19 November 2014 - Case #334
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Shweta Joshi and Dr. Nanda Patil, Krishna Institute of Medical Sciences (India), for contributing this case and the discussion.
Advertisement
Case #334
Clinical history:
A 70 year old woman with epilepsy presented with new onset vomiting. History and physical exam was normal but ultrasonography revealed a round to oval heteroechoic mass near the lower pole of right kidney, in the paracaval region. An exploratory laprotomy was performed and the mass was excised.
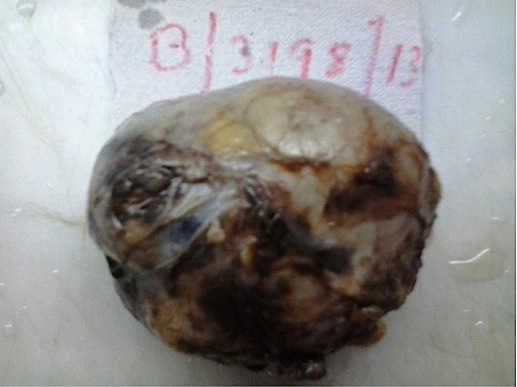
Gross description:
The mass was 7 x 6 x 4 cm, encapsulated, well circumscribed, globular, gray-white to gray-brown. The cut section revealed a variegated appearance with cystic areas, hemorrhage and areas of calcification.
Gross images:
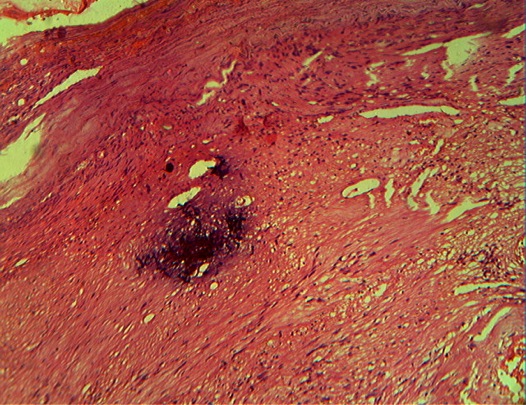
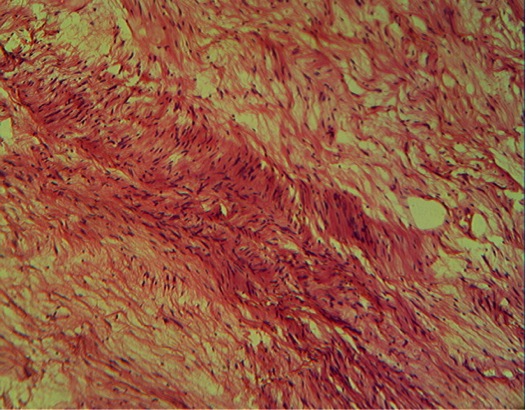
Microscopic images:
What is your diagnosis?
Diagnosis: Retroperitoneal schwannoma (ancient)
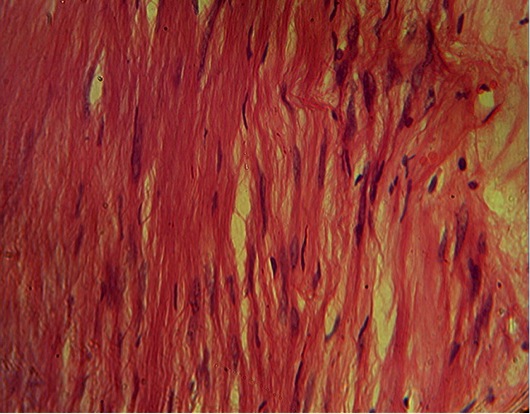
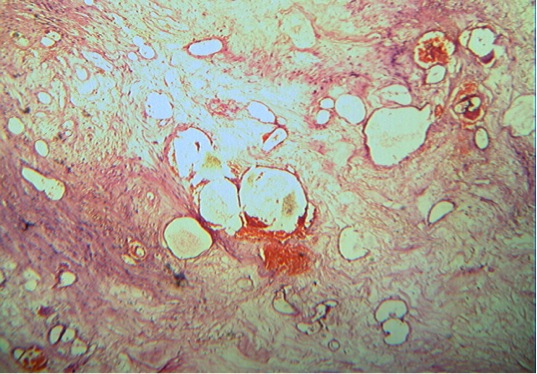
Stain images:
Discussion:
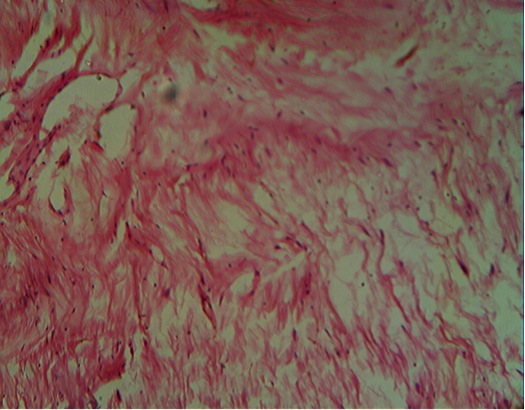
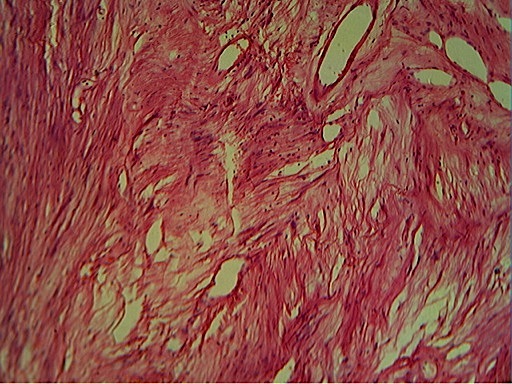
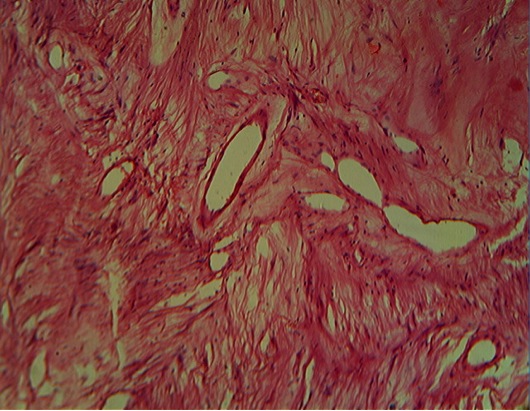
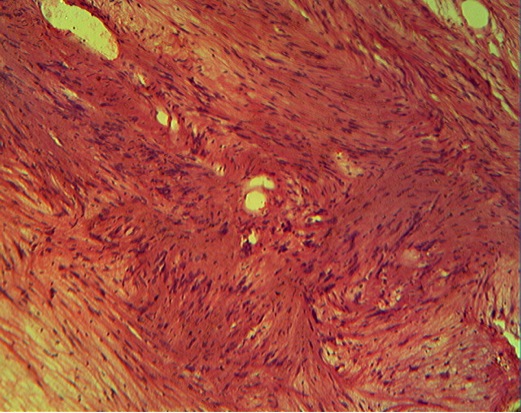
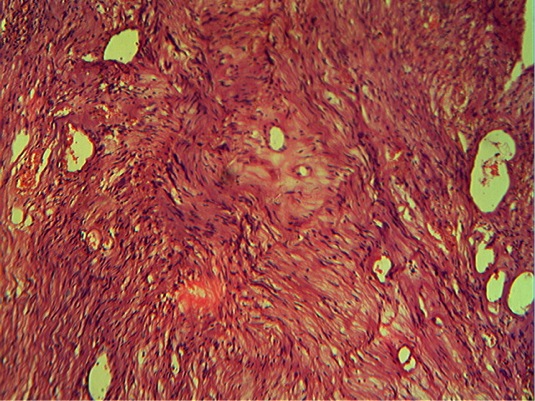
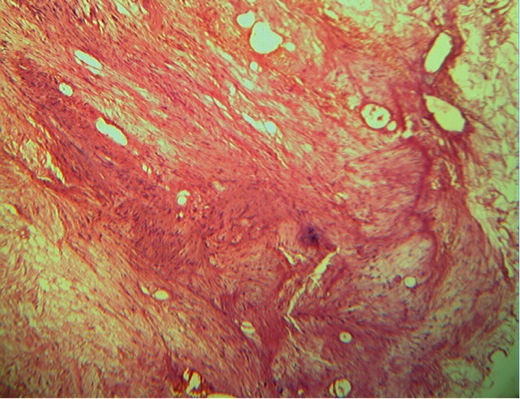
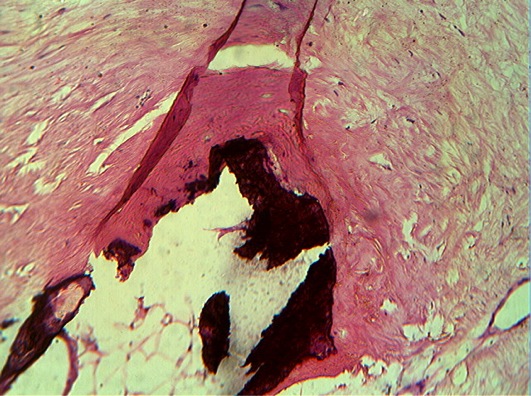
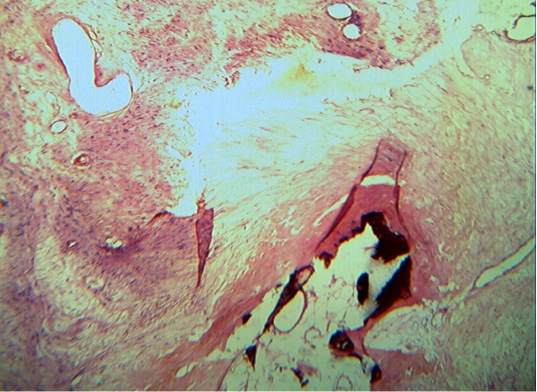
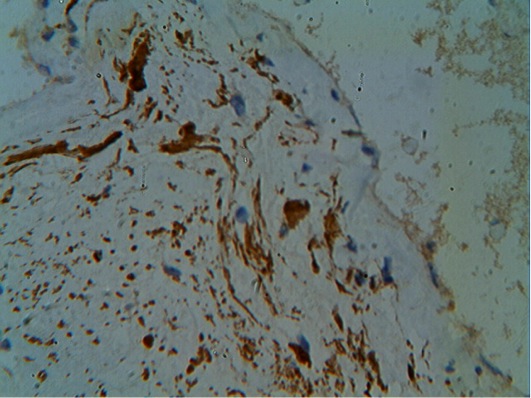
Histologically, the tumor was well circumscribed and encapsulated, showing hypercellular and hypocellular areas. Elongated spindle shaped neoplastic cells showed tapering nuclei with nuclear palisading. Occasional areas showed enlarged, hyperchromatic nuclei with very low mitotic activity. Areas of cystic degeneration, myxoid change and ossification were noted. The spindled cells were S100 immunoreactive.
Schwannoma (neurilemoma, less commonly called neurinoma or perineural fibroblastoma) is a benign tumor arising from the nerve sheath of Schwann cells, whose etiology is still unknown (OJHAS 2014;13:1, Neurol Sci 2010;27:353). It usually affects adults ages 20 - 50 years and is more common in men (Hong Kong Med J 2010;16:66). The most common sites are head and neck and flexor surfaces of extremities. The retroperitoneum is a rare site, with an incidence of 0.3 - 3%.
Retroperitoneal schwannomas account for 1 - 10% of all primary retroperitoneal tumors and typically have benign behavior (OJHAS 2014;13:1). They are usually detected incidentally after radiological examination. Neurological symptoms are rare. Rare cases present with abdominal and lower back pain and digestive disturbances.
Preoperative cross sectional imaging reveals a solid mass in the retroperitoneum with a few cystic areas. Although both ultrasound and computed tomography can detect the tumor, MRI allows better visualization and involvement of other organs. Radiological findings are usually nonspecific and often fail to give an accurate diagnosis (Am J Surg 2006;192:14). Definitive diagnosis requires histopathological examination. CT guided biopsy can be attempted for preoperative diagnosis but there is a risk of hemorrhage, infection and tumor seeding.
Retroperitoneal schwannomas are usually large with a glistening cut surface. Ancient schwannomas show infarct-like necrosis, cystic changes, calcification and ossification related to degeneration. Microscopically, conventional schwannomas are composed of elongated Schwann cells in hyper and hypocellular areas, with nuclear palisading (IARC: WHO Classification of Tumours of the Central Nervous System, 4th Edition, 2007). The stroma contains thick walled dilated vessels. Ancient schwannomas show nuclear polymorphism including bizarre forms with nuclear inclusions and other secondary changes such as calcification and ossification (Weiss: Enzinger and Weiss's Soft Tissue Tumors, 6th Edition, 2013).
The differential diagnosis includes paraganglioma, pheochromocytoma, liposarcoma, malignant fibrous histiocytoma and retroperitoneal cystic masses such as hemangioma and lymphangioma (OJHAS 2014;13:1). Immunohistochemistry is useful for confirmation. The Schwann cells are strongly S100+ and immunoreactive for GFAP / glial fibrillary acidic protein in some cases (Weiss: Enzinger and Weiss's Soft Tissue Tumors, 6th Edition, 2013, World J Gastroenterol 2011;17:3459).
Complete surgical excision is recommended. These tumors are not sensitive to radiotherapy and chemotherapy (Hong Kong Med J 2010;16:66). Prognosis is good, as only 5 - 10% recur due to incomplete excision (J Obstet Gynaecol 2007:33;371, Urology 2003;62:993, ANZ J Surg 2007;77:237).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Shweta Joshi and Dr. Nanda Patil, Krishna Institute of Medical Sciences (India), for contributing this case and the discussion.
Advertisement
Website news:
(1) We are seeking experts to serve on our Editorial Board to provide a secondary review of topics as they are updated. Editorial Board members are listed on the Reviewers page, on the relevant Chapter page and on all topics that they review.
(2) Our Feature page for November is Consumable Lab Products / Clinical Lab Analyzers and highlights our advertisers Leica Biosystems and Ventana Medical. It also contains an original short article, "Laboratory Consumables: Pathology Glass Slides", by Jaleh Mansouri, M.D.
(3) October traffic broke another record, with 661,468 total visits, 2,000,307 total page views and average daily visits of 21,337. Thanks for your support!
(4) We have now posted the Pathologist Jobs Report for the third quarter of 2014. For this quarter, there were 86 job postings for full time or part time pathologists at PathologyOutlines.com. This is a 19% increase from the 72 postings in the third quarter of 2013. For the first 3 quarters of 2014, there were 230 postings, a 17% increase from the 196 postings for the first 3 quarters of 2013. Click here for the full report.
Visit and follow our Blog to see recent updates to the website.
(1) We are seeking experts to serve on our Editorial Board to provide a secondary review of topics as they are updated. Editorial Board members are listed on the Reviewers page, on the relevant Chapter page and on all topics that they review.
(2) Our Feature page for November is Consumable Lab Products / Clinical Lab Analyzers and highlights our advertisers Leica Biosystems and Ventana Medical. It also contains an original short article, "Laboratory Consumables: Pathology Glass Slides", by Jaleh Mansouri, M.D.
(3) October traffic broke another record, with 661,468 total visits, 2,000,307 total page views and average daily visits of 21,337. Thanks for your support!
(4) We have now posted the Pathologist Jobs Report for the third quarter of 2014. For this quarter, there were 86 job postings for full time or part time pathologists at PathologyOutlines.com. This is a 19% increase from the 72 postings in the third quarter of 2013. For the first 3 quarters of 2014, there were 230 postings, a 17% increase from the 196 postings for the first 3 quarters of 2013. Click here for the full report.
Visit and follow our Blog to see recent updates to the website.
Case #334
Clinical history:
A 70 year old woman with epilepsy presented with new onset vomiting. History and physical exam was normal but ultrasonography revealed a round to oval heteroechoic mass near the lower pole of right kidney, in the paracaval region. An exploratory laprotomy was performed and the mass was excised.
Gross description:
The mass was 7 x 6 x 4 cm, encapsulated, well circumscribed, globular, gray-white to gray-brown. The cut section revealed a variegated appearance with cystic areas, hemorrhage and areas of calcification.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Retroperitoneal schwannoma (ancient)
Stain images:
Discussion:
Histologically, the tumor was well circumscribed and encapsulated, showing hypercellular and hypocellular areas. Elongated spindle shaped neoplastic cells showed tapering nuclei with nuclear palisading. Occasional areas showed enlarged, hyperchromatic nuclei with very low mitotic activity. Areas of cystic degeneration, myxoid change and ossification were noted. The spindled cells were S100 immunoreactive.
Schwannoma (neurilemoma, less commonly called neurinoma or perineural fibroblastoma) is a benign tumor arising from the nerve sheath of Schwann cells, whose etiology is still unknown (OJHAS 2014;13:1, Neurol Sci 2010;27:353). It usually affects adults ages 20 - 50 years and is more common in men (Hong Kong Med J 2010;16:66). The most common sites are head and neck and flexor surfaces of extremities. The retroperitoneum is a rare site, with an incidence of 0.3 - 3%.
Retroperitoneal schwannomas account for 1 - 10% of all primary retroperitoneal tumors and typically have benign behavior (OJHAS 2014;13:1). They are usually detected incidentally after radiological examination. Neurological symptoms are rare. Rare cases present with abdominal and lower back pain and digestive disturbances.
Preoperative cross sectional imaging reveals a solid mass in the retroperitoneum with a few cystic areas. Although both ultrasound and computed tomography can detect the tumor, MRI allows better visualization and involvement of other organs. Radiological findings are usually nonspecific and often fail to give an accurate diagnosis (Am J Surg 2006;192:14). Definitive diagnosis requires histopathological examination. CT guided biopsy can be attempted for preoperative diagnosis but there is a risk of hemorrhage, infection and tumor seeding.
Retroperitoneal schwannomas are usually large with a glistening cut surface. Ancient schwannomas show infarct-like necrosis, cystic changes, calcification and ossification related to degeneration. Microscopically, conventional schwannomas are composed of elongated Schwann cells in hyper and hypocellular areas, with nuclear palisading (IARC: WHO Classification of Tumours of the Central Nervous System, 4th Edition, 2007). The stroma contains thick walled dilated vessels. Ancient schwannomas show nuclear polymorphism including bizarre forms with nuclear inclusions and other secondary changes such as calcification and ossification (Weiss: Enzinger and Weiss's Soft Tissue Tumors, 6th Edition, 2013).
The differential diagnosis includes paraganglioma, pheochromocytoma, liposarcoma, malignant fibrous histiocytoma and retroperitoneal cystic masses such as hemangioma and lymphangioma (OJHAS 2014;13:1). Immunohistochemistry is useful for confirmation. The Schwann cells are strongly S100+ and immunoreactive for GFAP / glial fibrillary acidic protein in some cases (Weiss: Enzinger and Weiss's Soft Tissue Tumors, 6th Edition, 2013, World J Gastroenterol 2011;17:3459).
Complete surgical excision is recommended. These tumors are not sensitive to radiotherapy and chemotherapy (Hong Kong Med J 2010;16:66). Prognosis is good, as only 5 - 10% recur due to incomplete excision (J Obstet Gynaecol 2007:33;371, Urology 2003;62:993, ANZ J Surg 2007;77:237).