25 June 2014 - Case #317
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Mingyi Chen, University of California - Davis Medical Center (USA), for contributing this case and the discussion.
 Advertisement
Advertisement
Case #317
Clinical history:
A 37 year old man presented with fever and pancytopenia. His medical history was significant for Graves' hyperthyroidism, treated with radioiodine thyroid ablation, with subsequent hypothyroidism. CT detected right infraclavicular and axillary lymphadenopathy, hepatosplenomegaly, pleural and pericardial effusion and ascites. He underwent a right axillary node excisional biopsy.
Gross images:
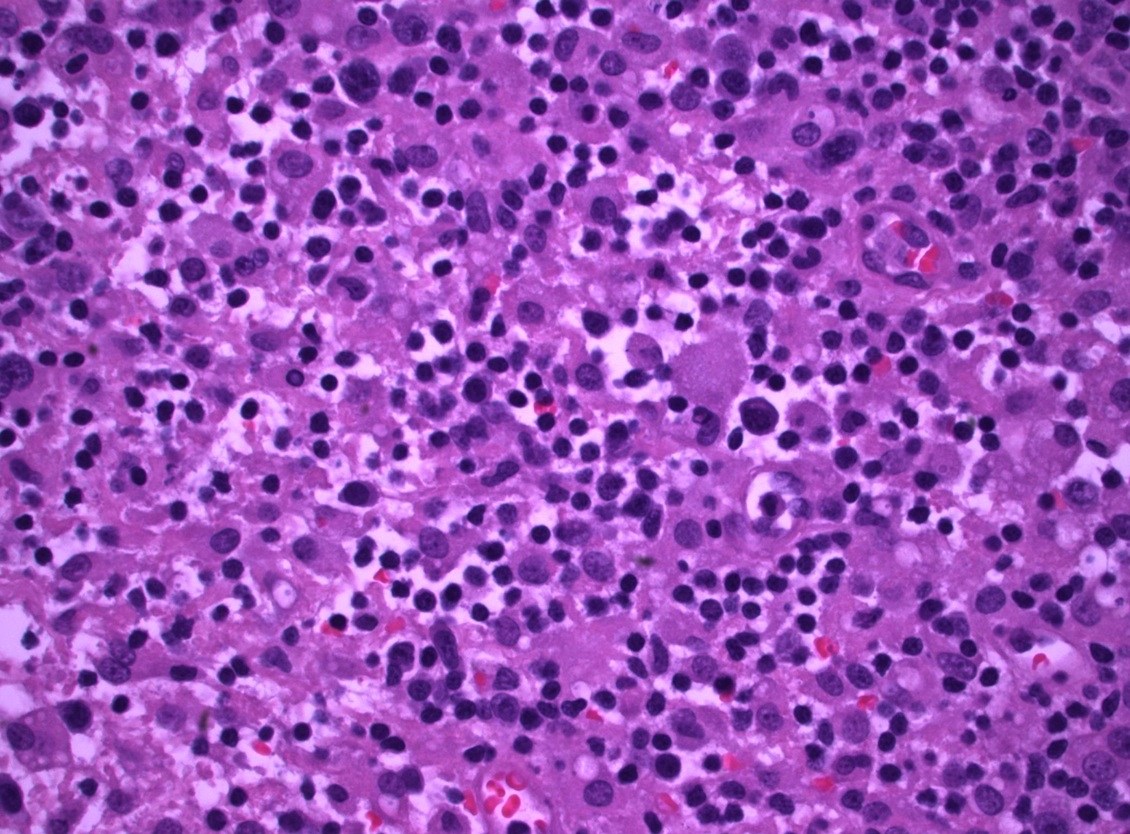
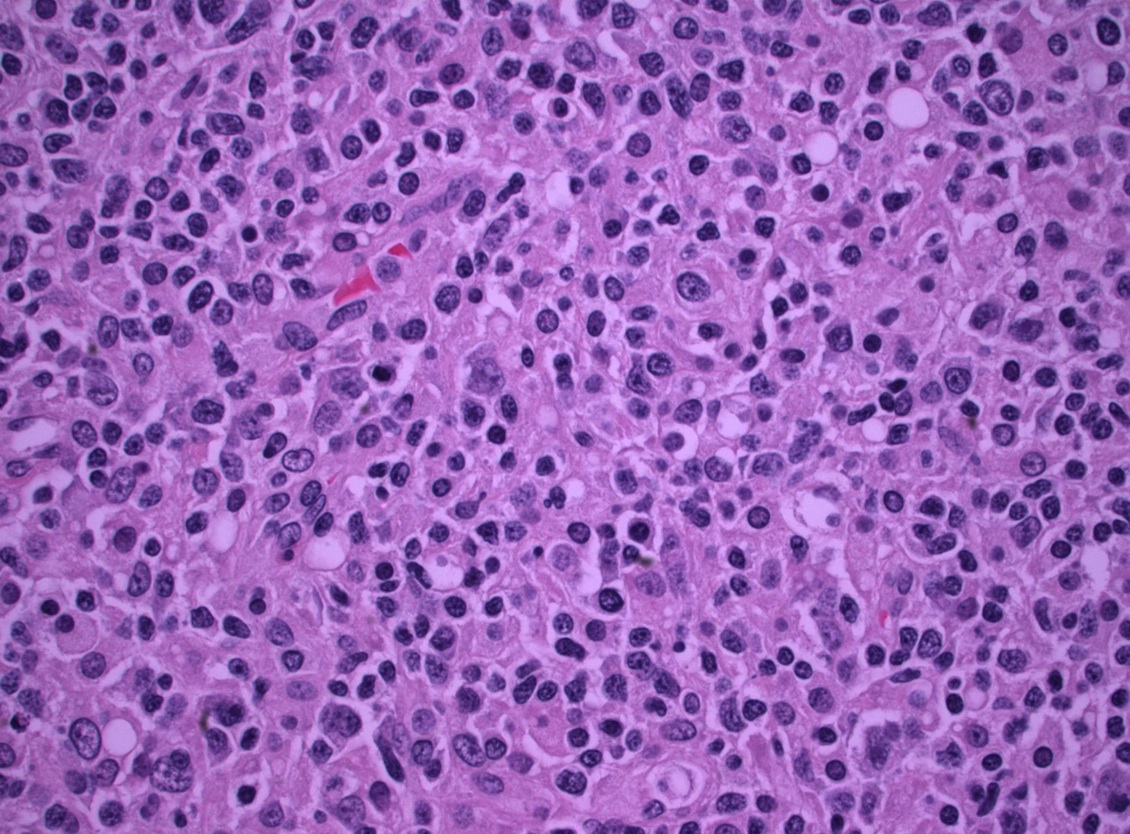
Microscopy images:
What is your diagnosis?
Diagnosis: T cell / histiocyte rich large B cell lymphoma
Immunostains:
Discussion:
The biopsy revealed an enlarged lymph node with a diffuse, atypical lymphoid infiltrate and effacement of the nodal architecture. There are numerous large atypical cells with eccentric nuclei, irregular nuclear contours, dispersed chromatin and occasional prominent nucleoli. Many histiocytes are present in the background. By immunohistochemistry, the large atypical lymphoid cells are positive for B cell markers (CD20, PAX5, BOB1 and OCT2) with coexpression of BCL2, BCL6 (weak), EMA and CD45 but are negative for CD3, CD15 and CD30 (rare positivity in B cells, not seen in above image). The background T cells are diffusely positive for CD3, CD4 and BCL2. The cell proliferation index marker Ki67 highlights the large cells. A bone marrow biopsy showed an interstitial atypical lymphoid and histiocytic infiltrate consistent with involvement by lymphoma.
T cell / histiocyte rich B cell lymphoma (T / HRBCL) is an uncommon morphologic variant of diffuse large B cell lymphoma (DLBCL). Pathologically, it is distinguished by < 10% malignant B cells amid a majority population of reactive T lymphocytes and histiocytes. Diagnosis of this entity is very challenging, as it may appear similar to T cell lymphoma and nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) (Mod Pathol 2013;26 Suppl 1:S57). Accurate diagnosis rests with careful immunohistochemical analysis of the tumor cells and the inflammatory microenvironment. In NLPHL with predominant nodular pattern, small B cells and CD57 positive cells are common, whereas in TCRBCL with diffuse pattern, TIA1 positive cytotoxic cells and histiocytes dominate, and small B cells are scarce or absent. A combination of the morphological characteristics and the reactivity of the background cells for CD57 and TIA1 seems to reliably discriminate between the entities, and should increase the interobserver reproducibility of diagnosis in the gray zone around Hodgkin lymphoma. Of note, a recent study found no consistent differences in the gene expression between these entities, suggesting that they may represent a spectrum of the same disease (PLoS One 2013;8:e78812). Clinically, T / HRBCL occurs in younger patients, predominantly affects men, and involves the liver, spleen and bone marrow with greater frequency than traditional DLBCL. Despite the unique clinical features and robust host inflammatory response, T / HRBCL follows a natural history similar to those of other DLBCLs, and responds similarly to therapy.
Comment:
I cannot help notice that the gross image shows a frankly nodular pattern of the lymph node cut surface. According to the WHO and in my own opinion, a thorough investigation of these areas should be done to exclude N-LP Hodgkin lymphoma, and a PD-1 stain should be performed, since it's very difficult to distinguish N-LPHL with diffuse areas from T / HRLBCL. The presence of small B cells in the nodular areas, together with the presence of numerous and sometimes rosette-forming Tfh cells should favor a diagnosis of N-LPHL. The use of CD57, as discussed in the text, seems really outdated now that better Tfh markers are available.
Response to comment:
We thank the constructive comment. Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) and T cell / histiocyte rich B cell lymphoma (T / HRBCL) are linked by a morphologic and probably a biologic continuum, which renders the differential diagnosis difficult. NLPHL may progress to a process indistinguishable from de novo T / HRLBCL. The relationship between primary and secondary T / HRLBCL is not fully resolved and in some instances the distinction between NLPHL and T / HRLBCL can be problematic. We agree that programmed death 1 (PD-1) shows greater sensitivity compared with CD57 across all variants of nodular lymphocyte predominant Hodgkin lymphoma. According to the literature, loss of programmed death 1 reactivity did not correlate with diffuse areas, progression, or the ability to differentiate NLPHL from T / HRBCL.
NLPHL can histologically and immunophenotypically resemble T / HRBCL. Besides the different clinical presentations of these lymphoma entities, there are variants of NLPHL with considerable histopathologic overlap to T / HRLBCL. T / HRLBCL-like NLPHL, a diffuse form of NLPHL, often presents a histopathologic pattern similar to T / HRLBCL, suggesting a close relationship between both lymphoma entities. In conclusion, NLPHL and T / HRLBCL may represent a spectrum of the same disease.
Features that favor T / HRLBCL include the lack of both small B cells and follicular dendritic cells / follicular structures. Despite the abundance of T cells in T / HRLBCL, well formed T cell rosettes are usually absent.
In contrast to the commonly indolent clinical behavior of nodular lymphocyte predominant Hodgkin lymphoma (NLPHL), T cell / histiocyte rich large B cell lymphoma (T / HRLBCL) is frequently diagnosed in advanced clinical stages and has a poor prognosis. The clinical picture is important because T / HRLBCL only rarely presents with localized stage I disease. By definition, small B cells are abundant in NLPHL but rare in T / HRBCL. The nature of the T cell background is also important: in NLPHL, T cells are mainly CD4+CD57+ follicular T cells that commonly form rosettes, while in T / HRBCL, CD8+ cytotoxic T cells and histiocytes predominate and T cell rosettes are rare.
In the current case, the essentially diffuse pattern, background CD4+ T cells, lack of small nodular B cells, and systemic involvement (hepatosplenomegaly, pleural and pericardial effusion) with high clinical stage and bone marrow involvement favor the diagnosis of T / HRLBCL versus NLPHL.
References: Haematologica 2010;95:352, Hum Pathol 2010;41:1726, Arch Pathol Lab Med 2010;134:1434, Blood 2003;102:3753
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Mingyi Chen, University of California - Davis Medical Center (USA), for contributing this case and the discussion.

Leica Biosystems releases two new customer apps for Immunohistochemistry (IHC) Education and Reference for Path Lead and IHC Antibody Catalog.
- PathLead is a mobile educational tool and pathology resource application, designed for use by healthcare professionals in the field of surgical pathology and diagnostic immunohistochemistry (IHC).
- IHC Antibody Catalog is an application for Laboratory Managers and Pathologists looking for both routine and innovative IHC antibodies and consumables.
- Both are currently available for download at the Apple App Store.
Click here for more information!
Website news:
(1) We are pleased to announce 2 special rates for Jobs-Related ads. These are ads for positions other than Pathologist / PhD, which appear on our Jobs-Related page. Through August 2014, the cost to post one of these ads (up to 300 words) is only $325 for up to 6 months. If you post a Job-Other ad within 2 days of posting a Pathologist / PhD ad, the cost is ZERO. Contact us at 248/646-0325 with any questions.
(2) See our featured books of the month for June, including WHO Classification of Tumours of Female Reproductive Organs and McGraw-Hill Specialty Board Review Anatomic Pathology.
Visit and follow our Blog to see recent updates to the website.
(1) We are pleased to announce 2 special rates for Jobs-Related ads. These are ads for positions other than Pathologist / PhD, which appear on our Jobs-Related page. Through August 2014, the cost to post one of these ads (up to 300 words) is only $325 for up to 6 months. If you post a Job-Other ad within 2 days of posting a Pathologist / PhD ad, the cost is ZERO. Contact us at 248/646-0325 with any questions.
(2) See our featured books of the month for June, including WHO Classification of Tumours of Female Reproductive Organs and McGraw-Hill Specialty Board Review Anatomic Pathology.
Visit and follow our Blog to see recent updates to the website.
Case #317
Clinical history:
A 37 year old man presented with fever and pancytopenia. His medical history was significant for Graves' hyperthyroidism, treated with radioiodine thyroid ablation, with subsequent hypothyroidism. CT detected right infraclavicular and axillary lymphadenopathy, hepatosplenomegaly, pleural and pericardial effusion and ascites. He underwent a right axillary node excisional biopsy.
Gross images:
Microscopy images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: T cell / histiocyte rich large B cell lymphoma
Immunostains:
Discussion:
The biopsy revealed an enlarged lymph node with a diffuse, atypical lymphoid infiltrate and effacement of the nodal architecture. There are numerous large atypical cells with eccentric nuclei, irregular nuclear contours, dispersed chromatin and occasional prominent nucleoli. Many histiocytes are present in the background. By immunohistochemistry, the large atypical lymphoid cells are positive for B cell markers (CD20, PAX5, BOB1 and OCT2) with coexpression of BCL2, BCL6 (weak), EMA and CD45 but are negative for CD3, CD15 and CD30 (rare positivity in B cells, not seen in above image). The background T cells are diffusely positive for CD3, CD4 and BCL2. The cell proliferation index marker Ki67 highlights the large cells. A bone marrow biopsy showed an interstitial atypical lymphoid and histiocytic infiltrate consistent with involvement by lymphoma.
T cell / histiocyte rich B cell lymphoma (T / HRBCL) is an uncommon morphologic variant of diffuse large B cell lymphoma (DLBCL). Pathologically, it is distinguished by < 10% malignant B cells amid a majority population of reactive T lymphocytes and histiocytes. Diagnosis of this entity is very challenging, as it may appear similar to T cell lymphoma and nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) (Mod Pathol 2013;26 Suppl 1:S57). Accurate diagnosis rests with careful immunohistochemical analysis of the tumor cells and the inflammatory microenvironment. In NLPHL with predominant nodular pattern, small B cells and CD57 positive cells are common, whereas in TCRBCL with diffuse pattern, TIA1 positive cytotoxic cells and histiocytes dominate, and small B cells are scarce or absent. A combination of the morphological characteristics and the reactivity of the background cells for CD57 and TIA1 seems to reliably discriminate between the entities, and should increase the interobserver reproducibility of diagnosis in the gray zone around Hodgkin lymphoma. Of note, a recent study found no consistent differences in the gene expression between these entities, suggesting that they may represent a spectrum of the same disease (PLoS One 2013;8:e78812). Clinically, T / HRBCL occurs in younger patients, predominantly affects men, and involves the liver, spleen and bone marrow with greater frequency than traditional DLBCL. Despite the unique clinical features and robust host inflammatory response, T / HRBCL follows a natural history similar to those of other DLBCLs, and responds similarly to therapy.
Comment:
I cannot help notice that the gross image shows a frankly nodular pattern of the lymph node cut surface. According to the WHO and in my own opinion, a thorough investigation of these areas should be done to exclude N-LP Hodgkin lymphoma, and a PD-1 stain should be performed, since it's very difficult to distinguish N-LPHL with diffuse areas from T / HRLBCL. The presence of small B cells in the nodular areas, together with the presence of numerous and sometimes rosette-forming Tfh cells should favor a diagnosis of N-LPHL. The use of CD57, as discussed in the text, seems really outdated now that better Tfh markers are available.
Response to comment:
We thank the constructive comment. Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) and T cell / histiocyte rich B cell lymphoma (T / HRBCL) are linked by a morphologic and probably a biologic continuum, which renders the differential diagnosis difficult. NLPHL may progress to a process indistinguishable from de novo T / HRLBCL. The relationship between primary and secondary T / HRLBCL is not fully resolved and in some instances the distinction between NLPHL and T / HRLBCL can be problematic. We agree that programmed death 1 (PD-1) shows greater sensitivity compared with CD57 across all variants of nodular lymphocyte predominant Hodgkin lymphoma. According to the literature, loss of programmed death 1 reactivity did not correlate with diffuse areas, progression, or the ability to differentiate NLPHL from T / HRBCL.
NLPHL can histologically and immunophenotypically resemble T / HRBCL. Besides the different clinical presentations of these lymphoma entities, there are variants of NLPHL with considerable histopathologic overlap to T / HRLBCL. T / HRLBCL-like NLPHL, a diffuse form of NLPHL, often presents a histopathologic pattern similar to T / HRLBCL, suggesting a close relationship between both lymphoma entities. In conclusion, NLPHL and T / HRLBCL may represent a spectrum of the same disease.
Features that favor T / HRLBCL include the lack of both small B cells and follicular dendritic cells / follicular structures. Despite the abundance of T cells in T / HRLBCL, well formed T cell rosettes are usually absent.
In contrast to the commonly indolent clinical behavior of nodular lymphocyte predominant Hodgkin lymphoma (NLPHL), T cell / histiocyte rich large B cell lymphoma (T / HRLBCL) is frequently diagnosed in advanced clinical stages and has a poor prognosis. The clinical picture is important because T / HRLBCL only rarely presents with localized stage I disease. By definition, small B cells are abundant in NLPHL but rare in T / HRBCL. The nature of the T cell background is also important: in NLPHL, T cells are mainly CD4+CD57+ follicular T cells that commonly form rosettes, while in T / HRBCL, CD8+ cytotoxic T cells and histiocytes predominate and T cell rosettes are rare.
In the current case, the essentially diffuse pattern, background CD4+ T cells, lack of small nodular B cells, and systemic involvement (hepatosplenomegaly, pleural and pericardial effusion) with high clinical stage and bone marrow involvement favor the diagnosis of T / HRLBCL versus NLPHL.
References: Haematologica 2010;95:352, Hum Pathol 2010;41:1726, Arch Pathol Lab Med 2010;134:1434, Blood 2003;102:3753