17 April 2014 - Case #349
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Koteeswaran Govindaswamy, Mahatma Gandhi Medical College and Research Institute (India), for contributing this case.
Advertisement
Case #349
Clinical history:
A 45 year old man presented with noise in his left ear and mild hearing loss for one year He was diagnosed clinically with a pulsating tinnitus. A MRI of the temporal bone showed a well defined soft tissue mass in the left middle ear cavity involving the meso- and hypo-tympanus and encasing the middle ear ossicle. A mastoidectomy was performed.
Gross description:
Soft dark tan nodules in aggregate measuring 6 mm.
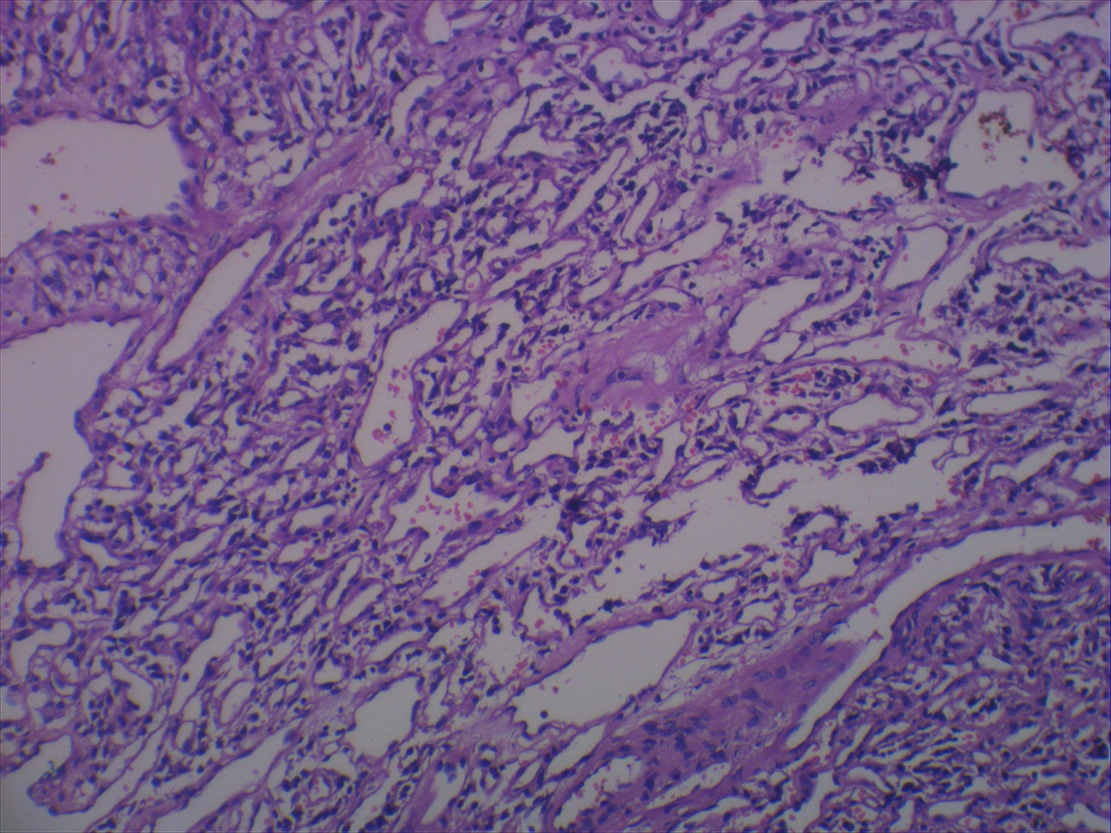
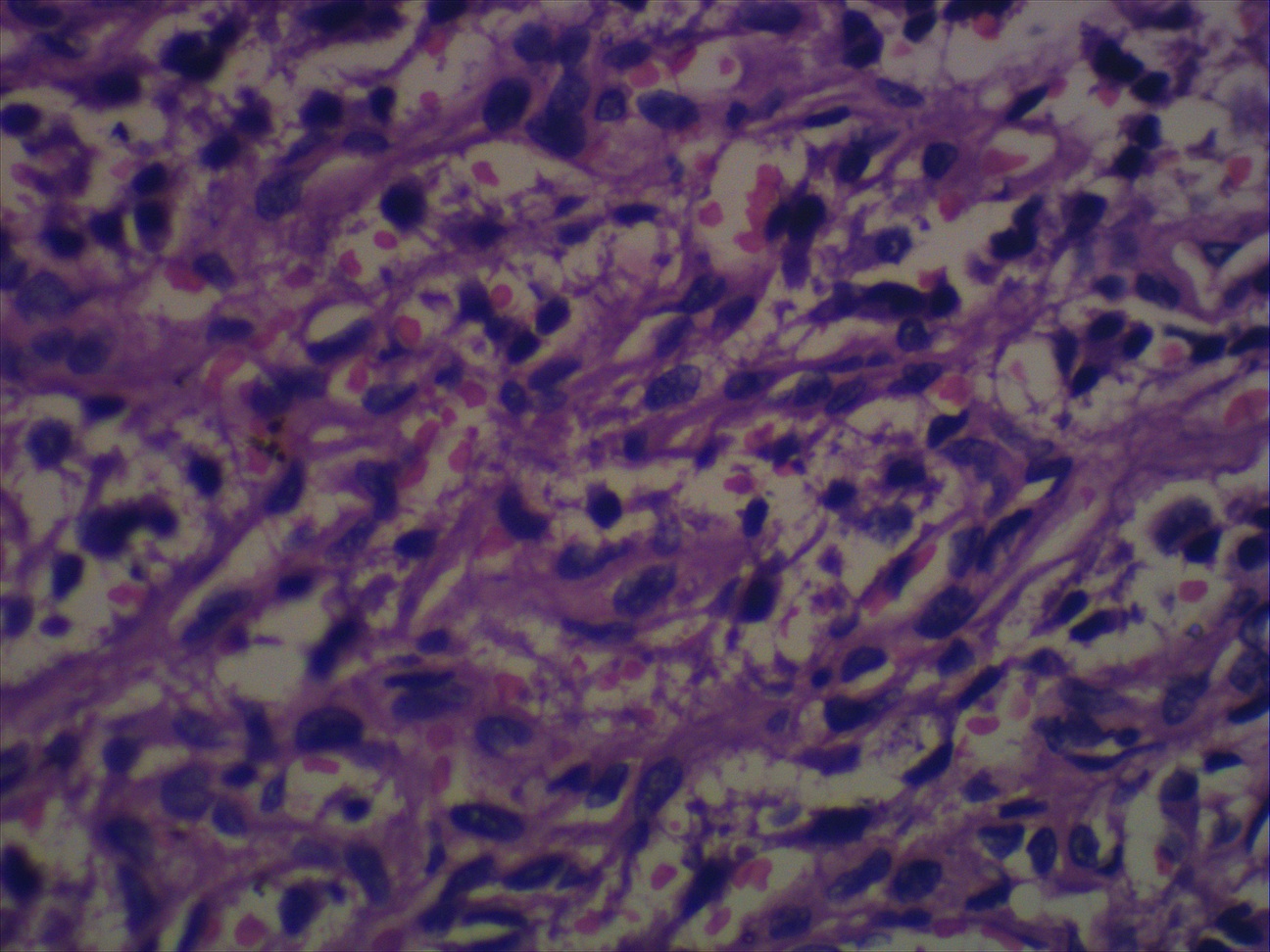
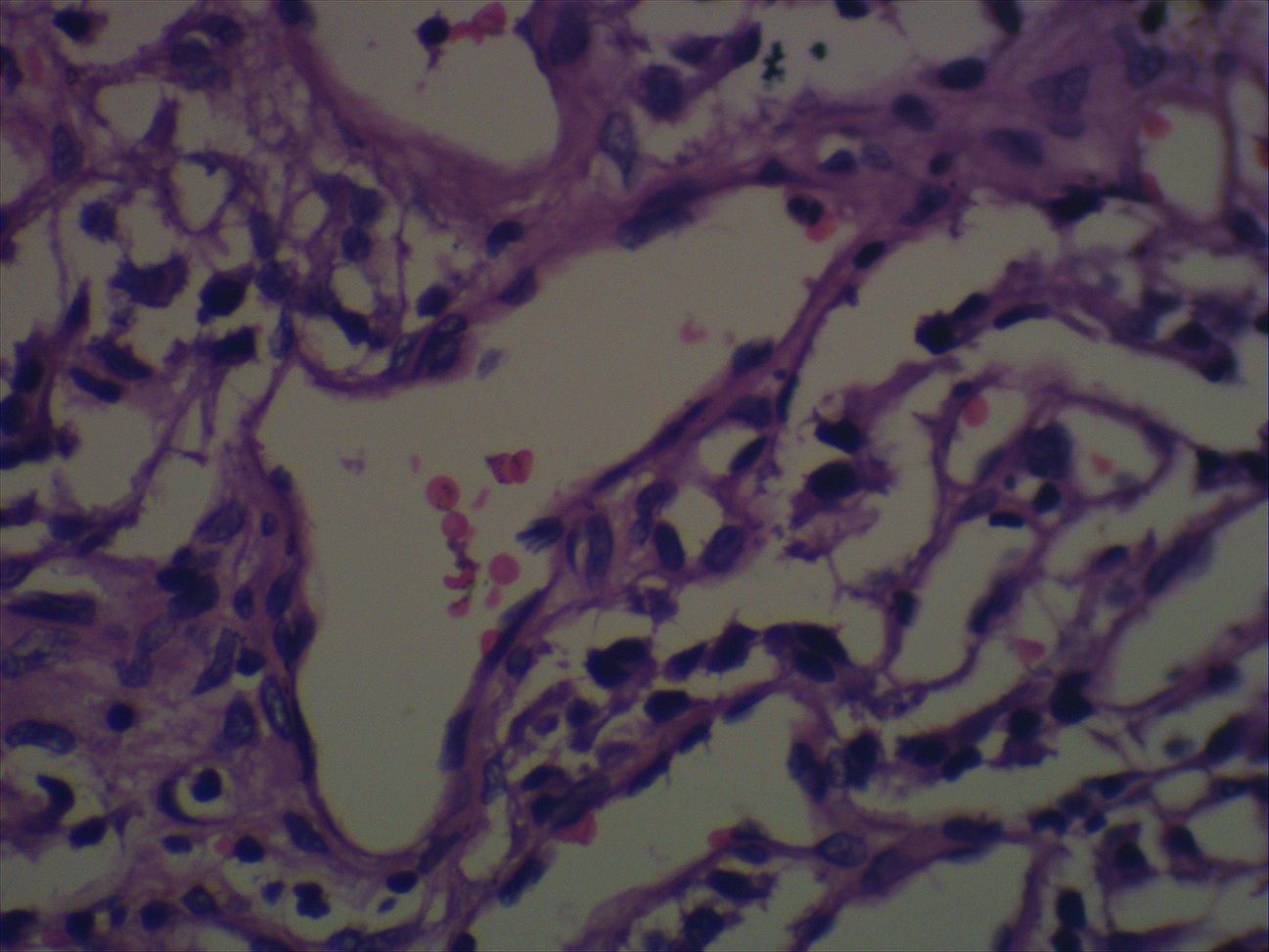
Microscopic images:
What is your diagnosis?
Diagnosis: Glomus tympanicum
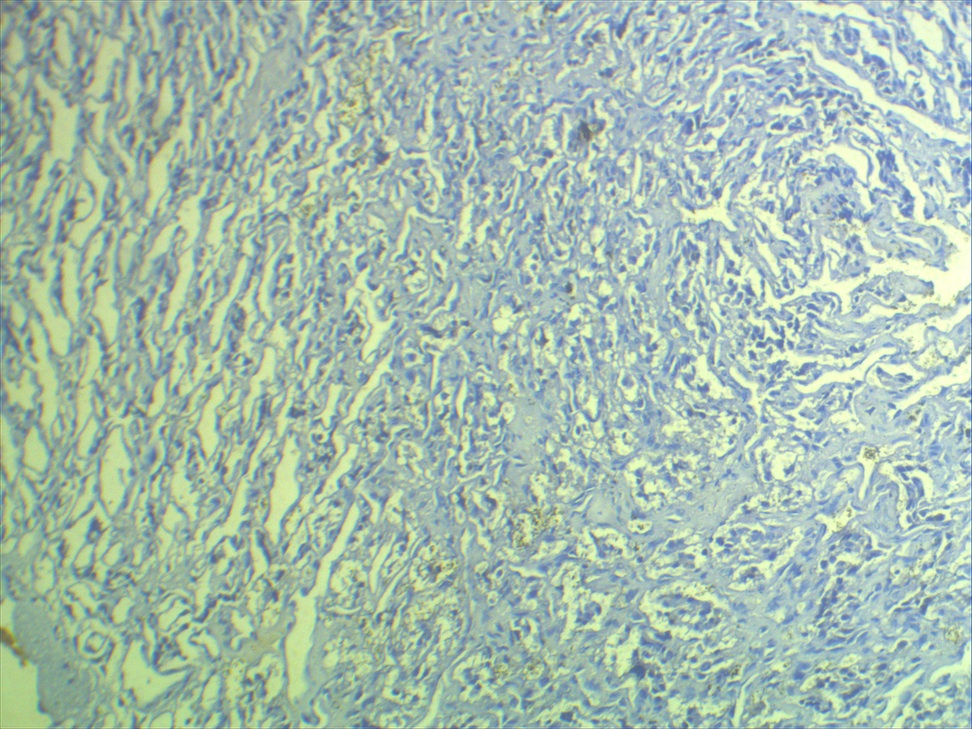
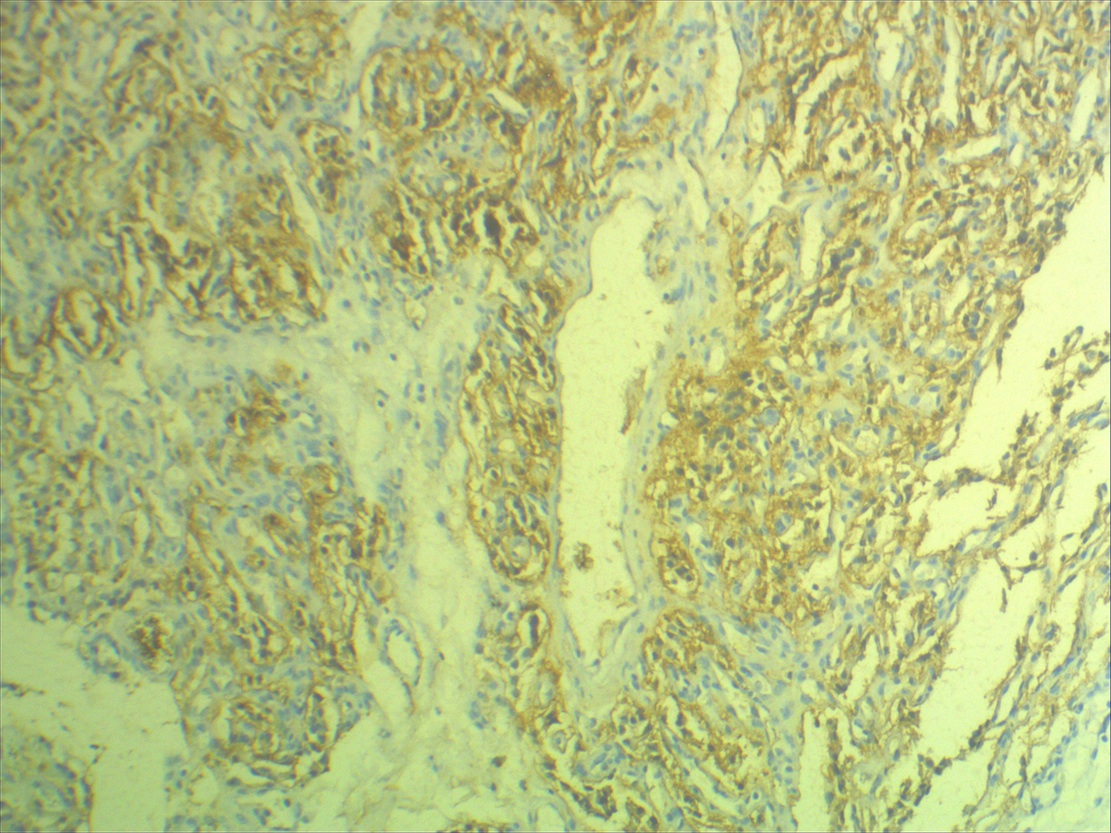
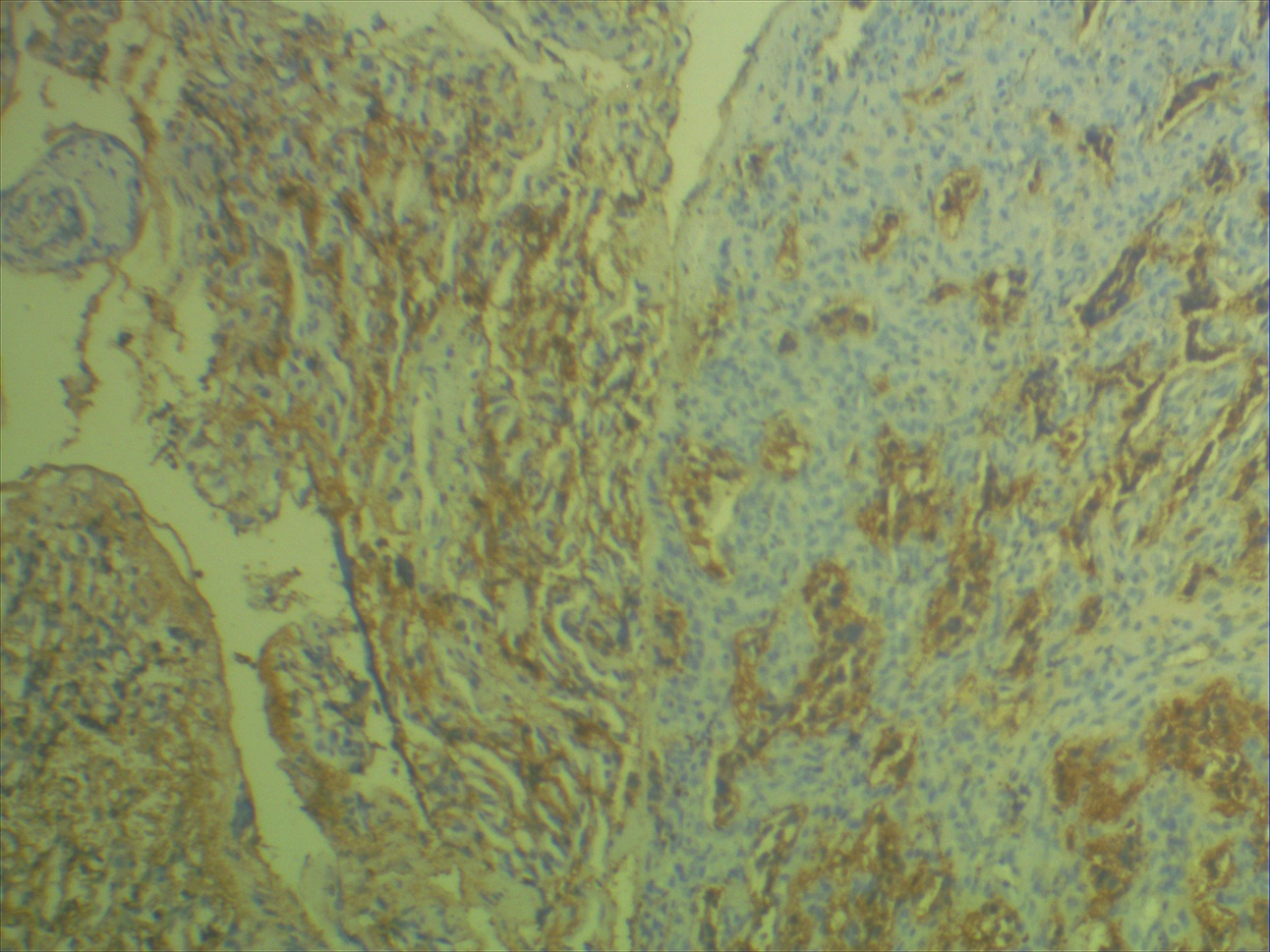
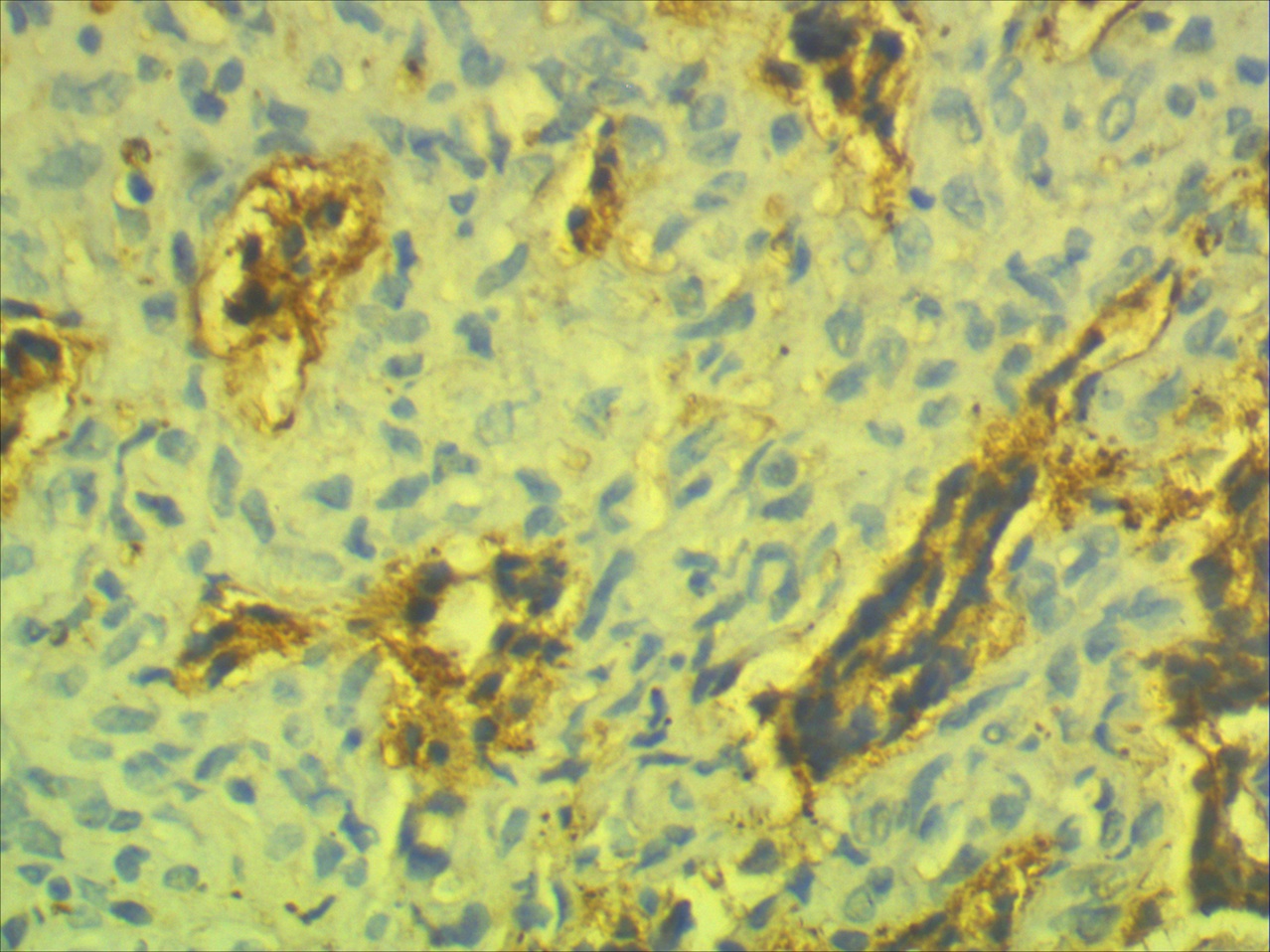
Immunostains:
Discussion:
Histology showed a neoplasm resembling a capillary hemangioma, composed primarily of variable sized capillary channels lined by a single layer of endothelial cells. An adjacent area was solid with closely packed small nests of round to epithelioid cells surrounded by capillaries. There were no mitoses.
S100 showed no definite sustentacular cells, likely obscured by capillaries. VEGF showed staining of vessels but no staining of most tumor cells.
Glomus tympanicum, also called jugulotympanic paraganglioma, is the most common tumor of the middle ear, usually occurring in women ages 40 - 69 years (eMedicine: Glomus Jugulare Tumors [Accessed 10 November 2023]). Most arise in the jugular bulb, causing a mass in the middle ear or external auditory canal. The remainder arise from the tympanic branch of the glossopharyngeal nerve, causing a middle ear mass or the posterior auricular branch of the vagus nerve, causing an external auditory canal mass. They usually cause a conductive hearing loss and may be locally invasive into the temporal bone and mastoid, causing cranial nerve palsies, cerebellar dysfunction, dysphagia or hoarseness.
Histologically, they have the classic organoid (zellballen) or nesting pattern of paragangliomas with central round / oval chief cells containing abundant eosinophilic granular or vacuolated cytoplasm and uniform nuclei with dispersed chromatin. Although difficult to identify in this case, sustentacular cells (spindled and basophilic) are usually present at the periphery of nests, which are separated by a fibrovascular stroma. Tumors typically have benign features but may have pleomorphism, dense fibrous stroma or apparent infiltration. Mitoses and necrosis are rare.
The chief cells in the tumor are immunoreactive for chromogranin and synaptophysin and typically the sustentacular cells are S100+. Reticulin stains the stroma and delineates the nesting pattern, which is particularly helpful with crushed specimens.
The differential diagnosis includes capillary hemangioma, which lack the organoid pattern and cellular composition (chief and sustentacular cells) of paragangliomas (Case Rep Otolaryngol 2012;2012:305172).
Common treatment options are surgery, which may be accompanied by profuse bleeding or radiosurgery / gamma knife, with low complication rates despite the location (Otolaryngol Head Neck Surg 2015;152:136, Auris Nasus Larynx 2010;37:661, Skull Base 2011;21:309, J Neurosurg 2014;121 Suppl:198). There is a low recurrence rate and occasional cases may have malignant behavior with metastases.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Koteeswaran Govindaswamy, Mahatma Gandhi Medical College and Research Institute (India), for contributing this case.
Advertisement
Website news:
(1) We now have a new server, which has an upgraded architecture, more memory and more storage. We apologize for the short down times the past few days but the new server should be a little faster and will support our expanded future capabilities.
(2) Our Feature page for April is Laboratory Accreditation / Education / CME and highlights our advertisers ARUP Laboratories, The American Society for Clinical Pathology (ASCP), Board Vitals, College of American Pathologists (CAP) and Educational Symposia. It also contains an original short article, "Laboratory Accreditation: The Business of Blood Banking", by Jaleh Mansouri, M.D.
(3) Thanks to your support, March 2015 had record traffic of 679,473 visits (average of 21,918 visits per day) and a record 2.62 million page views. Phase 2 of our Website upgrade will probably not start until mid May 2015.
Visit and follow our Blog to see recent updates to the website.
(1) We now have a new server, which has an upgraded architecture, more memory and more storage. We apologize for the short down times the past few days but the new server should be a little faster and will support our expanded future capabilities.
(2) Our Feature page for April is Laboratory Accreditation / Education / CME and highlights our advertisers ARUP Laboratories, The American Society for Clinical Pathology (ASCP), Board Vitals, College of American Pathologists (CAP) and Educational Symposia. It also contains an original short article, "Laboratory Accreditation: The Business of Blood Banking", by Jaleh Mansouri, M.D.
(3) Thanks to your support, March 2015 had record traffic of 679,473 visits (average of 21,918 visits per day) and a record 2.62 million page views. Phase 2 of our Website upgrade will probably not start until mid May 2015.
Visit and follow our Blog to see recent updates to the website.
Case #349
Clinical history:
A 45 year old man presented with noise in his left ear and mild hearing loss for one year He was diagnosed clinically with a pulsating tinnitus. A MRI of the temporal bone showed a well defined soft tissue mass in the left middle ear cavity involving the meso- and hypo-tympanus and encasing the middle ear ossicle. A mastoidectomy was performed.
Gross description:
Soft dark tan nodules in aggregate measuring 6 mm.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Glomus tympanicum
Immunostains:
Discussion:
Histology showed a neoplasm resembling a capillary hemangioma, composed primarily of variable sized capillary channels lined by a single layer of endothelial cells. An adjacent area was solid with closely packed small nests of round to epithelioid cells surrounded by capillaries. There were no mitoses.
S100 showed no definite sustentacular cells, likely obscured by capillaries. VEGF showed staining of vessels but no staining of most tumor cells.
Glomus tympanicum, also called jugulotympanic paraganglioma, is the most common tumor of the middle ear, usually occurring in women ages 40 - 69 years (eMedicine: Glomus Jugulare Tumors [Accessed 10 November 2023]). Most arise in the jugular bulb, causing a mass in the middle ear or external auditory canal. The remainder arise from the tympanic branch of the glossopharyngeal nerve, causing a middle ear mass or the posterior auricular branch of the vagus nerve, causing an external auditory canal mass. They usually cause a conductive hearing loss and may be locally invasive into the temporal bone and mastoid, causing cranial nerve palsies, cerebellar dysfunction, dysphagia or hoarseness.
Histologically, they have the classic organoid (zellballen) or nesting pattern of paragangliomas with central round / oval chief cells containing abundant eosinophilic granular or vacuolated cytoplasm and uniform nuclei with dispersed chromatin. Although difficult to identify in this case, sustentacular cells (spindled and basophilic) are usually present at the periphery of nests, which are separated by a fibrovascular stroma. Tumors typically have benign features but may have pleomorphism, dense fibrous stroma or apparent infiltration. Mitoses and necrosis are rare.
The chief cells in the tumor are immunoreactive for chromogranin and synaptophysin and typically the sustentacular cells are S100+. Reticulin stains the stroma and delineates the nesting pattern, which is particularly helpful with crushed specimens.
The differential diagnosis includes capillary hemangioma, which lack the organoid pattern and cellular composition (chief and sustentacular cells) of paragangliomas (Case Rep Otolaryngol 2012;2012:305172).
Common treatment options are surgery, which may be accompanied by profuse bleeding or radiosurgery / gamma knife, with low complication rates despite the location (Otolaryngol Head Neck Surg 2015;152:136, Auris Nasus Larynx 2010;37:661, Skull Base 2011;21:309, J Neurosurg 2014;121 Suppl:198). There is a low recurrence rate and occasional cases may have malignant behavior with metastases.