7 February 2013 - Case #265
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Joseph Fullmer, University of Wisconsin Hospital and Clinics (USA), for contributing this case and the discussion.
Advertisement
Case #265
Clinical history:
A 61 year old man had abdominal follicular lymphoma diagnosed 7 years ago, treated with chemotherapy and radiation, and thought to be in remission. He developed increasing difficulties with balance, dizziness, numbness over his left tongue and inside cheek spreading to his face, as well as clumsiness with his left hand and leg over a 7 week period. MRI revealed a 3.8 x 2.3 x 2.4 cm lesion with minimal edge enhancement (hence predominately non-enhancing) centered in the left middle cerebellar peduncle extending into the left paramedian pons and left cerebellar hemisphere. Preoperative differential diagnosis included demyelination, low grade glial neoplasm, and recurrent lymphoma. Biopsy of the mass was performed.
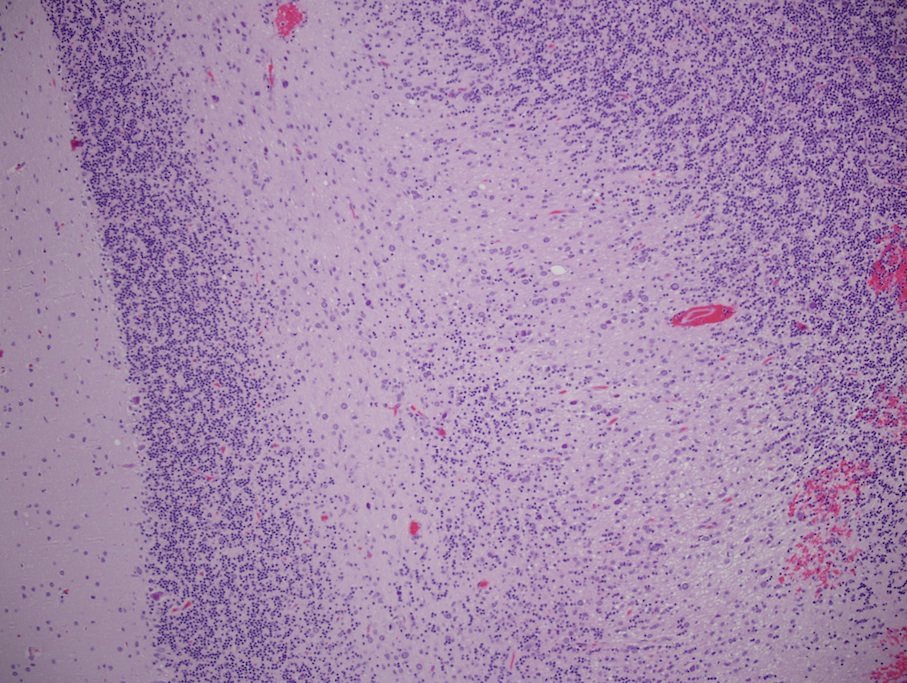
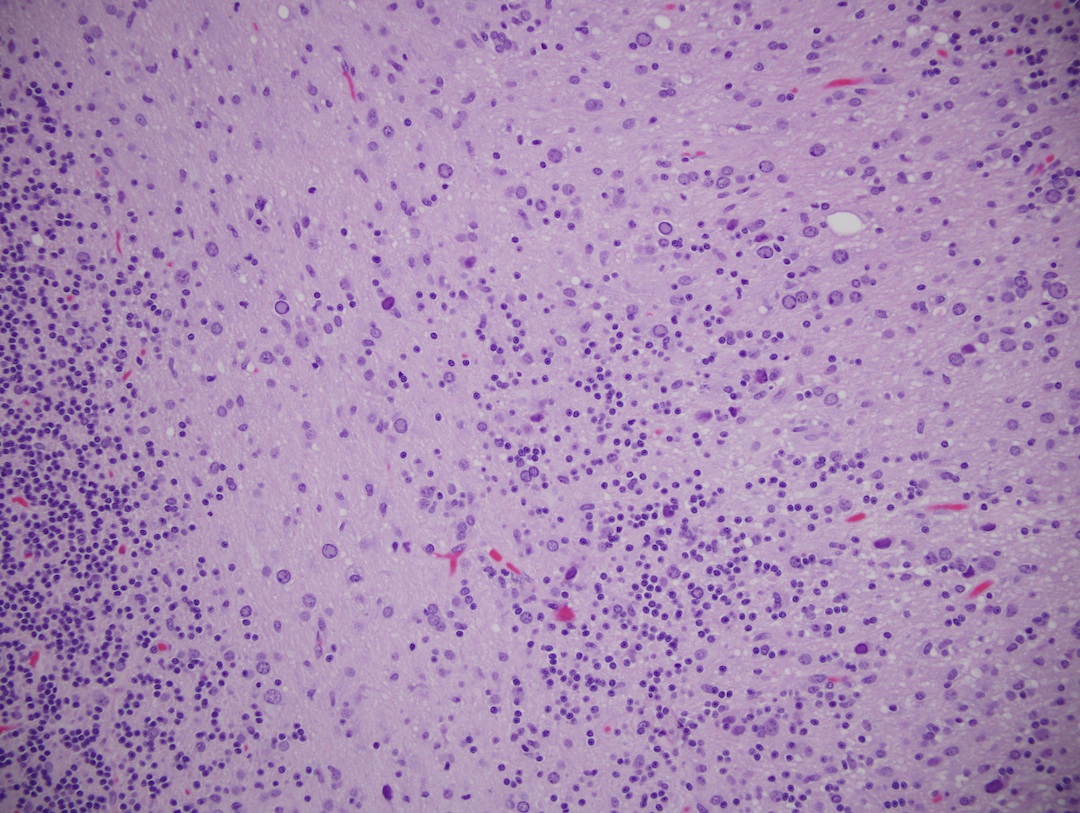
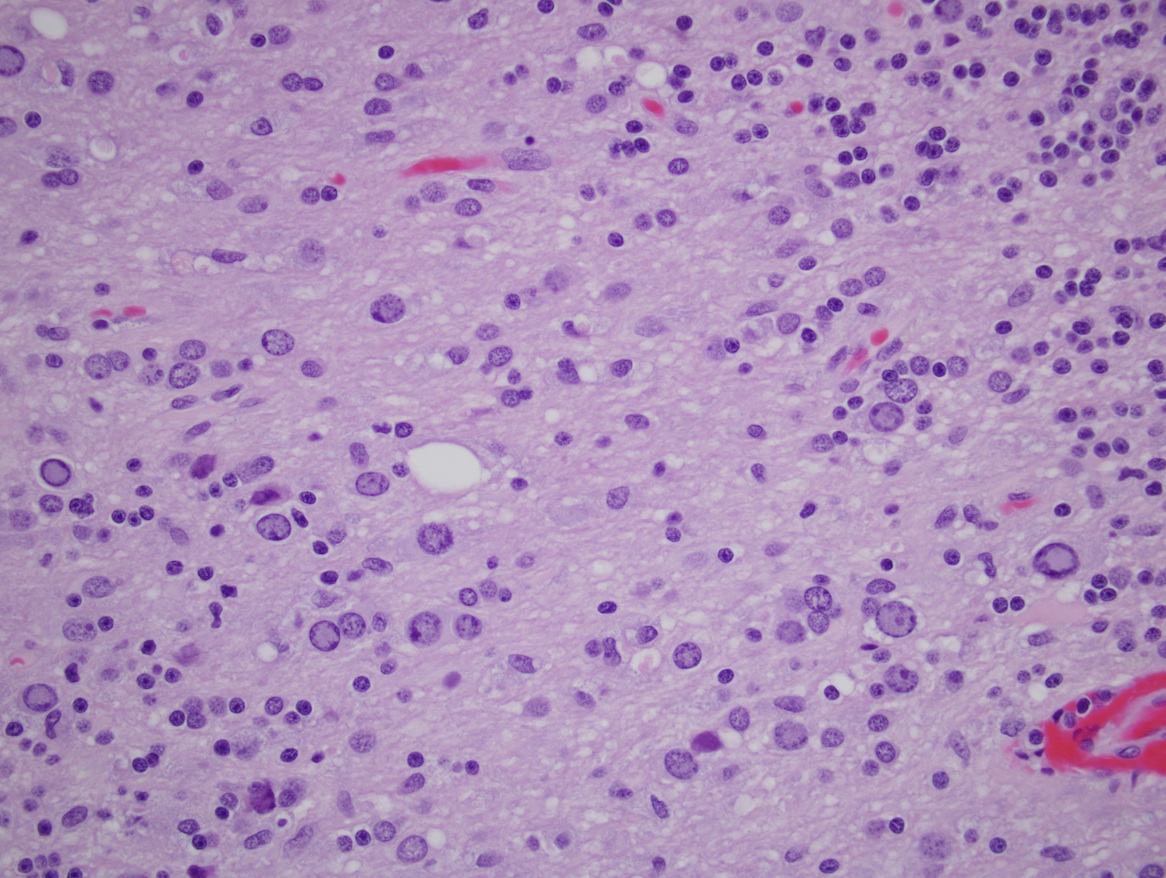
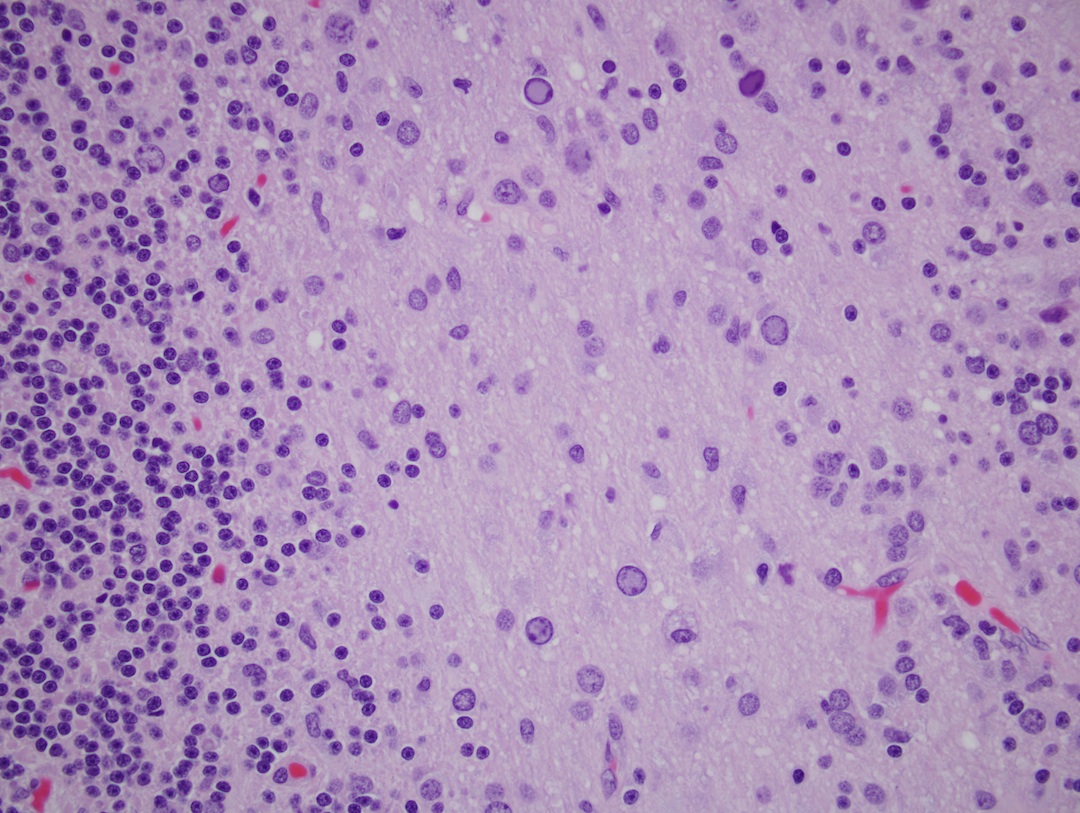
Microscopic images:
What is your diagnosis?
Diagnosis: Progressive multifocal leukoencephalopathy
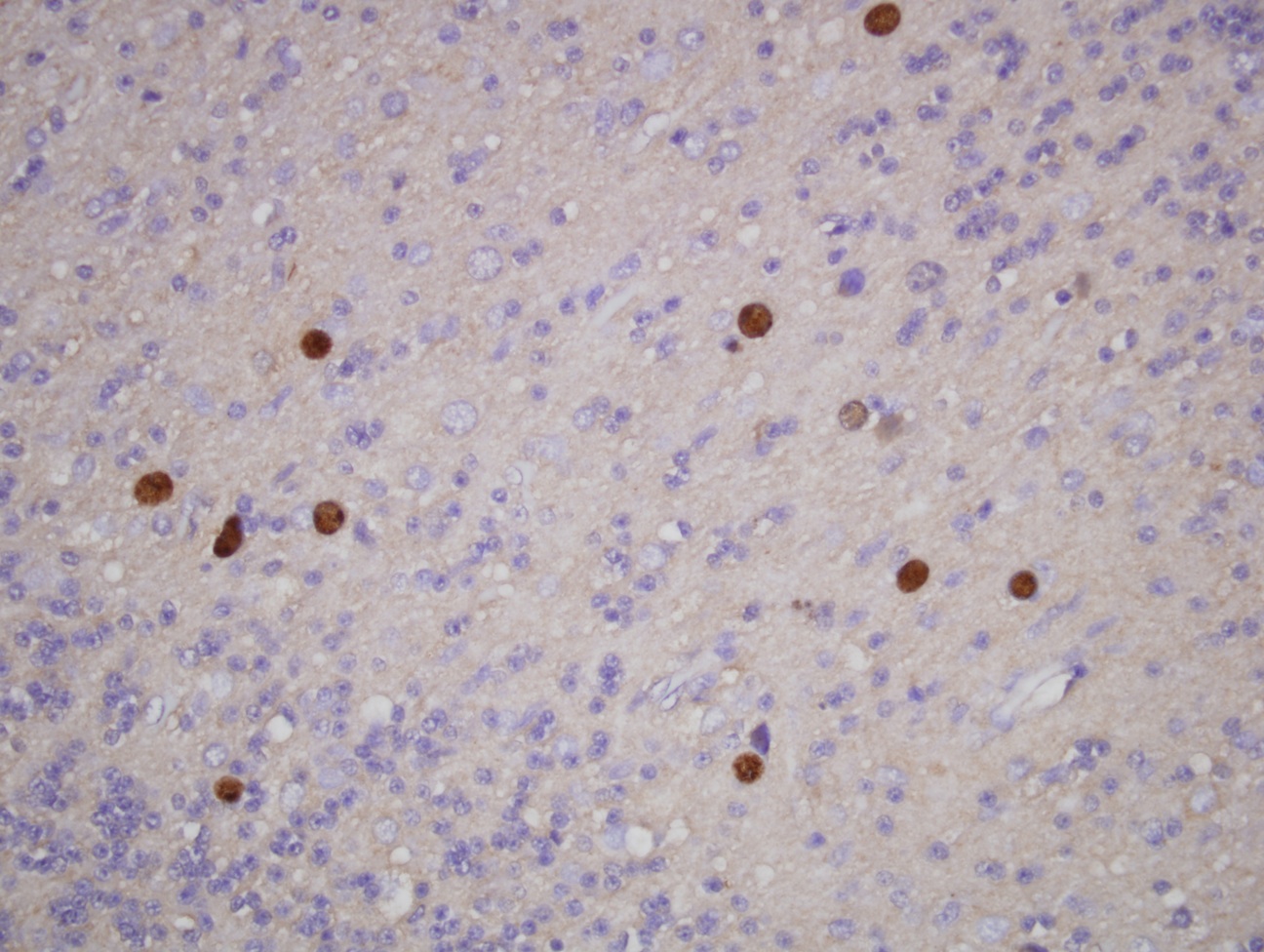
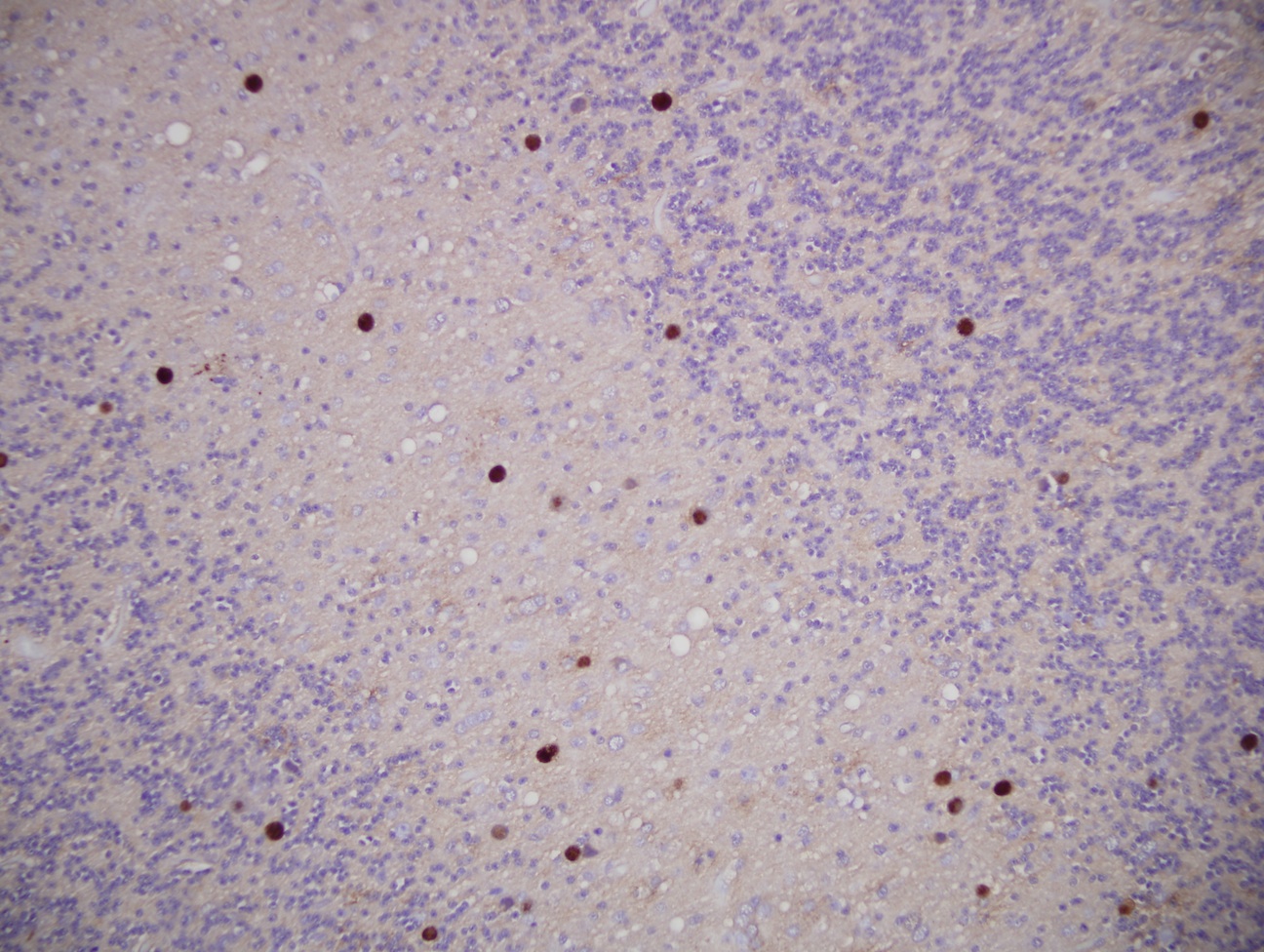
Immunostains:
Discussion:
Progressive multifocal leukoencephalopathy (PML), also known as progressive multifocal leukoencephalitis, is a rare and usually fatal demyelinating disease characterized by progressive multifocal white matter damage and inflammation, due to the JC virus (Discov Med 2011;12:495). It is almost always associated with immunosuppression, including immunosuppressive/biologic therapy for autoimmune diseases, such as natalizumab for multiple sclerosis and other agents for rheumatoid arthritis or lymphoma (Mult Scler 2012;18:143, Wikipedia: Progressive Multifocal Leukoencephalopathy [Accessed 8 April 2024], Joint Bone Spine 2012;79:351).
Lytic infection of CNS oligodendrocytes leads to their destruction and progressive demyelination, resulting in multifocal lesions. Although PML previously was relatively rare, it now occurs in 3 - 5% of HIV+ individuals, and is classified as an AIDS defining illness (Clin Microbiol Rev 2012;25:471).
Biopsies show multiple foci of demyelination with enlarged and bizzare astrocytes, which are often multinucleated and have multiple large processes. Oligodendrocytes may have eosinophilic or basophilic nuclear inclusions, due to virions (Acta Neuropathol 2010;120:403). Lymphocytic infiltration is variable. Necrosis with inflammation resembling an infarct may also be seen.
Treatment consists of reversal of the immunosuppression, if possible. Case reports now suggest some treatments may be effective (J Neurol Sci 2013;326:107, Ann Acad Med Singapore 2012;41:620).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Joseph Fullmer, University of Wisconsin Hospital and Clinics (USA), for contributing this case and the discussion.
Introducing 23 New Rabbit Monoclonal Antibodies: MSH2, CD25, RRM1, and others.
Epitomics is releasing 23 new EP Clones, high quality antibodies for anatomic pathology.
Our collection of EP Clones now includes new breast cancer markers: Aurora B and Mammaglobin; new Lymphoma markers CD25, RRM1, as well as various other Colon and Lung Cancer targets. Rabbit monoclonal antibodies (RabMAbs) are the product of true rabbit-rabbit hybridomas. The inherent qualities of the rabbit immune system allow us to select antibodies which include: 1) stronger binding affinity and 2) higher specificity.
Click here to view our new products or visit us at epitomics.com/diagnostics for our complete product listing.
Website news:
(1) New updates to our CME / Apps page include an advertisement for BoardVitals Pathology Question Bank and a free Apple app - Boardvitals Review for Clinical Pathology.
(2) We have updated the Lung tumor chapter based on reviews by Drs. Deepali Jain and Fulvio Lonardo and the Salivary glands chapter based on reviews by Fatima Aly, M.D. and Adriana Handra-Luca, M.D.
(3) We have removed the Topic search from the Home Page, since it wasn't working. We are developing a new architecture for the website, to first appear this summer, which will have a functioning topic search. For now, you can use the Google Search box to search for any text on the website. You can also use the Search feature of your browser (often Control F) to search for text on a particular page.
Visit and follow our Blog to see recent updates to the website.
(1) New updates to our CME / Apps page include an advertisement for BoardVitals Pathology Question Bank and a free Apple app - Boardvitals Review for Clinical Pathology.
(2) We have updated the Lung tumor chapter based on reviews by Drs. Deepali Jain and Fulvio Lonardo and the Salivary glands chapter based on reviews by Fatima Aly, M.D. and Adriana Handra-Luca, M.D.
(3) We have removed the Topic search from the Home Page, since it wasn't working. We are developing a new architecture for the website, to first appear this summer, which will have a functioning topic search. For now, you can use the Google Search box to search for any text on the website. You can also use the Search feature of your browser (often Control F) to search for text on a particular page.
Visit and follow our Blog to see recent updates to the website.
Case #265
Clinical history:
A 61 year old man had abdominal follicular lymphoma diagnosed 7 years ago, treated with chemotherapy and radiation, and thought to be in remission. He developed increasing difficulties with balance, dizziness, numbness over his left tongue and inside cheek spreading to his face, as well as clumsiness with his left hand and leg over a 7 week period. MRI revealed a 3.8 x 2.3 x 2.4 cm lesion with minimal edge enhancement (hence predominately non-enhancing) centered in the left middle cerebellar peduncle extending into the left paramedian pons and left cerebellar hemisphere. Preoperative differential diagnosis included demyelination, low grade glial neoplasm, and recurrent lymphoma. Biopsy of the mass was performed.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Progressive multifocal leukoencephalopathy
Immunostains:
Discussion:
Progressive multifocal leukoencephalopathy (PML), also known as progressive multifocal leukoencephalitis, is a rare and usually fatal demyelinating disease characterized by progressive multifocal white matter damage and inflammation, due to the JC virus (Discov Med 2011;12:495). It is almost always associated with immunosuppression, including immunosuppressive/biologic therapy for autoimmune diseases, such as natalizumab for multiple sclerosis and other agents for rheumatoid arthritis or lymphoma (Mult Scler 2012;18:143, Wikipedia: Progressive Multifocal Leukoencephalopathy [Accessed 8 April 2024], Joint Bone Spine 2012;79:351).
Lytic infection of CNS oligodendrocytes leads to their destruction and progressive demyelination, resulting in multifocal lesions. Although PML previously was relatively rare, it now occurs in 3 - 5% of HIV+ individuals, and is classified as an AIDS defining illness (Clin Microbiol Rev 2012;25:471).
Biopsies show multiple foci of demyelination with enlarged and bizzare astrocytes, which are often multinucleated and have multiple large processes. Oligodendrocytes may have eosinophilic or basophilic nuclear inclusions, due to virions (Acta Neuropathol 2010;120:403). Lymphocytic infiltration is variable. Necrosis with inflammation resembling an infarct may also be seen.
Treatment consists of reversal of the immunosuppression, if possible. Case reports now suggest some treatments may be effective (J Neurol Sci 2013;326:107, Ann Acad Med Singapore 2012;41:620).