6 May 2015 - Case #351
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Raul Gonzalez, University of Rochester Medical Center, New York (USA), for contributing this case.
Advertisement
Case #351
Clinical History:
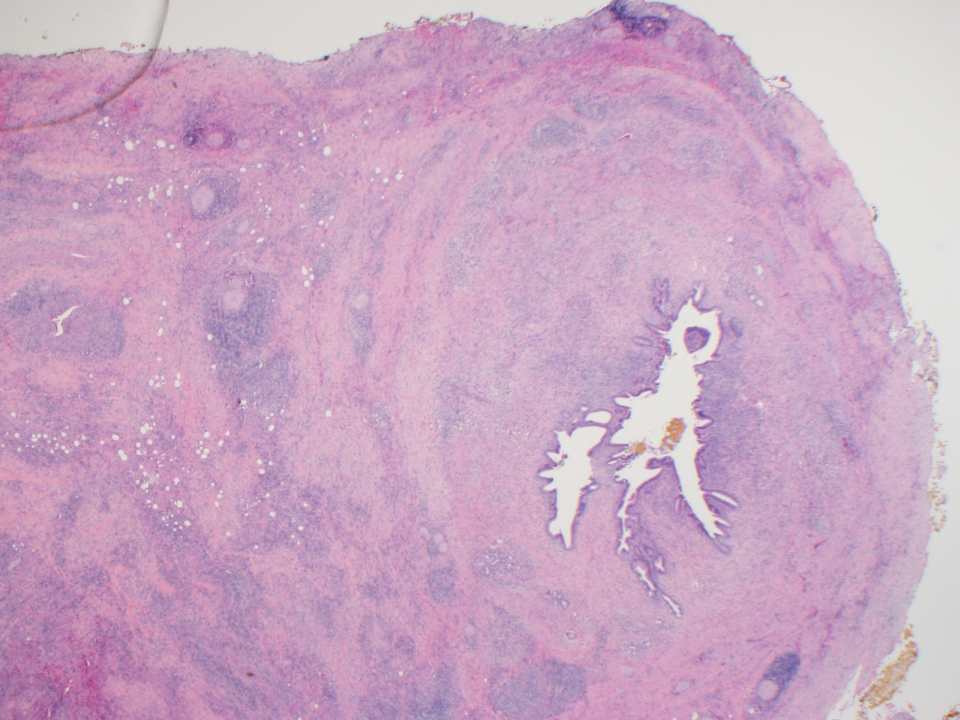
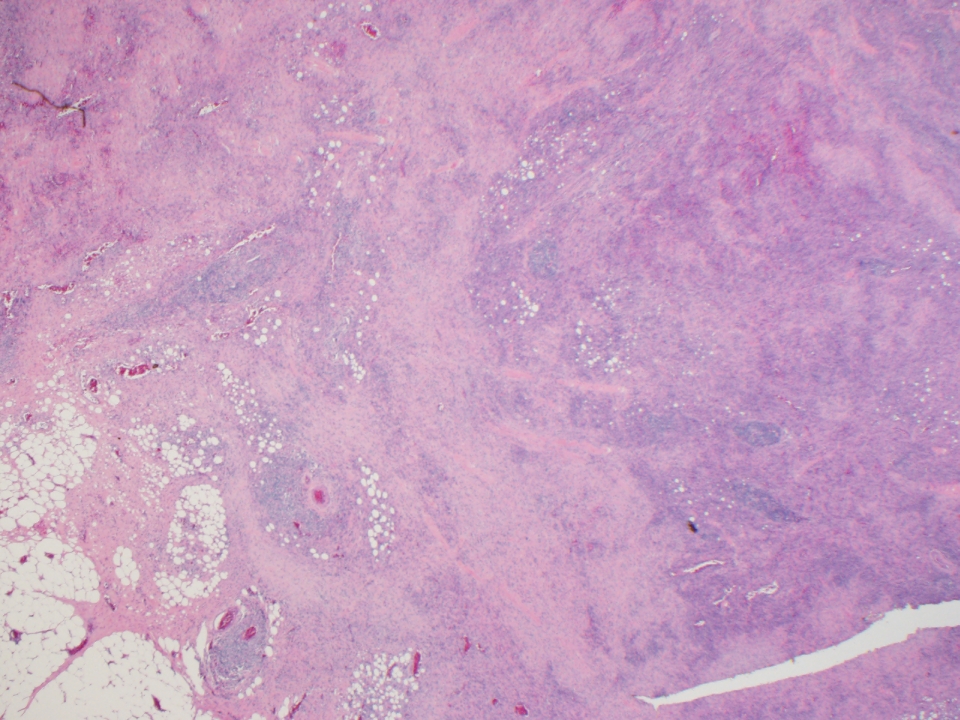
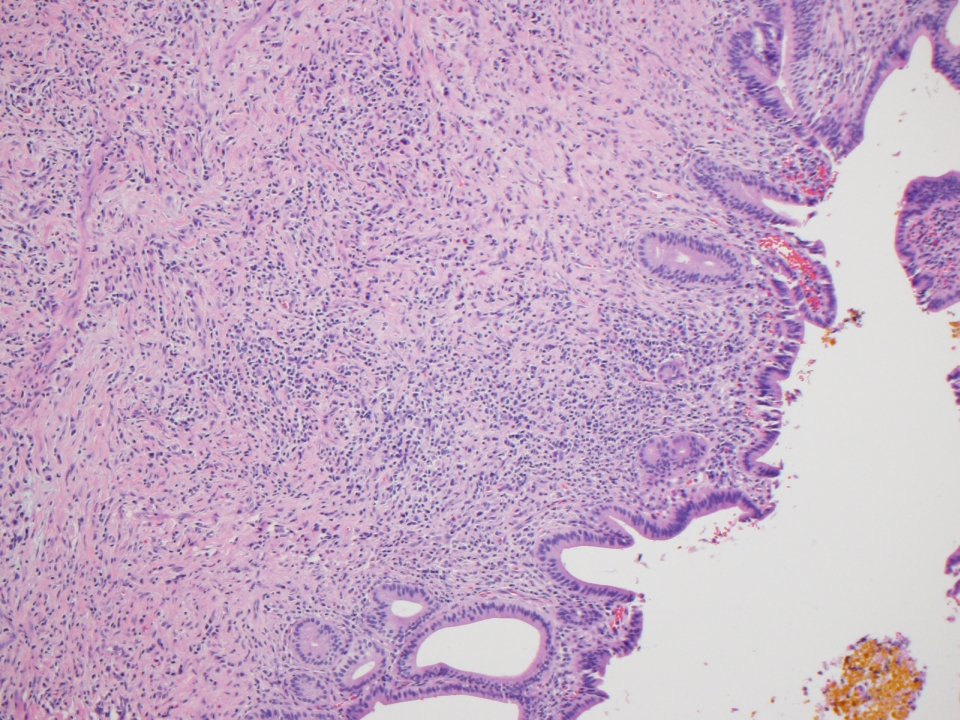
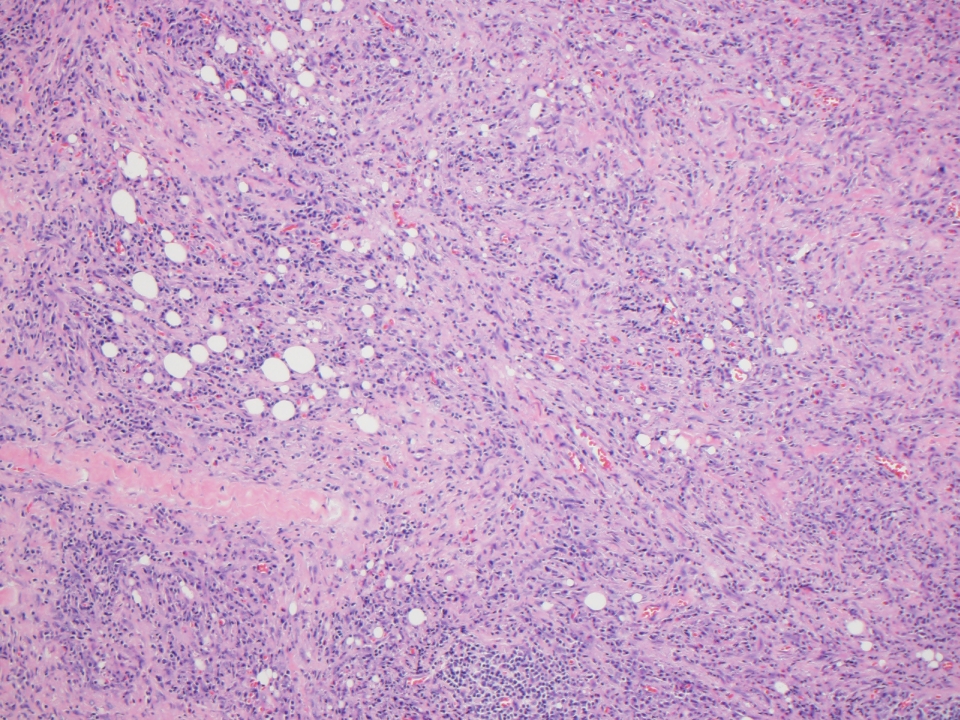
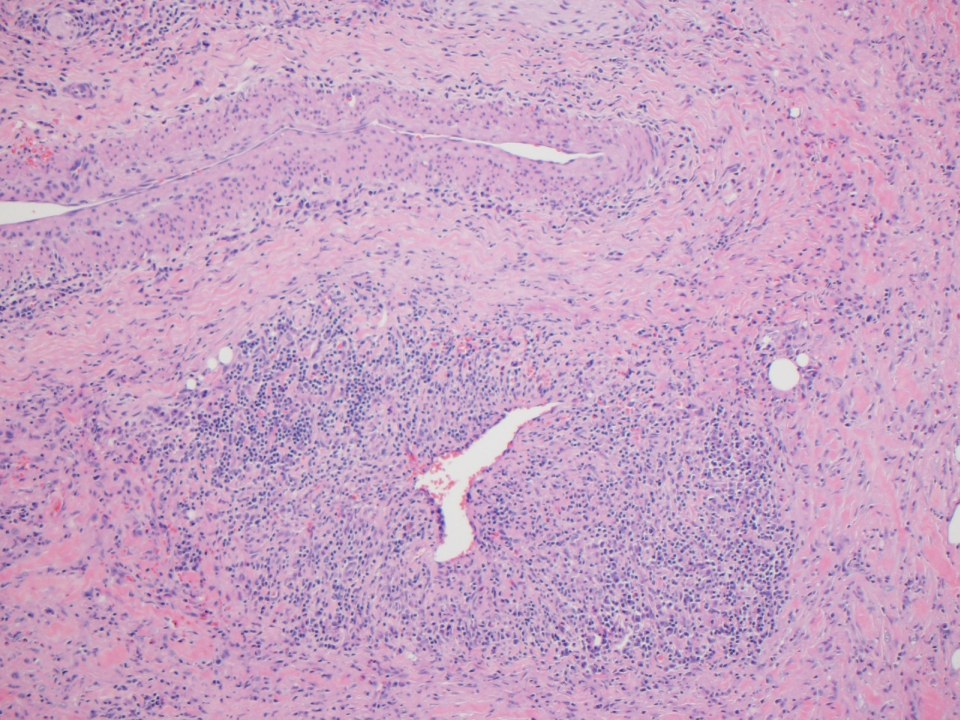
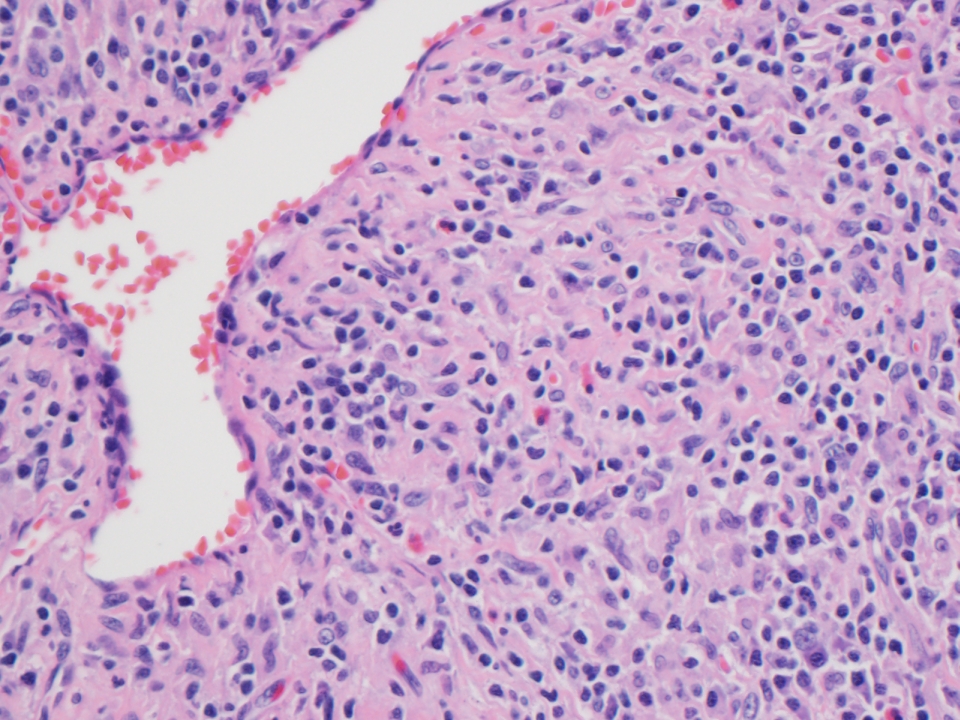
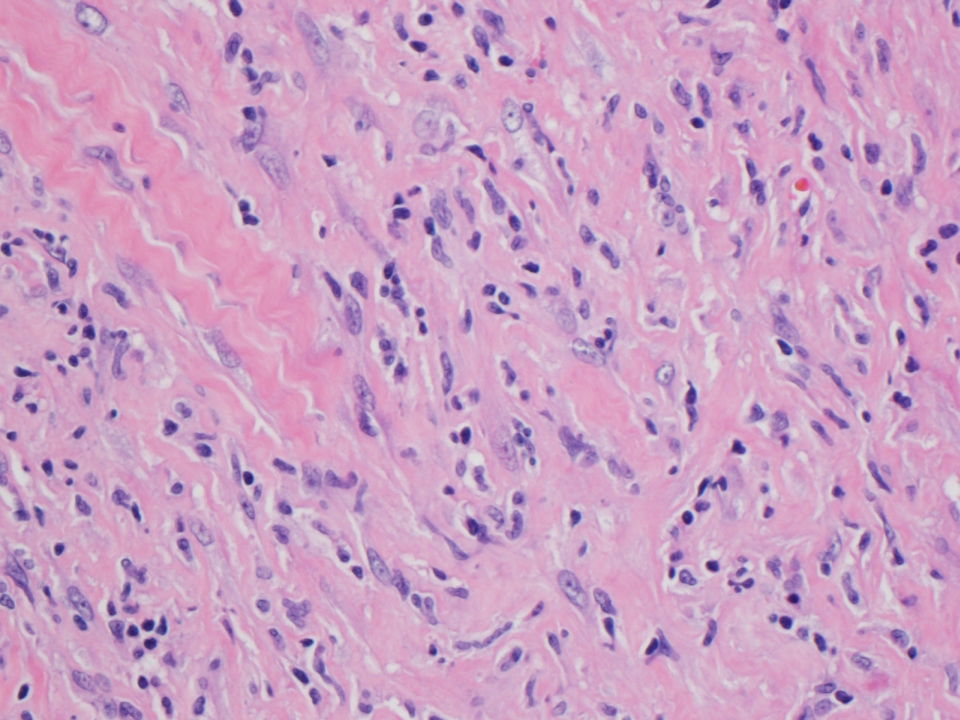
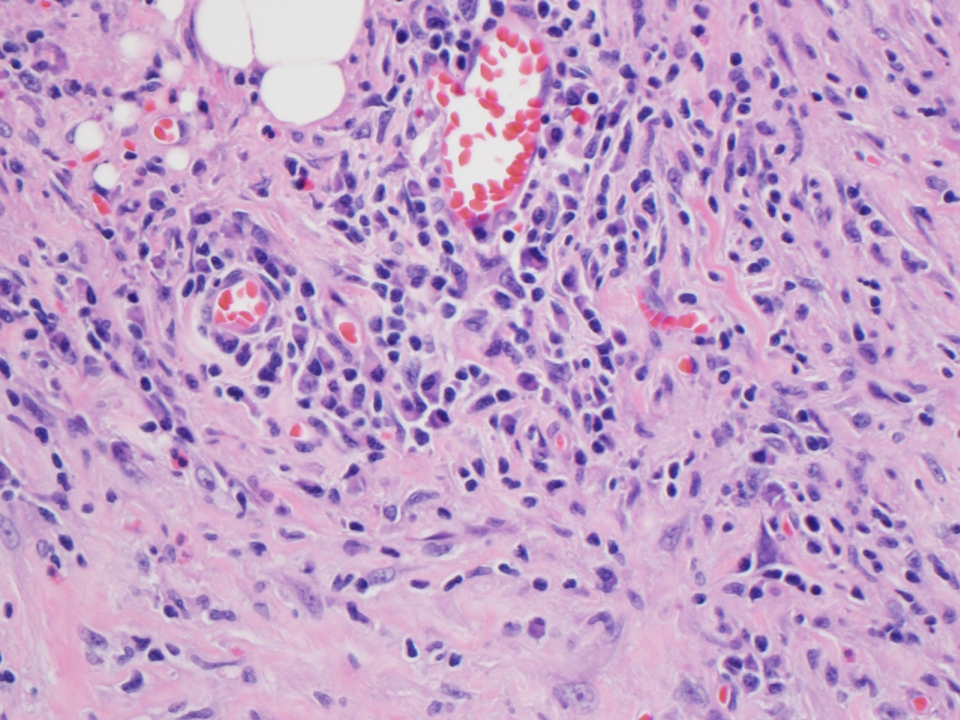
A 55 year old man had a common hepatic duct stricture, which was biopsied. Subsequently, he underwent a cholecystectomy and partial biliary tree resection, with sections below.
Microscopic images:
What is your diagnosis?
Diagnosis: IgG4 related sclerosing cholangitis
Discussion:
An IgG4 immunostain from the outside facility (image not available) showed > 100 IgG4+ plasma cells per HPF.
Primary sclerosing cholangitis occurs predominantly in men, usually under age 45 years. It often has an autoimmune origin, as 50 - 70% also have inflammatory bowel disease (particularly ulcerative colitis), although only 4% with ulcerative colitis have primary sclerosing cholangitis.
Histologic features include:
A newly recognized cause of secondary sclerosing cholangitis is IgG4 associated cholangitis. It is typically associated with autoimmune pancreatitis, although isolated intrapancreatic cases without autoimmune pancreatitis have been reported (World J Gastroenterol 2015;21:1334).
Patients with tissue IgG4 positivity have a more aggressive clinical course, including shorter time to transplant and higher likelihood of recurrence (Am J Surg Pathol 2010;34:88). Diagnostic criteria includes 10+ IgG4+ plasma cells/HPF at biopsy, although a cutoff of 50 has been recommended (Scand J Gastroenterol 2015;50:447).
Steroid treatment is standard. Assessment of steroid responsiveness, a diagnostic criteria, is recommended after initiation of treatment at 5 and 10 days, by testing serum total bilirubin, alanine aminotransferase and alkaline phosphatase and at 1 - 2 weeks by endoscopic retrograde cholangiography and magnetic resonance cholangiopancreatography (Adv Med Sci 2015;60:211).
The differential diagnosis includes cholangiocarcinoma / bile duct carcinoma because the entities may be clinically similar (Int Surg 2015;100:480, Hepatogastroenterology 2014;61:1852, Hum Pathol 2014;45:1722).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Raul Gonzalez, University of Rochester Medical Center, New York (USA), for contributing this case.

Scientific Symposiums International Summer CME Series
Critical Issues in Cutaneous Pathology: What's New as Critical New Information for Your Practice
June 22-25, 2015
The Kingsmill Resort, Williamsburg, VA
Register for our upcoming Dermatopathology course being held this June in order to learn the latest issues and tools affecting your practice.
Our world-renowned faculty includes Dirk M. Elston, M.D., Christine J. Ko M.D., Larry Gibson, M.D., and Tammy Ferringer, M.D.
This course is one not to be missed! Space is limited so register now!
Website news:
(1) We have now added the names of all the Case of the Week contributors to our main Case of the Week page. We thank all of our contributors once again - and don't forget to check out our upcoming cases for the next few weeks!
(2) Shop Amazon.com and Win! Win a $100, $50 or $25 Amazon Gift Card. To promote shopping at Amazon.com, particularly by going through our website, we will award Amazon gift cards of $100, $50 and $25 through a drawing of those who made purchases at Amazon in May or June 2015. Click here to see the contest rules.
Visit and follow our Blog to see recent updates to the website.
(1) We have now added the names of all the Case of the Week contributors to our main Case of the Week page. We thank all of our contributors once again - and don't forget to check out our upcoming cases for the next few weeks!
(2) Shop Amazon.com and Win! Win a $100, $50 or $25 Amazon Gift Card. To promote shopping at Amazon.com, particularly by going through our website, we will award Amazon gift cards of $100, $50 and $25 through a drawing of those who made purchases at Amazon in May or June 2015. Click here to see the contest rules.
Visit and follow our Blog to see recent updates to the website.
Case #351
Clinical History:
A 55 year old man had a common hepatic duct stricture, which was biopsied. Subsequently, he underwent a cholecystectomy and partial biliary tree resection, with sections below.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: IgG4 related sclerosing cholangitis
Discussion:
An IgG4 immunostain from the outside facility (image not available) showed > 100 IgG4+ plasma cells per HPF.
Primary sclerosing cholangitis occurs predominantly in men, usually under age 45 years. It often has an autoimmune origin, as 50 - 70% also have inflammatory bowel disease (particularly ulcerative colitis), although only 4% with ulcerative colitis have primary sclerosing cholangitis.
Histologic features include:
- Fibrosing cholangitis of intra and extrahepatic bile ducts (large and small) with lymphocytic infiltration
- Progressive atrophy of bile duct epithelium and obliteration of the lumen, with diffuse bile ductular proliferation
- Onion skin fibrosis around affected ducts, which later disappears, leaving a cord-like fibrous scar
- The remaining ducts are ectatic, inflamed and often elongated, with variable portal eosinophils
- Cirrhotic nodules, when present, have a jigsaw pattern due to portal to portal fibrosis; also present are gallbladder sclerosis and prominent lymphoid aggregates
- Post-transplant recurrences exhibit bile duct strictures and nonspecific autoimmune hepatitis with variable fibrosis (Eur Radiol 2014;24:1039)
A newly recognized cause of secondary sclerosing cholangitis is IgG4 associated cholangitis. It is typically associated with autoimmune pancreatitis, although isolated intrapancreatic cases without autoimmune pancreatitis have been reported (World J Gastroenterol 2015;21:1334).
Patients with tissue IgG4 positivity have a more aggressive clinical course, including shorter time to transplant and higher likelihood of recurrence (Am J Surg Pathol 2010;34:88). Diagnostic criteria includes 10+ IgG4+ plasma cells/HPF at biopsy, although a cutoff of 50 has been recommended (Scand J Gastroenterol 2015;50:447).
Steroid treatment is standard. Assessment of steroid responsiveness, a diagnostic criteria, is recommended after initiation of treatment at 5 and 10 days, by testing serum total bilirubin, alanine aminotransferase and alkaline phosphatase and at 1 - 2 weeks by endoscopic retrograde cholangiography and magnetic resonance cholangiopancreatography (Adv Med Sci 2015;60:211).
The differential diagnosis includes cholangiocarcinoma / bile duct carcinoma because the entities may be clinically similar (Int Surg 2015;100:480, Hepatogastroenterology 2014;61:1852, Hum Pathol 2014;45:1722).