18 January 2017 - Case of the Week #414
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Safa Alshaikh, Dr. Eman Aljufairi and Dr. Nisha Chandran, Department of Pathology, Salmaniya Medical Complex (Kingdom of Bahrain) for contributing this case. To contribute a Case of the Week, follow the guidelines on our main Case of the Week page.

Advertisement
Website news:
(1) Twice a year, PathologyOutlines.com donates 10% of our Amazon commission to a non-profit organization. For the first half of 2017, we will be contributing to Make-A-Wish. You can buy Pathology, non Pathology related books or any other items by using our Amazon link.
(2) To make a Print Friendly page for any page on our website, we suggest you visit www.PrintFriendly.com and follow the instructions. It sometimes looks a little odd with the images. Another possibility is to Print / Save the page as a PDF, and then print from the PDF (easier with a Mac). Let us know if you have any other comments / suggestions.
(3) We are seeking additional pathologist authors to write or edit the discussions of some of the pending Cases of the Week. Requirements include: (a) following our general format for case discussions, (b) turn around time of 1 week (in general) and (c) ability to write about most types of surgical pathology cases, not just a particular subspecialty. We would prefer you to meet the Author requirements indicated here. There is an honorarium of $75 per case. If interested, please send your CV and a writing sample of a case report or something similar to NatPernick@gmail.com.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #414
Clinical history:
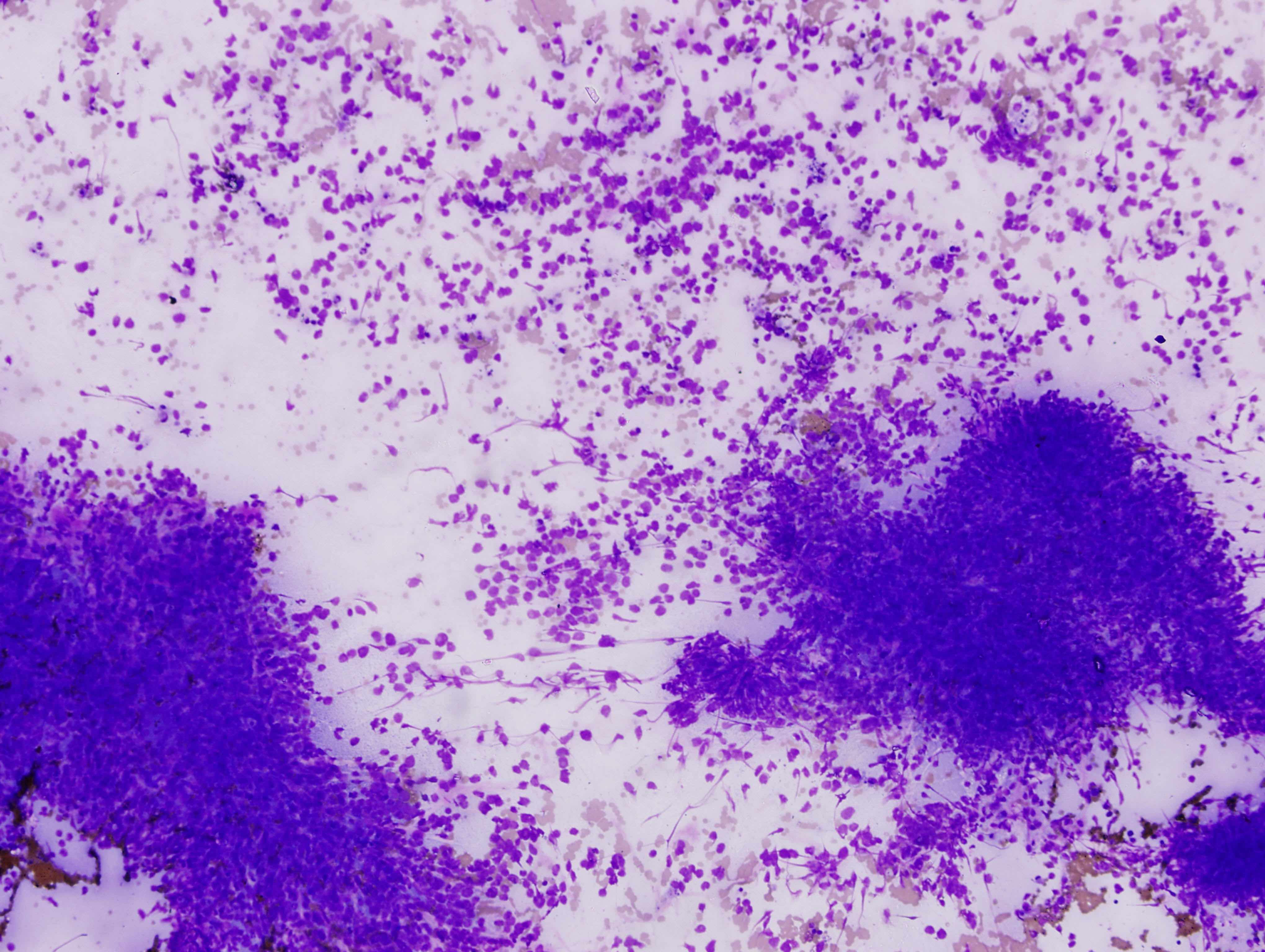
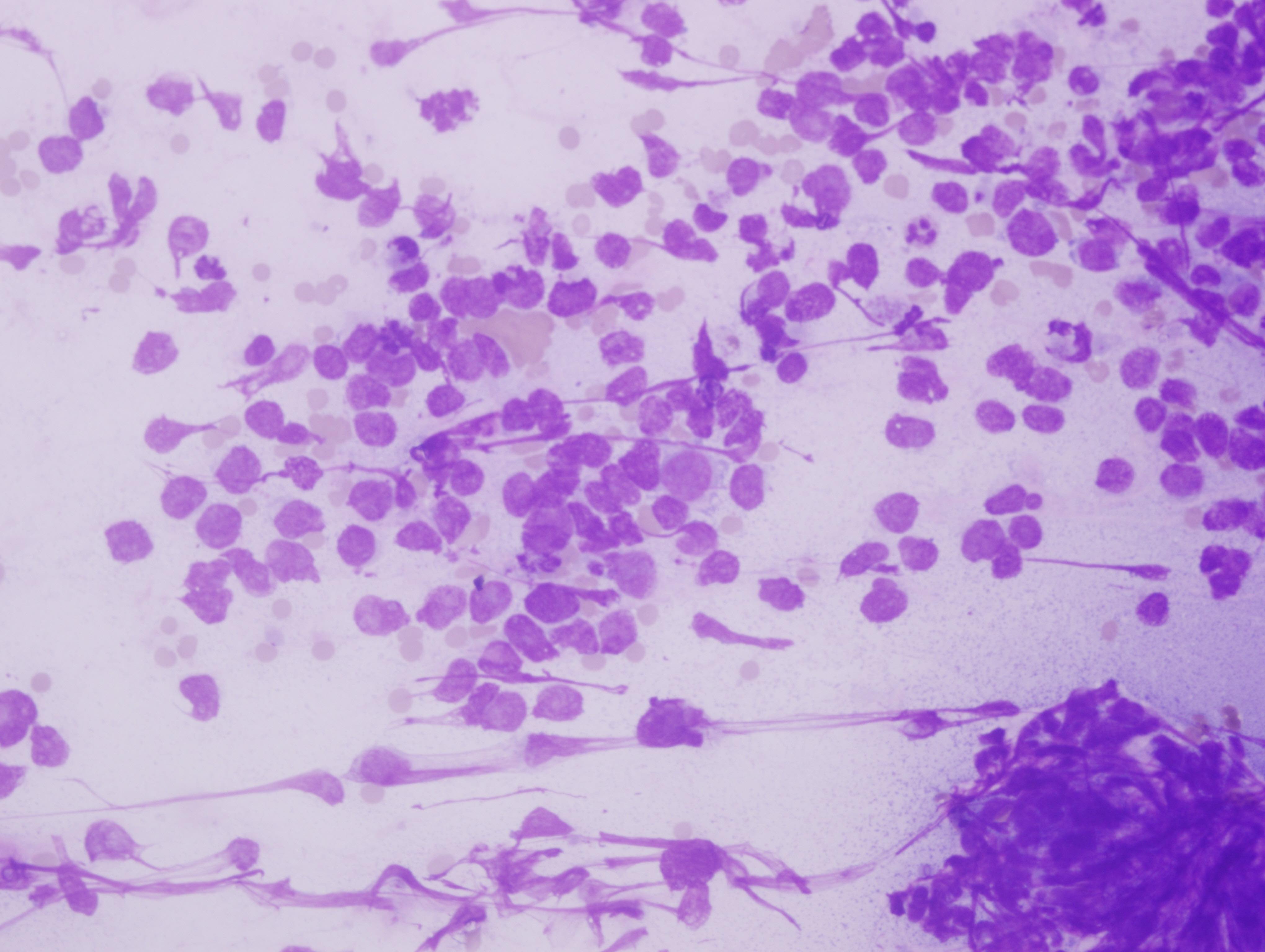
A 67 year old woman presented with a left arm ulcer for 6 months. She was treated with antibiotics for 4 months without improvement. Physical examination showed an ill defined, large, ulcerated and nodular mass measuring 5 x 5 cm, associated with multiple enlarged left axillary lymph nodes. An FNA was performed.
Cytology images:
Diagnosis:
Merkle cell carcinoma
Discussion:
Test question (answer at the end):
Which statement is true for Merkel cell carcinoma:
A. It typically is slow growing and has indolent behavior.
B. It is a small blue cell tumor and has prominent nucleoli.
C. It cytologically resembles small cell carcinoma, with poorly cohesive cells, molding and crush artifact.
D. A majority of cases, even those with a combined phenotype with other carcinomatous elements, are associated with Merkel cell polyomavirus.
Merkel cell carcinoma (MCC), also called primary cutaneous neuroendocrine carcinoma, is an aggressive neoplasm, typically presenting as a slow growing nodule on the sun exposed skin of older adults. It is rare, but increasing in incidence. There is a slight male predominance, and most patients are Caucasian. Immune compromise increases its risk (ACS - Merkel cell carcinoma risk factors). Clinically, the lesion is red to violet and 20% of cases are ulcerated (Wick: Silverberg's Principles and Practice of Surgical Pathology and Cytopathology, 5th ed, 2015).
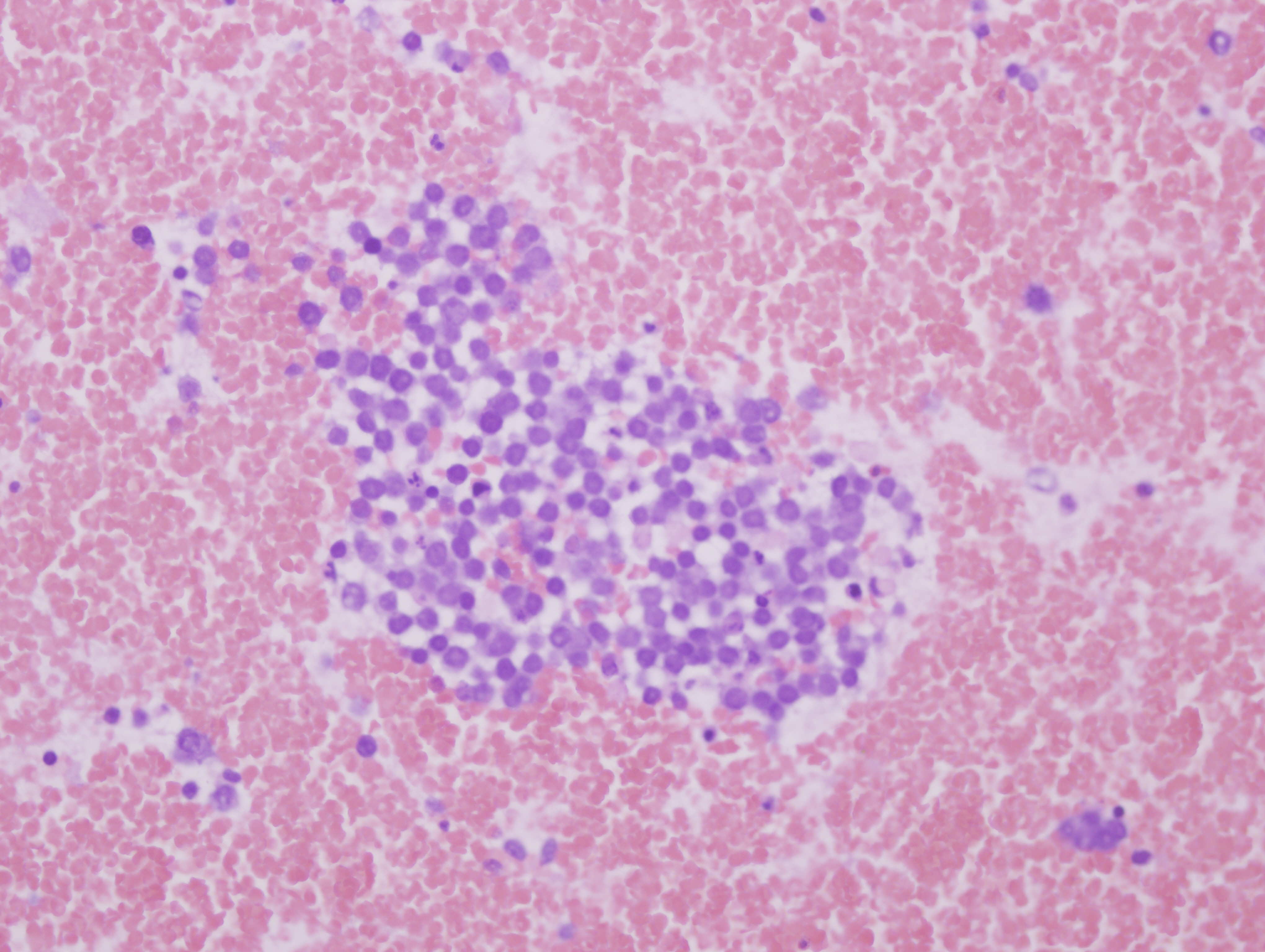
Microscopically, MCC falls into the "small round blue cell" category – the cells are monotonous with scant cytoplasm, rounded nuclei, fine chromatin and inconspicuous nuclei. There is generally a high mitotic rate with focal necrosis. "Blue buttons" – aggregates of intermediate filaments – can be seen in the cytoplasm but are not specific for MCC (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). Histologically the tumor cells can grow in sheets, nests and trabeculae (hence its original name, trabecular carcinoma) that are centered in the dermis, with invasion into the subcutis. The stroma can be mucinous.
Cytologically, as in this case, MCC resembles small cell carcinoma, with poorly cohesive cells, molding and crush artifact. Rare rosette-like structures can be seen in smears (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011, Coll Antropol 2010;34:691, Coll Antropol 2010;34:665).
MCC can show purely neuroendocrine differentiation, or can have a combined phenotype with other carcinomatous elements, such as squamous cell carcinoma and eccrine carcinoma, or can have sarcomatous elements (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). 80% of cases are associated with Merkel cell polyomavirus; however, tumors with combined phenotypes have been consistently negative for polyomavirus (Hum Pathol 2015;46:1290).
The differential diagnosis includes other small round blue cell tumors such as small cell carcinoma. On cytology, MCC typically shows less molding, less crush artifact and more monotony than small cell carcinoma (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). Neuroendocrine markers are positive in most MCCs, as they are in small cell carcinomas. Most, but not all, MCCs show a characteristic perinuclear dot-like positivity for CK20 (and other low molecular weight cytokeratins), corresponding to the "blue buttons". Up to 60% can stain positive for CD99 in a perinuclear dot-like pattern, membranous pattern or both (Int J Surg Pathol 2016;24:293). S100 can be positive, but TTF1 and CD45 should be negative (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). Some cases are positive for c-kit, but therapeutic trials of tyrosine kinase inhibitors in patients with advanced disease have not shown a benefit (Hum Pathol 2015;46:1290). A monoclonal antibody against the Merkel cell polyomavirus large T antigen, called CM2B4, has a sensitivity and specificity of 94% each for diagnosis when compared to real time PCR for the virus (Diagn Pathol 2014 20;9:65).
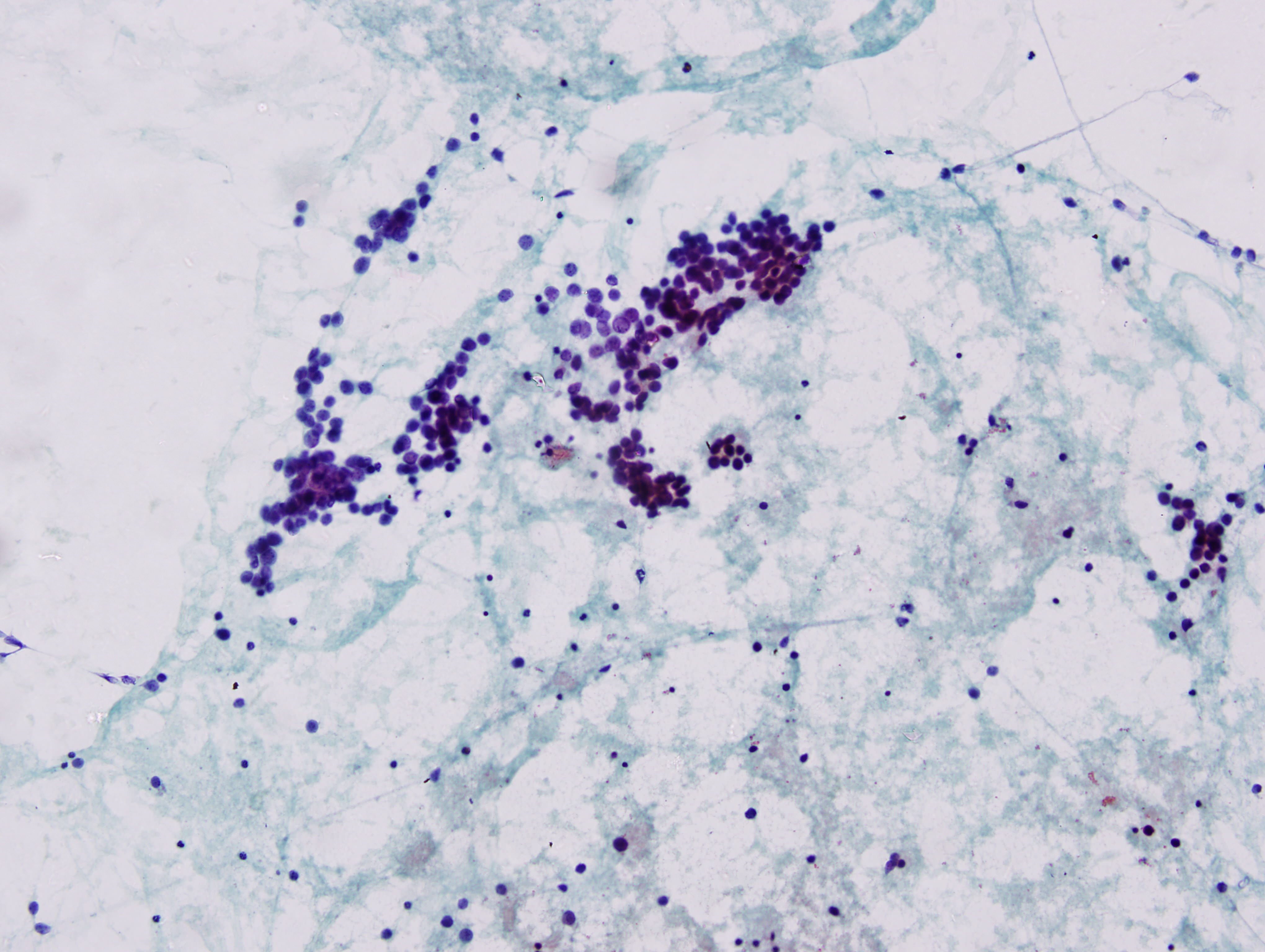
For this case, immunohistochemical stains were performed on the cell block. There was diffuse and intense perinuclear dot-like staining for CK20, and positivity for chromogranin and synaptophysin. No reactivity was detected for TTF1, CD45, p63, CK5, CK6, MelanA or S100. The cytologic findings were interpreted as malignant, small round blue cell tumor, consistent with MCC. Surgical excision of the mass and lymph nodes was performed. The histopathologic diagnosis was MCC. The lymph nodes were positive for metastatic disease. The patient was started on chemotherapy.
Five year survival decreases from 80% in early stage disease to 20% for advanced disease (ACS - Survival rates for Merkel cell carcinoma, by stage). Some studies have shown a worse prognosis if tumors are negative for Merkel cell polyomavirus (Hum Pathol 2015;46:1290). The mainstay of therapy is wide local excision, selective lymphadenectomy and radiation. Somatostatin analogs may provide palliative relief of neuroendocrine symptoms. A study of PD-1 immune checkpoint inhibitors in patients with advanced MCC showed a response rate of 62% in polyomavirus positive tumors and 44% in polyomavirus negative tumors. Interestingly, despite the aggressiveness of MCC, spontaneous complete regression occurs in up to 2% of cases (J Cutan Pathol 2016;43:1150).
Test Question Answer:
C. A is incorrect, because although it is typically slow growing, it has aggressive behavior. B is incorrect because although it is a small blue cell tumor, it has indistinct nucleoli. D is incorrect because cases with a combined phenotype are not associated with Merkel cell polyomavirus.
Discussion edited by: Dr. Hillary Z. Kimbrell, Myriad Genetics, Inc., Utah (USA)
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Safa Alshaikh, Dr. Eman Aljufairi and Dr. Nisha Chandran, Department of Pathology, Salmaniya Medical Complex (Kingdom of Bahrain) for contributing this case. To contribute a Case of the Week, follow the guidelines on our main Case of the Week page.

Advertisement
Website news:
(1) Twice a year, PathologyOutlines.com donates 10% of our Amazon commission to a non-profit organization. For the first half of 2017, we will be contributing to Make-A-Wish. You can buy Pathology, non Pathology related books or any other items by using our Amazon link.
(2) To make a Print Friendly page for any page on our website, we suggest you visit www.PrintFriendly.com and follow the instructions. It sometimes looks a little odd with the images. Another possibility is to Print / Save the page as a PDF, and then print from the PDF (easier with a Mac). Let us know if you have any other comments / suggestions.
(3) We are seeking additional pathologist authors to write or edit the discussions of some of the pending Cases of the Week. Requirements include: (a) following our general format for case discussions, (b) turn around time of 1 week (in general) and (c) ability to write about most types of surgical pathology cases, not just a particular subspecialty. We would prefer you to meet the Author requirements indicated here. There is an honorarium of $75 per case. If interested, please send your CV and a writing sample of a case report or something similar to NatPernick@gmail.com.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #414
Clinical history:
A 67 year old woman presented with a left arm ulcer for 6 months. She was treated with antibiotics for 4 months without improvement. Physical examination showed an ill defined, large, ulcerated and nodular mass measuring 5 x 5 cm, associated with multiple enlarged left axillary lymph nodes. An FNA was performed.
Cytology images:
Diagnosis:
Merkle cell carcinoma
Discussion:
Test question (answer at the end):
Which statement is true for Merkel cell carcinoma:
A. It typically is slow growing and has indolent behavior.
B. It is a small blue cell tumor and has prominent nucleoli.
C. It cytologically resembles small cell carcinoma, with poorly cohesive cells, molding and crush artifact.
D. A majority of cases, even those with a combined phenotype with other carcinomatous elements, are associated with Merkel cell polyomavirus.
Merkel cell carcinoma (MCC), also called primary cutaneous neuroendocrine carcinoma, is an aggressive neoplasm, typically presenting as a slow growing nodule on the sun exposed skin of older adults. It is rare, but increasing in incidence. There is a slight male predominance, and most patients are Caucasian. Immune compromise increases its risk (ACS - Merkel cell carcinoma risk factors). Clinically, the lesion is red to violet and 20% of cases are ulcerated (Wick: Silverberg's Principles and Practice of Surgical Pathology and Cytopathology, 5th ed, 2015).
Microscopically, MCC falls into the "small round blue cell" category – the cells are monotonous with scant cytoplasm, rounded nuclei, fine chromatin and inconspicuous nuclei. There is generally a high mitotic rate with focal necrosis. "Blue buttons" – aggregates of intermediate filaments – can be seen in the cytoplasm but are not specific for MCC (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). Histologically the tumor cells can grow in sheets, nests and trabeculae (hence its original name, trabecular carcinoma) that are centered in the dermis, with invasion into the subcutis. The stroma can be mucinous.
Cytologically, as in this case, MCC resembles small cell carcinoma, with poorly cohesive cells, molding and crush artifact. Rare rosette-like structures can be seen in smears (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011, Coll Antropol 2010;34:691, Coll Antropol 2010;34:665).
MCC can show purely neuroendocrine differentiation, or can have a combined phenotype with other carcinomatous elements, such as squamous cell carcinoma and eccrine carcinoma, or can have sarcomatous elements (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). 80% of cases are associated with Merkel cell polyomavirus; however, tumors with combined phenotypes have been consistently negative for polyomavirus (Hum Pathol 2015;46:1290).
The differential diagnosis includes other small round blue cell tumors such as small cell carcinoma. On cytology, MCC typically shows less molding, less crush artifact and more monotony than small cell carcinoma (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). Neuroendocrine markers are positive in most MCCs, as they are in small cell carcinomas. Most, but not all, MCCs show a characteristic perinuclear dot-like positivity for CK20 (and other low molecular weight cytokeratins), corresponding to the "blue buttons". Up to 60% can stain positive for CD99 in a perinuclear dot-like pattern, membranous pattern or both (Int J Surg Pathol 2016;24:293). S100 can be positive, but TTF1 and CD45 should be negative (DeMay: The Art & Science of Cytopathology, 2nd Ed, 2011). Some cases are positive for c-kit, but therapeutic trials of tyrosine kinase inhibitors in patients with advanced disease have not shown a benefit (Hum Pathol 2015;46:1290). A monoclonal antibody against the Merkel cell polyomavirus large T antigen, called CM2B4, has a sensitivity and specificity of 94% each for diagnosis when compared to real time PCR for the virus (Diagn Pathol 2014 20;9:65).
For this case, immunohistochemical stains were performed on the cell block. There was diffuse and intense perinuclear dot-like staining for CK20, and positivity for chromogranin and synaptophysin. No reactivity was detected for TTF1, CD45, p63, CK5, CK6, MelanA or S100. The cytologic findings were interpreted as malignant, small round blue cell tumor, consistent with MCC. Surgical excision of the mass and lymph nodes was performed. The histopathologic diagnosis was MCC. The lymph nodes were positive for metastatic disease. The patient was started on chemotherapy.
Five year survival decreases from 80% in early stage disease to 20% for advanced disease (ACS - Survival rates for Merkel cell carcinoma, by stage). Some studies have shown a worse prognosis if tumors are negative for Merkel cell polyomavirus (Hum Pathol 2015;46:1290). The mainstay of therapy is wide local excision, selective lymphadenectomy and radiation. Somatostatin analogs may provide palliative relief of neuroendocrine symptoms. A study of PD-1 immune checkpoint inhibitors in patients with advanced MCC showed a response rate of 62% in polyomavirus positive tumors and 44% in polyomavirus negative tumors. Interestingly, despite the aggressiveness of MCC, spontaneous complete regression occurs in up to 2% of cases (J Cutan Pathol 2016;43:1150).
Test Question Answer:
C. A is incorrect, because although it is typically slow growing, it has aggressive behavior. B is incorrect because although it is a small blue cell tumor, it has indistinct nucleoli. D is incorrect because cases with a combined phenotype are not associated with Merkel cell polyomavirus.
Discussion edited by: Dr. Hillary Z. Kimbrell, Myriad Genetics, Inc., Utah (USA)