13 March 2013 - Case #269
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Debra L. Zynger and Joshua J. Ebel, BS, The Ohio State University Medical Center, for contributing this case and the discussion.
Advertisement
Case #269
Clinical history:
A 59 year old man with a PSA of 7.9 had a prostatic needle biopsy, followed by a prostatectomy.
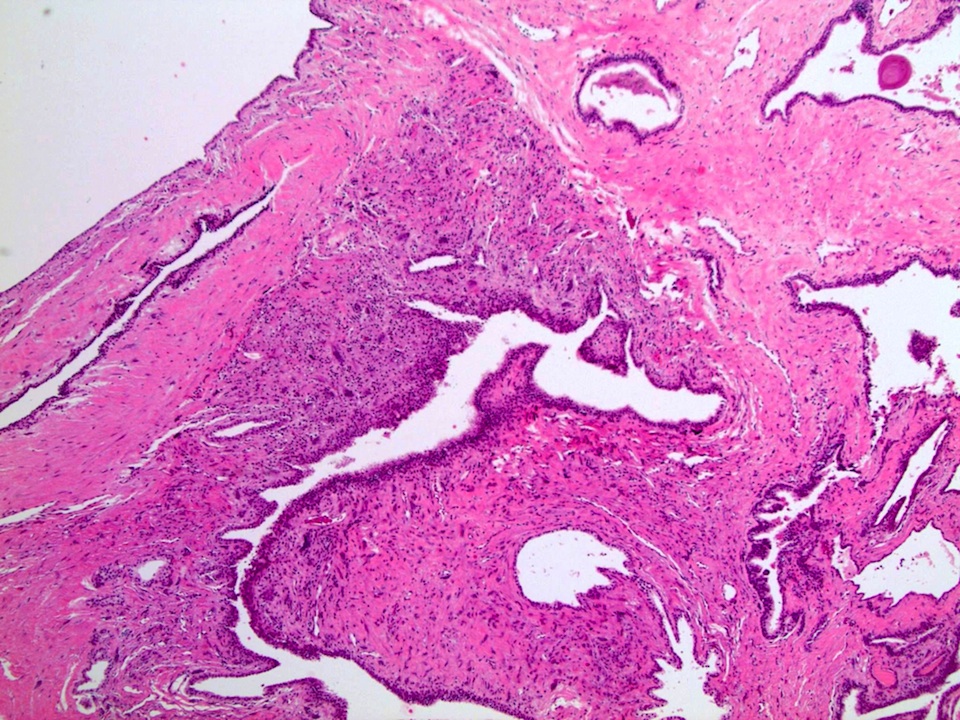
Gross images:
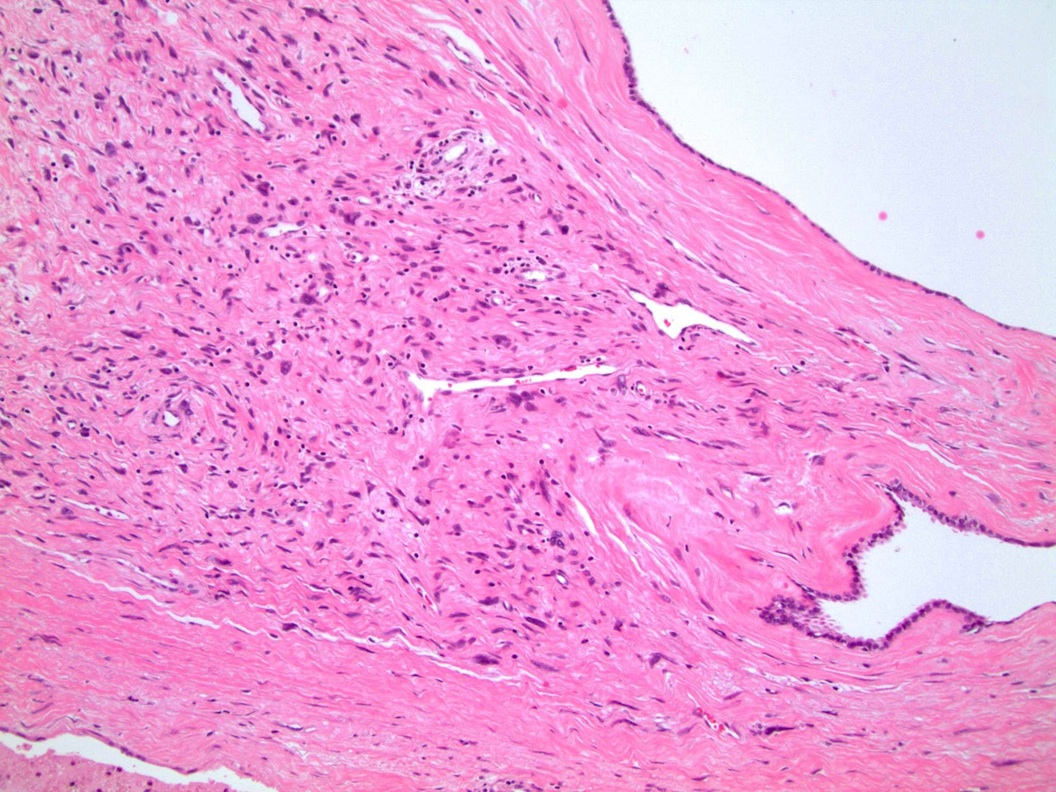
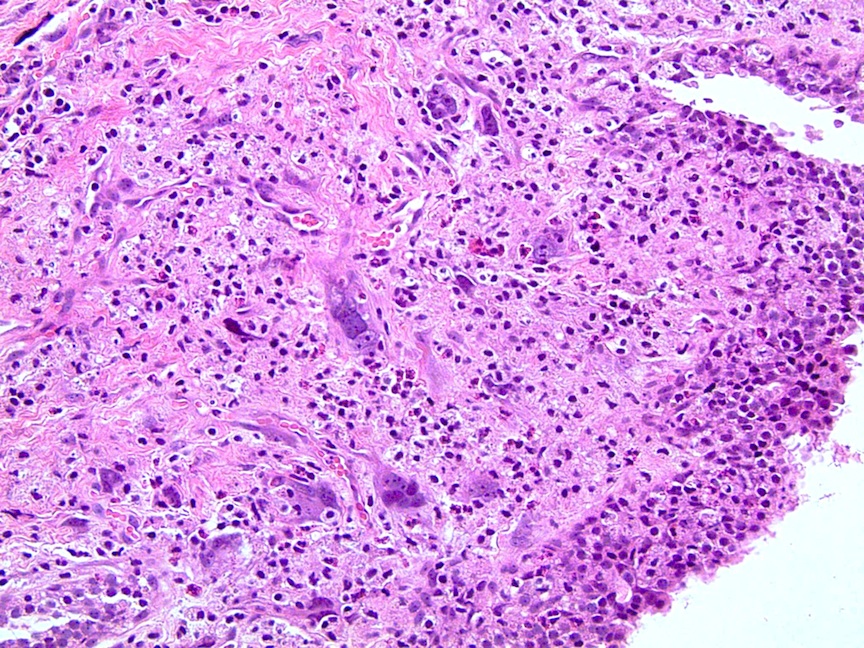
Microscopic images:
What is your diagnosis?
Diagnosis: Stromal tumor of uncertain malignant potential (STUMP)
Immunostains:
Discussion:
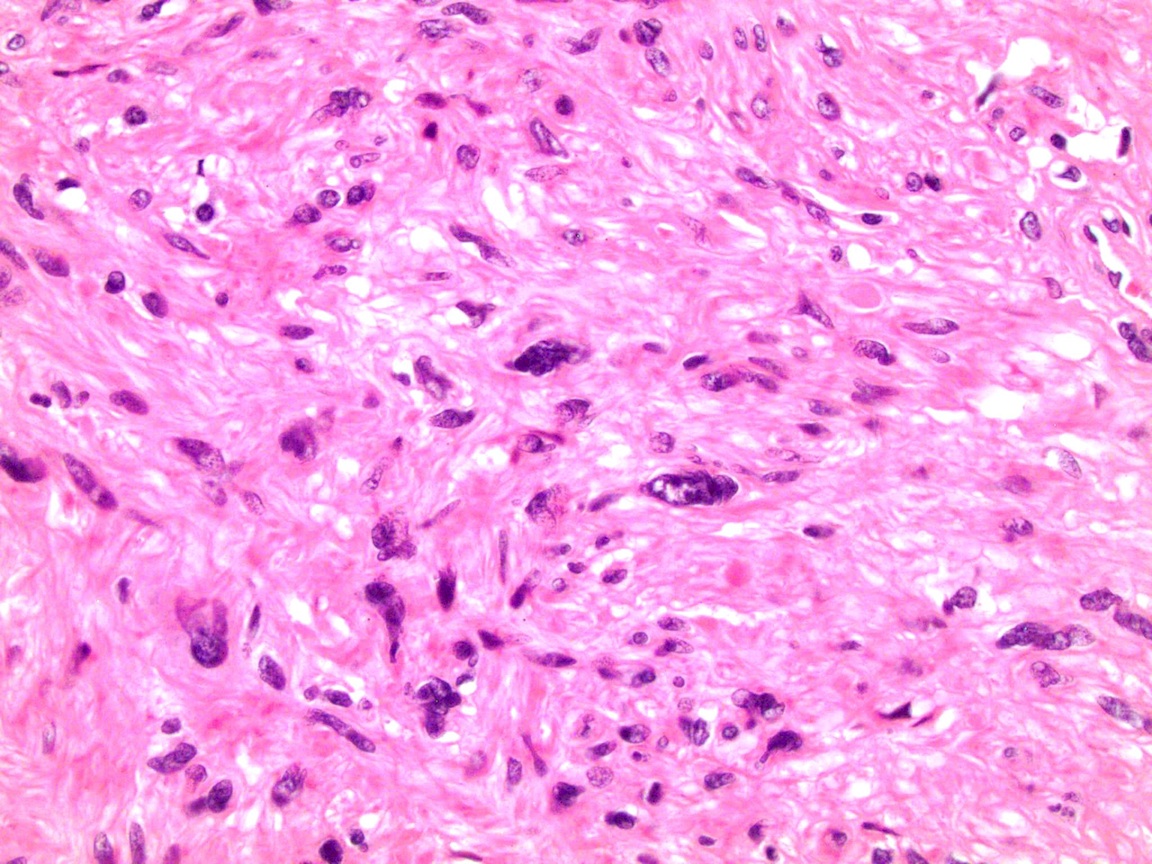
The initial needle core biopsy demonstrated STUMP. Prostatectomy showed STUMP diffusely involving the prostate with a minimal amount of prostatic adenocarcinoma (Gleason 3+3=6, 2% of the gland). The STUMP had degenerative atypia and phyllodes-like areas.
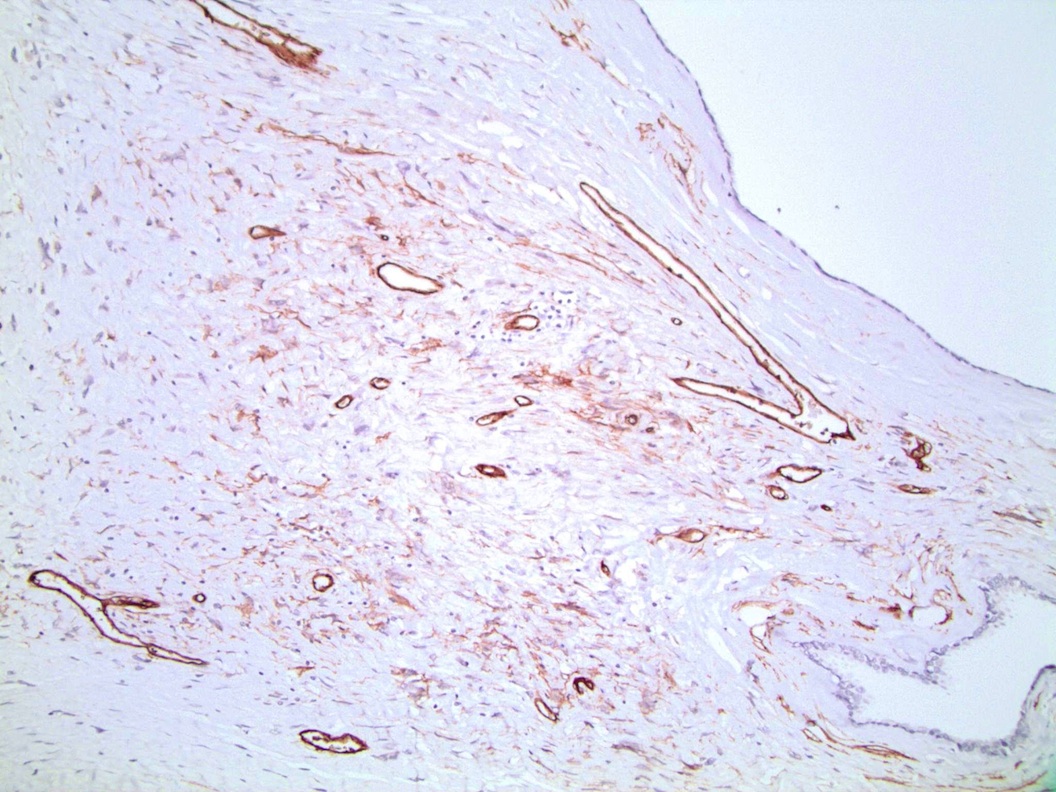
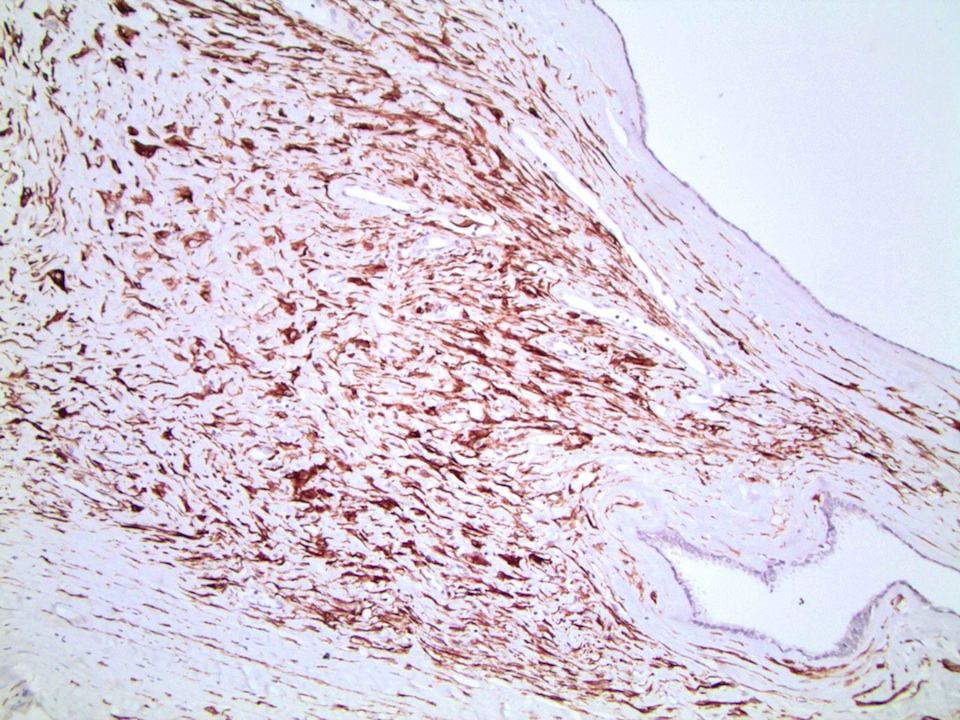
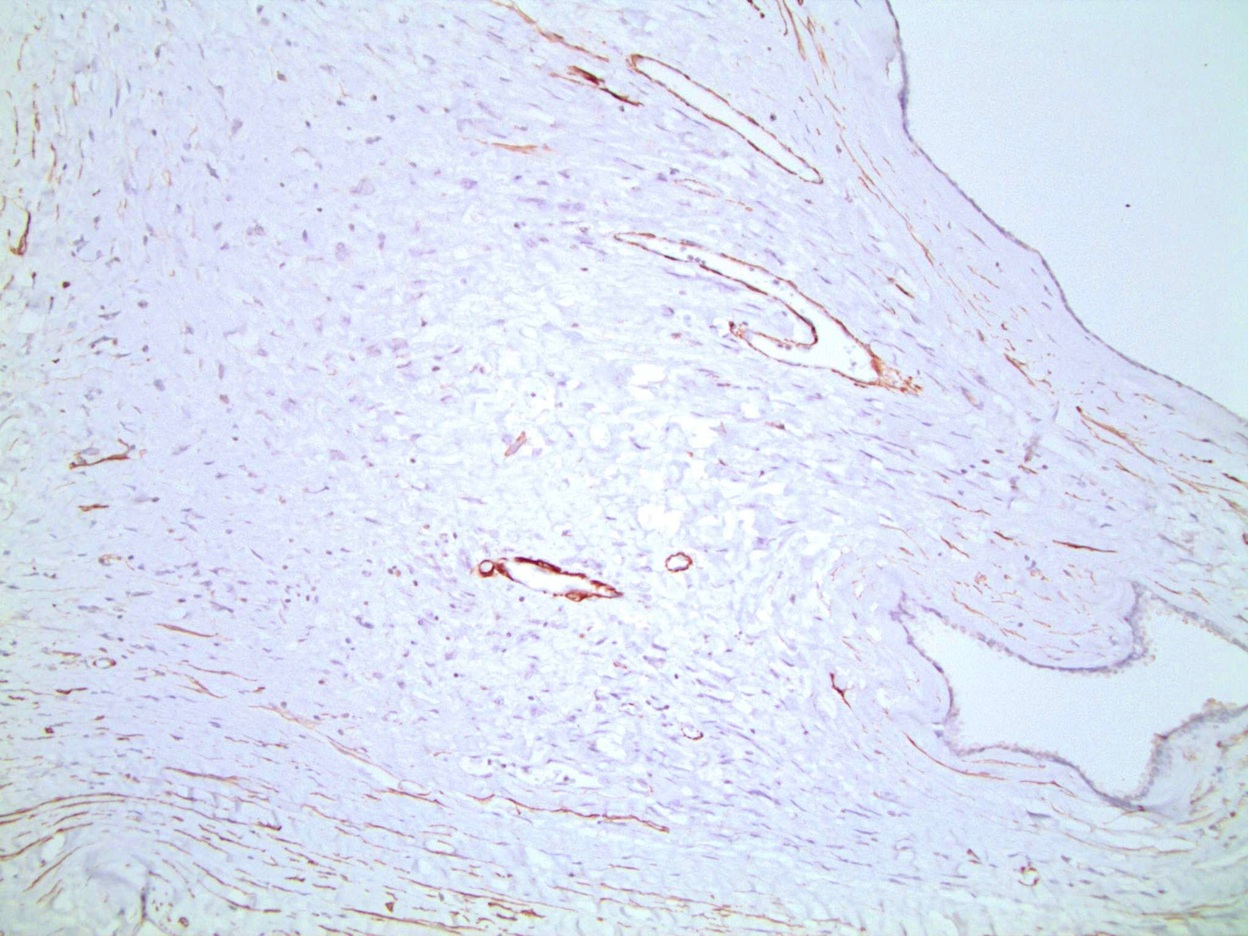
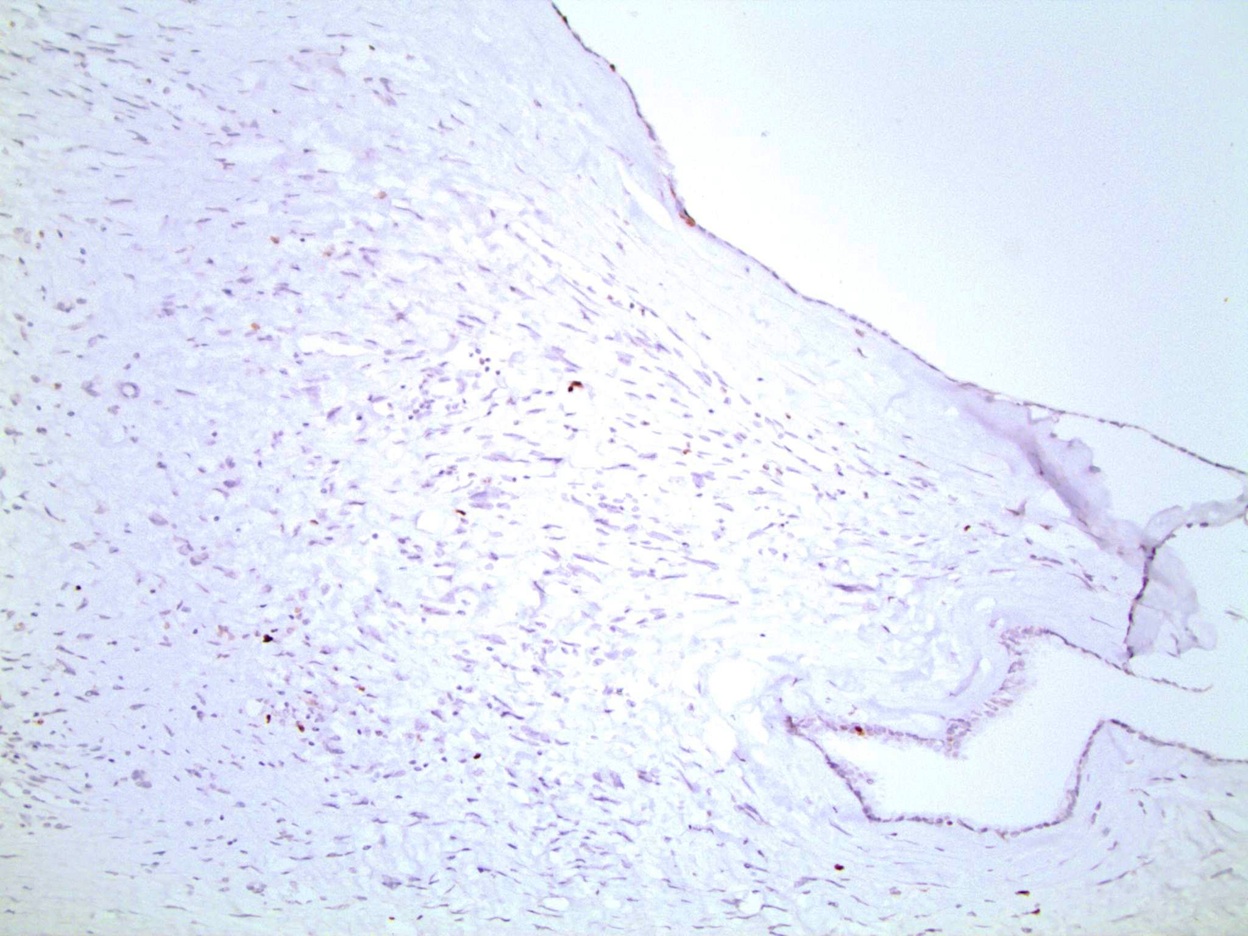
The STUMP was positive for CD34, desmin and PR with negative staining in the above image (variable staining elsewhere) and low staining for Ki67.
STUMP are rare prostatic tumors characterized by atypical stromal proliferation, that may resemble breast phyllodes tumors (Am J Surg Pathol 1998;22:148, Mod Pathol 2007;20:148). They are characterized by hypercellular stroma or cytologic atypia but without evidence of true sarcomatous transformation. The atypical stromal cells have enlarged nuclei with nuclear hyperchromasia and variable multinucleation. There are few / no mitotic figures and no atypical mitotic figures. Tumors may be associated with benign prostatic glands that may including crowding, a prominent basal cell layer or prominent papillary infolding (Am J Surg Pathol 2011;35:898).
STUMP tumors have 4 histologic patterns:
However, these patterns are not associated with behavior.
The differential diagnosis includes stromal sarcoma (greater cellularity, mitoses, necrosis and stromal overgrowth). Some authors consider phyllodes tumor to be a nonspecific pattern and recommend using a diagnosis of either STUMP or stromal sarcoma.
Treatment is somewhat controversial because of the small number of cases studied and since outcome varies from a benign course to recurrence and stromal sarcoma (Am J Surg Pathol 2006;30:694, eMedicine: Pathology of Prostatic Stromal Tumors of Uncertain Malignant Potential [Accessed 5 April 2024]).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Debra L. Zynger and Joshua J. Ebel, BS, The Ohio State University Medical Center, for contributing this case and the discussion.
Introducing MSH2: Rabbit Monoclonal Antibody
Epitomics has released MSH2, a high quality antibody for anatomic pathology. MutS homologue 2 (MSH2) is a DNA mismatch repair protein of the MutS family found in normal cells. Loss of MSH2 is linked to HNPCC and MSI-positive endometrial and ovarian cancers.
EP Clones are a line of high quality rabbit antibodies for anatomic pathology. We offer over 200 antibodies covering a range of 16 disease panels. Rabbit monoclonal antibodies (RabMAbs) are the product of true rabbit-rabbit hybridomas. The inherent qualities of the rabbit immune system allow for: 1) stronger binding affinity, and 2) higher specificity.
Website news:
(1) Thanks to everyone who stopped by our booth at USCAP and provided us with comments/suggestions.
(2) We are over 60% done with converting our 6,600 topics to our new easier to read format with thumbnails. We are also working on getting updated reviews every 1-2 years for each topic, and are expanding our editorial board to increase the quality of our content. Other future changes include additional newsletters for CME and Drugs of Interest to Pathologists.
Visit and follow our Blog to see recent updates to the website.
(1) Thanks to everyone who stopped by our booth at USCAP and provided us with comments/suggestions.
(2) We are over 60% done with converting our 6,600 topics to our new easier to read format with thumbnails. We are also working on getting updated reviews every 1-2 years for each topic, and are expanding our editorial board to increase the quality of our content. Other future changes include additional newsletters for CME and Drugs of Interest to Pathologists.
Visit and follow our Blog to see recent updates to the website.
Case #269
Clinical history:
A 59 year old man with a PSA of 7.9 had a prostatic needle biopsy, followed by a prostatectomy.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Stromal tumor of uncertain malignant potential (STUMP)
Immunostains:
Discussion:
The initial needle core biopsy demonstrated STUMP. Prostatectomy showed STUMP diffusely involving the prostate with a minimal amount of prostatic adenocarcinoma (Gleason 3+3=6, 2% of the gland). The STUMP had degenerative atypia and phyllodes-like areas.
The STUMP was positive for CD34, desmin and PR with negative staining in the above image (variable staining elsewhere) and low staining for Ki67.
STUMP are rare prostatic tumors characterized by atypical stromal proliferation, that may resemble breast phyllodes tumors (Am J Surg Pathol 1998;22:148, Mod Pathol 2007;20:148). They are characterized by hypercellular stroma or cytologic atypia but without evidence of true sarcomatous transformation. The atypical stromal cells have enlarged nuclei with nuclear hyperchromasia and variable multinucleation. There are few / no mitotic figures and no atypical mitotic figures. Tumors may be associated with benign prostatic glands that may including crowding, a prominent basal cell layer or prominent papillary infolding (Am J Surg Pathol 2011;35:898).
STUMP tumors have 4 histologic patterns:
- Hypercellular stroma with scattered cytologically atypical cells associated with benign glands
- Hypercellular stroma with minimal cytological atypia associated with benign glands
- Hypercellular stroma and benign glands in a leaf-like growth pattern resembling breast phyllodes tumor, with variable cytologic atypia
- Hypercellular stroma without cytologically atypical stromal cells and without glands
However, these patterns are not associated with behavior.
The differential diagnosis includes stromal sarcoma (greater cellularity, mitoses, necrosis and stromal overgrowth). Some authors consider phyllodes tumor to be a nonspecific pattern and recommend using a diagnosis of either STUMP or stromal sarcoma.
Treatment is somewhat controversial because of the small number of cases studied and since outcome varies from a benign course to recurrence and stromal sarcoma (Am J Surg Pathol 2006;30:694, eMedicine: Pathology of Prostatic Stromal Tumors of Uncertain Malignant Potential [Accessed 5 April 2024]).