5 September 2012 - Case #250
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Bassma Mohamed El Sabaa, Alexandria School of Medicine (Egypt), for contributing this case and the discussion.
Advertisement
Case #250
Clinical history:
A 4 month old boy had a 2 month history of manifestations of increased intracranial pressure. MRI showed a 1.5 x 1.5 cm solid mass in the hypothalamic area, which was biopsied.
Gross examination revealed a few tiny soft slimy tissue fragments collectively measuring 1.5 x 1.0 cm.
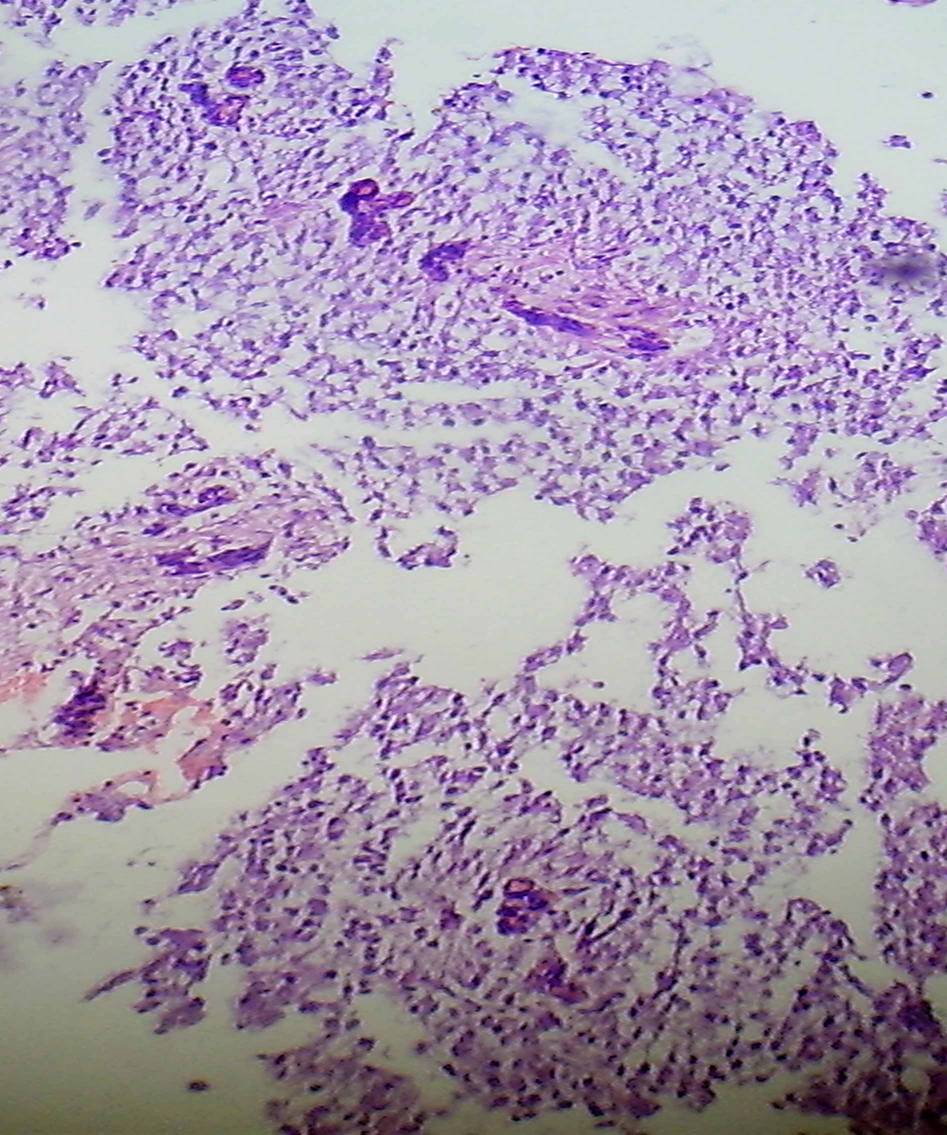
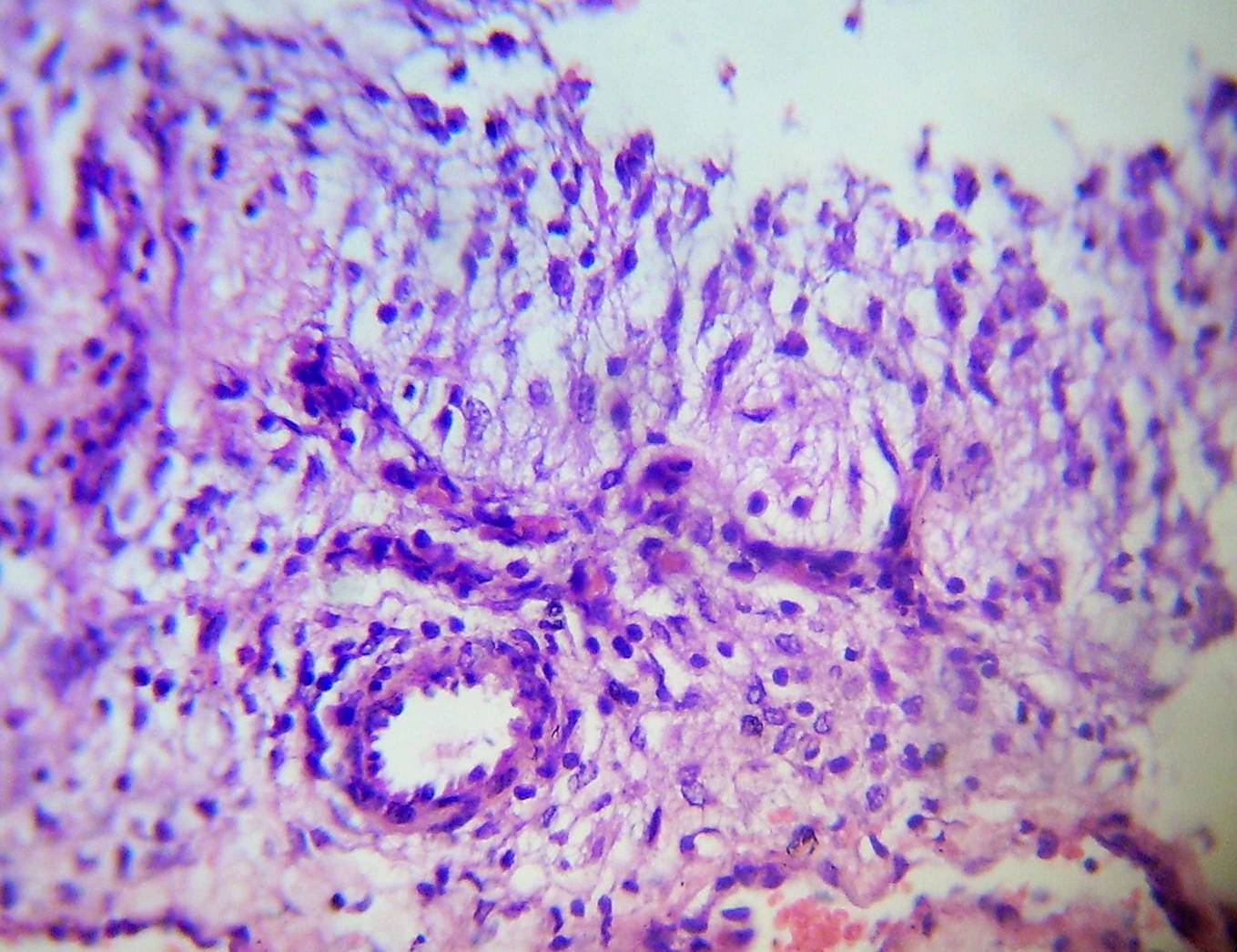
Microscopic images:
What is your diagnosis?
Diagnosis: Pilomyxoid astrocytoma (PMA), WHO grade II; ICD-O 9425/3
Discussion:
This hypothalamic tumor in a 4 month old is composed of monomorphic, spindled, bipolar, GFAP+ glial cells in a loose fibrillar and strikingly myxoid background, in a somewhat angiocentric pattern.
The differential diagnosis is based on patient age and tumor site, and includes pilocytic astrocytoma, pilomyxoid astrocytoma, low grade diffuse astrocytoma and ependymoma.
Pilocytic astrocytoma:
Diffuse infiltrating astrocytomas:
Ependymoma:
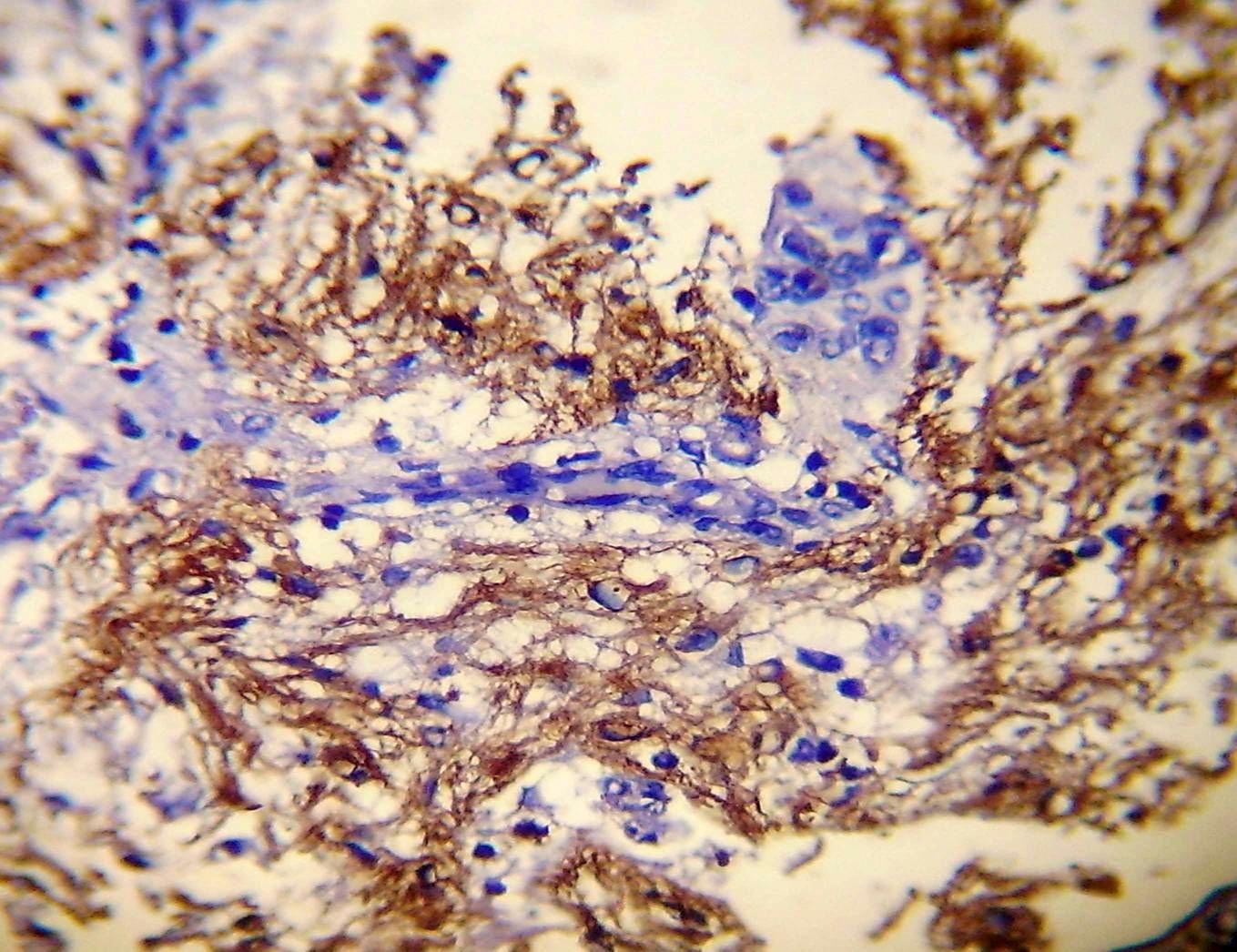
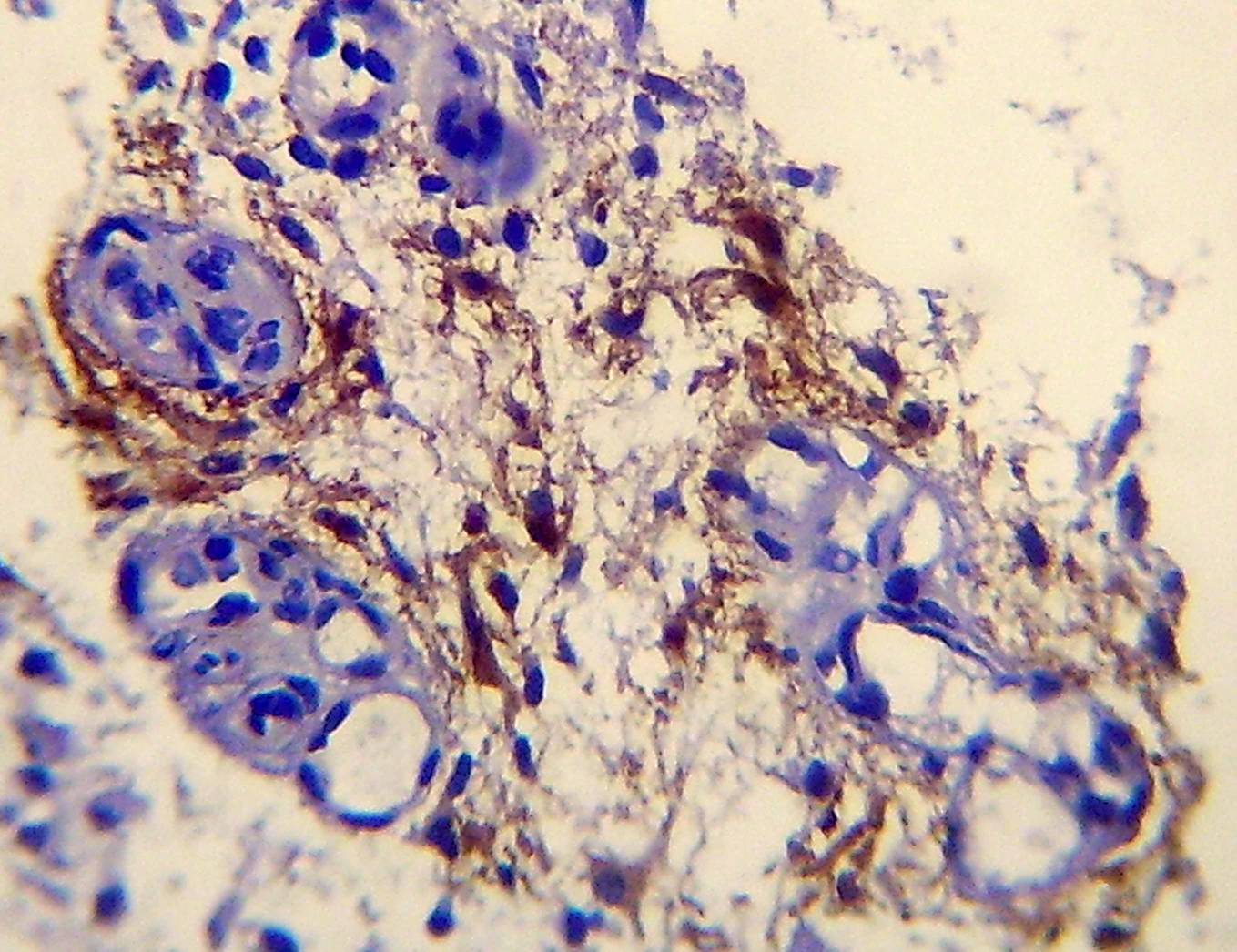
This case has characteristic features of pilomyxoid astrocytoma, including a prominent myxoid matrix, monomorphous bipolar spindle cells, a prominent angiocentric arrangement, some glomeruloid vessels and no mitotic figures / significant pleomorphism. The spindle cells are GFAP and vimentin positive and negative for synaptophysin, neuron specific nuclear protein (Neu-N), chromogranin, neruofilament and epithelial membrane antigen (EMA). The MIB1 (Ki67) labeling index varies between 0.9 - 6.1% with marked regional variations.
Pilomyxoid astrocytoma is an aggressive variant of pilocytic astrocytoma, with more local recurrence (55 - 76%) and CSF spread (11 - 14%). Up to 33% of patients die of disease within 2 years after diagnosis (J Neuropathol Exp Neurol 1999;58:1061, MedGenMed 2004;6:42). To date, no specific cytogenetic or molecular pathologic findings or associated syndromes have been identified.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Bassma Mohamed El Sabaa, Alexandria School of Medicine (Egypt), for contributing this case and the discussion.
November 10, 2012
The Henry, Autograph Collection
Dearborn, Michigan (USA)
8th Annual Course
Contemporary Issues In
Diagnostic Surgical Pathology

Sponsored by the Wayne State University School of Medicine,
Detroit Medical Center and Karmanos Cancer Institute

Course Director: Rouba Ali-Fehmi, M.D.
Website
Schedule
Hotel
Register
Telephone: 313 / 745-2520
Email: rali@med.wayne.edu
Website news:
(1) The Forensics chapter is now complete, written by Lindsey Harle, M.D. Recent chapter updates include Prostate gland and seminal vesicles, based on reviews by Ali Amin, M.D., Komal Arora, M.D. and Gladell Paner, M.D., and Kidney Tumor (adult malignant), now combined with Kidney tumor (children, benign), based on reviews by Sean Williamson, M.D.
(2) Recent new articles on our Management Page include, Medicare Changes Enrollment Guidelines From 30 days to 60 days, by Leigh Polk, PSA, LLC, click here and ACO's, Practice Buy-outs and Dj vu All over Again, by Mick Raich, Vachette Pathology, click here.
(3) Visit us at CAP, Booth #404, on September 9-10, 2012.
Visit and follow our Blog to see recent updates to the website.
(1) The Forensics chapter is now complete, written by Lindsey Harle, M.D. Recent chapter updates include Prostate gland and seminal vesicles, based on reviews by Ali Amin, M.D., Komal Arora, M.D. and Gladell Paner, M.D., and Kidney Tumor (adult malignant), now combined with Kidney tumor (children, benign), based on reviews by Sean Williamson, M.D.
(2) Recent new articles on our Management Page include, Medicare Changes Enrollment Guidelines From 30 days to 60 days, by Leigh Polk, PSA, LLC, click here and ACO's, Practice Buy-outs and Dj vu All over Again, by Mick Raich, Vachette Pathology, click here.
(3) Visit us at CAP, Booth #404, on September 9-10, 2012.
Visit and follow our Blog to see recent updates to the website.
Case #250
Clinical history:
A 4 month old boy had a 2 month history of manifestations of increased intracranial pressure. MRI showed a 1.5 x 1.5 cm solid mass in the hypothalamic area, which was biopsied.
Gross examination revealed a few tiny soft slimy tissue fragments collectively measuring 1.5 x 1.0 cm.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Pilomyxoid astrocytoma (PMA), WHO grade II; ICD-O 9425/3
Discussion:
This hypothalamic tumor in a 4 month old is composed of monomorphic, spindled, bipolar, GFAP+ glial cells in a loose fibrillar and strikingly myxoid background, in a somewhat angiocentric pattern.
The differential diagnosis is based on patient age and tumor site, and includes pilocytic astrocytoma, pilomyxoid astrocytoma, low grade diffuse astrocytoma and ependymoma.
Pilocytic astrocytoma:
- Features in this case that support this diagnosis:
- Age: children
- MRI: enhancing cyst with a mural nodule
- Histology: elongated, bipolar cells; glomeruloids of thin walled blood vessels
- Features of pilocytic astrocytoma not present in this case:
- Rosenthal fibers and eosinophilic granular bodies
- Myxoid changes are only focal
Diffuse infiltrating astrocytomas:
- Features in this case that support this diagnosis:
- Myxoid change can be seen in low grade astrocytoma (WHO grade II)
- Features of diffuse infiltrating astrocytoma not present in this case:
- Usually adults
- Myxoid stroma with perivascular bipolar cells is unusual
Ependymoma:
- Features of ependymoma not present in this case:
- Regular perivascular rosettes, true rosettes
- Extensive myxoid background unusual
This case has characteristic features of pilomyxoid astrocytoma, including a prominent myxoid matrix, monomorphous bipolar spindle cells, a prominent angiocentric arrangement, some glomeruloid vessels and no mitotic figures / significant pleomorphism. The spindle cells are GFAP and vimentin positive and negative for synaptophysin, neuron specific nuclear protein (Neu-N), chromogranin, neruofilament and epithelial membrane antigen (EMA). The MIB1 (Ki67) labeling index varies between 0.9 - 6.1% with marked regional variations.
Pilomyxoid astrocytoma is an aggressive variant of pilocytic astrocytoma, with more local recurrence (55 - 76%) and CSF spread (11 - 14%). Up to 33% of patients die of disease within 2 years after diagnosis (J Neuropathol Exp Neurol 1999;58:1061, MedGenMed 2004;6:42). To date, no specific cytogenetic or molecular pathologic findings or associated syndromes have been identified.