

Home
Case
of Week Home
Jobs
Conferences
Fellowships
Books
8 September 2011 Case of the Week #216
This email is only sent to subscribers. To subscribe or unsubscribe to this or our other email
lists, click
here.
All cases are archived on our website. To view them sorted by number, diagnosis or category,
visit our Home Page and click on the Case of the Week button on the left hand side.
Thanks to Dr. Bassma M. El Sabaa, Alexandria Faculty of Medicine, Egypt, for contributing this case. To contribute a Case of the Week, follow the guidelines on our Case of the Week page.

[#2664]
Advertisement
Website news:
(1) Visit us at CAP '11 at Booth #328, towards the back near the posters, left hand side (as you enter).
(2) Our Feature Page for September 2011 highlights Antibodies, and includes Biogenex, Covance, Epitomics and Leica Microsystems.
(3) We are looking for a reviewer for our new
CNS-nontumor chapter. Sections include normal / embryology,
malformations, infections, demyelinating disorders, dementia, stroke /
hemorrhage. Email us if interested.
(4) In August 2011, we had record traffic of
307,303 visits. Thanks to all of our supporters.
Case of the Week #216
Clinical History:
A 28 month old girl had a 2 month history of squinting, vomiting and ataxia. MRI showed lesions in the fourth ventricle and the left cerebellar hemisphere, which were excised.
Micro images:
What is your diagnosis?
Diagnosis:
Medulloepithelioma
Discussion:
Immunostains were negative for cytokeratin, EMA and GFAP, and positive for nestin and vimentin:


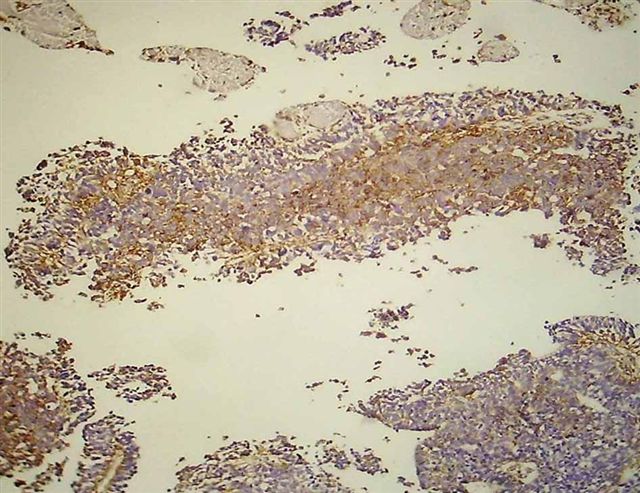
Nestin+ (left 2 images), vimentin+ (right image)
Medulloepithelioma is a rare, high grade (WHO grade IV), neoplasm containing epithelium resembling the embryonic neural tube. Most cases occur in the first 5 years of life, either supra- or infratentorially. It may also occur in the ciliary body / optic disc (Hum Pathol 2011 Jun 13 [Epub ahead of print]) or elsewhere in the body. Tumors are typically large, causing increased intracranial pressure or mass-type symptoms (Burger: Tumors of the Central Nervous System (AFIP Atlas of Tumor Pathology, Series 4, Vol 7, 2007).
Grossly, tumors are typically solid, gray-tan and soft, with variable cystic changes, hemorrhage, fibrosis or calcification. Classic histologic features are glands or tubules of primitive appearing epithelium that resembles the epithelium of the developing brain, with pseudostratification, small cytoplasmic blebs and mitotic figures. The outer surface has a well defined basement membrane, and the internal side has an ill-defined pseudomembrane. Other regions may have more undifferentiated tumor.
The basement membrane is strongly positive for PAS, type IV collagen and nestin, and tumor cells are immunoreactive for vimentin but negative for keratin, S100, GFAP and synaptophysin (Pediatr Pathol Lab Med 1997;17:913).
The differential diagnosis includes:
• choroid plexus carcinoma: papillary epithelium, S100+, cytokeratin+
• immature teratoma: has other fetal-appearing tissues, PLAP+, possibly AFP+ or CEA+
• ependymoblastoma: has rosettes with a lumen but without an outer or inner membrane
Most patients die within 1 year of diagnosis, although long term survival has been reported (J Neurosurg Pediatr 2008;2:339). In the above case, the patient received chemotherapy, and is alive and well one year post-diagnosis.
Nat Pernick, M.D., President
PathologyOutlines.com, Inc.
30100 Telegraph Road, Suite 408
Bingham Farms, Michigan (USA) 48025
Telephone: 248/646-0325
Email:
NatPernick@Hotmail.com
Alternate email: NatPernick@gmail.com