26 May 2011 - Case #207
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Kristin Olson, University of California, Los Angeles (USA), for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.

AccuCore Group invites you to a free 45 minute webinar:
Best Practices for Anatomic Pathology Quality Management
June 16th at 12:00pm Eastern
Webinar Agenda:
Sponsored by AccuPathology: Pathology Quality Management Software
AccuCore Group
(267) 564-5015
http://www.accucoregroup.com
Advertisement
Case #207
Clinical history:
An 8 year old girl presented to her primary care physician with precocious puberty. On physical examination, she had a large pelvic mass. The well circumscribed mass was resected. It weighed 413 grams and measured 13.5 x 9 x 6 cm. Sectioning demonstrated a variegated yellow-tan to red-brown cystic and hemorrhagic mass. One 2.5 cm cyst contained sebaceous material and scattered calcifications were identified.
Gross image:
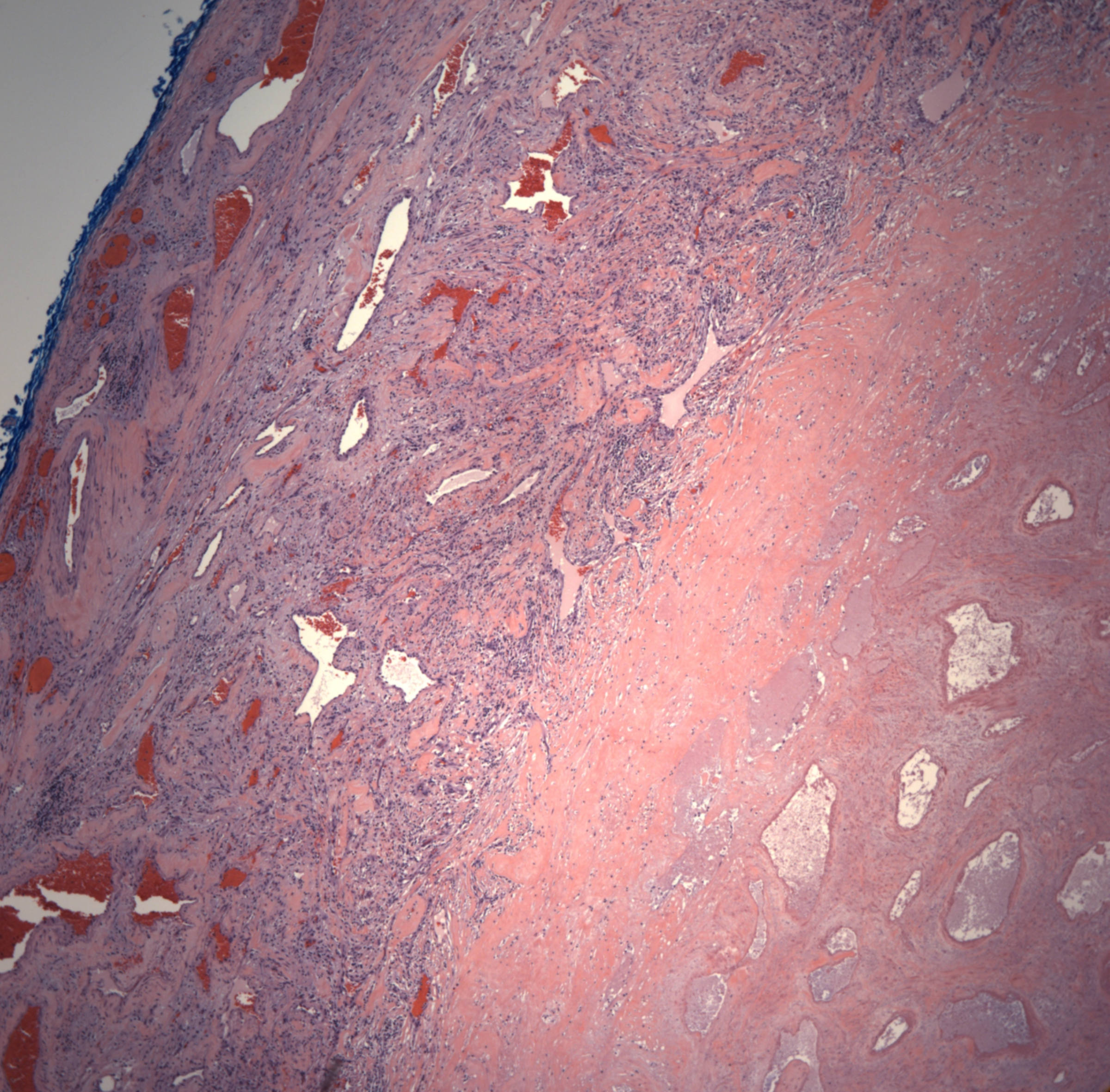
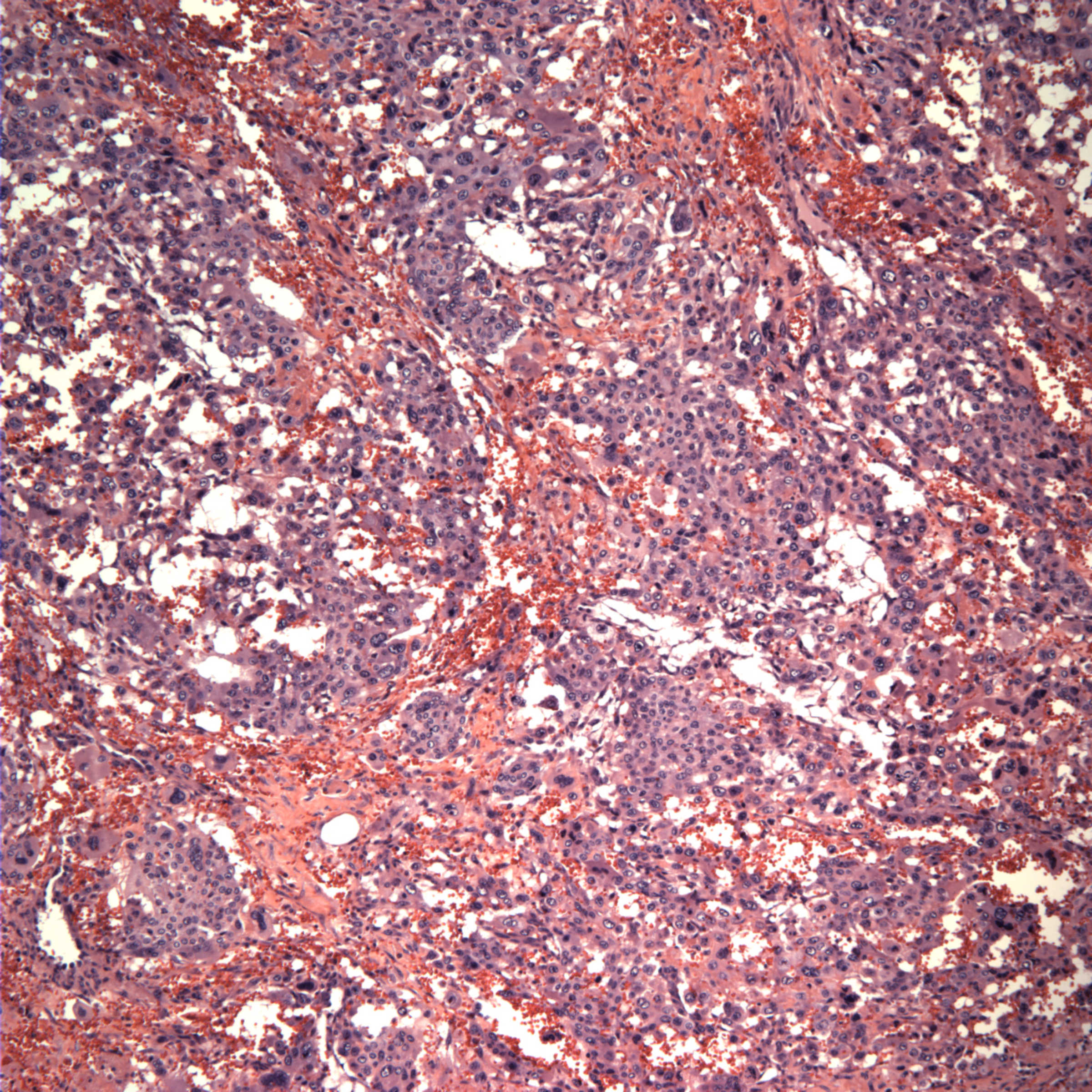
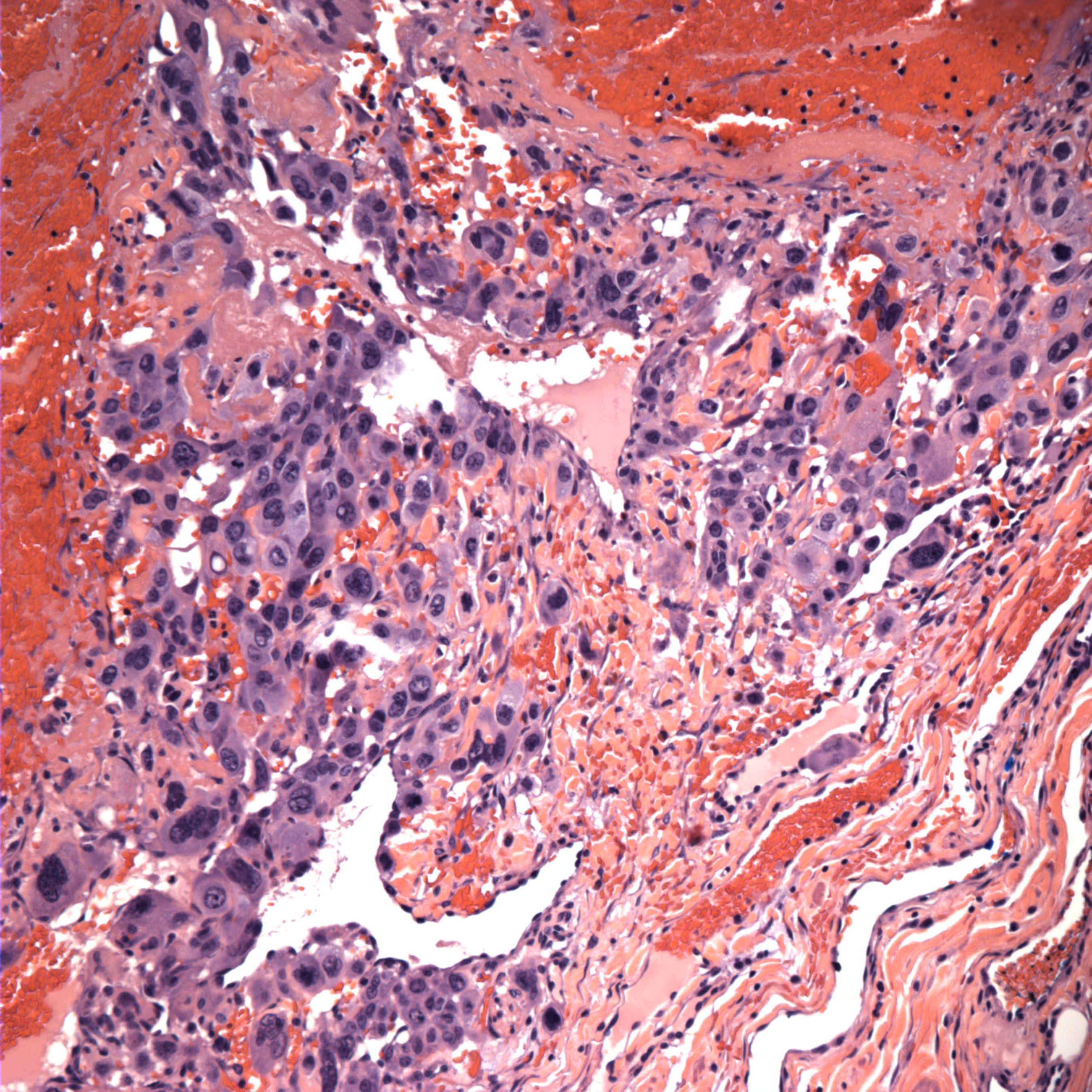
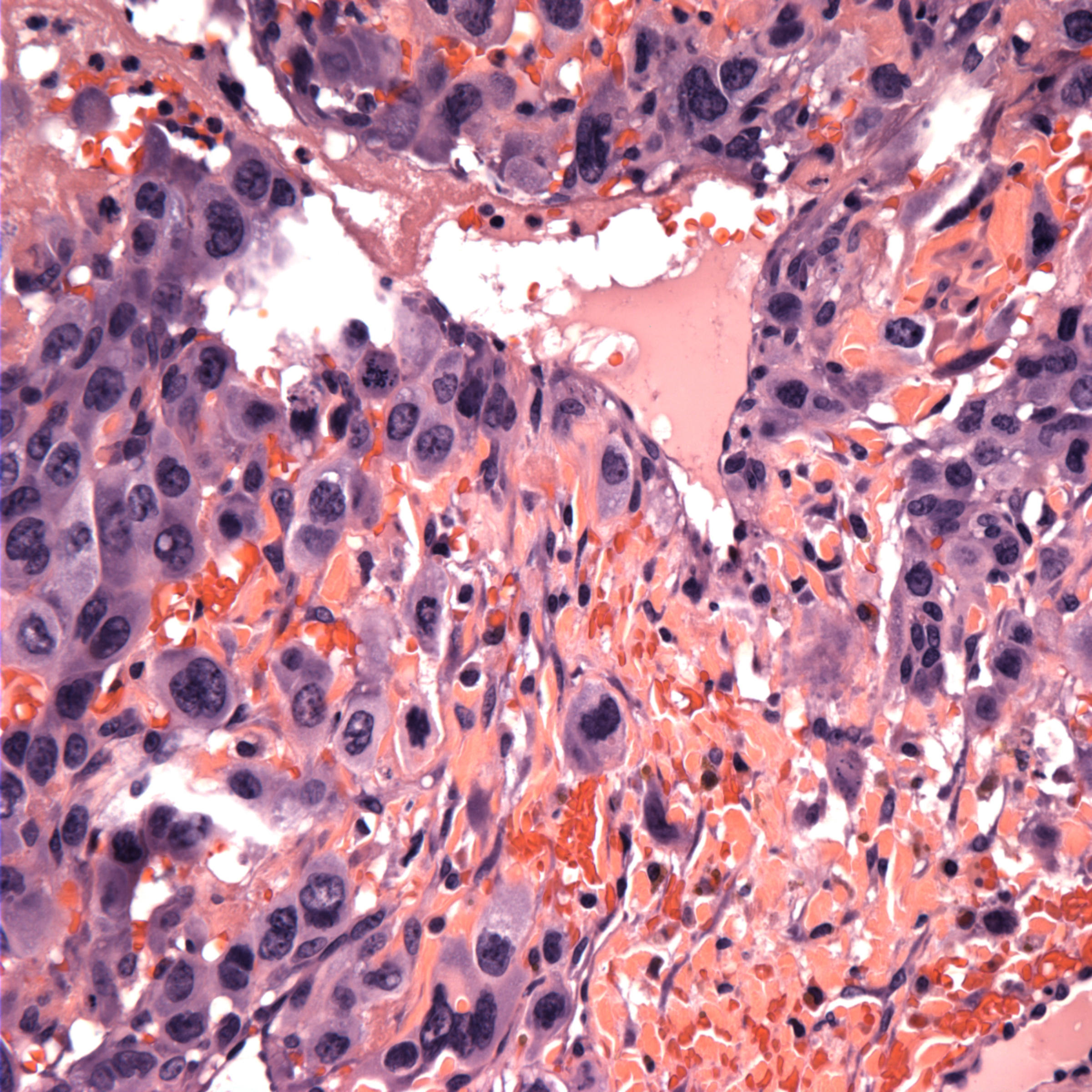
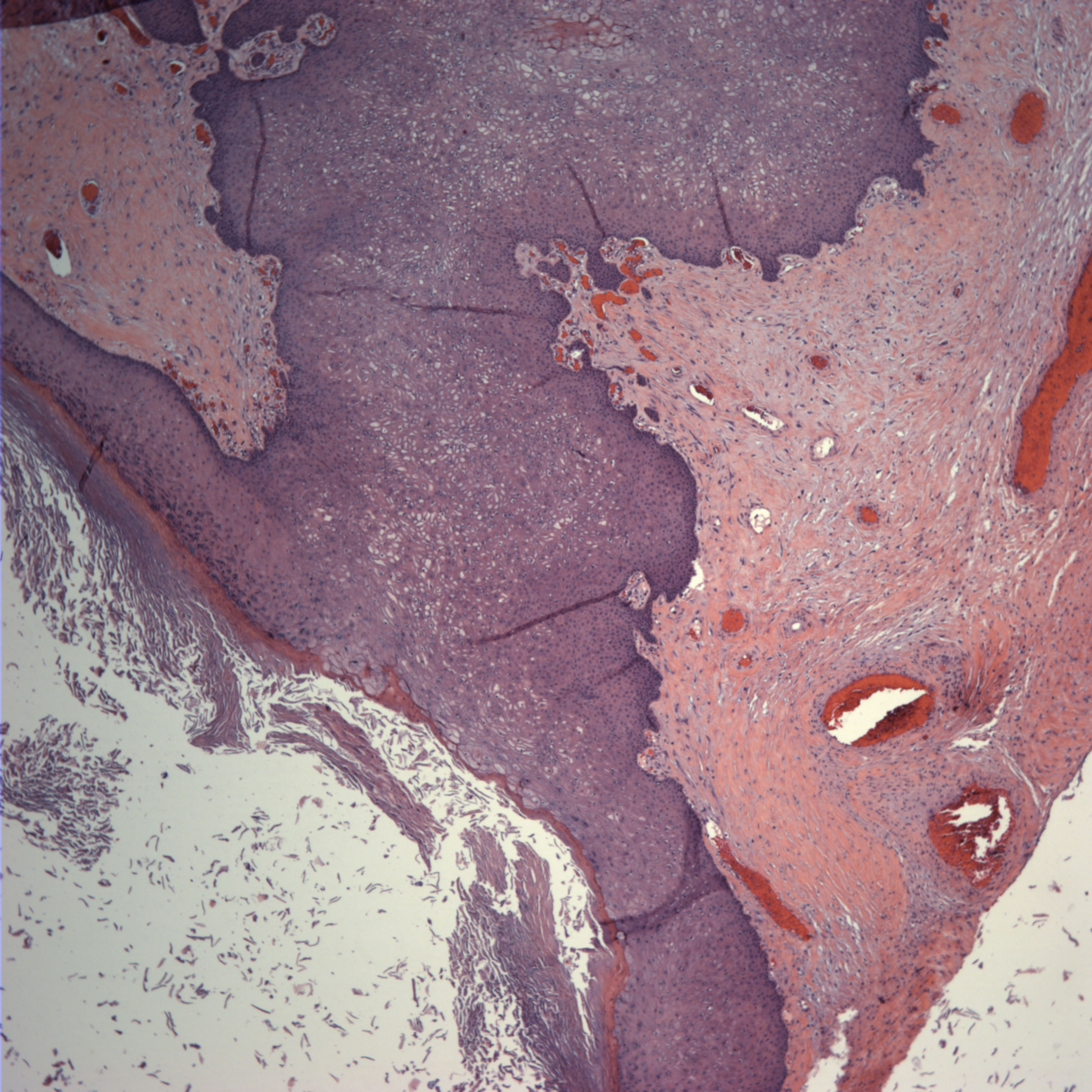
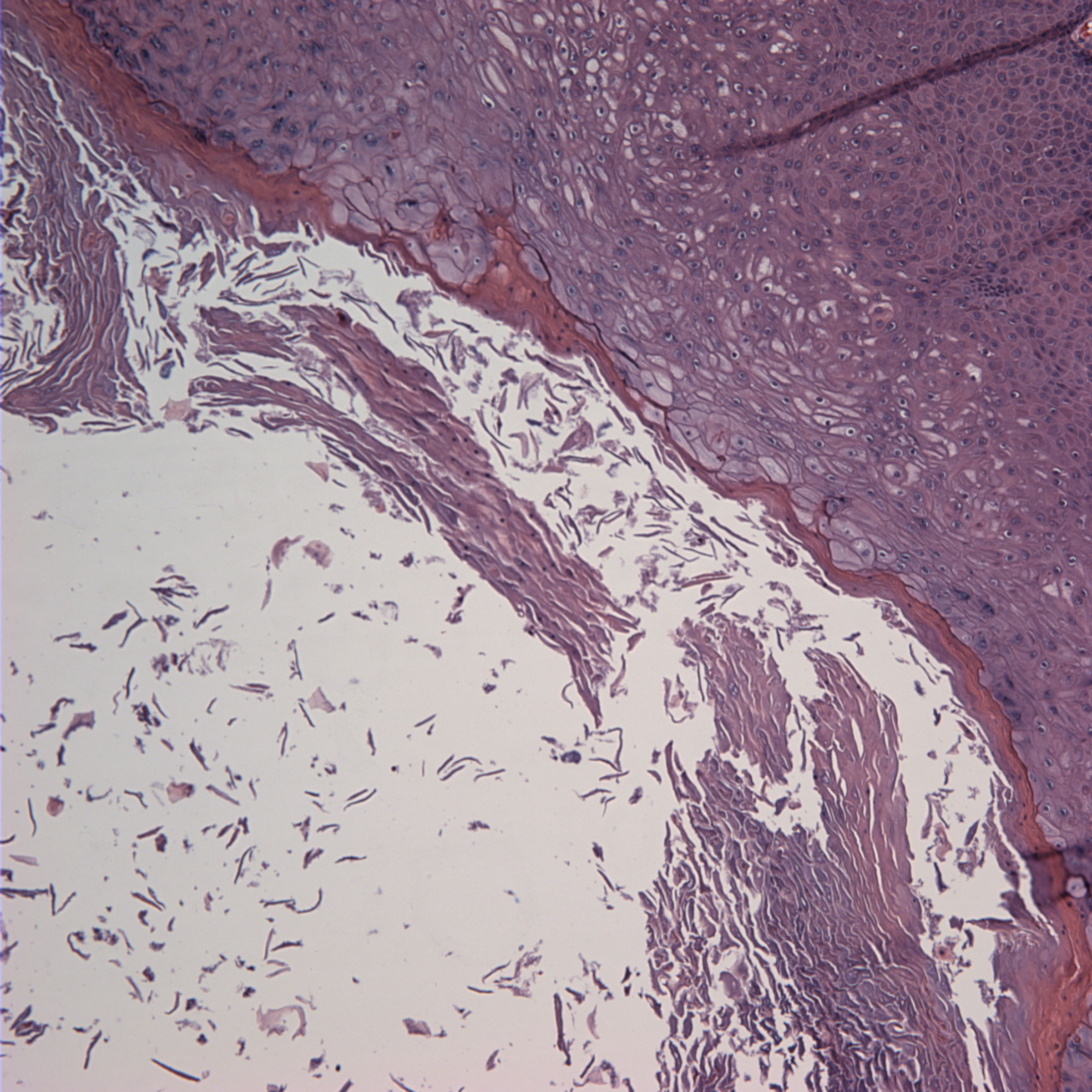
Microscopic images:
What is your diagnosis?
Diagnosis: Mixed malignant germ cell tumor; choriocarcinoma and mature teratoma
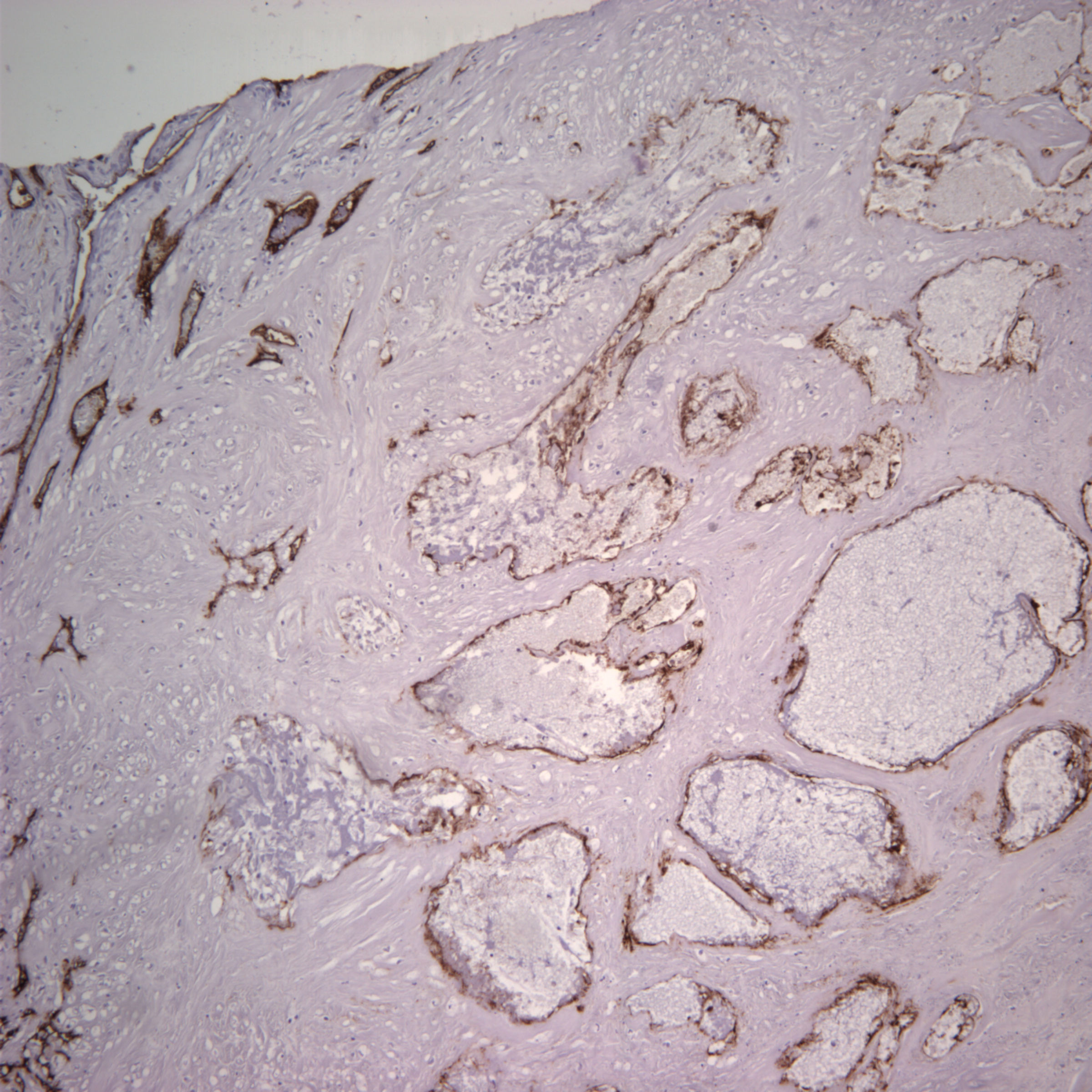
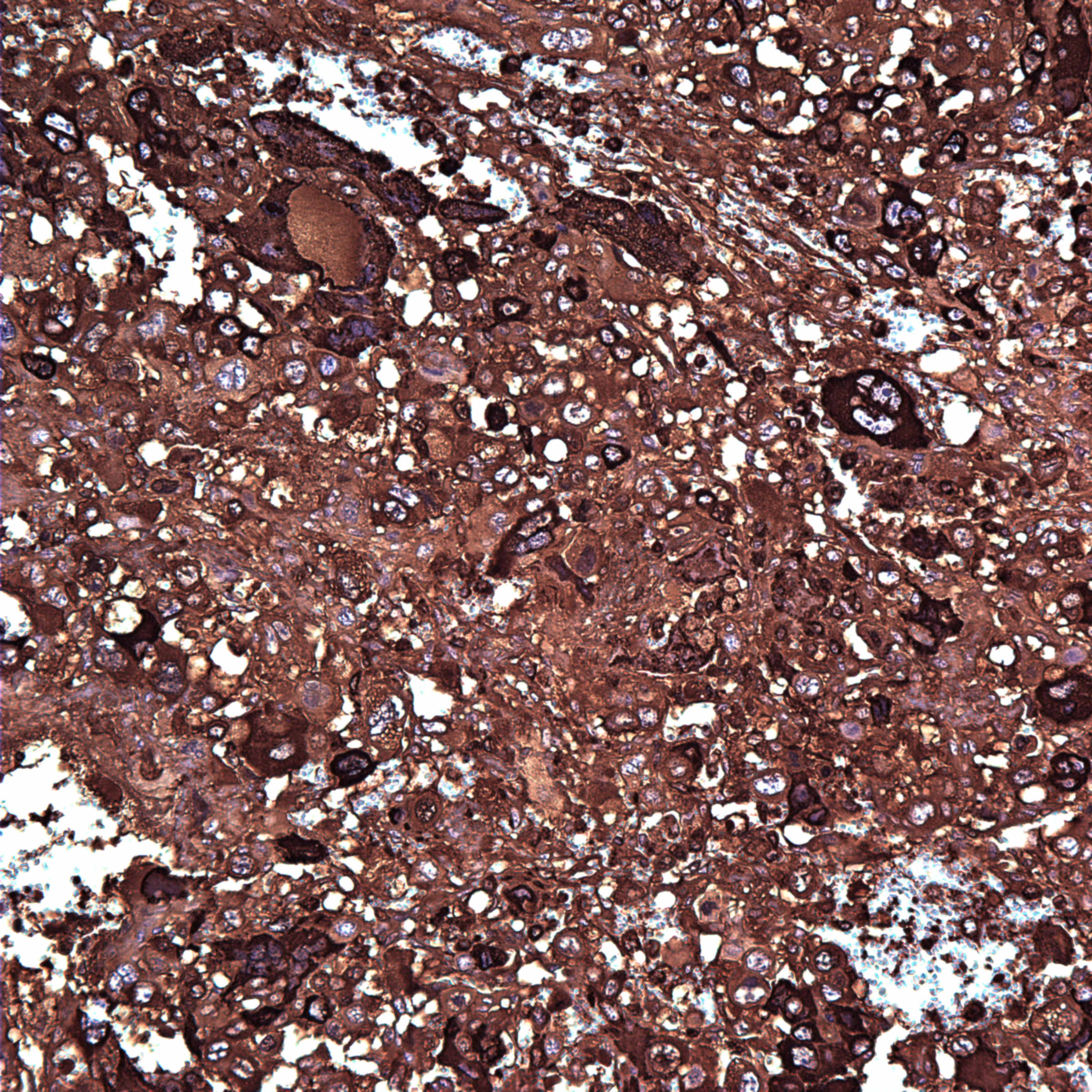
Immunostains:
Discussion:
Microscopic examination showed the mass to be a mixed malignant germ cell tumor consisting of choriocarcinoma (70%) and mature teratoma (30%). Angiolymphatic invasion is present, as shown on the CD34 stain. The choriocarcinoma component is highlighted with the beta hCG stain and is associated with extensive hemorrhagic necrosis. AFP is negative.
Ovarian choriocarcinoma is classified as gestational or nongestational. Tumors are definitively classified as nongestational only in a prepubertal patient (as in this case), in a woman unable to conceive or based on DNA analysis to determine if paternal DNA is present in the genome of the tumor.
Histologically, the tumor consists of a mixture of syncytiotrophoblastic and cytotrophoblastic elements in a hemorrhagic and necrotic background. Tumor cells are strongly immunoreactive for beta hCG and negative for AFP. However, these tumors are often part of a mixed germ cell tumor, which may contain components that are immunoreactive for AFP.
Nongestational choriocarcinoma is very rare. Historically, these tumors were usually fatal and unresponsive to chemotherapy. However, their prognosis has improved and it is currently unclear if their prognosis differs from the good prognosis of gestational choriocarcinoma (Int J Gynecol Cancer 2010;20:299, Gynecol Oncol 2001;80:262). Both types of choriocarcinoma have high levels of serum hCG and monitoring serum levels may be helpful in predicting recurrence.
In this case, at diagnosis, the beta hCG was 140,000. Radiologic evaluation for metastases was negative and the patient underwent 3 cycles of chemotherapy. 1 year after completing the therapeutic regimen, there was no evidence of recurrent or metastatic disease.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Kristin Olson, University of California, Los Angeles (USA), for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.

Best Practices for Anatomic Pathology Quality Management
June 16th at 12:00pm Eastern
Webinar Agenda:
- Anatomic Pathology issues and needs around QA and Peer Review
- External Demands: Standards Bodies (CAP and The Joint Commission) compliance
- Internal Demands: CMOs, Regulatory Affairs and PI demands for quality data
- Accurate Peer Reviews: Vetted details and automation
- QA for PAs, Histotechs, Transcriptionists, etc.
- Optimize your ability to provide accurate and timely diagnoses while improving QA
- Pathology Quality and Peer Review Mgmt. Best Practice: Example
- Discussion
Sponsored by AccuPathology: Pathology Quality Management Software
AccuCore Group
(267) 564-5015
http://www.accucoregroup.com
Website news:
(1) Congratulations to Dr. Pelin Bagci, Emory University (Atlanta, Georgia) and Dr. Teresita Zdunek, St. Joseph Hospital (Chicago, Illinois) for winning our Promotions contest. Each received a $25 Amazon.com gift card.
(2) For a "printer friendly page" of any part of our website, we recommend visiting http://www.printfriendly.com, which has options to print with or without images. As this works better than our "printer friendly" versions of chapters, we are removing the printer friendly versions as we update each chapter.
Visit and follow our Blog to see recent updates to the website.
(1) Congratulations to Dr. Pelin Bagci, Emory University (Atlanta, Georgia) and Dr. Teresita Zdunek, St. Joseph Hospital (Chicago, Illinois) for winning our Promotions contest. Each received a $25 Amazon.com gift card.
(2) For a "printer friendly page" of any part of our website, we recommend visiting http://www.printfriendly.com, which has options to print with or without images. As this works better than our "printer friendly" versions of chapters, we are removing the printer friendly versions as we update each chapter.
Visit and follow our Blog to see recent updates to the website.
Case #207
Clinical history:
An 8 year old girl presented to her primary care physician with precocious puberty. On physical examination, she had a large pelvic mass. The well circumscribed mass was resected. It weighed 413 grams and measured 13.5 x 9 x 6 cm. Sectioning demonstrated a variegated yellow-tan to red-brown cystic and hemorrhagic mass. One 2.5 cm cyst contained sebaceous material and scattered calcifications were identified.
Gross image:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Mixed malignant germ cell tumor; choriocarcinoma and mature teratoma
Immunostains:
Discussion:
Microscopic examination showed the mass to be a mixed malignant germ cell tumor consisting of choriocarcinoma (70%) and mature teratoma (30%). Angiolymphatic invasion is present, as shown on the CD34 stain. The choriocarcinoma component is highlighted with the beta hCG stain and is associated with extensive hemorrhagic necrosis. AFP is negative.
Ovarian choriocarcinoma is classified as gestational or nongestational. Tumors are definitively classified as nongestational only in a prepubertal patient (as in this case), in a woman unable to conceive or based on DNA analysis to determine if paternal DNA is present in the genome of the tumor.
Histologically, the tumor consists of a mixture of syncytiotrophoblastic and cytotrophoblastic elements in a hemorrhagic and necrotic background. Tumor cells are strongly immunoreactive for beta hCG and negative for AFP. However, these tumors are often part of a mixed germ cell tumor, which may contain components that are immunoreactive for AFP.
Nongestational choriocarcinoma is very rare. Historically, these tumors were usually fatal and unresponsive to chemotherapy. However, their prognosis has improved and it is currently unclear if their prognosis differs from the good prognosis of gestational choriocarcinoma (Int J Gynecol Cancer 2010;20:299, Gynecol Oncol 2001;80:262). Both types of choriocarcinoma have high levels of serum hCG and monitoring serum levels may be helpful in predicting recurrence.
In this case, at diagnosis, the beta hCG was 140,000. Radiologic evaluation for metastases was negative and the patient underwent 3 cycles of chemotherapy. 1 year after completing the therapeutic regimen, there was no evidence of recurrent or metastatic disease.