16 January 2020 - Case of the Month #487
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Andrey Bychkov, Kameda Medical Center, Kamogawa City, Chiba (Japan), for contributing this case and writing the discussion.
Case of the Month #487
Clinical history:
A 54 year old woman presented with a 3.5 cm midline neck mass. After imaging and FNA cytology, she underwent surgery.
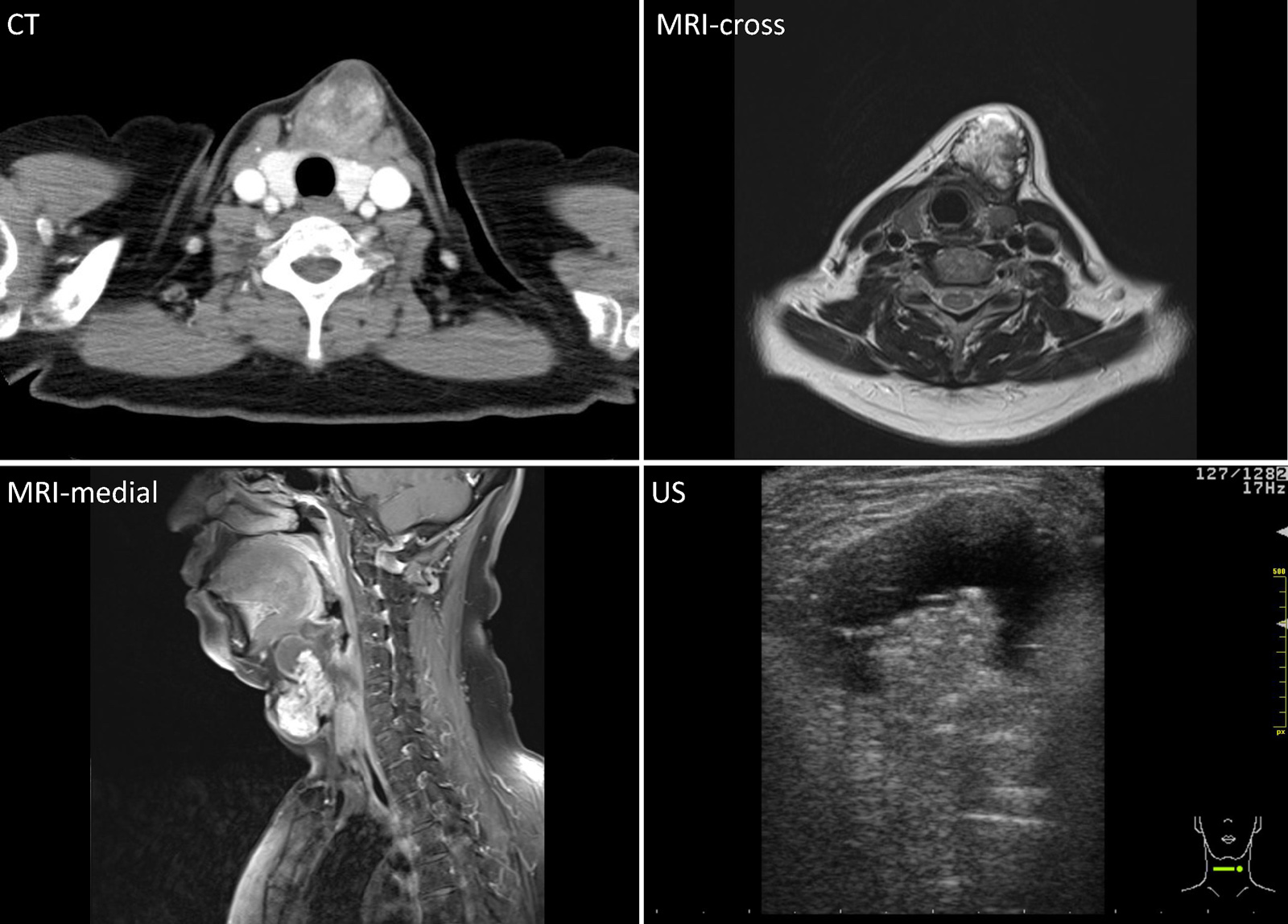
Imaging:
Cytology:
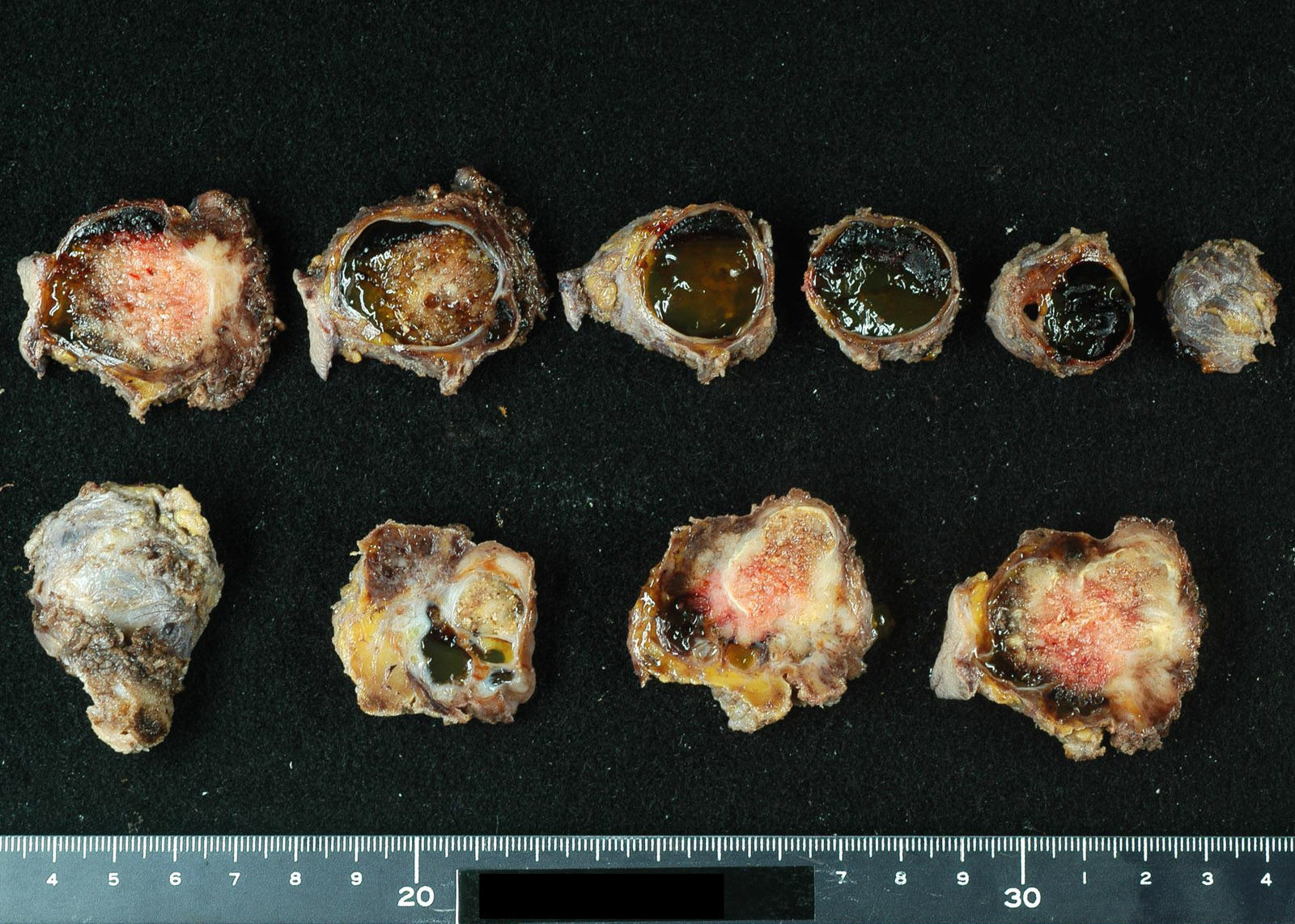
Gross image:
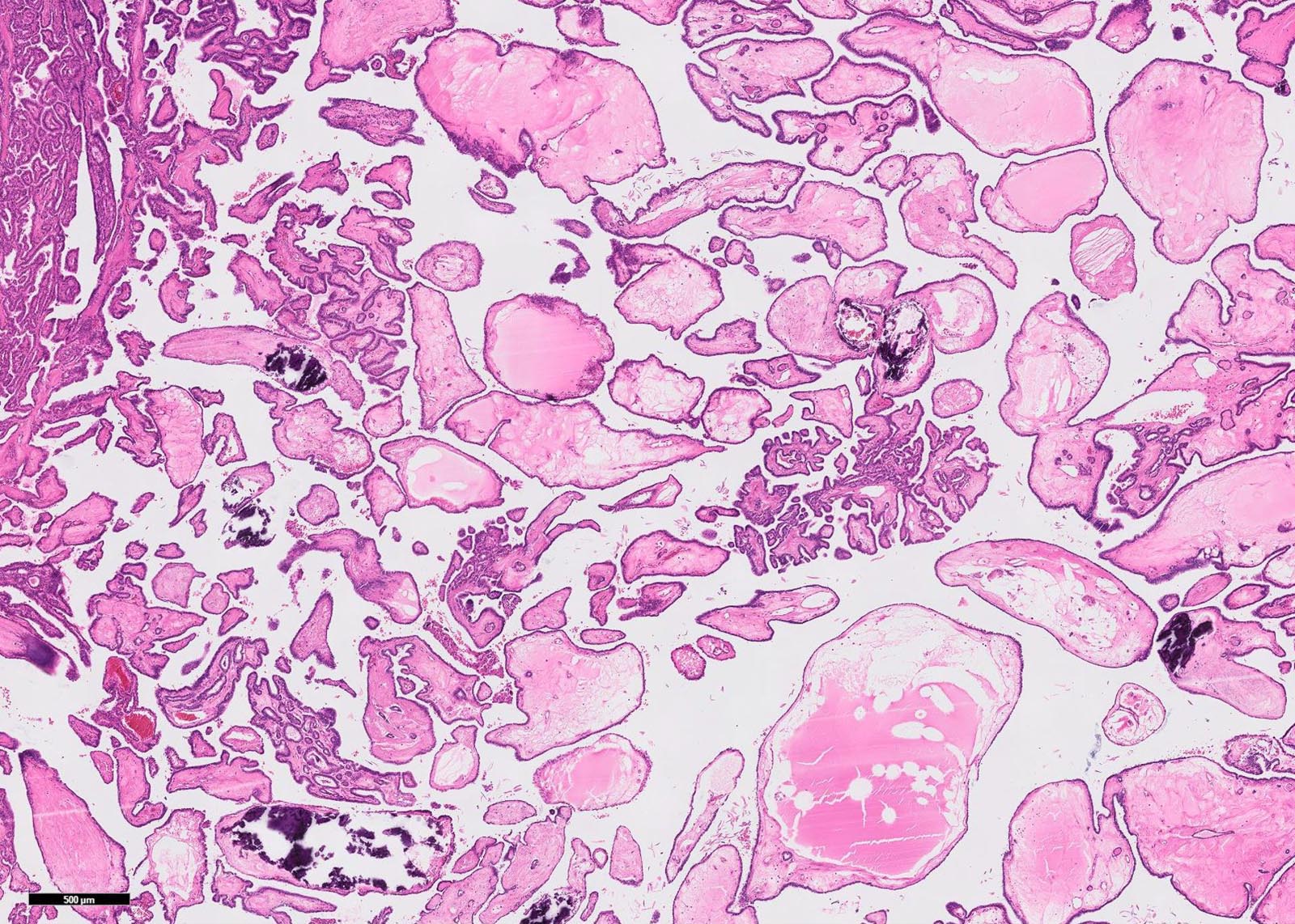
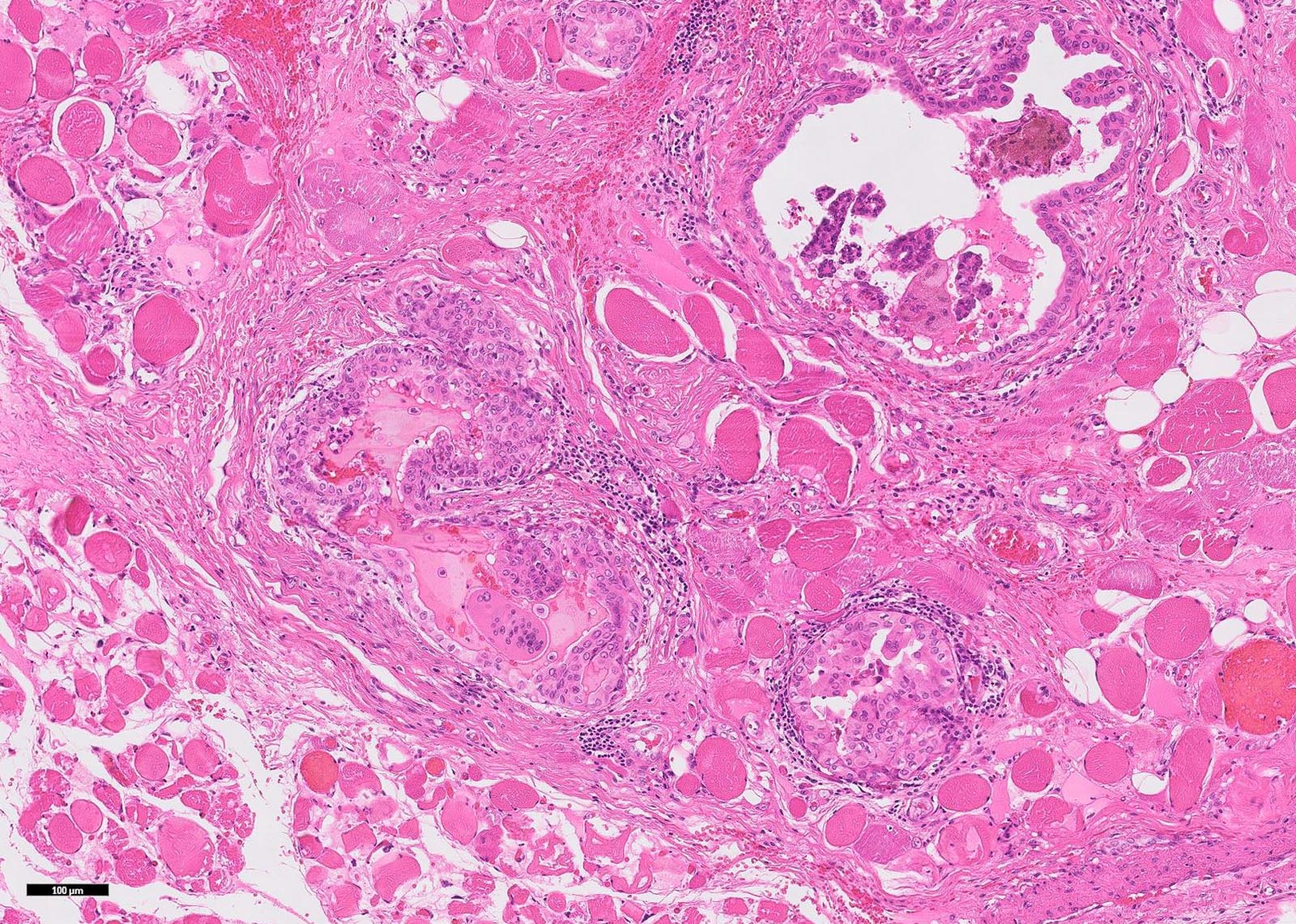
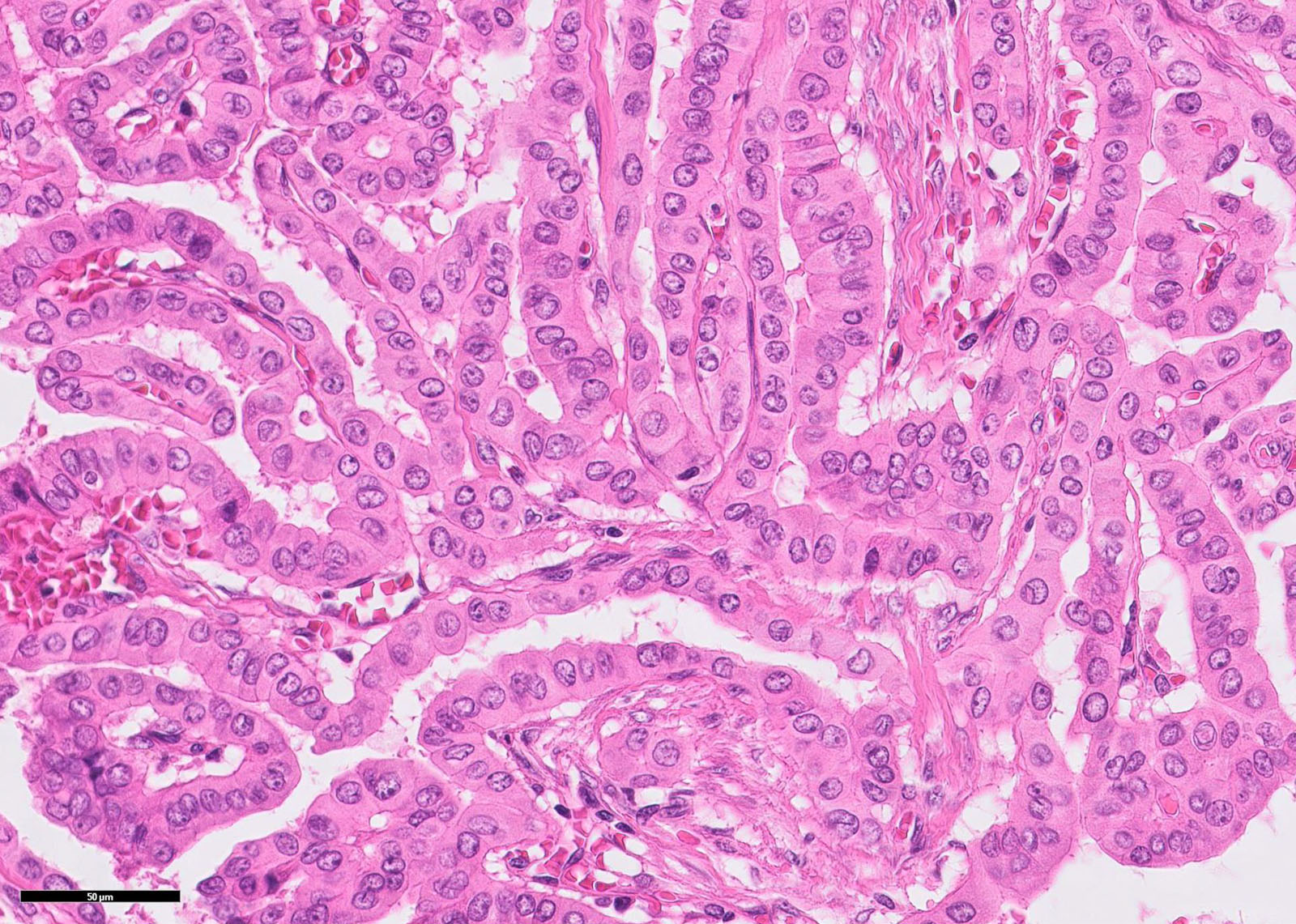
Histopathology images:
Virtual slide:
What is your diagnosis?
Diagnosis: Papillary carcinoma arising in the thyroglossal duct
Test question (answer at the end):
What histological type of thyroid cancer cannot develop in a thyroglossal duct cyst
A. Papillary carcinoma, conventional
B. Papillary carcinoma, follicular variant
C. Follicular carcinoma
D. Medullary carcinoma
E. Anaplastic carcinoma
Discussion:
Thyroglossal duct carcinoma is a rare malignancy arising from thyroid follicular cells of the thyroglossal duct. The thyroglossal duct is the embryonic tract between the initial area of development of the thyroid gland (foramen cecum of the tongue) and its final position in the lower neck. The thyroglossal duct disappears early during embryonic development. However its remnants may persist, undergo cystic dilation and manifest as a thyroglossal duct cyst, the most common congenital neck mass. It presents as a midline mass with epithelial lined remnants and heterotopic thyroid tissue.
Carcinoma develops in less than 1% of thyroglossal duct cysts, with a F:M ratio = 2:1 and a mean age of 40 years (Thyroid FNA Cytology 2019:143). Pediatric cases are uncommon, representing less than 15% of all thyroglossal duct cancers, with a mean age of 12 years (Thyroid 2004;14:777). The most common type is papillary thyroid carcinoma (90%), mainly classic variant, sometimes follicular and tall cell variant (J Clin Endocrinol Metab 2011;96:2684), and rarely anaplastic and mucoepidermoid carcinoma (Thyroid FNA Cytology 2019:143). Squamous cell carcinoma (5%) is derived from the actual cyst lining. Medullary carcinoma cannot develop in the thyroglossal duct because C cells are absent in this structure.
Most thyroglossal duct carcinomas are asymptomatic and discovered by the pathologist on routine histologic evaluation. Clinically, no clear distinction between a benign thyroglossal duct cyst and malignancy can be made (Head Neck Surg 1982;5:134). Nodal involvement is common while distant metastases are extremely rare.
Workup is similar to that for thyroglossal duct cyst, i.e. neck imaging (midline mass in the anterior neck on ultrasound, CT/MRI) and FNA cytology. FNA of the cyst may be helpful in confirming the clinical suspicion (most efficient in adults), but it has relatively low sensitivity and some institutions advocate intraoperative frozen sections (Endocrine 2014;46:160).
Most thyroglossal duct carcinomas are managed by the Sistrunk procedure of block excision of the entire thyroglossal duct to the foramen cecum and removal of the middle third of the hyoid bone. Further steps may include total thyroidectomy with neck dissection. Thyroglossal duct carcinoma has an excellent prognosis similar to conventional papillary thyroid carcinoma.
Microscopically, thyroglossal duct cancer has architectural, nuclear, IHC and molecular features of the specific histotype, in the context of a thyroglossal duct cyst with epithelial lining. Invasion of the hyoid bone and adjacent soft tissue is common.
Coexisting occult carcinoma in the thyroid gland has been found in half of cases with thyroidectomy, which means that thyroglossal duct cancer could represent metastasis from an occult thyroid primary (J Clin Endocrinol Metab 2013;98:458, Endocr Pathol 2015;26:75). Therefore, criteria for diagnosis of de novo thyroglossal duct carcinoma include histopathological confirmation of thyroglossal remnants in a specimen with carcinoma, plus absence of cancer in the thyroid gland. In addition, thyroglossal duct carcinoma should be distinguished from the primary cancer of the pyramidal thyroid lobe (no thyroglossal duct lining epithelium) or Delphian node metastasis (lymph node remnants).
Test question answer:
D.Medullary carcinoma
C cells are absent in thyroglossal duct cyst, therefore medullary carcinoma cannot develop. C cells are derived from lateral anlagen (ultimobranchial bodies) while the thyroglossal duct is a part of the medial thyroid anlage. Very recently, calcitonin-expressing neuroendocrine cells were found among the respiratory epithelium of the thyroglossal duct (Virchows Arch 2019;474:609). These cells can produce neuroendocrine tumors mimicking medullary carcinoma in mid-neck/median anlage derivatives.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Andrey Bychkov, Kameda Medical Center, Kamogawa City, Chiba (Japan), for contributing this case and writing the discussion.
We have created a Resident Advisory Board to determine how well we are meeting resident needs and to help us communicate with residents. This year's members are outstanding authors for PathologyOutlines.com:

Meaghan Morris, M.D., Ph.D., |
Farres Obeidin, M.D., |

Caroline Underwood, M.D., |
Case of the Month #487
Clinical history:
A 54 year old woman presented with a 3.5 cm midline neck mass. After imaging and FNA cytology, she underwent surgery.
Imaging:
Cytology:
Gross image:
Histopathology images:
Virtual slide:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Papillary carcinoma arising in the thyroglossal duct
Test question (answer at the end):
What histological type of thyroid cancer cannot develop in a thyroglossal duct cyst
A. Papillary carcinoma, conventional
B. Papillary carcinoma, follicular variant
C. Follicular carcinoma
D. Medullary carcinoma
E. Anaplastic carcinoma
Discussion:
Thyroglossal duct carcinoma is a rare malignancy arising from thyroid follicular cells of the thyroglossal duct. The thyroglossal duct is the embryonic tract between the initial area of development of the thyroid gland (foramen cecum of the tongue) and its final position in the lower neck. The thyroglossal duct disappears early during embryonic development. However its remnants may persist, undergo cystic dilation and manifest as a thyroglossal duct cyst, the most common congenital neck mass. It presents as a midline mass with epithelial lined remnants and heterotopic thyroid tissue.
Carcinoma develops in less than 1% of thyroglossal duct cysts, with a F:M ratio = 2:1 and a mean age of 40 years (Thyroid FNA Cytology 2019:143). Pediatric cases are uncommon, representing less than 15% of all thyroglossal duct cancers, with a mean age of 12 years (Thyroid 2004;14:777). The most common type is papillary thyroid carcinoma (90%), mainly classic variant, sometimes follicular and tall cell variant (J Clin Endocrinol Metab 2011;96:2684), and rarely anaplastic and mucoepidermoid carcinoma (Thyroid FNA Cytology 2019:143). Squamous cell carcinoma (5%) is derived from the actual cyst lining. Medullary carcinoma cannot develop in the thyroglossal duct because C cells are absent in this structure.
Most thyroglossal duct carcinomas are asymptomatic and discovered by the pathologist on routine histologic evaluation. Clinically, no clear distinction between a benign thyroglossal duct cyst and malignancy can be made (Head Neck Surg 1982;5:134). Nodal involvement is common while distant metastases are extremely rare.
Workup is similar to that for thyroglossal duct cyst, i.e. neck imaging (midline mass in the anterior neck on ultrasound, CT/MRI) and FNA cytology. FNA of the cyst may be helpful in confirming the clinical suspicion (most efficient in adults), but it has relatively low sensitivity and some institutions advocate intraoperative frozen sections (Endocrine 2014;46:160).
Most thyroglossal duct carcinomas are managed by the Sistrunk procedure of block excision of the entire thyroglossal duct to the foramen cecum and removal of the middle third of the hyoid bone. Further steps may include total thyroidectomy with neck dissection. Thyroglossal duct carcinoma has an excellent prognosis similar to conventional papillary thyroid carcinoma.
Microscopically, thyroglossal duct cancer has architectural, nuclear, IHC and molecular features of the specific histotype, in the context of a thyroglossal duct cyst with epithelial lining. Invasion of the hyoid bone and adjacent soft tissue is common.
Coexisting occult carcinoma in the thyroid gland has been found in half of cases with thyroidectomy, which means that thyroglossal duct cancer could represent metastasis from an occult thyroid primary (J Clin Endocrinol Metab 2013;98:458, Endocr Pathol 2015;26:75). Therefore, criteria for diagnosis of de novo thyroglossal duct carcinoma include histopathological confirmation of thyroglossal remnants in a specimen with carcinoma, plus absence of cancer in the thyroid gland. In addition, thyroglossal duct carcinoma should be distinguished from the primary cancer of the pyramidal thyroid lobe (no thyroglossal duct lining epithelium) or Delphian node metastasis (lymph node remnants).
Test question answer:
D.Medullary carcinoma
C cells are absent in thyroglossal duct cyst, therefore medullary carcinoma cannot develop. C cells are derived from lateral anlagen (ultimobranchial bodies) while the thyroglossal duct is a part of the medial thyroid anlage. Very recently, calcitonin-expressing neuroendocrine cells were found among the respiratory epithelium of the thyroglossal duct (Virchows Arch 2019;474:609). These cells can produce neuroendocrine tumors mimicking medullary carcinoma in mid-neck/median anlage derivatives.