28 September 2012 - Case #253
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Saroona Haroon, The Aga Khan University Hospital (Pakistan), for contributing this case.
Advertisement
Case #253
Clinical history:
A 70 year old woman presented with a painless cheek lesion for the past 4 months, which was increasing in size.
Gross images:
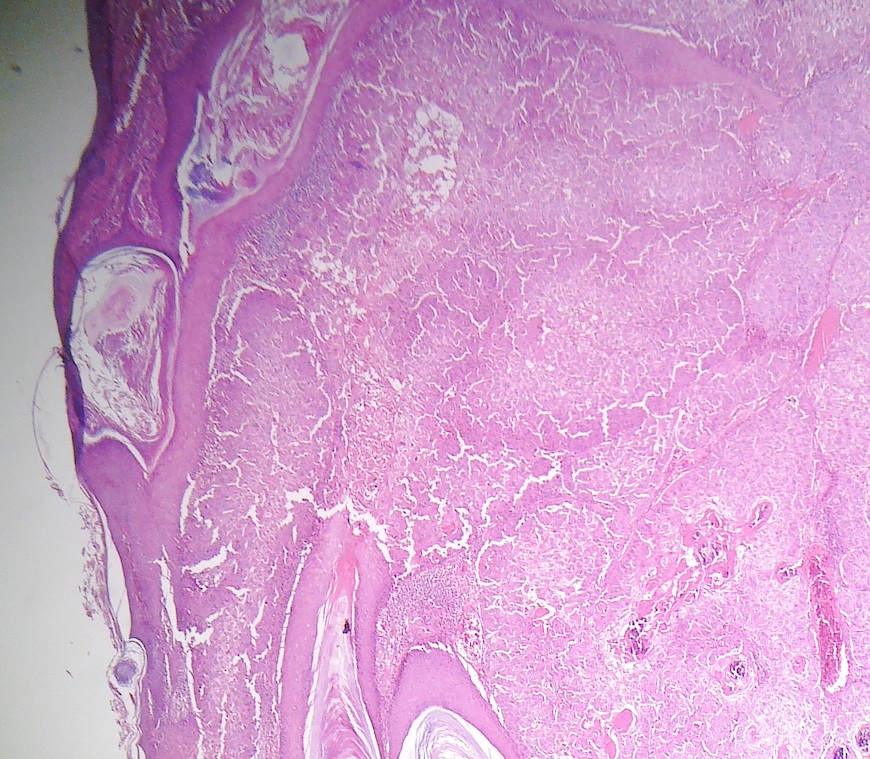
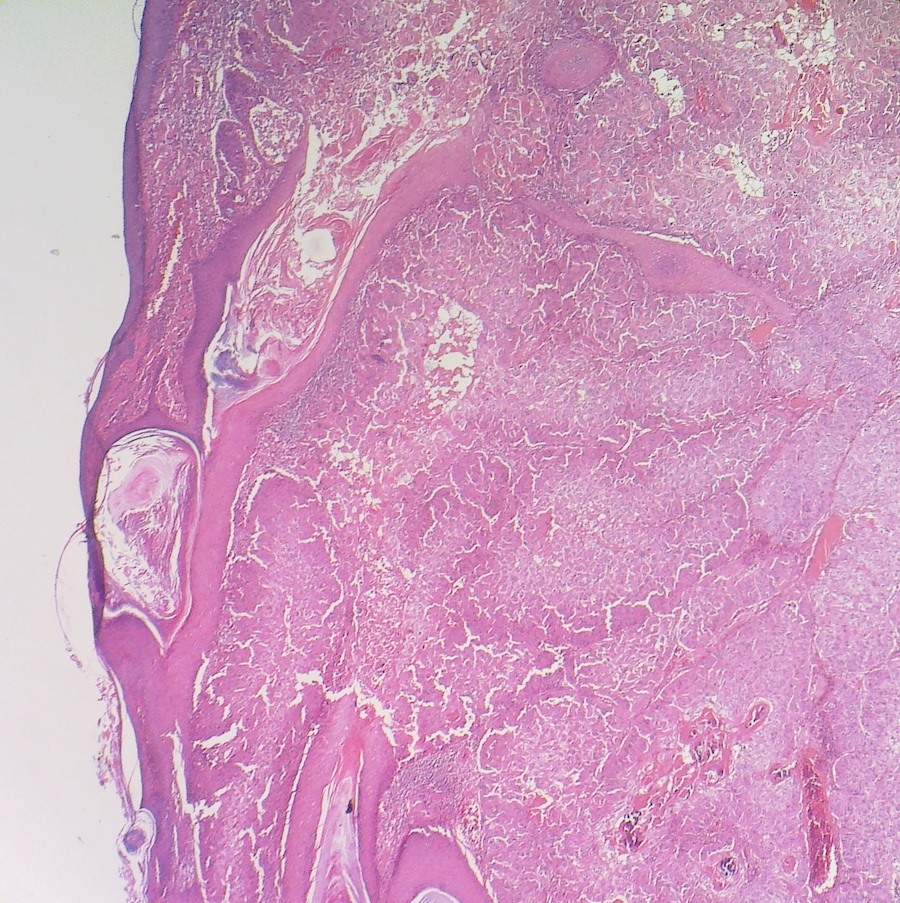
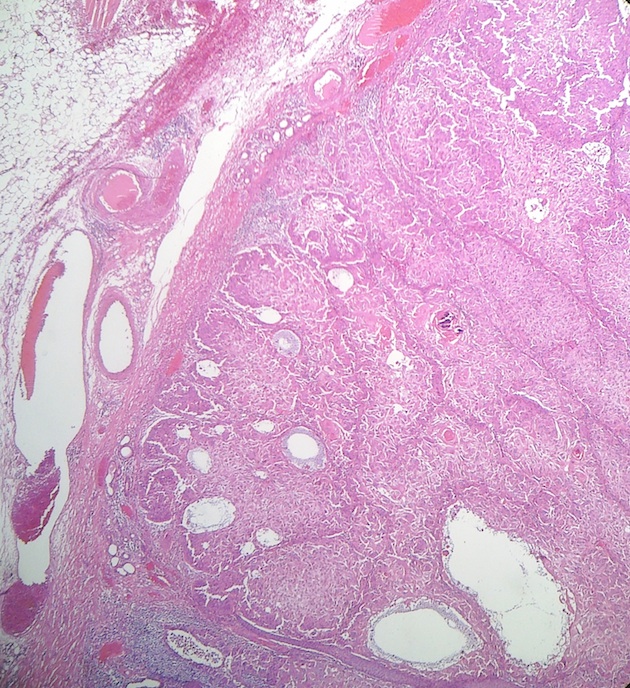
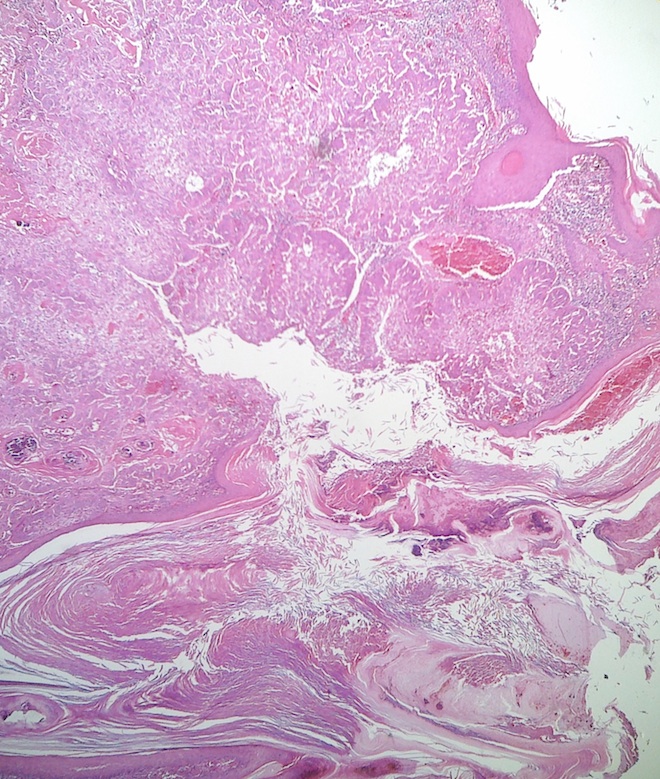
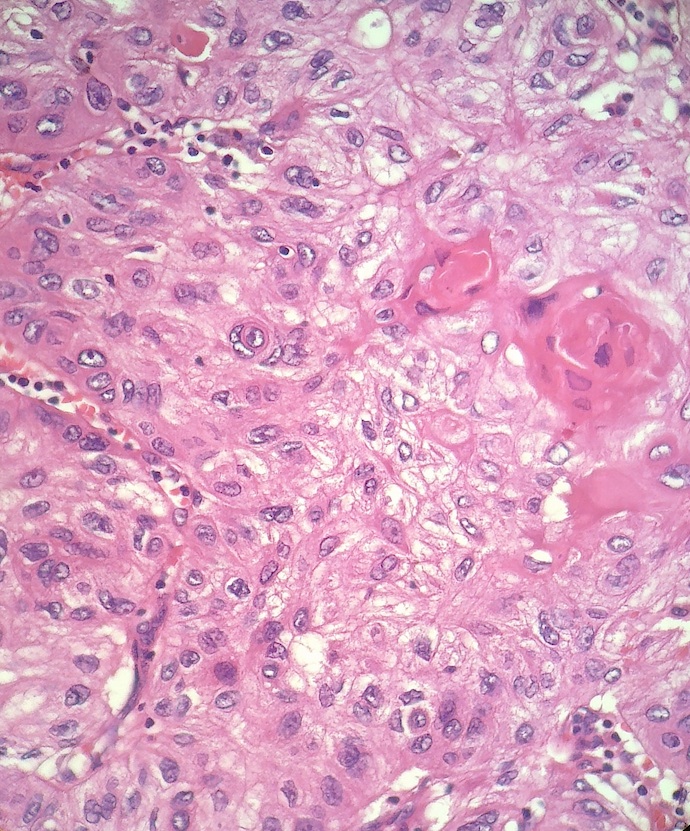
Microscopic images:
What is your diagnosis?
Diagnosis: Keratoacanthoma
Discussion:
Keratoacanthoma is considered by some to be a well differentiated cutaneous squamous cell carcinoma. It typically (80%) occurs in men on the sun exposed face, and is associated with inflammatory dermatoses, congenital lesions, genetic diseases and scars. Those affected are usually younger than in classic cutaneous squamous cell carcinoma. Clinically, most cases arises from normal skin, grow rapidly for 4 - 8 weeks, then regress over 6 months to leave a depressed, annular scar.
Histologically, the early phase is composed of well circumscribed solid lobules of large, pale squamous cells with little keratinization. The follicular infundibulum is distorted and there is mild atypia. The stable phase, which is often excised, has a central crater filled with keratin, but no granular layer. There are larger and more irregular infiltrating squamous nests and islands, accompanied by a marked inflammatory infiltrate with lichenoid features and eosinophils but no plasma cells. The squamous cells may be deeply infiltrative, with microabscesses of neutrophils and eosinophils approaching the surface. There is also often marked atypia with mitotic figures, atypical mitotic figures at the periphery, perineural invasion and rarely vascular invasion. The regressing (resolving) phase is characterized by a keratin filled crater but with mature epithelium without atypia. There is flattening of the cup shape, horizontal fibrosis in dermis, reduced inflammation and perforating elastic fibers (J Cutan Pathol 2012;39:243).
The differential diagnosis includes squamous cell carcinoma, which usually lacks the overhanging edges, the keratin filled crater and the hemispheric shape. Other diagnoses to consider basal cell carcinoma, nodular melanoma (non-pigmented), pilomatricoma and hypertrophic lichen planus (Sultan Qaboos Univ Med J 2012;12:360).
Most lesions regress, but show persistent crateriform architecture (J Am Acad Dermatol 2012;67:1008). Rare metastases have been reported (Semin Diagn Pathol 2009;26:150). Traditional treatment is surgical but intralesional methotrexate and topical imiquimod cream have also been effective (Can J Plast Surg 2011;19:e15, Ann Dermatol 2011;23:357).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Saroona Haroon, The Aga Khan University Hospital (Pakistan), for contributing this case.
Epitomics Rabbit Monoclonal Antibodies Show Optimal Staining in Third Party Assessments
In a series of independent assessments, Epitomics antibodies to MSH6, Her2, CD99, CD20, CK8, and CK19 were rated as "optimally" staining. With our proprietary RabMAb technology, Epitomics continues to develop high quality antibodies and IHC kits for anatomical pathology use.
See our full antibody listing and comparisons here.
EP Clones are a line of high quality antibodies for anatomical pathology. Each antibody was generated using Epitomics patented Rabbit Monoclonal Antibody (RabMAb) technology offering superior binding affinity and specificity. We now have over 150 antibodies, fully validated, ideal for FFPE tissues.
Website news:
(1) The Skin - Nonmelanocytic tumors chapter has now been updated, based on reviews by Christopher Hale, M.D., NYU Langone Medical Center, New York. We plan to have a recent update (since 2010) for all chapters by the USCAP meeting in March 2013, and then to update each chapter every 12-18 months. We also plan to add more images and references to each topic.
(2) We are cleaning up some technical issues with some of the thumbnail images, particularly in the Breast, Penis-Scrotum, Soft Tissue and Skin-Melanocytic tumor chapters, and to a lesser extent in other chapters. The links to the full images should be working even if the thumbnail is missing. We hope to have this completed as soon as possible, and apologize for any inconvenience.
Visit and follow our Blog to see recent updates to the website.
(1) The Skin - Nonmelanocytic tumors chapter has now been updated, based on reviews by Christopher Hale, M.D., NYU Langone Medical Center, New York. We plan to have a recent update (since 2010) for all chapters by the USCAP meeting in March 2013, and then to update each chapter every 12-18 months. We also plan to add more images and references to each topic.
(2) We are cleaning up some technical issues with some of the thumbnail images, particularly in the Breast, Penis-Scrotum, Soft Tissue and Skin-Melanocytic tumor chapters, and to a lesser extent in other chapters. The links to the full images should be working even if the thumbnail is missing. We hope to have this completed as soon as possible, and apologize for any inconvenience.
Visit and follow our Blog to see recent updates to the website.
Case #253
Clinical history:
A 70 year old woman presented with a painless cheek lesion for the past 4 months, which was increasing in size.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Keratoacanthoma
Discussion:
Keratoacanthoma is considered by some to be a well differentiated cutaneous squamous cell carcinoma. It typically (80%) occurs in men on the sun exposed face, and is associated with inflammatory dermatoses, congenital lesions, genetic diseases and scars. Those affected are usually younger than in classic cutaneous squamous cell carcinoma. Clinically, most cases arises from normal skin, grow rapidly for 4 - 8 weeks, then regress over 6 months to leave a depressed, annular scar.
Histologically, the early phase is composed of well circumscribed solid lobules of large, pale squamous cells with little keratinization. The follicular infundibulum is distorted and there is mild atypia. The stable phase, which is often excised, has a central crater filled with keratin, but no granular layer. There are larger and more irregular infiltrating squamous nests and islands, accompanied by a marked inflammatory infiltrate with lichenoid features and eosinophils but no plasma cells. The squamous cells may be deeply infiltrative, with microabscesses of neutrophils and eosinophils approaching the surface. There is also often marked atypia with mitotic figures, atypical mitotic figures at the periphery, perineural invasion and rarely vascular invasion. The regressing (resolving) phase is characterized by a keratin filled crater but with mature epithelium without atypia. There is flattening of the cup shape, horizontal fibrosis in dermis, reduced inflammation and perforating elastic fibers (J Cutan Pathol 2012;39:243).
The differential diagnosis includes squamous cell carcinoma, which usually lacks the overhanging edges, the keratin filled crater and the hemispheric shape. Other diagnoses to consider basal cell carcinoma, nodular melanoma (non-pigmented), pilomatricoma and hypertrophic lichen planus (Sultan Qaboos Univ Med J 2012;12:360).
Most lesions regress, but show persistent crateriform architecture (J Am Acad Dermatol 2012;67:1008). Rare metastases have been reported (Semin Diagn Pathol 2009;26:150). Traditional treatment is surgical but intralesional methotrexate and topical imiquimod cream have also been effective (Can J Plast Surg 2011;19:e15, Ann Dermatol 2011;23:357).