All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Sean Williamson, Indiana University School of Medicine, USA.
Learn how to:
www.accucoregroup.com, (267) 564-5015
Free 45 minute webinar
Best Practices for Anatomic Pathology Quality
and Document Management
Wednesday January 25th
12:00pm Eastern
Register here
Sponsored by AccuPathology
Pathology Quality Management Software
Manage and control documents mandated by CAP and TJC while meeting ISO 15189 standards
Identify pre-analytic and post-analytic variables that contribute to diagnostic errors
Integrate with your LIS to automate tasks, identifying potential QA to be performed
Automate OPPE, FPPE and Credentialing required processes
Leverage dashboards to gather and compile information for CAP and The Joint Commission audits
Spend less time, getting better information to make REAL changes while always being compliant
Advertisement
Case #229
Clinical History:
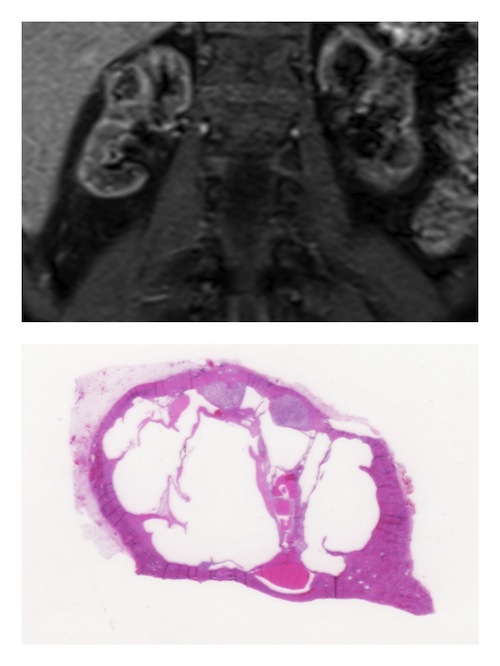
The patient is a 71 year old woman with end stage renal disease and acquired cystic kidney disease secondary to diabetes. 5 years after renal transplant, surveillance ultrasonography revealed complex cysts in the native right kidney, up to 1.9 cm in greatest dimension. Renal MRI confirmed the presence of multiple complex cystic lesions in the bilateral native kidneys, including an enhancing nodule within one of the lesions, concerning for malignancy. Bilateral nephrectomy was performed.
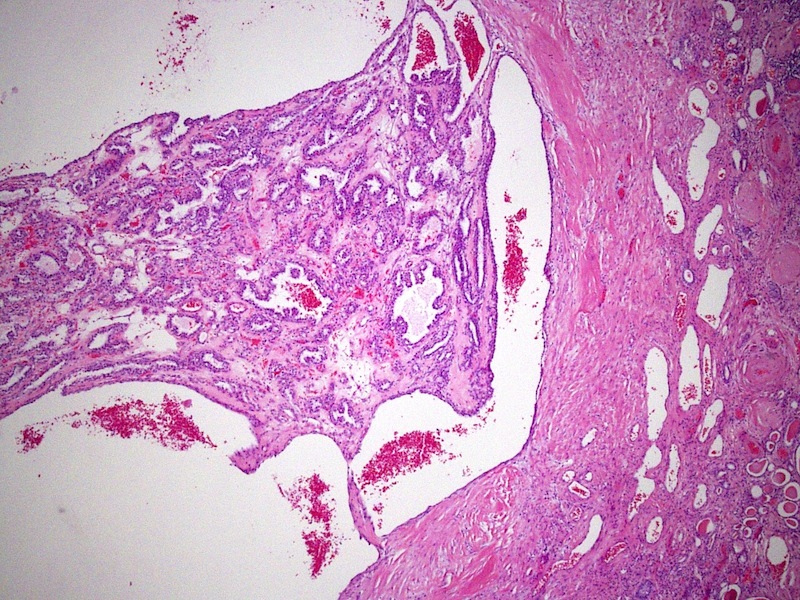
Gross examination of the native kidney nephrectomy specimens revealed multiple bilateral, complex cystic and focally solid lesions, ranging in size from 0.2 to 2.0 cm in greatest dimension. Microscopically, all of the tumors demonstrated similar histopathologic features.
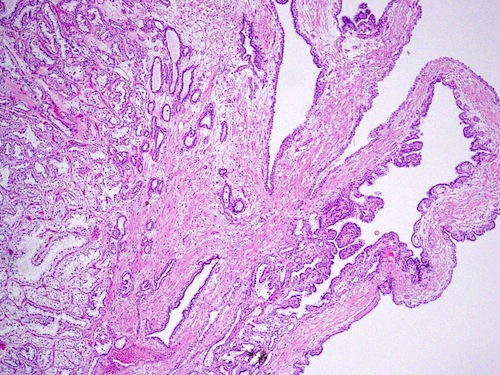
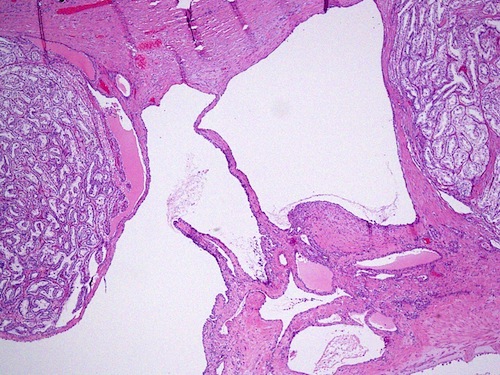
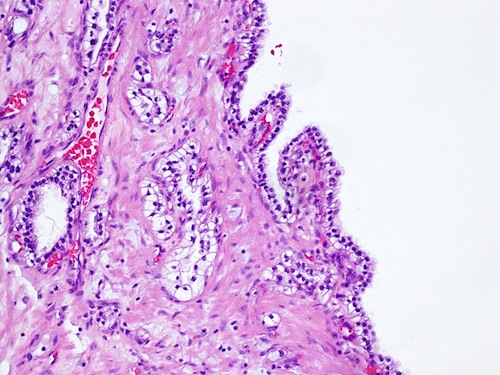
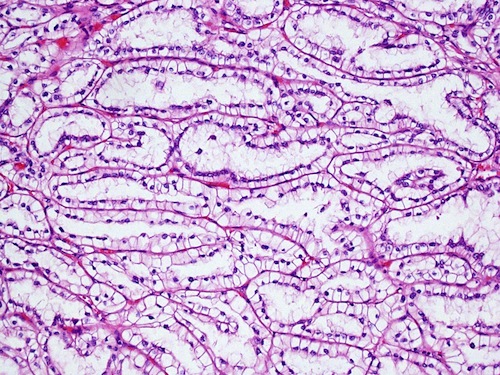
Microscopic images:
What is your diagnosis?
Diagnosis: Clear cell papillary renal cell carcinoma
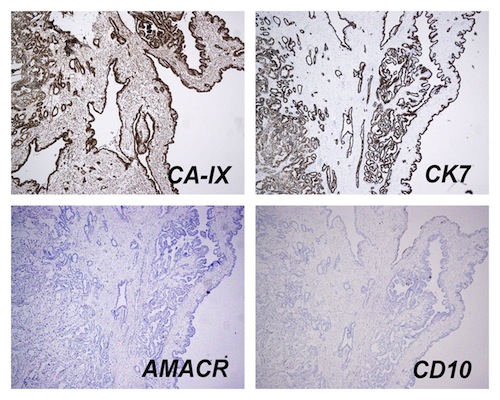
Stains images:
Discussion:
Clear cell papillary renal cell carcinoma is a recently identified renal neoplasm (also known as clear cell tubulopapillary renal cell carcinoma), originally described in the setting of end stage renal disease and acquired cystic kidney disease (Am J Surg Pathol 2006;30:141); however, tumors may also be found in patients with otherwise normal kidneys (Am J Surg Pathol 2008;32:1239).
Clear cell papillary renal cell carcinoma has distinctive histologic features, though sometimes showing significant morphologic overlap with clear cell carcinoma or papillary carcinoma. Architectural features include a mixture of cystic, solid tubular / ductular and branched papillary architectural components, combined cytologically with variable amounts of clear cytoplasm (Am J Surg Pathol 2010;34:1608, Histopathology 2011;58:1064, Am J Surg Pathol 2006;30:141). Often, at least focal areas show alignment of the tumor cell nuclei away from the basement membrane, similar to secretory endometrium. Other features include a branched configuration of the ductular / tubular component and occasional calcification within the fibrous septa. Although the tumor is named for the combination of clear cell cytology and papillary architecture, large, extensively branched papillae are not the predominant component in many cases. Some cases may be predominantly cystic, mimicking multilocular cystic renal cell carcinoma. Most show low grade nuclear features (Fuhrman grade 1 or 2).
By immunohistochemistry, tumors show expression of carbonic anhydrase IX (CAIX), similar to clear cell carcinoma, and cytokeratin 7, similar to papillary carcinoma; however, unlike clear cell and papillary carcinoma, CD10 and AMACR (P504S) are generally negative (Am J Surg Pathol 2008;32:1780).
A characteristic molecular genetic abnormality has not yet been identified. Some studies have found low copy number gains of chromosome 7 or 17 in a minority of cases, similar to although less frequent than papillary carcinoma. In contrast to clear cell carcinoma, abnormalities of chromosome 3p and the VHL gene are absent, although expression of CAIX, HIF1α and GLUT1 has led to the hypothesis that there is upregulation of the HIF pathway by a non-VHL dependent mechanism (Mod Pathol 2011;24:1207).
Prognosis in tumors reported thus far has been excellent, with no known metastases or aggressive behavior.