27 January 2016 - Case of the Week #377
All cases are archived on our website. To view them sorted by number, diagnosis or category, visit our Home Page and click on the Case of the Week button. To subscribe or unsubscribe to the Case of the Week or our other email lists, click here.
Thanks to Dr. Koteeswaran Govindaswamy, Mahatma Gandhi Medical College and Research Institute (India), for contributing this case. To contribute a Case of the Week, follow the guidelines on our main Case of the Week page.
Advertisement
Website news:
(1) Jason R. Rosen, D.O. of Winthrop-University Hospital has asked our help to publicize his survey for current residents, fellows and junior attendings about their experience with their program and professionalism. To complete the survey, click here.
(2) Our CD Markers chapter has been transferred to our new format. The new format has a table of contents for each topic, is mobile-friendly, has images sorted by reliability of links, and has been link checked to ensure all text and image links are valid, at least as of today.
(3) It is an overwhelming task to keep our free online textbook up to date, but we are working towards a goal of updating each topic every 2 years. At approximately 7,000 topics, this means posting 70 updates a week. Since we started keeping track in May 2015, we have updated 191 topics. Currently we are averaging 8 topic updates per week, so we have a ways to go.
We currently have 6 active Editors and 33 active Authors, with a goal of 20 Editors and 60 Authors by the end of 2016. Qualifications for Authors are listed on our Instructions for Authors page. If you meet these qualifications, want to help pathologists worldwide, and are NOT motivated primarily by money, please email NatPernick@gmail.com your CV and indicate your areas of interest.
Visit our Blog and Subscribe to our Posts or Follow by Email (click on the box on the right side) to see recent updates to the website.
Case of the Week #377
Clinical history:
A 29 year old old woman had a swelling at the nape of neck since 10 years of age, now measuring 2 x 1.5 cm and diagnosed clinically as lipoma. The lesion was excised.
Gross description:
The specimen was a skin covered nodule measuring 2 x 1.5 cm. The cut surface was cystic, containing gelatinous fluid and a central greyish white soft area measuring 1.0 x 0.3 cm.
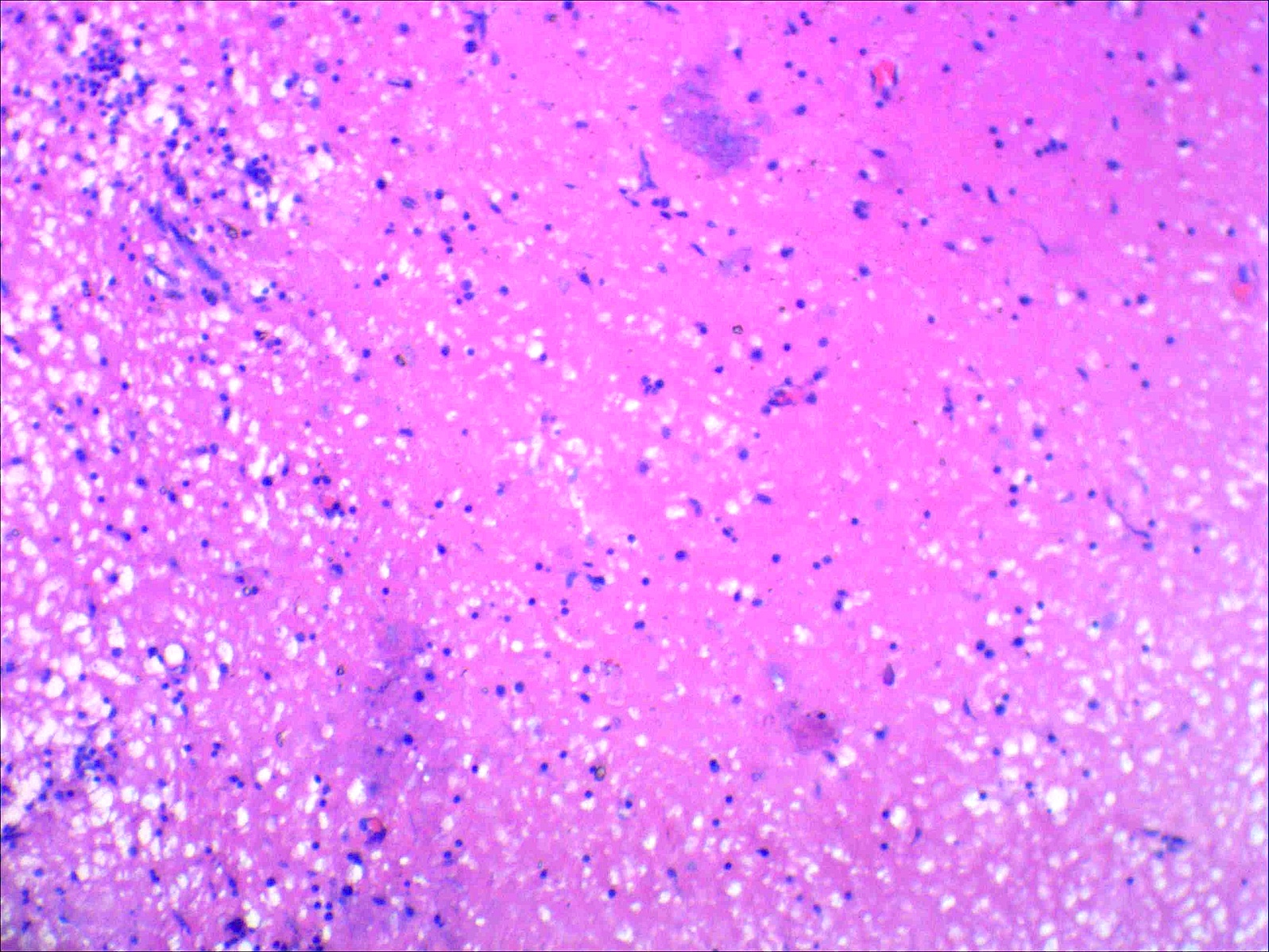
Micro images:
What is your diagnosis?
Diagnosis:
Lymphatic malformation with solid and cystic (mixed large and smaller) features
Discussion:
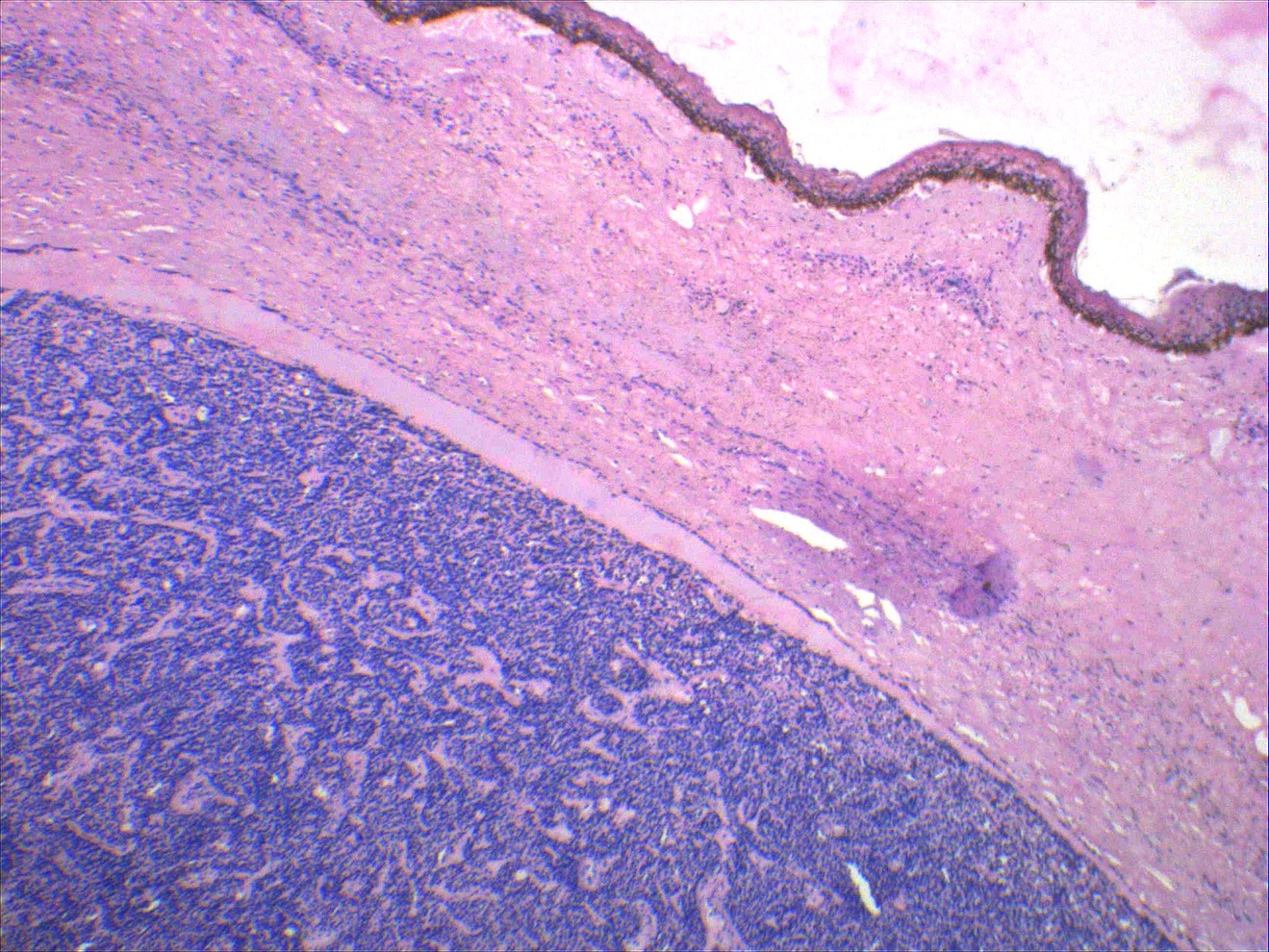
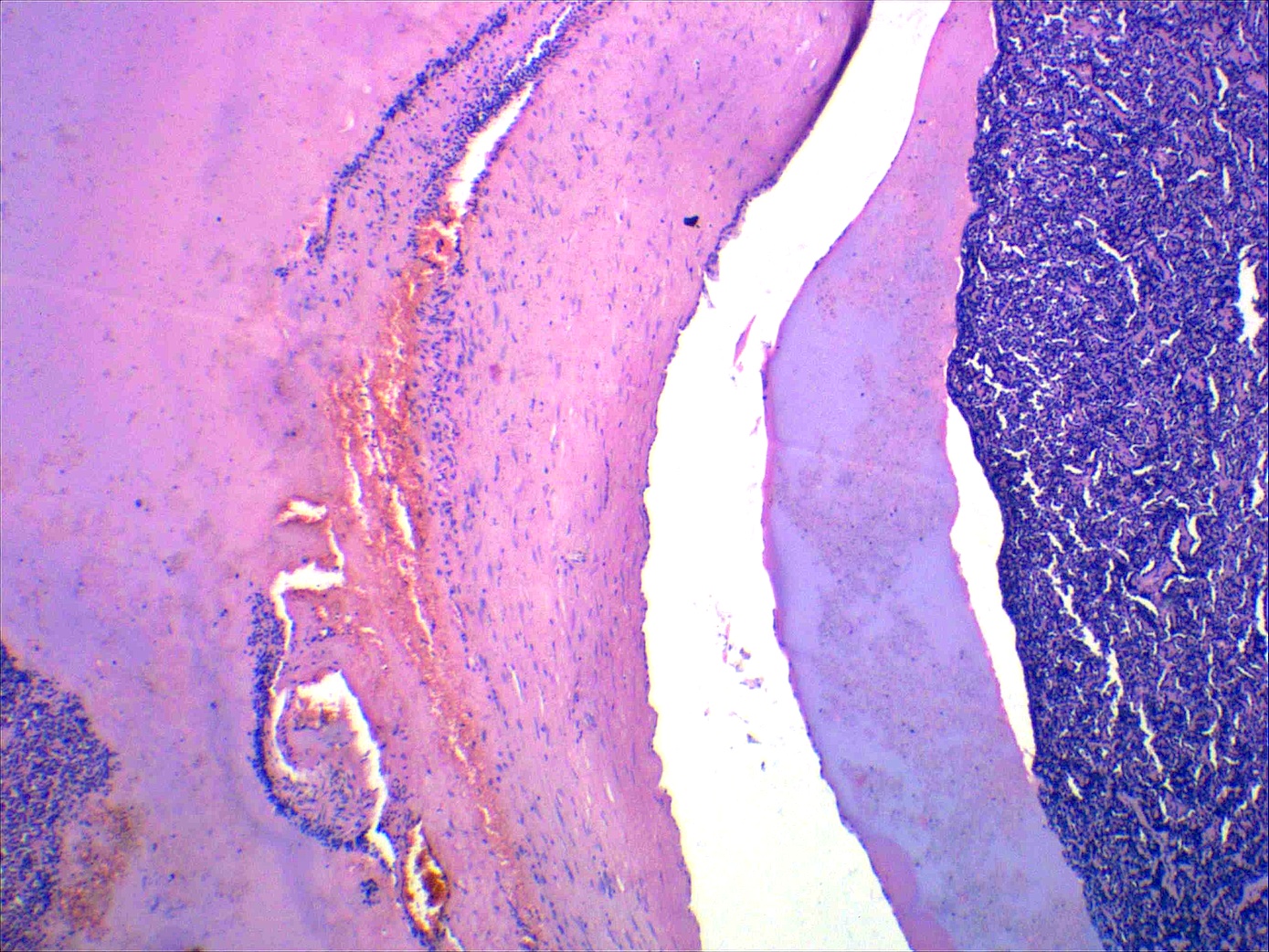
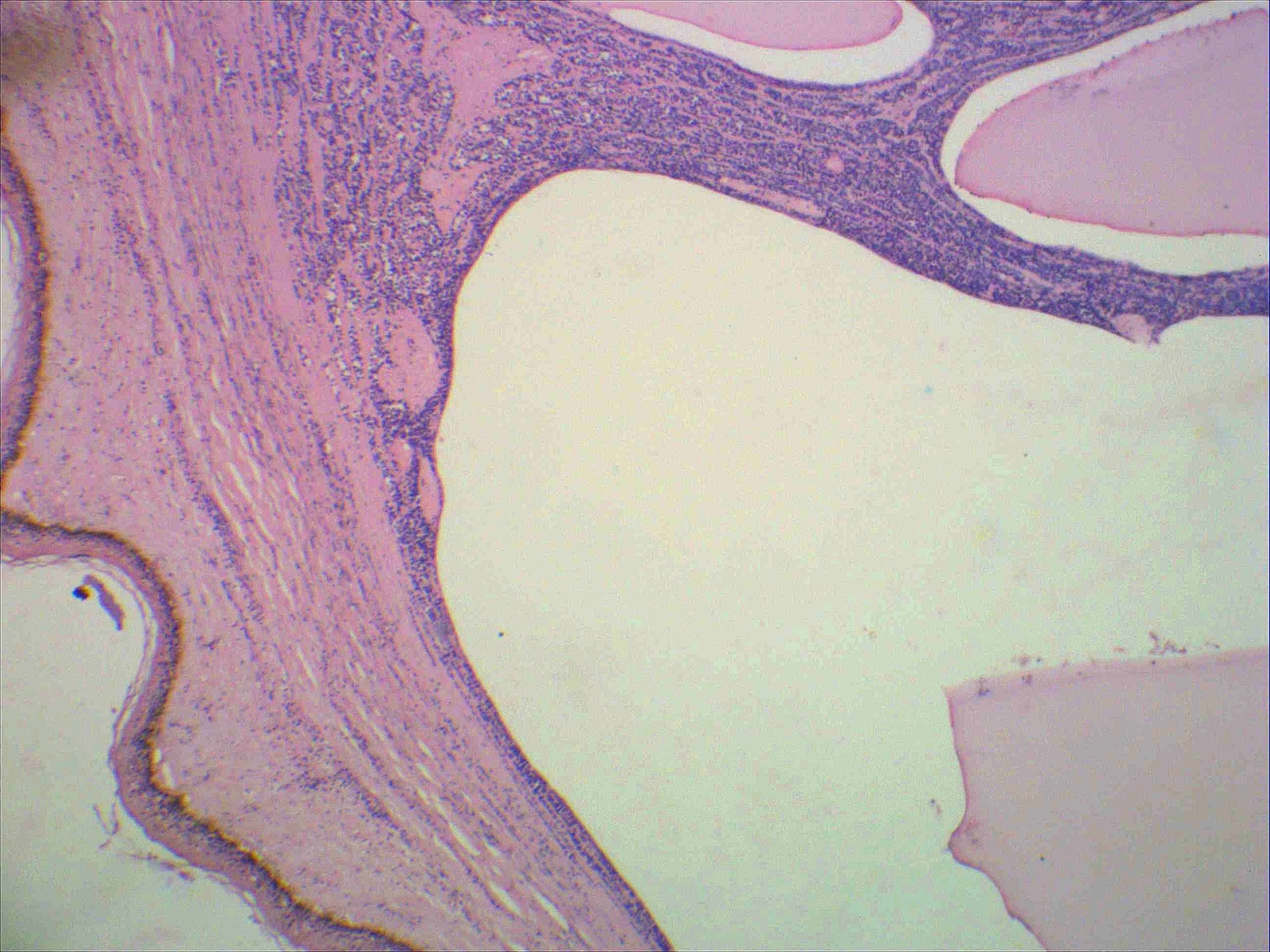
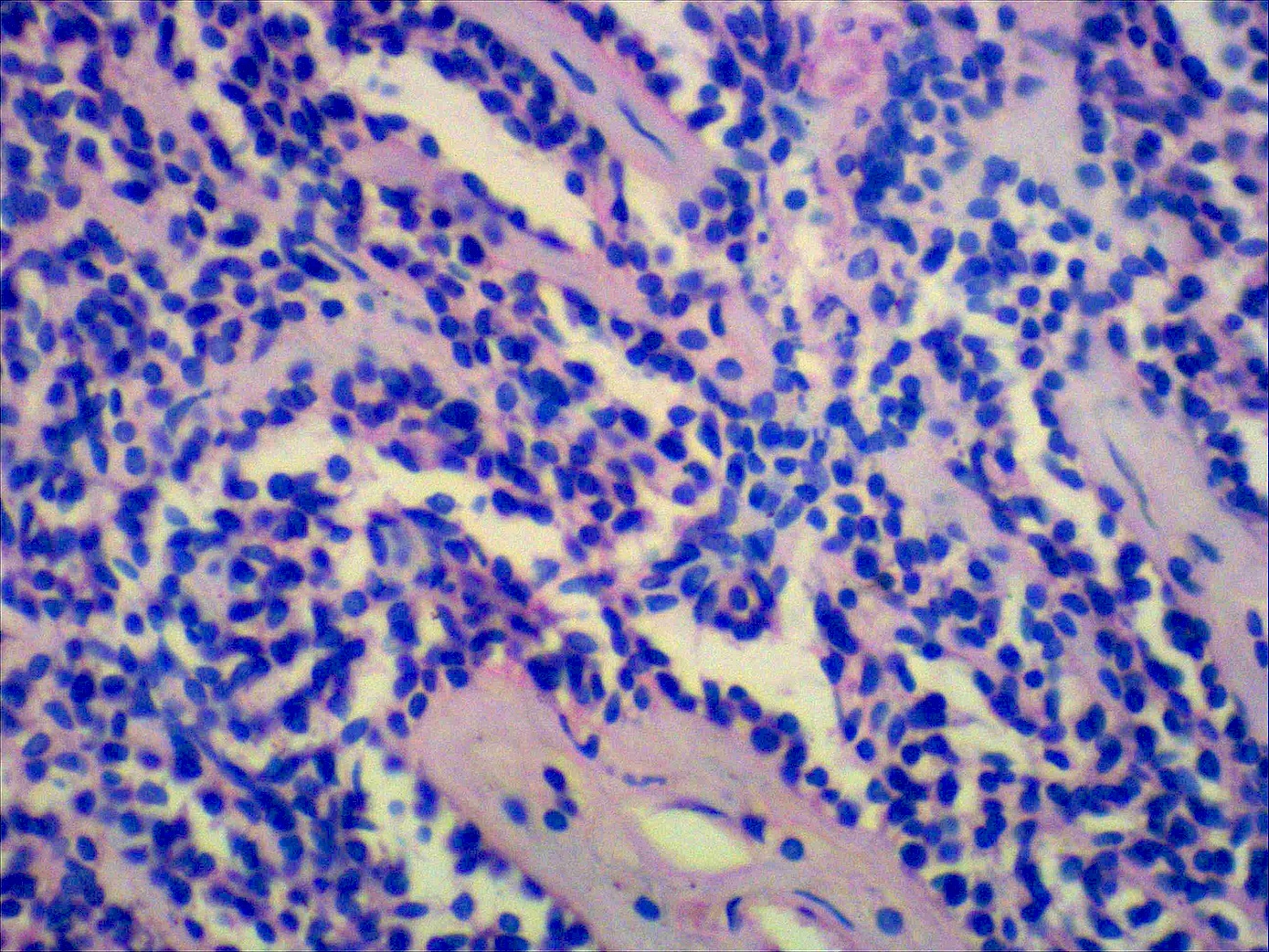
Histopathology shows skin with an attenuated epidermis and large, variably-sized cystic spaces in the dermis containing eosinophilic, proteinaceous lymphatic fluid. These cystic spaces are lined by flattened, banal endothelial cells. Within the interstitium are small lymphoid aggregates. The channels are highlighted by D2-40, a lymphatic endothelial marker.
Lymphatic malformations usually occur in the cervical region and involve the posterior triangle of the neck, and were classified by Mulliken and Young into microcystic, macrocystic and mixed types (Mulliken, Young: Vascular birthmarks: hemangiomas and malformations, 1988). The microcystic type includes lymphangioma circumscriptum, verrucous hemangioma and angiokeratoma circumscriptum. The macrocystic type includes cavernous lymphangioma and cystic hygroma and is often multiloculated with thin-walled septa. Focal lymphoid aggregates are often seen, which may also contain lymphatic spaces. Some cases, including the presented case, may have extensive lymphoid aggregates which can be mistaken for pseudolymphoma. Pseudolymphoma would demonstrate germinal centers mixed with plasma cells. A malignant vascular lesion can be excluded by the lack of significant cytologic atypia among endothelial cells and a reassuring growth pattern of the lesion (well-formed vascular channels and relative circumscription).
Treatment is usually by surgical excision, but nonsurgical techniques such as cryotherapy have been used with lesser results. The prognosis is excellent and there is no malignant transformation associated with lymphatic malformation. Of note, the term "lymphangioma" has the potential to cause anxiety to patients as it implies a neoplastic lesion; thus the designation "cystic lymphatic malformation" may be preferred for localized malformations of lymphatics.
References: Patterson: Weedon's Skin Pathology, 2015, J Cutan Aesthet Surg 2010;3:139, Barnhill: Dermatopathology: Third Edition, 2010, J Maxillofac Oral Surg 2010;9:284
Discussion edited by Dr. Jennifer R. Kaley, University of Arkansas for Medical Sciences (USA).
All cases are archived on our website. To view them sorted by number, diagnosis or category, visit our Home Page and click on the Case of the Week button. To subscribe or unsubscribe to the Case of the Week or our other email lists, click here.
Thanks to Dr. Koteeswaran Govindaswamy, Mahatma Gandhi Medical College and Research Institute (India), for contributing this case. To contribute a Case of the Week, follow the guidelines on our main Case of the Week page.
Advertisement
Website news:
(1) Jason R. Rosen, D.O. of Winthrop-University Hospital has asked our help to publicize his survey for current residents, fellows and junior attendings about their experience with their program and professionalism. To complete the survey, click here.
(2) Our CD Markers chapter has been transferred to our new format. The new format has a table of contents for each topic, is mobile-friendly, has images sorted by reliability of links, and has been link checked to ensure all text and image links are valid, at least as of today.
(3) It is an overwhelming task to keep our free online textbook up to date, but we are working towards a goal of updating each topic every 2 years. At approximately 7,000 topics, this means posting 70 updates a week. Since we started keeping track in May 2015, we have updated 191 topics. Currently we are averaging 8 topic updates per week, so we have a ways to go.
We currently have 6 active Editors and 33 active Authors, with a goal of 20 Editors and 60 Authors by the end of 2016. Qualifications for Authors are listed on our Instructions for Authors page. If you meet these qualifications, want to help pathologists worldwide, and are NOT motivated primarily by money, please email NatPernick@gmail.com your CV and indicate your areas of interest.
Visit our Blog and Subscribe to our Posts or Follow by Email (click on the box on the right side) to see recent updates to the website.
Case of the Week #377
Clinical history:
A 29 year old old woman had a swelling at the nape of neck since 10 years of age, now measuring 2 x 1.5 cm and diagnosed clinically as lipoma. The lesion was excised.
Gross description:
The specimen was a skin covered nodule measuring 2 x 1.5 cm. The cut surface was cystic, containing gelatinous fluid and a central greyish white soft area measuring 1.0 x 0.3 cm.
Micro images:
What is your diagnosis?
Diagnosis:
Lymphatic malformation with solid and cystic (mixed large and smaller) features
Discussion:
Histopathology shows skin with an attenuated epidermis and large, variably-sized cystic spaces in the dermis containing eosinophilic, proteinaceous lymphatic fluid. These cystic spaces are lined by flattened, banal endothelial cells. Within the interstitium are small lymphoid aggregates. The channels are highlighted by D2-40, a lymphatic endothelial marker.
Lymphatic malformations usually occur in the cervical region and involve the posterior triangle of the neck, and were classified by Mulliken and Young into microcystic, macrocystic and mixed types (Mulliken, Young: Vascular birthmarks: hemangiomas and malformations, 1988). The microcystic type includes lymphangioma circumscriptum, verrucous hemangioma and angiokeratoma circumscriptum. The macrocystic type includes cavernous lymphangioma and cystic hygroma and is often multiloculated with thin-walled septa. Focal lymphoid aggregates are often seen, which may also contain lymphatic spaces. Some cases, including the presented case, may have extensive lymphoid aggregates which can be mistaken for pseudolymphoma. Pseudolymphoma would demonstrate germinal centers mixed with plasma cells. A malignant vascular lesion can be excluded by the lack of significant cytologic atypia among endothelial cells and a reassuring growth pattern of the lesion (well-formed vascular channels and relative circumscription).
Treatment is usually by surgical excision, but nonsurgical techniques such as cryotherapy have been used with lesser results. The prognosis is excellent and there is no malignant transformation associated with lymphatic malformation. Of note, the term "lymphangioma" has the potential to cause anxiety to patients as it implies a neoplastic lesion; thus the designation "cystic lymphatic malformation" may be preferred for localized malformations of lymphatics.
References: Patterson: Weedon's Skin Pathology, 2015, J Cutan Aesthet Surg 2010;3:139, Barnhill: Dermatopathology: Third Edition, 2010, J Maxillofac Oral Surg 2010;9:284
Discussion edited by Dr. Jennifer R. Kaley, University of Arkansas for Medical Sciences (USA).