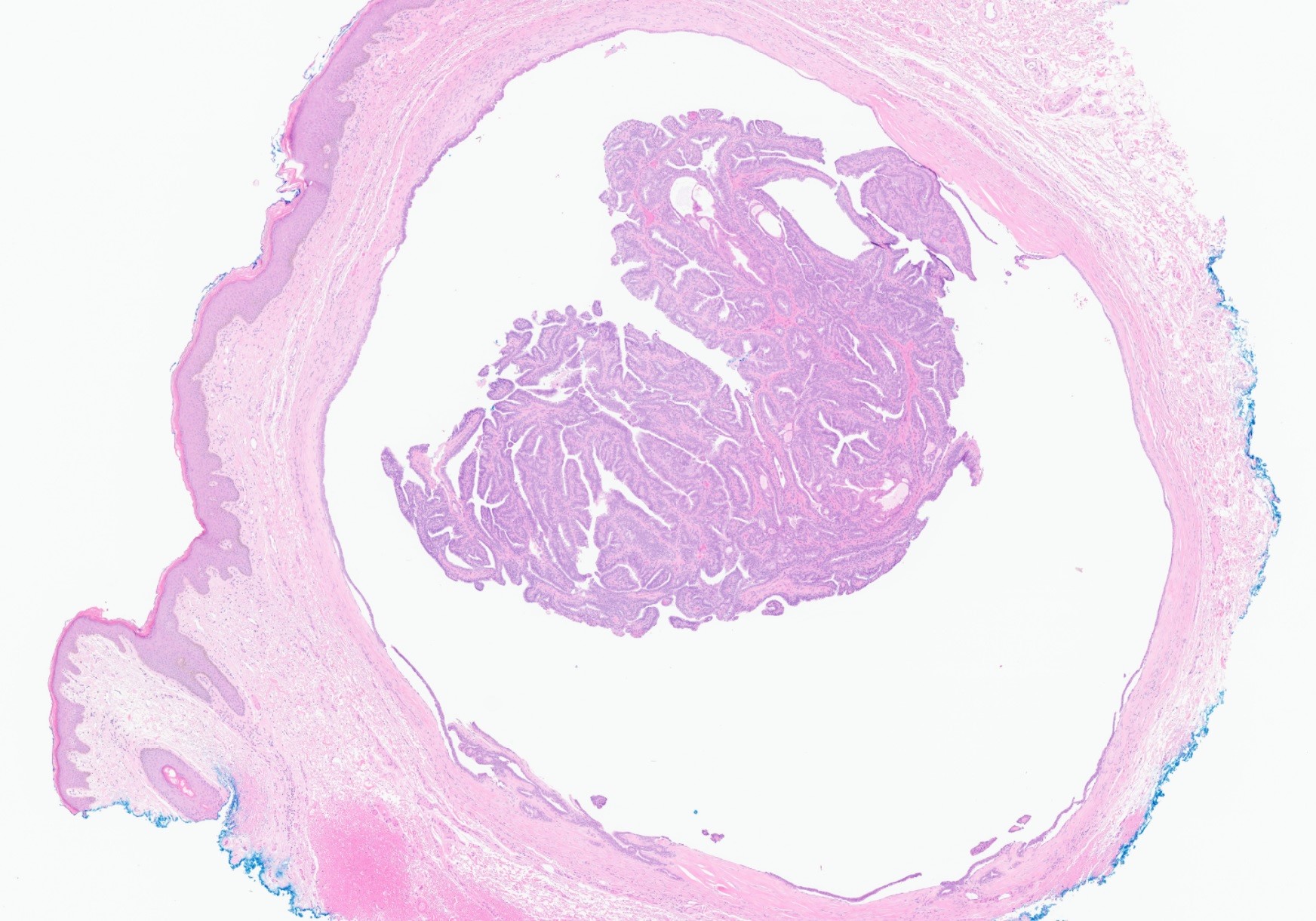
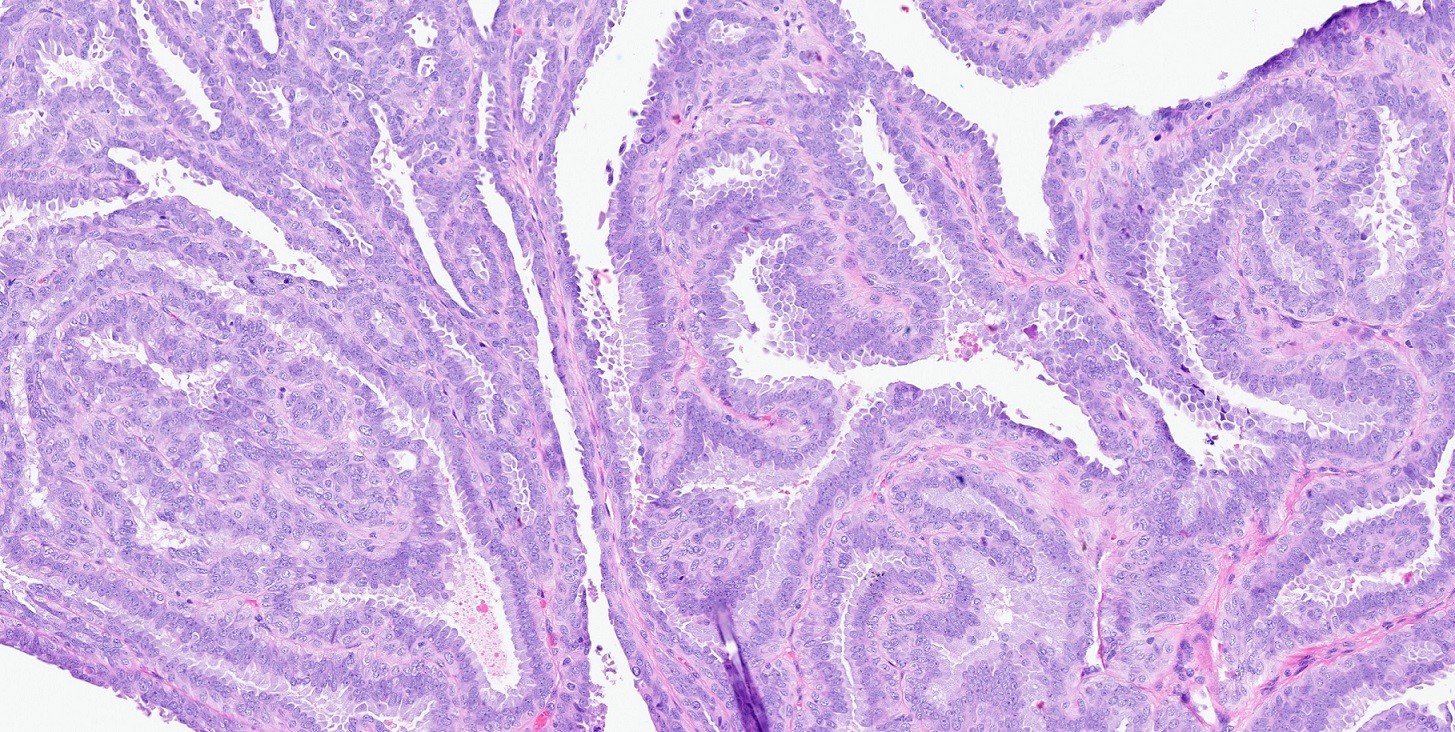
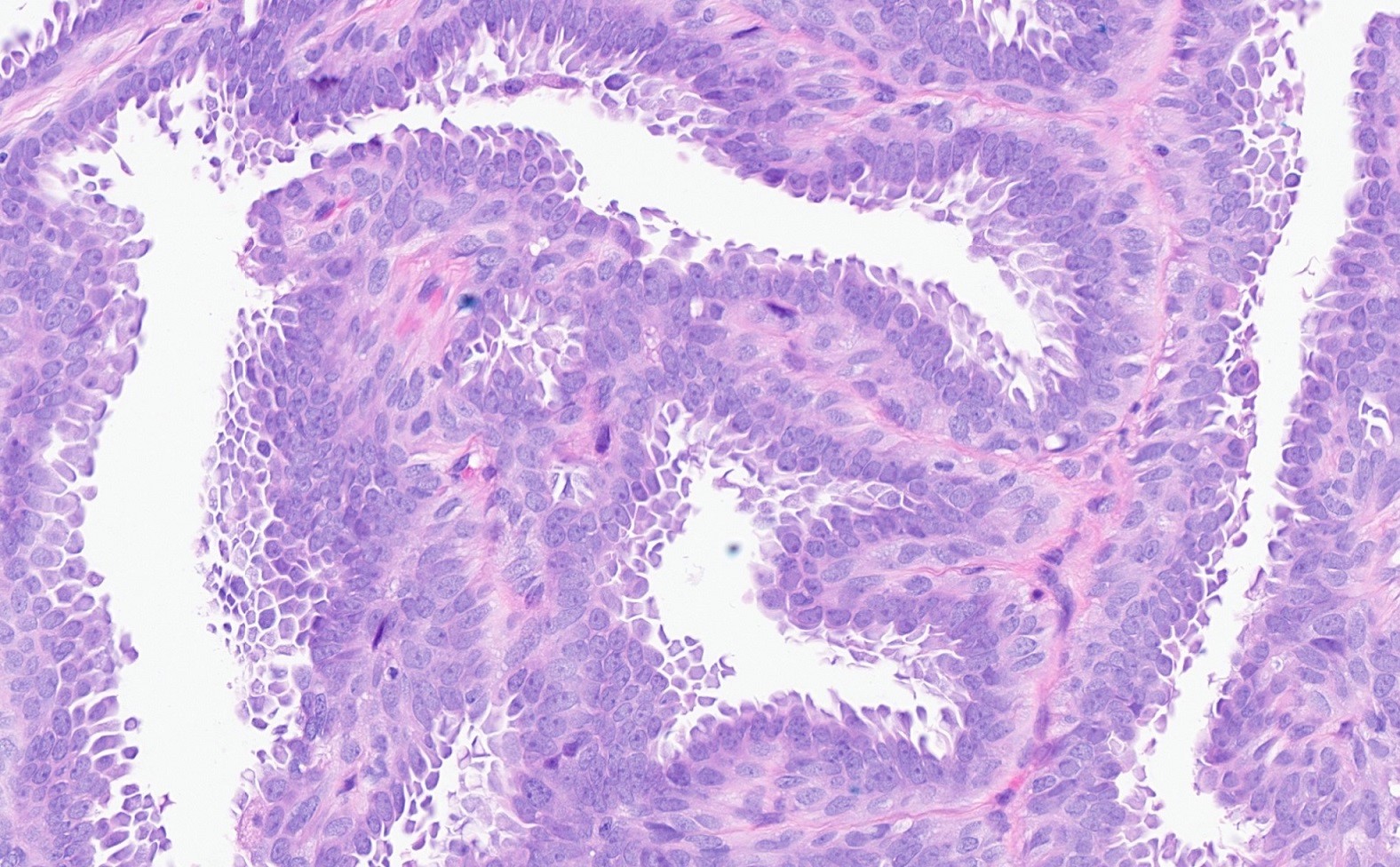
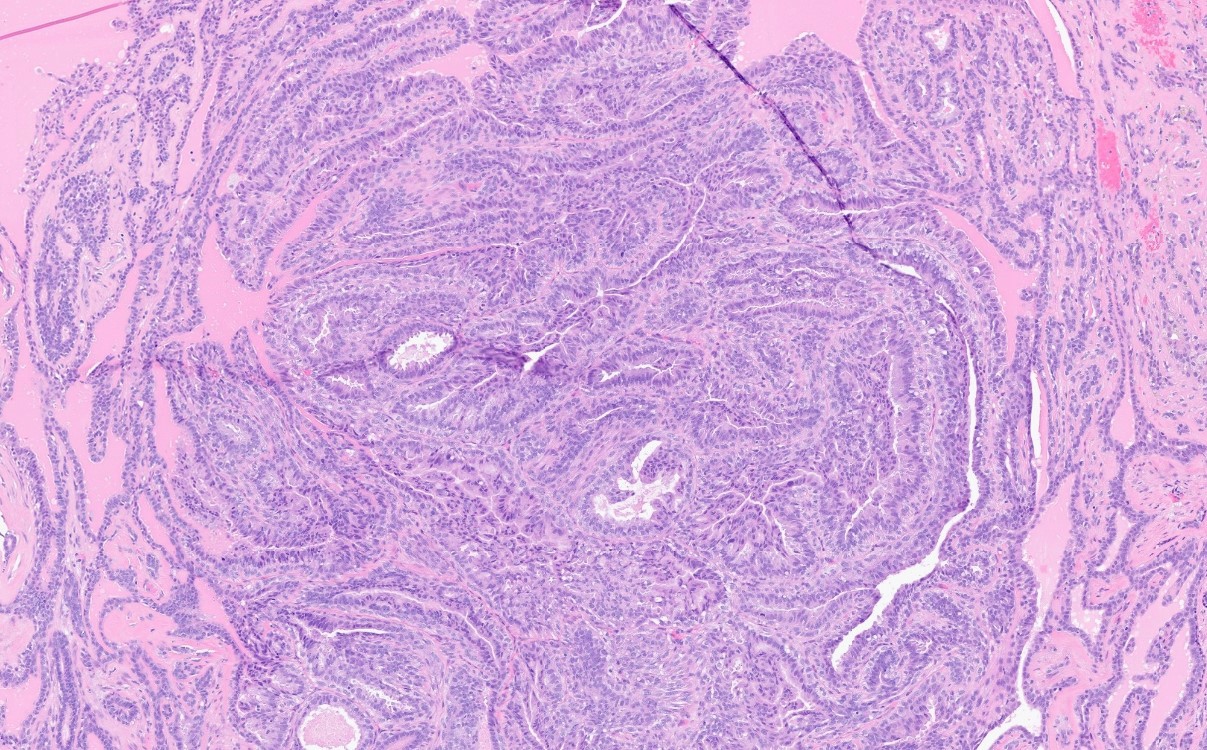
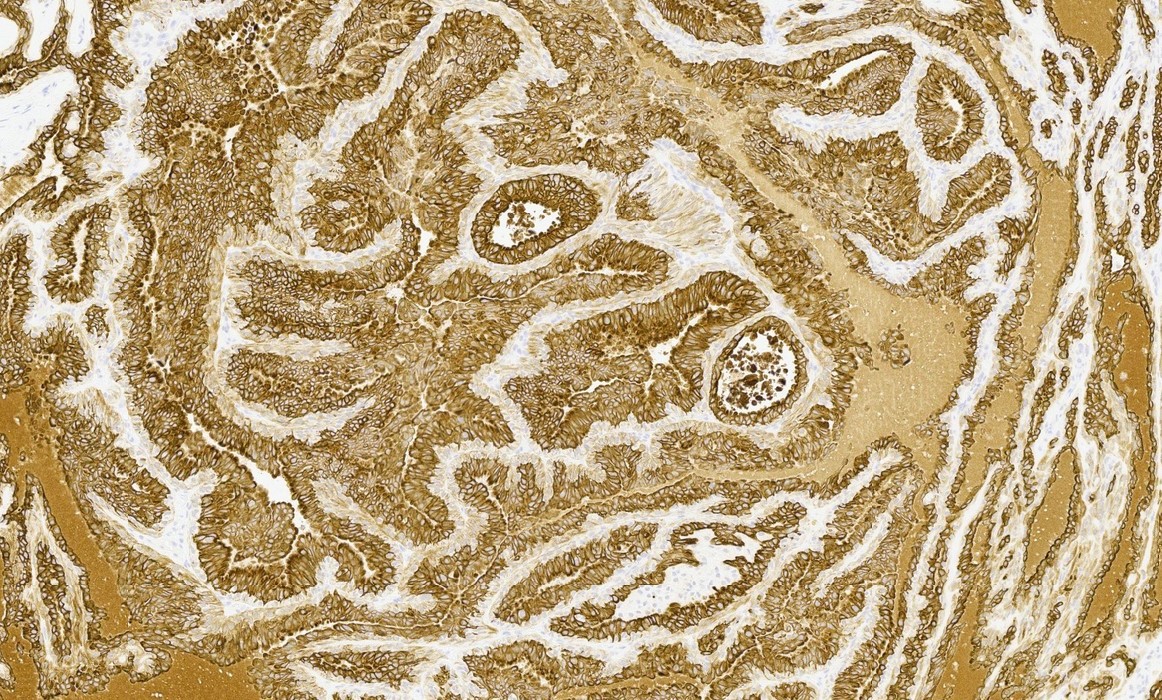
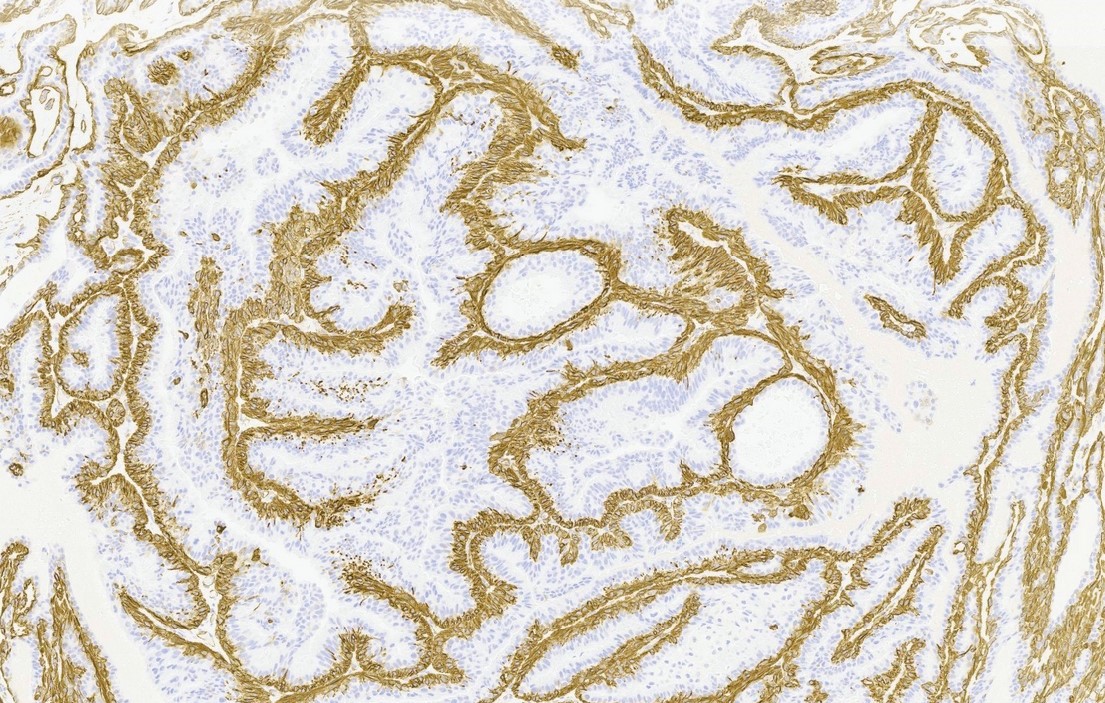
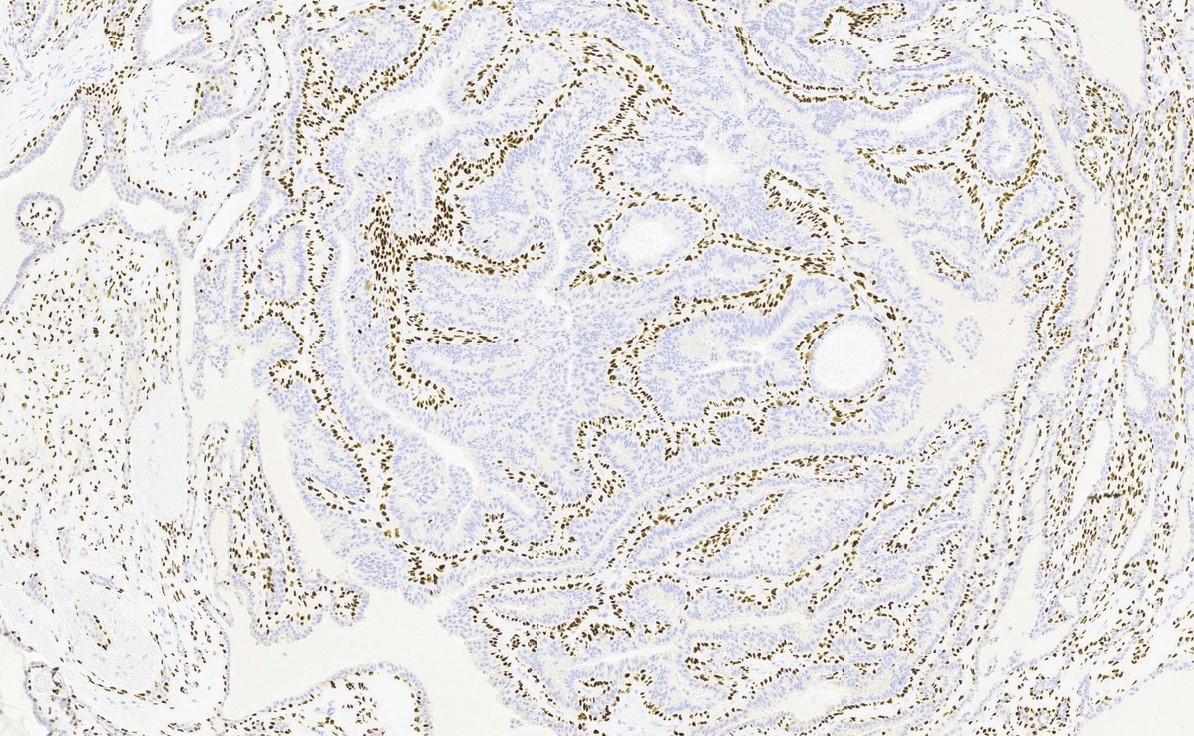







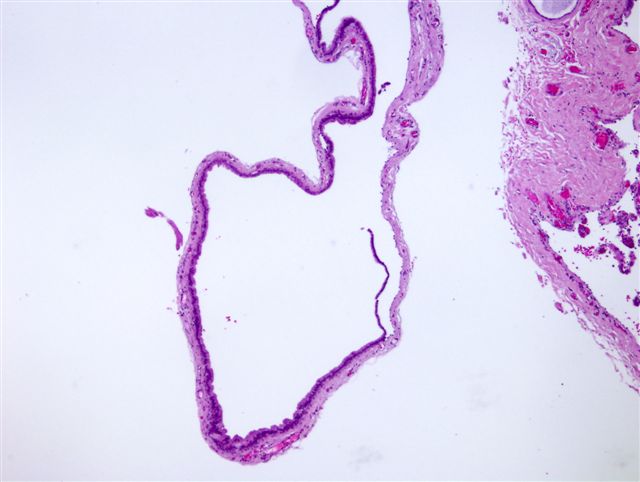
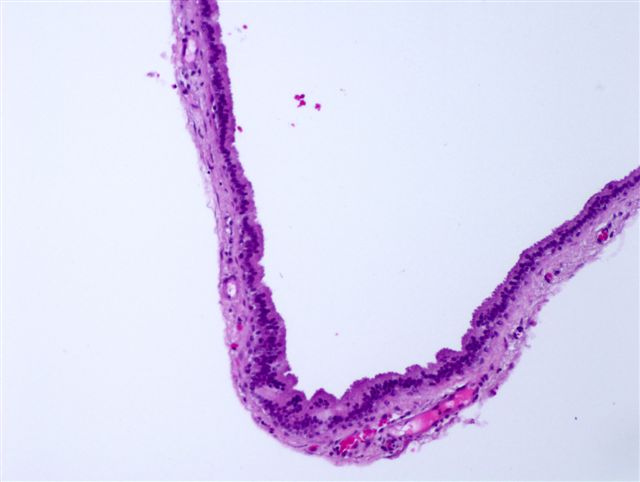

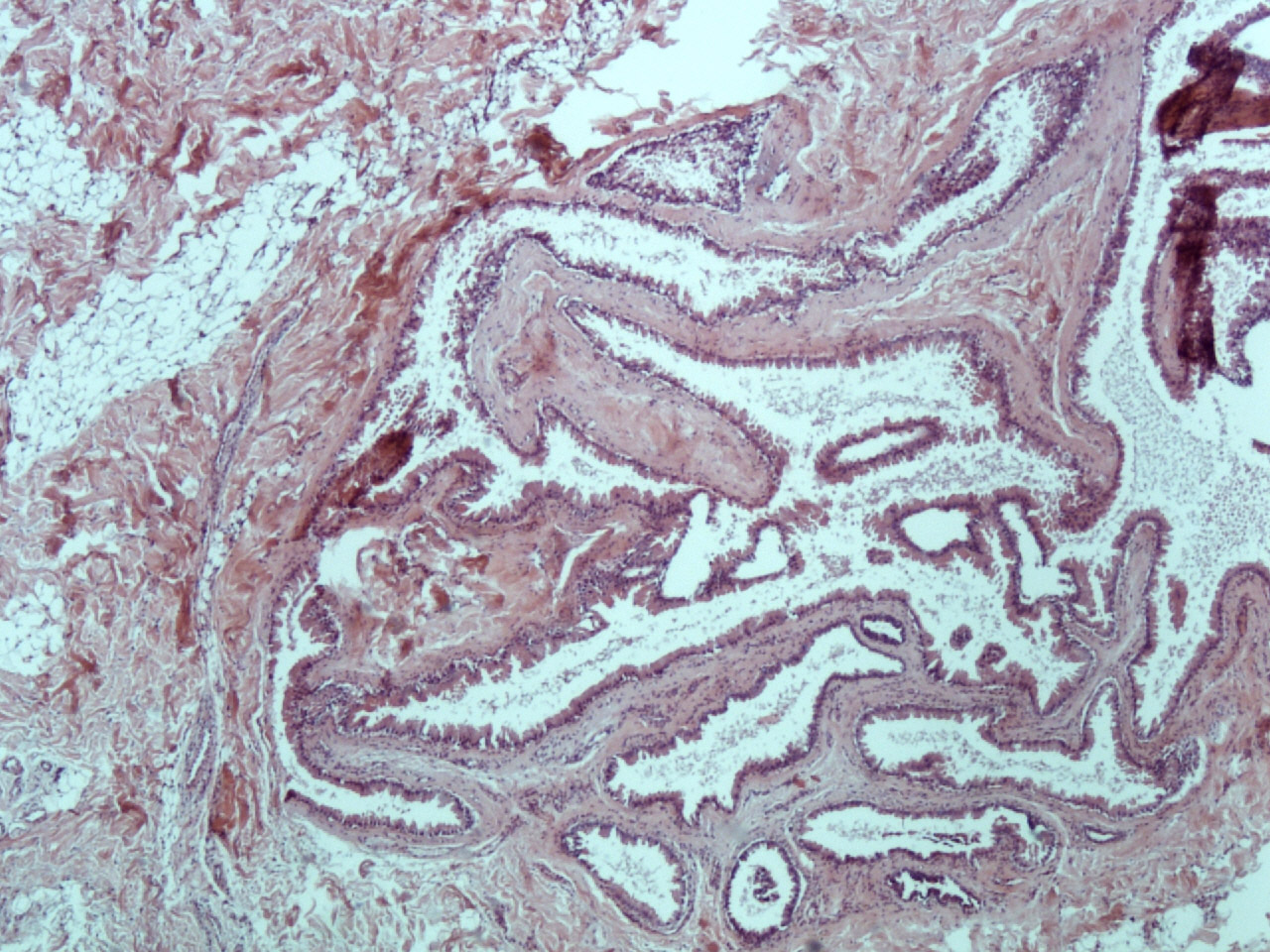

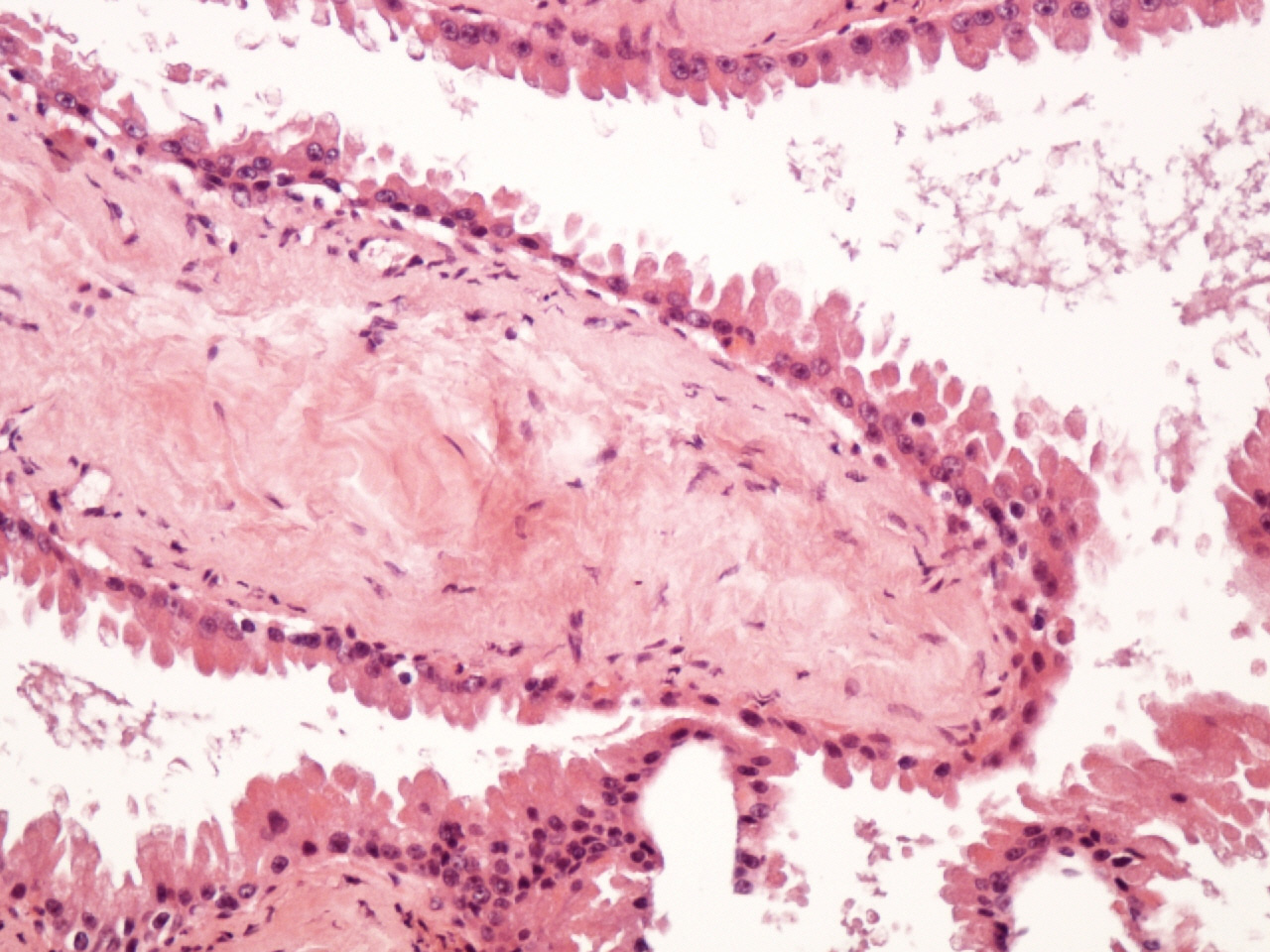






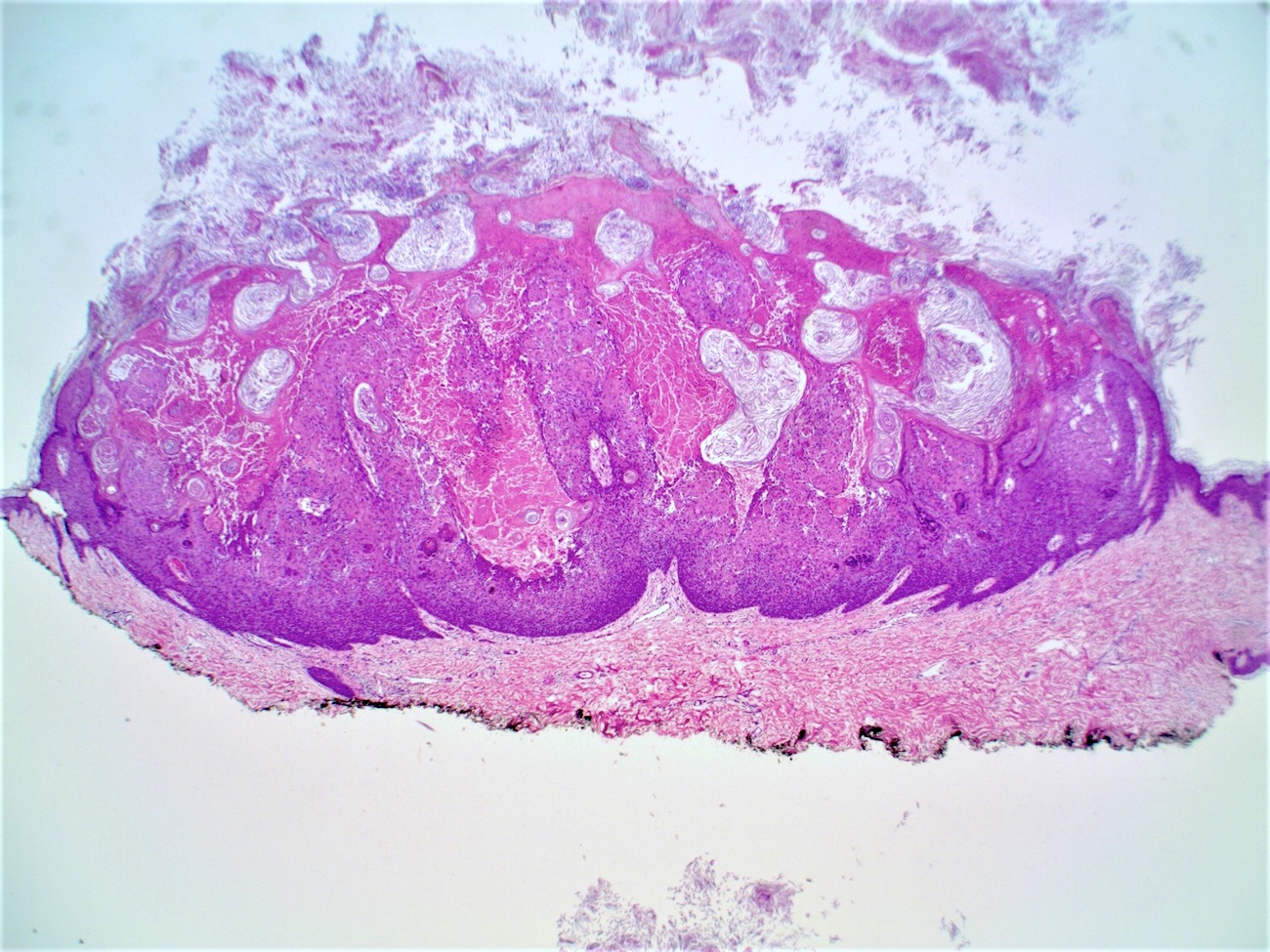

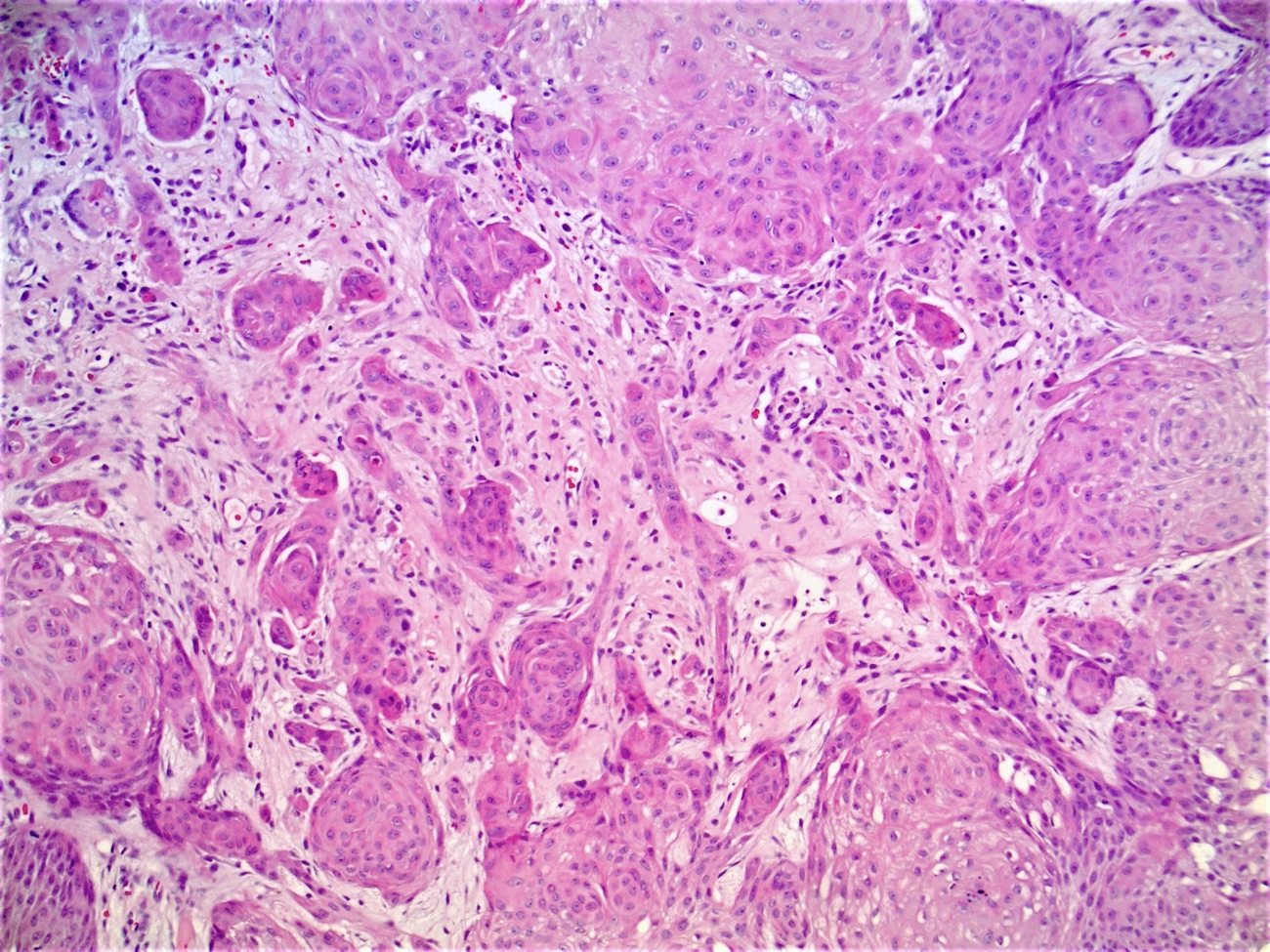
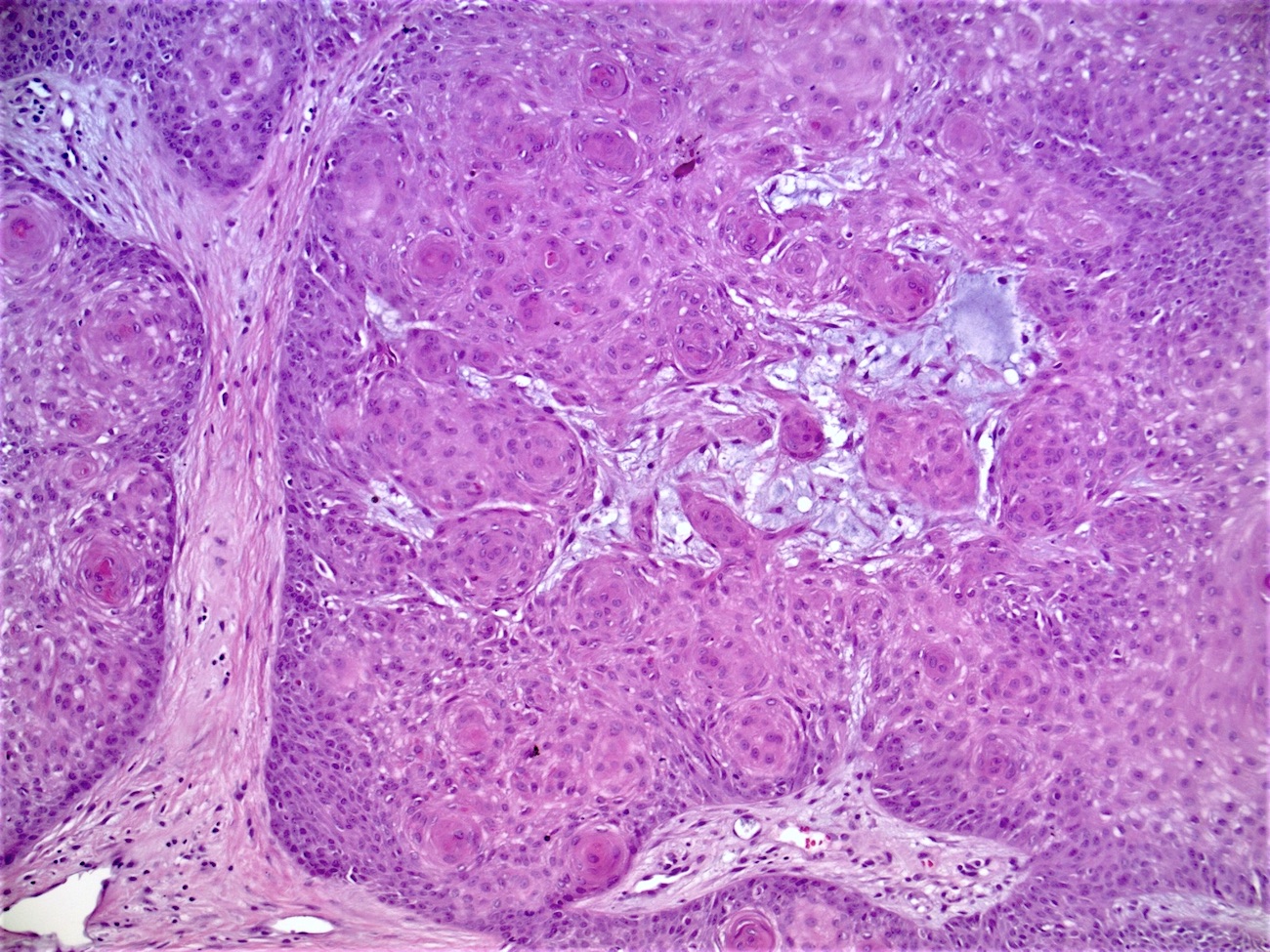
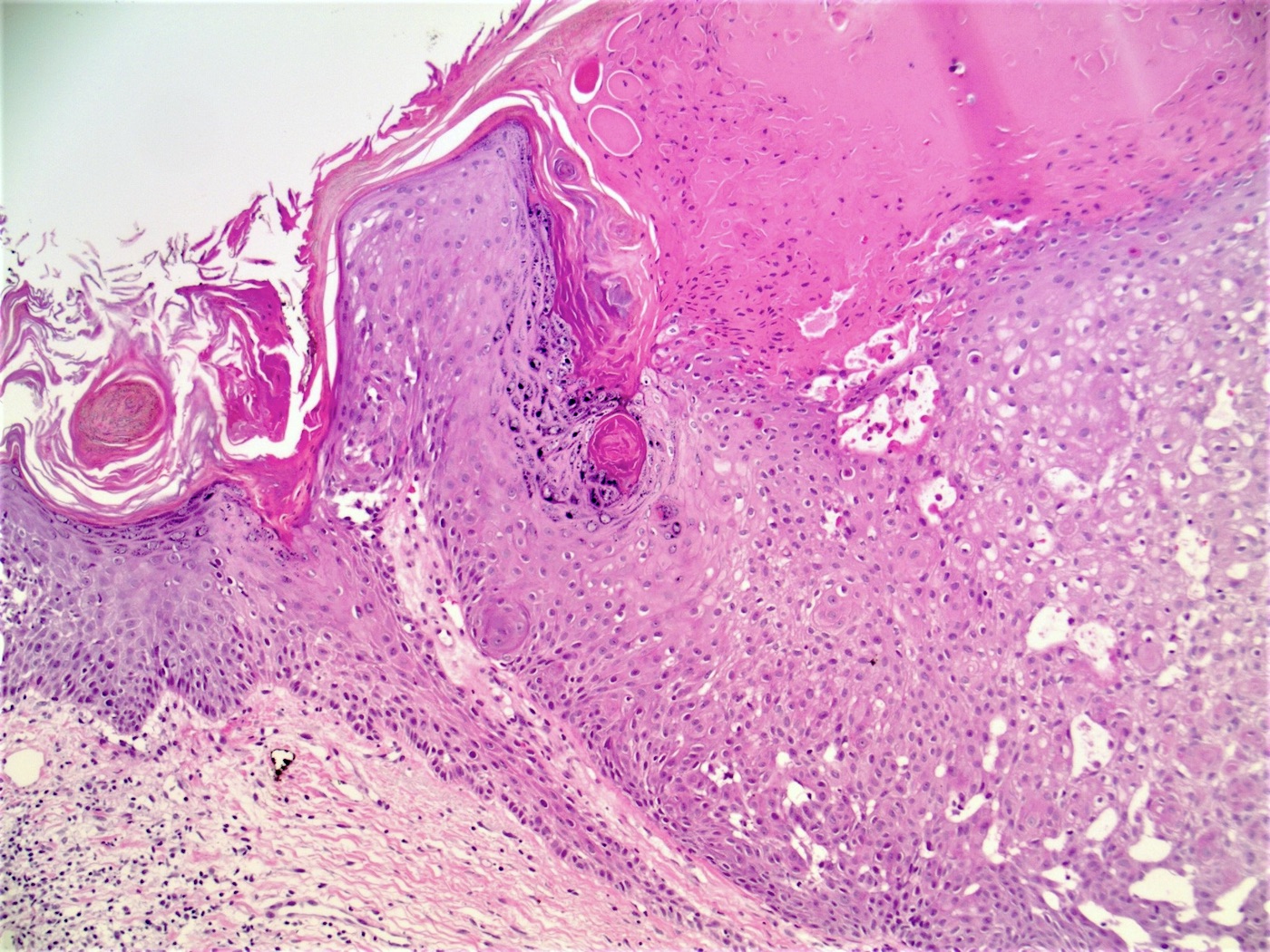

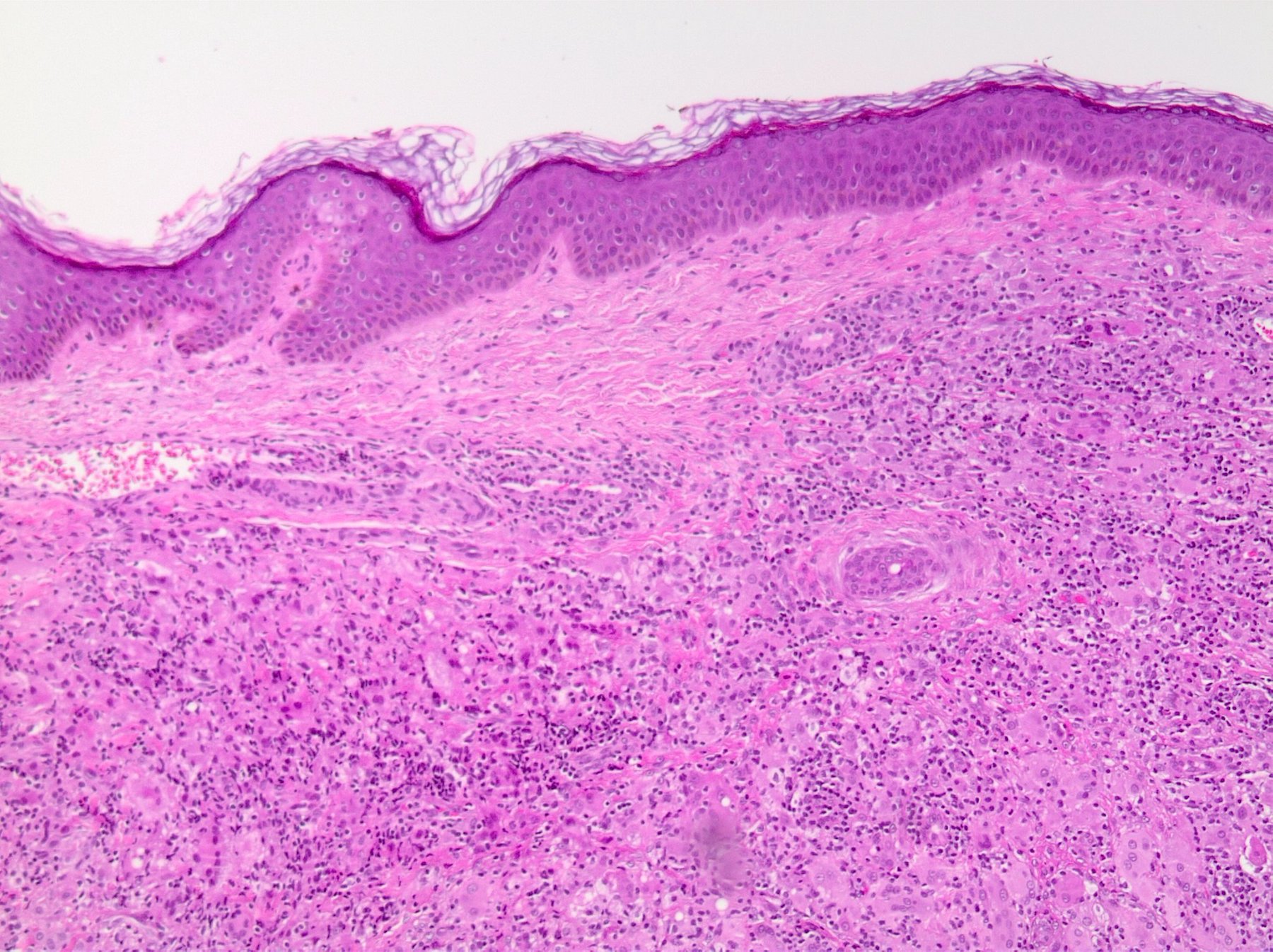

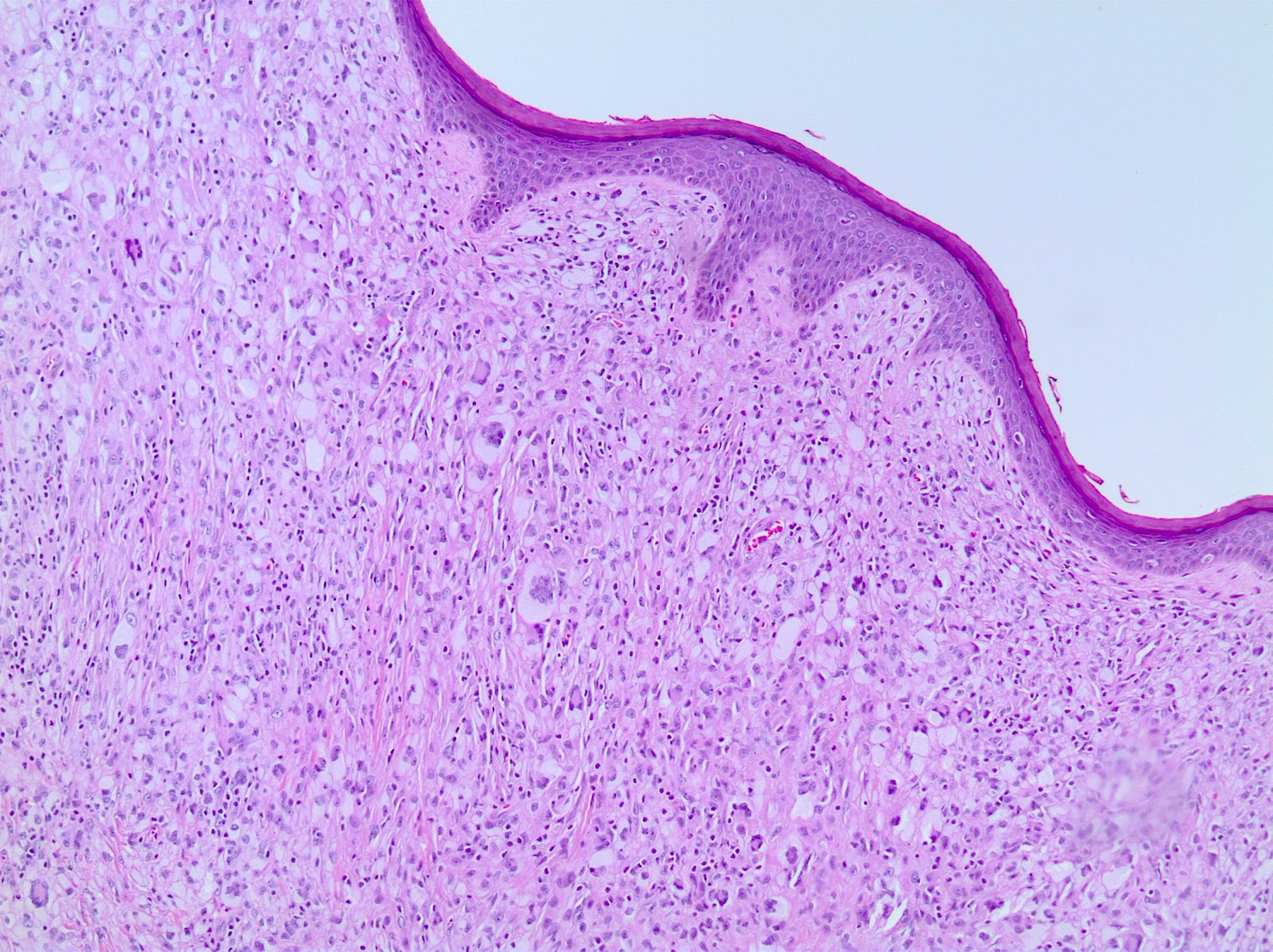
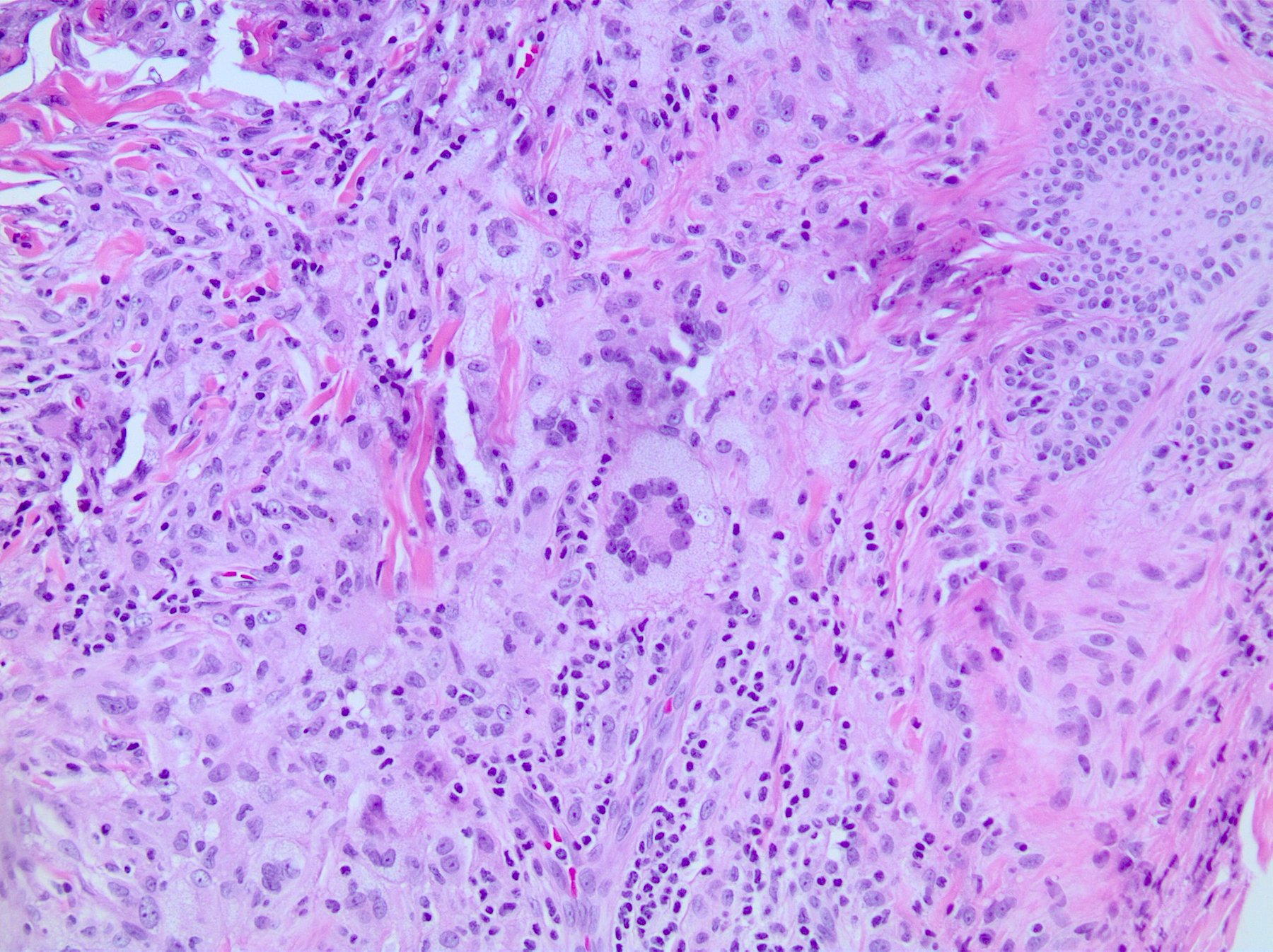
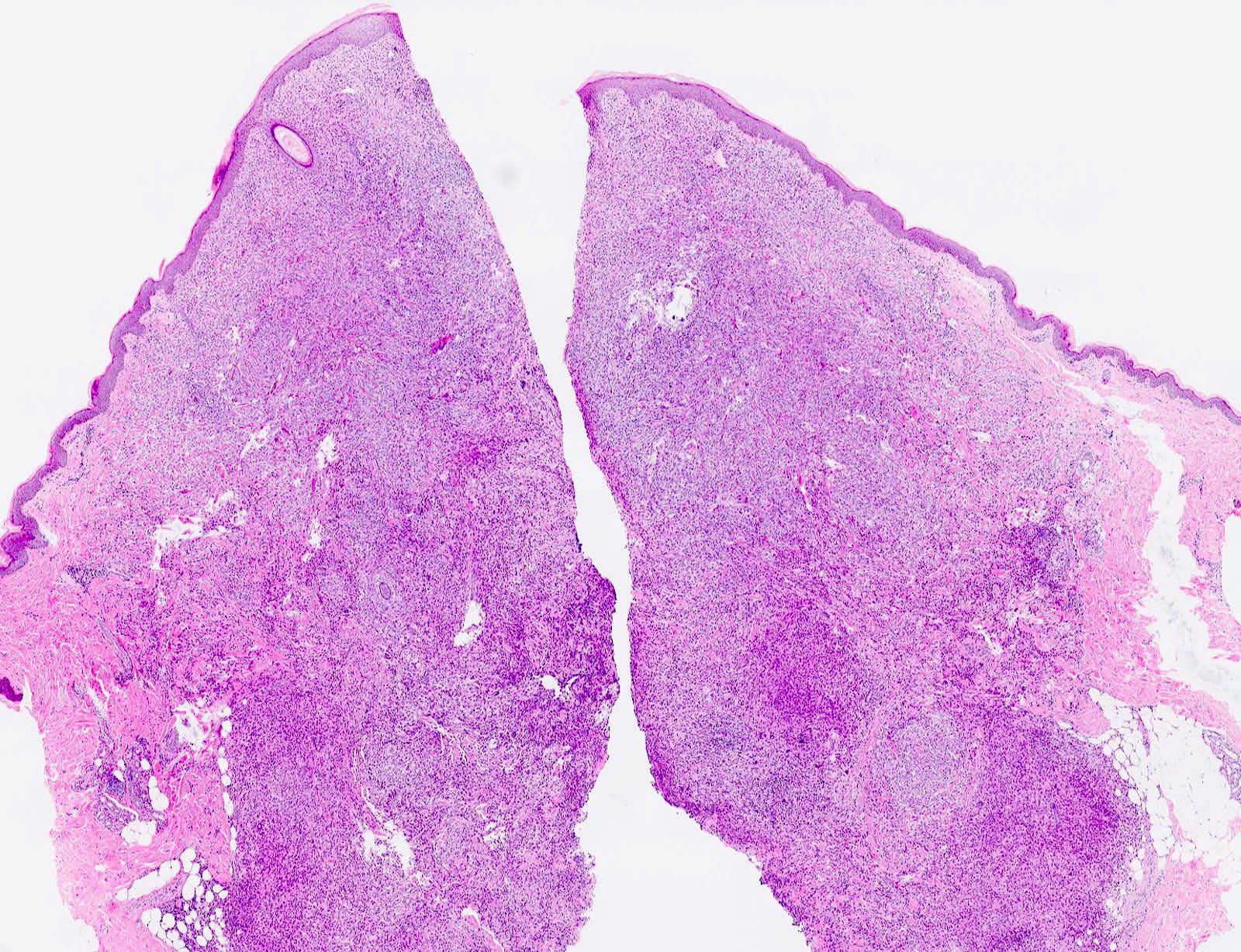
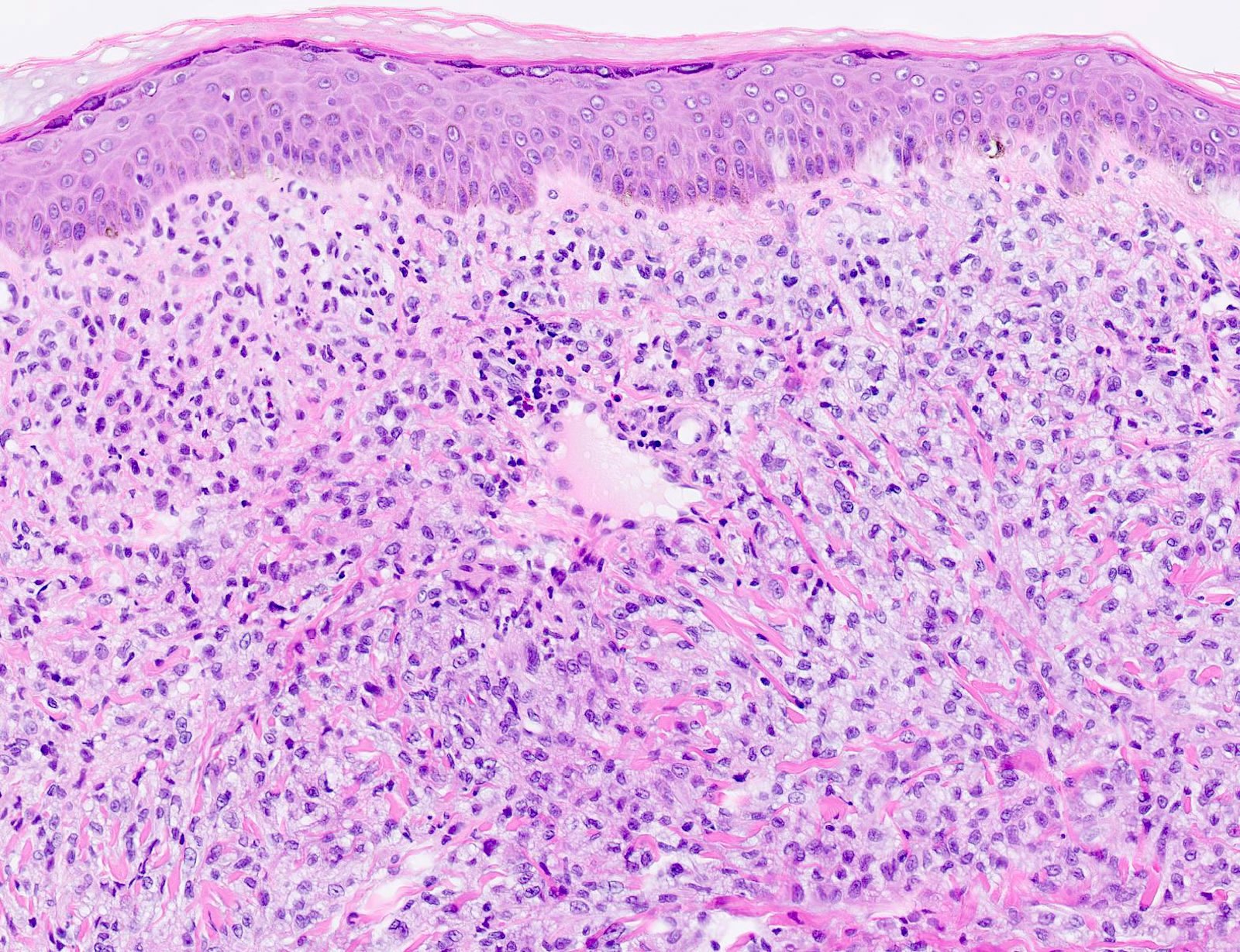
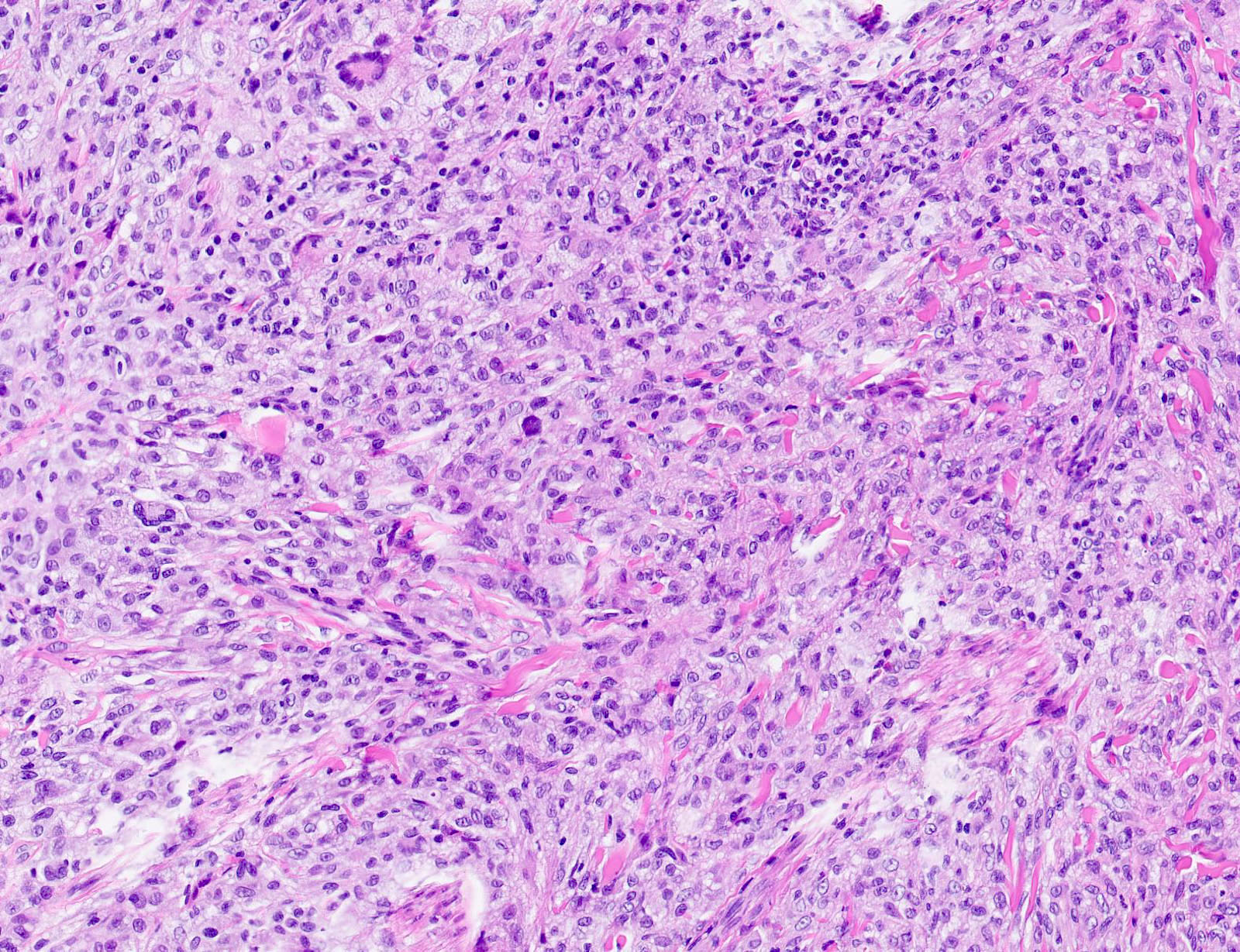
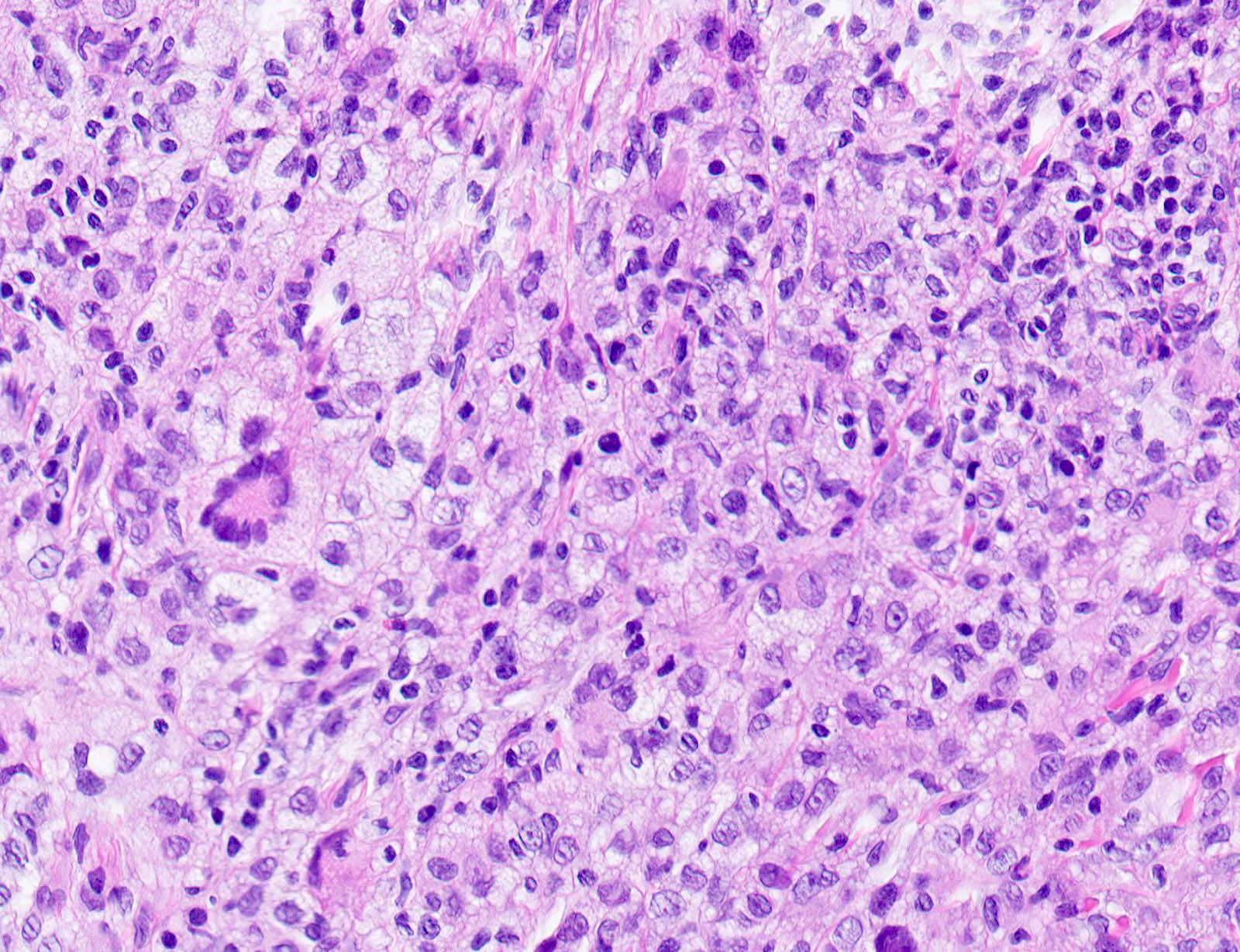
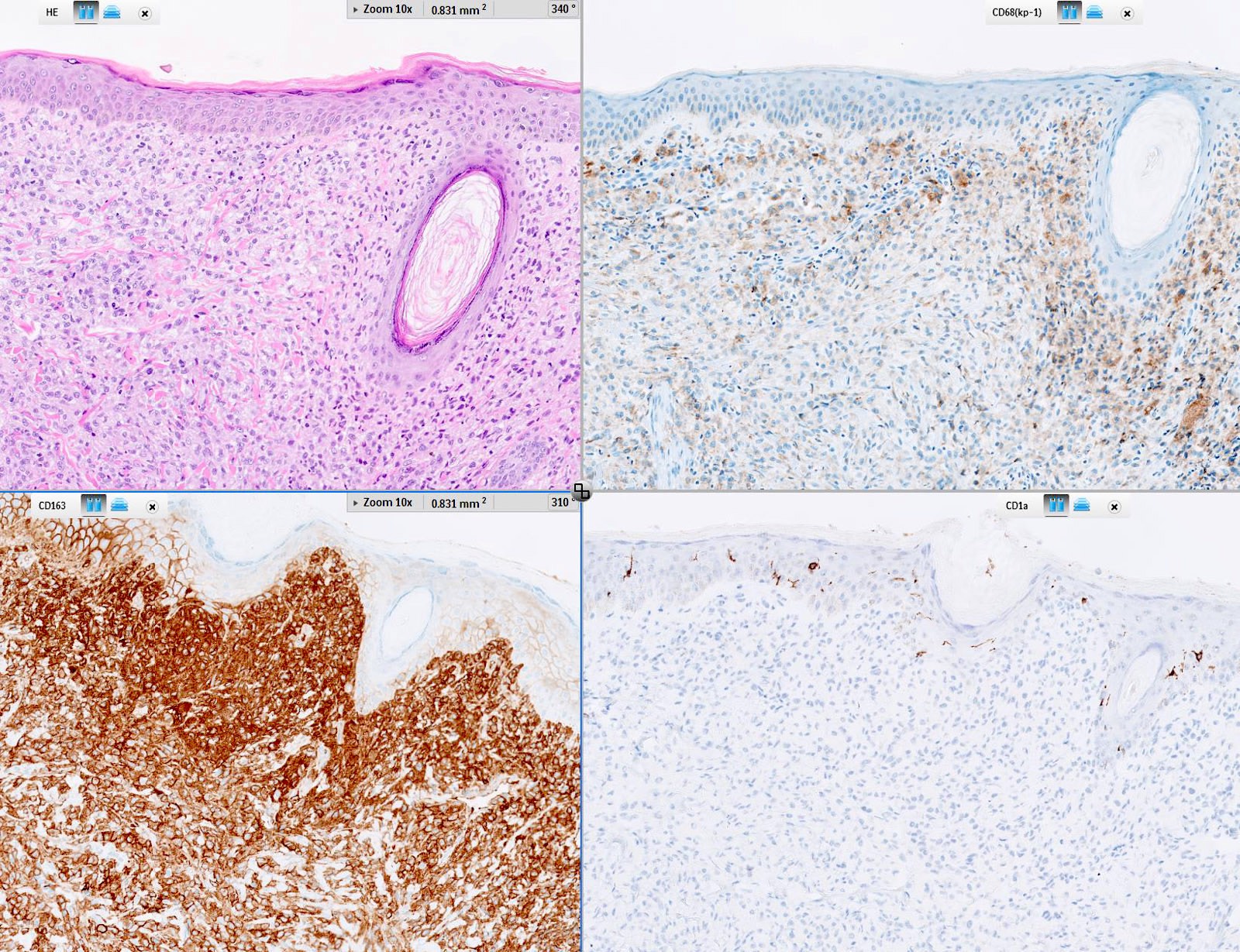


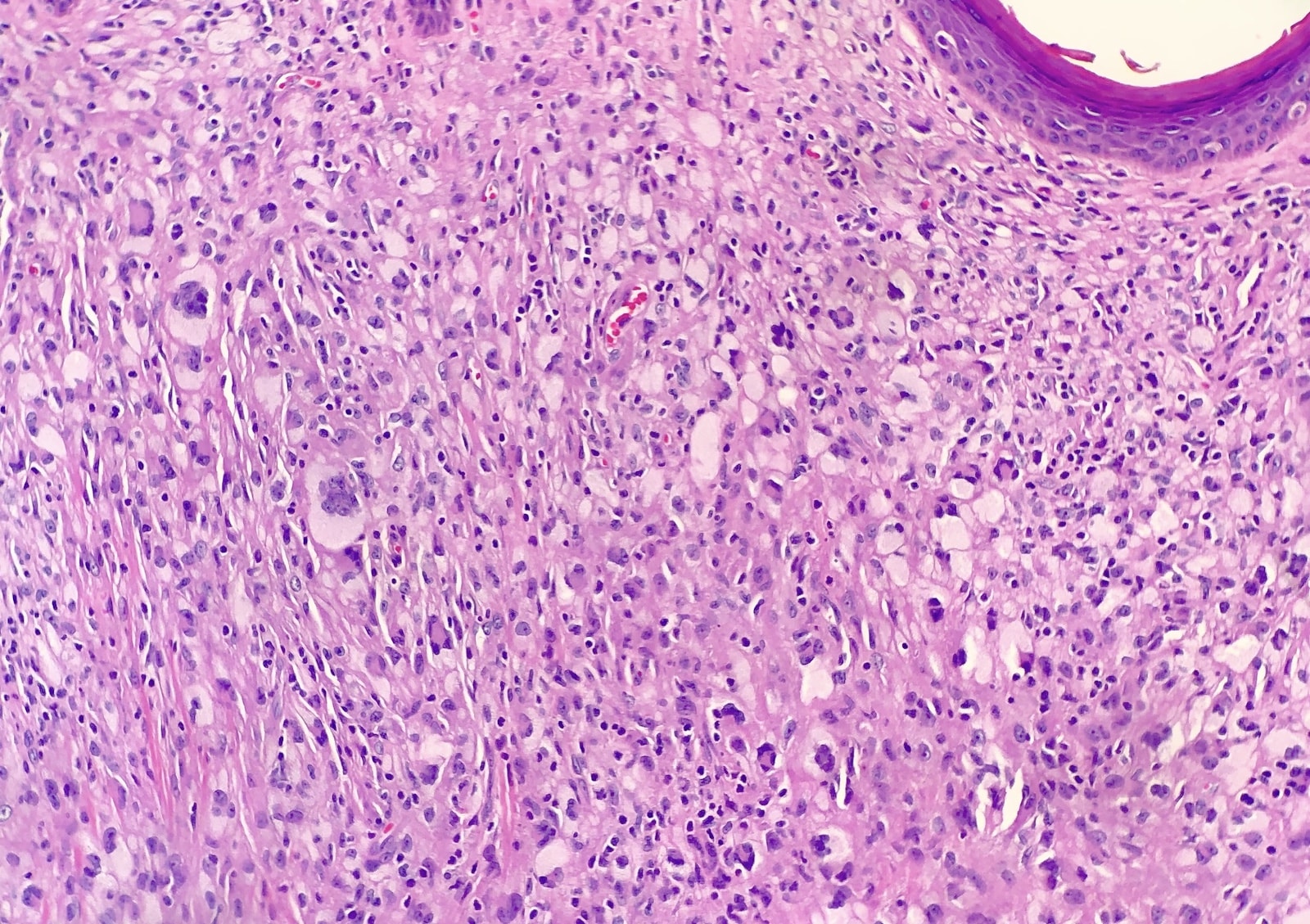
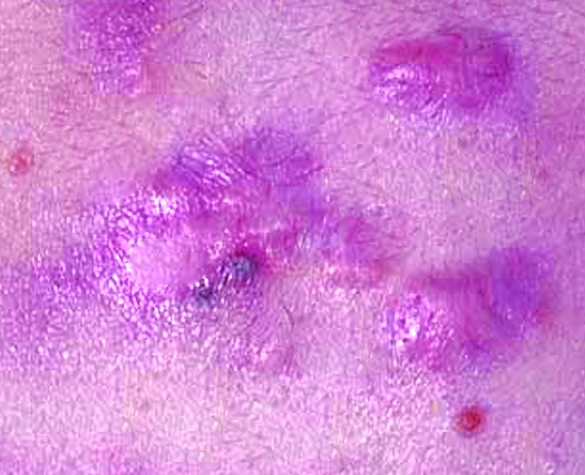
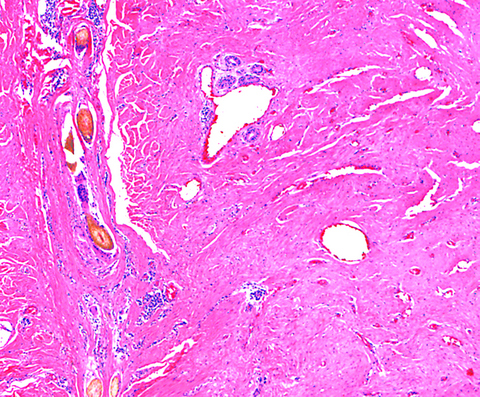














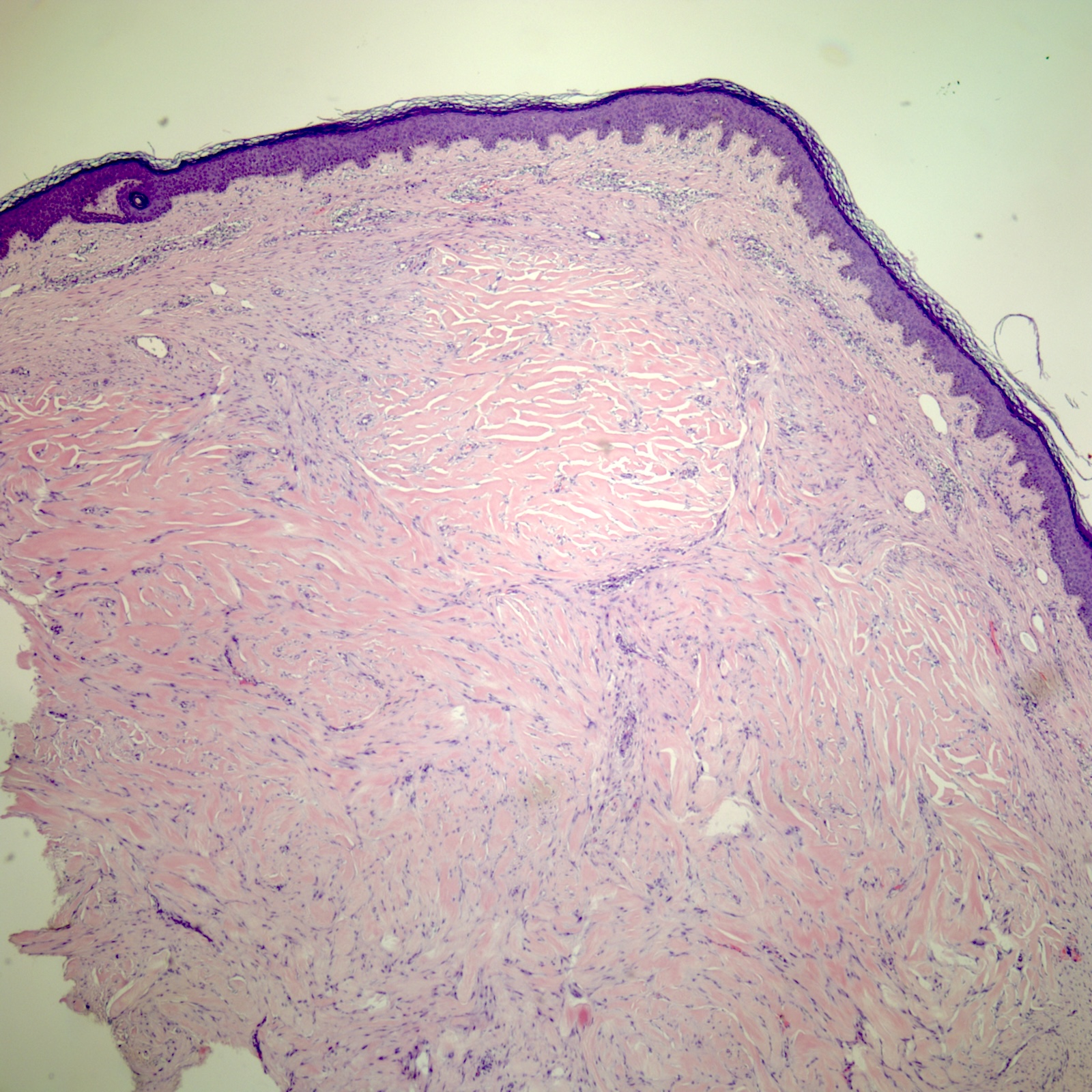
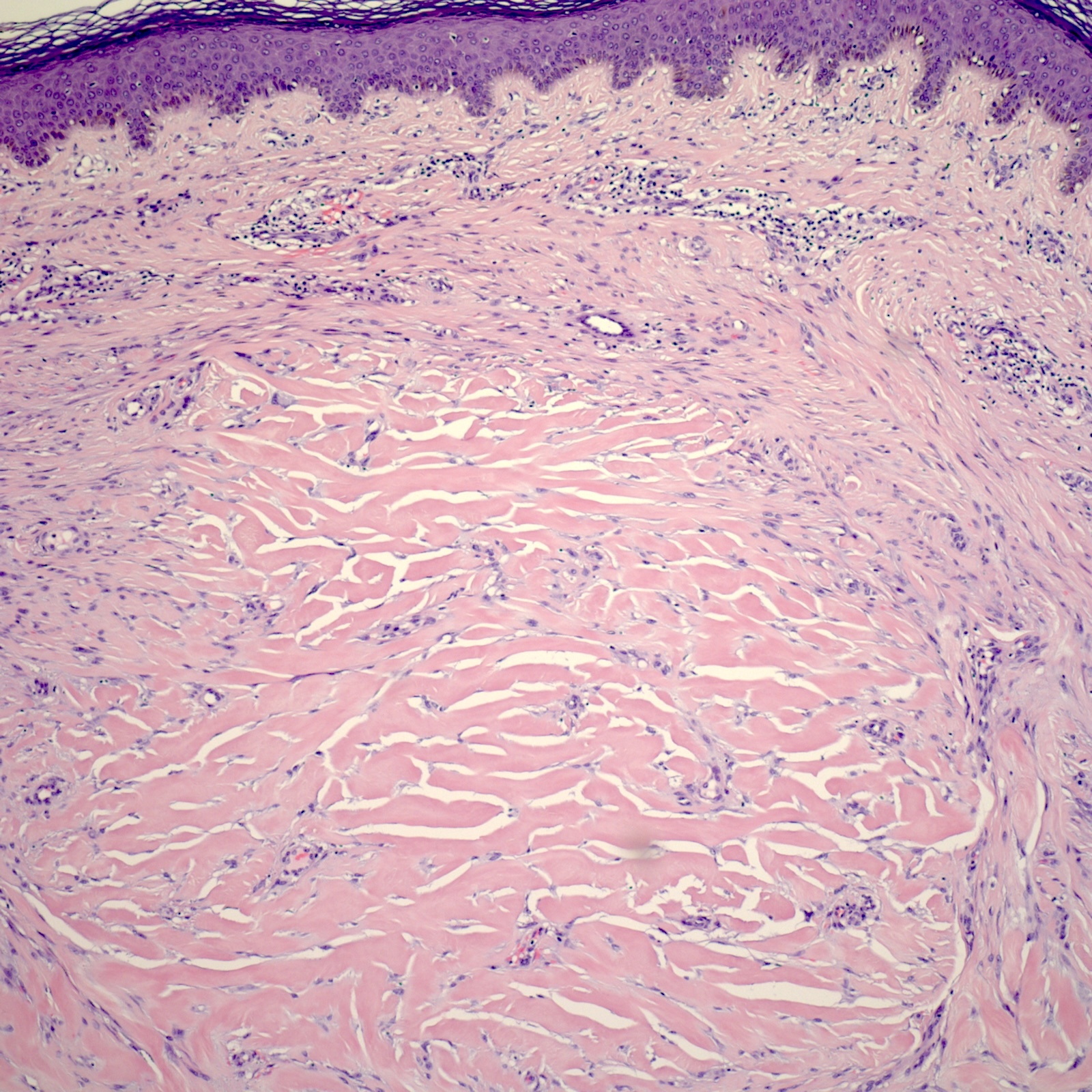
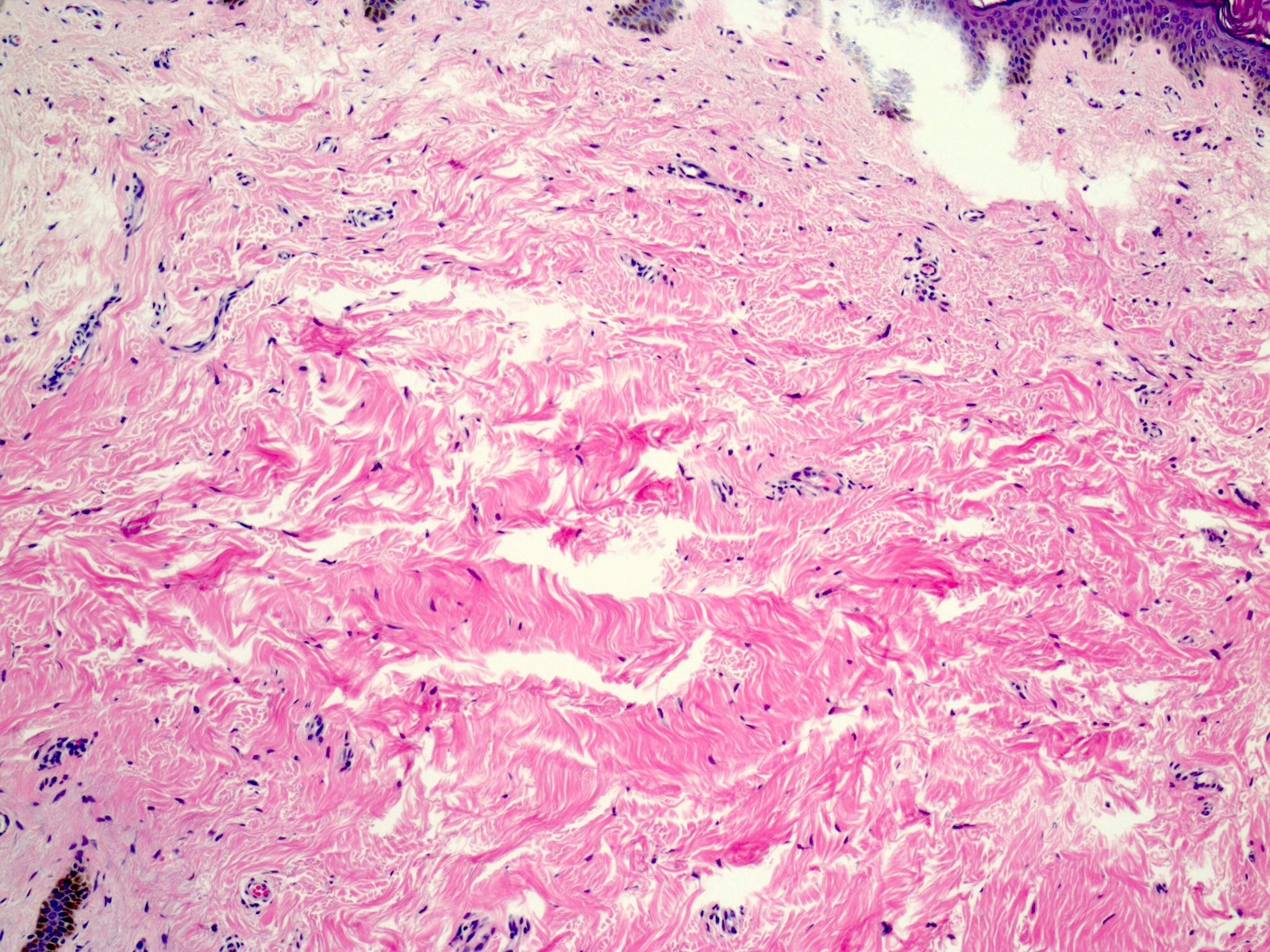
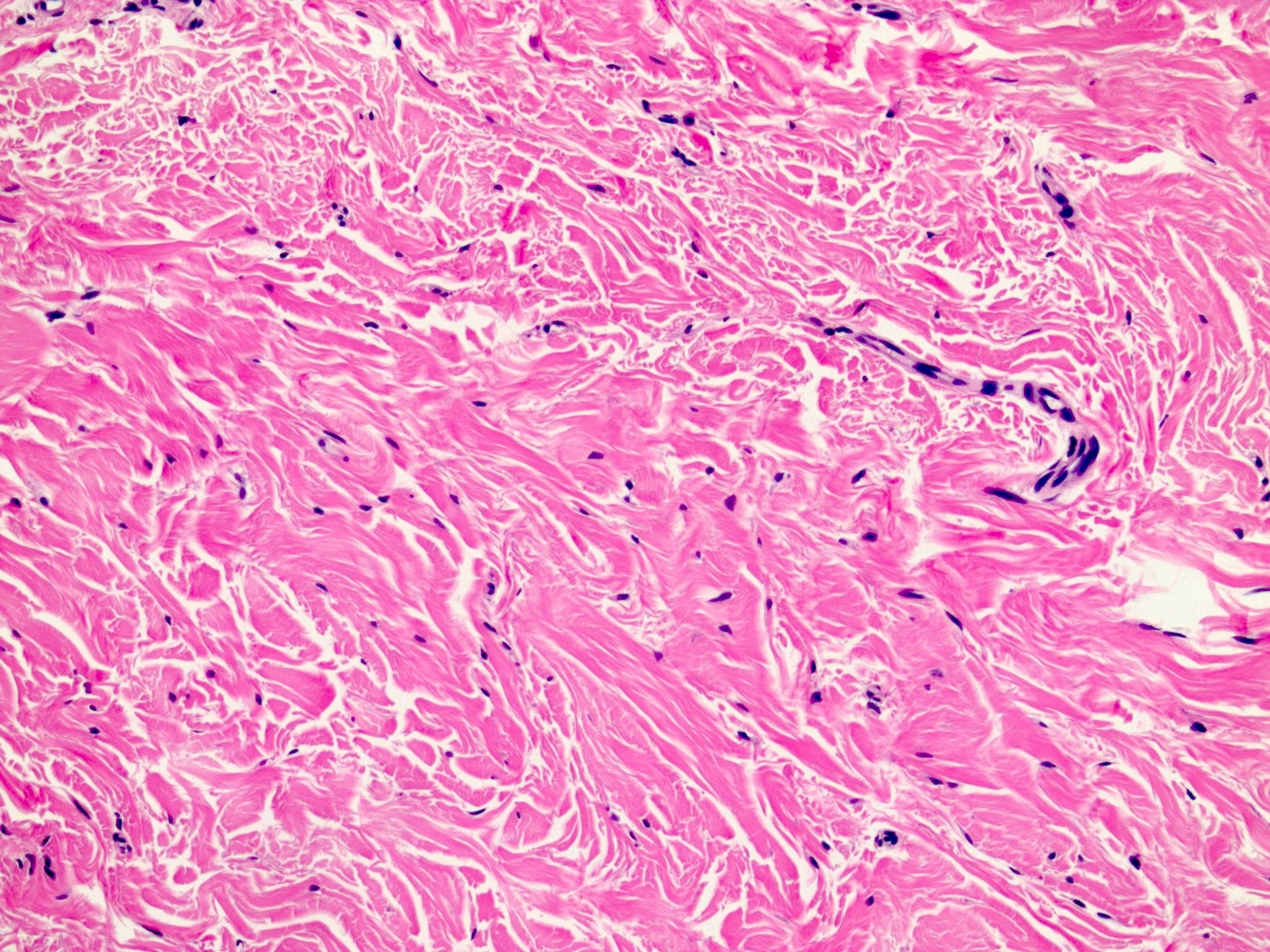
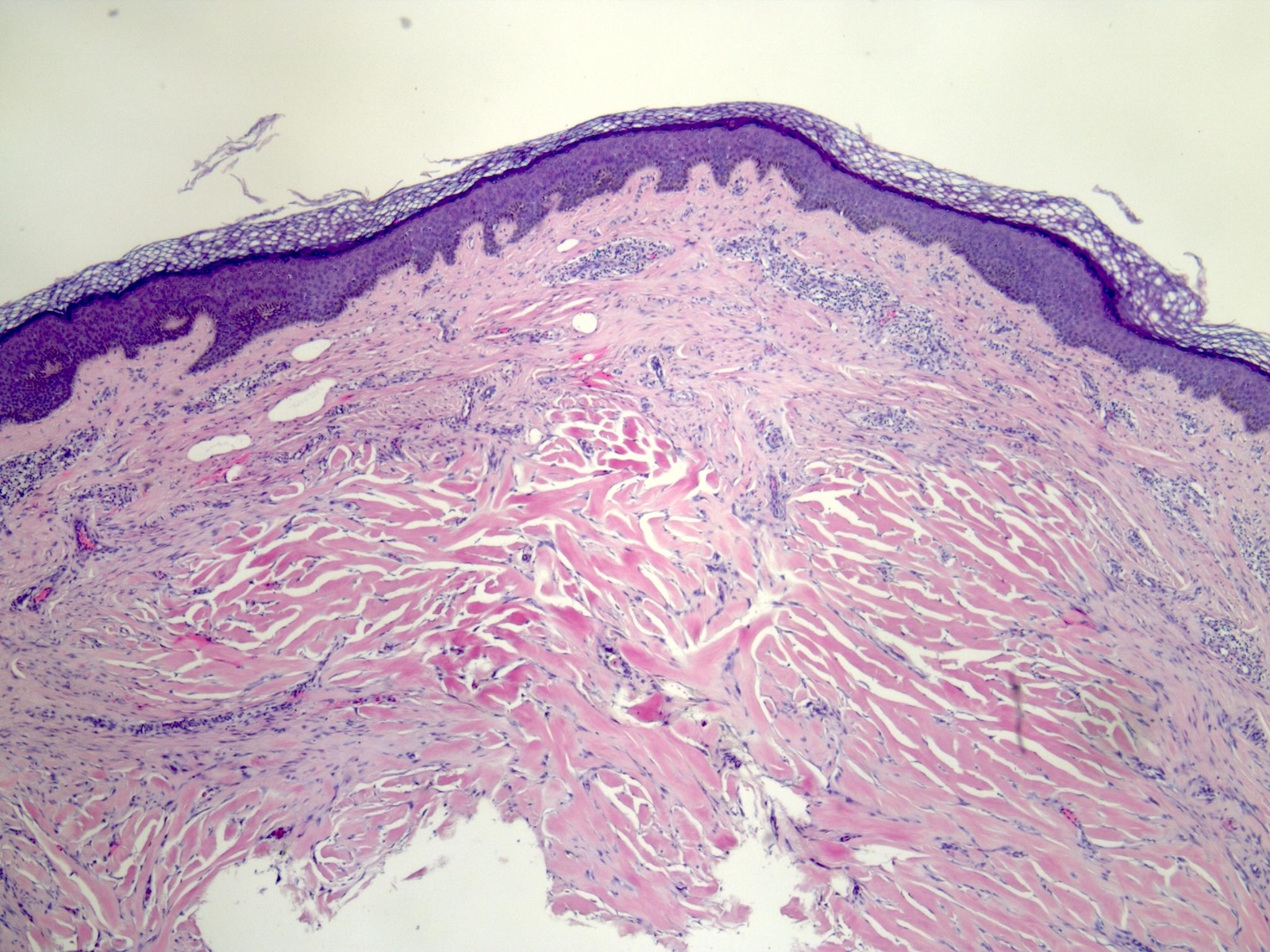
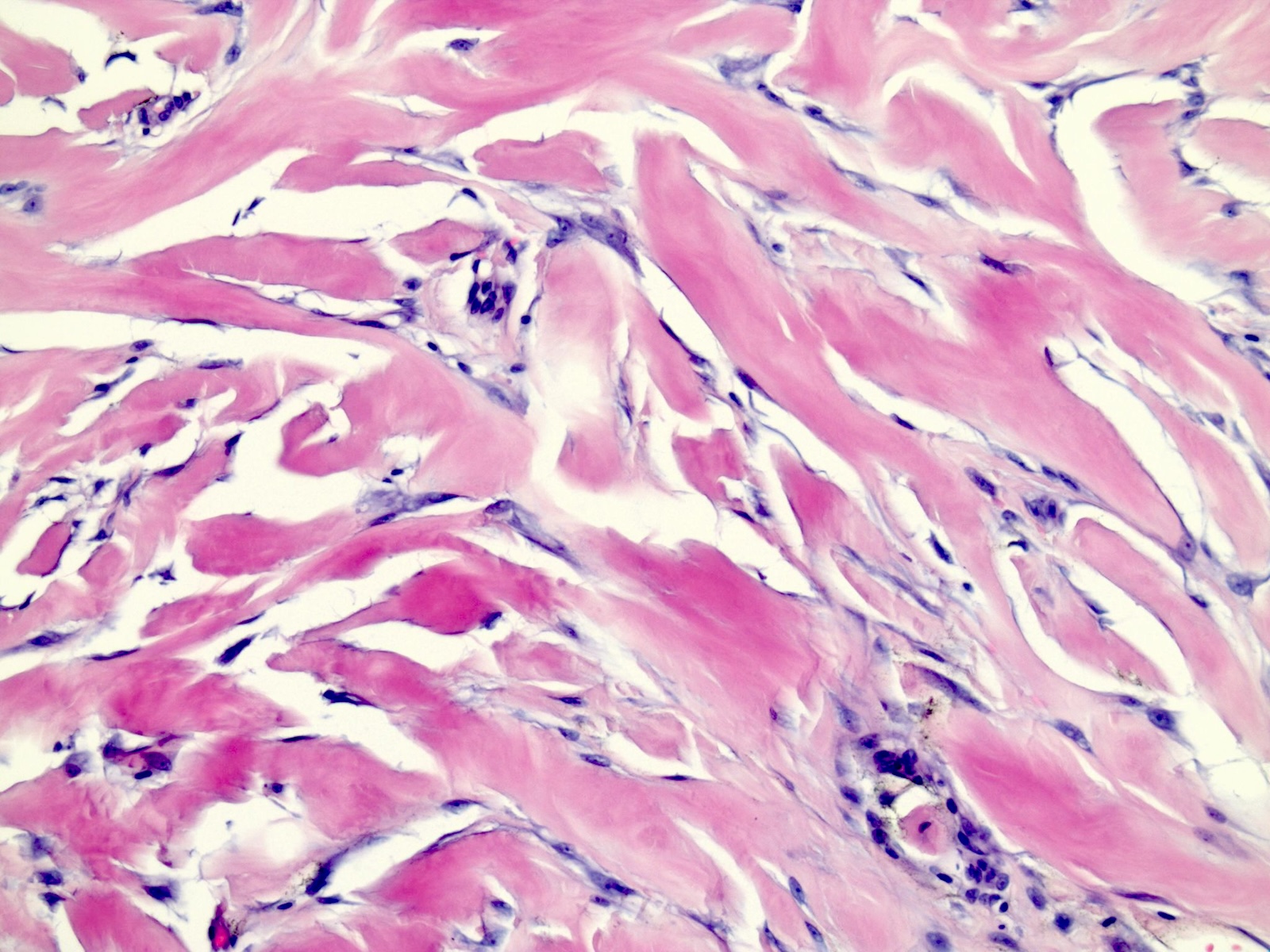

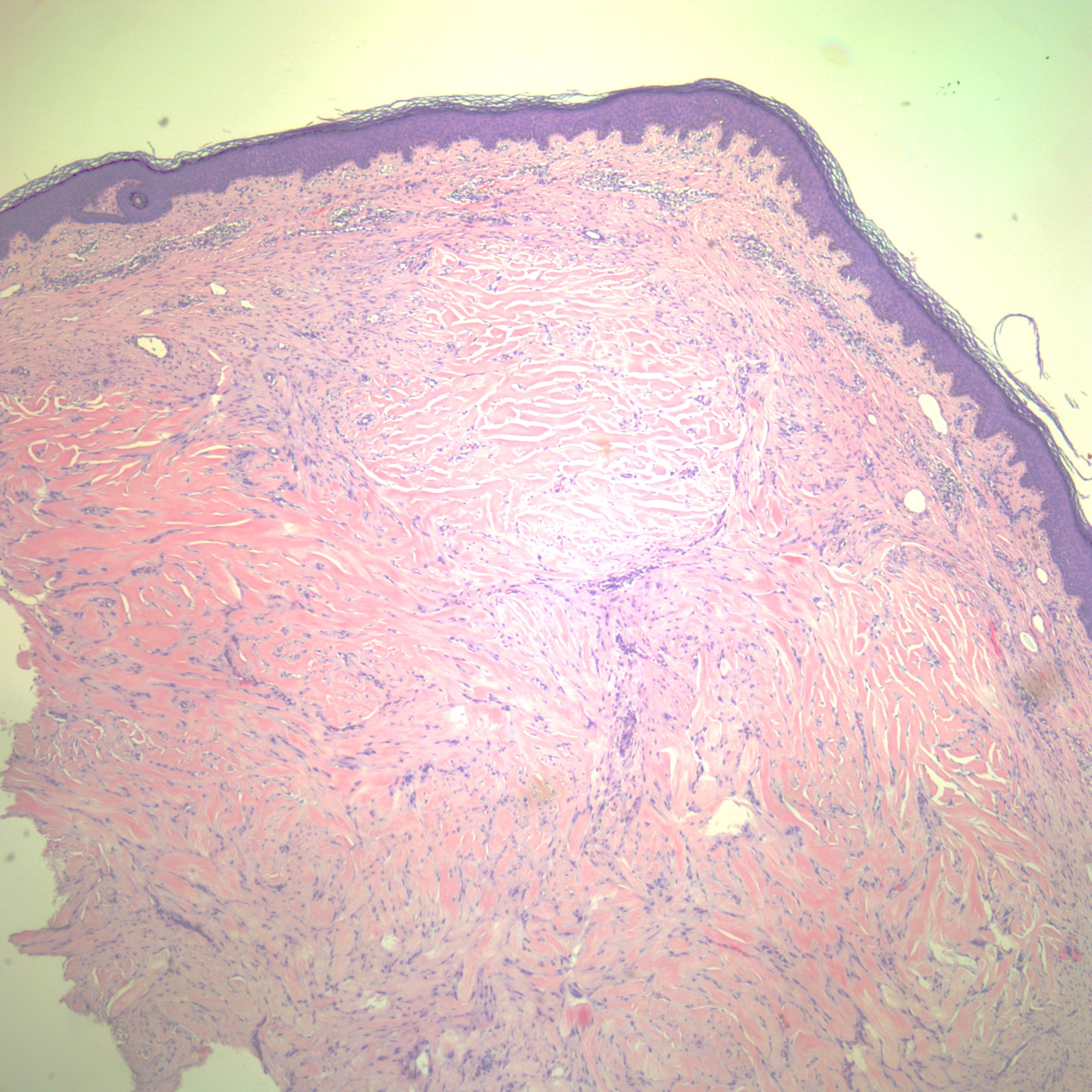



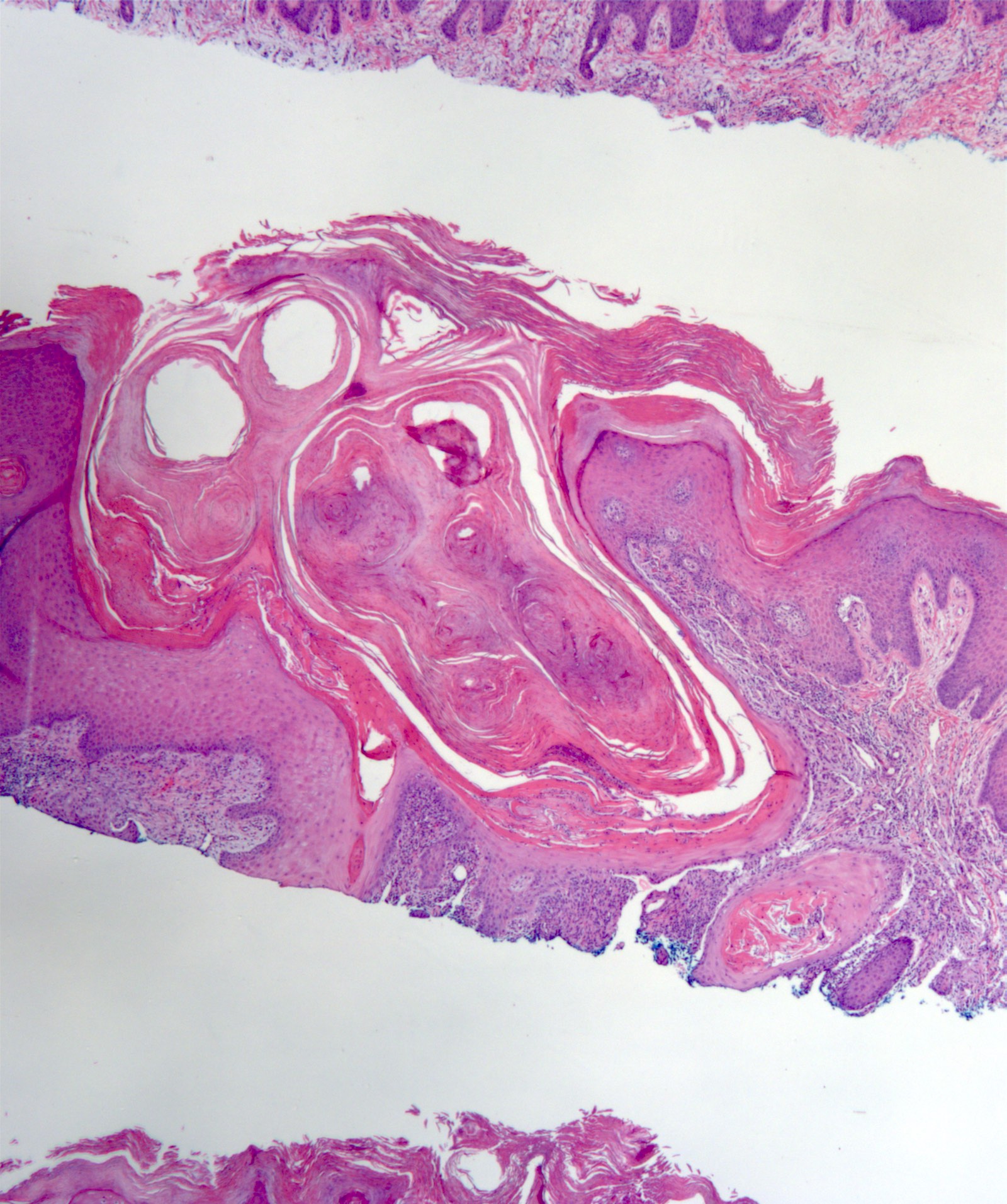
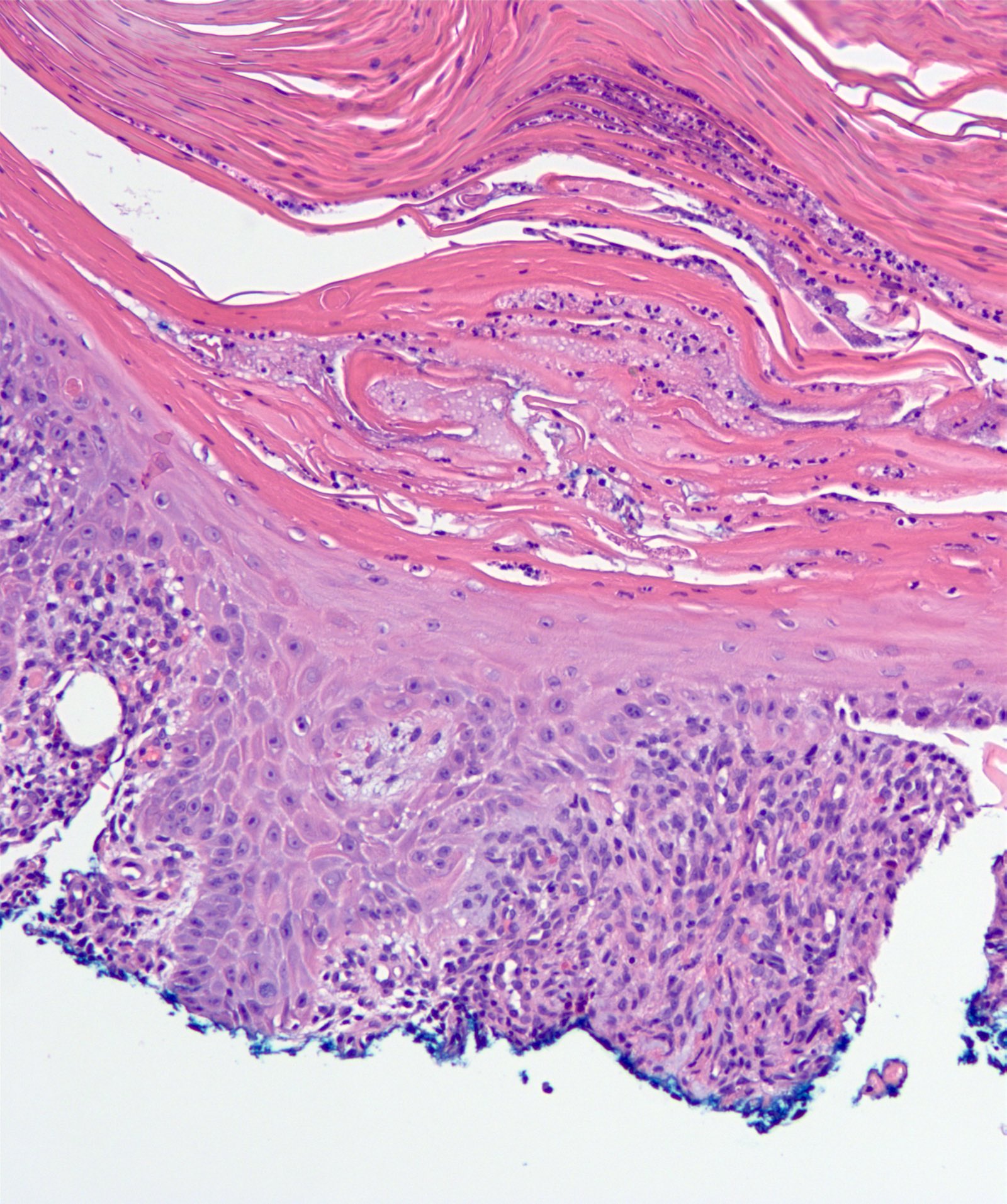
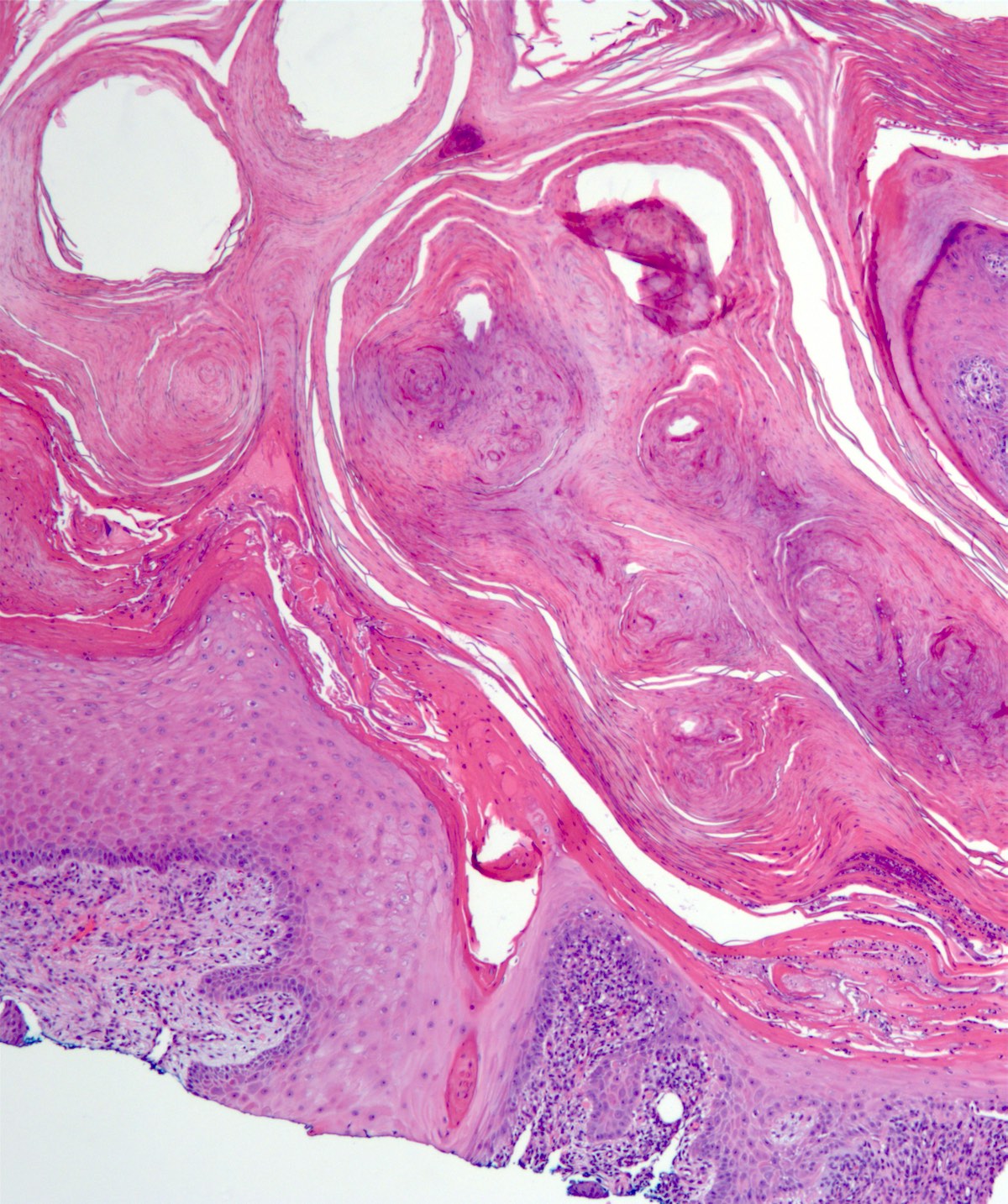






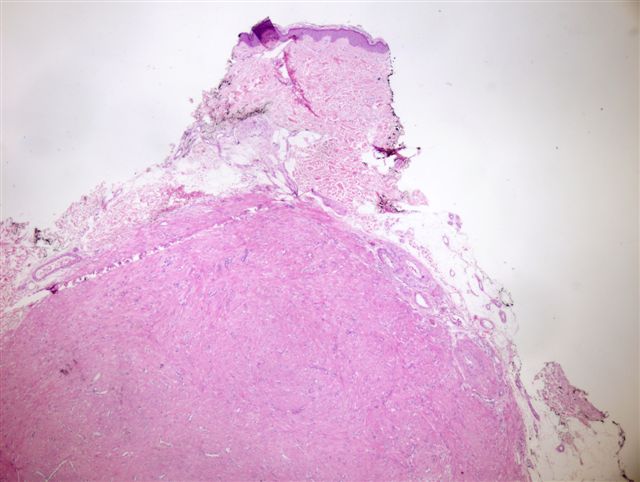
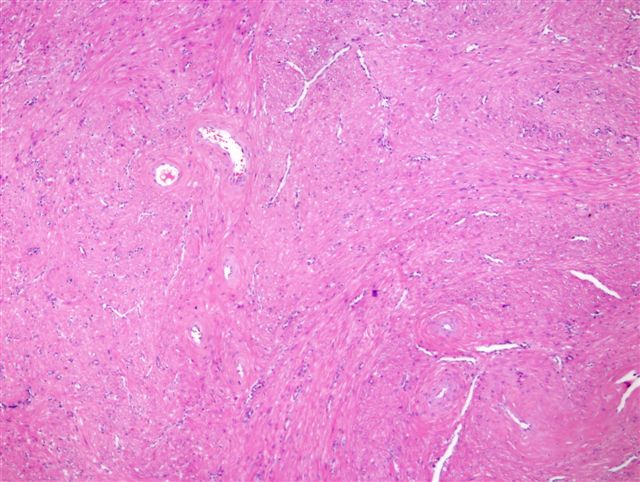
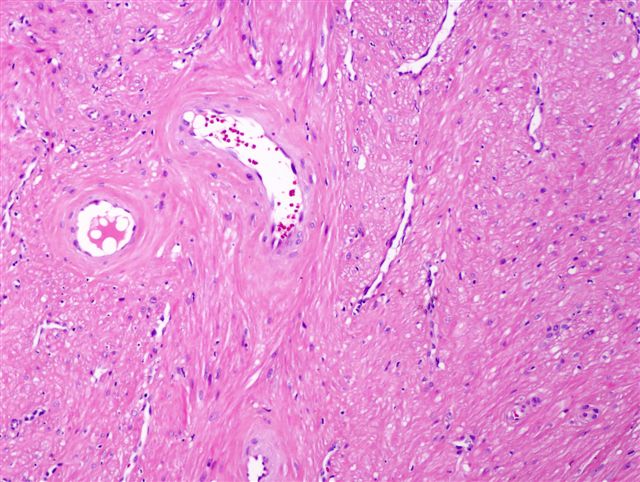




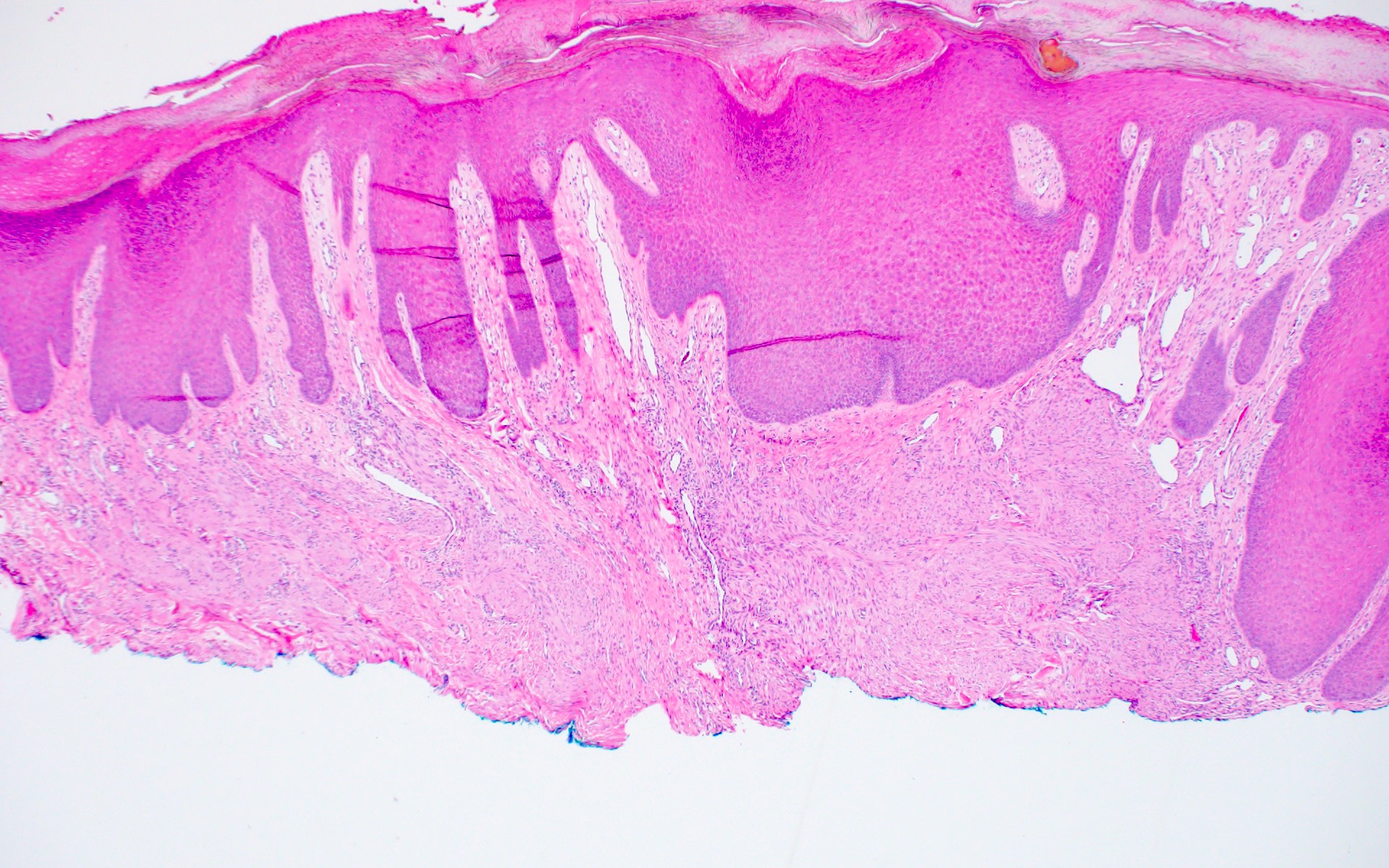
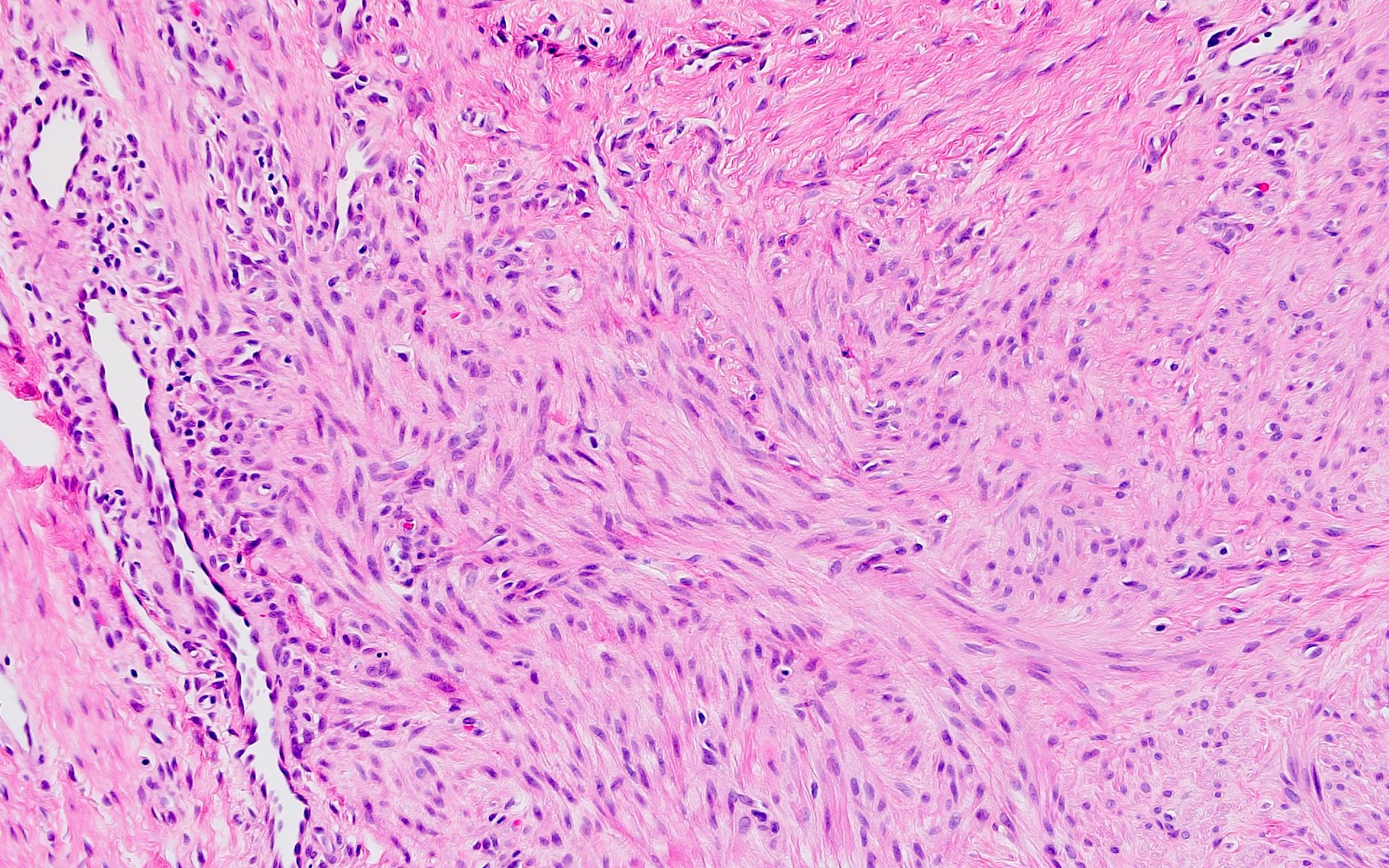
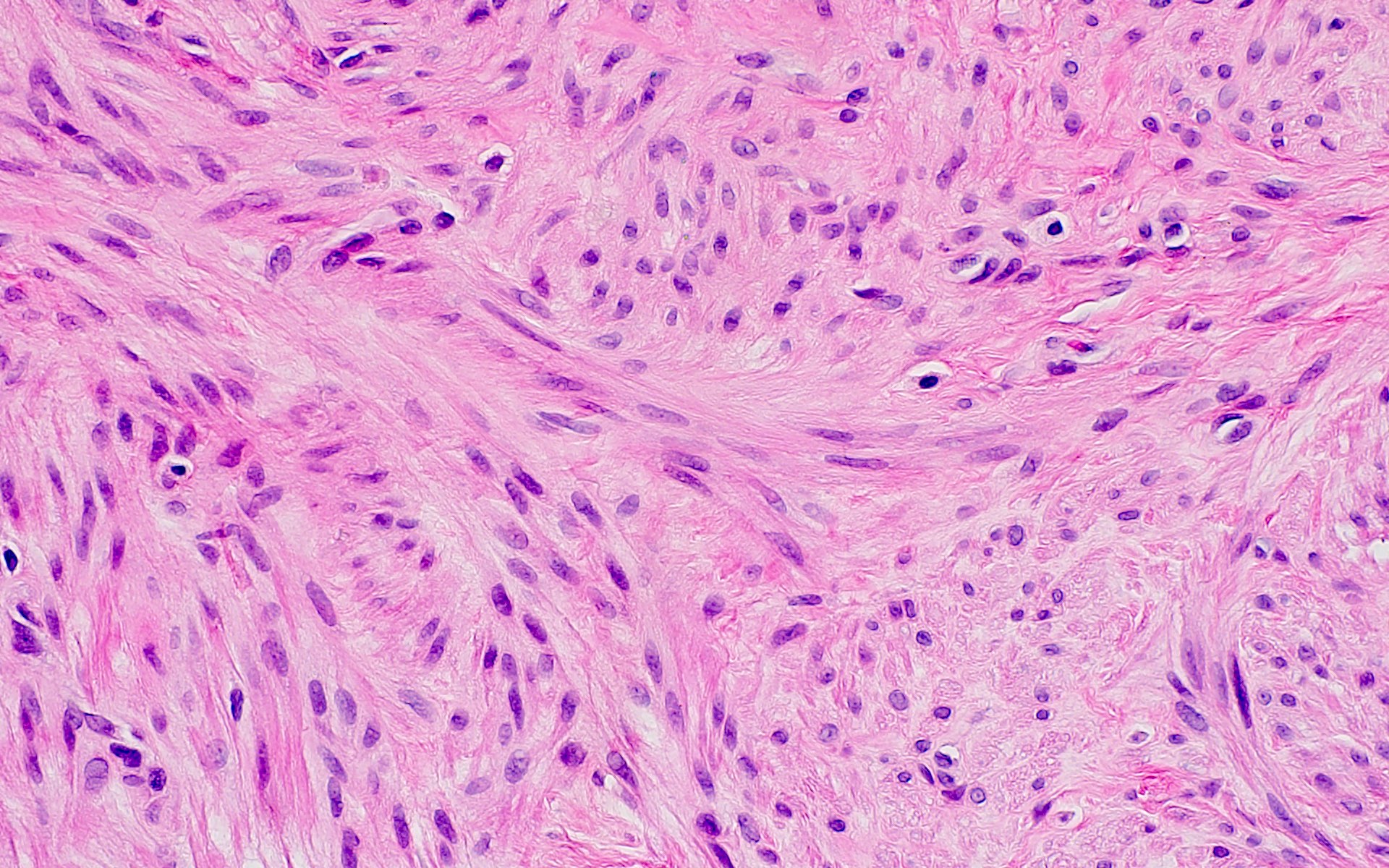
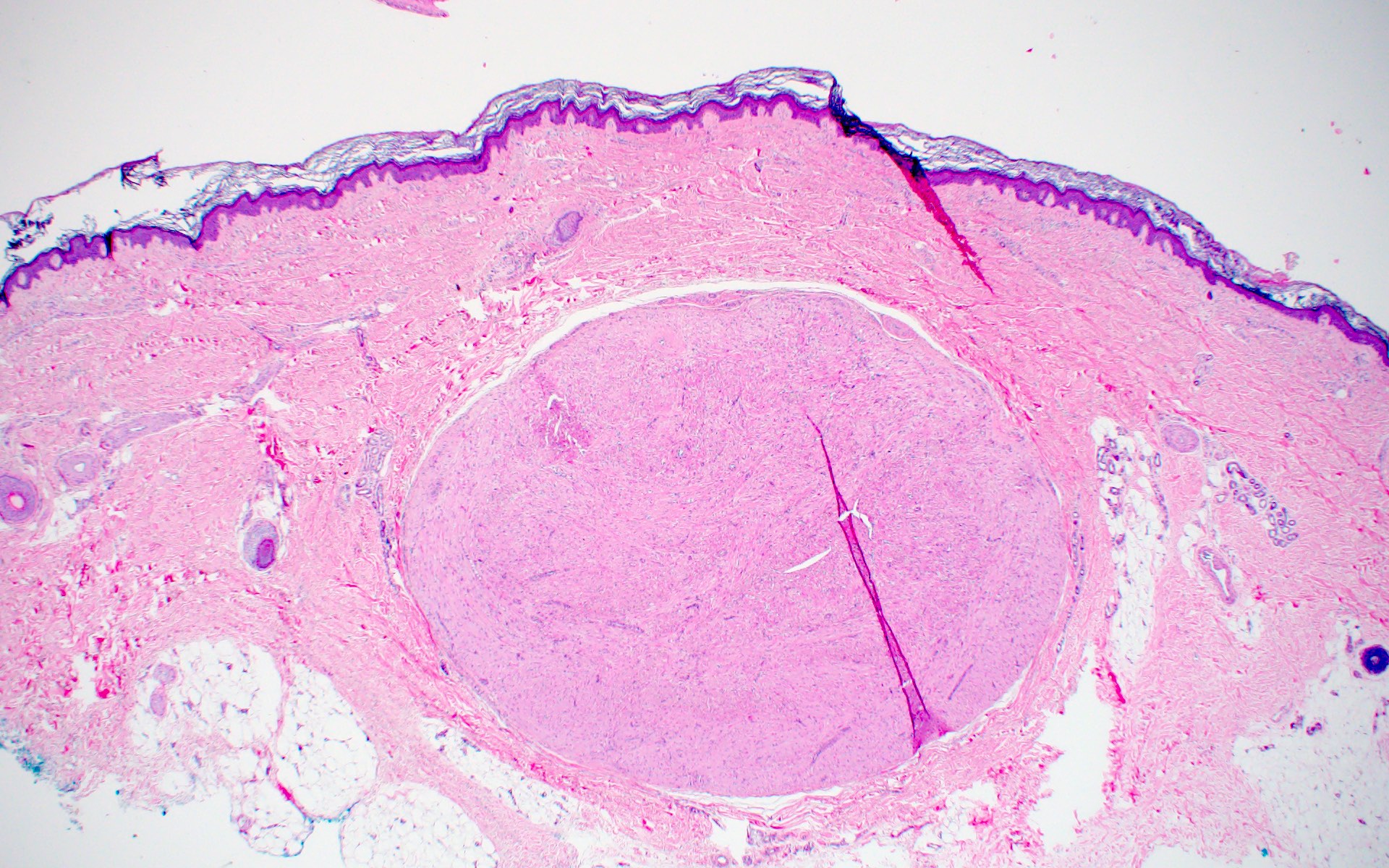
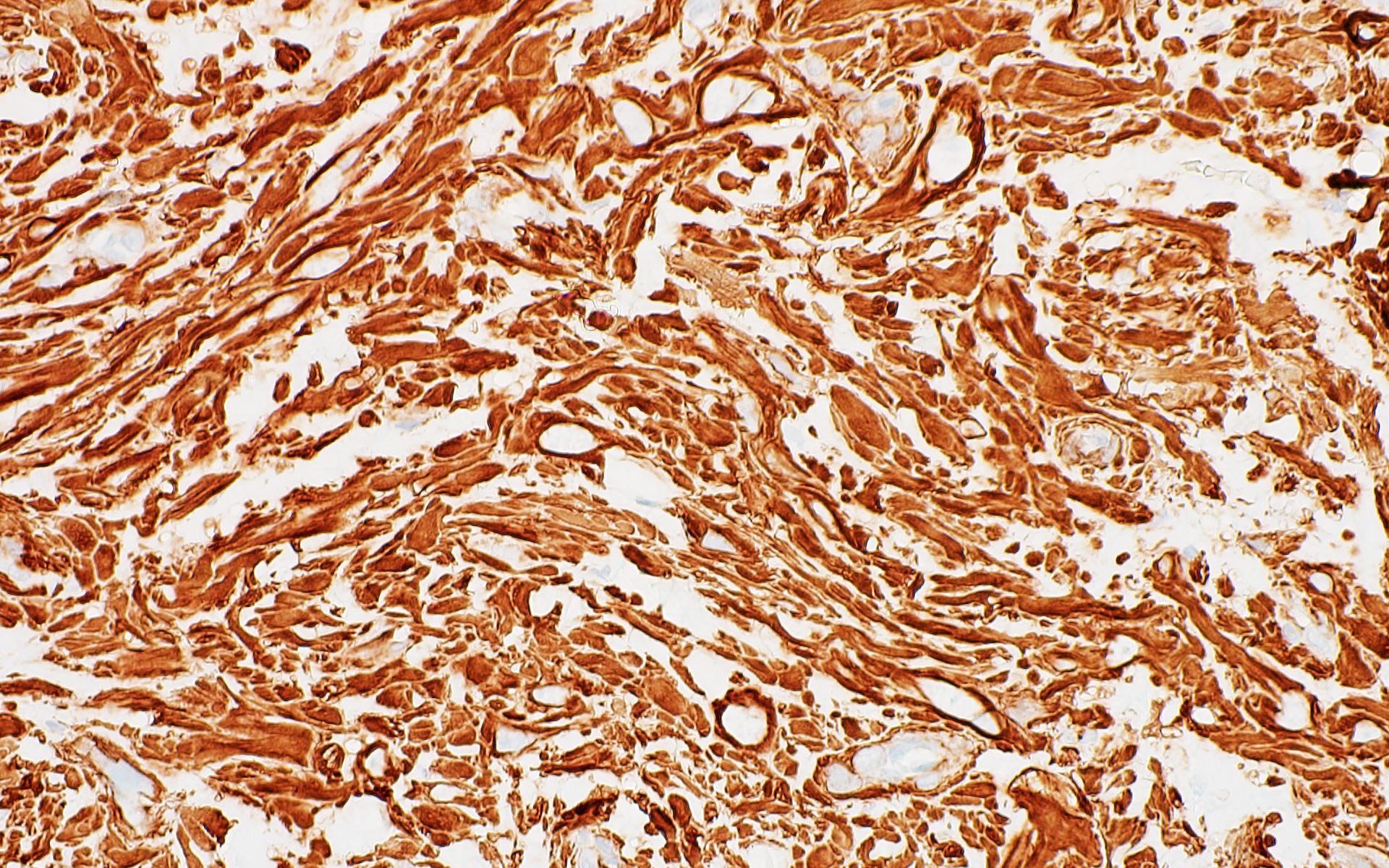
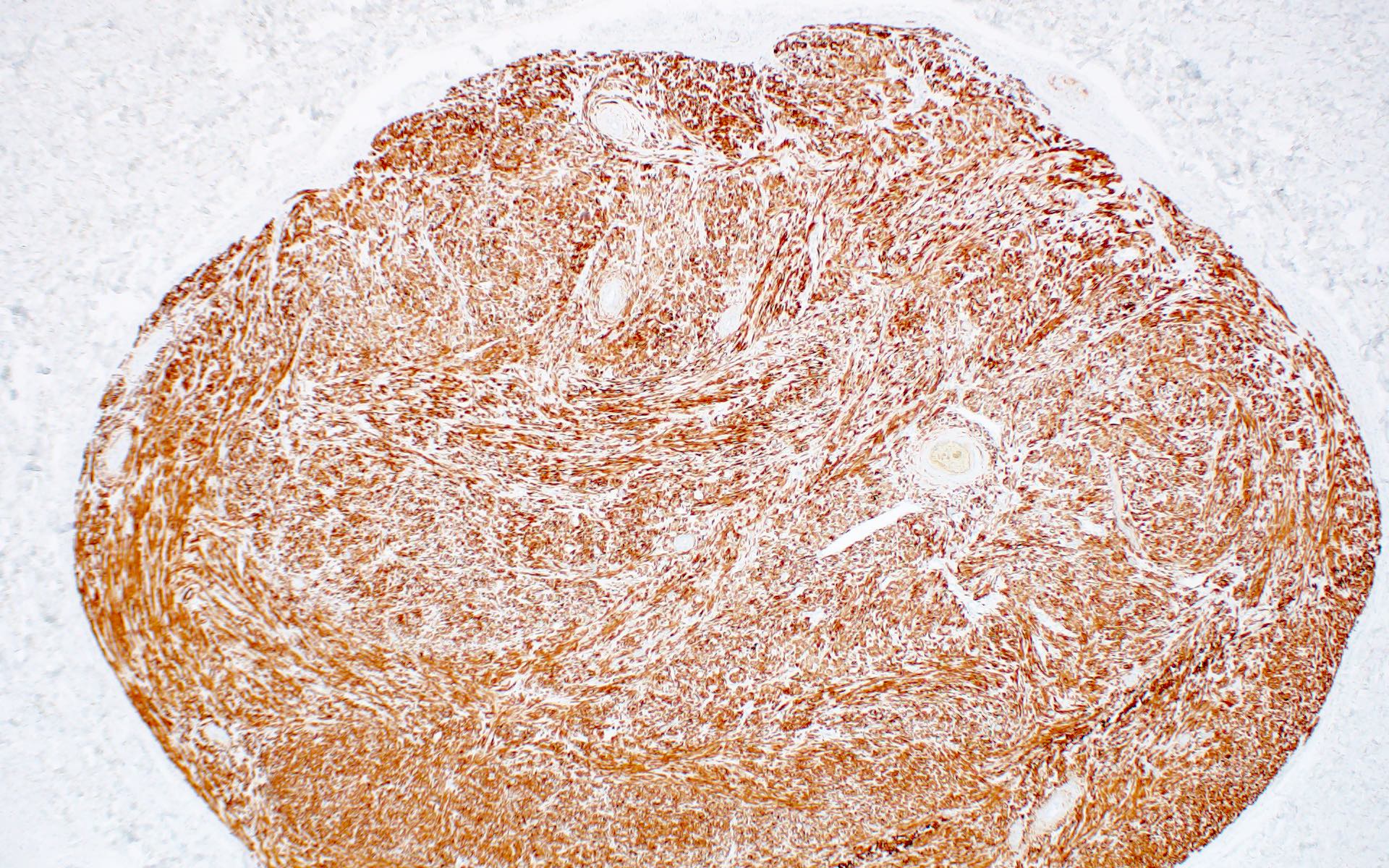




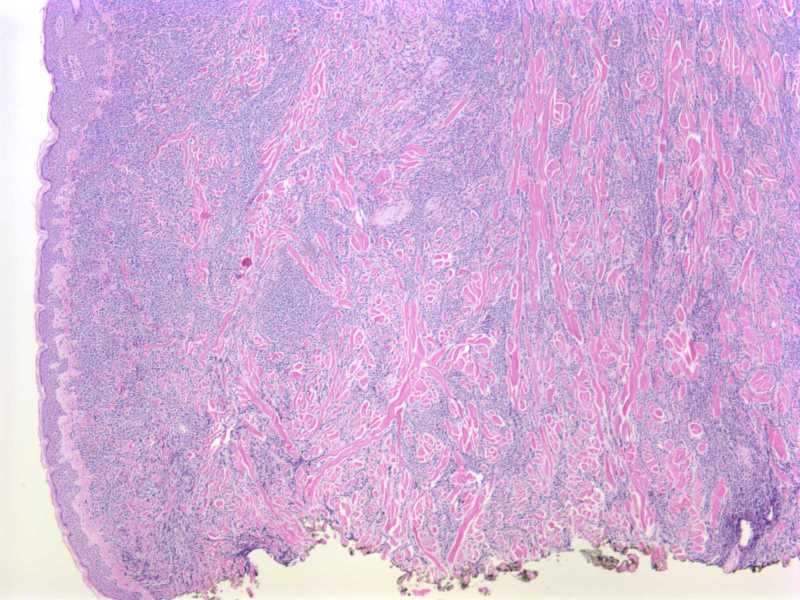

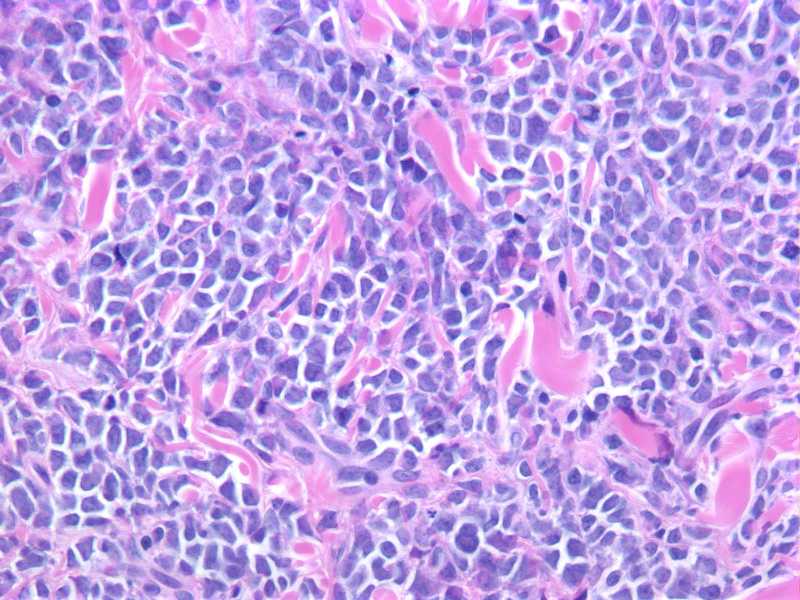
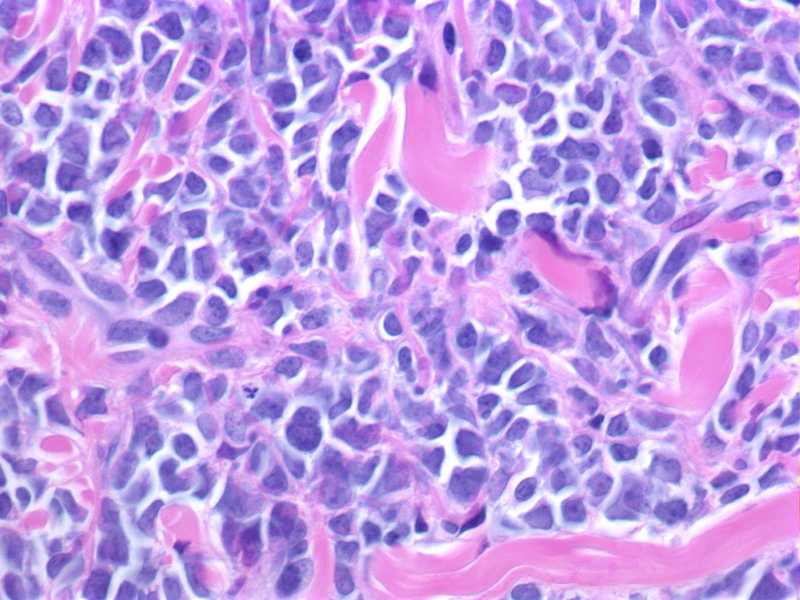
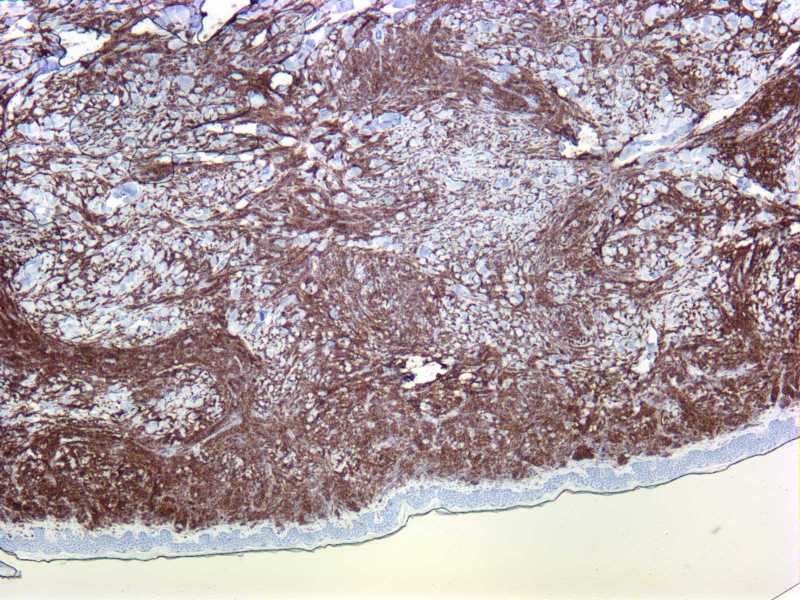
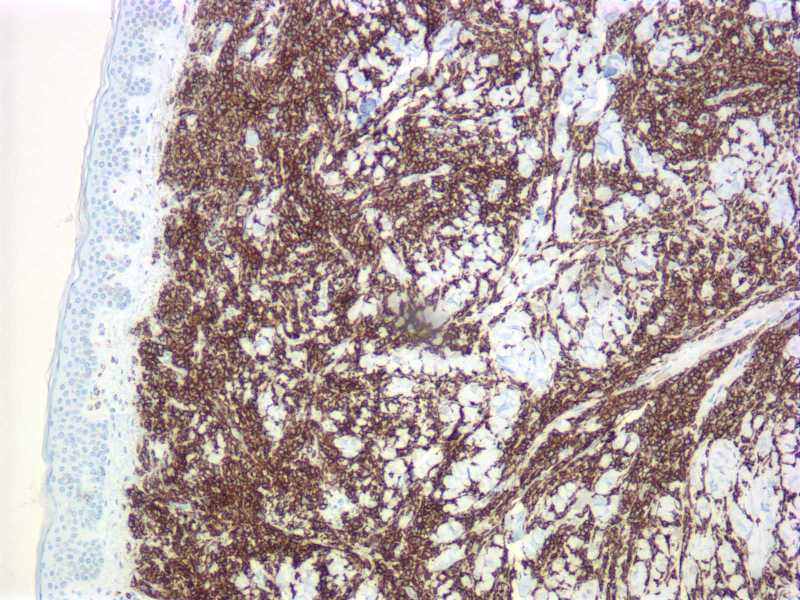

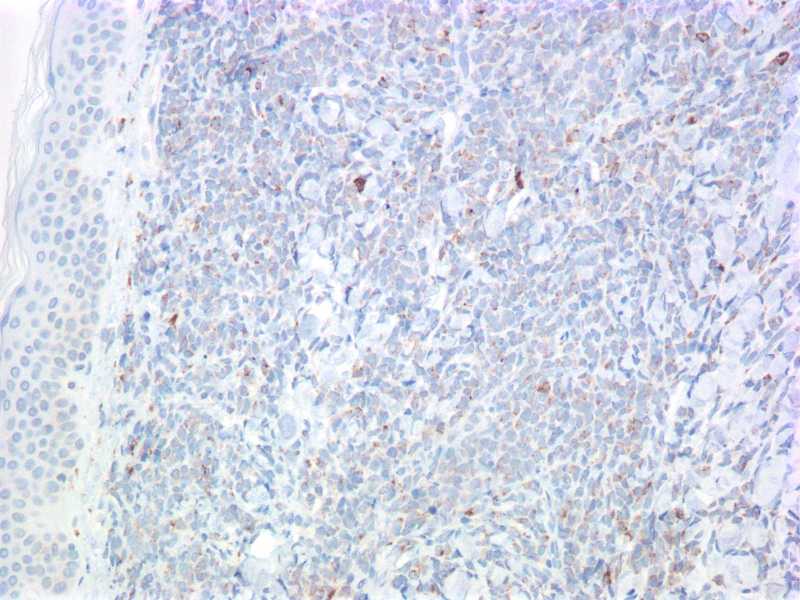
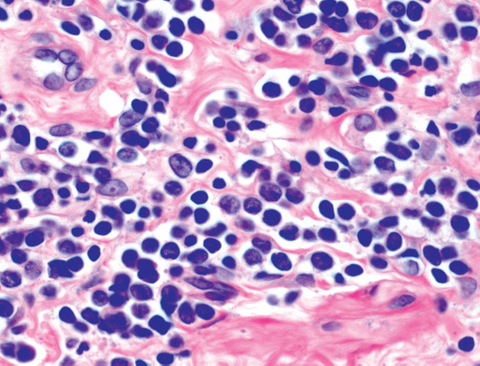
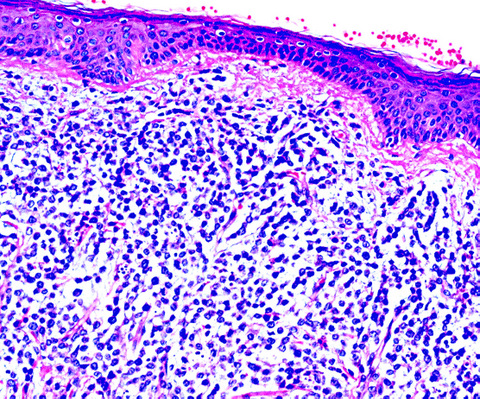
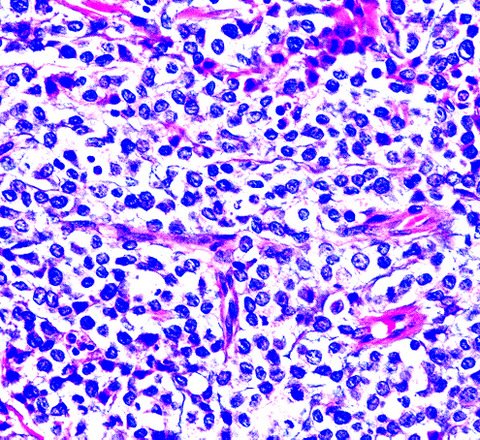
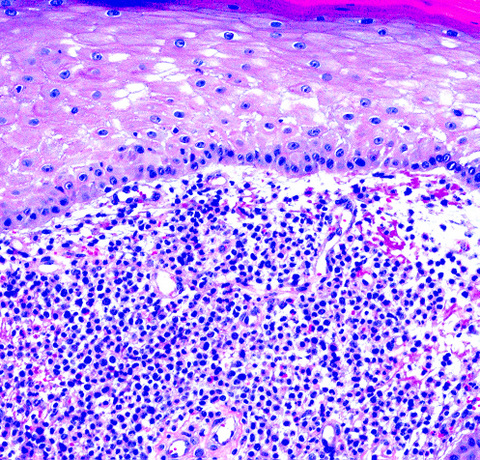

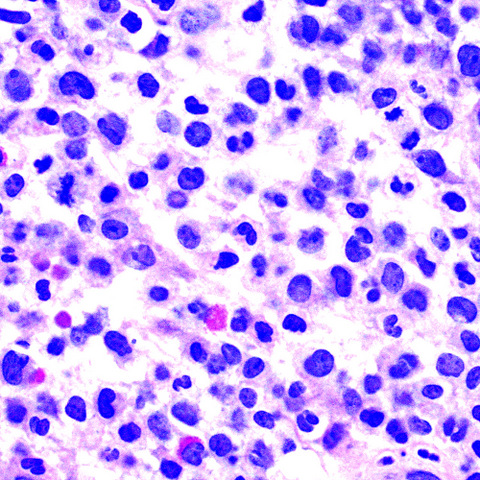
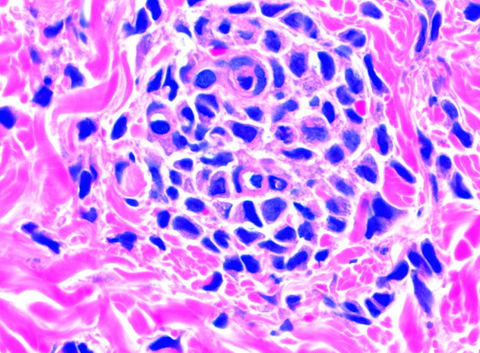

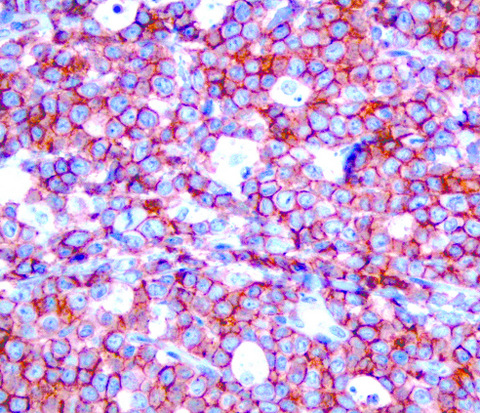
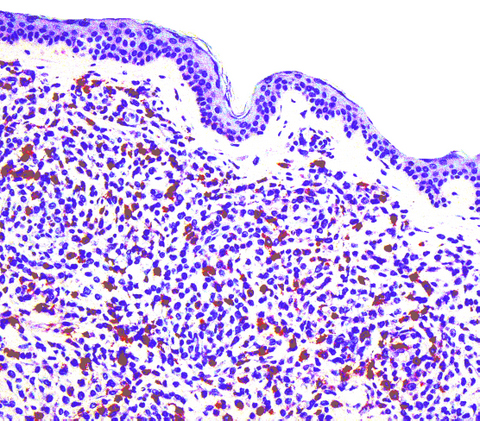
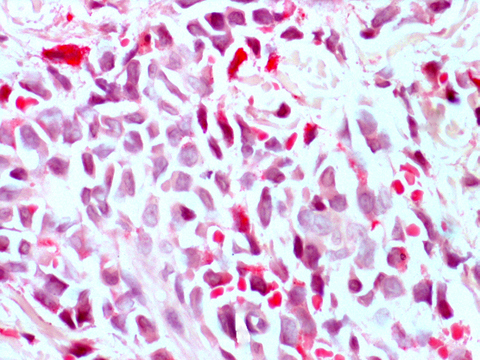
typeclin.jpg)

type.jpg)
typemicr.jpg)
typemicro.jpg)
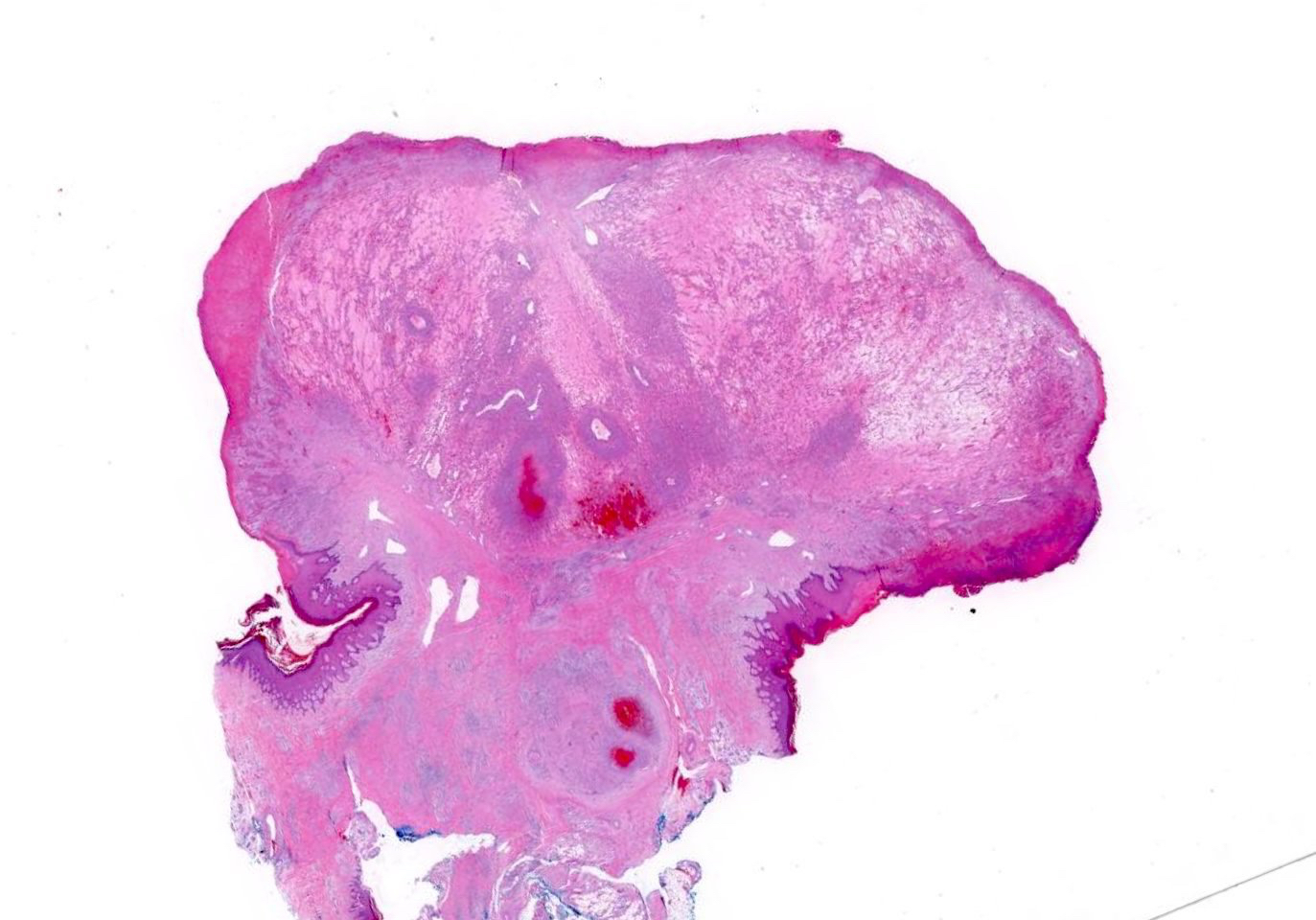
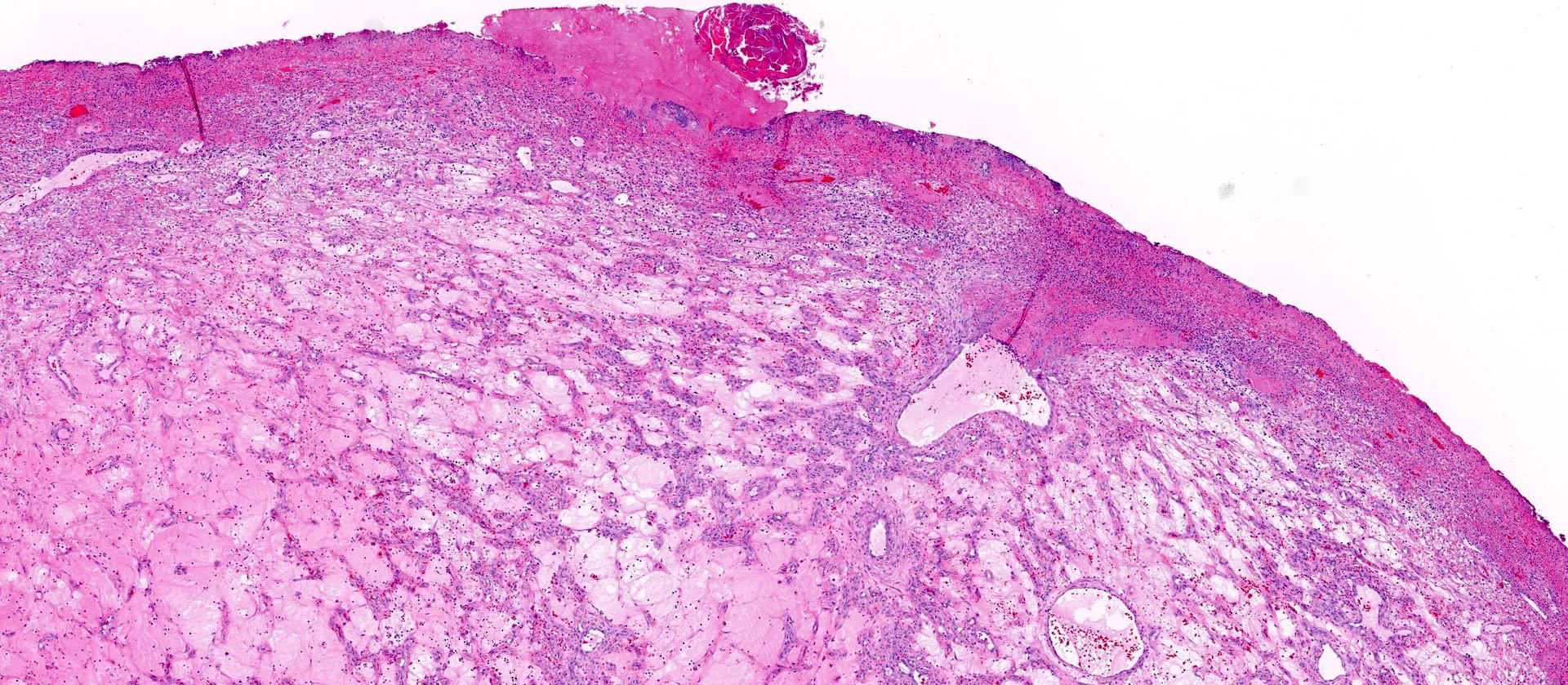
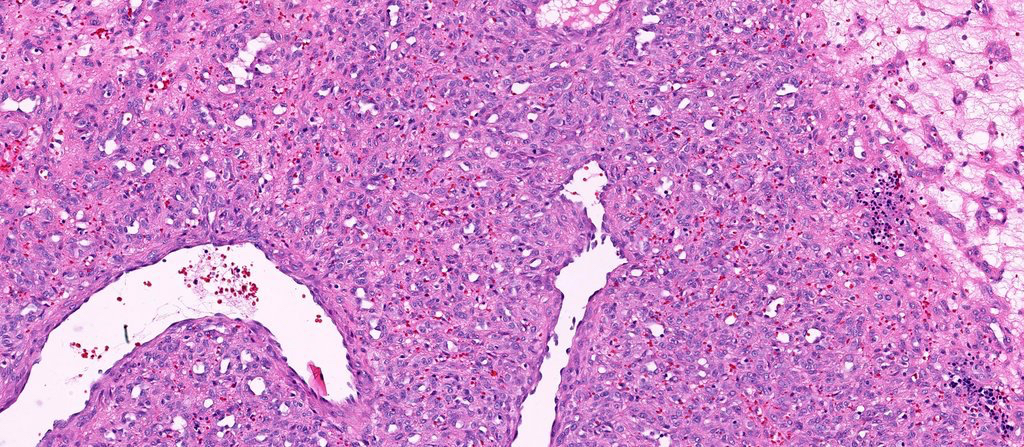



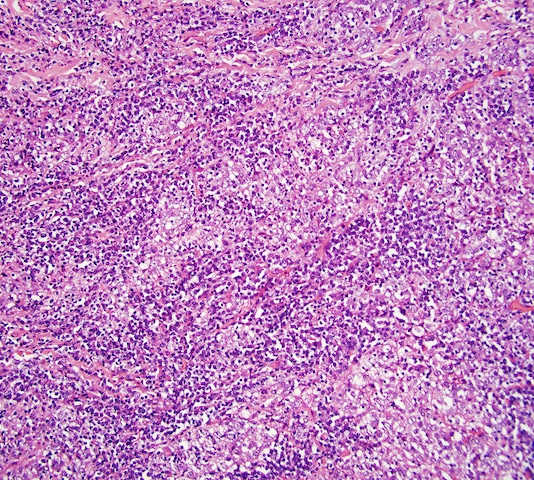
















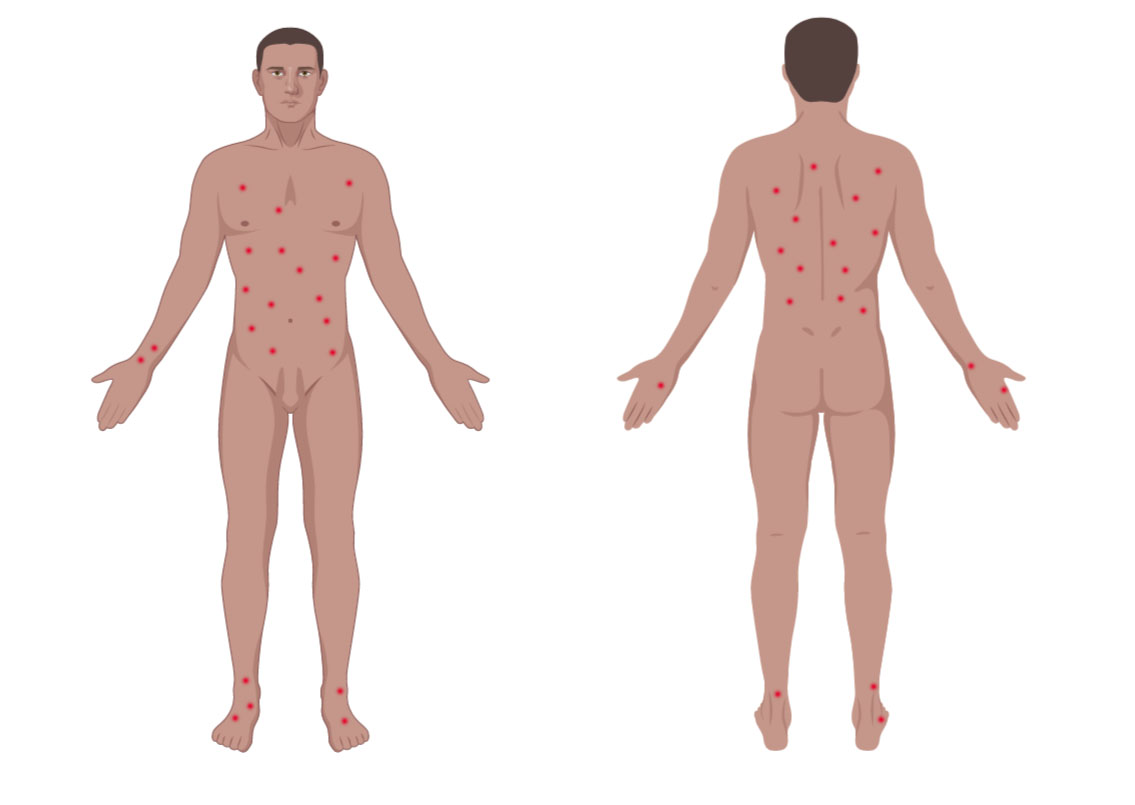





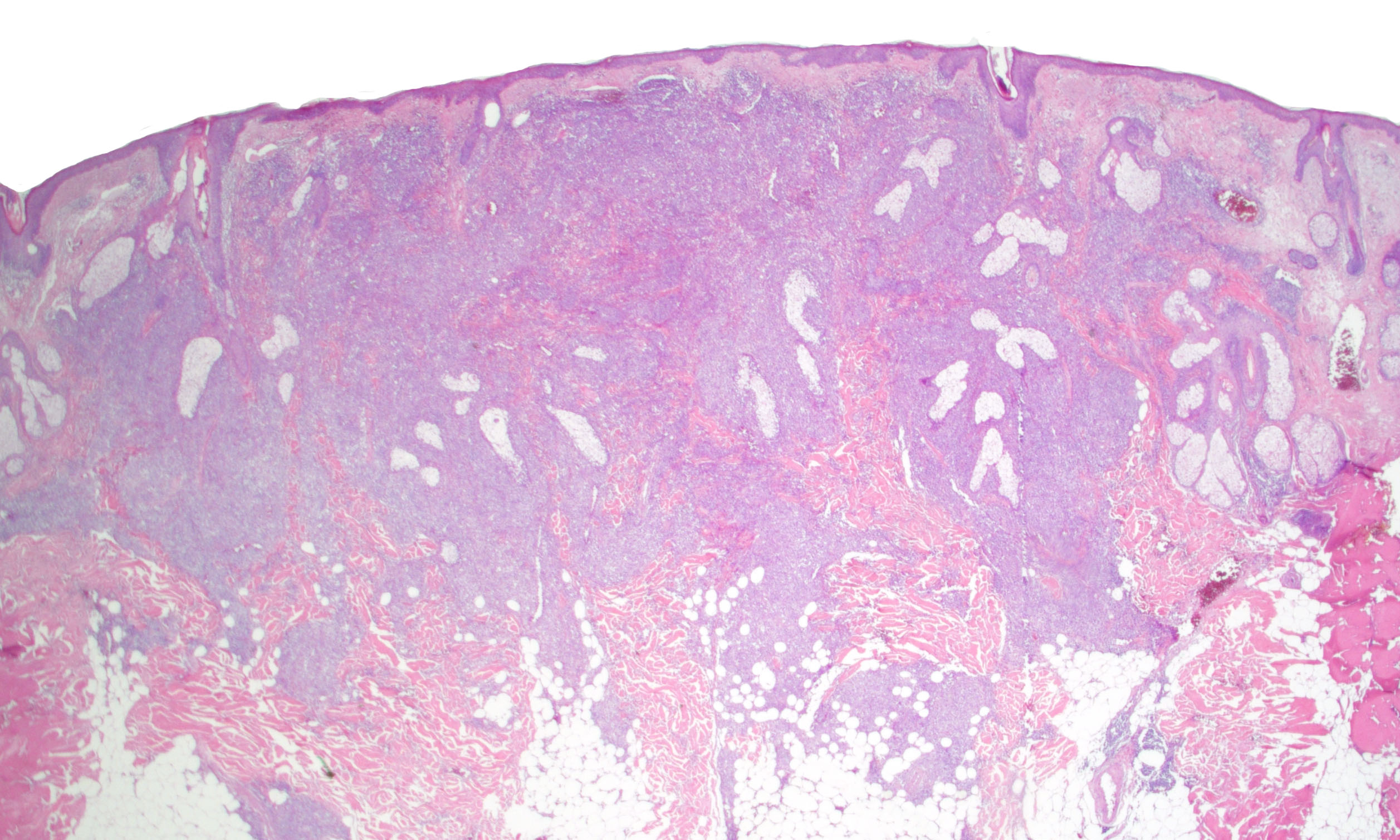
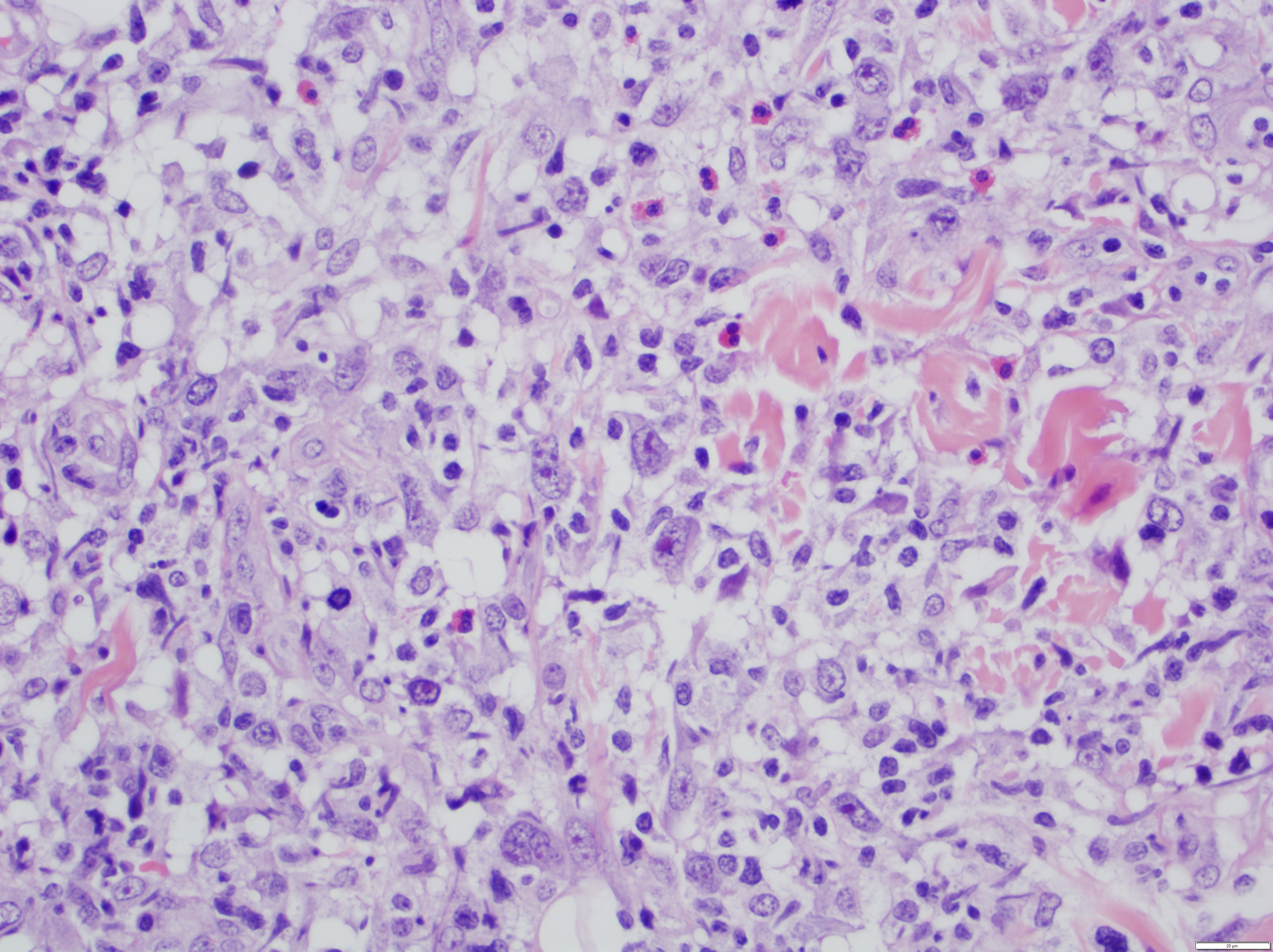

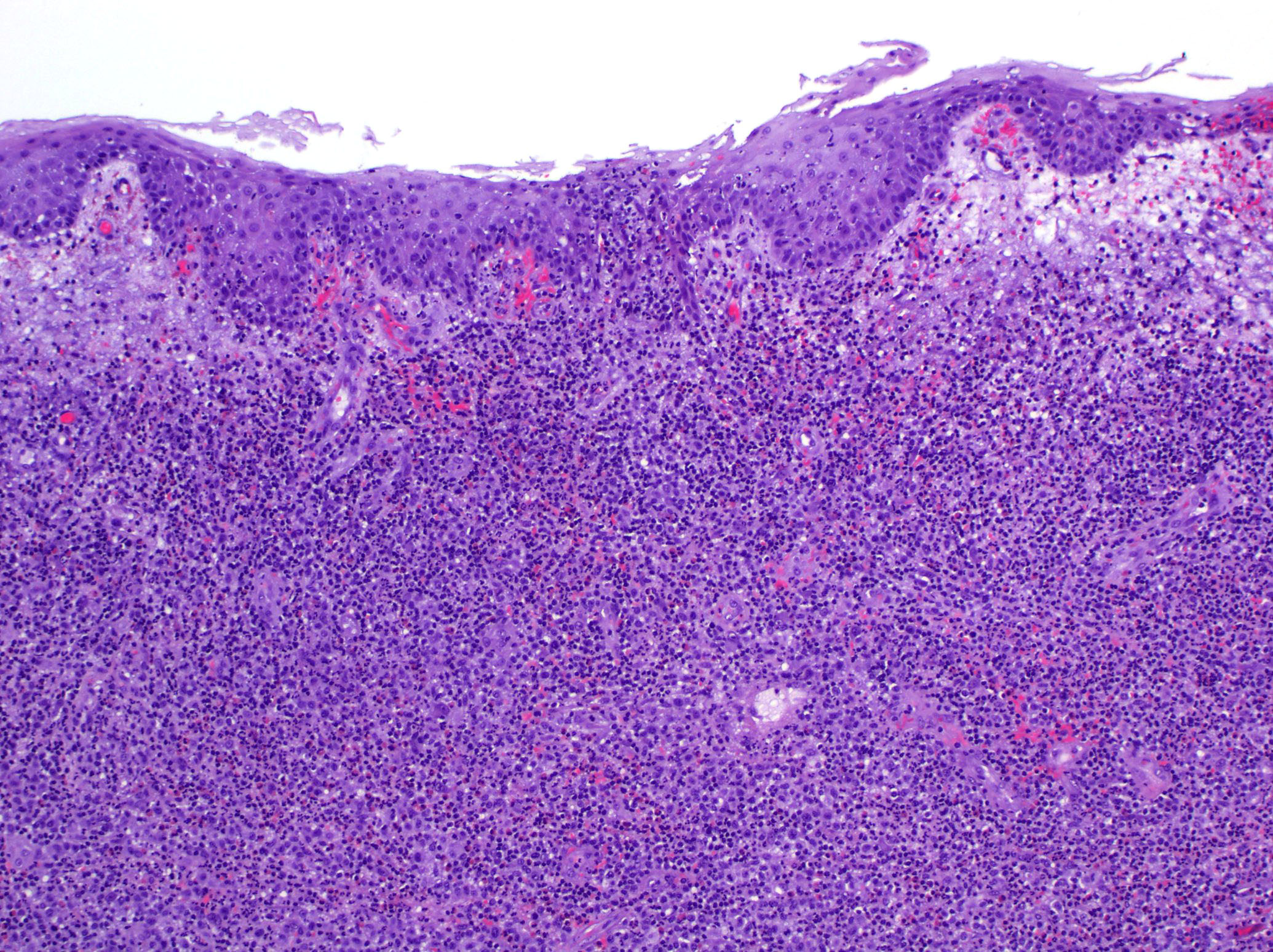
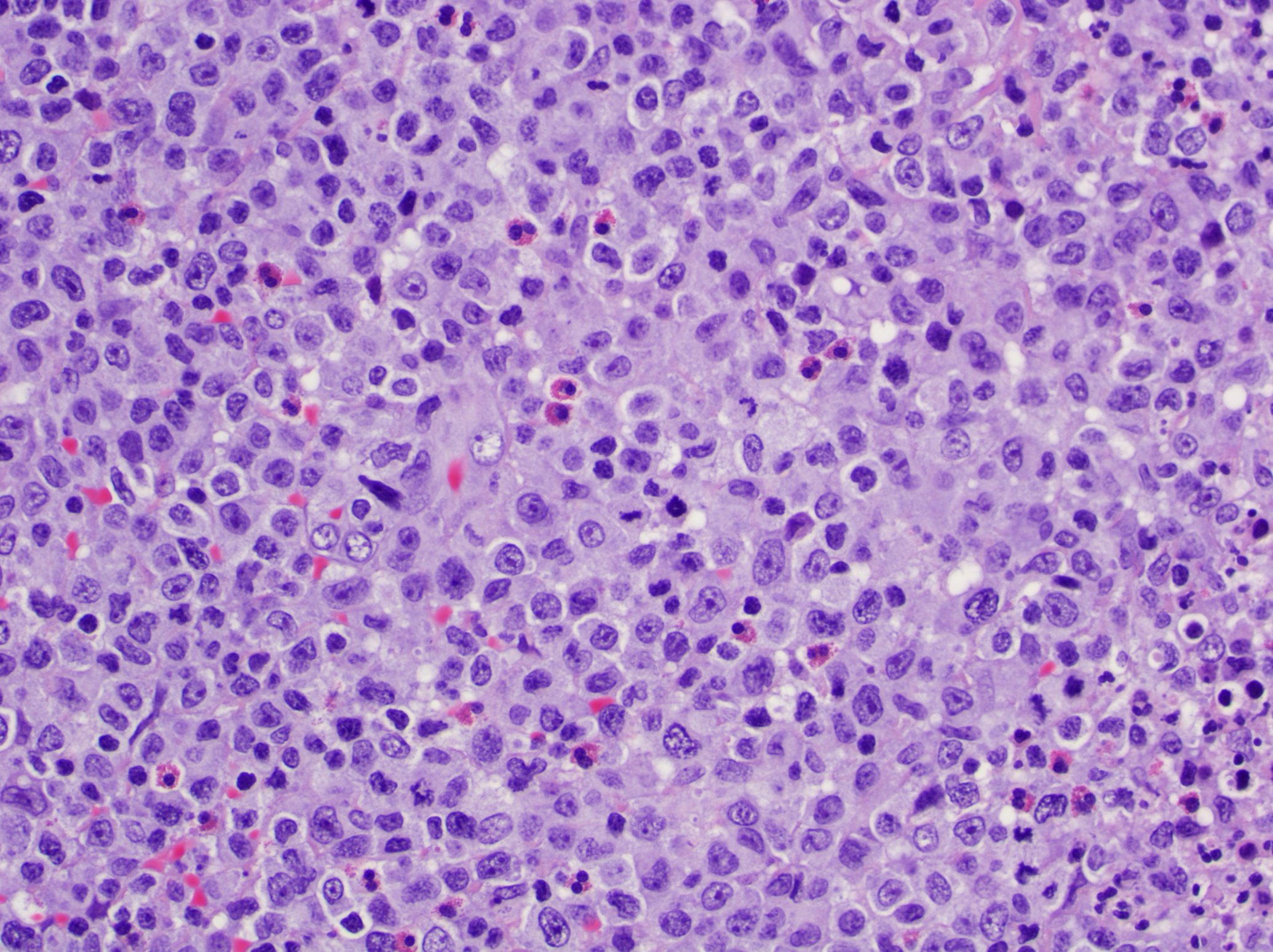
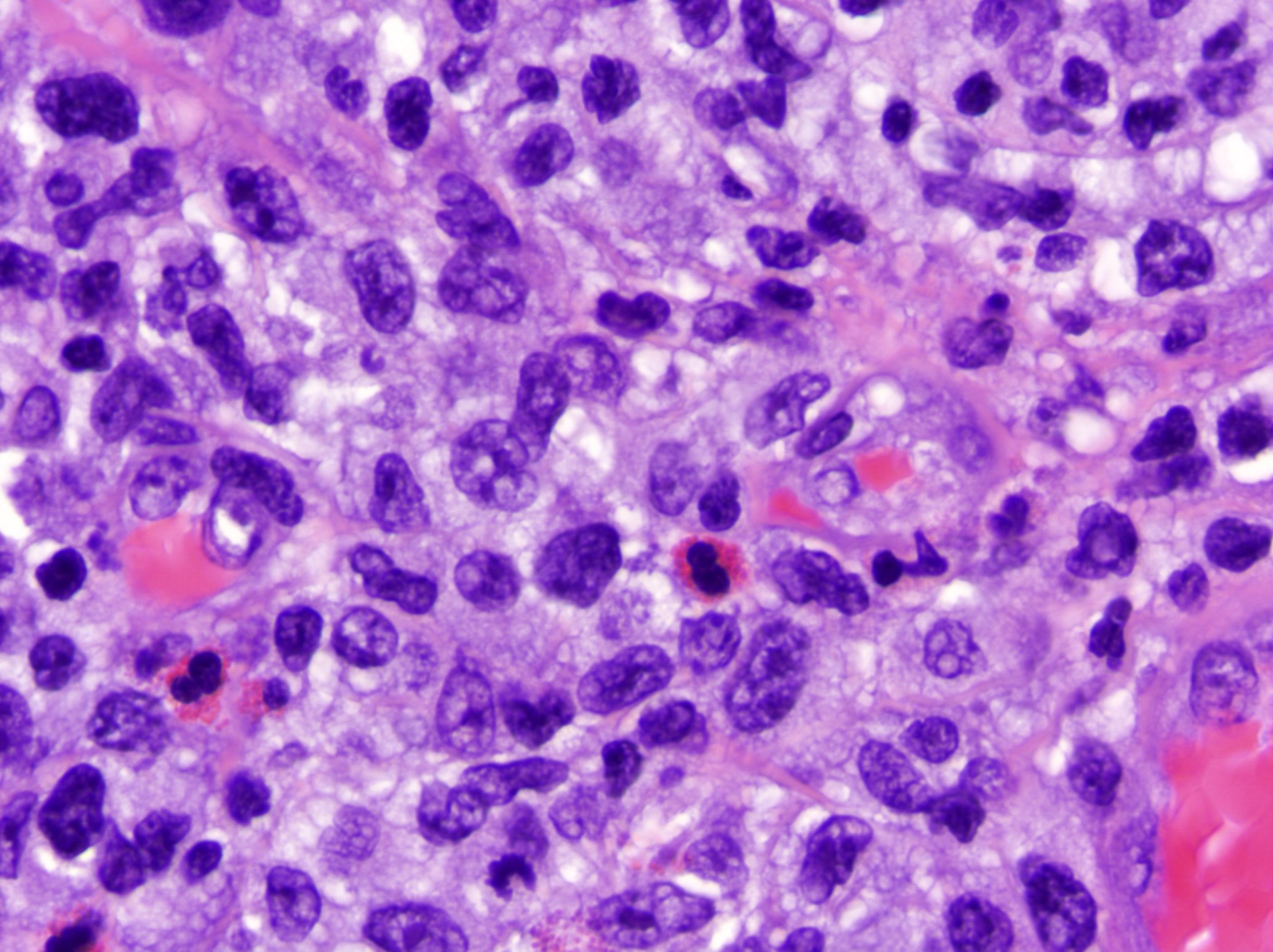
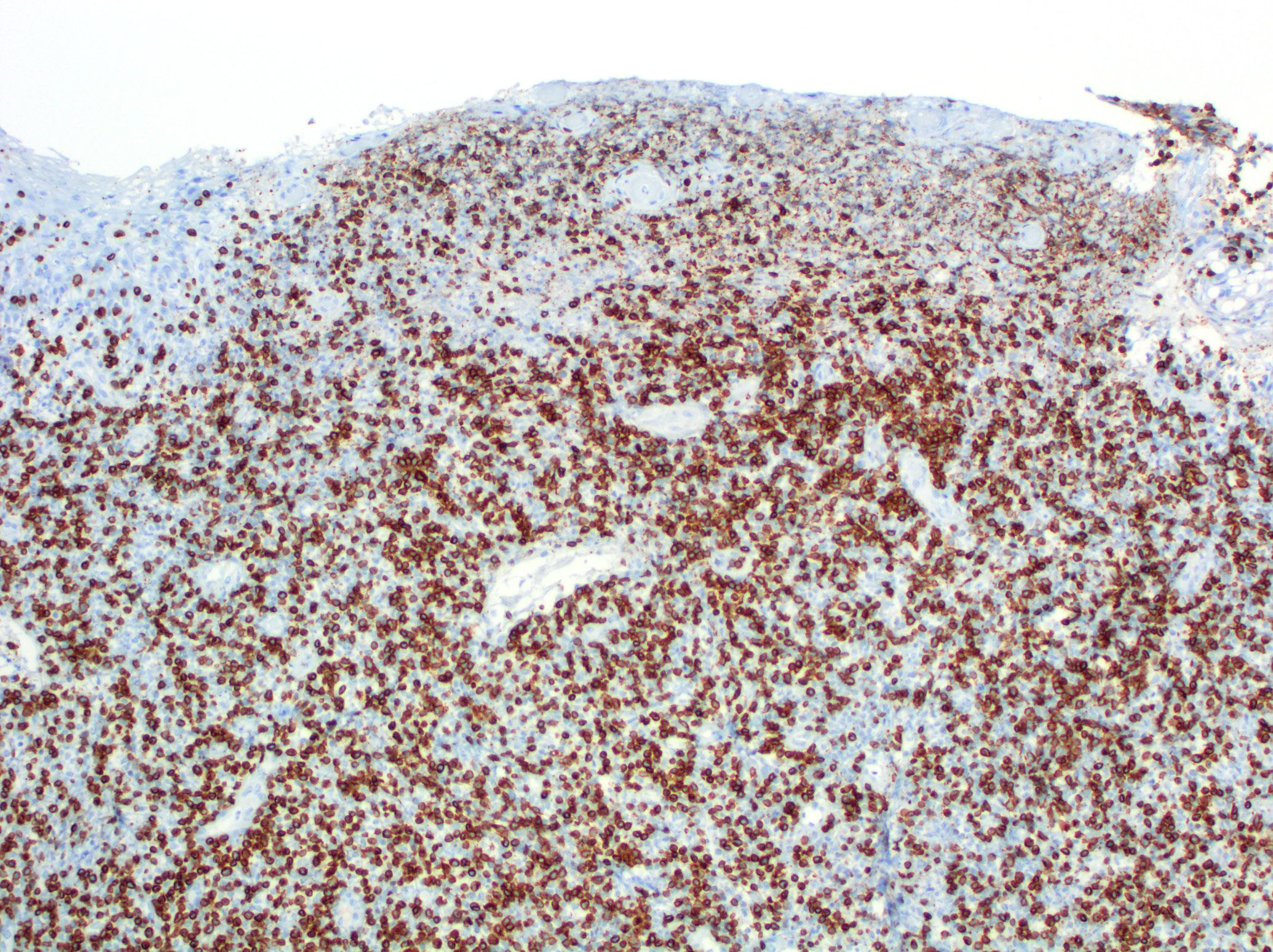
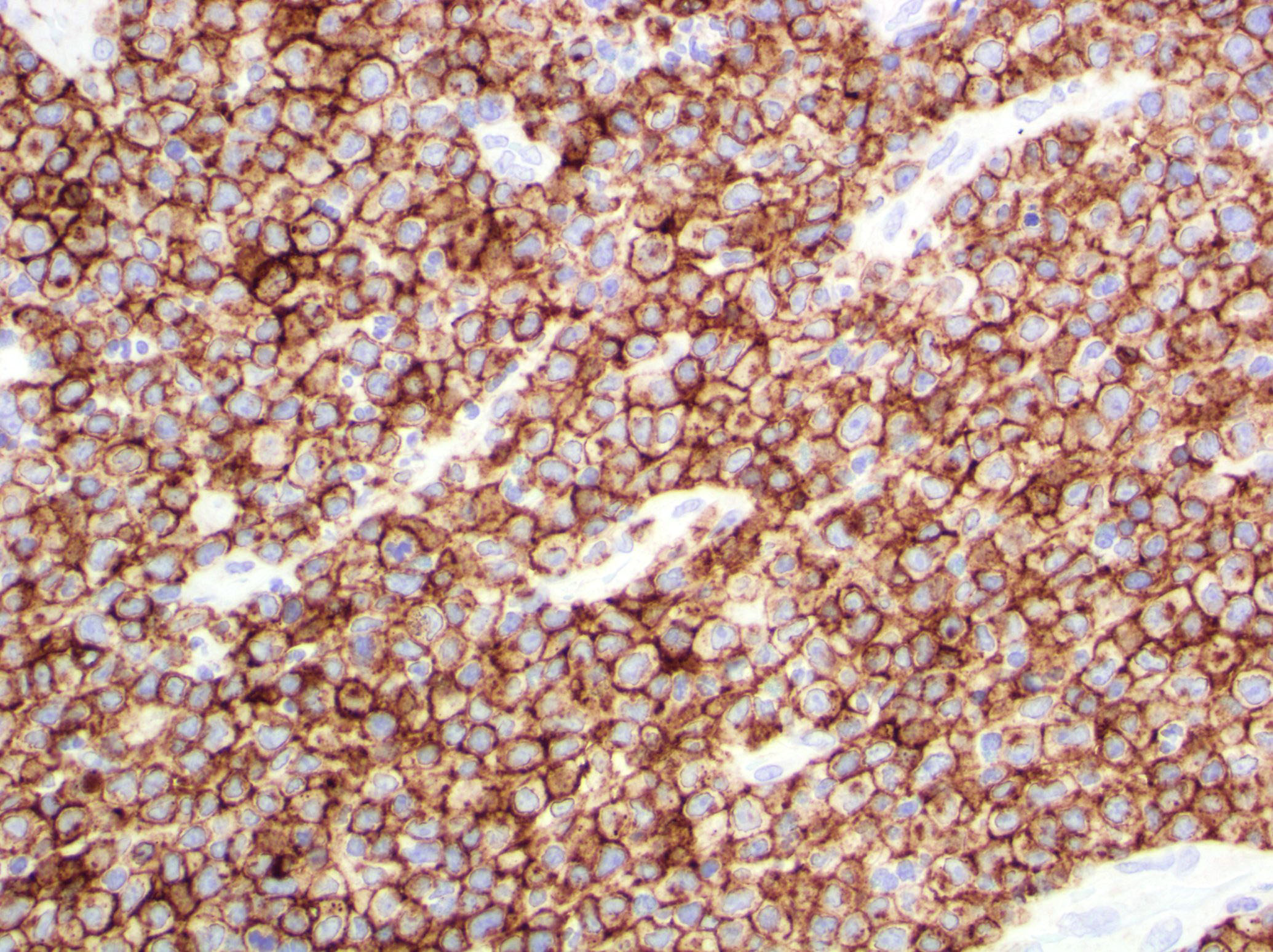
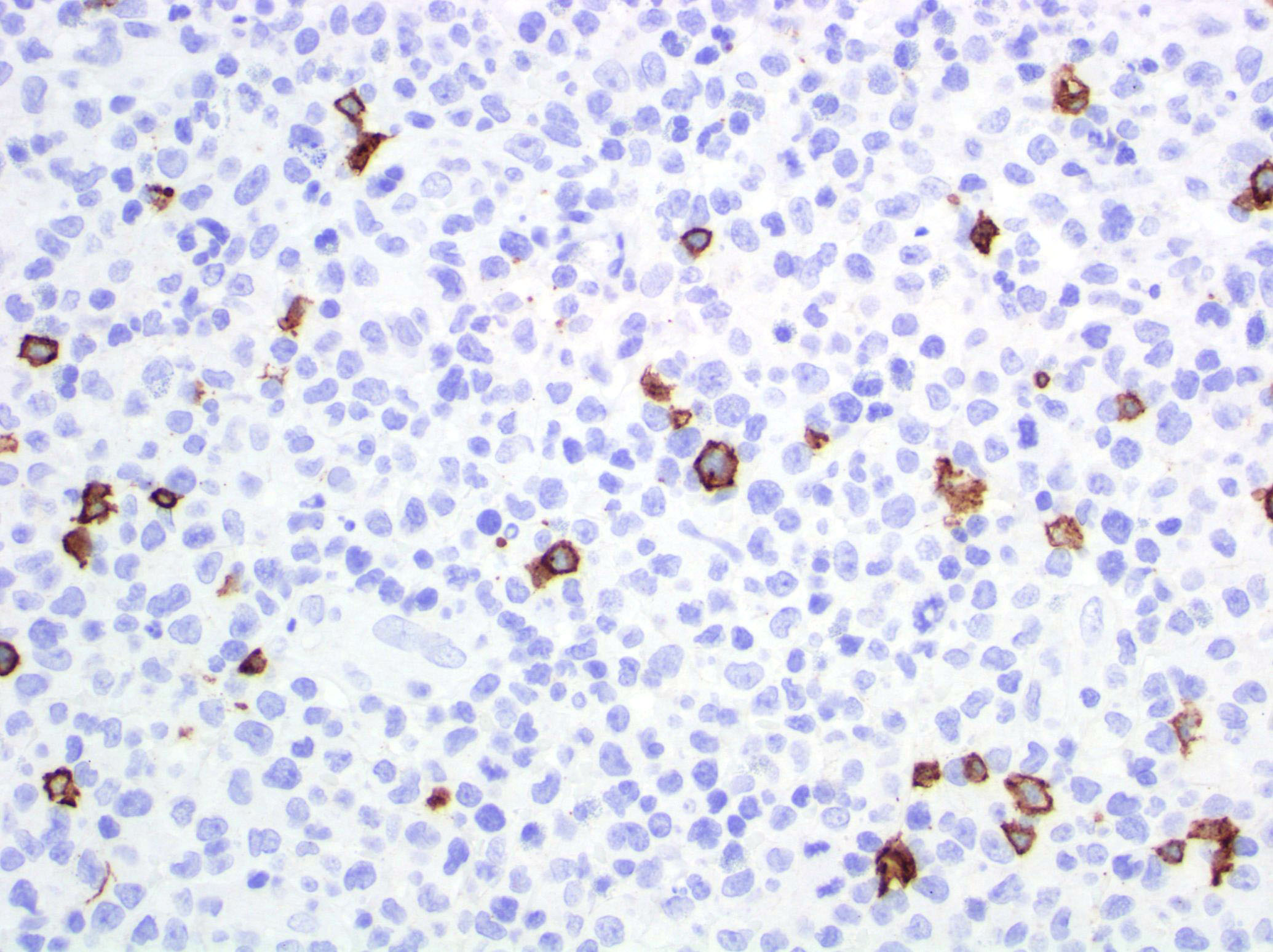
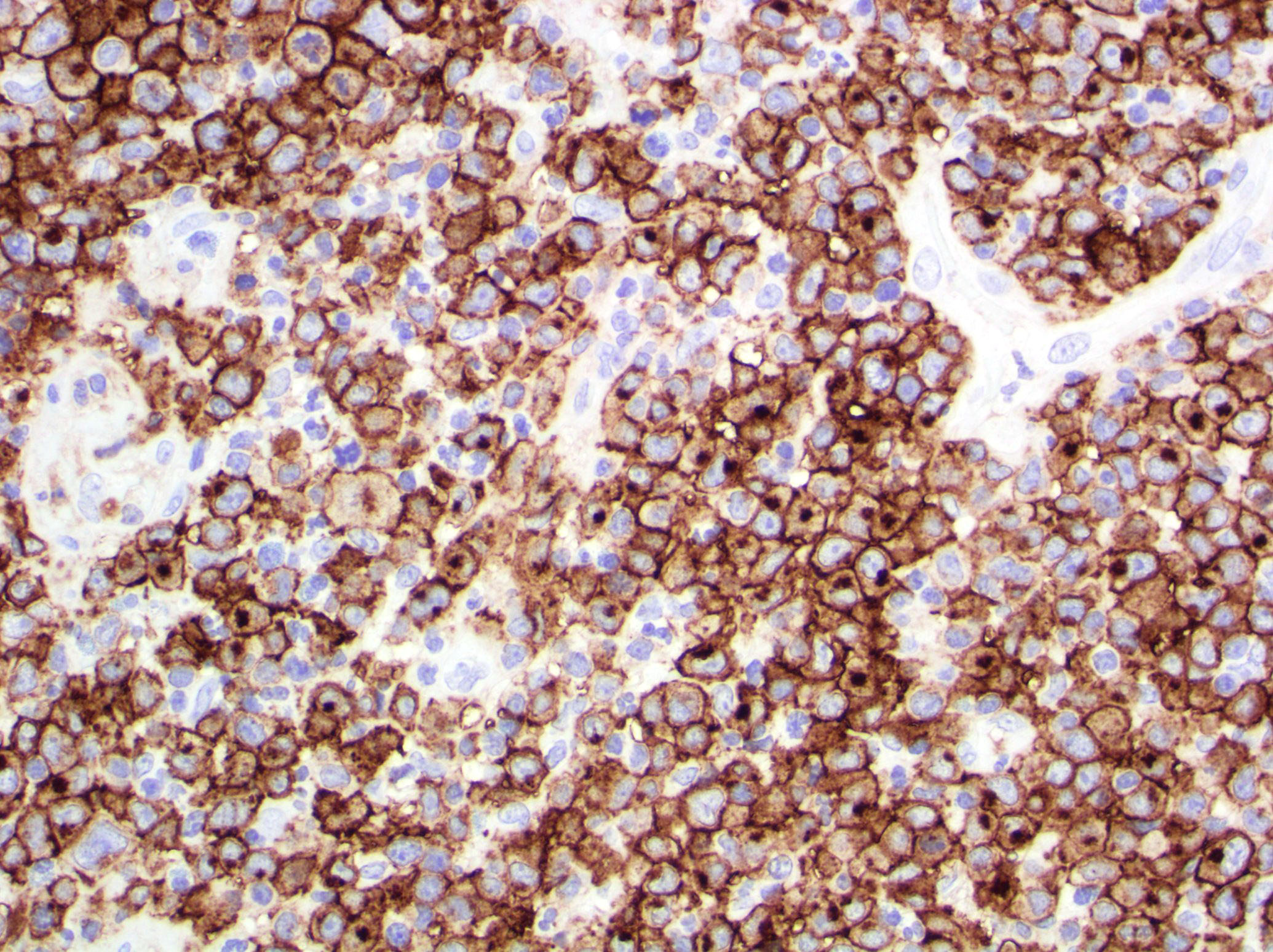
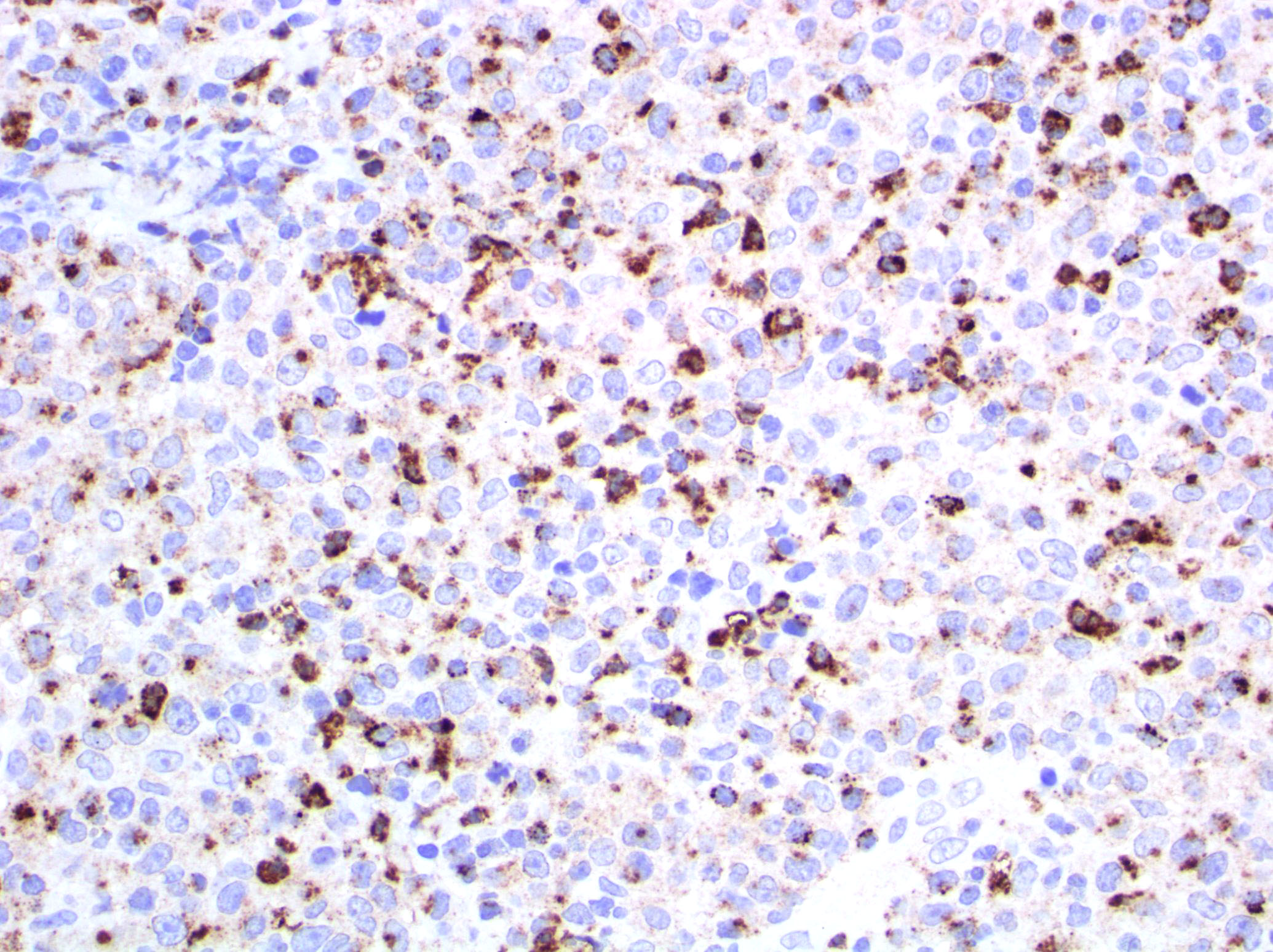
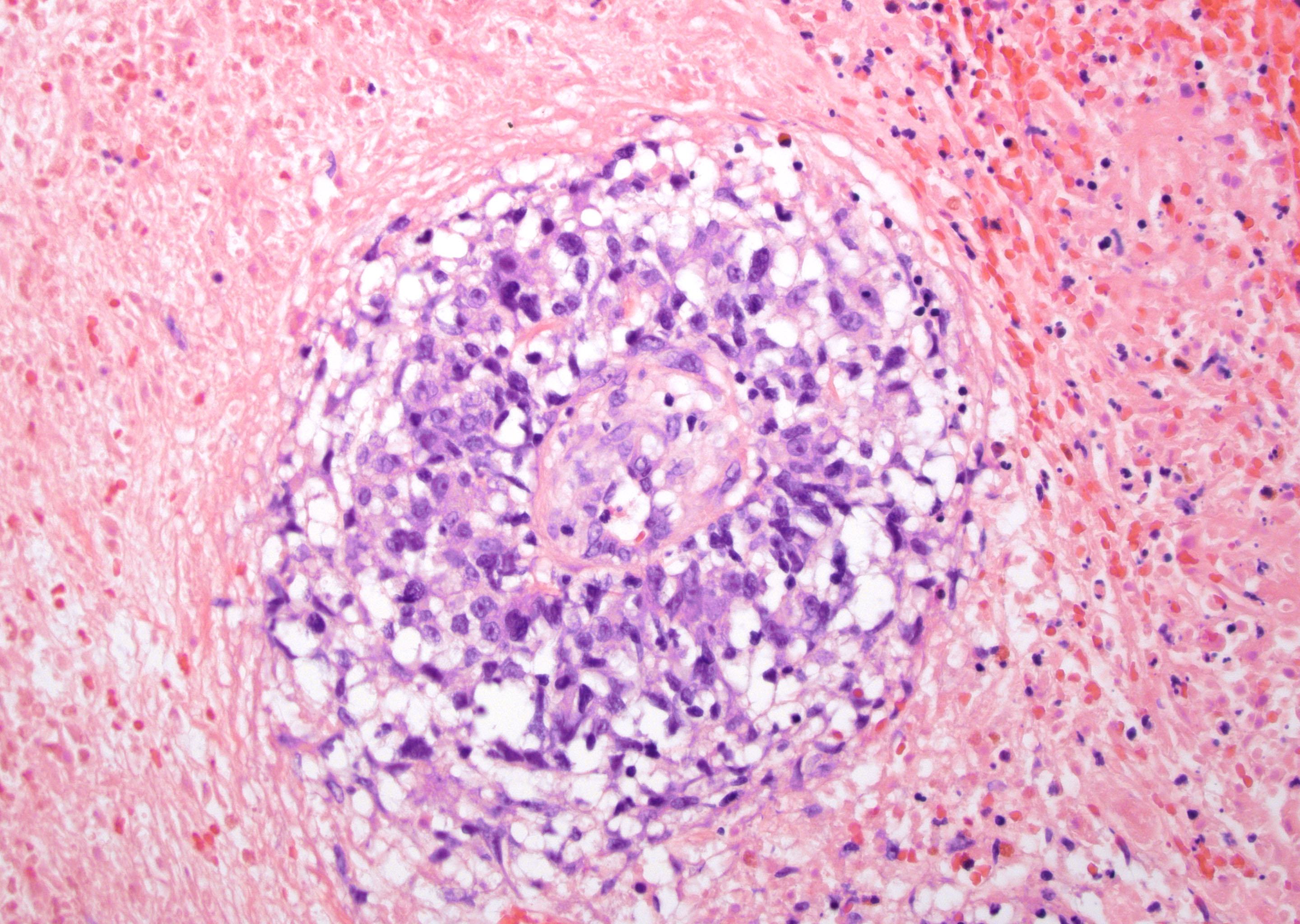
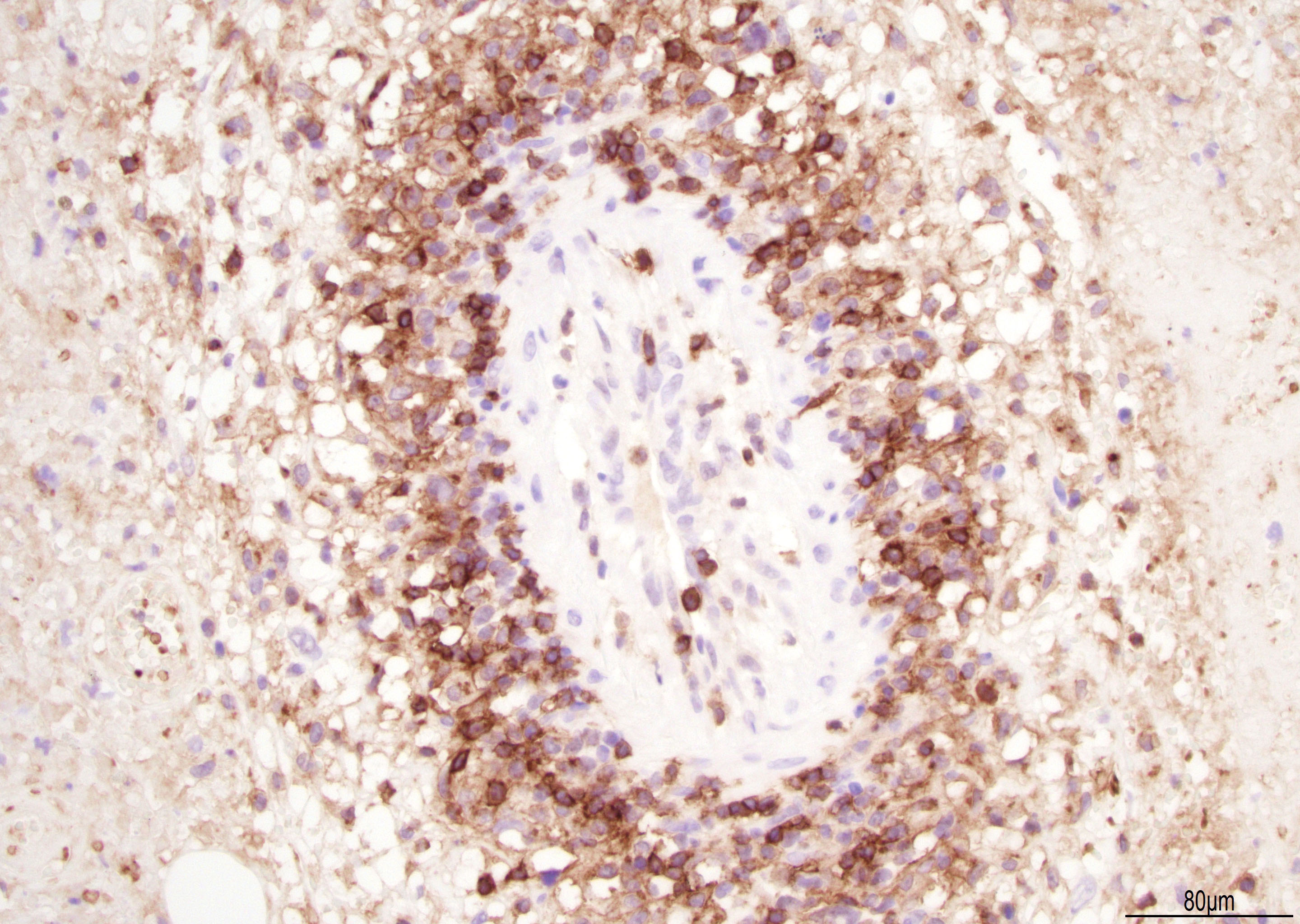
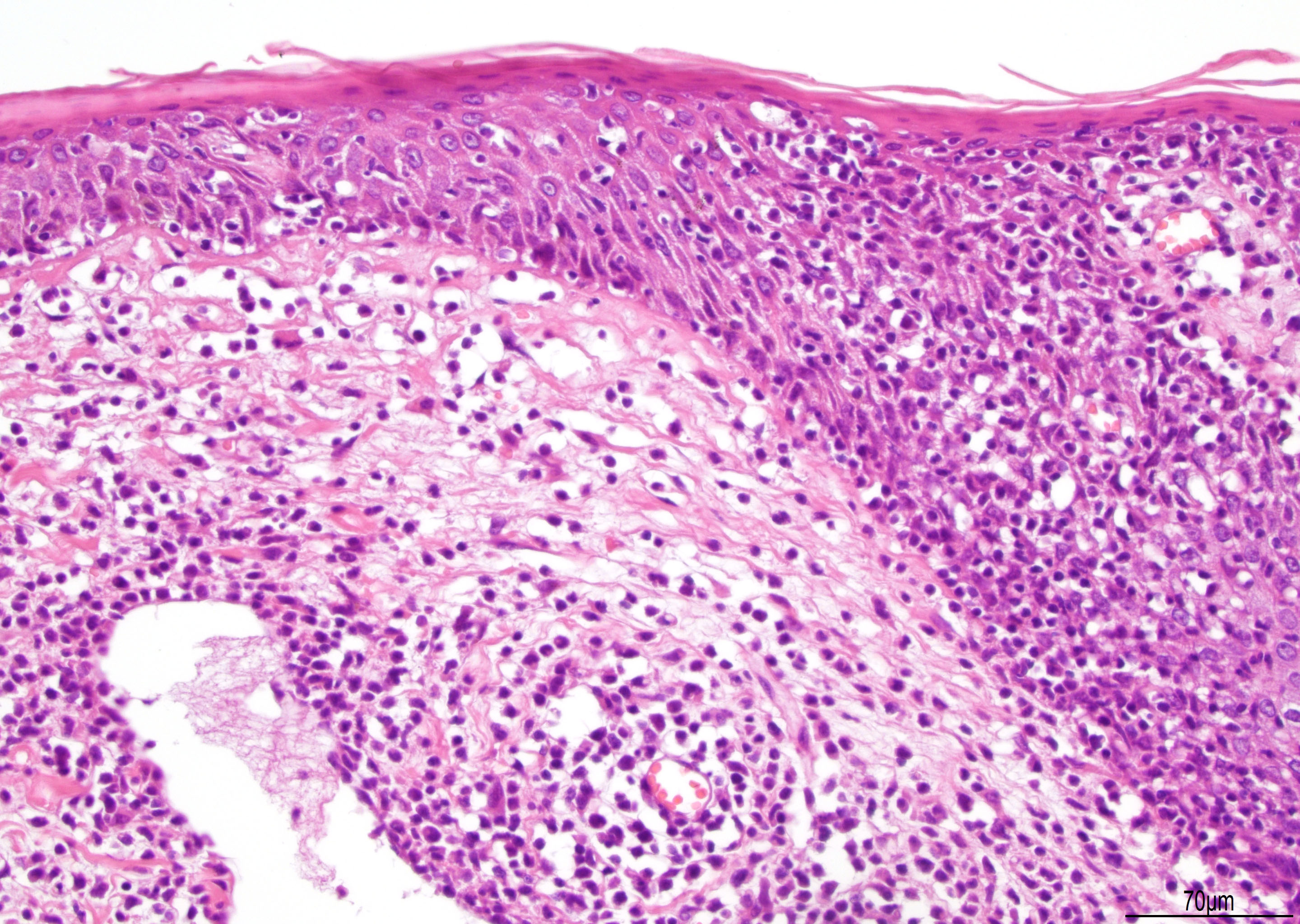












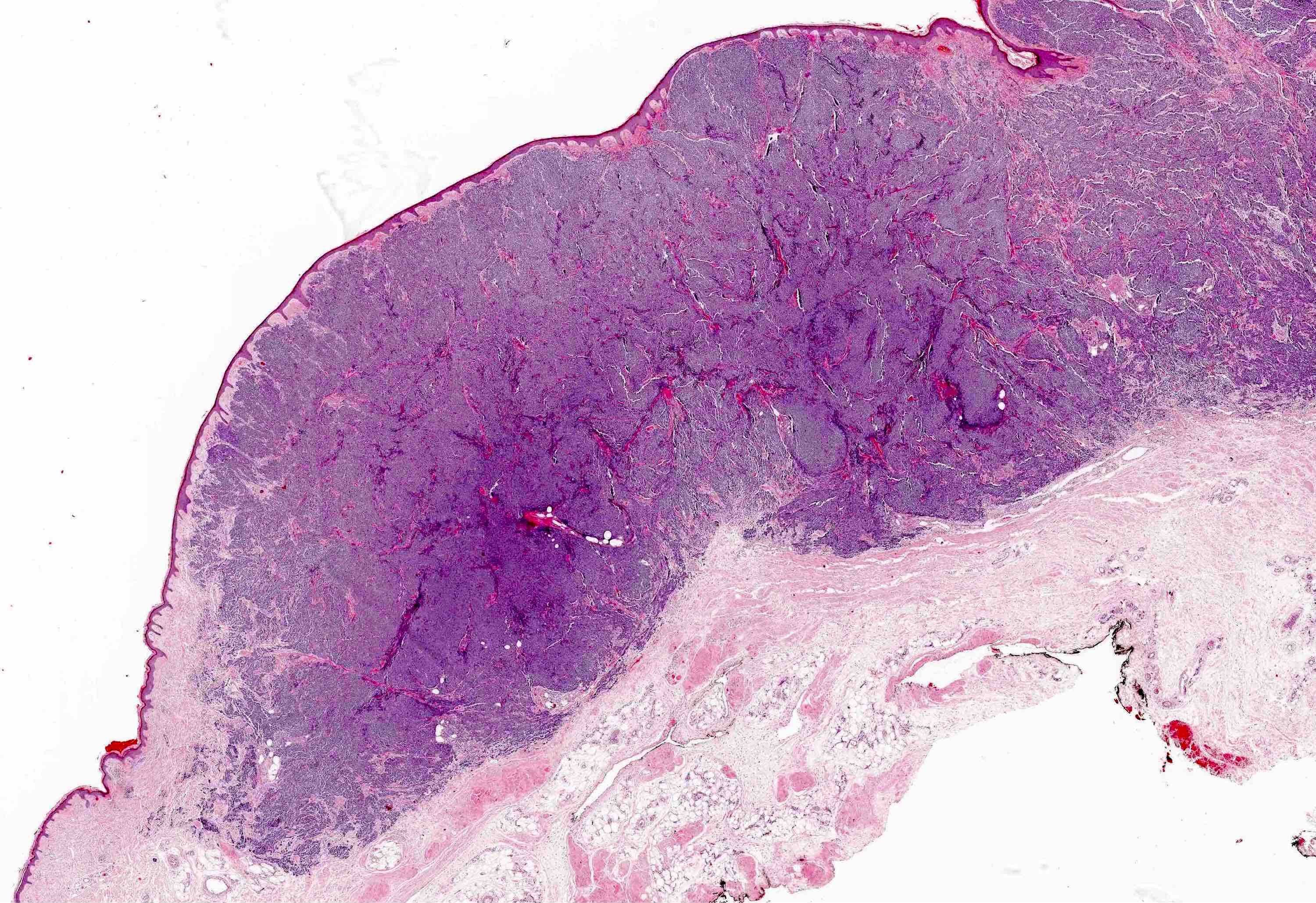
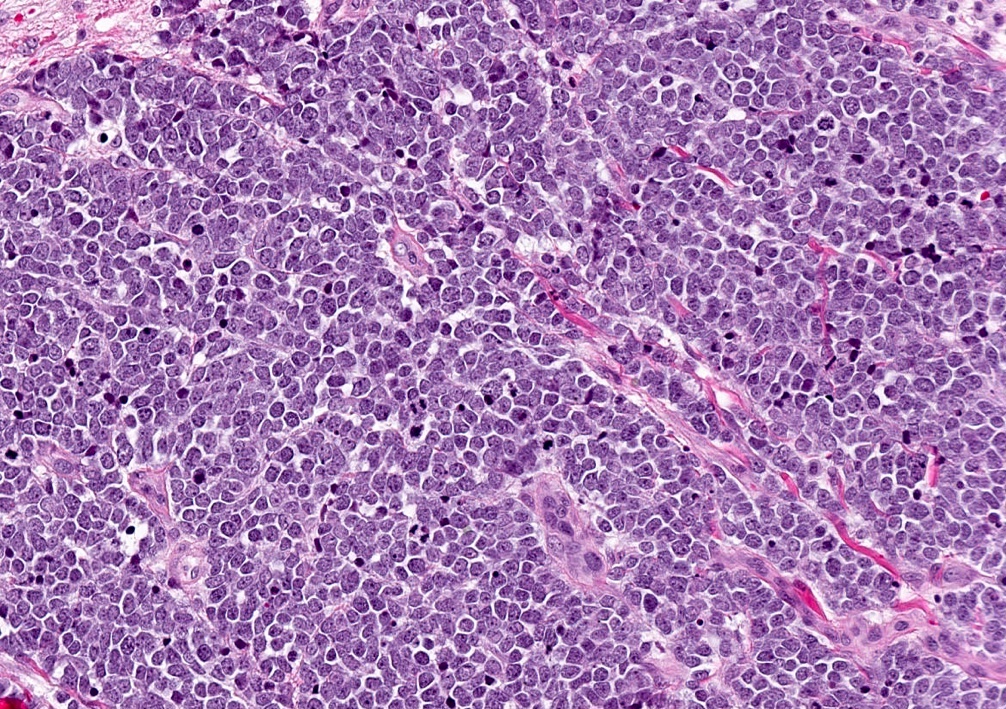
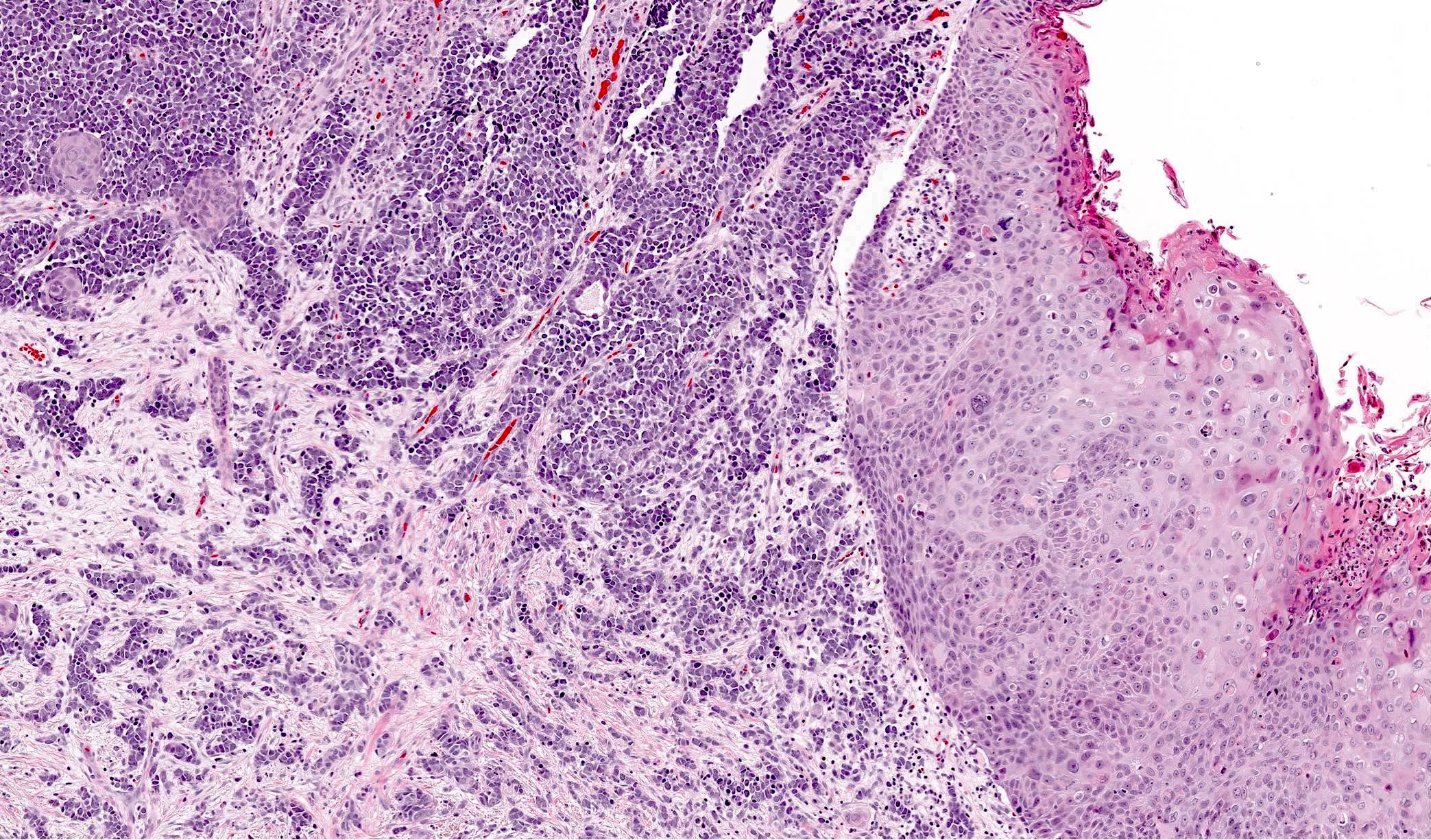
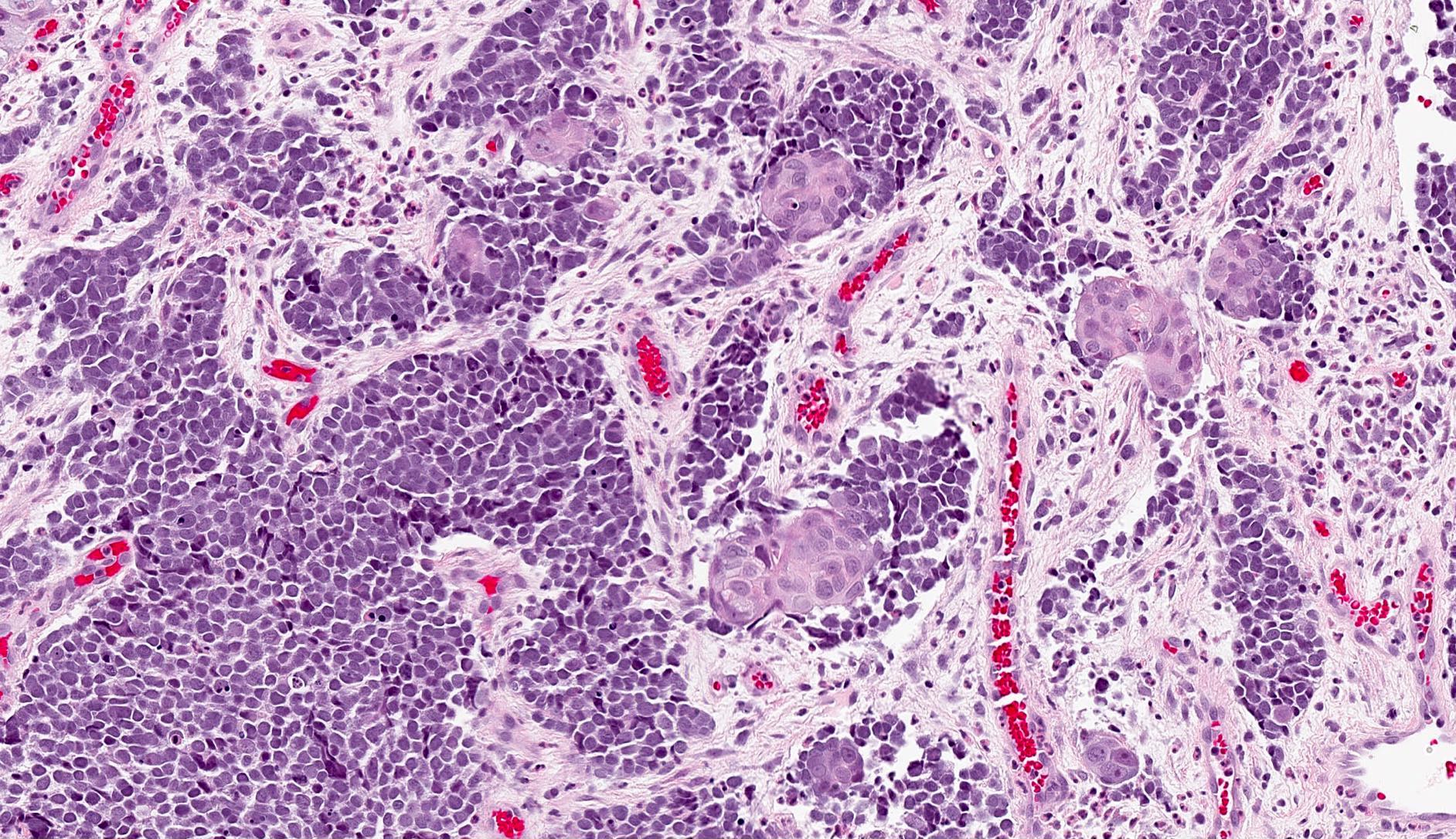
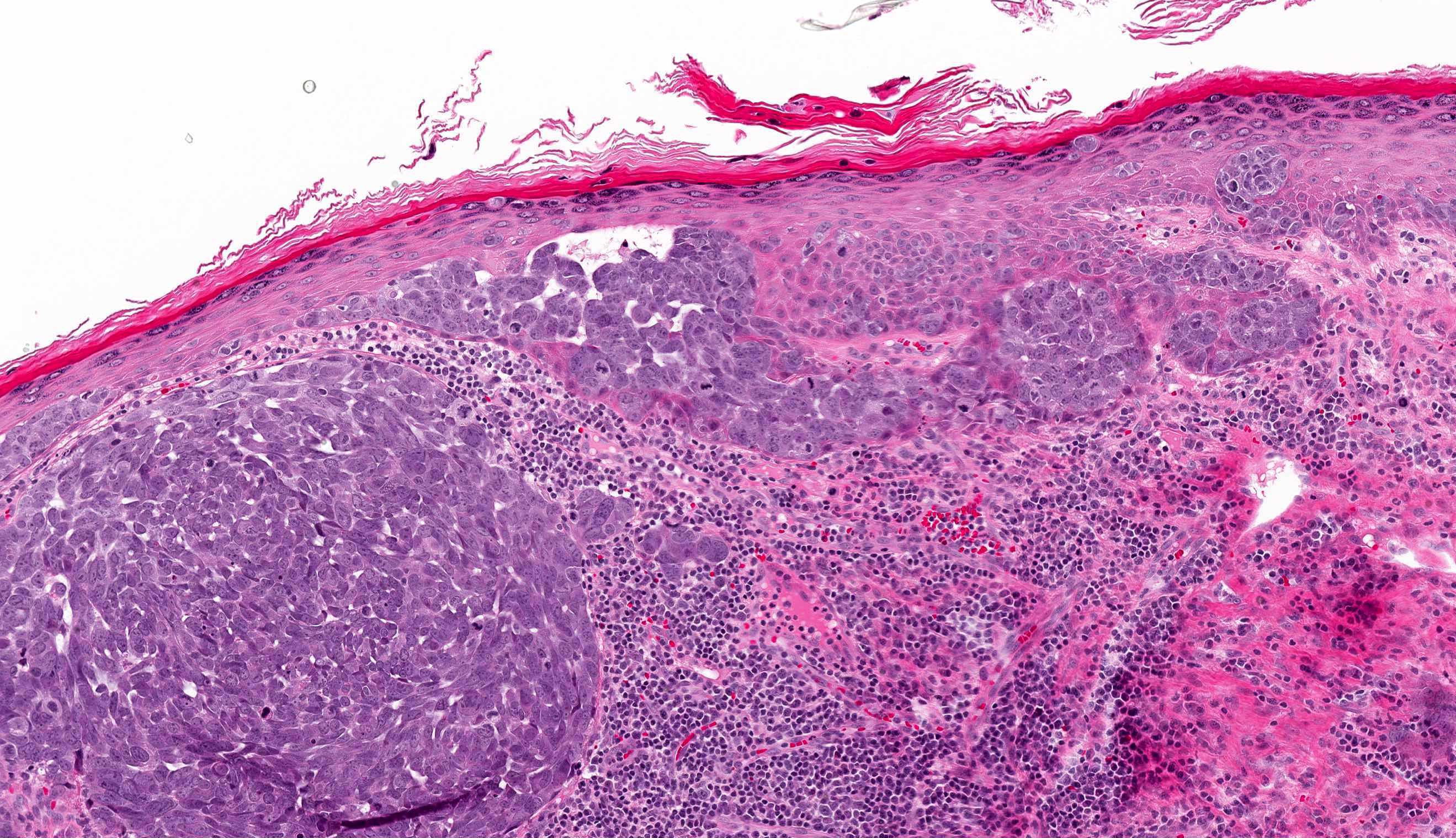
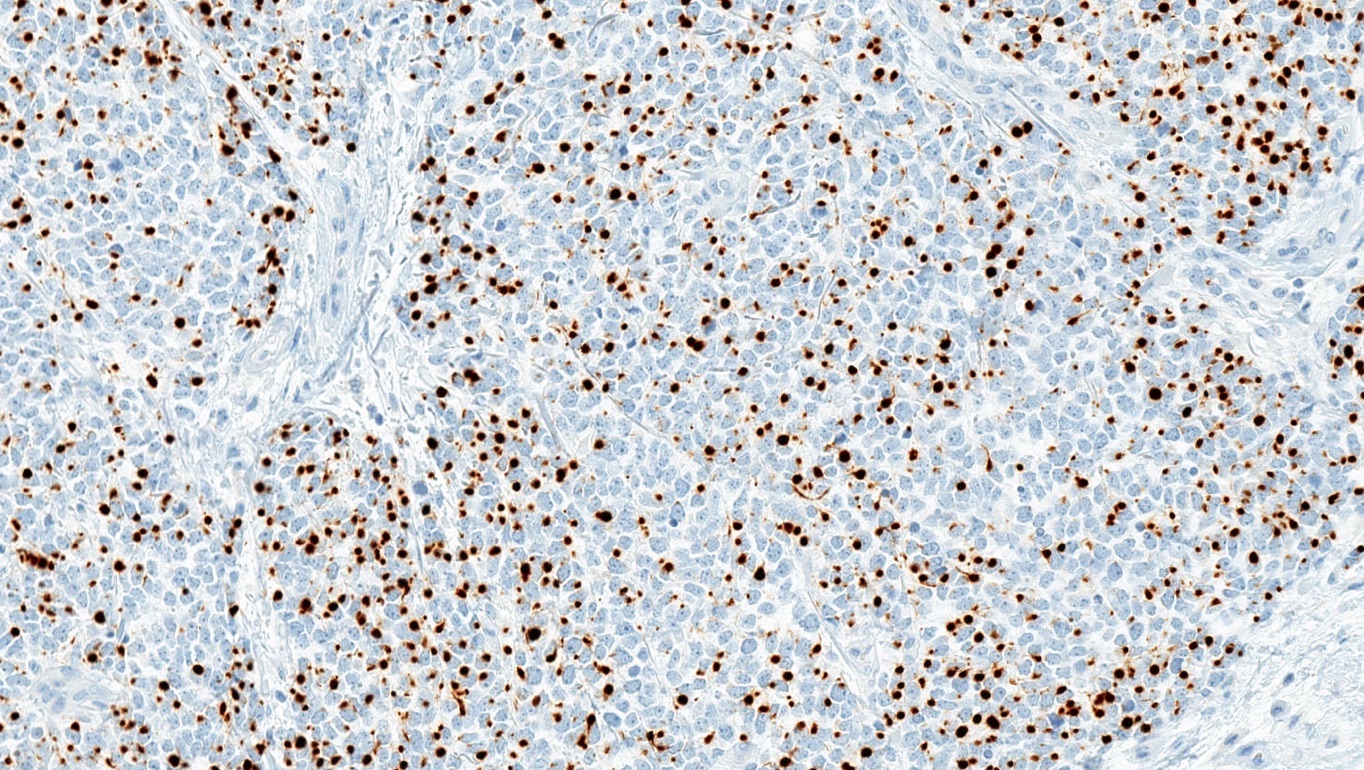
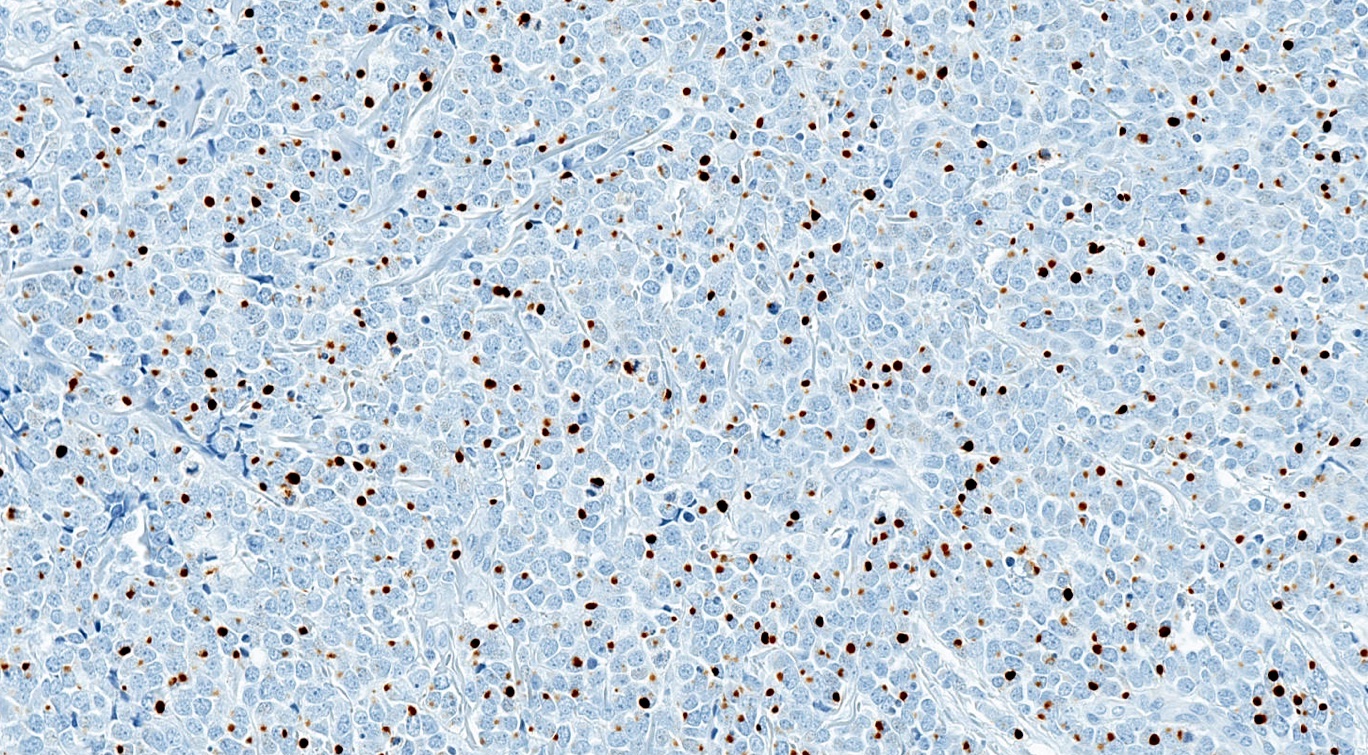
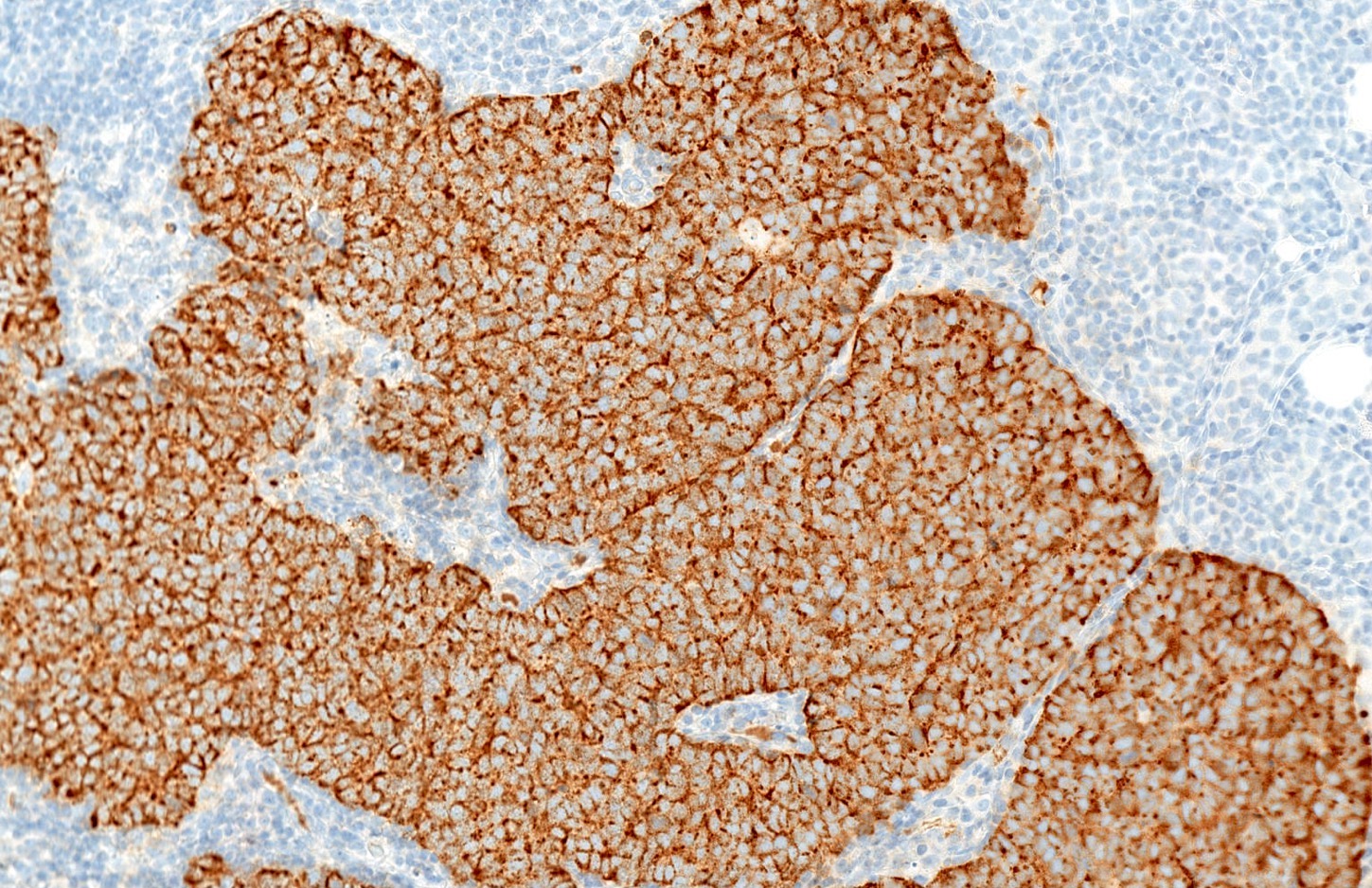
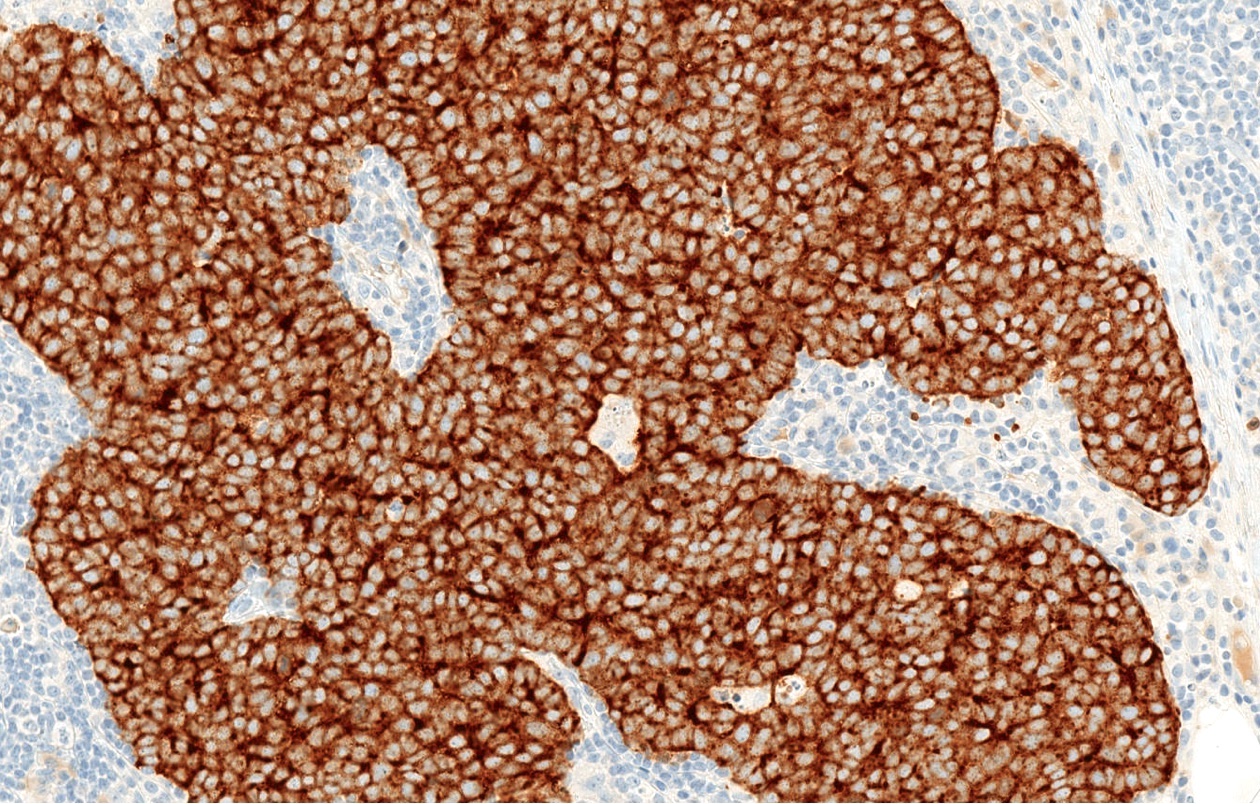
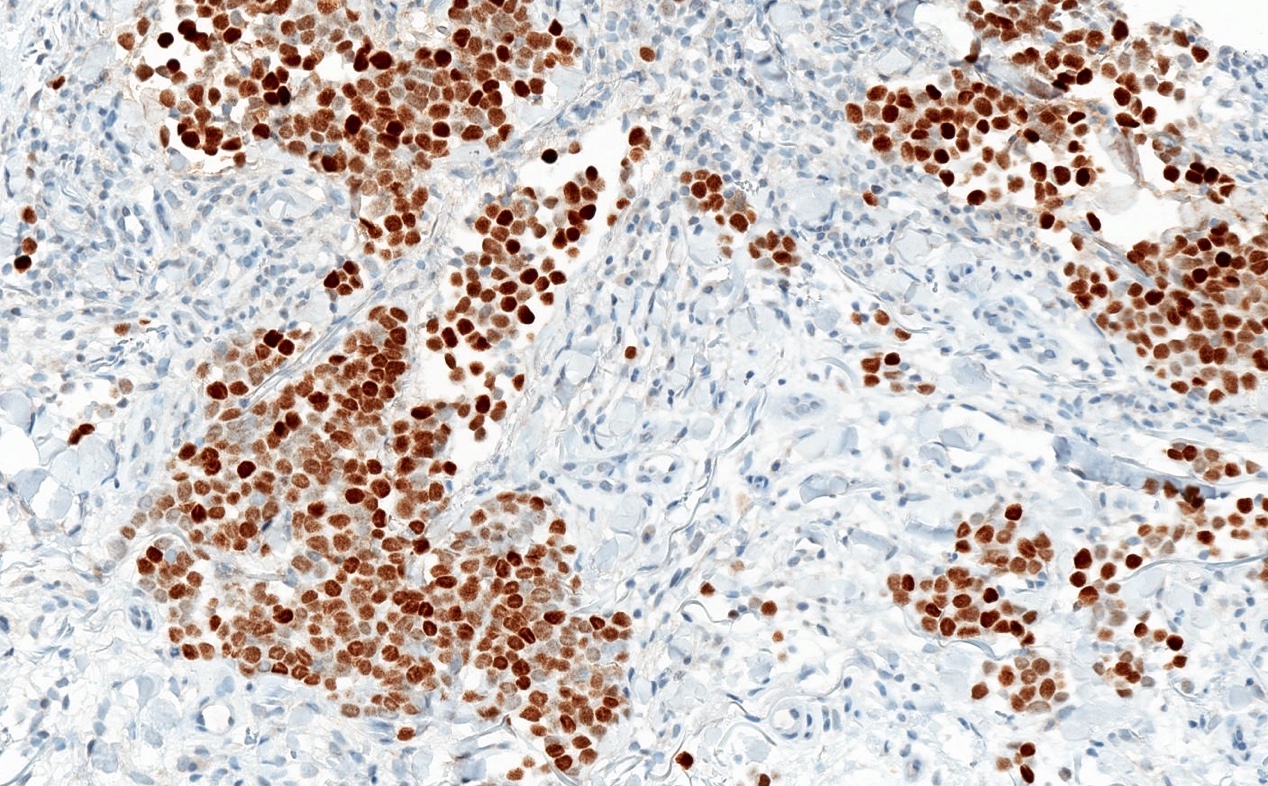


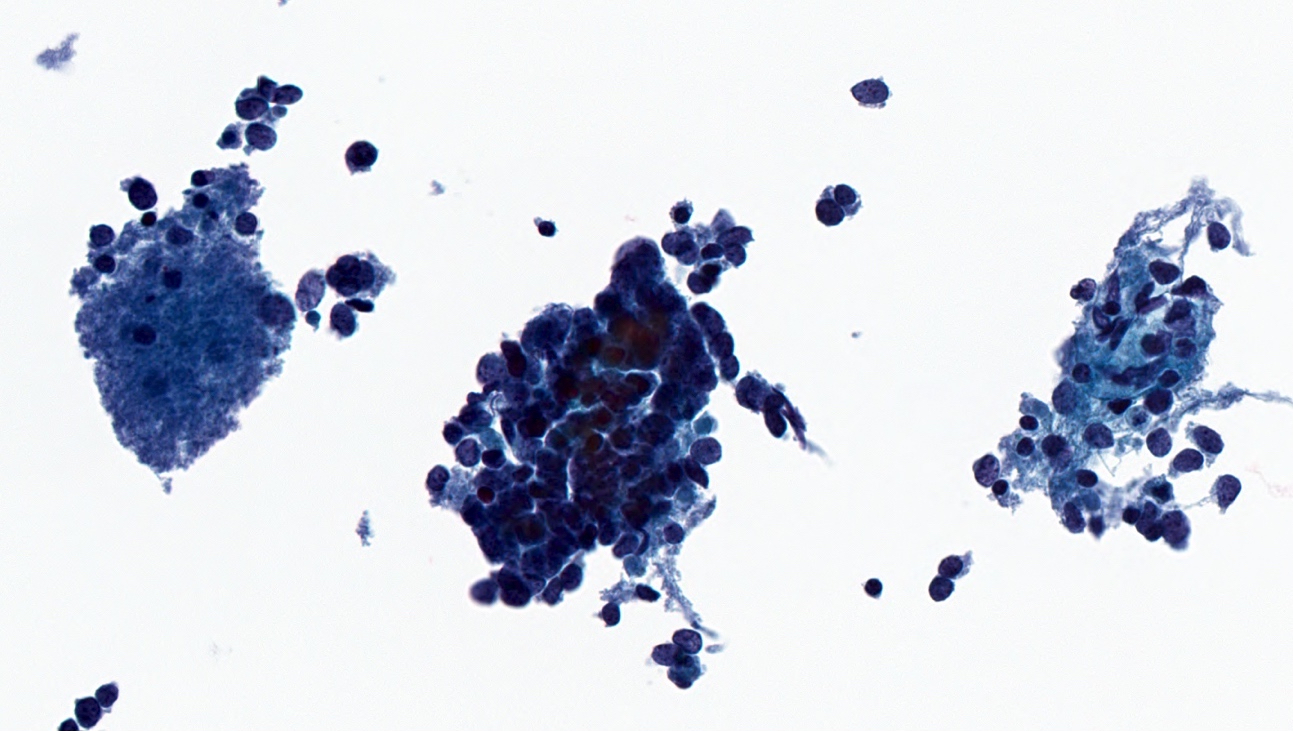
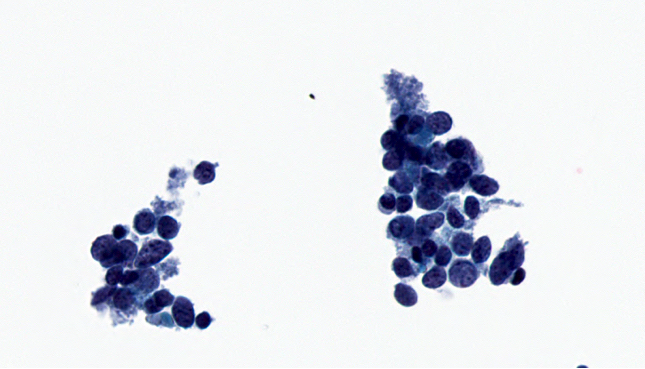





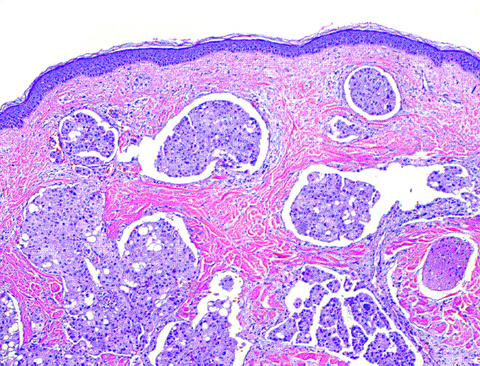









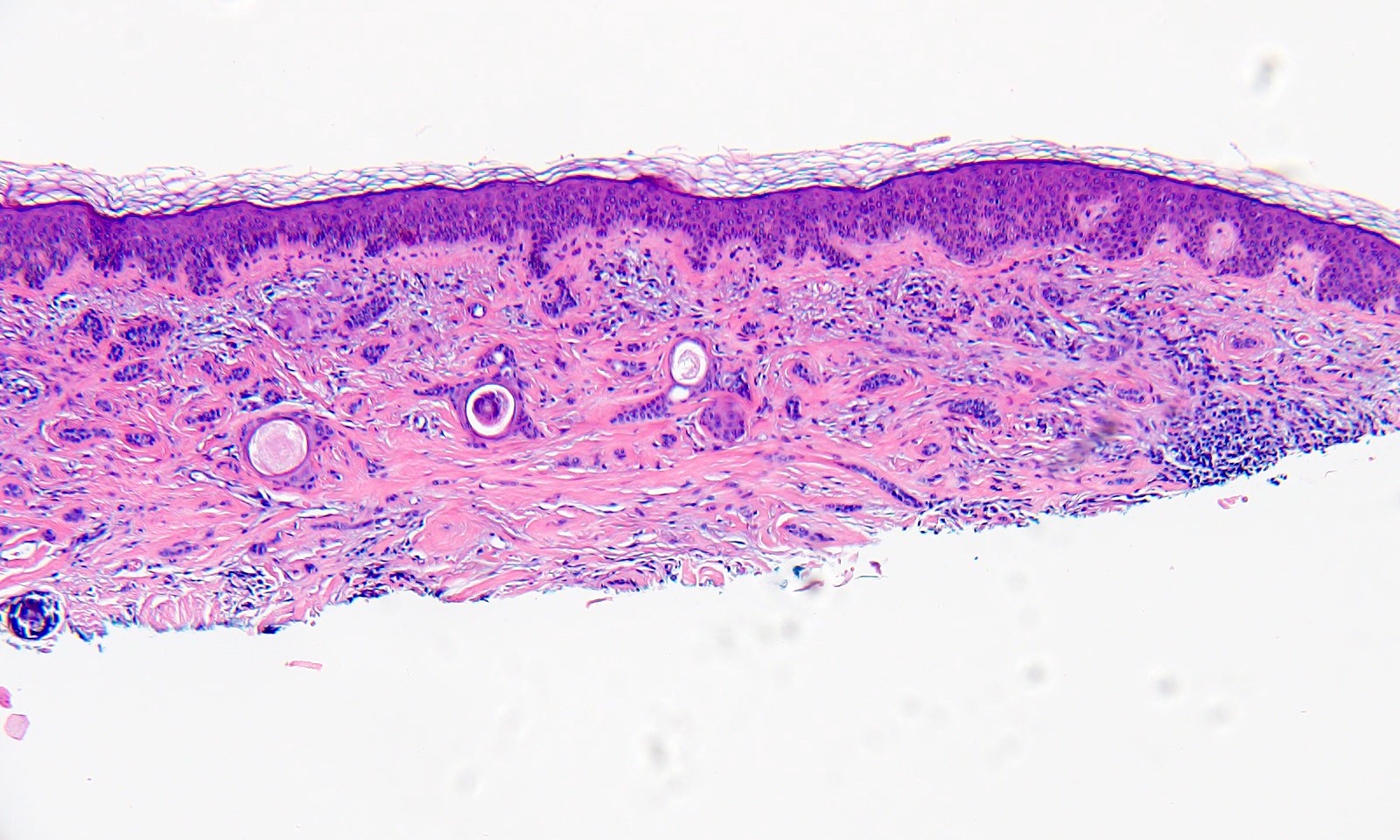
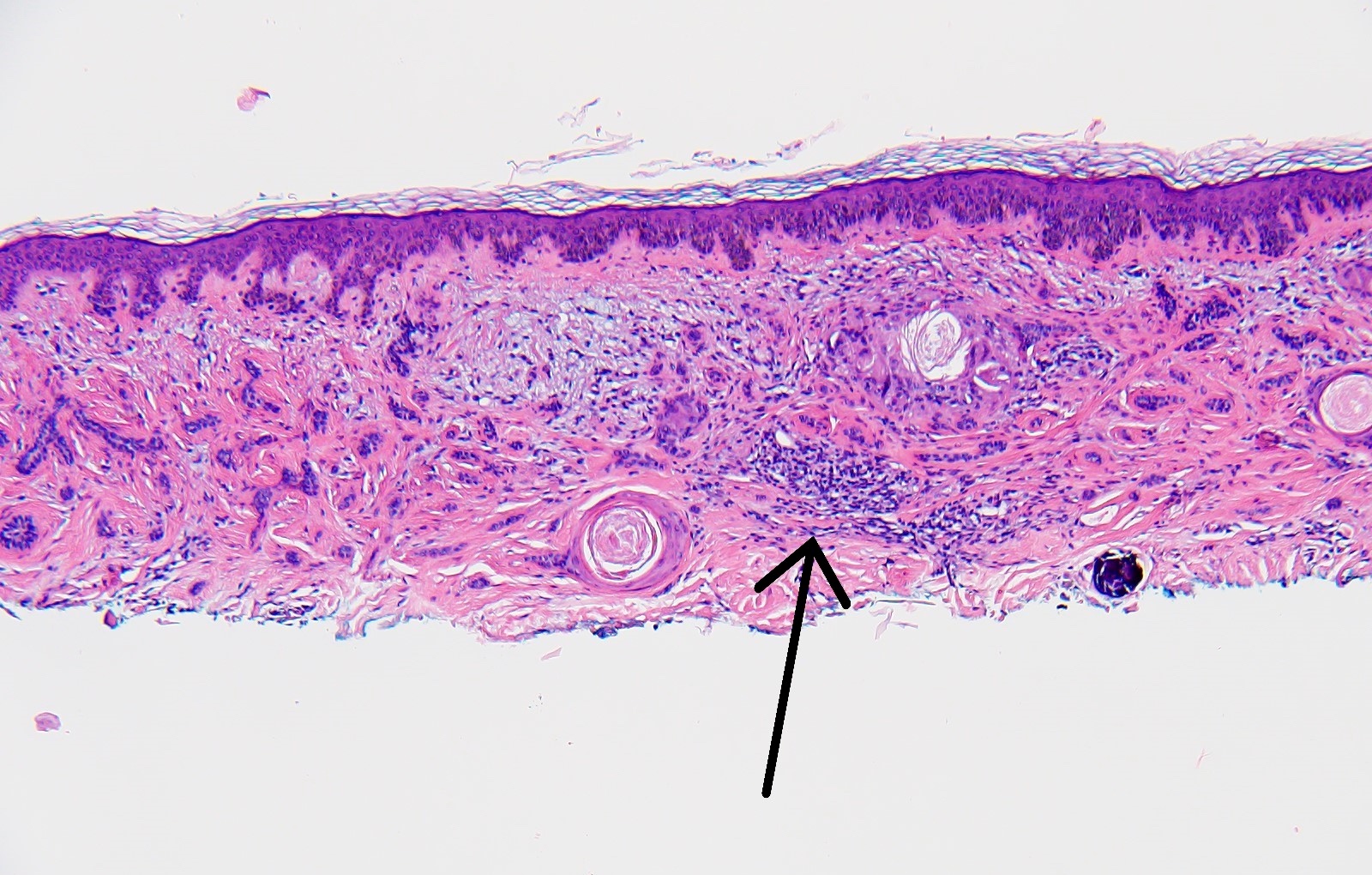
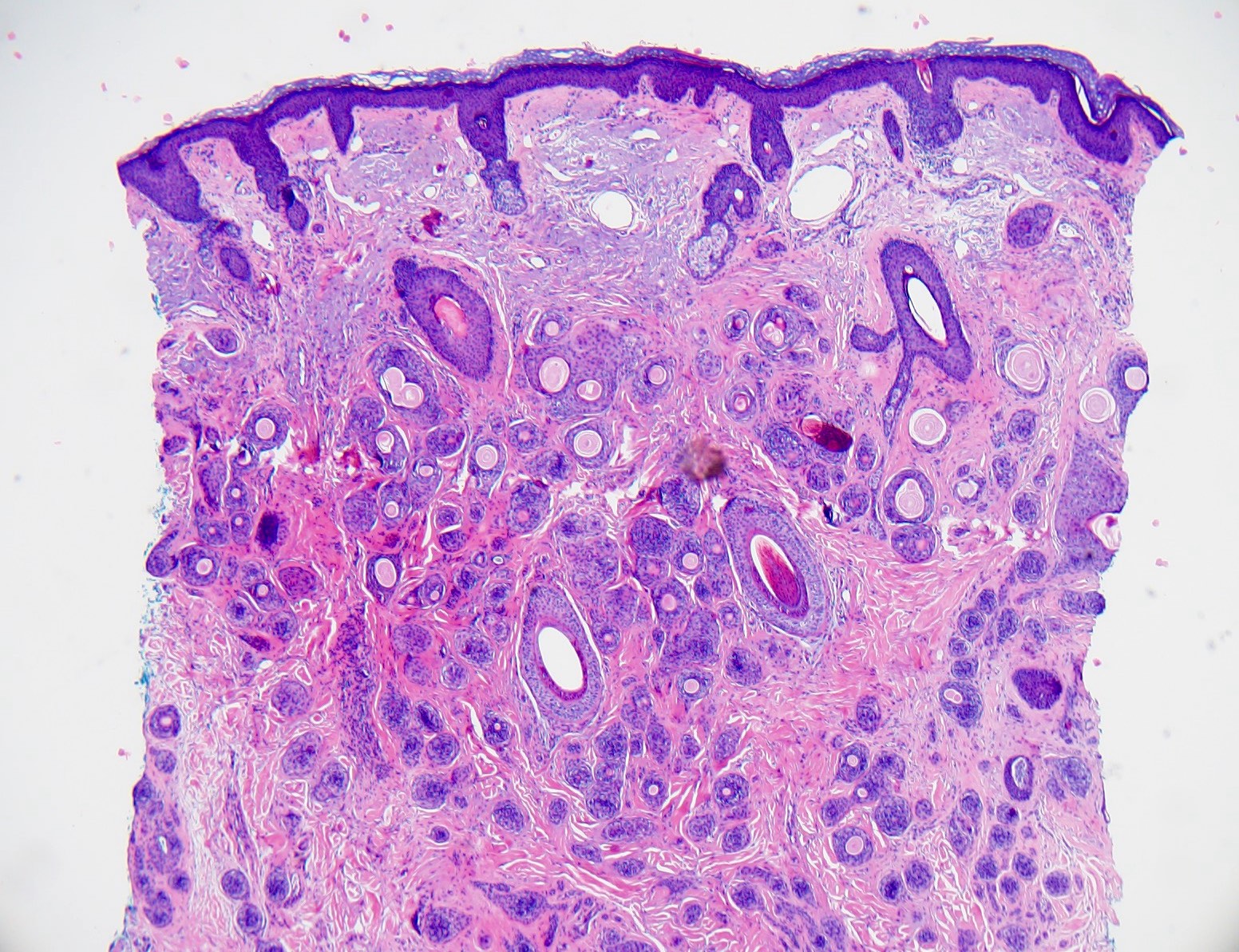
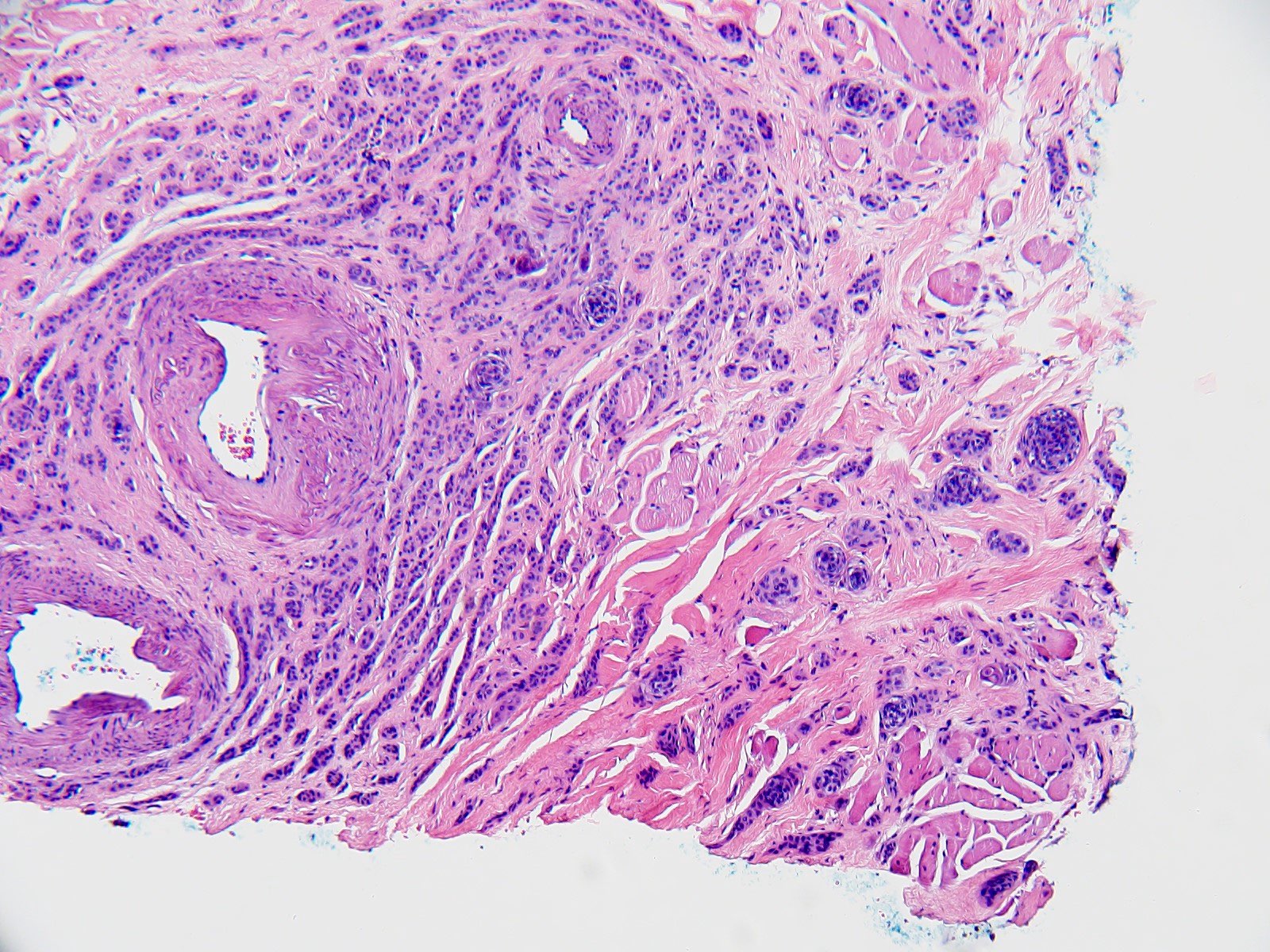
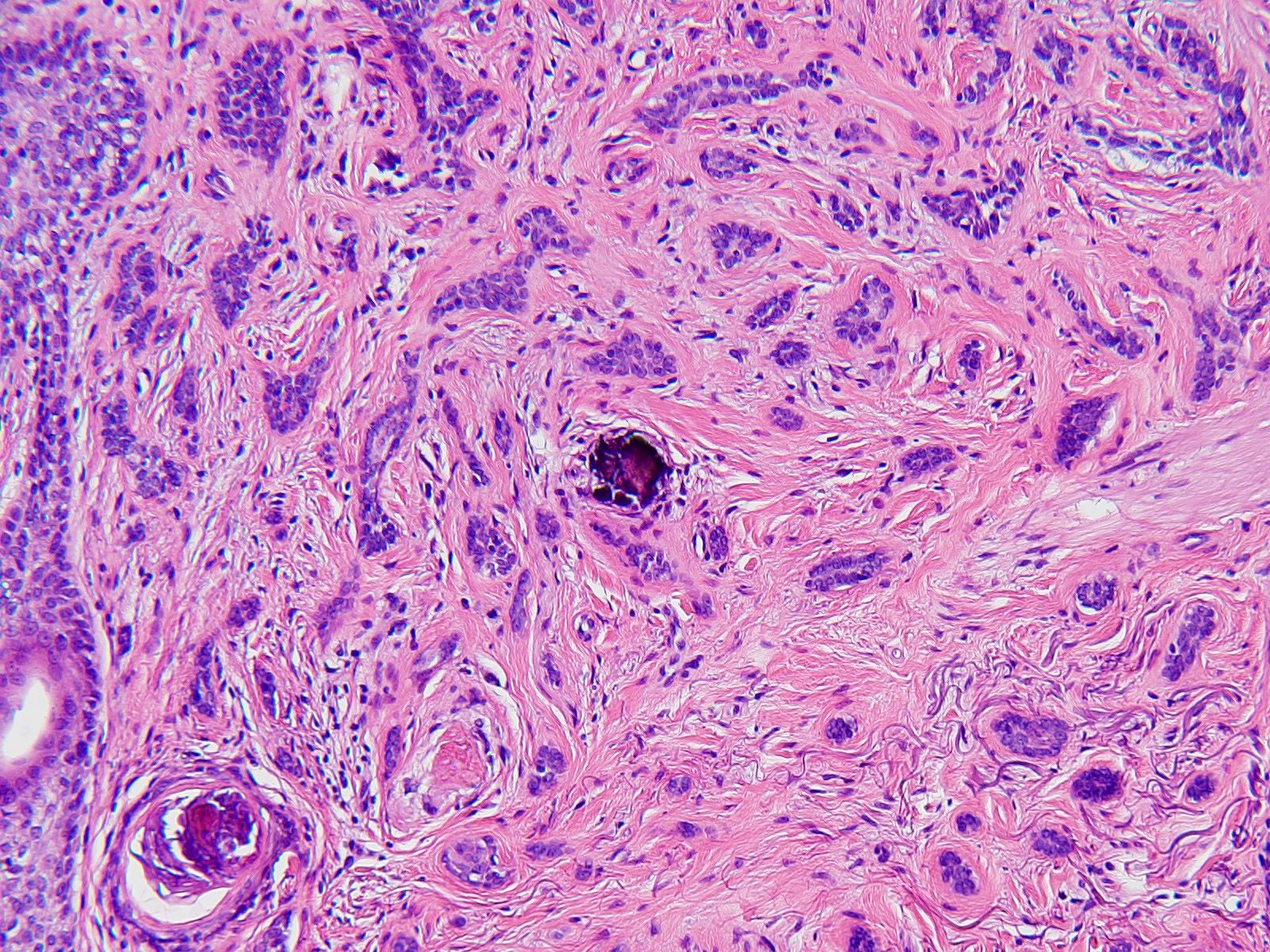
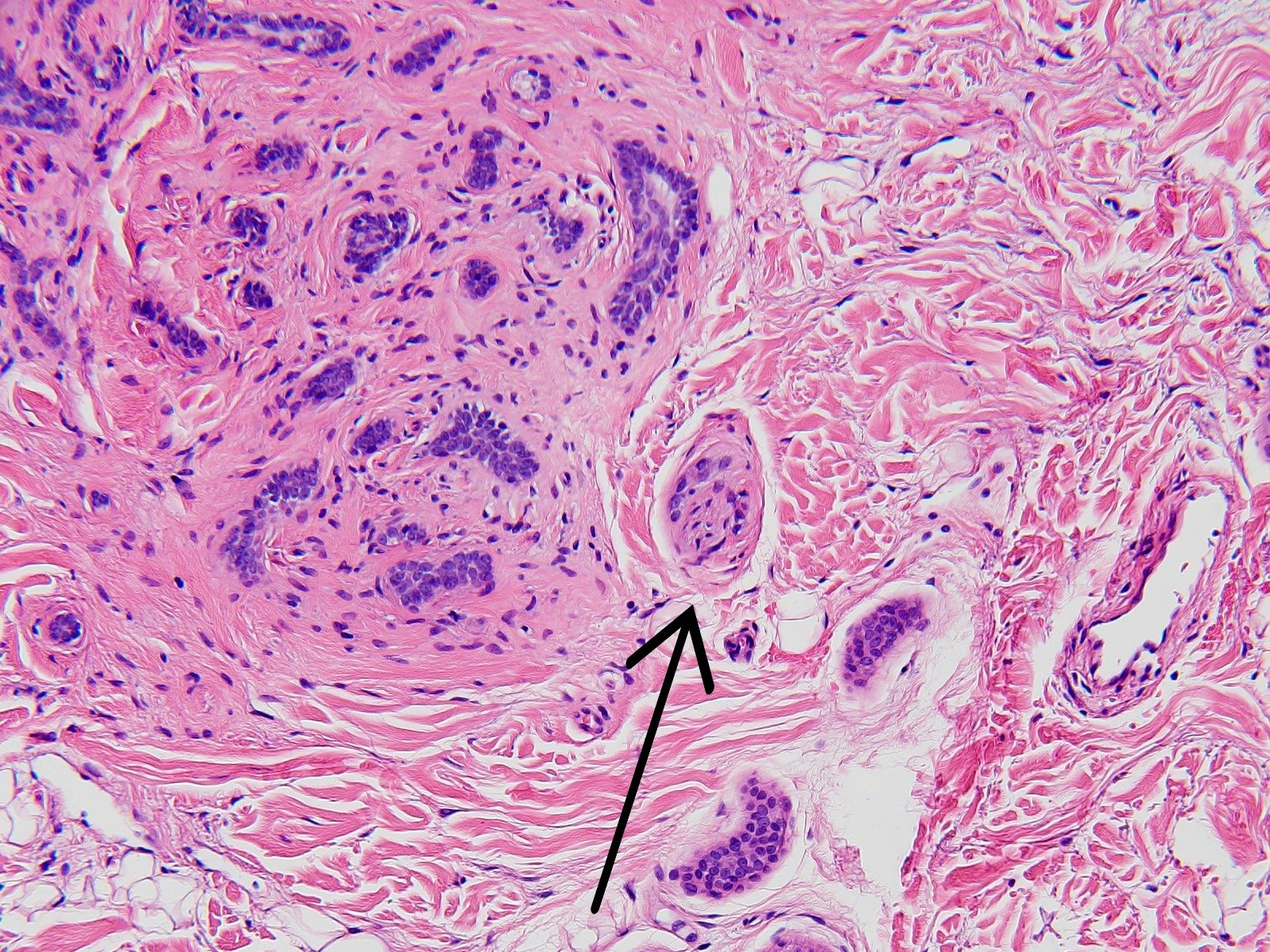

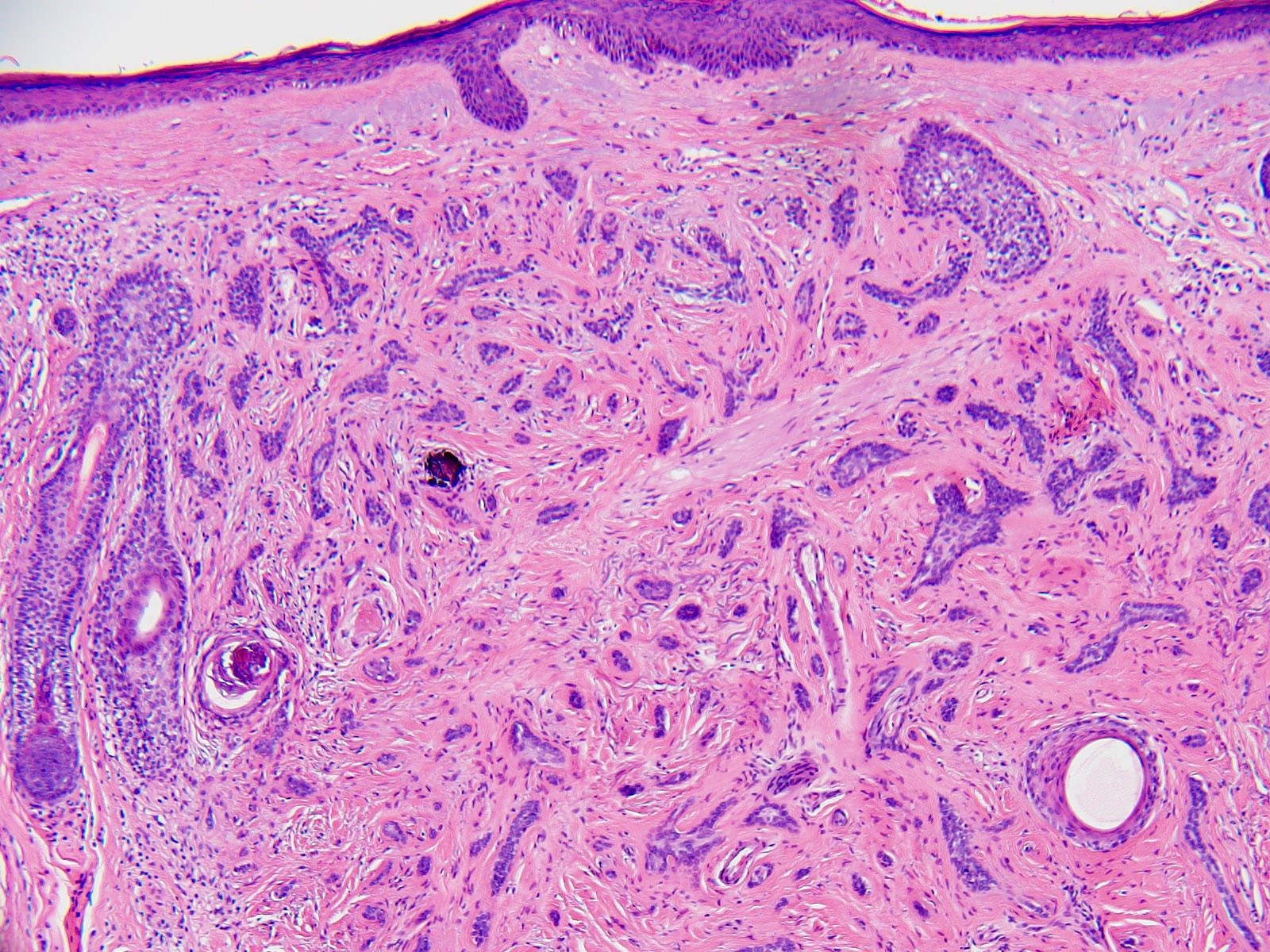

















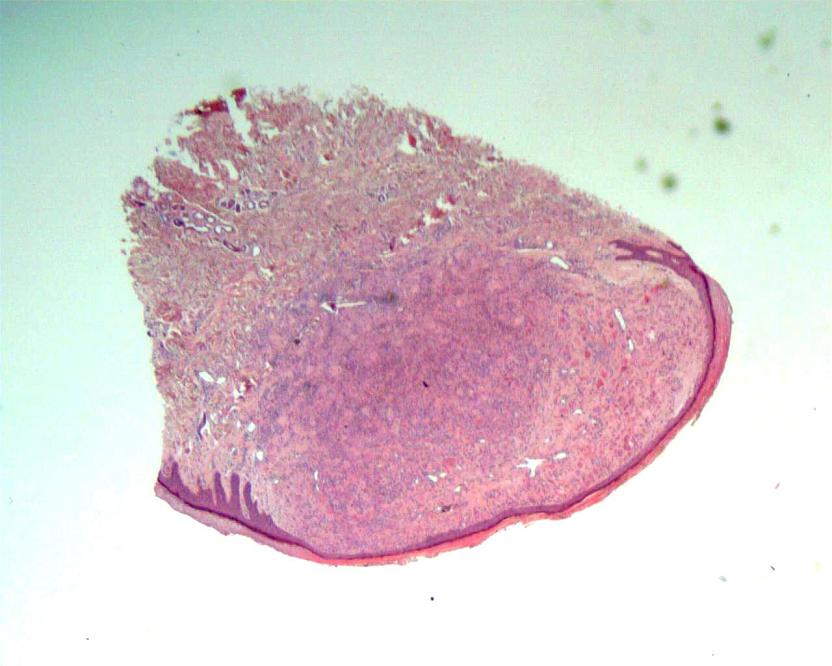
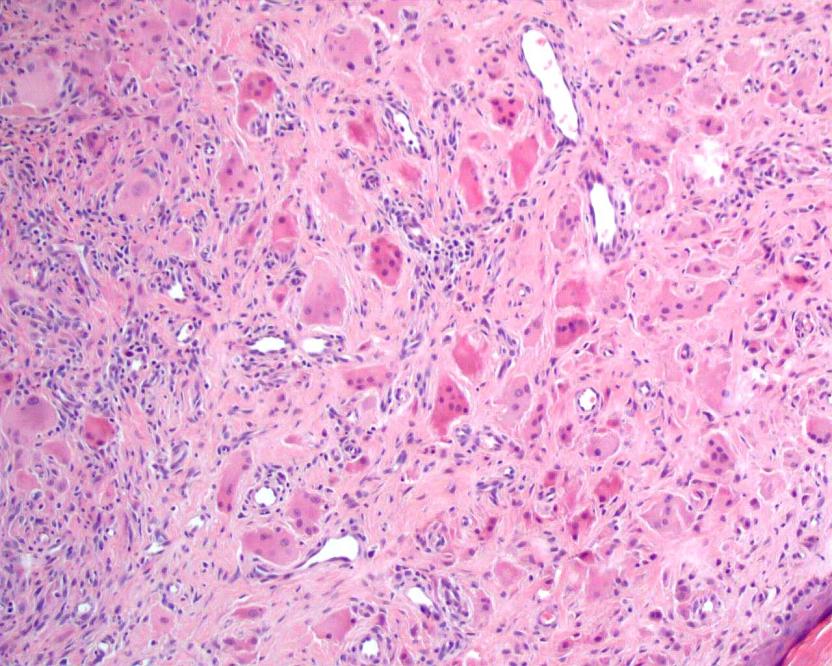
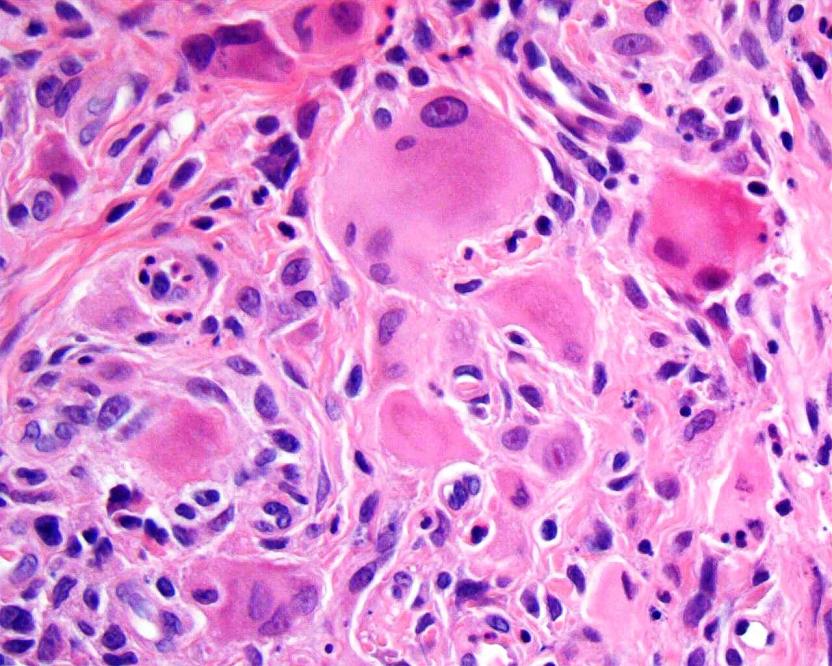
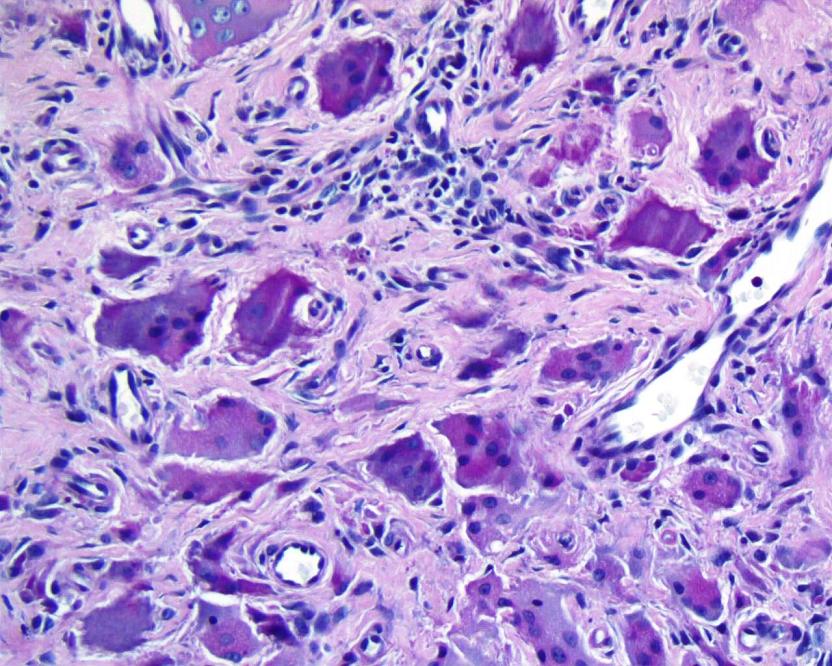
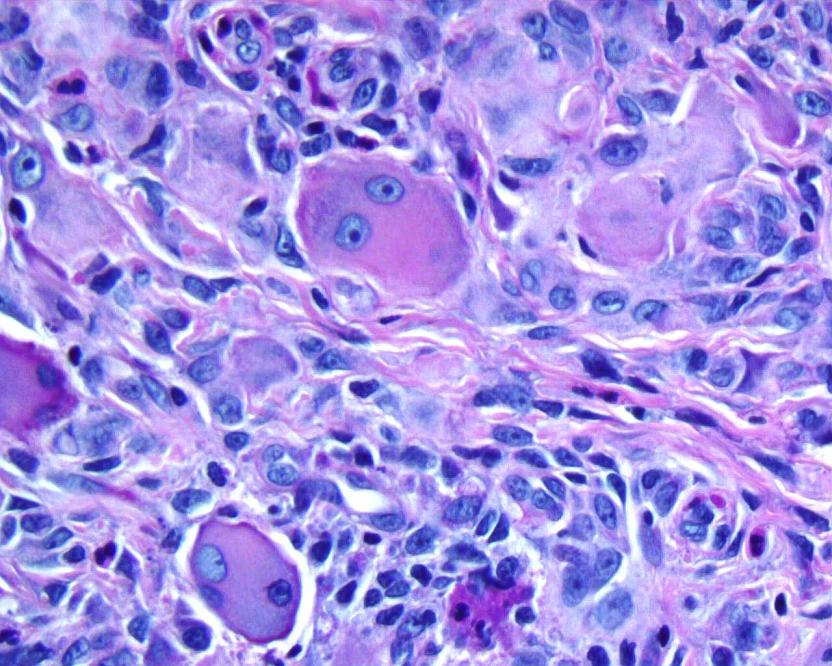





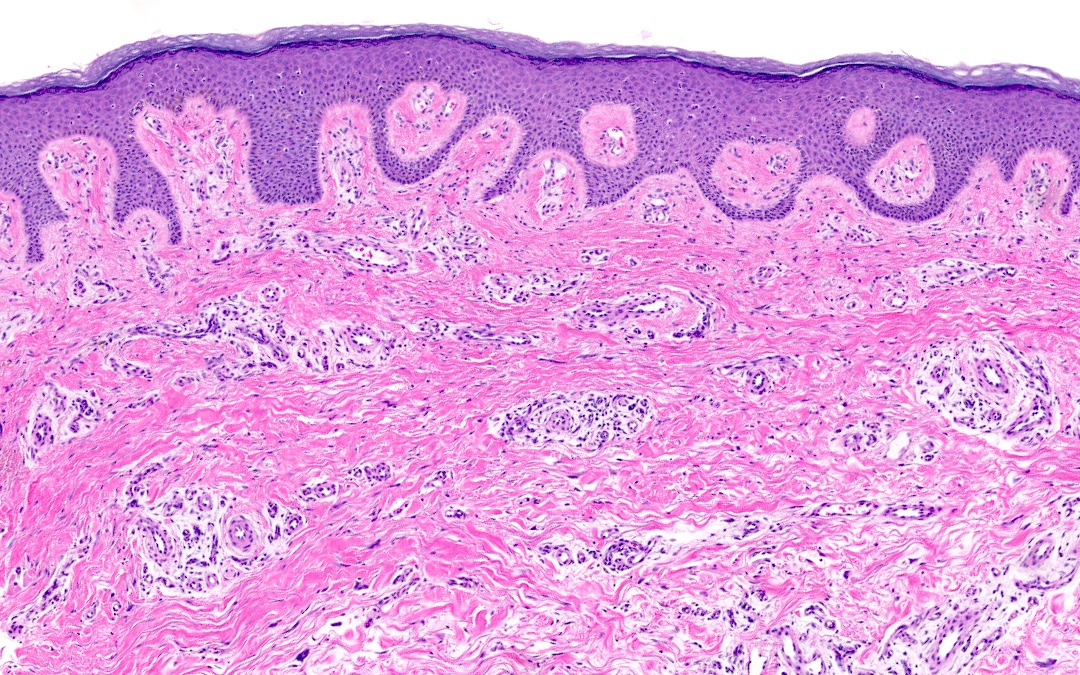
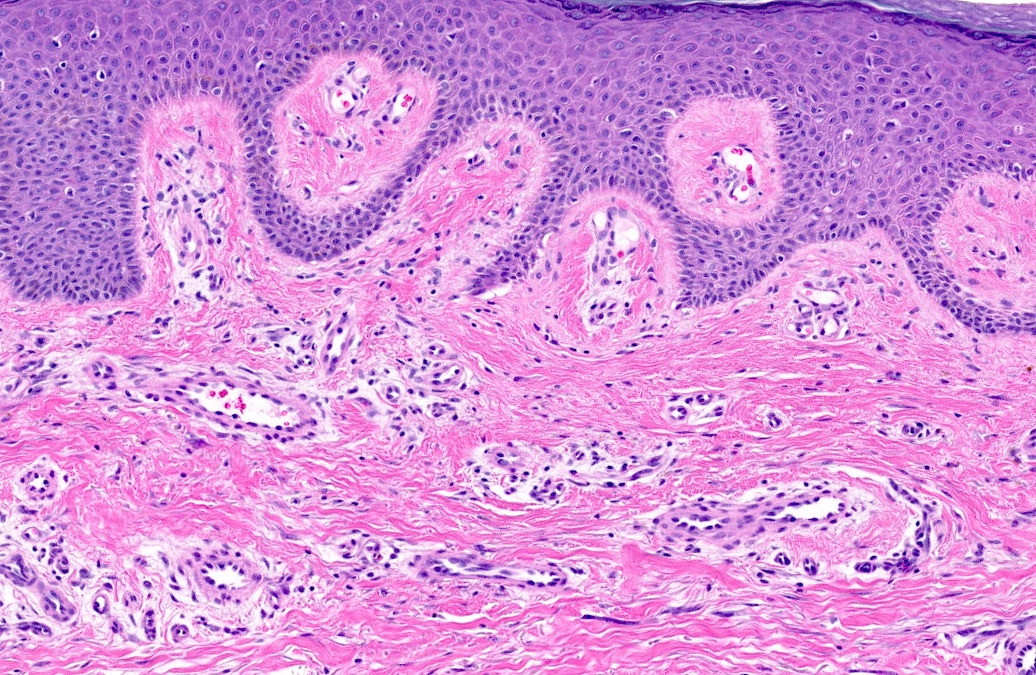
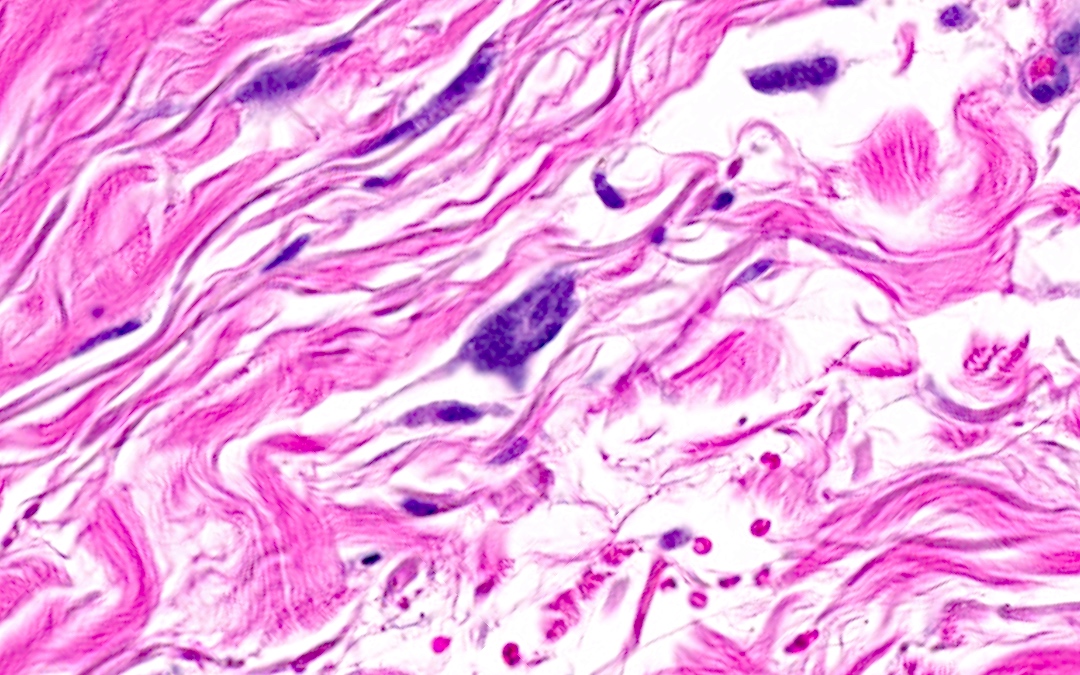
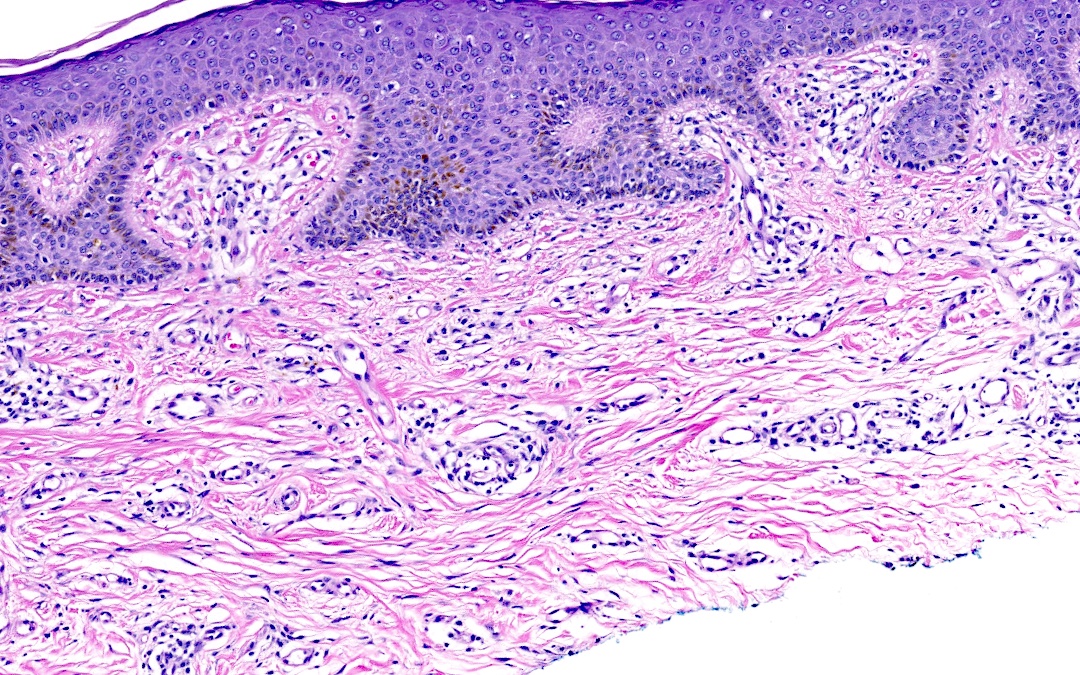











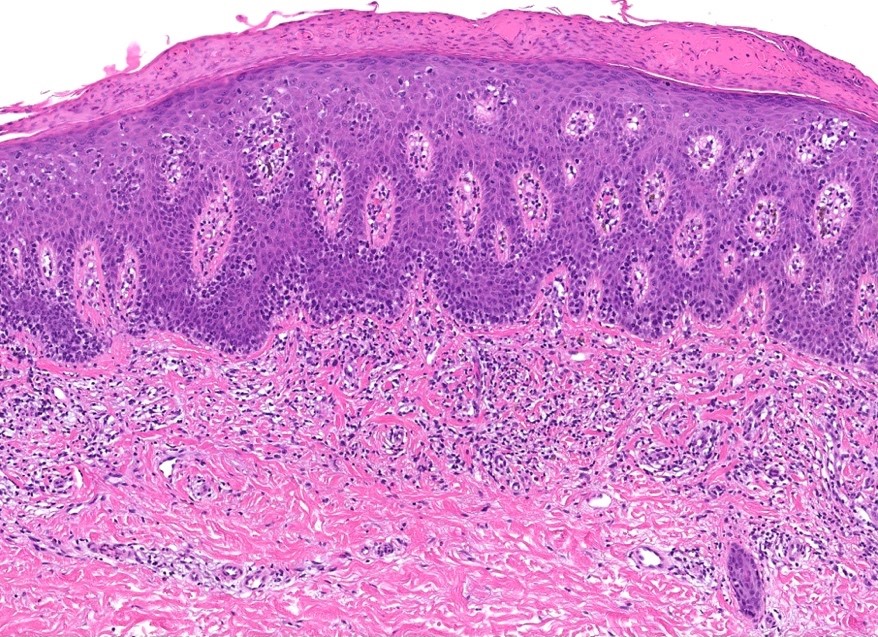

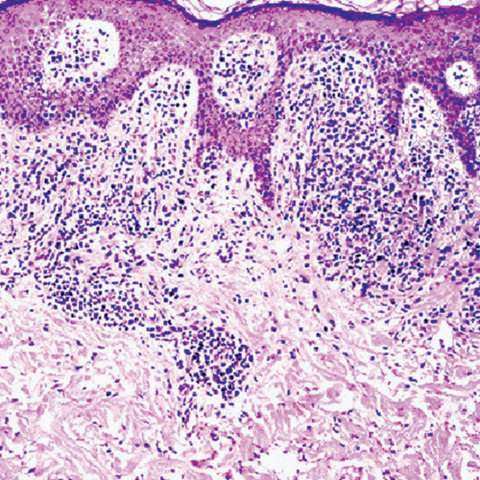
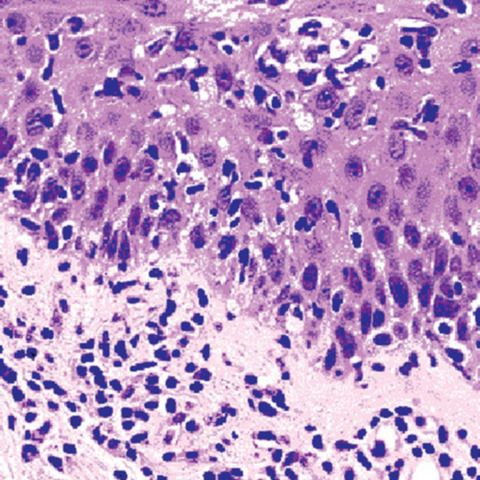
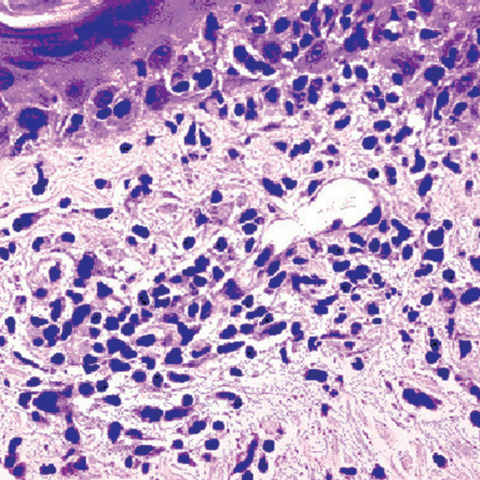
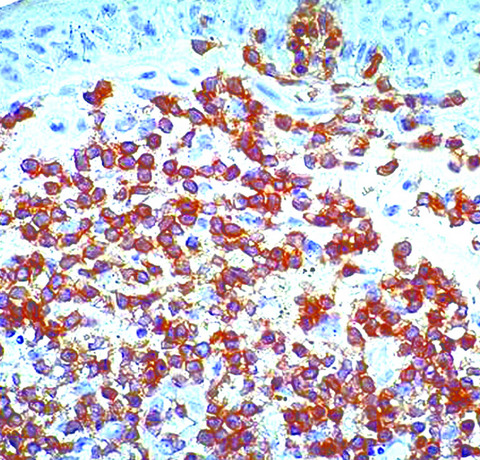
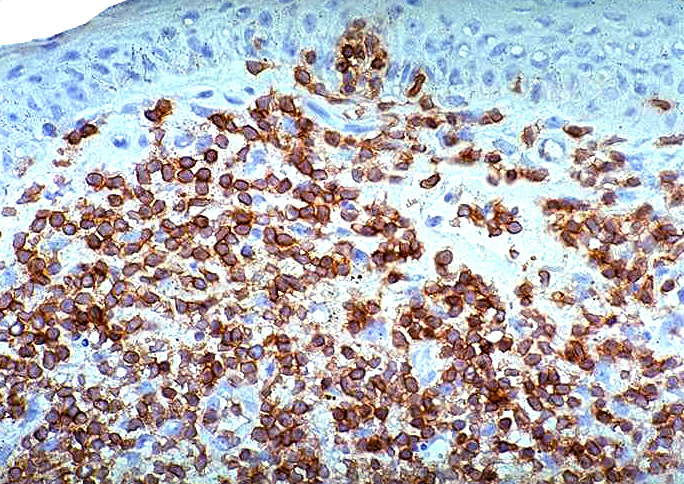
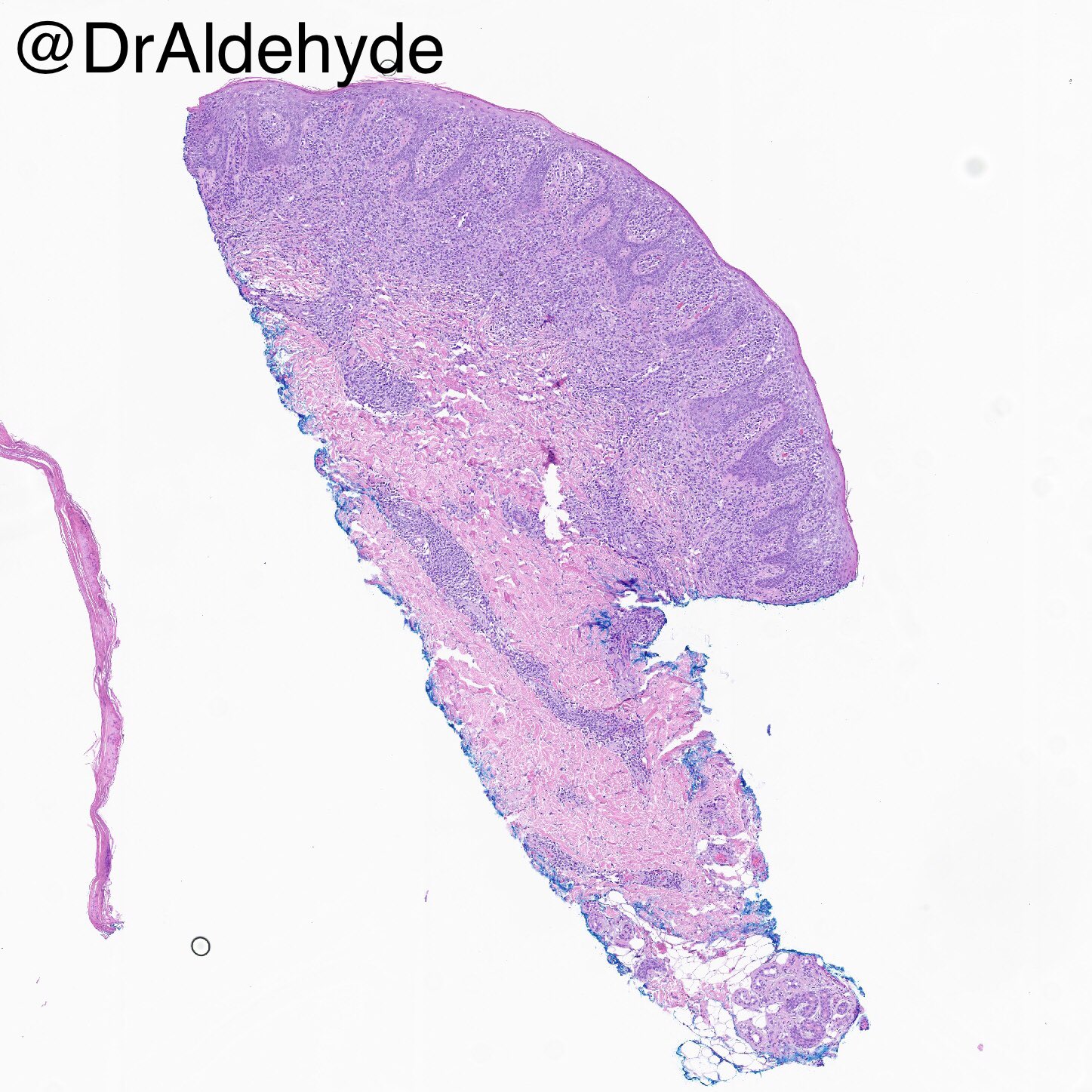
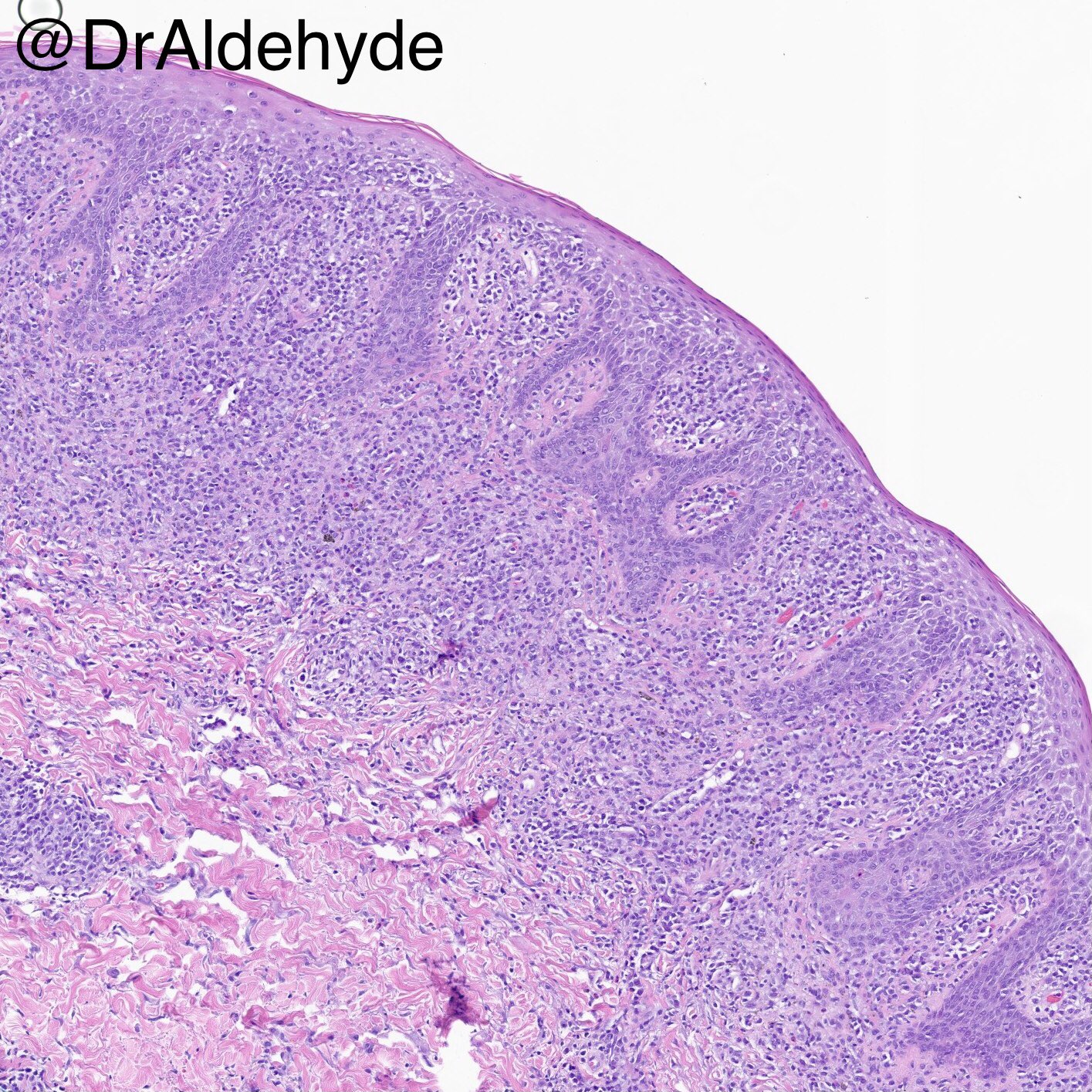
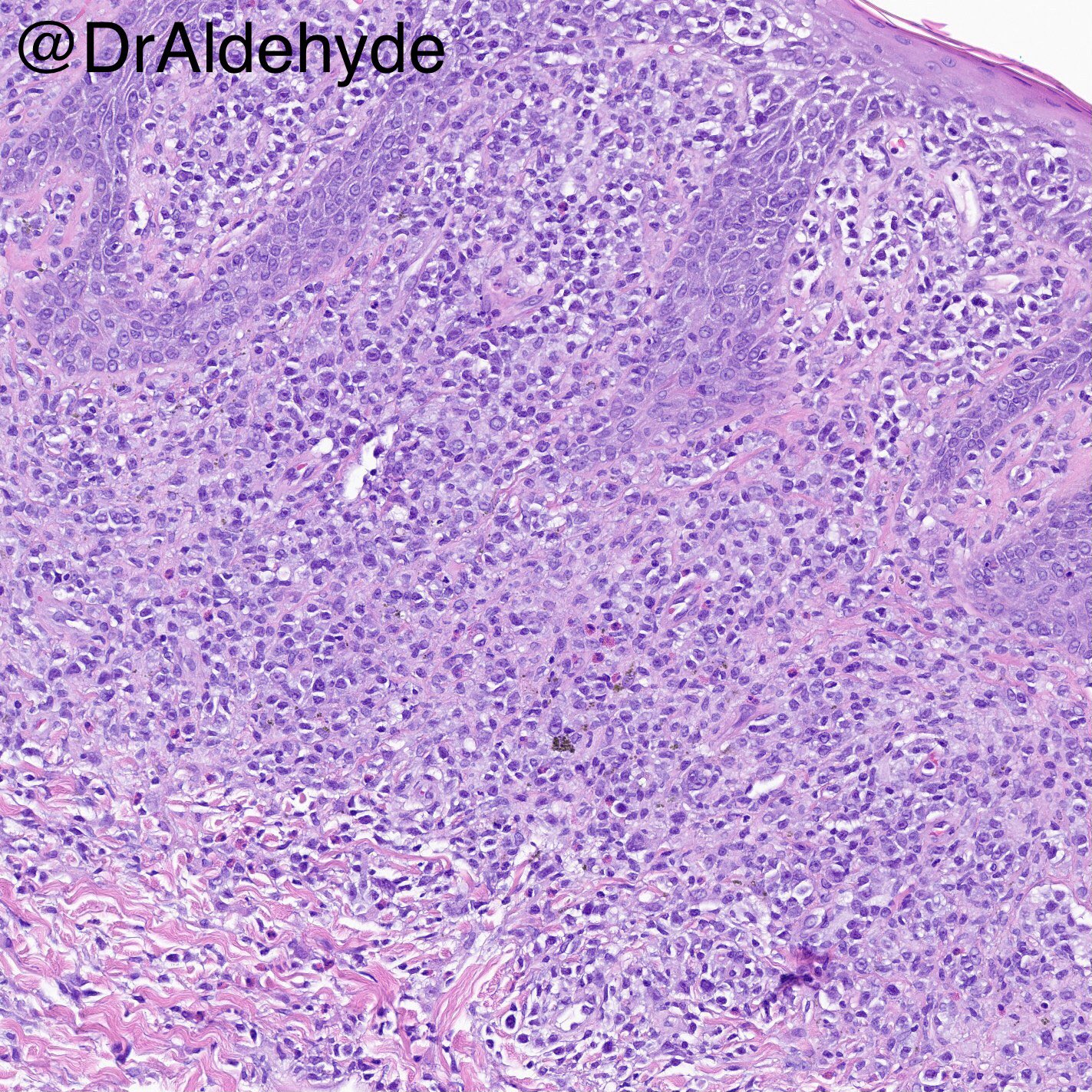
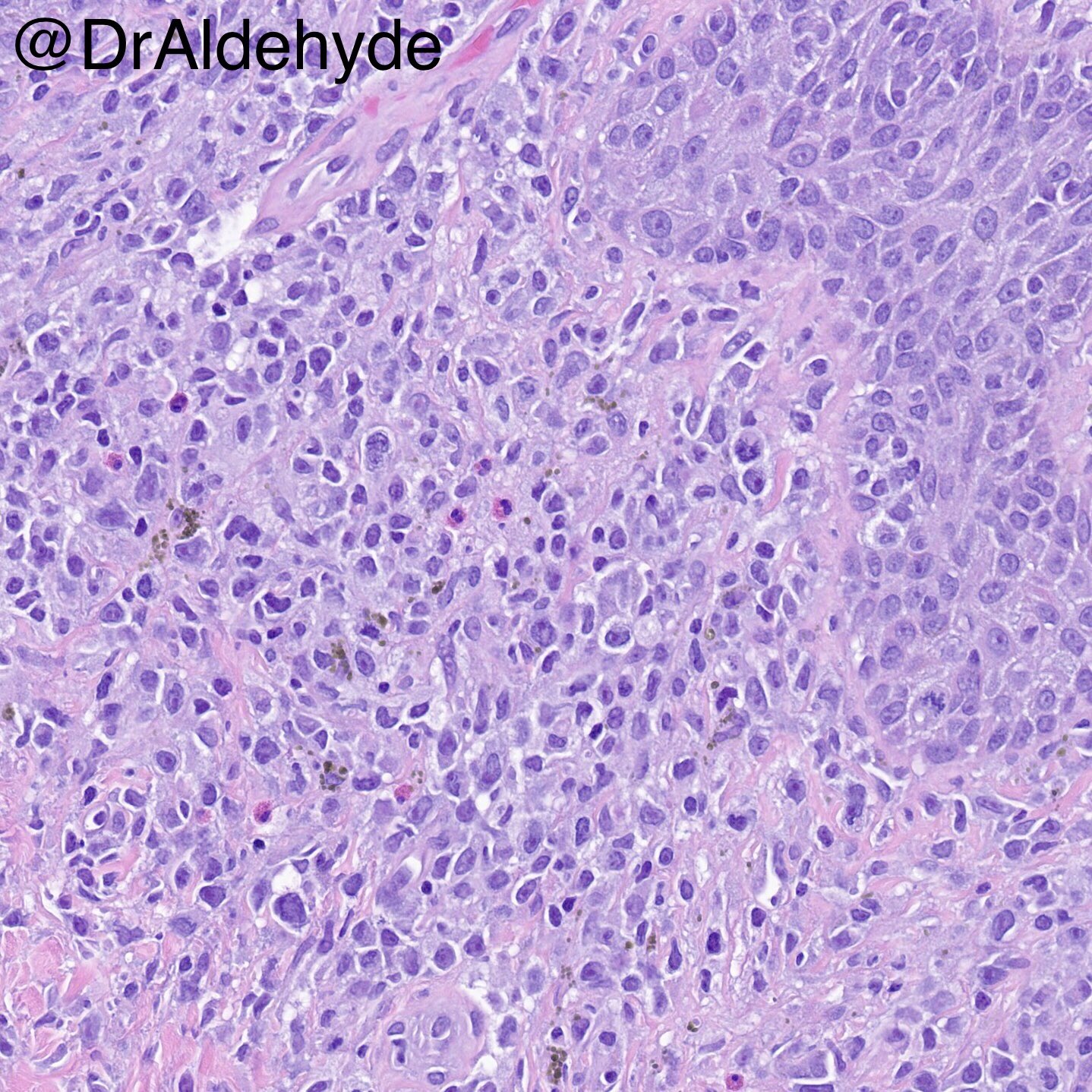
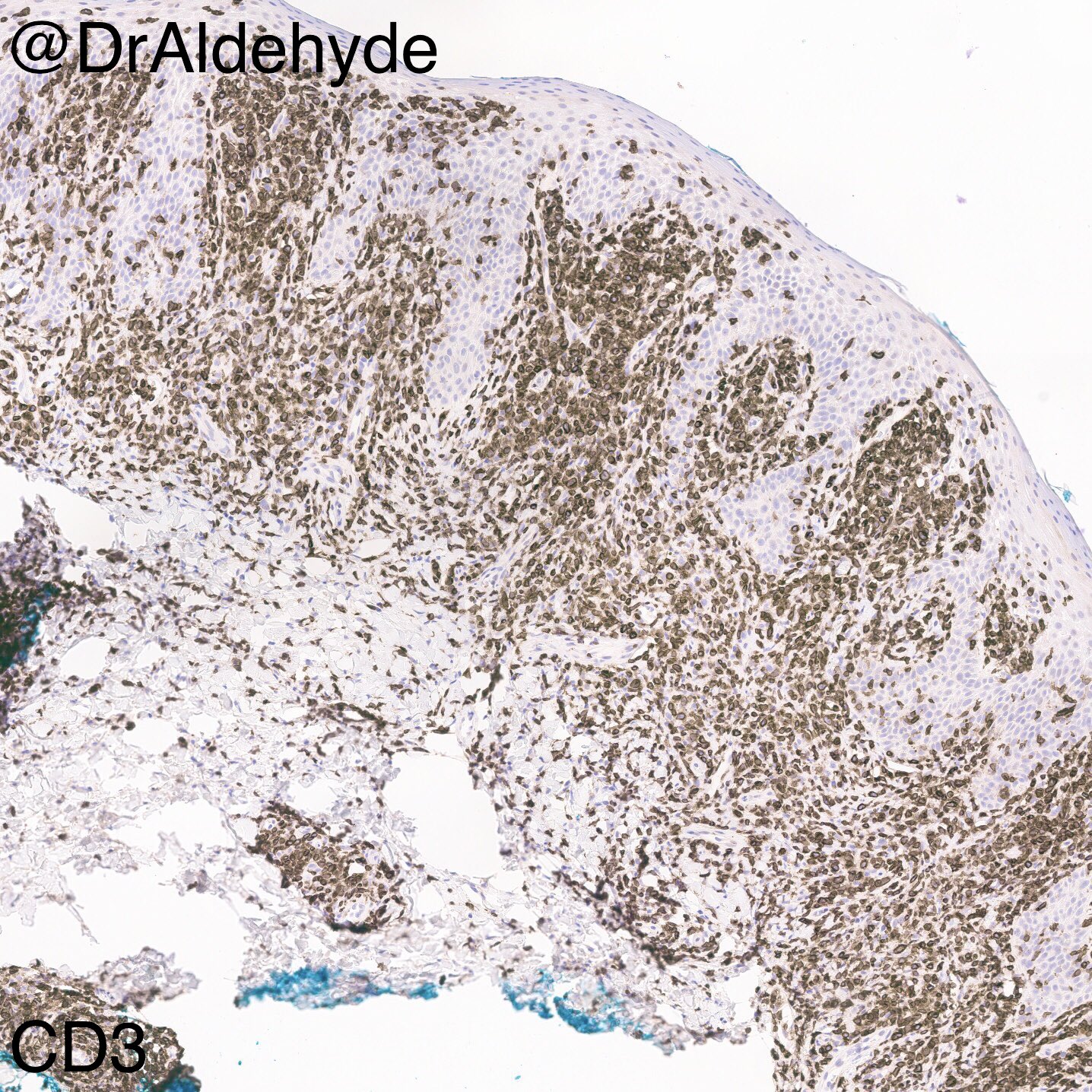
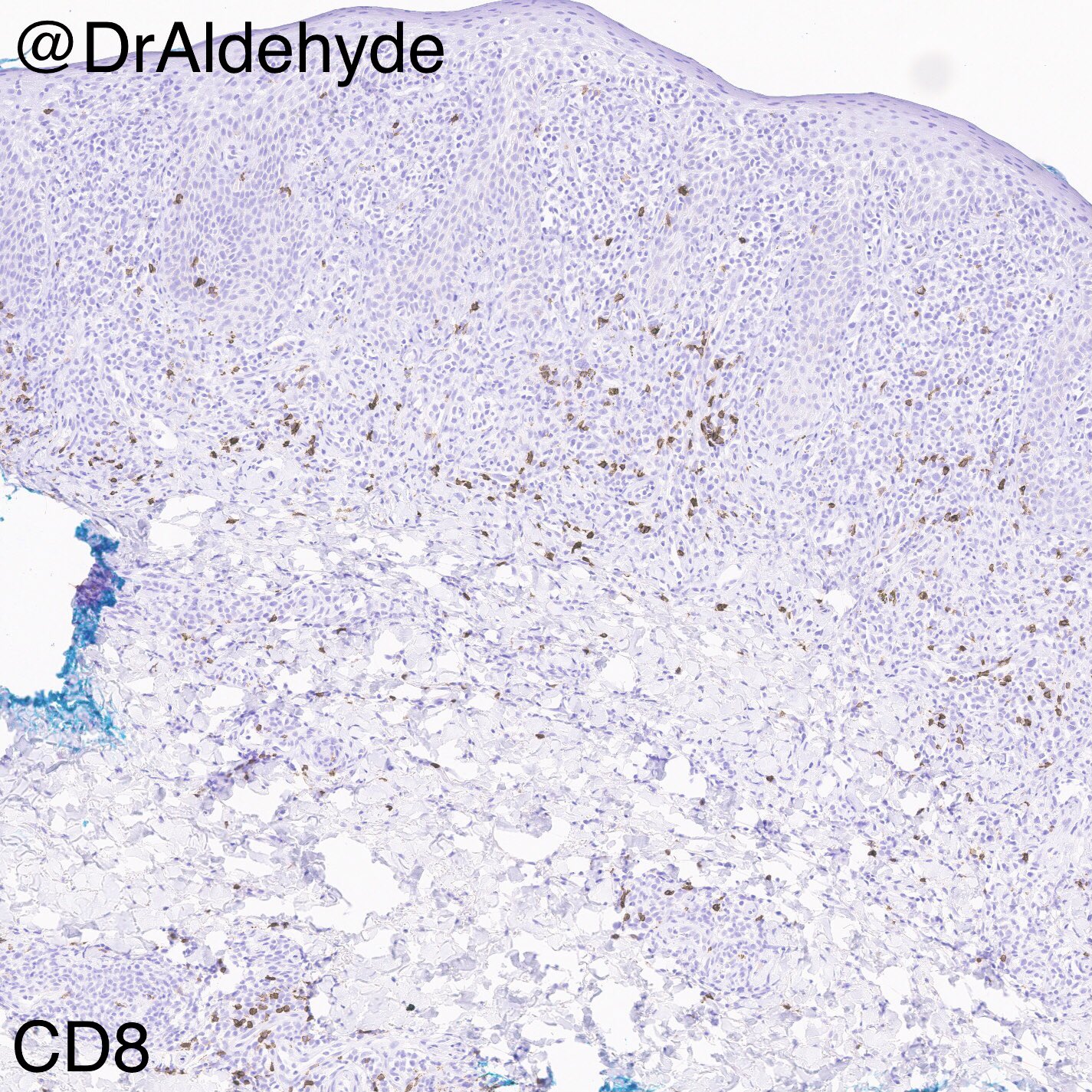
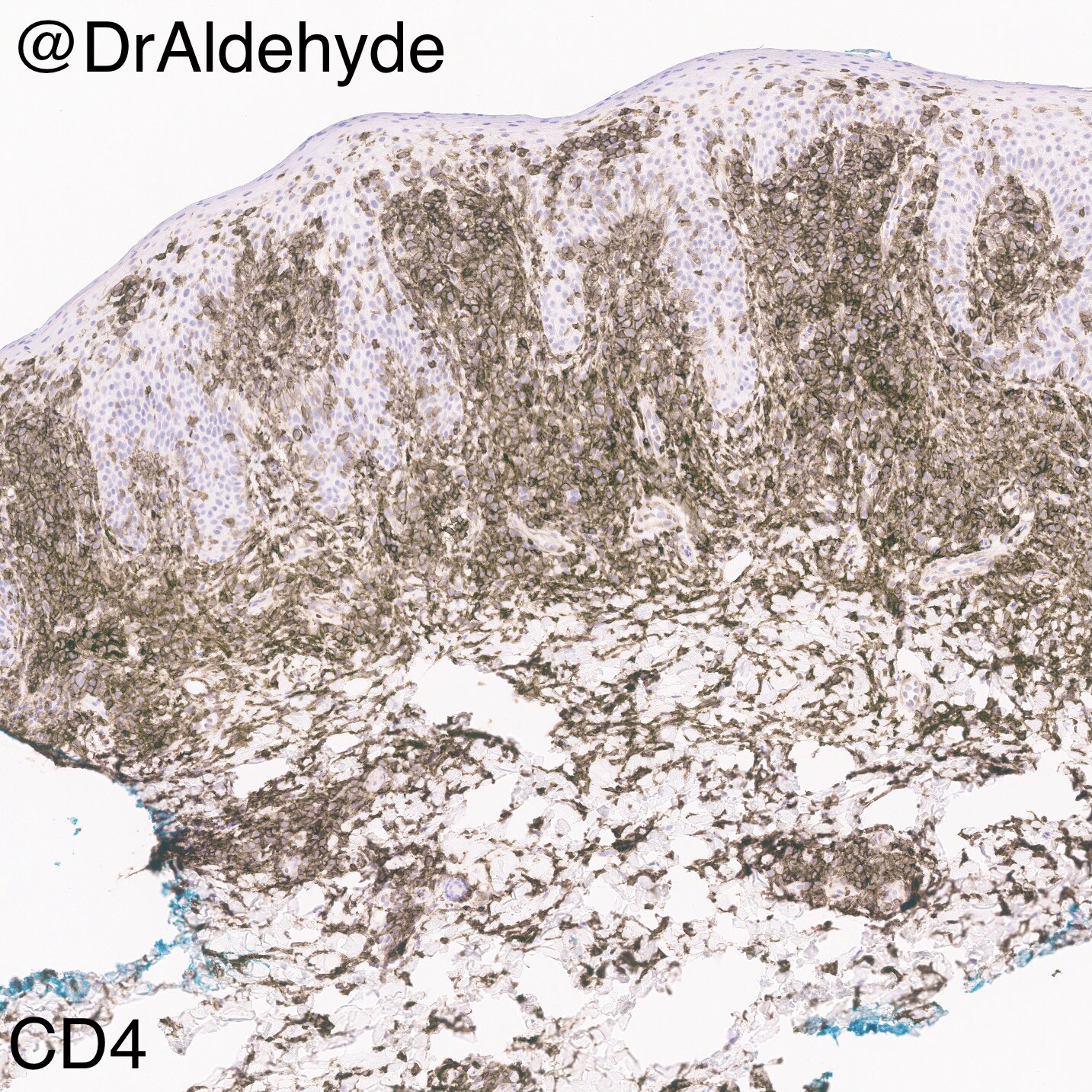
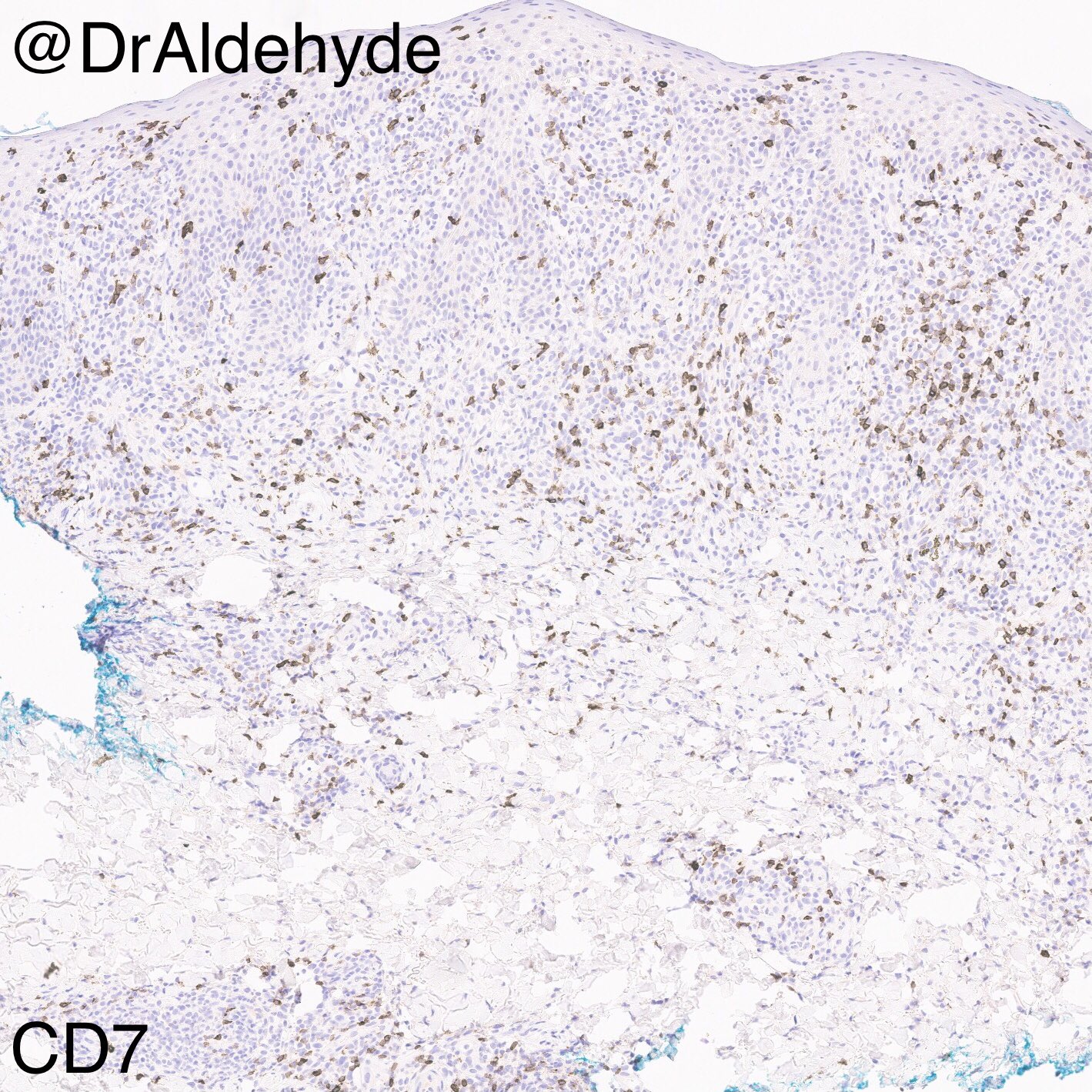
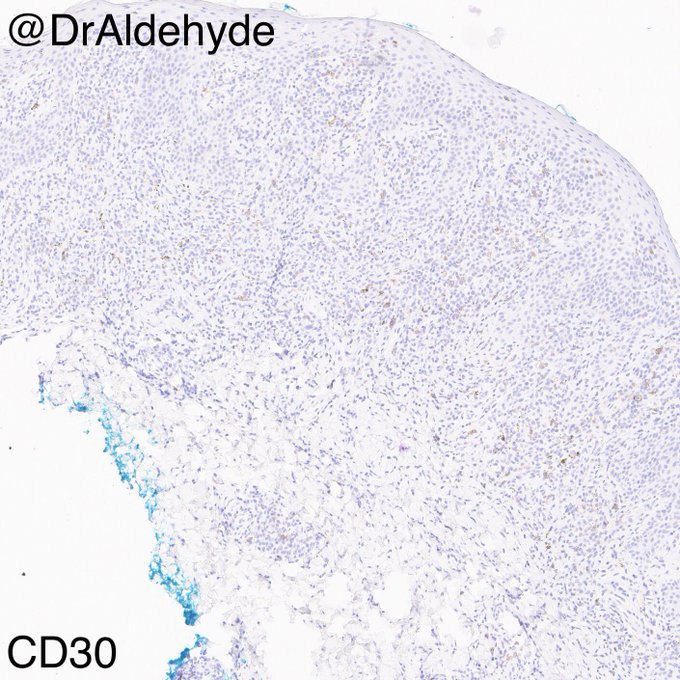


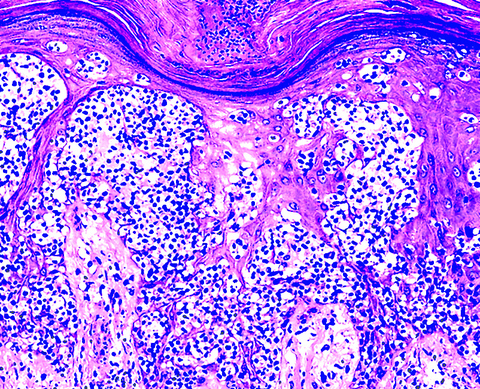





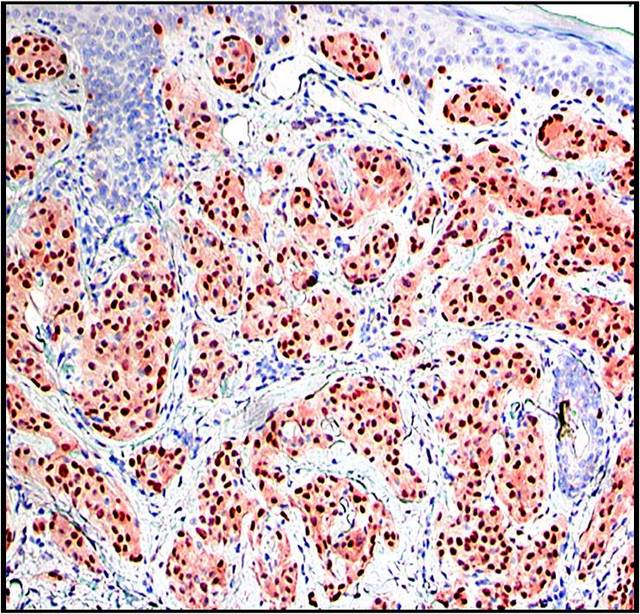

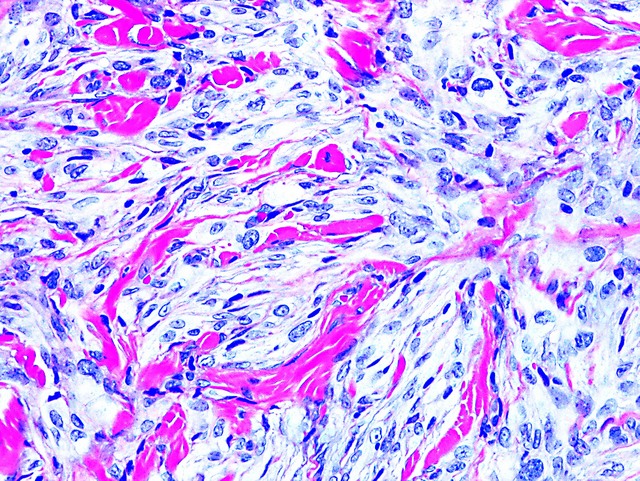

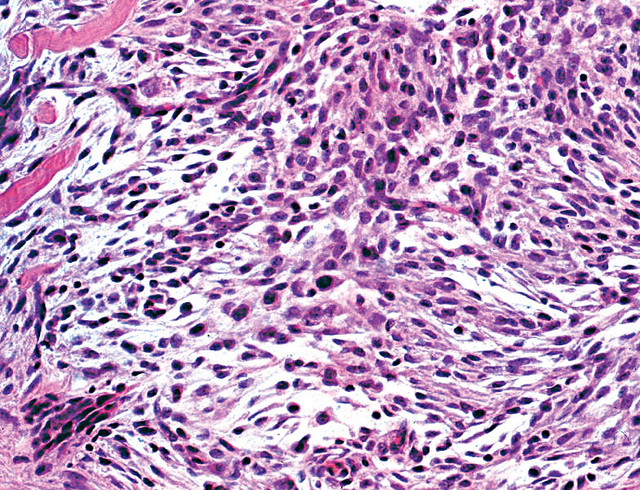
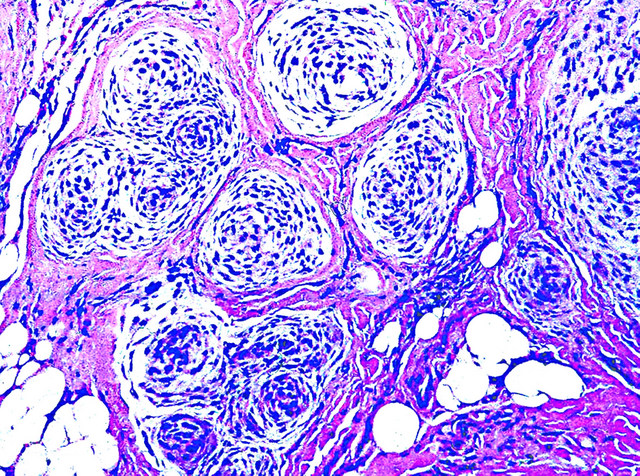
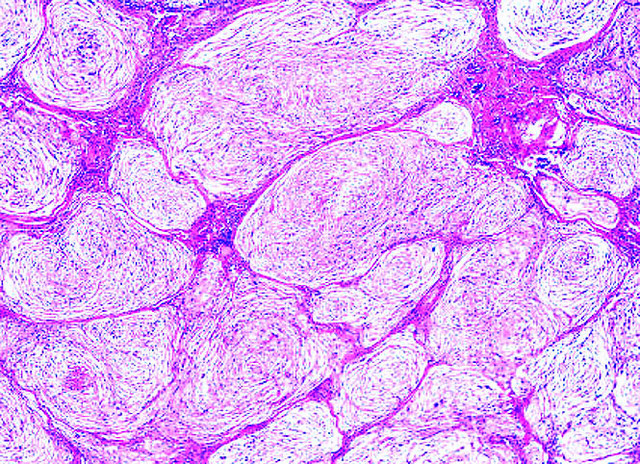















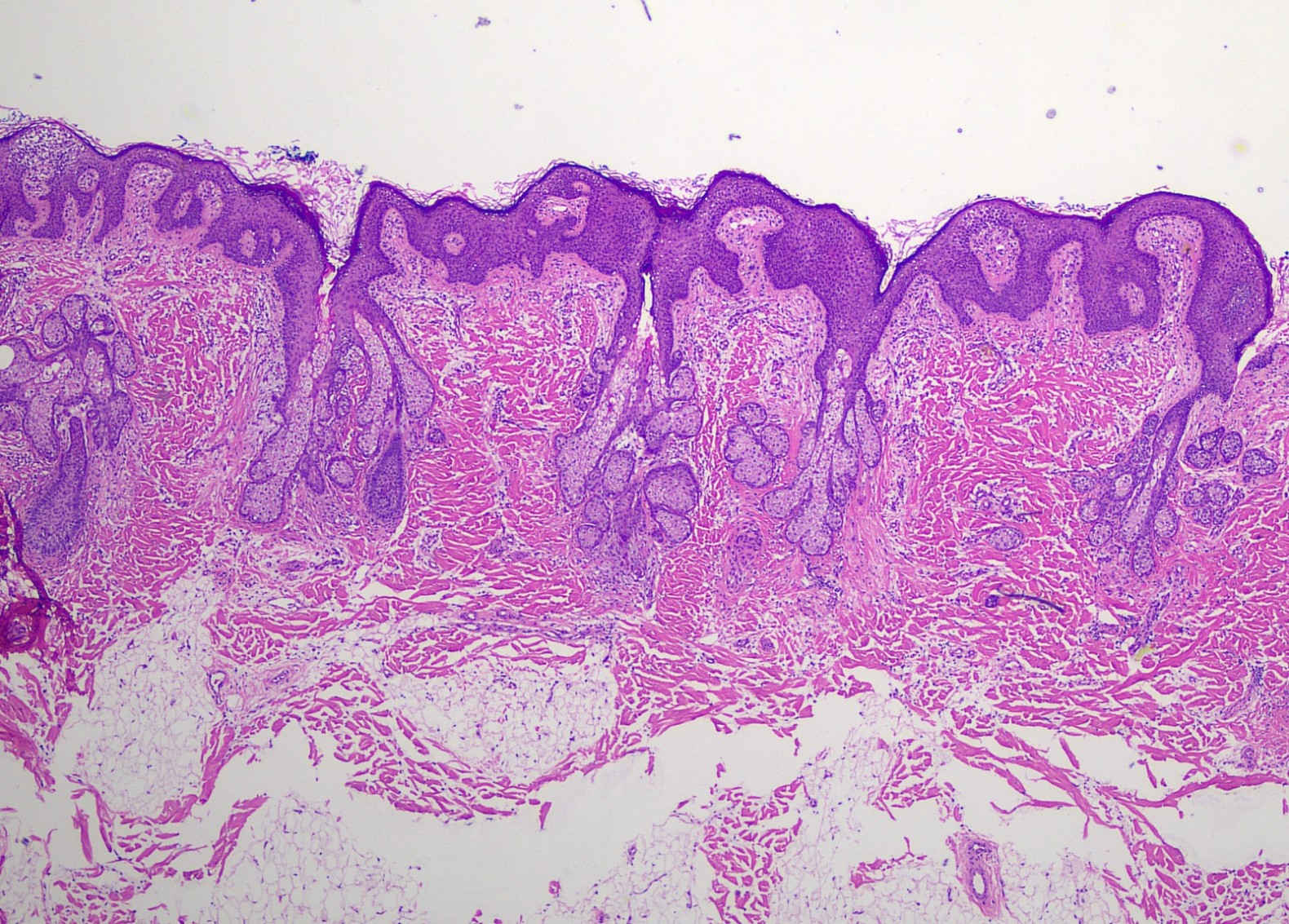
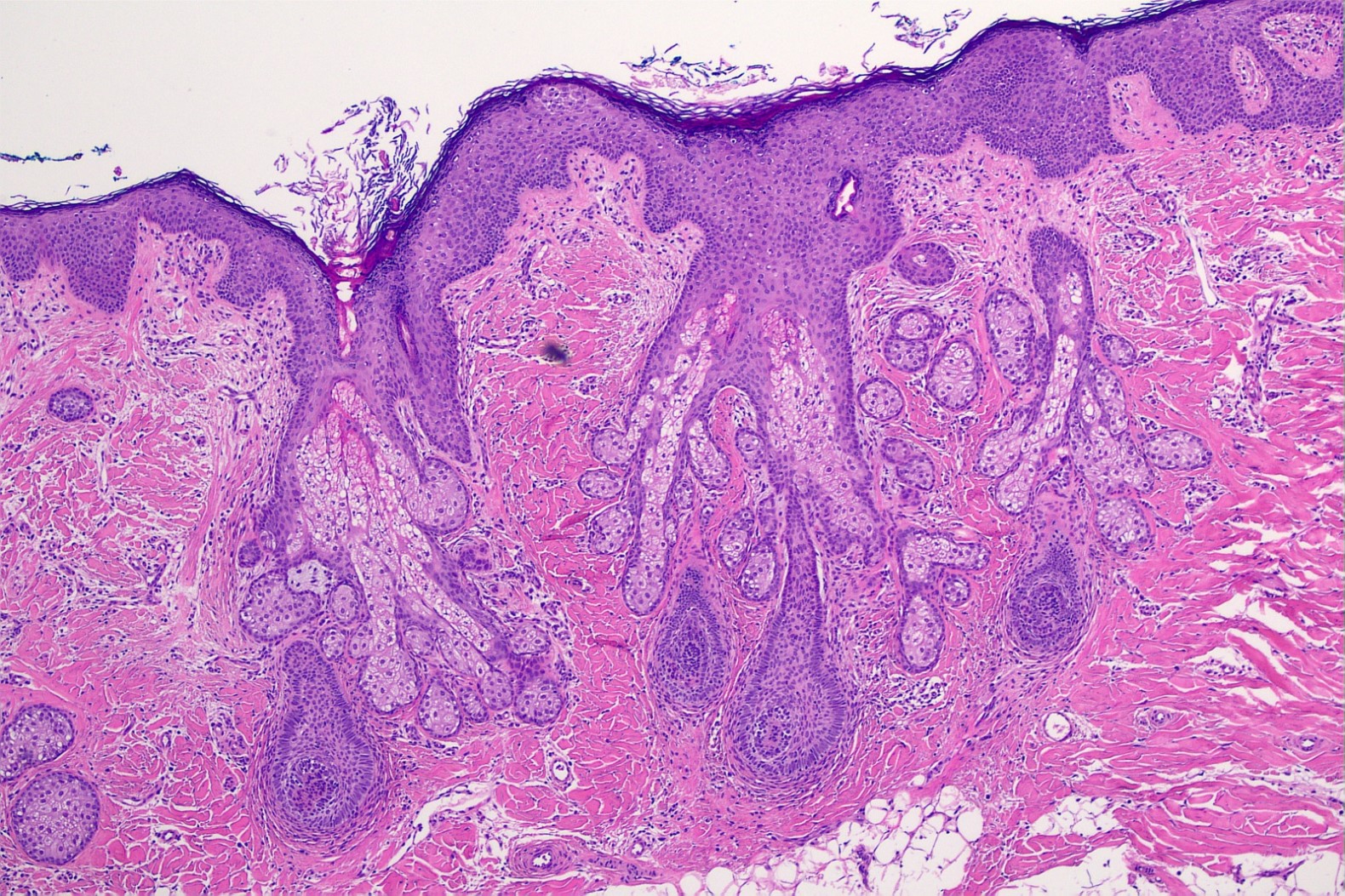

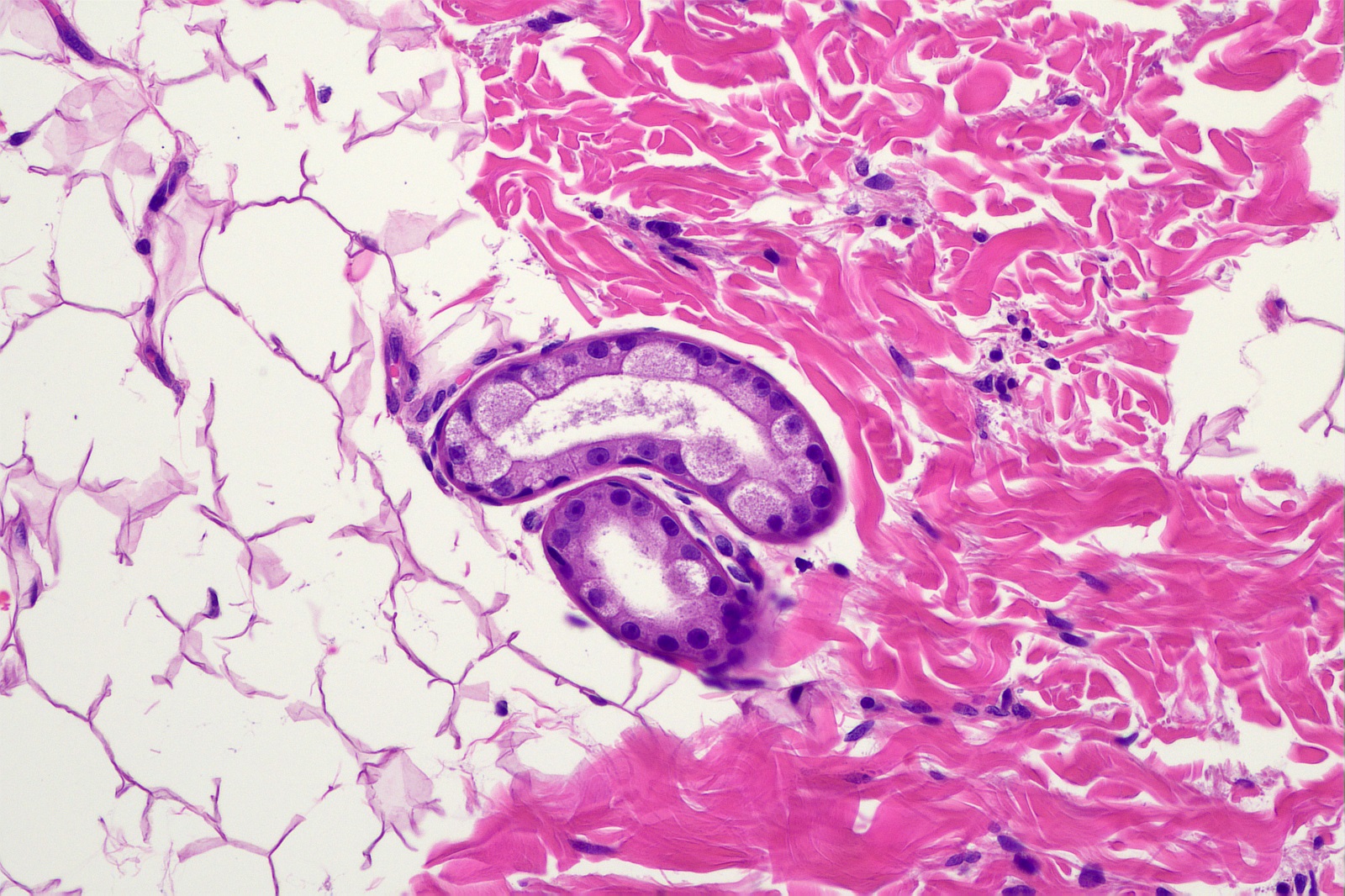
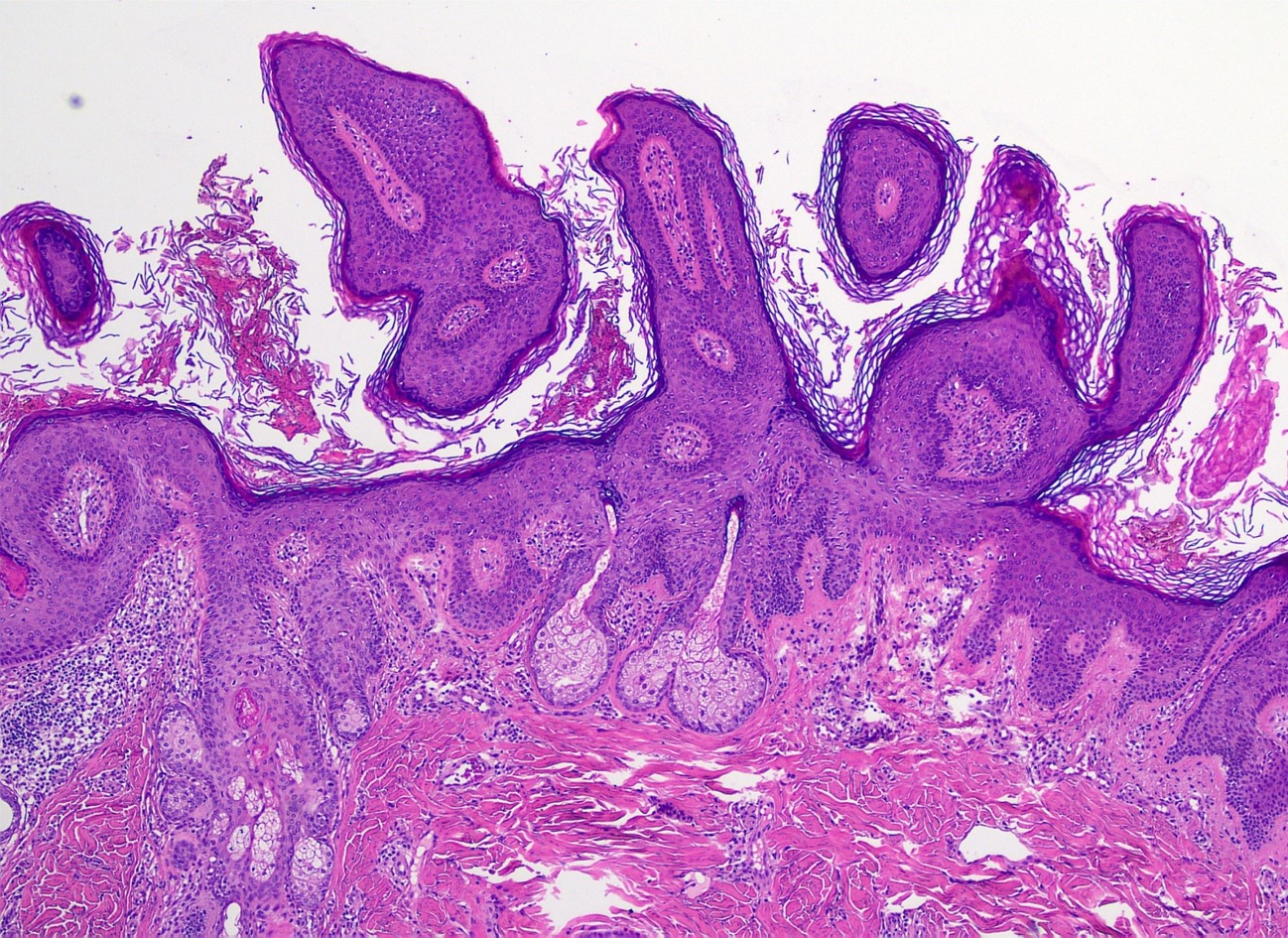
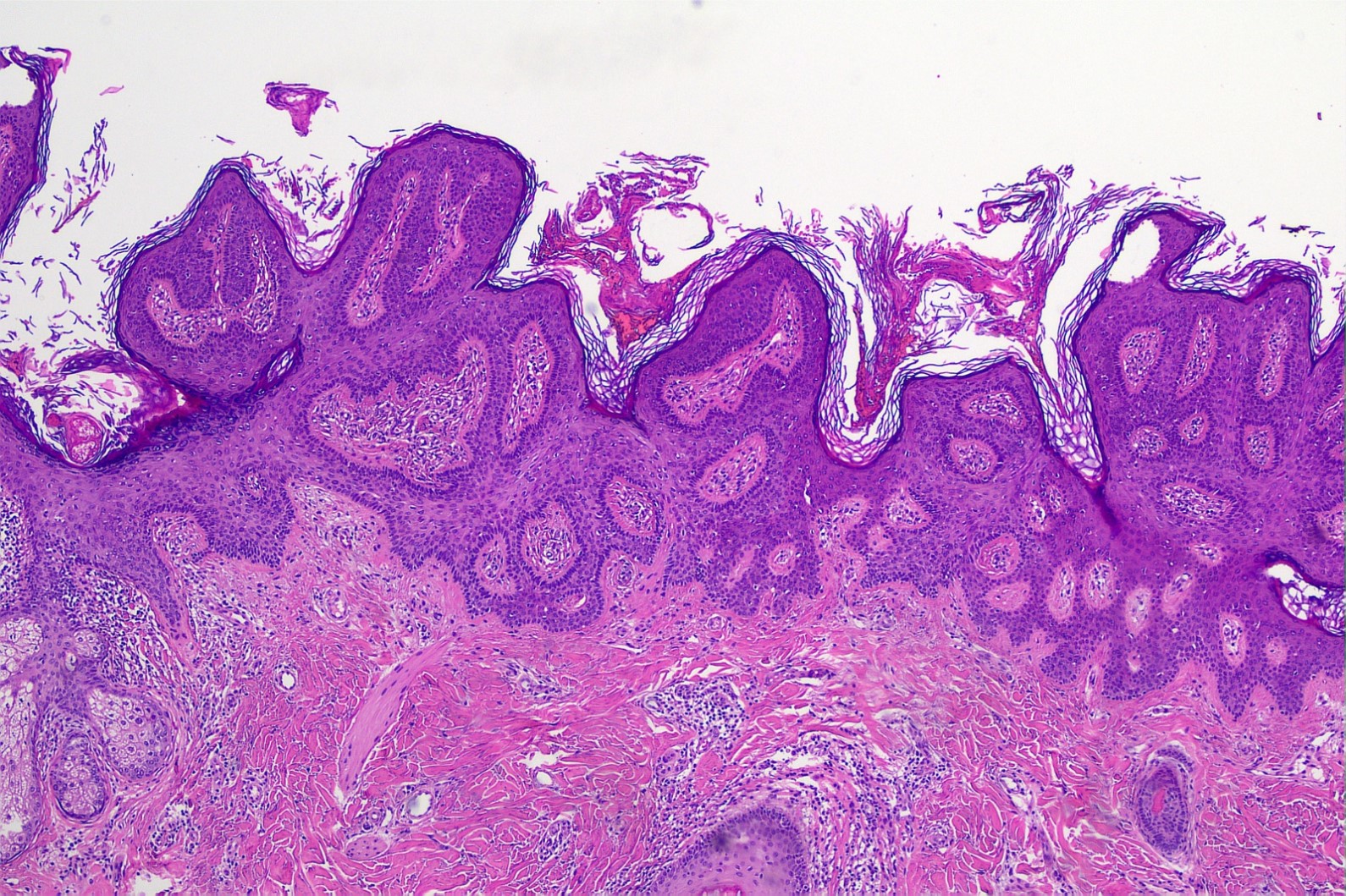
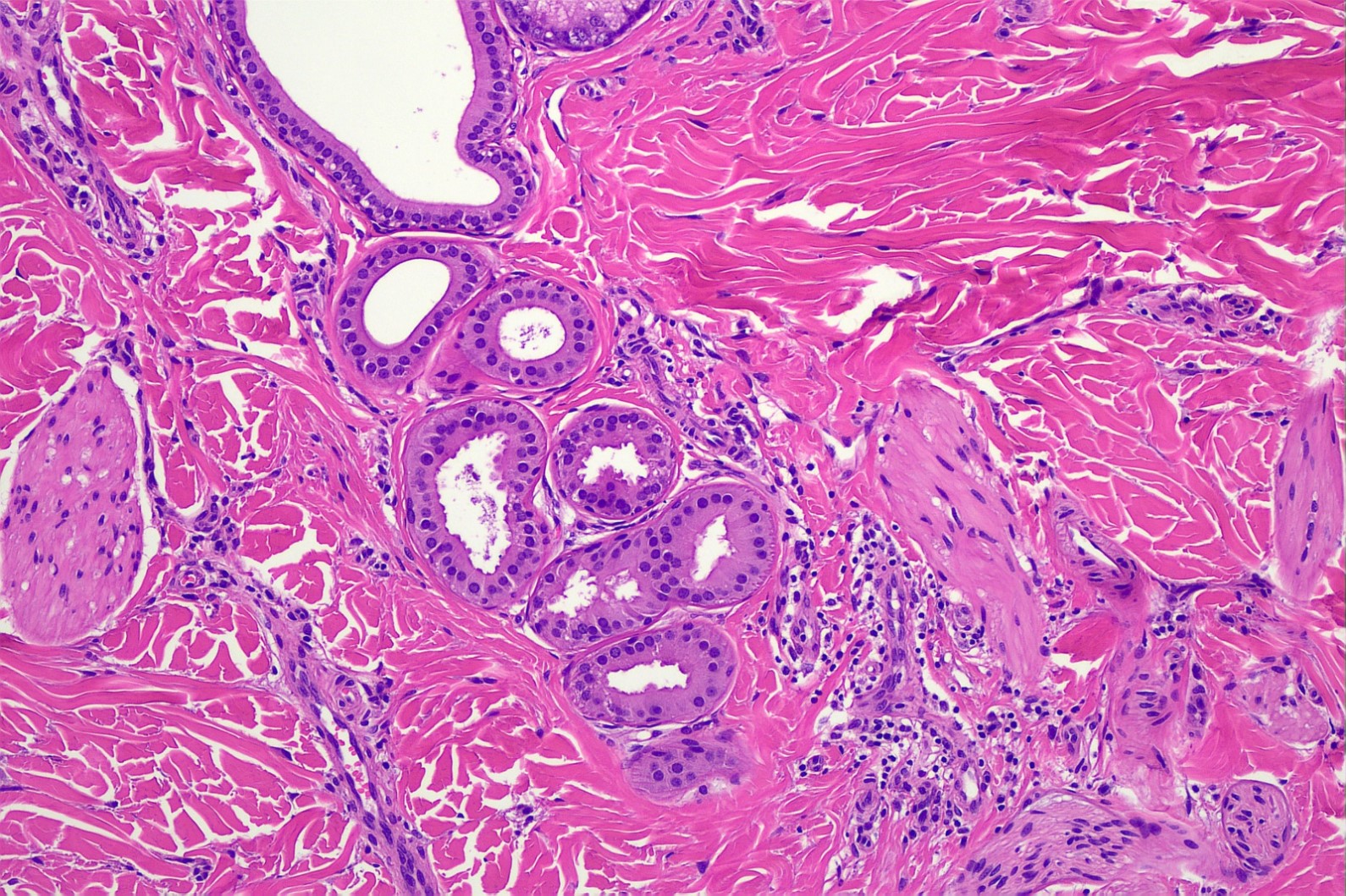
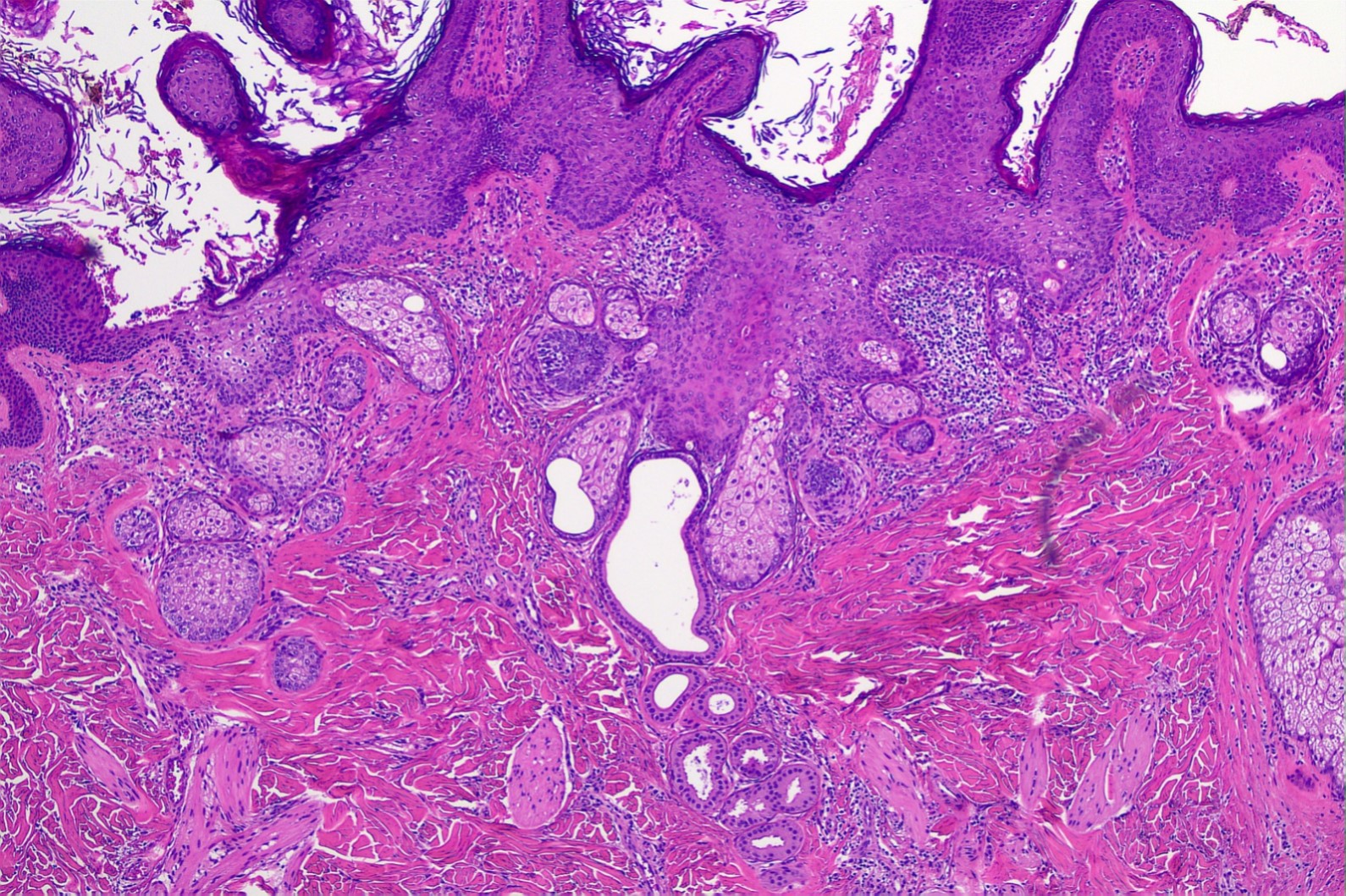
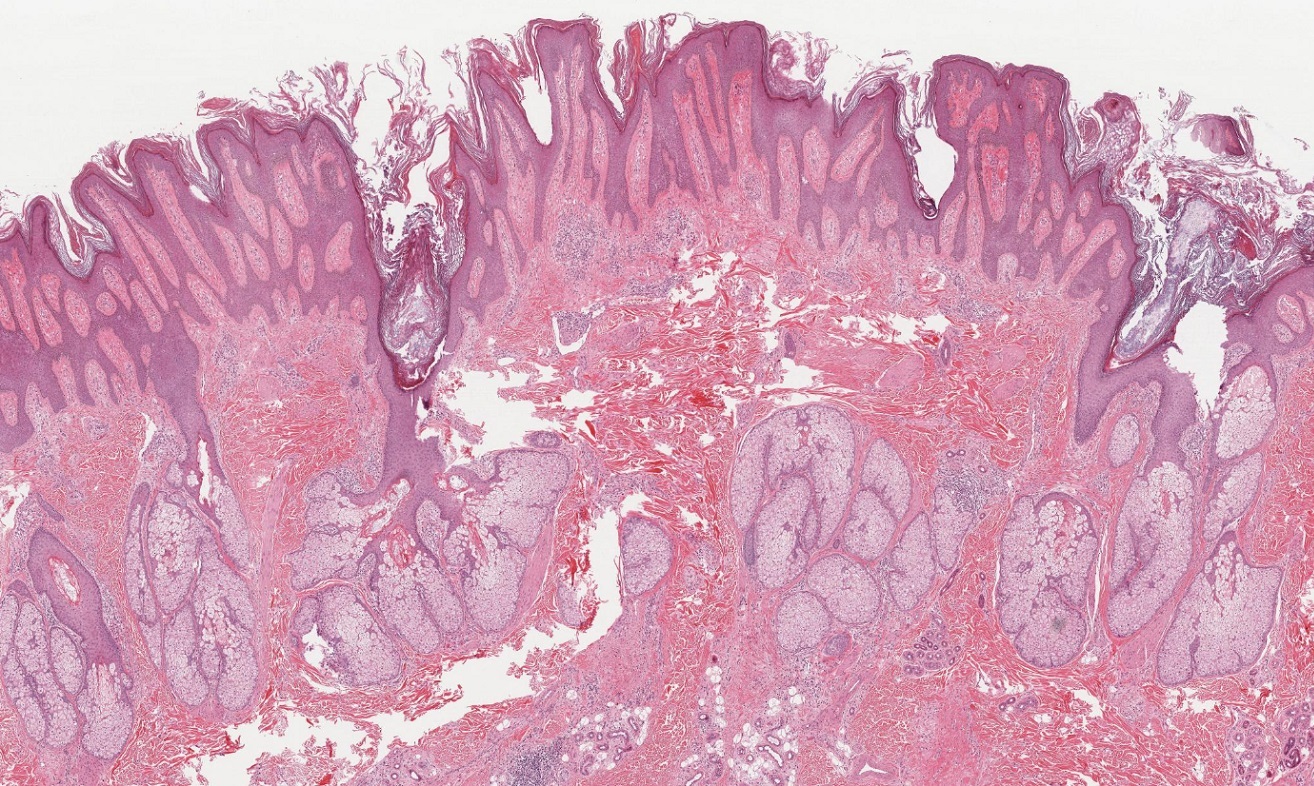
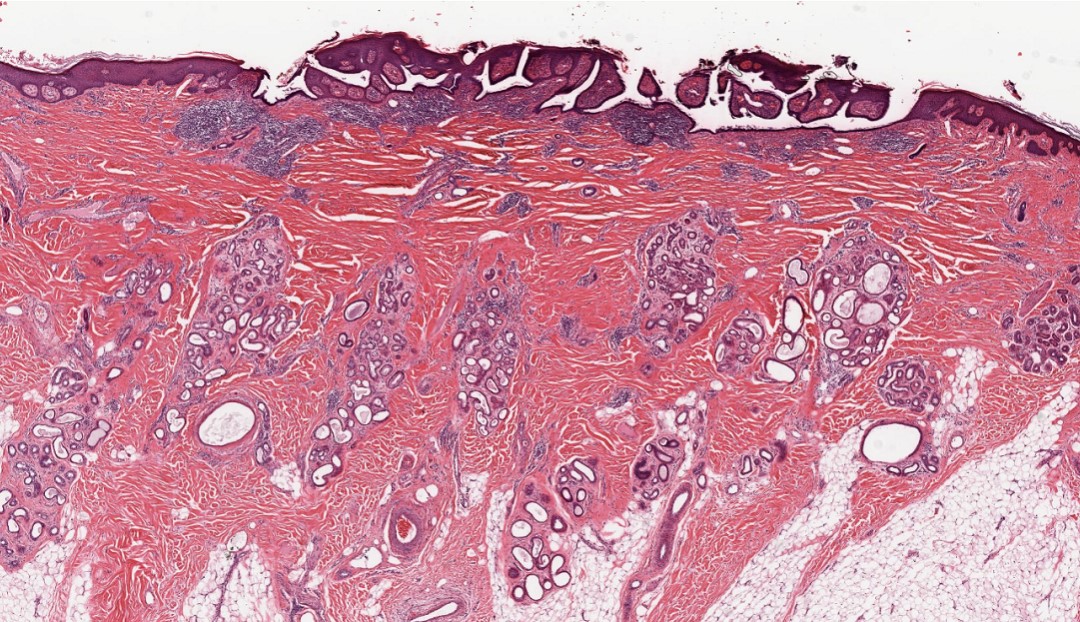
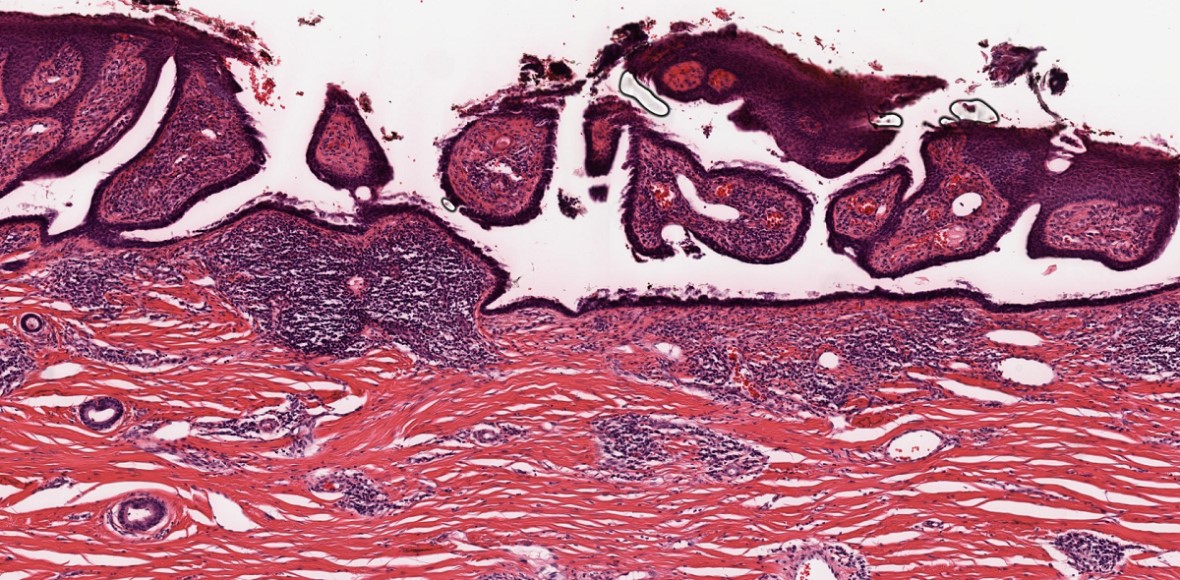
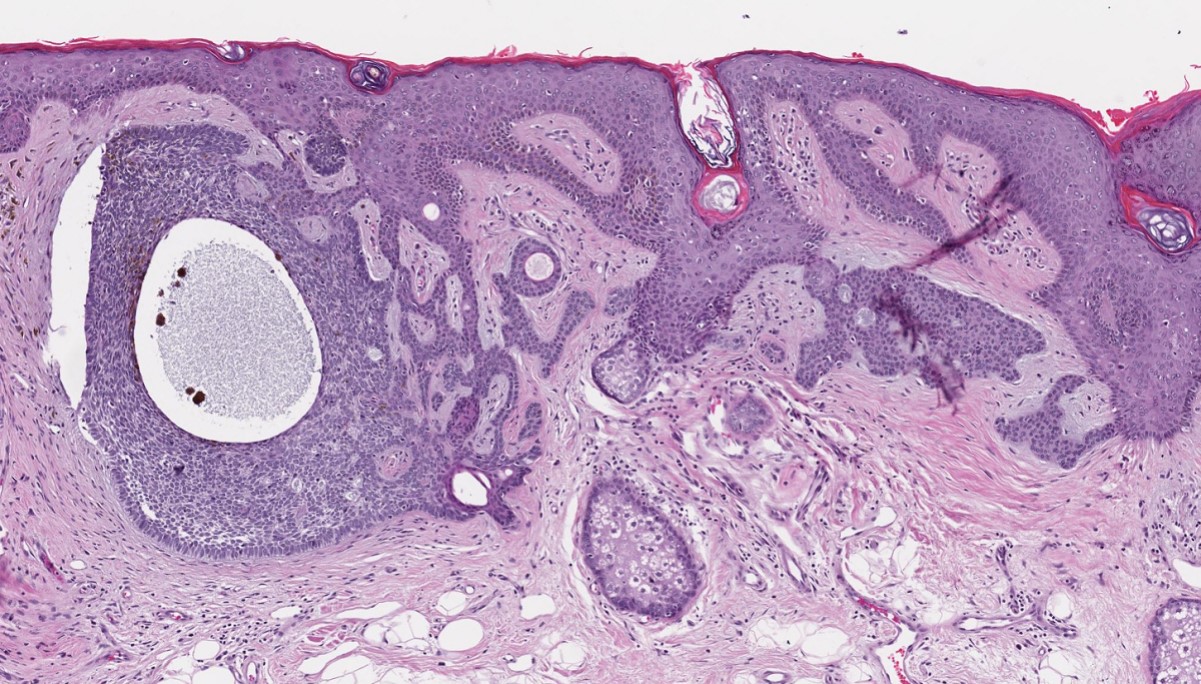
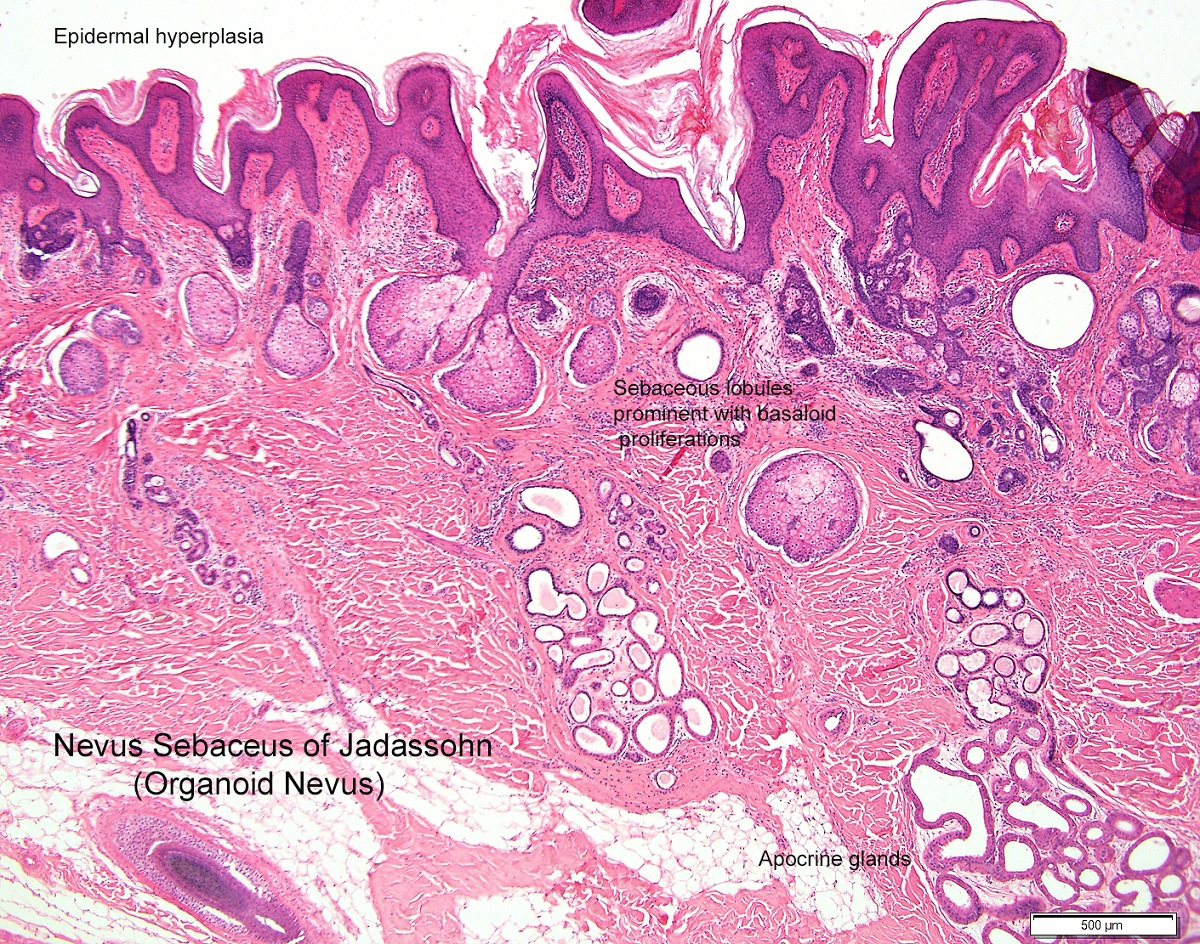
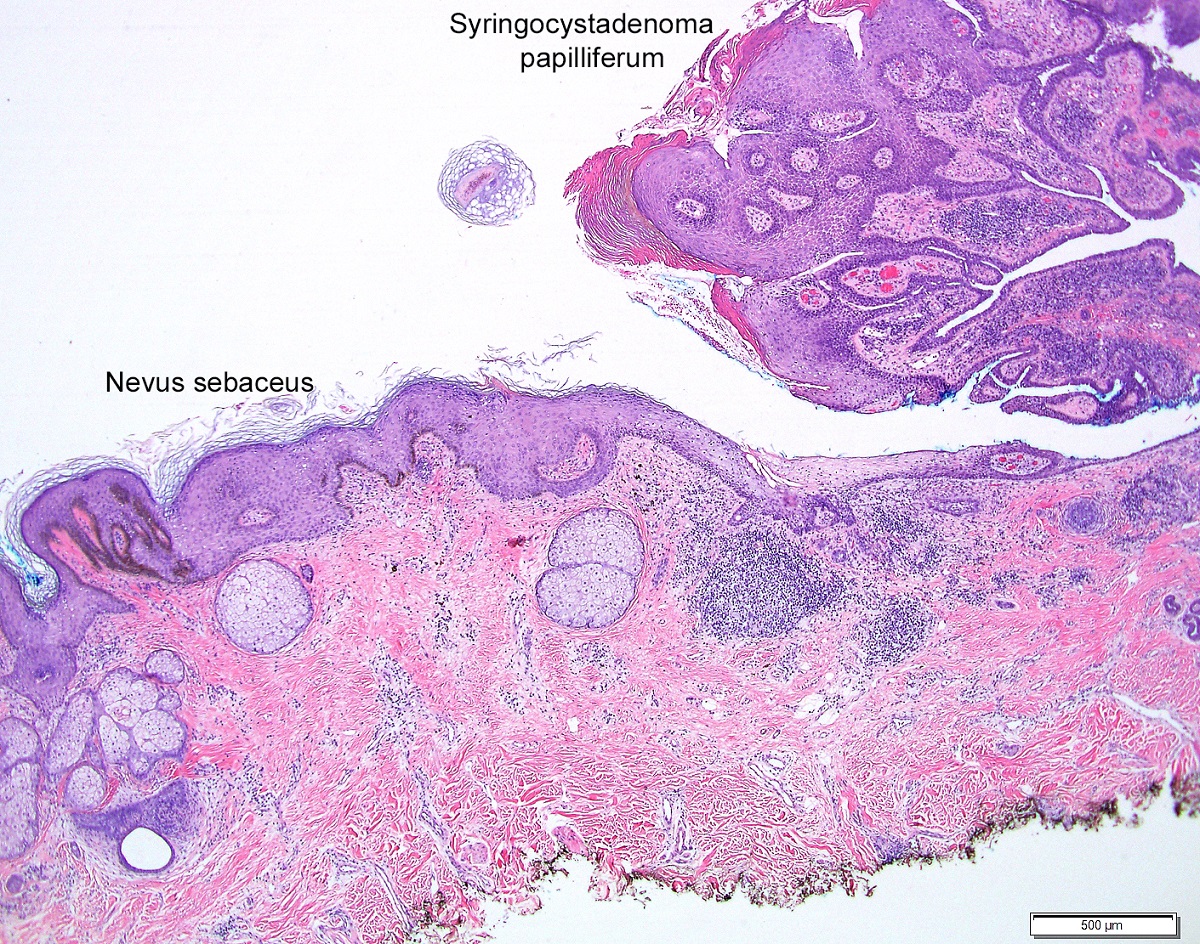
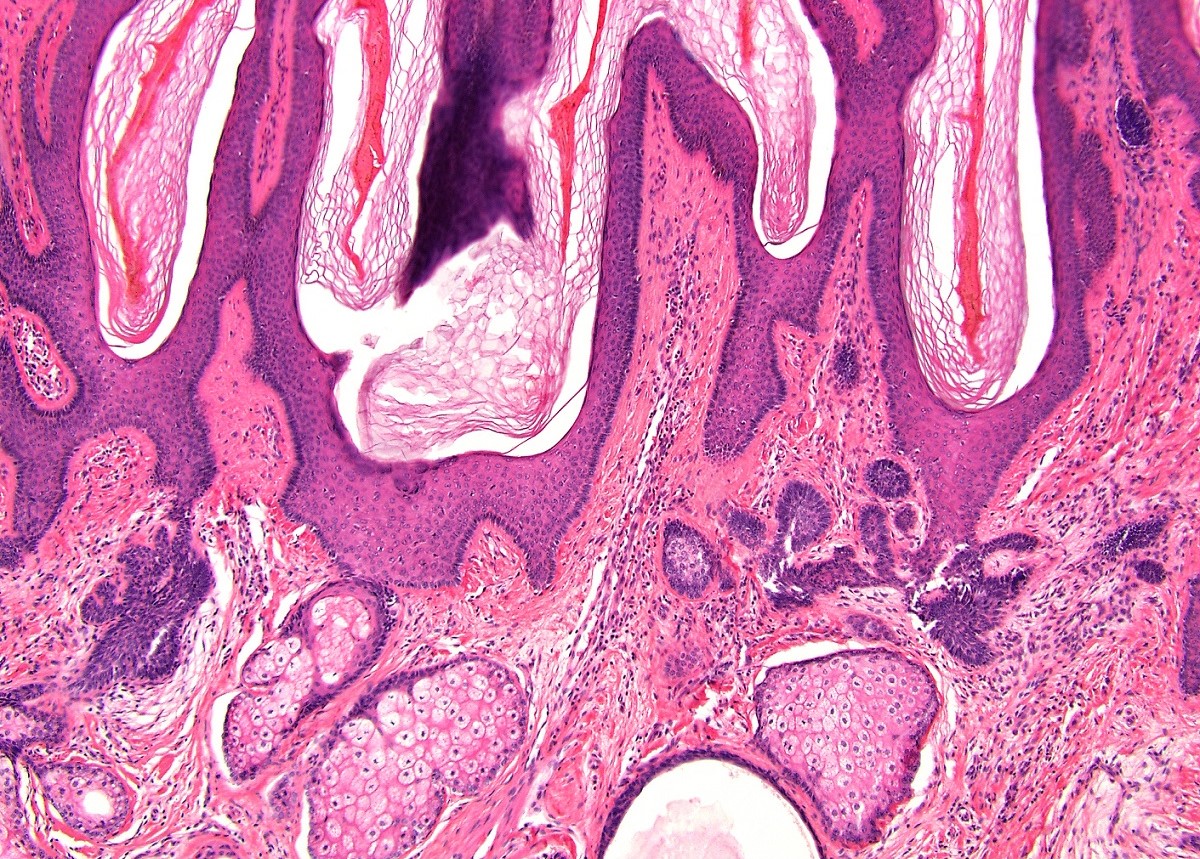
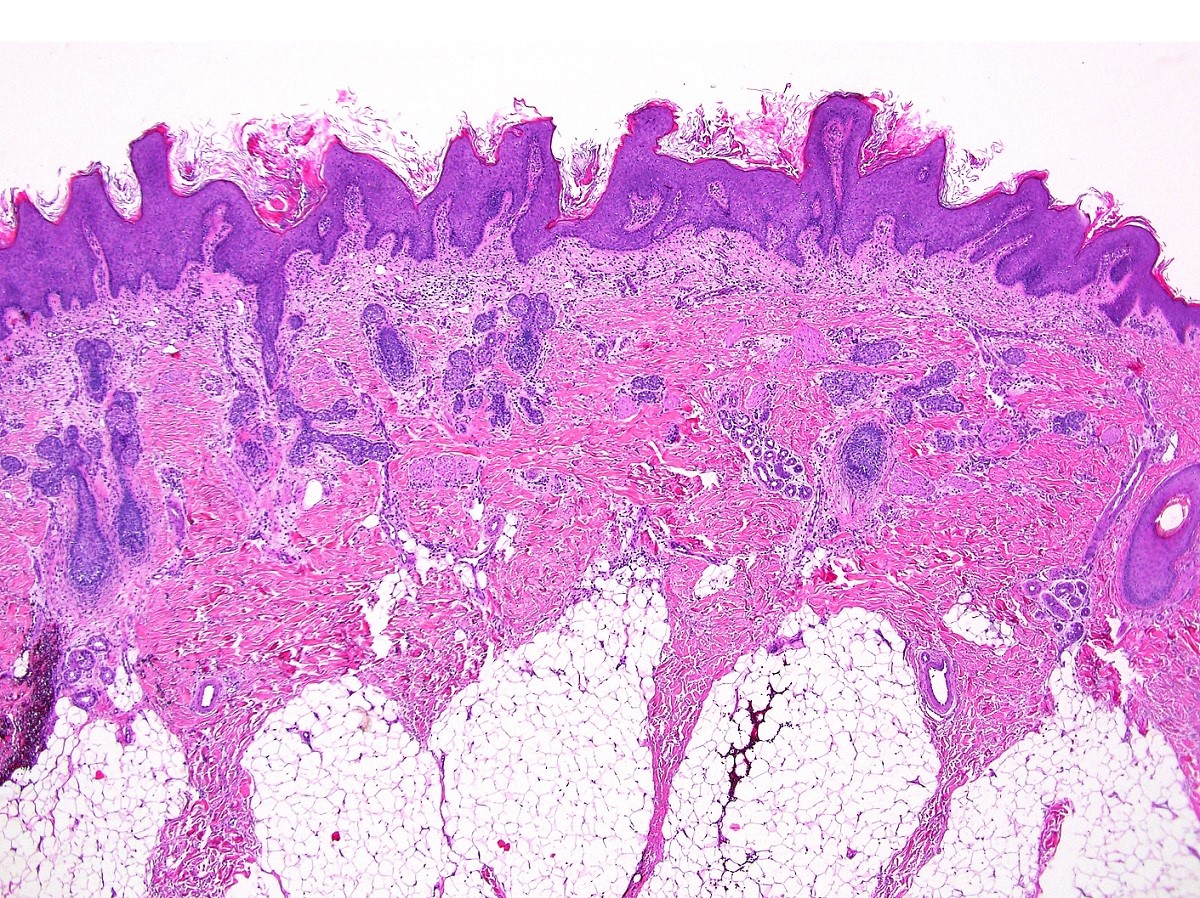
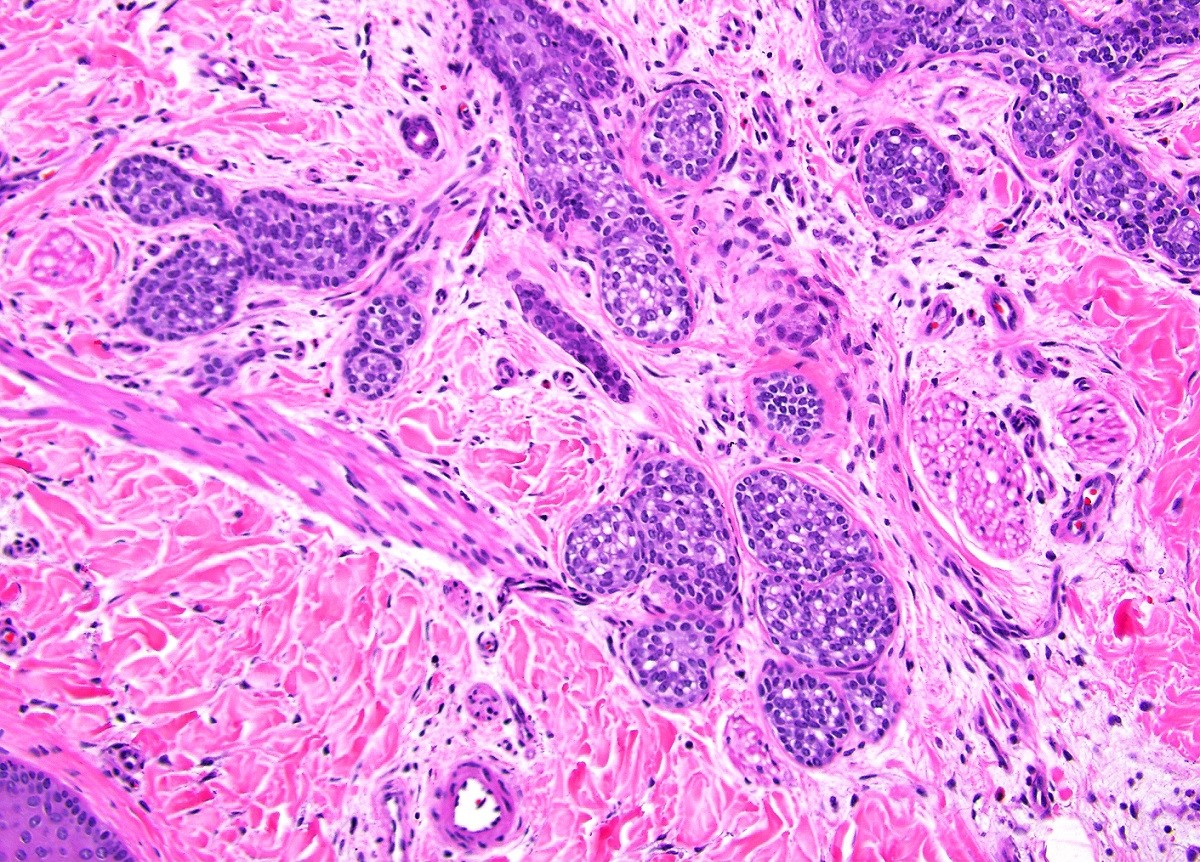
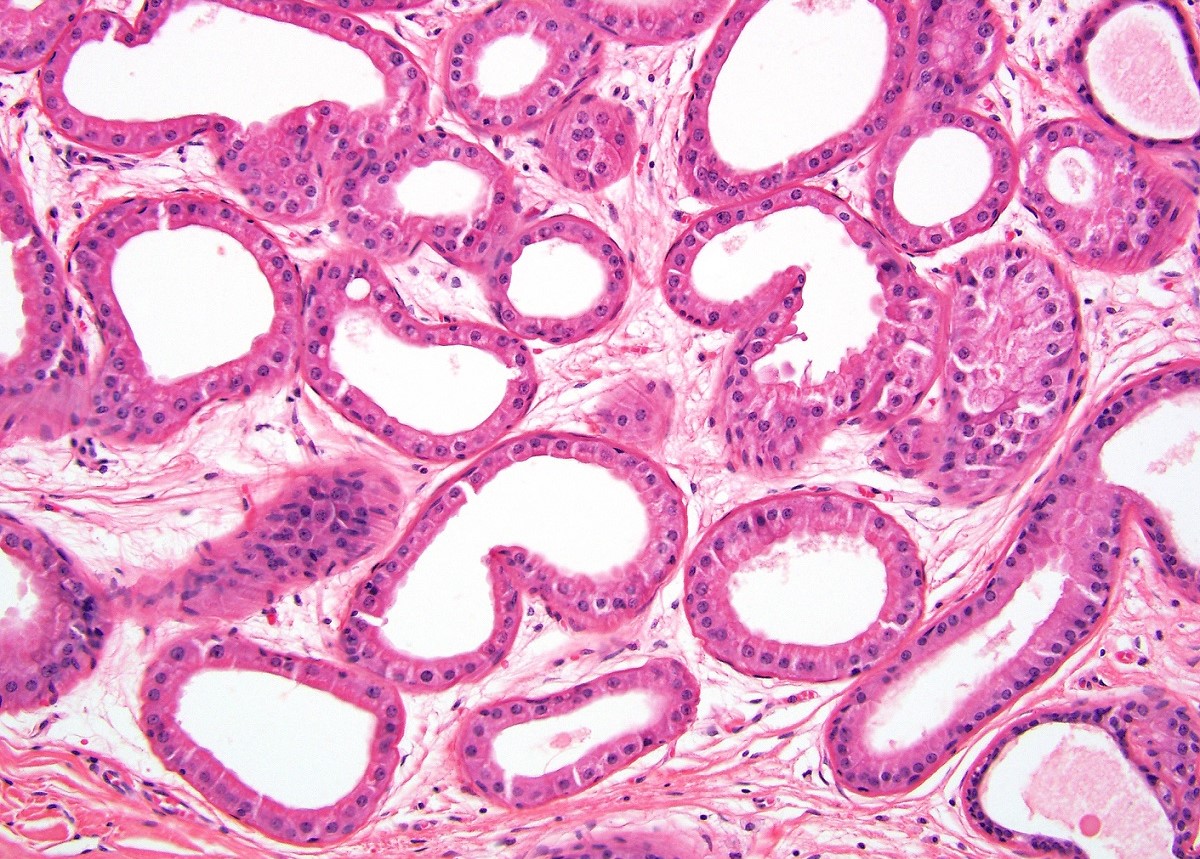





















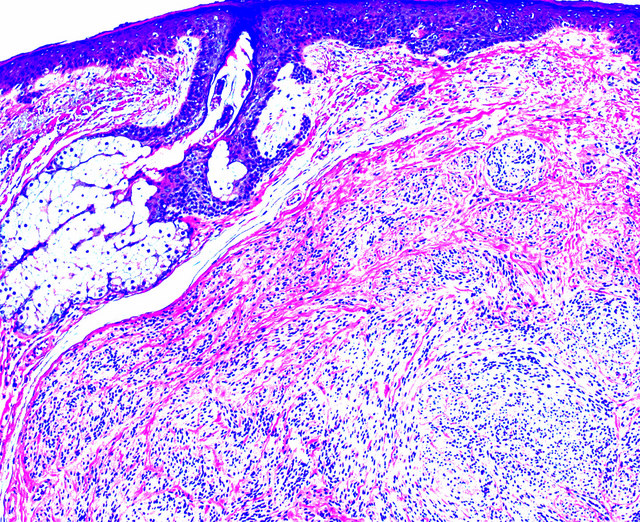
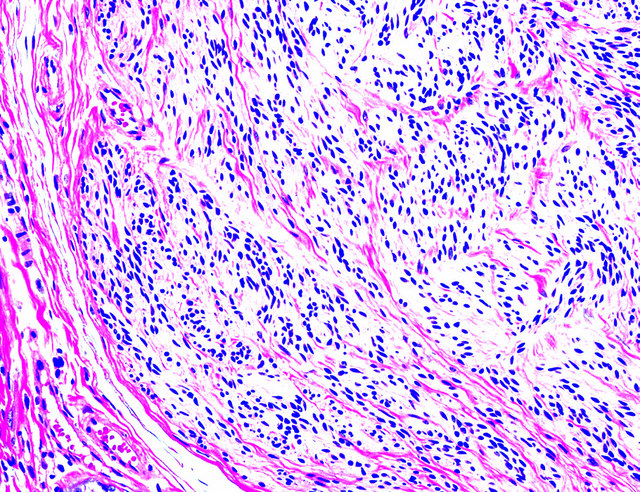
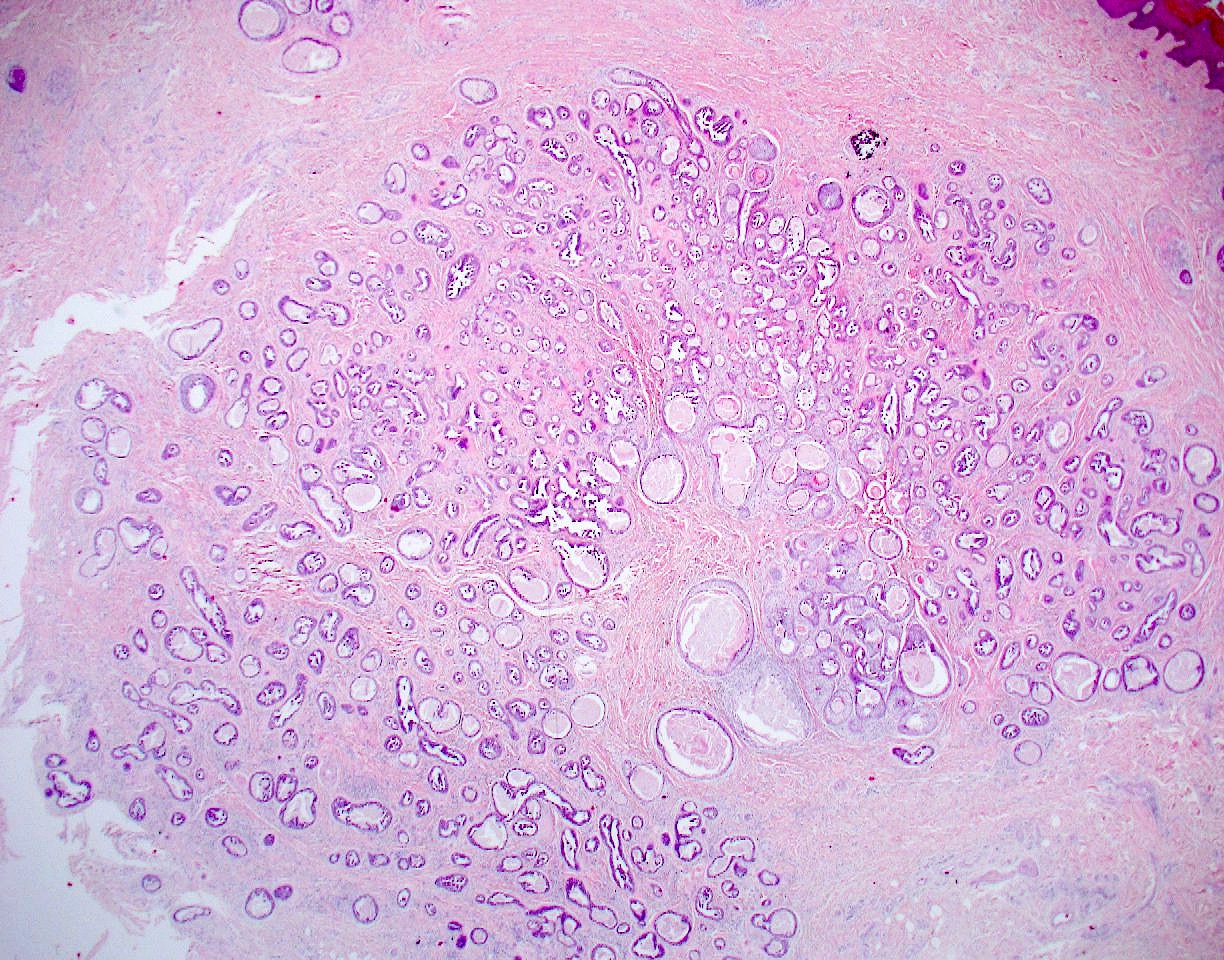
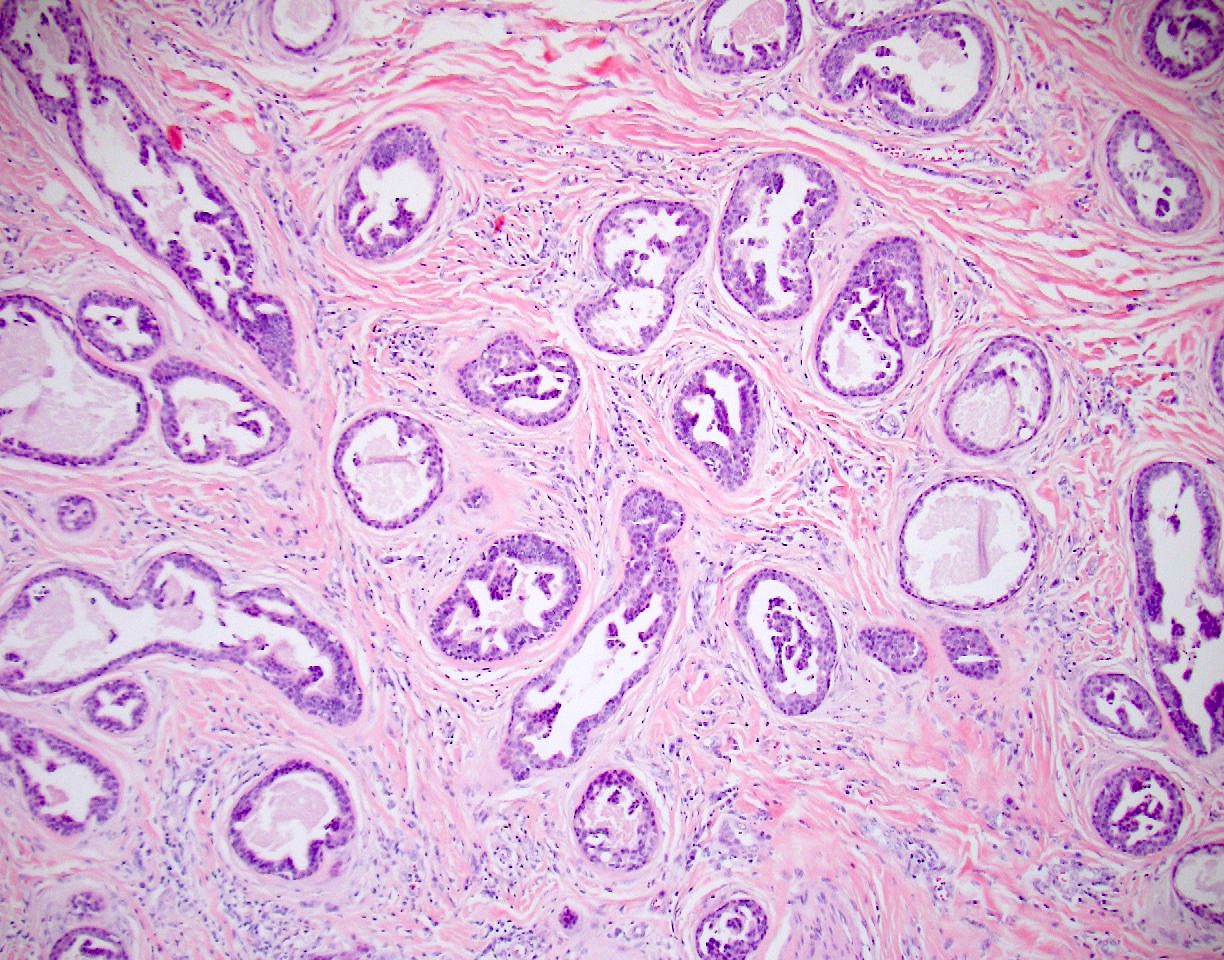
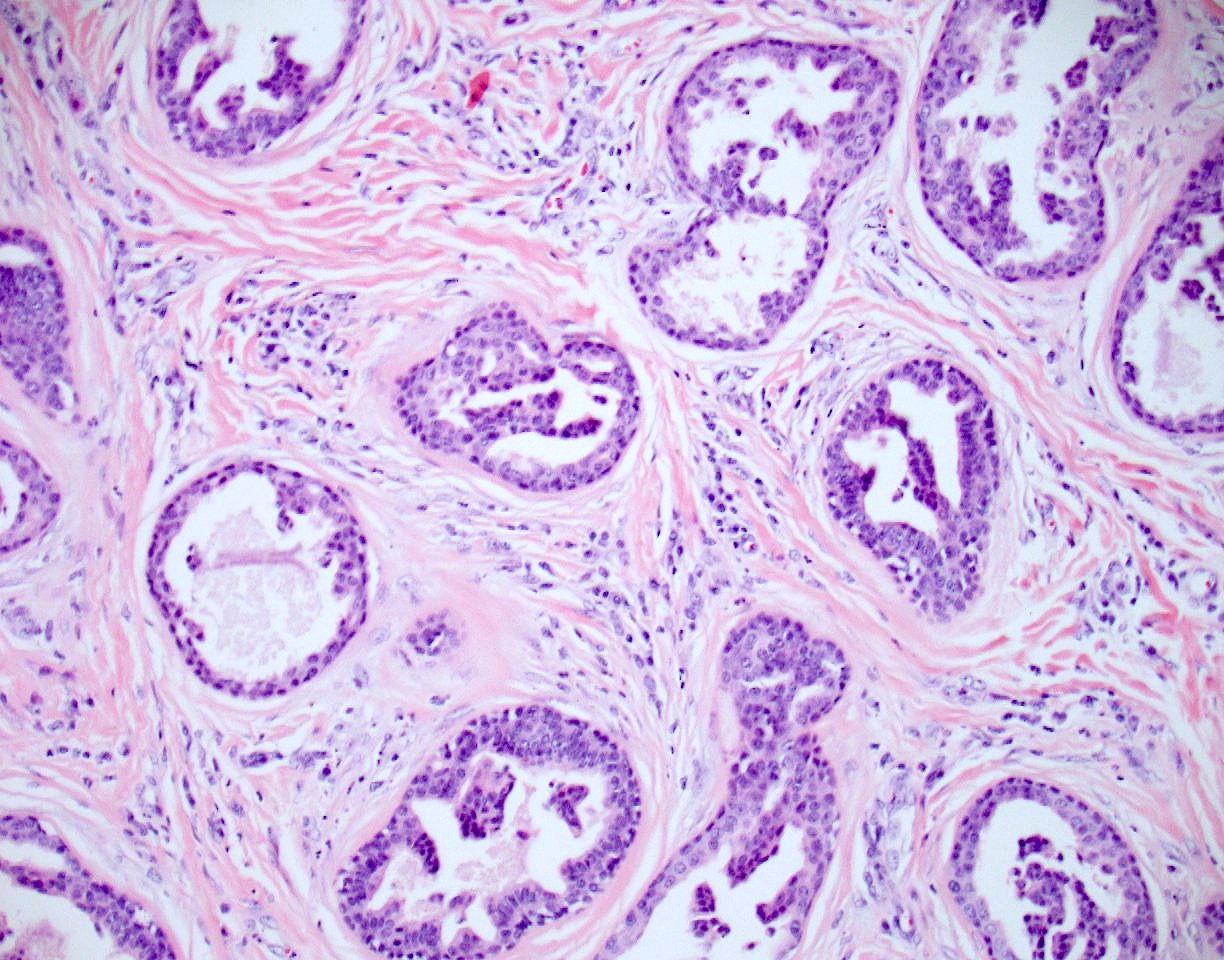
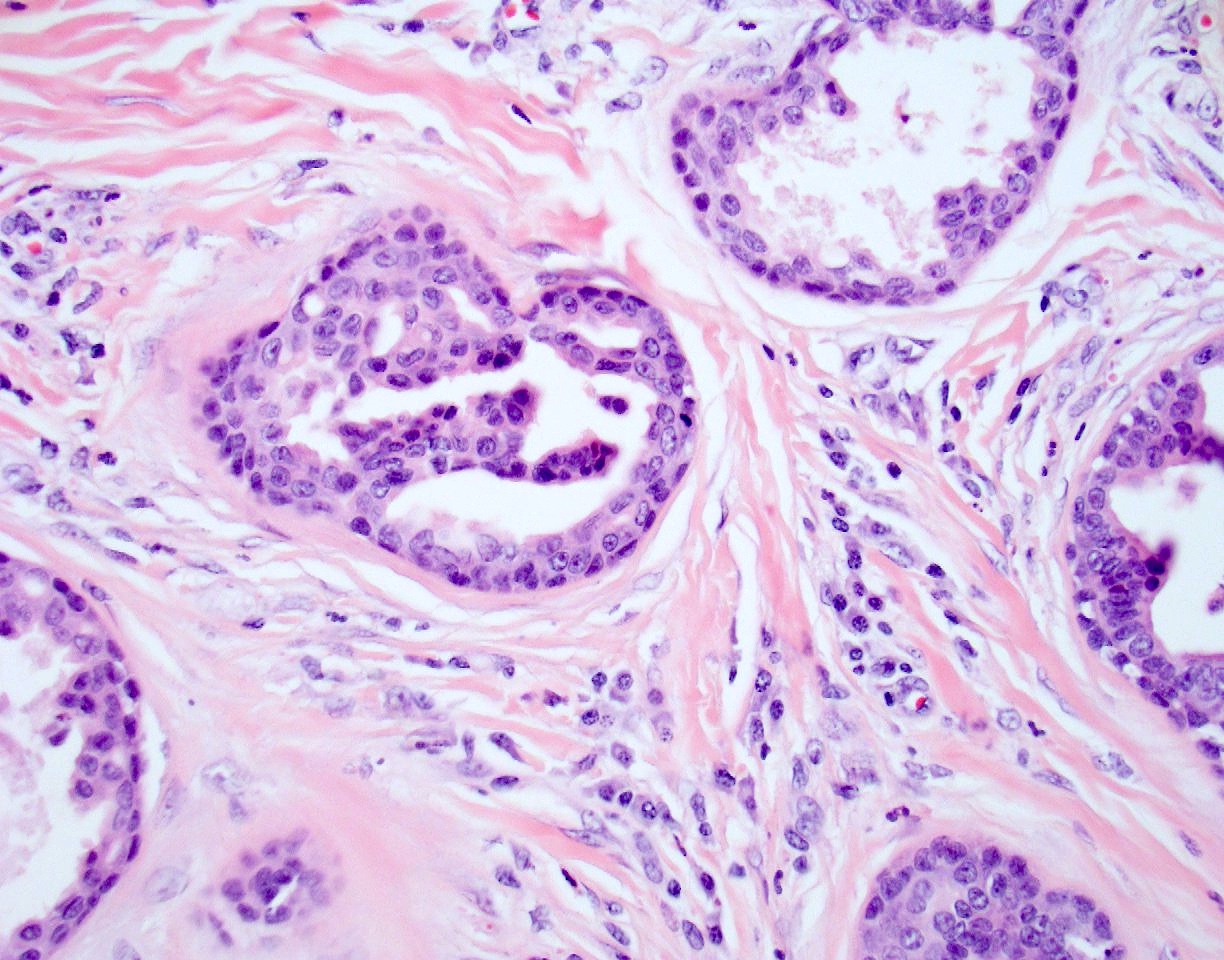
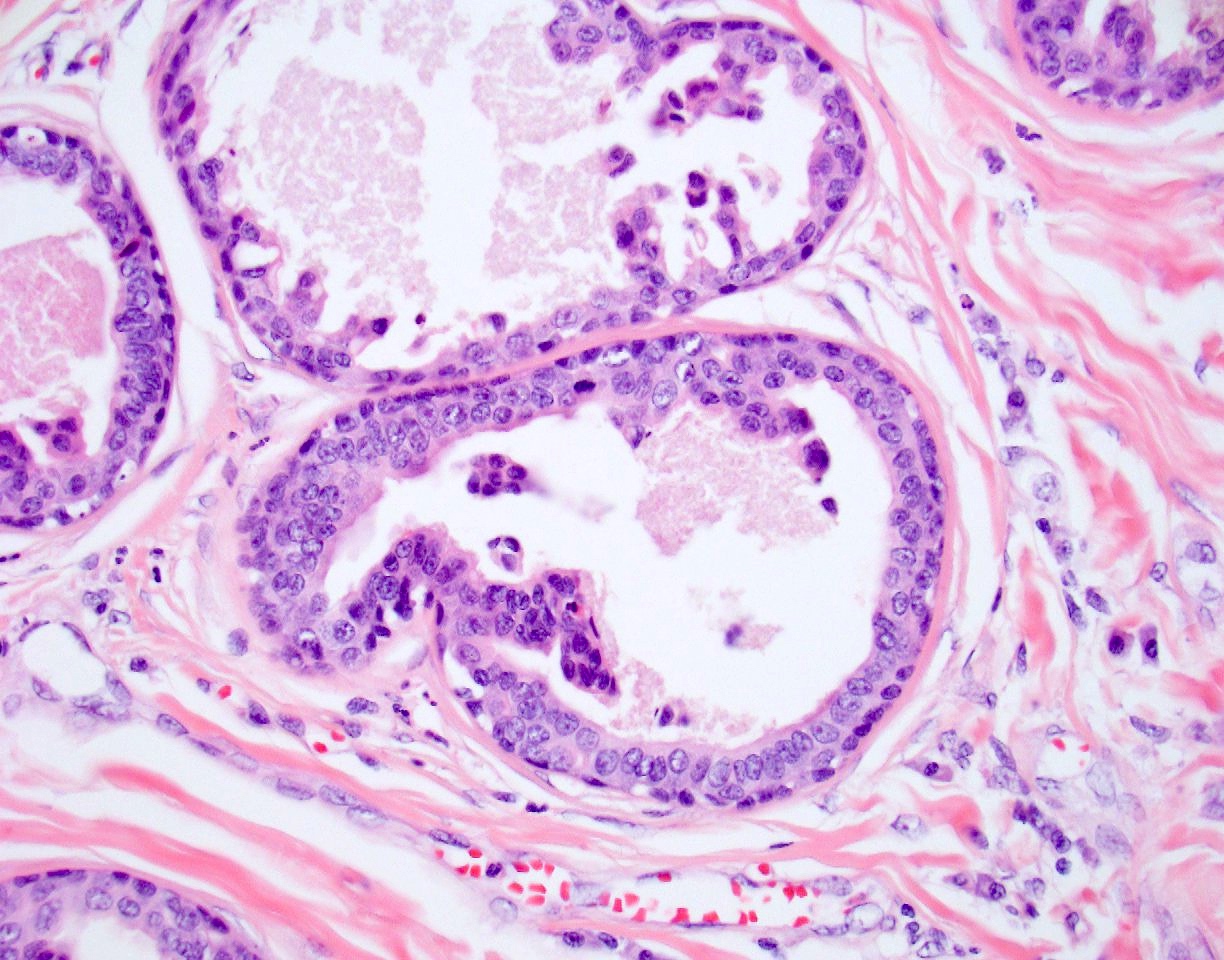
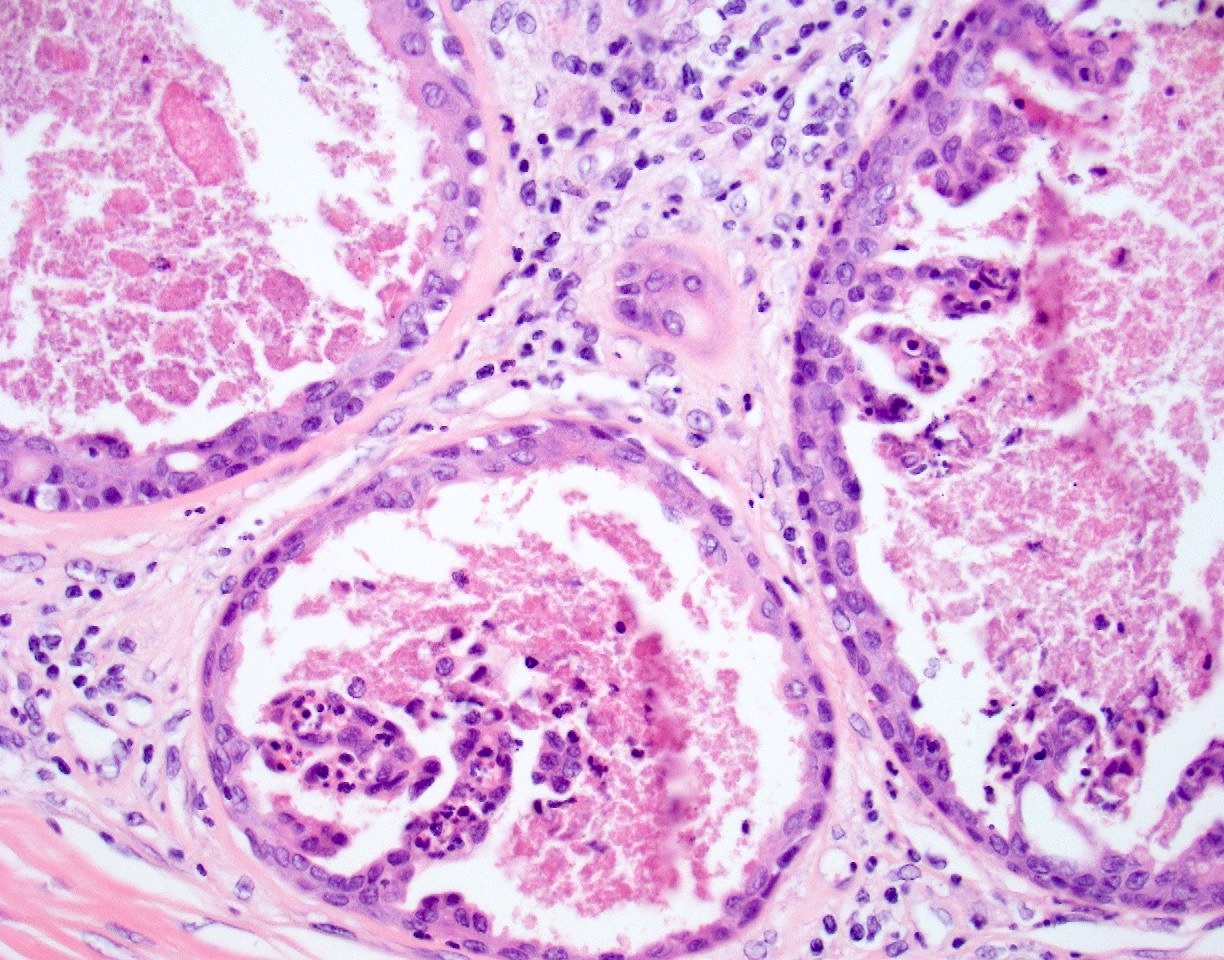
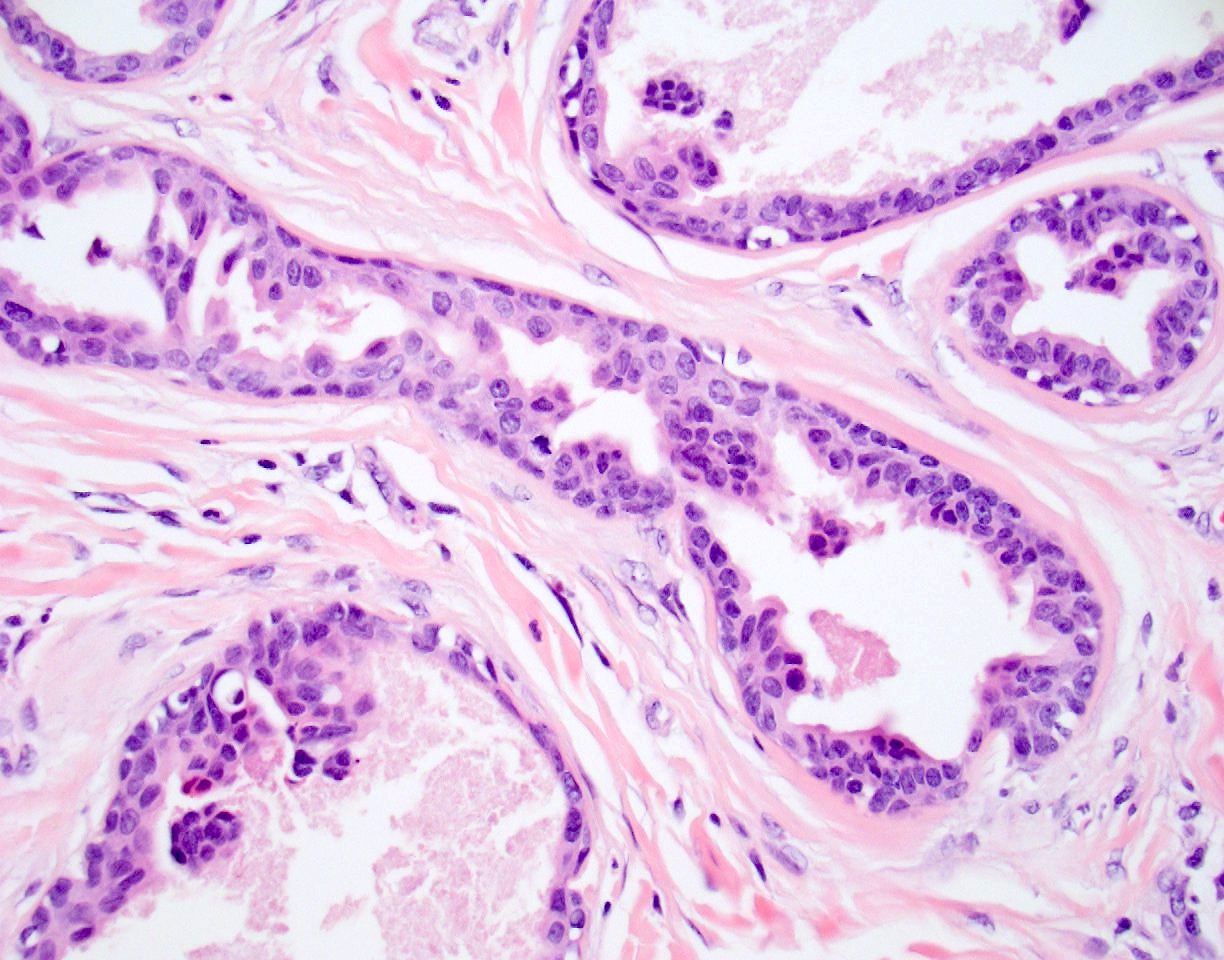
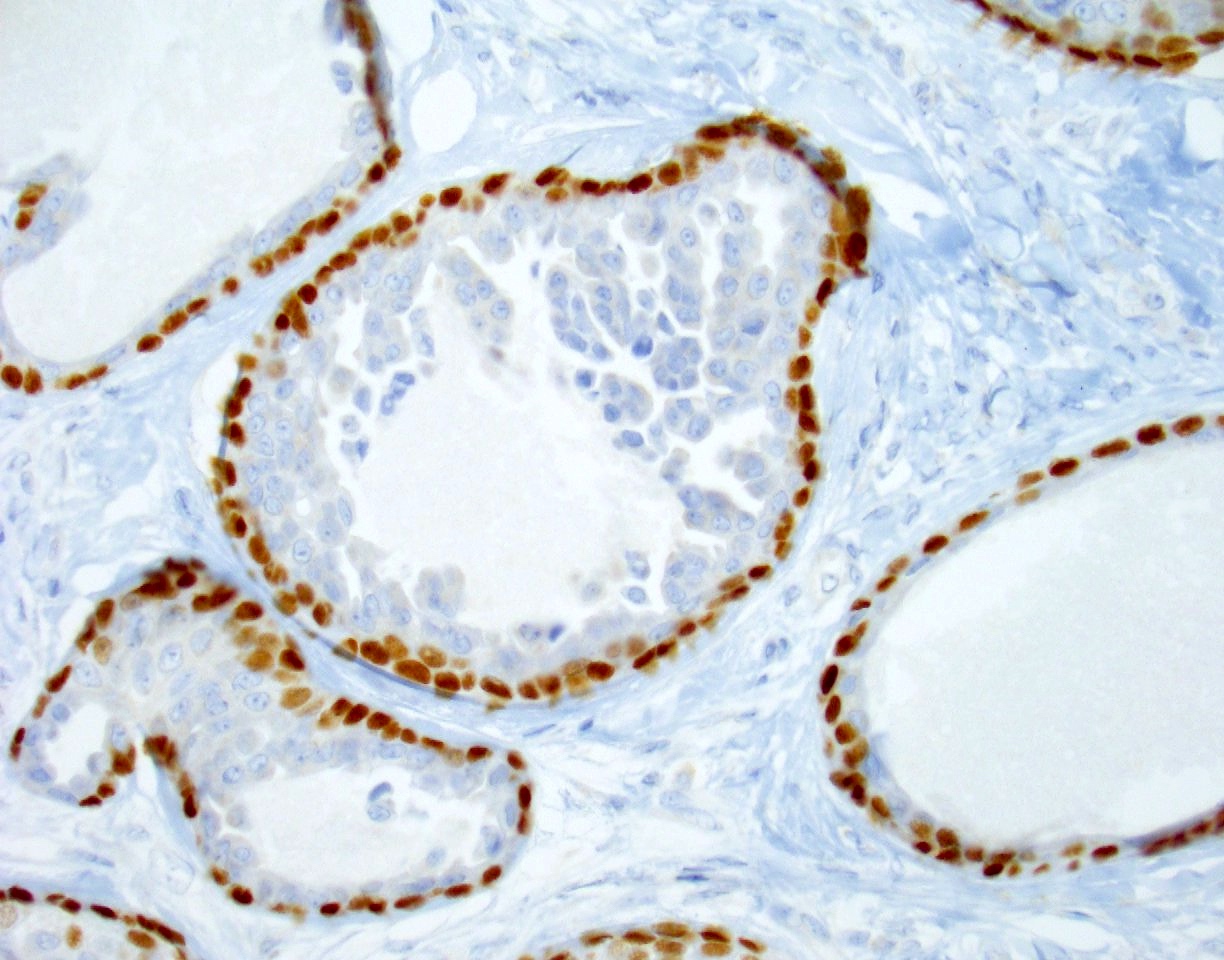


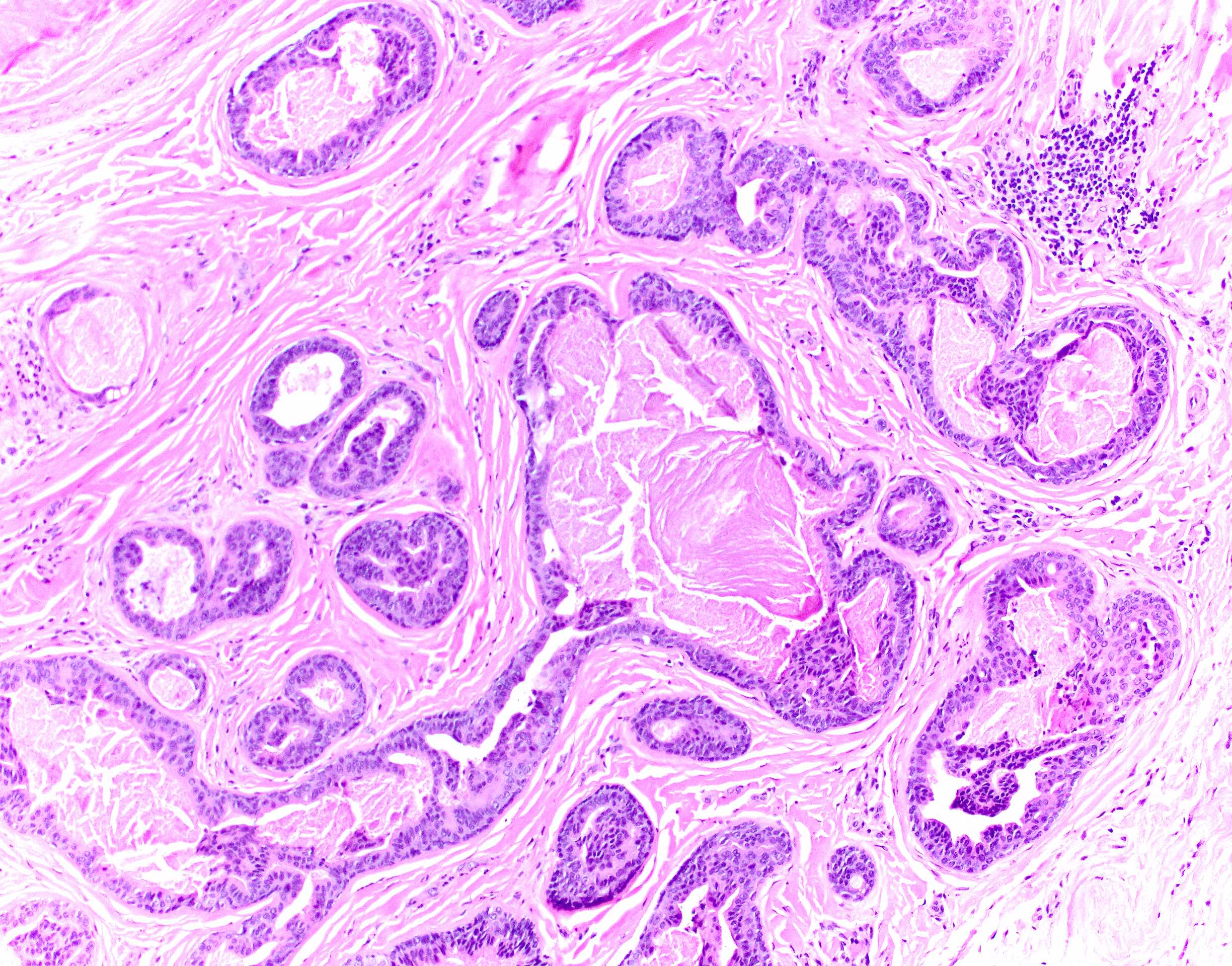
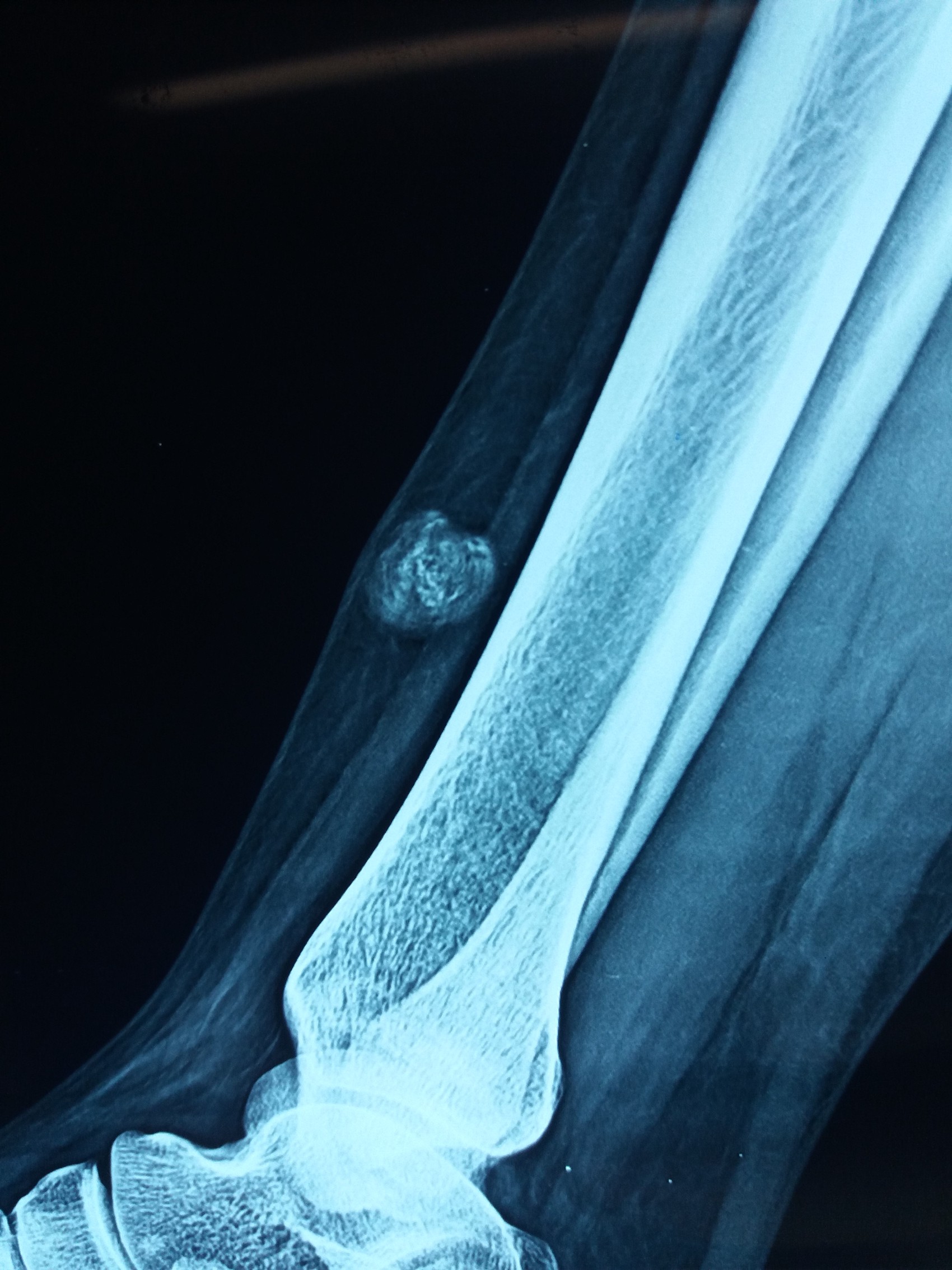









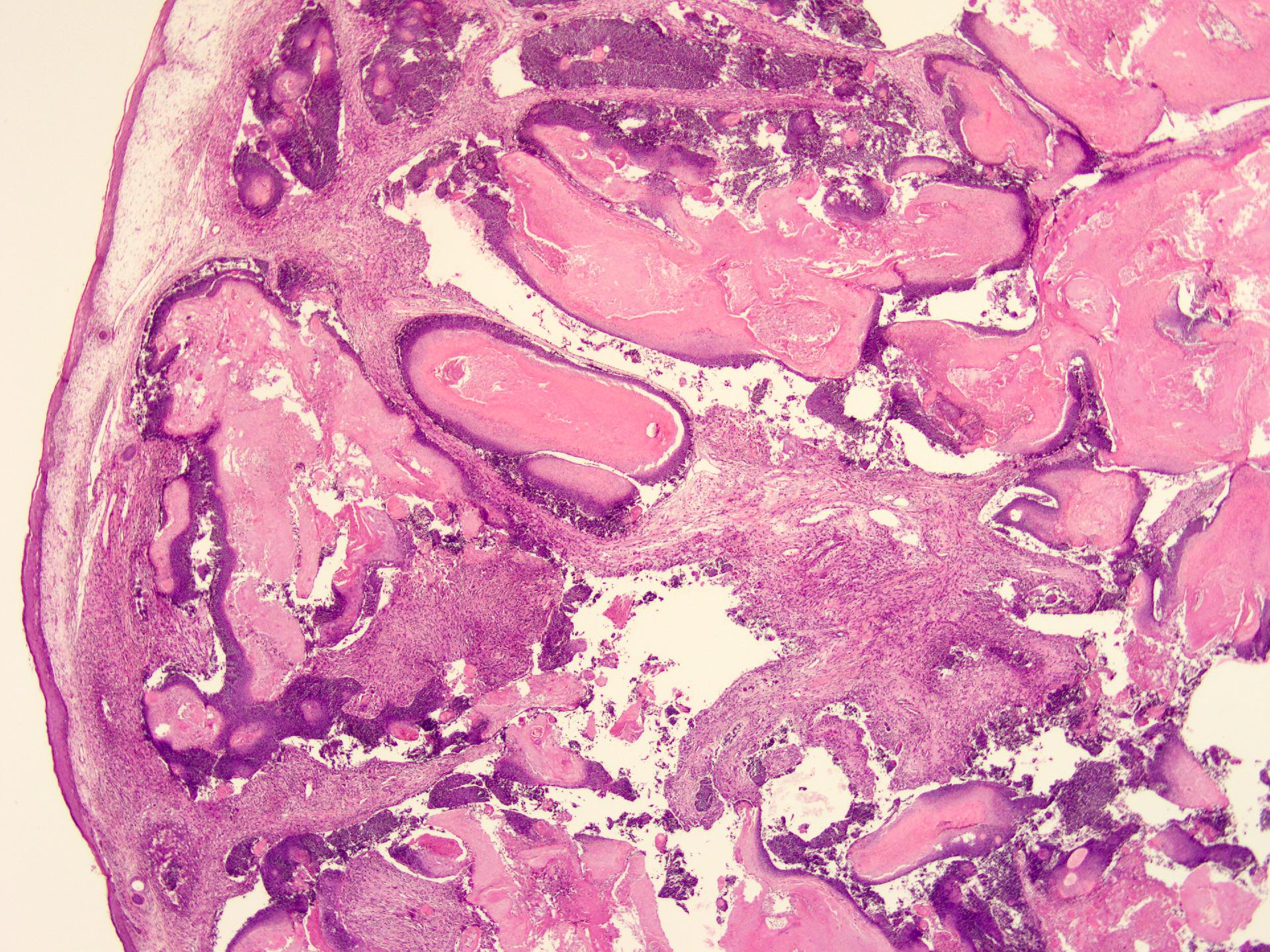
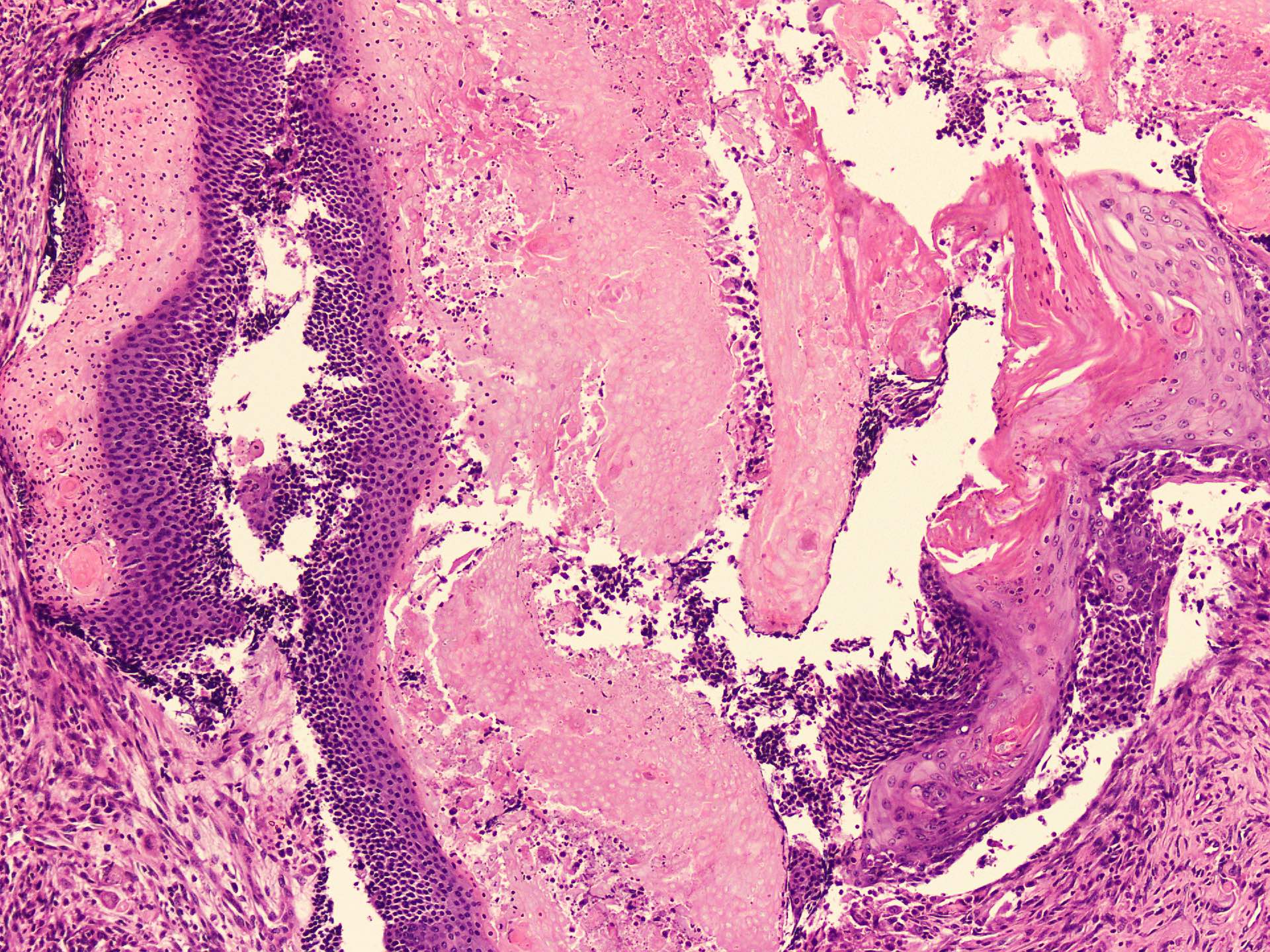
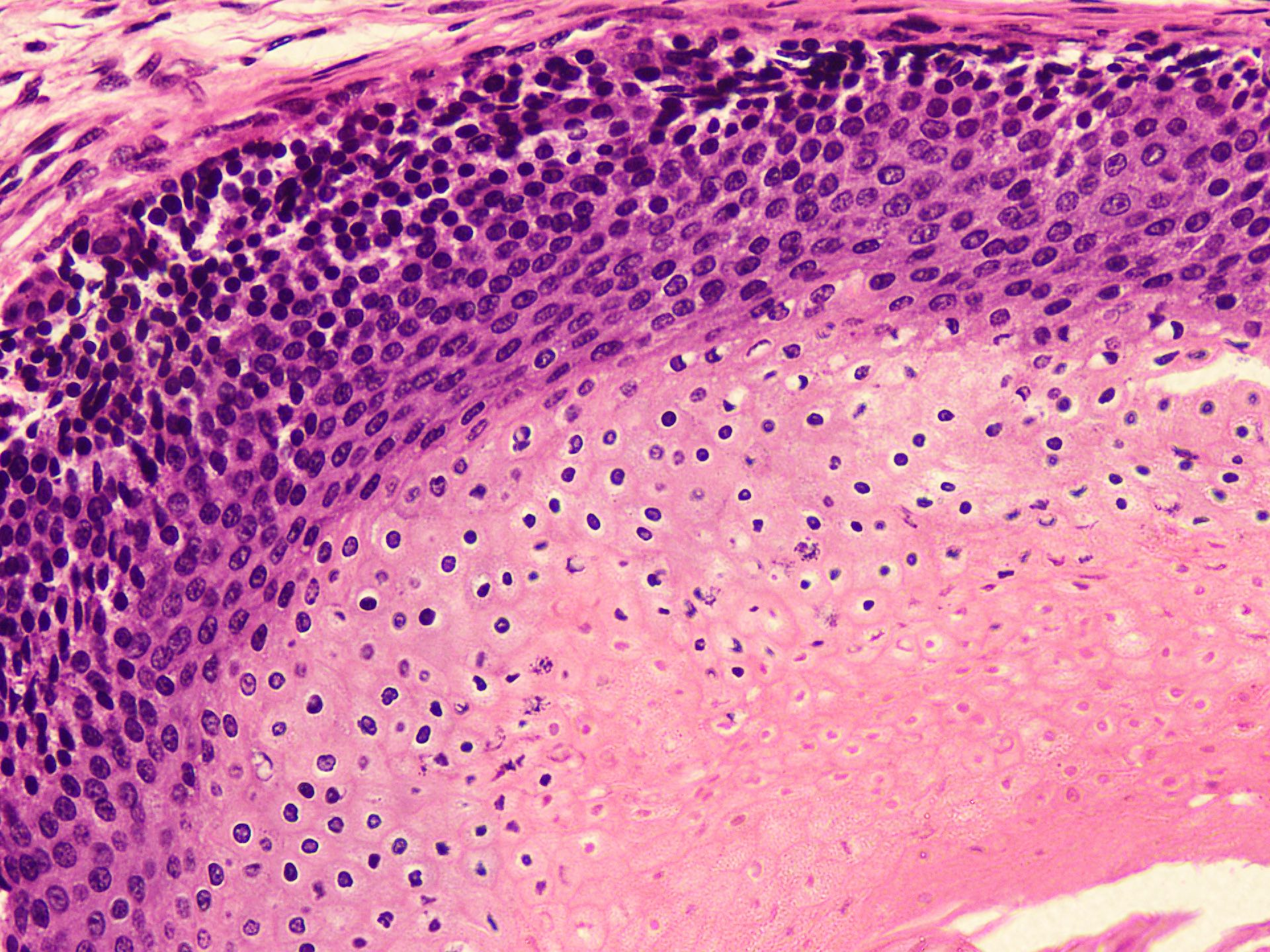
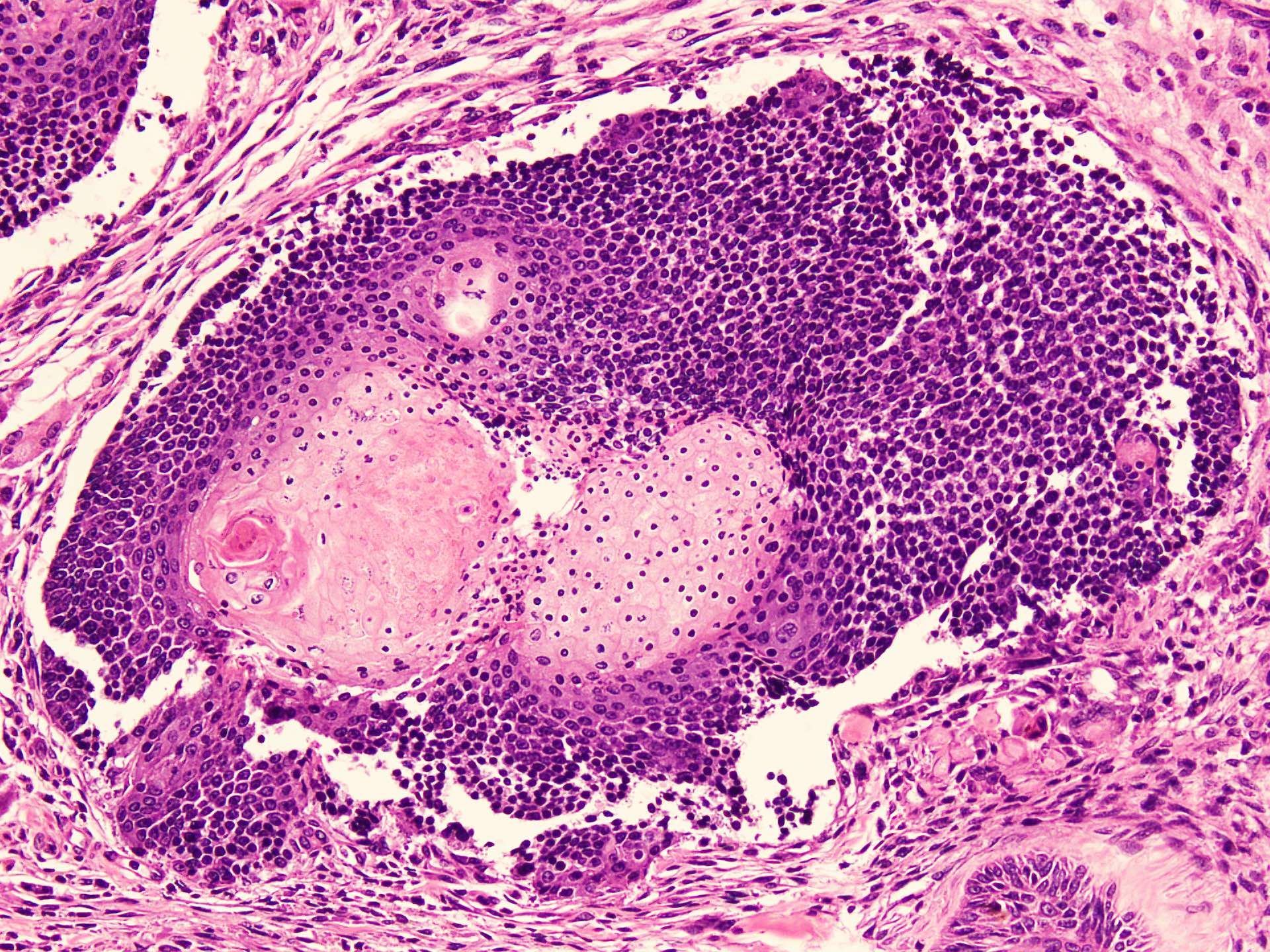
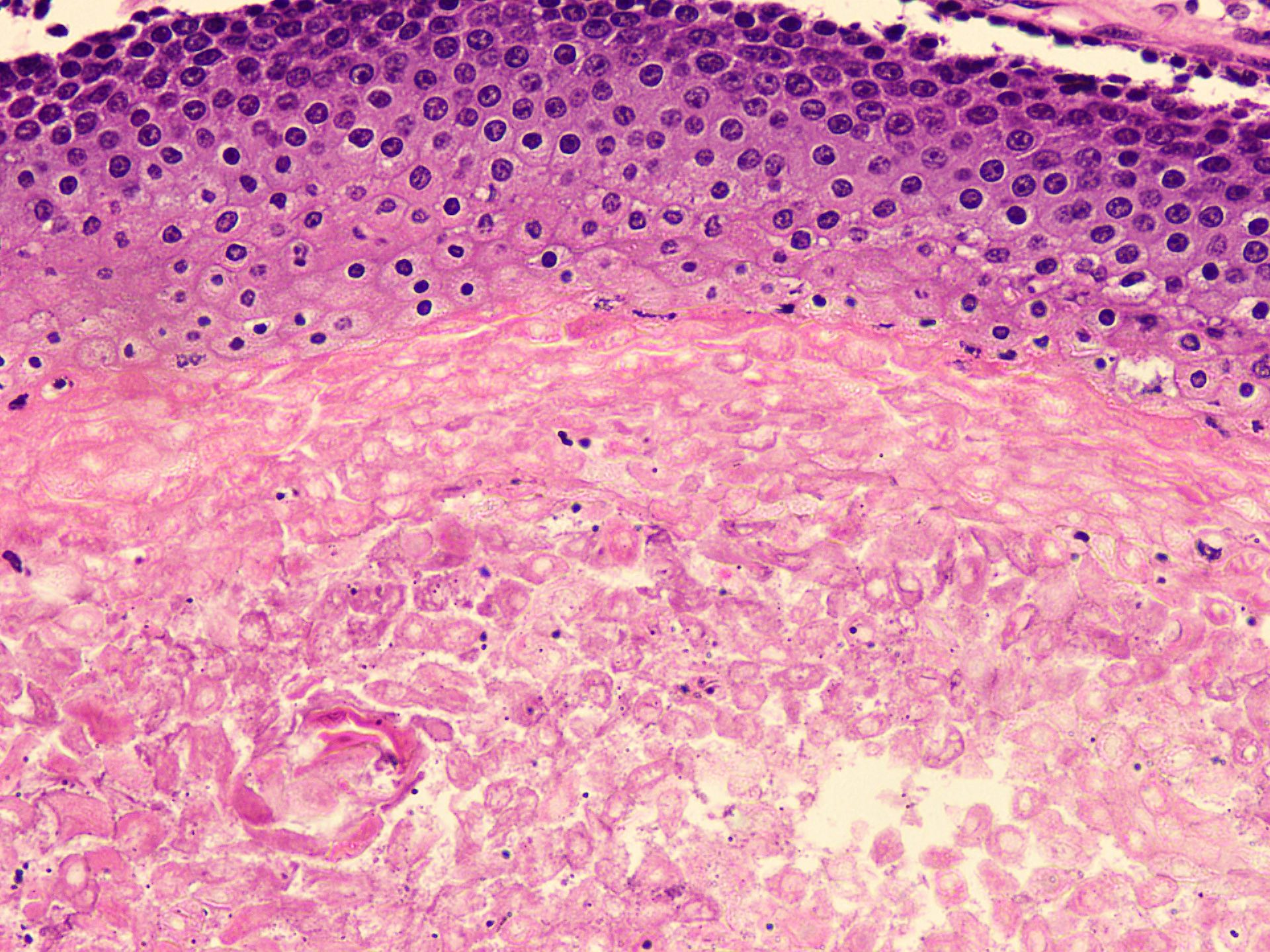
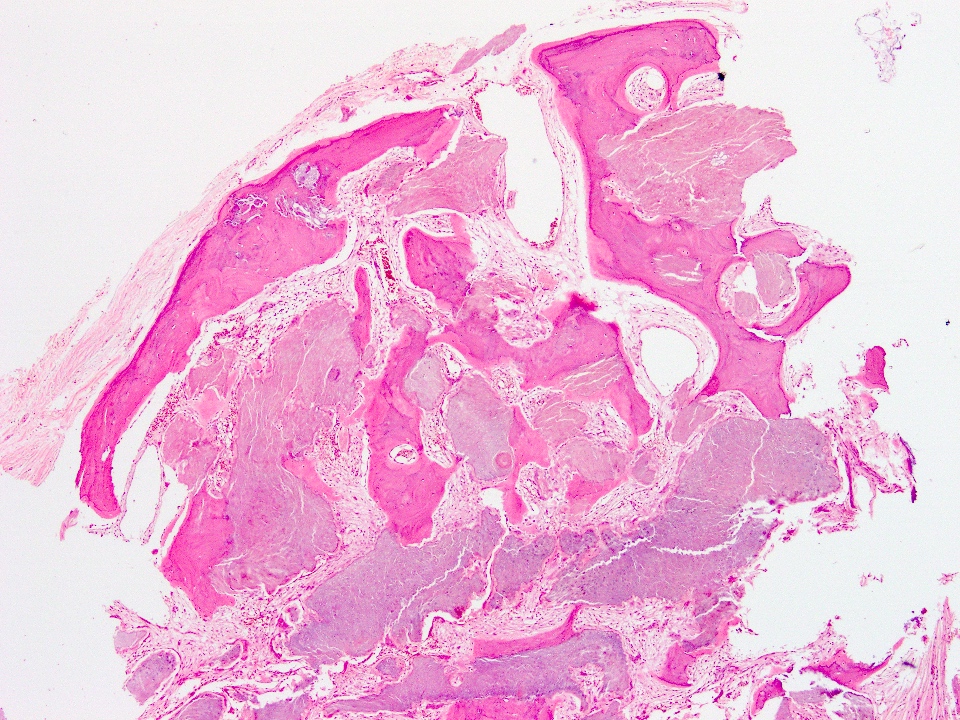
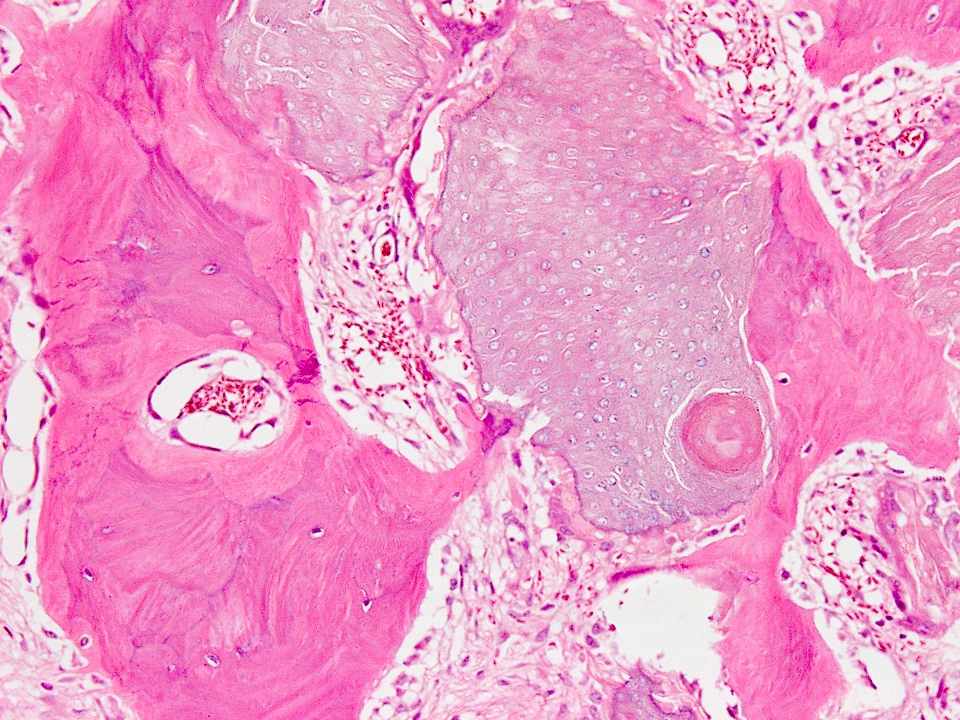
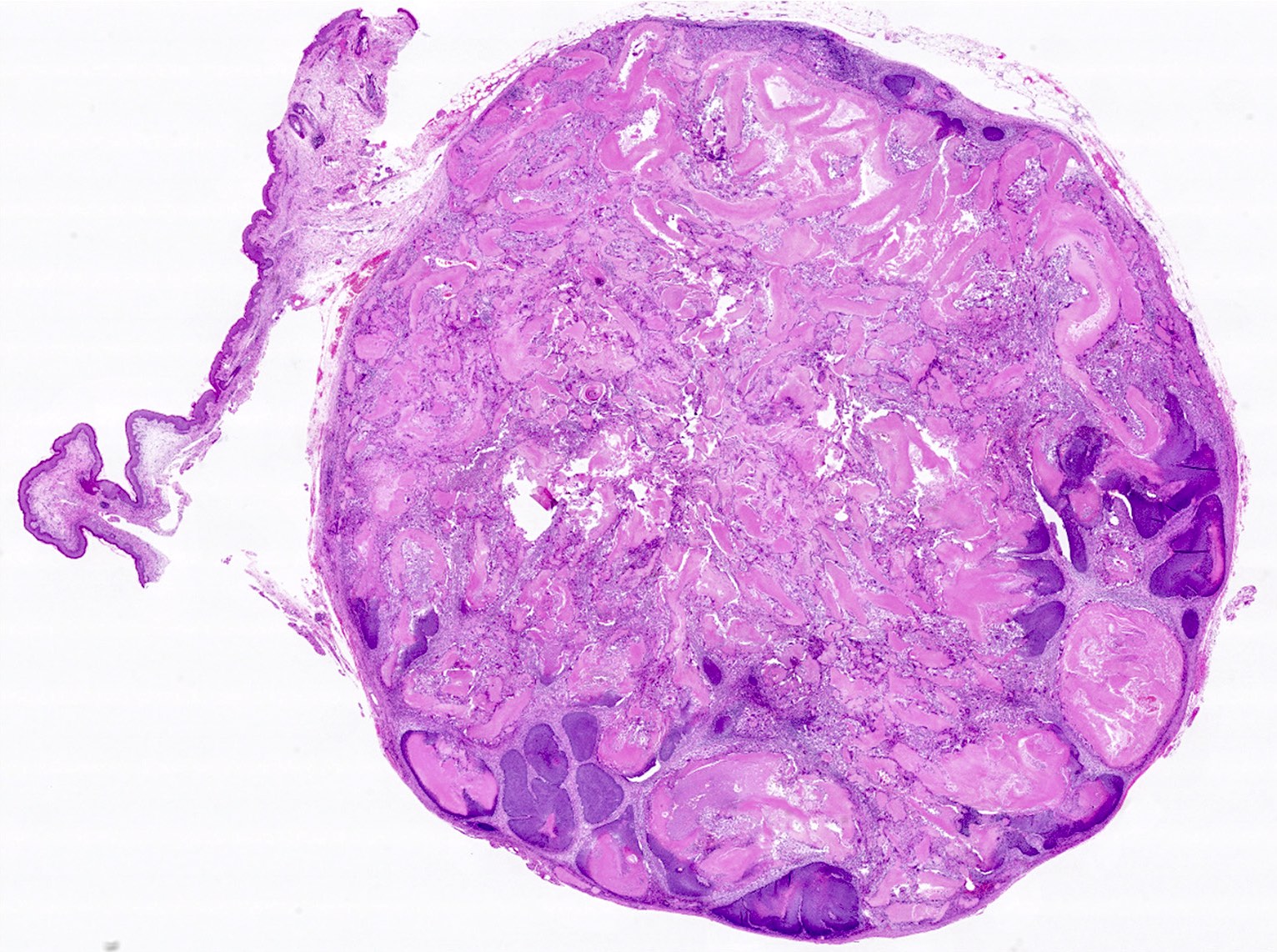
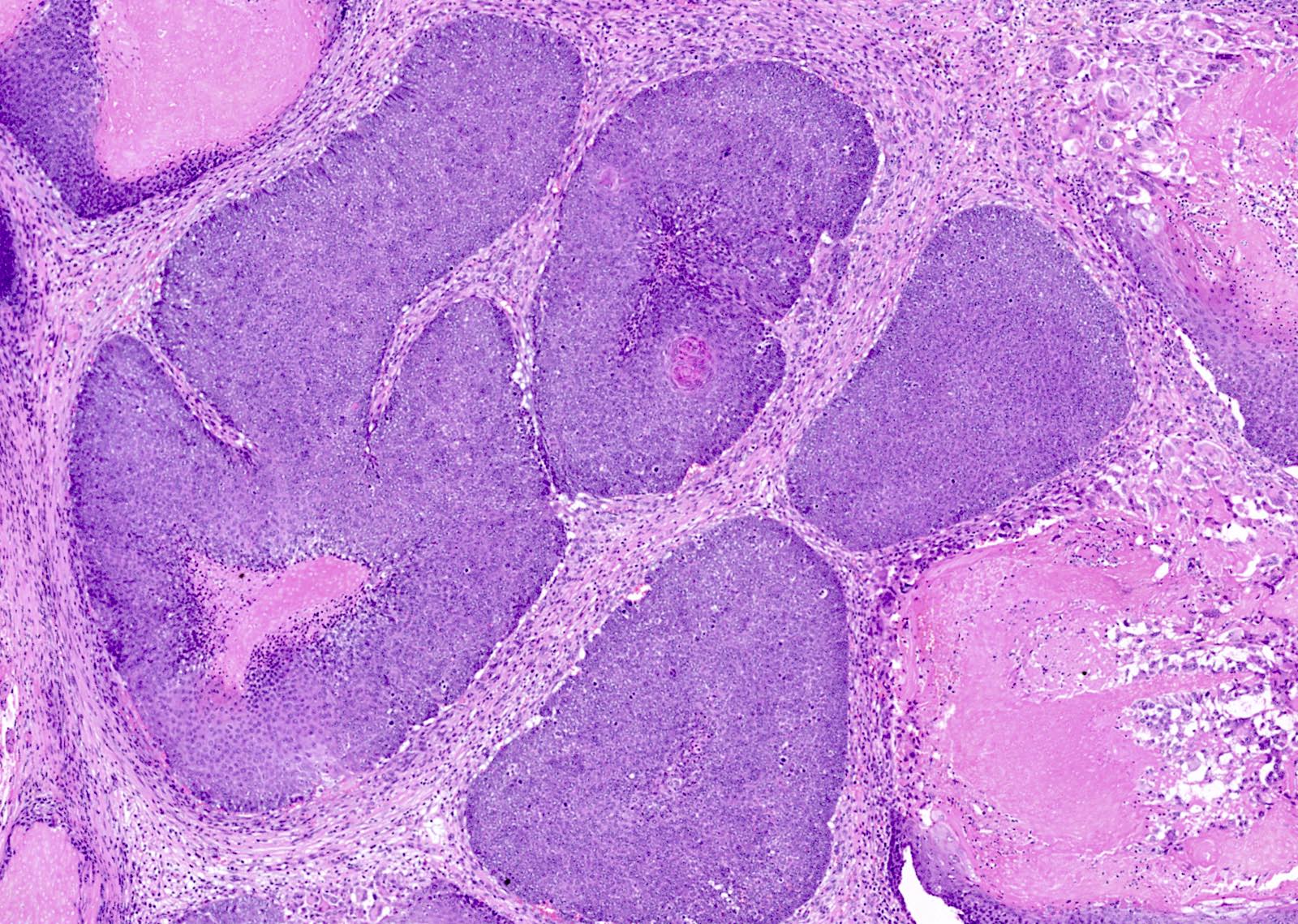
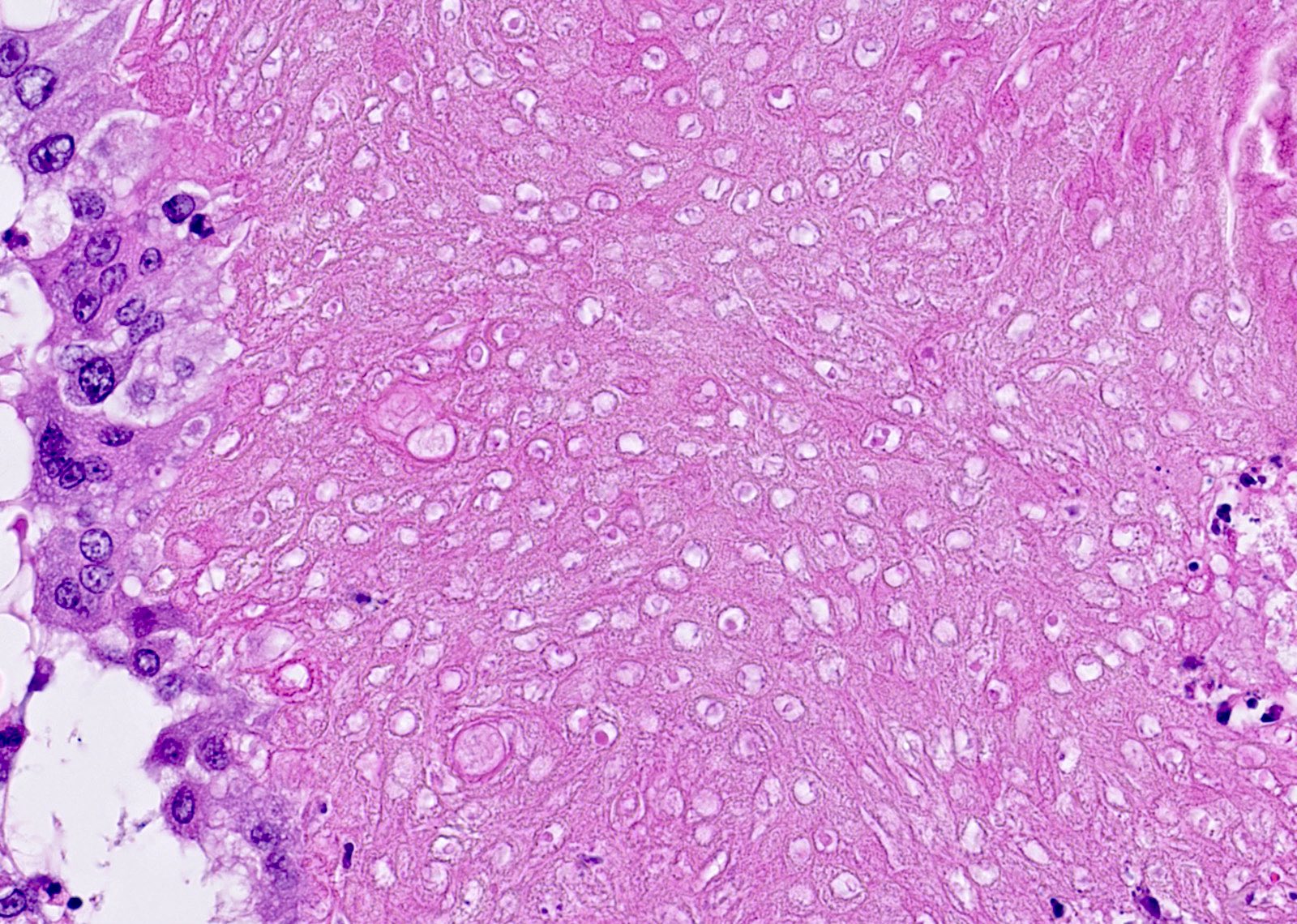
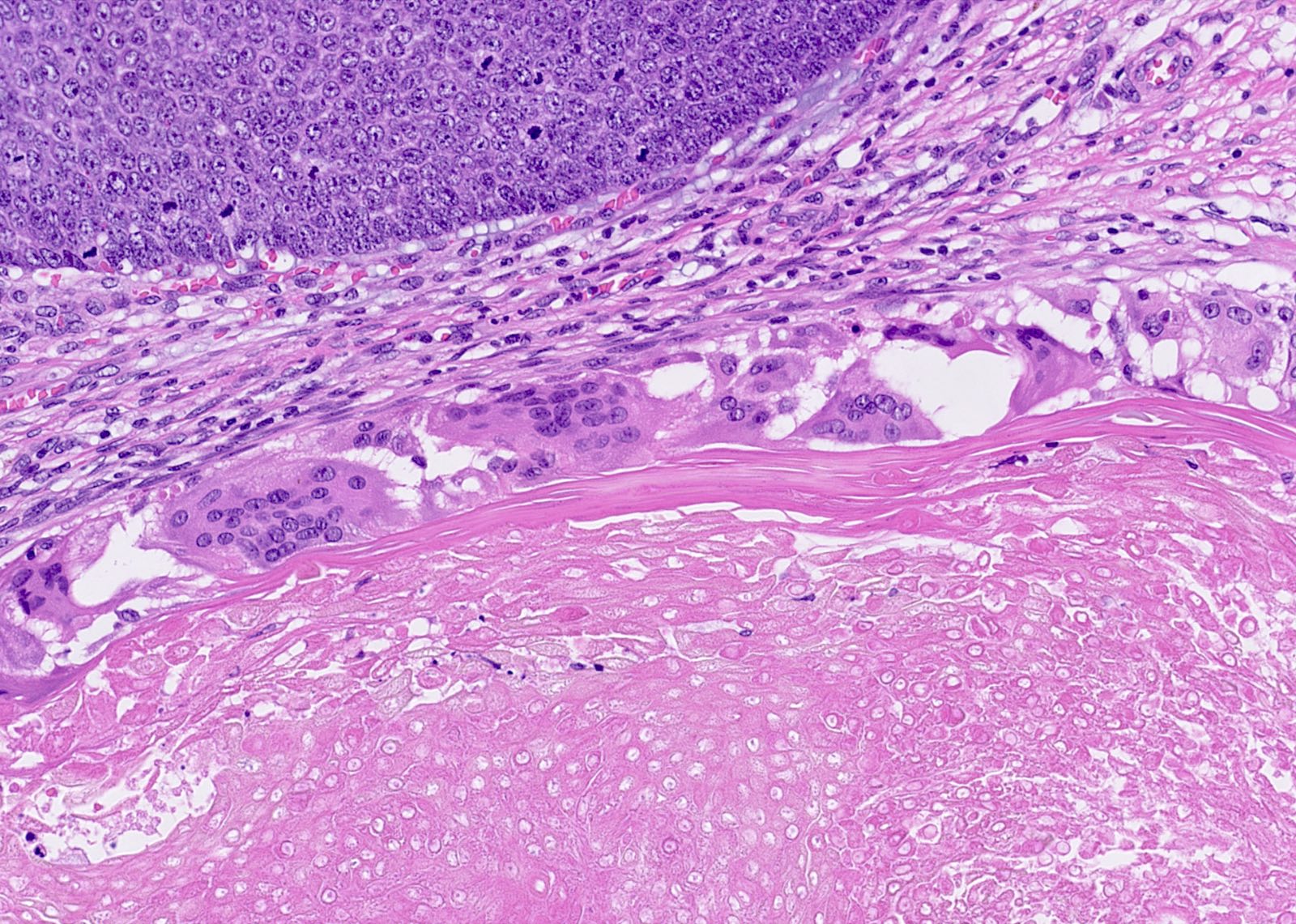


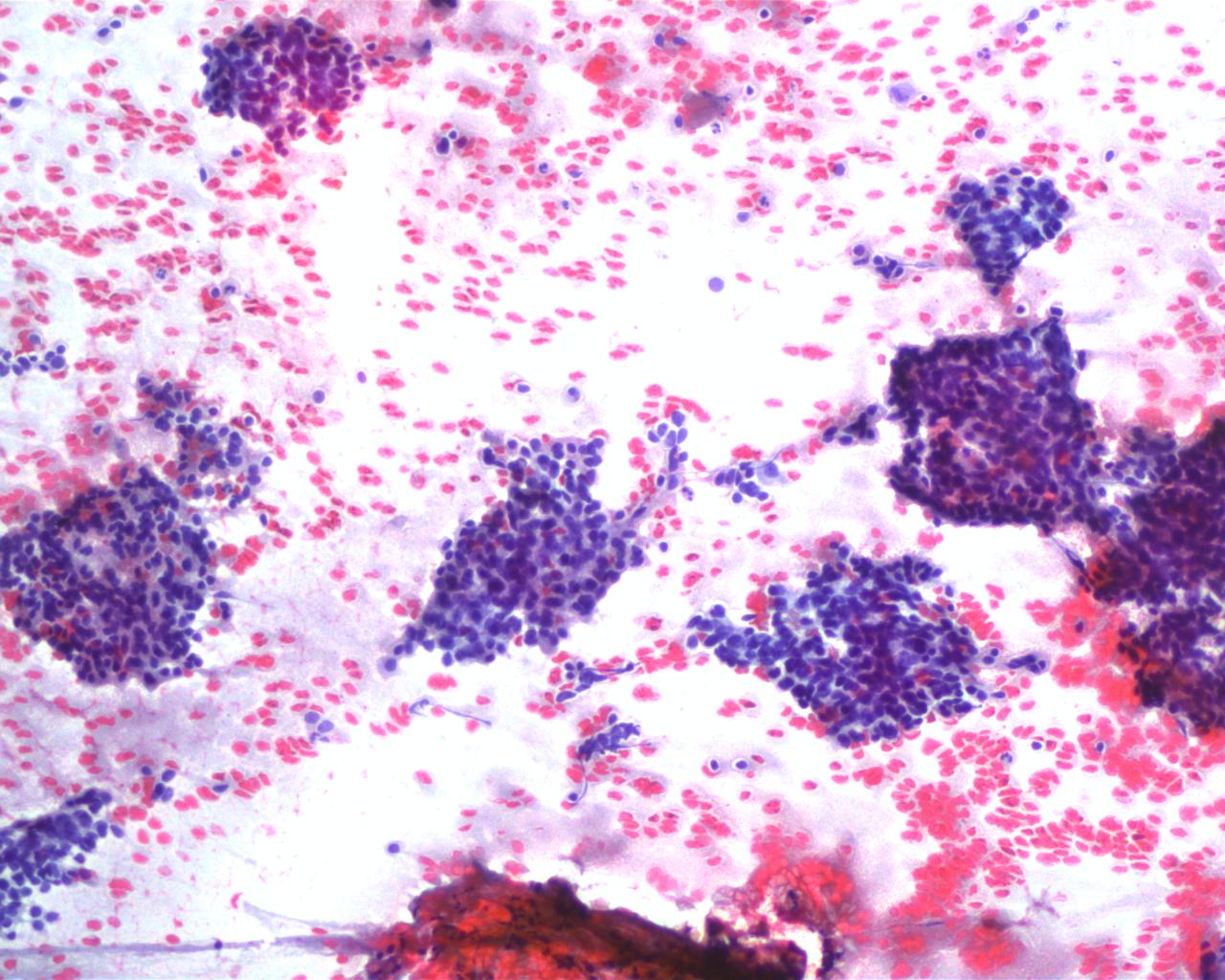
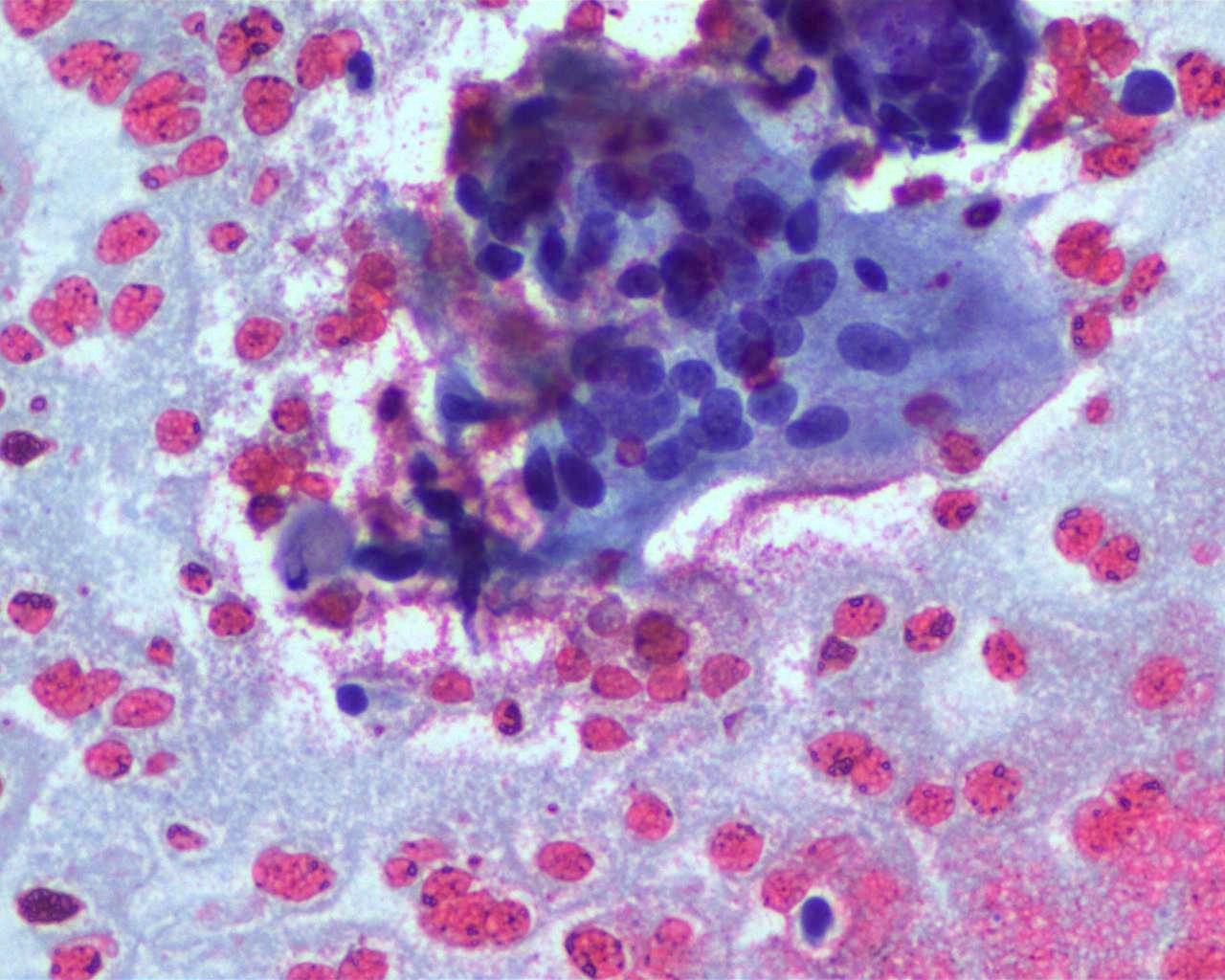








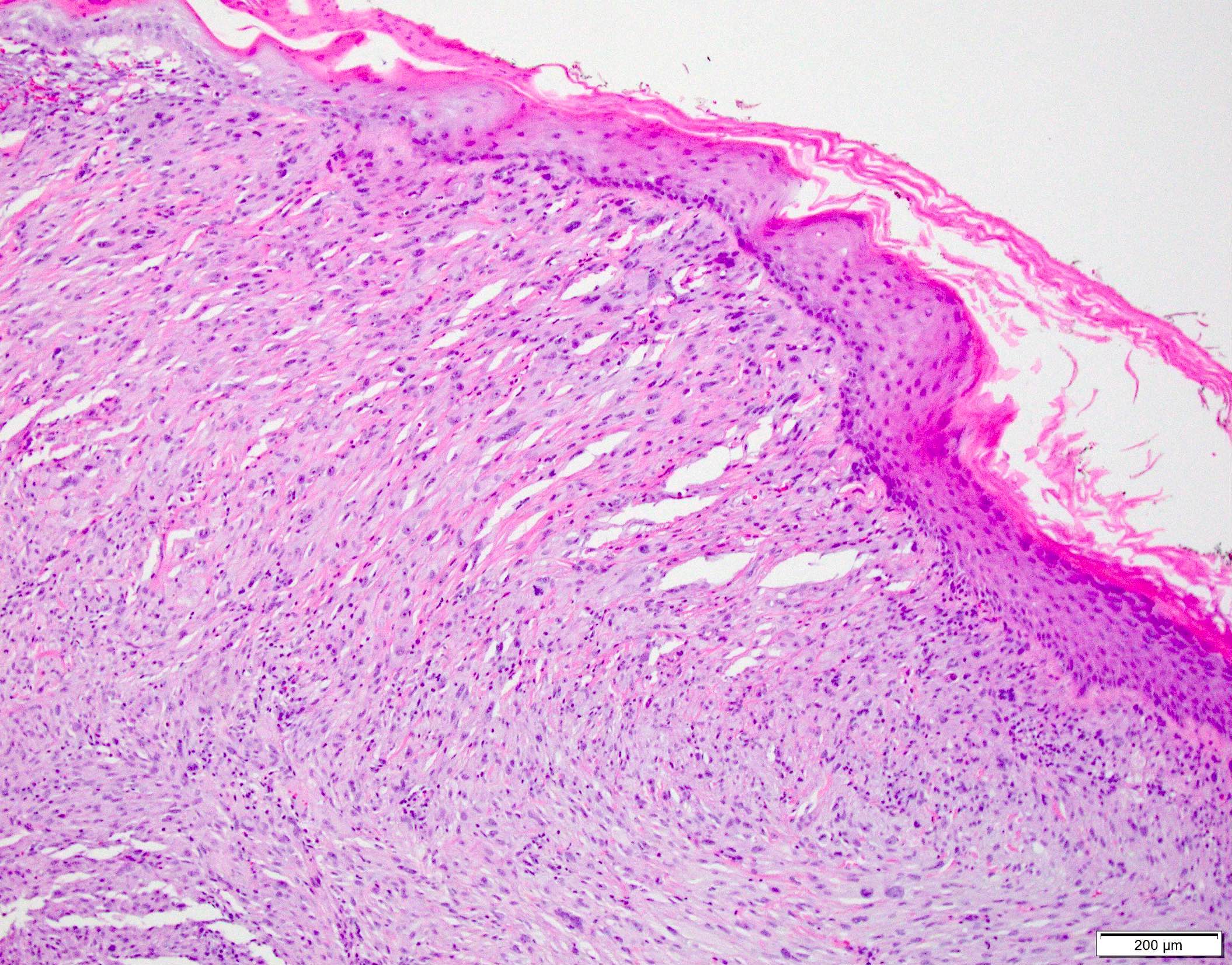
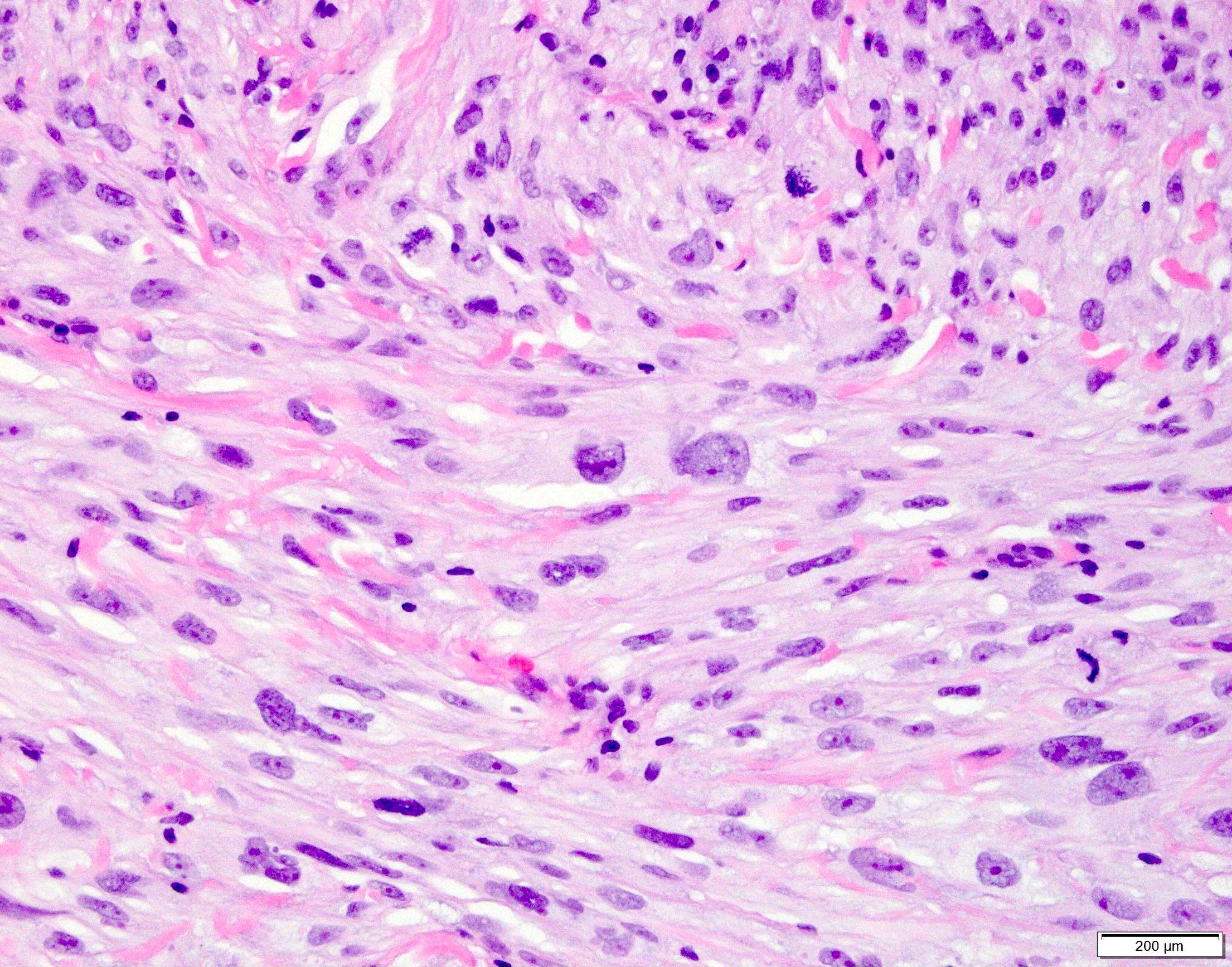
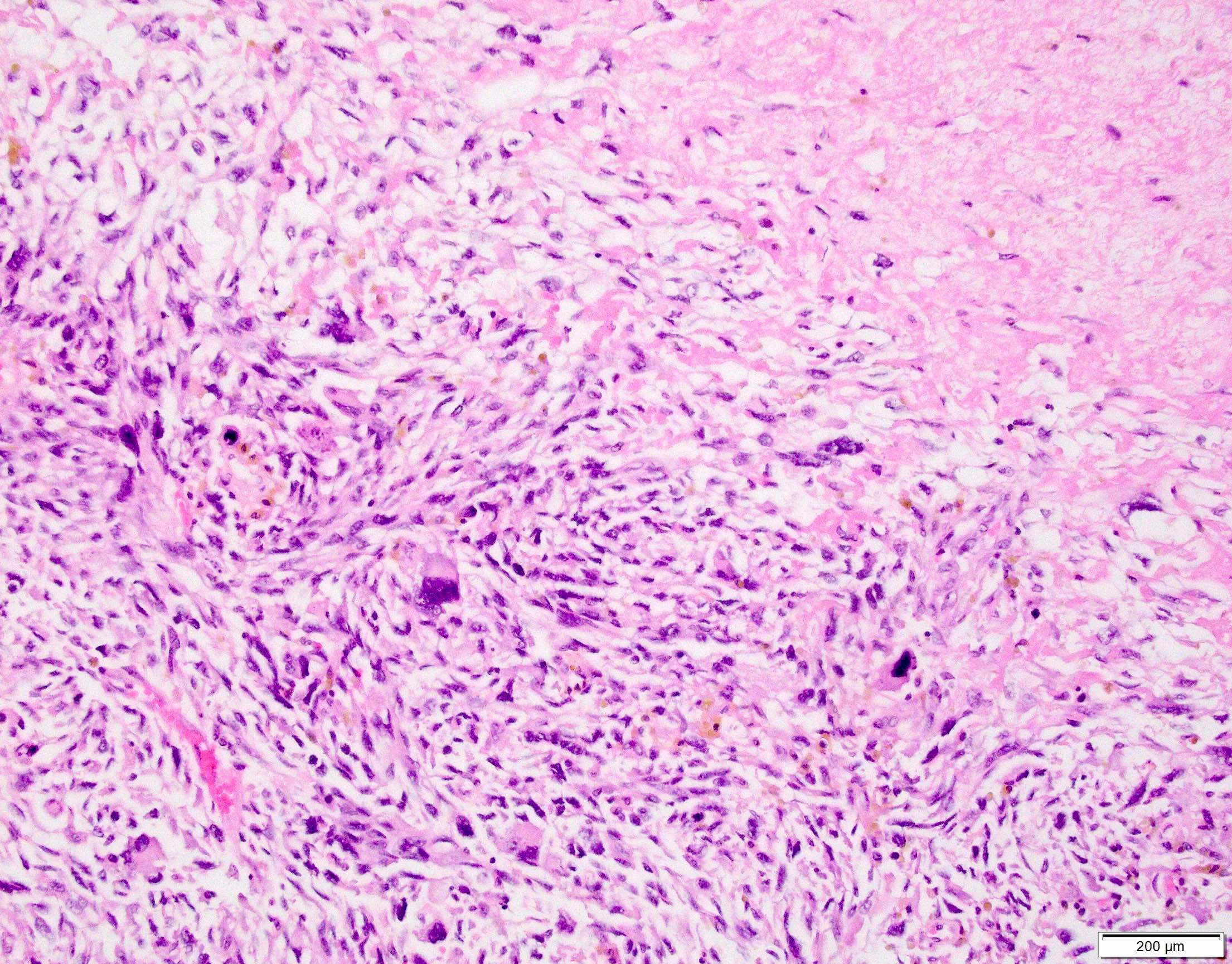

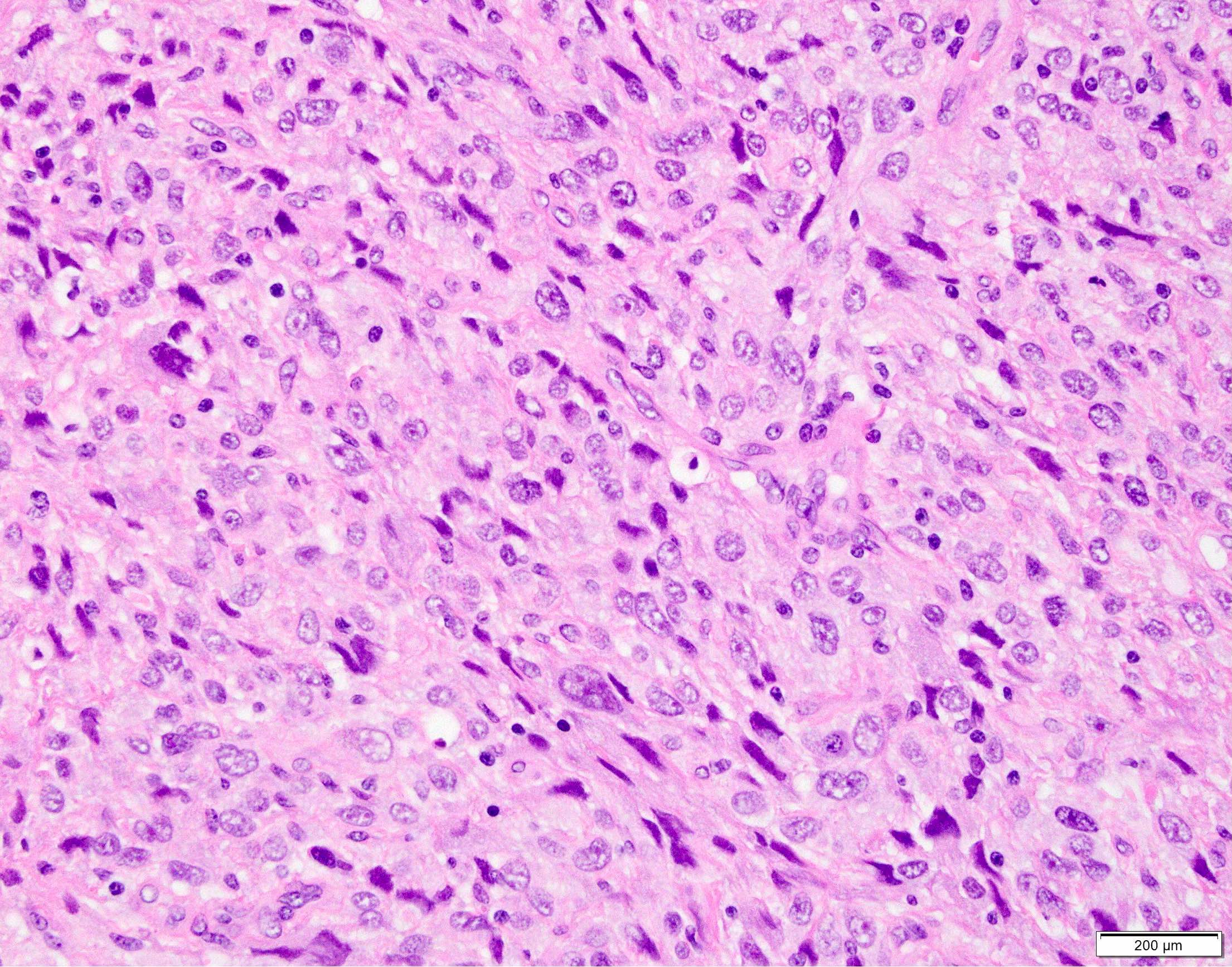

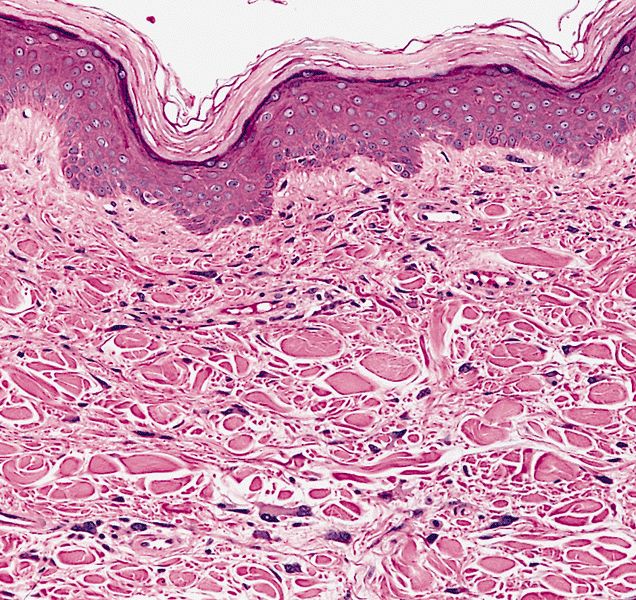
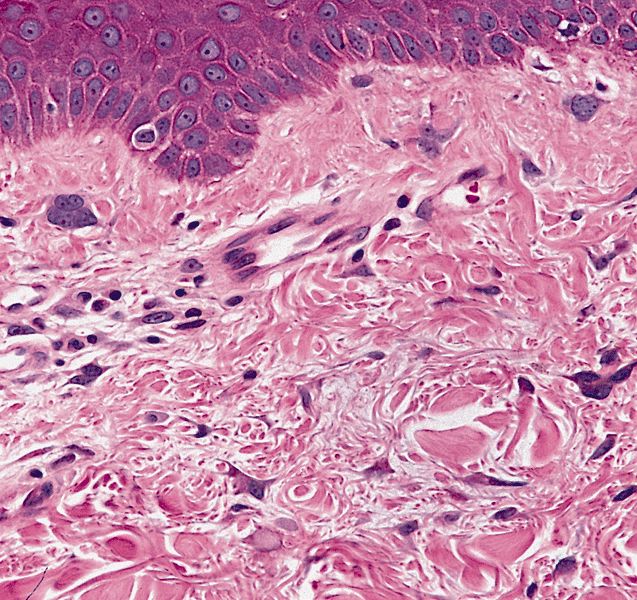





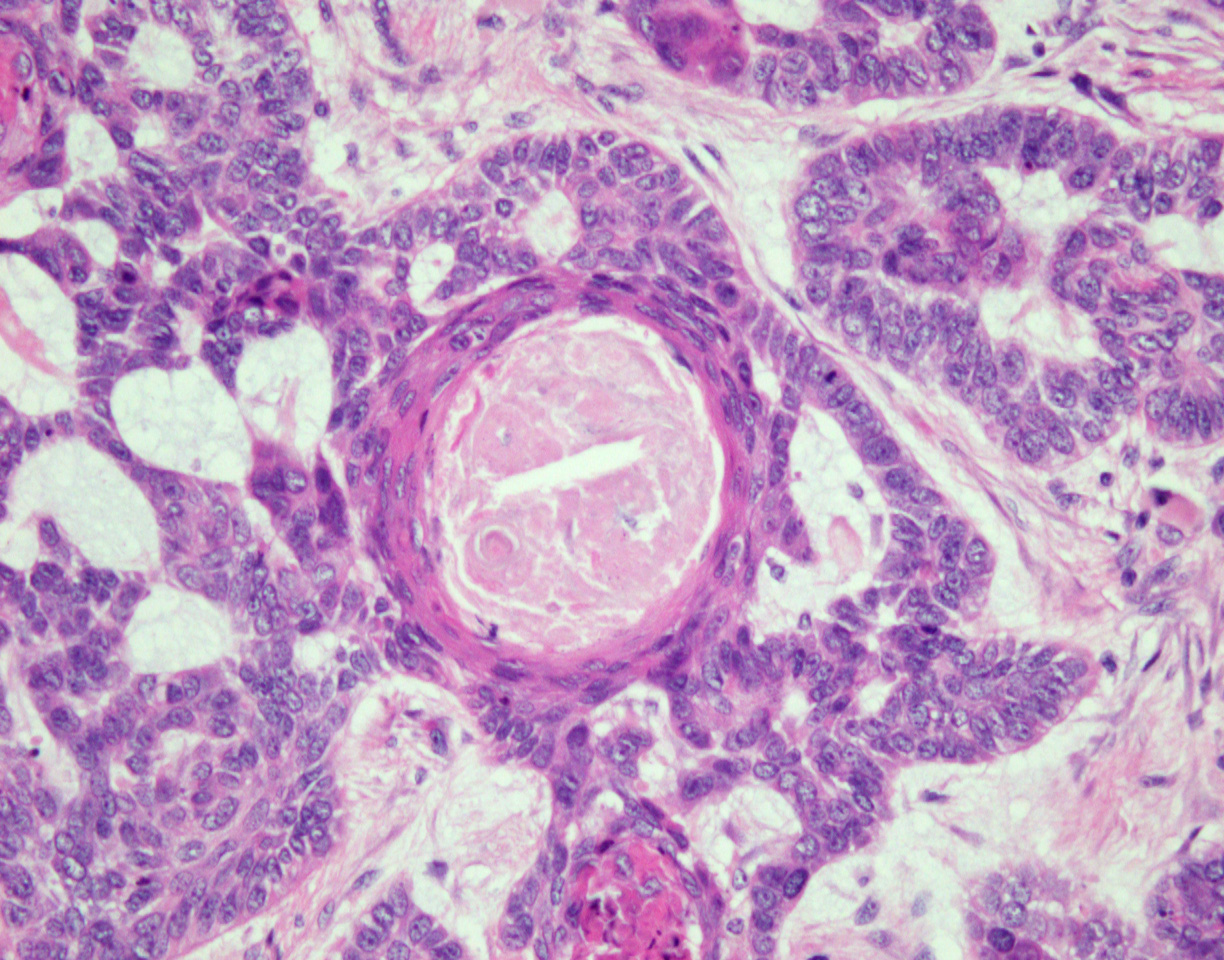
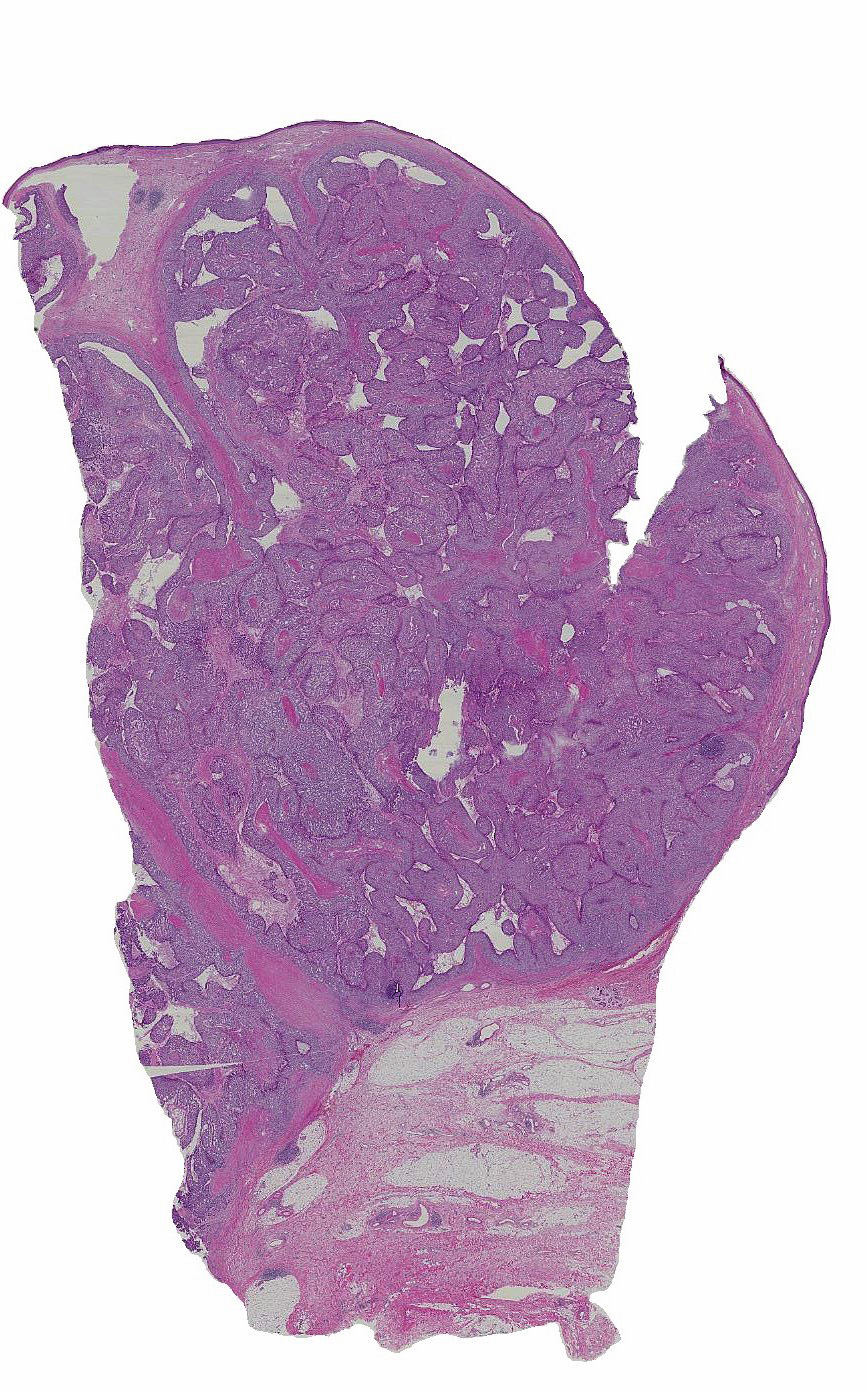
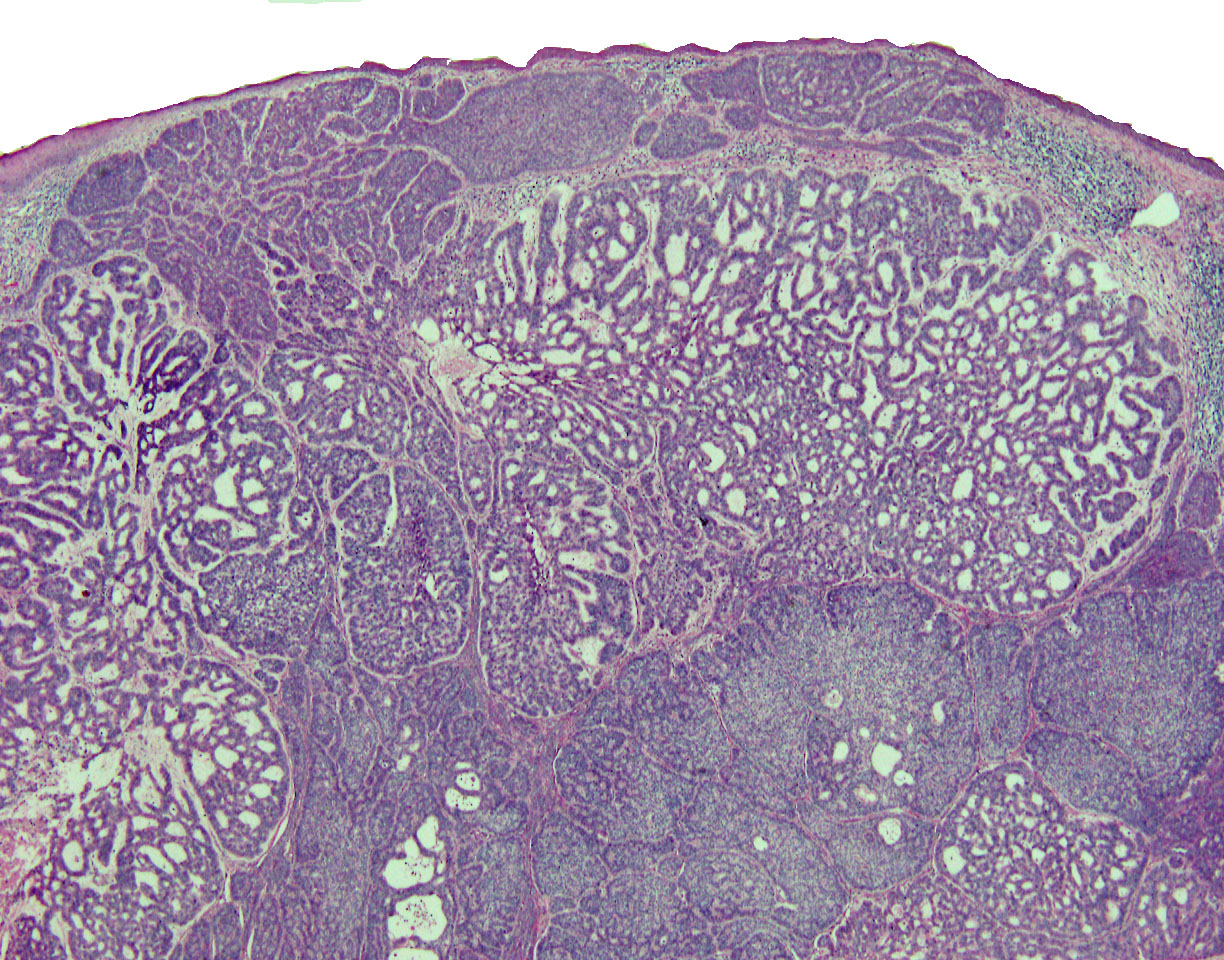
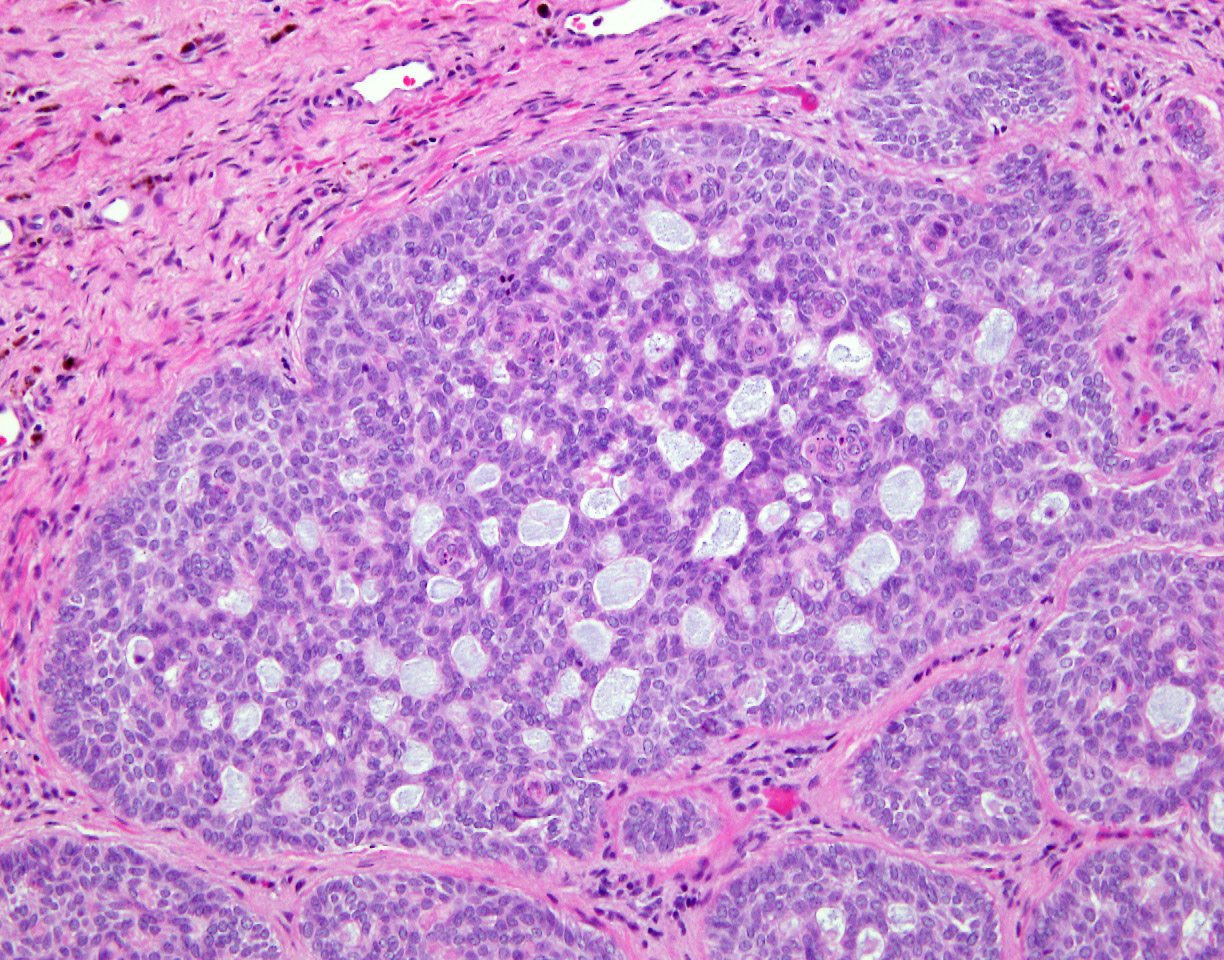
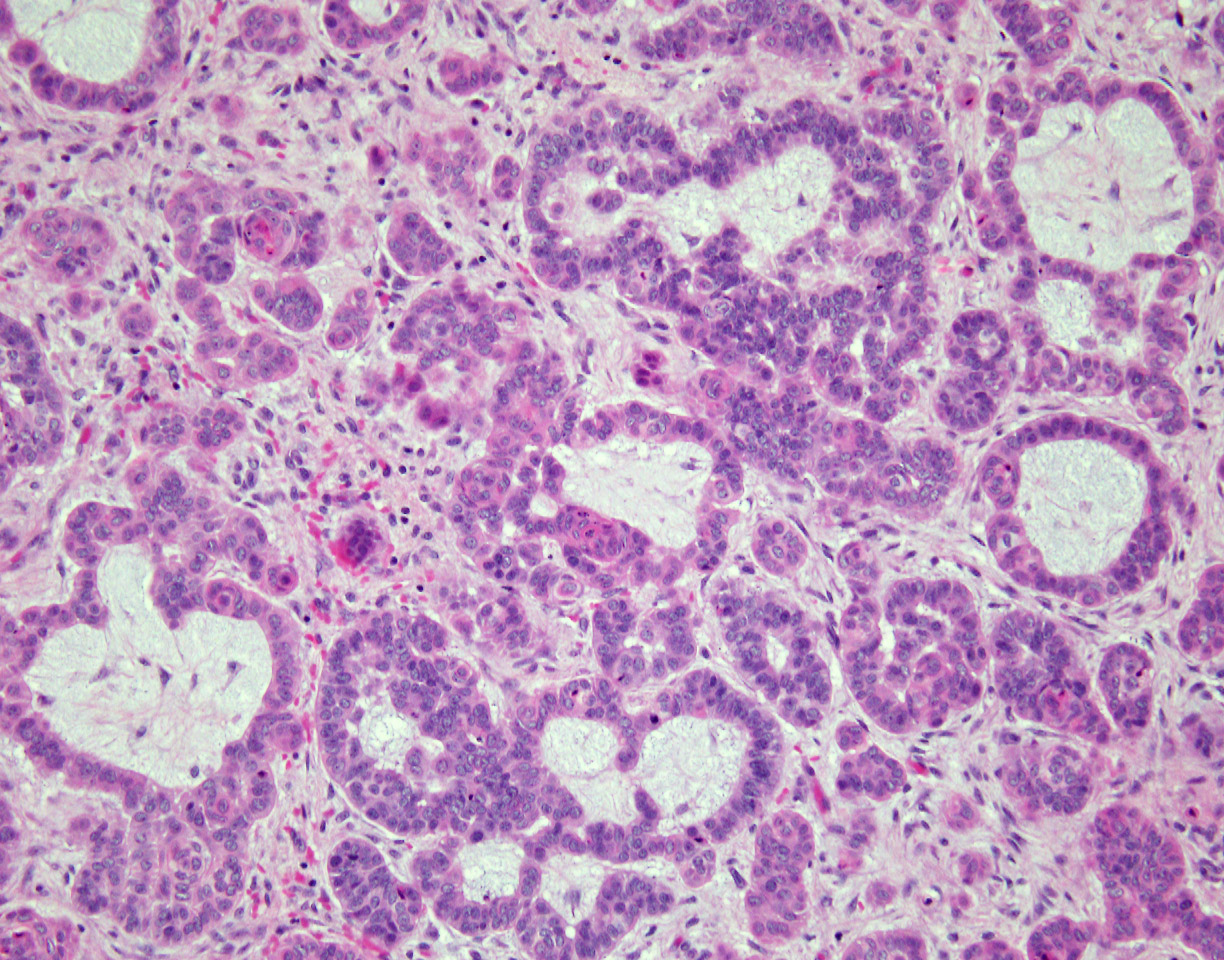
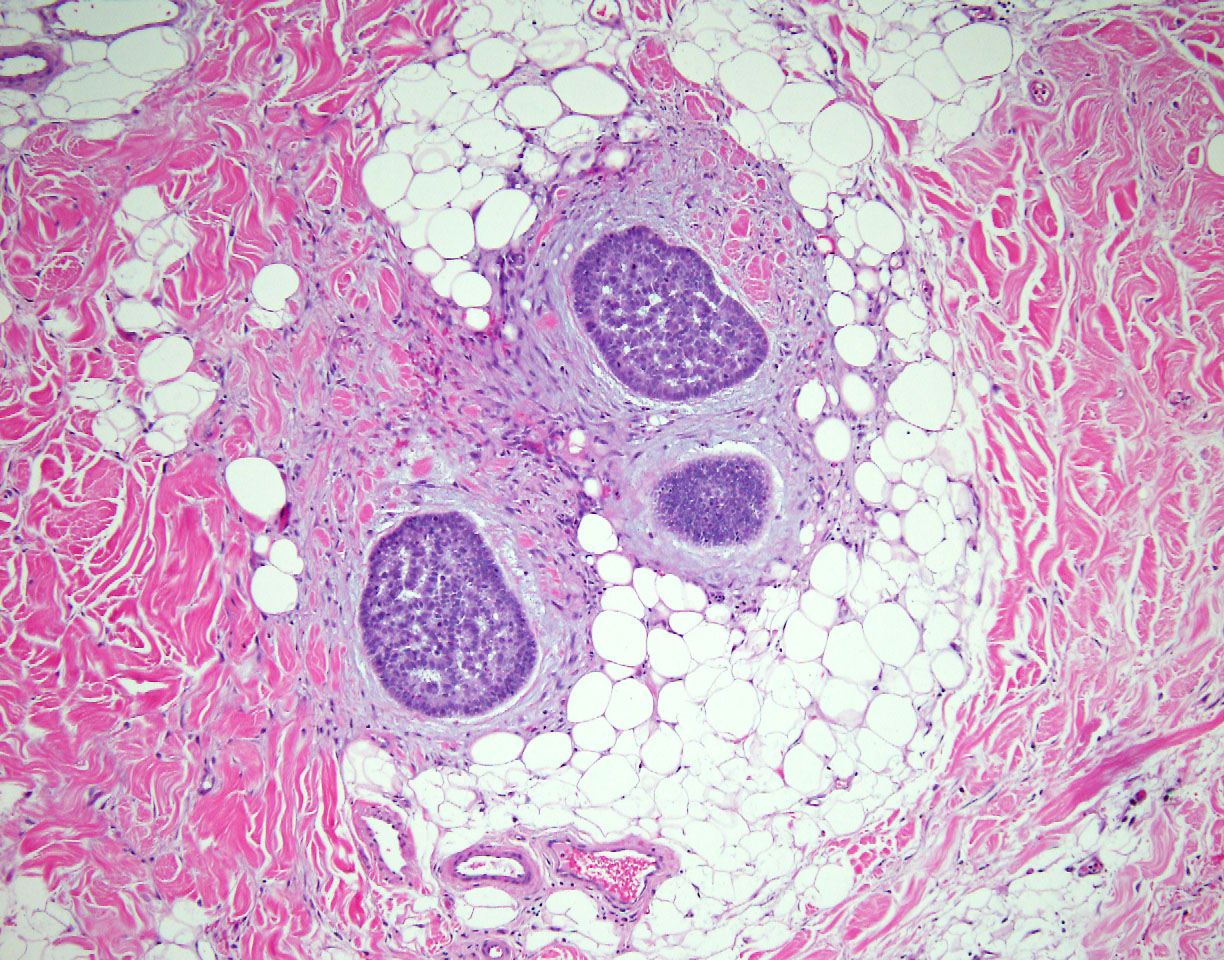
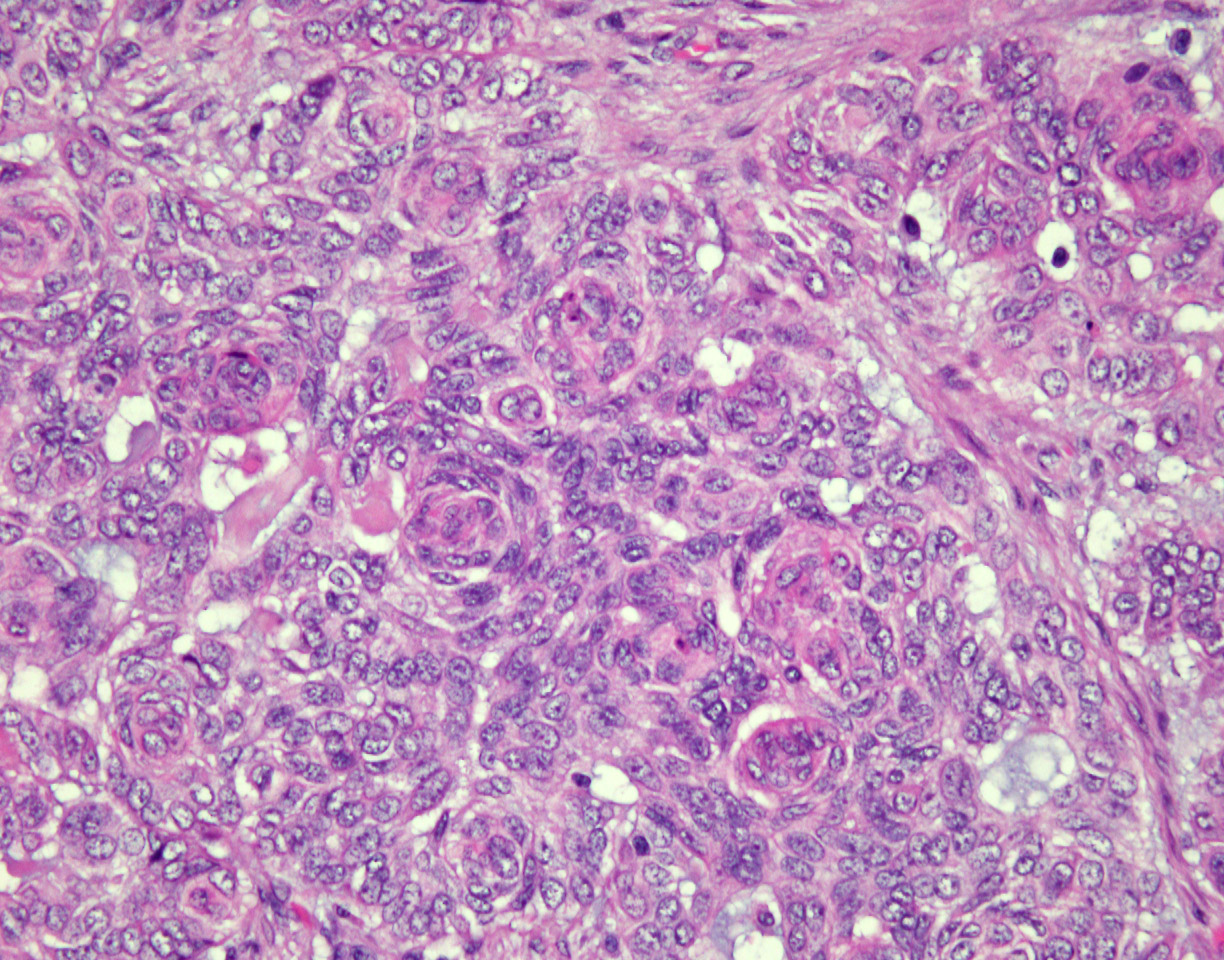
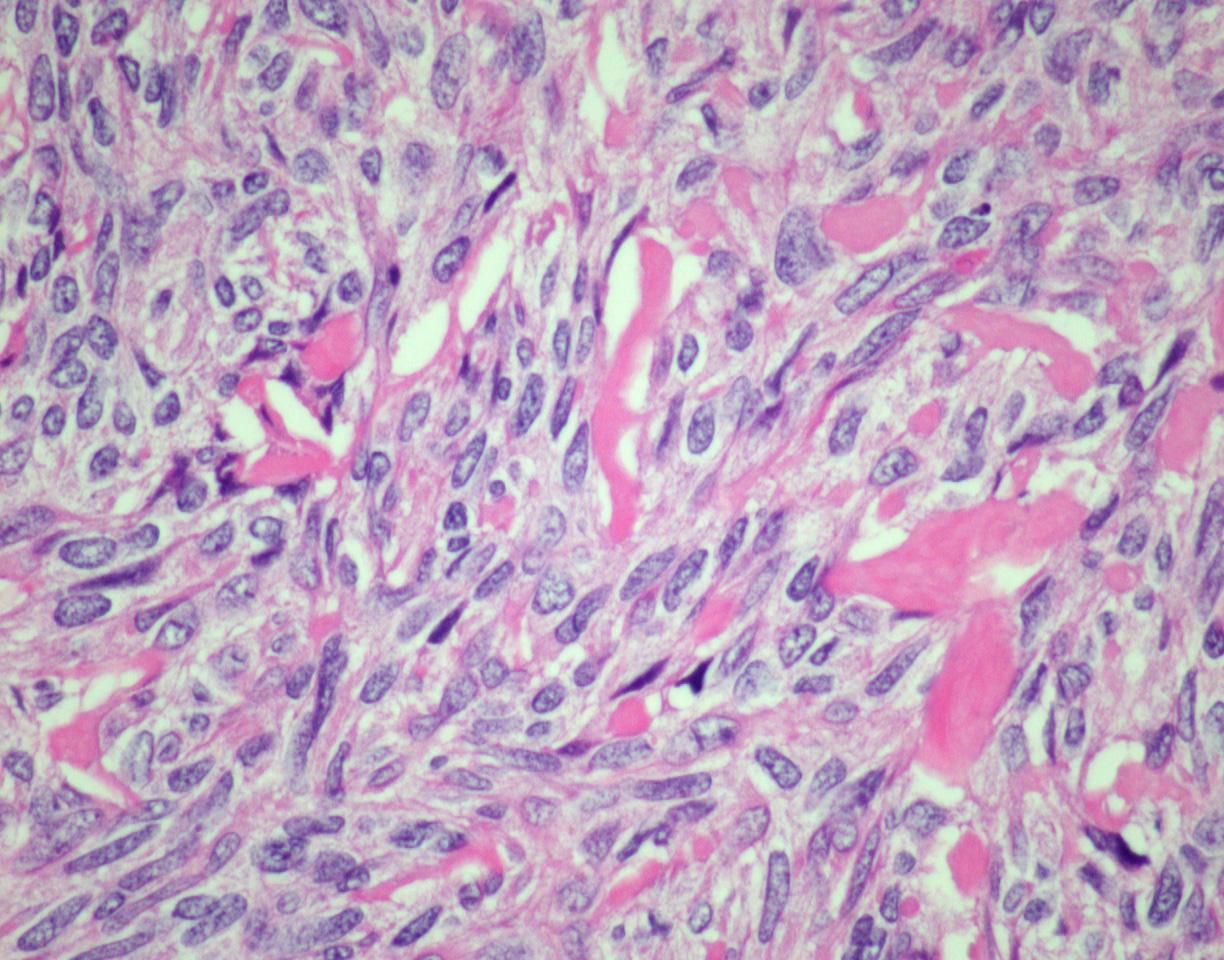
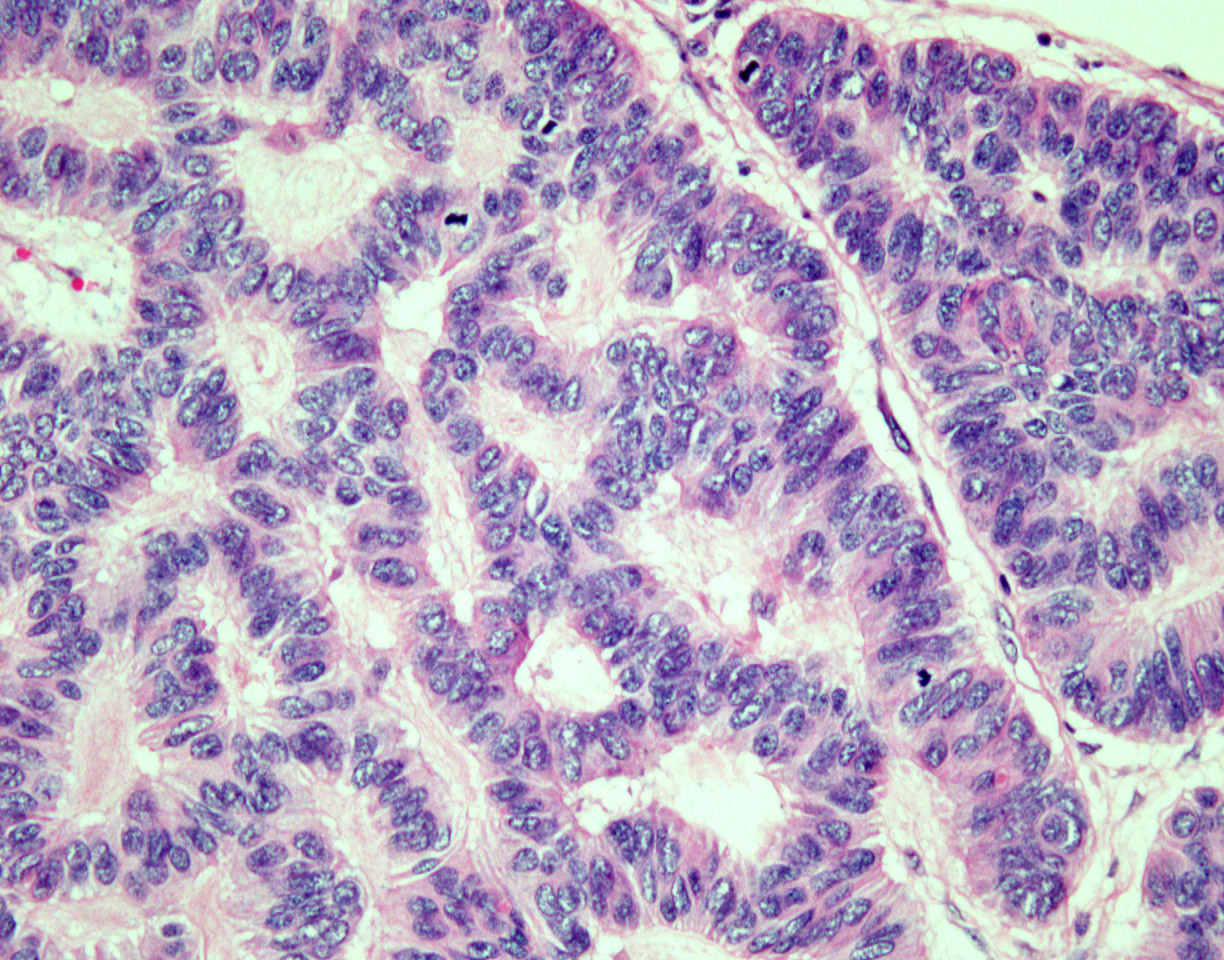
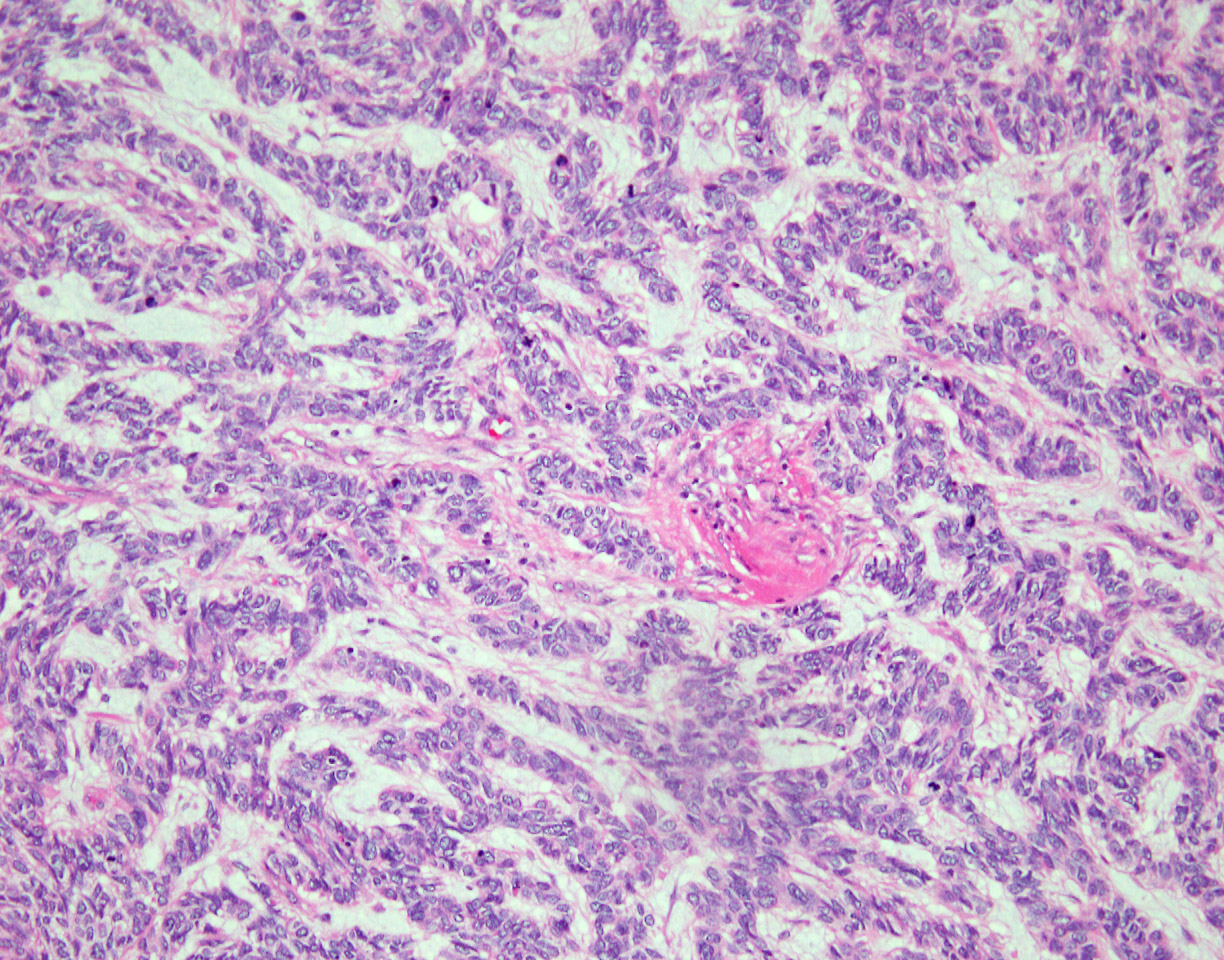
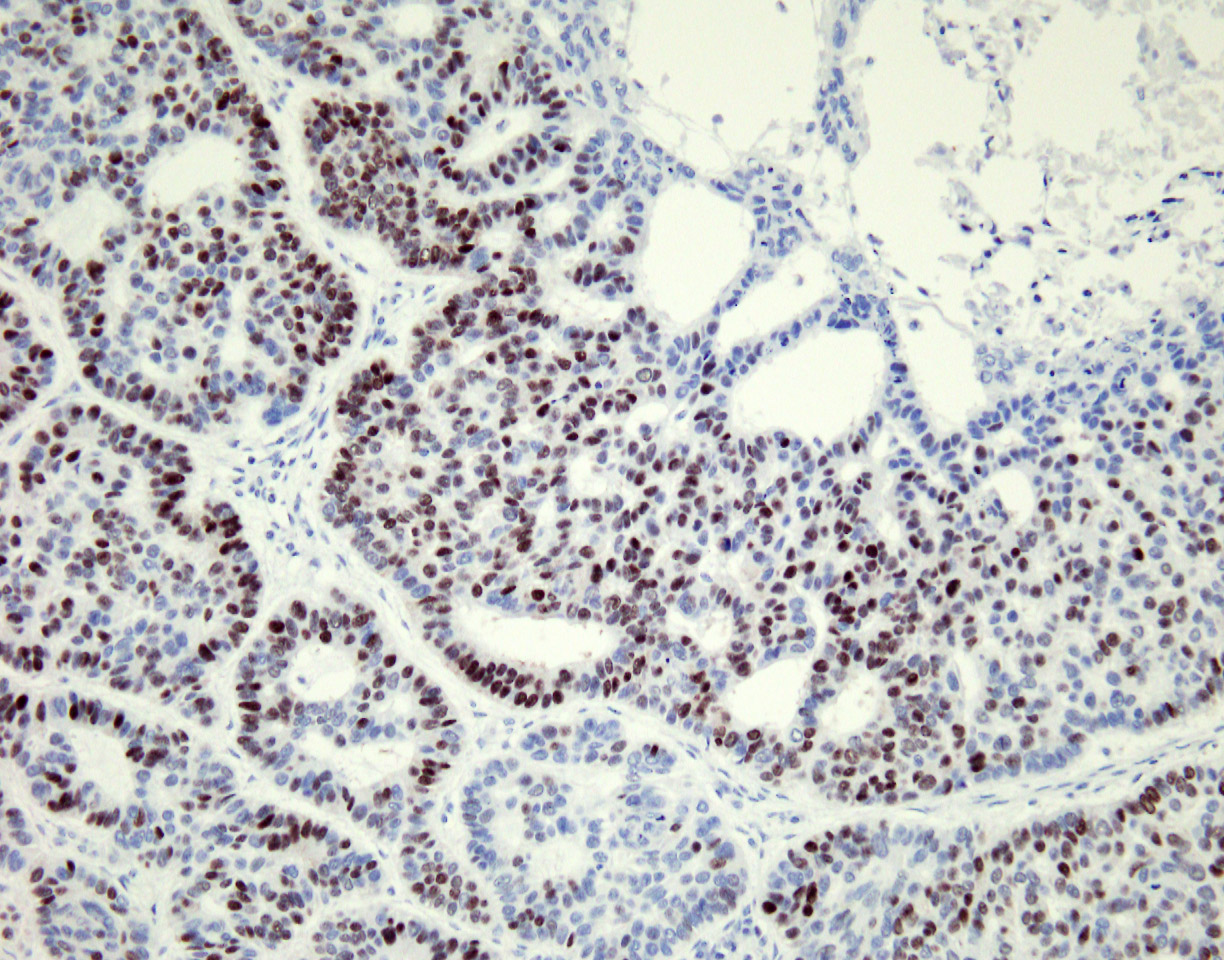
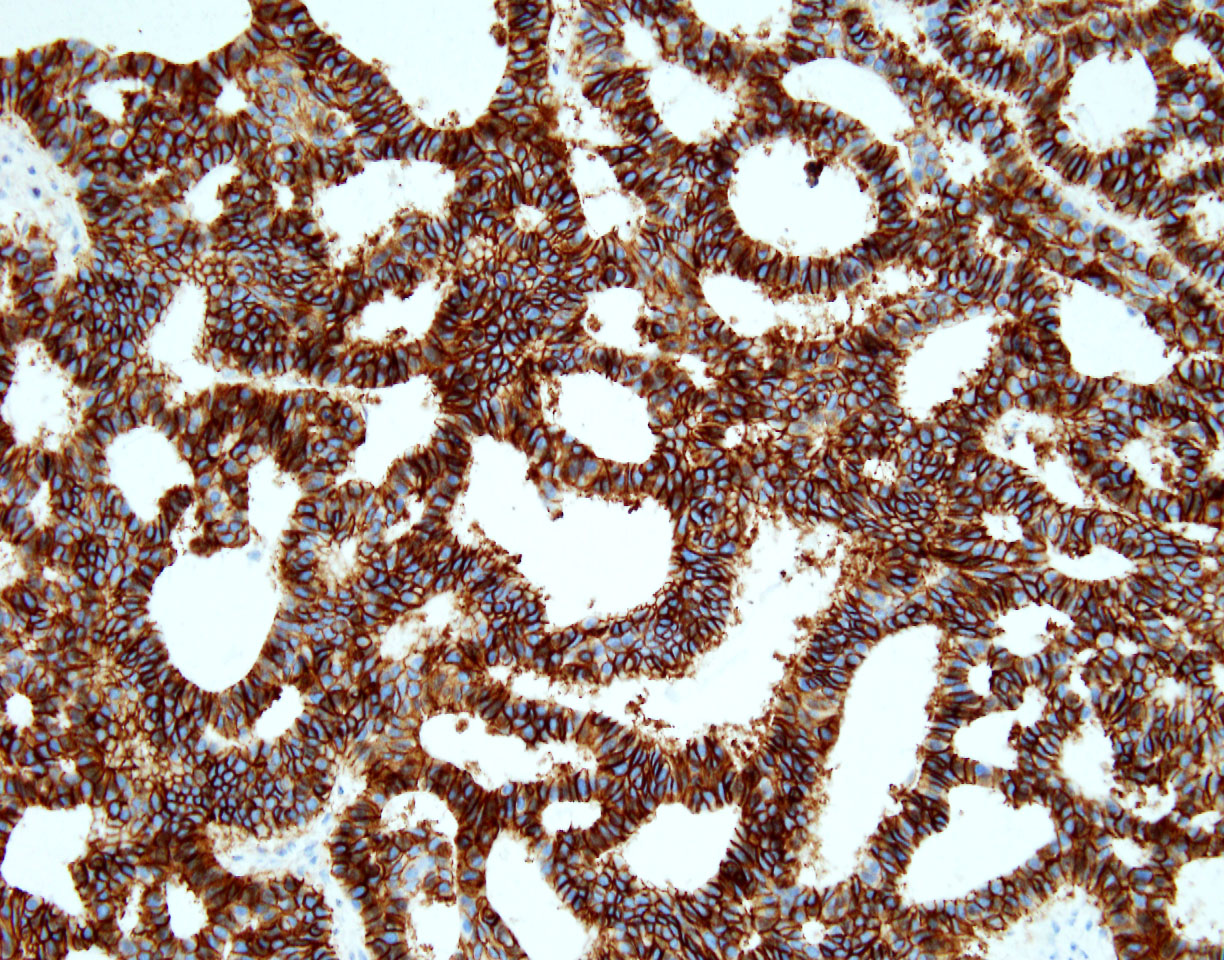
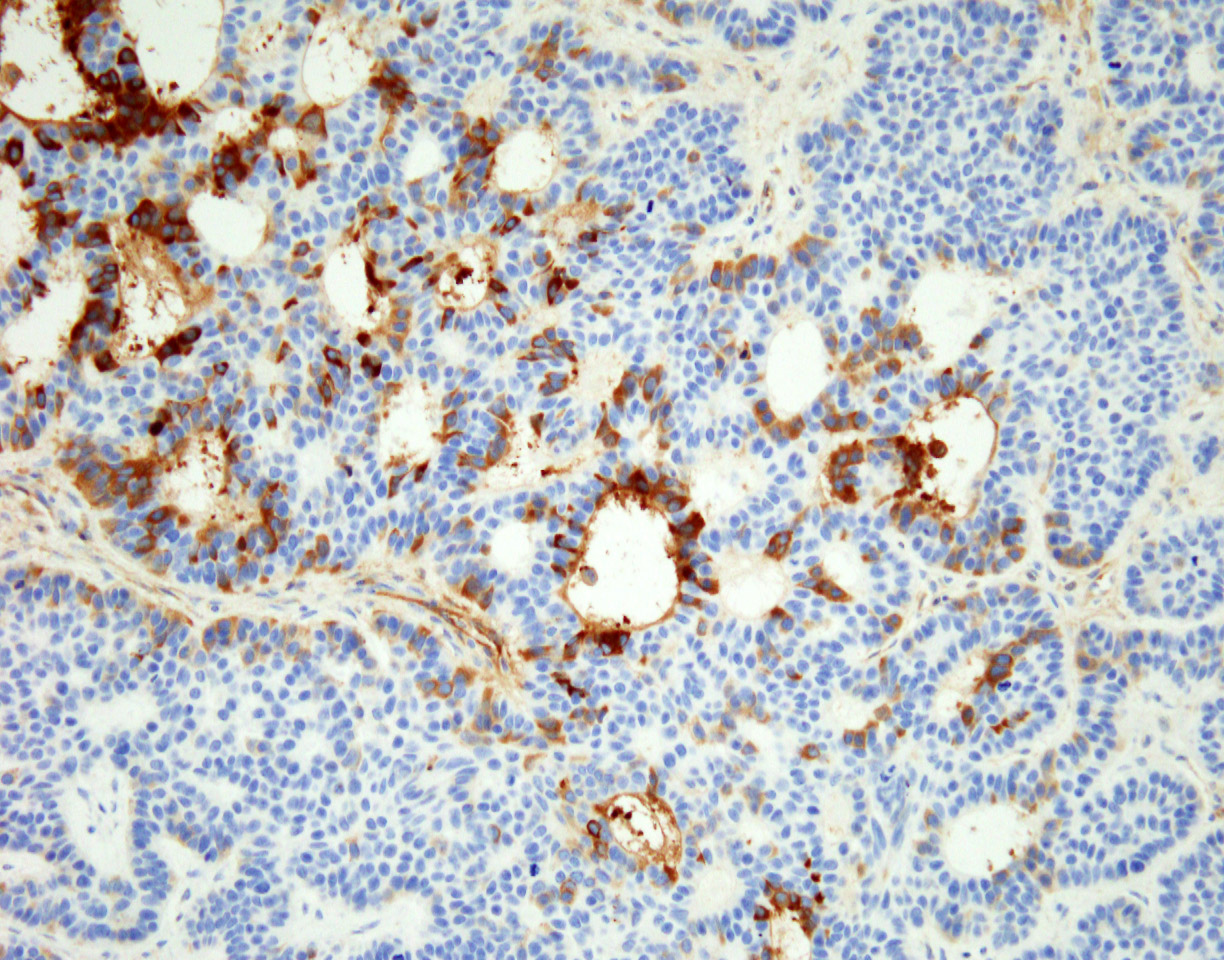
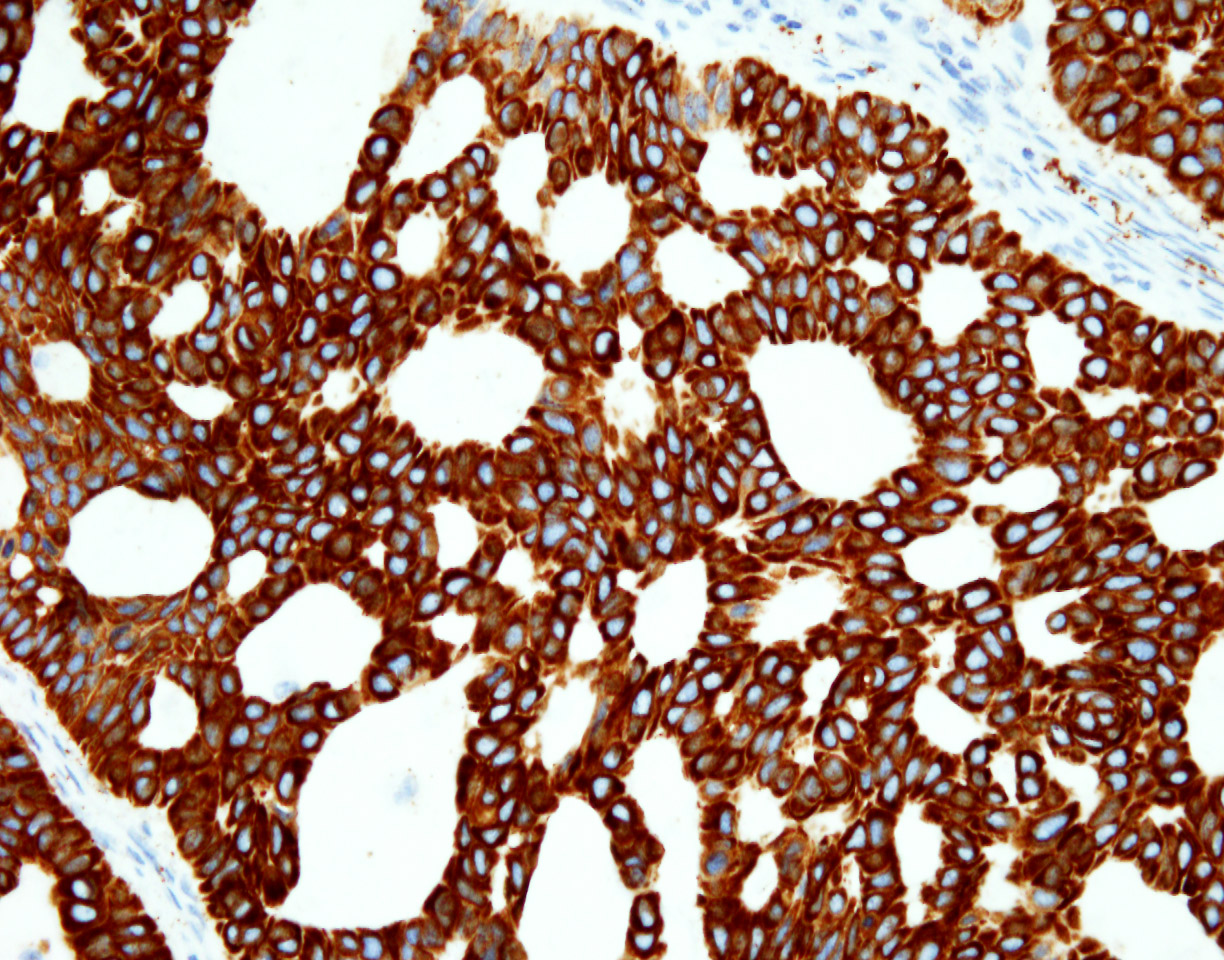
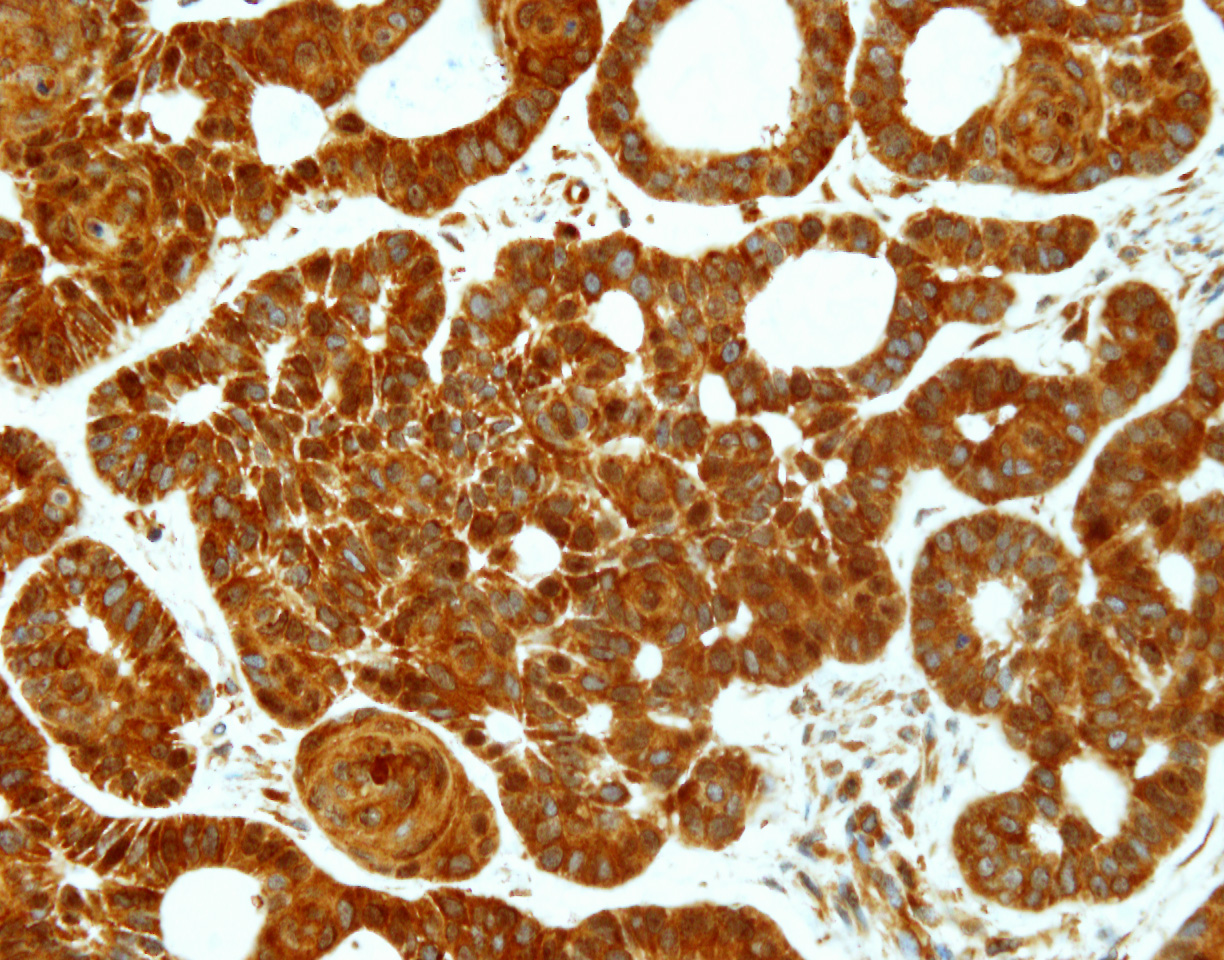









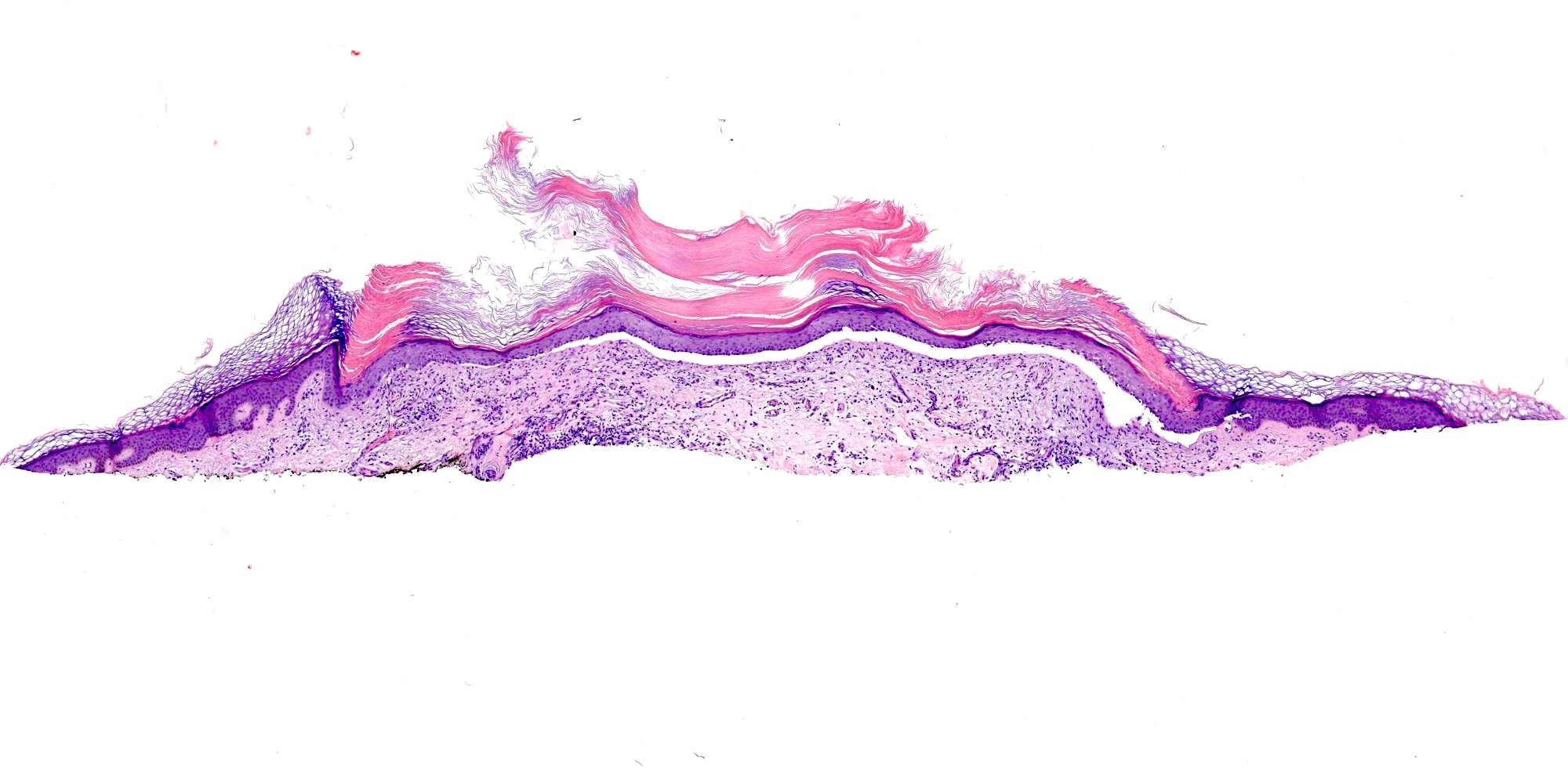

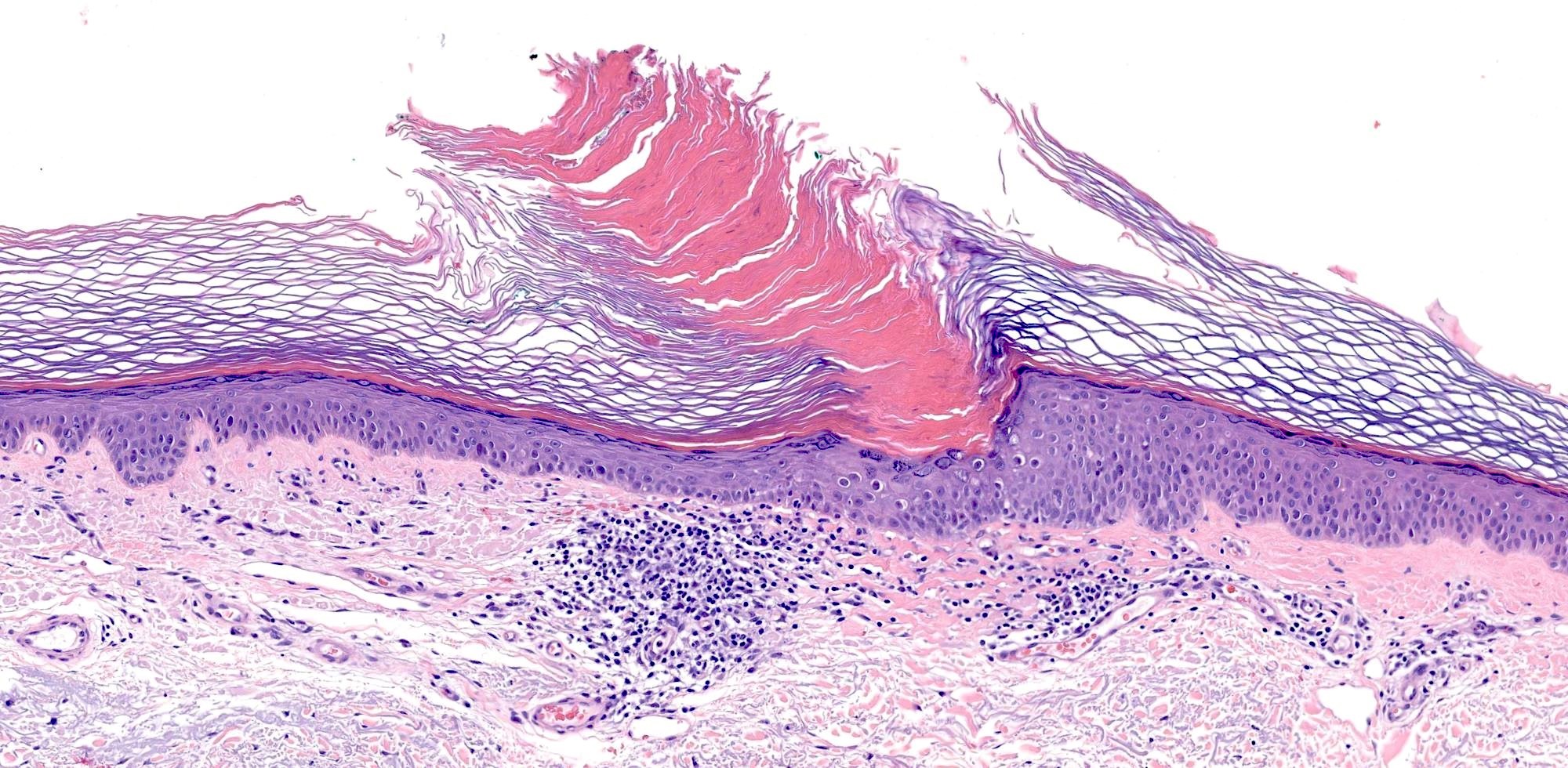
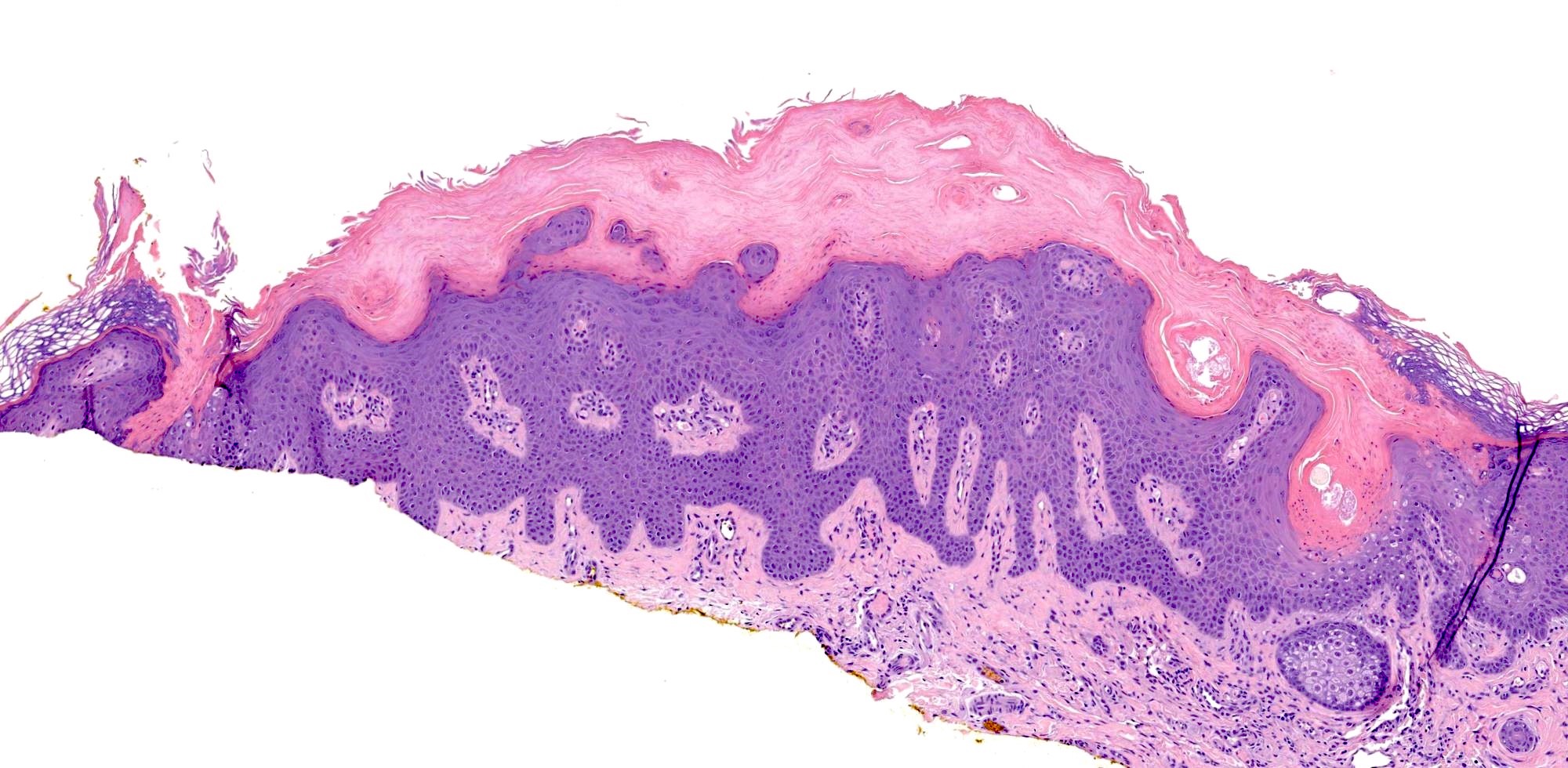
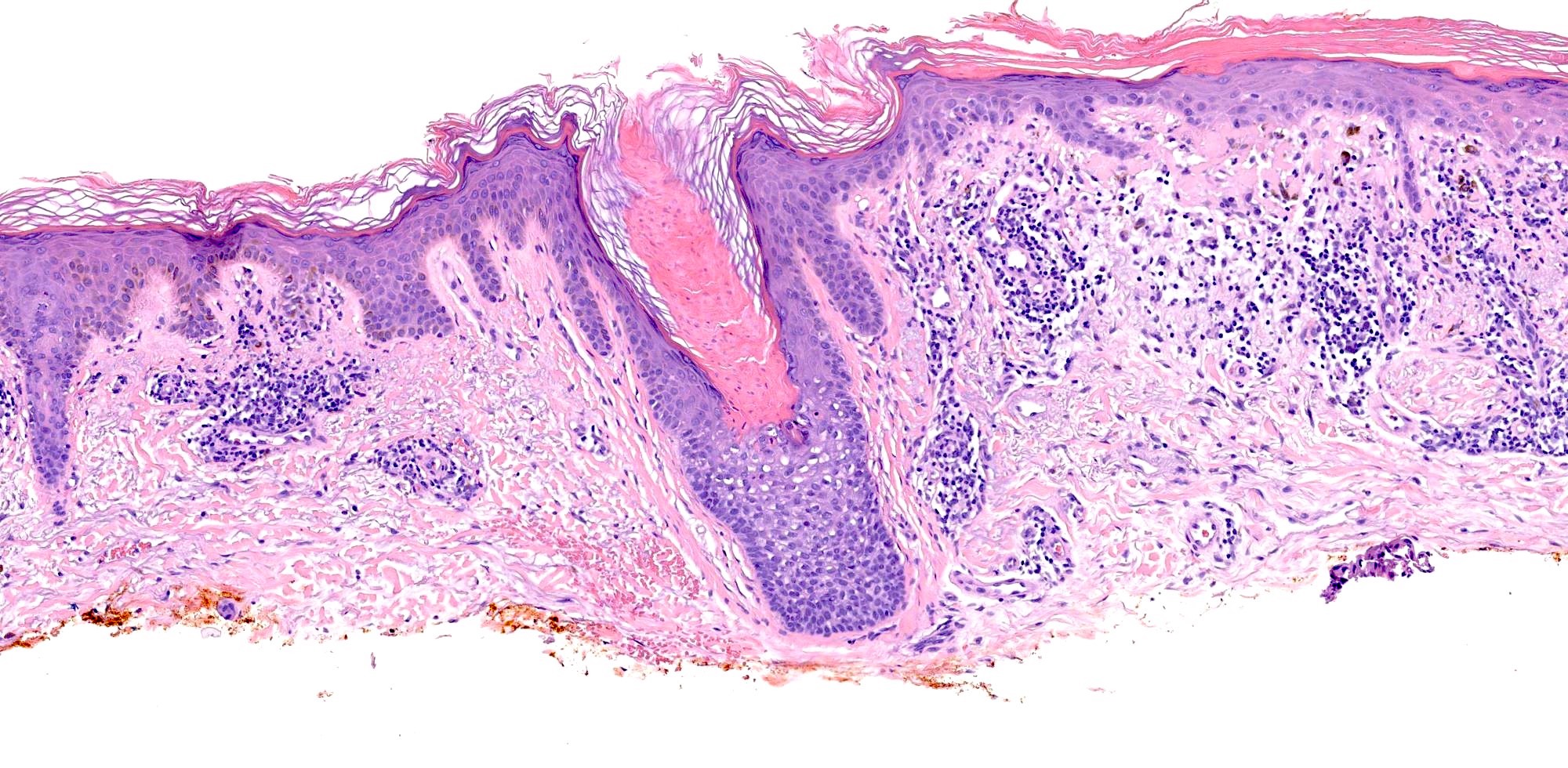
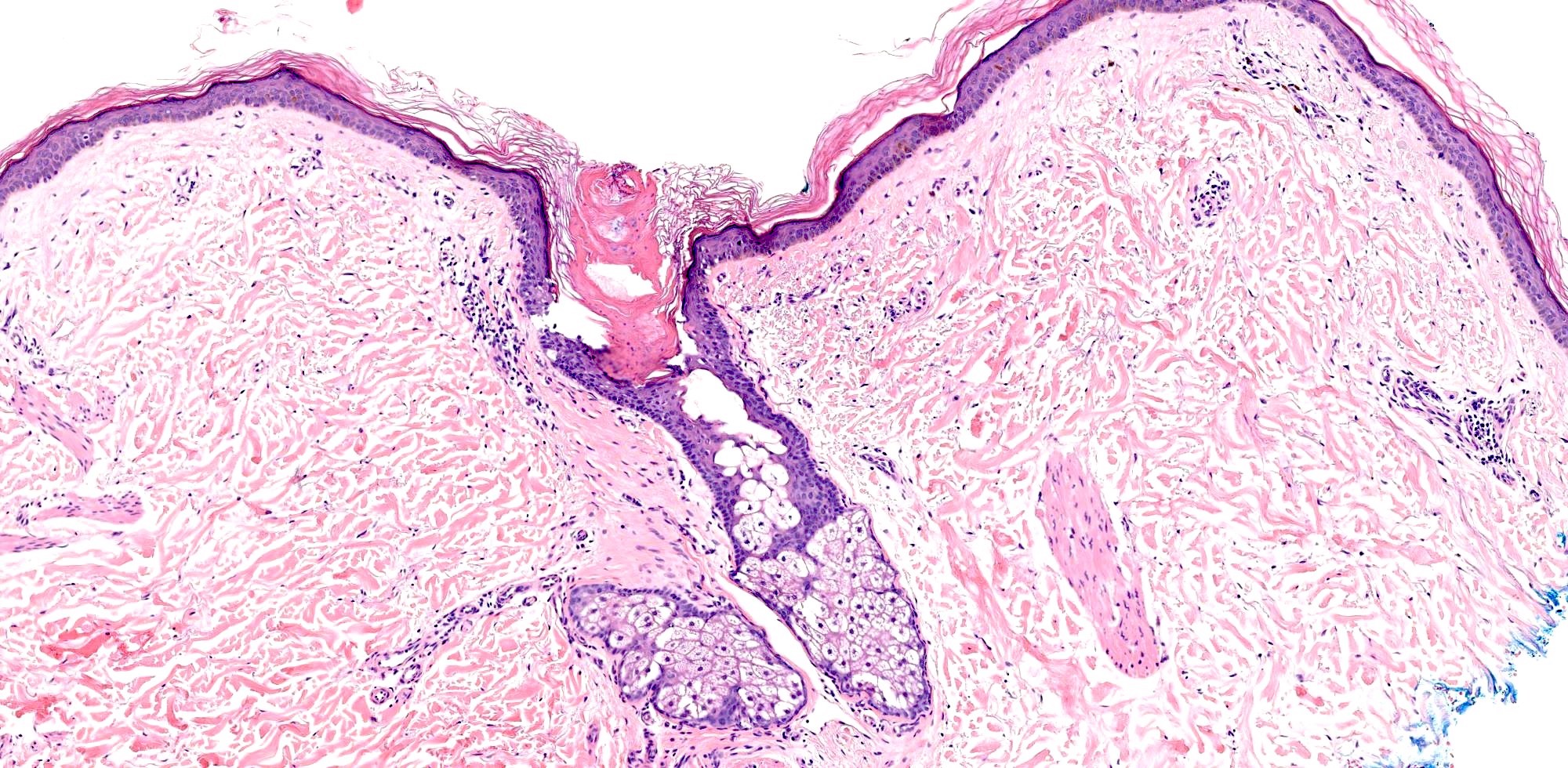
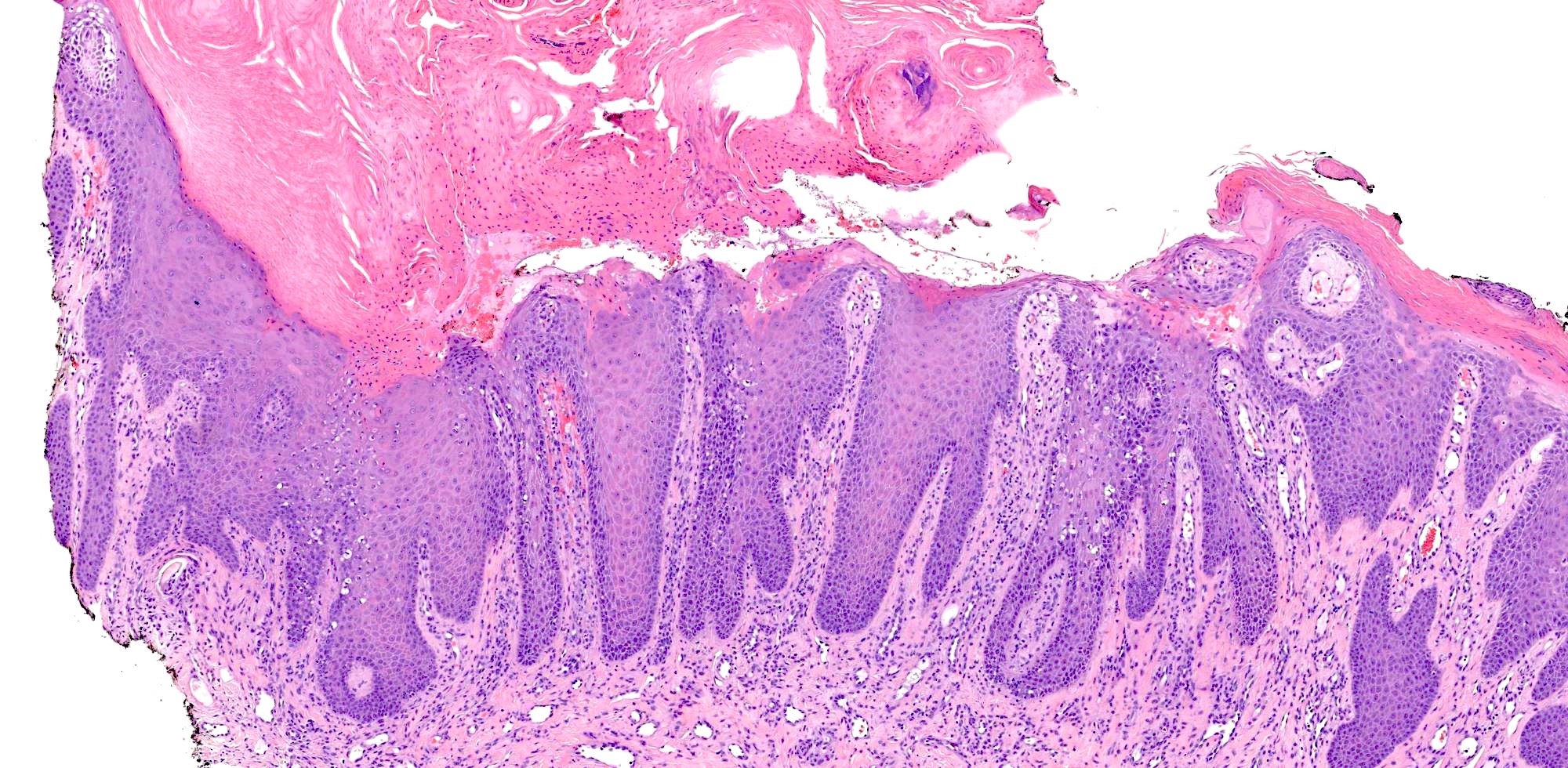




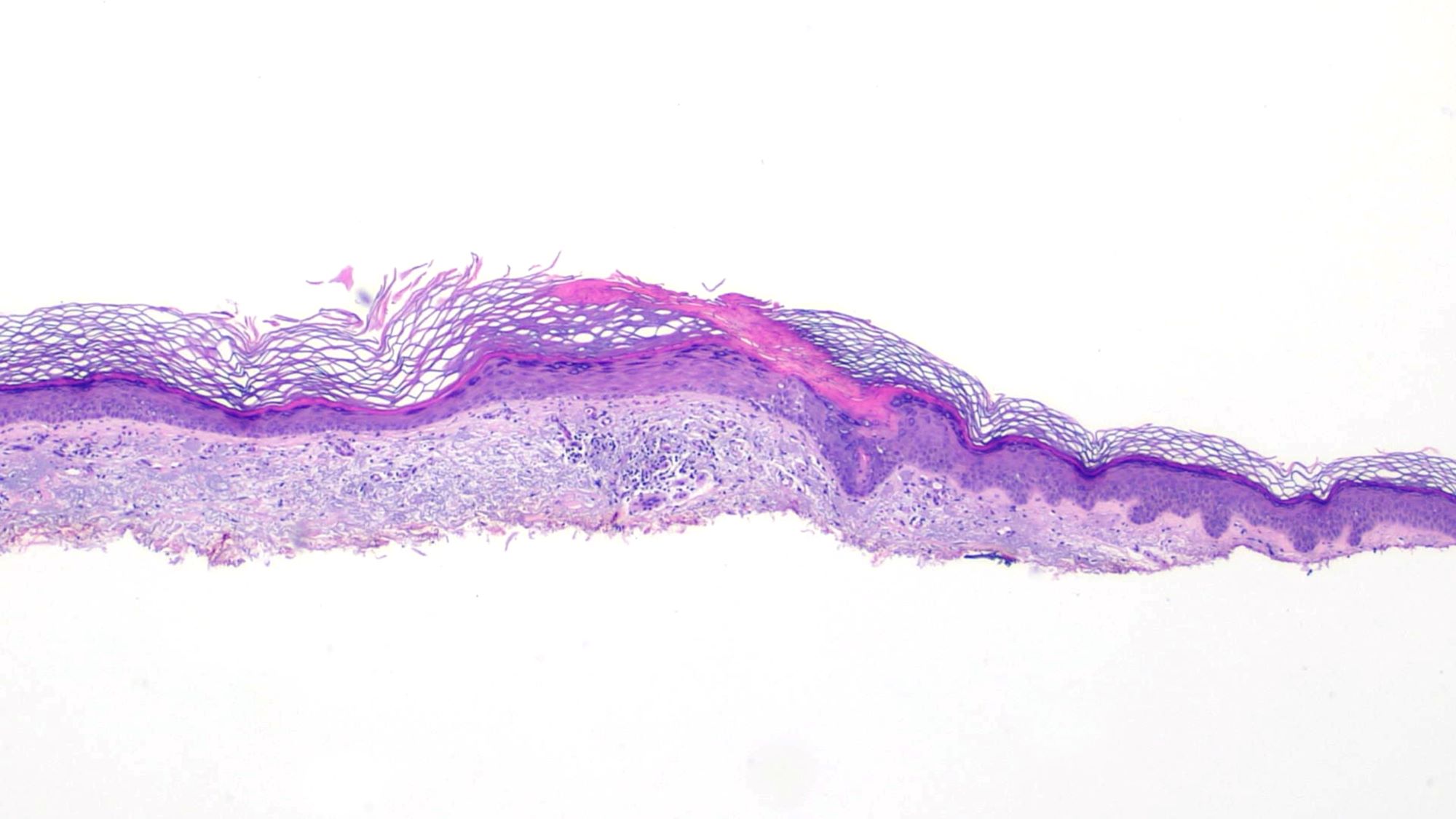
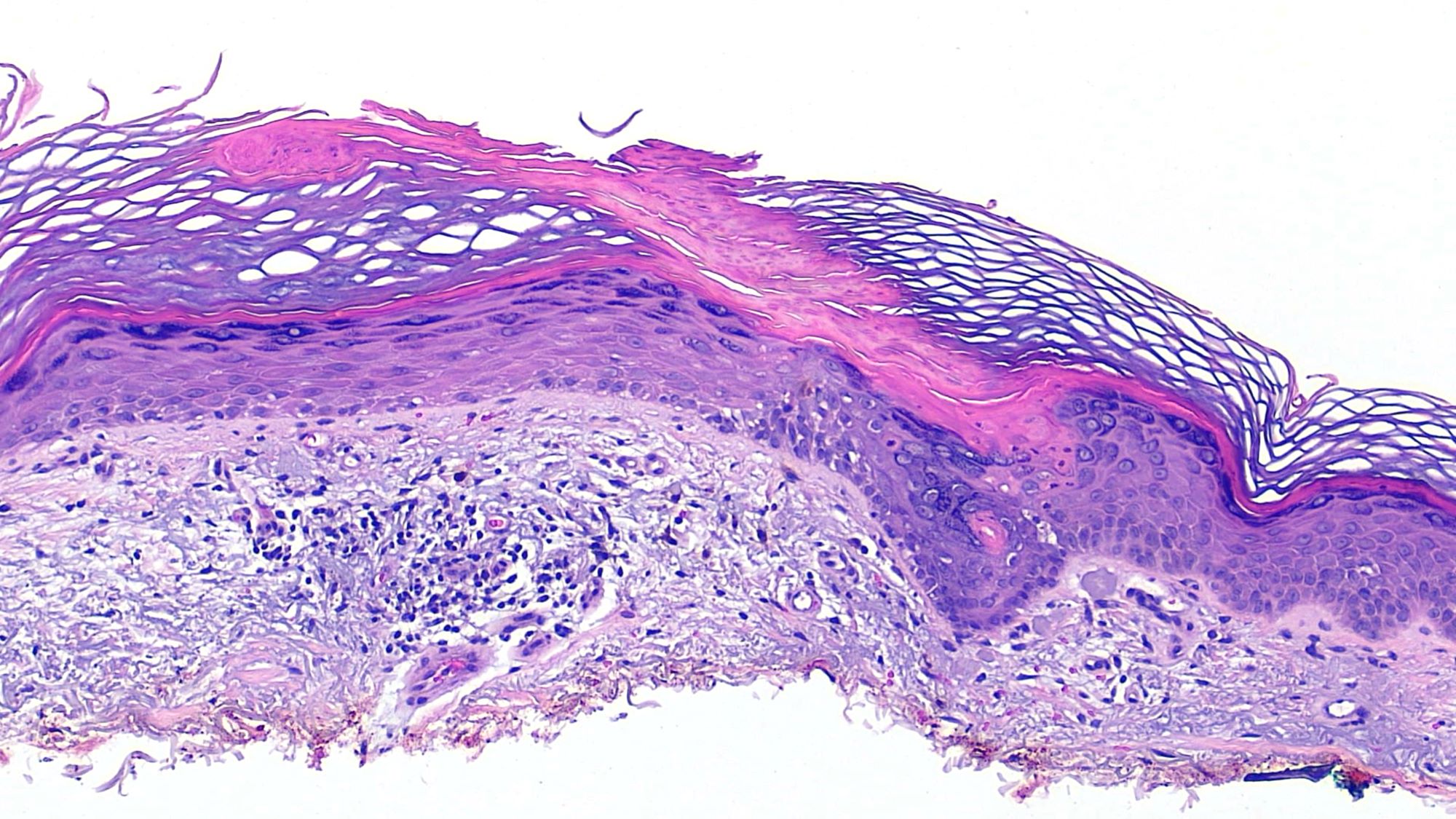



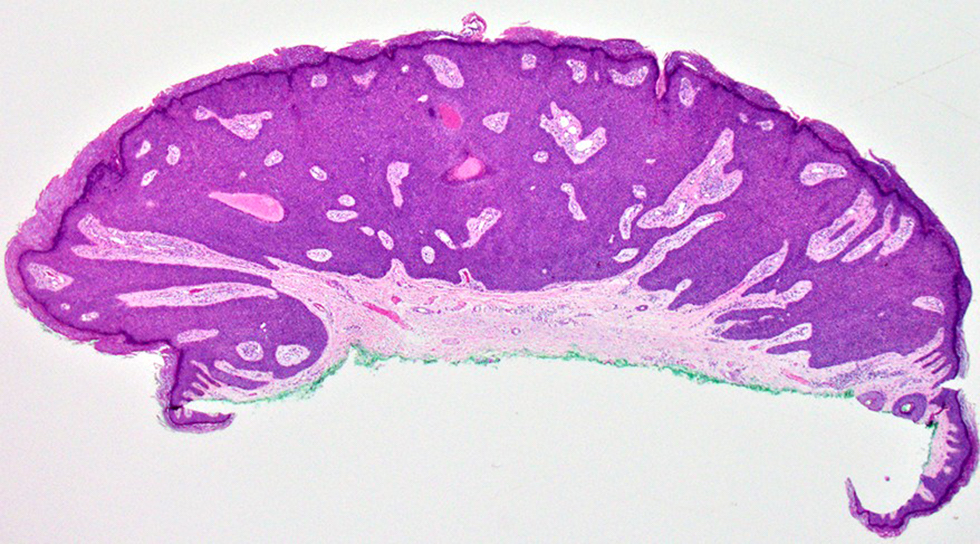
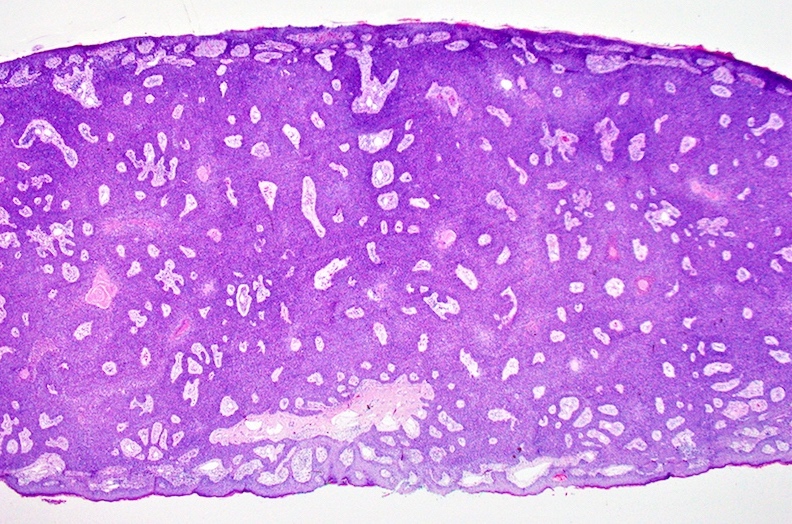
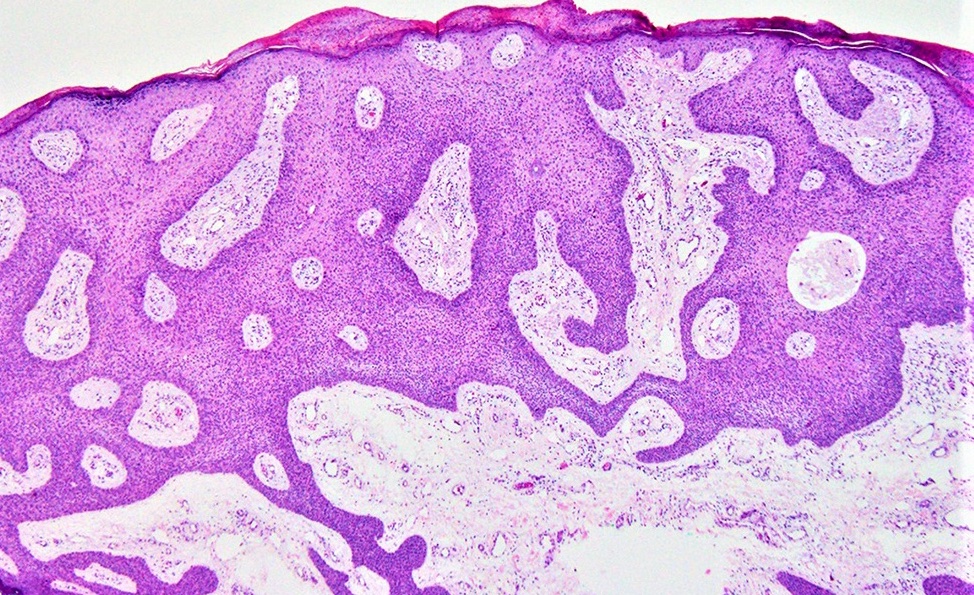
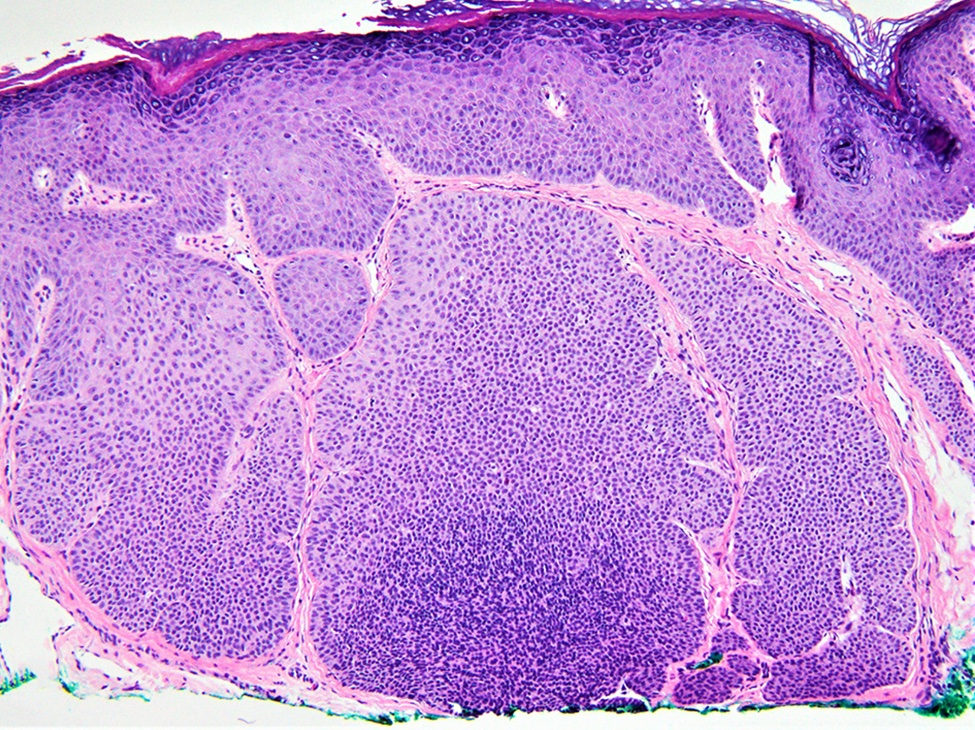
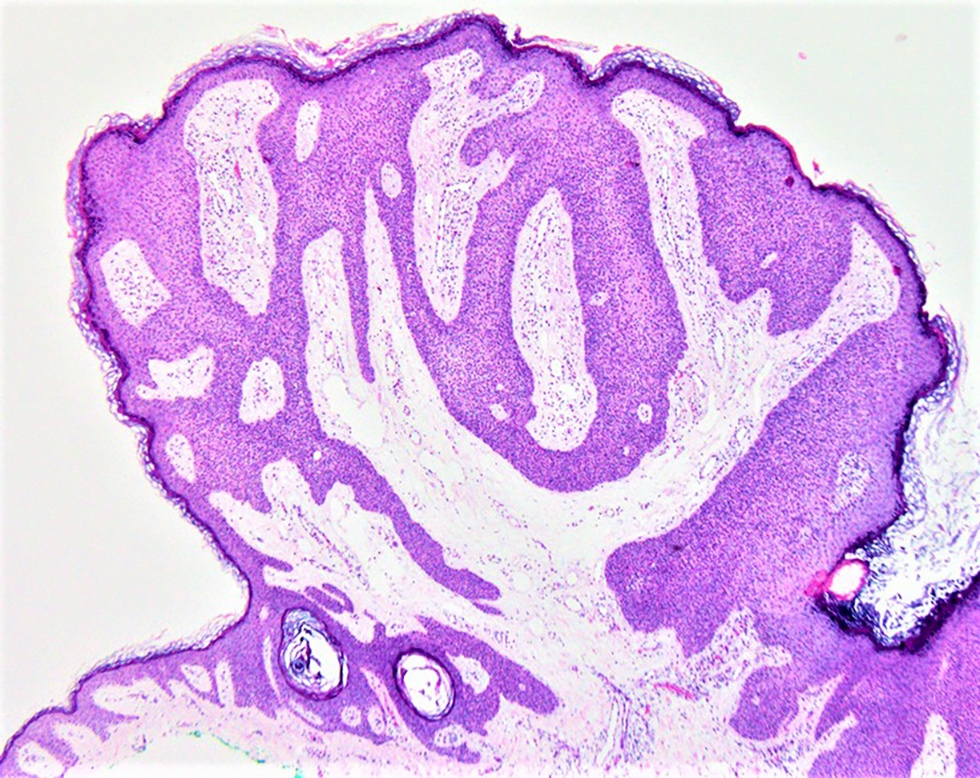
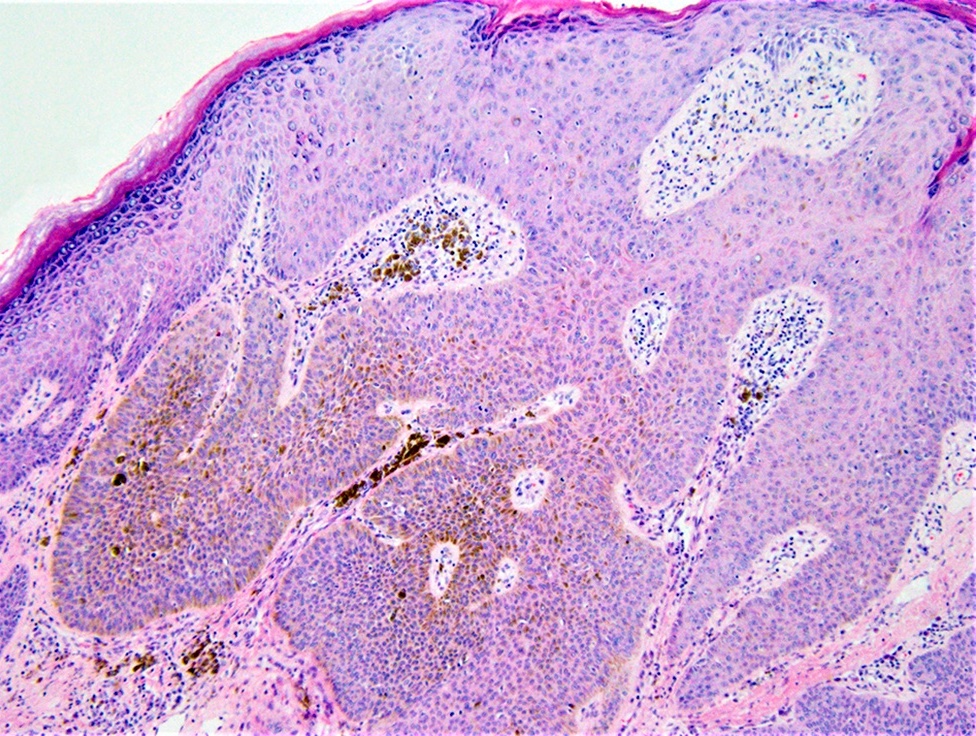
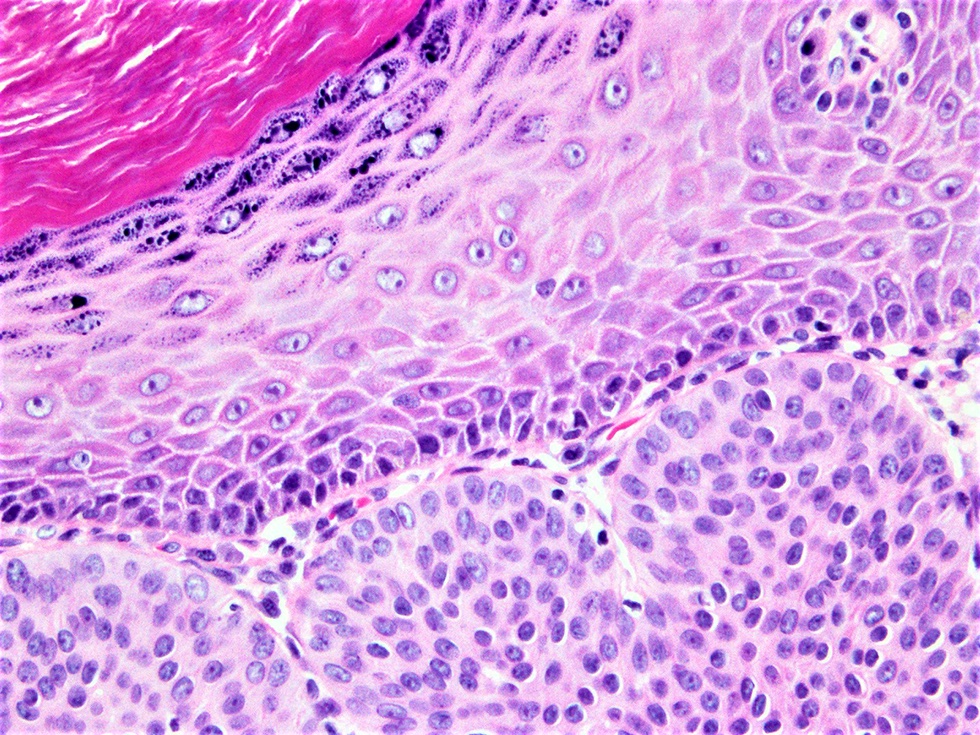
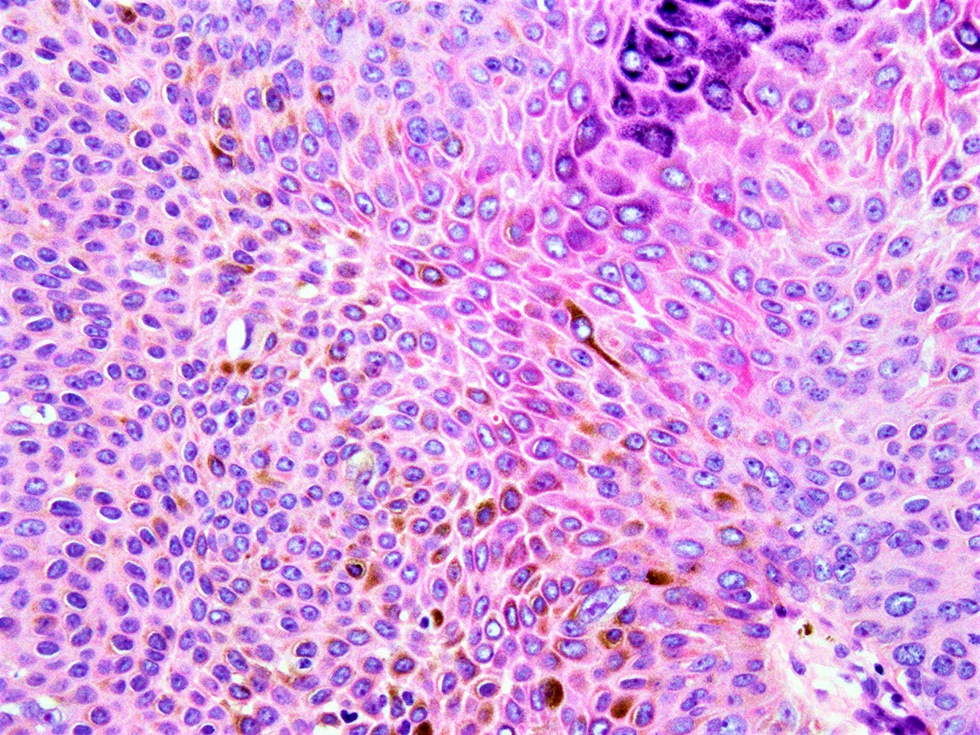
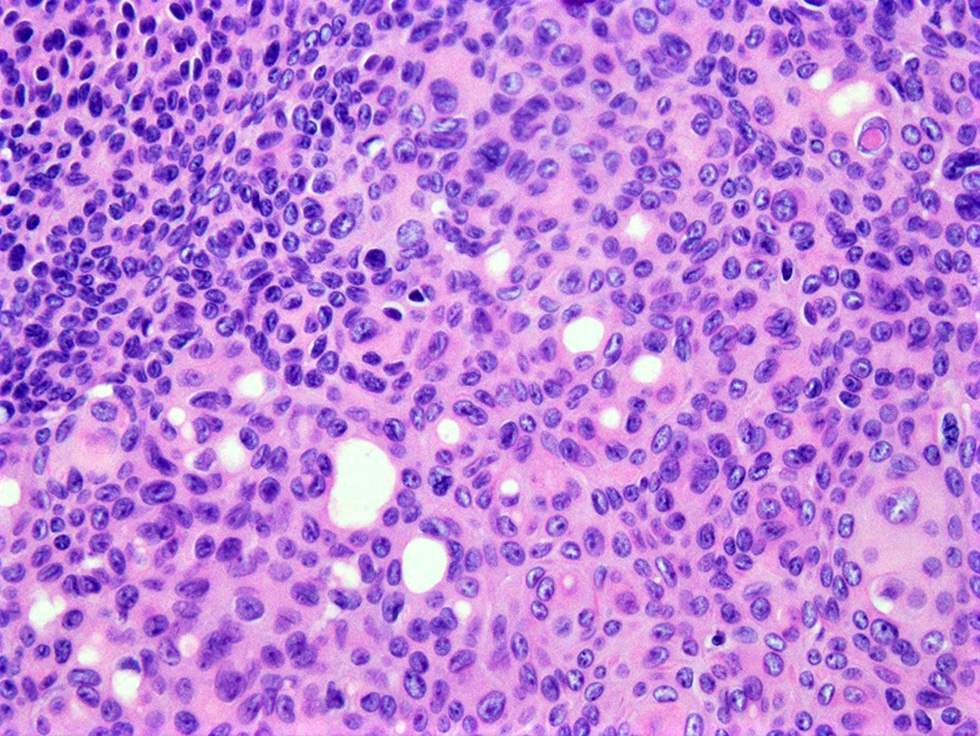
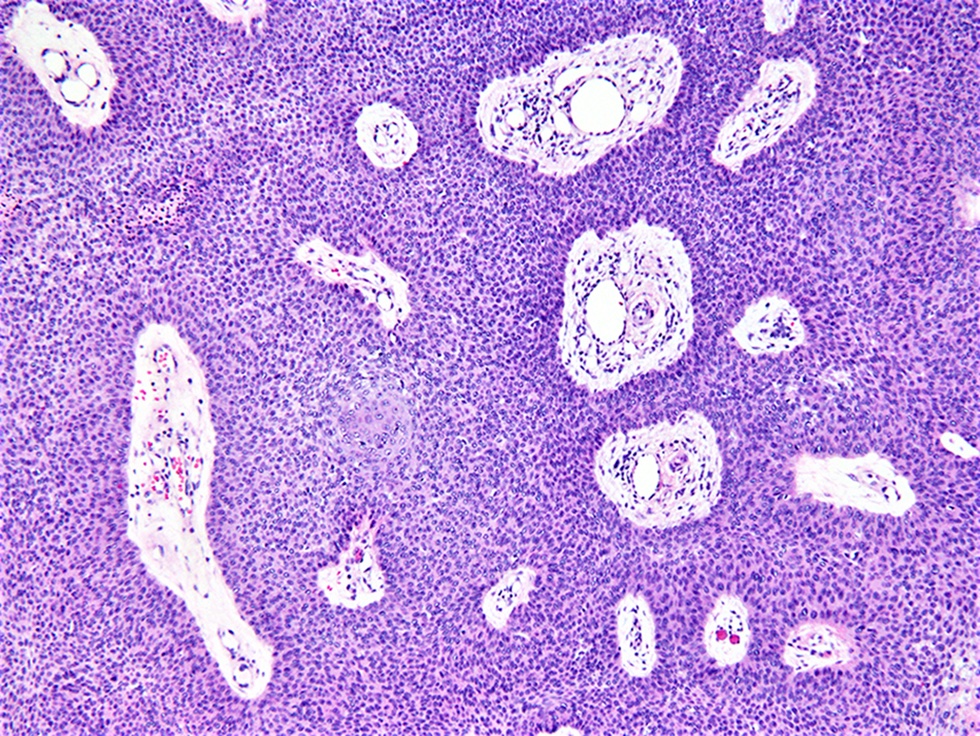
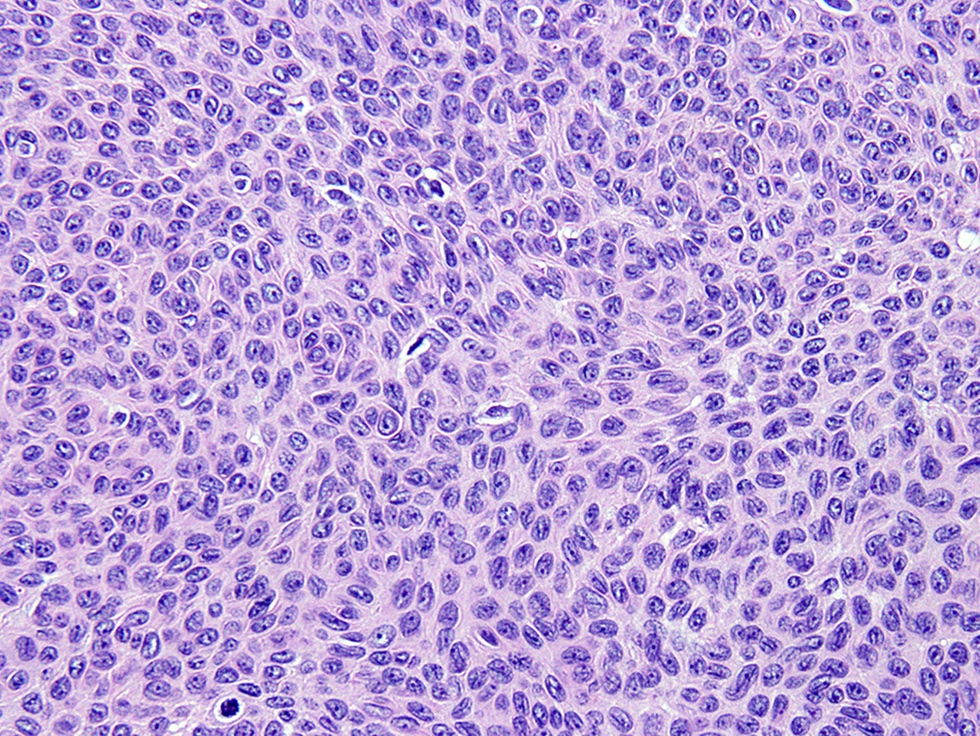
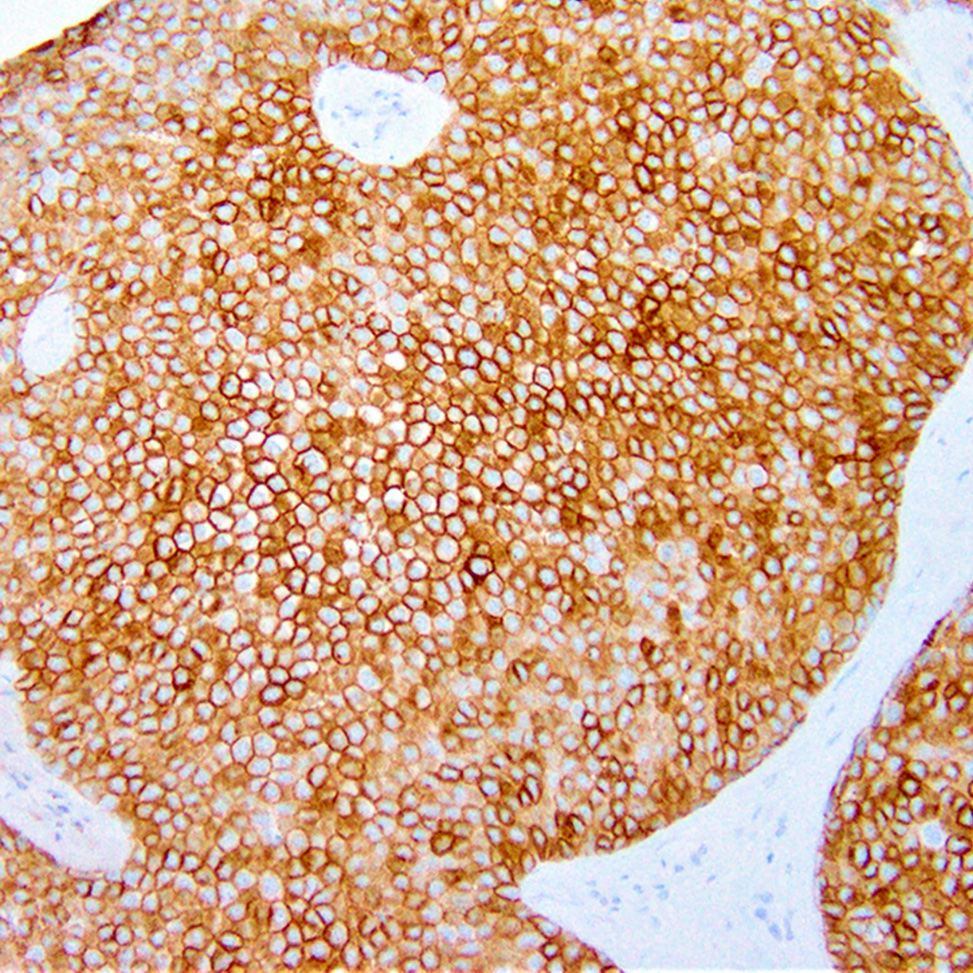
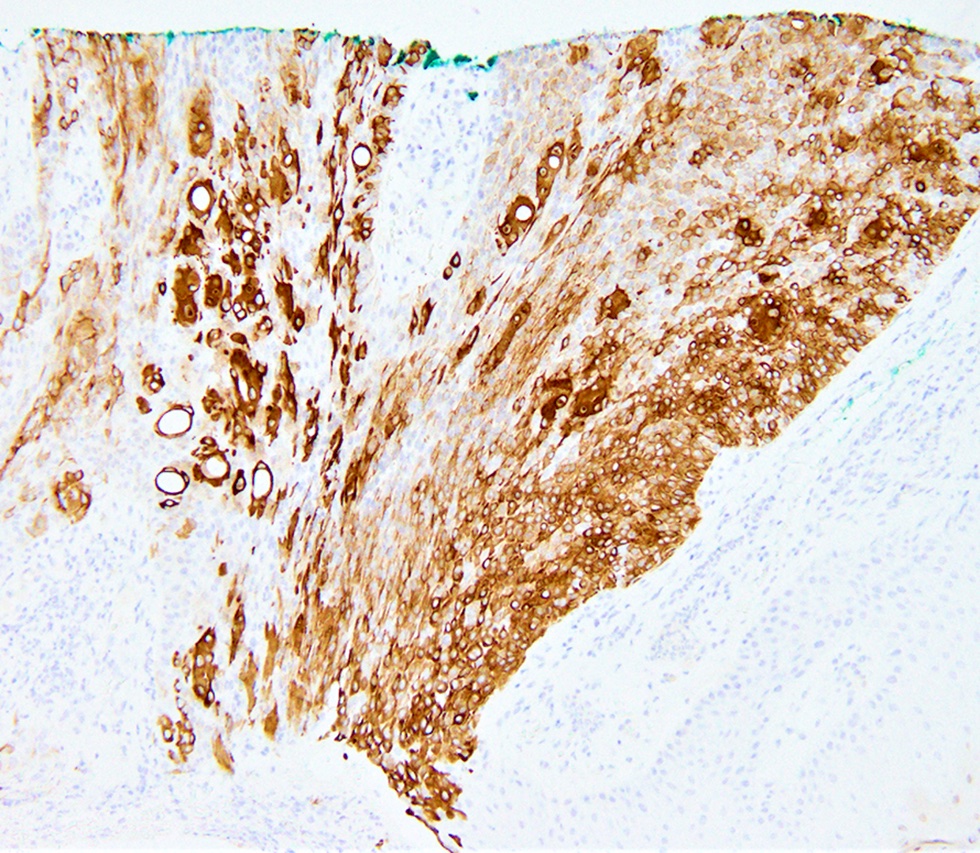
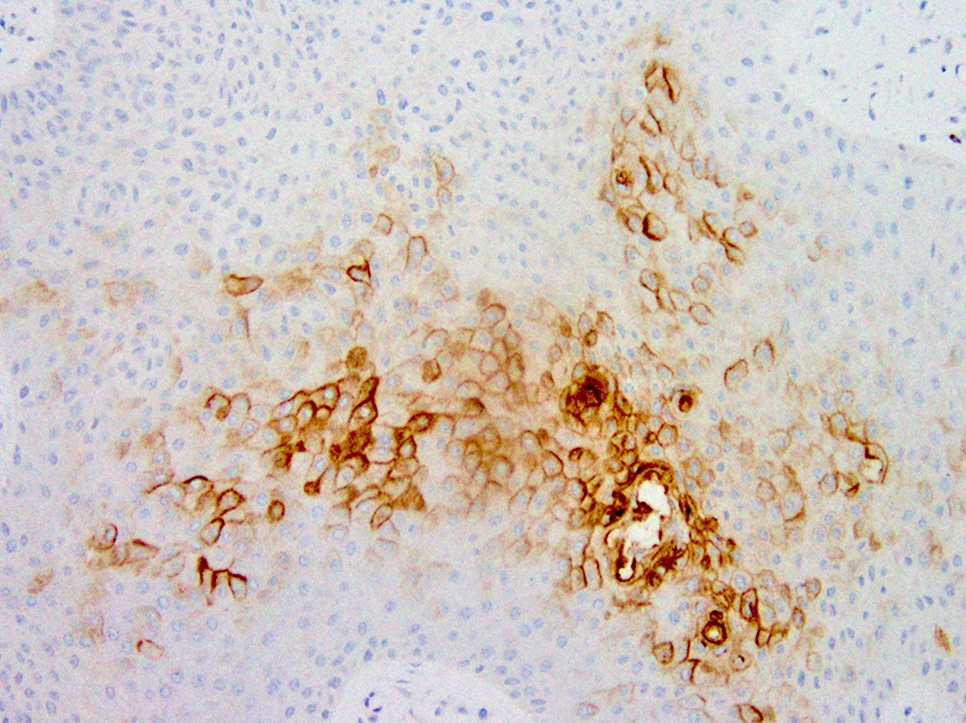
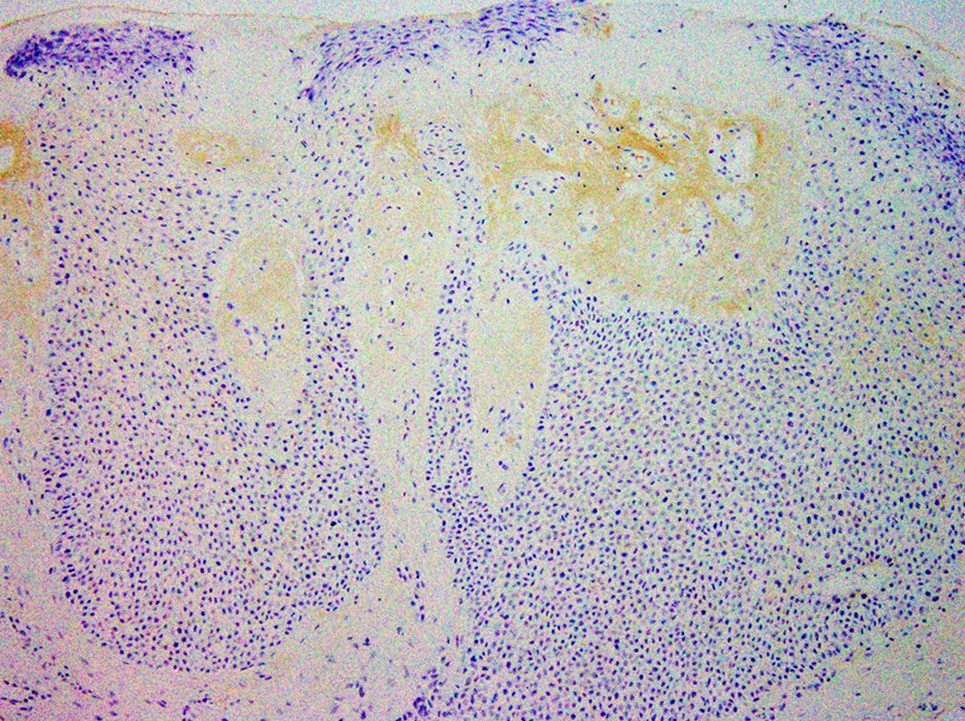

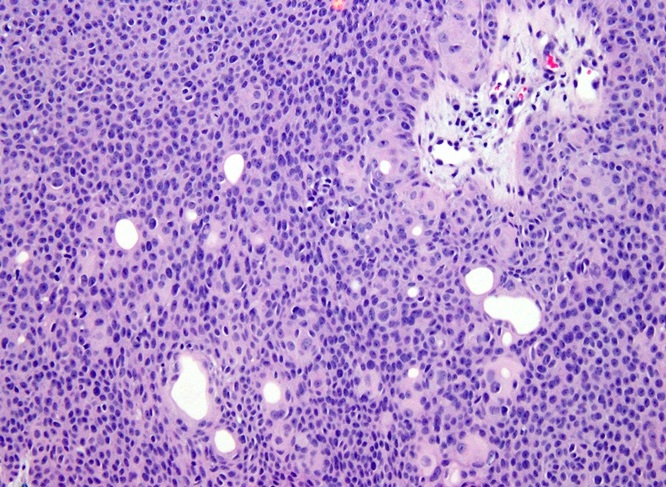


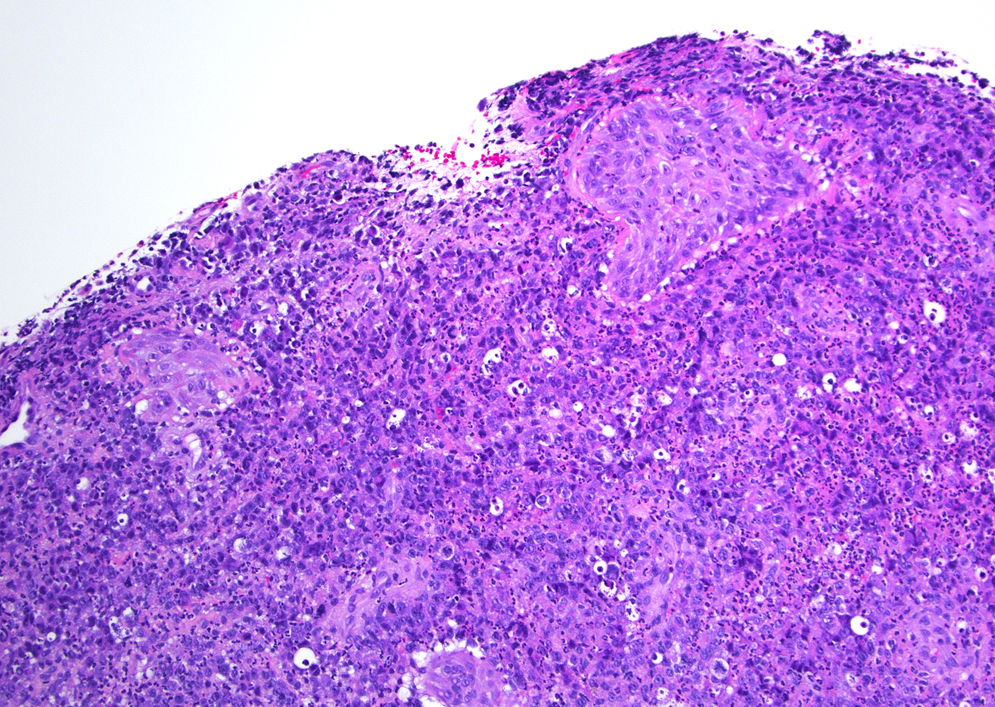
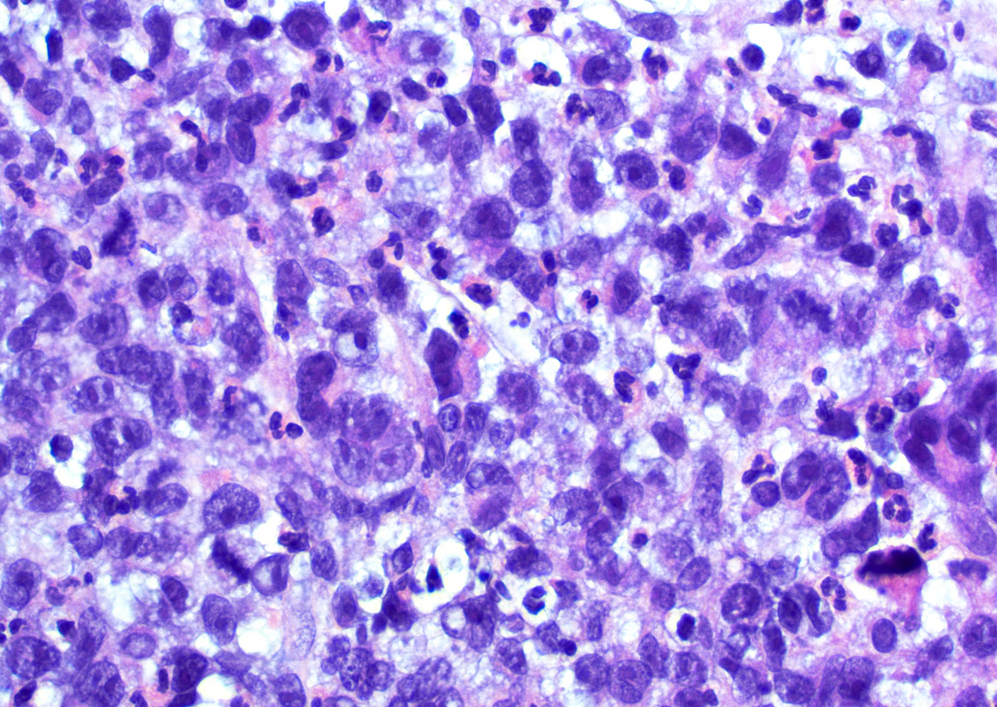

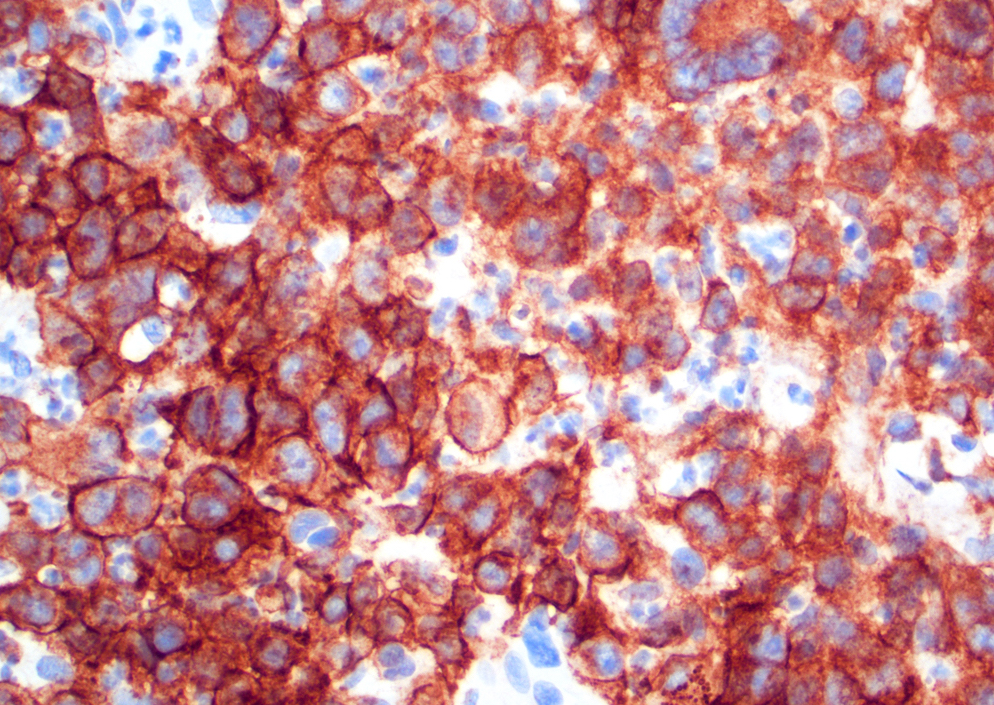
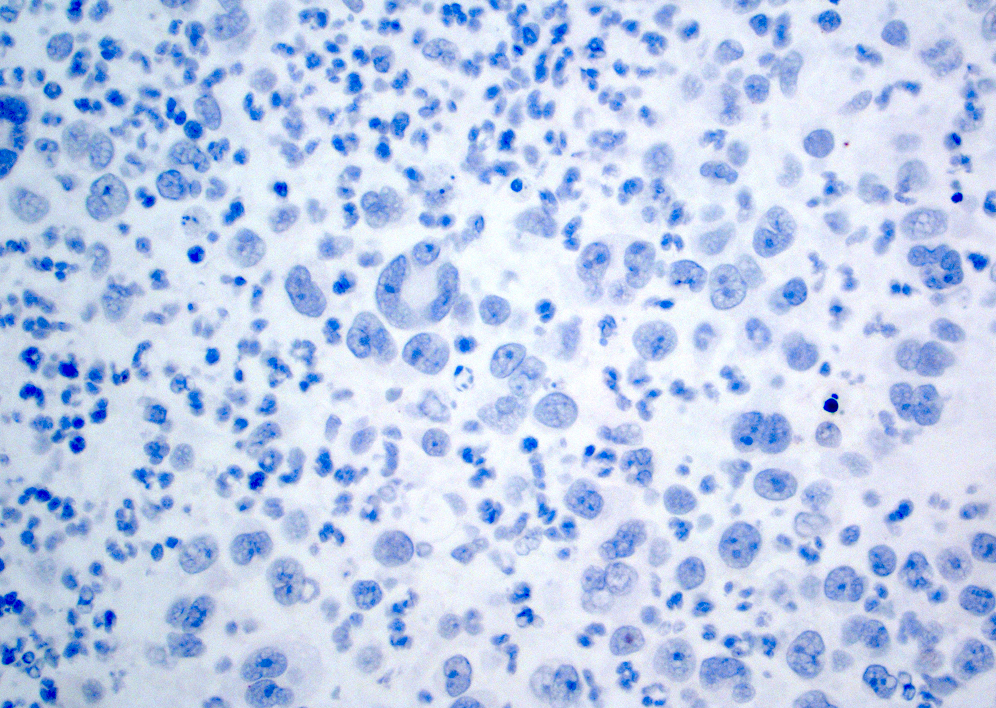
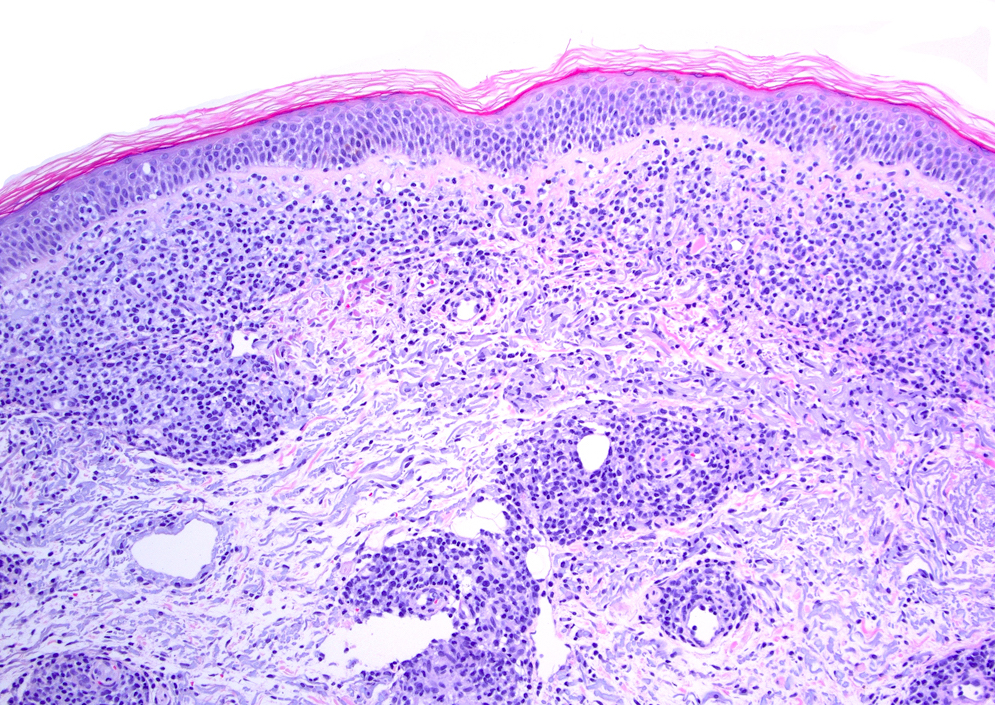

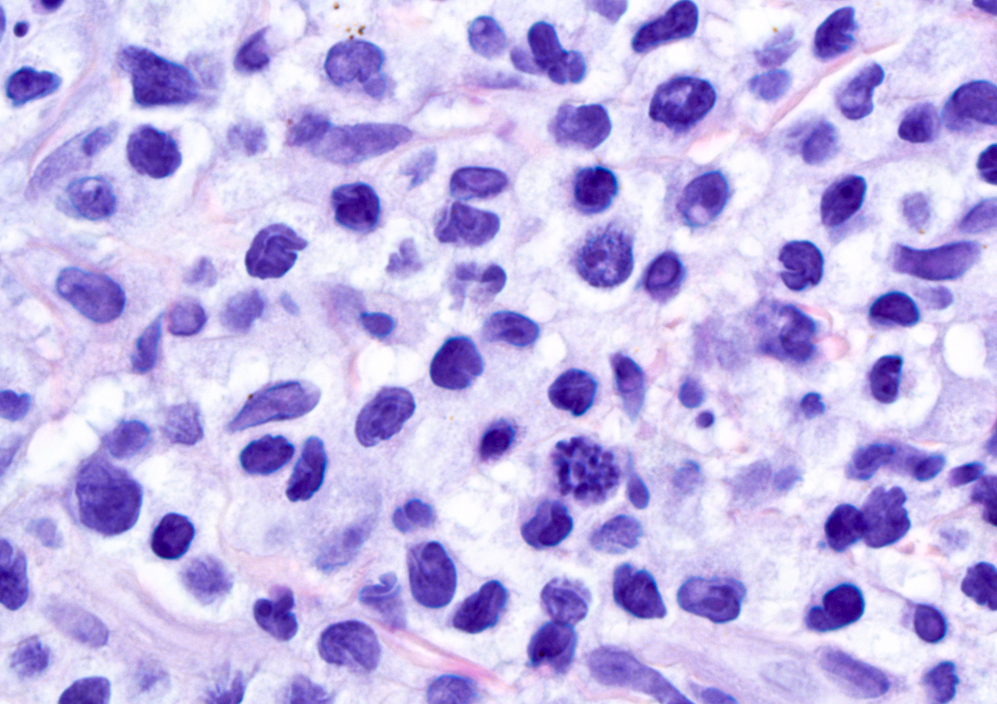
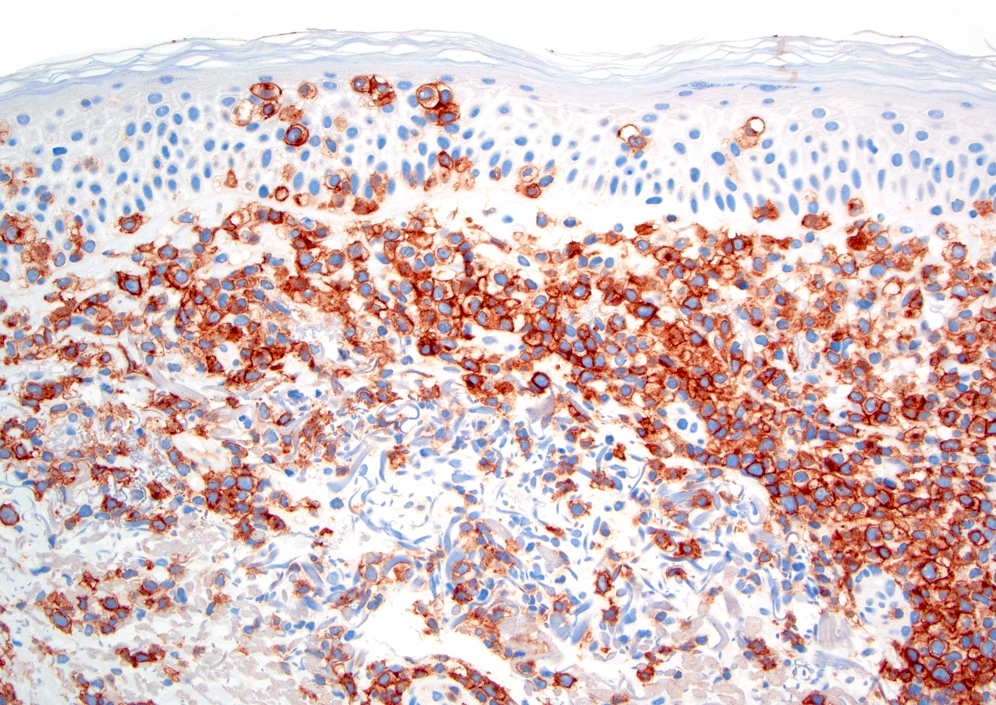







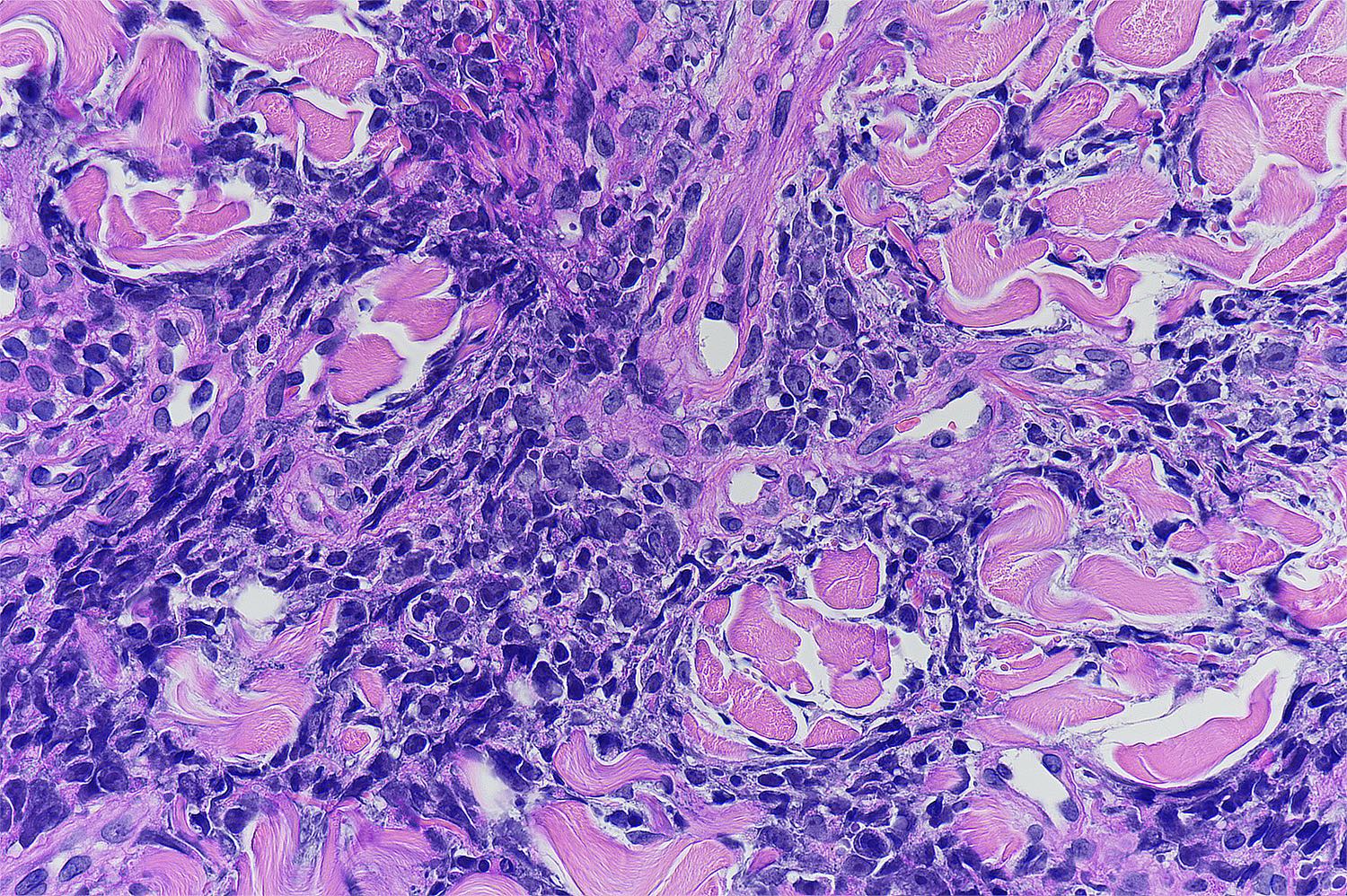
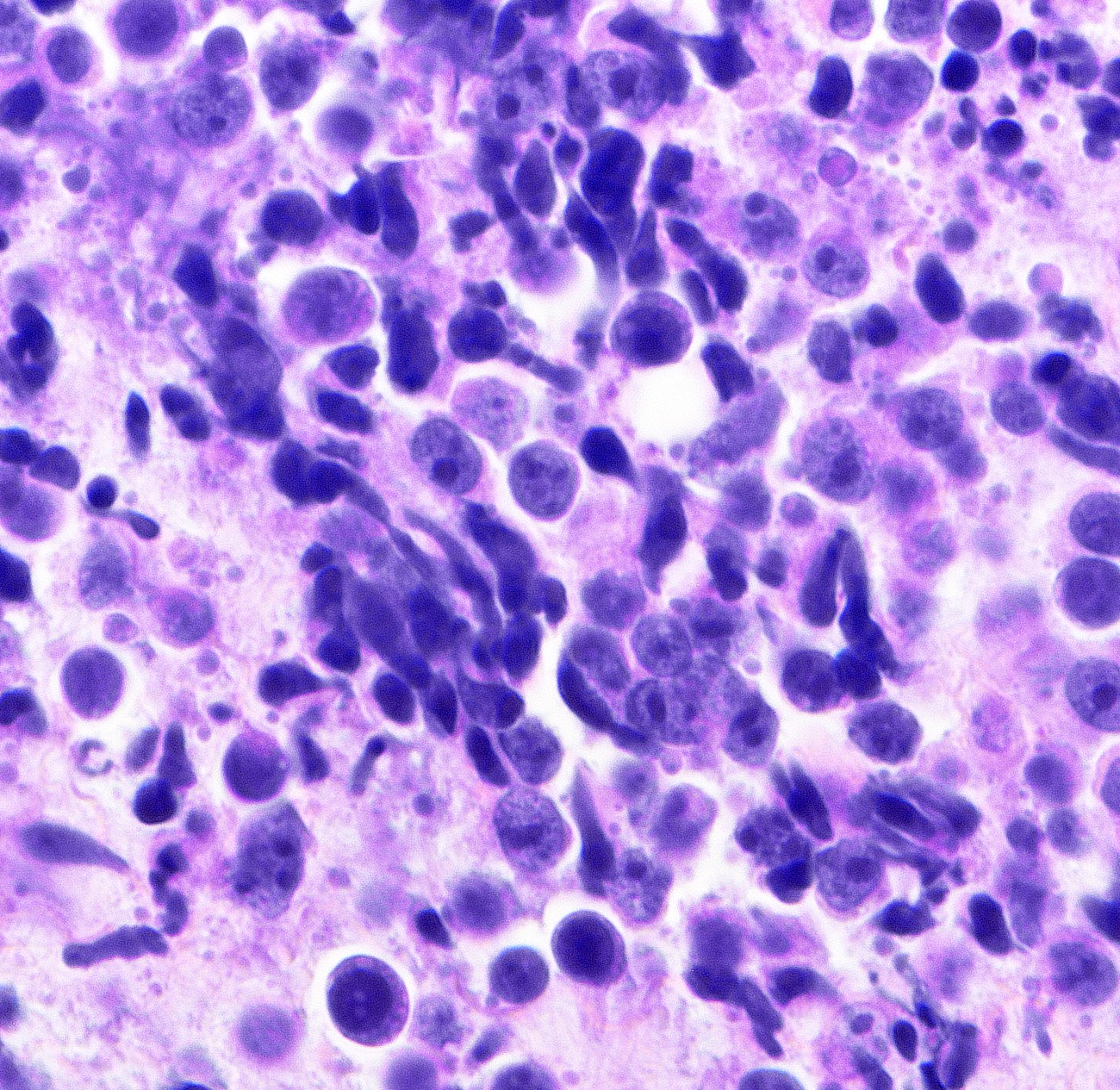
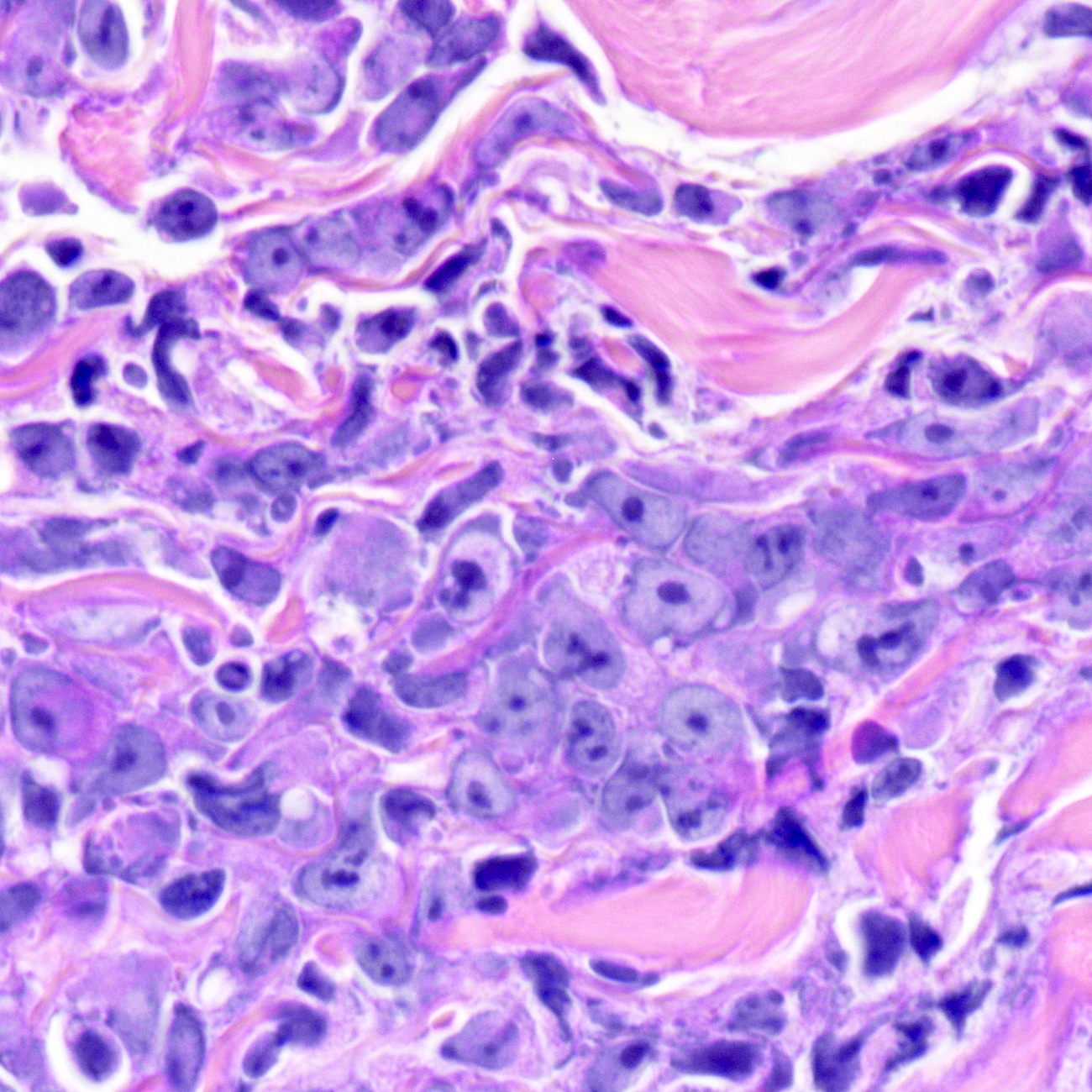
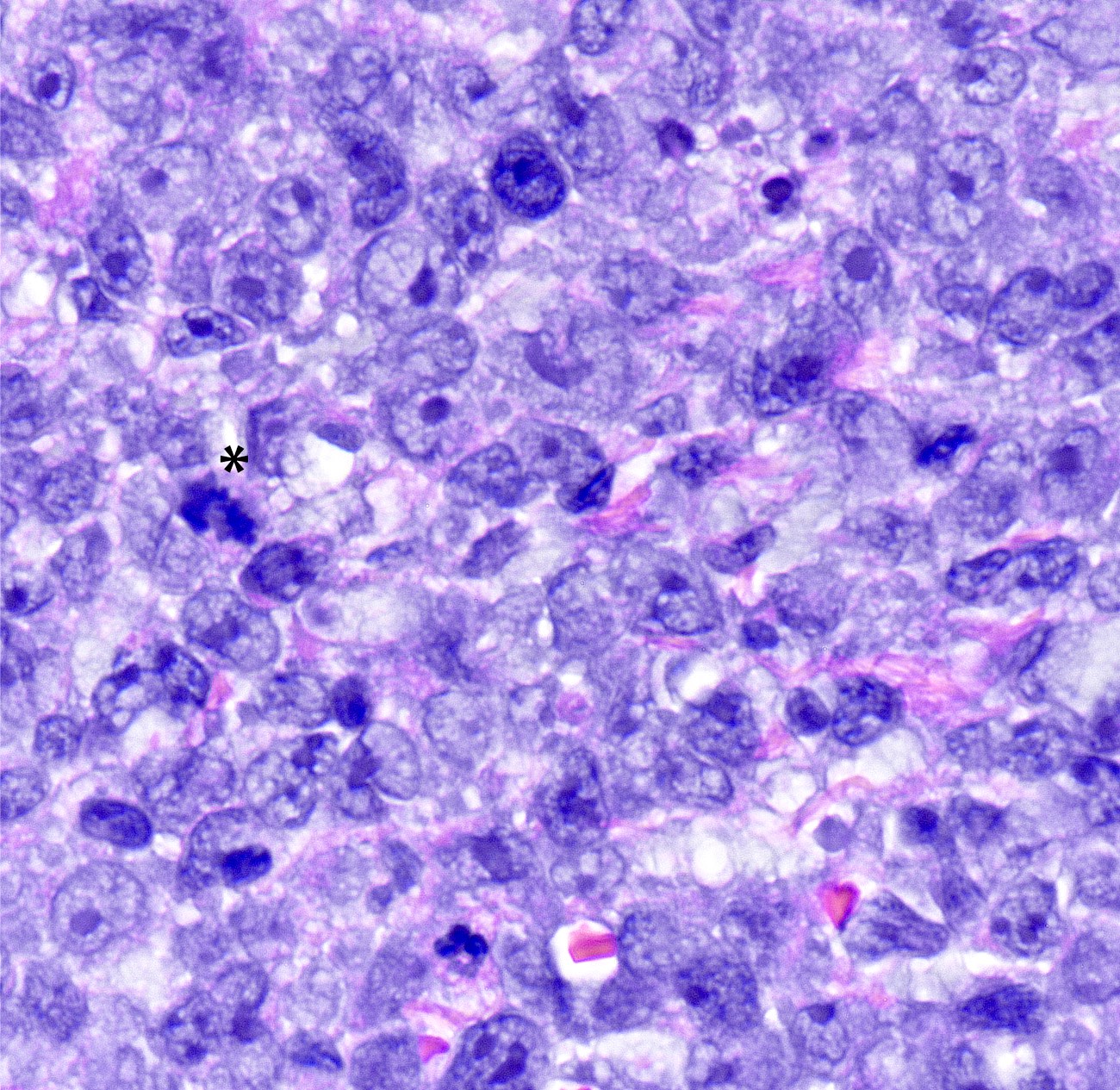
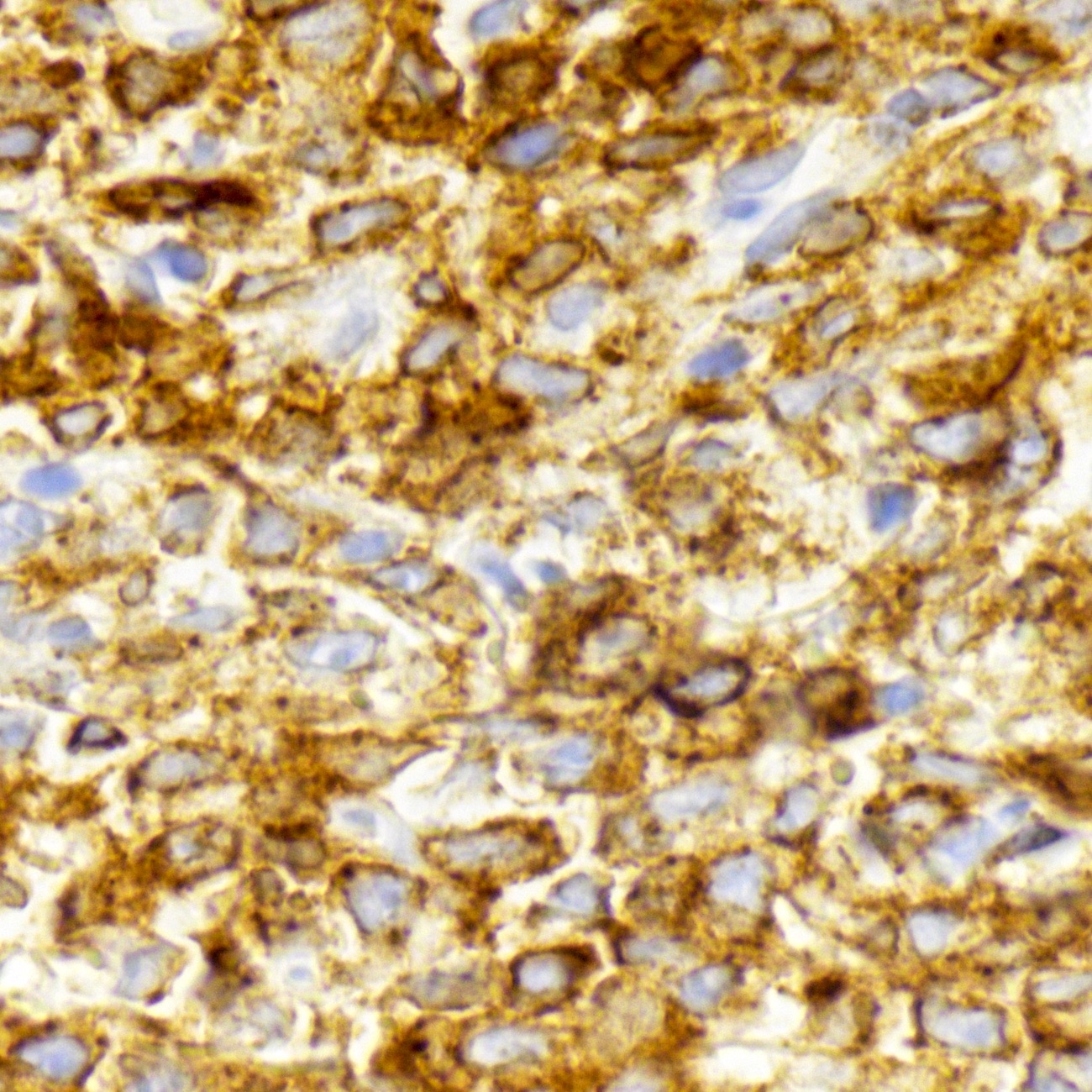




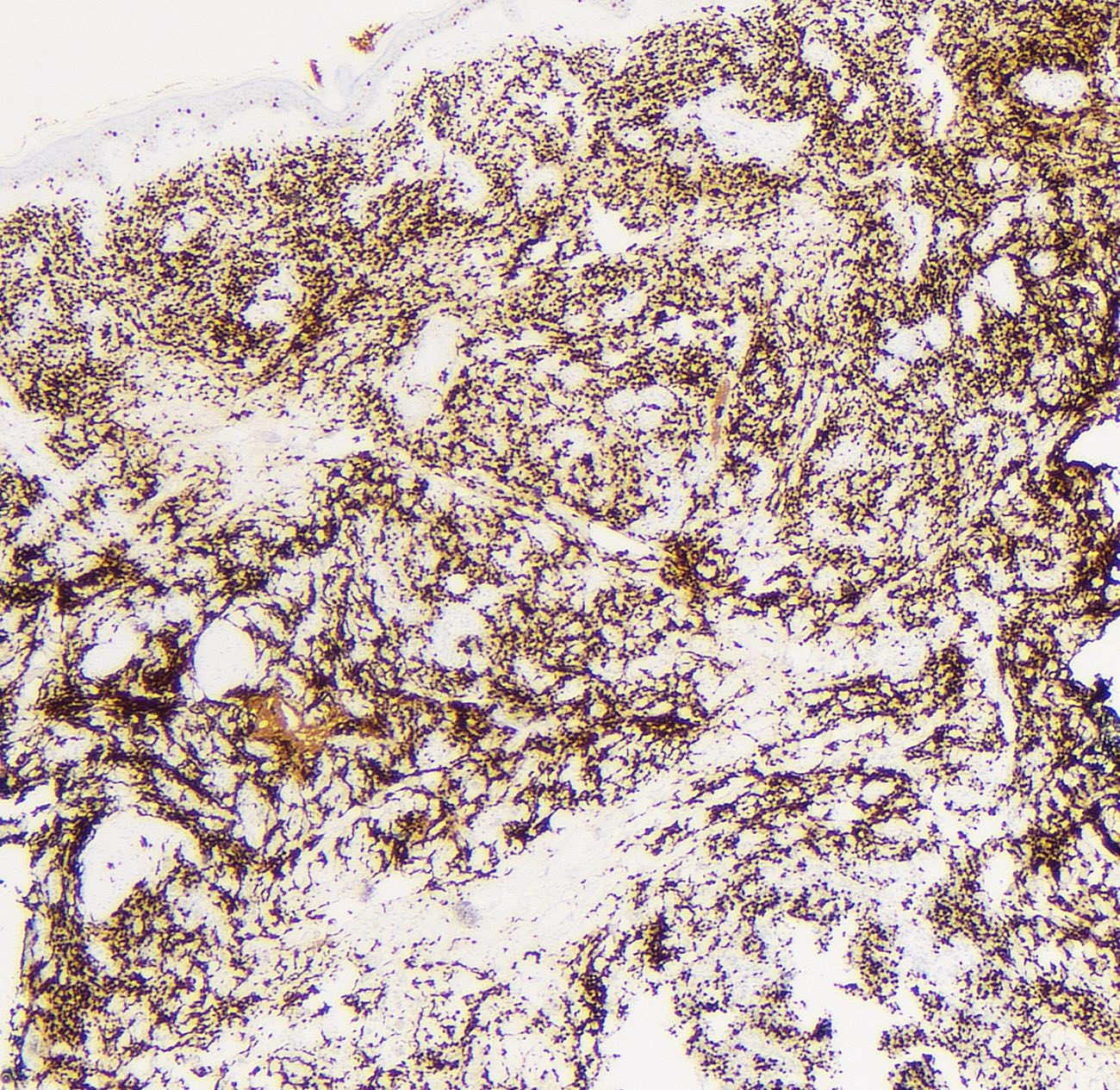
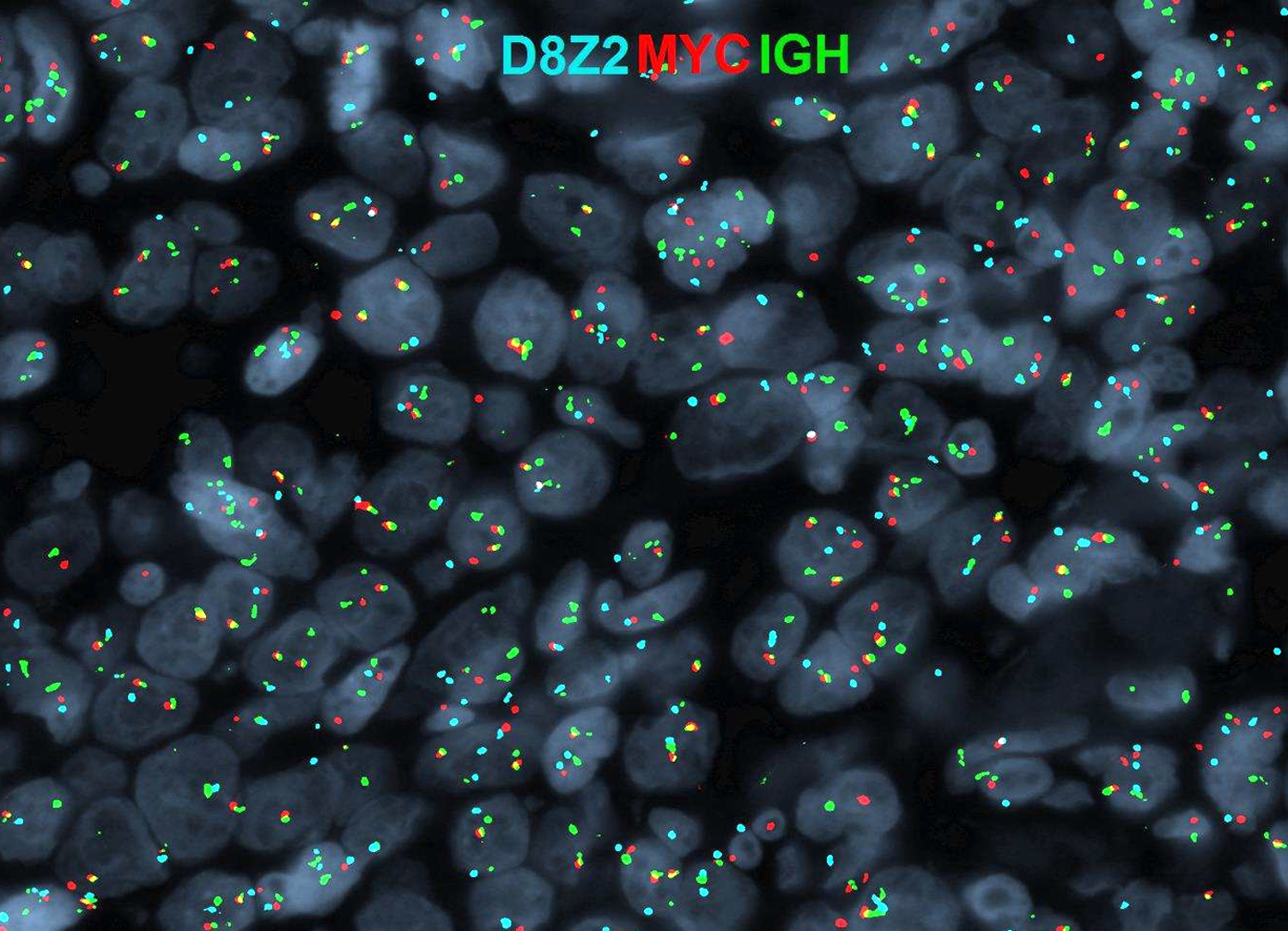

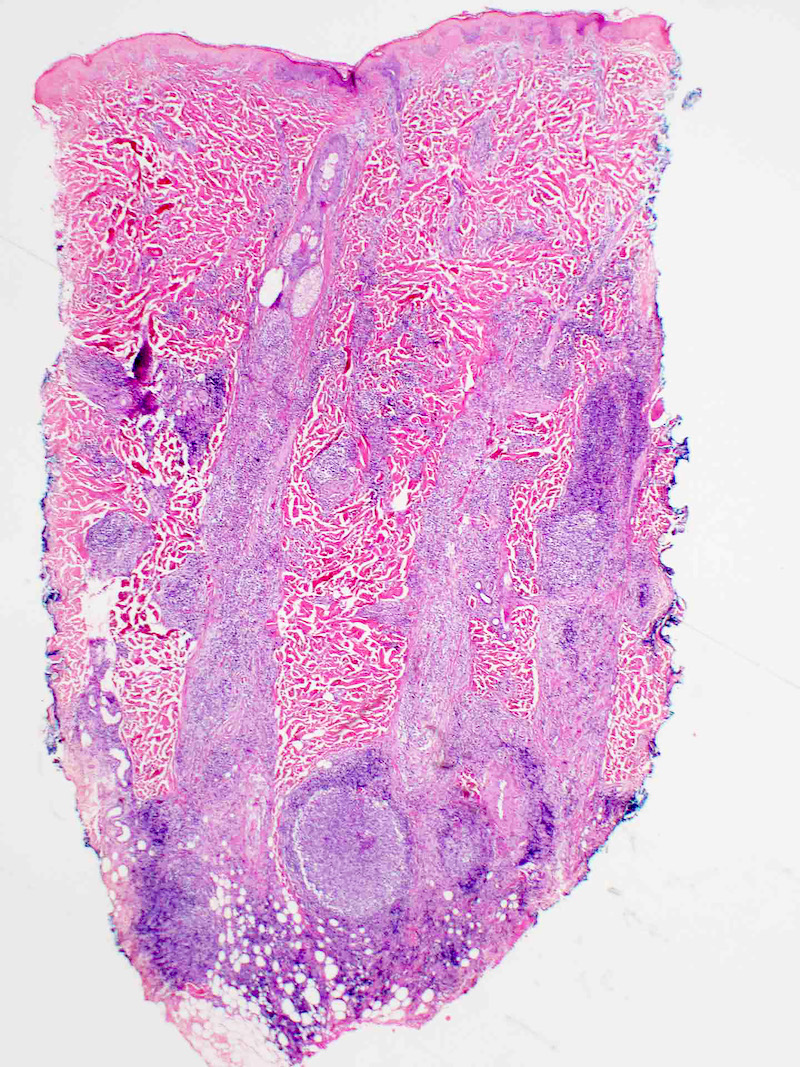
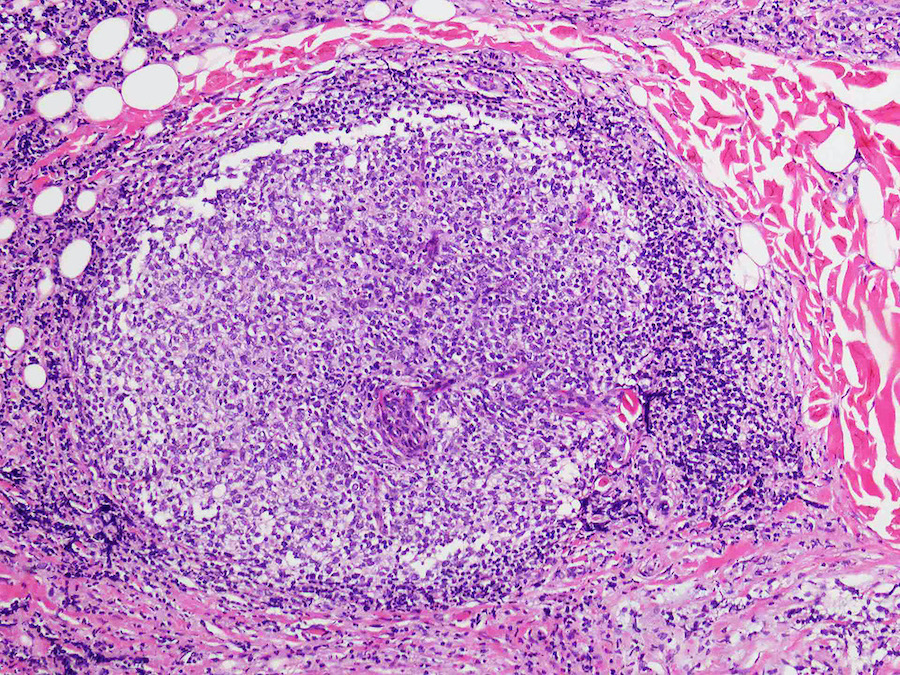


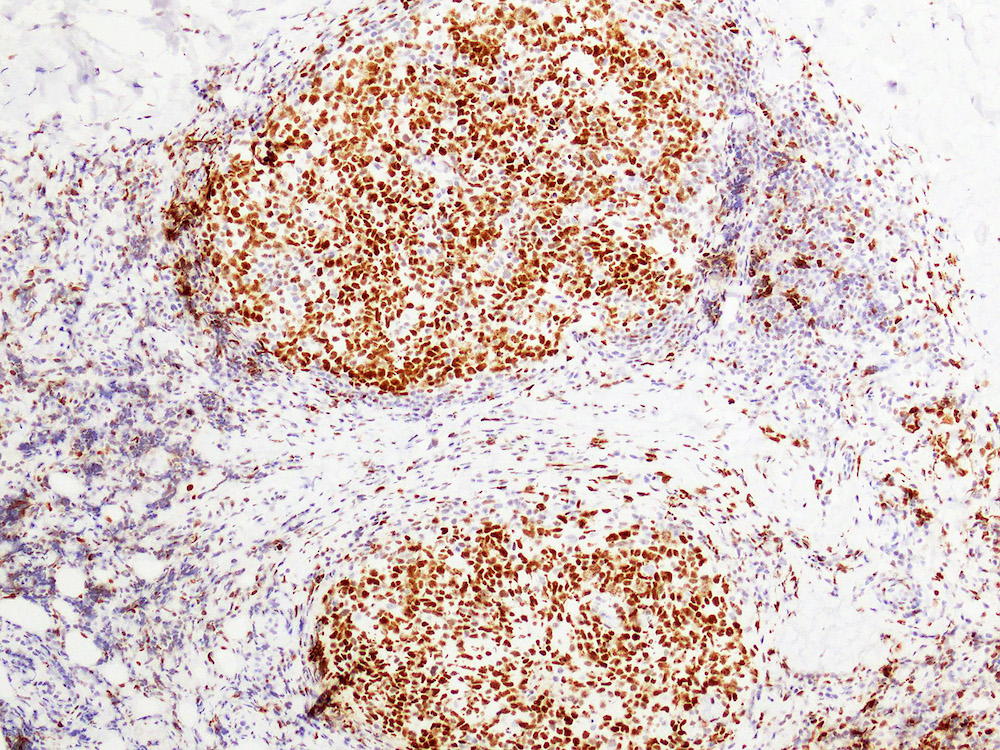
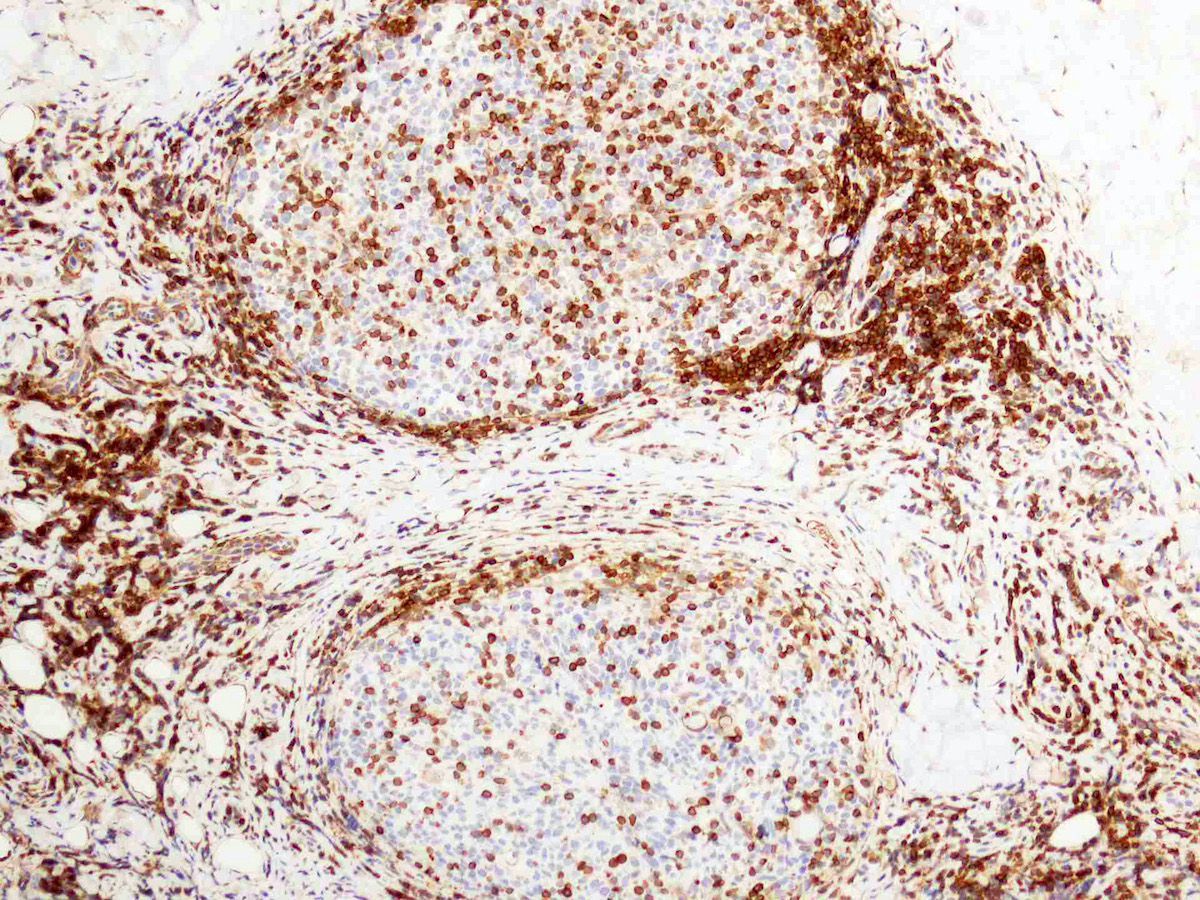

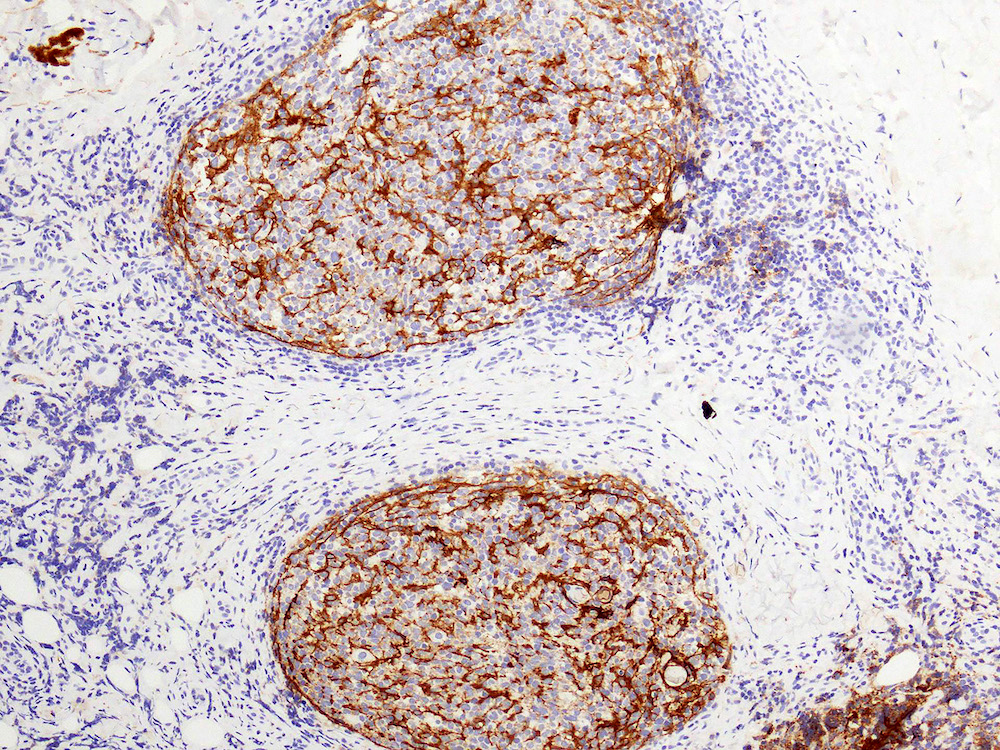


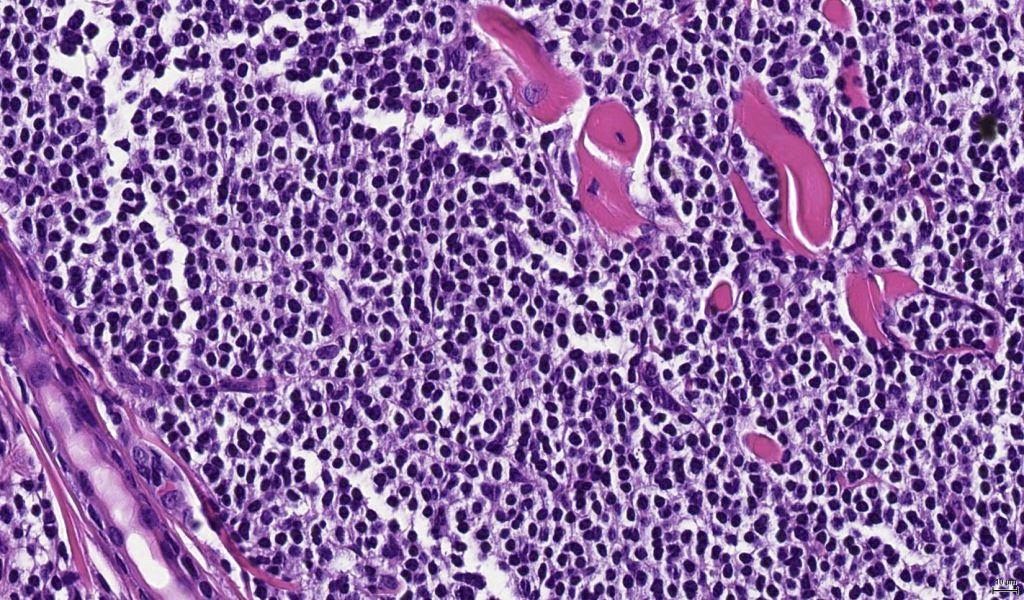
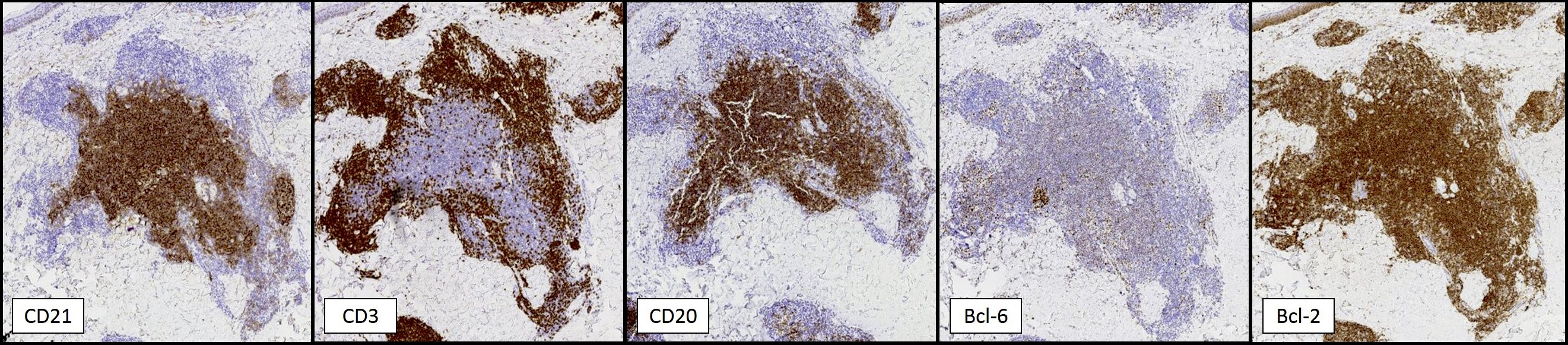
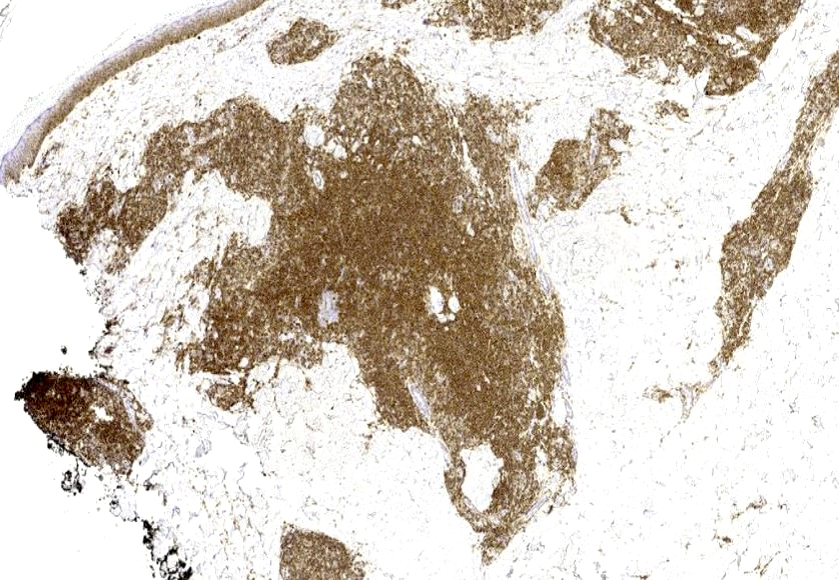
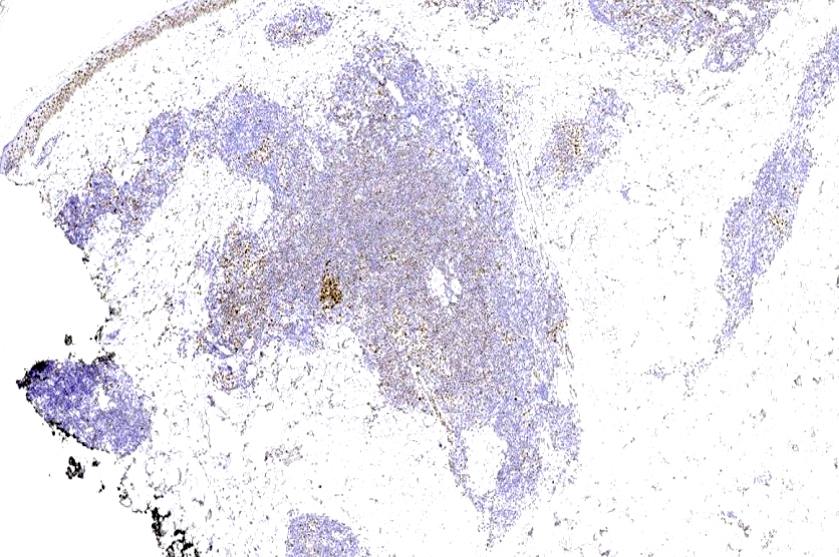
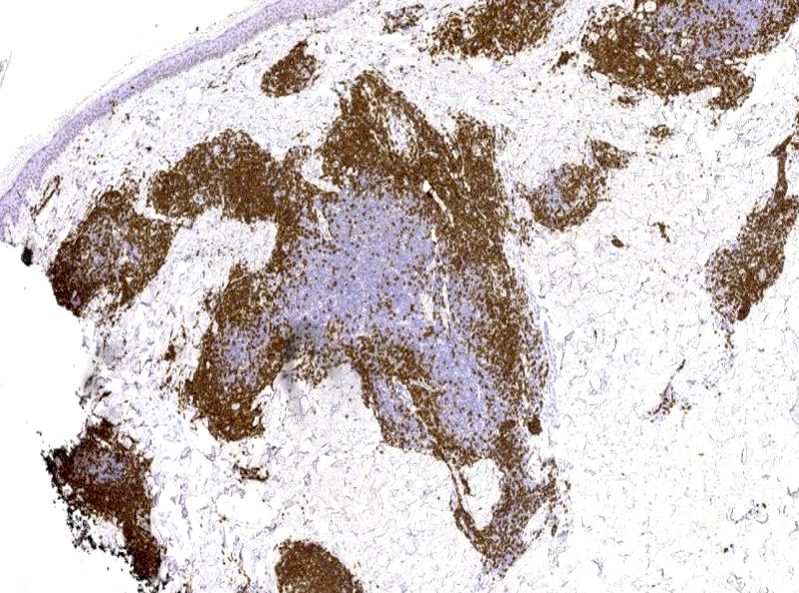

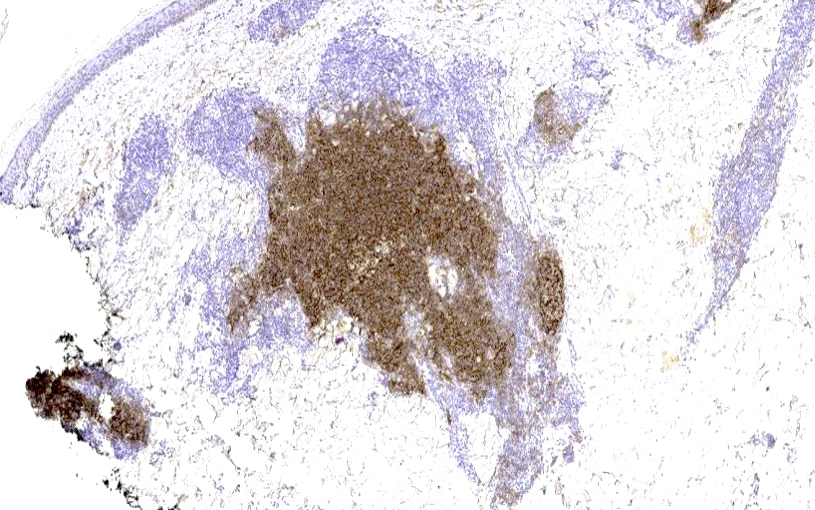

carcclin.jpg)
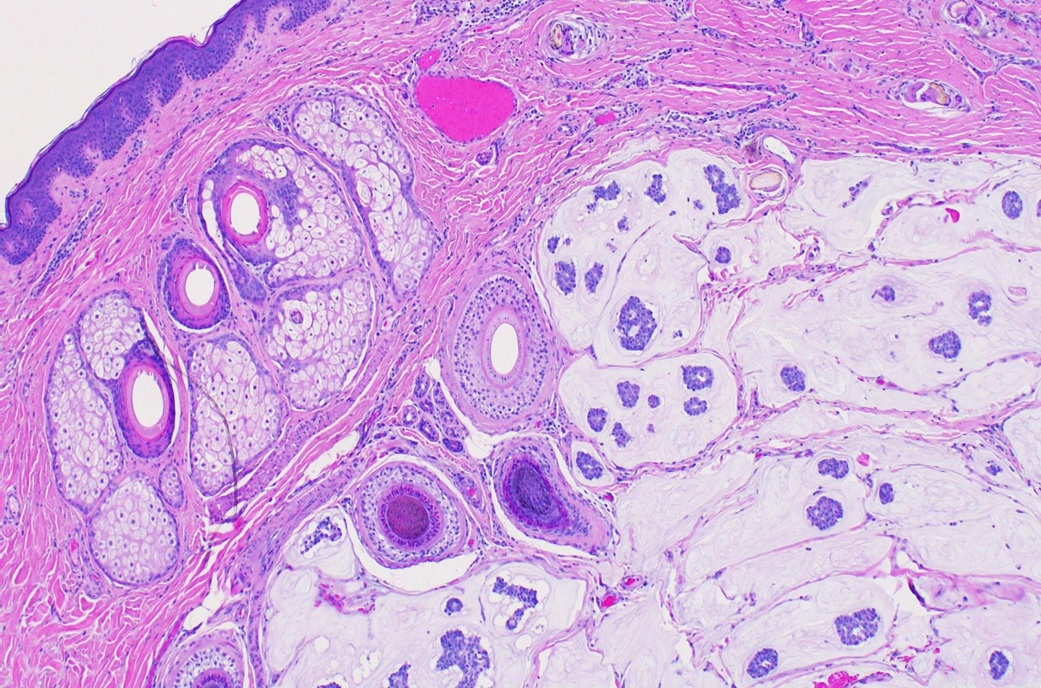
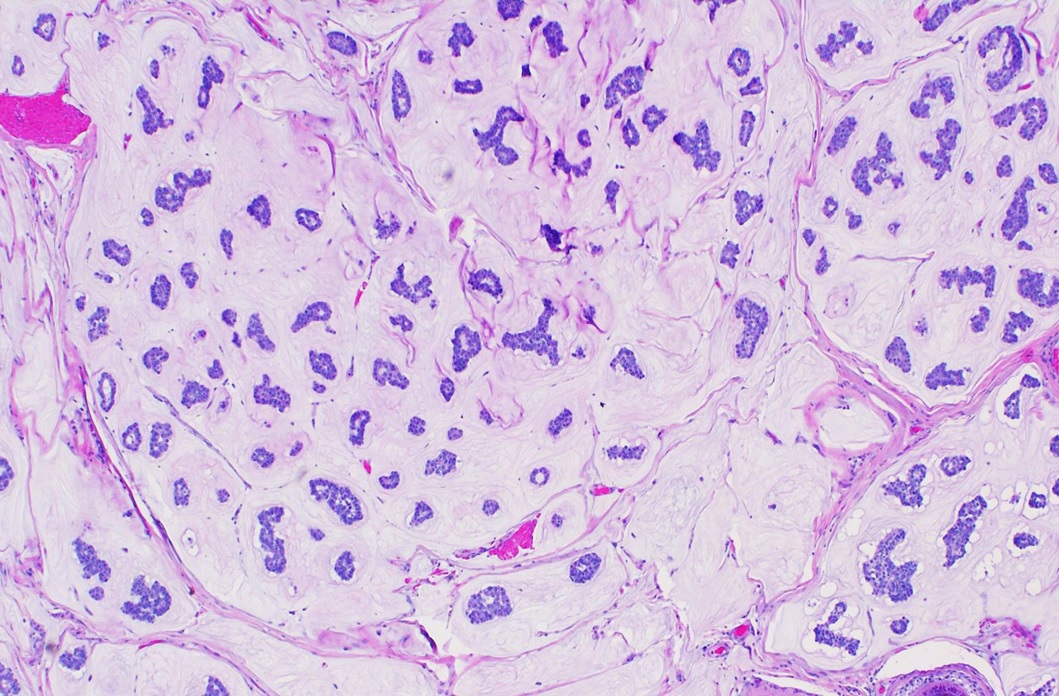
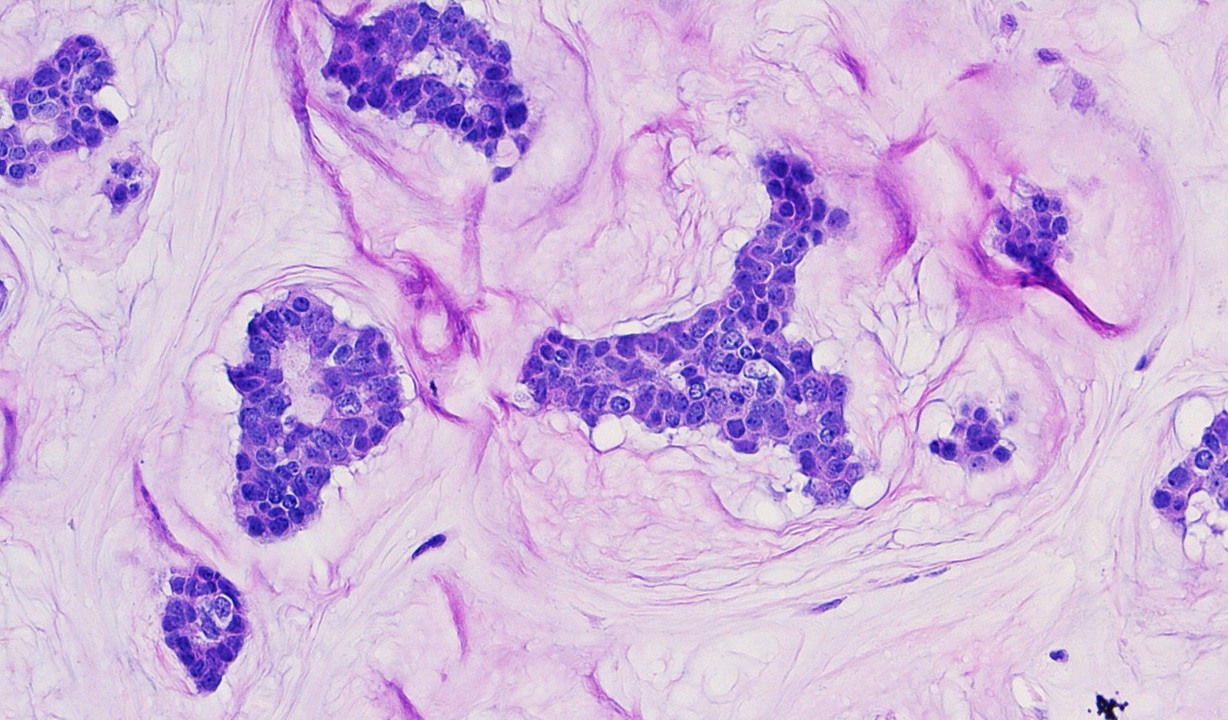
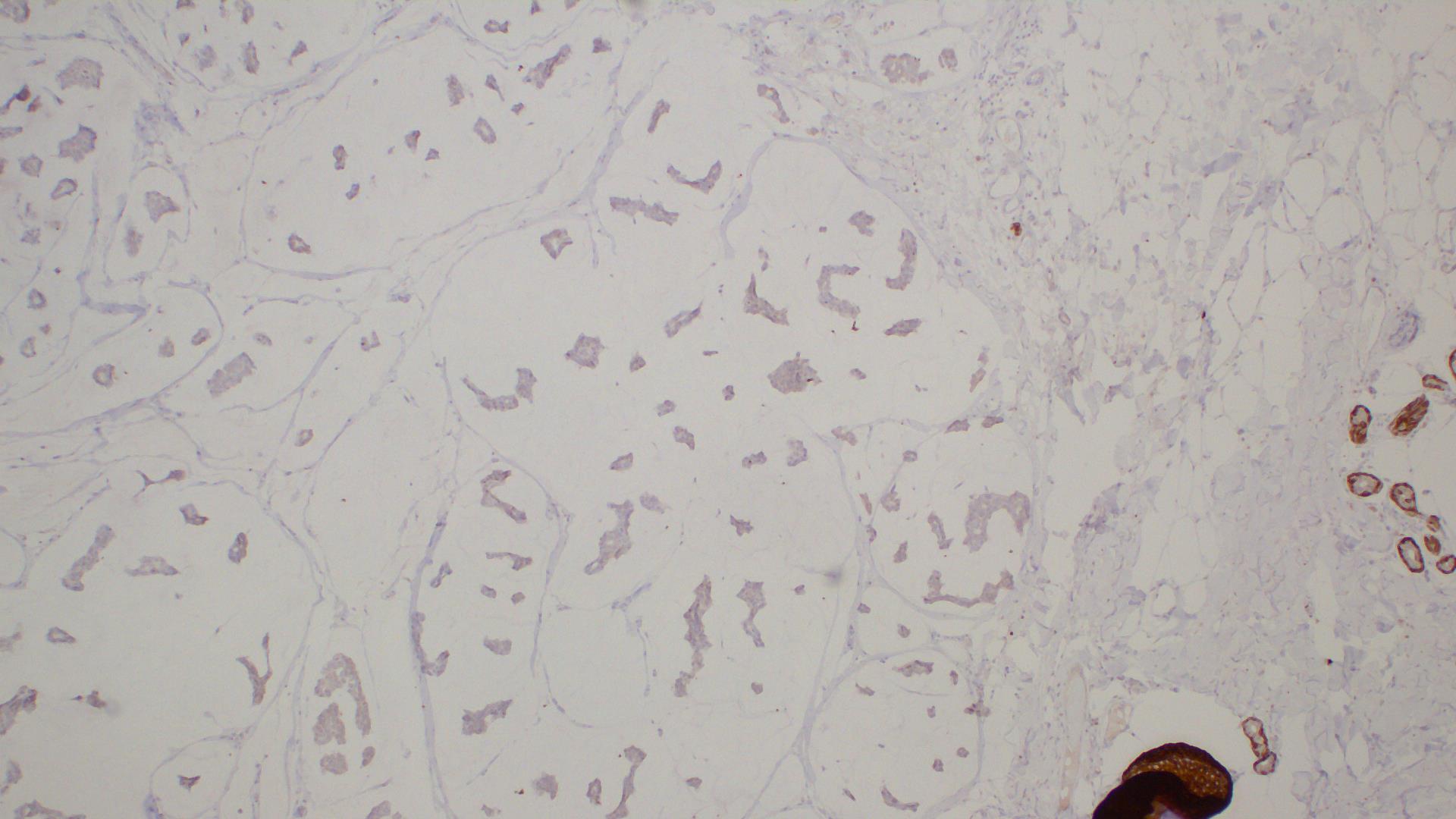
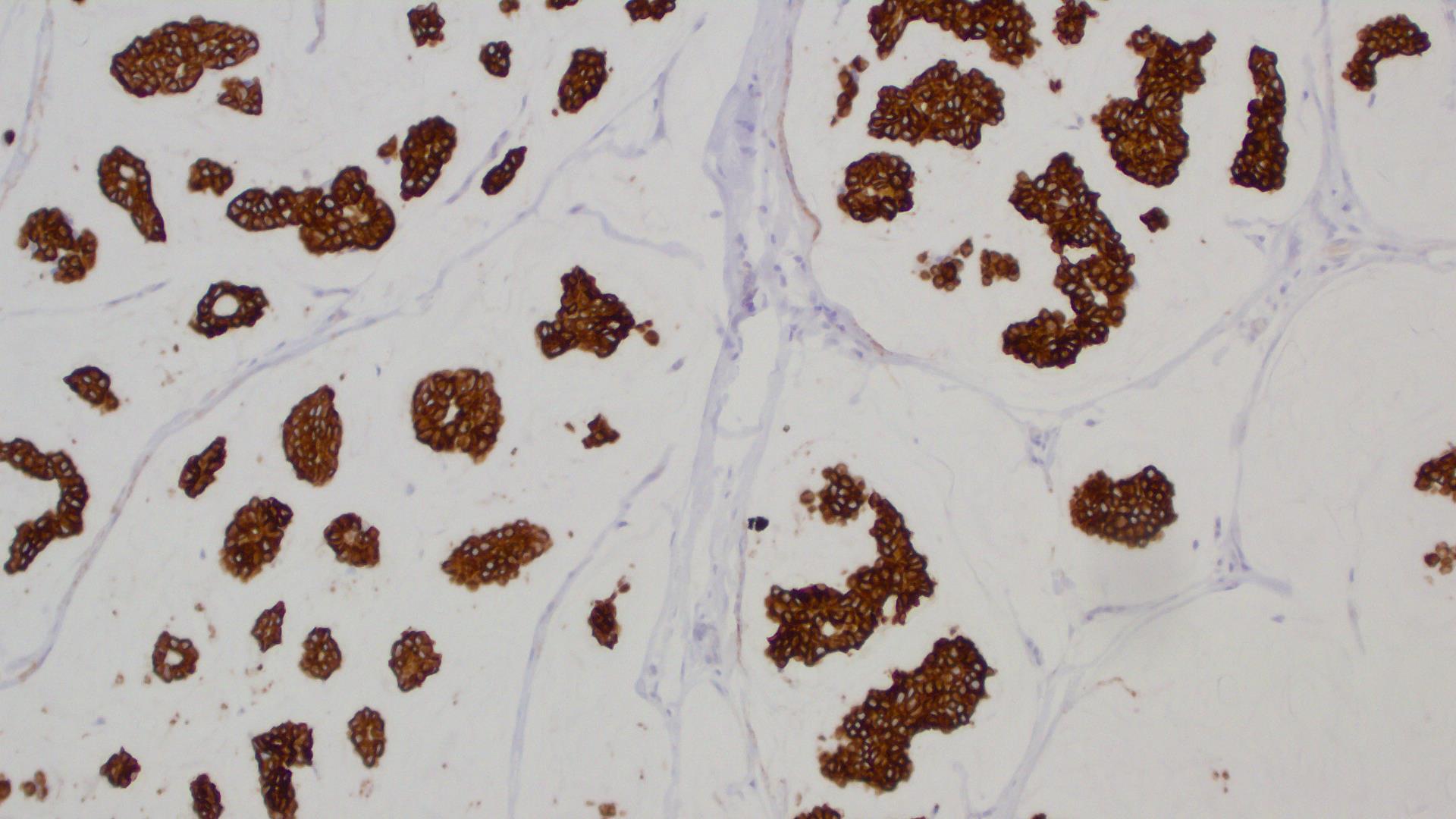

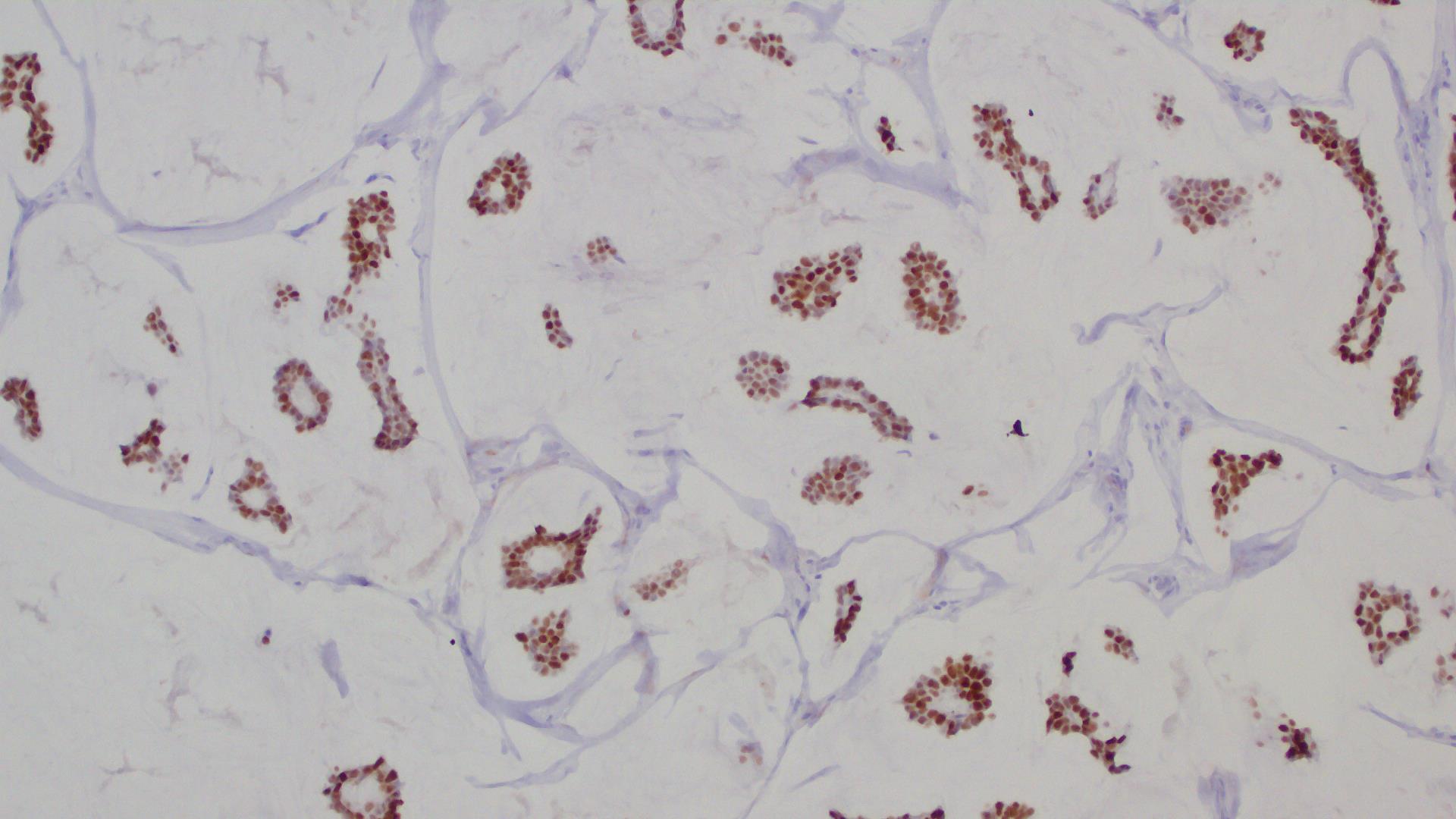

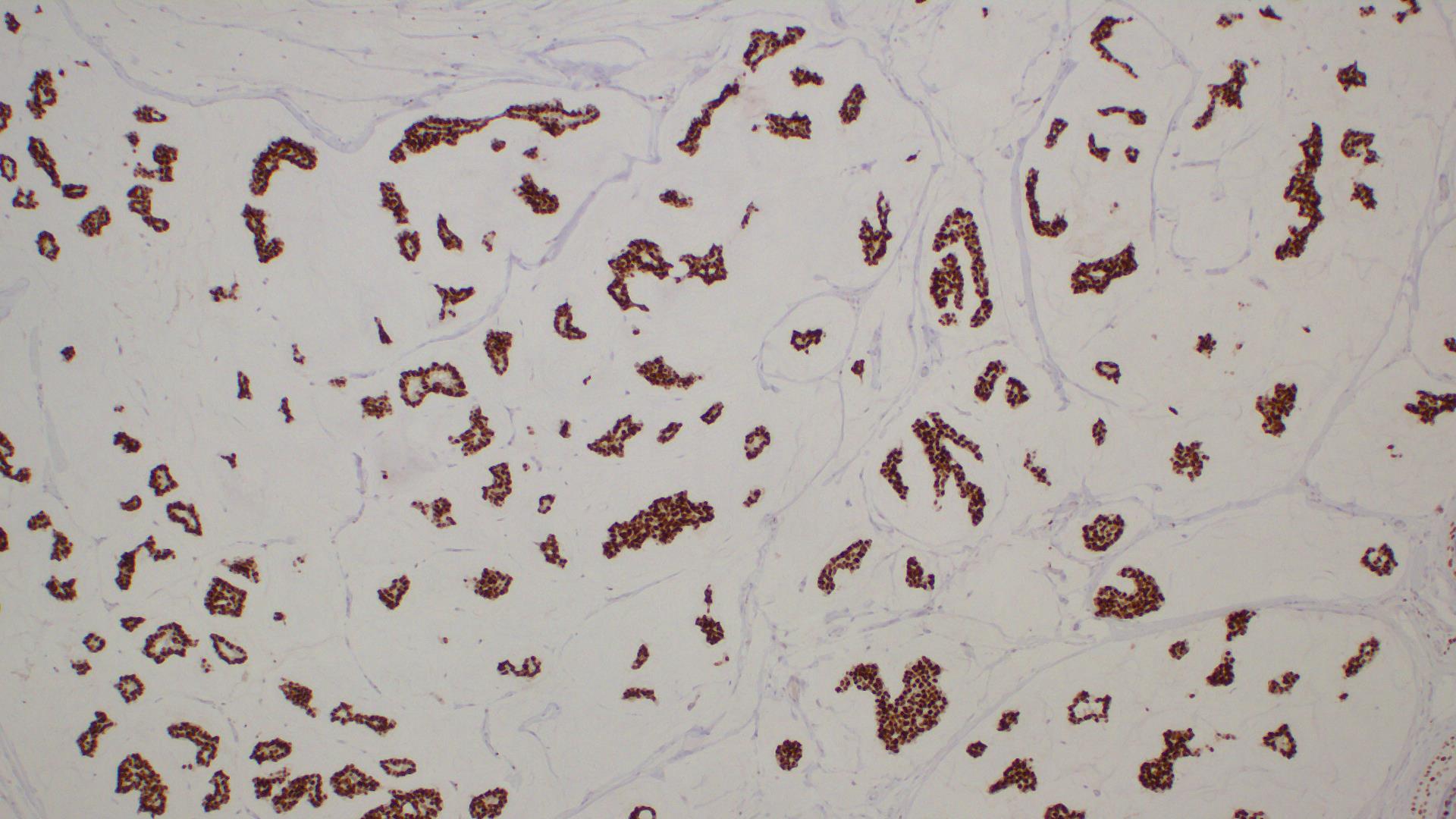
carc2.jpg)